User login
MRI Contralateral Volumetric Correlation Increases in Temporal Lobe Epilepsy
Volumetric correlation analysis of the brain can help detect subtle structural changes in patients with temporal lobe epilepsy (TLE). With that in mind, Conrad and associates performed T1 weighted 3T magnetic resonance imaging in 44 drug-resistant patients with unilateral TLE and in 44 healthy controls. They detected increased correlation in the contralateral areas to seizure foci and networks in several areas of the brains of patients with both left-sided and right-sided TLE. The areas, which included limbic, subcortical, and temporal regions, confirmed that there are coordinated volume changes in this population that are not confined to ipsilateral regions.
Conrad BN, Rogers BP, Abou-Khalil B et al. Increased MRI volumetric correlation contralateral to seizure focus in temporal lobe epilepsy. Epilepsy Res. 2016; 126:53-61.
Volumetric correlation analysis of the brain can help detect subtle structural changes in patients with temporal lobe epilepsy (TLE). With that in mind, Conrad and associates performed T1 weighted 3T magnetic resonance imaging in 44 drug-resistant patients with unilateral TLE and in 44 healthy controls. They detected increased correlation in the contralateral areas to seizure foci and networks in several areas of the brains of patients with both left-sided and right-sided TLE. The areas, which included limbic, subcortical, and temporal regions, confirmed that there are coordinated volume changes in this population that are not confined to ipsilateral regions.
Conrad BN, Rogers BP, Abou-Khalil B et al. Increased MRI volumetric correlation contralateral to seizure focus in temporal lobe epilepsy. Epilepsy Res. 2016; 126:53-61.
Volumetric correlation analysis of the brain can help detect subtle structural changes in patients with temporal lobe epilepsy (TLE). With that in mind, Conrad and associates performed T1 weighted 3T magnetic resonance imaging in 44 drug-resistant patients with unilateral TLE and in 44 healthy controls. They detected increased correlation in the contralateral areas to seizure foci and networks in several areas of the brains of patients with both left-sided and right-sided TLE. The areas, which included limbic, subcortical, and temporal regions, confirmed that there are coordinated volume changes in this population that are not confined to ipsilateral regions.
Conrad BN, Rogers BP, Abou-Khalil B et al. Increased MRI volumetric correlation contralateral to seizure focus in temporal lobe epilepsy. Epilepsy Res. 2016; 126:53-61.
Self-Management Programs May Prove Valuable for Patients With Epilepsy with Intellectual Disabilities
Patients with epilepsy who also have intellectual disabilities seem to fare better when they adhere to a self-management program suggests this pilot study. Since individuals with intellectual disabilities are 20 times more likely to have epilepsy, researchers wanted to determine if a self-management program could make a difference. Their review of pilot and randomized controlled feasibility studies suggests that patients find this type of intervention acceptable and that the programs improve seizure frequency and may improve their quality of life. Although their analysis highlights the potential for self-management programs, the investigators are currently conducting a randomized controlled trial to obtain more definitive results.
Dannenberg M, Mengoni SE, Gates B, Durand M. Self-management interventions for epilepsy in people with intellectual disabilities: A scoping review. Seizure. 2016;41:16-25.
Patients with epilepsy who also have intellectual disabilities seem to fare better when they adhere to a self-management program suggests this pilot study. Since individuals with intellectual disabilities are 20 times more likely to have epilepsy, researchers wanted to determine if a self-management program could make a difference. Their review of pilot and randomized controlled feasibility studies suggests that patients find this type of intervention acceptable and that the programs improve seizure frequency and may improve their quality of life. Although their analysis highlights the potential for self-management programs, the investigators are currently conducting a randomized controlled trial to obtain more definitive results.
Dannenberg M, Mengoni SE, Gates B, Durand M. Self-management interventions for epilepsy in people with intellectual disabilities: A scoping review. Seizure. 2016;41:16-25.
Patients with epilepsy who also have intellectual disabilities seem to fare better when they adhere to a self-management program suggests this pilot study. Since individuals with intellectual disabilities are 20 times more likely to have epilepsy, researchers wanted to determine if a self-management program could make a difference. Their review of pilot and randomized controlled feasibility studies suggests that patients find this type of intervention acceptable and that the programs improve seizure frequency and may improve their quality of life. Although their analysis highlights the potential for self-management programs, the investigators are currently conducting a randomized controlled trial to obtain more definitive results.
Dannenberg M, Mengoni SE, Gates B, Durand M. Self-management interventions for epilepsy in people with intellectual disabilities: A scoping review. Seizure. 2016;41:16-25.
Nodular Heterotopia Rarely Precipitates Seizures
Although ectopic tissue in certain regions of the brain has been linked to epilepsy, a recent review of the literature concluded that periventricular nodular heterotopia rarely causes clinical seizures. The review evaluated chronic invasive EEG recordings and found that nodules alone are rarely responsible for seizures. Their onset is more likely to be connected with overlying neocortex or mesial temporal structures. However, the analysis did find that substantial or complete ablation of nodules usually results in more favorable surgical outcomes.
Thompson SA, Kalamangalam GP, Tandon N. Intracranial evaluation and laser ablation for epilepsy with periventricular nodular heterotopia. Seizure. 2016;41:211-216.
Although ectopic tissue in certain regions of the brain has been linked to epilepsy, a recent review of the literature concluded that periventricular nodular heterotopia rarely causes clinical seizures. The review evaluated chronic invasive EEG recordings and found that nodules alone are rarely responsible for seizures. Their onset is more likely to be connected with overlying neocortex or mesial temporal structures. However, the analysis did find that substantial or complete ablation of nodules usually results in more favorable surgical outcomes.
Thompson SA, Kalamangalam GP, Tandon N. Intracranial evaluation and laser ablation for epilepsy with periventricular nodular heterotopia. Seizure. 2016;41:211-216.
Although ectopic tissue in certain regions of the brain has been linked to epilepsy, a recent review of the literature concluded that periventricular nodular heterotopia rarely causes clinical seizures. The review evaluated chronic invasive EEG recordings and found that nodules alone are rarely responsible for seizures. Their onset is more likely to be connected with overlying neocortex or mesial temporal structures. However, the analysis did find that substantial or complete ablation of nodules usually results in more favorable surgical outcomes.
Thompson SA, Kalamangalam GP, Tandon N. Intracranial evaluation and laser ablation for epilepsy with periventricular nodular heterotopia. Seizure. 2016;41:211-216.
Distinct Hand Gestures Linked to Different Seizure Types
Patients experiencing different types of seizures tend to present with distinct hand gestures during the attacks, according to a recent retrospective analysis published in Neurology. To reach that conclusion, researchers analyzed videotaped hand postures in patients with genetic generalized epilepsy, localization-related epilepsy, and non-epileptic attacks. They found that 96% of patients with localized epilepsy presented with index-finger pointing while 91.3% of patients with genetic generalized epilepsy presented with hand fanning, which only occurred at the onset of the seizures. The investigators also discovered that making a fist, fanning and index-finger pointing was more common among patients who were having epileptic seizures, when compared to those who were having non-epileptic attacks (74% vs 32%).
Siegel J, Tatum, WO. Hand postures in primary and secondary generalized tonic-clonic seizures. Neurology. 2016; Published online Sept 24.
Patients experiencing different types of seizures tend to present with distinct hand gestures during the attacks, according to a recent retrospective analysis published in Neurology. To reach that conclusion, researchers analyzed videotaped hand postures in patients with genetic generalized epilepsy, localization-related epilepsy, and non-epileptic attacks. They found that 96% of patients with localized epilepsy presented with index-finger pointing while 91.3% of patients with genetic generalized epilepsy presented with hand fanning, which only occurred at the onset of the seizures. The investigators also discovered that making a fist, fanning and index-finger pointing was more common among patients who were having epileptic seizures, when compared to those who were having non-epileptic attacks (74% vs 32%).
Siegel J, Tatum, WO. Hand postures in primary and secondary generalized tonic-clonic seizures. Neurology. 2016; Published online Sept 24.
Patients experiencing different types of seizures tend to present with distinct hand gestures during the attacks, according to a recent retrospective analysis published in Neurology. To reach that conclusion, researchers analyzed videotaped hand postures in patients with genetic generalized epilepsy, localization-related epilepsy, and non-epileptic attacks. They found that 96% of patients with localized epilepsy presented with index-finger pointing while 91.3% of patients with genetic generalized epilepsy presented with hand fanning, which only occurred at the onset of the seizures. The investigators also discovered that making a fist, fanning and index-finger pointing was more common among patients who were having epileptic seizures, when compared to those who were having non-epileptic attacks (74% vs 32%).
Siegel J, Tatum, WO. Hand postures in primary and secondary generalized tonic-clonic seizures. Neurology. 2016; Published online Sept 24.
VIDEO: Hepato-adrenal syndrome is an under-recognized source of ICU morbidity
BOSTON – Patients with serious liver disease who also had hepato-adrenal syndrome had significantly longer hospital stays; these patients had significantly longer ICU courses as well.
According to a recent study of this under-recognized syndrome, patients with cirrhosis, acute liver failure, or acute liver injury who also had clinically significant adrenocortical dysfunction had longer hospital stays when compared to patients without hepato-adrenal syndrome (HAS).
Presenting the study findings at a poster session at the annual meeting of the American Association for the Study of Liver Disease, Christina Lindenmeyer, MD, and her associates noted that the longer stays for HAS patients with serious liver disease held true even after adjustment for gender, blood glucose levels, and Child-Pugh score (median 29 days, HAS; 17 days, non-HAS; P = .001).
Further, the patients with HAS were more likely to have a prolonged ICU stay, after multivariable analysis adjusted for a variety of factors including the need for mechanical ventilation, age, bilirubin level, Model for End-stage Liver Disease (MELD) score, and severity of encephalopathy (13.5 vs. 4.9 days; P = .002).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Patients with cirrhosis commonly have hypotension, and I think it’s underrecognized that the elevated levels of endotoxin and the low levels of lipoprotein circulating in patients with cirrhosis can lead to adrenocortical dysfunction,” Dr. Lindenmeyer said in a video interview.
The single-center study enrolled ICU patients with cirrhosis, acute liver injury, and/or acute liver failure who had random cortisol or adrenocorticotropin-releasing hormone (ACTH) stimulation test results. From 2008 to 2014, the tertiary care center saw 69 patients meeting these criteria; 32 patients (46%) had HAS. The mean age was 57.4 years, and 63.8% of enrolled patients were male. There were no significant differences in these demographics between the groups. Serum bicarbonate was higher in patients with HAS (21.4 vs. 17.5 mEq/L; P = .020); other blood chemistries, mean arterial pressures, and the MELD and Child-Pugh scores did not differ significantly between groups.
Dr. Lindenmeyer, a fellow in the Cleveland Clinic’s department of gastroenterology and hepatology, said that the accepted definition of HAS is a random cortisol level of less than 15 mcg/dL in “patients who were highly stressed in the ICU, typically with respiratory failure or hypotension,” she said. For non-ICU patients, the random cortisol level should be less than 20 mcg/dL. An alternative criterion is a post-ACTH stimulation test cortisol level of less than 20 mcg/dL.
Though there was no statistically significant difference between in-hospital mortality for those patients meeting HAS criteria, the trend was actually for those patients to have lower in-hospital mortality (44% vs. 51%; P = .53). This was true even after correction for MELD scores and serum potassium levels. Dr. Lindenmeyer said these results were “a little surprising,” and noted that the study didn’t examine 90-day or 1-year mortality. “That would be something interesting to look at,” she said.
“Early recognition and treatment of HAS may improve judicious allocation of critical care and hospital resources,” wrote Dr. Lindenmeyer and her colleagues.
Dr. Lindenmeyer reported no conflicts of interest, and there were no outside sources of funding reported.
[email protected]
On Twitter @karioakes
BOSTON – Patients with serious liver disease who also had hepato-adrenal syndrome had significantly longer hospital stays; these patients had significantly longer ICU courses as well.
According to a recent study of this under-recognized syndrome, patients with cirrhosis, acute liver failure, or acute liver injury who also had clinically significant adrenocortical dysfunction had longer hospital stays when compared to patients without hepato-adrenal syndrome (HAS).
Presenting the study findings at a poster session at the annual meeting of the American Association for the Study of Liver Disease, Christina Lindenmeyer, MD, and her associates noted that the longer stays for HAS patients with serious liver disease held true even after adjustment for gender, blood glucose levels, and Child-Pugh score (median 29 days, HAS; 17 days, non-HAS; P = .001).
Further, the patients with HAS were more likely to have a prolonged ICU stay, after multivariable analysis adjusted for a variety of factors including the need for mechanical ventilation, age, bilirubin level, Model for End-stage Liver Disease (MELD) score, and severity of encephalopathy (13.5 vs. 4.9 days; P = .002).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Patients with cirrhosis commonly have hypotension, and I think it’s underrecognized that the elevated levels of endotoxin and the low levels of lipoprotein circulating in patients with cirrhosis can lead to adrenocortical dysfunction,” Dr. Lindenmeyer said in a video interview.
The single-center study enrolled ICU patients with cirrhosis, acute liver injury, and/or acute liver failure who had random cortisol or adrenocorticotropin-releasing hormone (ACTH) stimulation test results. From 2008 to 2014, the tertiary care center saw 69 patients meeting these criteria; 32 patients (46%) had HAS. The mean age was 57.4 years, and 63.8% of enrolled patients were male. There were no significant differences in these demographics between the groups. Serum bicarbonate was higher in patients with HAS (21.4 vs. 17.5 mEq/L; P = .020); other blood chemistries, mean arterial pressures, and the MELD and Child-Pugh scores did not differ significantly between groups.
Dr. Lindenmeyer, a fellow in the Cleveland Clinic’s department of gastroenterology and hepatology, said that the accepted definition of HAS is a random cortisol level of less than 15 mcg/dL in “patients who were highly stressed in the ICU, typically with respiratory failure or hypotension,” she said. For non-ICU patients, the random cortisol level should be less than 20 mcg/dL. An alternative criterion is a post-ACTH stimulation test cortisol level of less than 20 mcg/dL.
Though there was no statistically significant difference between in-hospital mortality for those patients meeting HAS criteria, the trend was actually for those patients to have lower in-hospital mortality (44% vs. 51%; P = .53). This was true even after correction for MELD scores and serum potassium levels. Dr. Lindenmeyer said these results were “a little surprising,” and noted that the study didn’t examine 90-day or 1-year mortality. “That would be something interesting to look at,” she said.
“Early recognition and treatment of HAS may improve judicious allocation of critical care and hospital resources,” wrote Dr. Lindenmeyer and her colleagues.
Dr. Lindenmeyer reported no conflicts of interest, and there were no outside sources of funding reported.
[email protected]
On Twitter @karioakes
BOSTON – Patients with serious liver disease who also had hepato-adrenal syndrome had significantly longer hospital stays; these patients had significantly longer ICU courses as well.
According to a recent study of this under-recognized syndrome, patients with cirrhosis, acute liver failure, or acute liver injury who also had clinically significant adrenocortical dysfunction had longer hospital stays when compared to patients without hepato-adrenal syndrome (HAS).
Presenting the study findings at a poster session at the annual meeting of the American Association for the Study of Liver Disease, Christina Lindenmeyer, MD, and her associates noted that the longer stays for HAS patients with serious liver disease held true even after adjustment for gender, blood glucose levels, and Child-Pugh score (median 29 days, HAS; 17 days, non-HAS; P = .001).
Further, the patients with HAS were more likely to have a prolonged ICU stay, after multivariable analysis adjusted for a variety of factors including the need for mechanical ventilation, age, bilirubin level, Model for End-stage Liver Disease (MELD) score, and severity of encephalopathy (13.5 vs. 4.9 days; P = .002).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Patients with cirrhosis commonly have hypotension, and I think it’s underrecognized that the elevated levels of endotoxin and the low levels of lipoprotein circulating in patients with cirrhosis can lead to adrenocortical dysfunction,” Dr. Lindenmeyer said in a video interview.
The single-center study enrolled ICU patients with cirrhosis, acute liver injury, and/or acute liver failure who had random cortisol or adrenocorticotropin-releasing hormone (ACTH) stimulation test results. From 2008 to 2014, the tertiary care center saw 69 patients meeting these criteria; 32 patients (46%) had HAS. The mean age was 57.4 years, and 63.8% of enrolled patients were male. There were no significant differences in these demographics between the groups. Serum bicarbonate was higher in patients with HAS (21.4 vs. 17.5 mEq/L; P = .020); other blood chemistries, mean arterial pressures, and the MELD and Child-Pugh scores did not differ significantly between groups.
Dr. Lindenmeyer, a fellow in the Cleveland Clinic’s department of gastroenterology and hepatology, said that the accepted definition of HAS is a random cortisol level of less than 15 mcg/dL in “patients who were highly stressed in the ICU, typically with respiratory failure or hypotension,” she said. For non-ICU patients, the random cortisol level should be less than 20 mcg/dL. An alternative criterion is a post-ACTH stimulation test cortisol level of less than 20 mcg/dL.
Though there was no statistically significant difference between in-hospital mortality for those patients meeting HAS criteria, the trend was actually for those patients to have lower in-hospital mortality (44% vs. 51%; P = .53). This was true even after correction for MELD scores and serum potassium levels. Dr. Lindenmeyer said these results were “a little surprising,” and noted that the study didn’t examine 90-day or 1-year mortality. “That would be something interesting to look at,” she said.
“Early recognition and treatment of HAS may improve judicious allocation of critical care and hospital resources,” wrote Dr. Lindenmeyer and her colleagues.
Dr. Lindenmeyer reported no conflicts of interest, and there were no outside sources of funding reported.
[email protected]
On Twitter @karioakes
AT THE LIVER MEETING 2016
Key clinical point:
Major finding: Patients with HAS had a longer length of hospital stay (median 29 days, HAS; 17 days, non-HAS; P = .001)
Data source: Single-center study of 69 consecutively enrolled ICU patients with serious liver disease and random cortisol or adrenocorticotropin-releasing hormone results.
Disclosures: The study investigators reported no disclosures, and no external sources of funding.
Alveolar stem cell failure implicated in pulmonary fibrosis
The failure of type 2 alveolar epithelial cells (AEC2s), which are critical to the repair and regeneration of lung tissue, appears to be a major cause of pulmonary fibrosis, according to a report published online in Nature Medicine.
Researchers performed a series of in vitro and murine studies to better understand the molecular mechanisms underlying pulmonary fibrosis, which is believed to result from repeated microinjuries to the alveolar epithelium that in turn promote excessive, sustained fibroblast activation with matrix-producing myofibroblasts. They found that expression of both hyaluronan (HA) and Toll-like receptor 4 (TLR4) on AEC2s is deficient in a mouse model of pulmonary fibrosis and in samples of lung tissue from patients with the disease, but not in samples from healthy control subjects or from patients with chronic obstructive pulmonary disease (COPD).
“The main finding here is that the endogenous matrix glycosaminoglycan HA and the innate immune receptor TLR4 are required for optimal AEC2 renewal and for limiting fibrosis after lung injury,” said Carol Liang, MD, of the department of medicine and the Women’s Guild Lung Institute, Cedars-Sinai Medical Center, Los Angeles, and her associates.
“These findings are the first published evidence that pulmonary fibrosis is primarily a disease of AEC2 stem cell failure,” Dr. Liang said, in a written statement.
The investigators began by showing that AEC2s engineered to stop expressing hyaluronan or TLR4 (by deleting the genes that encode for that expression) showed impaired self-renewal in vitro, compared with normal AEC2s. In a mouse model, the engineered AEC2s also caused impairment in the healing of deliberately induced lung injury.
In addition, the researchers developed a mouse model of pulmonary fibrosis and showed that treatment with exogenous interleukin 6 “enhanced AEC2 renewal and partially reversed the fibrotic phenotype” in vivo.
“To determine whether our observations in the mouse model of [deficient] AEC2s have relevance to human disease, we isolated AEC2s from lung explants of human subjects who had undergone lung transplantation because of [idiopathic pulmonary fibrosis],” the researchers said. These samples showed marked depletion in the number of AEC2s, compared with samples taken from healthy control subjects and from patients with COPD.
In addition, the few remaining AEC2s in the samples affected by pulmonary fibrosis were deficient in the expression of HA, compared with those in the samples from control subjects. This suggests that loss of cell-surface HA is unique to severe pulmonary fibrosis, the researchers said (Nature Med. 2016. doi: 10.1038/nm.4192).
Since pulmonary fibrosis is characterized by patchy areas of parenchymal fibrosis alternating with relatively normal lung tissue, the investigators then compared AEC2s taken from these two distinct types of tissue in the patient group. They found that AEC2 cells from affected areas of the lung showed much more markedly reduced expression of HA than those from healthy areas of the lung. Flow cytometry testing further demonstrated that the number of AEC2s also was greatly reduced in affected lung tissue but relatively higher in more normal lung tissue. However, even the “healthy” lung tissue from affected patients had lower numbers of AEC2s and impaired cell renewal when compared with tissue from unaffected control subjects, the researchers noted.
“In future studies, we will explore how the loss of hyaluronan promotes fibrosis and how it might be restored to cell surfaces. These endeavors could lead to new therapeutic approaches” for this progressive, fatal disease for which there is no effective treatment at present, Dr. Liang said, in the written statement.
The researchers reported having no relevant financial disclosures.
The failure of type 2 alveolar epithelial cells (AEC2s), which are critical to the repair and regeneration of lung tissue, appears to be a major cause of pulmonary fibrosis, according to a report published online in Nature Medicine.
Researchers performed a series of in vitro and murine studies to better understand the molecular mechanisms underlying pulmonary fibrosis, which is believed to result from repeated microinjuries to the alveolar epithelium that in turn promote excessive, sustained fibroblast activation with matrix-producing myofibroblasts. They found that expression of both hyaluronan (HA) and Toll-like receptor 4 (TLR4) on AEC2s is deficient in a mouse model of pulmonary fibrosis and in samples of lung tissue from patients with the disease, but not in samples from healthy control subjects or from patients with chronic obstructive pulmonary disease (COPD).
“The main finding here is that the endogenous matrix glycosaminoglycan HA and the innate immune receptor TLR4 are required for optimal AEC2 renewal and for limiting fibrosis after lung injury,” said Carol Liang, MD, of the department of medicine and the Women’s Guild Lung Institute, Cedars-Sinai Medical Center, Los Angeles, and her associates.
“These findings are the first published evidence that pulmonary fibrosis is primarily a disease of AEC2 stem cell failure,” Dr. Liang said, in a written statement.
The investigators began by showing that AEC2s engineered to stop expressing hyaluronan or TLR4 (by deleting the genes that encode for that expression) showed impaired self-renewal in vitro, compared with normal AEC2s. In a mouse model, the engineered AEC2s also caused impairment in the healing of deliberately induced lung injury.
In addition, the researchers developed a mouse model of pulmonary fibrosis and showed that treatment with exogenous interleukin 6 “enhanced AEC2 renewal and partially reversed the fibrotic phenotype” in vivo.
“To determine whether our observations in the mouse model of [deficient] AEC2s have relevance to human disease, we isolated AEC2s from lung explants of human subjects who had undergone lung transplantation because of [idiopathic pulmonary fibrosis],” the researchers said. These samples showed marked depletion in the number of AEC2s, compared with samples taken from healthy control subjects and from patients with COPD.
In addition, the few remaining AEC2s in the samples affected by pulmonary fibrosis were deficient in the expression of HA, compared with those in the samples from control subjects. This suggests that loss of cell-surface HA is unique to severe pulmonary fibrosis, the researchers said (Nature Med. 2016. doi: 10.1038/nm.4192).
Since pulmonary fibrosis is characterized by patchy areas of parenchymal fibrosis alternating with relatively normal lung tissue, the investigators then compared AEC2s taken from these two distinct types of tissue in the patient group. They found that AEC2 cells from affected areas of the lung showed much more markedly reduced expression of HA than those from healthy areas of the lung. Flow cytometry testing further demonstrated that the number of AEC2s also was greatly reduced in affected lung tissue but relatively higher in more normal lung tissue. However, even the “healthy” lung tissue from affected patients had lower numbers of AEC2s and impaired cell renewal when compared with tissue from unaffected control subjects, the researchers noted.
“In future studies, we will explore how the loss of hyaluronan promotes fibrosis and how it might be restored to cell surfaces. These endeavors could lead to new therapeutic approaches” for this progressive, fatal disease for which there is no effective treatment at present, Dr. Liang said, in the written statement.
The researchers reported having no relevant financial disclosures.
The failure of type 2 alveolar epithelial cells (AEC2s), which are critical to the repair and regeneration of lung tissue, appears to be a major cause of pulmonary fibrosis, according to a report published online in Nature Medicine.
Researchers performed a series of in vitro and murine studies to better understand the molecular mechanisms underlying pulmonary fibrosis, which is believed to result from repeated microinjuries to the alveolar epithelium that in turn promote excessive, sustained fibroblast activation with matrix-producing myofibroblasts. They found that expression of both hyaluronan (HA) and Toll-like receptor 4 (TLR4) on AEC2s is deficient in a mouse model of pulmonary fibrosis and in samples of lung tissue from patients with the disease, but not in samples from healthy control subjects or from patients with chronic obstructive pulmonary disease (COPD).
“The main finding here is that the endogenous matrix glycosaminoglycan HA and the innate immune receptor TLR4 are required for optimal AEC2 renewal and for limiting fibrosis after lung injury,” said Carol Liang, MD, of the department of medicine and the Women’s Guild Lung Institute, Cedars-Sinai Medical Center, Los Angeles, and her associates.
“These findings are the first published evidence that pulmonary fibrosis is primarily a disease of AEC2 stem cell failure,” Dr. Liang said, in a written statement.
The investigators began by showing that AEC2s engineered to stop expressing hyaluronan or TLR4 (by deleting the genes that encode for that expression) showed impaired self-renewal in vitro, compared with normal AEC2s. In a mouse model, the engineered AEC2s also caused impairment in the healing of deliberately induced lung injury.
In addition, the researchers developed a mouse model of pulmonary fibrosis and showed that treatment with exogenous interleukin 6 “enhanced AEC2 renewal and partially reversed the fibrotic phenotype” in vivo.
“To determine whether our observations in the mouse model of [deficient] AEC2s have relevance to human disease, we isolated AEC2s from lung explants of human subjects who had undergone lung transplantation because of [idiopathic pulmonary fibrosis],” the researchers said. These samples showed marked depletion in the number of AEC2s, compared with samples taken from healthy control subjects and from patients with COPD.
In addition, the few remaining AEC2s in the samples affected by pulmonary fibrosis were deficient in the expression of HA, compared with those in the samples from control subjects. This suggests that loss of cell-surface HA is unique to severe pulmonary fibrosis, the researchers said (Nature Med. 2016. doi: 10.1038/nm.4192).
Since pulmonary fibrosis is characterized by patchy areas of parenchymal fibrosis alternating with relatively normal lung tissue, the investigators then compared AEC2s taken from these two distinct types of tissue in the patient group. They found that AEC2 cells from affected areas of the lung showed much more markedly reduced expression of HA than those from healthy areas of the lung. Flow cytometry testing further demonstrated that the number of AEC2s also was greatly reduced in affected lung tissue but relatively higher in more normal lung tissue. However, even the “healthy” lung tissue from affected patients had lower numbers of AEC2s and impaired cell renewal when compared with tissue from unaffected control subjects, the researchers noted.
“In future studies, we will explore how the loss of hyaluronan promotes fibrosis and how it might be restored to cell surfaces. These endeavors could lead to new therapeutic approaches” for this progressive, fatal disease for which there is no effective treatment at present, Dr. Liang said, in the written statement.
The researchers reported having no relevant financial disclosures.
FROM NATURE MEDICINE
Key clinical point: The failure of type 2 alveolar epithelial cells, which are critical to lung tissue repair and regeneration, appears to be a major cause of pulmonary fibrosis.
Major finding: Lung samples from patients with pulmonary fibrosis showed marked depletion in the number of AEC2s, compared with samples taken from healthy control subjects and samples from patients with COPD.
Data source: A series of in vitro and murine studies, including testing of lung samples from patients with pulmonary fibrosis.
Disclosures: This study was supported by the National Institutes of Health and the California Institute for Regenerative Medicine. Dr. Liang and her associates reported having no relevant financial disclosures.
Sudden Unexpected Death in Epilepsy
Management of wound complications following obstetric anal sphincter injury (OASIS)
During vaginal delivery spontaneous perineal trauma and extension of episiotomy incisions are common. A severe perineal laceration that extends into or through the anal sphincter complex is referred to as an obstetric anal sphincter injury (OASIS) and requires meticulous repair. Following the repair of an OASIS, serious wound complications, including dehiscence and infection, may occur. In Europe the reported rate of OASIS varies widely among countries, with a rate of 0.1% in Romania, possibly due to underreporting, and 4.9% in Iceland.1 In the United States the rates of 3rd- and 4th-degree lacerations were reported to be 3.3% and 1.1%, respectively.2
Risk factors for OASIS include forceps delivery (odds ratio [OR], 5.50), vacuum-assisted delivery (OR, 3.98), and midline episiotomy (OR, 3.82).3 Additional risk factors for severe perineal injury at vaginal delivery include nulliparity (adjusted odds ratio [aOR], 2.58), delivery from a persistent occiput posterior position (aOR, 2.24), and above-average newborn birth weight (aOR, 1.28).4
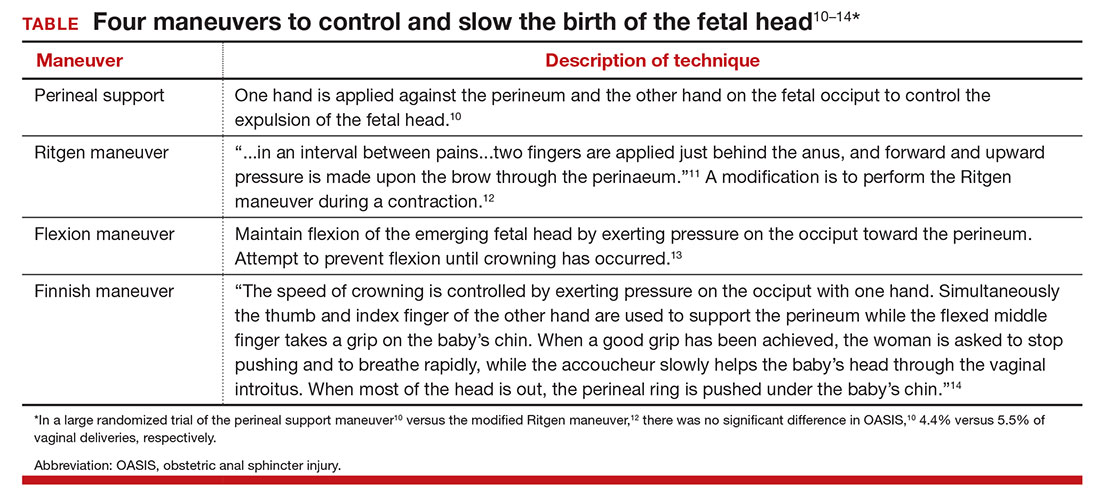
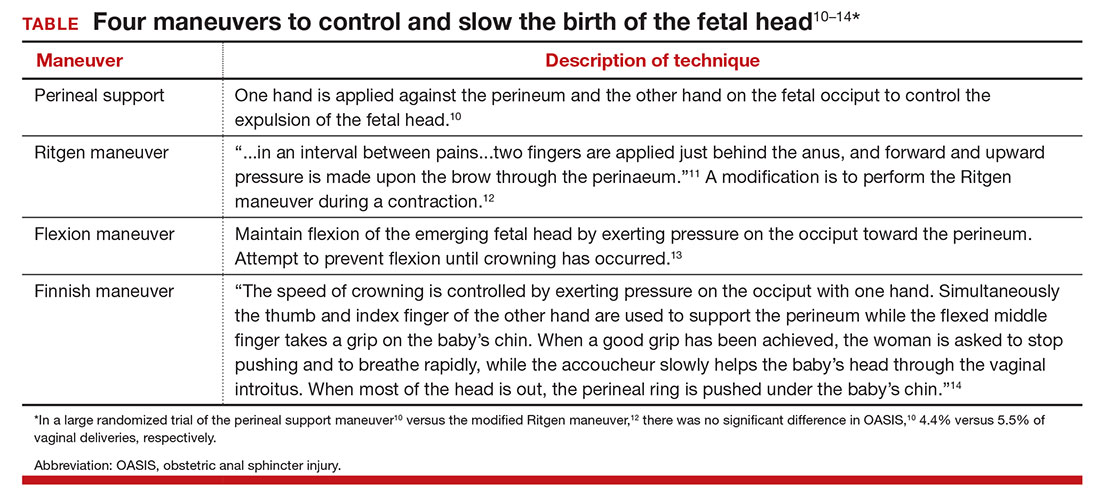
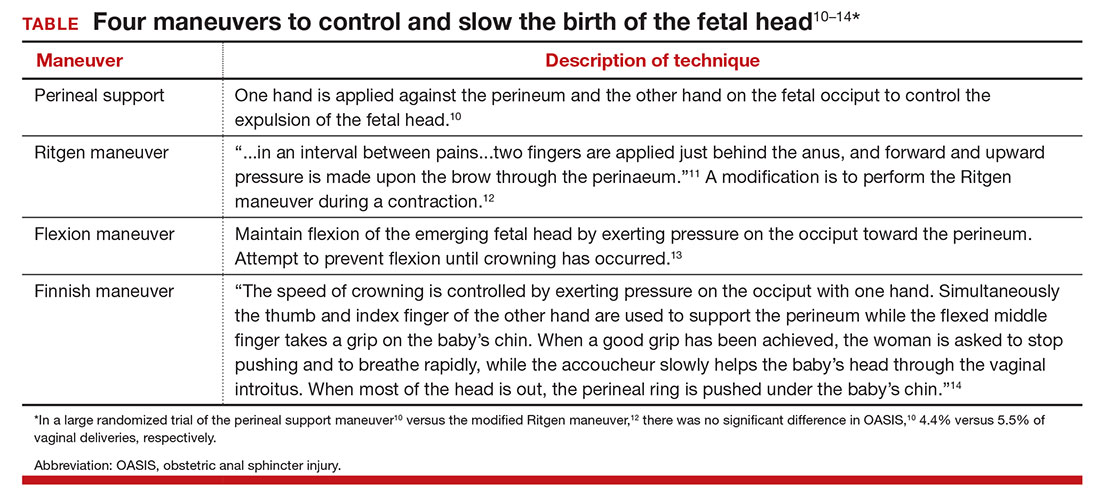
In a meta-analysis of randomized trials, the researchers reported that restrictive use of episiotomy reduced the risk of severe perineal trauma (relative risk [RR], 0.67) but increased the risk of anterior perineal trauma (RR, 1.84).5 The American College of Obstetricians and Gynecologists (ACOG) recommends that episiotomy should not be a routine practice and is best restricted to use in a limited number of cases where fetal and maternal benefit is likely.6 In addition, ACOG recommends that if episiotomy is indicated, a mediolateral incision is favored over a midline incision. In my practice I perform only mediolateral episiotomy incisions. However, mediolateral episiotomy may be associated with an increased risk of postpartum perineal pain and dyspareunia.7 Use of warm compresses applied to the perineum during the second stage of labor may reduce the risk of 3rd- and 4th-degree lacerations.8 Techniques to ensure that the fetal head and shoulders are birthed in a slow and controlled fashion may decrease the risk of OASIS.9 See the TABLE, “Four maneuvers to control and slow the birth of the fetal head.”10–14
Related article:
Stop performing median episiotomy!
Wound complications following the repair of a 3rd- or 4th-degree laceration are reported to occur in approximately 5% to 10% of cases.15 The most common wound complications are dehiscence, infection, abscess formation, pain, sexual dysfunction, and anal incontinence. Minor wound complications, including superficial epithelial separation, can be managed expectantly. However, major wound complications need intensive treatment.
In one study of 21 women who had a major wound complication following the repair of a 4th-degree laceration, 53% had dehiscence plus infection, 33% had dehiscence alone, and 14% had infection alone.16 Major wound complications present at a mean of 5 days after delivery, with a wide range from 1 to 17 days following delivery.17 In a study of 144 cases of wound breakdown following a perineal laceration repair, the major risk factors for wound breakdown were episiotomy (aOR, 11.1), smoking (aOR, 6.4), midwife repair of laceration (aOR, 4.7), use of chromic suture (aOR, 3.9), and operative vaginal delivery (aOR, 3.4).18 In one study of 66 women with a wound complication following the repair of a 3rd- or 4th-degree laceration, clinical risk factors for a wound complication were cigarette smoking (OR, 4.04), 4th-degree laceration (OR, 1.89), and operative vaginal delivery (OR, 1.76).19 The use of intrapartum antibiotics appears to be protective (OR, 0.29) against wound complications following a major perineal laceration.19
Approach to the patient with a dehisced and infected perineal wound
Historically, wound dehiscence following surgical repair of a perineal injury was managed by allowing the wound to slowly close. This approach adversely impacts the quality of life of the affected woman because it may take weeks for the wound to heal. One small randomized trial17 and multiple case series20–24 report that an active multistep management algorithm permits early closure of the majority of these wounds, thereby accelerating the patient’s full recovery. Delayed primary (within 72 hours postpartum) or early secondary reconstruction (within 14 days of delivery) has been demonstrated to be safe with acceptable long-term functional out-comes.25 The modern approach to the treatment of a patient with an infected wound dehiscence following a severe perineal injury involves 3 steps.
Related article:
It’s time to restrict the use of episiotomy
Step 1. Restore tissue to health
The dehisced wound is cultured and, if infection is present, treatment is initiated with intravenous antibiotics appropriate for an infection with colorectal flora. One antibiotic option includes a cephalosporin (cefotetan 2 g IV every 6 hours) plus metronidazole (500 mg IV every 8 hours).
In the operating room, the wound should be thoroughly assessed, cleansed, and debrided. This step includes irrigation of the wound with a warm fluid, mechanical debridement, and sharp dissection of necrotic tissue. If the wound is infected, removal of stitches that are visible in the open wound is recommended.
Often more than one session of debridement may be needed to obtain wound edges that are free from exudate and show granulation at the wound margins. Between debridement sessions, wet-to-dry dressings are utilized. Two to 10 days of wound care may be needed before an attempt is made to close the wound. The wound is suitable for repair when there is no infected tissue and granulation tissue is present. Some surgeons prefer a mechanical bowel preparation regimen just before surgically closing the open wound. This may prevent early bowel movements and provide for tissue healing after surgery.26 The same preparations recommended for colonoscopy can be considered prior to surgical repair.
Step 2. Surgically close the wound
The wound is surgically closed in the operating room. If in Step 1 the assessment of the wound shows major trauma, assistance from a urogynecologist may be warranted. Surgical management of a perineal wound dehiscence requires a clear understanding of perineal anatomy and the structures contained between the vagina and the anorectum.
Six key structures may be involved in perineal injury: the anorectal mucosa, internal anal sphincter, external anal sphincter, vaginal wall and perineal skin, bulbocavernosus muscle, and transverse perineal muscles. It is important to definitively identify the individual structures that need to be repaired. Careful dissection is then carried out to mobilize these structures for repair. Additional debridement may be necessary to remove excess granulation tissue.
Anorectal mucosa repair. With repair of a 4th-degree perineal wound dehiscence, the apex of the defect in the anorectal mucosa is identified. The defect is repaired beginning at the apex using closely spaced interrupted sutures or a running suture of 3-0 or 4-0 polyglactin 910. Adequate tissue bites that will resist tearing should be taken. If interrupted sutures are used, tying the knots within the anorectal canal prevents them from being located within the healing wound.
Internal anal sphincter repair. After the anorectal mucosa is closed, attention is turned to reapproximation of the internal anal sphincter. The ends of a torn internal anal sphincter are often located lateral to the anorectal mucosa and appear as shiny gray-white fibrous tissue. The surgeon’s gloved index finger can be placed within the anorectal canal to aid in identification of the internal anal sphincter, as it tends to have a rubbery feel. Additionally, while the surgeon’s gloved index finger is in the anorectal canal, the surgeon’s gloved thumb can be used to retract the anorectal mucosa slightly medial and inferior so that adequate bites of the internal anal sphincter can be taken on each side.
Alternatively, Allis clamps canbe placed on the ends of the retracted internal anal sphincter to facilitate repair. Suture selection for repair of the internal anal sphincter can include 3-0 polyglactin 910 or 3-0 monofilament, delayed-absorbable suture such as polydioxanone sulfate (PDS). Some surgeons prefer delayed-absorbable suture (PDS) for this layer given the internal anal sphincter is constantly contracting and relaxing as it samples stool.26 This layer also can be closed with either interrupted sutures or a running suture.
External anal sphincter repair. After the anorectal mucosa and internal anal sphincter defects are reapproximated, attention is turned to the external anal sphincter. Like the internal anal sphincter, the ends of the external anal sphincter are often retracted laterally and must be definitively identified and mobilized in order to ensure an adequate tension-free repair. It is important to include the fascial sheath in the repair of the external anal sphincter.27 Allis clamps can be used to grasp the ends of the torn muscle after they are identified.
We recommend 0 or 2-0 PDS for repair of the external sphincter. Repair can be performed using either an end-to-end or overlapping technique. An end-to-end repair traditionally involves reapproximating the ends of the torn muscle and its overlying fascial sheath using interrupted sutures placed at four quadrants (12:00, 3:00, 6:00, 9:00).
In contrast, in an overlapping repair, the ends of the muscle are brought together with mattress sutures. Suture is passed top down through the medial aspect of the more superior muscle flap and top down through the inferior muscle flap more laterally. The same suture is then passed bottom up through the inferior muscle flap more laterally and finally bottom up through the medial aspect of the more superior muscle flap. Two to four mattress sutures are usually placed. After all sutures are placed, they are tied securely.
An overlapping repair results in a greater amount of tissue contact between the two torn muscle ends. However, adequate mobility of the external anal sphincter is necessary to perform this type of repair.
Vaginal wall and perineal body repair. After the anal sphincters have been repaired, the vaginal wall and remainder of the perineal body are reconstructed using the same techniques involved in a 2nd-degree laceration repair. Care must be taken to retrieve and reapproximate the torn ends of the bulbocavernosus muscles, which are also often retracted laterally and superiorly. After the bulbocavernosus and transverse perineal muscles are brought together in the midline, the posterior vaginal wall should be perpendicular to the perineum.
An alternative to surgical closure of a 2nd-degree dehiscence is the use of vacuum-assisted wound closure. Disadvantages of this approach include difficulty in maintaining a vacuum seal in the perineal region and the risk of wound contamination with feces. In one case report, 3 weeks of vacuum-assisted wound closure resulted in healing of a 10-cm wound dehiscence that occurred 5 days following a forceps-assisted vaginal delivery with a mediolateral episiotomy.28
Step 3. Ensure complete healing of the wound
Superb postoperative wound care helps to ensure a quick return to full recovery. Wound care should include regularly scheduled sitz baths (at least 3 times daily) followed by drying the perineum. It is preferable to provide a liquid diet that avoids frequent bowel movements in the initial 3 postoperative days. Stool softeners and fiber supplementation are recommended when a full diet is resumed. Some surgeons have found mineral oil (1 to 2 tablespoons daily) effective in producing soft stools that are easy to pass.26 Ensuring soft stool consistency is important to help prevent repair breakdown that may occur with passage of hard stools, fecal impaction, and/or straining during defecation.
We recommend follow-up 1 to 2 weeks after surgery to assess wound healing. No vaginal intercourseis permitted until complete healing is achieved.
Use a surgical checklist
All obstetricians and midwives strive to reduce the risk of OASIS at vaginal birth. When OASIS occurs, it is often useful to use a surgical checklist to ensure the execution of all steps in the management of the repair and recovery process.29 It is heartbreaking to see an OASIS repair breakdown in the week following a vaginal delivery. But by following the 3 steps outlined here, the secondary repair is likely to be successful and will quickly return most patients to full health.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations

The authors report no financial relationships relevant to this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Blondel B, Alexander S, Bjarnadottir RI, et al; Euro-Peristat Scientific Committee. Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Perstat Project. Acta Obstet Gynecol Scand. 2016;95(7):746–754.
- Friedman AM, Ananth CV, Predergast E, D’Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927–937.
- Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G. Risk factors for severe perineal lacerations during childbirth. Int J Gynecol Obstet. 2014;125(1):6–14.
- Schmitz T, Alberti C, Andriss B, Moutafoff C, Oury JF, Sibony O. Identification of women at high risk for severe perineal lacerations. Eur J Obstet Gynecol Reprod Biol. 2014;182:11–15.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
- ACOG Committee on Practice Bulletins—Obstetrics. Practice bulletin no. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1–e15.
- Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–673.
- Aasheim V, Nilsen AB, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2011;(12):CD006672.
- Harvey MA, Pierce M, Alter JE, et al; Society of Obstetricians and Gynaecologists of Canada. Obstetrical anal sphincter injuries (OASIS): prevention, recognition and repair. J Obstet Gynaecol Can. 2015;37(12):1131–1148.
- Jonsson ER, Elfaghi I, Rydhstrom H, Herbst A. Modified Ritgen’s maneuver for anal sphincter injury at delivery: a randomized controlled trial. Obstet Gynecol. 2008;112(2 pt 1):212–217.
- Williams JW. Obstetrics: A Text-book for the Use of Students and Practitioners. New York, NY: D Appleton and Co; 1903:288.
- Cunningham FG. The Ritgen maneuver: another sacred cow questioned. Obstet Gynecol. 2008;112(2 pt 1):210–211.
- Myrfield K, Brook C, Creedy D. Reducing perineal trauma: implications of flexion and extension of the fetal head during birth. Midwifery. 1997;13:197–201.
- Ostergaard Poulsen M, Lund Madsen M, Skriver-Moller AC, Overgaard C. Does the Finnish intervention prevent obstetrical anal sphincter injuries? A systematic review of the literature. BMJ Open. 2015;5:e008346.
- Kamel A, Khaled M. Episiotomy and obstetric perineal wound dehiscence: beyond soreness. J Obstet Gynaecol. 2014;34(3):215–217.
- Goldaber KG, Wendel PJ, McIntire DD, Wendel GD Jr. Postpartum perineal morbidity after fourth-degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489–493.
- Monberg J, Hammen S. Ruptured episiotomia resutured primarily. Acta Obstet Gynecol Scand. 1987;66(2):163–164.
- Jallad K, Steele SE, Barber MD. Breakdown of perineal laceration repair after vaginal delivery: a case-control study. Female Pelvic Med Reconstr Surg. 2016;22(4):276–279.
- Stock L, Basham E, Gossett DR, Lewicky-Gaupp C. Factors associated with wound complications in women with obstetric anal sphincter injuries (OASIS). Am J Obstet Gynecol. 2013;208(4):327.e1–e8.
- Hauth JC, Gilstrap LC 3rd, Ward SC, Hankins GD. Early repair of an external sphincter ani muscle and rectal mucosal dehiscence. Obstet Gynecol. 1986;67(6):806–809.
- Hankins GD, Hauth JC, Gilstrap LC 3rd, Hammond TL, Yeomans ER, Snyder RR. Early repair of episiotomy dehiscence. Obstet Gynecol. 1990;75(1):48–51.
- Ramin SM, Ramus RM, Little BB, Gilstrap LC 3rd. Early repair of episiotomy dehiscence associated with infection. Am J Obstet Gynecol. 1992;167(4 pt 1):1104–1107.
- Arona AJ, Al-Marayati L, Grimes DA, Ballard CA. Early secondary repair of third- and fourth-degree perineal lacerations after outpatient wound preparation. Obstet Gynecol. 1995;86(2):294–296.
- Uygur D, Yesildaglar N, Kis S, Sipahi T. Early repair of episiotomy dehiscence. Aust N Z J Obstet Gynaecol. 2004;44(3):244–246.
- Soerensen MM, Bek KM, Buntzen S, Hojberg KE, Laurberg S. Long-term outcome of delayed primary or early secondary reconstruction of the anal sphincter after obstetrical injury. Dis Colon Rectum. 2008;51(3):312–317.
- Delancey JOL, Berger MB. Surgical approaches to postobstetrical perineal body defects (rectovaginal fistula and chronic third and fourth-degree lacerations). Clin Obstet Gynecol. 2010;53(1):134–144.
- Leeman L, Spearman M, Rogers R. Repair of obstetric perineal lacerations. Am Fam Physician. 2003;68(8):1585–1590.
- Aviki EM, Batalden RP, del Carmen MG, Berkowitz LR. Vacuum-assisted closure for episiotomy dehiscence. Obstet Gynecol. 2015;126(3):530–533.
- Barbieri RL. Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. OBG Manag. 2013;25(8):8–12.
During vaginal delivery spontaneous perineal trauma and extension of episiotomy incisions are common. A severe perineal laceration that extends into or through the anal sphincter complex is referred to as an obstetric anal sphincter injury (OASIS) and requires meticulous repair. Following the repair of an OASIS, serious wound complications, including dehiscence and infection, may occur. In Europe the reported rate of OASIS varies widely among countries, with a rate of 0.1% in Romania, possibly due to underreporting, and 4.9% in Iceland.1 In the United States the rates of 3rd- and 4th-degree lacerations were reported to be 3.3% and 1.1%, respectively.2
Risk factors for OASIS include forceps delivery (odds ratio [OR], 5.50), vacuum-assisted delivery (OR, 3.98), and midline episiotomy (OR, 3.82).3 Additional risk factors for severe perineal injury at vaginal delivery include nulliparity (adjusted odds ratio [aOR], 2.58), delivery from a persistent occiput posterior position (aOR, 2.24), and above-average newborn birth weight (aOR, 1.28).4
In a meta-analysis of randomized trials, the researchers reported that restrictive use of episiotomy reduced the risk of severe perineal trauma (relative risk [RR], 0.67) but increased the risk of anterior perineal trauma (RR, 1.84).5 The American College of Obstetricians and Gynecologists (ACOG) recommends that episiotomy should not be a routine practice and is best restricted to use in a limited number of cases where fetal and maternal benefit is likely.6 In addition, ACOG recommends that if episiotomy is indicated, a mediolateral incision is favored over a midline incision. In my practice I perform only mediolateral episiotomy incisions. However, mediolateral episiotomy may be associated with an increased risk of postpartum perineal pain and dyspareunia.7 Use of warm compresses applied to the perineum during the second stage of labor may reduce the risk of 3rd- and 4th-degree lacerations.8 Techniques to ensure that the fetal head and shoulders are birthed in a slow and controlled fashion may decrease the risk of OASIS.9 See the TABLE, “Four maneuvers to control and slow the birth of the fetal head.”10–14
Related article:
Stop performing median episiotomy!
Wound complications following the repair of a 3rd- or 4th-degree laceration are reported to occur in approximately 5% to 10% of cases.15 The most common wound complications are dehiscence, infection, abscess formation, pain, sexual dysfunction, and anal incontinence. Minor wound complications, including superficial epithelial separation, can be managed expectantly. However, major wound complications need intensive treatment.
In one study of 21 women who had a major wound complication following the repair of a 4th-degree laceration, 53% had dehiscence plus infection, 33% had dehiscence alone, and 14% had infection alone.16 Major wound complications present at a mean of 5 days after delivery, with a wide range from 1 to 17 days following delivery.17 In a study of 144 cases of wound breakdown following a perineal laceration repair, the major risk factors for wound breakdown were episiotomy (aOR, 11.1), smoking (aOR, 6.4), midwife repair of laceration (aOR, 4.7), use of chromic suture (aOR, 3.9), and operative vaginal delivery (aOR, 3.4).18 In one study of 66 women with a wound complication following the repair of a 3rd- or 4th-degree laceration, clinical risk factors for a wound complication were cigarette smoking (OR, 4.04), 4th-degree laceration (OR, 1.89), and operative vaginal delivery (OR, 1.76).19 The use of intrapartum antibiotics appears to be protective (OR, 0.29) against wound complications following a major perineal laceration.19
Approach to the patient with a dehisced and infected perineal wound
Historically, wound dehiscence following surgical repair of a perineal injury was managed by allowing the wound to slowly close. This approach adversely impacts the quality of life of the affected woman because it may take weeks for the wound to heal. One small randomized trial17 and multiple case series20–24 report that an active multistep management algorithm permits early closure of the majority of these wounds, thereby accelerating the patient’s full recovery. Delayed primary (within 72 hours postpartum) or early secondary reconstruction (within 14 days of delivery) has been demonstrated to be safe with acceptable long-term functional out-comes.25 The modern approach to the treatment of a patient with an infected wound dehiscence following a severe perineal injury involves 3 steps.
Related article:
It’s time to restrict the use of episiotomy
Step 1. Restore tissue to health
The dehisced wound is cultured and, if infection is present, treatment is initiated with intravenous antibiotics appropriate for an infection with colorectal flora. One antibiotic option includes a cephalosporin (cefotetan 2 g IV every 6 hours) plus metronidazole (500 mg IV every 8 hours).
In the operating room, the wound should be thoroughly assessed, cleansed, and debrided. This step includes irrigation of the wound with a warm fluid, mechanical debridement, and sharp dissection of necrotic tissue. If the wound is infected, removal of stitches that are visible in the open wound is recommended.
Often more than one session of debridement may be needed to obtain wound edges that are free from exudate and show granulation at the wound margins. Between debridement sessions, wet-to-dry dressings are utilized. Two to 10 days of wound care may be needed before an attempt is made to close the wound. The wound is suitable for repair when there is no infected tissue and granulation tissue is present. Some surgeons prefer a mechanical bowel preparation regimen just before surgically closing the open wound. This may prevent early bowel movements and provide for tissue healing after surgery.26 The same preparations recommended for colonoscopy can be considered prior to surgical repair.
Step 2. Surgically close the wound
The wound is surgically closed in the operating room. If in Step 1 the assessment of the wound shows major trauma, assistance from a urogynecologist may be warranted. Surgical management of a perineal wound dehiscence requires a clear understanding of perineal anatomy and the structures contained between the vagina and the anorectum.
Six key structures may be involved in perineal injury: the anorectal mucosa, internal anal sphincter, external anal sphincter, vaginal wall and perineal skin, bulbocavernosus muscle, and transverse perineal muscles. It is important to definitively identify the individual structures that need to be repaired. Careful dissection is then carried out to mobilize these structures for repair. Additional debridement may be necessary to remove excess granulation tissue.
Anorectal mucosa repair. With repair of a 4th-degree perineal wound dehiscence, the apex of the defect in the anorectal mucosa is identified. The defect is repaired beginning at the apex using closely spaced interrupted sutures or a running suture of 3-0 or 4-0 polyglactin 910. Adequate tissue bites that will resist tearing should be taken. If interrupted sutures are used, tying the knots within the anorectal canal prevents them from being located within the healing wound.
Internal anal sphincter repair. After the anorectal mucosa is closed, attention is turned to reapproximation of the internal anal sphincter. The ends of a torn internal anal sphincter are often located lateral to the anorectal mucosa and appear as shiny gray-white fibrous tissue. The surgeon’s gloved index finger can be placed within the anorectal canal to aid in identification of the internal anal sphincter, as it tends to have a rubbery feel. Additionally, while the surgeon’s gloved index finger is in the anorectal canal, the surgeon’s gloved thumb can be used to retract the anorectal mucosa slightly medial and inferior so that adequate bites of the internal anal sphincter can be taken on each side.
Alternatively, Allis clamps canbe placed on the ends of the retracted internal anal sphincter to facilitate repair. Suture selection for repair of the internal anal sphincter can include 3-0 polyglactin 910 or 3-0 monofilament, delayed-absorbable suture such as polydioxanone sulfate (PDS). Some surgeons prefer delayed-absorbable suture (PDS) for this layer given the internal anal sphincter is constantly contracting and relaxing as it samples stool.26 This layer also can be closed with either interrupted sutures or a running suture.
External anal sphincter repair. After the anorectal mucosa and internal anal sphincter defects are reapproximated, attention is turned to the external anal sphincter. Like the internal anal sphincter, the ends of the external anal sphincter are often retracted laterally and must be definitively identified and mobilized in order to ensure an adequate tension-free repair. It is important to include the fascial sheath in the repair of the external anal sphincter.27 Allis clamps can be used to grasp the ends of the torn muscle after they are identified.
We recommend 0 or 2-0 PDS for repair of the external sphincter. Repair can be performed using either an end-to-end or overlapping technique. An end-to-end repair traditionally involves reapproximating the ends of the torn muscle and its overlying fascial sheath using interrupted sutures placed at four quadrants (12:00, 3:00, 6:00, 9:00).
In contrast, in an overlapping repair, the ends of the muscle are brought together with mattress sutures. Suture is passed top down through the medial aspect of the more superior muscle flap and top down through the inferior muscle flap more laterally. The same suture is then passed bottom up through the inferior muscle flap more laterally and finally bottom up through the medial aspect of the more superior muscle flap. Two to four mattress sutures are usually placed. After all sutures are placed, they are tied securely.
An overlapping repair results in a greater amount of tissue contact between the two torn muscle ends. However, adequate mobility of the external anal sphincter is necessary to perform this type of repair.
Vaginal wall and perineal body repair. After the anal sphincters have been repaired, the vaginal wall and remainder of the perineal body are reconstructed using the same techniques involved in a 2nd-degree laceration repair. Care must be taken to retrieve and reapproximate the torn ends of the bulbocavernosus muscles, which are also often retracted laterally and superiorly. After the bulbocavernosus and transverse perineal muscles are brought together in the midline, the posterior vaginal wall should be perpendicular to the perineum.
An alternative to surgical closure of a 2nd-degree dehiscence is the use of vacuum-assisted wound closure. Disadvantages of this approach include difficulty in maintaining a vacuum seal in the perineal region and the risk of wound contamination with feces. In one case report, 3 weeks of vacuum-assisted wound closure resulted in healing of a 10-cm wound dehiscence that occurred 5 days following a forceps-assisted vaginal delivery with a mediolateral episiotomy.28
Step 3. Ensure complete healing of the wound
Superb postoperative wound care helps to ensure a quick return to full recovery. Wound care should include regularly scheduled sitz baths (at least 3 times daily) followed by drying the perineum. It is preferable to provide a liquid diet that avoids frequent bowel movements in the initial 3 postoperative days. Stool softeners and fiber supplementation are recommended when a full diet is resumed. Some surgeons have found mineral oil (1 to 2 tablespoons daily) effective in producing soft stools that are easy to pass.26 Ensuring soft stool consistency is important to help prevent repair breakdown that may occur with passage of hard stools, fecal impaction, and/or straining during defecation.
We recommend follow-up 1 to 2 weeks after surgery to assess wound healing. No vaginal intercourseis permitted until complete healing is achieved.
Use a surgical checklist
All obstetricians and midwives strive to reduce the risk of OASIS at vaginal birth. When OASIS occurs, it is often useful to use a surgical checklist to ensure the execution of all steps in the management of the repair and recovery process.29 It is heartbreaking to see an OASIS repair breakdown in the week following a vaginal delivery. But by following the 3 steps outlined here, the secondary repair is likely to be successful and will quickly return most patients to full health.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations

The authors report no financial relationships relevant to this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
During vaginal delivery spontaneous perineal trauma and extension of episiotomy incisions are common. A severe perineal laceration that extends into or through the anal sphincter complex is referred to as an obstetric anal sphincter injury (OASIS) and requires meticulous repair. Following the repair of an OASIS, serious wound complications, including dehiscence and infection, may occur. In Europe the reported rate of OASIS varies widely among countries, with a rate of 0.1% in Romania, possibly due to underreporting, and 4.9% in Iceland.1 In the United States the rates of 3rd- and 4th-degree lacerations were reported to be 3.3% and 1.1%, respectively.2
Risk factors for OASIS include forceps delivery (odds ratio [OR], 5.50), vacuum-assisted delivery (OR, 3.98), and midline episiotomy (OR, 3.82).3 Additional risk factors for severe perineal injury at vaginal delivery include nulliparity (adjusted odds ratio [aOR], 2.58), delivery from a persistent occiput posterior position (aOR, 2.24), and above-average newborn birth weight (aOR, 1.28).4
In a meta-analysis of randomized trials, the researchers reported that restrictive use of episiotomy reduced the risk of severe perineal trauma (relative risk [RR], 0.67) but increased the risk of anterior perineal trauma (RR, 1.84).5 The American College of Obstetricians and Gynecologists (ACOG) recommends that episiotomy should not be a routine practice and is best restricted to use in a limited number of cases where fetal and maternal benefit is likely.6 In addition, ACOG recommends that if episiotomy is indicated, a mediolateral incision is favored over a midline incision. In my practice I perform only mediolateral episiotomy incisions. However, mediolateral episiotomy may be associated with an increased risk of postpartum perineal pain and dyspareunia.7 Use of warm compresses applied to the perineum during the second stage of labor may reduce the risk of 3rd- and 4th-degree lacerations.8 Techniques to ensure that the fetal head and shoulders are birthed in a slow and controlled fashion may decrease the risk of OASIS.9 See the TABLE, “Four maneuvers to control and slow the birth of the fetal head.”10–14
Related article:
Stop performing median episiotomy!
Wound complications following the repair of a 3rd- or 4th-degree laceration are reported to occur in approximately 5% to 10% of cases.15 The most common wound complications are dehiscence, infection, abscess formation, pain, sexual dysfunction, and anal incontinence. Minor wound complications, including superficial epithelial separation, can be managed expectantly. However, major wound complications need intensive treatment.
In one study of 21 women who had a major wound complication following the repair of a 4th-degree laceration, 53% had dehiscence plus infection, 33% had dehiscence alone, and 14% had infection alone.16 Major wound complications present at a mean of 5 days after delivery, with a wide range from 1 to 17 days following delivery.17 In a study of 144 cases of wound breakdown following a perineal laceration repair, the major risk factors for wound breakdown were episiotomy (aOR, 11.1), smoking (aOR, 6.4), midwife repair of laceration (aOR, 4.7), use of chromic suture (aOR, 3.9), and operative vaginal delivery (aOR, 3.4).18 In one study of 66 women with a wound complication following the repair of a 3rd- or 4th-degree laceration, clinical risk factors for a wound complication were cigarette smoking (OR, 4.04), 4th-degree laceration (OR, 1.89), and operative vaginal delivery (OR, 1.76).19 The use of intrapartum antibiotics appears to be protective (OR, 0.29) against wound complications following a major perineal laceration.19
Approach to the patient with a dehisced and infected perineal wound
Historically, wound dehiscence following surgical repair of a perineal injury was managed by allowing the wound to slowly close. This approach adversely impacts the quality of life of the affected woman because it may take weeks for the wound to heal. One small randomized trial17 and multiple case series20–24 report that an active multistep management algorithm permits early closure of the majority of these wounds, thereby accelerating the patient’s full recovery. Delayed primary (within 72 hours postpartum) or early secondary reconstruction (within 14 days of delivery) has been demonstrated to be safe with acceptable long-term functional out-comes.25 The modern approach to the treatment of a patient with an infected wound dehiscence following a severe perineal injury involves 3 steps.
Related article:
It’s time to restrict the use of episiotomy
Step 1. Restore tissue to health
The dehisced wound is cultured and, if infection is present, treatment is initiated with intravenous antibiotics appropriate for an infection with colorectal flora. One antibiotic option includes a cephalosporin (cefotetan 2 g IV every 6 hours) plus metronidazole (500 mg IV every 8 hours).
In the operating room, the wound should be thoroughly assessed, cleansed, and debrided. This step includes irrigation of the wound with a warm fluid, mechanical debridement, and sharp dissection of necrotic tissue. If the wound is infected, removal of stitches that are visible in the open wound is recommended.
Often more than one session of debridement may be needed to obtain wound edges that are free from exudate and show granulation at the wound margins. Between debridement sessions, wet-to-dry dressings are utilized. Two to 10 days of wound care may be needed before an attempt is made to close the wound. The wound is suitable for repair when there is no infected tissue and granulation tissue is present. Some surgeons prefer a mechanical bowel preparation regimen just before surgically closing the open wound. This may prevent early bowel movements and provide for tissue healing after surgery.26 The same preparations recommended for colonoscopy can be considered prior to surgical repair.
Step 2. Surgically close the wound
The wound is surgically closed in the operating room. If in Step 1 the assessment of the wound shows major trauma, assistance from a urogynecologist may be warranted. Surgical management of a perineal wound dehiscence requires a clear understanding of perineal anatomy and the structures contained between the vagina and the anorectum.
Six key structures may be involved in perineal injury: the anorectal mucosa, internal anal sphincter, external anal sphincter, vaginal wall and perineal skin, bulbocavernosus muscle, and transverse perineal muscles. It is important to definitively identify the individual structures that need to be repaired. Careful dissection is then carried out to mobilize these structures for repair. Additional debridement may be necessary to remove excess granulation tissue.
Anorectal mucosa repair. With repair of a 4th-degree perineal wound dehiscence, the apex of the defect in the anorectal mucosa is identified. The defect is repaired beginning at the apex using closely spaced interrupted sutures or a running suture of 3-0 or 4-0 polyglactin 910. Adequate tissue bites that will resist tearing should be taken. If interrupted sutures are used, tying the knots within the anorectal canal prevents them from being located within the healing wound.
Internal anal sphincter repair. After the anorectal mucosa is closed, attention is turned to reapproximation of the internal anal sphincter. The ends of a torn internal anal sphincter are often located lateral to the anorectal mucosa and appear as shiny gray-white fibrous tissue. The surgeon’s gloved index finger can be placed within the anorectal canal to aid in identification of the internal anal sphincter, as it tends to have a rubbery feel. Additionally, while the surgeon’s gloved index finger is in the anorectal canal, the surgeon’s gloved thumb can be used to retract the anorectal mucosa slightly medial and inferior so that adequate bites of the internal anal sphincter can be taken on each side.
Alternatively, Allis clamps canbe placed on the ends of the retracted internal anal sphincter to facilitate repair. Suture selection for repair of the internal anal sphincter can include 3-0 polyglactin 910 or 3-0 monofilament, delayed-absorbable suture such as polydioxanone sulfate (PDS). Some surgeons prefer delayed-absorbable suture (PDS) for this layer given the internal anal sphincter is constantly contracting and relaxing as it samples stool.26 This layer also can be closed with either interrupted sutures or a running suture.
External anal sphincter repair. After the anorectal mucosa and internal anal sphincter defects are reapproximated, attention is turned to the external anal sphincter. Like the internal anal sphincter, the ends of the external anal sphincter are often retracted laterally and must be definitively identified and mobilized in order to ensure an adequate tension-free repair. It is important to include the fascial sheath in the repair of the external anal sphincter.27 Allis clamps can be used to grasp the ends of the torn muscle after they are identified.
We recommend 0 or 2-0 PDS for repair of the external sphincter. Repair can be performed using either an end-to-end or overlapping technique. An end-to-end repair traditionally involves reapproximating the ends of the torn muscle and its overlying fascial sheath using interrupted sutures placed at four quadrants (12:00, 3:00, 6:00, 9:00).
In contrast, in an overlapping repair, the ends of the muscle are brought together with mattress sutures. Suture is passed top down through the medial aspect of the more superior muscle flap and top down through the inferior muscle flap more laterally. The same suture is then passed bottom up through the inferior muscle flap more laterally and finally bottom up through the medial aspect of the more superior muscle flap. Two to four mattress sutures are usually placed. After all sutures are placed, they are tied securely.
An overlapping repair results in a greater amount of tissue contact between the two torn muscle ends. However, adequate mobility of the external anal sphincter is necessary to perform this type of repair.
Vaginal wall and perineal body repair. After the anal sphincters have been repaired, the vaginal wall and remainder of the perineal body are reconstructed using the same techniques involved in a 2nd-degree laceration repair. Care must be taken to retrieve and reapproximate the torn ends of the bulbocavernosus muscles, which are also often retracted laterally and superiorly. After the bulbocavernosus and transverse perineal muscles are brought together in the midline, the posterior vaginal wall should be perpendicular to the perineum.
An alternative to surgical closure of a 2nd-degree dehiscence is the use of vacuum-assisted wound closure. Disadvantages of this approach include difficulty in maintaining a vacuum seal in the perineal region and the risk of wound contamination with feces. In one case report, 3 weeks of vacuum-assisted wound closure resulted in healing of a 10-cm wound dehiscence that occurred 5 days following a forceps-assisted vaginal delivery with a mediolateral episiotomy.28
Step 3. Ensure complete healing of the wound
Superb postoperative wound care helps to ensure a quick return to full recovery. Wound care should include regularly scheduled sitz baths (at least 3 times daily) followed by drying the perineum. It is preferable to provide a liquid diet that avoids frequent bowel movements in the initial 3 postoperative days. Stool softeners and fiber supplementation are recommended when a full diet is resumed. Some surgeons have found mineral oil (1 to 2 tablespoons daily) effective in producing soft stools that are easy to pass.26 Ensuring soft stool consistency is important to help prevent repair breakdown that may occur with passage of hard stools, fecal impaction, and/or straining during defecation.
We recommend follow-up 1 to 2 weeks after surgery to assess wound healing. No vaginal intercourseis permitted until complete healing is achieved.
Use a surgical checklist
All obstetricians and midwives strive to reduce the risk of OASIS at vaginal birth. When OASIS occurs, it is often useful to use a surgical checklist to ensure the execution of all steps in the management of the repair and recovery process.29 It is heartbreaking to see an OASIS repair breakdown in the week following a vaginal delivery. But by following the 3 steps outlined here, the secondary repair is likely to be successful and will quickly return most patients to full health.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations

The authors report no financial relationships relevant to this article.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Blondel B, Alexander S, Bjarnadottir RI, et al; Euro-Peristat Scientific Committee. Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Perstat Project. Acta Obstet Gynecol Scand. 2016;95(7):746–754.
- Friedman AM, Ananth CV, Predergast E, D’Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927–937.
- Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G. Risk factors for severe perineal lacerations during childbirth. Int J Gynecol Obstet. 2014;125(1):6–14.
- Schmitz T, Alberti C, Andriss B, Moutafoff C, Oury JF, Sibony O. Identification of women at high risk for severe perineal lacerations. Eur J Obstet Gynecol Reprod Biol. 2014;182:11–15.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
- ACOG Committee on Practice Bulletins—Obstetrics. Practice bulletin no. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1–e15.
- Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–673.
- Aasheim V, Nilsen AB, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2011;(12):CD006672.
- Harvey MA, Pierce M, Alter JE, et al; Society of Obstetricians and Gynaecologists of Canada. Obstetrical anal sphincter injuries (OASIS): prevention, recognition and repair. J Obstet Gynaecol Can. 2015;37(12):1131–1148.
- Jonsson ER, Elfaghi I, Rydhstrom H, Herbst A. Modified Ritgen’s maneuver for anal sphincter injury at delivery: a randomized controlled trial. Obstet Gynecol. 2008;112(2 pt 1):212–217.
- Williams JW. Obstetrics: A Text-book for the Use of Students and Practitioners. New York, NY: D Appleton and Co; 1903:288.
- Cunningham FG. The Ritgen maneuver: another sacred cow questioned. Obstet Gynecol. 2008;112(2 pt 1):210–211.
- Myrfield K, Brook C, Creedy D. Reducing perineal trauma: implications of flexion and extension of the fetal head during birth. Midwifery. 1997;13:197–201.
- Ostergaard Poulsen M, Lund Madsen M, Skriver-Moller AC, Overgaard C. Does the Finnish intervention prevent obstetrical anal sphincter injuries? A systematic review of the literature. BMJ Open. 2015;5:e008346.
- Kamel A, Khaled M. Episiotomy and obstetric perineal wound dehiscence: beyond soreness. J Obstet Gynaecol. 2014;34(3):215–217.
- Goldaber KG, Wendel PJ, McIntire DD, Wendel GD Jr. Postpartum perineal morbidity after fourth-degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489–493.
- Monberg J, Hammen S. Ruptured episiotomia resutured primarily. Acta Obstet Gynecol Scand. 1987;66(2):163–164.
- Jallad K, Steele SE, Barber MD. Breakdown of perineal laceration repair after vaginal delivery: a case-control study. Female Pelvic Med Reconstr Surg. 2016;22(4):276–279.
- Stock L, Basham E, Gossett DR, Lewicky-Gaupp C. Factors associated with wound complications in women with obstetric anal sphincter injuries (OASIS). Am J Obstet Gynecol. 2013;208(4):327.e1–e8.
- Hauth JC, Gilstrap LC 3rd, Ward SC, Hankins GD. Early repair of an external sphincter ani muscle and rectal mucosal dehiscence. Obstet Gynecol. 1986;67(6):806–809.
- Hankins GD, Hauth JC, Gilstrap LC 3rd, Hammond TL, Yeomans ER, Snyder RR. Early repair of episiotomy dehiscence. Obstet Gynecol. 1990;75(1):48–51.
- Ramin SM, Ramus RM, Little BB, Gilstrap LC 3rd. Early repair of episiotomy dehiscence associated with infection. Am J Obstet Gynecol. 1992;167(4 pt 1):1104–1107.
- Arona AJ, Al-Marayati L, Grimes DA, Ballard CA. Early secondary repair of third- and fourth-degree perineal lacerations after outpatient wound preparation. Obstet Gynecol. 1995;86(2):294–296.
- Uygur D, Yesildaglar N, Kis S, Sipahi T. Early repair of episiotomy dehiscence. Aust N Z J Obstet Gynaecol. 2004;44(3):244–246.
- Soerensen MM, Bek KM, Buntzen S, Hojberg KE, Laurberg S. Long-term outcome of delayed primary or early secondary reconstruction of the anal sphincter after obstetrical injury. Dis Colon Rectum. 2008;51(3):312–317.
- Delancey JOL, Berger MB. Surgical approaches to postobstetrical perineal body defects (rectovaginal fistula and chronic third and fourth-degree lacerations). Clin Obstet Gynecol. 2010;53(1):134–144.
- Leeman L, Spearman M, Rogers R. Repair of obstetric perineal lacerations. Am Fam Physician. 2003;68(8):1585–1590.
- Aviki EM, Batalden RP, del Carmen MG, Berkowitz LR. Vacuum-assisted closure for episiotomy dehiscence. Obstet Gynecol. 2015;126(3):530–533.
- Barbieri RL. Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. OBG Manag. 2013;25(8):8–12.
- Blondel B, Alexander S, Bjarnadottir RI, et al; Euro-Peristat Scientific Committee. Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Perstat Project. Acta Obstet Gynecol Scand. 2016;95(7):746–754.
- Friedman AM, Ananth CV, Predergast E, D’Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927–937.
- Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G. Risk factors for severe perineal lacerations during childbirth. Int J Gynecol Obstet. 2014;125(1):6–14.
- Schmitz T, Alberti C, Andriss B, Moutafoff C, Oury JF, Sibony O. Identification of women at high risk for severe perineal lacerations. Eur J Obstet Gynecol Reprod Biol. 2014;182:11–15.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
- ACOG Committee on Practice Bulletins—Obstetrics. Practice bulletin no. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1–e15.
- Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–673.
- Aasheim V, Nilsen AB, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2011;(12):CD006672.
- Harvey MA, Pierce M, Alter JE, et al; Society of Obstetricians and Gynaecologists of Canada. Obstetrical anal sphincter injuries (OASIS): prevention, recognition and repair. J Obstet Gynaecol Can. 2015;37(12):1131–1148.
- Jonsson ER, Elfaghi I, Rydhstrom H, Herbst A. Modified Ritgen’s maneuver for anal sphincter injury at delivery: a randomized controlled trial. Obstet Gynecol. 2008;112(2 pt 1):212–217.
- Williams JW. Obstetrics: A Text-book for the Use of Students and Practitioners. New York, NY: D Appleton and Co; 1903:288.
- Cunningham FG. The Ritgen maneuver: another sacred cow questioned. Obstet Gynecol. 2008;112(2 pt 1):210–211.
- Myrfield K, Brook C, Creedy D. Reducing perineal trauma: implications of flexion and extension of the fetal head during birth. Midwifery. 1997;13:197–201.
- Ostergaard Poulsen M, Lund Madsen M, Skriver-Moller AC, Overgaard C. Does the Finnish intervention prevent obstetrical anal sphincter injuries? A systematic review of the literature. BMJ Open. 2015;5:e008346.
- Kamel A, Khaled M. Episiotomy and obstetric perineal wound dehiscence: beyond soreness. J Obstet Gynaecol. 2014;34(3):215–217.
- Goldaber KG, Wendel PJ, McIntire DD, Wendel GD Jr. Postpartum perineal morbidity after fourth-degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489–493.
- Monberg J, Hammen S. Ruptured episiotomia resutured primarily. Acta Obstet Gynecol Scand. 1987;66(2):163–164.
- Jallad K, Steele SE, Barber MD. Breakdown of perineal laceration repair after vaginal delivery: a case-control study. Female Pelvic Med Reconstr Surg. 2016;22(4):276–279.
- Stock L, Basham E, Gossett DR, Lewicky-Gaupp C. Factors associated with wound complications in women with obstetric anal sphincter injuries (OASIS). Am J Obstet Gynecol. 2013;208(4):327.e1–e8.
- Hauth JC, Gilstrap LC 3rd, Ward SC, Hankins GD. Early repair of an external sphincter ani muscle and rectal mucosal dehiscence. Obstet Gynecol. 1986;67(6):806–809.
- Hankins GD, Hauth JC, Gilstrap LC 3rd, Hammond TL, Yeomans ER, Snyder RR. Early repair of episiotomy dehiscence. Obstet Gynecol. 1990;75(1):48–51.
- Ramin SM, Ramus RM, Little BB, Gilstrap LC 3rd. Early repair of episiotomy dehiscence associated with infection. Am J Obstet Gynecol. 1992;167(4 pt 1):1104–1107.
- Arona AJ, Al-Marayati L, Grimes DA, Ballard CA. Early secondary repair of third- and fourth-degree perineal lacerations after outpatient wound preparation. Obstet Gynecol. 1995;86(2):294–296.
- Uygur D, Yesildaglar N, Kis S, Sipahi T. Early repair of episiotomy dehiscence. Aust N Z J Obstet Gynaecol. 2004;44(3):244–246.
- Soerensen MM, Bek KM, Buntzen S, Hojberg KE, Laurberg S. Long-term outcome of delayed primary or early secondary reconstruction of the anal sphincter after obstetrical injury. Dis Colon Rectum. 2008;51(3):312–317.
- Delancey JOL, Berger MB. Surgical approaches to postobstetrical perineal body defects (rectovaginal fistula and chronic third and fourth-degree lacerations). Clin Obstet Gynecol. 2010;53(1):134–144.
- Leeman L, Spearman M, Rogers R. Repair of obstetric perineal lacerations. Am Fam Physician. 2003;68(8):1585–1590.
- Aviki EM, Batalden RP, del Carmen MG, Berkowitz LR. Vacuum-assisted closure for episiotomy dehiscence. Obstet Gynecol. 2015;126(3):530–533.
- Barbieri RL. Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. OBG Manag. 2013;25(8):8–12.
SYNTAX analysis: Making the case for CABG over PCI
Whenever seminal clinical trials report results that challenge conventional thinking, physicians face the challenge of actually applying those findings in the clinic. A team of cardiac surgeons from Baylor University in Plano, Tex., has offered its take on the clinical implications of recent findings from the cause-of-death analysis of the SYNTAX trial that compared coronary artery bypass grafting with stenting: When counseling higher-risk patients with coronary artery disease about revascularization procedures, cardiologists and cardiac surgeons should clearly elucidate the dramatic advantage of coronary artery bypass grafting over stenting that SYNTAX had demonstrated.
Michael Mack, MD, and coauthors made their case in a featured expert opinion in the Journal of Thoracic and Cardiovascular Surgery (2016;152:1237-40).
“In fact, there was a significant survival advantage for CABG in the patients with intermediate and high SYNTAX scores, with the death rate of CABG versus PCI being 9.6% versus 16.3% (P less than .047) and 8.8% versus 17.8% (P less than .02), respectively,” they wrote.
The advantages of surgery “have been most striking for patients with intermediate or high SYNTAX scores, but seem to exist for patients with low scores as well, although requiring more follow-up,” Dr. Mack and colleagues said. But the situation is less clear in other subgroups, particularly in patients with less diffuse distal disease and lower SYNTAX scores, they added.
Complete revascularization after the procedure may explain the better outcomes with CABG, as 43.3% of those in the PCI arm had incomplete revascularization vs. 36.8% in the CABG arm. “Incomplete revascularization was associated with increased risk for major adverse cardiac or cerebrovascular events three years after PCI, but incomplete revascularization in the CABG group could not be identified as a predictor for worse outcomes,” Dr. Mack and colleagues noted.
The expert opinion authors debunk one of the recent criticisms of SYNTAX: that its reliance on first-generation drug-eluting stents is dated and not relevant today. They noted the more recent Bypass Surgery Vs. Everolimus-Eluting Stent Implantation for Multivessel Coronary Artery Disease trial found a similarly higher rate of death, heart attack, and target vessel revascularization occurred more frequently in the PCI group (15.3% vs. 10.6% in the CABG group) (N Engl J Med. 2015;372:1204-12).
Nonetheless, Dr. Mack and coauthors found room for improvement for CABG through increased use of atrial revascularization and appropriate measures to minimize stroke.
The latest SYNTAX findings can inform the approach surgeons take with high-risk patients, they said. This should include “a discussion of these data, particularly in regard to survival.” And physicians should base their therapeutic recommendations on these data. “At present, there are data seeming to indicate that the majority of patients with three-vessel disease receiving invasive treatment in the United States are being treated with PCI, an outcome that is not congruent with these outcome findings,” they said.
Taking into consideration other SYNTAX analyses that have shown that completeness of revascularization is a determining factor in post-PCI outcomes, Dr. Mack and coauthors said that physicians should calculate the degree of coronary artery disease (CAD) left untreated after intervention, “and those patients who are likely to have a high residual SYNTAX score should be strongly considered for CABG.” Doctors should also focus “intensive efforts” on adherence to optimal medical therapy after both CABG and PCI.
“Finally, although there is a strong patient preference for a less-invasive treatment of their CAD, patients with advanced disease should be made aware that the choice of PCI puts them at an increased risk of death relative to CABG, and a full and transparent discussion should occur regarding the implications of their decision,” Dr. Mack and coauthors concluded.
They had no relevant financial relationships to disclose.
In their invited editorial commentary, Saswata Deb, MD, and Stephen E. Fremes, MD, of the Schulich Heart Center at the University of Toronto, concurred with the conclusions of Dr. Mack and colleagues (J Thorac Cardiovasc Surg. 2016;152:1241-2). And Joseph F. Sabik III, MD, of the Cleveland Clinic arrived at a similar conclusion in an accompanying editorial (J. Thorac Cardiovasc Surg. 2016;152:1227-8).
Dr. Deb and Dr. Fremes found noteworthy the point Dr. Mack and coauthors raised about cardiologists and internists continuing to recommend PCI to patients with complex multivessel CAD despite evidence from SYNTAX and other trials. “This raises the importance of having a multidisciplinary heart team,” Dr. Deb and Dr. Fremes said.
But they also raised an important question about the difference in outcomes between CABG and PCI in complex multivessel disease. CABG should be the preferred intervention if the high rates of late fatal myocardial infarction after PCI are due to incomplete revascularization; however, if late stent thrombosis was the cause of this disparity in outcomes, then improvements in PCI could close that gap.
In his editorial, Dr. Sabik attributed the difference in outcomes between PCI and CABG to the ability of the former to both treat existing and prevent future stenosis. PCI can be “difficult, dangerous, and even impossible” when the target vessel is totally occluded or the stenosis is complex, hence leading to incomplete revascularization and residual ischemia. “Performing CABG to these vessels is no more difficult than for an isolated, noncomplex stenosis,” Dr. Sabik said.
Dr. Sabik disclosed he is the principal investigator for an Abbott Laboratories–sponsored trial of left main coronary disease, and is on the scientific advisory board of Medtronic.
Dr. Deb and Dr. Fremes had no relationships to disclose.
In their invited editorial commentary, Saswata Deb, MD, and Stephen E. Fremes, MD, of the Schulich Heart Center at the University of Toronto, concurred with the conclusions of Dr. Mack and colleagues (J Thorac Cardiovasc Surg. 2016;152:1241-2). And Joseph F. Sabik III, MD, of the Cleveland Clinic arrived at a similar conclusion in an accompanying editorial (J. Thorac Cardiovasc Surg. 2016;152:1227-8).
Dr. Deb and Dr. Fremes found noteworthy the point Dr. Mack and coauthors raised about cardiologists and internists continuing to recommend PCI to patients with complex multivessel CAD despite evidence from SYNTAX and other trials. “This raises the importance of having a multidisciplinary heart team,” Dr. Deb and Dr. Fremes said.
But they also raised an important question about the difference in outcomes between CABG and PCI in complex multivessel disease. CABG should be the preferred intervention if the high rates of late fatal myocardial infarction after PCI are due to incomplete revascularization; however, if late stent thrombosis was the cause of this disparity in outcomes, then improvements in PCI could close that gap.
In his editorial, Dr. Sabik attributed the difference in outcomes between PCI and CABG to the ability of the former to both treat existing and prevent future stenosis. PCI can be “difficult, dangerous, and even impossible” when the target vessel is totally occluded or the stenosis is complex, hence leading to incomplete revascularization and residual ischemia. “Performing CABG to these vessels is no more difficult than for an isolated, noncomplex stenosis,” Dr. Sabik said.
Dr. Sabik disclosed he is the principal investigator for an Abbott Laboratories–sponsored trial of left main coronary disease, and is on the scientific advisory board of Medtronic.
Dr. Deb and Dr. Fremes had no relationships to disclose.
In their invited editorial commentary, Saswata Deb, MD, and Stephen E. Fremes, MD, of the Schulich Heart Center at the University of Toronto, concurred with the conclusions of Dr. Mack and colleagues (J Thorac Cardiovasc Surg. 2016;152:1241-2). And Joseph F. Sabik III, MD, of the Cleveland Clinic arrived at a similar conclusion in an accompanying editorial (J. Thorac Cardiovasc Surg. 2016;152:1227-8).
Dr. Deb and Dr. Fremes found noteworthy the point Dr. Mack and coauthors raised about cardiologists and internists continuing to recommend PCI to patients with complex multivessel CAD despite evidence from SYNTAX and other trials. “This raises the importance of having a multidisciplinary heart team,” Dr. Deb and Dr. Fremes said.
But they also raised an important question about the difference in outcomes between CABG and PCI in complex multivessel disease. CABG should be the preferred intervention if the high rates of late fatal myocardial infarction after PCI are due to incomplete revascularization; however, if late stent thrombosis was the cause of this disparity in outcomes, then improvements in PCI could close that gap.
In his editorial, Dr. Sabik attributed the difference in outcomes between PCI and CABG to the ability of the former to both treat existing and prevent future stenosis. PCI can be “difficult, dangerous, and even impossible” when the target vessel is totally occluded or the stenosis is complex, hence leading to incomplete revascularization and residual ischemia. “Performing CABG to these vessels is no more difficult than for an isolated, noncomplex stenosis,” Dr. Sabik said.
Dr. Sabik disclosed he is the principal investigator for an Abbott Laboratories–sponsored trial of left main coronary disease, and is on the scientific advisory board of Medtronic.
Dr. Deb and Dr. Fremes had no relationships to disclose.
Whenever seminal clinical trials report results that challenge conventional thinking, physicians face the challenge of actually applying those findings in the clinic. A team of cardiac surgeons from Baylor University in Plano, Tex., has offered its take on the clinical implications of recent findings from the cause-of-death analysis of the SYNTAX trial that compared coronary artery bypass grafting with stenting: When counseling higher-risk patients with coronary artery disease about revascularization procedures, cardiologists and cardiac surgeons should clearly elucidate the dramatic advantage of coronary artery bypass grafting over stenting that SYNTAX had demonstrated.
Michael Mack, MD, and coauthors made their case in a featured expert opinion in the Journal of Thoracic and Cardiovascular Surgery (2016;152:1237-40).
“In fact, there was a significant survival advantage for CABG in the patients with intermediate and high SYNTAX scores, with the death rate of CABG versus PCI being 9.6% versus 16.3% (P less than .047) and 8.8% versus 17.8% (P less than .02), respectively,” they wrote.
The advantages of surgery “have been most striking for patients with intermediate or high SYNTAX scores, but seem to exist for patients with low scores as well, although requiring more follow-up,” Dr. Mack and colleagues said. But the situation is less clear in other subgroups, particularly in patients with less diffuse distal disease and lower SYNTAX scores, they added.
Complete revascularization after the procedure may explain the better outcomes with CABG, as 43.3% of those in the PCI arm had incomplete revascularization vs. 36.8% in the CABG arm. “Incomplete revascularization was associated with increased risk for major adverse cardiac or cerebrovascular events three years after PCI, but incomplete revascularization in the CABG group could not be identified as a predictor for worse outcomes,” Dr. Mack and colleagues noted.
The expert opinion authors debunk one of the recent criticisms of SYNTAX: that its reliance on first-generation drug-eluting stents is dated and not relevant today. They noted the more recent Bypass Surgery Vs. Everolimus-Eluting Stent Implantation for Multivessel Coronary Artery Disease trial found a similarly higher rate of death, heart attack, and target vessel revascularization occurred more frequently in the PCI group (15.3% vs. 10.6% in the CABG group) (N Engl J Med. 2015;372:1204-12).
Nonetheless, Dr. Mack and coauthors found room for improvement for CABG through increased use of atrial revascularization and appropriate measures to minimize stroke.
The latest SYNTAX findings can inform the approach surgeons take with high-risk patients, they said. This should include “a discussion of these data, particularly in regard to survival.” And physicians should base their therapeutic recommendations on these data. “At present, there are data seeming to indicate that the majority of patients with three-vessel disease receiving invasive treatment in the United States are being treated with PCI, an outcome that is not congruent with these outcome findings,” they said.
Taking into consideration other SYNTAX analyses that have shown that completeness of revascularization is a determining factor in post-PCI outcomes, Dr. Mack and coauthors said that physicians should calculate the degree of coronary artery disease (CAD) left untreated after intervention, “and those patients who are likely to have a high residual SYNTAX score should be strongly considered for CABG.” Doctors should also focus “intensive efforts” on adherence to optimal medical therapy after both CABG and PCI.
“Finally, although there is a strong patient preference for a less-invasive treatment of their CAD, patients with advanced disease should be made aware that the choice of PCI puts them at an increased risk of death relative to CABG, and a full and transparent discussion should occur regarding the implications of their decision,” Dr. Mack and coauthors concluded.
They had no relevant financial relationships to disclose.
Whenever seminal clinical trials report results that challenge conventional thinking, physicians face the challenge of actually applying those findings in the clinic. A team of cardiac surgeons from Baylor University in Plano, Tex., has offered its take on the clinical implications of recent findings from the cause-of-death analysis of the SYNTAX trial that compared coronary artery bypass grafting with stenting: When counseling higher-risk patients with coronary artery disease about revascularization procedures, cardiologists and cardiac surgeons should clearly elucidate the dramatic advantage of coronary artery bypass grafting over stenting that SYNTAX had demonstrated.
Michael Mack, MD, and coauthors made their case in a featured expert opinion in the Journal of Thoracic and Cardiovascular Surgery (2016;152:1237-40).
“In fact, there was a significant survival advantage for CABG in the patients with intermediate and high SYNTAX scores, with the death rate of CABG versus PCI being 9.6% versus 16.3% (P less than .047) and 8.8% versus 17.8% (P less than .02), respectively,” they wrote.
The advantages of surgery “have been most striking for patients with intermediate or high SYNTAX scores, but seem to exist for patients with low scores as well, although requiring more follow-up,” Dr. Mack and colleagues said. But the situation is less clear in other subgroups, particularly in patients with less diffuse distal disease and lower SYNTAX scores, they added.
Complete revascularization after the procedure may explain the better outcomes with CABG, as 43.3% of those in the PCI arm had incomplete revascularization vs. 36.8% in the CABG arm. “Incomplete revascularization was associated with increased risk for major adverse cardiac or cerebrovascular events three years after PCI, but incomplete revascularization in the CABG group could not be identified as a predictor for worse outcomes,” Dr. Mack and colleagues noted.
The expert opinion authors debunk one of the recent criticisms of SYNTAX: that its reliance on first-generation drug-eluting stents is dated and not relevant today. They noted the more recent Bypass Surgery Vs. Everolimus-Eluting Stent Implantation for Multivessel Coronary Artery Disease trial found a similarly higher rate of death, heart attack, and target vessel revascularization occurred more frequently in the PCI group (15.3% vs. 10.6% in the CABG group) (N Engl J Med. 2015;372:1204-12).
Nonetheless, Dr. Mack and coauthors found room for improvement for CABG through increased use of atrial revascularization and appropriate measures to minimize stroke.
The latest SYNTAX findings can inform the approach surgeons take with high-risk patients, they said. This should include “a discussion of these data, particularly in regard to survival.” And physicians should base their therapeutic recommendations on these data. “At present, there are data seeming to indicate that the majority of patients with three-vessel disease receiving invasive treatment in the United States are being treated with PCI, an outcome that is not congruent with these outcome findings,” they said.
Taking into consideration other SYNTAX analyses that have shown that completeness of revascularization is a determining factor in post-PCI outcomes, Dr. Mack and coauthors said that physicians should calculate the degree of coronary artery disease (CAD) left untreated after intervention, “and those patients who are likely to have a high residual SYNTAX score should be strongly considered for CABG.” Doctors should also focus “intensive efforts” on adherence to optimal medical therapy after both CABG and PCI.
“Finally, although there is a strong patient preference for a less-invasive treatment of their CAD, patients with advanced disease should be made aware that the choice of PCI puts them at an increased risk of death relative to CABG, and a full and transparent discussion should occur regarding the implications of their decision,” Dr. Mack and coauthors concluded.
They had no relevant financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Physicians should clearly communicate to patients with complex multivessel artery disease the key findings of the SYNTAX trial.
Major finding: The SYNTAX trials showed the risk of cardiac death from myocardial infarction after percutaneous coronary intervention (PCI) is 10 times greater than that after coronary artery bypass grafting in higher-risk patients.
Data source: A post hoc analysis of causes of death in all 3,075 trial and registry patients in the Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial.
Disclosures: Dr. Mack and coauthors reported having no financial disclosures.
Letters to the Editor: Update on contraception
“UPDATE ON CONTRACEPTION”
Mitchell D. Creinin, MD; Natasha R. Schimmoeller, MD, MPH, MA (August 2016)
Interesting anatomic variation and management for IUD placement
I recently saw a patient for insertion of an intrauterine device (IUD). On examination with a speculum, I could not find the patient’s cervix. On bimanual exam, I found the cervix to be extremely anterior. I again placed a speculum and, even knowing where to look, could not bring the cervix into view. I did a second bimanual exam and noticed that I could move the cervix into a more axial plane if I exerted suprapubic pressure. The patient’s uterus was retroverted and her cervix was behind her symphysis. When I placed the speculum again, I asked the patient to apply suprapubic pressure, as I just had. With this procedure I then found her cervix easily, grasped it with a tenaculum, and inserted the IUD, which went well.
Jeffrey Joseph, MD
Wakefield, Rhode Island
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“UPDATE ON CONTRACEPTION”
Mitchell D. Creinin, MD; Natasha R. Schimmoeller, MD, MPH, MA (August 2016)
Interesting anatomic variation and management for IUD placement
I recently saw a patient for insertion of an intrauterine device (IUD). On examination with a speculum, I could not find the patient’s cervix. On bimanual exam, I found the cervix to be extremely anterior. I again placed a speculum and, even knowing where to look, could not bring the cervix into view. I did a second bimanual exam and noticed that I could move the cervix into a more axial plane if I exerted suprapubic pressure. The patient’s uterus was retroverted and her cervix was behind her symphysis. When I placed the speculum again, I asked the patient to apply suprapubic pressure, as I just had. With this procedure I then found her cervix easily, grasped it with a tenaculum, and inserted the IUD, which went well.
Jeffrey Joseph, MD
Wakefield, Rhode Island
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“UPDATE ON CONTRACEPTION”
Mitchell D. Creinin, MD; Natasha R. Schimmoeller, MD, MPH, MA (August 2016)
Interesting anatomic variation and management for IUD placement
I recently saw a patient for insertion of an intrauterine device (IUD). On examination with a speculum, I could not find the patient’s cervix. On bimanual exam, I found the cervix to be extremely anterior. I again placed a speculum and, even knowing where to look, could not bring the cervix into view. I did a second bimanual exam and noticed that I could move the cervix into a more axial plane if I exerted suprapubic pressure. The patient’s uterus was retroverted and her cervix was behind her symphysis. When I placed the speculum again, I asked the patient to apply suprapubic pressure, as I just had. With this procedure I then found her cervix easily, grasped it with a tenaculum, and inserted the IUD, which went well.
Jeffrey Joseph, MD
Wakefield, Rhode Island
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.