User login
Large gallstone ileus
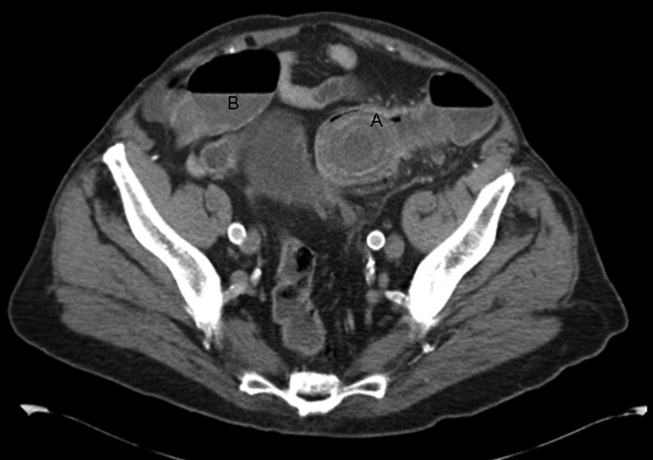
A 92‐year old man presented with a 5‐day history of obstipation, nausea, and vomiting. A computed tomography (CT) scan of the abdomen revealed a 4.1‐cm gallstone impacted in the sigmoid colon (Figure 1). The proximal colon was diffusely dilated in caliber consistent with obstruction (Figure 1B). The CT also showed a cholecystocolic fistula at the hepatic flexure of the colon (Figure 2) with an edematous gallbladder wall and a residual 3.8‐cm gallstone. Under colonoscopic guidance the stone was fragmented using intraluminal shock wave lithotripsy and other endoscopic techniques. The pieces were retrieved (Figure 3, shown reassembled). Cholecystectomy, common hepatic duct repair, and fistula takedown were electively performed to prevent recurrence.



Gallstone ileus is the mechanical impaction of gallstones within the gastrointestinal (GI) tract. It requires the formation of either a biliary‐enteric fistula or less often a choledocho‐enteric fistula. Usually the stone must be 2 cm or greater to cause obstruction.1 The site of obstruction is typically the terminal ileum or ileocecal valve because of the smaller diameter lumen and less active peristalsis. Although mortality rates approach 15%,2 this patient did remarkably well with early recognition, use of complex endoscopic removal, and avoidance of urgent laparotomy.
- ,.Gallstone ileus: a review of 1001 reported cases.Am Surg.1994;60:441–446.
- ,,,,,.[Gallstone Ileus: results of analysis of a series of 40 patients].Gastroenterol Hepatol.2001;24:489–494. In Spanish.
A 92‐year old man presented with a 5‐day history of obstipation, nausea, and vomiting. A computed tomography (CT) scan of the abdomen revealed a 4.1‐cm gallstone impacted in the sigmoid colon (Figure 1). The proximal colon was diffusely dilated in caliber consistent with obstruction (Figure 1B). The CT also showed a cholecystocolic fistula at the hepatic flexure of the colon (Figure 2) with an edematous gallbladder wall and a residual 3.8‐cm gallstone. Under colonoscopic guidance the stone was fragmented using intraluminal shock wave lithotripsy and other endoscopic techniques. The pieces were retrieved (Figure 3, shown reassembled). Cholecystectomy, common hepatic duct repair, and fistula takedown were electively performed to prevent recurrence.



Gallstone ileus is the mechanical impaction of gallstones within the gastrointestinal (GI) tract. It requires the formation of either a biliary‐enteric fistula or less often a choledocho‐enteric fistula. Usually the stone must be 2 cm or greater to cause obstruction.1 The site of obstruction is typically the terminal ileum or ileocecal valve because of the smaller diameter lumen and less active peristalsis. Although mortality rates approach 15%,2 this patient did remarkably well with early recognition, use of complex endoscopic removal, and avoidance of urgent laparotomy.
A 92‐year old man presented with a 5‐day history of obstipation, nausea, and vomiting. A computed tomography (CT) scan of the abdomen revealed a 4.1‐cm gallstone impacted in the sigmoid colon (Figure 1). The proximal colon was diffusely dilated in caliber consistent with obstruction (Figure 1B). The CT also showed a cholecystocolic fistula at the hepatic flexure of the colon (Figure 2) with an edematous gallbladder wall and a residual 3.8‐cm gallstone. Under colonoscopic guidance the stone was fragmented using intraluminal shock wave lithotripsy and other endoscopic techniques. The pieces were retrieved (Figure 3, shown reassembled). Cholecystectomy, common hepatic duct repair, and fistula takedown were electively performed to prevent recurrence.



Gallstone ileus is the mechanical impaction of gallstones within the gastrointestinal (GI) tract. It requires the formation of either a biliary‐enteric fistula or less often a choledocho‐enteric fistula. Usually the stone must be 2 cm or greater to cause obstruction.1 The site of obstruction is typically the terminal ileum or ileocecal valve because of the smaller diameter lumen and less active peristalsis. Although mortality rates approach 15%,2 this patient did remarkably well with early recognition, use of complex endoscopic removal, and avoidance of urgent laparotomy.
- ,.Gallstone ileus: a review of 1001 reported cases.Am Surg.1994;60:441–446.
- ,,,,,.[Gallstone Ileus: results of analysis of a series of 40 patients].Gastroenterol Hepatol.2001;24:489–494. In Spanish.
- ,.Gallstone ileus: a review of 1001 reported cases.Am Surg.1994;60:441–446.
- ,,,,,.[Gallstone Ileus: results of analysis of a series of 40 patients].Gastroenterol Hepatol.2001;24:489–494. In Spanish.
The Medicaid Gap
Amid the recent focus on Medicare’s spiraling costs and efforts to rein in government spending, media accounts have painted a grim picture of Medicaid financing as well:
- With record enrollment, Kentucky’s Medicaid program is facing a budget shortfall of nearly $500 million. In Arizona, the gap is expected to be $1 billion.
- In September, Washington state announced $112.8 million in Medicaid cuts, a reduction that the state’s Medicaid director described as “devastating.”
- According to the Kaiser Family Foundation, Louisiana cut Medicaid inpatient hospital rates 3.5% in fiscal year 2009, 12.1% in 2010, and an additional 4.6% for 2011 to help close budget gaps.
- Maine politicians are facing off over a $380 million state debt owed to hospitals providing Medicaid services.
Safety-net hospitals that care for a disproportionate share of uninsured and Medicaid patients are likely to feel the most pain. So what does that mean for hospitalists? Experts say they will be increasingly looked to for guidance and leadership in identifying cost-saving measures and in helping hospitals avoid further penalties by focusing on such critical metrics as readmission rates.
Political ‘Hot Potato’
The pressure isn’t likely to ease anytime soon. The American Recovery and Reinvestment Act provided $87 billion to help states pay for Medicaid costs from October 2008 through the end of this year by temporarily boosting the federal Medicaid matching rate, officially known as the Federal Medical Assistance Percentages (FMAP). In August, Congress passed legislation that provided an additional $16.1 billion to provide six more months of scaled-back relief through June, when the fiscal year ends in most states.
That’s when things could get really sticky. According to an annual survey conducted by the Kaiser Family Foundation, average state spending on Medicaid jumped 8.8% last year, the biggest increase in eight years and higher than the initial prediction of 6.3%. State Medicaid officials reported swelling ranks of eligible families due to the recession as a main reason for the rise. The pace is expected to cool slightly next year, but states that had relied heavily on federal aid to meet budget shortfalls are now facing the prospect of doing without amid a continued expansion of Medicaid enrollees.
“That’s the catch-22 that you’re in right now,” says Ellen Kugler, executive director of the National Association of Urban Hospitals, based in Sterling, Va. “There is increased demand and increasing numbers of uninsured. States are still in fiscal crisis, and there’s a delay before new dollars become available.”
New federal funds become available in 2014 to help pay for insuring those who currently lack insurance. That money will flow either through subsidies to state-administered exchanges or through direct Medicaid payments. But that same year, Kugler says, safety-net hospitals will begin seeing hefty reductions in Medicare disproportionate share (DSH) payments and possibly Medicaid DSH payments, too.
In theory, more people will have some form of health insurance by then, lessening the need to pay hospitals to help them recoup the cost of treating uninsured and underinsured patients. However, Kugler is urging caution on the DSH pay cuts, warning that it’s not clear what the ranks of the newly insured will be. Current projections, she says, suggest that half of those insured patients will fall under Medicaid programs, meaning that significant cuts could pose a financial hardship to hospitals that serve those populations.
Beyond reductions in services and reimbursement rates to doctors and hospitals, few politicians have had the stomach to propose major overhauls in how Medicaid is managed and financed. In New York state, however, a suite of proposals by Lt. Gov. Richard Ravitch has earned praise from The New York Times.1 One would streamline management of the program, now administered by 58 local governments and multiple state agencies. Ravitch also supports reducing the political wrangling over how reimbursement fees are calculated by wresting that power away from the state legislature and giving it to the state’s Medicaid director, who would be advised by an expert panel.
Another unresolved issue is how to pay for the long-term care of chronically ill patients, which in New York accounts for nearly half of its Medicaid spending. Kugler says the high incidence of chronic conditions, including mental illness, among patients in urban settings can contribute to the high readmission rates the new law is set to begin penalizing in 2012. Other studies have found that among Medicaid patients at high risk for frequent hospital admissions, substance abuse can be a major contributor.2
The difficult task, then, is to ensure that the hospitals serving these populations don’t lose even more resources through penalties due to subpar quality metrics. “Do the legwork now. Get your IT systems in place to be able to provide the coordinated care,” Kugler advises. Identifying efficiencies while maintaining the appropriate level of care will be key, whether in appropriate reductions in length of stay or in increased focus on communication with outpatient providers and other forms of outreach.
Hope for the Safety Net
Despite the financial and logistical challenges, Lenny Lopez, MD, MPH, a hospitalist at Brigham and Women’s Hospital and an assistant in health policy at Massachusetts General Hospital, both in Boston, says the situation is far from hopeless for safety-net hospitals. “The idea that if you’re a DSH hospital you’re somehow pegged and destined to provide low-quality care—that does not have to be the case,” he says. Nor do problems such as disparities in how patients are treated necessarily require expensive solutions.
In a recent paper in Academic Emergency Medicine, Dr. Lopez and his colleagues found that among patients with chest pain admitted to EDs, blacks, Hispanics, and those who lacked insurance or were on Medicare were less likely to receive urgent triage care.3 “These are problems that are fixable in a low-cost way,” he argues. “We don’t need another fancy machine to diagnose chest pain.” Rather, he suggests, the problem is really one of quality improvement that centers on boosting guidelines, not buying more equipment or involving more personnel.
Properly defining the problem, Dr. Lopez says, can lead to effective measures to boost quality. Amid the continuing budget crunch, pinpointing where interventions could provide the biggest bang for the buck also might prove enormously helpful.
Of the roughly 4,200 acute-care hospitals in the country, Dr. Lopez and his colleagues found that less than 10% care for the bulk of minority patients, and those on Medicaid or lacking insurance. That means such care is concentrated in about 400 hospitals, “which is a huge opportunity for intervention options for this kind of an issue,” he says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- 1. Benefits and burdens of Medicaid. The New York Times website. Available at: www.nytimes.com/2010/09/22/opinion/22wed2.html?_r=2&hp. Accessed Oct. 23, 2010.
- 2. Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009;86(2):230-241.
- 3. López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997-2006. Acad Emerg Med. 2010:17 (8):801-810.
Amid the recent focus on Medicare’s spiraling costs and efforts to rein in government spending, media accounts have painted a grim picture of Medicaid financing as well:
- With record enrollment, Kentucky’s Medicaid program is facing a budget shortfall of nearly $500 million. In Arizona, the gap is expected to be $1 billion.
- In September, Washington state announced $112.8 million in Medicaid cuts, a reduction that the state’s Medicaid director described as “devastating.”
- According to the Kaiser Family Foundation, Louisiana cut Medicaid inpatient hospital rates 3.5% in fiscal year 2009, 12.1% in 2010, and an additional 4.6% for 2011 to help close budget gaps.
- Maine politicians are facing off over a $380 million state debt owed to hospitals providing Medicaid services.
Safety-net hospitals that care for a disproportionate share of uninsured and Medicaid patients are likely to feel the most pain. So what does that mean for hospitalists? Experts say they will be increasingly looked to for guidance and leadership in identifying cost-saving measures and in helping hospitals avoid further penalties by focusing on such critical metrics as readmission rates.
Political ‘Hot Potato’
The pressure isn’t likely to ease anytime soon. The American Recovery and Reinvestment Act provided $87 billion to help states pay for Medicaid costs from October 2008 through the end of this year by temporarily boosting the federal Medicaid matching rate, officially known as the Federal Medical Assistance Percentages (FMAP). In August, Congress passed legislation that provided an additional $16.1 billion to provide six more months of scaled-back relief through June, when the fiscal year ends in most states.
That’s when things could get really sticky. According to an annual survey conducted by the Kaiser Family Foundation, average state spending on Medicaid jumped 8.8% last year, the biggest increase in eight years and higher than the initial prediction of 6.3%. State Medicaid officials reported swelling ranks of eligible families due to the recession as a main reason for the rise. The pace is expected to cool slightly next year, but states that had relied heavily on federal aid to meet budget shortfalls are now facing the prospect of doing without amid a continued expansion of Medicaid enrollees.
“That’s the catch-22 that you’re in right now,” says Ellen Kugler, executive director of the National Association of Urban Hospitals, based in Sterling, Va. “There is increased demand and increasing numbers of uninsured. States are still in fiscal crisis, and there’s a delay before new dollars become available.”
New federal funds become available in 2014 to help pay for insuring those who currently lack insurance. That money will flow either through subsidies to state-administered exchanges or through direct Medicaid payments. But that same year, Kugler says, safety-net hospitals will begin seeing hefty reductions in Medicare disproportionate share (DSH) payments and possibly Medicaid DSH payments, too.
In theory, more people will have some form of health insurance by then, lessening the need to pay hospitals to help them recoup the cost of treating uninsured and underinsured patients. However, Kugler is urging caution on the DSH pay cuts, warning that it’s not clear what the ranks of the newly insured will be. Current projections, she says, suggest that half of those insured patients will fall under Medicaid programs, meaning that significant cuts could pose a financial hardship to hospitals that serve those populations.
Beyond reductions in services and reimbursement rates to doctors and hospitals, few politicians have had the stomach to propose major overhauls in how Medicaid is managed and financed. In New York state, however, a suite of proposals by Lt. Gov. Richard Ravitch has earned praise from The New York Times.1 One would streamline management of the program, now administered by 58 local governments and multiple state agencies. Ravitch also supports reducing the political wrangling over how reimbursement fees are calculated by wresting that power away from the state legislature and giving it to the state’s Medicaid director, who would be advised by an expert panel.
Another unresolved issue is how to pay for the long-term care of chronically ill patients, which in New York accounts for nearly half of its Medicaid spending. Kugler says the high incidence of chronic conditions, including mental illness, among patients in urban settings can contribute to the high readmission rates the new law is set to begin penalizing in 2012. Other studies have found that among Medicaid patients at high risk for frequent hospital admissions, substance abuse can be a major contributor.2
The difficult task, then, is to ensure that the hospitals serving these populations don’t lose even more resources through penalties due to subpar quality metrics. “Do the legwork now. Get your IT systems in place to be able to provide the coordinated care,” Kugler advises. Identifying efficiencies while maintaining the appropriate level of care will be key, whether in appropriate reductions in length of stay or in increased focus on communication with outpatient providers and other forms of outreach.
Hope for the Safety Net
Despite the financial and logistical challenges, Lenny Lopez, MD, MPH, a hospitalist at Brigham and Women’s Hospital and an assistant in health policy at Massachusetts General Hospital, both in Boston, says the situation is far from hopeless for safety-net hospitals. “The idea that if you’re a DSH hospital you’re somehow pegged and destined to provide low-quality care—that does not have to be the case,” he says. Nor do problems such as disparities in how patients are treated necessarily require expensive solutions.
In a recent paper in Academic Emergency Medicine, Dr. Lopez and his colleagues found that among patients with chest pain admitted to EDs, blacks, Hispanics, and those who lacked insurance or were on Medicare were less likely to receive urgent triage care.3 “These are problems that are fixable in a low-cost way,” he argues. “We don’t need another fancy machine to diagnose chest pain.” Rather, he suggests, the problem is really one of quality improvement that centers on boosting guidelines, not buying more equipment or involving more personnel.
Properly defining the problem, Dr. Lopez says, can lead to effective measures to boost quality. Amid the continuing budget crunch, pinpointing where interventions could provide the biggest bang for the buck also might prove enormously helpful.
Of the roughly 4,200 acute-care hospitals in the country, Dr. Lopez and his colleagues found that less than 10% care for the bulk of minority patients, and those on Medicaid or lacking insurance. That means such care is concentrated in about 400 hospitals, “which is a huge opportunity for intervention options for this kind of an issue,” he says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- 1. Benefits and burdens of Medicaid. The New York Times website. Available at: www.nytimes.com/2010/09/22/opinion/22wed2.html?_r=2&hp. Accessed Oct. 23, 2010.
- 2. Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009;86(2):230-241.
- 3. López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997-2006. Acad Emerg Med. 2010:17 (8):801-810.
Amid the recent focus on Medicare’s spiraling costs and efforts to rein in government spending, media accounts have painted a grim picture of Medicaid financing as well:
- With record enrollment, Kentucky’s Medicaid program is facing a budget shortfall of nearly $500 million. In Arizona, the gap is expected to be $1 billion.
- In September, Washington state announced $112.8 million in Medicaid cuts, a reduction that the state’s Medicaid director described as “devastating.”
- According to the Kaiser Family Foundation, Louisiana cut Medicaid inpatient hospital rates 3.5% in fiscal year 2009, 12.1% in 2010, and an additional 4.6% for 2011 to help close budget gaps.
- Maine politicians are facing off over a $380 million state debt owed to hospitals providing Medicaid services.
Safety-net hospitals that care for a disproportionate share of uninsured and Medicaid patients are likely to feel the most pain. So what does that mean for hospitalists? Experts say they will be increasingly looked to for guidance and leadership in identifying cost-saving measures and in helping hospitals avoid further penalties by focusing on such critical metrics as readmission rates.
Political ‘Hot Potato’
The pressure isn’t likely to ease anytime soon. The American Recovery and Reinvestment Act provided $87 billion to help states pay for Medicaid costs from October 2008 through the end of this year by temporarily boosting the federal Medicaid matching rate, officially known as the Federal Medical Assistance Percentages (FMAP). In August, Congress passed legislation that provided an additional $16.1 billion to provide six more months of scaled-back relief through June, when the fiscal year ends in most states.
That’s when things could get really sticky. According to an annual survey conducted by the Kaiser Family Foundation, average state spending on Medicaid jumped 8.8% last year, the biggest increase in eight years and higher than the initial prediction of 6.3%. State Medicaid officials reported swelling ranks of eligible families due to the recession as a main reason for the rise. The pace is expected to cool slightly next year, but states that had relied heavily on federal aid to meet budget shortfalls are now facing the prospect of doing without amid a continued expansion of Medicaid enrollees.
“That’s the catch-22 that you’re in right now,” says Ellen Kugler, executive director of the National Association of Urban Hospitals, based in Sterling, Va. “There is increased demand and increasing numbers of uninsured. States are still in fiscal crisis, and there’s a delay before new dollars become available.”
New federal funds become available in 2014 to help pay for insuring those who currently lack insurance. That money will flow either through subsidies to state-administered exchanges or through direct Medicaid payments. But that same year, Kugler says, safety-net hospitals will begin seeing hefty reductions in Medicare disproportionate share (DSH) payments and possibly Medicaid DSH payments, too.
In theory, more people will have some form of health insurance by then, lessening the need to pay hospitals to help them recoup the cost of treating uninsured and underinsured patients. However, Kugler is urging caution on the DSH pay cuts, warning that it’s not clear what the ranks of the newly insured will be. Current projections, she says, suggest that half of those insured patients will fall under Medicaid programs, meaning that significant cuts could pose a financial hardship to hospitals that serve those populations.
Beyond reductions in services and reimbursement rates to doctors and hospitals, few politicians have had the stomach to propose major overhauls in how Medicaid is managed and financed. In New York state, however, a suite of proposals by Lt. Gov. Richard Ravitch has earned praise from The New York Times.1 One would streamline management of the program, now administered by 58 local governments and multiple state agencies. Ravitch also supports reducing the political wrangling over how reimbursement fees are calculated by wresting that power away from the state legislature and giving it to the state’s Medicaid director, who would be advised by an expert panel.
Another unresolved issue is how to pay for the long-term care of chronically ill patients, which in New York accounts for nearly half of its Medicaid spending. Kugler says the high incidence of chronic conditions, including mental illness, among patients in urban settings can contribute to the high readmission rates the new law is set to begin penalizing in 2012. Other studies have found that among Medicaid patients at high risk for frequent hospital admissions, substance abuse can be a major contributor.2
The difficult task, then, is to ensure that the hospitals serving these populations don’t lose even more resources through penalties due to subpar quality metrics. “Do the legwork now. Get your IT systems in place to be able to provide the coordinated care,” Kugler advises. Identifying efficiencies while maintaining the appropriate level of care will be key, whether in appropriate reductions in length of stay or in increased focus on communication with outpatient providers and other forms of outreach.
Hope for the Safety Net
Despite the financial and logistical challenges, Lenny Lopez, MD, MPH, a hospitalist at Brigham and Women’s Hospital and an assistant in health policy at Massachusetts General Hospital, both in Boston, says the situation is far from hopeless for safety-net hospitals. “The idea that if you’re a DSH hospital you’re somehow pegged and destined to provide low-quality care—that does not have to be the case,” he says. Nor do problems such as disparities in how patients are treated necessarily require expensive solutions.
In a recent paper in Academic Emergency Medicine, Dr. Lopez and his colleagues found that among patients with chest pain admitted to EDs, blacks, Hispanics, and those who lacked insurance or were on Medicare were less likely to receive urgent triage care.3 “These are problems that are fixable in a low-cost way,” he argues. “We don’t need another fancy machine to diagnose chest pain.” Rather, he suggests, the problem is really one of quality improvement that centers on boosting guidelines, not buying more equipment or involving more personnel.
Properly defining the problem, Dr. Lopez says, can lead to effective measures to boost quality. Amid the continuing budget crunch, pinpointing where interventions could provide the biggest bang for the buck also might prove enormously helpful.
Of the roughly 4,200 acute-care hospitals in the country, Dr. Lopez and his colleagues found that less than 10% care for the bulk of minority patients, and those on Medicaid or lacking insurance. That means such care is concentrated in about 400 hospitals, “which is a huge opportunity for intervention options for this kind of an issue,” he says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- 1. Benefits and burdens of Medicaid. The New York Times website. Available at: www.nytimes.com/2010/09/22/opinion/22wed2.html?_r=2&hp. Accessed Oct. 23, 2010.
- 2. Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009;86(2):230-241.
- 3. López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997-2006. Acad Emerg Med. 2010:17 (8):801-810.
ONLINE EXCLUSIVE: Audio interviews with experts in career advancement, training
Click here to listen to John Nelson, MD, MHM.
Click here to listen to Lakshmi Halasyamani, MD, SFHM.
Click here to listen to Win Whitcomb, MD, MHM.
Click here to listen to John Nelson, MD, MHM.
Click here to listen to Lakshmi Halasyamani, MD, SFHM.
Click here to listen to Win Whitcomb, MD, MHM.
Click here to listen to John Nelson, MD, MHM.
Click here to listen to Lakshmi Halasyamani, MD, SFHM.
Click here to listen to Win Whitcomb, MD, MHM.
Business Blueprint
Perhaps you’ve put in a few years of clinical practice in an HM group. Suddenly, your group needs a director—and everybody stepped back, except you. You now find yourself thrust into an unfamiliar world of bottom-line thinking, budgets, schedules, spreadsheets, decision-making, conflict resolution, recruiting, contract negotiations, and other managerial responsibilities. You’ve tried to learn how to perform most of these duties on the job. But you’ve learned that assuming direct responsibility for the fate of a hospitalist group with millions in annual billing requires skills that weren’t taught in medical school. And you’re struggling.
Maybe you’re a hospitalist residency program director in a teaching hospital setting, and you would like to transition into other hospital administrative leadership roles, such as chair of a medical staff or credentials committee, department chair, vice president of medical affairs, chief medical officer—maybe even CEO. But where do you begin?
The good news is that hospitalists are well positioned for such advancements, there is a core set of skills required for these various leadership positions that you can learn, and there are several places you can turn to for training. The trick is figuring out which skills and aptitudes you already possess, identifying those you need to strengthen, and selecting the training venues that best meet your goals. Your options vary widely, and include simply reading books on management to get up to speed quickly, investing in leadership training seminars and short courses, and pursuing advanced-degree programs in business leadership.
“Over the next 10 years, the single largest source of new CMOs might be hospitalists,” says John Nelson, MD, FACP, MHM, medical director of Overlake Hospital in Bellevue, Wash., and cofounder, past president, and past board member of SHM. “As many specialties focus more of their practice in the ambulatory care setting, that leaves behind those of us who will stay—e.g., hospitalists, radiologists, ER doctors, anesthesiologists—and who think of the hospital as their principal place of work. Of those doctors, hospitalists are probably the most interconnected and networked with all other doctors and all levels of hospital staff. That’s why hospitals are looking toward hospitalists for leadership.”
There is a growing need for HM to develop leaders, Dr. Nelson says, “not just for their own practice, but for various leadership activities within their hospital.”
Start at Self-Assessment
Hospitalist leadership is not for everyone, and you need to find out if you’re making the right decision by pursuing it. For one thing, you’ll need to facilitate consensus among physicians—a notoriously challenging group of professionals who are autonomous by training, conditioned to believe that they always wield veto power and that they don’t have to play by the rules established for everyone else, Dr. Nelson says.
Most daily leadership activities are much more open-ended and far less structured than physicians are used to, entailing simultaneous projects that need to be prioritized, says Dr. Nelson, who splits his time about 30% clinical and 70% administrative. He is a champion for his hospital’s technology initiative, medical director of his institution’s hospitalist practice, physician lead of its palliative-care program, principal of Nelson Flores Hospital Medicine Consultants, and a columnist for The Hospitalist.
How can you find out what you’re good at, what your weaknesses are, and what skills you need to build? There are several personality assessment instruments with which you can appraise your compatibility with leadership culture, says Julia S. Wright, MD, SFHM, FACP, senior medical officer for Canton, Ohio-based Hospitalists Management Group. And there are good self-assessment workbooks to test whether you have an inclination toward leadership, says Mary Jane Kornacki, MS, a partner in the Boston-based consulting firm Amicus Inc. You also can have a personal leadership assessment performed professionally (see “Leadership Self-Assessment,” p. 27).
Identify Core Leadership Requirements
There are various ways to categorize the leadership skills that a hospitalist needs, including these: financial and business literacy, technical savvy for projects like quality and patient safety improvement, planning acumen to identify external trends and implement appropriate change in one’s department or group, and emotional intelligence to engineer cooperative relationships, says Jack Silversin, DMD, DrPH, president of Amicus.
Indeed, the ability to manage the relationships with myriad stakeholders is a hospitalist leader’s central requirement, according to “Hospitalists: A Guide to Building and Sustaining a Successful Program.”1 Stakeholders include patients, families, referring physicians, medical subspecialists and surgeons, the hospital executive team (C-suite), the clinical team (nurses, case management, therapy departments, and others), the HM group itself, and the public.
The hospitalist leader is responsible for many tasks, the authors write, including:
- Blending marketplace needs with those of these various stakeholders;
- Managing budgets, billing and revenue cycles, resources, and performance metrics; and
- Overseeing such operational issues as scheduling, workload, census, staffing, and recruitment.
These duties will likely be time-consuming, but a hospitalist leader should nevertheless maintain a portion of his or her clinical practice to continue to be connected to the core work. “The foundation of your credibility as a leader is that you have excellent clinical skills,” says Winthrop F. Whitcomb, MD, MHM, medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., and SHM cofounder and past president.
Clinical excellence is the foundation of successful leadership because the best quality and safety practices will drive successful hospitalist business practices, according to Lakshmi K. Halasyamani, MD, SFHM, SHM board member and vice president for Quality and Systems Improvement at Saint Joseph Mercy Hospital in Ann Arbor, Mich. “As healthcare reform begins to financially incentivize things like safe patient handoffs and more evidence-based medicine,” she says, “the business part of running a practice is going to quickly align with quality and safety outcomes. That’s what hospital medicine leaders should be focusing on.”
Empathy and communication skills are essential for a leader, who must continually translate messages from hospital administration to rank-and-file physicians, and vice versa, Dr. Whitcomb says. For example, he says, the message that hospitalists want better work conditions and more staff should be presented so that administration hears something like this: “We don’t want care to be unsafe; that would hurt the hospital’s reputation. Some of the hospitalists are burning out, creating the risk of increasing turnover. In fact, length of stay would be lower if the group has better staffing, because they could get the patients earlier in the day and send them home sooner.”
Such “situational awareness” is necessary to win the trust and cooperation of others and avoid becoming marginalized by important allies, says Eric Howell, MD, SFHM, director of the Hospital Medicine Division at Johns Hopkins Bayview Medical Center in Baltimore. “I’ve seen very successful advocates of hospital medicine groups who were not very good leaders,” the SHM board member says, “because they could not see what the leadership above them needed.”
Pursue the Right Training Venues
Once you’ve identified your strengths and weaknesses, as well as the core requirements of your leadership duties, you are ready to pursue the right training path. Leadership can be learned, whether you’re thrust into it and find yourself in “damage control” mode, or you want to pursue new leadership opportunities for career advancement, Dr. Howell says.
Your first step might be to develop your leadership skill set through informal self-help training. The easiest way is by reading books that other hospitalist leaders have found to be valuable when they were starting out (see “Self-Training Resources,” below left).
The next step is to find a mentor. This person should be a good leader whom you trust and respect, and from whom you can seek advice. “A leadership position can be awfully lonely,” Dr. Nelson says. “I suggest that people find a confidant and mentor at their local institution, someone who is very accessible, who they see all the time, who works in the same environment and knows the local politics.” The mentor could be someone you trained with, or under, or perhaps a hospitalist program director at another institution. It could be the chief nursing officer at your institution. “It is reassuring to know that others are facing similar problems elsewhere,” Dr. Nelson adds.
A local mentor can help with technical matters like offering you a “crash course” in financial spreadsheets, says Patience Agborbesong, MD, SFHM, medical director of a 17-hospitalist program at Wake Forest University Baptist Medical Center in Winston-Salem, N.C. She notes that SHM provides networking resources to help you connect with other HM leaders (www.hospitalmedicine.org/leadership).
Large hospitalist groups frequently offer mentorship opportunities throughout their chain of operations, says Ethan B. Dunham, MBA, director of organizational development for Brentwood, Tenn.-based Cogent Healthcare. “If you find you’ve received something akin to a ‘battlefield promotion’ and are in over your head, you can turn to someone who has been there,” Dunham says.

Many larger health systems and academic medical centers—and even some community hospitals—offer in-house leadership training and mentorship programs, says David L. Klocke, MD, chair of the Division of Hospital Internal Medicine at Mayo Clinic in Rochester, Minn. In his institution, physician leaders are paired with partners from administration who fill in any gaps in their management or leadership skills, Dr. Klocke says. “You’re mentoring them as well about medical issues and skills,” he adds.
Another way to hone your skills is to join hospital committees. “Build up time in the saddle,” Dunham says. “Indicate your leadership potential and your interest in taking the next steps.” If you seek out committees, you’ll get on them, Dr. Nelson says. “And once on them, if you can distinguish yourself by helping to lead the committee in a good direction, your career will be off and running,” he explains. There are many kinds of hospital committee work to choose from, including peer review, performance improvement, practice guideline development, utilization review, pharmacy, and therapeutics.
Advanced Training
For hospitalists wanting a deeper dive, more formal business and leadership training is available through a variety of workshops and courses, many of which offer CME credit. “My favorite was the SHM Leadership Academy, which is fairly short and very practical. Every minute was directly relevant to me as a hospitalist,” Dr. Howell says of the four-day program. Covered topics include teamwork collaboration, communication strategies, hospital performance metrics, scheduling and compensation, strategic planning, financial reports, recruitment, negotiation, motivating others, and managing physician performance.
The American College of Physician Executives (ACPE) offers leadership training modules with certification, as well as MBA and MMM (master’s in medical management) programs through partnerships with universities, according to Dr. Agborbesong. There are several other organizations that offer leadership training, she notes, including The Institute for Medical Leadership, the Boot Camp on Leadership Fundamentals for Physicians, the Center for Creative Leadership, and the Carolinas Center for Medical Excellence (CCME) Physician Leadership Institute.
An MBA is an appropriate goal for many hospitalist leadership scenarios, such as entry-level program director, lead hospitalist at a healthcare system with multiple hospital medicine programs, or regional coordinator for a hospital medicine staffing company, says Michael Stahl, PhD, director of the Physician Executive MBA Program and professor of Strategy and Business Planning at the University of Tennessee in Knoxville.
“An MBA program is particularly well-suited to the physician who gets invited, all of a sudden, to be a leader and discovers they don’t have the knowledge, skill sets, tools and techniques, and ways of thinking about the business side of healthcare. It’s not unusual to see people at the start of their leadership careers saying, ‘I’m going to make an investment in my own human capital by earning an accredited MBA,’ ” Stahl says.
A rapidly changing healthcare landscape requires greater attention to business planning, capital and budget, revenue, and cost-containment principles, Stahl notes. “There will be incredible pressure on controlling the cost of healthcare in the future,” he says. “New reimbursement models are probably going to yield lower reimbursement. What we’re most interested in is equipping people with the tools and techniques of finance so that they can learn to model those new reimbursement types, whatever they are, and no matter how their regulations change.”
Although an MBA sounds daunting, many programs are tailored to a new leader’s busy schedule. For example, the Physician Executive MBA program at UT-Knoxville takes only one year to complete, focuses entirely on healthcare contexts, and combines four weeklong residence periods on campus with 40 Web-based classes, typically on Saturday mornings.
Traditional MBA programs typically take two years to complete and require more physical presence on campus. But in return, they offer ongoing face-to-face interaction with faculty and peers from a variety of business backgrounds that immerse you in the culture of business leadership, says Guy David, PhD, assistant professor of Healthcare Management at the Wharton School at the University of Pennsylvania in Philadelphia. Coursework includes finance, marketing, management, entrepreneurship, strategic development, data mining, economics, legal issues, IT, and other areas, David says. The coursework, he adds, gives physicians who have been trained to focus on the individual patient a much broader understanding of the system in which they operate.
Successful career advancement ultimately requires managerial and leadership acumen: proof that you can run the business, manage upstream and downstream communication, and handle administrative and liaison duties within the hospital, Dunham says. “An MBA is a shorthand, a way to signal to people that that skill set exists, maybe rather than having to prove it in the trenches,” he adds.
As the healthcare landscape continues to evolve, there will be a growing demand for physicians—particularly hospitalists—with greater procedural and conceptual understanding of healthcare systems and financials.
“Over time, it may become increasingly important to have received formal education in the business discipline,” Dunham says. “That’s something that time will tell.” TH
Chris Guadagnino is a freelance medical writer based in Philadelphia.
Reference
- Miller JA, Nelson JR, Whitcomb WF. Hospitalists: A Guide to Building and Sustaining a Successful Program. Health Administration Press: Chicago; 2008.
Perhaps you’ve put in a few years of clinical practice in an HM group. Suddenly, your group needs a director—and everybody stepped back, except you. You now find yourself thrust into an unfamiliar world of bottom-line thinking, budgets, schedules, spreadsheets, decision-making, conflict resolution, recruiting, contract negotiations, and other managerial responsibilities. You’ve tried to learn how to perform most of these duties on the job. But you’ve learned that assuming direct responsibility for the fate of a hospitalist group with millions in annual billing requires skills that weren’t taught in medical school. And you’re struggling.
Maybe you’re a hospitalist residency program director in a teaching hospital setting, and you would like to transition into other hospital administrative leadership roles, such as chair of a medical staff or credentials committee, department chair, vice president of medical affairs, chief medical officer—maybe even CEO. But where do you begin?
The good news is that hospitalists are well positioned for such advancements, there is a core set of skills required for these various leadership positions that you can learn, and there are several places you can turn to for training. The trick is figuring out which skills and aptitudes you already possess, identifying those you need to strengthen, and selecting the training venues that best meet your goals. Your options vary widely, and include simply reading books on management to get up to speed quickly, investing in leadership training seminars and short courses, and pursuing advanced-degree programs in business leadership.
“Over the next 10 years, the single largest source of new CMOs might be hospitalists,” says John Nelson, MD, FACP, MHM, medical director of Overlake Hospital in Bellevue, Wash., and cofounder, past president, and past board member of SHM. “As many specialties focus more of their practice in the ambulatory care setting, that leaves behind those of us who will stay—e.g., hospitalists, radiologists, ER doctors, anesthesiologists—and who think of the hospital as their principal place of work. Of those doctors, hospitalists are probably the most interconnected and networked with all other doctors and all levels of hospital staff. That’s why hospitals are looking toward hospitalists for leadership.”
There is a growing need for HM to develop leaders, Dr. Nelson says, “not just for their own practice, but for various leadership activities within their hospital.”
Start at Self-Assessment
Hospitalist leadership is not for everyone, and you need to find out if you’re making the right decision by pursuing it. For one thing, you’ll need to facilitate consensus among physicians—a notoriously challenging group of professionals who are autonomous by training, conditioned to believe that they always wield veto power and that they don’t have to play by the rules established for everyone else, Dr. Nelson says.
Most daily leadership activities are much more open-ended and far less structured than physicians are used to, entailing simultaneous projects that need to be prioritized, says Dr. Nelson, who splits his time about 30% clinical and 70% administrative. He is a champion for his hospital’s technology initiative, medical director of his institution’s hospitalist practice, physician lead of its palliative-care program, principal of Nelson Flores Hospital Medicine Consultants, and a columnist for The Hospitalist.
How can you find out what you’re good at, what your weaknesses are, and what skills you need to build? There are several personality assessment instruments with which you can appraise your compatibility with leadership culture, says Julia S. Wright, MD, SFHM, FACP, senior medical officer for Canton, Ohio-based Hospitalists Management Group. And there are good self-assessment workbooks to test whether you have an inclination toward leadership, says Mary Jane Kornacki, MS, a partner in the Boston-based consulting firm Amicus Inc. You also can have a personal leadership assessment performed professionally (see “Leadership Self-Assessment,” p. 27).
Identify Core Leadership Requirements
There are various ways to categorize the leadership skills that a hospitalist needs, including these: financial and business literacy, technical savvy for projects like quality and patient safety improvement, planning acumen to identify external trends and implement appropriate change in one’s department or group, and emotional intelligence to engineer cooperative relationships, says Jack Silversin, DMD, DrPH, president of Amicus.
Indeed, the ability to manage the relationships with myriad stakeholders is a hospitalist leader’s central requirement, according to “Hospitalists: A Guide to Building and Sustaining a Successful Program.”1 Stakeholders include patients, families, referring physicians, medical subspecialists and surgeons, the hospital executive team (C-suite), the clinical team (nurses, case management, therapy departments, and others), the HM group itself, and the public.
The hospitalist leader is responsible for many tasks, the authors write, including:
- Blending marketplace needs with those of these various stakeholders;
- Managing budgets, billing and revenue cycles, resources, and performance metrics; and
- Overseeing such operational issues as scheduling, workload, census, staffing, and recruitment.
These duties will likely be time-consuming, but a hospitalist leader should nevertheless maintain a portion of his or her clinical practice to continue to be connected to the core work. “The foundation of your credibility as a leader is that you have excellent clinical skills,” says Winthrop F. Whitcomb, MD, MHM, medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., and SHM cofounder and past president.
Clinical excellence is the foundation of successful leadership because the best quality and safety practices will drive successful hospitalist business practices, according to Lakshmi K. Halasyamani, MD, SFHM, SHM board member and vice president for Quality and Systems Improvement at Saint Joseph Mercy Hospital in Ann Arbor, Mich. “As healthcare reform begins to financially incentivize things like safe patient handoffs and more evidence-based medicine,” she says, “the business part of running a practice is going to quickly align with quality and safety outcomes. That’s what hospital medicine leaders should be focusing on.”
Empathy and communication skills are essential for a leader, who must continually translate messages from hospital administration to rank-and-file physicians, and vice versa, Dr. Whitcomb says. For example, he says, the message that hospitalists want better work conditions and more staff should be presented so that administration hears something like this: “We don’t want care to be unsafe; that would hurt the hospital’s reputation. Some of the hospitalists are burning out, creating the risk of increasing turnover. In fact, length of stay would be lower if the group has better staffing, because they could get the patients earlier in the day and send them home sooner.”
Such “situational awareness” is necessary to win the trust and cooperation of others and avoid becoming marginalized by important allies, says Eric Howell, MD, SFHM, director of the Hospital Medicine Division at Johns Hopkins Bayview Medical Center in Baltimore. “I’ve seen very successful advocates of hospital medicine groups who were not very good leaders,” the SHM board member says, “because they could not see what the leadership above them needed.”
Pursue the Right Training Venues
Once you’ve identified your strengths and weaknesses, as well as the core requirements of your leadership duties, you are ready to pursue the right training path. Leadership can be learned, whether you’re thrust into it and find yourself in “damage control” mode, or you want to pursue new leadership opportunities for career advancement, Dr. Howell says.
Your first step might be to develop your leadership skill set through informal self-help training. The easiest way is by reading books that other hospitalist leaders have found to be valuable when they were starting out (see “Self-Training Resources,” below left).
The next step is to find a mentor. This person should be a good leader whom you trust and respect, and from whom you can seek advice. “A leadership position can be awfully lonely,” Dr. Nelson says. “I suggest that people find a confidant and mentor at their local institution, someone who is very accessible, who they see all the time, who works in the same environment and knows the local politics.” The mentor could be someone you trained with, or under, or perhaps a hospitalist program director at another institution. It could be the chief nursing officer at your institution. “It is reassuring to know that others are facing similar problems elsewhere,” Dr. Nelson adds.
A local mentor can help with technical matters like offering you a “crash course” in financial spreadsheets, says Patience Agborbesong, MD, SFHM, medical director of a 17-hospitalist program at Wake Forest University Baptist Medical Center in Winston-Salem, N.C. She notes that SHM provides networking resources to help you connect with other HM leaders (www.hospitalmedicine.org/leadership).
Large hospitalist groups frequently offer mentorship opportunities throughout their chain of operations, says Ethan B. Dunham, MBA, director of organizational development for Brentwood, Tenn.-based Cogent Healthcare. “If you find you’ve received something akin to a ‘battlefield promotion’ and are in over your head, you can turn to someone who has been there,” Dunham says.

Many larger health systems and academic medical centers—and even some community hospitals—offer in-house leadership training and mentorship programs, says David L. Klocke, MD, chair of the Division of Hospital Internal Medicine at Mayo Clinic in Rochester, Minn. In his institution, physician leaders are paired with partners from administration who fill in any gaps in their management or leadership skills, Dr. Klocke says. “You’re mentoring them as well about medical issues and skills,” he adds.
Another way to hone your skills is to join hospital committees. “Build up time in the saddle,” Dunham says. “Indicate your leadership potential and your interest in taking the next steps.” If you seek out committees, you’ll get on them, Dr. Nelson says. “And once on them, if you can distinguish yourself by helping to lead the committee in a good direction, your career will be off and running,” he explains. There are many kinds of hospital committee work to choose from, including peer review, performance improvement, practice guideline development, utilization review, pharmacy, and therapeutics.
Advanced Training
For hospitalists wanting a deeper dive, more formal business and leadership training is available through a variety of workshops and courses, many of which offer CME credit. “My favorite was the SHM Leadership Academy, which is fairly short and very practical. Every minute was directly relevant to me as a hospitalist,” Dr. Howell says of the four-day program. Covered topics include teamwork collaboration, communication strategies, hospital performance metrics, scheduling and compensation, strategic planning, financial reports, recruitment, negotiation, motivating others, and managing physician performance.
The American College of Physician Executives (ACPE) offers leadership training modules with certification, as well as MBA and MMM (master’s in medical management) programs through partnerships with universities, according to Dr. Agborbesong. There are several other organizations that offer leadership training, she notes, including The Institute for Medical Leadership, the Boot Camp on Leadership Fundamentals for Physicians, the Center for Creative Leadership, and the Carolinas Center for Medical Excellence (CCME) Physician Leadership Institute.
An MBA is an appropriate goal for many hospitalist leadership scenarios, such as entry-level program director, lead hospitalist at a healthcare system with multiple hospital medicine programs, or regional coordinator for a hospital medicine staffing company, says Michael Stahl, PhD, director of the Physician Executive MBA Program and professor of Strategy and Business Planning at the University of Tennessee in Knoxville.
“An MBA program is particularly well-suited to the physician who gets invited, all of a sudden, to be a leader and discovers they don’t have the knowledge, skill sets, tools and techniques, and ways of thinking about the business side of healthcare. It’s not unusual to see people at the start of their leadership careers saying, ‘I’m going to make an investment in my own human capital by earning an accredited MBA,’ ” Stahl says.
A rapidly changing healthcare landscape requires greater attention to business planning, capital and budget, revenue, and cost-containment principles, Stahl notes. “There will be incredible pressure on controlling the cost of healthcare in the future,” he says. “New reimbursement models are probably going to yield lower reimbursement. What we’re most interested in is equipping people with the tools and techniques of finance so that they can learn to model those new reimbursement types, whatever they are, and no matter how their regulations change.”
Although an MBA sounds daunting, many programs are tailored to a new leader’s busy schedule. For example, the Physician Executive MBA program at UT-Knoxville takes only one year to complete, focuses entirely on healthcare contexts, and combines four weeklong residence periods on campus with 40 Web-based classes, typically on Saturday mornings.
Traditional MBA programs typically take two years to complete and require more physical presence on campus. But in return, they offer ongoing face-to-face interaction with faculty and peers from a variety of business backgrounds that immerse you in the culture of business leadership, says Guy David, PhD, assistant professor of Healthcare Management at the Wharton School at the University of Pennsylvania in Philadelphia. Coursework includes finance, marketing, management, entrepreneurship, strategic development, data mining, economics, legal issues, IT, and other areas, David says. The coursework, he adds, gives physicians who have been trained to focus on the individual patient a much broader understanding of the system in which they operate.
Successful career advancement ultimately requires managerial and leadership acumen: proof that you can run the business, manage upstream and downstream communication, and handle administrative and liaison duties within the hospital, Dunham says. “An MBA is a shorthand, a way to signal to people that that skill set exists, maybe rather than having to prove it in the trenches,” he adds.
As the healthcare landscape continues to evolve, there will be a growing demand for physicians—particularly hospitalists—with greater procedural and conceptual understanding of healthcare systems and financials.
“Over time, it may become increasingly important to have received formal education in the business discipline,” Dunham says. “That’s something that time will tell.” TH
Chris Guadagnino is a freelance medical writer based in Philadelphia.
Reference
- Miller JA, Nelson JR, Whitcomb WF. Hospitalists: A Guide to Building and Sustaining a Successful Program. Health Administration Press: Chicago; 2008.
Perhaps you’ve put in a few years of clinical practice in an HM group. Suddenly, your group needs a director—and everybody stepped back, except you. You now find yourself thrust into an unfamiliar world of bottom-line thinking, budgets, schedules, spreadsheets, decision-making, conflict resolution, recruiting, contract negotiations, and other managerial responsibilities. You’ve tried to learn how to perform most of these duties on the job. But you’ve learned that assuming direct responsibility for the fate of a hospitalist group with millions in annual billing requires skills that weren’t taught in medical school. And you’re struggling.
Maybe you’re a hospitalist residency program director in a teaching hospital setting, and you would like to transition into other hospital administrative leadership roles, such as chair of a medical staff or credentials committee, department chair, vice president of medical affairs, chief medical officer—maybe even CEO. But where do you begin?
The good news is that hospitalists are well positioned for such advancements, there is a core set of skills required for these various leadership positions that you can learn, and there are several places you can turn to for training. The trick is figuring out which skills and aptitudes you already possess, identifying those you need to strengthen, and selecting the training venues that best meet your goals. Your options vary widely, and include simply reading books on management to get up to speed quickly, investing in leadership training seminars and short courses, and pursuing advanced-degree programs in business leadership.
“Over the next 10 years, the single largest source of new CMOs might be hospitalists,” says John Nelson, MD, FACP, MHM, medical director of Overlake Hospital in Bellevue, Wash., and cofounder, past president, and past board member of SHM. “As many specialties focus more of their practice in the ambulatory care setting, that leaves behind those of us who will stay—e.g., hospitalists, radiologists, ER doctors, anesthesiologists—and who think of the hospital as their principal place of work. Of those doctors, hospitalists are probably the most interconnected and networked with all other doctors and all levels of hospital staff. That’s why hospitals are looking toward hospitalists for leadership.”
There is a growing need for HM to develop leaders, Dr. Nelson says, “not just for their own practice, but for various leadership activities within their hospital.”
Start at Self-Assessment
Hospitalist leadership is not for everyone, and you need to find out if you’re making the right decision by pursuing it. For one thing, you’ll need to facilitate consensus among physicians—a notoriously challenging group of professionals who are autonomous by training, conditioned to believe that they always wield veto power and that they don’t have to play by the rules established for everyone else, Dr. Nelson says.
Most daily leadership activities are much more open-ended and far less structured than physicians are used to, entailing simultaneous projects that need to be prioritized, says Dr. Nelson, who splits his time about 30% clinical and 70% administrative. He is a champion for his hospital’s technology initiative, medical director of his institution’s hospitalist practice, physician lead of its palliative-care program, principal of Nelson Flores Hospital Medicine Consultants, and a columnist for The Hospitalist.
How can you find out what you’re good at, what your weaknesses are, and what skills you need to build? There are several personality assessment instruments with which you can appraise your compatibility with leadership culture, says Julia S. Wright, MD, SFHM, FACP, senior medical officer for Canton, Ohio-based Hospitalists Management Group. And there are good self-assessment workbooks to test whether you have an inclination toward leadership, says Mary Jane Kornacki, MS, a partner in the Boston-based consulting firm Amicus Inc. You also can have a personal leadership assessment performed professionally (see “Leadership Self-Assessment,” p. 27).
Identify Core Leadership Requirements
There are various ways to categorize the leadership skills that a hospitalist needs, including these: financial and business literacy, technical savvy for projects like quality and patient safety improvement, planning acumen to identify external trends and implement appropriate change in one’s department or group, and emotional intelligence to engineer cooperative relationships, says Jack Silversin, DMD, DrPH, president of Amicus.
Indeed, the ability to manage the relationships with myriad stakeholders is a hospitalist leader’s central requirement, according to “Hospitalists: A Guide to Building and Sustaining a Successful Program.”1 Stakeholders include patients, families, referring physicians, medical subspecialists and surgeons, the hospital executive team (C-suite), the clinical team (nurses, case management, therapy departments, and others), the HM group itself, and the public.
The hospitalist leader is responsible for many tasks, the authors write, including:
- Blending marketplace needs with those of these various stakeholders;
- Managing budgets, billing and revenue cycles, resources, and performance metrics; and
- Overseeing such operational issues as scheduling, workload, census, staffing, and recruitment.
These duties will likely be time-consuming, but a hospitalist leader should nevertheless maintain a portion of his or her clinical practice to continue to be connected to the core work. “The foundation of your credibility as a leader is that you have excellent clinical skills,” says Winthrop F. Whitcomb, MD, MHM, medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., and SHM cofounder and past president.
Clinical excellence is the foundation of successful leadership because the best quality and safety practices will drive successful hospitalist business practices, according to Lakshmi K. Halasyamani, MD, SFHM, SHM board member and vice president for Quality and Systems Improvement at Saint Joseph Mercy Hospital in Ann Arbor, Mich. “As healthcare reform begins to financially incentivize things like safe patient handoffs and more evidence-based medicine,” she says, “the business part of running a practice is going to quickly align with quality and safety outcomes. That’s what hospital medicine leaders should be focusing on.”
Empathy and communication skills are essential for a leader, who must continually translate messages from hospital administration to rank-and-file physicians, and vice versa, Dr. Whitcomb says. For example, he says, the message that hospitalists want better work conditions and more staff should be presented so that administration hears something like this: “We don’t want care to be unsafe; that would hurt the hospital’s reputation. Some of the hospitalists are burning out, creating the risk of increasing turnover. In fact, length of stay would be lower if the group has better staffing, because they could get the patients earlier in the day and send them home sooner.”
Such “situational awareness” is necessary to win the trust and cooperation of others and avoid becoming marginalized by important allies, says Eric Howell, MD, SFHM, director of the Hospital Medicine Division at Johns Hopkins Bayview Medical Center in Baltimore. “I’ve seen very successful advocates of hospital medicine groups who were not very good leaders,” the SHM board member says, “because they could not see what the leadership above them needed.”
Pursue the Right Training Venues
Once you’ve identified your strengths and weaknesses, as well as the core requirements of your leadership duties, you are ready to pursue the right training path. Leadership can be learned, whether you’re thrust into it and find yourself in “damage control” mode, or you want to pursue new leadership opportunities for career advancement, Dr. Howell says.
Your first step might be to develop your leadership skill set through informal self-help training. The easiest way is by reading books that other hospitalist leaders have found to be valuable when they were starting out (see “Self-Training Resources,” below left).
The next step is to find a mentor. This person should be a good leader whom you trust and respect, and from whom you can seek advice. “A leadership position can be awfully lonely,” Dr. Nelson says. “I suggest that people find a confidant and mentor at their local institution, someone who is very accessible, who they see all the time, who works in the same environment and knows the local politics.” The mentor could be someone you trained with, or under, or perhaps a hospitalist program director at another institution. It could be the chief nursing officer at your institution. “It is reassuring to know that others are facing similar problems elsewhere,” Dr. Nelson adds.
A local mentor can help with technical matters like offering you a “crash course” in financial spreadsheets, says Patience Agborbesong, MD, SFHM, medical director of a 17-hospitalist program at Wake Forest University Baptist Medical Center in Winston-Salem, N.C. She notes that SHM provides networking resources to help you connect with other HM leaders (www.hospitalmedicine.org/leadership).
Large hospitalist groups frequently offer mentorship opportunities throughout their chain of operations, says Ethan B. Dunham, MBA, director of organizational development for Brentwood, Tenn.-based Cogent Healthcare. “If you find you’ve received something akin to a ‘battlefield promotion’ and are in over your head, you can turn to someone who has been there,” Dunham says.

Many larger health systems and academic medical centers—and even some community hospitals—offer in-house leadership training and mentorship programs, says David L. Klocke, MD, chair of the Division of Hospital Internal Medicine at Mayo Clinic in Rochester, Minn. In his institution, physician leaders are paired with partners from administration who fill in any gaps in their management or leadership skills, Dr. Klocke says. “You’re mentoring them as well about medical issues and skills,” he adds.
Another way to hone your skills is to join hospital committees. “Build up time in the saddle,” Dunham says. “Indicate your leadership potential and your interest in taking the next steps.” If you seek out committees, you’ll get on them, Dr. Nelson says. “And once on them, if you can distinguish yourself by helping to lead the committee in a good direction, your career will be off and running,” he explains. There are many kinds of hospital committee work to choose from, including peer review, performance improvement, practice guideline development, utilization review, pharmacy, and therapeutics.
Advanced Training
For hospitalists wanting a deeper dive, more formal business and leadership training is available through a variety of workshops and courses, many of which offer CME credit. “My favorite was the SHM Leadership Academy, which is fairly short and very practical. Every minute was directly relevant to me as a hospitalist,” Dr. Howell says of the four-day program. Covered topics include teamwork collaboration, communication strategies, hospital performance metrics, scheduling and compensation, strategic planning, financial reports, recruitment, negotiation, motivating others, and managing physician performance.
The American College of Physician Executives (ACPE) offers leadership training modules with certification, as well as MBA and MMM (master’s in medical management) programs through partnerships with universities, according to Dr. Agborbesong. There are several other organizations that offer leadership training, she notes, including The Institute for Medical Leadership, the Boot Camp on Leadership Fundamentals for Physicians, the Center for Creative Leadership, and the Carolinas Center for Medical Excellence (CCME) Physician Leadership Institute.
An MBA is an appropriate goal for many hospitalist leadership scenarios, such as entry-level program director, lead hospitalist at a healthcare system with multiple hospital medicine programs, or regional coordinator for a hospital medicine staffing company, says Michael Stahl, PhD, director of the Physician Executive MBA Program and professor of Strategy and Business Planning at the University of Tennessee in Knoxville.
“An MBA program is particularly well-suited to the physician who gets invited, all of a sudden, to be a leader and discovers they don’t have the knowledge, skill sets, tools and techniques, and ways of thinking about the business side of healthcare. It’s not unusual to see people at the start of their leadership careers saying, ‘I’m going to make an investment in my own human capital by earning an accredited MBA,’ ” Stahl says.
A rapidly changing healthcare landscape requires greater attention to business planning, capital and budget, revenue, and cost-containment principles, Stahl notes. “There will be incredible pressure on controlling the cost of healthcare in the future,” he says. “New reimbursement models are probably going to yield lower reimbursement. What we’re most interested in is equipping people with the tools and techniques of finance so that they can learn to model those new reimbursement types, whatever they are, and no matter how their regulations change.”
Although an MBA sounds daunting, many programs are tailored to a new leader’s busy schedule. For example, the Physician Executive MBA program at UT-Knoxville takes only one year to complete, focuses entirely on healthcare contexts, and combines four weeklong residence periods on campus with 40 Web-based classes, typically on Saturday mornings.
Traditional MBA programs typically take two years to complete and require more physical presence on campus. But in return, they offer ongoing face-to-face interaction with faculty and peers from a variety of business backgrounds that immerse you in the culture of business leadership, says Guy David, PhD, assistant professor of Healthcare Management at the Wharton School at the University of Pennsylvania in Philadelphia. Coursework includes finance, marketing, management, entrepreneurship, strategic development, data mining, economics, legal issues, IT, and other areas, David says. The coursework, he adds, gives physicians who have been trained to focus on the individual patient a much broader understanding of the system in which they operate.
Successful career advancement ultimately requires managerial and leadership acumen: proof that you can run the business, manage upstream and downstream communication, and handle administrative and liaison duties within the hospital, Dunham says. “An MBA is a shorthand, a way to signal to people that that skill set exists, maybe rather than having to prove it in the trenches,” he adds.
As the healthcare landscape continues to evolve, there will be a growing demand for physicians—particularly hospitalists—with greater procedural and conceptual understanding of healthcare systems and financials.
“Over time, it may become increasingly important to have received formal education in the business discipline,” Dunham says. “That’s something that time will tell.” TH
Chris Guadagnino is a freelance medical writer based in Philadelphia.
Reference
- Miller JA, Nelson JR, Whitcomb WF. Hospitalists: A Guide to Building and Sustaining a Successful Program. Health Administration Press: Chicago; 2008.
Infection-prevention professionals, hospital officials suggest steps to simplify and streamline HAI tracking system
Infection-prevention leaders and state hospital association representatives participated in regional meetings sponsored across the country during the summer of 2009 by the U.S. Department of Health and Human Services (HHS) and suggested ways that the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network (NHSN)—a leading federal system for tracking healthcare-associated infections (HAIs)—could be made easier for hospitals. Participants recommended steps to reduce data-collection burdens and to increase usefulness for hospital infection prevention and quality-improvement (QI) programs.
HHS convened the regional meetings to get stakeholders’ input into HHS’ Action Plan to Prevent Healthcare-Associated Infections (www.hhs.gov/ophs/initiatives/hai/index.html), as well as to hear about their experiences with the network. The action plan is a blueprint for HAI prevention and sets specific targets for monitoring and preventing HAIs nationally. Leaders from various HHS agencies, including the Agency for Healthcare Research and Quality (AHRQ), CDC, Centers for Medicare and Medicaid Services (CMS), the National Institutes of Health (NIH), and the Office of Public Health and Science joined me in discussing participants’ concerns at these meetings.
HHS uses NHSN data to help monitor progress toward the action plan goals. Twenty-eight states require hospitals to report HAIs publicly; most use the NHSN (www.cdc.gov/nhsn). Hospital enrollment in the NHSN has increased dramatically, to more than 2,700 hospitals in mid-2010 from 300 in 2005.
Daniel Pollock, MD, the surveillance branch chief for CDC’s Division of Healthcare Quality Promotion, and I reported on CDC’s efforts to update the NHSN and improve its ease of use. Simplifying and streamlining the system, and assuring sufficient technical capacity and user support, are top priorities. For example:
- CDC has instituted changes in data collection requirements for healthcare-associated urinary tract infections into the NHSN application;
- More NHSN staff were hired to perform comprehensive assessments and upgrades of the system’s technical infrastructure and usability, and to provide additional user support for enrollment and training;
- NHSN will begin migrating this fall to a new system of authenticating users; and
- NHSN Web pages are being redesigned to speed response times during peak use.
Dr. Pollock emphasized that the CDC is committed to accelerating the transition from manual to electronic case detection and reporting for the NHSN, and leveraging advances in health information technology as a primary strategy for enhancing the NHSN. As part of that effort, NHSN now is accepting electronic infection records submitted by hospitals that use commercial infection control surveillance systems.
The CDC continues to work closely with AHRQ, CMS, and the Office of the National Coordinator for Health Information Technology to coordinate integration efforts of federal information systems that provide HAI data. That is part of our commitment here in Washington to support hospitals’ efforts to reduce and eliminate HAIs, and to make healthcare safer for patients and families.
Don Wright, MD, MPH,
deputy assistant secretary for healthcare quality,
U.S. Department of Health and Human Services
Infection-prevention leaders and state hospital association representatives participated in regional meetings sponsored across the country during the summer of 2009 by the U.S. Department of Health and Human Services (HHS) and suggested ways that the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network (NHSN)—a leading federal system for tracking healthcare-associated infections (HAIs)—could be made easier for hospitals. Participants recommended steps to reduce data-collection burdens and to increase usefulness for hospital infection prevention and quality-improvement (QI) programs.
HHS convened the regional meetings to get stakeholders’ input into HHS’ Action Plan to Prevent Healthcare-Associated Infections (www.hhs.gov/ophs/initiatives/hai/index.html), as well as to hear about their experiences with the network. The action plan is a blueprint for HAI prevention and sets specific targets for monitoring and preventing HAIs nationally. Leaders from various HHS agencies, including the Agency for Healthcare Research and Quality (AHRQ), CDC, Centers for Medicare and Medicaid Services (CMS), the National Institutes of Health (NIH), and the Office of Public Health and Science joined me in discussing participants’ concerns at these meetings.
HHS uses NHSN data to help monitor progress toward the action plan goals. Twenty-eight states require hospitals to report HAIs publicly; most use the NHSN (www.cdc.gov/nhsn). Hospital enrollment in the NHSN has increased dramatically, to more than 2,700 hospitals in mid-2010 from 300 in 2005.
Daniel Pollock, MD, the surveillance branch chief for CDC’s Division of Healthcare Quality Promotion, and I reported on CDC’s efforts to update the NHSN and improve its ease of use. Simplifying and streamlining the system, and assuring sufficient technical capacity and user support, are top priorities. For example:
- CDC has instituted changes in data collection requirements for healthcare-associated urinary tract infections into the NHSN application;
- More NHSN staff were hired to perform comprehensive assessments and upgrades of the system’s technical infrastructure and usability, and to provide additional user support for enrollment and training;
- NHSN will begin migrating this fall to a new system of authenticating users; and
- NHSN Web pages are being redesigned to speed response times during peak use.
Dr. Pollock emphasized that the CDC is committed to accelerating the transition from manual to electronic case detection and reporting for the NHSN, and leveraging advances in health information technology as a primary strategy for enhancing the NHSN. As part of that effort, NHSN now is accepting electronic infection records submitted by hospitals that use commercial infection control surveillance systems.
The CDC continues to work closely with AHRQ, CMS, and the Office of the National Coordinator for Health Information Technology to coordinate integration efforts of federal information systems that provide HAI data. That is part of our commitment here in Washington to support hospitals’ efforts to reduce and eliminate HAIs, and to make healthcare safer for patients and families.
Don Wright, MD, MPH,
deputy assistant secretary for healthcare quality,
U.S. Department of Health and Human Services
Infection-prevention leaders and state hospital association representatives participated in regional meetings sponsored across the country during the summer of 2009 by the U.S. Department of Health and Human Services (HHS) and suggested ways that the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network (NHSN)—a leading federal system for tracking healthcare-associated infections (HAIs)—could be made easier for hospitals. Participants recommended steps to reduce data-collection burdens and to increase usefulness for hospital infection prevention and quality-improvement (QI) programs.
HHS convened the regional meetings to get stakeholders’ input into HHS’ Action Plan to Prevent Healthcare-Associated Infections (www.hhs.gov/ophs/initiatives/hai/index.html), as well as to hear about their experiences with the network. The action plan is a blueprint for HAI prevention and sets specific targets for monitoring and preventing HAIs nationally. Leaders from various HHS agencies, including the Agency for Healthcare Research and Quality (AHRQ), CDC, Centers for Medicare and Medicaid Services (CMS), the National Institutes of Health (NIH), and the Office of Public Health and Science joined me in discussing participants’ concerns at these meetings.
HHS uses NHSN data to help monitor progress toward the action plan goals. Twenty-eight states require hospitals to report HAIs publicly; most use the NHSN (www.cdc.gov/nhsn). Hospital enrollment in the NHSN has increased dramatically, to more than 2,700 hospitals in mid-2010 from 300 in 2005.
Daniel Pollock, MD, the surveillance branch chief for CDC’s Division of Healthcare Quality Promotion, and I reported on CDC’s efforts to update the NHSN and improve its ease of use. Simplifying and streamlining the system, and assuring sufficient technical capacity and user support, are top priorities. For example:
- CDC has instituted changes in data collection requirements for healthcare-associated urinary tract infections into the NHSN application;
- More NHSN staff were hired to perform comprehensive assessments and upgrades of the system’s technical infrastructure and usability, and to provide additional user support for enrollment and training;
- NHSN will begin migrating this fall to a new system of authenticating users; and
- NHSN Web pages are being redesigned to speed response times during peak use.
Dr. Pollock emphasized that the CDC is committed to accelerating the transition from manual to electronic case detection and reporting for the NHSN, and leveraging advances in health information technology as a primary strategy for enhancing the NHSN. As part of that effort, NHSN now is accepting electronic infection records submitted by hospitals that use commercial infection control surveillance systems.
The CDC continues to work closely with AHRQ, CMS, and the Office of the National Coordinator for Health Information Technology to coordinate integration efforts of federal information systems that provide HAI data. That is part of our commitment here in Washington to support hospitals’ efforts to reduce and eliminate HAIs, and to make healthcare safer for patients and families.
Don Wright, MD, MPH,
deputy assistant secretary for healthcare quality,
U.S. Department of Health and Human Services
Stage Presence
For hospitalist Robert Wachter, MD, MHM, the next annual SHM meeting will be particularly poignant, and not just because he’s HM11’s featured speaker.
Next year will mark the 15th anniversary of the New England Journal of Medicine article coauthored by Dr. Wachter that introduced the term “hospitalist” to the American healthcare lexicon. The specialty is growing and developing into adulthood nicely, he says, which will be part of his presentation in Grapevine, Texas.
“At age 15, that’s when you move to adolescence—you’re going to be off on adulthood and on your own,” says Dr. Wachter, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president and author of the blog Wachter’s World (www.wachtersworld.com).
Like a proud father, Dr. Wachter expects that he will reminisce about the past, speculate about HM’s bright future, and encourage hospitalists to continue their work.
“This will be an optimistic talk,” he says. “The growth has been extraordinary.”
At the outset of the specialty, Dr. Wachter says, he and colleagues predicted some of the current trends, but they underestimated how powerful some would become.
“We couldn’t have predicted that the pressures to increase quality and safety would be as intense as they are today, but we did a good job believing that these areas were important before they hit,” he says.
Looking forward, he says, other emerging forces will join quality and safety at the forefront of HM. “The next five years will likely bring similar pressures on efficiency and throughput,” he says. “I’m going to encourage folks to stay ahead of the curve.”
Having attended every annual conference since the beginning, Dr. Wachter looks forward to “polar things” about each meeting: catching up with the founders of the movement and seeing new faces.
“What’s more fun for me is the amount of youthful energy at the meetings,” he says, especially of the hospitalists he has mentored over the years. “When I come with my group from UCSF, it gives me tremendous pride.” TH
Brendon Shank is a freelance writer based in Philadelphia.
For hospitalist Robert Wachter, MD, MHM, the next annual SHM meeting will be particularly poignant, and not just because he’s HM11’s featured speaker.
Next year will mark the 15th anniversary of the New England Journal of Medicine article coauthored by Dr. Wachter that introduced the term “hospitalist” to the American healthcare lexicon. The specialty is growing and developing into adulthood nicely, he says, which will be part of his presentation in Grapevine, Texas.
“At age 15, that’s when you move to adolescence—you’re going to be off on adulthood and on your own,” says Dr. Wachter, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president and author of the blog Wachter’s World (www.wachtersworld.com).
Like a proud father, Dr. Wachter expects that he will reminisce about the past, speculate about HM’s bright future, and encourage hospitalists to continue their work.
“This will be an optimistic talk,” he says. “The growth has been extraordinary.”
At the outset of the specialty, Dr. Wachter says, he and colleagues predicted some of the current trends, but they underestimated how powerful some would become.
“We couldn’t have predicted that the pressures to increase quality and safety would be as intense as they are today, but we did a good job believing that these areas were important before they hit,” he says.
Looking forward, he says, other emerging forces will join quality and safety at the forefront of HM. “The next five years will likely bring similar pressures on efficiency and throughput,” he says. “I’m going to encourage folks to stay ahead of the curve.”
Having attended every annual conference since the beginning, Dr. Wachter looks forward to “polar things” about each meeting: catching up with the founders of the movement and seeing new faces.
“What’s more fun for me is the amount of youthful energy at the meetings,” he says, especially of the hospitalists he has mentored over the years. “When I come with my group from UCSF, it gives me tremendous pride.” TH
Brendon Shank is a freelance writer based in Philadelphia.
For hospitalist Robert Wachter, MD, MHM, the next annual SHM meeting will be particularly poignant, and not just because he’s HM11’s featured speaker.
Next year will mark the 15th anniversary of the New England Journal of Medicine article coauthored by Dr. Wachter that introduced the term “hospitalist” to the American healthcare lexicon. The specialty is growing and developing into adulthood nicely, he says, which will be part of his presentation in Grapevine, Texas.
“At age 15, that’s when you move to adolescence—you’re going to be off on adulthood and on your own,” says Dr. Wachter, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president and author of the blog Wachter’s World (www.wachtersworld.com).
Like a proud father, Dr. Wachter expects that he will reminisce about the past, speculate about HM’s bright future, and encourage hospitalists to continue their work.
“This will be an optimistic talk,” he says. “The growth has been extraordinary.”
At the outset of the specialty, Dr. Wachter says, he and colleagues predicted some of the current trends, but they underestimated how powerful some would become.
“We couldn’t have predicted that the pressures to increase quality and safety would be as intense as they are today, but we did a good job believing that these areas were important before they hit,” he says.
Looking forward, he says, other emerging forces will join quality and safety at the forefront of HM. “The next five years will likely bring similar pressures on efficiency and throughput,” he says. “I’m going to encourage folks to stay ahead of the curve.”
Having attended every annual conference since the beginning, Dr. Wachter looks forward to “polar things” about each meeting: catching up with the founders of the movement and seeing new faces.
“What’s more fun for me is the amount of youthful energy at the meetings,” he says, especially of the hospitalists he has mentored over the years. “When I come with my group from UCSF, it gives me tremendous pride.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Fellow in Hospital Medicine Spotlight
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Hospitalists Flock to Free HM App for iPhone, BlackBerry, and Other Handhelds
In less than a year, a smartphone application has attracted the attention of hospitalists across the country. Thousands of individuals have accessed the new “Hospitalist Connection” app since it launched in April.
Developed by Epocrates, one of the leaders in mobile applications in healthcare, “Hospitalist Connection” delivers fresh perspectives and unique content about leading research in hospital medicine. Topics include practice management, quality improvement, and care transitions.
Recent articles have covered the effect that financial incentives can have on HM operations and an editorial from Chad Whelan, MD, FHM, physician editor of “Hospitalist Connection,” about the effects of “presenteeism,” or physicians working when the know they are sick.
“When they are on the job, downtime for hospitalists is rare and valuable,” says Dr. Whelan, director of the Division of Hospital Medicine and associate professor of medicine at Loyola University’s Stritch School of Medicine in Chicago.
“‘Hospitalist Connection’ is an easy way to stay informed on best practices in the field—from anywhere at any time.”
To download and subscribe to “Hospitalist Connection,” visit www.hospitalmedicine.org/epocrates.
For SHM, delivering content to smartphones is a logical move.
“This advances the specialty, and we’re thrilled to make it as easy as possible for our members and others to subscribe,” says Todd Von Deak, MBA, CAE, vice president of operations and general manager of SHM. “This is another tangible way that SHM is helping hospitalists improve the quality, safety, and efficiency of care in the hospital.”
In less than a year, a smartphone application has attracted the attention of hospitalists across the country. Thousands of individuals have accessed the new “Hospitalist Connection” app since it launched in April.
Developed by Epocrates, one of the leaders in mobile applications in healthcare, “Hospitalist Connection” delivers fresh perspectives and unique content about leading research in hospital medicine. Topics include practice management, quality improvement, and care transitions.
Recent articles have covered the effect that financial incentives can have on HM operations and an editorial from Chad Whelan, MD, FHM, physician editor of “Hospitalist Connection,” about the effects of “presenteeism,” or physicians working when the know they are sick.
“When they are on the job, downtime for hospitalists is rare and valuable,” says Dr. Whelan, director of the Division of Hospital Medicine and associate professor of medicine at Loyola University’s Stritch School of Medicine in Chicago.
“‘Hospitalist Connection’ is an easy way to stay informed on best practices in the field—from anywhere at any time.”
To download and subscribe to “Hospitalist Connection,” visit www.hospitalmedicine.org/epocrates.
For SHM, delivering content to smartphones is a logical move.
“This advances the specialty, and we’re thrilled to make it as easy as possible for our members and others to subscribe,” says Todd Von Deak, MBA, CAE, vice president of operations and general manager of SHM. “This is another tangible way that SHM is helping hospitalists improve the quality, safety, and efficiency of care in the hospital.”
In less than a year, a smartphone application has attracted the attention of hospitalists across the country. Thousands of individuals have accessed the new “Hospitalist Connection” app since it launched in April.
Developed by Epocrates, one of the leaders in mobile applications in healthcare, “Hospitalist Connection” delivers fresh perspectives and unique content about leading research in hospital medicine. Topics include practice management, quality improvement, and care transitions.
Recent articles have covered the effect that financial incentives can have on HM operations and an editorial from Chad Whelan, MD, FHM, physician editor of “Hospitalist Connection,” about the effects of “presenteeism,” or physicians working when the know they are sick.
“When they are on the job, downtime for hospitalists is rare and valuable,” says Dr. Whelan, director of the Division of Hospital Medicine and associate professor of medicine at Loyola University’s Stritch School of Medicine in Chicago.
“‘Hospitalist Connection’ is an easy way to stay informed on best practices in the field—from anywhere at any time.”
To download and subscribe to “Hospitalist Connection,” visit www.hospitalmedicine.org/epocrates.
For SHM, delivering content to smartphones is a logical move.
“This advances the specialty, and we’re thrilled to make it as easy as possible for our members and others to subscribe,” says Todd Von Deak, MBA, CAE, vice president of operations and general manager of SHM. “This is another tangible way that SHM is helping hospitalists improve the quality, safety, and efficiency of care in the hospital.”
A New Look at Family Medicine Hospitalists
A new survey spearheaded by SHM’s Family Medicine Task Force gives the first glimpse into the demographics, settings, and scopes of practice of this growing HM segment.
The research found that hospitalists trained in family medicine are experienced physicians who likely work directly for their hospital. More than half (51%) completed residency training more than 10 years ago, although the largest single group of respondents (37%) finished residency six to 10 years ago.
Virtually all respondents (96%) work full-time and a third are hospital employees—the most prevalent staffing model found in the survey. In addition to clinical practice, half of family-medicine-trained hospitalists have teaching and other leadership responsibilities.
The survey is based on responses from 81 of the 263 SHM members registered as family medicine physicians.
“As the number of family-medicine-trained physicians grows within hospital medicine, it’s important for us to understand the people behind it,” said research coauthor Claudia Geyer, MD, FHM.
Family-medicine-trained hospitalists are a growing phenomenon in the specialty. Survey data from 2007 to 2008 revealed that 3.7% of U.S. hospitalists are trained in family medicine; however, SHM’s recent membership data show that more than 6% of SHM members are registered as family medicine physicians.
A new survey spearheaded by SHM’s Family Medicine Task Force gives the first glimpse into the demographics, settings, and scopes of practice of this growing HM segment.
The research found that hospitalists trained in family medicine are experienced physicians who likely work directly for their hospital. More than half (51%) completed residency training more than 10 years ago, although the largest single group of respondents (37%) finished residency six to 10 years ago.
Virtually all respondents (96%) work full-time and a third are hospital employees—the most prevalent staffing model found in the survey. In addition to clinical practice, half of family-medicine-trained hospitalists have teaching and other leadership responsibilities.
The survey is based on responses from 81 of the 263 SHM members registered as family medicine physicians.
“As the number of family-medicine-trained physicians grows within hospital medicine, it’s important for us to understand the people behind it,” said research coauthor Claudia Geyer, MD, FHM.
Family-medicine-trained hospitalists are a growing phenomenon in the specialty. Survey data from 2007 to 2008 revealed that 3.7% of U.S. hospitalists are trained in family medicine; however, SHM’s recent membership data show that more than 6% of SHM members are registered as family medicine physicians.
A new survey spearheaded by SHM’s Family Medicine Task Force gives the first glimpse into the demographics, settings, and scopes of practice of this growing HM segment.
The research found that hospitalists trained in family medicine are experienced physicians who likely work directly for their hospital. More than half (51%) completed residency training more than 10 years ago, although the largest single group of respondents (37%) finished residency six to 10 years ago.
Virtually all respondents (96%) work full-time and a third are hospital employees—the most prevalent staffing model found in the survey. In addition to clinical practice, half of family-medicine-trained hospitalists have teaching and other leadership responsibilities.
The survey is based on responses from 81 of the 263 SHM members registered as family medicine physicians.
“As the number of family-medicine-trained physicians grows within hospital medicine, it’s important for us to understand the people behind it,” said research coauthor Claudia Geyer, MD, FHM.
Family-medicine-trained hospitalists are a growing phenomenon in the specialty. Survey data from 2007 to 2008 revealed that 3.7% of U.S. hospitalists are trained in family medicine; however, SHM’s recent membership data show that more than 6% of SHM members are registered as family medicine physicians.
Fellows Program Application Deadline is Jan. 14
Next year’s annual meeting in Dallas marks the third induction of fellows into the SHM Fellows program. Candidates still have a few weeks to submit an application. The deadline for 2011 applications is Jan. 14.
More than 700 fellows and senior fellows have been inducted since the program began in 2009. “The success and enthusiasm for this program has been incredible,” says Todd Von Deak, SHM’s vice president of operations and general manager. “For individual hospitalists, it’s a simple way to demonstrate to patients and hospitals that you take your profession very seriously. For the specialty, it illustrates the growth and accomplishments of hospital medicine to the rest of the healthcare sector.”
In addition to additional rights and privileges from SHM, fellows can append their designation to their name and credentials.
The SHM Fellows program inducts three levels of fellows every year: Fellow in Hospital Medicine (FHM), Senior Fellow in Hospital Medicine (SFHM), and Master in Hospital Medicine (MHM).
To be nominated, both FHM and SFHM designations require five years as a practicing hospitalist and a demonstrated commitment to quality improvement, teamwork, and leadership. An FHM candidate must be an SHM member for at least three years; SFHM candidates must be members for at least five.
Introduced last year, the MHM designation is by invitation only and reserved for the specialty’s leaders and pioneers. The inaugural MHM designees were John Nelson (pictured left), MD, MHM, Robert Watcher (center), MD, MHM, and Winthrop Whitcomb (right), MD, MHM.
For more information or an application, visit www.hospitalmedicine.org/fellows.
FELLOW IN HOSPITAL MEDICINE SPOTLIGHT
Bradley M. Sherman, MD, FACP, FHM
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Next year’s annual meeting in Dallas marks the third induction of fellows into the SHM Fellows program. Candidates still have a few weeks to submit an application. The deadline for 2011 applications is Jan. 14.
More than 700 fellows and senior fellows have been inducted since the program began in 2009. “The success and enthusiasm for this program has been incredible,” says Todd Von Deak, SHM’s vice president of operations and general manager. “For individual hospitalists, it’s a simple way to demonstrate to patients and hospitals that you take your profession very seriously. For the specialty, it illustrates the growth and accomplishments of hospital medicine to the rest of the healthcare sector.”
In addition to additional rights and privileges from SHM, fellows can append their designation to their name and credentials.
The SHM Fellows program inducts three levels of fellows every year: Fellow in Hospital Medicine (FHM), Senior Fellow in Hospital Medicine (SFHM), and Master in Hospital Medicine (MHM).
To be nominated, both FHM and SFHM designations require five years as a practicing hospitalist and a demonstrated commitment to quality improvement, teamwork, and leadership. An FHM candidate must be an SHM member for at least three years; SFHM candidates must be members for at least five.
Introduced last year, the MHM designation is by invitation only and reserved for the specialty’s leaders and pioneers. The inaugural MHM designees were John Nelson (pictured left), MD, MHM, Robert Watcher (center), MD, MHM, and Winthrop Whitcomb (right), MD, MHM.
For more information or an application, visit www.hospitalmedicine.org/fellows.
FELLOW IN HOSPITAL MEDICINE SPOTLIGHT
Bradley M. Sherman, MD, FACP, FHM
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Next year’s annual meeting in Dallas marks the third induction of fellows into the SHM Fellows program. Candidates still have a few weeks to submit an application. The deadline for 2011 applications is Jan. 14.
More than 700 fellows and senior fellows have been inducted since the program began in 2009. “The success and enthusiasm for this program has been incredible,” says Todd Von Deak, SHM’s vice president of operations and general manager. “For individual hospitalists, it’s a simple way to demonstrate to patients and hospitals that you take your profession very seriously. For the specialty, it illustrates the growth and accomplishments of hospital medicine to the rest of the healthcare sector.”
In addition to additional rights and privileges from SHM, fellows can append their designation to their name and credentials.
The SHM Fellows program inducts three levels of fellows every year: Fellow in Hospital Medicine (FHM), Senior Fellow in Hospital Medicine (SFHM), and Master in Hospital Medicine (MHM).
To be nominated, both FHM and SFHM designations require five years as a practicing hospitalist and a demonstrated commitment to quality improvement, teamwork, and leadership. An FHM candidate must be an SHM member for at least three years; SFHM candidates must be members for at least five.
Introduced last year, the MHM designation is by invitation only and reserved for the specialty’s leaders and pioneers. The inaugural MHM designees were John Nelson (pictured left), MD, MHM, Robert Watcher (center), MD, MHM, and Winthrop Whitcomb (right), MD, MHM.
For more information or an application, visit www.hospitalmedicine.org/fellows.
FELLOW IN HOSPITAL MEDICINE SPOTLIGHT
Bradley M. Sherman, MD, FACP, FHM
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte