User login
FDA approves letermovir as CMV prophylaxis
The US Food and Drug Administration (FDA) has approved the oral and intravenous formulations of letermovir (PREVYMIS™).
Letermovir is a member of a new class of non-nucleoside CMV inhibitors known as 3,4 dihydro-quinazolines.
The FDA approved letermovir as prophylaxis for cytomegalovirus (CMV) infection and disease in adult recipients of allogeneic hematopoietic stem cell transplants (HSCTs) who are CMV-seropositive.
“PREVYMIS is the first new medicine for CMV infection approved in the US in 15 years,” said Roy Baynes, senior vice president, head of clinical development, and chief medical officer of Merck Research Laboratories, the company marketing letermovir.
Letermovir is expected to be available in December. The list price (wholesaler acquisition cost) per day is $195.00 for letermovir tablets and $270.00 for letermovir injections. (Wholesaler acquisition costs do not include discounts that may be paid on the product.)
The recommended dosage of letermovir is 480 mg once daily, initiated as early as day 0 and up to day 28 post-transplant (before or after engraftment) and continued through day 100. If letermovir is co-administered with cyclosporine, the dosage of letermovir should be decreased to 240 mg once daily.
Letermovir is available as 240 mg and 480 mg tablets, which may be administered with or without food. Letermovir is also available as a 240 mg and 480 mg injection for intravenous infusion via a peripheral catheter or central venous line at a constant rate over 1 hour.
For more details on letermovir, see the full prescribing information.
Trial results
The FDA’s approval of letermovir was supported by results of a phase 3 trial of adult recipients of allogeneic HSCTs who were CMV-seropositive. Patients were randomized (2:1) to receive either letermovir (at a dose of 480 mg once-daily, adjusted to 240 mg when co-administered with cyclosporine) or placebo.
Study drug was initiated after HSCT (at any time from day 0 to 28 post-transplant) and continued through week 14 post-transplant. Patients were monitored through week 24 post-HSCT for the primary efficacy endpoint, with continued follow-up through week 48.
Among the 565 treated patients, 34% were engrafted at baseline, and 30% had one or more factors associated with additional risk for CMV reactivation. The most common primary reasons for transplant were acute myeloid leukemia (38%), myelodysplastic syndromes (16%), and lymphoma (12%).
Thirty eight percent of patients in the letermovir arm and 61% in the placebo arm failed prophylaxis.
Reasons for failure (in the letermovir and placebo arms, respectively) included:
- Clinically significant CMV infection—18% vs 42%
- Initiation of PET based on documented CMV viremia—16% vs 40%
- CMV end-organ disease—2% for both
- Study discontinuation before week 24—17% vs 16%
- Missing outcome in week 24 visit window—3% for both.
The stratum-adjusted treatment difference for letermovir vs placebo was -23.5 (95% CI, -32.5, -14.6, P<0.0001).
The Kaplan-Meier event rate for all-cause mortality in the letermovir and placebo arms, respectively, was 12% and 17% at week 24 and 24% and 28% at week 48.
Common adverse events (in the letermovir and placebo arms, respectively) were nausea (27% vs 23%), diarrhea (26% vs 24%), vomiting (19% vs 14%), peripheral edema (14% vs 9%), cough (14% vs 10%), headache (14% vs 9%), fatigue (13% vs 11%), and abdominal pain (12% vs 9%).
The cardiac adverse event rate (regardless of investigator-assessed causality) was 13% in the letermovir arm and 6% in the placebo arm. The most common cardiac adverse events (in the letermovir and placebo arms, respectively) were tachycardia (4% vs 2%) and atrial fibrillation (3% vs 1%).
Results from this trial were presented at the 2017 BMT Tandem Meetings. ![]()
The US Food and Drug Administration (FDA) has approved the oral and intravenous formulations of letermovir (PREVYMIS™).
Letermovir is a member of a new class of non-nucleoside CMV inhibitors known as 3,4 dihydro-quinazolines.
The FDA approved letermovir as prophylaxis for cytomegalovirus (CMV) infection and disease in adult recipients of allogeneic hematopoietic stem cell transplants (HSCTs) who are CMV-seropositive.
“PREVYMIS is the first new medicine for CMV infection approved in the US in 15 years,” said Roy Baynes, senior vice president, head of clinical development, and chief medical officer of Merck Research Laboratories, the company marketing letermovir.
Letermovir is expected to be available in December. The list price (wholesaler acquisition cost) per day is $195.00 for letermovir tablets and $270.00 for letermovir injections. (Wholesaler acquisition costs do not include discounts that may be paid on the product.)
The recommended dosage of letermovir is 480 mg once daily, initiated as early as day 0 and up to day 28 post-transplant (before or after engraftment) and continued through day 100. If letermovir is co-administered with cyclosporine, the dosage of letermovir should be decreased to 240 mg once daily.
Letermovir is available as 240 mg and 480 mg tablets, which may be administered with or without food. Letermovir is also available as a 240 mg and 480 mg injection for intravenous infusion via a peripheral catheter or central venous line at a constant rate over 1 hour.
For more details on letermovir, see the full prescribing information.
Trial results
The FDA’s approval of letermovir was supported by results of a phase 3 trial of adult recipients of allogeneic HSCTs who were CMV-seropositive. Patients were randomized (2:1) to receive either letermovir (at a dose of 480 mg once-daily, adjusted to 240 mg when co-administered with cyclosporine) or placebo.
Study drug was initiated after HSCT (at any time from day 0 to 28 post-transplant) and continued through week 14 post-transplant. Patients were monitored through week 24 post-HSCT for the primary efficacy endpoint, with continued follow-up through week 48.
Among the 565 treated patients, 34% were engrafted at baseline, and 30% had one or more factors associated with additional risk for CMV reactivation. The most common primary reasons for transplant were acute myeloid leukemia (38%), myelodysplastic syndromes (16%), and lymphoma (12%).
Thirty eight percent of patients in the letermovir arm and 61% in the placebo arm failed prophylaxis.
Reasons for failure (in the letermovir and placebo arms, respectively) included:
- Clinically significant CMV infection—18% vs 42%
- Initiation of PET based on documented CMV viremia—16% vs 40%
- CMV end-organ disease—2% for both
- Study discontinuation before week 24—17% vs 16%
- Missing outcome in week 24 visit window—3% for both.
The stratum-adjusted treatment difference for letermovir vs placebo was -23.5 (95% CI, -32.5, -14.6, P<0.0001).
The Kaplan-Meier event rate for all-cause mortality in the letermovir and placebo arms, respectively, was 12% and 17% at week 24 and 24% and 28% at week 48.
Common adverse events (in the letermovir and placebo arms, respectively) were nausea (27% vs 23%), diarrhea (26% vs 24%), vomiting (19% vs 14%), peripheral edema (14% vs 9%), cough (14% vs 10%), headache (14% vs 9%), fatigue (13% vs 11%), and abdominal pain (12% vs 9%).
The cardiac adverse event rate (regardless of investigator-assessed causality) was 13% in the letermovir arm and 6% in the placebo arm. The most common cardiac adverse events (in the letermovir and placebo arms, respectively) were tachycardia (4% vs 2%) and atrial fibrillation (3% vs 1%).
Results from this trial were presented at the 2017 BMT Tandem Meetings. ![]()
The US Food and Drug Administration (FDA) has approved the oral and intravenous formulations of letermovir (PREVYMIS™).
Letermovir is a member of a new class of non-nucleoside CMV inhibitors known as 3,4 dihydro-quinazolines.
The FDA approved letermovir as prophylaxis for cytomegalovirus (CMV) infection and disease in adult recipients of allogeneic hematopoietic stem cell transplants (HSCTs) who are CMV-seropositive.
“PREVYMIS is the first new medicine for CMV infection approved in the US in 15 years,” said Roy Baynes, senior vice president, head of clinical development, and chief medical officer of Merck Research Laboratories, the company marketing letermovir.
Letermovir is expected to be available in December. The list price (wholesaler acquisition cost) per day is $195.00 for letermovir tablets and $270.00 for letermovir injections. (Wholesaler acquisition costs do not include discounts that may be paid on the product.)
The recommended dosage of letermovir is 480 mg once daily, initiated as early as day 0 and up to day 28 post-transplant (before or after engraftment) and continued through day 100. If letermovir is co-administered with cyclosporine, the dosage of letermovir should be decreased to 240 mg once daily.
Letermovir is available as 240 mg and 480 mg tablets, which may be administered with or without food. Letermovir is also available as a 240 mg and 480 mg injection for intravenous infusion via a peripheral catheter or central venous line at a constant rate over 1 hour.
For more details on letermovir, see the full prescribing information.
Trial results
The FDA’s approval of letermovir was supported by results of a phase 3 trial of adult recipients of allogeneic HSCTs who were CMV-seropositive. Patients were randomized (2:1) to receive either letermovir (at a dose of 480 mg once-daily, adjusted to 240 mg when co-administered with cyclosporine) or placebo.
Study drug was initiated after HSCT (at any time from day 0 to 28 post-transplant) and continued through week 14 post-transplant. Patients were monitored through week 24 post-HSCT for the primary efficacy endpoint, with continued follow-up through week 48.
Among the 565 treated patients, 34% were engrafted at baseline, and 30% had one or more factors associated with additional risk for CMV reactivation. The most common primary reasons for transplant were acute myeloid leukemia (38%), myelodysplastic syndromes (16%), and lymphoma (12%).
Thirty eight percent of patients in the letermovir arm and 61% in the placebo arm failed prophylaxis.
Reasons for failure (in the letermovir and placebo arms, respectively) included:
- Clinically significant CMV infection—18% vs 42%
- Initiation of PET based on documented CMV viremia—16% vs 40%
- CMV end-organ disease—2% for both
- Study discontinuation before week 24—17% vs 16%
- Missing outcome in week 24 visit window—3% for both.
The stratum-adjusted treatment difference for letermovir vs placebo was -23.5 (95% CI, -32.5, -14.6, P<0.0001).
The Kaplan-Meier event rate for all-cause mortality in the letermovir and placebo arms, respectively, was 12% and 17% at week 24 and 24% and 28% at week 48.
Common adverse events (in the letermovir and placebo arms, respectively) were nausea (27% vs 23%), diarrhea (26% vs 24%), vomiting (19% vs 14%), peripheral edema (14% vs 9%), cough (14% vs 10%), headache (14% vs 9%), fatigue (13% vs 11%), and abdominal pain (12% vs 9%).
The cardiac adverse event rate (regardless of investigator-assessed causality) was 13% in the letermovir arm and 6% in the placebo arm. The most common cardiac adverse events (in the letermovir and placebo arms, respectively) were tachycardia (4% vs 2%) and atrial fibrillation (3% vs 1%).
Results from this trial were presented at the 2017 BMT Tandem Meetings. ![]()
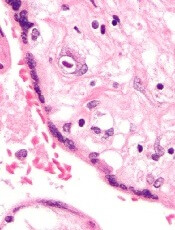
FDA approves brentuximab vedotin for pcALCL, MF
The US Food and Drug Administration (FDA) has expanded the approved use of brentuximab vedotin (BV, ADCETRIS).
BV is now approved for adults with primary cutaneous anaplastic large-cell lymphoma (pcALCL) and CD30-expressing mycosis fungoides (MF) who have received prior systemic therapy.
This is the fourth FDA-approved indication for BV. The drug has regular approval for 2 indications in classical Hodgkin lymphoma and accelerated approval for the treatment of systemic ALCL.
In November 2016, the FDA granted BV breakthrough therapy designation for the treatment of patients with pcALCL and CD30-expressing MF who require systemic therapy and have received one prior systemic therapy. The agency also granted the supplemental biologics license application priority review.
The approval for BV in pcALCL and CD30-expressing MF is based on data from the phase 3 ALCANZA trial and a pair of phase 2 investigator-sponsored trials.
Phase 3 trial
Results from ALCANZA were presented at the 9th Annual T-cell Lymphoma Forum in January and published in The Lancet in June.
There were 128 patients in the intent-to-treat and safety populations. Sixty-four patients (48 with MF and 16 with pcALCL) were randomized to receive BV at 1.8 mg/kg every 3 weeks for up to 48 weeks.
The other 64 patients (49 with MF and 15 with pcALCL) were randomized to receive standard of care (SOC)—methotrexate at 5 mg to 50 mg weekly or bexarotene at a target dose of 300 mg/m² daily for up to 48 weeks.
The study’s primary endpoint was the rate of objective response lasting at least 4 months (ORR4). The ORR4 rate was significantly higher with BV than with SOC—56.3% and 12.5%, respectively (P<0.0001).
For patients with MF, the ORR4 was 50% with BV and 10% with SOC. For patients with pcALCL, the ORR4 was 75% with BV and 20% with SOC.
Overall, the complete response (CR) rates were 15.6% in the BV arm and 1.6% in the SOC arm (P=0.0046).
For patients with MF, the CR rate was 10% with BV and 0% with SOC. For patients with pcALCL, the CR rate was 31% with BV and 7% with SOC.
Progression-free survival (PFS) was significantly longer in the BV arm than the SOC arm. The median PFS was 16.7 months and 3.5 months, respectively. The hazard ratio was 0.270 (P<0.0001).
For patients with MF, the median PFS was 15.9 months with BV and 3.5 months with SOC. For patients with pcALCL, the median PFS was 27.5 months with BV and 5.3 months with SOC.
The most common adverse events (AEs) of any grade (occurring in 15% or more of patients in the BV and SOC arms, respectively) were peripheral neuropathy (67% and 6%), nausea (36% and 13%), diarrhea (29% and 6%), fatigue (29% and 27%), vomiting (17% and 5%), alopecia (15% and 3%), pruritus (17% and 13%), pyrexia (17% and 18%), decreased appetite (15% and 5%), and hypertriglyceridemia (2% and 18%).
Phase 2 trials
Data from the investigator-sponsored trials were published in the Journal of Clinical Oncology in 2015.
The first study was published in July of that year. The trial enrolled 32 patients with MF or Sézary syndrome. Thirty patients were evaluable for efficacy, and more than half had received 3 or more prior systemic therapies.
Patients received BV (1.8 mg/kg) every 3 weeks for a maximum of 16 doses. The primary endpoint was objective clinical response rate.
Seventy percent of patients (21/30) achieved an objective response across all stages of disease. One patient had a CR, 20 had a partial response, 4 had stable disease, 5 had progressive disease, and 2 were not evaluable for response.
The most common related AEs of any grade were peripheral neuropathy (66%), fatigue (47%), nausea (28%), hair loss (22%), and neutropenia (19%). Grade 3/4 related AEs included neutropenia (n=4), rash (n=3), and peripheral neuropathy (n=1).
The second phase 2 trial was published in August 2015. This trial enrolled CD30-positive patients with lymphomatoid papulosis (LyP), pcALCL, and MF.
Fifty-four patients were enrolled, and 48 were evaluable at the time of analysis. Patients had received an infusion of BV (1.8 mg/kg) every 21 days.
Seventy-three percent of patients (35/48) achieved an objective response, including 100% (20/20) with LyP and/or pcALCL and 54% (15/28) with MF. The CR rate was 35% (n=17).
The most common AEs were peripheral neuropathy (67%), fatigue (35%), skin rash (24%), diarrhea (15%), muscle pain (17%), localized skin infection (15%), neutropenia (15%), and hair loss (11%).
Grade 3/4 AEs included neutropenia (n=3), nausea (n=2), unstable angina or myocardial infarction (n=2), infection (n=2), joint pain (n=2), fatigue (n=1), deep vein thrombosis (n=1), pulmonary embolism (n=1), aminotransferase elevation (n=1), and dehydration (n=1). ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of brentuximab vedotin (BV, ADCETRIS).
BV is now approved for adults with primary cutaneous anaplastic large-cell lymphoma (pcALCL) and CD30-expressing mycosis fungoides (MF) who have received prior systemic therapy.
This is the fourth FDA-approved indication for BV. The drug has regular approval for 2 indications in classical Hodgkin lymphoma and accelerated approval for the treatment of systemic ALCL.
In November 2016, the FDA granted BV breakthrough therapy designation for the treatment of patients with pcALCL and CD30-expressing MF who require systemic therapy and have received one prior systemic therapy. The agency also granted the supplemental biologics license application priority review.
The approval for BV in pcALCL and CD30-expressing MF is based on data from the phase 3 ALCANZA trial and a pair of phase 2 investigator-sponsored trials.
Phase 3 trial
Results from ALCANZA were presented at the 9th Annual T-cell Lymphoma Forum in January and published in The Lancet in June.
There were 128 patients in the intent-to-treat and safety populations. Sixty-four patients (48 with MF and 16 with pcALCL) were randomized to receive BV at 1.8 mg/kg every 3 weeks for up to 48 weeks.
The other 64 patients (49 with MF and 15 with pcALCL) were randomized to receive standard of care (SOC)—methotrexate at 5 mg to 50 mg weekly or bexarotene at a target dose of 300 mg/m² daily for up to 48 weeks.
The study’s primary endpoint was the rate of objective response lasting at least 4 months (ORR4). The ORR4 rate was significantly higher with BV than with SOC—56.3% and 12.5%, respectively (P<0.0001).
For patients with MF, the ORR4 was 50% with BV and 10% with SOC. For patients with pcALCL, the ORR4 was 75% with BV and 20% with SOC.
Overall, the complete response (CR) rates were 15.6% in the BV arm and 1.6% in the SOC arm (P=0.0046).
For patients with MF, the CR rate was 10% with BV and 0% with SOC. For patients with pcALCL, the CR rate was 31% with BV and 7% with SOC.
Progression-free survival (PFS) was significantly longer in the BV arm than the SOC arm. The median PFS was 16.7 months and 3.5 months, respectively. The hazard ratio was 0.270 (P<0.0001).
For patients with MF, the median PFS was 15.9 months with BV and 3.5 months with SOC. For patients with pcALCL, the median PFS was 27.5 months with BV and 5.3 months with SOC.
The most common adverse events (AEs) of any grade (occurring in 15% or more of patients in the BV and SOC arms, respectively) were peripheral neuropathy (67% and 6%), nausea (36% and 13%), diarrhea (29% and 6%), fatigue (29% and 27%), vomiting (17% and 5%), alopecia (15% and 3%), pruritus (17% and 13%), pyrexia (17% and 18%), decreased appetite (15% and 5%), and hypertriglyceridemia (2% and 18%).
Phase 2 trials
Data from the investigator-sponsored trials were published in the Journal of Clinical Oncology in 2015.
The first study was published in July of that year. The trial enrolled 32 patients with MF or Sézary syndrome. Thirty patients were evaluable for efficacy, and more than half had received 3 or more prior systemic therapies.
Patients received BV (1.8 mg/kg) every 3 weeks for a maximum of 16 doses. The primary endpoint was objective clinical response rate.
Seventy percent of patients (21/30) achieved an objective response across all stages of disease. One patient had a CR, 20 had a partial response, 4 had stable disease, 5 had progressive disease, and 2 were not evaluable for response.
The most common related AEs of any grade were peripheral neuropathy (66%), fatigue (47%), nausea (28%), hair loss (22%), and neutropenia (19%). Grade 3/4 related AEs included neutropenia (n=4), rash (n=3), and peripheral neuropathy (n=1).
The second phase 2 trial was published in August 2015. This trial enrolled CD30-positive patients with lymphomatoid papulosis (LyP), pcALCL, and MF.
Fifty-four patients were enrolled, and 48 were evaluable at the time of analysis. Patients had received an infusion of BV (1.8 mg/kg) every 21 days.
Seventy-three percent of patients (35/48) achieved an objective response, including 100% (20/20) with LyP and/or pcALCL and 54% (15/28) with MF. The CR rate was 35% (n=17).
The most common AEs were peripheral neuropathy (67%), fatigue (35%), skin rash (24%), diarrhea (15%), muscle pain (17%), localized skin infection (15%), neutropenia (15%), and hair loss (11%).
Grade 3/4 AEs included neutropenia (n=3), nausea (n=2), unstable angina or myocardial infarction (n=2), infection (n=2), joint pain (n=2), fatigue (n=1), deep vein thrombosis (n=1), pulmonary embolism (n=1), aminotransferase elevation (n=1), and dehydration (n=1). ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of brentuximab vedotin (BV, ADCETRIS).
BV is now approved for adults with primary cutaneous anaplastic large-cell lymphoma (pcALCL) and CD30-expressing mycosis fungoides (MF) who have received prior systemic therapy.
This is the fourth FDA-approved indication for BV. The drug has regular approval for 2 indications in classical Hodgkin lymphoma and accelerated approval for the treatment of systemic ALCL.
In November 2016, the FDA granted BV breakthrough therapy designation for the treatment of patients with pcALCL and CD30-expressing MF who require systemic therapy and have received one prior systemic therapy. The agency also granted the supplemental biologics license application priority review.
The approval for BV in pcALCL and CD30-expressing MF is based on data from the phase 3 ALCANZA trial and a pair of phase 2 investigator-sponsored trials.
Phase 3 trial
Results from ALCANZA were presented at the 9th Annual T-cell Lymphoma Forum in January and published in The Lancet in June.
There were 128 patients in the intent-to-treat and safety populations. Sixty-four patients (48 with MF and 16 with pcALCL) were randomized to receive BV at 1.8 mg/kg every 3 weeks for up to 48 weeks.
The other 64 patients (49 with MF and 15 with pcALCL) were randomized to receive standard of care (SOC)—methotrexate at 5 mg to 50 mg weekly or bexarotene at a target dose of 300 mg/m² daily for up to 48 weeks.
The study’s primary endpoint was the rate of objective response lasting at least 4 months (ORR4). The ORR4 rate was significantly higher with BV than with SOC—56.3% and 12.5%, respectively (P<0.0001).
For patients with MF, the ORR4 was 50% with BV and 10% with SOC. For patients with pcALCL, the ORR4 was 75% with BV and 20% with SOC.
Overall, the complete response (CR) rates were 15.6% in the BV arm and 1.6% in the SOC arm (P=0.0046).
For patients with MF, the CR rate was 10% with BV and 0% with SOC. For patients with pcALCL, the CR rate was 31% with BV and 7% with SOC.
Progression-free survival (PFS) was significantly longer in the BV arm than the SOC arm. The median PFS was 16.7 months and 3.5 months, respectively. The hazard ratio was 0.270 (P<0.0001).
For patients with MF, the median PFS was 15.9 months with BV and 3.5 months with SOC. For patients with pcALCL, the median PFS was 27.5 months with BV and 5.3 months with SOC.
The most common adverse events (AEs) of any grade (occurring in 15% or more of patients in the BV and SOC arms, respectively) were peripheral neuropathy (67% and 6%), nausea (36% and 13%), diarrhea (29% and 6%), fatigue (29% and 27%), vomiting (17% and 5%), alopecia (15% and 3%), pruritus (17% and 13%), pyrexia (17% and 18%), decreased appetite (15% and 5%), and hypertriglyceridemia (2% and 18%).
Phase 2 trials
Data from the investigator-sponsored trials were published in the Journal of Clinical Oncology in 2015.
The first study was published in July of that year. The trial enrolled 32 patients with MF or Sézary syndrome. Thirty patients were evaluable for efficacy, and more than half had received 3 or more prior systemic therapies.
Patients received BV (1.8 mg/kg) every 3 weeks for a maximum of 16 doses. The primary endpoint was objective clinical response rate.
Seventy percent of patients (21/30) achieved an objective response across all stages of disease. One patient had a CR, 20 had a partial response, 4 had stable disease, 5 had progressive disease, and 2 were not evaluable for response.
The most common related AEs of any grade were peripheral neuropathy (66%), fatigue (47%), nausea (28%), hair loss (22%), and neutropenia (19%). Grade 3/4 related AEs included neutropenia (n=4), rash (n=3), and peripheral neuropathy (n=1).
The second phase 2 trial was published in August 2015. This trial enrolled CD30-positive patients with lymphomatoid papulosis (LyP), pcALCL, and MF.
Fifty-four patients were enrolled, and 48 were evaluable at the time of analysis. Patients had received an infusion of BV (1.8 mg/kg) every 21 days.
Seventy-three percent of patients (35/48) achieved an objective response, including 100% (20/20) with LyP and/or pcALCL and 54% (15/28) with MF. The CR rate was 35% (n=17).
The most common AEs were peripheral neuropathy (67%), fatigue (35%), skin rash (24%), diarrhea (15%), muscle pain (17%), localized skin infection (15%), neutropenia (15%), and hair loss (11%).
Grade 3/4 AEs included neutropenia (n=3), nausea (n=2), unstable angina or myocardial infarction (n=2), infection (n=2), joint pain (n=2), fatigue (n=1), deep vein thrombosis (n=1), pulmonary embolism (n=1), aminotransferase elevation (n=1), and dehydration (n=1). ![]()
FDA approves IV formulation of aprepitant for CINV
The US Food and Drug Administration (FDA) has approved use of an intravenous (IV) formulation of aprepitant (CINVANTI™) to prevent chemotherapy-induced nausea and vomiting (CINV).
CINVANTI is intended to be used in combination with other antiemetic agents to prevent acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC).
CINVANTI is to be used in combination with a 5-HT3 receptor antagonist and dexamethasone.
The full prescribing information is available at www.cinvanti.com.
The US commercial launch of CINVANTI is planned for January 2018.
CINVANTI is the first IV formulation to directly deliver aprepitant, a substance P/neurokinin-1 (NK1) receptor antagonist.
Aprepitant is also the active ingredient in EMEND® capsules, which were approved by the FDA in 2003. EMEND IV®, which was approved in 2008, contains aprepitant’s prodrug, fosaprepitant.
Heron Therapeutics, Inc., developed CINVANTI in an attempt to provide an IV formulation of aprepitant that has the same efficacy as IV fosaprepitant but does not pose the risk of adverse events (AEs) related to polysorbate 80.
“Aprepitant has long been the standard in the NK1 class, and it remains the only single-agent NK1 with proven efficacy in preventing CINV in both the acute and delayed phases in HEC and MEC,” said Rudolph M. Navari, MD, PhD, of the University of Alabama Birmingham School of Medicine.
“Because CINVANTI is a novel, polysorbate 80-free, IV formulation of aprepitant, it enables physicians to provide patients with standard-of-care efficacy without the potential risk of polysorbate 80-related adverse events, such as infusion-site reactions.”
The FDA approved CINVANTI based on data demonstrating the bioequivalence of CINVANTI to EMEND IV.
A phase 1, randomized, 2-way cross-over study comparing the drugs enrolled 100 healthy subjects. The subjects received CINVANTI at 130 mg or EMEND IV at 150 mg, given over 30 minutes on day 1 of periods 1 and 2.
The researchers said 90% confidence intervals for CINVANTI AUC0-t (area under the time-concentration curve from time 0 to the last measurable concentration), AUC0-inf (area under the time-concentration curve from time 0 extrapolated to infinity), and C12h (plasma concentration at 12 hours) “were well within bioequivalence bounds,” which was 80% to 125%.
The team also found the incidence of treatment-emergent AEs was lower with CINVANTI than EMEND IV—21% and 28%, respectively. The same was true for related treatment-emergent AEs—15% and 28%, respectively.
These data were presented at the Hematology/Oncology Pharmacy Association Annual Conference in March/April and the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) Annual Meeting in June. ![]()
The US Food and Drug Administration (FDA) has approved use of an intravenous (IV) formulation of aprepitant (CINVANTI™) to prevent chemotherapy-induced nausea and vomiting (CINV).
CINVANTI is intended to be used in combination with other antiemetic agents to prevent acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC).
CINVANTI is to be used in combination with a 5-HT3 receptor antagonist and dexamethasone.
The full prescribing information is available at www.cinvanti.com.
The US commercial launch of CINVANTI is planned for January 2018.
CINVANTI is the first IV formulation to directly deliver aprepitant, a substance P/neurokinin-1 (NK1) receptor antagonist.
Aprepitant is also the active ingredient in EMEND® capsules, which were approved by the FDA in 2003. EMEND IV®, which was approved in 2008, contains aprepitant’s prodrug, fosaprepitant.
Heron Therapeutics, Inc., developed CINVANTI in an attempt to provide an IV formulation of aprepitant that has the same efficacy as IV fosaprepitant but does not pose the risk of adverse events (AEs) related to polysorbate 80.
“Aprepitant has long been the standard in the NK1 class, and it remains the only single-agent NK1 with proven efficacy in preventing CINV in both the acute and delayed phases in HEC and MEC,” said Rudolph M. Navari, MD, PhD, of the University of Alabama Birmingham School of Medicine.
“Because CINVANTI is a novel, polysorbate 80-free, IV formulation of aprepitant, it enables physicians to provide patients with standard-of-care efficacy without the potential risk of polysorbate 80-related adverse events, such as infusion-site reactions.”
The FDA approved CINVANTI based on data demonstrating the bioequivalence of CINVANTI to EMEND IV.
A phase 1, randomized, 2-way cross-over study comparing the drugs enrolled 100 healthy subjects. The subjects received CINVANTI at 130 mg or EMEND IV at 150 mg, given over 30 minutes on day 1 of periods 1 and 2.
The researchers said 90% confidence intervals for CINVANTI AUC0-t (area under the time-concentration curve from time 0 to the last measurable concentration), AUC0-inf (area under the time-concentration curve from time 0 extrapolated to infinity), and C12h (plasma concentration at 12 hours) “were well within bioequivalence bounds,” which was 80% to 125%.
The team also found the incidence of treatment-emergent AEs was lower with CINVANTI than EMEND IV—21% and 28%, respectively. The same was true for related treatment-emergent AEs—15% and 28%, respectively.
These data were presented at the Hematology/Oncology Pharmacy Association Annual Conference in March/April and the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) Annual Meeting in June. ![]()
The US Food and Drug Administration (FDA) has approved use of an intravenous (IV) formulation of aprepitant (CINVANTI™) to prevent chemotherapy-induced nausea and vomiting (CINV).
CINVANTI is intended to be used in combination with other antiemetic agents to prevent acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC).
CINVANTI is to be used in combination with a 5-HT3 receptor antagonist and dexamethasone.
The full prescribing information is available at www.cinvanti.com.
The US commercial launch of CINVANTI is planned for January 2018.
CINVANTI is the first IV formulation to directly deliver aprepitant, a substance P/neurokinin-1 (NK1) receptor antagonist.
Aprepitant is also the active ingredient in EMEND® capsules, which were approved by the FDA in 2003. EMEND IV®, which was approved in 2008, contains aprepitant’s prodrug, fosaprepitant.
Heron Therapeutics, Inc., developed CINVANTI in an attempt to provide an IV formulation of aprepitant that has the same efficacy as IV fosaprepitant but does not pose the risk of adverse events (AEs) related to polysorbate 80.
“Aprepitant has long been the standard in the NK1 class, and it remains the only single-agent NK1 with proven efficacy in preventing CINV in both the acute and delayed phases in HEC and MEC,” said Rudolph M. Navari, MD, PhD, of the University of Alabama Birmingham School of Medicine.
“Because CINVANTI is a novel, polysorbate 80-free, IV formulation of aprepitant, it enables physicians to provide patients with standard-of-care efficacy without the potential risk of polysorbate 80-related adverse events, such as infusion-site reactions.”
The FDA approved CINVANTI based on data demonstrating the bioequivalence of CINVANTI to EMEND IV.
A phase 1, randomized, 2-way cross-over study comparing the drugs enrolled 100 healthy subjects. The subjects received CINVANTI at 130 mg or EMEND IV at 150 mg, given over 30 minutes on day 1 of periods 1 and 2.
The researchers said 90% confidence intervals for CINVANTI AUC0-t (area under the time-concentration curve from time 0 to the last measurable concentration), AUC0-inf (area under the time-concentration curve from time 0 extrapolated to infinity), and C12h (plasma concentration at 12 hours) “were well within bioequivalence bounds,” which was 80% to 125%.
The team also found the incidence of treatment-emergent AEs was lower with CINVANTI than EMEND IV—21% and 28%, respectively. The same was true for related treatment-emergent AEs—15% and 28%, respectively.
These data were presented at the Hematology/Oncology Pharmacy Association Annual Conference in March/April and the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) Annual Meeting in June. ![]()
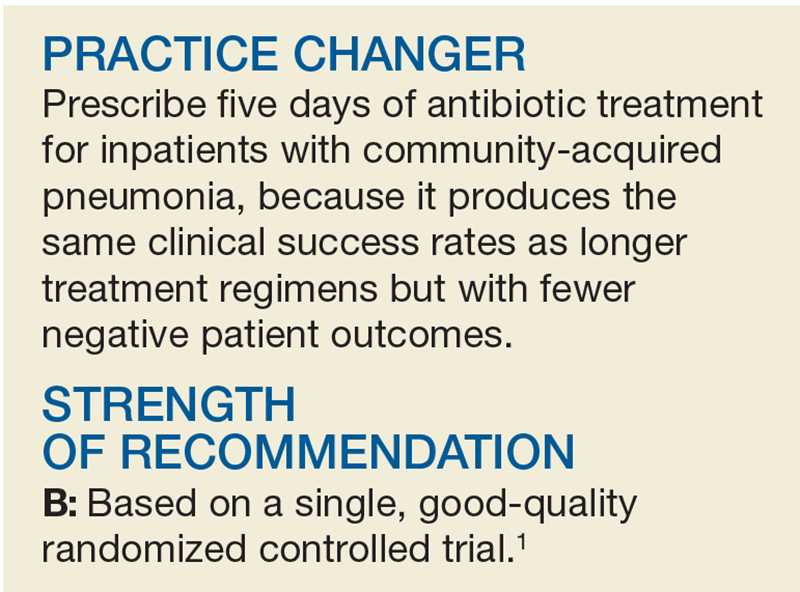
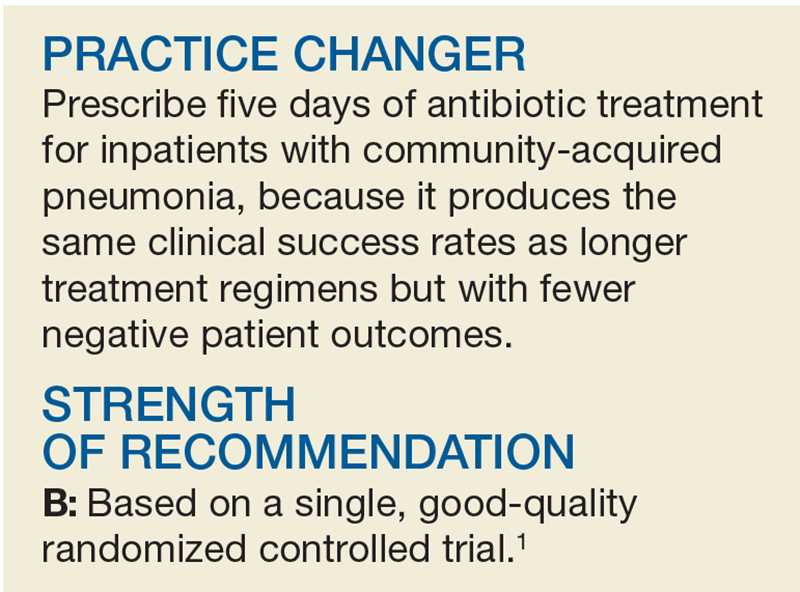
When to “CAP” Off Pneumonia Treatment
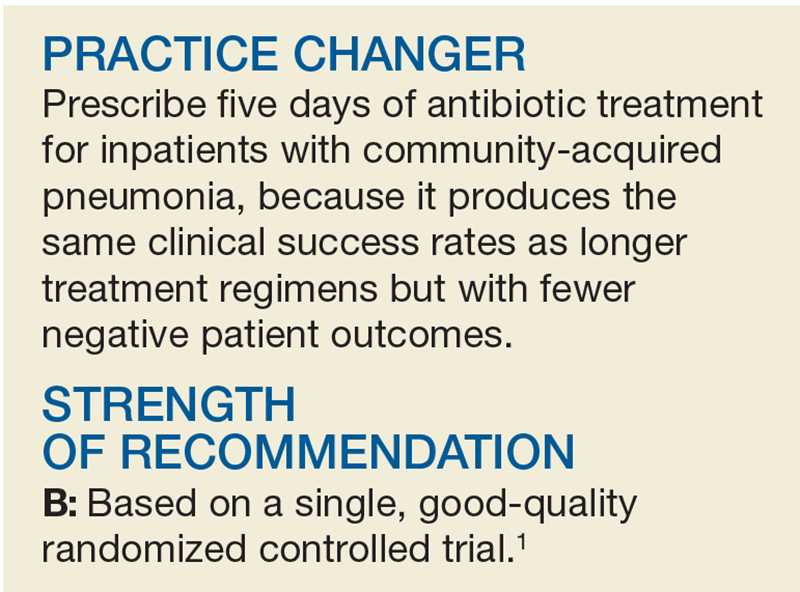
A 65-year-old woman is admitted to your inpatient service from the family health center. She is diagnosed with community-acquired pneumonia (CAP) based on a five-day history of cough and fever and a positive chest x-ray. She now requires oxygen at rest. She has a history of hypertension and diabetes, both of which have been controlled by oral medications. Antibiotic therapy is initiated—but what treatment duration is ideal?
The World Health Organization estimates that pneumonia is the third most common cause of mortality worldwide, causing 3.2 million deaths per year.2 Appropriate prescribing of antibiotics is critical for successful treatment of CAP.
In 2007, the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) created consensus guidelines for the treatment of CAP.3 These guidelines recommend a minimum five-day course of antibiotics if the patient is clinically stable (defined as afebrile for 48 h; heart rate ≤ 100 beats/min; respiratory rate ≤ 24 breaths/min-1
However, these recommendations are not routinely followed. Practitioners often make it their custom to prescribe longer courses of antibiotics.4 Yet, we know that there are several reasons to consider shorter courses of antibiotics, including lower health care costs, fewer adverse effects, and lower rates of bacterial resistance.5-7
Two meta-analyses were performed to compare the safety and efficacy of short- and long-course antibiotic therapy in CAP (≤ 7 d vs > 7 d, respectively).8,9 Both meta-analyses found no difference in efficacy or safety between shorter and longer courses of antibiotics for CAP. Secondary outcomes noted a trend toward decreased antibiotic-associated adverse events with shorter courses of therapy.8,9
However, there are limitations to broad implementation. Studies included in these analyses utilized a variety of antibiotic treatment regimens and longer courses (7 d vs 5 d) that are not recommended by the IDSA/ATS guidelines. Additionally, studies included both inpatient and outpatient treatment groups, so findings may not apply to an exclusively inpatient CAP population.8,9
This study sought to validate the IDSA/ATS guidelines recommending a five-day course of antibiotics for hospitalized patients with CAP.1

STUDY SUMMARY
No differences in clinical outcomes
This multicenter, double-blind, noninferiority randomized trial compared short-term antibiotic treatment duration (5 d) to physician-discretion antibiotic treatment duration among 312 patients (ages 18 and older) admitted for CAP to one of four teaching hospitals in Spain.1 Pneumonia was diagnosed on chest radiograph with at least one symptom: cough, fever, dyspnea, or chest pain. Patients were excluded if, among other things, they had an immunocompromising condition, lived in a nursing home, had a recent hospital stay, used antibiotics within the previous 30 days, or had an uncommon pathogen, such as Pseudomonas aeruginosa or Staphylococcus aureus.1
After receiving a minimum of five days of antibiotics, patients were randomly assigned to an intervention group (where, if clinically stable, no further antibiotics were given) or a control group (where physicians determined antibiotic duration).1
Primary outcomes were clinical success rate at days 10 and 30 from admission (defined as resolution of signs and symptoms of CAP without further antibiotics) and improvement of CAP-related symptoms (as determined by an 18-item questionnaire scored 0-90, with higher scores indicative of greater severity). Secondary outcomes included duration of antibiotic use, time to clinical improvement, mortality, hospital readmission, hospital length of stay, and CAP recurrence.1
Of the 312 participants, 162 were randomized to the intervention group and 150 to the control group. Mean age of patients in the intervention and control groups was 66.2 and 64.7, respectively. Other baseline demographics were similar between the groups. Nearly 80% of patients received quinolone treatment; < 10% received a ß-lactam plus a macrolide.1
Clinical success rates were similar for the control and intervention groups at day 10 (49% vs 56%, respectively) and day 30 (89% vs 92%). Median antibiotic treatment duration was shorter in the intervention group than in the control group (5 d vs 10 d); the intervention group also had a lower rate of 30-day hospital readmissions (1.4% vs 6.6%). There were no differences for other secondary outcomes.1
WHAT’S NEW
Clinical support for 2007 guidelines
This is the first study to clinically support the IDSA/ATS guidelines, which state that a five-day course of antibiotic therapy for hospitalized adults with CAP is effective and without increased risk for adverse events.
CAVEATS
Generalizability is unclear
This study focused on antibiotic duration for the treatment of CAP in hospitalized patients and mainly used quinolone antibiotics. It remains unclear if duration of therapy is as effective in the outpatient setting or when using alternative antibiotic regimens.
If patients continued to have symptoms (eg, fever or low oxygen saturation on room air) after five days of antibiotics, treatment was continued in the study. Thus, patients in real life who continue to have symptoms may need individualized therapy and may require more than five days of antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotics end before clinical improvement
In this study, it took an average of 12 days in both groups for patients to achieve clinical improvement, and upwards of 15 to 18 days for patients to return to normal activity. Patients and providers may be dissatisfied if the treatment course ends days before clinical improvement of symptoms. This may cause prescribers to lengthen the duration of antibiotic therapy inappropriately.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017; 66[10]:629-631).
1. Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257-1265.
2. World Health Organization. The top 10 causes of death. www.who.int/mediacentre/factsheets/fs310/en/index.html. Accessed October 18, 2017.
3. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Aliberti S, Blasi F, Zanaboni AM, et al. Duration of antibiotic therapy in hospitalised patients with community-acquired pneumonia. Eur Respir J. 2010;36:128-134.
5. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of ß-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998; 279:365-370.
6. Opmeer BC, el Moussaoui R, Bossuyt PM, et al. Costs associated with shorter duration of antibiotic therapy in hospitalized patients with mild-to-moderate severe community-acquired pneumonia. J Antimicrob Chemother. 2007;60: 1131-1136.
7. File TM Jr. Clinical efficacy of newer agents in short-duration therapy for community-acquired pneumonia. Clin Infect Dis. 2004;39(suppl 3):S159-S164.
8. Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
9. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68: 1841-1854.
A 65-year-old woman is admitted to your inpatient service from the family health center. She is diagnosed with community-acquired pneumonia (CAP) based on a five-day history of cough and fever and a positive chest x-ray. She now requires oxygen at rest. She has a history of hypertension and diabetes, both of which have been controlled by oral medications. Antibiotic therapy is initiated—but what treatment duration is ideal?
The World Health Organization estimates that pneumonia is the third most common cause of mortality worldwide, causing 3.2 million deaths per year.2 Appropriate prescribing of antibiotics is critical for successful treatment of CAP.
In 2007, the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) created consensus guidelines for the treatment of CAP.3 These guidelines recommend a minimum five-day course of antibiotics if the patient is clinically stable (defined as afebrile for 48 h; heart rate ≤ 100 beats/min; respiratory rate ≤ 24 breaths/min-1
However, these recommendations are not routinely followed. Practitioners often make it their custom to prescribe longer courses of antibiotics.4 Yet, we know that there are several reasons to consider shorter courses of antibiotics, including lower health care costs, fewer adverse effects, and lower rates of bacterial resistance.5-7
Two meta-analyses were performed to compare the safety and efficacy of short- and long-course antibiotic therapy in CAP (≤ 7 d vs > 7 d, respectively).8,9 Both meta-analyses found no difference in efficacy or safety between shorter and longer courses of antibiotics for CAP. Secondary outcomes noted a trend toward decreased antibiotic-associated adverse events with shorter courses of therapy.8,9
However, there are limitations to broad implementation. Studies included in these analyses utilized a variety of antibiotic treatment regimens and longer courses (7 d vs 5 d) that are not recommended by the IDSA/ATS guidelines. Additionally, studies included both inpatient and outpatient treatment groups, so findings may not apply to an exclusively inpatient CAP population.8,9
This study sought to validate the IDSA/ATS guidelines recommending a five-day course of antibiotics for hospitalized patients with CAP.1

STUDY SUMMARY
No differences in clinical outcomes
This multicenter, double-blind, noninferiority randomized trial compared short-term antibiotic treatment duration (5 d) to physician-discretion antibiotic treatment duration among 312 patients (ages 18 and older) admitted for CAP to one of four teaching hospitals in Spain.1 Pneumonia was diagnosed on chest radiograph with at least one symptom: cough, fever, dyspnea, or chest pain. Patients were excluded if, among other things, they had an immunocompromising condition, lived in a nursing home, had a recent hospital stay, used antibiotics within the previous 30 days, or had an uncommon pathogen, such as Pseudomonas aeruginosa or Staphylococcus aureus.1
After receiving a minimum of five days of antibiotics, patients were randomly assigned to an intervention group (where, if clinically stable, no further antibiotics were given) or a control group (where physicians determined antibiotic duration).1
Primary outcomes were clinical success rate at days 10 and 30 from admission (defined as resolution of signs and symptoms of CAP without further antibiotics) and improvement of CAP-related symptoms (as determined by an 18-item questionnaire scored 0-90, with higher scores indicative of greater severity). Secondary outcomes included duration of antibiotic use, time to clinical improvement, mortality, hospital readmission, hospital length of stay, and CAP recurrence.1
Of the 312 participants, 162 were randomized to the intervention group and 150 to the control group. Mean age of patients in the intervention and control groups was 66.2 and 64.7, respectively. Other baseline demographics were similar between the groups. Nearly 80% of patients received quinolone treatment; < 10% received a ß-lactam plus a macrolide.1
Clinical success rates were similar for the control and intervention groups at day 10 (49% vs 56%, respectively) and day 30 (89% vs 92%). Median antibiotic treatment duration was shorter in the intervention group than in the control group (5 d vs 10 d); the intervention group also had a lower rate of 30-day hospital readmissions (1.4% vs 6.6%). There were no differences for other secondary outcomes.1
WHAT’S NEW
Clinical support for 2007 guidelines
This is the first study to clinically support the IDSA/ATS guidelines, which state that a five-day course of antibiotic therapy for hospitalized adults with CAP is effective and without increased risk for adverse events.
CAVEATS
Generalizability is unclear
This study focused on antibiotic duration for the treatment of CAP in hospitalized patients and mainly used quinolone antibiotics. It remains unclear if duration of therapy is as effective in the outpatient setting or when using alternative antibiotic regimens.
If patients continued to have symptoms (eg, fever or low oxygen saturation on room air) after five days of antibiotics, treatment was continued in the study. Thus, patients in real life who continue to have symptoms may need individualized therapy and may require more than five days of antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotics end before clinical improvement
In this study, it took an average of 12 days in both groups for patients to achieve clinical improvement, and upwards of 15 to 18 days for patients to return to normal activity. Patients and providers may be dissatisfied if the treatment course ends days before clinical improvement of symptoms. This may cause prescribers to lengthen the duration of antibiotic therapy inappropriately.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017; 66[10]:629-631).
A 65-year-old woman is admitted to your inpatient service from the family health center. She is diagnosed with community-acquired pneumonia (CAP) based on a five-day history of cough and fever and a positive chest x-ray. She now requires oxygen at rest. She has a history of hypertension and diabetes, both of which have been controlled by oral medications. Antibiotic therapy is initiated—but what treatment duration is ideal?
The World Health Organization estimates that pneumonia is the third most common cause of mortality worldwide, causing 3.2 million deaths per year.2 Appropriate prescribing of antibiotics is critical for successful treatment of CAP.
In 2007, the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) created consensus guidelines for the treatment of CAP.3 These guidelines recommend a minimum five-day course of antibiotics if the patient is clinically stable (defined as afebrile for 48 h; heart rate ≤ 100 beats/min; respiratory rate ≤ 24 breaths/min-1
However, these recommendations are not routinely followed. Practitioners often make it their custom to prescribe longer courses of antibiotics.4 Yet, we know that there are several reasons to consider shorter courses of antibiotics, including lower health care costs, fewer adverse effects, and lower rates of bacterial resistance.5-7
Two meta-analyses were performed to compare the safety and efficacy of short- and long-course antibiotic therapy in CAP (≤ 7 d vs > 7 d, respectively).8,9 Both meta-analyses found no difference in efficacy or safety between shorter and longer courses of antibiotics for CAP. Secondary outcomes noted a trend toward decreased antibiotic-associated adverse events with shorter courses of therapy.8,9
However, there are limitations to broad implementation. Studies included in these analyses utilized a variety of antibiotic treatment regimens and longer courses (7 d vs 5 d) that are not recommended by the IDSA/ATS guidelines. Additionally, studies included both inpatient and outpatient treatment groups, so findings may not apply to an exclusively inpatient CAP population.8,9
This study sought to validate the IDSA/ATS guidelines recommending a five-day course of antibiotics for hospitalized patients with CAP.1

STUDY SUMMARY
No differences in clinical outcomes
This multicenter, double-blind, noninferiority randomized trial compared short-term antibiotic treatment duration (5 d) to physician-discretion antibiotic treatment duration among 312 patients (ages 18 and older) admitted for CAP to one of four teaching hospitals in Spain.1 Pneumonia was diagnosed on chest radiograph with at least one symptom: cough, fever, dyspnea, or chest pain. Patients were excluded if, among other things, they had an immunocompromising condition, lived in a nursing home, had a recent hospital stay, used antibiotics within the previous 30 days, or had an uncommon pathogen, such as Pseudomonas aeruginosa or Staphylococcus aureus.1
After receiving a minimum of five days of antibiotics, patients were randomly assigned to an intervention group (where, if clinically stable, no further antibiotics were given) or a control group (where physicians determined antibiotic duration).1
Primary outcomes were clinical success rate at days 10 and 30 from admission (defined as resolution of signs and symptoms of CAP without further antibiotics) and improvement of CAP-related symptoms (as determined by an 18-item questionnaire scored 0-90, with higher scores indicative of greater severity). Secondary outcomes included duration of antibiotic use, time to clinical improvement, mortality, hospital readmission, hospital length of stay, and CAP recurrence.1
Of the 312 participants, 162 were randomized to the intervention group and 150 to the control group. Mean age of patients in the intervention and control groups was 66.2 and 64.7, respectively. Other baseline demographics were similar between the groups. Nearly 80% of patients received quinolone treatment; < 10% received a ß-lactam plus a macrolide.1
Clinical success rates were similar for the control and intervention groups at day 10 (49% vs 56%, respectively) and day 30 (89% vs 92%). Median antibiotic treatment duration was shorter in the intervention group than in the control group (5 d vs 10 d); the intervention group also had a lower rate of 30-day hospital readmissions (1.4% vs 6.6%). There were no differences for other secondary outcomes.1
WHAT’S NEW
Clinical support for 2007 guidelines
This is the first study to clinically support the IDSA/ATS guidelines, which state that a five-day course of antibiotic therapy for hospitalized adults with CAP is effective and without increased risk for adverse events.
CAVEATS
Generalizability is unclear
This study focused on antibiotic duration for the treatment of CAP in hospitalized patients and mainly used quinolone antibiotics. It remains unclear if duration of therapy is as effective in the outpatient setting or when using alternative antibiotic regimens.
If patients continued to have symptoms (eg, fever or low oxygen saturation on room air) after five days of antibiotics, treatment was continued in the study. Thus, patients in real life who continue to have symptoms may need individualized therapy and may require more than five days of antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotics end before clinical improvement
In this study, it took an average of 12 days in both groups for patients to achieve clinical improvement, and upwards of 15 to 18 days for patients to return to normal activity. Patients and providers may be dissatisfied if the treatment course ends days before clinical improvement of symptoms. This may cause prescribers to lengthen the duration of antibiotic therapy inappropriately.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017; 66[10]:629-631).
1. Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257-1265.
2. World Health Organization. The top 10 causes of death. www.who.int/mediacentre/factsheets/fs310/en/index.html. Accessed October 18, 2017.
3. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Aliberti S, Blasi F, Zanaboni AM, et al. Duration of antibiotic therapy in hospitalised patients with community-acquired pneumonia. Eur Respir J. 2010;36:128-134.
5. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of ß-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998; 279:365-370.
6. Opmeer BC, el Moussaoui R, Bossuyt PM, et al. Costs associated with shorter duration of antibiotic therapy in hospitalized patients with mild-to-moderate severe community-acquired pneumonia. J Antimicrob Chemother. 2007;60: 1131-1136.
7. File TM Jr. Clinical efficacy of newer agents in short-duration therapy for community-acquired pneumonia. Clin Infect Dis. 2004;39(suppl 3):S159-S164.
8. Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
9. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68: 1841-1854.
1. Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257-1265.
2. World Health Organization. The top 10 causes of death. www.who.int/mediacentre/factsheets/fs310/en/index.html. Accessed October 18, 2017.
3. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Aliberti S, Blasi F, Zanaboni AM, et al. Duration of antibiotic therapy in hospitalised patients with community-acquired pneumonia. Eur Respir J. 2010;36:128-134.
5. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of ß-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998; 279:365-370.
6. Opmeer BC, el Moussaoui R, Bossuyt PM, et al. Costs associated with shorter duration of antibiotic therapy in hospitalized patients with mild-to-moderate severe community-acquired pneumonia. J Antimicrob Chemother. 2007;60: 1131-1136.
7. File TM Jr. Clinical efficacy of newer agents in short-duration therapy for community-acquired pneumonia. Clin Infect Dis. 2004;39(suppl 3):S159-S164.
8. Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
9. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68: 1841-1854.
FDA approves brentuximab vedotin for primary cutaneous anaplastic large cell lymphoma
Approval was based on a 56% objective response rate for brentuximab vedotin versus 12% for physician’s choice in a phase 3 trial (ALCANZA) of 131 patients with mycosis fungoides or pcALCL. All patients had received one prior systemic therapy and were randomized (1:1) to receive either brentuximab vedotin or the physician’s choice of methotrexate or bexarotene, the Food and Drug Administration said in a press statement.
The most common adverse reactions for patients in the brentuximab vedotin arm were anemia, peripheral sensory neuropathy, nausea, diarrhea, fatigue, and neutropenia. The most common adverse event leading to discontinuation of brentuximab vedotin was peripheral neuropathy.
The recommended dose of brentuximab vedotin is 1.8 mg/kg up to a maximum of 180 mg/kg as an IV infusion over 30 minutes every 3 weeks until a maximum of 16 cycles, disease progression, or unacceptable toxicity, the FDA wrote.
Brentuximab vedotin is marketed as Adcetris by Seattle Genetics.
ALCANZA results were presented at ASH 2016 and published in the Lancet in Aug. 5, 2017.
Approval was based on a 56% objective response rate for brentuximab vedotin versus 12% for physician’s choice in a phase 3 trial (ALCANZA) of 131 patients with mycosis fungoides or pcALCL. All patients had received one prior systemic therapy and were randomized (1:1) to receive either brentuximab vedotin or the physician’s choice of methotrexate or bexarotene, the Food and Drug Administration said in a press statement.
The most common adverse reactions for patients in the brentuximab vedotin arm were anemia, peripheral sensory neuropathy, nausea, diarrhea, fatigue, and neutropenia. The most common adverse event leading to discontinuation of brentuximab vedotin was peripheral neuropathy.
The recommended dose of brentuximab vedotin is 1.8 mg/kg up to a maximum of 180 mg/kg as an IV infusion over 30 minutes every 3 weeks until a maximum of 16 cycles, disease progression, or unacceptable toxicity, the FDA wrote.
Brentuximab vedotin is marketed as Adcetris by Seattle Genetics.
ALCANZA results were presented at ASH 2016 and published in the Lancet in Aug. 5, 2017.
Approval was based on a 56% objective response rate for brentuximab vedotin versus 12% for physician’s choice in a phase 3 trial (ALCANZA) of 131 patients with mycosis fungoides or pcALCL. All patients had received one prior systemic therapy and were randomized (1:1) to receive either brentuximab vedotin or the physician’s choice of methotrexate or bexarotene, the Food and Drug Administration said in a press statement.
The most common adverse reactions for patients in the brentuximab vedotin arm were anemia, peripheral sensory neuropathy, nausea, diarrhea, fatigue, and neutropenia. The most common adverse event leading to discontinuation of brentuximab vedotin was peripheral neuropathy.
The recommended dose of brentuximab vedotin is 1.8 mg/kg up to a maximum of 180 mg/kg as an IV infusion over 30 minutes every 3 weeks until a maximum of 16 cycles, disease progression, or unacceptable toxicity, the FDA wrote.
Brentuximab vedotin is marketed as Adcetris by Seattle Genetics.
ALCANZA results were presented at ASH 2016 and published in the Lancet in Aug. 5, 2017.
Adjunctive minocycline for schizophrenia found beneficial
PARIS – A report that adjunctive minocycline was found safe and effective for treatment of schizophrenia must be considered one of the year’s highlights in the field of psychosis, Pascal Steullet, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
The report came in the form of a meta-analysis conducted by investigators in China and Australia. This was the largest meta-analysis looking at the topic to date, and the only one to include a search of the Chinese language database, which provided three of the eight randomized, placebo-controlled clinical trials that were examined. Seven of the eight randomized trials were double-blind and deemed high quality by widely used criteria, including the Jadad scale and GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology, noted Dr. Steullet, a neuroscientist at the University of Lausanne (Switzerland).
The primary outcome was change in the PANSS (Positive and Negative Syndrome Scale) total psychopathology score, and the positive, negative, and general symptom subscale scores.
The biggest benefit was on PANSS negative symptoms. Minocycline brought significantly greater improvement in this domain than placebo, with a standard mean difference (SMD) of –0.69 and a P value of less than .00001 (Eur Psychopharmacol. 2017 Jan;27[1]:8-18).
“That’s quite a good effect size,” Dr. Steullet commented.
The benefit on PANSS positive symptoms, while statistically significant, was far less robust, with an SMD of –0.22 in favor of minocycline.
The PANSS total psychopathology score favored minocycline with an SMD of –0.64, which Dr. Steullet again deemed “a quite significant effect size.” The PANSS general symptom score also showed a significant benefit in favor of minocycline, with an SMD of –0.45.
Among various secondary endpoints that were evaluated: A significant benefit was found favoring minocycline on the Clinical Global Impressions scale (SMD of –0.53) and the Abnormal Involuntary Movement Scale (SMD of –0.56). However, no differences were found between the minocycline and control groups on the Global Assessment of Functioning Scale, the Extrapyramidal Symptom Rating Scale, or the Calgary Depression Scale for Schizophrenia.
Although the average dose of minocycline prescribed in the eight trials was 171.9 mg/day, dosing strategies varied widely from trial to trial, and the investigators concluded that future studies are needed in order to pin down the optimal dosing and duration.
There was no increase in adverse drug reactions in the minocycline-treated group.
Neurocognitive function as assessed by the MATRICS Consensus Cognitive Battery showed no differences between the minocycline and placebo groups in working memory, problem solving, attention/vigilance, or other elements.
Proposed mechanisms of minocycline’s benefit as adjunctive therapy alongside antipsychotics for schizophrenia include the antimicrobial’s good CNS penetration and its anti-inflammatory effects, which could reduce neuroinflammation, dampen activated microglia, and enhance glutamate neurotransmitters.
The meta-analysis was supported by the University of Macau. Its authors reported having no financial conflicts of interest. Dr. Steullet, who was not involved in the work, also reported having no financial conflicts of interest.
PARIS – A report that adjunctive minocycline was found safe and effective for treatment of schizophrenia must be considered one of the year’s highlights in the field of psychosis, Pascal Steullet, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
The report came in the form of a meta-analysis conducted by investigators in China and Australia. This was the largest meta-analysis looking at the topic to date, and the only one to include a search of the Chinese language database, which provided three of the eight randomized, placebo-controlled clinical trials that were examined. Seven of the eight randomized trials were double-blind and deemed high quality by widely used criteria, including the Jadad scale and GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology, noted Dr. Steullet, a neuroscientist at the University of Lausanne (Switzerland).
The primary outcome was change in the PANSS (Positive and Negative Syndrome Scale) total psychopathology score, and the positive, negative, and general symptom subscale scores.
The biggest benefit was on PANSS negative symptoms. Minocycline brought significantly greater improvement in this domain than placebo, with a standard mean difference (SMD) of –0.69 and a P value of less than .00001 (Eur Psychopharmacol. 2017 Jan;27[1]:8-18).
“That’s quite a good effect size,” Dr. Steullet commented.
The benefit on PANSS positive symptoms, while statistically significant, was far less robust, with an SMD of –0.22 in favor of minocycline.
The PANSS total psychopathology score favored minocycline with an SMD of –0.64, which Dr. Steullet again deemed “a quite significant effect size.” The PANSS general symptom score also showed a significant benefit in favor of minocycline, with an SMD of –0.45.
Among various secondary endpoints that were evaluated: A significant benefit was found favoring minocycline on the Clinical Global Impressions scale (SMD of –0.53) and the Abnormal Involuntary Movement Scale (SMD of –0.56). However, no differences were found between the minocycline and control groups on the Global Assessment of Functioning Scale, the Extrapyramidal Symptom Rating Scale, or the Calgary Depression Scale for Schizophrenia.
Although the average dose of minocycline prescribed in the eight trials was 171.9 mg/day, dosing strategies varied widely from trial to trial, and the investigators concluded that future studies are needed in order to pin down the optimal dosing and duration.
There was no increase in adverse drug reactions in the minocycline-treated group.
Neurocognitive function as assessed by the MATRICS Consensus Cognitive Battery showed no differences between the minocycline and placebo groups in working memory, problem solving, attention/vigilance, or other elements.
Proposed mechanisms of minocycline’s benefit as adjunctive therapy alongside antipsychotics for schizophrenia include the antimicrobial’s good CNS penetration and its anti-inflammatory effects, which could reduce neuroinflammation, dampen activated microglia, and enhance glutamate neurotransmitters.
The meta-analysis was supported by the University of Macau. Its authors reported having no financial conflicts of interest. Dr. Steullet, who was not involved in the work, also reported having no financial conflicts of interest.
PARIS – A report that adjunctive minocycline was found safe and effective for treatment of schizophrenia must be considered one of the year’s highlights in the field of psychosis, Pascal Steullet, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
The report came in the form of a meta-analysis conducted by investigators in China and Australia. This was the largest meta-analysis looking at the topic to date, and the only one to include a search of the Chinese language database, which provided three of the eight randomized, placebo-controlled clinical trials that were examined. Seven of the eight randomized trials were double-blind and deemed high quality by widely used criteria, including the Jadad scale and GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology, noted Dr. Steullet, a neuroscientist at the University of Lausanne (Switzerland).
The primary outcome was change in the PANSS (Positive and Negative Syndrome Scale) total psychopathology score, and the positive, negative, and general symptom subscale scores.
The biggest benefit was on PANSS negative symptoms. Minocycline brought significantly greater improvement in this domain than placebo, with a standard mean difference (SMD) of –0.69 and a P value of less than .00001 (Eur Psychopharmacol. 2017 Jan;27[1]:8-18).
“That’s quite a good effect size,” Dr. Steullet commented.
The benefit on PANSS positive symptoms, while statistically significant, was far less robust, with an SMD of –0.22 in favor of minocycline.
The PANSS total psychopathology score favored minocycline with an SMD of –0.64, which Dr. Steullet again deemed “a quite significant effect size.” The PANSS general symptom score also showed a significant benefit in favor of minocycline, with an SMD of –0.45.
Among various secondary endpoints that were evaluated: A significant benefit was found favoring minocycline on the Clinical Global Impressions scale (SMD of –0.53) and the Abnormal Involuntary Movement Scale (SMD of –0.56). However, no differences were found between the minocycline and control groups on the Global Assessment of Functioning Scale, the Extrapyramidal Symptom Rating Scale, or the Calgary Depression Scale for Schizophrenia.
Although the average dose of minocycline prescribed in the eight trials was 171.9 mg/day, dosing strategies varied widely from trial to trial, and the investigators concluded that future studies are needed in order to pin down the optimal dosing and duration.
There was no increase in adverse drug reactions in the minocycline-treated group.
Neurocognitive function as assessed by the MATRICS Consensus Cognitive Battery showed no differences between the minocycline and placebo groups in working memory, problem solving, attention/vigilance, or other elements.
Proposed mechanisms of minocycline’s benefit as adjunctive therapy alongside antipsychotics for schizophrenia include the antimicrobial’s good CNS penetration and its anti-inflammatory effects, which could reduce neuroinflammation, dampen activated microglia, and enhance glutamate neurotransmitters.
The meta-analysis was supported by the University of Macau. Its authors reported having no financial conflicts of interest. Dr. Steullet, who was not involved in the work, also reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE ECNP CONGRESS
Late-Breaking Science preview: Wednesday, Nov. 15
The final Late-Breaking Science session delves into innovative therapies and novel applications, including two phase 1-2 stem cell trials, an early trial in toxin treatments to prevent atrial fibrillation, a phase 1 test of an interatrial shunt device for heart failure with preserved ejection fraction, and more:
- TNT-POAF: Nathan Waldron, MD, of Duke University, Durham, N.C., will present results of a trial aiming to prevent postoperative atrial fibrillation with the use of temporary toxin treatment.
- REDUCE LAP–HF 1: In what the investigators call the first randomized controlled trial of a device-based therapy to reduce left atrial pressure in HFpEF, an inter-atrial shunt device designed to provide continuous and dynamic decompression of the left atrium. Sanjiv J Shah, MD, of Northwestern University will present the study, which holds the hypothesis that the device may reduce symptoms and slow the progression of heart failure.
- PROPEL: This study tested the hypothesis that granulocyte-macrophage colony-stimulating factor (GM-CSF) combined with supervised treadmill exercise in patients with peripheral artery disease would significantly improve functional performance more than GM-CSF alone or supervised treadmill exercise alone. Mary McDermott, MD, of Northwestern University, Chicago, will present the primary endpoint of change in 6-minute walk performance at 12-weeks’ follow-up, as well as several secondary outcomes.
- ALLSTAR: Timothy Henry, MD, of the Cedars-Sinai Heart Institute, Los Angeles, will present the phase 1-2 ALLSTAR (Allogeneic Heart Stem Cells to Achieve Myocardial Regeneration) study, which compared allogeneic cardiosphere-derived cells (CAP-1002) to placebo in order to find whether it is safe and effective in decreasing infarct size in patients with an MI.
- HOPE-Duchenne: This phase 1-2 study randomized men with cardiomyopathy secondary to Duchenne muscular dystrophy to receive CAP-1002 cells or usual care; its primary outcome is safety. Ronald Victor, MD, will present the results.
[email protected]
On Twitter @cardionews
The final Late-Breaking Science session delves into innovative therapies and novel applications, including two phase 1-2 stem cell trials, an early trial in toxin treatments to prevent atrial fibrillation, a phase 1 test of an interatrial shunt device for heart failure with preserved ejection fraction, and more:
- TNT-POAF: Nathan Waldron, MD, of Duke University, Durham, N.C., will present results of a trial aiming to prevent postoperative atrial fibrillation with the use of temporary toxin treatment.
- REDUCE LAP–HF 1: In what the investigators call the first randomized controlled trial of a device-based therapy to reduce left atrial pressure in HFpEF, an inter-atrial shunt device designed to provide continuous and dynamic decompression of the left atrium. Sanjiv J Shah, MD, of Northwestern University will present the study, which holds the hypothesis that the device may reduce symptoms and slow the progression of heart failure.
- PROPEL: This study tested the hypothesis that granulocyte-macrophage colony-stimulating factor (GM-CSF) combined with supervised treadmill exercise in patients with peripheral artery disease would significantly improve functional performance more than GM-CSF alone or supervised treadmill exercise alone. Mary McDermott, MD, of Northwestern University, Chicago, will present the primary endpoint of change in 6-minute walk performance at 12-weeks’ follow-up, as well as several secondary outcomes.
- ALLSTAR: Timothy Henry, MD, of the Cedars-Sinai Heart Institute, Los Angeles, will present the phase 1-2 ALLSTAR (Allogeneic Heart Stem Cells to Achieve Myocardial Regeneration) study, which compared allogeneic cardiosphere-derived cells (CAP-1002) to placebo in order to find whether it is safe and effective in decreasing infarct size in patients with an MI.
- HOPE-Duchenne: This phase 1-2 study randomized men with cardiomyopathy secondary to Duchenne muscular dystrophy to receive CAP-1002 cells or usual care; its primary outcome is safety. Ronald Victor, MD, will present the results.
[email protected]
On Twitter @cardionews
The final Late-Breaking Science session delves into innovative therapies and novel applications, including two phase 1-2 stem cell trials, an early trial in toxin treatments to prevent atrial fibrillation, a phase 1 test of an interatrial shunt device for heart failure with preserved ejection fraction, and more:
- TNT-POAF: Nathan Waldron, MD, of Duke University, Durham, N.C., will present results of a trial aiming to prevent postoperative atrial fibrillation with the use of temporary toxin treatment.
- REDUCE LAP–HF 1: In what the investigators call the first randomized controlled trial of a device-based therapy to reduce left atrial pressure in HFpEF, an inter-atrial shunt device designed to provide continuous and dynamic decompression of the left atrium. Sanjiv J Shah, MD, of Northwestern University will present the study, which holds the hypothesis that the device may reduce symptoms and slow the progression of heart failure.
- PROPEL: This study tested the hypothesis that granulocyte-macrophage colony-stimulating factor (GM-CSF) combined with supervised treadmill exercise in patients with peripheral artery disease would significantly improve functional performance more than GM-CSF alone or supervised treadmill exercise alone. Mary McDermott, MD, of Northwestern University, Chicago, will present the primary endpoint of change in 6-minute walk performance at 12-weeks’ follow-up, as well as several secondary outcomes.
- ALLSTAR: Timothy Henry, MD, of the Cedars-Sinai Heart Institute, Los Angeles, will present the phase 1-2 ALLSTAR (Allogeneic Heart Stem Cells to Achieve Myocardial Regeneration) study, which compared allogeneic cardiosphere-derived cells (CAP-1002) to placebo in order to find whether it is safe and effective in decreasing infarct size in patients with an MI.
- HOPE-Duchenne: This phase 1-2 study randomized men with cardiomyopathy secondary to Duchenne muscular dystrophy to receive CAP-1002 cells or usual care; its primary outcome is safety. Ronald Victor, MD, will present the results.
[email protected]
On Twitter @cardionews
AML candidate drug back in the pipeline
The Food and Drug Administration has given the biopharmaceutical company Cellectis permission to resume phase 1 trials of UCART123, a gene-edited T-cell investigational drug that targets CD123, as a potential treatment for acute myeloid leukemia (AML) and blastic plasmacytoid dendritic cell neoplasm (BPDCN), according to a press release from the company.
UCART123 is the first allogeneic, “off-the-shelf” gene-edited chimeric antigen receptor (CAR) T-cell product candidate that the FDA has approved for clinical trials. The agency had placed a clinical hold on phase 1 trials of the gene-edited CAR T-cell drug on Sept. 4, following a patient death in the BPDCN clinical study. In order to proceed with the trials, Cellectis agreed to several changes in the study protocols.
The changes include decreasing the dose of the UCART123 therapy to 6.25x104 cells/kg and lowering the dose of the lympho-depleting regimen of cyclophosphamide to 750 mg/m2 per day over 3 days with a maximum daily dose of 1.33 g. Additionally, there can be no uncontrolled infection after receipt of the lympho-depleting preconditioning regimen. Patients must be afebrile at the start of treatment, off all but a replacement dose of corticosteroids, and have no organ dysfunction. Plus, the next three patients treated in each study must be under age 65.
There’s also a condition that patient enrollments be staggered by at least 28 days.
The drug sponsor is working with investigators and each clinical site to obtain the Institutional Review Board’s approval of the revised protocols.
The hold followed the death of a 78-year-old man with relapsed/refractory BPDCN with 30% blasts in his bone marrow and cutaneous lesions. The first dose of UCART123 at 6.25x105 cells/kg was administered without complication, but at day 5 the patient began experiencing side effects, including cytokine release syndrome and a lung infection. At day 8, the cytokine release syndrome had worsened and the patient had also developed capillary leak syndrome. He died on day 9 of the study.
In the AML phase 1 study, a 58-year-old woman with AML and 84% blasts in her bone marrow received the same dose of UCART123. She also developed cytokine release syndrome and capillary leak syndrome but both resolved with treatment.
Both patients also received the same preconditioning treatment: 30 mg/m2 per day fludarabine for 4 days and 1g/m2 per day cyclophosphamide for 3 days.
[email protected]
On Twitter @maryellenny
The Food and Drug Administration has given the biopharmaceutical company Cellectis permission to resume phase 1 trials of UCART123, a gene-edited T-cell investigational drug that targets CD123, as a potential treatment for acute myeloid leukemia (AML) and blastic plasmacytoid dendritic cell neoplasm (BPDCN), according to a press release from the company.
UCART123 is the first allogeneic, “off-the-shelf” gene-edited chimeric antigen receptor (CAR) T-cell product candidate that the FDA has approved for clinical trials. The agency had placed a clinical hold on phase 1 trials of the gene-edited CAR T-cell drug on Sept. 4, following a patient death in the BPDCN clinical study. In order to proceed with the trials, Cellectis agreed to several changes in the study protocols.
The changes include decreasing the dose of the UCART123 therapy to 6.25x104 cells/kg and lowering the dose of the lympho-depleting regimen of cyclophosphamide to 750 mg/m2 per day over 3 days with a maximum daily dose of 1.33 g. Additionally, there can be no uncontrolled infection after receipt of the lympho-depleting preconditioning regimen. Patients must be afebrile at the start of treatment, off all but a replacement dose of corticosteroids, and have no organ dysfunction. Plus, the next three patients treated in each study must be under age 65.
There’s also a condition that patient enrollments be staggered by at least 28 days.
The drug sponsor is working with investigators and each clinical site to obtain the Institutional Review Board’s approval of the revised protocols.
The hold followed the death of a 78-year-old man with relapsed/refractory BPDCN with 30% blasts in his bone marrow and cutaneous lesions. The first dose of UCART123 at 6.25x105 cells/kg was administered without complication, but at day 5 the patient began experiencing side effects, including cytokine release syndrome and a lung infection. At day 8, the cytokine release syndrome had worsened and the patient had also developed capillary leak syndrome. He died on day 9 of the study.
In the AML phase 1 study, a 58-year-old woman with AML and 84% blasts in her bone marrow received the same dose of UCART123. She also developed cytokine release syndrome and capillary leak syndrome but both resolved with treatment.
Both patients also received the same preconditioning treatment: 30 mg/m2 per day fludarabine for 4 days and 1g/m2 per day cyclophosphamide for 3 days.
[email protected]
On Twitter @maryellenny
The Food and Drug Administration has given the biopharmaceutical company Cellectis permission to resume phase 1 trials of UCART123, a gene-edited T-cell investigational drug that targets CD123, as a potential treatment for acute myeloid leukemia (AML) and blastic plasmacytoid dendritic cell neoplasm (BPDCN), according to a press release from the company.
UCART123 is the first allogeneic, “off-the-shelf” gene-edited chimeric antigen receptor (CAR) T-cell product candidate that the FDA has approved for clinical trials. The agency had placed a clinical hold on phase 1 trials of the gene-edited CAR T-cell drug on Sept. 4, following a patient death in the BPDCN clinical study. In order to proceed with the trials, Cellectis agreed to several changes in the study protocols.
The changes include decreasing the dose of the UCART123 therapy to 6.25x104 cells/kg and lowering the dose of the lympho-depleting regimen of cyclophosphamide to 750 mg/m2 per day over 3 days with a maximum daily dose of 1.33 g. Additionally, there can be no uncontrolled infection after receipt of the lympho-depleting preconditioning regimen. Patients must be afebrile at the start of treatment, off all but a replacement dose of corticosteroids, and have no organ dysfunction. Plus, the next three patients treated in each study must be under age 65.
There’s also a condition that patient enrollments be staggered by at least 28 days.
The drug sponsor is working with investigators and each clinical site to obtain the Institutional Review Board’s approval of the revised protocols.
The hold followed the death of a 78-year-old man with relapsed/refractory BPDCN with 30% blasts in his bone marrow and cutaneous lesions. The first dose of UCART123 at 6.25x105 cells/kg was administered without complication, but at day 5 the patient began experiencing side effects, including cytokine release syndrome and a lung infection. At day 8, the cytokine release syndrome had worsened and the patient had also developed capillary leak syndrome. He died on day 9 of the study.
In the AML phase 1 study, a 58-year-old woman with AML and 84% blasts in her bone marrow received the same dose of UCART123. She also developed cytokine release syndrome and capillary leak syndrome but both resolved with treatment.
Both patients also received the same preconditioning treatment: 30 mg/m2 per day fludarabine for 4 days and 1g/m2 per day cyclophosphamide for 3 days.
[email protected]
On Twitter @maryellenny
Late-Breaking Science preview: Tuesday, Nov. 14
On the third day of the American Heart Association scientific sessions, antithrombotic therapy is the focus of the Late-Breaking Science 5 presentation, at 10:45 a.m.-12 p.m. on Tuesday, Nov. 14, followed by innovative investigations in evaluating quality improvement and patient-centered care interventions in the Late-Breaking Science 6 session, to be held at 3:45-5:15 p.m. Here are some highlights.
Late-Breaking Science 5, antithrombotic therapy
- RE-DUAL PCI: Jonas Oldgren, MD, of Uppsala (Sweden) University, will present an unspecified subgroup analysis from the RE-DUAL PCI (Dual Antithrombotic Therapy With Dabigatran in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary Intervention) trial, focusing on one arm of the study. The main results, presented in August, showed patients with atrial fibrillation who had undergone percutaneous coronary intervention had a lower risk of bleeding if they received dual therapy with dabigatran plus clopidogrel or ticagrelor than did those treated with warfarin, clopidogrel, or ticagrelor.
- POISE-2 PCI: Michelle M. Graham, MD, of the University of Alberta, Edmonton, will present a substudy of POISE-2 focusing on the patients in undergoing noncardiac surgery who had a previous percutaneous coronary intervention. POISE-2, published in 2014, showed that administering aspirin periprocedurally had no effect on the rate of a composite of death or nonfatal MI, but increased the risk of major bleeding.
Dr. Jonas Oldgren - GEMINI-ACS-1: In the main study, the risk of major bleeding was similar between ACS patients treated with a combination of low-dose rivaroxaban and a P2Y12 inhibitor and those treated with aspirin and P2Y12 inhibitor. Matthew T. Roe, MD, Duke Clinical Research Institute, Durham, N.C., will present the substudy focusing on P2Y12 inhibitor switching in response to routine notification of CYP2C19 clopidogrel metabolizer status following ACS.
- PRAGUE-18: Zuzana Motovska, MD, of Charles University in Prague, will present an unspecified substudy of PRAGUE-18, which in August 2016 showed no difference in safety or efficacy between prasugrel and ticagrelor in AMI patients undergoing primary angioplasty.
Late-Breaking Session 6, quality improvement and patient-centered care
The seven presentations in this session range from findings from the enormous SWEDEHEART registry on how treatments have improved for ST-elevation MI over 20 years, to STIC2IT, a cluster randomized, controlled trial to test whether a novel telepharmacist-based intervention for patients with metabolic syndrome improves medication adherence and disease control.
Other presentations include evaluation of a quality improvement toolkit on AMI in India called ACS QUIK; a trial of a decision support intervention for patients and caregivers offered a heart assist device as destination therapy called DECIDE-LVAD; a national rollout of a clinical guidance framework for the assessment of patients with possible ACS in emergency departments (iCARE-ACS); and a report from the American College of Cardiology’s Mission: Lifeline STEMI ACCELERATOR-2 study.
[email protected]
On Twitter @cardionews
On the third day of the American Heart Association scientific sessions, antithrombotic therapy is the focus of the Late-Breaking Science 5 presentation, at 10:45 a.m.-12 p.m. on Tuesday, Nov. 14, followed by innovative investigations in evaluating quality improvement and patient-centered care interventions in the Late-Breaking Science 6 session, to be held at 3:45-5:15 p.m. Here are some highlights.
Late-Breaking Science 5, antithrombotic therapy
- RE-DUAL PCI: Jonas Oldgren, MD, of Uppsala (Sweden) University, will present an unspecified subgroup analysis from the RE-DUAL PCI (Dual Antithrombotic Therapy With Dabigatran in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary Intervention) trial, focusing on one arm of the study. The main results, presented in August, showed patients with atrial fibrillation who had undergone percutaneous coronary intervention had a lower risk of bleeding if they received dual therapy with dabigatran plus clopidogrel or ticagrelor than did those treated with warfarin, clopidogrel, or ticagrelor.
- POISE-2 PCI: Michelle M. Graham, MD, of the University of Alberta, Edmonton, will present a substudy of POISE-2 focusing on the patients in undergoing noncardiac surgery who had a previous percutaneous coronary intervention. POISE-2, published in 2014, showed that administering aspirin periprocedurally had no effect on the rate of a composite of death or nonfatal MI, but increased the risk of major bleeding.
Dr. Jonas Oldgren - GEMINI-ACS-1: In the main study, the risk of major bleeding was similar between ACS patients treated with a combination of low-dose rivaroxaban and a P2Y12 inhibitor and those treated with aspirin and P2Y12 inhibitor. Matthew T. Roe, MD, Duke Clinical Research Institute, Durham, N.C., will present the substudy focusing on P2Y12 inhibitor switching in response to routine notification of CYP2C19 clopidogrel metabolizer status following ACS.
- PRAGUE-18: Zuzana Motovska, MD, of Charles University in Prague, will present an unspecified substudy of PRAGUE-18, which in August 2016 showed no difference in safety or efficacy between prasugrel and ticagrelor in AMI patients undergoing primary angioplasty.
Late-Breaking Session 6, quality improvement and patient-centered care
The seven presentations in this session range from findings from the enormous SWEDEHEART registry on how treatments have improved for ST-elevation MI over 20 years, to STIC2IT, a cluster randomized, controlled trial to test whether a novel telepharmacist-based intervention for patients with metabolic syndrome improves medication adherence and disease control.
Other presentations include evaluation of a quality improvement toolkit on AMI in India called ACS QUIK; a trial of a decision support intervention for patients and caregivers offered a heart assist device as destination therapy called DECIDE-LVAD; a national rollout of a clinical guidance framework for the assessment of patients with possible ACS in emergency departments (iCARE-ACS); and a report from the American College of Cardiology’s Mission: Lifeline STEMI ACCELERATOR-2 study.
[email protected]
On Twitter @cardionews
On the third day of the American Heart Association scientific sessions, antithrombotic therapy is the focus of the Late-Breaking Science 5 presentation, at 10:45 a.m.-12 p.m. on Tuesday, Nov. 14, followed by innovative investigations in evaluating quality improvement and patient-centered care interventions in the Late-Breaking Science 6 session, to be held at 3:45-5:15 p.m. Here are some highlights.
Late-Breaking Science 5, antithrombotic therapy
- RE-DUAL PCI: Jonas Oldgren, MD, of Uppsala (Sweden) University, will present an unspecified subgroup analysis from the RE-DUAL PCI (Dual Antithrombotic Therapy With Dabigatran in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary Intervention) trial, focusing on one arm of the study. The main results, presented in August, showed patients with atrial fibrillation who had undergone percutaneous coronary intervention had a lower risk of bleeding if they received dual therapy with dabigatran plus clopidogrel or ticagrelor than did those treated with warfarin, clopidogrel, or ticagrelor.
- POISE-2 PCI: Michelle M. Graham, MD, of the University of Alberta, Edmonton, will present a substudy of POISE-2 focusing on the patients in undergoing noncardiac surgery who had a previous percutaneous coronary intervention. POISE-2, published in 2014, showed that administering aspirin periprocedurally had no effect on the rate of a composite of death or nonfatal MI, but increased the risk of major bleeding.
Dr. Jonas Oldgren - GEMINI-ACS-1: In the main study, the risk of major bleeding was similar between ACS patients treated with a combination of low-dose rivaroxaban and a P2Y12 inhibitor and those treated with aspirin and P2Y12 inhibitor. Matthew T. Roe, MD, Duke Clinical Research Institute, Durham, N.C., will present the substudy focusing on P2Y12 inhibitor switching in response to routine notification of CYP2C19 clopidogrel metabolizer status following ACS.
- PRAGUE-18: Zuzana Motovska, MD, of Charles University in Prague, will present an unspecified substudy of PRAGUE-18, which in August 2016 showed no difference in safety or efficacy between prasugrel and ticagrelor in AMI patients undergoing primary angioplasty.
Late-Breaking Session 6, quality improvement and patient-centered care
The seven presentations in this session range from findings from the enormous SWEDEHEART registry on how treatments have improved for ST-elevation MI over 20 years, to STIC2IT, a cluster randomized, controlled trial to test whether a novel telepharmacist-based intervention for patients with metabolic syndrome improves medication adherence and disease control.
Other presentations include evaluation of a quality improvement toolkit on AMI in India called ACS QUIK; a trial of a decision support intervention for patients and caregivers offered a heart assist device as destination therapy called DECIDE-LVAD; a national rollout of a clinical guidance framework for the assessment of patients with possible ACS in emergency departments (iCARE-ACS); and a report from the American College of Cardiology’s Mission: Lifeline STEMI ACCELERATOR-2 study.
[email protected]
On Twitter @cardionews
Psych evaluation identifies bariatric surgery patients who do less well
NATIONAL HARBOR, MD. – Psychological screening prior to bariatric surgery is not effective for identifying who will do poorly after the procedure, but it can identify patients who are at risk for less weight loss and likely to benefit from additional support, according to one of the largest studies designed to evaluate the predictive accuracy of this screening. The results were presented at Obesity Week 2017.
“Psychological evaluations should not be used to exclude patients, because we do not appear to be very good at predicting who does well,” said Nina E. Boulard, PhD, a psychologist who currently performs preoperative psychological screening of bariatric surgery candidates at Eastern Maine Medical Center, Bangor. Rather, “our evaluations identify those who need to be followed more closely so we can intervene early when patients struggle,” she said at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
The two primary outcomes of interest were the ability to predict postsurgical mental health issues and the ability to predict difficulty in complying with behavioral changes. Percent excess weight loss (EWL) was also monitored. For mental health screening, the protocol included clinical interviews augmented with standardized testing, such as the Minnesota Multiphasic Personality Inventory-2-Restuctured Form (MMPI-2-RF). Patients were placed into five risk categories: low, low-moderate, moderate, moderate-high, and high.
For compliance, the patient evaluation was based primarily on interviews capturing self-reports of adherence to presurgical dietary and other lifestyle recommendations. Patients were also asked about eating behaviors, such as binge eating, and history of sexual abuse and attention-deficit/hyperactivity disorder and other neurodevelopmental issues.
The psychological screening report is provided to the surgeon, who ultimately decides whether patients go on to surgery. In this analysis, relatively few high-risk patients were included because these patients, such as those with active psychosis, uncontrolled binge eating, or severe depression, were excluded from surgery and therefore did not generate postsurgical follow-up data.
As has been reported by others, Dr. Boulard reported that no single standardized test or clinical variable was an effective predictor of “who will and will not struggle” psychologically after surgery. However, after adjusting for age, gender, presurgery weight, diabetes history, and surgery type, several variables were associated with reduced proportion EWL. These included anxiety (P = .02), ADHD (P = .01), and prior hospitalization of a psychological indication (P less than .05). History of sexual abuse was predictive of reduced percentage EWL 1 year but not 2 years after surgery.
“So, what this tells us is the clinical interpretation of the big picture might be important,” Dr. Boulard commented.
The presurgical psychological screening was not predictive of compliance, a result that Dr. Boulard labeled as “surprising.” She speculated that because weight loss in the first 2 years after bariatric surgery is relatively uniform, longer follow-up, such as 5 years, might be needed to capture the impact of patients predicted to have poor compliance.
Importantly, percent EWL remained high even among patients with risk factors associated with mental health challenges after surgery, according to Dr. Boulard. She stressed that even those with less weight loss “did not do poorly.” Rather, the relative differences in postsurgical weight loss for those who were predicted to struggle versus those who were not was “a matter of degrees.”
While Dr. Boulard acknowledged a prospective study using a standardized psychological screening protocol would be appropriate to validate the findings of this study, the study results have already changed practice at her institution.
“We are following the at-risk patients more closely, so we can intervene quickly if there are issues after surgery,” Dr. Boulard explained. The question raised by this study is, “can we bring them [patients at higher risk] to a higher level of response so they are just as successful” as those without risk factors identified in psychological screening.
Dr. Boulard reports no financial relationships relevant to this topic.
NATIONAL HARBOR, MD. – Psychological screening prior to bariatric surgery is not effective for identifying who will do poorly after the procedure, but it can identify patients who are at risk for less weight loss and likely to benefit from additional support, according to one of the largest studies designed to evaluate the predictive accuracy of this screening. The results were presented at Obesity Week 2017.
“Psychological evaluations should not be used to exclude patients, because we do not appear to be very good at predicting who does well,” said Nina E. Boulard, PhD, a psychologist who currently performs preoperative psychological screening of bariatric surgery candidates at Eastern Maine Medical Center, Bangor. Rather, “our evaluations identify those who need to be followed more closely so we can intervene early when patients struggle,” she said at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
The two primary outcomes of interest were the ability to predict postsurgical mental health issues and the ability to predict difficulty in complying with behavioral changes. Percent excess weight loss (EWL) was also monitored. For mental health screening, the protocol included clinical interviews augmented with standardized testing, such as the Minnesota Multiphasic Personality Inventory-2-Restuctured Form (MMPI-2-RF). Patients were placed into five risk categories: low, low-moderate, moderate, moderate-high, and high.
For compliance, the patient evaluation was based primarily on interviews capturing self-reports of adherence to presurgical dietary and other lifestyle recommendations. Patients were also asked about eating behaviors, such as binge eating, and history of sexual abuse and attention-deficit/hyperactivity disorder and other neurodevelopmental issues.
The psychological screening report is provided to the surgeon, who ultimately decides whether patients go on to surgery. In this analysis, relatively few high-risk patients were included because these patients, such as those with active psychosis, uncontrolled binge eating, or severe depression, were excluded from surgery and therefore did not generate postsurgical follow-up data.
As has been reported by others, Dr. Boulard reported that no single standardized test or clinical variable was an effective predictor of “who will and will not struggle” psychologically after surgery. However, after adjusting for age, gender, presurgery weight, diabetes history, and surgery type, several variables were associated with reduced proportion EWL. These included anxiety (P = .02), ADHD (P = .01), and prior hospitalization of a psychological indication (P less than .05). History of sexual abuse was predictive of reduced percentage EWL 1 year but not 2 years after surgery.
“So, what this tells us is the clinical interpretation of the big picture might be important,” Dr. Boulard commented.
The presurgical psychological screening was not predictive of compliance, a result that Dr. Boulard labeled as “surprising.” She speculated that because weight loss in the first 2 years after bariatric surgery is relatively uniform, longer follow-up, such as 5 years, might be needed to capture the impact of patients predicted to have poor compliance.
Importantly, percent EWL remained high even among patients with risk factors associated with mental health challenges after surgery, according to Dr. Boulard. She stressed that even those with less weight loss “did not do poorly.” Rather, the relative differences in postsurgical weight loss for those who were predicted to struggle versus those who were not was “a matter of degrees.”
While Dr. Boulard acknowledged a prospective study using a standardized psychological screening protocol would be appropriate to validate the findings of this study, the study results have already changed practice at her institution.
“We are following the at-risk patients more closely, so we can intervene quickly if there are issues after surgery,” Dr. Boulard explained. The question raised by this study is, “can we bring them [patients at higher risk] to a higher level of response so they are just as successful” as those without risk factors identified in psychological screening.
Dr. Boulard reports no financial relationships relevant to this topic.
NATIONAL HARBOR, MD. – Psychological screening prior to bariatric surgery is not effective for identifying who will do poorly after the procedure, but it can identify patients who are at risk for less weight loss and likely to benefit from additional support, according to one of the largest studies designed to evaluate the predictive accuracy of this screening. The results were presented at Obesity Week 2017.
“Psychological evaluations should not be used to exclude patients, because we do not appear to be very good at predicting who does well,” said Nina E. Boulard, PhD, a psychologist who currently performs preoperative psychological screening of bariatric surgery candidates at Eastern Maine Medical Center, Bangor. Rather, “our evaluations identify those who need to be followed more closely so we can intervene early when patients struggle,” she said at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
The two primary outcomes of interest were the ability to predict postsurgical mental health issues and the ability to predict difficulty in complying with behavioral changes. Percent excess weight loss (EWL) was also monitored. For mental health screening, the protocol included clinical interviews augmented with standardized testing, such as the Minnesota Multiphasic Personality Inventory-2-Restuctured Form (MMPI-2-RF). Patients were placed into five risk categories: low, low-moderate, moderate, moderate-high, and high.
For compliance, the patient evaluation was based primarily on interviews capturing self-reports of adherence to presurgical dietary and other lifestyle recommendations. Patients were also asked about eating behaviors, such as binge eating, and history of sexual abuse and attention-deficit/hyperactivity disorder and other neurodevelopmental issues.
The psychological screening report is provided to the surgeon, who ultimately decides whether patients go on to surgery. In this analysis, relatively few high-risk patients were included because these patients, such as those with active psychosis, uncontrolled binge eating, or severe depression, were excluded from surgery and therefore did not generate postsurgical follow-up data.
As has been reported by others, Dr. Boulard reported that no single standardized test or clinical variable was an effective predictor of “who will and will not struggle” psychologically after surgery. However, after adjusting for age, gender, presurgery weight, diabetes history, and surgery type, several variables were associated with reduced proportion EWL. These included anxiety (P = .02), ADHD (P = .01), and prior hospitalization of a psychological indication (P less than .05). History of sexual abuse was predictive of reduced percentage EWL 1 year but not 2 years after surgery.
“So, what this tells us is the clinical interpretation of the big picture might be important,” Dr. Boulard commented.
The presurgical psychological screening was not predictive of compliance, a result that Dr. Boulard labeled as “surprising.” She speculated that because weight loss in the first 2 years after bariatric surgery is relatively uniform, longer follow-up, such as 5 years, might be needed to capture the impact of patients predicted to have poor compliance.
Importantly, percent EWL remained high even among patients with risk factors associated with mental health challenges after surgery, according to Dr. Boulard. She stressed that even those with less weight loss “did not do poorly.” Rather, the relative differences in postsurgical weight loss for those who were predicted to struggle versus those who were not was “a matter of degrees.”
While Dr. Boulard acknowledged a prospective study using a standardized psychological screening protocol would be appropriate to validate the findings of this study, the study results have already changed practice at her institution.
“We are following the at-risk patients more closely, so we can intervene quickly if there are issues after surgery,” Dr. Boulard explained. The question raised by this study is, “can we bring them [patients at higher risk] to a higher level of response so they are just as successful” as those without risk factors identified in psychological screening.
Dr. Boulard reports no financial relationships relevant to this topic.
AT OBESITY WEEK 2017
Key clinical point: Psychological screening prior to bariatric surgery selects patients at risk for reduced postoperative weight loss.
Major finding: Prior psychological hospitalization (P less than .05) and number of previous psychological diagnoses (P = .04) are among markers of less postop weight loss.
Data source: Retrospective analysis.
Disclosures: Dr. Boulard reports no financial relationships relevant to this topic.