User login
Intimate partner violence, guns, and the ObGyn
On the afternoon of November 19, 2018, Dr. Tamara O’Neal was shot and killed by her ex-fiancé outside Mercy Hospital and Medical Center in Chicago, Illinois. After killing Dr. O’Neal, the gunman ran into the hospital where he exchanged gunfire with police, killing a pharmacy resident and a police officer, before he was killed by police.1
This horrific encounter between a woman and her former partner begs for a conversation about intimate partner violence (IPV). A data brief of The National Intimate Partner and Sexual Violence Survey was published in November 2018. According to this report, 30.6% of women experienced physical violence by an intimate partner in 2015, with 21.4% of women experiencing severe physical violence. In addition, 31.0% of men experienced physical violence by an intimate partner in 2015; 14.9% of men experienced severe physical violence.2

Intimate partner violence is “our lane”
The shooting at Mercy Hospital occurred amongst a backdrop of controversy between the National Rifle Association (NRA) and the medical community. On November 7, 2018, the NRA tweeted that doctors should “stay in their lane” with regard to gun control after a position paper from the American College of Physicians on reducing firearm deaths and injuries was published in the Annals of Internal Medicine.3 Doctors from every field and from all over the country responded through social media by stating that treating bullet wounds and caring for those affected by gun violence was “their lane.”4
It is time for us as a community to recognize that gun violence affects us all. The majority of mass shooters have a history of IPV and often target their current or prior partner during the shooting.5 At this intersection of IPV and gun control, the physician has a unique role. We not only treat those affected by gun violence and advocate for better gun control but we also have a duty to screen our patients for IPV. Part of the sacred patient-physician relationship is being present for our patients when they need us most. The American College of Obstetricians and Gynecologists (ACOG) recommends that ObGyns screen patients for IPV at regular intervals and recognizes that it may take several conversations before a patient discloses her history of IPV.6 Additionally, given the increased risk of gun injuries and death, it behooves us to also screen for gun safety in the home.
Ask patients about IPV, and ask again
The shooting at Mercy Hospital was a stark reminder that IPV can affect any of us. With nearly one-third of women and more than one-quarter of men experiencing IPV in their lifetime, action must be taken. The first step is to routinely screen patients for IPV, offering support and community resources. (see “Screening for intimate partner violence). The second step is to work to decrease the access perpetrators of IPV have to weapons with which to enact violence—through legislation, community engagement, and using our physician voices.
States that have passed legislation that prohibits persons with active restraining orders or a history of IPV or domestic violence from possessing firearms has seen a decrease in IPV firearm homicide rates.7 These policies can make a profound impact on the safety of our patients. Women who are in violent relationships are 5 times more likely to die if their partner has access to a firearm.5
Continue to: #BreakTheCycle...
#BreakTheCycle
The 116th Congress convened in January. We have an opportunity to make real gun legislation reform and work to keep our communities and our patients at risk for IPV safer. Tweet your representatives with #BreakTheCycle, and be on the lookout for important legislation to enact real change.
To sign the open letter from American Healthcare Professionals to the NRA regarding their recent comments and our medical experiences with gun violence, click here. Currently, there are more than 41,000 signatures.
There are numerous verified screening tools available to assess for intimate partner violence (IPV) for both pregnant and nonpregnant patients. Many recommended tools are accessible on the Centers for Disease Control and Prevention (CDC) website: https://www.cdc.gov/violenceprevention/pdf/ipv/ipvandsvscreening.pdf. In our office, the tool most commonly used is a 3-part question assessing domestic violence and IPV. It is important to recognize IPV can affect everyone—all races and religions regardless of socioeconomic background, sexual orientation, and pregnancy status. All patients deserve screening for IPV, and it should never be assumed a patient is not at risk. During an annual gynecology visit for return and new patients or a new obstetric intake visit, we use the following script obtained from ACOG’s Committee Opinion 518 on IPV1 :
Because violence is so common in many women’s lives and because there is help available for women being abused, I now ask every patient about domestic violence:
1. Within the past year (or since you have become pregnant) have you been hit, slapped, kicked, or otherwise physically hurt by someone?
2. Are you in a relationship with a person who threatens or physically hurts you?
3. Has anyone forced you to have sexual activities that made you feel uncomfortable?
If a patient screens positive, we assess their immediate safety. If a social worker is readily available, we arrange an urgent meeting with the patient. If offices do not have immediate access to this service, online information can be provided to patients, including the National Resource Center on Domestic Violence (https://nnedv.org/) and a toll-free number to the National Domestic Violence Hotline: 1-800-799-7233. Additionally, we ask patients about any history of verbal, physical, or sexual violence with prior partners, family members, acquaintances, coworkers, etc. Although the patient might not be at immediate risk, prior experiences with abuse can cause fear and anxiety around gynecologic and obstetric exams. Acknowledging this history can help the clinician adjust his or her physical exam and support the patient during, what may be, a triggering experience.
As an additional resource, Dr. Katherine Hicks-Courant, a resident at Tufts Medical Center, in Boston, Massachusetts, created a tool kit for providers working with pregnant patients with a history of sexual assault. It can be accessed without login online under the Junior Fellow Initiative Toolkit section at http://www.acog.org.
References
1. American College of Obstetricians and Gynecologists. Committee Opinion No. 518: intimate partner violence. Obstet Gynecol. 2012;119:412-417.
If you, or someone you know, needs help, please call The National Domestic Violence Hotline at 1-800-799-7233.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Buckley M, Gorner J, Greene M. “Chicago hospital shooting: Young cop, doctor, pharmacy resident and gunman die in Mercy Hospital attack. Chicago Tribune. Nov. 20, 2018.
2. Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner
and Sexual Violence Survey (NISVS): 2015 data brief – updated release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; November 2018.
3. Butkus R, Doherty R, Bornstein SS; for the Health and Public Policy Committee of the American College of Physicians. Reducing firearm injuries and deaths in the United States: a position paper from the American College of Physicians. Ann Intern Med. 2018;169:704-707.
4. Papenfuss M. NRA Tweets Warning to Anti-Gun Doctors: ‘Stay In Your Lane’. The Huffington Post. November 8, 2018.
5. Everytown for Gun Safety website. Mass Shootings in the United States: 2009–2016. Available at https://everytownresearch.org/reports/mass-shootings-analysis/. Accessed January 17, 2019.
6. The American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 518: intimate partner violence. Obstet Gynecol. 2012;119(2 pt 1):412-417. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Intimate-Partner-Violence.
7. Zeoli AM, McCourt A, Buggs S, et al. Analysis of the strength of legal firearms restrictions for perpetrators of domestic violence and their associations with intimate partner homicide. Am J Epidemiol. 2018;187:2365-2371.
On the afternoon of November 19, 2018, Dr. Tamara O’Neal was shot and killed by her ex-fiancé outside Mercy Hospital and Medical Center in Chicago, Illinois. After killing Dr. O’Neal, the gunman ran into the hospital where he exchanged gunfire with police, killing a pharmacy resident and a police officer, before he was killed by police.1
This horrific encounter between a woman and her former partner begs for a conversation about intimate partner violence (IPV). A data brief of The National Intimate Partner and Sexual Violence Survey was published in November 2018. According to this report, 30.6% of women experienced physical violence by an intimate partner in 2015, with 21.4% of women experiencing severe physical violence. In addition, 31.0% of men experienced physical violence by an intimate partner in 2015; 14.9% of men experienced severe physical violence.2

Intimate partner violence is “our lane”
The shooting at Mercy Hospital occurred amongst a backdrop of controversy between the National Rifle Association (NRA) and the medical community. On November 7, 2018, the NRA tweeted that doctors should “stay in their lane” with regard to gun control after a position paper from the American College of Physicians on reducing firearm deaths and injuries was published in the Annals of Internal Medicine.3 Doctors from every field and from all over the country responded through social media by stating that treating bullet wounds and caring for those affected by gun violence was “their lane.”4
It is time for us as a community to recognize that gun violence affects us all. The majority of mass shooters have a history of IPV and often target their current or prior partner during the shooting.5 At this intersection of IPV and gun control, the physician has a unique role. We not only treat those affected by gun violence and advocate for better gun control but we also have a duty to screen our patients for IPV. Part of the sacred patient-physician relationship is being present for our patients when they need us most. The American College of Obstetricians and Gynecologists (ACOG) recommends that ObGyns screen patients for IPV at regular intervals and recognizes that it may take several conversations before a patient discloses her history of IPV.6 Additionally, given the increased risk of gun injuries and death, it behooves us to also screen for gun safety in the home.
Ask patients about IPV, and ask again
The shooting at Mercy Hospital was a stark reminder that IPV can affect any of us. With nearly one-third of women and more than one-quarter of men experiencing IPV in their lifetime, action must be taken. The first step is to routinely screen patients for IPV, offering support and community resources. (see “Screening for intimate partner violence). The second step is to work to decrease the access perpetrators of IPV have to weapons with which to enact violence—through legislation, community engagement, and using our physician voices.
States that have passed legislation that prohibits persons with active restraining orders or a history of IPV or domestic violence from possessing firearms has seen a decrease in IPV firearm homicide rates.7 These policies can make a profound impact on the safety of our patients. Women who are in violent relationships are 5 times more likely to die if their partner has access to a firearm.5
Continue to: #BreakTheCycle...
#BreakTheCycle
The 116th Congress convened in January. We have an opportunity to make real gun legislation reform and work to keep our communities and our patients at risk for IPV safer. Tweet your representatives with #BreakTheCycle, and be on the lookout for important legislation to enact real change.
To sign the open letter from American Healthcare Professionals to the NRA regarding their recent comments and our medical experiences with gun violence, click here. Currently, there are more than 41,000 signatures.
There are numerous verified screening tools available to assess for intimate partner violence (IPV) for both pregnant and nonpregnant patients. Many recommended tools are accessible on the Centers for Disease Control and Prevention (CDC) website: https://www.cdc.gov/violenceprevention/pdf/ipv/ipvandsvscreening.pdf. In our office, the tool most commonly used is a 3-part question assessing domestic violence and IPV. It is important to recognize IPV can affect everyone—all races and religions regardless of socioeconomic background, sexual orientation, and pregnancy status. All patients deserve screening for IPV, and it should never be assumed a patient is not at risk. During an annual gynecology visit for return and new patients or a new obstetric intake visit, we use the following script obtained from ACOG’s Committee Opinion 518 on IPV1 :
Because violence is so common in many women’s lives and because there is help available for women being abused, I now ask every patient about domestic violence:
1. Within the past year (or since you have become pregnant) have you been hit, slapped, kicked, or otherwise physically hurt by someone?
2. Are you in a relationship with a person who threatens or physically hurts you?
3. Has anyone forced you to have sexual activities that made you feel uncomfortable?
If a patient screens positive, we assess their immediate safety. If a social worker is readily available, we arrange an urgent meeting with the patient. If offices do not have immediate access to this service, online information can be provided to patients, including the National Resource Center on Domestic Violence (https://nnedv.org/) and a toll-free number to the National Domestic Violence Hotline: 1-800-799-7233. Additionally, we ask patients about any history of verbal, physical, or sexual violence with prior partners, family members, acquaintances, coworkers, etc. Although the patient might not be at immediate risk, prior experiences with abuse can cause fear and anxiety around gynecologic and obstetric exams. Acknowledging this history can help the clinician adjust his or her physical exam and support the patient during, what may be, a triggering experience.
As an additional resource, Dr. Katherine Hicks-Courant, a resident at Tufts Medical Center, in Boston, Massachusetts, created a tool kit for providers working with pregnant patients with a history of sexual assault. It can be accessed without login online under the Junior Fellow Initiative Toolkit section at http://www.acog.org.
References
1. American College of Obstetricians and Gynecologists. Committee Opinion No. 518: intimate partner violence. Obstet Gynecol. 2012;119:412-417.
If you, or someone you know, needs help, please call The National Domestic Violence Hotline at 1-800-799-7233.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
On the afternoon of November 19, 2018, Dr. Tamara O’Neal was shot and killed by her ex-fiancé outside Mercy Hospital and Medical Center in Chicago, Illinois. After killing Dr. O’Neal, the gunman ran into the hospital where he exchanged gunfire with police, killing a pharmacy resident and a police officer, before he was killed by police.1
This horrific encounter between a woman and her former partner begs for a conversation about intimate partner violence (IPV). A data brief of The National Intimate Partner and Sexual Violence Survey was published in November 2018. According to this report, 30.6% of women experienced physical violence by an intimate partner in 2015, with 21.4% of women experiencing severe physical violence. In addition, 31.0% of men experienced physical violence by an intimate partner in 2015; 14.9% of men experienced severe physical violence.2

Intimate partner violence is “our lane”
The shooting at Mercy Hospital occurred amongst a backdrop of controversy between the National Rifle Association (NRA) and the medical community. On November 7, 2018, the NRA tweeted that doctors should “stay in their lane” with regard to gun control after a position paper from the American College of Physicians on reducing firearm deaths and injuries was published in the Annals of Internal Medicine.3 Doctors from every field and from all over the country responded through social media by stating that treating bullet wounds and caring for those affected by gun violence was “their lane.”4
It is time for us as a community to recognize that gun violence affects us all. The majority of mass shooters have a history of IPV and often target their current or prior partner during the shooting.5 At this intersection of IPV and gun control, the physician has a unique role. We not only treat those affected by gun violence and advocate for better gun control but we also have a duty to screen our patients for IPV. Part of the sacred patient-physician relationship is being present for our patients when they need us most. The American College of Obstetricians and Gynecologists (ACOG) recommends that ObGyns screen patients for IPV at regular intervals and recognizes that it may take several conversations before a patient discloses her history of IPV.6 Additionally, given the increased risk of gun injuries and death, it behooves us to also screen for gun safety in the home.
Ask patients about IPV, and ask again
The shooting at Mercy Hospital was a stark reminder that IPV can affect any of us. With nearly one-third of women and more than one-quarter of men experiencing IPV in their lifetime, action must be taken. The first step is to routinely screen patients for IPV, offering support and community resources. (see “Screening for intimate partner violence). The second step is to work to decrease the access perpetrators of IPV have to weapons with which to enact violence—through legislation, community engagement, and using our physician voices.
States that have passed legislation that prohibits persons with active restraining orders or a history of IPV or domestic violence from possessing firearms has seen a decrease in IPV firearm homicide rates.7 These policies can make a profound impact on the safety of our patients. Women who are in violent relationships are 5 times more likely to die if their partner has access to a firearm.5
Continue to: #BreakTheCycle...
#BreakTheCycle
The 116th Congress convened in January. We have an opportunity to make real gun legislation reform and work to keep our communities and our patients at risk for IPV safer. Tweet your representatives with #BreakTheCycle, and be on the lookout for important legislation to enact real change.
To sign the open letter from American Healthcare Professionals to the NRA regarding their recent comments and our medical experiences with gun violence, click here. Currently, there are more than 41,000 signatures.
There are numerous verified screening tools available to assess for intimate partner violence (IPV) for both pregnant and nonpregnant patients. Many recommended tools are accessible on the Centers for Disease Control and Prevention (CDC) website: https://www.cdc.gov/violenceprevention/pdf/ipv/ipvandsvscreening.pdf. In our office, the tool most commonly used is a 3-part question assessing domestic violence and IPV. It is important to recognize IPV can affect everyone—all races and religions regardless of socioeconomic background, sexual orientation, and pregnancy status. All patients deserve screening for IPV, and it should never be assumed a patient is not at risk. During an annual gynecology visit for return and new patients or a new obstetric intake visit, we use the following script obtained from ACOG’s Committee Opinion 518 on IPV1 :
Because violence is so common in many women’s lives and because there is help available for women being abused, I now ask every patient about domestic violence:
1. Within the past year (or since you have become pregnant) have you been hit, slapped, kicked, or otherwise physically hurt by someone?
2. Are you in a relationship with a person who threatens or physically hurts you?
3. Has anyone forced you to have sexual activities that made you feel uncomfortable?
If a patient screens positive, we assess their immediate safety. If a social worker is readily available, we arrange an urgent meeting with the patient. If offices do not have immediate access to this service, online information can be provided to patients, including the National Resource Center on Domestic Violence (https://nnedv.org/) and a toll-free number to the National Domestic Violence Hotline: 1-800-799-7233. Additionally, we ask patients about any history of verbal, physical, or sexual violence with prior partners, family members, acquaintances, coworkers, etc. Although the patient might not be at immediate risk, prior experiences with abuse can cause fear and anxiety around gynecologic and obstetric exams. Acknowledging this history can help the clinician adjust his or her physical exam and support the patient during, what may be, a triggering experience.
As an additional resource, Dr. Katherine Hicks-Courant, a resident at Tufts Medical Center, in Boston, Massachusetts, created a tool kit for providers working with pregnant patients with a history of sexual assault. It can be accessed without login online under the Junior Fellow Initiative Toolkit section at http://www.acog.org.
References
1. American College of Obstetricians and Gynecologists. Committee Opinion No. 518: intimate partner violence. Obstet Gynecol. 2012;119:412-417.
If you, or someone you know, needs help, please call The National Domestic Violence Hotline at 1-800-799-7233.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Buckley M, Gorner J, Greene M. “Chicago hospital shooting: Young cop, doctor, pharmacy resident and gunman die in Mercy Hospital attack. Chicago Tribune. Nov. 20, 2018.
2. Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner
and Sexual Violence Survey (NISVS): 2015 data brief – updated release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; November 2018.
3. Butkus R, Doherty R, Bornstein SS; for the Health and Public Policy Committee of the American College of Physicians. Reducing firearm injuries and deaths in the United States: a position paper from the American College of Physicians. Ann Intern Med. 2018;169:704-707.
4. Papenfuss M. NRA Tweets Warning to Anti-Gun Doctors: ‘Stay In Your Lane’. The Huffington Post. November 8, 2018.
5. Everytown for Gun Safety website. Mass Shootings in the United States: 2009–2016. Available at https://everytownresearch.org/reports/mass-shootings-analysis/. Accessed January 17, 2019.
6. The American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 518: intimate partner violence. Obstet Gynecol. 2012;119(2 pt 1):412-417. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Intimate-Partner-Violence.
7. Zeoli AM, McCourt A, Buggs S, et al. Analysis of the strength of legal firearms restrictions for perpetrators of domestic violence and their associations with intimate partner homicide. Am J Epidemiol. 2018;187:2365-2371.
1. Buckley M, Gorner J, Greene M. “Chicago hospital shooting: Young cop, doctor, pharmacy resident and gunman die in Mercy Hospital attack. Chicago Tribune. Nov. 20, 2018.
2. Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner
and Sexual Violence Survey (NISVS): 2015 data brief – updated release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; November 2018.
3. Butkus R, Doherty R, Bornstein SS; for the Health and Public Policy Committee of the American College of Physicians. Reducing firearm injuries and deaths in the United States: a position paper from the American College of Physicians. Ann Intern Med. 2018;169:704-707.
4. Papenfuss M. NRA Tweets Warning to Anti-Gun Doctors: ‘Stay In Your Lane’. The Huffington Post. November 8, 2018.
5. Everytown for Gun Safety website. Mass Shootings in the United States: 2009–2016. Available at https://everytownresearch.org/reports/mass-shootings-analysis/. Accessed January 17, 2019.
6. The American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 518: intimate partner violence. Obstet Gynecol. 2012;119(2 pt 1):412-417. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Intimate-Partner-Violence.
7. Zeoli AM, McCourt A, Buggs S, et al. Analysis of the strength of legal firearms restrictions for perpetrators of domestic violence and their associations with intimate partner homicide. Am J Epidemiol. 2018;187:2365-2371.
COPD linked to higher in-hospital death rates in patients with PAD
A growing body of evidence suggests that, along with other vascular beds, smoking and chronic obstructive pulmonary disease (COPD) affect the arteries of the lower limbs in terms of the development of peripheral arterial disease (PAD), reported Karsten Keller, MD, of the Johannes Gutenberg-University Mainz (Germany) and his colleagues.
This provided the rationale for their large database analysis of inpatients with concomitant COPD and PAD. They found that the additional presence of COPD was associated with increased in-hospital mortality in patients with PAD.
“Our data suggest that COPD increased the mortality of PAD patients by the factor 1.2-fold,” they wrote in Respiratory Medicine. “Unexpectedly, this increase was not driven by [myocardial infarction] as the life-threatening acute presentation of [coronary artery disease], but rather related to an increased risk for [pulmonary embolism] and a higher coprevalence of cancer.”
Dr. Keller and his colleagues inspected the German inpatient national database based on ICD codes. They identified 5,611,827 adult inpatients (64.8% men) diagnosed with PAD between January 2005 and December 2015, and of those, 13.6% also were coded for COPD. Overall, 277,894 PAD patients (5.0%) died in the hospital, Dr. Keller and his colleagues wrote.
The all-cause, in-hospital mortality was significantly higher in PAD patients with COPD, compared with those without COPD (6.5% vs. 4.7%, respectively; P less than .001), and cardiovascular events comprising pulmonary embolism (PE), deep vein thrombosis (DVT), and myocardial infarction (MI) occurred more often in coprevalence with PAD and COPD than in PAD without COPD.
In PAD patients, COPD was an independent predictor of in-hospital death (odds ratio, 1.16; 95% confidence interval, 1.15-1.17; P less than .001) as well as an independent predictor for PE (OR, 1.44; 95% CI, 1.40-1.49; P less than .001).
Overall, PAD patients with COPD were of similar age as (73 years), but stayed slightly longer in the hospital than (9 vs. 8 days), those without COPD. PAD patients without COPD revealed more often cardiovascular risk factors like essential arterial hypertension and diabetes, but the prevalence of cardiovascular diseases such as coronary artery disease and heart failure were more often found in PAD patients with COPD. In addition, cancer and renal insufficiency also were more common in PAD patients with COPD, according to the authors.
“Remarkably, PAD patients with COPD showed more frequently lower PAD stages than those without COPD. Especially, PAD stage IV was more prevalent in PAD patients without COPD (19.6% vs. 13.8%; P less than 0.001),” the authors stated. In addition, amputations were more often performed in PAD patients without COPD.
Dr. Keller and his colleagues had the following conclusions regarding the clinical implications of their study: “I) PAD patients with long-standing tobacco use might benefit from COPD screening and treatment. II) PAD patients with additional COPD should be monitored more intensively, and the treatment for COPD should be optimized. III) COPD increases the risk for PE, and it is critical not to overlook this life-threatening disease. IV) MI and PE are important causes of in-hospital death in PAD patients with and without COPD.”
The German Federal Ministry of Education and Research funded the study, and the authors reported having no conflicts.
SOURCE: Keller K et al. Respir Med. 2019 Feb;147:1-6.
A growing body of evidence suggests that, along with other vascular beds, smoking and chronic obstructive pulmonary disease (COPD) affect the arteries of the lower limbs in terms of the development of peripheral arterial disease (PAD), reported Karsten Keller, MD, of the Johannes Gutenberg-University Mainz (Germany) and his colleagues.
This provided the rationale for their large database analysis of inpatients with concomitant COPD and PAD. They found that the additional presence of COPD was associated with increased in-hospital mortality in patients with PAD.
“Our data suggest that COPD increased the mortality of PAD patients by the factor 1.2-fold,” they wrote in Respiratory Medicine. “Unexpectedly, this increase was not driven by [myocardial infarction] as the life-threatening acute presentation of [coronary artery disease], but rather related to an increased risk for [pulmonary embolism] and a higher coprevalence of cancer.”
Dr. Keller and his colleagues inspected the German inpatient national database based on ICD codes. They identified 5,611,827 adult inpatients (64.8% men) diagnosed with PAD between January 2005 and December 2015, and of those, 13.6% also were coded for COPD. Overall, 277,894 PAD patients (5.0%) died in the hospital, Dr. Keller and his colleagues wrote.
The all-cause, in-hospital mortality was significantly higher in PAD patients with COPD, compared with those without COPD (6.5% vs. 4.7%, respectively; P less than .001), and cardiovascular events comprising pulmonary embolism (PE), deep vein thrombosis (DVT), and myocardial infarction (MI) occurred more often in coprevalence with PAD and COPD than in PAD without COPD.
In PAD patients, COPD was an independent predictor of in-hospital death (odds ratio, 1.16; 95% confidence interval, 1.15-1.17; P less than .001) as well as an independent predictor for PE (OR, 1.44; 95% CI, 1.40-1.49; P less than .001).
Overall, PAD patients with COPD were of similar age as (73 years), but stayed slightly longer in the hospital than (9 vs. 8 days), those without COPD. PAD patients without COPD revealed more often cardiovascular risk factors like essential arterial hypertension and diabetes, but the prevalence of cardiovascular diseases such as coronary artery disease and heart failure were more often found in PAD patients with COPD. In addition, cancer and renal insufficiency also were more common in PAD patients with COPD, according to the authors.
“Remarkably, PAD patients with COPD showed more frequently lower PAD stages than those without COPD. Especially, PAD stage IV was more prevalent in PAD patients without COPD (19.6% vs. 13.8%; P less than 0.001),” the authors stated. In addition, amputations were more often performed in PAD patients without COPD.
Dr. Keller and his colleagues had the following conclusions regarding the clinical implications of their study: “I) PAD patients with long-standing tobacco use might benefit from COPD screening and treatment. II) PAD patients with additional COPD should be monitored more intensively, and the treatment for COPD should be optimized. III) COPD increases the risk for PE, and it is critical not to overlook this life-threatening disease. IV) MI and PE are important causes of in-hospital death in PAD patients with and without COPD.”
The German Federal Ministry of Education and Research funded the study, and the authors reported having no conflicts.
SOURCE: Keller K et al. Respir Med. 2019 Feb;147:1-6.
A growing body of evidence suggests that, along with other vascular beds, smoking and chronic obstructive pulmonary disease (COPD) affect the arteries of the lower limbs in terms of the development of peripheral arterial disease (PAD), reported Karsten Keller, MD, of the Johannes Gutenberg-University Mainz (Germany) and his colleagues.
This provided the rationale for their large database analysis of inpatients with concomitant COPD and PAD. They found that the additional presence of COPD was associated with increased in-hospital mortality in patients with PAD.
“Our data suggest that COPD increased the mortality of PAD patients by the factor 1.2-fold,” they wrote in Respiratory Medicine. “Unexpectedly, this increase was not driven by [myocardial infarction] as the life-threatening acute presentation of [coronary artery disease], but rather related to an increased risk for [pulmonary embolism] and a higher coprevalence of cancer.”
Dr. Keller and his colleagues inspected the German inpatient national database based on ICD codes. They identified 5,611,827 adult inpatients (64.8% men) diagnosed with PAD between January 2005 and December 2015, and of those, 13.6% also were coded for COPD. Overall, 277,894 PAD patients (5.0%) died in the hospital, Dr. Keller and his colleagues wrote.
The all-cause, in-hospital mortality was significantly higher in PAD patients with COPD, compared with those without COPD (6.5% vs. 4.7%, respectively; P less than .001), and cardiovascular events comprising pulmonary embolism (PE), deep vein thrombosis (DVT), and myocardial infarction (MI) occurred more often in coprevalence with PAD and COPD than in PAD without COPD.
In PAD patients, COPD was an independent predictor of in-hospital death (odds ratio, 1.16; 95% confidence interval, 1.15-1.17; P less than .001) as well as an independent predictor for PE (OR, 1.44; 95% CI, 1.40-1.49; P less than .001).
Overall, PAD patients with COPD were of similar age as (73 years), but stayed slightly longer in the hospital than (9 vs. 8 days), those without COPD. PAD patients without COPD revealed more often cardiovascular risk factors like essential arterial hypertension and diabetes, but the prevalence of cardiovascular diseases such as coronary artery disease and heart failure were more often found in PAD patients with COPD. In addition, cancer and renal insufficiency also were more common in PAD patients with COPD, according to the authors.
“Remarkably, PAD patients with COPD showed more frequently lower PAD stages than those without COPD. Especially, PAD stage IV was more prevalent in PAD patients without COPD (19.6% vs. 13.8%; P less than 0.001),” the authors stated. In addition, amputations were more often performed in PAD patients without COPD.
Dr. Keller and his colleagues had the following conclusions regarding the clinical implications of their study: “I) PAD patients with long-standing tobacco use might benefit from COPD screening and treatment. II) PAD patients with additional COPD should be monitored more intensively, and the treatment for COPD should be optimized. III) COPD increases the risk for PE, and it is critical not to overlook this life-threatening disease. IV) MI and PE are important causes of in-hospital death in PAD patients with and without COPD.”
The German Federal Ministry of Education and Research funded the study, and the authors reported having no conflicts.
SOURCE: Keller K et al. Respir Med. 2019 Feb;147:1-6.
FROM RESPIRATORY MEDICINE
Key clinical point:
Major finding: All-cause, in-hospital mortality was significantly higher in PAD patients with COPD, compared with those without (6.5% vs. 4.7%; P less than 0.001).
Study details: Database analysis of 5.6 million German PAD inpatients stratified for COPD.
Disclosures: The German Federal Ministry of Education and Research funded the study, and the authors reported having no conflicts.
Source: Keller K et al. Respir Med. 2019 Feb;147:1-6.
AML, myeloma risk higher for breast cancer survivors
Breast cancer survivors should continue to be monitored for hematologic malignancies, especially acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS), results of a population-based study from France suggest.
Among nearly 440,000 women with an incident breast cancer diagnosis, the incidence of AML was nearly three times higher and the incidence of MDS was five times higher than that of women in the general population. Women with breast cancer also were at higher risk for multiple myeloma (MM) and acute lymphoblastic leukemia/lymphocytic lymphoma (ALL/LL) compared with the background population, reported Marie Joelle Jabagi, PharmD, MPH, of the University of Paris Sud, France, and her colleagues.
“These findings serve to better inform practicing oncologists, and breast cancer survivors should be advised of the increased risk of developing certain hematologic malignant neoplasms after their first cancer diagnosis,” they wrote in JAMA Network Open.
Breast cancers are the malignant solid tumors most frequently associated with risk for myeloid neoplasms, but there is little information on the risk for secondary lymphoid malignancies among breast cancer patients, the investigators stated.
“In addition, real-life data on secondary hematologic malignant neoplasm incidence are scarce, especially in the recent period marked by major advances in breast cancer treatments,” they wrote.
To get better estimates of the incidence of myeloid and lymphoid neoplasms in this population, they conducted a retrospective review of information from the French National Health Data System on all French women from the ages of 20 to 85 years who had an incident breast cancer diagnosis from July 1, 2006, through Dec. 31, 2015.
In all, 439,704 women with a median age of 59 years were identified. They were followed until a diagnosis of a hematologic malignancy, death, or loss to follow-up, or until Dec. 31, 2016.
Data on the breast cancer patients were compared with those for all French women in the general population who were registered in the general national health insurance program from January 2007 through the end of 2016.
During a median follow-up of 5 years, there were 3,046 cases of hematologic neoplasms among the breast cancer patients, including 509 cases of AML, for a crude incidence rate (CIR) of 24.5 per 100,000 person-years (py); 832 cases of MDS for a CIR of 40.1/100,000 py; and 267 cases of myeloproliferative neoplasms (MPN), for a CIR of 12.8/100,000 py.
In addition, there were 420 cases of MM for a CIR of 20.3/100,000 py; 912 cases of Hodgkin or non-Hodgkin lymphoma (HL/NHL) for a CIR of 44.4/100,000 py, and 106 cases of ALL/LL for a CIR of 5.1/100,000 py.
Breast cancer survivors had significantly higher incidences, compared with the general population, of AML (standardized incidence ratio [SIR] 2.8, 95% confidence interval [CI], 2.5-3.2), MDS (SIR 5.0, CI, 4.4-5.7), MM (SIR 1.5, CI, 1.3-17), and ALL/LL (SIR 2.0, CI, 1.3-3.0). There was a trend toward significance for both MPN and HL/NHL, but the lower limit of the confidence intervals for these conditions either crossed or touched 1.
In a review of the literature, the authors found that “[s]everal studies linked AML and MDS to chemotherapeutic agents, radiation treatment, and supportive treatment with granulocyte colony-stimulating factor. These results are consistent with other available data showing a 2½-fold to 3½-fold increased risk of AML.”
They noted that their estimate of a five-fold increase in risk for MDS was higher than the 3.7-fold risk reported in a previous registry cohort analysis, suggesting that risk for MDS among breast cancer patients may be underestimated.
“The recent discovery of the gene signatures that guide treatment decisions in early-stage breast cancer might reduce the number of patients exposed to cytotoxic chemotherapy and its complications, including hematologic malignant neoplasm. Therefore, continuing to monitor hematologic malignant neoplasm trends is necessary, especially given that approaches to cancer treatment are rapidly evolving. Further research is also required to assess the modality of treatment for and the genetic predisposition to these secondary malignant neoplasms,” the authors concluded.
SOURCE: Jabagi MJ et al. JAMA Network Open. 2019 Jan 18. doi: 10.1001/jamanetworkopen.2018.7147.
Breast cancer survivors should continue to be monitored for hematologic malignancies, especially acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS), results of a population-based study from France suggest.
Among nearly 440,000 women with an incident breast cancer diagnosis, the incidence of AML was nearly three times higher and the incidence of MDS was five times higher than that of women in the general population. Women with breast cancer also were at higher risk for multiple myeloma (MM) and acute lymphoblastic leukemia/lymphocytic lymphoma (ALL/LL) compared with the background population, reported Marie Joelle Jabagi, PharmD, MPH, of the University of Paris Sud, France, and her colleagues.
“These findings serve to better inform practicing oncologists, and breast cancer survivors should be advised of the increased risk of developing certain hematologic malignant neoplasms after their first cancer diagnosis,” they wrote in JAMA Network Open.
Breast cancers are the malignant solid tumors most frequently associated with risk for myeloid neoplasms, but there is little information on the risk for secondary lymphoid malignancies among breast cancer patients, the investigators stated.
“In addition, real-life data on secondary hematologic malignant neoplasm incidence are scarce, especially in the recent period marked by major advances in breast cancer treatments,” they wrote.
To get better estimates of the incidence of myeloid and lymphoid neoplasms in this population, they conducted a retrospective review of information from the French National Health Data System on all French women from the ages of 20 to 85 years who had an incident breast cancer diagnosis from July 1, 2006, through Dec. 31, 2015.
In all, 439,704 women with a median age of 59 years were identified. They were followed until a diagnosis of a hematologic malignancy, death, or loss to follow-up, or until Dec. 31, 2016.
Data on the breast cancer patients were compared with those for all French women in the general population who were registered in the general national health insurance program from January 2007 through the end of 2016.
During a median follow-up of 5 years, there were 3,046 cases of hematologic neoplasms among the breast cancer patients, including 509 cases of AML, for a crude incidence rate (CIR) of 24.5 per 100,000 person-years (py); 832 cases of MDS for a CIR of 40.1/100,000 py; and 267 cases of myeloproliferative neoplasms (MPN), for a CIR of 12.8/100,000 py.
In addition, there were 420 cases of MM for a CIR of 20.3/100,000 py; 912 cases of Hodgkin or non-Hodgkin lymphoma (HL/NHL) for a CIR of 44.4/100,000 py, and 106 cases of ALL/LL for a CIR of 5.1/100,000 py.
Breast cancer survivors had significantly higher incidences, compared with the general population, of AML (standardized incidence ratio [SIR] 2.8, 95% confidence interval [CI], 2.5-3.2), MDS (SIR 5.0, CI, 4.4-5.7), MM (SIR 1.5, CI, 1.3-17), and ALL/LL (SIR 2.0, CI, 1.3-3.0). There was a trend toward significance for both MPN and HL/NHL, but the lower limit of the confidence intervals for these conditions either crossed or touched 1.
In a review of the literature, the authors found that “[s]everal studies linked AML and MDS to chemotherapeutic agents, radiation treatment, and supportive treatment with granulocyte colony-stimulating factor. These results are consistent with other available data showing a 2½-fold to 3½-fold increased risk of AML.”
They noted that their estimate of a five-fold increase in risk for MDS was higher than the 3.7-fold risk reported in a previous registry cohort analysis, suggesting that risk for MDS among breast cancer patients may be underestimated.
“The recent discovery of the gene signatures that guide treatment decisions in early-stage breast cancer might reduce the number of patients exposed to cytotoxic chemotherapy and its complications, including hematologic malignant neoplasm. Therefore, continuing to monitor hematologic malignant neoplasm trends is necessary, especially given that approaches to cancer treatment are rapidly evolving. Further research is also required to assess the modality of treatment for and the genetic predisposition to these secondary malignant neoplasms,” the authors concluded.
SOURCE: Jabagi MJ et al. JAMA Network Open. 2019 Jan 18. doi: 10.1001/jamanetworkopen.2018.7147.
Breast cancer survivors should continue to be monitored for hematologic malignancies, especially acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS), results of a population-based study from France suggest.
Among nearly 440,000 women with an incident breast cancer diagnosis, the incidence of AML was nearly three times higher and the incidence of MDS was five times higher than that of women in the general population. Women with breast cancer also were at higher risk for multiple myeloma (MM) and acute lymphoblastic leukemia/lymphocytic lymphoma (ALL/LL) compared with the background population, reported Marie Joelle Jabagi, PharmD, MPH, of the University of Paris Sud, France, and her colleagues.
“These findings serve to better inform practicing oncologists, and breast cancer survivors should be advised of the increased risk of developing certain hematologic malignant neoplasms after their first cancer diagnosis,” they wrote in JAMA Network Open.
Breast cancers are the malignant solid tumors most frequently associated with risk for myeloid neoplasms, but there is little information on the risk for secondary lymphoid malignancies among breast cancer patients, the investigators stated.
“In addition, real-life data on secondary hematologic malignant neoplasm incidence are scarce, especially in the recent period marked by major advances in breast cancer treatments,” they wrote.
To get better estimates of the incidence of myeloid and lymphoid neoplasms in this population, they conducted a retrospective review of information from the French National Health Data System on all French women from the ages of 20 to 85 years who had an incident breast cancer diagnosis from July 1, 2006, through Dec. 31, 2015.
In all, 439,704 women with a median age of 59 years were identified. They were followed until a diagnosis of a hematologic malignancy, death, or loss to follow-up, or until Dec. 31, 2016.
Data on the breast cancer patients were compared with those for all French women in the general population who were registered in the general national health insurance program from January 2007 through the end of 2016.
During a median follow-up of 5 years, there were 3,046 cases of hematologic neoplasms among the breast cancer patients, including 509 cases of AML, for a crude incidence rate (CIR) of 24.5 per 100,000 person-years (py); 832 cases of MDS for a CIR of 40.1/100,000 py; and 267 cases of myeloproliferative neoplasms (MPN), for a CIR of 12.8/100,000 py.
In addition, there were 420 cases of MM for a CIR of 20.3/100,000 py; 912 cases of Hodgkin or non-Hodgkin lymphoma (HL/NHL) for a CIR of 44.4/100,000 py, and 106 cases of ALL/LL for a CIR of 5.1/100,000 py.
Breast cancer survivors had significantly higher incidences, compared with the general population, of AML (standardized incidence ratio [SIR] 2.8, 95% confidence interval [CI], 2.5-3.2), MDS (SIR 5.0, CI, 4.4-5.7), MM (SIR 1.5, CI, 1.3-17), and ALL/LL (SIR 2.0, CI, 1.3-3.0). There was a trend toward significance for both MPN and HL/NHL, but the lower limit of the confidence intervals for these conditions either crossed or touched 1.
In a review of the literature, the authors found that “[s]everal studies linked AML and MDS to chemotherapeutic agents, radiation treatment, and supportive treatment with granulocyte colony-stimulating factor. These results are consistent with other available data showing a 2½-fold to 3½-fold increased risk of AML.”
They noted that their estimate of a five-fold increase in risk for MDS was higher than the 3.7-fold risk reported in a previous registry cohort analysis, suggesting that risk for MDS among breast cancer patients may be underestimated.
“The recent discovery of the gene signatures that guide treatment decisions in early-stage breast cancer might reduce the number of patients exposed to cytotoxic chemotherapy and its complications, including hematologic malignant neoplasm. Therefore, continuing to monitor hematologic malignant neoplasm trends is necessary, especially given that approaches to cancer treatment are rapidly evolving. Further research is also required to assess the modality of treatment for and the genetic predisposition to these secondary malignant neoplasms,” the authors concluded.
SOURCE: Jabagi MJ et al. JAMA Network Open. 2019 Jan 18. doi: 10.1001/jamanetworkopen.2018.7147.
FROM JAMA NETWORK OPEN
Key clinical point: Breast cancer survivors should be monitored for hematologic malignancies.
Major finding: The standardized incidence ratio for AML was 2.8 and the SIR for multiple myeloma was 5.0 among French breast cancer survivors compared with women in the general French population.
Study details: Retrospective analysis of data on 439,704 women aged 20-85 years with a breast cancer diagnosis.
Disclosures: The authors did not report a study funding source. Coauthor Anthony Goncalves, MD, reported nonfinancial support from Roche, Novartis, Pfizer, Celgene, MSD, Lilly, and Astra Zeneca outside of the submitted work. No other disclosures were reported.
Source: Jabagi MJ et al. JAMA Network Open. 2019 Jan 18. doi: 10.1001/jamanetworkopen.2018.7147.
COLOPEC: Adjuvant HIPEC for high-risk colon cancer disappoints
SAN FRANCISCO – according to primary results of the Dutch COLOPEC trial presented at the 2019 GI Cancers Symposium.
“Despite adjuvant systemic chemotherapy, locally advanced stage II and stage III colon cancer can give rise to metachronous peritoneal metastases in up to 25% of patients,” commented principal investigator Pieter J. Tanis, MD, PhD, a colorectal surgeon at the Academic Medical Center in Amsterdam. “These metastases are very difficult to detect, and when you detect them, they are difficult to treat.”
The 202 patients in COLOPEC, a multicenter, phase 3, randomized, controlled trial, underwent curative resection of primary colon tumors that were large (pT4 or cT4) or perforated, putting them at high risk for peritoneal metastases. All received routine adjuvant systemic chemotherapy.
At 18 months, the proportion of patients alive and free of peritoneal recurrence, assessed by laparoscopy, was 81% with addition of early postoperative oxaliplatin HIPEC and 76% without it, a nonsignificant difference.
“We couldn’t find any superiority of adjuvant HIPEC with oxaliplatin regarding peritoneal metastases–free survival in patients with T4 or perforated colon cancer,” Dr. Tanis summarized.
“We had a problem with the intention-to-treat analysis because 9% of patients already had recurrences before we performed the adjuvant HIPEC,” he added. “But I think we cannot perform an as-treated analysis in this trial because we don’t know the early recurrences in the control group.”
A symposium attendee wondered if the longer time to receiving systemic adjuvant systemic chemotherapy in the HIPEC group, a delay of about 4 weeks relative to the no-HIPEC group, was problematic and warranted consideration of neoadjuvant chemotherapy instead.
“The problem of the delay in chemotherapy, if you look in the literature, is there is no randomized trial looking at, for example, an 8- versus 12-week interval,” Dr. Tanis replied, noting that, in studies, adjuvant chemotherapy has most commonly been delayed because of patient comorbidities or surgical complications. “But you have to look very carefully at the expectation of the direct association between delay of chemotherapy and an effect. We have already looked at the disease-free survival and overall survival [in COLOPEC] and have not seen any difference … now at 23 months of follow-up,” he said.
End of the line for HIPEC?
Invited discussant Elin. R. Sigurdson, MD, PhD, a professor in the department of surgical oncology at the Fox Chase Cancer Center, Philadelphia, framed her discussion by drawing on the words of emeritus surgeon Blake Cady, MD. “ ‘In the world of surgical oncology, biology is the King, selection of cases is Queen, and the technical aspects of the surgical procedures are the Princes and Princesses who frequently try to overthrow the King and the Queen.’ ”
Staging systems, such as the Peritoneal Carcinomatosis Index, have improved patient selection. “It’s obviously very critical to assess these patients appropriately at the time of surgery, and that has influenced this study,” she maintained. “The very early recurrences I think fall into the lap of the surgeons.”
Trials in established disease have helped sort out the roles of tumor debulking and HIPEC. “In our attempt to overcome the biology of this disease, we can see that, in most of these studies, the debulking-only arm did much better than we would have thought. But controversies remain regarding both the duration of the HIPEC and the chemotherapy that we use,” Dr. Sigurdson commented. “Perhaps, as we move forward, more questions will be addressed in the near future as there are ongoing clinical trials both on our side and the European side.”
Symposium attendee Alan P. Venook, MD, of the University of California, San Francisco, noted that there have been three negative clinical trials of HIPEC in the last 3 years. “Is that enough to say enough, or do we still need to study the role of HIPEC in these patients?” he asked.
“The issue becomes, are there new possibilities in the way of new drugs in order to carry on?” Dr. Sigurdson replied. Also, “it clearly has been a learning curve in doing HIPEC, and we have failed to recognize how impactful the surgical part of HIPEC has been.”
“The trials shown today from Europe are the best-designed trials that we have, and I agree, yes, the negative trials are discouraging,” she elaborated. “But if there were drugs where the therapeutic index of giving them intraperitoneally would be beneficial, then it would be useful because it has worked in ovarian cancer, it has worked in other cancers. So hope remains. But I would argue that, in the absence of new drugs, we are getting to the point that repeating the clinical trials with those [same] drugs is not going to be positive.”
Study details
In COLOPEC, adjuvant HIPEC consisted of 30 minutes of intraperitoneal oxaliplatin plus intravenous 5-fluoruracil and leucovorin, Dr. Tanis reported at the symposium, which is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
HIPEC was usually performed 5-8 weeks after resection (91%) and laparoscopically (71%). Almost a fifth of patients were found to have extensive adhesions, making the procedure more difficult.
The rate of postoperative complications was 88% in the small number of patients having HIPEC at the time of resection, but only 6% in those having it 5-8 weeks after resection. A single patient developed encapsulating peritoneal sclerosis 8 months after HIPEC, requiring parenteral nutrition and surgery.
Patients in the HIPEC and control groups were similarly likely to receive adjuvant systemic chemotherapy (84% vs. 89%, P = .385), but the former had a longer time before starting this therapy (10.2 vs. 6.4 weeks, P less than .001).
Relative to counterparts in the control group, patients in the HIPEC group had a 14% reduction in risk of peritoneal recurrence or death at 18 months, but the difference was not significant (hazard ratio, 0.86; 95% confidence interval, 0.51-1.54). Findings were similar across a variety of subgroups.
In both trial groups, about two-thirds of patients in whom peritoneal metastases were detected underwent cytoreductive surgery and/or (additional) HIPEC to treat them.
“Overall, 21% of patients had peritoneal metastases detected after 23 months of follow-up, demonstrating the magnitude of this clinical problem,” noted Dr. Tanis, who reported that he had no relevant disclosures. The trial was sponsored by the Academic Medical Center, University of Amsterdam.
SOURCE: Tanis PJ et al. GI Cancers Symposium 2019, Abstract 482.
SAN FRANCISCO – according to primary results of the Dutch COLOPEC trial presented at the 2019 GI Cancers Symposium.
“Despite adjuvant systemic chemotherapy, locally advanced stage II and stage III colon cancer can give rise to metachronous peritoneal metastases in up to 25% of patients,” commented principal investigator Pieter J. Tanis, MD, PhD, a colorectal surgeon at the Academic Medical Center in Amsterdam. “These metastases are very difficult to detect, and when you detect them, they are difficult to treat.”
The 202 patients in COLOPEC, a multicenter, phase 3, randomized, controlled trial, underwent curative resection of primary colon tumors that were large (pT4 or cT4) or perforated, putting them at high risk for peritoneal metastases. All received routine adjuvant systemic chemotherapy.
At 18 months, the proportion of patients alive and free of peritoneal recurrence, assessed by laparoscopy, was 81% with addition of early postoperative oxaliplatin HIPEC and 76% without it, a nonsignificant difference.
“We couldn’t find any superiority of adjuvant HIPEC with oxaliplatin regarding peritoneal metastases–free survival in patients with T4 or perforated colon cancer,” Dr. Tanis summarized.
“We had a problem with the intention-to-treat analysis because 9% of patients already had recurrences before we performed the adjuvant HIPEC,” he added. “But I think we cannot perform an as-treated analysis in this trial because we don’t know the early recurrences in the control group.”
A symposium attendee wondered if the longer time to receiving systemic adjuvant systemic chemotherapy in the HIPEC group, a delay of about 4 weeks relative to the no-HIPEC group, was problematic and warranted consideration of neoadjuvant chemotherapy instead.
“The problem of the delay in chemotherapy, if you look in the literature, is there is no randomized trial looking at, for example, an 8- versus 12-week interval,” Dr. Tanis replied, noting that, in studies, adjuvant chemotherapy has most commonly been delayed because of patient comorbidities or surgical complications. “But you have to look very carefully at the expectation of the direct association between delay of chemotherapy and an effect. We have already looked at the disease-free survival and overall survival [in COLOPEC] and have not seen any difference … now at 23 months of follow-up,” he said.
End of the line for HIPEC?
Invited discussant Elin. R. Sigurdson, MD, PhD, a professor in the department of surgical oncology at the Fox Chase Cancer Center, Philadelphia, framed her discussion by drawing on the words of emeritus surgeon Blake Cady, MD. “ ‘In the world of surgical oncology, biology is the King, selection of cases is Queen, and the technical aspects of the surgical procedures are the Princes and Princesses who frequently try to overthrow the King and the Queen.’ ”
Staging systems, such as the Peritoneal Carcinomatosis Index, have improved patient selection. “It’s obviously very critical to assess these patients appropriately at the time of surgery, and that has influenced this study,” she maintained. “The very early recurrences I think fall into the lap of the surgeons.”
Trials in established disease have helped sort out the roles of tumor debulking and HIPEC. “In our attempt to overcome the biology of this disease, we can see that, in most of these studies, the debulking-only arm did much better than we would have thought. But controversies remain regarding both the duration of the HIPEC and the chemotherapy that we use,” Dr. Sigurdson commented. “Perhaps, as we move forward, more questions will be addressed in the near future as there are ongoing clinical trials both on our side and the European side.”
Symposium attendee Alan P. Venook, MD, of the University of California, San Francisco, noted that there have been three negative clinical trials of HIPEC in the last 3 years. “Is that enough to say enough, or do we still need to study the role of HIPEC in these patients?” he asked.
“The issue becomes, are there new possibilities in the way of new drugs in order to carry on?” Dr. Sigurdson replied. Also, “it clearly has been a learning curve in doing HIPEC, and we have failed to recognize how impactful the surgical part of HIPEC has been.”
“The trials shown today from Europe are the best-designed trials that we have, and I agree, yes, the negative trials are discouraging,” she elaborated. “But if there were drugs where the therapeutic index of giving them intraperitoneally would be beneficial, then it would be useful because it has worked in ovarian cancer, it has worked in other cancers. So hope remains. But I would argue that, in the absence of new drugs, we are getting to the point that repeating the clinical trials with those [same] drugs is not going to be positive.”
Study details
In COLOPEC, adjuvant HIPEC consisted of 30 minutes of intraperitoneal oxaliplatin plus intravenous 5-fluoruracil and leucovorin, Dr. Tanis reported at the symposium, which is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
HIPEC was usually performed 5-8 weeks after resection (91%) and laparoscopically (71%). Almost a fifth of patients were found to have extensive adhesions, making the procedure more difficult.
The rate of postoperative complications was 88% in the small number of patients having HIPEC at the time of resection, but only 6% in those having it 5-8 weeks after resection. A single patient developed encapsulating peritoneal sclerosis 8 months after HIPEC, requiring parenteral nutrition and surgery.
Patients in the HIPEC and control groups were similarly likely to receive adjuvant systemic chemotherapy (84% vs. 89%, P = .385), but the former had a longer time before starting this therapy (10.2 vs. 6.4 weeks, P less than .001).
Relative to counterparts in the control group, patients in the HIPEC group had a 14% reduction in risk of peritoneal recurrence or death at 18 months, but the difference was not significant (hazard ratio, 0.86; 95% confidence interval, 0.51-1.54). Findings were similar across a variety of subgroups.
In both trial groups, about two-thirds of patients in whom peritoneal metastases were detected underwent cytoreductive surgery and/or (additional) HIPEC to treat them.
“Overall, 21% of patients had peritoneal metastases detected after 23 months of follow-up, demonstrating the magnitude of this clinical problem,” noted Dr. Tanis, who reported that he had no relevant disclosures. The trial was sponsored by the Academic Medical Center, University of Amsterdam.
SOURCE: Tanis PJ et al. GI Cancers Symposium 2019, Abstract 482.
SAN FRANCISCO – according to primary results of the Dutch COLOPEC trial presented at the 2019 GI Cancers Symposium.
“Despite adjuvant systemic chemotherapy, locally advanced stage II and stage III colon cancer can give rise to metachronous peritoneal metastases in up to 25% of patients,” commented principal investigator Pieter J. Tanis, MD, PhD, a colorectal surgeon at the Academic Medical Center in Amsterdam. “These metastases are very difficult to detect, and when you detect them, they are difficult to treat.”
The 202 patients in COLOPEC, a multicenter, phase 3, randomized, controlled trial, underwent curative resection of primary colon tumors that were large (pT4 or cT4) or perforated, putting them at high risk for peritoneal metastases. All received routine adjuvant systemic chemotherapy.
At 18 months, the proportion of patients alive and free of peritoneal recurrence, assessed by laparoscopy, was 81% with addition of early postoperative oxaliplatin HIPEC and 76% without it, a nonsignificant difference.
“We couldn’t find any superiority of adjuvant HIPEC with oxaliplatin regarding peritoneal metastases–free survival in patients with T4 or perforated colon cancer,” Dr. Tanis summarized.
“We had a problem with the intention-to-treat analysis because 9% of patients already had recurrences before we performed the adjuvant HIPEC,” he added. “But I think we cannot perform an as-treated analysis in this trial because we don’t know the early recurrences in the control group.”
A symposium attendee wondered if the longer time to receiving systemic adjuvant systemic chemotherapy in the HIPEC group, a delay of about 4 weeks relative to the no-HIPEC group, was problematic and warranted consideration of neoadjuvant chemotherapy instead.
“The problem of the delay in chemotherapy, if you look in the literature, is there is no randomized trial looking at, for example, an 8- versus 12-week interval,” Dr. Tanis replied, noting that, in studies, adjuvant chemotherapy has most commonly been delayed because of patient comorbidities or surgical complications. “But you have to look very carefully at the expectation of the direct association between delay of chemotherapy and an effect. We have already looked at the disease-free survival and overall survival [in COLOPEC] and have not seen any difference … now at 23 months of follow-up,” he said.
End of the line for HIPEC?
Invited discussant Elin. R. Sigurdson, MD, PhD, a professor in the department of surgical oncology at the Fox Chase Cancer Center, Philadelphia, framed her discussion by drawing on the words of emeritus surgeon Blake Cady, MD. “ ‘In the world of surgical oncology, biology is the King, selection of cases is Queen, and the technical aspects of the surgical procedures are the Princes and Princesses who frequently try to overthrow the King and the Queen.’ ”
Staging systems, such as the Peritoneal Carcinomatosis Index, have improved patient selection. “It’s obviously very critical to assess these patients appropriately at the time of surgery, and that has influenced this study,” she maintained. “The very early recurrences I think fall into the lap of the surgeons.”
Trials in established disease have helped sort out the roles of tumor debulking and HIPEC. “In our attempt to overcome the biology of this disease, we can see that, in most of these studies, the debulking-only arm did much better than we would have thought. But controversies remain regarding both the duration of the HIPEC and the chemotherapy that we use,” Dr. Sigurdson commented. “Perhaps, as we move forward, more questions will be addressed in the near future as there are ongoing clinical trials both on our side and the European side.”
Symposium attendee Alan P. Venook, MD, of the University of California, San Francisco, noted that there have been three negative clinical trials of HIPEC in the last 3 years. “Is that enough to say enough, or do we still need to study the role of HIPEC in these patients?” he asked.
“The issue becomes, are there new possibilities in the way of new drugs in order to carry on?” Dr. Sigurdson replied. Also, “it clearly has been a learning curve in doing HIPEC, and we have failed to recognize how impactful the surgical part of HIPEC has been.”
“The trials shown today from Europe are the best-designed trials that we have, and I agree, yes, the negative trials are discouraging,” she elaborated. “But if there were drugs where the therapeutic index of giving them intraperitoneally would be beneficial, then it would be useful because it has worked in ovarian cancer, it has worked in other cancers. So hope remains. But I would argue that, in the absence of new drugs, we are getting to the point that repeating the clinical trials with those [same] drugs is not going to be positive.”
Study details
In COLOPEC, adjuvant HIPEC consisted of 30 minutes of intraperitoneal oxaliplatin plus intravenous 5-fluoruracil and leucovorin, Dr. Tanis reported at the symposium, which is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
HIPEC was usually performed 5-8 weeks after resection (91%) and laparoscopically (71%). Almost a fifth of patients were found to have extensive adhesions, making the procedure more difficult.
The rate of postoperative complications was 88% in the small number of patients having HIPEC at the time of resection, but only 6% in those having it 5-8 weeks after resection. A single patient developed encapsulating peritoneal sclerosis 8 months after HIPEC, requiring parenteral nutrition and surgery.
Patients in the HIPEC and control groups were similarly likely to receive adjuvant systemic chemotherapy (84% vs. 89%, P = .385), but the former had a longer time before starting this therapy (10.2 vs. 6.4 weeks, P less than .001).
Relative to counterparts in the control group, patients in the HIPEC group had a 14% reduction in risk of peritoneal recurrence or death at 18 months, but the difference was not significant (hazard ratio, 0.86; 95% confidence interval, 0.51-1.54). Findings were similar across a variety of subgroups.
In both trial groups, about two-thirds of patients in whom peritoneal metastases were detected underwent cytoreductive surgery and/or (additional) HIPEC to treat them.
“Overall, 21% of patients had peritoneal metastases detected after 23 months of follow-up, demonstrating the magnitude of this clinical problem,” noted Dr. Tanis, who reported that he had no relevant disclosures. The trial was sponsored by the Academic Medical Center, University of Amsterdam.
SOURCE: Tanis PJ et al. GI Cancers Symposium 2019, Abstract 482.
REPORTING FROM THE 2019 GI CANCERS SYMPOSIUM
Key clinical point: Adjuvant hyperthermic intraperitoneal chemotherapy (HIPEC) is not efficacious in patients undergoing curative resection of high-risk colon cancer.
Major finding: The rate of peritoneal metastasis–free survival at 18 months was 81% with HIPEC and 76% without HIPEC (hazard ratio, 0.86; 95% confidence interval, 0.51-1.54).
Study details: A phase 3, randomized, controlled trial among 202 patients who underwent curative resection of colon cancer having stage T4 or perforated tumors, all given adjuvant systemic chemotherapy (COLOPEC).
Disclosures: Dr. Tanis reported no relevant relationships. The trial was sponsored by the Academic Medical Center, University of Amsterdam.
Source: Tanis PJ et al. GI Cancers Symposium 2019, Abstract 482.
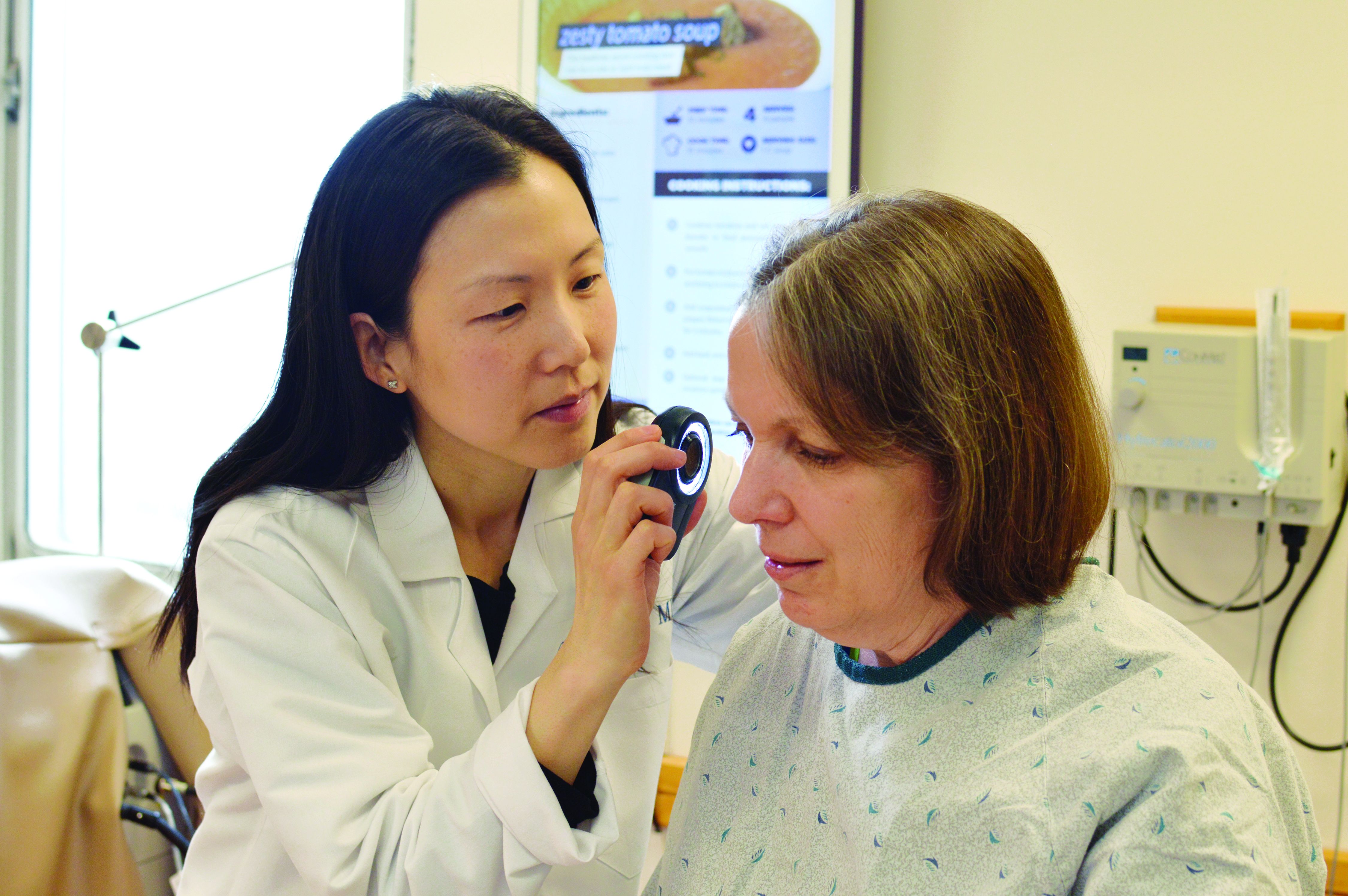
How not to miss the ‘invisible gorilla’: Visual intelligence in dermatology
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Perceptions of liver transplantation for ALD are evolving
“The findings suggest that early liver transplant for alcoholic hepatitis may be leading to broader acceptance of ALD for liver transplant,” Brian P. Lee, MD, of the University of California, San Francisco, and his colleagues wrote in JAMA Internal Medicine.
The researchers conducted a prospective cohort study of 9,438 patients with ALD who received a liver transplant from 2002 to 2016. Data were obtained from the United Network for Organ Sharing national database.
Study participants were evaluated for patterns, both nationally and regionally, related to liver transplant for the treatment of ALD. In addition, Dr. Lee and his colleagues completed a sensitivity analysis, which evaluated specific clinical parameters, including patient and graft survival, hepatocellular carcinoma (HCC), and hepatitis C viral (HCV) infection.
“Because there is no national policy regarding early liver transplant, we hypothesized that changes may vary regionally as liver transplant programs shifted their attitudes toward increased acceptance of early liver transplant for alcoholic hepatitis and ALD,” the researchers wrote.
After analysis, the researchers found that liver transplantation for patients with ALD increased proportionally from 24.2% to 36.7% from 2002 to 2016, respectively. With HCV-infected recipients included, the proportion of liver transplants rose from 15.3% to 30.6% over the same period, representing a twofold increase of transplants received for this indication.
The degree of increase was reported to vary based on geographic region and was linked with differences in patient-specific factors.
“There may be regional disparities in access to liver transplant for ALD; whether this is related to different attitudes toward ALD and requirements for sobriety is unknown,” they added.
The researchers acknowledged that a key limitation of the study was the use of registry data. As a result, Dr. Lee and his colleagues reported that all conclusions are not causal, but rather only by association.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interests.
SOURCE: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
One of the most significant findings of the study by Brian P. Lee, MD, and his colleagues is the major shift in attitudes surrounding the eligibility criteria for patients with ALD to undergo liver transplantation.
More than 3 decades ago, a group of surgical experts gathered together to discuss evaluation criteria for candidacy of individuals to undergo liver transplantation. They recommended that patients with ALD be required to restrict alcohol consumption for 6 months prior to being listed eligible for surgery. The group presumed that a period of complete avoidance may induce some degree of disease remission, circumventing the need for transplant altogether.
However, these suggestions were given without the use of evidence, formed largely on the basis of opinion, and recent data dispute these recommendations. On the contrary, relapse rates for alcohol use disorder has been shown to be due to factors other than length of abstinence. While these findings have lessened bias surrounding ALD and liver transplantation, the assumption still remains prevalent in clinical practice today.
These results highlight the unanswered question of how to best approach treatment of individuals with ALD, and whether the recent rise of patients undergoing liver transplantation for ALD, without a continued duration of abstinence, should be a concern of clinicians.
Mack C. Mitchell, MD, is affiliated with the department of internal medicine at the University of Texas in Dallas. Dr. Mitchell reported having financial affiliations with the National Institute of Alcohol and Alcohol Abuse. These comments are adapted from his accompanying editorial (JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6532 ).
One of the most significant findings of the study by Brian P. Lee, MD, and his colleagues is the major shift in attitudes surrounding the eligibility criteria for patients with ALD to undergo liver transplantation.
More than 3 decades ago, a group of surgical experts gathered together to discuss evaluation criteria for candidacy of individuals to undergo liver transplantation. They recommended that patients with ALD be required to restrict alcohol consumption for 6 months prior to being listed eligible for surgery. The group presumed that a period of complete avoidance may induce some degree of disease remission, circumventing the need for transplant altogether.
However, these suggestions were given without the use of evidence, formed largely on the basis of opinion, and recent data dispute these recommendations. On the contrary, relapse rates for alcohol use disorder has been shown to be due to factors other than length of abstinence. While these findings have lessened bias surrounding ALD and liver transplantation, the assumption still remains prevalent in clinical practice today.
These results highlight the unanswered question of how to best approach treatment of individuals with ALD, and whether the recent rise of patients undergoing liver transplantation for ALD, without a continued duration of abstinence, should be a concern of clinicians.
Mack C. Mitchell, MD, is affiliated with the department of internal medicine at the University of Texas in Dallas. Dr. Mitchell reported having financial affiliations with the National Institute of Alcohol and Alcohol Abuse. These comments are adapted from his accompanying editorial (JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6532 ).
One of the most significant findings of the study by Brian P. Lee, MD, and his colleagues is the major shift in attitudes surrounding the eligibility criteria for patients with ALD to undergo liver transplantation.
More than 3 decades ago, a group of surgical experts gathered together to discuss evaluation criteria for candidacy of individuals to undergo liver transplantation. They recommended that patients with ALD be required to restrict alcohol consumption for 6 months prior to being listed eligible for surgery. The group presumed that a period of complete avoidance may induce some degree of disease remission, circumventing the need for transplant altogether.
However, these suggestions were given without the use of evidence, formed largely on the basis of opinion, and recent data dispute these recommendations. On the contrary, relapse rates for alcohol use disorder has been shown to be due to factors other than length of abstinence. While these findings have lessened bias surrounding ALD and liver transplantation, the assumption still remains prevalent in clinical practice today.
These results highlight the unanswered question of how to best approach treatment of individuals with ALD, and whether the recent rise of patients undergoing liver transplantation for ALD, without a continued duration of abstinence, should be a concern of clinicians.
Mack C. Mitchell, MD, is affiliated with the department of internal medicine at the University of Texas in Dallas. Dr. Mitchell reported having financial affiliations with the National Institute of Alcohol and Alcohol Abuse. These comments are adapted from his accompanying editorial (JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6532 ).
“The findings suggest that early liver transplant for alcoholic hepatitis may be leading to broader acceptance of ALD for liver transplant,” Brian P. Lee, MD, of the University of California, San Francisco, and his colleagues wrote in JAMA Internal Medicine.
The researchers conducted a prospective cohort study of 9,438 patients with ALD who received a liver transplant from 2002 to 2016. Data were obtained from the United Network for Organ Sharing national database.
Study participants were evaluated for patterns, both nationally and regionally, related to liver transplant for the treatment of ALD. In addition, Dr. Lee and his colleagues completed a sensitivity analysis, which evaluated specific clinical parameters, including patient and graft survival, hepatocellular carcinoma (HCC), and hepatitis C viral (HCV) infection.
“Because there is no national policy regarding early liver transplant, we hypothesized that changes may vary regionally as liver transplant programs shifted their attitudes toward increased acceptance of early liver transplant for alcoholic hepatitis and ALD,” the researchers wrote.
After analysis, the researchers found that liver transplantation for patients with ALD increased proportionally from 24.2% to 36.7% from 2002 to 2016, respectively. With HCV-infected recipients included, the proportion of liver transplants rose from 15.3% to 30.6% over the same period, representing a twofold increase of transplants received for this indication.
The degree of increase was reported to vary based on geographic region and was linked with differences in patient-specific factors.
“There may be regional disparities in access to liver transplant for ALD; whether this is related to different attitudes toward ALD and requirements for sobriety is unknown,” they added.
The researchers acknowledged that a key limitation of the study was the use of registry data. As a result, Dr. Lee and his colleagues reported that all conclusions are not causal, but rather only by association.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interests.
SOURCE: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
“The findings suggest that early liver transplant for alcoholic hepatitis may be leading to broader acceptance of ALD for liver transplant,” Brian P. Lee, MD, of the University of California, San Francisco, and his colleagues wrote in JAMA Internal Medicine.
The researchers conducted a prospective cohort study of 9,438 patients with ALD who received a liver transplant from 2002 to 2016. Data were obtained from the United Network for Organ Sharing national database.
Study participants were evaluated for patterns, both nationally and regionally, related to liver transplant for the treatment of ALD. In addition, Dr. Lee and his colleagues completed a sensitivity analysis, which evaluated specific clinical parameters, including patient and graft survival, hepatocellular carcinoma (HCC), and hepatitis C viral (HCV) infection.
“Because there is no national policy regarding early liver transplant, we hypothesized that changes may vary regionally as liver transplant programs shifted their attitudes toward increased acceptance of early liver transplant for alcoholic hepatitis and ALD,” the researchers wrote.
After analysis, the researchers found that liver transplantation for patients with ALD increased proportionally from 24.2% to 36.7% from 2002 to 2016, respectively. With HCV-infected recipients included, the proportion of liver transplants rose from 15.3% to 30.6% over the same period, representing a twofold increase of transplants received for this indication.
The degree of increase was reported to vary based on geographic region and was linked with differences in patient-specific factors.
“There may be regional disparities in access to liver transplant for ALD; whether this is related to different attitudes toward ALD and requirements for sobriety is unknown,” they added.
The researchers acknowledged that a key limitation of the study was the use of registry data. As a result, Dr. Lee and his colleagues reported that all conclusions are not causal, but rather only by association.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interests.
SOURCE: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Liver transplantation for alcohol-associated liver disease (ALD) is occurring earlier and more frequently than before.
Major finding: The proportion of patients undergoing liver transplantation for ALD has nearly doubled from 2002 to 2016.
Study details: A prospective cohort study of 9,438 patients who underwent liver transplant for ALD in the United States from 2002 to 2016.
Disclosures: The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interest.
Source: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
Diet low in free sugars shows promise for adolescent NAFLD
after 8 weeks, compared with boys on a usual diet.
“Because of growing evidence implicating dietary sugars in NAFLD, well-controlled studies in children with NAFLD are needed to inform clinical practice and public policy,” wrote Jeffrey B. Schwimmer, MD, of the University of California, San Diego, La Jolla, and colleagues in JAMA.
The researchers randomized 40 boys aged 11-16 years with active NAFLD to a diet low in free sugars or their usual diet. The intervention diet involved personalized menu planning and provision of meals for the boys’ entire households that were designed to restrict free sugar intake to less than 3% of daily calories. Adherence to the diet was assessed by twice-weekly phone calls.
In the intervention group, hepatic steatosis decreased from an average of 25% at baseline to 17% after 8 weeks, compared with a change from 21% to 20% in the control group. The adjusted mean difference at 8 weeks was −6.23%, which was statistically significant (P less than .001).
The average age of the participants was 13 years, 95% were Hispanic. All 40 completed the study, and 18 of the 20 boys in the intervention group reported less than 3% of calories from free sugar during the study period. No adverse events were reported related to study participation.
The results were limited by several factors, including the small sample size and homogeneous population. In addition, neither hepatic steatosis or serum alanine aminotransferase (ALT) levels decreased enough to enter the normal range, the researchers noted. The findings, though preliminary, support the value of reducing free sugars, including glucose, fructose, and sucrose, to help manage NAFLD in adolescents, and “further research is required to assess long-term and clinical outcomes,” they said.
The study was supported by grants from multiple foundations and organizations, including the Nutrition Science Initiative, the University of California, San Diego, the National Institutes of Health, Children’s Healthcare of Atlanta and Emory University Pediatric Biostatistics Core, and the Georgia Clinical and Translational Science Alliance. Dr. Schwimmer reported receiving research support from Galmed and Intercept.
SOURCE: Schwimmer JB et al. JAMA. 2019;321(3):256-265.
after 8 weeks, compared with boys on a usual diet.
“Because of growing evidence implicating dietary sugars in NAFLD, well-controlled studies in children with NAFLD are needed to inform clinical practice and public policy,” wrote Jeffrey B. Schwimmer, MD, of the University of California, San Diego, La Jolla, and colleagues in JAMA.
The researchers randomized 40 boys aged 11-16 years with active NAFLD to a diet low in free sugars or their usual diet. The intervention diet involved personalized menu planning and provision of meals for the boys’ entire households that were designed to restrict free sugar intake to less than 3% of daily calories. Adherence to the diet was assessed by twice-weekly phone calls.
In the intervention group, hepatic steatosis decreased from an average of 25% at baseline to 17% after 8 weeks, compared with a change from 21% to 20% in the control group. The adjusted mean difference at 8 weeks was −6.23%, which was statistically significant (P less than .001).
The average age of the participants was 13 years, 95% were Hispanic. All 40 completed the study, and 18 of the 20 boys in the intervention group reported less than 3% of calories from free sugar during the study period. No adverse events were reported related to study participation.
The results were limited by several factors, including the small sample size and homogeneous population. In addition, neither hepatic steatosis or serum alanine aminotransferase (ALT) levels decreased enough to enter the normal range, the researchers noted. The findings, though preliminary, support the value of reducing free sugars, including glucose, fructose, and sucrose, to help manage NAFLD in adolescents, and “further research is required to assess long-term and clinical outcomes,” they said.
The study was supported by grants from multiple foundations and organizations, including the Nutrition Science Initiative, the University of California, San Diego, the National Institutes of Health, Children’s Healthcare of Atlanta and Emory University Pediatric Biostatistics Core, and the Georgia Clinical and Translational Science Alliance. Dr. Schwimmer reported receiving research support from Galmed and Intercept.
SOURCE: Schwimmer JB et al. JAMA. 2019;321(3):256-265.
after 8 weeks, compared with boys on a usual diet.
“Because of growing evidence implicating dietary sugars in NAFLD, well-controlled studies in children with NAFLD are needed to inform clinical practice and public policy,” wrote Jeffrey B. Schwimmer, MD, of the University of California, San Diego, La Jolla, and colleagues in JAMA.
The researchers randomized 40 boys aged 11-16 years with active NAFLD to a diet low in free sugars or their usual diet. The intervention diet involved personalized menu planning and provision of meals for the boys’ entire households that were designed to restrict free sugar intake to less than 3% of daily calories. Adherence to the diet was assessed by twice-weekly phone calls.
In the intervention group, hepatic steatosis decreased from an average of 25% at baseline to 17% after 8 weeks, compared with a change from 21% to 20% in the control group. The adjusted mean difference at 8 weeks was −6.23%, which was statistically significant (P less than .001).
The average age of the participants was 13 years, 95% were Hispanic. All 40 completed the study, and 18 of the 20 boys in the intervention group reported less than 3% of calories from free sugar during the study period. No adverse events were reported related to study participation.
The results were limited by several factors, including the small sample size and homogeneous population. In addition, neither hepatic steatosis or serum alanine aminotransferase (ALT) levels decreased enough to enter the normal range, the researchers noted. The findings, though preliminary, support the value of reducing free sugars, including glucose, fructose, and sucrose, to help manage NAFLD in adolescents, and “further research is required to assess long-term and clinical outcomes,” they said.
The study was supported by grants from multiple foundations and organizations, including the Nutrition Science Initiative, the University of California, San Diego, the National Institutes of Health, Children’s Healthcare of Atlanta and Emory University Pediatric Biostatistics Core, and the Georgia Clinical and Translational Science Alliance. Dr. Schwimmer reported receiving research support from Galmed and Intercept.
SOURCE: Schwimmer JB et al. JAMA. 2019;321(3):256-265.
FROM JAMA
Key clinical point: After 8 weeks, adolescent boys on a diet low in free sugars showed significant improvement in hepatic steatosis, compared with those on a usual diet.
Major finding: Hepatic steatosis decreased from an average of 25% at baseline to 17% after 8 weeks in the modified diet group, compared with a decrease from 21% to 20% in the usual diet group.
Study details: The data come from an open-label, randomized trial of 40 adolescent boys aged 11 to 16 years with active NAFLD.
Disclosures: The study was supported by grants from multiple foundations and organizations, including the Nutrition Science Initiative, the University of California, San Diego, the National Institutes of Health, Children’s Healthcare of Atlanta and Emory University Pediatric Biostatistics Core, and the Georgia Clinical and Translational Science Alliance. Dr. Schwimmer reported receiving research support from Galmed and Intercept.
Source: Schwimmer JB et al. JAMA. 2019;321(3):256-265.
Matched transplant improves stroke risk indicator in sickle cell anemia
, suggesting that this intervention may improve outcomes related to cerebral vasculopathy.
Matched sibling donor hematopoietic stem cell transplantation (MSD-HSCT) was linked to significantly lower transcranial Doppler (TCD) velocities at one year compared to standard care in the 9-center study, investigators reported in JAMA.
The study enrolled children with sickle cell anemia who required chronic transfusion due to persistently high TCD velocities, which are associated with increased stroke risk, researchers said.
“Further research is warranted to assess the effects of MSD-HSCT on clinical outcomes and over longer follow-up,” said the researchers, led by Françoise Bernaudin, MD, of Centre Hospitalier Intercommunal de Créteil, Créteil, France
In the non-randomized, prospective DREPAGREFFE study by Dr. Bernaudin and colleagues, 32 children with sickle cell anemia who had a matched sibling donor underwent transplantation, while another 35 children received standard therapy. The primary end point of the study was time-averaged mean of maximum velocities (TAMV) in cerebral arteries at one year.
The highest TAMV at one year was on average 129.6 cm/s in the MSD-HSCT group, versus 170.4 cm/s in the standard care group, for a difference of -40.8 cm/s (P less than .001), Dr. Bernaudin and co-investigators reported.
The improvement persisted at 3 years, with a TAMV of 112.4 cm/s in the transplantation group and 156.7 cm/s in the standard care group (P less than .001), which they also reported as a secondary outcome of the study.
These findings indicate that MSD-HSCT may allow patients with a history of abnormal TCD velocities to stop transfusions and hydroxyurea, Dr. Bernaudin and colleagues said.
The improvement in TCD velocities may be due in part to anemia correction, but also to the “exclusive presence” of normal red blood cells following transplantation, as opposed to simultaneous presence of normal and sickled cells as would be seen after transfusion, they added.
This study wasn’t powered to determine whether a 40 cm/s reduction in TCD velocities would translate into clinical benefits such as reduction in stenosis and silent infarct, or improved cognitive function, they said. Even so, there were no infarcts or stenoses in the MSD-HSCT group, whereas those event occurred in 9% and 6% of patients in the standard care group, respectively, they added.
Dr. Bernaudin reported disclosures related to Addmedica and bluebird bio. Co-authors reported disclosures with Addmedica, Novartis, Alexion, Amgen, Jazz Pharmaceuticals, and others.
SOURCE: Bernaudin F, et al. JAMA. 2019;321(3):266-276.
Results of DREPAGREFFE illustrate the benefits of matched sibling donor hematopoietic stem cell transplantation (HSCT) for a select group of children with sickle cell anemia, according to the author of an editorial on the study.
Matched sibling donor HSCT was well-tolerated in the study and linked to improved control of transcranial Doppler velocities compared to standard care, Janet L. Kwiatkowski, MD, said in the editorial.
“As a curative therapy, it also obviates the need for long-term treatment wrought with adherence challenges with the potential consequence of stroke, and morbidity from iron overload with transfusion therapy,” wrote Dr. Kwiatkowski.
Only a certain proportion of patients have matched sibling donor HSCT as a potential treatment choice, however, she added.
In this particular study, conducted at 9 sites in France, a higher-than-expected 48% of children with sickle cell anemia had a matched sibling donor, whereas in the United States, she said, less than 1 out of 5 such children would be expected to have an HLA-identical sibling donor.
Because many children don’t have an appropriate matched sibling donor, additional studies are needed not only to evaluate the role of HSCT using matched unrelated and haploidentical donors, Dr. Kwiatkowski said, but also to assess how gene therapy interventions impact cerebrovascular outcomes.
These comments are taken from the accompanying editorial in JAMA by Janet L. Kwiatkowski, MD, MSCE, of Children’s Hospital of Philadelphia, and the Department of Pediatrics at Perelman School of Medicine, University of Pennsylvania, Philadelphia. Dr. Kwiatowski disclosed relationships with bluebird bio, Apopharma, and Novartis.
Results of DREPAGREFFE illustrate the benefits of matched sibling donor hematopoietic stem cell transplantation (HSCT) for a select group of children with sickle cell anemia, according to the author of an editorial on the study.
Matched sibling donor HSCT was well-tolerated in the study and linked to improved control of transcranial Doppler velocities compared to standard care, Janet L. Kwiatkowski, MD, said in the editorial.
“As a curative therapy, it also obviates the need for long-term treatment wrought with adherence challenges with the potential consequence of stroke, and morbidity from iron overload with transfusion therapy,” wrote Dr. Kwiatkowski.
Only a certain proportion of patients have matched sibling donor HSCT as a potential treatment choice, however, she added.
In this particular study, conducted at 9 sites in France, a higher-than-expected 48% of children with sickle cell anemia had a matched sibling donor, whereas in the United States, she said, less than 1 out of 5 such children would be expected to have an HLA-identical sibling donor.
Because many children don’t have an appropriate matched sibling donor, additional studies are needed not only to evaluate the role of HSCT using matched unrelated and haploidentical donors, Dr. Kwiatkowski said, but also to assess how gene therapy interventions impact cerebrovascular outcomes.
These comments are taken from the accompanying editorial in JAMA by Janet L. Kwiatkowski, MD, MSCE, of Children’s Hospital of Philadelphia, and the Department of Pediatrics at Perelman School of Medicine, University of Pennsylvania, Philadelphia. Dr. Kwiatowski disclosed relationships with bluebird bio, Apopharma, and Novartis.
Results of DREPAGREFFE illustrate the benefits of matched sibling donor hematopoietic stem cell transplantation (HSCT) for a select group of children with sickle cell anemia, according to the author of an editorial on the study.
Matched sibling donor HSCT was well-tolerated in the study and linked to improved control of transcranial Doppler velocities compared to standard care, Janet L. Kwiatkowski, MD, said in the editorial.
“As a curative therapy, it also obviates the need for long-term treatment wrought with adherence challenges with the potential consequence of stroke, and morbidity from iron overload with transfusion therapy,” wrote Dr. Kwiatkowski.
Only a certain proportion of patients have matched sibling donor HSCT as a potential treatment choice, however, she added.
In this particular study, conducted at 9 sites in France, a higher-than-expected 48% of children with sickle cell anemia had a matched sibling donor, whereas in the United States, she said, less than 1 out of 5 such children would be expected to have an HLA-identical sibling donor.
Because many children don’t have an appropriate matched sibling donor, additional studies are needed not only to evaluate the role of HSCT using matched unrelated and haploidentical donors, Dr. Kwiatkowski said, but also to assess how gene therapy interventions impact cerebrovascular outcomes.
These comments are taken from the accompanying editorial in JAMA by Janet L. Kwiatkowski, MD, MSCE, of Children’s Hospital of Philadelphia, and the Department of Pediatrics at Perelman School of Medicine, University of Pennsylvania, Philadelphia. Dr. Kwiatowski disclosed relationships with bluebird bio, Apopharma, and Novartis.
, suggesting that this intervention may improve outcomes related to cerebral vasculopathy.
Matched sibling donor hematopoietic stem cell transplantation (MSD-HSCT) was linked to significantly lower transcranial Doppler (TCD) velocities at one year compared to standard care in the 9-center study, investigators reported in JAMA.
The study enrolled children with sickle cell anemia who required chronic transfusion due to persistently high TCD velocities, which are associated with increased stroke risk, researchers said.
“Further research is warranted to assess the effects of MSD-HSCT on clinical outcomes and over longer follow-up,” said the researchers, led by Françoise Bernaudin, MD, of Centre Hospitalier Intercommunal de Créteil, Créteil, France
In the non-randomized, prospective DREPAGREFFE study by Dr. Bernaudin and colleagues, 32 children with sickle cell anemia who had a matched sibling donor underwent transplantation, while another 35 children received standard therapy. The primary end point of the study was time-averaged mean of maximum velocities (TAMV) in cerebral arteries at one year.
The highest TAMV at one year was on average 129.6 cm/s in the MSD-HSCT group, versus 170.4 cm/s in the standard care group, for a difference of -40.8 cm/s (P less than .001), Dr. Bernaudin and co-investigators reported.
The improvement persisted at 3 years, with a TAMV of 112.4 cm/s in the transplantation group and 156.7 cm/s in the standard care group (P less than .001), which they also reported as a secondary outcome of the study.
These findings indicate that MSD-HSCT may allow patients with a history of abnormal TCD velocities to stop transfusions and hydroxyurea, Dr. Bernaudin and colleagues said.
The improvement in TCD velocities may be due in part to anemia correction, but also to the “exclusive presence” of normal red blood cells following transplantation, as opposed to simultaneous presence of normal and sickled cells as would be seen after transfusion, they added.
This study wasn’t powered to determine whether a 40 cm/s reduction in TCD velocities would translate into clinical benefits such as reduction in stenosis and silent infarct, or improved cognitive function, they said. Even so, there were no infarcts or stenoses in the MSD-HSCT group, whereas those event occurred in 9% and 6% of patients in the standard care group, respectively, they added.
Dr. Bernaudin reported disclosures related to Addmedica and bluebird bio. Co-authors reported disclosures with Addmedica, Novartis, Alexion, Amgen, Jazz Pharmaceuticals, and others.
SOURCE: Bernaudin F, et al. JAMA. 2019;321(3):266-276.
, suggesting that this intervention may improve outcomes related to cerebral vasculopathy.
Matched sibling donor hematopoietic stem cell transplantation (MSD-HSCT) was linked to significantly lower transcranial Doppler (TCD) velocities at one year compared to standard care in the 9-center study, investigators reported in JAMA.
The study enrolled children with sickle cell anemia who required chronic transfusion due to persistently high TCD velocities, which are associated with increased stroke risk, researchers said.
“Further research is warranted to assess the effects of MSD-HSCT on clinical outcomes and over longer follow-up,” said the researchers, led by Françoise Bernaudin, MD, of Centre Hospitalier Intercommunal de Créteil, Créteil, France
In the non-randomized, prospective DREPAGREFFE study by Dr. Bernaudin and colleagues, 32 children with sickle cell anemia who had a matched sibling donor underwent transplantation, while another 35 children received standard therapy. The primary end point of the study was time-averaged mean of maximum velocities (TAMV) in cerebral arteries at one year.
The highest TAMV at one year was on average 129.6 cm/s in the MSD-HSCT group, versus 170.4 cm/s in the standard care group, for a difference of -40.8 cm/s (P less than .001), Dr. Bernaudin and co-investigators reported.
The improvement persisted at 3 years, with a TAMV of 112.4 cm/s in the transplantation group and 156.7 cm/s in the standard care group (P less than .001), which they also reported as a secondary outcome of the study.
These findings indicate that MSD-HSCT may allow patients with a history of abnormal TCD velocities to stop transfusions and hydroxyurea, Dr. Bernaudin and colleagues said.
The improvement in TCD velocities may be due in part to anemia correction, but also to the “exclusive presence” of normal red blood cells following transplantation, as opposed to simultaneous presence of normal and sickled cells as would be seen after transfusion, they added.
This study wasn’t powered to determine whether a 40 cm/s reduction in TCD velocities would translate into clinical benefits such as reduction in stenosis and silent infarct, or improved cognitive function, they said. Even so, there were no infarcts or stenoses in the MSD-HSCT group, whereas those event occurred in 9% and 6% of patients in the standard care group, respectively, they added.
Dr. Bernaudin reported disclosures related to Addmedica and bluebird bio. Co-authors reported disclosures with Addmedica, Novartis, Alexion, Amgen, Jazz Pharmaceuticals, and others.
SOURCE: Bernaudin F, et al. JAMA. 2019;321(3):266-276.
FROM JAMA
Key clinical point: In children with sickle cell anemia, matched sibling donor hematopoietic stem cell transplants (HSCT) reduced an indicator of stroke risk, suggesting that the intervention may improve cerebrovascular outcomes.
Major finding: The primary end point, time-averaged mean of maximum velocities in cerebral arteries at one year, was on average 129.6 cm/s in the MSD-HSCT group, versus 170.4 cm/s in the standard care group (P less than .001).
Study details: A multicenter, non-randomized, prospective study (DREPAGREFFE) including 32 children with sickle cell anemia who underwent MSD-HSCT and 35 who received standard therapy.
Disclosures: Study authors provided disclosures related to Addmedica, bluebird bio, Novartis, Alexion, Amgen, Jazz Pharmaceuticals, and others.
Source: Bernaudin F, et al. JAMA. 2019;321(3):266-276.
Self-reporting extends lung cancer survival
Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance, according to a recent French study.
Self-reporting may notify care providers about adverse effects or recurrence earlier than imaging, suggested lead author, Fabrice Denis, MD, PhD, of Institut Inter-régional de Cancérologie Jean Bernard in Le Mans, France, and his colleagues. Findings were published in a letter in JAMA.
In 2017, a similar, single-center study showed that web-based symptom reporting could improve survival in patients undergoing chemotherapy. The lead investigator on that trial was Ethan Basch, MD, who coauthored the present publication.
The current, prospective study involved 121 patients treated at five centers in France between June 2014 and December 2017. Eligibility required a diagnosis of nonprogressive, metastatic lung cancer, including stage III or IV non–small cell or small cell disease. Patients were treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Patients in the control group had standard follow-up with imaging every 3-6 months. In contrast, the patient-reported outcomes (PRO) group completed a weekly online survey of 13 common symptoms between follow-up visits. If patients reported symptoms that matched with predefined criteria for severity or worsening, then the treating oncologist was notified.
When an 18-month interim analysis showed significant survival advantage in the PRO group, recruitment was stopped, and control patients were moved to the PRO group. After 2 years of follow-up, 40 patients (66.7%) in the control group had died, compared with 29 patients (47.5%) in the PRO group. Before censoring for crossover, median overall survival (OS) was 22.5 months in the PRO group, compared with 14.9 months in the control group (P = .03). Censoring for crossover widened the gap between groups by more than a month (22.5 vs. 13.5 months; P = .005).
“A potential mechanism of action is that symptoms suggesting adverse events or recurrence were detected earlier,” the investigators concluded.
The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer institute, Lilly, and others.
SOURCE: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance, according to a recent French study.
Self-reporting may notify care providers about adverse effects or recurrence earlier than imaging, suggested lead author, Fabrice Denis, MD, PhD, of Institut Inter-régional de Cancérologie Jean Bernard in Le Mans, France, and his colleagues. Findings were published in a letter in JAMA.
In 2017, a similar, single-center study showed that web-based symptom reporting could improve survival in patients undergoing chemotherapy. The lead investigator on that trial was Ethan Basch, MD, who coauthored the present publication.
The current, prospective study involved 121 patients treated at five centers in France between June 2014 and December 2017. Eligibility required a diagnosis of nonprogressive, metastatic lung cancer, including stage III or IV non–small cell or small cell disease. Patients were treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Patients in the control group had standard follow-up with imaging every 3-6 months. In contrast, the patient-reported outcomes (PRO) group completed a weekly online survey of 13 common symptoms between follow-up visits. If patients reported symptoms that matched with predefined criteria for severity or worsening, then the treating oncologist was notified.
When an 18-month interim analysis showed significant survival advantage in the PRO group, recruitment was stopped, and control patients were moved to the PRO group. After 2 years of follow-up, 40 patients (66.7%) in the control group had died, compared with 29 patients (47.5%) in the PRO group. Before censoring for crossover, median overall survival (OS) was 22.5 months in the PRO group, compared with 14.9 months in the control group (P = .03). Censoring for crossover widened the gap between groups by more than a month (22.5 vs. 13.5 months; P = .005).
“A potential mechanism of action is that symptoms suggesting adverse events or recurrence were detected earlier,” the investigators concluded.
The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer institute, Lilly, and others.
SOURCE: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance, according to a recent French study.
Self-reporting may notify care providers about adverse effects or recurrence earlier than imaging, suggested lead author, Fabrice Denis, MD, PhD, of Institut Inter-régional de Cancérologie Jean Bernard in Le Mans, France, and his colleagues. Findings were published in a letter in JAMA.
In 2017, a similar, single-center study showed that web-based symptom reporting could improve survival in patients undergoing chemotherapy. The lead investigator on that trial was Ethan Basch, MD, who coauthored the present publication.
The current, prospective study involved 121 patients treated at five centers in France between June 2014 and December 2017. Eligibility required a diagnosis of nonprogressive, metastatic lung cancer, including stage III or IV non–small cell or small cell disease. Patients were treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Patients in the control group had standard follow-up with imaging every 3-6 months. In contrast, the patient-reported outcomes (PRO) group completed a weekly online survey of 13 common symptoms between follow-up visits. If patients reported symptoms that matched with predefined criteria for severity or worsening, then the treating oncologist was notified.
When an 18-month interim analysis showed significant survival advantage in the PRO group, recruitment was stopped, and control patients were moved to the PRO group. After 2 years of follow-up, 40 patients (66.7%) in the control group had died, compared with 29 patients (47.5%) in the PRO group. Before censoring for crossover, median overall survival (OS) was 22.5 months in the PRO group, compared with 14.9 months in the control group (P = .03). Censoring for crossover widened the gap between groups by more than a month (22.5 vs. 13.5 months; P = .005).
“A potential mechanism of action is that symptoms suggesting adverse events or recurrence were detected earlier,” the investigators concluded.
The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer institute, Lilly, and others.
SOURCE: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
FROM JAMA
Key clinical point: Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance.
Major finding: Median overall survival (OS) of patients in the web-based monitoring group was 22.5 months versus 13.5 months for patients in the standard imaging group (P = .005).
Study details: A prospective study of 121 nonprogressive, metastatic lung cancer patients being treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Disclosures: The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer Institute, Lilly, and others.
Source: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
In the Literature: Short Takes
A second medical emergency team (MET) activation more likely in patients with recent MET activation
A prospective cohort study examined 471 MET activatios where the patient was not transferred to a higher level of care found that 18% had a second MET event. These second events were more likely to occur in the first 8-12 hours and to occur in patients recently discharged from the ICU.
Citation: Still MD et al. Predictors of a second medical emergency team activation within 24 hours of index event. J Nurs Care Qual 2018;33(2): 157-65
Risk of CV events in patients with TIA or minor stroke decreases significantly after first year
A prospective cohort study following TIA or minor stroke patients from the TIAregistry.org project shows that the risk of additional events (death from cardiovascular cause, nonfatal stroke, or nonfatal acute coronary syndrome) in the following 5 years is 12.9% with half of those events occuring in the first year.
Citation: Amarenco P et al. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378:2182-90.
Maintenance of certification associated with better physician performance scores
Physicians who still participated in Maintenance of Certification (MOC) programs 20 years after their initial certification scored higher on a variety of physician performance scores on Medicare patients.
Citation: Gray BG et al. Associations between American Board of Internal Medicine Maintenance of Certificate status and performance on a set of healthcare effectiveness data and information set (HEDIS) process measures. Ann Intern Med. 2018;169(2):97-105.
A second medical emergency team (MET) activation more likely in patients with recent MET activation
A prospective cohort study examined 471 MET activatios where the patient was not transferred to a higher level of care found that 18% had a second MET event. These second events were more likely to occur in the first 8-12 hours and to occur in patients recently discharged from the ICU.
Citation: Still MD et al. Predictors of a second medical emergency team activation within 24 hours of index event. J Nurs Care Qual 2018;33(2): 157-65
Risk of CV events in patients with TIA or minor stroke decreases significantly after first year
A prospective cohort study following TIA or minor stroke patients from the TIAregistry.org project shows that the risk of additional events (death from cardiovascular cause, nonfatal stroke, or nonfatal acute coronary syndrome) in the following 5 years is 12.9% with half of those events occuring in the first year.
Citation: Amarenco P et al. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378:2182-90.
Maintenance of certification associated with better physician performance scores
Physicians who still participated in Maintenance of Certification (MOC) programs 20 years after their initial certification scored higher on a variety of physician performance scores on Medicare patients.
Citation: Gray BG et al. Associations between American Board of Internal Medicine Maintenance of Certificate status and performance on a set of healthcare effectiveness data and information set (HEDIS) process measures. Ann Intern Med. 2018;169(2):97-105.
A second medical emergency team (MET) activation more likely in patients with recent MET activation
A prospective cohort study examined 471 MET activatios where the patient was not transferred to a higher level of care found that 18% had a second MET event. These second events were more likely to occur in the first 8-12 hours and to occur in patients recently discharged from the ICU.
Citation: Still MD et al. Predictors of a second medical emergency team activation within 24 hours of index event. J Nurs Care Qual 2018;33(2): 157-65
Risk of CV events in patients with TIA or minor stroke decreases significantly after first year
A prospective cohort study following TIA or minor stroke patients from the TIAregistry.org project shows that the risk of additional events (death from cardiovascular cause, nonfatal stroke, or nonfatal acute coronary syndrome) in the following 5 years is 12.9% with half of those events occuring in the first year.
Citation: Amarenco P et al. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378:2182-90.
Maintenance of certification associated with better physician performance scores
Physicians who still participated in Maintenance of Certification (MOC) programs 20 years after their initial certification scored higher on a variety of physician performance scores on Medicare patients.
Citation: Gray BG et al. Associations between American Board of Internal Medicine Maintenance of Certificate status and performance on a set of healthcare effectiveness data and information set (HEDIS) process measures. Ann Intern Med. 2018;169(2):97-105.