User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


DACA: Time to act
President Trump recently announced his decision to officially end the Deferred Action for Childhood Arrivals program, also known as DACA. The program has been controversial since its inception, almost as controversial as the decision to end it. What impact has DACA had on the medical community, including hospitalists, and what are the implications of ending it?
DACA is a program started in 2012 by an executive action under the Obama administration. The program currently protects approximately 800,000 undocumented immigrants in the United States from being deported. All DACA recipients were brought to this country illegally as children. When the DACA program began, in order to enroll, recipients had to prove that they had arrived to here before age 16, and that they had been living in the United States continuously since 2007. Once enrolled, the protections they receive from the program include the ability to legally work and to go to school, as well as obtain a social security number and driver’s license. These protections are then afforded for renewable 2-year periods of time.1
When Trump was elected, the controversy over continuing the DACA program accelerated. Understandably, the volume of applications rose substantially, with some estimating ~8,000 renewal requests being filed each week since the election. As such, many estimate the number of illegal immigrants affected by DACA has reached almost 1 million.1
One of the reasons the Trump administration feels compelled to dismantle the program is they contend that DACA is unconstitutional, as it was established purely by executive order. In the meantime, Trump is urging Congress to replace DACA with some type of equivalent legislation. According to his staffers, the dismantling of DACA means:
- No new applications will be accepted.
- All existing permits will be honored until they expire.
- All applications in process will continue to be processed.
They contend that no current DACA recipients will be affected before March 2018. Unfortunately for the Trump administration, this has been a very unpopular move, as two-thirds of Americans support allowing the Dreamers to stay in the United States.1
Impact on health care
The concern for the medical industry is that a “dismantling” of DACA could exacerbate an already existing physician shortage in the United States. For example, the Association of American Medical Colleges estimates the physician shortage will rise as the population ages and medical access increases; they currently estimate a physician shortage of approximately 40,000-104,000 by 2030.

But objectively evaluating the impact of the DACA program on the medical industry is difficult. We do know that most of the DACA recipients arrived from Mexico, El Salvador, Guatemala, and Honduras, as well as from Asia (primarily South Korea and the Philippines). We also know they reside in every state, with the largest numbers in California (222,795), Texas (124,300), New York (41,970), Illinois (42,376), and Florida (32,795). Most appear to be using DACA to work and to go to school; in a recent survey, 91% were employed, and 45% were enrolled in school.1
Pertaining specifically to medical school, during the 2016-2017 school year, there were 113 DACA applicants to U.S. medical schools, 65 of which were accepted and enrolled. The AAMC expects the 2017-2018 enrollment to be even higher. Almost half of medical school enrollees attend Loyola University Chicago, Maywood, Ill.; this year alone, Loyola Stritch Medical School enrolled 32 DACA medical students. This is because, in 2013, Loyola was the first medical school nationwide to openly accept students with DACA status. They did this by creating a mechanism for DACA medical students to get student loans.
One of the biggest challenges for DACA students is paying for school, as they are not eligible for federal student loans. To remove this barrier, Loyola created a loan program through the Illinois Finance Authority, which offers interest-free loans to DACA students if they commit to paying back the principal and working after medical school for 4 years in an underserved area in Illinois. It is clear that no medical school in the country will feel the effects of the DACA dismantling more than will Loyola.3
Another unintended issue that the dismantling of DACA can have on the medical industry is the temptation for undocumented immigrants to avoid seeking medical care, for fear of being discovered and deported. Such delays in seeking care can result in these patients presenting with significant and expensive medical issues.
So what are the options for Congress and what is the likely fate of these DACA recipients whose lives have been placed in limbo? Proposals introduced to date include:
- The Bridge Act, which effectively extends the present DACA program by 3 years.
- Recognizing America’s Children Act, which would allow people who meet DACA eligibility criteria to apply for conditional permanent residence with a path toward citizenship.
- The American Hope Act and updated DREAM Act, both of which propose broader eligibility criteria and faster pathways to citizenship.4
There is great hope that some definitive action can be employed by Congress, as most legislators on both sides of the aisle have expressed some support for at least one of the proposed policies (although that certainly does not guarantee sufficient votes to pass). There also is support from many Americans, given that most DACA recipients have been productive members of society, and most Americans believe that DACA recipients should not be held accountable “for the sins of their parents.”4
It appears that the dismantling of DACA would be quite unsettling and certainly would affect some areas of the country more severely than others. Regardless of political stance, everyone can agree that Congress needs to do something, as the ambiguity and uncertainty caused by a million undocumented immigrants living and working in the United States cannot be ignored or indefinitely deferred. Any of the above options that offer a pathway to citizenship would be welcomed by most Americans. Having Dreamers in limbo is bad for everyone; the time to act is now.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1. http://www.npr.org/2017/09/05/548754723/5-things-you-should-know-about-daca
2. https://www.forbes.com/sites/brucejapsen/2017/09/05/how-trumps-move-to-end-daca-worsens-the-doctor-shortage/#5143320d5b06
3. http://www.chicagomag.com/city-life/September-2017/DACA-Stritch-Medical-School/
4. http://www.nejm.org/doi/full/10.1056/NEJMp1711416?query=TOC
President Trump recently announced his decision to officially end the Deferred Action for Childhood Arrivals program, also known as DACA. The program has been controversial since its inception, almost as controversial as the decision to end it. What impact has DACA had on the medical community, including hospitalists, and what are the implications of ending it?
DACA is a program started in 2012 by an executive action under the Obama administration. The program currently protects approximately 800,000 undocumented immigrants in the United States from being deported. All DACA recipients were brought to this country illegally as children. When the DACA program began, in order to enroll, recipients had to prove that they had arrived to here before age 16, and that they had been living in the United States continuously since 2007. Once enrolled, the protections they receive from the program include the ability to legally work and to go to school, as well as obtain a social security number and driver’s license. These protections are then afforded for renewable 2-year periods of time.1
When Trump was elected, the controversy over continuing the DACA program accelerated. Understandably, the volume of applications rose substantially, with some estimating ~8,000 renewal requests being filed each week since the election. As such, many estimate the number of illegal immigrants affected by DACA has reached almost 1 million.1
One of the reasons the Trump administration feels compelled to dismantle the program is they contend that DACA is unconstitutional, as it was established purely by executive order. In the meantime, Trump is urging Congress to replace DACA with some type of equivalent legislation. According to his staffers, the dismantling of DACA means:
- No new applications will be accepted.
- All existing permits will be honored until they expire.
- All applications in process will continue to be processed.
They contend that no current DACA recipients will be affected before March 2018. Unfortunately for the Trump administration, this has been a very unpopular move, as two-thirds of Americans support allowing the Dreamers to stay in the United States.1
Impact on health care
The concern for the medical industry is that a “dismantling” of DACA could exacerbate an already existing physician shortage in the United States. For example, the Association of American Medical Colleges estimates the physician shortage will rise as the population ages and medical access increases; they currently estimate a physician shortage of approximately 40,000-104,000 by 2030.

But objectively evaluating the impact of the DACA program on the medical industry is difficult. We do know that most of the DACA recipients arrived from Mexico, El Salvador, Guatemala, and Honduras, as well as from Asia (primarily South Korea and the Philippines). We also know they reside in every state, with the largest numbers in California (222,795), Texas (124,300), New York (41,970), Illinois (42,376), and Florida (32,795). Most appear to be using DACA to work and to go to school; in a recent survey, 91% were employed, and 45% were enrolled in school.1
Pertaining specifically to medical school, during the 2016-2017 school year, there were 113 DACA applicants to U.S. medical schools, 65 of which were accepted and enrolled. The AAMC expects the 2017-2018 enrollment to be even higher. Almost half of medical school enrollees attend Loyola University Chicago, Maywood, Ill.; this year alone, Loyola Stritch Medical School enrolled 32 DACA medical students. This is because, in 2013, Loyola was the first medical school nationwide to openly accept students with DACA status. They did this by creating a mechanism for DACA medical students to get student loans.
One of the biggest challenges for DACA students is paying for school, as they are not eligible for federal student loans. To remove this barrier, Loyola created a loan program through the Illinois Finance Authority, which offers interest-free loans to DACA students if they commit to paying back the principal and working after medical school for 4 years in an underserved area in Illinois. It is clear that no medical school in the country will feel the effects of the DACA dismantling more than will Loyola.3
Another unintended issue that the dismantling of DACA can have on the medical industry is the temptation for undocumented immigrants to avoid seeking medical care, for fear of being discovered and deported. Such delays in seeking care can result in these patients presenting with significant and expensive medical issues.
So what are the options for Congress and what is the likely fate of these DACA recipients whose lives have been placed in limbo? Proposals introduced to date include:
- The Bridge Act, which effectively extends the present DACA program by 3 years.
- Recognizing America’s Children Act, which would allow people who meet DACA eligibility criteria to apply for conditional permanent residence with a path toward citizenship.
- The American Hope Act and updated DREAM Act, both of which propose broader eligibility criteria and faster pathways to citizenship.4
There is great hope that some definitive action can be employed by Congress, as most legislators on both sides of the aisle have expressed some support for at least one of the proposed policies (although that certainly does not guarantee sufficient votes to pass). There also is support from many Americans, given that most DACA recipients have been productive members of society, and most Americans believe that DACA recipients should not be held accountable “for the sins of their parents.”4
It appears that the dismantling of DACA would be quite unsettling and certainly would affect some areas of the country more severely than others. Regardless of political stance, everyone can agree that Congress needs to do something, as the ambiguity and uncertainty caused by a million undocumented immigrants living and working in the United States cannot be ignored or indefinitely deferred. Any of the above options that offer a pathway to citizenship would be welcomed by most Americans. Having Dreamers in limbo is bad for everyone; the time to act is now.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1. http://www.npr.org/2017/09/05/548754723/5-things-you-should-know-about-daca
2. https://www.forbes.com/sites/brucejapsen/2017/09/05/how-trumps-move-to-end-daca-worsens-the-doctor-shortage/#5143320d5b06
3. http://www.chicagomag.com/city-life/September-2017/DACA-Stritch-Medical-School/
4. http://www.nejm.org/doi/full/10.1056/NEJMp1711416?query=TOC
President Trump recently announced his decision to officially end the Deferred Action for Childhood Arrivals program, also known as DACA. The program has been controversial since its inception, almost as controversial as the decision to end it. What impact has DACA had on the medical community, including hospitalists, and what are the implications of ending it?
DACA is a program started in 2012 by an executive action under the Obama administration. The program currently protects approximately 800,000 undocumented immigrants in the United States from being deported. All DACA recipients were brought to this country illegally as children. When the DACA program began, in order to enroll, recipients had to prove that they had arrived to here before age 16, and that they had been living in the United States continuously since 2007. Once enrolled, the protections they receive from the program include the ability to legally work and to go to school, as well as obtain a social security number and driver’s license. These protections are then afforded for renewable 2-year periods of time.1
When Trump was elected, the controversy over continuing the DACA program accelerated. Understandably, the volume of applications rose substantially, with some estimating ~8,000 renewal requests being filed each week since the election. As such, many estimate the number of illegal immigrants affected by DACA has reached almost 1 million.1
One of the reasons the Trump administration feels compelled to dismantle the program is they contend that DACA is unconstitutional, as it was established purely by executive order. In the meantime, Trump is urging Congress to replace DACA with some type of equivalent legislation. According to his staffers, the dismantling of DACA means:
- No new applications will be accepted.
- All existing permits will be honored until they expire.
- All applications in process will continue to be processed.
They contend that no current DACA recipients will be affected before March 2018. Unfortunately for the Trump administration, this has been a very unpopular move, as two-thirds of Americans support allowing the Dreamers to stay in the United States.1
Impact on health care
The concern for the medical industry is that a “dismantling” of DACA could exacerbate an already existing physician shortage in the United States. For example, the Association of American Medical Colleges estimates the physician shortage will rise as the population ages and medical access increases; they currently estimate a physician shortage of approximately 40,000-104,000 by 2030.

But objectively evaluating the impact of the DACA program on the medical industry is difficult. We do know that most of the DACA recipients arrived from Mexico, El Salvador, Guatemala, and Honduras, as well as from Asia (primarily South Korea and the Philippines). We also know they reside in every state, with the largest numbers in California (222,795), Texas (124,300), New York (41,970), Illinois (42,376), and Florida (32,795). Most appear to be using DACA to work and to go to school; in a recent survey, 91% were employed, and 45% were enrolled in school.1
Pertaining specifically to medical school, during the 2016-2017 school year, there were 113 DACA applicants to U.S. medical schools, 65 of which were accepted and enrolled. The AAMC expects the 2017-2018 enrollment to be even higher. Almost half of medical school enrollees attend Loyola University Chicago, Maywood, Ill.; this year alone, Loyola Stritch Medical School enrolled 32 DACA medical students. This is because, in 2013, Loyola was the first medical school nationwide to openly accept students with DACA status. They did this by creating a mechanism for DACA medical students to get student loans.
One of the biggest challenges for DACA students is paying for school, as they are not eligible for federal student loans. To remove this barrier, Loyola created a loan program through the Illinois Finance Authority, which offers interest-free loans to DACA students if they commit to paying back the principal and working after medical school for 4 years in an underserved area in Illinois. It is clear that no medical school in the country will feel the effects of the DACA dismantling more than will Loyola.3
Another unintended issue that the dismantling of DACA can have on the medical industry is the temptation for undocumented immigrants to avoid seeking medical care, for fear of being discovered and deported. Such delays in seeking care can result in these patients presenting with significant and expensive medical issues.
So what are the options for Congress and what is the likely fate of these DACA recipients whose lives have been placed in limbo? Proposals introduced to date include:
- The Bridge Act, which effectively extends the present DACA program by 3 years.
- Recognizing America’s Children Act, which would allow people who meet DACA eligibility criteria to apply for conditional permanent residence with a path toward citizenship.
- The American Hope Act and updated DREAM Act, both of which propose broader eligibility criteria and faster pathways to citizenship.4
There is great hope that some definitive action can be employed by Congress, as most legislators on both sides of the aisle have expressed some support for at least one of the proposed policies (although that certainly does not guarantee sufficient votes to pass). There also is support from many Americans, given that most DACA recipients have been productive members of society, and most Americans believe that DACA recipients should not be held accountable “for the sins of their parents.”4
It appears that the dismantling of DACA would be quite unsettling and certainly would affect some areas of the country more severely than others. Regardless of political stance, everyone can agree that Congress needs to do something, as the ambiguity and uncertainty caused by a million undocumented immigrants living and working in the United States cannot be ignored or indefinitely deferred. Any of the above options that offer a pathway to citizenship would be welcomed by most Americans. Having Dreamers in limbo is bad for everyone; the time to act is now.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1. http://www.npr.org/2017/09/05/548754723/5-things-you-should-know-about-daca
2. https://www.forbes.com/sites/brucejapsen/2017/09/05/how-trumps-move-to-end-daca-worsens-the-doctor-shortage/#5143320d5b06
3. http://www.chicagomag.com/city-life/September-2017/DACA-Stritch-Medical-School/
4. http://www.nejm.org/doi/full/10.1056/NEJMp1711416?query=TOC
Renal dosing of non–vitamin K antagonist oral anticoagulants in atrial fibrillation is important in preventing thrombotic and bleeding complications
Clinical question: Does renal underdosing and overdosing of non–vitamin K antagonist oral anticoagulants (NOACs) impact the risk of thrombotic and bleeding complications?
Background: All of the NOACs have at least partial renal clearance, but compliance with Food and Drug Administration–labeled renal dosing recommendations is inconsistent. This study examines the risk of adverse thrombotic and bleeding events in patients with improper anticoagulant dosing.
Study design: Retrospective cohort study.
Setting: United States (OptumLabs data warehouse, a database of over 100 million patients hospitalized in the United States in the last 20 years).
Synopsis: With use of data from the OptumLabs data warehouse of privately insured and Medicare Advantage enrollees, 14,865 patients with nonvalvular atrial fibrillation who were started on NOACs (apixaban, dabigatran, or rivaroxaban) were identified. Creatinine values within the year before treatment were used to calculate an estimated glomerular filtration rate (eGFR).
Of patients qualifying for renal dose reduction, 43% received the standard dosing (overdose). Of patients not qualifying for renal dose reduction, 13% received a reduced dose (underdose). The overdosed group had a higher rate of bleeding events, compared with controls (hazard ratio, 2.19; 95% CI, 1.07-4.46). The underdosed group had a higher rate of stroke (HR, 4.87; 95% CI, 1.30-18.26).
Bottom line: Excessive dosing of NOACs in patients with renal insufficiency is common and is associated with bleeding.Citation: Yao X, Shah ND, Sangaralingham LR, Gersh BJ, and Noseworthy PA. Non–vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. JACC. 2017;69(23):2779-90.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does renal underdosing and overdosing of non–vitamin K antagonist oral anticoagulants (NOACs) impact the risk of thrombotic and bleeding complications?
Background: All of the NOACs have at least partial renal clearance, but compliance with Food and Drug Administration–labeled renal dosing recommendations is inconsistent. This study examines the risk of adverse thrombotic and bleeding events in patients with improper anticoagulant dosing.
Study design: Retrospective cohort study.
Setting: United States (OptumLabs data warehouse, a database of over 100 million patients hospitalized in the United States in the last 20 years).
Synopsis: With use of data from the OptumLabs data warehouse of privately insured and Medicare Advantage enrollees, 14,865 patients with nonvalvular atrial fibrillation who were started on NOACs (apixaban, dabigatran, or rivaroxaban) were identified. Creatinine values within the year before treatment were used to calculate an estimated glomerular filtration rate (eGFR).
Of patients qualifying for renal dose reduction, 43% received the standard dosing (overdose). Of patients not qualifying for renal dose reduction, 13% received a reduced dose (underdose). The overdosed group had a higher rate of bleeding events, compared with controls (hazard ratio, 2.19; 95% CI, 1.07-4.46). The underdosed group had a higher rate of stroke (HR, 4.87; 95% CI, 1.30-18.26).
Bottom line: Excessive dosing of NOACs in patients with renal insufficiency is common and is associated with bleeding.Citation: Yao X, Shah ND, Sangaralingham LR, Gersh BJ, and Noseworthy PA. Non–vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. JACC. 2017;69(23):2779-90.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does renal underdosing and overdosing of non–vitamin K antagonist oral anticoagulants (NOACs) impact the risk of thrombotic and bleeding complications?
Background: All of the NOACs have at least partial renal clearance, but compliance with Food and Drug Administration–labeled renal dosing recommendations is inconsistent. This study examines the risk of adverse thrombotic and bleeding events in patients with improper anticoagulant dosing.
Study design: Retrospective cohort study.
Setting: United States (OptumLabs data warehouse, a database of over 100 million patients hospitalized in the United States in the last 20 years).
Synopsis: With use of data from the OptumLabs data warehouse of privately insured and Medicare Advantage enrollees, 14,865 patients with nonvalvular atrial fibrillation who were started on NOACs (apixaban, dabigatran, or rivaroxaban) were identified. Creatinine values within the year before treatment were used to calculate an estimated glomerular filtration rate (eGFR).
Of patients qualifying for renal dose reduction, 43% received the standard dosing (overdose). Of patients not qualifying for renal dose reduction, 13% received a reduced dose (underdose). The overdosed group had a higher rate of bleeding events, compared with controls (hazard ratio, 2.19; 95% CI, 1.07-4.46). The underdosed group had a higher rate of stroke (HR, 4.87; 95% CI, 1.30-18.26).
Bottom line: Excessive dosing of NOACs in patients with renal insufficiency is common and is associated with bleeding.Citation: Yao X, Shah ND, Sangaralingham LR, Gersh BJ, and Noseworthy PA. Non–vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. JACC. 2017;69(23):2779-90.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
CABG and PCI with drug-eluting stents for left main coronary disease have superior outcomes to medical therapy alone
Clinical question: Does coronary artery bypass grafting (CABG) have superior mortality outcomes to percutaneous coronary intervention (PCI) for left main coronary disease, and how do these interventions compare with medical therapy alone?
Background: Optimal therapy for left main coronary disease is a highly researched topic with CABG having been standard therapy of choice for several decades. However, most studies have not included data comparing CABG to newer drug-eluting stent (DES) generations and no studies have directly compared PCI with DES to medical therapy alone (MTA).
Study design: Meta-analysis.
Setting: Largely European acute care hospitals as well as some VA hospitals.
Synopsis: With PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a review of PubMed and Cochrane databases was conducted, yielding eight RCTs, including a total of 4,850 patients. Six of the RCTs compared CABG with DES, while two compared CABG with MTA. Network meta-analysis was used to compare DES with MTA. At 5 years there were no differences in all-cause mortality between CABG and DES groups (RR, 0.94; 95% CI, 0.68-1.32), though both groups had lower mortality than MTA (RR, 0.21; 95% CI, 0.09-0.47 for CABG vs. MTA and RR, 0.20; 95% CI, 0.08-0.46 for DES vs MTA).
PCI did have higher risk of revascularization at 5 years (RR, 1.68; 95% CI, 1.36-2.08) and lower risk of stroke at 1 year (RR, 0.21; 95% CI, 0.07-0.63), compared with CABG, suggesting younger patients might prefer CABG to avoid revascularization, and older patients may prefer PCI to avoid postprocedural morbidity.
Bottom line: For patients with left main disease, CABG and PCI with DES appear equally effective with regards to prevention of all-cause mortality and both are superior to MTA.
Citation: Shah R, Morsy MS, Weiman DS, and Vetrovec GW. Meta-analysis comparing coronary artery bypass grafting to drug-eluting stents. Am J Cardiol. 2017;120:63-8.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does coronary artery bypass grafting (CABG) have superior mortality outcomes to percutaneous coronary intervention (PCI) for left main coronary disease, and how do these interventions compare with medical therapy alone?
Background: Optimal therapy for left main coronary disease is a highly researched topic with CABG having been standard therapy of choice for several decades. However, most studies have not included data comparing CABG to newer drug-eluting stent (DES) generations and no studies have directly compared PCI with DES to medical therapy alone (MTA).
Study design: Meta-analysis.
Setting: Largely European acute care hospitals as well as some VA hospitals.
Synopsis: With PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a review of PubMed and Cochrane databases was conducted, yielding eight RCTs, including a total of 4,850 patients. Six of the RCTs compared CABG with DES, while two compared CABG with MTA. Network meta-analysis was used to compare DES with MTA. At 5 years there were no differences in all-cause mortality between CABG and DES groups (RR, 0.94; 95% CI, 0.68-1.32), though both groups had lower mortality than MTA (RR, 0.21; 95% CI, 0.09-0.47 for CABG vs. MTA and RR, 0.20; 95% CI, 0.08-0.46 for DES vs MTA).
PCI did have higher risk of revascularization at 5 years (RR, 1.68; 95% CI, 1.36-2.08) and lower risk of stroke at 1 year (RR, 0.21; 95% CI, 0.07-0.63), compared with CABG, suggesting younger patients might prefer CABG to avoid revascularization, and older patients may prefer PCI to avoid postprocedural morbidity.
Bottom line: For patients with left main disease, CABG and PCI with DES appear equally effective with regards to prevention of all-cause mortality and both are superior to MTA.
Citation: Shah R, Morsy MS, Weiman DS, and Vetrovec GW. Meta-analysis comparing coronary artery bypass grafting to drug-eluting stents. Am J Cardiol. 2017;120:63-8.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does coronary artery bypass grafting (CABG) have superior mortality outcomes to percutaneous coronary intervention (PCI) for left main coronary disease, and how do these interventions compare with medical therapy alone?
Background: Optimal therapy for left main coronary disease is a highly researched topic with CABG having been standard therapy of choice for several decades. However, most studies have not included data comparing CABG to newer drug-eluting stent (DES) generations and no studies have directly compared PCI with DES to medical therapy alone (MTA).
Study design: Meta-analysis.
Setting: Largely European acute care hospitals as well as some VA hospitals.
Synopsis: With PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a review of PubMed and Cochrane databases was conducted, yielding eight RCTs, including a total of 4,850 patients. Six of the RCTs compared CABG with DES, while two compared CABG with MTA. Network meta-analysis was used to compare DES with MTA. At 5 years there were no differences in all-cause mortality between CABG and DES groups (RR, 0.94; 95% CI, 0.68-1.32), though both groups had lower mortality than MTA (RR, 0.21; 95% CI, 0.09-0.47 for CABG vs. MTA and RR, 0.20; 95% CI, 0.08-0.46 for DES vs MTA).
PCI did have higher risk of revascularization at 5 years (RR, 1.68; 95% CI, 1.36-2.08) and lower risk of stroke at 1 year (RR, 0.21; 95% CI, 0.07-0.63), compared with CABG, suggesting younger patients might prefer CABG to avoid revascularization, and older patients may prefer PCI to avoid postprocedural morbidity.
Bottom line: For patients with left main disease, CABG and PCI with DES appear equally effective with regards to prevention of all-cause mortality and both are superior to MTA.
Citation: Shah R, Morsy MS, Weiman DS, and Vetrovec GW. Meta-analysis comparing coronary artery bypass grafting to drug-eluting stents. Am J Cardiol. 2017;120:63-8.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Antiplatelet therapy can be continued through surgery without increased risk of reintervention for bleeding
Clinical question: Does continuing antiplatelet therapy through noncardiac surgery increase the risk of postoperative blood transfusion or surgical reintervention for bleeding?
Background: Many prior studies have analyzed the risks and benefits of holding versus continuing antiplatelet therapy in the perioperative setting, but heterogeneity in outcome reporting has limited the ability to compare and contrast studies.
Study design: Meta-analysis.
Setting: Both domestic and international studies were included in the meta-analysis.
Synopsis: With a MEDLINE search, 37 studies with over 30,000 patients total were identified and included in the meta-analysis. Studies compared outcomes of transfusion and surgical reintervention for bleeding in patients receiving noncardiac surgery. Patients were either on no antiplatelet therapy, single therapy, or dual-antiplatelet therapy (DAPT). Relative risk of transfusion escalated in proportion to the amount of antiplatelet therapy; there was a 14% increased risk (95% confidence interval, 1.03-1.26) with aspirin over control and a 33% (95% CI, 1.15-1.55) increased risk with DAPT over control.
Risk of surgical reintervention for bleeding, however, was not increased above control whether on aspirin (relative risk, 0.96; 95% CI, 0.76-1.22), clopidogrel (RR, 1.84; 95% CI, 0.87-3.87), or DAPT (RR, 1.51; (95% CI, 0.92-2.49).
Bottom line: In noncardiac surgery, continuing aspirin or DAPT perioperatively increases the need for transfusion, but not the need for surgical reintervention for bleeding.
Citation: Columbo JA, Lambour AJ, Sundling RA, et. al. A meta-analysis of the impact of aspirin, clopidogrel, and dual-antiplatelet therapy on bleeding complications in noncardiac surgery. Ann Surg. 2017;20(20):1-9.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does continuing antiplatelet therapy through noncardiac surgery increase the risk of postoperative blood transfusion or surgical reintervention for bleeding?
Background: Many prior studies have analyzed the risks and benefits of holding versus continuing antiplatelet therapy in the perioperative setting, but heterogeneity in outcome reporting has limited the ability to compare and contrast studies.
Study design: Meta-analysis.
Setting: Both domestic and international studies were included in the meta-analysis.
Synopsis: With a MEDLINE search, 37 studies with over 30,000 patients total were identified and included in the meta-analysis. Studies compared outcomes of transfusion and surgical reintervention for bleeding in patients receiving noncardiac surgery. Patients were either on no antiplatelet therapy, single therapy, or dual-antiplatelet therapy (DAPT). Relative risk of transfusion escalated in proportion to the amount of antiplatelet therapy; there was a 14% increased risk (95% confidence interval, 1.03-1.26) with aspirin over control and a 33% (95% CI, 1.15-1.55) increased risk with DAPT over control.
Risk of surgical reintervention for bleeding, however, was not increased above control whether on aspirin (relative risk, 0.96; 95% CI, 0.76-1.22), clopidogrel (RR, 1.84; 95% CI, 0.87-3.87), or DAPT (RR, 1.51; (95% CI, 0.92-2.49).
Bottom line: In noncardiac surgery, continuing aspirin or DAPT perioperatively increases the need for transfusion, but not the need for surgical reintervention for bleeding.
Citation: Columbo JA, Lambour AJ, Sundling RA, et. al. A meta-analysis of the impact of aspirin, clopidogrel, and dual-antiplatelet therapy on bleeding complications in noncardiac surgery. Ann Surg. 2017;20(20):1-9.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does continuing antiplatelet therapy through noncardiac surgery increase the risk of postoperative blood transfusion or surgical reintervention for bleeding?
Background: Many prior studies have analyzed the risks and benefits of holding versus continuing antiplatelet therapy in the perioperative setting, but heterogeneity in outcome reporting has limited the ability to compare and contrast studies.
Study design: Meta-analysis.
Setting: Both domestic and international studies were included in the meta-analysis.
Synopsis: With a MEDLINE search, 37 studies with over 30,000 patients total were identified and included in the meta-analysis. Studies compared outcomes of transfusion and surgical reintervention for bleeding in patients receiving noncardiac surgery. Patients were either on no antiplatelet therapy, single therapy, or dual-antiplatelet therapy (DAPT). Relative risk of transfusion escalated in proportion to the amount of antiplatelet therapy; there was a 14% increased risk (95% confidence interval, 1.03-1.26) with aspirin over control and a 33% (95% CI, 1.15-1.55) increased risk with DAPT over control.
Risk of surgical reintervention for bleeding, however, was not increased above control whether on aspirin (relative risk, 0.96; 95% CI, 0.76-1.22), clopidogrel (RR, 1.84; 95% CI, 0.87-3.87), or DAPT (RR, 1.51; (95% CI, 0.92-2.49).
Bottom line: In noncardiac surgery, continuing aspirin or DAPT perioperatively increases the need for transfusion, but not the need for surgical reintervention for bleeding.
Citation: Columbo JA, Lambour AJ, Sundling RA, et. al. A meta-analysis of the impact of aspirin, clopidogrel, and dual-antiplatelet therapy on bleeding complications in noncardiac surgery. Ann Surg. 2017;20(20):1-9.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Public health hazard: Bring your flu to work day
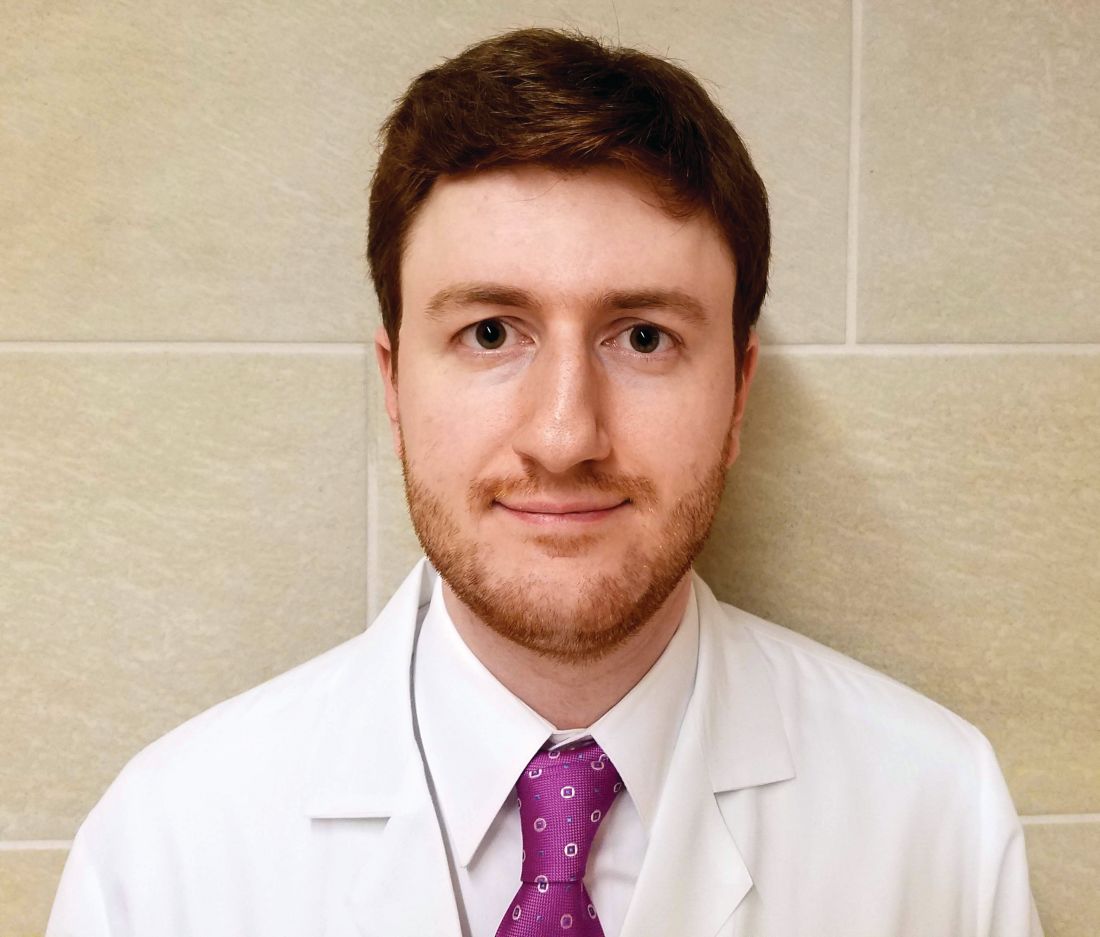
Slightly more than 41% of health care personnel who had the flu during the 2014-2015 influenza season went to work while they were ill, according to an annual survey.
Physicians, however, were well above this average, with 63% reporting they had worked with an influenza-like illness (ILI); they were not quite as far above average as pharmacists, though, who had a 67% rate of “presenteeism” – the highest among all of the health care occupations included in the survey, said Sophia Chiu, MD, MPH, of the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health, and her associates.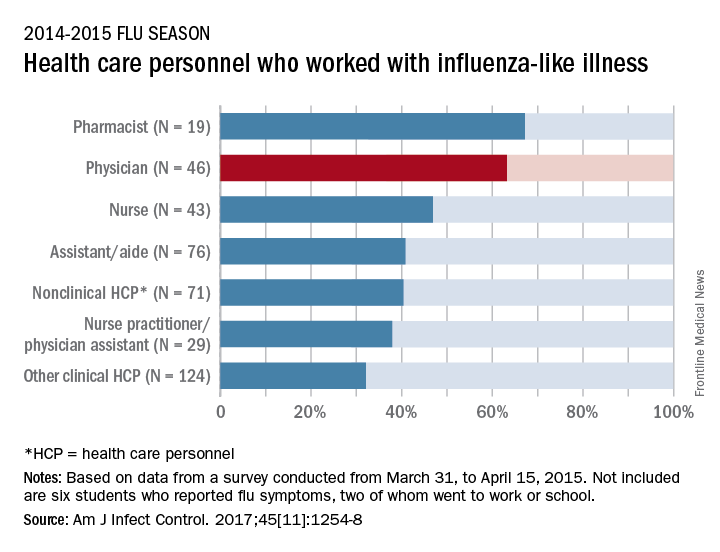
“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a health care worker who is sick are five times more likely to get a health care–associated infection,” Dr. Chiu said in a separate written statement.
For the study, ILI was defined as “fever (without a specified temperature cutoff) and sore throat or cough.” The “nonclinical personnel” category included managers, food service workers, and janitors, while the “other clinical personnel” category included technicians and technologists. The annual Internet panel survey was conducted from March 31, 2015, to April 15, 2015, and 414 of its 1,914 respondents self-reported having an ILI, of whom 183 said that they worked during their illness, Dr. Chiu and her associates said.
The investigators are all CDC employees. The respondents were recruited from Internet panels operated by Survey Sampling International through a contract with Abt Associates.
Slightly more than 41% of health care personnel who had the flu during the 2014-2015 influenza season went to work while they were ill, according to an annual survey.
Physicians, however, were well above this average, with 63% reporting they had worked with an influenza-like illness (ILI); they were not quite as far above average as pharmacists, though, who had a 67% rate of “presenteeism” – the highest among all of the health care occupations included in the survey, said Sophia Chiu, MD, MPH, of the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health, and her associates.
“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a health care worker who is sick are five times more likely to get a health care–associated infection,” Dr. Chiu said in a separate written statement.
For the study, ILI was defined as “fever (without a specified temperature cutoff) and sore throat or cough.” The “nonclinical personnel” category included managers, food service workers, and janitors, while the “other clinical personnel” category included technicians and technologists. The annual Internet panel survey was conducted from March 31, 2015, to April 15, 2015, and 414 of its 1,914 respondents self-reported having an ILI, of whom 183 said that they worked during their illness, Dr. Chiu and her associates said.
The investigators are all CDC employees. The respondents were recruited from Internet panels operated by Survey Sampling International through a contract with Abt Associates.
Slightly more than 41% of health care personnel who had the flu during the 2014-2015 influenza season went to work while they were ill, according to an annual survey.
Physicians, however, were well above this average, with 63% reporting they had worked with an influenza-like illness (ILI); they were not quite as far above average as pharmacists, though, who had a 67% rate of “presenteeism” – the highest among all of the health care occupations included in the survey, said Sophia Chiu, MD, MPH, of the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health, and her associates.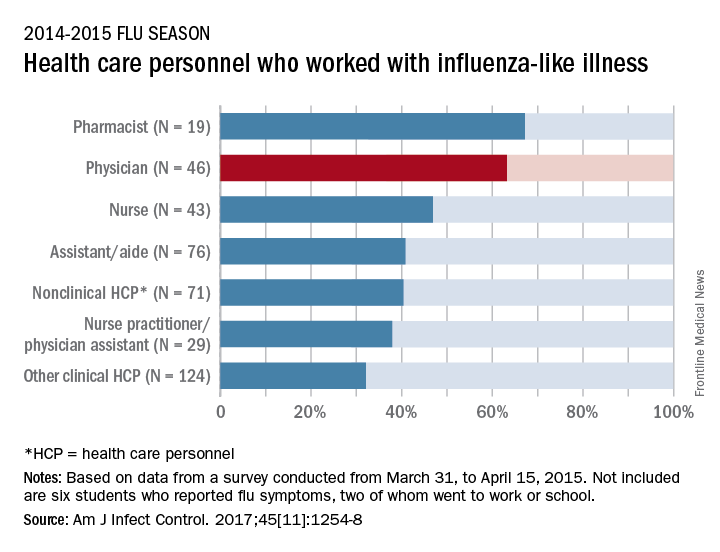
“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a health care worker who is sick are five times more likely to get a health care–associated infection,” Dr. Chiu said in a separate written statement.
For the study, ILI was defined as “fever (without a specified temperature cutoff) and sore throat or cough.” The “nonclinical personnel” category included managers, food service workers, and janitors, while the “other clinical personnel” category included technicians and technologists. The annual Internet panel survey was conducted from March 31, 2015, to April 15, 2015, and 414 of its 1,914 respondents self-reported having an ILI, of whom 183 said that they worked during their illness, Dr. Chiu and her associates said.
The investigators are all CDC employees. The respondents were recruited from Internet panels operated by Survey Sampling International through a contract with Abt Associates.
FROM THE AMERICAN JOURNAL OF INFECTION CONTROL
Identifying high-value care practices
A new tool can help where hospitalists need it most: at the bedside.
The focus on providing high-value care (HVC) continues to grow and expand in health care today. Still, most education around HVC currently happens in a formalized setting – lectures, modules, and so on, says Carolyn D. Sy, MD, interim director of the Hospital Medicine Service at the University of Washington, Seattle, and coauthor of a recent abstract about a new tool to address this shortcoming. “There are no instruments for measuring HVC discussions or practices at the bedside, confounding efforts to assess behavior changes associated with curricular interventions,” she said.
So she and other doctors undertook a study to identify 10 HVC topics in three domains (quality, cost, patient values), then measured their reliability with the goal of designing an HVC Rounding Tool and showing that it is an effective tool to measure observable markers of HVC at the bedside. “This is critical as it addresses an important educational gap in translating HVC from theoretical knowledge to bedside practice,” Dr. Sy said.
The tool is designed to capture multidisciplinary participation, she says, including involvement from not only faculty, fellows, or trainees, but also nursing, pharmacists, families, and other members of the health care team. The tool can be used as a peer feedback instrument to help physicians integrate HVC topics during bedside rounds or as a metric to assess the educational efficacy of future curriculum.
“The HVC Rounding Tool provides an opportunity for faculty development through peer observation and feedback on the integration and role modeling of HVC at the bedside,” Dr. Sy said. “It also is an instrument to help assess the educational efficacy of formal HVC curriculum and translation into bedside practice. Lastly, it is a tool that could be used to measure the relationship between HVC behaviors and actual patient outcomes such as length of stay, readmissions, cost of hospitalization – a feature with increasing importance given our move toward value-based health care.”
Reference
Sy CD, McDaniel C, Bradford M, et al. The Development and Validation of a High Value Care Rounding Tool Using the Delphi Method [abstract]. J Hosp Med. 2017; 12 (suppl 2). http://www.shmabstracts.com/abstract/the-development-and-validation-of-a-high-value-care-rounding-tool-using-the-delphi-method/. Accessed June 6, 2017.
A new tool can help where hospitalists need it most: at the bedside.
The focus on providing high-value care (HVC) continues to grow and expand in health care today. Still, most education around HVC currently happens in a formalized setting – lectures, modules, and so on, says Carolyn D. Sy, MD, interim director of the Hospital Medicine Service at the University of Washington, Seattle, and coauthor of a recent abstract about a new tool to address this shortcoming. “There are no instruments for measuring HVC discussions or practices at the bedside, confounding efforts to assess behavior changes associated with curricular interventions,” she said.
So she and other doctors undertook a study to identify 10 HVC topics in three domains (quality, cost, patient values), then measured their reliability with the goal of designing an HVC Rounding Tool and showing that it is an effective tool to measure observable markers of HVC at the bedside. “This is critical as it addresses an important educational gap in translating HVC from theoretical knowledge to bedside practice,” Dr. Sy said.
The tool is designed to capture multidisciplinary participation, she says, including involvement from not only faculty, fellows, or trainees, but also nursing, pharmacists, families, and other members of the health care team. The tool can be used as a peer feedback instrument to help physicians integrate HVC topics during bedside rounds or as a metric to assess the educational efficacy of future curriculum.
“The HVC Rounding Tool provides an opportunity for faculty development through peer observation and feedback on the integration and role modeling of HVC at the bedside,” Dr. Sy said. “It also is an instrument to help assess the educational efficacy of formal HVC curriculum and translation into bedside practice. Lastly, it is a tool that could be used to measure the relationship between HVC behaviors and actual patient outcomes such as length of stay, readmissions, cost of hospitalization – a feature with increasing importance given our move toward value-based health care.”
Reference
Sy CD, McDaniel C, Bradford M, et al. The Development and Validation of a High Value Care Rounding Tool Using the Delphi Method [abstract]. J Hosp Med. 2017; 12 (suppl 2). http://www.shmabstracts.com/abstract/the-development-and-validation-of-a-high-value-care-rounding-tool-using-the-delphi-method/. Accessed June 6, 2017.
A new tool can help where hospitalists need it most: at the bedside.
The focus on providing high-value care (HVC) continues to grow and expand in health care today. Still, most education around HVC currently happens in a formalized setting – lectures, modules, and so on, says Carolyn D. Sy, MD, interim director of the Hospital Medicine Service at the University of Washington, Seattle, and coauthor of a recent abstract about a new tool to address this shortcoming. “There are no instruments for measuring HVC discussions or practices at the bedside, confounding efforts to assess behavior changes associated with curricular interventions,” she said.
So she and other doctors undertook a study to identify 10 HVC topics in three domains (quality, cost, patient values), then measured their reliability with the goal of designing an HVC Rounding Tool and showing that it is an effective tool to measure observable markers of HVC at the bedside. “This is critical as it addresses an important educational gap in translating HVC from theoretical knowledge to bedside practice,” Dr. Sy said.
The tool is designed to capture multidisciplinary participation, she says, including involvement from not only faculty, fellows, or trainees, but also nursing, pharmacists, families, and other members of the health care team. The tool can be used as a peer feedback instrument to help physicians integrate HVC topics during bedside rounds or as a metric to assess the educational efficacy of future curriculum.
“The HVC Rounding Tool provides an opportunity for faculty development through peer observation and feedback on the integration and role modeling of HVC at the bedside,” Dr. Sy said. “It also is an instrument to help assess the educational efficacy of formal HVC curriculum and translation into bedside practice. Lastly, it is a tool that could be used to measure the relationship between HVC behaviors and actual patient outcomes such as length of stay, readmissions, cost of hospitalization – a feature with increasing importance given our move toward value-based health care.”
Reference
Sy CD, McDaniel C, Bradford M, et al. The Development and Validation of a High Value Care Rounding Tool Using the Delphi Method [abstract]. J Hosp Med. 2017; 12 (suppl 2). http://www.shmabstracts.com/abstract/the-development-and-validation-of-a-high-value-care-rounding-tool-using-the-delphi-method/. Accessed June 6, 2017.
SHORT TAKES
Cardiac testing of Emergency Department patients with chest pain leads to increased revascularization without reduction in admissions for acute MI
Retrospective cohort study of ED patients presenting with chest pain but without evidence of ischemia, shows that non-invasive cardiac testing of these patients lead to more coronary angiograms (92.1 per 1,000 patients) within 30 days, but no significant reduction of admissions for acute MI at 1 year (remained 7.8 per 1,000 patients tested).
Citation: Sandhu AT, Heidenreich PA, Bhattacharya J, Bundorf MK. Cardiovascular Testing and Clinical Outcomes in Emergency Department Patients With Chest Pain. JAMA Intern Med. Published online 2017 June 26. doi: 10.1001/jamainternmed.2017.2432.
Facebook star ratings and “likes” correlate with patient satisfaction scores
In a cross-sectional analysis of 136 New York State hospitals, the study found increased Facebook star ratings correlated (P less than .003) with overall increased HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) score (21/23 HCAHPS). HCAHPS measures also positively correlated (P less than .05) with adjusted number of “likes” on Facebook but to a lesser degree (3/21 HCAHPS). Neither star ratings nor number of “likes” correlate with Medicare spending or 30-day all-cause readmission rate.
Citation: Campbell L, Yue L. Are Facebook user ratings associated with hospital cost, quality, and patient satisfaction? BMJ Qual Saf. 2017 July 19. doi:10.1136/bmjqs-2016-006291.
Candida auris remains an ongoing health care facility transmission risk
Multidrug-resistant fungus Candida auris is an emerging pathogen and a transmission risk across health care facilities. From June 2016 through May 2017, 77 cases of clinical infection have been reported to the Centers for Disease Control and Prevention from seven states, though most (90%) cases are clustered in the New York City metropolitan area. Most patients had multiple medical conditions and extensive health care facility exposure. The CDC recommends contact precautions, private rooming, daily and terminal cleaning with disinfectant active against Clostridium difficile spores, and notification to receiving health care facilities about C. auris colonization or infection on transfer to help reduce the spread of C. auris throughout the United States.
Citation: Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities – United States, June 2016–May 2017. MMWR Morb Mortal Wkly Rep. 2017;66:51415.
Cardiac testing of Emergency Department patients with chest pain leads to increased revascularization without reduction in admissions for acute MI
Retrospective cohort study of ED patients presenting with chest pain but without evidence of ischemia, shows that non-invasive cardiac testing of these patients lead to more coronary angiograms (92.1 per 1,000 patients) within 30 days, but no significant reduction of admissions for acute MI at 1 year (remained 7.8 per 1,000 patients tested).
Citation: Sandhu AT, Heidenreich PA, Bhattacharya J, Bundorf MK. Cardiovascular Testing and Clinical Outcomes in Emergency Department Patients With Chest Pain. JAMA Intern Med. Published online 2017 June 26. doi: 10.1001/jamainternmed.2017.2432.
Facebook star ratings and “likes” correlate with patient satisfaction scores
In a cross-sectional analysis of 136 New York State hospitals, the study found increased Facebook star ratings correlated (P less than .003) with overall increased HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) score (21/23 HCAHPS). HCAHPS measures also positively correlated (P less than .05) with adjusted number of “likes” on Facebook but to a lesser degree (3/21 HCAHPS). Neither star ratings nor number of “likes” correlate with Medicare spending or 30-day all-cause readmission rate.
Citation: Campbell L, Yue L. Are Facebook user ratings associated with hospital cost, quality, and patient satisfaction? BMJ Qual Saf. 2017 July 19. doi:10.1136/bmjqs-2016-006291.
Candida auris remains an ongoing health care facility transmission risk
Multidrug-resistant fungus Candida auris is an emerging pathogen and a transmission risk across health care facilities. From June 2016 through May 2017, 77 cases of clinical infection have been reported to the Centers for Disease Control and Prevention from seven states, though most (90%) cases are clustered in the New York City metropolitan area. Most patients had multiple medical conditions and extensive health care facility exposure. The CDC recommends contact precautions, private rooming, daily and terminal cleaning with disinfectant active against Clostridium difficile spores, and notification to receiving health care facilities about C. auris colonization or infection on transfer to help reduce the spread of C. auris throughout the United States.
Citation: Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities – United States, June 2016–May 2017. MMWR Morb Mortal Wkly Rep. 2017;66:51415.
Cardiac testing of Emergency Department patients with chest pain leads to increased revascularization without reduction in admissions for acute MI
Retrospective cohort study of ED patients presenting with chest pain but without evidence of ischemia, shows that non-invasive cardiac testing of these patients lead to more coronary angiograms (92.1 per 1,000 patients) within 30 days, but no significant reduction of admissions for acute MI at 1 year (remained 7.8 per 1,000 patients tested).
Citation: Sandhu AT, Heidenreich PA, Bhattacharya J, Bundorf MK. Cardiovascular Testing and Clinical Outcomes in Emergency Department Patients With Chest Pain. JAMA Intern Med. Published online 2017 June 26. doi: 10.1001/jamainternmed.2017.2432.
Facebook star ratings and “likes” correlate with patient satisfaction scores
In a cross-sectional analysis of 136 New York State hospitals, the study found increased Facebook star ratings correlated (P less than .003) with overall increased HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) score (21/23 HCAHPS). HCAHPS measures also positively correlated (P less than .05) with adjusted number of “likes” on Facebook but to a lesser degree (3/21 HCAHPS). Neither star ratings nor number of “likes” correlate with Medicare spending or 30-day all-cause readmission rate.
Citation: Campbell L, Yue L. Are Facebook user ratings associated with hospital cost, quality, and patient satisfaction? BMJ Qual Saf. 2017 July 19. doi:10.1136/bmjqs-2016-006291.
Candida auris remains an ongoing health care facility transmission risk
Multidrug-resistant fungus Candida auris is an emerging pathogen and a transmission risk across health care facilities. From June 2016 through May 2017, 77 cases of clinical infection have been reported to the Centers for Disease Control and Prevention from seven states, though most (90%) cases are clustered in the New York City metropolitan area. Most patients had multiple medical conditions and extensive health care facility exposure. The CDC recommends contact precautions, private rooming, daily and terminal cleaning with disinfectant active against Clostridium difficile spores, and notification to receiving health care facilities about C. auris colonization or infection on transfer to help reduce the spread of C. auris throughout the United States.
Citation: Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities – United States, June 2016–May 2017. MMWR Morb Mortal Wkly Rep. 2017;66:51415.
Infections increase risk of idiopathic VTE
Infection and infection sites have been found to be associated with a significant increased risk of venous thromboembolism, according to results of a population-based, matched, case-control analysis of medical records covering the 13-year period 1988-2000.
Dr. Kevin P. Cohoon and his colleagues at the Mayo Clinic, Rochester, Minn., developed models using conditional logistic regression analysis to stratify the risk associated with specific infections and infection sites.
Five hundred thirteen (39.4%) cases and 189 (12.7%) controls had an infection within the previous 92 days (odds ratio, 4.5; P less than .0001). Known VTE risk factors and potentially confounding variables were used in the adjusted univariate and multivariate models, as reported in the American Journal of Medicine (2017. doi: 10.1016/j.amjmed.2017.09.015).
Dr. Cohoon and his colleagues reported that univariate analysis showed “most infection sites were strongly associated with venous thromboembolism” and the adjusted multivariate model resulted in 2.4-fold (P less than .0001) higher odds for VTE incidence, compared with uninfected controls.
Adjusted multivariate analysis ranked the odds of VTE according to specific infections. Dr. Cohoon and his colleagues reported that this modeling showed that the “highest magnitude of risk, compared with no infection, was imparted by intra-abdominal infection (OR, 18) followed by oral infection (OR, 12), systematic blood stream infection (OR, 11), lower respiratory infection such as pneumonia (OR, 3.6), and symptomatic urinary tract infection (OR, 2.2).”
The researchers concluded that their findings may allow for further refinement of inpatient VTE risk-prediction models such as the Padua prediction score and “future studies are required to assess the utility of venous thromboembolism prophylaxis among outpatients with high venous thromboembolism risk infections.”
The authors reported that they had no conflicts of interest.
Infection and infection sites have been found to be associated with a significant increased risk of venous thromboembolism, according to results of a population-based, matched, case-control analysis of medical records covering the 13-year period 1988-2000.
Dr. Kevin P. Cohoon and his colleagues at the Mayo Clinic, Rochester, Minn., developed models using conditional logistic regression analysis to stratify the risk associated with specific infections and infection sites.
Five hundred thirteen (39.4%) cases and 189 (12.7%) controls had an infection within the previous 92 days (odds ratio, 4.5; P less than .0001). Known VTE risk factors and potentially confounding variables were used in the adjusted univariate and multivariate models, as reported in the American Journal of Medicine (2017. doi: 10.1016/j.amjmed.2017.09.015).
Dr. Cohoon and his colleagues reported that univariate analysis showed “most infection sites were strongly associated with venous thromboembolism” and the adjusted multivariate model resulted in 2.4-fold (P less than .0001) higher odds for VTE incidence, compared with uninfected controls.
Adjusted multivariate analysis ranked the odds of VTE according to specific infections. Dr. Cohoon and his colleagues reported that this modeling showed that the “highest magnitude of risk, compared with no infection, was imparted by intra-abdominal infection (OR, 18) followed by oral infection (OR, 12), systematic blood stream infection (OR, 11), lower respiratory infection such as pneumonia (OR, 3.6), and symptomatic urinary tract infection (OR, 2.2).”
The researchers concluded that their findings may allow for further refinement of inpatient VTE risk-prediction models such as the Padua prediction score and “future studies are required to assess the utility of venous thromboembolism prophylaxis among outpatients with high venous thromboembolism risk infections.”
The authors reported that they had no conflicts of interest.
Infection and infection sites have been found to be associated with a significant increased risk of venous thromboembolism, according to results of a population-based, matched, case-control analysis of medical records covering the 13-year period 1988-2000.
Dr. Kevin P. Cohoon and his colleagues at the Mayo Clinic, Rochester, Minn., developed models using conditional logistic regression analysis to stratify the risk associated with specific infections and infection sites.
Five hundred thirteen (39.4%) cases and 189 (12.7%) controls had an infection within the previous 92 days (odds ratio, 4.5; P less than .0001). Known VTE risk factors and potentially confounding variables were used in the adjusted univariate and multivariate models, as reported in the American Journal of Medicine (2017. doi: 10.1016/j.amjmed.2017.09.015).
Dr. Cohoon and his colleagues reported that univariate analysis showed “most infection sites were strongly associated with venous thromboembolism” and the adjusted multivariate model resulted in 2.4-fold (P less than .0001) higher odds for VTE incidence, compared with uninfected controls.
Adjusted multivariate analysis ranked the odds of VTE according to specific infections. Dr. Cohoon and his colleagues reported that this modeling showed that the “highest magnitude of risk, compared with no infection, was imparted by intra-abdominal infection (OR, 18) followed by oral infection (OR, 12), systematic blood stream infection (OR, 11), lower respiratory infection such as pneumonia (OR, 3.6), and symptomatic urinary tract infection (OR, 2.2).”
The researchers concluded that their findings may allow for further refinement of inpatient VTE risk-prediction models such as the Padua prediction score and “future studies are required to assess the utility of venous thromboembolism prophylaxis among outpatients with high venous thromboembolism risk infections.”
The authors reported that they had no conflicts of interest.
FROM THE AMERICAN JOURNAL OF MEDICINE
Key clinical point:
Major finding: A significantly greater number of patients with infections developed VTE as compared with uninfected controls (OR, 4.5; P less than .0001).
Data source: Study was a retrospective database analysis of 1,303 VTE patients and 1,494 paired controls.
Disclosures: The authors reported that they had no conflicts of interest.
Developing machines that detect disease
Smells – of skin, breath, or bodily fluids – can, in some cases, reveal the presence of disease. This fact has led researchers to try to build an odor sensor that could make a fast, reliable diagnosis, and now the field may be on the verge of a breakthrough, according to a recent article in the New York Times.
In addition to various efforts in Austria, Switzerland, and Japan, an English manufacturer – Owlstone Medical – has been making headway with an odor analysis technology. It will be part of a National Health Service trial that will test the sensor for diagnosing lung cancer. The company also is conducting a trial using urine samples to detect colon cancer; its program allows changing the software to change what disease you detect.
Meanwhile, an Israeli chemical engineer, Hossam Haick, is using similar technology, with molecular receptors that have an affinity for certain biomarkers of disease found in the breath. Artificial intelligence allows the sensors to improve with each use, and a paper published last year showed that this system could distinguish among 17 different diseases with up to 86% accuracy.
And in the United States, researchers from the Monell Chemical Senses Center and the University of Pennsylvania are working on an odor sensor that detects ovarian cancer in samples of blood plasma. They chose plasma because it is less likely than breath or urine to be affected by other factors such as diet or environmental chemicals.
These technologies could be available to doctors in 3-5 years, experts say.
Reference
Murphy K. One Day, a Machine Will Smell Whether You’re Sick . New York Times. May 1, 2017. Accessed May 29, 2017.
Smells – of skin, breath, or bodily fluids – can, in some cases, reveal the presence of disease. This fact has led researchers to try to build an odor sensor that could make a fast, reliable diagnosis, and now the field may be on the verge of a breakthrough, according to a recent article in the New York Times.
In addition to various efforts in Austria, Switzerland, and Japan, an English manufacturer – Owlstone Medical – has been making headway with an odor analysis technology. It will be part of a National Health Service trial that will test the sensor for diagnosing lung cancer. The company also is conducting a trial using urine samples to detect colon cancer; its program allows changing the software to change what disease you detect.
Meanwhile, an Israeli chemical engineer, Hossam Haick, is using similar technology, with molecular receptors that have an affinity for certain biomarkers of disease found in the breath. Artificial intelligence allows the sensors to improve with each use, and a paper published last year showed that this system could distinguish among 17 different diseases with up to 86% accuracy.
And in the United States, researchers from the Monell Chemical Senses Center and the University of Pennsylvania are working on an odor sensor that detects ovarian cancer in samples of blood plasma. They chose plasma because it is less likely than breath or urine to be affected by other factors such as diet or environmental chemicals.
These technologies could be available to doctors in 3-5 years, experts say.
Reference
Murphy K. One Day, a Machine Will Smell Whether You’re Sick . New York Times. May 1, 2017. Accessed May 29, 2017.
Smells – of skin, breath, or bodily fluids – can, in some cases, reveal the presence of disease. This fact has led researchers to try to build an odor sensor that could make a fast, reliable diagnosis, and now the field may be on the verge of a breakthrough, according to a recent article in the New York Times.
In addition to various efforts in Austria, Switzerland, and Japan, an English manufacturer – Owlstone Medical – has been making headway with an odor analysis technology. It will be part of a National Health Service trial that will test the sensor for diagnosing lung cancer. The company also is conducting a trial using urine samples to detect colon cancer; its program allows changing the software to change what disease you detect.
Meanwhile, an Israeli chemical engineer, Hossam Haick, is using similar technology, with molecular receptors that have an affinity for certain biomarkers of disease found in the breath. Artificial intelligence allows the sensors to improve with each use, and a paper published last year showed that this system could distinguish among 17 different diseases with up to 86% accuracy.
And in the United States, researchers from the Monell Chemical Senses Center and the University of Pennsylvania are working on an odor sensor that detects ovarian cancer in samples of blood plasma. They chose plasma because it is less likely than breath or urine to be affected by other factors such as diet or environmental chemicals.
These technologies could be available to doctors in 3-5 years, experts say.
Reference
Murphy K. One Day, a Machine Will Smell Whether You’re Sick . New York Times. May 1, 2017. Accessed May 29, 2017.
Rates, predictors, and variability of interhospital transfers
Clinical question: What is the national frequency of interhospital transfers, and are there any patient or hospital factors that predict these transfers?
Background: Interhospital patient transfers may be due to the need for a specialized service, but the factors and patterns have not been well studied.
Setting: All acute care hospitals in the United States.
Synopsis: Using data from the 2013 Centers for Medicare & Medicaid Services and the 2013 American Hospital Association, this study showed that 1.5% of the 6.6 million eligible beneficiaries underwent interhospital transfer (IHT). Patient and hospital characteristics that increased the odds of IHT included age 74-85 years, nonblack race, higher comorbidity, lower diagnosis-related group weight, fewer recent hospitalizations, and hospitalization in the Northeast region of the United States. Lower case mix index was associated with increased odds of IHT. Rates of IHT remain variable, after adjusting for patient and hospital characteristics. This study was restricted to the Medicare population so did not represent all populations. IHT from the emergency room was not assessed, and those who were transferred more than once (to another hospital and back) were not included.
Bottom line: A large number of Medicare patients undergo IHT nationally, and the rate varies widely based on patient factors, geography, and other factors unrelated to patient or hospital characteristics.
Citation: Mueller SK, Jie Zheng, Orav EJ, Schnipper JL. Rates, predictors, and variability of interhospital transfers: A national evaluation. J Hosp Med. 2017;6:435-42.
Dr. Xu is assistant professor and hospitalist, Icahn School of Medicine of the Mount Sinai Health System, New York.
Clinical question: What is the national frequency of interhospital transfers, and are there any patient or hospital factors that predict these transfers?
Background: Interhospital patient transfers may be due to the need for a specialized service, but the factors and patterns have not been well studied.
Setting: All acute care hospitals in the United States.
Synopsis: Using data from the 2013 Centers for Medicare & Medicaid Services and the 2013 American Hospital Association, this study showed that 1.5% of the 6.6 million eligible beneficiaries underwent interhospital transfer (IHT). Patient and hospital characteristics that increased the odds of IHT included age 74-85 years, nonblack race, higher comorbidity, lower diagnosis-related group weight, fewer recent hospitalizations, and hospitalization in the Northeast region of the United States. Lower case mix index was associated with increased odds of IHT. Rates of IHT remain variable, after adjusting for patient and hospital characteristics. This study was restricted to the Medicare population so did not represent all populations. IHT from the emergency room was not assessed, and those who were transferred more than once (to another hospital and back) were not included.
Bottom line: A large number of Medicare patients undergo IHT nationally, and the rate varies widely based on patient factors, geography, and other factors unrelated to patient or hospital characteristics.
Citation: Mueller SK, Jie Zheng, Orav EJ, Schnipper JL. Rates, predictors, and variability of interhospital transfers: A national evaluation. J Hosp Med. 2017;6:435-42.
Dr. Xu is assistant professor and hospitalist, Icahn School of Medicine of the Mount Sinai Health System, New York.
Clinical question: What is the national frequency of interhospital transfers, and are there any patient or hospital factors that predict these transfers?
Background: Interhospital patient transfers may be due to the need for a specialized service, but the factors and patterns have not been well studied.
Setting: All acute care hospitals in the United States.
Synopsis: Using data from the 2013 Centers for Medicare & Medicaid Services and the 2013 American Hospital Association, this study showed that 1.5% of the 6.6 million eligible beneficiaries underwent interhospital transfer (IHT). Patient and hospital characteristics that increased the odds of IHT included age 74-85 years, nonblack race, higher comorbidity, lower diagnosis-related group weight, fewer recent hospitalizations, and hospitalization in the Northeast region of the United States. Lower case mix index was associated with increased odds of IHT. Rates of IHT remain variable, after adjusting for patient and hospital characteristics. This study was restricted to the Medicare population so did not represent all populations. IHT from the emergency room was not assessed, and those who were transferred more than once (to another hospital and back) were not included.
Bottom line: A large number of Medicare patients undergo IHT nationally, and the rate varies widely based on patient factors, geography, and other factors unrelated to patient or hospital characteristics.
Citation: Mueller SK, Jie Zheng, Orav EJ, Schnipper JL. Rates, predictors, and variability of interhospital transfers: A national evaluation. J Hosp Med. 2017;6:435-42.
Dr. Xu is assistant professor and hospitalist, Icahn School of Medicine of the Mount Sinai Health System, New York.