User login
QUIZ: What Is Your Risk from a Needlestick?
Later menopause lowers risk of later depression
The longer a woman’s reproductive years last, the less she may be prone to postmenopausal depression, a large meta-analysis has determined.
The risk of depression declined by 2% for every 2 premenopausal years after age 40. Women who entered menopause after age 40 experienced a 50% decrease in the risk of depression, compared with women who experienced premature menopause, Dr. Marios K. Georgakis and colleagues reported Jan. 6 in JAMA Psychiatry (2016. doi:10.1001/jamapsychiatry.2015.2653).
The findings suggest that longer exposure to endogenous estrogens mediates the pathophysiology of late-life depression, wrote Dr. Georgakis of the National and Kapodistrian University of Athens and coauthors.
“If confirmed in prospective and culturally diverse studies … these findings could have a significant clinical effect by allowing for the identification of a group of women at higher risk for depression who may benefit from psychiatric monitoring or estrogen-based therapies.”
The meta-analysis comprised 14 studies that included 67,714 women. They controlled for numerous factors, including age, body mass index, obesity, smoking, and hormone therapy. However, only two controlled for past depression – one of the biggest risk factors for recurring depression.
In addition to the 2% decline per 2 premenopausal years after 40, a subanalysis of three studies examining severe depression found a 5% decreased risk for the same time measure. Another analysis of women with premature menopause found a doubling in the risk of depression for those who experienced menopause before age 40.
Estrogen is known to have neuroprotective and antidepressive properties, and the brain is richly endowed with estrogen receptors, the authors said. The exact pathway of protection against depression, however, remains unknown. Potentiation of neurotransmitters and moderation of atherosclerosis might play protective roles.
“Given the results of our study, it remains to be investigated whether women with menopause at younger ages could benefit by preventive use of hormone therapy against late-life depression, provided that adverse effects associated with long-term use are considered,” the authors said. “In this context, the development of estrogen receptor subtype–specific ligands could decrease the proportion of estrogen therapy adverse effects.”
Neither Dr. Georgakis nor any of the coauthors declared any financial conflicts.
The study is a “commendable effort” to examine the role of reproductive hormones in postmenopausal depression, but several important caveats should temper enthusiasm for its conclusions, Dr. Hadine Joffe and Joyce T. Bromberger, Ph.D., wrote in an accompanying editorial.
In most of the studies, women were aged 55-60 years – considerably beyond the average menopausal age of 52. Additionally, most were at least 5 years past their menopause, reflecting a group that might have passed the period of highest risk for hormone-mediated depression.
“This meta-analysis does not address depression associated with the gonadal steroid fluctuations of the perimenopause or recent estradiol withdrawal of the immediate postmenopause,” the colleagues wrote. “Rather, the analysis applies to depression in older women whose brains have not recently been exposed to estradiol or other reproductive hormones and for whom hormonal risk factors have previously been considered less relevant.”
However, the study is one of the few to investigate the psychotropic effects of estrogen on aging women. “In contrast to the acute effects of reproductive hormones on mood in cycling women, the article highlights a potential neuroprotective effect of gonadal steroids on mood that is delayed and extends into the stable hypoestrogenic and hypoprogestinemic environment of the postmenopause.”
Its conclusions are strengthened by studies of nonpsychiatric diseases associated with earlier menopause, including cardiovascular disease, cognitive decline, and dementia. Nevertheless, it’s too early to recommend prophylactic hormone therapy, the authors concluded.
“Given the small effect size and limitations of the studies used in this analysis, more direct evidence supporting a sustained and delayed neuroprotective effect of extended exposure to estradiol, cyclic progestins, and their neurosteroid derivatives is required to support use of hormonal therapy as a therapeutic approach to protecting against postmenopausal depression.”
Dr. Joffe is director of the Women’s Hormone and Aging Research Program at Brigham and Women’s Hospital, Boston. Dr. Bromberger is a professor of epidemiology and psychiatry at the University of Pittsburgh.
The study is a “commendable effort” to examine the role of reproductive hormones in postmenopausal depression, but several important caveats should temper enthusiasm for its conclusions, Dr. Hadine Joffe and Joyce T. Bromberger, Ph.D., wrote in an accompanying editorial.
In most of the studies, women were aged 55-60 years – considerably beyond the average menopausal age of 52. Additionally, most were at least 5 years past their menopause, reflecting a group that might have passed the period of highest risk for hormone-mediated depression.
“This meta-analysis does not address depression associated with the gonadal steroid fluctuations of the perimenopause or recent estradiol withdrawal of the immediate postmenopause,” the colleagues wrote. “Rather, the analysis applies to depression in older women whose brains have not recently been exposed to estradiol or other reproductive hormones and for whom hormonal risk factors have previously been considered less relevant.”
However, the study is one of the few to investigate the psychotropic effects of estrogen on aging women. “In contrast to the acute effects of reproductive hormones on mood in cycling women, the article highlights a potential neuroprotective effect of gonadal steroids on mood that is delayed and extends into the stable hypoestrogenic and hypoprogestinemic environment of the postmenopause.”
Its conclusions are strengthened by studies of nonpsychiatric diseases associated with earlier menopause, including cardiovascular disease, cognitive decline, and dementia. Nevertheless, it’s too early to recommend prophylactic hormone therapy, the authors concluded.
“Given the small effect size and limitations of the studies used in this analysis, more direct evidence supporting a sustained and delayed neuroprotective effect of extended exposure to estradiol, cyclic progestins, and their neurosteroid derivatives is required to support use of hormonal therapy as a therapeutic approach to protecting against postmenopausal depression.”
Dr. Joffe is director of the Women’s Hormone and Aging Research Program at Brigham and Women’s Hospital, Boston. Dr. Bromberger is a professor of epidemiology and psychiatry at the University of Pittsburgh.
The study is a “commendable effort” to examine the role of reproductive hormones in postmenopausal depression, but several important caveats should temper enthusiasm for its conclusions, Dr. Hadine Joffe and Joyce T. Bromberger, Ph.D., wrote in an accompanying editorial.
In most of the studies, women were aged 55-60 years – considerably beyond the average menopausal age of 52. Additionally, most were at least 5 years past their menopause, reflecting a group that might have passed the period of highest risk for hormone-mediated depression.
“This meta-analysis does not address depression associated with the gonadal steroid fluctuations of the perimenopause or recent estradiol withdrawal of the immediate postmenopause,” the colleagues wrote. “Rather, the analysis applies to depression in older women whose brains have not recently been exposed to estradiol or other reproductive hormones and for whom hormonal risk factors have previously been considered less relevant.”
However, the study is one of the few to investigate the psychotropic effects of estrogen on aging women. “In contrast to the acute effects of reproductive hormones on mood in cycling women, the article highlights a potential neuroprotective effect of gonadal steroids on mood that is delayed and extends into the stable hypoestrogenic and hypoprogestinemic environment of the postmenopause.”
Its conclusions are strengthened by studies of nonpsychiatric diseases associated with earlier menopause, including cardiovascular disease, cognitive decline, and dementia. Nevertheless, it’s too early to recommend prophylactic hormone therapy, the authors concluded.
“Given the small effect size and limitations of the studies used in this analysis, more direct evidence supporting a sustained and delayed neuroprotective effect of extended exposure to estradiol, cyclic progestins, and their neurosteroid derivatives is required to support use of hormonal therapy as a therapeutic approach to protecting against postmenopausal depression.”
Dr. Joffe is director of the Women’s Hormone and Aging Research Program at Brigham and Women’s Hospital, Boston. Dr. Bromberger is a professor of epidemiology and psychiatry at the University of Pittsburgh.
The longer a woman’s reproductive years last, the less she may be prone to postmenopausal depression, a large meta-analysis has determined.
The risk of depression declined by 2% for every 2 premenopausal years after age 40. Women who entered menopause after age 40 experienced a 50% decrease in the risk of depression, compared with women who experienced premature menopause, Dr. Marios K. Georgakis and colleagues reported Jan. 6 in JAMA Psychiatry (2016. doi:10.1001/jamapsychiatry.2015.2653).
The findings suggest that longer exposure to endogenous estrogens mediates the pathophysiology of late-life depression, wrote Dr. Georgakis of the National and Kapodistrian University of Athens and coauthors.
“If confirmed in prospective and culturally diverse studies … these findings could have a significant clinical effect by allowing for the identification of a group of women at higher risk for depression who may benefit from psychiatric monitoring or estrogen-based therapies.”
The meta-analysis comprised 14 studies that included 67,714 women. They controlled for numerous factors, including age, body mass index, obesity, smoking, and hormone therapy. However, only two controlled for past depression – one of the biggest risk factors for recurring depression.
In addition to the 2% decline per 2 premenopausal years after 40, a subanalysis of three studies examining severe depression found a 5% decreased risk for the same time measure. Another analysis of women with premature menopause found a doubling in the risk of depression for those who experienced menopause before age 40.
Estrogen is known to have neuroprotective and antidepressive properties, and the brain is richly endowed with estrogen receptors, the authors said. The exact pathway of protection against depression, however, remains unknown. Potentiation of neurotransmitters and moderation of atherosclerosis might play protective roles.
“Given the results of our study, it remains to be investigated whether women with menopause at younger ages could benefit by preventive use of hormone therapy against late-life depression, provided that adverse effects associated with long-term use are considered,” the authors said. “In this context, the development of estrogen receptor subtype–specific ligands could decrease the proportion of estrogen therapy adverse effects.”
Neither Dr. Georgakis nor any of the coauthors declared any financial conflicts.
The longer a woman’s reproductive years last, the less she may be prone to postmenopausal depression, a large meta-analysis has determined.
The risk of depression declined by 2% for every 2 premenopausal years after age 40. Women who entered menopause after age 40 experienced a 50% decrease in the risk of depression, compared with women who experienced premature menopause, Dr. Marios K. Georgakis and colleagues reported Jan. 6 in JAMA Psychiatry (2016. doi:10.1001/jamapsychiatry.2015.2653).
The findings suggest that longer exposure to endogenous estrogens mediates the pathophysiology of late-life depression, wrote Dr. Georgakis of the National and Kapodistrian University of Athens and coauthors.
“If confirmed in prospective and culturally diverse studies … these findings could have a significant clinical effect by allowing for the identification of a group of women at higher risk for depression who may benefit from psychiatric monitoring or estrogen-based therapies.”
The meta-analysis comprised 14 studies that included 67,714 women. They controlled for numerous factors, including age, body mass index, obesity, smoking, and hormone therapy. However, only two controlled for past depression – one of the biggest risk factors for recurring depression.
In addition to the 2% decline per 2 premenopausal years after 40, a subanalysis of three studies examining severe depression found a 5% decreased risk for the same time measure. Another analysis of women with premature menopause found a doubling in the risk of depression for those who experienced menopause before age 40.
Estrogen is known to have neuroprotective and antidepressive properties, and the brain is richly endowed with estrogen receptors, the authors said. The exact pathway of protection against depression, however, remains unknown. Potentiation of neurotransmitters and moderation of atherosclerosis might play protective roles.
“Given the results of our study, it remains to be investigated whether women with menopause at younger ages could benefit by preventive use of hormone therapy against late-life depression, provided that adverse effects associated with long-term use are considered,” the authors said. “In this context, the development of estrogen receptor subtype–specific ligands could decrease the proportion of estrogen therapy adverse effects.”
Neither Dr. Georgakis nor any of the coauthors declared any financial conflicts.
FROM JAMA PSYCHIATRY
Key clinical point: Later menopause, with its longer estrogen exposure, appears tied to a lower risk of postmenopausal depression.
Major finding: The risk of depression decreased by 2% for each 2 premenopausal years after age 40.
Data source: The meta-analysis comprised 14 studies with more than 67,700 women.
Disclosures: Neither Dr. Georgakis nor any of the coauthors declared any financial conflicts.
A new year, a new wish list
It’s 2016. Where am I?
2015 was a mixed year for neurologists and doctors in general. The Sustainable Growth Rate was repealed in a rare moment of bipartisan cooperation. Whether this will stem the tide of doctors leaving Medicare remains to be seen. In my area, it seems like another internist changes to concierge practice every week.
Even with these changes, I can’t say the reimbursement rates have returned to previous levels. Neurologists, in a primarily thinking field, often take the brunt of cuts on the few procedures we have. Like other fields, we try to cram more things into limited time and hope it all somehow works out.
2016 brings an election year, and again doctors will be in the unenviable position of ping-pong balls whacked between both sides to score political points. It would be nice to have political parties willing to work out what’s best for the health of Americans as a whole rather than trying to fire up the extreme ends of the political spectrum.
2015 was the year a new International Classification of Diseases system was foisted on us for reasons I still don’t understand. With it came a whole new wave of codes and modifiers to learn. This in turn takes a lot of time, for which we aren’t paid. Time is something I, and most docs, don’t have a lot of. I’d like to focus on caring for patients, and nothing more, but the powers that be appear to have a dim view of such silliness. This brings me back to watching internists gradually shift to cash-pay models and wondering how big the demand would be for a general neurologist in that world. The only one I know who actually did it shut down in a few months.
What’s on my wish list in 2016? Obviously, the health and welfare of myself and those around me comes first. For my patients, it’s some breakthroughs for the terrible diseases we still have no real treatments for. For my practice, it’s staying strong enough to remain independent. Some better reimbursement and non–snake oil sources of revenue are always nice. I’m hoping that in 1 year I’ll be able to write something more optimistic.
Wishing you all a great 2016!
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
It’s 2016. Where am I?
2015 was a mixed year for neurologists and doctors in general. The Sustainable Growth Rate was repealed in a rare moment of bipartisan cooperation. Whether this will stem the tide of doctors leaving Medicare remains to be seen. In my area, it seems like another internist changes to concierge practice every week.
Even with these changes, I can’t say the reimbursement rates have returned to previous levels. Neurologists, in a primarily thinking field, often take the brunt of cuts on the few procedures we have. Like other fields, we try to cram more things into limited time and hope it all somehow works out.
2016 brings an election year, and again doctors will be in the unenviable position of ping-pong balls whacked between both sides to score political points. It would be nice to have political parties willing to work out what’s best for the health of Americans as a whole rather than trying to fire up the extreme ends of the political spectrum.
2015 was the year a new International Classification of Diseases system was foisted on us for reasons I still don’t understand. With it came a whole new wave of codes and modifiers to learn. This in turn takes a lot of time, for which we aren’t paid. Time is something I, and most docs, don’t have a lot of. I’d like to focus on caring for patients, and nothing more, but the powers that be appear to have a dim view of such silliness. This brings me back to watching internists gradually shift to cash-pay models and wondering how big the demand would be for a general neurologist in that world. The only one I know who actually did it shut down in a few months.
What’s on my wish list in 2016? Obviously, the health and welfare of myself and those around me comes first. For my patients, it’s some breakthroughs for the terrible diseases we still have no real treatments for. For my practice, it’s staying strong enough to remain independent. Some better reimbursement and non–snake oil sources of revenue are always nice. I’m hoping that in 1 year I’ll be able to write something more optimistic.
Wishing you all a great 2016!
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
It’s 2016. Where am I?
2015 was a mixed year for neurologists and doctors in general. The Sustainable Growth Rate was repealed in a rare moment of bipartisan cooperation. Whether this will stem the tide of doctors leaving Medicare remains to be seen. In my area, it seems like another internist changes to concierge practice every week.
Even with these changes, I can’t say the reimbursement rates have returned to previous levels. Neurologists, in a primarily thinking field, often take the brunt of cuts on the few procedures we have. Like other fields, we try to cram more things into limited time and hope it all somehow works out.
2016 brings an election year, and again doctors will be in the unenviable position of ping-pong balls whacked between both sides to score political points. It would be nice to have political parties willing to work out what’s best for the health of Americans as a whole rather than trying to fire up the extreme ends of the political spectrum.
2015 was the year a new International Classification of Diseases system was foisted on us for reasons I still don’t understand. With it came a whole new wave of codes and modifiers to learn. This in turn takes a lot of time, for which we aren’t paid. Time is something I, and most docs, don’t have a lot of. I’d like to focus on caring for patients, and nothing more, but the powers that be appear to have a dim view of such silliness. This brings me back to watching internists gradually shift to cash-pay models and wondering how big the demand would be for a general neurologist in that world. The only one I know who actually did it shut down in a few months.
What’s on my wish list in 2016? Obviously, the health and welfare of myself and those around me comes first. For my patients, it’s some breakthroughs for the terrible diseases we still have no real treatments for. For my practice, it’s staying strong enough to remain independent. Some better reimbursement and non–snake oil sources of revenue are always nice. I’m hoping that in 1 year I’ll be able to write something more optimistic.
Wishing you all a great 2016!
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Highlights of the January 2016 issue of The Hospitalist
Myth of the Month: Beta-blocker myths
A 59-year-old man is admitted to the ICU with a myocardial infarction. He is discharged after 5 days on enalapril, metoprolol, simvastatin, and aspirin. At a 3-month follow-up, he is noted to have marked anhedonia, complaints of insomnia, feelings of worthlessness, and psychomotor retardation.
What would you do?
A) Stop the enalapril.
B) Stop the metoprolol.
C) Stop the simvastatin.
D) Begin a tricyclic antidepressant.
E) Begin an SSRI.
When I was in medical school, the dogma was to never give beta-blockers to patients with systolic heart failure, because it would worsen the heart failure.1 As we all know, this dogma completely reversed, and beta-blocker therapy is a cornerstone of treatment of patients with systolic heart failure, with improvements in morbidity and mortality.2 Underutilization of beta-blockers for indicated conditions is likely due to fear of beta-blocker side effects.2
There has long been concern that beta-blockers can cause, or worsen, depression. As a result, beta-blockers are sometimes withheld from patients with a history of depression who may benefit, or beta-blockers are stopped in patients who develop depression.
Early reports of possible beta-blocker–induced depression surfaced soon after the beta-blocker propranolol became available in the 1960s. A frequently cited reference is a letter to the British Medical Journal in which H.J. Waal reported that 20 of 89 patients on propranolol volunteered or exhibited depressive symptoms.3 Almost half of those patients were diagnosed with grade I depression – symptoms of irritability, insomnia, nightmares, and fatigue. No control group of patients was evaluated to ascertain the prevalence of those symptoms in patients treated with other antihypertensives, or in nonhypertensive patients.
M. H. Pollack and colleagues reported on a series of three patients who developed symptoms of depression after starting propranolol, and the researchers concluded that depression following the administration of propranolol was a real phenomenon.4
Many subsequent studies have cast doubt on the association of beta-blockers and depression. Depression is common following myocardial infarction and in patients with coronary artery disease. Several studies have looked closely for association with beta-blocker use in this population.
Dr. Steven J. Schleifer and colleagues evaluated 190 patients who had sustained a myocardial infarction for evidence of depression. The patients were interviewed 8-10 days after the infarct and again at 3 months. No antianginal or antihypertensive medications, including beta-blockers, were associated with an increase in depression.5
Dr. Joost P. van Melle and colleagues participated in a multicenter study that looked at patients following myocardial infarction, assessing for depressive symptoms at baseline and at 3, 6, 9, and 12 months using the Beck depression inventory.6 A total of 254 patients receiving beta-blockers were matched with 127 control patients post MI not receiving beta-blockers. No significant differences were found between non–beta-blocker users and beta-blocker users on the presence of depressive symptoms.
Robert Carney, Ph.D., and colleagues evaluated 75 patients undergoing elective cardiac catheterization with psychiatric interview and psychological assessments.7 Half of the patients in the study were receiving beta-blockers. Thirty-three percent of the patients who were not receiving beta-blockers met DSM-III criteria for depression, and 21% of the beta-blocker–treated patients met criteria for depression.
Dr. Linda Battes and colleagues reported that beta-blocker use actually decreased the risk of depression in patients who had undergone a percutaneous intervention, with a risk reduction of 49% for depression in beta-blocker–treated patients.8 In a study of elderly patients, Dr. Hendrika Luijendijk and colleagues followed 5,104 elderly persons for episodes of incident depression. They found that beta-blocker use did not increase the risk of developing depression.9
Beta-blockers often have been avoided in patients with obstructive pulmonary disease – both in patients with asthma and those with COPD – because of concern for worsening obstructive pulmonary disease. There is strong evidence now that beta-blocker use is not problematic in patients with COPD.
Dr. Surya Bhatt and colleagues found that beta-blocker use decreased COPD exacerbations.10 Almost 3,500 patients were included. During a median of 2.1 years of follow-up, beta-blocker use was associated with a significantly lower rate of total exacerbations (incidence risk ratio, 0.73; 95% confidence interval, 0.60-0.90; P = .003) and severe exacerbations (IRR, 0.67, 95% CI, 0.48-0.93; P = .016).
Dr. Qingxia Du and colleagues found that beta-blocker use in patients with COPD both reduced exacerbations and reduced mortality.11 In another study, the use of beta-blockers in patients hospitalized for acute exacerbations of COPD reduced mortality.12 Most of the patients receiving beta-blockers in that study had severe cardiovascular disease.
There are far fewer data on beta-blocker use in patients with asthma. In general, beta-blockers are routinely avoided in patients with asthma. In one small study of asthmatic patients receiving propranolol, there was no effect on methacholine challenge response, histamine responsiveness, or asthma control questionnaire results.13 In a murine model of asthma, long-term administration of beta-blockers resulted in a decrease in airway hyperresponsiveness, suggesting an anti-inflammatory effect.14 This topic is an area of interest for further study in asthma control.
So much of what we thought we knew about beta-blockers has turned out to not be so. We keep our eyes open and welcome further enlightenment.
References
1. Circulation. 1983 Jun;67(6 Pt 2):I91.
2. Expert Opin Drug Saf. 2015 Dec;14(12):1855-63.
3. Br Med J. 1967 Apr 1;2(5543):50.
4. J Nerv Ment Dis. 1985 Feb;173(2):118-9.
5. Am Heart J. 1991 May;121(5):1397-402.
6. J Am Coll Cardiol. 2006 Dec 5;48(11):2209-14.
7. Am J Med. 1987 Aug;83(2):223-6.
8. J Affect Disord. 2012 Feb;136(3):751-7.
9. J Clin Psychopharmacol. 2011 Feb;31(1):45-50.
10. Thorax. 2016 Jan;71(1):8-14.
12. Thorax. 2008 Apr;63(4):301-5.
13. Am J Respir Crit Care Med. 2013 Jun 15;187(12):1308-14.
14. Int J Gen Med. 2013 Jul 8;6:549-55.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 59-year-old man is admitted to the ICU with a myocardial infarction. He is discharged after 5 days on enalapril, metoprolol, simvastatin, and aspirin. At a 3-month follow-up, he is noted to have marked anhedonia, complaints of insomnia, feelings of worthlessness, and psychomotor retardation.
What would you do?
A) Stop the enalapril.
B) Stop the metoprolol.
C) Stop the simvastatin.
D) Begin a tricyclic antidepressant.
E) Begin an SSRI.
When I was in medical school, the dogma was to never give beta-blockers to patients with systolic heart failure, because it would worsen the heart failure.1 As we all know, this dogma completely reversed, and beta-blocker therapy is a cornerstone of treatment of patients with systolic heart failure, with improvements in morbidity and mortality.2 Underutilization of beta-blockers for indicated conditions is likely due to fear of beta-blocker side effects.2
There has long been concern that beta-blockers can cause, or worsen, depression. As a result, beta-blockers are sometimes withheld from patients with a history of depression who may benefit, or beta-blockers are stopped in patients who develop depression.
Early reports of possible beta-blocker–induced depression surfaced soon after the beta-blocker propranolol became available in the 1960s. A frequently cited reference is a letter to the British Medical Journal in which H.J. Waal reported that 20 of 89 patients on propranolol volunteered or exhibited depressive symptoms.3 Almost half of those patients were diagnosed with grade I depression – symptoms of irritability, insomnia, nightmares, and fatigue. No control group of patients was evaluated to ascertain the prevalence of those symptoms in patients treated with other antihypertensives, or in nonhypertensive patients.
M. H. Pollack and colleagues reported on a series of three patients who developed symptoms of depression after starting propranolol, and the researchers concluded that depression following the administration of propranolol was a real phenomenon.4
Many subsequent studies have cast doubt on the association of beta-blockers and depression. Depression is common following myocardial infarction and in patients with coronary artery disease. Several studies have looked closely for association with beta-blocker use in this population.
Dr. Steven J. Schleifer and colleagues evaluated 190 patients who had sustained a myocardial infarction for evidence of depression. The patients were interviewed 8-10 days after the infarct and again at 3 months. No antianginal or antihypertensive medications, including beta-blockers, were associated with an increase in depression.5
Dr. Joost P. van Melle and colleagues participated in a multicenter study that looked at patients following myocardial infarction, assessing for depressive symptoms at baseline and at 3, 6, 9, and 12 months using the Beck depression inventory.6 A total of 254 patients receiving beta-blockers were matched with 127 control patients post MI not receiving beta-blockers. No significant differences were found between non–beta-blocker users and beta-blocker users on the presence of depressive symptoms.
Robert Carney, Ph.D., and colleagues evaluated 75 patients undergoing elective cardiac catheterization with psychiatric interview and psychological assessments.7 Half of the patients in the study were receiving beta-blockers. Thirty-three percent of the patients who were not receiving beta-blockers met DSM-III criteria for depression, and 21% of the beta-blocker–treated patients met criteria for depression.
Dr. Linda Battes and colleagues reported that beta-blocker use actually decreased the risk of depression in patients who had undergone a percutaneous intervention, with a risk reduction of 49% for depression in beta-blocker–treated patients.8 In a study of elderly patients, Dr. Hendrika Luijendijk and colleagues followed 5,104 elderly persons for episodes of incident depression. They found that beta-blocker use did not increase the risk of developing depression.9
Beta-blockers often have been avoided in patients with obstructive pulmonary disease – both in patients with asthma and those with COPD – because of concern for worsening obstructive pulmonary disease. There is strong evidence now that beta-blocker use is not problematic in patients with COPD.
Dr. Surya Bhatt and colleagues found that beta-blocker use decreased COPD exacerbations.10 Almost 3,500 patients were included. During a median of 2.1 years of follow-up, beta-blocker use was associated with a significantly lower rate of total exacerbations (incidence risk ratio, 0.73; 95% confidence interval, 0.60-0.90; P = .003) and severe exacerbations (IRR, 0.67, 95% CI, 0.48-0.93; P = .016).
Dr. Qingxia Du and colleagues found that beta-blocker use in patients with COPD both reduced exacerbations and reduced mortality.11 In another study, the use of beta-blockers in patients hospitalized for acute exacerbations of COPD reduced mortality.12 Most of the patients receiving beta-blockers in that study had severe cardiovascular disease.
There are far fewer data on beta-blocker use in patients with asthma. In general, beta-blockers are routinely avoided in patients with asthma. In one small study of asthmatic patients receiving propranolol, there was no effect on methacholine challenge response, histamine responsiveness, or asthma control questionnaire results.13 In a murine model of asthma, long-term administration of beta-blockers resulted in a decrease in airway hyperresponsiveness, suggesting an anti-inflammatory effect.14 This topic is an area of interest for further study in asthma control.
So much of what we thought we knew about beta-blockers has turned out to not be so. We keep our eyes open and welcome further enlightenment.
References
1. Circulation. 1983 Jun;67(6 Pt 2):I91.
2. Expert Opin Drug Saf. 2015 Dec;14(12):1855-63.
3. Br Med J. 1967 Apr 1;2(5543):50.
4. J Nerv Ment Dis. 1985 Feb;173(2):118-9.
5. Am Heart J. 1991 May;121(5):1397-402.
6. J Am Coll Cardiol. 2006 Dec 5;48(11):2209-14.
7. Am J Med. 1987 Aug;83(2):223-6.
8. J Affect Disord. 2012 Feb;136(3):751-7.
9. J Clin Psychopharmacol. 2011 Feb;31(1):45-50.
10. Thorax. 2016 Jan;71(1):8-14.
12. Thorax. 2008 Apr;63(4):301-5.
13. Am J Respir Crit Care Med. 2013 Jun 15;187(12):1308-14.
14. Int J Gen Med. 2013 Jul 8;6:549-55.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 59-year-old man is admitted to the ICU with a myocardial infarction. He is discharged after 5 days on enalapril, metoprolol, simvastatin, and aspirin. At a 3-month follow-up, he is noted to have marked anhedonia, complaints of insomnia, feelings of worthlessness, and psychomotor retardation.
What would you do?
A) Stop the enalapril.
B) Stop the metoprolol.
C) Stop the simvastatin.
D) Begin a tricyclic antidepressant.
E) Begin an SSRI.
When I was in medical school, the dogma was to never give beta-blockers to patients with systolic heart failure, because it would worsen the heart failure.1 As we all know, this dogma completely reversed, and beta-blocker therapy is a cornerstone of treatment of patients with systolic heart failure, with improvements in morbidity and mortality.2 Underutilization of beta-blockers for indicated conditions is likely due to fear of beta-blocker side effects.2
There has long been concern that beta-blockers can cause, or worsen, depression. As a result, beta-blockers are sometimes withheld from patients with a history of depression who may benefit, or beta-blockers are stopped in patients who develop depression.
Early reports of possible beta-blocker–induced depression surfaced soon after the beta-blocker propranolol became available in the 1960s. A frequently cited reference is a letter to the British Medical Journal in which H.J. Waal reported that 20 of 89 patients on propranolol volunteered or exhibited depressive symptoms.3 Almost half of those patients were diagnosed with grade I depression – symptoms of irritability, insomnia, nightmares, and fatigue. No control group of patients was evaluated to ascertain the prevalence of those symptoms in patients treated with other antihypertensives, or in nonhypertensive patients.
M. H. Pollack and colleagues reported on a series of three patients who developed symptoms of depression after starting propranolol, and the researchers concluded that depression following the administration of propranolol was a real phenomenon.4
Many subsequent studies have cast doubt on the association of beta-blockers and depression. Depression is common following myocardial infarction and in patients with coronary artery disease. Several studies have looked closely for association with beta-blocker use in this population.
Dr. Steven J. Schleifer and colleagues evaluated 190 patients who had sustained a myocardial infarction for evidence of depression. The patients were interviewed 8-10 days after the infarct and again at 3 months. No antianginal or antihypertensive medications, including beta-blockers, were associated with an increase in depression.5
Dr. Joost P. van Melle and colleagues participated in a multicenter study that looked at patients following myocardial infarction, assessing for depressive symptoms at baseline and at 3, 6, 9, and 12 months using the Beck depression inventory.6 A total of 254 patients receiving beta-blockers were matched with 127 control patients post MI not receiving beta-blockers. No significant differences were found between non–beta-blocker users and beta-blocker users on the presence of depressive symptoms.
Robert Carney, Ph.D., and colleagues evaluated 75 patients undergoing elective cardiac catheterization with psychiatric interview and psychological assessments.7 Half of the patients in the study were receiving beta-blockers. Thirty-three percent of the patients who were not receiving beta-blockers met DSM-III criteria for depression, and 21% of the beta-blocker–treated patients met criteria for depression.
Dr. Linda Battes and colleagues reported that beta-blocker use actually decreased the risk of depression in patients who had undergone a percutaneous intervention, with a risk reduction of 49% for depression in beta-blocker–treated patients.8 In a study of elderly patients, Dr. Hendrika Luijendijk and colleagues followed 5,104 elderly persons for episodes of incident depression. They found that beta-blocker use did not increase the risk of developing depression.9
Beta-blockers often have been avoided in patients with obstructive pulmonary disease – both in patients with asthma and those with COPD – because of concern for worsening obstructive pulmonary disease. There is strong evidence now that beta-blocker use is not problematic in patients with COPD.
Dr. Surya Bhatt and colleagues found that beta-blocker use decreased COPD exacerbations.10 Almost 3,500 patients were included. During a median of 2.1 years of follow-up, beta-blocker use was associated with a significantly lower rate of total exacerbations (incidence risk ratio, 0.73; 95% confidence interval, 0.60-0.90; P = .003) and severe exacerbations (IRR, 0.67, 95% CI, 0.48-0.93; P = .016).
Dr. Qingxia Du and colleagues found that beta-blocker use in patients with COPD both reduced exacerbations and reduced mortality.11 In another study, the use of beta-blockers in patients hospitalized for acute exacerbations of COPD reduced mortality.12 Most of the patients receiving beta-blockers in that study had severe cardiovascular disease.
There are far fewer data on beta-blocker use in patients with asthma. In general, beta-blockers are routinely avoided in patients with asthma. In one small study of asthmatic patients receiving propranolol, there was no effect on methacholine challenge response, histamine responsiveness, or asthma control questionnaire results.13 In a murine model of asthma, long-term administration of beta-blockers resulted in a decrease in airway hyperresponsiveness, suggesting an anti-inflammatory effect.14 This topic is an area of interest for further study in asthma control.
So much of what we thought we knew about beta-blockers has turned out to not be so. We keep our eyes open and welcome further enlightenment.
References
1. Circulation. 1983 Jun;67(6 Pt 2):I91.
2. Expert Opin Drug Saf. 2015 Dec;14(12):1855-63.
3. Br Med J. 1967 Apr 1;2(5543):50.
4. J Nerv Ment Dis. 1985 Feb;173(2):118-9.
5. Am Heart J. 1991 May;121(5):1397-402.
6. J Am Coll Cardiol. 2006 Dec 5;48(11):2209-14.
7. Am J Med. 1987 Aug;83(2):223-6.
8. J Affect Disord. 2012 Feb;136(3):751-7.
9. J Clin Psychopharmacol. 2011 Feb;31(1):45-50.
10. Thorax. 2016 Jan;71(1):8-14.
12. Thorax. 2008 Apr;63(4):301-5.
13. Am J Respir Crit Care Med. 2013 Jun 15;187(12):1308-14.
14. Int J Gen Med. 2013 Jul 8;6:549-55.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Cardiac abnormalities among childhood cancer survivors

Photo by Bill Branson
A new study has provided additional insight into the development of cardiac abnormalities in adult survivors of childhood cancer.
Researchers analyzed more than 1800 cancer survivors who were exposed to cardiotoxic therapies as children.
The team said they found evidence of cardiac abnormalities in a substantial number of these subjects, many of whom were younger and did not exhibit symptoms of abnormalities.
Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported these findings in Annals of Internal Medicine.
The team assessed cardiac outcomes among 1853 subjects who were 18 and older and had received cancer-related cardiotoxic therapy at least 10 years earlier.
The subjects were pretty evenly split along gender lines (52.3% male), their median age at cancer diagnosis was 8 (range, 0 to 24), and their median age at evaluation was 31 (range, 18 to 60).
At evaluation, 7.4% of subjects had cardiomyopathy (newly identified in 4.7%), 3.8% had coronary artery disease (newly identified in 2.2%), 28% had valvular regurgitation or stenosis (newly identified in 24.8%), and 4.4% had conduction or rhythm abnormalities (newly identified in 1.4%). All but 5 subjects were asymptomatic.
Multivariable analysis suggested the odds of developing cardiomyopathy were significantly associated with being male (odds ratio [OR]=1.9), receiving anthracycline doses of 250 mg/m2 or greater (OR=2.7), having cardiac radiation exposure greater than 1500 cGy (OR=1.9), and having hypertension (OR=3.0).
Being younger at diagnosis was associated with higher odds of valvular disease. The ORs were 1.5 for patients who were 0 to 4 years of age at diagnosis and 1.3 for patients who were 5 to 9 at diagnosis.
Receiving higher radiation doses was associated with higher odds of valvular disease as well. But associations between radiation and valvular disease varied according to a patient’s anthracycline exposure (interaction P<0.001). The highest odds were among survivors with the highest doses of radiation exposure and any anthracycline exposure (OR=4.5).
The researchers also noted a reduction in the OR for valvular disease among obese patients (OR=0.4) and those with dyslipidemia (OR=0.7).
The team said there were not enough cases of coronary artery disease and conduction or rhythm abnormalities to support a fully adjusted multivariable model. However, it seemed these outcomes were more common with older age (≥40 years) and among patients with cardiac radiation doses of 1500 cGy or greater.
The researchers said this study revealed “considerable cardiovascular disease” in a large cohort of adult survivors of childhood cancer, which suggests a substantial future healthcare burden.
The team believes their findings could guide stratification of risk factors, screening practices, health counseling, and potential therapeutic measures aimed at changing the disease trajectory in this young adult population. ![]()

Photo by Bill Branson
A new study has provided additional insight into the development of cardiac abnormalities in adult survivors of childhood cancer.
Researchers analyzed more than 1800 cancer survivors who were exposed to cardiotoxic therapies as children.
The team said they found evidence of cardiac abnormalities in a substantial number of these subjects, many of whom were younger and did not exhibit symptoms of abnormalities.
Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported these findings in Annals of Internal Medicine.
The team assessed cardiac outcomes among 1853 subjects who were 18 and older and had received cancer-related cardiotoxic therapy at least 10 years earlier.
The subjects were pretty evenly split along gender lines (52.3% male), their median age at cancer diagnosis was 8 (range, 0 to 24), and their median age at evaluation was 31 (range, 18 to 60).
At evaluation, 7.4% of subjects had cardiomyopathy (newly identified in 4.7%), 3.8% had coronary artery disease (newly identified in 2.2%), 28% had valvular regurgitation or stenosis (newly identified in 24.8%), and 4.4% had conduction or rhythm abnormalities (newly identified in 1.4%). All but 5 subjects were asymptomatic.
Multivariable analysis suggested the odds of developing cardiomyopathy were significantly associated with being male (odds ratio [OR]=1.9), receiving anthracycline doses of 250 mg/m2 or greater (OR=2.7), having cardiac radiation exposure greater than 1500 cGy (OR=1.9), and having hypertension (OR=3.0).
Being younger at diagnosis was associated with higher odds of valvular disease. The ORs were 1.5 for patients who were 0 to 4 years of age at diagnosis and 1.3 for patients who were 5 to 9 at diagnosis.
Receiving higher radiation doses was associated with higher odds of valvular disease as well. But associations between radiation and valvular disease varied according to a patient’s anthracycline exposure (interaction P<0.001). The highest odds were among survivors with the highest doses of radiation exposure and any anthracycline exposure (OR=4.5).
The researchers also noted a reduction in the OR for valvular disease among obese patients (OR=0.4) and those with dyslipidemia (OR=0.7).
The team said there were not enough cases of coronary artery disease and conduction or rhythm abnormalities to support a fully adjusted multivariable model. However, it seemed these outcomes were more common with older age (≥40 years) and among patients with cardiac radiation doses of 1500 cGy or greater.
The researchers said this study revealed “considerable cardiovascular disease” in a large cohort of adult survivors of childhood cancer, which suggests a substantial future healthcare burden.
The team believes their findings could guide stratification of risk factors, screening practices, health counseling, and potential therapeutic measures aimed at changing the disease trajectory in this young adult population. ![]()

Photo by Bill Branson
A new study has provided additional insight into the development of cardiac abnormalities in adult survivors of childhood cancer.
Researchers analyzed more than 1800 cancer survivors who were exposed to cardiotoxic therapies as children.
The team said they found evidence of cardiac abnormalities in a substantial number of these subjects, many of whom were younger and did not exhibit symptoms of abnormalities.
Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported these findings in Annals of Internal Medicine.
The team assessed cardiac outcomes among 1853 subjects who were 18 and older and had received cancer-related cardiotoxic therapy at least 10 years earlier.
The subjects were pretty evenly split along gender lines (52.3% male), their median age at cancer diagnosis was 8 (range, 0 to 24), and their median age at evaluation was 31 (range, 18 to 60).
At evaluation, 7.4% of subjects had cardiomyopathy (newly identified in 4.7%), 3.8% had coronary artery disease (newly identified in 2.2%), 28% had valvular regurgitation or stenosis (newly identified in 24.8%), and 4.4% had conduction or rhythm abnormalities (newly identified in 1.4%). All but 5 subjects were asymptomatic.
Multivariable analysis suggested the odds of developing cardiomyopathy were significantly associated with being male (odds ratio [OR]=1.9), receiving anthracycline doses of 250 mg/m2 or greater (OR=2.7), having cardiac radiation exposure greater than 1500 cGy (OR=1.9), and having hypertension (OR=3.0).
Being younger at diagnosis was associated with higher odds of valvular disease. The ORs were 1.5 for patients who were 0 to 4 years of age at diagnosis and 1.3 for patients who were 5 to 9 at diagnosis.
Receiving higher radiation doses was associated with higher odds of valvular disease as well. But associations between radiation and valvular disease varied according to a patient’s anthracycline exposure (interaction P<0.001). The highest odds were among survivors with the highest doses of radiation exposure and any anthracycline exposure (OR=4.5).
The researchers also noted a reduction in the OR for valvular disease among obese patients (OR=0.4) and those with dyslipidemia (OR=0.7).
The team said there were not enough cases of coronary artery disease and conduction or rhythm abnormalities to support a fully adjusted multivariable model. However, it seemed these outcomes were more common with older age (≥40 years) and among patients with cardiac radiation doses of 1500 cGy or greater.
The researchers said this study revealed “considerable cardiovascular disease” in a large cohort of adult survivors of childhood cancer, which suggests a substantial future healthcare burden.
The team believes their findings could guide stratification of risk factors, screening practices, health counseling, and potential therapeutic measures aimed at changing the disease trajectory in this young adult population. ![]()
Novel delivery system could treat MCL
Researchers say they have developed a system for delivering therapy at the site of mantle cell lymphoma (MCL).
The system harnesses nanoparticles coated with “GPS” antibodies that navigate toward cancerous cells, where they offload cyclin D1-blockers in the form of small interfering RNAs (siRNAs).
Experiments showed the system can halt the proliferation of cyclin D1 in both animal models and samples from MCL patients.
Dan Peer, PhD, of Tel Aviv University in Israel, and his colleagues reported these results in PNAS.
“MCL has a genetic hallmark,” Dr Peer noted. “In 85% of cases, the characteristic that defines this aggressive and prototypic B-cell lymphoma is the heightened activity of the gene CCND1, which leads to the extreme overexpression—a 3000- to 15,000-fold increase—of cyclin D1, a protein that controls the proliferation of cells. Downregulation of cyclin D1 using siRNAs is a potential therapeutic approach to this malignancy.”
For this research, Dr Peer and his colleagues designed lipid-based nanoparticles (LNPs) coated with anti-CD38 monoclonal antibodies that were taken up by human MCL cells in the bone marrow of affected mice.
When loaded with siRNAs against cyclin D1, the targeting LNPs induced gene silencing in MCL cells and prolonged the survival of tumor-bearing mice, with no observed adverse effects.
“In MCL, cyclin D1 is the exclusive cause of the overproduction of B lymphocytes, the cells responsible for generating antibodies,” Dr Peer said. “This makes the protein a perfect target for RNA therapy by siRNAs.”
“Normal, healthy cells don’t express the gene, so therapies that destroy the gene will only attack cancer cells. The RNA interference we have developed targets the faulty cyclin D1 within the cancerous cells. And when the cells are inhibited from proliferating, they sense they are being targeted and begin to die off.”
Dr Peer and his colleagues believe this work presents new opportunities for treating MCL and other similar B-cell malignancies.
“This research makes a definite contribution to the revolution of personalized medicine, whereby you tailor the drug based on the genetic profile of patient,” Dr Peer said. “In this case, MCL is a disease with a specific genetic hallmark, so you can sequence the patient to identify the mutation(s) and design RNA blockers to be placed inside a nanovehicle.”
“While the targeting antibodies—the ‘GPS’—can be used to target many different B-cell malignancies, the drug itself is designed to silence this specific disease. However, the delivery system can be used to accommodate any disease with a genetic profile. This could be the future. We are seeing it happen before our very eyes.” ![]()
Researchers say they have developed a system for delivering therapy at the site of mantle cell lymphoma (MCL).
The system harnesses nanoparticles coated with “GPS” antibodies that navigate toward cancerous cells, where they offload cyclin D1-blockers in the form of small interfering RNAs (siRNAs).
Experiments showed the system can halt the proliferation of cyclin D1 in both animal models and samples from MCL patients.
Dan Peer, PhD, of Tel Aviv University in Israel, and his colleagues reported these results in PNAS.
“MCL has a genetic hallmark,” Dr Peer noted. “In 85% of cases, the characteristic that defines this aggressive and prototypic B-cell lymphoma is the heightened activity of the gene CCND1, which leads to the extreme overexpression—a 3000- to 15,000-fold increase—of cyclin D1, a protein that controls the proliferation of cells. Downregulation of cyclin D1 using siRNAs is a potential therapeutic approach to this malignancy.”
For this research, Dr Peer and his colleagues designed lipid-based nanoparticles (LNPs) coated with anti-CD38 monoclonal antibodies that were taken up by human MCL cells in the bone marrow of affected mice.
When loaded with siRNAs against cyclin D1, the targeting LNPs induced gene silencing in MCL cells and prolonged the survival of tumor-bearing mice, with no observed adverse effects.
“In MCL, cyclin D1 is the exclusive cause of the overproduction of B lymphocytes, the cells responsible for generating antibodies,” Dr Peer said. “This makes the protein a perfect target for RNA therapy by siRNAs.”
“Normal, healthy cells don’t express the gene, so therapies that destroy the gene will only attack cancer cells. The RNA interference we have developed targets the faulty cyclin D1 within the cancerous cells. And when the cells are inhibited from proliferating, they sense they are being targeted and begin to die off.”
Dr Peer and his colleagues believe this work presents new opportunities for treating MCL and other similar B-cell malignancies.
“This research makes a definite contribution to the revolution of personalized medicine, whereby you tailor the drug based on the genetic profile of patient,” Dr Peer said. “In this case, MCL is a disease with a specific genetic hallmark, so you can sequence the patient to identify the mutation(s) and design RNA blockers to be placed inside a nanovehicle.”
“While the targeting antibodies—the ‘GPS’—can be used to target many different B-cell malignancies, the drug itself is designed to silence this specific disease. However, the delivery system can be used to accommodate any disease with a genetic profile. This could be the future. We are seeing it happen before our very eyes.” ![]()
Researchers say they have developed a system for delivering therapy at the site of mantle cell lymphoma (MCL).
The system harnesses nanoparticles coated with “GPS” antibodies that navigate toward cancerous cells, where they offload cyclin D1-blockers in the form of small interfering RNAs (siRNAs).
Experiments showed the system can halt the proliferation of cyclin D1 in both animal models and samples from MCL patients.
Dan Peer, PhD, of Tel Aviv University in Israel, and his colleagues reported these results in PNAS.
“MCL has a genetic hallmark,” Dr Peer noted. “In 85% of cases, the characteristic that defines this aggressive and prototypic B-cell lymphoma is the heightened activity of the gene CCND1, which leads to the extreme overexpression—a 3000- to 15,000-fold increase—of cyclin D1, a protein that controls the proliferation of cells. Downregulation of cyclin D1 using siRNAs is a potential therapeutic approach to this malignancy.”
For this research, Dr Peer and his colleagues designed lipid-based nanoparticles (LNPs) coated with anti-CD38 monoclonal antibodies that were taken up by human MCL cells in the bone marrow of affected mice.
When loaded with siRNAs against cyclin D1, the targeting LNPs induced gene silencing in MCL cells and prolonged the survival of tumor-bearing mice, with no observed adverse effects.
“In MCL, cyclin D1 is the exclusive cause of the overproduction of B lymphocytes, the cells responsible for generating antibodies,” Dr Peer said. “This makes the protein a perfect target for RNA therapy by siRNAs.”
“Normal, healthy cells don’t express the gene, so therapies that destroy the gene will only attack cancer cells. The RNA interference we have developed targets the faulty cyclin D1 within the cancerous cells. And when the cells are inhibited from proliferating, they sense they are being targeted and begin to die off.”
Dr Peer and his colleagues believe this work presents new opportunities for treating MCL and other similar B-cell malignancies.
“This research makes a definite contribution to the revolution of personalized medicine, whereby you tailor the drug based on the genetic profile of patient,” Dr Peer said. “In this case, MCL is a disease with a specific genetic hallmark, so you can sequence the patient to identify the mutation(s) and design RNA blockers to be placed inside a nanovehicle.”
“While the targeting antibodies—the ‘GPS’—can be used to target many different B-cell malignancies, the drug itself is designed to silence this specific disease. However, the delivery system can be used to accommodate any disease with a genetic profile. This could be the future. We are seeing it happen before our very eyes.” ![]()
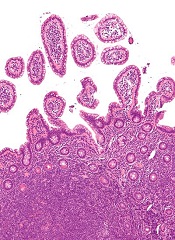
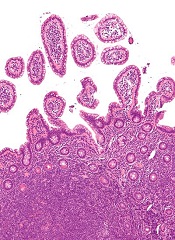
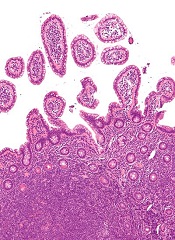
Paste may reduce radiation-induced fibrosis

woman for radiation
Photo by Rhoda Baer
A topical paste can reduce fibrosis caused by radiation therapy, according to preclinical research published in The FASEB Journal.
The study addressed a type of fibrosis called radiation dermatitis, in which radiation applied to the skin causes the buildup of fibrotic tissue and skin thickening.
To test their topical paste, researchers mimicked the development of radiation dermatitis in mice.
They exposed the mice’s skin to a single dose of 40 Gy, an amount of radiation similar to what patients undergoing anticancer radiation typically receive over 5 weeks.
Some of the irradiated animals were wild-type mice, while others were genetically engineered to lack the A2A receptor (A2AR). The researchers had previously shown that occupancy of A2AR induces collagen production.
The wild-type mice went on to receive placebo or daily treatment with ZM241385, a paste made with the research team’s patented A2AR blocker. The paste contains 2.5 milligrams of active ingredient per milliliter of 3% carboxymethyl cellulose, a gum “binder.”
A month after exposure, wild-type mice that received placebo had a nearly 2-fold increase in the amount of collagen and skin thickness. These mice also experienced epithelial hyperplasia.
On the other hand, mice treated with ZM241385 accumulated only 10% more skin-thickening collagen. ZM241385 treatment reduced the number of myofibroblasts, collagen fibrils, proliferating keratinocytes, and angiogenesis when compared to placebo. And the paste prevented epithelial hyperplasia.
Like ZM241385-treated mice, A2AR knockout mice did not have the excessive collagen production and skin thickening observed in placebo-treated wild-type mice. The knockout mice also exhibited reductions in myofibroblast content, angiogenesis, and epithelial hyperplasia.
The researchers noted that radiation-induced changes in the dermis and epidermis were accompanied by an infiltrate of T cells, which was prevented in both ZM241385-treated and A2AR knockout mice.
“Our latest study is the first to demonstrate that blocking or deleting the A2A receptor can be useful in reducing radiation-induced scarring in skin,” said study author Bruce Cronstein, MD, of New York University School of Medicine in New York, New York.
“The study also suggests that adenosine A2A receptor antagonists may have broad applications as drug therapies for preventing fibrosis and scarring, not just in the liver but also in the skin.”
If further experiments prove successful, Dr Cronstein said, clinicians treating early stage cancers with radiation could eventually prescribe an A2AR inhibitor paste to prevent fibrosis. He said his team next plans to study the mechanism underlying A2AR’s role in fibrosis. ![]()

woman for radiation
Photo by Rhoda Baer
A topical paste can reduce fibrosis caused by radiation therapy, according to preclinical research published in The FASEB Journal.
The study addressed a type of fibrosis called radiation dermatitis, in which radiation applied to the skin causes the buildup of fibrotic tissue and skin thickening.
To test their topical paste, researchers mimicked the development of radiation dermatitis in mice.
They exposed the mice’s skin to a single dose of 40 Gy, an amount of radiation similar to what patients undergoing anticancer radiation typically receive over 5 weeks.
Some of the irradiated animals were wild-type mice, while others were genetically engineered to lack the A2A receptor (A2AR). The researchers had previously shown that occupancy of A2AR induces collagen production.
The wild-type mice went on to receive placebo or daily treatment with ZM241385, a paste made with the research team’s patented A2AR blocker. The paste contains 2.5 milligrams of active ingredient per milliliter of 3% carboxymethyl cellulose, a gum “binder.”
A month after exposure, wild-type mice that received placebo had a nearly 2-fold increase in the amount of collagen and skin thickness. These mice also experienced epithelial hyperplasia.
On the other hand, mice treated with ZM241385 accumulated only 10% more skin-thickening collagen. ZM241385 treatment reduced the number of myofibroblasts, collagen fibrils, proliferating keratinocytes, and angiogenesis when compared to placebo. And the paste prevented epithelial hyperplasia.
Like ZM241385-treated mice, A2AR knockout mice did not have the excessive collagen production and skin thickening observed in placebo-treated wild-type mice. The knockout mice also exhibited reductions in myofibroblast content, angiogenesis, and epithelial hyperplasia.
The researchers noted that radiation-induced changes in the dermis and epidermis were accompanied by an infiltrate of T cells, which was prevented in both ZM241385-treated and A2AR knockout mice.
“Our latest study is the first to demonstrate that blocking or deleting the A2A receptor can be useful in reducing radiation-induced scarring in skin,” said study author Bruce Cronstein, MD, of New York University School of Medicine in New York, New York.
“The study also suggests that adenosine A2A receptor antagonists may have broad applications as drug therapies for preventing fibrosis and scarring, not just in the liver but also in the skin.”
If further experiments prove successful, Dr Cronstein said, clinicians treating early stage cancers with radiation could eventually prescribe an A2AR inhibitor paste to prevent fibrosis. He said his team next plans to study the mechanism underlying A2AR’s role in fibrosis. ![]()

woman for radiation
Photo by Rhoda Baer
A topical paste can reduce fibrosis caused by radiation therapy, according to preclinical research published in The FASEB Journal.
The study addressed a type of fibrosis called radiation dermatitis, in which radiation applied to the skin causes the buildup of fibrotic tissue and skin thickening.
To test their topical paste, researchers mimicked the development of radiation dermatitis in mice.
They exposed the mice’s skin to a single dose of 40 Gy, an amount of radiation similar to what patients undergoing anticancer radiation typically receive over 5 weeks.
Some of the irradiated animals were wild-type mice, while others were genetically engineered to lack the A2A receptor (A2AR). The researchers had previously shown that occupancy of A2AR induces collagen production.
The wild-type mice went on to receive placebo or daily treatment with ZM241385, a paste made with the research team’s patented A2AR blocker. The paste contains 2.5 milligrams of active ingredient per milliliter of 3% carboxymethyl cellulose, a gum “binder.”
A month after exposure, wild-type mice that received placebo had a nearly 2-fold increase in the amount of collagen and skin thickness. These mice also experienced epithelial hyperplasia.
On the other hand, mice treated with ZM241385 accumulated only 10% more skin-thickening collagen. ZM241385 treatment reduced the number of myofibroblasts, collagen fibrils, proliferating keratinocytes, and angiogenesis when compared to placebo. And the paste prevented epithelial hyperplasia.
Like ZM241385-treated mice, A2AR knockout mice did not have the excessive collagen production and skin thickening observed in placebo-treated wild-type mice. The knockout mice also exhibited reductions in myofibroblast content, angiogenesis, and epithelial hyperplasia.
The researchers noted that radiation-induced changes in the dermis and epidermis were accompanied by an infiltrate of T cells, which was prevented in both ZM241385-treated and A2AR knockout mice.
“Our latest study is the first to demonstrate that blocking or deleting the A2A receptor can be useful in reducing radiation-induced scarring in skin,” said study author Bruce Cronstein, MD, of New York University School of Medicine in New York, New York.
“The study also suggests that adenosine A2A receptor antagonists may have broad applications as drug therapies for preventing fibrosis and scarring, not just in the liver but also in the skin.”
If further experiments prove successful, Dr Cronstein said, clinicians treating early stage cancers with radiation could eventually prescribe an A2AR inhibitor paste to prevent fibrosis. He said his team next plans to study the mechanism underlying A2AR’s role in fibrosis. ![]()
Why cancer cells thrive when blood sugar is high

Photo by Andre Karwath
New research has revealed a mechanism that allows cancer cells to respond and grow rapidly when blood sugar levels rise.
This may help to explain why people who develop conditions in which they have chronically high blood sugar levels, such as obesity, also have an increased risk of developing certain cancers.
Susumu Hirabayashi, PhD, of Imperial College London in the UK, and Ross Cagan, PhD, of Mount Sinai Hospital in New York, New York, described the mechanism in eLife.
In a study published 2 years ago, the pair engineered fruit flies (Drosophila melanogaster) to activate the genes Ras and Src, which are activated in a range of malignancies.
The researchers activated Ras and Src in the flies’ developing eye tissue. Flies that were fed a normal diet grew small, benign tumors. But when flies were fed a high-sugar diet, they developed large, malignant tumors.
In flies fed a high-sugar diet, the normal cells became insulin-resistant, but the tumor cells didn’t. The tumor cells actually became more sensitive to insulin because they turned on a metabolic switch that triggered them to produce extra receptors for insulin. But this study did not explain how the tumor cells turned on this metabolic switch.
Now, after studying the same flies in more detail, Drs Hirabayashi and Cagan have found the tumor cells detect glucose availability indirectly, through a protein called salt-inducible kinase (SIK). When glucose levels are high, SIK sends a signal along the Hippo signaling pathway.
The Hippo signaling pathway is known to play a role in controlling cell growth. When it’s turned on, it keeps cell growth under control, but if it’s turned off, the cell can continue growing and may ultimately develop into a tumor.
Drs Hirabayashi and Cagan found that SIK acts like a sugar sensor, turning the Hippo signaling pathway off in response to raised glucose levels. This allows the tumor cells to continue to grow.
“Ras and Src co-activated tumors use SIK to sense that there’s lots of glucose available outside of their cells and to tell the cells to take advantage of that,” Dr Hirabayashi said. “Together, Ras and Src co-activated tumors use SIK to efficiently respond to glucose availability and ensure the tumors grow in nutrient-rich conditions such as obesity. We still don’t know if tumors caused by other genes respond to sugar in the same way.”
“Our results suggest that if we can develop drugs to target SIK, and stop it from alerting cancer cells in this way, then we may be able to stop cancer cells from thriving in an insulin-resistant environment and break the connection between obesity and cancer.” ![]()

Photo by Andre Karwath
New research has revealed a mechanism that allows cancer cells to respond and grow rapidly when blood sugar levels rise.
This may help to explain why people who develop conditions in which they have chronically high blood sugar levels, such as obesity, also have an increased risk of developing certain cancers.
Susumu Hirabayashi, PhD, of Imperial College London in the UK, and Ross Cagan, PhD, of Mount Sinai Hospital in New York, New York, described the mechanism in eLife.
In a study published 2 years ago, the pair engineered fruit flies (Drosophila melanogaster) to activate the genes Ras and Src, which are activated in a range of malignancies.
The researchers activated Ras and Src in the flies’ developing eye tissue. Flies that were fed a normal diet grew small, benign tumors. But when flies were fed a high-sugar diet, they developed large, malignant tumors.
In flies fed a high-sugar diet, the normal cells became insulin-resistant, but the tumor cells didn’t. The tumor cells actually became more sensitive to insulin because they turned on a metabolic switch that triggered them to produce extra receptors for insulin. But this study did not explain how the tumor cells turned on this metabolic switch.
Now, after studying the same flies in more detail, Drs Hirabayashi and Cagan have found the tumor cells detect glucose availability indirectly, through a protein called salt-inducible kinase (SIK). When glucose levels are high, SIK sends a signal along the Hippo signaling pathway.
The Hippo signaling pathway is known to play a role in controlling cell growth. When it’s turned on, it keeps cell growth under control, but if it’s turned off, the cell can continue growing and may ultimately develop into a tumor.
Drs Hirabayashi and Cagan found that SIK acts like a sugar sensor, turning the Hippo signaling pathway off in response to raised glucose levels. This allows the tumor cells to continue to grow.
“Ras and Src co-activated tumors use SIK to sense that there’s lots of glucose available outside of their cells and to tell the cells to take advantage of that,” Dr Hirabayashi said. “Together, Ras and Src co-activated tumors use SIK to efficiently respond to glucose availability and ensure the tumors grow in nutrient-rich conditions such as obesity. We still don’t know if tumors caused by other genes respond to sugar in the same way.”
“Our results suggest that if we can develop drugs to target SIK, and stop it from alerting cancer cells in this way, then we may be able to stop cancer cells from thriving in an insulin-resistant environment and break the connection between obesity and cancer.” ![]()

Photo by Andre Karwath
New research has revealed a mechanism that allows cancer cells to respond and grow rapidly when blood sugar levels rise.
This may help to explain why people who develop conditions in which they have chronically high blood sugar levels, such as obesity, also have an increased risk of developing certain cancers.
Susumu Hirabayashi, PhD, of Imperial College London in the UK, and Ross Cagan, PhD, of Mount Sinai Hospital in New York, New York, described the mechanism in eLife.
In a study published 2 years ago, the pair engineered fruit flies (Drosophila melanogaster) to activate the genes Ras and Src, which are activated in a range of malignancies.
The researchers activated Ras and Src in the flies’ developing eye tissue. Flies that were fed a normal diet grew small, benign tumors. But when flies were fed a high-sugar diet, they developed large, malignant tumors.
In flies fed a high-sugar diet, the normal cells became insulin-resistant, but the tumor cells didn’t. The tumor cells actually became more sensitive to insulin because they turned on a metabolic switch that triggered them to produce extra receptors for insulin. But this study did not explain how the tumor cells turned on this metabolic switch.
Now, after studying the same flies in more detail, Drs Hirabayashi and Cagan have found the tumor cells detect glucose availability indirectly, through a protein called salt-inducible kinase (SIK). When glucose levels are high, SIK sends a signal along the Hippo signaling pathway.
The Hippo signaling pathway is known to play a role in controlling cell growth. When it’s turned on, it keeps cell growth under control, but if it’s turned off, the cell can continue growing and may ultimately develop into a tumor.
Drs Hirabayashi and Cagan found that SIK acts like a sugar sensor, turning the Hippo signaling pathway off in response to raised glucose levels. This allows the tumor cells to continue to grow.
“Ras and Src co-activated tumors use SIK to sense that there’s lots of glucose available outside of their cells and to tell the cells to take advantage of that,” Dr Hirabayashi said. “Together, Ras and Src co-activated tumors use SIK to efficiently respond to glucose availability and ensure the tumors grow in nutrient-rich conditions such as obesity. We still don’t know if tumors caused by other genes respond to sugar in the same way.”
“Our results suggest that if we can develop drugs to target SIK, and stop it from alerting cancer cells in this way, then we may be able to stop cancer cells from thriving in an insulin-resistant environment and break the connection between obesity and cancer.” ![]()
Attending Workload, Teaching, and Safety
Teaching attending physicians must balance clinical workload and resident education simultaneously while supervising inpatient services. The workload of teaching attendings has been increasing due to many factors. As patient complexity has increased, length of stay has decreased, creating higher turnover and higher acuity of hospitalized patients.[1, 2, 3, 4, 5] The rising burden of clinical documentation has increased demands on inpatient attending physicians' time.[6] Additionally, resident duty hour restrictions have shifted the responsibility for patient care to the teaching attending.[7] These factors contribute to the perception of unsafe workloads among attending physicians[8] and could impact the ability to teach well.
Teaching effectiveness is an important facet of the graduate medical education (GME) learning environment.[9] Residents perceive that education suffers when their own workload increases,[10, 11, 12, 13, 14] and higher on‐call workload is associated with lower likelihood of participation in educational activities.[15] More contact between resident trainees and supervisory staff may improve the clinical value of inpatient rotations.[16] Program directors have expressed concern about the educational ramifications of work compression.[17, 18, 19, 20] Higher workload for attending physicians can negatively impact patient safety and quality of care,[21, 22] and perception of higher attending workload is associated with less time for teaching.[23] However, the impact of objective measures of attending physician workload on educational outcomes has not been explored. When attending physicians are responsible for increasingly complex clinical care in addition to resident education, teaching effectiveness may suffer. With growing emphasis on the educational environment's effect on healthcare quality and safety,[24] it is imperative to consider the influence of attending workload on patient care and resident education.
The combination of increasing clinical demands, fewer hours in‐house for residents, and less time for teaching has the potential to decrease attending physician teaching effectiveness. In this study, we aimed to evaluate relationships among objective measures of attending physician workload, resident perception of teaching effectiveness, and patient outcomes. We hypothesized that higher workload for attending physicians would be associated with lower ratings of teaching effectiveness and poorer outcomes for patients.
METHODS
We performed a retrospective study of attending physicians who supervised inpatient internal medicine teaching services at Mayo ClinicRochester from July 2005 through June 2011 (6 full academic years). The team structure for each service was 1 attending physician, 1 senior resident, and 3 interns. Senior residents were on call every fourth night, and interns were on call every sixth night. Up to 2 admissions per service were received during the daytime short call, and up to 5 admissions per service were received during the overnight long call. Attending physicians included all supervising physicians in appointment categories of attending/consultant, senior associate consultant, and chief medical resident at the Mayo Clinic. Maximum continuous on‐call time for residents during the study period was restricted to 30 hours continuously. The timeframe of this study was chosen to minimize variability in resident work schedules; effective July 1, 2011, duty hours for postgraduate year 1 residents were further restricted to a maximum of 16 hours in duration.[25]
Measures of Attending Physician Workload
To measure attending physician workload, we examined mean service census as reported at midnight, mean patient length of stay, mean number of daily admissions, and mean number of daily discharges. We also calculated mean daily outpatient relative value units (RVUs) generated as a measure of outpatient workload while the attending was supervising the inpatient service. Similar measures of workload have been used in previous research.[26] Attending physicians in this study functioned as hospitalists during their time supervising the teaching services; that is, they were not routinely assigned to any outpatient responsibilities. The only way for an outpatient RVU to be generated during their time supervising the hospital service was for the attending physician to specifically request to see an outpatient in the clinic. Attending physicians only supervised 1 teaching service at a time and had no concurrent nonteaching service obligations. Admissions were received on a rotating basis. Because patient illness severity may impact workload, we also examined mean expected mortality (per 1000 patients) for all patients on the attending physicians' hospital services.[27]
The above workload variables were measured in the specific timeframe that corresponded to the number of days an attending physician was supervising a particular team; for example, mean census was the mean number of patients on the attending physician's hospital service during his or her time supervising that resident team.
Teaching Effectiveness Outcome Measures
Teaching effectiveness was measured using residents' evaluations of their attending physicians with a 5‐point scale (1 = needs improvement, 3 = average, 5 = top 10% of attending physicians) that has been previously validated in similar contexts.[28, 29, 30, 31, 32] The evaluation questions are shown in Supporting Information, Appendix A, in the online version of this article.
Patient Outcome Measures
Patient outcomes included applicable patient safety indicators (PSIs) as defined by the Agency for Healthcare Research and Quality[33] (see Supporting Information, Appendix B, in the online version of this article), patient transfers to the intensive care unit (ICU), calls to the rapid response team/cardiopulmonary resuscitation team, and patient deaths. Each indicator and event was summarized as occurred or did not occur at the service‐team level. For example, for a particular attendingresident team, the occurrence of each of these events at any point during the time they worked together was recorded as occurred (1) or did not occur (0). Similar measures of patient outcomes have been used in previous research.[32]
Statistical Analysis
Mixed linear models with variance components covariance structure (including random effects to account for repeated ratings by residents and of faculty) were fit using restricted maximum likelihood to examine associations of attending workload and demographics with teaching scores. Generalized linear regression models, estimated via generalized estimating equations, were used to examine associations of attending workload and demographics with patient outcomes. Due to the binary nature of the outcomes, the binomial distribution and logit link function were used, producing odds ratios (ORs) for covariates akin to those found in standard logistic regression. Multivariate models were used to adjust for physician demographics including age, gender, teaching appointment (consultant, senior associate consultant/temporary clinical appointment, or chief medical resident) and academic rank (professor, associate professor, assistant professor, instructor/none).
To account for multiple comparisons, a significance level of P < 0.01 was used. All analyses were performed using SAS statistical software (version 9.3; SAS Institute Inc., Cary, NC). This study was deemed minimal risk after review by the Mayo Clinic Institutional Review Board.
RESULTS
Over the 6‐year study period, 107 attending physicians supervised internal medicine teaching services. Twenty‐three percent of teaching attending physicians were female. Mean attending age was 42.6 years. Attendings supervised a given service for between 2 and 19 days (mean [standard deviation] = 10.1 [4.1] days). There were 542 internal medicine residents on these teaching services who completed at least 1 teaching evaluation. A total of 69,386 teaching evaluation items were submitted by these residents during the study period.
In a multivariate analysis adjusted for faculty demographics and workload measures, teaching evaluation scores were significantly higher for attending physicians who had an academic rank of professor when compared to attendings who were assistant professors ( = 0.12, P = 0.007), or instructors/no academic rank ( = 0.23, P < 0.0001). The number of days an attending physician spent with the team showed a positive association with teaching evaluations ( = +0.015, P < 0.0001).
Associations between measures of attending physician workload and teaching evaluation scores are shown in Table 1. Mean midnight census and mean number of daily discharges were associated with lower teaching evaluation scores (both = 0.026, P < 0.0001). Mean number of daily admissions was associated with higher teaching scores ( = +0.021, P = 0.001). The mean expected mortality among hospitalized patients on the services supervised by teaching attendings and the outpatient RVUs generated by these attendings during the time they were supervising the hospital service showed no association with teaching scores. The average number of RVUs generated during an attending's entire time supervising hospital service was <1.
| Attending Physician Workload Measure | Mean (SD) | Multivariate Analysis* | |||
|---|---|---|---|---|---|
| SE | 99% CI | P | |||
| |||||
| Midnight census | 8.86 (1.8) | 0.026 | 0.002 | (0.03, 0.02) | <0.0001 |
| Length of stay, d | 6.91 (3.0) | +0.006 | 0.001 | (0.002, 0.009) | <0.0001 |
| Expected mortality (per 1,000 patients) | 51.94 (27.4) | 0.0001 | 0.0001 | (0.0004, 0.0001) | 0.19 |
| Daily admissions | 2.23 (0.54) | +0.021 | 0.006 | (0.004, 0.037) | 0.001 |
| Daily discharges | 2.13 (0.56) | 0.026 | 0.006 | (0.041, 0.010) | <0.0001 |
| Daily outpatient relative value units | 0.69 (1.2) | +0.004 | 0.003 | (0.002, 0.011) | 0.10 |
Table 2 shows relationships between attending physician workload and patient outcomes for the patients on hospital services supervised by 107 attending physicians during the study period. Patient outcome data showed positive associations between measures of higher workload and PSIs. Specifically, for each 1‐patient increase in the average number of daily admissions to the attending and resident services, the cohort of patients under the team's care was 1.8 times more likely to include at least 1 patient with a PSI event (OR = 1.81, 99% confidence interval [CI]: 1.21, 2.71, P = 0.0001). Likewise, for each 1‐day increase in average length of stay, the cohort of patients under the team's care was 1.16 times more likely to have at least 1 patient with a PSI (OR = 1.16, 99% CI: 1.07, 1.26, P < 0.0001). As anticipated, mean expected mortality was associated with actual mortality, cardiopulmonary resuscitation/rapid response team calls, and ICU transfers. There were no associations between patient outcomes and workload measures of midnight census and outpatient RVUs.
| Patient Outcomes, Multivariate Analysis* | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient Safety Indicators, n = 513 | Deaths, n = 352 | CPR/RRT Calls, n = 409 | ICU Transfers, n = 737 | |||||||||||||
| Workload measures | OR | SE | P | 99% CI | OR | SE | P | 99% CI | OR | SE | P | 99% CI | OR | SE | P | 99% CI |
| ||||||||||||||||
| Midnight census | 1.10 | 0.05 | 0.04 | (0.98, 1.24) | 0.91 | 0.04 | 0.03 | (0.81, 1.02) | 0.95 | 0.04 | 0.16 | (0.86, 1.05) | 1.06 | 0.04 | 0.16 | (0.96, 1.17) |
| Length of stay | 1.16 | 0.04 | <0.0001 | (1.07, 1.26) | 1.03 | 0.03 | 0.39 | (0.95, 1.12) | 0.99 | 0.03 | 0.63 | (0.92, 1.05) | 1.10 | 0.03 | 0.0001 | (1.03, 1.18) |
| Expected mortality (per 1,000 patients) | 1.00 | 0.003 | 0.24 | (0.99, 1.01) | 1.01 | 0.00 | 0.002 | (1.00, 1.02) | 1.02 | 0.00 | <0.0001 | (1.01, 1.02) | 1.01 | 0.00 | 0.003 | (1.00, 1.01) |
| Daily admissions | 1.81 | 0.28 | 0.0001 | (1.21, 2.71) | 0.78 | 0.14 | 0.16 | (0.49, 1.24) | 1.11 | 0.20 | 0.57 | (0.69, 1.77) | 1.34 | 0.24 | 0.09 | (0.85, 2.11) |
| Daily discharges | 1.06 | 0.13 | 0.61 | (0.78, 1.45) | 2.36 | 0.38 | <0.0001 | (1.56, 3.57) | 0.94 | 0.16 | 0.70 | (0.60, 1.46) | 1.09 | 0.16 | 0.53 | (0.75, 1.60) |
| Daily outpatient relative value units | 0.81 | 0.07 | 0.01 | (0.65, 1.00) | 1.02 | 0.04 | 0.56 | (0.92, 1.13) | 1.05 | 0.04 | 0.23 | (0.95, 1.17) | 0.92 | 0.06 | 0.23 | (0.77, 1.09) |
DISCUSSION
This study of internal medicine attending physician workload and resident education demonstrates that higher workload among attending physicians is associated with slightly lower teaching evaluation scores from residents as well as increased risks to patient safety.
The prior literature examining relationships between workload and teaching effectiveness is largely survey‐based and reliant upon physicians' self‐reported perceptions of workload.[10, 13, 23] The present study strengthens this evidence by using multiple objective measures of workload, objective measures of patient safety, and a large sample of teaching evaluations.
An interesting finding in this study was that the number of patient dismissals per day was associated with a significant decrease in teaching scores, whereas the number of admissions per day was associated with increased teaching scores. These findings may seem contradictory, because the number of admissions and discharges both measure physician workload. However, a likely explanation for this apparent inconsistency is that on internal medicine inpatient teaching services, much of the teaching of residents occurs at the time of a patient admission as residents are presenting cases to the attending physician, exploring differential diagnoses, and discussing management plans. By contrast, a patient dismissal tends to consist mainly of patient interaction, paperwork, and phone calls by the resident with less input required from the attending physician. Our findings suggest that although patient admissions remain a rich opportunity for resident education, patient dismissals may increase workload without improving teaching evaluations. As the inpatient hospital environment evolves, exploring options for nonphysician providers to assist with or complete patient dismissals may have a beneficial effect on resident education.[34] In addition, exploring more efficient teaching strategies may be beneficial in the fast‐paced inpatient learning milieu.[35]
There was a statistically significant positive association between the number of days an attending physician spent with the team and teaching evaluations. Although prior work has examined advantages and disadvantages of various resident schedules,[36, 37, 38] our results suggest scheduling models that emphasize continuity of the teaching attending and residents may be preferred to enhance teaching effectiveness. Further study would help elucidate potential implications of this finding for the scheduling of supervisory attendings to optimize education.
In this analysis, patient outcome measures were largely independent of attending physician workload, with the exception of PSIs. PSIs have been associated with longer stays in the hospital,[39, 40] which is consistent with our findings. However, mean daily admissions were also associated with PSIs. It could be expected that the more patients on a hospital service, the more PSIs will result. However, there was not a significant association between midnight census and PSIs when other variables were accounted for. Because new patient admissions are time consuming and contribute to the workload of both residents and attending physicians, it is possible that safety of the service's hospitalized patients is compromised when the team is putting time and effort toward new patients. Previous research has shown variability in PSI trends with changes in the workload environment.[41] Further studies are needed to fully explore relationships between admission volume and PSIs on teaching services.
It is worthwhile to note that attending physicians have specific responsibilities of supervision and documentation for new admissions. Although it could be argued that new admissions raise the workload for the entire team, and the higher team workload may impact teaching evaluations, previous research has demonstrated that resident burnout and well‐being, which are influenced by workload, do not impact residents' assessments of teachers.[42] In addition, metrics that could arguably be more apt to measure the workload of the team as a whole (eg, team census) did not show a significant association with patient outcomes.
This study has important limitations. First, the cohort of attending physicians, residents, and patients was from a large single institution and may not be generalizable to all settings. Second, most attending physicians in this sample were experienced teachers, so consequences of increased workload may have been managed effectively without a major impact on resident education in some cases. Third, the magnitude of change in teaching effectiveness, although statistically significant, was small and might call into question the educational significance of these findings. Fourth, although resident satisfaction does not influence teaching scores, it is possible that residents' perception of their own workload may have impacted teaching evaluations. Finally, data collection was intentionally closed at the end of the 2011 academic year because accreditation standards for resident duty hours changed again at that time.[43] Thus, these data may not directly reflect the evolving hospital learning environment but serve as a useful benchmark for future studies of workload and teaching effectiveness in the inpatient setting. Once hospitals have had sufficient time and experience with the new duty hour standards, additional studies exploring relationships between workload, teaching effectiveness, and patient outcomes may be warranted.
Limitations notwithstanding, this study shows that attending physician workload may adversely impact teaching and patient safety on internal medicine hospital services. Ongoing efforts by residency programs to optimize the learning environment should include strategies to manage the workload of supervising attendings.
Disclosures
This publication was made possible in part by Clinical and Translational Science Award grant number UL1 TR000135 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH. Authors also acknowledge support for the Mayo Clinic Department of Medicine Write‐up and Publish grant. In addition, this study was supported in part by the Mayo Clinic Internal Medicine Residency Office of Education Innovations as part of the Accreditation Council for Graduate Medical Education Educational Innovations Project. The information contained in this article was based in part on the performance package data maintained by the University HealthSystem Consortium. Copyright 2015 UHC. All rights reserved.
- , , . The future of residents' education in internal medicine. Am J Med. 2004;116(9):648–650.
- , , , , . Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine. Ann Intern Med. 2006;144(12):920–926.
- , , . Residency training in the modern era: the pipe dream of less time to learn more, care better, and be more professional. Arch Intern Med. 2005;165(22):2561–2562.
- , , , et al. Trends in Hospitalizations Among Medicare Survivors of Aortic Valve Replacement in the United States From 1999 to 2010. Ann Thorac Surg. 2015;99(2):509–517.
- , , . Restructuring an inpatient resident service to improve outcomes for residents, students, and patients. Acad Med. 2011;86(12):1500–1507.
- , , , . Clinical documentation in the 21st century: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;162(4):301–303.
- , . Effect of ACGME duty hours on attending physician teaching and satisfaction. Arch Intern Med. 2008;168(11):1226–1228.
- , , , , . Identifying potential predictors of a safe attending physician workload: a survey of hospitalists. J Hosp Med. 2013;8(11):644–646.
- , , . The clinical learning environment: the foundation of graduate medical education. JAMA. 2013;309(16):1687–1688.
- , , , , , . Better rested, but more stressed? Evidence of the effects of resident work hour restrictions. Acad Pediatr. 2012;12(4):335–343.
- , , , . Multifaceted longitudinal study of surgical resident education, quality of life, and patient care before and after July 2011. J Surg Educ. 2013;70(6):769–776.
- , , . Impact of the new 16‐hour duty period on pediatric interns' neonatal education. Clin Pediatr (Phila). 2014;53(1):51–59.
- , , , , , . Relationship between resident workload and self‐perceived learning on inpatient medicine wards: a longitudinal study. BMC Med Educ. 2006;6:35.
- , , , . Perceptions of educational experience and inpatient workload among pediatric residents. Hosp Pediatr. 2013;3(3):276–284.
- , , , et al. Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities. JAMA. 2008;300(10):1146–1153.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
- , , , , . Approval and perceived impact of duty hour regulations: survey of pediatric program directors. Pediatrics. 2013;132(5):819–824.
- , , , et al. Anticipated consequences of the 2011 duty hours standards: views of internal medicine and surgery program directors. Acad Med. 2012;87(7):895–903.
- , , , , . Training on the clock: family medicine residency directors' responses to resident duty hours reform. Acad Med. 2006;81(12):1032–1037.
- , , , et al. Duty hour recommendations and implications for meeting the ACGME core competencies: views of residency directors. Mayo Clin Proc. 2011;86(3):185–191.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–973.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. No time for teaching? Inpatient attending physicians' workload and teaching before and after the implementation of the 2003 duty hours regulations. Acad Med. 2013;88(9):1293–1298.
- Accreditation Council for Graduate Medical Education. Clinical Learning Environment Review (CLER) Program. Available at: http://www.acgme.org/acgmeweb/tabid/436/ProgramandInstitutionalAccreditation/NextAccreditationSystem/ClinicalLearningEnvironmentReviewProgram.aspx. Accessed April 27, 2015.
- Accreditation Council for Graduate Medical Education. Frequently Asked Questions: A ACGME common duty hour requirements. Available at: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh‐faqs 2011.pdf. Accessed April 27, 2015.
- , , , , . Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. 2014;174(5):786–793.
- University HealthSystem Consortium. UHC clinical database/resource manager for Mayo Clinic. Available at: http://www.uhc.edu. Data accessed August 25, 2011.
- , . The interpersonal, cognitive and efficiency domains of clinical teaching: construct validity of a multi‐dimensional scale. Med Educ. 2005;39(12):1221–1229.
- , , . Factor instability of clinical teaching assessment scores among general internists and cardiologists. Med Educ. 2006;40(12):1209–1216.
- , , , . Determining reliability of clinical assessment scores in real time. Teach Learn Med. 2009;21(3):188–194.
- , , , , , . Behaviors of highly professional resident physicians. JAMA. 2008;300(11):1326–1333.
- , , , et al. Service census caps and unit‐based admissions: resident workload, conference attendance, duty hour compliance, and patient safety. Mayo Clin Proc. 2012;87(4):320–327.
- Agency for Healthcare Research and Quality. Patient safety indicators technical specifications updates—Version 5.0, March 2015. Available at: http://www.qualityindicators.ahrq.gov/Modules/PSI_TechSpec.aspx. Accessed May 29, 2015.
- , , , , , . The impact of nonphysician clinicians: do they improve the quality and cost‐effectiveness of health care services? Med Care Res Rev. 2009;66(6 suppl):36S–89S.
- , , . Maximizing teaching on the wards: review and application of the One‐Minute Preceptor and SNAPPS models. J Hosp Med. 2015;10(2):125–130.
- , , , . Resident perceptions of the educational value of night float rotations. Teach Learn Med. 2010;22(3):196–201.
- , , , , , . An evaluation of internal medicine residency continuity clinic redesign to a 50/50 outpatient‐inpatient model. J Gen Intern Med. 2013;28(8):1014–1019.
- , , , et al. Revisiting the rotating call schedule in less than 80 hours per week. J Surg Educ. 2009;66(6):357–360.
- , . Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290(14):1868–1874.
- , , , . Agency for Healthcare Research and Quality patient safety indicators and mortality in surgical patients. Am Surg. 2014;80(8):801–804.
- , , , et al. Patient safety in the era of the 80‐hour workweek. J Surg Educ. 2014;71(4):551–559.
- , , , . Impact of resident well‐being and empathy on assessments of faculty physicians. J Gen Intern Med. 2010;25(1):52–56.
- , , , et al. Stress management training for surgeons‐a randomized, controlled, intervention study. Ann Surg. 2011;253(3):488–494.
Teaching attending physicians must balance clinical workload and resident education simultaneously while supervising inpatient services. The workload of teaching attendings has been increasing due to many factors. As patient complexity has increased, length of stay has decreased, creating higher turnover and higher acuity of hospitalized patients.[1, 2, 3, 4, 5] The rising burden of clinical documentation has increased demands on inpatient attending physicians' time.[6] Additionally, resident duty hour restrictions have shifted the responsibility for patient care to the teaching attending.[7] These factors contribute to the perception of unsafe workloads among attending physicians[8] and could impact the ability to teach well.
Teaching effectiveness is an important facet of the graduate medical education (GME) learning environment.[9] Residents perceive that education suffers when their own workload increases,[10, 11, 12, 13, 14] and higher on‐call workload is associated with lower likelihood of participation in educational activities.[15] More contact between resident trainees and supervisory staff may improve the clinical value of inpatient rotations.[16] Program directors have expressed concern about the educational ramifications of work compression.[17, 18, 19, 20] Higher workload for attending physicians can negatively impact patient safety and quality of care,[21, 22] and perception of higher attending workload is associated with less time for teaching.[23] However, the impact of objective measures of attending physician workload on educational outcomes has not been explored. When attending physicians are responsible for increasingly complex clinical care in addition to resident education, teaching effectiveness may suffer. With growing emphasis on the educational environment's effect on healthcare quality and safety,[24] it is imperative to consider the influence of attending workload on patient care and resident education.
The combination of increasing clinical demands, fewer hours in‐house for residents, and less time for teaching has the potential to decrease attending physician teaching effectiveness. In this study, we aimed to evaluate relationships among objective measures of attending physician workload, resident perception of teaching effectiveness, and patient outcomes. We hypothesized that higher workload for attending physicians would be associated with lower ratings of teaching effectiveness and poorer outcomes for patients.
METHODS
We performed a retrospective study of attending physicians who supervised inpatient internal medicine teaching services at Mayo ClinicRochester from July 2005 through June 2011 (6 full academic years). The team structure for each service was 1 attending physician, 1 senior resident, and 3 interns. Senior residents were on call every fourth night, and interns were on call every sixth night. Up to 2 admissions per service were received during the daytime short call, and up to 5 admissions per service were received during the overnight long call. Attending physicians included all supervising physicians in appointment categories of attending/consultant, senior associate consultant, and chief medical resident at the Mayo Clinic. Maximum continuous on‐call time for residents during the study period was restricted to 30 hours continuously. The timeframe of this study was chosen to minimize variability in resident work schedules; effective July 1, 2011, duty hours for postgraduate year 1 residents were further restricted to a maximum of 16 hours in duration.[25]
Measures of Attending Physician Workload
To measure attending physician workload, we examined mean service census as reported at midnight, mean patient length of stay, mean number of daily admissions, and mean number of daily discharges. We also calculated mean daily outpatient relative value units (RVUs) generated as a measure of outpatient workload while the attending was supervising the inpatient service. Similar measures of workload have been used in previous research.[26] Attending physicians in this study functioned as hospitalists during their time supervising the teaching services; that is, they were not routinely assigned to any outpatient responsibilities. The only way for an outpatient RVU to be generated during their time supervising the hospital service was for the attending physician to specifically request to see an outpatient in the clinic. Attending physicians only supervised 1 teaching service at a time and had no concurrent nonteaching service obligations. Admissions were received on a rotating basis. Because patient illness severity may impact workload, we also examined mean expected mortality (per 1000 patients) for all patients on the attending physicians' hospital services.[27]
The above workload variables were measured in the specific timeframe that corresponded to the number of days an attending physician was supervising a particular team; for example, mean census was the mean number of patients on the attending physician's hospital service during his or her time supervising that resident team.
Teaching Effectiveness Outcome Measures
Teaching effectiveness was measured using residents' evaluations of their attending physicians with a 5‐point scale (1 = needs improvement, 3 = average, 5 = top 10% of attending physicians) that has been previously validated in similar contexts.[28, 29, 30, 31, 32] The evaluation questions are shown in Supporting Information, Appendix A, in the online version of this article.
Patient Outcome Measures
Patient outcomes included applicable patient safety indicators (PSIs) as defined by the Agency for Healthcare Research and Quality[33] (see Supporting Information, Appendix B, in the online version of this article), patient transfers to the intensive care unit (ICU), calls to the rapid response team/cardiopulmonary resuscitation team, and patient deaths. Each indicator and event was summarized as occurred or did not occur at the service‐team level. For example, for a particular attendingresident team, the occurrence of each of these events at any point during the time they worked together was recorded as occurred (1) or did not occur (0). Similar measures of patient outcomes have been used in previous research.[32]
Statistical Analysis
Mixed linear models with variance components covariance structure (including random effects to account for repeated ratings by residents and of faculty) were fit using restricted maximum likelihood to examine associations of attending workload and demographics with teaching scores. Generalized linear regression models, estimated via generalized estimating equations, were used to examine associations of attending workload and demographics with patient outcomes. Due to the binary nature of the outcomes, the binomial distribution and logit link function were used, producing odds ratios (ORs) for covariates akin to those found in standard logistic regression. Multivariate models were used to adjust for physician demographics including age, gender, teaching appointment (consultant, senior associate consultant/temporary clinical appointment, or chief medical resident) and academic rank (professor, associate professor, assistant professor, instructor/none).
To account for multiple comparisons, a significance level of P < 0.01 was used. All analyses were performed using SAS statistical software (version 9.3; SAS Institute Inc., Cary, NC). This study was deemed minimal risk after review by the Mayo Clinic Institutional Review Board.
RESULTS
Over the 6‐year study period, 107 attending physicians supervised internal medicine teaching services. Twenty‐three percent of teaching attending physicians were female. Mean attending age was 42.6 years. Attendings supervised a given service for between 2 and 19 days (mean [standard deviation] = 10.1 [4.1] days). There were 542 internal medicine residents on these teaching services who completed at least 1 teaching evaluation. A total of 69,386 teaching evaluation items were submitted by these residents during the study period.
In a multivariate analysis adjusted for faculty demographics and workload measures, teaching evaluation scores were significantly higher for attending physicians who had an academic rank of professor when compared to attendings who were assistant professors ( = 0.12, P = 0.007), or instructors/no academic rank ( = 0.23, P < 0.0001). The number of days an attending physician spent with the team showed a positive association with teaching evaluations ( = +0.015, P < 0.0001).
Associations between measures of attending physician workload and teaching evaluation scores are shown in Table 1. Mean midnight census and mean number of daily discharges were associated with lower teaching evaluation scores (both = 0.026, P < 0.0001). Mean number of daily admissions was associated with higher teaching scores ( = +0.021, P = 0.001). The mean expected mortality among hospitalized patients on the services supervised by teaching attendings and the outpatient RVUs generated by these attendings during the time they were supervising the hospital service showed no association with teaching scores. The average number of RVUs generated during an attending's entire time supervising hospital service was <1.
| Attending Physician Workload Measure | Mean (SD) | Multivariate Analysis* | |||
|---|---|---|---|---|---|
| SE | 99% CI | P | |||
| |||||
| Midnight census | 8.86 (1.8) | 0.026 | 0.002 | (0.03, 0.02) | <0.0001 |
| Length of stay, d | 6.91 (3.0) | +0.006 | 0.001 | (0.002, 0.009) | <0.0001 |
| Expected mortality (per 1,000 patients) | 51.94 (27.4) | 0.0001 | 0.0001 | (0.0004, 0.0001) | 0.19 |
| Daily admissions | 2.23 (0.54) | +0.021 | 0.006 | (0.004, 0.037) | 0.001 |
| Daily discharges | 2.13 (0.56) | 0.026 | 0.006 | (0.041, 0.010) | <0.0001 |
| Daily outpatient relative value units | 0.69 (1.2) | +0.004 | 0.003 | (0.002, 0.011) | 0.10 |
Table 2 shows relationships between attending physician workload and patient outcomes for the patients on hospital services supervised by 107 attending physicians during the study period. Patient outcome data showed positive associations between measures of higher workload and PSIs. Specifically, for each 1‐patient increase in the average number of daily admissions to the attending and resident services, the cohort of patients under the team's care was 1.8 times more likely to include at least 1 patient with a PSI event (OR = 1.81, 99% confidence interval [CI]: 1.21, 2.71, P = 0.0001). Likewise, for each 1‐day increase in average length of stay, the cohort of patients under the team's care was 1.16 times more likely to have at least 1 patient with a PSI (OR = 1.16, 99% CI: 1.07, 1.26, P < 0.0001). As anticipated, mean expected mortality was associated with actual mortality, cardiopulmonary resuscitation/rapid response team calls, and ICU transfers. There were no associations between patient outcomes and workload measures of midnight census and outpatient RVUs.
| Patient Outcomes, Multivariate Analysis* | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient Safety Indicators, n = 513 | Deaths, n = 352 | CPR/RRT Calls, n = 409 | ICU Transfers, n = 737 | |||||||||||||
| Workload measures | OR | SE | P | 99% CI | OR | SE | P | 99% CI | OR | SE | P | 99% CI | OR | SE | P | 99% CI |
| ||||||||||||||||
| Midnight census | 1.10 | 0.05 | 0.04 | (0.98, 1.24) | 0.91 | 0.04 | 0.03 | (0.81, 1.02) | 0.95 | 0.04 | 0.16 | (0.86, 1.05) | 1.06 | 0.04 | 0.16 | (0.96, 1.17) |
| Length of stay | 1.16 | 0.04 | <0.0001 | (1.07, 1.26) | 1.03 | 0.03 | 0.39 | (0.95, 1.12) | 0.99 | 0.03 | 0.63 | (0.92, 1.05) | 1.10 | 0.03 | 0.0001 | (1.03, 1.18) |
| Expected mortality (per 1,000 patients) | 1.00 | 0.003 | 0.24 | (0.99, 1.01) | 1.01 | 0.00 | 0.002 | (1.00, 1.02) | 1.02 | 0.00 | <0.0001 | (1.01, 1.02) | 1.01 | 0.00 | 0.003 | (1.00, 1.01) |
| Daily admissions | 1.81 | 0.28 | 0.0001 | (1.21, 2.71) | 0.78 | 0.14 | 0.16 | (0.49, 1.24) | 1.11 | 0.20 | 0.57 | (0.69, 1.77) | 1.34 | 0.24 | 0.09 | (0.85, 2.11) |
| Daily discharges | 1.06 | 0.13 | 0.61 | (0.78, 1.45) | 2.36 | 0.38 | <0.0001 | (1.56, 3.57) | 0.94 | 0.16 | 0.70 | (0.60, 1.46) | 1.09 | 0.16 | 0.53 | (0.75, 1.60) |
| Daily outpatient relative value units | 0.81 | 0.07 | 0.01 | (0.65, 1.00) | 1.02 | 0.04 | 0.56 | (0.92, 1.13) | 1.05 | 0.04 | 0.23 | (0.95, 1.17) | 0.92 | 0.06 | 0.23 | (0.77, 1.09) |
DISCUSSION
This study of internal medicine attending physician workload and resident education demonstrates that higher workload among attending physicians is associated with slightly lower teaching evaluation scores from residents as well as increased risks to patient safety.
The prior literature examining relationships between workload and teaching effectiveness is largely survey‐based and reliant upon physicians' self‐reported perceptions of workload.[10, 13, 23] The present study strengthens this evidence by using multiple objective measures of workload, objective measures of patient safety, and a large sample of teaching evaluations.
An interesting finding in this study was that the number of patient dismissals per day was associated with a significant decrease in teaching scores, whereas the number of admissions per day was associated with increased teaching scores. These findings may seem contradictory, because the number of admissions and discharges both measure physician workload. However, a likely explanation for this apparent inconsistency is that on internal medicine inpatient teaching services, much of the teaching of residents occurs at the time of a patient admission as residents are presenting cases to the attending physician, exploring differential diagnoses, and discussing management plans. By contrast, a patient dismissal tends to consist mainly of patient interaction, paperwork, and phone calls by the resident with less input required from the attending physician. Our findings suggest that although patient admissions remain a rich opportunity for resident education, patient dismissals may increase workload without improving teaching evaluations. As the inpatient hospital environment evolves, exploring options for nonphysician providers to assist with or complete patient dismissals may have a beneficial effect on resident education.[34] In addition, exploring more efficient teaching strategies may be beneficial in the fast‐paced inpatient learning milieu.[35]
There was a statistically significant positive association between the number of days an attending physician spent with the team and teaching evaluations. Although prior work has examined advantages and disadvantages of various resident schedules,[36, 37, 38] our results suggest scheduling models that emphasize continuity of the teaching attending and residents may be preferred to enhance teaching effectiveness. Further study would help elucidate potential implications of this finding for the scheduling of supervisory attendings to optimize education.
In this analysis, patient outcome measures were largely independent of attending physician workload, with the exception of PSIs. PSIs have been associated with longer stays in the hospital,[39, 40] which is consistent with our findings. However, mean daily admissions were also associated with PSIs. It could be expected that the more patients on a hospital service, the more PSIs will result. However, there was not a significant association between midnight census and PSIs when other variables were accounted for. Because new patient admissions are time consuming and contribute to the workload of both residents and attending physicians, it is possible that safety of the service's hospitalized patients is compromised when the team is putting time and effort toward new patients. Previous research has shown variability in PSI trends with changes in the workload environment.[41] Further studies are needed to fully explore relationships between admission volume and PSIs on teaching services.
It is worthwhile to note that attending physicians have specific responsibilities of supervision and documentation for new admissions. Although it could be argued that new admissions raise the workload for the entire team, and the higher team workload may impact teaching evaluations, previous research has demonstrated that resident burnout and well‐being, which are influenced by workload, do not impact residents' assessments of teachers.[42] In addition, metrics that could arguably be more apt to measure the workload of the team as a whole (eg, team census) did not show a significant association with patient outcomes.
This study has important limitations. First, the cohort of attending physicians, residents, and patients was from a large single institution and may not be generalizable to all settings. Second, most attending physicians in this sample were experienced teachers, so consequences of increased workload may have been managed effectively without a major impact on resident education in some cases. Third, the magnitude of change in teaching effectiveness, although statistically significant, was small and might call into question the educational significance of these findings. Fourth, although resident satisfaction does not influence teaching scores, it is possible that residents' perception of their own workload may have impacted teaching evaluations. Finally, data collection was intentionally closed at the end of the 2011 academic year because accreditation standards for resident duty hours changed again at that time.[43] Thus, these data may not directly reflect the evolving hospital learning environment but serve as a useful benchmark for future studies of workload and teaching effectiveness in the inpatient setting. Once hospitals have had sufficient time and experience with the new duty hour standards, additional studies exploring relationships between workload, teaching effectiveness, and patient outcomes may be warranted.
Limitations notwithstanding, this study shows that attending physician workload may adversely impact teaching and patient safety on internal medicine hospital services. Ongoing efforts by residency programs to optimize the learning environment should include strategies to manage the workload of supervising attendings.
Disclosures
This publication was made possible in part by Clinical and Translational Science Award grant number UL1 TR000135 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH. Authors also acknowledge support for the Mayo Clinic Department of Medicine Write‐up and Publish grant. In addition, this study was supported in part by the Mayo Clinic Internal Medicine Residency Office of Education Innovations as part of the Accreditation Council for Graduate Medical Education Educational Innovations Project. The information contained in this article was based in part on the performance package data maintained by the University HealthSystem Consortium. Copyright 2015 UHC. All rights reserved.
Teaching attending physicians must balance clinical workload and resident education simultaneously while supervising inpatient services. The workload of teaching attendings has been increasing due to many factors. As patient complexity has increased, length of stay has decreased, creating higher turnover and higher acuity of hospitalized patients.[1, 2, 3, 4, 5] The rising burden of clinical documentation has increased demands on inpatient attending physicians' time.[6] Additionally, resident duty hour restrictions have shifted the responsibility for patient care to the teaching attending.[7] These factors contribute to the perception of unsafe workloads among attending physicians[8] and could impact the ability to teach well.
Teaching effectiveness is an important facet of the graduate medical education (GME) learning environment.[9] Residents perceive that education suffers when their own workload increases,[10, 11, 12, 13, 14] and higher on‐call workload is associated with lower likelihood of participation in educational activities.[15] More contact between resident trainees and supervisory staff may improve the clinical value of inpatient rotations.[16] Program directors have expressed concern about the educational ramifications of work compression.[17, 18, 19, 20] Higher workload for attending physicians can negatively impact patient safety and quality of care,[21, 22] and perception of higher attending workload is associated with less time for teaching.[23] However, the impact of objective measures of attending physician workload on educational outcomes has not been explored. When attending physicians are responsible for increasingly complex clinical care in addition to resident education, teaching effectiveness may suffer. With growing emphasis on the educational environment's effect on healthcare quality and safety,[24] it is imperative to consider the influence of attending workload on patient care and resident education.
The combination of increasing clinical demands, fewer hours in‐house for residents, and less time for teaching has the potential to decrease attending physician teaching effectiveness. In this study, we aimed to evaluate relationships among objective measures of attending physician workload, resident perception of teaching effectiveness, and patient outcomes. We hypothesized that higher workload for attending physicians would be associated with lower ratings of teaching effectiveness and poorer outcomes for patients.
METHODS
We performed a retrospective study of attending physicians who supervised inpatient internal medicine teaching services at Mayo ClinicRochester from July 2005 through June 2011 (6 full academic years). The team structure for each service was 1 attending physician, 1 senior resident, and 3 interns. Senior residents were on call every fourth night, and interns were on call every sixth night. Up to 2 admissions per service were received during the daytime short call, and up to 5 admissions per service were received during the overnight long call. Attending physicians included all supervising physicians in appointment categories of attending/consultant, senior associate consultant, and chief medical resident at the Mayo Clinic. Maximum continuous on‐call time for residents during the study period was restricted to 30 hours continuously. The timeframe of this study was chosen to minimize variability in resident work schedules; effective July 1, 2011, duty hours for postgraduate year 1 residents were further restricted to a maximum of 16 hours in duration.[25]
Measures of Attending Physician Workload
To measure attending physician workload, we examined mean service census as reported at midnight, mean patient length of stay, mean number of daily admissions, and mean number of daily discharges. We also calculated mean daily outpatient relative value units (RVUs) generated as a measure of outpatient workload while the attending was supervising the inpatient service. Similar measures of workload have been used in previous research.[26] Attending physicians in this study functioned as hospitalists during their time supervising the teaching services; that is, they were not routinely assigned to any outpatient responsibilities. The only way for an outpatient RVU to be generated during their time supervising the hospital service was for the attending physician to specifically request to see an outpatient in the clinic. Attending physicians only supervised 1 teaching service at a time and had no concurrent nonteaching service obligations. Admissions were received on a rotating basis. Because patient illness severity may impact workload, we also examined mean expected mortality (per 1000 patients) for all patients on the attending physicians' hospital services.[27]
The above workload variables were measured in the specific timeframe that corresponded to the number of days an attending physician was supervising a particular team; for example, mean census was the mean number of patients on the attending physician's hospital service during his or her time supervising that resident team.
Teaching Effectiveness Outcome Measures
Teaching effectiveness was measured using residents' evaluations of their attending physicians with a 5‐point scale (1 = needs improvement, 3 = average, 5 = top 10% of attending physicians) that has been previously validated in similar contexts.[28, 29, 30, 31, 32] The evaluation questions are shown in Supporting Information, Appendix A, in the online version of this article.
Patient Outcome Measures
Patient outcomes included applicable patient safety indicators (PSIs) as defined by the Agency for Healthcare Research and Quality[33] (see Supporting Information, Appendix B, in the online version of this article), patient transfers to the intensive care unit (ICU), calls to the rapid response team/cardiopulmonary resuscitation team, and patient deaths. Each indicator and event was summarized as occurred or did not occur at the service‐team level. For example, for a particular attendingresident team, the occurrence of each of these events at any point during the time they worked together was recorded as occurred (1) or did not occur (0). Similar measures of patient outcomes have been used in previous research.[32]
Statistical Analysis
Mixed linear models with variance components covariance structure (including random effects to account for repeated ratings by residents and of faculty) were fit using restricted maximum likelihood to examine associations of attending workload and demographics with teaching scores. Generalized linear regression models, estimated via generalized estimating equations, were used to examine associations of attending workload and demographics with patient outcomes. Due to the binary nature of the outcomes, the binomial distribution and logit link function were used, producing odds ratios (ORs) for covariates akin to those found in standard logistic regression. Multivariate models were used to adjust for physician demographics including age, gender, teaching appointment (consultant, senior associate consultant/temporary clinical appointment, or chief medical resident) and academic rank (professor, associate professor, assistant professor, instructor/none).
To account for multiple comparisons, a significance level of P < 0.01 was used. All analyses were performed using SAS statistical software (version 9.3; SAS Institute Inc., Cary, NC). This study was deemed minimal risk after review by the Mayo Clinic Institutional Review Board.
RESULTS
Over the 6‐year study period, 107 attending physicians supervised internal medicine teaching services. Twenty‐three percent of teaching attending physicians were female. Mean attending age was 42.6 years. Attendings supervised a given service for between 2 and 19 days (mean [standard deviation] = 10.1 [4.1] days). There were 542 internal medicine residents on these teaching services who completed at least 1 teaching evaluation. A total of 69,386 teaching evaluation items were submitted by these residents during the study period.
In a multivariate analysis adjusted for faculty demographics and workload measures, teaching evaluation scores were significantly higher for attending physicians who had an academic rank of professor when compared to attendings who were assistant professors ( = 0.12, P = 0.007), or instructors/no academic rank ( = 0.23, P < 0.0001). The number of days an attending physician spent with the team showed a positive association with teaching evaluations ( = +0.015, P < 0.0001).
Associations between measures of attending physician workload and teaching evaluation scores are shown in Table 1. Mean midnight census and mean number of daily discharges were associated with lower teaching evaluation scores (both = 0.026, P < 0.0001). Mean number of daily admissions was associated with higher teaching scores ( = +0.021, P = 0.001). The mean expected mortality among hospitalized patients on the services supervised by teaching attendings and the outpatient RVUs generated by these attendings during the time they were supervising the hospital service showed no association with teaching scores. The average number of RVUs generated during an attending's entire time supervising hospital service was <1.
| Attending Physician Workload Measure | Mean (SD) | Multivariate Analysis* | |||
|---|---|---|---|---|---|
| SE | 99% CI | P | |||
| |||||
| Midnight census | 8.86 (1.8) | 0.026 | 0.002 | (0.03, 0.02) | <0.0001 |
| Length of stay, d | 6.91 (3.0) | +0.006 | 0.001 | (0.002, 0.009) | <0.0001 |
| Expected mortality (per 1,000 patients) | 51.94 (27.4) | 0.0001 | 0.0001 | (0.0004, 0.0001) | 0.19 |
| Daily admissions | 2.23 (0.54) | +0.021 | 0.006 | (0.004, 0.037) | 0.001 |
| Daily discharges | 2.13 (0.56) | 0.026 | 0.006 | (0.041, 0.010) | <0.0001 |
| Daily outpatient relative value units | 0.69 (1.2) | +0.004 | 0.003 | (0.002, 0.011) | 0.10 |
Table 2 shows relationships between attending physician workload and patient outcomes for the patients on hospital services supervised by 107 attending physicians during the study period. Patient outcome data showed positive associations between measures of higher workload and PSIs. Specifically, for each 1‐patient increase in the average number of daily admissions to the attending and resident services, the cohort of patients under the team's care was 1.8 times more likely to include at least 1 patient with a PSI event (OR = 1.81, 99% confidence interval [CI]: 1.21, 2.71, P = 0.0001). Likewise, for each 1‐day increase in average length of stay, the cohort of patients under the team's care was 1.16 times more likely to have at least 1 patient with a PSI (OR = 1.16, 99% CI: 1.07, 1.26, P < 0.0001). As anticipated, mean expected mortality was associated with actual mortality, cardiopulmonary resuscitation/rapid response team calls, and ICU transfers. There were no associations between patient outcomes and workload measures of midnight census and outpatient RVUs.
| Patient Outcomes, Multivariate Analysis* | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient Safety Indicators, n = 513 | Deaths, n = 352 | CPR/RRT Calls, n = 409 | ICU Transfers, n = 737 | |||||||||||||
| Workload measures | OR | SE | P | 99% CI | OR | SE | P | 99% CI | OR | SE | P | 99% CI | OR | SE | P | 99% CI |
| ||||||||||||||||
| Midnight census | 1.10 | 0.05 | 0.04 | (0.98, 1.24) | 0.91 | 0.04 | 0.03 | (0.81, 1.02) | 0.95 | 0.04 | 0.16 | (0.86, 1.05) | 1.06 | 0.04 | 0.16 | (0.96, 1.17) |
| Length of stay | 1.16 | 0.04 | <0.0001 | (1.07, 1.26) | 1.03 | 0.03 | 0.39 | (0.95, 1.12) | 0.99 | 0.03 | 0.63 | (0.92, 1.05) | 1.10 | 0.03 | 0.0001 | (1.03, 1.18) |
| Expected mortality (per 1,000 patients) | 1.00 | 0.003 | 0.24 | (0.99, 1.01) | 1.01 | 0.00 | 0.002 | (1.00, 1.02) | 1.02 | 0.00 | <0.0001 | (1.01, 1.02) | 1.01 | 0.00 | 0.003 | (1.00, 1.01) |
| Daily admissions | 1.81 | 0.28 | 0.0001 | (1.21, 2.71) | 0.78 | 0.14 | 0.16 | (0.49, 1.24) | 1.11 | 0.20 | 0.57 | (0.69, 1.77) | 1.34 | 0.24 | 0.09 | (0.85, 2.11) |
| Daily discharges | 1.06 | 0.13 | 0.61 | (0.78, 1.45) | 2.36 | 0.38 | <0.0001 | (1.56, 3.57) | 0.94 | 0.16 | 0.70 | (0.60, 1.46) | 1.09 | 0.16 | 0.53 | (0.75, 1.60) |
| Daily outpatient relative value units | 0.81 | 0.07 | 0.01 | (0.65, 1.00) | 1.02 | 0.04 | 0.56 | (0.92, 1.13) | 1.05 | 0.04 | 0.23 | (0.95, 1.17) | 0.92 | 0.06 | 0.23 | (0.77, 1.09) |
DISCUSSION
This study of internal medicine attending physician workload and resident education demonstrates that higher workload among attending physicians is associated with slightly lower teaching evaluation scores from residents as well as increased risks to patient safety.
The prior literature examining relationships between workload and teaching effectiveness is largely survey‐based and reliant upon physicians' self‐reported perceptions of workload.[10, 13, 23] The present study strengthens this evidence by using multiple objective measures of workload, objective measures of patient safety, and a large sample of teaching evaluations.
An interesting finding in this study was that the number of patient dismissals per day was associated with a significant decrease in teaching scores, whereas the number of admissions per day was associated with increased teaching scores. These findings may seem contradictory, because the number of admissions and discharges both measure physician workload. However, a likely explanation for this apparent inconsistency is that on internal medicine inpatient teaching services, much of the teaching of residents occurs at the time of a patient admission as residents are presenting cases to the attending physician, exploring differential diagnoses, and discussing management plans. By contrast, a patient dismissal tends to consist mainly of patient interaction, paperwork, and phone calls by the resident with less input required from the attending physician. Our findings suggest that although patient admissions remain a rich opportunity for resident education, patient dismissals may increase workload without improving teaching evaluations. As the inpatient hospital environment evolves, exploring options for nonphysician providers to assist with or complete patient dismissals may have a beneficial effect on resident education.[34] In addition, exploring more efficient teaching strategies may be beneficial in the fast‐paced inpatient learning milieu.[35]
There was a statistically significant positive association between the number of days an attending physician spent with the team and teaching evaluations. Although prior work has examined advantages and disadvantages of various resident schedules,[36, 37, 38] our results suggest scheduling models that emphasize continuity of the teaching attending and residents may be preferred to enhance teaching effectiveness. Further study would help elucidate potential implications of this finding for the scheduling of supervisory attendings to optimize education.
In this analysis, patient outcome measures were largely independent of attending physician workload, with the exception of PSIs. PSIs have been associated with longer stays in the hospital,[39, 40] which is consistent with our findings. However, mean daily admissions were also associated with PSIs. It could be expected that the more patients on a hospital service, the more PSIs will result. However, there was not a significant association between midnight census and PSIs when other variables were accounted for. Because new patient admissions are time consuming and contribute to the workload of both residents and attending physicians, it is possible that safety of the service's hospitalized patients is compromised when the team is putting time and effort toward new patients. Previous research has shown variability in PSI trends with changes in the workload environment.[41] Further studies are needed to fully explore relationships between admission volume and PSIs on teaching services.
It is worthwhile to note that attending physicians have specific responsibilities of supervision and documentation for new admissions. Although it could be argued that new admissions raise the workload for the entire team, and the higher team workload may impact teaching evaluations, previous research has demonstrated that resident burnout and well‐being, which are influenced by workload, do not impact residents' assessments of teachers.[42] In addition, metrics that could arguably be more apt to measure the workload of the team as a whole (eg, team census) did not show a significant association with patient outcomes.
This study has important limitations. First, the cohort of attending physicians, residents, and patients was from a large single institution and may not be generalizable to all settings. Second, most attending physicians in this sample were experienced teachers, so consequences of increased workload may have been managed effectively without a major impact on resident education in some cases. Third, the magnitude of change in teaching effectiveness, although statistically significant, was small and might call into question the educational significance of these findings. Fourth, although resident satisfaction does not influence teaching scores, it is possible that residents' perception of their own workload may have impacted teaching evaluations. Finally, data collection was intentionally closed at the end of the 2011 academic year because accreditation standards for resident duty hours changed again at that time.[43] Thus, these data may not directly reflect the evolving hospital learning environment but serve as a useful benchmark for future studies of workload and teaching effectiveness in the inpatient setting. Once hospitals have had sufficient time and experience with the new duty hour standards, additional studies exploring relationships between workload, teaching effectiveness, and patient outcomes may be warranted.
Limitations notwithstanding, this study shows that attending physician workload may adversely impact teaching and patient safety on internal medicine hospital services. Ongoing efforts by residency programs to optimize the learning environment should include strategies to manage the workload of supervising attendings.
Disclosures
This publication was made possible in part by Clinical and Translational Science Award grant number UL1 TR000135 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH. Authors also acknowledge support for the Mayo Clinic Department of Medicine Write‐up and Publish grant. In addition, this study was supported in part by the Mayo Clinic Internal Medicine Residency Office of Education Innovations as part of the Accreditation Council for Graduate Medical Education Educational Innovations Project. The information contained in this article was based in part on the performance package data maintained by the University HealthSystem Consortium. Copyright 2015 UHC. All rights reserved.
- , , . The future of residents' education in internal medicine. Am J Med. 2004;116(9):648–650.
- , , , , . Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine. Ann Intern Med. 2006;144(12):920–926.
- , , . Residency training in the modern era: the pipe dream of less time to learn more, care better, and be more professional. Arch Intern Med. 2005;165(22):2561–2562.
- , , , et al. Trends in Hospitalizations Among Medicare Survivors of Aortic Valve Replacement in the United States From 1999 to 2010. Ann Thorac Surg. 2015;99(2):509–517.
- , , . Restructuring an inpatient resident service to improve outcomes for residents, students, and patients. Acad Med. 2011;86(12):1500–1507.
- , , , . Clinical documentation in the 21st century: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;162(4):301–303.
- , . Effect of ACGME duty hours on attending physician teaching and satisfaction. Arch Intern Med. 2008;168(11):1226–1228.
- , , , , . Identifying potential predictors of a safe attending physician workload: a survey of hospitalists. J Hosp Med. 2013;8(11):644–646.
- , , . The clinical learning environment: the foundation of graduate medical education. JAMA. 2013;309(16):1687–1688.
- , , , , , . Better rested, but more stressed? Evidence of the effects of resident work hour restrictions. Acad Pediatr. 2012;12(4):335–343.
- , , , . Multifaceted longitudinal study of surgical resident education, quality of life, and patient care before and after July 2011. J Surg Educ. 2013;70(6):769–776.
- , , . Impact of the new 16‐hour duty period on pediatric interns' neonatal education. Clin Pediatr (Phila). 2014;53(1):51–59.
- , , , , , . Relationship between resident workload and self‐perceived learning on inpatient medicine wards: a longitudinal study. BMC Med Educ. 2006;6:35.
- , , , . Perceptions of educational experience and inpatient workload among pediatric residents. Hosp Pediatr. 2013;3(3):276–284.
- , , , et al. Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities. JAMA. 2008;300(10):1146–1153.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
- , , , , . Approval and perceived impact of duty hour regulations: survey of pediatric program directors. Pediatrics. 2013;132(5):819–824.
- , , , et al. Anticipated consequences of the 2011 duty hours standards: views of internal medicine and surgery program directors. Acad Med. 2012;87(7):895–903.
- , , , , . Training on the clock: family medicine residency directors' responses to resident duty hours reform. Acad Med. 2006;81(12):1032–1037.
- , , , et al. Duty hour recommendations and implications for meeting the ACGME core competencies: views of residency directors. Mayo Clin Proc. 2011;86(3):185–191.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–973.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. No time for teaching? Inpatient attending physicians' workload and teaching before and after the implementation of the 2003 duty hours regulations. Acad Med. 2013;88(9):1293–1298.
- Accreditation Council for Graduate Medical Education. Clinical Learning Environment Review (CLER) Program. Available at: http://www.acgme.org/acgmeweb/tabid/436/ProgramandInstitutionalAccreditation/NextAccreditationSystem/ClinicalLearningEnvironmentReviewProgram.aspx. Accessed April 27, 2015.
- Accreditation Council for Graduate Medical Education. Frequently Asked Questions: A ACGME common duty hour requirements. Available at: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh‐faqs 2011.pdf. Accessed April 27, 2015.
- , , , , . Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. 2014;174(5):786–793.
- University HealthSystem Consortium. UHC clinical database/resource manager for Mayo Clinic. Available at: http://www.uhc.edu. Data accessed August 25, 2011.
- , . The interpersonal, cognitive and efficiency domains of clinical teaching: construct validity of a multi‐dimensional scale. Med Educ. 2005;39(12):1221–1229.
- , , . Factor instability of clinical teaching assessment scores among general internists and cardiologists. Med Educ. 2006;40(12):1209–1216.
- , , , . Determining reliability of clinical assessment scores in real time. Teach Learn Med. 2009;21(3):188–194.
- , , , , , . Behaviors of highly professional resident physicians. JAMA. 2008;300(11):1326–1333.
- , , , et al. Service census caps and unit‐based admissions: resident workload, conference attendance, duty hour compliance, and patient safety. Mayo Clin Proc. 2012;87(4):320–327.
- Agency for Healthcare Research and Quality. Patient safety indicators technical specifications updates—Version 5.0, March 2015. Available at: http://www.qualityindicators.ahrq.gov/Modules/PSI_TechSpec.aspx. Accessed May 29, 2015.
- , , , , , . The impact of nonphysician clinicians: do they improve the quality and cost‐effectiveness of health care services? Med Care Res Rev. 2009;66(6 suppl):36S–89S.
- , , . Maximizing teaching on the wards: review and application of the One‐Minute Preceptor and SNAPPS models. J Hosp Med. 2015;10(2):125–130.
- , , , . Resident perceptions of the educational value of night float rotations. Teach Learn Med. 2010;22(3):196–201.
- , , , , , . An evaluation of internal medicine residency continuity clinic redesign to a 50/50 outpatient‐inpatient model. J Gen Intern Med. 2013;28(8):1014–1019.
- , , , et al. Revisiting the rotating call schedule in less than 80 hours per week. J Surg Educ. 2009;66(6):357–360.
- , . Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290(14):1868–1874.
- , , , . Agency for Healthcare Research and Quality patient safety indicators and mortality in surgical patients. Am Surg. 2014;80(8):801–804.
- , , , et al. Patient safety in the era of the 80‐hour workweek. J Surg Educ. 2014;71(4):551–559.
- , , , . Impact of resident well‐being and empathy on assessments of faculty physicians. J Gen Intern Med. 2010;25(1):52–56.
- , , , et al. Stress management training for surgeons‐a randomized, controlled, intervention study. Ann Surg. 2011;253(3):488–494.
- , , . The future of residents' education in internal medicine. Am J Med. 2004;116(9):648–650.
- , , , , . Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine. Ann Intern Med. 2006;144(12):920–926.
- , , . Residency training in the modern era: the pipe dream of less time to learn more, care better, and be more professional. Arch Intern Med. 2005;165(22):2561–2562.
- , , , et al. Trends in Hospitalizations Among Medicare Survivors of Aortic Valve Replacement in the United States From 1999 to 2010. Ann Thorac Surg. 2015;99(2):509–517.
- , , . Restructuring an inpatient resident service to improve outcomes for residents, students, and patients. Acad Med. 2011;86(12):1500–1507.
- , , , . Clinical documentation in the 21st century: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;162(4):301–303.
- , . Effect of ACGME duty hours on attending physician teaching and satisfaction. Arch Intern Med. 2008;168(11):1226–1228.
- , , , , . Identifying potential predictors of a safe attending physician workload: a survey of hospitalists. J Hosp Med. 2013;8(11):644–646.
- , , . The clinical learning environment: the foundation of graduate medical education. JAMA. 2013;309(16):1687–1688.
- , , , , , . Better rested, but more stressed? Evidence of the effects of resident work hour restrictions. Acad Pediatr. 2012;12(4):335–343.
- , , , . Multifaceted longitudinal study of surgical resident education, quality of life, and patient care before and after July 2011. J Surg Educ. 2013;70(6):769–776.
- , , . Impact of the new 16‐hour duty period on pediatric interns' neonatal education. Clin Pediatr (Phila). 2014;53(1):51–59.
- , , , , , . Relationship between resident workload and self‐perceived learning on inpatient medicine wards: a longitudinal study. BMC Med Educ. 2006;6:35.
- , , , . Perceptions of educational experience and inpatient workload among pediatric residents. Hosp Pediatr. 2013;3(3):276–284.
- , , , et al. Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities. JAMA. 2008;300(10):1146–1153.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
- , , , , . Approval and perceived impact of duty hour regulations: survey of pediatric program directors. Pediatrics. 2013;132(5):819–824.
- , , , et al. Anticipated consequences of the 2011 duty hours standards: views of internal medicine and surgery program directors. Acad Med. 2012;87(7):895–903.
- , , , , . Training on the clock: family medicine residency directors' responses to resident duty hours reform. Acad Med. 2006;81(12):1032–1037.
- , , , et al. Duty hour recommendations and implications for meeting the ACGME core competencies: views of residency directors. Mayo Clin Proc. 2011;86(3):185–191.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–973.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. No time for teaching? Inpatient attending physicians' workload and teaching before and after the implementation of the 2003 duty hours regulations. Acad Med. 2013;88(9):1293–1298.
- Accreditation Council for Graduate Medical Education. Clinical Learning Environment Review (CLER) Program. Available at: http://www.acgme.org/acgmeweb/tabid/436/ProgramandInstitutionalAccreditation/NextAccreditationSystem/ClinicalLearningEnvironmentReviewProgram.aspx. Accessed April 27, 2015.
- Accreditation Council for Graduate Medical Education. Frequently Asked Questions: A ACGME common duty hour requirements. Available at: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh‐faqs 2011.pdf. Accessed April 27, 2015.
- , , , , . Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. 2014;174(5):786–793.
- University HealthSystem Consortium. UHC clinical database/resource manager for Mayo Clinic. Available at: http://www.uhc.edu. Data accessed August 25, 2011.
- , . The interpersonal, cognitive and efficiency domains of clinical teaching: construct validity of a multi‐dimensional scale. Med Educ. 2005;39(12):1221–1229.
- , , . Factor instability of clinical teaching assessment scores among general internists and cardiologists. Med Educ. 2006;40(12):1209–1216.
- , , , . Determining reliability of clinical assessment scores in real time. Teach Learn Med. 2009;21(3):188–194.
- , , , , , . Behaviors of highly professional resident physicians. JAMA. 2008;300(11):1326–1333.
- , , , et al. Service census caps and unit‐based admissions: resident workload, conference attendance, duty hour compliance, and patient safety. Mayo Clin Proc. 2012;87(4):320–327.
- Agency for Healthcare Research and Quality. Patient safety indicators technical specifications updates—Version 5.0, March 2015. Available at: http://www.qualityindicators.ahrq.gov/Modules/PSI_TechSpec.aspx. Accessed May 29, 2015.
- , , , , , . The impact of nonphysician clinicians: do they improve the quality and cost‐effectiveness of health care services? Med Care Res Rev. 2009;66(6 suppl):36S–89S.
- , , . Maximizing teaching on the wards: review and application of the One‐Minute Preceptor and SNAPPS models. J Hosp Med. 2015;10(2):125–130.
- , , , . Resident perceptions of the educational value of night float rotations. Teach Learn Med. 2010;22(3):196–201.
- , , , , , . An evaluation of internal medicine residency continuity clinic redesign to a 50/50 outpatient‐inpatient model. J Gen Intern Med. 2013;28(8):1014–1019.
- , , , et al. Revisiting the rotating call schedule in less than 80 hours per week. J Surg Educ. 2009;66(6):357–360.
- , . Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290(14):1868–1874.
- , , , . Agency for Healthcare Research and Quality patient safety indicators and mortality in surgical patients. Am Surg. 2014;80(8):801–804.
- , , , et al. Patient safety in the era of the 80‐hour workweek. J Surg Educ. 2014;71(4):551–559.
- , , , . Impact of resident well‐being and empathy on assessments of faculty physicians. J Gen Intern Med. 2010;25(1):52–56.
- , , , et al. Stress management training for surgeons‐a randomized, controlled, intervention study. Ann Surg. 2011;253(3):488–494.
© 2016 Society of Hospital Medicine




