User login
Identify and Treat Vitamin D Insufficiency
Many children and teenagers are not getting enough vitamin D, and this is a common problem.
I started seeing medical consequences years ago. We did a study of breastfed African American infants who developed rickets because they were so deficient in vitamin D (J. Pediatrics 2000;137:153-7). Based on these data, North Carolina Women, Infants, and Children Program clinics started distributing free multivitamin supplements to breastfeeding infants, and now we see fewer cases in our area.
What is new is that we are seeing the adverse effects of vitamin D deficiency in older kids. We've had vitamin D–deficient teenagers present with seizures, and we see osteoporosis in teenagers. We had one adolescent who broke his hip from just twisting around who was found to have a severe deficiency of vitamin D.
This is a preventable problem. But about 20% of children and teenagers get the recommended amounts of calcium and vitamin D.
Who do you screen for deficiency? We screen in our clinic with one useful question to ask parents and our kids: “How many glasses of milk do you drink a day?” For those who respond one glass or less, we check their serum vitamin D level.
When taking a history, determine if patients take medications that might interfere with vitamin D metabolism. For example, some antiseizure medicines cause vitamin D to break down more quickly. Obviously, if a child has a severe seizure disorder, that individual needs seizure medicine. But you may need to check the vitamin D level and increase supplementation accordingly.
We found 75% of 48 kids with a history of inadequate milk intake had a vitamin D level below 30 ng/mL; 30% of the children had deficient levels (below 20 ng/mL).
The key is prevention. I recommend that infants start drinking vitamin D–fortified milk after they wean off breast milk or formula. We are finding that a tremendous number of kids do not drink milk, and they go directly from the breast or formula to juice and soda. I tell them to drink a glass of milk with their breakfast, lunch, and supper, hoping they will get at least two glasses per day. I accept chocolate milk. It's not ideal, but it's better than no milk at all.
Make sure your patients get adequate calcium in their diet – about 700 mg/day for a young child anda1,200-1,300 mg for an adolescent. Recommend a multivitamin –, which typically has a minimum of 400 U of vitamin D – as well as a calcium supplement. This combination is important because vitamin D facilitates absorption of calcium from the gut.
I recommend milk with 1% or less fat. A lot of people believe that whole milk provides more vitamin D, but that is not the case. If you have lactose-intolerant patients, suggest that they drink a soy milk product fortified with vitamin D.
A good way to explain the importance of vitamin D to kids and parents is that we build up our bones until we're about 20 After that, if we live long enough, we're going to slide down the hill – we will all get osteoporosis. But if you've had your milk and followed recommendations, you'll start your slide downward from the top of the mountain.
In addition to those with poor diets, patients with chronic disease, with malabsorption, or who are confined to the indoors are at higher risk for vitamin D deficiency. If they are severely deficient, you will need to use higher doses of vitamin D or refer them to a specialist.
Specialists cannot see all these patients because vitamin D insufficiency is so common. It's becoming like obesity. We need the general pediatrician's help to screen and treat most of these patients. We can help via phone consultation or referral for severely deficient patients, particularly those who experience a seizure or multiple fractures because of their deficiency.
To diagnose a suspected deficiency of vitamin D, order a serum 25-hydroxyvitamin D level. With that you might want to get a calcium and phosphorus level and an alkaline phosphatase assay (a measure of bone formation).
Do not order a 1,25-dihydroxyvitamin D test. It is easily ordered by mistake with electronic test ordering. But the 1,25 form does not reflect true vitamin D sufficiency or insufficiency, and can confuse clinical diagnosis.
I do not recommend bone density measurements (such as dual-energy x-ray absorptiometry, or DXA) because many of these scans can be misread. You want to take a history, get a vitamin D level, and treat. Otherwise, you are just going to run up medical expenses.
No column on vitamin D would be complete without addressing sunlight. Ultraviolet light from sun exposuer week of sunshine if they are wearing only diapers, or 2 hours per week if fully clothed. That evidently provides an adequawe recommend sunscreen for people who are outdoors for more than just a short period. If children and teenagers are really out in the summer, when most get exposure, they're using sunscreens that block 95% of the rays. So we have become dependent on diet for our vitamin D, and we're not getting it.
Many children and teenagers are not getting enough vitamin D, and this is a common problem.
I started seeing medical consequences years ago. We did a study of breastfed African American infants who developed rickets because they were so deficient in vitamin D (J. Pediatrics 2000;137:153-7). Based on these data, North Carolina Women, Infants, and Children Program clinics started distributing free multivitamin supplements to breastfeeding infants, and now we see fewer cases in our area.
What is new is that we are seeing the adverse effects of vitamin D deficiency in older kids. We've had vitamin D–deficient teenagers present with seizures, and we see osteoporosis in teenagers. We had one adolescent who broke his hip from just twisting around who was found to have a severe deficiency of vitamin D.
This is a preventable problem. But about 20% of children and teenagers get the recommended amounts of calcium and vitamin D.
Who do you screen for deficiency? We screen in our clinic with one useful question to ask parents and our kids: “How many glasses of milk do you drink a day?” For those who respond one glass or less, we check their serum vitamin D level.
When taking a history, determine if patients take medications that might interfere with vitamin D metabolism. For example, some antiseizure medicines cause vitamin D to break down more quickly. Obviously, if a child has a severe seizure disorder, that individual needs seizure medicine. But you may need to check the vitamin D level and increase supplementation accordingly.
We found 75% of 48 kids with a history of inadequate milk intake had a vitamin D level below 30 ng/mL; 30% of the children had deficient levels (below 20 ng/mL).
The key is prevention. I recommend that infants start drinking vitamin D–fortified milk after they wean off breast milk or formula. We are finding that a tremendous number of kids do not drink milk, and they go directly from the breast or formula to juice and soda. I tell them to drink a glass of milk with their breakfast, lunch, and supper, hoping they will get at least two glasses per day. I accept chocolate milk. It's not ideal, but it's better than no milk at all.
Make sure your patients get adequate calcium in their diet – about 700 mg/day for a young child anda1,200-1,300 mg for an adolescent. Recommend a multivitamin –, which typically has a minimum of 400 U of vitamin D – as well as a calcium supplement. This combination is important because vitamin D facilitates absorption of calcium from the gut.
I recommend milk with 1% or less fat. A lot of people believe that whole milk provides more vitamin D, but that is not the case. If you have lactose-intolerant patients, suggest that they drink a soy milk product fortified with vitamin D.
A good way to explain the importance of vitamin D to kids and parents is that we build up our bones until we're about 20 After that, if we live long enough, we're going to slide down the hill – we will all get osteoporosis. But if you've had your milk and followed recommendations, you'll start your slide downward from the top of the mountain.
In addition to those with poor diets, patients with chronic disease, with malabsorption, or who are confined to the indoors are at higher risk for vitamin D deficiency. If they are severely deficient, you will need to use higher doses of vitamin D or refer them to a specialist.
Specialists cannot see all these patients because vitamin D insufficiency is so common. It's becoming like obesity. We need the general pediatrician's help to screen and treat most of these patients. We can help via phone consultation or referral for severely deficient patients, particularly those who experience a seizure or multiple fractures because of their deficiency.
To diagnose a suspected deficiency of vitamin D, order a serum 25-hydroxyvitamin D level. With that you might want to get a calcium and phosphorus level and an alkaline phosphatase assay (a measure of bone formation).
Do not order a 1,25-dihydroxyvitamin D test. It is easily ordered by mistake with electronic test ordering. But the 1,25 form does not reflect true vitamin D sufficiency or insufficiency, and can confuse clinical diagnosis.
I do not recommend bone density measurements (such as dual-energy x-ray absorptiometry, or DXA) because many of these scans can be misread. You want to take a history, get a vitamin D level, and treat. Otherwise, you are just going to run up medical expenses.
No column on vitamin D would be complete without addressing sunlight. Ultraviolet light from sun exposuer week of sunshine if they are wearing only diapers, or 2 hours per week if fully clothed. That evidently provides an adequawe recommend sunscreen for people who are outdoors for more than just a short period. If children and teenagers are really out in the summer, when most get exposure, they're using sunscreens that block 95% of the rays. So we have become dependent on diet for our vitamin D, and we're not getting it.
Many children and teenagers are not getting enough vitamin D, and this is a common problem.
I started seeing medical consequences years ago. We did a study of breastfed African American infants who developed rickets because they were so deficient in vitamin D (J. Pediatrics 2000;137:153-7). Based on these data, North Carolina Women, Infants, and Children Program clinics started distributing free multivitamin supplements to breastfeeding infants, and now we see fewer cases in our area.
What is new is that we are seeing the adverse effects of vitamin D deficiency in older kids. We've had vitamin D–deficient teenagers present with seizures, and we see osteoporosis in teenagers. We had one adolescent who broke his hip from just twisting around who was found to have a severe deficiency of vitamin D.
This is a preventable problem. But about 20% of children and teenagers get the recommended amounts of calcium and vitamin D.
Who do you screen for deficiency? We screen in our clinic with one useful question to ask parents and our kids: “How many glasses of milk do you drink a day?” For those who respond one glass or less, we check their serum vitamin D level.
When taking a history, determine if patients take medications that might interfere with vitamin D metabolism. For example, some antiseizure medicines cause vitamin D to break down more quickly. Obviously, if a child has a severe seizure disorder, that individual needs seizure medicine. But you may need to check the vitamin D level and increase supplementation accordingly.
We found 75% of 48 kids with a history of inadequate milk intake had a vitamin D level below 30 ng/mL; 30% of the children had deficient levels (below 20 ng/mL).
The key is prevention. I recommend that infants start drinking vitamin D–fortified milk after they wean off breast milk or formula. We are finding that a tremendous number of kids do not drink milk, and they go directly from the breast or formula to juice and soda. I tell them to drink a glass of milk with their breakfast, lunch, and supper, hoping they will get at least two glasses per day. I accept chocolate milk. It's not ideal, but it's better than no milk at all.
Make sure your patients get adequate calcium in their diet – about 700 mg/day for a young child anda1,200-1,300 mg for an adolescent. Recommend a multivitamin –, which typically has a minimum of 400 U of vitamin D – as well as a calcium supplement. This combination is important because vitamin D facilitates absorption of calcium from the gut.
I recommend milk with 1% or less fat. A lot of people believe that whole milk provides more vitamin D, but that is not the case. If you have lactose-intolerant patients, suggest that they drink a soy milk product fortified with vitamin D.
A good way to explain the importance of vitamin D to kids and parents is that we build up our bones until we're about 20 After that, if we live long enough, we're going to slide down the hill – we will all get osteoporosis. But if you've had your milk and followed recommendations, you'll start your slide downward from the top of the mountain.
In addition to those with poor diets, patients with chronic disease, with malabsorption, or who are confined to the indoors are at higher risk for vitamin D deficiency. If they are severely deficient, you will need to use higher doses of vitamin D or refer them to a specialist.
Specialists cannot see all these patients because vitamin D insufficiency is so common. It's becoming like obesity. We need the general pediatrician's help to screen and treat most of these patients. We can help via phone consultation or referral for severely deficient patients, particularly those who experience a seizure or multiple fractures because of their deficiency.
To diagnose a suspected deficiency of vitamin D, order a serum 25-hydroxyvitamin D level. With that you might want to get a calcium and phosphorus level and an alkaline phosphatase assay (a measure of bone formation).
Do not order a 1,25-dihydroxyvitamin D test. It is easily ordered by mistake with electronic test ordering. But the 1,25 form does not reflect true vitamin D sufficiency or insufficiency, and can confuse clinical diagnosis.
I do not recommend bone density measurements (such as dual-energy x-ray absorptiometry, or DXA) because many of these scans can be misread. You want to take a history, get a vitamin D level, and treat. Otherwise, you are just going to run up medical expenses.
No column on vitamin D would be complete without addressing sunlight. Ultraviolet light from sun exposuer week of sunshine if they are wearing only diapers, or 2 hours per week if fully clothed. That evidently provides an adequawe recommend sunscreen for people who are outdoors for more than just a short period. If children and teenagers are really out in the summer, when most get exposure, they're using sunscreens that block 95% of the rays. So we have become dependent on diet for our vitamin D, and we're not getting it.
Substance Use in Teens
Adolescent substance use is a big, difficult issue. Alcohol, cigarettes, and marijuana – and to a lesser extent, cocaine – are endemic to most high schools.
It's not at all unusual for high school juniors and seniors to drink or even to binge drink. In addition, about 15%-20% of them smoke cigarettes, depending on the community, and probably more than that try or intermittently smoke marijuana.
One approach is to educate parents about which children may be at higher risk for substance use.
For example, most teenagers are at some risk and need to be watched for any high-risk activities, especially drinking and driving or riding in a car with a friend who has been drinking. If parents begin to see a serious problem – such as binge drinking every weekend, obvious use of marijuana on a regular basis, or obvious use of cocaine – take it very seriously. Talk with patients and parents, and provide a referral for services as indicated.
Other kids might be at slightly higher risk in high school, based on their achievements. A good athlete who joins the varsity team in 9th or 10th grade, or the talented 9th-grader who lands the lead in the high school play, tend to spend more time with juniors and seniors. They get invited to parties and events outside their peer groups. Without the judgment of an older child and while trying to “keep up,” they might be more vulnerable to problematic substance use. The difference between a 14-year-old and a 17-year-old is enormous, and the peer pressure of being with seniors is considerable.
Recognize that some kids start high school already predisposed and at quite high risk for substance use problems: A patient with biologic or genetic risk factors; a patient with untreated depression or anxiety; and/or an adolescent with attention-deficit/hyperactivity disorder (ADHD) are examples.
Left unaddressed, these kids are predisposed to earlier and more serious substance use. Some children with genetic and/or biological risk factors begin drinking heavily before their 14th birthday. In contrast, the typical age of onset for alcohol use includes some experimentation at 15 or 16 years that becomes binge drinking for some a year or two later.
Biology predisposes some adolescents to nicotine addiction or heavy use of marijuana or alcohol. While adolescent brains are in development and experience the expected stress of puberty and building an identity, some teenagers' brains may be more susceptible to addiction than others. In addition, genetics and environment can play a role, evidenced by the higher risks for children whose parents have a personal or family history of substance use problems. If there is a strong history of alcoholism in the family or if a parent is a recovering alcoholic, discuss with parents how their past might influence how they treat their teenager. Advise them what information should be shared to alert the teenager to the potential risks. It might help a child at age 12 or 13 to know that he or she may be especially vulnerable to the dangers of substance use, and this may well open up an avenue of communication and trust that could be helpful later.
Anxiety and depression also have genetic roots in some patients. Asking parents about their family history of substance abuse, depression, or serious mental health disorder should be a routine part of pediatric practice.
In addition, implementing screening tests makes sense in adolescence. Such screening tests are publicly available and reviewed by the American Academy of Pediatrics Bright Futures: Mental Health effort (http://brightfutures.aap.org/3rd_Edition_Guidelines_and_Pocket_Guide.htmlwww.aap.org/pcorss/demos/mht.html
Children with ADHD make up another high-risk group. They also seem to be more vulnerable to cigarettes, alcohol, and marijuana. These teenagers can be driven to find relief in these substances because of brain biology and/or secondary to the stress of living with their ADHD symptoms.
On the plus side, ADHD kids treated appropriately with stimulants and support services have lower levels of substance use and probably higher self-esteem. Ensure they have the best treatment possible for their ADHD to minimize their substance use risk as much as possible.
As they become young teenagers, they should have a full review of all their ADHD treatment and how their typical day plays out at school and at home. Consider some additional preventative counseling to help these children face their substance use challenges throughout adolescence.
Offer such guidance to all children and parents, but especially to those in one of these high-risk groups. Suggest strategies that support and reinforce their resiliency. A warm, positive relationship with an adult is a protective factor. Also, kids who feel connected to a school, church, or sports team tend to be a little more resilient to some of these influences.
Facilitate open, honest communication between the parent and adolescent. Many parents might not realize that this is more effective than are attempts to control their teen's behavior 24/7. Over-control is impossible given the lifestyle of most 15-, 16- or 17-year-olds. Between cell phones, cars, and the amount of time they are out of the house, parents cannot control them to a level of stopping all substance use.
Even if more control is possible, the effort works against the adolescent's developmental trajectory toward increasing autonomy. The real goal of adolescence in our culture is to learn how to live in the real world and to prepare for autonomy as young adults. High school is a preparation for college life and adulthood where good judgment, safety, and socialization are important learned behaviors. Teaching adolescents how to navigate all this is an essential role for physicians and parents.
Part of growing autonomy is privacy. While it is tempting to invade that privacy to learn about substance use or to clarify other concerns, it is not clear that such efforts support the long-term goals of raising a teenager. Such efforts at control and investigation, including blood or urine testing, are best reserved when the benefits outweigh the risks, when there is a substance abuse problem that needs to be addressed.
Adolescent substance use is a big, difficult issue. Alcohol, cigarettes, and marijuana – and to a lesser extent, cocaine – are endemic to most high schools.
It's not at all unusual for high school juniors and seniors to drink or even to binge drink. In addition, about 15%-20% of them smoke cigarettes, depending on the community, and probably more than that try or intermittently smoke marijuana.
One approach is to educate parents about which children may be at higher risk for substance use.
For example, most teenagers are at some risk and need to be watched for any high-risk activities, especially drinking and driving or riding in a car with a friend who has been drinking. If parents begin to see a serious problem – such as binge drinking every weekend, obvious use of marijuana on a regular basis, or obvious use of cocaine – take it very seriously. Talk with patients and parents, and provide a referral for services as indicated.
Other kids might be at slightly higher risk in high school, based on their achievements. A good athlete who joins the varsity team in 9th or 10th grade, or the talented 9th-grader who lands the lead in the high school play, tend to spend more time with juniors and seniors. They get invited to parties and events outside their peer groups. Without the judgment of an older child and while trying to “keep up,” they might be more vulnerable to problematic substance use. The difference between a 14-year-old and a 17-year-old is enormous, and the peer pressure of being with seniors is considerable.
Recognize that some kids start high school already predisposed and at quite high risk for substance use problems: A patient with biologic or genetic risk factors; a patient with untreated depression or anxiety; and/or an adolescent with attention-deficit/hyperactivity disorder (ADHD) are examples.
Left unaddressed, these kids are predisposed to earlier and more serious substance use. Some children with genetic and/or biological risk factors begin drinking heavily before their 14th birthday. In contrast, the typical age of onset for alcohol use includes some experimentation at 15 or 16 years that becomes binge drinking for some a year or two later.
Biology predisposes some adolescents to nicotine addiction or heavy use of marijuana or alcohol. While adolescent brains are in development and experience the expected stress of puberty and building an identity, some teenagers' brains may be more susceptible to addiction than others. In addition, genetics and environment can play a role, evidenced by the higher risks for children whose parents have a personal or family history of substance use problems. If there is a strong history of alcoholism in the family or if a parent is a recovering alcoholic, discuss with parents how their past might influence how they treat their teenager. Advise them what information should be shared to alert the teenager to the potential risks. It might help a child at age 12 or 13 to know that he or she may be especially vulnerable to the dangers of substance use, and this may well open up an avenue of communication and trust that could be helpful later.
Anxiety and depression also have genetic roots in some patients. Asking parents about their family history of substance abuse, depression, or serious mental health disorder should be a routine part of pediatric practice.
In addition, implementing screening tests makes sense in adolescence. Such screening tests are publicly available and reviewed by the American Academy of Pediatrics Bright Futures: Mental Health effort (http://brightfutures.aap.org/3rd_Edition_Guidelines_and_Pocket_Guide.htmlwww.aap.org/pcorss/demos/mht.html
Children with ADHD make up another high-risk group. They also seem to be more vulnerable to cigarettes, alcohol, and marijuana. These teenagers can be driven to find relief in these substances because of brain biology and/or secondary to the stress of living with their ADHD symptoms.
On the plus side, ADHD kids treated appropriately with stimulants and support services have lower levels of substance use and probably higher self-esteem. Ensure they have the best treatment possible for their ADHD to minimize their substance use risk as much as possible.
As they become young teenagers, they should have a full review of all their ADHD treatment and how their typical day plays out at school and at home. Consider some additional preventative counseling to help these children face their substance use challenges throughout adolescence.
Offer such guidance to all children and parents, but especially to those in one of these high-risk groups. Suggest strategies that support and reinforce their resiliency. A warm, positive relationship with an adult is a protective factor. Also, kids who feel connected to a school, church, or sports team tend to be a little more resilient to some of these influences.
Facilitate open, honest communication between the parent and adolescent. Many parents might not realize that this is more effective than are attempts to control their teen's behavior 24/7. Over-control is impossible given the lifestyle of most 15-, 16- or 17-year-olds. Between cell phones, cars, and the amount of time they are out of the house, parents cannot control them to a level of stopping all substance use.
Even if more control is possible, the effort works against the adolescent's developmental trajectory toward increasing autonomy. The real goal of adolescence in our culture is to learn how to live in the real world and to prepare for autonomy as young adults. High school is a preparation for college life and adulthood where good judgment, safety, and socialization are important learned behaviors. Teaching adolescents how to navigate all this is an essential role for physicians and parents.
Part of growing autonomy is privacy. While it is tempting to invade that privacy to learn about substance use or to clarify other concerns, it is not clear that such efforts support the long-term goals of raising a teenager. Such efforts at control and investigation, including blood or urine testing, are best reserved when the benefits outweigh the risks, when there is a substance abuse problem that needs to be addressed.
Adolescent substance use is a big, difficult issue. Alcohol, cigarettes, and marijuana – and to a lesser extent, cocaine – are endemic to most high schools.
It's not at all unusual for high school juniors and seniors to drink or even to binge drink. In addition, about 15%-20% of them smoke cigarettes, depending on the community, and probably more than that try or intermittently smoke marijuana.
One approach is to educate parents about which children may be at higher risk for substance use.
For example, most teenagers are at some risk and need to be watched for any high-risk activities, especially drinking and driving or riding in a car with a friend who has been drinking. If parents begin to see a serious problem – such as binge drinking every weekend, obvious use of marijuana on a regular basis, or obvious use of cocaine – take it very seriously. Talk with patients and parents, and provide a referral for services as indicated.
Other kids might be at slightly higher risk in high school, based on their achievements. A good athlete who joins the varsity team in 9th or 10th grade, or the talented 9th-grader who lands the lead in the high school play, tend to spend more time with juniors and seniors. They get invited to parties and events outside their peer groups. Without the judgment of an older child and while trying to “keep up,” they might be more vulnerable to problematic substance use. The difference between a 14-year-old and a 17-year-old is enormous, and the peer pressure of being with seniors is considerable.
Recognize that some kids start high school already predisposed and at quite high risk for substance use problems: A patient with biologic or genetic risk factors; a patient with untreated depression or anxiety; and/or an adolescent with attention-deficit/hyperactivity disorder (ADHD) are examples.
Left unaddressed, these kids are predisposed to earlier and more serious substance use. Some children with genetic and/or biological risk factors begin drinking heavily before their 14th birthday. In contrast, the typical age of onset for alcohol use includes some experimentation at 15 or 16 years that becomes binge drinking for some a year or two later.
Biology predisposes some adolescents to nicotine addiction or heavy use of marijuana or alcohol. While adolescent brains are in development and experience the expected stress of puberty and building an identity, some teenagers' brains may be more susceptible to addiction than others. In addition, genetics and environment can play a role, evidenced by the higher risks for children whose parents have a personal or family history of substance use problems. If there is a strong history of alcoholism in the family or if a parent is a recovering alcoholic, discuss with parents how their past might influence how they treat their teenager. Advise them what information should be shared to alert the teenager to the potential risks. It might help a child at age 12 or 13 to know that he or she may be especially vulnerable to the dangers of substance use, and this may well open up an avenue of communication and trust that could be helpful later.
Anxiety and depression also have genetic roots in some patients. Asking parents about their family history of substance abuse, depression, or serious mental health disorder should be a routine part of pediatric practice.
In addition, implementing screening tests makes sense in adolescence. Such screening tests are publicly available and reviewed by the American Academy of Pediatrics Bright Futures: Mental Health effort (http://brightfutures.aap.org/3rd_Edition_Guidelines_and_Pocket_Guide.htmlwww.aap.org/pcorss/demos/mht.html
Children with ADHD make up another high-risk group. They also seem to be more vulnerable to cigarettes, alcohol, and marijuana. These teenagers can be driven to find relief in these substances because of brain biology and/or secondary to the stress of living with their ADHD symptoms.
On the plus side, ADHD kids treated appropriately with stimulants and support services have lower levels of substance use and probably higher self-esteem. Ensure they have the best treatment possible for their ADHD to minimize their substance use risk as much as possible.
As they become young teenagers, they should have a full review of all their ADHD treatment and how their typical day plays out at school and at home. Consider some additional preventative counseling to help these children face their substance use challenges throughout adolescence.
Offer such guidance to all children and parents, but especially to those in one of these high-risk groups. Suggest strategies that support and reinforce their resiliency. A warm, positive relationship with an adult is a protective factor. Also, kids who feel connected to a school, church, or sports team tend to be a little more resilient to some of these influences.
Facilitate open, honest communication between the parent and adolescent. Many parents might not realize that this is more effective than are attempts to control their teen's behavior 24/7. Over-control is impossible given the lifestyle of most 15-, 16- or 17-year-olds. Between cell phones, cars, and the amount of time they are out of the house, parents cannot control them to a level of stopping all substance use.
Even if more control is possible, the effort works against the adolescent's developmental trajectory toward increasing autonomy. The real goal of adolescence in our culture is to learn how to live in the real world and to prepare for autonomy as young adults. High school is a preparation for college life and adulthood where good judgment, safety, and socialization are important learned behaviors. Teaching adolescents how to navigate all this is an essential role for physicians and parents.
Part of growing autonomy is privacy. While it is tempting to invade that privacy to learn about substance use or to clarify other concerns, it is not clear that such efforts support the long-term goals of raising a teenager. Such efforts at control and investigation, including blood or urine testing, are best reserved when the benefits outweigh the risks, when there is a substance abuse problem that needs to be addressed.
BCBS of North Carolina’s refund to customers due to changes in health reform legislation
Bryn Nelson in the October issue of The Hospitalist (see “A Taxing Future for HM?,” p. 16) incorrectly states that Blue Cross Blue Shield of North Carolina’s refund to customers was a result of an overcharge. In point of fact, the refund is a result of a one-time opportunity due to the changes brought about by the health reform law. The new rating and grandfathering rules in the Patient Protection and Affordable Care Act create a one-time circumstance enabling these refunds.
The funds come from active life reserves, which are portions of the premium set aside in the early years of a policy to pay future claims and keep rates stable as customers’ medical expenses rise during the life of the policy. However, policies purchased or substantially modified after March 23, 2010, will end in 2014 under the new healthcare reform law, which is when the new products under health reform will be introduced. Therefore, the reserves held for these products will cover a much shorter period of time, allowing for these funds to be released.
Lew Borman,
media relations,
Blue Cross Blue Shield of North Carolina
Bryn Nelson in the October issue of The Hospitalist (see “A Taxing Future for HM?,” p. 16) incorrectly states that Blue Cross Blue Shield of North Carolina’s refund to customers was a result of an overcharge. In point of fact, the refund is a result of a one-time opportunity due to the changes brought about by the health reform law. The new rating and grandfathering rules in the Patient Protection and Affordable Care Act create a one-time circumstance enabling these refunds.
The funds come from active life reserves, which are portions of the premium set aside in the early years of a policy to pay future claims and keep rates stable as customers’ medical expenses rise during the life of the policy. However, policies purchased or substantially modified after March 23, 2010, will end in 2014 under the new healthcare reform law, which is when the new products under health reform will be introduced. Therefore, the reserves held for these products will cover a much shorter period of time, allowing for these funds to be released.
Lew Borman,
media relations,
Blue Cross Blue Shield of North Carolina
Bryn Nelson in the October issue of The Hospitalist (see “A Taxing Future for HM?,” p. 16) incorrectly states that Blue Cross Blue Shield of North Carolina’s refund to customers was a result of an overcharge. In point of fact, the refund is a result of a one-time opportunity due to the changes brought about by the health reform law. The new rating and grandfathering rules in the Patient Protection and Affordable Care Act create a one-time circumstance enabling these refunds.
The funds come from active life reserves, which are portions of the premium set aside in the early years of a policy to pay future claims and keep rates stable as customers’ medical expenses rise during the life of the policy. However, policies purchased or substantially modified after March 23, 2010, will end in 2014 under the new healthcare reform law, which is when the new products under health reform will be introduced. Therefore, the reserves held for these products will cover a much shorter period of time, allowing for these funds to be released.
Lew Borman,
media relations,
Blue Cross Blue Shield of North Carolina
Night or Weekend Admission and Outcomes
The hospitalist movement and increasingly stringent resident work hour restrictions have led to the utilization of shift work in many hospitals.1 Use of nocturnist and night float systems, while often necessary, results in increased patient hand‐offs. Research suggests that hand‐offs in the inpatient setting can adversely affect patient outcomes as lack of continuity may increase the possibility of medical error.2, 3 In 2001, Bell et al.4 found that mortality was higher among patients admitted on weekends as compared to weekdays. Uneven staffing, lack of supervision, and fragmented care were cited as potential contributing factors.4 Similarly, Peberdy et al.5 in 2008 revealed that patients were less likely to survive a cardiac arrest if it occurred at night or on weekends, again attributed in part to fragmented patient care and understaffing.
The results of these studies raise concerns as to whether increased reliance on shift work and resulting handoffs compromises patient care.6, 7 The aim of this study was to evaluate the potential association between night admission and hospitalization‐relevant outcomes (length of stay [LOS], hospital charges, intensive care unit [ICU] transfer during hospitalization, repeat emergency department [ED] visit within 30 days of discharge, readmission within 30 days of discharge, and poor outcome [transfer to the ICU, cardiac arrest, or death] within the first 24 hours of admission) at an institution that exclusively uses nocturnists (night‐shift based hospitalists) and a resident night float system for patients admitted at night to the general medicine service. A secondary aim was to determine the potential association between weekend admission and hospitalization‐relevant outcomes.
Methods
Study Sample and Selection
We conducted a retrospective medical record review at a large urban academic hospital. Using an administrative hospital data set, we assembled a list of approximately 9000 admissions to the general medicine service from the ED between January 2008 and October 2008. We sampled consecutive admissions from 3 distinct periods beginning in January, April, and July to capture outcomes at various points in the academic year. We attempted to review approximately 10% of all charts equally distributed among the 3 sampling periods (ie, 900 charts total with one‐third from each period) based on time available to the reviewers. We excluded patients not admitted to the general medicine service and patients without complete demographic or outcome information. We also excluded patients not admitted from the ED given that the vast majority of admissions to our hospital during the night (96%) or weekend (93%) are from the ED. Patients admitted to the general medicine service are cared for either by a hospitalist or by a teaching team comprised of 1 attending (about 40% of whom are hospitalists), 1 resident, 1 to 2 interns, and 1 to 3 medical students. From 7 am to 6:59 pm patients are admitted to the care of 1 of the primary daytime admitting teams. From 7 pm to 6:59 am patients are admitted by nocturnists (hospitalist service) or night float residents (teaching service). These patients are handed off to day teams at 7 am. Hospitalist teams change service on a weekly to biweekly basis and resident teams switch on a monthly basis; there is no difference in physician staffing between the weekend and weekdays. The Northwestern University Institutional Review Board approved this study.
Data Acquisition and Medical Records Reviews
We obtained demographic data including gender, age, race and ethnicity, patient insurance, admission day (weekday vs. weekend), admission time (defined as the time that a patient receives a hospital bed, which at our institution is also the time that admitting teams receive report and assume care for the patient), and the International Classification of Disease codes required to determine the Major Diagnostic Category (MDC) and calculate the Charlson Comorbidity Index8, 9 as part of an administrative data set. We divided the admission time into night admission (defined as 7 pm to 6:59 am) and day admission (defined as 7:00 am to 6:59 pm). We created a chart abstraction tool to allow manual recording of the additional fields of admitting team (hospitalist vs. resident), 30 day repeat ED visit, 30 day readmission, and poor outcomes within the first 24 hours of admission, directly from the electronic record.
Study Outcomes
We evaluated each admission for the following 6 primary outcomes which were specified a priori: LOS (defined as discharge date and time minus admission date and time), hospital charges (defined as charges billed as recorded in the administrative data set), ICU transfer during hospitalization (defined as 1 ICU day in the administrative data set), 30 day repeat ED visit (defined as a visit to our ED within 30 days of discharge as assessed by chart abstraction), 30 day readmission (defined as any planned or unplanned admission to any inpatient service at our institution within 30 days of discharge as assessed by chart abstraction), and poor outcome within 24 hours of admission (defined as transfer to the ICU, cardiac arrest, or death as assessed by chart abstraction). Each of these outcomes has been used in prior work to assess the quality of inpatient care.10, 11
Statistical Analysis
Interrater reliability between the 3 physician reviewers was assessed for 20 randomly selected admissions across the 4 separate review measures using interclass correlation coefficients. Comparisons between night admissions and day admissions, and between weekend and weekday admissions, for the continuous primary outcomes (LOS, hospital charges) were assessed using 2‐tailed t‐tests as well as Wilcoxon rank sum test. In the multivariable modeling, these outcomes were assessed by linear regression controlling for age, gender, race and ethnicity, Medicaid or self‐pay insurance, admission to the hospitalist or teaching service, most common MDC categories, and Charlson Comorbidity Index. Because both outcomes were right‐skewed, we separately assessed each after log‐transformation controlling for the same variables.
All comparisons of the dichotomous primary outcomes (ICU transfer during hospitalization, 30 day repeat ED visit, 30 day readmission, and poor outcome within the first 24 hours after admission) were assessed at the univariate level by chi‐squared test, and in the multivariable models using logistic regression, controlling for the same variables as the linear models above. All adjustments were specified a priori. All data analyses were conducted using Stata (College Station, TX; Version 11).
Results
We reviewed 857 records. After excluding 33 records lacking administrative data regarding gender, race and ethnicity, and other demographic variables, there were 824 medical records available for analysis. We reviewed a similar number of records from each time period: 274 from January 2008, 265 from April 2008, and 285 from July 2008. A total of 345 (42%) patients were admitted during the day, and 479 (58%) at night; 641 (78%) were admitted on weekdays, and 183 (22%) on weekends. The 33 excluded charts were similar to the included charts for both time of admission and outcomes. Results for parametric testing and nonparametric testing, as well as for log‐transformation and non‐log‐transformation of the continuous outcomes were similar in both magnitude and statistical significance, so we present the parametric and nonlog‐transformed results below for ease of interpretation.
Interrater reliability among the 3 reviewers was very high. There were no disagreements among the 20 multiple reviews for either poor outcomes within 24 hours of admission or admitting service; the interclass correlation coefficients for 30 day repeat ED visit and 30 day readmission were 0.97 and 0.87, respectively.
Patients admitted at night or on the weekend were similar to patients admitted during the day and week across age, gender, insurance class, MDC, and Charlson Comorbidity Index (Table 1). For unadjusted outcomes, patients admitted at night has a similar LOS, hospital charges, 30 day repeat ED visits, 30 day readmissions, and poor outcome within 24 hours of admission as those patients admitted during the day. They had a potentially lower chance of any ICU transfer during hospitalization though this did not reach statistical significance at P < 0.05 (night admission 6%, day admission 3%, P = 0.06) (Table 2).
| Characteristics | Time of Day | Day of the Week | ||
|---|---|---|---|---|
| Day Admission (n = 345) | Night Admission (n = 479) | Weekday Admission (n = 641) | Weekend Admission (n = 183) | |
| ||||
| Age (years) | 60.8 | 59.7 | 60.6 | 58.7 |
| Gender (% male) | 47 | 43 | 45 | 46 |
| Race/Ethnicity (%) | ||||
| White, Asian, other | 61 | 54 | 57 | 55 |
| Black | 34 | 38 | 37 | 34 |
| Hispanic | 5 | 8 | 6 | 10 |
| Medicaid or self pay (%) | 9 | 10 | 10 | 11 |
| Major diagnostic category (%) | ||||
| Respiratory disease | 14 | 13 | 14 | 13 |
| Circulatory disease | 28 | 23 | 26 | 24 |
| Digestive disease | 12 | 12 | 12 | 12 |
| Other | 45 | 52 | 48 | 51 |
| Charlson Comorbidity Index | 3.71 | 3.60 | 3.66 | 3.60 |
| Outcomes | Time of Day | Day of the Week | ||
|---|---|---|---|---|
| Day Admission (n = 345) | Night Admission (n = 479) | Weekday Admission (n = 641) | Weekend Admission (n = 183) | |
| ||||
| Length of stay | 4.3 | 4.1 | 4.3 | 3.8 |
| Hospital charges | $27,500 | $25,200 | $27,200* | $22,700* |
| ICU transfer during hospitalization (%) | 6 | 3 | 5* | 1* |
| Repeat ED visit at 30 days (%) | 20 | 22 | 22 | 21 |
| Readmission at 30 days (%) | 17 | 20 | 20 | 17 |
| Poor outcome at 24 hours (ICU transfer, cardiac arrest, or death)(%) | 2 | 1 | 2 | 1 |
Patients admitted to the hospital during the weekend were similar to patients admitted during the week for unadjusted LOS, 30 day repeat ED visit or readmission rate, and poor outcomes within 24 hours of admission as those admitted during the week; however, they had lower hospital charges (weekend admission $22,700, weekday admission $27,200; P = 0.02), and a lower chance of ICU transfer during hospitalization (weekend admission 1%, weekday admission 5%; P = 0.02) (Table 2).
In the multivariable linear and logistic regression models (Tables 3 and 4), we assessed the independent association between night admission or weekend admission and each hospitalization‐relevant outcome except for poor outcome within 24 hours of admission (poor outcome within 24 hours of admission was not modeled to avoid the risk of overfitting because there were only 13 total events). After adjustment for age, gender, race and ethnicity, admitting service (hospitalist or teaching), Medicaid or self‐pay insurance, MDC, and Charlson Comorbidity Index, there was no statistically significant association between night admission and worse outcomes for LOS, hospital charges, 30 day repeat ED visit, or 30 day readmission. Night admission was associated with a decreased chance of ICU transfer during hospitalization, but the difference was not statistically significant (odds ratio, 0.54; 95% confidence interval [CI], 0.26‐1.11, P = 0.09). Weekend admission was not associated with worse outcomes for LOS or 30 day repeat ED visit or readmission; however, weekend admission was associated with a decrease in overall charges ($4400; 95% CI, $8300 to $600) and a decreased chance of ICU transfer during hospitalization (odds ratio, 0.20; 95% CI, 0.050.88).
| Predictors | Length of Stay (days), Coefficient (95% CI) | Hospital Charges (dollars), Coefficient (95% CI) |
|---|---|---|
| ||
| Night admission | 0.23 (0.77 to 0.32) | 2100 (5400 to 1100) |
| Weekend admission | 0.42 (1.07 to 0.23) | 4400 (8300 to 600)* |
| Age | 0.01 (0.01 to 0.03) | 0 (100 to 100) |
| Male gender | 0.15 (0.70 to 0.39) | 400 (3700 to 2800) |
| Race, Black | 0.18 (0.41 to 0.78) | 200 (3700 to 3400) |
| Ethnicity, Hispanic | 0.62 (1.73 to 0.49) | 2300 (8900 to 4300) |
| Medicaid or self‐pay insurance | 1.87 (0.93 to 2.82)* | 8900 (3300 to 14600)* |
| Hospitalist service | 0.26 (0.29 to 0.81) | 600 (3900 to 2700) |
| MDC: respiratory | 0.36 (1.18 to 0.46) | 700 (4200 to 5600) |
| MDC: circulatory | 1.36 (2.04 to 0.68)* | 600 (4600 to 3400) |
| MDC: digestive | 1.22 (2.08 to 0.35)* | 6800 (12000 to 1700)* |
| Charlson Comorbidity Index | 0.35 (0.22 to 0.49)* | 2200 (1400 to 3000)* |
| Predictors | ICU Transfer during Hospitalization, Odds Ratio (95% CI) | Repeat ED Visit at 30 days, Odds Ratio (95% CI) | Readmission at 30 days, Odds Ratio (95% CI) |
|---|---|---|---|
| |||
| Night admission | 0.53 (0.26 to 1.11) | 1.13 (0.80 to 1.60) | 1.23 (0.86 to 1.78) |
| Weekend admission | 0.20 (0.05 to 0.88)* | 0.95 (0.63 to 1.44) | 0.80 (0.51 to 1.25) |
| Age | 1.00 (0.98 to 1.02) | 0.99 (0.98 to 1.002) | 1.00 (0.99 to 1.01) |
| Male gender | 0.98 (0.47 to 2.02) | 1.09 (0.78 to 1.54) | 0.91 (0.64 to 1.31) |
| Race, Black | 0.75 (0.33 to 1.70) | 1.48 (1.02 to 2.14)* | 1.12 (0.76 to 1.65) |
| Ethnicity, Hispanic | 0.76 (0.16 to 3.73) | 1.09 (0.55 to 2.17) | 1.11 (0.55 to 2.22) |
| Medicaid or self‐pay insurance | 0.75 (0.16 to 3.49) | 1.61 (0.95 to 2.72) | 2.14 (1.24 to 3.67)* |
| Hospitalist service | 0.68 (0.33 to 1.44) | 1.15 (0.81 to 1.63) | 0.99 (0.69 to 1.43) |
| MDC: respiratory | 1.18 (0.41 to 3.38) | 1.02 (0.61 to 1.69) | 1.16 (0.69 to 1.95) |
| MDC: circulatory | 1.22 (0.52 to 2.87) | 0.79 (0.51 to 1.22) | 0.80 (0.51 to 1.27) |
| MDC: digestive | 0.51 (0.11 to 2.32) | 0.83 (0.47 to 1.46) | 1.08 (0.62 to 1.91) |
| Charlson Comobrbidity Index | 1.25 (1.09 to 1.45)* | 1.09 (1.01 to 1.19)* | 1.11 (1.02 to 1.21)* |
Our multivariate models explained very little of the variance in patient outcomes. For LOS and hospital charges, adjusted R2 values were 0.06 and 0.05, respectively. For ICU transfer during hospitalization, 30 day repeat ED visit, and 30 day readmission, the areas under the receiver operator curves were 0.75, 0.51, and 0.61 respectively.
To assess the robustness of our conclusions regarding night admission, we redefined night to include only patients admitted between the hours of 8 pm and 5:59 am. This did not change our conclusions. We also tested for interaction between night admission and weekend admission for all outcomes to assess whether night admissions on the weekend were in fact at increased risk of worse outcomes; we found no evidence of interaction (P > 0.3 for the interaction terms in each model).
Discussion
Among patients admitted to the medicine services at our academic medical center, night or weekend admission was not associated with worse hospitalization‐relevant outcomes. In some cases, night or weekend admission was associated with better outcomes, particularly in terms of ICU transfer during hospitalization and hospital charges. Prior research indicates worse outcomes during off‐hours,5 but we did not replicate this finding in our study.
The finding that admission at night was not associated with worse outcomes, particularly proximal outcomes such as LOS or ICU transfer during hospitalization, was surprising, though reassuring in view of the fact that more than half of our patients are admitted at night. We believe a few factors may be responsible. First, our general medicine service is staffed during the night (7 pm to 7 am) by in‐house nocturnists and night float residents. Second, our staffing ratio, while lower at night than during the day, remains the same on weekends and may be higher than in other settings. In continuously well‐staffed settings such as the ED12 and ICU,13 night and weekend admissions are only inconsistently associated with worse outcomes, which may be the same phenomena we observed in the current study. Third, the hospital used as the site of this study has received Nursing Magnet recognition and numerous quality awards such as the National Research Corporation's Consumer Choice Award and recognition as a Distinguished Hospital for Clinical Excellence by HealthGrades. Fourth, our integrated electronic medical record, computerized physician order entry system, and automatically generated sign out serve as complements to the morning hand off. Fifth, hospitalists and teaching teams rotate on a weekly, biweekly, or every 4 week basis, which may protect against discontinuity associated with the weekend. We believe that all of these factors may facilitate alert, comprehensive care during the night and weekend as well as safe and efficient transfer of patients from the night to the day providers.
We were also surprised by the association between weekend admission and lower charges and a lower chance of ICU transfer during hospitalization. We believe many of the same factors noted above may have played a role in these findings. In terms of hospital charges, it is possible that some workups were completed outside of the hospital rather than during the hospitalization, and that some tests were not ordered at all due to unavailability on weekends. The decreased chance of ICU transfer is unexplained. We hypothesize that there may have been a more conservative admission strategy within the ED, such that patients with high baseline severity were admitted directly to the ICU on the weekend rather than being admitted first to the general medicine floor. This hypothesis requires further study.
Our study had important limitations. It was a retrospective study from a single academic hospital. The sample size lacked sufficient power to detect differences in the low frequency of certain outcomes such as poor outcomes within 24 hours of admission (2% vs. 1%), and also for more frequent outcomes such as 30 day readmission; it is possible that with a larger sample there would have been statistically significant differences. Further, we recognize that the Charlson Comorbidity Index, which was developed to predict 1‐year mortality for medicine service patients, does not adjust for severity of illness at presentation, particularly for outcomes such as readmission. If patients admitted at night and during the weekend were less acutely ill despite having similar comorbidities and MDCs at admission, true associations between time of admission and worse outcomes could have been masked. Furthermore, the multivariable modeling explained very little of the variance in patient outcomes such that significant unmeasured confounding may still be present, and consequently our results cannot be interpreted in a causal way. Data was collected from electronic records, so it is possible that some adverse events were not recorded. However, it seems unlikely that major events such as death and transfer to an ICU would have been missed.
Several aspects of the study strengthen our confidence in the findings, including a large sample size, relevance of the outcomes, the adjustment for confounders, and an assessment for robustness of the conclusions based on restricting the definition of night and also testing for interaction between night and weekend admission. Our patient demographics and insurance mix resemble that of other academic hospitals,10 and perhaps our results may be generalizable to these settings, if not to non‐urban or community hospitals. Furthermore, the Charlson Comorbidity Index was associated with all 5 of the modeled outcomes we chose for our study, reaffirming their utility in assessing the quality of hospital care. Future directions for investigation may include examining the association of night admission with hospitalization‐relevant outcomes in nonacademic, nonurban settings, and examining whether the lack of association between night and weekend admission and worse outcomes persists with adjustment for initial severity of illness.
In summary, at a large, well‐staffed urban academic hospital, day or time of admission were not associated with worse hospitalization‐relevant outcomes. The use of nocturnists and night float teams for night admissions and continuity across weekends appears to be a safe approach to handling the increased volume of patients admitted at night, and a viable alternative to overnight call in the era of work hour restrictions.
- ,,, et al.Three‐year results of mandated work hour restrictions: attending and resident perspectives and effects in a community hospital.Am Surg.2008;74(6):542–546; discussion 546–547.
- ,,, et al.Handoffs causing patient harm: a survey of medical and surgical house staff.Jt Comm J Qual Patient Saf.2008;34(10):563–570.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121(11):866–872.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345(9):663–668.
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299(7):785–792.
- ,,,.Continuity of care and intensive care unit use at the end of life.Arch Intern Med.2009;169(1):81–86.
- ,,,,,.Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301(16):1671–1680.
- ,,,.Why predictive indexes perform less well in validation studies: is it magic or methods?Arch Intern Med.1987;147:2155–2161.
- ,,.Adapting a clinical comorbidity index for use with ICD‐9‐CM administrative databases.J Clin Epidemiol.1992;45(6):613–619.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,, et al.Use of an admission early warning score to predict patient morbidity and mortality and treatment success.Emerg Med J.2008;25(12):803–806.
- ,,.The impact of weekends on outcome for emergency patients.Clin Med.2005;5(6):621–625.
- ,,,,,.Off hour admission to an intensivist‐led ICU is not associated with increased mortality.Crit Care.2009;13(3):R84.
The hospitalist movement and increasingly stringent resident work hour restrictions have led to the utilization of shift work in many hospitals.1 Use of nocturnist and night float systems, while often necessary, results in increased patient hand‐offs. Research suggests that hand‐offs in the inpatient setting can adversely affect patient outcomes as lack of continuity may increase the possibility of medical error.2, 3 In 2001, Bell et al.4 found that mortality was higher among patients admitted on weekends as compared to weekdays. Uneven staffing, lack of supervision, and fragmented care were cited as potential contributing factors.4 Similarly, Peberdy et al.5 in 2008 revealed that patients were less likely to survive a cardiac arrest if it occurred at night or on weekends, again attributed in part to fragmented patient care and understaffing.
The results of these studies raise concerns as to whether increased reliance on shift work and resulting handoffs compromises patient care.6, 7 The aim of this study was to evaluate the potential association between night admission and hospitalization‐relevant outcomes (length of stay [LOS], hospital charges, intensive care unit [ICU] transfer during hospitalization, repeat emergency department [ED] visit within 30 days of discharge, readmission within 30 days of discharge, and poor outcome [transfer to the ICU, cardiac arrest, or death] within the first 24 hours of admission) at an institution that exclusively uses nocturnists (night‐shift based hospitalists) and a resident night float system for patients admitted at night to the general medicine service. A secondary aim was to determine the potential association between weekend admission and hospitalization‐relevant outcomes.
Methods
Study Sample and Selection
We conducted a retrospective medical record review at a large urban academic hospital. Using an administrative hospital data set, we assembled a list of approximately 9000 admissions to the general medicine service from the ED between January 2008 and October 2008. We sampled consecutive admissions from 3 distinct periods beginning in January, April, and July to capture outcomes at various points in the academic year. We attempted to review approximately 10% of all charts equally distributed among the 3 sampling periods (ie, 900 charts total with one‐third from each period) based on time available to the reviewers. We excluded patients not admitted to the general medicine service and patients without complete demographic or outcome information. We also excluded patients not admitted from the ED given that the vast majority of admissions to our hospital during the night (96%) or weekend (93%) are from the ED. Patients admitted to the general medicine service are cared for either by a hospitalist or by a teaching team comprised of 1 attending (about 40% of whom are hospitalists), 1 resident, 1 to 2 interns, and 1 to 3 medical students. From 7 am to 6:59 pm patients are admitted to the care of 1 of the primary daytime admitting teams. From 7 pm to 6:59 am patients are admitted by nocturnists (hospitalist service) or night float residents (teaching service). These patients are handed off to day teams at 7 am. Hospitalist teams change service on a weekly to biweekly basis and resident teams switch on a monthly basis; there is no difference in physician staffing between the weekend and weekdays. The Northwestern University Institutional Review Board approved this study.
Data Acquisition and Medical Records Reviews
We obtained demographic data including gender, age, race and ethnicity, patient insurance, admission day (weekday vs. weekend), admission time (defined as the time that a patient receives a hospital bed, which at our institution is also the time that admitting teams receive report and assume care for the patient), and the International Classification of Disease codes required to determine the Major Diagnostic Category (MDC) and calculate the Charlson Comorbidity Index8, 9 as part of an administrative data set. We divided the admission time into night admission (defined as 7 pm to 6:59 am) and day admission (defined as 7:00 am to 6:59 pm). We created a chart abstraction tool to allow manual recording of the additional fields of admitting team (hospitalist vs. resident), 30 day repeat ED visit, 30 day readmission, and poor outcomes within the first 24 hours of admission, directly from the electronic record.
Study Outcomes
We evaluated each admission for the following 6 primary outcomes which were specified a priori: LOS (defined as discharge date and time minus admission date and time), hospital charges (defined as charges billed as recorded in the administrative data set), ICU transfer during hospitalization (defined as 1 ICU day in the administrative data set), 30 day repeat ED visit (defined as a visit to our ED within 30 days of discharge as assessed by chart abstraction), 30 day readmission (defined as any planned or unplanned admission to any inpatient service at our institution within 30 days of discharge as assessed by chart abstraction), and poor outcome within 24 hours of admission (defined as transfer to the ICU, cardiac arrest, or death as assessed by chart abstraction). Each of these outcomes has been used in prior work to assess the quality of inpatient care.10, 11
Statistical Analysis
Interrater reliability between the 3 physician reviewers was assessed for 20 randomly selected admissions across the 4 separate review measures using interclass correlation coefficients. Comparisons between night admissions and day admissions, and between weekend and weekday admissions, for the continuous primary outcomes (LOS, hospital charges) were assessed using 2‐tailed t‐tests as well as Wilcoxon rank sum test. In the multivariable modeling, these outcomes were assessed by linear regression controlling for age, gender, race and ethnicity, Medicaid or self‐pay insurance, admission to the hospitalist or teaching service, most common MDC categories, and Charlson Comorbidity Index. Because both outcomes were right‐skewed, we separately assessed each after log‐transformation controlling for the same variables.
All comparisons of the dichotomous primary outcomes (ICU transfer during hospitalization, 30 day repeat ED visit, 30 day readmission, and poor outcome within the first 24 hours after admission) were assessed at the univariate level by chi‐squared test, and in the multivariable models using logistic regression, controlling for the same variables as the linear models above. All adjustments were specified a priori. All data analyses were conducted using Stata (College Station, TX; Version 11).
Results
We reviewed 857 records. After excluding 33 records lacking administrative data regarding gender, race and ethnicity, and other demographic variables, there were 824 medical records available for analysis. We reviewed a similar number of records from each time period: 274 from January 2008, 265 from April 2008, and 285 from July 2008. A total of 345 (42%) patients were admitted during the day, and 479 (58%) at night; 641 (78%) were admitted on weekdays, and 183 (22%) on weekends. The 33 excluded charts were similar to the included charts for both time of admission and outcomes. Results for parametric testing and nonparametric testing, as well as for log‐transformation and non‐log‐transformation of the continuous outcomes were similar in both magnitude and statistical significance, so we present the parametric and nonlog‐transformed results below for ease of interpretation.
Interrater reliability among the 3 reviewers was very high. There were no disagreements among the 20 multiple reviews for either poor outcomes within 24 hours of admission or admitting service; the interclass correlation coefficients for 30 day repeat ED visit and 30 day readmission were 0.97 and 0.87, respectively.
Patients admitted at night or on the weekend were similar to patients admitted during the day and week across age, gender, insurance class, MDC, and Charlson Comorbidity Index (Table 1). For unadjusted outcomes, patients admitted at night has a similar LOS, hospital charges, 30 day repeat ED visits, 30 day readmissions, and poor outcome within 24 hours of admission as those patients admitted during the day. They had a potentially lower chance of any ICU transfer during hospitalization though this did not reach statistical significance at P < 0.05 (night admission 6%, day admission 3%, P = 0.06) (Table 2).
| Characteristics | Time of Day | Day of the Week | ||
|---|---|---|---|---|
| Day Admission (n = 345) | Night Admission (n = 479) | Weekday Admission (n = 641) | Weekend Admission (n = 183) | |
| ||||
| Age (years) | 60.8 | 59.7 | 60.6 | 58.7 |
| Gender (% male) | 47 | 43 | 45 | 46 |
| Race/Ethnicity (%) | ||||
| White, Asian, other | 61 | 54 | 57 | 55 |
| Black | 34 | 38 | 37 | 34 |
| Hispanic | 5 | 8 | 6 | 10 |
| Medicaid or self pay (%) | 9 | 10 | 10 | 11 |
| Major diagnostic category (%) | ||||
| Respiratory disease | 14 | 13 | 14 | 13 |
| Circulatory disease | 28 | 23 | 26 | 24 |
| Digestive disease | 12 | 12 | 12 | 12 |
| Other | 45 | 52 | 48 | 51 |
| Charlson Comorbidity Index | 3.71 | 3.60 | 3.66 | 3.60 |
| Outcomes | Time of Day | Day of the Week | ||
|---|---|---|---|---|
| Day Admission (n = 345) | Night Admission (n = 479) | Weekday Admission (n = 641) | Weekend Admission (n = 183) | |
| ||||
| Length of stay | 4.3 | 4.1 | 4.3 | 3.8 |
| Hospital charges | $27,500 | $25,200 | $27,200* | $22,700* |
| ICU transfer during hospitalization (%) | 6 | 3 | 5* | 1* |
| Repeat ED visit at 30 days (%) | 20 | 22 | 22 | 21 |
| Readmission at 30 days (%) | 17 | 20 | 20 | 17 |
| Poor outcome at 24 hours (ICU transfer, cardiac arrest, or death)(%) | 2 | 1 | 2 | 1 |
Patients admitted to the hospital during the weekend were similar to patients admitted during the week for unadjusted LOS, 30 day repeat ED visit or readmission rate, and poor outcomes within 24 hours of admission as those admitted during the week; however, they had lower hospital charges (weekend admission $22,700, weekday admission $27,200; P = 0.02), and a lower chance of ICU transfer during hospitalization (weekend admission 1%, weekday admission 5%; P = 0.02) (Table 2).
In the multivariable linear and logistic regression models (Tables 3 and 4), we assessed the independent association between night admission or weekend admission and each hospitalization‐relevant outcome except for poor outcome within 24 hours of admission (poor outcome within 24 hours of admission was not modeled to avoid the risk of overfitting because there were only 13 total events). After adjustment for age, gender, race and ethnicity, admitting service (hospitalist or teaching), Medicaid or self‐pay insurance, MDC, and Charlson Comorbidity Index, there was no statistically significant association between night admission and worse outcomes for LOS, hospital charges, 30 day repeat ED visit, or 30 day readmission. Night admission was associated with a decreased chance of ICU transfer during hospitalization, but the difference was not statistically significant (odds ratio, 0.54; 95% confidence interval [CI], 0.26‐1.11, P = 0.09). Weekend admission was not associated with worse outcomes for LOS or 30 day repeat ED visit or readmission; however, weekend admission was associated with a decrease in overall charges ($4400; 95% CI, $8300 to $600) and a decreased chance of ICU transfer during hospitalization (odds ratio, 0.20; 95% CI, 0.050.88).
| Predictors | Length of Stay (days), Coefficient (95% CI) | Hospital Charges (dollars), Coefficient (95% CI) |
|---|---|---|
| ||
| Night admission | 0.23 (0.77 to 0.32) | 2100 (5400 to 1100) |
| Weekend admission | 0.42 (1.07 to 0.23) | 4400 (8300 to 600)* |
| Age | 0.01 (0.01 to 0.03) | 0 (100 to 100) |
| Male gender | 0.15 (0.70 to 0.39) | 400 (3700 to 2800) |
| Race, Black | 0.18 (0.41 to 0.78) | 200 (3700 to 3400) |
| Ethnicity, Hispanic | 0.62 (1.73 to 0.49) | 2300 (8900 to 4300) |
| Medicaid or self‐pay insurance | 1.87 (0.93 to 2.82)* | 8900 (3300 to 14600)* |
| Hospitalist service | 0.26 (0.29 to 0.81) | 600 (3900 to 2700) |
| MDC: respiratory | 0.36 (1.18 to 0.46) | 700 (4200 to 5600) |
| MDC: circulatory | 1.36 (2.04 to 0.68)* | 600 (4600 to 3400) |
| MDC: digestive | 1.22 (2.08 to 0.35)* | 6800 (12000 to 1700)* |
| Charlson Comorbidity Index | 0.35 (0.22 to 0.49)* | 2200 (1400 to 3000)* |
| Predictors | ICU Transfer during Hospitalization, Odds Ratio (95% CI) | Repeat ED Visit at 30 days, Odds Ratio (95% CI) | Readmission at 30 days, Odds Ratio (95% CI) |
|---|---|---|---|
| |||
| Night admission | 0.53 (0.26 to 1.11) | 1.13 (0.80 to 1.60) | 1.23 (0.86 to 1.78) |
| Weekend admission | 0.20 (0.05 to 0.88)* | 0.95 (0.63 to 1.44) | 0.80 (0.51 to 1.25) |
| Age | 1.00 (0.98 to 1.02) | 0.99 (0.98 to 1.002) | 1.00 (0.99 to 1.01) |
| Male gender | 0.98 (0.47 to 2.02) | 1.09 (0.78 to 1.54) | 0.91 (0.64 to 1.31) |
| Race, Black | 0.75 (0.33 to 1.70) | 1.48 (1.02 to 2.14)* | 1.12 (0.76 to 1.65) |
| Ethnicity, Hispanic | 0.76 (0.16 to 3.73) | 1.09 (0.55 to 2.17) | 1.11 (0.55 to 2.22) |
| Medicaid or self‐pay insurance | 0.75 (0.16 to 3.49) | 1.61 (0.95 to 2.72) | 2.14 (1.24 to 3.67)* |
| Hospitalist service | 0.68 (0.33 to 1.44) | 1.15 (0.81 to 1.63) | 0.99 (0.69 to 1.43) |
| MDC: respiratory | 1.18 (0.41 to 3.38) | 1.02 (0.61 to 1.69) | 1.16 (0.69 to 1.95) |
| MDC: circulatory | 1.22 (0.52 to 2.87) | 0.79 (0.51 to 1.22) | 0.80 (0.51 to 1.27) |
| MDC: digestive | 0.51 (0.11 to 2.32) | 0.83 (0.47 to 1.46) | 1.08 (0.62 to 1.91) |
| Charlson Comobrbidity Index | 1.25 (1.09 to 1.45)* | 1.09 (1.01 to 1.19)* | 1.11 (1.02 to 1.21)* |
Our multivariate models explained very little of the variance in patient outcomes. For LOS and hospital charges, adjusted R2 values were 0.06 and 0.05, respectively. For ICU transfer during hospitalization, 30 day repeat ED visit, and 30 day readmission, the areas under the receiver operator curves were 0.75, 0.51, and 0.61 respectively.
To assess the robustness of our conclusions regarding night admission, we redefined night to include only patients admitted between the hours of 8 pm and 5:59 am. This did not change our conclusions. We also tested for interaction between night admission and weekend admission for all outcomes to assess whether night admissions on the weekend were in fact at increased risk of worse outcomes; we found no evidence of interaction (P > 0.3 for the interaction terms in each model).
Discussion
Among patients admitted to the medicine services at our academic medical center, night or weekend admission was not associated with worse hospitalization‐relevant outcomes. In some cases, night or weekend admission was associated with better outcomes, particularly in terms of ICU transfer during hospitalization and hospital charges. Prior research indicates worse outcomes during off‐hours,5 but we did not replicate this finding in our study.
The finding that admission at night was not associated with worse outcomes, particularly proximal outcomes such as LOS or ICU transfer during hospitalization, was surprising, though reassuring in view of the fact that more than half of our patients are admitted at night. We believe a few factors may be responsible. First, our general medicine service is staffed during the night (7 pm to 7 am) by in‐house nocturnists and night float residents. Second, our staffing ratio, while lower at night than during the day, remains the same on weekends and may be higher than in other settings. In continuously well‐staffed settings such as the ED12 and ICU,13 night and weekend admissions are only inconsistently associated with worse outcomes, which may be the same phenomena we observed in the current study. Third, the hospital used as the site of this study has received Nursing Magnet recognition and numerous quality awards such as the National Research Corporation's Consumer Choice Award and recognition as a Distinguished Hospital for Clinical Excellence by HealthGrades. Fourth, our integrated electronic medical record, computerized physician order entry system, and automatically generated sign out serve as complements to the morning hand off. Fifth, hospitalists and teaching teams rotate on a weekly, biweekly, or every 4 week basis, which may protect against discontinuity associated with the weekend. We believe that all of these factors may facilitate alert, comprehensive care during the night and weekend as well as safe and efficient transfer of patients from the night to the day providers.
We were also surprised by the association between weekend admission and lower charges and a lower chance of ICU transfer during hospitalization. We believe many of the same factors noted above may have played a role in these findings. In terms of hospital charges, it is possible that some workups were completed outside of the hospital rather than during the hospitalization, and that some tests were not ordered at all due to unavailability on weekends. The decreased chance of ICU transfer is unexplained. We hypothesize that there may have been a more conservative admission strategy within the ED, such that patients with high baseline severity were admitted directly to the ICU on the weekend rather than being admitted first to the general medicine floor. This hypothesis requires further study.
Our study had important limitations. It was a retrospective study from a single academic hospital. The sample size lacked sufficient power to detect differences in the low frequency of certain outcomes such as poor outcomes within 24 hours of admission (2% vs. 1%), and also for more frequent outcomes such as 30 day readmission; it is possible that with a larger sample there would have been statistically significant differences. Further, we recognize that the Charlson Comorbidity Index, which was developed to predict 1‐year mortality for medicine service patients, does not adjust for severity of illness at presentation, particularly for outcomes such as readmission. If patients admitted at night and during the weekend were less acutely ill despite having similar comorbidities and MDCs at admission, true associations between time of admission and worse outcomes could have been masked. Furthermore, the multivariable modeling explained very little of the variance in patient outcomes such that significant unmeasured confounding may still be present, and consequently our results cannot be interpreted in a causal way. Data was collected from electronic records, so it is possible that some adverse events were not recorded. However, it seems unlikely that major events such as death and transfer to an ICU would have been missed.
Several aspects of the study strengthen our confidence in the findings, including a large sample size, relevance of the outcomes, the adjustment for confounders, and an assessment for robustness of the conclusions based on restricting the definition of night and also testing for interaction between night and weekend admission. Our patient demographics and insurance mix resemble that of other academic hospitals,10 and perhaps our results may be generalizable to these settings, if not to non‐urban or community hospitals. Furthermore, the Charlson Comorbidity Index was associated with all 5 of the modeled outcomes we chose for our study, reaffirming their utility in assessing the quality of hospital care. Future directions for investigation may include examining the association of night admission with hospitalization‐relevant outcomes in nonacademic, nonurban settings, and examining whether the lack of association between night and weekend admission and worse outcomes persists with adjustment for initial severity of illness.
In summary, at a large, well‐staffed urban academic hospital, day or time of admission were not associated with worse hospitalization‐relevant outcomes. The use of nocturnists and night float teams for night admissions and continuity across weekends appears to be a safe approach to handling the increased volume of patients admitted at night, and a viable alternative to overnight call in the era of work hour restrictions.
The hospitalist movement and increasingly stringent resident work hour restrictions have led to the utilization of shift work in many hospitals.1 Use of nocturnist and night float systems, while often necessary, results in increased patient hand‐offs. Research suggests that hand‐offs in the inpatient setting can adversely affect patient outcomes as lack of continuity may increase the possibility of medical error.2, 3 In 2001, Bell et al.4 found that mortality was higher among patients admitted on weekends as compared to weekdays. Uneven staffing, lack of supervision, and fragmented care were cited as potential contributing factors.4 Similarly, Peberdy et al.5 in 2008 revealed that patients were less likely to survive a cardiac arrest if it occurred at night or on weekends, again attributed in part to fragmented patient care and understaffing.
The results of these studies raise concerns as to whether increased reliance on shift work and resulting handoffs compromises patient care.6, 7 The aim of this study was to evaluate the potential association between night admission and hospitalization‐relevant outcomes (length of stay [LOS], hospital charges, intensive care unit [ICU] transfer during hospitalization, repeat emergency department [ED] visit within 30 days of discharge, readmission within 30 days of discharge, and poor outcome [transfer to the ICU, cardiac arrest, or death] within the first 24 hours of admission) at an institution that exclusively uses nocturnists (night‐shift based hospitalists) and a resident night float system for patients admitted at night to the general medicine service. A secondary aim was to determine the potential association between weekend admission and hospitalization‐relevant outcomes.
Methods
Study Sample and Selection
We conducted a retrospective medical record review at a large urban academic hospital. Using an administrative hospital data set, we assembled a list of approximately 9000 admissions to the general medicine service from the ED between January 2008 and October 2008. We sampled consecutive admissions from 3 distinct periods beginning in January, April, and July to capture outcomes at various points in the academic year. We attempted to review approximately 10% of all charts equally distributed among the 3 sampling periods (ie, 900 charts total with one‐third from each period) based on time available to the reviewers. We excluded patients not admitted to the general medicine service and patients without complete demographic or outcome information. We also excluded patients not admitted from the ED given that the vast majority of admissions to our hospital during the night (96%) or weekend (93%) are from the ED. Patients admitted to the general medicine service are cared for either by a hospitalist or by a teaching team comprised of 1 attending (about 40% of whom are hospitalists), 1 resident, 1 to 2 interns, and 1 to 3 medical students. From 7 am to 6:59 pm patients are admitted to the care of 1 of the primary daytime admitting teams. From 7 pm to 6:59 am patients are admitted by nocturnists (hospitalist service) or night float residents (teaching service). These patients are handed off to day teams at 7 am. Hospitalist teams change service on a weekly to biweekly basis and resident teams switch on a monthly basis; there is no difference in physician staffing between the weekend and weekdays. The Northwestern University Institutional Review Board approved this study.
Data Acquisition and Medical Records Reviews
We obtained demographic data including gender, age, race and ethnicity, patient insurance, admission day (weekday vs. weekend), admission time (defined as the time that a patient receives a hospital bed, which at our institution is also the time that admitting teams receive report and assume care for the patient), and the International Classification of Disease codes required to determine the Major Diagnostic Category (MDC) and calculate the Charlson Comorbidity Index8, 9 as part of an administrative data set. We divided the admission time into night admission (defined as 7 pm to 6:59 am) and day admission (defined as 7:00 am to 6:59 pm). We created a chart abstraction tool to allow manual recording of the additional fields of admitting team (hospitalist vs. resident), 30 day repeat ED visit, 30 day readmission, and poor outcomes within the first 24 hours of admission, directly from the electronic record.
Study Outcomes
We evaluated each admission for the following 6 primary outcomes which were specified a priori: LOS (defined as discharge date and time minus admission date and time), hospital charges (defined as charges billed as recorded in the administrative data set), ICU transfer during hospitalization (defined as 1 ICU day in the administrative data set), 30 day repeat ED visit (defined as a visit to our ED within 30 days of discharge as assessed by chart abstraction), 30 day readmission (defined as any planned or unplanned admission to any inpatient service at our institution within 30 days of discharge as assessed by chart abstraction), and poor outcome within 24 hours of admission (defined as transfer to the ICU, cardiac arrest, or death as assessed by chart abstraction). Each of these outcomes has been used in prior work to assess the quality of inpatient care.10, 11
Statistical Analysis
Interrater reliability between the 3 physician reviewers was assessed for 20 randomly selected admissions across the 4 separate review measures using interclass correlation coefficients. Comparisons between night admissions and day admissions, and between weekend and weekday admissions, for the continuous primary outcomes (LOS, hospital charges) were assessed using 2‐tailed t‐tests as well as Wilcoxon rank sum test. In the multivariable modeling, these outcomes were assessed by linear regression controlling for age, gender, race and ethnicity, Medicaid or self‐pay insurance, admission to the hospitalist or teaching service, most common MDC categories, and Charlson Comorbidity Index. Because both outcomes were right‐skewed, we separately assessed each after log‐transformation controlling for the same variables.
All comparisons of the dichotomous primary outcomes (ICU transfer during hospitalization, 30 day repeat ED visit, 30 day readmission, and poor outcome within the first 24 hours after admission) were assessed at the univariate level by chi‐squared test, and in the multivariable models using logistic regression, controlling for the same variables as the linear models above. All adjustments were specified a priori. All data analyses were conducted using Stata (College Station, TX; Version 11).
Results
We reviewed 857 records. After excluding 33 records lacking administrative data regarding gender, race and ethnicity, and other demographic variables, there were 824 medical records available for analysis. We reviewed a similar number of records from each time period: 274 from January 2008, 265 from April 2008, and 285 from July 2008. A total of 345 (42%) patients were admitted during the day, and 479 (58%) at night; 641 (78%) were admitted on weekdays, and 183 (22%) on weekends. The 33 excluded charts were similar to the included charts for both time of admission and outcomes. Results for parametric testing and nonparametric testing, as well as for log‐transformation and non‐log‐transformation of the continuous outcomes were similar in both magnitude and statistical significance, so we present the parametric and nonlog‐transformed results below for ease of interpretation.
Interrater reliability among the 3 reviewers was very high. There were no disagreements among the 20 multiple reviews for either poor outcomes within 24 hours of admission or admitting service; the interclass correlation coefficients for 30 day repeat ED visit and 30 day readmission were 0.97 and 0.87, respectively.
Patients admitted at night or on the weekend were similar to patients admitted during the day and week across age, gender, insurance class, MDC, and Charlson Comorbidity Index (Table 1). For unadjusted outcomes, patients admitted at night has a similar LOS, hospital charges, 30 day repeat ED visits, 30 day readmissions, and poor outcome within 24 hours of admission as those patients admitted during the day. They had a potentially lower chance of any ICU transfer during hospitalization though this did not reach statistical significance at P < 0.05 (night admission 6%, day admission 3%, P = 0.06) (Table 2).
| Characteristics | Time of Day | Day of the Week | ||
|---|---|---|---|---|
| Day Admission (n = 345) | Night Admission (n = 479) | Weekday Admission (n = 641) | Weekend Admission (n = 183) | |
| ||||
| Age (years) | 60.8 | 59.7 | 60.6 | 58.7 |
| Gender (% male) | 47 | 43 | 45 | 46 |
| Race/Ethnicity (%) | ||||
| White, Asian, other | 61 | 54 | 57 | 55 |
| Black | 34 | 38 | 37 | 34 |
| Hispanic | 5 | 8 | 6 | 10 |
| Medicaid or self pay (%) | 9 | 10 | 10 | 11 |
| Major diagnostic category (%) | ||||
| Respiratory disease | 14 | 13 | 14 | 13 |
| Circulatory disease | 28 | 23 | 26 | 24 |
| Digestive disease | 12 | 12 | 12 | 12 |
| Other | 45 | 52 | 48 | 51 |
| Charlson Comorbidity Index | 3.71 | 3.60 | 3.66 | 3.60 |
| Outcomes | Time of Day | Day of the Week | ||
|---|---|---|---|---|
| Day Admission (n = 345) | Night Admission (n = 479) | Weekday Admission (n = 641) | Weekend Admission (n = 183) | |
| ||||
| Length of stay | 4.3 | 4.1 | 4.3 | 3.8 |
| Hospital charges | $27,500 | $25,200 | $27,200* | $22,700* |
| ICU transfer during hospitalization (%) | 6 | 3 | 5* | 1* |
| Repeat ED visit at 30 days (%) | 20 | 22 | 22 | 21 |
| Readmission at 30 days (%) | 17 | 20 | 20 | 17 |
| Poor outcome at 24 hours (ICU transfer, cardiac arrest, or death)(%) | 2 | 1 | 2 | 1 |
Patients admitted to the hospital during the weekend were similar to patients admitted during the week for unadjusted LOS, 30 day repeat ED visit or readmission rate, and poor outcomes within 24 hours of admission as those admitted during the week; however, they had lower hospital charges (weekend admission $22,700, weekday admission $27,200; P = 0.02), and a lower chance of ICU transfer during hospitalization (weekend admission 1%, weekday admission 5%; P = 0.02) (Table 2).
In the multivariable linear and logistic regression models (Tables 3 and 4), we assessed the independent association between night admission or weekend admission and each hospitalization‐relevant outcome except for poor outcome within 24 hours of admission (poor outcome within 24 hours of admission was not modeled to avoid the risk of overfitting because there were only 13 total events). After adjustment for age, gender, race and ethnicity, admitting service (hospitalist or teaching), Medicaid or self‐pay insurance, MDC, and Charlson Comorbidity Index, there was no statistically significant association between night admission and worse outcomes for LOS, hospital charges, 30 day repeat ED visit, or 30 day readmission. Night admission was associated with a decreased chance of ICU transfer during hospitalization, but the difference was not statistically significant (odds ratio, 0.54; 95% confidence interval [CI], 0.26‐1.11, P = 0.09). Weekend admission was not associated with worse outcomes for LOS or 30 day repeat ED visit or readmission; however, weekend admission was associated with a decrease in overall charges ($4400; 95% CI, $8300 to $600) and a decreased chance of ICU transfer during hospitalization (odds ratio, 0.20; 95% CI, 0.050.88).
| Predictors | Length of Stay (days), Coefficient (95% CI) | Hospital Charges (dollars), Coefficient (95% CI) |
|---|---|---|
| ||
| Night admission | 0.23 (0.77 to 0.32) | 2100 (5400 to 1100) |
| Weekend admission | 0.42 (1.07 to 0.23) | 4400 (8300 to 600)* |
| Age | 0.01 (0.01 to 0.03) | 0 (100 to 100) |
| Male gender | 0.15 (0.70 to 0.39) | 400 (3700 to 2800) |
| Race, Black | 0.18 (0.41 to 0.78) | 200 (3700 to 3400) |
| Ethnicity, Hispanic | 0.62 (1.73 to 0.49) | 2300 (8900 to 4300) |
| Medicaid or self‐pay insurance | 1.87 (0.93 to 2.82)* | 8900 (3300 to 14600)* |
| Hospitalist service | 0.26 (0.29 to 0.81) | 600 (3900 to 2700) |
| MDC: respiratory | 0.36 (1.18 to 0.46) | 700 (4200 to 5600) |
| MDC: circulatory | 1.36 (2.04 to 0.68)* | 600 (4600 to 3400) |
| MDC: digestive | 1.22 (2.08 to 0.35)* | 6800 (12000 to 1700)* |
| Charlson Comorbidity Index | 0.35 (0.22 to 0.49)* | 2200 (1400 to 3000)* |
| Predictors | ICU Transfer during Hospitalization, Odds Ratio (95% CI) | Repeat ED Visit at 30 days, Odds Ratio (95% CI) | Readmission at 30 days, Odds Ratio (95% CI) |
|---|---|---|---|
| |||
| Night admission | 0.53 (0.26 to 1.11) | 1.13 (0.80 to 1.60) | 1.23 (0.86 to 1.78) |
| Weekend admission | 0.20 (0.05 to 0.88)* | 0.95 (0.63 to 1.44) | 0.80 (0.51 to 1.25) |
| Age | 1.00 (0.98 to 1.02) | 0.99 (0.98 to 1.002) | 1.00 (0.99 to 1.01) |
| Male gender | 0.98 (0.47 to 2.02) | 1.09 (0.78 to 1.54) | 0.91 (0.64 to 1.31) |
| Race, Black | 0.75 (0.33 to 1.70) | 1.48 (1.02 to 2.14)* | 1.12 (0.76 to 1.65) |
| Ethnicity, Hispanic | 0.76 (0.16 to 3.73) | 1.09 (0.55 to 2.17) | 1.11 (0.55 to 2.22) |
| Medicaid or self‐pay insurance | 0.75 (0.16 to 3.49) | 1.61 (0.95 to 2.72) | 2.14 (1.24 to 3.67)* |
| Hospitalist service | 0.68 (0.33 to 1.44) | 1.15 (0.81 to 1.63) | 0.99 (0.69 to 1.43) |
| MDC: respiratory | 1.18 (0.41 to 3.38) | 1.02 (0.61 to 1.69) | 1.16 (0.69 to 1.95) |
| MDC: circulatory | 1.22 (0.52 to 2.87) | 0.79 (0.51 to 1.22) | 0.80 (0.51 to 1.27) |
| MDC: digestive | 0.51 (0.11 to 2.32) | 0.83 (0.47 to 1.46) | 1.08 (0.62 to 1.91) |
| Charlson Comobrbidity Index | 1.25 (1.09 to 1.45)* | 1.09 (1.01 to 1.19)* | 1.11 (1.02 to 1.21)* |
Our multivariate models explained very little of the variance in patient outcomes. For LOS and hospital charges, adjusted R2 values were 0.06 and 0.05, respectively. For ICU transfer during hospitalization, 30 day repeat ED visit, and 30 day readmission, the areas under the receiver operator curves were 0.75, 0.51, and 0.61 respectively.
To assess the robustness of our conclusions regarding night admission, we redefined night to include only patients admitted between the hours of 8 pm and 5:59 am. This did not change our conclusions. We also tested for interaction between night admission and weekend admission for all outcomes to assess whether night admissions on the weekend were in fact at increased risk of worse outcomes; we found no evidence of interaction (P > 0.3 for the interaction terms in each model).
Discussion
Among patients admitted to the medicine services at our academic medical center, night or weekend admission was not associated with worse hospitalization‐relevant outcomes. In some cases, night or weekend admission was associated with better outcomes, particularly in terms of ICU transfer during hospitalization and hospital charges. Prior research indicates worse outcomes during off‐hours,5 but we did not replicate this finding in our study.
The finding that admission at night was not associated with worse outcomes, particularly proximal outcomes such as LOS or ICU transfer during hospitalization, was surprising, though reassuring in view of the fact that more than half of our patients are admitted at night. We believe a few factors may be responsible. First, our general medicine service is staffed during the night (7 pm to 7 am) by in‐house nocturnists and night float residents. Second, our staffing ratio, while lower at night than during the day, remains the same on weekends and may be higher than in other settings. In continuously well‐staffed settings such as the ED12 and ICU,13 night and weekend admissions are only inconsistently associated with worse outcomes, which may be the same phenomena we observed in the current study. Third, the hospital used as the site of this study has received Nursing Magnet recognition and numerous quality awards such as the National Research Corporation's Consumer Choice Award and recognition as a Distinguished Hospital for Clinical Excellence by HealthGrades. Fourth, our integrated electronic medical record, computerized physician order entry system, and automatically generated sign out serve as complements to the morning hand off. Fifth, hospitalists and teaching teams rotate on a weekly, biweekly, or every 4 week basis, which may protect against discontinuity associated with the weekend. We believe that all of these factors may facilitate alert, comprehensive care during the night and weekend as well as safe and efficient transfer of patients from the night to the day providers.
We were also surprised by the association between weekend admission and lower charges and a lower chance of ICU transfer during hospitalization. We believe many of the same factors noted above may have played a role in these findings. In terms of hospital charges, it is possible that some workups were completed outside of the hospital rather than during the hospitalization, and that some tests were not ordered at all due to unavailability on weekends. The decreased chance of ICU transfer is unexplained. We hypothesize that there may have been a more conservative admission strategy within the ED, such that patients with high baseline severity were admitted directly to the ICU on the weekend rather than being admitted first to the general medicine floor. This hypothesis requires further study.
Our study had important limitations. It was a retrospective study from a single academic hospital. The sample size lacked sufficient power to detect differences in the low frequency of certain outcomes such as poor outcomes within 24 hours of admission (2% vs. 1%), and also for more frequent outcomes such as 30 day readmission; it is possible that with a larger sample there would have been statistically significant differences. Further, we recognize that the Charlson Comorbidity Index, which was developed to predict 1‐year mortality for medicine service patients, does not adjust for severity of illness at presentation, particularly for outcomes such as readmission. If patients admitted at night and during the weekend were less acutely ill despite having similar comorbidities and MDCs at admission, true associations between time of admission and worse outcomes could have been masked. Furthermore, the multivariable modeling explained very little of the variance in patient outcomes such that significant unmeasured confounding may still be present, and consequently our results cannot be interpreted in a causal way. Data was collected from electronic records, so it is possible that some adverse events were not recorded. However, it seems unlikely that major events such as death and transfer to an ICU would have been missed.
Several aspects of the study strengthen our confidence in the findings, including a large sample size, relevance of the outcomes, the adjustment for confounders, and an assessment for robustness of the conclusions based on restricting the definition of night and also testing for interaction between night and weekend admission. Our patient demographics and insurance mix resemble that of other academic hospitals,10 and perhaps our results may be generalizable to these settings, if not to non‐urban or community hospitals. Furthermore, the Charlson Comorbidity Index was associated with all 5 of the modeled outcomes we chose for our study, reaffirming their utility in assessing the quality of hospital care. Future directions for investigation may include examining the association of night admission with hospitalization‐relevant outcomes in nonacademic, nonurban settings, and examining whether the lack of association between night and weekend admission and worse outcomes persists with adjustment for initial severity of illness.
In summary, at a large, well‐staffed urban academic hospital, day or time of admission were not associated with worse hospitalization‐relevant outcomes. The use of nocturnists and night float teams for night admissions and continuity across weekends appears to be a safe approach to handling the increased volume of patients admitted at night, and a viable alternative to overnight call in the era of work hour restrictions.
- ,,, et al.Three‐year results of mandated work hour restrictions: attending and resident perspectives and effects in a community hospital.Am Surg.2008;74(6):542–546; discussion 546–547.
- ,,, et al.Handoffs causing patient harm: a survey of medical and surgical house staff.Jt Comm J Qual Patient Saf.2008;34(10):563–570.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121(11):866–872.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345(9):663–668.
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299(7):785–792.
- ,,,.Continuity of care and intensive care unit use at the end of life.Arch Intern Med.2009;169(1):81–86.
- ,,,,,.Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301(16):1671–1680.
- ,,,.Why predictive indexes perform less well in validation studies: is it magic or methods?Arch Intern Med.1987;147:2155–2161.
- ,,.Adapting a clinical comorbidity index for use with ICD‐9‐CM administrative databases.J Clin Epidemiol.1992;45(6):613–619.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,, et al.Use of an admission early warning score to predict patient morbidity and mortality and treatment success.Emerg Med J.2008;25(12):803–806.
- ,,.The impact of weekends on outcome for emergency patients.Clin Med.2005;5(6):621–625.
- ,,,,,.Off hour admission to an intensivist‐led ICU is not associated with increased mortality.Crit Care.2009;13(3):R84.
- ,,, et al.Three‐year results of mandated work hour restrictions: attending and resident perspectives and effects in a community hospital.Am Surg.2008;74(6):542–546; discussion 546–547.
- ,,, et al.Handoffs causing patient harm: a survey of medical and surgical house staff.Jt Comm J Qual Patient Saf.2008;34(10):563–570.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121(11):866–872.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345(9):663–668.
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299(7):785–792.
- ,,,.Continuity of care and intensive care unit use at the end of life.Arch Intern Med.2009;169(1):81–86.
- ,,,,,.Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301(16):1671–1680.
- ,,,.Why predictive indexes perform less well in validation studies: is it magic or methods?Arch Intern Med.1987;147:2155–2161.
- ,,.Adapting a clinical comorbidity index for use with ICD‐9‐CM administrative databases.J Clin Epidemiol.1992;45(6):613–619.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,, et al.Use of an admission early warning score to predict patient morbidity and mortality and treatment success.Emerg Med J.2008;25(12):803–806.
- ,,.The impact of weekends on outcome for emergency patients.Clin Med.2005;5(6):621–625.
- ,,,,,.Off hour admission to an intensivist‐led ICU is not associated with increased mortality.Crit Care.2009;13(3):R84.
Copyright © 2010 Society of Hospital Medicine
Hospital‐Based Tobacco Treatment Service
Hospitalization can be considered a teachable moment for smoking cessation13 for the 6.5 million adult smokers who are hospitalized in the United States each year.4 Smokers who receive tobacco treatment during hospitalization and outpatient follow‐up treatment for at least 1 month are more likely to quit than patients who receive no treatment.5, 6
Unless tobacco treatment is explicitly delegated to other providers, physicians shoulder the responsibility of encouraging smokers to quit and prescribing smoking cessation medications. This is problematic in that physicians sometimes fail to counsel their patients about quitting smoking7, 8 or recommend outpatient follow‐up.9 Few hospitals provide comprehensive treatment. In a review of 33 studies on the prevalence of smoking care delivery in hospitals, 3 hospitals reported they provided advice to quit alone, 29 provided advice plus counseling and assistance in quitting, and 8 provided advice or prescription for cessation pharmacotherapy.9 Although post‐discharge support is a key component of effective treatment for hospitalized smokers,6 only 11 reported providing follow‐up treatment, or referral for follow‐up treatment, after discharge. Among these 11 hospitals, respondents reported they provided referral or follow‐up to 1% to 74% of their smokers, with a median percentage of 24%. The 1 study that specified the type of outpatient treatment provided reported the hospital provided the state quitline number to smokers.
Instituting a dedicated smoking cessation program may enhance inpatient treatment, outpatient follow‐up, and treatment outcomes. Two studies have found that institutional smoking cessation programs increased the likelihood that patients would receive treatment and quit compared to hospitals without dedicated programs.10, 11
Although many US hospitals are developing programs to provide systematic treatment for tobacco dependence,9 little is known regarding how programs structure their staff, enroll patients, or provide treatment to patients that smoke. Instituting tobacco treatment services usually requires policy change and system‐wide approaches with quality improvement endpoint goals.8, 1214 In the United States, elements of these services include: 1) developing a cadre of trained tobacco treatment specialists, 2) implementing hospital systems for identifying smokers and referring them to the service, 3) providing inpatient treatment based on current treatment guidelines15 and 4) providing or facilitating follow‐up treatment after discharge, often via fax‐referral to tobacco quitlines. This systematic approach is still lacking in many hospitals.
To date, few evaluations of dedicated hospital‐based smoking cessation programs have been reported in the literature.8, 11 The purpose of this study is to describe patient characteristics and outcomes of a dedicated tobacco treatment service, with paid staff, in a large academic medical center. We describe treatment protocols, profile patients served, treatments provided, and summarization of 6‐month post‐discharge outcomes for smokers referred to the UKanQuit service over a 1‐year period. We close with lessons learned on how to improve the delivery of tobacco treatment to hospitalized patients.
Methods
Design and Setting
This is a descriptive observational study of a tobacco treatment program in a large Midwestern academic medical center between September 1, 2007 and August 31, 2008. The specialty tobacco treatment service (UKanQuit) was established when the hospital campus went smoke free on September 1, 2006. Patients are referred to the service via the hospital electronic medical record (EMR). As nurses complete electronic forms on patients admitted to their units, the EMR prompts nurses to ask patients if they smoke, ask smokers if they would like tobacco treatment medication to prevent withdrawal symptoms while in the hospital, and ask smokers if they would like to talk to a tobacco treatment specialist during their hospital stay. Those who respond yes to the final question are placed on an electronic list for UKanQuit services. Physicians and other health care providers can also order consultation from the UKanQuit service. A description of smokers admitted to the hospital and predictors of referral to UKanQuit within the first year of service is presented elsewhere.16, 17
The UKanQuit staff consists of an interdisciplinary team of counselors with a Ph.D., Masters degrees, and/or substantial experience in case management and substance abuse treatment. All have received intensive training and supervision in treating tobacco dependence. All participate in UKanQuit counseling on a part‐time basis, and spend the remainder of their effort as research assistants and counselors on smoking cessation research projects in the medical center. Hence, staffing consists of 1 full‐time equivalent counselor, 0.15 full‐time equivalent director (Richter), and 0.05 full‐time equivalent medical director (Ellerbeck). The program is funded through a contract with the hospital. We are in the process of hiring a nurse practitioner to create a more sustainable funding stream for the program because nurse practitioners can bill cessation services.
UKanQuit provides hospital counseling from 9 AM to 5 PM on weekdays. UKanQuit staff meets weekly for counseling supervision, strategic planning, continuing education, and troubleshooting difficult cases. In addition to treating smokers, the UKanQuit staff provides training and consultation to hospital personnel via grand rounds and other presentations. The service also provides a platform for medical students and residents to conduct focused research related to quality improvement. To facilitate systematic treatment of tobacco, UKanQuit developed the hospital treatment protocol for nursing staff, developed evidence‐based written self‐help materials that are accessible to hospital staff via the hospital printing system, and developed and instituted a tobacco treatment order set that was recently integrated into the EMR and automatically becomes prioritized as a recommended order set for all patients who report they have smoked in the past 30 days.
Procedures
UKanQuit staff retrieves patient details from the EMR and visits patients at their bedside. All hospital services refer to UKanQuit. UKanQuit provides counseling to Spanish speakers through bilingual/bicultural staff and hospital translators assist UKanQuit staff in counseling patients who speak other languages. The staff conducts a brief assessment at the bedside to inform treatment and contacts patients 6 months following inpatient treatment to assess outcomes and provide additional support and referral. This study evaluating the UKanQuit program was approved by the medical center's Institutional Review Board.
Program Intervention
UKanQuit staff visit patients at the bedside to deliver tobacco treatment. This consists of: (a) assessing withdrawal; (b) working with the health care team to adjust nicotine replacement to keep the patient comfortable; (c) assessing patients' interest in quitting smoking; (d) providing brief motivational intervention to patients not interested in quitting; and (e) providing assistance in quitting (developing a quit plan, arranging for medications on discharge) to patients interested in quitting (Figure 1). UKanQuit staff recommend medications based on the patients' level of dependence, history of cessation, and cessation medication preferences. The recommendation is communicated in person and by chart documentation to the medical team, usually by the nursing staff. The patients' resident or attending physician makes the final determination regarding medication provided. The hospital has nicotine replacement therapy (NRT; patch, gum, and lozenge), bupropion, and varenicline in its formulary. Patients are then offered an option of fax referral to the state tobacco quitline for follow‐up counseling. UKanQuit staff documents the services provided in the EMR via SOAR (Subjective, Objective, Assessment and Referral) notes.
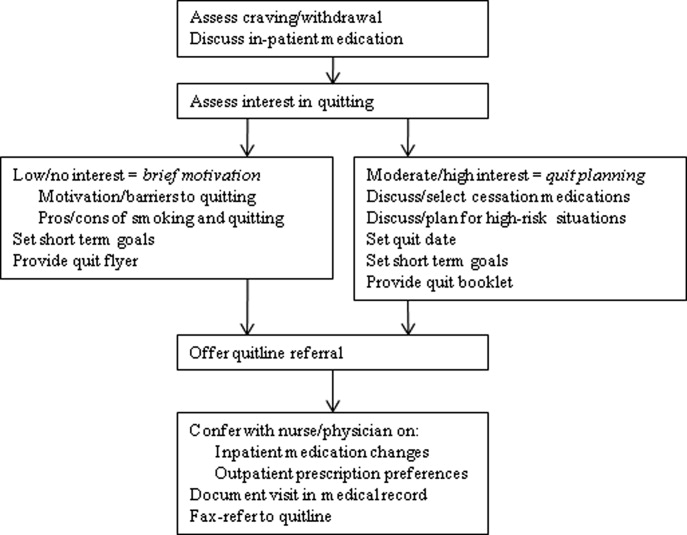
Measures
Baseline Measures
These were collected from the UKanQuit 1‐page program intake form, which UKanQuit designed to collect the minimal information necessary to conduct medication and behavioral counseling, to maximize counseling time, and to fit into the dense schedule of each patient's hospital stay. Demographic measures include age, gender and ethnicity. Smoking behavior measures include number of years smoked, number of cigarettes per day, a single item from the Fagerstrom Test for Nicotine Dependence that assesses time to first cigarette after waking,18, 19 interest in quitting smoking (on a 0‐10 scale, with 10 being very interested in quitting), and a single item from the self report version of the Minnesota Nicotine Withdrawal Scale (MNWS) that asks smokers to rate their desire or craving to smoke over a specified period. The single item craving measure from the MNWS has been found to have high reliability and good construct validity and is neither less sensitive to abstinence nor less reliable than the ten‐item brief questionnaire of smoking urges (QSU‐brief) used in laboratory and clinical trials.20 We asked about craving over the past 24 hours on a scale from 0 (none) to 4 (severe).21
Process Measures
Counselors also document the treatment they provided to smokers including the time spent with patients during counseling, provision of written self‐help materials, whether smokers set goals for quitting, hospital staff had already placed the smoker on a tobacco treatment medication, smokers are interested in increasing or changing their medication, the smoker wants smoking cessation medication on discharge, UKanQuit staff submitted a recommendation to hospital staff to make a medication change and/or provide a prescription for medication on discharge, plans for post‐discharge follow‐up (fax‐referral of patients to the state tobacco quitline or acceptance of UKanQuit counseling after discharge), and the patient agrees to be contacted at 6 months post‐discharge for follow‐up assessment and assistance.
Follow‐Up Measures
Outcome measures were collected by telephone 6 months post‐discharge by study staff who were not involved in the in‐hospital counseling. Call attempts to reach each patient ranged from 1 to 11. Measures included self‐reported 7‐day point prevalence abstinence rates, the number of quit attempts lasting over 24 hours, and cigarettes smoked per day among continuing smokers. Patients are asked if they participated in counseling through the tobacco quitline. Scaled (0‐10) items assess how important it is to the patients to quit smoking or remain quit, how confident they are in being able to quit or remain quit, and how satisfied they were with the assistance provided by UKanQuit. A yes/no item assesses whether patients think the program should be continued. In addition, UKanQuit asked two open‐ended questions to qualitatively assess satisfaction with the program and elicit suggestions for improvements. The questions were: What, if anything, was helpful to you about our services? and How can UKanQuit better help people stop smoking?
Analyses
Categorical variables were summarized by frequencies and percentages; continuous variables were summarized by means and standard deviations (SDs). We compared baseline characteristic differences between respondents and nonrespondents at 6 months follow‐up using chi‐square for categorical variables and t‐test for continuous variables. We also compared cigarettes per day at baseline and 6 months post‐discharge in smokers who were not able to quit using paired t‐test. All analyses were done with SPSS 17.0 statistical package. Open‐ended questions were analyzed using the framework synthesis method.22 Following examination and familiarization with the data, we developed an initial list of themes. We then categorized the responses by these themes using numerical codes. Each thematic code was summarized as a percentage of all responses. Those responses that fit into multiple thematic codes were multiply coded.
Results
Baseline
Within the study period (September 1, 2007 to August 31, 2008), 22,624 patients were admitted to the medical center (Figure 2). A total of 4150 were current smokers (ie, smoked within the past 30 days). UKanQuit staff met with 513 (68%) of 753 patients referred to the service. Some of the reasons why 32% of referred patients were not seen by the UKanQuit staff have been described in our previous paper.17 These include patient was asleep, doctor in the room, out of bed for procedure, and unable to speak. Table 1 displays the characteristics of 513 smokers treated by UKanQuit from September 1, 2007 to August 31, 2008. Patients were predominantly white (74%) with mean age of 50 years. Slightly more than half of smokers were male (57%). They had smoked an average of 18 cigarettes per day for a mean duration of 29 years, and over half (58%) smoked within 5 minutes of waking suggesting a high level of dependence. On a scale of 1 to 10 the mean interest in quitting was 7.9 (SD 2.9) and the mean craving score on a scale of 0 to 4 was 1.2 (SD 1.4) suggesting slight to mild craving.
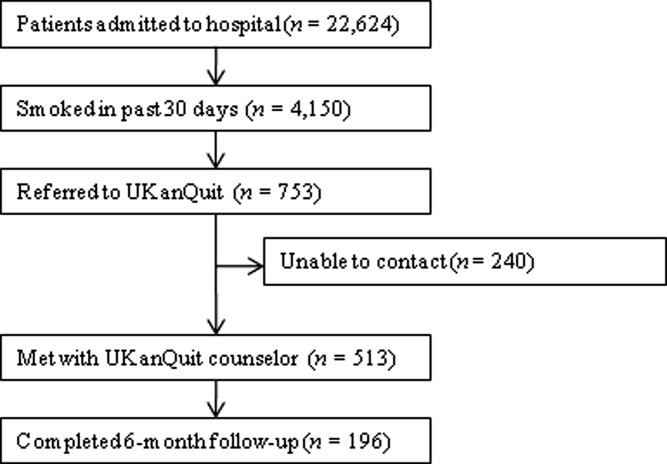
| Characteristics | Treated (n = 513) |
|---|---|
| |
| Demographics | |
| Mean age (SD), years | 50.2 (13.6) |
| Male, n (%) | 291 (56.7) |
| Ethnicity, n (%) | |
| White | 371 (73.6) |
| AA | 107 (21.2) |
| Latino | 18 (3.6) |
| Other | 8 (1.6) |
| Referral source, n (%) | |
| Nursing profile | 477 (94.1) |
| Physician | 5 (1.0) |
| Other | 25 (4.9) |
| Smoking characteristics | |
| Mean number of years smoked (SD) | 28.9 (14.6) |
| Smokes within 5 minutes of waking n (%) | 270 (58.3) |
| Mean cigarettes smoked per day (SD) | 18.4 (12.6) |
| Mean interest in quitting (SD)* | 7.9 (2.9) |
| Mean craving (SD) | 1.2 (1.4) |
| Tobacco treatment provided | |
| Counseling | |
| Average time spent with patients (SD) | 19.9 (9.1) |
| Received information packet, n (%) | 490 (97.4) |
| Set goals for quitting, n (%) | 352 (73.3) |
| Had quit plan, n (%) | 151 (33.2) |
| Accepted fax referral to quitline, n (%) | 277 (55.8) |
| Opted for UKanQuit counseling, n (%) | 29 (5.9) |
| Medication | |
| On smoking cessation medication, n (%) | 133 (26.2) |
| Interested in receiving or changing smoking cessation medication, n (%) | 132 (26.7) |
| Added or changed smoking cessation medication, n (%) | 195 (40.5) |
| Discharge med, n (%) | 196 (40.2) |
In‐Hospital Treatment
Hospital staff had placed 1 in 4 of the patients on smoking cessation medication prior to the UKanQuit staff visit. Nineteen percent were on NRT (16.2% transdermal patch, 2.5% on lozenge, 0.8% on nicotine gum); 5% on bupropion, 16.5% on varenicline, and 2.5% on clonidine. A total of 1.7% used a combination of Patch and bupropion while 2.5% used a combination of patch and gum. Staff provided 97% of the patients with written materials. Most patients (73%) set a goal for quitting or cutting down, and one‐third developed quit plans. Fifty‐six percent accepted fax referral to their state quitline, and 6% opted for follow‐up counseling with a UKanQuit counselor. Average time spent by UKanQuit with the patient was 20 minutes. Most of the patients treated (n = 426, 86%) agreed that UKanQuit staff can contact them for follow‐up assessment at 6 months.
Outcomes
Staff successfully contacted 196 (46%) of the 426 patients who agreed to 6‐month follow‐up. Responders were older (mean age 53 years, SD 12.6 vs. mean age 48 years, SD 13.8; P < 0.001); were more interested in quitting (mean interest in quitting 8.4, SD 2.5 vs. 7.6, SD 3.1 P = 0.001); and had a lower craving score at baseline (mean craving score 0.99, SD 1.3 vs. 1.29, SD 1.5; P < 0.001) compared to nonresponders. There were no differences between responders and nonresponders by gender, number of cigarettes smoked per day, years of smoking, referral source, inpatient smoking cessation medication used or time spent with UKanQuit hospital staff during the inpatient visit.
Table 2 displays smoking behavior and smoking cessation‐related characteristics of the respondents 6‐month post‐discharge. Over 70% attempted a quit attempt lasting at least 24 hours. The self reported 7‐day point prevalence abstinence rate was 31.8% among respondents. The intent‐to‐treat quit rate was 14.6% among all participants who agreed to follow‐up, counting those who we could not contact as smokers. While 34% used pharmacotherapy, only 5% of those who were fax‐referred to the quitline utilized the service. Most of the patients seen by the UKanQuit counselor considered quitting and staying quit important, mean 8.7, SD 2.3, and their confidence to quit or stay quit was above average, mean 6.6, SD 3.6. They rated the UKanQuit program very high, at 8.3, SD 2.8, on a scale of 0 to 10, and 98% of them wanted the program to continue. Of those who were not able to quit at 6 months, the mean number of cigarettes smoked per day decreased significantly from 17.8, SD 12.0 at baseline to 14.0, SD 9.7 at 6 months follow‐up (P < 0.001).
| Variables | |
|---|---|
| |
| Smoking characteristics | |
| 7 day point prevalence abstinence rate, n (%) | 62 (31.8) |
| Among current smokers at 6 months follow‐up, n = 134 | |
| Proportion of smokers who attempted to quit within 6 months, n (%) | 99 (73.9) |
| Mean CPD for smokers at 6 months (SD) | 14.0 (9.7) |
| Used formal quit smoking program | |
| Quit smoking medication, n (%) | 65 (34.4) |
| Quitline use among those faxed to quitline, n (%)* | 6 (5.0) |
| Importance/ Confidence | |
| How important is it to quit or stay quit, mean (SD) | 8.7 (2.3) |
| How confident are you to quit or stay quit, mean (SD) | 6.6 (3.6) |
| Views about service | |
| Satisfaction with UKanQuit service, mean (SD) | 8.3 (2.8) |
| Wants the UKanQuit program to continue, n (%) | 165 (97.6) |
Satisfaction and Recommendations for Improvement
Most (96%) of participants contacted at follow‐up commented on what was helpful about the services. Table 3 displays the distribution of themes and illustrative comments. Themes included staff encouragement, support and counseling (41.8%); other (27%); information and education materials (20.9%); medication advice and referral (2.6%), and referral to quitline (0.5%)
| n (%) | |
|---|---|
| |
| Staff encouragement, support and counseling | 82 (41.8) |
| You guys did excellent. The friendliness of the people who visited me. | |
| Her outlook and her encouragement | |
| Other | 53 (27.1) |
| I don't remember the visit because I was heavily medicated, | |
| A lot was helpful but I couldn't tell you exactly what part was the most helpful | |
| Information/education material | 41 (20.9) |
| Provided me with a lot of info and the packet was helpful. | |
| The information packet | |
| Program not helpful | 14 (7.1) |
| I really didn't need their information, I was able to quit without it. | |
| Nothing helpful except the companionship | |
| Medication advice/referral | 5 (2.6) |
| They took the time and set up the patches for me | |
| She helped me with questions about medication, especially Chantix | |
| Referral to Quitline | 1 (0.5) |
| Talking on the phone | |
Discussion
Among patients served by this inpatient program, interest in quitting was high but administration of inpatient medications upon admission was low (26%). Nearly all patients were provided with written materials, a majority set some form of goal for quitting or cutting down, and many developed quit plans and received assistance adjusting inpatient and/or discharge medications. After discharge, the majority of study participants made unassisted quit attempts, as utilization of medications and quitline services was suboptimal. Fax‐referral to quitline may not, on its own, fulfill guideline recommendations for post‐discharge follow‐up.
Our intent‐to‐treat quit rate was about half of what was found in Taylor et al.'s11 hospital program dissemination trial. Their program may have had better effects as it was somewhat more intensive. It included at least 1 follow‐up phone call immediately after discharge, as well as an accompanying video and relaxation audiotape or compact disc. However, differences in outcomes may also be due to large differences between the study populations. Hospitals participating in Taylor's study only conducted intervention and outcome assessment among smokers who were ready to quit, willing to enroll in a clinical trial, and willing to complete informed consent. Our intervention and outcome data included patients who agreed to speak with UKanQuit staff, regardless of readiness to quit. Our participants did not have to complete informed consent and enroll in a trial as our analyses were conducted post hoc. Our study outcomes might better reflect quit rates for a program serving all smokers, at all levels of readiness to quit, in actual hospital practices. The mean reduction in cigarette smoking among smokers who continued to smoke at 6 months' follow‐up was statistically significant. However, findings from a lung health study show that 50% or more reduction in smoking was ultimately related to successful quitting.23
Strengths and Limitations
The strengths of the study include the fact that the program attempts to intervene with all smokers, and provides stage‐appropriate intervention based on readiness to quit. It provides a snapshot of how a program is incorporated into clinical practice and describes implementation of protocol components.
This study has a number of limitations. We do not know exactly how many patients received the in‐hospital medication change agreed upon by the counselor and medical team immediately following the patient encounter. Our follow‐up rate was low and abstinence rates were based on self‐report, which limits our ability to draw conclusions about cessation outcomes. Process of care measures are based on counselor self‐report, without verification of services rendered. We are not able to identify the impact of our intervention above and beyond our patients' hospital experience, because we did not have a control group. We collected limited data from study participants so we are not able to better understand causes of nonadherence to quitline or poor pharmacotherapy utilization. Lastly, when the respondents were asked to comment about what was helpful about UKanQuit, 23% of the respondents said they could not remember the UKanQuit visit during their hospital stay. Many hospital medications induce brief amnesia, and patients have numerous consults during their stay and might not be able to separate one from the other. The 6‐month interval between their visit and follow‐up call may also account for their inability to remember the cessation consult.
Our patient population is in fact a subset of all smokers admitted (11% of smokers) because they are motivated enough to agree to talk with a counselor. Our intervention procedures, and results, might be quite different if all smokers were visited by the counselor. Efficacy trials of tobacco treatment in hospitals have focused on smokers who are ready to quit.24 Hence, procedures for working with unmotivated smokers in hospitals are less well established. Policymakers, hospitals, and hospital tobacco treatment programs should examine the most efficient (ie, effective and cost‐effective) approaches for addressing smoking in hospitals and specifically focus on whether all smokers should be treated by dedicated tobacco treatment staff, or only those who agree to a consult.
Lessons Learned
Linking Patients With In‐Hospital Cessation Medications Requires Collaboration With the Entire Health Care Team
Only 1 in 4 UKanQuit participants had been given smoking cessation medication to ameliorate withdrawal before counselors met with the patients. Although we have not systematically collected reasons patients do not receive cessation medication on admission, the 2 most common causes are that patients refuse it or physicians refuse it. Patients refuse medication perhaps because they do not want to quit, they feel they will cope without smoking during their hospital stay, or they are paying out of pocket and want to reduce costs. Physicians do not permit it because they believe it is contraindicated for the patient's health condition, it is contraindicated for the procedure the patient is receiving in the hospital, or they believe it will interfere with wound healing. There is also a considerable delay between ordering and receiving medications; patients who become uncomfortable during their stay sometimes change their minds, but end up being discharged before their medication arrives. Most of these issues pertain to nicotine replacement. Although patients not eligible for NRT may be good candidates for bupropion, varenicline, or even the second line cessation medications of clonidine or nortryptiline, these medications do not provide immediate relief from tobacco withdrawal symptoms and staff are reluctant to start patients on medications they may not receive on an outpatient basis. It is not clear what proportion of hospitalized patients should receive ameliorative medication. Not every hospitalized smoker is a candidate for NRT, due to contraindicated medical conditions, patients' level of dependence, and patients' willingness to accept cessation medication in order to prevent withdrawal. Koplan et al.25 achieved hospital‐wide increases in NRT orders from 1.6% to 2.5% after the introduction of an electronic tobacco treatment order set. These percentages seem low but actually were calculated from all hospital admissions, including smokers and nonsmokers. Moreover, their hospital population had a relatively low smoking rate of 12%. Our in‐hospital and post‐discharge (26.2% and 34.4% respectively) pharmacotherapy utilization rates were based only on smokers who had been seen by our service. Even though 1 in 4 smokers were already on medication when they were seen by counselors, 1 in 4 of patients seen wanted to either add a cessation medication or change their current dose. There is clearly room for improvement in how we offer and administer cessation medications on admission. Also, assessing medication efficacy and adjusting as needed appears to be an important role for in‐hospital counselors.
Facilitating Medications Post‐Discharge Will Require Creativity and Outpatient Follow‐Up
Post‐discharge, only 1 in 3 of our patients reported they used cessation medications. This may, again, be a function of patients' readiness to quit. However, it could also be related to knowledge/attitudes regarding the efficacy of medications or access to low‐cost medications. Some of our patients commented that making medication affordable would be helpful. Although our materials provide information on sources for free or low‐cost medications, this information may not have been salient during the hospital stay. To increase access to medications post‐discharge, programs should consider providing a booster mailer to the home with information on sources for free or reduced medications, providing take‐home starter pharmacotherapy kits lasting 1 to 2 weeks to bridge the gap between hospital discharge and finding another source of medications, and/or a follow‐up call shortly after discharge to verify use of pharmacotherapy and troubleshoot problems with medications or procurement.
Providing Follow‐Up Via Fax Referral to Quitlines Is Not as Simple as It Seems
Although our overall quitline fax‐referral rate was high (over half of all patients seen), rate of enrollment among those referred is much lower than the rates reported elsewhere, which range from 16% to 53%.2628 In our sample of fax‐referred smokers, we do not know how many were not enrolled due to failure to make contact vs. patient refusal once contact was made. One possible factor impacting enrollment rates is whether or not smokers are prescreened for readiness to quit. Nearly half of US quitlines require smokers to be ready to quit in order to receive a full course of treatment,29 but only 20% of smokers are ready to quit at any given time.30 In the cited studies with higher conversion rates, counselors prescreened patients for readiness to quit and only offered fax‐referral to those ready to quit in the next 30 days. Our program offers fax‐referral to all smokers. Our findings suggest that doing so results in high rates of referral but low rates of enrollment among those referred. Future studies should examine the impact of prescreening for readiness versus offering referral to all smokers on net enrollment and cessation.
Linking hospitalized smokers with tobacco quitlines has many potential benefits.31, 32 Proactive tobacco quitlines are effective15 and cost effective33 for smoking cessation; they are available, free, to all US smokers; services are delivered via telephone which minimizes many access barriers; hospitals do not have to bear the costs of the services; and many quitlines are undersubscribed and eager to increase their reach.34 Potential methods for increasing conversion to enrollment include building motivation to accept counseling and preparing patients for the quitline intake procedures. Our program is considering providing a warm handoff to patients by calling the quitline during the bedside consult to permit the quitline to enroll the patient during their hospital stay.
Hospital‐based cessation programs have the potential to deliver tobacco treatment to millions of hospitalized smokers annually. To deliver high‐quality, effective care, hospital cessation programs will have to solve problems inherent in hospital‐based carehow best to integrate into existing hospital systems, how to effectively communicate with other hospital care providers, and how to facilitate transitions in care to ensure patients receive evidence‐based post‐discharge care. We offer this report as the first of hopefully many that address quality improvement for specialized programs dedicated to treating tobacco in hospitals.
Acknowledgements
The authors gratefully acknowledge the contributions of the following UKanQuit Counselors in the planning and development of this manuscript: Brian Hernandez, Alex Perez‐Estrada, Grace Meikenhous, Meredith Benson, Terri Tapp. We also thank Chip Hulen, Albers Bart and Chris Wittkopp of the Organizational Improvement Department of KU Hospital; Marilyn Painter, Joanne McNair and Karisa Deculus of the KU Preventive Medicine and Public Health Department.
- ,.Smokers who are hospitalized: a window of opportunity for cessation interventions.Prev Med.1992;21:262–269.
- ,,.Understanding the potential of teachable moments: the case of smoking cessation.Health Educ Res.2003;18(2):156–170.
- ,.Teachable moments for promoting smoking cessation: the context of cancer care and survivorship.Cancer Control.2003;10(4):325–333.
- ,,.Helping hospitalized smokers quit: new directions for treatment and research.J Consul Clin Psychol.1993;61(5):778–789.
- ,,.Smoking cessation interventions for hospitalized smokers: a systematic review.Arch Intern Med.2008;168(18):1950–1960.
- ,,.Interventions for smoking cessation in hospitalised patients.Cochrane Database Syst Rev.2007(3):CD001837.
- CDC.Physician and other health‐care professional counseling of smokers to quit‐‐United States, 1991.MMWR Morb Mortal Wkly Rep.1993;42(44):854–857.
- ,,,,,.Implementing tobacco interventions in the real world of managed care.Tob Control.2000;9Suppl 1:I18–I24.
- ,,, et al.Smoking care provision in hospitals: a review of prevalence.Nicotine Tob Res.2008;10(5):757–774.
- ,,,,,.Predictors of smoking cessation after a myocardial infarction: the role of institutional smoking cessation programs in improving success.Arch Intern Med.2008;168(18):1961–1967.
- ,,,,.Dissemination of an effective inpatient tobacco use cessation program.Nicotine Tob Res.2005;7(1):129–137.
- ,,,,.Application of a nurse‐managed inpatient smoking cessation program.Nicotine Tob Res.2002;4(2):211–222.
- ,,,,,.Delivering clinical preventive services is a systems problem.Ann Behav Med.1997;19(3):271–278.
- ,,, et al.Lessons from experienced guideline implementers: attend to many factors and use multiple strategies.Jt Comm J Qual Improv.2000;26(4):171–188.
- U.S. Department of Health and Human Services (USDHHS).Treating Tobacco Use and Dependence: Clinical Practice Guideline 2008 Update.
- ,,,,.Referral and treatment for nicotine dependence among hospitalized patients.Subst Abus.2009;30(1):94–95.
- ,,,,.Prevalence and predictors of tobacco treatment in an academic medical center.Jt Comm J Qual Patient Saf.2009;35(11):551–557.
- ,,,.The Fagerstrom Test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire.Br J Addict.1991;86(9):1119–1127.
- ,,, et al.Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence.Nicotine Tob Res.2007;9 Supp 4:555–570.
- ,.Is the ten‐item Questionnaire of Smoking Urges (QSU‐brief) more sensitive to abstinence than shorter craving measures?Psychopharmacology (Berl).2010;208(3):427–432.
- ,.Signs and symptoms of tobacco withdrawal.Arch Gen Psychiatry.1986;43(3):289–294.
- ,,.Qualitative research in health care. Analysing qualitative data.BMJ.2000;320(7227):114–116.
- ,,,.Smoking reduction in the Lung Health Study.Nicotine Tob Res.2004;6(2):275–280.
- ,,.Interventions for smoking cessation in hospitalised patients.Cochrane Database Syst Rev.2007(3):CD001837.
- ,,,,.A computerized aid to support smoking cessation treatment for hospital patients.J Gen Intern Med.2008;23(8):1214–1217.
- ,,,,,.The feasibility of connecting physician offices to a state‐level tobacco quit line.Am J Prev Med.2006;30(1):31–37.
- ,,, et al.Clinical faxed referrals to a tobacco quitline: reach, enrollment, and participant characteristics.Am J Prev Med.2009;36(4):337–340.
- ,,, et al.Feasibility of a Spanish/English computerized decision aid to facilitate smoking cessation efforts in underserved communities.J Health Care Poor Underserved.2010;21(2):504–517.
- North American Quitline Consortium. Available at: http://www.naquitline. org. Accessed July2010.
- ,,,,,.Distribution of smokers by stage in three representative samples.Prev Med.1995;24:401–411.
- ,,.Telephone counselling for smoking cessation.Cochrane Database Syst Rev.2006;3:CD002850.
- ,.The potential of quitlines to increase smoking cessation.Drug Alcohol Rev.2006;25(1):73–78.
- ,,, et al.Evidence of real‐world effectiveness of a telephone quitline for smokers.N Engl J Med.2002;347(14):1087–1093.
- Campaign for Tobacco Free Kids Fact Sheets 2008. Quitlines Help Smokers Quit. Available at: http://www.tobaccofreekids.org/research/factsheets/pdf/0326.pdf. Accessed July2010.
Hospitalization can be considered a teachable moment for smoking cessation13 for the 6.5 million adult smokers who are hospitalized in the United States each year.4 Smokers who receive tobacco treatment during hospitalization and outpatient follow‐up treatment for at least 1 month are more likely to quit than patients who receive no treatment.5, 6
Unless tobacco treatment is explicitly delegated to other providers, physicians shoulder the responsibility of encouraging smokers to quit and prescribing smoking cessation medications. This is problematic in that physicians sometimes fail to counsel their patients about quitting smoking7, 8 or recommend outpatient follow‐up.9 Few hospitals provide comprehensive treatment. In a review of 33 studies on the prevalence of smoking care delivery in hospitals, 3 hospitals reported they provided advice to quit alone, 29 provided advice plus counseling and assistance in quitting, and 8 provided advice or prescription for cessation pharmacotherapy.9 Although post‐discharge support is a key component of effective treatment for hospitalized smokers,6 only 11 reported providing follow‐up treatment, or referral for follow‐up treatment, after discharge. Among these 11 hospitals, respondents reported they provided referral or follow‐up to 1% to 74% of their smokers, with a median percentage of 24%. The 1 study that specified the type of outpatient treatment provided reported the hospital provided the state quitline number to smokers.
Instituting a dedicated smoking cessation program may enhance inpatient treatment, outpatient follow‐up, and treatment outcomes. Two studies have found that institutional smoking cessation programs increased the likelihood that patients would receive treatment and quit compared to hospitals without dedicated programs.10, 11
Although many US hospitals are developing programs to provide systematic treatment for tobacco dependence,9 little is known regarding how programs structure their staff, enroll patients, or provide treatment to patients that smoke. Instituting tobacco treatment services usually requires policy change and system‐wide approaches with quality improvement endpoint goals.8, 1214 In the United States, elements of these services include: 1) developing a cadre of trained tobacco treatment specialists, 2) implementing hospital systems for identifying smokers and referring them to the service, 3) providing inpatient treatment based on current treatment guidelines15 and 4) providing or facilitating follow‐up treatment after discharge, often via fax‐referral to tobacco quitlines. This systematic approach is still lacking in many hospitals.
To date, few evaluations of dedicated hospital‐based smoking cessation programs have been reported in the literature.8, 11 The purpose of this study is to describe patient characteristics and outcomes of a dedicated tobacco treatment service, with paid staff, in a large academic medical center. We describe treatment protocols, profile patients served, treatments provided, and summarization of 6‐month post‐discharge outcomes for smokers referred to the UKanQuit service over a 1‐year period. We close with lessons learned on how to improve the delivery of tobacco treatment to hospitalized patients.
Methods
Design and Setting
This is a descriptive observational study of a tobacco treatment program in a large Midwestern academic medical center between September 1, 2007 and August 31, 2008. The specialty tobacco treatment service (UKanQuit) was established when the hospital campus went smoke free on September 1, 2006. Patients are referred to the service via the hospital electronic medical record (EMR). As nurses complete electronic forms on patients admitted to their units, the EMR prompts nurses to ask patients if they smoke, ask smokers if they would like tobacco treatment medication to prevent withdrawal symptoms while in the hospital, and ask smokers if they would like to talk to a tobacco treatment specialist during their hospital stay. Those who respond yes to the final question are placed on an electronic list for UKanQuit services. Physicians and other health care providers can also order consultation from the UKanQuit service. A description of smokers admitted to the hospital and predictors of referral to UKanQuit within the first year of service is presented elsewhere.16, 17
The UKanQuit staff consists of an interdisciplinary team of counselors with a Ph.D., Masters degrees, and/or substantial experience in case management and substance abuse treatment. All have received intensive training and supervision in treating tobacco dependence. All participate in UKanQuit counseling on a part‐time basis, and spend the remainder of their effort as research assistants and counselors on smoking cessation research projects in the medical center. Hence, staffing consists of 1 full‐time equivalent counselor, 0.15 full‐time equivalent director (Richter), and 0.05 full‐time equivalent medical director (Ellerbeck). The program is funded through a contract with the hospital. We are in the process of hiring a nurse practitioner to create a more sustainable funding stream for the program because nurse practitioners can bill cessation services.
UKanQuit provides hospital counseling from 9 AM to 5 PM on weekdays. UKanQuit staff meets weekly for counseling supervision, strategic planning, continuing education, and troubleshooting difficult cases. In addition to treating smokers, the UKanQuit staff provides training and consultation to hospital personnel via grand rounds and other presentations. The service also provides a platform for medical students and residents to conduct focused research related to quality improvement. To facilitate systematic treatment of tobacco, UKanQuit developed the hospital treatment protocol for nursing staff, developed evidence‐based written self‐help materials that are accessible to hospital staff via the hospital printing system, and developed and instituted a tobacco treatment order set that was recently integrated into the EMR and automatically becomes prioritized as a recommended order set for all patients who report they have smoked in the past 30 days.
Procedures
UKanQuit staff retrieves patient details from the EMR and visits patients at their bedside. All hospital services refer to UKanQuit. UKanQuit provides counseling to Spanish speakers through bilingual/bicultural staff and hospital translators assist UKanQuit staff in counseling patients who speak other languages. The staff conducts a brief assessment at the bedside to inform treatment and contacts patients 6 months following inpatient treatment to assess outcomes and provide additional support and referral. This study evaluating the UKanQuit program was approved by the medical center's Institutional Review Board.
Program Intervention
UKanQuit staff visit patients at the bedside to deliver tobacco treatment. This consists of: (a) assessing withdrawal; (b) working with the health care team to adjust nicotine replacement to keep the patient comfortable; (c) assessing patients' interest in quitting smoking; (d) providing brief motivational intervention to patients not interested in quitting; and (e) providing assistance in quitting (developing a quit plan, arranging for medications on discharge) to patients interested in quitting (Figure 1). UKanQuit staff recommend medications based on the patients' level of dependence, history of cessation, and cessation medication preferences. The recommendation is communicated in person and by chart documentation to the medical team, usually by the nursing staff. The patients' resident or attending physician makes the final determination regarding medication provided. The hospital has nicotine replacement therapy (NRT; patch, gum, and lozenge), bupropion, and varenicline in its formulary. Patients are then offered an option of fax referral to the state tobacco quitline for follow‐up counseling. UKanQuit staff documents the services provided in the EMR via SOAR (Subjective, Objective, Assessment and Referral) notes.
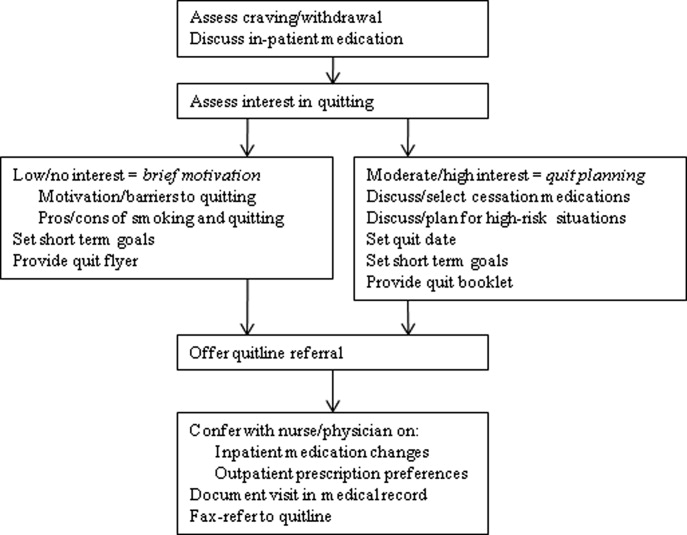
Measures
Baseline Measures
These were collected from the UKanQuit 1‐page program intake form, which UKanQuit designed to collect the minimal information necessary to conduct medication and behavioral counseling, to maximize counseling time, and to fit into the dense schedule of each patient's hospital stay. Demographic measures include age, gender and ethnicity. Smoking behavior measures include number of years smoked, number of cigarettes per day, a single item from the Fagerstrom Test for Nicotine Dependence that assesses time to first cigarette after waking,18, 19 interest in quitting smoking (on a 0‐10 scale, with 10 being very interested in quitting), and a single item from the self report version of the Minnesota Nicotine Withdrawal Scale (MNWS) that asks smokers to rate their desire or craving to smoke over a specified period. The single item craving measure from the MNWS has been found to have high reliability and good construct validity and is neither less sensitive to abstinence nor less reliable than the ten‐item brief questionnaire of smoking urges (QSU‐brief) used in laboratory and clinical trials.20 We asked about craving over the past 24 hours on a scale from 0 (none) to 4 (severe).21
Process Measures
Counselors also document the treatment they provided to smokers including the time spent with patients during counseling, provision of written self‐help materials, whether smokers set goals for quitting, hospital staff had already placed the smoker on a tobacco treatment medication, smokers are interested in increasing or changing their medication, the smoker wants smoking cessation medication on discharge, UKanQuit staff submitted a recommendation to hospital staff to make a medication change and/or provide a prescription for medication on discharge, plans for post‐discharge follow‐up (fax‐referral of patients to the state tobacco quitline or acceptance of UKanQuit counseling after discharge), and the patient agrees to be contacted at 6 months post‐discharge for follow‐up assessment and assistance.
Follow‐Up Measures
Outcome measures were collected by telephone 6 months post‐discharge by study staff who were not involved in the in‐hospital counseling. Call attempts to reach each patient ranged from 1 to 11. Measures included self‐reported 7‐day point prevalence abstinence rates, the number of quit attempts lasting over 24 hours, and cigarettes smoked per day among continuing smokers. Patients are asked if they participated in counseling through the tobacco quitline. Scaled (0‐10) items assess how important it is to the patients to quit smoking or remain quit, how confident they are in being able to quit or remain quit, and how satisfied they were with the assistance provided by UKanQuit. A yes/no item assesses whether patients think the program should be continued. In addition, UKanQuit asked two open‐ended questions to qualitatively assess satisfaction with the program and elicit suggestions for improvements. The questions were: What, if anything, was helpful to you about our services? and How can UKanQuit better help people stop smoking?
Analyses
Categorical variables were summarized by frequencies and percentages; continuous variables were summarized by means and standard deviations (SDs). We compared baseline characteristic differences between respondents and nonrespondents at 6 months follow‐up using chi‐square for categorical variables and t‐test for continuous variables. We also compared cigarettes per day at baseline and 6 months post‐discharge in smokers who were not able to quit using paired t‐test. All analyses were done with SPSS 17.0 statistical package. Open‐ended questions were analyzed using the framework synthesis method.22 Following examination and familiarization with the data, we developed an initial list of themes. We then categorized the responses by these themes using numerical codes. Each thematic code was summarized as a percentage of all responses. Those responses that fit into multiple thematic codes were multiply coded.
Results
Baseline
Within the study period (September 1, 2007 to August 31, 2008), 22,624 patients were admitted to the medical center (Figure 2). A total of 4150 were current smokers (ie, smoked within the past 30 days). UKanQuit staff met with 513 (68%) of 753 patients referred to the service. Some of the reasons why 32% of referred patients were not seen by the UKanQuit staff have been described in our previous paper.17 These include patient was asleep, doctor in the room, out of bed for procedure, and unable to speak. Table 1 displays the characteristics of 513 smokers treated by UKanQuit from September 1, 2007 to August 31, 2008. Patients were predominantly white (74%) with mean age of 50 years. Slightly more than half of smokers were male (57%). They had smoked an average of 18 cigarettes per day for a mean duration of 29 years, and over half (58%) smoked within 5 minutes of waking suggesting a high level of dependence. On a scale of 1 to 10 the mean interest in quitting was 7.9 (SD 2.9) and the mean craving score on a scale of 0 to 4 was 1.2 (SD 1.4) suggesting slight to mild craving.
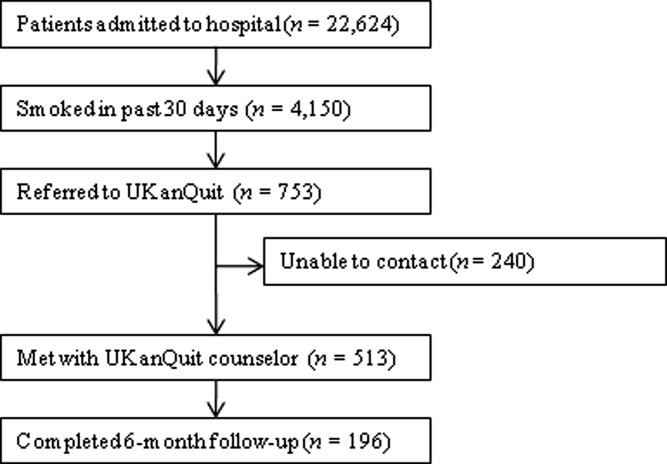
| Characteristics | Treated (n = 513) |
|---|---|
| |
| Demographics | |
| Mean age (SD), years | 50.2 (13.6) |
| Male, n (%) | 291 (56.7) |
| Ethnicity, n (%) | |
| White | 371 (73.6) |
| AA | 107 (21.2) |
| Latino | 18 (3.6) |
| Other | 8 (1.6) |
| Referral source, n (%) | |
| Nursing profile | 477 (94.1) |
| Physician | 5 (1.0) |
| Other | 25 (4.9) |
| Smoking characteristics | |
| Mean number of years smoked (SD) | 28.9 (14.6) |
| Smokes within 5 minutes of waking n (%) | 270 (58.3) |
| Mean cigarettes smoked per day (SD) | 18.4 (12.6) |
| Mean interest in quitting (SD)* | 7.9 (2.9) |
| Mean craving (SD) | 1.2 (1.4) |
| Tobacco treatment provided | |
| Counseling | |
| Average time spent with patients (SD) | 19.9 (9.1) |
| Received information packet, n (%) | 490 (97.4) |
| Set goals for quitting, n (%) | 352 (73.3) |
| Had quit plan, n (%) | 151 (33.2) |
| Accepted fax referral to quitline, n (%) | 277 (55.8) |
| Opted for UKanQuit counseling, n (%) | 29 (5.9) |
| Medication | |
| On smoking cessation medication, n (%) | 133 (26.2) |
| Interested in receiving or changing smoking cessation medication, n (%) | 132 (26.7) |
| Added or changed smoking cessation medication, n (%) | 195 (40.5) |
| Discharge med, n (%) | 196 (40.2) |
In‐Hospital Treatment
Hospital staff had placed 1 in 4 of the patients on smoking cessation medication prior to the UKanQuit staff visit. Nineteen percent were on NRT (16.2% transdermal patch, 2.5% on lozenge, 0.8% on nicotine gum); 5% on bupropion, 16.5% on varenicline, and 2.5% on clonidine. A total of 1.7% used a combination of Patch and bupropion while 2.5% used a combination of patch and gum. Staff provided 97% of the patients with written materials. Most patients (73%) set a goal for quitting or cutting down, and one‐third developed quit plans. Fifty‐six percent accepted fax referral to their state quitline, and 6% opted for follow‐up counseling with a UKanQuit counselor. Average time spent by UKanQuit with the patient was 20 minutes. Most of the patients treated (n = 426, 86%) agreed that UKanQuit staff can contact them for follow‐up assessment at 6 months.
Outcomes
Staff successfully contacted 196 (46%) of the 426 patients who agreed to 6‐month follow‐up. Responders were older (mean age 53 years, SD 12.6 vs. mean age 48 years, SD 13.8; P < 0.001); were more interested in quitting (mean interest in quitting 8.4, SD 2.5 vs. 7.6, SD 3.1 P = 0.001); and had a lower craving score at baseline (mean craving score 0.99, SD 1.3 vs. 1.29, SD 1.5; P < 0.001) compared to nonresponders. There were no differences between responders and nonresponders by gender, number of cigarettes smoked per day, years of smoking, referral source, inpatient smoking cessation medication used or time spent with UKanQuit hospital staff during the inpatient visit.
Table 2 displays smoking behavior and smoking cessation‐related characteristics of the respondents 6‐month post‐discharge. Over 70% attempted a quit attempt lasting at least 24 hours. The self reported 7‐day point prevalence abstinence rate was 31.8% among respondents. The intent‐to‐treat quit rate was 14.6% among all participants who agreed to follow‐up, counting those who we could not contact as smokers. While 34% used pharmacotherapy, only 5% of those who were fax‐referred to the quitline utilized the service. Most of the patients seen by the UKanQuit counselor considered quitting and staying quit important, mean 8.7, SD 2.3, and their confidence to quit or stay quit was above average, mean 6.6, SD 3.6. They rated the UKanQuit program very high, at 8.3, SD 2.8, on a scale of 0 to 10, and 98% of them wanted the program to continue. Of those who were not able to quit at 6 months, the mean number of cigarettes smoked per day decreased significantly from 17.8, SD 12.0 at baseline to 14.0, SD 9.7 at 6 months follow‐up (P < 0.001).
| Variables | |
|---|---|
| |
| Smoking characteristics | |
| 7 day point prevalence abstinence rate, n (%) | 62 (31.8) |
| Among current smokers at 6 months follow‐up, n = 134 | |
| Proportion of smokers who attempted to quit within 6 months, n (%) | 99 (73.9) |
| Mean CPD for smokers at 6 months (SD) | 14.0 (9.7) |
| Used formal quit smoking program | |
| Quit smoking medication, n (%) | 65 (34.4) |
| Quitline use among those faxed to quitline, n (%)* | 6 (5.0) |
| Importance/ Confidence | |
| How important is it to quit or stay quit, mean (SD) | 8.7 (2.3) |
| How confident are you to quit or stay quit, mean (SD) | 6.6 (3.6) |
| Views about service | |
| Satisfaction with UKanQuit service, mean (SD) | 8.3 (2.8) |
| Wants the UKanQuit program to continue, n (%) | 165 (97.6) |
Satisfaction and Recommendations for Improvement
Most (96%) of participants contacted at follow‐up commented on what was helpful about the services. Table 3 displays the distribution of themes and illustrative comments. Themes included staff encouragement, support and counseling (41.8%); other (27%); information and education materials (20.9%); medication advice and referral (2.6%), and referral to quitline (0.5%)
| n (%) | |
|---|---|
| |
| Staff encouragement, support and counseling | 82 (41.8) |
| You guys did excellent. The friendliness of the people who visited me. | |
| Her outlook and her encouragement | |
| Other | 53 (27.1) |
| I don't remember the visit because I was heavily medicated, | |
| A lot was helpful but I couldn't tell you exactly what part was the most helpful | |
| Information/education material | 41 (20.9) |
| Provided me with a lot of info and the packet was helpful. | |
| The information packet | |
| Program not helpful | 14 (7.1) |
| I really didn't need their information, I was able to quit without it. | |
| Nothing helpful except the companionship | |
| Medication advice/referral | 5 (2.6) |
| They took the time and set up the patches for me | |
| She helped me with questions about medication, especially Chantix | |
| Referral to Quitline | 1 (0.5) |
| Talking on the phone | |
Discussion
Among patients served by this inpatient program, interest in quitting was high but administration of inpatient medications upon admission was low (26%). Nearly all patients were provided with written materials, a majority set some form of goal for quitting or cutting down, and many developed quit plans and received assistance adjusting inpatient and/or discharge medications. After discharge, the majority of study participants made unassisted quit attempts, as utilization of medications and quitline services was suboptimal. Fax‐referral to quitline may not, on its own, fulfill guideline recommendations for post‐discharge follow‐up.
Our intent‐to‐treat quit rate was about half of what was found in Taylor et al.'s11 hospital program dissemination trial. Their program may have had better effects as it was somewhat more intensive. It included at least 1 follow‐up phone call immediately after discharge, as well as an accompanying video and relaxation audiotape or compact disc. However, differences in outcomes may also be due to large differences between the study populations. Hospitals participating in Taylor's study only conducted intervention and outcome assessment among smokers who were ready to quit, willing to enroll in a clinical trial, and willing to complete informed consent. Our intervention and outcome data included patients who agreed to speak with UKanQuit staff, regardless of readiness to quit. Our participants did not have to complete informed consent and enroll in a trial as our analyses were conducted post hoc. Our study outcomes might better reflect quit rates for a program serving all smokers, at all levels of readiness to quit, in actual hospital practices. The mean reduction in cigarette smoking among smokers who continued to smoke at 6 months' follow‐up was statistically significant. However, findings from a lung health study show that 50% or more reduction in smoking was ultimately related to successful quitting.23
Strengths and Limitations
The strengths of the study include the fact that the program attempts to intervene with all smokers, and provides stage‐appropriate intervention based on readiness to quit. It provides a snapshot of how a program is incorporated into clinical practice and describes implementation of protocol components.
This study has a number of limitations. We do not know exactly how many patients received the in‐hospital medication change agreed upon by the counselor and medical team immediately following the patient encounter. Our follow‐up rate was low and abstinence rates were based on self‐report, which limits our ability to draw conclusions about cessation outcomes. Process of care measures are based on counselor self‐report, without verification of services rendered. We are not able to identify the impact of our intervention above and beyond our patients' hospital experience, because we did not have a control group. We collected limited data from study participants so we are not able to better understand causes of nonadherence to quitline or poor pharmacotherapy utilization. Lastly, when the respondents were asked to comment about what was helpful about UKanQuit, 23% of the respondents said they could not remember the UKanQuit visit during their hospital stay. Many hospital medications induce brief amnesia, and patients have numerous consults during their stay and might not be able to separate one from the other. The 6‐month interval between their visit and follow‐up call may also account for their inability to remember the cessation consult.
Our patient population is in fact a subset of all smokers admitted (11% of smokers) because they are motivated enough to agree to talk with a counselor. Our intervention procedures, and results, might be quite different if all smokers were visited by the counselor. Efficacy trials of tobacco treatment in hospitals have focused on smokers who are ready to quit.24 Hence, procedures for working with unmotivated smokers in hospitals are less well established. Policymakers, hospitals, and hospital tobacco treatment programs should examine the most efficient (ie, effective and cost‐effective) approaches for addressing smoking in hospitals and specifically focus on whether all smokers should be treated by dedicated tobacco treatment staff, or only those who agree to a consult.
Lessons Learned
Linking Patients With In‐Hospital Cessation Medications Requires Collaboration With the Entire Health Care Team
Only 1 in 4 UKanQuit participants had been given smoking cessation medication to ameliorate withdrawal before counselors met with the patients. Although we have not systematically collected reasons patients do not receive cessation medication on admission, the 2 most common causes are that patients refuse it or physicians refuse it. Patients refuse medication perhaps because they do not want to quit, they feel they will cope without smoking during their hospital stay, or they are paying out of pocket and want to reduce costs. Physicians do not permit it because they believe it is contraindicated for the patient's health condition, it is contraindicated for the procedure the patient is receiving in the hospital, or they believe it will interfere with wound healing. There is also a considerable delay between ordering and receiving medications; patients who become uncomfortable during their stay sometimes change their minds, but end up being discharged before their medication arrives. Most of these issues pertain to nicotine replacement. Although patients not eligible for NRT may be good candidates for bupropion, varenicline, or even the second line cessation medications of clonidine or nortryptiline, these medications do not provide immediate relief from tobacco withdrawal symptoms and staff are reluctant to start patients on medications they may not receive on an outpatient basis. It is not clear what proportion of hospitalized patients should receive ameliorative medication. Not every hospitalized smoker is a candidate for NRT, due to contraindicated medical conditions, patients' level of dependence, and patients' willingness to accept cessation medication in order to prevent withdrawal. Koplan et al.25 achieved hospital‐wide increases in NRT orders from 1.6% to 2.5% after the introduction of an electronic tobacco treatment order set. These percentages seem low but actually were calculated from all hospital admissions, including smokers and nonsmokers. Moreover, their hospital population had a relatively low smoking rate of 12%. Our in‐hospital and post‐discharge (26.2% and 34.4% respectively) pharmacotherapy utilization rates were based only on smokers who had been seen by our service. Even though 1 in 4 smokers were already on medication when they were seen by counselors, 1 in 4 of patients seen wanted to either add a cessation medication or change their current dose. There is clearly room for improvement in how we offer and administer cessation medications on admission. Also, assessing medication efficacy and adjusting as needed appears to be an important role for in‐hospital counselors.
Facilitating Medications Post‐Discharge Will Require Creativity and Outpatient Follow‐Up
Post‐discharge, only 1 in 3 of our patients reported they used cessation medications. This may, again, be a function of patients' readiness to quit. However, it could also be related to knowledge/attitudes regarding the efficacy of medications or access to low‐cost medications. Some of our patients commented that making medication affordable would be helpful. Although our materials provide information on sources for free or low‐cost medications, this information may not have been salient during the hospital stay. To increase access to medications post‐discharge, programs should consider providing a booster mailer to the home with information on sources for free or reduced medications, providing take‐home starter pharmacotherapy kits lasting 1 to 2 weeks to bridge the gap between hospital discharge and finding another source of medications, and/or a follow‐up call shortly after discharge to verify use of pharmacotherapy and troubleshoot problems with medications or procurement.
Providing Follow‐Up Via Fax Referral to Quitlines Is Not as Simple as It Seems
Although our overall quitline fax‐referral rate was high (over half of all patients seen), rate of enrollment among those referred is much lower than the rates reported elsewhere, which range from 16% to 53%.2628 In our sample of fax‐referred smokers, we do not know how many were not enrolled due to failure to make contact vs. patient refusal once contact was made. One possible factor impacting enrollment rates is whether or not smokers are prescreened for readiness to quit. Nearly half of US quitlines require smokers to be ready to quit in order to receive a full course of treatment,29 but only 20% of smokers are ready to quit at any given time.30 In the cited studies with higher conversion rates, counselors prescreened patients for readiness to quit and only offered fax‐referral to those ready to quit in the next 30 days. Our program offers fax‐referral to all smokers. Our findings suggest that doing so results in high rates of referral but low rates of enrollment among those referred. Future studies should examine the impact of prescreening for readiness versus offering referral to all smokers on net enrollment and cessation.
Linking hospitalized smokers with tobacco quitlines has many potential benefits.31, 32 Proactive tobacco quitlines are effective15 and cost effective33 for smoking cessation; they are available, free, to all US smokers; services are delivered via telephone which minimizes many access barriers; hospitals do not have to bear the costs of the services; and many quitlines are undersubscribed and eager to increase their reach.34 Potential methods for increasing conversion to enrollment include building motivation to accept counseling and preparing patients for the quitline intake procedures. Our program is considering providing a warm handoff to patients by calling the quitline during the bedside consult to permit the quitline to enroll the patient during their hospital stay.
Hospital‐based cessation programs have the potential to deliver tobacco treatment to millions of hospitalized smokers annually. To deliver high‐quality, effective care, hospital cessation programs will have to solve problems inherent in hospital‐based carehow best to integrate into existing hospital systems, how to effectively communicate with other hospital care providers, and how to facilitate transitions in care to ensure patients receive evidence‐based post‐discharge care. We offer this report as the first of hopefully many that address quality improvement for specialized programs dedicated to treating tobacco in hospitals.
Acknowledgements
The authors gratefully acknowledge the contributions of the following UKanQuit Counselors in the planning and development of this manuscript: Brian Hernandez, Alex Perez‐Estrada, Grace Meikenhous, Meredith Benson, Terri Tapp. We also thank Chip Hulen, Albers Bart and Chris Wittkopp of the Organizational Improvement Department of KU Hospital; Marilyn Painter, Joanne McNair and Karisa Deculus of the KU Preventive Medicine and Public Health Department.
Hospitalization can be considered a teachable moment for smoking cessation13 for the 6.5 million adult smokers who are hospitalized in the United States each year.4 Smokers who receive tobacco treatment during hospitalization and outpatient follow‐up treatment for at least 1 month are more likely to quit than patients who receive no treatment.5, 6
Unless tobacco treatment is explicitly delegated to other providers, physicians shoulder the responsibility of encouraging smokers to quit and prescribing smoking cessation medications. This is problematic in that physicians sometimes fail to counsel their patients about quitting smoking7, 8 or recommend outpatient follow‐up.9 Few hospitals provide comprehensive treatment. In a review of 33 studies on the prevalence of smoking care delivery in hospitals, 3 hospitals reported they provided advice to quit alone, 29 provided advice plus counseling and assistance in quitting, and 8 provided advice or prescription for cessation pharmacotherapy.9 Although post‐discharge support is a key component of effective treatment for hospitalized smokers,6 only 11 reported providing follow‐up treatment, or referral for follow‐up treatment, after discharge. Among these 11 hospitals, respondents reported they provided referral or follow‐up to 1% to 74% of their smokers, with a median percentage of 24%. The 1 study that specified the type of outpatient treatment provided reported the hospital provided the state quitline number to smokers.
Instituting a dedicated smoking cessation program may enhance inpatient treatment, outpatient follow‐up, and treatment outcomes. Two studies have found that institutional smoking cessation programs increased the likelihood that patients would receive treatment and quit compared to hospitals without dedicated programs.10, 11
Although many US hospitals are developing programs to provide systematic treatment for tobacco dependence,9 little is known regarding how programs structure their staff, enroll patients, or provide treatment to patients that smoke. Instituting tobacco treatment services usually requires policy change and system‐wide approaches with quality improvement endpoint goals.8, 1214 In the United States, elements of these services include: 1) developing a cadre of trained tobacco treatment specialists, 2) implementing hospital systems for identifying smokers and referring them to the service, 3) providing inpatient treatment based on current treatment guidelines15 and 4) providing or facilitating follow‐up treatment after discharge, often via fax‐referral to tobacco quitlines. This systematic approach is still lacking in many hospitals.
To date, few evaluations of dedicated hospital‐based smoking cessation programs have been reported in the literature.8, 11 The purpose of this study is to describe patient characteristics and outcomes of a dedicated tobacco treatment service, with paid staff, in a large academic medical center. We describe treatment protocols, profile patients served, treatments provided, and summarization of 6‐month post‐discharge outcomes for smokers referred to the UKanQuit service over a 1‐year period. We close with lessons learned on how to improve the delivery of tobacco treatment to hospitalized patients.
Methods
Design and Setting
This is a descriptive observational study of a tobacco treatment program in a large Midwestern academic medical center between September 1, 2007 and August 31, 2008. The specialty tobacco treatment service (UKanQuit) was established when the hospital campus went smoke free on September 1, 2006. Patients are referred to the service via the hospital electronic medical record (EMR). As nurses complete electronic forms on patients admitted to their units, the EMR prompts nurses to ask patients if they smoke, ask smokers if they would like tobacco treatment medication to prevent withdrawal symptoms while in the hospital, and ask smokers if they would like to talk to a tobacco treatment specialist during their hospital stay. Those who respond yes to the final question are placed on an electronic list for UKanQuit services. Physicians and other health care providers can also order consultation from the UKanQuit service. A description of smokers admitted to the hospital and predictors of referral to UKanQuit within the first year of service is presented elsewhere.16, 17
The UKanQuit staff consists of an interdisciplinary team of counselors with a Ph.D., Masters degrees, and/or substantial experience in case management and substance abuse treatment. All have received intensive training and supervision in treating tobacco dependence. All participate in UKanQuit counseling on a part‐time basis, and spend the remainder of their effort as research assistants and counselors on smoking cessation research projects in the medical center. Hence, staffing consists of 1 full‐time equivalent counselor, 0.15 full‐time equivalent director (Richter), and 0.05 full‐time equivalent medical director (Ellerbeck). The program is funded through a contract with the hospital. We are in the process of hiring a nurse practitioner to create a more sustainable funding stream for the program because nurse practitioners can bill cessation services.
UKanQuit provides hospital counseling from 9 AM to 5 PM on weekdays. UKanQuit staff meets weekly for counseling supervision, strategic planning, continuing education, and troubleshooting difficult cases. In addition to treating smokers, the UKanQuit staff provides training and consultation to hospital personnel via grand rounds and other presentations. The service also provides a platform for medical students and residents to conduct focused research related to quality improvement. To facilitate systematic treatment of tobacco, UKanQuit developed the hospital treatment protocol for nursing staff, developed evidence‐based written self‐help materials that are accessible to hospital staff via the hospital printing system, and developed and instituted a tobacco treatment order set that was recently integrated into the EMR and automatically becomes prioritized as a recommended order set for all patients who report they have smoked in the past 30 days.
Procedures
UKanQuit staff retrieves patient details from the EMR and visits patients at their bedside. All hospital services refer to UKanQuit. UKanQuit provides counseling to Spanish speakers through bilingual/bicultural staff and hospital translators assist UKanQuit staff in counseling patients who speak other languages. The staff conducts a brief assessment at the bedside to inform treatment and contacts patients 6 months following inpatient treatment to assess outcomes and provide additional support and referral. This study evaluating the UKanQuit program was approved by the medical center's Institutional Review Board.
Program Intervention
UKanQuit staff visit patients at the bedside to deliver tobacco treatment. This consists of: (a) assessing withdrawal; (b) working with the health care team to adjust nicotine replacement to keep the patient comfortable; (c) assessing patients' interest in quitting smoking; (d) providing brief motivational intervention to patients not interested in quitting; and (e) providing assistance in quitting (developing a quit plan, arranging for medications on discharge) to patients interested in quitting (Figure 1). UKanQuit staff recommend medications based on the patients' level of dependence, history of cessation, and cessation medication preferences. The recommendation is communicated in person and by chart documentation to the medical team, usually by the nursing staff. The patients' resident or attending physician makes the final determination regarding medication provided. The hospital has nicotine replacement therapy (NRT; patch, gum, and lozenge), bupropion, and varenicline in its formulary. Patients are then offered an option of fax referral to the state tobacco quitline for follow‐up counseling. UKanQuit staff documents the services provided in the EMR via SOAR (Subjective, Objective, Assessment and Referral) notes.
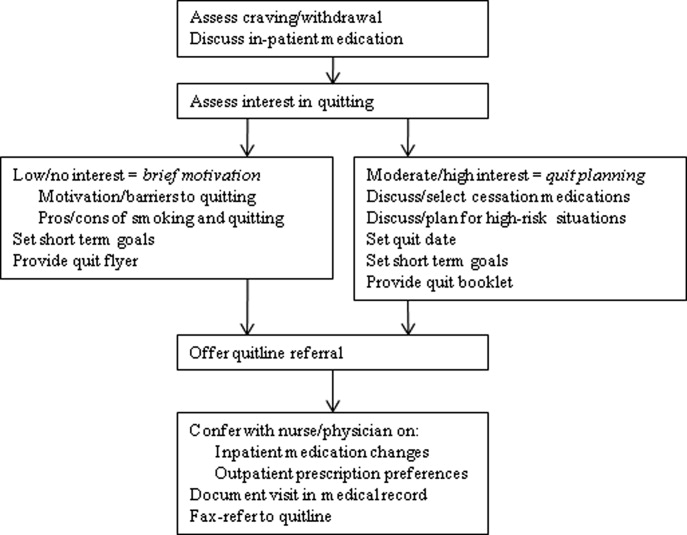
Measures
Baseline Measures
These were collected from the UKanQuit 1‐page program intake form, which UKanQuit designed to collect the minimal information necessary to conduct medication and behavioral counseling, to maximize counseling time, and to fit into the dense schedule of each patient's hospital stay. Demographic measures include age, gender and ethnicity. Smoking behavior measures include number of years smoked, number of cigarettes per day, a single item from the Fagerstrom Test for Nicotine Dependence that assesses time to first cigarette after waking,18, 19 interest in quitting smoking (on a 0‐10 scale, with 10 being very interested in quitting), and a single item from the self report version of the Minnesota Nicotine Withdrawal Scale (MNWS) that asks smokers to rate their desire or craving to smoke over a specified period. The single item craving measure from the MNWS has been found to have high reliability and good construct validity and is neither less sensitive to abstinence nor less reliable than the ten‐item brief questionnaire of smoking urges (QSU‐brief) used in laboratory and clinical trials.20 We asked about craving over the past 24 hours on a scale from 0 (none) to 4 (severe).21
Process Measures
Counselors also document the treatment they provided to smokers including the time spent with patients during counseling, provision of written self‐help materials, whether smokers set goals for quitting, hospital staff had already placed the smoker on a tobacco treatment medication, smokers are interested in increasing or changing their medication, the smoker wants smoking cessation medication on discharge, UKanQuit staff submitted a recommendation to hospital staff to make a medication change and/or provide a prescription for medication on discharge, plans for post‐discharge follow‐up (fax‐referral of patients to the state tobacco quitline or acceptance of UKanQuit counseling after discharge), and the patient agrees to be contacted at 6 months post‐discharge for follow‐up assessment and assistance.
Follow‐Up Measures
Outcome measures were collected by telephone 6 months post‐discharge by study staff who were not involved in the in‐hospital counseling. Call attempts to reach each patient ranged from 1 to 11. Measures included self‐reported 7‐day point prevalence abstinence rates, the number of quit attempts lasting over 24 hours, and cigarettes smoked per day among continuing smokers. Patients are asked if they participated in counseling through the tobacco quitline. Scaled (0‐10) items assess how important it is to the patients to quit smoking or remain quit, how confident they are in being able to quit or remain quit, and how satisfied they were with the assistance provided by UKanQuit. A yes/no item assesses whether patients think the program should be continued. In addition, UKanQuit asked two open‐ended questions to qualitatively assess satisfaction with the program and elicit suggestions for improvements. The questions were: What, if anything, was helpful to you about our services? and How can UKanQuit better help people stop smoking?
Analyses
Categorical variables were summarized by frequencies and percentages; continuous variables were summarized by means and standard deviations (SDs). We compared baseline characteristic differences between respondents and nonrespondents at 6 months follow‐up using chi‐square for categorical variables and t‐test for continuous variables. We also compared cigarettes per day at baseline and 6 months post‐discharge in smokers who were not able to quit using paired t‐test. All analyses were done with SPSS 17.0 statistical package. Open‐ended questions were analyzed using the framework synthesis method.22 Following examination and familiarization with the data, we developed an initial list of themes. We then categorized the responses by these themes using numerical codes. Each thematic code was summarized as a percentage of all responses. Those responses that fit into multiple thematic codes were multiply coded.
Results
Baseline
Within the study period (September 1, 2007 to August 31, 2008), 22,624 patients were admitted to the medical center (Figure 2). A total of 4150 were current smokers (ie, smoked within the past 30 days). UKanQuit staff met with 513 (68%) of 753 patients referred to the service. Some of the reasons why 32% of referred patients were not seen by the UKanQuit staff have been described in our previous paper.17 These include patient was asleep, doctor in the room, out of bed for procedure, and unable to speak. Table 1 displays the characteristics of 513 smokers treated by UKanQuit from September 1, 2007 to August 31, 2008. Patients were predominantly white (74%) with mean age of 50 years. Slightly more than half of smokers were male (57%). They had smoked an average of 18 cigarettes per day for a mean duration of 29 years, and over half (58%) smoked within 5 minutes of waking suggesting a high level of dependence. On a scale of 1 to 10 the mean interest in quitting was 7.9 (SD 2.9) and the mean craving score on a scale of 0 to 4 was 1.2 (SD 1.4) suggesting slight to mild craving.
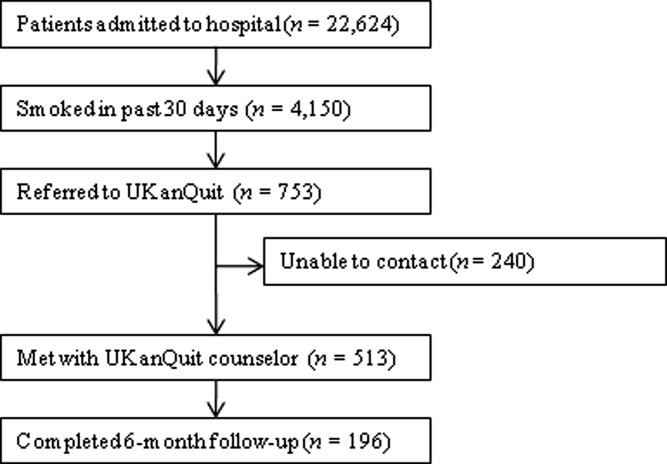
| Characteristics | Treated (n = 513) |
|---|---|
| |
| Demographics | |
| Mean age (SD), years | 50.2 (13.6) |
| Male, n (%) | 291 (56.7) |
| Ethnicity, n (%) | |
| White | 371 (73.6) |
| AA | 107 (21.2) |
| Latino | 18 (3.6) |
| Other | 8 (1.6) |
| Referral source, n (%) | |
| Nursing profile | 477 (94.1) |
| Physician | 5 (1.0) |
| Other | 25 (4.9) |
| Smoking characteristics | |
| Mean number of years smoked (SD) | 28.9 (14.6) |
| Smokes within 5 minutes of waking n (%) | 270 (58.3) |
| Mean cigarettes smoked per day (SD) | 18.4 (12.6) |
| Mean interest in quitting (SD)* | 7.9 (2.9) |
| Mean craving (SD) | 1.2 (1.4) |
| Tobacco treatment provided | |
| Counseling | |
| Average time spent with patients (SD) | 19.9 (9.1) |
| Received information packet, n (%) | 490 (97.4) |
| Set goals for quitting, n (%) | 352 (73.3) |
| Had quit plan, n (%) | 151 (33.2) |
| Accepted fax referral to quitline, n (%) | 277 (55.8) |
| Opted for UKanQuit counseling, n (%) | 29 (5.9) |
| Medication | |
| On smoking cessation medication, n (%) | 133 (26.2) |
| Interested in receiving or changing smoking cessation medication, n (%) | 132 (26.7) |
| Added or changed smoking cessation medication, n (%) | 195 (40.5) |
| Discharge med, n (%) | 196 (40.2) |
In‐Hospital Treatment
Hospital staff had placed 1 in 4 of the patients on smoking cessation medication prior to the UKanQuit staff visit. Nineteen percent were on NRT (16.2% transdermal patch, 2.5% on lozenge, 0.8% on nicotine gum); 5% on bupropion, 16.5% on varenicline, and 2.5% on clonidine. A total of 1.7% used a combination of Patch and bupropion while 2.5% used a combination of patch and gum. Staff provided 97% of the patients with written materials. Most patients (73%) set a goal for quitting or cutting down, and one‐third developed quit plans. Fifty‐six percent accepted fax referral to their state quitline, and 6% opted for follow‐up counseling with a UKanQuit counselor. Average time spent by UKanQuit with the patient was 20 minutes. Most of the patients treated (n = 426, 86%) agreed that UKanQuit staff can contact them for follow‐up assessment at 6 months.
Outcomes
Staff successfully contacted 196 (46%) of the 426 patients who agreed to 6‐month follow‐up. Responders were older (mean age 53 years, SD 12.6 vs. mean age 48 years, SD 13.8; P < 0.001); were more interested in quitting (mean interest in quitting 8.4, SD 2.5 vs. 7.6, SD 3.1 P = 0.001); and had a lower craving score at baseline (mean craving score 0.99, SD 1.3 vs. 1.29, SD 1.5; P < 0.001) compared to nonresponders. There were no differences between responders and nonresponders by gender, number of cigarettes smoked per day, years of smoking, referral source, inpatient smoking cessation medication used or time spent with UKanQuit hospital staff during the inpatient visit.
Table 2 displays smoking behavior and smoking cessation‐related characteristics of the respondents 6‐month post‐discharge. Over 70% attempted a quit attempt lasting at least 24 hours. The self reported 7‐day point prevalence abstinence rate was 31.8% among respondents. The intent‐to‐treat quit rate was 14.6% among all participants who agreed to follow‐up, counting those who we could not contact as smokers. While 34% used pharmacotherapy, only 5% of those who were fax‐referred to the quitline utilized the service. Most of the patients seen by the UKanQuit counselor considered quitting and staying quit important, mean 8.7, SD 2.3, and their confidence to quit or stay quit was above average, mean 6.6, SD 3.6. They rated the UKanQuit program very high, at 8.3, SD 2.8, on a scale of 0 to 10, and 98% of them wanted the program to continue. Of those who were not able to quit at 6 months, the mean number of cigarettes smoked per day decreased significantly from 17.8, SD 12.0 at baseline to 14.0, SD 9.7 at 6 months follow‐up (P < 0.001).
| Variables | |
|---|---|
| |
| Smoking characteristics | |
| 7 day point prevalence abstinence rate, n (%) | 62 (31.8) |
| Among current smokers at 6 months follow‐up, n = 134 | |
| Proportion of smokers who attempted to quit within 6 months, n (%) | 99 (73.9) |
| Mean CPD for smokers at 6 months (SD) | 14.0 (9.7) |
| Used formal quit smoking program | |
| Quit smoking medication, n (%) | 65 (34.4) |
| Quitline use among those faxed to quitline, n (%)* | 6 (5.0) |
| Importance/ Confidence | |
| How important is it to quit or stay quit, mean (SD) | 8.7 (2.3) |
| How confident are you to quit or stay quit, mean (SD) | 6.6 (3.6) |
| Views about service | |
| Satisfaction with UKanQuit service, mean (SD) | 8.3 (2.8) |
| Wants the UKanQuit program to continue, n (%) | 165 (97.6) |
Satisfaction and Recommendations for Improvement
Most (96%) of participants contacted at follow‐up commented on what was helpful about the services. Table 3 displays the distribution of themes and illustrative comments. Themes included staff encouragement, support and counseling (41.8%); other (27%); information and education materials (20.9%); medication advice and referral (2.6%), and referral to quitline (0.5%)
| n (%) | |
|---|---|
| |
| Staff encouragement, support and counseling | 82 (41.8) |
| You guys did excellent. The friendliness of the people who visited me. | |
| Her outlook and her encouragement | |
| Other | 53 (27.1) |
| I don't remember the visit because I was heavily medicated, | |
| A lot was helpful but I couldn't tell you exactly what part was the most helpful | |
| Information/education material | 41 (20.9) |
| Provided me with a lot of info and the packet was helpful. | |
| The information packet | |
| Program not helpful | 14 (7.1) |
| I really didn't need their information, I was able to quit without it. | |
| Nothing helpful except the companionship | |
| Medication advice/referral | 5 (2.6) |
| They took the time and set up the patches for me | |
| She helped me with questions about medication, especially Chantix | |
| Referral to Quitline | 1 (0.5) |
| Talking on the phone | |
Discussion
Among patients served by this inpatient program, interest in quitting was high but administration of inpatient medications upon admission was low (26%). Nearly all patients were provided with written materials, a majority set some form of goal for quitting or cutting down, and many developed quit plans and received assistance adjusting inpatient and/or discharge medications. After discharge, the majority of study participants made unassisted quit attempts, as utilization of medications and quitline services was suboptimal. Fax‐referral to quitline may not, on its own, fulfill guideline recommendations for post‐discharge follow‐up.
Our intent‐to‐treat quit rate was about half of what was found in Taylor et al.'s11 hospital program dissemination trial. Their program may have had better effects as it was somewhat more intensive. It included at least 1 follow‐up phone call immediately after discharge, as well as an accompanying video and relaxation audiotape or compact disc. However, differences in outcomes may also be due to large differences between the study populations. Hospitals participating in Taylor's study only conducted intervention and outcome assessment among smokers who were ready to quit, willing to enroll in a clinical trial, and willing to complete informed consent. Our intervention and outcome data included patients who agreed to speak with UKanQuit staff, regardless of readiness to quit. Our participants did not have to complete informed consent and enroll in a trial as our analyses were conducted post hoc. Our study outcomes might better reflect quit rates for a program serving all smokers, at all levels of readiness to quit, in actual hospital practices. The mean reduction in cigarette smoking among smokers who continued to smoke at 6 months' follow‐up was statistically significant. However, findings from a lung health study show that 50% or more reduction in smoking was ultimately related to successful quitting.23
Strengths and Limitations
The strengths of the study include the fact that the program attempts to intervene with all smokers, and provides stage‐appropriate intervention based on readiness to quit. It provides a snapshot of how a program is incorporated into clinical practice and describes implementation of protocol components.
This study has a number of limitations. We do not know exactly how many patients received the in‐hospital medication change agreed upon by the counselor and medical team immediately following the patient encounter. Our follow‐up rate was low and abstinence rates were based on self‐report, which limits our ability to draw conclusions about cessation outcomes. Process of care measures are based on counselor self‐report, without verification of services rendered. We are not able to identify the impact of our intervention above and beyond our patients' hospital experience, because we did not have a control group. We collected limited data from study participants so we are not able to better understand causes of nonadherence to quitline or poor pharmacotherapy utilization. Lastly, when the respondents were asked to comment about what was helpful about UKanQuit, 23% of the respondents said they could not remember the UKanQuit visit during their hospital stay. Many hospital medications induce brief amnesia, and patients have numerous consults during their stay and might not be able to separate one from the other. The 6‐month interval between their visit and follow‐up call may also account for their inability to remember the cessation consult.
Our patient population is in fact a subset of all smokers admitted (11% of smokers) because they are motivated enough to agree to talk with a counselor. Our intervention procedures, and results, might be quite different if all smokers were visited by the counselor. Efficacy trials of tobacco treatment in hospitals have focused on smokers who are ready to quit.24 Hence, procedures for working with unmotivated smokers in hospitals are less well established. Policymakers, hospitals, and hospital tobacco treatment programs should examine the most efficient (ie, effective and cost‐effective) approaches for addressing smoking in hospitals and specifically focus on whether all smokers should be treated by dedicated tobacco treatment staff, or only those who agree to a consult.
Lessons Learned
Linking Patients With In‐Hospital Cessation Medications Requires Collaboration With the Entire Health Care Team
Only 1 in 4 UKanQuit participants had been given smoking cessation medication to ameliorate withdrawal before counselors met with the patients. Although we have not systematically collected reasons patients do not receive cessation medication on admission, the 2 most common causes are that patients refuse it or physicians refuse it. Patients refuse medication perhaps because they do not want to quit, they feel they will cope without smoking during their hospital stay, or they are paying out of pocket and want to reduce costs. Physicians do not permit it because they believe it is contraindicated for the patient's health condition, it is contraindicated for the procedure the patient is receiving in the hospital, or they believe it will interfere with wound healing. There is also a considerable delay between ordering and receiving medications; patients who become uncomfortable during their stay sometimes change their minds, but end up being discharged before their medication arrives. Most of these issues pertain to nicotine replacement. Although patients not eligible for NRT may be good candidates for bupropion, varenicline, or even the second line cessation medications of clonidine or nortryptiline, these medications do not provide immediate relief from tobacco withdrawal symptoms and staff are reluctant to start patients on medications they may not receive on an outpatient basis. It is not clear what proportion of hospitalized patients should receive ameliorative medication. Not every hospitalized smoker is a candidate for NRT, due to contraindicated medical conditions, patients' level of dependence, and patients' willingness to accept cessation medication in order to prevent withdrawal. Koplan et al.25 achieved hospital‐wide increases in NRT orders from 1.6% to 2.5% after the introduction of an electronic tobacco treatment order set. These percentages seem low but actually were calculated from all hospital admissions, including smokers and nonsmokers. Moreover, their hospital population had a relatively low smoking rate of 12%. Our in‐hospital and post‐discharge (26.2% and 34.4% respectively) pharmacotherapy utilization rates were based only on smokers who had been seen by our service. Even though 1 in 4 smokers were already on medication when they were seen by counselors, 1 in 4 of patients seen wanted to either add a cessation medication or change their current dose. There is clearly room for improvement in how we offer and administer cessation medications on admission. Also, assessing medication efficacy and adjusting as needed appears to be an important role for in‐hospital counselors.
Facilitating Medications Post‐Discharge Will Require Creativity and Outpatient Follow‐Up
Post‐discharge, only 1 in 3 of our patients reported they used cessation medications. This may, again, be a function of patients' readiness to quit. However, it could also be related to knowledge/attitudes regarding the efficacy of medications or access to low‐cost medications. Some of our patients commented that making medication affordable would be helpful. Although our materials provide information on sources for free or low‐cost medications, this information may not have been salient during the hospital stay. To increase access to medications post‐discharge, programs should consider providing a booster mailer to the home with information on sources for free or reduced medications, providing take‐home starter pharmacotherapy kits lasting 1 to 2 weeks to bridge the gap between hospital discharge and finding another source of medications, and/or a follow‐up call shortly after discharge to verify use of pharmacotherapy and troubleshoot problems with medications or procurement.
Providing Follow‐Up Via Fax Referral to Quitlines Is Not as Simple as It Seems
Although our overall quitline fax‐referral rate was high (over half of all patients seen), rate of enrollment among those referred is much lower than the rates reported elsewhere, which range from 16% to 53%.2628 In our sample of fax‐referred smokers, we do not know how many were not enrolled due to failure to make contact vs. patient refusal once contact was made. One possible factor impacting enrollment rates is whether or not smokers are prescreened for readiness to quit. Nearly half of US quitlines require smokers to be ready to quit in order to receive a full course of treatment,29 but only 20% of smokers are ready to quit at any given time.30 In the cited studies with higher conversion rates, counselors prescreened patients for readiness to quit and only offered fax‐referral to those ready to quit in the next 30 days. Our program offers fax‐referral to all smokers. Our findings suggest that doing so results in high rates of referral but low rates of enrollment among those referred. Future studies should examine the impact of prescreening for readiness versus offering referral to all smokers on net enrollment and cessation.
Linking hospitalized smokers with tobacco quitlines has many potential benefits.31, 32 Proactive tobacco quitlines are effective15 and cost effective33 for smoking cessation; they are available, free, to all US smokers; services are delivered via telephone which minimizes many access barriers; hospitals do not have to bear the costs of the services; and many quitlines are undersubscribed and eager to increase their reach.34 Potential methods for increasing conversion to enrollment include building motivation to accept counseling and preparing patients for the quitline intake procedures. Our program is considering providing a warm handoff to patients by calling the quitline during the bedside consult to permit the quitline to enroll the patient during their hospital stay.
Hospital‐based cessation programs have the potential to deliver tobacco treatment to millions of hospitalized smokers annually. To deliver high‐quality, effective care, hospital cessation programs will have to solve problems inherent in hospital‐based carehow best to integrate into existing hospital systems, how to effectively communicate with other hospital care providers, and how to facilitate transitions in care to ensure patients receive evidence‐based post‐discharge care. We offer this report as the first of hopefully many that address quality improvement for specialized programs dedicated to treating tobacco in hospitals.
Acknowledgements
The authors gratefully acknowledge the contributions of the following UKanQuit Counselors in the planning and development of this manuscript: Brian Hernandez, Alex Perez‐Estrada, Grace Meikenhous, Meredith Benson, Terri Tapp. We also thank Chip Hulen, Albers Bart and Chris Wittkopp of the Organizational Improvement Department of KU Hospital; Marilyn Painter, Joanne McNair and Karisa Deculus of the KU Preventive Medicine and Public Health Department.
- ,.Smokers who are hospitalized: a window of opportunity for cessation interventions.Prev Med.1992;21:262–269.
- ,,.Understanding the potential of teachable moments: the case of smoking cessation.Health Educ Res.2003;18(2):156–170.
- ,.Teachable moments for promoting smoking cessation: the context of cancer care and survivorship.Cancer Control.2003;10(4):325–333.
- ,,.Helping hospitalized smokers quit: new directions for treatment and research.J Consul Clin Psychol.1993;61(5):778–789.
- ,,.Smoking cessation interventions for hospitalized smokers: a systematic review.Arch Intern Med.2008;168(18):1950–1960.
- ,,.Interventions for smoking cessation in hospitalised patients.Cochrane Database Syst Rev.2007(3):CD001837.
- CDC.Physician and other health‐care professional counseling of smokers to quit‐‐United States, 1991.MMWR Morb Mortal Wkly Rep.1993;42(44):854–857.
- ,,,,,.Implementing tobacco interventions in the real world of managed care.Tob Control.2000;9Suppl 1:I18–I24.
- ,,, et al.Smoking care provision in hospitals: a review of prevalence.Nicotine Tob Res.2008;10(5):757–774.
- ,,,,,.Predictors of smoking cessation after a myocardial infarction: the role of institutional smoking cessation programs in improving success.Arch Intern Med.2008;168(18):1961–1967.
- ,,,,.Dissemination of an effective inpatient tobacco use cessation program.Nicotine Tob Res.2005;7(1):129–137.
- ,,,,.Application of a nurse‐managed inpatient smoking cessation program.Nicotine Tob Res.2002;4(2):211–222.
- ,,,,,.Delivering clinical preventive services is a systems problem.Ann Behav Med.1997;19(3):271–278.
- ,,, et al.Lessons from experienced guideline implementers: attend to many factors and use multiple strategies.Jt Comm J Qual Improv.2000;26(4):171–188.
- U.S. Department of Health and Human Services (USDHHS).Treating Tobacco Use and Dependence: Clinical Practice Guideline 2008 Update.
- ,,,,.Referral and treatment for nicotine dependence among hospitalized patients.Subst Abus.2009;30(1):94–95.
- ,,,,.Prevalence and predictors of tobacco treatment in an academic medical center.Jt Comm J Qual Patient Saf.2009;35(11):551–557.
- ,,,.The Fagerstrom Test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire.Br J Addict.1991;86(9):1119–1127.
- ,,, et al.Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence.Nicotine Tob Res.2007;9 Supp 4:555–570.
- ,.Is the ten‐item Questionnaire of Smoking Urges (QSU‐brief) more sensitive to abstinence than shorter craving measures?Psychopharmacology (Berl).2010;208(3):427–432.
- ,.Signs and symptoms of tobacco withdrawal.Arch Gen Psychiatry.1986;43(3):289–294.
- ,,.Qualitative research in health care. Analysing qualitative data.BMJ.2000;320(7227):114–116.
- ,,,.Smoking reduction in the Lung Health Study.Nicotine Tob Res.2004;6(2):275–280.
- ,,.Interventions for smoking cessation in hospitalised patients.Cochrane Database Syst Rev.2007(3):CD001837.
- ,,,,.A computerized aid to support smoking cessation treatment for hospital patients.J Gen Intern Med.2008;23(8):1214–1217.
- ,,,,,.The feasibility of connecting physician offices to a state‐level tobacco quit line.Am J Prev Med.2006;30(1):31–37.
- ,,, et al.Clinical faxed referrals to a tobacco quitline: reach, enrollment, and participant characteristics.Am J Prev Med.2009;36(4):337–340.
- ,,, et al.Feasibility of a Spanish/English computerized decision aid to facilitate smoking cessation efforts in underserved communities.J Health Care Poor Underserved.2010;21(2):504–517.
- North American Quitline Consortium. Available at: http://www.naquitline. org. Accessed July2010.
- ,,,,,.Distribution of smokers by stage in three representative samples.Prev Med.1995;24:401–411.
- ,,.Telephone counselling for smoking cessation.Cochrane Database Syst Rev.2006;3:CD002850.
- ,.The potential of quitlines to increase smoking cessation.Drug Alcohol Rev.2006;25(1):73–78.
- ,,, et al.Evidence of real‐world effectiveness of a telephone quitline for smokers.N Engl J Med.2002;347(14):1087–1093.
- Campaign for Tobacco Free Kids Fact Sheets 2008. Quitlines Help Smokers Quit. Available at: http://www.tobaccofreekids.org/research/factsheets/pdf/0326.pdf. Accessed July2010.
- ,.Smokers who are hospitalized: a window of opportunity for cessation interventions.Prev Med.1992;21:262–269.
- ,,.Understanding the potential of teachable moments: the case of smoking cessation.Health Educ Res.2003;18(2):156–170.
- ,.Teachable moments for promoting smoking cessation: the context of cancer care and survivorship.Cancer Control.2003;10(4):325–333.
- ,,.Helping hospitalized smokers quit: new directions for treatment and research.J Consul Clin Psychol.1993;61(5):778–789.
- ,,.Smoking cessation interventions for hospitalized smokers: a systematic review.Arch Intern Med.2008;168(18):1950–1960.
- ,,.Interventions for smoking cessation in hospitalised patients.Cochrane Database Syst Rev.2007(3):CD001837.
- CDC.Physician and other health‐care professional counseling of smokers to quit‐‐United States, 1991.MMWR Morb Mortal Wkly Rep.1993;42(44):854–857.
- ,,,,,.Implementing tobacco interventions in the real world of managed care.Tob Control.2000;9Suppl 1:I18–I24.
- ,,, et al.Smoking care provision in hospitals: a review of prevalence.Nicotine Tob Res.2008;10(5):757–774.
- ,,,,,.Predictors of smoking cessation after a myocardial infarction: the role of institutional smoking cessation programs in improving success.Arch Intern Med.2008;168(18):1961–1967.
- ,,,,.Dissemination of an effective inpatient tobacco use cessation program.Nicotine Tob Res.2005;7(1):129–137.
- ,,,,.Application of a nurse‐managed inpatient smoking cessation program.Nicotine Tob Res.2002;4(2):211–222.
- ,,,,,.Delivering clinical preventive services is a systems problem.Ann Behav Med.1997;19(3):271–278.
- ,,, et al.Lessons from experienced guideline implementers: attend to many factors and use multiple strategies.Jt Comm J Qual Improv.2000;26(4):171–188.
- U.S. Department of Health and Human Services (USDHHS).Treating Tobacco Use and Dependence: Clinical Practice Guideline 2008 Update.
- ,,,,.Referral and treatment for nicotine dependence among hospitalized patients.Subst Abus.2009;30(1):94–95.
- ,,,,.Prevalence and predictors of tobacco treatment in an academic medical center.Jt Comm J Qual Patient Saf.2009;35(11):551–557.
- ,,,.The Fagerstrom Test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire.Br J Addict.1991;86(9):1119–1127.
- ,,, et al.Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence.Nicotine Tob Res.2007;9 Supp 4:555–570.
- ,.Is the ten‐item Questionnaire of Smoking Urges (QSU‐brief) more sensitive to abstinence than shorter craving measures?Psychopharmacology (Berl).2010;208(3):427–432.
- ,.Signs and symptoms of tobacco withdrawal.Arch Gen Psychiatry.1986;43(3):289–294.
- ,,.Qualitative research in health care. Analysing qualitative data.BMJ.2000;320(7227):114–116.
- ,,,.Smoking reduction in the Lung Health Study.Nicotine Tob Res.2004;6(2):275–280.
- ,,.Interventions for smoking cessation in hospitalised patients.Cochrane Database Syst Rev.2007(3):CD001837.
- ,,,,.A computerized aid to support smoking cessation treatment for hospital patients.J Gen Intern Med.2008;23(8):1214–1217.
- ,,,,,.The feasibility of connecting physician offices to a state‐level tobacco quit line.Am J Prev Med.2006;30(1):31–37.
- ,,, et al.Clinical faxed referrals to a tobacco quitline: reach, enrollment, and participant characteristics.Am J Prev Med.2009;36(4):337–340.
- ,,, et al.Feasibility of a Spanish/English computerized decision aid to facilitate smoking cessation efforts in underserved communities.J Health Care Poor Underserved.2010;21(2):504–517.
- North American Quitline Consortium. Available at: http://www.naquitline. org. Accessed July2010.
- ,,,,,.Distribution of smokers by stage in three representative samples.Prev Med.1995;24:401–411.
- ,,.Telephone counselling for smoking cessation.Cochrane Database Syst Rev.2006;3:CD002850.
- ,.The potential of quitlines to increase smoking cessation.Drug Alcohol Rev.2006;25(1):73–78.
- ,,, et al.Evidence of real‐world effectiveness of a telephone quitline for smokers.N Engl J Med.2002;347(14):1087–1093.
- Campaign for Tobacco Free Kids Fact Sheets 2008. Quitlines Help Smokers Quit. Available at: http://www.tobaccofreekids.org/research/factsheets/pdf/0326.pdf. Accessed July2010.
Copyright © 2010 Society of Hospital Medicine
Emergency Response at a Children's Hospital
The incidence of sudden pediatric cardiac or respiratory arrest is low.1 Most inpatient pediatric arrests appear to occur as progression of respiratory distress or shock.2 The outcome of inpatient pediatric cardiorespiratory arrests continues to be poor, emphasizing the need for early recognition and intervention. In 2006, as part of its 100,000 Lives Campaign the Institute for Healthcare Improvement recommended the implementation of Rapid Response Teams (RRT) as 1 of the strategies to reduce the number of preventable inpatient deaths.3 We reviewed all emergency response team (ERT) activations for last 13 years at The Children's Hospital in Denver, CO to assist in the development of a new RRT and to identify at risk populations, situations, and system processes the RRT should address.
This is a retrospective review of 13 years of data collection on ERT activations at The Children's Hospital in Denver, CO. We describe demographic and clinical variables, including outcomes of ERT activations at a free‐standing tertiary care children's hospital.
Background/Methods
The Children's Hospital (TCH) is a 270 inpatient bed tertiary care free standing children's hospital associated with University of Colorado at Denver Health Sciences Center. The current distribution of inpatient beds includes: 168 medical/surgical beds, 102 critical care beds (26 pediatric intensive care unit, 16 cardiac intensive care unit, and 60 neonatal intensive care unit). In 2006, nearly 10,000 patients were admitted for care at this hospital with an average inpatient stay of 6 days. TCH is a Level One Regional Trauma Center serving a catchment area of seven states, and a major transplant center for heart, solid organs, and bone marrow.
The history of the TCH Emergency Response Team dates back to 1990 when we first began to follow cardiorespiratory arrests in noncritical care areas of the hospital. In 1992, a Cardiac Or Respiratory event (COR) team including the most senior in‐house specialist was available 24 hours a day, 7 days a week to respond to all arrests within the hospital. The COR committee provided oversight and monitoring of the arrest events, including standardization of crash carts and the development of mock codes to ensure that the responding personnel were qualified in resuscitation practices. The COR team has evolved over the ensuing years, including a name change to the Emergency Response Team (ERT); now a single number activated by any medical staff is used to call the operator who activates the ERT via overhead paging and via code pager system. The 14 member Emergency Response Team consists of PICU/CICU/anesthesia/surgical fellows, ED attending, in‐house residents, PICU/CICU/ED charge nurse, nursing supervisor, resource RN, pharmacist, respiratory therapist, and a messenger.
A database has been maintained by 1 of the authors (DBH) since the inception of the COR/ERT at TCH 16 years ago. This is a retrospective review of this database of ERT activations. An ERT activation could have been triggered by any event that was felt to be emergent, life threatening, and/or needing immediate medical attention. After the event, a debriefing form was filled out about the event. Data collected included date, time, medical record number, location, primary care service, age, sex, primary and secondary diagnoses, and disposition. Data not captured in this database included initial rhythm, need for compressions, cardiac medications, defibrillation or intubation.
Analyses were performed on data collected from January 1993 through April 2007. Medical records of the documented ERT activations were reviewed for missing information and/or clarification of the events. Categories entered in Statistical Package for Social Statistics (SPSS) were similar to information included in the debriefing form: age, sex, admission diagnosis, precipitating event, percentage of admissions, acute vs. chronic diagnosis, winter vs. nonwinter months (October‐March/April‐September), day (6 am‐6 pm) and night (6 pm‐6 am) shifts, survival of ERT activation, survival to discharge, and primary attending service. Data were analyzed using SPSS 16.0 (2007, Chicago, IL). The study was approved by the Colorado Multiple Institutional Review Board.
Results/Conclusion
There were 1537 ERT activations in the database. A total of 203 ERT activations were eliminated from the database: 177 were eliminated from analysis because of missing age, admission diagnosis or time of day of activation, and 26 were ERT activations that had been triggered on adult visitors or adult employees. The remaining 1334 ERT activations were included for analysis.
Table 1 shows the demographics of the patients. The median age was 1.8 years, with a range of 0 to 29 years. A total of 39%(511) of all ERT activations occurred in patients under the age of 1 year with the highest incidence between 1 month and 1 year. Overall, the children at highest risk were males less than 1 year of age with a chronic diagnosis. In addition, time of day and time of year of ERT activations were analyzed as shown. There was no statistical difference between nonwinter (April‐September) and winter (October‐March) months. Statistically, there were significantly more ERT activations during day shifts (6 am‐6 pm) as compared to night shifts (P < 0.001).
| Variable (n = 1334) | n (%) |
|---|---|
| |
| Age | |
| Neonate | 127 (10) |
| <1 year | 384 (29) |
| 1‐3 years | 324 (24) |
| 4‐6 years | 137 (10) |
| 7‐10 years | 120 (9) |
| 11‐13 years | 84 (6) |
| 14‐17 years | 120 (9) |
| >17 years | 38 (3) |
| Gender | |
| Male | 807 (60) |
| Time of day* | |
| Day (06:00‐18:00) | 784 (59) |
| Night (18:00‐06:00) | 550 (41) |
| Time of Year | |
| April‐September | 669 (50) |
| October‐March | 665 (50) |
The most common admission diagnosis (Table 2) and underlying chronic condition was cardiac disease; other common admission diagnoses were infectious disease, trauma, and pulmonary disease. The medical categories of admission diagnosis included congenital/metabolic (39%), gastrointestinal (29%), renal (18%), rheumatology (4%), toxicology (4%), psychiatry (3%), endocrine (2%), and allergy (1%). The surgery category of admission diagnosis included otolaryngology (63%), orthopedics (28%), urology (4%), dental (4%), and ophthalmology (1%).
| Admission Diagnosis (n = 1334) | n (%) |
|---|---|
| |
| Cardiac | 370 (28) |
| Infectious disease | 197 (15) |
| Trauma | 192 (14) |
| Other medical | 137 (10) |
| Pulmonary | 109 (8) |
| Neurology | 79 (6) |
| Other surgery | 76 (6) |
| Neurosurgery | 68 (5) |
| Hematology/oncology | 53 (4) |
| Surgery | 53 (4) |
Finally, the patients' survival rate after an ERT itself was to be 90% (Table 3), with an overall survival rate to discharge of 78% (Table 4). Survival rate to discharge of those patients who survived the ERT event was 87%. Two patients were missing survival event data and 137 patients were missing survival to discharge data.
| Admission Diagnosis | Survival of Event n (%) |
|---|---|
| |
| Cardiac (n = 370) | 315 (85) |
| Infectious disease (n = 197) | 186 (94) |
| Trauma (n = 191) | 168 (88) |
| Other medical (n = 136) | 125 (92) |
| Pulmonary (n = 109) | 97 (89) |
| Neurology (n = 79) | 75 (95) |
| Other surgery (n = 76) | 75 (99) |
| Neurosurgery (n = 68) | 63 (93) |
| Surgery (n = 53) | 50 (94) |
| Hematology/oncology (n = 53) | 46 (87) |
| Total (n = 1332)* | 1200 (90) |
Discussion
We present a retrospective review of 1334 emergency response team activations over 13 years at an academic free‐standing tertiary care children's hospital. In keeping with previous reports, we found that children less than 1 year of age were at the highest risk for activation of the emergency response team.1, 4, 5
The National Registry for CardioPulmonary Resuscitation (NRCPR) database cite respiratory failure (asphyxia) and circulatory shock (ischemia) as the most common causes of in‐hospital cardiac arrests.1 Additionally, more than half of pediatric patients that experience a cardiopulmonary arrest have an underlying chronic illness.1, 2, 4, 5, 6 These are similar to our findings that chronic pulmonary and cardiac diseases were among the most frequent admission diagnosis.
Unlike Peberdy et al.,7we did not find an increase in the number of emergency response team activations at night or on weekends. Instead, we found that an ERT activation was more likely to be requested during the day shifts (6 am‐6 pm) which is a similar to that reported by Jones et al.8 Similarly, Jones et al.8 reported that the hourly rate of their medical emergency team activation was greater during the time between 8 am and 6 pm.
Our overall survival rate (78%) to discharge after an ERT event was much higher than what has been reported by Topjian et al.9 (25%). This likely reflects our inclusion of all emergency response team activations, not just apneic and asystolic arrests. The improved survival rate may also be influenced by the 24/7 presence of pediatric fellows, residents and surgeons in our hospital, which has been associated with improved 24‐hour survival for children receiving in‐hospital cardiopulmonary resuscitation.10
There are several limitations to our data collection and this report. This was a retrospective review and as previously noted some medical details were absent resulting in the exclusion of some cases. We also found that the original debriefing form which was used as the basis for the database did not include some important clinical variable, such as vital signs, more detailed events such as rhythm, medications used, and deficits or changes in baseline function. We suggest including multiple variables in a future multicenter study of pediatric RRT's: facility, admitting service, admission diagnosis, age (chronologic and gestational), sex, how long patient has been in hospital prior to the event, past medical history, vitals signs before and after activation, time/date, location, any precipitating events and actions taken by the RRT (eg, cardiopulmonary resuscitation, defibrillation, emergent intubation, and other emergent interventions), medications, survival of event, survival to discharge, deficits or changes in baseline function after the event and to discharge. In particular, information about history of prematurity would have been helpful in assessing further risk factors. Analysis of survival with or without significant deficits or changes in baseline function would be another useful outcome measure. Figure 1 is an example of a debriefing form a multi‐institutional study or hospitalist led quality improvement project may use to collect this data.
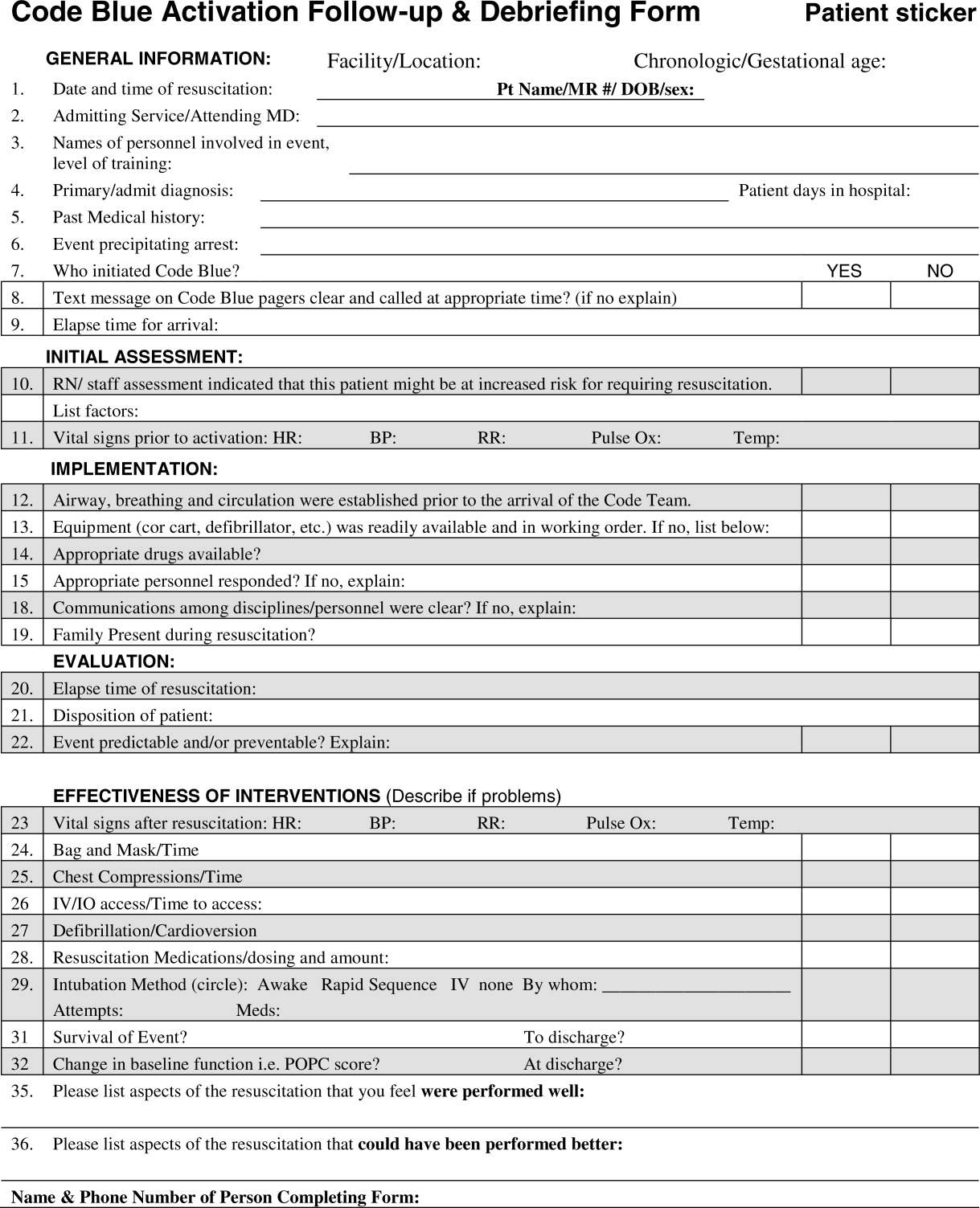
We were able to identify a population of higher‐risk patients (less than 1 year of age with comorbidities and an admission diagnosis of cardiac or respiratory disease) to focus our educational efforts on earlier recognition of patient deterioration for both inpatient ward staff and RRT responders. These findings may assist in future quality assurance issues such as patient placement and early ICU admissions depending on age, chronic conditions, and/or admission diagnosis. Future directions should include multi‐center study of RRT to improve external validity. In addition, a more careful analysis of events surrounding the activation, including incorporating such tools as the Pediatric Early Warning (PEW) Score,11 may further assist hospitals and practitioners identify hospitalized children at risk for deterioration on the inpatient ward.
| Admission Diagnosis | Survival to Discharge n (%) |
|---|---|
| |
| Cardiac (n = 317) | 217 (69) |
| Infectious disease (n = 175) | 139 (79) |
| Trauma (n = 182) | 151 (83) |
| Other medical (n = 125) | 99 (79) |
| Pulmonary (n = 98) | 76 (78) |
| Neurology (n = 71) | 63 (89) |
| Other surgery (n = 74) | 70 (95) |
| Neurosurgery (n = 64) | 53 (83) |
| Surgery (n = 47) | 39 (83) |
| Hematology/oncology (n = 44) | 24 (55) |
| Total (n = 1197)* | 931 (78) |
Acknowledgements
The acknowledge Dr. Genie Roosevelt MD, MPH, and Sara Deakyne MPH for their assistance in data analysis.
- ,,,.In‐hospital pediatric arrest.Pediatr Clin North Am.2008;55(3):589–604.
- ,,, et al.First documented rhythm and clinical outcome from in‐hospital cardiac arrest among children and adults.JAMA.2006;295:50–57.
- 57100K Lives Campaign‐getting started Kit: Rapid response Teams. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1 Accessed July2010.
- ,,, et al.Higher survival rates among younger patients after pediatric intensive care unity cardiac arrests.Pediatrics2006;118:2424–2433.
- , et al.A prospective investigation into the epidemiology of in‐hospital pediatric cardiopulmonary resuscitation using the internationalUtseinReporting Style.Pediatrics.2002;109:200–209.
- ,,,,.Results of inpatient pediatric resuscitation.Crit Care Med.1986;14:469–471
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299:785–792.
- ,,, et al.Circadian pattern of activation of the medical emergency team in a teaching hospital.Crit Care.2005;9:R303–R306.
- ,,.Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes.Pediatrics.2008;122;1086–1098
- ,,, et al.Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the National Registry of Cardiopulmonary Resuscitation.Pediatrics.2006;118:995–1001.
- ,,.The Pediatric Early Warning System score: a severity of illness score to predict urgent medical need in hospitalized children.J Crit Care.2006;21(3):271–278.
The incidence of sudden pediatric cardiac or respiratory arrest is low.1 Most inpatient pediatric arrests appear to occur as progression of respiratory distress or shock.2 The outcome of inpatient pediatric cardiorespiratory arrests continues to be poor, emphasizing the need for early recognition and intervention. In 2006, as part of its 100,000 Lives Campaign the Institute for Healthcare Improvement recommended the implementation of Rapid Response Teams (RRT) as 1 of the strategies to reduce the number of preventable inpatient deaths.3 We reviewed all emergency response team (ERT) activations for last 13 years at The Children's Hospital in Denver, CO to assist in the development of a new RRT and to identify at risk populations, situations, and system processes the RRT should address.
This is a retrospective review of 13 years of data collection on ERT activations at The Children's Hospital in Denver, CO. We describe demographic and clinical variables, including outcomes of ERT activations at a free‐standing tertiary care children's hospital.
Background/Methods
The Children's Hospital (TCH) is a 270 inpatient bed tertiary care free standing children's hospital associated with University of Colorado at Denver Health Sciences Center. The current distribution of inpatient beds includes: 168 medical/surgical beds, 102 critical care beds (26 pediatric intensive care unit, 16 cardiac intensive care unit, and 60 neonatal intensive care unit). In 2006, nearly 10,000 patients were admitted for care at this hospital with an average inpatient stay of 6 days. TCH is a Level One Regional Trauma Center serving a catchment area of seven states, and a major transplant center for heart, solid organs, and bone marrow.
The history of the TCH Emergency Response Team dates back to 1990 when we first began to follow cardiorespiratory arrests in noncritical care areas of the hospital. In 1992, a Cardiac Or Respiratory event (COR) team including the most senior in‐house specialist was available 24 hours a day, 7 days a week to respond to all arrests within the hospital. The COR committee provided oversight and monitoring of the arrest events, including standardization of crash carts and the development of mock codes to ensure that the responding personnel were qualified in resuscitation practices. The COR team has evolved over the ensuing years, including a name change to the Emergency Response Team (ERT); now a single number activated by any medical staff is used to call the operator who activates the ERT via overhead paging and via code pager system. The 14 member Emergency Response Team consists of PICU/CICU/anesthesia/surgical fellows, ED attending, in‐house residents, PICU/CICU/ED charge nurse, nursing supervisor, resource RN, pharmacist, respiratory therapist, and a messenger.
A database has been maintained by 1 of the authors (DBH) since the inception of the COR/ERT at TCH 16 years ago. This is a retrospective review of this database of ERT activations. An ERT activation could have been triggered by any event that was felt to be emergent, life threatening, and/or needing immediate medical attention. After the event, a debriefing form was filled out about the event. Data collected included date, time, medical record number, location, primary care service, age, sex, primary and secondary diagnoses, and disposition. Data not captured in this database included initial rhythm, need for compressions, cardiac medications, defibrillation or intubation.
Analyses were performed on data collected from January 1993 through April 2007. Medical records of the documented ERT activations were reviewed for missing information and/or clarification of the events. Categories entered in Statistical Package for Social Statistics (SPSS) were similar to information included in the debriefing form: age, sex, admission diagnosis, precipitating event, percentage of admissions, acute vs. chronic diagnosis, winter vs. nonwinter months (October‐March/April‐September), day (6 am‐6 pm) and night (6 pm‐6 am) shifts, survival of ERT activation, survival to discharge, and primary attending service. Data were analyzed using SPSS 16.0 (2007, Chicago, IL). The study was approved by the Colorado Multiple Institutional Review Board.
Results/Conclusion
There were 1537 ERT activations in the database. A total of 203 ERT activations were eliminated from the database: 177 were eliminated from analysis because of missing age, admission diagnosis or time of day of activation, and 26 were ERT activations that had been triggered on adult visitors or adult employees. The remaining 1334 ERT activations were included for analysis.
Table 1 shows the demographics of the patients. The median age was 1.8 years, with a range of 0 to 29 years. A total of 39%(511) of all ERT activations occurred in patients under the age of 1 year with the highest incidence between 1 month and 1 year. Overall, the children at highest risk were males less than 1 year of age with a chronic diagnosis. In addition, time of day and time of year of ERT activations were analyzed as shown. There was no statistical difference between nonwinter (April‐September) and winter (October‐March) months. Statistically, there were significantly more ERT activations during day shifts (6 am‐6 pm) as compared to night shifts (P < 0.001).
| Variable (n = 1334) | n (%) |
|---|---|
| |
| Age | |
| Neonate | 127 (10) |
| <1 year | 384 (29) |
| 1‐3 years | 324 (24) |
| 4‐6 years | 137 (10) |
| 7‐10 years | 120 (9) |
| 11‐13 years | 84 (6) |
| 14‐17 years | 120 (9) |
| >17 years | 38 (3) |
| Gender | |
| Male | 807 (60) |
| Time of day* | |
| Day (06:00‐18:00) | 784 (59) |
| Night (18:00‐06:00) | 550 (41) |
| Time of Year | |
| April‐September | 669 (50) |
| October‐March | 665 (50) |
The most common admission diagnosis (Table 2) and underlying chronic condition was cardiac disease; other common admission diagnoses were infectious disease, trauma, and pulmonary disease. The medical categories of admission diagnosis included congenital/metabolic (39%), gastrointestinal (29%), renal (18%), rheumatology (4%), toxicology (4%), psychiatry (3%), endocrine (2%), and allergy (1%). The surgery category of admission diagnosis included otolaryngology (63%), orthopedics (28%), urology (4%), dental (4%), and ophthalmology (1%).
| Admission Diagnosis (n = 1334) | n (%) |
|---|---|
| |
| Cardiac | 370 (28) |
| Infectious disease | 197 (15) |
| Trauma | 192 (14) |
| Other medical | 137 (10) |
| Pulmonary | 109 (8) |
| Neurology | 79 (6) |
| Other surgery | 76 (6) |
| Neurosurgery | 68 (5) |
| Hematology/oncology | 53 (4) |
| Surgery | 53 (4) |
Finally, the patients' survival rate after an ERT itself was to be 90% (Table 3), with an overall survival rate to discharge of 78% (Table 4). Survival rate to discharge of those patients who survived the ERT event was 87%. Two patients were missing survival event data and 137 patients were missing survival to discharge data.
| Admission Diagnosis | Survival of Event n (%) |
|---|---|
| |
| Cardiac (n = 370) | 315 (85) |
| Infectious disease (n = 197) | 186 (94) |
| Trauma (n = 191) | 168 (88) |
| Other medical (n = 136) | 125 (92) |
| Pulmonary (n = 109) | 97 (89) |
| Neurology (n = 79) | 75 (95) |
| Other surgery (n = 76) | 75 (99) |
| Neurosurgery (n = 68) | 63 (93) |
| Surgery (n = 53) | 50 (94) |
| Hematology/oncology (n = 53) | 46 (87) |
| Total (n = 1332)* | 1200 (90) |
Discussion
We present a retrospective review of 1334 emergency response team activations over 13 years at an academic free‐standing tertiary care children's hospital. In keeping with previous reports, we found that children less than 1 year of age were at the highest risk for activation of the emergency response team.1, 4, 5
The National Registry for CardioPulmonary Resuscitation (NRCPR) database cite respiratory failure (asphyxia) and circulatory shock (ischemia) as the most common causes of in‐hospital cardiac arrests.1 Additionally, more than half of pediatric patients that experience a cardiopulmonary arrest have an underlying chronic illness.1, 2, 4, 5, 6 These are similar to our findings that chronic pulmonary and cardiac diseases were among the most frequent admission diagnosis.
Unlike Peberdy et al.,7we did not find an increase in the number of emergency response team activations at night or on weekends. Instead, we found that an ERT activation was more likely to be requested during the day shifts (6 am‐6 pm) which is a similar to that reported by Jones et al.8 Similarly, Jones et al.8 reported that the hourly rate of their medical emergency team activation was greater during the time between 8 am and 6 pm.
Our overall survival rate (78%) to discharge after an ERT event was much higher than what has been reported by Topjian et al.9 (25%). This likely reflects our inclusion of all emergency response team activations, not just apneic and asystolic arrests. The improved survival rate may also be influenced by the 24/7 presence of pediatric fellows, residents and surgeons in our hospital, which has been associated with improved 24‐hour survival for children receiving in‐hospital cardiopulmonary resuscitation.10
There are several limitations to our data collection and this report. This was a retrospective review and as previously noted some medical details were absent resulting in the exclusion of some cases. We also found that the original debriefing form which was used as the basis for the database did not include some important clinical variable, such as vital signs, more detailed events such as rhythm, medications used, and deficits or changes in baseline function. We suggest including multiple variables in a future multicenter study of pediatric RRT's: facility, admitting service, admission diagnosis, age (chronologic and gestational), sex, how long patient has been in hospital prior to the event, past medical history, vitals signs before and after activation, time/date, location, any precipitating events and actions taken by the RRT (eg, cardiopulmonary resuscitation, defibrillation, emergent intubation, and other emergent interventions), medications, survival of event, survival to discharge, deficits or changes in baseline function after the event and to discharge. In particular, information about history of prematurity would have been helpful in assessing further risk factors. Analysis of survival with or without significant deficits or changes in baseline function would be another useful outcome measure. Figure 1 is an example of a debriefing form a multi‐institutional study or hospitalist led quality improvement project may use to collect this data.
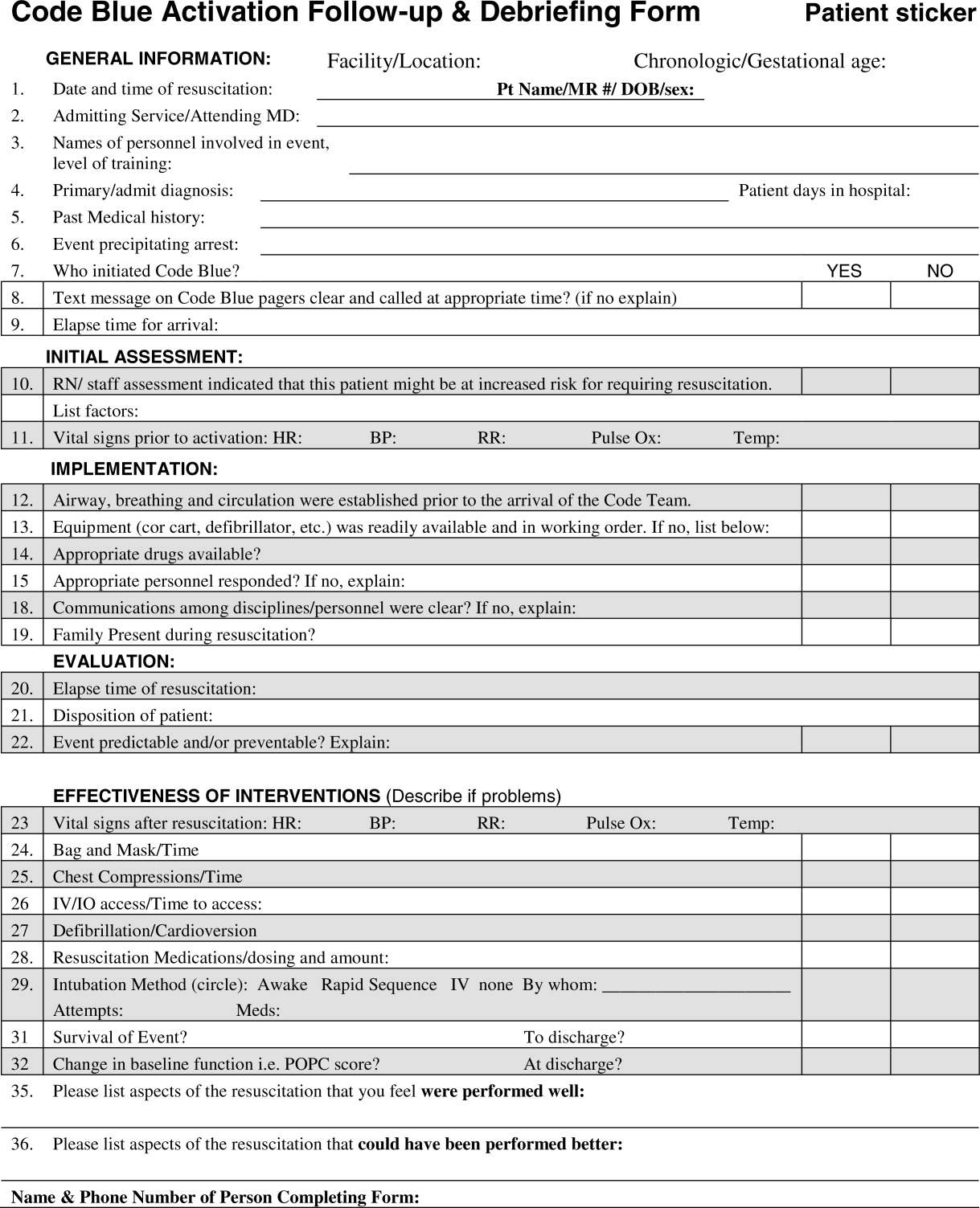
We were able to identify a population of higher‐risk patients (less than 1 year of age with comorbidities and an admission diagnosis of cardiac or respiratory disease) to focus our educational efforts on earlier recognition of patient deterioration for both inpatient ward staff and RRT responders. These findings may assist in future quality assurance issues such as patient placement and early ICU admissions depending on age, chronic conditions, and/or admission diagnosis. Future directions should include multi‐center study of RRT to improve external validity. In addition, a more careful analysis of events surrounding the activation, including incorporating such tools as the Pediatric Early Warning (PEW) Score,11 may further assist hospitals and practitioners identify hospitalized children at risk for deterioration on the inpatient ward.
| Admission Diagnosis | Survival to Discharge n (%) |
|---|---|
| |
| Cardiac (n = 317) | 217 (69) |
| Infectious disease (n = 175) | 139 (79) |
| Trauma (n = 182) | 151 (83) |
| Other medical (n = 125) | 99 (79) |
| Pulmonary (n = 98) | 76 (78) |
| Neurology (n = 71) | 63 (89) |
| Other surgery (n = 74) | 70 (95) |
| Neurosurgery (n = 64) | 53 (83) |
| Surgery (n = 47) | 39 (83) |
| Hematology/oncology (n = 44) | 24 (55) |
| Total (n = 1197)* | 931 (78) |
Acknowledgements
The acknowledge Dr. Genie Roosevelt MD, MPH, and Sara Deakyne MPH for their assistance in data analysis.
The incidence of sudden pediatric cardiac or respiratory arrest is low.1 Most inpatient pediatric arrests appear to occur as progression of respiratory distress or shock.2 The outcome of inpatient pediatric cardiorespiratory arrests continues to be poor, emphasizing the need for early recognition and intervention. In 2006, as part of its 100,000 Lives Campaign the Institute for Healthcare Improvement recommended the implementation of Rapid Response Teams (RRT) as 1 of the strategies to reduce the number of preventable inpatient deaths.3 We reviewed all emergency response team (ERT) activations for last 13 years at The Children's Hospital in Denver, CO to assist in the development of a new RRT and to identify at risk populations, situations, and system processes the RRT should address.
This is a retrospective review of 13 years of data collection on ERT activations at The Children's Hospital in Denver, CO. We describe demographic and clinical variables, including outcomes of ERT activations at a free‐standing tertiary care children's hospital.
Background/Methods
The Children's Hospital (TCH) is a 270 inpatient bed tertiary care free standing children's hospital associated with University of Colorado at Denver Health Sciences Center. The current distribution of inpatient beds includes: 168 medical/surgical beds, 102 critical care beds (26 pediatric intensive care unit, 16 cardiac intensive care unit, and 60 neonatal intensive care unit). In 2006, nearly 10,000 patients were admitted for care at this hospital with an average inpatient stay of 6 days. TCH is a Level One Regional Trauma Center serving a catchment area of seven states, and a major transplant center for heart, solid organs, and bone marrow.
The history of the TCH Emergency Response Team dates back to 1990 when we first began to follow cardiorespiratory arrests in noncritical care areas of the hospital. In 1992, a Cardiac Or Respiratory event (COR) team including the most senior in‐house specialist was available 24 hours a day, 7 days a week to respond to all arrests within the hospital. The COR committee provided oversight and monitoring of the arrest events, including standardization of crash carts and the development of mock codes to ensure that the responding personnel were qualified in resuscitation practices. The COR team has evolved over the ensuing years, including a name change to the Emergency Response Team (ERT); now a single number activated by any medical staff is used to call the operator who activates the ERT via overhead paging and via code pager system. The 14 member Emergency Response Team consists of PICU/CICU/anesthesia/surgical fellows, ED attending, in‐house residents, PICU/CICU/ED charge nurse, nursing supervisor, resource RN, pharmacist, respiratory therapist, and a messenger.
A database has been maintained by 1 of the authors (DBH) since the inception of the COR/ERT at TCH 16 years ago. This is a retrospective review of this database of ERT activations. An ERT activation could have been triggered by any event that was felt to be emergent, life threatening, and/or needing immediate medical attention. After the event, a debriefing form was filled out about the event. Data collected included date, time, medical record number, location, primary care service, age, sex, primary and secondary diagnoses, and disposition. Data not captured in this database included initial rhythm, need for compressions, cardiac medications, defibrillation or intubation.
Analyses were performed on data collected from January 1993 through April 2007. Medical records of the documented ERT activations were reviewed for missing information and/or clarification of the events. Categories entered in Statistical Package for Social Statistics (SPSS) were similar to information included in the debriefing form: age, sex, admission diagnosis, precipitating event, percentage of admissions, acute vs. chronic diagnosis, winter vs. nonwinter months (October‐March/April‐September), day (6 am‐6 pm) and night (6 pm‐6 am) shifts, survival of ERT activation, survival to discharge, and primary attending service. Data were analyzed using SPSS 16.0 (2007, Chicago, IL). The study was approved by the Colorado Multiple Institutional Review Board.
Results/Conclusion
There were 1537 ERT activations in the database. A total of 203 ERT activations were eliminated from the database: 177 were eliminated from analysis because of missing age, admission diagnosis or time of day of activation, and 26 were ERT activations that had been triggered on adult visitors or adult employees. The remaining 1334 ERT activations were included for analysis.
Table 1 shows the demographics of the patients. The median age was 1.8 years, with a range of 0 to 29 years. A total of 39%(511) of all ERT activations occurred in patients under the age of 1 year with the highest incidence between 1 month and 1 year. Overall, the children at highest risk were males less than 1 year of age with a chronic diagnosis. In addition, time of day and time of year of ERT activations were analyzed as shown. There was no statistical difference between nonwinter (April‐September) and winter (October‐March) months. Statistically, there were significantly more ERT activations during day shifts (6 am‐6 pm) as compared to night shifts (P < 0.001).
| Variable (n = 1334) | n (%) |
|---|---|
| |
| Age | |
| Neonate | 127 (10) |
| <1 year | 384 (29) |
| 1‐3 years | 324 (24) |
| 4‐6 years | 137 (10) |
| 7‐10 years | 120 (9) |
| 11‐13 years | 84 (6) |
| 14‐17 years | 120 (9) |
| >17 years | 38 (3) |
| Gender | |
| Male | 807 (60) |
| Time of day* | |
| Day (06:00‐18:00) | 784 (59) |
| Night (18:00‐06:00) | 550 (41) |
| Time of Year | |
| April‐September | 669 (50) |
| October‐March | 665 (50) |
The most common admission diagnosis (Table 2) and underlying chronic condition was cardiac disease; other common admission diagnoses were infectious disease, trauma, and pulmonary disease. The medical categories of admission diagnosis included congenital/metabolic (39%), gastrointestinal (29%), renal (18%), rheumatology (4%), toxicology (4%), psychiatry (3%), endocrine (2%), and allergy (1%). The surgery category of admission diagnosis included otolaryngology (63%), orthopedics (28%), urology (4%), dental (4%), and ophthalmology (1%).
| Admission Diagnosis (n = 1334) | n (%) |
|---|---|
| |
| Cardiac | 370 (28) |
| Infectious disease | 197 (15) |
| Trauma | 192 (14) |
| Other medical | 137 (10) |
| Pulmonary | 109 (8) |
| Neurology | 79 (6) |
| Other surgery | 76 (6) |
| Neurosurgery | 68 (5) |
| Hematology/oncology | 53 (4) |
| Surgery | 53 (4) |
Finally, the patients' survival rate after an ERT itself was to be 90% (Table 3), with an overall survival rate to discharge of 78% (Table 4). Survival rate to discharge of those patients who survived the ERT event was 87%. Two patients were missing survival event data and 137 patients were missing survival to discharge data.
| Admission Diagnosis | Survival of Event n (%) |
|---|---|
| |
| Cardiac (n = 370) | 315 (85) |
| Infectious disease (n = 197) | 186 (94) |
| Trauma (n = 191) | 168 (88) |
| Other medical (n = 136) | 125 (92) |
| Pulmonary (n = 109) | 97 (89) |
| Neurology (n = 79) | 75 (95) |
| Other surgery (n = 76) | 75 (99) |
| Neurosurgery (n = 68) | 63 (93) |
| Surgery (n = 53) | 50 (94) |
| Hematology/oncology (n = 53) | 46 (87) |
| Total (n = 1332)* | 1200 (90) |
Discussion
We present a retrospective review of 1334 emergency response team activations over 13 years at an academic free‐standing tertiary care children's hospital. In keeping with previous reports, we found that children less than 1 year of age were at the highest risk for activation of the emergency response team.1, 4, 5
The National Registry for CardioPulmonary Resuscitation (NRCPR) database cite respiratory failure (asphyxia) and circulatory shock (ischemia) as the most common causes of in‐hospital cardiac arrests.1 Additionally, more than half of pediatric patients that experience a cardiopulmonary arrest have an underlying chronic illness.1, 2, 4, 5, 6 These are similar to our findings that chronic pulmonary and cardiac diseases were among the most frequent admission diagnosis.
Unlike Peberdy et al.,7we did not find an increase in the number of emergency response team activations at night or on weekends. Instead, we found that an ERT activation was more likely to be requested during the day shifts (6 am‐6 pm) which is a similar to that reported by Jones et al.8 Similarly, Jones et al.8 reported that the hourly rate of their medical emergency team activation was greater during the time between 8 am and 6 pm.
Our overall survival rate (78%) to discharge after an ERT event was much higher than what has been reported by Topjian et al.9 (25%). This likely reflects our inclusion of all emergency response team activations, not just apneic and asystolic arrests. The improved survival rate may also be influenced by the 24/7 presence of pediatric fellows, residents and surgeons in our hospital, which has been associated with improved 24‐hour survival for children receiving in‐hospital cardiopulmonary resuscitation.10
There are several limitations to our data collection and this report. This was a retrospective review and as previously noted some medical details were absent resulting in the exclusion of some cases. We also found that the original debriefing form which was used as the basis for the database did not include some important clinical variable, such as vital signs, more detailed events such as rhythm, medications used, and deficits or changes in baseline function. We suggest including multiple variables in a future multicenter study of pediatric RRT's: facility, admitting service, admission diagnosis, age (chronologic and gestational), sex, how long patient has been in hospital prior to the event, past medical history, vitals signs before and after activation, time/date, location, any precipitating events and actions taken by the RRT (eg, cardiopulmonary resuscitation, defibrillation, emergent intubation, and other emergent interventions), medications, survival of event, survival to discharge, deficits or changes in baseline function after the event and to discharge. In particular, information about history of prematurity would have been helpful in assessing further risk factors. Analysis of survival with or without significant deficits or changes in baseline function would be another useful outcome measure. Figure 1 is an example of a debriefing form a multi‐institutional study or hospitalist led quality improvement project may use to collect this data.
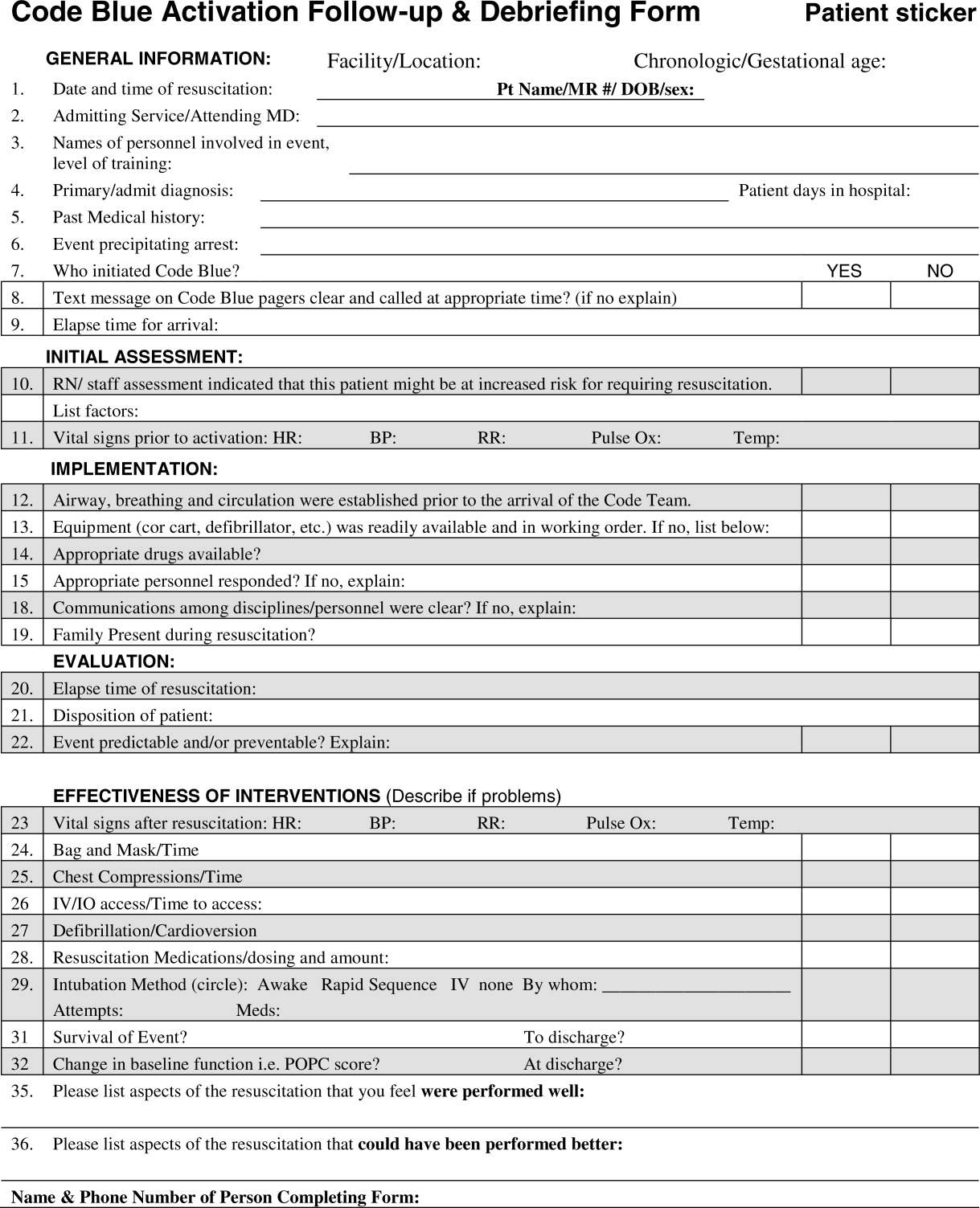
We were able to identify a population of higher‐risk patients (less than 1 year of age with comorbidities and an admission diagnosis of cardiac or respiratory disease) to focus our educational efforts on earlier recognition of patient deterioration for both inpatient ward staff and RRT responders. These findings may assist in future quality assurance issues such as patient placement and early ICU admissions depending on age, chronic conditions, and/or admission diagnosis. Future directions should include multi‐center study of RRT to improve external validity. In addition, a more careful analysis of events surrounding the activation, including incorporating such tools as the Pediatric Early Warning (PEW) Score,11 may further assist hospitals and practitioners identify hospitalized children at risk for deterioration on the inpatient ward.
| Admission Diagnosis | Survival to Discharge n (%) |
|---|---|
| |
| Cardiac (n = 317) | 217 (69) |
| Infectious disease (n = 175) | 139 (79) |
| Trauma (n = 182) | 151 (83) |
| Other medical (n = 125) | 99 (79) |
| Pulmonary (n = 98) | 76 (78) |
| Neurology (n = 71) | 63 (89) |
| Other surgery (n = 74) | 70 (95) |
| Neurosurgery (n = 64) | 53 (83) |
| Surgery (n = 47) | 39 (83) |
| Hematology/oncology (n = 44) | 24 (55) |
| Total (n = 1197)* | 931 (78) |
Acknowledgements
The acknowledge Dr. Genie Roosevelt MD, MPH, and Sara Deakyne MPH for their assistance in data analysis.
- ,,,.In‐hospital pediatric arrest.Pediatr Clin North Am.2008;55(3):589–604.
- ,,, et al.First documented rhythm and clinical outcome from in‐hospital cardiac arrest among children and adults.JAMA.2006;295:50–57.
- 57100K Lives Campaign‐getting started Kit: Rapid response Teams. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1 Accessed July2010.
- ,,, et al.Higher survival rates among younger patients after pediatric intensive care unity cardiac arrests.Pediatrics2006;118:2424–2433.
- , et al.A prospective investigation into the epidemiology of in‐hospital pediatric cardiopulmonary resuscitation using the internationalUtseinReporting Style.Pediatrics.2002;109:200–209.
- ,,,,.Results of inpatient pediatric resuscitation.Crit Care Med.1986;14:469–471
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299:785–792.
- ,,, et al.Circadian pattern of activation of the medical emergency team in a teaching hospital.Crit Care.2005;9:R303–R306.
- ,,.Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes.Pediatrics.2008;122;1086–1098
- ,,, et al.Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the National Registry of Cardiopulmonary Resuscitation.Pediatrics.2006;118:995–1001.
- ,,.The Pediatric Early Warning System score: a severity of illness score to predict urgent medical need in hospitalized children.J Crit Care.2006;21(3):271–278.
- ,,,.In‐hospital pediatric arrest.Pediatr Clin North Am.2008;55(3):589–604.
- ,,, et al.First documented rhythm and clinical outcome from in‐hospital cardiac arrest among children and adults.JAMA.2006;295:50–57.
- 57100K Lives Campaign‐getting started Kit: Rapid response Teams. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1 Accessed July2010.
- ,,, et al.Higher survival rates among younger patients after pediatric intensive care unity cardiac arrests.Pediatrics2006;118:2424–2433.
- , et al.A prospective investigation into the epidemiology of in‐hospital pediatric cardiopulmonary resuscitation using the internationalUtseinReporting Style.Pediatrics.2002;109:200–209.
- ,,,,.Results of inpatient pediatric resuscitation.Crit Care Med.1986;14:469–471
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299:785–792.
- ,,, et al.Circadian pattern of activation of the medical emergency team in a teaching hospital.Crit Care.2005;9:R303–R306.
- ,,.Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes.Pediatrics.2008;122;1086–1098
- ,,, et al.Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the National Registry of Cardiopulmonary Resuscitation.Pediatrics.2006;118:995–1001.
- ,,.The Pediatric Early Warning System score: a severity of illness score to predict urgent medical need in hospitalized children.J Crit Care.2006;21(3):271–278.
Copyright © 2010 Society of Hospital Medicine
Study Associates Inflammatory Bowel Disease with VTE
Hospitalists should pay attention to a new study that shows patients with inflammatory bowel disease (IBD) are at increased risk of recurrent VTE, according to a veteran hospitalist who studies the topic. Until research advances to the point it can identify weighted risk, however, it’s difficult to emphasize the results too much, he adds.
Still, Alpesh Amin, MD, MBA, SFHM, FACP, professor and chairman of the Department of Medicine and executive director of the HM program at the University of California at Irvine, says the new research solidifies the idea that HM groups should know whether a patient has IBD when doing a risk assessment.
"Now the question is, 'Which risk factors are most significant?'" Dr. Amin says. "More information needs to come to help define that."
The 14-center cohort study found that the probability of recurrence five years after discontinuation of anticoagulation therapy was higher among patients with IBD than patients without IBD (33.4%; 95% confidence interval [CI]: 21.8–45.0 vs. 21.7%; 95% CI: 18.8–24.6; P=0.01) (Gastroenterology. 2010;139(3):779-787). In addition, after adjustment for potential confounders, IBD also rates as an independent risk factor of recurrence (hazard ratio=2.5; 95% CI: 1.4–4.2; P=0.001).
Dr. Amin would like to see data that delineate the risk differential between hospitalized patients with IBD and hospitalized patients admitted for acute flare-ups of their IBD. For example, an IBD patient admitted with bloody diarrhea is usually steered away from anticoagulants for fear of increased bleeding. In some of those cases, hospitalists may instead use an inferior vena cava (IVC) filter. Those devices recently drew attention after an Archives of Internal Medicine report (PDF) and an FDA advisory questioned their long-term safety implications.
"We don't have strong evidence whether having acute flare-ups makes the risk worse or not," Dr. Amin says. "We need to figure out how to deal with that issue."
Hospitalists should pay attention to a new study that shows patients with inflammatory bowel disease (IBD) are at increased risk of recurrent VTE, according to a veteran hospitalist who studies the topic. Until research advances to the point it can identify weighted risk, however, it’s difficult to emphasize the results too much, he adds.
Still, Alpesh Amin, MD, MBA, SFHM, FACP, professor and chairman of the Department of Medicine and executive director of the HM program at the University of California at Irvine, says the new research solidifies the idea that HM groups should know whether a patient has IBD when doing a risk assessment.
"Now the question is, 'Which risk factors are most significant?'" Dr. Amin says. "More information needs to come to help define that."
The 14-center cohort study found that the probability of recurrence five years after discontinuation of anticoagulation therapy was higher among patients with IBD than patients without IBD (33.4%; 95% confidence interval [CI]: 21.8–45.0 vs. 21.7%; 95% CI: 18.8–24.6; P=0.01) (Gastroenterology. 2010;139(3):779-787). In addition, after adjustment for potential confounders, IBD also rates as an independent risk factor of recurrence (hazard ratio=2.5; 95% CI: 1.4–4.2; P=0.001).
Dr. Amin would like to see data that delineate the risk differential between hospitalized patients with IBD and hospitalized patients admitted for acute flare-ups of their IBD. For example, an IBD patient admitted with bloody diarrhea is usually steered away from anticoagulants for fear of increased bleeding. In some of those cases, hospitalists may instead use an inferior vena cava (IVC) filter. Those devices recently drew attention after an Archives of Internal Medicine report (PDF) and an FDA advisory questioned their long-term safety implications.
"We don't have strong evidence whether having acute flare-ups makes the risk worse or not," Dr. Amin says. "We need to figure out how to deal with that issue."
Hospitalists should pay attention to a new study that shows patients with inflammatory bowel disease (IBD) are at increased risk of recurrent VTE, according to a veteran hospitalist who studies the topic. Until research advances to the point it can identify weighted risk, however, it’s difficult to emphasize the results too much, he adds.
Still, Alpesh Amin, MD, MBA, SFHM, FACP, professor and chairman of the Department of Medicine and executive director of the HM program at the University of California at Irvine, says the new research solidifies the idea that HM groups should know whether a patient has IBD when doing a risk assessment.
"Now the question is, 'Which risk factors are most significant?'" Dr. Amin says. "More information needs to come to help define that."
The 14-center cohort study found that the probability of recurrence five years after discontinuation of anticoagulation therapy was higher among patients with IBD than patients without IBD (33.4%; 95% confidence interval [CI]: 21.8–45.0 vs. 21.7%; 95% CI: 18.8–24.6; P=0.01) (Gastroenterology. 2010;139(3):779-787). In addition, after adjustment for potential confounders, IBD also rates as an independent risk factor of recurrence (hazard ratio=2.5; 95% CI: 1.4–4.2; P=0.001).
Dr. Amin would like to see data that delineate the risk differential between hospitalized patients with IBD and hospitalized patients admitted for acute flare-ups of their IBD. For example, an IBD patient admitted with bloody diarrhea is usually steered away from anticoagulants for fear of increased bleeding. In some of those cases, hospitalists may instead use an inferior vena cava (IVC) filter. Those devices recently drew attention after an Archives of Internal Medicine report (PDF) and an FDA advisory questioned their long-term safety implications.
"We don't have strong evidence whether having acute flare-ups makes the risk worse or not," Dr. Amin says. "We need to figure out how to deal with that issue."
In the Literature: Research You Need to Know
Clinical question: Are beta-blockers safe to use in patients with chest pain and recent cocaine use?
Background: Beta-blockers are known to improve outcomes after myocardial infarction, yet are contraindicated in chest pain associated with recent cocaine use. Recommendations against beta-blocker use in the setting of cocaine-induced chest pain are based on case reports, small-scale human experiments, and the theoretical concern that beta-blockers may potentiate cocaine toxicity by creating unopposed alpha-adrenergic stimulation. Clinical outcomes of beta-blocker use in patients with cocaine use and chest pain are unknown.
Study design: Retrospective cohort study.
Setting: San Francisco General Hospital, San Francisco.
Synopsis: Three hundred thirty-one patients with chest pain and positive urine toxicologic screening for cocaine were admitted during the study period. One hundred fifty-one (46%) received a beta-blocker in the ED, per the discretion of the treating physicians. There were no differences in ECG abnormalities, troponin levels, length of stay, intubation, ventricular arrhythmias, use of vasopressors, or death in those patients who did and who did not receive a beta-blocker. Over a median follow-up of 972 days, patients who had been discharged on a beta-blocker did have a significant reduction in cardiovascular death (hazard ratio 0.29, 95% CI, 0.09-0.98, P= 0.047).
Because this was an observational study and post-discharge data were limited only to vital status, definitive conclusions regarding the safety of beta-blockers in cocaine-associated chest pain cannot be made. The authors acknowledge that more rigorous study is indicated given the potential benefit of beta-blockers in this population.
Bottom line: Use of beta-blockers in patients with chest pain and positive urine drug screen for cocaine is not associated with immediate adverse outcomes and might actually reduce cardiovascular mortality over time.
Citation: Rangel C, Shu RG, Lazar LD, Vittinghoff E, Hsue P, Marcus GM. Beta-blockers for chest pain associated with recent cocaine use. Arch Intern Med. 2010;170(10):874-879.
Reviewed for TH eWire by Kelly Cunningham, MD, Joshua LaBrin, MD, Amanda Salanitro, MD, MSPH, Kelly Sopko, MD, Shelley Ellis, MD, MPH, and Elizabeth Rice, MD, Section of Hospital Medicine, Vanderbilt University, Nashville, Tenn.
For more physician reviews of literature, visit our website.
Clinical question: Are beta-blockers safe to use in patients with chest pain and recent cocaine use?
Background: Beta-blockers are known to improve outcomes after myocardial infarction, yet are contraindicated in chest pain associated with recent cocaine use. Recommendations against beta-blocker use in the setting of cocaine-induced chest pain are based on case reports, small-scale human experiments, and the theoretical concern that beta-blockers may potentiate cocaine toxicity by creating unopposed alpha-adrenergic stimulation. Clinical outcomes of beta-blocker use in patients with cocaine use and chest pain are unknown.
Study design: Retrospective cohort study.
Setting: San Francisco General Hospital, San Francisco.
Synopsis: Three hundred thirty-one patients with chest pain and positive urine toxicologic screening for cocaine were admitted during the study period. One hundred fifty-one (46%) received a beta-blocker in the ED, per the discretion of the treating physicians. There were no differences in ECG abnormalities, troponin levels, length of stay, intubation, ventricular arrhythmias, use of vasopressors, or death in those patients who did and who did not receive a beta-blocker. Over a median follow-up of 972 days, patients who had been discharged on a beta-blocker did have a significant reduction in cardiovascular death (hazard ratio 0.29, 95% CI, 0.09-0.98, P= 0.047).
Because this was an observational study and post-discharge data were limited only to vital status, definitive conclusions regarding the safety of beta-blockers in cocaine-associated chest pain cannot be made. The authors acknowledge that more rigorous study is indicated given the potential benefit of beta-blockers in this population.
Bottom line: Use of beta-blockers in patients with chest pain and positive urine drug screen for cocaine is not associated with immediate adverse outcomes and might actually reduce cardiovascular mortality over time.
Citation: Rangel C, Shu RG, Lazar LD, Vittinghoff E, Hsue P, Marcus GM. Beta-blockers for chest pain associated with recent cocaine use. Arch Intern Med. 2010;170(10):874-879.
Reviewed for TH eWire by Kelly Cunningham, MD, Joshua LaBrin, MD, Amanda Salanitro, MD, MSPH, Kelly Sopko, MD, Shelley Ellis, MD, MPH, and Elizabeth Rice, MD, Section of Hospital Medicine, Vanderbilt University, Nashville, Tenn.
For more physician reviews of literature, visit our website.
Clinical question: Are beta-blockers safe to use in patients with chest pain and recent cocaine use?
Background: Beta-blockers are known to improve outcomes after myocardial infarction, yet are contraindicated in chest pain associated with recent cocaine use. Recommendations against beta-blocker use in the setting of cocaine-induced chest pain are based on case reports, small-scale human experiments, and the theoretical concern that beta-blockers may potentiate cocaine toxicity by creating unopposed alpha-adrenergic stimulation. Clinical outcomes of beta-blocker use in patients with cocaine use and chest pain are unknown.
Study design: Retrospective cohort study.
Setting: San Francisco General Hospital, San Francisco.
Synopsis: Three hundred thirty-one patients with chest pain and positive urine toxicologic screening for cocaine were admitted during the study period. One hundred fifty-one (46%) received a beta-blocker in the ED, per the discretion of the treating physicians. There were no differences in ECG abnormalities, troponin levels, length of stay, intubation, ventricular arrhythmias, use of vasopressors, or death in those patients who did and who did not receive a beta-blocker. Over a median follow-up of 972 days, patients who had been discharged on a beta-blocker did have a significant reduction in cardiovascular death (hazard ratio 0.29, 95% CI, 0.09-0.98, P= 0.047).
Because this was an observational study and post-discharge data were limited only to vital status, definitive conclusions regarding the safety of beta-blockers in cocaine-associated chest pain cannot be made. The authors acknowledge that more rigorous study is indicated given the potential benefit of beta-blockers in this population.
Bottom line: Use of beta-blockers in patients with chest pain and positive urine drug screen for cocaine is not associated with immediate adverse outcomes and might actually reduce cardiovascular mortality over time.
Citation: Rangel C, Shu RG, Lazar LD, Vittinghoff E, Hsue P, Marcus GM. Beta-blockers for chest pain associated with recent cocaine use. Arch Intern Med. 2010;170(10):874-879.
Reviewed for TH eWire by Kelly Cunningham, MD, Joshua LaBrin, MD, Amanda Salanitro, MD, MSPH, Kelly Sopko, MD, Shelley Ellis, MD, MPH, and Elizabeth Rice, MD, Section of Hospital Medicine, Vanderbilt University, Nashville, Tenn.
For more physician reviews of literature, visit our website.
Dabigatran: lower hemorrhage risk than warfarin

A recent analysis of previous data found that while warfarin and dabigatran are comparable at preventing stroke in patients with atrial fibrillation who have previously had a stroke or transient ischemic attack, the risk of developing intracranial bleeding is lower with dabigatran.
The study, led by Hans-Christoph Diener, MD, of University Hospital Essen in Germany, aimed to analyze a subgroup of patients from the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial.
The RE-LY trial found that 110 mg dabigatran twice daily was as effective as warfarin in reducing the occurrence of stroke, and that 150 mg dabigatran twice daily was better than warfarin in patients who had atrial fibrillation.
Twenty percent of the participants had previously had a stroke or transient ischemic attack, which increases the risk of having another stroke. Dr Diener and colleagues decided to look at this subgroup because they are more susceptible to adverse events from anticoagulation, especially cerebral hemorrhage.
It is important to note that one of warfarin’s negative side effects is bleeding.
The investigators found that warfarin and both dosages of dabigatran were equally effective in preventing stroke or systemic embolism in patients with a previous transient ischemic attack or stroke.
Compared with warfarin, the relative risk (RR) of stroke or systemic embolism with the 150 mg dose of dabigatran was 0.75 and for the 110 mg dose was 0.84.
The rate of major bleeding was significantly lower in patients on 110 mg dabigatran (RR 0.66) and similar in those on 150 mg dabigatran (RR 1.01) compared with those on warfarin.
The 110 mg dose of dabigatran was also associated with a significant reduction in the rate of vascular death (RR 0.63) and all-cause mortality (0.70).
According to the authors, “The exact mechanism for the lower rate of intracranial bleeding with dabigatran compared with warfarin, beyond a more stable anticoagulation, is not yet known. One possible explanation is that dabigatran does not cross the blood-brain barrier.”
When it comes to choosing a dosage, the authors concluded, “The dose of 150 mg dabigatran twice daily could be preferred to 110 mg twice daily because it significantly reduces the risk of ischemic stroke without increasing the risk of hemorrhagic stroke."
The study was funded by Boehringer Ingelheim and published online first by The Lancet Neurology. ![]()

A recent analysis of previous data found that while warfarin and dabigatran are comparable at preventing stroke in patients with atrial fibrillation who have previously had a stroke or transient ischemic attack, the risk of developing intracranial bleeding is lower with dabigatran.
The study, led by Hans-Christoph Diener, MD, of University Hospital Essen in Germany, aimed to analyze a subgroup of patients from the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial.
The RE-LY trial found that 110 mg dabigatran twice daily was as effective as warfarin in reducing the occurrence of stroke, and that 150 mg dabigatran twice daily was better than warfarin in patients who had atrial fibrillation.
Twenty percent of the participants had previously had a stroke or transient ischemic attack, which increases the risk of having another stroke. Dr Diener and colleagues decided to look at this subgroup because they are more susceptible to adverse events from anticoagulation, especially cerebral hemorrhage.
It is important to note that one of warfarin’s negative side effects is bleeding.
The investigators found that warfarin and both dosages of dabigatran were equally effective in preventing stroke or systemic embolism in patients with a previous transient ischemic attack or stroke.
Compared with warfarin, the relative risk (RR) of stroke or systemic embolism with the 150 mg dose of dabigatran was 0.75 and for the 110 mg dose was 0.84.
The rate of major bleeding was significantly lower in patients on 110 mg dabigatran (RR 0.66) and similar in those on 150 mg dabigatran (RR 1.01) compared with those on warfarin.
The 110 mg dose of dabigatran was also associated with a significant reduction in the rate of vascular death (RR 0.63) and all-cause mortality (0.70).
According to the authors, “The exact mechanism for the lower rate of intracranial bleeding with dabigatran compared with warfarin, beyond a more stable anticoagulation, is not yet known. One possible explanation is that dabigatran does not cross the blood-brain barrier.”
When it comes to choosing a dosage, the authors concluded, “The dose of 150 mg dabigatran twice daily could be preferred to 110 mg twice daily because it significantly reduces the risk of ischemic stroke without increasing the risk of hemorrhagic stroke."
The study was funded by Boehringer Ingelheim and published online first by The Lancet Neurology. ![]()

A recent analysis of previous data found that while warfarin and dabigatran are comparable at preventing stroke in patients with atrial fibrillation who have previously had a stroke or transient ischemic attack, the risk of developing intracranial bleeding is lower with dabigatran.
The study, led by Hans-Christoph Diener, MD, of University Hospital Essen in Germany, aimed to analyze a subgroup of patients from the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial.
The RE-LY trial found that 110 mg dabigatran twice daily was as effective as warfarin in reducing the occurrence of stroke, and that 150 mg dabigatran twice daily was better than warfarin in patients who had atrial fibrillation.
Twenty percent of the participants had previously had a stroke or transient ischemic attack, which increases the risk of having another stroke. Dr Diener and colleagues decided to look at this subgroup because they are more susceptible to adverse events from anticoagulation, especially cerebral hemorrhage.
It is important to note that one of warfarin’s negative side effects is bleeding.
The investigators found that warfarin and both dosages of dabigatran were equally effective in preventing stroke or systemic embolism in patients with a previous transient ischemic attack or stroke.
Compared with warfarin, the relative risk (RR) of stroke or systemic embolism with the 150 mg dose of dabigatran was 0.75 and for the 110 mg dose was 0.84.
The rate of major bleeding was significantly lower in patients on 110 mg dabigatran (RR 0.66) and similar in those on 150 mg dabigatran (RR 1.01) compared with those on warfarin.
The 110 mg dose of dabigatran was also associated with a significant reduction in the rate of vascular death (RR 0.63) and all-cause mortality (0.70).
According to the authors, “The exact mechanism for the lower rate of intracranial bleeding with dabigatran compared with warfarin, beyond a more stable anticoagulation, is not yet known. One possible explanation is that dabigatran does not cross the blood-brain barrier.”
When it comes to choosing a dosage, the authors concluded, “The dose of 150 mg dabigatran twice daily could be preferred to 110 mg twice daily because it significantly reduces the risk of ischemic stroke without increasing the risk of hemorrhagic stroke."
The study was funded by Boehringer Ingelheim and published online first by The Lancet Neurology. ![]()
Joint Commission: U.S. Hospitals Make "Core Measure" Gains
The Joint Commission's annual report on quality initiatives in American hospitals could be more valuable to hospitalist groups if they look at where rankings show room for improvement, one hospitalist says.
Eduard Vasilevskis, MD, assistant professor of medicine in the Section of Hospital Medicine at Vanderbilt University and the Tennessee Valley-Nashville VA Hospital, says substantial gains in core-measure categories are great in aggregate but do little to spur QI in individual hospitals.
"As a group, we're doing pretty well with these core measures," Dr. Vasilevskis says. "But at an institution, it's critical you understand your individual numbers."
"Improving America’s Hospitals” (PDF), released in September, reported composite 2009 care results of 97.7% for heart attacks and 92.9% for pneumonia. Both were the highest measures since the report began tabulating the data in 2002.
Dr. Vasilevskis sees the news as a great sign for patient care but thinks the value of QI is to apply the techniques that have boosted those measures to other issues, such as interdisciplinary and transitional care. Those areas are more difficult to quantify and study, but that makes them ripe for HM group leaders to tackle, he says.
“This is going to take leadership; we need a quarterback on the team,” he adds. “Hospitalists can step up and be that quarterback.”
Dr. Vasilevskis also advocates for stiffer compliance requirements. For example, he says, while the current report lists a 99.4% compliance rate for physicians giving smoking cessation advice, the report includes no data or follow-up to show how that advice pans out. He notes that approach would be costly and time-consuming but could reap a valuable return on the investment.
"The first step is data," he says. "Then it's going to take leadership."
The Joint Commission's annual report on quality initiatives in American hospitals could be more valuable to hospitalist groups if they look at where rankings show room for improvement, one hospitalist says.
Eduard Vasilevskis, MD, assistant professor of medicine in the Section of Hospital Medicine at Vanderbilt University and the Tennessee Valley-Nashville VA Hospital, says substantial gains in core-measure categories are great in aggregate but do little to spur QI in individual hospitals.
"As a group, we're doing pretty well with these core measures," Dr. Vasilevskis says. "But at an institution, it's critical you understand your individual numbers."
"Improving America’s Hospitals” (PDF), released in September, reported composite 2009 care results of 97.7% for heart attacks and 92.9% for pneumonia. Both were the highest measures since the report began tabulating the data in 2002.
Dr. Vasilevskis sees the news as a great sign for patient care but thinks the value of QI is to apply the techniques that have boosted those measures to other issues, such as interdisciplinary and transitional care. Those areas are more difficult to quantify and study, but that makes them ripe for HM group leaders to tackle, he says.
“This is going to take leadership; we need a quarterback on the team,” he adds. “Hospitalists can step up and be that quarterback.”
Dr. Vasilevskis also advocates for stiffer compliance requirements. For example, he says, while the current report lists a 99.4% compliance rate for physicians giving smoking cessation advice, the report includes no data or follow-up to show how that advice pans out. He notes that approach would be costly and time-consuming but could reap a valuable return on the investment.
"The first step is data," he says. "Then it's going to take leadership."
The Joint Commission's annual report on quality initiatives in American hospitals could be more valuable to hospitalist groups if they look at where rankings show room for improvement, one hospitalist says.
Eduard Vasilevskis, MD, assistant professor of medicine in the Section of Hospital Medicine at Vanderbilt University and the Tennessee Valley-Nashville VA Hospital, says substantial gains in core-measure categories are great in aggregate but do little to spur QI in individual hospitals.
"As a group, we're doing pretty well with these core measures," Dr. Vasilevskis says. "But at an institution, it's critical you understand your individual numbers."
"Improving America’s Hospitals” (PDF), released in September, reported composite 2009 care results of 97.7% for heart attacks and 92.9% for pneumonia. Both were the highest measures since the report began tabulating the data in 2002.
Dr. Vasilevskis sees the news as a great sign for patient care but thinks the value of QI is to apply the techniques that have boosted those measures to other issues, such as interdisciplinary and transitional care. Those areas are more difficult to quantify and study, but that makes them ripe for HM group leaders to tackle, he says.
“This is going to take leadership; we need a quarterback on the team,” he adds. “Hospitalists can step up and be that quarterback.”
Dr. Vasilevskis also advocates for stiffer compliance requirements. For example, he says, while the current report lists a 99.4% compliance rate for physicians giving smoking cessation advice, the report includes no data or follow-up to show how that advice pans out. He notes that approach would be costly and time-consuming but could reap a valuable return on the investment.
"The first step is data," he says. "Then it's going to take leadership."