User login
Factors Tied to Photoprotection ID'd for Organ Recipients
Article Type
Changed
Display Headline
Factors Tied to Photoprotection ID'd for Organ Recipients
Issue
Cutis - 90(2)
Publications
Page Number
4
Legacy Keywords
photoprotection, skin cancer, aging skin
Issue
Cutis - 90(2)
Issue
Cutis - 90(2)
Page Number
4
Page Number
4
Publications
Publications
Article Type
Display Headline
Factors Tied to Photoprotection ID'd for Organ Recipients
Display Headline
Factors Tied to Photoprotection ID'd for Organ Recipients
Legacy Keywords
photoprotection, skin cancer, aging skin
Legacy Keywords
photoprotection, skin cancer, aging skin
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
Neurotoxin Treatment of the Upper Face
Article Type
Changed
Display Headline
Neurotoxin Treatment of the Upper Face
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
427-432
Legacy Keywords
neurotoxin injections of the face, Botulinum toxin type A preparations, topical and injectable forms of botox, injection techniques for the upper face, botulinum toxin mechanism of action,
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
427-432
Page Number
427-432
Publications
Publications
Topics
Article Type
Display Headline
Neurotoxin Treatment of the Upper Face
Display Headline
Neurotoxin Treatment of the Upper Face
Legacy Keywords
neurotoxin injections of the face, Botulinum toxin type A preparations, topical and injectable forms of botox, injection techniques for the upper face, botulinum toxin mechanism of action,
Legacy Keywords
neurotoxin injections of the face, Botulinum toxin type A preparations, topical and injectable forms of botox, injection techniques for the upper face, botulinum toxin mechanism of action,
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
Article PDF Media
Document
An Overview of Injectable Fillers With Special Consideration to the Periorbital Area
Article Type
Changed
Display Headline
An Overview of Injectable Fillers With Special Consideration to the Periorbital Area
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
421-426
Legacy Keywords
soft tissue augmentation with temporary fillers, history of injectable fillers in dermatology, injectable facial fillers, injection technique for dermal fillers, ideal characteristics of facial fillers, synthetic extracellular matrix materials
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
421-426
Page Number
421-426
Publications
Publications
Topics
Article Type
Display Headline
An Overview of Injectable Fillers With Special Consideration to the Periorbital Area
Display Headline
An Overview of Injectable Fillers With Special Consideration to the Periorbital Area
Legacy Keywords
soft tissue augmentation with temporary fillers, history of injectable fillers in dermatology, injectable facial fillers, injection technique for dermal fillers, ideal characteristics of facial fillers, synthetic extracellular matrix materials
Legacy Keywords
soft tissue augmentation with temporary fillers, history of injectable fillers in dermatology, injectable facial fillers, injection technique for dermal fillers, ideal characteristics of facial fillers, synthetic extracellular matrix materials
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
Article PDF Media
Document
Devices for Rejuvenation of the Aging Face
Article Type
Changed
Display Headline
Devices for Rejuvenation of the Aging Face
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
412-418
Legacy Keywords
photorejuvenation devices, ablative resurfacing techniques, nonablative resurfacing techniques, reversing signs of aging, treating signs of skin aging, technology and facial rejuvenation
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
412-418
Page Number
412-418
Publications
Publications
Topics
Article Type
Display Headline
Devices for Rejuvenation of the Aging Face
Display Headline
Devices for Rejuvenation of the Aging Face
Legacy Keywords
photorejuvenation devices, ablative resurfacing techniques, nonablative resurfacing techniques, reversing signs of aging, treating signs of skin aging, technology and facial rejuvenation
Legacy Keywords
photorejuvenation devices, ablative resurfacing techniques, nonablative resurfacing techniques, reversing signs of aging, treating signs of skin aging, technology and facial rejuvenation
Citation Override
Originally published in Cosmetic Dermatology
Disallow All Ads
Article PDF Media
Document
Vitamin-Based Cosmeceuticals
Article Type
Changed
Display Headline
Vitamin-Based Cosmeceuticals
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
405-410
Legacy Keywords
cosmeceutical product testing and development, antiaging skin care market, botanicals and vitamins in cosmetic products, vitamins in topical skin care formulations
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
405-410
Page Number
405-410
Publications
Publications
Topics
Article Type
Display Headline
Vitamin-Based Cosmeceuticals
Display Headline
Vitamin-Based Cosmeceuticals
Legacy Keywords
cosmeceutical product testing and development, antiaging skin care market, botanicals and vitamins in cosmetic products, vitamins in topical skin care formulations
Legacy Keywords
cosmeceutical product testing and development, antiaging skin care market, botanicals and vitamins in cosmetic products, vitamins in topical skin care formulations
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
Article PDF Media
Document
Mechanisms of Skin Aging
Article Type
Changed
Display Headline
Mechanisms of Skin Aging
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
399-402
Legacy Keywords
extrinsic signs of aging, intrinsic signs of aging, extrinsic facial aging, free radical theory of aging, UV radiation and skin aging, photoaging
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
399-402
Page Number
399-402
Publications
Publications
Topics
Article Type
Display Headline
Mechanisms of Skin Aging
Display Headline
Mechanisms of Skin Aging
Legacy Keywords
extrinsic signs of aging, intrinsic signs of aging, extrinsic facial aging, free radical theory of aging, UV radiation and skin aging, photoaging
Legacy Keywords
extrinsic signs of aging, intrinsic signs of aging, extrinsic facial aging, free radical theory of aging, UV radiation and skin aging, photoaging
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
Article PDF Media
Document
Plant Stem Cells and Skin Care
Article Type
Changed
Display Headline
Plant Stem Cells and Skin Care
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
395-396
Legacy Keywords
preparation of plant extracts, stem cell cultivation and cosmetics, berry extracts and cosmetics, stem cells and cosmeceutical ingredients
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
395-396
Page Number
395-396
Publications
Publications
Topics
Article Type
Display Headline
Plant Stem Cells and Skin Care
Display Headline
Plant Stem Cells and Skin Care
Legacy Keywords
preparation of plant extracts, stem cell cultivation and cosmetics, berry extracts and cosmetics, stem cells and cosmeceutical ingredients
Legacy Keywords
preparation of plant extracts, stem cell cultivation and cosmetics, berry extracts and cosmetics, stem cells and cosmeceutical ingredients
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
Article PDF Media
Document
Training in Cosmetic Dermatology [editorial]
Article Type
Changed
Display Headline
Training in Cosmetic Dermatology [editorial]
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
392-393
Legacy Keywords
development of cosmetic procedures, dermatology residents in training, dermatologists and technology development, cosmetic dermatology training programs, teaching dermatologic techniques
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
392-393
Page Number
392-393
Publications
Publications
Topics
Article Type
Display Headline
Training in Cosmetic Dermatology [editorial]
Display Headline
Training in Cosmetic Dermatology [editorial]
Legacy Keywords
development of cosmetic procedures, dermatology residents in training, dermatologists and technology development, cosmetic dermatology training programs, teaching dermatologic techniques
Legacy Keywords
development of cosmetic procedures, dermatology residents in training, dermatologists and technology development, cosmetic dermatology training programs, teaching dermatologic techniques
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
Article PDF Media
Document
Reasons for Discontinuation Vary by Psoriasis Treatment
Article Type
Changed
Display Headline
Reasons for Discontinuation Vary by Psoriasis Treatment
Issue
Cutis - 90(2)
Publications
Page Number
3
Legacy Keywords
psoriasis treatment, plaque psoriasis
Issue
Cutis - 90(2)
Issue
Cutis - 90(2)
Page Number
3
Page Number
3
Publications
Publications
Article Type
Display Headline
Reasons for Discontinuation Vary by Psoriasis Treatment
Display Headline
Reasons for Discontinuation Vary by Psoriasis Treatment
Legacy Keywords
psoriasis treatment, plaque psoriasis
Legacy Keywords
psoriasis treatment, plaque psoriasis
Article Source
Citation Override
Originally published in Cosmetic Dermatology
PURLs Copyright
Inside the Article
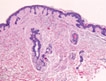
Primary Systemic Amyloidosis
Article Type
Changed
Display Headline
Primary Systemic Amyloidosis
Article PDF
Issue
Cutis - 90(3)
Publications
Topics
Page Number
119, 123-124
Legacy Keywords
primary systemic amyloidosis and underlying plasma cell dyscrasia, primary systemic amyloidosis and organ involvement, histopathology of primary systemic amyloidosis,
Sections
Article PDF
Article PDF
Issue
Cutis - 90(3)
Issue
Cutis - 90(3)
Page Number
119, 123-124
Page Number
119, 123-124
Publications
Publications
Topics
Article Type
Display Headline
Primary Systemic Amyloidosis
Display Headline
Primary Systemic Amyloidosis
Legacy Keywords
primary systemic amyloidosis and underlying plasma cell dyscrasia, primary systemic amyloidosis and organ involvement, histopathology of primary systemic amyloidosis,
Legacy Keywords
primary systemic amyloidosis and underlying plasma cell dyscrasia, primary systemic amyloidosis and organ involvement, histopathology of primary systemic amyloidosis,
Sections
Article Source
PURLs Copyright
Inside the Article
Article PDF Media
Document