User login
Sneak Peak: The Hospital Leader Blog “The Impact of Hospital Design on Health – for Patients AND Providers”
I was rounding on the inpatient general medicine teaching service last weekend and offered to meet my team of students and residents in the “resident library” on Saturday morning. (Although it holds the name “library,” there were no books or periodicals to be seen.) I had not been in the library for many months and was struck by a few things as I entered.
It is a dimly lit space, lined on three of the four walls with rickety desks and desktop computers all facing the walls. The walls are painted an off-white color with innumerable dings and nicks, presumably accumulated over the course of years. There was a string of garland in the shape of a Christmas tree pinned to the wall (P.S. It is March), the entire left side of which was sagging and misshapen. There were various tattered and coffee-stained papers scattered haphazardly throughout the room, including what appeared to be progress notes and test results printed from the EHR; a few worn ECGs; a telemetry strip; even a few (REALLY old, no doubt) chest x-ray films. Lining the fourth wall was a large foldable table, topped with crumbs and food scraps, a half-eaten chocolate Bundt cake, and scattered napkins and utensils, some of which appeared to be used. The one exterior-facing wall had a row of windows with crinkled blinds, some completely closed, others opened at awkward angles and seemingly stuck in place. There was a cadre of chairs in the room, none matching, all in various stages of disrepair, with one completely missing an armrest and another tucked in the corner, probably needing the addition of a handwritten sign “BRokEn.”
This library is a place where the students, interns, and residents go for a bit of a safe haven. They can take their coats off, sit down, have their own computer space, answer pages, and complain about their woes. They can bounce questions off each other, vent frustrations, find the humor in a situation, and just be themselves. So,But what struck me about their sanctuary is that it is totally and utterly depressing. And it was as if they didn’t even notice the chaos and filth laying everywhere around them. I find it impossible to believe that it does not have an effect on their mood and outlook. Although we are all social animals, and we have a real need to congregate and connect with one another, is this really the best environment to do that?
Read the full text of this blog post at hospitalleader.org.
Dr. Scheurer is a clinical hospitalist and the medical director of quality and safety at the Medical University of South Carolina in Charleston.
Also on The Hospital Leader…
- Should Overuse Be Considered an Adverse Event By Chris Moriates, MD
- Pulling the Welcome Mat Out from Under Our Colleagues By Brett Hendel-Paterson, MD
- The Upside of Anger By Tracy Cardin, ACNP-BC, SFHM
- Does Your Onboarding Process Really Get Folks on Board? By Leslie Flores, MH, SFHM
- A GIF Is Worth 3000 Words: Introducing #Visual Abstract for #JHMChat By Charlie Wray, DO
I was rounding on the inpatient general medicine teaching service last weekend and offered to meet my team of students and residents in the “resident library” on Saturday morning. (Although it holds the name “library,” there were no books or periodicals to be seen.) I had not been in the library for many months and was struck by a few things as I entered.
It is a dimly lit space, lined on three of the four walls with rickety desks and desktop computers all facing the walls. The walls are painted an off-white color with innumerable dings and nicks, presumably accumulated over the course of years. There was a string of garland in the shape of a Christmas tree pinned to the wall (P.S. It is March), the entire left side of which was sagging and misshapen. There were various tattered and coffee-stained papers scattered haphazardly throughout the room, including what appeared to be progress notes and test results printed from the EHR; a few worn ECGs; a telemetry strip; even a few (REALLY old, no doubt) chest x-ray films. Lining the fourth wall was a large foldable table, topped with crumbs and food scraps, a half-eaten chocolate Bundt cake, and scattered napkins and utensils, some of which appeared to be used. The one exterior-facing wall had a row of windows with crinkled blinds, some completely closed, others opened at awkward angles and seemingly stuck in place. There was a cadre of chairs in the room, none matching, all in various stages of disrepair, with one completely missing an armrest and another tucked in the corner, probably needing the addition of a handwritten sign “BRokEn.”
This library is a place where the students, interns, and residents go for a bit of a safe haven. They can take their coats off, sit down, have their own computer space, answer pages, and complain about their woes. They can bounce questions off each other, vent frustrations, find the humor in a situation, and just be themselves. So,But what struck me about their sanctuary is that it is totally and utterly depressing. And it was as if they didn’t even notice the chaos and filth laying everywhere around them. I find it impossible to believe that it does not have an effect on their mood and outlook. Although we are all social animals, and we have a real need to congregate and connect with one another, is this really the best environment to do that?
Read the full text of this blog post at hospitalleader.org.
Dr. Scheurer is a clinical hospitalist and the medical director of quality and safety at the Medical University of South Carolina in Charleston.
Also on The Hospital Leader…
- Should Overuse Be Considered an Adverse Event By Chris Moriates, MD
- Pulling the Welcome Mat Out from Under Our Colleagues By Brett Hendel-Paterson, MD
- The Upside of Anger By Tracy Cardin, ACNP-BC, SFHM
- Does Your Onboarding Process Really Get Folks on Board? By Leslie Flores, MH, SFHM
- A GIF Is Worth 3000 Words: Introducing #Visual Abstract for #JHMChat By Charlie Wray, DO
I was rounding on the inpatient general medicine teaching service last weekend and offered to meet my team of students and residents in the “resident library” on Saturday morning. (Although it holds the name “library,” there were no books or periodicals to be seen.) I had not been in the library for many months and was struck by a few things as I entered.
It is a dimly lit space, lined on three of the four walls with rickety desks and desktop computers all facing the walls. The walls are painted an off-white color with innumerable dings and nicks, presumably accumulated over the course of years. There was a string of garland in the shape of a Christmas tree pinned to the wall (P.S. It is March), the entire left side of which was sagging and misshapen. There were various tattered and coffee-stained papers scattered haphazardly throughout the room, including what appeared to be progress notes and test results printed from the EHR; a few worn ECGs; a telemetry strip; even a few (REALLY old, no doubt) chest x-ray films. Lining the fourth wall was a large foldable table, topped with crumbs and food scraps, a half-eaten chocolate Bundt cake, and scattered napkins and utensils, some of which appeared to be used. The one exterior-facing wall had a row of windows with crinkled blinds, some completely closed, others opened at awkward angles and seemingly stuck in place. There was a cadre of chairs in the room, none matching, all in various stages of disrepair, with one completely missing an armrest and another tucked in the corner, probably needing the addition of a handwritten sign “BRokEn.”
This library is a place where the students, interns, and residents go for a bit of a safe haven. They can take their coats off, sit down, have their own computer space, answer pages, and complain about their woes. They can bounce questions off each other, vent frustrations, find the humor in a situation, and just be themselves. So,But what struck me about their sanctuary is that it is totally and utterly depressing. And it was as if they didn’t even notice the chaos and filth laying everywhere around them. I find it impossible to believe that it does not have an effect on their mood and outlook. Although we are all social animals, and we have a real need to congregate and connect with one another, is this really the best environment to do that?
Read the full text of this blog post at hospitalleader.org.
Dr. Scheurer is a clinical hospitalist and the medical director of quality and safety at the Medical University of South Carolina in Charleston.
Also on The Hospital Leader…
- Should Overuse Be Considered an Adverse Event By Chris Moriates, MD
- Pulling the Welcome Mat Out from Under Our Colleagues By Brett Hendel-Paterson, MD
- The Upside of Anger By Tracy Cardin, ACNP-BC, SFHM
- Does Your Onboarding Process Really Get Folks on Board? By Leslie Flores, MH, SFHM
- A GIF Is Worth 3000 Words: Introducing #Visual Abstract for #JHMChat By Charlie Wray, DO
Trump overturns Title X family planning rule
President Donald Trump has signed a resolution that could strip public funding from U.S. clinics that provide abortions, including Planned Parenthood.
The April 13 action overturns a rule imposed by the Obama administration regarding how states can distribute Title X funds, money that assists low-income patients in accessing family planning and preventive health services. The Obama administration’s rule had reinforced existing law that states cannot withhold Title X funding from medical providers for reasons other than poor performance or noncompliance. In recent years, states have begun restricting participation by certain types of providers in the Title X program, such as those that provide abortions.
“Our federal system was set up to allow states to address the unique needs of their own populations when possible, especially [when it] comes to programs as important and sensitive as family planning,” Mr. Spicer said. “With the bill signing, the president has restored respect to states’ rights on this particular issue.”
The Planned Parenthood Federation of America condemned President Trump’s measure, calling it an effort to undermine women’s health and overturn a rule that reinforced protections for millions of patients who rely on Title X for health care.
“Four million people depend on the Title X family planning program, and by signing this bill, President Trump disregards their health and well-being,” Dawn Laguens, executive vice president of the Planned Parenthood Federation of America said in a statement. “We should build on the tremendous progress made in this country with expanded access to birth control, instead of enacting policies that take us backward. Too many women still face barriers to health care, especially young women, women of color, those who live in rural areas, and women with low incomes.”
Since 2011, 13 states have restricted participation in the Title X program based on reasons other than the providers’ ability to provide the services, according to a summary of the 2016 rule. For example, Texas in 2011 reduced its contribution to family planning services, and also restructured Title X funds using a tiered approach. The combination of these actions decreased the Title X provider network in Texas from 48 to 36 providers and reduced the number of patients served from 259,606 in 2011 to 166,538 in 2015.
By statute, Title X funds cannot be used for abortions. Title X provides family planning and related reproductive health services such as testing and counseling for sexually transmitted diseases, contraceptive methods including method-specific counseling, breast and cervical cancer screening, and pregnancy tests and counseling.
The Susan B. Anthony List, an antiabortion organization, praised President Trump’s resolution and said it’s another step toward defunding Planned Parenthood and keeping taxpayer dollars away from abortion businesses.
“Prioritizing funding away from Planned Parenthood to comprehensive health care alternatives is a winning issue,” Susan B. Anthony List president, Marjorie Dannenfelser, said in a statement. “We expect to see Congress continue its efforts to redirect additional taxpayer funding away from Planned Parenthood through pro-life health care reform after the spring recess.”
[email protected]
On Twitter @legal_med
President Donald Trump has signed a resolution that could strip public funding from U.S. clinics that provide abortions, including Planned Parenthood.
The April 13 action overturns a rule imposed by the Obama administration regarding how states can distribute Title X funds, money that assists low-income patients in accessing family planning and preventive health services. The Obama administration’s rule had reinforced existing law that states cannot withhold Title X funding from medical providers for reasons other than poor performance or noncompliance. In recent years, states have begun restricting participation by certain types of providers in the Title X program, such as those that provide abortions.
“Our federal system was set up to allow states to address the unique needs of their own populations when possible, especially [when it] comes to programs as important and sensitive as family planning,” Mr. Spicer said. “With the bill signing, the president has restored respect to states’ rights on this particular issue.”
The Planned Parenthood Federation of America condemned President Trump’s measure, calling it an effort to undermine women’s health and overturn a rule that reinforced protections for millions of patients who rely on Title X for health care.
“Four million people depend on the Title X family planning program, and by signing this bill, President Trump disregards their health and well-being,” Dawn Laguens, executive vice president of the Planned Parenthood Federation of America said in a statement. “We should build on the tremendous progress made in this country with expanded access to birth control, instead of enacting policies that take us backward. Too many women still face barriers to health care, especially young women, women of color, those who live in rural areas, and women with low incomes.”
Since 2011, 13 states have restricted participation in the Title X program based on reasons other than the providers’ ability to provide the services, according to a summary of the 2016 rule. For example, Texas in 2011 reduced its contribution to family planning services, and also restructured Title X funds using a tiered approach. The combination of these actions decreased the Title X provider network in Texas from 48 to 36 providers and reduced the number of patients served from 259,606 in 2011 to 166,538 in 2015.
By statute, Title X funds cannot be used for abortions. Title X provides family planning and related reproductive health services such as testing and counseling for sexually transmitted diseases, contraceptive methods including method-specific counseling, breast and cervical cancer screening, and pregnancy tests and counseling.
The Susan B. Anthony List, an antiabortion organization, praised President Trump’s resolution and said it’s another step toward defunding Planned Parenthood and keeping taxpayer dollars away from abortion businesses.
“Prioritizing funding away from Planned Parenthood to comprehensive health care alternatives is a winning issue,” Susan B. Anthony List president, Marjorie Dannenfelser, said in a statement. “We expect to see Congress continue its efforts to redirect additional taxpayer funding away from Planned Parenthood through pro-life health care reform after the spring recess.”
[email protected]
On Twitter @legal_med
President Donald Trump has signed a resolution that could strip public funding from U.S. clinics that provide abortions, including Planned Parenthood.
The April 13 action overturns a rule imposed by the Obama administration regarding how states can distribute Title X funds, money that assists low-income patients in accessing family planning and preventive health services. The Obama administration’s rule had reinforced existing law that states cannot withhold Title X funding from medical providers for reasons other than poor performance or noncompliance. In recent years, states have begun restricting participation by certain types of providers in the Title X program, such as those that provide abortions.
“Our federal system was set up to allow states to address the unique needs of their own populations when possible, especially [when it] comes to programs as important and sensitive as family planning,” Mr. Spicer said. “With the bill signing, the president has restored respect to states’ rights on this particular issue.”
The Planned Parenthood Federation of America condemned President Trump’s measure, calling it an effort to undermine women’s health and overturn a rule that reinforced protections for millions of patients who rely on Title X for health care.
“Four million people depend on the Title X family planning program, and by signing this bill, President Trump disregards their health and well-being,” Dawn Laguens, executive vice president of the Planned Parenthood Federation of America said in a statement. “We should build on the tremendous progress made in this country with expanded access to birth control, instead of enacting policies that take us backward. Too many women still face barriers to health care, especially young women, women of color, those who live in rural areas, and women with low incomes.”
Since 2011, 13 states have restricted participation in the Title X program based on reasons other than the providers’ ability to provide the services, according to a summary of the 2016 rule. For example, Texas in 2011 reduced its contribution to family planning services, and also restructured Title X funds using a tiered approach. The combination of these actions decreased the Title X provider network in Texas from 48 to 36 providers and reduced the number of patients served from 259,606 in 2011 to 166,538 in 2015.
By statute, Title X funds cannot be used for abortions. Title X provides family planning and related reproductive health services such as testing and counseling for sexually transmitted diseases, contraceptive methods including method-specific counseling, breast and cervical cancer screening, and pregnancy tests and counseling.
The Susan B. Anthony List, an antiabortion organization, praised President Trump’s resolution and said it’s another step toward defunding Planned Parenthood and keeping taxpayer dollars away from abortion businesses.
“Prioritizing funding away from Planned Parenthood to comprehensive health care alternatives is a winning issue,” Susan B. Anthony List president, Marjorie Dannenfelser, said in a statement. “We expect to see Congress continue its efforts to redirect additional taxpayer funding away from Planned Parenthood through pro-life health care reform after the spring recess.”
[email protected]
On Twitter @legal_med
Arthritis Is On the Rise—But There Are Ways to Help Reduce the Effects
Arthritis aches and pains are not a normal part of aging. Nonetheless, approximately 54 million American adults who took the CDC’s National Health Survey said their doctor had diagnosed them with arthritis. That’s about 1 in 4 US adults, the majority of whom are of working age.
Related: Taking Steps to Reduce Arthritis Pain
Arthritis can make it hard to lift a cup, let alone a bag of groceries or a heavy briefcase. The percentage of adults with arthritis who have activity limitations grew from 35.9% in 2002 to 42.8% in 2014, a 20% increase independent of the aging of the population.
Research has shown that engaging in physical activity can reduce arthritis symptoms by up to 40%. But one third of adults with arthritis say they don’t engage in physical activity during leisure time. And, while they also can reduce their symptoms by participating in disease management education programs, only 1 in 10 has taken part in such programs.
Related: Lessons Learned From the RACAT Trial: A Comparison of Rheumatoid Arthritis Therapies
“It’s extremely important for primary care providers to encourage their patients with arthritis to be physically active,” says CDC epidemiologist Kamil Barbour, PhD. But Barbour adds that it’s just as important to motivate patients to attend education programs. The CDC says adults with arthritis are significantly more likely to attend an education program when a health care provider has recommended it.
Arthritis aches and pains are not a normal part of aging. Nonetheless, approximately 54 million American adults who took the CDC’s National Health Survey said their doctor had diagnosed them with arthritis. That’s about 1 in 4 US adults, the majority of whom are of working age.
Related: Taking Steps to Reduce Arthritis Pain
Arthritis can make it hard to lift a cup, let alone a bag of groceries or a heavy briefcase. The percentage of adults with arthritis who have activity limitations grew from 35.9% in 2002 to 42.8% in 2014, a 20% increase independent of the aging of the population.
Research has shown that engaging in physical activity can reduce arthritis symptoms by up to 40%. But one third of adults with arthritis say they don’t engage in physical activity during leisure time. And, while they also can reduce their symptoms by participating in disease management education programs, only 1 in 10 has taken part in such programs.
Related: Lessons Learned From the RACAT Trial: A Comparison of Rheumatoid Arthritis Therapies
“It’s extremely important for primary care providers to encourage their patients with arthritis to be physically active,” says CDC epidemiologist Kamil Barbour, PhD. But Barbour adds that it’s just as important to motivate patients to attend education programs. The CDC says adults with arthritis are significantly more likely to attend an education program when a health care provider has recommended it.
Arthritis aches and pains are not a normal part of aging. Nonetheless, approximately 54 million American adults who took the CDC’s National Health Survey said their doctor had diagnosed them with arthritis. That’s about 1 in 4 US adults, the majority of whom are of working age.
Related: Taking Steps to Reduce Arthritis Pain
Arthritis can make it hard to lift a cup, let alone a bag of groceries or a heavy briefcase. The percentage of adults with arthritis who have activity limitations grew from 35.9% in 2002 to 42.8% in 2014, a 20% increase independent of the aging of the population.
Research has shown that engaging in physical activity can reduce arthritis symptoms by up to 40%. But one third of adults with arthritis say they don’t engage in physical activity during leisure time. And, while they also can reduce their symptoms by participating in disease management education programs, only 1 in 10 has taken part in such programs.
Related: Lessons Learned From the RACAT Trial: A Comparison of Rheumatoid Arthritis Therapies
“It’s extremely important for primary care providers to encourage their patients with arthritis to be physically active,” says CDC epidemiologist Kamil Barbour, PhD. But Barbour adds that it’s just as important to motivate patients to attend education programs. The CDC says adults with arthritis are significantly more likely to attend an education program when a health care provider has recommended it.
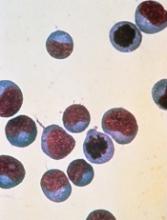
Nanoparticles allow for creation of CAR T cells in vivo
Researchers say they have developed biodegradable nanoparticles that can be used to genetically reprogram T cells while they are still in the body.
The nanoparticles were able to program T cells with genes encoding leukemia-specific chimeric antigen receptors (CARs).
The resulting CAR T cells were able to eliminate leukemia or slow the progression of disease in a mouse model of B-cell acute lymphoblastic leukemia (B-ALL).
Researchers reported these results in Nature Nanotechnology.
“Our technology is the first that we know of to quickly program tumor-recognizing capabilities into T cells without extracting them for laboratory manipulation,” said Matthias Stephan, MD, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“The reprogrammed cells begin to work within 24 to 48 hours and continue to produce these receptors for weeks. This suggests that our technology has the potential to allow the immune system to quickly mount a strong enough response to destroy cancerous cells before the disease becomes fatal.”
Dr Stephan and his colleagues designed their nanoparticles to carry genes that encode for CARs intended to target and eliminate B-ALL. The nanoparticles are coated with ligands that make them seek out and bind to T cells.
When a nanoparticle binds to a T cell, the cell engulfs the particle. The nanoparticle then travels to the cell’s nucleus and dissolves.
The CAR genes integrate into chromosomes housed in the nucleus, making it possible for the T cells to begin decoding the new genes and producing CARs within 1 or 2 days.
Once they determined their CAR-carrying nanoparticles reprogrammed a noticeable percentage of T cells, the researchers tested the T cells’ efficacy in a mouse model of B-ALL.
The team infused the nanoparticles into 10 mice and found the treatment eradicated tumors in 7 of the animals. The other 3 mice “showed substantial regression” of leukemia, the researchers said.
On average, mice that received CAR-carrying nanoparticles had a 58-day improvement in survival compared to control mice.
Mice that received the nanoparticles also had “dramatically reduced” B-cell numbers in their spleens. The researchers noted that this is consistent with the reversible B-cell aplasia observed in patients who receive conventional CD19 CAR T-cell therapy.
Dr Stephan and his colleagues also tested conventional CAR T-cell therapy in the B-ALL mouse model. The mice received cyclophosphamide followed by CAR T cells created ex vivo.
These mice had significantly better survival than controls, but their survival was comparable to that of the mice that received the CAR-carrying nanoparticles.
Although these nanoparticles are several steps away from the clinic, Dr Stephan said he imagines a future in which nanoparticles transform cell-based immunotherapies into easily administered, off-the-shelf treatments that are available anywhere.
“I’ve never had cancer, but if I did get a cancer diagnosis, I would want to start treatment right away,” Dr Stephan said. “I want to make cellular immunotherapy a treatment option the day of diagnosis and have it able to be done in an outpatient setting near where people live.” ![]()
Researchers say they have developed biodegradable nanoparticles that can be used to genetically reprogram T cells while they are still in the body.
The nanoparticles were able to program T cells with genes encoding leukemia-specific chimeric antigen receptors (CARs).
The resulting CAR T cells were able to eliminate leukemia or slow the progression of disease in a mouse model of B-cell acute lymphoblastic leukemia (B-ALL).
Researchers reported these results in Nature Nanotechnology.
“Our technology is the first that we know of to quickly program tumor-recognizing capabilities into T cells without extracting them for laboratory manipulation,” said Matthias Stephan, MD, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“The reprogrammed cells begin to work within 24 to 48 hours and continue to produce these receptors for weeks. This suggests that our technology has the potential to allow the immune system to quickly mount a strong enough response to destroy cancerous cells before the disease becomes fatal.”
Dr Stephan and his colleagues designed their nanoparticles to carry genes that encode for CARs intended to target and eliminate B-ALL. The nanoparticles are coated with ligands that make them seek out and bind to T cells.
When a nanoparticle binds to a T cell, the cell engulfs the particle. The nanoparticle then travels to the cell’s nucleus and dissolves.
The CAR genes integrate into chromosomes housed in the nucleus, making it possible for the T cells to begin decoding the new genes and producing CARs within 1 or 2 days.
Once they determined their CAR-carrying nanoparticles reprogrammed a noticeable percentage of T cells, the researchers tested the T cells’ efficacy in a mouse model of B-ALL.
The team infused the nanoparticles into 10 mice and found the treatment eradicated tumors in 7 of the animals. The other 3 mice “showed substantial regression” of leukemia, the researchers said.
On average, mice that received CAR-carrying nanoparticles had a 58-day improvement in survival compared to control mice.
Mice that received the nanoparticles also had “dramatically reduced” B-cell numbers in their spleens. The researchers noted that this is consistent with the reversible B-cell aplasia observed in patients who receive conventional CD19 CAR T-cell therapy.
Dr Stephan and his colleagues also tested conventional CAR T-cell therapy in the B-ALL mouse model. The mice received cyclophosphamide followed by CAR T cells created ex vivo.
These mice had significantly better survival than controls, but their survival was comparable to that of the mice that received the CAR-carrying nanoparticles.
Although these nanoparticles are several steps away from the clinic, Dr Stephan said he imagines a future in which nanoparticles transform cell-based immunotherapies into easily administered, off-the-shelf treatments that are available anywhere.
“I’ve never had cancer, but if I did get a cancer diagnosis, I would want to start treatment right away,” Dr Stephan said. “I want to make cellular immunotherapy a treatment option the day of diagnosis and have it able to be done in an outpatient setting near where people live.” ![]()
Researchers say they have developed biodegradable nanoparticles that can be used to genetically reprogram T cells while they are still in the body.
The nanoparticles were able to program T cells with genes encoding leukemia-specific chimeric antigen receptors (CARs).
The resulting CAR T cells were able to eliminate leukemia or slow the progression of disease in a mouse model of B-cell acute lymphoblastic leukemia (B-ALL).
Researchers reported these results in Nature Nanotechnology.
“Our technology is the first that we know of to quickly program tumor-recognizing capabilities into T cells without extracting them for laboratory manipulation,” said Matthias Stephan, MD, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“The reprogrammed cells begin to work within 24 to 48 hours and continue to produce these receptors for weeks. This suggests that our technology has the potential to allow the immune system to quickly mount a strong enough response to destroy cancerous cells before the disease becomes fatal.”
Dr Stephan and his colleagues designed their nanoparticles to carry genes that encode for CARs intended to target and eliminate B-ALL. The nanoparticles are coated with ligands that make them seek out and bind to T cells.
When a nanoparticle binds to a T cell, the cell engulfs the particle. The nanoparticle then travels to the cell’s nucleus and dissolves.
The CAR genes integrate into chromosomes housed in the nucleus, making it possible for the T cells to begin decoding the new genes and producing CARs within 1 or 2 days.
Once they determined their CAR-carrying nanoparticles reprogrammed a noticeable percentage of T cells, the researchers tested the T cells’ efficacy in a mouse model of B-ALL.
The team infused the nanoparticles into 10 mice and found the treatment eradicated tumors in 7 of the animals. The other 3 mice “showed substantial regression” of leukemia, the researchers said.
On average, mice that received CAR-carrying nanoparticles had a 58-day improvement in survival compared to control mice.
Mice that received the nanoparticles also had “dramatically reduced” B-cell numbers in their spleens. The researchers noted that this is consistent with the reversible B-cell aplasia observed in patients who receive conventional CD19 CAR T-cell therapy.
Dr Stephan and his colleagues also tested conventional CAR T-cell therapy in the B-ALL mouse model. The mice received cyclophosphamide followed by CAR T cells created ex vivo.
These mice had significantly better survival than controls, but their survival was comparable to that of the mice that received the CAR-carrying nanoparticles.
Although these nanoparticles are several steps away from the clinic, Dr Stephan said he imagines a future in which nanoparticles transform cell-based immunotherapies into easily administered, off-the-shelf treatments that are available anywhere.
“I’ve never had cancer, but if I did get a cancer diagnosis, I would want to start treatment right away,” Dr Stephan said. “I want to make cellular immunotherapy a treatment option the day of diagnosis and have it able to be done in an outpatient setting near where people live.” ![]()
Health Canada expands approval of daratumumab in MM
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat MM patients who have received at least 1 prior therapy.
Health Canada granted daratumumab priority review for this indication due to a high unmet medical need in patients with MM.
When a drug is granted priority review, Health Canada aims to complete its review of the drug within 180 days from the time an application is submitted.
Health Canada grants priority review to products intended for the treatment, prevention, or diagnosis of serious, life-threatening, or severely debilitating diseases or conditions.
About daratumumab
Daratumumab is a human IgG1k monoclonal antibody that binds to CD38, which is highly expressed on the surface of MM cells.
The drug is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab.
Daratumumab received conditional approval in Canada last year.
In June 2016, Health Canada issued a Notice of Compliance with Conditions approving daratumumab for MM patients who had received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or patients who are refractory to both a proteasome inhibitor and an immunomodulatory agent.
Phase 3 trial data
Health Canada’s expanded approval for daratumumab is based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October 2016.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August 2016. ![]()
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat MM patients who have received at least 1 prior therapy.
Health Canada granted daratumumab priority review for this indication due to a high unmet medical need in patients with MM.
When a drug is granted priority review, Health Canada aims to complete its review of the drug within 180 days from the time an application is submitted.
Health Canada grants priority review to products intended for the treatment, prevention, or diagnosis of serious, life-threatening, or severely debilitating diseases or conditions.
About daratumumab
Daratumumab is a human IgG1k monoclonal antibody that binds to CD38, which is highly expressed on the surface of MM cells.
The drug is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab.
Daratumumab received conditional approval in Canada last year.
In June 2016, Health Canada issued a Notice of Compliance with Conditions approving daratumumab for MM patients who had received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or patients who are refractory to both a proteasome inhibitor and an immunomodulatory agent.
Phase 3 trial data
Health Canada’s expanded approval for daratumumab is based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October 2016.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August 2016. ![]()
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat MM patients who have received at least 1 prior therapy.
Health Canada granted daratumumab priority review for this indication due to a high unmet medical need in patients with MM.
When a drug is granted priority review, Health Canada aims to complete its review of the drug within 180 days from the time an application is submitted.
Health Canada grants priority review to products intended for the treatment, prevention, or diagnosis of serious, life-threatening, or severely debilitating diseases or conditions.
About daratumumab
Daratumumab is a human IgG1k monoclonal antibody that binds to CD38, which is highly expressed on the surface of MM cells.
The drug is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab.
Daratumumab received conditional approval in Canada last year.
In June 2016, Health Canada issued a Notice of Compliance with Conditions approving daratumumab for MM patients who had received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or patients who are refractory to both a proteasome inhibitor and an immunomodulatory agent.
Phase 3 trial data
Health Canada’s expanded approval for daratumumab is based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October 2016.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August 2016. ![]()
Inhibitor exhibits activity against hematologic malignancies
A dual kinase inhibitor is active against a range of hematologic malignancies, according to preclinical research.
Investigators found that ASN002, a SYK/JAK inhibitor, exhibited “potent” antiproliferative activity in leukemia, lymphoma, and myeloma cell lines.
ASN002 also inhibited tumor growth in mouse models of these malignancies and proved active against ibrutinib-resistant diffuse large B-cell lymphoma (DLBCL).
The investigators presented these results at the AACR Annual Meeting 2017 (abstract 4204).
The work was conducted by employees of Asana BioSciences, the company developing ASN002.
The investigators tested ASN002 in 178 cell lines and found the drug exhibited “strong antiproliferative activity” in a range of hematologic cancer cell lines, including:
- Leukemia—HEL31, HL60, Jurkat, MOLM-13, and MOLM-16
- Lymphoma—KARPAS-299, OCI-LY10, OCI-LY-19, Pfeiffer, Raji, Ramos, SU-DHL-1, SU-DHL-6, and SU-DHL-10
- Myeloma—H929, JJN3, OPM2, and U266.
In addition, ASN002 was active against ibrutinib-resistant clones derived from the DLBCL cell line SU-DHL-6.
In a SU-DHL-6 xenograft model, the combination of ASN002 and ibrutinib was more effective than either compound alone.
The investigators also found that ASN002 alone demonstrated “strong tumor growth inhibition” in mouse models of DLBCL (Pfeiffer and SU-DHL-6), myeloma (H929), and erythroleukemia (HEL).
The team pointed out that ASN002 is currently under investigation in a phase 1/2 study of patients with B-cell lymphomas (DLBCL, mantle cell lymphoma, and follicular lymphoma) as well as solid tumors.
The investigators said that, to date, ASN002 has been well tolerated and has shown encouraging early evidence of clinical activity and symptomatic benefit in the lymphoma patients. ![]()
A dual kinase inhibitor is active against a range of hematologic malignancies, according to preclinical research.
Investigators found that ASN002, a SYK/JAK inhibitor, exhibited “potent” antiproliferative activity in leukemia, lymphoma, and myeloma cell lines.
ASN002 also inhibited tumor growth in mouse models of these malignancies and proved active against ibrutinib-resistant diffuse large B-cell lymphoma (DLBCL).
The investigators presented these results at the AACR Annual Meeting 2017 (abstract 4204).
The work was conducted by employees of Asana BioSciences, the company developing ASN002.
The investigators tested ASN002 in 178 cell lines and found the drug exhibited “strong antiproliferative activity” in a range of hematologic cancer cell lines, including:
- Leukemia—HEL31, HL60, Jurkat, MOLM-13, and MOLM-16
- Lymphoma—KARPAS-299, OCI-LY10, OCI-LY-19, Pfeiffer, Raji, Ramos, SU-DHL-1, SU-DHL-6, and SU-DHL-10
- Myeloma—H929, JJN3, OPM2, and U266.
In addition, ASN002 was active against ibrutinib-resistant clones derived from the DLBCL cell line SU-DHL-6.
In a SU-DHL-6 xenograft model, the combination of ASN002 and ibrutinib was more effective than either compound alone.
The investigators also found that ASN002 alone demonstrated “strong tumor growth inhibition” in mouse models of DLBCL (Pfeiffer and SU-DHL-6), myeloma (H929), and erythroleukemia (HEL).
The team pointed out that ASN002 is currently under investigation in a phase 1/2 study of patients with B-cell lymphomas (DLBCL, mantle cell lymphoma, and follicular lymphoma) as well as solid tumors.
The investigators said that, to date, ASN002 has been well tolerated and has shown encouraging early evidence of clinical activity and symptomatic benefit in the lymphoma patients. ![]()
A dual kinase inhibitor is active against a range of hematologic malignancies, according to preclinical research.
Investigators found that ASN002, a SYK/JAK inhibitor, exhibited “potent” antiproliferative activity in leukemia, lymphoma, and myeloma cell lines.
ASN002 also inhibited tumor growth in mouse models of these malignancies and proved active against ibrutinib-resistant diffuse large B-cell lymphoma (DLBCL).
The investigators presented these results at the AACR Annual Meeting 2017 (abstract 4204).
The work was conducted by employees of Asana BioSciences, the company developing ASN002.
The investigators tested ASN002 in 178 cell lines and found the drug exhibited “strong antiproliferative activity” in a range of hematologic cancer cell lines, including:
- Leukemia—HEL31, HL60, Jurkat, MOLM-13, and MOLM-16
- Lymphoma—KARPAS-299, OCI-LY10, OCI-LY-19, Pfeiffer, Raji, Ramos, SU-DHL-1, SU-DHL-6, and SU-DHL-10
- Myeloma—H929, JJN3, OPM2, and U266.
In addition, ASN002 was active against ibrutinib-resistant clones derived from the DLBCL cell line SU-DHL-6.
In a SU-DHL-6 xenograft model, the combination of ASN002 and ibrutinib was more effective than either compound alone.
The investigators also found that ASN002 alone demonstrated “strong tumor growth inhibition” in mouse models of DLBCL (Pfeiffer and SU-DHL-6), myeloma (H929), and erythroleukemia (HEL).
The team pointed out that ASN002 is currently under investigation in a phase 1/2 study of patients with B-cell lymphomas (DLBCL, mantle cell lymphoma, and follicular lymphoma) as well as solid tumors.
The investigators said that, to date, ASN002 has been well tolerated and has shown encouraging early evidence of clinical activity and symptomatic benefit in the lymphoma patients. ![]()
50 years of pediatric residency: What has changed?
When Eileen Ouellette, MD, graduated from Boston’s Harvard Medical School in 1962, she was one of seven women in her class of 141 students. She went on to become one of only three women in pediatric residency at Massachusetts General Hospital later that year.
Free room and board was included in the program, Dr. Ouellette recalled, but her cramped room was poorly insulated and so small that she had to kneel on the bed to open her chest of drawers. The young doctor also soon learned that the women residents made less money than their male counterparts.
Dr. Ouellette, 79, now can laugh at the memory of her tiny room and tinier paycheck. The pediatric residents of today are entering a vastly different environment, she said. For starters, the average pay for medical residents in 2017 is $54,107. Women pediatric residents today far outnumber male residents. And most residents enjoy standard-sized rooms or apartments when completing their residencies.
Technology, for instance, greatly aids pediatric residents in their education today, said Renee Jenkins, MD, a professor at Howard University in Washington and a past AAP president.
Fewer hours, more hand-offs
During Dr. Ouellette’s residency from 1962 to 1965, sleep became a luxury. Of 168 hours in a week, residents were sometimes off for only 26 of them, she said.
“That was absolutely brutal,” she said. “You could not think of anything other than sleep. That became the primary focus of your whole life.”
“It didn’t seem crazy at the time,” said Dr. Stanton, founding dean of Seton Hall University Hackensack Meridian School of Medicine, South Orange, N.J. ”You developed the kind of bond with these families that it wouldn’t occur to you to go home.”
In the 1960s, there were no explicit limits on duty hours, according to Susan White, director of external communications for the Accreditation Council of Graduate Medical Education (ACGME). A “Guide for Residency Programs in Pediatrics,” published in 1968, recommended that “time off should be taken only when the service needs of the patients are assured and that “night and weekend duty provides a valuable educational experience. ... Duty of this type every second or third night and weekend is desirable.”
The guide predates the existence of the ACGME – established in 1981 – but it originated from a committee approved by the American Academy of Pediatrics, the American Board of Pediatrics, and the Council on Medical Education of the American Medical Association, according to Ms. White. While some residency programs changed their work hours over the years, the first mandated requirements for duty hours came in 1990 when ACGME set an 80-hour work week for four specialties: internal medicine, dermatology, ophthalmology, and preventive medicine. The council also limited on-call to every third night that year. In 2003, ACGME put in place duty hour requirements for all specialties.
“The pediatric requirements currently in effect provide safeguards for the resident, guidelines for educational programs, specific competencies and medical knowledge, as well as communication skills, professionalism requirements, and standardized assessment,” Ms. White said.
Current limitations for duty hours are beneficial in terms of resident safety, but the restrictions can be a double-edged sword, Dr. Jenkins said.
A changing gender demographic
By the time Dr. Stanton graduated from Yale in 1976, about 15% of her class were women, a marked shift from just a few years earlier, she said.
“In my residency program, women made up a quarter of our group,” she recalled. “That was a big change.”
The number of women going into pediatric residency has steadily increased in the last 5 decades, now far surpassing the number of men. Of 8,933 pediatric residents from 2015 to 2016, 67% were female and 25% were male, (with 8% not reporting), according to ACGME data.
“
Pediatrics is a natural selection for women, especially for those who plan to raise families, said Antoinette Eaton, MD, a retired pediatrician who completed her residency in the late 1950s at what is now Nationwide Children’s Hospital in Columbus, Ohio. Pediatrics is a prime specialty for career and family balance, she said.
“I worked part time a lot during my career,” said Dr. Eaton, a past AAP president. “Always being responsible as a mother and to the house were very high priorities.”
Dr. Stanton agrees that pediatric practices are much more tolerant of part time work, allowing women to better juggle children and career. However, she notes that the decline of male pediatricians also can be negative for the field overall.
New focus, growing debt
The curriculum focus for pediatric residency, meanwhile, has changed significantly over the years, pediatricians say. Dr. Eaton recalls her residency being almost entirely focused on inpatient care. In fact, insurance companies often refused to pay for outpatient care in sharp contrast to today, she said.
“You had to admit the patient if you wanted insurance to pay for it,” she said. “For example, if you had a patient with cerebral palsy or special needs, I had to admit that patient for 3, 4, 5 days. It was really different than what you have today.”
As time has passed, pediatric requirements have changed to emphasize the need for balance between inpatient and outpatient care, with a focus on continuity of care in either setting, Ms. White said. Newer additions to the requirements include the competencies of professionalism, communication, and life-long learning.
“Over the years these setting have expanded to include inpatients in hospitals, clinics, emergency centers, intensive care units, and in the community, [including] schools and other settings,” she said. “The requirements have always emphasized the importance of having high-quality, board-certified faculty to provide bedside teaching and deliver lectures at conferences.”
Another marked change for pediatric residents is the accumulation of debt. After her medical education, Dr. Jenkins owed about $1,500, she recalls.
“Today, that’s a drop in the bucket,” she said. “For the most part, you stayed out of [debt] trouble. It was nothing compared to that kids have to pay now.”
In 2014, the average medical school student graduated with a median debt of $180,000, according to data from the Association of American Medical Colleges. The wide debt differences are attributed to more expensive medical education today, Dr. Jenkins said.
While debt has risen, clinical responsibilities for residents have dropped as physician extenders and advanced equipment have become commonplace.
When Dr. Ouellette was a resident in the 1960s, there were few technicians to assist and no CT scans or MRIs for imaging. Residents drew blood from and gave blood to patients themselves. They took x-rays and developed them, she said.
“We had to use our brains and figure out what was going on,” she said. “People don’t think so much now. They send x-rays or scans to someone else, rather than figuring out the answer. Medicine may not be as much fun now as it was back then.”
Dr. Eaton added that residents have more technical demands today, more regulations to follow, and more paperwork to complete than the residents of the past. However, she believes pediatrics remains a worthwhile medical path. Three of her four children became doctors, one of whom went into pediatrics.
“I’m very disturbed when people try to convince children not to go into medicine,” she said. “I think it’s still a wonderful and rewarding career.”
[email protected]
On Twitter @legal_med
*Clarification made on 4/21/17
When Eileen Ouellette, MD, graduated from Boston’s Harvard Medical School in 1962, she was one of seven women in her class of 141 students. She went on to become one of only three women in pediatric residency at Massachusetts General Hospital later that year.
Free room and board was included in the program, Dr. Ouellette recalled, but her cramped room was poorly insulated and so small that she had to kneel on the bed to open her chest of drawers. The young doctor also soon learned that the women residents made less money than their male counterparts.
Dr. Ouellette, 79, now can laugh at the memory of her tiny room and tinier paycheck. The pediatric residents of today are entering a vastly different environment, she said. For starters, the average pay for medical residents in 2017 is $54,107. Women pediatric residents today far outnumber male residents. And most residents enjoy standard-sized rooms or apartments when completing their residencies.
Technology, for instance, greatly aids pediatric residents in their education today, said Renee Jenkins, MD, a professor at Howard University in Washington and a past AAP president.
Fewer hours, more hand-offs
During Dr. Ouellette’s residency from 1962 to 1965, sleep became a luxury. Of 168 hours in a week, residents were sometimes off for only 26 of them, she said.
“That was absolutely brutal,” she said. “You could not think of anything other than sleep. That became the primary focus of your whole life.”
“It didn’t seem crazy at the time,” said Dr. Stanton, founding dean of Seton Hall University Hackensack Meridian School of Medicine, South Orange, N.J. ”You developed the kind of bond with these families that it wouldn’t occur to you to go home.”
In the 1960s, there were no explicit limits on duty hours, according to Susan White, director of external communications for the Accreditation Council of Graduate Medical Education (ACGME). A “Guide for Residency Programs in Pediatrics,” published in 1968, recommended that “time off should be taken only when the service needs of the patients are assured and that “night and weekend duty provides a valuable educational experience. ... Duty of this type every second or third night and weekend is desirable.”
The guide predates the existence of the ACGME – established in 1981 – but it originated from a committee approved by the American Academy of Pediatrics, the American Board of Pediatrics, and the Council on Medical Education of the American Medical Association, according to Ms. White. While some residency programs changed their work hours over the years, the first mandated requirements for duty hours came in 1990 when ACGME set an 80-hour work week for four specialties: internal medicine, dermatology, ophthalmology, and preventive medicine. The council also limited on-call to every third night that year. In 2003, ACGME put in place duty hour requirements for all specialties.
“The pediatric requirements currently in effect provide safeguards for the resident, guidelines for educational programs, specific competencies and medical knowledge, as well as communication skills, professionalism requirements, and standardized assessment,” Ms. White said.
Current limitations for duty hours are beneficial in terms of resident safety, but the restrictions can be a double-edged sword, Dr. Jenkins said.
A changing gender demographic
By the time Dr. Stanton graduated from Yale in 1976, about 15% of her class were women, a marked shift from just a few years earlier, she said.
“In my residency program, women made up a quarter of our group,” she recalled. “That was a big change.”
The number of women going into pediatric residency has steadily increased in the last 5 decades, now far surpassing the number of men. Of 8,933 pediatric residents from 2015 to 2016, 67% were female and 25% were male, (with 8% not reporting), according to ACGME data.
“
Pediatrics is a natural selection for women, especially for those who plan to raise families, said Antoinette Eaton, MD, a retired pediatrician who completed her residency in the late 1950s at what is now Nationwide Children’s Hospital in Columbus, Ohio. Pediatrics is a prime specialty for career and family balance, she said.
“I worked part time a lot during my career,” said Dr. Eaton, a past AAP president. “Always being responsible as a mother and to the house were very high priorities.”
Dr. Stanton agrees that pediatric practices are much more tolerant of part time work, allowing women to better juggle children and career. However, she notes that the decline of male pediatricians also can be negative for the field overall.
New focus, growing debt
The curriculum focus for pediatric residency, meanwhile, has changed significantly over the years, pediatricians say. Dr. Eaton recalls her residency being almost entirely focused on inpatient care. In fact, insurance companies often refused to pay for outpatient care in sharp contrast to today, she said.
“You had to admit the patient if you wanted insurance to pay for it,” she said. “For example, if you had a patient with cerebral palsy or special needs, I had to admit that patient for 3, 4, 5 days. It was really different than what you have today.”
As time has passed, pediatric requirements have changed to emphasize the need for balance between inpatient and outpatient care, with a focus on continuity of care in either setting, Ms. White said. Newer additions to the requirements include the competencies of professionalism, communication, and life-long learning.
“Over the years these setting have expanded to include inpatients in hospitals, clinics, emergency centers, intensive care units, and in the community, [including] schools and other settings,” she said. “The requirements have always emphasized the importance of having high-quality, board-certified faculty to provide bedside teaching and deliver lectures at conferences.”
Another marked change for pediatric residents is the accumulation of debt. After her medical education, Dr. Jenkins owed about $1,500, she recalls.
“Today, that’s a drop in the bucket,” she said. “For the most part, you stayed out of [debt] trouble. It was nothing compared to that kids have to pay now.”
In 2014, the average medical school student graduated with a median debt of $180,000, according to data from the Association of American Medical Colleges. The wide debt differences are attributed to more expensive medical education today, Dr. Jenkins said.
While debt has risen, clinical responsibilities for residents have dropped as physician extenders and advanced equipment have become commonplace.
When Dr. Ouellette was a resident in the 1960s, there were few technicians to assist and no CT scans or MRIs for imaging. Residents drew blood from and gave blood to patients themselves. They took x-rays and developed them, she said.
“We had to use our brains and figure out what was going on,” she said. “People don’t think so much now. They send x-rays or scans to someone else, rather than figuring out the answer. Medicine may not be as much fun now as it was back then.”
Dr. Eaton added that residents have more technical demands today, more regulations to follow, and more paperwork to complete than the residents of the past. However, she believes pediatrics remains a worthwhile medical path. Three of her four children became doctors, one of whom went into pediatrics.
“I’m very disturbed when people try to convince children not to go into medicine,” she said. “I think it’s still a wonderful and rewarding career.”
[email protected]
On Twitter @legal_med
*Clarification made on 4/21/17
When Eileen Ouellette, MD, graduated from Boston’s Harvard Medical School in 1962, she was one of seven women in her class of 141 students. She went on to become one of only three women in pediatric residency at Massachusetts General Hospital later that year.
Free room and board was included in the program, Dr. Ouellette recalled, but her cramped room was poorly insulated and so small that she had to kneel on the bed to open her chest of drawers. The young doctor also soon learned that the women residents made less money than their male counterparts.
Dr. Ouellette, 79, now can laugh at the memory of her tiny room and tinier paycheck. The pediatric residents of today are entering a vastly different environment, she said. For starters, the average pay for medical residents in 2017 is $54,107. Women pediatric residents today far outnumber male residents. And most residents enjoy standard-sized rooms or apartments when completing their residencies.
Technology, for instance, greatly aids pediatric residents in their education today, said Renee Jenkins, MD, a professor at Howard University in Washington and a past AAP president.
Fewer hours, more hand-offs
During Dr. Ouellette’s residency from 1962 to 1965, sleep became a luxury. Of 168 hours in a week, residents were sometimes off for only 26 of them, she said.
“That was absolutely brutal,” she said. “You could not think of anything other than sleep. That became the primary focus of your whole life.”
“It didn’t seem crazy at the time,” said Dr. Stanton, founding dean of Seton Hall University Hackensack Meridian School of Medicine, South Orange, N.J. ”You developed the kind of bond with these families that it wouldn’t occur to you to go home.”
In the 1960s, there were no explicit limits on duty hours, according to Susan White, director of external communications for the Accreditation Council of Graduate Medical Education (ACGME). A “Guide for Residency Programs in Pediatrics,” published in 1968, recommended that “time off should be taken only when the service needs of the patients are assured and that “night and weekend duty provides a valuable educational experience. ... Duty of this type every second or third night and weekend is desirable.”
The guide predates the existence of the ACGME – established in 1981 – but it originated from a committee approved by the American Academy of Pediatrics, the American Board of Pediatrics, and the Council on Medical Education of the American Medical Association, according to Ms. White. While some residency programs changed their work hours over the years, the first mandated requirements for duty hours came in 1990 when ACGME set an 80-hour work week for four specialties: internal medicine, dermatology, ophthalmology, and preventive medicine. The council also limited on-call to every third night that year. In 2003, ACGME put in place duty hour requirements for all specialties.
“The pediatric requirements currently in effect provide safeguards for the resident, guidelines for educational programs, specific competencies and medical knowledge, as well as communication skills, professionalism requirements, and standardized assessment,” Ms. White said.
Current limitations for duty hours are beneficial in terms of resident safety, but the restrictions can be a double-edged sword, Dr. Jenkins said.
A changing gender demographic
By the time Dr. Stanton graduated from Yale in 1976, about 15% of her class were women, a marked shift from just a few years earlier, she said.
“In my residency program, women made up a quarter of our group,” she recalled. “That was a big change.”
The number of women going into pediatric residency has steadily increased in the last 5 decades, now far surpassing the number of men. Of 8,933 pediatric residents from 2015 to 2016, 67% were female and 25% were male, (with 8% not reporting), according to ACGME data.
“
Pediatrics is a natural selection for women, especially for those who plan to raise families, said Antoinette Eaton, MD, a retired pediatrician who completed her residency in the late 1950s at what is now Nationwide Children’s Hospital in Columbus, Ohio. Pediatrics is a prime specialty for career and family balance, she said.
“I worked part time a lot during my career,” said Dr. Eaton, a past AAP president. “Always being responsible as a mother and to the house were very high priorities.”
Dr. Stanton agrees that pediatric practices are much more tolerant of part time work, allowing women to better juggle children and career. However, she notes that the decline of male pediatricians also can be negative for the field overall.
New focus, growing debt
The curriculum focus for pediatric residency, meanwhile, has changed significantly over the years, pediatricians say. Dr. Eaton recalls her residency being almost entirely focused on inpatient care. In fact, insurance companies often refused to pay for outpatient care in sharp contrast to today, she said.
“You had to admit the patient if you wanted insurance to pay for it,” she said. “For example, if you had a patient with cerebral palsy or special needs, I had to admit that patient for 3, 4, 5 days. It was really different than what you have today.”
As time has passed, pediatric requirements have changed to emphasize the need for balance between inpatient and outpatient care, with a focus on continuity of care in either setting, Ms. White said. Newer additions to the requirements include the competencies of professionalism, communication, and life-long learning.
“Over the years these setting have expanded to include inpatients in hospitals, clinics, emergency centers, intensive care units, and in the community, [including] schools and other settings,” she said. “The requirements have always emphasized the importance of having high-quality, board-certified faculty to provide bedside teaching and deliver lectures at conferences.”
Another marked change for pediatric residents is the accumulation of debt. After her medical education, Dr. Jenkins owed about $1,500, she recalls.
“Today, that’s a drop in the bucket,” she said. “For the most part, you stayed out of [debt] trouble. It was nothing compared to that kids have to pay now.”
In 2014, the average medical school student graduated with a median debt of $180,000, according to data from the Association of American Medical Colleges. The wide debt differences are attributed to more expensive medical education today, Dr. Jenkins said.
While debt has risen, clinical responsibilities for residents have dropped as physician extenders and advanced equipment have become commonplace.
When Dr. Ouellette was a resident in the 1960s, there were few technicians to assist and no CT scans or MRIs for imaging. Residents drew blood from and gave blood to patients themselves. They took x-rays and developed them, she said.
“We had to use our brains and figure out what was going on,” she said. “People don’t think so much now. They send x-rays or scans to someone else, rather than figuring out the answer. Medicine may not be as much fun now as it was back then.”
Dr. Eaton added that residents have more technical demands today, more regulations to follow, and more paperwork to complete than the residents of the past. However, she believes pediatrics remains a worthwhile medical path. Three of her four children became doctors, one of whom went into pediatrics.
“I’m very disturbed when people try to convince children not to go into medicine,” she said. “I think it’s still a wonderful and rewarding career.”
[email protected]
On Twitter @legal_med
*Clarification made on 4/21/17
Apply By May 1 for International Scholarships for Surgical Education
Two international scholarships focused on surgical education and sponsored by the American College of Surgeons (ACS) Division of Education and the International Relations Committee will offer faculty members from countries outside the U.S. and Canada the opportunity to participate in a variety of faculty development activities. All application materials and supporting documents are due May 1.
The scholars will participate in the Surgical Education: Principles and Practice Course at the Clinical Congress 2017, October 22–26 in San Diego, CA. In addition, the scholars will attend plenary sessions and courses that address surgical education and training across the continuum of professional development. The scholars, in turn, will use the knowledge and skills they acquire to improve surgical education and training in their home institutions and countries. The scholarships include a stipend of $10,000 to cover travel, per diem expenses, and the cost of Clinical Congress courses. The registration cost for Clinical Congress and fees for the surgical education courses will be provided free to the scholars.
View the scholarship requirements and access the application on the ACS website at facs.org/member-services/scholarships/international/issurged. Direct questions to the ACS International Liaison at [email protected].
Two international scholarships focused on surgical education and sponsored by the American College of Surgeons (ACS) Division of Education and the International Relations Committee will offer faculty members from countries outside the U.S. and Canada the opportunity to participate in a variety of faculty development activities. All application materials and supporting documents are due May 1.
The scholars will participate in the Surgical Education: Principles and Practice Course at the Clinical Congress 2017, October 22–26 in San Diego, CA. In addition, the scholars will attend plenary sessions and courses that address surgical education and training across the continuum of professional development. The scholars, in turn, will use the knowledge and skills they acquire to improve surgical education and training in their home institutions and countries. The scholarships include a stipend of $10,000 to cover travel, per diem expenses, and the cost of Clinical Congress courses. The registration cost for Clinical Congress and fees for the surgical education courses will be provided free to the scholars.
View the scholarship requirements and access the application on the ACS website at facs.org/member-services/scholarships/international/issurged. Direct questions to the ACS International Liaison at [email protected].
Two international scholarships focused on surgical education and sponsored by the American College of Surgeons (ACS) Division of Education and the International Relations Committee will offer faculty members from countries outside the U.S. and Canada the opportunity to participate in a variety of faculty development activities. All application materials and supporting documents are due May 1.
The scholars will participate in the Surgical Education: Principles and Practice Course at the Clinical Congress 2017, October 22–26 in San Diego, CA. In addition, the scholars will attend plenary sessions and courses that address surgical education and training across the continuum of professional development. The scholars, in turn, will use the knowledge and skills they acquire to improve surgical education and training in their home institutions and countries. The scholarships include a stipend of $10,000 to cover travel, per diem expenses, and the cost of Clinical Congress courses. The registration cost for Clinical Congress and fees for the surgical education courses will be provided free to the scholars.
View the scholarship requirements and access the application on the ACS website at facs.org/member-services/scholarships/international/issurged. Direct questions to the ACS International Liaison at [email protected].
From the Washington Office: Advocacy in Action
Fellows frequently ask how they can get more involved in the advocacy efforts of the ACS. Whether you are new to the arena of policy and advocacy or an experienced veteran of innumerable efforts directed at ensuring access to quality surgical care, I can think of no better way to learn new skills and exercise old ones than by attending the ACS’ annual Leadership and Advocacy Summit.
The 2017 Leadership and Advocacy Summit will take place May 6–9 at the Renaissance Washington, DC Downtown Hotel. More than 300 individuals have already registered and you can join them by registering via the link found here: https://www.facs.org/advocacy/participate/summit-2017/register
The Advocacy Summit portion of the meeting will kick-off on the evening of May 7 with a reception and dinner featuring bestselling author, MSNBC political analyst, and former Communications Chief for President George W. Bush, Nicolle Wallace as the Keynote Speaker.
A robust agenda is planned for Monday, May 8. The morning will lead off with a panel entitled, Perspectives on 2017 Health Care Reform, featuring health policy experts from the Georgetown University Law Center, the George Washington University Milken Institute School of Public Health, the American Enterprise Institute, and the Heritage Foundation. The Monday agenda will also feature a panel of senior staffers from Capitol Hill discussing issues of particular interest to Fellows, a Medicare physician payment panel, and an address from a leading authority on effective communications strategies designed to make your interaction with legislators and their staff more effective.
The luncheon speaker for Monday will be Fox News contributor and Washington Examiner columnist, Lisa Boothe. The afternoon agenda will conclude with a series of issue briefings from ACS staff (in preparation for the Hill visits to legislator’s offices scheduled for Tuesday, May 9) and remarks from several United States Senators. ACSPA-SurgeonsPAC will host a reception on Monday evening, May 8 for all 2017 PAC contributors and a guest.
On Tuesday morning, May 9, attendees will be transported to Capitol Hill to visit the offices of their individual Member of Congress, Senators and staff with visits concluding in time to make flights out of Washington that afternoon.
I encourage all Fellows who are able to set aside time for the event to do so as I believe all will find the program educational and the experience rewarding.
For information about the Leadership Summit, contact Connie Bura at [email protected], or 312-919-5290. For information about the Advocacy Summit, contact Michael Carmody at [email protected], or 202-672-1511.
Until next month ….
Dr. Bailey is a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
Fellows frequently ask how they can get more involved in the advocacy efforts of the ACS. Whether you are new to the arena of policy and advocacy or an experienced veteran of innumerable efforts directed at ensuring access to quality surgical care, I can think of no better way to learn new skills and exercise old ones than by attending the ACS’ annual Leadership and Advocacy Summit.
The 2017 Leadership and Advocacy Summit will take place May 6–9 at the Renaissance Washington, DC Downtown Hotel. More than 300 individuals have already registered and you can join them by registering via the link found here: https://www.facs.org/advocacy/participate/summit-2017/register
The Advocacy Summit portion of the meeting will kick-off on the evening of May 7 with a reception and dinner featuring bestselling author, MSNBC political analyst, and former Communications Chief for President George W. Bush, Nicolle Wallace as the Keynote Speaker.
A robust agenda is planned for Monday, May 8. The morning will lead off with a panel entitled, Perspectives on 2017 Health Care Reform, featuring health policy experts from the Georgetown University Law Center, the George Washington University Milken Institute School of Public Health, the American Enterprise Institute, and the Heritage Foundation. The Monday agenda will also feature a panel of senior staffers from Capitol Hill discussing issues of particular interest to Fellows, a Medicare physician payment panel, and an address from a leading authority on effective communications strategies designed to make your interaction with legislators and their staff more effective.
The luncheon speaker for Monday will be Fox News contributor and Washington Examiner columnist, Lisa Boothe. The afternoon agenda will conclude with a series of issue briefings from ACS staff (in preparation for the Hill visits to legislator’s offices scheduled for Tuesday, May 9) and remarks from several United States Senators. ACSPA-SurgeonsPAC will host a reception on Monday evening, May 8 for all 2017 PAC contributors and a guest.
On Tuesday morning, May 9, attendees will be transported to Capitol Hill to visit the offices of their individual Member of Congress, Senators and staff with visits concluding in time to make flights out of Washington that afternoon.
I encourage all Fellows who are able to set aside time for the event to do so as I believe all will find the program educational and the experience rewarding.
For information about the Leadership Summit, contact Connie Bura at [email protected], or 312-919-5290. For information about the Advocacy Summit, contact Michael Carmody at [email protected], or 202-672-1511.
Until next month ….
Dr. Bailey is a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
Fellows frequently ask how they can get more involved in the advocacy efforts of the ACS. Whether you are new to the arena of policy and advocacy or an experienced veteran of innumerable efforts directed at ensuring access to quality surgical care, I can think of no better way to learn new skills and exercise old ones than by attending the ACS’ annual Leadership and Advocacy Summit.
The 2017 Leadership and Advocacy Summit will take place May 6–9 at the Renaissance Washington, DC Downtown Hotel. More than 300 individuals have already registered and you can join them by registering via the link found here: https://www.facs.org/advocacy/participate/summit-2017/register
The Advocacy Summit portion of the meeting will kick-off on the evening of May 7 with a reception and dinner featuring bestselling author, MSNBC political analyst, and former Communications Chief for President George W. Bush, Nicolle Wallace as the Keynote Speaker.
A robust agenda is planned for Monday, May 8. The morning will lead off with a panel entitled, Perspectives on 2017 Health Care Reform, featuring health policy experts from the Georgetown University Law Center, the George Washington University Milken Institute School of Public Health, the American Enterprise Institute, and the Heritage Foundation. The Monday agenda will also feature a panel of senior staffers from Capitol Hill discussing issues of particular interest to Fellows, a Medicare physician payment panel, and an address from a leading authority on effective communications strategies designed to make your interaction with legislators and their staff more effective.
The luncheon speaker for Monday will be Fox News contributor and Washington Examiner columnist, Lisa Boothe. The afternoon agenda will conclude with a series of issue briefings from ACS staff (in preparation for the Hill visits to legislator’s offices scheduled for Tuesday, May 9) and remarks from several United States Senators. ACSPA-SurgeonsPAC will host a reception on Monday evening, May 8 for all 2017 PAC contributors and a guest.
On Tuesday morning, May 9, attendees will be transported to Capitol Hill to visit the offices of their individual Member of Congress, Senators and staff with visits concluding in time to make flights out of Washington that afternoon.
I encourage all Fellows who are able to set aside time for the event to do so as I believe all will find the program educational and the experience rewarding.
For information about the Leadership Summit, contact Connie Bura at [email protected], or 312-919-5290. For information about the Advocacy Summit, contact Michael Carmody at [email protected], or 202-672-1511.
Until next month ….
Dr. Bailey is a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
2017 Claude H. Organ, Jr., MD, FACS Traveling Fellowship Applications due June 1
The family and friends of the late Dr. Claude H. Organ, Jr., established an endowment through the American College of Surgeons (ACS) Foundation to provide funding for an annual fellowship to be awarded to an outstanding young surgeon from the Society of Black Academic Surgeons, the Association of Women Surgeons, or the Surgical Section of the National Medical Association.
The fellowship, in the amount of $5,000, enables a U.S. or Canadian Fellow or Associate Fellow under age 45 who is a member of one of the above societies to attend an educational meeting or make an extended visit to an institution of his or her choice, tailored to his or her research interests.
Past awardees have used their fellowships to develop their careers in creative ways. The 2016 fellow, Stephanie Bonne, MD, is researching a successful hospital-based violence program in San Francisco in order to develop one at her home institution.
View the full requirements for the Claude H. Organ Traveling Fellowship at facs.org/member-services/scholarships/special/organ. The deadline for receipt of all application materials is June 1, with decisions to be made by August 2017. Questions and application materials should be submitted to the attention of the ACS Scholarships Administrator at [email protected].
The family and friends of the late Dr. Claude H. Organ, Jr., established an endowment through the American College of Surgeons (ACS) Foundation to provide funding for an annual fellowship to be awarded to an outstanding young surgeon from the Society of Black Academic Surgeons, the Association of Women Surgeons, or the Surgical Section of the National Medical Association.
The fellowship, in the amount of $5,000, enables a U.S. or Canadian Fellow or Associate Fellow under age 45 who is a member of one of the above societies to attend an educational meeting or make an extended visit to an institution of his or her choice, tailored to his or her research interests.
Past awardees have used their fellowships to develop their careers in creative ways. The 2016 fellow, Stephanie Bonne, MD, is researching a successful hospital-based violence program in San Francisco in order to develop one at her home institution.
View the full requirements for the Claude H. Organ Traveling Fellowship at facs.org/member-services/scholarships/special/organ. The deadline for receipt of all application materials is June 1, with decisions to be made by August 2017. Questions and application materials should be submitted to the attention of the ACS Scholarships Administrator at [email protected].
The family and friends of the late Dr. Claude H. Organ, Jr., established an endowment through the American College of Surgeons (ACS) Foundation to provide funding for an annual fellowship to be awarded to an outstanding young surgeon from the Society of Black Academic Surgeons, the Association of Women Surgeons, or the Surgical Section of the National Medical Association.
The fellowship, in the amount of $5,000, enables a U.S. or Canadian Fellow or Associate Fellow under age 45 who is a member of one of the above societies to attend an educational meeting or make an extended visit to an institution of his or her choice, tailored to his or her research interests.
Past awardees have used their fellowships to develop their careers in creative ways. The 2016 fellow, Stephanie Bonne, MD, is researching a successful hospital-based violence program in San Francisco in order to develop one at her home institution.
View the full requirements for the Claude H. Organ Traveling Fellowship at facs.org/member-services/scholarships/special/organ. The deadline for receipt of all application materials is June 1, with decisions to be made by August 2017. Questions and application materials should be submitted to the attention of the ACS Scholarships Administrator at [email protected].