User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
CME in the time of COVID-19
As the COVID-19 pandemic spreads, it now seems like the norm is that large medical conferences are being canceled.
The American Psychiatric Association (APA) canceled its 2020 annual meeting, which was scheduled for late April. The cancellation disappointed many, because we will miss out on the camaraderie and professional invigoration that comes from gathering with psychiatrists and other mental health professionals from across the United States and around the world. After the APA’s decision was announced, the White House released guidelines advising Americans to avoid social gatherings of 10 or more people.
On a practical level, many psychiatrists will not be able to earn up to 35 continuing medical education credits (CME) from attending the meeting and fulfilling the administrative requirements to obtain a CME certificate. Not only have meetings been canceled, but events many other clinicians count on for CME, such as journal clubs and department grand rounds, have been canceled until they can be moved to a virtual space.
The CME requirements for state medical licenses vary widely. On average, most states require at least 25 credits per year or 60 to 100 credits every 2 years, and the American Board of Psychiatry and Neurology requires diplomates to complete an average of 30 specialty and/or subspecialty CME credits per year, averaged over 3 years. Usually, annual medical conferences would be a great way to get an infusion of CME credits, brush up on cutting-edge treatments, and review the basics.
On top of everything else we have to worry about with COVID-19, getting enough CME credits has been added to the list for many psychiatrists and mental health clinicians. As our schedules and daily lives are disrupted, it’s important to find relief in routine activities that are not affected by social distancing and fears of isolation and quarantine. A routine activity to lean into might include learning or practicing a skill that we enjoy, such as psychiatry (hopefully!) and the practice of medicine. The CME could be focused on a psychiatric topic or perhaps learning about the specifics of COVID-19 or brushing up on medical knowledge that might be a bit rusty after many years of practicing solely psychiatry.
As you start to gather CME credits online, it’s helpful to sign up for a service that stores your CME credits and helps you keep track of the number. When it comes time to renew your medical license or apply for maintenance of certification (MOC), who wants to be the person searching through their email for PDFs of CME certificates or taking pictures or scanning paper certificates? The APA has a section under education and MOC to track certificates earned by watching online modules from its “Learning Center.” The website also allows users to upload external certificates. The American Medical Association offers a similar service on its “Ed Hub,” in which users can log in to watch, listen, or download articles to earn CME credits after finishing the associated quiz. Medscape, in the CME and Education section, also offers an easy-to-use CME dashboard, in which clinicians can filter by their specialty, topic, duration of learning activity – ranging from 0.25 to 3 CME credits. Clinicians also can track their credits as they complete activities.
If you’re someone who’s having trouble focusing on anything besides COVID-19, there are COVID-19-specific CME activities that are available and can help psychiatrists feel comfortable talking with patients, family, and their institutions about the risks of COVID-19. The AMA Ed Hub has a featured 8-credit CME course about the novel coronavirus with updates about diagnosis, treatment, and public health strategies.
For the psychiatrists who may have procrastinated in-depth learning about the opioid crisis or getting their buprenorphine waivers, AMA Ed Hub offers a 42-credit course about opioids and pain management covering guidelines, research, and treatment.
For fun refreshers on general medicine, the New England Journal of Medicine offers up to 20 online CME exams based on quizzes from interesting clinical cases ranging from “regular” medicine to rare clinical scenarios. The APA Learning Center has an easy-to-use search function allowing users to select content from more than 200 modules covering a wide range of general topics; from reviewing recent treatment guidelines to specialized psychiatric topics such as geriatric bipolar disorder. A psychiatrist who has been quickly pushed to telepsychiatry because of the current pandemic could use the APA Learning Center to find educational modules about risk management in telepsychiatry or learn the special considerations of using telepsychiatry to treat patients with serious mental illness.
Using podcasts to earn CME is becoming increasingly common, with such as outlets as JAMA Networks offering podcasts in many specialties in which subscribers can take a quiz through the JAMA app and obtain CME credits.
As our clinical boundaries as psychiatrists are pushed by an ever-changing public health situation, now is the time to earn CME focused on new topics to meet the demands placed on health care workers at the front lines of clinical care.
If the COVID-19 pandemic reaches the number of cases predicted by public health officials, our health care system is going to be under extreme stress. All specialties face the threat of losing part of their working capacity as clinicians get sick with the virus, or as they stay home because of exposure or to take care of a loved one. CME can be a way to empower ourselves by staying current on the cutting edge of our specialties, but also brushing up on the medicine that we may be asked to practice in a time of great need.
Dr. Posada is consultation-liaison psychiatry fellow with the Inova Fairfax Hospital/George Washington University program in Falls Church, Va. She also is associate producer of the MDedge Psychcast. Dr. Posada has no disclosures.
As the COVID-19 pandemic spreads, it now seems like the norm is that large medical conferences are being canceled.
The American Psychiatric Association (APA) canceled its 2020 annual meeting, which was scheduled for late April. The cancellation disappointed many, because we will miss out on the camaraderie and professional invigoration that comes from gathering with psychiatrists and other mental health professionals from across the United States and around the world. After the APA’s decision was announced, the White House released guidelines advising Americans to avoid social gatherings of 10 or more people.
On a practical level, many psychiatrists will not be able to earn up to 35 continuing medical education credits (CME) from attending the meeting and fulfilling the administrative requirements to obtain a CME certificate. Not only have meetings been canceled, but events many other clinicians count on for CME, such as journal clubs and department grand rounds, have been canceled until they can be moved to a virtual space.
The CME requirements for state medical licenses vary widely. On average, most states require at least 25 credits per year or 60 to 100 credits every 2 years, and the American Board of Psychiatry and Neurology requires diplomates to complete an average of 30 specialty and/or subspecialty CME credits per year, averaged over 3 years. Usually, annual medical conferences would be a great way to get an infusion of CME credits, brush up on cutting-edge treatments, and review the basics.
On top of everything else we have to worry about with COVID-19, getting enough CME credits has been added to the list for many psychiatrists and mental health clinicians. As our schedules and daily lives are disrupted, it’s important to find relief in routine activities that are not affected by social distancing and fears of isolation and quarantine. A routine activity to lean into might include learning or practicing a skill that we enjoy, such as psychiatry (hopefully!) and the practice of medicine. The CME could be focused on a psychiatric topic or perhaps learning about the specifics of COVID-19 or brushing up on medical knowledge that might be a bit rusty after many years of practicing solely psychiatry.
As you start to gather CME credits online, it’s helpful to sign up for a service that stores your CME credits and helps you keep track of the number. When it comes time to renew your medical license or apply for maintenance of certification (MOC), who wants to be the person searching through their email for PDFs of CME certificates or taking pictures or scanning paper certificates? The APA has a section under education and MOC to track certificates earned by watching online modules from its “Learning Center.” The website also allows users to upload external certificates. The American Medical Association offers a similar service on its “Ed Hub,” in which users can log in to watch, listen, or download articles to earn CME credits after finishing the associated quiz. Medscape, in the CME and Education section, also offers an easy-to-use CME dashboard, in which clinicians can filter by their specialty, topic, duration of learning activity – ranging from 0.25 to 3 CME credits. Clinicians also can track their credits as they complete activities.
If you’re someone who’s having trouble focusing on anything besides COVID-19, there are COVID-19-specific CME activities that are available and can help psychiatrists feel comfortable talking with patients, family, and their institutions about the risks of COVID-19. The AMA Ed Hub has a featured 8-credit CME course about the novel coronavirus with updates about diagnosis, treatment, and public health strategies.
For the psychiatrists who may have procrastinated in-depth learning about the opioid crisis or getting their buprenorphine waivers, AMA Ed Hub offers a 42-credit course about opioids and pain management covering guidelines, research, and treatment.
For fun refreshers on general medicine, the New England Journal of Medicine offers up to 20 online CME exams based on quizzes from interesting clinical cases ranging from “regular” medicine to rare clinical scenarios. The APA Learning Center has an easy-to-use search function allowing users to select content from more than 200 modules covering a wide range of general topics; from reviewing recent treatment guidelines to specialized psychiatric topics such as geriatric bipolar disorder. A psychiatrist who has been quickly pushed to telepsychiatry because of the current pandemic could use the APA Learning Center to find educational modules about risk management in telepsychiatry or learn the special considerations of using telepsychiatry to treat patients with serious mental illness.
Using podcasts to earn CME is becoming increasingly common, with such as outlets as JAMA Networks offering podcasts in many specialties in which subscribers can take a quiz through the JAMA app and obtain CME credits.
As our clinical boundaries as psychiatrists are pushed by an ever-changing public health situation, now is the time to earn CME focused on new topics to meet the demands placed on health care workers at the front lines of clinical care.
If the COVID-19 pandemic reaches the number of cases predicted by public health officials, our health care system is going to be under extreme stress. All specialties face the threat of losing part of their working capacity as clinicians get sick with the virus, or as they stay home because of exposure or to take care of a loved one. CME can be a way to empower ourselves by staying current on the cutting edge of our specialties, but also brushing up on the medicine that we may be asked to practice in a time of great need.
Dr. Posada is consultation-liaison psychiatry fellow with the Inova Fairfax Hospital/George Washington University program in Falls Church, Va. She also is associate producer of the MDedge Psychcast. Dr. Posada has no disclosures.
As the COVID-19 pandemic spreads, it now seems like the norm is that large medical conferences are being canceled.
The American Psychiatric Association (APA) canceled its 2020 annual meeting, which was scheduled for late April. The cancellation disappointed many, because we will miss out on the camaraderie and professional invigoration that comes from gathering with psychiatrists and other mental health professionals from across the United States and around the world. After the APA’s decision was announced, the White House released guidelines advising Americans to avoid social gatherings of 10 or more people.
On a practical level, many psychiatrists will not be able to earn up to 35 continuing medical education credits (CME) from attending the meeting and fulfilling the administrative requirements to obtain a CME certificate. Not only have meetings been canceled, but events many other clinicians count on for CME, such as journal clubs and department grand rounds, have been canceled until they can be moved to a virtual space.
The CME requirements for state medical licenses vary widely. On average, most states require at least 25 credits per year or 60 to 100 credits every 2 years, and the American Board of Psychiatry and Neurology requires diplomates to complete an average of 30 specialty and/or subspecialty CME credits per year, averaged over 3 years. Usually, annual medical conferences would be a great way to get an infusion of CME credits, brush up on cutting-edge treatments, and review the basics.
On top of everything else we have to worry about with COVID-19, getting enough CME credits has been added to the list for many psychiatrists and mental health clinicians. As our schedules and daily lives are disrupted, it’s important to find relief in routine activities that are not affected by social distancing and fears of isolation and quarantine. A routine activity to lean into might include learning or practicing a skill that we enjoy, such as psychiatry (hopefully!) and the practice of medicine. The CME could be focused on a psychiatric topic or perhaps learning about the specifics of COVID-19 or brushing up on medical knowledge that might be a bit rusty after many years of practicing solely psychiatry.
As you start to gather CME credits online, it’s helpful to sign up for a service that stores your CME credits and helps you keep track of the number. When it comes time to renew your medical license or apply for maintenance of certification (MOC), who wants to be the person searching through their email for PDFs of CME certificates or taking pictures or scanning paper certificates? The APA has a section under education and MOC to track certificates earned by watching online modules from its “Learning Center.” The website also allows users to upload external certificates. The American Medical Association offers a similar service on its “Ed Hub,” in which users can log in to watch, listen, or download articles to earn CME credits after finishing the associated quiz. Medscape, in the CME and Education section, also offers an easy-to-use CME dashboard, in which clinicians can filter by their specialty, topic, duration of learning activity – ranging from 0.25 to 3 CME credits. Clinicians also can track their credits as they complete activities.
If you’re someone who’s having trouble focusing on anything besides COVID-19, there are COVID-19-specific CME activities that are available and can help psychiatrists feel comfortable talking with patients, family, and their institutions about the risks of COVID-19. The AMA Ed Hub has a featured 8-credit CME course about the novel coronavirus with updates about diagnosis, treatment, and public health strategies.
For the psychiatrists who may have procrastinated in-depth learning about the opioid crisis or getting their buprenorphine waivers, AMA Ed Hub offers a 42-credit course about opioids and pain management covering guidelines, research, and treatment.
For fun refreshers on general medicine, the New England Journal of Medicine offers up to 20 online CME exams based on quizzes from interesting clinical cases ranging from “regular” medicine to rare clinical scenarios. The APA Learning Center has an easy-to-use search function allowing users to select content from more than 200 modules covering a wide range of general topics; from reviewing recent treatment guidelines to specialized psychiatric topics such as geriatric bipolar disorder. A psychiatrist who has been quickly pushed to telepsychiatry because of the current pandemic could use the APA Learning Center to find educational modules about risk management in telepsychiatry or learn the special considerations of using telepsychiatry to treat patients with serious mental illness.
Using podcasts to earn CME is becoming increasingly common, with such as outlets as JAMA Networks offering podcasts in many specialties in which subscribers can take a quiz through the JAMA app and obtain CME credits.
As our clinical boundaries as psychiatrists are pushed by an ever-changing public health situation, now is the time to earn CME focused on new topics to meet the demands placed on health care workers at the front lines of clinical care.
If the COVID-19 pandemic reaches the number of cases predicted by public health officials, our health care system is going to be under extreme stress. All specialties face the threat of losing part of their working capacity as clinicians get sick with the virus, or as they stay home because of exposure or to take care of a loved one. CME can be a way to empower ourselves by staying current on the cutting edge of our specialties, but also brushing up on the medicine that we may be asked to practice in a time of great need.
Dr. Posada is consultation-liaison psychiatry fellow with the Inova Fairfax Hospital/George Washington University program in Falls Church, Va. She also is associate producer of the MDedge Psychcast. Dr. Posada has no disclosures.
Coronavirus stays in aerosols for hours, on surfaces for days
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
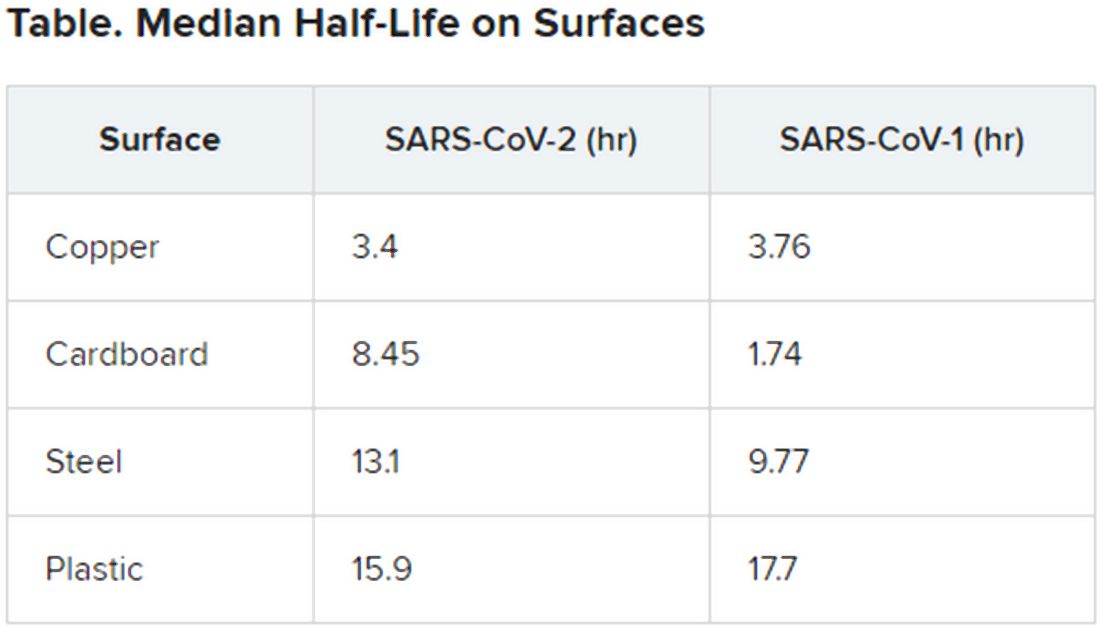
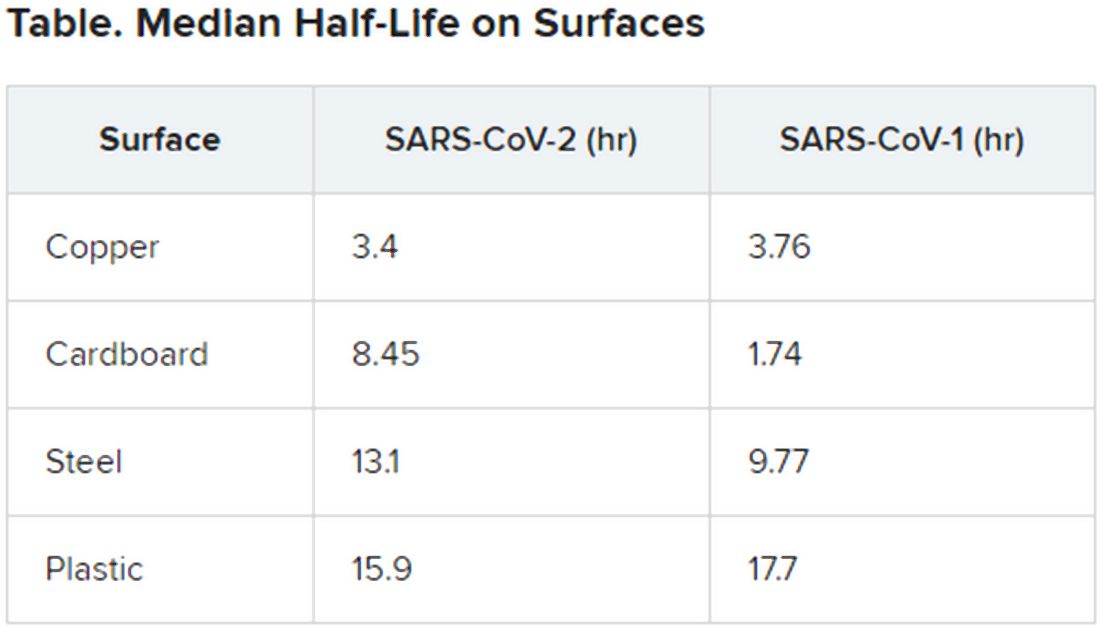
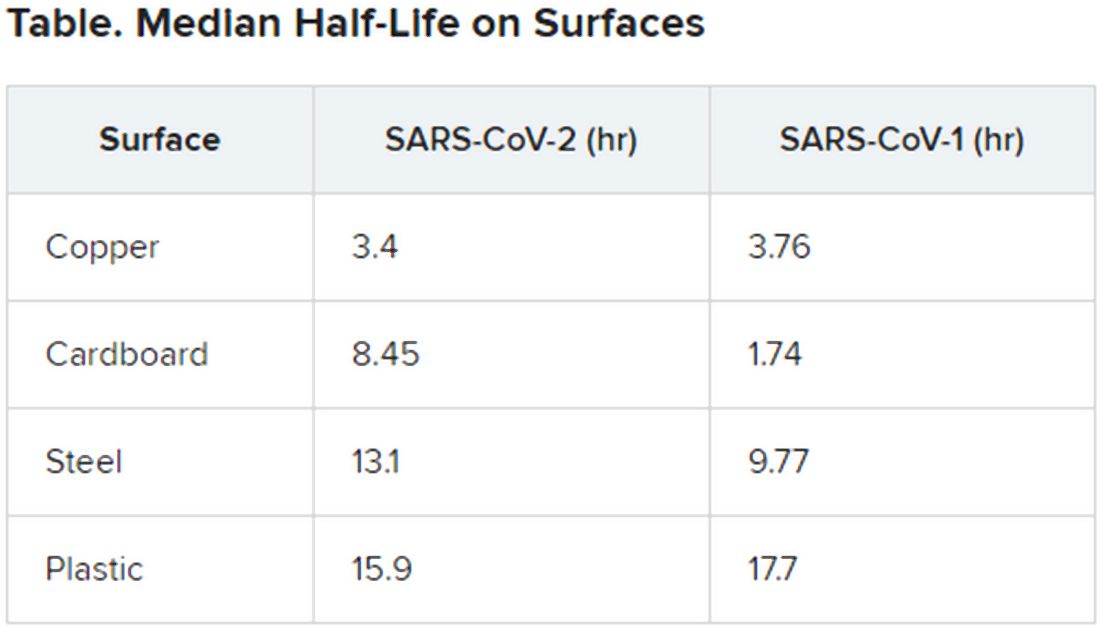
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Potential GI manifestation, transmission of coronavirus
The novel coronavirus (2019-nCoV) shows evidence of causing gastrointestinal symptoms and has the potential to be transmitted by the fecal-oral route, according to a new report from physicians at Shanghai Jiao Tong University, published online (Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054).
The virus’s respiratory symptoms are well documented and suggest primary transmission by droplet or contact, while other symptoms such as diarrhea, nausea, vomiting, and abdominal discomfort are less common and appear to vary between populations. The SARS coronavirus showed up in stool, even sometimes in patients discharged from the hospital. In a study of hospitalized patients in Wuhan, China, 10.1% of coronavirus patients had diarrhea and nausea in the 1-2 days before onset of fever and dyspnea. The first U.S. patient to be diagnosed had a 2-day history of nausea and vomiting, and had a loose bowel movement on the second day in the hospital. Clinicians later confirmed the presence of viral RNA in both the patient’s stool and airway.
The authors say that researchers in China have isolated viral RNA from the stool of two patients (unpublished), and it has been found in saliva, suggesting the possibility of the salivary gland as an infection or transmission route.
The authors maintain that previous studies likely overlooked or neglected patients who had mild intestinal symptoms. “Many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” the authors wrote.
Like other coronaviruses, it appears that 2019-nCoV infects cells through an interaction between viral transmembrane spike glycoprotein (S-protein) receptor-binding domain, and the cell receptors angiotensin-converting enzyme 2 (ACE-2) and host cellular transmembrane serine protease (TMPRSS). Transcriptome analysis has shown that human lung AT2 cells express ACE-2 and TMPRSS, but esophagus upper and stratified epithelial cells also express both factors, as do stratified epithelial cells and absorptive enterocytes in the ileum and colon.
The researchers call for investigation into ACE-2 fusion proteins and TMPRSS inhibitors for diagnosis, prophylaxis, or treatment of COVID-19.
The authors also noted that COVID-19 has been linked to mild to moderate liver injury as revealed by elevated aminotransferases, hypoproteinemia and prothrombin time prolongation. This also has precedent in that the SARS coronavirus can infect the liver, and biopsies revealed mitoses and apoptosis, along with other abnormalities. SARS-associated hepatitis may be the result of viral hepatitis, immune overreaction, or a secondary effect of antiviral medications or other drugs. Little is known to date about the ability of 2019-nCoV to infect the liver, but single-cell RNA sequencing data from two distinct cohorts showed more ACE-2 expression in cholangiocytes (59.7%) than hepatocytes (2.6%), which indicates that the virus might directly affect intrahepatic bile ducts.
The authors had no sources of funding or financial conflicts.
SOURCE: GU J et al. Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054.
*This story was updated on 4/10.2020.
The novel coronavirus (2019-nCoV) shows evidence of causing gastrointestinal symptoms and has the potential to be transmitted by the fecal-oral route, according to a new report from physicians at Shanghai Jiao Tong University, published online (Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054).
The virus’s respiratory symptoms are well documented and suggest primary transmission by droplet or contact, while other symptoms such as diarrhea, nausea, vomiting, and abdominal discomfort are less common and appear to vary between populations. The SARS coronavirus showed up in stool, even sometimes in patients discharged from the hospital. In a study of hospitalized patients in Wuhan, China, 10.1% of coronavirus patients had diarrhea and nausea in the 1-2 days before onset of fever and dyspnea. The first U.S. patient to be diagnosed had a 2-day history of nausea and vomiting, and had a loose bowel movement on the second day in the hospital. Clinicians later confirmed the presence of viral RNA in both the patient’s stool and airway.
The authors say that researchers in China have isolated viral RNA from the stool of two patients (unpublished), and it has been found in saliva, suggesting the possibility of the salivary gland as an infection or transmission route.
The authors maintain that previous studies likely overlooked or neglected patients who had mild intestinal symptoms. “Many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” the authors wrote.
Like other coronaviruses, it appears that 2019-nCoV infects cells through an interaction between viral transmembrane spike glycoprotein (S-protein) receptor-binding domain, and the cell receptors angiotensin-converting enzyme 2 (ACE-2) and host cellular transmembrane serine protease (TMPRSS). Transcriptome analysis has shown that human lung AT2 cells express ACE-2 and TMPRSS, but esophagus upper and stratified epithelial cells also express both factors, as do stratified epithelial cells and absorptive enterocytes in the ileum and colon.
The researchers call for investigation into ACE-2 fusion proteins and TMPRSS inhibitors for diagnosis, prophylaxis, or treatment of COVID-19.
The authors also noted that COVID-19 has been linked to mild to moderate liver injury as revealed by elevated aminotransferases, hypoproteinemia and prothrombin time prolongation. This also has precedent in that the SARS coronavirus can infect the liver, and biopsies revealed mitoses and apoptosis, along with other abnormalities. SARS-associated hepatitis may be the result of viral hepatitis, immune overreaction, or a secondary effect of antiviral medications or other drugs. Little is known to date about the ability of 2019-nCoV to infect the liver, but single-cell RNA sequencing data from two distinct cohorts showed more ACE-2 expression in cholangiocytes (59.7%) than hepatocytes (2.6%), which indicates that the virus might directly affect intrahepatic bile ducts.
The authors had no sources of funding or financial conflicts.
SOURCE: GU J et al. Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054.
*This story was updated on 4/10.2020.
The novel coronavirus (2019-nCoV) shows evidence of causing gastrointestinal symptoms and has the potential to be transmitted by the fecal-oral route, according to a new report from physicians at Shanghai Jiao Tong University, published online (Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054).
The virus’s respiratory symptoms are well documented and suggest primary transmission by droplet or contact, while other symptoms such as diarrhea, nausea, vomiting, and abdominal discomfort are less common and appear to vary between populations. The SARS coronavirus showed up in stool, even sometimes in patients discharged from the hospital. In a study of hospitalized patients in Wuhan, China, 10.1% of coronavirus patients had diarrhea and nausea in the 1-2 days before onset of fever and dyspnea. The first U.S. patient to be diagnosed had a 2-day history of nausea and vomiting, and had a loose bowel movement on the second day in the hospital. Clinicians later confirmed the presence of viral RNA in both the patient’s stool and airway.
The authors say that researchers in China have isolated viral RNA from the stool of two patients (unpublished), and it has been found in saliva, suggesting the possibility of the salivary gland as an infection or transmission route.
The authors maintain that previous studies likely overlooked or neglected patients who had mild intestinal symptoms. “Many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” the authors wrote.
Like other coronaviruses, it appears that 2019-nCoV infects cells through an interaction between viral transmembrane spike glycoprotein (S-protein) receptor-binding domain, and the cell receptors angiotensin-converting enzyme 2 (ACE-2) and host cellular transmembrane serine protease (TMPRSS). Transcriptome analysis has shown that human lung AT2 cells express ACE-2 and TMPRSS, but esophagus upper and stratified epithelial cells also express both factors, as do stratified epithelial cells and absorptive enterocytes in the ileum and colon.
The researchers call for investigation into ACE-2 fusion proteins and TMPRSS inhibitors for diagnosis, prophylaxis, or treatment of COVID-19.
The authors also noted that COVID-19 has been linked to mild to moderate liver injury as revealed by elevated aminotransferases, hypoproteinemia and prothrombin time prolongation. This also has precedent in that the SARS coronavirus can infect the liver, and biopsies revealed mitoses and apoptosis, along with other abnormalities. SARS-associated hepatitis may be the result of viral hepatitis, immune overreaction, or a secondary effect of antiviral medications or other drugs. Little is known to date about the ability of 2019-nCoV to infect the liver, but single-cell RNA sequencing data from two distinct cohorts showed more ACE-2 expression in cholangiocytes (59.7%) than hepatocytes (2.6%), which indicates that the virus might directly affect intrahepatic bile ducts.
The authors had no sources of funding or financial conflicts.
SOURCE: GU J et al. Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054.
*This story was updated on 4/10.2020.
FROM GASTROENTEROLOGY
COVID-19: Extra caution needed for patients with diabetes
Patients with diabetes may have an increased risk of developing coronavirus infection (COVID-19), along with increased risks of morbidity and mortality, according to researchers writing in Diabetes & Metabolic Syndrome.
Although relevant clinical data remain scarce, patients with diabetes should take extra precautions to avoid infection and, if infected, may require special care, reported Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues.
“The disease severity [with COVID-19] has varied from mild, self-limiting, flu-like illness to fulminant pneumonia, respiratory failure, and death,” the authors wrote.
As of March 16, 2020, the World Health Organization reported 167,515 confirmed cases of COVID-19 and 6,606 deaths from around the world, with a mortality rate of 3.9%. But the actual mortality rate may be lower, the authors suggested, because a study involving more than 1,000 confirmed cases reported a mortality rate of 1.4%.
“Considering that the number of unreported and unconfirmed cases is likely to be much higher than the reported cases, the actual mortality may be less than 1%, which is similar to that of severe seasonal influenza,” the authors said, in reference to an editorial by Anthony S. Fauci, MD, and colleagues in the New England Journal of Medicine. In addition, they noted, mortality rates may vary by region.
The largest study relevant to patients with diabetes, which involved 72,314 cases of COVID-19, showed that patients with diabetes had a threefold higher mortality rate than did those without diabetes (7.3% vs. 2.3%, respectively). These figures were reported by the Chinese Centre for Disease Control and Prevention.
However, data from smaller cohorts with diabetes and COVID-19 have yielded mixed results. For instance, one study, involving 140 patients from Wuhan, suggested that diabetes was not a risk factor for severe disease, and in an analysis of 11 studies reporting on laboratory abnormalities in patients with a diagnosis of COVID-19, raised blood sugar levels or diabetes were not mentioned among the predictors of severe disease.
“Our knowledge about the prevalence of COVID-19 and disease course in people with diabetes will evolve as more detailed analyses are carried out,” the authors wrote. “For now, it is reasonable to assume that people with diabetes are at increased risk of developing infection. Coexisting heart disease, kidney disease, advanced age, and frailty are likely to further increase the severity of disease.”
Prevention first
“It is important that people with diabetes maintain good glycemic control, because it might help in reducing the risk of infection and the severity,” the authors wrote.
In addition to more frequent monitoring of blood glucose levels, they recommended other preventive measures, such as getting adequate nutrition, exercising, and being current with vaccinations for influenza and pneumonia. The latter, they said, may also reduce the risk of secondary bacterial pneumonia after a respiratory viral infection.
In regard to nutrition, adequate protein intake is important and “any deficiencies of minerals and vitamins need to be taken care of,” they advised. Likewise, exercise is known to improve immunity and should continue, but they suggest avoiding gyms and swimming pools.
For patients with coexisting heart and/or kidney disease, they also recommended efforts to stabilize cardiac/renal status.
In addition, the general preventive measures, such as regular and thorough hand washing with soap and water, practicing good respiratory hygiene by sneezing and coughing into a bent elbow or a facial tissue, and avoiding contact with anyone who is infected, should be observed.
As with other patients with chronic diseases that are managed long-term medications, patients with diabetes should always ensure that they have a sufficient supply of their medications and refills, if possible.
After a diagnosis
If patients with diabetes develop COVID-19, then home management may still be possible, wrote the authors, who recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve.
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often. “Frequent changes in dosage and correctional bolus may be required to maintain normoglycemia,” they cautioned.
Concerning diabetic drug regimens, they suggest patients avoid antihyperglycemic agents that can cause volume depletion or hypoglycemia and, if necessary, that they reduce oral antidiabetic drugs and follow sick-day guidelines.
For hospitalized patients, the investigators strengthened that statement, advising that oral agents need to be stopped, particularly sodium-glucose cotransporter 2 inhibitors and metformin. “Insulin is the preferred agent for control of hyperglycemia in hospitalized sick patients,” they wrote.
Untested therapies
The authors also discussed a range of untested therapies that may help fight COVID-19, such as antiviral drugs (such as lopinavir and ritonavir), zinc nanoparticles, and vitamin C. Supplementing those recommendations, Dr. Gupta and colleagues provided a concise review of COVID-19 epidemiology and extant data relevant to patients with diabetes.
The investigators reported no conflicts of interest.
SOURCE: Gupta et al. Diabetes Metab Syndr. 2020;14(3):211-12.
Patients with diabetes may have an increased risk of developing coronavirus infection (COVID-19), along with increased risks of morbidity and mortality, according to researchers writing in Diabetes & Metabolic Syndrome.
Although relevant clinical data remain scarce, patients with diabetes should take extra precautions to avoid infection and, if infected, may require special care, reported Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues.
“The disease severity [with COVID-19] has varied from mild, self-limiting, flu-like illness to fulminant pneumonia, respiratory failure, and death,” the authors wrote.
As of March 16, 2020, the World Health Organization reported 167,515 confirmed cases of COVID-19 and 6,606 deaths from around the world, with a mortality rate of 3.9%. But the actual mortality rate may be lower, the authors suggested, because a study involving more than 1,000 confirmed cases reported a mortality rate of 1.4%.
“Considering that the number of unreported and unconfirmed cases is likely to be much higher than the reported cases, the actual mortality may be less than 1%, which is similar to that of severe seasonal influenza,” the authors said, in reference to an editorial by Anthony S. Fauci, MD, and colleagues in the New England Journal of Medicine. In addition, they noted, mortality rates may vary by region.
The largest study relevant to patients with diabetes, which involved 72,314 cases of COVID-19, showed that patients with diabetes had a threefold higher mortality rate than did those without diabetes (7.3% vs. 2.3%, respectively). These figures were reported by the Chinese Centre for Disease Control and Prevention.
However, data from smaller cohorts with diabetes and COVID-19 have yielded mixed results. For instance, one study, involving 140 patients from Wuhan, suggested that diabetes was not a risk factor for severe disease, and in an analysis of 11 studies reporting on laboratory abnormalities in patients with a diagnosis of COVID-19, raised blood sugar levels or diabetes were not mentioned among the predictors of severe disease.
“Our knowledge about the prevalence of COVID-19 and disease course in people with diabetes will evolve as more detailed analyses are carried out,” the authors wrote. “For now, it is reasonable to assume that people with diabetes are at increased risk of developing infection. Coexisting heart disease, kidney disease, advanced age, and frailty are likely to further increase the severity of disease.”
Prevention first
“It is important that people with diabetes maintain good glycemic control, because it might help in reducing the risk of infection and the severity,” the authors wrote.
In addition to more frequent monitoring of blood glucose levels, they recommended other preventive measures, such as getting adequate nutrition, exercising, and being current with vaccinations for influenza and pneumonia. The latter, they said, may also reduce the risk of secondary bacterial pneumonia after a respiratory viral infection.
In regard to nutrition, adequate protein intake is important and “any deficiencies of minerals and vitamins need to be taken care of,” they advised. Likewise, exercise is known to improve immunity and should continue, but they suggest avoiding gyms and swimming pools.
For patients with coexisting heart and/or kidney disease, they also recommended efforts to stabilize cardiac/renal status.
In addition, the general preventive measures, such as regular and thorough hand washing with soap and water, practicing good respiratory hygiene by sneezing and coughing into a bent elbow or a facial tissue, and avoiding contact with anyone who is infected, should be observed.
As with other patients with chronic diseases that are managed long-term medications, patients with diabetes should always ensure that they have a sufficient supply of their medications and refills, if possible.
After a diagnosis
If patients with diabetes develop COVID-19, then home management may still be possible, wrote the authors, who recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve.
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often. “Frequent changes in dosage and correctional bolus may be required to maintain normoglycemia,” they cautioned.
Concerning diabetic drug regimens, they suggest patients avoid antihyperglycemic agents that can cause volume depletion or hypoglycemia and, if necessary, that they reduce oral antidiabetic drugs and follow sick-day guidelines.
For hospitalized patients, the investigators strengthened that statement, advising that oral agents need to be stopped, particularly sodium-glucose cotransporter 2 inhibitors and metformin. “Insulin is the preferred agent for control of hyperglycemia in hospitalized sick patients,” they wrote.
Untested therapies
The authors also discussed a range of untested therapies that may help fight COVID-19, such as antiviral drugs (such as lopinavir and ritonavir), zinc nanoparticles, and vitamin C. Supplementing those recommendations, Dr. Gupta and colleagues provided a concise review of COVID-19 epidemiology and extant data relevant to patients with diabetes.
The investigators reported no conflicts of interest.
SOURCE: Gupta et al. Diabetes Metab Syndr. 2020;14(3):211-12.
Patients with diabetes may have an increased risk of developing coronavirus infection (COVID-19), along with increased risks of morbidity and mortality, according to researchers writing in Diabetes & Metabolic Syndrome.
Although relevant clinical data remain scarce, patients with diabetes should take extra precautions to avoid infection and, if infected, may require special care, reported Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues.
“The disease severity [with COVID-19] has varied from mild, self-limiting, flu-like illness to fulminant pneumonia, respiratory failure, and death,” the authors wrote.
As of March 16, 2020, the World Health Organization reported 167,515 confirmed cases of COVID-19 and 6,606 deaths from around the world, with a mortality rate of 3.9%. But the actual mortality rate may be lower, the authors suggested, because a study involving more than 1,000 confirmed cases reported a mortality rate of 1.4%.
“Considering that the number of unreported and unconfirmed cases is likely to be much higher than the reported cases, the actual mortality may be less than 1%, which is similar to that of severe seasonal influenza,” the authors said, in reference to an editorial by Anthony S. Fauci, MD, and colleagues in the New England Journal of Medicine. In addition, they noted, mortality rates may vary by region.
The largest study relevant to patients with diabetes, which involved 72,314 cases of COVID-19, showed that patients with diabetes had a threefold higher mortality rate than did those without diabetes (7.3% vs. 2.3%, respectively). These figures were reported by the Chinese Centre for Disease Control and Prevention.
However, data from smaller cohorts with diabetes and COVID-19 have yielded mixed results. For instance, one study, involving 140 patients from Wuhan, suggested that diabetes was not a risk factor for severe disease, and in an analysis of 11 studies reporting on laboratory abnormalities in patients with a diagnosis of COVID-19, raised blood sugar levels or diabetes were not mentioned among the predictors of severe disease.
“Our knowledge about the prevalence of COVID-19 and disease course in people with diabetes will evolve as more detailed analyses are carried out,” the authors wrote. “For now, it is reasonable to assume that people with diabetes are at increased risk of developing infection. Coexisting heart disease, kidney disease, advanced age, and frailty are likely to further increase the severity of disease.”
Prevention first
“It is important that people with diabetes maintain good glycemic control, because it might help in reducing the risk of infection and the severity,” the authors wrote.
In addition to more frequent monitoring of blood glucose levels, they recommended other preventive measures, such as getting adequate nutrition, exercising, and being current with vaccinations for influenza and pneumonia. The latter, they said, may also reduce the risk of secondary bacterial pneumonia after a respiratory viral infection.
In regard to nutrition, adequate protein intake is important and “any deficiencies of minerals and vitamins need to be taken care of,” they advised. Likewise, exercise is known to improve immunity and should continue, but they suggest avoiding gyms and swimming pools.
For patients with coexisting heart and/or kidney disease, they also recommended efforts to stabilize cardiac/renal status.
In addition, the general preventive measures, such as regular and thorough hand washing with soap and water, practicing good respiratory hygiene by sneezing and coughing into a bent elbow or a facial tissue, and avoiding contact with anyone who is infected, should be observed.
As with other patients with chronic diseases that are managed long-term medications, patients with diabetes should always ensure that they have a sufficient supply of their medications and refills, if possible.
After a diagnosis
If patients with diabetes develop COVID-19, then home management may still be possible, wrote the authors, who recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve.
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often. “Frequent changes in dosage and correctional bolus may be required to maintain normoglycemia,” they cautioned.
Concerning diabetic drug regimens, they suggest patients avoid antihyperglycemic agents that can cause volume depletion or hypoglycemia and, if necessary, that they reduce oral antidiabetic drugs and follow sick-day guidelines.
For hospitalized patients, the investigators strengthened that statement, advising that oral agents need to be stopped, particularly sodium-glucose cotransporter 2 inhibitors and metformin. “Insulin is the preferred agent for control of hyperglycemia in hospitalized sick patients,” they wrote.
Untested therapies
The authors also discussed a range of untested therapies that may help fight COVID-19, such as antiviral drugs (such as lopinavir and ritonavir), zinc nanoparticles, and vitamin C. Supplementing those recommendations, Dr. Gupta and colleagues provided a concise review of COVID-19 epidemiology and extant data relevant to patients with diabetes.
The investigators reported no conflicts of interest.
SOURCE: Gupta et al. Diabetes Metab Syndr. 2020;14(3):211-12.
FROM DIABETES & METABOLIC SYNDROME
FDA provides flexibility to improve COVID-19 test availability
First, the FDA is giving states more flexibility to approve and implement testing for COVID-19.
“States can set up a system in which they take responsibility for authorizing such tests and the laboratories will not engage with the FDA,” agency Commissioner Stephen Hahn, MD, said in a March 16 statement announcing the policy updates. “Laboratories developing tests in these states can engage directly with the appropriate state authorities, instead of with the FDA.”
A copy of the updated guidance document can be found here.
Dr. Hahn added that laboratories working within this authority granted to states will not have to pursue an emergency use authorization (EUA). New York state was previously granted a waiver to allow for more state oversight over the introduction of diagnostic testing.
Second, the FDA is expanding guidance issued on Feb. 29 on who can develop diagnostic tests. Originally, the Feb. 29 guidance was aimed at labs certified to perform high-complexity testing consistent with requirements outlined in the Clinical Laboratory Improvement Amendments.
“Under the update published today, the agency does not intend to object to commercial manufacturers distributing and labs using new commercially developed tests prior to the FDA granting an EUA, under certain circumstances,” Commissioner Hahn said, adding that a number of commercial manufacturers are developing tests for the coronavirus with the intent of submitting an EUA request.
“During this public health emergency, the FDA does not intend to object to the distribution and use of these tests for specimen testing for a reasonable period of time after the manufacturer’s validation of the test while the manufacturer is preparing its EUA request,” he added.
The updated guidance also provides recommendations for test developers working on serologic tests for COVID-19.
During a March 16 conference call with reporters, Commissioner Hahn said the flexibility would add a “significant number of tests and we believe this will be a surge to meet the demand that we expect to see, although it is somewhat difficult” to quantify the number of tests this new flexibility will bring to the market.
First, the FDA is giving states more flexibility to approve and implement testing for COVID-19.
“States can set up a system in which they take responsibility for authorizing such tests and the laboratories will not engage with the FDA,” agency Commissioner Stephen Hahn, MD, said in a March 16 statement announcing the policy updates. “Laboratories developing tests in these states can engage directly with the appropriate state authorities, instead of with the FDA.”
A copy of the updated guidance document can be found here.
Dr. Hahn added that laboratories working within this authority granted to states will not have to pursue an emergency use authorization (EUA). New York state was previously granted a waiver to allow for more state oversight over the introduction of diagnostic testing.
Second, the FDA is expanding guidance issued on Feb. 29 on who can develop diagnostic tests. Originally, the Feb. 29 guidance was aimed at labs certified to perform high-complexity testing consistent with requirements outlined in the Clinical Laboratory Improvement Amendments.
“Under the update published today, the agency does not intend to object to commercial manufacturers distributing and labs using new commercially developed tests prior to the FDA granting an EUA, under certain circumstances,” Commissioner Hahn said, adding that a number of commercial manufacturers are developing tests for the coronavirus with the intent of submitting an EUA request.
“During this public health emergency, the FDA does not intend to object to the distribution and use of these tests for specimen testing for a reasonable period of time after the manufacturer’s validation of the test while the manufacturer is preparing its EUA request,” he added.
The updated guidance also provides recommendations for test developers working on serologic tests for COVID-19.
During a March 16 conference call with reporters, Commissioner Hahn said the flexibility would add a “significant number of tests and we believe this will be a surge to meet the demand that we expect to see, although it is somewhat difficult” to quantify the number of tests this new flexibility will bring to the market.
First, the FDA is giving states more flexibility to approve and implement testing for COVID-19.
“States can set up a system in which they take responsibility for authorizing such tests and the laboratories will not engage with the FDA,” agency Commissioner Stephen Hahn, MD, said in a March 16 statement announcing the policy updates. “Laboratories developing tests in these states can engage directly with the appropriate state authorities, instead of with the FDA.”
A copy of the updated guidance document can be found here.
Dr. Hahn added that laboratories working within this authority granted to states will not have to pursue an emergency use authorization (EUA). New York state was previously granted a waiver to allow for more state oversight over the introduction of diagnostic testing.
Second, the FDA is expanding guidance issued on Feb. 29 on who can develop diagnostic tests. Originally, the Feb. 29 guidance was aimed at labs certified to perform high-complexity testing consistent with requirements outlined in the Clinical Laboratory Improvement Amendments.
“Under the update published today, the agency does not intend to object to commercial manufacturers distributing and labs using new commercially developed tests prior to the FDA granting an EUA, under certain circumstances,” Commissioner Hahn said, adding that a number of commercial manufacturers are developing tests for the coronavirus with the intent of submitting an EUA request.
“During this public health emergency, the FDA does not intend to object to the distribution and use of these tests for specimen testing for a reasonable period of time after the manufacturer’s validation of the test while the manufacturer is preparing its EUA request,” he added.
The updated guidance also provides recommendations for test developers working on serologic tests for COVID-19.
During a March 16 conference call with reporters, Commissioner Hahn said the flexibility would add a “significant number of tests and we believe this will be a surge to meet the demand that we expect to see, although it is somewhat difficult” to quantify the number of tests this new flexibility will bring to the market.
CDC expert answers top COVID-19 questions
With new developments daily and lingering uncertainty about COVID-19, questions about testing and treatment for the coronavirus are at the forefront.
To address these top questions, Jay C. Butler, MD, deputy director for infectious diseases at the Centers for Disease Control and Prevention, sat down with JAMA editor Howard Bauchner, MD, to discuss the latest data on COVID-19 and to outline updated guidance from the agency. The following question-and-answer session was part of a live stream interview hosted by JAMA on March 16, 2020. The questions have been edited for length and clarity.
What test is being used to identify COVID-19?
In the United States, the most common and widely available test is the RT-polymerase chain reaction (rRT-PCR), which over the past few weeks has become available at public health labs across the country, Dr. Butler said during the JAMA interview. Capacity for the test is now possible in all 50 states and in Washington, D.C.
“More recently, there’s been a number of commercial labs that have come online to be able to do the testing,” Dr. Butler said. “Additionally, a number of academic centers are now able to run [Food and Drug Administration]–approved testing using slightly different PCR platforms.”
How accurate is the test?
Dr. Butler called PCR the “gold standard,” for testing COVID-19, and said it’s safe to say the test’s likelihood of identifying infection or past infection is extremely high. However, data on test sensitivity is limited.
“This may be frustrating to those of us who really like to know specifics of how to interpret the test results, but it’s important to keep in mind, we’re talking about a virus that we didn’t know existed 3 months ago,” he said.
At what point does a person with coronavirus test positive?
When exactly a test becomes positive is an unknown, Dr. Butler said. The assumption is that a patient who tests positive is more likely to be infectious, and data suggest the level of infectiousness is greatest after the onset of symptoms.
“There is at least some anecdotal reports that suggest that transmission could occur before onset of symptoms, but the data is still very limited,” he said. “Of course that has big implications in terms of how well we can really slow the spread of the virus.”
Who should get tested?
Dr. Butler said the focus should be individuals who are symptomatic with evidence of respiratory tract infection. People who are concerned about the virus and want a test are not the target.
“It’s important when talking to patients to help them to understand, this is different than a test for HIV or hepatitis C, where much of the message is: ‘Please get tested.’ ” he said. “This a situation where we’re trying to diagnose an acute infection. We do have a resource that may become limited again as some of the equipment required for running the test or collecting the specimen may come into short supply, so we want to focus on those people who are symptomatic and particularly on people who may be at higher risk of more severe illness.”
If a previously infected patient tests negative, can they still shed virus?
The CDC is currently analyzing how a negative PCR test relates to viral load, according to Dr. Butler. He added there have been situations in which a patient has twice tested negative for the virus, but a third swab resulted in a weakly positive result.
“It’s not clear if those are people who are actually infectious,” he said. “The PCR is detecting viral RNA, it doesn’t necessarily indicate there is viable virus present in the respiratory tract. So in general, I think it is safe to go back to work, but a positive test in a situation like that can be very difficult to interpret because we think it probably doesn’t reflect infectivity, but we don’t know for sure.”
Do we have an adequate supply of tests in the United States?
The CDC has addressed supply concerns by broadening the number of PCR platforms that can be used to run COVID-19 analyses, Dr. Butler said. Expansion of these platforms has been one way the government is furthering testing options and enabling consumer labs and academic centers to contribute to testing.
When can people who test positive go back to work?
The CDC is still researching that question and reviewing the data, Dr. Butler said. The current recommendation is that a patient who tests positive is considered clear to return to work after two negative tests at least 24 hours apart, following the resolution of symptoms. The CDC has not yet made an official recommendation on an exact time frame, but the CDC is considering a 14-day minimum of quarantine.
“The one caveat I’ll add is that someone who is a health care worker, even if they have resolved symptoms, it’s still a good idea to wear a surgical mask [when they return to work], just as an extra precaution.”
What do we know about immunity? Can patients get reinfected?
Long-term immunity after exposure and infection is virtually unknown, Dr. Butler said. Investigators know those with COVID-19 have an antibody response, but whether that is protective or not, is unclear. In regard to older coronaviruses, such as those that cause colds, patients generally develop an antibody response and may have a period of immunity, but that immunity eventually wanes and reinfection can occur.
What is the latest on therapies?
A number of trials are underway in China and in the United States to test possible therapies for COVID-19, Dr. Butler said. One of the candidate drugs is the broad spectrum antiviral drug remdesivir, which was developed for the treatment of the Ebola virus. Additionally, the National Institutes of Health is studying the potential for monoclonal antibodies to treat COVID-19.
“Of course these are drugs not yet FDA approved,” he said. “We all want to have them in our toolbox as soon as possible, but we want to make sure these drugs are going to benefit and not harm, and that they really do have the utility that we hope for.”
Is there specific guidance for healthcare workers about COVID-19?
Health care workers have a much higher likelihood of being exposed or exposing others who are at high risk of severe infection, Dr. Butler said. That’s why, if a health care worker becomes infected and recovers, it’s still important to take extra precautions when going back to work, such as wearing a mask.
“These are recommendations that are in-draft,” he said. “I want to be clear, I’m floating concepts out there that people can consider. ... I recognize as a former infection control medical director at a hospital that sometimes you have to adapt those guidelines based on your local conditions.”
With new developments daily and lingering uncertainty about COVID-19, questions about testing and treatment for the coronavirus are at the forefront.
To address these top questions, Jay C. Butler, MD, deputy director for infectious diseases at the Centers for Disease Control and Prevention, sat down with JAMA editor Howard Bauchner, MD, to discuss the latest data on COVID-19 and to outline updated guidance from the agency. The following question-and-answer session was part of a live stream interview hosted by JAMA on March 16, 2020. The questions have been edited for length and clarity.
What test is being used to identify COVID-19?
In the United States, the most common and widely available test is the RT-polymerase chain reaction (rRT-PCR), which over the past few weeks has become available at public health labs across the country, Dr. Butler said during the JAMA interview. Capacity for the test is now possible in all 50 states and in Washington, D.C.
“More recently, there’s been a number of commercial labs that have come online to be able to do the testing,” Dr. Butler said. “Additionally, a number of academic centers are now able to run [Food and Drug Administration]–approved testing using slightly different PCR platforms.”
How accurate is the test?
Dr. Butler called PCR the “gold standard,” for testing COVID-19, and said it’s safe to say the test’s likelihood of identifying infection or past infection is extremely high. However, data on test sensitivity is limited.
“This may be frustrating to those of us who really like to know specifics of how to interpret the test results, but it’s important to keep in mind, we’re talking about a virus that we didn’t know existed 3 months ago,” he said.
At what point does a person with coronavirus test positive?
When exactly a test becomes positive is an unknown, Dr. Butler said. The assumption is that a patient who tests positive is more likely to be infectious, and data suggest the level of infectiousness is greatest after the onset of symptoms.
“There is at least some anecdotal reports that suggest that transmission could occur before onset of symptoms, but the data is still very limited,” he said. “Of course that has big implications in terms of how well we can really slow the spread of the virus.”
Who should get tested?
Dr. Butler said the focus should be individuals who are symptomatic with evidence of respiratory tract infection. People who are concerned about the virus and want a test are not the target.
“It’s important when talking to patients to help them to understand, this is different than a test for HIV or hepatitis C, where much of the message is: ‘Please get tested.’ ” he said. “This a situation where we’re trying to diagnose an acute infection. We do have a resource that may become limited again as some of the equipment required for running the test or collecting the specimen may come into short supply, so we want to focus on those people who are symptomatic and particularly on people who may be at higher risk of more severe illness.”
If a previously infected patient tests negative, can they still shed virus?
The CDC is currently analyzing how a negative PCR test relates to viral load, according to Dr. Butler. He added there have been situations in which a patient has twice tested negative for the virus, but a third swab resulted in a weakly positive result.
“It’s not clear if those are people who are actually infectious,” he said. “The PCR is detecting viral RNA, it doesn’t necessarily indicate there is viable virus present in the respiratory tract. So in general, I think it is safe to go back to work, but a positive test in a situation like that can be very difficult to interpret because we think it probably doesn’t reflect infectivity, but we don’t know for sure.”
Do we have an adequate supply of tests in the United States?
The CDC has addressed supply concerns by broadening the number of PCR platforms that can be used to run COVID-19 analyses, Dr. Butler said. Expansion of these platforms has been one way the government is furthering testing options and enabling consumer labs and academic centers to contribute to testing.
When can people who test positive go back to work?
The CDC is still researching that question and reviewing the data, Dr. Butler said. The current recommendation is that a patient who tests positive is considered clear to return to work after two negative tests at least 24 hours apart, following the resolution of symptoms. The CDC has not yet made an official recommendation on an exact time frame, but the CDC is considering a 14-day minimum of quarantine.
“The one caveat I’ll add is that someone who is a health care worker, even if they have resolved symptoms, it’s still a good idea to wear a surgical mask [when they return to work], just as an extra precaution.”
What do we know about immunity? Can patients get reinfected?
Long-term immunity after exposure and infection is virtually unknown, Dr. Butler said. Investigators know those with COVID-19 have an antibody response, but whether that is protective or not, is unclear. In regard to older coronaviruses, such as those that cause colds, patients generally develop an antibody response and may have a period of immunity, but that immunity eventually wanes and reinfection can occur.
What is the latest on therapies?
A number of trials are underway in China and in the United States to test possible therapies for COVID-19, Dr. Butler said. One of the candidate drugs is the broad spectrum antiviral drug remdesivir, which was developed for the treatment of the Ebola virus. Additionally, the National Institutes of Health is studying the potential for monoclonal antibodies to treat COVID-19.
“Of course these are drugs not yet FDA approved,” he said. “We all want to have them in our toolbox as soon as possible, but we want to make sure these drugs are going to benefit and not harm, and that they really do have the utility that we hope for.”
Is there specific guidance for healthcare workers about COVID-19?
Health care workers have a much higher likelihood of being exposed or exposing others who are at high risk of severe infection, Dr. Butler said. That’s why, if a health care worker becomes infected and recovers, it’s still important to take extra precautions when going back to work, such as wearing a mask.
“These are recommendations that are in-draft,” he said. “I want to be clear, I’m floating concepts out there that people can consider. ... I recognize as a former infection control medical director at a hospital that sometimes you have to adapt those guidelines based on your local conditions.”
With new developments daily and lingering uncertainty about COVID-19, questions about testing and treatment for the coronavirus are at the forefront.
To address these top questions, Jay C. Butler, MD, deputy director for infectious diseases at the Centers for Disease Control and Prevention, sat down with JAMA editor Howard Bauchner, MD, to discuss the latest data on COVID-19 and to outline updated guidance from the agency. The following question-and-answer session was part of a live stream interview hosted by JAMA on March 16, 2020. The questions have been edited for length and clarity.
What test is being used to identify COVID-19?
In the United States, the most common and widely available test is the RT-polymerase chain reaction (rRT-PCR), which over the past few weeks has become available at public health labs across the country, Dr. Butler said during the JAMA interview. Capacity for the test is now possible in all 50 states and in Washington, D.C.
“More recently, there’s been a number of commercial labs that have come online to be able to do the testing,” Dr. Butler said. “Additionally, a number of academic centers are now able to run [Food and Drug Administration]–approved testing using slightly different PCR platforms.”
How accurate is the test?
Dr. Butler called PCR the “gold standard,” for testing COVID-19, and said it’s safe to say the test’s likelihood of identifying infection or past infection is extremely high. However, data on test sensitivity is limited.
“This may be frustrating to those of us who really like to know specifics of how to interpret the test results, but it’s important to keep in mind, we’re talking about a virus that we didn’t know existed 3 months ago,” he said.
At what point does a person with coronavirus test positive?
When exactly a test becomes positive is an unknown, Dr. Butler said. The assumption is that a patient who tests positive is more likely to be infectious, and data suggest the level of infectiousness is greatest after the onset of symptoms.
“There is at least some anecdotal reports that suggest that transmission could occur before onset of symptoms, but the data is still very limited,” he said. “Of course that has big implications in terms of how well we can really slow the spread of the virus.”
Who should get tested?
Dr. Butler said the focus should be individuals who are symptomatic with evidence of respiratory tract infection. People who are concerned about the virus and want a test are not the target.
“It’s important when talking to patients to help them to understand, this is different than a test for HIV or hepatitis C, where much of the message is: ‘Please get tested.’ ” he said. “This a situation where we’re trying to diagnose an acute infection. We do have a resource that may become limited again as some of the equipment required for running the test or collecting the specimen may come into short supply, so we want to focus on those people who are symptomatic and particularly on people who may be at higher risk of more severe illness.”
If a previously infected patient tests negative, can they still shed virus?
The CDC is currently analyzing how a negative PCR test relates to viral load, according to Dr. Butler. He added there have been situations in which a patient has twice tested negative for the virus, but a third swab resulted in a weakly positive result.
“It’s not clear if those are people who are actually infectious,” he said. “The PCR is detecting viral RNA, it doesn’t necessarily indicate there is viable virus present in the respiratory tract. So in general, I think it is safe to go back to work, but a positive test in a situation like that can be very difficult to interpret because we think it probably doesn’t reflect infectivity, but we don’t know for sure.”
Do we have an adequate supply of tests in the United States?
The CDC has addressed supply concerns by broadening the number of PCR platforms that can be used to run COVID-19 analyses, Dr. Butler said. Expansion of these platforms has been one way the government is furthering testing options and enabling consumer labs and academic centers to contribute to testing.
When can people who test positive go back to work?
The CDC is still researching that question and reviewing the data, Dr. Butler said. The current recommendation is that a patient who tests positive is considered clear to return to work after two negative tests at least 24 hours apart, following the resolution of symptoms. The CDC has not yet made an official recommendation on an exact time frame, but the CDC is considering a 14-day minimum of quarantine.
“The one caveat I’ll add is that someone who is a health care worker, even if they have resolved symptoms, it’s still a good idea to wear a surgical mask [when they return to work], just as an extra precaution.”
What do we know about immunity? Can patients get reinfected?
Long-term immunity after exposure and infection is virtually unknown, Dr. Butler said. Investigators know those with COVID-19 have an antibody response, but whether that is protective or not, is unclear. In regard to older coronaviruses, such as those that cause colds, patients generally develop an antibody response and may have a period of immunity, but that immunity eventually wanes and reinfection can occur.
What is the latest on therapies?
A number of trials are underway in China and in the United States to test possible therapies for COVID-19, Dr. Butler said. One of the candidate drugs is the broad spectrum antiviral drug remdesivir, which was developed for the treatment of the Ebola virus. Additionally, the National Institutes of Health is studying the potential for monoclonal antibodies to treat COVID-19.
“Of course these are drugs not yet FDA approved,” he said. “We all want to have them in our toolbox as soon as possible, but we want to make sure these drugs are going to benefit and not harm, and that they really do have the utility that we hope for.”
Is there specific guidance for healthcare workers about COVID-19?
Health care workers have a much higher likelihood of being exposed or exposing others who are at high risk of severe infection, Dr. Butler said. That’s why, if a health care worker becomes infected and recovers, it’s still important to take extra precautions when going back to work, such as wearing a mask.
“These are recommendations that are in-draft,” he said. “I want to be clear, I’m floating concepts out there that people can consider. ... I recognize as a former infection control medical director at a hospital that sometimes you have to adapt those guidelines based on your local conditions.”
Trump to governors: Don’t wait for feds on medical supplies
President Donald Trump has advised state governors not to wait on the federal government when it comes to ensuring readiness for a surge in patients from the COVID-19 outbreak.
“If they are able to get ventilators, respirators, if they are able to get certain things without having to go through the longer process of federal government,” they should order on their own and bypass the federal government ordering system, the president stated during a March 16 press briefing.
That being said, he noted that the federal government is “ordering tremendous numbers of ventilators, respirators, [and] masks,” although he could not give a specific number on how much has been ordered or how many has already been stockpiled.
“It is always going to be faster if they can get them directly, if they need them, and I have given them authorization to order directly,” President Trump said.
The comments came as the White House revised recommendations on gatherings. The new guidelines now limit gatherings to no more than 10 people. Officials are further advising Americans to self-quarantine for 2 weeks if they are sick, if someone in their house is sick, or if someone in their house has tested positive for COVID-19.
Additionally, the White House called on Americans to limit discretionary travel and to avoid eating and drinking in restaurants, bars, and food courts during the next 15 days, even if they are feeling healthy and are asymptomatic.
“With several weeks of focused action, we can turn the corner and turn it quickly,” the president said.
In terms of testing, the Food and Drug Administration has granted emergency use authorization to two commercial diagnostic tests: Thermo Fisher for its TaqPath COVID-19 Combo Kit and Roche for its cobas SARS-CoV-2 test. White House officials said up to 1 million tests will be available this week, with 2 million next week.
The president also announced that phase 1 testing of a vaccine has begun. The test involves more than 40 healthy volunteers in the Seattle area who will receive three shots over the trial period. Phase 1 testing is generally conducted to determine safety of a new therapeutic.
President Donald Trump has advised state governors not to wait on the federal government when it comes to ensuring readiness for a surge in patients from the COVID-19 outbreak.
“If they are able to get ventilators, respirators, if they are able to get certain things without having to go through the longer process of federal government,” they should order on their own and bypass the federal government ordering system, the president stated during a March 16 press briefing.
That being said, he noted that the federal government is “ordering tremendous numbers of ventilators, respirators, [and] masks,” although he could not give a specific number on how much has been ordered or how many has already been stockpiled.
“It is always going to be faster if they can get them directly, if they need them, and I have given them authorization to order directly,” President Trump said.
The comments came as the White House revised recommendations on gatherings. The new guidelines now limit gatherings to no more than 10 people. Officials are further advising Americans to self-quarantine for 2 weeks if they are sick, if someone in their house is sick, or if someone in their house has tested positive for COVID-19.
Additionally, the White House called on Americans to limit discretionary travel and to avoid eating and drinking in restaurants, bars, and food courts during the next 15 days, even if they are feeling healthy and are asymptomatic.
“With several weeks of focused action, we can turn the corner and turn it quickly,” the president said.
In terms of testing, the Food and Drug Administration has granted emergency use authorization to two commercial diagnostic tests: Thermo Fisher for its TaqPath COVID-19 Combo Kit and Roche for its cobas SARS-CoV-2 test. White House officials said up to 1 million tests will be available this week, with 2 million next week.
The president also announced that phase 1 testing of a vaccine has begun. The test involves more than 40 healthy volunteers in the Seattle area who will receive three shots over the trial period. Phase 1 testing is generally conducted to determine safety of a new therapeutic.
President Donald Trump has advised state governors not to wait on the federal government when it comes to ensuring readiness for a surge in patients from the COVID-19 outbreak.
“If they are able to get ventilators, respirators, if they are able to get certain things without having to go through the longer process of federal government,” they should order on their own and bypass the federal government ordering system, the president stated during a March 16 press briefing.
That being said, he noted that the federal government is “ordering tremendous numbers of ventilators, respirators, [and] masks,” although he could not give a specific number on how much has been ordered or how many has already been stockpiled.
“It is always going to be faster if they can get them directly, if they need them, and I have given them authorization to order directly,” President Trump said.
The comments came as the White House revised recommendations on gatherings. The new guidelines now limit gatherings to no more than 10 people. Officials are further advising Americans to self-quarantine for 2 weeks if they are sick, if someone in their house is sick, or if someone in their house has tested positive for COVID-19.
Additionally, the White House called on Americans to limit discretionary travel and to avoid eating and drinking in restaurants, bars, and food courts during the next 15 days, even if they are feeling healthy and are asymptomatic.
“With several weeks of focused action, we can turn the corner and turn it quickly,” the president said.
In terms of testing, the Food and Drug Administration has granted emergency use authorization to two commercial diagnostic tests: Thermo Fisher for its TaqPath COVID-19 Combo Kit and Roche for its cobas SARS-CoV-2 test. White House officials said up to 1 million tests will be available this week, with 2 million next week.
The president also announced that phase 1 testing of a vaccine has begun. The test involves more than 40 healthy volunteers in the Seattle area who will receive three shots over the trial period. Phase 1 testing is generally conducted to determine safety of a new therapeutic.
ESC says continue hypertension meds despite COVID-19 concern
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
The European Society of Cardiology (ESC) has issued a statement urging physicians and patients to continue treatment with angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), in light of a newly described theory that those agents could increase the risk of developing COVID-19 and/or worsen its severity.
The concern arises from the observation that the new coronavirus SARS-CoV-2 causing COVID-19 binds to angiotensin-converting enzyme 2 (ACE2) to infect cells, and both ACE inhibitors and ARBs increase ACE2 levels.
This mechanism has been theorized as a possible risk factor for facilitating the acquisition of COVID-19 infection and worsening its severity. However, paradoxically, it has also been hypothesized to protect against acute lung injury from the disease.
Meanwhile, a Lancet Respiratory Medicine article was published March 11 entitled, “Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?”
“We ... hypothesize that diabetes and hypertension treatment with ACE2-stimulating drugs increases the risk of developing severe and fatal COVID-19,” said the authors.
This prompted some media coverage in the United Kingdom and “social media-related amplification,” leading to concern and, in some cases, discontinuation of the drugs by patients.
But on March 13, the ESC Council on Hypertension dismissed the concerns as entirely speculative, in a statement posted to the ESC website.
It said that the council “strongly recommend that physicians and patients should continue treatment with their usual antihypertensive therapy because there is no clinical or scientific evidence to suggest that treatment with ACE inhibitors or ARBs should be discontinued because of the COVID-19 infection.”
The statement, signed by Council Chair Professor Giovanni de Simone, MD, on behalf of the nucleus members, also says that in regard to the theorized protective effect against serious lung complications in individuals with COVID-19, the data come only from animal, and not human, studies.
“Speculation about the safety of ACE-inhibitor or ARB treatment in relation to COVID-19 does not have a sound scientific basis or evidence to support it,” the ESC panel concludes.
This article first appeared on Medscape.com.
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
The European Society of Cardiology (ESC) has issued a statement urging physicians and patients to continue treatment with angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), in light of a newly described theory that those agents could increase the risk of developing COVID-19 and/or worsen its severity.
The concern arises from the observation that the new coronavirus SARS-CoV-2 causing COVID-19 binds to angiotensin-converting enzyme 2 (ACE2) to infect cells, and both ACE inhibitors and ARBs increase ACE2 levels.
This mechanism has been theorized as a possible risk factor for facilitating the acquisition of COVID-19 infection and worsening its severity. However, paradoxically, it has also been hypothesized to protect against acute lung injury from the disease.
Meanwhile, a Lancet Respiratory Medicine article was published March 11 entitled, “Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?”
“We ... hypothesize that diabetes and hypertension treatment with ACE2-stimulating drugs increases the risk of developing severe and fatal COVID-19,” said the authors.
This prompted some media coverage in the United Kingdom and “social media-related amplification,” leading to concern and, in some cases, discontinuation of the drugs by patients.
But on March 13, the ESC Council on Hypertension dismissed the concerns as entirely speculative, in a statement posted to the ESC website.
It said that the council “strongly recommend that physicians and patients should continue treatment with their usual antihypertensive therapy because there is no clinical or scientific evidence to suggest that treatment with ACE inhibitors or ARBs should be discontinued because of the COVID-19 infection.”
The statement, signed by Council Chair Professor Giovanni de Simone, MD, on behalf of the nucleus members, also says that in regard to the theorized protective effect against serious lung complications in individuals with COVID-19, the data come only from animal, and not human, studies.
“Speculation about the safety of ACE-inhibitor or ARB treatment in relation to COVID-19 does not have a sound scientific basis or evidence to support it,” the ESC panel concludes.
This article first appeared on Medscape.com.
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
The European Society of Cardiology (ESC) has issued a statement urging physicians and patients to continue treatment with angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), in light of a newly described theory that those agents could increase the risk of developing COVID-19 and/or worsen its severity.
The concern arises from the observation that the new coronavirus SARS-CoV-2 causing COVID-19 binds to angiotensin-converting enzyme 2 (ACE2) to infect cells, and both ACE inhibitors and ARBs increase ACE2 levels.
This mechanism has been theorized as a possible risk factor for facilitating the acquisition of COVID-19 infection and worsening its severity. However, paradoxically, it has also been hypothesized to protect against acute lung injury from the disease.
Meanwhile, a Lancet Respiratory Medicine article was published March 11 entitled, “Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?”
“We ... hypothesize that diabetes and hypertension treatment with ACE2-stimulating drugs increases the risk of developing severe and fatal COVID-19,” said the authors.
This prompted some media coverage in the United Kingdom and “social media-related amplification,” leading to concern and, in some cases, discontinuation of the drugs by patients.
But on March 13, the ESC Council on Hypertension dismissed the concerns as entirely speculative, in a statement posted to the ESC website.
It said that the council “strongly recommend that physicians and patients should continue treatment with their usual antihypertensive therapy because there is no clinical or scientific evidence to suggest that treatment with ACE inhibitors or ARBs should be discontinued because of the COVID-19 infection.”
The statement, signed by Council Chair Professor Giovanni de Simone, MD, on behalf of the nucleus members, also says that in regard to the theorized protective effect against serious lung complications in individuals with COVID-19, the data come only from animal, and not human, studies.
“Speculation about the safety of ACE-inhibitor or ARB treatment in relation to COVID-19 does not have a sound scientific basis or evidence to support it,” the ESC panel concludes.
This article first appeared on Medscape.com.
Nearly half of STI events go without HIV testing
according to Danielle Petsis, MPH, of the Children’s Hospital of Philadelphia, and associates.
In a study published in Pediatrics, the investigators conducted a retrospective analysis of 1,816 acute STI events from 1,313 patients aged 13-24 years admitted between July 2014 and Dec. 2017 at two urban health care clinics. The most common STIs in the analysis were Chlamydia, gonorrhea, trichomoniasis, and syphilis; the mean age at diagnosis was 17 years, 71% of episodes occurred in females, and 97% occurred in African American patients.
Of the 1,816 events, HIV testing was completed within 90 days of the STI diagnosis for only 55%; there was 1 confirmed HIV diagnosis among the completed tests. When HIV testing did occur, in 38% of cases it was completed concurrently with STI testing or HIV testing was performed in 35% of the 872 follow-up cases. Of the 815 events where HIV testing was not performed, 27% had a test ordered by the provider but not completed by the patient; the patient leaving the laboratory before the test could be performed was the most common reason for test noncompletion (67%), followed by not showing up at all (18%) and errors in the medical record or laboratory (5%); the remaining patients gave as reasons for test noncompletion: declining an HIV test, a closed lab, or no reason.
Logistic regression showed that participants who were female and those with a previous history of STIs had significantly lower adjusted odds of HIV test completion, compared with males and those with no previous history of STIs, respectively, the investigators said. In addition, having insurance and having a family planning visit were associated with decreased odds of HIV testing, compared with not having insurance or a family planning visit.
“As we enter the fourth decade of the HIV epidemic, it remains clear that missed opportunities for diagnosis have the potential to delay HIV diagnosis and linkage to antiretroviral therapy or PrEP and prevention services, thus increasing the population risk of HIV transmission. Our data underscore the need for improved HIV testing education for providers of all levels of training and the need for public health agencies to clearly communicate the need for testing at the time of STI infection to reduce the number of missed opportunities for testing,” Ms. Petsis and colleagues concluded.
The study was supported by the National Institutes of Mental Health and the Children’s Hospital of Philadelphia Research Institute K-Readiness Award. One coauthor reported receiving funding from Bayer Healthcare, the Templeton Foundation, the National Institutes of Health, and Janssen Biotech. She also serves on expert advisory boards for Mylan Pharmaceuticals and Merck. The other authors have no relevant financial disclosures.
SOURCE: Wood S et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2019-2265.
according to Danielle Petsis, MPH, of the Children’s Hospital of Philadelphia, and associates.
In a study published in Pediatrics, the investigators conducted a retrospective analysis of 1,816 acute STI events from 1,313 patients aged 13-24 years admitted between July 2014 and Dec. 2017 at two urban health care clinics. The most common STIs in the analysis were Chlamydia, gonorrhea, trichomoniasis, and syphilis; the mean age at diagnosis was 17 years, 71% of episodes occurred in females, and 97% occurred in African American patients.
Of the 1,816 events, HIV testing was completed within 90 days of the STI diagnosis for only 55%; there was 1 confirmed HIV diagnosis among the completed tests. When HIV testing did occur, in 38% of cases it was completed concurrently with STI testing or HIV testing was performed in 35% of the 872 follow-up cases. Of the 815 events where HIV testing was not performed, 27% had a test ordered by the provider but not completed by the patient; the patient leaving the laboratory before the test could be performed was the most common reason for test noncompletion (67%), followed by not showing up at all (18%) and errors in the medical record or laboratory (5%); the remaining patients gave as reasons for test noncompletion: declining an HIV test, a closed lab, or no reason.
Logistic regression showed that participants who were female and those with a previous history of STIs had significantly lower adjusted odds of HIV test completion, compared with males and those with no previous history of STIs, respectively, the investigators said. In addition, having insurance and having a family planning visit were associated with decreased odds of HIV testing, compared with not having insurance or a family planning visit.
“As we enter the fourth decade of the HIV epidemic, it remains clear that missed opportunities for diagnosis have the potential to delay HIV diagnosis and linkage to antiretroviral therapy or PrEP and prevention services, thus increasing the population risk of HIV transmission. Our data underscore the need for improved HIV testing education for providers of all levels of training and the need for public health agencies to clearly communicate the need for testing at the time of STI infection to reduce the number of missed opportunities for testing,” Ms. Petsis and colleagues concluded.
The study was supported by the National Institutes of Mental Health and the Children’s Hospital of Philadelphia Research Institute K-Readiness Award. One coauthor reported receiving funding from Bayer Healthcare, the Templeton Foundation, the National Institutes of Health, and Janssen Biotech. She also serves on expert advisory boards for Mylan Pharmaceuticals and Merck. The other authors have no relevant financial disclosures.
SOURCE: Wood S et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2019-2265.
according to Danielle Petsis, MPH, of the Children’s Hospital of Philadelphia, and associates.
In a study published in Pediatrics, the investigators conducted a retrospective analysis of 1,816 acute STI events from 1,313 patients aged 13-24 years admitted between July 2014 and Dec. 2017 at two urban health care clinics. The most common STIs in the analysis were Chlamydia, gonorrhea, trichomoniasis, and syphilis; the mean age at diagnosis was 17 years, 71% of episodes occurred in females, and 97% occurred in African American patients.
Of the 1,816 events, HIV testing was completed within 90 days of the STI diagnosis for only 55%; there was 1 confirmed HIV diagnosis among the completed tests. When HIV testing did occur, in 38% of cases it was completed concurrently with STI testing or HIV testing was performed in 35% of the 872 follow-up cases. Of the 815 events where HIV testing was not performed, 27% had a test ordered by the provider but not completed by the patient; the patient leaving the laboratory before the test could be performed was the most common reason for test noncompletion (67%), followed by not showing up at all (18%) and errors in the medical record or laboratory (5%); the remaining patients gave as reasons for test noncompletion: declining an HIV test, a closed lab, or no reason.
Logistic regression showed that participants who were female and those with a previous history of STIs had significantly lower adjusted odds of HIV test completion, compared with males and those with no previous history of STIs, respectively, the investigators said. In addition, having insurance and having a family planning visit were associated with decreased odds of HIV testing, compared with not having insurance or a family planning visit.
“As we enter the fourth decade of the HIV epidemic, it remains clear that missed opportunities for diagnosis have the potential to delay HIV diagnosis and linkage to antiretroviral therapy or PrEP and prevention services, thus increasing the population risk of HIV transmission. Our data underscore the need for improved HIV testing education for providers of all levels of training and the need for public health agencies to clearly communicate the need for testing at the time of STI infection to reduce the number of missed opportunities for testing,” Ms. Petsis and colleagues concluded.
The study was supported by the National Institutes of Mental Health and the Children’s Hospital of Philadelphia Research Institute K-Readiness Award. One coauthor reported receiving funding from Bayer Healthcare, the Templeton Foundation, the National Institutes of Health, and Janssen Biotech. She also serves on expert advisory boards for Mylan Pharmaceuticals and Merck. The other authors have no relevant financial disclosures.
SOURCE: Wood S et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2019-2265.
FROM PEDIATRICS
Stick with the full 12-week DAA course for acute HCV
The first randomized trial to see if a short course of a direct-acting antiviral works as well for acute hepatitis C virus (HCV) infection as the standard 12-week course was stopped early after it became clear that it did not, according to a report at the Conference on Retroviruses & Opportunistic Infections.
In the end, 6 weeks of sofosbuvir-velpatasvir (Epclusa) “was inferior” to 12 weeks, said investigators led by Gail Matthews, MD, PhD, an associate professor in the Viral Hepatitis Clinical Research Program at the Kirby Institute, in Sydney, New South Wales, Australia.
Guidelines recommend 12 weeks of direct-acting antiviral treatment, but a few observational studies have suggested that 6 weeks might be enough. Since that would make it easier for physicians and patients, and would save money, Dr. Matthews and her team set out to resolve the uncertainty with a randomized trial.
Enrollment was halted short of the 250 target because of an “unacceptably high” relapse rate of 9.7% among 93 people randomized to 6 weeks of sofosbuvir-velpatasvir versus 2% among 99 subjects randomized to the standard 12-week regimen. All the relapse patients except for one in the 12-week arm were more than 95% adherent to treatment, she at the meeting, which was scheduled to be in Boston, but was held online this year because of concerns about spreading the COVID-19 virus.
There were 17 treatment failures (18.3%) in the short arm: two deaths, three reinfections, three lost to follow-up, and the nine relapses 12 weeks out from the end of treatment. There were eight failures (8%) in the long arm, including two reinfections, two lost to follow-up, and the two relapses, but no deaths. Excluding patients with no virologic reason for failure, Dr. Matthews said, “we see the difference in the two arms even more clearly,” with viral RNA undetectable in 98% of the 12-week patients – which is in keeping with label data – versus 89% in the short arm.
The groups were well balanced. Almost all the subjects were men and the majority were white; the median age was 43 years. Almost two-thirds had a primary infection at baseline and HCV genotype 1 a/b was the most common in both groups. Patients had been infected for a year or less, with a median of 25 weeks.
The majority of subjects picked up the virus through homosexual sex, but about 20% by injection drug use. Over two-thirds had well-controlled HIV. There were no treatment related discontinuations, and all the relapsed patients were successfully treated with subsequent therapy, Dr. Matthews said.
The study was conducted in the United States, Europe, Canada, New Zealand, and Australia, and funded by the National Institutes of Health. Dr. Matthews reported research grants to her institution form Abbvie and Gilead, maker of Epclusa.
SOURCE: Matthews G. CROI 2020 abstract 121.
The first randomized trial to see if a short course of a direct-acting antiviral works as well for acute hepatitis C virus (HCV) infection as the standard 12-week course was stopped early after it became clear that it did not, according to a report at the Conference on Retroviruses & Opportunistic Infections.
In the end, 6 weeks of sofosbuvir-velpatasvir (Epclusa) “was inferior” to 12 weeks, said investigators led by Gail Matthews, MD, PhD, an associate professor in the Viral Hepatitis Clinical Research Program at the Kirby Institute, in Sydney, New South Wales, Australia.
Guidelines recommend 12 weeks of direct-acting antiviral treatment, but a few observational studies have suggested that 6 weeks might be enough. Since that would make it easier for physicians and patients, and would save money, Dr. Matthews and her team set out to resolve the uncertainty with a randomized trial.
Enrollment was halted short of the 250 target because of an “unacceptably high” relapse rate of 9.7% among 93 people randomized to 6 weeks of sofosbuvir-velpatasvir versus 2% among 99 subjects randomized to the standard 12-week regimen. All the relapse patients except for one in the 12-week arm were more than 95% adherent to treatment, she at the meeting, which was scheduled to be in Boston, but was held online this year because of concerns about spreading the COVID-19 virus.
There were 17 treatment failures (18.3%) in the short arm: two deaths, three reinfections, three lost to follow-up, and the nine relapses 12 weeks out from the end of treatment. There were eight failures (8%) in the long arm, including two reinfections, two lost to follow-up, and the two relapses, but no deaths. Excluding patients with no virologic reason for failure, Dr. Matthews said, “we see the difference in the two arms even more clearly,” with viral RNA undetectable in 98% of the 12-week patients – which is in keeping with label data – versus 89% in the short arm.
The groups were well balanced. Almost all the subjects were men and the majority were white; the median age was 43 years. Almost two-thirds had a primary infection at baseline and HCV genotype 1 a/b was the most common in both groups. Patients had been infected for a year or less, with a median of 25 weeks.
The majority of subjects picked up the virus through homosexual sex, but about 20% by injection drug use. Over two-thirds had well-controlled HIV. There were no treatment related discontinuations, and all the relapsed patients were successfully treated with subsequent therapy, Dr. Matthews said.
The study was conducted in the United States, Europe, Canada, New Zealand, and Australia, and funded by the National Institutes of Health. Dr. Matthews reported research grants to her institution form Abbvie and Gilead, maker of Epclusa.
SOURCE: Matthews G. CROI 2020 abstract 121.
The first randomized trial to see if a short course of a direct-acting antiviral works as well for acute hepatitis C virus (HCV) infection as the standard 12-week course was stopped early after it became clear that it did not, according to a report at the Conference on Retroviruses & Opportunistic Infections.
In the end, 6 weeks of sofosbuvir-velpatasvir (Epclusa) “was inferior” to 12 weeks, said investigators led by Gail Matthews, MD, PhD, an associate professor in the Viral Hepatitis Clinical Research Program at the Kirby Institute, in Sydney, New South Wales, Australia.
Guidelines recommend 12 weeks of direct-acting antiviral treatment, but a few observational studies have suggested that 6 weeks might be enough. Since that would make it easier for physicians and patients, and would save money, Dr. Matthews and her team set out to resolve the uncertainty with a randomized trial.
Enrollment was halted short of the 250 target because of an “unacceptably high” relapse rate of 9.7% among 93 people randomized to 6 weeks of sofosbuvir-velpatasvir versus 2% among 99 subjects randomized to the standard 12-week regimen. All the relapse patients except for one in the 12-week arm were more than 95% adherent to treatment, she at the meeting, which was scheduled to be in Boston, but was held online this year because of concerns about spreading the COVID-19 virus.
There were 17 treatment failures (18.3%) in the short arm: two deaths, three reinfections, three lost to follow-up, and the nine relapses 12 weeks out from the end of treatment. There were eight failures (8%) in the long arm, including two reinfections, two lost to follow-up, and the two relapses, but no deaths. Excluding patients with no virologic reason for failure, Dr. Matthews said, “we see the difference in the two arms even more clearly,” with viral RNA undetectable in 98% of the 12-week patients – which is in keeping with label data – versus 89% in the short arm.
The groups were well balanced. Almost all the subjects were men and the majority were white; the median age was 43 years. Almost two-thirds had a primary infection at baseline and HCV genotype 1 a/b was the most common in both groups. Patients had been infected for a year or less, with a median of 25 weeks.
The majority of subjects picked up the virus through homosexual sex, but about 20% by injection drug use. Over two-thirds had well-controlled HIV. There were no treatment related discontinuations, and all the relapsed patients were successfully treated with subsequent therapy, Dr. Matthews said.
The study was conducted in the United States, Europe, Canada, New Zealand, and Australia, and funded by the National Institutes of Health. Dr. Matthews reported research grants to her institution form Abbvie and Gilead, maker of Epclusa.
SOURCE: Matthews G. CROI 2020 abstract 121.
FROM CROI 2020