User login
Stem cells can help form blood vessels

A novel technique can jump-start the creation of blood vessels, researchers have reported in Nature Biotechnology.
The team used human embryonic stem cells (hESCs) and induced pluripotent stem cells (hiPSCs) to create endothelial colony-forming cells (ECFCs).
These lab-generated ECFCs successfully produced human blood vessels in mice and restored blood flow to damaged retinas and limbs, without posing a risk of teratoma formation.
ECFCs can lose their ability to proliferate into new blood vessels as patients age or develop diseases such as peripheral arterial disease, said Mervin C. Yoder Jr, MD, of the Indiana University School of Medicine in Indianapolis.
He and his colleagues theorized that injecting patients with “younger,” more “enthusiastic” ECFCs might jump-start the process of creating new blood vessels. Such cells are difficult to find in adults but are common in umbilical cord blood.
With that in mind, the researchers developed a novel method to mature hiPSCs or hESCs into cells with the characteristics of ECFCs found in cord blood.
Both hiPSC-ECFCs and hESC-ECFCs exhibited properties of cord blood-derived ECFCs, including a homogenous monolayer with a cobblestone appearance and high clonal proliferative potential.
In addition, hiPSC-ECFCs and hESC-ECFCs formed capillary structures when cultured on Matrigel, and they generated in vivo inosculated vessels when implanted in immune-deficient mice.
In other murine experiments, hiPSC-ECFCs contributed to vascular repair of experimentally induced ischemic limbs and injured retinas. The cells’ effects were similar to those observed with cord blood-derived ECFCs and superior to effects observed with endothelial cells isolated using other published protocols.
Furthermore, hiPSC-ECFCs did not transition to nonendothelial cells over prolonged culture, and they could expand to more than 1 trillion endothelial cells in less than 3 months.
“This is one of the first studies using induced pluripotent stem cells that has been able to produce new cells in clinically relevant numbers, enough to enable a clinical trial,” Dr Yoder said.
He added that one of the next steps for this research is reaching an agreement with a facility approved to produce cells for use in human testing. ![]()

A novel technique can jump-start the creation of blood vessels, researchers have reported in Nature Biotechnology.
The team used human embryonic stem cells (hESCs) and induced pluripotent stem cells (hiPSCs) to create endothelial colony-forming cells (ECFCs).
These lab-generated ECFCs successfully produced human blood vessels in mice and restored blood flow to damaged retinas and limbs, without posing a risk of teratoma formation.
ECFCs can lose their ability to proliferate into new blood vessels as patients age or develop diseases such as peripheral arterial disease, said Mervin C. Yoder Jr, MD, of the Indiana University School of Medicine in Indianapolis.
He and his colleagues theorized that injecting patients with “younger,” more “enthusiastic” ECFCs might jump-start the process of creating new blood vessels. Such cells are difficult to find in adults but are common in umbilical cord blood.
With that in mind, the researchers developed a novel method to mature hiPSCs or hESCs into cells with the characteristics of ECFCs found in cord blood.
Both hiPSC-ECFCs and hESC-ECFCs exhibited properties of cord blood-derived ECFCs, including a homogenous monolayer with a cobblestone appearance and high clonal proliferative potential.
In addition, hiPSC-ECFCs and hESC-ECFCs formed capillary structures when cultured on Matrigel, and they generated in vivo inosculated vessels when implanted in immune-deficient mice.
In other murine experiments, hiPSC-ECFCs contributed to vascular repair of experimentally induced ischemic limbs and injured retinas. The cells’ effects were similar to those observed with cord blood-derived ECFCs and superior to effects observed with endothelial cells isolated using other published protocols.
Furthermore, hiPSC-ECFCs did not transition to nonendothelial cells over prolonged culture, and they could expand to more than 1 trillion endothelial cells in less than 3 months.
“This is one of the first studies using induced pluripotent stem cells that has been able to produce new cells in clinically relevant numbers, enough to enable a clinical trial,” Dr Yoder said.
He added that one of the next steps for this research is reaching an agreement with a facility approved to produce cells for use in human testing. ![]()

A novel technique can jump-start the creation of blood vessels, researchers have reported in Nature Biotechnology.
The team used human embryonic stem cells (hESCs) and induced pluripotent stem cells (hiPSCs) to create endothelial colony-forming cells (ECFCs).
These lab-generated ECFCs successfully produced human blood vessels in mice and restored blood flow to damaged retinas and limbs, without posing a risk of teratoma formation.
ECFCs can lose their ability to proliferate into new blood vessels as patients age or develop diseases such as peripheral arterial disease, said Mervin C. Yoder Jr, MD, of the Indiana University School of Medicine in Indianapolis.
He and his colleagues theorized that injecting patients with “younger,” more “enthusiastic” ECFCs might jump-start the process of creating new blood vessels. Such cells are difficult to find in adults but are common in umbilical cord blood.
With that in mind, the researchers developed a novel method to mature hiPSCs or hESCs into cells with the characteristics of ECFCs found in cord blood.
Both hiPSC-ECFCs and hESC-ECFCs exhibited properties of cord blood-derived ECFCs, including a homogenous monolayer with a cobblestone appearance and high clonal proliferative potential.
In addition, hiPSC-ECFCs and hESC-ECFCs formed capillary structures when cultured on Matrigel, and they generated in vivo inosculated vessels when implanted in immune-deficient mice.
In other murine experiments, hiPSC-ECFCs contributed to vascular repair of experimentally induced ischemic limbs and injured retinas. The cells’ effects were similar to those observed with cord blood-derived ECFCs and superior to effects observed with endothelial cells isolated using other published protocols.
Furthermore, hiPSC-ECFCs did not transition to nonendothelial cells over prolonged culture, and they could expand to more than 1 trillion endothelial cells in less than 3 months.
“This is one of the first studies using induced pluripotent stem cells that has been able to produce new cells in clinically relevant numbers, enough to enable a clinical trial,” Dr Yoder said.
He added that one of the next steps for this research is reaching an agreement with a facility approved to produce cells for use in human testing. ![]()
Invention allows for precise gene control

Credit: NIGMS
A new way to control genes may provide a better understanding of cancers and aid the development of new therapies.
The key to the method is an invention called SunTag, a series of molecular hooks for hanging multiple copies of biologically active molecules onto a single protein scaffold used to target genes or other molecules.
Compared to molecules assembled without these hooks, those incorporating SunTag can greatly amplify biological activity.
SunTag was developed by researchers in the lab of Ron Vale, PhD, of the University of California, San Francisco (UCSF), and described in two papers published in Cell.
In one paper, the authors recount how they used SunTag to greatly amplify the light-emitting signal from the green fluorescent protein commonly used to label molecules within cells.
In another paper, the researchers explain how they used SunTag to supercharge a variation of a biochemical approach known as CRISPR.
CRISPR is a technique that emerged a few years ago as a way to edit DNA anywhere within the genome.
The UCSF researchers adapted CRISPR to activate genes or interfere with their activity in a reversible way without altering DNA. The team believes this capability might make previous methods for probing poorly understood cellular functions obsolete.
“With these techniques, we can fine-tune the activity of genes within cells, and this has broad implications for the reprogramming of cells,” said Jonathan Weissman, PhD, also of UCSF.
Scientists previously reported ways to activate or interfere with genes using CRISPR, but Dr Vale said these methods were inefficient, especially for activating genes.
“It depends on the gene, but this new approach appears to amplify gene-switching by as much as 50-fold,” he said. “It’s a much more robust way of activating genes.”
CRISPR with SunTag sheds light on cancers
CRISPR is a natural system that bacteria use to defend themselves against viruses. The basis for CRISPR applications in the lab is a protein called Cas9, a chassis into which scientists can insert any specific RNA partner molecule.
The selected RNA serves as an adaptor that determines the target anywhere within the genome. The researchers attached SunTag to this chassis, enabling one Cas9 to recruit many copies of a protein to a specific DNA sequence.
The adaptation of SunTag for CRISPR activation makes it possible to systematically probe the biological roles of all genes within the genome in a single experiment, the team said.
They used CRISPR activation to identify a number of tumor suppressor genes that inhibit the growth of cancer cells. In future studies, they plan to use CRISPR activation to reveal mechanisms by which cancer cells develop resistance to anticancer drugs, a process that typically involves gene activation.
Will RNA interference become obsolete?
CRISPR interference has the potential to render RNA interference obsolete, according to Dr Weissman.
Unlike conventional RNA interference techniques, CRISPR interference allows any number of individual genes to be silenced at the same time. In addition, there is little risk of turning off untargeted genes the way RNA interference techniques do.
RNA interference blocks the messenger RNA that drives protein protection based on the blueprint contained within a gene’s DNA sequence. By preventing protein production, RNA interference may be used to get around the problem of difficult-to-target proteins, a frequent challenge in drug development.
But CRISPR interference acts one step earlier in the cell’s protein-manufacturing process.
“The horse has already left the barn with RNA interference, in the sense that the RNA message already has been transcribed from DNA,” Dr Weissman said. “With CRISPR interference, we can prevent the message from being written.” ![]()

Credit: NIGMS
A new way to control genes may provide a better understanding of cancers and aid the development of new therapies.
The key to the method is an invention called SunTag, a series of molecular hooks for hanging multiple copies of biologically active molecules onto a single protein scaffold used to target genes or other molecules.
Compared to molecules assembled without these hooks, those incorporating SunTag can greatly amplify biological activity.
SunTag was developed by researchers in the lab of Ron Vale, PhD, of the University of California, San Francisco (UCSF), and described in two papers published in Cell.
In one paper, the authors recount how they used SunTag to greatly amplify the light-emitting signal from the green fluorescent protein commonly used to label molecules within cells.
In another paper, the researchers explain how they used SunTag to supercharge a variation of a biochemical approach known as CRISPR.
CRISPR is a technique that emerged a few years ago as a way to edit DNA anywhere within the genome.
The UCSF researchers adapted CRISPR to activate genes or interfere with their activity in a reversible way without altering DNA. The team believes this capability might make previous methods for probing poorly understood cellular functions obsolete.
“With these techniques, we can fine-tune the activity of genes within cells, and this has broad implications for the reprogramming of cells,” said Jonathan Weissman, PhD, also of UCSF.
Scientists previously reported ways to activate or interfere with genes using CRISPR, but Dr Vale said these methods were inefficient, especially for activating genes.
“It depends on the gene, but this new approach appears to amplify gene-switching by as much as 50-fold,” he said. “It’s a much more robust way of activating genes.”
CRISPR with SunTag sheds light on cancers
CRISPR is a natural system that bacteria use to defend themselves against viruses. The basis for CRISPR applications in the lab is a protein called Cas9, a chassis into which scientists can insert any specific RNA partner molecule.
The selected RNA serves as an adaptor that determines the target anywhere within the genome. The researchers attached SunTag to this chassis, enabling one Cas9 to recruit many copies of a protein to a specific DNA sequence.
The adaptation of SunTag for CRISPR activation makes it possible to systematically probe the biological roles of all genes within the genome in a single experiment, the team said.
They used CRISPR activation to identify a number of tumor suppressor genes that inhibit the growth of cancer cells. In future studies, they plan to use CRISPR activation to reveal mechanisms by which cancer cells develop resistance to anticancer drugs, a process that typically involves gene activation.
Will RNA interference become obsolete?
CRISPR interference has the potential to render RNA interference obsolete, according to Dr Weissman.
Unlike conventional RNA interference techniques, CRISPR interference allows any number of individual genes to be silenced at the same time. In addition, there is little risk of turning off untargeted genes the way RNA interference techniques do.
RNA interference blocks the messenger RNA that drives protein protection based on the blueprint contained within a gene’s DNA sequence. By preventing protein production, RNA interference may be used to get around the problem of difficult-to-target proteins, a frequent challenge in drug development.
But CRISPR interference acts one step earlier in the cell’s protein-manufacturing process.
“The horse has already left the barn with RNA interference, in the sense that the RNA message already has been transcribed from DNA,” Dr Weissman said. “With CRISPR interference, we can prevent the message from being written.” ![]()

Credit: NIGMS
A new way to control genes may provide a better understanding of cancers and aid the development of new therapies.
The key to the method is an invention called SunTag, a series of molecular hooks for hanging multiple copies of biologically active molecules onto a single protein scaffold used to target genes or other molecules.
Compared to molecules assembled without these hooks, those incorporating SunTag can greatly amplify biological activity.
SunTag was developed by researchers in the lab of Ron Vale, PhD, of the University of California, San Francisco (UCSF), and described in two papers published in Cell.
In one paper, the authors recount how they used SunTag to greatly amplify the light-emitting signal from the green fluorescent protein commonly used to label molecules within cells.
In another paper, the researchers explain how they used SunTag to supercharge a variation of a biochemical approach known as CRISPR.
CRISPR is a technique that emerged a few years ago as a way to edit DNA anywhere within the genome.
The UCSF researchers adapted CRISPR to activate genes or interfere with their activity in a reversible way without altering DNA. The team believes this capability might make previous methods for probing poorly understood cellular functions obsolete.
“With these techniques, we can fine-tune the activity of genes within cells, and this has broad implications for the reprogramming of cells,” said Jonathan Weissman, PhD, also of UCSF.
Scientists previously reported ways to activate or interfere with genes using CRISPR, but Dr Vale said these methods were inefficient, especially for activating genes.
“It depends on the gene, but this new approach appears to amplify gene-switching by as much as 50-fold,” he said. “It’s a much more robust way of activating genes.”
CRISPR with SunTag sheds light on cancers
CRISPR is a natural system that bacteria use to defend themselves against viruses. The basis for CRISPR applications in the lab is a protein called Cas9, a chassis into which scientists can insert any specific RNA partner molecule.
The selected RNA serves as an adaptor that determines the target anywhere within the genome. The researchers attached SunTag to this chassis, enabling one Cas9 to recruit many copies of a protein to a specific DNA sequence.
The adaptation of SunTag for CRISPR activation makes it possible to systematically probe the biological roles of all genes within the genome in a single experiment, the team said.
They used CRISPR activation to identify a number of tumor suppressor genes that inhibit the growth of cancer cells. In future studies, they plan to use CRISPR activation to reveal mechanisms by which cancer cells develop resistance to anticancer drugs, a process that typically involves gene activation.
Will RNA interference become obsolete?
CRISPR interference has the potential to render RNA interference obsolete, according to Dr Weissman.
Unlike conventional RNA interference techniques, CRISPR interference allows any number of individual genes to be silenced at the same time. In addition, there is little risk of turning off untargeted genes the way RNA interference techniques do.
RNA interference blocks the messenger RNA that drives protein protection based on the blueprint contained within a gene’s DNA sequence. By preventing protein production, RNA interference may be used to get around the problem of difficult-to-target proteins, a frequent challenge in drug development.
But CRISPR interference acts one step earlier in the cell’s protein-manufacturing process.
“The horse has already left the barn with RNA interference, in the sense that the RNA message already has been transcribed from DNA,” Dr Weissman said. “With CRISPR interference, we can prevent the message from being written.” ![]()
‘Nano-cocoons’ offer targeted drug delivery

Photo courtesy of the Gu lab
Biomedical engineers have developed a drug delivery system in which cancer cells are “tricked” into absorbing nanoscale “cocoons” before
they unleash anticancer drugs.
Each cocoon is made of a deoxyribonuclease (DNase)-degradable DNA nanoclew embedded with an acid-responsive DNase I nanocapsule.
A cancer cell’s acidic environment prompts the DNase to degrade the cocoon and release the drug encapsulated in the endolysosomal compartment.
The engineers described the creation of these nano-cocoons and in vitro experiments testing the delivery of doxorubicin in the Journal of the American Chemical Society.
“This drug delivery system is DNA-based, which means it is biocompatible and less toxic to patients than systems that use synthetic materials,” said study author Zhen Gu, PhD, of the University of North Carolina Chapel Hill.
“This technique also specifically targets cancer cells, can carry a large drug load, and releases the drugs very quickly once inside the cancer cell.”
“In addition, because we used self-assembling DNA techniques, it is relatively easy to manufacture,” added Wujin Sun, a PhD student in Dr Gu’s lab.
Each nano-cocoon is made of a single strand of DNA that self-assembles into a structure measuring 150 nanometers across.
The core of the nano-cocoon contains the anticancer drug doxorubicin and DNase. The DNase, an enzyme that would normally dismantle the DNA cocoon, is contained by a thin polymer coating.
The surface of the nano-cocoon is studded with folic acid ligands. When the nano-cocoon encounters a cancer cell, the ligands bind the nano-cocoon to receptors on the surface of the cell, causing the cell to engulf the nano-cocoon.
Once the cocoon is inside the cancer cell, the cell’s acidic environment destroys the polymer sheath containing the DNase. The DNase then slices through the DNA cocoon, spilling doxorubicin into the cancer cell and killing it.
“We’re preparing to launch preclinical testing now,” Dr Gu said. “We’re very excited about this system and think it holds promise for delivering a variety of drugs targeting cancer and other diseases.” ![]()

Photo courtesy of the Gu lab
Biomedical engineers have developed a drug delivery system in which cancer cells are “tricked” into absorbing nanoscale “cocoons” before
they unleash anticancer drugs.
Each cocoon is made of a deoxyribonuclease (DNase)-degradable DNA nanoclew embedded with an acid-responsive DNase I nanocapsule.
A cancer cell’s acidic environment prompts the DNase to degrade the cocoon and release the drug encapsulated in the endolysosomal compartment.
The engineers described the creation of these nano-cocoons and in vitro experiments testing the delivery of doxorubicin in the Journal of the American Chemical Society.
“This drug delivery system is DNA-based, which means it is biocompatible and less toxic to patients than systems that use synthetic materials,” said study author Zhen Gu, PhD, of the University of North Carolina Chapel Hill.
“This technique also specifically targets cancer cells, can carry a large drug load, and releases the drugs very quickly once inside the cancer cell.”
“In addition, because we used self-assembling DNA techniques, it is relatively easy to manufacture,” added Wujin Sun, a PhD student in Dr Gu’s lab.
Each nano-cocoon is made of a single strand of DNA that self-assembles into a structure measuring 150 nanometers across.
The core of the nano-cocoon contains the anticancer drug doxorubicin and DNase. The DNase, an enzyme that would normally dismantle the DNA cocoon, is contained by a thin polymer coating.
The surface of the nano-cocoon is studded with folic acid ligands. When the nano-cocoon encounters a cancer cell, the ligands bind the nano-cocoon to receptors on the surface of the cell, causing the cell to engulf the nano-cocoon.
Once the cocoon is inside the cancer cell, the cell’s acidic environment destroys the polymer sheath containing the DNase. The DNase then slices through the DNA cocoon, spilling doxorubicin into the cancer cell and killing it.
“We’re preparing to launch preclinical testing now,” Dr Gu said. “We’re very excited about this system and think it holds promise for delivering a variety of drugs targeting cancer and other diseases.” ![]()

Photo courtesy of the Gu lab
Biomedical engineers have developed a drug delivery system in which cancer cells are “tricked” into absorbing nanoscale “cocoons” before
they unleash anticancer drugs.
Each cocoon is made of a deoxyribonuclease (DNase)-degradable DNA nanoclew embedded with an acid-responsive DNase I nanocapsule.
A cancer cell’s acidic environment prompts the DNase to degrade the cocoon and release the drug encapsulated in the endolysosomal compartment.
The engineers described the creation of these nano-cocoons and in vitro experiments testing the delivery of doxorubicin in the Journal of the American Chemical Society.
“This drug delivery system is DNA-based, which means it is biocompatible and less toxic to patients than systems that use synthetic materials,” said study author Zhen Gu, PhD, of the University of North Carolina Chapel Hill.
“This technique also specifically targets cancer cells, can carry a large drug load, and releases the drugs very quickly once inside the cancer cell.”
“In addition, because we used self-assembling DNA techniques, it is relatively easy to manufacture,” added Wujin Sun, a PhD student in Dr Gu’s lab.
Each nano-cocoon is made of a single strand of DNA that self-assembles into a structure measuring 150 nanometers across.
The core of the nano-cocoon contains the anticancer drug doxorubicin and DNase. The DNase, an enzyme that would normally dismantle the DNA cocoon, is contained by a thin polymer coating.
The surface of the nano-cocoon is studded with folic acid ligands. When the nano-cocoon encounters a cancer cell, the ligands bind the nano-cocoon to receptors on the surface of the cell, causing the cell to engulf the nano-cocoon.
Once the cocoon is inside the cancer cell, the cell’s acidic environment destroys the polymer sheath containing the DNase. The DNase then slices through the DNA cocoon, spilling doxorubicin into the cancer cell and killing it.
“We’re preparing to launch preclinical testing now,” Dr Gu said. “We’re very excited about this system and think it holds promise for delivering a variety of drugs targeting cancer and other diseases.” ![]()
CAR T cells can produce durable remissions

Credit: Penn Medicine
In a small study, 90% of children and adults with relapsed or refractory acute lymphoblastic leukemia (ALL) achieved remission after receiving CTL019, a chimeric antigen receptor (CAR) T-cell therapy.
Seven of these 27 patients ultimately relapsed, and 5 went on to receive additional therapy, including stem cell transplant.
Still, 15 of these heavily pretreated patients remained in remission at a median of 7 months of follow-up and did not require further treatment.
“[Patients] had relapsed as many as 4 times, including 60% whose cancers came back even after stem cell transplants,” said Stephan Grupp, MD, PhD, of the Children’s Hospital of Philadelphia in Pennsylvania.
“Their cancers were so aggressive they had no treatment options left. The durable responses we have observed with CTL019 therapy are unprecedented.”
Dr Grupp and his colleagues reported these results in NEJM. The new data build on preliminary findings presented at the 2013 ASH Annual Meeting and the 2012 ASH Annual Meeting.
CTL019 cells are a patient’s own T cells genetically engineered to express an anti-CD19 scFv coupled to CD3ζ signaling and 4-1BB co-stimulatory domains. The cells are activated and expanded ex vivo with anti-CD3 and anti-CD28 beads, then infused into patients.
In all, 30 patients received CTL019, including 25 children and young adults (ages 5 to 22) and 5 adults (ages 26 to 60). Three patients had primary refractory disease, 5 had relapsed once, and 22 patients had relapsed 2 or more times. Eighteen patients had received an allogeneic stem cell transplant.
Twenty-seven patients achieved a complete remission after an infusion of CTL019. Nineteen patients remain in remission, 15 of whom received CTL019 alone. Follow-up ranged from 1.4 months to 24 months.
Tests in patients who experienced complete remissions showed that their normal B cells had been eliminated along with their tumors. The researchers noted that persistent absence of normal B cells following CTL019 treatment indicates continued activity of the CAR T cells.
“Our results support that CTL019 can produce long-lasting remissions for certain heavily pretreated ALL patients without further therapy,” said Noelle Frey, MD, of the University of Pennsylvania in Philadelphia.
However, 5 patients did seek additional therapy, 3 of whom proceeded to allogeneic stem cell transplants while in remission.
Seven patients relapsed, between 6 weeks and 8.5 months after their infusions, including 3 whose cancers returned as CD19-negative leukemia that would not have been targeted by CTL019.
At 6 months, the overall survival rate was 78%, and the event-free survival rate was 67%.
All of the patients experienced cytokine release syndrome (CRS) within a few days of receiving CTL019, but they all fully recovered.
Twenty-two patients experienced mild to moderate CRS, which included varying degrees of flu-like symptoms, with high fevers, nausea, and muscle pain. Eight patients developed severe CRS, which required treatment for low blood pressure and breathing difficulties.
Nine patients were treated with tocilizumab, an immunosuppressant that inhibits the effects of the inflammatory cytokine IL-6, which have been found to spike during the most robust phase of the CAR T cells’ expansion in the body. Six patients also received short courses of steroids to combat CRS symptoms.
CTL019 was invented at The University of Pennsylvania but has been licensed to Novartis. In July, the US Food and Drug Administration granted CTL019 breakthrough therapy designation for the treatment of relapsed and refractory adult and pediatric ALL.
The first multicenter trial of CTL019 recently opened in the US, and additional multisite trials are expected to begin by the end of the year. ![]()

Credit: Penn Medicine
In a small study, 90% of children and adults with relapsed or refractory acute lymphoblastic leukemia (ALL) achieved remission after receiving CTL019, a chimeric antigen receptor (CAR) T-cell therapy.
Seven of these 27 patients ultimately relapsed, and 5 went on to receive additional therapy, including stem cell transplant.
Still, 15 of these heavily pretreated patients remained in remission at a median of 7 months of follow-up and did not require further treatment.
“[Patients] had relapsed as many as 4 times, including 60% whose cancers came back even after stem cell transplants,” said Stephan Grupp, MD, PhD, of the Children’s Hospital of Philadelphia in Pennsylvania.
“Their cancers were so aggressive they had no treatment options left. The durable responses we have observed with CTL019 therapy are unprecedented.”
Dr Grupp and his colleagues reported these results in NEJM. The new data build on preliminary findings presented at the 2013 ASH Annual Meeting and the 2012 ASH Annual Meeting.
CTL019 cells are a patient’s own T cells genetically engineered to express an anti-CD19 scFv coupled to CD3ζ signaling and 4-1BB co-stimulatory domains. The cells are activated and expanded ex vivo with anti-CD3 and anti-CD28 beads, then infused into patients.
In all, 30 patients received CTL019, including 25 children and young adults (ages 5 to 22) and 5 adults (ages 26 to 60). Three patients had primary refractory disease, 5 had relapsed once, and 22 patients had relapsed 2 or more times. Eighteen patients had received an allogeneic stem cell transplant.
Twenty-seven patients achieved a complete remission after an infusion of CTL019. Nineteen patients remain in remission, 15 of whom received CTL019 alone. Follow-up ranged from 1.4 months to 24 months.
Tests in patients who experienced complete remissions showed that their normal B cells had been eliminated along with their tumors. The researchers noted that persistent absence of normal B cells following CTL019 treatment indicates continued activity of the CAR T cells.
“Our results support that CTL019 can produce long-lasting remissions for certain heavily pretreated ALL patients without further therapy,” said Noelle Frey, MD, of the University of Pennsylvania in Philadelphia.
However, 5 patients did seek additional therapy, 3 of whom proceeded to allogeneic stem cell transplants while in remission.
Seven patients relapsed, between 6 weeks and 8.5 months after their infusions, including 3 whose cancers returned as CD19-negative leukemia that would not have been targeted by CTL019.
At 6 months, the overall survival rate was 78%, and the event-free survival rate was 67%.
All of the patients experienced cytokine release syndrome (CRS) within a few days of receiving CTL019, but they all fully recovered.
Twenty-two patients experienced mild to moderate CRS, which included varying degrees of flu-like symptoms, with high fevers, nausea, and muscle pain. Eight patients developed severe CRS, which required treatment for low blood pressure and breathing difficulties.
Nine patients were treated with tocilizumab, an immunosuppressant that inhibits the effects of the inflammatory cytokine IL-6, which have been found to spike during the most robust phase of the CAR T cells’ expansion in the body. Six patients also received short courses of steroids to combat CRS symptoms.
CTL019 was invented at The University of Pennsylvania but has been licensed to Novartis. In July, the US Food and Drug Administration granted CTL019 breakthrough therapy designation for the treatment of relapsed and refractory adult and pediatric ALL.
The first multicenter trial of CTL019 recently opened in the US, and additional multisite trials are expected to begin by the end of the year. ![]()

Credit: Penn Medicine
In a small study, 90% of children and adults with relapsed or refractory acute lymphoblastic leukemia (ALL) achieved remission after receiving CTL019, a chimeric antigen receptor (CAR) T-cell therapy.
Seven of these 27 patients ultimately relapsed, and 5 went on to receive additional therapy, including stem cell transplant.
Still, 15 of these heavily pretreated patients remained in remission at a median of 7 months of follow-up and did not require further treatment.
“[Patients] had relapsed as many as 4 times, including 60% whose cancers came back even after stem cell transplants,” said Stephan Grupp, MD, PhD, of the Children’s Hospital of Philadelphia in Pennsylvania.
“Their cancers were so aggressive they had no treatment options left. The durable responses we have observed with CTL019 therapy are unprecedented.”
Dr Grupp and his colleagues reported these results in NEJM. The new data build on preliminary findings presented at the 2013 ASH Annual Meeting and the 2012 ASH Annual Meeting.
CTL019 cells are a patient’s own T cells genetically engineered to express an anti-CD19 scFv coupled to CD3ζ signaling and 4-1BB co-stimulatory domains. The cells are activated and expanded ex vivo with anti-CD3 and anti-CD28 beads, then infused into patients.
In all, 30 patients received CTL019, including 25 children and young adults (ages 5 to 22) and 5 adults (ages 26 to 60). Three patients had primary refractory disease, 5 had relapsed once, and 22 patients had relapsed 2 or more times. Eighteen patients had received an allogeneic stem cell transplant.
Twenty-seven patients achieved a complete remission after an infusion of CTL019. Nineteen patients remain in remission, 15 of whom received CTL019 alone. Follow-up ranged from 1.4 months to 24 months.
Tests in patients who experienced complete remissions showed that their normal B cells had been eliminated along with their tumors. The researchers noted that persistent absence of normal B cells following CTL019 treatment indicates continued activity of the CAR T cells.
“Our results support that CTL019 can produce long-lasting remissions for certain heavily pretreated ALL patients without further therapy,” said Noelle Frey, MD, of the University of Pennsylvania in Philadelphia.
However, 5 patients did seek additional therapy, 3 of whom proceeded to allogeneic stem cell transplants while in remission.
Seven patients relapsed, between 6 weeks and 8.5 months after their infusions, including 3 whose cancers returned as CD19-negative leukemia that would not have been targeted by CTL019.
At 6 months, the overall survival rate was 78%, and the event-free survival rate was 67%.
All of the patients experienced cytokine release syndrome (CRS) within a few days of receiving CTL019, but they all fully recovered.
Twenty-two patients experienced mild to moderate CRS, which included varying degrees of flu-like symptoms, with high fevers, nausea, and muscle pain. Eight patients developed severe CRS, which required treatment for low blood pressure and breathing difficulties.
Nine patients were treated with tocilizumab, an immunosuppressant that inhibits the effects of the inflammatory cytokine IL-6, which have been found to spike during the most robust phase of the CAR T cells’ expansion in the body. Six patients also received short courses of steroids to combat CRS symptoms.
CTL019 was invented at The University of Pennsylvania but has been licensed to Novartis. In July, the US Food and Drug Administration granted CTL019 breakthrough therapy designation for the treatment of relapsed and refractory adult and pediatric ALL.
The first multicenter trial of CTL019 recently opened in the US, and additional multisite trials are expected to begin by the end of the year. ![]()
NICE doesn’t support pomalidomide for MM

Credit: CDC
The UK’s National Institute for Health and Care Excellence (NICE) has issued a preliminary draft guidance rejecting the use of pomalidomide
(Imnovid) to treat patients with relapsed or refractory multiple myeloma (MM).
NICE said the drug’s maker, Celgene, did not provide sufficient evidence of pomalidomide’s effectiveness as compared to current treatment.
Furthermore, the drug did not offer enough of a benefit to justify its high price.
“We are disappointed not to be able to recommend pomalidomide in this preliminary guidance, but the analyses submitted by Celgene, the company that makes the drug, did not show how well the drug works compared to the other treatments available,” said Sir Andrew Dillon, NICE chief executive.
Specifically, NICE said it cannot recommend pomalidomide in combination with dexamethasone for treating relapsed and refractory MM in adults who have had at least 2 prior treatments, including lenalidomide and bortezomib, and whose disease has progressed on their last therapy.
A committee advising NICE concluded that, because of the design of the MM-003 study, the extent of the benefits associated with pomalidomide was uncertain. In addition, the MM-003 results were of limited value in comparing pomalidomide with “established practice without pomalidomide.”
The recommended dose of pomalidomide is 4 mg once daily, taken on days 1 to 21 of repeated 28-day cycles. Treatment should continue until disease progression.
The price of a pack (21 tablets) of 1 mg, 2 mg, 3 mg, or 4 mg tablets is £8884 (excluding value-added tax). Costs may vary in different settings because of negotiated procurement discounts.
The cost per quality-adjusted life-year (QALY) gained presented by Celgene was over £50,000 compared with bortezomib.
The committee heard from a clinical expert that, although there is no standard of care for people with relapsed or refractory MM, bendamustine was likely to be the most commonly used therapy in this setting in England.
When comparing pomalidomide with bendamustine plus thalidomide and dexamethasone, all costs per QALYs presented were over £70,000.
The committee was not persuaded that the estimates of the extension to life were robust, objective, or plausible based on the company’s economic modeling. It therefore concluded that pomalidomide did not fulfill the criteria for being a life-extending, end-of-life treatment.
The committee further concluded that, even if pomalidomide fulfilled these criteria, the weight that would have to be placed on the QALYs would be too high for pomalidomide to be considered a cost-effective use of National Health Service resources.
Consultees, including the manufacturer, healthcare professionals, and members of the public are now able to comment on these preliminary recommendations.
Until a final guidance is issued, National Health Service bodies should make decisions locally on the funding of specific treatments. Once NICE issues its final guidance on a technology, it replaces local recommendations. ![]()

Credit: CDC
The UK’s National Institute for Health and Care Excellence (NICE) has issued a preliminary draft guidance rejecting the use of pomalidomide
(Imnovid) to treat patients with relapsed or refractory multiple myeloma (MM).
NICE said the drug’s maker, Celgene, did not provide sufficient evidence of pomalidomide’s effectiveness as compared to current treatment.
Furthermore, the drug did not offer enough of a benefit to justify its high price.
“We are disappointed not to be able to recommend pomalidomide in this preliminary guidance, but the analyses submitted by Celgene, the company that makes the drug, did not show how well the drug works compared to the other treatments available,” said Sir Andrew Dillon, NICE chief executive.
Specifically, NICE said it cannot recommend pomalidomide in combination with dexamethasone for treating relapsed and refractory MM in adults who have had at least 2 prior treatments, including lenalidomide and bortezomib, and whose disease has progressed on their last therapy.
A committee advising NICE concluded that, because of the design of the MM-003 study, the extent of the benefits associated with pomalidomide was uncertain. In addition, the MM-003 results were of limited value in comparing pomalidomide with “established practice without pomalidomide.”
The recommended dose of pomalidomide is 4 mg once daily, taken on days 1 to 21 of repeated 28-day cycles. Treatment should continue until disease progression.
The price of a pack (21 tablets) of 1 mg, 2 mg, 3 mg, or 4 mg tablets is £8884 (excluding value-added tax). Costs may vary in different settings because of negotiated procurement discounts.
The cost per quality-adjusted life-year (QALY) gained presented by Celgene was over £50,000 compared with bortezomib.
The committee heard from a clinical expert that, although there is no standard of care for people with relapsed or refractory MM, bendamustine was likely to be the most commonly used therapy in this setting in England.
When comparing pomalidomide with bendamustine plus thalidomide and dexamethasone, all costs per QALYs presented were over £70,000.
The committee was not persuaded that the estimates of the extension to life were robust, objective, or plausible based on the company’s economic modeling. It therefore concluded that pomalidomide did not fulfill the criteria for being a life-extending, end-of-life treatment.
The committee further concluded that, even if pomalidomide fulfilled these criteria, the weight that would have to be placed on the QALYs would be too high for pomalidomide to be considered a cost-effective use of National Health Service resources.
Consultees, including the manufacturer, healthcare professionals, and members of the public are now able to comment on these preliminary recommendations.
Until a final guidance is issued, National Health Service bodies should make decisions locally on the funding of specific treatments. Once NICE issues its final guidance on a technology, it replaces local recommendations. ![]()

Credit: CDC
The UK’s National Institute for Health and Care Excellence (NICE) has issued a preliminary draft guidance rejecting the use of pomalidomide
(Imnovid) to treat patients with relapsed or refractory multiple myeloma (MM).
NICE said the drug’s maker, Celgene, did not provide sufficient evidence of pomalidomide’s effectiveness as compared to current treatment.
Furthermore, the drug did not offer enough of a benefit to justify its high price.
“We are disappointed not to be able to recommend pomalidomide in this preliminary guidance, but the analyses submitted by Celgene, the company that makes the drug, did not show how well the drug works compared to the other treatments available,” said Sir Andrew Dillon, NICE chief executive.
Specifically, NICE said it cannot recommend pomalidomide in combination with dexamethasone for treating relapsed and refractory MM in adults who have had at least 2 prior treatments, including lenalidomide and bortezomib, and whose disease has progressed on their last therapy.
A committee advising NICE concluded that, because of the design of the MM-003 study, the extent of the benefits associated with pomalidomide was uncertain. In addition, the MM-003 results were of limited value in comparing pomalidomide with “established practice without pomalidomide.”
The recommended dose of pomalidomide is 4 mg once daily, taken on days 1 to 21 of repeated 28-day cycles. Treatment should continue until disease progression.
The price of a pack (21 tablets) of 1 mg, 2 mg, 3 mg, or 4 mg tablets is £8884 (excluding value-added tax). Costs may vary in different settings because of negotiated procurement discounts.
The cost per quality-adjusted life-year (QALY) gained presented by Celgene was over £50,000 compared with bortezomib.
The committee heard from a clinical expert that, although there is no standard of care for people with relapsed or refractory MM, bendamustine was likely to be the most commonly used therapy in this setting in England.
When comparing pomalidomide with bendamustine plus thalidomide and dexamethasone, all costs per QALYs presented were over £70,000.
The committee was not persuaded that the estimates of the extension to life were robust, objective, or plausible based on the company’s economic modeling. It therefore concluded that pomalidomide did not fulfill the criteria for being a life-extending, end-of-life treatment.
The committee further concluded that, even if pomalidomide fulfilled these criteria, the weight that would have to be placed on the QALYs would be too high for pomalidomide to be considered a cost-effective use of National Health Service resources.
Consultees, including the manufacturer, healthcare professionals, and members of the public are now able to comment on these preliminary recommendations.
Until a final guidance is issued, National Health Service bodies should make decisions locally on the funding of specific treatments. Once NICE issues its final guidance on a technology, it replaces local recommendations. ![]()
Amoeba could help fight cancers

Experiments in a soil-dwelling amoeba have provided insight that could help us treat cancers characterized by PTEN mutations, researchers have reported in PLOS ONE.
The team discovered that this amoeba has two genes that function like the human tumor suppressor PTEN.
And increasing expression of one of these genes compensated for a mutation in the other gene.
If the same method works in humans with mutated PTEN, this finding could have implications for a range of cancers.
PTEN mutations are thought to be involved in nearly half of all leukemia cases, 40% of breast cancer cases, and up to 70% of prostate cancer cases.
“If you look at tumors across the board . . . , you find that PTEN is the most generally mutated gene, and, when you mutate PTEN in mice, you cause tumors,” said study author David Soll, PhD, of the University of Iowa in Iowa City.
He and his colleagues found that the amoeba Dictyostelium discoideum has the gene ptenA, which mutates similarly to the human PTEN gene and causes behavioral defects in the cell.
They also found a close relative of ptenA in the amoeba, called lpten, that performs the same functions of ptenA but to a lesser degree.
The researchers hypothesized that ramping up the presence of lpten could compensate for the mutated ptenA.
They tested this theory by placing lpten in a plasmid behind a powerful promoter designed to overexpress the gene. They then introduced the super-charged lpten into a cell with the mutated ptenA gene.
The team found that the overexpressed lpten gene fully compensated for all of the defects in the ptenA mutant.
If this method works in human cells, it could lead to a new way to treat cancers, the researchers said. They are now aiming to identify a drug that would activate the promoter for one of PTEN’s close relatives.
Once a patient is diagnosed with cancer caused by a PTEN mutation, the patient could take the drug, overexpress the PTEN replacement gene, and potentially stop cancer in its tracks, Dr Soll said.
This research has also led Dr Soll and his colleagues to study other human genes that may be able to step in for the mutated PTEN gene and perform the same tumor-suppressing role. The team is currently studying 2 close relatives of PTEN.
“And nature might have put them there just for that; that’s the curious thing,” Dr Soll said. “Somewhere, there may be a backup system, what we call ‘redundancy,’ that might be the basis for better identifying tumors and possibly creating cancer-fighting drugs. You have another gene which might be able to step in for the broken gene to keep things normal, and that’s what we’re playing with here. It’s very sophisticated.” ![]()

Experiments in a soil-dwelling amoeba have provided insight that could help us treat cancers characterized by PTEN mutations, researchers have reported in PLOS ONE.
The team discovered that this amoeba has two genes that function like the human tumor suppressor PTEN.
And increasing expression of one of these genes compensated for a mutation in the other gene.
If the same method works in humans with mutated PTEN, this finding could have implications for a range of cancers.
PTEN mutations are thought to be involved in nearly half of all leukemia cases, 40% of breast cancer cases, and up to 70% of prostate cancer cases.
“If you look at tumors across the board . . . , you find that PTEN is the most generally mutated gene, and, when you mutate PTEN in mice, you cause tumors,” said study author David Soll, PhD, of the University of Iowa in Iowa City.
He and his colleagues found that the amoeba Dictyostelium discoideum has the gene ptenA, which mutates similarly to the human PTEN gene and causes behavioral defects in the cell.
They also found a close relative of ptenA in the amoeba, called lpten, that performs the same functions of ptenA but to a lesser degree.
The researchers hypothesized that ramping up the presence of lpten could compensate for the mutated ptenA.
They tested this theory by placing lpten in a plasmid behind a powerful promoter designed to overexpress the gene. They then introduced the super-charged lpten into a cell with the mutated ptenA gene.
The team found that the overexpressed lpten gene fully compensated for all of the defects in the ptenA mutant.
If this method works in human cells, it could lead to a new way to treat cancers, the researchers said. They are now aiming to identify a drug that would activate the promoter for one of PTEN’s close relatives.
Once a patient is diagnosed with cancer caused by a PTEN mutation, the patient could take the drug, overexpress the PTEN replacement gene, and potentially stop cancer in its tracks, Dr Soll said.
This research has also led Dr Soll and his colleagues to study other human genes that may be able to step in for the mutated PTEN gene and perform the same tumor-suppressing role. The team is currently studying 2 close relatives of PTEN.
“And nature might have put them there just for that; that’s the curious thing,” Dr Soll said. “Somewhere, there may be a backup system, what we call ‘redundancy,’ that might be the basis for better identifying tumors and possibly creating cancer-fighting drugs. You have another gene which might be able to step in for the broken gene to keep things normal, and that’s what we’re playing with here. It’s very sophisticated.” ![]()

Experiments in a soil-dwelling amoeba have provided insight that could help us treat cancers characterized by PTEN mutations, researchers have reported in PLOS ONE.
The team discovered that this amoeba has two genes that function like the human tumor suppressor PTEN.
And increasing expression of one of these genes compensated for a mutation in the other gene.
If the same method works in humans with mutated PTEN, this finding could have implications for a range of cancers.
PTEN mutations are thought to be involved in nearly half of all leukemia cases, 40% of breast cancer cases, and up to 70% of prostate cancer cases.
“If you look at tumors across the board . . . , you find that PTEN is the most generally mutated gene, and, when you mutate PTEN in mice, you cause tumors,” said study author David Soll, PhD, of the University of Iowa in Iowa City.
He and his colleagues found that the amoeba Dictyostelium discoideum has the gene ptenA, which mutates similarly to the human PTEN gene and causes behavioral defects in the cell.
They also found a close relative of ptenA in the amoeba, called lpten, that performs the same functions of ptenA but to a lesser degree.
The researchers hypothesized that ramping up the presence of lpten could compensate for the mutated ptenA.
They tested this theory by placing lpten in a plasmid behind a powerful promoter designed to overexpress the gene. They then introduced the super-charged lpten into a cell with the mutated ptenA gene.
The team found that the overexpressed lpten gene fully compensated for all of the defects in the ptenA mutant.
If this method works in human cells, it could lead to a new way to treat cancers, the researchers said. They are now aiming to identify a drug that would activate the promoter for one of PTEN’s close relatives.
Once a patient is diagnosed with cancer caused by a PTEN mutation, the patient could take the drug, overexpress the PTEN replacement gene, and potentially stop cancer in its tracks, Dr Soll said.
This research has also led Dr Soll and his colleagues to study other human genes that may be able to step in for the mutated PTEN gene and perform the same tumor-suppressing role. The team is currently studying 2 close relatives of PTEN.
“And nature might have put them there just for that; that’s the curious thing,” Dr Soll said. “Somewhere, there may be a backup system, what we call ‘redundancy,’ that might be the basis for better identifying tumors and possibly creating cancer-fighting drugs. You have another gene which might be able to step in for the broken gene to keep things normal, and that’s what we’re playing with here. It’s very sophisticated.” ![]()
Malpractice reform may not reduce ‘defensive medicine’

Credit: CDC
Making it more difficult for patients to sue physicians for medical malpractice may not reduce the amount of “defensive medicine” physicians
practice, new research suggests.
Investigators studied patient records in 3 states that raised the standard for malpractice in the emergency room to gross negligence.
And they found that strong new legal protections did not significantly reduce the use of common defensive medicine practices or the cost of care.
The team detailed these findings in NEJM.
“Our findings suggest that malpractice reform may have less effect on costs than has been projected by conventional wisdom,” said lead study author Daniel A. Waxman, MD, PhD, of RAND Health in Santa Monica, California.
“Physicians say they order unnecessary tests strictly out of fear of being sued, but our results suggest the story is more complicated.”
The investigators evaluated the results of malpractice reform in 3 states—Georgia, Texas, and South Carolina.
About a decade ago, these states changed the legal malpractice standard for emergency care to gross negligence. The higher standard means plaintiffs must prove that doctors consciously disregarded the need to use reasonable care, knowing full well that their actions were likely to cause serious injury.
“These malpractice reforms have been said to provide virtual immunity against lawsuits,” Dr Waxman noted.
He and his colleagues examined 3.8 million Medicare patient records from 1166 hospital emergency departments spanning the period from 1997 to 2011. They compared care in the 3 reform states, before and after the statutes took effect, to care in neighboring states that did not pass malpractice reform.
The team assessed whether physicians ordered an advanced imaging study (CT or MRI scan), whether the patient was hospitalized after the emergency visit, and total charges for the visit.
Advanced imaging and hospitalization are among the most costly consequences of an emergency room visit, and physicians have identified them as common defensive medicine practices.
The malpractice reform laws had no effect on the use of imaging or the rate of hospitalization following emergency visits.
For 2 of the states, Texas and South Carolina, the law did not appear to cause any reduction in charges. Relative to neighboring states, Georgia saw a drop of 3.6% in average emergency room charges following its 2005 reform.
“This study suggests that, even when the risk of being sued for malpractice decreases, the path of least resistance still may favor resource-intensive care, at least in hospital emergency departments,” Dr Waxman said. ![]()

Credit: CDC
Making it more difficult for patients to sue physicians for medical malpractice may not reduce the amount of “defensive medicine” physicians
practice, new research suggests.
Investigators studied patient records in 3 states that raised the standard for malpractice in the emergency room to gross negligence.
And they found that strong new legal protections did not significantly reduce the use of common defensive medicine practices or the cost of care.
The team detailed these findings in NEJM.
“Our findings suggest that malpractice reform may have less effect on costs than has been projected by conventional wisdom,” said lead study author Daniel A. Waxman, MD, PhD, of RAND Health in Santa Monica, California.
“Physicians say they order unnecessary tests strictly out of fear of being sued, but our results suggest the story is more complicated.”
The investigators evaluated the results of malpractice reform in 3 states—Georgia, Texas, and South Carolina.
About a decade ago, these states changed the legal malpractice standard for emergency care to gross negligence. The higher standard means plaintiffs must prove that doctors consciously disregarded the need to use reasonable care, knowing full well that their actions were likely to cause serious injury.
“These malpractice reforms have been said to provide virtual immunity against lawsuits,” Dr Waxman noted.
He and his colleagues examined 3.8 million Medicare patient records from 1166 hospital emergency departments spanning the period from 1997 to 2011. They compared care in the 3 reform states, before and after the statutes took effect, to care in neighboring states that did not pass malpractice reform.
The team assessed whether physicians ordered an advanced imaging study (CT or MRI scan), whether the patient was hospitalized after the emergency visit, and total charges for the visit.
Advanced imaging and hospitalization are among the most costly consequences of an emergency room visit, and physicians have identified them as common defensive medicine practices.
The malpractice reform laws had no effect on the use of imaging or the rate of hospitalization following emergency visits.
For 2 of the states, Texas and South Carolina, the law did not appear to cause any reduction in charges. Relative to neighboring states, Georgia saw a drop of 3.6% in average emergency room charges following its 2005 reform.
“This study suggests that, even when the risk of being sued for malpractice decreases, the path of least resistance still may favor resource-intensive care, at least in hospital emergency departments,” Dr Waxman said. ![]()

Credit: CDC
Making it more difficult for patients to sue physicians for medical malpractice may not reduce the amount of “defensive medicine” physicians
practice, new research suggests.
Investigators studied patient records in 3 states that raised the standard for malpractice in the emergency room to gross negligence.
And they found that strong new legal protections did not significantly reduce the use of common defensive medicine practices or the cost of care.
The team detailed these findings in NEJM.
“Our findings suggest that malpractice reform may have less effect on costs than has been projected by conventional wisdom,” said lead study author Daniel A. Waxman, MD, PhD, of RAND Health in Santa Monica, California.
“Physicians say they order unnecessary tests strictly out of fear of being sued, but our results suggest the story is more complicated.”
The investigators evaluated the results of malpractice reform in 3 states—Georgia, Texas, and South Carolina.
About a decade ago, these states changed the legal malpractice standard for emergency care to gross negligence. The higher standard means plaintiffs must prove that doctors consciously disregarded the need to use reasonable care, knowing full well that their actions were likely to cause serious injury.
“These malpractice reforms have been said to provide virtual immunity against lawsuits,” Dr Waxman noted.
He and his colleagues examined 3.8 million Medicare patient records from 1166 hospital emergency departments spanning the period from 1997 to 2011. They compared care in the 3 reform states, before and after the statutes took effect, to care in neighboring states that did not pass malpractice reform.
The team assessed whether physicians ordered an advanced imaging study (CT or MRI scan), whether the patient was hospitalized after the emergency visit, and total charges for the visit.
Advanced imaging and hospitalization are among the most costly consequences of an emergency room visit, and physicians have identified them as common defensive medicine practices.
The malpractice reform laws had no effect on the use of imaging or the rate of hospitalization following emergency visits.
For 2 of the states, Texas and South Carolina, the law did not appear to cause any reduction in charges. Relative to neighboring states, Georgia saw a drop of 3.6% in average emergency room charges following its 2005 reform.
“This study suggests that, even when the risk of being sued for malpractice decreases, the path of least resistance still may favor resource-intensive care, at least in hospital emergency departments,” Dr Waxman said.
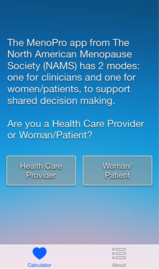
New mobile app assists clinicians in assessing menopausal patients
A new mobile app for iPhone and iPad enables both clinicians and patients to make decisions about menopausal therapies for moderate to severe hot flashes, night sweats, and/or genitourinary symptoms. The app also aids in assessing the patient’s risk of cardiovascular disease, breast cancer, and fracture.

|
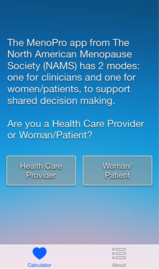
|
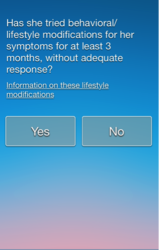
|
The MenoPro app, developed in association with the North American Menopause Society (NAMS), is available free of charge from Apple. The app is designed to aid in the assessment and management of bothersome menopausal symptoms in women aged 45 and older.
Designed for both clinician and patient
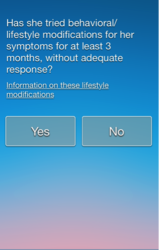
A novel feature of the app is its two modes—one for the clinician and another for the patient. The clinician mode enables risk assessment and decision-making to determine whether hormonal therapy might be indicated and to determine the formulation and dosage of the therapy selected. It also features assessment of the patient’s 10-year risk of cardiovascular disease, her risk of breast cancer using the Gail model, and her fracture risk using the FRAX tool. When hormonal therapies are not appropriate, the app steers the clinician to nonhormonal options.
The patient can make use of the app to learn about her different treatment options, including lifestyle modifications. The app guides her through a self-assessment to gauge how far along she is in the menopausal transition, the severity of her symptoms, and her interest in hormonal or nonhormonal therapy. The app begins by recommending lifestyle changes and behavioral factors that can reduce menopausal symptoms. After a 3-month trial of these modifications, the patient is prompted to visit her health-care provider if further relief is needed.
Only FDA-approved drugs are recommended
“The app is completely up to date in terms of information about the newest medications that have been approved by the US Food and Drug Administration,” says JoAnn E. Manson, MD, DrPH, current chair of the NAMS Scientific Program and a past president of NAMS. Dr. Manson is Chief of the Division of Preventive Medicine at Brigham and Women’s Hospital in Boston. She also is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health at Harvard Medical School.
“The app focuses on FDA-approved medications, including off-label use of medications that may be commonly prescribed in practice to treat hot flashes, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs),” she says.
“I think another big advantage is that very often clinicians who are managing patients during the menopausal transition or in early menopause may not be thinking that much about cardiovascular risk or even know how to evaluate it or make use of a 10-year risk score. So the app really helps them to become very familiar with the evaluation of cardiovascular risk, breast cancer risk, and fracture risk, and provides them with the resources to make use of the information.”
An algorithm is available within the app
The app is based on an algorithm that can be accessed within the app by choosing the “About” button. Another feature: the clinician can email a summary of the patient’s assessment directly to her, along with links to resources on a variety of relevant topics.
“In the future, there is a plan to have the app available for other mobile phones and tablet devices in addition to the iPhone and iPad,” says Dr. Manson. “We also hope to have it incorporated into electronic health records, where it could be used for clinical decision-making within the record.”
The app is not intended to replace clinical judgment, she adds. “I think clinicians are really familiar with the concept that, when you’re using an app, clinical judgment remains paramount. The app is not going to replace the clinician’s own discernment of what is going on with the patient.”
For detailed information, see an article on the app in the journal Menopause, available at http://www.menopause.org/docs/default-source/professional/our-new-paper.pdf
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
A new mobile app for iPhone and iPad enables both clinicians and patients to make decisions about menopausal therapies for moderate to severe hot flashes, night sweats, and/or genitourinary symptoms. The app also aids in assessing the patient’s risk of cardiovascular disease, breast cancer, and fracture.

|
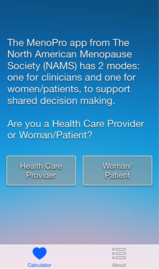
|
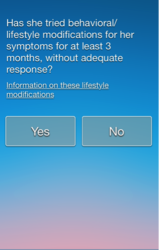
|
The MenoPro app, developed in association with the North American Menopause Society (NAMS), is available free of charge from Apple. The app is designed to aid in the assessment and management of bothersome menopausal symptoms in women aged 45 and older.
Designed for both clinician and patient
A novel feature of the app is its two modes—one for the clinician and another for the patient. The clinician mode enables risk assessment and decision-making to determine whether hormonal therapy might be indicated and to determine the formulation and dosage of the therapy selected. It also features assessment of the patient’s 10-year risk of cardiovascular disease, her risk of breast cancer using the Gail model, and her fracture risk using the FRAX tool. When hormonal therapies are not appropriate, the app steers the clinician to nonhormonal options.
The patient can make use of the app to learn about her different treatment options, including lifestyle modifications. The app guides her through a self-assessment to gauge how far along she is in the menopausal transition, the severity of her symptoms, and her interest in hormonal or nonhormonal therapy. The app begins by recommending lifestyle changes and behavioral factors that can reduce menopausal symptoms. After a 3-month trial of these modifications, the patient is prompted to visit her health-care provider if further relief is needed.
Only FDA-approved drugs are recommended
“The app is completely up to date in terms of information about the newest medications that have been approved by the US Food and Drug Administration,” says JoAnn E. Manson, MD, DrPH, current chair of the NAMS Scientific Program and a past president of NAMS. Dr. Manson is Chief of the Division of Preventive Medicine at Brigham and Women’s Hospital in Boston. She also is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health at Harvard Medical School.
“The app focuses on FDA-approved medications, including off-label use of medications that may be commonly prescribed in practice to treat hot flashes, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs),” she says.
“I think another big advantage is that very often clinicians who are managing patients during the menopausal transition or in early menopause may not be thinking that much about cardiovascular risk or even know how to evaluate it or make use of a 10-year risk score. So the app really helps them to become very familiar with the evaluation of cardiovascular risk, breast cancer risk, and fracture risk, and provides them with the resources to make use of the information.”
An algorithm is available within the app
The app is based on an algorithm that can be accessed within the app by choosing the “About” button. Another feature: the clinician can email a summary of the patient’s assessment directly to her, along with links to resources on a variety of relevant topics.
“In the future, there is a plan to have the app available for other mobile phones and tablet devices in addition to the iPhone and iPad,” says Dr. Manson. “We also hope to have it incorporated into electronic health records, where it could be used for clinical decision-making within the record.”
The app is not intended to replace clinical judgment, she adds. “I think clinicians are really familiar with the concept that, when you’re using an app, clinical judgment remains paramount. The app is not going to replace the clinician’s own discernment of what is going on with the patient.”
For detailed information, see an article on the app in the journal Menopause, available at http://www.menopause.org/docs/default-source/professional/our-new-paper.pdf
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
A new mobile app for iPhone and iPad enables both clinicians and patients to make decisions about menopausal therapies for moderate to severe hot flashes, night sweats, and/or genitourinary symptoms. The app also aids in assessing the patient’s risk of cardiovascular disease, breast cancer, and fracture.

|
|
|
The MenoPro app, developed in association with the North American Menopause Society (NAMS), is available free of charge from Apple. The app is designed to aid in the assessment and management of bothersome menopausal symptoms in women aged 45 and older.
Designed for both clinician and patient
A novel feature of the app is its two modes—one for the clinician and another for the patient. The clinician mode enables risk assessment and decision-making to determine whether hormonal therapy might be indicated and to determine the formulation and dosage of the therapy selected. It also features assessment of the patient’s 10-year risk of cardiovascular disease, her risk of breast cancer using the Gail model, and her fracture risk using the FRAX tool. When hormonal therapies are not appropriate, the app steers the clinician to nonhormonal options.
The patient can make use of the app to learn about her different treatment options, including lifestyle modifications. The app guides her through a self-assessment to gauge how far along she is in the menopausal transition, the severity of her symptoms, and her interest in hormonal or nonhormonal therapy. The app begins by recommending lifestyle changes and behavioral factors that can reduce menopausal symptoms. After a 3-month trial of these modifications, the patient is prompted to visit her health-care provider if further relief is needed.
Only FDA-approved drugs are recommended
“The app is completely up to date in terms of information about the newest medications that have been approved by the US Food and Drug Administration,” says JoAnn E. Manson, MD, DrPH, current chair of the NAMS Scientific Program and a past president of NAMS. Dr. Manson is Chief of the Division of Preventive Medicine at Brigham and Women’s Hospital in Boston. She also is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health at Harvard Medical School.
“The app focuses on FDA-approved medications, including off-label use of medications that may be commonly prescribed in practice to treat hot flashes, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs),” she says.
“I think another big advantage is that very often clinicians who are managing patients during the menopausal transition or in early menopause may not be thinking that much about cardiovascular risk or even know how to evaluate it or make use of a 10-year risk score. So the app really helps them to become very familiar with the evaluation of cardiovascular risk, breast cancer risk, and fracture risk, and provides them with the resources to make use of the information.”
An algorithm is available within the app
The app is based on an algorithm that can be accessed within the app by choosing the “About” button. Another feature: the clinician can email a summary of the patient’s assessment directly to her, along with links to resources on a variety of relevant topics.
“In the future, there is a plan to have the app available for other mobile phones and tablet devices in addition to the iPhone and iPad,” says Dr. Manson. “We also hope to have it incorporated into electronic health records, where it could be used for clinical decision-making within the record.”
The app is not intended to replace clinical judgment, she adds. “I think clinicians are really familiar with the concept that, when you’re using an app, clinical judgment remains paramount. The app is not going to replace the clinician’s own discernment of what is going on with the patient.”
For detailed information, see an article on the app in the journal Menopause, available at http://www.menopause.org/docs/default-source/professional/our-new-paper.pdf
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Positive CvLPRIT results lead ACC to change guidelines
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
On Twitter @naseemmiller
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
On Twitter @naseemmiller
BARCELONA – Heart attack patients who had complete revascularization of all blocked arteries had better outcomes than those who had only the “culprit” artery unblocked, according to results from the CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial) study.
The open label, randomized trial showed that among patients with acute ST-segment elevation myocardial infarction (STEMI), those who had stenting of significant coronary stenoses not responsible for the infarction as well as the infarct-producing lesion had a 55% reduction in major adverse cardiac events (MACE) at 1 year, compared with the group that had only the infarct-related artery treated. The results were presented at the annual congress of the European Society of Cardiology.
The positive results mirror the results of the PRAMI trial presented at last year’s ESC annual congress, and seem to be the tipping point for the American College of Cardiology to withdraw one of its Choosing Wisely recommendations, which had questioned any intervention beyond unblocking just the artery responsible for the heart attack.
“The newest findings regarding coronary revascularization are great examples of science on the move, and we are responding accordingly,” wrote ACC President Patrick T. O’Gara in a statement issued on Sept. 22, not too long after the results of CvLPRIT were presented.
Dr. Anthony Gershlick, who presented the results of CvLPRIT at ESC, also concluded that “this strategy may be needed to be considered for future STEMI guidelines committees.”
But the topic remains controversial, and not all experts agree that it’s time for a change in clinical practice.
Dr. Shamir R. Mehta of McMaster University in Hamilton, Ont., said that both the CvLPRIT and PRAMI trials are still relatively small to measure up to the results of large meta-analyses, which show that revascularization of nonculprit arteries at the time of primary percutaneous coronary intervention (PCI) could be associated with higher mortality rates.
“The important question is, was there a significant hazard with doing revascularization at a later time point, and unfortunately this trial was too small to answer that question,” Dr. Mehta said at ESC. Dr. Gershlick, of University Hospitals of Leicester NHS Trust in England, disagreed.
“One question for me was, if a clinician is presented with angiographically significant stenoses in a non–infarct-related artery, should these be treated on that admission?” said Dr. Gershlick in a press conference. He said although retrospective registry data suggest otherwise, the results of PRAMI showed a 65% reduction in MACE with total revascularization at the time of primary PCI.
For CvLPRIT, he and his colleagues randomized 296 heart attack patients to receive either revascularization of only the infarct-related artery (146 patients), or have complete revascularization at the time of primary PCI.
The primary endpoint was MACE, which is a composite of total mortality, recurrent myocardial infarction (MI), heart failure, and ischemia-driven revascularization at 12 months.
Patients were on average 65 years old and mostly male. More than 80% had stenoses of a non–infarct-related artery, and more than 70% were treated via the radial approach.
In the complete revascularization group, the non–infarct-related arteries were treated after the infarct-related artery during the same sitting or during the same hospital admission.
At 12 months, there was a 55% reduction in MACE among patients who had complete revascularization. All components of the composite endpoint also showed a decrease, although they didn’t reach significance, compared with the group that received stenting of only the infarct-related artery.
There also was a reduction in all-cause mortality, recurrent MI, heart failure, and repeat revascularization in the complete revascularization group.
In addition, there were no safety signals, Dr. Gershlick said.
The study had several limitations, including its small size, combined endpoint, and loss to follow-up.
Experts agreed that there’s a need for larger randomized trials, such as the COMPLETE trial, which is currently enrolling patients.
Dr. Gershlick and Dr. Mehta had no disclosures.
On Twitter @naseemmiller
AT THE ESC CONGRESS 2014
Key clinical point: Complete revascularization at the time of primary PCI may be considered by future STEMI guidelines committees.
Major finding: There was a 55% reduction in MACE among heart attack patients who received complete revascularization at the time of primary PCI.
Data source: An open-label, randomized trial of 296 heart attack patients.
Disclosures: Dr. Gershlick and Dr. Mehta had no disclosures.
Selling your practice
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor, and the practice would continue on as before. Occasionally that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. The buyer of a medical practice today is more likely to be an institution, such as a hospital, an HMO, or a large practice group, rather than an individual physician.
Also, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail last month. For the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation, such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, such as mine (New Jersey), the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, or merger.
Buyers, especially institutional buyers, prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave the seller with a bunch of “odd lots” to dispose of. But depending on the circumstances, an asset sale may be to the advantage of both parties.
Sellers typically prefer to sell stock because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity. I’ll cover some of the more common merger variants in a future column.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain which will be taxed (under current law) at 28%. As the saying goes, it’s not what you earn, it’s what you keep; so it may benefit the seller to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently around 40% – plus a social security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid. However, such payments may be mistaken by the Internal Revenue Service for payments for referrals, which is illegal. And there is always the problem of making certain all the payments are made.
The seller may wish to continue working at the practice as an employee, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News. Additional columns are available online at edermatologynews.com.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor, and the practice would continue on as before. Occasionally that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. The buyer of a medical practice today is more likely to be an institution, such as a hospital, an HMO, or a large practice group, rather than an individual physician.
Also, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail last month. For the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation, such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, such as mine (New Jersey), the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, or merger.
Buyers, especially institutional buyers, prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave the seller with a bunch of “odd lots” to dispose of. But depending on the circumstances, an asset sale may be to the advantage of both parties.
Sellers typically prefer to sell stock because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity. I’ll cover some of the more common merger variants in a future column.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain which will be taxed (under current law) at 28%. As the saying goes, it’s not what you earn, it’s what you keep; so it may benefit the seller to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently around 40% – plus a social security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid. However, such payments may be mistaken by the Internal Revenue Service for payments for referrals, which is illegal. And there is always the problem of making certain all the payments are made.
The seller may wish to continue working at the practice as an employee, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News. Additional columns are available online at edermatologynews.com.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor, and the practice would continue on as before. Occasionally that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. The buyer of a medical practice today is more likely to be an institution, such as a hospital, an HMO, or a large practice group, rather than an individual physician.
Also, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail last month. For the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation, such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, such as mine (New Jersey), the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, or merger.
Buyers, especially institutional buyers, prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave the seller with a bunch of “odd lots” to dispose of. But depending on the circumstances, an asset sale may be to the advantage of both parties.
Sellers typically prefer to sell stock because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity. I’ll cover some of the more common merger variants in a future column.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain which will be taxed (under current law) at 28%. As the saying goes, it’s not what you earn, it’s what you keep; so it may benefit the seller to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently around 40% – plus a social security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid. However, such payments may be mistaken by the Internal Revenue Service for payments for referrals, which is illegal. And there is always the problem of making certain all the payments are made.
The seller may wish to continue working at the practice as an employee, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News. Additional columns are available online at edermatologynews.com.



