User login
Marriage of Necessity
Doctors and hospitals need each other. Healthcare reform is requiring hospitals to rely more heavily on physicians to help them meet quality, safety, and efficiency goals. But in return, doctors are demanding more financial security and a larger role in hospital leadership.
Just how far are they willing to take their mutual relationship to meet their individual needs? A new report by professional services company PwC (formerly PricewaterhouseCoopers) examines the mindsets of potential partners, including an online survey of more than 1,000 doctors and in-depth interviews with 28 healthcare executives. The results suggest plenty of opportunities for alignment, though perhaps also the need for serious pre-marriage counseling.
“From Courtship to Marriage Part II” (www.PwC.com/us/PhysicianHospitalAlignment) follows an initial report that emphasizes the element of trust that’s necessary for any doctor-hospital alignment to succeed. This time around, the sequel is focusing on more concrete steps needed to take the budding relationship to the next level and sustain it. In particular, the new report focuses on sharing power (governance), sharing resources (compensation), and sharing outcomes (guidelines).
The PwC report preempts the naysayers by acknowledging at the outset that “hospitals and physicians have been to the altar before, but many of those marriages ended in divorce.” So what’s different from the 1990s, that decade of broken marriages doomed by the irreconcilable differences over capitation?
“Number one is that back in the ’90s, there wasn’t a clear consensus in defining and determining what is quality,” says Warren Skea, a director in the PwC Health Enterprise Growth Practice. In the intervening years, he says, membership societies—SHM among them—and nonprofit organizations, such as the National Quality Forum, have helped address the need to define and measure healthcare quality. The Centers for Medicare & Medicaid Services (CMS) followed up by adopting and implementing some of those measures in programs, including hospital value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
Another missing component in the ’90s, Skea says, was an adequate set of tools for gauging quality. “Even if we did agree what quality was, we couldn’t go back in there and measure it in a valid way,” he explains. “We just didn’t have that capacity.”
A third lesson learned the hard way is that decision-making should involve all physicians, from primary-care doctors to specialists. That power-sharing will be critical, Skea says, as reimbursement models move away from fee-for-service, transaction-based compensation methods and toward paying for outcomes and quality. Silos of care are out, and transitioning patients across a continuum of care is definitely in.
Sound familiar? It should, and the similarity to the hospitalist job description isn’t lost on Skea. “I think hospitalists have served as a very good illustrative example of how physicians can add value to that efficiency equation, improve quality, increase [good] outcomes—all of those things,” he says. In fact, Skea says, the question now is how the quarterback role assumed by hospitalists can be translated or projected to the larger industry and other settings (e.g. outpatient clinics, home care rehabilitation, and continuing care facilities).
Accountable-care organizations (ACOs) are a hot topic in any discussion of better patient transitions and closer doctor-hospital alignments, but they’re hardly the only wedding chapels in town. The new report sketches out the corresponding amenities of a comanagement model and provider-owned plan, and Skea notes that part of the new Center for Medicare & Medicaid Innovation’s mandate will be to investigate other promising methods for encouraging providers to work together.
Leaders, Partners
For most doctors, according to the survey, working together means making joint decisions. More than 90% said they should be involved in “hospital governance activities such as serving on boards, being in management, and taking part in performance.”
“That didn’t surprise me at all; there’s a huge appetite for physicians to be involved in strategic governance and oversight,” Skea says. “That’s where hospitalists have been really good: taking it to that next level of strategy and leadership.”
Next to compensation, he says, governance is the biggest issue for many hospital-affiliated physicians. One wrinkle, however, is what the report’s authors heard from hospital executives. “There’s a recognition by hospital executives that they need those physicians in those governance roles,” Skea says. But the executives felt that more physicians should be trained and educated in business and financial decision-making.
Some of the training strategies, he says, are homegrown. One hospital client, for example, is providing its physicians with courses in statistical analysis, financial modeling, and change management, and referring to the educational package as “MBA in a box.” Other hospitals are steering their physicians toward outside sources of instruction. SHM’s four-day Leadership Academy (www.hospitalmedicine.org/leadership) offers another resource for hospitalists seeking more prominent roles within their institutions.
Along with a desire for more power-sharing, doctors looking to a hospital setting have clearly indicated that they expect to hold their own financially. According to the survey, 83% of doctors considering hospital employment expect to be paid as much as or more than they are currently earning.
And therein lies another potential sticking point. Based on past experience, doctors might expect that hospitals’ financial resources will still allow them to maximize their compensation. But as health reform plays out, Skea cautions, “everybody is going to have to do more with less.”
Compromise Ahead
But other survey results hint at the potential for compromise. According to the report, physicians agreed that half of their compensation should be a fixed salary, while the remaining half could be based on meeting productivity, quality, patient satisfaction, and cost-of-care goals, with the potential for performance rewards. “This shows that physicians realize the health system is changing to track and reward performance and that they can influence the quality and cost of care delivery at the institutional level,” the report states.
And as for the guidelines doctors follow while delivering healthcare, 62% of those surveyed believe nationally accepted guidelines should guide the way they practice medicine; 30% prefer local guidelines.
Skea says he was a bit surprised that nearly 1 in 3 doctors are still resistant to national guidelines, though he believes that number is on the wane. After an initial pushback, he says, doctors seem to be gravitating toward the national standards, due in part to physician societies taking active roles in the discussions.
So what should hospitalists take away from all of this? Skea says they should continue to highlight and demonstrate the value they provide in standardizing care, measuring quality, and improving efficiencies in the four walls of the hospital. “They’ve had a track record, I think they have the mindset, and they’ve had the relationship with hospital executives,” he says.
Hospitalists likely will be called upon to help educate their physician colleagues in other specialties. Because of their background and history of success, Skea says, “they could be one of the real leaders and catalysts for change within an ACO or some of these other more integrated and aligned delivery models, and then move into governance.”
With a little assistance, perhaps this marriage might work after all. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Doctors and hospitals need each other. Healthcare reform is requiring hospitals to rely more heavily on physicians to help them meet quality, safety, and efficiency goals. But in return, doctors are demanding more financial security and a larger role in hospital leadership.
Just how far are they willing to take their mutual relationship to meet their individual needs? A new report by professional services company PwC (formerly PricewaterhouseCoopers) examines the mindsets of potential partners, including an online survey of more than 1,000 doctors and in-depth interviews with 28 healthcare executives. The results suggest plenty of opportunities for alignment, though perhaps also the need for serious pre-marriage counseling.
“From Courtship to Marriage Part II” (www.PwC.com/us/PhysicianHospitalAlignment) follows an initial report that emphasizes the element of trust that’s necessary for any doctor-hospital alignment to succeed. This time around, the sequel is focusing on more concrete steps needed to take the budding relationship to the next level and sustain it. In particular, the new report focuses on sharing power (governance), sharing resources (compensation), and sharing outcomes (guidelines).
The PwC report preempts the naysayers by acknowledging at the outset that “hospitals and physicians have been to the altar before, but many of those marriages ended in divorce.” So what’s different from the 1990s, that decade of broken marriages doomed by the irreconcilable differences over capitation?
“Number one is that back in the ’90s, there wasn’t a clear consensus in defining and determining what is quality,” says Warren Skea, a director in the PwC Health Enterprise Growth Practice. In the intervening years, he says, membership societies—SHM among them—and nonprofit organizations, such as the National Quality Forum, have helped address the need to define and measure healthcare quality. The Centers for Medicare & Medicaid Services (CMS) followed up by adopting and implementing some of those measures in programs, including hospital value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
Another missing component in the ’90s, Skea says, was an adequate set of tools for gauging quality. “Even if we did agree what quality was, we couldn’t go back in there and measure it in a valid way,” he explains. “We just didn’t have that capacity.”
A third lesson learned the hard way is that decision-making should involve all physicians, from primary-care doctors to specialists. That power-sharing will be critical, Skea says, as reimbursement models move away from fee-for-service, transaction-based compensation methods and toward paying for outcomes and quality. Silos of care are out, and transitioning patients across a continuum of care is definitely in.
Sound familiar? It should, and the similarity to the hospitalist job description isn’t lost on Skea. “I think hospitalists have served as a very good illustrative example of how physicians can add value to that efficiency equation, improve quality, increase [good] outcomes—all of those things,” he says. In fact, Skea says, the question now is how the quarterback role assumed by hospitalists can be translated or projected to the larger industry and other settings (e.g. outpatient clinics, home care rehabilitation, and continuing care facilities).
Accountable-care organizations (ACOs) are a hot topic in any discussion of better patient transitions and closer doctor-hospital alignments, but they’re hardly the only wedding chapels in town. The new report sketches out the corresponding amenities of a comanagement model and provider-owned plan, and Skea notes that part of the new Center for Medicare & Medicaid Innovation’s mandate will be to investigate other promising methods for encouraging providers to work together.
Leaders, Partners
For most doctors, according to the survey, working together means making joint decisions. More than 90% said they should be involved in “hospital governance activities such as serving on boards, being in management, and taking part in performance.”
“That didn’t surprise me at all; there’s a huge appetite for physicians to be involved in strategic governance and oversight,” Skea says. “That’s where hospitalists have been really good: taking it to that next level of strategy and leadership.”
Next to compensation, he says, governance is the biggest issue for many hospital-affiliated physicians. One wrinkle, however, is what the report’s authors heard from hospital executives. “There’s a recognition by hospital executives that they need those physicians in those governance roles,” Skea says. But the executives felt that more physicians should be trained and educated in business and financial decision-making.
Some of the training strategies, he says, are homegrown. One hospital client, for example, is providing its physicians with courses in statistical analysis, financial modeling, and change management, and referring to the educational package as “MBA in a box.” Other hospitals are steering their physicians toward outside sources of instruction. SHM’s four-day Leadership Academy (www.hospitalmedicine.org/leadership) offers another resource for hospitalists seeking more prominent roles within their institutions.
Along with a desire for more power-sharing, doctors looking to a hospital setting have clearly indicated that they expect to hold their own financially. According to the survey, 83% of doctors considering hospital employment expect to be paid as much as or more than they are currently earning.
And therein lies another potential sticking point. Based on past experience, doctors might expect that hospitals’ financial resources will still allow them to maximize their compensation. But as health reform plays out, Skea cautions, “everybody is going to have to do more with less.”
Compromise Ahead
But other survey results hint at the potential for compromise. According to the report, physicians agreed that half of their compensation should be a fixed salary, while the remaining half could be based on meeting productivity, quality, patient satisfaction, and cost-of-care goals, with the potential for performance rewards. “This shows that physicians realize the health system is changing to track and reward performance and that they can influence the quality and cost of care delivery at the institutional level,” the report states.
And as for the guidelines doctors follow while delivering healthcare, 62% of those surveyed believe nationally accepted guidelines should guide the way they practice medicine; 30% prefer local guidelines.
Skea says he was a bit surprised that nearly 1 in 3 doctors are still resistant to national guidelines, though he believes that number is on the wane. After an initial pushback, he says, doctors seem to be gravitating toward the national standards, due in part to physician societies taking active roles in the discussions.
So what should hospitalists take away from all of this? Skea says they should continue to highlight and demonstrate the value they provide in standardizing care, measuring quality, and improving efficiencies in the four walls of the hospital. “They’ve had a track record, I think they have the mindset, and they’ve had the relationship with hospital executives,” he says.
Hospitalists likely will be called upon to help educate their physician colleagues in other specialties. Because of their background and history of success, Skea says, “they could be one of the real leaders and catalysts for change within an ACO or some of these other more integrated and aligned delivery models, and then move into governance.”
With a little assistance, perhaps this marriage might work after all. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Doctors and hospitals need each other. Healthcare reform is requiring hospitals to rely more heavily on physicians to help them meet quality, safety, and efficiency goals. But in return, doctors are demanding more financial security and a larger role in hospital leadership.
Just how far are they willing to take their mutual relationship to meet their individual needs? A new report by professional services company PwC (formerly PricewaterhouseCoopers) examines the mindsets of potential partners, including an online survey of more than 1,000 doctors and in-depth interviews with 28 healthcare executives. The results suggest plenty of opportunities for alignment, though perhaps also the need for serious pre-marriage counseling.
“From Courtship to Marriage Part II” (www.PwC.com/us/PhysicianHospitalAlignment) follows an initial report that emphasizes the element of trust that’s necessary for any doctor-hospital alignment to succeed. This time around, the sequel is focusing on more concrete steps needed to take the budding relationship to the next level and sustain it. In particular, the new report focuses on sharing power (governance), sharing resources (compensation), and sharing outcomes (guidelines).
The PwC report preempts the naysayers by acknowledging at the outset that “hospitals and physicians have been to the altar before, but many of those marriages ended in divorce.” So what’s different from the 1990s, that decade of broken marriages doomed by the irreconcilable differences over capitation?
“Number one is that back in the ’90s, there wasn’t a clear consensus in defining and determining what is quality,” says Warren Skea, a director in the PwC Health Enterprise Growth Practice. In the intervening years, he says, membership societies—SHM among them—and nonprofit organizations, such as the National Quality Forum, have helped address the need to define and measure healthcare quality. The Centers for Medicare & Medicaid Services (CMS) followed up by adopting and implementing some of those measures in programs, including hospital value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
Another missing component in the ’90s, Skea says, was an adequate set of tools for gauging quality. “Even if we did agree what quality was, we couldn’t go back in there and measure it in a valid way,” he explains. “We just didn’t have that capacity.”
A third lesson learned the hard way is that decision-making should involve all physicians, from primary-care doctors to specialists. That power-sharing will be critical, Skea says, as reimbursement models move away from fee-for-service, transaction-based compensation methods and toward paying for outcomes and quality. Silos of care are out, and transitioning patients across a continuum of care is definitely in.
Sound familiar? It should, and the similarity to the hospitalist job description isn’t lost on Skea. “I think hospitalists have served as a very good illustrative example of how physicians can add value to that efficiency equation, improve quality, increase [good] outcomes—all of those things,” he says. In fact, Skea says, the question now is how the quarterback role assumed by hospitalists can be translated or projected to the larger industry and other settings (e.g. outpatient clinics, home care rehabilitation, and continuing care facilities).
Accountable-care organizations (ACOs) are a hot topic in any discussion of better patient transitions and closer doctor-hospital alignments, but they’re hardly the only wedding chapels in town. The new report sketches out the corresponding amenities of a comanagement model and provider-owned plan, and Skea notes that part of the new Center for Medicare & Medicaid Innovation’s mandate will be to investigate other promising methods for encouraging providers to work together.
Leaders, Partners
For most doctors, according to the survey, working together means making joint decisions. More than 90% said they should be involved in “hospital governance activities such as serving on boards, being in management, and taking part in performance.”
“That didn’t surprise me at all; there’s a huge appetite for physicians to be involved in strategic governance and oversight,” Skea says. “That’s where hospitalists have been really good: taking it to that next level of strategy and leadership.”
Next to compensation, he says, governance is the biggest issue for many hospital-affiliated physicians. One wrinkle, however, is what the report’s authors heard from hospital executives. “There’s a recognition by hospital executives that they need those physicians in those governance roles,” Skea says. But the executives felt that more physicians should be trained and educated in business and financial decision-making.
Some of the training strategies, he says, are homegrown. One hospital client, for example, is providing its physicians with courses in statistical analysis, financial modeling, and change management, and referring to the educational package as “MBA in a box.” Other hospitals are steering their physicians toward outside sources of instruction. SHM’s four-day Leadership Academy (www.hospitalmedicine.org/leadership) offers another resource for hospitalists seeking more prominent roles within their institutions.
Along with a desire for more power-sharing, doctors looking to a hospital setting have clearly indicated that they expect to hold their own financially. According to the survey, 83% of doctors considering hospital employment expect to be paid as much as or more than they are currently earning.
And therein lies another potential sticking point. Based on past experience, doctors might expect that hospitals’ financial resources will still allow them to maximize their compensation. But as health reform plays out, Skea cautions, “everybody is going to have to do more with less.”
Compromise Ahead
But other survey results hint at the potential for compromise. According to the report, physicians agreed that half of their compensation should be a fixed salary, while the remaining half could be based on meeting productivity, quality, patient satisfaction, and cost-of-care goals, with the potential for performance rewards. “This shows that physicians realize the health system is changing to track and reward performance and that they can influence the quality and cost of care delivery at the institutional level,” the report states.
And as for the guidelines doctors follow while delivering healthcare, 62% of those surveyed believe nationally accepted guidelines should guide the way they practice medicine; 30% prefer local guidelines.
Skea says he was a bit surprised that nearly 1 in 3 doctors are still resistant to national guidelines, though he believes that number is on the wane. After an initial pushback, he says, doctors seem to be gravitating toward the national standards, due in part to physician societies taking active roles in the discussions.
So what should hospitalists take away from all of this? Skea says they should continue to highlight and demonstrate the value they provide in standardizing care, measuring quality, and improving efficiencies in the four walls of the hospital. “They’ve had a track record, I think they have the mindset, and they’ve had the relationship with hospital executives,” he says.
Hospitalists likely will be called upon to help educate their physician colleagues in other specialties. Because of their background and history of success, Skea says, “they could be one of the real leaders and catalysts for change within an ACO or some of these other more integrated and aligned delivery models, and then move into governance.”
With a little assistance, perhaps this marriage might work after all. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Medical Industry Takes Notice of Social Media
Most companies recognize that social media have become established as viable business tools. Many leaders are using sites like Facebook, Twitter, and LinkedIn to connect to their customers, recruit followers, and promote their services in real time. But the opportunity to connect the dots and utilize social media in a safe and meaningful way has yet to be fully realized. Whoever gets there first has the opportunity to revolutionize and forever change the medical industry.
The Current Situation
Social media sites for the medical industry range from broad, open platforms to niche, narrowly concentrated forums. Facebook, Twitter, and YouTube are broad platforms for individuals and corporations alike to broadcast experiences and opinions large and small. CancerDoc, HealthLine, and RevolutionHealth are more narrowly targeted places for rapidly communicating and connecting to those who are sharing similar experiences, communicating information, and sharing ideas amongst patients and medical industry peers. Expert Q&A sites, such as WebMD and AskDrWiki, are popular with patients who can find credible answers to their health-related questions. Physician networks (e.g. Sermo and Ozmosis) serve as “virtual water coolers” where physicians can collaborate in real time.
But no matter what portal is being used by patient or provider, the single most beneficial aspect of social media is the collaboration enabled by the openness of vast numbers. Most are trying to get their message out, educate, inform, and simply share. The portals themselves, empowered by the strength of their members, are positioning themselves as the source of true, real-time data and insight. Many healthcare facilities use social media to crowdsource, or basically ask for input from users to help develop or improve products and services quickly and efficiently. Others are enabling real-time learning through podcasts of surgeries, which medical students can attend remotely.
In 2010 specifically, we saw a significant jump in medical companies utilizing social media tools. The Mayo Clinic has gained more than 33,000 Facebook fans in a little more than a year. The Mayo “wall” is filled with patients’ thanks, interviews, advice, industry news, and nearly 150 videos. Its presence in this space has strengthened the Mayo name as a thought leader in medical care and innovation.
Future Opportunities
While all this is important to building relationships and brands, these building blocks could be the source for more revolutionary advancements. Over time, the intimate knowledge of a contributor, a regional demographic, or an international group of sufferers could be used as proactive triggers for action. Imagine a device that collects signs of your general well-being, then the data from this blends with your Facebook postings on location, time, diet, and feeling while aggregating information from other users and facilities. When linked to your medical facility and medication status, your pharmacy, your caregiver, or your gym could generate guidance and suggestions, which are sent back to you daily. If a hazardous situation is suspected by auto-analysis of the data, then this could directly alert your doctor to provide personal, quick advice and instructions. The potential to use social media and connected, aware devices for well-being and preventative care is huge, as are the possibilities for predicting and tracking patterns in health globally.
Social media offer unique opportunities for scalable interaction and collaboration, a key reason medical and lifestyle device manufacturers have much opportunity ahead of them. By developing products that become part of the user’s daily lives (think how important your smartphone is to you now), manufacturers will find themselves building a loyal customer base that is not only using their device, but is also interacting with them and providing unparalleled insight into their habits in real time.
Nike is one company that has been quick to the punch. The NikePlus Running Monitor is an application that meshes telehealth devices with social media, monitoring and posting running information on Facebook. All of this tracking and communication serves as a great promoter of the manufacturer, as it’s advertised every time the user posts a status update.
Despite all the progress, challenges remain for medical companies when diving into social media. It remains a very new horizon for an industry that faces hurdles posed by the traditions of the medical and insurance industries. Companies who are agile and able to pivot likely will be the winners. It’s easy to imagine Google as the CDC’s biggest information source in the future, aggregating and reporting clusters of users searching for key disease symptoms through an app portal or tweeting about illnesses. Used as tools for triggers, social media can take the temperature of societal health, allowing the medical community to watch population density or pollution patterns unfold.
If device manufacturers and the medical community figure out how to harness and leverage the power of people’s desire to connect and share, they could achieve groundbreaking contributions to healthcare and the connected world as a whole in the coming years.
Tim Morton,
design director,
Product Development Technologies,
Lake Zurich, Ill.
Journal Venues for Safety and Quality-Improvement Publications
The message is clear: Conducting business as usual is no longer tenable, nor the “right thing to do” for our patients. In a recent survey of departments of medicine chairs, Staiger et al summarize: “Top-performing academic institutions have recognized that quality improvement/patient safety (QI/PS) activities, leading to improved and measurable patient outcomes, are imperative for strategic survival.”1
Long before this report, the Society of General Internal Medicine’s Academic Hospitalist Task Force provided a framework to document the scholarship for promotion in academic medical centers and to document improvement activities.2 Since then, major academic institutions have incorporated such principles to support academic promotion.
Table 1 (see p. 6) provides venues for publication to advance the science of safety and QI; each is Medline-indexed. The list is not exhaustive and is meant to serve as a starting point of reference. We have not included many other excellent clinical journals that publish QI and patient safety work. When conducting improvement studies, we encourage hospitalists to use the Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines for publication of quality-improvement articles.3,4,5
Enjoy a new era in academic medical centers.
Adolfo Peña, MD,
hospitalist,
Saint Joseph Hospital,
London, Ky.;
Benjamin Taylor, MD, MPH,
chief quality officer,
University Hospital,
The University of Alabama at Birmingham,
SGIM Academic Hospitalist Task Force member;
Pat Patrician, RN, PhD,
senior scholar,
Birmingham VA Quality Scholars Program;
Carlos A. Estrada, MD, MS,
senior scholar,
Birmingham VA Quality Scholars Program
References
- Staiger TO, Wong EY, Schleyer AM, Martin DP, Levinson W, Bremner WJ. The role of quality improvement and patient safety in academic promotion: results of a survey of chairs of departments of internal medicine in North America. Am J Med. 2011;124:277-280.
- Society of General Internal Medicine (SGIM) Academic Hospitalist Task Force. Quality Portfolio. SGIM website. Available at: www.sgim.org/index.cfm?pageId=844. Accessed May 3, 2011.
- Davidoff D, Batalden P, Stevens D, Ogrinc D, Mooney S. Publication guidelines for quality improvement in health care: evolution of the SQUIRE project. Qual Saf Health Care. 2008;17 Suppl 1:i3-i9.
- Ogrinc G, Mooney S, Estrada C, et al. The SQUIRE (Standards for QUality Improvement Reporting Excellence) guidelines for quality improvement reporting: explanation and elaboration. Qual Saf Health Care. 2008;17 Suppl 1:i13-i32.
- Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines for publication of quality improvement articles. SQUIRE website. Available at: http://squire-statement.org. Accessed May 3, 2011.
Most companies recognize that social media have become established as viable business tools. Many leaders are using sites like Facebook, Twitter, and LinkedIn to connect to their customers, recruit followers, and promote their services in real time. But the opportunity to connect the dots and utilize social media in a safe and meaningful way has yet to be fully realized. Whoever gets there first has the opportunity to revolutionize and forever change the medical industry.
The Current Situation
Social media sites for the medical industry range from broad, open platforms to niche, narrowly concentrated forums. Facebook, Twitter, and YouTube are broad platforms for individuals and corporations alike to broadcast experiences and opinions large and small. CancerDoc, HealthLine, and RevolutionHealth are more narrowly targeted places for rapidly communicating and connecting to those who are sharing similar experiences, communicating information, and sharing ideas amongst patients and medical industry peers. Expert Q&A sites, such as WebMD and AskDrWiki, are popular with patients who can find credible answers to their health-related questions. Physician networks (e.g. Sermo and Ozmosis) serve as “virtual water coolers” where physicians can collaborate in real time.
But no matter what portal is being used by patient or provider, the single most beneficial aspect of social media is the collaboration enabled by the openness of vast numbers. Most are trying to get their message out, educate, inform, and simply share. The portals themselves, empowered by the strength of their members, are positioning themselves as the source of true, real-time data and insight. Many healthcare facilities use social media to crowdsource, or basically ask for input from users to help develop or improve products and services quickly and efficiently. Others are enabling real-time learning through podcasts of surgeries, which medical students can attend remotely.
In 2010 specifically, we saw a significant jump in medical companies utilizing social media tools. The Mayo Clinic has gained more than 33,000 Facebook fans in a little more than a year. The Mayo “wall” is filled with patients’ thanks, interviews, advice, industry news, and nearly 150 videos. Its presence in this space has strengthened the Mayo name as a thought leader in medical care and innovation.
Future Opportunities
While all this is important to building relationships and brands, these building blocks could be the source for more revolutionary advancements. Over time, the intimate knowledge of a contributor, a regional demographic, or an international group of sufferers could be used as proactive triggers for action. Imagine a device that collects signs of your general well-being, then the data from this blends with your Facebook postings on location, time, diet, and feeling while aggregating information from other users and facilities. When linked to your medical facility and medication status, your pharmacy, your caregiver, or your gym could generate guidance and suggestions, which are sent back to you daily. If a hazardous situation is suspected by auto-analysis of the data, then this could directly alert your doctor to provide personal, quick advice and instructions. The potential to use social media and connected, aware devices for well-being and preventative care is huge, as are the possibilities for predicting and tracking patterns in health globally.
Social media offer unique opportunities for scalable interaction and collaboration, a key reason medical and lifestyle device manufacturers have much opportunity ahead of them. By developing products that become part of the user’s daily lives (think how important your smartphone is to you now), manufacturers will find themselves building a loyal customer base that is not only using their device, but is also interacting with them and providing unparalleled insight into their habits in real time.
Nike is one company that has been quick to the punch. The NikePlus Running Monitor is an application that meshes telehealth devices with social media, monitoring and posting running information on Facebook. All of this tracking and communication serves as a great promoter of the manufacturer, as it’s advertised every time the user posts a status update.
Despite all the progress, challenges remain for medical companies when diving into social media. It remains a very new horizon for an industry that faces hurdles posed by the traditions of the medical and insurance industries. Companies who are agile and able to pivot likely will be the winners. It’s easy to imagine Google as the CDC’s biggest information source in the future, aggregating and reporting clusters of users searching for key disease symptoms through an app portal or tweeting about illnesses. Used as tools for triggers, social media can take the temperature of societal health, allowing the medical community to watch population density or pollution patterns unfold.
If device manufacturers and the medical community figure out how to harness and leverage the power of people’s desire to connect and share, they could achieve groundbreaking contributions to healthcare and the connected world as a whole in the coming years.
Tim Morton,
design director,
Product Development Technologies,
Lake Zurich, Ill.
Journal Venues for Safety and Quality-Improvement Publications
The message is clear: Conducting business as usual is no longer tenable, nor the “right thing to do” for our patients. In a recent survey of departments of medicine chairs, Staiger et al summarize: “Top-performing academic institutions have recognized that quality improvement/patient safety (QI/PS) activities, leading to improved and measurable patient outcomes, are imperative for strategic survival.”1
Long before this report, the Society of General Internal Medicine’s Academic Hospitalist Task Force provided a framework to document the scholarship for promotion in academic medical centers and to document improvement activities.2 Since then, major academic institutions have incorporated such principles to support academic promotion.
Table 1 (see p. 6) provides venues for publication to advance the science of safety and QI; each is Medline-indexed. The list is not exhaustive and is meant to serve as a starting point of reference. We have not included many other excellent clinical journals that publish QI and patient safety work. When conducting improvement studies, we encourage hospitalists to use the Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines for publication of quality-improvement articles.3,4,5
Enjoy a new era in academic medical centers.
Adolfo Peña, MD,
hospitalist,
Saint Joseph Hospital,
London, Ky.;
Benjamin Taylor, MD, MPH,
chief quality officer,
University Hospital,
The University of Alabama at Birmingham,
SGIM Academic Hospitalist Task Force member;
Pat Patrician, RN, PhD,
senior scholar,
Birmingham VA Quality Scholars Program;
Carlos A. Estrada, MD, MS,
senior scholar,
Birmingham VA Quality Scholars Program
References
- Staiger TO, Wong EY, Schleyer AM, Martin DP, Levinson W, Bremner WJ. The role of quality improvement and patient safety in academic promotion: results of a survey of chairs of departments of internal medicine in North America. Am J Med. 2011;124:277-280.
- Society of General Internal Medicine (SGIM) Academic Hospitalist Task Force. Quality Portfolio. SGIM website. Available at: www.sgim.org/index.cfm?pageId=844. Accessed May 3, 2011.
- Davidoff D, Batalden P, Stevens D, Ogrinc D, Mooney S. Publication guidelines for quality improvement in health care: evolution of the SQUIRE project. Qual Saf Health Care. 2008;17 Suppl 1:i3-i9.
- Ogrinc G, Mooney S, Estrada C, et al. The SQUIRE (Standards for QUality Improvement Reporting Excellence) guidelines for quality improvement reporting: explanation and elaboration. Qual Saf Health Care. 2008;17 Suppl 1:i13-i32.
- Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines for publication of quality improvement articles. SQUIRE website. Available at: http://squire-statement.org. Accessed May 3, 2011.
Most companies recognize that social media have become established as viable business tools. Many leaders are using sites like Facebook, Twitter, and LinkedIn to connect to their customers, recruit followers, and promote their services in real time. But the opportunity to connect the dots and utilize social media in a safe and meaningful way has yet to be fully realized. Whoever gets there first has the opportunity to revolutionize and forever change the medical industry.
The Current Situation
Social media sites for the medical industry range from broad, open platforms to niche, narrowly concentrated forums. Facebook, Twitter, and YouTube are broad platforms for individuals and corporations alike to broadcast experiences and opinions large and small. CancerDoc, HealthLine, and RevolutionHealth are more narrowly targeted places for rapidly communicating and connecting to those who are sharing similar experiences, communicating information, and sharing ideas amongst patients and medical industry peers. Expert Q&A sites, such as WebMD and AskDrWiki, are popular with patients who can find credible answers to their health-related questions. Physician networks (e.g. Sermo and Ozmosis) serve as “virtual water coolers” where physicians can collaborate in real time.
But no matter what portal is being used by patient or provider, the single most beneficial aspect of social media is the collaboration enabled by the openness of vast numbers. Most are trying to get their message out, educate, inform, and simply share. The portals themselves, empowered by the strength of their members, are positioning themselves as the source of true, real-time data and insight. Many healthcare facilities use social media to crowdsource, or basically ask for input from users to help develop or improve products and services quickly and efficiently. Others are enabling real-time learning through podcasts of surgeries, which medical students can attend remotely.
In 2010 specifically, we saw a significant jump in medical companies utilizing social media tools. The Mayo Clinic has gained more than 33,000 Facebook fans in a little more than a year. The Mayo “wall” is filled with patients’ thanks, interviews, advice, industry news, and nearly 150 videos. Its presence in this space has strengthened the Mayo name as a thought leader in medical care and innovation.
Future Opportunities
While all this is important to building relationships and brands, these building blocks could be the source for more revolutionary advancements. Over time, the intimate knowledge of a contributor, a regional demographic, or an international group of sufferers could be used as proactive triggers for action. Imagine a device that collects signs of your general well-being, then the data from this blends with your Facebook postings on location, time, diet, and feeling while aggregating information from other users and facilities. When linked to your medical facility and medication status, your pharmacy, your caregiver, or your gym could generate guidance and suggestions, which are sent back to you daily. If a hazardous situation is suspected by auto-analysis of the data, then this could directly alert your doctor to provide personal, quick advice and instructions. The potential to use social media and connected, aware devices for well-being and preventative care is huge, as are the possibilities for predicting and tracking patterns in health globally.
Social media offer unique opportunities for scalable interaction and collaboration, a key reason medical and lifestyle device manufacturers have much opportunity ahead of them. By developing products that become part of the user’s daily lives (think how important your smartphone is to you now), manufacturers will find themselves building a loyal customer base that is not only using their device, but is also interacting with them and providing unparalleled insight into their habits in real time.
Nike is one company that has been quick to the punch. The NikePlus Running Monitor is an application that meshes telehealth devices with social media, monitoring and posting running information on Facebook. All of this tracking and communication serves as a great promoter of the manufacturer, as it’s advertised every time the user posts a status update.
Despite all the progress, challenges remain for medical companies when diving into social media. It remains a very new horizon for an industry that faces hurdles posed by the traditions of the medical and insurance industries. Companies who are agile and able to pivot likely will be the winners. It’s easy to imagine Google as the CDC’s biggest information source in the future, aggregating and reporting clusters of users searching for key disease symptoms through an app portal or tweeting about illnesses. Used as tools for triggers, social media can take the temperature of societal health, allowing the medical community to watch population density or pollution patterns unfold.
If device manufacturers and the medical community figure out how to harness and leverage the power of people’s desire to connect and share, they could achieve groundbreaking contributions to healthcare and the connected world as a whole in the coming years.
Tim Morton,
design director,
Product Development Technologies,
Lake Zurich, Ill.
Journal Venues for Safety and Quality-Improvement Publications
The message is clear: Conducting business as usual is no longer tenable, nor the “right thing to do” for our patients. In a recent survey of departments of medicine chairs, Staiger et al summarize: “Top-performing academic institutions have recognized that quality improvement/patient safety (QI/PS) activities, leading to improved and measurable patient outcomes, are imperative for strategic survival.”1
Long before this report, the Society of General Internal Medicine’s Academic Hospitalist Task Force provided a framework to document the scholarship for promotion in academic medical centers and to document improvement activities.2 Since then, major academic institutions have incorporated such principles to support academic promotion.
Table 1 (see p. 6) provides venues for publication to advance the science of safety and QI; each is Medline-indexed. The list is not exhaustive and is meant to serve as a starting point of reference. We have not included many other excellent clinical journals that publish QI and patient safety work. When conducting improvement studies, we encourage hospitalists to use the Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines for publication of quality-improvement articles.3,4,5
Enjoy a new era in academic medical centers.
Adolfo Peña, MD,
hospitalist,
Saint Joseph Hospital,
London, Ky.;
Benjamin Taylor, MD, MPH,
chief quality officer,
University Hospital,
The University of Alabama at Birmingham,
SGIM Academic Hospitalist Task Force member;
Pat Patrician, RN, PhD,
senior scholar,
Birmingham VA Quality Scholars Program;
Carlos A. Estrada, MD, MS,
senior scholar,
Birmingham VA Quality Scholars Program
References
- Staiger TO, Wong EY, Schleyer AM, Martin DP, Levinson W, Bremner WJ. The role of quality improvement and patient safety in academic promotion: results of a survey of chairs of departments of internal medicine in North America. Am J Med. 2011;124:277-280.
- Society of General Internal Medicine (SGIM) Academic Hospitalist Task Force. Quality Portfolio. SGIM website. Available at: www.sgim.org/index.cfm?pageId=844. Accessed May 3, 2011.
- Davidoff D, Batalden P, Stevens D, Ogrinc D, Mooney S. Publication guidelines for quality improvement in health care: evolution of the SQUIRE project. Qual Saf Health Care. 2008;17 Suppl 1:i3-i9.
- Ogrinc G, Mooney S, Estrada C, et al. The SQUIRE (Standards for QUality Improvement Reporting Excellence) guidelines for quality improvement reporting: explanation and elaboration. Qual Saf Health Care. 2008;17 Suppl 1:i13-i32.
- Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines for publication of quality improvement articles. SQUIRE website. Available at: http://squire-statement.org. Accessed May 3, 2011.
Virtual Mentorship
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
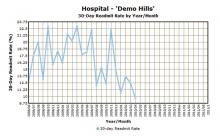
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
POLICY CORNER: SHM Pledges Support to Patient-Safety Initiative
On April 12, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius joined the Centers for Medicare & Medicaid Services (CMS) administrator Donald Berwick, MD, in announcing a major patient-safety initiative bringing together hospitals, clinicians, consumers, employers, federal and state governments, and many more groups around two common goals: reducing harm caused to patients in hospitals and reducing hospital readmissions.
SHM was one of the first physician groups to sign on to the Pledge of Support, which aims to reduce hospital-acquired conditions by 40% and decrease preventable readmissions within 30 days of discharge by 20%, both by the end of 2013.
The pledge includes specific expectations for each of the different healthcare entities signing on. By signing, SHM agrees on behalf of hospitalists that they will work together to redesign activities within the hospital to reduce harm, learn from experiences and share best practices, and engage with patients and families to implement practices that foster more patient-centered care that improves safety, communication, and care coordination.
HHS is committing a total of $1 billion from the Patient Protection and Affordable Care Act of 2010 (ACA) to support hospitals and other providers in their efforts to reach these goals. Of the funding, $500 million will come through the Community-Based Care Transitions Program (CCTP) created in the ACA to help community-based organizations partnering with eligible hospitals to improve transitions between settings of care. The other $500 million will come from the Centers for Medicare and Medicaid Innovation (CMMI) to test different models of improving patient care, patient engagement, and collaboration in order to reduce hospital-acquired conditions and improve care transitions nationwide.
The partnership takes the best ideas from the public and private sectors and accelerates their spread to achieve a safer, higher-quality healthcare system for all Americans. It aligns Dr. Berwick’s triple aim (improve care, improve people’s health, and reduce the overall cost of healthcare) with SHM’s efforts to improve quality and patient safety through innovation and collaboration.
SHM’s Project BOOST (www.hospitalmedicine.org/boost) is listed in the solicitation for applications for the CCTP, and SHM’s VTE resource room is among the resources posted on the partnership website.
For more information on the initiative, visit www.healthcare.gov. TH
On April 12, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius joined the Centers for Medicare & Medicaid Services (CMS) administrator Donald Berwick, MD, in announcing a major patient-safety initiative bringing together hospitals, clinicians, consumers, employers, federal and state governments, and many more groups around two common goals: reducing harm caused to patients in hospitals and reducing hospital readmissions.
SHM was one of the first physician groups to sign on to the Pledge of Support, which aims to reduce hospital-acquired conditions by 40% and decrease preventable readmissions within 30 days of discharge by 20%, both by the end of 2013.
The pledge includes specific expectations for each of the different healthcare entities signing on. By signing, SHM agrees on behalf of hospitalists that they will work together to redesign activities within the hospital to reduce harm, learn from experiences and share best practices, and engage with patients and families to implement practices that foster more patient-centered care that improves safety, communication, and care coordination.
HHS is committing a total of $1 billion from the Patient Protection and Affordable Care Act of 2010 (ACA) to support hospitals and other providers in their efforts to reach these goals. Of the funding, $500 million will come through the Community-Based Care Transitions Program (CCTP) created in the ACA to help community-based organizations partnering with eligible hospitals to improve transitions between settings of care. The other $500 million will come from the Centers for Medicare and Medicaid Innovation (CMMI) to test different models of improving patient care, patient engagement, and collaboration in order to reduce hospital-acquired conditions and improve care transitions nationwide.
The partnership takes the best ideas from the public and private sectors and accelerates their spread to achieve a safer, higher-quality healthcare system for all Americans. It aligns Dr. Berwick’s triple aim (improve care, improve people’s health, and reduce the overall cost of healthcare) with SHM’s efforts to improve quality and patient safety through innovation and collaboration.
SHM’s Project BOOST (www.hospitalmedicine.org/boost) is listed in the solicitation for applications for the CCTP, and SHM’s VTE resource room is among the resources posted on the partnership website.
For more information on the initiative, visit www.healthcare.gov. TH
On April 12, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius joined the Centers for Medicare & Medicaid Services (CMS) administrator Donald Berwick, MD, in announcing a major patient-safety initiative bringing together hospitals, clinicians, consumers, employers, federal and state governments, and many more groups around two common goals: reducing harm caused to patients in hospitals and reducing hospital readmissions.
SHM was one of the first physician groups to sign on to the Pledge of Support, which aims to reduce hospital-acquired conditions by 40% and decrease preventable readmissions within 30 days of discharge by 20%, both by the end of 2013.
The pledge includes specific expectations for each of the different healthcare entities signing on. By signing, SHM agrees on behalf of hospitalists that they will work together to redesign activities within the hospital to reduce harm, learn from experiences and share best practices, and engage with patients and families to implement practices that foster more patient-centered care that improves safety, communication, and care coordination.
HHS is committing a total of $1 billion from the Patient Protection and Affordable Care Act of 2010 (ACA) to support hospitals and other providers in their efforts to reach these goals. Of the funding, $500 million will come through the Community-Based Care Transitions Program (CCTP) created in the ACA to help community-based organizations partnering with eligible hospitals to improve transitions between settings of care. The other $500 million will come from the Centers for Medicare and Medicaid Innovation (CMMI) to test different models of improving patient care, patient engagement, and collaboration in order to reduce hospital-acquired conditions and improve care transitions nationwide.
The partnership takes the best ideas from the public and private sectors and accelerates their spread to achieve a safer, higher-quality healthcare system for all Americans. It aligns Dr. Berwick’s triple aim (improve care, improve people’s health, and reduce the overall cost of healthcare) with SHM’s efforts to improve quality and patient safety through innovation and collaboration.
SHM’s Project BOOST (www.hospitalmedicine.org/boost) is listed in the solicitation for applications for the CCTP, and SHM’s VTE resource room is among the resources posted on the partnership website.
For more information on the initiative, visit www.healthcare.gov. TH
Hospitalists on the Move: June 2011
Robert Harrington Jr., MD, SFHM, and Erin Stucky Fisher, MD, MHM, have been elected to SHM’s board of directors. Dr. Harrington, chief medical officer for Locum Leaders, serves as chair of SHM’s Family Medicine Task Force and board liaison to the IT Core Committee. Dr. Fisher, professor of clinical pediatrics at the University of California at San Diego, is actively involved with quality initiatives for the American Academy of Pediatrics, the Institute for Healthcare Improvement, and the National Association of Children’s Hospitals.
Jasen W. Gundersen, MD, MBA, CPE, SFHM, has been appointed chief medical officer for TeamHealth Hospital Medicine.
IPC: The Hospitalist Company Inc. has appointed Kerry Weiner, MD, to the newly created position of chief clinical officer. Dr. Weiner will lead the clinical functions of the company and continue the development of hospitalist leaders throughout IPC.
Steven Pantilat, MD, FACP, SFHM, has received a 2011 James Irvine Foundation Leadership Award. Dr. Pantilat, one of five recipients, is professor of clinical medicine, the Alan M. Kates and John M. Burnard Endowed Chair in Palliative Care, and director of the Palliative Care Leadership Center at UCSF. Now in its sixth year, the award celebrates extraordinary leaders who are applying innovative and effective solutions to significant state issues. Dr. Pantilat, a past SHM president, will receive $125,000 in organizational support.
Hospitalist Patrick O’Neil, DO, has been named Lake Regional Health System’s 2011 Physician of the Year. The 116-bed health system serves 1,300 employees in the Land of the Ozarks, Mo., area.
Hospitalist Wiley Robinson, MD, has been named president-elect of the Tennessee Medical Association and will head the organization for 2012-2013. An internal-medicine specialist, Dr. Robinson is cofounder and president of Inpatient Physicians of the Mid-South, a Memphis-based hospitalist group.
The Association of Specialty Professors announced Robert M. Wachter, MD, MHM, will receive the 2011 ASP Eric G. Neilson, MD, Distinguished Professor Award. Dr. Wachter is professor of medicine and the Marc and Lynne Benioff Endowed Chair in Hospital Medicine at the University of California at San Francisco (UCSF) School of Medicine, and a past president of SHM. The Neilson Award is presented annually to a leader who has shaped the internal-medicine landscape and promotes the work of leaders who bring about change for specialty medicine. TH
Robert Harrington Jr., MD, SFHM, and Erin Stucky Fisher, MD, MHM, have been elected to SHM’s board of directors. Dr. Harrington, chief medical officer for Locum Leaders, serves as chair of SHM’s Family Medicine Task Force and board liaison to the IT Core Committee. Dr. Fisher, professor of clinical pediatrics at the University of California at San Diego, is actively involved with quality initiatives for the American Academy of Pediatrics, the Institute for Healthcare Improvement, and the National Association of Children’s Hospitals.
Jasen W. Gundersen, MD, MBA, CPE, SFHM, has been appointed chief medical officer for TeamHealth Hospital Medicine.
IPC: The Hospitalist Company Inc. has appointed Kerry Weiner, MD, to the newly created position of chief clinical officer. Dr. Weiner will lead the clinical functions of the company and continue the development of hospitalist leaders throughout IPC.
Steven Pantilat, MD, FACP, SFHM, has received a 2011 James Irvine Foundation Leadership Award. Dr. Pantilat, one of five recipients, is professor of clinical medicine, the Alan M. Kates and John M. Burnard Endowed Chair in Palliative Care, and director of the Palliative Care Leadership Center at UCSF. Now in its sixth year, the award celebrates extraordinary leaders who are applying innovative and effective solutions to significant state issues. Dr. Pantilat, a past SHM president, will receive $125,000 in organizational support.
Hospitalist Patrick O’Neil, DO, has been named Lake Regional Health System’s 2011 Physician of the Year. The 116-bed health system serves 1,300 employees in the Land of the Ozarks, Mo., area.
Hospitalist Wiley Robinson, MD, has been named president-elect of the Tennessee Medical Association and will head the organization for 2012-2013. An internal-medicine specialist, Dr. Robinson is cofounder and president of Inpatient Physicians of the Mid-South, a Memphis-based hospitalist group.
The Association of Specialty Professors announced Robert M. Wachter, MD, MHM, will receive the 2011 ASP Eric G. Neilson, MD, Distinguished Professor Award. Dr. Wachter is professor of medicine and the Marc and Lynne Benioff Endowed Chair in Hospital Medicine at the University of California at San Francisco (UCSF) School of Medicine, and a past president of SHM. The Neilson Award is presented annually to a leader who has shaped the internal-medicine landscape and promotes the work of leaders who bring about change for specialty medicine. TH
Robert Harrington Jr., MD, SFHM, and Erin Stucky Fisher, MD, MHM, have been elected to SHM’s board of directors. Dr. Harrington, chief medical officer for Locum Leaders, serves as chair of SHM’s Family Medicine Task Force and board liaison to the IT Core Committee. Dr. Fisher, professor of clinical pediatrics at the University of California at San Diego, is actively involved with quality initiatives for the American Academy of Pediatrics, the Institute for Healthcare Improvement, and the National Association of Children’s Hospitals.
Jasen W. Gundersen, MD, MBA, CPE, SFHM, has been appointed chief medical officer for TeamHealth Hospital Medicine.
IPC: The Hospitalist Company Inc. has appointed Kerry Weiner, MD, to the newly created position of chief clinical officer. Dr. Weiner will lead the clinical functions of the company and continue the development of hospitalist leaders throughout IPC.
Steven Pantilat, MD, FACP, SFHM, has received a 2011 James Irvine Foundation Leadership Award. Dr. Pantilat, one of five recipients, is professor of clinical medicine, the Alan M. Kates and John M. Burnard Endowed Chair in Palliative Care, and director of the Palliative Care Leadership Center at UCSF. Now in its sixth year, the award celebrates extraordinary leaders who are applying innovative and effective solutions to significant state issues. Dr. Pantilat, a past SHM president, will receive $125,000 in organizational support.
Hospitalist Patrick O’Neil, DO, has been named Lake Regional Health System’s 2011 Physician of the Year. The 116-bed health system serves 1,300 employees in the Land of the Ozarks, Mo., area.
Hospitalist Wiley Robinson, MD, has been named president-elect of the Tennessee Medical Association and will head the organization for 2012-2013. An internal-medicine specialist, Dr. Robinson is cofounder and president of Inpatient Physicians of the Mid-South, a Memphis-based hospitalist group.
The Association of Specialty Professors announced Robert M. Wachter, MD, MHM, will receive the 2011 ASP Eric G. Neilson, MD, Distinguished Professor Award. Dr. Wachter is professor of medicine and the Marc and Lynne Benioff Endowed Chair in Hospital Medicine at the University of California at San Francisco (UCSF) School of Medicine, and a past president of SHM. The Neilson Award is presented annually to a leader who has shaped the internal-medicine landscape and promotes the work of leaders who bring about change for specialty medicine. TH
Med Students’ Simple Idea Has Serious Potential
The difficulties in routinely recalling each and every action to take with a patient has encouraged hospitalists to abide by checklists that remind them of just what to do. So why shouldn’t patients have the same systematic prodding? That’s exactly what two first-year students at the University of Michigan Medical School in Ann Arbor—Andrew Lin and Aaron Farberg—thought two years ago, prompting them to invent Dear Doctor.
With the help of senior physicians, including former SHM president Scott Flanders, MD, SFHM, FACP, Lin and Farberg conducted a three-month study that provided bedside notepads to patients. The patients were encouraged to jot down questions for their doctors whenever a question occurred to them, not just when the physician was in the room. The students produced 1,000 notepads, even shrink-wrapping them with companion pens.
The simple yet seemingly effective approach worked so well that “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication” earned the budding physicians the 2010 Innovation Poster award in the Research, Innovations, and Clinical Vignettes competition at HM10.
“This isn’t groundbreaking work here,” Lin says. “It’s a notepad, scraps of paper. Look around your desk and you’ve got sticky notes around. That’s what this is.”
Lin and Farberg both say they were surprised no one had crafted a similar communication tool as a potential quality-improvement (QI) measure. To wit, they are now working on publishing their research in the Journal of Hospital Medicine to further draw attention to the concept. They envision a day when the notes patients write down could be included in electronic medical records.
The ultimate goal is to give hospitalists and other physicians another way to communicate with their patients. “We want to institutionalize [Dear Doctor] to the point it’s a recognized necessity for the hospital system,” Lin says.—RQ
Toolkit Addresses Small-Business Security Concerns
The Healthcare Information and Management Systems Society (HIMSS) has had a privacy and security toolkit for physicians for a decade, but after its last annual security survey with the Medical Group Management Association (MGMA), it became clear that small- to medium-sized organizations were behind in implementation.
And so was born the HIMSS Privacy and Security Toolkit for Small Provider Organizations. The joint initiative is one that HM groups in rural or small settings should take advantage of, says Lisa Gallagher, HIMSS’ senior director of privacy and security.
Hospitalists “need to understand the reporting environment,” Gallagher says. “They are the subject of a lot of the policies and technology. We need them to be knowledgeable about it. They’re the ones who have access.”
HM’s role at the juncture of different departments and physicians, particularly at smaller hospitals that rely on hospitalists as traffic cops, makes it all the more important for hospitalists to understand the nuances of both privacy and security.
The interactive toolkit allows users to submit their own suggestions for improved processes and features introductions to the Centers for Medicare & Medicaid Services’ (CMS) “meaningful use” standard. Gallagher is hopeful that an engaged physician response to the toolkit will only bolster its efficacy in the coming months. “This is going to continue to evolve,” she says.—RQ
QUALITY RESEARCH
Care Transitions, Readmissions Concern Other Countries
International studies suggest that the recent torrent of attention toward improving care transitions and preventing hospital readmissions is not just an American trend. For example, a literature survey of physician “handovers” (aka handoffs) in international hospitals published in the British Medical Journal for Quality and Safety identified 32 papers on the subject.1 The authors conclude that the existing literature rarely examines pre- and post-handover phases or evaluates the quality of handover practices, and thus “does not fully identify where communication failures typically occur.” More systematic analysis of all stages of handoffs by physicians is warranted, the authors suggest.
In the same journal, a literature search of English-language publications from 1990 to 2010 found a dozen studies—eight from the U.S.—documenting failure to perform adequate follow-up for patients’ test results.2 The lack of follow-up ranged from 20% to 62% for hospitalized patients, and from 1% to 75% for patients treated in the ED. Two areas where problems were particularly evident were critical test results and results for patients moving across healthcare settings. “The existing evidence suggests that the problem of missed test results is considerable and reported negative impacts on patients warrant the exploration of solutions,” the authors conclude. They recommend further study of the effectiveness of such interventions as online endorsement of results, and integration of information technology into clinical work practices.
The World Alliance for Patient Safety, which was convened in 2004 by the World Health Organization, recently pointed to poor test result follow-up as one of the major processes contributing to unsafe patient care internationally.1 The organization has identified nine “patient-safety solutions,” one of which is ensuring medication accuracy at transitions of care.
For more information on the alliance and WHO’s interest in patient safety, visit http://www.who.int/topics/patient_safety/en/. —LB
References
- Raduma-Tomás MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospi- tals: a literature review. BMJ Qual Saf. 2011;20:128-133.
- Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194-199.
The difficulties in routinely recalling each and every action to take with a patient has encouraged hospitalists to abide by checklists that remind them of just what to do. So why shouldn’t patients have the same systematic prodding? That’s exactly what two first-year students at the University of Michigan Medical School in Ann Arbor—Andrew Lin and Aaron Farberg—thought two years ago, prompting them to invent Dear Doctor.
With the help of senior physicians, including former SHM president Scott Flanders, MD, SFHM, FACP, Lin and Farberg conducted a three-month study that provided bedside notepads to patients. The patients were encouraged to jot down questions for their doctors whenever a question occurred to them, not just when the physician was in the room. The students produced 1,000 notepads, even shrink-wrapping them with companion pens.
The simple yet seemingly effective approach worked so well that “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication” earned the budding physicians the 2010 Innovation Poster award in the Research, Innovations, and Clinical Vignettes competition at HM10.
“This isn’t groundbreaking work here,” Lin says. “It’s a notepad, scraps of paper. Look around your desk and you’ve got sticky notes around. That’s what this is.”
Lin and Farberg both say they were surprised no one had crafted a similar communication tool as a potential quality-improvement (QI) measure. To wit, they are now working on publishing their research in the Journal of Hospital Medicine to further draw attention to the concept. They envision a day when the notes patients write down could be included in electronic medical records.
The ultimate goal is to give hospitalists and other physicians another way to communicate with their patients. “We want to institutionalize [Dear Doctor] to the point it’s a recognized necessity for the hospital system,” Lin says.—RQ
Toolkit Addresses Small-Business Security Concerns
The Healthcare Information and Management Systems Society (HIMSS) has had a privacy and security toolkit for physicians for a decade, but after its last annual security survey with the Medical Group Management Association (MGMA), it became clear that small- to medium-sized organizations were behind in implementation.
And so was born the HIMSS Privacy and Security Toolkit for Small Provider Organizations. The joint initiative is one that HM groups in rural or small settings should take advantage of, says Lisa Gallagher, HIMSS’ senior director of privacy and security.
Hospitalists “need to understand the reporting environment,” Gallagher says. “They are the subject of a lot of the policies and technology. We need them to be knowledgeable about it. They’re the ones who have access.”
HM’s role at the juncture of different departments and physicians, particularly at smaller hospitals that rely on hospitalists as traffic cops, makes it all the more important for hospitalists to understand the nuances of both privacy and security.
The interactive toolkit allows users to submit their own suggestions for improved processes and features introductions to the Centers for Medicare & Medicaid Services’ (CMS) “meaningful use” standard. Gallagher is hopeful that an engaged physician response to the toolkit will only bolster its efficacy in the coming months. “This is going to continue to evolve,” she says.—RQ
QUALITY RESEARCH
Care Transitions, Readmissions Concern Other Countries
International studies suggest that the recent torrent of attention toward improving care transitions and preventing hospital readmissions is not just an American trend. For example, a literature survey of physician “handovers” (aka handoffs) in international hospitals published in the British Medical Journal for Quality and Safety identified 32 papers on the subject.1 The authors conclude that the existing literature rarely examines pre- and post-handover phases or evaluates the quality of handover practices, and thus “does not fully identify where communication failures typically occur.” More systematic analysis of all stages of handoffs by physicians is warranted, the authors suggest.
In the same journal, a literature search of English-language publications from 1990 to 2010 found a dozen studies—eight from the U.S.—documenting failure to perform adequate follow-up for patients’ test results.2 The lack of follow-up ranged from 20% to 62% for hospitalized patients, and from 1% to 75% for patients treated in the ED. Two areas where problems were particularly evident were critical test results and results for patients moving across healthcare settings. “The existing evidence suggests that the problem of missed test results is considerable and reported negative impacts on patients warrant the exploration of solutions,” the authors conclude. They recommend further study of the effectiveness of such interventions as online endorsement of results, and integration of information technology into clinical work practices.
The World Alliance for Patient Safety, which was convened in 2004 by the World Health Organization, recently pointed to poor test result follow-up as one of the major processes contributing to unsafe patient care internationally.1 The organization has identified nine “patient-safety solutions,” one of which is ensuring medication accuracy at transitions of care.
For more information on the alliance and WHO’s interest in patient safety, visit http://www.who.int/topics/patient_safety/en/. —LB
References
- Raduma-Tomás MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospi- tals: a literature review. BMJ Qual Saf. 2011;20:128-133.
- Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194-199.
The difficulties in routinely recalling each and every action to take with a patient has encouraged hospitalists to abide by checklists that remind them of just what to do. So why shouldn’t patients have the same systematic prodding? That’s exactly what two first-year students at the University of Michigan Medical School in Ann Arbor—Andrew Lin and Aaron Farberg—thought two years ago, prompting them to invent Dear Doctor.
With the help of senior physicians, including former SHM president Scott Flanders, MD, SFHM, FACP, Lin and Farberg conducted a three-month study that provided bedside notepads to patients. The patients were encouraged to jot down questions for their doctors whenever a question occurred to them, not just when the physician was in the room. The students produced 1,000 notepads, even shrink-wrapping them with companion pens.
The simple yet seemingly effective approach worked so well that “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication” earned the budding physicians the 2010 Innovation Poster award in the Research, Innovations, and Clinical Vignettes competition at HM10.
“This isn’t groundbreaking work here,” Lin says. “It’s a notepad, scraps of paper. Look around your desk and you’ve got sticky notes around. That’s what this is.”
Lin and Farberg both say they were surprised no one had crafted a similar communication tool as a potential quality-improvement (QI) measure. To wit, they are now working on publishing their research in the Journal of Hospital Medicine to further draw attention to the concept. They envision a day when the notes patients write down could be included in electronic medical records.
The ultimate goal is to give hospitalists and other physicians another way to communicate with their patients. “We want to institutionalize [Dear Doctor] to the point it’s a recognized necessity for the hospital system,” Lin says.—RQ
Toolkit Addresses Small-Business Security Concerns
The Healthcare Information and Management Systems Society (HIMSS) has had a privacy and security toolkit for physicians for a decade, but after its last annual security survey with the Medical Group Management Association (MGMA), it became clear that small- to medium-sized organizations were behind in implementation.
And so was born the HIMSS Privacy and Security Toolkit for Small Provider Organizations. The joint initiative is one that HM groups in rural or small settings should take advantage of, says Lisa Gallagher, HIMSS’ senior director of privacy and security.
Hospitalists “need to understand the reporting environment,” Gallagher says. “They are the subject of a lot of the policies and technology. We need them to be knowledgeable about it. They’re the ones who have access.”
HM’s role at the juncture of different departments and physicians, particularly at smaller hospitals that rely on hospitalists as traffic cops, makes it all the more important for hospitalists to understand the nuances of both privacy and security.
The interactive toolkit allows users to submit their own suggestions for improved processes and features introductions to the Centers for Medicare & Medicaid Services’ (CMS) “meaningful use” standard. Gallagher is hopeful that an engaged physician response to the toolkit will only bolster its efficacy in the coming months. “This is going to continue to evolve,” she says.—RQ
QUALITY RESEARCH
Care Transitions, Readmissions Concern Other Countries
International studies suggest that the recent torrent of attention toward improving care transitions and preventing hospital readmissions is not just an American trend. For example, a literature survey of physician “handovers” (aka handoffs) in international hospitals published in the British Medical Journal for Quality and Safety identified 32 papers on the subject.1 The authors conclude that the existing literature rarely examines pre- and post-handover phases or evaluates the quality of handover practices, and thus “does not fully identify where communication failures typically occur.” More systematic analysis of all stages of handoffs by physicians is warranted, the authors suggest.
In the same journal, a literature search of English-language publications from 1990 to 2010 found a dozen studies—eight from the U.S.—documenting failure to perform adequate follow-up for patients’ test results.2 The lack of follow-up ranged from 20% to 62% for hospitalized patients, and from 1% to 75% for patients treated in the ED. Two areas where problems were particularly evident were critical test results and results for patients moving across healthcare settings. “The existing evidence suggests that the problem of missed test results is considerable and reported negative impacts on patients warrant the exploration of solutions,” the authors conclude. They recommend further study of the effectiveness of such interventions as online endorsement of results, and integration of information technology into clinical work practices.
The World Alliance for Patient Safety, which was convened in 2004 by the World Health Organization, recently pointed to poor test result follow-up as one of the major processes contributing to unsafe patient care internationally.1 The organization has identified nine “patient-safety solutions,” one of which is ensuring medication accuracy at transitions of care.
For more information on the alliance and WHO’s interest in patient safety, visit http://www.who.int/topics/patient_safety/en/. —LB
References
- Raduma-Tomás MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospi- tals: a literature review. BMJ Qual Saf. 2011;20:128-133.
- Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194-199.
The Future Is Forward
GRAPEVINE, Texas—New SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, asked a question at HM11 that might be a first for the relatively nascent field. After explaining to the crowd in the ballroom at the Gaylord Texan Resort and Convention Center that the average hospitalist is 37 years old, Dr. Li asked: “What’s going to happen when the hospitalist gets older and their priorities change?”
A hopeful, if wary, eye on the future of the still-growing field was a common thread throughout HM11, as SHM leaders from the new president to CEO Larry Wellikson, MD, SFHM, laid out the pathway of growth for a 15-year-old specialty. Although each acknowledged uncertainties as they adjust to a domestic healthcare system in the throes of its largest reform in a generation, they agree on a few mainstays.
First, HM should continue to take ownership of quality-improvement (QI) and patient-safety initiatives that improve outcomes and reduce costs for hospitals, as the dual reward of better care for patients and lower costs for chief financial officers can serve as change agents for healthcare and leverage for the next contract.
Second, hospitalists should be careful to balance expansion of their duties—be it via such “hyphenated hospitalists” as laborists, say, or through comanagement of surgical and ED patients—with an appropriate amount of dedicated resources.
Finally, academic hospitalists, from residents to attendings, should continue to plan for this summer’s reduction in work hours and patient caps for residents, new rules from the Accreditation Council for Graduate Medical Education (ACGME) that some fear could create a future cast of ill-prepared internists.
“There’s a lot that’s bearing down on physicians and it’s been compressed in a short period of time,” said AMA President Cecil Wilson, MD. “We cannot go back to where we were and we cannot stay where we are. … We may not have a choice about change, but we do have a choice on how we respond to change and how we influence it.”
Dr. Li sees SHM sitting at the intersection of practical application and influence. He wants to continue with society-sponsored training academies and leadership programs that both impress upon hospitalists how important it is for them to take leadership roles in their hospitals and make sure they have the skills to do so. Dr. Li says the field needs to look no further than other fields adopting the in-hospital practice model as proof that the care model is vital to improving equality.
“We need to be laser-focused in terms of what we want to do. [We] want to improve the quality of care of patients both inside and outside the hospital,” he adds. “I say both inside and outside because, oftentimes, that transition is somewhere in between it. We have many hospitalists, like at my place, who provide care in the outpatient setting, in post-discharge clinics, and other places.”
Dr. Li also says that collaborations with fellow medical societies and organizations are key to SHM’s advocacy role. Society leaders are attending other specialty conferences to build and strengthen relationships that help extend HM’s reach into policy circles. In perhaps one of the strongest relationships, SHM leadership is meeting this summer with Donald Berwick, MD, administrator of the Centers for Medicare & Medicaid Services (CMS). The meeting is even more valuable in context of Dr. Berwick’s recent selection of Patrick Conway, MD, MSc, SFHM, a pediatric hospitalist and director of hospital medicine at Cincinnati Children’s Hospital Medical Center, as CMS’ chief medical officer. The government position is the highest-ranking policy role ever held by a hospitalist (see “Hospitalist Takes Charge” p. 28).
“We’re in a position going forward where we don’t talk alone,” says immediate past SHM president Jeff Wiese, MD, FACP, SFHM, associate professor of medicine at Tulane University Health Sciences Center in New Orleans. “It’s us and our partners talking together. That moves what is currently a loud voice to a stentorian voice. You can imagine where SHM and ACP [American College of Physicians] and the VA [Veterans Administration] and Society of Critical Care Medicine … if they’re all saying the same thing, that’s a very different message than if one organization is saying it alone.”
Adds SHM board member and former SHM Public Policy Committee chairman Eric Siegal, MD, SFHM, a critical-care fellow at the University of Wisconsin School of Medicine and Public Health in Madison, “We’re absolutely at the table in a way that’s, frankly, almost stunning how fast we have evolved [from] several years ago, when we first went to Washington, D.C., for our first advocacy day, and we had to explain to people that hospitalists were not in the hospitality industry. We punch well above our weight class right now.”
It’s a tall order for any specialty society to push the national healthcare discussion, but Dr. Li sees HM as perfectly perched “to train the trainers.” The field has grown to more than 30,000 hospitalists, well beyond the estimated ceiling of 20,000 hospitalists forecasted in the field’s earliest days. That rapid-fire growth–hospitalists are now present in the vast majority of hospitals that can either afford them or need them–means the field can now evolve past simply swelling numbers to creating better physicians. By encouraging more rank-and-file practitioners to become leaders, the logic goes, the number of groups will increase as practices sprout in those remaining hospitals without HM services: more practices, more hospitalists, more presence in future policy discussions.
To that end, Dr. Wellikson notes that SHM continues to introduce training courses and research repositories. Two recent additions are eQUIPS (Electronic Quality Improvement Programs), a series of QI and patient toolkits aimed at transitional care, glycemic control, and VTE prevention, and SQUINT, SHM’s new QI repository, which allows users to upload research projects to a searchable database that other physicians can then mine for data.
“We’re really only at the very beginning,” Dr. Li says. “All of hospital medicine only started 10, 15 years ago. For some folks, they believe that’s a long time. But this really is the very beginning of this movement.”
Richard Quinn is a freelance writer based in New Jersey.
GRAPEVINE, Texas—New SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, asked a question at HM11 that might be a first for the relatively nascent field. After explaining to the crowd in the ballroom at the Gaylord Texan Resort and Convention Center that the average hospitalist is 37 years old, Dr. Li asked: “What’s going to happen when the hospitalist gets older and their priorities change?”
A hopeful, if wary, eye on the future of the still-growing field was a common thread throughout HM11, as SHM leaders from the new president to CEO Larry Wellikson, MD, SFHM, laid out the pathway of growth for a 15-year-old specialty. Although each acknowledged uncertainties as they adjust to a domestic healthcare system in the throes of its largest reform in a generation, they agree on a few mainstays.
First, HM should continue to take ownership of quality-improvement (QI) and patient-safety initiatives that improve outcomes and reduce costs for hospitals, as the dual reward of better care for patients and lower costs for chief financial officers can serve as change agents for healthcare and leverage for the next contract.
Second, hospitalists should be careful to balance expansion of their duties—be it via such “hyphenated hospitalists” as laborists, say, or through comanagement of surgical and ED patients—with an appropriate amount of dedicated resources.
Finally, academic hospitalists, from residents to attendings, should continue to plan for this summer’s reduction in work hours and patient caps for residents, new rules from the Accreditation Council for Graduate Medical Education (ACGME) that some fear could create a future cast of ill-prepared internists.
“There’s a lot that’s bearing down on physicians and it’s been compressed in a short period of time,” said AMA President Cecil Wilson, MD. “We cannot go back to where we were and we cannot stay where we are. … We may not have a choice about change, but we do have a choice on how we respond to change and how we influence it.”
Dr. Li sees SHM sitting at the intersection of practical application and influence. He wants to continue with society-sponsored training academies and leadership programs that both impress upon hospitalists how important it is for them to take leadership roles in their hospitals and make sure they have the skills to do so. Dr. Li says the field needs to look no further than other fields adopting the in-hospital practice model as proof that the care model is vital to improving equality.
“We need to be laser-focused in terms of what we want to do. [We] want to improve the quality of care of patients both inside and outside the hospital,” he adds. “I say both inside and outside because, oftentimes, that transition is somewhere in between it. We have many hospitalists, like at my place, who provide care in the outpatient setting, in post-discharge clinics, and other places.”
Dr. Li also says that collaborations with fellow medical societies and organizations are key to SHM’s advocacy role. Society leaders are attending other specialty conferences to build and strengthen relationships that help extend HM’s reach into policy circles. In perhaps one of the strongest relationships, SHM leadership is meeting this summer with Donald Berwick, MD, administrator of the Centers for Medicare & Medicaid Services (CMS). The meeting is even more valuable in context of Dr. Berwick’s recent selection of Patrick Conway, MD, MSc, SFHM, a pediatric hospitalist and director of hospital medicine at Cincinnati Children’s Hospital Medical Center, as CMS’ chief medical officer. The government position is the highest-ranking policy role ever held by a hospitalist (see “Hospitalist Takes Charge” p. 28).
“We’re in a position going forward where we don’t talk alone,” says immediate past SHM president Jeff Wiese, MD, FACP, SFHM, associate professor of medicine at Tulane University Health Sciences Center in New Orleans. “It’s us and our partners talking together. That moves what is currently a loud voice to a stentorian voice. You can imagine where SHM and ACP [American College of Physicians] and the VA [Veterans Administration] and Society of Critical Care Medicine … if they’re all saying the same thing, that’s a very different message than if one organization is saying it alone.”
Adds SHM board member and former SHM Public Policy Committee chairman Eric Siegal, MD, SFHM, a critical-care fellow at the University of Wisconsin School of Medicine and Public Health in Madison, “We’re absolutely at the table in a way that’s, frankly, almost stunning how fast we have evolved [from] several years ago, when we first went to Washington, D.C., for our first advocacy day, and we had to explain to people that hospitalists were not in the hospitality industry. We punch well above our weight class right now.”
It’s a tall order for any specialty society to push the national healthcare discussion, but Dr. Li sees HM as perfectly perched “to train the trainers.” The field has grown to more than 30,000 hospitalists, well beyond the estimated ceiling of 20,000 hospitalists forecasted in the field’s earliest days. That rapid-fire growth–hospitalists are now present in the vast majority of hospitals that can either afford them or need them–means the field can now evolve past simply swelling numbers to creating better physicians. By encouraging more rank-and-file practitioners to become leaders, the logic goes, the number of groups will increase as practices sprout in those remaining hospitals without HM services: more practices, more hospitalists, more presence in future policy discussions.
To that end, Dr. Wellikson notes that SHM continues to introduce training courses and research repositories. Two recent additions are eQUIPS (Electronic Quality Improvement Programs), a series of QI and patient toolkits aimed at transitional care, glycemic control, and VTE prevention, and SQUINT, SHM’s new QI repository, which allows users to upload research projects to a searchable database that other physicians can then mine for data.
“We’re really only at the very beginning,” Dr. Li says. “All of hospital medicine only started 10, 15 years ago. For some folks, they believe that’s a long time. But this really is the very beginning of this movement.”
Richard Quinn is a freelance writer based in New Jersey.
GRAPEVINE, Texas—New SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, asked a question at HM11 that might be a first for the relatively nascent field. After explaining to the crowd in the ballroom at the Gaylord Texan Resort and Convention Center that the average hospitalist is 37 years old, Dr. Li asked: “What’s going to happen when the hospitalist gets older and their priorities change?”
A hopeful, if wary, eye on the future of the still-growing field was a common thread throughout HM11, as SHM leaders from the new president to CEO Larry Wellikson, MD, SFHM, laid out the pathway of growth for a 15-year-old specialty. Although each acknowledged uncertainties as they adjust to a domestic healthcare system in the throes of its largest reform in a generation, they agree on a few mainstays.
First, HM should continue to take ownership of quality-improvement (QI) and patient-safety initiatives that improve outcomes and reduce costs for hospitals, as the dual reward of better care for patients and lower costs for chief financial officers can serve as change agents for healthcare and leverage for the next contract.
Second, hospitalists should be careful to balance expansion of their duties—be it via such “hyphenated hospitalists” as laborists, say, or through comanagement of surgical and ED patients—with an appropriate amount of dedicated resources.
Finally, academic hospitalists, from residents to attendings, should continue to plan for this summer’s reduction in work hours and patient caps for residents, new rules from the Accreditation Council for Graduate Medical Education (ACGME) that some fear could create a future cast of ill-prepared internists.
“There’s a lot that’s bearing down on physicians and it’s been compressed in a short period of time,” said AMA President Cecil Wilson, MD. “We cannot go back to where we were and we cannot stay where we are. … We may not have a choice about change, but we do have a choice on how we respond to change and how we influence it.”
Dr. Li sees SHM sitting at the intersection of practical application and influence. He wants to continue with society-sponsored training academies and leadership programs that both impress upon hospitalists how important it is for them to take leadership roles in their hospitals and make sure they have the skills to do so. Dr. Li says the field needs to look no further than other fields adopting the in-hospital practice model as proof that the care model is vital to improving equality.
“We need to be laser-focused in terms of what we want to do. [We] want to improve the quality of care of patients both inside and outside the hospital,” he adds. “I say both inside and outside because, oftentimes, that transition is somewhere in between it. We have many hospitalists, like at my place, who provide care in the outpatient setting, in post-discharge clinics, and other places.”
Dr. Li also says that collaborations with fellow medical societies and organizations are key to SHM’s advocacy role. Society leaders are attending other specialty conferences to build and strengthen relationships that help extend HM’s reach into policy circles. In perhaps one of the strongest relationships, SHM leadership is meeting this summer with Donald Berwick, MD, administrator of the Centers for Medicare & Medicaid Services (CMS). The meeting is even more valuable in context of Dr. Berwick’s recent selection of Patrick Conway, MD, MSc, SFHM, a pediatric hospitalist and director of hospital medicine at Cincinnati Children’s Hospital Medical Center, as CMS’ chief medical officer. The government position is the highest-ranking policy role ever held by a hospitalist (see “Hospitalist Takes Charge” p. 28).
“We’re in a position going forward where we don’t talk alone,” says immediate past SHM president Jeff Wiese, MD, FACP, SFHM, associate professor of medicine at Tulane University Health Sciences Center in New Orleans. “It’s us and our partners talking together. That moves what is currently a loud voice to a stentorian voice. You can imagine where SHM and ACP [American College of Physicians] and the VA [Veterans Administration] and Society of Critical Care Medicine … if they’re all saying the same thing, that’s a very different message than if one organization is saying it alone.”
Adds SHM board member and former SHM Public Policy Committee chairman Eric Siegal, MD, SFHM, a critical-care fellow at the University of Wisconsin School of Medicine and Public Health in Madison, “We’re absolutely at the table in a way that’s, frankly, almost stunning how fast we have evolved [from] several years ago, when we first went to Washington, D.C., for our first advocacy day, and we had to explain to people that hospitalists were not in the hospitality industry. We punch well above our weight class right now.”
It’s a tall order for any specialty society to push the national healthcare discussion, but Dr. Li sees HM as perfectly perched “to train the trainers.” The field has grown to more than 30,000 hospitalists, well beyond the estimated ceiling of 20,000 hospitalists forecasted in the field’s earliest days. That rapid-fire growth–hospitalists are now present in the vast majority of hospitals that can either afford them or need them–means the field can now evolve past simply swelling numbers to creating better physicians. By encouraging more rank-and-file practitioners to become leaders, the logic goes, the number of groups will increase as practices sprout in those remaining hospitals without HM services: more practices, more hospitalists, more presence in future policy discussions.
To that end, Dr. Wellikson notes that SHM continues to introduce training courses and research repositories. Two recent additions are eQUIPS (Electronic Quality Improvement Programs), a series of QI and patient toolkits aimed at transitional care, glycemic control, and VTE prevention, and SQUINT, SHM’s new QI repository, which allows users to upload research projects to a searchable database that other physicians can then mine for data.
“We’re really only at the very beginning,” Dr. Li says. “All of hospital medicine only started 10, 15 years ago. For some folks, they believe that’s a long time. But this really is the very beginning of this movement.”
Richard Quinn is a freelance writer based in New Jersey.
The Future of Better Patient Care
GRAPEVINE, Texas—Hospitalist Michael Monge, MD, of Cogent Healthcare in San Bernardino, Calif., watched an instructor squeeze the lubricating gel on the transponder and press it gently, but firmly, into the crook of a woman’s arm. Veins practically popped off an ultrasound monitor, serving as a literal road map for vascular access.
And he thought: Wouldn’t it be great if I had this technology all the time, just like I remember from my residency?
“A lot of my ER attendings were able to do a study at the bedside in a manner of minutes, not 30 or 45 minutes,” says Dr. Monge, who practices at Saint Bernardine Medical Center. “If they saw something abnormal, sure enough, they got the full study. But they were able to get that glimpse. Ultimately, it’s just better patient care.”
Dr. Monge’s ultrasound lesson was a first for the SHM annual meeting. In past years, training on ultrasounds was wrapped into the “Medical Procedures for the Hospitalist” pre-course. But at HM11, thanks to the growing prevalence and portability of the technology, the training was expanded into its own half-day pre-course, appropriately dubbed “Portable Ultrasound for the Hospitalist.”
“The ultrasound will be the stethoscope of the 21st century,” says Mark Ault, director of the Division of General Internal Medicine and assistant chairman for clinical affairs of the Department of Medicine at Cedars-Sinai Medical Center in Los Angeles. “And the goal will be to have an ultrasound in the hands of every internist.”
Only time will tell whether portable ultrasound becomes as commonplace as Dr. Ault envisions, but what is clear is that the evolution of the technology makes it widely applicable to hospitalists, says Bradley Rosen, MD, MBA, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Medical Center.
Pricing is one such example. In years past, ultrasound machines were bulky and costly, with price tags in the hundreds of thousands of dollars. Now, portable units, depending on the number of transducers and functionality, can come as low as $20,000, though more-advanced machines quickly jump into the $40,000 to $60,000 range.
Still, Dr. Rosen views the practical uses of the technology as almost endless, and could include vascular access, placing central and PICC lines, and insertion and removal of catheters. Most hospitalists, however, continue to have limited experience with portable ultrasound, meaning those interested in learning more likely have to seek out physicians in other departments to provide the training and mentorship required. Dr. Rosen suggests working with ED physicians, OB-GYNs, and radiologists, although he notes you should be careful to be clear that the HM community is not looking to supplant anyone, or take billing opportunities away.
Hospitalists “don’t know how to use it, and people don’t know where to go to learn how to use it,” he says. “This is a starting point that will allow people … to take these ideas back and, hopefully, generate enough of a critical mass that it becomes a louder and louder chorus asking for this technology.”
GRAPEVINE, Texas—Hospitalist Michael Monge, MD, of Cogent Healthcare in San Bernardino, Calif., watched an instructor squeeze the lubricating gel on the transponder and press it gently, but firmly, into the crook of a woman’s arm. Veins practically popped off an ultrasound monitor, serving as a literal road map for vascular access.
And he thought: Wouldn’t it be great if I had this technology all the time, just like I remember from my residency?
“A lot of my ER attendings were able to do a study at the bedside in a manner of minutes, not 30 or 45 minutes,” says Dr. Monge, who practices at Saint Bernardine Medical Center. “If they saw something abnormal, sure enough, they got the full study. But they were able to get that glimpse. Ultimately, it’s just better patient care.”
Dr. Monge’s ultrasound lesson was a first for the SHM annual meeting. In past years, training on ultrasounds was wrapped into the “Medical Procedures for the Hospitalist” pre-course. But at HM11, thanks to the growing prevalence and portability of the technology, the training was expanded into its own half-day pre-course, appropriately dubbed “Portable Ultrasound for the Hospitalist.”
“The ultrasound will be the stethoscope of the 21st century,” says Mark Ault, director of the Division of General Internal Medicine and assistant chairman for clinical affairs of the Department of Medicine at Cedars-Sinai Medical Center in Los Angeles. “And the goal will be to have an ultrasound in the hands of every internist.”
Only time will tell whether portable ultrasound becomes as commonplace as Dr. Ault envisions, but what is clear is that the evolution of the technology makes it widely applicable to hospitalists, says Bradley Rosen, MD, MBA, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Medical Center.
Pricing is one such example. In years past, ultrasound machines were bulky and costly, with price tags in the hundreds of thousands of dollars. Now, portable units, depending on the number of transducers and functionality, can come as low as $20,000, though more-advanced machines quickly jump into the $40,000 to $60,000 range.
Still, Dr. Rosen views the practical uses of the technology as almost endless, and could include vascular access, placing central and PICC lines, and insertion and removal of catheters. Most hospitalists, however, continue to have limited experience with portable ultrasound, meaning those interested in learning more likely have to seek out physicians in other departments to provide the training and mentorship required. Dr. Rosen suggests working with ED physicians, OB-GYNs, and radiologists, although he notes you should be careful to be clear that the HM community is not looking to supplant anyone, or take billing opportunities away.
Hospitalists “don’t know how to use it, and people don’t know where to go to learn how to use it,” he says. “This is a starting point that will allow people … to take these ideas back and, hopefully, generate enough of a critical mass that it becomes a louder and louder chorus asking for this technology.”
GRAPEVINE, Texas—Hospitalist Michael Monge, MD, of Cogent Healthcare in San Bernardino, Calif., watched an instructor squeeze the lubricating gel on the transponder and press it gently, but firmly, into the crook of a woman’s arm. Veins practically popped off an ultrasound monitor, serving as a literal road map for vascular access.
And he thought: Wouldn’t it be great if I had this technology all the time, just like I remember from my residency?
“A lot of my ER attendings were able to do a study at the bedside in a manner of minutes, not 30 or 45 minutes,” says Dr. Monge, who practices at Saint Bernardine Medical Center. “If they saw something abnormal, sure enough, they got the full study. But they were able to get that glimpse. Ultimately, it’s just better patient care.”
Dr. Monge’s ultrasound lesson was a first for the SHM annual meeting. In past years, training on ultrasounds was wrapped into the “Medical Procedures for the Hospitalist” pre-course. But at HM11, thanks to the growing prevalence and portability of the technology, the training was expanded into its own half-day pre-course, appropriately dubbed “Portable Ultrasound for the Hospitalist.”
“The ultrasound will be the stethoscope of the 21st century,” says Mark Ault, director of the Division of General Internal Medicine and assistant chairman for clinical affairs of the Department of Medicine at Cedars-Sinai Medical Center in Los Angeles. “And the goal will be to have an ultrasound in the hands of every internist.”
Only time will tell whether portable ultrasound becomes as commonplace as Dr. Ault envisions, but what is clear is that the evolution of the technology makes it widely applicable to hospitalists, says Bradley Rosen, MD, MBA, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Medical Center.
Pricing is one such example. In years past, ultrasound machines were bulky and costly, with price tags in the hundreds of thousands of dollars. Now, portable units, depending on the number of transducers and functionality, can come as low as $20,000, though more-advanced machines quickly jump into the $40,000 to $60,000 range.
Still, Dr. Rosen views the practical uses of the technology as almost endless, and could include vascular access, placing central and PICC lines, and insertion and removal of catheters. Most hospitalists, however, continue to have limited experience with portable ultrasound, meaning those interested in learning more likely have to seek out physicians in other departments to provide the training and mentorship required. Dr. Rosen suggests working with ED physicians, OB-GYNs, and radiologists, although he notes you should be careful to be clear that the HM community is not looking to supplant anyone, or take billing opportunities away.
Hospitalists “don’t know how to use it, and people don’t know where to go to learn how to use it,” he says. “This is a starting point that will allow people … to take these ideas back and, hopefully, generate enough of a critical mass that it becomes a louder and louder chorus asking for this technology.”
The Suggestions Box: SHM's Special Interest Forums
It was only natural when SHM started hosting Special Interest Forums a few meetings ago that a chat devoted to quality would emerge. So it was no surprise when some 60 HM11 attendees crowded into a room to talk about just that. But part of preaching the value of quality is knowing how to preach.
To that end, Mangla Gulati, MD, FACP, assistant professor in the Department of Medicine at the University of Maryland School of Medicine in Baltimore, wants resources to teach her how to talk with administrators on their level. “We need to know the language to parlay with our CFO or CEO,” she says. “That’s what’s helpful for us.”
Joe Miller, SHM’s senior vice president and chief solutions officer, suggested the society could create a microsite within www.hospitalmedicine.org dedicated to the topic. He says there are online toolkits the society has developed in the past, and will continue to develop, that will help introduce hospitalists to already-existing quality initiatives they simply don’t know about. He particularly noted SQUINT, SHM’s searchable database for quality projects that is just getting off the ground.
“The stuff that’s there, I use and I love it,” says Dorothy Pusateri, MD, of Allegheny Hospitalist Service in Pittsburgh. “The stuff on Project BOOST [Better Outcomes for Older Adults through Safer Transitions] was enough to teach me.”
Rural Hospitalists
Small-town hospitalists from every corner of the country discussed recruiting issues, scheduling solutions, advocacy concerns, and more. A group of 15 rural hospitalists shared concerns about brutal, “72-hour” shifts and potential solutions to hiring and staffing issues, including growing your own hospitalists and hiring nonphysician providers (NPPs) to supplement 24/7 coverage.
“You can’t sustain mentally if you are doing all of it by yourself all day, all night,” said Martin Johns, MD, a hospitalist at 25-bed Gifford Medical Center in Randolph, Vt. Dr. Johns suggested rural groups think about utilizing NPPs and physician assistants (PAs) to fill coverage gaps; however, the opinions varied widely in what was considered proper compensation and responsibilities for nonphysicians.
“Our PAs make almost as much as our docs,” said Dale Vizcarra, MD, medical director of the hospitalist group at St. Mary’s Healthcare, a 68-bed critical-care hospital in Pierre, S.D.
The group also discussed at length the difficulties in bringing doctors to small towns. Although compensation can be higher than in large urban centers, the group agreed that the “one-man show” aspect of working as a small-town hospitalist is a detractor.
“I hear it all the time,” said forum moderator Alan Himmelstein, a regional vice president for Sound Physicians. “I can take care of gunshot wounds, but I forgot everything I know about community-acquired pneumonia. You aren’t surrounded by 23 specialists; in rural communities, you guys are the top of the heap. Your skill set, by definition, has to make you comfortable to take care of everything that comes through the door. You don’t have another facility a half-hour away; a lot of your geography doesn’t allow helicopters to fly 365 days.”
Rural hospitalists, who as a group admit nearly 40% of all hospital admissions nationwide, also are looking for a voice. “We’re a huge constituency,” Dr. Johns said, “and we are under-represented.”
Jason Carris, editor of The Hospitalist, contributed to this report.
It was only natural when SHM started hosting Special Interest Forums a few meetings ago that a chat devoted to quality would emerge. So it was no surprise when some 60 HM11 attendees crowded into a room to talk about just that. But part of preaching the value of quality is knowing how to preach.
To that end, Mangla Gulati, MD, FACP, assistant professor in the Department of Medicine at the University of Maryland School of Medicine in Baltimore, wants resources to teach her how to talk with administrators on their level. “We need to know the language to parlay with our CFO or CEO,” she says. “That’s what’s helpful for us.”
Joe Miller, SHM’s senior vice president and chief solutions officer, suggested the society could create a microsite within www.hospitalmedicine.org dedicated to the topic. He says there are online toolkits the society has developed in the past, and will continue to develop, that will help introduce hospitalists to already-existing quality initiatives they simply don’t know about. He particularly noted SQUINT, SHM’s searchable database for quality projects that is just getting off the ground.
“The stuff that’s there, I use and I love it,” says Dorothy Pusateri, MD, of Allegheny Hospitalist Service in Pittsburgh. “The stuff on Project BOOST [Better Outcomes for Older Adults through Safer Transitions] was enough to teach me.”
Rural Hospitalists
Small-town hospitalists from every corner of the country discussed recruiting issues, scheduling solutions, advocacy concerns, and more. A group of 15 rural hospitalists shared concerns about brutal, “72-hour” shifts and potential solutions to hiring and staffing issues, including growing your own hospitalists and hiring nonphysician providers (NPPs) to supplement 24/7 coverage.
“You can’t sustain mentally if you are doing all of it by yourself all day, all night,” said Martin Johns, MD, a hospitalist at 25-bed Gifford Medical Center in Randolph, Vt. Dr. Johns suggested rural groups think about utilizing NPPs and physician assistants (PAs) to fill coverage gaps; however, the opinions varied widely in what was considered proper compensation and responsibilities for nonphysicians.
“Our PAs make almost as much as our docs,” said Dale Vizcarra, MD, medical director of the hospitalist group at St. Mary’s Healthcare, a 68-bed critical-care hospital in Pierre, S.D.
The group also discussed at length the difficulties in bringing doctors to small towns. Although compensation can be higher than in large urban centers, the group agreed that the “one-man show” aspect of working as a small-town hospitalist is a detractor.
“I hear it all the time,” said forum moderator Alan Himmelstein, a regional vice president for Sound Physicians. “I can take care of gunshot wounds, but I forgot everything I know about community-acquired pneumonia. You aren’t surrounded by 23 specialists; in rural communities, you guys are the top of the heap. Your skill set, by definition, has to make you comfortable to take care of everything that comes through the door. You don’t have another facility a half-hour away; a lot of your geography doesn’t allow helicopters to fly 365 days.”
Rural hospitalists, who as a group admit nearly 40% of all hospital admissions nationwide, also are looking for a voice. “We’re a huge constituency,” Dr. Johns said, “and we are under-represented.”
Jason Carris, editor of The Hospitalist, contributed to this report.
It was only natural when SHM started hosting Special Interest Forums a few meetings ago that a chat devoted to quality would emerge. So it was no surprise when some 60 HM11 attendees crowded into a room to talk about just that. But part of preaching the value of quality is knowing how to preach.
To that end, Mangla Gulati, MD, FACP, assistant professor in the Department of Medicine at the University of Maryland School of Medicine in Baltimore, wants resources to teach her how to talk with administrators on their level. “We need to know the language to parlay with our CFO or CEO,” she says. “That’s what’s helpful for us.”
Joe Miller, SHM’s senior vice president and chief solutions officer, suggested the society could create a microsite within www.hospitalmedicine.org dedicated to the topic. He says there are online toolkits the society has developed in the past, and will continue to develop, that will help introduce hospitalists to already-existing quality initiatives they simply don’t know about. He particularly noted SQUINT, SHM’s searchable database for quality projects that is just getting off the ground.
“The stuff that’s there, I use and I love it,” says Dorothy Pusateri, MD, of Allegheny Hospitalist Service in Pittsburgh. “The stuff on Project BOOST [Better Outcomes for Older Adults through Safer Transitions] was enough to teach me.”
Rural Hospitalists
Small-town hospitalists from every corner of the country discussed recruiting issues, scheduling solutions, advocacy concerns, and more. A group of 15 rural hospitalists shared concerns about brutal, “72-hour” shifts and potential solutions to hiring and staffing issues, including growing your own hospitalists and hiring nonphysician providers (NPPs) to supplement 24/7 coverage.
“You can’t sustain mentally if you are doing all of it by yourself all day, all night,” said Martin Johns, MD, a hospitalist at 25-bed Gifford Medical Center in Randolph, Vt. Dr. Johns suggested rural groups think about utilizing NPPs and physician assistants (PAs) to fill coverage gaps; however, the opinions varied widely in what was considered proper compensation and responsibilities for nonphysicians.
“Our PAs make almost as much as our docs,” said Dale Vizcarra, MD, medical director of the hospitalist group at St. Mary’s Healthcare, a 68-bed critical-care hospital in Pierre, S.D.
The group also discussed at length the difficulties in bringing doctors to small towns. Although compensation can be higher than in large urban centers, the group agreed that the “one-man show” aspect of working as a small-town hospitalist is a detractor.
“I hear it all the time,” said forum moderator Alan Himmelstein, a regional vice president for Sound Physicians. “I can take care of gunshot wounds, but I forgot everything I know about community-acquired pneumonia. You aren’t surrounded by 23 specialists; in rural communities, you guys are the top of the heap. Your skill set, by definition, has to make you comfortable to take care of everything that comes through the door. You don’t have another facility a half-hour away; a lot of your geography doesn’t allow helicopters to fly 365 days.”
Rural hospitalists, who as a group admit nearly 40% of all hospital admissions nationwide, also are looking for a voice. “We’re a huge constituency,” Dr. Johns said, “and we are under-represented.”
Jason Carris, editor of The Hospitalist, contributed to this report.
HM=Improved Patient Care
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”