User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Early data for experimental THC drug ‘promising’ for Tourette’s
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Health care workers eager for COVID booster shots
As COVID vaccine boosters move closer to reality, most physicians and nurses are ready and willing to get another shot in the arm, according to a new Medscape survey.
Altogether, 93% of physicians and 87% of nurses/advanced practice nurses (APNs) said they wanted to get a booster, although the timing of when they wanted the shots differed somewhat between the two groups surveyed Aug. 4-15.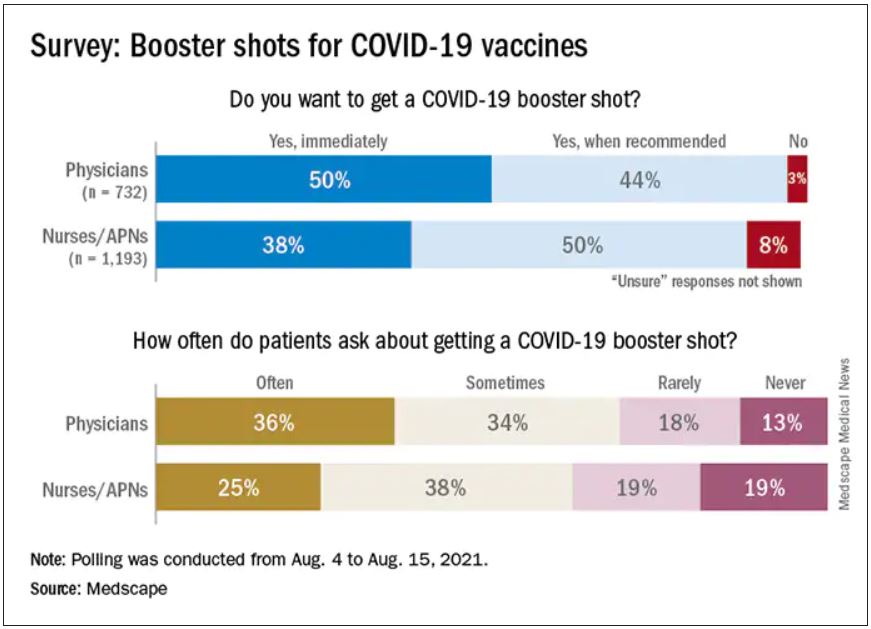
Among the 732 physicians polled, 50% wanted to get their shot immediately, compared with 38% of the 1,193 nurses/APNs who responded, while 44% of physicians and 50% of nurses/APNs said that they would wait until the vaccine booster was authorized and recommended.
At this point in time, almost all of the health care workers surveyed – 98% of physicians and 94% of nurses/APNs – have been fully vaccinated against COVID-19. A small proportion of each group, however, received the Johnson & Johnson vaccine (1% of physicians and 3% of nurses) and are not included in the current plan for booster shots.
The Medscape survey sample did include one group that is already eligible for a third dose: About 20% of physicians and 26% of nurses/ANPs said they have a condition or take a medication that compromises their immune system.
Respondents’ experiences with patient requests for boosters suggest a somewhat lower level of interest. About two-thirds of the health care workers (69% of physicians and 63% of nurses) said that patients frequently or sometimes asked about COVID boosters, compared with 13% (physicians) and 19% (nurses) who said their patients had never asked.
Interest lower among general population
In a separate survey conducted by WebMD, 82% of those who have been at least partially vaccinated said they want to get a COVID vaccine booster (14% immediately and 68% after authorization and recommendation). Of the remaining vaccinees, 7% said they do not want to get a booster and 11% were unsure.
The full sample of 592 respondents surveyed Aug. 5-10, however, included 19% who do not plan to get vaccinated and 6% who are planning to be vaccinated but have not yet done so.
The proportion of immunocompromised individuals in the two survey groups was similar, with about 25% of those in the WebMD survey reporting they have a condition or take a medication that compromises their immune system. Those respondents were more than twice as likely to want to get a booster immediately, compared to those with an uncompromised immune system (24% vs. 11%).
The distribution of vaccines received by brand was also comparable between the two groups surveyed. Of health care workers and readers, over half of each group received the Pfizer/BioNTech vaccine (59% vs. 54%), followed by Moderna (38% vs. 40%) and Johnson & Johnson (3% vs. 5%).
A version of this article first appeared on Medscape.com.
As COVID vaccine boosters move closer to reality, most physicians and nurses are ready and willing to get another shot in the arm, according to a new Medscape survey.
Altogether, 93% of physicians and 87% of nurses/advanced practice nurses (APNs) said they wanted to get a booster, although the timing of when they wanted the shots differed somewhat between the two groups surveyed Aug. 4-15.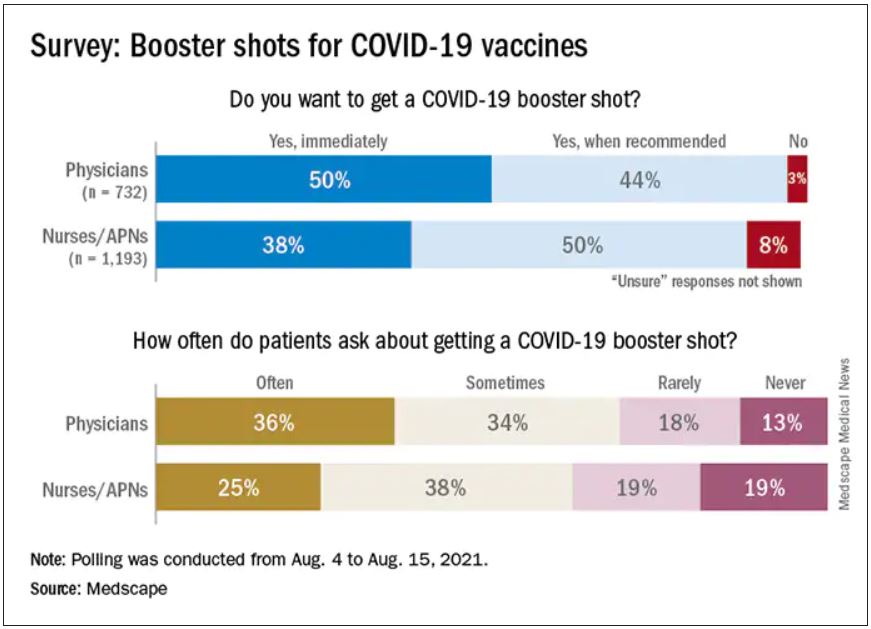
Among the 732 physicians polled, 50% wanted to get their shot immediately, compared with 38% of the 1,193 nurses/APNs who responded, while 44% of physicians and 50% of nurses/APNs said that they would wait until the vaccine booster was authorized and recommended.
At this point in time, almost all of the health care workers surveyed – 98% of physicians and 94% of nurses/APNs – have been fully vaccinated against COVID-19. A small proportion of each group, however, received the Johnson & Johnson vaccine (1% of physicians and 3% of nurses) and are not included in the current plan for booster shots.
The Medscape survey sample did include one group that is already eligible for a third dose: About 20% of physicians and 26% of nurses/ANPs said they have a condition or take a medication that compromises their immune system.
Respondents’ experiences with patient requests for boosters suggest a somewhat lower level of interest. About two-thirds of the health care workers (69% of physicians and 63% of nurses) said that patients frequently or sometimes asked about COVID boosters, compared with 13% (physicians) and 19% (nurses) who said their patients had never asked.
Interest lower among general population
In a separate survey conducted by WebMD, 82% of those who have been at least partially vaccinated said they want to get a COVID vaccine booster (14% immediately and 68% after authorization and recommendation). Of the remaining vaccinees, 7% said they do not want to get a booster and 11% were unsure.
The full sample of 592 respondents surveyed Aug. 5-10, however, included 19% who do not plan to get vaccinated and 6% who are planning to be vaccinated but have not yet done so.
The proportion of immunocompromised individuals in the two survey groups was similar, with about 25% of those in the WebMD survey reporting they have a condition or take a medication that compromises their immune system. Those respondents were more than twice as likely to want to get a booster immediately, compared to those with an uncompromised immune system (24% vs. 11%).
The distribution of vaccines received by brand was also comparable between the two groups surveyed. Of health care workers and readers, over half of each group received the Pfizer/BioNTech vaccine (59% vs. 54%), followed by Moderna (38% vs. 40%) and Johnson & Johnson (3% vs. 5%).
A version of this article first appeared on Medscape.com.
As COVID vaccine boosters move closer to reality, most physicians and nurses are ready and willing to get another shot in the arm, according to a new Medscape survey.
Altogether, 93% of physicians and 87% of nurses/advanced practice nurses (APNs) said they wanted to get a booster, although the timing of when they wanted the shots differed somewhat between the two groups surveyed Aug. 4-15.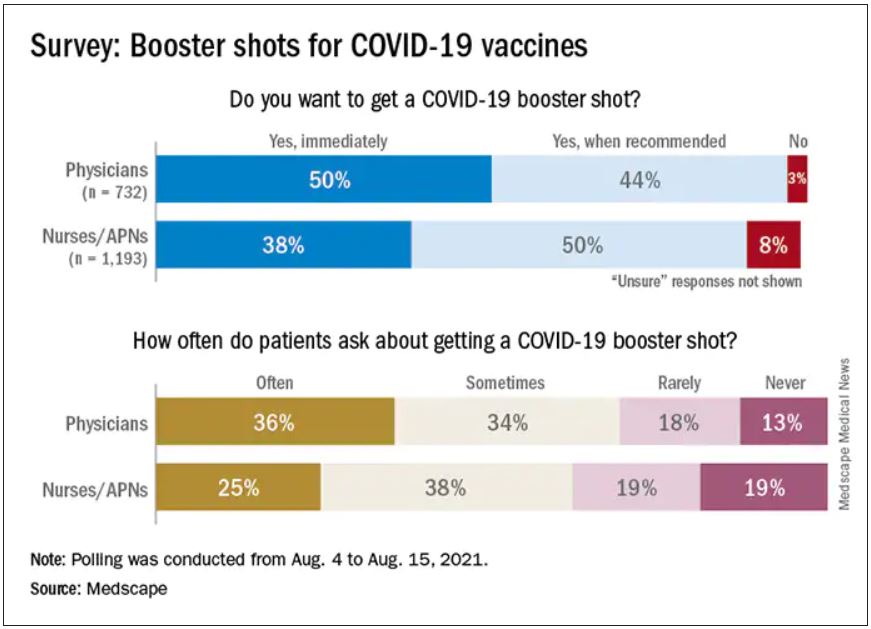
Among the 732 physicians polled, 50% wanted to get their shot immediately, compared with 38% of the 1,193 nurses/APNs who responded, while 44% of physicians and 50% of nurses/APNs said that they would wait until the vaccine booster was authorized and recommended.
At this point in time, almost all of the health care workers surveyed – 98% of physicians and 94% of nurses/APNs – have been fully vaccinated against COVID-19. A small proportion of each group, however, received the Johnson & Johnson vaccine (1% of physicians and 3% of nurses) and are not included in the current plan for booster shots.
The Medscape survey sample did include one group that is already eligible for a third dose: About 20% of physicians and 26% of nurses/ANPs said they have a condition or take a medication that compromises their immune system.
Respondents’ experiences with patient requests for boosters suggest a somewhat lower level of interest. About two-thirds of the health care workers (69% of physicians and 63% of nurses) said that patients frequently or sometimes asked about COVID boosters, compared with 13% (physicians) and 19% (nurses) who said their patients had never asked.
Interest lower among general population
In a separate survey conducted by WebMD, 82% of those who have been at least partially vaccinated said they want to get a COVID vaccine booster (14% immediately and 68% after authorization and recommendation). Of the remaining vaccinees, 7% said they do not want to get a booster and 11% were unsure.
The full sample of 592 respondents surveyed Aug. 5-10, however, included 19% who do not plan to get vaccinated and 6% who are planning to be vaccinated but have not yet done so.
The proportion of immunocompromised individuals in the two survey groups was similar, with about 25% of those in the WebMD survey reporting they have a condition or take a medication that compromises their immune system. Those respondents were more than twice as likely to want to get a booster immediately, compared to those with an uncompromised immune system (24% vs. 11%).
The distribution of vaccines received by brand was also comparable between the two groups surveyed. Of health care workers and readers, over half of each group received the Pfizer/BioNTech vaccine (59% vs. 54%), followed by Moderna (38% vs. 40%) and Johnson & Johnson (3% vs. 5%).
A version of this article first appeared on Medscape.com.
Guidance on additional COVID-19 vaccine dose for MS patients
Patients aged 12 years and older with multiple sclerosis (MS) who are fully immunized against COVID-19 with either the Pfizer-BioNTech or Moderna mRNA vaccine may be eligible to receive an additional dose now, the National Multiple Sclerosis Society has announced.
New guidance, which is “based on available data from studies and expert consensus opinion” by a panel of MS neurologists and experts, was published Aug. 19 on the organization’s website.
The Food and Drug Administration has authorized an additional dose of the coronavirus vaccine for patients who are expected to not have a normal or adequate immune response to the first two doses. Patients with MS who use certain treatments have a reduced or absent antibody response to the vaccine, according to recent data.
“We want people living with MS to be aware of this additional dose and discuss when they need an additional dose or booster dose with their health care provider,” Julie Fiol, RN, MSW, associate vice president of health care access, National MS Society, said in an interview.
Those who may benefit from an additional dose include patients with MS who use sphingosine 1-phosphate receptor modulators, anti-CD20 monoclonal antibodies, or alemtuzumab (Lemtrada), the National MS Society noted. These particular disease modifying therapies (DMTs) have a stronger effect on the immune system than do other treatments.
Protecting ‘the most vulnerable’
Sphingosine 1-phosphate receptor modulators include fingolimod (Gilenya), siponimod (Mayzent), ozanimod (Zeposia), and ponesimod (Ponvory).
Anti-CD20 monoclonal antibodies include ocrelizumab (Ocrevus), ofatumumab (Kesimpta), rituximab (Rituxan), and corresponding biosimilars.
Current data do not support an additional dose for immunocompromised patients who received the Johnson & Johnson vaccine. The FDA and the Centers for Disease Control and Prevention are developing recommendations for these patients, and the National MS Society will update its guidance as needed, the organization noted in its statement.
“Like other medical decisions, the decision to get an additional dose is best made in partnership with your health care provider,” said Ms. Fiol. “Talk to your MS health care provider to determine what is best for you.”
MS itself does not compromise the immune system, but some MS therapies alter the immune system and reduce the body’s response to vaccination. Patients with MS who use B cell-depleting therapies have a better antibody response when they receive the vaccine 3 months or more after the last dose of MS therapy, according to the National MS Society.
Data suggest that patients with MS are not more susceptible to COVID-19 infection, severe illness, or death than are patients without MS. However, certain groups of patients with MS, such as those who receive B cell-depleting treatments, are more susceptible to having a severe case of COVID-19.
That said, “everyone will need a booster at some point. Those who take DMTs that have greater impact on the immune system are the most urgent need now,” the organization noted.
“Vaccination against COVID-19 is critical for public safety and, especially, the safety of the most vulnerable among us,” said Ms. Fiol. “We encourage everyone with MS get vaccinated.”
A version of this article first appeared on Medscape.com.
Patients aged 12 years and older with multiple sclerosis (MS) who are fully immunized against COVID-19 with either the Pfizer-BioNTech or Moderna mRNA vaccine may be eligible to receive an additional dose now, the National Multiple Sclerosis Society has announced.
New guidance, which is “based on available data from studies and expert consensus opinion” by a panel of MS neurologists and experts, was published Aug. 19 on the organization’s website.
The Food and Drug Administration has authorized an additional dose of the coronavirus vaccine for patients who are expected to not have a normal or adequate immune response to the first two doses. Patients with MS who use certain treatments have a reduced or absent antibody response to the vaccine, according to recent data.
“We want people living with MS to be aware of this additional dose and discuss when they need an additional dose or booster dose with their health care provider,” Julie Fiol, RN, MSW, associate vice president of health care access, National MS Society, said in an interview.
Those who may benefit from an additional dose include patients with MS who use sphingosine 1-phosphate receptor modulators, anti-CD20 monoclonal antibodies, or alemtuzumab (Lemtrada), the National MS Society noted. These particular disease modifying therapies (DMTs) have a stronger effect on the immune system than do other treatments.
Protecting ‘the most vulnerable’
Sphingosine 1-phosphate receptor modulators include fingolimod (Gilenya), siponimod (Mayzent), ozanimod (Zeposia), and ponesimod (Ponvory).
Anti-CD20 monoclonal antibodies include ocrelizumab (Ocrevus), ofatumumab (Kesimpta), rituximab (Rituxan), and corresponding biosimilars.
Current data do not support an additional dose for immunocompromised patients who received the Johnson & Johnson vaccine. The FDA and the Centers for Disease Control and Prevention are developing recommendations for these patients, and the National MS Society will update its guidance as needed, the organization noted in its statement.
“Like other medical decisions, the decision to get an additional dose is best made in partnership with your health care provider,” said Ms. Fiol. “Talk to your MS health care provider to determine what is best for you.”
MS itself does not compromise the immune system, but some MS therapies alter the immune system and reduce the body’s response to vaccination. Patients with MS who use B cell-depleting therapies have a better antibody response when they receive the vaccine 3 months or more after the last dose of MS therapy, according to the National MS Society.
Data suggest that patients with MS are not more susceptible to COVID-19 infection, severe illness, or death than are patients without MS. However, certain groups of patients with MS, such as those who receive B cell-depleting treatments, are more susceptible to having a severe case of COVID-19.
That said, “everyone will need a booster at some point. Those who take DMTs that have greater impact on the immune system are the most urgent need now,” the organization noted.
“Vaccination against COVID-19 is critical for public safety and, especially, the safety of the most vulnerable among us,” said Ms. Fiol. “We encourage everyone with MS get vaccinated.”
A version of this article first appeared on Medscape.com.
Patients aged 12 years and older with multiple sclerosis (MS) who are fully immunized against COVID-19 with either the Pfizer-BioNTech or Moderna mRNA vaccine may be eligible to receive an additional dose now, the National Multiple Sclerosis Society has announced.
New guidance, which is “based on available data from studies and expert consensus opinion” by a panel of MS neurologists and experts, was published Aug. 19 on the organization’s website.
The Food and Drug Administration has authorized an additional dose of the coronavirus vaccine for patients who are expected to not have a normal or adequate immune response to the first two doses. Patients with MS who use certain treatments have a reduced or absent antibody response to the vaccine, according to recent data.
“We want people living with MS to be aware of this additional dose and discuss when they need an additional dose or booster dose with their health care provider,” Julie Fiol, RN, MSW, associate vice president of health care access, National MS Society, said in an interview.
Those who may benefit from an additional dose include patients with MS who use sphingosine 1-phosphate receptor modulators, anti-CD20 monoclonal antibodies, or alemtuzumab (Lemtrada), the National MS Society noted. These particular disease modifying therapies (DMTs) have a stronger effect on the immune system than do other treatments.
Protecting ‘the most vulnerable’
Sphingosine 1-phosphate receptor modulators include fingolimod (Gilenya), siponimod (Mayzent), ozanimod (Zeposia), and ponesimod (Ponvory).
Anti-CD20 monoclonal antibodies include ocrelizumab (Ocrevus), ofatumumab (Kesimpta), rituximab (Rituxan), and corresponding biosimilars.
Current data do not support an additional dose for immunocompromised patients who received the Johnson & Johnson vaccine. The FDA and the Centers for Disease Control and Prevention are developing recommendations for these patients, and the National MS Society will update its guidance as needed, the organization noted in its statement.
“Like other medical decisions, the decision to get an additional dose is best made in partnership with your health care provider,” said Ms. Fiol. “Talk to your MS health care provider to determine what is best for you.”
MS itself does not compromise the immune system, but some MS therapies alter the immune system and reduce the body’s response to vaccination. Patients with MS who use B cell-depleting therapies have a better antibody response when they receive the vaccine 3 months or more after the last dose of MS therapy, according to the National MS Society.
Data suggest that patients with MS are not more susceptible to COVID-19 infection, severe illness, or death than are patients without MS. However, certain groups of patients with MS, such as those who receive B cell-depleting treatments, are more susceptible to having a severe case of COVID-19.
That said, “everyone will need a booster at some point. Those who take DMTs that have greater impact on the immune system are the most urgent need now,” the organization noted.
“Vaccination against COVID-19 is critical for public safety and, especially, the safety of the most vulnerable among us,” said Ms. Fiol. “We encourage everyone with MS get vaccinated.”
A version of this article first appeared on Medscape.com.
Walking the dog and fetching happiness
To go back to last week’s column, some of the best advice I ever got came from those early days when I was just starting my solo practice.
One of the family docs I met was a bit off the path. He was in a small medical building, maybe three to four offices total. It wasn’t rundown, but was obviously an older building, and not located near the hospital.
When I went in, it was clear he’d been there a while, and hadn’t bothered to redecorate at all (granted, in 2021, neither have I). The lobby reminded me more of my grandparents’ living room than a medical practice. I watched as the receptionist artfully ran through answering several lines, putting people on hold, and scheduling appointments, before she turned to me.
As soon as I started my spiel (“Hi, I’m a new neurologist in the area”) she got up and went to get the doctor. She said he always wanted to meet the new doctors who came in.
Dr. Charlie took me back to his office. His desk was covered with charts in no obvious order, and the bookcases with various journals. There was a feeling of comfortable, intentional, messiness.
He was 67 at the time, obviously still enjoying his work. He told me he’d been in solo practice since day 1, recommended it to all starting out (23 years later I’ll agree with that), and offered me this piece of advice:
“Treat your practice like you would your dog. Enjoy it, take care of it, and it will serve you well. But never, ever, let it be your master. If you do, you’ll be miserable. Raise it the right way and you’ll always be happy.”
After the brief meeting he walked me up front and I went on to the next office.
In the years to come I encountered him on and off rounding at the hospital or sending each other letters about a patient. He retired a few years later and died in 2007.
I still think about him. I’ve had one practice and owned several dogs during that time, and he was really right.
In solo practice I probably haven’t made as much money as I would have in a larger group. But I have more time to do as I wish, no one else to argue with me about a new direction for the practice, computer upgrades, or staff changes. I see, within the limits allowed by my overhead, as many or as few patients as I want. I can take vacations and days off. I have time to goof off with my staff and spend extra minutes with patients who need it. Medicine is a high-stress field, but at least I can keep the stress as low as possible.
On the flip side, I see the people he warned me about. New docs who come out with guns blazing, cramming their schedule as full as possible until they can’t possibly see more patients. Their staff gets overworked and has a high turnover. They themselves burn out quickly and either melt down or close down.
So I’ll pass the same advice to all others starting out. I still recommend solo practice. And
As I say to my dogs every day, “you guys are awesome.”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
To go back to last week’s column, some of the best advice I ever got came from those early days when I was just starting my solo practice.
One of the family docs I met was a bit off the path. He was in a small medical building, maybe three to four offices total. It wasn’t rundown, but was obviously an older building, and not located near the hospital.
When I went in, it was clear he’d been there a while, and hadn’t bothered to redecorate at all (granted, in 2021, neither have I). The lobby reminded me more of my grandparents’ living room than a medical practice. I watched as the receptionist artfully ran through answering several lines, putting people on hold, and scheduling appointments, before she turned to me.
As soon as I started my spiel (“Hi, I’m a new neurologist in the area”) she got up and went to get the doctor. She said he always wanted to meet the new doctors who came in.
Dr. Charlie took me back to his office. His desk was covered with charts in no obvious order, and the bookcases with various journals. There was a feeling of comfortable, intentional, messiness.
He was 67 at the time, obviously still enjoying his work. He told me he’d been in solo practice since day 1, recommended it to all starting out (23 years later I’ll agree with that), and offered me this piece of advice:
“Treat your practice like you would your dog. Enjoy it, take care of it, and it will serve you well. But never, ever, let it be your master. If you do, you’ll be miserable. Raise it the right way and you’ll always be happy.”
After the brief meeting he walked me up front and I went on to the next office.
In the years to come I encountered him on and off rounding at the hospital or sending each other letters about a patient. He retired a few years later and died in 2007.
I still think about him. I’ve had one practice and owned several dogs during that time, and he was really right.
In solo practice I probably haven’t made as much money as I would have in a larger group. But I have more time to do as I wish, no one else to argue with me about a new direction for the practice, computer upgrades, or staff changes. I see, within the limits allowed by my overhead, as many or as few patients as I want. I can take vacations and days off. I have time to goof off with my staff and spend extra minutes with patients who need it. Medicine is a high-stress field, but at least I can keep the stress as low as possible.
On the flip side, I see the people he warned me about. New docs who come out with guns blazing, cramming their schedule as full as possible until they can’t possibly see more patients. Their staff gets overworked and has a high turnover. They themselves burn out quickly and either melt down or close down.
So I’ll pass the same advice to all others starting out. I still recommend solo practice. And
As I say to my dogs every day, “you guys are awesome.”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
To go back to last week’s column, some of the best advice I ever got came from those early days when I was just starting my solo practice.
One of the family docs I met was a bit off the path. He was in a small medical building, maybe three to four offices total. It wasn’t rundown, but was obviously an older building, and not located near the hospital.
When I went in, it was clear he’d been there a while, and hadn’t bothered to redecorate at all (granted, in 2021, neither have I). The lobby reminded me more of my grandparents’ living room than a medical practice. I watched as the receptionist artfully ran through answering several lines, putting people on hold, and scheduling appointments, before she turned to me.
As soon as I started my spiel (“Hi, I’m a new neurologist in the area”) she got up and went to get the doctor. She said he always wanted to meet the new doctors who came in.
Dr. Charlie took me back to his office. His desk was covered with charts in no obvious order, and the bookcases with various journals. There was a feeling of comfortable, intentional, messiness.
He was 67 at the time, obviously still enjoying his work. He told me he’d been in solo practice since day 1, recommended it to all starting out (23 years later I’ll agree with that), and offered me this piece of advice:
“Treat your practice like you would your dog. Enjoy it, take care of it, and it will serve you well. But never, ever, let it be your master. If you do, you’ll be miserable. Raise it the right way and you’ll always be happy.”
After the brief meeting he walked me up front and I went on to the next office.
In the years to come I encountered him on and off rounding at the hospital or sending each other letters about a patient. He retired a few years later and died in 2007.
I still think about him. I’ve had one practice and owned several dogs during that time, and he was really right.
In solo practice I probably haven’t made as much money as I would have in a larger group. But I have more time to do as I wish, no one else to argue with me about a new direction for the practice, computer upgrades, or staff changes. I see, within the limits allowed by my overhead, as many or as few patients as I want. I can take vacations and days off. I have time to goof off with my staff and spend extra minutes with patients who need it. Medicine is a high-stress field, but at least I can keep the stress as low as possible.
On the flip side, I see the people he warned me about. New docs who come out with guns blazing, cramming their schedule as full as possible until they can’t possibly see more patients. Their staff gets overworked and has a high turnover. They themselves burn out quickly and either melt down or close down.
So I’ll pass the same advice to all others starting out. I still recommend solo practice. And
As I say to my dogs every day, “you guys are awesome.”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
FDA fully approves Pfizer COVID-19 vaccine
The Food and Drug Administration has granted a biological license application, more commonly known as “full approval,” to the Pfizer-BioNTech COVID-19 vaccine.
It is the first COVID-19 vaccine to be fully licensed in the United States. It will be marketed under the trade name Comirnaty.
The approval applies to individuals ages 16 years and older. The vaccine is still available for emergency use for those ages 12-15.
The FDA’s stamp of approval is somewhat anticlimactic, following months of real-world use and millions of doses doled out to the general population. It comes after months of scrutiny by the agency of the clinical trial data.
Still, the approval puts the vaccines on firmer legal footing and is expected to spur a raft of new vaccination requirements by employers, schools, and universities.
“The FDA approval is the gold standard,” President Joe Biden said from the White House. “Those who have been waiting for full approval should go and get your shot now.”
“It could save your life or the lives of those you love,” he said.
Biden also called on businesses to mandate COVID vaccines for their employees.
Indeed, soon after the approval was announced, Defense Secretary Lloyd Austin said the vaccines would be required for all 1.4 million active duty service members.
Public health advocates have seen full approval as an important tool to increase U.S. vaccination rates and had criticized the FDA for taking so long to grant the license.
In a news briefing on the approval, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said the agency had not dragged its feet.
Marks noted that his team had reviewed tens of thousands of pages of clinical trial data -- down to the level of individual patients. They also inspected clinical trial sites and manufacturing facilities, and reviewed information gathered after the vaccines were authorized for use.
“It’s been 97 days since Pfizer completed the role of its [application for approval] and the clock started, which means that we completed this in about 40% of the normal clock time for a submission of this magnitude,” he said. “People worked day and night.”
The agency resisted pressure to speed up its process, saying a thorough review was necessary to ensure public confidence.
“While millions of people have already safely received COVID-19 vaccines, we recognize that for some, the FDA approval of a vaccine may now instill additional confidence to get vaccinated. Today’s milestone puts us one step closer to altering the course of this pandemic in the U.S.,” acting FDA Commissioner Janet Woodcock said in a FDA news release.
Experts agreed the move would increase public confidence.
“I don't expect a big line outside of vaccination sites this afternoon or tomorrow morning, but it will persuade some,” said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University in Nashville.
A recent Kaiser Family Foundation poll found that 3 in 10 unvaccinated adults said they would be more likely to get vaccinated if the vaccines were given full approval.
More importantly, Schaffner said, the FDA’s approval would lay the groundwork for vaccine mandates. “I think those kinds of mandates are going to be necessary to get us up over 80% vaccinated.”
In granting the approval, the agency reviewed a record amount of data from more than 40,000 people who took part in clinical trials. About 12,000 recipients have been followed for at least 6 months, the agency said.
The FDA also reviewed safety data collected since it issued its emergency use authorization for the shots in December.
Based on the results from the clinical trials, the vaccine was 91% effective at preventing COVID-19 disease. But that estimate came from data collected before the Delta variant became widespread.
The most commonly reported side effects in the clinical trials were pain, redness and swelling at the injection site, fatigue, headache, muscle or joint pain, chills, and fever.
The FDA said the vaccine is effective in preventing COVID-19 and potentially serious outcomes, including hospitalization and death.
Based on safety data reviewed since the two-dose vaccine was approved, the FDA said the data demonstrates a higher risk for heart inflammation -- clinically known as myocarditis or pericarditis -- especially within 7 days after the second dose of the shots. The risk is highest for men under age 40, compared to women and older men.
The prescription information includes warnings about these risks. The FDA said the drugmakers must continue to study the risks and long-term effects on people who have myocarditis after vaccination.
A version of this article first appeared on Medscape.com.
This article was updated on 8/24/21.
The Food and Drug Administration has granted a biological license application, more commonly known as “full approval,” to the Pfizer-BioNTech COVID-19 vaccine.
It is the first COVID-19 vaccine to be fully licensed in the United States. It will be marketed under the trade name Comirnaty.
The approval applies to individuals ages 16 years and older. The vaccine is still available for emergency use for those ages 12-15.
The FDA’s stamp of approval is somewhat anticlimactic, following months of real-world use and millions of doses doled out to the general population. It comes after months of scrutiny by the agency of the clinical trial data.
Still, the approval puts the vaccines on firmer legal footing and is expected to spur a raft of new vaccination requirements by employers, schools, and universities.
“The FDA approval is the gold standard,” President Joe Biden said from the White House. “Those who have been waiting for full approval should go and get your shot now.”
“It could save your life or the lives of those you love,” he said.
Biden also called on businesses to mandate COVID vaccines for their employees.
Indeed, soon after the approval was announced, Defense Secretary Lloyd Austin said the vaccines would be required for all 1.4 million active duty service members.
Public health advocates have seen full approval as an important tool to increase U.S. vaccination rates and had criticized the FDA for taking so long to grant the license.
In a news briefing on the approval, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said the agency had not dragged its feet.
Marks noted that his team had reviewed tens of thousands of pages of clinical trial data -- down to the level of individual patients. They also inspected clinical trial sites and manufacturing facilities, and reviewed information gathered after the vaccines were authorized for use.
“It’s been 97 days since Pfizer completed the role of its [application for approval] and the clock started, which means that we completed this in about 40% of the normal clock time for a submission of this magnitude,” he said. “People worked day and night.”
The agency resisted pressure to speed up its process, saying a thorough review was necessary to ensure public confidence.
“While millions of people have already safely received COVID-19 vaccines, we recognize that for some, the FDA approval of a vaccine may now instill additional confidence to get vaccinated. Today’s milestone puts us one step closer to altering the course of this pandemic in the U.S.,” acting FDA Commissioner Janet Woodcock said in a FDA news release.
Experts agreed the move would increase public confidence.
“I don't expect a big line outside of vaccination sites this afternoon or tomorrow morning, but it will persuade some,” said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University in Nashville.
A recent Kaiser Family Foundation poll found that 3 in 10 unvaccinated adults said they would be more likely to get vaccinated if the vaccines were given full approval.
More importantly, Schaffner said, the FDA’s approval would lay the groundwork for vaccine mandates. “I think those kinds of mandates are going to be necessary to get us up over 80% vaccinated.”
In granting the approval, the agency reviewed a record amount of data from more than 40,000 people who took part in clinical trials. About 12,000 recipients have been followed for at least 6 months, the agency said.
The FDA also reviewed safety data collected since it issued its emergency use authorization for the shots in December.
Based on the results from the clinical trials, the vaccine was 91% effective at preventing COVID-19 disease. But that estimate came from data collected before the Delta variant became widespread.
The most commonly reported side effects in the clinical trials were pain, redness and swelling at the injection site, fatigue, headache, muscle or joint pain, chills, and fever.
The FDA said the vaccine is effective in preventing COVID-19 and potentially serious outcomes, including hospitalization and death.
Based on safety data reviewed since the two-dose vaccine was approved, the FDA said the data demonstrates a higher risk for heart inflammation -- clinically known as myocarditis or pericarditis -- especially within 7 days after the second dose of the shots. The risk is highest for men under age 40, compared to women and older men.
The prescription information includes warnings about these risks. The FDA said the drugmakers must continue to study the risks and long-term effects on people who have myocarditis after vaccination.
A version of this article first appeared on Medscape.com.
This article was updated on 8/24/21.
The Food and Drug Administration has granted a biological license application, more commonly known as “full approval,” to the Pfizer-BioNTech COVID-19 vaccine.
It is the first COVID-19 vaccine to be fully licensed in the United States. It will be marketed under the trade name Comirnaty.
The approval applies to individuals ages 16 years and older. The vaccine is still available for emergency use for those ages 12-15.
The FDA’s stamp of approval is somewhat anticlimactic, following months of real-world use and millions of doses doled out to the general population. It comes after months of scrutiny by the agency of the clinical trial data.
Still, the approval puts the vaccines on firmer legal footing and is expected to spur a raft of new vaccination requirements by employers, schools, and universities.
“The FDA approval is the gold standard,” President Joe Biden said from the White House. “Those who have been waiting for full approval should go and get your shot now.”
“It could save your life or the lives of those you love,” he said.
Biden also called on businesses to mandate COVID vaccines for their employees.
Indeed, soon after the approval was announced, Defense Secretary Lloyd Austin said the vaccines would be required for all 1.4 million active duty service members.
Public health advocates have seen full approval as an important tool to increase U.S. vaccination rates and had criticized the FDA for taking so long to grant the license.
In a news briefing on the approval, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said the agency had not dragged its feet.
Marks noted that his team had reviewed tens of thousands of pages of clinical trial data -- down to the level of individual patients. They also inspected clinical trial sites and manufacturing facilities, and reviewed information gathered after the vaccines were authorized for use.
“It’s been 97 days since Pfizer completed the role of its [application for approval] and the clock started, which means that we completed this in about 40% of the normal clock time for a submission of this magnitude,” he said. “People worked day and night.”
The agency resisted pressure to speed up its process, saying a thorough review was necessary to ensure public confidence.
“While millions of people have already safely received COVID-19 vaccines, we recognize that for some, the FDA approval of a vaccine may now instill additional confidence to get vaccinated. Today’s milestone puts us one step closer to altering the course of this pandemic in the U.S.,” acting FDA Commissioner Janet Woodcock said in a FDA news release.
Experts agreed the move would increase public confidence.
“I don't expect a big line outside of vaccination sites this afternoon or tomorrow morning, but it will persuade some,” said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University in Nashville.
A recent Kaiser Family Foundation poll found that 3 in 10 unvaccinated adults said they would be more likely to get vaccinated if the vaccines were given full approval.
More importantly, Schaffner said, the FDA’s approval would lay the groundwork for vaccine mandates. “I think those kinds of mandates are going to be necessary to get us up over 80% vaccinated.”
In granting the approval, the agency reviewed a record amount of data from more than 40,000 people who took part in clinical trials. About 12,000 recipients have been followed for at least 6 months, the agency said.
The FDA also reviewed safety data collected since it issued its emergency use authorization for the shots in December.
Based on the results from the clinical trials, the vaccine was 91% effective at preventing COVID-19 disease. But that estimate came from data collected before the Delta variant became widespread.
The most commonly reported side effects in the clinical trials were pain, redness and swelling at the injection site, fatigue, headache, muscle or joint pain, chills, and fever.
The FDA said the vaccine is effective in preventing COVID-19 and potentially serious outcomes, including hospitalization and death.
Based on safety data reviewed since the two-dose vaccine was approved, the FDA said the data demonstrates a higher risk for heart inflammation -- clinically known as myocarditis or pericarditis -- especially within 7 days after the second dose of the shots. The risk is highest for men under age 40, compared to women and older men.
The prescription information includes warnings about these risks. The FDA said the drugmakers must continue to study the risks and long-term effects on people who have myocarditis after vaccination.
A version of this article first appeared on Medscape.com.
This article was updated on 8/24/21.
Psychotic features among older adults tied to Parkinson’s
Adults aged 65 years and older who develop psychotic manifestations are significantly more likely than those without such manifestations to develop prodromal Parkinson’s disease, data from 925 individuals suggest.
“The presence of perceptual abnormalities and/or delusional ideation among community-dwelling elderly individuals is more widespread than considered in the past,” wrote Ioanna Pachi, MD, of National and Kapodistrian University of Athens Medical School and colleagues. However, those psychoses and their potential impact on prodromal Parkinson’s disease (PD) have not been well studied in community-dwelling populations, they noted in the study, published in Parkinsonism and Related Disorders.
In the study, Dr. Pachi and colleagues reviewed data from 914 participants in the Hellenic Longitudinal Investigation of Aging and Diet study (HELIAD), a cross-sectional, population-based cohort study of older adults in Greece. The average age of the participants was 76 years, and 41% were men. Participants had no delusional features at baseline; delusional features were assessed using the Neuropsychiatric Inventory scale and the Columbia University Scale for Psychopathology in Alzheimer’s disease. The researchers calculated the probability of prodromal PD (pPD) for each participant based on the 2019 International Parkinson and Movement Disorders Society research criteria for prodromal PD.
Over a 3-year follow-up period, 20 participants developed psychotic manifestations and were 1.3 times more likely to have pPD, compared with those without psychoses (P = .006). Those with new-onset psychotic features were categorized together as the NPSY group, regardless of symptom severity or frequency; those with no symptoms at either baseline or during follow-up were categorized as unaffected (UPSY). Most of the NPSY participants showed isolated delusional features, although some expressed hallucinations. Most symptoms were mild.
New-onset psychosis was associated with a fivefold increased risk of both subthreshold parkinsonism and depression (adjusted odds ratios, 4.5 and 5.0, respectively) and with a threefold increased risk of constipation (aOR 2.6). Other factors, including nonsmoking, global cognitive deficit, and anxiety were not significantly associated with new-onset psychotic symptoms after adjusting for confounding factors.
Although the mechanism behind the association remains unclear,
The study findings were limited by several factors, including the administration of neuropsychiatric questionnaires by nonpsychiatrists, and lack of detailed psychiatric history, including complete information on medication use, the researchers noted. The small size of the NPSY group also prevented evaluation of the potential associations between pPD and different modalities of hallucinations, they said.
However, the results were strengthened by the overall large and population-based sample size, and the comprehensive evaluation of psychotic features, they wrote. More follow-up evaluations in the HELIAD cohort are planned to further explore the underlying mechanism of the association between late-life psychosis and pPD.
“Provided that these results are confirmed in other community cohorts of elderly subjects, psychotic features may be added to the list of manifestations of pPD,” they concluded.
The study was supported in part by grants from the Alzheimer’s Association, ARISTEIA, and the ESPA-EU program Excellence Grant. It was cofunded by the European Social Fund and Greek National resources, the Ministry for Health and Social Solidarity, Greece, and the Greek State Scholarships Foundation. Dr. Pachi had no disclosures.
Adults aged 65 years and older who develop psychotic manifestations are significantly more likely than those without such manifestations to develop prodromal Parkinson’s disease, data from 925 individuals suggest.
“The presence of perceptual abnormalities and/or delusional ideation among community-dwelling elderly individuals is more widespread than considered in the past,” wrote Ioanna Pachi, MD, of National and Kapodistrian University of Athens Medical School and colleagues. However, those psychoses and their potential impact on prodromal Parkinson’s disease (PD) have not been well studied in community-dwelling populations, they noted in the study, published in Parkinsonism and Related Disorders.
In the study, Dr. Pachi and colleagues reviewed data from 914 participants in the Hellenic Longitudinal Investigation of Aging and Diet study (HELIAD), a cross-sectional, population-based cohort study of older adults in Greece. The average age of the participants was 76 years, and 41% were men. Participants had no delusional features at baseline; delusional features were assessed using the Neuropsychiatric Inventory scale and the Columbia University Scale for Psychopathology in Alzheimer’s disease. The researchers calculated the probability of prodromal PD (pPD) for each participant based on the 2019 International Parkinson and Movement Disorders Society research criteria for prodromal PD.
Over a 3-year follow-up period, 20 participants developed psychotic manifestations and were 1.3 times more likely to have pPD, compared with those without psychoses (P = .006). Those with new-onset psychotic features were categorized together as the NPSY group, regardless of symptom severity or frequency; those with no symptoms at either baseline or during follow-up were categorized as unaffected (UPSY). Most of the NPSY participants showed isolated delusional features, although some expressed hallucinations. Most symptoms were mild.
New-onset psychosis was associated with a fivefold increased risk of both subthreshold parkinsonism and depression (adjusted odds ratios, 4.5 and 5.0, respectively) and with a threefold increased risk of constipation (aOR 2.6). Other factors, including nonsmoking, global cognitive deficit, and anxiety were not significantly associated with new-onset psychotic symptoms after adjusting for confounding factors.
Although the mechanism behind the association remains unclear,
The study findings were limited by several factors, including the administration of neuropsychiatric questionnaires by nonpsychiatrists, and lack of detailed psychiatric history, including complete information on medication use, the researchers noted. The small size of the NPSY group also prevented evaluation of the potential associations between pPD and different modalities of hallucinations, they said.
However, the results were strengthened by the overall large and population-based sample size, and the comprehensive evaluation of psychotic features, they wrote. More follow-up evaluations in the HELIAD cohort are planned to further explore the underlying mechanism of the association between late-life psychosis and pPD.
“Provided that these results are confirmed in other community cohorts of elderly subjects, psychotic features may be added to the list of manifestations of pPD,” they concluded.
The study was supported in part by grants from the Alzheimer’s Association, ARISTEIA, and the ESPA-EU program Excellence Grant. It was cofunded by the European Social Fund and Greek National resources, the Ministry for Health and Social Solidarity, Greece, and the Greek State Scholarships Foundation. Dr. Pachi had no disclosures.
Adults aged 65 years and older who develop psychotic manifestations are significantly more likely than those without such manifestations to develop prodromal Parkinson’s disease, data from 925 individuals suggest.
“The presence of perceptual abnormalities and/or delusional ideation among community-dwelling elderly individuals is more widespread than considered in the past,” wrote Ioanna Pachi, MD, of National and Kapodistrian University of Athens Medical School and colleagues. However, those psychoses and their potential impact on prodromal Parkinson’s disease (PD) have not been well studied in community-dwelling populations, they noted in the study, published in Parkinsonism and Related Disorders.
In the study, Dr. Pachi and colleagues reviewed data from 914 participants in the Hellenic Longitudinal Investigation of Aging and Diet study (HELIAD), a cross-sectional, population-based cohort study of older adults in Greece. The average age of the participants was 76 years, and 41% were men. Participants had no delusional features at baseline; delusional features were assessed using the Neuropsychiatric Inventory scale and the Columbia University Scale for Psychopathology in Alzheimer’s disease. The researchers calculated the probability of prodromal PD (pPD) for each participant based on the 2019 International Parkinson and Movement Disorders Society research criteria for prodromal PD.
Over a 3-year follow-up period, 20 participants developed psychotic manifestations and were 1.3 times more likely to have pPD, compared with those without psychoses (P = .006). Those with new-onset psychotic features were categorized together as the NPSY group, regardless of symptom severity or frequency; those with no symptoms at either baseline or during follow-up were categorized as unaffected (UPSY). Most of the NPSY participants showed isolated delusional features, although some expressed hallucinations. Most symptoms were mild.
New-onset psychosis was associated with a fivefold increased risk of both subthreshold parkinsonism and depression (adjusted odds ratios, 4.5 and 5.0, respectively) and with a threefold increased risk of constipation (aOR 2.6). Other factors, including nonsmoking, global cognitive deficit, and anxiety were not significantly associated with new-onset psychotic symptoms after adjusting for confounding factors.
Although the mechanism behind the association remains unclear,
The study findings were limited by several factors, including the administration of neuropsychiatric questionnaires by nonpsychiatrists, and lack of detailed psychiatric history, including complete information on medication use, the researchers noted. The small size of the NPSY group also prevented evaluation of the potential associations between pPD and different modalities of hallucinations, they said.
However, the results were strengthened by the overall large and population-based sample size, and the comprehensive evaluation of psychotic features, they wrote. More follow-up evaluations in the HELIAD cohort are planned to further explore the underlying mechanism of the association between late-life psychosis and pPD.
“Provided that these results are confirmed in other community cohorts of elderly subjects, psychotic features may be added to the list of manifestations of pPD,” they concluded.
The study was supported in part by grants from the Alzheimer’s Association, ARISTEIA, and the ESPA-EU program Excellence Grant. It was cofunded by the European Social Fund and Greek National resources, the Ministry for Health and Social Solidarity, Greece, and the Greek State Scholarships Foundation. Dr. Pachi had no disclosures.
FROM PARKINSONISM AND RELATED DISORDERS
Managing sleep in the elderly
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
FROM FOCUS ON NEUROPSYCHIATRY 2021
Doctor wins restraining order against CVS after prescription ban
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
Increased risk of hospitalization and death with Parkinson’s drug
, according to a new study.
A retrospective cohort study of elderly patients with Parkinson’s disease who were in long-term care facilities found that the use of pimavanserin (Nuplazid) was associated with an increased risk of 30-day hospitalization and mortality for up to a year.
“Given that a previous study showed typical and atypical antipsychotics more than doubled mortality risk in patients with Parkinson’s disease, we aimed to assess the risk of hospitalization and death associated with pimavanserin,” wrote lead author Y. Joseph Hwang, MD, Johns Hopkins University, Baltimore, and colleagues in the paper. “These findings, in a large real-world cohort within long-term care facilities, may help to inform decisions regarding its risk-benefit balance among patients with Parkinson’s disease.”
The findings were published online Aug. 13 in Neurology.
The researchers enrolled 2,186 patients with Parkinson’s disease aged 65 years and older in Medicare-certified long-term care facilities who also had a pimavanserin prescription and 18,212 nonusers of pimavanserin between Nov. 1, 2015, and December 31, 2018. Patients in the pimavanserin group used the drug over the course of the entire study period. Hospitalization and mortality were calculated from the date of pimavanserin prescription. Propensity score–based inverse probability of treatment weighting (IPTW) was used to balance the two groups on 24 baseline characteristics such as age, sex, and comorbidities.
Pimavanserin use was associated with a 24% higher risk of 30-day hospitalization (adjusted hazard ratio, 1.24; 95% confidence interval, 1.06-1.43). However, “the association did not reach statistical significance in a smaller subcohort of propensity score-matched users and nonusers,” Dr. Hwang and colleagues wrote.
Pimavanserin use was also linked to higher mortality at:
- 90 days (aHR, 1.20; 95% CI, 1.02-1.41).
- 180 days (aHR, 1.28; 95% CI, 1.13-1.45).
- 365 days (aHR, 1.56; 95% CI, 1.42-1.72).
No associations were found between pimavanserin use and 90-day hospitalization (aHR, 1.10; 95% CI, 0.99-1.24) nor with 30-day mortality (aHR, 0.76; 95% CI, 0.56-1.03).
Important considerations
“This study raises three important points to consider for any practicing neurology provider: 1) how to address and interpret risks associated with pimavanserin use in this patient population 2) utility of pimavanserin 3) interpretation of data showing increased mortality in patients being treated for Parkinson’s disease psychosis,” wrote Farwa Ali, MBBS, of the Mayo Clinic, Rochester, Minn., in an accompanying editorial published in Neurology.
Hallucinations and delusions are highly prevalent in Parkinson’s disease; as many as 60% of patients will develop psychosis over the course of their illness. Pimavanserin is a selective serotonin inverse agonist which targets 5-HT2A serotonin receptors in the brain, decreasing their activity in order to attenuate hallucinations and delusions.
“Pimavanserin has been approved by the FDA [Food and Drug Administration] for Parkinson’s disease psychosis, but its safety has been called into question based on previous reports of increased mortality risk, compared with a rather modest benefit seen in a 6-week clinical trial, the duration of which limits determination of long-term safety,” wrote Dr. Ali.
Pimavanserin carries a boxed warning that elderly patients with dementia may be at an increased risk of death. After its approval in 2016, the U.S. FDA later reviewed 893 deaths in association with pimavanserin during the postmarketing surveillance period – “an unexpected number in a new drug,” Dr. Hwang and colleagues noted. “It [the FDA] noted that most reports occurred in a population with high underlying death rates and did not signal any additional risk beyond the current warning for all antipsychotics, which could have resulted in annual mortality rates of up to 60%.”
As the first cohort study to examine hospitalization and death between pimavanserin users and nonusers, “the study confirms previous concerns regarding safety of pimavanserin and more importantly brings to attention the importance of carefully considering risks and benefits of pharmacotherapy in Parkinson’s disease psychosis, clear communication with patients and families, and close observation to ensure safety,” wrote Dr. Ali.
The study limitations include its observational design, which subjected the findings to residual confounding.
“While we developed models to maximize the strength of causal inference, our comparison group was pimavanserin nonusers and the very reason for prescription of pimavanserin could have predisposed its users to the outcomes of hospitalization and death, introducing confounding by indication,” Dr. Hwang and colleagues wrote in the paper.
Additionally, “while robust analyses were conducted to ensure pimavanserin users and nonusers were comparable, Dr. Hwang et al. did find that pimavanserin users were more likely to concomitantly use other antipsychotic drugs which has been demonstrated as increasing the mortality risk,” Dr. Ali pointed out.
Since patients living in long-term care facilities may have a higher risk of mortality because of more severe or later-stage Parkinson’s disease, the study results “may not be generalizable to community-dwelling PD patients,” Dr. Ali wrote. “These factors are important to consider while making individual management decisions.”
Dr. Hwang and Dr. Ali disclosed no relevant financial relationships. The study authors reported no targeted funding.
, according to a new study.
A retrospective cohort study of elderly patients with Parkinson’s disease who were in long-term care facilities found that the use of pimavanserin (Nuplazid) was associated with an increased risk of 30-day hospitalization and mortality for up to a year.
“Given that a previous study showed typical and atypical antipsychotics more than doubled mortality risk in patients with Parkinson’s disease, we aimed to assess the risk of hospitalization and death associated with pimavanserin,” wrote lead author Y. Joseph Hwang, MD, Johns Hopkins University, Baltimore, and colleagues in the paper. “These findings, in a large real-world cohort within long-term care facilities, may help to inform decisions regarding its risk-benefit balance among patients with Parkinson’s disease.”
The findings were published online Aug. 13 in Neurology.
The researchers enrolled 2,186 patients with Parkinson’s disease aged 65 years and older in Medicare-certified long-term care facilities who also had a pimavanserin prescription and 18,212 nonusers of pimavanserin between Nov. 1, 2015, and December 31, 2018. Patients in the pimavanserin group used the drug over the course of the entire study period. Hospitalization and mortality were calculated from the date of pimavanserin prescription. Propensity score–based inverse probability of treatment weighting (IPTW) was used to balance the two groups on 24 baseline characteristics such as age, sex, and comorbidities.
Pimavanserin use was associated with a 24% higher risk of 30-day hospitalization (adjusted hazard ratio, 1.24; 95% confidence interval, 1.06-1.43). However, “the association did not reach statistical significance in a smaller subcohort of propensity score-matched users and nonusers,” Dr. Hwang and colleagues wrote.
Pimavanserin use was also linked to higher mortality at:
- 90 days (aHR, 1.20; 95% CI, 1.02-1.41).
- 180 days (aHR, 1.28; 95% CI, 1.13-1.45).
- 365 days (aHR, 1.56; 95% CI, 1.42-1.72).
No associations were found between pimavanserin use and 90-day hospitalization (aHR, 1.10; 95% CI, 0.99-1.24) nor with 30-day mortality (aHR, 0.76; 95% CI, 0.56-1.03).
Important considerations
“This study raises three important points to consider for any practicing neurology provider: 1) how to address and interpret risks associated with pimavanserin use in this patient population 2) utility of pimavanserin 3) interpretation of data showing increased mortality in patients being treated for Parkinson’s disease psychosis,” wrote Farwa Ali, MBBS, of the Mayo Clinic, Rochester, Minn., in an accompanying editorial published in Neurology.
Hallucinations and delusions are highly prevalent in Parkinson’s disease; as many as 60% of patients will develop psychosis over the course of their illness. Pimavanserin is a selective serotonin inverse agonist which targets 5-HT2A serotonin receptors in the brain, decreasing their activity in order to attenuate hallucinations and delusions.
“Pimavanserin has been approved by the FDA [Food and Drug Administration] for Parkinson’s disease psychosis, but its safety has been called into question based on previous reports of increased mortality risk, compared with a rather modest benefit seen in a 6-week clinical trial, the duration of which limits determination of long-term safety,” wrote Dr. Ali.
Pimavanserin carries a boxed warning that elderly patients with dementia may be at an increased risk of death. After its approval in 2016, the U.S. FDA later reviewed 893 deaths in association with pimavanserin during the postmarketing surveillance period – “an unexpected number in a new drug,” Dr. Hwang and colleagues noted. “It [the FDA] noted that most reports occurred in a population with high underlying death rates and did not signal any additional risk beyond the current warning for all antipsychotics, which could have resulted in annual mortality rates of up to 60%.”
As the first cohort study to examine hospitalization and death between pimavanserin users and nonusers, “the study confirms previous concerns regarding safety of pimavanserin and more importantly brings to attention the importance of carefully considering risks and benefits of pharmacotherapy in Parkinson’s disease psychosis, clear communication with patients and families, and close observation to ensure safety,” wrote Dr. Ali.
The study limitations include its observational design, which subjected the findings to residual confounding.
“While we developed models to maximize the strength of causal inference, our comparison group was pimavanserin nonusers and the very reason for prescription of pimavanserin could have predisposed its users to the outcomes of hospitalization and death, introducing confounding by indication,” Dr. Hwang and colleagues wrote in the paper.
Additionally, “while robust analyses were conducted to ensure pimavanserin users and nonusers were comparable, Dr. Hwang et al. did find that pimavanserin users were more likely to concomitantly use other antipsychotic drugs which has been demonstrated as increasing the mortality risk,” Dr. Ali pointed out.
Since patients living in long-term care facilities may have a higher risk of mortality because of more severe or later-stage Parkinson’s disease, the study results “may not be generalizable to community-dwelling PD patients,” Dr. Ali wrote. “These factors are important to consider while making individual management decisions.”
Dr. Hwang and Dr. Ali disclosed no relevant financial relationships. The study authors reported no targeted funding.
, according to a new study.
A retrospective cohort study of elderly patients with Parkinson’s disease who were in long-term care facilities found that the use of pimavanserin (Nuplazid) was associated with an increased risk of 30-day hospitalization and mortality for up to a year.
“Given that a previous study showed typical and atypical antipsychotics more than doubled mortality risk in patients with Parkinson’s disease, we aimed to assess the risk of hospitalization and death associated with pimavanserin,” wrote lead author Y. Joseph Hwang, MD, Johns Hopkins University, Baltimore, and colleagues in the paper. “These findings, in a large real-world cohort within long-term care facilities, may help to inform decisions regarding its risk-benefit balance among patients with Parkinson’s disease.”
The findings were published online Aug. 13 in Neurology.
The researchers enrolled 2,186 patients with Parkinson’s disease aged 65 years and older in Medicare-certified long-term care facilities who also had a pimavanserin prescription and 18,212 nonusers of pimavanserin between Nov. 1, 2015, and December 31, 2018. Patients in the pimavanserin group used the drug over the course of the entire study period. Hospitalization and mortality were calculated from the date of pimavanserin prescription. Propensity score–based inverse probability of treatment weighting (IPTW) was used to balance the two groups on 24 baseline characteristics such as age, sex, and comorbidities.
Pimavanserin use was associated with a 24% higher risk of 30-day hospitalization (adjusted hazard ratio, 1.24; 95% confidence interval, 1.06-1.43). However, “the association did not reach statistical significance in a smaller subcohort of propensity score-matched users and nonusers,” Dr. Hwang and colleagues wrote.
Pimavanserin use was also linked to higher mortality at:
- 90 days (aHR, 1.20; 95% CI, 1.02-1.41).
- 180 days (aHR, 1.28; 95% CI, 1.13-1.45).
- 365 days (aHR, 1.56; 95% CI, 1.42-1.72).
No associations were found between pimavanserin use and 90-day hospitalization (aHR, 1.10; 95% CI, 0.99-1.24) nor with 30-day mortality (aHR, 0.76; 95% CI, 0.56-1.03).
Important considerations
“This study raises three important points to consider for any practicing neurology provider: 1) how to address and interpret risks associated with pimavanserin use in this patient population 2) utility of pimavanserin 3) interpretation of data showing increased mortality in patients being treated for Parkinson’s disease psychosis,” wrote Farwa Ali, MBBS, of the Mayo Clinic, Rochester, Minn., in an accompanying editorial published in Neurology.
Hallucinations and delusions are highly prevalent in Parkinson’s disease; as many as 60% of patients will develop psychosis over the course of their illness. Pimavanserin is a selective serotonin inverse agonist which targets 5-HT2A serotonin receptors in the brain, decreasing their activity in order to attenuate hallucinations and delusions.
“Pimavanserin has been approved by the FDA [Food and Drug Administration] for Parkinson’s disease psychosis, but its safety has been called into question based on previous reports of increased mortality risk, compared with a rather modest benefit seen in a 6-week clinical trial, the duration of which limits determination of long-term safety,” wrote Dr. Ali.
Pimavanserin carries a boxed warning that elderly patients with dementia may be at an increased risk of death. After its approval in 2016, the U.S. FDA later reviewed 893 deaths in association with pimavanserin during the postmarketing surveillance period – “an unexpected number in a new drug,” Dr. Hwang and colleagues noted. “It [the FDA] noted that most reports occurred in a population with high underlying death rates and did not signal any additional risk beyond the current warning for all antipsychotics, which could have resulted in annual mortality rates of up to 60%.”
As the first cohort study to examine hospitalization and death between pimavanserin users and nonusers, “the study confirms previous concerns regarding safety of pimavanserin and more importantly brings to attention the importance of carefully considering risks and benefits of pharmacotherapy in Parkinson’s disease psychosis, clear communication with patients and families, and close observation to ensure safety,” wrote Dr. Ali.
The study limitations include its observational design, which subjected the findings to residual confounding.
“While we developed models to maximize the strength of causal inference, our comparison group was pimavanserin nonusers and the very reason for prescription of pimavanserin could have predisposed its users to the outcomes of hospitalization and death, introducing confounding by indication,” Dr. Hwang and colleagues wrote in the paper.
Additionally, “while robust analyses were conducted to ensure pimavanserin users and nonusers were comparable, Dr. Hwang et al. did find that pimavanserin users were more likely to concomitantly use other antipsychotic drugs which has been demonstrated as increasing the mortality risk,” Dr. Ali pointed out.
Since patients living in long-term care facilities may have a higher risk of mortality because of more severe or later-stage Parkinson’s disease, the study results “may not be generalizable to community-dwelling PD patients,” Dr. Ali wrote. “These factors are important to consider while making individual management decisions.”
Dr. Hwang and Dr. Ali disclosed no relevant financial relationships. The study authors reported no targeted funding.
FROM NEUROLOGY
Medicinal liquor and edited mosquitoes
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.








