User login
Failing the 15-minute suicide watch: Guidelines to monitor inpatients
Patient commits suicide after 15-minute checks are stopped
Honolulu County (HI) Circuit Court
A patient was brought to a hospital and interviewed by a psychiatrist. She was found to be at moderate risk for suicide, was admitted, and ordered to be monitored every 15 minutes. The patient attempted suicide 2 days later by closing a drawer on her neck. She died from the injuries the following day.
The patient’s family claimed that a hospital nurse misread the psychiatrist’s instructions and stopped the 15-minute checks on the morning of the incident, believing that the order was limited to 15-minute checks for the first 24 hours, even though they had been done for almost 2 days. The patient refused medication on the first day of admission, and the psychiatrist had started the procedure to obtain a court order committing the patient and allowing injection of necessary medication. The claims against the hospital were settled for a confidential amount.
The patient’s family claimed the psychiatrist diagnosed the patient with major depression with recurrent suicide ideation but failed to properly assess her for suicide monitoring. The family also said the patient should have been determined to be at least at high risk and required to be within sight of staff.
The psychiatrist claimed to be unaware the 15-minute monitoring had ceased. The psychiatrist saw the patient 30 minutes before she was found collapsed with her head in the drawer. The hospital staff checked the patient approximately 15 to 30 minutes before she was found.
- A defense verdict was returned
Reduced observation blamed for suicide by hanging
Kings County (NY) Supreme Court
A 45-year-old police lieutenant who suffered from alcohol abuse and depression was admitted to a psychiatric care facility. He was classiffied “Q15,” a category assigned to patients who must be visually inspected every 15 minutes, cannot have access to sharp objects or any other material or object they can use to inflict bodily harm, and must request permission to use restrooms. The next day the psychiatrist examined the patient and moved him to a “Q30” status, which halved the frequency of visual inspections, gave him unrestricted access to restrooms, and allowed him to have a bathrobe with a belt. The patient hanged himself the next day, using a restroom door to support a noose he made from the bathrobe belt.
The patient’s family faulted the hospital and psychiatrist for prematurely advancing the patient to “Q30” status. The hospital and psychiatrist claimed the suicide could not have been predicted and argued that given his background as a police lieutenant, the patient would have interpreted more stringent restrictions as incarceration. The psychiatrist argued that such a perception would have impeded the patient’s progress.
- A $71,989 verdict was returned, apportioning fault 65% to the hospital and 35% to the psychiatrist
Constant patient observation—such as one-to-one staffing or 15-minute checks—is used to protect patients from harming themselves or others. One study of a psychiatric hospital1 reported that 13% of psychiatric inpatients required constant observation.
Even 15 minutes is sufficient time to complete a suicide.3 Common methods of inpatient suicide include hanging, overdosing, and jumping from high places.4,5 One study found that 73% of inpatient suicides in a psychiatric ward occurred after 28 days of admission.5
The cost of constant observation may account for as much as 20% of the total nursing budget at a psychiatric hospital and up to 10% at a long-term care facility or general hospital.6 The annual cost of constant observation can exceed $500,000, depending on the hospital’s size and monitoring frequency.6
Determining responsibility
The outcomes of these 2 cases may appear inconsistent. In the first, the psychiatrist who assessed the patient as a moderate suicide risk was not negligent, even though the family claimed the patient was at high risk. In the second case, the psychiatrist was found partly liable for not maintaining a higher vigilance of suicide risk assessment.
Physicians cannot put every patient on one-to-one monitoring or 15-minute checks because of fear of suicide and malpractice litigation. These 2 cases demonstrate that if a suicide occurs, the courts will look for clinical reasons for the level of observation. The level of suicide precautions—one-to-one vs 15-minute checks—should be based on the patient’s clinical presentation and supported by clinical rationale.7
Risk analysis
The courts look to see if the suicide assessment was “clinically reasonable”.8 To meet this standard, perform a “suicide risk-benefit analysis” each time you make a significant clinical decision, such as ordering 15-minute checks. The record should include information sources you used (such as family members or previous medical records), factors that entered the clinical decision, and how you balanced these factors in a risk-benefit assessment (Box 1).9
Document decisions. Mistakes in clinical judgment do not necessarily constitute negligence,8 but deviations in the standard of care cannot be adequately determined in a court of law unless the clinician had documented his or her thought processes at the time of the decision.
Predicting which patients will re-experience or deny suicidal ideation is impossible,7 but if the patient is determined to be at high risk for suicide, then implement and document a plan to address this risk. In addition, communicate information regarding the risk-benefit assessment to staff responsible for implementing these precautions.
- Suicidal thoughts or behaviors—ideas, plans, attempts
- Psychiatric diagnoses—depression, bipolar disorder, schizophrenia, substance use, Cluster B personality disorders
- Physical illnesses—HIV, malignant cancers, pain syndromes
- Psychosocial features—lack of support, unemployment
- Childhood traumas
- Genetic and familial effects—family history of suicide
- Psychological features—hopelessness, agitation, impulsiveness
- Cognitive features—polarized thinking
- Demographic features—adolescents, young adults, and elderly patients
- Other factors—access to firearms, intoxication.
Source: Reference 7
- a patient is admitted for inpatient treatment
- observation status changes
- a patient’s clinical condition changes substantially
- acute psychosocial stressors are discovered during the hospitalization.7
1. Shugar G, Rehaluk R. Continuous observation for psychiatric inpatients. Compr Psychiatry 1990;30:48-55.
2. Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry 2003;64:14-9.
3. Bowers L, Gournay K, Dufy D. Suicide and self-harm in inpatient psychiatric units: a national survey of observation policies. J Adv Nursing 2000;32:437-44.
4. Proulx F, Lesage AD, Grunberg F. One hundred in-patient suicides. Br J Psychiatry 1997;171:247-50.
5. Shah AK, Ganesvaran T. Inpatient suicides in an Australian mental hospital. Aust NZ J Psychiatr 1997;31:291-8.
6. Moore P, Berman K, Knight M, Devine J. Constant observation: implications for nursing practice. J Psychosoc Nurs Ment Health Serv 1995;33:46-50.
7. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Available at: http://www.psych.org/psych_pract/treatg/pg/SuicidalBehavior_05-15-06.pdf. Accessed April 19, 2007.
8. Simon RI. The suicidal patient. In Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:166-86.
9. Abille v United States, 482 F Supp 703 (ND Cal 1980).
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
Patient commits suicide after 15-minute checks are stopped
Honolulu County (HI) Circuit Court
A patient was brought to a hospital and interviewed by a psychiatrist. She was found to be at moderate risk for suicide, was admitted, and ordered to be monitored every 15 minutes. The patient attempted suicide 2 days later by closing a drawer on her neck. She died from the injuries the following day.
The patient’s family claimed that a hospital nurse misread the psychiatrist’s instructions and stopped the 15-minute checks on the morning of the incident, believing that the order was limited to 15-minute checks for the first 24 hours, even though they had been done for almost 2 days. The patient refused medication on the first day of admission, and the psychiatrist had started the procedure to obtain a court order committing the patient and allowing injection of necessary medication. The claims against the hospital were settled for a confidential amount.
The patient’s family claimed the psychiatrist diagnosed the patient with major depression with recurrent suicide ideation but failed to properly assess her for suicide monitoring. The family also said the patient should have been determined to be at least at high risk and required to be within sight of staff.
The psychiatrist claimed to be unaware the 15-minute monitoring had ceased. The psychiatrist saw the patient 30 minutes before she was found collapsed with her head in the drawer. The hospital staff checked the patient approximately 15 to 30 minutes before she was found.
- A defense verdict was returned
Reduced observation blamed for suicide by hanging
Kings County (NY) Supreme Court
A 45-year-old police lieutenant who suffered from alcohol abuse and depression was admitted to a psychiatric care facility. He was classiffied “Q15,” a category assigned to patients who must be visually inspected every 15 minutes, cannot have access to sharp objects or any other material or object they can use to inflict bodily harm, and must request permission to use restrooms. The next day the psychiatrist examined the patient and moved him to a “Q30” status, which halved the frequency of visual inspections, gave him unrestricted access to restrooms, and allowed him to have a bathrobe with a belt. The patient hanged himself the next day, using a restroom door to support a noose he made from the bathrobe belt.
The patient’s family faulted the hospital and psychiatrist for prematurely advancing the patient to “Q30” status. The hospital and psychiatrist claimed the suicide could not have been predicted and argued that given his background as a police lieutenant, the patient would have interpreted more stringent restrictions as incarceration. The psychiatrist argued that such a perception would have impeded the patient’s progress.
- A $71,989 verdict was returned, apportioning fault 65% to the hospital and 35% to the psychiatrist
Constant patient observation—such as one-to-one staffing or 15-minute checks—is used to protect patients from harming themselves or others. One study of a psychiatric hospital1 reported that 13% of psychiatric inpatients required constant observation.
Even 15 minutes is sufficient time to complete a suicide.3 Common methods of inpatient suicide include hanging, overdosing, and jumping from high places.4,5 One study found that 73% of inpatient suicides in a psychiatric ward occurred after 28 days of admission.5
The cost of constant observation may account for as much as 20% of the total nursing budget at a psychiatric hospital and up to 10% at a long-term care facility or general hospital.6 The annual cost of constant observation can exceed $500,000, depending on the hospital’s size and monitoring frequency.6
Determining responsibility
The outcomes of these 2 cases may appear inconsistent. In the first, the psychiatrist who assessed the patient as a moderate suicide risk was not negligent, even though the family claimed the patient was at high risk. In the second case, the psychiatrist was found partly liable for not maintaining a higher vigilance of suicide risk assessment.
Physicians cannot put every patient on one-to-one monitoring or 15-minute checks because of fear of suicide and malpractice litigation. These 2 cases demonstrate that if a suicide occurs, the courts will look for clinical reasons for the level of observation. The level of suicide precautions—one-to-one vs 15-minute checks—should be based on the patient’s clinical presentation and supported by clinical rationale.7
Risk analysis
The courts look to see if the suicide assessment was “clinically reasonable”.8 To meet this standard, perform a “suicide risk-benefit analysis” each time you make a significant clinical decision, such as ordering 15-minute checks. The record should include information sources you used (such as family members or previous medical records), factors that entered the clinical decision, and how you balanced these factors in a risk-benefit assessment (Box 1).9
Document decisions. Mistakes in clinical judgment do not necessarily constitute negligence,8 but deviations in the standard of care cannot be adequately determined in a court of law unless the clinician had documented his or her thought processes at the time of the decision.
Predicting which patients will re-experience or deny suicidal ideation is impossible,7 but if the patient is determined to be at high risk for suicide, then implement and document a plan to address this risk. In addition, communicate information regarding the risk-benefit assessment to staff responsible for implementing these precautions.
- Suicidal thoughts or behaviors—ideas, plans, attempts
- Psychiatric diagnoses—depression, bipolar disorder, schizophrenia, substance use, Cluster B personality disorders
- Physical illnesses—HIV, malignant cancers, pain syndromes
- Psychosocial features—lack of support, unemployment
- Childhood traumas
- Genetic and familial effects—family history of suicide
- Psychological features—hopelessness, agitation, impulsiveness
- Cognitive features—polarized thinking
- Demographic features—adolescents, young adults, and elderly patients
- Other factors—access to firearms, intoxication.
Source: Reference 7
- a patient is admitted for inpatient treatment
- observation status changes
- a patient’s clinical condition changes substantially
- acute psychosocial stressors are discovered during the hospitalization.7
Patient commits suicide after 15-minute checks are stopped
Honolulu County (HI) Circuit Court
A patient was brought to a hospital and interviewed by a psychiatrist. She was found to be at moderate risk for suicide, was admitted, and ordered to be monitored every 15 minutes. The patient attempted suicide 2 days later by closing a drawer on her neck. She died from the injuries the following day.
The patient’s family claimed that a hospital nurse misread the psychiatrist’s instructions and stopped the 15-minute checks on the morning of the incident, believing that the order was limited to 15-minute checks for the first 24 hours, even though they had been done for almost 2 days. The patient refused medication on the first day of admission, and the psychiatrist had started the procedure to obtain a court order committing the patient and allowing injection of necessary medication. The claims against the hospital were settled for a confidential amount.
The patient’s family claimed the psychiatrist diagnosed the patient with major depression with recurrent suicide ideation but failed to properly assess her for suicide monitoring. The family also said the patient should have been determined to be at least at high risk and required to be within sight of staff.
The psychiatrist claimed to be unaware the 15-minute monitoring had ceased. The psychiatrist saw the patient 30 minutes before she was found collapsed with her head in the drawer. The hospital staff checked the patient approximately 15 to 30 minutes before she was found.
- A defense verdict was returned
Reduced observation blamed for suicide by hanging
Kings County (NY) Supreme Court
A 45-year-old police lieutenant who suffered from alcohol abuse and depression was admitted to a psychiatric care facility. He was classiffied “Q15,” a category assigned to patients who must be visually inspected every 15 minutes, cannot have access to sharp objects or any other material or object they can use to inflict bodily harm, and must request permission to use restrooms. The next day the psychiatrist examined the patient and moved him to a “Q30” status, which halved the frequency of visual inspections, gave him unrestricted access to restrooms, and allowed him to have a bathrobe with a belt. The patient hanged himself the next day, using a restroom door to support a noose he made from the bathrobe belt.
The patient’s family faulted the hospital and psychiatrist for prematurely advancing the patient to “Q30” status. The hospital and psychiatrist claimed the suicide could not have been predicted and argued that given his background as a police lieutenant, the patient would have interpreted more stringent restrictions as incarceration. The psychiatrist argued that such a perception would have impeded the patient’s progress.
- A $71,989 verdict was returned, apportioning fault 65% to the hospital and 35% to the psychiatrist
Constant patient observation—such as one-to-one staffing or 15-minute checks—is used to protect patients from harming themselves or others. One study of a psychiatric hospital1 reported that 13% of psychiatric inpatients required constant observation.
Even 15 minutes is sufficient time to complete a suicide.3 Common methods of inpatient suicide include hanging, overdosing, and jumping from high places.4,5 One study found that 73% of inpatient suicides in a psychiatric ward occurred after 28 days of admission.5
The cost of constant observation may account for as much as 20% of the total nursing budget at a psychiatric hospital and up to 10% at a long-term care facility or general hospital.6 The annual cost of constant observation can exceed $500,000, depending on the hospital’s size and monitoring frequency.6
Determining responsibility
The outcomes of these 2 cases may appear inconsistent. In the first, the psychiatrist who assessed the patient as a moderate suicide risk was not negligent, even though the family claimed the patient was at high risk. In the second case, the psychiatrist was found partly liable for not maintaining a higher vigilance of suicide risk assessment.
Physicians cannot put every patient on one-to-one monitoring or 15-minute checks because of fear of suicide and malpractice litigation. These 2 cases demonstrate that if a suicide occurs, the courts will look for clinical reasons for the level of observation. The level of suicide precautions—one-to-one vs 15-minute checks—should be based on the patient’s clinical presentation and supported by clinical rationale.7
Risk analysis
The courts look to see if the suicide assessment was “clinically reasonable”.8 To meet this standard, perform a “suicide risk-benefit analysis” each time you make a significant clinical decision, such as ordering 15-minute checks. The record should include information sources you used (such as family members or previous medical records), factors that entered the clinical decision, and how you balanced these factors in a risk-benefit assessment (Box 1).9
Document decisions. Mistakes in clinical judgment do not necessarily constitute negligence,8 but deviations in the standard of care cannot be adequately determined in a court of law unless the clinician had documented his or her thought processes at the time of the decision.
Predicting which patients will re-experience or deny suicidal ideation is impossible,7 but if the patient is determined to be at high risk for suicide, then implement and document a plan to address this risk. In addition, communicate information regarding the risk-benefit assessment to staff responsible for implementing these precautions.
- Suicidal thoughts or behaviors—ideas, plans, attempts
- Psychiatric diagnoses—depression, bipolar disorder, schizophrenia, substance use, Cluster B personality disorders
- Physical illnesses—HIV, malignant cancers, pain syndromes
- Psychosocial features—lack of support, unemployment
- Childhood traumas
- Genetic and familial effects—family history of suicide
- Psychological features—hopelessness, agitation, impulsiveness
- Cognitive features—polarized thinking
- Demographic features—adolescents, young adults, and elderly patients
- Other factors—access to firearms, intoxication.
Source: Reference 7
- a patient is admitted for inpatient treatment
- observation status changes
- a patient’s clinical condition changes substantially
- acute psychosocial stressors are discovered during the hospitalization.7
1. Shugar G, Rehaluk R. Continuous observation for psychiatric inpatients. Compr Psychiatry 1990;30:48-55.
2. Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry 2003;64:14-9.
3. Bowers L, Gournay K, Dufy D. Suicide and self-harm in inpatient psychiatric units: a national survey of observation policies. J Adv Nursing 2000;32:437-44.
4. Proulx F, Lesage AD, Grunberg F. One hundred in-patient suicides. Br J Psychiatry 1997;171:247-50.
5. Shah AK, Ganesvaran T. Inpatient suicides in an Australian mental hospital. Aust NZ J Psychiatr 1997;31:291-8.
6. Moore P, Berman K, Knight M, Devine J. Constant observation: implications for nursing practice. J Psychosoc Nurs Ment Health Serv 1995;33:46-50.
7. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Available at: http://www.psych.org/psych_pract/treatg/pg/SuicidalBehavior_05-15-06.pdf. Accessed April 19, 2007.
8. Simon RI. The suicidal patient. In Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:166-86.
9. Abille v United States, 482 F Supp 703 (ND Cal 1980).
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
1. Shugar G, Rehaluk R. Continuous observation for psychiatric inpatients. Compr Psychiatry 1990;30:48-55.
2. Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry 2003;64:14-9.
3. Bowers L, Gournay K, Dufy D. Suicide and self-harm in inpatient psychiatric units: a national survey of observation policies. J Adv Nursing 2000;32:437-44.
4. Proulx F, Lesage AD, Grunberg F. One hundred in-patient suicides. Br J Psychiatry 1997;171:247-50.
5. Shah AK, Ganesvaran T. Inpatient suicides in an Australian mental hospital. Aust NZ J Psychiatr 1997;31:291-8.
6. Moore P, Berman K, Knight M, Devine J. Constant observation: implications for nursing practice. J Psychosoc Nurs Ment Health Serv 1995;33:46-50.
7. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Available at: http://www.psych.org/psych_pract/treatg/pg/SuicidalBehavior_05-15-06.pdf. Accessed April 19, 2007.
8. Simon RI. The suicidal patient. In Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:166-86.
9. Abille v United States, 482 F Supp 703 (ND Cal 1980).
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
ADHD: Only half the diagnosis in an adult with inattention?
Overlapping symptoms may obscure comorbid bipolar illness
An adult with function-impairing inattention could have attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or both. Comorbid ADHD and BD often is unrecognized, however, because patients are more likely to report ADHD-related symptoms than manic symptoms.1
To help you recognize comorbid ADHD/BD—and protect adults who might switch into mania if given stimulants or antidepressants—this article describes a hierarchy to diagnose and treat this comorbidity. Based on the evidence and our experience, we:
- discuss how to differentiate between these disorders with overlapping symptoms
- provide tools and suggestions to screen for BD and adult ADHD
- offer 3 algorithms to guide your diagnosis and choice of medications.
Clinical challenges
Prevalence is unclear. Adult ADHD—with an estimated prevalence of 4.4%2—is more common than BD. Lifetime prevalences of BD types I and II are 1.6% and 0.5%, respectively.3 Studies of ADHD/BD comorbidity suggest wide-ranging prevalence rates:
Underdiagnosis. Adult ADHD/BD is a more severe illness than ADHD or BD alone and is highly comorbid with agoraphobia, social phobia, posttraumatic stress disorder, and alcohol or drug addiction. Adults with ADHD/BD have more frequent affective episodes, suicide attempts, violence, and legal problems.4 Diagnosing this comorbidity remains a challenge, however, because:
- identifying which symptoms are caused by which disorder can be difficult
- BD tends to be underdiagnosed9
- patients often misidentify, underreport, or deny manic symptoms1,10,11
- if a patient presents with active bipolar symptoms, DSM-IV-TR criteria require that ADHD not be diagnosed until mood symptoms are resolved.
Overlapping symptoms. ADHD and bipolar mania share some DSM-IV-TR diagnostic criteria, including talkativeness, distractibility, increased activity or physical restlessness, and loss of social inhibitions (Table 1).12 Overlapping symptoms also are notable within ADHD diagnostic criteria (Table 2). In the inattention category, for example, “easily distracted by extraneous stimuli,” “difficulty sustaining attention in tasks,” and “fails to give close attention to details” are considered 3 separate symptoms. In the hyperactivity category, “often leaves seat,” “often runs about or climbs excessively,” and “often on the go, or often acts as if driven by a motor” are 3 separate symptoms.
Given ADHD’s relatively loose diagnostic criteria and high comorbidity in adults with mood disorders, the question of whether adult ADHD/BD represents comorbidity or diagnostic overlap remains unresolved. For the clinician, the disorders’ nonoverlapping features (Table 1) can assist with the differential diagnosis. For example:
- ADHD symptoms tend to be chronic and BD symptoms episodic.
- ADHD patients may have high energy but lack increased productivity seen in BD patients.
- ADHD patients do not need less sleep or have inflated self-esteem like symptomatic BD patients.
- Psychotic symptoms such as hallucinations or delusions might be present in severe BD but are absent in ADHD.
Table 1
Overlap between DSM-IV-TR diagnostic criteria for ADHD and bipolar mania
| Overlapping symptoms | |
|---|---|
| ADHD | Bipolar mania |
| Talks excessively | More talkative than usual |
| Easily distracted/jumps from one activity to the next | Distractibility or constant changes in activity or plans |
| Fidgets Difficulty remaining seated Runs or climbs about inappropriately Difficulty playing quietly On the go as if driven by a motor | Increased activity or physical restlessness |
| Interrupts or butts in uninvited Blurts out answers | Loss of normal social inhibitions |
| Nonoverlapping symptoms | |
| ADHD Forgetful in daily activities Difficulty awaiting turn Difficulty organizing self Loses things Avoids sustained mental effort Does not seem to listen Difficulty following through on instructions/fails to finish work Difficulty sustaining attention Fails to give close attention to details/makes careless mistakes | |
| Bipolar mania Inflated self-esteem/grandiosity Increase in goal-directed activity Flight of ideas Decreased need for sleep Excessive involvement in pleasurable activities with disregard for potential adverse consequences Marked sexual energy or sexual indiscretions | |
| ADHD: attention-deficit/hyperactivity disorder | |
| Source: Adapted and reprinted with permission from reference 12 | |
Table 2
DSM-IV-TR diagnostic criteria for attention-deficit/ hyperactivity disorder
| Inattention |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Hyperactivity/impulsivity |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Diagnosis requires evidence of inattention or hyperactivity/impulsivity or both |
| Some hyperactive/impulsive or inattentive symptoms that caused impairment were present before age 7 |
| Some impairment from symptoms is present in ≥2 settings (such as at school, work, or home) |
| Symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorder and are not better accounted for by another mental disorder (mood disorder, anxiety disorder, dissociative disorder, or a personality disorder) |
| Source: DSM-IV-TR |
Mood symptoms first
A diagnostic hierarchy is implicit in DSM-IV-TR; anxiety disorders are not diagnosed during an active major depressive or manic episode, and schizophrenia is not diagnosed on the basis of psychotic symptoms during an active major depressive or manic episode. Mood disorders sit atop this implied diagnostic hierarchy and must be ruled out before psychotic or anxiety disorders are diagnosed. Similarly, most personality disorders are not diagnosed during an active mood or psychotic episode.
Diagnosing adult ADHD when a patient is actively depressed or manic is inconsistent with this hierarchy and conflicts with extensive nosologic literature.13 We suggest that ADHD—a cognitive-behavioral problem—not be diagnosed solely on symptoms observed when a patient is experiencing a mood episode or psychotic illness.
Bipolar disorder. Two useful mnemonics (Table 3) assist in screening for DSM-IV-TR symptoms of BD type I:
- Pure mania consists of euphoric mood and ≥3 of 7 DIGFAST criteria, or irritable mood and ≥4 of 7 DIGFAST criteria
- Mixed mania consists of depressed mood with ≥4 of 7 DIGFAST criteria and ≥4 of 8 SIGECAPS criteria.
To be diagnostic, these symptoms must cause substantial social or occupational dysfunction and be present at least 1 week. Diagnose BD type I if a patient has experienced a single pure or mixed manic episode at any time, unless the episode had a medical cause such as hyperthyroidism or antidepressant use. Because patients with mixed episodes experience depressed mood, assess any patient with clinical depression for manic symptoms. Otherwise, a patient with a mixed episode could be misdiagnosed as having unipolar depression instead of BD type I.14
BD type II also has been observed in patients with comorbid adult ADHD/BD.4,6 The main difference between BD types I and II is that manic symptoms in type II are not severe enough to cause functional impairment or psychotic symptoms.15
Adult ADHD. The clinical interview seeking evidence of inattention and hyperactivity/impulsivity remains the basis of adult ADHD diagnosis (Table 2). Key areas are:
- the patient’s past and current functional impairment
- whether substantial impairment occurs in at least 2 areas of life (such as school, work, or home).
Take medical, educational, social, psychological, and vocational histories, and rule out other conditions before concluding that adult ADHD is the appropriate diagnosis.16 In adult ADHD, inattentive symptoms become far more prominent, about twice as common as hyperactive symptoms.17 Inattentive symptoms may manifest as neglect, poor time management, motivational deficits, or poor concentration that results in forgetfulness, distractibility, item misplacement, or excessive mistakes in paperwork.18 When impulsive symptoms persist in adults, they may manifest as automobile accidents or low tolerance for frustration, which may lead to frequent job changes and unstable, interrupted interpersonal relationships.18
Neuropsychological testing is not required to make an adult ADHD diagnosis but can help establish the breadth of symptoms or comorbidity.17 Rating scales can screen, gather data (including presence and severity of symptoms), and measure treatment response.16 Commonly used rating scales include:
- Conners’ Adult ADHD Rating Scales19
- Brown Attention Deficit Disorder Rating Scale for Adults20
- Adult ADHD Self-Report Scale.21
When using rating scales, remember that adult psychopathology can distort perceptions, and some self-report scales have questionable reliability.16
Table 3
Mnemonics for diagnostic symptoms of pure and mixed bipolar mania
| DIGFAST* for bipolar mania symptoms | SIGECAPS† bipolar depression symptoms |
|---|---|
| Distractibility Insomnia Grandiosity Flight of ideas Activities Speech Thoughtlessness | Sleep Interest Guilt Energy Concentration Appetite Psychomotor Suicide |
| Pure mania: Euphoric mood with ≥3 DIGFAST criteria or irritable mood with ≥4 DIGFAST criteria. | |
| Mixed mania: Depressed mood with ≥4 DIGFAST criteria and ≥4 SIGECAPS criteria. | |
| * Developed by William Falk, MD | |
| †Developed by Carey Gross, MD | |
| Source: Adapted from Ghaemi SN. Mood disorders. New York: Lippincott, Williams, & Wilkins; 2003 | |
Treatment recommendations
Limited data. We found only 1 study on adult ADHD/BD treatment. In this open trial,22 36 adults with comorbid ADHD and BD received bupropion SR, up to 200 mg bid, for ADHD symptoms while maintained on mood stabilizers, antipsychotics, or both. Improvement was defined as ≥30% reduction in ADHD Symptom Checklist Scale scores, without concurrent mania. After 6 weeks, 82% of patients had improved; 1 dropped out at week 2 because of hypomanic activation. Methodologic limitations included trial design (non-randomized, nonblinded, short duration) and patient selection (90% of subjects had BD type II).
In the absence of adequate data on adult ADHD/BD, studies in children suggest:
- stimulants may not be effective for ADHD symptoms in patients with active manic or depressive symptoms
- mood stabilization is a prerequisite for successful pharmacologic treatment of ADHD in patients with both ADHD and manic or depressive symptoms.23,24
Follow the hierarchy. First treat acute mood symptoms, then reevaluate and possibly treat ADHD symptoms if they persist during euthymia (Algorithm 1). When a patient meets criteria for adult ADHD/BD, first stabilize bipolar manic or depressive symptoms (Algorithm 2). For acute mania, treat with standard mood stabilizers (lithium, valproate, lamotrigine, or carbamazepine) with or without a second-generation antipsychotic.25 Starting stimulants for ADHD when patients have active mood symptoms is sub-optimal and potentially harmful because of the risk of inducing mania. For acute bipolar depression, adjunctive antidepressant treatment has been found to be no more effective than a mood stabilizer alone.26
After bipolar symptoms respond or remit, reassess for adult ADHD. If ADHD symptoms persist during euthymia, additional treatment may be indicated.
Very little evidence exists on treating adult ADHD/BD; as mentioned, bupropion is the only medication studied in this population. For adult ADHD alone, clinical trials have showed varying efficacy with bupropion,27,28 atomoxetine,29 venlafaxine,30,31 desipramine,32 methylphenidate,33 mixed amphetamine salts,34 and guanfacine.35 Whether these treatments can be generalized as safe and efficacious for comorbid adult ADHD/BD is unclear. Nonetheless, we suggest using bupropion first, followed by atomoxetine or guanfacine before you consider amphetamine stimulants (Algorithm 3).
Algorithm 1
Hierarchy for diagnosis and treatment of adult ADHD/BD
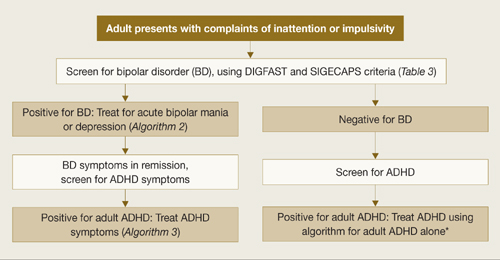
ADHD: attention-deficit/hyperactivity disorder; BD: bipolar disorder
*Adler LA, Chua HC. Management of ADHD in adults. J Clin Psychiatry 2002;63(suppl 12):29-35.
Algorithm 2
Treating acute episodes of bipolar disorder
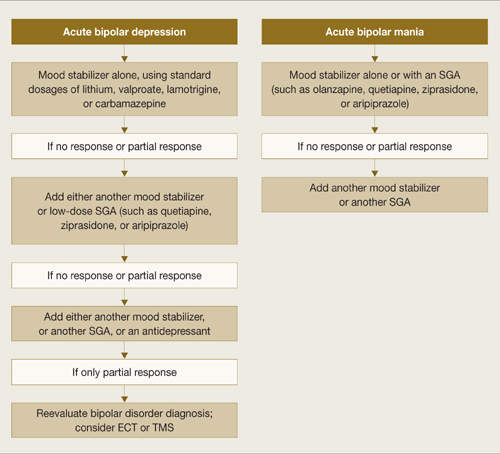
ECT: electroconvulsive therapy; SGA: second-generation antipsychotic; TMS: transcranial magnetic stimulation
Algorithm 3
Suggested approach to adult ADHD with comorbid BD*
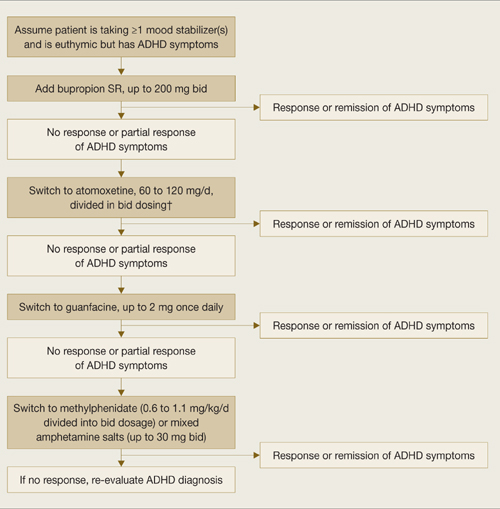
* Based on data extrapolated from samples of patients with ADHD alone because of very limited data in ADHD/BD samples.
† We recommend against combining antidepressants and stimulants because of additive risks of mania in BD. Discontinue stimulant or antidepressant if manic symptoms appear or rapid cycling emerges.
Reducing mania risk
Antidepressants and stimulants may help adults with ADHD alone, but risks of mania and rapid cycling limit their use in adults with ADHD/BD.
Stimulants and mania. One study found a 17% manic switch rate when methylphenidate (≤10 mg bid) was given to 14 bipolar depressed adults (10 BD type I, 2 BD type II, and 2 with secondary mania) taking mood stabilizers.36 A chart review of 82 bipolar children not taking mood stabilizers found an 18% switch rate with methylphenidate or amphetamine.37 Another chart review of 80 children with BD type I found that past amphetamine treatment (but not history of ADHD diagnosis or antidepressant treatment) was associated with more severe bipolar illness.38
No studies have examined predictors of amphetamine-induced mania. In our clinical experience, triggers are similar to those that can cause antidepressant-induced mania, such as:
- recent manic episodes
- current rapid cycling
- past antidepressant-induced mania.
Antidepressants and mania. When 64 patients with acute bipolar depression received both antidepressants and mood stabilizers in a randomized, double-blind trial, switch rates into mania or hypomania were 10% for bupropion, 9% for sertraline, and 29% for venlafaxine.39 In a meta analysis of clinical trials using selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants (TCAs), the manic switch rate was threefold higher with TCAs than SSRIs.40 Antidepressant use in bipolar patients was associated with rapid cycling in the only randomized study of this topic.41
Insufficient data exist to clarify whether mania induction with antidepressants is dose-dependent.42 Factors associated with antidepressant-induced mania include:
- previous antidepressant-induced mania
- family history of BD
- exposure to multiple antidepressant trials42
- history of substance abuse and/or dependence.43
Related resources
- Bipolar disorder information and resources. www.psycheducation.org.
- ADHD Information and resources. www.adhdnews.com.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. New York: McGraw-Hill; 2006.
Drug brand names
- Amphetamine/Dextroamphetamine • Adderall
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methylphenidate • Ritalin
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Valproate • Depakote
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Wingo reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ghaemi receives research grants from GlaxoSmithKline and Pfizer and is a speaker for GlaxoSmithKline, AstraZeneca, Pfizer, and Abbott Laboratories. Neither he nor his family hold equity positions in pharmaceutical companies.
1. Ghaemi SN, Stoll AL, Pope HG, Jr, et al. Lack of insight in bipolar disorder. The acute manic episode. J Nerv Ment Dis 1995;183(7):464-7.
2. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163(4):716-23.
3. Sadock BJ, Sadock VA, eds. Synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.
4. Nierenberg AA, Miyahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry 2005;57(11):1467-73.
5. Tamam L, Tuglu C, Karatas G, et al. Adult attention-deficit hyperactivity disorder in patients with bipolar I disorder in remission: preliminary study. Psychiatry Clin Neurosci 2006;60(4):480-5.
6. Wilens TE, Biederman J, Wozniak J, et al. Can adults with attention-deficit/hyperactivity disorder be distinguished from those with comorbid bipolar disorder? Findings from a sample of clinically referred adults. Biol Psychiatry 2003;54(1):1-8.
7. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry 2005;162(9):1621-7.
8. Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry 2006;163(10):1720-9.
9. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord 1999;52(1-3):135-44.
10. Keitner GI, Solomon DA, Ryan CE, et al. Prodromal and residual symptoms in bipolar I disorder. Compr Psychiatry 1996;37(5):362-7.
11. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv 2001;52(1):51-5.
12. Kent L, Craddock N. Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? J Affect Disord 2003;73(3):211-21.
13. Surtees PG, Kendell RE. The hierarchy model of psychiatric symptomatology: an investigation based on present state examination ratings. Br J Psychiatry 1979;135:438-43.
14. Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog Neuropsychopharmacol Biol Psychiatry 2006;30(3):471-7.
15. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text rev. Washington, DC: American Psychiatric Association; 2000.
16. Murphy KR, Adler LA. Assessing attention-deficit hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry 2004;65(suppl 3):12-17.
17. Adler LA. Diagnosing adult attention deficit hyperactivity disorder. Primary Psychiatry 2006;13(suppl 3):9-10.
18. Montano B. Diagnosis and treatment of ADHD in adults in primary care. J Clin Psychiatry 2004;65(suppl 3):18-21.
19. Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS). North Tonawanda, NY: Multi-Health Systems; 1999.
20. Brown TE. Brown Attention Deficit Disorder Scales. San Antonio, TX: The Psychological Corporation; 1996.
21. Adler LA, Kessler RC, Spencer T. Adult ADHD Self-report Scale v1.1 (ASRS-v1.1) Symptom Checklist. World Health Organization. Available at: http://www.med.nyu.edu/psych/assets/adhdscreen18.pdf. Accessed May 7, 2007.
22. Wilens TE, Prince JB, Spencer T, et al. An open trial of bupropion for the treatment of adults with attention-deficit/hyperactivity disorder and bipolar disorder. Biol Psychiatry 2003;54(1):9-16.
23. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
24. Daviss WB, Bentivoglio P, Racusin R, et al. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry 2001;40(3):307-14.
25. Scherk H, Pajonk FG, Leucht SL. Second-generation antipsychotic agents in the treatment of acute mania. Arch Gen Psychiatry 2007;64:442-55.
26. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 2007:356:(17):1711-22.
27. Wilens TE, Haight BR, Horrigan JP, et al. Bupropion XL in adults with attention deficit hyperactivity disorder: a randomized, placebo controlled study. Biol Psychiatry 2005;57:793-801.
28. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
29. Michelson D, Adler LA, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo controlled studies. Biol Psychiatry 2003;53:112-20.
30. Adler LA, Resnick S, Kunz M, Devinsky O. Open-label trial of venlafaxine in adults with attention deficit disorder. Psychopharmacol Bull 1995;31(4):785-8.
31. Hedges D, Reimherr FW, Rogers A, et al. An open trial of venlafaxine in adult patients with attention deficit hyperactivity disorder. Psychopharmacol Bull 1995;31(4):779-83.
32. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry 1996;153(9):1147-53.
33. Faraone SV, Spencer T, Aleardi M, et al. Meta analysis of the efficacy of methylphenidate for treating adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2004;24(1):24-8.
34. Spencer T, Biederman J, Wilens TE, et al. Efficacy of a mixed amphetamine salts compound in adults with attention deficit hyperactivity disorder. Arch Gen Psychiatry 2001;58:775-82.
35. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2000;21(2):223-8.
36. El-Mallakh RS. An open study of methylphenidate in bipolar depression. Bipolar Disord 2000;2(1):56-9.
37. Faedda GL, Baldessarini RJ, Glovinsky IP, et al. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord 2004;82(1):149-58.
38. Soutullo CA, DelBello MP, Ochsner JE, et al. Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment. J Affect Disord 2002;70(3):323-7.
39. Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 2006;189:124-31.
40. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry 1994;164(4):549-50.
41. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145(2):179-84.
42. Goldberg JF. When do antidepressants worsen the course of bipolar disorder? J Psychiatr Pract. 2003;9(3):181-94.
43. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry 2002;63(9):791-5.
Overlapping symptoms may obscure comorbid bipolar illness
An adult with function-impairing inattention could have attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or both. Comorbid ADHD and BD often is unrecognized, however, because patients are more likely to report ADHD-related symptoms than manic symptoms.1
To help you recognize comorbid ADHD/BD—and protect adults who might switch into mania if given stimulants or antidepressants—this article describes a hierarchy to diagnose and treat this comorbidity. Based on the evidence and our experience, we:
- discuss how to differentiate between these disorders with overlapping symptoms
- provide tools and suggestions to screen for BD and adult ADHD
- offer 3 algorithms to guide your diagnosis and choice of medications.
Clinical challenges
Prevalence is unclear. Adult ADHD—with an estimated prevalence of 4.4%2—is more common than BD. Lifetime prevalences of BD types I and II are 1.6% and 0.5%, respectively.3 Studies of ADHD/BD comorbidity suggest wide-ranging prevalence rates:
Underdiagnosis. Adult ADHD/BD is a more severe illness than ADHD or BD alone and is highly comorbid with agoraphobia, social phobia, posttraumatic stress disorder, and alcohol or drug addiction. Adults with ADHD/BD have more frequent affective episodes, suicide attempts, violence, and legal problems.4 Diagnosing this comorbidity remains a challenge, however, because:
- identifying which symptoms are caused by which disorder can be difficult
- BD tends to be underdiagnosed9
- patients often misidentify, underreport, or deny manic symptoms1,10,11
- if a patient presents with active bipolar symptoms, DSM-IV-TR criteria require that ADHD not be diagnosed until mood symptoms are resolved.
Overlapping symptoms. ADHD and bipolar mania share some DSM-IV-TR diagnostic criteria, including talkativeness, distractibility, increased activity or physical restlessness, and loss of social inhibitions (Table 1).12 Overlapping symptoms also are notable within ADHD diagnostic criteria (Table 2). In the inattention category, for example, “easily distracted by extraneous stimuli,” “difficulty sustaining attention in tasks,” and “fails to give close attention to details” are considered 3 separate symptoms. In the hyperactivity category, “often leaves seat,” “often runs about or climbs excessively,” and “often on the go, or often acts as if driven by a motor” are 3 separate symptoms.
Given ADHD’s relatively loose diagnostic criteria and high comorbidity in adults with mood disorders, the question of whether adult ADHD/BD represents comorbidity or diagnostic overlap remains unresolved. For the clinician, the disorders’ nonoverlapping features (Table 1) can assist with the differential diagnosis. For example:
- ADHD symptoms tend to be chronic and BD symptoms episodic.
- ADHD patients may have high energy but lack increased productivity seen in BD patients.
- ADHD patients do not need less sleep or have inflated self-esteem like symptomatic BD patients.
- Psychotic symptoms such as hallucinations or delusions might be present in severe BD but are absent in ADHD.
Table 1
Overlap between DSM-IV-TR diagnostic criteria for ADHD and bipolar mania
| Overlapping symptoms | |
|---|---|
| ADHD | Bipolar mania |
| Talks excessively | More talkative than usual |
| Easily distracted/jumps from one activity to the next | Distractibility or constant changes in activity or plans |
| Fidgets Difficulty remaining seated Runs or climbs about inappropriately Difficulty playing quietly On the go as if driven by a motor | Increased activity or physical restlessness |
| Interrupts or butts in uninvited Blurts out answers | Loss of normal social inhibitions |
| Nonoverlapping symptoms | |
| ADHD Forgetful in daily activities Difficulty awaiting turn Difficulty organizing self Loses things Avoids sustained mental effort Does not seem to listen Difficulty following through on instructions/fails to finish work Difficulty sustaining attention Fails to give close attention to details/makes careless mistakes | |
| Bipolar mania Inflated self-esteem/grandiosity Increase in goal-directed activity Flight of ideas Decreased need for sleep Excessive involvement in pleasurable activities with disregard for potential adverse consequences Marked sexual energy or sexual indiscretions | |
| ADHD: attention-deficit/hyperactivity disorder | |
| Source: Adapted and reprinted with permission from reference 12 | |
Table 2
DSM-IV-TR diagnostic criteria for attention-deficit/ hyperactivity disorder
| Inattention |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Hyperactivity/impulsivity |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Diagnosis requires evidence of inattention or hyperactivity/impulsivity or both |
| Some hyperactive/impulsive or inattentive symptoms that caused impairment were present before age 7 |
| Some impairment from symptoms is present in ≥2 settings (such as at school, work, or home) |
| Symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorder and are not better accounted for by another mental disorder (mood disorder, anxiety disorder, dissociative disorder, or a personality disorder) |
| Source: DSM-IV-TR |
Mood symptoms first
A diagnostic hierarchy is implicit in DSM-IV-TR; anxiety disorders are not diagnosed during an active major depressive or manic episode, and schizophrenia is not diagnosed on the basis of psychotic symptoms during an active major depressive or manic episode. Mood disorders sit atop this implied diagnostic hierarchy and must be ruled out before psychotic or anxiety disorders are diagnosed. Similarly, most personality disorders are not diagnosed during an active mood or psychotic episode.
Diagnosing adult ADHD when a patient is actively depressed or manic is inconsistent with this hierarchy and conflicts with extensive nosologic literature.13 We suggest that ADHD—a cognitive-behavioral problem—not be diagnosed solely on symptoms observed when a patient is experiencing a mood episode or psychotic illness.
Bipolar disorder. Two useful mnemonics (Table 3) assist in screening for DSM-IV-TR symptoms of BD type I:
- Pure mania consists of euphoric mood and ≥3 of 7 DIGFAST criteria, or irritable mood and ≥4 of 7 DIGFAST criteria
- Mixed mania consists of depressed mood with ≥4 of 7 DIGFAST criteria and ≥4 of 8 SIGECAPS criteria.
To be diagnostic, these symptoms must cause substantial social or occupational dysfunction and be present at least 1 week. Diagnose BD type I if a patient has experienced a single pure or mixed manic episode at any time, unless the episode had a medical cause such as hyperthyroidism or antidepressant use. Because patients with mixed episodes experience depressed mood, assess any patient with clinical depression for manic symptoms. Otherwise, a patient with a mixed episode could be misdiagnosed as having unipolar depression instead of BD type I.14
BD type II also has been observed in patients with comorbid adult ADHD/BD.4,6 The main difference between BD types I and II is that manic symptoms in type II are not severe enough to cause functional impairment or psychotic symptoms.15
Adult ADHD. The clinical interview seeking evidence of inattention and hyperactivity/impulsivity remains the basis of adult ADHD diagnosis (Table 2). Key areas are:
- the patient’s past and current functional impairment
- whether substantial impairment occurs in at least 2 areas of life (such as school, work, or home).
Take medical, educational, social, psychological, and vocational histories, and rule out other conditions before concluding that adult ADHD is the appropriate diagnosis.16 In adult ADHD, inattentive symptoms become far more prominent, about twice as common as hyperactive symptoms.17 Inattentive symptoms may manifest as neglect, poor time management, motivational deficits, or poor concentration that results in forgetfulness, distractibility, item misplacement, or excessive mistakes in paperwork.18 When impulsive symptoms persist in adults, they may manifest as automobile accidents or low tolerance for frustration, which may lead to frequent job changes and unstable, interrupted interpersonal relationships.18
Neuropsychological testing is not required to make an adult ADHD diagnosis but can help establish the breadth of symptoms or comorbidity.17 Rating scales can screen, gather data (including presence and severity of symptoms), and measure treatment response.16 Commonly used rating scales include:
- Conners’ Adult ADHD Rating Scales19
- Brown Attention Deficit Disorder Rating Scale for Adults20
- Adult ADHD Self-Report Scale.21
When using rating scales, remember that adult psychopathology can distort perceptions, and some self-report scales have questionable reliability.16
Table 3
Mnemonics for diagnostic symptoms of pure and mixed bipolar mania
| DIGFAST* for bipolar mania symptoms | SIGECAPS† bipolar depression symptoms |
|---|---|
| Distractibility Insomnia Grandiosity Flight of ideas Activities Speech Thoughtlessness | Sleep Interest Guilt Energy Concentration Appetite Psychomotor Suicide |
| Pure mania: Euphoric mood with ≥3 DIGFAST criteria or irritable mood with ≥4 DIGFAST criteria. | |
| Mixed mania: Depressed mood with ≥4 DIGFAST criteria and ≥4 SIGECAPS criteria. | |
| * Developed by William Falk, MD | |
| †Developed by Carey Gross, MD | |
| Source: Adapted from Ghaemi SN. Mood disorders. New York: Lippincott, Williams, & Wilkins; 2003 | |
Treatment recommendations
Limited data. We found only 1 study on adult ADHD/BD treatment. In this open trial,22 36 adults with comorbid ADHD and BD received bupropion SR, up to 200 mg bid, for ADHD symptoms while maintained on mood stabilizers, antipsychotics, or both. Improvement was defined as ≥30% reduction in ADHD Symptom Checklist Scale scores, without concurrent mania. After 6 weeks, 82% of patients had improved; 1 dropped out at week 2 because of hypomanic activation. Methodologic limitations included trial design (non-randomized, nonblinded, short duration) and patient selection (90% of subjects had BD type II).
In the absence of adequate data on adult ADHD/BD, studies in children suggest:
- stimulants may not be effective for ADHD symptoms in patients with active manic or depressive symptoms
- mood stabilization is a prerequisite for successful pharmacologic treatment of ADHD in patients with both ADHD and manic or depressive symptoms.23,24
Follow the hierarchy. First treat acute mood symptoms, then reevaluate and possibly treat ADHD symptoms if they persist during euthymia (Algorithm 1). When a patient meets criteria for adult ADHD/BD, first stabilize bipolar manic or depressive symptoms (Algorithm 2). For acute mania, treat with standard mood stabilizers (lithium, valproate, lamotrigine, or carbamazepine) with or without a second-generation antipsychotic.25 Starting stimulants for ADHD when patients have active mood symptoms is sub-optimal and potentially harmful because of the risk of inducing mania. For acute bipolar depression, adjunctive antidepressant treatment has been found to be no more effective than a mood stabilizer alone.26
After bipolar symptoms respond or remit, reassess for adult ADHD. If ADHD symptoms persist during euthymia, additional treatment may be indicated.
Very little evidence exists on treating adult ADHD/BD; as mentioned, bupropion is the only medication studied in this population. For adult ADHD alone, clinical trials have showed varying efficacy with bupropion,27,28 atomoxetine,29 venlafaxine,30,31 desipramine,32 methylphenidate,33 mixed amphetamine salts,34 and guanfacine.35 Whether these treatments can be generalized as safe and efficacious for comorbid adult ADHD/BD is unclear. Nonetheless, we suggest using bupropion first, followed by atomoxetine or guanfacine before you consider amphetamine stimulants (Algorithm 3).
Algorithm 1
Hierarchy for diagnosis and treatment of adult ADHD/BD
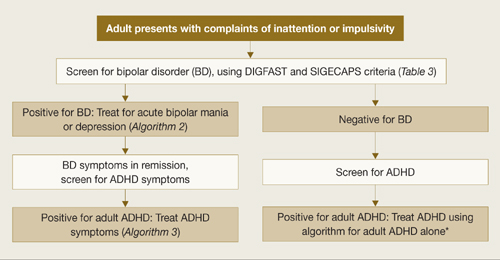
ADHD: attention-deficit/hyperactivity disorder; BD: bipolar disorder
*Adler LA, Chua HC. Management of ADHD in adults. J Clin Psychiatry 2002;63(suppl 12):29-35.
Algorithm 2
Treating acute episodes of bipolar disorder
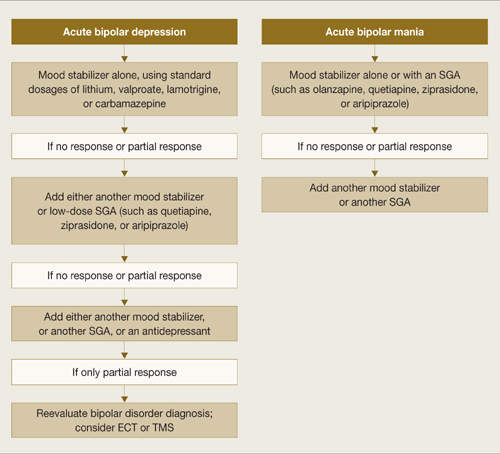
ECT: electroconvulsive therapy; SGA: second-generation antipsychotic; TMS: transcranial magnetic stimulation
Algorithm 3
Suggested approach to adult ADHD with comorbid BD*
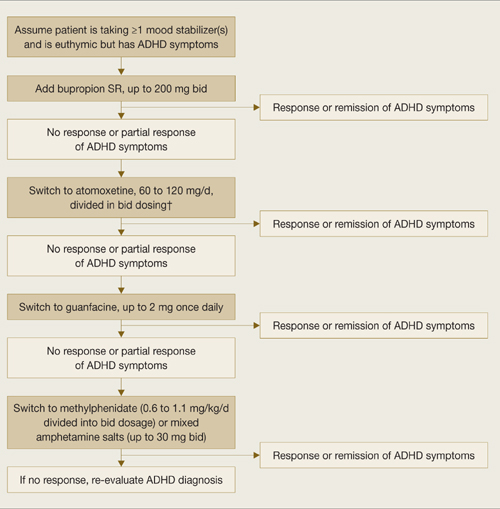
* Based on data extrapolated from samples of patients with ADHD alone because of very limited data in ADHD/BD samples.
† We recommend against combining antidepressants and stimulants because of additive risks of mania in BD. Discontinue stimulant or antidepressant if manic symptoms appear or rapid cycling emerges.
Reducing mania risk
Antidepressants and stimulants may help adults with ADHD alone, but risks of mania and rapid cycling limit their use in adults with ADHD/BD.
Stimulants and mania. One study found a 17% manic switch rate when methylphenidate (≤10 mg bid) was given to 14 bipolar depressed adults (10 BD type I, 2 BD type II, and 2 with secondary mania) taking mood stabilizers.36 A chart review of 82 bipolar children not taking mood stabilizers found an 18% switch rate with methylphenidate or amphetamine.37 Another chart review of 80 children with BD type I found that past amphetamine treatment (but not history of ADHD diagnosis or antidepressant treatment) was associated with more severe bipolar illness.38
No studies have examined predictors of amphetamine-induced mania. In our clinical experience, triggers are similar to those that can cause antidepressant-induced mania, such as:
- recent manic episodes
- current rapid cycling
- past antidepressant-induced mania.
Antidepressants and mania. When 64 patients with acute bipolar depression received both antidepressants and mood stabilizers in a randomized, double-blind trial, switch rates into mania or hypomania were 10% for bupropion, 9% for sertraline, and 29% for venlafaxine.39 In a meta analysis of clinical trials using selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants (TCAs), the manic switch rate was threefold higher with TCAs than SSRIs.40 Antidepressant use in bipolar patients was associated with rapid cycling in the only randomized study of this topic.41
Insufficient data exist to clarify whether mania induction with antidepressants is dose-dependent.42 Factors associated with antidepressant-induced mania include:
- previous antidepressant-induced mania
- family history of BD
- exposure to multiple antidepressant trials42
- history of substance abuse and/or dependence.43
Related resources
- Bipolar disorder information and resources. www.psycheducation.org.
- ADHD Information and resources. www.adhdnews.com.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. New York: McGraw-Hill; 2006.
Drug brand names
- Amphetamine/Dextroamphetamine • Adderall
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methylphenidate • Ritalin
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Valproate • Depakote
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Wingo reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ghaemi receives research grants from GlaxoSmithKline and Pfizer and is a speaker for GlaxoSmithKline, AstraZeneca, Pfizer, and Abbott Laboratories. Neither he nor his family hold equity positions in pharmaceutical companies.
Overlapping symptoms may obscure comorbid bipolar illness
An adult with function-impairing inattention could have attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or both. Comorbid ADHD and BD often is unrecognized, however, because patients are more likely to report ADHD-related symptoms than manic symptoms.1
To help you recognize comorbid ADHD/BD—and protect adults who might switch into mania if given stimulants or antidepressants—this article describes a hierarchy to diagnose and treat this comorbidity. Based on the evidence and our experience, we:
- discuss how to differentiate between these disorders with overlapping symptoms
- provide tools and suggestions to screen for BD and adult ADHD
- offer 3 algorithms to guide your diagnosis and choice of medications.
Clinical challenges
Prevalence is unclear. Adult ADHD—with an estimated prevalence of 4.4%2—is more common than BD. Lifetime prevalences of BD types I and II are 1.6% and 0.5%, respectively.3 Studies of ADHD/BD comorbidity suggest wide-ranging prevalence rates:
Underdiagnosis. Adult ADHD/BD is a more severe illness than ADHD or BD alone and is highly comorbid with agoraphobia, social phobia, posttraumatic stress disorder, and alcohol or drug addiction. Adults with ADHD/BD have more frequent affective episodes, suicide attempts, violence, and legal problems.4 Diagnosing this comorbidity remains a challenge, however, because:
- identifying which symptoms are caused by which disorder can be difficult
- BD tends to be underdiagnosed9
- patients often misidentify, underreport, or deny manic symptoms1,10,11
- if a patient presents with active bipolar symptoms, DSM-IV-TR criteria require that ADHD not be diagnosed until mood symptoms are resolved.
Overlapping symptoms. ADHD and bipolar mania share some DSM-IV-TR diagnostic criteria, including talkativeness, distractibility, increased activity or physical restlessness, and loss of social inhibitions (Table 1).12 Overlapping symptoms also are notable within ADHD diagnostic criteria (Table 2). In the inattention category, for example, “easily distracted by extraneous stimuli,” “difficulty sustaining attention in tasks,” and “fails to give close attention to details” are considered 3 separate symptoms. In the hyperactivity category, “often leaves seat,” “often runs about or climbs excessively,” and “often on the go, or often acts as if driven by a motor” are 3 separate symptoms.
Given ADHD’s relatively loose diagnostic criteria and high comorbidity in adults with mood disorders, the question of whether adult ADHD/BD represents comorbidity or diagnostic overlap remains unresolved. For the clinician, the disorders’ nonoverlapping features (Table 1) can assist with the differential diagnosis. For example:
- ADHD symptoms tend to be chronic and BD symptoms episodic.
- ADHD patients may have high energy but lack increased productivity seen in BD patients.
- ADHD patients do not need less sleep or have inflated self-esteem like symptomatic BD patients.
- Psychotic symptoms such as hallucinations or delusions might be present in severe BD but are absent in ADHD.
Table 1
Overlap between DSM-IV-TR diagnostic criteria for ADHD and bipolar mania
| Overlapping symptoms | |
|---|---|
| ADHD | Bipolar mania |
| Talks excessively | More talkative than usual |
| Easily distracted/jumps from one activity to the next | Distractibility or constant changes in activity or plans |
| Fidgets Difficulty remaining seated Runs or climbs about inappropriately Difficulty playing quietly On the go as if driven by a motor | Increased activity or physical restlessness |
| Interrupts or butts in uninvited Blurts out answers | Loss of normal social inhibitions |
| Nonoverlapping symptoms | |
| ADHD Forgetful in daily activities Difficulty awaiting turn Difficulty organizing self Loses things Avoids sustained mental effort Does not seem to listen Difficulty following through on instructions/fails to finish work Difficulty sustaining attention Fails to give close attention to details/makes careless mistakes | |
| Bipolar mania Inflated self-esteem/grandiosity Increase in goal-directed activity Flight of ideas Decreased need for sleep Excessive involvement in pleasurable activities with disregard for potential adverse consequences Marked sexual energy or sexual indiscretions | |
| ADHD: attention-deficit/hyperactivity disorder | |
| Source: Adapted and reprinted with permission from reference 12 | |
Table 2
DSM-IV-TR diagnostic criteria for attention-deficit/ hyperactivity disorder
| Inattention |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Hyperactivity/impulsivity |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Diagnosis requires evidence of inattention or hyperactivity/impulsivity or both |
| Some hyperactive/impulsive or inattentive symptoms that caused impairment were present before age 7 |
| Some impairment from symptoms is present in ≥2 settings (such as at school, work, or home) |
| Symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorder and are not better accounted for by another mental disorder (mood disorder, anxiety disorder, dissociative disorder, or a personality disorder) |
| Source: DSM-IV-TR |
Mood symptoms first
A diagnostic hierarchy is implicit in DSM-IV-TR; anxiety disorders are not diagnosed during an active major depressive or manic episode, and schizophrenia is not diagnosed on the basis of psychotic symptoms during an active major depressive or manic episode. Mood disorders sit atop this implied diagnostic hierarchy and must be ruled out before psychotic or anxiety disorders are diagnosed. Similarly, most personality disorders are not diagnosed during an active mood or psychotic episode.
Diagnosing adult ADHD when a patient is actively depressed or manic is inconsistent with this hierarchy and conflicts with extensive nosologic literature.13 We suggest that ADHD—a cognitive-behavioral problem—not be diagnosed solely on symptoms observed when a patient is experiencing a mood episode or psychotic illness.
Bipolar disorder. Two useful mnemonics (Table 3) assist in screening for DSM-IV-TR symptoms of BD type I:
- Pure mania consists of euphoric mood and ≥3 of 7 DIGFAST criteria, or irritable mood and ≥4 of 7 DIGFAST criteria
- Mixed mania consists of depressed mood with ≥4 of 7 DIGFAST criteria and ≥4 of 8 SIGECAPS criteria.
To be diagnostic, these symptoms must cause substantial social or occupational dysfunction and be present at least 1 week. Diagnose BD type I if a patient has experienced a single pure or mixed manic episode at any time, unless the episode had a medical cause such as hyperthyroidism or antidepressant use. Because patients with mixed episodes experience depressed mood, assess any patient with clinical depression for manic symptoms. Otherwise, a patient with a mixed episode could be misdiagnosed as having unipolar depression instead of BD type I.14
BD type II also has been observed in patients with comorbid adult ADHD/BD.4,6 The main difference between BD types I and II is that manic symptoms in type II are not severe enough to cause functional impairment or psychotic symptoms.15
Adult ADHD. The clinical interview seeking evidence of inattention and hyperactivity/impulsivity remains the basis of adult ADHD diagnosis (Table 2). Key areas are:
- the patient’s past and current functional impairment
- whether substantial impairment occurs in at least 2 areas of life (such as school, work, or home).
Take medical, educational, social, psychological, and vocational histories, and rule out other conditions before concluding that adult ADHD is the appropriate diagnosis.16 In adult ADHD, inattentive symptoms become far more prominent, about twice as common as hyperactive symptoms.17 Inattentive symptoms may manifest as neglect, poor time management, motivational deficits, or poor concentration that results in forgetfulness, distractibility, item misplacement, or excessive mistakes in paperwork.18 When impulsive symptoms persist in adults, they may manifest as automobile accidents or low tolerance for frustration, which may lead to frequent job changes and unstable, interrupted interpersonal relationships.18
Neuropsychological testing is not required to make an adult ADHD diagnosis but can help establish the breadth of symptoms or comorbidity.17 Rating scales can screen, gather data (including presence and severity of symptoms), and measure treatment response.16 Commonly used rating scales include:
- Conners’ Adult ADHD Rating Scales19
- Brown Attention Deficit Disorder Rating Scale for Adults20
- Adult ADHD Self-Report Scale.21
When using rating scales, remember that adult psychopathology can distort perceptions, and some self-report scales have questionable reliability.16
Table 3
Mnemonics for diagnostic symptoms of pure and mixed bipolar mania
| DIGFAST* for bipolar mania symptoms | SIGECAPS† bipolar depression symptoms |
|---|---|
| Distractibility Insomnia Grandiosity Flight of ideas Activities Speech Thoughtlessness | Sleep Interest Guilt Energy Concentration Appetite Psychomotor Suicide |
| Pure mania: Euphoric mood with ≥3 DIGFAST criteria or irritable mood with ≥4 DIGFAST criteria. | |
| Mixed mania: Depressed mood with ≥4 DIGFAST criteria and ≥4 SIGECAPS criteria. | |
| * Developed by William Falk, MD | |
| †Developed by Carey Gross, MD | |
| Source: Adapted from Ghaemi SN. Mood disorders. New York: Lippincott, Williams, & Wilkins; 2003 | |
Treatment recommendations
Limited data. We found only 1 study on adult ADHD/BD treatment. In this open trial,22 36 adults with comorbid ADHD and BD received bupropion SR, up to 200 mg bid, for ADHD symptoms while maintained on mood stabilizers, antipsychotics, or both. Improvement was defined as ≥30% reduction in ADHD Symptom Checklist Scale scores, without concurrent mania. After 6 weeks, 82% of patients had improved; 1 dropped out at week 2 because of hypomanic activation. Methodologic limitations included trial design (non-randomized, nonblinded, short duration) and patient selection (90% of subjects had BD type II).
In the absence of adequate data on adult ADHD/BD, studies in children suggest:
- stimulants may not be effective for ADHD symptoms in patients with active manic or depressive symptoms
- mood stabilization is a prerequisite for successful pharmacologic treatment of ADHD in patients with both ADHD and manic or depressive symptoms.23,24
Follow the hierarchy. First treat acute mood symptoms, then reevaluate and possibly treat ADHD symptoms if they persist during euthymia (Algorithm 1). When a patient meets criteria for adult ADHD/BD, first stabilize bipolar manic or depressive symptoms (Algorithm 2). For acute mania, treat with standard mood stabilizers (lithium, valproate, lamotrigine, or carbamazepine) with or without a second-generation antipsychotic.25 Starting stimulants for ADHD when patients have active mood symptoms is sub-optimal and potentially harmful because of the risk of inducing mania. For acute bipolar depression, adjunctive antidepressant treatment has been found to be no more effective than a mood stabilizer alone.26
After bipolar symptoms respond or remit, reassess for adult ADHD. If ADHD symptoms persist during euthymia, additional treatment may be indicated.
Very little evidence exists on treating adult ADHD/BD; as mentioned, bupropion is the only medication studied in this population. For adult ADHD alone, clinical trials have showed varying efficacy with bupropion,27,28 atomoxetine,29 venlafaxine,30,31 desipramine,32 methylphenidate,33 mixed amphetamine salts,34 and guanfacine.35 Whether these treatments can be generalized as safe and efficacious for comorbid adult ADHD/BD is unclear. Nonetheless, we suggest using bupropion first, followed by atomoxetine or guanfacine before you consider amphetamine stimulants (Algorithm 3).
Algorithm 1
Hierarchy for diagnosis and treatment of adult ADHD/BD
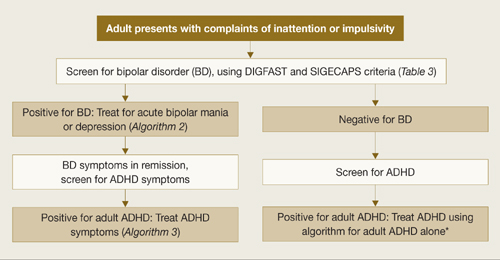
ADHD: attention-deficit/hyperactivity disorder; BD: bipolar disorder
*Adler LA, Chua HC. Management of ADHD in adults. J Clin Psychiatry 2002;63(suppl 12):29-35.
Algorithm 2
Treating acute episodes of bipolar disorder
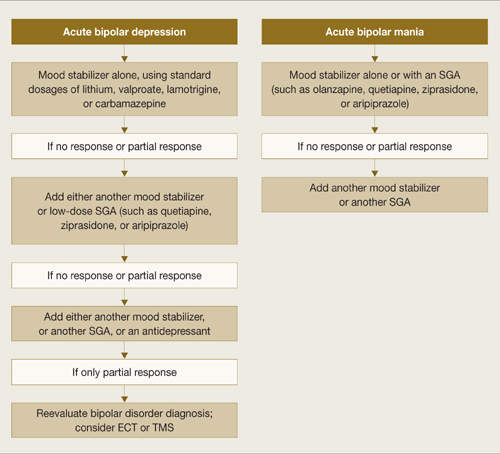
ECT: electroconvulsive therapy; SGA: second-generation antipsychotic; TMS: transcranial magnetic stimulation
Algorithm 3
Suggested approach to adult ADHD with comorbid BD*
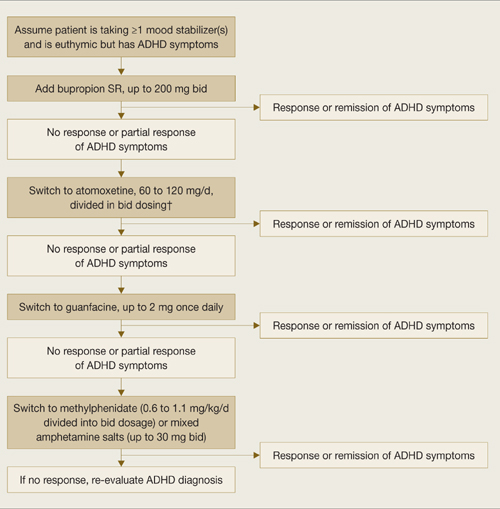
* Based on data extrapolated from samples of patients with ADHD alone because of very limited data in ADHD/BD samples.
† We recommend against combining antidepressants and stimulants because of additive risks of mania in BD. Discontinue stimulant or antidepressant if manic symptoms appear or rapid cycling emerges.
Reducing mania risk
Antidepressants and stimulants may help adults with ADHD alone, but risks of mania and rapid cycling limit their use in adults with ADHD/BD.
Stimulants and mania. One study found a 17% manic switch rate when methylphenidate (≤10 mg bid) was given to 14 bipolar depressed adults (10 BD type I, 2 BD type II, and 2 with secondary mania) taking mood stabilizers.36 A chart review of 82 bipolar children not taking mood stabilizers found an 18% switch rate with methylphenidate or amphetamine.37 Another chart review of 80 children with BD type I found that past amphetamine treatment (but not history of ADHD diagnosis or antidepressant treatment) was associated with more severe bipolar illness.38
No studies have examined predictors of amphetamine-induced mania. In our clinical experience, triggers are similar to those that can cause antidepressant-induced mania, such as:
- recent manic episodes
- current rapid cycling
- past antidepressant-induced mania.
Antidepressants and mania. When 64 patients with acute bipolar depression received both antidepressants and mood stabilizers in a randomized, double-blind trial, switch rates into mania or hypomania were 10% for bupropion, 9% for sertraline, and 29% for venlafaxine.39 In a meta analysis of clinical trials using selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants (TCAs), the manic switch rate was threefold higher with TCAs than SSRIs.40 Antidepressant use in bipolar patients was associated with rapid cycling in the only randomized study of this topic.41
Insufficient data exist to clarify whether mania induction with antidepressants is dose-dependent.42 Factors associated with antidepressant-induced mania include:
- previous antidepressant-induced mania
- family history of BD
- exposure to multiple antidepressant trials42
- history of substance abuse and/or dependence.43
Related resources
- Bipolar disorder information and resources. www.psycheducation.org.
- ADHD Information and resources. www.adhdnews.com.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. New York: McGraw-Hill; 2006.
Drug brand names
- Amphetamine/Dextroamphetamine • Adderall
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methylphenidate • Ritalin
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Valproate • Depakote
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Wingo reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ghaemi receives research grants from GlaxoSmithKline and Pfizer and is a speaker for GlaxoSmithKline, AstraZeneca, Pfizer, and Abbott Laboratories. Neither he nor his family hold equity positions in pharmaceutical companies.
1. Ghaemi SN, Stoll AL, Pope HG, Jr, et al. Lack of insight in bipolar disorder. The acute manic episode. J Nerv Ment Dis 1995;183(7):464-7.
2. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163(4):716-23.
3. Sadock BJ, Sadock VA, eds. Synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.
4. Nierenberg AA, Miyahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry 2005;57(11):1467-73.
5. Tamam L, Tuglu C, Karatas G, et al. Adult attention-deficit hyperactivity disorder in patients with bipolar I disorder in remission: preliminary study. Psychiatry Clin Neurosci 2006;60(4):480-5.
6. Wilens TE, Biederman J, Wozniak J, et al. Can adults with attention-deficit/hyperactivity disorder be distinguished from those with comorbid bipolar disorder? Findings from a sample of clinically referred adults. Biol Psychiatry 2003;54(1):1-8.
7. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry 2005;162(9):1621-7.
8. Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry 2006;163(10):1720-9.
9. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord 1999;52(1-3):135-44.
10. Keitner GI, Solomon DA, Ryan CE, et al. Prodromal and residual symptoms in bipolar I disorder. Compr Psychiatry 1996;37(5):362-7.
11. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv 2001;52(1):51-5.
12. Kent L, Craddock N. Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? J Affect Disord 2003;73(3):211-21.
13. Surtees PG, Kendell RE. The hierarchy model of psychiatric symptomatology: an investigation based on present state examination ratings. Br J Psychiatry 1979;135:438-43.
14. Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog Neuropsychopharmacol Biol Psychiatry 2006;30(3):471-7.
15. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text rev. Washington, DC: American Psychiatric Association; 2000.
16. Murphy KR, Adler LA. Assessing attention-deficit hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry 2004;65(suppl 3):12-17.
17. Adler LA. Diagnosing adult attention deficit hyperactivity disorder. Primary Psychiatry 2006;13(suppl 3):9-10.
18. Montano B. Diagnosis and treatment of ADHD in adults in primary care. J Clin Psychiatry 2004;65(suppl 3):18-21.
19. Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS). North Tonawanda, NY: Multi-Health Systems; 1999.
20. Brown TE. Brown Attention Deficit Disorder Scales. San Antonio, TX: The Psychological Corporation; 1996.
21. Adler LA, Kessler RC, Spencer T. Adult ADHD Self-report Scale v1.1 (ASRS-v1.1) Symptom Checklist. World Health Organization. Available at: http://www.med.nyu.edu/psych/assets/adhdscreen18.pdf. Accessed May 7, 2007.
22. Wilens TE, Prince JB, Spencer T, et al. An open trial of bupropion for the treatment of adults with attention-deficit/hyperactivity disorder and bipolar disorder. Biol Psychiatry 2003;54(1):9-16.
23. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
24. Daviss WB, Bentivoglio P, Racusin R, et al. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry 2001;40(3):307-14.
25. Scherk H, Pajonk FG, Leucht SL. Second-generation antipsychotic agents in the treatment of acute mania. Arch Gen Psychiatry 2007;64:442-55.
26. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 2007:356:(17):1711-22.
27. Wilens TE, Haight BR, Horrigan JP, et al. Bupropion XL in adults with attention deficit hyperactivity disorder: a randomized, placebo controlled study. Biol Psychiatry 2005;57:793-801.
28. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
29. Michelson D, Adler LA, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo controlled studies. Biol Psychiatry 2003;53:112-20.
30. Adler LA, Resnick S, Kunz M, Devinsky O. Open-label trial of venlafaxine in adults with attention deficit disorder. Psychopharmacol Bull 1995;31(4):785-8.
31. Hedges D, Reimherr FW, Rogers A, et al. An open trial of venlafaxine in adult patients with attention deficit hyperactivity disorder. Psychopharmacol Bull 1995;31(4):779-83.
32. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry 1996;153(9):1147-53.
33. Faraone SV, Spencer T, Aleardi M, et al. Meta analysis of the efficacy of methylphenidate for treating adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2004;24(1):24-8.
34. Spencer T, Biederman J, Wilens TE, et al. Efficacy of a mixed amphetamine salts compound in adults with attention deficit hyperactivity disorder. Arch Gen Psychiatry 2001;58:775-82.
35. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2000;21(2):223-8.
36. El-Mallakh RS. An open study of methylphenidate in bipolar depression. Bipolar Disord 2000;2(1):56-9.
37. Faedda GL, Baldessarini RJ, Glovinsky IP, et al. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord 2004;82(1):149-58.
38. Soutullo CA, DelBello MP, Ochsner JE, et al. Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment. J Affect Disord 2002;70(3):323-7.
39. Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 2006;189:124-31.
40. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry 1994;164(4):549-50.
41. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145(2):179-84.
42. Goldberg JF. When do antidepressants worsen the course of bipolar disorder? J Psychiatr Pract. 2003;9(3):181-94.
43. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry 2002;63(9):791-5.
1. Ghaemi SN, Stoll AL, Pope HG, Jr, et al. Lack of insight in bipolar disorder. The acute manic episode. J Nerv Ment Dis 1995;183(7):464-7.
2. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163(4):716-23.
3. Sadock BJ, Sadock VA, eds. Synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.
4. Nierenberg AA, Miyahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry 2005;57(11):1467-73.
5. Tamam L, Tuglu C, Karatas G, et al. Adult attention-deficit hyperactivity disorder in patients with bipolar I disorder in remission: preliminary study. Psychiatry Clin Neurosci 2006;60(4):480-5.
6. Wilens TE, Biederman J, Wozniak J, et al. Can adults with attention-deficit/hyperactivity disorder be distinguished from those with comorbid bipolar disorder? Findings from a sample of clinically referred adults. Biol Psychiatry 2003;54(1):1-8.
7. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry 2005;162(9):1621-7.
8. Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry 2006;163(10):1720-9.
9. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord 1999;52(1-3):135-44.
10. Keitner GI, Solomon DA, Ryan CE, et al. Prodromal and residual symptoms in bipolar I disorder. Compr Psychiatry 1996;37(5):362-7.
11. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv 2001;52(1):51-5.
12. Kent L, Craddock N. Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? J Affect Disord 2003;73(3):211-21.
13. Surtees PG, Kendell RE. The hierarchy model of psychiatric symptomatology: an investigation based on present state examination ratings. Br J Psychiatry 1979;135:438-43.
14. Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog Neuropsychopharmacol Biol Psychiatry 2006;30(3):471-7.
15. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text rev. Washington, DC: American Psychiatric Association; 2000.
16. Murphy KR, Adler LA. Assessing attention-deficit hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry 2004;65(suppl 3):12-17.
17. Adler LA. Diagnosing adult attention deficit hyperactivity disorder. Primary Psychiatry 2006;13(suppl 3):9-10.
18. Montano B. Diagnosis and treatment of ADHD in adults in primary care. J Clin Psychiatry 2004;65(suppl 3):18-21.
19. Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS). North Tonawanda, NY: Multi-Health Systems; 1999.
20. Brown TE. Brown Attention Deficit Disorder Scales. San Antonio, TX: The Psychological Corporation; 1996.
21. Adler LA, Kessler RC, Spencer T. Adult ADHD Self-report Scale v1.1 (ASRS-v1.1) Symptom Checklist. World Health Organization. Available at: http://www.med.nyu.edu/psych/assets/adhdscreen18.pdf. Accessed May 7, 2007.
22. Wilens TE, Prince JB, Spencer T, et al. An open trial of bupropion for the treatment of adults with attention-deficit/hyperactivity disorder and bipolar disorder. Biol Psychiatry 2003;54(1):9-16.
23. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
24. Daviss WB, Bentivoglio P, Racusin R, et al. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry 2001;40(3):307-14.
25. Scherk H, Pajonk FG, Leucht SL. Second-generation antipsychotic agents in the treatment of acute mania. Arch Gen Psychiatry 2007;64:442-55.
26. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 2007:356:(17):1711-22.
27. Wilens TE, Haight BR, Horrigan JP, et al. Bupropion XL in adults with attention deficit hyperactivity disorder: a randomized, placebo controlled study. Biol Psychiatry 2005;57:793-801.
28. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
29. Michelson D, Adler LA, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo controlled studies. Biol Psychiatry 2003;53:112-20.
30. Adler LA, Resnick S, Kunz M, Devinsky O. Open-label trial of venlafaxine in adults with attention deficit disorder. Psychopharmacol Bull 1995;31(4):785-8.
31. Hedges D, Reimherr FW, Rogers A, et al. An open trial of venlafaxine in adult patients with attention deficit hyperactivity disorder. Psychopharmacol Bull 1995;31(4):779-83.
32. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry 1996;153(9):1147-53.
33. Faraone SV, Spencer T, Aleardi M, et al. Meta analysis of the efficacy of methylphenidate for treating adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2004;24(1):24-8.
34. Spencer T, Biederman J, Wilens TE, et al. Efficacy of a mixed amphetamine salts compound in adults with attention deficit hyperactivity disorder. Arch Gen Psychiatry 2001;58:775-82.
35. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2000;21(2):223-8.
36. El-Mallakh RS. An open study of methylphenidate in bipolar depression. Bipolar Disord 2000;2(1):56-9.
37. Faedda GL, Baldessarini RJ, Glovinsky IP, et al. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord 2004;82(1):149-58.
38. Soutullo CA, DelBello MP, Ochsner JE, et al. Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment. J Affect Disord 2002;70(3):323-7.
39. Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 2006;189:124-31.
40. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry 1994;164(4):549-50.
41. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145(2):179-84.
42. Goldberg JF. When do antidepressants worsen the course of bipolar disorder? J Psychiatr Pract. 2003;9(3):181-94.
43. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry 2002;63(9):791-5.
The Hospital as College
The hospital is the only proper college in which to rear a true disciple of Aesculapius.—John Abernethy (1764-1831), surgeon and teacher
With this quote Sir William Osler began his address, “The Hospital as a College?” to the Academy of Medicine in New York in 1903. His second quote for this report was from the famed physician Oliver Wendell Holmes Sr. in 1867:
“The most essential part of a student’s instruction is obtained, as I believe, not in the lecture room, but at the bedside. Nothing seen there is lost: the rhythms of disease are learned by frequent repetition: its unforeseen occurrence stamp themselves indelibly on the memory. Before the student is aware of what he had acquired he has learned the aspects and causes and probable issue of the disease he has seen with his teacher and the proper mode of dealing with them, as far as his master knows.”
In his report Osler was celebrating a quarter century’s success in education. He demanded a better general education for students, a lengthened period for professional study, and the substitution of theoretical by practical learning. He wanted the student not to learn only from dissecting the sympathetic nervous system but to learn to “take a blood pressure observation” with a kymograph (an instrument used to record the temporal variations of any physiological or muscular process; it consists essentially of a revolving drum, bearing a record sheet on which a stylus travels).
Osler observed that there should be no teaching without a patient for a text: “The whole of medicine is in observation” that the teacher’s art is educating the student’s finger to feel and eyes to see. Give the student good methods and a proper point of view, and experience will do the rest.
Osler expressed confidence that students would keep the hospital physician from slovenliness and improve the care of patients. He was also concerned that “we ask too much of the resident physicians, whose number has not increased in proportion to the enormous amount of work thrust upon them.” Students were the answer, the proto-scut-monkey.
The practicality of working out of a teaching hospital was outlined at length in Osler’s report. The student’s third year should begin with a systematic physical diagnosis course, first in history taking, then in writing reports. Concurrently, a physical examination course should be given several days a week with individual cases assigned to students to follow, and instruction is accessing the literature. Next comes clinical microscopy—an essential in an era where there was often no lab to call upon. In general, medical clinic occurs one day a week when interesting cases are brought from the wards. Of note, committees were appointed to report on every case of pneumonia.
In revamping medical education Osler brought the third-year students to the outpatient clinic and the fourth-year students to the wards. What implication does this have for us as hospitalists?
I have no pretensions about being another Osler (I am barely a Newman on my best days), but still my colleagues and I trudge along in our teaching duties. What education do we really do? I sat down after reading Osler’s paper, stimulated by a tangential question from the esteemed Tom Baudenistel, MD, and decided to see exactly whom we were teaching.
First there are medical students. We are faculty on their first-year selectives, offering a shadow experience. We staff the introduction to physical exam courses in second year. Third-year students rotate on our services, and seniors take our elective as well as taking acting internships on our teaching services. We act as mentors and interest group leaders. There is certainly more to this list. We also spend time teaching NP and PA students.
The internal medicine residents rotate on our hospitalist services, and we staff the general medical services. We interact with them daily when they are on consult services, trying to set a role model. General medicine, geriatric, and hospital medicine fellows rotate through as well.
We also teach the nurses on services and through in-services and daily rounds to cement the working relationship and improve communication. We teach each other. A day rarely goes by without a colleague passing on a tasty medical tidbit. (Of course, for me, a tabla blanca, no shortage of space for pearls). And finally we teach our patients and their families. Every day we do this, and if we don’t then we are missing the point of our profession entirely.
Each party—patient or student—has something to learn from us, but more importantly we have something to learn from them. Osler wrote that “The stimulus of their presence (the student) neutralizes the clinical apathy certain, sooner or later, to beset the man who makes lonely “rounds” with his house physician.”
One hundred years plus later, much of what was written is still true: Whether in a teaching institution or making “lonely rounds” we must strive to continue to educate ourselves, our colleagues, and our patients. And what better place to do it than the hospital? TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
Osler W (Sir) Aequanimitas. 1945. The Blakiston Company, Philadelphia. p. 311-327.
The hospital is the only proper college in which to rear a true disciple of Aesculapius.—John Abernethy (1764-1831), surgeon and teacher
With this quote Sir William Osler began his address, “The Hospital as a College?” to the Academy of Medicine in New York in 1903. His second quote for this report was from the famed physician Oliver Wendell Holmes Sr. in 1867:
“The most essential part of a student’s instruction is obtained, as I believe, not in the lecture room, but at the bedside. Nothing seen there is lost: the rhythms of disease are learned by frequent repetition: its unforeseen occurrence stamp themselves indelibly on the memory. Before the student is aware of what he had acquired he has learned the aspects and causes and probable issue of the disease he has seen with his teacher and the proper mode of dealing with them, as far as his master knows.”
In his report Osler was celebrating a quarter century’s success in education. He demanded a better general education for students, a lengthened period for professional study, and the substitution of theoretical by practical learning. He wanted the student not to learn only from dissecting the sympathetic nervous system but to learn to “take a blood pressure observation” with a kymograph (an instrument used to record the temporal variations of any physiological or muscular process; it consists essentially of a revolving drum, bearing a record sheet on which a stylus travels).
Osler observed that there should be no teaching without a patient for a text: “The whole of medicine is in observation” that the teacher’s art is educating the student’s finger to feel and eyes to see. Give the student good methods and a proper point of view, and experience will do the rest.
Osler expressed confidence that students would keep the hospital physician from slovenliness and improve the care of patients. He was also concerned that “we ask too much of the resident physicians, whose number has not increased in proportion to the enormous amount of work thrust upon them.” Students were the answer, the proto-scut-monkey.
The practicality of working out of a teaching hospital was outlined at length in Osler’s report. The student’s third year should begin with a systematic physical diagnosis course, first in history taking, then in writing reports. Concurrently, a physical examination course should be given several days a week with individual cases assigned to students to follow, and instruction is accessing the literature. Next comes clinical microscopy—an essential in an era where there was often no lab to call upon. In general, medical clinic occurs one day a week when interesting cases are brought from the wards. Of note, committees were appointed to report on every case of pneumonia.
In revamping medical education Osler brought the third-year students to the outpatient clinic and the fourth-year students to the wards. What implication does this have for us as hospitalists?
I have no pretensions about being another Osler (I am barely a Newman on my best days), but still my colleagues and I trudge along in our teaching duties. What education do we really do? I sat down after reading Osler’s paper, stimulated by a tangential question from the esteemed Tom Baudenistel, MD, and decided to see exactly whom we were teaching.
First there are medical students. We are faculty on their first-year selectives, offering a shadow experience. We staff the introduction to physical exam courses in second year. Third-year students rotate on our services, and seniors take our elective as well as taking acting internships on our teaching services. We act as mentors and interest group leaders. There is certainly more to this list. We also spend time teaching NP and PA students.
The internal medicine residents rotate on our hospitalist services, and we staff the general medical services. We interact with them daily when they are on consult services, trying to set a role model. General medicine, geriatric, and hospital medicine fellows rotate through as well.
We also teach the nurses on services and through in-services and daily rounds to cement the working relationship and improve communication. We teach each other. A day rarely goes by without a colleague passing on a tasty medical tidbit. (Of course, for me, a tabla blanca, no shortage of space for pearls). And finally we teach our patients and their families. Every day we do this, and if we don’t then we are missing the point of our profession entirely.
Each party—patient or student—has something to learn from us, but more importantly we have something to learn from them. Osler wrote that “The stimulus of their presence (the student) neutralizes the clinical apathy certain, sooner or later, to beset the man who makes lonely “rounds” with his house physician.”
One hundred years plus later, much of what was written is still true: Whether in a teaching institution or making “lonely rounds” we must strive to continue to educate ourselves, our colleagues, and our patients. And what better place to do it than the hospital? TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
Osler W (Sir) Aequanimitas. 1945. The Blakiston Company, Philadelphia. p. 311-327.
The hospital is the only proper college in which to rear a true disciple of Aesculapius.—John Abernethy (1764-1831), surgeon and teacher
With this quote Sir William Osler began his address, “The Hospital as a College?” to the Academy of Medicine in New York in 1903. His second quote for this report was from the famed physician Oliver Wendell Holmes Sr. in 1867:
“The most essential part of a student’s instruction is obtained, as I believe, not in the lecture room, but at the bedside. Nothing seen there is lost: the rhythms of disease are learned by frequent repetition: its unforeseen occurrence stamp themselves indelibly on the memory. Before the student is aware of what he had acquired he has learned the aspects and causes and probable issue of the disease he has seen with his teacher and the proper mode of dealing with them, as far as his master knows.”
In his report Osler was celebrating a quarter century’s success in education. He demanded a better general education for students, a lengthened period for professional study, and the substitution of theoretical by practical learning. He wanted the student not to learn only from dissecting the sympathetic nervous system but to learn to “take a blood pressure observation” with a kymograph (an instrument used to record the temporal variations of any physiological or muscular process; it consists essentially of a revolving drum, bearing a record sheet on which a stylus travels).
Osler observed that there should be no teaching without a patient for a text: “The whole of medicine is in observation” that the teacher’s art is educating the student’s finger to feel and eyes to see. Give the student good methods and a proper point of view, and experience will do the rest.
Osler expressed confidence that students would keep the hospital physician from slovenliness and improve the care of patients. He was also concerned that “we ask too much of the resident physicians, whose number has not increased in proportion to the enormous amount of work thrust upon them.” Students were the answer, the proto-scut-monkey.
The practicality of working out of a teaching hospital was outlined at length in Osler’s report. The student’s third year should begin with a systematic physical diagnosis course, first in history taking, then in writing reports. Concurrently, a physical examination course should be given several days a week with individual cases assigned to students to follow, and instruction is accessing the literature. Next comes clinical microscopy—an essential in an era where there was often no lab to call upon. In general, medical clinic occurs one day a week when interesting cases are brought from the wards. Of note, committees were appointed to report on every case of pneumonia.
In revamping medical education Osler brought the third-year students to the outpatient clinic and the fourth-year students to the wards. What implication does this have for us as hospitalists?
I have no pretensions about being another Osler (I am barely a Newman on my best days), but still my colleagues and I trudge along in our teaching duties. What education do we really do? I sat down after reading Osler’s paper, stimulated by a tangential question from the esteemed Tom Baudenistel, MD, and decided to see exactly whom we were teaching.
First there are medical students. We are faculty on their first-year selectives, offering a shadow experience. We staff the introduction to physical exam courses in second year. Third-year students rotate on our services, and seniors take our elective as well as taking acting internships on our teaching services. We act as mentors and interest group leaders. There is certainly more to this list. We also spend time teaching NP and PA students.
The internal medicine residents rotate on our hospitalist services, and we staff the general medical services. We interact with them daily when they are on consult services, trying to set a role model. General medicine, geriatric, and hospital medicine fellows rotate through as well.
We also teach the nurses on services and through in-services and daily rounds to cement the working relationship and improve communication. We teach each other. A day rarely goes by without a colleague passing on a tasty medical tidbit. (Of course, for me, a tabla blanca, no shortage of space for pearls). And finally we teach our patients and their families. Every day we do this, and if we don’t then we are missing the point of our profession entirely.
Each party—patient or student—has something to learn from us, but more importantly we have something to learn from them. Osler wrote that “The stimulus of their presence (the student) neutralizes the clinical apathy certain, sooner or later, to beset the man who makes lonely “rounds” with his house physician.”
One hundred years plus later, much of what was written is still true: Whether in a teaching institution or making “lonely rounds” we must strive to continue to educate ourselves, our colleagues, and our patients. And what better place to do it than the hospital? TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
Osler W (Sir) Aequanimitas. 1945. The Blakiston Company, Philadelphia. p. 311-327.
Trendsetting Hospitalists Receive SHM’s Top Honors
SHM has presented the 2008 Awards of Excellence to four hospitalists and one quality improvement team. Their work and research have contributed significantly to hospital medicine and the betterment of patient care and quality improvement. The winners were recognized at Hospital Medicine 2008.
Award for Clinical Excellence: Kevin O’Leary, MD, associate professor of medicine and the associate chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. O’Leary leads strategic initiatives for the division in his job as associate chief of the Division of Hospital Medicine, especially in patient safety and quality. He also chairs the department’s Quality Management Committee.
An active member of SHM since 2002, Dr. O’Leary has served on the Core Competencies Task Force, the Annual Meeting Planning Committee, and the Annual Meeting Precourse Planning Committee. He also is active in SHM’s Chicago chapter, where he serves as vice president. He serves as an assistant editor for the Journal of Hospital Medicine.
Dr. O’Leary received his bachelor’s inbiology and medical degree from the University of Illinois. He completed his residency at Northwestern University.
Award for Excellence in Research: Peter Lindenauer, MD, MSc, medical director of clinical and quality informatics at Baystate Health in Springfield, Mass., and associate professor of medicine at Tufts University School of Medicine in Boston.
Dr. Lindenauer is responsible for lending the development of an electronic medical record at a large integrated delivery network in western Massachusetts in his job as medical director of clinical and quality informatics.
He has served on technical expert panels for Medicare, patient safety, monitoring systems, and surgical care improvement projects. He also has been a part of the National Quality Forum’s Hospital Quality Measures Development Group and has served on the inpatient functionality work group of the Certifying Committee for Healthcare Information Technology.
As a founding member of SHM, Dr. Lindenauer has served on the society’s board of directors and is a member of the Hospital Quality and Patient Safety Standards Committee.
A graduate of the University of Chicago, Dr. Lindenauer received his bachelor’s in history and received his graduate degree from the Herndon School of Economics and Political Science in Health Planning and Financing. He received his medical degree from the University of Pennsylvania and completed residency training at the University of California, San Francisco.
Award for Excellence in Teaching: Anjala Tess, MD, associate program director for the Internal Medicine Residency Program and director of education for the hospital medicine program, as well as a medical unit director and practicing hospitalist at Beth Israel Deaconess Medical Center in Boston.
Dr. Tess is in charge of the quality improvement teaching program and curriculum for the entire residency program at Beth Israel Deaconess. She also helps oversee the resident elective in hospital medicine and directs educational activities for the group. Her goal is to involve residents in process improvement in the hospital by giving them a hands-on role in quality improvement and peer review.
She has received numerous awards, including the Hermann Blumgart Teaching Award at Beth Israel Deaconess and first prize in SHM’s Innovations Poster Competition.
As an undergraduate, Dr. Tess earned her degree from Brown University, in Rhode Island, and received her medical degree at Washington University’s St. Louis School of Medicine. She completed her residency at Beth Israel Deaconess. She also completed fellowships at Harvard Medical School, the Carl J. Shapiro Institute for Education Research and Beth Israel Deaconess Medical Center.
Award for Outstanding Service in Hospital Medicine: David Zipes, MD, director of pediatric hospitalist service at the Peyton Manning Children’s Hospital in Indianapolis, Ind.
Dr. Zipes oversees all hospitalists and staff, leads strategic planning for the group and the hospital, oversees the business and financial issues of the group and provides general medical direction and leadership of the pediatric units at both the Peyton Manning’s Children’s Hospital and its suburban campus.
As a founding member of SHM, Dr. Zipes is active on its Annual Meeting Planning Committee, Pediatrics Committee, and Pediatrics Core Competencies Task Force. He is also a contributing author for Pediatric Hospital Medicine and the Textbook of Pediatric Hospital Medicine, and a founding member of the annual pediatric hospital medicine meeting.
He also has been the recipient of several awards, including the Family Medicine Teacher of the Year Annual Award (2002, 2005, and 2006) and the St. Vincent Spirit of Caring Award for Service and Dedication to the Hospital (2006 and 2007.)
Dr. Zipes earned his bachelor’s and medical degrees from Indiana University. He completed his residency at Children’s Hospital Medicine Center in Cincinnati, Ohio.
Award for Team Approaches in Quality Improvement: Team Leader, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
Dr. Maynard and his team (Ian Jenkins, MD, Sarah Stone, MD, Josh Lee, MD, Ed Fink, Tim Morris, MD, Peter Fedullo, MD, Robert Schoenhaus, PharmD, Doug Humber, PharmD, Marian Renvall, Pat Cal, and Isabella London) are the recipients of the first Team Approaches in Quality Improvement Award for their project “Optimizing Prevention of Hospital-Acquired Venous Thromboembolism.”
Dr. Maynard led the three-year project, which has been implemented at more than 25 sites. Using proven performance-improvement methods and a multidisciplinary team structure, Maynard and his team designed a VTE-prevention protocol for all adult inpatients at their academic center. The protocol integrated a simple VTE risk assessment with a menu of prophylaxis options preferred at each level of risk.
During three years of study, the percentage of patients with adequate VTE prophylaxis regimens increased from 55% to 98%, and the number of patients suffering from hospital-acquired VTE decreased dramatically.
SHM has presented the 2008 Awards of Excellence to four hospitalists and one quality improvement team. Their work and research have contributed significantly to hospital medicine and the betterment of patient care and quality improvement. The winners were recognized at Hospital Medicine 2008.
Award for Clinical Excellence: Kevin O’Leary, MD, associate professor of medicine and the associate chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. O’Leary leads strategic initiatives for the division in his job as associate chief of the Division of Hospital Medicine, especially in patient safety and quality. He also chairs the department’s Quality Management Committee.
An active member of SHM since 2002, Dr. O’Leary has served on the Core Competencies Task Force, the Annual Meeting Planning Committee, and the Annual Meeting Precourse Planning Committee. He also is active in SHM’s Chicago chapter, where he serves as vice president. He serves as an assistant editor for the Journal of Hospital Medicine.
Dr. O’Leary received his bachelor’s inbiology and medical degree from the University of Illinois. He completed his residency at Northwestern University.
Award for Excellence in Research: Peter Lindenauer, MD, MSc, medical director of clinical and quality informatics at Baystate Health in Springfield, Mass., and associate professor of medicine at Tufts University School of Medicine in Boston.
Dr. Lindenauer is responsible for lending the development of an electronic medical record at a large integrated delivery network in western Massachusetts in his job as medical director of clinical and quality informatics.
He has served on technical expert panels for Medicare, patient safety, monitoring systems, and surgical care improvement projects. He also has been a part of the National Quality Forum’s Hospital Quality Measures Development Group and has served on the inpatient functionality work group of the Certifying Committee for Healthcare Information Technology.
As a founding member of SHM, Dr. Lindenauer has served on the society’s board of directors and is a member of the Hospital Quality and Patient Safety Standards Committee.
A graduate of the University of Chicago, Dr. Lindenauer received his bachelor’s in history and received his graduate degree from the Herndon School of Economics and Political Science in Health Planning and Financing. He received his medical degree from the University of Pennsylvania and completed residency training at the University of California, San Francisco.
Award for Excellence in Teaching: Anjala Tess, MD, associate program director for the Internal Medicine Residency Program and director of education for the hospital medicine program, as well as a medical unit director and practicing hospitalist at Beth Israel Deaconess Medical Center in Boston.
Dr. Tess is in charge of the quality improvement teaching program and curriculum for the entire residency program at Beth Israel Deaconess. She also helps oversee the resident elective in hospital medicine and directs educational activities for the group. Her goal is to involve residents in process improvement in the hospital by giving them a hands-on role in quality improvement and peer review.
She has received numerous awards, including the Hermann Blumgart Teaching Award at Beth Israel Deaconess and first prize in SHM’s Innovations Poster Competition.
As an undergraduate, Dr. Tess earned her degree from Brown University, in Rhode Island, and received her medical degree at Washington University’s St. Louis School of Medicine. She completed her residency at Beth Israel Deaconess. She also completed fellowships at Harvard Medical School, the Carl J. Shapiro Institute for Education Research and Beth Israel Deaconess Medical Center.
Award for Outstanding Service in Hospital Medicine: David Zipes, MD, director of pediatric hospitalist service at the Peyton Manning Children’s Hospital in Indianapolis, Ind.
Dr. Zipes oversees all hospitalists and staff, leads strategic planning for the group and the hospital, oversees the business and financial issues of the group and provides general medical direction and leadership of the pediatric units at both the Peyton Manning’s Children’s Hospital and its suburban campus.
As a founding member of SHM, Dr. Zipes is active on its Annual Meeting Planning Committee, Pediatrics Committee, and Pediatrics Core Competencies Task Force. He is also a contributing author for Pediatric Hospital Medicine and the Textbook of Pediatric Hospital Medicine, and a founding member of the annual pediatric hospital medicine meeting.
He also has been the recipient of several awards, including the Family Medicine Teacher of the Year Annual Award (2002, 2005, and 2006) and the St. Vincent Spirit of Caring Award for Service and Dedication to the Hospital (2006 and 2007.)
Dr. Zipes earned his bachelor’s and medical degrees from Indiana University. He completed his residency at Children’s Hospital Medicine Center in Cincinnati, Ohio.
Award for Team Approaches in Quality Improvement: Team Leader, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
Dr. Maynard and his team (Ian Jenkins, MD, Sarah Stone, MD, Josh Lee, MD, Ed Fink, Tim Morris, MD, Peter Fedullo, MD, Robert Schoenhaus, PharmD, Doug Humber, PharmD, Marian Renvall, Pat Cal, and Isabella London) are the recipients of the first Team Approaches in Quality Improvement Award for their project “Optimizing Prevention of Hospital-Acquired Venous Thromboembolism.”
Dr. Maynard led the three-year project, which has been implemented at more than 25 sites. Using proven performance-improvement methods and a multidisciplinary team structure, Maynard and his team designed a VTE-prevention protocol for all adult inpatients at their academic center. The protocol integrated a simple VTE risk assessment with a menu of prophylaxis options preferred at each level of risk.
During three years of study, the percentage of patients with adequate VTE prophylaxis regimens increased from 55% to 98%, and the number of patients suffering from hospital-acquired VTE decreased dramatically.
SHM has presented the 2008 Awards of Excellence to four hospitalists and one quality improvement team. Their work and research have contributed significantly to hospital medicine and the betterment of patient care and quality improvement. The winners were recognized at Hospital Medicine 2008.
Award for Clinical Excellence: Kevin O’Leary, MD, associate professor of medicine and the associate chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. O’Leary leads strategic initiatives for the division in his job as associate chief of the Division of Hospital Medicine, especially in patient safety and quality. He also chairs the department’s Quality Management Committee.
An active member of SHM since 2002, Dr. O’Leary has served on the Core Competencies Task Force, the Annual Meeting Planning Committee, and the Annual Meeting Precourse Planning Committee. He also is active in SHM’s Chicago chapter, where he serves as vice president. He serves as an assistant editor for the Journal of Hospital Medicine.
Dr. O’Leary received his bachelor’s inbiology and medical degree from the University of Illinois. He completed his residency at Northwestern University.
Award for Excellence in Research: Peter Lindenauer, MD, MSc, medical director of clinical and quality informatics at Baystate Health in Springfield, Mass., and associate professor of medicine at Tufts University School of Medicine in Boston.
Dr. Lindenauer is responsible for lending the development of an electronic medical record at a large integrated delivery network in western Massachusetts in his job as medical director of clinical and quality informatics.
He has served on technical expert panels for Medicare, patient safety, monitoring systems, and surgical care improvement projects. He also has been a part of the National Quality Forum’s Hospital Quality Measures Development Group and has served on the inpatient functionality work group of the Certifying Committee for Healthcare Information Technology.
As a founding member of SHM, Dr. Lindenauer has served on the society’s board of directors and is a member of the Hospital Quality and Patient Safety Standards Committee.
A graduate of the University of Chicago, Dr. Lindenauer received his bachelor’s in history and received his graduate degree from the Herndon School of Economics and Political Science in Health Planning and Financing. He received his medical degree from the University of Pennsylvania and completed residency training at the University of California, San Francisco.
Award for Excellence in Teaching: Anjala Tess, MD, associate program director for the Internal Medicine Residency Program and director of education for the hospital medicine program, as well as a medical unit director and practicing hospitalist at Beth Israel Deaconess Medical Center in Boston.
Dr. Tess is in charge of the quality improvement teaching program and curriculum for the entire residency program at Beth Israel Deaconess. She also helps oversee the resident elective in hospital medicine and directs educational activities for the group. Her goal is to involve residents in process improvement in the hospital by giving them a hands-on role in quality improvement and peer review.
She has received numerous awards, including the Hermann Blumgart Teaching Award at Beth Israel Deaconess and first prize in SHM’s Innovations Poster Competition.
As an undergraduate, Dr. Tess earned her degree from Brown University, in Rhode Island, and received her medical degree at Washington University’s St. Louis School of Medicine. She completed her residency at Beth Israel Deaconess. She also completed fellowships at Harvard Medical School, the Carl J. Shapiro Institute for Education Research and Beth Israel Deaconess Medical Center.
Award for Outstanding Service in Hospital Medicine: David Zipes, MD, director of pediatric hospitalist service at the Peyton Manning Children’s Hospital in Indianapolis, Ind.
Dr. Zipes oversees all hospitalists and staff, leads strategic planning for the group and the hospital, oversees the business and financial issues of the group and provides general medical direction and leadership of the pediatric units at both the Peyton Manning’s Children’s Hospital and its suburban campus.
As a founding member of SHM, Dr. Zipes is active on its Annual Meeting Planning Committee, Pediatrics Committee, and Pediatrics Core Competencies Task Force. He is also a contributing author for Pediatric Hospital Medicine and the Textbook of Pediatric Hospital Medicine, and a founding member of the annual pediatric hospital medicine meeting.
He also has been the recipient of several awards, including the Family Medicine Teacher of the Year Annual Award (2002, 2005, and 2006) and the St. Vincent Spirit of Caring Award for Service and Dedication to the Hospital (2006 and 2007.)
Dr. Zipes earned his bachelor’s and medical degrees from Indiana University. He completed his residency at Children’s Hospital Medicine Center in Cincinnati, Ohio.
Award for Team Approaches in Quality Improvement: Team Leader, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
Dr. Maynard and his team (Ian Jenkins, MD, Sarah Stone, MD, Josh Lee, MD, Ed Fink, Tim Morris, MD, Peter Fedullo, MD, Robert Schoenhaus, PharmD, Doug Humber, PharmD, Marian Renvall, Pat Cal, and Isabella London) are the recipients of the first Team Approaches in Quality Improvement Award for their project “Optimizing Prevention of Hospital-Acquired Venous Thromboembolism.”
Dr. Maynard led the three-year project, which has been implemented at more than 25 sites. Using proven performance-improvement methods and a multidisciplinary team structure, Maynard and his team designed a VTE-prevention protocol for all adult inpatients at their academic center. The protocol integrated a simple VTE risk assessment with a menu of prophylaxis options preferred at each level of risk.
During three years of study, the percentage of patients with adequate VTE prophylaxis regimens increased from 55% to 98%, and the number of patients suffering from hospital-acquired VTE decreased dramatically.
Dodging Disaster
I became a hospitalist in the 1980s, in the same year CDs outsold vinyl records for the first time. During the next eight to 10 years, I watched and participated in the growth of hospitalist practices around the country. But, by the late 1990s, a new phenomenon had begun to appear occasionally: failed hospitalist practices. I became interested in the relatively few practices that started up only to fail and dissolve. I wanted to know why they had failed and what happens at a hospital that loses its hospitalist practice?
It is worth remembering that the whole idea of hospitalist practice was more controversial in the late 1990s than it is today. Many doctors saw the concept as an invention of managed care, with the sole aim of reducing costs. When a practice collapsed, some doctors at the institution were usually delighted because, as far as they were concerned, this proved that hospitalist practice was a bad idea. Yet, to the dismay of these critics, the failure of a practice was reliably followed by an intense—sometimes even frenzied—effort to create a new and improved hospitalist practice. In fact, I’m not aware of any institution in which a hospitalist practice failed and a new one didn’t replace it. I suspect such places exist, but they’re not common.
Creating a replacement hospitalist practice is usually stressful and expensive, so of course it’s better to get it right the first time. To that end, I think every institution should be aware of the most common reasons practices fail and should work to avoid these problems. What follows are the issues I’ve seen come up regularly. While they may not cause the failure of a whole practice, they are likely to result in physician dissatisfaction and/or increased turnover.
1) Failure to appreciate rapid growth in volume in a new practice: Unquestionably, this is the most common mistake made by new hospitalist practices. Patient volume often grows dramatically—even within the first weeks a new practice is in operation. Some institutions mistakenly plan on growth rates similar to those experienced in other types of practices. When growth proves much more rapid, the first few hospitalists in the practice can become worn out and might even quit. This has led to the collapse of some practices. There are two ways to guard against this problem. One is to continue recruiting (even with no clear need for additional staff), anticipating the length of time it can take to recruit new hospitalists. In other words, most practices should never stop recruiting.
The other, less desirable but sometimes unavoidable strategy is to have the practice start with a limited scope of work that increases as new hospitalists are added to the group. For example, the practice might accept only unassigned medical admissions from the emergency department (ED) at the outset; once a predetermined number of hospitalists has joined the group, it is ready to start accepting referrals from primary care doctors and other sources.
2) Hospitalists who have an employee mentality, rather than that of a practice owner: Hospitalist practices tend to attract doctors who simply want to see patients, leaving the management of the practice and its financial health to others. This tendency may be exacerbated in practices that compensate hospitalists in a way that is not connected to the overall financial health of the practice (e.g., a straight salary).
Unfortunately, this situation can create a culture in which a hospitalist feels that the only job that is important is to see the next patient. These hospitalists may be reluctant to participate in efforts to ensure the financial health of the practice. Examples: 1) They may not be attentive to optimal documentation and coding, and the practice may lose significant billing revenue; 2) They may not want to accept new referrals or encourage growth in the practice; or 3) They may be too quick to add doctors to the group, with the aim of working fewer hours.
Even if the doctors are employees of a hospital or other large entity, make every effort to encourage them to think of themselves as owners of their practice. One way to create this environment is to have a tight connection between the economic health of the practice and the hospitalists’ income (e.g., production-based incentive compensation). This should lead to greater autonomy in decision-making, as well as hospitalist satisfaction.
3) Poor leadership: Many hospitalist practices start with doctors who have no prior hospitalist experience. This may result in physician leaders poorly suited for their roles. For a practice that is uncertain whether it has an appropriate medical director among the initial doctors it has hired, it might be a good idea to wait a year or two to select the leader. An interim leadership model can be implemented, taking advantage of physician leaders in the hospital, perhaps including the vice president for medical affairs, respected primary care physicians, or emergency physicians. Establishing a hospitalist oversight committee that is made up of leaders among the medical staff can also provide guidance for the new program until there is an effective hospitalist leader in place.
4) Excessive or inappropriate hospitalist overhead: This can take two forms. First, excessive overhead results from securing too much office space and/or staff support. Because the majority of a hospitalist’s work is done on the hospital wards, it is usually sufficient for a hospitalist group to share a single office with enough seating and workstations, including computers, for one-third to one-half of the total number of doctors in the group. For example, a 12-hospitalist group might share an office with four to six workstations. A small group—six or fewer doctors—might function effectively with a single clerical assistant supporting the hospitalists and some other department at the same time.
Second, inappropriate overhead may occur in multispecialty groups that charge hospitalists the same overhead paid by office physicians. This high overhead rate—more than 50%—may leave insufficient funds to pay the hospitalists a competitive salary. Thus, it is important for the group to assess hospitalists’ overhead based on what they actually consume. In general, this should include the cost of billing and collections, malpractice insurance, and modest clerical support. The hospitalist collections should not ordinarily go to support office-based expenses such as support staff and building/equipment expenses.
5) Initial tolerance of inappropriate expectations of hospitalists: To gain support from the medical staff in the early stages of a program, hospitalists sometimes overcommit, assuming responsibility for the scut work that no one wants to perform. This is not a sustainable model. Eventually, it will be hard to tell physicians that they must take back responsibility for something the hospitalists have been doing. This is likely to lead to unhappiness for everyone involved.
One common example of this problem is when hospitalists assume responsibility for tuck-in admissions—those in which the hospitalist admits a physician’s patient overnight and then transfers the patient back to that physician the next day. Another example involves hospitalists who assist with paperwork on patients they did not care for; for example, the hospitalist is expected to do a discharge summary for a heart surgeon, even though the hospitalist wasn’t involved in that particular patient’s care.
The best strategy to use in avoiding this pitfall is to identify the most important services for hospitalists to provide, keeping the list relatively small initially (e.g., admit unassigned emergency medical patients, accept referrals from primary care physicians, and perform consults from other doctors). Other services, such as co-management of some surgical admissions, can be added as hospitalist staffing allows and after hospitalists have had an opportunity to participate in deciding which services are the most appropriate to add.
6) Excessive workload, leading to hospitalist dissatisfaction: A variety of factors can lead to excessive hospitalist workloads or patient volumes. The most common reason (mentioned above) is referral volume that grows faster than staff can be added. In other cases, hospitalists can make the mistake of scheduling each doctor to work relatively few annual days or shifts; this practice results in a high workload for each day worked, even though the annual patient volume may not be excessive.
Hospitalists, like other professionals, seek balance in their jobs. The biggest threat to this goal is an excessive workload, which can hinder a hospitalist’s ability to devote adequate attention to ensuring the satisfaction of the patient and the referring physician. It also limits the hospitalist’s ability to assume non-clinical responsibilities like protocol development and hospital committees. Some data suggest that, at some point, an increasing patient load begins to result in an increased length of stay. And, over time, it is likely to result in poor job satisfaction, burnout, and turnover among physicians in the group.
7) Insufficient financial support: SHM survey data from 2006 show that, in addition to collected professional fees, 97% of hospitalist practices receive financial support and/or services in kind. This money usually comes from the hospital in which the hospitalists work. The few practices that don’t receive such support usually have some combination of the following factors:
- Hospitalists who work only weekday hours;
- Hospitalists who are not responsible for emergency, unassigned patients; and
- A hospital with an excellent payer mix.
Practices that accept all the unassigned medical admissions from the ED and keep a doctor in the hospital 24 hours a day for seven days a week usually have professional fee collections that fall far short of the amount needed to pay competitive salaries. They usually need financial support from a source such as their hospital to supplement their fee collections. Without it, they must maintain high patient volumes to collect professional fee revenue that is adequate to pay reasonable salaries and benefits to the doctors. These practices are at risk of poor performance or collapse.
To Succeed, Avoid Failure
So why go to the trouble of starting over when you can get it right the first time? Setting clear and realistic expectations from the beginning gives any hospitalist practice a better chance of succeeding. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
I became a hospitalist in the 1980s, in the same year CDs outsold vinyl records for the first time. During the next eight to 10 years, I watched and participated in the growth of hospitalist practices around the country. But, by the late 1990s, a new phenomenon had begun to appear occasionally: failed hospitalist practices. I became interested in the relatively few practices that started up only to fail and dissolve. I wanted to know why they had failed and what happens at a hospital that loses its hospitalist practice?
It is worth remembering that the whole idea of hospitalist practice was more controversial in the late 1990s than it is today. Many doctors saw the concept as an invention of managed care, with the sole aim of reducing costs. When a practice collapsed, some doctors at the institution were usually delighted because, as far as they were concerned, this proved that hospitalist practice was a bad idea. Yet, to the dismay of these critics, the failure of a practice was reliably followed by an intense—sometimes even frenzied—effort to create a new and improved hospitalist practice. In fact, I’m not aware of any institution in which a hospitalist practice failed and a new one didn’t replace it. I suspect such places exist, but they’re not common.
Creating a replacement hospitalist practice is usually stressful and expensive, so of course it’s better to get it right the first time. To that end, I think every institution should be aware of the most common reasons practices fail and should work to avoid these problems. What follows are the issues I’ve seen come up regularly. While they may not cause the failure of a whole practice, they are likely to result in physician dissatisfaction and/or increased turnover.
1) Failure to appreciate rapid growth in volume in a new practice: Unquestionably, this is the most common mistake made by new hospitalist practices. Patient volume often grows dramatically—even within the first weeks a new practice is in operation. Some institutions mistakenly plan on growth rates similar to those experienced in other types of practices. When growth proves much more rapid, the first few hospitalists in the practice can become worn out and might even quit. This has led to the collapse of some practices. There are two ways to guard against this problem. One is to continue recruiting (even with no clear need for additional staff), anticipating the length of time it can take to recruit new hospitalists. In other words, most practices should never stop recruiting.
The other, less desirable but sometimes unavoidable strategy is to have the practice start with a limited scope of work that increases as new hospitalists are added to the group. For example, the practice might accept only unassigned medical admissions from the emergency department (ED) at the outset; once a predetermined number of hospitalists has joined the group, it is ready to start accepting referrals from primary care doctors and other sources.
2) Hospitalists who have an employee mentality, rather than that of a practice owner: Hospitalist practices tend to attract doctors who simply want to see patients, leaving the management of the practice and its financial health to others. This tendency may be exacerbated in practices that compensate hospitalists in a way that is not connected to the overall financial health of the practice (e.g., a straight salary).
Unfortunately, this situation can create a culture in which a hospitalist feels that the only job that is important is to see the next patient. These hospitalists may be reluctant to participate in efforts to ensure the financial health of the practice. Examples: 1) They may not be attentive to optimal documentation and coding, and the practice may lose significant billing revenue; 2) They may not want to accept new referrals or encourage growth in the practice; or 3) They may be too quick to add doctors to the group, with the aim of working fewer hours.
Even if the doctors are employees of a hospital or other large entity, make every effort to encourage them to think of themselves as owners of their practice. One way to create this environment is to have a tight connection between the economic health of the practice and the hospitalists’ income (e.g., production-based incentive compensation). This should lead to greater autonomy in decision-making, as well as hospitalist satisfaction.
3) Poor leadership: Many hospitalist practices start with doctors who have no prior hospitalist experience. This may result in physician leaders poorly suited for their roles. For a practice that is uncertain whether it has an appropriate medical director among the initial doctors it has hired, it might be a good idea to wait a year or two to select the leader. An interim leadership model can be implemented, taking advantage of physician leaders in the hospital, perhaps including the vice president for medical affairs, respected primary care physicians, or emergency physicians. Establishing a hospitalist oversight committee that is made up of leaders among the medical staff can also provide guidance for the new program until there is an effective hospitalist leader in place.
4) Excessive or inappropriate hospitalist overhead: This can take two forms. First, excessive overhead results from securing too much office space and/or staff support. Because the majority of a hospitalist’s work is done on the hospital wards, it is usually sufficient for a hospitalist group to share a single office with enough seating and workstations, including computers, for one-third to one-half of the total number of doctors in the group. For example, a 12-hospitalist group might share an office with four to six workstations. A small group—six or fewer doctors—might function effectively with a single clerical assistant supporting the hospitalists and some other department at the same time.
Second, inappropriate overhead may occur in multispecialty groups that charge hospitalists the same overhead paid by office physicians. This high overhead rate—more than 50%—may leave insufficient funds to pay the hospitalists a competitive salary. Thus, it is important for the group to assess hospitalists’ overhead based on what they actually consume. In general, this should include the cost of billing and collections, malpractice insurance, and modest clerical support. The hospitalist collections should not ordinarily go to support office-based expenses such as support staff and building/equipment expenses.
5) Initial tolerance of inappropriate expectations of hospitalists: To gain support from the medical staff in the early stages of a program, hospitalists sometimes overcommit, assuming responsibility for the scut work that no one wants to perform. This is not a sustainable model. Eventually, it will be hard to tell physicians that they must take back responsibility for something the hospitalists have been doing. This is likely to lead to unhappiness for everyone involved.
One common example of this problem is when hospitalists assume responsibility for tuck-in admissions—those in which the hospitalist admits a physician’s patient overnight and then transfers the patient back to that physician the next day. Another example involves hospitalists who assist with paperwork on patients they did not care for; for example, the hospitalist is expected to do a discharge summary for a heart surgeon, even though the hospitalist wasn’t involved in that particular patient’s care.
The best strategy to use in avoiding this pitfall is to identify the most important services for hospitalists to provide, keeping the list relatively small initially (e.g., admit unassigned emergency medical patients, accept referrals from primary care physicians, and perform consults from other doctors). Other services, such as co-management of some surgical admissions, can be added as hospitalist staffing allows and after hospitalists have had an opportunity to participate in deciding which services are the most appropriate to add.
6) Excessive workload, leading to hospitalist dissatisfaction: A variety of factors can lead to excessive hospitalist workloads or patient volumes. The most common reason (mentioned above) is referral volume that grows faster than staff can be added. In other cases, hospitalists can make the mistake of scheduling each doctor to work relatively few annual days or shifts; this practice results in a high workload for each day worked, even though the annual patient volume may not be excessive.
Hospitalists, like other professionals, seek balance in their jobs. The biggest threat to this goal is an excessive workload, which can hinder a hospitalist’s ability to devote adequate attention to ensuring the satisfaction of the patient and the referring physician. It also limits the hospitalist’s ability to assume non-clinical responsibilities like protocol development and hospital committees. Some data suggest that, at some point, an increasing patient load begins to result in an increased length of stay. And, over time, it is likely to result in poor job satisfaction, burnout, and turnover among physicians in the group.
7) Insufficient financial support: SHM survey data from 2006 show that, in addition to collected professional fees, 97% of hospitalist practices receive financial support and/or services in kind. This money usually comes from the hospital in which the hospitalists work. The few practices that don’t receive such support usually have some combination of the following factors:
- Hospitalists who work only weekday hours;
- Hospitalists who are not responsible for emergency, unassigned patients; and
- A hospital with an excellent payer mix.
Practices that accept all the unassigned medical admissions from the ED and keep a doctor in the hospital 24 hours a day for seven days a week usually have professional fee collections that fall far short of the amount needed to pay competitive salaries. They usually need financial support from a source such as their hospital to supplement their fee collections. Without it, they must maintain high patient volumes to collect professional fee revenue that is adequate to pay reasonable salaries and benefits to the doctors. These practices are at risk of poor performance or collapse.
To Succeed, Avoid Failure
So why go to the trouble of starting over when you can get it right the first time? Setting clear and realistic expectations from the beginning gives any hospitalist practice a better chance of succeeding. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
I became a hospitalist in the 1980s, in the same year CDs outsold vinyl records for the first time. During the next eight to 10 years, I watched and participated in the growth of hospitalist practices around the country. But, by the late 1990s, a new phenomenon had begun to appear occasionally: failed hospitalist practices. I became interested in the relatively few practices that started up only to fail and dissolve. I wanted to know why they had failed and what happens at a hospital that loses its hospitalist practice?
It is worth remembering that the whole idea of hospitalist practice was more controversial in the late 1990s than it is today. Many doctors saw the concept as an invention of managed care, with the sole aim of reducing costs. When a practice collapsed, some doctors at the institution were usually delighted because, as far as they were concerned, this proved that hospitalist practice was a bad idea. Yet, to the dismay of these critics, the failure of a practice was reliably followed by an intense—sometimes even frenzied—effort to create a new and improved hospitalist practice. In fact, I’m not aware of any institution in which a hospitalist practice failed and a new one didn’t replace it. I suspect such places exist, but they’re not common.
Creating a replacement hospitalist practice is usually stressful and expensive, so of course it’s better to get it right the first time. To that end, I think every institution should be aware of the most common reasons practices fail and should work to avoid these problems. What follows are the issues I’ve seen come up regularly. While they may not cause the failure of a whole practice, they are likely to result in physician dissatisfaction and/or increased turnover.
1) Failure to appreciate rapid growth in volume in a new practice: Unquestionably, this is the most common mistake made by new hospitalist practices. Patient volume often grows dramatically—even within the first weeks a new practice is in operation. Some institutions mistakenly plan on growth rates similar to those experienced in other types of practices. When growth proves much more rapid, the first few hospitalists in the practice can become worn out and might even quit. This has led to the collapse of some practices. There are two ways to guard against this problem. One is to continue recruiting (even with no clear need for additional staff), anticipating the length of time it can take to recruit new hospitalists. In other words, most practices should never stop recruiting.
The other, less desirable but sometimes unavoidable strategy is to have the practice start with a limited scope of work that increases as new hospitalists are added to the group. For example, the practice might accept only unassigned medical admissions from the emergency department (ED) at the outset; once a predetermined number of hospitalists has joined the group, it is ready to start accepting referrals from primary care doctors and other sources.
2) Hospitalists who have an employee mentality, rather than that of a practice owner: Hospitalist practices tend to attract doctors who simply want to see patients, leaving the management of the practice and its financial health to others. This tendency may be exacerbated in practices that compensate hospitalists in a way that is not connected to the overall financial health of the practice (e.g., a straight salary).
Unfortunately, this situation can create a culture in which a hospitalist feels that the only job that is important is to see the next patient. These hospitalists may be reluctant to participate in efforts to ensure the financial health of the practice. Examples: 1) They may not be attentive to optimal documentation and coding, and the practice may lose significant billing revenue; 2) They may not want to accept new referrals or encourage growth in the practice; or 3) They may be too quick to add doctors to the group, with the aim of working fewer hours.
Even if the doctors are employees of a hospital or other large entity, make every effort to encourage them to think of themselves as owners of their practice. One way to create this environment is to have a tight connection between the economic health of the practice and the hospitalists’ income (e.g., production-based incentive compensation). This should lead to greater autonomy in decision-making, as well as hospitalist satisfaction.
3) Poor leadership: Many hospitalist practices start with doctors who have no prior hospitalist experience. This may result in physician leaders poorly suited for their roles. For a practice that is uncertain whether it has an appropriate medical director among the initial doctors it has hired, it might be a good idea to wait a year or two to select the leader. An interim leadership model can be implemented, taking advantage of physician leaders in the hospital, perhaps including the vice president for medical affairs, respected primary care physicians, or emergency physicians. Establishing a hospitalist oversight committee that is made up of leaders among the medical staff can also provide guidance for the new program until there is an effective hospitalist leader in place.
4) Excessive or inappropriate hospitalist overhead: This can take two forms. First, excessive overhead results from securing too much office space and/or staff support. Because the majority of a hospitalist’s work is done on the hospital wards, it is usually sufficient for a hospitalist group to share a single office with enough seating and workstations, including computers, for one-third to one-half of the total number of doctors in the group. For example, a 12-hospitalist group might share an office with four to six workstations. A small group—six or fewer doctors—might function effectively with a single clerical assistant supporting the hospitalists and some other department at the same time.
Second, inappropriate overhead may occur in multispecialty groups that charge hospitalists the same overhead paid by office physicians. This high overhead rate—more than 50%—may leave insufficient funds to pay the hospitalists a competitive salary. Thus, it is important for the group to assess hospitalists’ overhead based on what they actually consume. In general, this should include the cost of billing and collections, malpractice insurance, and modest clerical support. The hospitalist collections should not ordinarily go to support office-based expenses such as support staff and building/equipment expenses.
5) Initial tolerance of inappropriate expectations of hospitalists: To gain support from the medical staff in the early stages of a program, hospitalists sometimes overcommit, assuming responsibility for the scut work that no one wants to perform. This is not a sustainable model. Eventually, it will be hard to tell physicians that they must take back responsibility for something the hospitalists have been doing. This is likely to lead to unhappiness for everyone involved.
One common example of this problem is when hospitalists assume responsibility for tuck-in admissions—those in which the hospitalist admits a physician’s patient overnight and then transfers the patient back to that physician the next day. Another example involves hospitalists who assist with paperwork on patients they did not care for; for example, the hospitalist is expected to do a discharge summary for a heart surgeon, even though the hospitalist wasn’t involved in that particular patient’s care.
The best strategy to use in avoiding this pitfall is to identify the most important services for hospitalists to provide, keeping the list relatively small initially (e.g., admit unassigned emergency medical patients, accept referrals from primary care physicians, and perform consults from other doctors). Other services, such as co-management of some surgical admissions, can be added as hospitalist staffing allows and after hospitalists have had an opportunity to participate in deciding which services are the most appropriate to add.
6) Excessive workload, leading to hospitalist dissatisfaction: A variety of factors can lead to excessive hospitalist workloads or patient volumes. The most common reason (mentioned above) is referral volume that grows faster than staff can be added. In other cases, hospitalists can make the mistake of scheduling each doctor to work relatively few annual days or shifts; this practice results in a high workload for each day worked, even though the annual patient volume may not be excessive.
Hospitalists, like other professionals, seek balance in their jobs. The biggest threat to this goal is an excessive workload, which can hinder a hospitalist’s ability to devote adequate attention to ensuring the satisfaction of the patient and the referring physician. It also limits the hospitalist’s ability to assume non-clinical responsibilities like protocol development and hospital committees. Some data suggest that, at some point, an increasing patient load begins to result in an increased length of stay. And, over time, it is likely to result in poor job satisfaction, burnout, and turnover among physicians in the group.
7) Insufficient financial support: SHM survey data from 2006 show that, in addition to collected professional fees, 97% of hospitalist practices receive financial support and/or services in kind. This money usually comes from the hospital in which the hospitalists work. The few practices that don’t receive such support usually have some combination of the following factors:
- Hospitalists who work only weekday hours;
- Hospitalists who are not responsible for emergency, unassigned patients; and
- A hospital with an excellent payer mix.
Practices that accept all the unassigned medical admissions from the ED and keep a doctor in the hospital 24 hours a day for seven days a week usually have professional fee collections that fall far short of the amount needed to pay competitive salaries. They usually need financial support from a source such as their hospital to supplement their fee collections. Without it, they must maintain high patient volumes to collect professional fee revenue that is adequate to pay reasonable salaries and benefits to the doctors. These practices are at risk of poor performance or collapse.
To Succeed, Avoid Failure
So why go to the trouble of starting over when you can get it right the first time? Setting clear and realistic expectations from the beginning gives any hospitalist practice a better chance of succeeding. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Big D Births an HM Program
When hospitalists stepped into Parkland Hospital (Dallas) a few months ago, they knew they were taking up a new challenge. Initially, they were known as the doctors without a team in a place where everyone was used to seeing no fewer than six to eight physicians rounding in a group.
Soon our hospitalists realized that a lot of teaching and awareness was needed among the nursing and support staff of the hospital to get them ready for this new breed of physicians.
A Case of Nerves
After four years of administrative planning and developing, the hospitalist program finally started in July 2006. Parkland started a hospitalist program due to the new restrictions on resident work hours and the number of patients a resident can admit. There used to be a considerable delay in the admission process causing patients to wait in our emergency department (ED) for hours until an admitting team could see them. This led to higher patient load in the ED. This load not only affected our patient care adversely, but it also caused considerable financial loss to the hospital because we couldn’t bill for admission until the patients were assigned a bed.
Our hospitalists help ease this overcrowding because they don’t work under these restrictions and can increase the ED throughput of the patients. Parkland also instituted a hospital medicine program to decrease length of stay.
Initially there was a lot of excitement, nervousness, and anxiety about the program. When I say nervousness and anxiety, it was primarily related to the nursing and administrative staff’s skepticism about how they would deal with full-time attending physicians. They wondered whether hospitalists would be easily approachable or not. How would they compare with medical residents?
Fortunately, during the next few months, this anxiety gave way to a new trust between the nurses and the hospitalists as the nurses realized that their concerns were answered promptly. Nursing staff also enjoyed a new benefit: the ability to communicate directly with the attending physicians and, in the process, the potential to play a greater role in the medical management of their patients.
Initially we hired eight hospitalists (actually we started with two because the others were in the process of getting credentialed). We handled the workload in the beginning by limiting the number of admissions each day for each hospitalist until everyone was on board. One hospitalist was already a Parkland doc; the rest were hired from outside.
Details
Like many new hospital medicine programs, Parkland’s hospitalists were venturing into a place where the nursing staff’s involvement in patient care was different from that of their private counterparts.
Background: Parkland Hospital is the main teaching site for the University of Texas Southwestern Medical School and Residency Training Program. The residents and medical students are involved to a great extent in patient care. They assume most patient care responsibilities, including placing PPDs (tuberculosis skin tests), caring for wounds, taking arterial blood gases (ABGs), and removing peripherally inserted central catheter (PICC) lines—to name just a few.
As a result of the residents’ involvement, our nursing staff took a back seat in these aspects of care. But once our hospitalists entered the picture they didn’t have the support of medical students or residents. Therefore, to increase the hospitalists’ efficiency in seeing more patients, the onus of doing those procedures fell on the shoulders of the nursing and paramedic staff. Educating the nursing and paramedical staff to help them regain autonomy and play a great role in patient care was a new challenge for the hospitalists.
We achieved this goal by holding a series of meetings in which physicians, including hospitalists and administrators, worked continuously on these concerns. Also, more operational issues were identified. Among them:
- Giving telephonic verbal orders to nurses for medications, laboratory studies, and radiology procedures, which was not the case with residents;
- Easing restrictions on the use of different medicines that usually require approval of attending faculty for the resident teams; and
- Setting up new dictation lines for our hospitalists (residents have to write their own patient histories and physical assessments).
We resolved to ensure that the program would run like any other private hospitalist program.
Modifications and Scheduling
Other services, including pharmacy, wound care, medical records, and pathology, were also approached by the hospitalists—including the medical director and chief of general internal medicine. The pharmacy was approached to ease restrictions on the medicine prescribed by hospitalists (as opposed to rules for residents, who have to work under different restrictions because they are training.)
Wound-care nurses were asked to implement their orders after telephone approval by the hospitalists (again, this is not the case with resident services). The Medical Records Department created a separate way to handle incomplete medical records for hospitalists—one that takes into account their week-on/week-off schedule. All these requests are now in different phases of approval and implementation.
Overall Parkland has responded well to these changes by appointing senior leadership to fast-track several of these recommendations. Many more policies are under review to complete the transformation from a resident-run model to one that is run by hospitalists.
Scheduling
Like any other new program, the hospitalist program at Parkland went through the growing pains of choosing the right kind of schedule to meet the expectations of the hospital as well as the professional expectations of its doctors. As mentioned above, we currently employ eight hospitalists. Four hospitalists work a week of 12- to 13-hour shifts; they are then off the following week. At that time the other four hospitalists take over for their counterparts. We cover nights using nocturnists.
When the program was not fully staffed there were fewer teams, depending on the number of hospitalists on shift. After the first two hospitalists were hired, we added one team to bring the total number of teams to four. Our teams worked the week-on/week-off schedule. During our initial start-up, the odd-numbered hospitalist who didn’t have a partner to work in week-on/week-off mode worked Monday through Friday each week with weekends covered by one of the main teams.
One of the most important considerations in a hospitalist’s job is the need for flexibility in working hours as compared with the schedule used in a traditional internal medicine practice. At Parkland, hospitalists see 10 to 12 patients in a week. During their week off from patient duties, they are free from all clinical duties and can handle administrative duties, conduct research projects, and accomplish any other tasks awaiting their attention.
Dual Launch Benefits Both Hospitals
At the same time the Parkland Hospital Medicine Program was launched, the Southwestern University also started a hospitalist program at St. Paul University Hospital, Dallas. The Department of Medicine of the University of Texas Southwestern oversees both the programs. All hospitalists are hired by Southwestern University and are part of the Department of General Internal medicine.
The common leadership of both of these programs in the Department of Medicine led to the implementation of a variety of policies derived from the best practices of the two groups. The interaction between these programs has been fruitful. The exchange of physicians credentialed at both hospitals has also reduced the staffing problems that tend to occur due to vacations, holidays, and illness.
Working toward the Future
As we settle down, fully staffed with eight hospitalists, we have started participating in the hospital’s administration by joining various committees. Our hospitalists participate on the pathology clinical advisory committee, the antibiotic committee, the medical reconciliation committee, and the utilization review committee.
Every day brings new challenges and continuous hard work. To make a successful program, it is not only important to grow out of the teething problems, but also to provide exceptional care so that the idea of a hospitalist program is well thought of by the hospital administration. Two of our teething issues included:
- General acceptance of our hospitalists as attending physicians by nursing, support staff, and the other physicians—not as trainees interacting with residents for patient care; and
- Recognition of the distinction between residents who traditionally work under several restrictions as a part of their training as compared with hospitalists who have already undergone training in their field.
Naturally, the hospital wants improvements in both short-term and long-term quality of care. The advantages the hospitalists provide include rendering consistent quality of care, developing new clinical pathways to provide efficient care, and ensuring greater continuity of care.
Regarding specific expectations, for example, SHM advocates 10 to 12 patient encounters per day as adequate. And so we expect our hospitalists to see that number of patients. Other expectations we have:
- That our hospitalists be involved in research projects on patient safety and quality of care; and
- That our hospitalists be involved in developing clinical pathways.
Conclusion
The future of the hospitalist program at Parkland Hospital is bright. As part of the university’s teaching faculty, our hospitalists will be progressively more involved in resident and medical student teaching. As a result, as time goes on, the schedule will have to change in order to provide both continuity of patient care and continuity in the teaching service. While our schedule now works well, we expect to get involved in a resident teaching service to a greater extent, as well as medical consult service and perioperative consult and care. These additional responsibilities may change our schedule.
The hospitalists are actively involved in developing an inpatient curriculum for the residents, along with a new set of standard orders suited to hospitalist practice. Other areas the hospitalists will become more involved in include pre- and perioperative consultations and co-management of surgical and orthopedic patients. We are also working on special hospital projects, focusing on patient safety and hospital efficiency.
The hospitalists at the University of Texas Southwestern put in nothing less than their best efforts. After all, “High achievement always takes place in a framework of high expectation” (Jack Kinder, motivational author). TH
Dr. Mohan is the medical director of the hospital medicine program at Parkland Hospital, Dallas.
When hospitalists stepped into Parkland Hospital (Dallas) a few months ago, they knew they were taking up a new challenge. Initially, they were known as the doctors without a team in a place where everyone was used to seeing no fewer than six to eight physicians rounding in a group.
Soon our hospitalists realized that a lot of teaching and awareness was needed among the nursing and support staff of the hospital to get them ready for this new breed of physicians.
A Case of Nerves
After four years of administrative planning and developing, the hospitalist program finally started in July 2006. Parkland started a hospitalist program due to the new restrictions on resident work hours and the number of patients a resident can admit. There used to be a considerable delay in the admission process causing patients to wait in our emergency department (ED) for hours until an admitting team could see them. This led to higher patient load in the ED. This load not only affected our patient care adversely, but it also caused considerable financial loss to the hospital because we couldn’t bill for admission until the patients were assigned a bed.
Our hospitalists help ease this overcrowding because they don’t work under these restrictions and can increase the ED throughput of the patients. Parkland also instituted a hospital medicine program to decrease length of stay.
Initially there was a lot of excitement, nervousness, and anxiety about the program. When I say nervousness and anxiety, it was primarily related to the nursing and administrative staff’s skepticism about how they would deal with full-time attending physicians. They wondered whether hospitalists would be easily approachable or not. How would they compare with medical residents?
Fortunately, during the next few months, this anxiety gave way to a new trust between the nurses and the hospitalists as the nurses realized that their concerns were answered promptly. Nursing staff also enjoyed a new benefit: the ability to communicate directly with the attending physicians and, in the process, the potential to play a greater role in the medical management of their patients.
Initially we hired eight hospitalists (actually we started with two because the others were in the process of getting credentialed). We handled the workload in the beginning by limiting the number of admissions each day for each hospitalist until everyone was on board. One hospitalist was already a Parkland doc; the rest were hired from outside.
Details
Like many new hospital medicine programs, Parkland’s hospitalists were venturing into a place where the nursing staff’s involvement in patient care was different from that of their private counterparts.
Background: Parkland Hospital is the main teaching site for the University of Texas Southwestern Medical School and Residency Training Program. The residents and medical students are involved to a great extent in patient care. They assume most patient care responsibilities, including placing PPDs (tuberculosis skin tests), caring for wounds, taking arterial blood gases (ABGs), and removing peripherally inserted central catheter (PICC) lines—to name just a few.
As a result of the residents’ involvement, our nursing staff took a back seat in these aspects of care. But once our hospitalists entered the picture they didn’t have the support of medical students or residents. Therefore, to increase the hospitalists’ efficiency in seeing more patients, the onus of doing those procedures fell on the shoulders of the nursing and paramedic staff. Educating the nursing and paramedical staff to help them regain autonomy and play a great role in patient care was a new challenge for the hospitalists.
We achieved this goal by holding a series of meetings in which physicians, including hospitalists and administrators, worked continuously on these concerns. Also, more operational issues were identified. Among them:
- Giving telephonic verbal orders to nurses for medications, laboratory studies, and radiology procedures, which was not the case with residents;
- Easing restrictions on the use of different medicines that usually require approval of attending faculty for the resident teams; and
- Setting up new dictation lines for our hospitalists (residents have to write their own patient histories and physical assessments).
We resolved to ensure that the program would run like any other private hospitalist program.
Modifications and Scheduling
Other services, including pharmacy, wound care, medical records, and pathology, were also approached by the hospitalists—including the medical director and chief of general internal medicine. The pharmacy was approached to ease restrictions on the medicine prescribed by hospitalists (as opposed to rules for residents, who have to work under different restrictions because they are training.)
Wound-care nurses were asked to implement their orders after telephone approval by the hospitalists (again, this is not the case with resident services). The Medical Records Department created a separate way to handle incomplete medical records for hospitalists—one that takes into account their week-on/week-off schedule. All these requests are now in different phases of approval and implementation.
Overall Parkland has responded well to these changes by appointing senior leadership to fast-track several of these recommendations. Many more policies are under review to complete the transformation from a resident-run model to one that is run by hospitalists.
Scheduling
Like any other new program, the hospitalist program at Parkland went through the growing pains of choosing the right kind of schedule to meet the expectations of the hospital as well as the professional expectations of its doctors. As mentioned above, we currently employ eight hospitalists. Four hospitalists work a week of 12- to 13-hour shifts; they are then off the following week. At that time the other four hospitalists take over for their counterparts. We cover nights using nocturnists.
When the program was not fully staffed there were fewer teams, depending on the number of hospitalists on shift. After the first two hospitalists were hired, we added one team to bring the total number of teams to four. Our teams worked the week-on/week-off schedule. During our initial start-up, the odd-numbered hospitalist who didn’t have a partner to work in week-on/week-off mode worked Monday through Friday each week with weekends covered by one of the main teams.
One of the most important considerations in a hospitalist’s job is the need for flexibility in working hours as compared with the schedule used in a traditional internal medicine practice. At Parkland, hospitalists see 10 to 12 patients in a week. During their week off from patient duties, they are free from all clinical duties and can handle administrative duties, conduct research projects, and accomplish any other tasks awaiting their attention.
Dual Launch Benefits Both Hospitals
At the same time the Parkland Hospital Medicine Program was launched, the Southwestern University also started a hospitalist program at St. Paul University Hospital, Dallas. The Department of Medicine of the University of Texas Southwestern oversees both the programs. All hospitalists are hired by Southwestern University and are part of the Department of General Internal medicine.
The common leadership of both of these programs in the Department of Medicine led to the implementation of a variety of policies derived from the best practices of the two groups. The interaction between these programs has been fruitful. The exchange of physicians credentialed at both hospitals has also reduced the staffing problems that tend to occur due to vacations, holidays, and illness.
Working toward the Future
As we settle down, fully staffed with eight hospitalists, we have started participating in the hospital’s administration by joining various committees. Our hospitalists participate on the pathology clinical advisory committee, the antibiotic committee, the medical reconciliation committee, and the utilization review committee.
Every day brings new challenges and continuous hard work. To make a successful program, it is not only important to grow out of the teething problems, but also to provide exceptional care so that the idea of a hospitalist program is well thought of by the hospital administration. Two of our teething issues included:
- General acceptance of our hospitalists as attending physicians by nursing, support staff, and the other physicians—not as trainees interacting with residents for patient care; and
- Recognition of the distinction between residents who traditionally work under several restrictions as a part of their training as compared with hospitalists who have already undergone training in their field.
Naturally, the hospital wants improvements in both short-term and long-term quality of care. The advantages the hospitalists provide include rendering consistent quality of care, developing new clinical pathways to provide efficient care, and ensuring greater continuity of care.
Regarding specific expectations, for example, SHM advocates 10 to 12 patient encounters per day as adequate. And so we expect our hospitalists to see that number of patients. Other expectations we have:
- That our hospitalists be involved in research projects on patient safety and quality of care; and
- That our hospitalists be involved in developing clinical pathways.
Conclusion
The future of the hospitalist program at Parkland Hospital is bright. As part of the university’s teaching faculty, our hospitalists will be progressively more involved in resident and medical student teaching. As a result, as time goes on, the schedule will have to change in order to provide both continuity of patient care and continuity in the teaching service. While our schedule now works well, we expect to get involved in a resident teaching service to a greater extent, as well as medical consult service and perioperative consult and care. These additional responsibilities may change our schedule.
The hospitalists are actively involved in developing an inpatient curriculum for the residents, along with a new set of standard orders suited to hospitalist practice. Other areas the hospitalists will become more involved in include pre- and perioperative consultations and co-management of surgical and orthopedic patients. We are also working on special hospital projects, focusing on patient safety and hospital efficiency.
The hospitalists at the University of Texas Southwestern put in nothing less than their best efforts. After all, “High achievement always takes place in a framework of high expectation” (Jack Kinder, motivational author). TH
Dr. Mohan is the medical director of the hospital medicine program at Parkland Hospital, Dallas.
When hospitalists stepped into Parkland Hospital (Dallas) a few months ago, they knew they were taking up a new challenge. Initially, they were known as the doctors without a team in a place where everyone was used to seeing no fewer than six to eight physicians rounding in a group.
Soon our hospitalists realized that a lot of teaching and awareness was needed among the nursing and support staff of the hospital to get them ready for this new breed of physicians.
A Case of Nerves
After four years of administrative planning and developing, the hospitalist program finally started in July 2006. Parkland started a hospitalist program due to the new restrictions on resident work hours and the number of patients a resident can admit. There used to be a considerable delay in the admission process causing patients to wait in our emergency department (ED) for hours until an admitting team could see them. This led to higher patient load in the ED. This load not only affected our patient care adversely, but it also caused considerable financial loss to the hospital because we couldn’t bill for admission until the patients were assigned a bed.
Our hospitalists help ease this overcrowding because they don’t work under these restrictions and can increase the ED throughput of the patients. Parkland also instituted a hospital medicine program to decrease length of stay.
Initially there was a lot of excitement, nervousness, and anxiety about the program. When I say nervousness and anxiety, it was primarily related to the nursing and administrative staff’s skepticism about how they would deal with full-time attending physicians. They wondered whether hospitalists would be easily approachable or not. How would they compare with medical residents?
Fortunately, during the next few months, this anxiety gave way to a new trust between the nurses and the hospitalists as the nurses realized that their concerns were answered promptly. Nursing staff also enjoyed a new benefit: the ability to communicate directly with the attending physicians and, in the process, the potential to play a greater role in the medical management of their patients.
Initially we hired eight hospitalists (actually we started with two because the others were in the process of getting credentialed). We handled the workload in the beginning by limiting the number of admissions each day for each hospitalist until everyone was on board. One hospitalist was already a Parkland doc; the rest were hired from outside.
Details
Like many new hospital medicine programs, Parkland’s hospitalists were venturing into a place where the nursing staff’s involvement in patient care was different from that of their private counterparts.
Background: Parkland Hospital is the main teaching site for the University of Texas Southwestern Medical School and Residency Training Program. The residents and medical students are involved to a great extent in patient care. They assume most patient care responsibilities, including placing PPDs (tuberculosis skin tests), caring for wounds, taking arterial blood gases (ABGs), and removing peripherally inserted central catheter (PICC) lines—to name just a few.
As a result of the residents’ involvement, our nursing staff took a back seat in these aspects of care. But once our hospitalists entered the picture they didn’t have the support of medical students or residents. Therefore, to increase the hospitalists’ efficiency in seeing more patients, the onus of doing those procedures fell on the shoulders of the nursing and paramedic staff. Educating the nursing and paramedical staff to help them regain autonomy and play a great role in patient care was a new challenge for the hospitalists.
We achieved this goal by holding a series of meetings in which physicians, including hospitalists and administrators, worked continuously on these concerns. Also, more operational issues were identified. Among them:
- Giving telephonic verbal orders to nurses for medications, laboratory studies, and radiology procedures, which was not the case with residents;
- Easing restrictions on the use of different medicines that usually require approval of attending faculty for the resident teams; and
- Setting up new dictation lines for our hospitalists (residents have to write their own patient histories and physical assessments).
We resolved to ensure that the program would run like any other private hospitalist program.
Modifications and Scheduling
Other services, including pharmacy, wound care, medical records, and pathology, were also approached by the hospitalists—including the medical director and chief of general internal medicine. The pharmacy was approached to ease restrictions on the medicine prescribed by hospitalists (as opposed to rules for residents, who have to work under different restrictions because they are training.)
Wound-care nurses were asked to implement their orders after telephone approval by the hospitalists (again, this is not the case with resident services). The Medical Records Department created a separate way to handle incomplete medical records for hospitalists—one that takes into account their week-on/week-off schedule. All these requests are now in different phases of approval and implementation.
Overall Parkland has responded well to these changes by appointing senior leadership to fast-track several of these recommendations. Many more policies are under review to complete the transformation from a resident-run model to one that is run by hospitalists.
Scheduling
Like any other new program, the hospitalist program at Parkland went through the growing pains of choosing the right kind of schedule to meet the expectations of the hospital as well as the professional expectations of its doctors. As mentioned above, we currently employ eight hospitalists. Four hospitalists work a week of 12- to 13-hour shifts; they are then off the following week. At that time the other four hospitalists take over for their counterparts. We cover nights using nocturnists.
When the program was not fully staffed there were fewer teams, depending on the number of hospitalists on shift. After the first two hospitalists were hired, we added one team to bring the total number of teams to four. Our teams worked the week-on/week-off schedule. During our initial start-up, the odd-numbered hospitalist who didn’t have a partner to work in week-on/week-off mode worked Monday through Friday each week with weekends covered by one of the main teams.
One of the most important considerations in a hospitalist’s job is the need for flexibility in working hours as compared with the schedule used in a traditional internal medicine practice. At Parkland, hospitalists see 10 to 12 patients in a week. During their week off from patient duties, they are free from all clinical duties and can handle administrative duties, conduct research projects, and accomplish any other tasks awaiting their attention.
Dual Launch Benefits Both Hospitals
At the same time the Parkland Hospital Medicine Program was launched, the Southwestern University also started a hospitalist program at St. Paul University Hospital, Dallas. The Department of Medicine of the University of Texas Southwestern oversees both the programs. All hospitalists are hired by Southwestern University and are part of the Department of General Internal medicine.
The common leadership of both of these programs in the Department of Medicine led to the implementation of a variety of policies derived from the best practices of the two groups. The interaction between these programs has been fruitful. The exchange of physicians credentialed at both hospitals has also reduced the staffing problems that tend to occur due to vacations, holidays, and illness.
Working toward the Future
As we settle down, fully staffed with eight hospitalists, we have started participating in the hospital’s administration by joining various committees. Our hospitalists participate on the pathology clinical advisory committee, the antibiotic committee, the medical reconciliation committee, and the utilization review committee.
Every day brings new challenges and continuous hard work. To make a successful program, it is not only important to grow out of the teething problems, but also to provide exceptional care so that the idea of a hospitalist program is well thought of by the hospital administration. Two of our teething issues included:
- General acceptance of our hospitalists as attending physicians by nursing, support staff, and the other physicians—not as trainees interacting with residents for patient care; and
- Recognition of the distinction between residents who traditionally work under several restrictions as a part of their training as compared with hospitalists who have already undergone training in their field.
Naturally, the hospital wants improvements in both short-term and long-term quality of care. The advantages the hospitalists provide include rendering consistent quality of care, developing new clinical pathways to provide efficient care, and ensuring greater continuity of care.
Regarding specific expectations, for example, SHM advocates 10 to 12 patient encounters per day as adequate. And so we expect our hospitalists to see that number of patients. Other expectations we have:
- That our hospitalists be involved in research projects on patient safety and quality of care; and
- That our hospitalists be involved in developing clinical pathways.
Conclusion
The future of the hospitalist program at Parkland Hospital is bright. As part of the university’s teaching faculty, our hospitalists will be progressively more involved in resident and medical student teaching. As a result, as time goes on, the schedule will have to change in order to provide both continuity of patient care and continuity in the teaching service. While our schedule now works well, we expect to get involved in a resident teaching service to a greater extent, as well as medical consult service and perioperative consult and care. These additional responsibilities may change our schedule.
The hospitalists are actively involved in developing an inpatient curriculum for the residents, along with a new set of standard orders suited to hospitalist practice. Other areas the hospitalists will become more involved in include pre- and perioperative consultations and co-management of surgical and orthopedic patients. We are also working on special hospital projects, focusing on patient safety and hospital efficiency.
The hospitalists at the University of Texas Southwestern put in nothing less than their best efforts. After all, “High achievement always takes place in a framework of high expectation” (Jack Kinder, motivational author). TH
Dr. Mohan is the medical director of the hospital medicine program at Parkland Hospital, Dallas.
Town & Gown
Centers of academia and learning have been physically located within urban communities since the time of the ancient Greeks. During the Middle Ages, church-supported universities were established in Italian cities, in Paris, and in Britain at Oxford. Typically, the university community resided in a sequestered segment of the city. As a result of financial endowment and protection granted by the Church, they were largely independent of civil laws and regulations.
In the Middle Ages, students and teachers wore gowns over their attire for warmth in the drafty libraries as well as to identify themselves as scholars; hence the distinction of “town,” a term referring to the townspeople, from “gown,” the people associated with the university.1 For a host of reasons, the traditional relationship between the local community and associated centers of academia has been one of suspicion and hostility.
Establishing Alliances
Over the years, better communication and cooperation between the academic communities and their host cities has eased some of these tensions and—in some cases—has resulted in positive and cordial relationships. Some academic institutions endeavor to contribute to the general community by providing access to evening study events and lectures and by inviting the community to participate in fine arts performances.
These overtures are welcome, but it is important to recognize the potential for universities to exert a dominating influence within a community. The impact of a university on the local community can vary, depending on the size and reputation of the university as well as the size of the town. A large, powerful university has a more profound influence when it is located in a moderate-size city (one with a population less than 250,000) than if it is located in a major metropolitan community. In this situation, the onus is upon the university to recognize its position with respect to the local community and its obligation to contribute to the general societal good.
Most universities recognize the value of establishing strong alliances and trusting relationships with their host communities. Located in Gainesville, Fla., a city with a population of 186,000, the University of Florida is a large university with a major medical school and a 576-bed teaching hospital. In response to community concerns about neighborhood issues, the university’s president appointed a University of Florida Town/Gown Task Force to identify problems and make recommendations to initiate change.2 The task force members included individuals representing the student body, the university faculty, and various representatives of the local community.
Other universities also recognize the importance of working together for the common good. Situated in a town of 13,000, South Carolina’s Clemson University, which has 17,100 students, developed a town-and-gown symposium in 2006 called Community Is a Contact Sport: Universities and Cities Reaching Common Ground. Designed to address neighborhood issues, it also provided a forum for concerns, as well as an opportunity for conflict resolution (www.clemson.edu/town-gown).
From Concern to Conflict
The conflict escalates on multiple levels when town-and-gown issues are set in the context of academic versus private practice medicine. University physicians and community doctors compete for the same patient population. Primary care physicians across the country have complained that when they refer their patients to academic teaching hospitals for specialized care, the patients are absorbed by the university hospitals. They complain that they are not afforded the courtesy of a follow-up letter, nor does the patient return to their care when the acute event is resolved.3 Private practice physicians and community-based hospitals provide important services and are necessary within any community. When the local, private medical community becomes concerned that a university-based medical center seeks to usurp their patients and their livelihood, a heated conflict may ensue.
University-based, research-oriented academic medical centers, with training programs involved in cutting edge technology and highly specialized patient care services, are clearly a positive adjunct to any local community’s—or state’s, for that matter—capability to provide top-notch patient care and services. No one can deny the benefits afforded by this level of expertise. Problems arise when university-based medical centers set a powerful and lustful gaze upon the medical community at large.
During the 1990s, large medical centers across the country bought up community hospitals and medical practices. At that time, and continuing into the present, office overhead—building costs, liability insurance, personnel costs—for private practice groups has often exceeded the ability of these primary care groups to survive. Not unexpectedly, once incorporated into the system, these practices are used to support the subspecialty services at the university medical center, bypassing the community-based subspecialty physicians.
Additionally, large, academic medical centers set up funded and university-supported subspecialty groups that compete head-on with independent practitioners. Private practitioners view these circumstances as stacked competition. The primary-care doctor’s decision in selecting a subspecialty doctor for a patient is no longer based on service, timeliness, and competence, but is instead a result of proscribed referral patterns delineated by the academic institution. Discriminatory referral patterns—not based on merit—result in local discontent, frustration, and unhealthy competition.
Short-Term Savings, Long-Term Loss
These issues are complex. A case can always be made to consolidate resources at the university hospital and avoid duplication of services by stripping away departments in the community hospitals. If pursued to its logical end, this operational model effectively starves community hospitals until they evolve into low acuity, “feeder” stations for the main academic hospital facility. On paper, this plan presents economic advantages. In practice, it not only deprives the metropolitan area of community-based hospital options, but it also results in a dwindling population base and the general decline and disenchantment of the local medical community. As the medical community contracts, so does the patient-base referral radius.
University-owned community hospitals are subject to the discretion of the university medical center. Decision making is attributed to maximum utilization of resources and certification of need, but most observers see the basic principle as economic: ways of garnering a larger portion of the healthcare dollar in the university coffers. Services and even departments provided by community hospitals are likewise subject to the benevolence of the university medical system. Hospitals function like living organisms: If a department such as pediatrics is withdrawn, the hospital continues—but with a limp. Few children can be seen and evaluated in the emergency department; likewise, high-risk obstetrics must be transferred to a major university hospital because the patient may need a neonatal intensive care unit. Hospitalists and internists who happen to be double boarded in medicine and pediatrics steer away from hospitals without a pediatric department. The changes are subtle but, over time, the effects of the loss are apparent.
Hospitalists need to be cognizant of these issues when pursuing employment opportunities. Many career-minded hospitalists seek employment in community-based, full-service hospitals with university medical center affiliations. This combination can provide the best of both worlds: autonomy, opportunities for growth and development, and opportunities for working with house staff and teaching. Checking the status of the relationship between the community hospital and the affiliated university medical center may be an important factor in pre-contract negotiations and decision-making for career hospitalists.
The Bottom Line
The turf battle between community medicine and academic medicine is primarily one of economics. Interesting parallels may be drawn between this conflict and the teachings of Adam Smith. Prior to Smith, economic theory was based on the idea that every dollar you have is one less dollar for me. Smith proposed an entirely different concept: If I help you earn dollars, the economic house will grow, and I, too, will make more dollars, and then you will make more dollars. In this way, the entire system generates more than anyone could have previously imagined. This economic concept extrapolates well to the present discussion of the university medical center versus community medicine.
University health systems do not seem to realize that real growth happens when communities grow together. A robust and vibrant community hospital supports a university medical center with more vigor than an anemic, waning, and disenchanted community hospital that perceives its woes as a result of the powerful—and perhaps dogmatic—university health system. There are enough patients to grow both systems together—the patient base radius grows wider with cooperation and growth—but this cannot happen if the university engenders distrust among local practitioners and the local community. This is a situation that will either be win-win or lose-lose.
Although the crux of the conflict is economic, other aspects of town-and-gown medicine can contribute to better cooperation and understanding. Some academic medical centers have explored ways to incorporate local physicians in university-based clinical trials. These programs offer cutting edge medicine and an opportunity to participate in intellectually stimulating work; at the same time, physicians retain their private practices.
This research opportunity is being offered and supported by a number of academic institutions, including Columbia-Presbyterian in New York City, Duke in Durham, N.C., Partners HealthCare in Boston, the University of Pittsburgh, the University of Rochester (N.Y.), and Washington University (St. Louis, Mo.).4 This is a good-faith start in mending the relationship between the academic and private medical sectors. To achieve a lasting positive relationship, community physicians must trust the academic community to respect their autonomy and to recognize that they have the right to provide full-service care to their patients and to serve their patients without the fear of being unfairly disenfranchised.
The lack of integration of the academic medical community and private practitioners of medicine—the proverbial town and gown—is an old dilemma. It is time to lay it to rest. The solutions are straightforward. Empowering community hospitals and physicians will not diminish the influence of university-based hospitals, nor will there be loss of reimbursement. Just the opposite will occur. In the end, with cooperation, everyone wins; with adversarial actions, all parties lose, especially the patients. TH
Dr. Brezina is a member of the consulting clinical faculty at Duke University, Durham, N.C.
References
- Town and gown in the Middle Ages. Available at: http://en.wikipedia.org/wiki/Town_and_gown. Last accessed March 29, 2007.
- University of Florida Web site. Town/gown task force. Available at: www.facilities.ufl.edu/cp/towngown.htm. Last accessed March 29, 2007.
- Adams D, Croasdale M. Town and gown: turning rivalries into relationships [American Medical News Web site]. January 13, 2003. Available at: www.ama-assn.org/amednews/2003/01/13/prsa0113.htm. Last accessed March 20, 2007.
- Maguire P. Marriage of town and gown brings clinical research to busy practices [ACP-ASIM Observer Web site]. February 2001. Available at: www.acponline.org/journals/news/feb01/clinresearch.htm. Last accessed March 20, 2007.
Centers of academia and learning have been physically located within urban communities since the time of the ancient Greeks. During the Middle Ages, church-supported universities were established in Italian cities, in Paris, and in Britain at Oxford. Typically, the university community resided in a sequestered segment of the city. As a result of financial endowment and protection granted by the Church, they were largely independent of civil laws and regulations.
In the Middle Ages, students and teachers wore gowns over their attire for warmth in the drafty libraries as well as to identify themselves as scholars; hence the distinction of “town,” a term referring to the townspeople, from “gown,” the people associated with the university.1 For a host of reasons, the traditional relationship between the local community and associated centers of academia has been one of suspicion and hostility.
Establishing Alliances
Over the years, better communication and cooperation between the academic communities and their host cities has eased some of these tensions and—in some cases—has resulted in positive and cordial relationships. Some academic institutions endeavor to contribute to the general community by providing access to evening study events and lectures and by inviting the community to participate in fine arts performances.
These overtures are welcome, but it is important to recognize the potential for universities to exert a dominating influence within a community. The impact of a university on the local community can vary, depending on the size and reputation of the university as well as the size of the town. A large, powerful university has a more profound influence when it is located in a moderate-size city (one with a population less than 250,000) than if it is located in a major metropolitan community. In this situation, the onus is upon the university to recognize its position with respect to the local community and its obligation to contribute to the general societal good.
Most universities recognize the value of establishing strong alliances and trusting relationships with their host communities. Located in Gainesville, Fla., a city with a population of 186,000, the University of Florida is a large university with a major medical school and a 576-bed teaching hospital. In response to community concerns about neighborhood issues, the university’s president appointed a University of Florida Town/Gown Task Force to identify problems and make recommendations to initiate change.2 The task force members included individuals representing the student body, the university faculty, and various representatives of the local community.
Other universities also recognize the importance of working together for the common good. Situated in a town of 13,000, South Carolina’s Clemson University, which has 17,100 students, developed a town-and-gown symposium in 2006 called Community Is a Contact Sport: Universities and Cities Reaching Common Ground. Designed to address neighborhood issues, it also provided a forum for concerns, as well as an opportunity for conflict resolution (www.clemson.edu/town-gown).
From Concern to Conflict
The conflict escalates on multiple levels when town-and-gown issues are set in the context of academic versus private practice medicine. University physicians and community doctors compete for the same patient population. Primary care physicians across the country have complained that when they refer their patients to academic teaching hospitals for specialized care, the patients are absorbed by the university hospitals. They complain that they are not afforded the courtesy of a follow-up letter, nor does the patient return to their care when the acute event is resolved.3 Private practice physicians and community-based hospitals provide important services and are necessary within any community. When the local, private medical community becomes concerned that a university-based medical center seeks to usurp their patients and their livelihood, a heated conflict may ensue.
University-based, research-oriented academic medical centers, with training programs involved in cutting edge technology and highly specialized patient care services, are clearly a positive adjunct to any local community’s—or state’s, for that matter—capability to provide top-notch patient care and services. No one can deny the benefits afforded by this level of expertise. Problems arise when university-based medical centers set a powerful and lustful gaze upon the medical community at large.
During the 1990s, large medical centers across the country bought up community hospitals and medical practices. At that time, and continuing into the present, office overhead—building costs, liability insurance, personnel costs—for private practice groups has often exceeded the ability of these primary care groups to survive. Not unexpectedly, once incorporated into the system, these practices are used to support the subspecialty services at the university medical center, bypassing the community-based subspecialty physicians.
Additionally, large, academic medical centers set up funded and university-supported subspecialty groups that compete head-on with independent practitioners. Private practitioners view these circumstances as stacked competition. The primary-care doctor’s decision in selecting a subspecialty doctor for a patient is no longer based on service, timeliness, and competence, but is instead a result of proscribed referral patterns delineated by the academic institution. Discriminatory referral patterns—not based on merit—result in local discontent, frustration, and unhealthy competition.
Short-Term Savings, Long-Term Loss
These issues are complex. A case can always be made to consolidate resources at the university hospital and avoid duplication of services by stripping away departments in the community hospitals. If pursued to its logical end, this operational model effectively starves community hospitals until they evolve into low acuity, “feeder” stations for the main academic hospital facility. On paper, this plan presents economic advantages. In practice, it not only deprives the metropolitan area of community-based hospital options, but it also results in a dwindling population base and the general decline and disenchantment of the local medical community. As the medical community contracts, so does the patient-base referral radius.
University-owned community hospitals are subject to the discretion of the university medical center. Decision making is attributed to maximum utilization of resources and certification of need, but most observers see the basic principle as economic: ways of garnering a larger portion of the healthcare dollar in the university coffers. Services and even departments provided by community hospitals are likewise subject to the benevolence of the university medical system. Hospitals function like living organisms: If a department such as pediatrics is withdrawn, the hospital continues—but with a limp. Few children can be seen and evaluated in the emergency department; likewise, high-risk obstetrics must be transferred to a major university hospital because the patient may need a neonatal intensive care unit. Hospitalists and internists who happen to be double boarded in medicine and pediatrics steer away from hospitals without a pediatric department. The changes are subtle but, over time, the effects of the loss are apparent.
Hospitalists need to be cognizant of these issues when pursuing employment opportunities. Many career-minded hospitalists seek employment in community-based, full-service hospitals with university medical center affiliations. This combination can provide the best of both worlds: autonomy, opportunities for growth and development, and opportunities for working with house staff and teaching. Checking the status of the relationship between the community hospital and the affiliated university medical center may be an important factor in pre-contract negotiations and decision-making for career hospitalists.
The Bottom Line
The turf battle between community medicine and academic medicine is primarily one of economics. Interesting parallels may be drawn between this conflict and the teachings of Adam Smith. Prior to Smith, economic theory was based on the idea that every dollar you have is one less dollar for me. Smith proposed an entirely different concept: If I help you earn dollars, the economic house will grow, and I, too, will make more dollars, and then you will make more dollars. In this way, the entire system generates more than anyone could have previously imagined. This economic concept extrapolates well to the present discussion of the university medical center versus community medicine.
University health systems do not seem to realize that real growth happens when communities grow together. A robust and vibrant community hospital supports a university medical center with more vigor than an anemic, waning, and disenchanted community hospital that perceives its woes as a result of the powerful—and perhaps dogmatic—university health system. There are enough patients to grow both systems together—the patient base radius grows wider with cooperation and growth—but this cannot happen if the university engenders distrust among local practitioners and the local community. This is a situation that will either be win-win or lose-lose.
Although the crux of the conflict is economic, other aspects of town-and-gown medicine can contribute to better cooperation and understanding. Some academic medical centers have explored ways to incorporate local physicians in university-based clinical trials. These programs offer cutting edge medicine and an opportunity to participate in intellectually stimulating work; at the same time, physicians retain their private practices.
This research opportunity is being offered and supported by a number of academic institutions, including Columbia-Presbyterian in New York City, Duke in Durham, N.C., Partners HealthCare in Boston, the University of Pittsburgh, the University of Rochester (N.Y.), and Washington University (St. Louis, Mo.).4 This is a good-faith start in mending the relationship between the academic and private medical sectors. To achieve a lasting positive relationship, community physicians must trust the academic community to respect their autonomy and to recognize that they have the right to provide full-service care to their patients and to serve their patients without the fear of being unfairly disenfranchised.
The lack of integration of the academic medical community and private practitioners of medicine—the proverbial town and gown—is an old dilemma. It is time to lay it to rest. The solutions are straightforward. Empowering community hospitals and physicians will not diminish the influence of university-based hospitals, nor will there be loss of reimbursement. Just the opposite will occur. In the end, with cooperation, everyone wins; with adversarial actions, all parties lose, especially the patients. TH
Dr. Brezina is a member of the consulting clinical faculty at Duke University, Durham, N.C.
References
- Town and gown in the Middle Ages. Available at: http://en.wikipedia.org/wiki/Town_and_gown. Last accessed March 29, 2007.
- University of Florida Web site. Town/gown task force. Available at: www.facilities.ufl.edu/cp/towngown.htm. Last accessed March 29, 2007.
- Adams D, Croasdale M. Town and gown: turning rivalries into relationships [American Medical News Web site]. January 13, 2003. Available at: www.ama-assn.org/amednews/2003/01/13/prsa0113.htm. Last accessed March 20, 2007.
- Maguire P. Marriage of town and gown brings clinical research to busy practices [ACP-ASIM Observer Web site]. February 2001. Available at: www.acponline.org/journals/news/feb01/clinresearch.htm. Last accessed March 20, 2007.
Centers of academia and learning have been physically located within urban communities since the time of the ancient Greeks. During the Middle Ages, church-supported universities were established in Italian cities, in Paris, and in Britain at Oxford. Typically, the university community resided in a sequestered segment of the city. As a result of financial endowment and protection granted by the Church, they were largely independent of civil laws and regulations.
In the Middle Ages, students and teachers wore gowns over their attire for warmth in the drafty libraries as well as to identify themselves as scholars; hence the distinction of “town,” a term referring to the townspeople, from “gown,” the people associated with the university.1 For a host of reasons, the traditional relationship between the local community and associated centers of academia has been one of suspicion and hostility.
Establishing Alliances
Over the years, better communication and cooperation between the academic communities and their host cities has eased some of these tensions and—in some cases—has resulted in positive and cordial relationships. Some academic institutions endeavor to contribute to the general community by providing access to evening study events and lectures and by inviting the community to participate in fine arts performances.
These overtures are welcome, but it is important to recognize the potential for universities to exert a dominating influence within a community. The impact of a university on the local community can vary, depending on the size and reputation of the university as well as the size of the town. A large, powerful university has a more profound influence when it is located in a moderate-size city (one with a population less than 250,000) than if it is located in a major metropolitan community. In this situation, the onus is upon the university to recognize its position with respect to the local community and its obligation to contribute to the general societal good.
Most universities recognize the value of establishing strong alliances and trusting relationships with their host communities. Located in Gainesville, Fla., a city with a population of 186,000, the University of Florida is a large university with a major medical school and a 576-bed teaching hospital. In response to community concerns about neighborhood issues, the university’s president appointed a University of Florida Town/Gown Task Force to identify problems and make recommendations to initiate change.2 The task force members included individuals representing the student body, the university faculty, and various representatives of the local community.
Other universities also recognize the importance of working together for the common good. Situated in a town of 13,000, South Carolina’s Clemson University, which has 17,100 students, developed a town-and-gown symposium in 2006 called Community Is a Contact Sport: Universities and Cities Reaching Common Ground. Designed to address neighborhood issues, it also provided a forum for concerns, as well as an opportunity for conflict resolution (www.clemson.edu/town-gown).
From Concern to Conflict
The conflict escalates on multiple levels when town-and-gown issues are set in the context of academic versus private practice medicine. University physicians and community doctors compete for the same patient population. Primary care physicians across the country have complained that when they refer their patients to academic teaching hospitals for specialized care, the patients are absorbed by the university hospitals. They complain that they are not afforded the courtesy of a follow-up letter, nor does the patient return to their care when the acute event is resolved.3 Private practice physicians and community-based hospitals provide important services and are necessary within any community. When the local, private medical community becomes concerned that a university-based medical center seeks to usurp their patients and their livelihood, a heated conflict may ensue.
University-based, research-oriented academic medical centers, with training programs involved in cutting edge technology and highly specialized patient care services, are clearly a positive adjunct to any local community’s—or state’s, for that matter—capability to provide top-notch patient care and services. No one can deny the benefits afforded by this level of expertise. Problems arise when university-based medical centers set a powerful and lustful gaze upon the medical community at large.
During the 1990s, large medical centers across the country bought up community hospitals and medical practices. At that time, and continuing into the present, office overhead—building costs, liability insurance, personnel costs—for private practice groups has often exceeded the ability of these primary care groups to survive. Not unexpectedly, once incorporated into the system, these practices are used to support the subspecialty services at the university medical center, bypassing the community-based subspecialty physicians.
Additionally, large, academic medical centers set up funded and university-supported subspecialty groups that compete head-on with independent practitioners. Private practitioners view these circumstances as stacked competition. The primary-care doctor’s decision in selecting a subspecialty doctor for a patient is no longer based on service, timeliness, and competence, but is instead a result of proscribed referral patterns delineated by the academic institution. Discriminatory referral patterns—not based on merit—result in local discontent, frustration, and unhealthy competition.
Short-Term Savings, Long-Term Loss
These issues are complex. A case can always be made to consolidate resources at the university hospital and avoid duplication of services by stripping away departments in the community hospitals. If pursued to its logical end, this operational model effectively starves community hospitals until they evolve into low acuity, “feeder” stations for the main academic hospital facility. On paper, this plan presents economic advantages. In practice, it not only deprives the metropolitan area of community-based hospital options, but it also results in a dwindling population base and the general decline and disenchantment of the local medical community. As the medical community contracts, so does the patient-base referral radius.
University-owned community hospitals are subject to the discretion of the university medical center. Decision making is attributed to maximum utilization of resources and certification of need, but most observers see the basic principle as economic: ways of garnering a larger portion of the healthcare dollar in the university coffers. Services and even departments provided by community hospitals are likewise subject to the benevolence of the university medical system. Hospitals function like living organisms: If a department such as pediatrics is withdrawn, the hospital continues—but with a limp. Few children can be seen and evaluated in the emergency department; likewise, high-risk obstetrics must be transferred to a major university hospital because the patient may need a neonatal intensive care unit. Hospitalists and internists who happen to be double boarded in medicine and pediatrics steer away from hospitals without a pediatric department. The changes are subtle but, over time, the effects of the loss are apparent.
Hospitalists need to be cognizant of these issues when pursuing employment opportunities. Many career-minded hospitalists seek employment in community-based, full-service hospitals with university medical center affiliations. This combination can provide the best of both worlds: autonomy, opportunities for growth and development, and opportunities for working with house staff and teaching. Checking the status of the relationship between the community hospital and the affiliated university medical center may be an important factor in pre-contract negotiations and decision-making for career hospitalists.
The Bottom Line
The turf battle between community medicine and academic medicine is primarily one of economics. Interesting parallels may be drawn between this conflict and the teachings of Adam Smith. Prior to Smith, economic theory was based on the idea that every dollar you have is one less dollar for me. Smith proposed an entirely different concept: If I help you earn dollars, the economic house will grow, and I, too, will make more dollars, and then you will make more dollars. In this way, the entire system generates more than anyone could have previously imagined. This economic concept extrapolates well to the present discussion of the university medical center versus community medicine.
University health systems do not seem to realize that real growth happens when communities grow together. A robust and vibrant community hospital supports a university medical center with more vigor than an anemic, waning, and disenchanted community hospital that perceives its woes as a result of the powerful—and perhaps dogmatic—university health system. There are enough patients to grow both systems together—the patient base radius grows wider with cooperation and growth—but this cannot happen if the university engenders distrust among local practitioners and the local community. This is a situation that will either be win-win or lose-lose.
Although the crux of the conflict is economic, other aspects of town-and-gown medicine can contribute to better cooperation and understanding. Some academic medical centers have explored ways to incorporate local physicians in university-based clinical trials. These programs offer cutting edge medicine and an opportunity to participate in intellectually stimulating work; at the same time, physicians retain their private practices.
This research opportunity is being offered and supported by a number of academic institutions, including Columbia-Presbyterian in New York City, Duke in Durham, N.C., Partners HealthCare in Boston, the University of Pittsburgh, the University of Rochester (N.Y.), and Washington University (St. Louis, Mo.).4 This is a good-faith start in mending the relationship between the academic and private medical sectors. To achieve a lasting positive relationship, community physicians must trust the academic community to respect their autonomy and to recognize that they have the right to provide full-service care to their patients and to serve their patients without the fear of being unfairly disenfranchised.
The lack of integration of the academic medical community and private practitioners of medicine—the proverbial town and gown—is an old dilemma. It is time to lay it to rest. The solutions are straightforward. Empowering community hospitals and physicians will not diminish the influence of university-based hospitals, nor will there be loss of reimbursement. Just the opposite will occur. In the end, with cooperation, everyone wins; with adversarial actions, all parties lose, especially the patients. TH
Dr. Brezina is a member of the consulting clinical faculty at Duke University, Durham, N.C.
References
- Town and gown in the Middle Ages. Available at: http://en.wikipedia.org/wiki/Town_and_gown. Last accessed March 29, 2007.
- University of Florida Web site. Town/gown task force. Available at: www.facilities.ufl.edu/cp/towngown.htm. Last accessed March 29, 2007.
- Adams D, Croasdale M. Town and gown: turning rivalries into relationships [American Medical News Web site]. January 13, 2003. Available at: www.ama-assn.org/amednews/2003/01/13/prsa0113.htm. Last accessed March 20, 2007.
- Maguire P. Marriage of town and gown brings clinical research to busy practices [ACP-ASIM Observer Web site]. February 2001. Available at: www.acponline.org/journals/news/feb01/clinresearch.htm. Last accessed March 20, 2007.
Scapular Pain
Case
A 67-year-old female was referred for two weeks of left shoulder pain that kept her from sleeping and moving her arm and interfered with her job as a typist. The pain was located in the posterior shoulder just medial to the scapula, radiated down her left arm, and was positional. She had not noticed a decreased range of motion.
After failure of steroids and NSAIDs, she was referred to a chiropractor, who did not improve her shoulder pain. When she got up from the table, she noticed that she was having crushing chest pain bilaterally on each side of the sternum at the level of the first and second ribs. Since then, she had been on significant doses of opiates and oral steroids without pain resolution.
Physical Exam
A shoulder exam revealed bilateral normal range of motion with no crepitus. The patient’s head was slightly tilted, her back laterally rotated. There was a palpable tender mass over the medial aspect of her left scapula. Palpation of the rhomboid muscle caused intense acute pain that radiated down her arm and reproduced her symptoms (See sample photos 1 & 2).
Rhomboid Spasm
Etiology: A rhomboid muscle strain or spasm is usually caused by overuse of the shoulder and arm, especially during repetitive overhead activities like serving a tennis ball or reaching to put objects on a high shelf. It can also result from activities such as the prolonged use of a computer, the problem experienced by this patient.
Anatomy: The rhomboids originate on the last (seventh) cervical and first five thoracic vertebrae and insert on the medial border of the scapula. They work with the levator scapulae and the upper trapezius to elevate and retract the scapula. Spasms of the rhomboids refer pain to a local and limited area, as well as down the lateral aspect of the arm, and are often accompanied by trigger points in levator scapulae, trapezius, and pectoralis major and minor. (See photos 3a, 3b, and 4).
Treatment
Rhomboid spasm should be treated by local lidocaine injection and a depot corticosteroid into the rhomboid muscle. The lidocaine provides the direct effect of reducing the current spasm, and the anti-inflammatory effect of the steroid reduces recurrence.
Rhomboid Injection
To administer a rhomboid injection, first locate the rhomboid muscle just medial to the scapula on the posterior shoulder. A rhomboid muscle in spasm often presents as a painful, palpable mass. Next, identify an area of point tenderness. Inject lidocaine and a corticosteroid. The correct location will be confirmed by immediate pain relief; the steroid, however, may take up to a week to provide pain relief.
Three-Month Follow-Up
The patient returned three months after her rhomboid muscle was injected with lidocaine and a depo-steroid preparation. She has resumed her job as a typist and performs rhomboid spasm prevention exercises. She sleeps well and can move her arm without pain. She is active in her daily activities and enjoys shopping with her friends.
Prevention
Prevention can be achieved through the following rhomboid exercises:
- Sit with your legs stretched in front of you. Bend your right knee and place your right foot on the left/outside of your left knee. With your right hand, grab and hold on to your right ankle. Holding on to your right ankle, lean back. (See 5A.)
- The key: Press your right elbow into your right knee and point/push your right shoulder toward the floor in front of you. (See 5B.)
- Stand with your arms at your sides. Stretch one arm across your body and pull it in toward your body with your other hand. (See 5C.)
- Sit on a chair firmly planted on the floor. Lift your right leg and put the right ankle onto the knee of the left leg. Grab your right ankle with your right hand and rest your right elbow on your right knee. With your left hand, grasp the chair back behind you and rotate your torso to the left to look over your left hand. (See 5D.)
Dr. Ficalora is an associate professor of medicine at the Mayo Clinic College of Medicine, and Gerhart is a third-year medical student at the Mayo Clinic College of Medicine, Rochester, Minn.
Case
A 67-year-old female was referred for two weeks of left shoulder pain that kept her from sleeping and moving her arm and interfered with her job as a typist. The pain was located in the posterior shoulder just medial to the scapula, radiated down her left arm, and was positional. She had not noticed a decreased range of motion.
After failure of steroids and NSAIDs, she was referred to a chiropractor, who did not improve her shoulder pain. When she got up from the table, she noticed that she was having crushing chest pain bilaterally on each side of the sternum at the level of the first and second ribs. Since then, she had been on significant doses of opiates and oral steroids without pain resolution.
Physical Exam
A shoulder exam revealed bilateral normal range of motion with no crepitus. The patient’s head was slightly tilted, her back laterally rotated. There was a palpable tender mass over the medial aspect of her left scapula. Palpation of the rhomboid muscle caused intense acute pain that radiated down her arm and reproduced her symptoms (See sample photos 1 & 2).
Rhomboid Spasm
Etiology: A rhomboid muscle strain or spasm is usually caused by overuse of the shoulder and arm, especially during repetitive overhead activities like serving a tennis ball or reaching to put objects on a high shelf. It can also result from activities such as the prolonged use of a computer, the problem experienced by this patient.
Anatomy: The rhomboids originate on the last (seventh) cervical and first five thoracic vertebrae and insert on the medial border of the scapula. They work with the levator scapulae and the upper trapezius to elevate and retract the scapula. Spasms of the rhomboids refer pain to a local and limited area, as well as down the lateral aspect of the arm, and are often accompanied by trigger points in levator scapulae, trapezius, and pectoralis major and minor. (See photos 3a, 3b, and 4).
Treatment
Rhomboid spasm should be treated by local lidocaine injection and a depot corticosteroid into the rhomboid muscle. The lidocaine provides the direct effect of reducing the current spasm, and the anti-inflammatory effect of the steroid reduces recurrence.
Rhomboid Injection
To administer a rhomboid injection, first locate the rhomboid muscle just medial to the scapula on the posterior shoulder. A rhomboid muscle in spasm often presents as a painful, palpable mass. Next, identify an area of point tenderness. Inject lidocaine and a corticosteroid. The correct location will be confirmed by immediate pain relief; the steroid, however, may take up to a week to provide pain relief.
Three-Month Follow-Up
The patient returned three months after her rhomboid muscle was injected with lidocaine and a depo-steroid preparation. She has resumed her job as a typist and performs rhomboid spasm prevention exercises. She sleeps well and can move her arm without pain. She is active in her daily activities and enjoys shopping with her friends.
Prevention
Prevention can be achieved through the following rhomboid exercises:
- Sit with your legs stretched in front of you. Bend your right knee and place your right foot on the left/outside of your left knee. With your right hand, grab and hold on to your right ankle. Holding on to your right ankle, lean back. (See 5A.)
- The key: Press your right elbow into your right knee and point/push your right shoulder toward the floor in front of you. (See 5B.)
- Stand with your arms at your sides. Stretch one arm across your body and pull it in toward your body with your other hand. (See 5C.)
- Sit on a chair firmly planted on the floor. Lift your right leg and put the right ankle onto the knee of the left leg. Grab your right ankle with your right hand and rest your right elbow on your right knee. With your left hand, grasp the chair back behind you and rotate your torso to the left to look over your left hand. (See 5D.)
Dr. Ficalora is an associate professor of medicine at the Mayo Clinic College of Medicine, and Gerhart is a third-year medical student at the Mayo Clinic College of Medicine, Rochester, Minn.
Case
A 67-year-old female was referred for two weeks of left shoulder pain that kept her from sleeping and moving her arm and interfered with her job as a typist. The pain was located in the posterior shoulder just medial to the scapula, radiated down her left arm, and was positional. She had not noticed a decreased range of motion.
After failure of steroids and NSAIDs, she was referred to a chiropractor, who did not improve her shoulder pain. When she got up from the table, she noticed that she was having crushing chest pain bilaterally on each side of the sternum at the level of the first and second ribs. Since then, she had been on significant doses of opiates and oral steroids without pain resolution.
Physical Exam
A shoulder exam revealed bilateral normal range of motion with no crepitus. The patient’s head was slightly tilted, her back laterally rotated. There was a palpable tender mass over the medial aspect of her left scapula. Palpation of the rhomboid muscle caused intense acute pain that radiated down her arm and reproduced her symptoms (See sample photos 1 & 2).
Rhomboid Spasm
Etiology: A rhomboid muscle strain or spasm is usually caused by overuse of the shoulder and arm, especially during repetitive overhead activities like serving a tennis ball or reaching to put objects on a high shelf. It can also result from activities such as the prolonged use of a computer, the problem experienced by this patient.
Anatomy: The rhomboids originate on the last (seventh) cervical and first five thoracic vertebrae and insert on the medial border of the scapula. They work with the levator scapulae and the upper trapezius to elevate and retract the scapula. Spasms of the rhomboids refer pain to a local and limited area, as well as down the lateral aspect of the arm, and are often accompanied by trigger points in levator scapulae, trapezius, and pectoralis major and minor. (See photos 3a, 3b, and 4).
Treatment
Rhomboid spasm should be treated by local lidocaine injection and a depot corticosteroid into the rhomboid muscle. The lidocaine provides the direct effect of reducing the current spasm, and the anti-inflammatory effect of the steroid reduces recurrence.
Rhomboid Injection
To administer a rhomboid injection, first locate the rhomboid muscle just medial to the scapula on the posterior shoulder. A rhomboid muscle in spasm often presents as a painful, palpable mass. Next, identify an area of point tenderness. Inject lidocaine and a corticosteroid. The correct location will be confirmed by immediate pain relief; the steroid, however, may take up to a week to provide pain relief.
Three-Month Follow-Up
The patient returned three months after her rhomboid muscle was injected with lidocaine and a depo-steroid preparation. She has resumed her job as a typist and performs rhomboid spasm prevention exercises. She sleeps well and can move her arm without pain. She is active in her daily activities and enjoys shopping with her friends.
Prevention
Prevention can be achieved through the following rhomboid exercises:
- Sit with your legs stretched in front of you. Bend your right knee and place your right foot on the left/outside of your left knee. With your right hand, grab and hold on to your right ankle. Holding on to your right ankle, lean back. (See 5A.)
- The key: Press your right elbow into your right knee and point/push your right shoulder toward the floor in front of you. (See 5B.)
- Stand with your arms at your sides. Stretch one arm across your body and pull it in toward your body with your other hand. (See 5C.)
- Sit on a chair firmly planted on the floor. Lift your right leg and put the right ankle onto the knee of the left leg. Grab your right ankle with your right hand and rest your right elbow on your right knee. With your left hand, grasp the chair back behind you and rotate your torso to the left to look over your left hand. (See 5D.)
Dr. Ficalora is an associate professor of medicine at the Mayo Clinic College of Medicine, and Gerhart is a third-year medical student at the Mayo Clinic College of Medicine, Rochester, Minn.
Vacuum-Assisted Closure Therapy
Vacuum-assisted closure (VAC) therapy has been used to manage wounds for 20 years and has taken wound treatment to a higher level. Clinical applications include chronic and acute wounds. Wound treatment has become easier with VAC. It improves the quality of life of the patient and reduces hospitalization time and expenses.
With the development of a portable vacuum device, treating patients with wounds is possible even in the home. We have been treating admitted and home care patients with VAC for five years in our Wound Centre. In this article, we discuss our experiences with VAC and review the procedure’s current applications and complications.
Background
Before the introduction of VAC therapy, the treatment and management of difficult wounds mainly belonged in the arena of plastic and reconstructive surgery.1 When Morykwas and colleagues developed VAC, however, they could have hoped only that it would take the treatment of acute and chronic wounds to a higher level.2 VAC is also known as TNP (topical negative pressure), as SPD (sub-atmospheric pressure), as VST (vacuum sealing technique), and as SSS (sealed surface wound suction).3 It is a technique that is easy to use in a clinical setting, and it has a low complication rate.4 The portable VAC system has made wound treatment possible in a home care setting, a development that improves quality of life and reduces hospitalization time.5,6 The portable VAC system (V.A.C. Freedom) is the size of a regular handbag. (See Figure 1, left.)
In this paper, we will discuss the working mechanisms of VAC, its current clinical applications, and the complications that might occur during VAC treatment.
How Does It Work?
Normally, wounds heal by approximation of the wound edges—for example, by suturing or by the formation of a matrix of small blood vessels and connective tissue, when wound edges are not opposed, for the migration of keratinocytes across the surface and the re-epithelialization of the defect. This is a complex process; its main objectives can be considered minimization of blood loss, replacement of any defects with new tissue (granulation), and the restoration of an intact epithelial barrier. For this process to occur, healing debris must be removed, infection must be controlled, and inflammation must be cleared.4 Further disturbance of the rate of healing may occur due to inadequate vascular supply and incapacity of the wound to form new capillaries or matrix. Any disruption in the processes involved in wound healing, such as debridement, granulation, and epithelialization, can lead to the formation of a chronic wound. In our Wound Centre, VAC is mainly used in the granulation phase of a wound, as well as for securing split skin grafts.7
VAC uses medical-grade, open cell polyurethane ether foam.2,4 The pore size is generally 400-600 micrometers. This foam is cut to fit the wound bed before it is applied to the wound. If necessary, multiple pieces of foam can be used to connect separate wounds or to fill up any remaining gaps. Adhesive tape is then applied over an additional three to five cm border of intact skin to provide a seal.4 Then a track pad is placed over a small hole in the adhesive tape. A tube connects the track pad to an adjustable vacuum pump and a canister for collecting effluent fluids. The pump can be adjusted for both the timing (intermittent vs. continuous) and the magnitude of the vacuum effect.4 In general, an intermittent cycle (five minutes on, two minutes off) is used; this has been shown to be most beneficial.2 The VAC system is easy to apply, even on difficult wounds like the open abdomen. (See Figure 2, left.)
With the VAC technique, the open wound is converted into a controlled and temporarily closed environment. Animal studies have shown that VAC optimizes blood flow, decreases local edema, reduces bacteria levels, and removes excess fluids from the wound.2,8 (See Figure 3, above.) The cyclical application of sub-atmospheric pressure alters the cytoskeleton of the cells in the wound bed, triggering a cascade of intracellular signals that increases the rate of cell division and, thus, the formation of granulation tissue.9 This results in faster healing of the wounds than would have occurred with regular therapy; further, it significantly reduces hospitalization time and expenses.
Indications
VAC can be used on several types of wounds; however, before starting VAC therapy; adequate debridement for the formation of granulation tissue is essential.10 An overview of current clinical applications follows.
Chronic Wounds
The VAC system was originally designed to treat chronic wounds and to simplify the treatment of patients with chronic wounds both inside and outside the hospital.11 Around 10% of the general population will develop a chronic wound in the course of a lifetime; mortality resulting from these wounds amounts to 2.5%.12 VAC therapy has changed the clinical approach to and management of chronic wounds such as venous stasis ulcers, pressure ulcers, surgical dehisced wounds, arterial and diabetic ulcers, and a wide variety of other types of lingering wounds.12-15 Chronic wounds should be adequately debrided, either surgically or using another approach such as maggot debridement.16-18 This converts a chronic wound into a semi-acute wound. Such wounds respond better to VAC therapy than non-debrided wounds.11
Acute Wounds
VAC has become widely accepted in the treatment of large soft-tissue injuries with compromised tissue; it is also used for contaminated wounds, hematomas, and gunshot wounds. It has successfully been used in the treatment of extremities and orthopedic trauma and in treating degloving injuries and burns.19,21-25 (See Figure 4, p. 41.) When using VAC on traumatic injuries, nonviable tissue must be debrided, foreign bodies removed, and hemostasis obtained. Coverage of vital structures such as major vessels, viscera, and nerves by mobilization of local muscle or soft tissue is preferential. Wounds are then treated with VAC, and dressings are changed at appropriate intervals; if there is any suspicion of significant contamination, or if the patient develops signs of infection, adequate action, such as antibiotics or more dressing changes, must be taken.11
VAC therapy can also be used on a wide variety of surgical wounds and in treating surgical complications. It has successfully been used in sternal infections and mediastinitis, abdominal wall defects, enterocutaneous fistula, and perineal surgical wounds.11,26-35 The application of VAC in both chronic and acute wounds shows that it is a technique that facilitates wound management and wound healing for a wide variety of wound types.
Complications
When used within recommendations, complications resulting from VAC are infrequent.4 As the vacuum system device is more frequently adapted to multiple problems, however, the complication rate increases, probably due to co-morbidity and mortality.11 Localized superficial skin irritation is the most common complication reported in the literature.36 Further complications involve pain, infection, bleeding, and fluid depletion.4,12,35-37 Rare, severe complications, such as toxic shock syndrome, anaerobic sepsis, or thrombosis have been described as well.38-39(Also see M. Leijnen, MD, MSc, and colleagues, unpublished data, 2007.)
Conclusion
After 20 years of experience with vacuum-assisted closure, we can state that VAC therapy contributes positively to wound treatment. Wounds treated with this procedure are easier to manage, both in the hospital and at home. It can be used on a wide variety of chronic and acute wounds, and more applications are being developed. The procedure also reduces hospitalization time and expenses, and perhaps most important, it improves the patient’s quality of life. TH
M. Leijnen, MD, MSc, and S.A. da Costa, MD, PhD, practice in the Department of Surgery, Rijnland Hospital, Leiderdorp, The Netherlands. L. van Doorn, MA-NPA, practices in the Rijnland Wound Centre, Leiderdorp, The Netherlands. P. Steenvoorde, MD, MSc, and J. Oskam, MD, PhD practice in the Department of Surgery, Rijnland Hospital, Leiderdorp, The Netherlands, and in the Rijnland Wound Center, Leiderdorp, The Netherlands.
References
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997 Jun;38(6):563-576; discussion 577. Ann Plast Surg. 2000 Sep;45(3):332-334; discussion 335-336.
- Morykwas MJ, Argenta LC, Shelton-Brown EI, et al. Vacuum assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997 Jun;38(6):553-562. Comment in: Ann Plast Surg. 2000 Sep;45(3):332-334; discussion 335-336.
- Banwell PE, Teot L. Topical negative pressure (TNP): the evolution of a novel wound therapy. J Wound Care. 2003;12(1):22-28. Review.
- Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg. 2005 Mar;29(3):219-226.
- Baradarian S, Stahovich M, Krause S, et al. Case series: clinical management of persistent mechanical assist device driveline drainage using vacuum-assisted closure therapy. ASAIO J. 2006;52:354-356.
- Sposato G, Molea G, Di Caprio G, et al. Ambulant vacuum-assisted closure of skin-graft dressing in the lower limbs using a portable mini-VAC device. Br J Plast Surg. 2001 Apr;54(3):235-237.
- Scherer LA, Shiver S, Chang M, et al. The vacuum assisted closure device: a method of securing skin grafts and improving graft survival. Arch Surg. 2002 Aug;137(8):930-933.
- Chen SZ, Li J, Li XY, et al. Effects of vacuum-assisted closure on wound microcirculation: an experimental study. Asian J Surg. 2005 Jul;28(3):211-217.
- Venturi ML, Attinger CE, Mesbahi AN, et al. Mechanisms and clinical applications of the vacuum-assisted closure (VAC) device: a review. Am J Clin Dermatol. 2005;6(3):185-194. Review.
- Philbeck TE Jr, Whittington KT, Millsap MH, et al. The clinical and cost effectiveness of externally applied negative pressure wound therapy in the treatment of wounds in home healthcare Medicare patients. Ostomy Wound Manage. 1999 Nov;45(11):41-50.
- Argenta LC, Morykwas MJ, Marks MW, et al. Vacuum-assisted closure: state of clinic art. Plast Reconstr Surg. 2006 Jun;117(7 Suppl):127S-142S.
- Karl T, Modic PK, Voss EU. Indications and results of VAC therapy treatments in vascular surgery - state of the art in the treatment of chronic wounds [in German]. Zentralbl Chir. 2004 May;129 Suppl 1:S74-S79.
- Ford CN, Reinhard ER, Yeh D, et al. Interim analysis of a prospective, randomized trial of vacuum-assisted closure versus the healthpoint system in the management of pressure ulcers. Ann Plast Surg. 2002 Jul;49(1):55-61.
- Joseph E, Hamori CA, Bergman S, et al. A prospective randomized trial of vacuum-assisted closure versus standard therapy of chronic non-healing wounds. Wounds. 2000;12:60-67.
- Rozeboom AL, Steenvoorde P, Hartgrink HH, et al. Necrotizing fasciitis of the leg following a simple pelvic fracture: case report and literature review. J Wound Care. 2006;15:117-120.
- Steenvoorde P, Calame JJ, Oskam J. Maggot-treated wounds follow normal wound healing phases. Int J Dermatol. 2006;45:1477-1479.
- Mumcuoglu KY. Clinical applications for maggots in wound care. Am J Clin Dermatol. 2001;2(4):219-227.
- Attinger CE, Bulan EJ. Debridement. The key initial first step in wound healing. Foot Ankle Clin. 2001 Dec;6(4):627-660.
- Stannard JP, Robinson JT, Anderson ER, et al. Negative pressure wound therapy to treat hematomas and surgical incisions following high-energy trauma. J Trauma. 2006 Jun;60(6):1301-1306.
- Webb LX, Laver D, DeFranzo A. Negative pressure wound therapy in the management of orthopedic wounds. Ostomy Wound Manage. 2004 Apr;50(4A Suppl):26-27.
- Herscovici D Jr, Sanders RW, Scaduto JM, et al. Vacuum-assisted wound closure (VAC therapy) for the management of patients with high-energy soft tissue injuries. J Orthop Trauma. 2003 Nov-Dec;17(10):683-688.
- Wong LK, Nesbit RD, Turner LA, et al. Management of a circumferential lower extremity degloving injury with the use of vacuum-assisted closure. South Med J. 2006;99:628-630.
- Josty IC, Ramaswamy R, Laing JH. Vacuum assisted closure: an alternative strategy in the management of degloving injuries of the foot. Br J Plast Surg. 2001 Jun;54(4):363-365.
- Adamkova M, Tymonova J, Zamecnikova I, et al. First experience with the use of vacuum assisted closure in the treatment of skin defects at the burn center. Acta Chir Plast. 2005;47(1):24-27.
- Kamolz LP, Andel H, Haslik W, et al. Use of subatmospheric pressure therapy to prevent burn wound progression in human: first experiences. Burns. 2004;30:253-258.
- Obdeijn MC, de Lange MY, Lichtendahl DH, et al. Vacuum-assisted closure in the treatment of poststernotomy mediastinitis. Ann Thorac Surg. 1999;68:2358-2360.
- Agarwal JP, Ogilvie M, Wu LC, et al. Vacuum-assisted closure for sternal wounds: a first-line therapeutic management approach. Plast Reconstr Surg. 2005;116:1035-1040.
- Scholl L, Chang E, Reitz B, et al. Sternal osteomyelitis: use of vacuum-assisted closure device as an adjunct to definitive closure with sternectomy and muscle flap reconstruction. J Card Surg. 2004 Sep-Oct;19(5):453-461.
- DeFranzo AJ, Argenta L. Vacuum-assisted closure for the treatment of abdominal wounds. Clin Plast Surg. 2006;33:213-224.
- Nienhuijs SW, Manupassa R, Strobbe LJ, et al. Can topical negative pressure be used to control complex enterocutaneous fistulae? J Wound Care. 2003;12:343-345.
- Alvarez AA, Maxwell GL, Rodriguez GC. Vacuum-assisted closure for cutaneous gastrointestinal fistula management. Gynecol Oncol. 2001;80:413-416.
- Erdmann D, Drye C, Heller L, et al. Abdominal wall defect and enterocutaneous fistula treatment with the Vacuum-Assisted Closure (V.A.C.) system. Plast Reconstr Surg. 2001;108:2066-2068.
- Schaffzin DM, Douglas JM, Stahl TJ, et al. Vacuum-assisted closure of complex perineal wounds. Dis Colon Rectum. 2004;47:1745-1748.
- Jethwa P, Lake SP. Using topical negative pressure therapy to resolve wound failure following perineal resection. J Wound Care. 2005;14:166-167.
- McGuinness JG, Winter DC, O’Connell PR. Vacuum-assisted closure of a complex pilonidal sinus. Dis Colon Rectum. 2003;46:274-276.
- Steenvoorde P, van Engeland A. Oskam J. Vacuum-assisted closure therapy and oral anticoagulation therapy. Plast Reconstr Surg. 2004;113:2220-2221.
- Negative pressure wound therapy: Morykwas approach [adverse events data]. Available at: www.npwt.com/morykwas.htm. Last accessed March 20, 2007.
- Carson SN, Overall K, Lee-Jahshan S, et al. Vacuum-assisted closure used for healing chronic wounds and skin grafts in the lower extremities. Ostomy Wound Manage. 2004;50:52-58.
- Gwan-Nulla D, Casal RS. Toxic shock syndrome associated with the use of the vacuum-assisted closure device. Ann Plast Surg. 2001;47:552-554.
Vacuum-assisted closure (VAC) therapy has been used to manage wounds for 20 years and has taken wound treatment to a higher level. Clinical applications include chronic and acute wounds. Wound treatment has become easier with VAC. It improves the quality of life of the patient and reduces hospitalization time and expenses.
With the development of a portable vacuum device, treating patients with wounds is possible even in the home. We have been treating admitted and home care patients with VAC for five years in our Wound Centre. In this article, we discuss our experiences with VAC and review the procedure’s current applications and complications.
Background
Before the introduction of VAC therapy, the treatment and management of difficult wounds mainly belonged in the arena of plastic and reconstructive surgery.1 When Morykwas and colleagues developed VAC, however, they could have hoped only that it would take the treatment of acute and chronic wounds to a higher level.2 VAC is also known as TNP (topical negative pressure), as SPD (sub-atmospheric pressure), as VST (vacuum sealing technique), and as SSS (sealed surface wound suction).3 It is a technique that is easy to use in a clinical setting, and it has a low complication rate.4 The portable VAC system has made wound treatment possible in a home care setting, a development that improves quality of life and reduces hospitalization time.5,6 The portable VAC system (V.A.C. Freedom) is the size of a regular handbag. (See Figure 1, left.)
In this paper, we will discuss the working mechanisms of VAC, its current clinical applications, and the complications that might occur during VAC treatment.
How Does It Work?
Normally, wounds heal by approximation of the wound edges—for example, by suturing or by the formation of a matrix of small blood vessels and connective tissue, when wound edges are not opposed, for the migration of keratinocytes across the surface and the re-epithelialization of the defect. This is a complex process; its main objectives can be considered minimization of blood loss, replacement of any defects with new tissue (granulation), and the restoration of an intact epithelial barrier. For this process to occur, healing debris must be removed, infection must be controlled, and inflammation must be cleared.4 Further disturbance of the rate of healing may occur due to inadequate vascular supply and incapacity of the wound to form new capillaries or matrix. Any disruption in the processes involved in wound healing, such as debridement, granulation, and epithelialization, can lead to the formation of a chronic wound. In our Wound Centre, VAC is mainly used in the granulation phase of a wound, as well as for securing split skin grafts.7
VAC uses medical-grade, open cell polyurethane ether foam.2,4 The pore size is generally 400-600 micrometers. This foam is cut to fit the wound bed before it is applied to the wound. If necessary, multiple pieces of foam can be used to connect separate wounds or to fill up any remaining gaps. Adhesive tape is then applied over an additional three to five cm border of intact skin to provide a seal.4 Then a track pad is placed over a small hole in the adhesive tape. A tube connects the track pad to an adjustable vacuum pump and a canister for collecting effluent fluids. The pump can be adjusted for both the timing (intermittent vs. continuous) and the magnitude of the vacuum effect.4 In general, an intermittent cycle (five minutes on, two minutes off) is used; this has been shown to be most beneficial.2 The VAC system is easy to apply, even on difficult wounds like the open abdomen. (See Figure 2, left.)
With the VAC technique, the open wound is converted into a controlled and temporarily closed environment. Animal studies have shown that VAC optimizes blood flow, decreases local edema, reduces bacteria levels, and removes excess fluids from the wound.2,8 (See Figure 3, above.) The cyclical application of sub-atmospheric pressure alters the cytoskeleton of the cells in the wound bed, triggering a cascade of intracellular signals that increases the rate of cell division and, thus, the formation of granulation tissue.9 This results in faster healing of the wounds than would have occurred with regular therapy; further, it significantly reduces hospitalization time and expenses.
Indications
VAC can be used on several types of wounds; however, before starting VAC therapy; adequate debridement for the formation of granulation tissue is essential.10 An overview of current clinical applications follows.
Chronic Wounds
The VAC system was originally designed to treat chronic wounds and to simplify the treatment of patients with chronic wounds both inside and outside the hospital.11 Around 10% of the general population will develop a chronic wound in the course of a lifetime; mortality resulting from these wounds amounts to 2.5%.12 VAC therapy has changed the clinical approach to and management of chronic wounds such as venous stasis ulcers, pressure ulcers, surgical dehisced wounds, arterial and diabetic ulcers, and a wide variety of other types of lingering wounds.12-15 Chronic wounds should be adequately debrided, either surgically or using another approach such as maggot debridement.16-18 This converts a chronic wound into a semi-acute wound. Such wounds respond better to VAC therapy than non-debrided wounds.11
Acute Wounds
VAC has become widely accepted in the treatment of large soft-tissue injuries with compromised tissue; it is also used for contaminated wounds, hematomas, and gunshot wounds. It has successfully been used in the treatment of extremities and orthopedic trauma and in treating degloving injuries and burns.19,21-25 (See Figure 4, p. 41.) When using VAC on traumatic injuries, nonviable tissue must be debrided, foreign bodies removed, and hemostasis obtained. Coverage of vital structures such as major vessels, viscera, and nerves by mobilization of local muscle or soft tissue is preferential. Wounds are then treated with VAC, and dressings are changed at appropriate intervals; if there is any suspicion of significant contamination, or if the patient develops signs of infection, adequate action, such as antibiotics or more dressing changes, must be taken.11
VAC therapy can also be used on a wide variety of surgical wounds and in treating surgical complications. It has successfully been used in sternal infections and mediastinitis, abdominal wall defects, enterocutaneous fistula, and perineal surgical wounds.11,26-35 The application of VAC in both chronic and acute wounds shows that it is a technique that facilitates wound management and wound healing for a wide variety of wound types.
Complications
When used within recommendations, complications resulting from VAC are infrequent.4 As the vacuum system device is more frequently adapted to multiple problems, however, the complication rate increases, probably due to co-morbidity and mortality.11 Localized superficial skin irritation is the most common complication reported in the literature.36 Further complications involve pain, infection, bleeding, and fluid depletion.4,12,35-37 Rare, severe complications, such as toxic shock syndrome, anaerobic sepsis, or thrombosis have been described as well.38-39(Also see M. Leijnen, MD, MSc, and colleagues, unpublished data, 2007.)
Conclusion
After 20 years of experience with vacuum-assisted closure, we can state that VAC therapy contributes positively to wound treatment. Wounds treated with this procedure are easier to manage, both in the hospital and at home. It can be used on a wide variety of chronic and acute wounds, and more applications are being developed. The procedure also reduces hospitalization time and expenses, and perhaps most important, it improves the patient’s quality of life. TH
M. Leijnen, MD, MSc, and S.A. da Costa, MD, PhD, practice in the Department of Surgery, Rijnland Hospital, Leiderdorp, The Netherlands. L. van Doorn, MA-NPA, practices in the Rijnland Wound Centre, Leiderdorp, The Netherlands. P. Steenvoorde, MD, MSc, and J. Oskam, MD, PhD practice in the Department of Surgery, Rijnland Hospital, Leiderdorp, The Netherlands, and in the Rijnland Wound Center, Leiderdorp, The Netherlands.
References
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997 Jun;38(6):563-576; discussion 577. Ann Plast Surg. 2000 Sep;45(3):332-334; discussion 335-336.
- Morykwas MJ, Argenta LC, Shelton-Brown EI, et al. Vacuum assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997 Jun;38(6):553-562. Comment in: Ann Plast Surg. 2000 Sep;45(3):332-334; discussion 335-336.
- Banwell PE, Teot L. Topical negative pressure (TNP): the evolution of a novel wound therapy. J Wound Care. 2003;12(1):22-28. Review.
- Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg. 2005 Mar;29(3):219-226.
- Baradarian S, Stahovich M, Krause S, et al. Case series: clinical management of persistent mechanical assist device driveline drainage using vacuum-assisted closure therapy. ASAIO J. 2006;52:354-356.
- Sposato G, Molea G, Di Caprio G, et al. Ambulant vacuum-assisted closure of skin-graft dressing in the lower limbs using a portable mini-VAC device. Br J Plast Surg. 2001 Apr;54(3):235-237.
- Scherer LA, Shiver S, Chang M, et al. The vacuum assisted closure device: a method of securing skin grafts and improving graft survival. Arch Surg. 2002 Aug;137(8):930-933.
- Chen SZ, Li J, Li XY, et al. Effects of vacuum-assisted closure on wound microcirculation: an experimental study. Asian J Surg. 2005 Jul;28(3):211-217.
- Venturi ML, Attinger CE, Mesbahi AN, et al. Mechanisms and clinical applications of the vacuum-assisted closure (VAC) device: a review. Am J Clin Dermatol. 2005;6(3):185-194. Review.
- Philbeck TE Jr, Whittington KT, Millsap MH, et al. The clinical and cost effectiveness of externally applied negative pressure wound therapy in the treatment of wounds in home healthcare Medicare patients. Ostomy Wound Manage. 1999 Nov;45(11):41-50.
- Argenta LC, Morykwas MJ, Marks MW, et al. Vacuum-assisted closure: state of clinic art. Plast Reconstr Surg. 2006 Jun;117(7 Suppl):127S-142S.
- Karl T, Modic PK, Voss EU. Indications and results of VAC therapy treatments in vascular surgery - state of the art in the treatment of chronic wounds [in German]. Zentralbl Chir. 2004 May;129 Suppl 1:S74-S79.
- Ford CN, Reinhard ER, Yeh D, et al. Interim analysis of a prospective, randomized trial of vacuum-assisted closure versus the healthpoint system in the management of pressure ulcers. Ann Plast Surg. 2002 Jul;49(1):55-61.
- Joseph E, Hamori CA, Bergman S, et al. A prospective randomized trial of vacuum-assisted closure versus standard therapy of chronic non-healing wounds. Wounds. 2000;12:60-67.
- Rozeboom AL, Steenvoorde P, Hartgrink HH, et al. Necrotizing fasciitis of the leg following a simple pelvic fracture: case report and literature review. J Wound Care. 2006;15:117-120.
- Steenvoorde P, Calame JJ, Oskam J. Maggot-treated wounds follow normal wound healing phases. Int J Dermatol. 2006;45:1477-1479.
- Mumcuoglu KY. Clinical applications for maggots in wound care. Am J Clin Dermatol. 2001;2(4):219-227.
- Attinger CE, Bulan EJ. Debridement. The key initial first step in wound healing. Foot Ankle Clin. 2001 Dec;6(4):627-660.
- Stannard JP, Robinson JT, Anderson ER, et al. Negative pressure wound therapy to treat hematomas and surgical incisions following high-energy trauma. J Trauma. 2006 Jun;60(6):1301-1306.
- Webb LX, Laver D, DeFranzo A. Negative pressure wound therapy in the management of orthopedic wounds. Ostomy Wound Manage. 2004 Apr;50(4A Suppl):26-27.
- Herscovici D Jr, Sanders RW, Scaduto JM, et al. Vacuum-assisted wound closure (VAC therapy) for the management of patients with high-energy soft tissue injuries. J Orthop Trauma. 2003 Nov-Dec;17(10):683-688.
- Wong LK, Nesbit RD, Turner LA, et al. Management of a circumferential lower extremity degloving injury with the use of vacuum-assisted closure. South Med J. 2006;99:628-630.
- Josty IC, Ramaswamy R, Laing JH. Vacuum assisted closure: an alternative strategy in the management of degloving injuries of the foot. Br J Plast Surg. 2001 Jun;54(4):363-365.
- Adamkova M, Tymonova J, Zamecnikova I, et al. First experience with the use of vacuum assisted closure in the treatment of skin defects at the burn center. Acta Chir Plast. 2005;47(1):24-27.
- Kamolz LP, Andel H, Haslik W, et al. Use of subatmospheric pressure therapy to prevent burn wound progression in human: first experiences. Burns. 2004;30:253-258.
- Obdeijn MC, de Lange MY, Lichtendahl DH, et al. Vacuum-assisted closure in the treatment of poststernotomy mediastinitis. Ann Thorac Surg. 1999;68:2358-2360.
- Agarwal JP, Ogilvie M, Wu LC, et al. Vacuum-assisted closure for sternal wounds: a first-line therapeutic management approach. Plast Reconstr Surg. 2005;116:1035-1040.
- Scholl L, Chang E, Reitz B, et al. Sternal osteomyelitis: use of vacuum-assisted closure device as an adjunct to definitive closure with sternectomy and muscle flap reconstruction. J Card Surg. 2004 Sep-Oct;19(5):453-461.
- DeFranzo AJ, Argenta L. Vacuum-assisted closure for the treatment of abdominal wounds. Clin Plast Surg. 2006;33:213-224.
- Nienhuijs SW, Manupassa R, Strobbe LJ, et al. Can topical negative pressure be used to control complex enterocutaneous fistulae? J Wound Care. 2003;12:343-345.
- Alvarez AA, Maxwell GL, Rodriguez GC. Vacuum-assisted closure for cutaneous gastrointestinal fistula management. Gynecol Oncol. 2001;80:413-416.
- Erdmann D, Drye C, Heller L, et al. Abdominal wall defect and enterocutaneous fistula treatment with the Vacuum-Assisted Closure (V.A.C.) system. Plast Reconstr Surg. 2001;108:2066-2068.
- Schaffzin DM, Douglas JM, Stahl TJ, et al. Vacuum-assisted closure of complex perineal wounds. Dis Colon Rectum. 2004;47:1745-1748.
- Jethwa P, Lake SP. Using topical negative pressure therapy to resolve wound failure following perineal resection. J Wound Care. 2005;14:166-167.
- McGuinness JG, Winter DC, O’Connell PR. Vacuum-assisted closure of a complex pilonidal sinus. Dis Colon Rectum. 2003;46:274-276.
- Steenvoorde P, van Engeland A. Oskam J. Vacuum-assisted closure therapy and oral anticoagulation therapy. Plast Reconstr Surg. 2004;113:2220-2221.
- Negative pressure wound therapy: Morykwas approach [adverse events data]. Available at: www.npwt.com/morykwas.htm. Last accessed March 20, 2007.
- Carson SN, Overall K, Lee-Jahshan S, et al. Vacuum-assisted closure used for healing chronic wounds and skin grafts in the lower extremities. Ostomy Wound Manage. 2004;50:52-58.
- Gwan-Nulla D, Casal RS. Toxic shock syndrome associated with the use of the vacuum-assisted closure device. Ann Plast Surg. 2001;47:552-554.
Vacuum-assisted closure (VAC) therapy has been used to manage wounds for 20 years and has taken wound treatment to a higher level. Clinical applications include chronic and acute wounds. Wound treatment has become easier with VAC. It improves the quality of life of the patient and reduces hospitalization time and expenses.
With the development of a portable vacuum device, treating patients with wounds is possible even in the home. We have been treating admitted and home care patients with VAC for five years in our Wound Centre. In this article, we discuss our experiences with VAC and review the procedure’s current applications and complications.
Background
Before the introduction of VAC therapy, the treatment and management of difficult wounds mainly belonged in the arena of plastic and reconstructive surgery.1 When Morykwas and colleagues developed VAC, however, they could have hoped only that it would take the treatment of acute and chronic wounds to a higher level.2 VAC is also known as TNP (topical negative pressure), as SPD (sub-atmospheric pressure), as VST (vacuum sealing technique), and as SSS (sealed surface wound suction).3 It is a technique that is easy to use in a clinical setting, and it has a low complication rate.4 The portable VAC system has made wound treatment possible in a home care setting, a development that improves quality of life and reduces hospitalization time.5,6 The portable VAC system (V.A.C. Freedom) is the size of a regular handbag. (See Figure 1, left.)
In this paper, we will discuss the working mechanisms of VAC, its current clinical applications, and the complications that might occur during VAC treatment.
How Does It Work?
Normally, wounds heal by approximation of the wound edges—for example, by suturing or by the formation of a matrix of small blood vessels and connective tissue, when wound edges are not opposed, for the migration of keratinocytes across the surface and the re-epithelialization of the defect. This is a complex process; its main objectives can be considered minimization of blood loss, replacement of any defects with new tissue (granulation), and the restoration of an intact epithelial barrier. For this process to occur, healing debris must be removed, infection must be controlled, and inflammation must be cleared.4 Further disturbance of the rate of healing may occur due to inadequate vascular supply and incapacity of the wound to form new capillaries or matrix. Any disruption in the processes involved in wound healing, such as debridement, granulation, and epithelialization, can lead to the formation of a chronic wound. In our Wound Centre, VAC is mainly used in the granulation phase of a wound, as well as for securing split skin grafts.7
VAC uses medical-grade, open cell polyurethane ether foam.2,4 The pore size is generally 400-600 micrometers. This foam is cut to fit the wound bed before it is applied to the wound. If necessary, multiple pieces of foam can be used to connect separate wounds or to fill up any remaining gaps. Adhesive tape is then applied over an additional three to five cm border of intact skin to provide a seal.4 Then a track pad is placed over a small hole in the adhesive tape. A tube connects the track pad to an adjustable vacuum pump and a canister for collecting effluent fluids. The pump can be adjusted for both the timing (intermittent vs. continuous) and the magnitude of the vacuum effect.4 In general, an intermittent cycle (five minutes on, two minutes off) is used; this has been shown to be most beneficial.2 The VAC system is easy to apply, even on difficult wounds like the open abdomen. (See Figure 2, left.)
With the VAC technique, the open wound is converted into a controlled and temporarily closed environment. Animal studies have shown that VAC optimizes blood flow, decreases local edema, reduces bacteria levels, and removes excess fluids from the wound.2,8 (See Figure 3, above.) The cyclical application of sub-atmospheric pressure alters the cytoskeleton of the cells in the wound bed, triggering a cascade of intracellular signals that increases the rate of cell division and, thus, the formation of granulation tissue.9 This results in faster healing of the wounds than would have occurred with regular therapy; further, it significantly reduces hospitalization time and expenses.
Indications
VAC can be used on several types of wounds; however, before starting VAC therapy; adequate debridement for the formation of granulation tissue is essential.10 An overview of current clinical applications follows.
Chronic Wounds
The VAC system was originally designed to treat chronic wounds and to simplify the treatment of patients with chronic wounds both inside and outside the hospital.11 Around 10% of the general population will develop a chronic wound in the course of a lifetime; mortality resulting from these wounds amounts to 2.5%.12 VAC therapy has changed the clinical approach to and management of chronic wounds such as venous stasis ulcers, pressure ulcers, surgical dehisced wounds, arterial and diabetic ulcers, and a wide variety of other types of lingering wounds.12-15 Chronic wounds should be adequately debrided, either surgically or using another approach such as maggot debridement.16-18 This converts a chronic wound into a semi-acute wound. Such wounds respond better to VAC therapy than non-debrided wounds.11
Acute Wounds
VAC has become widely accepted in the treatment of large soft-tissue injuries with compromised tissue; it is also used for contaminated wounds, hematomas, and gunshot wounds. It has successfully been used in the treatment of extremities and orthopedic trauma and in treating degloving injuries and burns.19,21-25 (See Figure 4, p. 41.) When using VAC on traumatic injuries, nonviable tissue must be debrided, foreign bodies removed, and hemostasis obtained. Coverage of vital structures such as major vessels, viscera, and nerves by mobilization of local muscle or soft tissue is preferential. Wounds are then treated with VAC, and dressings are changed at appropriate intervals; if there is any suspicion of significant contamination, or if the patient develops signs of infection, adequate action, such as antibiotics or more dressing changes, must be taken.11
VAC therapy can also be used on a wide variety of surgical wounds and in treating surgical complications. It has successfully been used in sternal infections and mediastinitis, abdominal wall defects, enterocutaneous fistula, and perineal surgical wounds.11,26-35 The application of VAC in both chronic and acute wounds shows that it is a technique that facilitates wound management and wound healing for a wide variety of wound types.
Complications
When used within recommendations, complications resulting from VAC are infrequent.4 As the vacuum system device is more frequently adapted to multiple problems, however, the complication rate increases, probably due to co-morbidity and mortality.11 Localized superficial skin irritation is the most common complication reported in the literature.36 Further complications involve pain, infection, bleeding, and fluid depletion.4,12,35-37 Rare, severe complications, such as toxic shock syndrome, anaerobic sepsis, or thrombosis have been described as well.38-39(Also see M. Leijnen, MD, MSc, and colleagues, unpublished data, 2007.)
Conclusion
After 20 years of experience with vacuum-assisted closure, we can state that VAC therapy contributes positively to wound treatment. Wounds treated with this procedure are easier to manage, both in the hospital and at home. It can be used on a wide variety of chronic and acute wounds, and more applications are being developed. The procedure also reduces hospitalization time and expenses, and perhaps most important, it improves the patient’s quality of life. TH
M. Leijnen, MD, MSc, and S.A. da Costa, MD, PhD, practice in the Department of Surgery, Rijnland Hospital, Leiderdorp, The Netherlands. L. van Doorn, MA-NPA, practices in the Rijnland Wound Centre, Leiderdorp, The Netherlands. P. Steenvoorde, MD, MSc, and J. Oskam, MD, PhD practice in the Department of Surgery, Rijnland Hospital, Leiderdorp, The Netherlands, and in the Rijnland Wound Center, Leiderdorp, The Netherlands.
References
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997 Jun;38(6):563-576; discussion 577. Ann Plast Surg. 2000 Sep;45(3):332-334; discussion 335-336.
- Morykwas MJ, Argenta LC, Shelton-Brown EI, et al. Vacuum assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997 Jun;38(6):553-562. Comment in: Ann Plast Surg. 2000 Sep;45(3):332-334; discussion 335-336.
- Banwell PE, Teot L. Topical negative pressure (TNP): the evolution of a novel wound therapy. J Wound Care. 2003;12(1):22-28. Review.
- Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg. 2005 Mar;29(3):219-226.
- Baradarian S, Stahovich M, Krause S, et al. Case series: clinical management of persistent mechanical assist device driveline drainage using vacuum-assisted closure therapy. ASAIO J. 2006;52:354-356.
- Sposato G, Molea G, Di Caprio G, et al. Ambulant vacuum-assisted closure of skin-graft dressing in the lower limbs using a portable mini-VAC device. Br J Plast Surg. 2001 Apr;54(3):235-237.
- Scherer LA, Shiver S, Chang M, et al. The vacuum assisted closure device: a method of securing skin grafts and improving graft survival. Arch Surg. 2002 Aug;137(8):930-933.
- Chen SZ, Li J, Li XY, et al. Effects of vacuum-assisted closure on wound microcirculation: an experimental study. Asian J Surg. 2005 Jul;28(3):211-217.
- Venturi ML, Attinger CE, Mesbahi AN, et al. Mechanisms and clinical applications of the vacuum-assisted closure (VAC) device: a review. Am J Clin Dermatol. 2005;6(3):185-194. Review.
- Philbeck TE Jr, Whittington KT, Millsap MH, et al. The clinical and cost effectiveness of externally applied negative pressure wound therapy in the treatment of wounds in home healthcare Medicare patients. Ostomy Wound Manage. 1999 Nov;45(11):41-50.
- Argenta LC, Morykwas MJ, Marks MW, et al. Vacuum-assisted closure: state of clinic art. Plast Reconstr Surg. 2006 Jun;117(7 Suppl):127S-142S.
- Karl T, Modic PK, Voss EU. Indications and results of VAC therapy treatments in vascular surgery - state of the art in the treatment of chronic wounds [in German]. Zentralbl Chir. 2004 May;129 Suppl 1:S74-S79.
- Ford CN, Reinhard ER, Yeh D, et al. Interim analysis of a prospective, randomized trial of vacuum-assisted closure versus the healthpoint system in the management of pressure ulcers. Ann Plast Surg. 2002 Jul;49(1):55-61.
- Joseph E, Hamori CA, Bergman S, et al. A prospective randomized trial of vacuum-assisted closure versus standard therapy of chronic non-healing wounds. Wounds. 2000;12:60-67.
- Rozeboom AL, Steenvoorde P, Hartgrink HH, et al. Necrotizing fasciitis of the leg following a simple pelvic fracture: case report and literature review. J Wound Care. 2006;15:117-120.
- Steenvoorde P, Calame JJ, Oskam J. Maggot-treated wounds follow normal wound healing phases. Int J Dermatol. 2006;45:1477-1479.
- Mumcuoglu KY. Clinical applications for maggots in wound care. Am J Clin Dermatol. 2001;2(4):219-227.
- Attinger CE, Bulan EJ. Debridement. The key initial first step in wound healing. Foot Ankle Clin. 2001 Dec;6(4):627-660.
- Stannard JP, Robinson JT, Anderson ER, et al. Negative pressure wound therapy to treat hematomas and surgical incisions following high-energy trauma. J Trauma. 2006 Jun;60(6):1301-1306.
- Webb LX, Laver D, DeFranzo A. Negative pressure wound therapy in the management of orthopedic wounds. Ostomy Wound Manage. 2004 Apr;50(4A Suppl):26-27.
- Herscovici D Jr, Sanders RW, Scaduto JM, et al. Vacuum-assisted wound closure (VAC therapy) for the management of patients with high-energy soft tissue injuries. J Orthop Trauma. 2003 Nov-Dec;17(10):683-688.
- Wong LK, Nesbit RD, Turner LA, et al. Management of a circumferential lower extremity degloving injury with the use of vacuum-assisted closure. South Med J. 2006;99:628-630.
- Josty IC, Ramaswamy R, Laing JH. Vacuum assisted closure: an alternative strategy in the management of degloving injuries of the foot. Br J Plast Surg. 2001 Jun;54(4):363-365.
- Adamkova M, Tymonova J, Zamecnikova I, et al. First experience with the use of vacuum assisted closure in the treatment of skin defects at the burn center. Acta Chir Plast. 2005;47(1):24-27.
- Kamolz LP, Andel H, Haslik W, et al. Use of subatmospheric pressure therapy to prevent burn wound progression in human: first experiences. Burns. 2004;30:253-258.
- Obdeijn MC, de Lange MY, Lichtendahl DH, et al. Vacuum-assisted closure in the treatment of poststernotomy mediastinitis. Ann Thorac Surg. 1999;68:2358-2360.
- Agarwal JP, Ogilvie M, Wu LC, et al. Vacuum-assisted closure for sternal wounds: a first-line therapeutic management approach. Plast Reconstr Surg. 2005;116:1035-1040.
- Scholl L, Chang E, Reitz B, et al. Sternal osteomyelitis: use of vacuum-assisted closure device as an adjunct to definitive closure with sternectomy and muscle flap reconstruction. J Card Surg. 2004 Sep-Oct;19(5):453-461.
- DeFranzo AJ, Argenta L. Vacuum-assisted closure for the treatment of abdominal wounds. Clin Plast Surg. 2006;33:213-224.
- Nienhuijs SW, Manupassa R, Strobbe LJ, et al. Can topical negative pressure be used to control complex enterocutaneous fistulae? J Wound Care. 2003;12:343-345.
- Alvarez AA, Maxwell GL, Rodriguez GC. Vacuum-assisted closure for cutaneous gastrointestinal fistula management. Gynecol Oncol. 2001;80:413-416.
- Erdmann D, Drye C, Heller L, et al. Abdominal wall defect and enterocutaneous fistula treatment with the Vacuum-Assisted Closure (V.A.C.) system. Plast Reconstr Surg. 2001;108:2066-2068.
- Schaffzin DM, Douglas JM, Stahl TJ, et al. Vacuum-assisted closure of complex perineal wounds. Dis Colon Rectum. 2004;47:1745-1748.
- Jethwa P, Lake SP. Using topical negative pressure therapy to resolve wound failure following perineal resection. J Wound Care. 2005;14:166-167.
- McGuinness JG, Winter DC, O’Connell PR. Vacuum-assisted closure of a complex pilonidal sinus. Dis Colon Rectum. 2003;46:274-276.
- Steenvoorde P, van Engeland A. Oskam J. Vacuum-assisted closure therapy and oral anticoagulation therapy. Plast Reconstr Surg. 2004;113:2220-2221.
- Negative pressure wound therapy: Morykwas approach [adverse events data]. Available at: www.npwt.com/morykwas.htm. Last accessed March 20, 2007.
- Carson SN, Overall K, Lee-Jahshan S, et al. Vacuum-assisted closure used for healing chronic wounds and skin grafts in the lower extremities. Ostomy Wound Manage. 2004;50:52-58.
- Gwan-Nulla D, Casal RS. Toxic shock syndrome associated with the use of the vacuum-assisted closure device. Ann Plast Surg. 2001;47:552-554.
New Moves
The transition from hospital to home or to another care site is a high-risk period for the patient for a number of reasons, as we have discussed in The Hospitalist this year. Ineffective communication with the patient and between healthcare practitioners at discharge is common. In addition, primary care providers increasingly delegate inpatient care to hospitalists. This delegation of care can lead to gaps in knowledge that present risks to patient safety.
Further, information transfer among healthcare practitioners—whether they be primary care providers or hospitalists—and their patients is often compromised by record inaccuracies, omissions, illegibility, information never delivered, and delays in generation or transmission.
The Agency for Healthcare Research and Quality (AHRQ) has identified recall error, increased clinician workloads, interface failures between physicians and clerical staff, and inadequate training of physicians to respect the discharge process as the root causes of deficiencies in the current process of information transfer at discharge. While an interoperable health information technology infrastructure for the nation could effectively address many issues related to discharge planning, such a solution is certainly many years away.
New Approaches
Given the fact that a nationwide, interoperable health information technology infrastructure is not yet a reality, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is exploring multiple approaches for improving communication with patients and among practitioners in the discharge planning process. This article details those strategies and is meant to stimulate discussion and elicit suggestions for future approaches.
If you have any suggestions for improving the discharge planning process, e-mail us at [email protected]. We’ll publish the most effective and intriguing responses in a future issue of The Hospitalist.
Discharge Planning Standards
Patients may be discharged from the hospital entirely or transferred to another level of care, treatment, and services; they may be reassigned to different professionals or settings for continued services. JCAHO standards require that the hospital’s processes for transfer or discharge be based on the patient’s assessed needs. To facilitate discharge or transfer, the hospital should assess the patient’s needs, plan for discharge or transfer, facilitate the discharge or transfer process, and help to ensure that continuity of care, treatment, and services is maintained.
These standards (found in the Provision of Care (PC), Ethics, Rights and Responsibilities (RI), and Management of Information (IM) chapters of the hospital accreditation manual) will be updated in July 2007. The changes include both new language and new requirements meant to improve communication with patients and among providers during the discharge planning process. Rather than a significant overhaul, these changes can be viewed as refinements to the existing standards that will help hospitals ensure that the intent of each standard is actually carried out to benefit patients. For example, an element of performance for standard PC.4.10 that addresses development of a plan of care now specifies that this process should be individualized to the patient’s needs. Another example is standard IM.6.20, for which an element of performance will require that the medical record contain medications dispensed or prescribed at discharge.
It is also important to note that JCAHO standards underscore the importance of the patient retaining information. Today, JCAHO requires—through its National Patient Safety Goals—that a list of current medications be provided to the patient at discharge. For patients who have been treated by a hospitalist, this requirement is especially important when they return to their primary care physicians for follow-up treatment.
Discharge Planning During the On-Site Survey
JCAHO began more closely examining discharge planning in 2005 by piloting a new process that surveyors used to evaluate standards compliance in 2006. The first option tested is a concurrent review in which surveyors observe the discharge instructions as they are being taught to the patient and then interview the patient about the content. The second option is a retrospective review and entails calling patients 24 to 48 hours after discharge to ascertain their understanding of the medication regimen and other instructions provided. Both options are used by JCAHO surveyors to understand how practitioners, nurses, and other caregivers carry out the hospital’s policies.
To help hospitalists understand how surveyors approach this process, the following summary provides information about the two review options.
Discharge Planning—Active Review
- Ask for a list of patients who will be discharged during the survey.
- Review the patient’s medical/clinical record for discharge orders.
- Request that the organization obtain patient permission to observe the discharge process.
- Observe the clinician providing discharge instructions. Components of the discharge instruction may include:
- Activity;
- Diet;
- Medications (post-discharge);
- Plans for physician follow-up;
- Wound care, if applicable;
- Signs and symptoms to be aware of (i.e., elevated temperature, medication side effects);
- The name and telephone number of a physician to call should a problem or question arise following discharge; and
- Patient repetition of information to confirm understanding.
- Review the written discharge instructions given to the patient. The discharge instructions are written in a language the patient can read and understand.
- Interview the patient to determine the patient’s level of understanding of discharge instructions. If applicable to the instructions given to the patient being observed, the patient should understand:
- The purpose for taking any new medication;
- How to take the medication, including dose and frequency;
- Possible side effects of medication;
- The medication regimen, including continuation or discontinuation of medications taken prior to hospital admission;
- Contraindications between prescribed medications and over-the-counter medications and herbal remedies;
- Changes in diet and dietary restric- tions or supplements;
- Signs and symptoms of potential problems and who to call with questions and concerns;
- Information regarding continued self-care (i.e., wound care, activity);
- Follow-up process with physician(s); and
- Arrangements made for home-health needs (i.e., oxygen therapy, physical therapy).
- Interview the nurse/clinician to ascertain the origination of discharge information (physician-nurse communication regarding discharge instruction).
Discharge Planning—Retrospective Review
- Ask for a list of patients discharged during the past 48 hours.
- Review the patient’s old medical record for discharge orders.
- Request that the organization stay with the surveyor as phone calls are made. The organization should first talk with the patient to explain the purpose of the call and obtain permission for a phone interview.
- Interview the patient to determine understanding of discharge instructions provided. If applicable to the instructions given to the patient being observed, the patient should understand:
- The purpose for taking any new medication;
- How to take the medication, including dose and frequency;
- The medication regimen, including continuation or discontinuation of medications taken prior to hospital admission;
- Possible side effects of medication;
- Contraindications between prescribed medications and over-the-counter medications and herbal remedies;
- Changes in diet and dietary restrictions or supplements;
- Signs and symptoms of potential problems and whom to call with questions and concerns;
- Information regarding continued self-care (i.e., wound care, activity);
- Follow-up process with physician(s); and
- Arrangements made for home health needs (i.e., oxygen therapy, physical therapy).
- Explore the patient’s perception of the discharge instructions. Does the patient believe the necessary information was given?
Continuity of Care Record
Recognizing that patients remain the primary vehicle for transporting basic health information between providers, JCAHO is exploring strategies related to the Continuity of Care Record (CCR). This approach acknowledges that electronic health records are—at this time—a goal rather than the norm. Patients typically transport basic health information between providers in the context of completing a basic set of information on a registration form that is attached to a medical clipboard, prior to outpatient appointments and admissions.
An accurate minimum data set, containing such items as medication lists, allergies, conditions, and procedures, would provide substantial value to providers and patients. JCAHO already requires that an accurate medication list be updated at discharge and made available to the patient and the subsequent provider of care, but other key pieces of patient data, such as diagnosis and procedures, as well as the means required to make these data available to the patient or to the next caregiver, are not currently required.
JCAHO is now considering how hospitals and other healthcare organizations could provide or update a clinically relevant minimum data set of summarized health information, such as that contained in the CCR. The CCR is a standard specification being developed jointly by ASTM International, the Massachusetts Medical Society, the Healthcare Information Management Systems Society (HIMSS), the American Academy of Family Physicians, and the American Academy of Pediatrics.
JCAHO envisions a minimum data set that includes an accurate list of demographics, medical insurance, medications, diagnosis, past procedures, allergies, and current healthcare providers. It also desires a data set that can be provided to the patient or the patient’s authorized representatives—both as paper and in a fully transportable and interoperable digital format—that could be presented to subsequent caregivers. This summary health record would permit care providers within or outside the organization to review the patient’s important clinical information at the point of care and near the time of clinical decision-making. Subsequent care providers would then be able to update the patient’s minimum data set as appropriate.
In addition to providing caregivers with the most essential and relevant information necessary to ensure safe, quality care, such an approach would minimize the effort necessary to keep such information current. Healthcare providers would have easy access to the most recent patient assessment and the recommendations of the caregiver who last treated the patient.
Patient Involvement
JCAHO has sought to help healthcare organizations in assisting patients with the discharge planning process through its Speak Up education program, which urges people to take an active role in their own healthcare. “Planning Your Recovery” provides tips to help people get more involved in their care and obtain the information they need for the best possible recovery. Patients who understand and follow directions about their follow-up care have a greater chance of getting better faster; they are also less likely to go back to the hospital.
Specifically, the JCAHO education campaign advises patients to:
1. Find out about their condition. This includes knowing how soon they should feel better, getting information about their ability to do everyday activities such as walking or preparing meals, knowing warning signs and symptoms to watch for, enlisting the help of a family member of friend in the discharge process from the hospital, and getting the phone number of a person to call at the hospital if a problem arises.
2. Find out about new medicines. It is important to request written directions about new medicines and ask any questions before leaving the hospital. Other issues that JCAHO advises patients to consider include finding out whether other medicines, vitamins, and herbs could interfere with the new drugs and knowing whether there are any specific foods or drinks to avoid. Understanding the side effects of medications and any necessary restrictions on daily activities because of the potential for dizziness or sleepiness is also crucial.
3. Find out about follow-up care. This includes asking for written directions about cleaning and bandaging wounds, using special equipment, or doing any required exercises; finding out about follow-up visits to the hospital and making transportation arrangements for those visits; reviewing insurance to find out whether the cost of medicines and equipment needed for recovery will be covered; and determining whether home care services or a nursing home or assisted living center will be necessary for follow-up care.
JCAHO is joined in encouraging people to play an active role in planning their recovery by the National Alliance for Caregiving and the Centers for Medicare and Medicaid Services’ Care Planner. Practitioners who want to share this advice with their patients or wish to direct their patients to the information can go to JCAHO’s Web site, www.jointcommission.org, to download a free Speak Up brochure.
Conclusion
Ideally, discharge planning should be a smooth process facilitated by a personal health record that is controlled by the patient and that provides ready access to all of the patient’s health data that have been compiled from all the patient’s healthcare providers. Such a record would be accessible anywhere and at any time, over a lifetime. This concept remains in its infancy, however. Until such time as communication with patients and among providers is more transparent and less prone to error, The Joint Commission will continue to seek methods to better address this important aspect of providing safe, effective care. TH
Dr. Jacott, special advisor for professional relations at JCAHO, is the organization’s liaison to SHM. He also reaches out to state and specialty physician societies, hospital medical staffs, and other professional organizations.
The transition from hospital to home or to another care site is a high-risk period for the patient for a number of reasons, as we have discussed in The Hospitalist this year. Ineffective communication with the patient and between healthcare practitioners at discharge is common. In addition, primary care providers increasingly delegate inpatient care to hospitalists. This delegation of care can lead to gaps in knowledge that present risks to patient safety.
Further, information transfer among healthcare practitioners—whether they be primary care providers or hospitalists—and their patients is often compromised by record inaccuracies, omissions, illegibility, information never delivered, and delays in generation or transmission.
The Agency for Healthcare Research and Quality (AHRQ) has identified recall error, increased clinician workloads, interface failures between physicians and clerical staff, and inadequate training of physicians to respect the discharge process as the root causes of deficiencies in the current process of information transfer at discharge. While an interoperable health information technology infrastructure for the nation could effectively address many issues related to discharge planning, such a solution is certainly many years away.
New Approaches
Given the fact that a nationwide, interoperable health information technology infrastructure is not yet a reality, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is exploring multiple approaches for improving communication with patients and among practitioners in the discharge planning process. This article details those strategies and is meant to stimulate discussion and elicit suggestions for future approaches.
If you have any suggestions for improving the discharge planning process, e-mail us at [email protected]. We’ll publish the most effective and intriguing responses in a future issue of The Hospitalist.
Discharge Planning Standards
Patients may be discharged from the hospital entirely or transferred to another level of care, treatment, and services; they may be reassigned to different professionals or settings for continued services. JCAHO standards require that the hospital’s processes for transfer or discharge be based on the patient’s assessed needs. To facilitate discharge or transfer, the hospital should assess the patient’s needs, plan for discharge or transfer, facilitate the discharge or transfer process, and help to ensure that continuity of care, treatment, and services is maintained.
These standards (found in the Provision of Care (PC), Ethics, Rights and Responsibilities (RI), and Management of Information (IM) chapters of the hospital accreditation manual) will be updated in July 2007. The changes include both new language and new requirements meant to improve communication with patients and among providers during the discharge planning process. Rather than a significant overhaul, these changes can be viewed as refinements to the existing standards that will help hospitals ensure that the intent of each standard is actually carried out to benefit patients. For example, an element of performance for standard PC.4.10 that addresses development of a plan of care now specifies that this process should be individualized to the patient’s needs. Another example is standard IM.6.20, for which an element of performance will require that the medical record contain medications dispensed or prescribed at discharge.
It is also important to note that JCAHO standards underscore the importance of the patient retaining information. Today, JCAHO requires—through its National Patient Safety Goals—that a list of current medications be provided to the patient at discharge. For patients who have been treated by a hospitalist, this requirement is especially important when they return to their primary care physicians for follow-up treatment.
Discharge Planning During the On-Site Survey
JCAHO began more closely examining discharge planning in 2005 by piloting a new process that surveyors used to evaluate standards compliance in 2006. The first option tested is a concurrent review in which surveyors observe the discharge instructions as they are being taught to the patient and then interview the patient about the content. The second option is a retrospective review and entails calling patients 24 to 48 hours after discharge to ascertain their understanding of the medication regimen and other instructions provided. Both options are used by JCAHO surveyors to understand how practitioners, nurses, and other caregivers carry out the hospital’s policies.
To help hospitalists understand how surveyors approach this process, the following summary provides information about the two review options.
Discharge Planning—Active Review
- Ask for a list of patients who will be discharged during the survey.
- Review the patient’s medical/clinical record for discharge orders.
- Request that the organization obtain patient permission to observe the discharge process.
- Observe the clinician providing discharge instructions. Components of the discharge instruction may include:
- Activity;
- Diet;
- Medications (post-discharge);
- Plans for physician follow-up;
- Wound care, if applicable;
- Signs and symptoms to be aware of (i.e., elevated temperature, medication side effects);
- The name and telephone number of a physician to call should a problem or question arise following discharge; and
- Patient repetition of information to confirm understanding.
- Review the written discharge instructions given to the patient. The discharge instructions are written in a language the patient can read and understand.
- Interview the patient to determine the patient’s level of understanding of discharge instructions. If applicable to the instructions given to the patient being observed, the patient should understand:
- The purpose for taking any new medication;
- How to take the medication, including dose and frequency;
- Possible side effects of medication;
- The medication regimen, including continuation or discontinuation of medications taken prior to hospital admission;
- Contraindications between prescribed medications and over-the-counter medications and herbal remedies;
- Changes in diet and dietary restric- tions or supplements;
- Signs and symptoms of potential problems and who to call with questions and concerns;
- Information regarding continued self-care (i.e., wound care, activity);
- Follow-up process with physician(s); and
- Arrangements made for home-health needs (i.e., oxygen therapy, physical therapy).
- Interview the nurse/clinician to ascertain the origination of discharge information (physician-nurse communication regarding discharge instruction).
Discharge Planning—Retrospective Review
- Ask for a list of patients discharged during the past 48 hours.
- Review the patient’s old medical record for discharge orders.
- Request that the organization stay with the surveyor as phone calls are made. The organization should first talk with the patient to explain the purpose of the call and obtain permission for a phone interview.
- Interview the patient to determine understanding of discharge instructions provided. If applicable to the instructions given to the patient being observed, the patient should understand:
- The purpose for taking any new medication;
- How to take the medication, including dose and frequency;
- The medication regimen, including continuation or discontinuation of medications taken prior to hospital admission;
- Possible side effects of medication;
- Contraindications between prescribed medications and over-the-counter medications and herbal remedies;
- Changes in diet and dietary restrictions or supplements;
- Signs and symptoms of potential problems and whom to call with questions and concerns;
- Information regarding continued self-care (i.e., wound care, activity);
- Follow-up process with physician(s); and
- Arrangements made for home health needs (i.e., oxygen therapy, physical therapy).
- Explore the patient’s perception of the discharge instructions. Does the patient believe the necessary information was given?
Continuity of Care Record
Recognizing that patients remain the primary vehicle for transporting basic health information between providers, JCAHO is exploring strategies related to the Continuity of Care Record (CCR). This approach acknowledges that electronic health records are—at this time—a goal rather than the norm. Patients typically transport basic health information between providers in the context of completing a basic set of information on a registration form that is attached to a medical clipboard, prior to outpatient appointments and admissions.
An accurate minimum data set, containing such items as medication lists, allergies, conditions, and procedures, would provide substantial value to providers and patients. JCAHO already requires that an accurate medication list be updated at discharge and made available to the patient and the subsequent provider of care, but other key pieces of patient data, such as diagnosis and procedures, as well as the means required to make these data available to the patient or to the next caregiver, are not currently required.
JCAHO is now considering how hospitals and other healthcare organizations could provide or update a clinically relevant minimum data set of summarized health information, such as that contained in the CCR. The CCR is a standard specification being developed jointly by ASTM International, the Massachusetts Medical Society, the Healthcare Information Management Systems Society (HIMSS), the American Academy of Family Physicians, and the American Academy of Pediatrics.
JCAHO envisions a minimum data set that includes an accurate list of demographics, medical insurance, medications, diagnosis, past procedures, allergies, and current healthcare providers. It also desires a data set that can be provided to the patient or the patient’s authorized representatives—both as paper and in a fully transportable and interoperable digital format—that could be presented to subsequent caregivers. This summary health record would permit care providers within or outside the organization to review the patient’s important clinical information at the point of care and near the time of clinical decision-making. Subsequent care providers would then be able to update the patient’s minimum data set as appropriate.
In addition to providing caregivers with the most essential and relevant information necessary to ensure safe, quality care, such an approach would minimize the effort necessary to keep such information current. Healthcare providers would have easy access to the most recent patient assessment and the recommendations of the caregiver who last treated the patient.
Patient Involvement
JCAHO has sought to help healthcare organizations in assisting patients with the discharge planning process through its Speak Up education program, which urges people to take an active role in their own healthcare. “Planning Your Recovery” provides tips to help people get more involved in their care and obtain the information they need for the best possible recovery. Patients who understand and follow directions about their follow-up care have a greater chance of getting better faster; they are also less likely to go back to the hospital.
Specifically, the JCAHO education campaign advises patients to:
1. Find out about their condition. This includes knowing how soon they should feel better, getting information about their ability to do everyday activities such as walking or preparing meals, knowing warning signs and symptoms to watch for, enlisting the help of a family member of friend in the discharge process from the hospital, and getting the phone number of a person to call at the hospital if a problem arises.
2. Find out about new medicines. It is important to request written directions about new medicines and ask any questions before leaving the hospital. Other issues that JCAHO advises patients to consider include finding out whether other medicines, vitamins, and herbs could interfere with the new drugs and knowing whether there are any specific foods or drinks to avoid. Understanding the side effects of medications and any necessary restrictions on daily activities because of the potential for dizziness or sleepiness is also crucial.
3. Find out about follow-up care. This includes asking for written directions about cleaning and bandaging wounds, using special equipment, or doing any required exercises; finding out about follow-up visits to the hospital and making transportation arrangements for those visits; reviewing insurance to find out whether the cost of medicines and equipment needed for recovery will be covered; and determining whether home care services or a nursing home or assisted living center will be necessary for follow-up care.
JCAHO is joined in encouraging people to play an active role in planning their recovery by the National Alliance for Caregiving and the Centers for Medicare and Medicaid Services’ Care Planner. Practitioners who want to share this advice with their patients or wish to direct their patients to the information can go to JCAHO’s Web site, www.jointcommission.org, to download a free Speak Up brochure.
Conclusion
Ideally, discharge planning should be a smooth process facilitated by a personal health record that is controlled by the patient and that provides ready access to all of the patient’s health data that have been compiled from all the patient’s healthcare providers. Such a record would be accessible anywhere and at any time, over a lifetime. This concept remains in its infancy, however. Until such time as communication with patients and among providers is more transparent and less prone to error, The Joint Commission will continue to seek methods to better address this important aspect of providing safe, effective care. TH
Dr. Jacott, special advisor for professional relations at JCAHO, is the organization’s liaison to SHM. He also reaches out to state and specialty physician societies, hospital medical staffs, and other professional organizations.
The transition from hospital to home or to another care site is a high-risk period for the patient for a number of reasons, as we have discussed in The Hospitalist this year. Ineffective communication with the patient and between healthcare practitioners at discharge is common. In addition, primary care providers increasingly delegate inpatient care to hospitalists. This delegation of care can lead to gaps in knowledge that present risks to patient safety.
Further, information transfer among healthcare practitioners—whether they be primary care providers or hospitalists—and their patients is often compromised by record inaccuracies, omissions, illegibility, information never delivered, and delays in generation or transmission.
The Agency for Healthcare Research and Quality (AHRQ) has identified recall error, increased clinician workloads, interface failures between physicians and clerical staff, and inadequate training of physicians to respect the discharge process as the root causes of deficiencies in the current process of information transfer at discharge. While an interoperable health information technology infrastructure for the nation could effectively address many issues related to discharge planning, such a solution is certainly many years away.
New Approaches
Given the fact that a nationwide, interoperable health information technology infrastructure is not yet a reality, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is exploring multiple approaches for improving communication with patients and among practitioners in the discharge planning process. This article details those strategies and is meant to stimulate discussion and elicit suggestions for future approaches.
If you have any suggestions for improving the discharge planning process, e-mail us at [email protected]. We’ll publish the most effective and intriguing responses in a future issue of The Hospitalist.
Discharge Planning Standards
Patients may be discharged from the hospital entirely or transferred to another level of care, treatment, and services; they may be reassigned to different professionals or settings for continued services. JCAHO standards require that the hospital’s processes for transfer or discharge be based on the patient’s assessed needs. To facilitate discharge or transfer, the hospital should assess the patient’s needs, plan for discharge or transfer, facilitate the discharge or transfer process, and help to ensure that continuity of care, treatment, and services is maintained.
These standards (found in the Provision of Care (PC), Ethics, Rights and Responsibilities (RI), and Management of Information (IM) chapters of the hospital accreditation manual) will be updated in July 2007. The changes include both new language and new requirements meant to improve communication with patients and among providers during the discharge planning process. Rather than a significant overhaul, these changes can be viewed as refinements to the existing standards that will help hospitals ensure that the intent of each standard is actually carried out to benefit patients. For example, an element of performance for standard PC.4.10 that addresses development of a plan of care now specifies that this process should be individualized to the patient’s needs. Another example is standard IM.6.20, for which an element of performance will require that the medical record contain medications dispensed or prescribed at discharge.
It is also important to note that JCAHO standards underscore the importance of the patient retaining information. Today, JCAHO requires—through its National Patient Safety Goals—that a list of current medications be provided to the patient at discharge. For patients who have been treated by a hospitalist, this requirement is especially important when they return to their primary care physicians for follow-up treatment.
Discharge Planning During the On-Site Survey
JCAHO began more closely examining discharge planning in 2005 by piloting a new process that surveyors used to evaluate standards compliance in 2006. The first option tested is a concurrent review in which surveyors observe the discharge instructions as they are being taught to the patient and then interview the patient about the content. The second option is a retrospective review and entails calling patients 24 to 48 hours after discharge to ascertain their understanding of the medication regimen and other instructions provided. Both options are used by JCAHO surveyors to understand how practitioners, nurses, and other caregivers carry out the hospital’s policies.
To help hospitalists understand how surveyors approach this process, the following summary provides information about the two review options.
Discharge Planning—Active Review
- Ask for a list of patients who will be discharged during the survey.
- Review the patient’s medical/clinical record for discharge orders.
- Request that the organization obtain patient permission to observe the discharge process.
- Observe the clinician providing discharge instructions. Components of the discharge instruction may include:
- Activity;
- Diet;
- Medications (post-discharge);
- Plans for physician follow-up;
- Wound care, if applicable;
- Signs and symptoms to be aware of (i.e., elevated temperature, medication side effects);
- The name and telephone number of a physician to call should a problem or question arise following discharge; and
- Patient repetition of information to confirm understanding.
- Review the written discharge instructions given to the patient. The discharge instructions are written in a language the patient can read and understand.
- Interview the patient to determine the patient’s level of understanding of discharge instructions. If applicable to the instructions given to the patient being observed, the patient should understand:
- The purpose for taking any new medication;
- How to take the medication, including dose and frequency;
- Possible side effects of medication;
- The medication regimen, including continuation or discontinuation of medications taken prior to hospital admission;
- Contraindications between prescribed medications and over-the-counter medications and herbal remedies;
- Changes in diet and dietary restric- tions or supplements;
- Signs and symptoms of potential problems and who to call with questions and concerns;
- Information regarding continued self-care (i.e., wound care, activity);
- Follow-up process with physician(s); and
- Arrangements made for home-health needs (i.e., oxygen therapy, physical therapy).
- Interview the nurse/clinician to ascertain the origination of discharge information (physician-nurse communication regarding discharge instruction).
Discharge Planning—Retrospective Review
- Ask for a list of patients discharged during the past 48 hours.
- Review the patient’s old medical record for discharge orders.
- Request that the organization stay with the surveyor as phone calls are made. The organization should first talk with the patient to explain the purpose of the call and obtain permission for a phone interview.
- Interview the patient to determine understanding of discharge instructions provided. If applicable to the instructions given to the patient being observed, the patient should understand:
- The purpose for taking any new medication;
- How to take the medication, including dose and frequency;
- The medication regimen, including continuation or discontinuation of medications taken prior to hospital admission;
- Possible side effects of medication;
- Contraindications between prescribed medications and over-the-counter medications and herbal remedies;
- Changes in diet and dietary restrictions or supplements;
- Signs and symptoms of potential problems and whom to call with questions and concerns;
- Information regarding continued self-care (i.e., wound care, activity);
- Follow-up process with physician(s); and
- Arrangements made for home health needs (i.e., oxygen therapy, physical therapy).
- Explore the patient’s perception of the discharge instructions. Does the patient believe the necessary information was given?
Continuity of Care Record
Recognizing that patients remain the primary vehicle for transporting basic health information between providers, JCAHO is exploring strategies related to the Continuity of Care Record (CCR). This approach acknowledges that electronic health records are—at this time—a goal rather than the norm. Patients typically transport basic health information between providers in the context of completing a basic set of information on a registration form that is attached to a medical clipboard, prior to outpatient appointments and admissions.
An accurate minimum data set, containing such items as medication lists, allergies, conditions, and procedures, would provide substantial value to providers and patients. JCAHO already requires that an accurate medication list be updated at discharge and made available to the patient and the subsequent provider of care, but other key pieces of patient data, such as diagnosis and procedures, as well as the means required to make these data available to the patient or to the next caregiver, are not currently required.
JCAHO is now considering how hospitals and other healthcare organizations could provide or update a clinically relevant minimum data set of summarized health information, such as that contained in the CCR. The CCR is a standard specification being developed jointly by ASTM International, the Massachusetts Medical Society, the Healthcare Information Management Systems Society (HIMSS), the American Academy of Family Physicians, and the American Academy of Pediatrics.
JCAHO envisions a minimum data set that includes an accurate list of demographics, medical insurance, medications, diagnosis, past procedures, allergies, and current healthcare providers. It also desires a data set that can be provided to the patient or the patient’s authorized representatives—both as paper and in a fully transportable and interoperable digital format—that could be presented to subsequent caregivers. This summary health record would permit care providers within or outside the organization to review the patient’s important clinical information at the point of care and near the time of clinical decision-making. Subsequent care providers would then be able to update the patient’s minimum data set as appropriate.
In addition to providing caregivers with the most essential and relevant information necessary to ensure safe, quality care, such an approach would minimize the effort necessary to keep such information current. Healthcare providers would have easy access to the most recent patient assessment and the recommendations of the caregiver who last treated the patient.
Patient Involvement
JCAHO has sought to help healthcare organizations in assisting patients with the discharge planning process through its Speak Up education program, which urges people to take an active role in their own healthcare. “Planning Your Recovery” provides tips to help people get more involved in their care and obtain the information they need for the best possible recovery. Patients who understand and follow directions about their follow-up care have a greater chance of getting better faster; they are also less likely to go back to the hospital.
Specifically, the JCAHO education campaign advises patients to:
1. Find out about their condition. This includes knowing how soon they should feel better, getting information about their ability to do everyday activities such as walking or preparing meals, knowing warning signs and symptoms to watch for, enlisting the help of a family member of friend in the discharge process from the hospital, and getting the phone number of a person to call at the hospital if a problem arises.
2. Find out about new medicines. It is important to request written directions about new medicines and ask any questions before leaving the hospital. Other issues that JCAHO advises patients to consider include finding out whether other medicines, vitamins, and herbs could interfere with the new drugs and knowing whether there are any specific foods or drinks to avoid. Understanding the side effects of medications and any necessary restrictions on daily activities because of the potential for dizziness or sleepiness is also crucial.
3. Find out about follow-up care. This includes asking for written directions about cleaning and bandaging wounds, using special equipment, or doing any required exercises; finding out about follow-up visits to the hospital and making transportation arrangements for those visits; reviewing insurance to find out whether the cost of medicines and equipment needed for recovery will be covered; and determining whether home care services or a nursing home or assisted living center will be necessary for follow-up care.
JCAHO is joined in encouraging people to play an active role in planning their recovery by the National Alliance for Caregiving and the Centers for Medicare and Medicaid Services’ Care Planner. Practitioners who want to share this advice with their patients or wish to direct their patients to the information can go to JCAHO’s Web site, www.jointcommission.org, to download a free Speak Up brochure.
Conclusion
Ideally, discharge planning should be a smooth process facilitated by a personal health record that is controlled by the patient and that provides ready access to all of the patient’s health data that have been compiled from all the patient’s healthcare providers. Such a record would be accessible anywhere and at any time, over a lifetime. This concept remains in its infancy, however. Until such time as communication with patients and among providers is more transparent and less prone to error, The Joint Commission will continue to seek methods to better address this important aspect of providing safe, effective care. TH
Dr. Jacott, special advisor for professional relations at JCAHO, is the organization’s liaison to SHM. He also reaches out to state and specialty physician societies, hospital medical staffs, and other professional organizations.