User login
Ginger, Cinnamon, Cumin Improve Glycemic Control
TOPLINE:
The spices and aromatic herbs of the Mediterranean diet with significant benefits in improving glycemic health in type 2 diabetes are limited to ginger, cinnamon, black cumin, turmeric, and saffron, with ginger, black cumin, and cinnamon having the strongest effects on fasting glucose, according to a systematic review and meta-analysis of research.
The meta-analysis also evaluated clove, thyme, turmeric, and various other spices and herbs common in the diet but showed no other correlations with glycemic benefits.
METHODOLOGY:
- In the analysis of 77 studies, 45, involving 3050 participants, were included in the meta-analysis and 32 studies in the systematic review.
- The studies’ inclusion criteria included adult patients with type 2 diabetes, with data on fasting glucose and/or A1c and/or , and involving any supplementation with black cumin, clove, , saffron, thyme, ginger, black pepper, , curcumin, cinnamon, basil, and/or oregano.
- The number of studies involving clove, parsley, thyme, black pepper, rosemary, basil, or oregano and their association with glycemic factors in people with type 2 diabetes was insufficient, hence the analysis primarily focused on the remaining five ingredients of cinnamon, curcumin, ginger, black cumin, saffron, and rosemary.
TAKEAWAY:
- However, the most significant decreases in fasting glucose, between 17 mg/dL and 27 mg/dL, occurred after supplementation with black cumin, followed by cinnamon and ginger.
- Notably, only ginger and black cumin were associated with a significant improvement in A1c.
- Only cinnamon and ginger were associated with a significant decrease in insulin values.
- Of the 11 studies including cinnamon in the meta-analysis, 6 reported significant differences in fasting glucose, while 4 had differences in A1c after the supplementation.
- However, ginger was the only component associated with a significant decrease in each of the 3 outcomes examined of fasting glucose, A1c, and insulin.
IN PRACTICE:
“The Mediterranean Diet is the dietary pattern par excellence for managing and preventing metabolic diseases, such as type 2 diabetes,” the authors reported.
“As far as we are aware, this is the first systematic review and meta-analysis aiming to evaluate the effect of aromatic herbs and spices included in the Mediterranean Diet, such as black cumin, clove [and others], on the glycemic profile of individuals with type 2 diabetes,” they added.
“When focusing on HbA1c, only ginger and black cumin demonstrated therapeutic effects,” the authors noted. “However, our meta-analysis highlights ginger as an herb with substantial translational potential for diabetes treatment, impacting all three glycemic parameters.”
“Regarding clove, parsley, thyme, black pepper, rosemary, basil, and oregano, more studies are needed to analyze the effect of these herbs on the glycemic profile in type 2 diabetes subjects,” the authors concluded.
SOURCE:
The study was published on March 7, 2024, in Nutrients. The first author was Maria Carmen Garza, PhD, of the Department of Human Anatomy and Histology, School Medicine, University of Zaragoza, Zaragoza, Spain.
LIMITATIONS:
Despite the results, a variety of other factors can affect fasting glucose levels, including changes in body weight or body mass index, as well as the combination of spice or aromatic herb supplementation with physical activity or lifestyle changes, the authors noted.
Due to the studies’ differences, the determination of effective dosages of the herbs and spices was not possible.
Furthermore, the studies had wide variations in quality, with few studies including adequate statistical analysis.
DISCLOSURES:
The authors had no disclosures to report.
A version of this article appeared on Medscape.com.
TOPLINE:
The spices and aromatic herbs of the Mediterranean diet with significant benefits in improving glycemic health in type 2 diabetes are limited to ginger, cinnamon, black cumin, turmeric, and saffron, with ginger, black cumin, and cinnamon having the strongest effects on fasting glucose, according to a systematic review and meta-analysis of research.
The meta-analysis also evaluated clove, thyme, turmeric, and various other spices and herbs common in the diet but showed no other correlations with glycemic benefits.
METHODOLOGY:
- In the analysis of 77 studies, 45, involving 3050 participants, were included in the meta-analysis and 32 studies in the systematic review.
- The studies’ inclusion criteria included adult patients with type 2 diabetes, with data on fasting glucose and/or A1c and/or , and involving any supplementation with black cumin, clove, , saffron, thyme, ginger, black pepper, , curcumin, cinnamon, basil, and/or oregano.
- The number of studies involving clove, parsley, thyme, black pepper, rosemary, basil, or oregano and their association with glycemic factors in people with type 2 diabetes was insufficient, hence the analysis primarily focused on the remaining five ingredients of cinnamon, curcumin, ginger, black cumin, saffron, and rosemary.
TAKEAWAY:
- However, the most significant decreases in fasting glucose, between 17 mg/dL and 27 mg/dL, occurred after supplementation with black cumin, followed by cinnamon and ginger.
- Notably, only ginger and black cumin were associated with a significant improvement in A1c.
- Only cinnamon and ginger were associated with a significant decrease in insulin values.
- Of the 11 studies including cinnamon in the meta-analysis, 6 reported significant differences in fasting glucose, while 4 had differences in A1c after the supplementation.
- However, ginger was the only component associated with a significant decrease in each of the 3 outcomes examined of fasting glucose, A1c, and insulin.
IN PRACTICE:
“The Mediterranean Diet is the dietary pattern par excellence for managing and preventing metabolic diseases, such as type 2 diabetes,” the authors reported.
“As far as we are aware, this is the first systematic review and meta-analysis aiming to evaluate the effect of aromatic herbs and spices included in the Mediterranean Diet, such as black cumin, clove [and others], on the glycemic profile of individuals with type 2 diabetes,” they added.
“When focusing on HbA1c, only ginger and black cumin demonstrated therapeutic effects,” the authors noted. “However, our meta-analysis highlights ginger as an herb with substantial translational potential for diabetes treatment, impacting all three glycemic parameters.”
“Regarding clove, parsley, thyme, black pepper, rosemary, basil, and oregano, more studies are needed to analyze the effect of these herbs on the glycemic profile in type 2 diabetes subjects,” the authors concluded.
SOURCE:
The study was published on March 7, 2024, in Nutrients. The first author was Maria Carmen Garza, PhD, of the Department of Human Anatomy and Histology, School Medicine, University of Zaragoza, Zaragoza, Spain.
LIMITATIONS:
Despite the results, a variety of other factors can affect fasting glucose levels, including changes in body weight or body mass index, as well as the combination of spice or aromatic herb supplementation with physical activity or lifestyle changes, the authors noted.
Due to the studies’ differences, the determination of effective dosages of the herbs and spices was not possible.
Furthermore, the studies had wide variations in quality, with few studies including adequate statistical analysis.
DISCLOSURES:
The authors had no disclosures to report.
A version of this article appeared on Medscape.com.
TOPLINE:
The spices and aromatic herbs of the Mediterranean diet with significant benefits in improving glycemic health in type 2 diabetes are limited to ginger, cinnamon, black cumin, turmeric, and saffron, with ginger, black cumin, and cinnamon having the strongest effects on fasting glucose, according to a systematic review and meta-analysis of research.
The meta-analysis also evaluated clove, thyme, turmeric, and various other spices and herbs common in the diet but showed no other correlations with glycemic benefits.
METHODOLOGY:
- In the analysis of 77 studies, 45, involving 3050 participants, were included in the meta-analysis and 32 studies in the systematic review.
- The studies’ inclusion criteria included adult patients with type 2 diabetes, with data on fasting glucose and/or A1c and/or , and involving any supplementation with black cumin, clove, , saffron, thyme, ginger, black pepper, , curcumin, cinnamon, basil, and/or oregano.
- The number of studies involving clove, parsley, thyme, black pepper, rosemary, basil, or oregano and their association with glycemic factors in people with type 2 diabetes was insufficient, hence the analysis primarily focused on the remaining five ingredients of cinnamon, curcumin, ginger, black cumin, saffron, and rosemary.
TAKEAWAY:
- However, the most significant decreases in fasting glucose, between 17 mg/dL and 27 mg/dL, occurred after supplementation with black cumin, followed by cinnamon and ginger.
- Notably, only ginger and black cumin were associated with a significant improvement in A1c.
- Only cinnamon and ginger were associated with a significant decrease in insulin values.
- Of the 11 studies including cinnamon in the meta-analysis, 6 reported significant differences in fasting glucose, while 4 had differences in A1c after the supplementation.
- However, ginger was the only component associated with a significant decrease in each of the 3 outcomes examined of fasting glucose, A1c, and insulin.
IN PRACTICE:
“The Mediterranean Diet is the dietary pattern par excellence for managing and preventing metabolic diseases, such as type 2 diabetes,” the authors reported.
“As far as we are aware, this is the first systematic review and meta-analysis aiming to evaluate the effect of aromatic herbs and spices included in the Mediterranean Diet, such as black cumin, clove [and others], on the glycemic profile of individuals with type 2 diabetes,” they added.
“When focusing on HbA1c, only ginger and black cumin demonstrated therapeutic effects,” the authors noted. “However, our meta-analysis highlights ginger as an herb with substantial translational potential for diabetes treatment, impacting all three glycemic parameters.”
“Regarding clove, parsley, thyme, black pepper, rosemary, basil, and oregano, more studies are needed to analyze the effect of these herbs on the glycemic profile in type 2 diabetes subjects,” the authors concluded.
SOURCE:
The study was published on March 7, 2024, in Nutrients. The first author was Maria Carmen Garza, PhD, of the Department of Human Anatomy and Histology, School Medicine, University of Zaragoza, Zaragoza, Spain.
LIMITATIONS:
Despite the results, a variety of other factors can affect fasting glucose levels, including changes in body weight or body mass index, as well as the combination of spice or aromatic herb supplementation with physical activity or lifestyle changes, the authors noted.
Due to the studies’ differences, the determination of effective dosages of the herbs and spices was not possible.
Furthermore, the studies had wide variations in quality, with few studies including adequate statistical analysis.
DISCLOSURES:
The authors had no disclosures to report.
A version of this article appeared on Medscape.com.
Can Treating Depression Mitigate CVD Risk?
TOPLINE:
Depression is linked to a significantly increased risk for cardiovascular disease (CVD), particularly in women, new data from a large retrospective cohort study show.
METHODOLOGY:
- Researchers analyzed health insurance claims from more than 4 million Japanese patients filed between 2005 and 2022.
- Participants were 18-75 (median age, 44) without a history of CVD or stroke, heart failure, or atrial fibrillation.
- Investigators followed participants for a mean period of 2.5-3.5 years to observe the number of CVD events in those who had a diagnosis of depression.
- During the follow-up period, there were 119,000 CVD events in men (14 per 10,000 person-years) and 61,800 CVD events in women (111 per 10,000 person-years).
TAKEAWAY:
- Compared with women without depression, those with depression had a 64% higher risk for CVD (hazard ratio [HR], 1.64), while men with depression had a 39% higher risk for CVD vs their counterparts without depression (HR, 1.39; P < .001).
- This association was significant even after controlling for various factors such as body mass index, diabetes, smoking, alcohol consumption, and physical inactivity.
- Investigators offered several theories about the increased risk for CVD in women with depression, including how depression during hormonal shifts can contribute to a greater impact on cardiovascular health.
IN PRACTICE:
“Healthcare professionals must recognize the important role of depression in the development of CVD and emphasize the importance of a comprehensive, patient-centered approach to its prevention and management,” study author Hidehiro Kaneko, MD, said in a press release. “Assessing the risk of CVD in depressed patients and treating and preventing depression may lead to a decrease of CVD cases.”
SOURCE:
Keitaro Senoo, MD, of the Kyoto Prefectural University of Medicine, Kyoto, Japan, led the study, which was published online on March 12 in JACC: Asia.
LIMITATIONS:
The study is observational, so causality between depression and subsequent CVD events cannot be established. In addition, depression severity is unknown.
DISCLOSURES:
The study was funded by the Ministry of Health, Labour, and Welfare, Japan, and the Ministry of Education, Culture, Sports, Science, and Technology, Japan. There were no disclosures reported.
A version of this article appeared on Medscape.com.
TOPLINE:
Depression is linked to a significantly increased risk for cardiovascular disease (CVD), particularly in women, new data from a large retrospective cohort study show.
METHODOLOGY:
- Researchers analyzed health insurance claims from more than 4 million Japanese patients filed between 2005 and 2022.
- Participants were 18-75 (median age, 44) without a history of CVD or stroke, heart failure, or atrial fibrillation.
- Investigators followed participants for a mean period of 2.5-3.5 years to observe the number of CVD events in those who had a diagnosis of depression.
- During the follow-up period, there were 119,000 CVD events in men (14 per 10,000 person-years) and 61,800 CVD events in women (111 per 10,000 person-years).
TAKEAWAY:
- Compared with women without depression, those with depression had a 64% higher risk for CVD (hazard ratio [HR], 1.64), while men with depression had a 39% higher risk for CVD vs their counterparts without depression (HR, 1.39; P < .001).
- This association was significant even after controlling for various factors such as body mass index, diabetes, smoking, alcohol consumption, and physical inactivity.
- Investigators offered several theories about the increased risk for CVD in women with depression, including how depression during hormonal shifts can contribute to a greater impact on cardiovascular health.
IN PRACTICE:
“Healthcare professionals must recognize the important role of depression in the development of CVD and emphasize the importance of a comprehensive, patient-centered approach to its prevention and management,” study author Hidehiro Kaneko, MD, said in a press release. “Assessing the risk of CVD in depressed patients and treating and preventing depression may lead to a decrease of CVD cases.”
SOURCE:
Keitaro Senoo, MD, of the Kyoto Prefectural University of Medicine, Kyoto, Japan, led the study, which was published online on March 12 in JACC: Asia.
LIMITATIONS:
The study is observational, so causality between depression and subsequent CVD events cannot be established. In addition, depression severity is unknown.
DISCLOSURES:
The study was funded by the Ministry of Health, Labour, and Welfare, Japan, and the Ministry of Education, Culture, Sports, Science, and Technology, Japan. There were no disclosures reported.
A version of this article appeared on Medscape.com.
TOPLINE:
Depression is linked to a significantly increased risk for cardiovascular disease (CVD), particularly in women, new data from a large retrospective cohort study show.
METHODOLOGY:
- Researchers analyzed health insurance claims from more than 4 million Japanese patients filed between 2005 and 2022.
- Participants were 18-75 (median age, 44) without a history of CVD or stroke, heart failure, or atrial fibrillation.
- Investigators followed participants for a mean period of 2.5-3.5 years to observe the number of CVD events in those who had a diagnosis of depression.
- During the follow-up period, there were 119,000 CVD events in men (14 per 10,000 person-years) and 61,800 CVD events in women (111 per 10,000 person-years).
TAKEAWAY:
- Compared with women without depression, those with depression had a 64% higher risk for CVD (hazard ratio [HR], 1.64), while men with depression had a 39% higher risk for CVD vs their counterparts without depression (HR, 1.39; P < .001).
- This association was significant even after controlling for various factors such as body mass index, diabetes, smoking, alcohol consumption, and physical inactivity.
- Investigators offered several theories about the increased risk for CVD in women with depression, including how depression during hormonal shifts can contribute to a greater impact on cardiovascular health.
IN PRACTICE:
“Healthcare professionals must recognize the important role of depression in the development of CVD and emphasize the importance of a comprehensive, patient-centered approach to its prevention and management,” study author Hidehiro Kaneko, MD, said in a press release. “Assessing the risk of CVD in depressed patients and treating and preventing depression may lead to a decrease of CVD cases.”
SOURCE:
Keitaro Senoo, MD, of the Kyoto Prefectural University of Medicine, Kyoto, Japan, led the study, which was published online on March 12 in JACC: Asia.
LIMITATIONS:
The study is observational, so causality between depression and subsequent CVD events cannot be established. In addition, depression severity is unknown.
DISCLOSURES:
The study was funded by the Ministry of Health, Labour, and Welfare, Japan, and the Ministry of Education, Culture, Sports, Science, and Technology, Japan. There were no disclosures reported.
A version of this article appeared on Medscape.com.
When the Next Big Thing Falls Short
Recently, Acadia Pharmaceuticals announced it was stopping trials on Nuplazid for indications outside of Parkinson’s disease psychosis.
I was impressed with what I saw in my office. Although I know there’s some controversy over the drug, the majority of studies do show efficacy, and in my little practice I clearly noticed improvements in patients with Parkinson’s disease who’d previously failed the more standard agents (note - I have no financial affiliation with Acadia Pharmaceuticals).
So, as a lay-neurologist, I expected the drug to work for other kinds of psychosis, particularly Alzheimer’s disease. All of us in practice know how much we need new options for that.
But when the clinical trials came, the drug didn’t work. It didn’t work for schizophrenia, either, Finally, Acadia threw in the towel and gave up.
I have no idea what happened. I’m sure others are wondering the same thing. On paper, I’d have thought it would work for Alzheimer’s psychosis, but in the real world it didn’t.
Is psychosis between the two disorders that different, with different neurotransmitter causes? Are the benefits in my patients with Parkinson’s disease really just from my own selection bias? Or is there just a lot we still don’t know?
Look at the graveyard full of amyloid-targeting drugs. Yeah, I know Leqembi is out there, and donanemab is in the wings, but are they anywhere near as good as we thought they’d be? Not at all.
At the same time, we’ve been waiting for the BTK drugs (not to be confused with a Korean pop band) for multiple sclerosis. They sounded like they were the Next Big Thing.
They may be, but recent data on one of them, evobrutinib, was less than encouraging. Of course, that shouldn’t extrapolate to the group as a whole, but it does leave you wondering why.
Medicine is always improving, but it’s also still a trial-and-error process. Just because something should work doesn’t mean it will, and it may be years before we know why.
It’s just a reminder that, here in 2024, we still have a lot to learn.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, Acadia Pharmaceuticals announced it was stopping trials on Nuplazid for indications outside of Parkinson’s disease psychosis.
I was impressed with what I saw in my office. Although I know there’s some controversy over the drug, the majority of studies do show efficacy, and in my little practice I clearly noticed improvements in patients with Parkinson’s disease who’d previously failed the more standard agents (note - I have no financial affiliation with Acadia Pharmaceuticals).
So, as a lay-neurologist, I expected the drug to work for other kinds of psychosis, particularly Alzheimer’s disease. All of us in practice know how much we need new options for that.
But when the clinical trials came, the drug didn’t work. It didn’t work for schizophrenia, either, Finally, Acadia threw in the towel and gave up.
I have no idea what happened. I’m sure others are wondering the same thing. On paper, I’d have thought it would work for Alzheimer’s psychosis, but in the real world it didn’t.
Is psychosis between the two disorders that different, with different neurotransmitter causes? Are the benefits in my patients with Parkinson’s disease really just from my own selection bias? Or is there just a lot we still don’t know?
Look at the graveyard full of amyloid-targeting drugs. Yeah, I know Leqembi is out there, and donanemab is in the wings, but are they anywhere near as good as we thought they’d be? Not at all.
At the same time, we’ve been waiting for the BTK drugs (not to be confused with a Korean pop band) for multiple sclerosis. They sounded like they were the Next Big Thing.
They may be, but recent data on one of them, evobrutinib, was less than encouraging. Of course, that shouldn’t extrapolate to the group as a whole, but it does leave you wondering why.
Medicine is always improving, but it’s also still a trial-and-error process. Just because something should work doesn’t mean it will, and it may be years before we know why.
It’s just a reminder that, here in 2024, we still have a lot to learn.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, Acadia Pharmaceuticals announced it was stopping trials on Nuplazid for indications outside of Parkinson’s disease psychosis.
I was impressed with what I saw in my office. Although I know there’s some controversy over the drug, the majority of studies do show efficacy, and in my little practice I clearly noticed improvements in patients with Parkinson’s disease who’d previously failed the more standard agents (note - I have no financial affiliation with Acadia Pharmaceuticals).
So, as a lay-neurologist, I expected the drug to work for other kinds of psychosis, particularly Alzheimer’s disease. All of us in practice know how much we need new options for that.
But when the clinical trials came, the drug didn’t work. It didn’t work for schizophrenia, either, Finally, Acadia threw in the towel and gave up.
I have no idea what happened. I’m sure others are wondering the same thing. On paper, I’d have thought it would work for Alzheimer’s psychosis, but in the real world it didn’t.
Is psychosis between the two disorders that different, with different neurotransmitter causes? Are the benefits in my patients with Parkinson’s disease really just from my own selection bias? Or is there just a lot we still don’t know?
Look at the graveyard full of amyloid-targeting drugs. Yeah, I know Leqembi is out there, and donanemab is in the wings, but are they anywhere near as good as we thought they’d be? Not at all.
At the same time, we’ve been waiting for the BTK drugs (not to be confused with a Korean pop band) for multiple sclerosis. They sounded like they were the Next Big Thing.
They may be, but recent data on one of them, evobrutinib, was less than encouraging. Of course, that shouldn’t extrapolate to the group as a whole, but it does leave you wondering why.
Medicine is always improving, but it’s also still a trial-and-error process. Just because something should work doesn’t mean it will, and it may be years before we know why.
It’s just a reminder that, here in 2024, we still have a lot to learn.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Why a New Inhalable Lung Cancer Treatment Is So Promising
Cells in the human body chat with each other all the time. One major way they communicate is by releasing tiny spheres called exosomes. These carry fats, proteins, and genetic material that help regulate everything from pregnancy and immune responses to heart health and kidney function.
“Exosomes work like text messages between cells , sending and receiving information,” said lead researcher Ke Cheng, PhD, professor of biomedical engineering at Columbia. “The significance of this study is that exosomes can bring mRNA-based treatment to lung cancer cells locally, unlike systemic chemotherapy that can have side effects throughout the body. And inhalation is totally noninvasive. You don’t need a nurse to use an IV needle to pierce your skin.”
Dr. Cheng expects a human trial could launch within 5 years. For now, his study is attracting attention because it marks an advance in three areas of intense interest by researchers and biotech companies alike: Therapeutic uses of exosomes, inhalable treatments for lung conditions, and the safe delivery of powerful interleukin-12 (IL-12) immunotherapy.
Inside the Study
Dr. Cheng, who has been developing exosome and stem cell therapies for more than 15 years, and his lab team focused on lung cancer because the disease, often detected in later stages, “has a huge mortality rate,” he said. “Therapies have been suboptimal and leave the organ so damaged.”
He wanted to explore new alternatives to systemic treatments. Most are given intravenously, but Dr. Cheng thinks exosomes — also called extracellular vesicles (EVs) — could change that.
“One of the advantages of exosomes is that they are naturally secreted by the body or cultured cells,” he noted. “They have low toxicity and have multiple ways of getting their message into cells.”
The scientists borrowed an approach that captured public attention during the pandemic: Using messenger RNA, which directs cells to make proteins for tasks — including boosting immune response.
IL-12 has shown promise against cancer for decades, but early human trials triggered serious side effects and several deaths. Researchers are now trying new delivery methods that target tumor cells without affecting healthy tissue. Dr. Cheng’s team took a new approach, inserting mRNA for IL-12 into exosomes.
One aim of the study was to compare the effectiveness of inhaled exosomes vs inhaled liposomes, engineered fat droplets also under investigation as drug carriers. The team’s question: Which would work better at introducing IL-12 to the lungs to affect cancer, without triggering side effects?
After lab mice inhaled the particles through the nose, the researchers found that exosomes delivered more mRNA into cancer cells in the lungs and fought lung cancer with few side effects. Three days after treatment, researchers saw an influx of cancer-fighting T cells within tumors — with higher levels for exosome-based treatment. Plus, the exosomes led to more cancer-destroying nature killer cells and more monocytes, a sign of immune-system activation.
Researchers also found the treatment acted as a vaccine, training the immune system to battle newly introduced cancers. Little of the exosome-delivered drug escaped into the bloodstream, and the study found minimal side effects. Inhalation didn’t affect normal breathing, Dr. Cheng added.
The study’s use of inhaled exosomes makes it significant, said Raghu Kalluri, MD, PhD, professor and chair of the Department of Cancer Biology at MD Anderson Cancer Center. “This is an interesting study that explores the inhalable delivery of engineered EVs for the treatment of lung cancer and offers insights into focused delivery of EV-based drugs…with implications for diseases beyond cancer,” he said. Dr. Kalluri is also an exosome researcher.
New Frontiers
Once seen as a “quirky biological phenomenon” or just cellular trash, exosomes are now the subject of intense medical research for their potential as drug carriers, as treatments in their own right for everything from wound healing and pneumonia to heart attacks and bowel disorders, and as measurable biological markers that could lead to new tests for cancer and other conditions. One exosome-based prostate cancer test, the ExoDx Prostate Test, is already on the market.
The explosion in exosome research — the number of published studies has grown from just a handful in the early 1980s to more than 9000 — spotlights a particular focus on cancer. According to a 2021 paper in Annals of Oncology, clinical trials for exosomes in cancer treatments and tests far out-paces those for diabetes, heart disease, or neurologic conditions. Currently, 52 clinical trials using exosomes in cancer diagnosis or treatment have been completed, are underway, or are looking for participants, according to clinicaltrials.gov.
Dr. Cheng’s approach could also be used to deliver other drugs to the lungs and other organs via inhalation. “We’re testing inhalation for a different type of lung disease, acute lung injury,” Dr. Cheng said. Other potential targets include lung disorders like pulmonary hypertension. Inhaled exosomes could potentially reach the brain via the olfactory bulb or the heart as it receives oxygenated blood from the lungs.
Breathing in Medicine
So far, inhalable cancer treatments are not available outside research studies in the United States or Europe , said Remi Rosiere, PhD, a lecturer at the Université libre de Bruxelles in Brussels, Belgium, and chief scientific officer of InhaTarget Therapeutics, a company developing its own inhaled treatments for severe respiratory diseases. “Oncologists are very interested,” he said. “If you concentrate the drug on the tumor site, you can avoid distribution to the body.”
Early research into inhalable chemotherapy began in the 1960s but was unsuccessful because breathing equipment dispersed toxic cancer drugs into the air or delivered only small amounts to the lungs, he said.
New delivery techniques aim to change that. Dr. Rosiere’s company is starting a human trial of a dry powder inhaler with the chemotherapy drug cisplatin for lung cancer. Also in the pipeline is an immunotherapy treatment for lung cancer inserted in lipid nanoparticles, which are tiny fat particles similar to liposomes.
He said Dr. Cheng’s study shows the advantages of sending in exosomes. “The data are very persuasive,” Dr. Rosier said of the study. “Exosomes have a good safety profile and are able to remain in the lung for quite a long time. This prolongs exposure to the drug for greater effectiveness, without causing toxicities.”
Getting from a mouse study to a human trial will take time. “You need to understand this is very early stage,” Dr. Rosiere added. “There will be many challenges to overcome.”
One is purely practical: If the drug approaches human trials, he said, regulators will ask whether the exosomes can be produced in large quantities to meet the huge demand for new lung cancer treatments. “Lung cancer is the number one fatal cancer in the world,” Dr. Rosiere said.
A New Route for ‘Powerful’ Cancer Treatment
Meanwhile, the Columbia University study showed that inhalable exosomes are a unique delivery method for IL-12 — and could help solve a major problem that’s plagued this promising cancer treatment for decades.
Called “one of the most powerful immunotherapy agents ever discovered” in a 2022 literature review, IL-12 showed serious side effects that stalled research in the 1980s , sparking an ongoing search for new delivery methods that continues today. In 2022 and 2023, Big Pharma companies including AstraZenca, Moderna, and Bristol Myers Squib reduced their involvement with IL-12 treatment research, leaving the field open to smaller biotech companies working on a variety of drug-delivery approaches that could make IL-12 safe and effective in humans.
These include injecting it directly into tumors, encasing it in various types of particles, masking the drug so it is activated only in cancer cells, and using IL-12 mRNA, which essentially turns tumor cells into IL-12–producing factories. Another IL-12 mRNA drug, from Pittsburgh-based Krystal Biotech, received a fast-track designation from the US Food and Drug Administration in February 2024 for an inhaled lung cancer treatment that packages mRNA for IL-12 and IL-2 inside an engineered virus.
And of course, there is Dr. Cheng’s inhalable treatment, culminating decades of work across three burgeoning fields.
A version of this article appeared on Medscape.com.
Cells in the human body chat with each other all the time. One major way they communicate is by releasing tiny spheres called exosomes. These carry fats, proteins, and genetic material that help regulate everything from pregnancy and immune responses to heart health and kidney function.
“Exosomes work like text messages between cells , sending and receiving information,” said lead researcher Ke Cheng, PhD, professor of biomedical engineering at Columbia. “The significance of this study is that exosomes can bring mRNA-based treatment to lung cancer cells locally, unlike systemic chemotherapy that can have side effects throughout the body. And inhalation is totally noninvasive. You don’t need a nurse to use an IV needle to pierce your skin.”
Dr. Cheng expects a human trial could launch within 5 years. For now, his study is attracting attention because it marks an advance in three areas of intense interest by researchers and biotech companies alike: Therapeutic uses of exosomes, inhalable treatments for lung conditions, and the safe delivery of powerful interleukin-12 (IL-12) immunotherapy.
Inside the Study
Dr. Cheng, who has been developing exosome and stem cell therapies for more than 15 years, and his lab team focused on lung cancer because the disease, often detected in later stages, “has a huge mortality rate,” he said. “Therapies have been suboptimal and leave the organ so damaged.”
He wanted to explore new alternatives to systemic treatments. Most are given intravenously, but Dr. Cheng thinks exosomes — also called extracellular vesicles (EVs) — could change that.
“One of the advantages of exosomes is that they are naturally secreted by the body or cultured cells,” he noted. “They have low toxicity and have multiple ways of getting their message into cells.”
The scientists borrowed an approach that captured public attention during the pandemic: Using messenger RNA, which directs cells to make proteins for tasks — including boosting immune response.
IL-12 has shown promise against cancer for decades, but early human trials triggered serious side effects and several deaths. Researchers are now trying new delivery methods that target tumor cells without affecting healthy tissue. Dr. Cheng’s team took a new approach, inserting mRNA for IL-12 into exosomes.
One aim of the study was to compare the effectiveness of inhaled exosomes vs inhaled liposomes, engineered fat droplets also under investigation as drug carriers. The team’s question: Which would work better at introducing IL-12 to the lungs to affect cancer, without triggering side effects?
After lab mice inhaled the particles through the nose, the researchers found that exosomes delivered more mRNA into cancer cells in the lungs and fought lung cancer with few side effects. Three days after treatment, researchers saw an influx of cancer-fighting T cells within tumors — with higher levels for exosome-based treatment. Plus, the exosomes led to more cancer-destroying nature killer cells and more monocytes, a sign of immune-system activation.
Researchers also found the treatment acted as a vaccine, training the immune system to battle newly introduced cancers. Little of the exosome-delivered drug escaped into the bloodstream, and the study found minimal side effects. Inhalation didn’t affect normal breathing, Dr. Cheng added.
The study’s use of inhaled exosomes makes it significant, said Raghu Kalluri, MD, PhD, professor and chair of the Department of Cancer Biology at MD Anderson Cancer Center. “This is an interesting study that explores the inhalable delivery of engineered EVs for the treatment of lung cancer and offers insights into focused delivery of EV-based drugs…with implications for diseases beyond cancer,” he said. Dr. Kalluri is also an exosome researcher.
New Frontiers
Once seen as a “quirky biological phenomenon” or just cellular trash, exosomes are now the subject of intense medical research for their potential as drug carriers, as treatments in their own right for everything from wound healing and pneumonia to heart attacks and bowel disorders, and as measurable biological markers that could lead to new tests for cancer and other conditions. One exosome-based prostate cancer test, the ExoDx Prostate Test, is already on the market.
The explosion in exosome research — the number of published studies has grown from just a handful in the early 1980s to more than 9000 — spotlights a particular focus on cancer. According to a 2021 paper in Annals of Oncology, clinical trials for exosomes in cancer treatments and tests far out-paces those for diabetes, heart disease, or neurologic conditions. Currently, 52 clinical trials using exosomes in cancer diagnosis or treatment have been completed, are underway, or are looking for participants, according to clinicaltrials.gov.
Dr. Cheng’s approach could also be used to deliver other drugs to the lungs and other organs via inhalation. “We’re testing inhalation for a different type of lung disease, acute lung injury,” Dr. Cheng said. Other potential targets include lung disorders like pulmonary hypertension. Inhaled exosomes could potentially reach the brain via the olfactory bulb or the heart as it receives oxygenated blood from the lungs.
Breathing in Medicine
So far, inhalable cancer treatments are not available outside research studies in the United States or Europe , said Remi Rosiere, PhD, a lecturer at the Université libre de Bruxelles in Brussels, Belgium, and chief scientific officer of InhaTarget Therapeutics, a company developing its own inhaled treatments for severe respiratory diseases. “Oncologists are very interested,” he said. “If you concentrate the drug on the tumor site, you can avoid distribution to the body.”
Early research into inhalable chemotherapy began in the 1960s but was unsuccessful because breathing equipment dispersed toxic cancer drugs into the air or delivered only small amounts to the lungs, he said.
New delivery techniques aim to change that. Dr. Rosiere’s company is starting a human trial of a dry powder inhaler with the chemotherapy drug cisplatin for lung cancer. Also in the pipeline is an immunotherapy treatment for lung cancer inserted in lipid nanoparticles, which are tiny fat particles similar to liposomes.
He said Dr. Cheng’s study shows the advantages of sending in exosomes. “The data are very persuasive,” Dr. Rosier said of the study. “Exosomes have a good safety profile and are able to remain in the lung for quite a long time. This prolongs exposure to the drug for greater effectiveness, without causing toxicities.”
Getting from a mouse study to a human trial will take time. “You need to understand this is very early stage,” Dr. Rosiere added. “There will be many challenges to overcome.”
One is purely practical: If the drug approaches human trials, he said, regulators will ask whether the exosomes can be produced in large quantities to meet the huge demand for new lung cancer treatments. “Lung cancer is the number one fatal cancer in the world,” Dr. Rosiere said.
A New Route for ‘Powerful’ Cancer Treatment
Meanwhile, the Columbia University study showed that inhalable exosomes are a unique delivery method for IL-12 — and could help solve a major problem that’s plagued this promising cancer treatment for decades.
Called “one of the most powerful immunotherapy agents ever discovered” in a 2022 literature review, IL-12 showed serious side effects that stalled research in the 1980s , sparking an ongoing search for new delivery methods that continues today. In 2022 and 2023, Big Pharma companies including AstraZenca, Moderna, and Bristol Myers Squib reduced their involvement with IL-12 treatment research, leaving the field open to smaller biotech companies working on a variety of drug-delivery approaches that could make IL-12 safe and effective in humans.
These include injecting it directly into tumors, encasing it in various types of particles, masking the drug so it is activated only in cancer cells, and using IL-12 mRNA, which essentially turns tumor cells into IL-12–producing factories. Another IL-12 mRNA drug, from Pittsburgh-based Krystal Biotech, received a fast-track designation from the US Food and Drug Administration in February 2024 for an inhaled lung cancer treatment that packages mRNA for IL-12 and IL-2 inside an engineered virus.
And of course, there is Dr. Cheng’s inhalable treatment, culminating decades of work across three burgeoning fields.
A version of this article appeared on Medscape.com.
Cells in the human body chat with each other all the time. One major way they communicate is by releasing tiny spheres called exosomes. These carry fats, proteins, and genetic material that help regulate everything from pregnancy and immune responses to heart health and kidney function.
“Exosomes work like text messages between cells , sending and receiving information,” said lead researcher Ke Cheng, PhD, professor of biomedical engineering at Columbia. “The significance of this study is that exosomes can bring mRNA-based treatment to lung cancer cells locally, unlike systemic chemotherapy that can have side effects throughout the body. And inhalation is totally noninvasive. You don’t need a nurse to use an IV needle to pierce your skin.”
Dr. Cheng expects a human trial could launch within 5 years. For now, his study is attracting attention because it marks an advance in three areas of intense interest by researchers and biotech companies alike: Therapeutic uses of exosomes, inhalable treatments for lung conditions, and the safe delivery of powerful interleukin-12 (IL-12) immunotherapy.
Inside the Study
Dr. Cheng, who has been developing exosome and stem cell therapies for more than 15 years, and his lab team focused on lung cancer because the disease, often detected in later stages, “has a huge mortality rate,” he said. “Therapies have been suboptimal and leave the organ so damaged.”
He wanted to explore new alternatives to systemic treatments. Most are given intravenously, but Dr. Cheng thinks exosomes — also called extracellular vesicles (EVs) — could change that.
“One of the advantages of exosomes is that they are naturally secreted by the body or cultured cells,” he noted. “They have low toxicity and have multiple ways of getting their message into cells.”
The scientists borrowed an approach that captured public attention during the pandemic: Using messenger RNA, which directs cells to make proteins for tasks — including boosting immune response.
IL-12 has shown promise against cancer for decades, but early human trials triggered serious side effects and several deaths. Researchers are now trying new delivery methods that target tumor cells without affecting healthy tissue. Dr. Cheng’s team took a new approach, inserting mRNA for IL-12 into exosomes.
One aim of the study was to compare the effectiveness of inhaled exosomes vs inhaled liposomes, engineered fat droplets also under investigation as drug carriers. The team’s question: Which would work better at introducing IL-12 to the lungs to affect cancer, without triggering side effects?
After lab mice inhaled the particles through the nose, the researchers found that exosomes delivered more mRNA into cancer cells in the lungs and fought lung cancer with few side effects. Three days after treatment, researchers saw an influx of cancer-fighting T cells within tumors — with higher levels for exosome-based treatment. Plus, the exosomes led to more cancer-destroying nature killer cells and more monocytes, a sign of immune-system activation.
Researchers also found the treatment acted as a vaccine, training the immune system to battle newly introduced cancers. Little of the exosome-delivered drug escaped into the bloodstream, and the study found minimal side effects. Inhalation didn’t affect normal breathing, Dr. Cheng added.
The study’s use of inhaled exosomes makes it significant, said Raghu Kalluri, MD, PhD, professor and chair of the Department of Cancer Biology at MD Anderson Cancer Center. “This is an interesting study that explores the inhalable delivery of engineered EVs for the treatment of lung cancer and offers insights into focused delivery of EV-based drugs…with implications for diseases beyond cancer,” he said. Dr. Kalluri is also an exosome researcher.
New Frontiers
Once seen as a “quirky biological phenomenon” or just cellular trash, exosomes are now the subject of intense medical research for their potential as drug carriers, as treatments in their own right for everything from wound healing and pneumonia to heart attacks and bowel disorders, and as measurable biological markers that could lead to new tests for cancer and other conditions. One exosome-based prostate cancer test, the ExoDx Prostate Test, is already on the market.
The explosion in exosome research — the number of published studies has grown from just a handful in the early 1980s to more than 9000 — spotlights a particular focus on cancer. According to a 2021 paper in Annals of Oncology, clinical trials for exosomes in cancer treatments and tests far out-paces those for diabetes, heart disease, or neurologic conditions. Currently, 52 clinical trials using exosomes in cancer diagnosis or treatment have been completed, are underway, or are looking for participants, according to clinicaltrials.gov.
Dr. Cheng’s approach could also be used to deliver other drugs to the lungs and other organs via inhalation. “We’re testing inhalation for a different type of lung disease, acute lung injury,” Dr. Cheng said. Other potential targets include lung disorders like pulmonary hypertension. Inhaled exosomes could potentially reach the brain via the olfactory bulb or the heart as it receives oxygenated blood from the lungs.
Breathing in Medicine
So far, inhalable cancer treatments are not available outside research studies in the United States or Europe , said Remi Rosiere, PhD, a lecturer at the Université libre de Bruxelles in Brussels, Belgium, and chief scientific officer of InhaTarget Therapeutics, a company developing its own inhaled treatments for severe respiratory diseases. “Oncologists are very interested,” he said. “If you concentrate the drug on the tumor site, you can avoid distribution to the body.”
Early research into inhalable chemotherapy began in the 1960s but was unsuccessful because breathing equipment dispersed toxic cancer drugs into the air or delivered only small amounts to the lungs, he said.
New delivery techniques aim to change that. Dr. Rosiere’s company is starting a human trial of a dry powder inhaler with the chemotherapy drug cisplatin for lung cancer. Also in the pipeline is an immunotherapy treatment for lung cancer inserted in lipid nanoparticles, which are tiny fat particles similar to liposomes.
He said Dr. Cheng’s study shows the advantages of sending in exosomes. “The data are very persuasive,” Dr. Rosier said of the study. “Exosomes have a good safety profile and are able to remain in the lung for quite a long time. This prolongs exposure to the drug for greater effectiveness, without causing toxicities.”
Getting from a mouse study to a human trial will take time. “You need to understand this is very early stage,” Dr. Rosiere added. “There will be many challenges to overcome.”
One is purely practical: If the drug approaches human trials, he said, regulators will ask whether the exosomes can be produced in large quantities to meet the huge demand for new lung cancer treatments. “Lung cancer is the number one fatal cancer in the world,” Dr. Rosiere said.
A New Route for ‘Powerful’ Cancer Treatment
Meanwhile, the Columbia University study showed that inhalable exosomes are a unique delivery method for IL-12 — and could help solve a major problem that’s plagued this promising cancer treatment for decades.
Called “one of the most powerful immunotherapy agents ever discovered” in a 2022 literature review, IL-12 showed serious side effects that stalled research in the 1980s , sparking an ongoing search for new delivery methods that continues today. In 2022 and 2023, Big Pharma companies including AstraZenca, Moderna, and Bristol Myers Squib reduced their involvement with IL-12 treatment research, leaving the field open to smaller biotech companies working on a variety of drug-delivery approaches that could make IL-12 safe and effective in humans.
These include injecting it directly into tumors, encasing it in various types of particles, masking the drug so it is activated only in cancer cells, and using IL-12 mRNA, which essentially turns tumor cells into IL-12–producing factories. Another IL-12 mRNA drug, from Pittsburgh-based Krystal Biotech, received a fast-track designation from the US Food and Drug Administration in February 2024 for an inhaled lung cancer treatment that packages mRNA for IL-12 and IL-2 inside an engineered virus.
And of course, there is Dr. Cheng’s inhalable treatment, culminating decades of work across three burgeoning fields.
A version of this article appeared on Medscape.com.
FROM NATURE NANOTECHNOLOGY
Paid Parental Leave: Impact on Maternal Mental Health and Child Wellbeing
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Topical Roflumilast Effective in 4 Weeks for Atopic Dermatitis in Young Children
SAN DIEGO — Treatment with (AD), according to the results of a phase 3 study reported at the annual meeting of the American Academy of Dermatology.
Among patients treated with roflumilast cream, 0.05%, 25.4% reached the primary endpoint of “clear” or “almost clear” plus a two-grade improvement from baseline at week 4 vs 10.7% among those in the vehicle group (P < .0001) in a phase 3 randomized controlled trial of children. The findings were released in a late-breaker session at the meeting.
Roflumilast cream, 0.3% (Zoryve), is approved by the Food and Drug Administration (FDA) for treating psoriasis in patients 6 years and older, and lower doses are being evaluated for AD: 0.15% for adults and children ages 6 and older, and 0.05% for ages 2-5. Roflumilast is a phosphodiesterase-4 inhibitor. In 2023, the FDA accepted a supplemental drug application from the manufacturer, Arcutis, for roflumilast, 0.15%, for treating AD in patients ages 6 and older, based on the results from two recently published phase 3 trials, INTEGUMENT-1 and INTEGUMENT-2.
The study of younger children, INTEGUMENT-PED, recruited 652 patients aged 2-5 with mild to moderate AD, with a Validated Investigator Global Assessment scale for AD (vlGA-AD) score of 2 or 3, a mean body surface area of 22% overall (range, 3%-82%), and an Eczema Area and Severity Index (EASI) score of at least 5. Of the patients enrolled, 437 were assigned to 0.05% roflumilast cream, applied once a day for 4 weeks (mean age, 3.3 years; 51.6% male; 67.4% White; 15.6% Black; 8.5% Asian; 8.5% other or more than one race; 80.5% not Latino/Hispanic). The remaining 215 children were assigned to vehicle cream and had similar characteristics.
About 52% of the patients in both groups had an inadequate response, intolerance, or contraindications to topical corticosteroids (and about 17% for topical calcineurin inhibitors and about 9% for crisaborole).
The proportions of patients who reached “clear” (0) or “almost clear” (1) on the vlGA-AD scale were 35.4% and 14.6%, respectively, at week 4 (P < .0001) for roflumilast and vehicle, respectively, according to the lead author of the study, Lawrence M. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, who presented the results at the meeting. In addition, 39.4% and 20.6% achieved an EASI-75 (a secondary endpoint), respectively (P < .0001), and itch also improved within 24 hours of starting treatment.
With regard to safety, 29.7% of patients taking roflumilast had treatment-emergent adverse effects (including upper respiratory tract infections in 4.1%) vs 21.9% of those in the vehicle arm (including upper respiratory tract infections in 1.4%). Reports of pain at the administration site were low (1.6% for roflumilast vs 1.9% for vehicle). Only one patient, a 2-year-old girl, had a treatment-emergent serious adverse event. The child, who was in the roflumilast group, had cellulitis involving noneczematous skin and was treated with antibiotics in the hospital for 3 days. The event was not attributed to roflumilast, which was stopped for 5 days, according to Dr. Eichenfield.
In an interview, Fairfield, Connecticut–based dermatologist Brittany Craiglow, MD, who was not involved in the study, said topical roflumilast would be an “important” new treatment because there are still few nonsteroidal options for the treatment of AD in children under 12. “The excellent local tolerability combined with early improvements in itch and skin clearance will make this a particularly attractive option, if approved,” she said.
Dr. Eichenfield disclosed multiple relationships with various drugmakers. He and several other study authors are investigators and/or consultants for Arcutis and received grants/research funding and/or honoraria. Two authors are Arcutis employees. Other disclosure information for the authors was not immediately available. Dr. Craiglow had no disclosures.
A version of this article appeared on Medscape.com .
SAN DIEGO — Treatment with (AD), according to the results of a phase 3 study reported at the annual meeting of the American Academy of Dermatology.
Among patients treated with roflumilast cream, 0.05%, 25.4% reached the primary endpoint of “clear” or “almost clear” plus a two-grade improvement from baseline at week 4 vs 10.7% among those in the vehicle group (P < .0001) in a phase 3 randomized controlled trial of children. The findings were released in a late-breaker session at the meeting.
Roflumilast cream, 0.3% (Zoryve), is approved by the Food and Drug Administration (FDA) for treating psoriasis in patients 6 years and older, and lower doses are being evaluated for AD: 0.15% for adults and children ages 6 and older, and 0.05% for ages 2-5. Roflumilast is a phosphodiesterase-4 inhibitor. In 2023, the FDA accepted a supplemental drug application from the manufacturer, Arcutis, for roflumilast, 0.15%, for treating AD in patients ages 6 and older, based on the results from two recently published phase 3 trials, INTEGUMENT-1 and INTEGUMENT-2.
The study of younger children, INTEGUMENT-PED, recruited 652 patients aged 2-5 with mild to moderate AD, with a Validated Investigator Global Assessment scale for AD (vlGA-AD) score of 2 or 3, a mean body surface area of 22% overall (range, 3%-82%), and an Eczema Area and Severity Index (EASI) score of at least 5. Of the patients enrolled, 437 were assigned to 0.05% roflumilast cream, applied once a day for 4 weeks (mean age, 3.3 years; 51.6% male; 67.4% White; 15.6% Black; 8.5% Asian; 8.5% other or more than one race; 80.5% not Latino/Hispanic). The remaining 215 children were assigned to vehicle cream and had similar characteristics.
About 52% of the patients in both groups had an inadequate response, intolerance, or contraindications to topical corticosteroids (and about 17% for topical calcineurin inhibitors and about 9% for crisaborole).
The proportions of patients who reached “clear” (0) or “almost clear” (1) on the vlGA-AD scale were 35.4% and 14.6%, respectively, at week 4 (P < .0001) for roflumilast and vehicle, respectively, according to the lead author of the study, Lawrence M. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, who presented the results at the meeting. In addition, 39.4% and 20.6% achieved an EASI-75 (a secondary endpoint), respectively (P < .0001), and itch also improved within 24 hours of starting treatment.
With regard to safety, 29.7% of patients taking roflumilast had treatment-emergent adverse effects (including upper respiratory tract infections in 4.1%) vs 21.9% of those in the vehicle arm (including upper respiratory tract infections in 1.4%). Reports of pain at the administration site were low (1.6% for roflumilast vs 1.9% for vehicle). Only one patient, a 2-year-old girl, had a treatment-emergent serious adverse event. The child, who was in the roflumilast group, had cellulitis involving noneczematous skin and was treated with antibiotics in the hospital for 3 days. The event was not attributed to roflumilast, which was stopped for 5 days, according to Dr. Eichenfield.
In an interview, Fairfield, Connecticut–based dermatologist Brittany Craiglow, MD, who was not involved in the study, said topical roflumilast would be an “important” new treatment because there are still few nonsteroidal options for the treatment of AD in children under 12. “The excellent local tolerability combined with early improvements in itch and skin clearance will make this a particularly attractive option, if approved,” she said.
Dr. Eichenfield disclosed multiple relationships with various drugmakers. He and several other study authors are investigators and/or consultants for Arcutis and received grants/research funding and/or honoraria. Two authors are Arcutis employees. Other disclosure information for the authors was not immediately available. Dr. Craiglow had no disclosures.
A version of this article appeared on Medscape.com .
SAN DIEGO — Treatment with (AD), according to the results of a phase 3 study reported at the annual meeting of the American Academy of Dermatology.
Among patients treated with roflumilast cream, 0.05%, 25.4% reached the primary endpoint of “clear” or “almost clear” plus a two-grade improvement from baseline at week 4 vs 10.7% among those in the vehicle group (P < .0001) in a phase 3 randomized controlled trial of children. The findings were released in a late-breaker session at the meeting.
Roflumilast cream, 0.3% (Zoryve), is approved by the Food and Drug Administration (FDA) for treating psoriasis in patients 6 years and older, and lower doses are being evaluated for AD: 0.15% for adults and children ages 6 and older, and 0.05% for ages 2-5. Roflumilast is a phosphodiesterase-4 inhibitor. In 2023, the FDA accepted a supplemental drug application from the manufacturer, Arcutis, for roflumilast, 0.15%, for treating AD in patients ages 6 and older, based on the results from two recently published phase 3 trials, INTEGUMENT-1 and INTEGUMENT-2.
The study of younger children, INTEGUMENT-PED, recruited 652 patients aged 2-5 with mild to moderate AD, with a Validated Investigator Global Assessment scale for AD (vlGA-AD) score of 2 or 3, a mean body surface area of 22% overall (range, 3%-82%), and an Eczema Area and Severity Index (EASI) score of at least 5. Of the patients enrolled, 437 were assigned to 0.05% roflumilast cream, applied once a day for 4 weeks (mean age, 3.3 years; 51.6% male; 67.4% White; 15.6% Black; 8.5% Asian; 8.5% other or more than one race; 80.5% not Latino/Hispanic). The remaining 215 children were assigned to vehicle cream and had similar characteristics.
About 52% of the patients in both groups had an inadequate response, intolerance, or contraindications to topical corticosteroids (and about 17% for topical calcineurin inhibitors and about 9% for crisaborole).
The proportions of patients who reached “clear” (0) or “almost clear” (1) on the vlGA-AD scale were 35.4% and 14.6%, respectively, at week 4 (P < .0001) for roflumilast and vehicle, respectively, according to the lead author of the study, Lawrence M. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, who presented the results at the meeting. In addition, 39.4% and 20.6% achieved an EASI-75 (a secondary endpoint), respectively (P < .0001), and itch also improved within 24 hours of starting treatment.
With regard to safety, 29.7% of patients taking roflumilast had treatment-emergent adverse effects (including upper respiratory tract infections in 4.1%) vs 21.9% of those in the vehicle arm (including upper respiratory tract infections in 1.4%). Reports of pain at the administration site were low (1.6% for roflumilast vs 1.9% for vehicle). Only one patient, a 2-year-old girl, had a treatment-emergent serious adverse event. The child, who was in the roflumilast group, had cellulitis involving noneczematous skin and was treated with antibiotics in the hospital for 3 days. The event was not attributed to roflumilast, which was stopped for 5 days, according to Dr. Eichenfield.
In an interview, Fairfield, Connecticut–based dermatologist Brittany Craiglow, MD, who was not involved in the study, said topical roflumilast would be an “important” new treatment because there are still few nonsteroidal options for the treatment of AD in children under 12. “The excellent local tolerability combined with early improvements in itch and skin clearance will make this a particularly attractive option, if approved,” she said.
Dr. Eichenfield disclosed multiple relationships with various drugmakers. He and several other study authors are investigators and/or consultants for Arcutis and received grants/research funding and/or honoraria. Two authors are Arcutis employees. Other disclosure information for the authors was not immediately available. Dr. Craiglow had no disclosures.
A version of this article appeared on Medscape.com .
FROM AAD 2024
New Research Dissects Transgenerational Obesity and Diabetes
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1).
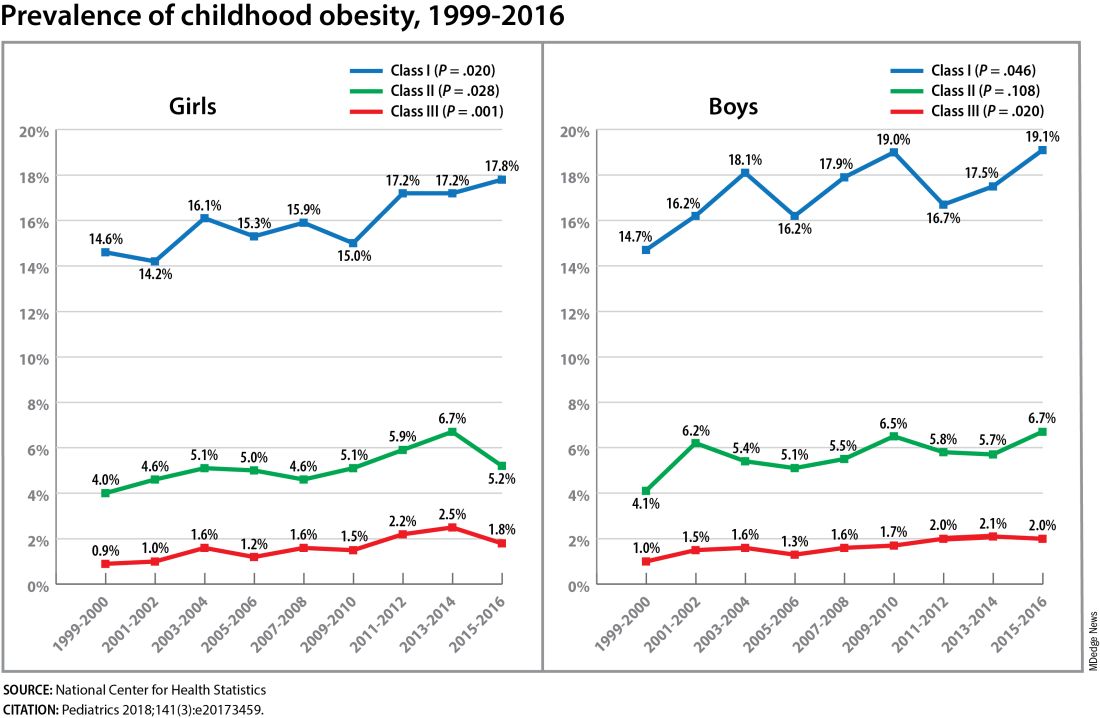
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1).
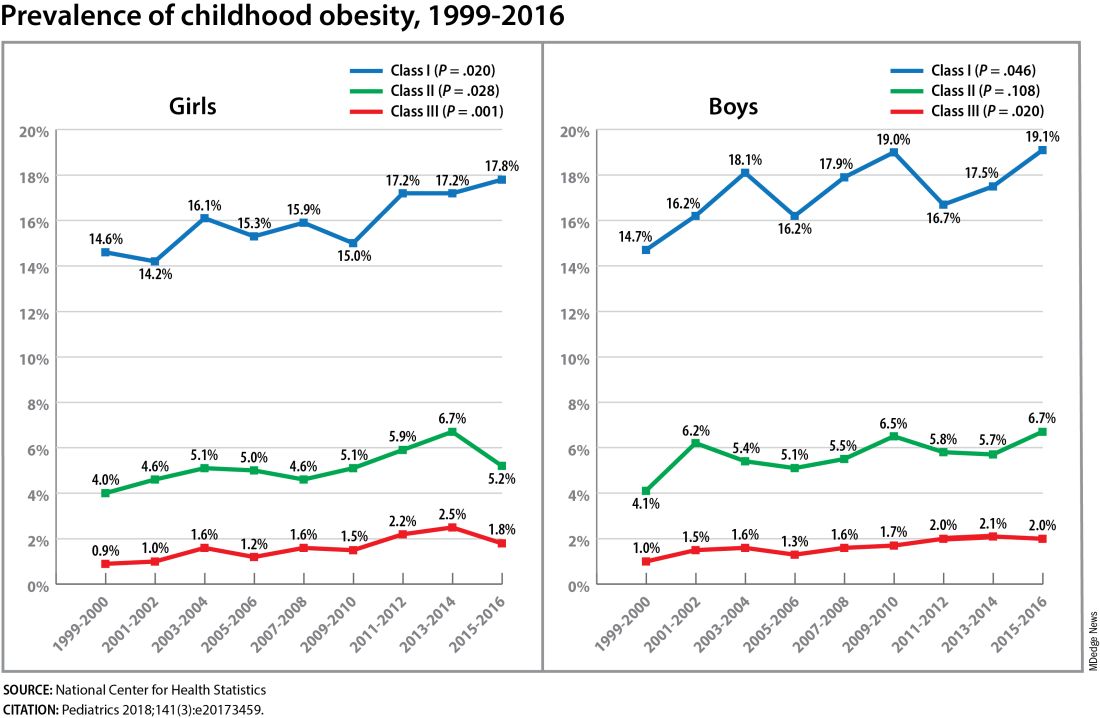
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1).
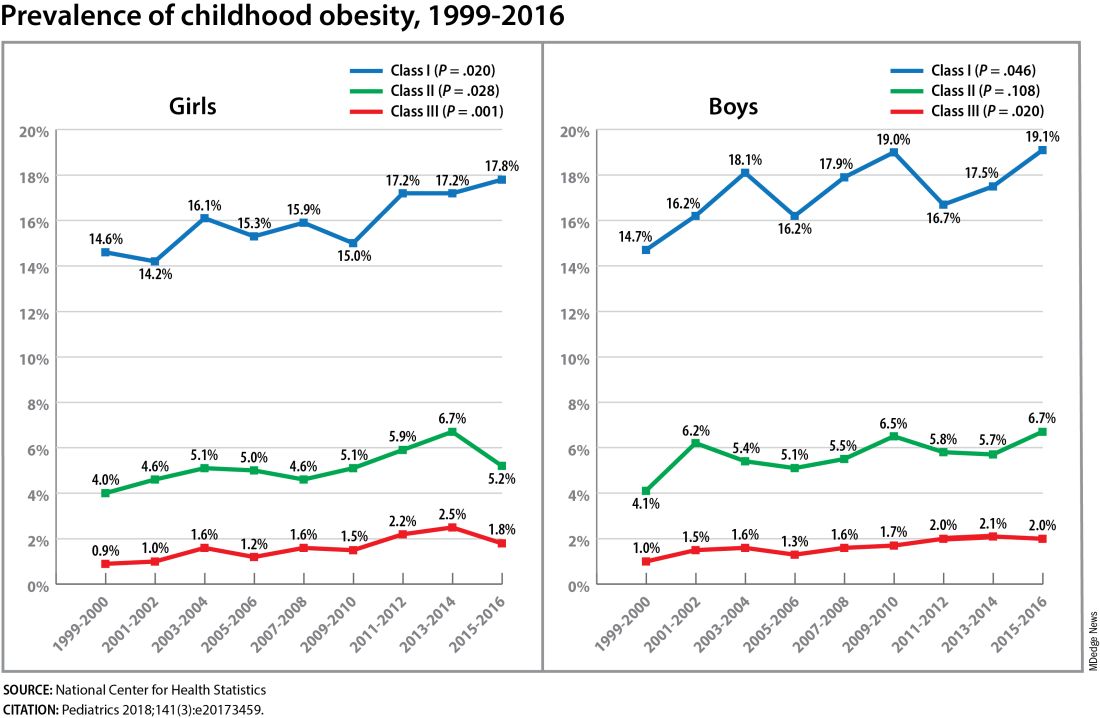
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FROM DPSG-NA 2023
Web-Based Aid Educates Women on Tubal Sterilization
Although tubal sterilization is common, especially among those with lower income and education levels, misunderstandings persist about the reversibility of the procedure, and previous studies suggest that many pregnant individuals are not making well-informed decisions, wrote Sonya Borrero, MD, of the University of Pittsburgh, and colleagues.
In a study published in JAMA Network Open, the researchers randomized 350 pregnant individuals with Medicaid insurance to usual care or usual care plus a web-based decision aid in English or Spanish called MyDecision/MiDecisión that included written, audio, and video information about tubal sterilization. The tool also included an interactive table comparing tubal sterilization to other contraceptive options, exercises to clarify patients’ values, knowledge checks, and a final summary report.
The two primary outcomes were knowledge of tubal sterilization based on a 10-question true/false test and decisional conflict about contraceptive choices using the low-literacy Decision Conflict Scale. The participants ranged in age from 21 to 45 years, with a mean age of 29.7 years. Participants were randomized prior to 24 weeks’ gestation, and those in the intervention group completed the intervention immediately using a personal device or a university device in the clinical setting. Further assessments occurred by phone during the third trimester and at 3 months postpartum.
Participants in the decision aid group showed significantly greater knowledge of tubal sterilization compared with controls, with a mean of 76.5% correct responses to the knowledge questions, vs. 55.6% in the control group (P < .001). Decisional conflict scores also were significantly lower in the intervention group compared with controls (mean 12.7 vs. 18.7, P = .002).
The most dramatic knowledge gap related to permanence of tubal sterilization; 90.1% of participants in the intervention group answered correctly that the procedure is not easily reversible, compared to 39.3% of the controls. Similarly, 86.6% of the intervention group responded correctly that the tubes do not “come untied” spontaneously, vs. 33.7% of controls (P < .001 for both).
The findings were limited by several factors including the focus only on pregnant Medicaid patients, the presentation of the decision tool only at a point early in pregnancy, which may have been too soon for some participants to consider tubal sterilization, and a lack of data on long-term satisfaction or regret about tubal sterilization decisions, the researchers noted.
However, the knowledge differences between the intervention and control groups remained significant at the third trimester assessment, they said.
More research is needed in other populations and using other time points, but the current study results suggest that use of the MyDecision/MiDecisión tool in a real-world clinical setting at the actual time of decision-making could improve knowledge and inform patients’ choices, the researchers concluded. Improved patient education also could inform policy decisions about the potential elimination of the 30-day waiting period for sterilization procedures, they said.
The study was supported by the National Institute on Minority Health and Health Disparities. The researchers had no financial conflicts to disclose.
Although tubal sterilization is common, especially among those with lower income and education levels, misunderstandings persist about the reversibility of the procedure, and previous studies suggest that many pregnant individuals are not making well-informed decisions, wrote Sonya Borrero, MD, of the University of Pittsburgh, and colleagues.
In a study published in JAMA Network Open, the researchers randomized 350 pregnant individuals with Medicaid insurance to usual care or usual care plus a web-based decision aid in English or Spanish called MyDecision/MiDecisión that included written, audio, and video information about tubal sterilization. The tool also included an interactive table comparing tubal sterilization to other contraceptive options, exercises to clarify patients’ values, knowledge checks, and a final summary report.
The two primary outcomes were knowledge of tubal sterilization based on a 10-question true/false test and decisional conflict about contraceptive choices using the low-literacy Decision Conflict Scale. The participants ranged in age from 21 to 45 years, with a mean age of 29.7 years. Participants were randomized prior to 24 weeks’ gestation, and those in the intervention group completed the intervention immediately using a personal device or a university device in the clinical setting. Further assessments occurred by phone during the third trimester and at 3 months postpartum.
Participants in the decision aid group showed significantly greater knowledge of tubal sterilization compared with controls, with a mean of 76.5% correct responses to the knowledge questions, vs. 55.6% in the control group (P < .001). Decisional conflict scores also were significantly lower in the intervention group compared with controls (mean 12.7 vs. 18.7, P = .002).
The most dramatic knowledge gap related to permanence of tubal sterilization; 90.1% of participants in the intervention group answered correctly that the procedure is not easily reversible, compared to 39.3% of the controls. Similarly, 86.6% of the intervention group responded correctly that the tubes do not “come untied” spontaneously, vs. 33.7% of controls (P < .001 for both).
The findings were limited by several factors including the focus only on pregnant Medicaid patients, the presentation of the decision tool only at a point early in pregnancy, which may have been too soon for some participants to consider tubal sterilization, and a lack of data on long-term satisfaction or regret about tubal sterilization decisions, the researchers noted.
However, the knowledge differences between the intervention and control groups remained significant at the third trimester assessment, they said.
More research is needed in other populations and using other time points, but the current study results suggest that use of the MyDecision/MiDecisión tool in a real-world clinical setting at the actual time of decision-making could improve knowledge and inform patients’ choices, the researchers concluded. Improved patient education also could inform policy decisions about the potential elimination of the 30-day waiting period for sterilization procedures, they said.
The study was supported by the National Institute on Minority Health and Health Disparities. The researchers had no financial conflicts to disclose.
Although tubal sterilization is common, especially among those with lower income and education levels, misunderstandings persist about the reversibility of the procedure, and previous studies suggest that many pregnant individuals are not making well-informed decisions, wrote Sonya Borrero, MD, of the University of Pittsburgh, and colleagues.
In a study published in JAMA Network Open, the researchers randomized 350 pregnant individuals with Medicaid insurance to usual care or usual care plus a web-based decision aid in English or Spanish called MyDecision/MiDecisión that included written, audio, and video information about tubal sterilization. The tool also included an interactive table comparing tubal sterilization to other contraceptive options, exercises to clarify patients’ values, knowledge checks, and a final summary report.
The two primary outcomes were knowledge of tubal sterilization based on a 10-question true/false test and decisional conflict about contraceptive choices using the low-literacy Decision Conflict Scale. The participants ranged in age from 21 to 45 years, with a mean age of 29.7 years. Participants were randomized prior to 24 weeks’ gestation, and those in the intervention group completed the intervention immediately using a personal device or a university device in the clinical setting. Further assessments occurred by phone during the third trimester and at 3 months postpartum.
Participants in the decision aid group showed significantly greater knowledge of tubal sterilization compared with controls, with a mean of 76.5% correct responses to the knowledge questions, vs. 55.6% in the control group (P < .001). Decisional conflict scores also were significantly lower in the intervention group compared with controls (mean 12.7 vs. 18.7, P = .002).
The most dramatic knowledge gap related to permanence of tubal sterilization; 90.1% of participants in the intervention group answered correctly that the procedure is not easily reversible, compared to 39.3% of the controls. Similarly, 86.6% of the intervention group responded correctly that the tubes do not “come untied” spontaneously, vs. 33.7% of controls (P < .001 for both).
The findings were limited by several factors including the focus only on pregnant Medicaid patients, the presentation of the decision tool only at a point early in pregnancy, which may have been too soon for some participants to consider tubal sterilization, and a lack of data on long-term satisfaction or regret about tubal sterilization decisions, the researchers noted.
However, the knowledge differences between the intervention and control groups remained significant at the third trimester assessment, they said.
More research is needed in other populations and using other time points, but the current study results suggest that use of the MyDecision/MiDecisión tool in a real-world clinical setting at the actual time of decision-making could improve knowledge and inform patients’ choices, the researchers concluded. Improved patient education also could inform policy decisions about the potential elimination of the 30-day waiting period for sterilization procedures, they said.
The study was supported by the National Institute on Minority Health and Health Disparities. The researchers had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
No Excess Cancer Risk Seen with Non-TNF Inhibitor Biologics in RA
TOPLINE:
Treatment of patients with rheumatoid arthritis (RA) with non–tumor necrosis factor inhibitor (TNFi) biologic disease-modifying antirheumatic drugs (bDMARDs) may not pose an increased risk for cancer, compared with TNFis and conventional synthetic DMARDs.
METHODOLOGY:
- Previous research has presented conflicting results on the association between non-TNFi bDMARDs and the risk for cancer, with abatacept drawing particular attention owing to its mode of action.
- By utilizing information from Danish registers (January 2006-December 2020), researchers compared the risk for cancer in 14,944 patients with RA (age > 18 years) who were initiated on non-TNFi bDMARDs (tocilizumab/sarilumab, abatacept, or rituximab), TNFis, or were in the conventional synthetic DMARDs (bDMARD-naive) group.
- The patient population contributed to 21,982 treatment initiations, which corresponded to 1457, 1016, 690, 7458, and 11,361 treatment initiations for the tocilizumab/sarilumab, abatacept, rituximab, TNFi, and bDMARD-naive groups, respectively.
- Patients were followed up until a diagnosis was obtained for cancer, death, emigration, the initiation of a different bDMARD or a targeted synthetic DMARD, or the end of the study, whichever was earlier.
- The primary outcome was defined as any primary cancer diagnosis (except nonmelanoma skin cancer).
TAKEAWAY:
- The risk for overall cancer was not significantly higher in the tocilizumab/sarilumab-, abatacept-, or rituximab-initiated groups than in the TNFi-treated and bDMARD-naive groups.
- The likelihood of cancer appeared to be higher in patients with more than 5 years of exposure to abatacept than in the TNFi-treated (hazard ratio [HR], 1.41; 95% CI, 0.60-2.60) and bDMARD-naive groups (HR, 1.14; 95% CI, 0.51-2.33). However, the results were not statistically significant.
- Treatment with rituximab may be associated with a lower risk for hematologic cancers than for TNFi-treated (HR, 0.09; 95% CI, 0.00-2.06) or bDMARD-naive groups (HR, 0.13; 95% CI, 0.00-1.89), although the findings did not show statistical significance.
IN PRACTICE:
The authors wrote, “bDMARD-associated cancer risk remains a clinically important research question, and more future studies specifically investigating non-TNFi bDMARDs in terms of cancer risk in patients with RA are warranted.”
SOURCE:
The investigation, led by Rasmus Westermann, MD, of Aalborg University Hospital, Aalborg, Denmark, was published online on March 7 in Rheumatology.
LIMITATIONS:
Many patients received more than one type of non-TNFi bDMARD treatment during the study. Because the temporal relationship of DMARD treatment with cancer was not certain, potential carcinogenic treatment effects could not be distinguished. Limited data were available on cancer risk factors.
DISCLOSURES:
The study was supported by the Danish Rheumatism Association and the Danish Cancer Society. Some authors reported financial relationships with pharmaceutical companies outside of the submitted work.
A version of this article appeared on Medscape.com.
TOPLINE:
Treatment of patients with rheumatoid arthritis (RA) with non–tumor necrosis factor inhibitor (TNFi) biologic disease-modifying antirheumatic drugs (bDMARDs) may not pose an increased risk for cancer, compared with TNFis and conventional synthetic DMARDs.
METHODOLOGY:
- Previous research has presented conflicting results on the association between non-TNFi bDMARDs and the risk for cancer, with abatacept drawing particular attention owing to its mode of action.
- By utilizing information from Danish registers (January 2006-December 2020), researchers compared the risk for cancer in 14,944 patients with RA (age > 18 years) who were initiated on non-TNFi bDMARDs (tocilizumab/sarilumab, abatacept, or rituximab), TNFis, or were in the conventional synthetic DMARDs (bDMARD-naive) group.
- The patient population contributed to 21,982 treatment initiations, which corresponded to 1457, 1016, 690, 7458, and 11,361 treatment initiations for the tocilizumab/sarilumab, abatacept, rituximab, TNFi, and bDMARD-naive groups, respectively.
- Patients were followed up until a diagnosis was obtained for cancer, death, emigration, the initiation of a different bDMARD or a targeted synthetic DMARD, or the end of the study, whichever was earlier.
- The primary outcome was defined as any primary cancer diagnosis (except nonmelanoma skin cancer).
TAKEAWAY:
- The risk for overall cancer was not significantly higher in the tocilizumab/sarilumab-, abatacept-, or rituximab-initiated groups than in the TNFi-treated and bDMARD-naive groups.
- The likelihood of cancer appeared to be higher in patients with more than 5 years of exposure to abatacept than in the TNFi-treated (hazard ratio [HR], 1.41; 95% CI, 0.60-2.60) and bDMARD-naive groups (HR, 1.14; 95% CI, 0.51-2.33). However, the results were not statistically significant.
- Treatment with rituximab may be associated with a lower risk for hematologic cancers than for TNFi-treated (HR, 0.09; 95% CI, 0.00-2.06) or bDMARD-naive groups (HR, 0.13; 95% CI, 0.00-1.89), although the findings did not show statistical significance.
IN PRACTICE:
The authors wrote, “bDMARD-associated cancer risk remains a clinically important research question, and more future studies specifically investigating non-TNFi bDMARDs in terms of cancer risk in patients with RA are warranted.”
SOURCE:
The investigation, led by Rasmus Westermann, MD, of Aalborg University Hospital, Aalborg, Denmark, was published online on March 7 in Rheumatology.
LIMITATIONS:
Many patients received more than one type of non-TNFi bDMARD treatment during the study. Because the temporal relationship of DMARD treatment with cancer was not certain, potential carcinogenic treatment effects could not be distinguished. Limited data were available on cancer risk factors.
DISCLOSURES:
The study was supported by the Danish Rheumatism Association and the Danish Cancer Society. Some authors reported financial relationships with pharmaceutical companies outside of the submitted work.
A version of this article appeared on Medscape.com.
TOPLINE:
Treatment of patients with rheumatoid arthritis (RA) with non–tumor necrosis factor inhibitor (TNFi) biologic disease-modifying antirheumatic drugs (bDMARDs) may not pose an increased risk for cancer, compared with TNFis and conventional synthetic DMARDs.
METHODOLOGY:
- Previous research has presented conflicting results on the association between non-TNFi bDMARDs and the risk for cancer, with abatacept drawing particular attention owing to its mode of action.
- By utilizing information from Danish registers (January 2006-December 2020), researchers compared the risk for cancer in 14,944 patients with RA (age > 18 years) who were initiated on non-TNFi bDMARDs (tocilizumab/sarilumab, abatacept, or rituximab), TNFis, or were in the conventional synthetic DMARDs (bDMARD-naive) group.
- The patient population contributed to 21,982 treatment initiations, which corresponded to 1457, 1016, 690, 7458, and 11,361 treatment initiations for the tocilizumab/sarilumab, abatacept, rituximab, TNFi, and bDMARD-naive groups, respectively.
- Patients were followed up until a diagnosis was obtained for cancer, death, emigration, the initiation of a different bDMARD or a targeted synthetic DMARD, or the end of the study, whichever was earlier.
- The primary outcome was defined as any primary cancer diagnosis (except nonmelanoma skin cancer).
TAKEAWAY:
- The risk for overall cancer was not significantly higher in the tocilizumab/sarilumab-, abatacept-, or rituximab-initiated groups than in the TNFi-treated and bDMARD-naive groups.
- The likelihood of cancer appeared to be higher in patients with more than 5 years of exposure to abatacept than in the TNFi-treated (hazard ratio [HR], 1.41; 95% CI, 0.60-2.60) and bDMARD-naive groups (HR, 1.14; 95% CI, 0.51-2.33). However, the results were not statistically significant.
- Treatment with rituximab may be associated with a lower risk for hematologic cancers than for TNFi-treated (HR, 0.09; 95% CI, 0.00-2.06) or bDMARD-naive groups (HR, 0.13; 95% CI, 0.00-1.89), although the findings did not show statistical significance.
IN PRACTICE:
The authors wrote, “bDMARD-associated cancer risk remains a clinically important research question, and more future studies specifically investigating non-TNFi bDMARDs in terms of cancer risk in patients with RA are warranted.”
SOURCE:
The investigation, led by Rasmus Westermann, MD, of Aalborg University Hospital, Aalborg, Denmark, was published online on March 7 in Rheumatology.
LIMITATIONS:
Many patients received more than one type of non-TNFi bDMARD treatment during the study. Because the temporal relationship of DMARD treatment with cancer was not certain, potential carcinogenic treatment effects could not be distinguished. Limited data were available on cancer risk factors.
DISCLOSURES:
The study was supported by the Danish Rheumatism Association and the Danish Cancer Society. Some authors reported financial relationships with pharmaceutical companies outside of the submitted work.
A version of this article appeared on Medscape.com.
Early Diagnosis Improves Clinical Outcomes in Psoriatic Arthritis
TOPLINE:
An earlier diagnosis of psoriatic arthritis (PsA) following symptom onset increases the likelihood of achieving improved clinical outcomes, highlighting the presence of a diagnostic window of opportunity in PsA.
METHODOLOGY:
- A diagnostic delay in PsA leads to increased joint erosions and functional impairment; however, whether a “window of opportunity” (< 12 weeks) exists in PsA requires further evaluation.
- Researchers assessed the impact of diagnostic delay on clinical outcomes in 708 newly diagnosed, disease-modifying antirheumatic drug-naive patients with PsA from the Dutch southwest Early PsA cohort.
- Total diagnostic delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist.
- On the basis of the total diagnostic delay, patients were categorized into those with a short delay of < 12 weeks (n = 136), intermediate delay of 12 weeks to 1 year (n = 237), and a long delay of > 1 year (n = 335).
- The groups were compared for clinical (Minimal Disease Activity [MDA] and Disease Activity index for Psoriatic Arthritis [DAPSA] remission) and patient-reported outcomes during 3 years of follow-up.
TAKEAWAY:
- The probability of achieving MDA was higher in patients with a short vs long diagnostic delay (odds ratio [OR], 2.55; 95% CI, 1.37-4.76).
- Compared with patients in the long diagnostic delay group, those in the short (OR, 2.35; 95% CI, 1.32-4.19) and intermediate (OR, 1.94; 95% CI, 1.19-3.15) diagnostic delay groups were more likely to achieve DAPSA remission.
- Compared with patients in the long diagnostic delay group, those in the short (estimated mean difference [Δ], −1.09; 95% CI, −1.88 to −0.30) or intermediate (Δ, −0.85; 95% CI, −1.50 to −0.19) groups had slightly less tender joints.
IN PRACTICE:
“A delay of > 1 year is associated with worse clinical outcomes, which includes almost 50% of the PsA population” in this study, wrote the authors, adding that for better long-term outcomes, “it is important that PsA patients are diagnosed by a rheumatologist within 1 year after symptom onset.”
SOURCE:
This study, led by Selinde V.J. Snoeck Henkemans, MD, of the department of rheumatology at Erasmus University Medical Center, Rotterdam, the Netherlands, was published online February 27, 2024, in RMD Open.
LIMITATIONS:
The study’s dropout rates (25%-31% across groups) may have influenced the findings. Patients with a long diagnostic delay might have dropped out owing to treatment dissatisfaction, and those with a short or intermediate delay might have dropped out due to inactive disease.
DISCLOSURES:
This study did not declare any specific source of funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
An earlier diagnosis of psoriatic arthritis (PsA) following symptom onset increases the likelihood of achieving improved clinical outcomes, highlighting the presence of a diagnostic window of opportunity in PsA.
METHODOLOGY:
- A diagnostic delay in PsA leads to increased joint erosions and functional impairment; however, whether a “window of opportunity” (< 12 weeks) exists in PsA requires further evaluation.
- Researchers assessed the impact of diagnostic delay on clinical outcomes in 708 newly diagnosed, disease-modifying antirheumatic drug-naive patients with PsA from the Dutch southwest Early PsA cohort.
- Total diagnostic delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist.
- On the basis of the total diagnostic delay, patients were categorized into those with a short delay of < 12 weeks (n = 136), intermediate delay of 12 weeks to 1 year (n = 237), and a long delay of > 1 year (n = 335).
- The groups were compared for clinical (Minimal Disease Activity [MDA] and Disease Activity index for Psoriatic Arthritis [DAPSA] remission) and patient-reported outcomes during 3 years of follow-up.
TAKEAWAY:
- The probability of achieving MDA was higher in patients with a short vs long diagnostic delay (odds ratio [OR], 2.55; 95% CI, 1.37-4.76).
- Compared with patients in the long diagnostic delay group, those in the short (OR, 2.35; 95% CI, 1.32-4.19) and intermediate (OR, 1.94; 95% CI, 1.19-3.15) diagnostic delay groups were more likely to achieve DAPSA remission.
- Compared with patients in the long diagnostic delay group, those in the short (estimated mean difference [Δ], −1.09; 95% CI, −1.88 to −0.30) or intermediate (Δ, −0.85; 95% CI, −1.50 to −0.19) groups had slightly less tender joints.
IN PRACTICE:
“A delay of > 1 year is associated with worse clinical outcomes, which includes almost 50% of the PsA population” in this study, wrote the authors, adding that for better long-term outcomes, “it is important that PsA patients are diagnosed by a rheumatologist within 1 year after symptom onset.”
SOURCE:
This study, led by Selinde V.J. Snoeck Henkemans, MD, of the department of rheumatology at Erasmus University Medical Center, Rotterdam, the Netherlands, was published online February 27, 2024, in RMD Open.
LIMITATIONS:
The study’s dropout rates (25%-31% across groups) may have influenced the findings. Patients with a long diagnostic delay might have dropped out owing to treatment dissatisfaction, and those with a short or intermediate delay might have dropped out due to inactive disease.
DISCLOSURES:
This study did not declare any specific source of funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
An earlier diagnosis of psoriatic arthritis (PsA) following symptom onset increases the likelihood of achieving improved clinical outcomes, highlighting the presence of a diagnostic window of opportunity in PsA.
METHODOLOGY:
- A diagnostic delay in PsA leads to increased joint erosions and functional impairment; however, whether a “window of opportunity” (< 12 weeks) exists in PsA requires further evaluation.
- Researchers assessed the impact of diagnostic delay on clinical outcomes in 708 newly diagnosed, disease-modifying antirheumatic drug-naive patients with PsA from the Dutch southwest Early PsA cohort.
- Total diagnostic delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist.
- On the basis of the total diagnostic delay, patients were categorized into those with a short delay of < 12 weeks (n = 136), intermediate delay of 12 weeks to 1 year (n = 237), and a long delay of > 1 year (n = 335).
- The groups were compared for clinical (Minimal Disease Activity [MDA] and Disease Activity index for Psoriatic Arthritis [DAPSA] remission) and patient-reported outcomes during 3 years of follow-up.
TAKEAWAY:
- The probability of achieving MDA was higher in patients with a short vs long diagnostic delay (odds ratio [OR], 2.55; 95% CI, 1.37-4.76).
- Compared with patients in the long diagnostic delay group, those in the short (OR, 2.35; 95% CI, 1.32-4.19) and intermediate (OR, 1.94; 95% CI, 1.19-3.15) diagnostic delay groups were more likely to achieve DAPSA remission.
- Compared with patients in the long diagnostic delay group, those in the short (estimated mean difference [Δ], −1.09; 95% CI, −1.88 to −0.30) or intermediate (Δ, −0.85; 95% CI, −1.50 to −0.19) groups had slightly less tender joints.
IN PRACTICE:
“A delay of > 1 year is associated with worse clinical outcomes, which includes almost 50% of the PsA population” in this study, wrote the authors, adding that for better long-term outcomes, “it is important that PsA patients are diagnosed by a rheumatologist within 1 year after symptom onset.”
SOURCE:
This study, led by Selinde V.J. Snoeck Henkemans, MD, of the department of rheumatology at Erasmus University Medical Center, Rotterdam, the Netherlands, was published online February 27, 2024, in RMD Open.
LIMITATIONS:
The study’s dropout rates (25%-31% across groups) may have influenced the findings. Patients with a long diagnostic delay might have dropped out owing to treatment dissatisfaction, and those with a short or intermediate delay might have dropped out due to inactive disease.
DISCLOSURES:
This study did not declare any specific source of funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.




