User login
Generic clofarabine injection hits the market
The generic clofarabine injection for treatment of children with relapsed or refractory acute lymphoblastic leukemia (ALL) is now available on the U.S. market.
The generic version of the drug was approved by the Food and Drug Administration in May 2017 for children up to age 21 years with relapsed or refractory ALL after at least two prior regimens.
The injection, marketed by Mylan N.V., is available in 20 mg/20 mL (1 mg/mL) single-dose vials. It is a generic version of Genzyme’s Clolar.
[email protected]
On Twitter @maryellenny
The generic clofarabine injection for treatment of children with relapsed or refractory acute lymphoblastic leukemia (ALL) is now available on the U.S. market.
The generic version of the drug was approved by the Food and Drug Administration in May 2017 for children up to age 21 years with relapsed or refractory ALL after at least two prior regimens.
The injection, marketed by Mylan N.V., is available in 20 mg/20 mL (1 mg/mL) single-dose vials. It is a generic version of Genzyme’s Clolar.
[email protected]
On Twitter @maryellenny
The generic clofarabine injection for treatment of children with relapsed or refractory acute lymphoblastic leukemia (ALL) is now available on the U.S. market.
The generic version of the drug was approved by the Food and Drug Administration in May 2017 for children up to age 21 years with relapsed or refractory ALL after at least two prior regimens.
The injection, marketed by Mylan N.V., is available in 20 mg/20 mL (1 mg/mL) single-dose vials. It is a generic version of Genzyme’s Clolar.
[email protected]
On Twitter @maryellenny
FDA approves first two-dose HBV vaccine
When the Food and Drug Administration approved Heplisav-B Nov. 9, it marked the first new vaccine for hepatitis B virus (HBV) to be sanctioned in over 25 years.
Heplisav-B is the only two-dose regimen that protects against all known subtypes of HBV in adults 18 years and older, according to a statement released by Dynavax Technologies, the creator of the drug.
“Heplisav-B is the first FDA-approved product for Dynavax and demonstrates our ability to develop innovative products and progress them from discovery to commercialization,” according to Eddie Gray, chief executive officer of Dynavax. “We expect that it will become an essential tool in the public health community’s fight to prevent hepatitis B [infection], and we look forward to making Heplisav-B available to clinicians and their adult patients.”
Incidence of HBV has increased sharply from 2012 to 2015 in the United States, with reported cases rising from 2,895 to 3,370, according to the Centers for Disease Control and Prevention.
From 2014 to 2015, acute HBV infection increased 20.7%, according to the CDC report.
The new vaccine’s approval came after review of safety and efficacy data from three phase 3 trials comparing Heplisav-B with Engerix-B, another HBV vaccine currently available, that is given in a three-dose regimen.
In one study of 2,032 patients between the ages of 18 and 55 years, seroprotection rate in the Heplisav-B group (1,511) was 95%, compared with 81.5% in the Engerix-B group (521).
Heplisav-B patients were given a two-dose regimen of the drug at 0 and 1 months, followed by a placebo at 6 months, while investigators administered Engerix-B at all three intervals in the comparator subjects.
The FDA’s decision to green-light the new vaccine follows a recommendation for approval from the FDA’s Vaccines and Related Biological Products Advisory Committee, held at the end of July this year.
During the advisory committee meeting, members were concerned about an increased relative risk for acute myocardial infarction of 6.97 in Heplisav-B patients (14), compared with Engerix-B patients (1).
The recommendation for approval came with the caveat of conducting postmarketing analysis for the risk of AMI in Heplisav-B patients, which Dynavax is conducting through the Kaiser Permanente system in California.
“To evaluate the risk of AMIs, the study will enroll 25,000 Heplisav-B patients and 25,000 Engerix-B patients over approximately 10 months and follow them for 1 year after vaccination,” according to a statement from Dynavax. “In addition we will evaluate the rate of immune-mediated diseases in these patients in an additional 5,000 Heplisav-B recipients and 5,000 Engerix-B recipients.”
Dynavax is currently set to introduce Heplisav-B commercially in the United States in 2018, with the cost of the drug set to be released soon.
“Dynavax is in the process of finalizing the price of a two-dose series of Heplisav-B, and they plan to disclose it shortly after approval,” according to the company. “Their pricing and access strategy will be aimed at ensuring that populations at risk of infection are able to access this new vaccine, while recognizing the value it brings to the health care system with a two-dose regimen and higher rates of protection compared to Engerix-B.”
[email protected]
On Twitter @eaztweets
When the Food and Drug Administration approved Heplisav-B Nov. 9, it marked the first new vaccine for hepatitis B virus (HBV) to be sanctioned in over 25 years.
Heplisav-B is the only two-dose regimen that protects against all known subtypes of HBV in adults 18 years and older, according to a statement released by Dynavax Technologies, the creator of the drug.
“Heplisav-B is the first FDA-approved product for Dynavax and demonstrates our ability to develop innovative products and progress them from discovery to commercialization,” according to Eddie Gray, chief executive officer of Dynavax. “We expect that it will become an essential tool in the public health community’s fight to prevent hepatitis B [infection], and we look forward to making Heplisav-B available to clinicians and their adult patients.”
Incidence of HBV has increased sharply from 2012 to 2015 in the United States, with reported cases rising from 2,895 to 3,370, according to the Centers for Disease Control and Prevention.
From 2014 to 2015, acute HBV infection increased 20.7%, according to the CDC report.
The new vaccine’s approval came after review of safety and efficacy data from three phase 3 trials comparing Heplisav-B with Engerix-B, another HBV vaccine currently available, that is given in a three-dose regimen.
In one study of 2,032 patients between the ages of 18 and 55 years, seroprotection rate in the Heplisav-B group (1,511) was 95%, compared with 81.5% in the Engerix-B group (521).
Heplisav-B patients were given a two-dose regimen of the drug at 0 and 1 months, followed by a placebo at 6 months, while investigators administered Engerix-B at all three intervals in the comparator subjects.
The FDA’s decision to green-light the new vaccine follows a recommendation for approval from the FDA’s Vaccines and Related Biological Products Advisory Committee, held at the end of July this year.
During the advisory committee meeting, members were concerned about an increased relative risk for acute myocardial infarction of 6.97 in Heplisav-B patients (14), compared with Engerix-B patients (1).
The recommendation for approval came with the caveat of conducting postmarketing analysis for the risk of AMI in Heplisav-B patients, which Dynavax is conducting through the Kaiser Permanente system in California.
“To evaluate the risk of AMIs, the study will enroll 25,000 Heplisav-B patients and 25,000 Engerix-B patients over approximately 10 months and follow them for 1 year after vaccination,” according to a statement from Dynavax. “In addition we will evaluate the rate of immune-mediated diseases in these patients in an additional 5,000 Heplisav-B recipients and 5,000 Engerix-B recipients.”
Dynavax is currently set to introduce Heplisav-B commercially in the United States in 2018, with the cost of the drug set to be released soon.
“Dynavax is in the process of finalizing the price of a two-dose series of Heplisav-B, and they plan to disclose it shortly after approval,” according to the company. “Their pricing and access strategy will be aimed at ensuring that populations at risk of infection are able to access this new vaccine, while recognizing the value it brings to the health care system with a two-dose regimen and higher rates of protection compared to Engerix-B.”
[email protected]
On Twitter @eaztweets
When the Food and Drug Administration approved Heplisav-B Nov. 9, it marked the first new vaccine for hepatitis B virus (HBV) to be sanctioned in over 25 years.
Heplisav-B is the only two-dose regimen that protects against all known subtypes of HBV in adults 18 years and older, according to a statement released by Dynavax Technologies, the creator of the drug.
“Heplisav-B is the first FDA-approved product for Dynavax and demonstrates our ability to develop innovative products and progress them from discovery to commercialization,” according to Eddie Gray, chief executive officer of Dynavax. “We expect that it will become an essential tool in the public health community’s fight to prevent hepatitis B [infection], and we look forward to making Heplisav-B available to clinicians and their adult patients.”
Incidence of HBV has increased sharply from 2012 to 2015 in the United States, with reported cases rising from 2,895 to 3,370, according to the Centers for Disease Control and Prevention.
From 2014 to 2015, acute HBV infection increased 20.7%, according to the CDC report.
The new vaccine’s approval came after review of safety and efficacy data from three phase 3 trials comparing Heplisav-B with Engerix-B, another HBV vaccine currently available, that is given in a three-dose regimen.
In one study of 2,032 patients between the ages of 18 and 55 years, seroprotection rate in the Heplisav-B group (1,511) was 95%, compared with 81.5% in the Engerix-B group (521).
Heplisav-B patients were given a two-dose regimen of the drug at 0 and 1 months, followed by a placebo at 6 months, while investigators administered Engerix-B at all three intervals in the comparator subjects.
The FDA’s decision to green-light the new vaccine follows a recommendation for approval from the FDA’s Vaccines and Related Biological Products Advisory Committee, held at the end of July this year.
During the advisory committee meeting, members were concerned about an increased relative risk for acute myocardial infarction of 6.97 in Heplisav-B patients (14), compared with Engerix-B patients (1).
The recommendation for approval came with the caveat of conducting postmarketing analysis for the risk of AMI in Heplisav-B patients, which Dynavax is conducting through the Kaiser Permanente system in California.
“To evaluate the risk of AMIs, the study will enroll 25,000 Heplisav-B patients and 25,000 Engerix-B patients over approximately 10 months and follow them for 1 year after vaccination,” according to a statement from Dynavax. “In addition we will evaluate the rate of immune-mediated diseases in these patients in an additional 5,000 Heplisav-B recipients and 5,000 Engerix-B recipients.”
Dynavax is currently set to introduce Heplisav-B commercially in the United States in 2018, with the cost of the drug set to be released soon.
“Dynavax is in the process of finalizing the price of a two-dose series of Heplisav-B, and they plan to disclose it shortly after approval,” according to the company. “Their pricing and access strategy will be aimed at ensuring that populations at risk of infection are able to access this new vaccine, while recognizing the value it brings to the health care system with a two-dose regimen and higher rates of protection compared to Engerix-B.”
[email protected]
On Twitter @eaztweets
Lung injury risk higher with apheresis blood products
SAN DIEGO – , according to research presented at the annual meeting of the American Association of Blood Banks.
Compared with other RBC products, those derived from apheresis significantly increased pulmonary cell interleukin (IL)–6 and IL-8 production, and this was further exacerbated by cell stretching. Conversely, red cell–filtered products appeared to be the least likely to cause cell injury.
“Several studies have shown that red blood cell transfusion is associated with acute lung injury, and transfusion induces leakage in ICU patients,” said lead study author Mathijs Wirtz, MD, of the Academic Medical Center, Amsterdam.
ICU patients who did not receive any transfusions had significantly lower leakage than those who were transfused. “There also seems to be a synergy between transfusion and mechanical ventilation,” Dr. Wirtz said.
Studies have also shown that there are differences in the prevalence of transfusion-related acute lung injury, when comparing Europe to the United States. Storage and manufacturing methods do differ between Europe and the United States, Dr. Wirtz noted. “This led to our hypothesis that lung injury inflicted by red blood cell transfusion is influenced by manufacturing methods.”
In this study, Dr. Wirtz and his colleagues investigated the response of pulmonary cells to the different methods of manufacturing RBC products. Using type A or B blood obtained from eight donors, a variety of RBC products were manufactured for the study, including whole-blood filtered, red-cell filtered, apheresis derived, and whole-blood derived.
For measuring thrombin generation and analyzing extracellular vesicles (EV), supernatants were prepared after 4-5 days of storage for fresh and 41-42 days for stored. The researchers selected A549 type II alveolar cells to seed onto flexible membranes, which were then incubated with RBC supernatant also stretched 25% using a cell stretcher.
After 24 hours, the production of IL-8 and IL-6 was measured.
Both fresh and stored supernatants that were derived from apheresis significantly increased the production of IL-6 and IL-8 in pulmonary cells, compared with nonincubated controls and most of the other RBC products. The production of IL-6 and IL-8 was exacerbated by cell stretching.
Average IL-6 production in nonstretched cells was 91 pg/mL for fresh and 87 pg/mL for expired (P less than .05 vs. control and other RBC products). For stretched cells, it was 130 pg/mL and 150 pg/mL (P less than .05 vs. control). For controls, mean nonstretched and stretched production was 21 pg/mL and 85 pg/mL.
Mean IL-8 production in nonstretched cells was 2,100 pg/mL for fresh and 1,900 pg/mL for stored (P less than .05 vs. control and other RBC products). For stretched cells, the means were 4,100 pg/mL for fresh and 5,200 pg/mL for stored (P less than .05 vs. control).
The average nonstretched and stretched control IL-8 production was 1,200 pg/mL for fresh and 4,300 pg/mL for stored.
Products derived from apheresis also demonstrated a significantly higher ability to generate thrombin, compared with other RBC products, and a significantly increased number of RBC-derived EVs, compared with filtered red cell and whole blood–derived products (P less than .05).
However, incubated stretched cells from stored whole blood–filtered products had higher IL-8 production (16,000 pg/mL), compared with other products and stretched controls. The lowest mean levels of IL-6 were observed in supernatants derived from red cell–filtered products (nonstretched fresh and expired, 12 pg/mL and 8 pg/mL; stretched, 40 pg/mL and 36 pg/mL) and they did not appear to activate pulmonary cells. Levels of EVs were also low, compared with other blood products.
“We can conclude that manufacturing methods contribute to the differences in inducing lung injury, and especially the apheresis-derived products, which induced the most consistent injury in our model,” Dr. Wirtz said. “The red cell–filtered products appeared to be the safest.”
Dr. Wirtz had no disclosures.
SAN DIEGO – , according to research presented at the annual meeting of the American Association of Blood Banks.
Compared with other RBC products, those derived from apheresis significantly increased pulmonary cell interleukin (IL)–6 and IL-8 production, and this was further exacerbated by cell stretching. Conversely, red cell–filtered products appeared to be the least likely to cause cell injury.
“Several studies have shown that red blood cell transfusion is associated with acute lung injury, and transfusion induces leakage in ICU patients,” said lead study author Mathijs Wirtz, MD, of the Academic Medical Center, Amsterdam.
ICU patients who did not receive any transfusions had significantly lower leakage than those who were transfused. “There also seems to be a synergy between transfusion and mechanical ventilation,” Dr. Wirtz said.
Studies have also shown that there are differences in the prevalence of transfusion-related acute lung injury, when comparing Europe to the United States. Storage and manufacturing methods do differ between Europe and the United States, Dr. Wirtz noted. “This led to our hypothesis that lung injury inflicted by red blood cell transfusion is influenced by manufacturing methods.”
In this study, Dr. Wirtz and his colleagues investigated the response of pulmonary cells to the different methods of manufacturing RBC products. Using type A or B blood obtained from eight donors, a variety of RBC products were manufactured for the study, including whole-blood filtered, red-cell filtered, apheresis derived, and whole-blood derived.
For measuring thrombin generation and analyzing extracellular vesicles (EV), supernatants were prepared after 4-5 days of storage for fresh and 41-42 days for stored. The researchers selected A549 type II alveolar cells to seed onto flexible membranes, which were then incubated with RBC supernatant also stretched 25% using a cell stretcher.
After 24 hours, the production of IL-8 and IL-6 was measured.
Both fresh and stored supernatants that were derived from apheresis significantly increased the production of IL-6 and IL-8 in pulmonary cells, compared with nonincubated controls and most of the other RBC products. The production of IL-6 and IL-8 was exacerbated by cell stretching.
Average IL-6 production in nonstretched cells was 91 pg/mL for fresh and 87 pg/mL for expired (P less than .05 vs. control and other RBC products). For stretched cells, it was 130 pg/mL and 150 pg/mL (P less than .05 vs. control). For controls, mean nonstretched and stretched production was 21 pg/mL and 85 pg/mL.
Mean IL-8 production in nonstretched cells was 2,100 pg/mL for fresh and 1,900 pg/mL for stored (P less than .05 vs. control and other RBC products). For stretched cells, the means were 4,100 pg/mL for fresh and 5,200 pg/mL for stored (P less than .05 vs. control).
The average nonstretched and stretched control IL-8 production was 1,200 pg/mL for fresh and 4,300 pg/mL for stored.
Products derived from apheresis also demonstrated a significantly higher ability to generate thrombin, compared with other RBC products, and a significantly increased number of RBC-derived EVs, compared with filtered red cell and whole blood–derived products (P less than .05).
However, incubated stretched cells from stored whole blood–filtered products had higher IL-8 production (16,000 pg/mL), compared with other products and stretched controls. The lowest mean levels of IL-6 were observed in supernatants derived from red cell–filtered products (nonstretched fresh and expired, 12 pg/mL and 8 pg/mL; stretched, 40 pg/mL and 36 pg/mL) and they did not appear to activate pulmonary cells. Levels of EVs were also low, compared with other blood products.
“We can conclude that manufacturing methods contribute to the differences in inducing lung injury, and especially the apheresis-derived products, which induced the most consistent injury in our model,” Dr. Wirtz said. “The red cell–filtered products appeared to be the safest.”
Dr. Wirtz had no disclosures.
SAN DIEGO – , according to research presented at the annual meeting of the American Association of Blood Banks.
Compared with other RBC products, those derived from apheresis significantly increased pulmonary cell interleukin (IL)–6 and IL-8 production, and this was further exacerbated by cell stretching. Conversely, red cell–filtered products appeared to be the least likely to cause cell injury.
“Several studies have shown that red blood cell transfusion is associated with acute lung injury, and transfusion induces leakage in ICU patients,” said lead study author Mathijs Wirtz, MD, of the Academic Medical Center, Amsterdam.
ICU patients who did not receive any transfusions had significantly lower leakage than those who were transfused. “There also seems to be a synergy between transfusion and mechanical ventilation,” Dr. Wirtz said.
Studies have also shown that there are differences in the prevalence of transfusion-related acute lung injury, when comparing Europe to the United States. Storage and manufacturing methods do differ between Europe and the United States, Dr. Wirtz noted. “This led to our hypothesis that lung injury inflicted by red blood cell transfusion is influenced by manufacturing methods.”
In this study, Dr. Wirtz and his colleagues investigated the response of pulmonary cells to the different methods of manufacturing RBC products. Using type A or B blood obtained from eight donors, a variety of RBC products were manufactured for the study, including whole-blood filtered, red-cell filtered, apheresis derived, and whole-blood derived.
For measuring thrombin generation and analyzing extracellular vesicles (EV), supernatants were prepared after 4-5 days of storage for fresh and 41-42 days for stored. The researchers selected A549 type II alveolar cells to seed onto flexible membranes, which were then incubated with RBC supernatant also stretched 25% using a cell stretcher.
After 24 hours, the production of IL-8 and IL-6 was measured.
Both fresh and stored supernatants that were derived from apheresis significantly increased the production of IL-6 and IL-8 in pulmonary cells, compared with nonincubated controls and most of the other RBC products. The production of IL-6 and IL-8 was exacerbated by cell stretching.
Average IL-6 production in nonstretched cells was 91 pg/mL for fresh and 87 pg/mL for expired (P less than .05 vs. control and other RBC products). For stretched cells, it was 130 pg/mL and 150 pg/mL (P less than .05 vs. control). For controls, mean nonstretched and stretched production was 21 pg/mL and 85 pg/mL.
Mean IL-8 production in nonstretched cells was 2,100 pg/mL for fresh and 1,900 pg/mL for stored (P less than .05 vs. control and other RBC products). For stretched cells, the means were 4,100 pg/mL for fresh and 5,200 pg/mL for stored (P less than .05 vs. control).
The average nonstretched and stretched control IL-8 production was 1,200 pg/mL for fresh and 4,300 pg/mL for stored.
Products derived from apheresis also demonstrated a significantly higher ability to generate thrombin, compared with other RBC products, and a significantly increased number of RBC-derived EVs, compared with filtered red cell and whole blood–derived products (P less than .05).
However, incubated stretched cells from stored whole blood–filtered products had higher IL-8 production (16,000 pg/mL), compared with other products and stretched controls. The lowest mean levels of IL-6 were observed in supernatants derived from red cell–filtered products (nonstretched fresh and expired, 12 pg/mL and 8 pg/mL; stretched, 40 pg/mL and 36 pg/mL) and they did not appear to activate pulmonary cells. Levels of EVs were also low, compared with other blood products.
“We can conclude that manufacturing methods contribute to the differences in inducing lung injury, and especially the apheresis-derived products, which induced the most consistent injury in our model,” Dr. Wirtz said. “The red cell–filtered products appeared to be the safest.”
Dr. Wirtz had no disclosures.
From AABB17
Key clinical point: The method of manufacturing blood products can markedly influence the interaction of RBC products with lung cells, especially in patients on mechanical ventilation.
Major finding: Apheresis-derived products are the most consistent in causing injuries, while red cell–filtered products appear to be the safest in avoiding lung injury.
Data source: An experimental study that investigated different manufacturing methods of RBC products and the response of pulmonary cells in an in vitro model of mechanical ventilation.
Disclosures: Dr. Wirtz had no disclosures.
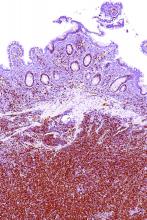
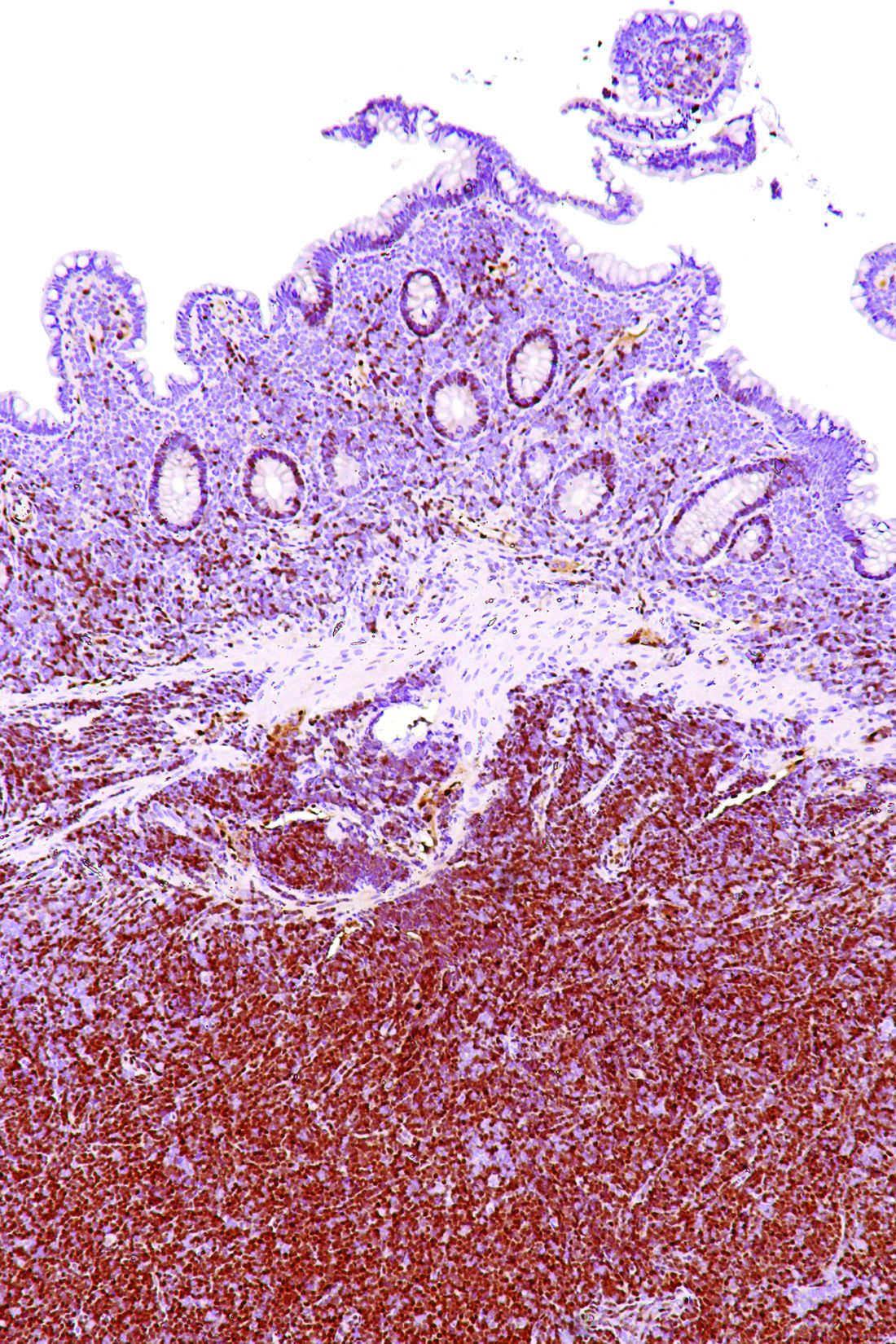
MMR deficiency testing remains low in colorectal cancer patients
Overall utilization of mismatch repair (MMR) deficiency testing is poor among patients with colorectal cancer, and utilization also remains low among young adults despite national guidelines calling for universal testing, according to an analysis of cases from the National Cancer Database.
The findings suggest that interventions that target groups at risk for nonadherence to guidelines may be warranted, wrote Talha Shaikh, MD, and colleagues at Fox Chase Cancer Center, Philadelphia. The report was published in JAMA Oncology (2017 Nov 9. doi: 10.1001/jamaoncol.2017.3580).
Of 152,993 adults with colorectal cancer (CRC) who were included in the study, only 28% underwent MMR deficiency testing, and of 17,218 aged 30-49 years, only 43% were tested. The proportion of patients tested in both groups increased between 2010 and 2012 (from about 22% to 33%, and from about 36% to 48%, respectively).
After the researchers controlled for all other covariates, factors significantly associated with being tested were higher educational level (odds ratio, 1.38), later diagnosis year (OR, 1.81), early-stage disease (OR, 1.24), and number of regional lymph nodes examined (OR, 1.44 for 12 or more lymph nodes). Factors associated with underuse of testing were older age (OR, 0.31), insurance status (Medicare, Medicaid, uninsured; ORs, 0.89, 0.83, and 0.78, respectively), research facility type (nonacademic vs. academic; OR, 0.44), rectosigmoid or rectal tumor location (OR, 0.76), unknown grade (OR, 0.61), and nonreceipt of definitive surgery (OR, 0.33).
MMR deficiency occurs in up to 15% of sporadic CRC and is a feature of Lynch syndrome, which occurs most often in patients under age 50 years. National guidelines have long recommended routine MMR deficiency testing for CRC patients in that age group, and universal testing has been recommended since 2014.
“Although the proportions of patients tested increased during the study period, our results suggest that underutilization of MMR deficiency testing was significant and pervasive, even among young patients with CRC with a well-established risk of Lynch syndrome. Our study ... identifies significant groups at risk for potential nonadherence to newly implemented universal testing guidelines moving forward,” the investigators said, noting that the associations between type and utilization of patient testing and socioeconomic status, insurance status, and cancer program location are of particular concern.
Ongoing analyses to track progress toward “closing this important clinical service gap,” will be needed, they concluded.
This study was funded by a grant from the National Institutes of Health, National Cancer Institute. The authors reported having no conflicts of interest.
The findings by Shaikh et al. are sobering, given the overwhelming published evidence regarding the importance of MMR deficiency testing, and they underscore a need to determine the causes of the low testing rates, according to Stanley R. Hamilton, MD.
Importantly, they also highlight areas that are “potentially actionable.” For example, the higher frequency of testing among those with higher educational levels, and underuse of testing in older patients and those from nonacademic facilities suggest that better education of physicians and patients about the value of testing could improve adherence to guidelines, Dr. Hamilton wrote in an editorial (JAMA Oncol. 2017 Nov 9. doi: 10.1001/jamaoncol.2017.3574).
Further, the lower frequency of testing among certain demographic groups suggests a need to address underserved and underresourced patient populations, he said, concluding that efforts must continue to meet the goal of universal testing and that those efforts must be accompanied by studies to evaluate the clinical utility of testing in reducing CRC mortality.
Dr. Hamilton is with the University of Texas MD Anderson Cancer Center, Houston. He is a member of the Fred Hutchinson Cancer Research Scientific Advisory Committee, a consultant for LOXO Oncology, and a member of the HalioDx Scientific Advisory Committee. He has a financial relationship with The Johns Hopkins University School of Medicine and with Merck.
The findings by Shaikh et al. are sobering, given the overwhelming published evidence regarding the importance of MMR deficiency testing, and they underscore a need to determine the causes of the low testing rates, according to Stanley R. Hamilton, MD.
Importantly, they also highlight areas that are “potentially actionable.” For example, the higher frequency of testing among those with higher educational levels, and underuse of testing in older patients and those from nonacademic facilities suggest that better education of physicians and patients about the value of testing could improve adherence to guidelines, Dr. Hamilton wrote in an editorial (JAMA Oncol. 2017 Nov 9. doi: 10.1001/jamaoncol.2017.3574).
Further, the lower frequency of testing among certain demographic groups suggests a need to address underserved and underresourced patient populations, he said, concluding that efforts must continue to meet the goal of universal testing and that those efforts must be accompanied by studies to evaluate the clinical utility of testing in reducing CRC mortality.
Dr. Hamilton is with the University of Texas MD Anderson Cancer Center, Houston. He is a member of the Fred Hutchinson Cancer Research Scientific Advisory Committee, a consultant for LOXO Oncology, and a member of the HalioDx Scientific Advisory Committee. He has a financial relationship with The Johns Hopkins University School of Medicine and with Merck.
The findings by Shaikh et al. are sobering, given the overwhelming published evidence regarding the importance of MMR deficiency testing, and they underscore a need to determine the causes of the low testing rates, according to Stanley R. Hamilton, MD.
Importantly, they also highlight areas that are “potentially actionable.” For example, the higher frequency of testing among those with higher educational levels, and underuse of testing in older patients and those from nonacademic facilities suggest that better education of physicians and patients about the value of testing could improve adherence to guidelines, Dr. Hamilton wrote in an editorial (JAMA Oncol. 2017 Nov 9. doi: 10.1001/jamaoncol.2017.3574).
Further, the lower frequency of testing among certain demographic groups suggests a need to address underserved and underresourced patient populations, he said, concluding that efforts must continue to meet the goal of universal testing and that those efforts must be accompanied by studies to evaluate the clinical utility of testing in reducing CRC mortality.
Dr. Hamilton is with the University of Texas MD Anderson Cancer Center, Houston. He is a member of the Fred Hutchinson Cancer Research Scientific Advisory Committee, a consultant for LOXO Oncology, and a member of the HalioDx Scientific Advisory Committee. He has a financial relationship with The Johns Hopkins University School of Medicine and with Merck.
Overall utilization of mismatch repair (MMR) deficiency testing is poor among patients with colorectal cancer, and utilization also remains low among young adults despite national guidelines calling for universal testing, according to an analysis of cases from the National Cancer Database.
The findings suggest that interventions that target groups at risk for nonadherence to guidelines may be warranted, wrote Talha Shaikh, MD, and colleagues at Fox Chase Cancer Center, Philadelphia. The report was published in JAMA Oncology (2017 Nov 9. doi: 10.1001/jamaoncol.2017.3580).
Of 152,993 adults with colorectal cancer (CRC) who were included in the study, only 28% underwent MMR deficiency testing, and of 17,218 aged 30-49 years, only 43% were tested. The proportion of patients tested in both groups increased between 2010 and 2012 (from about 22% to 33%, and from about 36% to 48%, respectively).
After the researchers controlled for all other covariates, factors significantly associated with being tested were higher educational level (odds ratio, 1.38), later diagnosis year (OR, 1.81), early-stage disease (OR, 1.24), and number of regional lymph nodes examined (OR, 1.44 for 12 or more lymph nodes). Factors associated with underuse of testing were older age (OR, 0.31), insurance status (Medicare, Medicaid, uninsured; ORs, 0.89, 0.83, and 0.78, respectively), research facility type (nonacademic vs. academic; OR, 0.44), rectosigmoid or rectal tumor location (OR, 0.76), unknown grade (OR, 0.61), and nonreceipt of definitive surgery (OR, 0.33).
MMR deficiency occurs in up to 15% of sporadic CRC and is a feature of Lynch syndrome, which occurs most often in patients under age 50 years. National guidelines have long recommended routine MMR deficiency testing for CRC patients in that age group, and universal testing has been recommended since 2014.
“Although the proportions of patients tested increased during the study period, our results suggest that underutilization of MMR deficiency testing was significant and pervasive, even among young patients with CRC with a well-established risk of Lynch syndrome. Our study ... identifies significant groups at risk for potential nonadherence to newly implemented universal testing guidelines moving forward,” the investigators said, noting that the associations between type and utilization of patient testing and socioeconomic status, insurance status, and cancer program location are of particular concern.
Ongoing analyses to track progress toward “closing this important clinical service gap,” will be needed, they concluded.
This study was funded by a grant from the National Institutes of Health, National Cancer Institute. The authors reported having no conflicts of interest.
Overall utilization of mismatch repair (MMR) deficiency testing is poor among patients with colorectal cancer, and utilization also remains low among young adults despite national guidelines calling for universal testing, according to an analysis of cases from the National Cancer Database.
The findings suggest that interventions that target groups at risk for nonadherence to guidelines may be warranted, wrote Talha Shaikh, MD, and colleagues at Fox Chase Cancer Center, Philadelphia. The report was published in JAMA Oncology (2017 Nov 9. doi: 10.1001/jamaoncol.2017.3580).
Of 152,993 adults with colorectal cancer (CRC) who were included in the study, only 28% underwent MMR deficiency testing, and of 17,218 aged 30-49 years, only 43% were tested. The proportion of patients tested in both groups increased between 2010 and 2012 (from about 22% to 33%, and from about 36% to 48%, respectively).
After the researchers controlled for all other covariates, factors significantly associated with being tested were higher educational level (odds ratio, 1.38), later diagnosis year (OR, 1.81), early-stage disease (OR, 1.24), and number of regional lymph nodes examined (OR, 1.44 for 12 or more lymph nodes). Factors associated with underuse of testing were older age (OR, 0.31), insurance status (Medicare, Medicaid, uninsured; ORs, 0.89, 0.83, and 0.78, respectively), research facility type (nonacademic vs. academic; OR, 0.44), rectosigmoid or rectal tumor location (OR, 0.76), unknown grade (OR, 0.61), and nonreceipt of definitive surgery (OR, 0.33).
MMR deficiency occurs in up to 15% of sporadic CRC and is a feature of Lynch syndrome, which occurs most often in patients under age 50 years. National guidelines have long recommended routine MMR deficiency testing for CRC patients in that age group, and universal testing has been recommended since 2014.
“Although the proportions of patients tested increased during the study period, our results suggest that underutilization of MMR deficiency testing was significant and pervasive, even among young patients with CRC with a well-established risk of Lynch syndrome. Our study ... identifies significant groups at risk for potential nonadherence to newly implemented universal testing guidelines moving forward,” the investigators said, noting that the associations between type and utilization of patient testing and socioeconomic status, insurance status, and cancer program location are of particular concern.
Ongoing analyses to track progress toward “closing this important clinical service gap,” will be needed, they concluded.
This study was funded by a grant from the National Institutes of Health, National Cancer Institute. The authors reported having no conflicts of interest.
FROM JAMA ONCOLOGY
Key clinical point:
Major finding: Only 28% of patients overall, and only 43% of younger patients, underwent MMR deficiency testing.
Data source: 152,993 cases from the National Cancer Database.
Disclosures: This study was funded by a grant from the National Institutes of Health, National Cancer Institute. The authors reported having no conflicts of interest.
TP53 mutations could help stratify MCL patients
TP53 mutations identified a phenotypically distinct and aggressive form of mantle cell lymphoma (MCL) that did not respond to standard-of-care treatments, according to results from 183 patients younger than 66 years from the Nordic MCL2 and MCL3 trials.
, and that patients with the mutations should be considered for experimental trials of novel agents, wrote Christian W. Eskelund of the department of hematology at Rigshospitalet, Copenhagen, and colleagues.
The researchers collected DNA from the Nordic MCL2 and MCL3 trials and 183 samples were of sufficient quality for genetic analyses. They examined the prognostic value of eight recurrently mutated and two recurrently deleted genes. Only TP53 mutations showed an independent prognostic effect for overall survival (hazard ratio 6.2; P less than .0001) in multivariate Cox regression analyses.
“Our data show that TP53 mutations identify a unique MCL subtype associated with high-risk baseline characteristics, dismal response to standard treatment, and poor clinical outcome,” the researchers wrote.
Read the full study in Blood (2017 Oct 26;130[17]:1903-10).
[email protected]
On Twitter @maryellenny
TP53 mutations identified a phenotypically distinct and aggressive form of mantle cell lymphoma (MCL) that did not respond to standard-of-care treatments, according to results from 183 patients younger than 66 years from the Nordic MCL2 and MCL3 trials.
, and that patients with the mutations should be considered for experimental trials of novel agents, wrote Christian W. Eskelund of the department of hematology at Rigshospitalet, Copenhagen, and colleagues.
The researchers collected DNA from the Nordic MCL2 and MCL3 trials and 183 samples were of sufficient quality for genetic analyses. They examined the prognostic value of eight recurrently mutated and two recurrently deleted genes. Only TP53 mutations showed an independent prognostic effect for overall survival (hazard ratio 6.2; P less than .0001) in multivariate Cox regression analyses.
“Our data show that TP53 mutations identify a unique MCL subtype associated with high-risk baseline characteristics, dismal response to standard treatment, and poor clinical outcome,” the researchers wrote.
Read the full study in Blood (2017 Oct 26;130[17]:1903-10).
[email protected]
On Twitter @maryellenny
TP53 mutations identified a phenotypically distinct and aggressive form of mantle cell lymphoma (MCL) that did not respond to standard-of-care treatments, according to results from 183 patients younger than 66 years from the Nordic MCL2 and MCL3 trials.
, and that patients with the mutations should be considered for experimental trials of novel agents, wrote Christian W. Eskelund of the department of hematology at Rigshospitalet, Copenhagen, and colleagues.
The researchers collected DNA from the Nordic MCL2 and MCL3 trials and 183 samples were of sufficient quality for genetic analyses. They examined the prognostic value of eight recurrently mutated and two recurrently deleted genes. Only TP53 mutations showed an independent prognostic effect for overall survival (hazard ratio 6.2; P less than .0001) in multivariate Cox regression analyses.
“Our data show that TP53 mutations identify a unique MCL subtype associated with high-risk baseline characteristics, dismal response to standard treatment, and poor clinical outcome,” the researchers wrote.
Read the full study in Blood (2017 Oct 26;130[17]:1903-10).
[email protected]
On Twitter @maryellenny
FROM BLOOD
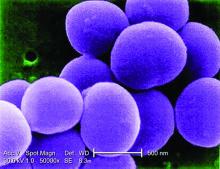
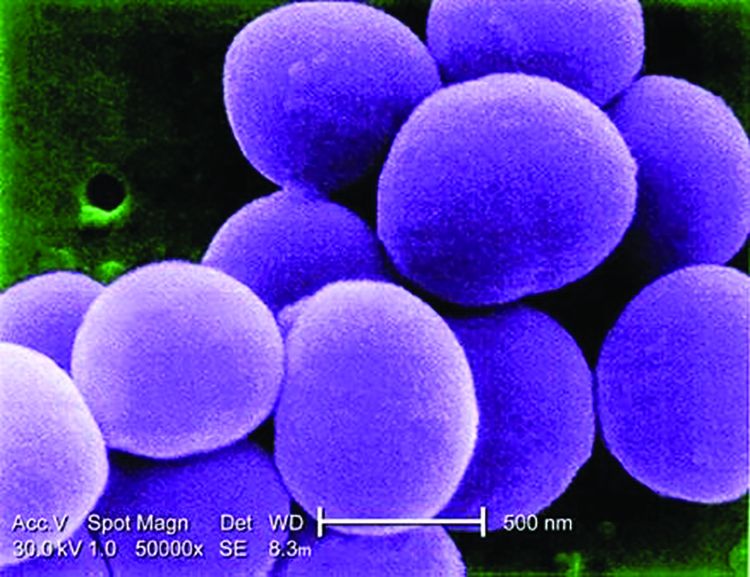
Concerning rise of staphylococcal scalded skin syndrome has U.S. doctors on alert
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point:
Major finding: The annual incidence rate of SSSS was 7.67 per million U.S. children.
Data source: Analysis of the U.S. Nationwide Inpatient Sample of 6,149,864 pediatric admissions from 2008 to 2012, including 589 cases of SSSS.
Disclosures: The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
Lenalidomide shows clinical activity in relapsed/refractory MCL
Lenalidomide alone and in combination showed “clinically significant activity” and no new safety signals in patients with mantle cell lymphoma (MCL) who had previously failed on ibrutinib, according to findings from a retrospective, observational study.
Michael Wang, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues enrolled 58 MCL patients across 11 study sites. The patients had a median age of 71 years and 88% of patients had received three or more prior therapies. Most had received ibrutinib as monotherapy and used a lenalidomide-containing therapy next.
The overall response rate was 29% (95% confidence interval, 18%-43%). The rate was similar between patients with MCL refractory to ibrutinib and patients who relapsed/progressed on or following ibrutinib use (32% versus 30%, respectively). There was a 14% complete response, though it varied by subgroup with 8% among MCL patients refractory to ibrutinib and 22% among relapsed/progressed patients. There was a 20-week median duration of response, but 82% of responders were censored so the researchers urged caution in interpreting that finding.
Among the 58 patients, more than 80% reported one or more treatment-emergent adverse events during lenalidomide treatment and 20 patients (34%) had serious events. Nine patients (16%) discontinued the drug because of adverse events.
“Lenalidomide addresses an unmet medical need and widens the therapeutic options in a difficult-to-treat patient population,” the researchers wrote.
Read the full study in the Journal of Hematology Oncology (2017 Nov 2;10[1]:171).
[email protected]
On Twitter @maryellenny
Lenalidomide alone and in combination showed “clinically significant activity” and no new safety signals in patients with mantle cell lymphoma (MCL) who had previously failed on ibrutinib, according to findings from a retrospective, observational study.
Michael Wang, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues enrolled 58 MCL patients across 11 study sites. The patients had a median age of 71 years and 88% of patients had received three or more prior therapies. Most had received ibrutinib as monotherapy and used a lenalidomide-containing therapy next.
The overall response rate was 29% (95% confidence interval, 18%-43%). The rate was similar between patients with MCL refractory to ibrutinib and patients who relapsed/progressed on or following ibrutinib use (32% versus 30%, respectively). There was a 14% complete response, though it varied by subgroup with 8% among MCL patients refractory to ibrutinib and 22% among relapsed/progressed patients. There was a 20-week median duration of response, but 82% of responders were censored so the researchers urged caution in interpreting that finding.
Among the 58 patients, more than 80% reported one or more treatment-emergent adverse events during lenalidomide treatment and 20 patients (34%) had serious events. Nine patients (16%) discontinued the drug because of adverse events.
“Lenalidomide addresses an unmet medical need and widens the therapeutic options in a difficult-to-treat patient population,” the researchers wrote.
Read the full study in the Journal of Hematology Oncology (2017 Nov 2;10[1]:171).
[email protected]
On Twitter @maryellenny
Lenalidomide alone and in combination showed “clinically significant activity” and no new safety signals in patients with mantle cell lymphoma (MCL) who had previously failed on ibrutinib, according to findings from a retrospective, observational study.
Michael Wang, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues enrolled 58 MCL patients across 11 study sites. The patients had a median age of 71 years and 88% of patients had received three or more prior therapies. Most had received ibrutinib as monotherapy and used a lenalidomide-containing therapy next.
The overall response rate was 29% (95% confidence interval, 18%-43%). The rate was similar between patients with MCL refractory to ibrutinib and patients who relapsed/progressed on or following ibrutinib use (32% versus 30%, respectively). There was a 14% complete response, though it varied by subgroup with 8% among MCL patients refractory to ibrutinib and 22% among relapsed/progressed patients. There was a 20-week median duration of response, but 82% of responders were censored so the researchers urged caution in interpreting that finding.
Among the 58 patients, more than 80% reported one or more treatment-emergent adverse events during lenalidomide treatment and 20 patients (34%) had serious events. Nine patients (16%) discontinued the drug because of adverse events.
“Lenalidomide addresses an unmet medical need and widens the therapeutic options in a difficult-to-treat patient population,” the researchers wrote.
Read the full study in the Journal of Hematology Oncology (2017 Nov 2;10[1]:171).
[email protected]
On Twitter @maryellenny
FROM THE JOURNAL OF HEMATOLOGY & ONCOLOGY
Gastrectomy mortality risk increased fivefold with same-day discharge
NATIONAL HARBOR, MD. – Laparoscopic sleeve gastrectomy has been associated with low mortality, but the mortality is even lower when it includes overnight observation, according to a national database evaluation.
Among patients discharged on the same day, 30-day mortality was 0.1%, but it fell to 0.02% among patients discharged the following day, according to Colette Inaba, MD, a surgery resident at the University of California, Irvine.*
“Surgeons who are considering same-day discharge in sleeve gastrectomy patients should have a low threshold to admit these patients for overnight observation given our findings,” Dr. Inaba reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
Same-day discharge has been associated with an increased mortality risk in previously published descriptive institutional reviews, but this is the first study to evaluate this question through analysis of a national database, according to Dr. Inaba. It was based on 37,301 laparoscopic sleeve gastrectomy cases performed in 2015 and submitted to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. All participants in this database are accredited bariatric centers.
There were baseline differences between same-day and next-day discharges, but many of these differences conferred the next-day group with higher risk. In particular, the next-day group had significantly higher rates of hypertension, diabetes mellitus, hypercholesterolemia, chronic obstructive pulmonary disease, and sleep apnea. On average, the procedure time was 13 minutes longer in the next-day versus the same-day discharge groups.
In addition to mortality, 30-day morbidity and need for revisions were compared between the two groups, but there were no significant differences between groups in the rates of these outcomes.
Overall, the baseline demographics of the patients in same-day and next-day groups were comparable, according to Dr. Inaba. She described the population as predominantly female and white with an average body mass index of 45 kg/m2. In this analysis, only primary procedures (excluding redos and revisions) were included.
Relative to the next-day discharge cases, a significantly higher percentage of same-day discharge procedures were performed with a surgical tech or another provider rather than a designated first-assist surgeon, according to Dr. Inaba. For next-day cases, a higher percentage was performed with the participation of fellows or surgical residents. There were fewer swallow studies performed before discharge in the same-day discharge group.
Very similar results were generated by a study evaluating same-day discharge after laparoscopic Roux-en-Y gastric bypass, according to John M. Morton, MD, chief of bariatric and minimally invasive surgery, Stanford (Calif.) University. Dr. Morton, first author of the study and moderator of the session in which Dr. Inaba presented the LSG data, reported that same-day discharge in that study was also associated with a trend for an increased risk of serious complications (Ann Surg. 2014;259:286-92).
“Same-day discharge is often reimbursed at a lower rate, so there is less pay and patients are at greater risk of harm,” Dr. Morton said.
The reasons that same-day discharge is associated with higher mortality cannot be derived from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, but, Dr. Inaba said, “Our thought is it is a function of failure to rescue patients from respiratory complications.” She acknowledged that this is a speculative assessment not supported by data, but she suggested that history of sleep apnea might be a particular indication to consider next-day discharge.
Dr. Inaba reports no financial relationships relevant to this topic.
Correction, 12/4/17: An earlier version of this article misstated the 30-day mortality among patients discharged the next day.
NATIONAL HARBOR, MD. – Laparoscopic sleeve gastrectomy has been associated with low mortality, but the mortality is even lower when it includes overnight observation, according to a national database evaluation.
Among patients discharged on the same day, 30-day mortality was 0.1%, but it fell to 0.02% among patients discharged the following day, according to Colette Inaba, MD, a surgery resident at the University of California, Irvine.*
“Surgeons who are considering same-day discharge in sleeve gastrectomy patients should have a low threshold to admit these patients for overnight observation given our findings,” Dr. Inaba reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
Same-day discharge has been associated with an increased mortality risk in previously published descriptive institutional reviews, but this is the first study to evaluate this question through analysis of a national database, according to Dr. Inaba. It was based on 37,301 laparoscopic sleeve gastrectomy cases performed in 2015 and submitted to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. All participants in this database are accredited bariatric centers.
There were baseline differences between same-day and next-day discharges, but many of these differences conferred the next-day group with higher risk. In particular, the next-day group had significantly higher rates of hypertension, diabetes mellitus, hypercholesterolemia, chronic obstructive pulmonary disease, and sleep apnea. On average, the procedure time was 13 minutes longer in the next-day versus the same-day discharge groups.
In addition to mortality, 30-day morbidity and need for revisions were compared between the two groups, but there were no significant differences between groups in the rates of these outcomes.
Overall, the baseline demographics of the patients in same-day and next-day groups were comparable, according to Dr. Inaba. She described the population as predominantly female and white with an average body mass index of 45 kg/m2. In this analysis, only primary procedures (excluding redos and revisions) were included.
Relative to the next-day discharge cases, a significantly higher percentage of same-day discharge procedures were performed with a surgical tech or another provider rather than a designated first-assist surgeon, according to Dr. Inaba. For next-day cases, a higher percentage was performed with the participation of fellows or surgical residents. There were fewer swallow studies performed before discharge in the same-day discharge group.
Very similar results were generated by a study evaluating same-day discharge after laparoscopic Roux-en-Y gastric bypass, according to John M. Morton, MD, chief of bariatric and minimally invasive surgery, Stanford (Calif.) University. Dr. Morton, first author of the study and moderator of the session in which Dr. Inaba presented the LSG data, reported that same-day discharge in that study was also associated with a trend for an increased risk of serious complications (Ann Surg. 2014;259:286-92).
“Same-day discharge is often reimbursed at a lower rate, so there is less pay and patients are at greater risk of harm,” Dr. Morton said.
The reasons that same-day discharge is associated with higher mortality cannot be derived from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, but, Dr. Inaba said, “Our thought is it is a function of failure to rescue patients from respiratory complications.” She acknowledged that this is a speculative assessment not supported by data, but she suggested that history of sleep apnea might be a particular indication to consider next-day discharge.
Dr. Inaba reports no financial relationships relevant to this topic.
Correction, 12/4/17: An earlier version of this article misstated the 30-day mortality among patients discharged the next day.
NATIONAL HARBOR, MD. – Laparoscopic sleeve gastrectomy has been associated with low mortality, but the mortality is even lower when it includes overnight observation, according to a national database evaluation.
Among patients discharged on the same day, 30-day mortality was 0.1%, but it fell to 0.02% among patients discharged the following day, according to Colette Inaba, MD, a surgery resident at the University of California, Irvine.*
“Surgeons who are considering same-day discharge in sleeve gastrectomy patients should have a low threshold to admit these patients for overnight observation given our findings,” Dr. Inaba reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
Same-day discharge has been associated with an increased mortality risk in previously published descriptive institutional reviews, but this is the first study to evaluate this question through analysis of a national database, according to Dr. Inaba. It was based on 37,301 laparoscopic sleeve gastrectomy cases performed in 2015 and submitted to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. All participants in this database are accredited bariatric centers.
There were baseline differences between same-day and next-day discharges, but many of these differences conferred the next-day group with higher risk. In particular, the next-day group had significantly higher rates of hypertension, diabetes mellitus, hypercholesterolemia, chronic obstructive pulmonary disease, and sleep apnea. On average, the procedure time was 13 minutes longer in the next-day versus the same-day discharge groups.
In addition to mortality, 30-day morbidity and need for revisions were compared between the two groups, but there were no significant differences between groups in the rates of these outcomes.
Overall, the baseline demographics of the patients in same-day and next-day groups were comparable, according to Dr. Inaba. She described the population as predominantly female and white with an average body mass index of 45 kg/m2. In this analysis, only primary procedures (excluding redos and revisions) were included.
Relative to the next-day discharge cases, a significantly higher percentage of same-day discharge procedures were performed with a surgical tech or another provider rather than a designated first-assist surgeon, according to Dr. Inaba. For next-day cases, a higher percentage was performed with the participation of fellows or surgical residents. There were fewer swallow studies performed before discharge in the same-day discharge group.
Very similar results were generated by a study evaluating same-day discharge after laparoscopic Roux-en-Y gastric bypass, according to John M. Morton, MD, chief of bariatric and minimally invasive surgery, Stanford (Calif.) University. Dr. Morton, first author of the study and moderator of the session in which Dr. Inaba presented the LSG data, reported that same-day discharge in that study was also associated with a trend for an increased risk of serious complications (Ann Surg. 2014;259:286-92).
“Same-day discharge is often reimbursed at a lower rate, so there is less pay and patients are at greater risk of harm,” Dr. Morton said.
The reasons that same-day discharge is associated with higher mortality cannot be derived from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, but, Dr. Inaba said, “Our thought is it is a function of failure to rescue patients from respiratory complications.” She acknowledged that this is a speculative assessment not supported by data, but she suggested that history of sleep apnea might be a particular indication to consider next-day discharge.
Dr. Inaba reports no financial relationships relevant to this topic.
Correction, 12/4/17: An earlier version of this article misstated the 30-day mortality among patients discharged the next day.
AT OBESITY WEEK 2017
Key clinical point: Thirty-day mortality after laparoscopic sleeve gastrectomy is several times higher with same-day discharge relative to an overnight stay.
Major finding: In an analysis of a national database with more than 35,000 cases, the mortality odds ratio for same-day discharge was 5.7 (P = .032) relative to next-day discharge.
Data source: Retrospective database analysis.
Disclosures: Dr. Inaba reports no financial relationships relevant to this topic.
FDA approves letermovir for CMV prophylaxis
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
OSA home testing less expensive than polysomnography
Home respiratory polygraphy had similar efficacy with substantially lower per-patient cost, compared with traditional polysomnography for diagnosing obstructive sleep apnea, a study showed.
Obstructive sleep apnea (OSA) is a common chronic disease associated with higher risk of cardiovascular disease and traffic accidents and a lower quality of life. Although expensive and time intensive, the polysomnography (PSG) has been the preferred test for diagnosing OSA. Home respiratory polygraphy (HRP) uses portable devices that are less complex than polysomnography and has been shown to have similar effectiveness in diagnosing OSA, compared with PSG, in patients with a high clinical suspicion of OSA. However, there is limited evidence for the cost effectiveness of HRP, compared with PSG (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1181-90).
The investigators conducted a multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis comparing PSG with HRP. Inclusion criteria included snoring or observed sleep apnea, Epworth Sleepiness Scale (ESS)of 10 or higher, and no suspicion of alternative causes for daytime sleepiness. Patients with a suspicion for OSA were randomized to polysomnography or respiratory polygraphy protocols. Both arms received counseling on proper sleep hygiene; counseling on weight loss, if overweight; and auto-CPAP titration if continuous positive airway pressure (CPAP) was clinically indicated.
Assessment of CPAP compliance or dietary and sleep hygiene compliance was assessed at months 1 and 3. ESS, quality of life measures, well-being measures, 24-hour blood pressure monitoring, auto accidents, and cardiovascular events were assessed at baseline and at month 6.
CPAP treatment was indicated in 68% of the PSG arm, compared with 53% of the HRP arm. After intention-to-treat analysis, there was no statistically significant difference between the two groups for ESS improvement (HRP mean, –4.2, vs. PSG mean, –4.9; P = .14). The groups demonstrated similar results for quality of life, blood pressure, polysomnographic assessment at 6 months, CPAP compliance, and rates of cardiovascular events and accidents at follow-up.
The cost-effective analysis demonstrated respiratory polygraphy was less expensive, saving more than 400 euros/patient. “Because the effectiveness (ESS and QALYs [quality-adjusted life-years]) was similar between arms, the HRP protocol is preferable due to its lower cost,” the authors wrote.
In all, 430 patients were randomized to HRP or PSG and consisted mostly of men (70.5%) with a mean body mass index of 30.7 kg/m2. The groups had similar rates of alcohol consumption and hypertension.
Limitations of the study included unblinded randomization to the participants and researchers and the possibility of variability in therapeutic decisions. However, the authors noted that intraobserver variability was minimized by using the Spanish Sleep Network guidelines and centralized assessment.
“[The] HRP management protocol is not inferior to PSG and presents substantially lower costs. Therefore, PSG is not necessary for most patients with suspicion of OSA. This finding could change established clinical practice, with a clear economic benefit,” the authors concluded.
Home respiratory polygraphy continues to impress
This study adds strong evidence to support the use of home respiratory polygraphy for the diagnosis of obstructive sleep apnea in patients without major comorbidities such as severe chronic restrictive or obstructive lung disease, heart failure or unstable cardiovascular disease, major psychiatric diagnoses, and neuromuscular conditions, noted Ching Li Chai-Coetzer, MBBS, PhD, and R.
Doug McEvoy, MBBS, MD, in an accompanying editorial (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1096-8). However, lower-cost methods to diagnose OSA would still not address unmet needs such as the cost of continuous positive airway pressure and scarcity of sleep physicians to assess patients with OSA, and still may be too expensive for underresourced populations, they said.
Dr. Chai-Coetzer and Dr. McEvoy are affiliated with the Adelaide Institute for Sleep Health at Flinders University and the Sleep Health Service, Southern Adelaide Local Health Network, both in South Australia.
The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The investigators report no disclosures.
Dr. Chai-Coetzer reported grants from National Health and Medical Research Council of Australia and nonfinancial support from Biotech Pharmaceuticals. Dr. McEvoy reported grants and nonfinancial support from Philips Respironics, nonfinancial support from ResMed, and grants from Fisher & Paykel.
Home respiratory polygraphy had similar efficacy with substantially lower per-patient cost, compared with traditional polysomnography for diagnosing obstructive sleep apnea, a study showed.
Obstructive sleep apnea (OSA) is a common chronic disease associated with higher risk of cardiovascular disease and traffic accidents and a lower quality of life. Although expensive and time intensive, the polysomnography (PSG) has been the preferred test for diagnosing OSA. Home respiratory polygraphy (HRP) uses portable devices that are less complex than polysomnography and has been shown to have similar effectiveness in diagnosing OSA, compared with PSG, in patients with a high clinical suspicion of OSA. However, there is limited evidence for the cost effectiveness of HRP, compared with PSG (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1181-90).
The investigators conducted a multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis comparing PSG with HRP. Inclusion criteria included snoring or observed sleep apnea, Epworth Sleepiness Scale (ESS)of 10 or higher, and no suspicion of alternative causes for daytime sleepiness. Patients with a suspicion for OSA were randomized to polysomnography or respiratory polygraphy protocols. Both arms received counseling on proper sleep hygiene; counseling on weight loss, if overweight; and auto-CPAP titration if continuous positive airway pressure (CPAP) was clinically indicated.
Assessment of CPAP compliance or dietary and sleep hygiene compliance was assessed at months 1 and 3. ESS, quality of life measures, well-being measures, 24-hour blood pressure monitoring, auto accidents, and cardiovascular events were assessed at baseline and at month 6.
CPAP treatment was indicated in 68% of the PSG arm, compared with 53% of the HRP arm. After intention-to-treat analysis, there was no statistically significant difference between the two groups for ESS improvement (HRP mean, –4.2, vs. PSG mean, –4.9; P = .14). The groups demonstrated similar results for quality of life, blood pressure, polysomnographic assessment at 6 months, CPAP compliance, and rates of cardiovascular events and accidents at follow-up.
The cost-effective analysis demonstrated respiratory polygraphy was less expensive, saving more than 400 euros/patient. “Because the effectiveness (ESS and QALYs [quality-adjusted life-years]) was similar between arms, the HRP protocol is preferable due to its lower cost,” the authors wrote.
In all, 430 patients were randomized to HRP or PSG and consisted mostly of men (70.5%) with a mean body mass index of 30.7 kg/m2. The groups had similar rates of alcohol consumption and hypertension.
Limitations of the study included unblinded randomization to the participants and researchers and the possibility of variability in therapeutic decisions. However, the authors noted that intraobserver variability was minimized by using the Spanish Sleep Network guidelines and centralized assessment.
“[The] HRP management protocol is not inferior to PSG and presents substantially lower costs. Therefore, PSG is not necessary for most patients with suspicion of OSA. This finding could change established clinical practice, with a clear economic benefit,” the authors concluded.
Home respiratory polygraphy continues to impress
This study adds strong evidence to support the use of home respiratory polygraphy for the diagnosis of obstructive sleep apnea in patients without major comorbidities such as severe chronic restrictive or obstructive lung disease, heart failure or unstable cardiovascular disease, major psychiatric diagnoses, and neuromuscular conditions, noted Ching Li Chai-Coetzer, MBBS, PhD, and R.
Doug McEvoy, MBBS, MD, in an accompanying editorial (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1096-8). However, lower-cost methods to diagnose OSA would still not address unmet needs such as the cost of continuous positive airway pressure and scarcity of sleep physicians to assess patients with OSA, and still may be too expensive for underresourced populations, they said.
Dr. Chai-Coetzer and Dr. McEvoy are affiliated with the Adelaide Institute for Sleep Health at Flinders University and the Sleep Health Service, Southern Adelaide Local Health Network, both in South Australia.
The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The investigators report no disclosures.
Dr. Chai-Coetzer reported grants from National Health and Medical Research Council of Australia and nonfinancial support from Biotech Pharmaceuticals. Dr. McEvoy reported grants and nonfinancial support from Philips Respironics, nonfinancial support from ResMed, and grants from Fisher & Paykel.
Home respiratory polygraphy had similar efficacy with substantially lower per-patient cost, compared with traditional polysomnography for diagnosing obstructive sleep apnea, a study showed.
Obstructive sleep apnea (OSA) is a common chronic disease associated with higher risk of cardiovascular disease and traffic accidents and a lower quality of life. Although expensive and time intensive, the polysomnography (PSG) has been the preferred test for diagnosing OSA. Home respiratory polygraphy (HRP) uses portable devices that are less complex than polysomnography and has been shown to have similar effectiveness in diagnosing OSA, compared with PSG, in patients with a high clinical suspicion of OSA. However, there is limited evidence for the cost effectiveness of HRP, compared with PSG (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1181-90).
The investigators conducted a multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis comparing PSG with HRP. Inclusion criteria included snoring or observed sleep apnea, Epworth Sleepiness Scale (ESS)of 10 or higher, and no suspicion of alternative causes for daytime sleepiness. Patients with a suspicion for OSA were randomized to polysomnography or respiratory polygraphy protocols. Both arms received counseling on proper sleep hygiene; counseling on weight loss, if overweight; and auto-CPAP titration if continuous positive airway pressure (CPAP) was clinically indicated.
Assessment of CPAP compliance or dietary and sleep hygiene compliance was assessed at months 1 and 3. ESS, quality of life measures, well-being measures, 24-hour blood pressure monitoring, auto accidents, and cardiovascular events were assessed at baseline and at month 6.
CPAP treatment was indicated in 68% of the PSG arm, compared with 53% of the HRP arm. After intention-to-treat analysis, there was no statistically significant difference between the two groups for ESS improvement (HRP mean, –4.2, vs. PSG mean, –4.9; P = .14). The groups demonstrated similar results for quality of life, blood pressure, polysomnographic assessment at 6 months, CPAP compliance, and rates of cardiovascular events and accidents at follow-up.
The cost-effective analysis demonstrated respiratory polygraphy was less expensive, saving more than 400 euros/patient. “Because the effectiveness (ESS and QALYs [quality-adjusted life-years]) was similar between arms, the HRP protocol is preferable due to its lower cost,” the authors wrote.
In all, 430 patients were randomized to HRP or PSG and consisted mostly of men (70.5%) with a mean body mass index of 30.7 kg/m2. The groups had similar rates of alcohol consumption and hypertension.
Limitations of the study included unblinded randomization to the participants and researchers and the possibility of variability in therapeutic decisions. However, the authors noted that intraobserver variability was minimized by using the Spanish Sleep Network guidelines and centralized assessment.
“[The] HRP management protocol is not inferior to PSG and presents substantially lower costs. Therefore, PSG is not necessary for most patients with suspicion of OSA. This finding could change established clinical practice, with a clear economic benefit,” the authors concluded.
Home respiratory polygraphy continues to impress
This study adds strong evidence to support the use of home respiratory polygraphy for the diagnosis of obstructive sleep apnea in patients without major comorbidities such as severe chronic restrictive or obstructive lung disease, heart failure or unstable cardiovascular disease, major psychiatric diagnoses, and neuromuscular conditions, noted Ching Li Chai-Coetzer, MBBS, PhD, and R.
Doug McEvoy, MBBS, MD, in an accompanying editorial (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1096-8). However, lower-cost methods to diagnose OSA would still not address unmet needs such as the cost of continuous positive airway pressure and scarcity of sleep physicians to assess patients with OSA, and still may be too expensive for underresourced populations, they said.
Dr. Chai-Coetzer and Dr. McEvoy are affiliated with the Adelaide Institute for Sleep Health at Flinders University and the Sleep Health Service, Southern Adelaide Local Health Network, both in South Australia.
The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The investigators report no disclosures.
Dr. Chai-Coetzer reported grants from National Health and Medical Research Council of Australia and nonfinancial support from Biotech Pharmaceuticals. Dr. McEvoy reported grants and nonfinancial support from Philips Respironics, nonfinancial support from ResMed, and grants from Fisher & Paykel.
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Key clinical point: Home obstructive sleep apnea testing was less costly and noninferior to polysomnography.
Major finding: Using respiratory polygraphy instead of polysomnography results in savings of more than 400 euros/patient.
Data source: A multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis of 430 patients suspected of having OSA.
Disclosures: The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The authors report no disclosures.