User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Daily Recap: Headache as COVID evolution predictor; psoriasis drug treats canker sores
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Headache may predict clinical evolution of COVID-19
new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19 and could resemble tension-type or migraine headache.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period. In a subgroup of participants, headache persisted even after the symptoms of COVID-19 had been resolved.
Investigators noted that understanding the pathophysiology of headache in COVID-19 could improve understanding of migraine and other headache disorders. “It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection by SARS-CoV-2,” lead investigator Patricia Pozo-Rosich, MD, PhD, head of the headache and craniofacial pain unit at Vall d’Hebron University Hospital, Barcelona, said in an interview.
She presented the findings at the virtual annual meeting of the American Headache Society.
Systemic inflammation
Headache is one of the main symptoms of COVID-19. A recent study of 214 patients with COVID-19 showed that approximately 13% of the participants had headache and 5% had anosmia.
SARS-CoV-2 penetrates the cells through the ACE2 receptor, which is present throughout the body. “SARS-CoV-2 enters the body through the nasal cavity and it probably penetrates the nervous system in the periphery through afferent branches of the olfactory and trigeminal nerve,” Dr. Pozo-Rosich said. It travels to the lungs and, later, the bloodstream. This generates systemic inflammation that may turn into a cytokine storm. Evidence has identified cortical hyperintensities and olfactory bulb hyperintensities in patients with COVID-19, suggesting that the virus directly infects the CNS.
Interleukin-6, one of the main inflammatory molecules, has been proven to be related to COVID-19 and has become a therapeutic target. Levels of IL-6 may be lower and tend to be more stable in patients with both COVID-19 and headache than in patients with COVID-19 only.
The researchers observed 130 patients (51% women; mean age, 54 years) with COVID-19 who were attended by neurologists at Vall d’Hebron. In this group, 74.4% had headache. Patients with headache tended to be younger than those without headache (mean age, 50 years vs. 63 years, respectively) and tended to be women (58.6% vs. 29.4%).
Approximately one-third of patients with headache had a history of migraine. Most reported mild to moderate pain that resembled tension-type headache. In participants with severe pain and migraine-like features, headache more often began during the asymptomatic phase of COVID-19.
Disease evolution predictor?
The investigators followed up on 100 of the 130 patients with COVID-19, of whom 74 had headache. About 38% of these patients had ongoing headache after 6 weeks, which suggests that some patients may develop a new daily persistent headache once a 3-month period has elapsed. Half of this group had no previous headache history. Headache had been the prodromal symptom of COVID-19 for 21.4% of these patients.
Results showed that headache predicted the clinical evolution of COVID-19. The symptomatic phase of COVID-19 was 7 days shorter for patients with headache than for those without headache. In addition, the period of hospitalization was 7 days shorter for patients with headache and anosmia, compared with patients who had neither headache nor anosmia.
Most therapies, including ibuprofen, candesartan, and anti–calcitonin gene–related peptide (CGRP) monoclonal antibodies, are safe for treating headache in COVID-19, the investigators noted. “We should just try to initially avoid steroids to avoid interference with the body’s reaction to SARS-CoV-2,” Dr. Pozo-Rosich said.
Researchers at Sidney Kimmel Medical College, Philadelphia, are currently studying intranasal vazegepant, an anti-CGRP therapy, as a way to potentially blunt the severe inflammatory response in the lungs of patients with COVID-19, she noted, adding that this peptide may have a future role not only in headache, but also in COVID-19.
Historical link to viral infections
Commenting on the study, Matthew S. Robbins, MD, associate professor of neurology at Weill Cornell Medicine, New York, said the findings associating headache with a shorter symptomatic phase of COVID-19 were “interesting.”
“Headache is common with mild viral infections. More severe viral infections may simply feature more overwhelming respiratory symptoms and fever that lead to underreporting or underascertainment of headache,” said Dr. Robbins, who was not involved with the research.
He noted that the finding showing an association of headache and COVID-19 with a younger age and in women “may be related to a higher prevalence of migraine biology in such patients, and being triggered by the virus or the psychological stress associated with it.”
Dr. Robbins added that viral illnesses have long been associated with new daily persistent headache, “dating back to the early 1980s,” when it was first described in association with Epstein-Barr virus. These infections have also been implicated in the progression of migraine to chronic migraine in adolescents.
“In my view, treatment should be aimed at the symptomatic headache type for which new daily persistent headache resembles, regardless of the potential inciting factor,” Dr. Robbins said.
Dr. Pozo-Rosich has received consulting fees from Allergan, Amgen, Almirall, Biohaven, Chiesi, Eli Lilly, Medscape, Novartis, and Teva Pharmaceuticals. Dr. Robbins has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19 and could resemble tension-type or migraine headache.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period. In a subgroup of participants, headache persisted even after the symptoms of COVID-19 had been resolved.
Investigators noted that understanding the pathophysiology of headache in COVID-19 could improve understanding of migraine and other headache disorders. “It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection by SARS-CoV-2,” lead investigator Patricia Pozo-Rosich, MD, PhD, head of the headache and craniofacial pain unit at Vall d’Hebron University Hospital, Barcelona, said in an interview.
She presented the findings at the virtual annual meeting of the American Headache Society.
Systemic inflammation
Headache is one of the main symptoms of COVID-19. A recent study of 214 patients with COVID-19 showed that approximately 13% of the participants had headache and 5% had anosmia.
SARS-CoV-2 penetrates the cells through the ACE2 receptor, which is present throughout the body. “SARS-CoV-2 enters the body through the nasal cavity and it probably penetrates the nervous system in the periphery through afferent branches of the olfactory and trigeminal nerve,” Dr. Pozo-Rosich said. It travels to the lungs and, later, the bloodstream. This generates systemic inflammation that may turn into a cytokine storm. Evidence has identified cortical hyperintensities and olfactory bulb hyperintensities in patients with COVID-19, suggesting that the virus directly infects the CNS.
Interleukin-6, one of the main inflammatory molecules, has been proven to be related to COVID-19 and has become a therapeutic target. Levels of IL-6 may be lower and tend to be more stable in patients with both COVID-19 and headache than in patients with COVID-19 only.
The researchers observed 130 patients (51% women; mean age, 54 years) with COVID-19 who were attended by neurologists at Vall d’Hebron. In this group, 74.4% had headache. Patients with headache tended to be younger than those without headache (mean age, 50 years vs. 63 years, respectively) and tended to be women (58.6% vs. 29.4%).
Approximately one-third of patients with headache had a history of migraine. Most reported mild to moderate pain that resembled tension-type headache. In participants with severe pain and migraine-like features, headache more often began during the asymptomatic phase of COVID-19.
Disease evolution predictor?
The investigators followed up on 100 of the 130 patients with COVID-19, of whom 74 had headache. About 38% of these patients had ongoing headache after 6 weeks, which suggests that some patients may develop a new daily persistent headache once a 3-month period has elapsed. Half of this group had no previous headache history. Headache had been the prodromal symptom of COVID-19 for 21.4% of these patients.
Results showed that headache predicted the clinical evolution of COVID-19. The symptomatic phase of COVID-19 was 7 days shorter for patients with headache than for those without headache. In addition, the period of hospitalization was 7 days shorter for patients with headache and anosmia, compared with patients who had neither headache nor anosmia.
Most therapies, including ibuprofen, candesartan, and anti–calcitonin gene–related peptide (CGRP) monoclonal antibodies, are safe for treating headache in COVID-19, the investigators noted. “We should just try to initially avoid steroids to avoid interference with the body’s reaction to SARS-CoV-2,” Dr. Pozo-Rosich said.
Researchers at Sidney Kimmel Medical College, Philadelphia, are currently studying intranasal vazegepant, an anti-CGRP therapy, as a way to potentially blunt the severe inflammatory response in the lungs of patients with COVID-19, she noted, adding that this peptide may have a future role not only in headache, but also in COVID-19.
Historical link to viral infections
Commenting on the study, Matthew S. Robbins, MD, associate professor of neurology at Weill Cornell Medicine, New York, said the findings associating headache with a shorter symptomatic phase of COVID-19 were “interesting.”
“Headache is common with mild viral infections. More severe viral infections may simply feature more overwhelming respiratory symptoms and fever that lead to underreporting or underascertainment of headache,” said Dr. Robbins, who was not involved with the research.
He noted that the finding showing an association of headache and COVID-19 with a younger age and in women “may be related to a higher prevalence of migraine biology in such patients, and being triggered by the virus or the psychological stress associated with it.”
Dr. Robbins added that viral illnesses have long been associated with new daily persistent headache, “dating back to the early 1980s,” when it was first described in association with Epstein-Barr virus. These infections have also been implicated in the progression of migraine to chronic migraine in adolescents.
“In my view, treatment should be aimed at the symptomatic headache type for which new daily persistent headache resembles, regardless of the potential inciting factor,” Dr. Robbins said.
Dr. Pozo-Rosich has received consulting fees from Allergan, Amgen, Almirall, Biohaven, Chiesi, Eli Lilly, Medscape, Novartis, and Teva Pharmaceuticals. Dr. Robbins has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19 and could resemble tension-type or migraine headache.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period. In a subgroup of participants, headache persisted even after the symptoms of COVID-19 had been resolved.
Investigators noted that understanding the pathophysiology of headache in COVID-19 could improve understanding of migraine and other headache disorders. “It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection by SARS-CoV-2,” lead investigator Patricia Pozo-Rosich, MD, PhD, head of the headache and craniofacial pain unit at Vall d’Hebron University Hospital, Barcelona, said in an interview.
She presented the findings at the virtual annual meeting of the American Headache Society.
Systemic inflammation
Headache is one of the main symptoms of COVID-19. A recent study of 214 patients with COVID-19 showed that approximately 13% of the participants had headache and 5% had anosmia.
SARS-CoV-2 penetrates the cells through the ACE2 receptor, which is present throughout the body. “SARS-CoV-2 enters the body through the nasal cavity and it probably penetrates the nervous system in the periphery through afferent branches of the olfactory and trigeminal nerve,” Dr. Pozo-Rosich said. It travels to the lungs and, later, the bloodstream. This generates systemic inflammation that may turn into a cytokine storm. Evidence has identified cortical hyperintensities and olfactory bulb hyperintensities in patients with COVID-19, suggesting that the virus directly infects the CNS.
Interleukin-6, one of the main inflammatory molecules, has been proven to be related to COVID-19 and has become a therapeutic target. Levels of IL-6 may be lower and tend to be more stable in patients with both COVID-19 and headache than in patients with COVID-19 only.
The researchers observed 130 patients (51% women; mean age, 54 years) with COVID-19 who were attended by neurologists at Vall d’Hebron. In this group, 74.4% had headache. Patients with headache tended to be younger than those without headache (mean age, 50 years vs. 63 years, respectively) and tended to be women (58.6% vs. 29.4%).
Approximately one-third of patients with headache had a history of migraine. Most reported mild to moderate pain that resembled tension-type headache. In participants with severe pain and migraine-like features, headache more often began during the asymptomatic phase of COVID-19.
Disease evolution predictor?
The investigators followed up on 100 of the 130 patients with COVID-19, of whom 74 had headache. About 38% of these patients had ongoing headache after 6 weeks, which suggests that some patients may develop a new daily persistent headache once a 3-month period has elapsed. Half of this group had no previous headache history. Headache had been the prodromal symptom of COVID-19 for 21.4% of these patients.
Results showed that headache predicted the clinical evolution of COVID-19. The symptomatic phase of COVID-19 was 7 days shorter for patients with headache than for those without headache. In addition, the period of hospitalization was 7 days shorter for patients with headache and anosmia, compared with patients who had neither headache nor anosmia.
Most therapies, including ibuprofen, candesartan, and anti–calcitonin gene–related peptide (CGRP) monoclonal antibodies, are safe for treating headache in COVID-19, the investigators noted. “We should just try to initially avoid steroids to avoid interference with the body’s reaction to SARS-CoV-2,” Dr. Pozo-Rosich said.
Researchers at Sidney Kimmel Medical College, Philadelphia, are currently studying intranasal vazegepant, an anti-CGRP therapy, as a way to potentially blunt the severe inflammatory response in the lungs of patients with COVID-19, she noted, adding that this peptide may have a future role not only in headache, but also in COVID-19.
Historical link to viral infections
Commenting on the study, Matthew S. Robbins, MD, associate professor of neurology at Weill Cornell Medicine, New York, said the findings associating headache with a shorter symptomatic phase of COVID-19 were “interesting.”
“Headache is common with mild viral infections. More severe viral infections may simply feature more overwhelming respiratory symptoms and fever that lead to underreporting or underascertainment of headache,” said Dr. Robbins, who was not involved with the research.
He noted that the finding showing an association of headache and COVID-19 with a younger age and in women “may be related to a higher prevalence of migraine biology in such patients, and being triggered by the virus or the psychological stress associated with it.”
Dr. Robbins added that viral illnesses have long been associated with new daily persistent headache, “dating back to the early 1980s,” when it was first described in association with Epstein-Barr virus. These infections have also been implicated in the progression of migraine to chronic migraine in adolescents.
“In my view, treatment should be aimed at the symptomatic headache type for which new daily persistent headache resembles, regardless of the potential inciting factor,” Dr. Robbins said.
Dr. Pozo-Rosich has received consulting fees from Allergan, Amgen, Almirall, Biohaven, Chiesi, Eli Lilly, Medscape, Novartis, and Teva Pharmaceuticals. Dr. Robbins has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM AHS 2020
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
Corresponding author Marie E. McDonnell, MD, director of the diabetes program at Brigham and Women’s Hospital, Boston, Massachusetts, discussed the recommendations with Medscape Medical News and also spoke about the news this week that the corticosteroid dexamethasone reduced death rates in severely ill patients with COVID-19.
The full JCEM article, by lead author Nadine E. Palermo, DO, Division of Endocrinology, Diabetes, and Hypertension, also at Brigham and Women’s Hospital, covers DKA diagnosis and triage, and emphasizes that usual hospital protocols for DKA management may need to be adjusted during COVID-19 to help preserve personal protective equipment and ICU beds.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” McDonnell said in an Endocrine Society statement.
What about dexamethasone for severe COVID-19 in diabetes?
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors.
But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
McDonnell told Medscape Medical News that she would need to see formal results to better understand exactly which patients were studied and which ones benefited.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” she said. “If they all had acute respiratory distress syndrome [ARDS],” that’s different.
“There are already some data supporting steroid use in ARDS,” she noted, but added that not all of it suggests benefit.
She pointed to one of several studies now showing that diabetes, and hyperglycemia among people without a prior diabetes diagnosis, are both strong predictors of mortality in hospitalized patients with COVID-19.
“There was a very clear relationship between hyperglycemia and outcomes. We really shouldn’t put people at risk until we have clear data,” she said.
If, once the data are reviewed and appropriate dexamethasone becomes an established treatment for severe COVID-19, hyperglycemia would be a concern among all patients, not just those with previously diagnosed diabetes, she noted.
“We know a good number of people with prediabetes develop hyperglycemia when put on steroids. They can push people over the edge. We’re not going to miss anybody, but treating steroid-induced hyperglycemia is really hard,” McDonnell explained.
She also recommended 2014 guidance from Diabetes UK and the Association of British Clinical Diabetologists, which addresses management of inpatient steroid-induced DKA in patients with and without pre-existing diabetes.
Another major concern, she said, is “patients trying to get dexamethasone when they start to get sick” because this is not the right population to use this agent.
“We worry about people who do not need this drug. If they have diabetes, they put themselves at risk of hyperglycemia, which then increases the risk of severe COVID-19. And then they’re also putting themselves at risk of DKA. It would just be bad medicine,” she said.
Managing DKA in the face of COVID-19: Flexibility is key
In the JCEM article, Palermo and colleagues emphasize that the usual hospital protocols for DKA management may need to be adjusted during COVID-19 in the interest of reducing transmission risk and preserving scare resources.
They provide evidence for alternative treatment strategies, such as the use of subcutaneous rather than intravenous insulin when appropriate.
“We wanted to outline when exactly you should consider nonintensive management strategies for DKA,” McDonnell further explained to Medscape Medical News.
“That would include those with mild or some with moderate DKA. ... The idea is to remind our colleagues about that because hospitals tend to operate on a protocol-driven algorithmic methodology, they can forget to step off the usual care pathway even if evidence supports that,” she said.
But on the other hand, she also said that, in some very complex or severely ill patients with COVID-19, classical intravenous insulin therapy makes the most sense even if their DKA is mild.
The outpatient setting: Prevention and preparation
The new article also addresses several concerns regarding DKA prevention in the outpatient setting.
As with other guidelines, it includes a reminder that patients with diabetes should be advised to discontinue sodium-glucose cotransporter 2 (SGLT2) inhibitors if they become ill with COVID-19, especially if they’re not eating or drinking normally, because they raise the risk for DKA.
Also, for patients with type 1 diabetes, particularly those with a history of repeated DKA, “this is the time to make sure we reach out to patients to refill their insulin prescriptions and address issues related to cost and other access difficulties,” McDonnell said.
The authors also emphasize that insulin starts and education should not be postponed during the pandemic. “Patients identified as meeting criteria to start insulin should be referred for urgent education, either in person or, whenever possible and practical, via video teleconferencing,” they urge.
McDonnell has reported receiving research funding from Novo Nordisk. The other two authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
Corresponding author Marie E. McDonnell, MD, director of the diabetes program at Brigham and Women’s Hospital, Boston, Massachusetts, discussed the recommendations with Medscape Medical News and also spoke about the news this week that the corticosteroid dexamethasone reduced death rates in severely ill patients with COVID-19.
The full JCEM article, by lead author Nadine E. Palermo, DO, Division of Endocrinology, Diabetes, and Hypertension, also at Brigham and Women’s Hospital, covers DKA diagnosis and triage, and emphasizes that usual hospital protocols for DKA management may need to be adjusted during COVID-19 to help preserve personal protective equipment and ICU beds.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” McDonnell said in an Endocrine Society statement.
What about dexamethasone for severe COVID-19 in diabetes?
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors.
But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
McDonnell told Medscape Medical News that she would need to see formal results to better understand exactly which patients were studied and which ones benefited.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” she said. “If they all had acute respiratory distress syndrome [ARDS],” that’s different.
“There are already some data supporting steroid use in ARDS,” she noted, but added that not all of it suggests benefit.
She pointed to one of several studies now showing that diabetes, and hyperglycemia among people without a prior diabetes diagnosis, are both strong predictors of mortality in hospitalized patients with COVID-19.
“There was a very clear relationship between hyperglycemia and outcomes. We really shouldn’t put people at risk until we have clear data,” she said.
If, once the data are reviewed and appropriate dexamethasone becomes an established treatment for severe COVID-19, hyperglycemia would be a concern among all patients, not just those with previously diagnosed diabetes, she noted.
“We know a good number of people with prediabetes develop hyperglycemia when put on steroids. They can push people over the edge. We’re not going to miss anybody, but treating steroid-induced hyperglycemia is really hard,” McDonnell explained.
She also recommended 2014 guidance from Diabetes UK and the Association of British Clinical Diabetologists, which addresses management of inpatient steroid-induced DKA in patients with and without pre-existing diabetes.
Another major concern, she said, is “patients trying to get dexamethasone when they start to get sick” because this is not the right population to use this agent.
“We worry about people who do not need this drug. If they have diabetes, they put themselves at risk of hyperglycemia, which then increases the risk of severe COVID-19. And then they’re also putting themselves at risk of DKA. It would just be bad medicine,” she said.
Managing DKA in the face of COVID-19: Flexibility is key
In the JCEM article, Palermo and colleagues emphasize that the usual hospital protocols for DKA management may need to be adjusted during COVID-19 in the interest of reducing transmission risk and preserving scare resources.
They provide evidence for alternative treatment strategies, such as the use of subcutaneous rather than intravenous insulin when appropriate.
“We wanted to outline when exactly you should consider nonintensive management strategies for DKA,” McDonnell further explained to Medscape Medical News.
“That would include those with mild or some with moderate DKA. ... The idea is to remind our colleagues about that because hospitals tend to operate on a protocol-driven algorithmic methodology, they can forget to step off the usual care pathway even if evidence supports that,” she said.
But on the other hand, she also said that, in some very complex or severely ill patients with COVID-19, classical intravenous insulin therapy makes the most sense even if their DKA is mild.
The outpatient setting: Prevention and preparation
The new article also addresses several concerns regarding DKA prevention in the outpatient setting.
As with other guidelines, it includes a reminder that patients with diabetes should be advised to discontinue sodium-glucose cotransporter 2 (SGLT2) inhibitors if they become ill with COVID-19, especially if they’re not eating or drinking normally, because they raise the risk for DKA.
Also, for patients with type 1 diabetes, particularly those with a history of repeated DKA, “this is the time to make sure we reach out to patients to refill their insulin prescriptions and address issues related to cost and other access difficulties,” McDonnell said.
The authors also emphasize that insulin starts and education should not be postponed during the pandemic. “Patients identified as meeting criteria to start insulin should be referred for urgent education, either in person or, whenever possible and practical, via video teleconferencing,” they urge.
McDonnell has reported receiving research funding from Novo Nordisk. The other two authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
Corresponding author Marie E. McDonnell, MD, director of the diabetes program at Brigham and Women’s Hospital, Boston, Massachusetts, discussed the recommendations with Medscape Medical News and also spoke about the news this week that the corticosteroid dexamethasone reduced death rates in severely ill patients with COVID-19.
The full JCEM article, by lead author Nadine E. Palermo, DO, Division of Endocrinology, Diabetes, and Hypertension, also at Brigham and Women’s Hospital, covers DKA diagnosis and triage, and emphasizes that usual hospital protocols for DKA management may need to be adjusted during COVID-19 to help preserve personal protective equipment and ICU beds.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” McDonnell said in an Endocrine Society statement.
What about dexamethasone for severe COVID-19 in diabetes?
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors.
But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
McDonnell told Medscape Medical News that she would need to see formal results to better understand exactly which patients were studied and which ones benefited.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” she said. “If they all had acute respiratory distress syndrome [ARDS],” that’s different.
“There are already some data supporting steroid use in ARDS,” she noted, but added that not all of it suggests benefit.
She pointed to one of several studies now showing that diabetes, and hyperglycemia among people without a prior diabetes diagnosis, are both strong predictors of mortality in hospitalized patients with COVID-19.
“There was a very clear relationship between hyperglycemia and outcomes. We really shouldn’t put people at risk until we have clear data,” she said.
If, once the data are reviewed and appropriate dexamethasone becomes an established treatment for severe COVID-19, hyperglycemia would be a concern among all patients, not just those with previously diagnosed diabetes, she noted.
“We know a good number of people with prediabetes develop hyperglycemia when put on steroids. They can push people over the edge. We’re not going to miss anybody, but treating steroid-induced hyperglycemia is really hard,” McDonnell explained.
She also recommended 2014 guidance from Diabetes UK and the Association of British Clinical Diabetologists, which addresses management of inpatient steroid-induced DKA in patients with and without pre-existing diabetes.
Another major concern, she said, is “patients trying to get dexamethasone when they start to get sick” because this is not the right population to use this agent.
“We worry about people who do not need this drug. If they have diabetes, they put themselves at risk of hyperglycemia, which then increases the risk of severe COVID-19. And then they’re also putting themselves at risk of DKA. It would just be bad medicine,” she said.
Managing DKA in the face of COVID-19: Flexibility is key
In the JCEM article, Palermo and colleagues emphasize that the usual hospital protocols for DKA management may need to be adjusted during COVID-19 in the interest of reducing transmission risk and preserving scare resources.
They provide evidence for alternative treatment strategies, such as the use of subcutaneous rather than intravenous insulin when appropriate.
“We wanted to outline when exactly you should consider nonintensive management strategies for DKA,” McDonnell further explained to Medscape Medical News.
“That would include those with mild or some with moderate DKA. ... The idea is to remind our colleagues about that because hospitals tend to operate on a protocol-driven algorithmic methodology, they can forget to step off the usual care pathway even if evidence supports that,” she said.
But on the other hand, she also said that, in some very complex or severely ill patients with COVID-19, classical intravenous insulin therapy makes the most sense even if their DKA is mild.
The outpatient setting: Prevention and preparation
The new article also addresses several concerns regarding DKA prevention in the outpatient setting.
As with other guidelines, it includes a reminder that patients with diabetes should be advised to discontinue sodium-glucose cotransporter 2 (SGLT2) inhibitors if they become ill with COVID-19, especially if they’re not eating or drinking normally, because they raise the risk for DKA.
Also, for patients with type 1 diabetes, particularly those with a history of repeated DKA, “this is the time to make sure we reach out to patients to refill their insulin prescriptions and address issues related to cost and other access difficulties,” McDonnell said.
The authors also emphasize that insulin starts and education should not be postponed during the pandemic. “Patients identified as meeting criteria to start insulin should be referred for urgent education, either in person or, whenever possible and practical, via video teleconferencing,” they urge.
McDonnell has reported receiving research funding from Novo Nordisk. The other two authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Daily Recap: From hospitalist to ‘COVIDist’; Systolic BP -- How low should you go?
Here are the stories our MDedge editors across specialties think you need to know about today:
A ‘Fraternity of People Who Are Struggling’
Kathleen Ronan spent a week in a New Jersey hospital, including 5 days in the ICU, battling the novel coronavirus.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, 51, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article. “It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, researchers have documented what they call post–intensive care syndrome (PICS) — a constellation of physical, cognitive, and psychiatric symptoms that result from an ICU stay. Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her. Read more.
The evolution of ‘COVIDists’
At the start of the pandemic earlier this year hospitalists at Baystate Health in Western Massachusetts realized the necessity of a new model of care for COVID-19 patients. Challenges included a massive surge of COVID-19 patients, a limited supply of PPE, an inadequate number of intensivists for managing the anticipated ventilated patients, and the potential of losing some of our workforce if they became infected. Hospitalists there came up with an elaborate plan to manage the disease burden and the strain on resources effectively.
A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them. The group underwent rapid training in various treatment protocols and ongoing clinical trials.
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. Read more.
How low should you go?
Cardiovascular risk continues to reduce as systolic blood pressure decreases right down to levels as low as 90 mm Hg, according to a new study.
Researchers analyzed data from a cohort of 1,457 participants (mean age, 58 years) who did not have any traditional cardiovascular risk factors and had a systolic blood pressure level between 90 and 129 mm Hg at baseline. Results showed that, during a mean follow-up of 14.5 years, there was an increase in traditional cardiovascular risk factors, coronary artery calcium, and incident cardiovascular events with increasing systolic blood pressure levels.
“We modeled systolic blood pressure on a continuous scale and saw the risk increasing in a linear fashion as blood pressure increased and this occurred right down to 90 mm Hg. We didn’t see any nadir or J-point where there may be an increased risk at lower pressures,” said lead author Seamus Whelton, MD, assistant professor of medicine at the division of cardiology at Johns Hopkins Medicine, Baltimore.
“From an individual level we can now say that in healthy individuals, a systolic pressure in the 90s is not too low. It is a positive thing. And it is recommended to try and keep systolic pressure at these levels if possible by maintaining a healthy lifestyle,” Dr. Whelton said in an interview. Read more.
Asthma tops spending on avoidable pediatric inpatient stays
Asthma costs nearly equaled potentially avoidable hospital bills for diabetes, gastroenteritis, and UTIs combined in a study of in-patient stays among children aged 3 months to 17 years.
Indeed, hospital charges for the treatment of children with asthma made up nearly half of all potentially avoidable pediatric inpatient costs in 2017, according to the Agency for Healthcare Research and Quality.
The cost of potentially avoidable visits for asthma that year was $278 million, versus $284 million combined for the other three conditions, Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, reported in an AHRQ statistical brief.
The state inpatient databases of the AHRQ’s Healthcare Cost and Utilization Project included 1.4 million inpatient stays among children aged 3 months to 17 years in 2017, of which 8% (108,300) were deemed potentially preventable.
Rates of potentially avoidable stays for asthma (159 per 100,000 population), gastroenteritis (90 per 100,000), and UTIs (41 per 100,000) were highest for children aged 0-4 years and generally decreased with age, but diabetes stays increased with age, rising from 12 per 100,000 in children aged 5-9 years to 38 per 100,000 for those 15-17 years old, the researchers said. Read more.
Adding monoclonal antibodies to Botox for migraine prevention
Adjunctive preventive therapy with a calcitonin gene–related peptide monoclonal antibody (CGRP-mAb) medication is safe and effective in patients with chronic migraine who have only achieved a partial response to onabotulinumtoxinA (Botox) treatment.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed. Three CGRP-mAbs have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. Patients treated with Botox had been excluded from these earlier trials, however. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
A ‘Fraternity of People Who Are Struggling’
Kathleen Ronan spent a week in a New Jersey hospital, including 5 days in the ICU, battling the novel coronavirus.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, 51, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article. “It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, researchers have documented what they call post–intensive care syndrome (PICS) — a constellation of physical, cognitive, and psychiatric symptoms that result from an ICU stay. Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her. Read more.
The evolution of ‘COVIDists’
At the start of the pandemic earlier this year hospitalists at Baystate Health in Western Massachusetts realized the necessity of a new model of care for COVID-19 patients. Challenges included a massive surge of COVID-19 patients, a limited supply of PPE, an inadequate number of intensivists for managing the anticipated ventilated patients, and the potential of losing some of our workforce if they became infected. Hospitalists there came up with an elaborate plan to manage the disease burden and the strain on resources effectively.
A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them. The group underwent rapid training in various treatment protocols and ongoing clinical trials.
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. Read more.
How low should you go?
Cardiovascular risk continues to reduce as systolic blood pressure decreases right down to levels as low as 90 mm Hg, according to a new study.
Researchers analyzed data from a cohort of 1,457 participants (mean age, 58 years) who did not have any traditional cardiovascular risk factors and had a systolic blood pressure level between 90 and 129 mm Hg at baseline. Results showed that, during a mean follow-up of 14.5 years, there was an increase in traditional cardiovascular risk factors, coronary artery calcium, and incident cardiovascular events with increasing systolic blood pressure levels.
“We modeled systolic blood pressure on a continuous scale and saw the risk increasing in a linear fashion as blood pressure increased and this occurred right down to 90 mm Hg. We didn’t see any nadir or J-point where there may be an increased risk at lower pressures,” said lead author Seamus Whelton, MD, assistant professor of medicine at the division of cardiology at Johns Hopkins Medicine, Baltimore.
“From an individual level we can now say that in healthy individuals, a systolic pressure in the 90s is not too low. It is a positive thing. And it is recommended to try and keep systolic pressure at these levels if possible by maintaining a healthy lifestyle,” Dr. Whelton said in an interview. Read more.
Asthma tops spending on avoidable pediatric inpatient stays
Asthma costs nearly equaled potentially avoidable hospital bills for diabetes, gastroenteritis, and UTIs combined in a study of in-patient stays among children aged 3 months to 17 years.
Indeed, hospital charges for the treatment of children with asthma made up nearly half of all potentially avoidable pediatric inpatient costs in 2017, according to the Agency for Healthcare Research and Quality.
The cost of potentially avoidable visits for asthma that year was $278 million, versus $284 million combined for the other three conditions, Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, reported in an AHRQ statistical brief.
The state inpatient databases of the AHRQ’s Healthcare Cost and Utilization Project included 1.4 million inpatient stays among children aged 3 months to 17 years in 2017, of which 8% (108,300) were deemed potentially preventable.
Rates of potentially avoidable stays for asthma (159 per 100,000 population), gastroenteritis (90 per 100,000), and UTIs (41 per 100,000) were highest for children aged 0-4 years and generally decreased with age, but diabetes stays increased with age, rising from 12 per 100,000 in children aged 5-9 years to 38 per 100,000 for those 15-17 years old, the researchers said. Read more.
Adding monoclonal antibodies to Botox for migraine prevention
Adjunctive preventive therapy with a calcitonin gene–related peptide monoclonal antibody (CGRP-mAb) medication is safe and effective in patients with chronic migraine who have only achieved a partial response to onabotulinumtoxinA (Botox) treatment.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed. Three CGRP-mAbs have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. Patients treated with Botox had been excluded from these earlier trials, however. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
A ‘Fraternity of People Who Are Struggling’
Kathleen Ronan spent a week in a New Jersey hospital, including 5 days in the ICU, battling the novel coronavirus.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, 51, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article. “It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, researchers have documented what they call post–intensive care syndrome (PICS) — a constellation of physical, cognitive, and psychiatric symptoms that result from an ICU stay. Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her. Read more.
The evolution of ‘COVIDists’
At the start of the pandemic earlier this year hospitalists at Baystate Health in Western Massachusetts realized the necessity of a new model of care for COVID-19 patients. Challenges included a massive surge of COVID-19 patients, a limited supply of PPE, an inadequate number of intensivists for managing the anticipated ventilated patients, and the potential of losing some of our workforce if they became infected. Hospitalists there came up with an elaborate plan to manage the disease burden and the strain on resources effectively.
A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them. The group underwent rapid training in various treatment protocols and ongoing clinical trials.
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. Read more.
How low should you go?
Cardiovascular risk continues to reduce as systolic blood pressure decreases right down to levels as low as 90 mm Hg, according to a new study.
Researchers analyzed data from a cohort of 1,457 participants (mean age, 58 years) who did not have any traditional cardiovascular risk factors and had a systolic blood pressure level between 90 and 129 mm Hg at baseline. Results showed that, during a mean follow-up of 14.5 years, there was an increase in traditional cardiovascular risk factors, coronary artery calcium, and incident cardiovascular events with increasing systolic blood pressure levels.
“We modeled systolic blood pressure on a continuous scale and saw the risk increasing in a linear fashion as blood pressure increased and this occurred right down to 90 mm Hg. We didn’t see any nadir or J-point where there may be an increased risk at lower pressures,” said lead author Seamus Whelton, MD, assistant professor of medicine at the division of cardiology at Johns Hopkins Medicine, Baltimore.
“From an individual level we can now say that in healthy individuals, a systolic pressure in the 90s is not too low. It is a positive thing. And it is recommended to try and keep systolic pressure at these levels if possible by maintaining a healthy lifestyle,” Dr. Whelton said in an interview. Read more.
Asthma tops spending on avoidable pediatric inpatient stays
Asthma costs nearly equaled potentially avoidable hospital bills for diabetes, gastroenteritis, and UTIs combined in a study of in-patient stays among children aged 3 months to 17 years.
Indeed, hospital charges for the treatment of children with asthma made up nearly half of all potentially avoidable pediatric inpatient costs in 2017, according to the Agency for Healthcare Research and Quality.
The cost of potentially avoidable visits for asthma that year was $278 million, versus $284 million combined for the other three conditions, Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, reported in an AHRQ statistical brief.
The state inpatient databases of the AHRQ’s Healthcare Cost and Utilization Project included 1.4 million inpatient stays among children aged 3 months to 17 years in 2017, of which 8% (108,300) were deemed potentially preventable.
Rates of potentially avoidable stays for asthma (159 per 100,000 population), gastroenteritis (90 per 100,000), and UTIs (41 per 100,000) were highest for children aged 0-4 years and generally decreased with age, but diabetes stays increased with age, rising from 12 per 100,000 in children aged 5-9 years to 38 per 100,000 for those 15-17 years old, the researchers said. Read more.
Adding monoclonal antibodies to Botox for migraine prevention
Adjunctive preventive therapy with a calcitonin gene–related peptide monoclonal antibody (CGRP-mAb) medication is safe and effective in patients with chronic migraine who have only achieved a partial response to onabotulinumtoxinA (Botox) treatment.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed. Three CGRP-mAbs have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. Patients treated with Botox had been excluded from these earlier trials, however. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
After the ICU: A ‘fraternity of people who are struggling’
By the time she was discharged from a suburban New Jersey hospital on April 10, Kathleen Ronan thought the worst was behind her. For a week before her husband rushed her to the emergency department (ED), incoherent and struggling to breathe, the novel coronavirus had ravaged her body. She tried to treat her fevers with acetaminophen and ice packs. Despite taking enough Tylenol to risk liver damage and packing herself on ice like the catch of the day, Ronan’s fever continued to rise. By the time her temperature reached 104.5° F, Ronan knew the time had come for more drastic measures.
A team of masked and gowned nurses greeted her at a triage tent outside the ED, and from there, everything becomes hazy for Ronan. She was immediately rushed to the hospital’s special COVID-19 intensive care unit (ICU), where she spent 5 days. But she has few distinct memories from this time. What she does remember is the exhaustion, the pain, the loneliness, and the fear. Her family couldn’t visit, and though Ronan works as a home health nurse, her brain was so addled with fever that she couldn’t make sense of what was happening. After a week in the hospital, 5 days of which were spent in the ICU, 51-year-old Ronan was discharged.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, who had supplemented long days on her feet caring for others as a nurse with regular trips to the gym, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article.
“It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, . Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
Nor is PICS simply a set of side effects that will go away on their own. It includes ongoing cognitive difficulties and physical weakness, both of which can lead to employment problems. Beyond that, depression and anxiety can exacerbate – and be exacerbated by – these challenges. Psychologist Jim Jackson, PsyD, assistant director of the ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tennessee, recently spoke with a former ICU patient who has struggled since her discharge 30 years ago.
“Her life essentially stopped with her critical care stay. She hasn’t been able to move forward,” he said. “She’s part of a whole fraternity of people who are struggling.”
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her.
Surviving the ICU
Although the new coronavirus has pushed the world’s critical care system to its limits, it was an outbreak in 1952 that inspired the creation of intensive care units. That summer, a wave of paralytic polio swept over Copenhagen, Denmark, and anesthesiologist Bjørn Ibsen, MD, PhD, used mechanical ventilation — physically operated by medical and dental students – to help 316 children breathe for weeks at a time while their small bodies worked to fight off the virus. The effort halved the mortality rate from polio that affected breathing, from 80% to 40%.
In these wards, dedicated to the very sickest, each patient was assigned his or her own nurse. Over the next decade, hospitals in the United Kingdom and the United States established their own ICUs to treat patients with a variety of conditions. Although it helped improve survival, mortality rates in critical care units remained stubbornly high, owing to the patients’ severe underlying illnesses.
“We thought we were doing a good job if the patient survived, but we had no idea what happened after discharge,” said Carla Sevin, MD, medical director of Vanderbilt’s ICU Recovery Center. Nor did their efforts to find out always bring answers. “We struggled to get people to come in for support — they were debilitated, physically burdened, and weak.”
Through further advances in life support, by the early 2000s, the average mortality rates in American ICUs had dropped to 8% to 19%. As the number of critical care survivors began to climb, clinical researchers noticed that the lives of these patients and their families were profoundly altered by their severe illness.
As Dale Needham, MD, PhD, began his pulmonology and critical care residency in Toronto, Canada, in 2005, a group of physicians there began a 5-year longitudinal study to assess long-term outcomes of patients who developed acute respiratory distress syndrome (ARDS). Although ARDS is an acute condition, the investigators found that patients felt effects for years. Younger patients recovered better than older ones, but none of the patients› physical functioning was equivalent to that of age-matched control persons. Even 5 years later, former ICU patients only reached 76% of expected physical functioning, according to results published in the New England Journal of Medicine. The study was a wake-up call.
At a meeting in Chicago in 2010, Needham, now an intensivist at Johns Hopkins Hospital in Baltimore, Maryland, gathered an interdisciplinary group of colleagues, including patients and caregivers, to clarify the phenomena they were seeing. What emerged from that meeting, published in 2012 in Critical Care Medicine, were the diagnostic criteria for PICS: According to the new definition, PICS is characterized by new or worsening physical and neuropsychiatric deficits that range from forgetfulness and loss of motivation to physical weakness and insomnia.
The issue, Needham says, is that although the trouble starts in the ICU, it only becomes clear once patients leave. “ICU doctors aren’t the ones dealing with this,” Needham said. “We need to build stronger bridges between critical care and other professions.” That’s where PICS comes in, a definition that exists explicitly to alert healthcare providers about the constellation of challenges many of these individuals face as they try to reenter “normal” life.
Defining the problem
As an ICU nurse at the Mayo Clinic in Rochester, Minnesota, Annie Johnson, ACNP-BC, knew lots about helping hospitalized patients, but she says she didn’t know anything about what to do after discharge – at least not until her own mother became a patient.
On the first day of retirement in October 2014, Johnson’s mother flatlined. Quick-thinking paramedics resuscitated her, and after several days in critical care, she was discharged. Since then, her heart has remained healthy. Johnson’s sister, who spent time worrying over her mother at the hospital, also had lingering effects. Both have since struggled, plagued by nightmares, flashbacks, and insomnia.
Johnson initially believed her mom’s and sister’s neuropsychiatric, post-ICU struggles were unique to her family. It was only a year later, at a seminar she was attending, that she first heard the words “post–intensive care syndrome.” Suddenly, Johnson had a name for her family’s experiences, and she began to create support groups and resources to help other families like hers.
“I thought of all the patients I had treated over the years who had been on ventilators for days and days and days. And if this happened to my mom after 48 hours, what must they be going through?” she asked.
Once physicians formally defined PICS, the Society for Critical Care Medicine helped create programs to educate ICU staff, patients, and families about potential post-discharge challenges. Researchers also began to investigate factors affecting post-ICU functioning. Follow-up studies of patients with delirium (ranging from general confusion about time and place to extreme agitation and violence) showed they had striking cognitive deficits. Problems with short-term memory, flexible thinking, and motivation plagued patients for years after their critical illness, similar to the physical deficiencies seen after ARDS. Delirium was one of the strongest risk factors for neuropsychiatric problems.
“Delirium is basically a stress test for the brain,” said Babar Khan, MD, a critical care specialist at Indiana University’s Regenstrief Institute, in Bloomington. But whether delirium accentuates preexisting cognitive difficulties or creates them afresh isn’t yet clear.
Sophia Wang, MD, a geriatric psychiatrist at Indiana University who works with many critical care patients, says patients who had experienced delirium in the ICU showed significant defects in memory and executive functioning long after their hospital stay. She points to a 2015 study that followed 47 ICU patients for a year post discharge. Among those who experienced delirium, brain volumes, as measured by MRI, were smaller at 3 months, something associated with cognitive problems at 1 year. Many struggled at work, and unemployment was common. Depression and posttraumatic stress compounded these difficulties. Among those with acute respiratory distress, ICU patients who are young, female, and unemployed are most likely to suffer from posttraumatic stress disorder after they are discharge.
Critical care medicine may have given these patients a second chance at life, Wang says, but the life they return to often looks nothing like the one they had before their illness.
Prolonged mechanical ventilation and the heavy sedation that often accompanies it are predictors of PICS severity. Some of these links could be explained by the gravity of the illness that landed someone in critical care, but others are more likely to be iatrogenic, says Gerald Weinhouse, MD, a pulmonology and critical care physician and co-director of the Critical Illness Recovery Program at the Brigham and Women’s Hospital in Boston. The involvement of loved ones at the patient’s bedside, however, improved the entire family’s outcome.
When Weinhouse saw those data, he and his colleagues founded a peer support program for ICU survivors. In a study published in 2019 in Critical Care Medicine, they identified six different models for peer support for those with PICS and their families, including both online and in-person approaches. An ongoing challenge for physicians, Weinhouse says, is getting patients to engage with these programs, given that their calendars are crowded with medical appointments and that they suffer from increased physical and mental disability.
Studies such as these led critical care physicians to form the ICU Liberation Collaborative to rethink critical care medicine. At Vanderbilt, Sevin and Jackson headed up one of the world’s first post-ICU clinics, which uses an interdisciplinary team to help patients maximize their functioning. They redesigned their critical care unit in a way that allows families to spend the night and that encourages patient mobility. Both Needham and Weinhouse continue tracking patient outcomes.
Even before the novel coronavirus struck, the United States — and the world — had begun to realize that graduating from the ICU was only the start of what was often an extensive recovery.
The long road back
When COVID-19 patients began flooding intensive care wards around the world, physicians scrambled to meet their complex and desperate acute medical needs. Over the past few months, physicians have focused on keeping these patients alive. “We’ve never seen anything like it ― not even during polio — with the sheer number of patients, all with respiratory distress,” Needham said.
But he and his colleagues know this is only the beginning.
“We’re aware that survivorship issues are coming. There’s going to be a wave of sick people who survived the coronavirus but are going to need more help,” Weinhouse said.
Intensivists have been drawing on PICS research in their fight to help COVID-19 patients. Work from the past few years has shown that although sedation is required during intubation itself, not everyone needs it while on a ventilator. Titrating down sedating medication helps reduce delirium, Wang says. Such medication has been shown to contribute to later cognitive problems. Needham’s studies showing that prolonged bedrest by ICU patients causes muscular atrophy has led him to encourage patients to move as much as possible. With the help of physical therapists, many patients on ventilators can be awake, alert, and moving around the ward.
One of the biggest challenges critical-care coronavirus patients face is prolonged isolation. The constant presence of a familiar face helps orient confused and delirious patients and provides emotional support during a frightening time. But because the immediate need for infection control outweighs these benefits, few hospitals allow visitors, especially for COVID-19 patients.
To address this, some units have been using video technology to allow loved ones to call in. At Johns Hopkins, physicians have also been relying on the expertise of occupational therapists (OTs). Needham says that one OT found that rubbing the hand and back of an agitated, delirious patient helped soothe and calm him better than many medications.
Ronan, who spent 5 days in intensive care, echoes that problem. She says she found the relative lack of human contact to be one of the most challenging parts of being in a bed on a COVID-19 ward. Separated from her husband and daughter, suffering from high fever and severe illness, she lost all track of time.
Her return home was difficult, too. Although her job as a home health nurse had prepared her on some level for the challenges she would face after discharge, Ronan says the hospital provided little practical help.
“Everything is so much harder at home, even little things like going to the bathroom,” she said. “I feel like I’m trying to bail out a sinking ship with a teacup.”
Khan and other physicians, aware of the challenges Ronan and others face once home, aim to create post-ICU clinics specifically for COVID-19 patients. They want to build what Khan calls a “one-stop shop” for all the support patients need to recover. Some of that can be provided via telehealth, which may also help ease the physical burden.
Because there’s so much physicians don’t know about the coronavirus, Johnson says, such clinics are not only a chance to help the sickest COVID-19 patients, they will also help researchers learn more about the virus and improve critical care for other illnesses.
Today, nearly 2 months after discharge, Ronan is back on the job but struggles with a persistent cough — likely due to the lung damage she sustained while ill. She has constant fatigue, as well as ongoing upset stomach from all the medications she took to reduce fever and body aches. When she dons a mask for work, the tangible reminder of her hospital stay sends her into a panic attack. Physically, she’s weaker than before.
Researchers are still trying to understand everything that Ronan and other COVID-19 patients need to move on with their lives after being in the ICU. Mysteries abound, but the ground laid by Sevin, Needham, Weinhouse, and others has provided a solid foundation on which to build.
This article first appeared on Medscape.com.
By the time she was discharged from a suburban New Jersey hospital on April 10, Kathleen Ronan thought the worst was behind her. For a week before her husband rushed her to the emergency department (ED), incoherent and struggling to breathe, the novel coronavirus had ravaged her body. She tried to treat her fevers with acetaminophen and ice packs. Despite taking enough Tylenol to risk liver damage and packing herself on ice like the catch of the day, Ronan’s fever continued to rise. By the time her temperature reached 104.5° F, Ronan knew the time had come for more drastic measures.
A team of masked and gowned nurses greeted her at a triage tent outside the ED, and from there, everything becomes hazy for Ronan. She was immediately rushed to the hospital’s special COVID-19 intensive care unit (ICU), where she spent 5 days. But she has few distinct memories from this time. What she does remember is the exhaustion, the pain, the loneliness, and the fear. Her family couldn’t visit, and though Ronan works as a home health nurse, her brain was so addled with fever that she couldn’t make sense of what was happening. After a week in the hospital, 5 days of which were spent in the ICU, 51-year-old Ronan was discharged.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, who had supplemented long days on her feet caring for others as a nurse with regular trips to the gym, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article.
“It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, . Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
Nor is PICS simply a set of side effects that will go away on their own. It includes ongoing cognitive difficulties and physical weakness, both of which can lead to employment problems. Beyond that, depression and anxiety can exacerbate – and be exacerbated by – these challenges. Psychologist Jim Jackson, PsyD, assistant director of the ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tennessee, recently spoke with a former ICU patient who has struggled since her discharge 30 years ago.
“Her life essentially stopped with her critical care stay. She hasn’t been able to move forward,” he said. “She’s part of a whole fraternity of people who are struggling.”
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her.
Surviving the ICU
Although the new coronavirus has pushed the world’s critical care system to its limits, it was an outbreak in 1952 that inspired the creation of intensive care units. That summer, a wave of paralytic polio swept over Copenhagen, Denmark, and anesthesiologist Bjørn Ibsen, MD, PhD, used mechanical ventilation — physically operated by medical and dental students – to help 316 children breathe for weeks at a time while their small bodies worked to fight off the virus. The effort halved the mortality rate from polio that affected breathing, from 80% to 40%.
In these wards, dedicated to the very sickest, each patient was assigned his or her own nurse. Over the next decade, hospitals in the United Kingdom and the United States established their own ICUs to treat patients with a variety of conditions. Although it helped improve survival, mortality rates in critical care units remained stubbornly high, owing to the patients’ severe underlying illnesses.
“We thought we were doing a good job if the patient survived, but we had no idea what happened after discharge,” said Carla Sevin, MD, medical director of Vanderbilt’s ICU Recovery Center. Nor did their efforts to find out always bring answers. “We struggled to get people to come in for support — they were debilitated, physically burdened, and weak.”
Through further advances in life support, by the early 2000s, the average mortality rates in American ICUs had dropped to 8% to 19%. As the number of critical care survivors began to climb, clinical researchers noticed that the lives of these patients and their families were profoundly altered by their severe illness.
As Dale Needham, MD, PhD, began his pulmonology and critical care residency in Toronto, Canada, in 2005, a group of physicians there began a 5-year longitudinal study to assess long-term outcomes of patients who developed acute respiratory distress syndrome (ARDS). Although ARDS is an acute condition, the investigators found that patients felt effects for years. Younger patients recovered better than older ones, but none of the patients› physical functioning was equivalent to that of age-matched control persons. Even 5 years later, former ICU patients only reached 76% of expected physical functioning, according to results published in the New England Journal of Medicine. The study was a wake-up call.
At a meeting in Chicago in 2010, Needham, now an intensivist at Johns Hopkins Hospital in Baltimore, Maryland, gathered an interdisciplinary group of colleagues, including patients and caregivers, to clarify the phenomena they were seeing. What emerged from that meeting, published in 2012 in Critical Care Medicine, were the diagnostic criteria for PICS: According to the new definition, PICS is characterized by new or worsening physical and neuropsychiatric deficits that range from forgetfulness and loss of motivation to physical weakness and insomnia.
The issue, Needham says, is that although the trouble starts in the ICU, it only becomes clear once patients leave. “ICU doctors aren’t the ones dealing with this,” Needham said. “We need to build stronger bridges between critical care and other professions.” That’s where PICS comes in, a definition that exists explicitly to alert healthcare providers about the constellation of challenges many of these individuals face as they try to reenter “normal” life.
Defining the problem
As an ICU nurse at the Mayo Clinic in Rochester, Minnesota, Annie Johnson, ACNP-BC, knew lots about helping hospitalized patients, but she says she didn’t know anything about what to do after discharge – at least not until her own mother became a patient.
On the first day of retirement in October 2014, Johnson’s mother flatlined. Quick-thinking paramedics resuscitated her, and after several days in critical care, she was discharged. Since then, her heart has remained healthy. Johnson’s sister, who spent time worrying over her mother at the hospital, also had lingering effects. Both have since struggled, plagued by nightmares, flashbacks, and insomnia.
Johnson initially believed her mom’s and sister’s neuropsychiatric, post-ICU struggles were unique to her family. It was only a year later, at a seminar she was attending, that she first heard the words “post–intensive care syndrome.” Suddenly, Johnson had a name for her family’s experiences, and she began to create support groups and resources to help other families like hers.
“I thought of all the patients I had treated over the years who had been on ventilators for days and days and days. And if this happened to my mom after 48 hours, what must they be going through?” she asked.
Once physicians formally defined PICS, the Society for Critical Care Medicine helped create programs to educate ICU staff, patients, and families about potential post-discharge challenges. Researchers also began to investigate factors affecting post-ICU functioning. Follow-up studies of patients with delirium (ranging from general confusion about time and place to extreme agitation and violence) showed they had striking cognitive deficits. Problems with short-term memory, flexible thinking, and motivation plagued patients for years after their critical illness, similar to the physical deficiencies seen after ARDS. Delirium was one of the strongest risk factors for neuropsychiatric problems.
“Delirium is basically a stress test for the brain,” said Babar Khan, MD, a critical care specialist at Indiana University’s Regenstrief Institute, in Bloomington. But whether delirium accentuates preexisting cognitive difficulties or creates them afresh isn’t yet clear.
Sophia Wang, MD, a geriatric psychiatrist at Indiana University who works with many critical care patients, says patients who had experienced delirium in the ICU showed significant defects in memory and executive functioning long after their hospital stay. She points to a 2015 study that followed 47 ICU patients for a year post discharge. Among those who experienced delirium, brain volumes, as measured by MRI, were smaller at 3 months, something associated with cognitive problems at 1 year. Many struggled at work, and unemployment was common. Depression and posttraumatic stress compounded these difficulties. Among those with acute respiratory distress, ICU patients who are young, female, and unemployed are most likely to suffer from posttraumatic stress disorder after they are discharge.
Critical care medicine may have given these patients a second chance at life, Wang says, but the life they return to often looks nothing like the one they had before their illness.
Prolonged mechanical ventilation and the heavy sedation that often accompanies it are predictors of PICS severity. Some of these links could be explained by the gravity of the illness that landed someone in critical care, but others are more likely to be iatrogenic, says Gerald Weinhouse, MD, a pulmonology and critical care physician and co-director of the Critical Illness Recovery Program at the Brigham and Women’s Hospital in Boston. The involvement of loved ones at the patient’s bedside, however, improved the entire family’s outcome.
When Weinhouse saw those data, he and his colleagues founded a peer support program for ICU survivors. In a study published in 2019 in Critical Care Medicine, they identified six different models for peer support for those with PICS and their families, including both online and in-person approaches. An ongoing challenge for physicians, Weinhouse says, is getting patients to engage with these programs, given that their calendars are crowded with medical appointments and that they suffer from increased physical and mental disability.
Studies such as these led critical care physicians to form the ICU Liberation Collaborative to rethink critical care medicine. At Vanderbilt, Sevin and Jackson headed up one of the world’s first post-ICU clinics, which uses an interdisciplinary team to help patients maximize their functioning. They redesigned their critical care unit in a way that allows families to spend the night and that encourages patient mobility. Both Needham and Weinhouse continue tracking patient outcomes.
Even before the novel coronavirus struck, the United States — and the world — had begun to realize that graduating from the ICU was only the start of what was often an extensive recovery.
The long road back
When COVID-19 patients began flooding intensive care wards around the world, physicians scrambled to meet their complex and desperate acute medical needs. Over the past few months, physicians have focused on keeping these patients alive. “We’ve never seen anything like it ― not even during polio — with the sheer number of patients, all with respiratory distress,” Needham said.
But he and his colleagues know this is only the beginning.
“We’re aware that survivorship issues are coming. There’s going to be a wave of sick people who survived the coronavirus but are going to need more help,” Weinhouse said.
Intensivists have been drawing on PICS research in their fight to help COVID-19 patients. Work from the past few years has shown that although sedation is required during intubation itself, not everyone needs it while on a ventilator. Titrating down sedating medication helps reduce delirium, Wang says. Such medication has been shown to contribute to later cognitive problems. Needham’s studies showing that prolonged bedrest by ICU patients causes muscular atrophy has led him to encourage patients to move as much as possible. With the help of physical therapists, many patients on ventilators can be awake, alert, and moving around the ward.
One of the biggest challenges critical-care coronavirus patients face is prolonged isolation. The constant presence of a familiar face helps orient confused and delirious patients and provides emotional support during a frightening time. But because the immediate need for infection control outweighs these benefits, few hospitals allow visitors, especially for COVID-19 patients.
To address this, some units have been using video technology to allow loved ones to call in. At Johns Hopkins, physicians have also been relying on the expertise of occupational therapists (OTs). Needham says that one OT found that rubbing the hand and back of an agitated, delirious patient helped soothe and calm him better than many medications.
Ronan, who spent 5 days in intensive care, echoes that problem. She says she found the relative lack of human contact to be one of the most challenging parts of being in a bed on a COVID-19 ward. Separated from her husband and daughter, suffering from high fever and severe illness, she lost all track of time.
Her return home was difficult, too. Although her job as a home health nurse had prepared her on some level for the challenges she would face after discharge, Ronan says the hospital provided little practical help.
“Everything is so much harder at home, even little things like going to the bathroom,” she said. “I feel like I’m trying to bail out a sinking ship with a teacup.”
Khan and other physicians, aware of the challenges Ronan and others face once home, aim to create post-ICU clinics specifically for COVID-19 patients. They want to build what Khan calls a “one-stop shop” for all the support patients need to recover. Some of that can be provided via telehealth, which may also help ease the physical burden.
Because there’s so much physicians don’t know about the coronavirus, Johnson says, such clinics are not only a chance to help the sickest COVID-19 patients, they will also help researchers learn more about the virus and improve critical care for other illnesses.
Today, nearly 2 months after discharge, Ronan is back on the job but struggles with a persistent cough — likely due to the lung damage she sustained while ill. She has constant fatigue, as well as ongoing upset stomach from all the medications she took to reduce fever and body aches. When she dons a mask for work, the tangible reminder of her hospital stay sends her into a panic attack. Physically, she’s weaker than before.
Researchers are still trying to understand everything that Ronan and other COVID-19 patients need to move on with their lives after being in the ICU. Mysteries abound, but the ground laid by Sevin, Needham, Weinhouse, and others has provided a solid foundation on which to build.
This article first appeared on Medscape.com.
By the time she was discharged from a suburban New Jersey hospital on April 10, Kathleen Ronan thought the worst was behind her. For a week before her husband rushed her to the emergency department (ED), incoherent and struggling to breathe, the novel coronavirus had ravaged her body. She tried to treat her fevers with acetaminophen and ice packs. Despite taking enough Tylenol to risk liver damage and packing herself on ice like the catch of the day, Ronan’s fever continued to rise. By the time her temperature reached 104.5° F, Ronan knew the time had come for more drastic measures.
A team of masked and gowned nurses greeted her at a triage tent outside the ED, and from there, everything becomes hazy for Ronan. She was immediately rushed to the hospital’s special COVID-19 intensive care unit (ICU), where she spent 5 days. But she has few distinct memories from this time. What she does remember is the exhaustion, the pain, the loneliness, and the fear. Her family couldn’t visit, and though Ronan works as a home health nurse, her brain was so addled with fever that she couldn’t make sense of what was happening. After a week in the hospital, 5 days of which were spent in the ICU, 51-year-old Ronan was discharged.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, who had supplemented long days on her feet caring for others as a nurse with regular trips to the gym, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article.
“It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, . Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
Nor is PICS simply a set of side effects that will go away on their own. It includes ongoing cognitive difficulties and physical weakness, both of which can lead to employment problems. Beyond that, depression and anxiety can exacerbate – and be exacerbated by – these challenges. Psychologist Jim Jackson, PsyD, assistant director of the ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tennessee, recently spoke with a former ICU patient who has struggled since her discharge 30 years ago.
“Her life essentially stopped with her critical care stay. She hasn’t been able to move forward,” he said. “She’s part of a whole fraternity of people who are struggling.”
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her.
Surviving the ICU
Although the new coronavirus has pushed the world’s critical care system to its limits, it was an outbreak in 1952 that inspired the creation of intensive care units. That summer, a wave of paralytic polio swept over Copenhagen, Denmark, and anesthesiologist Bjørn Ibsen, MD, PhD, used mechanical ventilation — physically operated by medical and dental students – to help 316 children breathe for weeks at a time while their small bodies worked to fight off the virus. The effort halved the mortality rate from polio that affected breathing, from 80% to 40%.
In these wards, dedicated to the very sickest, each patient was assigned his or her own nurse. Over the next decade, hospitals in the United Kingdom and the United States established their own ICUs to treat patients with a variety of conditions. Although it helped improve survival, mortality rates in critical care units remained stubbornly high, owing to the patients’ severe underlying illnesses.
“We thought we were doing a good job if the patient survived, but we had no idea what happened after discharge,” said Carla Sevin, MD, medical director of Vanderbilt’s ICU Recovery Center. Nor did their efforts to find out always bring answers. “We struggled to get people to come in for support — they were debilitated, physically burdened, and weak.”
Through further advances in life support, by the early 2000s, the average mortality rates in American ICUs had dropped to 8% to 19%. As the number of critical care survivors began to climb, clinical researchers noticed that the lives of these patients and their families were profoundly altered by their severe illness.
As Dale Needham, MD, PhD, began his pulmonology and critical care residency in Toronto, Canada, in 2005, a group of physicians there began a 5-year longitudinal study to assess long-term outcomes of patients who developed acute respiratory distress syndrome (ARDS). Although ARDS is an acute condition, the investigators found that patients felt effects for years. Younger patients recovered better than older ones, but none of the patients› physical functioning was equivalent to that of age-matched control persons. Even 5 years later, former ICU patients only reached 76% of expected physical functioning, according to results published in the New England Journal of Medicine. The study was a wake-up call.
At a meeting in Chicago in 2010, Needham, now an intensivist at Johns Hopkins Hospital in Baltimore, Maryland, gathered an interdisciplinary group of colleagues, including patients and caregivers, to clarify the phenomena they were seeing. What emerged from that meeting, published in 2012 in Critical Care Medicine, were the diagnostic criteria for PICS: According to the new definition, PICS is characterized by new or worsening physical and neuropsychiatric deficits that range from forgetfulness and loss of motivation to physical weakness and insomnia.
The issue, Needham says, is that although the trouble starts in the ICU, it only becomes clear once patients leave. “ICU doctors aren’t the ones dealing with this,” Needham said. “We need to build stronger bridges between critical care and other professions.” That’s where PICS comes in, a definition that exists explicitly to alert healthcare providers about the constellation of challenges many of these individuals face as they try to reenter “normal” life.
Defining the problem
As an ICU nurse at the Mayo Clinic in Rochester, Minnesota, Annie Johnson, ACNP-BC, knew lots about helping hospitalized patients, but she says she didn’t know anything about what to do after discharge – at least not until her own mother became a patient.
On the first day of retirement in October 2014, Johnson’s mother flatlined. Quick-thinking paramedics resuscitated her, and after several days in critical care, she was discharged. Since then, her heart has remained healthy. Johnson’s sister, who spent time worrying over her mother at the hospital, also had lingering effects. Both have since struggled, plagued by nightmares, flashbacks, and insomnia.
Johnson initially believed her mom’s and sister’s neuropsychiatric, post-ICU struggles were unique to her family. It was only a year later, at a seminar she was attending, that she first heard the words “post–intensive care syndrome.” Suddenly, Johnson had a name for her family’s experiences, and she began to create support groups and resources to help other families like hers.
“I thought of all the patients I had treated over the years who had been on ventilators for days and days and days. And if this happened to my mom after 48 hours, what must they be going through?” she asked.
Once physicians formally defined PICS, the Society for Critical Care Medicine helped create programs to educate ICU staff, patients, and families about potential post-discharge challenges. Researchers also began to investigate factors affecting post-ICU functioning. Follow-up studies of patients with delirium (ranging from general confusion about time and place to extreme agitation and violence) showed they had striking cognitive deficits. Problems with short-term memory, flexible thinking, and motivation plagued patients for years after their critical illness, similar to the physical deficiencies seen after ARDS. Delirium was one of the strongest risk factors for neuropsychiatric problems.
“Delirium is basically a stress test for the brain,” said Babar Khan, MD, a critical care specialist at Indiana University’s Regenstrief Institute, in Bloomington. But whether delirium accentuates preexisting cognitive difficulties or creates them afresh isn’t yet clear.
Sophia Wang, MD, a geriatric psychiatrist at Indiana University who works with many critical care patients, says patients who had experienced delirium in the ICU showed significant defects in memory and executive functioning long after their hospital stay. She points to a 2015 study that followed 47 ICU patients for a year post discharge. Among those who experienced delirium, brain volumes, as measured by MRI, were smaller at 3 months, something associated with cognitive problems at 1 year. Many struggled at work, and unemployment was common. Depression and posttraumatic stress compounded these difficulties. Among those with acute respiratory distress, ICU patients who are young, female, and unemployed are most likely to suffer from posttraumatic stress disorder after they are discharge.
Critical care medicine may have given these patients a second chance at life, Wang says, but the life they return to often looks nothing like the one they had before their illness.
Prolonged mechanical ventilation and the heavy sedation that often accompanies it are predictors of PICS severity. Some of these links could be explained by the gravity of the illness that landed someone in critical care, but others are more likely to be iatrogenic, says Gerald Weinhouse, MD, a pulmonology and critical care physician and co-director of the Critical Illness Recovery Program at the Brigham and Women’s Hospital in Boston. The involvement of loved ones at the patient’s bedside, however, improved the entire family’s outcome.
When Weinhouse saw those data, he and his colleagues founded a peer support program for ICU survivors. In a study published in 2019 in Critical Care Medicine, they identified six different models for peer support for those with PICS and their families, including both online and in-person approaches. An ongoing challenge for physicians, Weinhouse says, is getting patients to engage with these programs, given that their calendars are crowded with medical appointments and that they suffer from increased physical and mental disability.
Studies such as these led critical care physicians to form the ICU Liberation Collaborative to rethink critical care medicine. At Vanderbilt, Sevin and Jackson headed up one of the world’s first post-ICU clinics, which uses an interdisciplinary team to help patients maximize their functioning. They redesigned their critical care unit in a way that allows families to spend the night and that encourages patient mobility. Both Needham and Weinhouse continue tracking patient outcomes.
Even before the novel coronavirus struck, the United States — and the world — had begun to realize that graduating from the ICU was only the start of what was often an extensive recovery.
The long road back
When COVID-19 patients began flooding intensive care wards around the world, physicians scrambled to meet their complex and desperate acute medical needs. Over the past few months, physicians have focused on keeping these patients alive. “We’ve never seen anything like it ― not even during polio — with the sheer number of patients, all with respiratory distress,” Needham said.
But he and his colleagues know this is only the beginning.
“We’re aware that survivorship issues are coming. There’s going to be a wave of sick people who survived the coronavirus but are going to need more help,” Weinhouse said.
Intensivists have been drawing on PICS research in their fight to help COVID-19 patients. Work from the past few years has shown that although sedation is required during intubation itself, not everyone needs it while on a ventilator. Titrating down sedating medication helps reduce delirium, Wang says. Such medication has been shown to contribute to later cognitive problems. Needham’s studies showing that prolonged bedrest by ICU patients causes muscular atrophy has led him to encourage patients to move as much as possible. With the help of physical therapists, many patients on ventilators can be awake, alert, and moving around the ward.
One of the biggest challenges critical-care coronavirus patients face is prolonged isolation. The constant presence of a familiar face helps orient confused and delirious patients and provides emotional support during a frightening time. But because the immediate need for infection control outweighs these benefits, few hospitals allow visitors, especially for COVID-19 patients.
To address this, some units have been using video technology to allow loved ones to call in. At Johns Hopkins, physicians have also been relying on the expertise of occupational therapists (OTs). Needham says that one OT found that rubbing the hand and back of an agitated, delirious patient helped soothe and calm him better than many medications.
Ronan, who spent 5 days in intensive care, echoes that problem. She says she found the relative lack of human contact to be one of the most challenging parts of being in a bed on a COVID-19 ward. Separated from her husband and daughter, suffering from high fever and severe illness, she lost all track of time.
Her return home was difficult, too. Although her job as a home health nurse had prepared her on some level for the challenges she would face after discharge, Ronan says the hospital provided little practical help.
“Everything is so much harder at home, even little things like going to the bathroom,” she said. “I feel like I’m trying to bail out a sinking ship with a teacup.”
Khan and other physicians, aware of the challenges Ronan and others face once home, aim to create post-ICU clinics specifically for COVID-19 patients. They want to build what Khan calls a “one-stop shop” for all the support patients need to recover. Some of that can be provided via telehealth, which may also help ease the physical burden.
Because there’s so much physicians don’t know about the coronavirus, Johnson says, such clinics are not only a chance to help the sickest COVID-19 patients, they will also help researchers learn more about the virus and improve critical care for other illnesses.
Today, nearly 2 months after discharge, Ronan is back on the job but struggles with a persistent cough — likely due to the lung damage she sustained while ill. She has constant fatigue, as well as ongoing upset stomach from all the medications she took to reduce fever and body aches. When she dons a mask for work, the tangible reminder of her hospital stay sends her into a panic attack. Physically, she’s weaker than before.
Researchers are still trying to understand everything that Ronan and other COVID-19 patients need to move on with their lives after being in the ICU. Mysteries abound, but the ground laid by Sevin, Needham, Weinhouse, and others has provided a solid foundation on which to build.
This article first appeared on Medscape.com.
CMSC MRI guidelines evolve into international consensus protocol
, with the hope that internationally accepted consensus guidelines will improve lagging conformity with the recommendations.
“We’ve always envisioned the guidelines as being international, but now we have harmony with the groups, so this is truly a global protocol,” Anthony Traboulsee, MD, a professor of neurology and director of the MS clinic and neuromyelitis optica clinic at the University of British Columbia in Vancouver, said in presenting the proposed updates during the virtual meeting of the CMSC.
The updates reflect the input of an international expert panel convened by the CMSC in October 2019, made up of neurologists, radiologists, magnetic resonance technologists, and imaging scientists with expertise in MS. Attendees represented groups including the European-based Magnetic Resonance Imaging in MS (MAGNIMS), North American Imaging in Multiple Sclerosis Cooperative, National MS Society, Multiple Sclerosis Association of America, MRI manufacturers, and commercial image analysis.
Standardizing scans
While the mission was to review and update the current guidelines, an important overriding objective was to boost universal acceptance and improve the utilization of the protocol, which research shows is surprisingly low. According to one poster presented at the meeting, a real-world MRI dataset of 1,233 sessions showed only 8% satisfied criteria for the T1 sequence outlined in the 2018 guidelines, and only 7% satisfied criteria for the T2 sequence. “In a real-world MRI dataset of patients with MS, the conformance to the CMSC brain MRI guidelines was extremely low,” concluded the authors, who were with Icometrix, in Chicago and Belgium.
David Li, MD, also of the University of British Columbia and cochair of the MRI guideline committee, said the nonconformity has important implications. “Nonstandardized scans, with inconsistent slice thickness and gaps, nonstandardized slice acquisition (not in the subcallosal plane), and incomplete brain coverage, all contribute to scans that are difficult to compare,” he said. Those factors, “allow for assessment of new lesions and lesion activity that are invaluable for diagnosis as well as determining the effectiveness of therapy or the need for initiating/changing therapy.”
Dr. Traboulsee said the lack of adherence to guidelines may simply have to do with a mistaken perception of complexity. “Part of the challenge is MRI centers don’t realize how easy it is to implement these guidelines,” he said in presenting the proposed updates.
Dr. Traboulsee noted that the CMSC has been working with manufacturers to try to incorporate the protocol into the scanners “so that it’s just a button to press” for the MRI. “I think that will get us over a major hurdle of adaptation,” Dr. Traboulsee said. “Most radiologists said once they started using it they were really happy with it. They found they were using it beyond MS for other basic neurologic imaging, so just raising awareness and making things more of a one-step process for individuals to use will be helpful,” he said.
Repositioning consistency is key
Among key suggestions that the expert panel proposed for guideline updates include the use of the subcallosal plane for consistent repositioning, which should allow for more accuracy and consistency in the identification of lesions in MS, Dr. Traboulsee said. “A major change reflecting improvements in MRI technology is the ability to acquire high-resolution 3-D images and that’s particularly helpful with fluid attenuation inversion recovery (FLAIR) sequences, which is what we do to identify lesions,” he explained. “The repositioning along the subcallosal line is important because it allows us to easily compare studies over time. It takes very little time but allows us to prepare studies over time much more easily,” he said.
Central vein sign
Another update is the establishment of a new category of optimum plus sequences allowing for the monitoring of brain atrophy and identifying lesions with a central vein sign, which has gained high interest as a marker on 3T MRI of demyelinating plaques in MS. As described in recent research, the central vein sign shows high accuracy in differentiating between MS and non-MS lesions.
“Many people have a few white spots on neuroimaging, but with MRI so much more available around the world, many of them are being misdiagnosed with MS,” Dr. Traboulsee said. “But the central vein sign, using a very simple MRI technique, can identify lesions with a vein in the center that (distinguishes them as) MS lesions.”
Though the process is still several years from routine clinical use, the proposed update would better implement susceptibility weighted imaging, which has traditionally been used for functional MRI.
PML Surveillance
The updates also include recommendations to help in the detection of the rare but potentially serious complication of some disease-modifying therapies of progressive multifocal leukoencephalopathy (PML). “We need a very quick and comprehensive way to monitor patients for PML before symptoms develop,” Dr. Traboulsee said. “The sequences we recommended were based on expert opinion of people who have worked quite a bit with PML in MS, and if one wants to survey for PML it’s only about a 10-minute scan.”
International protocol
Corey Ford, MD, a professor of neurology and director of the MS Specialty Clinic at the University of New Mexico Health Sciences Center in Albuquerque, commented that, with imaging playing such an important role in MS, the lack of adherence to the protocol can be a significant hindrance. “MRI is the most important imaging tool we have in the diagnosing and management of MS, but ... it’s quite amazing how different the sequences that are used can be when imaging centers are asked to image someone with a diagnosis of MS, so it’s a problem,” he said.
Dr. Ford speculated that part of the problem is simply inertia at some imaging centers. “Practices will have been programmed into their protocol for a long time, so when a patient comes in for imaging regarding MS, they may [turn to] their typical sequence,” he said. “There is an inertial barrier to upgrading that sequence, which can involve testing it out on the machine, training the techs to do it that way, and interpreting it for the physician clients who requested the imaging.”
In addition, there is a lack of exposure of MS imaging guidelines in the radiology literature, Dr. Ford added. “Maybe it’s a matter of giving more presentations at meetings that include radiologists, or getting the information out through the manufacturers. I think at the end of the day it could be a combination of all of those things,” he said.
However, the CMSC collaboration could make a big difference, Dr. Ford noted. “This is where the international protocol could be important in terms of making all of this happen,” he said. “What we’re seeing is the confluence of representatives of the U.S. and European centers hash out a consensus, and if it’s international, I think that adds a lot of weight to an eventual implementation on a wider basis.”
“I think the group has done a stellar job, and we should not try to be too focused on adding everyone’s little tweak,” he noted. “If we can get a good baseline foundational imaging sequence that can be implemented worldwide, we would be much better off.”
The CMSC updated imaging guidelines are expected to be published in coming months. The most recent previous updates are available online.
Dr. Traboulsee disclosed relationships with Biogen, Chugai, Roche, Sanofi, and Teva. Dr. Ford and Dr. Li have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, with the hope that internationally accepted consensus guidelines will improve lagging conformity with the recommendations.
“We’ve always envisioned the guidelines as being international, but now we have harmony with the groups, so this is truly a global protocol,” Anthony Traboulsee, MD, a professor of neurology and director of the MS clinic and neuromyelitis optica clinic at the University of British Columbia in Vancouver, said in presenting the proposed updates during the virtual meeting of the CMSC.
The updates reflect the input of an international expert panel convened by the CMSC in October 2019, made up of neurologists, radiologists, magnetic resonance technologists, and imaging scientists with expertise in MS. Attendees represented groups including the European-based Magnetic Resonance Imaging in MS (MAGNIMS), North American Imaging in Multiple Sclerosis Cooperative, National MS Society, Multiple Sclerosis Association of America, MRI manufacturers, and commercial image analysis.
Standardizing scans
While the mission was to review and update the current guidelines, an important overriding objective was to boost universal acceptance and improve the utilization of the protocol, which research shows is surprisingly low. According to one poster presented at the meeting, a real-world MRI dataset of 1,233 sessions showed only 8% satisfied criteria for the T1 sequence outlined in the 2018 guidelines, and only 7% satisfied criteria for the T2 sequence. “In a real-world MRI dataset of patients with MS, the conformance to the CMSC brain MRI guidelines was extremely low,” concluded the authors, who were with Icometrix, in Chicago and Belgium.
David Li, MD, also of the University of British Columbia and cochair of the MRI guideline committee, said the nonconformity has important implications. “Nonstandardized scans, with inconsistent slice thickness and gaps, nonstandardized slice acquisition (not in the subcallosal plane), and incomplete brain coverage, all contribute to scans that are difficult to compare,” he said. Those factors, “allow for assessment of new lesions and lesion activity that are invaluable for diagnosis as well as determining the effectiveness of therapy or the need for initiating/changing therapy.”
Dr. Traboulsee said the lack of adherence to guidelines may simply have to do with a mistaken perception of complexity. “Part of the challenge is MRI centers don’t realize how easy it is to implement these guidelines,” he said in presenting the proposed updates.
Dr. Traboulsee noted that the CMSC has been working with manufacturers to try to incorporate the protocol into the scanners “so that it’s just a button to press” for the MRI. “I think that will get us over a major hurdle of adaptation,” Dr. Traboulsee said. “Most radiologists said once they started using it they were really happy with it. They found they were using it beyond MS for other basic neurologic imaging, so just raising awareness and making things more of a one-step process for individuals to use will be helpful,” he said.
Repositioning consistency is key
Among key suggestions that the expert panel proposed for guideline updates include the use of the subcallosal plane for consistent repositioning, which should allow for more accuracy and consistency in the identification of lesions in MS, Dr. Traboulsee said. “A major change reflecting improvements in MRI technology is the ability to acquire high-resolution 3-D images and that’s particularly helpful with fluid attenuation inversion recovery (FLAIR) sequences, which is what we do to identify lesions,” he explained. “The repositioning along the subcallosal line is important because it allows us to easily compare studies over time. It takes very little time but allows us to prepare studies over time much more easily,” he said.
Central vein sign
Another update is the establishment of a new category of optimum plus sequences allowing for the monitoring of brain atrophy and identifying lesions with a central vein sign, which has gained high interest as a marker on 3T MRI of demyelinating plaques in MS. As described in recent research, the central vein sign shows high accuracy in differentiating between MS and non-MS lesions.
“Many people have a few white spots on neuroimaging, but with MRI so much more available around the world, many of them are being misdiagnosed with MS,” Dr. Traboulsee said. “But the central vein sign, using a very simple MRI technique, can identify lesions with a vein in the center that (distinguishes them as) MS lesions.”
Though the process is still several years from routine clinical use, the proposed update would better implement susceptibility weighted imaging, which has traditionally been used for functional MRI.
PML Surveillance
The updates also include recommendations to help in the detection of the rare but potentially serious complication of some disease-modifying therapies of progressive multifocal leukoencephalopathy (PML). “We need a very quick and comprehensive way to monitor patients for PML before symptoms develop,” Dr. Traboulsee said. “The sequences we recommended were based on expert opinion of people who have worked quite a bit with PML in MS, and if one wants to survey for PML it’s only about a 10-minute scan.”
International protocol
Corey Ford, MD, a professor of neurology and director of the MS Specialty Clinic at the University of New Mexico Health Sciences Center in Albuquerque, commented that, with imaging playing such an important role in MS, the lack of adherence to the protocol can be a significant hindrance. “MRI is the most important imaging tool we have in the diagnosing and management of MS, but ... it’s quite amazing how different the sequences that are used can be when imaging centers are asked to image someone with a diagnosis of MS, so it’s a problem,” he said.
Dr. Ford speculated that part of the problem is simply inertia at some imaging centers. “Practices will have been programmed into their protocol for a long time, so when a patient comes in for imaging regarding MS, they may [turn to] their typical sequence,” he said. “There is an inertial barrier to upgrading that sequence, which can involve testing it out on the machine, training the techs to do it that way, and interpreting it for the physician clients who requested the imaging.”
In addition, there is a lack of exposure of MS imaging guidelines in the radiology literature, Dr. Ford added. “Maybe it’s a matter of giving more presentations at meetings that include radiologists, or getting the information out through the manufacturers. I think at the end of the day it could be a combination of all of those things,” he said.
However, the CMSC collaboration could make a big difference, Dr. Ford noted. “This is where the international protocol could be important in terms of making all of this happen,” he said. “What we’re seeing is the confluence of representatives of the U.S. and European centers hash out a consensus, and if it’s international, I think that adds a lot of weight to an eventual implementation on a wider basis.”
“I think the group has done a stellar job, and we should not try to be too focused on adding everyone’s little tweak,” he noted. “If we can get a good baseline foundational imaging sequence that can be implemented worldwide, we would be much better off.”
The CMSC updated imaging guidelines are expected to be published in coming months. The most recent previous updates are available online.
Dr. Traboulsee disclosed relationships with Biogen, Chugai, Roche, Sanofi, and Teva. Dr. Ford and Dr. Li have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, with the hope that internationally accepted consensus guidelines will improve lagging conformity with the recommendations.
“We’ve always envisioned the guidelines as being international, but now we have harmony with the groups, so this is truly a global protocol,” Anthony Traboulsee, MD, a professor of neurology and director of the MS clinic and neuromyelitis optica clinic at the University of British Columbia in Vancouver, said in presenting the proposed updates during the virtual meeting of the CMSC.
The updates reflect the input of an international expert panel convened by the CMSC in October 2019, made up of neurologists, radiologists, magnetic resonance technologists, and imaging scientists with expertise in MS. Attendees represented groups including the European-based Magnetic Resonance Imaging in MS (MAGNIMS), North American Imaging in Multiple Sclerosis Cooperative, National MS Society, Multiple Sclerosis Association of America, MRI manufacturers, and commercial image analysis.
Standardizing scans
While the mission was to review and update the current guidelines, an important overriding objective was to boost universal acceptance and improve the utilization of the protocol, which research shows is surprisingly low. According to one poster presented at the meeting, a real-world MRI dataset of 1,233 sessions showed only 8% satisfied criteria for the T1 sequence outlined in the 2018 guidelines, and only 7% satisfied criteria for the T2 sequence. “In a real-world MRI dataset of patients with MS, the conformance to the CMSC brain MRI guidelines was extremely low,” concluded the authors, who were with Icometrix, in Chicago and Belgium.
David Li, MD, also of the University of British Columbia and cochair of the MRI guideline committee, said the nonconformity has important implications. “Nonstandardized scans, with inconsistent slice thickness and gaps, nonstandardized slice acquisition (not in the subcallosal plane), and incomplete brain coverage, all contribute to scans that are difficult to compare,” he said. Those factors, “allow for assessment of new lesions and lesion activity that are invaluable for diagnosis as well as determining the effectiveness of therapy or the need for initiating/changing therapy.”
Dr. Traboulsee said the lack of adherence to guidelines may simply have to do with a mistaken perception of complexity. “Part of the challenge is MRI centers don’t realize how easy it is to implement these guidelines,” he said in presenting the proposed updates.
Dr. Traboulsee noted that the CMSC has been working with manufacturers to try to incorporate the protocol into the scanners “so that it’s just a button to press” for the MRI. “I think that will get us over a major hurdle of adaptation,” Dr. Traboulsee said. “Most radiologists said once they started using it they were really happy with it. They found they were using it beyond MS for other basic neurologic imaging, so just raising awareness and making things more of a one-step process for individuals to use will be helpful,” he said.
Repositioning consistency is key
Among key suggestions that the expert panel proposed for guideline updates include the use of the subcallosal plane for consistent repositioning, which should allow for more accuracy and consistency in the identification of lesions in MS, Dr. Traboulsee said. “A major change reflecting improvements in MRI technology is the ability to acquire high-resolution 3-D images and that’s particularly helpful with fluid attenuation inversion recovery (FLAIR) sequences, which is what we do to identify lesions,” he explained. “The repositioning along the subcallosal line is important because it allows us to easily compare studies over time. It takes very little time but allows us to prepare studies over time much more easily,” he said.
Central vein sign
Another update is the establishment of a new category of optimum plus sequences allowing for the monitoring of brain atrophy and identifying lesions with a central vein sign, which has gained high interest as a marker on 3T MRI of demyelinating plaques in MS. As described in recent research, the central vein sign shows high accuracy in differentiating between MS and non-MS lesions.
“Many people have a few white spots on neuroimaging, but with MRI so much more available around the world, many of them are being misdiagnosed with MS,” Dr. Traboulsee said. “But the central vein sign, using a very simple MRI technique, can identify lesions with a vein in the center that (distinguishes them as) MS lesions.”
Though the process is still several years from routine clinical use, the proposed update would better implement susceptibility weighted imaging, which has traditionally been used for functional MRI.
PML Surveillance
The updates also include recommendations to help in the detection of the rare but potentially serious complication of some disease-modifying therapies of progressive multifocal leukoencephalopathy (PML). “We need a very quick and comprehensive way to monitor patients for PML before symptoms develop,” Dr. Traboulsee said. “The sequences we recommended were based on expert opinion of people who have worked quite a bit with PML in MS, and if one wants to survey for PML it’s only about a 10-minute scan.”
International protocol
Corey Ford, MD, a professor of neurology and director of the MS Specialty Clinic at the University of New Mexico Health Sciences Center in Albuquerque, commented that, with imaging playing such an important role in MS, the lack of adherence to the protocol can be a significant hindrance. “MRI is the most important imaging tool we have in the diagnosing and management of MS, but ... it’s quite amazing how different the sequences that are used can be when imaging centers are asked to image someone with a diagnosis of MS, so it’s a problem,” he said.
Dr. Ford speculated that part of the problem is simply inertia at some imaging centers. “Practices will have been programmed into their protocol for a long time, so when a patient comes in for imaging regarding MS, they may [turn to] their typical sequence,” he said. “There is an inertial barrier to upgrading that sequence, which can involve testing it out on the machine, training the techs to do it that way, and interpreting it for the physician clients who requested the imaging.”
In addition, there is a lack of exposure of MS imaging guidelines in the radiology literature, Dr. Ford added. “Maybe it’s a matter of giving more presentations at meetings that include radiologists, or getting the information out through the manufacturers. I think at the end of the day it could be a combination of all of those things,” he said.
However, the CMSC collaboration could make a big difference, Dr. Ford noted. “This is where the international protocol could be important in terms of making all of this happen,” he said. “What we’re seeing is the confluence of representatives of the U.S. and European centers hash out a consensus, and if it’s international, I think that adds a lot of weight to an eventual implementation on a wider basis.”
“I think the group has done a stellar job, and we should not try to be too focused on adding everyone’s little tweak,” he noted. “If we can get a good baseline foundational imaging sequence that can be implemented worldwide, we would be much better off.”
The CMSC updated imaging guidelines are expected to be published in coming months. The most recent previous updates are available online.
Dr. Traboulsee disclosed relationships with Biogen, Chugai, Roche, Sanofi, and Teva. Dr. Ford and Dr. Li have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
From CMSC 2020
Adding CGRP to Botox is safe and effective for migraine prevention
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
“The addition of a CGRP monoclonal antibody provided statistically significantly fewer monthly headache days,” said study investigator Fred Cohen, MD, an internal medicine resident physician at Montefiore Health System, New York. “However, this was a retrospective chart review, which is hindered by elements such as recall bias. Therefore, future prospective studies are warranted for higher quality data.”
The findings were presented at the virtual annual meeting of the American Headache Society.
Fewer headache days
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed.
The CGRP-mAbs fremanezumab, galcanezumab, and erenumab, have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. However, patients treated with Botox were excluded from these trials and to date there are no data on combination treatment with Botox and CGRP-mAbs.
To determine whether adjunctive treatment with CGRP-mAbs augments Botox therapy in chronic migraine the investigators conducted a retrospective chart review of patients receiving Botox and prescribed a CGRP-mAb.
Eligible patients met the International Classification of Headache Disorders, 3rd edition, criteria for chronic migraine; were age 18 years or older; and presented at a single headache center between May 2018 and May 2019. Patients who received another new therapy during the study or those taking CGRP-mAb treatment for less than 2 months were excluded.
The study’s primary outcome was change in the number of reported monthly headache days, and change in pain severity was the secondary outcome.
The final analysis included data on 153 patients. The population’s mean age was 47.1 years, and 139 patients (90.8%) were women. In all, 89 patients (58.0%) received erenumab (35 received 70 mg and 54 received 140 mg), 51 (33.0%) received galcanezumab, and 13 (9.0%) received fremanezumab.
Overall, 114 (74.5%) patients reported a decrease in monthly headache days or pain severity. In the group of 66 patients for whom quantitative data were available, the average number of monthly headache days before Botox treatment was 25.7. After Botox treatment, patients had an average decrease of 10.9 monthly headache days, a 42.4% reduction, so on average study participants continued to have an average of 14.8 monthly headache days.
After treatment with a CGRP-mAb the number decreased by 5.6 additional days (37.8%). Patients receiving combined therapy had an average of 9.1 monthly headache days. The total decrease from baseline was 16.6 fewer monthly headache days, a 64.6% reduction.
The number of headache days per month was reduced to 9.3 for erenumab and galcanezumab and 5.8 for fremanezumab. However, few patients in the study took fremanezumab so this result had less statistical power than the results for the other CGRP-mAbs.
A total of 13 patients (8.5%) reported side effects associated with the CGRP-mAbs, which included constipation, injection-site reaction, and fatigue.
More evidence is needed
Commenting on the findings, Peter McAllister, MD, medical director of the New England Institute for Neurology and Headache in Stamford, Conn., said the study’s main limitation is that it is a retrospective chart review, which yields lower level evidence than a prospective, double-blind, placebo-controlled study. Dr. McAllister, who was not involved in the research, also noted that the sample size was small, particularly with respect to fremanezumab.
“This study, despite its limitations, shows that addition of a monoclonal antibody to onabotulinumtoxinA is safe and well tolerated, and may confer additional reduction in migraine or headache days. The authors correctly state that more evidence via prospective study is warranted,” said Dr. McAllister, who is also chief medical officer of the New England Institute for Clinical Research and was not involved in the investigation.
Dr. Cohen has reported no relevant financial relationships. Dr. McAllister was an investigator in the PREEMPT trial of onabotulinumtoxinA, as well as in all of the phase 3 monoclonal antibody studies.
A version of this article originally appeared on Medscape.com.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
“The addition of a CGRP monoclonal antibody provided statistically significantly fewer monthly headache days,” said study investigator Fred Cohen, MD, an internal medicine resident physician at Montefiore Health System, New York. “However, this was a retrospective chart review, which is hindered by elements such as recall bias. Therefore, future prospective studies are warranted for higher quality data.”
The findings were presented at the virtual annual meeting of the American Headache Society.
Fewer headache days
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed.
The CGRP-mAbs fremanezumab, galcanezumab, and erenumab, have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. However, patients treated with Botox were excluded from these trials and to date there are no data on combination treatment with Botox and CGRP-mAbs.
To determine whether adjunctive treatment with CGRP-mAbs augments Botox therapy in chronic migraine the investigators conducted a retrospective chart review of patients receiving Botox and prescribed a CGRP-mAb.
Eligible patients met the International Classification of Headache Disorders, 3rd edition, criteria for chronic migraine; were age 18 years or older; and presented at a single headache center between May 2018 and May 2019. Patients who received another new therapy during the study or those taking CGRP-mAb treatment for less than 2 months were excluded.
The study’s primary outcome was change in the number of reported monthly headache days, and change in pain severity was the secondary outcome.
The final analysis included data on 153 patients. The population’s mean age was 47.1 years, and 139 patients (90.8%) were women. In all, 89 patients (58.0%) received erenumab (35 received 70 mg and 54 received 140 mg), 51 (33.0%) received galcanezumab, and 13 (9.0%) received fremanezumab.
Overall, 114 (74.5%) patients reported a decrease in monthly headache days or pain severity. In the group of 66 patients for whom quantitative data were available, the average number of monthly headache days before Botox treatment was 25.7. After Botox treatment, patients had an average decrease of 10.9 monthly headache days, a 42.4% reduction, so on average study participants continued to have an average of 14.8 monthly headache days.
After treatment with a CGRP-mAb the number decreased by 5.6 additional days (37.8%). Patients receiving combined therapy had an average of 9.1 monthly headache days. The total decrease from baseline was 16.6 fewer monthly headache days, a 64.6% reduction.
The number of headache days per month was reduced to 9.3 for erenumab and galcanezumab and 5.8 for fremanezumab. However, few patients in the study took fremanezumab so this result had less statistical power than the results for the other CGRP-mAbs.
A total of 13 patients (8.5%) reported side effects associated with the CGRP-mAbs, which included constipation, injection-site reaction, and fatigue.
More evidence is needed
Commenting on the findings, Peter McAllister, MD, medical director of the New England Institute for Neurology and Headache in Stamford, Conn., said the study’s main limitation is that it is a retrospective chart review, which yields lower level evidence than a prospective, double-blind, placebo-controlled study. Dr. McAllister, who was not involved in the research, also noted that the sample size was small, particularly with respect to fremanezumab.
“This study, despite its limitations, shows that addition of a monoclonal antibody to onabotulinumtoxinA is safe and well tolerated, and may confer additional reduction in migraine or headache days. The authors correctly state that more evidence via prospective study is warranted,” said Dr. McAllister, who is also chief medical officer of the New England Institute for Clinical Research and was not involved in the investigation.
Dr. Cohen has reported no relevant financial relationships. Dr. McAllister was an investigator in the PREEMPT trial of onabotulinumtoxinA, as well as in all of the phase 3 monoclonal antibody studies.
A version of this article originally appeared on Medscape.com.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
“The addition of a CGRP monoclonal antibody provided statistically significantly fewer monthly headache days,” said study investigator Fred Cohen, MD, an internal medicine resident physician at Montefiore Health System, New York. “However, this was a retrospective chart review, which is hindered by elements such as recall bias. Therefore, future prospective studies are warranted for higher quality data.”
The findings were presented at the virtual annual meeting of the American Headache Society.
Fewer headache days
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed.
The CGRP-mAbs fremanezumab, galcanezumab, and erenumab, have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. However, patients treated with Botox were excluded from these trials and to date there are no data on combination treatment with Botox and CGRP-mAbs.
To determine whether adjunctive treatment with CGRP-mAbs augments Botox therapy in chronic migraine the investigators conducted a retrospective chart review of patients receiving Botox and prescribed a CGRP-mAb.
Eligible patients met the International Classification of Headache Disorders, 3rd edition, criteria for chronic migraine; were age 18 years or older; and presented at a single headache center between May 2018 and May 2019. Patients who received another new therapy during the study or those taking CGRP-mAb treatment for less than 2 months were excluded.
The study’s primary outcome was change in the number of reported monthly headache days, and change in pain severity was the secondary outcome.
The final analysis included data on 153 patients. The population’s mean age was 47.1 years, and 139 patients (90.8%) were women. In all, 89 patients (58.0%) received erenumab (35 received 70 mg and 54 received 140 mg), 51 (33.0%) received galcanezumab, and 13 (9.0%) received fremanezumab.
Overall, 114 (74.5%) patients reported a decrease in monthly headache days or pain severity. In the group of 66 patients for whom quantitative data were available, the average number of monthly headache days before Botox treatment was 25.7. After Botox treatment, patients had an average decrease of 10.9 monthly headache days, a 42.4% reduction, so on average study participants continued to have an average of 14.8 monthly headache days.
After treatment with a CGRP-mAb the number decreased by 5.6 additional days (37.8%). Patients receiving combined therapy had an average of 9.1 monthly headache days. The total decrease from baseline was 16.6 fewer monthly headache days, a 64.6% reduction.
The number of headache days per month was reduced to 9.3 for erenumab and galcanezumab and 5.8 for fremanezumab. However, few patients in the study took fremanezumab so this result had less statistical power than the results for the other CGRP-mAbs.
A total of 13 patients (8.5%) reported side effects associated with the CGRP-mAbs, which included constipation, injection-site reaction, and fatigue.
More evidence is needed
Commenting on the findings, Peter McAllister, MD, medical director of the New England Institute for Neurology and Headache in Stamford, Conn., said the study’s main limitation is that it is a retrospective chart review, which yields lower level evidence than a prospective, double-blind, placebo-controlled study. Dr. McAllister, who was not involved in the research, also noted that the sample size was small, particularly with respect to fremanezumab.
“This study, despite its limitations, shows that addition of a monoclonal antibody to onabotulinumtoxinA is safe and well tolerated, and may confer additional reduction in migraine or headache days. The authors correctly state that more evidence via prospective study is warranted,” said Dr. McAllister, who is also chief medical officer of the New England Institute for Clinical Research and was not involved in the investigation.
Dr. Cohen has reported no relevant financial relationships. Dr. McAllister was an investigator in the PREEMPT trial of onabotulinumtoxinA, as well as in all of the phase 3 monoclonal antibody studies.
A version of this article originally appeared on Medscape.com.
FROM AHS 2020
Commonalities challenge the threshold of high-frequency episodic and low-frequency chronic migraine
according to an analysis of almost 17,000 patients from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study presented at the virtual annual meeting of the American Headache Society.
“The results showed substantial overlap in levels of burden, anxiety, depression and health utilization, including outpatient, inpatient and emergency department visits, among CaMEO respondents with high-frequency episodic migraine and those with low-frequency chronic migraine,” said Richard B. Lipton, MD, of the Albert Einstein College of Medicine, New York.
The study analyzed data on 16,789 respondents to CaMEO, the longitudinal, web-based study designed to characterize the course of episodic and chronic migraine. The study population consisted of four subgroups based on the number of self-reporting monthly headache days (MHDs):
- Low- and moderate-frequency episodic migraine (LFEM; zero to seven MHDs; n = 13,473).
- High-frequency episodic migraine (HFEM; 8-14 MHDs; n = 1,840).
- Low-frequency chronic migraine (LFCM; 15-23 MHDs; n = 1,035).
- High-frequency chronic migraine (HFCM; 24 or more MHDs; n = 441).
Dr. Lipton pointed out that the International Classification of Headache Disorders, 3rd edition, defines chronic migraine as 15 or more MHDs for 3 months or more with criteria for migraine with or without aura met on 8 days a month or more. It defines episodic migraine as less than 15 MHDs.
The study characterized migraine subgroups by various demographics. “The more frequent headache categories were associated with slightly older age of onset with a higher proportion of BMI [body mass index] in the obese range and overall with lower levels of household income and education,” Dr. Lipton said.
Similar headache characteristics
A comparison of headache characteristics and headache-related disabilities across subgroups revealed a number of commonalities between the HFEM and LFCM subgroups, Dr. Lipton said. Among them were presence of mild to severe allodynia, disability grade, interictal burden, and anxiety and depression scores. For example, 47.3% of the HFEM subgroup and 54.9% of the LFCM subgroup had Patient Health Questionnaire–9 depression test scores greater than 10.
The study also evaluated patterns of consultation, diagnosis, and health resource utilization and found similar rates between the HFEM and LCFM subgroups, Dr. Lipton said. Rates of overnight hospital stay in the past 6 months were almost identical between the two subgroups: 4.1% for the former and 4.2% for the latter. One striking difference between the two subgroups: the rate of medication overuse per ICHD-3 recommendations was 40.5% in HFEM and 63% in LFCM.
“These finding suggest that the treatment needs of people with HFEM may be similar to those of people with LFCM, suggesting that the 15-MHD threshold currently recommended by the ICHD-3 may merit reconsideration,” Dr. Lipton said.
An arbitrary cutoff?
The findings raise a valid point about reevaluating the thresholds for low- and high-frequency migraine, said Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles. “My own personal view is that they’re the same thing,” he said of HFEM and LFCM; The 15-day cutoff, he said, is “somewhat arbitrary.”
Dr. Charles suggested migraine categories address frequency and not characteristics – episodic versus chronic – and use a range rather than a threshold. “Define a range that’s more like 10-20 days per month rather than having that point at 15,” Dr. Charles said. “People sometimes make the mistake of thinking that that classification reflects some underlying pathophysiology, and that may not be necessarily true.”
Dr. Lipton disclosed financial relationships with Alder Biopharmaceuticals, Allergan (now AbbVie), Amgen, Biohaven Pharmaceuticals, Dr. Reddy’s/Promius, Electrocore, Eli Lilly, eNeura Therapeutics, GlaxoSmithKline, Lundbeck (Alder), Merck, Pernix Therapeutics, Pfizer, Supernus, Teva, Trigemina, Axsome Therapeutics, Vector, and Vedanta. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
according to an analysis of almost 17,000 patients from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study presented at the virtual annual meeting of the American Headache Society.
“The results showed substantial overlap in levels of burden, anxiety, depression and health utilization, including outpatient, inpatient and emergency department visits, among CaMEO respondents with high-frequency episodic migraine and those with low-frequency chronic migraine,” said Richard B. Lipton, MD, of the Albert Einstein College of Medicine, New York.
The study analyzed data on 16,789 respondents to CaMEO, the longitudinal, web-based study designed to characterize the course of episodic and chronic migraine. The study population consisted of four subgroups based on the number of self-reporting monthly headache days (MHDs):
- Low- and moderate-frequency episodic migraine (LFEM; zero to seven MHDs; n = 13,473).
- High-frequency episodic migraine (HFEM; 8-14 MHDs; n = 1,840).
- Low-frequency chronic migraine (LFCM; 15-23 MHDs; n = 1,035).
- High-frequency chronic migraine (HFCM; 24 or more MHDs; n = 441).
Dr. Lipton pointed out that the International Classification of Headache Disorders, 3rd edition, defines chronic migraine as 15 or more MHDs for 3 months or more with criteria for migraine with or without aura met on 8 days a month or more. It defines episodic migraine as less than 15 MHDs.
The study characterized migraine subgroups by various demographics. “The more frequent headache categories were associated with slightly older age of onset with a higher proportion of BMI [body mass index] in the obese range and overall with lower levels of household income and education,” Dr. Lipton said.
Similar headache characteristics
A comparison of headache characteristics and headache-related disabilities across subgroups revealed a number of commonalities between the HFEM and LFCM subgroups, Dr. Lipton said. Among them were presence of mild to severe allodynia, disability grade, interictal burden, and anxiety and depression scores. For example, 47.3% of the HFEM subgroup and 54.9% of the LFCM subgroup had Patient Health Questionnaire–9 depression test scores greater than 10.
The study also evaluated patterns of consultation, diagnosis, and health resource utilization and found similar rates between the HFEM and LCFM subgroups, Dr. Lipton said. Rates of overnight hospital stay in the past 6 months were almost identical between the two subgroups: 4.1% for the former and 4.2% for the latter. One striking difference between the two subgroups: the rate of medication overuse per ICHD-3 recommendations was 40.5% in HFEM and 63% in LFCM.
“These finding suggest that the treatment needs of people with HFEM may be similar to those of people with LFCM, suggesting that the 15-MHD threshold currently recommended by the ICHD-3 may merit reconsideration,” Dr. Lipton said.
An arbitrary cutoff?
The findings raise a valid point about reevaluating the thresholds for low- and high-frequency migraine, said Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles. “My own personal view is that they’re the same thing,” he said of HFEM and LFCM; The 15-day cutoff, he said, is “somewhat arbitrary.”
Dr. Charles suggested migraine categories address frequency and not characteristics – episodic versus chronic – and use a range rather than a threshold. “Define a range that’s more like 10-20 days per month rather than having that point at 15,” Dr. Charles said. “People sometimes make the mistake of thinking that that classification reflects some underlying pathophysiology, and that may not be necessarily true.”
Dr. Lipton disclosed financial relationships with Alder Biopharmaceuticals, Allergan (now AbbVie), Amgen, Biohaven Pharmaceuticals, Dr. Reddy’s/Promius, Electrocore, Eli Lilly, eNeura Therapeutics, GlaxoSmithKline, Lundbeck (Alder), Merck, Pernix Therapeutics, Pfizer, Supernus, Teva, Trigemina, Axsome Therapeutics, Vector, and Vedanta. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
according to an analysis of almost 17,000 patients from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study presented at the virtual annual meeting of the American Headache Society.
“The results showed substantial overlap in levels of burden, anxiety, depression and health utilization, including outpatient, inpatient and emergency department visits, among CaMEO respondents with high-frequency episodic migraine and those with low-frequency chronic migraine,” said Richard B. Lipton, MD, of the Albert Einstein College of Medicine, New York.
The study analyzed data on 16,789 respondents to CaMEO, the longitudinal, web-based study designed to characterize the course of episodic and chronic migraine. The study population consisted of four subgroups based on the number of self-reporting monthly headache days (MHDs):
- Low- and moderate-frequency episodic migraine (LFEM; zero to seven MHDs; n = 13,473).
- High-frequency episodic migraine (HFEM; 8-14 MHDs; n = 1,840).
- Low-frequency chronic migraine (LFCM; 15-23 MHDs; n = 1,035).
- High-frequency chronic migraine (HFCM; 24 or more MHDs; n = 441).
Dr. Lipton pointed out that the International Classification of Headache Disorders, 3rd edition, defines chronic migraine as 15 or more MHDs for 3 months or more with criteria for migraine with or without aura met on 8 days a month or more. It defines episodic migraine as less than 15 MHDs.
The study characterized migraine subgroups by various demographics. “The more frequent headache categories were associated with slightly older age of onset with a higher proportion of BMI [body mass index] in the obese range and overall with lower levels of household income and education,” Dr. Lipton said.
Similar headache characteristics
A comparison of headache characteristics and headache-related disabilities across subgroups revealed a number of commonalities between the HFEM and LFCM subgroups, Dr. Lipton said. Among them were presence of mild to severe allodynia, disability grade, interictal burden, and anxiety and depression scores. For example, 47.3% of the HFEM subgroup and 54.9% of the LFCM subgroup had Patient Health Questionnaire–9 depression test scores greater than 10.
The study also evaluated patterns of consultation, diagnosis, and health resource utilization and found similar rates between the HFEM and LCFM subgroups, Dr. Lipton said. Rates of overnight hospital stay in the past 6 months were almost identical between the two subgroups: 4.1% for the former and 4.2% for the latter. One striking difference between the two subgroups: the rate of medication overuse per ICHD-3 recommendations was 40.5% in HFEM and 63% in LFCM.
“These finding suggest that the treatment needs of people with HFEM may be similar to those of people with LFCM, suggesting that the 15-MHD threshold currently recommended by the ICHD-3 may merit reconsideration,” Dr. Lipton said.
An arbitrary cutoff?
The findings raise a valid point about reevaluating the thresholds for low- and high-frequency migraine, said Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles. “My own personal view is that they’re the same thing,” he said of HFEM and LFCM; The 15-day cutoff, he said, is “somewhat arbitrary.”
Dr. Charles suggested migraine categories address frequency and not characteristics – episodic versus chronic – and use a range rather than a threshold. “Define a range that’s more like 10-20 days per month rather than having that point at 15,” Dr. Charles said. “People sometimes make the mistake of thinking that that classification reflects some underlying pathophysiology, and that may not be necessarily true.”
Dr. Lipton disclosed financial relationships with Alder Biopharmaceuticals, Allergan (now AbbVie), Amgen, Biohaven Pharmaceuticals, Dr. Reddy’s/Promius, Electrocore, Eli Lilly, eNeura Therapeutics, GlaxoSmithKline, Lundbeck (Alder), Merck, Pernix Therapeutics, Pfizer, Supernus, Teva, Trigemina, Axsome Therapeutics, Vector, and Vedanta. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
FROM AHS 2020
The evolution of “COVIDists”
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).
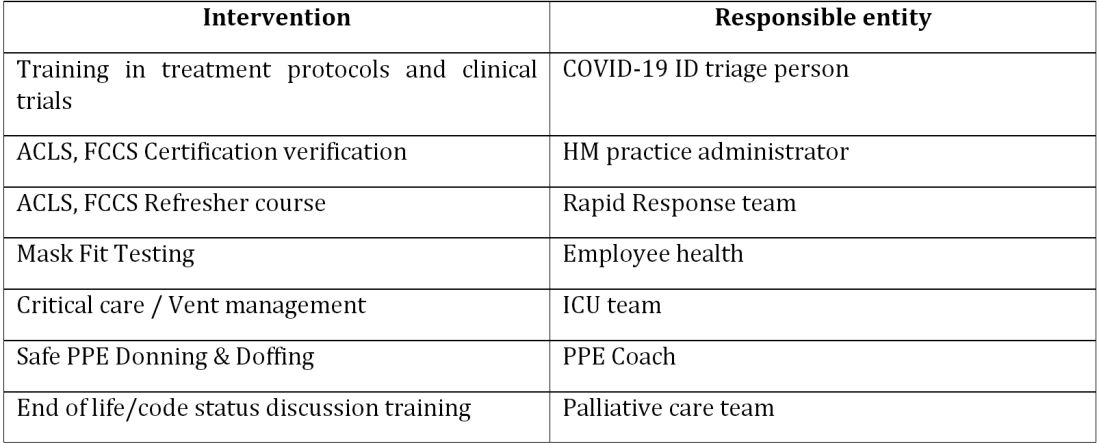
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).
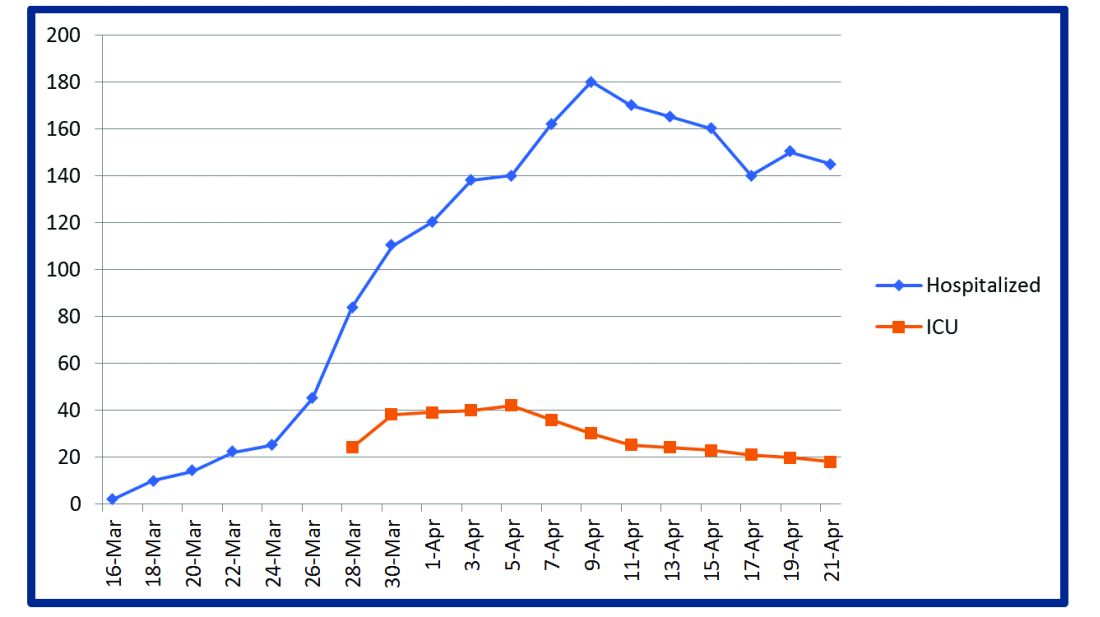
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
Adapting to the demands placed on hospital resources by COVID-19
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).
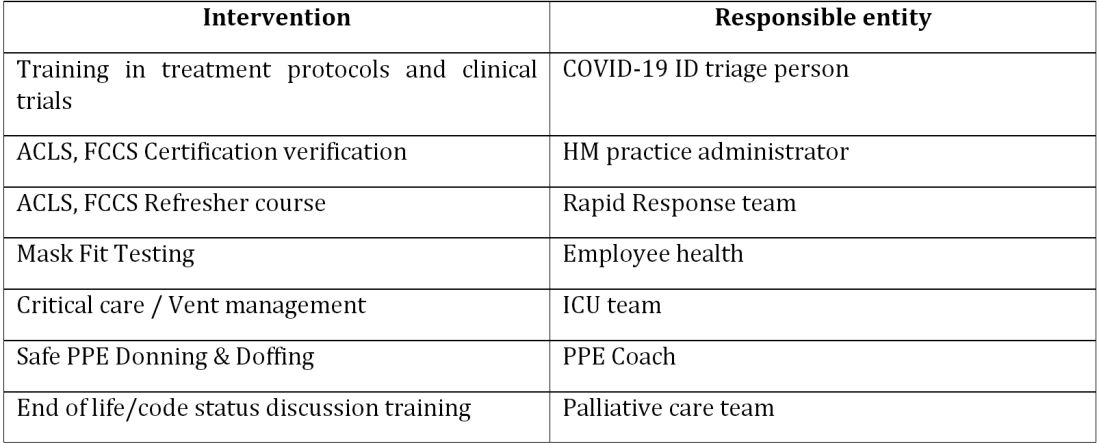
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).
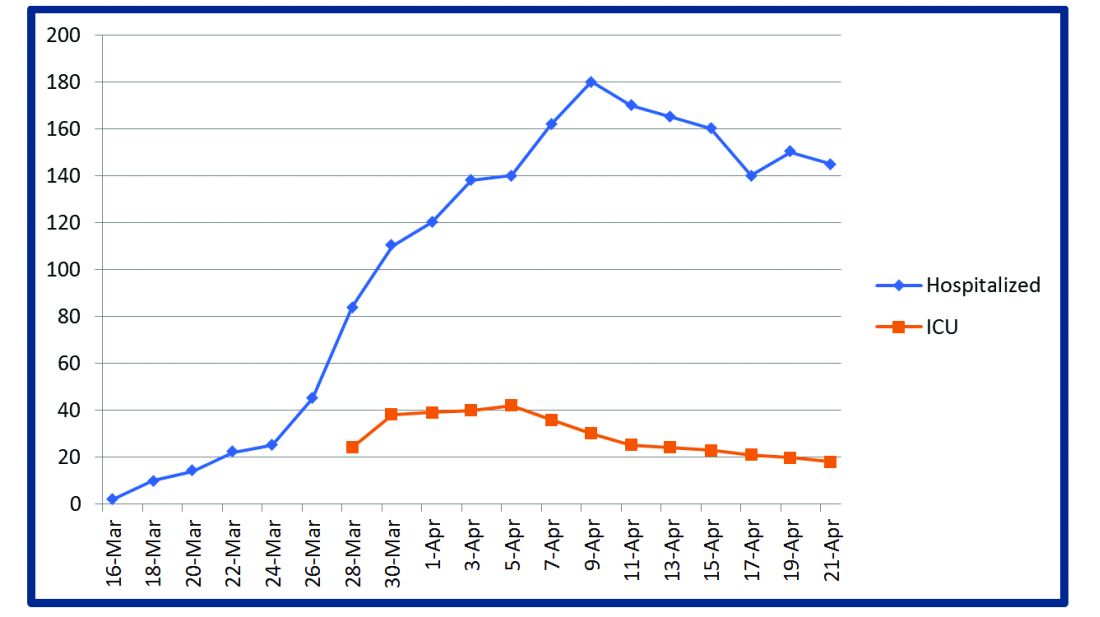
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).
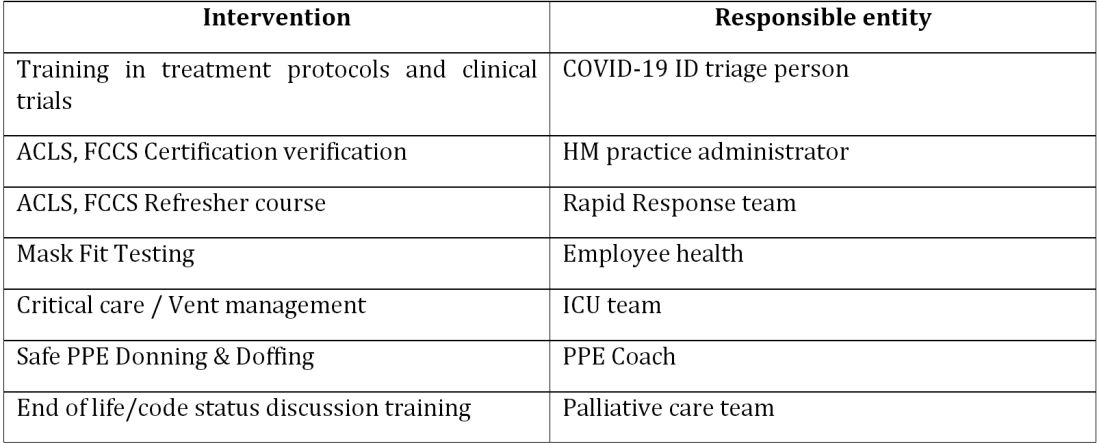
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).
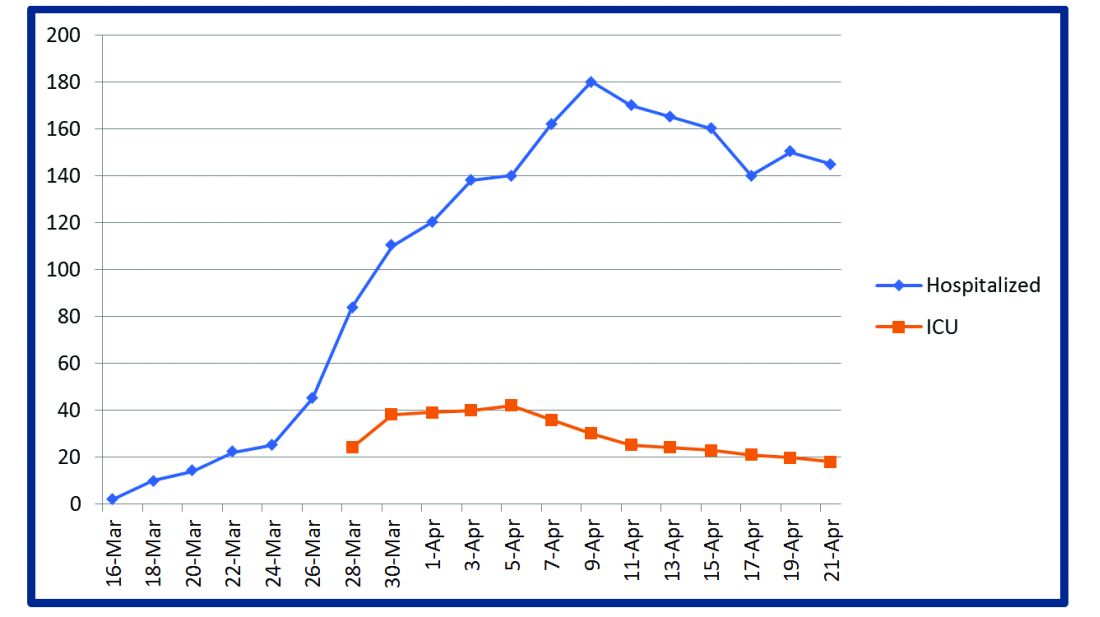
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
Daily Recap: Lung ultrasound helps diagnose COVID-19 in kids, first treatment approved for adult-onset Still’s disease
Here are the stories our MDedge editors across specialties think you need to know about today:
Lung ultrasound works well in children with COVID-19
Lung ultrasound has “high concordance” with radiologic findings in children with COVID-19 and offers benefits over other imaging techniques, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” wrote Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy. “Secondly, when performed at the bedside, [lung ultrasound] allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].” The findings of the small, observational study were published in Pediatrics. Read more.
New hypertension definitions reveal preclampsia risk
Using the new clinical definitions of hypertension, pregnant women with even modest elevations in blood pressure are at increased risk for preeclampsia, according to results from a large retrospective cohort study. Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby. The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy, which are not well studied” in comparison to nonpregnant hypertensive states. Read more.
Face mask type matters when sterilizing
When sterilizing face masks, the type of mask and the method of sterilization have a bearing on subsequent filtration efficiency, according to new research published in JAMA Network Open. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks. With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%. Read more.
FDA approves first treatment for adult-onset Still’s disease
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA). That makes Ilaris the first approved treatment for AOSD. The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab. Read more.
Intranasal DHE shows promise in migraine
An intranasal form of dihydroergotamine (DHE) targeting the upper nasal region is safe and effective for the treatment of migraine, according to results from a phase 3 clinical trial. The new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE. The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). A total of 66.3% of participants reported pain relief by 2 hours following a dose, and 38% had freedom from pain. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Lung ultrasound works well in children with COVID-19
Lung ultrasound has “high concordance” with radiologic findings in children with COVID-19 and offers benefits over other imaging techniques, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” wrote Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy. “Secondly, when performed at the bedside, [lung ultrasound] allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].” The findings of the small, observational study were published in Pediatrics. Read more.
New hypertension definitions reveal preclampsia risk
Using the new clinical definitions of hypertension, pregnant women with even modest elevations in blood pressure are at increased risk for preeclampsia, according to results from a large retrospective cohort study. Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby. The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy, which are not well studied” in comparison to nonpregnant hypertensive states. Read more.
Face mask type matters when sterilizing
When sterilizing face masks, the type of mask and the method of sterilization have a bearing on subsequent filtration efficiency, according to new research published in JAMA Network Open. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks. With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%. Read more.
FDA approves first treatment for adult-onset Still’s disease
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA). That makes Ilaris the first approved treatment for AOSD. The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab. Read more.
Intranasal DHE shows promise in migraine
An intranasal form of dihydroergotamine (DHE) targeting the upper nasal region is safe and effective for the treatment of migraine, according to results from a phase 3 clinical trial. The new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE. The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). A total of 66.3% of participants reported pain relief by 2 hours following a dose, and 38% had freedom from pain. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Lung ultrasound works well in children with COVID-19
Lung ultrasound has “high concordance” with radiologic findings in children with COVID-19 and offers benefits over other imaging techniques, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” wrote Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy. “Secondly, when performed at the bedside, [lung ultrasound] allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].” The findings of the small, observational study were published in Pediatrics. Read more.
New hypertension definitions reveal preclampsia risk
Using the new clinical definitions of hypertension, pregnant women with even modest elevations in blood pressure are at increased risk for preeclampsia, according to results from a large retrospective cohort study. Elizabeth F. Sutton, PhD, of the University of Pittsburgh and colleagues looked at records from 18,162 women who had given birth to a single baby. The authors found preeclampsia risk increased with increasing blood pressure elevation. Among women with normal blood pressure before 20 weeks’ gestation, 5% had preeclampsia, while 7% of those with elevated blood pressure did, as did 12% of women with stage 1 hypertension and 30% of women with stage 2 hypertension. The increase in risk of preeclampsia was because of preterm preeclampsia in the women with elevated blood pressure. Preeclampsia researcher Mark Santillan, MD, PhD, of the University of Iowa in Iowa City, said in an interview that the results “open the door to considering these new blood pressure categories as a prognosticator” for preeclampsia. “This paper furthers the field by applying these new categories to hypertensive diseases in pregnancy, which are not well studied” in comparison to nonpregnant hypertensive states. Read more.
Face mask type matters when sterilizing
When sterilizing face masks, the type of mask and the method of sterilization have a bearing on subsequent filtration efficiency, according to new research published in JAMA Network Open. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks. With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%. Read more.
FDA approves first treatment for adult-onset Still’s disease
The Food and Drug Administration has expanded the indications for canakinumab (Ilaris) to include all patients with active Still’s disease older than 2 years, adding adult-onset Still’s disease (AOSD) to a previous approval for juvenile-onset Still’s disease, also known as systemic juvenile idiopathic arthritis (sJIA). That makes Ilaris the first approved treatment for AOSD. The results from a randomized, double-blind, placebo-controlled study of 36 patients with AOSD aged 22-70 years showed that the efficacy and safety data in AOSD were generally consistent with the results of a pooled analysis of sJIA patients, according to Novartis, which markets canakinumab. Read more.
Intranasal DHE shows promise in migraine
An intranasal form of dihydroergotamine (DHE) targeting the upper nasal region is safe and effective for the treatment of migraine, according to results from a phase 3 clinical trial. The new formulation could offer patients an at-home alternative to intramuscular infusions or intravenous injections currently used to deliver DHE. The STOP 301 phase 3 open-label safety and tolerability trial treated over 5,650 migraine attacks in 354 patients who self-administered INP104 for up to 52 weeks. They were provided up to three doses per week (1.45 mg in a dose of two puffs, one per nostril). A total of 66.3% of participants reported pain relief by 2 hours following a dose, and 38% had freedom from pain. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.