User login
Ibrutinib linked to hypertension in B-cell malignancies
The incidence and severity of hypertension was considerably higher in patients with B-cell malignancies treated with ibrutinib, according to a retrospective analysis.
Additionally, new or worsening hypertension was associated with a greater risk of major adverse cardiac events (MACE), including stroke, myocardial infarction, and cardiovascular-related death (hazard ratio, 2.17; 95% confidence interval, 1.08-4.38; P = .03).
“Despite ibrutinib’s benefits, cardiotoxicity has emerged as an increasingly important complication of this life-saving therapy,” Tyler Dickerson, PhD, of the Ohio State University, Columbus, and colleagues wrote in Blood.
The researchers retrospectively studied 562 consecutive patients with a lymphoid malignancy who received ibrutinib. Data was collected from patients treated at The Ohio State University’s Comprehensive Cancer Center during 2009-2016.
The mean age of study participants was 63.8 years, with a mean body mass index of 28.0 kg/m2. Most of the patients included in the analysis were men.
The team assessed rates of new or worsening hypertension, as well as rates of other MACE. The observed rates were compared with Framingham Heart Study–predicted incident-hypertension rates. The effects of various antihypertensive drugs on ibrutinib-linked hypertension were also evaluated.
After a median follow-up of 30 months, 78.3% of patients who received ibrutinib had new or worsening hypertension using a systolic blood pressure cutoff of 130 mm Hg. Of these, 84.8% of cases had an “at least probable association with ibrutinib,” they reported.
Among the 215 patients with no baseline hypertension, 71.6% developed hypertension while on ibrutinib, with a mean increase in systolic blood pressure of 13.4 mm Hg. Among the 347 patients with baseline hypertension, 82.4% experienced a worsening of their hypertension.
“This relationship remained even after accounting for ibrutinib dose, and was not attenuated by the use of any specific anti-hypertensive class,” the researchers wrote.
The researchers observed MACE among 93 patients. This included 84 patients with new or worsening hypertension and 9 patients with stable or no hypertension. Most MACE events were of at least probable ibrutinib association, the researchers reported.
Overall, the cumulative incidence of new hypertension at 1 year was 442 per 1,000 person-years in the current study. This value is 12.9-fold higher than the Framingham Heart Study risk–predicted rate of 34 per 1,000 person-years.
“Given the expected continued increase in ibrutinib use, further studies characterizing the mechanisms, treatment, and implications of [hypertension] during ibrutinib use are needed,” the researchers wrote.
The study was funded by the National Institutes of Health, the D. Warren Brown Family Foundation, the Four Winds Foundation, and the Connie Brown CLL Research Fund. The authors reported financial affiliations with Janssen, Pharmacyclics, and other companies.
SOURCE: Dickerson T et al. Blood. 2019 Oct 3. doi: 10.1182/blood.2019000840.
The incidence and severity of hypertension was considerably higher in patients with B-cell malignancies treated with ibrutinib, according to a retrospective analysis.
Additionally, new or worsening hypertension was associated with a greater risk of major adverse cardiac events (MACE), including stroke, myocardial infarction, and cardiovascular-related death (hazard ratio, 2.17; 95% confidence interval, 1.08-4.38; P = .03).
“Despite ibrutinib’s benefits, cardiotoxicity has emerged as an increasingly important complication of this life-saving therapy,” Tyler Dickerson, PhD, of the Ohio State University, Columbus, and colleagues wrote in Blood.
The researchers retrospectively studied 562 consecutive patients with a lymphoid malignancy who received ibrutinib. Data was collected from patients treated at The Ohio State University’s Comprehensive Cancer Center during 2009-2016.
The mean age of study participants was 63.8 years, with a mean body mass index of 28.0 kg/m2. Most of the patients included in the analysis were men.
The team assessed rates of new or worsening hypertension, as well as rates of other MACE. The observed rates were compared with Framingham Heart Study–predicted incident-hypertension rates. The effects of various antihypertensive drugs on ibrutinib-linked hypertension were also evaluated.
After a median follow-up of 30 months, 78.3% of patients who received ibrutinib had new or worsening hypertension using a systolic blood pressure cutoff of 130 mm Hg. Of these, 84.8% of cases had an “at least probable association with ibrutinib,” they reported.
Among the 215 patients with no baseline hypertension, 71.6% developed hypertension while on ibrutinib, with a mean increase in systolic blood pressure of 13.4 mm Hg. Among the 347 patients with baseline hypertension, 82.4% experienced a worsening of their hypertension.
“This relationship remained even after accounting for ibrutinib dose, and was not attenuated by the use of any specific anti-hypertensive class,” the researchers wrote.
The researchers observed MACE among 93 patients. This included 84 patients with new or worsening hypertension and 9 patients with stable or no hypertension. Most MACE events were of at least probable ibrutinib association, the researchers reported.
Overall, the cumulative incidence of new hypertension at 1 year was 442 per 1,000 person-years in the current study. This value is 12.9-fold higher than the Framingham Heart Study risk–predicted rate of 34 per 1,000 person-years.
“Given the expected continued increase in ibrutinib use, further studies characterizing the mechanisms, treatment, and implications of [hypertension] during ibrutinib use are needed,” the researchers wrote.
The study was funded by the National Institutes of Health, the D. Warren Brown Family Foundation, the Four Winds Foundation, and the Connie Brown CLL Research Fund. The authors reported financial affiliations with Janssen, Pharmacyclics, and other companies.
SOURCE: Dickerson T et al. Blood. 2019 Oct 3. doi: 10.1182/blood.2019000840.
The incidence and severity of hypertension was considerably higher in patients with B-cell malignancies treated with ibrutinib, according to a retrospective analysis.
Additionally, new or worsening hypertension was associated with a greater risk of major adverse cardiac events (MACE), including stroke, myocardial infarction, and cardiovascular-related death (hazard ratio, 2.17; 95% confidence interval, 1.08-4.38; P = .03).
“Despite ibrutinib’s benefits, cardiotoxicity has emerged as an increasingly important complication of this life-saving therapy,” Tyler Dickerson, PhD, of the Ohio State University, Columbus, and colleagues wrote in Blood.
The researchers retrospectively studied 562 consecutive patients with a lymphoid malignancy who received ibrutinib. Data was collected from patients treated at The Ohio State University’s Comprehensive Cancer Center during 2009-2016.
The mean age of study participants was 63.8 years, with a mean body mass index of 28.0 kg/m2. Most of the patients included in the analysis were men.
The team assessed rates of new or worsening hypertension, as well as rates of other MACE. The observed rates were compared with Framingham Heart Study–predicted incident-hypertension rates. The effects of various antihypertensive drugs on ibrutinib-linked hypertension were also evaluated.
After a median follow-up of 30 months, 78.3% of patients who received ibrutinib had new or worsening hypertension using a systolic blood pressure cutoff of 130 mm Hg. Of these, 84.8% of cases had an “at least probable association with ibrutinib,” they reported.
Among the 215 patients with no baseline hypertension, 71.6% developed hypertension while on ibrutinib, with a mean increase in systolic blood pressure of 13.4 mm Hg. Among the 347 patients with baseline hypertension, 82.4% experienced a worsening of their hypertension.
“This relationship remained even after accounting for ibrutinib dose, and was not attenuated by the use of any specific anti-hypertensive class,” the researchers wrote.
The researchers observed MACE among 93 patients. This included 84 patients with new or worsening hypertension and 9 patients with stable or no hypertension. Most MACE events were of at least probable ibrutinib association, the researchers reported.
Overall, the cumulative incidence of new hypertension at 1 year was 442 per 1,000 person-years in the current study. This value is 12.9-fold higher than the Framingham Heart Study risk–predicted rate of 34 per 1,000 person-years.
“Given the expected continued increase in ibrutinib use, further studies characterizing the mechanisms, treatment, and implications of [hypertension] during ibrutinib use are needed,” the researchers wrote.
The study was funded by the National Institutes of Health, the D. Warren Brown Family Foundation, the Four Winds Foundation, and the Connie Brown CLL Research Fund. The authors reported financial affiliations with Janssen, Pharmacyclics, and other companies.
SOURCE: Dickerson T et al. Blood. 2019 Oct 3. doi: 10.1182/blood.2019000840.
FROM BLOOD
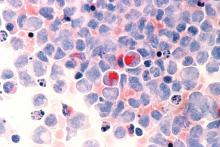
Adverse cytogenetics trump molecular risk in NPM1-mutated AML
A pooled analysis suggests adverse cytogenetics are a key factor negatively impacting outcomes in patients with NPM1mut/FLT3-ITDneg/low acute myeloid leukemia (AML).
In patients with adverse chromosomal abnormalities, NPM1 mutational status was found not to confer a favorable outcome. The findings suggest cytogenetic risk outweighs molecular risk in patients with NPM1 mutations and the FLT3-ITDneg/low genotype.
“Patients carrying adverse-risk cytogenetics shared a virtually identical unfavorable outcome, regardless of whether the otherwise beneficial NPM1mut/FLT3-ITDneg/low status was present. The type of the adverse chromosomal abnormality did not seem to influence this effect, although low numbers might obscure detection of heterogeneity among individual aberrations,” Linus Angenendt, MD, of University Hospital Munster (Germany) and colleagues, wrote in the Journal of Clinical Oncology.
The researchers retrospectively analyzed 2,426 patients with NPM1mut/FLT3-ITDneg/low AML. Of these, 17.6% had an abnormal karyotype, and 3.4% had adverse-risk chromosomal aberrations.
Prior to analysis, individual patient data were pooled from nine international AML study group registries or treatment centers.
After analysis, the researchers found that adverse cytogenetics were associated with inferior complete remission rates (66.3%), compared with in patients with normal karyotype or intermediate-risk cytogenetic abnormalities (87.7% and 86.0%, respectively; P less than .001). The complete remission rates for the NPM1mut/FLT3-ITDneg/low AML adverse cytogenetics group was similar to patients with NPM1wt/FLT3-ITDneg/low and adverse cytogenetic abnormalities (66.3% vs. 57.5%).
Five-year event-free survival rates and overall survival rates were also lower in patients with NPM1mut/FLT3-ITDneg/low AML and adverse cytogenetics, compared with patients with normal karyotype or intermediate-risk cytogenetic abnormalities (P less than .001).
“Even though the combination of an NPM1 mutation with these abnormalities is rare, the prognostic effect of adverse cytogenetics in NPM1mut AML has important implications for postremission treatment decisions, in particular, the current recommendation that patients who are NPM1mut/FLT3-ITDneg/low not receive allogeneic hematopoietic stem cell transplantation (HSCT), given their presumed low risk of relapse might be altered if the adverse karyotype increased the risk,” they wrote.
The type of chromosomal aberration did not appear to impact this effect, but the small sample size may have hindered the ability to detect a difference between different abnormalities, the researchers noted.
One key limitation of the study was the retrospective design. As a result, in patients with an abnormal karyotype, some genetic analyses could have been underutilized.
“These results demand additional validation within prospective trials,” the researchers concluded.
The study was funded by the University of Munster Medical School, the German Research Foundation, the French government, the Ministry of Health of the Czech Republic, and others. The authors reported financial affiliations with numerous pharmaceutical companies.
SOURCE: Angenendt L et al. J Clin Oncol. 2019 Oct 10;37(29):2632-42.
A pooled analysis suggests adverse cytogenetics are a key factor negatively impacting outcomes in patients with NPM1mut/FLT3-ITDneg/low acute myeloid leukemia (AML).
In patients with adverse chromosomal abnormalities, NPM1 mutational status was found not to confer a favorable outcome. The findings suggest cytogenetic risk outweighs molecular risk in patients with NPM1 mutations and the FLT3-ITDneg/low genotype.
“Patients carrying adverse-risk cytogenetics shared a virtually identical unfavorable outcome, regardless of whether the otherwise beneficial NPM1mut/FLT3-ITDneg/low status was present. The type of the adverse chromosomal abnormality did not seem to influence this effect, although low numbers might obscure detection of heterogeneity among individual aberrations,” Linus Angenendt, MD, of University Hospital Munster (Germany) and colleagues, wrote in the Journal of Clinical Oncology.
The researchers retrospectively analyzed 2,426 patients with NPM1mut/FLT3-ITDneg/low AML. Of these, 17.6% had an abnormal karyotype, and 3.4% had adverse-risk chromosomal aberrations.
Prior to analysis, individual patient data were pooled from nine international AML study group registries or treatment centers.
After analysis, the researchers found that adverse cytogenetics were associated with inferior complete remission rates (66.3%), compared with in patients with normal karyotype or intermediate-risk cytogenetic abnormalities (87.7% and 86.0%, respectively; P less than .001). The complete remission rates for the NPM1mut/FLT3-ITDneg/low AML adverse cytogenetics group was similar to patients with NPM1wt/FLT3-ITDneg/low and adverse cytogenetic abnormalities (66.3% vs. 57.5%).
Five-year event-free survival rates and overall survival rates were also lower in patients with NPM1mut/FLT3-ITDneg/low AML and adverse cytogenetics, compared with patients with normal karyotype or intermediate-risk cytogenetic abnormalities (P less than .001).
“Even though the combination of an NPM1 mutation with these abnormalities is rare, the prognostic effect of adverse cytogenetics in NPM1mut AML has important implications for postremission treatment decisions, in particular, the current recommendation that patients who are NPM1mut/FLT3-ITDneg/low not receive allogeneic hematopoietic stem cell transplantation (HSCT), given their presumed low risk of relapse might be altered if the adverse karyotype increased the risk,” they wrote.
The type of chromosomal aberration did not appear to impact this effect, but the small sample size may have hindered the ability to detect a difference between different abnormalities, the researchers noted.
One key limitation of the study was the retrospective design. As a result, in patients with an abnormal karyotype, some genetic analyses could have been underutilized.
“These results demand additional validation within prospective trials,” the researchers concluded.
The study was funded by the University of Munster Medical School, the German Research Foundation, the French government, the Ministry of Health of the Czech Republic, and others. The authors reported financial affiliations with numerous pharmaceutical companies.
SOURCE: Angenendt L et al. J Clin Oncol. 2019 Oct 10;37(29):2632-42.
A pooled analysis suggests adverse cytogenetics are a key factor negatively impacting outcomes in patients with NPM1mut/FLT3-ITDneg/low acute myeloid leukemia (AML).
In patients with adverse chromosomal abnormalities, NPM1 mutational status was found not to confer a favorable outcome. The findings suggest cytogenetic risk outweighs molecular risk in patients with NPM1 mutations and the FLT3-ITDneg/low genotype.
“Patients carrying adverse-risk cytogenetics shared a virtually identical unfavorable outcome, regardless of whether the otherwise beneficial NPM1mut/FLT3-ITDneg/low status was present. The type of the adverse chromosomal abnormality did not seem to influence this effect, although low numbers might obscure detection of heterogeneity among individual aberrations,” Linus Angenendt, MD, of University Hospital Munster (Germany) and colleagues, wrote in the Journal of Clinical Oncology.
The researchers retrospectively analyzed 2,426 patients with NPM1mut/FLT3-ITDneg/low AML. Of these, 17.6% had an abnormal karyotype, and 3.4% had adverse-risk chromosomal aberrations.
Prior to analysis, individual patient data were pooled from nine international AML study group registries or treatment centers.
After analysis, the researchers found that adverse cytogenetics were associated with inferior complete remission rates (66.3%), compared with in patients with normal karyotype or intermediate-risk cytogenetic abnormalities (87.7% and 86.0%, respectively; P less than .001). The complete remission rates for the NPM1mut/FLT3-ITDneg/low AML adverse cytogenetics group was similar to patients with NPM1wt/FLT3-ITDneg/low and adverse cytogenetic abnormalities (66.3% vs. 57.5%).
Five-year event-free survival rates and overall survival rates were also lower in patients with NPM1mut/FLT3-ITDneg/low AML and adverse cytogenetics, compared with patients with normal karyotype or intermediate-risk cytogenetic abnormalities (P less than .001).
“Even though the combination of an NPM1 mutation with these abnormalities is rare, the prognostic effect of adverse cytogenetics in NPM1mut AML has important implications for postremission treatment decisions, in particular, the current recommendation that patients who are NPM1mut/FLT3-ITDneg/low not receive allogeneic hematopoietic stem cell transplantation (HSCT), given their presumed low risk of relapse might be altered if the adverse karyotype increased the risk,” they wrote.
The type of chromosomal aberration did not appear to impact this effect, but the small sample size may have hindered the ability to detect a difference between different abnormalities, the researchers noted.
One key limitation of the study was the retrospective design. As a result, in patients with an abnormal karyotype, some genetic analyses could have been underutilized.
“These results demand additional validation within prospective trials,” the researchers concluded.
The study was funded by the University of Munster Medical School, the German Research Foundation, the French government, the Ministry of Health of the Czech Republic, and others. The authors reported financial affiliations with numerous pharmaceutical companies.
SOURCE: Angenendt L et al. J Clin Oncol. 2019 Oct 10;37(29):2632-42.
REPORTING FROM THE JOURNAL OF CLINICAL ONCOLOGY
Calendar
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Dec. 9-10, 11-12, 18-19, 2019; Jan. 15-16, 22-23; Feb. 12-13, Mar. 10-11, 11-12, 25-26; Apr. 15-16; May 13-14, 2020
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a 2-day, in-depth training course provided by McVey Associates, Inc.
Anaheim, Calif. (12/9-10); Houston, Tex. (12/11-12); New Orleans, La. (12/18-19); Phoenix, Ariz. (12/18-19); Pittsburgh, Pa. (1/15-16); Dallas, Tex. (1/22-23); Hartford, Conn. (2/12-13); Orlando, Fla. (3/10-11); Novi, Mich. (3/11-12); Charlotte, N.C. (3/25-26); Columbus, Ohio (4/15-16); Chicago, Ill. (5/13-14)
Jan. 23–25, 2020
2020 Crohn’s & Colitis Congress®
Gain a multidisciplinary perspective on treating inflammatory bowel diseases (IBD). Join health care professionals and researchers at the Crohn’s & Colitis Congress® for the premier conference on IBD. Discover different perspectives, leave with practical information you can immediately implement, and hear about potential treatments on the horizon.
Austin, Tex.
Jan. 23–25, 2020
Gastrointestinal Cancers Symposium
Designed for clinicians, scientists, and all other members of the cancer care and research community, the 2020 Gastrointestinal Cancers Symposium will feature a wide array of multidisciplinary topics and expert faculty will offer insights on the application of gastrointestinal advances in: cancers of the esophagus and stomach, pancreas, small bowel and hepatobiliary tract, and the colon, rectum, and anus.
San Francisco, Calif.
Feb. 8-9, 2020
2020 Academic Skills Workshop
A free biannual meeting for fellows and early-career GIs that is implemented in conjunction with the AASLD. Topics range from leveraging mentor-mentee relationships, promotion strategies, and insights on writing grants. The application deadline is Nov. 18, 2019.
Charlotte, N.C.
Feb. 20; Mar. 24, 2020
Coding and Reimbursement Solutions by McVey Associates, Inc.
Improve the efficiency and performance of your practice by staying current on the latest reimbursement, coding and compliance changes.
Knoxville, Tenn. (2/20); Birmingham, Ala. (3/24)
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Ill.
June 3-6, 2020
2020 AGA Tech Summit
Visit https://techsummit.gastro.org/ for more details.
San Francisco, Calif.
AWARDS DEADLINES
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD, or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Dec. 9-10, 11-12, 18-19, 2019; Jan. 15-16, 22-23; Feb. 12-13, Mar. 10-11, 11-12, 25-26; Apr. 15-16; May 13-14, 2020
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a 2-day, in-depth training course provided by McVey Associates, Inc.
Anaheim, Calif. (12/9-10); Houston, Tex. (12/11-12); New Orleans, La. (12/18-19); Phoenix, Ariz. (12/18-19); Pittsburgh, Pa. (1/15-16); Dallas, Tex. (1/22-23); Hartford, Conn. (2/12-13); Orlando, Fla. (3/10-11); Novi, Mich. (3/11-12); Charlotte, N.C. (3/25-26); Columbus, Ohio (4/15-16); Chicago, Ill. (5/13-14)
Jan. 23–25, 2020
2020 Crohn’s & Colitis Congress®
Gain a multidisciplinary perspective on treating inflammatory bowel diseases (IBD). Join health care professionals and researchers at the Crohn’s & Colitis Congress® for the premier conference on IBD. Discover different perspectives, leave with practical information you can immediately implement, and hear about potential treatments on the horizon.
Austin, Tex.
Jan. 23–25, 2020
Gastrointestinal Cancers Symposium
Designed for clinicians, scientists, and all other members of the cancer care and research community, the 2020 Gastrointestinal Cancers Symposium will feature a wide array of multidisciplinary topics and expert faculty will offer insights on the application of gastrointestinal advances in: cancers of the esophagus and stomach, pancreas, small bowel and hepatobiliary tract, and the colon, rectum, and anus.
San Francisco, Calif.
Feb. 8-9, 2020
2020 Academic Skills Workshop
A free biannual meeting for fellows and early-career GIs that is implemented in conjunction with the AASLD. Topics range from leveraging mentor-mentee relationships, promotion strategies, and insights on writing grants. The application deadline is Nov. 18, 2019.
Charlotte, N.C.
Feb. 20; Mar. 24, 2020
Coding and Reimbursement Solutions by McVey Associates, Inc.
Improve the efficiency and performance of your practice by staying current on the latest reimbursement, coding and compliance changes.
Knoxville, Tenn. (2/20); Birmingham, Ala. (3/24)
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Ill.
June 3-6, 2020
2020 AGA Tech Summit
Visit https://techsummit.gastro.org/ for more details.
San Francisco, Calif.
AWARDS DEADLINES
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD, or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Dec. 9-10, 11-12, 18-19, 2019; Jan. 15-16, 22-23; Feb. 12-13, Mar. 10-11, 11-12, 25-26; Apr. 15-16; May 13-14, 2020
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a 2-day, in-depth training course provided by McVey Associates, Inc.
Anaheim, Calif. (12/9-10); Houston, Tex. (12/11-12); New Orleans, La. (12/18-19); Phoenix, Ariz. (12/18-19); Pittsburgh, Pa. (1/15-16); Dallas, Tex. (1/22-23); Hartford, Conn. (2/12-13); Orlando, Fla. (3/10-11); Novi, Mich. (3/11-12); Charlotte, N.C. (3/25-26); Columbus, Ohio (4/15-16); Chicago, Ill. (5/13-14)
Jan. 23–25, 2020
2020 Crohn’s & Colitis Congress®
Gain a multidisciplinary perspective on treating inflammatory bowel diseases (IBD). Join health care professionals and researchers at the Crohn’s & Colitis Congress® for the premier conference on IBD. Discover different perspectives, leave with practical information you can immediately implement, and hear about potential treatments on the horizon.
Austin, Tex.
Jan. 23–25, 2020
Gastrointestinal Cancers Symposium
Designed for clinicians, scientists, and all other members of the cancer care and research community, the 2020 Gastrointestinal Cancers Symposium will feature a wide array of multidisciplinary topics and expert faculty will offer insights on the application of gastrointestinal advances in: cancers of the esophagus and stomach, pancreas, small bowel and hepatobiliary tract, and the colon, rectum, and anus.
San Francisco, Calif.
Feb. 8-9, 2020
2020 Academic Skills Workshop
A free biannual meeting for fellows and early-career GIs that is implemented in conjunction with the AASLD. Topics range from leveraging mentor-mentee relationships, promotion strategies, and insights on writing grants. The application deadline is Nov. 18, 2019.
Charlotte, N.C.
Feb. 20; Mar. 24, 2020
Coding and Reimbursement Solutions by McVey Associates, Inc.
Improve the efficiency and performance of your practice by staying current on the latest reimbursement, coding and compliance changes.
Knoxville, Tenn. (2/20); Birmingham, Ala. (3/24)
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Ill.
June 3-6, 2020
2020 AGA Tech Summit
Visit https://techsummit.gastro.org/ for more details.
San Francisco, Calif.
AWARDS DEADLINES
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD, or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
Don’t let knowledge gaps hold back fracture prevention efforts, experts say
ORLANDO – Clinicians shouldn't let the lack of research on osteoporosis treatment compliance and barriers to care keep them from acting on what's already known about drug therapies' effectiveness in preventing fractures.
That's the advice from leaders at the American Society for Bone and Mineral Research, who discussed recent recommendations issued from a National Institutes of Health Pathways to Prevention Workshop on the “Appropriate Use of Drug Therapies for Osteoporotic Fracture Prevention.”
Speakers at a special session of the annual meeting were in agreement on the need for more research into current barriers of osteoporosis care and new methods for increasing patient and physician compliance with recommendations.
But the focus should also be on what researchers in bone health have already learned about treating osteoporosis, “which is quite a bit,” said Benjamin Z. Leder, MD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, who gave the ASBMR’s perspective at the session. Dr. Leder was also first author on a perspective paper that outlined the society’s concerns about the recommendations coming from the workshop (J Bone Miner Res. 2019;34[9]:1549-51).
Gaps in knowledge and treatment
“We thought that [not focusing on what is already known about osteoporosis treatment] perhaps would have the potential to exacerbate the treatment gap that exists in osteoporosis therapy,” Dr. Leder said in his presentation. “We also felt that any knowledge deficits must be understood in the context of what has been unequivocally demonstrated in terms of our knowledge of osteoporosis therapies.”
That includes knowing how to identify patients at the highest risk of fracture, which medications reduce the risk of osteoporotic and osteopenic fractures, and that using these medications saves lives, Dr. Leder noted.
With limited resources in osteoporosis and the absence of any large, randomized, controlled trials or new therapies because of lack of interest from industry, stakeholders should be examining what can be done outside of trials. In osteoporosis, as is the case with any other therapeutic area or disease state, the results of randomized, placebo-controlled trials will not address every patient subgroup of interest, he said.
“Some extrapolation is always required,” Dr. Leder said. “We have to – as we treat, as we practice medicine – use the evidence we have and then try to use that to guide us when the randomized, controlled trial doesn’t answer that specific question.”
Dr. Leder also emphasized that fear of side effects such as osteonecrosis of the jaw and atypical femoral fracture are not the only barriers in osteoporosis care. Adherence is generally poor with osteoporosis treatment, and physicians usually have competing priorities when seeing their patients. “Even in the absence of the idea that these side effects are potentially paralyzing patients and physicians, we have to remember that we started from a fairly low baseline,” Dr. Leder said.
Other issues that complicate the issue of osteoporosis care are misinformation available online that may cause patients to not use medications, overestimations of the benefits of not using osteoporosis medication in favor of nondrug interventions, and conflicting, faulty, or unhelpful guidelines from medical societies, he said.
“There are a lot of issues that need to be addressed. The [Pathways to Prevention] has really done us a great service, and the ASBMR hopes to continue supporting their efforts moving forward,” he said.
Recommendations for secondary fracture prevention
Although there are gaps in osteoporosis treatment, there is still room to act, which the ASBMR aimed to accomplish in its Secondary Fracture Prevention Initiative, Douglas P. Kiel, MD, MPH, said in his presentation.
In 2016, the ASBMR put out a Call to Action to intensify screening for high-risk patients to prevent fractures, and 39 organizations signed on to the effort. The target population for the initiative is men and women aged 65 years or older who have experienced a vertebral or hip fracture who would ideally be appropriately evaluated, managed, and treated in a multidisciplinary clinical system with case management through systems like a fracture liaison service.
“The bottom line is, if you have a patient in this age group who has already experienced one of these fractures, they should be treated,” said Dr. Kiel, director of the Musculoskeletal Research Center at the Institute for Aging Research at Hebrew SeniorLife in Boston and a professor of medicine at Harvard Medical School. “It doesn’t mean we should ignore other populations, but we need to start somewhere, and this was a well-defined, at-risk population.”
Consensus clinical recommendations for the initiative were recently published in the Journal of Bone and Mineral Research (J Bone Miner Res. 2019 Sep 20. doi: 10.1002/jbmr.3877), and the ASBMR plans to spread the recommendations in a wide number of areas, including through stakeholder organizations, social media, webinars, educational sessions, and in other guidelines.
The next step for the initiative is to execute the ASBMR’s Action Plan, which prioritizes challenges such as reimbursement for fracture liaison services and care coordination, establishment of a national fracture registry, and sharing the society’s messaging on osteoporosis fracture–prevention in guidelines and education services. The ASBMR is also examining whether it could take advantage of a new National Institutes of Health grant for dissemination and implementation research in health to help fund the Secondary Fracture Prevention Initiative, Dr. Kiel said.
Dr. Leder and Dr. Kiel reported no relevant financial disclosures.
ORLANDO – Clinicians shouldn't let the lack of research on osteoporosis treatment compliance and barriers to care keep them from acting on what's already known about drug therapies' effectiveness in preventing fractures.
That's the advice from leaders at the American Society for Bone and Mineral Research, who discussed recent recommendations issued from a National Institutes of Health Pathways to Prevention Workshop on the “Appropriate Use of Drug Therapies for Osteoporotic Fracture Prevention.”
Speakers at a special session of the annual meeting were in agreement on the need for more research into current barriers of osteoporosis care and new methods for increasing patient and physician compliance with recommendations.
But the focus should also be on what researchers in bone health have already learned about treating osteoporosis, “which is quite a bit,” said Benjamin Z. Leder, MD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, who gave the ASBMR’s perspective at the session. Dr. Leder was also first author on a perspective paper that outlined the society’s concerns about the recommendations coming from the workshop (J Bone Miner Res. 2019;34[9]:1549-51).
Gaps in knowledge and treatment
“We thought that [not focusing on what is already known about osteoporosis treatment] perhaps would have the potential to exacerbate the treatment gap that exists in osteoporosis therapy,” Dr. Leder said in his presentation. “We also felt that any knowledge deficits must be understood in the context of what has been unequivocally demonstrated in terms of our knowledge of osteoporosis therapies.”
That includes knowing how to identify patients at the highest risk of fracture, which medications reduce the risk of osteoporotic and osteopenic fractures, and that using these medications saves lives, Dr. Leder noted.
With limited resources in osteoporosis and the absence of any large, randomized, controlled trials or new therapies because of lack of interest from industry, stakeholders should be examining what can be done outside of trials. In osteoporosis, as is the case with any other therapeutic area or disease state, the results of randomized, placebo-controlled trials will not address every patient subgroup of interest, he said.
“Some extrapolation is always required,” Dr. Leder said. “We have to – as we treat, as we practice medicine – use the evidence we have and then try to use that to guide us when the randomized, controlled trial doesn’t answer that specific question.”
Dr. Leder also emphasized that fear of side effects such as osteonecrosis of the jaw and atypical femoral fracture are not the only barriers in osteoporosis care. Adherence is generally poor with osteoporosis treatment, and physicians usually have competing priorities when seeing their patients. “Even in the absence of the idea that these side effects are potentially paralyzing patients and physicians, we have to remember that we started from a fairly low baseline,” Dr. Leder said.
Other issues that complicate the issue of osteoporosis care are misinformation available online that may cause patients to not use medications, overestimations of the benefits of not using osteoporosis medication in favor of nondrug interventions, and conflicting, faulty, or unhelpful guidelines from medical societies, he said.
“There are a lot of issues that need to be addressed. The [Pathways to Prevention] has really done us a great service, and the ASBMR hopes to continue supporting their efforts moving forward,” he said.
Recommendations for secondary fracture prevention
Although there are gaps in osteoporosis treatment, there is still room to act, which the ASBMR aimed to accomplish in its Secondary Fracture Prevention Initiative, Douglas P. Kiel, MD, MPH, said in his presentation.
In 2016, the ASBMR put out a Call to Action to intensify screening for high-risk patients to prevent fractures, and 39 organizations signed on to the effort. The target population for the initiative is men and women aged 65 years or older who have experienced a vertebral or hip fracture who would ideally be appropriately evaluated, managed, and treated in a multidisciplinary clinical system with case management through systems like a fracture liaison service.
“The bottom line is, if you have a patient in this age group who has already experienced one of these fractures, they should be treated,” said Dr. Kiel, director of the Musculoskeletal Research Center at the Institute for Aging Research at Hebrew SeniorLife in Boston and a professor of medicine at Harvard Medical School. “It doesn’t mean we should ignore other populations, but we need to start somewhere, and this was a well-defined, at-risk population.”
Consensus clinical recommendations for the initiative were recently published in the Journal of Bone and Mineral Research (J Bone Miner Res. 2019 Sep 20. doi: 10.1002/jbmr.3877), and the ASBMR plans to spread the recommendations in a wide number of areas, including through stakeholder organizations, social media, webinars, educational sessions, and in other guidelines.
The next step for the initiative is to execute the ASBMR’s Action Plan, which prioritizes challenges such as reimbursement for fracture liaison services and care coordination, establishment of a national fracture registry, and sharing the society’s messaging on osteoporosis fracture–prevention in guidelines and education services. The ASBMR is also examining whether it could take advantage of a new National Institutes of Health grant for dissemination and implementation research in health to help fund the Secondary Fracture Prevention Initiative, Dr. Kiel said.
Dr. Leder and Dr. Kiel reported no relevant financial disclosures.
ORLANDO – Clinicians shouldn't let the lack of research on osteoporosis treatment compliance and barriers to care keep them from acting on what's already known about drug therapies' effectiveness in preventing fractures.
That's the advice from leaders at the American Society for Bone and Mineral Research, who discussed recent recommendations issued from a National Institutes of Health Pathways to Prevention Workshop on the “Appropriate Use of Drug Therapies for Osteoporotic Fracture Prevention.”
Speakers at a special session of the annual meeting were in agreement on the need for more research into current barriers of osteoporosis care and new methods for increasing patient and physician compliance with recommendations.
But the focus should also be on what researchers in bone health have already learned about treating osteoporosis, “which is quite a bit,” said Benjamin Z. Leder, MD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, who gave the ASBMR’s perspective at the session. Dr. Leder was also first author on a perspective paper that outlined the society’s concerns about the recommendations coming from the workshop (J Bone Miner Res. 2019;34[9]:1549-51).
Gaps in knowledge and treatment
“We thought that [not focusing on what is already known about osteoporosis treatment] perhaps would have the potential to exacerbate the treatment gap that exists in osteoporosis therapy,” Dr. Leder said in his presentation. “We also felt that any knowledge deficits must be understood in the context of what has been unequivocally demonstrated in terms of our knowledge of osteoporosis therapies.”
That includes knowing how to identify patients at the highest risk of fracture, which medications reduce the risk of osteoporotic and osteopenic fractures, and that using these medications saves lives, Dr. Leder noted.
With limited resources in osteoporosis and the absence of any large, randomized, controlled trials or new therapies because of lack of interest from industry, stakeholders should be examining what can be done outside of trials. In osteoporosis, as is the case with any other therapeutic area or disease state, the results of randomized, placebo-controlled trials will not address every patient subgroup of interest, he said.
“Some extrapolation is always required,” Dr. Leder said. “We have to – as we treat, as we practice medicine – use the evidence we have and then try to use that to guide us when the randomized, controlled trial doesn’t answer that specific question.”
Dr. Leder also emphasized that fear of side effects such as osteonecrosis of the jaw and atypical femoral fracture are not the only barriers in osteoporosis care. Adherence is generally poor with osteoporosis treatment, and physicians usually have competing priorities when seeing their patients. “Even in the absence of the idea that these side effects are potentially paralyzing patients and physicians, we have to remember that we started from a fairly low baseline,” Dr. Leder said.
Other issues that complicate the issue of osteoporosis care are misinformation available online that may cause patients to not use medications, overestimations of the benefits of not using osteoporosis medication in favor of nondrug interventions, and conflicting, faulty, or unhelpful guidelines from medical societies, he said.
“There are a lot of issues that need to be addressed. The [Pathways to Prevention] has really done us a great service, and the ASBMR hopes to continue supporting their efforts moving forward,” he said.
Recommendations for secondary fracture prevention
Although there are gaps in osteoporosis treatment, there is still room to act, which the ASBMR aimed to accomplish in its Secondary Fracture Prevention Initiative, Douglas P. Kiel, MD, MPH, said in his presentation.
In 2016, the ASBMR put out a Call to Action to intensify screening for high-risk patients to prevent fractures, and 39 organizations signed on to the effort. The target population for the initiative is men and women aged 65 years or older who have experienced a vertebral or hip fracture who would ideally be appropriately evaluated, managed, and treated in a multidisciplinary clinical system with case management through systems like a fracture liaison service.
“The bottom line is, if you have a patient in this age group who has already experienced one of these fractures, they should be treated,” said Dr. Kiel, director of the Musculoskeletal Research Center at the Institute for Aging Research at Hebrew SeniorLife in Boston and a professor of medicine at Harvard Medical School. “It doesn’t mean we should ignore other populations, but we need to start somewhere, and this was a well-defined, at-risk population.”
Consensus clinical recommendations for the initiative were recently published in the Journal of Bone and Mineral Research (J Bone Miner Res. 2019 Sep 20. doi: 10.1002/jbmr.3877), and the ASBMR plans to spread the recommendations in a wide number of areas, including through stakeholder organizations, social media, webinars, educational sessions, and in other guidelines.
The next step for the initiative is to execute the ASBMR’s Action Plan, which prioritizes challenges such as reimbursement for fracture liaison services and care coordination, establishment of a national fracture registry, and sharing the society’s messaging on osteoporosis fracture–prevention in guidelines and education services. The ASBMR is also examining whether it could take advantage of a new National Institutes of Health grant for dissemination and implementation research in health to help fund the Secondary Fracture Prevention Initiative, Dr. Kiel said.
Dr. Leder and Dr. Kiel reported no relevant financial disclosures.
EXPERT ANALYSIS FROM ASBMR 2019
Coronary Artery Calcification Scores in Migraine Patients
No significant differences were demonstrated in the amount of coronary calcifications in patients with and without migraine, a new study found. Researchers evaluated if the increased cardiovascular (CV) risk in migraineurs is attributed to an increased coronary artery calcification (CAC). They found:
- The CAC score was assessed by computed tomography of the heart in 1,437 patients, of which 337 were migraineurs.
- All patients had a similar CV risk profile, so that the risk for CAC could be considered similar between migraineurs and non-migraineurs.
- There were no significant differences in the amount of CAC in patients with or without migraine.
Filippopulos FM, et al. Coronary artery calcification score in migraine patients. [Published online ahead of print October 1, 2019]. Sci Rep. doi: 10.1038/s41598-019-50660-9.
No significant differences were demonstrated in the amount of coronary calcifications in patients with and without migraine, a new study found. Researchers evaluated if the increased cardiovascular (CV) risk in migraineurs is attributed to an increased coronary artery calcification (CAC). They found:
- The CAC score was assessed by computed tomography of the heart in 1,437 patients, of which 337 were migraineurs.
- All patients had a similar CV risk profile, so that the risk for CAC could be considered similar between migraineurs and non-migraineurs.
- There were no significant differences in the amount of CAC in patients with or without migraine.
Filippopulos FM, et al. Coronary artery calcification score in migraine patients. [Published online ahead of print October 1, 2019]. Sci Rep. doi: 10.1038/s41598-019-50660-9.
No significant differences were demonstrated in the amount of coronary calcifications in patients with and without migraine, a new study found. Researchers evaluated if the increased cardiovascular (CV) risk in migraineurs is attributed to an increased coronary artery calcification (CAC). They found:
- The CAC score was assessed by computed tomography of the heart in 1,437 patients, of which 337 were migraineurs.
- All patients had a similar CV risk profile, so that the risk for CAC could be considered similar between migraineurs and non-migraineurs.
- There were no significant differences in the amount of CAC in patients with or without migraine.
Filippopulos FM, et al. Coronary artery calcification score in migraine patients. [Published online ahead of print October 1, 2019]. Sci Rep. doi: 10.1038/s41598-019-50660-9.
Abnormal CV Response to Nitroglycerin in Migraine
Patients with migraine who developed a migraine-like attack in response to nitroglycerin demonstrated stronger systemic cardiovascular (CV) responses compared to non-headache controls, a new study found. In 16 women with migraine without aura and 10 age- and gender-matched controls, intravenous nitroglycerin was administered. Researchers found:
- Nitroglycerin provoked a migraine-like attack in 81.2% of migraineurs but not in controls.
- Migraineurs who later developed a migraine-like attack showed different responses in all parameters vs controls.
- The decreases in cardiac output and stroke volume were more rapid and longer lasting, heart rate increased, mean arterial pressure and total peripheral resistance were higher and decreased after an initial increase.
van Oosterhout WPJ, et al. Abnormal cardiovascular response to nitroglycerin in migraine. [Published online ahead of print October 9, 2019]. Cephalalgia. doi: 10.1177/0333102419881657.
Patients with migraine who developed a migraine-like attack in response to nitroglycerin demonstrated stronger systemic cardiovascular (CV) responses compared to non-headache controls, a new study found. In 16 women with migraine without aura and 10 age- and gender-matched controls, intravenous nitroglycerin was administered. Researchers found:
- Nitroglycerin provoked a migraine-like attack in 81.2% of migraineurs but not in controls.
- Migraineurs who later developed a migraine-like attack showed different responses in all parameters vs controls.
- The decreases in cardiac output and stroke volume were more rapid and longer lasting, heart rate increased, mean arterial pressure and total peripheral resistance were higher and decreased after an initial increase.
van Oosterhout WPJ, et al. Abnormal cardiovascular response to nitroglycerin in migraine. [Published online ahead of print October 9, 2019]. Cephalalgia. doi: 10.1177/0333102419881657.
Patients with migraine who developed a migraine-like attack in response to nitroglycerin demonstrated stronger systemic cardiovascular (CV) responses compared to non-headache controls, a new study found. In 16 women with migraine without aura and 10 age- and gender-matched controls, intravenous nitroglycerin was administered. Researchers found:
- Nitroglycerin provoked a migraine-like attack in 81.2% of migraineurs but not in controls.
- Migraineurs who later developed a migraine-like attack showed different responses in all parameters vs controls.
- The decreases in cardiac output and stroke volume were more rapid and longer lasting, heart rate increased, mean arterial pressure and total peripheral resistance were higher and decreased after an initial increase.
van Oosterhout WPJ, et al. Abnormal cardiovascular response to nitroglycerin in migraine. [Published online ahead of print October 9, 2019]. Cephalalgia. doi: 10.1177/0333102419881657.
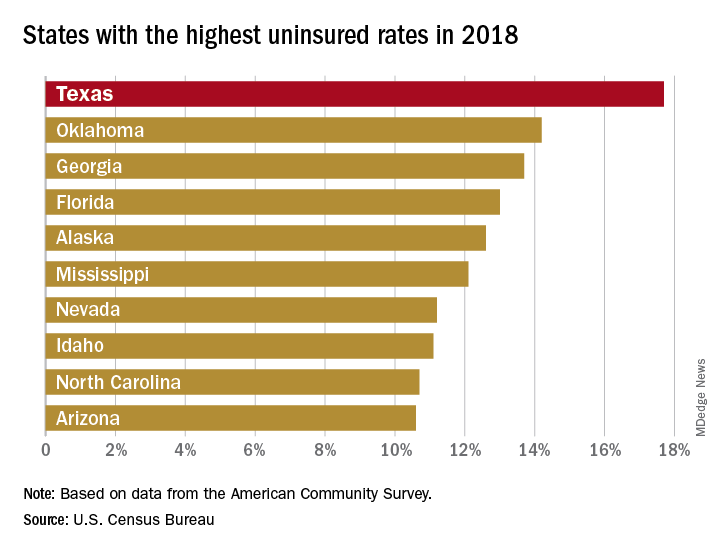
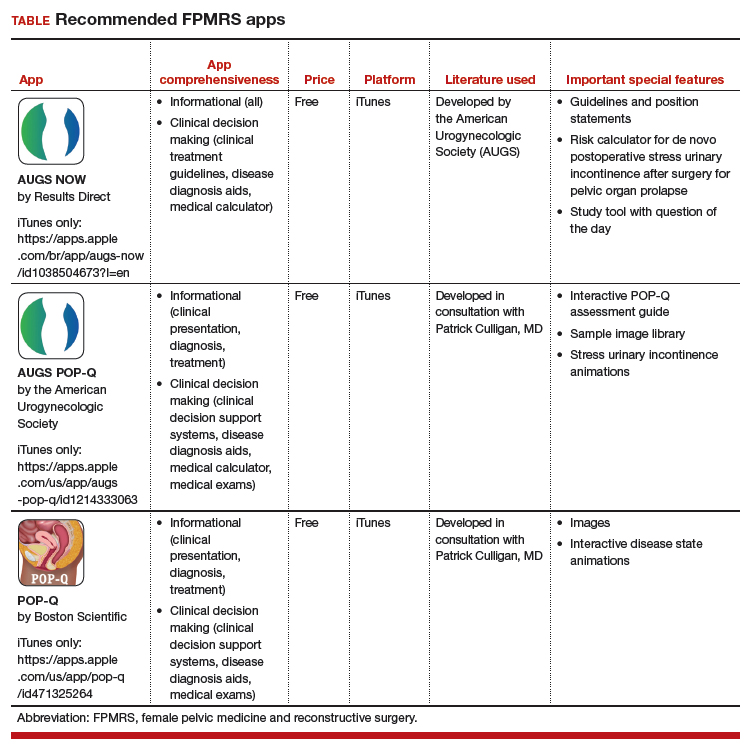
Three free apps for urogynecology providers
Thousands of medical apps are available for smart mobile devices; however, identifying accurate and high-quality apps poses a challenge to health care providers. In the field of urogynecology, also known as female pelvic medicine and reconstructive surgery (FPMRS), the authors of a recent study identified and rated a number of apps for use by urogynecologists.1
The 3 apps featured here are all free and are both informational and clinical decision-making apps.
Informational apps include one or more of the following datasets in a given condition: epidemiology, etiology/pathophysiology, histology/pathology, clinical presentation, treatment, follow-up care, prevention, and/or prognosis.
Clinical decision-making apps may have the following functionalities within the app: clinical decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, medical calculators, laboratory test ordering, laboratory test interpretation, and/or medical exams.
The TABLE details the features of these recommended apps based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).2 I hope urogynecologists view these apps as innovative educational resources that provide quick medical knowledge and pelvic floor patient education.
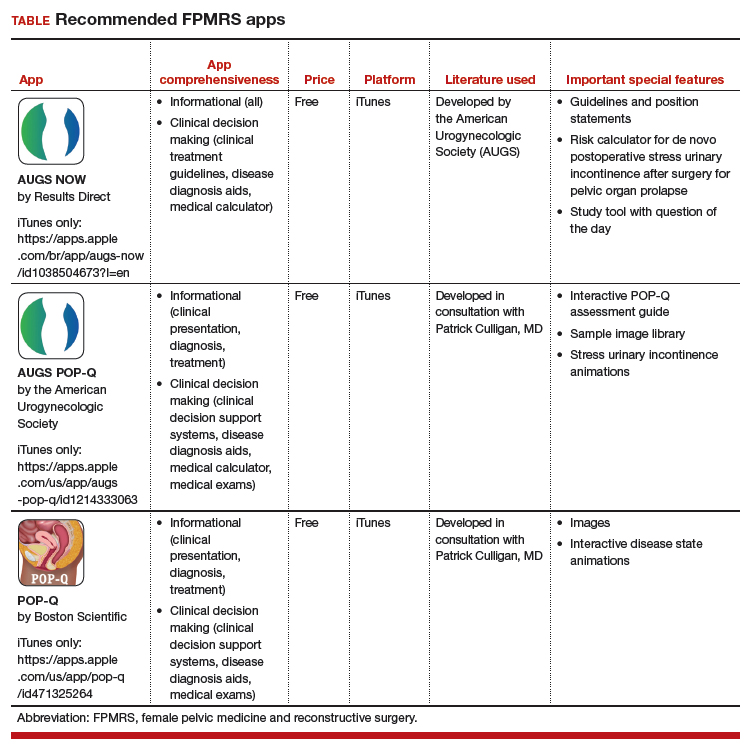
1. Wallace SL, Mehta S, Farag S, et al. In search of mobile applications for urogynecology providers. Female Pelvic Med Reconstr Surg. 2018. doi:10.1097/SPV.0000000000000580.
2. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
Thousands of medical apps are available for smart mobile devices; however, identifying accurate and high-quality apps poses a challenge to health care providers. In the field of urogynecology, also known as female pelvic medicine and reconstructive surgery (FPMRS), the authors of a recent study identified and rated a number of apps for use by urogynecologists.1
The 3 apps featured here are all free and are both informational and clinical decision-making apps.
Informational apps include one or more of the following datasets in a given condition: epidemiology, etiology/pathophysiology, histology/pathology, clinical presentation, treatment, follow-up care, prevention, and/or prognosis.
Clinical decision-making apps may have the following functionalities within the app: clinical decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, medical calculators, laboratory test ordering, laboratory test interpretation, and/or medical exams.
The TABLE details the features of these recommended apps based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).2 I hope urogynecologists view these apps as innovative educational resources that provide quick medical knowledge and pelvic floor patient education.
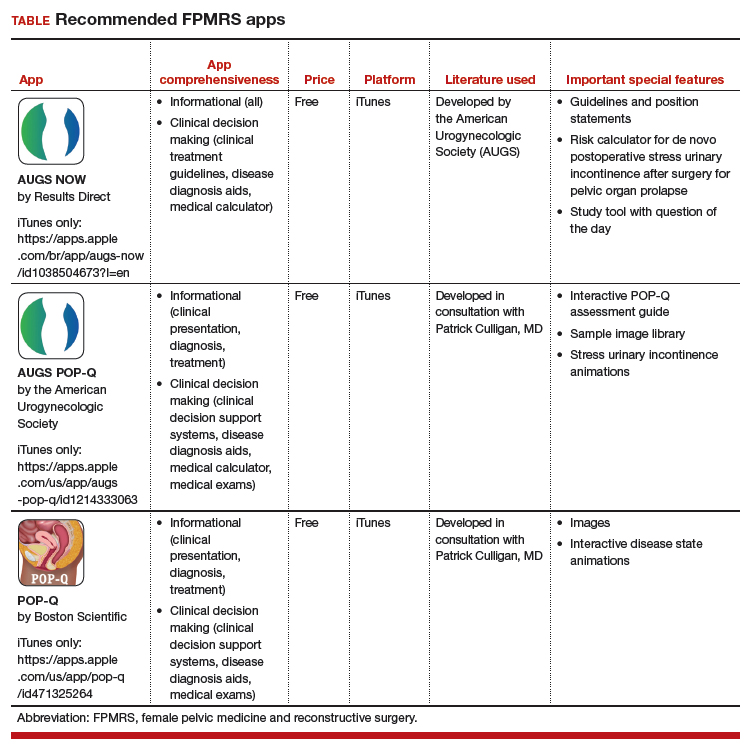
Thousands of medical apps are available for smart mobile devices; however, identifying accurate and high-quality apps poses a challenge to health care providers. In the field of urogynecology, also known as female pelvic medicine and reconstructive surgery (FPMRS), the authors of a recent study identified and rated a number of apps for use by urogynecologists.1
The 3 apps featured here are all free and are both informational and clinical decision-making apps.
Informational apps include one or more of the following datasets in a given condition: epidemiology, etiology/pathophysiology, histology/pathology, clinical presentation, treatment, follow-up care, prevention, and/or prognosis.
Clinical decision-making apps may have the following functionalities within the app: clinical decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, medical calculators, laboratory test ordering, laboratory test interpretation, and/or medical exams.
The TABLE details the features of these recommended apps based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).2 I hope urogynecologists view these apps as innovative educational resources that provide quick medical knowledge and pelvic floor patient education.
1. Wallace SL, Mehta S, Farag S, et al. In search of mobile applications for urogynecology providers. Female Pelvic Med Reconstr Surg. 2018. doi:10.1097/SPV.0000000000000580.
2. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
1. Wallace SL, Mehta S, Farag S, et al. In search of mobile applications for urogynecology providers. Female Pelvic Med Reconstr Surg. 2018. doi:10.1097/SPV.0000000000000580.
2. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
Poor Patient Awareness Common in Migraine
Poor awareness of migraine is common among patients in several countries, a new study found. The multicenter study was conducted in 12 headache centers in 7 countries with each center recruiting 100 or less patients referred for a first visit and diagnosed with migraine. Participants were given a structured clinical questionnaire-based interview about perceptions of the type of headache they suffer from, its cause, previous diagnoses, investigations, and treatments. Researchers found:
- Of the 1,161 patients who completed the study, 28% of participants were aware they suffer from migraine.
- 64% of participants called their migraine “headache,” less commonly used terms such as “cervical pain,” “tension headache,” and “sinusitis.”
- 8% of general practitioners and 35% of specialists consulted for migraine formulated the correct diagnosis.
Viana M, et al. Poor patient awareness and frequent misdiagnosis of migraine: findings from a large transcontinental cohort. [Published online ahead of print October 1, 2019]. Eur J Neurol. doi: 10.1111/ene.14098.
Poor awareness of migraine is common among patients in several countries, a new study found. The multicenter study was conducted in 12 headache centers in 7 countries with each center recruiting 100 or less patients referred for a first visit and diagnosed with migraine. Participants were given a structured clinical questionnaire-based interview about perceptions of the type of headache they suffer from, its cause, previous diagnoses, investigations, and treatments. Researchers found:
- Of the 1,161 patients who completed the study, 28% of participants were aware they suffer from migraine.
- 64% of participants called their migraine “headache,” less commonly used terms such as “cervical pain,” “tension headache,” and “sinusitis.”
- 8% of general practitioners and 35% of specialists consulted for migraine formulated the correct diagnosis.
Viana M, et al. Poor patient awareness and frequent misdiagnosis of migraine: findings from a large transcontinental cohort. [Published online ahead of print October 1, 2019]. Eur J Neurol. doi: 10.1111/ene.14098.
Poor awareness of migraine is common among patients in several countries, a new study found. The multicenter study was conducted in 12 headache centers in 7 countries with each center recruiting 100 or less patients referred for a first visit and diagnosed with migraine. Participants were given a structured clinical questionnaire-based interview about perceptions of the type of headache they suffer from, its cause, previous diagnoses, investigations, and treatments. Researchers found:
- Of the 1,161 patients who completed the study, 28% of participants were aware they suffer from migraine.
- 64% of participants called their migraine “headache,” less commonly used terms such as “cervical pain,” “tension headache,” and “sinusitis.”
- 8% of general practitioners and 35% of specialists consulted for migraine formulated the correct diagnosis.
Viana M, et al. Poor patient awareness and frequent misdiagnosis of migraine: findings from a large transcontinental cohort. [Published online ahead of print October 1, 2019]. Eur J Neurol. doi: 10.1111/ene.14098.
Minimize blood pressure peaks, variability after stroke reperfusion
ST. LOUIS – Albuquerque. Investigators found that every 10–mm Hg increase in peak systolic pressure boosted the risk of in-hospital death 24% (P = .01) and reduced the chance of being discharged home or to a inpatient rehabilitation facility 13% (P = .03). Results were even stronger for peak mean arterial pressure, at 76% (P = .01) and 29% (P = .04), respectively; trends in the same direction for peak diastolic pressure were not statistically significant.
Also, every 10–mm Hg increase in blood pressure variability again increased the risk of dying in the hospital, whether it was systolic (33%; P = .002), diastolic (33%; P = .03), or mean arterial pressure variability (58%; P = .02). Higher variability also reduced the chance of being discharged home or to a rehab 10%-20%, but the findings, although close, were not statistically significant.
Neurologists generally do what they can to control blood pressure after stroke, and the study confirms the need to do that. What’s new is that the work was limited to reperfusion patients – intravenous thrombolysis with alteplase in 83.5%, mechanical thrombectomy in 60%, with some having both – which has not been the specific focus of much research.
“Be much more aggressive in terms of making sure the variability is limited and limiting the peaks,” especially within 24 hours of reperfusion, said lead investigator and stroke neurologist Dinesh Jillella, MD, of Emory University, Atlanta, at the annual meeting of the American Neurological Association. “We want to be much more aggressive [with these patients]; it might limit our worse outcomes,” Dr. Jillella said. He conducted the review while in training at the University of New Mexico.
What led to the study is that Dr. Jillella and colleagues noticed that similar reperfusion patients can have very different outcomes, and he wanted to find modifiable risk factors that could account for the differences. The study did not address why high peaks and variability lead to worse outcomes, but he said hemorrhagic conversion might play a role.
It is also possible that higher pressures could be a marker of bad outcomes, as opposed to a direct cause, but the findings were adjusted for two significant confounders: age and the National Institutes of Health Stroke Scale score, which were both significantly higher in patients who did not do well. But after adjustment, “we [still] found an independent association with blood pressures and worse outcomes,” he said.
Higher peak systolic pressures and variability were also associated with about a 15% lower odds of leaving the hospital with a modified Rankin Scale score of 3 or less, which means the patient has some moderate disability but is still able to walk without assistance.
Patients were 69 years old on average, and about 60% were men. The majority were white. About a third had a modified Rankin Scale score at or below 3 at discharge, and about two-thirds were discharged home or to a rehabilitation facility; 17% of patients died in the hospital.
Differences in antihypertensive regimens were not associated with outcomes on univariate analysis. Dr. Jillella said that, ideally, he would like to run a multicenter, prospective trial of blood pressure reduction targets after reperfusion.
There was no external funding, and Dr. Jillella didn’t have any relevant disclosures.
ST. LOUIS – Albuquerque. Investigators found that every 10–mm Hg increase in peak systolic pressure boosted the risk of in-hospital death 24% (P = .01) and reduced the chance of being discharged home or to a inpatient rehabilitation facility 13% (P = .03). Results were even stronger for peak mean arterial pressure, at 76% (P = .01) and 29% (P = .04), respectively; trends in the same direction for peak diastolic pressure were not statistically significant.
Also, every 10–mm Hg increase in blood pressure variability again increased the risk of dying in the hospital, whether it was systolic (33%; P = .002), diastolic (33%; P = .03), or mean arterial pressure variability (58%; P = .02). Higher variability also reduced the chance of being discharged home or to a rehab 10%-20%, but the findings, although close, were not statistically significant.
Neurologists generally do what they can to control blood pressure after stroke, and the study confirms the need to do that. What’s new is that the work was limited to reperfusion patients – intravenous thrombolysis with alteplase in 83.5%, mechanical thrombectomy in 60%, with some having both – which has not been the specific focus of much research.
“Be much more aggressive in terms of making sure the variability is limited and limiting the peaks,” especially within 24 hours of reperfusion, said lead investigator and stroke neurologist Dinesh Jillella, MD, of Emory University, Atlanta, at the annual meeting of the American Neurological Association. “We want to be much more aggressive [with these patients]; it might limit our worse outcomes,” Dr. Jillella said. He conducted the review while in training at the University of New Mexico.
What led to the study is that Dr. Jillella and colleagues noticed that similar reperfusion patients can have very different outcomes, and he wanted to find modifiable risk factors that could account for the differences. The study did not address why high peaks and variability lead to worse outcomes, but he said hemorrhagic conversion might play a role.
It is also possible that higher pressures could be a marker of bad outcomes, as opposed to a direct cause, but the findings were adjusted for two significant confounders: age and the National Institutes of Health Stroke Scale score, which were both significantly higher in patients who did not do well. But after adjustment, “we [still] found an independent association with blood pressures and worse outcomes,” he said.
Higher peak systolic pressures and variability were also associated with about a 15% lower odds of leaving the hospital with a modified Rankin Scale score of 3 or less, which means the patient has some moderate disability but is still able to walk without assistance.
Patients were 69 years old on average, and about 60% were men. The majority were white. About a third had a modified Rankin Scale score at or below 3 at discharge, and about two-thirds were discharged home or to a rehabilitation facility; 17% of patients died in the hospital.
Differences in antihypertensive regimens were not associated with outcomes on univariate analysis. Dr. Jillella said that, ideally, he would like to run a multicenter, prospective trial of blood pressure reduction targets after reperfusion.
There was no external funding, and Dr. Jillella didn’t have any relevant disclosures.
ST. LOUIS – Albuquerque. Investigators found that every 10–mm Hg increase in peak systolic pressure boosted the risk of in-hospital death 24% (P = .01) and reduced the chance of being discharged home or to a inpatient rehabilitation facility 13% (P = .03). Results were even stronger for peak mean arterial pressure, at 76% (P = .01) and 29% (P = .04), respectively; trends in the same direction for peak diastolic pressure were not statistically significant.
Also, every 10–mm Hg increase in blood pressure variability again increased the risk of dying in the hospital, whether it was systolic (33%; P = .002), diastolic (33%; P = .03), or mean arterial pressure variability (58%; P = .02). Higher variability also reduced the chance of being discharged home or to a rehab 10%-20%, but the findings, although close, were not statistically significant.
Neurologists generally do what they can to control blood pressure after stroke, and the study confirms the need to do that. What’s new is that the work was limited to reperfusion patients – intravenous thrombolysis with alteplase in 83.5%, mechanical thrombectomy in 60%, with some having both – which has not been the specific focus of much research.
“Be much more aggressive in terms of making sure the variability is limited and limiting the peaks,” especially within 24 hours of reperfusion, said lead investigator and stroke neurologist Dinesh Jillella, MD, of Emory University, Atlanta, at the annual meeting of the American Neurological Association. “We want to be much more aggressive [with these patients]; it might limit our worse outcomes,” Dr. Jillella said. He conducted the review while in training at the University of New Mexico.
What led to the study is that Dr. Jillella and colleagues noticed that similar reperfusion patients can have very different outcomes, and he wanted to find modifiable risk factors that could account for the differences. The study did not address why high peaks and variability lead to worse outcomes, but he said hemorrhagic conversion might play a role.
It is also possible that higher pressures could be a marker of bad outcomes, as opposed to a direct cause, but the findings were adjusted for two significant confounders: age and the National Institutes of Health Stroke Scale score, which were both significantly higher in patients who did not do well. But after adjustment, “we [still] found an independent association with blood pressures and worse outcomes,” he said.
Higher peak systolic pressures and variability were also associated with about a 15% lower odds of leaving the hospital with a modified Rankin Scale score of 3 or less, which means the patient has some moderate disability but is still able to walk without assistance.
Patients were 69 years old on average, and about 60% were men. The majority were white. About a third had a modified Rankin Scale score at or below 3 at discharge, and about two-thirds were discharged home or to a rehabilitation facility; 17% of patients died in the hospital.
Differences in antihypertensive regimens were not associated with outcomes on univariate analysis. Dr. Jillella said that, ideally, he would like to run a multicenter, prospective trial of blood pressure reduction targets after reperfusion.
There was no external funding, and Dr. Jillella didn’t have any relevant disclosures.
REPORTING FROM ANA 2019
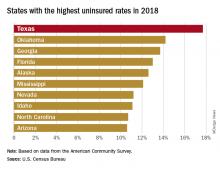
Uninsured population is big in Texas
There were just over 5 million uninsured people in the Lone Star State last year, representing an increase from 17.3% of the total population in 2017 to 17.7%, and that works out to an additional 186,000 residents with no health care coverage, the Census Bureau said in a recent report.
That 17.7% rate for 2018 gave Texas the highest proportion of uninsured population, putting it ahead of Oklahoma (14.2%), Georgia (13.7%), Florida (13.0%), Alaska (12.6%), and Mississippi (12.1%). Oklahoma had basically no change from 2017, while the other three each had a small but nonsignificant increase. Nationally, the rate of uninsured population went from 7.9% in 2017 to 8.5% in 2018, the Census Bureau investigators said.
On the other end of the coverage spectrum was Massachusetts, where only 2.8% of the population, or about 189,000 people, lacked health insurance in 2018. Washington, D.C., was next with an uninsured rate of 3.2%, followed by Vermont (4.0%), Hawaii (4.1%), Rhode Island (4.1%), and Minnesota (4.4%), they said, based on data from the American Community Survey.
A separate analysis of Census Bureau data by the personal finance website WalletHub showed that states that expanded Medicaid along with their Affordable Care Act implementation had an average uninsured rate of 7.0% in 2018, compared with 11.1% for states that did not expand eligibility.
All 50 states were in negative territory when changes in uninsured rates were calculated over a longer time period, 2010-2018, as the national rate fell by 6.6%. The largest drops among the states came in Nevada (–11.4%), California (–11.3%), Oregon (–10.1%), and New Mexico (–10.1%), while Massachusetts (–1.7%), Maine (–2.1%), and North Dakota (–2.5%) had the smallest declines, WalletHub reported.
There were just over 5 million uninsured people in the Lone Star State last year, representing an increase from 17.3% of the total population in 2017 to 17.7%, and that works out to an additional 186,000 residents with no health care coverage, the Census Bureau said in a recent report.
That 17.7% rate for 2018 gave Texas the highest proportion of uninsured population, putting it ahead of Oklahoma (14.2%), Georgia (13.7%), Florida (13.0%), Alaska (12.6%), and Mississippi (12.1%). Oklahoma had basically no change from 2017, while the other three each had a small but nonsignificant increase. Nationally, the rate of uninsured population went from 7.9% in 2017 to 8.5% in 2018, the Census Bureau investigators said.
On the other end of the coverage spectrum was Massachusetts, where only 2.8% of the population, or about 189,000 people, lacked health insurance in 2018. Washington, D.C., was next with an uninsured rate of 3.2%, followed by Vermont (4.0%), Hawaii (4.1%), Rhode Island (4.1%), and Minnesota (4.4%), they said, based on data from the American Community Survey.
A separate analysis of Census Bureau data by the personal finance website WalletHub showed that states that expanded Medicaid along with their Affordable Care Act implementation had an average uninsured rate of 7.0% in 2018, compared with 11.1% for states that did not expand eligibility.
All 50 states were in negative territory when changes in uninsured rates were calculated over a longer time period, 2010-2018, as the national rate fell by 6.6%. The largest drops among the states came in Nevada (–11.4%), California (–11.3%), Oregon (–10.1%), and New Mexico (–10.1%), while Massachusetts (–1.7%), Maine (–2.1%), and North Dakota (–2.5%) had the smallest declines, WalletHub reported.
There were just over 5 million uninsured people in the Lone Star State last year, representing an increase from 17.3% of the total population in 2017 to 17.7%, and that works out to an additional 186,000 residents with no health care coverage, the Census Bureau said in a recent report.
That 17.7% rate for 2018 gave Texas the highest proportion of uninsured population, putting it ahead of Oklahoma (14.2%), Georgia (13.7%), Florida (13.0%), Alaska (12.6%), and Mississippi (12.1%). Oklahoma had basically no change from 2017, while the other three each had a small but nonsignificant increase. Nationally, the rate of uninsured population went from 7.9% in 2017 to 8.5% in 2018, the Census Bureau investigators said.
On the other end of the coverage spectrum was Massachusetts, where only 2.8% of the population, or about 189,000 people, lacked health insurance in 2018. Washington, D.C., was next with an uninsured rate of 3.2%, followed by Vermont (4.0%), Hawaii (4.1%), Rhode Island (4.1%), and Minnesota (4.4%), they said, based on data from the American Community Survey.
A separate analysis of Census Bureau data by the personal finance website WalletHub showed that states that expanded Medicaid along with their Affordable Care Act implementation had an average uninsured rate of 7.0% in 2018, compared with 11.1% for states that did not expand eligibility.
All 50 states were in negative territory when changes in uninsured rates were calculated over a longer time period, 2010-2018, as the national rate fell by 6.6%. The largest drops among the states came in Nevada (–11.4%), California (–11.3%), Oregon (–10.1%), and New Mexico (–10.1%), while Massachusetts (–1.7%), Maine (–2.1%), and North Dakota (–2.5%) had the smallest declines, WalletHub reported.