User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Every click you make, the EHR is watching you
This transcript has been edited for clarity.
When I close my eyes and imagine what it is I do for a living, I see a computer screen.
I’m primarily a clinical researcher, so much of what I do is looking at statistical software, or, more recently, writing grant applications. But even when I think of my clinical duties, I see that computer screen.
The reason? The electronic health record (EHR) – the hot, beating heart of medical care in the modern era. Our most powerful tool and our greatest enemy.
The EHR records everything – not just the vital signs and lab values of our patients, not just our notes and billing codes. Everything. Every interaction we have is tracked and can be analyzed. The EHR is basically Sting in the song “Every Breath You Take.” Every click you make, it is watching you.
Researchers are leveraging that panopticon to give insight into something we don’t talk about frequently: the issue of racial bias in medicine. Is our true nature revealed by our interactions with the EHR?
We’re talking about this study in JAMA Network Open.
Researchers leveraged huge amounts of EHR data from two big academic medical centers, Vanderbilt University Medical Center and Northwestern University Medical Center. All told, there are data from nearly 250,000 hospitalizations here.
The researchers created a metric for EHR engagement. Basically, they summed the amount of clicks and other EHR interactions that occurred during the hospitalization, divided by the length of stay in days, to create a sort of average “engagement per day” metric. This number was categorized into four groups: low engagement, medium engagement, high engagement, and very high engagement.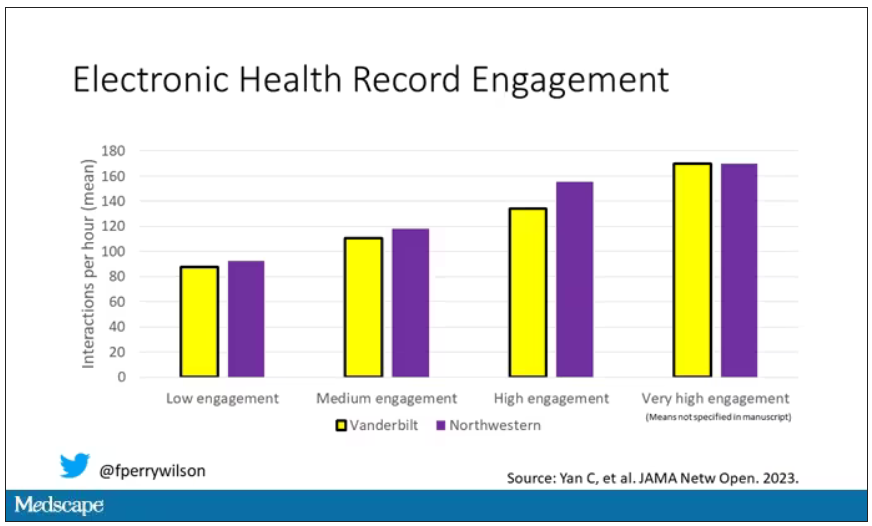
What factors would predict higher engagement? Well, , except among Black patients who actually got a bit more engagement.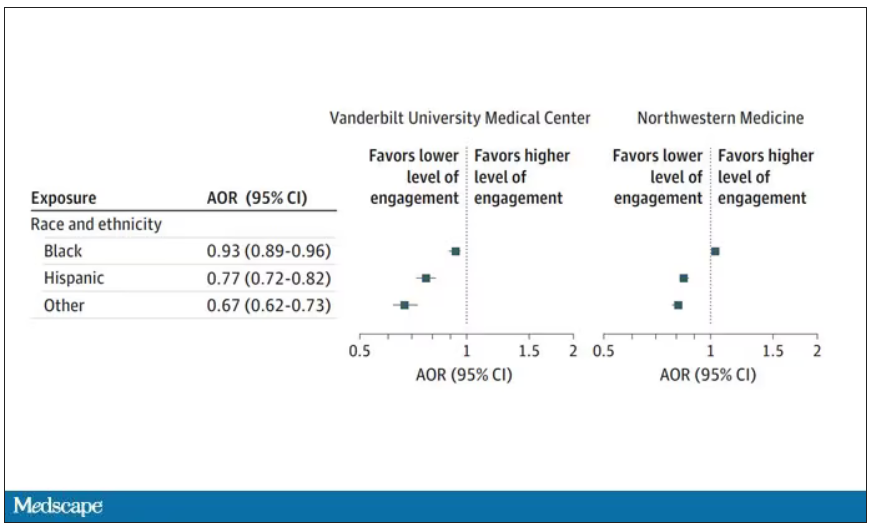
So, right away we need to be concerned about the obvious implications. Less engagement with the EHR may mean lower-quality care, right? Less attention to medical issues. And if that differs systematically by race, that’s a problem.
But we need to be careful here, because engagement in the health record is not random. Many factors would lead you to spend more time in one patient’s chart vs. another. Medical complexity is the most obvious one. The authors did their best to account for this, adjusting for patients’ age, sex, insurance status, comorbidity score, and social deprivation index based on their ZIP code. But notably, they did not account for the acuity of illness during the hospitalization. If individuals identifying as a minority were, all else being equal, less likely to be severely ill by the time they were hospitalized, you might see results like this.
The authors also restrict their analysis to individuals who were discharged alive. I’m not entirely clear why they made this choice. Most people don’t die in the hospital; the inpatient mortality rate at most centers is 1%-1.5%. But excluding those patients could potentially bias these results, especially if race is, all else being equal, a predictor of inpatient mortality, as some studies have shown.
But the truth is, these data aren’t coming out of nowhere; they don’t exist in a vacuum. Numerous studies demonstrate different intensity of care among minority vs. nonminority individuals. There is this study, which shows that minority populations are less likely to be placed on the liver transplant waitlist.
There is this study, which found that minority kids with type 1 diabetes were less likely to get insulin pumps than were their White counterparts. And this one, which showed that kids with acute appendicitis were less likely to get pain-control medications if they were Black.
This study shows that although life expectancy decreased across all races during the pandemic, it decreased the most among minority populations.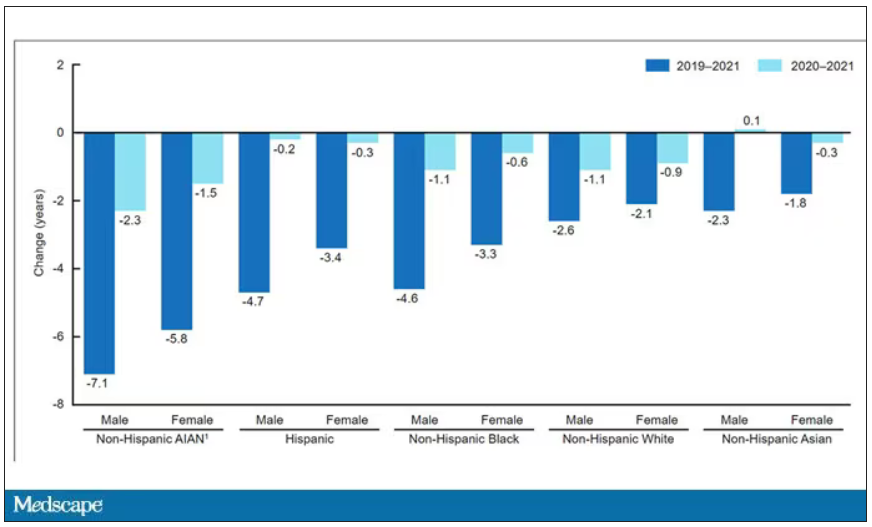
This list goes on. It’s why the CDC has called racism a “fundamental cause of ... disease.”
So, yes, it is clear that there are racial disparities in health care outcomes. It is clear that there are racial disparities in treatments. It is also clear that virtually every physician believes they deliver equitable care. Somewhere, this disconnect arises. Could the actions we take in the EHR reveal the unconscious biases we have? Does the all-seeing eye of the EHR see not only into our brains but into our hearts? And if it can, are we ready to confront what it sees?
F. Perry Wilson, MD, MSCE, is associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When I close my eyes and imagine what it is I do for a living, I see a computer screen.
I’m primarily a clinical researcher, so much of what I do is looking at statistical software, or, more recently, writing grant applications. But even when I think of my clinical duties, I see that computer screen.
The reason? The electronic health record (EHR) – the hot, beating heart of medical care in the modern era. Our most powerful tool and our greatest enemy.
The EHR records everything – not just the vital signs and lab values of our patients, not just our notes and billing codes. Everything. Every interaction we have is tracked and can be analyzed. The EHR is basically Sting in the song “Every Breath You Take.” Every click you make, it is watching you.
Researchers are leveraging that panopticon to give insight into something we don’t talk about frequently: the issue of racial bias in medicine. Is our true nature revealed by our interactions with the EHR?
We’re talking about this study in JAMA Network Open.
Researchers leveraged huge amounts of EHR data from two big academic medical centers, Vanderbilt University Medical Center and Northwestern University Medical Center. All told, there are data from nearly 250,000 hospitalizations here.
The researchers created a metric for EHR engagement. Basically, they summed the amount of clicks and other EHR interactions that occurred during the hospitalization, divided by the length of stay in days, to create a sort of average “engagement per day” metric. This number was categorized into four groups: low engagement, medium engagement, high engagement, and very high engagement.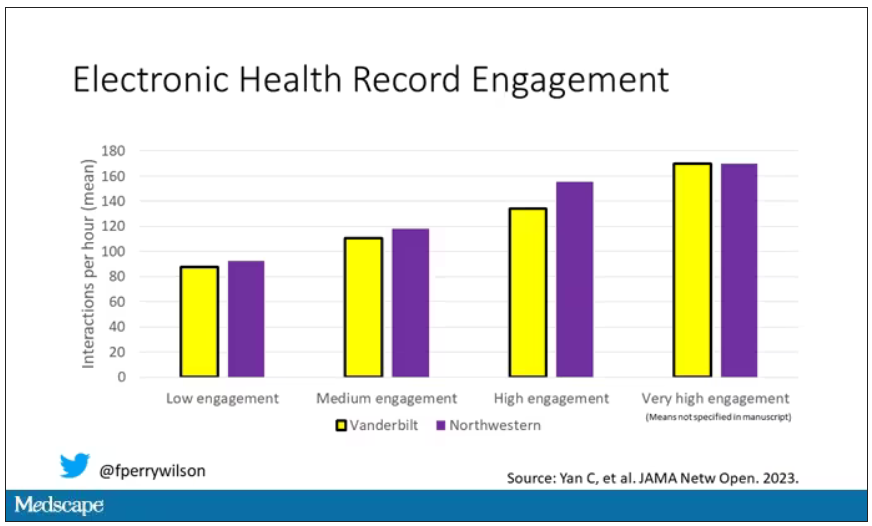
What factors would predict higher engagement? Well, , except among Black patients who actually got a bit more engagement.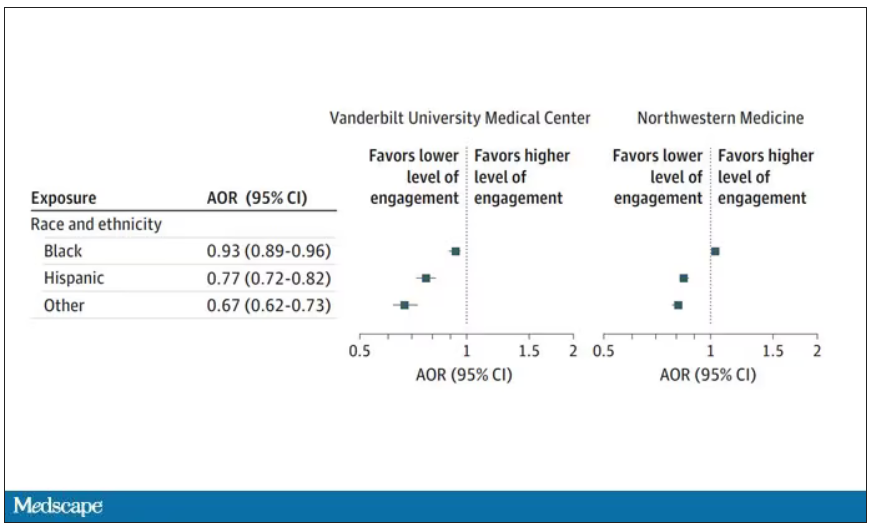
So, right away we need to be concerned about the obvious implications. Less engagement with the EHR may mean lower-quality care, right? Less attention to medical issues. And if that differs systematically by race, that’s a problem.
But we need to be careful here, because engagement in the health record is not random. Many factors would lead you to spend more time in one patient’s chart vs. another. Medical complexity is the most obvious one. The authors did their best to account for this, adjusting for patients’ age, sex, insurance status, comorbidity score, and social deprivation index based on their ZIP code. But notably, they did not account for the acuity of illness during the hospitalization. If individuals identifying as a minority were, all else being equal, less likely to be severely ill by the time they were hospitalized, you might see results like this.
The authors also restrict their analysis to individuals who were discharged alive. I’m not entirely clear why they made this choice. Most people don’t die in the hospital; the inpatient mortality rate at most centers is 1%-1.5%. But excluding those patients could potentially bias these results, especially if race is, all else being equal, a predictor of inpatient mortality, as some studies have shown.
But the truth is, these data aren’t coming out of nowhere; they don’t exist in a vacuum. Numerous studies demonstrate different intensity of care among minority vs. nonminority individuals. There is this study, which shows that minority populations are less likely to be placed on the liver transplant waitlist.
There is this study, which found that minority kids with type 1 diabetes were less likely to get insulin pumps than were their White counterparts. And this one, which showed that kids with acute appendicitis were less likely to get pain-control medications if they were Black.
This study shows that although life expectancy decreased across all races during the pandemic, it decreased the most among minority populations.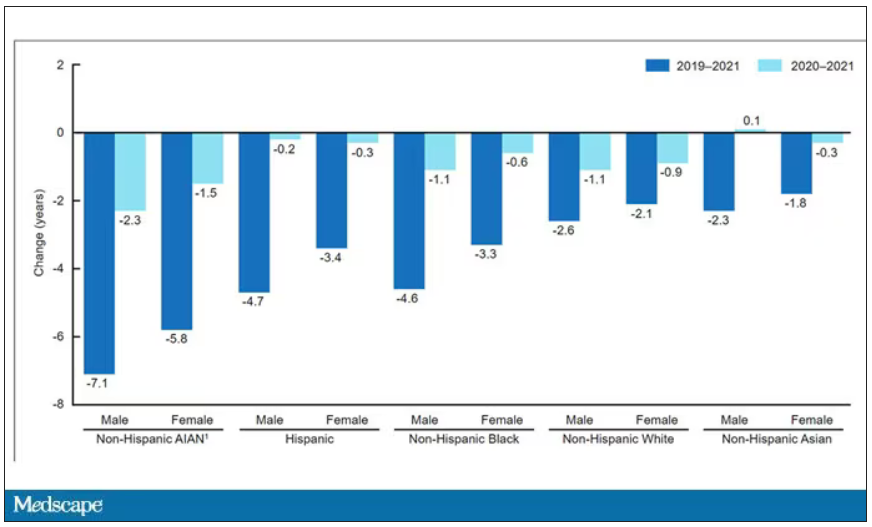
This list goes on. It’s why the CDC has called racism a “fundamental cause of ... disease.”
So, yes, it is clear that there are racial disparities in health care outcomes. It is clear that there are racial disparities in treatments. It is also clear that virtually every physician believes they deliver equitable care. Somewhere, this disconnect arises. Could the actions we take in the EHR reveal the unconscious biases we have? Does the all-seeing eye of the EHR see not only into our brains but into our hearts? And if it can, are we ready to confront what it sees?
F. Perry Wilson, MD, MSCE, is associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When I close my eyes and imagine what it is I do for a living, I see a computer screen.
I’m primarily a clinical researcher, so much of what I do is looking at statistical software, or, more recently, writing grant applications. But even when I think of my clinical duties, I see that computer screen.
The reason? The electronic health record (EHR) – the hot, beating heart of medical care in the modern era. Our most powerful tool and our greatest enemy.
The EHR records everything – not just the vital signs and lab values of our patients, not just our notes and billing codes. Everything. Every interaction we have is tracked and can be analyzed. The EHR is basically Sting in the song “Every Breath You Take.” Every click you make, it is watching you.
Researchers are leveraging that panopticon to give insight into something we don’t talk about frequently: the issue of racial bias in medicine. Is our true nature revealed by our interactions with the EHR?
We’re talking about this study in JAMA Network Open.
Researchers leveraged huge amounts of EHR data from two big academic medical centers, Vanderbilt University Medical Center and Northwestern University Medical Center. All told, there are data from nearly 250,000 hospitalizations here.
The researchers created a metric for EHR engagement. Basically, they summed the amount of clicks and other EHR interactions that occurred during the hospitalization, divided by the length of stay in days, to create a sort of average “engagement per day” metric. This number was categorized into four groups: low engagement, medium engagement, high engagement, and very high engagement.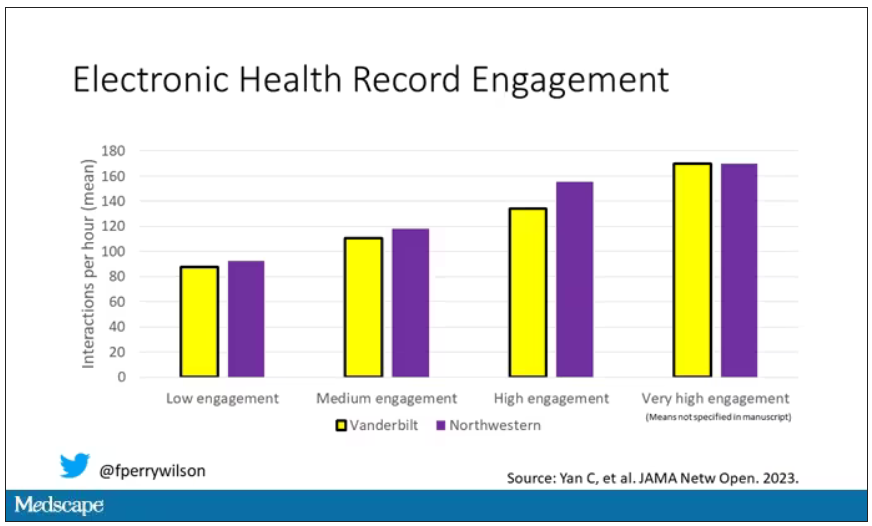
What factors would predict higher engagement? Well, , except among Black patients who actually got a bit more engagement.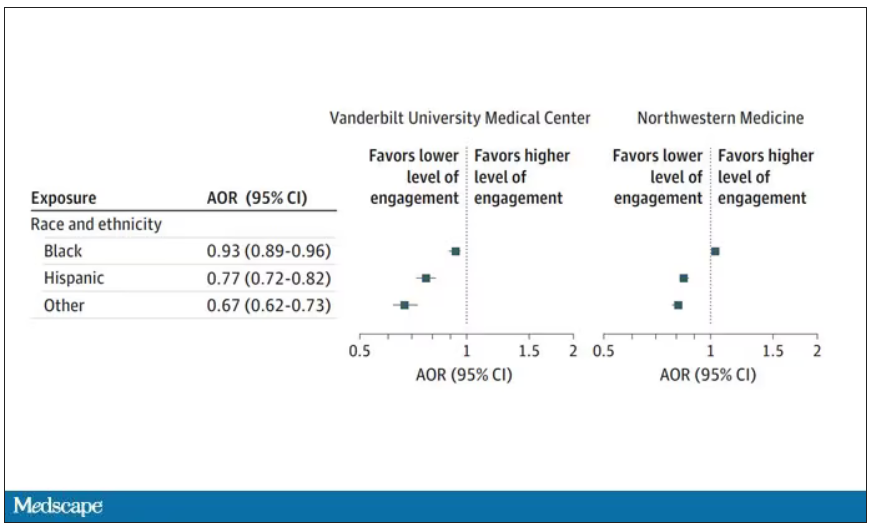
So, right away we need to be concerned about the obvious implications. Less engagement with the EHR may mean lower-quality care, right? Less attention to medical issues. And if that differs systematically by race, that’s a problem.
But we need to be careful here, because engagement in the health record is not random. Many factors would lead you to spend more time in one patient’s chart vs. another. Medical complexity is the most obvious one. The authors did their best to account for this, adjusting for patients’ age, sex, insurance status, comorbidity score, and social deprivation index based on their ZIP code. But notably, they did not account for the acuity of illness during the hospitalization. If individuals identifying as a minority were, all else being equal, less likely to be severely ill by the time they were hospitalized, you might see results like this.
The authors also restrict their analysis to individuals who were discharged alive. I’m not entirely clear why they made this choice. Most people don’t die in the hospital; the inpatient mortality rate at most centers is 1%-1.5%. But excluding those patients could potentially bias these results, especially if race is, all else being equal, a predictor of inpatient mortality, as some studies have shown.
But the truth is, these data aren’t coming out of nowhere; they don’t exist in a vacuum. Numerous studies demonstrate different intensity of care among minority vs. nonminority individuals. There is this study, which shows that minority populations are less likely to be placed on the liver transplant waitlist.
There is this study, which found that minority kids with type 1 diabetes were less likely to get insulin pumps than were their White counterparts. And this one, which showed that kids with acute appendicitis were less likely to get pain-control medications if they were Black.
This study shows that although life expectancy decreased across all races during the pandemic, it decreased the most among minority populations.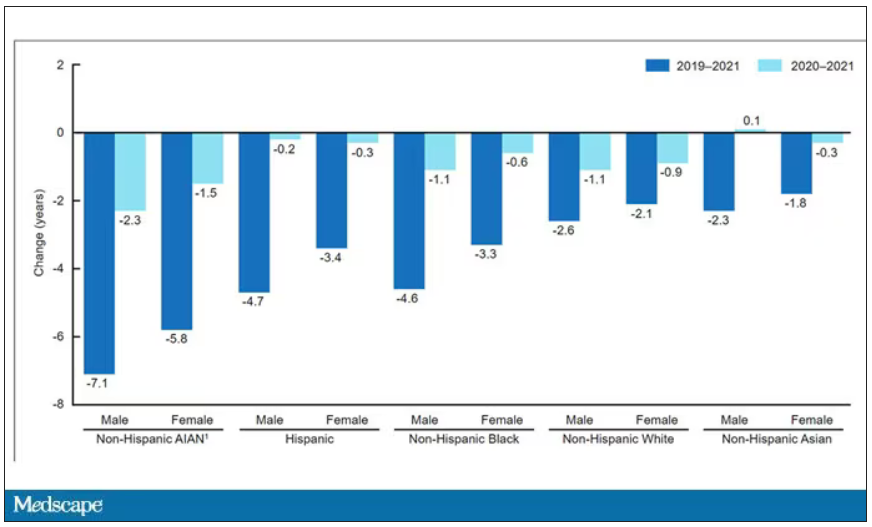
This list goes on. It’s why the CDC has called racism a “fundamental cause of ... disease.”
So, yes, it is clear that there are racial disparities in health care outcomes. It is clear that there are racial disparities in treatments. It is also clear that virtually every physician believes they deliver equitable care. Somewhere, this disconnect arises. Could the actions we take in the EHR reveal the unconscious biases we have? Does the all-seeing eye of the EHR see not only into our brains but into our hearts? And if it can, are we ready to confront what it sees?
F. Perry Wilson, MD, MSCE, is associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Young women rate top sources for STI self-testing
, based on surveys from 92 individuals.
Direct-to-consumer (DTC) sexually transmitted infection (STI) screening methods involve the use of self-collected samples outside of a clinical setting, and may help reach women who avoid screening or lack access to clinical care, wrote Stacey B. Griner, PhD, of the University of North Texas Health Science Center, Fort Worth, and colleagues.
However, data on the methods used to promote DTC to the young female population are limited, and the goal of the current study was to identify preferred sources and communication channels for DTC STI information in this population, they said.
In a study published in Sexually Transmitted Diseases, the researchers reviewed data from 92 women aged 18-24 years at a single university who participated in an online survey. Of these, 24 also participated in in-depth interviews. The mean age of the participants was 20.0 years, and all reported being sexually active in the past year. Approximately two-thirds (68.5%) were White, 24% were Hispanic, 13% were Black or African American; 63.0% overall were heterosexual.
Participants received a description of DTC methods and were asked whether they were interested in receiving more information, and if so, what were their preferred sources for receiving the information. Potential sources included health care providers, friends, family members, partners, the Internet, college resources, classes, and other, and participants were asked to rank these choices in order of preference.
More than half of the participants identified health care providers as their preferred source of information (56.5%), followed by trusted websites (25%), and university-based resources or friends (6.5% for both).
Overall, participants who underwent STI screening in the past 12 months ranked college resources higher than those who had not undergone screening.
Race played a significant role in ranking partners and family members as resources. Compared with Black participants, White participants and those who were biracial/multiracial/another race ranked partners as a significantly more preferred source, but the differences between White and biracial/multiracial/another race were not significant. White participants and Black participants were similar in ranking family as a preferred information source, but White participants, compared with biracial/multiracial/other participants, ranked family as a significantly more preferred source.
Differences in rankings were similar across sexual orientations.
In-depth interviews were conducted on the college campus prior to the COVID-19 pandemic. The mean age of the interview participants was 19.5 years, and most were non-Hispanic White. Sexual orientation was varied, with 50% identifying as heterosexual and 50% identifying as a sexual minority.
In the interviews, health care providers were seen as influential for considering DTC methods, with gynecologists, other specialists, and more experienced physicians deemed the most trustworthy. Interviewees noted social media sites as a way to provide information and raise awareness of DTC methods, such as through the advertisements feature on Instagram. They also identified university orientation as a way to reach students and provide information about DTC options in the context of other health-related orientation topics such as sexual consent and alcohol use.
Many interviewees also mentioned friends as a resource for discussing sex, sexuality, and STI screening, and said they would be accepting of information, knowledge, and emotional support when learning about DTC from friends.
The findings were limited by several factors, including the cross-sectional design, use of data from a single campus setting, and the overrepresentation of White women, and more studies are needed to identify differences by region and campus type that might guide interventions, the researchers noted. The study also was limited by “the lack of specificity of what participants considered to be credible Internet information sources,” they said.
However, the results suggest that using health care providers, trusted websites, and established college resources as dissemination channels may help increase the awareness and use of DTC methods for STI screening in young women, they concluded.
The study was supported in part by the Doug Kirby Adolescent Sexual Health Research Grant from the Rural Center for AIDS/STD Prevention at Indiana University and by the University of South Florida College of Public Health. The researchers had no financial conflicts to disclose.
, based on surveys from 92 individuals.
Direct-to-consumer (DTC) sexually transmitted infection (STI) screening methods involve the use of self-collected samples outside of a clinical setting, and may help reach women who avoid screening or lack access to clinical care, wrote Stacey B. Griner, PhD, of the University of North Texas Health Science Center, Fort Worth, and colleagues.
However, data on the methods used to promote DTC to the young female population are limited, and the goal of the current study was to identify preferred sources and communication channels for DTC STI information in this population, they said.
In a study published in Sexually Transmitted Diseases, the researchers reviewed data from 92 women aged 18-24 years at a single university who participated in an online survey. Of these, 24 also participated in in-depth interviews. The mean age of the participants was 20.0 years, and all reported being sexually active in the past year. Approximately two-thirds (68.5%) were White, 24% were Hispanic, 13% were Black or African American; 63.0% overall were heterosexual.
Participants received a description of DTC methods and were asked whether they were interested in receiving more information, and if so, what were their preferred sources for receiving the information. Potential sources included health care providers, friends, family members, partners, the Internet, college resources, classes, and other, and participants were asked to rank these choices in order of preference.
More than half of the participants identified health care providers as their preferred source of information (56.5%), followed by trusted websites (25%), and university-based resources or friends (6.5% for both).
Overall, participants who underwent STI screening in the past 12 months ranked college resources higher than those who had not undergone screening.
Race played a significant role in ranking partners and family members as resources. Compared with Black participants, White participants and those who were biracial/multiracial/another race ranked partners as a significantly more preferred source, but the differences between White and biracial/multiracial/another race were not significant. White participants and Black participants were similar in ranking family as a preferred information source, but White participants, compared with biracial/multiracial/other participants, ranked family as a significantly more preferred source.
Differences in rankings were similar across sexual orientations.
In-depth interviews were conducted on the college campus prior to the COVID-19 pandemic. The mean age of the interview participants was 19.5 years, and most were non-Hispanic White. Sexual orientation was varied, with 50% identifying as heterosexual and 50% identifying as a sexual minority.
In the interviews, health care providers were seen as influential for considering DTC methods, with gynecologists, other specialists, and more experienced physicians deemed the most trustworthy. Interviewees noted social media sites as a way to provide information and raise awareness of DTC methods, such as through the advertisements feature on Instagram. They also identified university orientation as a way to reach students and provide information about DTC options in the context of other health-related orientation topics such as sexual consent and alcohol use.
Many interviewees also mentioned friends as a resource for discussing sex, sexuality, and STI screening, and said they would be accepting of information, knowledge, and emotional support when learning about DTC from friends.
The findings were limited by several factors, including the cross-sectional design, use of data from a single campus setting, and the overrepresentation of White women, and more studies are needed to identify differences by region and campus type that might guide interventions, the researchers noted. The study also was limited by “the lack of specificity of what participants considered to be credible Internet information sources,” they said.
However, the results suggest that using health care providers, trusted websites, and established college resources as dissemination channels may help increase the awareness and use of DTC methods for STI screening in young women, they concluded.
The study was supported in part by the Doug Kirby Adolescent Sexual Health Research Grant from the Rural Center for AIDS/STD Prevention at Indiana University and by the University of South Florida College of Public Health. The researchers had no financial conflicts to disclose.
, based on surveys from 92 individuals.
Direct-to-consumer (DTC) sexually transmitted infection (STI) screening methods involve the use of self-collected samples outside of a clinical setting, and may help reach women who avoid screening or lack access to clinical care, wrote Stacey B. Griner, PhD, of the University of North Texas Health Science Center, Fort Worth, and colleagues.
However, data on the methods used to promote DTC to the young female population are limited, and the goal of the current study was to identify preferred sources and communication channels for DTC STI information in this population, they said.
In a study published in Sexually Transmitted Diseases, the researchers reviewed data from 92 women aged 18-24 years at a single university who participated in an online survey. Of these, 24 also participated in in-depth interviews. The mean age of the participants was 20.0 years, and all reported being sexually active in the past year. Approximately two-thirds (68.5%) were White, 24% were Hispanic, 13% were Black or African American; 63.0% overall were heterosexual.
Participants received a description of DTC methods and were asked whether they were interested in receiving more information, and if so, what were their preferred sources for receiving the information. Potential sources included health care providers, friends, family members, partners, the Internet, college resources, classes, and other, and participants were asked to rank these choices in order of preference.
More than half of the participants identified health care providers as their preferred source of information (56.5%), followed by trusted websites (25%), and university-based resources or friends (6.5% for both).
Overall, participants who underwent STI screening in the past 12 months ranked college resources higher than those who had not undergone screening.
Race played a significant role in ranking partners and family members as resources. Compared with Black participants, White participants and those who were biracial/multiracial/another race ranked partners as a significantly more preferred source, but the differences between White and biracial/multiracial/another race were not significant. White participants and Black participants were similar in ranking family as a preferred information source, but White participants, compared with biracial/multiracial/other participants, ranked family as a significantly more preferred source.
Differences in rankings were similar across sexual orientations.
In-depth interviews were conducted on the college campus prior to the COVID-19 pandemic. The mean age of the interview participants was 19.5 years, and most were non-Hispanic White. Sexual orientation was varied, with 50% identifying as heterosexual and 50% identifying as a sexual minority.
In the interviews, health care providers were seen as influential for considering DTC methods, with gynecologists, other specialists, and more experienced physicians deemed the most trustworthy. Interviewees noted social media sites as a way to provide information and raise awareness of DTC methods, such as through the advertisements feature on Instagram. They also identified university orientation as a way to reach students and provide information about DTC options in the context of other health-related orientation topics such as sexual consent and alcohol use.
Many interviewees also mentioned friends as a resource for discussing sex, sexuality, and STI screening, and said they would be accepting of information, knowledge, and emotional support when learning about DTC from friends.
The findings were limited by several factors, including the cross-sectional design, use of data from a single campus setting, and the overrepresentation of White women, and more studies are needed to identify differences by region and campus type that might guide interventions, the researchers noted. The study also was limited by “the lack of specificity of what participants considered to be credible Internet information sources,” they said.
However, the results suggest that using health care providers, trusted websites, and established college resources as dissemination channels may help increase the awareness and use of DTC methods for STI screening in young women, they concluded.
The study was supported in part by the Doug Kirby Adolescent Sexual Health Research Grant from the Rural Center for AIDS/STD Prevention at Indiana University and by the University of South Florida College of Public Health. The researchers had no financial conflicts to disclose.
FROM SEXUALLY TRANSMITTED DISEASES
Paxlovid tied to benefits in high-risk patients with COVID
In a cohort study from British Columbia that included nearly 7,000 patients with COVID-19, nirmatrelvir-ritonavir was associated with a 2.5% reduction in risk for death or emergency hospitalization in clinically extremely vulnerable (CEV) patients who were severely immunocompromised. No significant benefit was observed in patients who were not immunocompromised.
“This finding could help substantially limit unnecessary use of nirmatrelvir and ritonavir in older, otherwise healthy individuals,” lead author Colin R. Dormuth, ScD, associate professor of anesthesiology, pharmacology, and therapeutics at the University of British Columbia, Vancouver, told this news organization. “Another finding that was surprising and might help place the role of nirmatrelvir and ritonavir in context is that even in severely immunocompromised individuals who did not take [the drug], the risk of death or hospitalization with COVID-19 was less than 4% in our study population.”
The study was published online in JAMA Network Open.
Who benefits?
The investigators analyzed medical records for 6,866 patients in British Columbia (median age, 70 years; 57% women) who presented between Feb. 1, 2022, and Feb. 3, 2023. Eligible patients belonged to one of four higher-risk groups who received priority for COVID-19 vaccination.
Two groups included CEV patients who were severely (CEV1) or moderately (CEV2) immunocompromised. The CEV3 group was not immunocompromised but had medical conditions associated with a high risk for complications from COVID-19. A fourth expanded eligibility (EXEL) group included higher-risk patients who were not in one of the other groups, such as unvaccinated patients older than age 70 years.
The investigators matched treated patients to untreated patients in the same vulnerability group according to age, sex, and month of infection. The primary outcome was death from any cause or emergency hospitalization with COVID-19 within 28 days.
Treatment with nirmatrelvir-ritonavir was associated with statistically significant relative reductions in the primary outcome, compared with no treatment, for patients in the CEV1 (risk difference, −2.5%) and CEV2 (RD, −1.7%) groups. In the CEV3 group, the RD of −1.3% was not statistically significant. In the EXEL group, treatment was associated with a higher risk for the primary outcome (RD, 1.0%), but the result was not statistically significant.
The results were “robust across sex and older vs. younger age,” the authors note. “No reduction in the primary outcome was observed in lower-risk individuals, including those aged 70 years or older without serious comorbidities.”
The combination of nirmatrelvir-ritonavir was approved for use in Canada based on interim efficacy and safety data from the Evaluation of Inhibition for COVID-19 in High-Risk Patients (EPIC-HR) trial, said Dr. Dormuth.
British Columbia’s eligibility criteria for nirmatrelvir-ritonavir coverage differ substantially from the criteria for participants in the EPIC-HR trial, he noted. Those patients were unvaccinated, had no natural immunity from a previous COVID-19 infection, and were infected with COVID-19 variants that were different from those now circulating. The current study was prompted by the need to look at a broader population of individuals in British Columbia with varying risks of complications from COVID-19 infection.
Before the study, a common view was that patients aged 70 and older would benefit from the drug, said Dr. Dormuth. “Our study, which accounted for medical conditions related to an individual’s vulnerability to complications, showed that older age on its own was not a reason to use nirmatrelvir and ritonavir once relevant medical conditions were taken into consideration.”
The researchers are working on a study to identify with greater specificity which comorbid conditions are most associated with nirmatrelvir-ritonavir effectiveness, he added. “It could be that a relatively small number of conditions can be used to identify most individuals who would benefit from the drug.”
‘Signal toward benefit’
Commenting on the findings for this news organization, Abhijit Duggal, MD, vice chair of critical care at the Cleveland Clinic, who was not involved in this study, said, “I’m always very wary when we look at observational data and we start saying the effectiveness is not really as high as was seen in other studies. We are seeing an effect with all these studies that seems to be in the right direction.
“Having said that,” he added, “is the effect going to be potentially more in patients at higher risk? Absolutely. I think these postmarket studies are really showing that after vaccination, if someone does get infected, this is a secondary option available to us that can prevent progression of the disease, which would likely be more severe in immunocompromised patients.”
Dr. Duggal was a coinvestigator on a recent study of more than 68,000 patients that showed that nirmatrelvir-ritonavir or molnupiravir was associated with reductions in mortality and hospitalization in nonhospitalized patients infected with the Omicron variant, regardless of age, race and ethnicity, virus strain, vaccination status, previous infection status, or coexisting conditions.
“In all groups, there was a signal toward benefit,” said Dr. Duggal. “These studies tell us that these drugs do remain valid options. But their use needs to be discussed on a case-by-case basis with patients we feel are deteriorating or at a higher risk because of underlying disease processes.”
The study was supported by funding from the British Columbia Ministry of Health. Dr. Dormuth and Dr. Duggal report no relevant financial relationships.
A version of this article appeared on Medscape.com.
In a cohort study from British Columbia that included nearly 7,000 patients with COVID-19, nirmatrelvir-ritonavir was associated with a 2.5% reduction in risk for death or emergency hospitalization in clinically extremely vulnerable (CEV) patients who were severely immunocompromised. No significant benefit was observed in patients who were not immunocompromised.
“This finding could help substantially limit unnecessary use of nirmatrelvir and ritonavir in older, otherwise healthy individuals,” lead author Colin R. Dormuth, ScD, associate professor of anesthesiology, pharmacology, and therapeutics at the University of British Columbia, Vancouver, told this news organization. “Another finding that was surprising and might help place the role of nirmatrelvir and ritonavir in context is that even in severely immunocompromised individuals who did not take [the drug], the risk of death or hospitalization with COVID-19 was less than 4% in our study population.”
The study was published online in JAMA Network Open.
Who benefits?
The investigators analyzed medical records for 6,866 patients in British Columbia (median age, 70 years; 57% women) who presented between Feb. 1, 2022, and Feb. 3, 2023. Eligible patients belonged to one of four higher-risk groups who received priority for COVID-19 vaccination.
Two groups included CEV patients who were severely (CEV1) or moderately (CEV2) immunocompromised. The CEV3 group was not immunocompromised but had medical conditions associated with a high risk for complications from COVID-19. A fourth expanded eligibility (EXEL) group included higher-risk patients who were not in one of the other groups, such as unvaccinated patients older than age 70 years.
The investigators matched treated patients to untreated patients in the same vulnerability group according to age, sex, and month of infection. The primary outcome was death from any cause or emergency hospitalization with COVID-19 within 28 days.
Treatment with nirmatrelvir-ritonavir was associated with statistically significant relative reductions in the primary outcome, compared with no treatment, for patients in the CEV1 (risk difference, −2.5%) and CEV2 (RD, −1.7%) groups. In the CEV3 group, the RD of −1.3% was not statistically significant. In the EXEL group, treatment was associated with a higher risk for the primary outcome (RD, 1.0%), but the result was not statistically significant.
The results were “robust across sex and older vs. younger age,” the authors note. “No reduction in the primary outcome was observed in lower-risk individuals, including those aged 70 years or older without serious comorbidities.”
The combination of nirmatrelvir-ritonavir was approved for use in Canada based on interim efficacy and safety data from the Evaluation of Inhibition for COVID-19 in High-Risk Patients (EPIC-HR) trial, said Dr. Dormuth.
British Columbia’s eligibility criteria for nirmatrelvir-ritonavir coverage differ substantially from the criteria for participants in the EPIC-HR trial, he noted. Those patients were unvaccinated, had no natural immunity from a previous COVID-19 infection, and were infected with COVID-19 variants that were different from those now circulating. The current study was prompted by the need to look at a broader population of individuals in British Columbia with varying risks of complications from COVID-19 infection.
Before the study, a common view was that patients aged 70 and older would benefit from the drug, said Dr. Dormuth. “Our study, which accounted for medical conditions related to an individual’s vulnerability to complications, showed that older age on its own was not a reason to use nirmatrelvir and ritonavir once relevant medical conditions were taken into consideration.”
The researchers are working on a study to identify with greater specificity which comorbid conditions are most associated with nirmatrelvir-ritonavir effectiveness, he added. “It could be that a relatively small number of conditions can be used to identify most individuals who would benefit from the drug.”
‘Signal toward benefit’
Commenting on the findings for this news organization, Abhijit Duggal, MD, vice chair of critical care at the Cleveland Clinic, who was not involved in this study, said, “I’m always very wary when we look at observational data and we start saying the effectiveness is not really as high as was seen in other studies. We are seeing an effect with all these studies that seems to be in the right direction.
“Having said that,” he added, “is the effect going to be potentially more in patients at higher risk? Absolutely. I think these postmarket studies are really showing that after vaccination, if someone does get infected, this is a secondary option available to us that can prevent progression of the disease, which would likely be more severe in immunocompromised patients.”
Dr. Duggal was a coinvestigator on a recent study of more than 68,000 patients that showed that nirmatrelvir-ritonavir or molnupiravir was associated with reductions in mortality and hospitalization in nonhospitalized patients infected with the Omicron variant, regardless of age, race and ethnicity, virus strain, vaccination status, previous infection status, or coexisting conditions.
“In all groups, there was a signal toward benefit,” said Dr. Duggal. “These studies tell us that these drugs do remain valid options. But their use needs to be discussed on a case-by-case basis with patients we feel are deteriorating or at a higher risk because of underlying disease processes.”
The study was supported by funding from the British Columbia Ministry of Health. Dr. Dormuth and Dr. Duggal report no relevant financial relationships.
A version of this article appeared on Medscape.com.
In a cohort study from British Columbia that included nearly 7,000 patients with COVID-19, nirmatrelvir-ritonavir was associated with a 2.5% reduction in risk for death or emergency hospitalization in clinically extremely vulnerable (CEV) patients who were severely immunocompromised. No significant benefit was observed in patients who were not immunocompromised.
“This finding could help substantially limit unnecessary use of nirmatrelvir and ritonavir in older, otherwise healthy individuals,” lead author Colin R. Dormuth, ScD, associate professor of anesthesiology, pharmacology, and therapeutics at the University of British Columbia, Vancouver, told this news organization. “Another finding that was surprising and might help place the role of nirmatrelvir and ritonavir in context is that even in severely immunocompromised individuals who did not take [the drug], the risk of death or hospitalization with COVID-19 was less than 4% in our study population.”
The study was published online in JAMA Network Open.
Who benefits?
The investigators analyzed medical records for 6,866 patients in British Columbia (median age, 70 years; 57% women) who presented between Feb. 1, 2022, and Feb. 3, 2023. Eligible patients belonged to one of four higher-risk groups who received priority for COVID-19 vaccination.
Two groups included CEV patients who were severely (CEV1) or moderately (CEV2) immunocompromised. The CEV3 group was not immunocompromised but had medical conditions associated with a high risk for complications from COVID-19. A fourth expanded eligibility (EXEL) group included higher-risk patients who were not in one of the other groups, such as unvaccinated patients older than age 70 years.
The investigators matched treated patients to untreated patients in the same vulnerability group according to age, sex, and month of infection. The primary outcome was death from any cause or emergency hospitalization with COVID-19 within 28 days.
Treatment with nirmatrelvir-ritonavir was associated with statistically significant relative reductions in the primary outcome, compared with no treatment, for patients in the CEV1 (risk difference, −2.5%) and CEV2 (RD, −1.7%) groups. In the CEV3 group, the RD of −1.3% was not statistically significant. In the EXEL group, treatment was associated with a higher risk for the primary outcome (RD, 1.0%), but the result was not statistically significant.
The results were “robust across sex and older vs. younger age,” the authors note. “No reduction in the primary outcome was observed in lower-risk individuals, including those aged 70 years or older without serious comorbidities.”
The combination of nirmatrelvir-ritonavir was approved for use in Canada based on interim efficacy and safety data from the Evaluation of Inhibition for COVID-19 in High-Risk Patients (EPIC-HR) trial, said Dr. Dormuth.
British Columbia’s eligibility criteria for nirmatrelvir-ritonavir coverage differ substantially from the criteria for participants in the EPIC-HR trial, he noted. Those patients were unvaccinated, had no natural immunity from a previous COVID-19 infection, and were infected with COVID-19 variants that were different from those now circulating. The current study was prompted by the need to look at a broader population of individuals in British Columbia with varying risks of complications from COVID-19 infection.
Before the study, a common view was that patients aged 70 and older would benefit from the drug, said Dr. Dormuth. “Our study, which accounted for medical conditions related to an individual’s vulnerability to complications, showed that older age on its own was not a reason to use nirmatrelvir and ritonavir once relevant medical conditions were taken into consideration.”
The researchers are working on a study to identify with greater specificity which comorbid conditions are most associated with nirmatrelvir-ritonavir effectiveness, he added. “It could be that a relatively small number of conditions can be used to identify most individuals who would benefit from the drug.”
‘Signal toward benefit’
Commenting on the findings for this news organization, Abhijit Duggal, MD, vice chair of critical care at the Cleveland Clinic, who was not involved in this study, said, “I’m always very wary when we look at observational data and we start saying the effectiveness is not really as high as was seen in other studies. We are seeing an effect with all these studies that seems to be in the right direction.
“Having said that,” he added, “is the effect going to be potentially more in patients at higher risk? Absolutely. I think these postmarket studies are really showing that after vaccination, if someone does get infected, this is a secondary option available to us that can prevent progression of the disease, which would likely be more severe in immunocompromised patients.”
Dr. Duggal was a coinvestigator on a recent study of more than 68,000 patients that showed that nirmatrelvir-ritonavir or molnupiravir was associated with reductions in mortality and hospitalization in nonhospitalized patients infected with the Omicron variant, regardless of age, race and ethnicity, virus strain, vaccination status, previous infection status, or coexisting conditions.
“In all groups, there was a signal toward benefit,” said Dr. Duggal. “These studies tell us that these drugs do remain valid options. But their use needs to be discussed on a case-by-case basis with patients we feel are deteriorating or at a higher risk because of underlying disease processes.”
The study was supported by funding from the British Columbia Ministry of Health. Dr. Dormuth and Dr. Duggal report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Severity score predicts mortality in pulmonary tuberculosis
, based on data from approximately 400 individuals.
Although a mortality risk-prediction score could improve treatment for pulmonary tuberculosis patients, such a score has not been previously reported, wrote Takeshi Osawa, MD, of Fukujuji Hospital, Tokyo, and colleagues.
In a study published in the journal CHEST, the researchers used 252 patients from a previous perspective study of newly diagnosed pulmonary tuberculosis as the development cohort, and recruited 165 additional patients between March 2021 and September 2022.
The primary endpoint was all-cause in-hospital mortality. Based on data from the development group, the researchers found that age 65 years and older and age 80 years and older, hypoxemia, activities of daily living, bilateral pulmonary lesions, lymphocyte count of less than 720 microliters, serum albumin less than 2.86 mg/dL, C-reactive protein (CRP) 3.97 mg/dL or higher, and procalcitonin (PCT) 0.130 ng/mL or higher were predictors of all-cause in hospital mortality.
The researchers used this information to create the disease severity score, known as the AHL score. The AHL included three clinical parameters: activity in daily living (semi-dependent, 1 point; totally dependent, 2 points); hypoxemia (1 point) and lymphocytes (< 720 /mcL, 1 point).
The scoring systems for the three parameters were, respectively, 1 point for semi-dependent and 2 points totally dependent (for activity in daily living), 1 point for presence of hypoxemia, and 1 point for lymphocytes less than 720 per microliter. The researchers stratified the scores into levels of low, intermediate, and high risk, with scores of 0, 1-2, and 3-4, respectively.
All-cause in hospital mortality occurred in 39 (15.5%) and 17 (10.3%) of patients in the developmental and validation cohorts, respectively.
The AHL score effectively predicted mortality, dividing patients into three groups of 1.3% low-risk, 8.9% intermediate risk, and 39.3% high-risk in the validation cohort, with a Harrell’s c-statistic of 0.842.
The corresponding numbers for the development cohort were 0, 13.5%, and 55.8%, with a c-statistic of 0.902.
The findings were limited by several factors, including the lack of data from “smear-negative” patients who were treated as outpatients, and more research is needed to determine the applicability of the AHL score in an outpatient population, the researchers noted. Other limitations included the lack of data on long-term mortality in surviving patients who were discharged, and the reliance on assessments that can be performed only in clinical settings in developed countries, they said.
However, the results support the feasibility of the AHL score in clinical settings to accurately predict mortality in patients with pulmonary TB, and may help optimize treatments for this population, they concluded.
The study received no outside funding. All authors disclosed nonfinancial support in the form of measuring reagents from Fujifilm Wako Pure Chemical Corporation during the study but had no relevant financial conflicts to disclose.
, based on data from approximately 400 individuals.
Although a mortality risk-prediction score could improve treatment for pulmonary tuberculosis patients, such a score has not been previously reported, wrote Takeshi Osawa, MD, of Fukujuji Hospital, Tokyo, and colleagues.
In a study published in the journal CHEST, the researchers used 252 patients from a previous perspective study of newly diagnosed pulmonary tuberculosis as the development cohort, and recruited 165 additional patients between March 2021 and September 2022.
The primary endpoint was all-cause in-hospital mortality. Based on data from the development group, the researchers found that age 65 years and older and age 80 years and older, hypoxemia, activities of daily living, bilateral pulmonary lesions, lymphocyte count of less than 720 microliters, serum albumin less than 2.86 mg/dL, C-reactive protein (CRP) 3.97 mg/dL or higher, and procalcitonin (PCT) 0.130 ng/mL or higher were predictors of all-cause in hospital mortality.
The researchers used this information to create the disease severity score, known as the AHL score. The AHL included three clinical parameters: activity in daily living (semi-dependent, 1 point; totally dependent, 2 points); hypoxemia (1 point) and lymphocytes (< 720 /mcL, 1 point).
The scoring systems for the three parameters were, respectively, 1 point for semi-dependent and 2 points totally dependent (for activity in daily living), 1 point for presence of hypoxemia, and 1 point for lymphocytes less than 720 per microliter. The researchers stratified the scores into levels of low, intermediate, and high risk, with scores of 0, 1-2, and 3-4, respectively.
All-cause in hospital mortality occurred in 39 (15.5%) and 17 (10.3%) of patients in the developmental and validation cohorts, respectively.
The AHL score effectively predicted mortality, dividing patients into three groups of 1.3% low-risk, 8.9% intermediate risk, and 39.3% high-risk in the validation cohort, with a Harrell’s c-statistic of 0.842.
The corresponding numbers for the development cohort were 0, 13.5%, and 55.8%, with a c-statistic of 0.902.
The findings were limited by several factors, including the lack of data from “smear-negative” patients who were treated as outpatients, and more research is needed to determine the applicability of the AHL score in an outpatient population, the researchers noted. Other limitations included the lack of data on long-term mortality in surviving patients who were discharged, and the reliance on assessments that can be performed only in clinical settings in developed countries, they said.
However, the results support the feasibility of the AHL score in clinical settings to accurately predict mortality in patients with pulmonary TB, and may help optimize treatments for this population, they concluded.
The study received no outside funding. All authors disclosed nonfinancial support in the form of measuring reagents from Fujifilm Wako Pure Chemical Corporation during the study but had no relevant financial conflicts to disclose.
, based on data from approximately 400 individuals.
Although a mortality risk-prediction score could improve treatment for pulmonary tuberculosis patients, such a score has not been previously reported, wrote Takeshi Osawa, MD, of Fukujuji Hospital, Tokyo, and colleagues.
In a study published in the journal CHEST, the researchers used 252 patients from a previous perspective study of newly diagnosed pulmonary tuberculosis as the development cohort, and recruited 165 additional patients between March 2021 and September 2022.
The primary endpoint was all-cause in-hospital mortality. Based on data from the development group, the researchers found that age 65 years and older and age 80 years and older, hypoxemia, activities of daily living, bilateral pulmonary lesions, lymphocyte count of less than 720 microliters, serum albumin less than 2.86 mg/dL, C-reactive protein (CRP) 3.97 mg/dL or higher, and procalcitonin (PCT) 0.130 ng/mL or higher were predictors of all-cause in hospital mortality.
The researchers used this information to create the disease severity score, known as the AHL score. The AHL included three clinical parameters: activity in daily living (semi-dependent, 1 point; totally dependent, 2 points); hypoxemia (1 point) and lymphocytes (< 720 /mcL, 1 point).
The scoring systems for the three parameters were, respectively, 1 point for semi-dependent and 2 points totally dependent (for activity in daily living), 1 point for presence of hypoxemia, and 1 point for lymphocytes less than 720 per microliter. The researchers stratified the scores into levels of low, intermediate, and high risk, with scores of 0, 1-2, and 3-4, respectively.
All-cause in hospital mortality occurred in 39 (15.5%) and 17 (10.3%) of patients in the developmental and validation cohorts, respectively.
The AHL score effectively predicted mortality, dividing patients into three groups of 1.3% low-risk, 8.9% intermediate risk, and 39.3% high-risk in the validation cohort, with a Harrell’s c-statistic of 0.842.
The corresponding numbers for the development cohort were 0, 13.5%, and 55.8%, with a c-statistic of 0.902.
The findings were limited by several factors, including the lack of data from “smear-negative” patients who were treated as outpatients, and more research is needed to determine the applicability of the AHL score in an outpatient population, the researchers noted. Other limitations included the lack of data on long-term mortality in surviving patients who were discharged, and the reliance on assessments that can be performed only in clinical settings in developed countries, they said.
However, the results support the feasibility of the AHL score in clinical settings to accurately predict mortality in patients with pulmonary TB, and may help optimize treatments for this population, they concluded.
The study received no outside funding. All authors disclosed nonfinancial support in the form of measuring reagents from Fujifilm Wako Pure Chemical Corporation during the study but had no relevant financial conflicts to disclose.
FROM THE JOURNAL CHEST
Pulmonary aspergillosis predicts poor outcomes in critically ill flu patients
Critically ill influenza patients with associated pulmonary aspergillosis were more than twice as likely to die in intensive care than those without the added infection, based on data from a meta-analysis of more than 1,700 individuals.
Reports of influenza-associated pulmonary aspergillosis (IAPA) are rising in critically ill patients, but data on risk factors, clinical features, and outcomes are limited, Lawrence Y. Lu, MD, of The Prince Charles Hospital, Brisbane, Australia, and colleagues wrote. In addition, diagnosis of IAPA can be challenging, and many clinicians report low awareness of the condition.
In a study published in the journal Chest, the researchers reviewed data from 10 observational studies including 1,720 critically ill influenza patients aged 16 years and older; of these, 331 had IAPA, for a prevalence of 19.2%. The primary outcomes were all-cause mortality in the hospital and in the ICU. Secondary outcomes included ICU length of stay, hospital length of stay, and the need for supportive care (invasive and noninvasive mechanical ventilation, renal replacement therapy, pressor support, and extracorporeal membranous oxygenation).
Overall, mortality among flu patients in the ICU was significantly higher for those with IAPA than those without IAPA (45.0% vs. 23.8%, respectively), as was all-cause mortality (46.4% vs. 26.2%, respectively; odds ratio, 2.6 and P < .001 for both ICU and all-cause mortality).
Factors significantly associated with an increased risk for IAPA included organ transplant (OR, 4.8), hematogenous malignancy (OR, 2.5), being immunocompromised in some way (OR, 2.2), and prolonged corticosteroid use prior to hospital admission (OR, 2.4).
IAPA also was associated with more severe disease, a higher rate of complications, longer ICU stays, and a greater need for organ supports, the researchers noted. Clinical features not significantly more common in patients with IAPA included fever, hemoptysis, and acute respiratory distress syndrome.
The findings were limited by several factors including the retrospective design of the included studies and inability to control for all potential confounders, the researchers noted. Other limitations included the variations in study design, variability of practice patterns across locations, and inclusion of data mainly from countries of high socioeconomic status.
“Given the apparent waning of the COVID-19 pandemic and re-emergence of influenza, our analysis also revealed other gaps in the current literature, including the need to validate newer diagnostic methods and to develop a system to measure severity of IAPA,” the researchers added.
However, the current study results reflect IAPA prevalence from previous studies, and support the need to have a lower threshold for IAPA testing and initiation of antifungal treatment, even with limited data for clinical guidance, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Critically ill influenza patients with associated pulmonary aspergillosis were more than twice as likely to die in intensive care than those without the added infection, based on data from a meta-analysis of more than 1,700 individuals.
Reports of influenza-associated pulmonary aspergillosis (IAPA) are rising in critically ill patients, but data on risk factors, clinical features, and outcomes are limited, Lawrence Y. Lu, MD, of The Prince Charles Hospital, Brisbane, Australia, and colleagues wrote. In addition, diagnosis of IAPA can be challenging, and many clinicians report low awareness of the condition.
In a study published in the journal Chest, the researchers reviewed data from 10 observational studies including 1,720 critically ill influenza patients aged 16 years and older; of these, 331 had IAPA, for a prevalence of 19.2%. The primary outcomes were all-cause mortality in the hospital and in the ICU. Secondary outcomes included ICU length of stay, hospital length of stay, and the need for supportive care (invasive and noninvasive mechanical ventilation, renal replacement therapy, pressor support, and extracorporeal membranous oxygenation).
Overall, mortality among flu patients in the ICU was significantly higher for those with IAPA than those without IAPA (45.0% vs. 23.8%, respectively), as was all-cause mortality (46.4% vs. 26.2%, respectively; odds ratio, 2.6 and P < .001 for both ICU and all-cause mortality).
Factors significantly associated with an increased risk for IAPA included organ transplant (OR, 4.8), hematogenous malignancy (OR, 2.5), being immunocompromised in some way (OR, 2.2), and prolonged corticosteroid use prior to hospital admission (OR, 2.4).
IAPA also was associated with more severe disease, a higher rate of complications, longer ICU stays, and a greater need for organ supports, the researchers noted. Clinical features not significantly more common in patients with IAPA included fever, hemoptysis, and acute respiratory distress syndrome.
The findings were limited by several factors including the retrospective design of the included studies and inability to control for all potential confounders, the researchers noted. Other limitations included the variations in study design, variability of practice patterns across locations, and inclusion of data mainly from countries of high socioeconomic status.
“Given the apparent waning of the COVID-19 pandemic and re-emergence of influenza, our analysis also revealed other gaps in the current literature, including the need to validate newer diagnostic methods and to develop a system to measure severity of IAPA,” the researchers added.
However, the current study results reflect IAPA prevalence from previous studies, and support the need to have a lower threshold for IAPA testing and initiation of antifungal treatment, even with limited data for clinical guidance, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Critically ill influenza patients with associated pulmonary aspergillosis were more than twice as likely to die in intensive care than those without the added infection, based on data from a meta-analysis of more than 1,700 individuals.
Reports of influenza-associated pulmonary aspergillosis (IAPA) are rising in critically ill patients, but data on risk factors, clinical features, and outcomes are limited, Lawrence Y. Lu, MD, of The Prince Charles Hospital, Brisbane, Australia, and colleagues wrote. In addition, diagnosis of IAPA can be challenging, and many clinicians report low awareness of the condition.
In a study published in the journal Chest, the researchers reviewed data from 10 observational studies including 1,720 critically ill influenza patients aged 16 years and older; of these, 331 had IAPA, for a prevalence of 19.2%. The primary outcomes were all-cause mortality in the hospital and in the ICU. Secondary outcomes included ICU length of stay, hospital length of stay, and the need for supportive care (invasive and noninvasive mechanical ventilation, renal replacement therapy, pressor support, and extracorporeal membranous oxygenation).
Overall, mortality among flu patients in the ICU was significantly higher for those with IAPA than those without IAPA (45.0% vs. 23.8%, respectively), as was all-cause mortality (46.4% vs. 26.2%, respectively; odds ratio, 2.6 and P < .001 for both ICU and all-cause mortality).
Factors significantly associated with an increased risk for IAPA included organ transplant (OR, 4.8), hematogenous malignancy (OR, 2.5), being immunocompromised in some way (OR, 2.2), and prolonged corticosteroid use prior to hospital admission (OR, 2.4).
IAPA also was associated with more severe disease, a higher rate of complications, longer ICU stays, and a greater need for organ supports, the researchers noted. Clinical features not significantly more common in patients with IAPA included fever, hemoptysis, and acute respiratory distress syndrome.
The findings were limited by several factors including the retrospective design of the included studies and inability to control for all potential confounders, the researchers noted. Other limitations included the variations in study design, variability of practice patterns across locations, and inclusion of data mainly from countries of high socioeconomic status.
“Given the apparent waning of the COVID-19 pandemic and re-emergence of influenza, our analysis also revealed other gaps in the current literature, including the need to validate newer diagnostic methods and to develop a system to measure severity of IAPA,” the researchers added.
However, the current study results reflect IAPA prevalence from previous studies, and support the need to have a lower threshold for IAPA testing and initiation of antifungal treatment, even with limited data for clinical guidance, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL CHEST
What’s right and wrong for doctors on social media
She went by the name “Dr. Roxy” on social media and became something of a sensation on TikTok, where she livestreamed her patients’ operations. Ultimately, however, plastic surgeon Katharine Roxanne Grawe, MD, lost her medical license based partly on her “life-altering, reckless treatment,” heightened by her social media fame. In July, the Ohio state medical board permanently revoked Dr. Grawe’s license after twice reprimanding her for her failure to meet the standard of care. The board also determined that, by livestreaming procedures, she placed her patients in danger of immediate and serious harm.
Although most doctors don’t use social media to the degree that Dr. Grawe did, using the various platforms – from X (formerly Twitter) to Facebook, Instagram, and TikTok – can be a slippery slope. Medscape’s Physician Behavior Report 2023 revealed that doctors have seen their share of unprofessional or offensive social media use from their peers. Nearly 7 in 10 said it is unethical for a doctor to act rudely, offensively, or unprofessionally on social media, even if their medical practice isn’t mentioned. As one physician put it: “Professional is not a 9-to-5 descriptor.”
“There’s still a stigma attached,” said Liudmila Schafer, MD, an oncologist with The Doctor Connect, a career consulting firm. “Physicians face a tougher challenge due to societal expectations of perfection, with greater consequences for mistakes. We’re under constant ‘observation’ from peers, employers, and patients.”
Beverly Hills plastic surgeon Jay Calvert, MD, says he holds firm boundaries with how he uses social media. “I do comedy on the side, but it’s not acceptable for me as a doctor to share that on social media,” he said. “People want doctors who are professional, and I’m always concerned about how I present myself.”
Dr. Calvert said it is fairly easy to spot doctors who cross the line with social media. “You have to hold yourself back when posting. Doing things like dancing in the OR are out of whack with the profession.”
According to Dr. Schafer, a definite line to avoid crossing is offering medical advice or guidance on social media. “You also can’t discuss confidential practice details, respond to unfamiliar contacts, or discuss institutional policies without permission,” she said. “It’s important to add disclaimers if a personal scientific opinion is shared without reference [or] research or with unchecked sources.”
Navigating the many social media sites
Each social media platform has its pros and cons. Doctors need to determine why to use them and what the payback of each might be. Dr. Schafer uses multiple sites, including LinkedIn, Facebook, Instagram, X, Threads, YouTube, and, to a lesser degree, Clubhouse. How and what she posts on each varies. “I use them almost 95% professionally,” she said. “It’s challenging to meet and engage in person, so that is where social media helps.”
Stephen Pribut, MD, a Washington-based podiatrist, likes to use X as an information source. He follows pretty simple rules when it comes to what he tweets and shares on various sites: “I stay away from politics and religion,” he said. “I also avoid controversial topics online, such as vaccines.”
Joseph Daibes, DO, who specializes in cardiovascular medicine at New Jersey Heart and Vein, Clifton, said he has changed how he uses social media. “Initially, I was a passive consumer, but as I recognized the importance of accurate medical information online, I became more active in weighing in responsibly, occasionally sharing studies, debunking myths, and engaging in meaningful conversations,” he said. “Social media can get dangerous, so we have a duty to use it responsibly, and I cannot stress that enough.”
For plastic surgeons like Dr. Calvert, the visual platforms such as Instagram can prove invaluable for marketing purposes. “I’ve been using Instagram since 2012, and it’s been my most positive experience,” he said. “I don’t generate business from it, but I use it to back up my qualifications as a surgeon.”
Potential patients like to scroll through posts by plastic surgeons to learn what their finished product looks like, Dr. Calvert said. In many cases, plastic surgeons hire social media experts to cultivate their content. “I’ve hired and fired social media managers over the years, ultimately deciding I should develop my own content,” he said. “I want people to see the same doctor on social media that they will see in the office. I like an authentic presentation, not glitzy.”
Social media gone wrong
Dr. Calvert said that in the world of plastic surgery, some doctors use social media to present “before and after” compilations that in his opinion aren’t necessarily fully authentic, and this rubs him wrong. “There’s a bit of ‘cheating’ in some of these posts, using filters, making the ‘befores’ particularly bad, and other tricks,” he said.
Dr. Daibes has also seen his share of social media misuse: ”Red flags include oversharing personal indulgences, engaging in online spats, or making unfounded medical claims,” he said. “It’s essential to remember our role as educators and advocates, and to present ourselves in a way that upholds the dignity of our profession.”
At the end of the day, social media can have positive uses for physicians, and it is clearly here to stay. The onus for responsible use ultimately falls to the physicians using it.
Dr. Daibes emphasizes the fact that a doctor’s words carry weight – perhaps more so than those of other professionals. “The added scrutiny is good because it keeps us accountable; it’s crucial that our information is accurate,” he said. “The downside is that the scrutiny can be stifling at times and lead to self-censorship, even on nonmedical matters.”
Physicians have suggested eight guidelines for doctors to follow when using social media:
- Remember that you represent your profession, even if posting on personal accounts.
- Never post from the operating room, the emergency department, or any sort of medical space.
- If you’re employed, before you post, check with your employer to see whether they have any rules or guidance surrounding social media.
- Never use social media to badmouth colleagues, hospitals, or other healthcare organizations.
- Never use social media to dispense medical advice.
- Steer clear of the obvious hot-button issues, like religion and politics.
- Always protect patient privacy when posting.
- Be careful with how and whom you engage on social media.
A version of this article first appeared on Medscape.com.
She went by the name “Dr. Roxy” on social media and became something of a sensation on TikTok, where she livestreamed her patients’ operations. Ultimately, however, plastic surgeon Katharine Roxanne Grawe, MD, lost her medical license based partly on her “life-altering, reckless treatment,” heightened by her social media fame. In July, the Ohio state medical board permanently revoked Dr. Grawe’s license after twice reprimanding her for her failure to meet the standard of care. The board also determined that, by livestreaming procedures, she placed her patients in danger of immediate and serious harm.
Although most doctors don’t use social media to the degree that Dr. Grawe did, using the various platforms – from X (formerly Twitter) to Facebook, Instagram, and TikTok – can be a slippery slope. Medscape’s Physician Behavior Report 2023 revealed that doctors have seen their share of unprofessional or offensive social media use from their peers. Nearly 7 in 10 said it is unethical for a doctor to act rudely, offensively, or unprofessionally on social media, even if their medical practice isn’t mentioned. As one physician put it: “Professional is not a 9-to-5 descriptor.”
“There’s still a stigma attached,” said Liudmila Schafer, MD, an oncologist with The Doctor Connect, a career consulting firm. “Physicians face a tougher challenge due to societal expectations of perfection, with greater consequences for mistakes. We’re under constant ‘observation’ from peers, employers, and patients.”
Beverly Hills plastic surgeon Jay Calvert, MD, says he holds firm boundaries with how he uses social media. “I do comedy on the side, but it’s not acceptable for me as a doctor to share that on social media,” he said. “People want doctors who are professional, and I’m always concerned about how I present myself.”
Dr. Calvert said it is fairly easy to spot doctors who cross the line with social media. “You have to hold yourself back when posting. Doing things like dancing in the OR are out of whack with the profession.”
According to Dr. Schafer, a definite line to avoid crossing is offering medical advice or guidance on social media. “You also can’t discuss confidential practice details, respond to unfamiliar contacts, or discuss institutional policies without permission,” she said. “It’s important to add disclaimers if a personal scientific opinion is shared without reference [or] research or with unchecked sources.”
Navigating the many social media sites
Each social media platform has its pros and cons. Doctors need to determine why to use them and what the payback of each might be. Dr. Schafer uses multiple sites, including LinkedIn, Facebook, Instagram, X, Threads, YouTube, and, to a lesser degree, Clubhouse. How and what she posts on each varies. “I use them almost 95% professionally,” she said. “It’s challenging to meet and engage in person, so that is where social media helps.”
Stephen Pribut, MD, a Washington-based podiatrist, likes to use X as an information source. He follows pretty simple rules when it comes to what he tweets and shares on various sites: “I stay away from politics and religion,” he said. “I also avoid controversial topics online, such as vaccines.”
Joseph Daibes, DO, who specializes in cardiovascular medicine at New Jersey Heart and Vein, Clifton, said he has changed how he uses social media. “Initially, I was a passive consumer, but as I recognized the importance of accurate medical information online, I became more active in weighing in responsibly, occasionally sharing studies, debunking myths, and engaging in meaningful conversations,” he said. “Social media can get dangerous, so we have a duty to use it responsibly, and I cannot stress that enough.”
For plastic surgeons like Dr. Calvert, the visual platforms such as Instagram can prove invaluable for marketing purposes. “I’ve been using Instagram since 2012, and it’s been my most positive experience,” he said. “I don’t generate business from it, but I use it to back up my qualifications as a surgeon.”
Potential patients like to scroll through posts by plastic surgeons to learn what their finished product looks like, Dr. Calvert said. In many cases, plastic surgeons hire social media experts to cultivate their content. “I’ve hired and fired social media managers over the years, ultimately deciding I should develop my own content,” he said. “I want people to see the same doctor on social media that they will see in the office. I like an authentic presentation, not glitzy.”
Social media gone wrong
Dr. Calvert said that in the world of plastic surgery, some doctors use social media to present “before and after” compilations that in his opinion aren’t necessarily fully authentic, and this rubs him wrong. “There’s a bit of ‘cheating’ in some of these posts, using filters, making the ‘befores’ particularly bad, and other tricks,” he said.
Dr. Daibes has also seen his share of social media misuse: ”Red flags include oversharing personal indulgences, engaging in online spats, or making unfounded medical claims,” he said. “It’s essential to remember our role as educators and advocates, and to present ourselves in a way that upholds the dignity of our profession.”
At the end of the day, social media can have positive uses for physicians, and it is clearly here to stay. The onus for responsible use ultimately falls to the physicians using it.
Dr. Daibes emphasizes the fact that a doctor’s words carry weight – perhaps more so than those of other professionals. “The added scrutiny is good because it keeps us accountable; it’s crucial that our information is accurate,” he said. “The downside is that the scrutiny can be stifling at times and lead to self-censorship, even on nonmedical matters.”
Physicians have suggested eight guidelines for doctors to follow when using social media:
- Remember that you represent your profession, even if posting on personal accounts.
- Never post from the operating room, the emergency department, or any sort of medical space.
- If you’re employed, before you post, check with your employer to see whether they have any rules or guidance surrounding social media.
- Never use social media to badmouth colleagues, hospitals, or other healthcare organizations.
- Never use social media to dispense medical advice.
- Steer clear of the obvious hot-button issues, like religion and politics.
- Always protect patient privacy when posting.
- Be careful with how and whom you engage on social media.
A version of this article first appeared on Medscape.com.
She went by the name “Dr. Roxy” on social media and became something of a sensation on TikTok, where she livestreamed her patients’ operations. Ultimately, however, plastic surgeon Katharine Roxanne Grawe, MD, lost her medical license based partly on her “life-altering, reckless treatment,” heightened by her social media fame. In July, the Ohio state medical board permanently revoked Dr. Grawe’s license after twice reprimanding her for her failure to meet the standard of care. The board also determined that, by livestreaming procedures, she placed her patients in danger of immediate and serious harm.
Although most doctors don’t use social media to the degree that Dr. Grawe did, using the various platforms – from X (formerly Twitter) to Facebook, Instagram, and TikTok – can be a slippery slope. Medscape’s Physician Behavior Report 2023 revealed that doctors have seen their share of unprofessional or offensive social media use from their peers. Nearly 7 in 10 said it is unethical for a doctor to act rudely, offensively, or unprofessionally on social media, even if their medical practice isn’t mentioned. As one physician put it: “Professional is not a 9-to-5 descriptor.”
“There’s still a stigma attached,” said Liudmila Schafer, MD, an oncologist with The Doctor Connect, a career consulting firm. “Physicians face a tougher challenge due to societal expectations of perfection, with greater consequences for mistakes. We’re under constant ‘observation’ from peers, employers, and patients.”
Beverly Hills plastic surgeon Jay Calvert, MD, says he holds firm boundaries with how he uses social media. “I do comedy on the side, but it’s not acceptable for me as a doctor to share that on social media,” he said. “People want doctors who are professional, and I’m always concerned about how I present myself.”
Dr. Calvert said it is fairly easy to spot doctors who cross the line with social media. “You have to hold yourself back when posting. Doing things like dancing in the OR are out of whack with the profession.”
According to Dr. Schafer, a definite line to avoid crossing is offering medical advice or guidance on social media. “You also can’t discuss confidential practice details, respond to unfamiliar contacts, or discuss institutional policies without permission,” she said. “It’s important to add disclaimers if a personal scientific opinion is shared without reference [or] research or with unchecked sources.”
Navigating the many social media sites
Each social media platform has its pros and cons. Doctors need to determine why to use them and what the payback of each might be. Dr. Schafer uses multiple sites, including LinkedIn, Facebook, Instagram, X, Threads, YouTube, and, to a lesser degree, Clubhouse. How and what she posts on each varies. “I use them almost 95% professionally,” she said. “It’s challenging to meet and engage in person, so that is where social media helps.”
Stephen Pribut, MD, a Washington-based podiatrist, likes to use X as an information source. He follows pretty simple rules when it comes to what he tweets and shares on various sites: “I stay away from politics and religion,” he said. “I also avoid controversial topics online, such as vaccines.”
Joseph Daibes, DO, who specializes in cardiovascular medicine at New Jersey Heart and Vein, Clifton, said he has changed how he uses social media. “Initially, I was a passive consumer, but as I recognized the importance of accurate medical information online, I became more active in weighing in responsibly, occasionally sharing studies, debunking myths, and engaging in meaningful conversations,” he said. “Social media can get dangerous, so we have a duty to use it responsibly, and I cannot stress that enough.”
For plastic surgeons like Dr. Calvert, the visual platforms such as Instagram can prove invaluable for marketing purposes. “I’ve been using Instagram since 2012, and it’s been my most positive experience,” he said. “I don’t generate business from it, but I use it to back up my qualifications as a surgeon.”
Potential patients like to scroll through posts by plastic surgeons to learn what their finished product looks like, Dr. Calvert said. In many cases, plastic surgeons hire social media experts to cultivate their content. “I’ve hired and fired social media managers over the years, ultimately deciding I should develop my own content,” he said. “I want people to see the same doctor on social media that they will see in the office. I like an authentic presentation, not glitzy.”
Social media gone wrong
Dr. Calvert said that in the world of plastic surgery, some doctors use social media to present “before and after” compilations that in his opinion aren’t necessarily fully authentic, and this rubs him wrong. “There’s a bit of ‘cheating’ in some of these posts, using filters, making the ‘befores’ particularly bad, and other tricks,” he said.
Dr. Daibes has also seen his share of social media misuse: ”Red flags include oversharing personal indulgences, engaging in online spats, or making unfounded medical claims,” he said. “It’s essential to remember our role as educators and advocates, and to present ourselves in a way that upholds the dignity of our profession.”
At the end of the day, social media can have positive uses for physicians, and it is clearly here to stay. The onus for responsible use ultimately falls to the physicians using it.
Dr. Daibes emphasizes the fact that a doctor’s words carry weight – perhaps more so than those of other professionals. “The added scrutiny is good because it keeps us accountable; it’s crucial that our information is accurate,” he said. “The downside is that the scrutiny can be stifling at times and lead to self-censorship, even on nonmedical matters.”
Physicians have suggested eight guidelines for doctors to follow when using social media:
- Remember that you represent your profession, even if posting on personal accounts.
- Never post from the operating room, the emergency department, or any sort of medical space.
- If you’re employed, before you post, check with your employer to see whether they have any rules or guidance surrounding social media.
- Never use social media to badmouth colleagues, hospitals, or other healthcare organizations.
- Never use social media to dispense medical advice.
- Steer clear of the obvious hot-button issues, like religion and politics.
- Always protect patient privacy when posting.
- Be careful with how and whom you engage on social media.
A version of this article first appeared on Medscape.com.
COVID-19 virus infects coronary vasculature
TOPLINE:
, which could help explain why people with COVID-19 have an increased risk for ischemic cardiovascular complications up to 1 year after infection.
METHODOLOGY:
- Researchers obtained 27 coronary autopsy specimens from eight patients who died from COVID-19, mean age 70 years and 75% male. All had coronary artery disease and most had cardiovascular risk factors such as hypertension, were overweight or obese, and had hyperlipidemia and type 2 diabetes.
- All but one patient, who was pronounced dead before hospital admission, were hospitalized for an average of 17.6 days.
- To identify SARS-CoV-2 viral RNA (vRNA) in the autoptic coronary vasculature, researchers performed RNA fluorescence in situ hybridization (RNA-FISH) analysis for the vRNA encoding the spike (S) protein; they also probed the antisense strand of the S gene (S antisense), which is only produced during viral replication.
TAKEAWAY:
- The study found evidence of SARS-CoV-2 replication in all analyzed human autopsy coronaries regardless of their pathological classification, although viral replication was highest in early-stage lesions that progress to more advanced atherosclerotic plaques.
- Findings indicated that more than 79% of macrophages (white blood cells that help remove lipids) and more than 90% of foam cells (lipid-laden macrophages that are a hallmark of atherosclerosis at all stages of the disease) are S+, and more than 40% of both cell types are S antisense+, indicating SARS-CoV-2 can infect macrophages at a high rate.
- SARS-CoV-2 induced a strong inflammatory response as evidenced by release of cytokines (including interleukin-1 beta and interluekin-6 that are linked to myocardial infarction) in both macrophages and foam cells, which may contribute to the ischemic cardiovascular complications in patients with COVID-19.
IN PRACTICE:
“Our data conclusively demonstrate that SARS-CoV-2 is capable of infecting and replicating in macrophages within the coronary vasculature of patients with COVID-19,” write the authors, adding that SARS-CoV-2 preferentially replicates in foam cells, compared with other macrophages, suggesting these cells “might act as a reservoir of SARS-CoV-2 viral debris in the atherosclerotic plaque.”
SOURCE:
The study was led by Natalia Eberhardt, PhD, postdoctoral fellow, department of medicine, division of cardiology, New York University, and colleagues. It was published online in Nature Cardiovascular Research.
LIMITATIONS:
Findings are relevant only to the original strains of SARS-CoV-2 that circulated in New York between May 2020 and May 2021, and are not generalizable to patients younger and healthier than those from whom samples were obtained for the study.
DISCLOSURES:
The study received support from the National Institutes of Health. The authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, which could help explain why people with COVID-19 have an increased risk for ischemic cardiovascular complications up to 1 year after infection.
METHODOLOGY:
- Researchers obtained 27 coronary autopsy specimens from eight patients who died from COVID-19, mean age 70 years and 75% male. All had coronary artery disease and most had cardiovascular risk factors such as hypertension, were overweight or obese, and had hyperlipidemia and type 2 diabetes.
- All but one patient, who was pronounced dead before hospital admission, were hospitalized for an average of 17.6 days.
- To identify SARS-CoV-2 viral RNA (vRNA) in the autoptic coronary vasculature, researchers performed RNA fluorescence in situ hybridization (RNA-FISH) analysis for the vRNA encoding the spike (S) protein; they also probed the antisense strand of the S gene (S antisense), which is only produced during viral replication.
TAKEAWAY:
- The study found evidence of SARS-CoV-2 replication in all analyzed human autopsy coronaries regardless of their pathological classification, although viral replication was highest in early-stage lesions that progress to more advanced atherosclerotic plaques.
- Findings indicated that more than 79% of macrophages (white blood cells that help remove lipids) and more than 90% of foam cells (lipid-laden macrophages that are a hallmark of atherosclerosis at all stages of the disease) are S+, and more than 40% of both cell types are S antisense+, indicating SARS-CoV-2 can infect macrophages at a high rate.
- SARS-CoV-2 induced a strong inflammatory response as evidenced by release of cytokines (including interleukin-1 beta and interluekin-6 that are linked to myocardial infarction) in both macrophages and foam cells, which may contribute to the ischemic cardiovascular complications in patients with COVID-19.
IN PRACTICE:
“Our data conclusively demonstrate that SARS-CoV-2 is capable of infecting and replicating in macrophages within the coronary vasculature of patients with COVID-19,” write the authors, adding that SARS-CoV-2 preferentially replicates in foam cells, compared with other macrophages, suggesting these cells “might act as a reservoir of SARS-CoV-2 viral debris in the atherosclerotic plaque.”
SOURCE:
The study was led by Natalia Eberhardt, PhD, postdoctoral fellow, department of medicine, division of cardiology, New York University, and colleagues. It was published online in Nature Cardiovascular Research.
LIMITATIONS:
Findings are relevant only to the original strains of SARS-CoV-2 that circulated in New York between May 2020 and May 2021, and are not generalizable to patients younger and healthier than those from whom samples were obtained for the study.
DISCLOSURES:
The study received support from the National Institutes of Health. The authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, which could help explain why people with COVID-19 have an increased risk for ischemic cardiovascular complications up to 1 year after infection.
METHODOLOGY:
- Researchers obtained 27 coronary autopsy specimens from eight patients who died from COVID-19, mean age 70 years and 75% male. All had coronary artery disease and most had cardiovascular risk factors such as hypertension, were overweight or obese, and had hyperlipidemia and type 2 diabetes.
- All but one patient, who was pronounced dead before hospital admission, were hospitalized for an average of 17.6 days.
- To identify SARS-CoV-2 viral RNA (vRNA) in the autoptic coronary vasculature, researchers performed RNA fluorescence in situ hybridization (RNA-FISH) analysis for the vRNA encoding the spike (S) protein; they also probed the antisense strand of the S gene (S antisense), which is only produced during viral replication.
TAKEAWAY:
- The study found evidence of SARS-CoV-2 replication in all analyzed human autopsy coronaries regardless of their pathological classification, although viral replication was highest in early-stage lesions that progress to more advanced atherosclerotic plaques.
- Findings indicated that more than 79% of macrophages (white blood cells that help remove lipids) and more than 90% of foam cells (lipid-laden macrophages that are a hallmark of atherosclerosis at all stages of the disease) are S+, and more than 40% of both cell types are S antisense+, indicating SARS-CoV-2 can infect macrophages at a high rate.
- SARS-CoV-2 induced a strong inflammatory response as evidenced by release of cytokines (including interleukin-1 beta and interluekin-6 that are linked to myocardial infarction) in both macrophages and foam cells, which may contribute to the ischemic cardiovascular complications in patients with COVID-19.
IN PRACTICE:
“Our data conclusively demonstrate that SARS-CoV-2 is capable of infecting and replicating in macrophages within the coronary vasculature of patients with COVID-19,” write the authors, adding that SARS-CoV-2 preferentially replicates in foam cells, compared with other macrophages, suggesting these cells “might act as a reservoir of SARS-CoV-2 viral debris in the atherosclerotic plaque.”
SOURCE:
The study was led by Natalia Eberhardt, PhD, postdoctoral fellow, department of medicine, division of cardiology, New York University, and colleagues. It was published online in Nature Cardiovascular Research.
LIMITATIONS:
Findings are relevant only to the original strains of SARS-CoV-2 that circulated in New York between May 2020 and May 2021, and are not generalizable to patients younger and healthier than those from whom samples were obtained for the study.
DISCLOSURES:
The study received support from the National Institutes of Health. The authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Study: Unexpected vaginal bleeding rises after COVID vaccination
The researchers suggested it could have been connected to the SARS-CoV-2 spike protein in the vaccines. The study was published in Science Advances.
After vaccinations became widely available, many women reported heavier menstrual bleeding than normal. Researchers at the Norwegian Institute of Public Health in Oslo examined the data, particularly among women who do not have periods, such as those who have been through menopause or are taking contraceptives.
The researchers used an ongoing population health survey called the Norwegian Mother, Father, and Child Cohort Study, Nature reported. They examined more than 21,000 responses from postmenopausal, perimenopausal, and nonmenstruating premenopausal women. Some were on long-term hormonal contraceptives.
They learned that 252 postmenopausal women, 1,008 perimenopausal women, and 924 premenopausal women reported having unexpected vaginal bleeding.
About half said the bleeding occurred within 4 weeks of the first or second shot or both. The risk of bleeding was up three to five times for premenopausal and perimenopausal women, and two to three times for postmenopausal women, the researchers found.
Postmenopausal bleeding is usually serious and can be a sign of cancer. “Knowing a patient’s vaccination status could put their bleeding incidence into context,” said Kate Clancy, a biological anthropologist at the University of Illinois at Urbana-Champaign.
The study received funding through the Norwegian Institute of Public Health and Research Council of Norway. The researchers reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
The researchers suggested it could have been connected to the SARS-CoV-2 spike protein in the vaccines. The study was published in Science Advances.
After vaccinations became widely available, many women reported heavier menstrual bleeding than normal. Researchers at the Norwegian Institute of Public Health in Oslo examined the data, particularly among women who do not have periods, such as those who have been through menopause or are taking contraceptives.
The researchers used an ongoing population health survey called the Norwegian Mother, Father, and Child Cohort Study, Nature reported. They examined more than 21,000 responses from postmenopausal, perimenopausal, and nonmenstruating premenopausal women. Some were on long-term hormonal contraceptives.
They learned that 252 postmenopausal women, 1,008 perimenopausal women, and 924 premenopausal women reported having unexpected vaginal bleeding.
About half said the bleeding occurred within 4 weeks of the first or second shot or both. The risk of bleeding was up three to five times for premenopausal and perimenopausal women, and two to three times for postmenopausal women, the researchers found.
Postmenopausal bleeding is usually serious and can be a sign of cancer. “Knowing a patient’s vaccination status could put their bleeding incidence into context,” said Kate Clancy, a biological anthropologist at the University of Illinois at Urbana-Champaign.
The study received funding through the Norwegian Institute of Public Health and Research Council of Norway. The researchers reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
The researchers suggested it could have been connected to the SARS-CoV-2 spike protein in the vaccines. The study was published in Science Advances.
After vaccinations became widely available, many women reported heavier menstrual bleeding than normal. Researchers at the Norwegian Institute of Public Health in Oslo examined the data, particularly among women who do not have periods, such as those who have been through menopause or are taking contraceptives.
The researchers used an ongoing population health survey called the Norwegian Mother, Father, and Child Cohort Study, Nature reported. They examined more than 21,000 responses from postmenopausal, perimenopausal, and nonmenstruating premenopausal women. Some were on long-term hormonal contraceptives.
They learned that 252 postmenopausal women, 1,008 perimenopausal women, and 924 premenopausal women reported having unexpected vaginal bleeding.
About half said the bleeding occurred within 4 weeks of the first or second shot or both. The risk of bleeding was up three to five times for premenopausal and perimenopausal women, and two to three times for postmenopausal women, the researchers found.
Postmenopausal bleeding is usually serious and can be a sign of cancer. “Knowing a patient’s vaccination status could put their bleeding incidence into context,” said Kate Clancy, a biological anthropologist at the University of Illinois at Urbana-Champaign.
The study received funding through the Norwegian Institute of Public Health and Research Council of Norway. The researchers reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
FROM SCIENCE ADVANCES
Overburdened: Health care workers more likely to die by suicide
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study.
If you run into a health care provider these days and ask, “How are you doing?” you’re likely to get a response like this one: “You know, hanging in there.” You smile and move on. But it may be time to go a step further. If you ask that next question – “No, really, how are you doing?” Well, you might need to carve out some time.
It’s been a rough few years for those of us in the health care professions. Our lives, dominated by COVID-related concerns at home, were equally dominated by COVID concerns at work. On the job, there were fewer and fewer of us around as exploitation and COVID-related stressors led doctors, nurses, and others to leave the profession entirely or take early retirement. Even now, I’m not sure we’ve recovered. Staffing in the hospitals is still a huge problem, and the persistence of impersonal meetings via teleconference – which not only prevent any sort of human connection but, audaciously, run from one into another without a break – robs us of even the subtle joy of walking from one hallway to another for 5 minutes of reflection before sitting down to view the next hastily cobbled together PowerPoint.
I’m speaking in generalities, of course.
I’m talking about how bad things are now because, in truth, they’ve never been great. And that may be why health care workers – people with jobs focused on serving others – are nevertheless at substantially increased risk for suicide.
Analyses through the years have shown that physicians tend to have higher rates of death from suicide than the general population. There are reasons for this that may not entirely be because of work-related stress. Doctors’ suicide attempts are more often lethal – we know what is likely to work, after all.
And, according to this paper in JAMA, it is those people who may be suffering most of all.
The study is a nationally representative sample based on the 2008 American Community Survey. Records were linked to the National Death Index through 2019.
Survey respondents were classified into five categories of health care worker, as you can see here. And 1,666,000 non–health care workers served as the control group.
Let’s take a look at the numbers.
I’m showing you age- and sex-standardized rates of death from suicide, starting with non–health care workers. In this study, physicians have similar rates of death from suicide to the general population. Nurses have higher rates, but health care support workers – nurses’ aides, home health aides – have rates nearly twice that of the general population.
Only social and behavioral health workers had rates lower than those in the general population, perhaps because they know how to access life-saving resources.
Of course, these groups differ in a lot of ways – education and income, for example. But even after adjustment for these factors as well as for sex, race, and marital status, the results persist. The only group with even a trend toward lower suicide rates are social and behavioral health workers.
There has been much hand-wringing about rates of physician suicide in the past. It is still a very real problem. But this paper finally highlights that there is a lot more to the health care profession than physicians. It’s time we acknowledge and support the people in our profession who seem to be suffering more than any of us: the aides, the techs, the support staff – the overworked and underpaid who have to deal with all the stresses that physicians like me face and then some.
There’s more to suicide risk than just your job; I know that. Family matters. Relationships matter. Medical and psychiatric illnesses matter. But to ignore this problem when it is right here, in our own house so to speak, can’t continue.
Might I suggest we start by asking someone in our profession – whether doctor, nurse, aide, or tech – how they are doing. How they are really doing. And when we are done listening, we use what we hear to advocate for real change.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study.
If you run into a health care provider these days and ask, “How are you doing?” you’re likely to get a response like this one: “You know, hanging in there.” You smile and move on. But it may be time to go a step further. If you ask that next question – “No, really, how are you doing?” Well, you might need to carve out some time.
It’s been a rough few years for those of us in the health care professions. Our lives, dominated by COVID-related concerns at home, were equally dominated by COVID concerns at work. On the job, there were fewer and fewer of us around as exploitation and COVID-related stressors led doctors, nurses, and others to leave the profession entirely or take early retirement. Even now, I’m not sure we’ve recovered. Staffing in the hospitals is still a huge problem, and the persistence of impersonal meetings via teleconference – which not only prevent any sort of human connection but, audaciously, run from one into another without a break – robs us of even the subtle joy of walking from one hallway to another for 5 minutes of reflection before sitting down to view the next hastily cobbled together PowerPoint.
I’m speaking in generalities, of course.
I’m talking about how bad things are now because, in truth, they’ve never been great. And that may be why health care workers – people with jobs focused on serving others – are nevertheless at substantially increased risk for suicide.
Analyses through the years have shown that physicians tend to have higher rates of death from suicide than the general population. There are reasons for this that may not entirely be because of work-related stress. Doctors’ suicide attempts are more often lethal – we know what is likely to work, after all.
And, according to this paper in JAMA, it is those people who may be suffering most of all.
The study is a nationally representative sample based on the 2008 American Community Survey. Records were linked to the National Death Index through 2019.
Survey respondents were classified into five categories of health care worker, as you can see here. And 1,666,000 non–health care workers served as the control group.
Let’s take a look at the numbers.
I’m showing you age- and sex-standardized rates of death from suicide, starting with non–health care workers. In this study, physicians have similar rates of death from suicide to the general population. Nurses have higher rates, but health care support workers – nurses’ aides, home health aides – have rates nearly twice that of the general population.
Only social and behavioral health workers had rates lower than those in the general population, perhaps because they know how to access life-saving resources.
Of course, these groups differ in a lot of ways – education and income, for example. But even after adjustment for these factors as well as for sex, race, and marital status, the results persist. The only group with even a trend toward lower suicide rates are social and behavioral health workers.
There has been much hand-wringing about rates of physician suicide in the past. It is still a very real problem. But this paper finally highlights that there is a lot more to the health care profession than physicians. It’s time we acknowledge and support the people in our profession who seem to be suffering more than any of us: the aides, the techs, the support staff – the overworked and underpaid who have to deal with all the stresses that physicians like me face and then some.
There’s more to suicide risk than just your job; I know that. Family matters. Relationships matter. Medical and psychiatric illnesses matter. But to ignore this problem when it is right here, in our own house so to speak, can’t continue.
Might I suggest we start by asking someone in our profession – whether doctor, nurse, aide, or tech – how they are doing. How they are really doing. And when we are done listening, we use what we hear to advocate for real change.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study.
If you run into a health care provider these days and ask, “How are you doing?” you’re likely to get a response like this one: “You know, hanging in there.” You smile and move on. But it may be time to go a step further. If you ask that next question – “No, really, how are you doing?” Well, you might need to carve out some time.
It’s been a rough few years for those of us in the health care professions. Our lives, dominated by COVID-related concerns at home, were equally dominated by COVID concerns at work. On the job, there were fewer and fewer of us around as exploitation and COVID-related stressors led doctors, nurses, and others to leave the profession entirely or take early retirement. Even now, I’m not sure we’ve recovered. Staffing in the hospitals is still a huge problem, and the persistence of impersonal meetings via teleconference – which not only prevent any sort of human connection but, audaciously, run from one into another without a break – robs us of even the subtle joy of walking from one hallway to another for 5 minutes of reflection before sitting down to view the next hastily cobbled together PowerPoint.
I’m speaking in generalities, of course.
I’m talking about how bad things are now because, in truth, they’ve never been great. And that may be why health care workers – people with jobs focused on serving others – are nevertheless at substantially increased risk for suicide.
Analyses through the years have shown that physicians tend to have higher rates of death from suicide than the general population. There are reasons for this that may not entirely be because of work-related stress. Doctors’ suicide attempts are more often lethal – we know what is likely to work, after all.
And, according to this paper in JAMA, it is those people who may be suffering most of all.
The study is a nationally representative sample based on the 2008 American Community Survey. Records were linked to the National Death Index through 2019.
Survey respondents were classified into five categories of health care worker, as you can see here. And 1,666,000 non–health care workers served as the control group.
Let’s take a look at the numbers.
I’m showing you age- and sex-standardized rates of death from suicide, starting with non–health care workers. In this study, physicians have similar rates of death from suicide to the general population. Nurses have higher rates, but health care support workers – nurses’ aides, home health aides – have rates nearly twice that of the general population.
Only social and behavioral health workers had rates lower than those in the general population, perhaps because they know how to access life-saving resources.
Of course, these groups differ in a lot of ways – education and income, for example. But even after adjustment for these factors as well as for sex, race, and marital status, the results persist. The only group with even a trend toward lower suicide rates are social and behavioral health workers.
There has been much hand-wringing about rates of physician suicide in the past. It is still a very real problem. But this paper finally highlights that there is a lot more to the health care profession than physicians. It’s time we acknowledge and support the people in our profession who seem to be suffering more than any of us: the aides, the techs, the support staff – the overworked and underpaid who have to deal with all the stresses that physicians like me face and then some.
There’s more to suicide risk than just your job; I know that. Family matters. Relationships matter. Medical and psychiatric illnesses matter. But to ignore this problem when it is right here, in our own house so to speak, can’t continue.
Might I suggest we start by asking someone in our profession – whether doctor, nurse, aide, or tech – how they are doing. How they are really doing. And when we are done listening, we use what we hear to advocate for real change.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
How to get paid if your patient passes on
The death of a patient comes with many challenges for physicians, including a range of emotional and professional issues. Beyond those concerns,
“When a patient passes away, obviously there is, unfortunately, a lot of paperwork and stress for families, and it’s a very difficult situation,” says Shikha Jain, MD, an oncologist and associate professor of medicine at the University of Illinois at Chicago. “Talking about finances in that moment can be difficult and uncomfortable, and one thing I’d recommend is that the physicians themselves not get involved.”
Instead, Dr. Jain said, someone in the billing department in the practice or the hospital should take a lead on dealing with any outstanding debts.
“That doctor-patient relationship is a very precious relationship, so you don’t want to mix that financial aspect of providing care with the doctor-patient relationship,” Dr. Jain said. “That’s one thing that’s really important.”
The best approach in such situations is for practices to have a standing policy in place that dictates how to handle bills once a patient has died.
In most cases, the executor of the patient’s will must inform all creditors, including doctors, that the decedent has died, but sometimes there’s a delay.
Hoping the doctor’s office writes it off
“Even though the person in charge of the estate is supposed to contact the doctor’s office and let them know when a patient has passed, that doesn’t always happen,” says Hope Wen, head of billing at practice management platform Soundry Health. “It can be very challenging to track down that information, and sometimes they’re just crossing their fingers hoping that the doctor’s office will just write off the balance, which they often do.”
Some offices use a service that compares accounts receivable lists to Social Security death files and state records to identify deaths more quickly. Some physicians might also use a debt collection agency or an attorney who has experience collecting decedent debts and dealing with executors and probate courts.
Once the practice becomes aware that a patient has died, it can no longer send communications to the name and address on file, although it can continue to go through the billing process with the insurer for any bills incurred up to the date of the death.
At that point, the estate becomes responsible for the debt, and all communication must go to the executor of the estate (in some states, this might be called a personal representative). The office can reach out to any contacts on file to see if they are able to identify the executor.
“You want to do that in a compassionate way,” says Jack Brown III, JD, MBA, president of Gulf Coast Collection Bureau. “You’ll tell them you’re sorry for their loss, but you’re wondering who is responsible for the estate. Once you’ve identified that person and gotten their letter of administration from the probate court or a power of attorney, then you can speak with that person as if they were the patient.”
The names of executors are also public record and are available through the probate court (sometimes called the surrogate court) in the county where the decedent lived.
“Even if there’s no will or no executive named, the court will appoint an administrator for the estate, which is usually a family member,” said Robert Bernstein, an estate lawyer in Parsippany, N.J. “Their information will be on file in the court.”
Insurance coverage
Typically, insurance will pay for treatment (after deductibles and copays) up until the date of the patient’s death. But, of course, it can take months for some insurance companies to make their final payments, allowing physicians to know exactly how much they’re owed by that estate. In such cases, it’s important for physicians to know the rules in the decedent’s state for how long they have to file a claim.
Most states require that claims occur within 6-9 months of the person’s death. However, in some states, claimants can continue to file for much longer if the estate has not yet paid out all of its assets.
“Sometimes there is real estate to sell or a business to wind down, and it can take years for the estate to distribute all of the assets,” Mr. Bernstein says. “If it’s a year later and they still haven’t distributed the assets, the physician can still file the claim and should be paid.”
In some cases, especially if the decedent received compassionate, quality care, their family will want to make good on any outstanding debts to the health care providers who took care of their loved ones in their final days. In other cases, especially when a family member has had a long illness, their assets have been depleted over time or were transferred to other family members so that there is little left in the estate itself when the patient dies.
Regardless of other circumstances, the estate alone is responsible for such payments, and family members, including spouses and children, typically have no liability. (Though rarely enforced, some states do have filial responsibility laws that could hold children responsible for their parents’ debts, including unpaid medical bills. In addition, states with community property laws might require a surviving spouse to cover their partner’s debt, even after death.)
The probate process varies from state to state, but in general, the probate system and the executor will gather all existing assets and then notify all creditors about how to submit a claim. Typically, the claim will need to include information about how much is owed and documentation, such as bills and an explanation of benefits to back up the claim. It should be borne in mind that even those who’ve passed away have privacy protections under the Health Insurance Portability and Accountability Act, so practices must be careful as to how much information they’re sharing through their claim.
Once the estate has received all the claims, the executor will follow a priority of claims, starting with secured creditors. Typically, medical bills, especially those incurred in the last 90 days of the decedent’s life, have priority in the probate process, Mr. Brown says.
How to minimize losses
In that case, the practice would write off the unpaid debt as a business loss. If there are not enough assets in the estate to pay all claims, the executor will follow a state schedule that apportions those assets that are available.
There are some steps that practices can take to protect themselves from incurring such losses. For example, before beginning treatment, practices might consider asking patients to name a guarantor, who will essentially promise to cover any outstanding debts that the patient incurs.
To be binding, the office will need a signature from both the patient and the guarantor. Some offices may also keep a patient credit card number on file with written authorization that they can use to pay bills that are past due, although this payment method would no longer be valid after a patient dies.
While it’s important for all physicians to document and verify the financial information for their patients, oncologists often must consider an additional layer of fiduciary responsibility when it comes to their patients. Ms. Wen suggests that oncology offices check in with insurance companies to determine whether a patient has exhausted their benefits.
“That can happen with cancer patients, depending on how long they’ve been receiving treatment and what type of treatment they’ve been getting,” she said. “Some of the clinical trials, insurance will pay for them, but they’re really expensive and can get toward that max. So knowing where they are with their insurance coverage is big.”
When time is of the essence, some patients will choose to go forward with a treatment before receiving insurance approval. In those cases, the office must have an additional conversation in which the costs of the treatment are discussed. The office should obtain written confirmation of who will pay if the insurer does not, Ms. Wen said. While it’s the patient’s responsibility to keep track of their insurance benefits, oncology practices and hospitals must also exercise due diligence in monitoring the benefits that are available.
“That’s part of their contract with insurance companies if they’re in network, helping patients understand their benefits,” Ms. Wen saids.
It’s also important for practices to keep clear, consistent records to make it easier to identify outstanding bills and the correct contact information for them. If bills had gone unpaid prior to a patient’s death and the office started legal action and received a judgment, that claim would typically go ahead of other creditors’ claims.
Dr. Jain says that some practices might also consider keeping a financial adviser or social worker on staff who can assist patients and their families with understanding their out-of-pocket costs for treatment.
“Financial toxicity in oncology and medical care is a very real problem,” she says. “At the beginning of the relationship, I recommend that my patients get set up with a financial specialist that can help them navigate that aspect, not only when a patient passes away but during the process of receiving treatment, so they’re not shocked by the bills.”
A version of this article first appeared on Medscape.com.
The death of a patient comes with many challenges for physicians, including a range of emotional and professional issues. Beyond those concerns,
“When a patient passes away, obviously there is, unfortunately, a lot of paperwork and stress for families, and it’s a very difficult situation,” says Shikha Jain, MD, an oncologist and associate professor of medicine at the University of Illinois at Chicago. “Talking about finances in that moment can be difficult and uncomfortable, and one thing I’d recommend is that the physicians themselves not get involved.”
Instead, Dr. Jain said, someone in the billing department in the practice or the hospital should take a lead on dealing with any outstanding debts.
“That doctor-patient relationship is a very precious relationship, so you don’t want to mix that financial aspect of providing care with the doctor-patient relationship,” Dr. Jain said. “That’s one thing that’s really important.”
The best approach in such situations is for practices to have a standing policy in place that dictates how to handle bills once a patient has died.
In most cases, the executor of the patient’s will must inform all creditors, including doctors, that the decedent has died, but sometimes there’s a delay.
Hoping the doctor’s office writes it off
“Even though the person in charge of the estate is supposed to contact the doctor’s office and let them know when a patient has passed, that doesn’t always happen,” says Hope Wen, head of billing at practice management platform Soundry Health. “It can be very challenging to track down that information, and sometimes they’re just crossing their fingers hoping that the doctor’s office will just write off the balance, which they often do.”
Some offices use a service that compares accounts receivable lists to Social Security death files and state records to identify deaths more quickly. Some physicians might also use a debt collection agency or an attorney who has experience collecting decedent debts and dealing with executors and probate courts.
Once the practice becomes aware that a patient has died, it can no longer send communications to the name and address on file, although it can continue to go through the billing process with the insurer for any bills incurred up to the date of the death.
At that point, the estate becomes responsible for the debt, and all communication must go to the executor of the estate (in some states, this might be called a personal representative). The office can reach out to any contacts on file to see if they are able to identify the executor.
“You want to do that in a compassionate way,” says Jack Brown III, JD, MBA, president of Gulf Coast Collection Bureau. “You’ll tell them you’re sorry for their loss, but you’re wondering who is responsible for the estate. Once you’ve identified that person and gotten their letter of administration from the probate court or a power of attorney, then you can speak with that person as if they were the patient.”
The names of executors are also public record and are available through the probate court (sometimes called the surrogate court) in the county where the decedent lived.
“Even if there’s no will or no executive named, the court will appoint an administrator for the estate, which is usually a family member,” said Robert Bernstein, an estate lawyer in Parsippany, N.J. “Their information will be on file in the court.”
Insurance coverage
Typically, insurance will pay for treatment (after deductibles and copays) up until the date of the patient’s death. But, of course, it can take months for some insurance companies to make their final payments, allowing physicians to know exactly how much they’re owed by that estate. In such cases, it’s important for physicians to know the rules in the decedent’s state for how long they have to file a claim.
Most states require that claims occur within 6-9 months of the person’s death. However, in some states, claimants can continue to file for much longer if the estate has not yet paid out all of its assets.
“Sometimes there is real estate to sell or a business to wind down, and it can take years for the estate to distribute all of the assets,” Mr. Bernstein says. “If it’s a year later and they still haven’t distributed the assets, the physician can still file the claim and should be paid.”
In some cases, especially if the decedent received compassionate, quality care, their family will want to make good on any outstanding debts to the health care providers who took care of their loved ones in their final days. In other cases, especially when a family member has had a long illness, their assets have been depleted over time or were transferred to other family members so that there is little left in the estate itself when the patient dies.
Regardless of other circumstances, the estate alone is responsible for such payments, and family members, including spouses and children, typically have no liability. (Though rarely enforced, some states do have filial responsibility laws that could hold children responsible for their parents’ debts, including unpaid medical bills. In addition, states with community property laws might require a surviving spouse to cover their partner’s debt, even after death.)
The probate process varies from state to state, but in general, the probate system and the executor will gather all existing assets and then notify all creditors about how to submit a claim. Typically, the claim will need to include information about how much is owed and documentation, such as bills and an explanation of benefits to back up the claim. It should be borne in mind that even those who’ve passed away have privacy protections under the Health Insurance Portability and Accountability Act, so practices must be careful as to how much information they’re sharing through their claim.
Once the estate has received all the claims, the executor will follow a priority of claims, starting with secured creditors. Typically, medical bills, especially those incurred in the last 90 days of the decedent’s life, have priority in the probate process, Mr. Brown says.
How to minimize losses
In that case, the practice would write off the unpaid debt as a business loss. If there are not enough assets in the estate to pay all claims, the executor will follow a state schedule that apportions those assets that are available.
There are some steps that practices can take to protect themselves from incurring such losses. For example, before beginning treatment, practices might consider asking patients to name a guarantor, who will essentially promise to cover any outstanding debts that the patient incurs.
To be binding, the office will need a signature from both the patient and the guarantor. Some offices may also keep a patient credit card number on file with written authorization that they can use to pay bills that are past due, although this payment method would no longer be valid after a patient dies.
While it’s important for all physicians to document and verify the financial information for their patients, oncologists often must consider an additional layer of fiduciary responsibility when it comes to their patients. Ms. Wen suggests that oncology offices check in with insurance companies to determine whether a patient has exhausted their benefits.
“That can happen with cancer patients, depending on how long they’ve been receiving treatment and what type of treatment they’ve been getting,” she said. “Some of the clinical trials, insurance will pay for them, but they’re really expensive and can get toward that max. So knowing where they are with their insurance coverage is big.”
When time is of the essence, some patients will choose to go forward with a treatment before receiving insurance approval. In those cases, the office must have an additional conversation in which the costs of the treatment are discussed. The office should obtain written confirmation of who will pay if the insurer does not, Ms. Wen said. While it’s the patient’s responsibility to keep track of their insurance benefits, oncology practices and hospitals must also exercise due diligence in monitoring the benefits that are available.
“That’s part of their contract with insurance companies if they’re in network, helping patients understand their benefits,” Ms. Wen saids.
It’s also important for practices to keep clear, consistent records to make it easier to identify outstanding bills and the correct contact information for them. If bills had gone unpaid prior to a patient’s death and the office started legal action and received a judgment, that claim would typically go ahead of other creditors’ claims.
Dr. Jain says that some practices might also consider keeping a financial adviser or social worker on staff who can assist patients and their families with understanding their out-of-pocket costs for treatment.
“Financial toxicity in oncology and medical care is a very real problem,” she says. “At the beginning of the relationship, I recommend that my patients get set up with a financial specialist that can help them navigate that aspect, not only when a patient passes away but during the process of receiving treatment, so they’re not shocked by the bills.”
A version of this article first appeared on Medscape.com.
The death of a patient comes with many challenges for physicians, including a range of emotional and professional issues. Beyond those concerns,
“When a patient passes away, obviously there is, unfortunately, a lot of paperwork and stress for families, and it’s a very difficult situation,” says Shikha Jain, MD, an oncologist and associate professor of medicine at the University of Illinois at Chicago. “Talking about finances in that moment can be difficult and uncomfortable, and one thing I’d recommend is that the physicians themselves not get involved.”
Instead, Dr. Jain said, someone in the billing department in the practice or the hospital should take a lead on dealing with any outstanding debts.
“That doctor-patient relationship is a very precious relationship, so you don’t want to mix that financial aspect of providing care with the doctor-patient relationship,” Dr. Jain said. “That’s one thing that’s really important.”
The best approach in such situations is for practices to have a standing policy in place that dictates how to handle bills once a patient has died.
In most cases, the executor of the patient’s will must inform all creditors, including doctors, that the decedent has died, but sometimes there’s a delay.
Hoping the doctor’s office writes it off
“Even though the person in charge of the estate is supposed to contact the doctor’s office and let them know when a patient has passed, that doesn’t always happen,” says Hope Wen, head of billing at practice management platform Soundry Health. “It can be very challenging to track down that information, and sometimes they’re just crossing their fingers hoping that the doctor’s office will just write off the balance, which they often do.”
Some offices use a service that compares accounts receivable lists to Social Security death files and state records to identify deaths more quickly. Some physicians might also use a debt collection agency or an attorney who has experience collecting decedent debts and dealing with executors and probate courts.
Once the practice becomes aware that a patient has died, it can no longer send communications to the name and address on file, although it can continue to go through the billing process with the insurer for any bills incurred up to the date of the death.
At that point, the estate becomes responsible for the debt, and all communication must go to the executor of the estate (in some states, this might be called a personal representative). The office can reach out to any contacts on file to see if they are able to identify the executor.
“You want to do that in a compassionate way,” says Jack Brown III, JD, MBA, president of Gulf Coast Collection Bureau. “You’ll tell them you’re sorry for their loss, but you’re wondering who is responsible for the estate. Once you’ve identified that person and gotten their letter of administration from the probate court or a power of attorney, then you can speak with that person as if they were the patient.”
The names of executors are also public record and are available through the probate court (sometimes called the surrogate court) in the county where the decedent lived.
“Even if there’s no will or no executive named, the court will appoint an administrator for the estate, which is usually a family member,” said Robert Bernstein, an estate lawyer in Parsippany, N.J. “Their information will be on file in the court.”
Insurance coverage
Typically, insurance will pay for treatment (after deductibles and copays) up until the date of the patient’s death. But, of course, it can take months for some insurance companies to make their final payments, allowing physicians to know exactly how much they’re owed by that estate. In such cases, it’s important for physicians to know the rules in the decedent’s state for how long they have to file a claim.
Most states require that claims occur within 6-9 months of the person’s death. However, in some states, claimants can continue to file for much longer if the estate has not yet paid out all of its assets.
“Sometimes there is real estate to sell or a business to wind down, and it can take years for the estate to distribute all of the assets,” Mr. Bernstein says. “If it’s a year later and they still haven’t distributed the assets, the physician can still file the claim and should be paid.”
In some cases, especially if the decedent received compassionate, quality care, their family will want to make good on any outstanding debts to the health care providers who took care of their loved ones in their final days. In other cases, especially when a family member has had a long illness, their assets have been depleted over time or were transferred to other family members so that there is little left in the estate itself when the patient dies.
Regardless of other circumstances, the estate alone is responsible for such payments, and family members, including spouses and children, typically have no liability. (Though rarely enforced, some states do have filial responsibility laws that could hold children responsible for their parents’ debts, including unpaid medical bills. In addition, states with community property laws might require a surviving spouse to cover their partner’s debt, even after death.)
The probate process varies from state to state, but in general, the probate system and the executor will gather all existing assets and then notify all creditors about how to submit a claim. Typically, the claim will need to include information about how much is owed and documentation, such as bills and an explanation of benefits to back up the claim. It should be borne in mind that even those who’ve passed away have privacy protections under the Health Insurance Portability and Accountability Act, so practices must be careful as to how much information they’re sharing through their claim.
Once the estate has received all the claims, the executor will follow a priority of claims, starting with secured creditors. Typically, medical bills, especially those incurred in the last 90 days of the decedent’s life, have priority in the probate process, Mr. Brown says.
How to minimize losses
In that case, the practice would write off the unpaid debt as a business loss. If there are not enough assets in the estate to pay all claims, the executor will follow a state schedule that apportions those assets that are available.
There are some steps that practices can take to protect themselves from incurring such losses. For example, before beginning treatment, practices might consider asking patients to name a guarantor, who will essentially promise to cover any outstanding debts that the patient incurs.
To be binding, the office will need a signature from both the patient and the guarantor. Some offices may also keep a patient credit card number on file with written authorization that they can use to pay bills that are past due, although this payment method would no longer be valid after a patient dies.
While it’s important for all physicians to document and verify the financial information for their patients, oncologists often must consider an additional layer of fiduciary responsibility when it comes to their patients. Ms. Wen suggests that oncology offices check in with insurance companies to determine whether a patient has exhausted their benefits.
“That can happen with cancer patients, depending on how long they’ve been receiving treatment and what type of treatment they’ve been getting,” she said. “Some of the clinical trials, insurance will pay for them, but they’re really expensive and can get toward that max. So knowing where they are with their insurance coverage is big.”
When time is of the essence, some patients will choose to go forward with a treatment before receiving insurance approval. In those cases, the office must have an additional conversation in which the costs of the treatment are discussed. The office should obtain written confirmation of who will pay if the insurer does not, Ms. Wen said. While it’s the patient’s responsibility to keep track of their insurance benefits, oncology practices and hospitals must also exercise due diligence in monitoring the benefits that are available.
“That’s part of their contract with insurance companies if they’re in network, helping patients understand their benefits,” Ms. Wen saids.
It’s also important for practices to keep clear, consistent records to make it easier to identify outstanding bills and the correct contact information for them. If bills had gone unpaid prior to a patient’s death and the office started legal action and received a judgment, that claim would typically go ahead of other creditors’ claims.
Dr. Jain says that some practices might also consider keeping a financial adviser or social worker on staff who can assist patients and their families with understanding their out-of-pocket costs for treatment.
“Financial toxicity in oncology and medical care is a very real problem,” she says. “At the beginning of the relationship, I recommend that my patients get set up with a financial specialist that can help them navigate that aspect, not only when a patient passes away but during the process of receiving treatment, so they’re not shocked by the bills.”
A version of this article first appeared on Medscape.com.

