User login
The Official Newspaper of the American Association for Thoracic Surgery
Docs still don’t get MACRA
Seven months into the first year of the Quality Payment Program, the new value-based payment plan set up by the Medicare Access and CHIP Reauthorization Act (MACRA), and doctors’ knowledge of the program is still light.
“Physicians, especially those in small practices, need more help in preparing” for participation in QPP either through the Merit-Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs), according to a new report issued by the American Medical Association and consulting firm KPMG.
That said, about 70% of those surveyed responded that they have begun preparing to meet the requirements of the QPP in 2017. The survey did not make clear whether this meant meeting the minimum requirements to avoid any penalties or doing more to become eligible for potential bonus Medicare payments.
“Even those who feel prepared still don’t fully understand the financial ramifications of the program,” the report said. “In short, they may be prepared to ‘check the box’ of reporting requirements, but may lack the long-term strategic financial vision to succeed in 2018 and beyond,” noting that only 8% of the respondents said they are “very prepared” for long-term financial success. On the other side of the that spectrum, 26% said they are not at all prepared and 58% said they were slightly prepared.
Survey respondents indicated a number of areas where they need help:
• Time required to accurately capture and report performance data (66%)
• Understanding reporting requirements (58%)
• Understanding the overall MIPS scoring process (57%)
• Cost required to accurately capture and report performance data (53%)
• Organizational infrastructure needed to report performance (49%)
The report also noted the significant differences when it comes to practice size, although the differences were “not unexpected.” For example, solo practices, compared to those groups of 50 or more physicians, were “significantly more likely (56%) to view reporting requirements as very burdensome, ... significantly more like to feel ‘not at all prepared’ for long-term financial success, ... less likely to be participating in an advanced APM, [and] less likely to have begun preparing.”
Specialists, more so than primary care physicians were “slightly more likely to be deeply knowledgeable about MACRA/QPP, [and] more likely to expect to participate in MIPS (61% versus 48%) and less likely to participate in an advanced APM (15% versus 22%),” the report adds.
“Ongoing educational assistance from CMS, as well as those in the private sector, should focus on the areas where physicians need the most help: understanding requirements and potential financial impact, selection of quality measures, and clinical practice transformation strategies,” the report states.
The survey comes on the heels of CMS releasing its proposed update to the regulations surrounding the QPP for 2018. Comments on the proposed regulatory update are due to CMS on Aug. 21, 2017.
Seven months into the first year of the Quality Payment Program, the new value-based payment plan set up by the Medicare Access and CHIP Reauthorization Act (MACRA), and doctors’ knowledge of the program is still light.
“Physicians, especially those in small practices, need more help in preparing” for participation in QPP either through the Merit-Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs), according to a new report issued by the American Medical Association and consulting firm KPMG.
That said, about 70% of those surveyed responded that they have begun preparing to meet the requirements of the QPP in 2017. The survey did not make clear whether this meant meeting the minimum requirements to avoid any penalties or doing more to become eligible for potential bonus Medicare payments.
“Even those who feel prepared still don’t fully understand the financial ramifications of the program,” the report said. “In short, they may be prepared to ‘check the box’ of reporting requirements, but may lack the long-term strategic financial vision to succeed in 2018 and beyond,” noting that only 8% of the respondents said they are “very prepared” for long-term financial success. On the other side of the that spectrum, 26% said they are not at all prepared and 58% said they were slightly prepared.
Survey respondents indicated a number of areas where they need help:
• Time required to accurately capture and report performance data (66%)
• Understanding reporting requirements (58%)
• Understanding the overall MIPS scoring process (57%)
• Cost required to accurately capture and report performance data (53%)
• Organizational infrastructure needed to report performance (49%)
The report also noted the significant differences when it comes to practice size, although the differences were “not unexpected.” For example, solo practices, compared to those groups of 50 or more physicians, were “significantly more likely (56%) to view reporting requirements as very burdensome, ... significantly more like to feel ‘not at all prepared’ for long-term financial success, ... less likely to be participating in an advanced APM, [and] less likely to have begun preparing.”
Specialists, more so than primary care physicians were “slightly more likely to be deeply knowledgeable about MACRA/QPP, [and] more likely to expect to participate in MIPS (61% versus 48%) and less likely to participate in an advanced APM (15% versus 22%),” the report adds.
“Ongoing educational assistance from CMS, as well as those in the private sector, should focus on the areas where physicians need the most help: understanding requirements and potential financial impact, selection of quality measures, and clinical practice transformation strategies,” the report states.
The survey comes on the heels of CMS releasing its proposed update to the regulations surrounding the QPP for 2018. Comments on the proposed regulatory update are due to CMS on Aug. 21, 2017.
Seven months into the first year of the Quality Payment Program, the new value-based payment plan set up by the Medicare Access and CHIP Reauthorization Act (MACRA), and doctors’ knowledge of the program is still light.
“Physicians, especially those in small practices, need more help in preparing” for participation in QPP either through the Merit-Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs), according to a new report issued by the American Medical Association and consulting firm KPMG.
That said, about 70% of those surveyed responded that they have begun preparing to meet the requirements of the QPP in 2017. The survey did not make clear whether this meant meeting the minimum requirements to avoid any penalties or doing more to become eligible for potential bonus Medicare payments.
“Even those who feel prepared still don’t fully understand the financial ramifications of the program,” the report said. “In short, they may be prepared to ‘check the box’ of reporting requirements, but may lack the long-term strategic financial vision to succeed in 2018 and beyond,” noting that only 8% of the respondents said they are “very prepared” for long-term financial success. On the other side of the that spectrum, 26% said they are not at all prepared and 58% said they were slightly prepared.
Survey respondents indicated a number of areas where they need help:
• Time required to accurately capture and report performance data (66%)
• Understanding reporting requirements (58%)
• Understanding the overall MIPS scoring process (57%)
• Cost required to accurately capture and report performance data (53%)
• Organizational infrastructure needed to report performance (49%)
The report also noted the significant differences when it comes to practice size, although the differences were “not unexpected.” For example, solo practices, compared to those groups of 50 or more physicians, were “significantly more likely (56%) to view reporting requirements as very burdensome, ... significantly more like to feel ‘not at all prepared’ for long-term financial success, ... less likely to be participating in an advanced APM, [and] less likely to have begun preparing.”
Specialists, more so than primary care physicians were “slightly more likely to be deeply knowledgeable about MACRA/QPP, [and] more likely to expect to participate in MIPS (61% versus 48%) and less likely to participate in an advanced APM (15% versus 22%),” the report adds.
“Ongoing educational assistance from CMS, as well as those in the private sector, should focus on the areas where physicians need the most help: understanding requirements and potential financial impact, selection of quality measures, and clinical practice transformation strategies,” the report states.
The survey comes on the heels of CMS releasing its proposed update to the regulations surrounding the QPP for 2018. Comments on the proposed regulatory update are due to CMS on Aug. 21, 2017.
Medicaid expansion produced opposing cost effects
States that expanded Medicaid in 2014 both increased and decreased their Medicaid spending that year, compared with the nonexpansion states, according to an analysis from the Centers for Medicare & Medicaid Services.
The 26 states, along with the District of Columbia, that expanded Medicaid eligibility by the end of 2014 had an increase in total Medicaid spending of 12.3% over 2013, compared with an increase of 6.2% in nonexpansion states.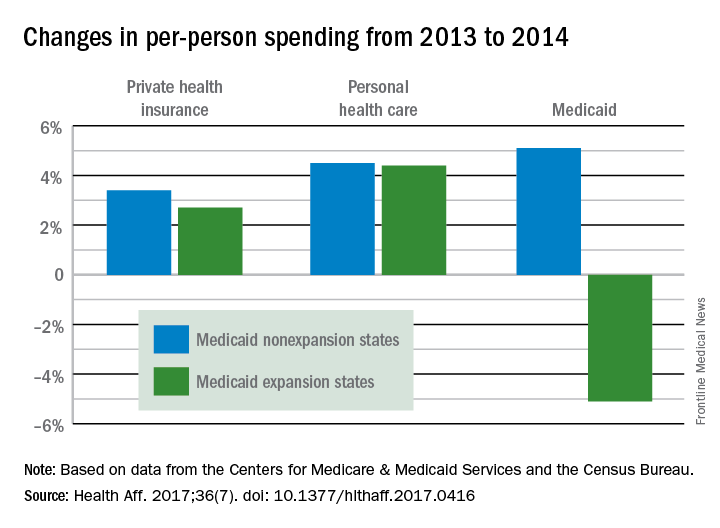
The expansion of coverage “increased the share of ... less expensive enrollees relative to the previous Medicaid beneficiary population mix,” the investigators said. Medicaid expansion brought in more relatively inexpensive adults – 43% of total enrollment in 2014, compared with 32% in 2013 – and reduced the proportion of disabled and aged enrollees, whose cost per person is much higher, they explained.
Private health insurance spending showed a different pattern: Nonexpansion states had larger increases in both higher per-person and overall costs than did expansion states. Per-person costs were up 3.4% for nonexpanders and 2.7% for expanders, and total costs rose 6.8% in nonexpansion states and 4.6% in the Medicaid expanders, Mr. Lassman and his associates said. Higher per-person spending growth for enrollees in the state and federal marketplaces, compared with nonmarketplace individual coverage, was partially responsible for this trend, they pointed out.
States that expanded Medicaid in 2014 both increased and decreased their Medicaid spending that year, compared with the nonexpansion states, according to an analysis from the Centers for Medicare & Medicaid Services.
The 26 states, along with the District of Columbia, that expanded Medicaid eligibility by the end of 2014 had an increase in total Medicaid spending of 12.3% over 2013, compared with an increase of 6.2% in nonexpansion states.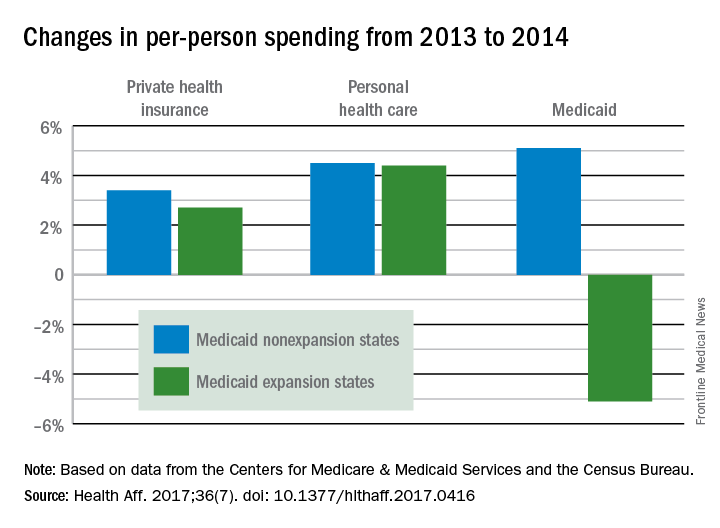
The expansion of coverage “increased the share of ... less expensive enrollees relative to the previous Medicaid beneficiary population mix,” the investigators said. Medicaid expansion brought in more relatively inexpensive adults – 43% of total enrollment in 2014, compared with 32% in 2013 – and reduced the proportion of disabled and aged enrollees, whose cost per person is much higher, they explained.
Private health insurance spending showed a different pattern: Nonexpansion states had larger increases in both higher per-person and overall costs than did expansion states. Per-person costs were up 3.4% for nonexpanders and 2.7% for expanders, and total costs rose 6.8% in nonexpansion states and 4.6% in the Medicaid expanders, Mr. Lassman and his associates said. Higher per-person spending growth for enrollees in the state and federal marketplaces, compared with nonmarketplace individual coverage, was partially responsible for this trend, they pointed out.
States that expanded Medicaid in 2014 both increased and decreased their Medicaid spending that year, compared with the nonexpansion states, according to an analysis from the Centers for Medicare & Medicaid Services.
The 26 states, along with the District of Columbia, that expanded Medicaid eligibility by the end of 2014 had an increase in total Medicaid spending of 12.3% over 2013, compared with an increase of 6.2% in nonexpansion states.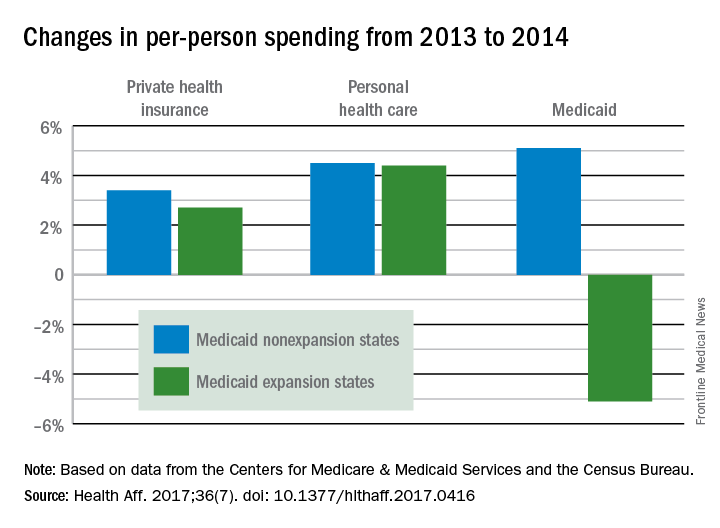
The expansion of coverage “increased the share of ... less expensive enrollees relative to the previous Medicaid beneficiary population mix,” the investigators said. Medicaid expansion brought in more relatively inexpensive adults – 43% of total enrollment in 2014, compared with 32% in 2013 – and reduced the proportion of disabled and aged enrollees, whose cost per person is much higher, they explained.
Private health insurance spending showed a different pattern: Nonexpansion states had larger increases in both higher per-person and overall costs than did expansion states. Per-person costs were up 3.4% for nonexpanders and 2.7% for expanders, and total costs rose 6.8% in nonexpansion states and 4.6% in the Medicaid expanders, Mr. Lassman and his associates said. Higher per-person spending growth for enrollees in the state and federal marketplaces, compared with nonmarketplace individual coverage, was partially responsible for this trend, they pointed out.
FROM HEALTH AFFAIRS
Poll: Most voters oppose House and Senate health care bills
Voters in nearly every region of the United States are opposed to the health reform bills that have been proposed in the House and Senate, according to a poll by the American Medical Association.
Surveys conducted in Alaska, Arkansas, Colorado, Nevada, Ohio, Tennessee, and West Virginia showed that voters in each state had an overall low opinion of the House-passed American Health Care Act (AHCA), according to an AMA analysis released June 27.
When asked whether the reform bill was a “good idea” or a “bad idea,” the most common response in each state was “bad idea,” ranging from 40% in Arkansas to 58% in Colorado. The majority of respondents in Alaska, Arkansas, Colorado, Nevada, and Ohio replied that the Senate should not pass the House legislation and the ACA should remain in place.
The plurality of Tennessee voters said the Senate should make major changes to the AHCA and pass it, while voters in West Virginia were split on what should happen to the AHCA.
Voters were not asked their views on the Senate’s Better Care Reconciliation Act (BCRA), but they were asked about specific provisions of the proposal.
When asked if federal funding for Medicaid expansion should be eliminated or reduced – as both the House and Senate propose – the majority of respondents in each state were opposed, ranging from 54% to 63%.
Voters in each state also strongly opposed BCRA provisions that would allow insurers to offer low-cost health plans, referred to as “skinny plans,” that would limit coverage for prescription drugs, mental health care, and other areas. When asked if low-income people should be provided with federal assistance to purchase inexpensive plans that would cover expensive illnesses, but not include preventive health care, a plurality of respondents were opposed, ranging from 43% in Arkansas to 58% in Ohio.
Respondents were supportive of the ACA’s individual mandate. When asked whether the ACA’s individual mandate should be eliminated and replaced with allowing health insurance companies to charge people 30% higher premiums for a year if they have not had continuous coverage, the majority of voters surveyed in all seven states were strongly opposed.
However, most voters were supportive of changing the Medicaid program to a federal grant program. When asked whether the government should change Medicaid from an entitlement program to a federal grant program and allow states to decide how to best use federal dollars to cover their low-income population, most voters agreed, ranging from 45% in Ohio to 52% in West Virginia.
The survey was conducted by phone in Alaska, Arkansas, Colorado, Nevada, Ohio, and Tennessee June 13-20, 2017. Samples were drawn from the voter file proportional to the statewide registered voter population. Quotas were set by specific demographics such as region, age, gender, and ethnicity based on data from the U.S. Census and the voter file to ensure a representative sample. Polling in West Virginia was conducted June 19-22, 2017.
[email protected]
On Twitter @legal_med
Voters in nearly every region of the United States are opposed to the health reform bills that have been proposed in the House and Senate, according to a poll by the American Medical Association.
Surveys conducted in Alaska, Arkansas, Colorado, Nevada, Ohio, Tennessee, and West Virginia showed that voters in each state had an overall low opinion of the House-passed American Health Care Act (AHCA), according to an AMA analysis released June 27.
When asked whether the reform bill was a “good idea” or a “bad idea,” the most common response in each state was “bad idea,” ranging from 40% in Arkansas to 58% in Colorado. The majority of respondents in Alaska, Arkansas, Colorado, Nevada, and Ohio replied that the Senate should not pass the House legislation and the ACA should remain in place.
The plurality of Tennessee voters said the Senate should make major changes to the AHCA and pass it, while voters in West Virginia were split on what should happen to the AHCA.
Voters were not asked their views on the Senate’s Better Care Reconciliation Act (BCRA), but they were asked about specific provisions of the proposal.
When asked if federal funding for Medicaid expansion should be eliminated or reduced – as both the House and Senate propose – the majority of respondents in each state were opposed, ranging from 54% to 63%.
Voters in each state also strongly opposed BCRA provisions that would allow insurers to offer low-cost health plans, referred to as “skinny plans,” that would limit coverage for prescription drugs, mental health care, and other areas. When asked if low-income people should be provided with federal assistance to purchase inexpensive plans that would cover expensive illnesses, but not include preventive health care, a plurality of respondents were opposed, ranging from 43% in Arkansas to 58% in Ohio.
Respondents were supportive of the ACA’s individual mandate. When asked whether the ACA’s individual mandate should be eliminated and replaced with allowing health insurance companies to charge people 30% higher premiums for a year if they have not had continuous coverage, the majority of voters surveyed in all seven states were strongly opposed.
However, most voters were supportive of changing the Medicaid program to a federal grant program. When asked whether the government should change Medicaid from an entitlement program to a federal grant program and allow states to decide how to best use federal dollars to cover their low-income population, most voters agreed, ranging from 45% in Ohio to 52% in West Virginia.
The survey was conducted by phone in Alaska, Arkansas, Colorado, Nevada, Ohio, and Tennessee June 13-20, 2017. Samples were drawn from the voter file proportional to the statewide registered voter population. Quotas were set by specific demographics such as region, age, gender, and ethnicity based on data from the U.S. Census and the voter file to ensure a representative sample. Polling in West Virginia was conducted June 19-22, 2017.
[email protected]
On Twitter @legal_med
Voters in nearly every region of the United States are opposed to the health reform bills that have been proposed in the House and Senate, according to a poll by the American Medical Association.
Surveys conducted in Alaska, Arkansas, Colorado, Nevada, Ohio, Tennessee, and West Virginia showed that voters in each state had an overall low opinion of the House-passed American Health Care Act (AHCA), according to an AMA analysis released June 27.
When asked whether the reform bill was a “good idea” or a “bad idea,” the most common response in each state was “bad idea,” ranging from 40% in Arkansas to 58% in Colorado. The majority of respondents in Alaska, Arkansas, Colorado, Nevada, and Ohio replied that the Senate should not pass the House legislation and the ACA should remain in place.
The plurality of Tennessee voters said the Senate should make major changes to the AHCA and pass it, while voters in West Virginia were split on what should happen to the AHCA.
Voters were not asked their views on the Senate’s Better Care Reconciliation Act (BCRA), but they were asked about specific provisions of the proposal.
When asked if federal funding for Medicaid expansion should be eliminated or reduced – as both the House and Senate propose – the majority of respondents in each state were opposed, ranging from 54% to 63%.
Voters in each state also strongly opposed BCRA provisions that would allow insurers to offer low-cost health plans, referred to as “skinny plans,” that would limit coverage for prescription drugs, mental health care, and other areas. When asked if low-income people should be provided with federal assistance to purchase inexpensive plans that would cover expensive illnesses, but not include preventive health care, a plurality of respondents were opposed, ranging from 43% in Arkansas to 58% in Ohio.
Respondents were supportive of the ACA’s individual mandate. When asked whether the ACA’s individual mandate should be eliminated and replaced with allowing health insurance companies to charge people 30% higher premiums for a year if they have not had continuous coverage, the majority of voters surveyed in all seven states were strongly opposed.
However, most voters were supportive of changing the Medicaid program to a federal grant program. When asked whether the government should change Medicaid from an entitlement program to a federal grant program and allow states to decide how to best use federal dollars to cover their low-income population, most voters agreed, ranging from 45% in Ohio to 52% in West Virginia.
The survey was conducted by phone in Alaska, Arkansas, Colorado, Nevada, Ohio, and Tennessee June 13-20, 2017. Samples were drawn from the voter file proportional to the statewide registered voter population. Quotas were set by specific demographics such as region, age, gender, and ethnicity based on data from the U.S. Census and the voter file to ensure a representative sample. Polling in West Virginia was conducted June 19-22, 2017.
[email protected]
On Twitter @legal_med
CBO: Senate health care proposal marginally better than House-passed bill
The Senate health care proposal is only marginally better in terms of the number of uninsured Americans, compared with the House-passed bill it aims to replace, but it still would leave 22 million more Americans without insurance coverage, according to a June 26 analysis by the Congressional Budget Office.
The analysis raised voices of opposition from the medical community.
BCRA would lower the federal deficit by $321 billion between 2017-2026, driven by the dramatic cuts in spending on Medicaid (estimated to be $772 billion), as well as $408 billion saved from reduced tax credits and other subsidies to help people afford health insurance.
The CBO’s estimate also addresses how the bill could impact access to health care.
Initially, patients can expect another short-term spike in insurance premiums, with average premiums in 2018 increasing by 20%, compared with current law, “mainly because the penalty for not having insurance would be eliminated, inducing fewer comparatively healthy people to sign up.” In 2019, premiums are predicted to be about 10% higher than under current law; however, by 2020, premiums for benchmark plans would be 30% lower than with current law.
However, as premiums come down, deductibles would continue to rise for plans that would offer lower levels of coverage, according to the CBO report. Additionally, “starting in 2020, the premium for a silver plan would typically be a relatively high percentage of income for low income people. The deductible for a plan ... would be a significantly higher percentage of income – also making such a plan unattractive but for a different reason. As a result, despite being eligible for premium tax credits, few low-income people would purchase any plan.”
The report also notes that the Senate proposal would not necessarily reverse current concerns regarding consumer choice in the individual markets, stating that “a small fraction of the population resides in areas which – because of this legislation, for at least some of the years after 2019 – no insurers will participate in the nongroup market or insurance would be offered only with very high premiums.” Additionally, removing the employer mandate could result in employers forgoing offering health insurance to their employees.
The bill faces an uphill battle in the Senate as there seemingly are not enough votes to pass the bill at this time. The measure is using the budget reconciliation process, meaning it will need 50 of the 52 Senate Republicans to pass it (all 48 Democrats are expected to vote against it). At least six GOP senators have said they are not ready to start debate. Senate Majority Leader Mitch McConnell (R-Ky) will not present the bill to the chamber for consideration until after the July 4 recess in an effort to tweak the language to garner the 50 votes needed to pass.*
Medical societies are pushing back against the bill as well.
The American Medical Association, in a letter to Senate leaders, notes that the first principal that medical professionals operate under is to do no harm. “The draft legislation violates that standard on many levels,” according to the AMA letter.
The American Osteopathic Association reiterated its objections to BCRA in a statement, citing the CBO’s determination that 22 million would lose coverage.
“As patient advocates, we cannot accept that under [BCRA] patients in need will no longer have the coverage they require to access health care services,” the association said in a statement. “The BCRA does nothing to control health costs but instead focuses on reducing federal health care expenditures by cutting coverage of our nation’s most vulnerable individuals and eliminating policies that promote access to preventive care services that can actually drive down expenses while improving patient outcomes.”
The American College of Cardiology noted that CBO analysis “makes it clear that the [BCRA] would lead to loss of coverage for millions of Americans and limit access to care for our most vulnerable populations. ... The ACC opposes the BCRA as it does not align with our Principles for Health Reform, which stress the need for patient access to meaningful insurance coverage and high-quality care.”
*This article was updated on June 27, 2017.
The Senate health care proposal is only marginally better in terms of the number of uninsured Americans, compared with the House-passed bill it aims to replace, but it still would leave 22 million more Americans without insurance coverage, according to a June 26 analysis by the Congressional Budget Office.
The analysis raised voices of opposition from the medical community.
BCRA would lower the federal deficit by $321 billion between 2017-2026, driven by the dramatic cuts in spending on Medicaid (estimated to be $772 billion), as well as $408 billion saved from reduced tax credits and other subsidies to help people afford health insurance.
The CBO’s estimate also addresses how the bill could impact access to health care.
Initially, patients can expect another short-term spike in insurance premiums, with average premiums in 2018 increasing by 20%, compared with current law, “mainly because the penalty for not having insurance would be eliminated, inducing fewer comparatively healthy people to sign up.” In 2019, premiums are predicted to be about 10% higher than under current law; however, by 2020, premiums for benchmark plans would be 30% lower than with current law.
However, as premiums come down, deductibles would continue to rise for plans that would offer lower levels of coverage, according to the CBO report. Additionally, “starting in 2020, the premium for a silver plan would typically be a relatively high percentage of income for low income people. The deductible for a plan ... would be a significantly higher percentage of income – also making such a plan unattractive but for a different reason. As a result, despite being eligible for premium tax credits, few low-income people would purchase any plan.”
The report also notes that the Senate proposal would not necessarily reverse current concerns regarding consumer choice in the individual markets, stating that “a small fraction of the population resides in areas which – because of this legislation, for at least some of the years after 2019 – no insurers will participate in the nongroup market or insurance would be offered only with very high premiums.” Additionally, removing the employer mandate could result in employers forgoing offering health insurance to their employees.
The bill faces an uphill battle in the Senate as there seemingly are not enough votes to pass the bill at this time. The measure is using the budget reconciliation process, meaning it will need 50 of the 52 Senate Republicans to pass it (all 48 Democrats are expected to vote against it). At least six GOP senators have said they are not ready to start debate. Senate Majority Leader Mitch McConnell (R-Ky) will not present the bill to the chamber for consideration until after the July 4 recess in an effort to tweak the language to garner the 50 votes needed to pass.*
Medical societies are pushing back against the bill as well.
The American Medical Association, in a letter to Senate leaders, notes that the first principal that medical professionals operate under is to do no harm. “The draft legislation violates that standard on many levels,” according to the AMA letter.
The American Osteopathic Association reiterated its objections to BCRA in a statement, citing the CBO’s determination that 22 million would lose coverage.
“As patient advocates, we cannot accept that under [BCRA] patients in need will no longer have the coverage they require to access health care services,” the association said in a statement. “The BCRA does nothing to control health costs but instead focuses on reducing federal health care expenditures by cutting coverage of our nation’s most vulnerable individuals and eliminating policies that promote access to preventive care services that can actually drive down expenses while improving patient outcomes.”
The American College of Cardiology noted that CBO analysis “makes it clear that the [BCRA] would lead to loss of coverage for millions of Americans and limit access to care for our most vulnerable populations. ... The ACC opposes the BCRA as it does not align with our Principles for Health Reform, which stress the need for patient access to meaningful insurance coverage and high-quality care.”
*This article was updated on June 27, 2017.
The Senate health care proposal is only marginally better in terms of the number of uninsured Americans, compared with the House-passed bill it aims to replace, but it still would leave 22 million more Americans without insurance coverage, according to a June 26 analysis by the Congressional Budget Office.
The analysis raised voices of opposition from the medical community.
BCRA would lower the federal deficit by $321 billion between 2017-2026, driven by the dramatic cuts in spending on Medicaid (estimated to be $772 billion), as well as $408 billion saved from reduced tax credits and other subsidies to help people afford health insurance.
The CBO’s estimate also addresses how the bill could impact access to health care.
Initially, patients can expect another short-term spike in insurance premiums, with average premiums in 2018 increasing by 20%, compared with current law, “mainly because the penalty for not having insurance would be eliminated, inducing fewer comparatively healthy people to sign up.” In 2019, premiums are predicted to be about 10% higher than under current law; however, by 2020, premiums for benchmark plans would be 30% lower than with current law.
However, as premiums come down, deductibles would continue to rise for plans that would offer lower levels of coverage, according to the CBO report. Additionally, “starting in 2020, the premium for a silver plan would typically be a relatively high percentage of income for low income people. The deductible for a plan ... would be a significantly higher percentage of income – also making such a plan unattractive but for a different reason. As a result, despite being eligible for premium tax credits, few low-income people would purchase any plan.”
The report also notes that the Senate proposal would not necessarily reverse current concerns regarding consumer choice in the individual markets, stating that “a small fraction of the population resides in areas which – because of this legislation, for at least some of the years after 2019 – no insurers will participate in the nongroup market or insurance would be offered only with very high premiums.” Additionally, removing the employer mandate could result in employers forgoing offering health insurance to their employees.
The bill faces an uphill battle in the Senate as there seemingly are not enough votes to pass the bill at this time. The measure is using the budget reconciliation process, meaning it will need 50 of the 52 Senate Republicans to pass it (all 48 Democrats are expected to vote against it). At least six GOP senators have said they are not ready to start debate. Senate Majority Leader Mitch McConnell (R-Ky) will not present the bill to the chamber for consideration until after the July 4 recess in an effort to tweak the language to garner the 50 votes needed to pass.*
Medical societies are pushing back against the bill as well.
The American Medical Association, in a letter to Senate leaders, notes that the first principal that medical professionals operate under is to do no harm. “The draft legislation violates that standard on many levels,” according to the AMA letter.
The American Osteopathic Association reiterated its objections to BCRA in a statement, citing the CBO’s determination that 22 million would lose coverage.
“As patient advocates, we cannot accept that under [BCRA] patients in need will no longer have the coverage they require to access health care services,” the association said in a statement. “The BCRA does nothing to control health costs but instead focuses on reducing federal health care expenditures by cutting coverage of our nation’s most vulnerable individuals and eliminating policies that promote access to preventive care services that can actually drive down expenses while improving patient outcomes.”
The American College of Cardiology noted that CBO analysis “makes it clear that the [BCRA] would lead to loss of coverage for millions of Americans and limit access to care for our most vulnerable populations. ... The ACC opposes the BCRA as it does not align with our Principles for Health Reform, which stress the need for patient access to meaningful insurance coverage and high-quality care.”
*This article was updated on June 27, 2017.
MV disease in children requires modified strategies
NEW YORK – Repairing mitral valves in pediatric patients must overcome two issues: the wide variability in their anatomy and their growth. Using strategies and techniques common in adult mitral surgery can accomplish good mitral valve function in children, but some techniques in children differ, like using combined resorbable material with autologous tissue or transferring native chords instead of placing artificial chords to a malfunctioning leaflet.
Pedro del Nido, MD, of Boston Children’s Hospital, said the spectrum of mitral valve pathology in children goes from congenital mitral stenosis with a thick annulus with leaflet immobility to leaflet hypermobility that involves anterior leaflet prolapse and can involve a cleft that causes regurgitation. Dr. del Nido explained his surgical approaches for mitral valve disease in children at the 2017 Mitral Conclave, sponsored by the American Association of Thoracic Surgery.
Accessing the mitral valve in children requires a different approach than in adults, Dr. del Nido said. “Going through the left atrium is generally difficult, so we often enter through a trans-septal incision,” he said. “The main reason for that is because the tricuspid valve is often associated with the mitral valve problem and this gives us the most direct exposure.”
Once the surgeon gains exposure, the surgical analysis for a diseased adult or child valve is almost identical, with the exception that adult disease is acquired whereas childhood disease tends to be congenital, Dr. del Nido said. “In the congenital patient, we often find fibroelastic tissue that the child is born with,” he said. “We see this in neonates and young infants. It thickens over time; it doesn’t often calcify, but it does often restrict the leaflets and it tends to fuse the chords, so in essence you have direct attachments of the leaflets to the papillaries.”
He explained that this pathology requires an approach similar to that for rheumatic mitral disease in adults. “Start splitting the commissures and start resecting the tissue off the chords creating fenestrations in order to improve the inflow.” Dr. del Nido added, “If you don’t do this, the child will always have a gradient, and if you think about an adult having problems and symptoms with a gradient, think about a 10-year-old running around trying to do athletics; it’s impossible.”
Dysfunctional chords also require a somewhat different approach in children than they require in adults. “We find elongation of the chords and the anterior support structure is abnormal; the secondary chords are totally intact,” Dr. del Nido said. When confronting a torn-edge chord, resection is often an option in adults, but is uncommon in children. “We don’t usually have very much leaflet tissue,” he said. Artificial chords do not accommodate growth.
“We tend to use native tissue,” said Dr. del Nido. “You can transfer the strut chord; you can transfer the secondary chord in order to achieve support for the edge of that prolapsed leaflet.”
Leaflet problems are probably the biggest single source of recurrence in children, Dr. del Nido said. A cleft on the anterior leaflet can be particularly vexing. For example, cleft edges attached to the septum can prevent the valve leaflet from coaptation with the posterior leaflet. “If you don’t recognize that on 3-D echocardiography, you’re going to have a problem; that leaflet will never create the coaptation surface that you want,” he said.
The solution may lie underneath the leaflet. Said Dr. del Nido, “We tend to want to close a cleft, and, yes, that will get you relief of regurgitation in the central portion, but if you end up with immobility of that leaflet, then look underneath. Most often there are very abnormal attachments to the edges of that cleft to the septum. You have to get rid of that; if you don’t resect all that, you’ll never have a leaflet that truly floats up to coapt against the posterior leaflet.”
Annular dilation in children can also challenge a cardiothoracic surgeon’s skill.
In rare cases, a suture commissuroplasty may correct the problem. Sometimes Dr. del Nido will use the DeVega suture annuloplasty – “even though it is very much user dependent; it’s very easy in pediatrics to create stenosis with the DeVega.” As an alternative, synthetic ring annuloplasties can confine valve growth and are rarely used.
Dr. del Nido’s preference is to use a hybrid approach of tissue and resorbable material. “The advantage of the resorbable material is that it will go away, but that’s also the problem with the resorbable material,” he said. “Once it does go away, there’s nothing there to support the annulus, so a combination of tissue and resorbable suture is probably the best answer.”
In posterior leaflet deficiency, a patch of pericardium posteriorly can augment the dysfunctional leaflet. You can also use pericardium as an annuloplasty ring. “You can use it circumferentially,” Dr. del Nido said. “It’s a soft ring; you can certainly use this material which is autologous; it does provide strength to the fibrous annulus; it does support that valve; and you do see growth.” He added that bovine pericardium is not ideal for this use.
Dr. del Nido reported no relevant financial relationships.
NEW YORK – Repairing mitral valves in pediatric patients must overcome two issues: the wide variability in their anatomy and their growth. Using strategies and techniques common in adult mitral surgery can accomplish good mitral valve function in children, but some techniques in children differ, like using combined resorbable material with autologous tissue or transferring native chords instead of placing artificial chords to a malfunctioning leaflet.
Pedro del Nido, MD, of Boston Children’s Hospital, said the spectrum of mitral valve pathology in children goes from congenital mitral stenosis with a thick annulus with leaflet immobility to leaflet hypermobility that involves anterior leaflet prolapse and can involve a cleft that causes regurgitation. Dr. del Nido explained his surgical approaches for mitral valve disease in children at the 2017 Mitral Conclave, sponsored by the American Association of Thoracic Surgery.
Accessing the mitral valve in children requires a different approach than in adults, Dr. del Nido said. “Going through the left atrium is generally difficult, so we often enter through a trans-septal incision,” he said. “The main reason for that is because the tricuspid valve is often associated with the mitral valve problem and this gives us the most direct exposure.”
Once the surgeon gains exposure, the surgical analysis for a diseased adult or child valve is almost identical, with the exception that adult disease is acquired whereas childhood disease tends to be congenital, Dr. del Nido said. “In the congenital patient, we often find fibroelastic tissue that the child is born with,” he said. “We see this in neonates and young infants. It thickens over time; it doesn’t often calcify, but it does often restrict the leaflets and it tends to fuse the chords, so in essence you have direct attachments of the leaflets to the papillaries.”
He explained that this pathology requires an approach similar to that for rheumatic mitral disease in adults. “Start splitting the commissures and start resecting the tissue off the chords creating fenestrations in order to improve the inflow.” Dr. del Nido added, “If you don’t do this, the child will always have a gradient, and if you think about an adult having problems and symptoms with a gradient, think about a 10-year-old running around trying to do athletics; it’s impossible.”
Dysfunctional chords also require a somewhat different approach in children than they require in adults. “We find elongation of the chords and the anterior support structure is abnormal; the secondary chords are totally intact,” Dr. del Nido said. When confronting a torn-edge chord, resection is often an option in adults, but is uncommon in children. “We don’t usually have very much leaflet tissue,” he said. Artificial chords do not accommodate growth.
“We tend to use native tissue,” said Dr. del Nido. “You can transfer the strut chord; you can transfer the secondary chord in order to achieve support for the edge of that prolapsed leaflet.”
Leaflet problems are probably the biggest single source of recurrence in children, Dr. del Nido said. A cleft on the anterior leaflet can be particularly vexing. For example, cleft edges attached to the septum can prevent the valve leaflet from coaptation with the posterior leaflet. “If you don’t recognize that on 3-D echocardiography, you’re going to have a problem; that leaflet will never create the coaptation surface that you want,” he said.
The solution may lie underneath the leaflet. Said Dr. del Nido, “We tend to want to close a cleft, and, yes, that will get you relief of regurgitation in the central portion, but if you end up with immobility of that leaflet, then look underneath. Most often there are very abnormal attachments to the edges of that cleft to the septum. You have to get rid of that; if you don’t resect all that, you’ll never have a leaflet that truly floats up to coapt against the posterior leaflet.”
Annular dilation in children can also challenge a cardiothoracic surgeon’s skill.
In rare cases, a suture commissuroplasty may correct the problem. Sometimes Dr. del Nido will use the DeVega suture annuloplasty – “even though it is very much user dependent; it’s very easy in pediatrics to create stenosis with the DeVega.” As an alternative, synthetic ring annuloplasties can confine valve growth and are rarely used.
Dr. del Nido’s preference is to use a hybrid approach of tissue and resorbable material. “The advantage of the resorbable material is that it will go away, but that’s also the problem with the resorbable material,” he said. “Once it does go away, there’s nothing there to support the annulus, so a combination of tissue and resorbable suture is probably the best answer.”
In posterior leaflet deficiency, a patch of pericardium posteriorly can augment the dysfunctional leaflet. You can also use pericardium as an annuloplasty ring. “You can use it circumferentially,” Dr. del Nido said. “It’s a soft ring; you can certainly use this material which is autologous; it does provide strength to the fibrous annulus; it does support that valve; and you do see growth.” He added that bovine pericardium is not ideal for this use.
Dr. del Nido reported no relevant financial relationships.
NEW YORK – Repairing mitral valves in pediatric patients must overcome two issues: the wide variability in their anatomy and their growth. Using strategies and techniques common in adult mitral surgery can accomplish good mitral valve function in children, but some techniques in children differ, like using combined resorbable material with autologous tissue or transferring native chords instead of placing artificial chords to a malfunctioning leaflet.
Pedro del Nido, MD, of Boston Children’s Hospital, said the spectrum of mitral valve pathology in children goes from congenital mitral stenosis with a thick annulus with leaflet immobility to leaflet hypermobility that involves anterior leaflet prolapse and can involve a cleft that causes regurgitation. Dr. del Nido explained his surgical approaches for mitral valve disease in children at the 2017 Mitral Conclave, sponsored by the American Association of Thoracic Surgery.
Accessing the mitral valve in children requires a different approach than in adults, Dr. del Nido said. “Going through the left atrium is generally difficult, so we often enter through a trans-septal incision,” he said. “The main reason for that is because the tricuspid valve is often associated with the mitral valve problem and this gives us the most direct exposure.”
Once the surgeon gains exposure, the surgical analysis for a diseased adult or child valve is almost identical, with the exception that adult disease is acquired whereas childhood disease tends to be congenital, Dr. del Nido said. “In the congenital patient, we often find fibroelastic tissue that the child is born with,” he said. “We see this in neonates and young infants. It thickens over time; it doesn’t often calcify, but it does often restrict the leaflets and it tends to fuse the chords, so in essence you have direct attachments of the leaflets to the papillaries.”
He explained that this pathology requires an approach similar to that for rheumatic mitral disease in adults. “Start splitting the commissures and start resecting the tissue off the chords creating fenestrations in order to improve the inflow.” Dr. del Nido added, “If you don’t do this, the child will always have a gradient, and if you think about an adult having problems and symptoms with a gradient, think about a 10-year-old running around trying to do athletics; it’s impossible.”
Dysfunctional chords also require a somewhat different approach in children than they require in adults. “We find elongation of the chords and the anterior support structure is abnormal; the secondary chords are totally intact,” Dr. del Nido said. When confronting a torn-edge chord, resection is often an option in adults, but is uncommon in children. “We don’t usually have very much leaflet tissue,” he said. Artificial chords do not accommodate growth.
“We tend to use native tissue,” said Dr. del Nido. “You can transfer the strut chord; you can transfer the secondary chord in order to achieve support for the edge of that prolapsed leaflet.”
Leaflet problems are probably the biggest single source of recurrence in children, Dr. del Nido said. A cleft on the anterior leaflet can be particularly vexing. For example, cleft edges attached to the septum can prevent the valve leaflet from coaptation with the posterior leaflet. “If you don’t recognize that on 3-D echocardiography, you’re going to have a problem; that leaflet will never create the coaptation surface that you want,” he said.
The solution may lie underneath the leaflet. Said Dr. del Nido, “We tend to want to close a cleft, and, yes, that will get you relief of regurgitation in the central portion, but if you end up with immobility of that leaflet, then look underneath. Most often there are very abnormal attachments to the edges of that cleft to the septum. You have to get rid of that; if you don’t resect all that, you’ll never have a leaflet that truly floats up to coapt against the posterior leaflet.”
Annular dilation in children can also challenge a cardiothoracic surgeon’s skill.
In rare cases, a suture commissuroplasty may correct the problem. Sometimes Dr. del Nido will use the DeVega suture annuloplasty – “even though it is very much user dependent; it’s very easy in pediatrics to create stenosis with the DeVega.” As an alternative, synthetic ring annuloplasties can confine valve growth and are rarely used.
Dr. del Nido’s preference is to use a hybrid approach of tissue and resorbable material. “The advantage of the resorbable material is that it will go away, but that’s also the problem with the resorbable material,” he said. “Once it does go away, there’s nothing there to support the annulus, so a combination of tissue and resorbable suture is probably the best answer.”
In posterior leaflet deficiency, a patch of pericardium posteriorly can augment the dysfunctional leaflet. You can also use pericardium as an annuloplasty ring. “You can use it circumferentially,” Dr. del Nido said. “It’s a soft ring; you can certainly use this material which is autologous; it does provide strength to the fibrous annulus; it does support that valve; and you do see growth.” He added that bovine pericardium is not ideal for this use.
Dr. del Nido reported no relevant financial relationships.
AT THE 2017 MITRAL VALVE CONCLAVE
Key clinical point: Operating on mitral valves in pediatric patients must overcome the wide variability in anatomy among young patients and accommodate growth.
Major finding: Strategies that involve a combination of resorbable material with autologous tissue can accomplish repair in most of these patients.
Data source: Review based on Dr. del Nido’s experience.
Disclosures: Dr. del Nido reported having no relevant financial disclosures.
Supreme Court allows partial travel ban to proceed
The U.S. Supreme Court has allowed a limited version of President Trump’s travel ban to move forward, prohibiting certain foreign nationals from six majority-Muslim countries from entering the country.
The justices’ June 26 order means that travelers from the affected countries who do not have a bona fide relationship with U.S. nationals or U.S. entities may not enter the United States. Conversely, it means that foreign physicians who have accepted a job at a U.S. institution or students who have been accepted to a U.S. medical school will be allowed to take those positions.
“In practical terms, this means that [the executive order] may not be enforced against foreign nationals who have a credible claim of a bona fide relationship with a person or entity in the United States,” justices wrote in their order. “All other foreign nationals are subject to the provisions. For individuals, a close familial relationship is required. A foreign national who wishes to enter the United States to live with or visit a family member ... clearly has such a relationship. As for entities, the relationship must be formal, documented, and formed in the ordinary course, rather than for the purpose of evading [the executive order].”
In a dissenting statement, Associate Justice Clarence Thomas wrote that the full ban should have gone into effect. Associate Justice Samuel Alito and Associate Justice Neil Gorsuch joined the dissent.
“I agree with the court’s implicit conclusion that the government has made a strong showing that it is likely to succeed on the merits – that is, that the [lower] judgments will be reversed,”Associate Justice Thomas wrote. “The government has also established that failure to stay the injunctions will cause irreparable harm by interfering with its compelling need to provide for the nation’s security. Finally, weighing the government’s interest in preserving national security against the hardships caused to respondents by temporary denials of entry into the country, the balance of the equities favors the government. I would thus grant the government’s applications for a stay in their entirety.”
President Trump’s revised executive order, signed March 6, bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from the affected countries from entering the U.S. for 120 days. The executive measure superseded President Trump’s original Jan. 27 travel ban. The revised order clarified that citizens of the six countries who are legal permanent U.S. residents or who have current visas to enter the country are exempt from the travel prohibition. Federal judges in Hawaii and Maryland ruled that the revised order was discriminatory and blocked the order from taking effect, a decision upheld by the 9th U.S. Circuit Court of Appeals.
Justices will hear oral arguments in the case this fall.
[email protected]
On Twitter @legal_med
The U.S. Supreme Court has allowed a limited version of President Trump’s travel ban to move forward, prohibiting certain foreign nationals from six majority-Muslim countries from entering the country.
The justices’ June 26 order means that travelers from the affected countries who do not have a bona fide relationship with U.S. nationals or U.S. entities may not enter the United States. Conversely, it means that foreign physicians who have accepted a job at a U.S. institution or students who have been accepted to a U.S. medical school will be allowed to take those positions.
“In practical terms, this means that [the executive order] may not be enforced against foreign nationals who have a credible claim of a bona fide relationship with a person or entity in the United States,” justices wrote in their order. “All other foreign nationals are subject to the provisions. For individuals, a close familial relationship is required. A foreign national who wishes to enter the United States to live with or visit a family member ... clearly has such a relationship. As for entities, the relationship must be formal, documented, and formed in the ordinary course, rather than for the purpose of evading [the executive order].”
In a dissenting statement, Associate Justice Clarence Thomas wrote that the full ban should have gone into effect. Associate Justice Samuel Alito and Associate Justice Neil Gorsuch joined the dissent.
“I agree with the court’s implicit conclusion that the government has made a strong showing that it is likely to succeed on the merits – that is, that the [lower] judgments will be reversed,”Associate Justice Thomas wrote. “The government has also established that failure to stay the injunctions will cause irreparable harm by interfering with its compelling need to provide for the nation’s security. Finally, weighing the government’s interest in preserving national security against the hardships caused to respondents by temporary denials of entry into the country, the balance of the equities favors the government. I would thus grant the government’s applications for a stay in their entirety.”
President Trump’s revised executive order, signed March 6, bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from the affected countries from entering the U.S. for 120 days. The executive measure superseded President Trump’s original Jan. 27 travel ban. The revised order clarified that citizens of the six countries who are legal permanent U.S. residents or who have current visas to enter the country are exempt from the travel prohibition. Federal judges in Hawaii and Maryland ruled that the revised order was discriminatory and blocked the order from taking effect, a decision upheld by the 9th U.S. Circuit Court of Appeals.
Justices will hear oral arguments in the case this fall.
[email protected]
On Twitter @legal_med
The U.S. Supreme Court has allowed a limited version of President Trump’s travel ban to move forward, prohibiting certain foreign nationals from six majority-Muslim countries from entering the country.
The justices’ June 26 order means that travelers from the affected countries who do not have a bona fide relationship with U.S. nationals or U.S. entities may not enter the United States. Conversely, it means that foreign physicians who have accepted a job at a U.S. institution or students who have been accepted to a U.S. medical school will be allowed to take those positions.
“In practical terms, this means that [the executive order] may not be enforced against foreign nationals who have a credible claim of a bona fide relationship with a person or entity in the United States,” justices wrote in their order. “All other foreign nationals are subject to the provisions. For individuals, a close familial relationship is required. A foreign national who wishes to enter the United States to live with or visit a family member ... clearly has such a relationship. As for entities, the relationship must be formal, documented, and formed in the ordinary course, rather than for the purpose of evading [the executive order].”
In a dissenting statement, Associate Justice Clarence Thomas wrote that the full ban should have gone into effect. Associate Justice Samuel Alito and Associate Justice Neil Gorsuch joined the dissent.
“I agree with the court’s implicit conclusion that the government has made a strong showing that it is likely to succeed on the merits – that is, that the [lower] judgments will be reversed,”Associate Justice Thomas wrote. “The government has also established that failure to stay the injunctions will cause irreparable harm by interfering with its compelling need to provide for the nation’s security. Finally, weighing the government’s interest in preserving national security against the hardships caused to respondents by temporary denials of entry into the country, the balance of the equities favors the government. I would thus grant the government’s applications for a stay in their entirety.”
President Trump’s revised executive order, signed March 6, bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from the affected countries from entering the U.S. for 120 days. The executive measure superseded President Trump’s original Jan. 27 travel ban. The revised order clarified that citizens of the six countries who are legal permanent U.S. residents or who have current visas to enter the country are exempt from the travel prohibition. Federal judges in Hawaii and Maryland ruled that the revised order was discriminatory and blocked the order from taking effect, a decision upheld by the 9th U.S. Circuit Court of Appeals.
Justices will hear oral arguments in the case this fall.
[email protected]
On Twitter @legal_med
Endosonography can help eliminate false negatives
BOSTON – Patients at high risk for non–small cell lung cancer (NSCLC) metastases were found to have a significant rate of unsuspected lymph node metastases upon endosonographic assessment, even in the presence of radiologically normal mediastinal lymph nodes, according to a study reported by Pravachan Hegde, MD, of the University of Montreal. Dr. Hegde presented the results at the 2017 AATS Centennial meeting.
Positron-emission tomography (PET) with computed tomography (CT) is routinely utilized to investigate lymph node (LN) metastases in non-small cell lung cancer, according to Dr. Hegde. However, this method has been found to be less sensitive in normal-sized LNs.
Dr. Hegde and his colleagues retrospectively reviewed a single-institution prospectively maintained database. Patients were identified from a cohort between January 2009 and December 2014. Consecutive patients with NSCLC were identified in whom both the pre-endosonography CT and PET-CT were negative for mediastinal LN metastases.
Patients were staged if they had central tumor, tumor size greater than 3 cm, N1 lymph node involvement on PET-CT/CT, or if there was low SUV in the primary tumor. Combined endosonography (EBUS+EUS-FNA) was performed in all patients.
A total of 22 out of 161 patients with radiologically normal mediastinum were found to be positive on combined EBUS/EUS staging. Out of 21 patients upstaged, 71% had tumor size greater than 3 cm; 28% had N1 disease; 61% had N2 disease; and 9% had adrenal involvement. None of the patients that were upstaged had N1 LN involvement on PET-CT or CT scan, according to Dr. Hegde.
A total of 416 lymph nodes were biopsied in the 161 patients by combined endosonography, 147 by EBUS and 269 by EUS. Of the 22 patients upstaged with endosonography, 12 were upstaged with EBUS and 10 were upstaged with EUS.
“Given the significant rate of unsuspected lymph node metastases, combined endosonographic lymph node staging should be routinely performed in staging of NSCLC in high risk patients even in the presence of radiologically normal mediastinal lymph nodes,” Dr. Hegde concluded.
In an interview, Moishe Liberman, MD, a coauthor of the study stated: “Pre-operative lymph node staging of lung cancer has dramatically changed over the last decade due to the availability and improvements in technology in PET, CT, EBUS, and EUS. While imaging (CT and PET) definitely help in staging, these tests are imperfect with significant false-negative rates as seen in our study.
“Minimally invasive, endoscopic techniques can help to significantly decrease these false- negative rates by providing biopsy of the target lymph nodes. Surprise intra-operative findings not accurately picked up by PET and CT should be almost nonexistant in 2017 with aggressive endosonographic pre-operative staging. This ensures that patients who actually benefit from surgery undergo resection and those with higher stage disease get appropriate treatment,” Dr. Liberman added. ■
BOSTON – Patients at high risk for non–small cell lung cancer (NSCLC) metastases were found to have a significant rate of unsuspected lymph node metastases upon endosonographic assessment, even in the presence of radiologically normal mediastinal lymph nodes, according to a study reported by Pravachan Hegde, MD, of the University of Montreal. Dr. Hegde presented the results at the 2017 AATS Centennial meeting.
Positron-emission tomography (PET) with computed tomography (CT) is routinely utilized to investigate lymph node (LN) metastases in non-small cell lung cancer, according to Dr. Hegde. However, this method has been found to be less sensitive in normal-sized LNs.
Dr. Hegde and his colleagues retrospectively reviewed a single-institution prospectively maintained database. Patients were identified from a cohort between January 2009 and December 2014. Consecutive patients with NSCLC were identified in whom both the pre-endosonography CT and PET-CT were negative for mediastinal LN metastases.
Patients were staged if they had central tumor, tumor size greater than 3 cm, N1 lymph node involvement on PET-CT/CT, or if there was low SUV in the primary tumor. Combined endosonography (EBUS+EUS-FNA) was performed in all patients.
A total of 22 out of 161 patients with radiologically normal mediastinum were found to be positive on combined EBUS/EUS staging. Out of 21 patients upstaged, 71% had tumor size greater than 3 cm; 28% had N1 disease; 61% had N2 disease; and 9% had adrenal involvement. None of the patients that were upstaged had N1 LN involvement on PET-CT or CT scan, according to Dr. Hegde.
A total of 416 lymph nodes were biopsied in the 161 patients by combined endosonography, 147 by EBUS and 269 by EUS. Of the 22 patients upstaged with endosonography, 12 were upstaged with EBUS and 10 were upstaged with EUS.
“Given the significant rate of unsuspected lymph node metastases, combined endosonographic lymph node staging should be routinely performed in staging of NSCLC in high risk patients even in the presence of radiologically normal mediastinal lymph nodes,” Dr. Hegde concluded.
In an interview, Moishe Liberman, MD, a coauthor of the study stated: “Pre-operative lymph node staging of lung cancer has dramatically changed over the last decade due to the availability and improvements in technology in PET, CT, EBUS, and EUS. While imaging (CT and PET) definitely help in staging, these tests are imperfect with significant false-negative rates as seen in our study.
“Minimally invasive, endoscopic techniques can help to significantly decrease these false- negative rates by providing biopsy of the target lymph nodes. Surprise intra-operative findings not accurately picked up by PET and CT should be almost nonexistant in 2017 with aggressive endosonographic pre-operative staging. This ensures that patients who actually benefit from surgery undergo resection and those with higher stage disease get appropriate treatment,” Dr. Liberman added. ■
BOSTON – Patients at high risk for non–small cell lung cancer (NSCLC) metastases were found to have a significant rate of unsuspected lymph node metastases upon endosonographic assessment, even in the presence of radiologically normal mediastinal lymph nodes, according to a study reported by Pravachan Hegde, MD, of the University of Montreal. Dr. Hegde presented the results at the 2017 AATS Centennial meeting.
Positron-emission tomography (PET) with computed tomography (CT) is routinely utilized to investigate lymph node (LN) metastases in non-small cell lung cancer, according to Dr. Hegde. However, this method has been found to be less sensitive in normal-sized LNs.
Dr. Hegde and his colleagues retrospectively reviewed a single-institution prospectively maintained database. Patients were identified from a cohort between January 2009 and December 2014. Consecutive patients with NSCLC were identified in whom both the pre-endosonography CT and PET-CT were negative for mediastinal LN metastases.
Patients were staged if they had central tumor, tumor size greater than 3 cm, N1 lymph node involvement on PET-CT/CT, or if there was low SUV in the primary tumor. Combined endosonography (EBUS+EUS-FNA) was performed in all patients.
A total of 22 out of 161 patients with radiologically normal mediastinum were found to be positive on combined EBUS/EUS staging. Out of 21 patients upstaged, 71% had tumor size greater than 3 cm; 28% had N1 disease; 61% had N2 disease; and 9% had adrenal involvement. None of the patients that were upstaged had N1 LN involvement on PET-CT or CT scan, according to Dr. Hegde.
A total of 416 lymph nodes were biopsied in the 161 patients by combined endosonography, 147 by EBUS and 269 by EUS. Of the 22 patients upstaged with endosonography, 12 were upstaged with EBUS and 10 were upstaged with EUS.
“Given the significant rate of unsuspected lymph node metastases, combined endosonographic lymph node staging should be routinely performed in staging of NSCLC in high risk patients even in the presence of radiologically normal mediastinal lymph nodes,” Dr. Hegde concluded.
In an interview, Moishe Liberman, MD, a coauthor of the study stated: “Pre-operative lymph node staging of lung cancer has dramatically changed over the last decade due to the availability and improvements in technology in PET, CT, EBUS, and EUS. While imaging (CT and PET) definitely help in staging, these tests are imperfect with significant false-negative rates as seen in our study.
“Minimally invasive, endoscopic techniques can help to significantly decrease these false- negative rates by providing biopsy of the target lymph nodes. Surprise intra-operative findings not accurately picked up by PET and CT should be almost nonexistant in 2017 with aggressive endosonographic pre-operative staging. This ensures that patients who actually benefit from surgery undergo resection and those with higher stage disease get appropriate treatment,” Dr. Liberman added. ■
Study suggests surgery is relatively safe for pediatric AAOCA
It’s relatively safe to surgically treat anomalous aortic origin of a coronary artery in children and adolescents, with essentially all patients cleared for full activity after 3 months, according to a study presented by Carlos M. Mery, MD.
Anomalous aortic origin of a coronary artery (AAOCA) is the second leading cause of sudden cardiac death (SCD) in young people, noted Dr. Mery of Texas Children’s Hospital at the plenary session of the 2017 AATS Centennial meeting.
Surgical indications included an anomalous left coronary artery, ischemic symptoms, a positive nuclear perfusion test (NPT), or high-risk anatomy such as long intramural segment or ostial stenosis identified via CT angiography. Median patient age was 14 years.
Nine of the patients (20%) underwent surgery for an anomalous left coronary artery, with 32 patients (80%) receiving surgical intervention for an anomalous right coronary artery.
A total of 34 surgical procedures (77%) were unroofing of intramural segments, 7 were coronary translocations (16%), and 2 were ostioplasties (4%).
There were no operative deaths. One patient required coronary artery bypass grafting after developing ischemia following a coronary translocation. Minor complications were seen in eight other patients (18%).
One patient presented with a second episode of aborted sudden cardiac death 1 year after unroofing of an anomalous left coronary artery with a short intramural segment, and underwent successful coronary translocation and unroofing of a previously identified myocardial bridge.
At follow-up (median 2 years), 40 patients were asymptomatic (91%), while 4 patients had nonspecific chest pain (9%). Forty-one patients (93%) had returned to full activity, while 3 patients were waiting for their 3-month clearance to return to full activity. ■
[email protected]
It’s relatively safe to surgically treat anomalous aortic origin of a coronary artery in children and adolescents, with essentially all patients cleared for full activity after 3 months, according to a study presented by Carlos M. Mery, MD.
Anomalous aortic origin of a coronary artery (AAOCA) is the second leading cause of sudden cardiac death (SCD) in young people, noted Dr. Mery of Texas Children’s Hospital at the plenary session of the 2017 AATS Centennial meeting.
Surgical indications included an anomalous left coronary artery, ischemic symptoms, a positive nuclear perfusion test (NPT), or high-risk anatomy such as long intramural segment or ostial stenosis identified via CT angiography. Median patient age was 14 years.
Nine of the patients (20%) underwent surgery for an anomalous left coronary artery, with 32 patients (80%) receiving surgical intervention for an anomalous right coronary artery.
A total of 34 surgical procedures (77%) were unroofing of intramural segments, 7 were coronary translocations (16%), and 2 were ostioplasties (4%).
There were no operative deaths. One patient required coronary artery bypass grafting after developing ischemia following a coronary translocation. Minor complications were seen in eight other patients (18%).
One patient presented with a second episode of aborted sudden cardiac death 1 year after unroofing of an anomalous left coronary artery with a short intramural segment, and underwent successful coronary translocation and unroofing of a previously identified myocardial bridge.
At follow-up (median 2 years), 40 patients were asymptomatic (91%), while 4 patients had nonspecific chest pain (9%). Forty-one patients (93%) had returned to full activity, while 3 patients were waiting for their 3-month clearance to return to full activity. ■
[email protected]
It’s relatively safe to surgically treat anomalous aortic origin of a coronary artery in children and adolescents, with essentially all patients cleared for full activity after 3 months, according to a study presented by Carlos M. Mery, MD.
Anomalous aortic origin of a coronary artery (AAOCA) is the second leading cause of sudden cardiac death (SCD) in young people, noted Dr. Mery of Texas Children’s Hospital at the plenary session of the 2017 AATS Centennial meeting.
Surgical indications included an anomalous left coronary artery, ischemic symptoms, a positive nuclear perfusion test (NPT), or high-risk anatomy such as long intramural segment or ostial stenosis identified via CT angiography. Median patient age was 14 years.
Nine of the patients (20%) underwent surgery for an anomalous left coronary artery, with 32 patients (80%) receiving surgical intervention for an anomalous right coronary artery.
A total of 34 surgical procedures (77%) were unroofing of intramural segments, 7 were coronary translocations (16%), and 2 were ostioplasties (4%).
There were no operative deaths. One patient required coronary artery bypass grafting after developing ischemia following a coronary translocation. Minor complications were seen in eight other patients (18%).
One patient presented with a second episode of aborted sudden cardiac death 1 year after unroofing of an anomalous left coronary artery with a short intramural segment, and underwent successful coronary translocation and unroofing of a previously identified myocardial bridge.
At follow-up (median 2 years), 40 patients were asymptomatic (91%), while 4 patients had nonspecific chest pain (9%). Forty-one patients (93%) had returned to full activity, while 3 patients were waiting for their 3-month clearance to return to full activity. ■
[email protected]
High TAVR rates linked to fewer readmissions
WASHINGTON – Hospitals with a higher volume of transcatheter aortic valve replacements (TAVRs) have significantly lower 30-day readmission rates, according to an observational study.
In a study of 129 hospitals, those that performed more than 100 TAVR procedures had a 24% and 25% lower readmission rate compared with hospitals that performed 50 to100 TAVRs (P less than .001) and hospitals that performed fewer that 50 TAVRs (P = .007) respectively (JAMA Cardiol. 2017 May 11. doi: 10.1001/jamacardio.2017.1630).
This finding could have serious financial and medical implications for hospitals that are deciding whether or not to focus on this minimally invasive procedure, according to Sahil Khera, MD, MPH, chief resident and cardiology fellow at New York Medical College, Valhalla, and his colleagues.
“Lower readmission rates at high-volume hospitals substantially reduce health care expenditure,” said Dr. Khera and colleagues. “As new TAVR programs open across the country, these data will guide policymakers to identify targets for optimizing and standardizing TAVR outcomes across hospitals.”
To study the correlation between TAVR procedures and readmission rates, the investigators gathered records on hospitals that performed at least five TAVRs in 2014, which were then categorized into high-, medium-, or low-volume categories, and cross-referenced with the 2014 Nationwide Readmissions Database.
Of the 16,252 TAVR procedures conducted in 2014, 663 (4%), 3,067 (19%), and 12,522 (77%) were performed at low-, medium-, and high-volume hospitals, respectively, according to the investigators.
Patients undergoing these procedures were on average 81 years of age, with an average of four Elixhauser comorbidities, most commonly dyslipidemia (64%), hypertension (80%), heart failure (75%), and known coronary artery disease (69%), with a majority having undergone an endovascular procedure (83%).
However, the researchers found the population of TAVR patients of high volume hospitals were slightly younger, had fewer women, were more likely to be in a higher income household, and were less likely to undergo a transapical procedure than in low volume hospitals, which Dr. Khera and fellow researchers believe may have some impact on their findings.
“Low-volume hospitals were more likely to operate on patients with a higher number of comorbidities compared with high-volume hospitals and were more likely to use the TA approach,” according to investigators, “Transapical TAVR is associated with poorer short- and intermediate-term mortality, increased use of skilled nursing care facilities, longer hospital stays, and readmissions when compared with transfemoral TAVR.”
Overall, there were 2,667 readmissions reported, among which high volume hospitals reported a 30-day readmission rate of 15.6%, while low- and medium-volume hospitals reported similarly higher rates of 19.5% and 19%.
When looking into the causes for these readmissions, the investigators found that 1,619 (61%) were due to noncardiac causes, which appeared in all three hospitals, despite a larger proportion present in low-volume hospitals as opposed to medium and high-volume hospitals (65.6% vs. 60.1% and 60.6%, respectively).
“Infection, respiratory, endocrine/metabolic, renal, and trauma problems were more common in low-volume hospitals,” according to the researchers. “Whereas gastrointestinal and TIA/stroke issues were more common in medium and high volume hospitals.”
While price and length of stay did not differ among the volume categories, the investigators estimate the lower rate of readmissions saved high-volume hospitals approximately $6.5 million.
They found that while the difference of readmissions between hospital classifications narrowed when controlling for experience, the margin was still significant. They admitted, however, that the possibility of greater access to more technologically advanced TAVR in high-volume hospitals may affect the findings.
This study was limited by administrative nature of the database used, which does not make available information such as valve type, patient risk scores, or medications.
One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.
[email protected]
On Twitter @eaztweets
Considering the idea of using readmissions in comparison to rate of TAVR procedures is interesting, the number of confounds are too great to give any kind of accurate representation of medical practice. While the authors of this study do address its limitations, including a learning curve as it relates to the risk of inpatient mortality, the number of adjustments that must be made to account for the additional confounding factors are simply too insurmountable to give an accurate estimate of statistical and clinical importance.
For example, researchers found TAVR readmissions were associated with certain baseline comorbidities, access sites, and complications. However, association does not mean causation and so the categorization of cardiac-related vs. noncardiac-related readmissions must be approached with some caution.
If one were to try to use readmission rates after TAVR to argue for reimbursement of the procedure, one would need to determine a well established, validated reimbursement rate for TAVR readmissions, which has not been done.
Also, the advancing nature of this procedure, combined with a constant focus from hospitals to reduce readmission rates means any baseline for readmissions used would most likely be out of date.
It would be unlikely for investigators to factor in the cause of reduced readmission rates, which could be a factor of increased technology, more experienced physicians, lower-risk patients, or any combination thereof.
Holding TAVR sites accountable for quality of care is of course important, but using readmission rates to determine something like funding is not appropriate when the measurement being used is so complex.
Perhaps a better approach would be to widen access for low volume hospitals to resources that would improve the TAVR processes and encourage using financial incentives.
Evaluations by physical therapists or a similar procedure should be put into place before discharge to assess a patient’s risk of readmission.
Overall, this is a multifaceted issue that would be better helped by promoting TAVR best practices and encouraging hospitals to compare themselves against each other to reduce unnecessary readmissions.
John D. Carroll, MD, is professor of medicine and director of the Cardiac and Vascular Center at the University of Colorado, Denver. He made his remarks in an editorial in JAMA Cardiology ( doi: 10.1001/jamacardio.2017.1650 ).
Considering the idea of using readmissions in comparison to rate of TAVR procedures is interesting, the number of confounds are too great to give any kind of accurate representation of medical practice. While the authors of this study do address its limitations, including a learning curve as it relates to the risk of inpatient mortality, the number of adjustments that must be made to account for the additional confounding factors are simply too insurmountable to give an accurate estimate of statistical and clinical importance.
For example, researchers found TAVR readmissions were associated with certain baseline comorbidities, access sites, and complications. However, association does not mean causation and so the categorization of cardiac-related vs. noncardiac-related readmissions must be approached with some caution.
If one were to try to use readmission rates after TAVR to argue for reimbursement of the procedure, one would need to determine a well established, validated reimbursement rate for TAVR readmissions, which has not been done.
Also, the advancing nature of this procedure, combined with a constant focus from hospitals to reduce readmission rates means any baseline for readmissions used would most likely be out of date.
It would be unlikely for investigators to factor in the cause of reduced readmission rates, which could be a factor of increased technology, more experienced physicians, lower-risk patients, or any combination thereof.
Holding TAVR sites accountable for quality of care is of course important, but using readmission rates to determine something like funding is not appropriate when the measurement being used is so complex.
Perhaps a better approach would be to widen access for low volume hospitals to resources that would improve the TAVR processes and encourage using financial incentives.
Evaluations by physical therapists or a similar procedure should be put into place before discharge to assess a patient’s risk of readmission.
Overall, this is a multifaceted issue that would be better helped by promoting TAVR best practices and encouraging hospitals to compare themselves against each other to reduce unnecessary readmissions.
John D. Carroll, MD, is professor of medicine and director of the Cardiac and Vascular Center at the University of Colorado, Denver. He made his remarks in an editorial in JAMA Cardiology ( doi: 10.1001/jamacardio.2017.1650 ).
Considering the idea of using readmissions in comparison to rate of TAVR procedures is interesting, the number of confounds are too great to give any kind of accurate representation of medical practice. While the authors of this study do address its limitations, including a learning curve as it relates to the risk of inpatient mortality, the number of adjustments that must be made to account for the additional confounding factors are simply too insurmountable to give an accurate estimate of statistical and clinical importance.
For example, researchers found TAVR readmissions were associated with certain baseline comorbidities, access sites, and complications. However, association does not mean causation and so the categorization of cardiac-related vs. noncardiac-related readmissions must be approached with some caution.
If one were to try to use readmission rates after TAVR to argue for reimbursement of the procedure, one would need to determine a well established, validated reimbursement rate for TAVR readmissions, which has not been done.
Also, the advancing nature of this procedure, combined with a constant focus from hospitals to reduce readmission rates means any baseline for readmissions used would most likely be out of date.
It would be unlikely for investigators to factor in the cause of reduced readmission rates, which could be a factor of increased technology, more experienced physicians, lower-risk patients, or any combination thereof.
Holding TAVR sites accountable for quality of care is of course important, but using readmission rates to determine something like funding is not appropriate when the measurement being used is so complex.
Perhaps a better approach would be to widen access for low volume hospitals to resources that would improve the TAVR processes and encourage using financial incentives.
Evaluations by physical therapists or a similar procedure should be put into place before discharge to assess a patient’s risk of readmission.
Overall, this is a multifaceted issue that would be better helped by promoting TAVR best practices and encouraging hospitals to compare themselves against each other to reduce unnecessary readmissions.
John D. Carroll, MD, is professor of medicine and director of the Cardiac and Vascular Center at the University of Colorado, Denver. He made his remarks in an editorial in JAMA Cardiology ( doi: 10.1001/jamacardio.2017.1650 ).
WASHINGTON – Hospitals with a higher volume of transcatheter aortic valve replacements (TAVRs) have significantly lower 30-day readmission rates, according to an observational study.
In a study of 129 hospitals, those that performed more than 100 TAVR procedures had a 24% and 25% lower readmission rate compared with hospitals that performed 50 to100 TAVRs (P less than .001) and hospitals that performed fewer that 50 TAVRs (P = .007) respectively (JAMA Cardiol. 2017 May 11. doi: 10.1001/jamacardio.2017.1630).
This finding could have serious financial and medical implications for hospitals that are deciding whether or not to focus on this minimally invasive procedure, according to Sahil Khera, MD, MPH, chief resident and cardiology fellow at New York Medical College, Valhalla, and his colleagues.
“Lower readmission rates at high-volume hospitals substantially reduce health care expenditure,” said Dr. Khera and colleagues. “As new TAVR programs open across the country, these data will guide policymakers to identify targets for optimizing and standardizing TAVR outcomes across hospitals.”
To study the correlation between TAVR procedures and readmission rates, the investigators gathered records on hospitals that performed at least five TAVRs in 2014, which were then categorized into high-, medium-, or low-volume categories, and cross-referenced with the 2014 Nationwide Readmissions Database.
Of the 16,252 TAVR procedures conducted in 2014, 663 (4%), 3,067 (19%), and 12,522 (77%) were performed at low-, medium-, and high-volume hospitals, respectively, according to the investigators.
Patients undergoing these procedures were on average 81 years of age, with an average of four Elixhauser comorbidities, most commonly dyslipidemia (64%), hypertension (80%), heart failure (75%), and known coronary artery disease (69%), with a majority having undergone an endovascular procedure (83%).
However, the researchers found the population of TAVR patients of high volume hospitals were slightly younger, had fewer women, were more likely to be in a higher income household, and were less likely to undergo a transapical procedure than in low volume hospitals, which Dr. Khera and fellow researchers believe may have some impact on their findings.
“Low-volume hospitals were more likely to operate on patients with a higher number of comorbidities compared with high-volume hospitals and were more likely to use the TA approach,” according to investigators, “Transapical TAVR is associated with poorer short- and intermediate-term mortality, increased use of skilled nursing care facilities, longer hospital stays, and readmissions when compared with transfemoral TAVR.”
Overall, there were 2,667 readmissions reported, among which high volume hospitals reported a 30-day readmission rate of 15.6%, while low- and medium-volume hospitals reported similarly higher rates of 19.5% and 19%.
When looking into the causes for these readmissions, the investigators found that 1,619 (61%) were due to noncardiac causes, which appeared in all three hospitals, despite a larger proportion present in low-volume hospitals as opposed to medium and high-volume hospitals (65.6% vs. 60.1% and 60.6%, respectively).
“Infection, respiratory, endocrine/metabolic, renal, and trauma problems were more common in low-volume hospitals,” according to the researchers. “Whereas gastrointestinal and TIA/stroke issues were more common in medium and high volume hospitals.”
While price and length of stay did not differ among the volume categories, the investigators estimate the lower rate of readmissions saved high-volume hospitals approximately $6.5 million.
They found that while the difference of readmissions between hospital classifications narrowed when controlling for experience, the margin was still significant. They admitted, however, that the possibility of greater access to more technologically advanced TAVR in high-volume hospitals may affect the findings.
This study was limited by administrative nature of the database used, which does not make available information such as valve type, patient risk scores, or medications.
One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.
[email protected]
On Twitter @eaztweets
WASHINGTON – Hospitals with a higher volume of transcatheter aortic valve replacements (TAVRs) have significantly lower 30-day readmission rates, according to an observational study.
In a study of 129 hospitals, those that performed more than 100 TAVR procedures had a 24% and 25% lower readmission rate compared with hospitals that performed 50 to100 TAVRs (P less than .001) and hospitals that performed fewer that 50 TAVRs (P = .007) respectively (JAMA Cardiol. 2017 May 11. doi: 10.1001/jamacardio.2017.1630).
This finding could have serious financial and medical implications for hospitals that are deciding whether or not to focus on this minimally invasive procedure, according to Sahil Khera, MD, MPH, chief resident and cardiology fellow at New York Medical College, Valhalla, and his colleagues.
“Lower readmission rates at high-volume hospitals substantially reduce health care expenditure,” said Dr. Khera and colleagues. “As new TAVR programs open across the country, these data will guide policymakers to identify targets for optimizing and standardizing TAVR outcomes across hospitals.”
To study the correlation between TAVR procedures and readmission rates, the investigators gathered records on hospitals that performed at least five TAVRs in 2014, which were then categorized into high-, medium-, or low-volume categories, and cross-referenced with the 2014 Nationwide Readmissions Database.
Of the 16,252 TAVR procedures conducted in 2014, 663 (4%), 3,067 (19%), and 12,522 (77%) were performed at low-, medium-, and high-volume hospitals, respectively, according to the investigators.
Patients undergoing these procedures were on average 81 years of age, with an average of four Elixhauser comorbidities, most commonly dyslipidemia (64%), hypertension (80%), heart failure (75%), and known coronary artery disease (69%), with a majority having undergone an endovascular procedure (83%).
However, the researchers found the population of TAVR patients of high volume hospitals were slightly younger, had fewer women, were more likely to be in a higher income household, and were less likely to undergo a transapical procedure than in low volume hospitals, which Dr. Khera and fellow researchers believe may have some impact on their findings.
“Low-volume hospitals were more likely to operate on patients with a higher number of comorbidities compared with high-volume hospitals and were more likely to use the TA approach,” according to investigators, “Transapical TAVR is associated with poorer short- and intermediate-term mortality, increased use of skilled nursing care facilities, longer hospital stays, and readmissions when compared with transfemoral TAVR.”
Overall, there were 2,667 readmissions reported, among which high volume hospitals reported a 30-day readmission rate of 15.6%, while low- and medium-volume hospitals reported similarly higher rates of 19.5% and 19%.
When looking into the causes for these readmissions, the investigators found that 1,619 (61%) were due to noncardiac causes, which appeared in all three hospitals, despite a larger proportion present in low-volume hospitals as opposed to medium and high-volume hospitals (65.6% vs. 60.1% and 60.6%, respectively).
“Infection, respiratory, endocrine/metabolic, renal, and trauma problems were more common in low-volume hospitals,” according to the researchers. “Whereas gastrointestinal and TIA/stroke issues were more common in medium and high volume hospitals.”
While price and length of stay did not differ among the volume categories, the investigators estimate the lower rate of readmissions saved high-volume hospitals approximately $6.5 million.
They found that while the difference of readmissions between hospital classifications narrowed when controlling for experience, the margin was still significant. They admitted, however, that the possibility of greater access to more technologically advanced TAVR in high-volume hospitals may affect the findings.
This study was limited by administrative nature of the database used, which does not make available information such as valve type, patient risk scores, or medications.
One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.
[email protected]
On Twitter @eaztweets
FROM JAMA CARDIOLOGY
Key clinical point:
Major finding: Hospitals that performed more than 100 TAVR procedures reported significantly lower 30-day readmission rates, compared with those that performed 50-100 procedures and hospitals that performed less than 50.
Data source: Observational study of 129 hospitals that performed at least five TAVRs in 2015, and documents gathered from the 2014 Nationwide Readmissions Database.
Disclosures: One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.
FDA approves dabrafenib and trametinib for BRAF V600E+ metastatic NSCLC
The FDA also approved a diagnostic, the Oncomine Dx Target Test, a next-generation sequencing test to detect gene mutations or alterations, including BRAF, from a single tissue specimen, the FDA reported in a statement.
The approvals are based on overall response rate (ORR) for the combination in a phase II, nonrandomized, noncomparative, open-label trial of patients with locally confirmed BRAF V600E mutation-positive metastatic NSCLC. The ORR for the combination treatment was 61% (95% confidence interval, 44%-77%) among 36 patients who had received no prior systemic therapy for metastatic NSCLC, and 63% (95% CI, 49%-76%) among 57 patients who had received at least one platinum-based chemotherapy regimen with demonstrated disease progression before enrollment. Those 93 patients were all treated with the combination of dabrafenib (150 mg orally twice daily) and trametinib (2 mg orally once daily).
The ORR was 27% (95% CI, 18%-38%) among a third cohort of 78 patients with previously treated BRAF V600E mutation-positive NSCLC who received single-agent dabrafenib.
The most common adverse reactions were similar to those reported in prior approvals for patients with melanoma, including pyrexia, fatigue, nausea, vomiting, diarrhea, dry skin, decreased appetite, edema, rash, chills, hemorrhage, cough, and dyspnea. The most common grade 3-4 adverse reactions were pyrexia, fatigue, dyspnea, vomiting, rash, hemorrhage, and diarrhea. The most common grade 3-4 laboratory abnormalities were hyponatremia, lymphopenia, anemia, hyperglycemia, neutropenia, leukopenia, hypophosphatemia, and increased alanine aminotransferase. Dabrafenib and trametinib were discontinued for adverse reactions in 18% and 19% of patients, respectively, the FDA said.
Novartis is marketing Dabrafenib as Tafinlar and trametinib as Mekinist.
The recommended doses are dabrafenib 150 mg orally twice daily, approximately 12 hours apart, with trametinib 2 mg orally once daily, following confirmation of BRAF V600E mutation in a tumor specimen by an FDA-approved test.
The FDA also approved a diagnostic, the Oncomine Dx Target Test, a next-generation sequencing test to detect gene mutations or alterations, including BRAF, from a single tissue specimen, the FDA reported in a statement.
The approvals are based on overall response rate (ORR) for the combination in a phase II, nonrandomized, noncomparative, open-label trial of patients with locally confirmed BRAF V600E mutation-positive metastatic NSCLC. The ORR for the combination treatment was 61% (95% confidence interval, 44%-77%) among 36 patients who had received no prior systemic therapy for metastatic NSCLC, and 63% (95% CI, 49%-76%) among 57 patients who had received at least one platinum-based chemotherapy regimen with demonstrated disease progression before enrollment. Those 93 patients were all treated with the combination of dabrafenib (150 mg orally twice daily) and trametinib (2 mg orally once daily).
The ORR was 27% (95% CI, 18%-38%) among a third cohort of 78 patients with previously treated BRAF V600E mutation-positive NSCLC who received single-agent dabrafenib.
The most common adverse reactions were similar to those reported in prior approvals for patients with melanoma, including pyrexia, fatigue, nausea, vomiting, diarrhea, dry skin, decreased appetite, edema, rash, chills, hemorrhage, cough, and dyspnea. The most common grade 3-4 adverse reactions were pyrexia, fatigue, dyspnea, vomiting, rash, hemorrhage, and diarrhea. The most common grade 3-4 laboratory abnormalities were hyponatremia, lymphopenia, anemia, hyperglycemia, neutropenia, leukopenia, hypophosphatemia, and increased alanine aminotransferase. Dabrafenib and trametinib were discontinued for adverse reactions in 18% and 19% of patients, respectively, the FDA said.
Novartis is marketing Dabrafenib as Tafinlar and trametinib as Mekinist.
The recommended doses are dabrafenib 150 mg orally twice daily, approximately 12 hours apart, with trametinib 2 mg orally once daily, following confirmation of BRAF V600E mutation in a tumor specimen by an FDA-approved test.
The FDA also approved a diagnostic, the Oncomine Dx Target Test, a next-generation sequencing test to detect gene mutations or alterations, including BRAF, from a single tissue specimen, the FDA reported in a statement.
The approvals are based on overall response rate (ORR) for the combination in a phase II, nonrandomized, noncomparative, open-label trial of patients with locally confirmed BRAF V600E mutation-positive metastatic NSCLC. The ORR for the combination treatment was 61% (95% confidence interval, 44%-77%) among 36 patients who had received no prior systemic therapy for metastatic NSCLC, and 63% (95% CI, 49%-76%) among 57 patients who had received at least one platinum-based chemotherapy regimen with demonstrated disease progression before enrollment. Those 93 patients were all treated with the combination of dabrafenib (150 mg orally twice daily) and trametinib (2 mg orally once daily).
The ORR was 27% (95% CI, 18%-38%) among a third cohort of 78 patients with previously treated BRAF V600E mutation-positive NSCLC who received single-agent dabrafenib.
The most common adverse reactions were similar to those reported in prior approvals for patients with melanoma, including pyrexia, fatigue, nausea, vomiting, diarrhea, dry skin, decreased appetite, edema, rash, chills, hemorrhage, cough, and dyspnea. The most common grade 3-4 adverse reactions were pyrexia, fatigue, dyspnea, vomiting, rash, hemorrhage, and diarrhea. The most common grade 3-4 laboratory abnormalities were hyponatremia, lymphopenia, anemia, hyperglycemia, neutropenia, leukopenia, hypophosphatemia, and increased alanine aminotransferase. Dabrafenib and trametinib were discontinued for adverse reactions in 18% and 19% of patients, respectively, the FDA said.
Novartis is marketing Dabrafenib as Tafinlar and trametinib as Mekinist.
The recommended doses are dabrafenib 150 mg orally twice daily, approximately 12 hours apart, with trametinib 2 mg orally once daily, following confirmation of BRAF V600E mutation in a tumor specimen by an FDA-approved test.








