User login
Quality Pays [editorial]
Adviser ONLY on the Web
In-office lab test is not an occasion for a modifier
I suspect that your problem may not be a global issue, but one of coverage for a lab test performed by your practice under CLIA (Clinical Laboratory Improvement Amendments). [Editor’s note: Details about coding for office lab tests (eg, wet mounts and KOH preps) in relation to CLIA certificate requirements were discussed in Reimbursement Adviser in the August 2006 issue of OBG Management. Read this installment at obgmanagement.com by linking to “Past Issues” on the top navigation bar of the home page.]
To sort out this situation, you first need to contact the payer to find out whether it considers a lab test global to an office visit, which should never be the case. Perhaps your billing staff misinterpreted the denial message. Or maybe this payer does, in fact, require a modifier for any service billed at the same time as an office visit.
On the other hand, it could also be that you do not have the required CLIA certificate to bill for the wet mount using code 87210.
Payer may balk at modified biophysical profile
- Code for the complete biophysical profile (76818) but add a modifier -52 for a reduced service. The problem? Not all payers permit use of this modifier with an imaging code.
- Itemize your services by reporting 59025 for the fetal non-stress test and 76815 (limited pelvic ultrasound) for evaluation of amniotic fluid volume. The problem here? Code 59025 is bundled into code 76815; although you are allowed to use the modifier -59 (distinct procedural service) to bypass the edit, you can only do so if you can meet the criteria for doing so (eg, care involves a different incision or excision, a different patient encounter, or a different injury or site). Some payers may not accept that you’ve met those requirements, although I would disagree with that decision: Each test is performed independently and measures different things. So, to bill this combination of tests, add modifier -59 to the bundled code: 76815, 59025-59.
Hysteroscopy before but not during thermoablation
Modifier -59 is defined as follows in CPT: “…used to identify procedures/services that are not normally reported together, but are appropriate under the circumstances. This may represent a different session or patient encounter, different procedure or surgery, different site or organ system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive injuries) not ordinarily encountered or performed on the same day by the same physician.”
In the situation that you describe, the hysteroscope was inserted in the same area as the ablation, not at a different site; no separate excision or incision was made when inserting the hysteroscope; this was not a different surgical session; and, last, although hysteroscopy might, technically, be a distinct procedure from the ablation, it was directly related to the performance of the ablation in that it represented initial “exploration.”
I believe, therefore, that correct coding in this case is to report the all-inclusive 58563 (Hysteroscopy, surgical; with endometrial ablation [eg, endometrial resection, electrosurgical ablation, thermoablation]). Support for this opinion is found in ACOG’s Ob/GYN Coding Manual: Components of Correct Procedural Coding 2007. A comment included with code 58353 states: “If hysteroscopy is also performed, report code 58563 instead.”
In-office lab test is not an occasion for a modifier
I suspect that your problem may not be a global issue, but one of coverage for a lab test performed by your practice under CLIA (Clinical Laboratory Improvement Amendments). [Editor’s note: Details about coding for office lab tests (eg, wet mounts and KOH preps) in relation to CLIA certificate requirements were discussed in Reimbursement Adviser in the August 2006 issue of OBG Management. Read this installment at obgmanagement.com by linking to “Past Issues” on the top navigation bar of the home page.]
To sort out this situation, you first need to contact the payer to find out whether it considers a lab test global to an office visit, which should never be the case. Perhaps your billing staff misinterpreted the denial message. Or maybe this payer does, in fact, require a modifier for any service billed at the same time as an office visit.
On the other hand, it could also be that you do not have the required CLIA certificate to bill for the wet mount using code 87210.
Payer may balk at modified biophysical profile
- Code for the complete biophysical profile (76818) but add a modifier -52 for a reduced service. The problem? Not all payers permit use of this modifier with an imaging code.
- Itemize your services by reporting 59025 for the fetal non-stress test and 76815 (limited pelvic ultrasound) for evaluation of amniotic fluid volume. The problem here? Code 59025 is bundled into code 76815; although you are allowed to use the modifier -59 (distinct procedural service) to bypass the edit, you can only do so if you can meet the criteria for doing so (eg, care involves a different incision or excision, a different patient encounter, or a different injury or site). Some payers may not accept that you’ve met those requirements, although I would disagree with that decision: Each test is performed independently and measures different things. So, to bill this combination of tests, add modifier -59 to the bundled code: 76815, 59025-59.
Hysteroscopy before but not during thermoablation
Modifier -59 is defined as follows in CPT: “…used to identify procedures/services that are not normally reported together, but are appropriate under the circumstances. This may represent a different session or patient encounter, different procedure or surgery, different site or organ system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive injuries) not ordinarily encountered or performed on the same day by the same physician.”
In the situation that you describe, the hysteroscope was inserted in the same area as the ablation, not at a different site; no separate excision or incision was made when inserting the hysteroscope; this was not a different surgical session; and, last, although hysteroscopy might, technically, be a distinct procedure from the ablation, it was directly related to the performance of the ablation in that it represented initial “exploration.”
I believe, therefore, that correct coding in this case is to report the all-inclusive 58563 (Hysteroscopy, surgical; with endometrial ablation [eg, endometrial resection, electrosurgical ablation, thermoablation]). Support for this opinion is found in ACOG’s Ob/GYN Coding Manual: Components of Correct Procedural Coding 2007. A comment included with code 58353 states: “If hysteroscopy is also performed, report code 58563 instead.”
In-office lab test is not an occasion for a modifier
I suspect that your problem may not be a global issue, but one of coverage for a lab test performed by your practice under CLIA (Clinical Laboratory Improvement Amendments). [Editor’s note: Details about coding for office lab tests (eg, wet mounts and KOH preps) in relation to CLIA certificate requirements were discussed in Reimbursement Adviser in the August 2006 issue of OBG Management. Read this installment at obgmanagement.com by linking to “Past Issues” on the top navigation bar of the home page.]
To sort out this situation, you first need to contact the payer to find out whether it considers a lab test global to an office visit, which should never be the case. Perhaps your billing staff misinterpreted the denial message. Or maybe this payer does, in fact, require a modifier for any service billed at the same time as an office visit.
On the other hand, it could also be that you do not have the required CLIA certificate to bill for the wet mount using code 87210.
Payer may balk at modified biophysical profile
- Code for the complete biophysical profile (76818) but add a modifier -52 for a reduced service. The problem? Not all payers permit use of this modifier with an imaging code.
- Itemize your services by reporting 59025 for the fetal non-stress test and 76815 (limited pelvic ultrasound) for evaluation of amniotic fluid volume. The problem here? Code 59025 is bundled into code 76815; although you are allowed to use the modifier -59 (distinct procedural service) to bypass the edit, you can only do so if you can meet the criteria for doing so (eg, care involves a different incision or excision, a different patient encounter, or a different injury or site). Some payers may not accept that you’ve met those requirements, although I would disagree with that decision: Each test is performed independently and measures different things. So, to bill this combination of tests, add modifier -59 to the bundled code: 76815, 59025-59.
Hysteroscopy before but not during thermoablation
Modifier -59 is defined as follows in CPT: “…used to identify procedures/services that are not normally reported together, but are appropriate under the circumstances. This may represent a different session or patient encounter, different procedure or surgery, different site or organ system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive injuries) not ordinarily encountered or performed on the same day by the same physician.”
In the situation that you describe, the hysteroscope was inserted in the same area as the ablation, not at a different site; no separate excision or incision was made when inserting the hysteroscope; this was not a different surgical session; and, last, although hysteroscopy might, technically, be a distinct procedure from the ablation, it was directly related to the performance of the ablation in that it represented initial “exploration.”
I believe, therefore, that correct coding in this case is to report the all-inclusive 58563 (Hysteroscopy, surgical; with endometrial ablation [eg, endometrial resection, electrosurgical ablation, thermoablation]). Support for this opinion is found in ACOG’s Ob/GYN Coding Manual: Components of Correct Procedural Coding 2007. A comment included with code 58353 states: “If hysteroscopy is also performed, report code 58563 instead.”
More Reimbursement Adviser
“The fifth-digits, which are appropriate for each code number, are listed in brackets under each code. The fifth digits on each code should all be consistent with each other. That is, should a delivery occur all of the fifth digits should indicate the delivery.”
In this case, although the patient was still in the antepartum period during initial care, she did deliver during that hospitalization. That means a fifth digit of “3” (antepartum condition or complication) is incompatible with a fifth digit of “1” (delivered, with or without mention of antepartum condition), which is probably what generated the denial message. You have 2 choices:
- Resubmit a corrected claim, indicating a fifth digit of “1” for both diagnostic codes
- Appeal the denial, indicating the diagnostic correction and supplying information regarding the additional care for this patient.
Bundle codes for repair of a pelvic floor defect?
Based on the definition of the addon mesh code, it is appropriate for you to bill for a quantity of 2: 1 for the anterior compartment repair and 1 for the posterior compartment repair, which includes the rectocele and enterocele.
As for reporting the cystoscopy (with 52000 [cystourethroscopy (separate procedure)]), the reason that you provide for the procedure will determine whether you are reimbursed. There must be a medical indication for cystoscopy beyond your simply checking your work, which is considered a standard of surgical care by most payers.
“The fifth-digits, which are appropriate for each code number, are listed in brackets under each code. The fifth digits on each code should all be consistent with each other. That is, should a delivery occur all of the fifth digits should indicate the delivery.”
In this case, although the patient was still in the antepartum period during initial care, she did deliver during that hospitalization. That means a fifth digit of “3” (antepartum condition or complication) is incompatible with a fifth digit of “1” (delivered, with or without mention of antepartum condition), which is probably what generated the denial message. You have 2 choices:
- Resubmit a corrected claim, indicating a fifth digit of “1” for both diagnostic codes
- Appeal the denial, indicating the diagnostic correction and supplying information regarding the additional care for this patient.
Bundle codes for repair of a pelvic floor defect?
Based on the definition of the addon mesh code, it is appropriate for you to bill for a quantity of 2: 1 for the anterior compartment repair and 1 for the posterior compartment repair, which includes the rectocele and enterocele.
As for reporting the cystoscopy (with 52000 [cystourethroscopy (separate procedure)]), the reason that you provide for the procedure will determine whether you are reimbursed. There must be a medical indication for cystoscopy beyond your simply checking your work, which is considered a standard of surgical care by most payers.
“The fifth-digits, which are appropriate for each code number, are listed in brackets under each code. The fifth digits on each code should all be consistent with each other. That is, should a delivery occur all of the fifth digits should indicate the delivery.”
In this case, although the patient was still in the antepartum period during initial care, she did deliver during that hospitalization. That means a fifth digit of “3” (antepartum condition or complication) is incompatible with a fifth digit of “1” (delivered, with or without mention of antepartum condition), which is probably what generated the denial message. You have 2 choices:
- Resubmit a corrected claim, indicating a fifth digit of “1” for both diagnostic codes
- Appeal the denial, indicating the diagnostic correction and supplying information regarding the additional care for this patient.
Bundle codes for repair of a pelvic floor defect?
Based on the definition of the addon mesh code, it is appropriate for you to bill for a quantity of 2: 1 for the anterior compartment repair and 1 for the posterior compartment repair, which includes the rectocele and enterocele.
As for reporting the cystoscopy (with 52000 [cystourethroscopy (separate procedure)]), the reason that you provide for the procedure will determine whether you are reimbursed. There must be a medical indication for cystoscopy beyond your simply checking your work, which is considered a standard of surgical care by most payers.
Lisdexamfetamine for ADHD
Lisdexamfetamine—FDA-approved to treat attention-deficit/hyperactivity disorder (ADHD) in children ages 6 to 12 (Table 1)—reduces ADHD symptoms during and after school and may be less likely to be abused than other psychostimulants, particularly immediate-release preparations, clinical data suggest.
Table 1
Lisdexamfetamine: Fast facts
| Brand name: Vyvanse |
| Indication: ADHD in children ages 6 to 12 |
| Approval date: February 23, 2007 |
| Manufacturers: New River Pharmaceuticals and Shire |
| Dosing forms: 30-, 50-, and 70-mg capsules |
| Recommended dosage: Start at 30 mg/d. If necessary, titrate by 20 mg every 3 to 7 days to a maximum 70 mg/d. |
Clinical implications
Because it is effective for about 12 hours, lisdexamfetamine might improve the child’s ability to complete homework and participate in extracurricular activities, which in turn might enhance academic performance and/or socialization skills.
Lisdexamfetamine could help the child with ADHD who shows no contraindications to the drug —particularly if he or she needs daylong coverage.
How it works
Lisdexamfetamine—a dextroamphetamine derivative—is rapidly absorbed and converted to dextroamphetamine, which is believed to exert therapeutic effect by:
- blocking norepinephrine and dopamine reuptake into presynaptic neurons
- increasing the neurotransmitters’ release into the extraneuronal space.
The medication’s amphetamine release is highly predictable, which contributes to its therapeutic benefit in ADHD. Amphetamine is released through GI metabolism of lisdexamfetamine, which produces the active d-amphetamine moiety that reaches the bloodstream. The medication is derived from d-amphetamine, with negligible amounts of lysine cleaved.
Lisdexamfetamine requires in vivo metabolism (in the GI tract) to its active constituent d-amphetamine. As a result, the medication will not produce high d-amphetamine blood levels—and should not cause euphoria or other reinforcing effects—if injected or snorted. Its abuse potential is lower overall compared with immediate-release psychostimulant formulations.
Pharmacokinetics
Dextroamphetamine’s plasma elimination half-life is approximately 9½ hours—which accounts for lisdexamfetamine’s extended action. The drug reaches steady-state concentrations in 2 to 3 days.
Food does not affect absorption and delays maximum concentration by 1 hour or less, so taking lisdexamfetamine during breakfast should not slow its therapeutic effect. Because dextroamphetamine reaches maximum concentration in approximately 3½ hours, the medication should take effect by the time the child gets to school. In one randomized, phase-2 trial, children with ADHD who received lisdexamfetamine, 30 to 70 mg/d, showed overall improvement within 2 hours after dosing.1
Efficacy
Lisdexamfetamine reduced ADHD symptoms in 2 double-blind studies: a phase-2 crossover study and a phase-3 random-dose trial.
Phase-2 crossover study.2 Fifty-two children ages 6 to 12 with combined or hyperactive-impulsive type ADHD received extended-release mixed amphetamine salts (MAS) for 3 weeks. Subjects received 10 mg/d or dosages titrated to 20 or 30 mg/d based on response to medication.
The youths then were divided into 3 groups based on optimal MAS dosage and received 3 treatments for 1 week each:
- group 1: placebo; MAS, 10 mg/d; lisdexamfetamine, 30 mg/d
- group 2: placebo; MAS, 20 mg/d; lisdexamfetamine, 50 mg/d
- group 3: placebo; MAS, 30 mg/d; lisdexamfetamine, 70 mg/d.
While taking lisdexamfetamine or MAS, subjects showed similar improvement in behavior, based on Swanson, Kotkin, Agler, M-Flynn, and Pelham (SKAMP) scores, and inattention, based on SKAMP and Permanent Product Measure of Performance scores.
Both psychostimulants outperformed placebo in both measures, and both improved behavior more decisively than inattention. Based on post-hoc analysis, improvement 12 hours after dosing was more substantial with lisdexamfetamine than with MAS.
Phase-3 random-dose trial.3 A total of 290 children ages 6 to 12 with combined or hyperactive-impulsive type ADHD were “washed out” from prior medications over 1 week, then received lisdexamfetamine or placebo for 4 weeks. Treatment-group children were started at 30 mg/d; some received dosages titrated at random to 50 or 70 mg/d in weekly 20-mg increments.
Over 4 weeks, ADHD Rating Scale Version IV (ADHD-RS-IV) scores fell 50% to 59% among the 3 lisdexamfetamine dosage groups, compared with a 15% reduction in the placebo group. Substantial ADHD-RS-IV score improvements after 1 week of lisdexamfetamine were maintained throughout the trial, suggesting the medication sustains ADHD symptom improvement. Controlled trials have not addressed lisdexamfetamine use >4 weeks, however.
Based on parents’ and guardians’ reports, treatment-group patients’ ADHD symptoms were notably less severe at 10 AM, 2 PM, and 6 PM compared with placebo-group children.3 This suggests that lisdexamfetamine offers a daylong therapeutic effect.
Tolerability
In the phase-3 study,3 162 of 218 (74%) children receiving any dosage of lisdexamfetamine reported an adverse event, compared with 34 of 72 (47%) children in the placebo group. Overall, 39% of lisdexamfetamine-group patients reported decreased appetite. Also common were insomnia, headaches, irritability, upper abdominal pain, vomiting, and weight loss (Table 2).
Although most adverse events were mild to moderate, 9.2% of treatment-group children dropped out because of intolerability, compared with 1.4% of the placebo group. The investigators increased dosages quickly, regardless of efficacy or tolerability,3 which might have increased side-effect incidence among the treatment groups.
In the phase-2 crossover trial,2 adverse event rates were similar among the lisdexamfetamine, extended-release MAS, and placebo groups (15% to 18%). Among youths receiving lisdexamfetamine, 8% reported insomnia and 6% reported appetite loss, compared with 2% and 4% of the MAS group, respectively.
Table 2
Rates of commonly reported adverse effects
during phase-3 lisdexamfetamine (LDX) study
| Adverse effect | LDX 30 mg/d | LDX 50 mg/d* | LDX 70 mg/d* | LDX all dosages | Placebo |
|---|---|---|---|---|---|
| All adverse effects | 72% | 68% | 84% | 74% | 47% |
| Decreased appetite | 37% | 31% | 49% | 39% | 4% |
| Insomnia | 16% | 16% | 25% | 19% | 3% |
| Upper abdominal pain | 14% | 7% | 15% | 12% | 6% |
| Headache | 10% | 10% | 16% | 12% | 10% |
| Irritability | 11% | 8% | 10% | 10% | 0% |
| Vomiting | 7% | 5% | 14% | 9% | 4% |
| Weight loss | 6% | 3% | 19% | 9% | 1% |
| *Dosages were randomly titrated regardless of efficacy or tolerability. | |||||
| Source: Reference 3 | |||||
Safety
Findling et al4 found a larger change in corrected QT interval with lisdexamfetamine (7 to 14 msec) than with extended-release MAS (5 to 10 msec) 5 and 10½ hours after dosing. The authors reasoned that these findings are atypical, and no children suffered serious adverse events during the trial. Nonetheless, more research on whether lisdexamfetamine increases cardiac risk is needed.
In a lethal-dose study in rats,5 oral lisdexamfetamine doses up to 1,000 mg/kg did not result in death, suggesting the medication might undergo saturation kinetics in the GI tract that may protect against overdose or abuse at higher dosages. By comparison, the median lethal oral dosage of d-amphetamine in rats was 96.8 mg/kg.5
Abuse potential
As with other psychostimulants indicated for ADHD, the Drug Enforcement Administration has classified lisdexamfetamine as a schedule II drug, which applies to addictive prescription-only medications with an accepted medical use.
Clinical data suggest, however, that lisdexamfetamine might be less “enjoyable”—and less likely to be abused intravenously, orally, or intranasally—than equipotent d-amphetamine. In an abuse liability study,6 12 adults with histories of stimulant abuse received intravenous immediate-release (IR) d-amphetamine, 10 or 20 mg. Two days later, they received a comparable dose of IV lisdexamfetamine, 25 or 50 mg. The researchers found that:
- Plasma d-amphetamine peaked within 5 minutes after injection, compared with 2 to 3 hours after lisdexamfetamine dosing.
- Subjects who received IR d-amphetamine said they felt euphoria within 15 minutes of injection. By contrast, no one reported euphoria or amphetamine-like subjective effects after receiving lisdexamfetamine.
When asked which medication they would try again, 9 of 12 subjects chose IR d-amphetamine and 1 chose lisdexamfetamine.
In a double-blind, randomized, placebo-controlled study,7 oral lisdexamfetamine, 50 or 100 mg, was not more “likeable” than placebo. Subjects reported “liking” effects with 150 mg of lisdexamfetamine, however, suggesting the medication could be misused or abused at higher-than-therapeutic dosages.
As with other psychostimulants, do not give lisdexamfetamine to youths with preexisting serious structural cardiac abnormalities or other heart problems. Assess patient and family history of heart disease before prescribing this medication.
Do not prescribe lisdexamfetamine to patients taking a monoamine oxidase inhibitor (MAOI). By slowing amphetamine metabolism, these antidepressants intensify amphetamines’ effect on monoamine release, which can cause headaches and lead to hypertensive crisis. Before starting lisdexamfetamine, ask if the patient is taking an MAOI or has taken one within 2 weeks of presentation.
Use caution when prescribing lisdexamfetamine to patients with:
- a comorbid eating disorder or sleep disturbance. Determine whether to address the comorbidity before treating ADHD symptoms, and make sure lisdexamfetamine is not worsening the comorbid symptoms.
- untreated hypertension or other cardiovascular conditions, as stimulant medications can increase blood pressure and heart rate. Watch for significant heart rate and blood pressure changes in patients taking lisdexamfetamine, which probably would not cause sustained blood pressure increase in patients taking antihypertensives.8
Related resources
- Lisdexamfetamine Web site. www.vyvanse.com.
Drug brand names
- Extended-release mixed amphetamine salts • Adderall XR
- Lisdexamfetamine • Vyvanse
Disclosure
Dr. Wilens receives research/grant support from Abbott Laboratories, Eli Lilly and Company, National Institute on Drug Abuse, NeuroSearch, Ortho-McNeil, and Shire; is a speaker for Novartis Pharmaceuticals Corp., Ortho-McNeil, and Shire; and is a consultant to Abbott Laboratories, Eli Lilly and Company, GlaxoSmithKline, National Institute on Drug Abuse, Novartis Pharmaceuticals Corp., Ortho-McNeil, Pfizer, and Shire.
1. Lopez FA, Boellner SW, Childress A, et al. ADHD symptom improvement in children treated with lisdexamfetamine dimesylate (LDX). Poster presented at: Annual Meeting of the American Academy of Child and Adolescent Psychiatry; October 24-29, 2006; San Diego, CA.
2. Biederman J, Boellner SW, Childress A, et al. Improvements in symptoms of attention-deficit/hyperactivity disorder in school-aged children with lisdexamfetamine (NRP 104) and mixed amphetamine salts, extended-release versus placebo. Poster presented at: Annual Meeting of the American Psychiatric Association; May 20-25, 2006; Toronto, Canada.
3. Biederman J, Krishnan S, Zhang Y, et al. Efficacy and tolerability of lisdexamfetamine dimesylate (NRP 104) in children with attention-deficit/hyperactivity disorder: a phase III, multicenter, randomized, double-blind, forced-dose, parallel-group study. Clin Ther 2007;29:450-63.
4. Findling FL, Biederman J, Wilens TE, et al. Short- and long-term cardiovascular effects of mixed amphetamine salts extended release in children. J Pediatr 2005;147:348-54.
5. Krishnan S. Toxicity profile of lisdexamfetamine dimesylate (LDX NRP104) in three independent rat toxicology studies. Basic Clin Phamacol Toxicol. In press.
6. Jasinski DR. Abuse liability of intravenous L-lysine-d-amphetamine (NRP 104). Poster presented at: Annual Meeting of the College on Problems of Drug Dependence; June 17-22, 2006; Scottsdale, AZ. Available at: http://xml.10kwizard.com/filing_raw.php?repo=tenk&ipage=4234033. Accessed April 5, 2007.
7. Jasinski D, Krishnan S. A double-blind, randomized, placebo and active-controlled, six-period crossover study to evaluate the likeability, safety, and abuse liability of NRP 104 in healthy adult volunteers with histories of stimulant abuse (NRP104. A03). Poster presented at: Annual Meeting of the College on Problems of Drug Dependence; June 17-22, 2006; Scottsdale, AZ. Available at: http://www.secinfo.com/d12Pk6.v9Ac.d.htm. Accessed May 14, 2007.
8. Wilens TE, Zusman RM, Hammerness PG, et al. An open-label study of the tolerability of mixed amphetamine salts in adults with attention-deficit/hyperactivity disorder and treated primary essential hypertension. J Clin Psychiatry 2006;67:696-702.
Lisdexamfetamine—FDA-approved to treat attention-deficit/hyperactivity disorder (ADHD) in children ages 6 to 12 (Table 1)—reduces ADHD symptoms during and after school and may be less likely to be abused than other psychostimulants, particularly immediate-release preparations, clinical data suggest.
Table 1
Lisdexamfetamine: Fast facts
| Brand name: Vyvanse |
| Indication: ADHD in children ages 6 to 12 |
| Approval date: February 23, 2007 |
| Manufacturers: New River Pharmaceuticals and Shire |
| Dosing forms: 30-, 50-, and 70-mg capsules |
| Recommended dosage: Start at 30 mg/d. If necessary, titrate by 20 mg every 3 to 7 days to a maximum 70 mg/d. |
Clinical implications
Because it is effective for about 12 hours, lisdexamfetamine might improve the child’s ability to complete homework and participate in extracurricular activities, which in turn might enhance academic performance and/or socialization skills.
Lisdexamfetamine could help the child with ADHD who shows no contraindications to the drug —particularly if he or she needs daylong coverage.
How it works
Lisdexamfetamine—a dextroamphetamine derivative—is rapidly absorbed and converted to dextroamphetamine, which is believed to exert therapeutic effect by:
- blocking norepinephrine and dopamine reuptake into presynaptic neurons
- increasing the neurotransmitters’ release into the extraneuronal space.
The medication’s amphetamine release is highly predictable, which contributes to its therapeutic benefit in ADHD. Amphetamine is released through GI metabolism of lisdexamfetamine, which produces the active d-amphetamine moiety that reaches the bloodstream. The medication is derived from d-amphetamine, with negligible amounts of lysine cleaved.
Lisdexamfetamine requires in vivo metabolism (in the GI tract) to its active constituent d-amphetamine. As a result, the medication will not produce high d-amphetamine blood levels—and should not cause euphoria or other reinforcing effects—if injected or snorted. Its abuse potential is lower overall compared with immediate-release psychostimulant formulations.
Pharmacokinetics
Dextroamphetamine’s plasma elimination half-life is approximately 9½ hours—which accounts for lisdexamfetamine’s extended action. The drug reaches steady-state concentrations in 2 to 3 days.
Food does not affect absorption and delays maximum concentration by 1 hour or less, so taking lisdexamfetamine during breakfast should not slow its therapeutic effect. Because dextroamphetamine reaches maximum concentration in approximately 3½ hours, the medication should take effect by the time the child gets to school. In one randomized, phase-2 trial, children with ADHD who received lisdexamfetamine, 30 to 70 mg/d, showed overall improvement within 2 hours after dosing.1
Efficacy
Lisdexamfetamine reduced ADHD symptoms in 2 double-blind studies: a phase-2 crossover study and a phase-3 random-dose trial.
Phase-2 crossover study.2 Fifty-two children ages 6 to 12 with combined or hyperactive-impulsive type ADHD received extended-release mixed amphetamine salts (MAS) for 3 weeks. Subjects received 10 mg/d or dosages titrated to 20 or 30 mg/d based on response to medication.
The youths then were divided into 3 groups based on optimal MAS dosage and received 3 treatments for 1 week each:
- group 1: placebo; MAS, 10 mg/d; lisdexamfetamine, 30 mg/d
- group 2: placebo; MAS, 20 mg/d; lisdexamfetamine, 50 mg/d
- group 3: placebo; MAS, 30 mg/d; lisdexamfetamine, 70 mg/d.
While taking lisdexamfetamine or MAS, subjects showed similar improvement in behavior, based on Swanson, Kotkin, Agler, M-Flynn, and Pelham (SKAMP) scores, and inattention, based on SKAMP and Permanent Product Measure of Performance scores.
Both psychostimulants outperformed placebo in both measures, and both improved behavior more decisively than inattention. Based on post-hoc analysis, improvement 12 hours after dosing was more substantial with lisdexamfetamine than with MAS.
Phase-3 random-dose trial.3 A total of 290 children ages 6 to 12 with combined or hyperactive-impulsive type ADHD were “washed out” from prior medications over 1 week, then received lisdexamfetamine or placebo for 4 weeks. Treatment-group children were started at 30 mg/d; some received dosages titrated at random to 50 or 70 mg/d in weekly 20-mg increments.
Over 4 weeks, ADHD Rating Scale Version IV (ADHD-RS-IV) scores fell 50% to 59% among the 3 lisdexamfetamine dosage groups, compared with a 15% reduction in the placebo group. Substantial ADHD-RS-IV score improvements after 1 week of lisdexamfetamine were maintained throughout the trial, suggesting the medication sustains ADHD symptom improvement. Controlled trials have not addressed lisdexamfetamine use >4 weeks, however.
Based on parents’ and guardians’ reports, treatment-group patients’ ADHD symptoms were notably less severe at 10 AM, 2 PM, and 6 PM compared with placebo-group children.3 This suggests that lisdexamfetamine offers a daylong therapeutic effect.
Tolerability
In the phase-3 study,3 162 of 218 (74%) children receiving any dosage of lisdexamfetamine reported an adverse event, compared with 34 of 72 (47%) children in the placebo group. Overall, 39% of lisdexamfetamine-group patients reported decreased appetite. Also common were insomnia, headaches, irritability, upper abdominal pain, vomiting, and weight loss (Table 2).
Although most adverse events were mild to moderate, 9.2% of treatment-group children dropped out because of intolerability, compared with 1.4% of the placebo group. The investigators increased dosages quickly, regardless of efficacy or tolerability,3 which might have increased side-effect incidence among the treatment groups.
In the phase-2 crossover trial,2 adverse event rates were similar among the lisdexamfetamine, extended-release MAS, and placebo groups (15% to 18%). Among youths receiving lisdexamfetamine, 8% reported insomnia and 6% reported appetite loss, compared with 2% and 4% of the MAS group, respectively.
Table 2
Rates of commonly reported adverse effects
during phase-3 lisdexamfetamine (LDX) study
| Adverse effect | LDX 30 mg/d | LDX 50 mg/d* | LDX 70 mg/d* | LDX all dosages | Placebo |
|---|---|---|---|---|---|
| All adverse effects | 72% | 68% | 84% | 74% | 47% |
| Decreased appetite | 37% | 31% | 49% | 39% | 4% |
| Insomnia | 16% | 16% | 25% | 19% | 3% |
| Upper abdominal pain | 14% | 7% | 15% | 12% | 6% |
| Headache | 10% | 10% | 16% | 12% | 10% |
| Irritability | 11% | 8% | 10% | 10% | 0% |
| Vomiting | 7% | 5% | 14% | 9% | 4% |
| Weight loss | 6% | 3% | 19% | 9% | 1% |
| *Dosages were randomly titrated regardless of efficacy or tolerability. | |||||
| Source: Reference 3 | |||||
Safety
Findling et al4 found a larger change in corrected QT interval with lisdexamfetamine (7 to 14 msec) than with extended-release MAS (5 to 10 msec) 5 and 10½ hours after dosing. The authors reasoned that these findings are atypical, and no children suffered serious adverse events during the trial. Nonetheless, more research on whether lisdexamfetamine increases cardiac risk is needed.
In a lethal-dose study in rats,5 oral lisdexamfetamine doses up to 1,000 mg/kg did not result in death, suggesting the medication might undergo saturation kinetics in the GI tract that may protect against overdose or abuse at higher dosages. By comparison, the median lethal oral dosage of d-amphetamine in rats was 96.8 mg/kg.5
Abuse potential
As with other psychostimulants indicated for ADHD, the Drug Enforcement Administration has classified lisdexamfetamine as a schedule II drug, which applies to addictive prescription-only medications with an accepted medical use.
Clinical data suggest, however, that lisdexamfetamine might be less “enjoyable”—and less likely to be abused intravenously, orally, or intranasally—than equipotent d-amphetamine. In an abuse liability study,6 12 adults with histories of stimulant abuse received intravenous immediate-release (IR) d-amphetamine, 10 or 20 mg. Two days later, they received a comparable dose of IV lisdexamfetamine, 25 or 50 mg. The researchers found that:
- Plasma d-amphetamine peaked within 5 minutes after injection, compared with 2 to 3 hours after lisdexamfetamine dosing.
- Subjects who received IR d-amphetamine said they felt euphoria within 15 minutes of injection. By contrast, no one reported euphoria or amphetamine-like subjective effects after receiving lisdexamfetamine.
When asked which medication they would try again, 9 of 12 subjects chose IR d-amphetamine and 1 chose lisdexamfetamine.
In a double-blind, randomized, placebo-controlled study,7 oral lisdexamfetamine, 50 or 100 mg, was not more “likeable” than placebo. Subjects reported “liking” effects with 150 mg of lisdexamfetamine, however, suggesting the medication could be misused or abused at higher-than-therapeutic dosages.
As with other psychostimulants, do not give lisdexamfetamine to youths with preexisting serious structural cardiac abnormalities or other heart problems. Assess patient and family history of heart disease before prescribing this medication.
Do not prescribe lisdexamfetamine to patients taking a monoamine oxidase inhibitor (MAOI). By slowing amphetamine metabolism, these antidepressants intensify amphetamines’ effect on monoamine release, which can cause headaches and lead to hypertensive crisis. Before starting lisdexamfetamine, ask if the patient is taking an MAOI or has taken one within 2 weeks of presentation.
Use caution when prescribing lisdexamfetamine to patients with:
- a comorbid eating disorder or sleep disturbance. Determine whether to address the comorbidity before treating ADHD symptoms, and make sure lisdexamfetamine is not worsening the comorbid symptoms.
- untreated hypertension or other cardiovascular conditions, as stimulant medications can increase blood pressure and heart rate. Watch for significant heart rate and blood pressure changes in patients taking lisdexamfetamine, which probably would not cause sustained blood pressure increase in patients taking antihypertensives.8
Related resources
- Lisdexamfetamine Web site. www.vyvanse.com.
Drug brand names
- Extended-release mixed amphetamine salts • Adderall XR
- Lisdexamfetamine • Vyvanse
Disclosure
Dr. Wilens receives research/grant support from Abbott Laboratories, Eli Lilly and Company, National Institute on Drug Abuse, NeuroSearch, Ortho-McNeil, and Shire; is a speaker for Novartis Pharmaceuticals Corp., Ortho-McNeil, and Shire; and is a consultant to Abbott Laboratories, Eli Lilly and Company, GlaxoSmithKline, National Institute on Drug Abuse, Novartis Pharmaceuticals Corp., Ortho-McNeil, Pfizer, and Shire.
Lisdexamfetamine—FDA-approved to treat attention-deficit/hyperactivity disorder (ADHD) in children ages 6 to 12 (Table 1)—reduces ADHD symptoms during and after school and may be less likely to be abused than other psychostimulants, particularly immediate-release preparations, clinical data suggest.
Table 1
Lisdexamfetamine: Fast facts
| Brand name: Vyvanse |
| Indication: ADHD in children ages 6 to 12 |
| Approval date: February 23, 2007 |
| Manufacturers: New River Pharmaceuticals and Shire |
| Dosing forms: 30-, 50-, and 70-mg capsules |
| Recommended dosage: Start at 30 mg/d. If necessary, titrate by 20 mg every 3 to 7 days to a maximum 70 mg/d. |
Clinical implications
Because it is effective for about 12 hours, lisdexamfetamine might improve the child’s ability to complete homework and participate in extracurricular activities, which in turn might enhance academic performance and/or socialization skills.
Lisdexamfetamine could help the child with ADHD who shows no contraindications to the drug —particularly if he or she needs daylong coverage.
How it works
Lisdexamfetamine—a dextroamphetamine derivative—is rapidly absorbed and converted to dextroamphetamine, which is believed to exert therapeutic effect by:
- blocking norepinephrine and dopamine reuptake into presynaptic neurons
- increasing the neurotransmitters’ release into the extraneuronal space.
The medication’s amphetamine release is highly predictable, which contributes to its therapeutic benefit in ADHD. Amphetamine is released through GI metabolism of lisdexamfetamine, which produces the active d-amphetamine moiety that reaches the bloodstream. The medication is derived from d-amphetamine, with negligible amounts of lysine cleaved.
Lisdexamfetamine requires in vivo metabolism (in the GI tract) to its active constituent d-amphetamine. As a result, the medication will not produce high d-amphetamine blood levels—and should not cause euphoria or other reinforcing effects—if injected or snorted. Its abuse potential is lower overall compared with immediate-release psychostimulant formulations.
Pharmacokinetics
Dextroamphetamine’s plasma elimination half-life is approximately 9½ hours—which accounts for lisdexamfetamine’s extended action. The drug reaches steady-state concentrations in 2 to 3 days.
Food does not affect absorption and delays maximum concentration by 1 hour or less, so taking lisdexamfetamine during breakfast should not slow its therapeutic effect. Because dextroamphetamine reaches maximum concentration in approximately 3½ hours, the medication should take effect by the time the child gets to school. In one randomized, phase-2 trial, children with ADHD who received lisdexamfetamine, 30 to 70 mg/d, showed overall improvement within 2 hours after dosing.1
Efficacy
Lisdexamfetamine reduced ADHD symptoms in 2 double-blind studies: a phase-2 crossover study and a phase-3 random-dose trial.
Phase-2 crossover study.2 Fifty-two children ages 6 to 12 with combined or hyperactive-impulsive type ADHD received extended-release mixed amphetamine salts (MAS) for 3 weeks. Subjects received 10 mg/d or dosages titrated to 20 or 30 mg/d based on response to medication.
The youths then were divided into 3 groups based on optimal MAS dosage and received 3 treatments for 1 week each:
- group 1: placebo; MAS, 10 mg/d; lisdexamfetamine, 30 mg/d
- group 2: placebo; MAS, 20 mg/d; lisdexamfetamine, 50 mg/d
- group 3: placebo; MAS, 30 mg/d; lisdexamfetamine, 70 mg/d.
While taking lisdexamfetamine or MAS, subjects showed similar improvement in behavior, based on Swanson, Kotkin, Agler, M-Flynn, and Pelham (SKAMP) scores, and inattention, based on SKAMP and Permanent Product Measure of Performance scores.
Both psychostimulants outperformed placebo in both measures, and both improved behavior more decisively than inattention. Based on post-hoc analysis, improvement 12 hours after dosing was more substantial with lisdexamfetamine than with MAS.
Phase-3 random-dose trial.3 A total of 290 children ages 6 to 12 with combined or hyperactive-impulsive type ADHD were “washed out” from prior medications over 1 week, then received lisdexamfetamine or placebo for 4 weeks. Treatment-group children were started at 30 mg/d; some received dosages titrated at random to 50 or 70 mg/d in weekly 20-mg increments.
Over 4 weeks, ADHD Rating Scale Version IV (ADHD-RS-IV) scores fell 50% to 59% among the 3 lisdexamfetamine dosage groups, compared with a 15% reduction in the placebo group. Substantial ADHD-RS-IV score improvements after 1 week of lisdexamfetamine were maintained throughout the trial, suggesting the medication sustains ADHD symptom improvement. Controlled trials have not addressed lisdexamfetamine use >4 weeks, however.
Based on parents’ and guardians’ reports, treatment-group patients’ ADHD symptoms were notably less severe at 10 AM, 2 PM, and 6 PM compared with placebo-group children.3 This suggests that lisdexamfetamine offers a daylong therapeutic effect.
Tolerability
In the phase-3 study,3 162 of 218 (74%) children receiving any dosage of lisdexamfetamine reported an adverse event, compared with 34 of 72 (47%) children in the placebo group. Overall, 39% of lisdexamfetamine-group patients reported decreased appetite. Also common were insomnia, headaches, irritability, upper abdominal pain, vomiting, and weight loss (Table 2).
Although most adverse events were mild to moderate, 9.2% of treatment-group children dropped out because of intolerability, compared with 1.4% of the placebo group. The investigators increased dosages quickly, regardless of efficacy or tolerability,3 which might have increased side-effect incidence among the treatment groups.
In the phase-2 crossover trial,2 adverse event rates were similar among the lisdexamfetamine, extended-release MAS, and placebo groups (15% to 18%). Among youths receiving lisdexamfetamine, 8% reported insomnia and 6% reported appetite loss, compared with 2% and 4% of the MAS group, respectively.
Table 2
Rates of commonly reported adverse effects
during phase-3 lisdexamfetamine (LDX) study
| Adverse effect | LDX 30 mg/d | LDX 50 mg/d* | LDX 70 mg/d* | LDX all dosages | Placebo |
|---|---|---|---|---|---|
| All adverse effects | 72% | 68% | 84% | 74% | 47% |
| Decreased appetite | 37% | 31% | 49% | 39% | 4% |
| Insomnia | 16% | 16% | 25% | 19% | 3% |
| Upper abdominal pain | 14% | 7% | 15% | 12% | 6% |
| Headache | 10% | 10% | 16% | 12% | 10% |
| Irritability | 11% | 8% | 10% | 10% | 0% |
| Vomiting | 7% | 5% | 14% | 9% | 4% |
| Weight loss | 6% | 3% | 19% | 9% | 1% |
| *Dosages were randomly titrated regardless of efficacy or tolerability. | |||||
| Source: Reference 3 | |||||
Safety
Findling et al4 found a larger change in corrected QT interval with lisdexamfetamine (7 to 14 msec) than with extended-release MAS (5 to 10 msec) 5 and 10½ hours after dosing. The authors reasoned that these findings are atypical, and no children suffered serious adverse events during the trial. Nonetheless, more research on whether lisdexamfetamine increases cardiac risk is needed.
In a lethal-dose study in rats,5 oral lisdexamfetamine doses up to 1,000 mg/kg did not result in death, suggesting the medication might undergo saturation kinetics in the GI tract that may protect against overdose or abuse at higher dosages. By comparison, the median lethal oral dosage of d-amphetamine in rats was 96.8 mg/kg.5
Abuse potential
As with other psychostimulants indicated for ADHD, the Drug Enforcement Administration has classified lisdexamfetamine as a schedule II drug, which applies to addictive prescription-only medications with an accepted medical use.
Clinical data suggest, however, that lisdexamfetamine might be less “enjoyable”—and less likely to be abused intravenously, orally, or intranasally—than equipotent d-amphetamine. In an abuse liability study,6 12 adults with histories of stimulant abuse received intravenous immediate-release (IR) d-amphetamine, 10 or 20 mg. Two days later, they received a comparable dose of IV lisdexamfetamine, 25 or 50 mg. The researchers found that:
- Plasma d-amphetamine peaked within 5 minutes after injection, compared with 2 to 3 hours after lisdexamfetamine dosing.
- Subjects who received IR d-amphetamine said they felt euphoria within 15 minutes of injection. By contrast, no one reported euphoria or amphetamine-like subjective effects after receiving lisdexamfetamine.
When asked which medication they would try again, 9 of 12 subjects chose IR d-amphetamine and 1 chose lisdexamfetamine.
In a double-blind, randomized, placebo-controlled study,7 oral lisdexamfetamine, 50 or 100 mg, was not more “likeable” than placebo. Subjects reported “liking” effects with 150 mg of lisdexamfetamine, however, suggesting the medication could be misused or abused at higher-than-therapeutic dosages.
As with other psychostimulants, do not give lisdexamfetamine to youths with preexisting serious structural cardiac abnormalities or other heart problems. Assess patient and family history of heart disease before prescribing this medication.
Do not prescribe lisdexamfetamine to patients taking a monoamine oxidase inhibitor (MAOI). By slowing amphetamine metabolism, these antidepressants intensify amphetamines’ effect on monoamine release, which can cause headaches and lead to hypertensive crisis. Before starting lisdexamfetamine, ask if the patient is taking an MAOI or has taken one within 2 weeks of presentation.
Use caution when prescribing lisdexamfetamine to patients with:
- a comorbid eating disorder or sleep disturbance. Determine whether to address the comorbidity before treating ADHD symptoms, and make sure lisdexamfetamine is not worsening the comorbid symptoms.
- untreated hypertension or other cardiovascular conditions, as stimulant medications can increase blood pressure and heart rate. Watch for significant heart rate and blood pressure changes in patients taking lisdexamfetamine, which probably would not cause sustained blood pressure increase in patients taking antihypertensives.8
Related resources
- Lisdexamfetamine Web site. www.vyvanse.com.
Drug brand names
- Extended-release mixed amphetamine salts • Adderall XR
- Lisdexamfetamine • Vyvanse
Disclosure
Dr. Wilens receives research/grant support from Abbott Laboratories, Eli Lilly and Company, National Institute on Drug Abuse, NeuroSearch, Ortho-McNeil, and Shire; is a speaker for Novartis Pharmaceuticals Corp., Ortho-McNeil, and Shire; and is a consultant to Abbott Laboratories, Eli Lilly and Company, GlaxoSmithKline, National Institute on Drug Abuse, Novartis Pharmaceuticals Corp., Ortho-McNeil, Pfizer, and Shire.
1. Lopez FA, Boellner SW, Childress A, et al. ADHD symptom improvement in children treated with lisdexamfetamine dimesylate (LDX). Poster presented at: Annual Meeting of the American Academy of Child and Adolescent Psychiatry; October 24-29, 2006; San Diego, CA.
2. Biederman J, Boellner SW, Childress A, et al. Improvements in symptoms of attention-deficit/hyperactivity disorder in school-aged children with lisdexamfetamine (NRP 104) and mixed amphetamine salts, extended-release versus placebo. Poster presented at: Annual Meeting of the American Psychiatric Association; May 20-25, 2006; Toronto, Canada.
3. Biederman J, Krishnan S, Zhang Y, et al. Efficacy and tolerability of lisdexamfetamine dimesylate (NRP 104) in children with attention-deficit/hyperactivity disorder: a phase III, multicenter, randomized, double-blind, forced-dose, parallel-group study. Clin Ther 2007;29:450-63.
4. Findling FL, Biederman J, Wilens TE, et al. Short- and long-term cardiovascular effects of mixed amphetamine salts extended release in children. J Pediatr 2005;147:348-54.
5. Krishnan S. Toxicity profile of lisdexamfetamine dimesylate (LDX NRP104) in three independent rat toxicology studies. Basic Clin Phamacol Toxicol. In press.
6. Jasinski DR. Abuse liability of intravenous L-lysine-d-amphetamine (NRP 104). Poster presented at: Annual Meeting of the College on Problems of Drug Dependence; June 17-22, 2006; Scottsdale, AZ. Available at: http://xml.10kwizard.com/filing_raw.php?repo=tenk&ipage=4234033. Accessed April 5, 2007.
7. Jasinski D, Krishnan S. A double-blind, randomized, placebo and active-controlled, six-period crossover study to evaluate the likeability, safety, and abuse liability of NRP 104 in healthy adult volunteers with histories of stimulant abuse (NRP104. A03). Poster presented at: Annual Meeting of the College on Problems of Drug Dependence; June 17-22, 2006; Scottsdale, AZ. Available at: http://www.secinfo.com/d12Pk6.v9Ac.d.htm. Accessed May 14, 2007.
8. Wilens TE, Zusman RM, Hammerness PG, et al. An open-label study of the tolerability of mixed amphetamine salts in adults with attention-deficit/hyperactivity disorder and treated primary essential hypertension. J Clin Psychiatry 2006;67:696-702.
1. Lopez FA, Boellner SW, Childress A, et al. ADHD symptom improvement in children treated with lisdexamfetamine dimesylate (LDX). Poster presented at: Annual Meeting of the American Academy of Child and Adolescent Psychiatry; October 24-29, 2006; San Diego, CA.
2. Biederman J, Boellner SW, Childress A, et al. Improvements in symptoms of attention-deficit/hyperactivity disorder in school-aged children with lisdexamfetamine (NRP 104) and mixed amphetamine salts, extended-release versus placebo. Poster presented at: Annual Meeting of the American Psychiatric Association; May 20-25, 2006; Toronto, Canada.
3. Biederman J, Krishnan S, Zhang Y, et al. Efficacy and tolerability of lisdexamfetamine dimesylate (NRP 104) in children with attention-deficit/hyperactivity disorder: a phase III, multicenter, randomized, double-blind, forced-dose, parallel-group study. Clin Ther 2007;29:450-63.
4. Findling FL, Biederman J, Wilens TE, et al. Short- and long-term cardiovascular effects of mixed amphetamine salts extended release in children. J Pediatr 2005;147:348-54.
5. Krishnan S. Toxicity profile of lisdexamfetamine dimesylate (LDX NRP104) in three independent rat toxicology studies. Basic Clin Phamacol Toxicol. In press.
6. Jasinski DR. Abuse liability of intravenous L-lysine-d-amphetamine (NRP 104). Poster presented at: Annual Meeting of the College on Problems of Drug Dependence; June 17-22, 2006; Scottsdale, AZ. Available at: http://xml.10kwizard.com/filing_raw.php?repo=tenk&ipage=4234033. Accessed April 5, 2007.
7. Jasinski D, Krishnan S. A double-blind, randomized, placebo and active-controlled, six-period crossover study to evaluate the likeability, safety, and abuse liability of NRP 104 in healthy adult volunteers with histories of stimulant abuse (NRP104. A03). Poster presented at: Annual Meeting of the College on Problems of Drug Dependence; June 17-22, 2006; Scottsdale, AZ. Available at: http://www.secinfo.com/d12Pk6.v9Ac.d.htm. Accessed May 14, 2007.
8. Wilens TE, Zusman RM, Hammerness PG, et al. An open-label study of the tolerability of mixed amphetamine salts in adults with attention-deficit/hyperactivity disorder and treated primary essential hypertension. J Clin Psychiatry 2006;67:696-702.
Failing the 15-minute suicide watch: Guidelines to monitor inpatients
Patient commits suicide after 15-minute checks are stopped
Honolulu County (HI) Circuit Court
A patient was brought to a hospital and interviewed by a psychiatrist. She was found to be at moderate risk for suicide, was admitted, and ordered to be monitored every 15 minutes. The patient attempted suicide 2 days later by closing a drawer on her neck. She died from the injuries the following day.
The patient’s family claimed that a hospital nurse misread the psychiatrist’s instructions and stopped the 15-minute checks on the morning of the incident, believing that the order was limited to 15-minute checks for the first 24 hours, even though they had been done for almost 2 days. The patient refused medication on the first day of admission, and the psychiatrist had started the procedure to obtain a court order committing the patient and allowing injection of necessary medication. The claims against the hospital were settled for a confidential amount.
The patient’s family claimed the psychiatrist diagnosed the patient with major depression with recurrent suicide ideation but failed to properly assess her for suicide monitoring. The family also said the patient should have been determined to be at least at high risk and required to be within sight of staff.
The psychiatrist claimed to be unaware the 15-minute monitoring had ceased. The psychiatrist saw the patient 30 minutes before she was found collapsed with her head in the drawer. The hospital staff checked the patient approximately 15 to 30 minutes before she was found.
- A defense verdict was returned
Reduced observation blamed for suicide by hanging
Kings County (NY) Supreme Court
A 45-year-old police lieutenant who suffered from alcohol abuse and depression was admitted to a psychiatric care facility. He was classiffied “Q15,” a category assigned to patients who must be visually inspected every 15 minutes, cannot have access to sharp objects or any other material or object they can use to inflict bodily harm, and must request permission to use restrooms. The next day the psychiatrist examined the patient and moved him to a “Q30” status, which halved the frequency of visual inspections, gave him unrestricted access to restrooms, and allowed him to have a bathrobe with a belt. The patient hanged himself the next day, using a restroom door to support a noose he made from the bathrobe belt.
The patient’s family faulted the hospital and psychiatrist for prematurely advancing the patient to “Q30” status. The hospital and psychiatrist claimed the suicide could not have been predicted and argued that given his background as a police lieutenant, the patient would have interpreted more stringent restrictions as incarceration. The psychiatrist argued that such a perception would have impeded the patient’s progress.
- A $71,989 verdict was returned, apportioning fault 65% to the hospital and 35% to the psychiatrist
Constant patient observation—such as one-to-one staffing or 15-minute checks—is used to protect patients from harming themselves or others. One study of a psychiatric hospital1 reported that 13% of psychiatric inpatients required constant observation.
Even 15 minutes is sufficient time to complete a suicide.3 Common methods of inpatient suicide include hanging, overdosing, and jumping from high places.4,5 One study found that 73% of inpatient suicides in a psychiatric ward occurred after 28 days of admission.5
The cost of constant observation may account for as much as 20% of the total nursing budget at a psychiatric hospital and up to 10% at a long-term care facility or general hospital.6 The annual cost of constant observation can exceed $500,000, depending on the hospital’s size and monitoring frequency.6
Determining responsibility
The outcomes of these 2 cases may appear inconsistent. In the first, the psychiatrist who assessed the patient as a moderate suicide risk was not negligent, even though the family claimed the patient was at high risk. In the second case, the psychiatrist was found partly liable for not maintaining a higher vigilance of suicide risk assessment.
Physicians cannot put every patient on one-to-one monitoring or 15-minute checks because of fear of suicide and malpractice litigation. These 2 cases demonstrate that if a suicide occurs, the courts will look for clinical reasons for the level of observation. The level of suicide precautions—one-to-one vs 15-minute checks—should be based on the patient’s clinical presentation and supported by clinical rationale.7
Risk analysis
The courts look to see if the suicide assessment was “clinically reasonable”.8 To meet this standard, perform a “suicide risk-benefit analysis” each time you make a significant clinical decision, such as ordering 15-minute checks. The record should include information sources you used (such as family members or previous medical records), factors that entered the clinical decision, and how you balanced these factors in a risk-benefit assessment (Box 1).9
Document decisions. Mistakes in clinical judgment do not necessarily constitute negligence,8 but deviations in the standard of care cannot be adequately determined in a court of law unless the clinician had documented his or her thought processes at the time of the decision.
Predicting which patients will re-experience or deny suicidal ideation is impossible,7 but if the patient is determined to be at high risk for suicide, then implement and document a plan to address this risk. In addition, communicate information regarding the risk-benefit assessment to staff responsible for implementing these precautions.
- Suicidal thoughts or behaviors—ideas, plans, attempts
- Psychiatric diagnoses—depression, bipolar disorder, schizophrenia, substance use, Cluster B personality disorders
- Physical illnesses—HIV, malignant cancers, pain syndromes
- Psychosocial features—lack of support, unemployment
- Childhood traumas
- Genetic and familial effects—family history of suicide
- Psychological features—hopelessness, agitation, impulsiveness
- Cognitive features—polarized thinking
- Demographic features—adolescents, young adults, and elderly patients
- Other factors—access to firearms, intoxication.
Source: Reference 7
- a patient is admitted for inpatient treatment
- observation status changes
- a patient’s clinical condition changes substantially
- acute psychosocial stressors are discovered during the hospitalization.7
1. Shugar G, Rehaluk R. Continuous observation for psychiatric inpatients. Compr Psychiatry 1990;30:48-55.
2. Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry 2003;64:14-9.
3. Bowers L, Gournay K, Dufy D. Suicide and self-harm in inpatient psychiatric units: a national survey of observation policies. J Adv Nursing 2000;32:437-44.
4. Proulx F, Lesage AD, Grunberg F. One hundred in-patient suicides. Br J Psychiatry 1997;171:247-50.
5. Shah AK, Ganesvaran T. Inpatient suicides in an Australian mental hospital. Aust NZ J Psychiatr 1997;31:291-8.
6. Moore P, Berman K, Knight M, Devine J. Constant observation: implications for nursing practice. J Psychosoc Nurs Ment Health Serv 1995;33:46-50.
7. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Available at: http://www.psych.org/psych_pract/treatg/pg/SuicidalBehavior_05-15-06.pdf. Accessed April 19, 2007.
8. Simon RI. The suicidal patient. In Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:166-86.
9. Abille v United States, 482 F Supp 703 (ND Cal 1980).
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
Patient commits suicide after 15-minute checks are stopped
Honolulu County (HI) Circuit Court
A patient was brought to a hospital and interviewed by a psychiatrist. She was found to be at moderate risk for suicide, was admitted, and ordered to be monitored every 15 minutes. The patient attempted suicide 2 days later by closing a drawer on her neck. She died from the injuries the following day.
The patient’s family claimed that a hospital nurse misread the psychiatrist’s instructions and stopped the 15-minute checks on the morning of the incident, believing that the order was limited to 15-minute checks for the first 24 hours, even though they had been done for almost 2 days. The patient refused medication on the first day of admission, and the psychiatrist had started the procedure to obtain a court order committing the patient and allowing injection of necessary medication. The claims against the hospital were settled for a confidential amount.
The patient’s family claimed the psychiatrist diagnosed the patient with major depression with recurrent suicide ideation but failed to properly assess her for suicide monitoring. The family also said the patient should have been determined to be at least at high risk and required to be within sight of staff.
The psychiatrist claimed to be unaware the 15-minute monitoring had ceased. The psychiatrist saw the patient 30 minutes before she was found collapsed with her head in the drawer. The hospital staff checked the patient approximately 15 to 30 minutes before she was found.
- A defense verdict was returned
Reduced observation blamed for suicide by hanging
Kings County (NY) Supreme Court
A 45-year-old police lieutenant who suffered from alcohol abuse and depression was admitted to a psychiatric care facility. He was classiffied “Q15,” a category assigned to patients who must be visually inspected every 15 minutes, cannot have access to sharp objects or any other material or object they can use to inflict bodily harm, and must request permission to use restrooms. The next day the psychiatrist examined the patient and moved him to a “Q30” status, which halved the frequency of visual inspections, gave him unrestricted access to restrooms, and allowed him to have a bathrobe with a belt. The patient hanged himself the next day, using a restroom door to support a noose he made from the bathrobe belt.
The patient’s family faulted the hospital and psychiatrist for prematurely advancing the patient to “Q30” status. The hospital and psychiatrist claimed the suicide could not have been predicted and argued that given his background as a police lieutenant, the patient would have interpreted more stringent restrictions as incarceration. The psychiatrist argued that such a perception would have impeded the patient’s progress.
- A $71,989 verdict was returned, apportioning fault 65% to the hospital and 35% to the psychiatrist
Constant patient observation—such as one-to-one staffing or 15-minute checks—is used to protect patients from harming themselves or others. One study of a psychiatric hospital1 reported that 13% of psychiatric inpatients required constant observation.
Even 15 minutes is sufficient time to complete a suicide.3 Common methods of inpatient suicide include hanging, overdosing, and jumping from high places.4,5 One study found that 73% of inpatient suicides in a psychiatric ward occurred after 28 days of admission.5
The cost of constant observation may account for as much as 20% of the total nursing budget at a psychiatric hospital and up to 10% at a long-term care facility or general hospital.6 The annual cost of constant observation can exceed $500,000, depending on the hospital’s size and monitoring frequency.6
Determining responsibility
The outcomes of these 2 cases may appear inconsistent. In the first, the psychiatrist who assessed the patient as a moderate suicide risk was not negligent, even though the family claimed the patient was at high risk. In the second case, the psychiatrist was found partly liable for not maintaining a higher vigilance of suicide risk assessment.
Physicians cannot put every patient on one-to-one monitoring or 15-minute checks because of fear of suicide and malpractice litigation. These 2 cases demonstrate that if a suicide occurs, the courts will look for clinical reasons for the level of observation. The level of suicide precautions—one-to-one vs 15-minute checks—should be based on the patient’s clinical presentation and supported by clinical rationale.7
Risk analysis
The courts look to see if the suicide assessment was “clinically reasonable”.8 To meet this standard, perform a “suicide risk-benefit analysis” each time you make a significant clinical decision, such as ordering 15-minute checks. The record should include information sources you used (such as family members or previous medical records), factors that entered the clinical decision, and how you balanced these factors in a risk-benefit assessment (Box 1).9
Document decisions. Mistakes in clinical judgment do not necessarily constitute negligence,8 but deviations in the standard of care cannot be adequately determined in a court of law unless the clinician had documented his or her thought processes at the time of the decision.
Predicting which patients will re-experience or deny suicidal ideation is impossible,7 but if the patient is determined to be at high risk for suicide, then implement and document a plan to address this risk. In addition, communicate information regarding the risk-benefit assessment to staff responsible for implementing these precautions.
- Suicidal thoughts or behaviors—ideas, plans, attempts
- Psychiatric diagnoses—depression, bipolar disorder, schizophrenia, substance use, Cluster B personality disorders
- Physical illnesses—HIV, malignant cancers, pain syndromes
- Psychosocial features—lack of support, unemployment
- Childhood traumas
- Genetic and familial effects—family history of suicide
- Psychological features—hopelessness, agitation, impulsiveness
- Cognitive features—polarized thinking
- Demographic features—adolescents, young adults, and elderly patients
- Other factors—access to firearms, intoxication.
Source: Reference 7
- a patient is admitted for inpatient treatment
- observation status changes
- a patient’s clinical condition changes substantially
- acute psychosocial stressors are discovered during the hospitalization.7
Patient commits suicide after 15-minute checks are stopped
Honolulu County (HI) Circuit Court
A patient was brought to a hospital and interviewed by a psychiatrist. She was found to be at moderate risk for suicide, was admitted, and ordered to be monitored every 15 minutes. The patient attempted suicide 2 days later by closing a drawer on her neck. She died from the injuries the following day.
The patient’s family claimed that a hospital nurse misread the psychiatrist’s instructions and stopped the 15-minute checks on the morning of the incident, believing that the order was limited to 15-minute checks for the first 24 hours, even though they had been done for almost 2 days. The patient refused medication on the first day of admission, and the psychiatrist had started the procedure to obtain a court order committing the patient and allowing injection of necessary medication. The claims against the hospital were settled for a confidential amount.
The patient’s family claimed the psychiatrist diagnosed the patient with major depression with recurrent suicide ideation but failed to properly assess her for suicide monitoring. The family also said the patient should have been determined to be at least at high risk and required to be within sight of staff.
The psychiatrist claimed to be unaware the 15-minute monitoring had ceased. The psychiatrist saw the patient 30 minutes before she was found collapsed with her head in the drawer. The hospital staff checked the patient approximately 15 to 30 minutes before she was found.
- A defense verdict was returned
Reduced observation blamed for suicide by hanging
Kings County (NY) Supreme Court
A 45-year-old police lieutenant who suffered from alcohol abuse and depression was admitted to a psychiatric care facility. He was classiffied “Q15,” a category assigned to patients who must be visually inspected every 15 minutes, cannot have access to sharp objects or any other material or object they can use to inflict bodily harm, and must request permission to use restrooms. The next day the psychiatrist examined the patient and moved him to a “Q30” status, which halved the frequency of visual inspections, gave him unrestricted access to restrooms, and allowed him to have a bathrobe with a belt. The patient hanged himself the next day, using a restroom door to support a noose he made from the bathrobe belt.
The patient’s family faulted the hospital and psychiatrist for prematurely advancing the patient to “Q30” status. The hospital and psychiatrist claimed the suicide could not have been predicted and argued that given his background as a police lieutenant, the patient would have interpreted more stringent restrictions as incarceration. The psychiatrist argued that such a perception would have impeded the patient’s progress.
- A $71,989 verdict was returned, apportioning fault 65% to the hospital and 35% to the psychiatrist
Constant patient observation—such as one-to-one staffing or 15-minute checks—is used to protect patients from harming themselves or others. One study of a psychiatric hospital1 reported that 13% of psychiatric inpatients required constant observation.
Even 15 minutes is sufficient time to complete a suicide.3 Common methods of inpatient suicide include hanging, overdosing, and jumping from high places.4,5 One study found that 73% of inpatient suicides in a psychiatric ward occurred after 28 days of admission.5
The cost of constant observation may account for as much as 20% of the total nursing budget at a psychiatric hospital and up to 10% at a long-term care facility or general hospital.6 The annual cost of constant observation can exceed $500,000, depending on the hospital’s size and monitoring frequency.6
Determining responsibility
The outcomes of these 2 cases may appear inconsistent. In the first, the psychiatrist who assessed the patient as a moderate suicide risk was not negligent, even though the family claimed the patient was at high risk. In the second case, the psychiatrist was found partly liable for not maintaining a higher vigilance of suicide risk assessment.
Physicians cannot put every patient on one-to-one monitoring or 15-minute checks because of fear of suicide and malpractice litigation. These 2 cases demonstrate that if a suicide occurs, the courts will look for clinical reasons for the level of observation. The level of suicide precautions—one-to-one vs 15-minute checks—should be based on the patient’s clinical presentation and supported by clinical rationale.7
Risk analysis
The courts look to see if the suicide assessment was “clinically reasonable”.8 To meet this standard, perform a “suicide risk-benefit analysis” each time you make a significant clinical decision, such as ordering 15-minute checks. The record should include information sources you used (such as family members or previous medical records), factors that entered the clinical decision, and how you balanced these factors in a risk-benefit assessment (Box 1).9
Document decisions. Mistakes in clinical judgment do not necessarily constitute negligence,8 but deviations in the standard of care cannot be adequately determined in a court of law unless the clinician had documented his or her thought processes at the time of the decision.
Predicting which patients will re-experience or deny suicidal ideation is impossible,7 but if the patient is determined to be at high risk for suicide, then implement and document a plan to address this risk. In addition, communicate information regarding the risk-benefit assessment to staff responsible for implementing these precautions.
- Suicidal thoughts or behaviors—ideas, plans, attempts
- Psychiatric diagnoses—depression, bipolar disorder, schizophrenia, substance use, Cluster B personality disorders
- Physical illnesses—HIV, malignant cancers, pain syndromes
- Psychosocial features—lack of support, unemployment
- Childhood traumas
- Genetic and familial effects—family history of suicide
- Psychological features—hopelessness, agitation, impulsiveness
- Cognitive features—polarized thinking
- Demographic features—adolescents, young adults, and elderly patients
- Other factors—access to firearms, intoxication.
Source: Reference 7
- a patient is admitted for inpatient treatment
- observation status changes
- a patient’s clinical condition changes substantially
- acute psychosocial stressors are discovered during the hospitalization.7
1. Shugar G, Rehaluk R. Continuous observation for psychiatric inpatients. Compr Psychiatry 1990;30:48-55.
2. Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry 2003;64:14-9.
3. Bowers L, Gournay K, Dufy D. Suicide and self-harm in inpatient psychiatric units: a national survey of observation policies. J Adv Nursing 2000;32:437-44.
4. Proulx F, Lesage AD, Grunberg F. One hundred in-patient suicides. Br J Psychiatry 1997;171:247-50.
5. Shah AK, Ganesvaran T. Inpatient suicides in an Australian mental hospital. Aust NZ J Psychiatr 1997;31:291-8.
6. Moore P, Berman K, Knight M, Devine J. Constant observation: implications for nursing practice. J Psychosoc Nurs Ment Health Serv 1995;33:46-50.
7. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Available at: http://www.psych.org/psych_pract/treatg/pg/SuicidalBehavior_05-15-06.pdf. Accessed April 19, 2007.
8. Simon RI. The suicidal patient. In Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:166-86.
9. Abille v United States, 482 F Supp 703 (ND Cal 1980).
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
1. Shugar G, Rehaluk R. Continuous observation for psychiatric inpatients. Compr Psychiatry 1990;30:48-55.
2. Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry 2003;64:14-9.
3. Bowers L, Gournay K, Dufy D. Suicide and self-harm in inpatient psychiatric units: a national survey of observation policies. J Adv Nursing 2000;32:437-44.
4. Proulx F, Lesage AD, Grunberg F. One hundred in-patient suicides. Br J Psychiatry 1997;171:247-50.
5. Shah AK, Ganesvaran T. Inpatient suicides in an Australian mental hospital. Aust NZ J Psychiatr 1997;31:291-8.
6. Moore P, Berman K, Knight M, Devine J. Constant observation: implications for nursing practice. J Psychosoc Nurs Ment Health Serv 1995;33:46-50.
7. American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Available at: http://www.psych.org/psych_pract/treatg/pg/SuicidalBehavior_05-15-06.pdf. Accessed April 19, 2007.
8. Simon RI. The suicidal patient. In Lifson LE, Simon RI, eds. The mental health practitioner and the law. Cambridge, MA: Harvard University Press; 1998:166-86.
9. Abille v United States, 482 F Supp 703 (ND Cal 1980).
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
ADHD: Only half the diagnosis in an adult with inattention?
Overlapping symptoms may obscure comorbid bipolar illness
An adult with function-impairing inattention could have attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or both. Comorbid ADHD and BD often is unrecognized, however, because patients are more likely to report ADHD-related symptoms than manic symptoms.1
To help you recognize comorbid ADHD/BD—and protect adults who might switch into mania if given stimulants or antidepressants—this article describes a hierarchy to diagnose and treat this comorbidity. Based on the evidence and our experience, we:
- discuss how to differentiate between these disorders with overlapping symptoms
- provide tools and suggestions to screen for BD and adult ADHD
- offer 3 algorithms to guide your diagnosis and choice of medications.
Clinical challenges
Prevalence is unclear. Adult ADHD—with an estimated prevalence of 4.4%2—is more common than BD. Lifetime prevalences of BD types I and II are 1.6% and 0.5%, respectively.3 Studies of ADHD/BD comorbidity suggest wide-ranging prevalence rates:
Underdiagnosis. Adult ADHD/BD is a more severe illness than ADHD or BD alone and is highly comorbid with agoraphobia, social phobia, posttraumatic stress disorder, and alcohol or drug addiction. Adults with ADHD/BD have more frequent affective episodes, suicide attempts, violence, and legal problems.4 Diagnosing this comorbidity remains a challenge, however, because:
- identifying which symptoms are caused by which disorder can be difficult
- BD tends to be underdiagnosed9
- patients often misidentify, underreport, or deny manic symptoms1,10,11
- if a patient presents with active bipolar symptoms, DSM-IV-TR criteria require that ADHD not be diagnosed until mood symptoms are resolved.
Overlapping symptoms. ADHD and bipolar mania share some DSM-IV-TR diagnostic criteria, including talkativeness, distractibility, increased activity or physical restlessness, and loss of social inhibitions (Table 1).12 Overlapping symptoms also are notable within ADHD diagnostic criteria (Table 2). In the inattention category, for example, “easily distracted by extraneous stimuli,” “difficulty sustaining attention in tasks,” and “fails to give close attention to details” are considered 3 separate symptoms. In the hyperactivity category, “often leaves seat,” “often runs about or climbs excessively,” and “often on the go, or often acts as if driven by a motor” are 3 separate symptoms.
Given ADHD’s relatively loose diagnostic criteria and high comorbidity in adults with mood disorders, the question of whether adult ADHD/BD represents comorbidity or diagnostic overlap remains unresolved. For the clinician, the disorders’ nonoverlapping features (Table 1) can assist with the differential diagnosis. For example:
- ADHD symptoms tend to be chronic and BD symptoms episodic.
- ADHD patients may have high energy but lack increased productivity seen in BD patients.
- ADHD patients do not need less sleep or have inflated self-esteem like symptomatic BD patients.
- Psychotic symptoms such as hallucinations or delusions might be present in severe BD but are absent in ADHD.
Table 1
Overlap between DSM-IV-TR diagnostic criteria for ADHD and bipolar mania
| Overlapping symptoms | |
|---|---|
| ADHD | Bipolar mania |
| Talks excessively | More talkative than usual |
| Easily distracted/jumps from one activity to the next | Distractibility or constant changes in activity or plans |
| Fidgets Difficulty remaining seated Runs or climbs about inappropriately Difficulty playing quietly On the go as if driven by a motor | Increased activity or physical restlessness |
| Interrupts or butts in uninvited Blurts out answers | Loss of normal social inhibitions |
| Nonoverlapping symptoms | |
| ADHD Forgetful in daily activities Difficulty awaiting turn Difficulty organizing self Loses things Avoids sustained mental effort Does not seem to listen Difficulty following through on instructions/fails to finish work Difficulty sustaining attention Fails to give close attention to details/makes careless mistakes | |
| Bipolar mania Inflated self-esteem/grandiosity Increase in goal-directed activity Flight of ideas Decreased need for sleep Excessive involvement in pleasurable activities with disregard for potential adverse consequences Marked sexual energy or sexual indiscretions | |
| ADHD: attention-deficit/hyperactivity disorder | |
| Source: Adapted and reprinted with permission from reference 12 | |
Table 2
DSM-IV-TR diagnostic criteria for attention-deficit/ hyperactivity disorder
| Inattention |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Hyperactivity/impulsivity |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Diagnosis requires evidence of inattention or hyperactivity/impulsivity or both |
| Some hyperactive/impulsive or inattentive symptoms that caused impairment were present before age 7 |
| Some impairment from symptoms is present in ≥2 settings (such as at school, work, or home) |
| Symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorder and are not better accounted for by another mental disorder (mood disorder, anxiety disorder, dissociative disorder, or a personality disorder) |
| Source: DSM-IV-TR |
Mood symptoms first
A diagnostic hierarchy is implicit in DSM-IV-TR; anxiety disorders are not diagnosed during an active major depressive or manic episode, and schizophrenia is not diagnosed on the basis of psychotic symptoms during an active major depressive or manic episode. Mood disorders sit atop this implied diagnostic hierarchy and must be ruled out before psychotic or anxiety disorders are diagnosed. Similarly, most personality disorders are not diagnosed during an active mood or psychotic episode.
Diagnosing adult ADHD when a patient is actively depressed or manic is inconsistent with this hierarchy and conflicts with extensive nosologic literature.13 We suggest that ADHD—a cognitive-behavioral problem—not be diagnosed solely on symptoms observed when a patient is experiencing a mood episode or psychotic illness.
Bipolar disorder. Two useful mnemonics (Table 3) assist in screening for DSM-IV-TR symptoms of BD type I:
- Pure mania consists of euphoric mood and ≥3 of 7 DIGFAST criteria, or irritable mood and ≥4 of 7 DIGFAST criteria
- Mixed mania consists of depressed mood with ≥4 of 7 DIGFAST criteria and ≥4 of 8 SIGECAPS criteria.
To be diagnostic, these symptoms must cause substantial social or occupational dysfunction and be present at least 1 week. Diagnose BD type I if a patient has experienced a single pure or mixed manic episode at any time, unless the episode had a medical cause such as hyperthyroidism or antidepressant use. Because patients with mixed episodes experience depressed mood, assess any patient with clinical depression for manic symptoms. Otherwise, a patient with a mixed episode could be misdiagnosed as having unipolar depression instead of BD type I.14
BD type II also has been observed in patients with comorbid adult ADHD/BD.4,6 The main difference between BD types I and II is that manic symptoms in type II are not severe enough to cause functional impairment or psychotic symptoms.15
Adult ADHD. The clinical interview seeking evidence of inattention and hyperactivity/impulsivity remains the basis of adult ADHD diagnosis (Table 2). Key areas are:
- the patient’s past and current functional impairment
- whether substantial impairment occurs in at least 2 areas of life (such as school, work, or home).
Take medical, educational, social, psychological, and vocational histories, and rule out other conditions before concluding that adult ADHD is the appropriate diagnosis.16 In adult ADHD, inattentive symptoms become far more prominent, about twice as common as hyperactive symptoms.17 Inattentive symptoms may manifest as neglect, poor time management, motivational deficits, or poor concentration that results in forgetfulness, distractibility, item misplacement, or excessive mistakes in paperwork.18 When impulsive symptoms persist in adults, they may manifest as automobile accidents or low tolerance for frustration, which may lead to frequent job changes and unstable, interrupted interpersonal relationships.18
Neuropsychological testing is not required to make an adult ADHD diagnosis but can help establish the breadth of symptoms or comorbidity.17 Rating scales can screen, gather data (including presence and severity of symptoms), and measure treatment response.16 Commonly used rating scales include:
- Conners’ Adult ADHD Rating Scales19
- Brown Attention Deficit Disorder Rating Scale for Adults20
- Adult ADHD Self-Report Scale.21
When using rating scales, remember that adult psychopathology can distort perceptions, and some self-report scales have questionable reliability.16
Table 3
Mnemonics for diagnostic symptoms of pure and mixed bipolar mania
| DIGFAST* for bipolar mania symptoms | SIGECAPS† bipolar depression symptoms |
|---|---|
| Distractibility Insomnia Grandiosity Flight of ideas Activities Speech Thoughtlessness | Sleep Interest Guilt Energy Concentration Appetite Psychomotor Suicide |
| Pure mania: Euphoric mood with ≥3 DIGFAST criteria or irritable mood with ≥4 DIGFAST criteria. | |
| Mixed mania: Depressed mood with ≥4 DIGFAST criteria and ≥4 SIGECAPS criteria. | |
| * Developed by William Falk, MD | |
| †Developed by Carey Gross, MD | |
| Source: Adapted from Ghaemi SN. Mood disorders. New York: Lippincott, Williams, & Wilkins; 2003 | |
Treatment recommendations
Limited data. We found only 1 study on adult ADHD/BD treatment. In this open trial,22 36 adults with comorbid ADHD and BD received bupropion SR, up to 200 mg bid, for ADHD symptoms while maintained on mood stabilizers, antipsychotics, or both. Improvement was defined as ≥30% reduction in ADHD Symptom Checklist Scale scores, without concurrent mania. After 6 weeks, 82% of patients had improved; 1 dropped out at week 2 because of hypomanic activation. Methodologic limitations included trial design (non-randomized, nonblinded, short duration) and patient selection (90% of subjects had BD type II).
In the absence of adequate data on adult ADHD/BD, studies in children suggest:
- stimulants may not be effective for ADHD symptoms in patients with active manic or depressive symptoms
- mood stabilization is a prerequisite for successful pharmacologic treatment of ADHD in patients with both ADHD and manic or depressive symptoms.23,24
Follow the hierarchy. First treat acute mood symptoms, then reevaluate and possibly treat ADHD symptoms if they persist during euthymia (Algorithm 1). When a patient meets criteria for adult ADHD/BD, first stabilize bipolar manic or depressive symptoms (Algorithm 2). For acute mania, treat with standard mood stabilizers (lithium, valproate, lamotrigine, or carbamazepine) with or without a second-generation antipsychotic.25 Starting stimulants for ADHD when patients have active mood symptoms is sub-optimal and potentially harmful because of the risk of inducing mania. For acute bipolar depression, adjunctive antidepressant treatment has been found to be no more effective than a mood stabilizer alone.26
After bipolar symptoms respond or remit, reassess for adult ADHD. If ADHD symptoms persist during euthymia, additional treatment may be indicated.
Very little evidence exists on treating adult ADHD/BD; as mentioned, bupropion is the only medication studied in this population. For adult ADHD alone, clinical trials have showed varying efficacy with bupropion,27,28 atomoxetine,29 venlafaxine,30,31 desipramine,32 methylphenidate,33 mixed amphetamine salts,34 and guanfacine.35 Whether these treatments can be generalized as safe and efficacious for comorbid adult ADHD/BD is unclear. Nonetheless, we suggest using bupropion first, followed by atomoxetine or guanfacine before you consider amphetamine stimulants (Algorithm 3).
Algorithm 1
Hierarchy for diagnosis and treatment of adult ADHD/BD
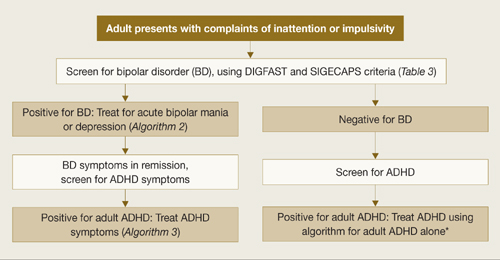
ADHD: attention-deficit/hyperactivity disorder; BD: bipolar disorder
*Adler LA, Chua HC. Management of ADHD in adults. J Clin Psychiatry 2002;63(suppl 12):29-35.
Algorithm 2
Treating acute episodes of bipolar disorder
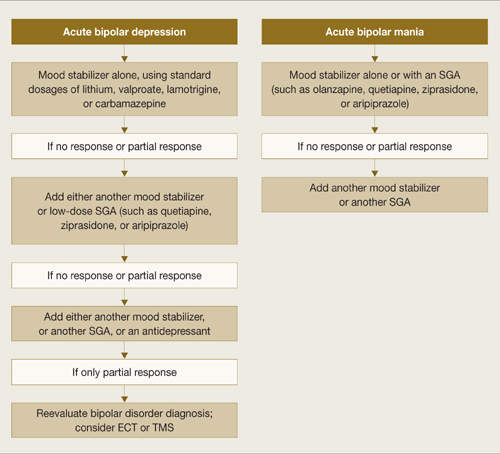
ECT: electroconvulsive therapy; SGA: second-generation antipsychotic; TMS: transcranial magnetic stimulation
Algorithm 3
Suggested approach to adult ADHD with comorbid BD*
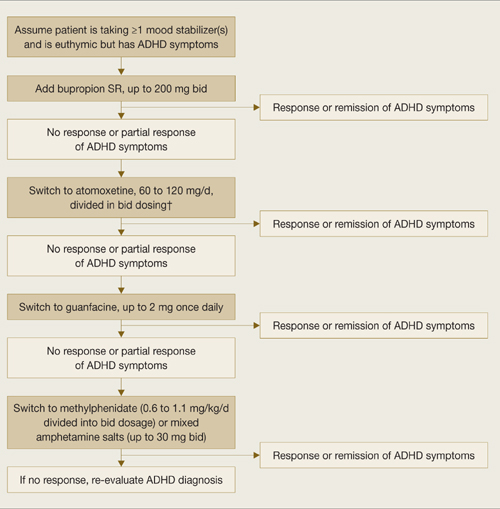
* Based on data extrapolated from samples of patients with ADHD alone because of very limited data in ADHD/BD samples.
† We recommend against combining antidepressants and stimulants because of additive risks of mania in BD. Discontinue stimulant or antidepressant if manic symptoms appear or rapid cycling emerges.
Reducing mania risk
Antidepressants and stimulants may help adults with ADHD alone, but risks of mania and rapid cycling limit their use in adults with ADHD/BD.
Stimulants and mania. One study found a 17% manic switch rate when methylphenidate (≤10 mg bid) was given to 14 bipolar depressed adults (10 BD type I, 2 BD type II, and 2 with secondary mania) taking mood stabilizers.36 A chart review of 82 bipolar children not taking mood stabilizers found an 18% switch rate with methylphenidate or amphetamine.37 Another chart review of 80 children with BD type I found that past amphetamine treatment (but not history of ADHD diagnosis or antidepressant treatment) was associated with more severe bipolar illness.38
No studies have examined predictors of amphetamine-induced mania. In our clinical experience, triggers are similar to those that can cause antidepressant-induced mania, such as:
- recent manic episodes
- current rapid cycling
- past antidepressant-induced mania.
Antidepressants and mania. When 64 patients with acute bipolar depression received both antidepressants and mood stabilizers in a randomized, double-blind trial, switch rates into mania or hypomania were 10% for bupropion, 9% for sertraline, and 29% for venlafaxine.39 In a meta analysis of clinical trials using selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants (TCAs), the manic switch rate was threefold higher with TCAs than SSRIs.40 Antidepressant use in bipolar patients was associated with rapid cycling in the only randomized study of this topic.41
Insufficient data exist to clarify whether mania induction with antidepressants is dose-dependent.42 Factors associated with antidepressant-induced mania include:
- previous antidepressant-induced mania
- family history of BD
- exposure to multiple antidepressant trials42
- history of substance abuse and/or dependence.43
Related resources
- Bipolar disorder information and resources. www.psycheducation.org.
- ADHD Information and resources. www.adhdnews.com.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. New York: McGraw-Hill; 2006.
Drug brand names
- Amphetamine/Dextroamphetamine • Adderall
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methylphenidate • Ritalin
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Valproate • Depakote
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Wingo reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ghaemi receives research grants from GlaxoSmithKline and Pfizer and is a speaker for GlaxoSmithKline, AstraZeneca, Pfizer, and Abbott Laboratories. Neither he nor his family hold equity positions in pharmaceutical companies.
1. Ghaemi SN, Stoll AL, Pope HG, Jr, et al. Lack of insight in bipolar disorder. The acute manic episode. J Nerv Ment Dis 1995;183(7):464-7.
2. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163(4):716-23.
3. Sadock BJ, Sadock VA, eds. Synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.
4. Nierenberg AA, Miyahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry 2005;57(11):1467-73.
5. Tamam L, Tuglu C, Karatas G, et al. Adult attention-deficit hyperactivity disorder in patients with bipolar I disorder in remission: preliminary study. Psychiatry Clin Neurosci 2006;60(4):480-5.
6. Wilens TE, Biederman J, Wozniak J, et al. Can adults with attention-deficit/hyperactivity disorder be distinguished from those with comorbid bipolar disorder? Findings from a sample of clinically referred adults. Biol Psychiatry 2003;54(1):1-8.
7. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry 2005;162(9):1621-7.
8. Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry 2006;163(10):1720-9.
9. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord 1999;52(1-3):135-44.
10. Keitner GI, Solomon DA, Ryan CE, et al. Prodromal and residual symptoms in bipolar I disorder. Compr Psychiatry 1996;37(5):362-7.
11. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv 2001;52(1):51-5.
12. Kent L, Craddock N. Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? J Affect Disord 2003;73(3):211-21.
13. Surtees PG, Kendell RE. The hierarchy model of psychiatric symptomatology: an investigation based on present state examination ratings. Br J Psychiatry 1979;135:438-43.
14. Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog Neuropsychopharmacol Biol Psychiatry 2006;30(3):471-7.
15. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text rev. Washington, DC: American Psychiatric Association; 2000.
16. Murphy KR, Adler LA. Assessing attention-deficit hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry 2004;65(suppl 3):12-17.
17. Adler LA. Diagnosing adult attention deficit hyperactivity disorder. Primary Psychiatry 2006;13(suppl 3):9-10.
18. Montano B. Diagnosis and treatment of ADHD in adults in primary care. J Clin Psychiatry 2004;65(suppl 3):18-21.
19. Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS). North Tonawanda, NY: Multi-Health Systems; 1999.
20. Brown TE. Brown Attention Deficit Disorder Scales. San Antonio, TX: The Psychological Corporation; 1996.
21. Adler LA, Kessler RC, Spencer T. Adult ADHD Self-report Scale v1.1 (ASRS-v1.1) Symptom Checklist. World Health Organization. Available at: http://www.med.nyu.edu/psych/assets/adhdscreen18.pdf. Accessed May 7, 2007.
22. Wilens TE, Prince JB, Spencer T, et al. An open trial of bupropion for the treatment of adults with attention-deficit/hyperactivity disorder and bipolar disorder. Biol Psychiatry 2003;54(1):9-16.
23. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
24. Daviss WB, Bentivoglio P, Racusin R, et al. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry 2001;40(3):307-14.
25. Scherk H, Pajonk FG, Leucht SL. Second-generation antipsychotic agents in the treatment of acute mania. Arch Gen Psychiatry 2007;64:442-55.
26. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 2007:356:(17):1711-22.
27. Wilens TE, Haight BR, Horrigan JP, et al. Bupropion XL in adults with attention deficit hyperactivity disorder: a randomized, placebo controlled study. Biol Psychiatry 2005;57:793-801.
28. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
29. Michelson D, Adler LA, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo controlled studies. Biol Psychiatry 2003;53:112-20.
30. Adler LA, Resnick S, Kunz M, Devinsky O. Open-label trial of venlafaxine in adults with attention deficit disorder. Psychopharmacol Bull 1995;31(4):785-8.
31. Hedges D, Reimherr FW, Rogers A, et al. An open trial of venlafaxine in adult patients with attention deficit hyperactivity disorder. Psychopharmacol Bull 1995;31(4):779-83.
32. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry 1996;153(9):1147-53.
33. Faraone SV, Spencer T, Aleardi M, et al. Meta analysis of the efficacy of methylphenidate for treating adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2004;24(1):24-8.
34. Spencer T, Biederman J, Wilens TE, et al. Efficacy of a mixed amphetamine salts compound in adults with attention deficit hyperactivity disorder. Arch Gen Psychiatry 2001;58:775-82.
35. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2000;21(2):223-8.
36. El-Mallakh RS. An open study of methylphenidate in bipolar depression. Bipolar Disord 2000;2(1):56-9.
37. Faedda GL, Baldessarini RJ, Glovinsky IP, et al. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord 2004;82(1):149-58.
38. Soutullo CA, DelBello MP, Ochsner JE, et al. Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment. J Affect Disord 2002;70(3):323-7.
39. Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 2006;189:124-31.
40. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry 1994;164(4):549-50.
41. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145(2):179-84.
42. Goldberg JF. When do antidepressants worsen the course of bipolar disorder? J Psychiatr Pract. 2003;9(3):181-94.
43. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry 2002;63(9):791-5.
Overlapping symptoms may obscure comorbid bipolar illness
An adult with function-impairing inattention could have attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or both. Comorbid ADHD and BD often is unrecognized, however, because patients are more likely to report ADHD-related symptoms than manic symptoms.1
To help you recognize comorbid ADHD/BD—and protect adults who might switch into mania if given stimulants or antidepressants—this article describes a hierarchy to diagnose and treat this comorbidity. Based on the evidence and our experience, we:
- discuss how to differentiate between these disorders with overlapping symptoms
- provide tools and suggestions to screen for BD and adult ADHD
- offer 3 algorithms to guide your diagnosis and choice of medications.
Clinical challenges
Prevalence is unclear. Adult ADHD—with an estimated prevalence of 4.4%2—is more common than BD. Lifetime prevalences of BD types I and II are 1.6% and 0.5%, respectively.3 Studies of ADHD/BD comorbidity suggest wide-ranging prevalence rates:
Underdiagnosis. Adult ADHD/BD is a more severe illness than ADHD or BD alone and is highly comorbid with agoraphobia, social phobia, posttraumatic stress disorder, and alcohol or drug addiction. Adults with ADHD/BD have more frequent affective episodes, suicide attempts, violence, and legal problems.4 Diagnosing this comorbidity remains a challenge, however, because:
- identifying which symptoms are caused by which disorder can be difficult
- BD tends to be underdiagnosed9
- patients often misidentify, underreport, or deny manic symptoms1,10,11
- if a patient presents with active bipolar symptoms, DSM-IV-TR criteria require that ADHD not be diagnosed until mood symptoms are resolved.
Overlapping symptoms. ADHD and bipolar mania share some DSM-IV-TR diagnostic criteria, including talkativeness, distractibility, increased activity or physical restlessness, and loss of social inhibitions (Table 1).12 Overlapping symptoms also are notable within ADHD diagnostic criteria (Table 2). In the inattention category, for example, “easily distracted by extraneous stimuli,” “difficulty sustaining attention in tasks,” and “fails to give close attention to details” are considered 3 separate symptoms. In the hyperactivity category, “often leaves seat,” “often runs about or climbs excessively,” and “often on the go, or often acts as if driven by a motor” are 3 separate symptoms.
Given ADHD’s relatively loose diagnostic criteria and high comorbidity in adults with mood disorders, the question of whether adult ADHD/BD represents comorbidity or diagnostic overlap remains unresolved. For the clinician, the disorders’ nonoverlapping features (Table 1) can assist with the differential diagnosis. For example:
- ADHD symptoms tend to be chronic and BD symptoms episodic.
- ADHD patients may have high energy but lack increased productivity seen in BD patients.
- ADHD patients do not need less sleep or have inflated self-esteem like symptomatic BD patients.
- Psychotic symptoms such as hallucinations or delusions might be present in severe BD but are absent in ADHD.
Table 1
Overlap between DSM-IV-TR diagnostic criteria for ADHD and bipolar mania
| Overlapping symptoms | |
|---|---|
| ADHD | Bipolar mania |
| Talks excessively | More talkative than usual |
| Easily distracted/jumps from one activity to the next | Distractibility or constant changes in activity or plans |
| Fidgets Difficulty remaining seated Runs or climbs about inappropriately Difficulty playing quietly On the go as if driven by a motor | Increased activity or physical restlessness |
| Interrupts or butts in uninvited Blurts out answers | Loss of normal social inhibitions |
| Nonoverlapping symptoms | |
| ADHD Forgetful in daily activities Difficulty awaiting turn Difficulty organizing self Loses things Avoids sustained mental effort Does not seem to listen Difficulty following through on instructions/fails to finish work Difficulty sustaining attention Fails to give close attention to details/makes careless mistakes | |
| Bipolar mania Inflated self-esteem/grandiosity Increase in goal-directed activity Flight of ideas Decreased need for sleep Excessive involvement in pleasurable activities with disregard for potential adverse consequences Marked sexual energy or sexual indiscretions | |
| ADHD: attention-deficit/hyperactivity disorder | |
| Source: Adapted and reprinted with permission from reference 12 | |
Table 2
DSM-IV-TR diagnostic criteria for attention-deficit/ hyperactivity disorder
| Inattention |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Hyperactivity/impulsivity |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Diagnosis requires evidence of inattention or hyperactivity/impulsivity or both |
| Some hyperactive/impulsive or inattentive symptoms that caused impairment were present before age 7 |
| Some impairment from symptoms is present in ≥2 settings (such as at school, work, or home) |
| Symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorder and are not better accounted for by another mental disorder (mood disorder, anxiety disorder, dissociative disorder, or a personality disorder) |
| Source: DSM-IV-TR |
Mood symptoms first
A diagnostic hierarchy is implicit in DSM-IV-TR; anxiety disorders are not diagnosed during an active major depressive or manic episode, and schizophrenia is not diagnosed on the basis of psychotic symptoms during an active major depressive or manic episode. Mood disorders sit atop this implied diagnostic hierarchy and must be ruled out before psychotic or anxiety disorders are diagnosed. Similarly, most personality disorders are not diagnosed during an active mood or psychotic episode.
Diagnosing adult ADHD when a patient is actively depressed or manic is inconsistent with this hierarchy and conflicts with extensive nosologic literature.13 We suggest that ADHD—a cognitive-behavioral problem—not be diagnosed solely on symptoms observed when a patient is experiencing a mood episode or psychotic illness.
Bipolar disorder. Two useful mnemonics (Table 3) assist in screening for DSM-IV-TR symptoms of BD type I:
- Pure mania consists of euphoric mood and ≥3 of 7 DIGFAST criteria, or irritable mood and ≥4 of 7 DIGFAST criteria
- Mixed mania consists of depressed mood with ≥4 of 7 DIGFAST criteria and ≥4 of 8 SIGECAPS criteria.
To be diagnostic, these symptoms must cause substantial social or occupational dysfunction and be present at least 1 week. Diagnose BD type I if a patient has experienced a single pure or mixed manic episode at any time, unless the episode had a medical cause such as hyperthyroidism or antidepressant use. Because patients with mixed episodes experience depressed mood, assess any patient with clinical depression for manic symptoms. Otherwise, a patient with a mixed episode could be misdiagnosed as having unipolar depression instead of BD type I.14
BD type II also has been observed in patients with comorbid adult ADHD/BD.4,6 The main difference between BD types I and II is that manic symptoms in type II are not severe enough to cause functional impairment or psychotic symptoms.15
Adult ADHD. The clinical interview seeking evidence of inattention and hyperactivity/impulsivity remains the basis of adult ADHD diagnosis (Table 2). Key areas are:
- the patient’s past and current functional impairment
- whether substantial impairment occurs in at least 2 areas of life (such as school, work, or home).
Take medical, educational, social, psychological, and vocational histories, and rule out other conditions before concluding that adult ADHD is the appropriate diagnosis.16 In adult ADHD, inattentive symptoms become far more prominent, about twice as common as hyperactive symptoms.17 Inattentive symptoms may manifest as neglect, poor time management, motivational deficits, or poor concentration that results in forgetfulness, distractibility, item misplacement, or excessive mistakes in paperwork.18 When impulsive symptoms persist in adults, they may manifest as automobile accidents or low tolerance for frustration, which may lead to frequent job changes and unstable, interrupted interpersonal relationships.18
Neuropsychological testing is not required to make an adult ADHD diagnosis but can help establish the breadth of symptoms or comorbidity.17 Rating scales can screen, gather data (including presence and severity of symptoms), and measure treatment response.16 Commonly used rating scales include:
- Conners’ Adult ADHD Rating Scales19
- Brown Attention Deficit Disorder Rating Scale for Adults20
- Adult ADHD Self-Report Scale.21
When using rating scales, remember that adult psychopathology can distort perceptions, and some self-report scales have questionable reliability.16
Table 3
Mnemonics for diagnostic symptoms of pure and mixed bipolar mania
| DIGFAST* for bipolar mania symptoms | SIGECAPS† bipolar depression symptoms |
|---|---|
| Distractibility Insomnia Grandiosity Flight of ideas Activities Speech Thoughtlessness | Sleep Interest Guilt Energy Concentration Appetite Psychomotor Suicide |
| Pure mania: Euphoric mood with ≥3 DIGFAST criteria or irritable mood with ≥4 DIGFAST criteria. | |
| Mixed mania: Depressed mood with ≥4 DIGFAST criteria and ≥4 SIGECAPS criteria. | |
| * Developed by William Falk, MD | |
| †Developed by Carey Gross, MD | |
| Source: Adapted from Ghaemi SN. Mood disorders. New York: Lippincott, Williams, & Wilkins; 2003 | |
Treatment recommendations
Limited data. We found only 1 study on adult ADHD/BD treatment. In this open trial,22 36 adults with comorbid ADHD and BD received bupropion SR, up to 200 mg bid, for ADHD symptoms while maintained on mood stabilizers, antipsychotics, or both. Improvement was defined as ≥30% reduction in ADHD Symptom Checklist Scale scores, without concurrent mania. After 6 weeks, 82% of patients had improved; 1 dropped out at week 2 because of hypomanic activation. Methodologic limitations included trial design (non-randomized, nonblinded, short duration) and patient selection (90% of subjects had BD type II).
In the absence of adequate data on adult ADHD/BD, studies in children suggest:
- stimulants may not be effective for ADHD symptoms in patients with active manic or depressive symptoms
- mood stabilization is a prerequisite for successful pharmacologic treatment of ADHD in patients with both ADHD and manic or depressive symptoms.23,24
Follow the hierarchy. First treat acute mood symptoms, then reevaluate and possibly treat ADHD symptoms if they persist during euthymia (Algorithm 1). When a patient meets criteria for adult ADHD/BD, first stabilize bipolar manic or depressive symptoms (Algorithm 2). For acute mania, treat with standard mood stabilizers (lithium, valproate, lamotrigine, or carbamazepine) with or without a second-generation antipsychotic.25 Starting stimulants for ADHD when patients have active mood symptoms is sub-optimal and potentially harmful because of the risk of inducing mania. For acute bipolar depression, adjunctive antidepressant treatment has been found to be no more effective than a mood stabilizer alone.26
After bipolar symptoms respond or remit, reassess for adult ADHD. If ADHD symptoms persist during euthymia, additional treatment may be indicated.
Very little evidence exists on treating adult ADHD/BD; as mentioned, bupropion is the only medication studied in this population. For adult ADHD alone, clinical trials have showed varying efficacy with bupropion,27,28 atomoxetine,29 venlafaxine,30,31 desipramine,32 methylphenidate,33 mixed amphetamine salts,34 and guanfacine.35 Whether these treatments can be generalized as safe and efficacious for comorbid adult ADHD/BD is unclear. Nonetheless, we suggest using bupropion first, followed by atomoxetine or guanfacine before you consider amphetamine stimulants (Algorithm 3).
Algorithm 1
Hierarchy for diagnosis and treatment of adult ADHD/BD
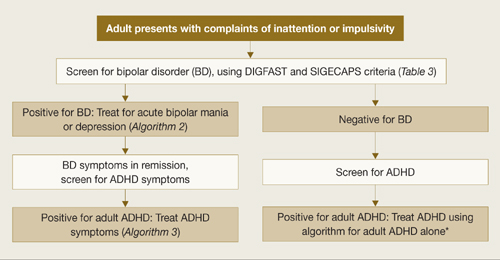
ADHD: attention-deficit/hyperactivity disorder; BD: bipolar disorder
*Adler LA, Chua HC. Management of ADHD in adults. J Clin Psychiatry 2002;63(suppl 12):29-35.
Algorithm 2
Treating acute episodes of bipolar disorder
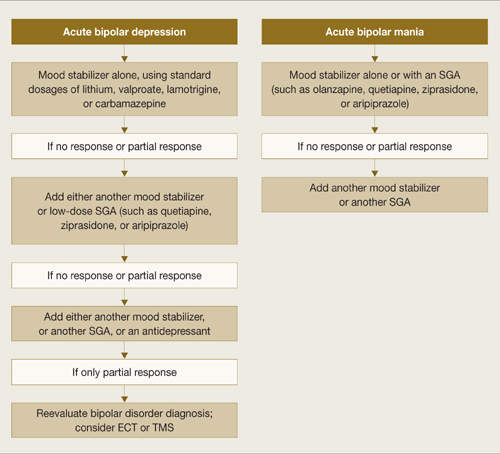
ECT: electroconvulsive therapy; SGA: second-generation antipsychotic; TMS: transcranial magnetic stimulation
Algorithm 3
Suggested approach to adult ADHD with comorbid BD*
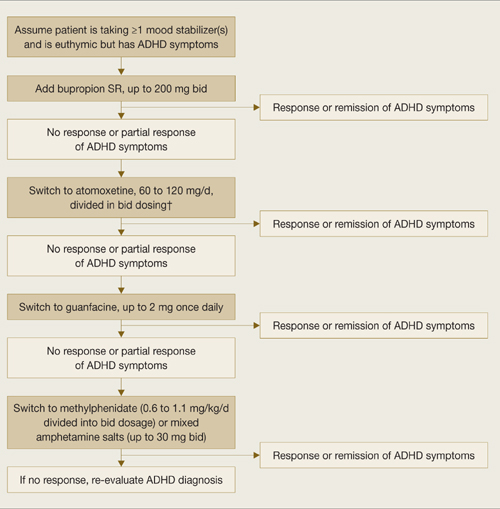
* Based on data extrapolated from samples of patients with ADHD alone because of very limited data in ADHD/BD samples.
† We recommend against combining antidepressants and stimulants because of additive risks of mania in BD. Discontinue stimulant or antidepressant if manic symptoms appear or rapid cycling emerges.
Reducing mania risk
Antidepressants and stimulants may help adults with ADHD alone, but risks of mania and rapid cycling limit their use in adults with ADHD/BD.
Stimulants and mania. One study found a 17% manic switch rate when methylphenidate (≤10 mg bid) was given to 14 bipolar depressed adults (10 BD type I, 2 BD type II, and 2 with secondary mania) taking mood stabilizers.36 A chart review of 82 bipolar children not taking mood stabilizers found an 18% switch rate with methylphenidate or amphetamine.37 Another chart review of 80 children with BD type I found that past amphetamine treatment (but not history of ADHD diagnosis or antidepressant treatment) was associated with more severe bipolar illness.38
No studies have examined predictors of amphetamine-induced mania. In our clinical experience, triggers are similar to those that can cause antidepressant-induced mania, such as:
- recent manic episodes
- current rapid cycling
- past antidepressant-induced mania.
Antidepressants and mania. When 64 patients with acute bipolar depression received both antidepressants and mood stabilizers in a randomized, double-blind trial, switch rates into mania or hypomania were 10% for bupropion, 9% for sertraline, and 29% for venlafaxine.39 In a meta analysis of clinical trials using selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants (TCAs), the manic switch rate was threefold higher with TCAs than SSRIs.40 Antidepressant use in bipolar patients was associated with rapid cycling in the only randomized study of this topic.41
Insufficient data exist to clarify whether mania induction with antidepressants is dose-dependent.42 Factors associated with antidepressant-induced mania include:
- previous antidepressant-induced mania
- family history of BD
- exposure to multiple antidepressant trials42
- history of substance abuse and/or dependence.43
Related resources
- Bipolar disorder information and resources. www.psycheducation.org.
- ADHD Information and resources. www.adhdnews.com.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. New York: McGraw-Hill; 2006.
Drug brand names
- Amphetamine/Dextroamphetamine • Adderall
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methylphenidate • Ritalin
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Valproate • Depakote
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Wingo reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ghaemi receives research grants from GlaxoSmithKline and Pfizer and is a speaker for GlaxoSmithKline, AstraZeneca, Pfizer, and Abbott Laboratories. Neither he nor his family hold equity positions in pharmaceutical companies.
Overlapping symptoms may obscure comorbid bipolar illness
An adult with function-impairing inattention could have attention-deficit/hyperactivity disorder (ADHD), bipolar disorder (BD), or both. Comorbid ADHD and BD often is unrecognized, however, because patients are more likely to report ADHD-related symptoms than manic symptoms.1
To help you recognize comorbid ADHD/BD—and protect adults who might switch into mania if given stimulants or antidepressants—this article describes a hierarchy to diagnose and treat this comorbidity. Based on the evidence and our experience, we:
- discuss how to differentiate between these disorders with overlapping symptoms
- provide tools and suggestions to screen for BD and adult ADHD
- offer 3 algorithms to guide your diagnosis and choice of medications.
Clinical challenges
Prevalence is unclear. Adult ADHD—with an estimated prevalence of 4.4%2—is more common than BD. Lifetime prevalences of BD types I and II are 1.6% and 0.5%, respectively.3 Studies of ADHD/BD comorbidity suggest wide-ranging prevalence rates:
Underdiagnosis. Adult ADHD/BD is a more severe illness than ADHD or BD alone and is highly comorbid with agoraphobia, social phobia, posttraumatic stress disorder, and alcohol or drug addiction. Adults with ADHD/BD have more frequent affective episodes, suicide attempts, violence, and legal problems.4 Diagnosing this comorbidity remains a challenge, however, because:
- identifying which symptoms are caused by which disorder can be difficult
- BD tends to be underdiagnosed9
- patients often misidentify, underreport, or deny manic symptoms1,10,11
- if a patient presents with active bipolar symptoms, DSM-IV-TR criteria require that ADHD not be diagnosed until mood symptoms are resolved.
Overlapping symptoms. ADHD and bipolar mania share some DSM-IV-TR diagnostic criteria, including talkativeness, distractibility, increased activity or physical restlessness, and loss of social inhibitions (Table 1).12 Overlapping symptoms also are notable within ADHD diagnostic criteria (Table 2). In the inattention category, for example, “easily distracted by extraneous stimuli,” “difficulty sustaining attention in tasks,” and “fails to give close attention to details” are considered 3 separate symptoms. In the hyperactivity category, “often leaves seat,” “often runs about or climbs excessively,” and “often on the go, or often acts as if driven by a motor” are 3 separate symptoms.
Given ADHD’s relatively loose diagnostic criteria and high comorbidity in adults with mood disorders, the question of whether adult ADHD/BD represents comorbidity or diagnostic overlap remains unresolved. For the clinician, the disorders’ nonoverlapping features (Table 1) can assist with the differential diagnosis. For example:
- ADHD symptoms tend to be chronic and BD symptoms episodic.
- ADHD patients may have high energy but lack increased productivity seen in BD patients.
- ADHD patients do not need less sleep or have inflated self-esteem like symptomatic BD patients.
- Psychotic symptoms such as hallucinations or delusions might be present in severe BD but are absent in ADHD.
Table 1
Overlap between DSM-IV-TR diagnostic criteria for ADHD and bipolar mania
| Overlapping symptoms | |
|---|---|
| ADHD | Bipolar mania |
| Talks excessively | More talkative than usual |
| Easily distracted/jumps from one activity to the next | Distractibility or constant changes in activity or plans |
| Fidgets Difficulty remaining seated Runs or climbs about inappropriately Difficulty playing quietly On the go as if driven by a motor | Increased activity or physical restlessness |
| Interrupts or butts in uninvited Blurts out answers | Loss of normal social inhibitions |
| Nonoverlapping symptoms | |
| ADHD Forgetful in daily activities Difficulty awaiting turn Difficulty organizing self Loses things Avoids sustained mental effort Does not seem to listen Difficulty following through on instructions/fails to finish work Difficulty sustaining attention Fails to give close attention to details/makes careless mistakes | |
| Bipolar mania Inflated self-esteem/grandiosity Increase in goal-directed activity Flight of ideas Decreased need for sleep Excessive involvement in pleasurable activities with disregard for potential adverse consequences Marked sexual energy or sexual indiscretions | |
| ADHD: attention-deficit/hyperactivity disorder | |
| Source: Adapted and reprinted with permission from reference 12 | |
Table 2
DSM-IV-TR diagnostic criteria for attention-deficit/ hyperactivity disorder
| Inattention |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Hyperactivity/impulsivity |
≥6 symptoms have persisted ≥6 months to a degree that is maladaptive and inconsistent with developmental level. The patient often:
|
| Diagnosis requires evidence of inattention or hyperactivity/impulsivity or both |
| Some hyperactive/impulsive or inattentive symptoms that caused impairment were present before age 7 |
| Some impairment from symptoms is present in ≥2 settings (such as at school, work, or home) |
| Symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorder and are not better accounted for by another mental disorder (mood disorder, anxiety disorder, dissociative disorder, or a personality disorder) |
| Source: DSM-IV-TR |
Mood symptoms first
A diagnostic hierarchy is implicit in DSM-IV-TR; anxiety disorders are not diagnosed during an active major depressive or manic episode, and schizophrenia is not diagnosed on the basis of psychotic symptoms during an active major depressive or manic episode. Mood disorders sit atop this implied diagnostic hierarchy and must be ruled out before psychotic or anxiety disorders are diagnosed. Similarly, most personality disorders are not diagnosed during an active mood or psychotic episode.
Diagnosing adult ADHD when a patient is actively depressed or manic is inconsistent with this hierarchy and conflicts with extensive nosologic literature.13 We suggest that ADHD—a cognitive-behavioral problem—not be diagnosed solely on symptoms observed when a patient is experiencing a mood episode or psychotic illness.
Bipolar disorder. Two useful mnemonics (Table 3) assist in screening for DSM-IV-TR symptoms of BD type I:
- Pure mania consists of euphoric mood and ≥3 of 7 DIGFAST criteria, or irritable mood and ≥4 of 7 DIGFAST criteria
- Mixed mania consists of depressed mood with ≥4 of 7 DIGFAST criteria and ≥4 of 8 SIGECAPS criteria.
To be diagnostic, these symptoms must cause substantial social or occupational dysfunction and be present at least 1 week. Diagnose BD type I if a patient has experienced a single pure or mixed manic episode at any time, unless the episode had a medical cause such as hyperthyroidism or antidepressant use. Because patients with mixed episodes experience depressed mood, assess any patient with clinical depression for manic symptoms. Otherwise, a patient with a mixed episode could be misdiagnosed as having unipolar depression instead of BD type I.14
BD type II also has been observed in patients with comorbid adult ADHD/BD.4,6 The main difference between BD types I and II is that manic symptoms in type II are not severe enough to cause functional impairment or psychotic symptoms.15
Adult ADHD. The clinical interview seeking evidence of inattention and hyperactivity/impulsivity remains the basis of adult ADHD diagnosis (Table 2). Key areas are:
- the patient’s past and current functional impairment
- whether substantial impairment occurs in at least 2 areas of life (such as school, work, or home).
Take medical, educational, social, psychological, and vocational histories, and rule out other conditions before concluding that adult ADHD is the appropriate diagnosis.16 In adult ADHD, inattentive symptoms become far more prominent, about twice as common as hyperactive symptoms.17 Inattentive symptoms may manifest as neglect, poor time management, motivational deficits, or poor concentration that results in forgetfulness, distractibility, item misplacement, or excessive mistakes in paperwork.18 When impulsive symptoms persist in adults, they may manifest as automobile accidents or low tolerance for frustration, which may lead to frequent job changes and unstable, interrupted interpersonal relationships.18
Neuropsychological testing is not required to make an adult ADHD diagnosis but can help establish the breadth of symptoms or comorbidity.17 Rating scales can screen, gather data (including presence and severity of symptoms), and measure treatment response.16 Commonly used rating scales include:
- Conners’ Adult ADHD Rating Scales19
- Brown Attention Deficit Disorder Rating Scale for Adults20
- Adult ADHD Self-Report Scale.21
When using rating scales, remember that adult psychopathology can distort perceptions, and some self-report scales have questionable reliability.16
Table 3
Mnemonics for diagnostic symptoms of pure and mixed bipolar mania
| DIGFAST* for bipolar mania symptoms | SIGECAPS† bipolar depression symptoms |
|---|---|
| Distractibility Insomnia Grandiosity Flight of ideas Activities Speech Thoughtlessness | Sleep Interest Guilt Energy Concentration Appetite Psychomotor Suicide |
| Pure mania: Euphoric mood with ≥3 DIGFAST criteria or irritable mood with ≥4 DIGFAST criteria. | |
| Mixed mania: Depressed mood with ≥4 DIGFAST criteria and ≥4 SIGECAPS criteria. | |
| * Developed by William Falk, MD | |
| †Developed by Carey Gross, MD | |
| Source: Adapted from Ghaemi SN. Mood disorders. New York: Lippincott, Williams, & Wilkins; 2003 | |
Treatment recommendations
Limited data. We found only 1 study on adult ADHD/BD treatment. In this open trial,22 36 adults with comorbid ADHD and BD received bupropion SR, up to 200 mg bid, for ADHD symptoms while maintained on mood stabilizers, antipsychotics, or both. Improvement was defined as ≥30% reduction in ADHD Symptom Checklist Scale scores, without concurrent mania. After 6 weeks, 82% of patients had improved; 1 dropped out at week 2 because of hypomanic activation. Methodologic limitations included trial design (non-randomized, nonblinded, short duration) and patient selection (90% of subjects had BD type II).
In the absence of adequate data on adult ADHD/BD, studies in children suggest:
- stimulants may not be effective for ADHD symptoms in patients with active manic or depressive symptoms
- mood stabilization is a prerequisite for successful pharmacologic treatment of ADHD in patients with both ADHD and manic or depressive symptoms.23,24
Follow the hierarchy. First treat acute mood symptoms, then reevaluate and possibly treat ADHD symptoms if they persist during euthymia (Algorithm 1). When a patient meets criteria for adult ADHD/BD, first stabilize bipolar manic or depressive symptoms (Algorithm 2). For acute mania, treat with standard mood stabilizers (lithium, valproate, lamotrigine, or carbamazepine) with or without a second-generation antipsychotic.25 Starting stimulants for ADHD when patients have active mood symptoms is sub-optimal and potentially harmful because of the risk of inducing mania. For acute bipolar depression, adjunctive antidepressant treatment has been found to be no more effective than a mood stabilizer alone.26
After bipolar symptoms respond or remit, reassess for adult ADHD. If ADHD symptoms persist during euthymia, additional treatment may be indicated.
Very little evidence exists on treating adult ADHD/BD; as mentioned, bupropion is the only medication studied in this population. For adult ADHD alone, clinical trials have showed varying efficacy with bupropion,27,28 atomoxetine,29 venlafaxine,30,31 desipramine,32 methylphenidate,33 mixed amphetamine salts,34 and guanfacine.35 Whether these treatments can be generalized as safe and efficacious for comorbid adult ADHD/BD is unclear. Nonetheless, we suggest using bupropion first, followed by atomoxetine or guanfacine before you consider amphetamine stimulants (Algorithm 3).
Algorithm 1
Hierarchy for diagnosis and treatment of adult ADHD/BD
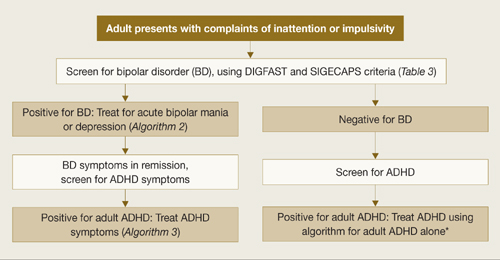
ADHD: attention-deficit/hyperactivity disorder; BD: bipolar disorder
*Adler LA, Chua HC. Management of ADHD in adults. J Clin Psychiatry 2002;63(suppl 12):29-35.
Algorithm 2
Treating acute episodes of bipolar disorder
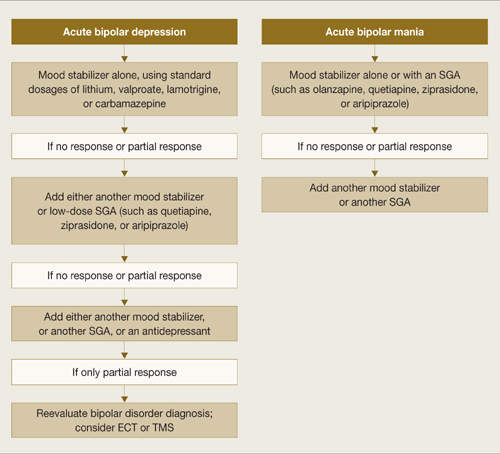
ECT: electroconvulsive therapy; SGA: second-generation antipsychotic; TMS: transcranial magnetic stimulation
Algorithm 3
Suggested approach to adult ADHD with comorbid BD*
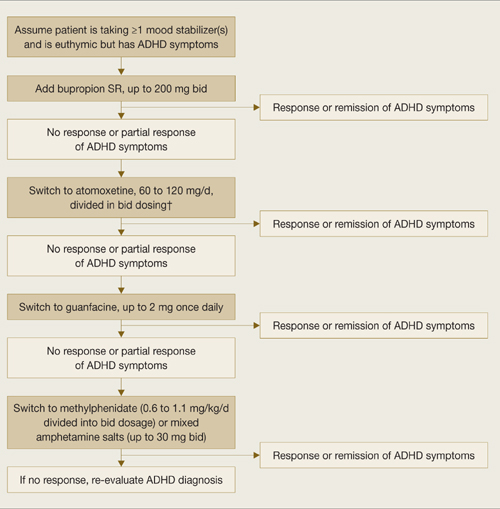
* Based on data extrapolated from samples of patients with ADHD alone because of very limited data in ADHD/BD samples.
† We recommend against combining antidepressants and stimulants because of additive risks of mania in BD. Discontinue stimulant or antidepressant if manic symptoms appear or rapid cycling emerges.
Reducing mania risk
Antidepressants and stimulants may help adults with ADHD alone, but risks of mania and rapid cycling limit their use in adults with ADHD/BD.
Stimulants and mania. One study found a 17% manic switch rate when methylphenidate (≤10 mg bid) was given to 14 bipolar depressed adults (10 BD type I, 2 BD type II, and 2 with secondary mania) taking mood stabilizers.36 A chart review of 82 bipolar children not taking mood stabilizers found an 18% switch rate with methylphenidate or amphetamine.37 Another chart review of 80 children with BD type I found that past amphetamine treatment (but not history of ADHD diagnosis or antidepressant treatment) was associated with more severe bipolar illness.38
No studies have examined predictors of amphetamine-induced mania. In our clinical experience, triggers are similar to those that can cause antidepressant-induced mania, such as:
- recent manic episodes
- current rapid cycling
- past antidepressant-induced mania.
Antidepressants and mania. When 64 patients with acute bipolar depression received both antidepressants and mood stabilizers in a randomized, double-blind trial, switch rates into mania or hypomania were 10% for bupropion, 9% for sertraline, and 29% for venlafaxine.39 In a meta analysis of clinical trials using selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants (TCAs), the manic switch rate was threefold higher with TCAs than SSRIs.40 Antidepressant use in bipolar patients was associated with rapid cycling in the only randomized study of this topic.41
Insufficient data exist to clarify whether mania induction with antidepressants is dose-dependent.42 Factors associated with antidepressant-induced mania include:
- previous antidepressant-induced mania
- family history of BD
- exposure to multiple antidepressant trials42
- history of substance abuse and/or dependence.43
Related resources
- Bipolar disorder information and resources. www.psycheducation.org.
- ADHD Information and resources. www.adhdnews.com.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. New York: McGraw-Hill; 2006.
Drug brand names
- Amphetamine/Dextroamphetamine • Adderall
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Methylphenidate • Ritalin
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Valproate • Depakote
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosures
Dr. Wingo reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Ghaemi receives research grants from GlaxoSmithKline and Pfizer and is a speaker for GlaxoSmithKline, AstraZeneca, Pfizer, and Abbott Laboratories. Neither he nor his family hold equity positions in pharmaceutical companies.
1. Ghaemi SN, Stoll AL, Pope HG, Jr, et al. Lack of insight in bipolar disorder. The acute manic episode. J Nerv Ment Dis 1995;183(7):464-7.
2. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163(4):716-23.
3. Sadock BJ, Sadock VA, eds. Synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.
4. Nierenberg AA, Miyahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry 2005;57(11):1467-73.
5. Tamam L, Tuglu C, Karatas G, et al. Adult attention-deficit hyperactivity disorder in patients with bipolar I disorder in remission: preliminary study. Psychiatry Clin Neurosci 2006;60(4):480-5.
6. Wilens TE, Biederman J, Wozniak J, et al. Can adults with attention-deficit/hyperactivity disorder be distinguished from those with comorbid bipolar disorder? Findings from a sample of clinically referred adults. Biol Psychiatry 2003;54(1):1-8.
7. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry 2005;162(9):1621-7.
8. Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry 2006;163(10):1720-9.
9. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord 1999;52(1-3):135-44.
10. Keitner GI, Solomon DA, Ryan CE, et al. Prodromal and residual symptoms in bipolar I disorder. Compr Psychiatry 1996;37(5):362-7.
11. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv 2001;52(1):51-5.
12. Kent L, Craddock N. Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? J Affect Disord 2003;73(3):211-21.
13. Surtees PG, Kendell RE. The hierarchy model of psychiatric symptomatology: an investigation based on present state examination ratings. Br J Psychiatry 1979;135:438-43.
14. Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog Neuropsychopharmacol Biol Psychiatry 2006;30(3):471-7.
15. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text rev. Washington, DC: American Psychiatric Association; 2000.
16. Murphy KR, Adler LA. Assessing attention-deficit hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry 2004;65(suppl 3):12-17.
17. Adler LA. Diagnosing adult attention deficit hyperactivity disorder. Primary Psychiatry 2006;13(suppl 3):9-10.
18. Montano B. Diagnosis and treatment of ADHD in adults in primary care. J Clin Psychiatry 2004;65(suppl 3):18-21.
19. Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS). North Tonawanda, NY: Multi-Health Systems; 1999.
20. Brown TE. Brown Attention Deficit Disorder Scales. San Antonio, TX: The Psychological Corporation; 1996.
21. Adler LA, Kessler RC, Spencer T. Adult ADHD Self-report Scale v1.1 (ASRS-v1.1) Symptom Checklist. World Health Organization. Available at: http://www.med.nyu.edu/psych/assets/adhdscreen18.pdf. Accessed May 7, 2007.
22. Wilens TE, Prince JB, Spencer T, et al. An open trial of bupropion for the treatment of adults with attention-deficit/hyperactivity disorder and bipolar disorder. Biol Psychiatry 2003;54(1):9-16.
23. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
24. Daviss WB, Bentivoglio P, Racusin R, et al. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry 2001;40(3):307-14.
25. Scherk H, Pajonk FG, Leucht SL. Second-generation antipsychotic agents in the treatment of acute mania. Arch Gen Psychiatry 2007;64:442-55.
26. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 2007:356:(17):1711-22.
27. Wilens TE, Haight BR, Horrigan JP, et al. Bupropion XL in adults with attention deficit hyperactivity disorder: a randomized, placebo controlled study. Biol Psychiatry 2005;57:793-801.
28. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
29. Michelson D, Adler LA, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo controlled studies. Biol Psychiatry 2003;53:112-20.
30. Adler LA, Resnick S, Kunz M, Devinsky O. Open-label trial of venlafaxine in adults with attention deficit disorder. Psychopharmacol Bull 1995;31(4):785-8.
31. Hedges D, Reimherr FW, Rogers A, et al. An open trial of venlafaxine in adult patients with attention deficit hyperactivity disorder. Psychopharmacol Bull 1995;31(4):779-83.
32. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry 1996;153(9):1147-53.
33. Faraone SV, Spencer T, Aleardi M, et al. Meta analysis of the efficacy of methylphenidate for treating adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2004;24(1):24-8.
34. Spencer T, Biederman J, Wilens TE, et al. Efficacy of a mixed amphetamine salts compound in adults with attention deficit hyperactivity disorder. Arch Gen Psychiatry 2001;58:775-82.
35. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2000;21(2):223-8.
36. El-Mallakh RS. An open study of methylphenidate in bipolar depression. Bipolar Disord 2000;2(1):56-9.
37. Faedda GL, Baldessarini RJ, Glovinsky IP, et al. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord 2004;82(1):149-58.
38. Soutullo CA, DelBello MP, Ochsner JE, et al. Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment. J Affect Disord 2002;70(3):323-7.
39. Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 2006;189:124-31.
40. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry 1994;164(4):549-50.
41. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145(2):179-84.
42. Goldberg JF. When do antidepressants worsen the course of bipolar disorder? J Psychiatr Pract. 2003;9(3):181-94.
43. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry 2002;63(9):791-5.
1. Ghaemi SN, Stoll AL, Pope HG, Jr, et al. Lack of insight in bipolar disorder. The acute manic episode. J Nerv Ment Dis 1995;183(7):464-7.
2. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163(4):716-23.
3. Sadock BJ, Sadock VA, eds. Synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.
4. Nierenberg AA, Miyahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry 2005;57(11):1467-73.
5. Tamam L, Tuglu C, Karatas G, et al. Adult attention-deficit hyperactivity disorder in patients with bipolar I disorder in remission: preliminary study. Psychiatry Clin Neurosci 2006;60(4):480-5.
6. Wilens TE, Biederman J, Wozniak J, et al. Can adults with attention-deficit/hyperactivity disorder be distinguished from those with comorbid bipolar disorder? Findings from a sample of clinically referred adults. Biol Psychiatry 2003;54(1):1-8.
7. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry 2005;162(9):1621-7.
8. Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry 2006;163(10):1720-9.
9. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord 1999;52(1-3):135-44.
10. Keitner GI, Solomon DA, Ryan CE, et al. Prodromal and residual symptoms in bipolar I disorder. Compr Psychiatry 1996;37(5):362-7.
11. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv 2001;52(1):51-5.
12. Kent L, Craddock N. Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? J Affect Disord 2003;73(3):211-21.
13. Surtees PG, Kendell RE. The hierarchy model of psychiatric symptomatology: an investigation based on present state examination ratings. Br J Psychiatry 1979;135:438-43.
14. Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog Neuropsychopharmacol Biol Psychiatry 2006;30(3):471-7.
15. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text rev. Washington, DC: American Psychiatric Association; 2000.
16. Murphy KR, Adler LA. Assessing attention-deficit hyperactivity disorder in adults: focus on rating scales. J Clin Psychiatry 2004;65(suppl 3):12-17.
17. Adler LA. Diagnosing adult attention deficit hyperactivity disorder. Primary Psychiatry 2006;13(suppl 3):9-10.
18. Montano B. Diagnosis and treatment of ADHD in adults in primary care. J Clin Psychiatry 2004;65(suppl 3):18-21.
19. Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS). North Tonawanda, NY: Multi-Health Systems; 1999.
20. Brown TE. Brown Attention Deficit Disorder Scales. San Antonio, TX: The Psychological Corporation; 1996.
21. Adler LA, Kessler RC, Spencer T. Adult ADHD Self-report Scale v1.1 (ASRS-v1.1) Symptom Checklist. World Health Organization. Available at: http://www.med.nyu.edu/psych/assets/adhdscreen18.pdf. Accessed May 7, 2007.
22. Wilens TE, Prince JB, Spencer T, et al. An open trial of bupropion for the treatment of adults with attention-deficit/hyperactivity disorder and bipolar disorder. Biol Psychiatry 2003;54(1):9-16.
23. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
24. Daviss WB, Bentivoglio P, Racusin R, et al. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry 2001;40(3):307-14.
25. Scherk H, Pajonk FG, Leucht SL. Second-generation antipsychotic agents in the treatment of acute mania. Arch Gen Psychiatry 2007;64:442-55.
26. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 2007:356:(17):1711-22.
27. Wilens TE, Haight BR, Horrigan JP, et al. Bupropion XL in adults with attention deficit hyperactivity disorder: a randomized, placebo controlled study. Biol Psychiatry 2005;57:793-801.
28. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
29. Michelson D, Adler LA, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo controlled studies. Biol Psychiatry 2003;53:112-20.
30. Adler LA, Resnick S, Kunz M, Devinsky O. Open-label trial of venlafaxine in adults with attention deficit disorder. Psychopharmacol Bull 1995;31(4):785-8.
31. Hedges D, Reimherr FW, Rogers A, et al. An open trial of venlafaxine in adult patients with attention deficit hyperactivity disorder. Psychopharmacol Bull 1995;31(4):779-83.
32. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry 1996;153(9):1147-53.
33. Faraone SV, Spencer T, Aleardi M, et al. Meta analysis of the efficacy of methylphenidate for treating adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2004;24(1):24-8.
34. Spencer T, Biederman J, Wilens TE, et al. Efficacy of a mixed amphetamine salts compound in adults with attention deficit hyperactivity disorder. Arch Gen Psychiatry 2001;58:775-82.
35. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit hyperactivity disorder. J Clin Psychopharmacol 2000;21(2):223-8.
36. El-Mallakh RS. An open study of methylphenidate in bipolar depression. Bipolar Disord 2000;2(1):56-9.
37. Faedda GL, Baldessarini RJ, Glovinsky IP, et al. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord 2004;82(1):149-58.
38. Soutullo CA, DelBello MP, Ochsner JE, et al. Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment. J Affect Disord 2002;70(3):323-7.
39. Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 2006;189:124-31.
40. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry 1994;164(4):549-50.
41. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145(2):179-84.
42. Goldberg JF. When do antidepressants worsen the course of bipolar disorder? J Psychiatr Pract. 2003;9(3):181-94.
43. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry 2002;63(9):791-5.
The Hospital as College
The hospital is the only proper college in which to rear a true disciple of Aesculapius.—John Abernethy (1764-1831), surgeon and teacher
With this quote Sir William Osler began his address, “The Hospital as a College?” to the Academy of Medicine in New York in 1903. His second quote for this report was from the famed physician Oliver Wendell Holmes Sr. in 1867:
“The most essential part of a student’s instruction is obtained, as I believe, not in the lecture room, but at the bedside. Nothing seen there is lost: the rhythms of disease are learned by frequent repetition: its unforeseen occurrence stamp themselves indelibly on the memory. Before the student is aware of what he had acquired he has learned the aspects and causes and probable issue of the disease he has seen with his teacher and the proper mode of dealing with them, as far as his master knows.”
In his report Osler was celebrating a quarter century’s success in education. He demanded a better general education for students, a lengthened period for professional study, and the substitution of theoretical by practical learning. He wanted the student not to learn only from dissecting the sympathetic nervous system but to learn to “take a blood pressure observation” with a kymograph (an instrument used to record the temporal variations of any physiological or muscular process; it consists essentially of a revolving drum, bearing a record sheet on which a stylus travels).
Osler observed that there should be no teaching without a patient for a text: “The whole of medicine is in observation” that the teacher’s art is educating the student’s finger to feel and eyes to see. Give the student good methods and a proper point of view, and experience will do the rest.
Osler expressed confidence that students would keep the hospital physician from slovenliness and improve the care of patients. He was also concerned that “we ask too much of the resident physicians, whose number has not increased in proportion to the enormous amount of work thrust upon them.” Students were the answer, the proto-scut-monkey.
The practicality of working out of a teaching hospital was outlined at length in Osler’s report. The student’s third year should begin with a systematic physical diagnosis course, first in history taking, then in writing reports. Concurrently, a physical examination course should be given several days a week with individual cases assigned to students to follow, and instruction is accessing the literature. Next comes clinical microscopy—an essential in an era where there was often no lab to call upon. In general, medical clinic occurs one day a week when interesting cases are brought from the wards. Of note, committees were appointed to report on every case of pneumonia.
In revamping medical education Osler brought the third-year students to the outpatient clinic and the fourth-year students to the wards. What implication does this have for us as hospitalists?
I have no pretensions about being another Osler (I am barely a Newman on my best days), but still my colleagues and I trudge along in our teaching duties. What education do we really do? I sat down after reading Osler’s paper, stimulated by a tangential question from the esteemed Tom Baudenistel, MD, and decided to see exactly whom we were teaching.
First there are medical students. We are faculty on their first-year selectives, offering a shadow experience. We staff the introduction to physical exam courses in second year. Third-year students rotate on our services, and seniors take our elective as well as taking acting internships on our teaching services. We act as mentors and interest group leaders. There is certainly more to this list. We also spend time teaching NP and PA students.
The internal medicine residents rotate on our hospitalist services, and we staff the general medical services. We interact with them daily when they are on consult services, trying to set a role model. General medicine, geriatric, and hospital medicine fellows rotate through as well.
We also teach the nurses on services and through in-services and daily rounds to cement the working relationship and improve communication. We teach each other. A day rarely goes by without a colleague passing on a tasty medical tidbit. (Of course, for me, a tabla blanca, no shortage of space for pearls). And finally we teach our patients and their families. Every day we do this, and if we don’t then we are missing the point of our profession entirely.
Each party—patient or student—has something to learn from us, but more importantly we have something to learn from them. Osler wrote that “The stimulus of their presence (the student) neutralizes the clinical apathy certain, sooner or later, to beset the man who makes lonely “rounds” with his house physician.”
One hundred years plus later, much of what was written is still true: Whether in a teaching institution or making “lonely rounds” we must strive to continue to educate ourselves, our colleagues, and our patients. And what better place to do it than the hospital? TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
Osler W (Sir) Aequanimitas. 1945. The Blakiston Company, Philadelphia. p. 311-327.
The hospital is the only proper college in which to rear a true disciple of Aesculapius.—John Abernethy (1764-1831), surgeon and teacher
With this quote Sir William Osler began his address, “The Hospital as a College?” to the Academy of Medicine in New York in 1903. His second quote for this report was from the famed physician Oliver Wendell Holmes Sr. in 1867:
“The most essential part of a student’s instruction is obtained, as I believe, not in the lecture room, but at the bedside. Nothing seen there is lost: the rhythms of disease are learned by frequent repetition: its unforeseen occurrence stamp themselves indelibly on the memory. Before the student is aware of what he had acquired he has learned the aspects and causes and probable issue of the disease he has seen with his teacher and the proper mode of dealing with them, as far as his master knows.”
In his report Osler was celebrating a quarter century’s success in education. He demanded a better general education for students, a lengthened period for professional study, and the substitution of theoretical by practical learning. He wanted the student not to learn only from dissecting the sympathetic nervous system but to learn to “take a blood pressure observation” with a kymograph (an instrument used to record the temporal variations of any physiological or muscular process; it consists essentially of a revolving drum, bearing a record sheet on which a stylus travels).
Osler observed that there should be no teaching without a patient for a text: “The whole of medicine is in observation” that the teacher’s art is educating the student’s finger to feel and eyes to see. Give the student good methods and a proper point of view, and experience will do the rest.
Osler expressed confidence that students would keep the hospital physician from slovenliness and improve the care of patients. He was also concerned that “we ask too much of the resident physicians, whose number has not increased in proportion to the enormous amount of work thrust upon them.” Students were the answer, the proto-scut-monkey.
The practicality of working out of a teaching hospital was outlined at length in Osler’s report. The student’s third year should begin with a systematic physical diagnosis course, first in history taking, then in writing reports. Concurrently, a physical examination course should be given several days a week with individual cases assigned to students to follow, and instruction is accessing the literature. Next comes clinical microscopy—an essential in an era where there was often no lab to call upon. In general, medical clinic occurs one day a week when interesting cases are brought from the wards. Of note, committees were appointed to report on every case of pneumonia.
In revamping medical education Osler brought the third-year students to the outpatient clinic and the fourth-year students to the wards. What implication does this have for us as hospitalists?
I have no pretensions about being another Osler (I am barely a Newman on my best days), but still my colleagues and I trudge along in our teaching duties. What education do we really do? I sat down after reading Osler’s paper, stimulated by a tangential question from the esteemed Tom Baudenistel, MD, and decided to see exactly whom we were teaching.
First there are medical students. We are faculty on their first-year selectives, offering a shadow experience. We staff the introduction to physical exam courses in second year. Third-year students rotate on our services, and seniors take our elective as well as taking acting internships on our teaching services. We act as mentors and interest group leaders. There is certainly more to this list. We also spend time teaching NP and PA students.
The internal medicine residents rotate on our hospitalist services, and we staff the general medical services. We interact with them daily when they are on consult services, trying to set a role model. General medicine, geriatric, and hospital medicine fellows rotate through as well.
We also teach the nurses on services and through in-services and daily rounds to cement the working relationship and improve communication. We teach each other. A day rarely goes by without a colleague passing on a tasty medical tidbit. (Of course, for me, a tabla blanca, no shortage of space for pearls). And finally we teach our patients and their families. Every day we do this, and if we don’t then we are missing the point of our profession entirely.
Each party—patient or student—has something to learn from us, but more importantly we have something to learn from them. Osler wrote that “The stimulus of their presence (the student) neutralizes the clinical apathy certain, sooner or later, to beset the man who makes lonely “rounds” with his house physician.”
One hundred years plus later, much of what was written is still true: Whether in a teaching institution or making “lonely rounds” we must strive to continue to educate ourselves, our colleagues, and our patients. And what better place to do it than the hospital? TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
Osler W (Sir) Aequanimitas. 1945. The Blakiston Company, Philadelphia. p. 311-327.
The hospital is the only proper college in which to rear a true disciple of Aesculapius.—John Abernethy (1764-1831), surgeon and teacher
With this quote Sir William Osler began his address, “The Hospital as a College?” to the Academy of Medicine in New York in 1903. His second quote for this report was from the famed physician Oliver Wendell Holmes Sr. in 1867:
“The most essential part of a student’s instruction is obtained, as I believe, not in the lecture room, but at the bedside. Nothing seen there is lost: the rhythms of disease are learned by frequent repetition: its unforeseen occurrence stamp themselves indelibly on the memory. Before the student is aware of what he had acquired he has learned the aspects and causes and probable issue of the disease he has seen with his teacher and the proper mode of dealing with them, as far as his master knows.”
In his report Osler was celebrating a quarter century’s success in education. He demanded a better general education for students, a lengthened period for professional study, and the substitution of theoretical by practical learning. He wanted the student not to learn only from dissecting the sympathetic nervous system but to learn to “take a blood pressure observation” with a kymograph (an instrument used to record the temporal variations of any physiological or muscular process; it consists essentially of a revolving drum, bearing a record sheet on which a stylus travels).
Osler observed that there should be no teaching without a patient for a text: “The whole of medicine is in observation” that the teacher’s art is educating the student’s finger to feel and eyes to see. Give the student good methods and a proper point of view, and experience will do the rest.
Osler expressed confidence that students would keep the hospital physician from slovenliness and improve the care of patients. He was also concerned that “we ask too much of the resident physicians, whose number has not increased in proportion to the enormous amount of work thrust upon them.” Students were the answer, the proto-scut-monkey.
The practicality of working out of a teaching hospital was outlined at length in Osler’s report. The student’s third year should begin with a systematic physical diagnosis course, first in history taking, then in writing reports. Concurrently, a physical examination course should be given several days a week with individual cases assigned to students to follow, and instruction is accessing the literature. Next comes clinical microscopy—an essential in an era where there was often no lab to call upon. In general, medical clinic occurs one day a week when interesting cases are brought from the wards. Of note, committees were appointed to report on every case of pneumonia.
In revamping medical education Osler brought the third-year students to the outpatient clinic and the fourth-year students to the wards. What implication does this have for us as hospitalists?
I have no pretensions about being another Osler (I am barely a Newman on my best days), but still my colleagues and I trudge along in our teaching duties. What education do we really do? I sat down after reading Osler’s paper, stimulated by a tangential question from the esteemed Tom Baudenistel, MD, and decided to see exactly whom we were teaching.
First there are medical students. We are faculty on their first-year selectives, offering a shadow experience. We staff the introduction to physical exam courses in second year. Third-year students rotate on our services, and seniors take our elective as well as taking acting internships on our teaching services. We act as mentors and interest group leaders. There is certainly more to this list. We also spend time teaching NP and PA students.
The internal medicine residents rotate on our hospitalist services, and we staff the general medical services. We interact with them daily when they are on consult services, trying to set a role model. General medicine, geriatric, and hospital medicine fellows rotate through as well.
We also teach the nurses on services and through in-services and daily rounds to cement the working relationship and improve communication. We teach each other. A day rarely goes by without a colleague passing on a tasty medical tidbit. (Of course, for me, a tabla blanca, no shortage of space for pearls). And finally we teach our patients and their families. Every day we do this, and if we don’t then we are missing the point of our profession entirely.
Each party—patient or student—has something to learn from us, but more importantly we have something to learn from them. Osler wrote that “The stimulus of their presence (the student) neutralizes the clinical apathy certain, sooner or later, to beset the man who makes lonely “rounds” with his house physician.”
One hundred years plus later, much of what was written is still true: Whether in a teaching institution or making “lonely rounds” we must strive to continue to educate ourselves, our colleagues, and our patients. And what better place to do it than the hospital? TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Bibliography
Osler W (Sir) Aequanimitas. 1945. The Blakiston Company, Philadelphia. p. 311-327.
Trendsetting Hospitalists Receive SHM’s Top Honors
SHM has presented the 2008 Awards of Excellence to four hospitalists and one quality improvement team. Their work and research have contributed significantly to hospital medicine and the betterment of patient care and quality improvement. The winners were recognized at Hospital Medicine 2008.
Award for Clinical Excellence: Kevin O’Leary, MD, associate professor of medicine and the associate chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. O’Leary leads strategic initiatives for the division in his job as associate chief of the Division of Hospital Medicine, especially in patient safety and quality. He also chairs the department’s Quality Management Committee.
An active member of SHM since 2002, Dr. O’Leary has served on the Core Competencies Task Force, the Annual Meeting Planning Committee, and the Annual Meeting Precourse Planning Committee. He also is active in SHM’s Chicago chapter, where he serves as vice president. He serves as an assistant editor for the Journal of Hospital Medicine.
Dr. O’Leary received his bachelor’s inbiology and medical degree from the University of Illinois. He completed his residency at Northwestern University.
Award for Excellence in Research: Peter Lindenauer, MD, MSc, medical director of clinical and quality informatics at Baystate Health in Springfield, Mass., and associate professor of medicine at Tufts University School of Medicine in Boston.
Dr. Lindenauer is responsible for lending the development of an electronic medical record at a large integrated delivery network in western Massachusetts in his job as medical director of clinical and quality informatics.
He has served on technical expert panels for Medicare, patient safety, monitoring systems, and surgical care improvement projects. He also has been a part of the National Quality Forum’s Hospital Quality Measures Development Group and has served on the inpatient functionality work group of the Certifying Committee for Healthcare Information Technology.
As a founding member of SHM, Dr. Lindenauer has served on the society’s board of directors and is a member of the Hospital Quality and Patient Safety Standards Committee.
A graduate of the University of Chicago, Dr. Lindenauer received his bachelor’s in history and received his graduate degree from the Herndon School of Economics and Political Science in Health Planning and Financing. He received his medical degree from the University of Pennsylvania and completed residency training at the University of California, San Francisco.
Award for Excellence in Teaching: Anjala Tess, MD, associate program director for the Internal Medicine Residency Program and director of education for the hospital medicine program, as well as a medical unit director and practicing hospitalist at Beth Israel Deaconess Medical Center in Boston.
Dr. Tess is in charge of the quality improvement teaching program and curriculum for the entire residency program at Beth Israel Deaconess. She also helps oversee the resident elective in hospital medicine and directs educational activities for the group. Her goal is to involve residents in process improvement in the hospital by giving them a hands-on role in quality improvement and peer review.
She has received numerous awards, including the Hermann Blumgart Teaching Award at Beth Israel Deaconess and first prize in SHM’s Innovations Poster Competition.
As an undergraduate, Dr. Tess earned her degree from Brown University, in Rhode Island, and received her medical degree at Washington University’s St. Louis School of Medicine. She completed her residency at Beth Israel Deaconess. She also completed fellowships at Harvard Medical School, the Carl J. Shapiro Institute for Education Research and Beth Israel Deaconess Medical Center.
Award for Outstanding Service in Hospital Medicine: David Zipes, MD, director of pediatric hospitalist service at the Peyton Manning Children’s Hospital in Indianapolis, Ind.
Dr. Zipes oversees all hospitalists and staff, leads strategic planning for the group and the hospital, oversees the business and financial issues of the group and provides general medical direction and leadership of the pediatric units at both the Peyton Manning’s Children’s Hospital and its suburban campus.
As a founding member of SHM, Dr. Zipes is active on its Annual Meeting Planning Committee, Pediatrics Committee, and Pediatrics Core Competencies Task Force. He is also a contributing author for Pediatric Hospital Medicine and the Textbook of Pediatric Hospital Medicine, and a founding member of the annual pediatric hospital medicine meeting.
He also has been the recipient of several awards, including the Family Medicine Teacher of the Year Annual Award (2002, 2005, and 2006) and the St. Vincent Spirit of Caring Award for Service and Dedication to the Hospital (2006 and 2007.)
Dr. Zipes earned his bachelor’s and medical degrees from Indiana University. He completed his residency at Children’s Hospital Medicine Center in Cincinnati, Ohio.
Award for Team Approaches in Quality Improvement: Team Leader, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
Dr. Maynard and his team (Ian Jenkins, MD, Sarah Stone, MD, Josh Lee, MD, Ed Fink, Tim Morris, MD, Peter Fedullo, MD, Robert Schoenhaus, PharmD, Doug Humber, PharmD, Marian Renvall, Pat Cal, and Isabella London) are the recipients of the first Team Approaches in Quality Improvement Award for their project “Optimizing Prevention of Hospital-Acquired Venous Thromboembolism.”
Dr. Maynard led the three-year project, which has been implemented at more than 25 sites. Using proven performance-improvement methods and a multidisciplinary team structure, Maynard and his team designed a VTE-prevention protocol for all adult inpatients at their academic center. The protocol integrated a simple VTE risk assessment with a menu of prophylaxis options preferred at each level of risk.
During three years of study, the percentage of patients with adequate VTE prophylaxis regimens increased from 55% to 98%, and the number of patients suffering from hospital-acquired VTE decreased dramatically.
SHM has presented the 2008 Awards of Excellence to four hospitalists and one quality improvement team. Their work and research have contributed significantly to hospital medicine and the betterment of patient care and quality improvement. The winners were recognized at Hospital Medicine 2008.
Award for Clinical Excellence: Kevin O’Leary, MD, associate professor of medicine and the associate chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. O’Leary leads strategic initiatives for the division in his job as associate chief of the Division of Hospital Medicine, especially in patient safety and quality. He also chairs the department’s Quality Management Committee.
An active member of SHM since 2002, Dr. O’Leary has served on the Core Competencies Task Force, the Annual Meeting Planning Committee, and the Annual Meeting Precourse Planning Committee. He also is active in SHM’s Chicago chapter, where he serves as vice president. He serves as an assistant editor for the Journal of Hospital Medicine.
Dr. O’Leary received his bachelor’s inbiology and medical degree from the University of Illinois. He completed his residency at Northwestern University.
Award for Excellence in Research: Peter Lindenauer, MD, MSc, medical director of clinical and quality informatics at Baystate Health in Springfield, Mass., and associate professor of medicine at Tufts University School of Medicine in Boston.
Dr. Lindenauer is responsible for lending the development of an electronic medical record at a large integrated delivery network in western Massachusetts in his job as medical director of clinical and quality informatics.
He has served on technical expert panels for Medicare, patient safety, monitoring systems, and surgical care improvement projects. He also has been a part of the National Quality Forum’s Hospital Quality Measures Development Group and has served on the inpatient functionality work group of the Certifying Committee for Healthcare Information Technology.
As a founding member of SHM, Dr. Lindenauer has served on the society’s board of directors and is a member of the Hospital Quality and Patient Safety Standards Committee.
A graduate of the University of Chicago, Dr. Lindenauer received his bachelor’s in history and received his graduate degree from the Herndon School of Economics and Political Science in Health Planning and Financing. He received his medical degree from the University of Pennsylvania and completed residency training at the University of California, San Francisco.
Award for Excellence in Teaching: Anjala Tess, MD, associate program director for the Internal Medicine Residency Program and director of education for the hospital medicine program, as well as a medical unit director and practicing hospitalist at Beth Israel Deaconess Medical Center in Boston.
Dr. Tess is in charge of the quality improvement teaching program and curriculum for the entire residency program at Beth Israel Deaconess. She also helps oversee the resident elective in hospital medicine and directs educational activities for the group. Her goal is to involve residents in process improvement in the hospital by giving them a hands-on role in quality improvement and peer review.
She has received numerous awards, including the Hermann Blumgart Teaching Award at Beth Israel Deaconess and first prize in SHM’s Innovations Poster Competition.
As an undergraduate, Dr. Tess earned her degree from Brown University, in Rhode Island, and received her medical degree at Washington University’s St. Louis School of Medicine. She completed her residency at Beth Israel Deaconess. She also completed fellowships at Harvard Medical School, the Carl J. Shapiro Institute for Education Research and Beth Israel Deaconess Medical Center.
Award for Outstanding Service in Hospital Medicine: David Zipes, MD, director of pediatric hospitalist service at the Peyton Manning Children’s Hospital in Indianapolis, Ind.
Dr. Zipes oversees all hospitalists and staff, leads strategic planning for the group and the hospital, oversees the business and financial issues of the group and provides general medical direction and leadership of the pediatric units at both the Peyton Manning’s Children’s Hospital and its suburban campus.
As a founding member of SHM, Dr. Zipes is active on its Annual Meeting Planning Committee, Pediatrics Committee, and Pediatrics Core Competencies Task Force. He is also a contributing author for Pediatric Hospital Medicine and the Textbook of Pediatric Hospital Medicine, and a founding member of the annual pediatric hospital medicine meeting.
He also has been the recipient of several awards, including the Family Medicine Teacher of the Year Annual Award (2002, 2005, and 2006) and the St. Vincent Spirit of Caring Award for Service and Dedication to the Hospital (2006 and 2007.)
Dr. Zipes earned his bachelor’s and medical degrees from Indiana University. He completed his residency at Children’s Hospital Medicine Center in Cincinnati, Ohio.
Award for Team Approaches in Quality Improvement: Team Leader, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
Dr. Maynard and his team (Ian Jenkins, MD, Sarah Stone, MD, Josh Lee, MD, Ed Fink, Tim Morris, MD, Peter Fedullo, MD, Robert Schoenhaus, PharmD, Doug Humber, PharmD, Marian Renvall, Pat Cal, and Isabella London) are the recipients of the first Team Approaches in Quality Improvement Award for their project “Optimizing Prevention of Hospital-Acquired Venous Thromboembolism.”
Dr. Maynard led the three-year project, which has been implemented at more than 25 sites. Using proven performance-improvement methods and a multidisciplinary team structure, Maynard and his team designed a VTE-prevention protocol for all adult inpatients at their academic center. The protocol integrated a simple VTE risk assessment with a menu of prophylaxis options preferred at each level of risk.
During three years of study, the percentage of patients with adequate VTE prophylaxis regimens increased from 55% to 98%, and the number of patients suffering from hospital-acquired VTE decreased dramatically.
SHM has presented the 2008 Awards of Excellence to four hospitalists and one quality improvement team. Their work and research have contributed significantly to hospital medicine and the betterment of patient care and quality improvement. The winners were recognized at Hospital Medicine 2008.
Award for Clinical Excellence: Kevin O’Leary, MD, associate professor of medicine and the associate chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. O’Leary leads strategic initiatives for the division in his job as associate chief of the Division of Hospital Medicine, especially in patient safety and quality. He also chairs the department’s Quality Management Committee.
An active member of SHM since 2002, Dr. O’Leary has served on the Core Competencies Task Force, the Annual Meeting Planning Committee, and the Annual Meeting Precourse Planning Committee. He also is active in SHM’s Chicago chapter, where he serves as vice president. He serves as an assistant editor for the Journal of Hospital Medicine.
Dr. O’Leary received his bachelor’s inbiology and medical degree from the University of Illinois. He completed his residency at Northwestern University.
Award for Excellence in Research: Peter Lindenauer, MD, MSc, medical director of clinical and quality informatics at Baystate Health in Springfield, Mass., and associate professor of medicine at Tufts University School of Medicine in Boston.
Dr. Lindenauer is responsible for lending the development of an electronic medical record at a large integrated delivery network in western Massachusetts in his job as medical director of clinical and quality informatics.
He has served on technical expert panels for Medicare, patient safety, monitoring systems, and surgical care improvement projects. He also has been a part of the National Quality Forum’s Hospital Quality Measures Development Group and has served on the inpatient functionality work group of the Certifying Committee for Healthcare Information Technology.
As a founding member of SHM, Dr. Lindenauer has served on the society’s board of directors and is a member of the Hospital Quality and Patient Safety Standards Committee.
A graduate of the University of Chicago, Dr. Lindenauer received his bachelor’s in history and received his graduate degree from the Herndon School of Economics and Political Science in Health Planning and Financing. He received his medical degree from the University of Pennsylvania and completed residency training at the University of California, San Francisco.
Award for Excellence in Teaching: Anjala Tess, MD, associate program director for the Internal Medicine Residency Program and director of education for the hospital medicine program, as well as a medical unit director and practicing hospitalist at Beth Israel Deaconess Medical Center in Boston.
Dr. Tess is in charge of the quality improvement teaching program and curriculum for the entire residency program at Beth Israel Deaconess. She also helps oversee the resident elective in hospital medicine and directs educational activities for the group. Her goal is to involve residents in process improvement in the hospital by giving them a hands-on role in quality improvement and peer review.
She has received numerous awards, including the Hermann Blumgart Teaching Award at Beth Israel Deaconess and first prize in SHM’s Innovations Poster Competition.
As an undergraduate, Dr. Tess earned her degree from Brown University, in Rhode Island, and received her medical degree at Washington University’s St. Louis School of Medicine. She completed her residency at Beth Israel Deaconess. She also completed fellowships at Harvard Medical School, the Carl J. Shapiro Institute for Education Research and Beth Israel Deaconess Medical Center.
Award for Outstanding Service in Hospital Medicine: David Zipes, MD, director of pediatric hospitalist service at the Peyton Manning Children’s Hospital in Indianapolis, Ind.
Dr. Zipes oversees all hospitalists and staff, leads strategic planning for the group and the hospital, oversees the business and financial issues of the group and provides general medical direction and leadership of the pediatric units at both the Peyton Manning’s Children’s Hospital and its suburban campus.
As a founding member of SHM, Dr. Zipes is active on its Annual Meeting Planning Committee, Pediatrics Committee, and Pediatrics Core Competencies Task Force. He is also a contributing author for Pediatric Hospital Medicine and the Textbook of Pediatric Hospital Medicine, and a founding member of the annual pediatric hospital medicine meeting.
He also has been the recipient of several awards, including the Family Medicine Teacher of the Year Annual Award (2002, 2005, and 2006) and the St. Vincent Spirit of Caring Award for Service and Dedication to the Hospital (2006 and 2007.)
Dr. Zipes earned his bachelor’s and medical degrees from Indiana University. He completed his residency at Children’s Hospital Medicine Center in Cincinnati, Ohio.
Award for Team Approaches in Quality Improvement: Team Leader, Greg Maynard, MD, MSc, professor of clinical medicine and chief of the division of hospital medicine at the University of California, San Diego.
Dr. Maynard and his team (Ian Jenkins, MD, Sarah Stone, MD, Josh Lee, MD, Ed Fink, Tim Morris, MD, Peter Fedullo, MD, Robert Schoenhaus, PharmD, Doug Humber, PharmD, Marian Renvall, Pat Cal, and Isabella London) are the recipients of the first Team Approaches in Quality Improvement Award for their project “Optimizing Prevention of Hospital-Acquired Venous Thromboembolism.”
Dr. Maynard led the three-year project, which has been implemented at more than 25 sites. Using proven performance-improvement methods and a multidisciplinary team structure, Maynard and his team designed a VTE-prevention protocol for all adult inpatients at their academic center. The protocol integrated a simple VTE risk assessment with a menu of prophylaxis options preferred at each level of risk.
During three years of study, the percentage of patients with adequate VTE prophylaxis regimens increased from 55% to 98%, and the number of patients suffering from hospital-acquired VTE decreased dramatically.
Dodging Disaster
I became a hospitalist in the 1980s, in the same year CDs outsold vinyl records for the first time. During the next eight to 10 years, I watched and participated in the growth of hospitalist practices around the country. But, by the late 1990s, a new phenomenon had begun to appear occasionally: failed hospitalist practices. I became interested in the relatively few practices that started up only to fail and dissolve. I wanted to know why they had failed and what happens at a hospital that loses its hospitalist practice?
It is worth remembering that the whole idea of hospitalist practice was more controversial in the late 1990s than it is today. Many doctors saw the concept as an invention of managed care, with the sole aim of reducing costs. When a practice collapsed, some doctors at the institution were usually delighted because, as far as they were concerned, this proved that hospitalist practice was a bad idea. Yet, to the dismay of these critics, the failure of a practice was reliably followed by an intense—sometimes even frenzied—effort to create a new and improved hospitalist practice. In fact, I’m not aware of any institution in which a hospitalist practice failed and a new one didn’t replace it. I suspect such places exist, but they’re not common.
Creating a replacement hospitalist practice is usually stressful and expensive, so of course it’s better to get it right the first time. To that end, I think every institution should be aware of the most common reasons practices fail and should work to avoid these problems. What follows are the issues I’ve seen come up regularly. While they may not cause the failure of a whole practice, they are likely to result in physician dissatisfaction and/or increased turnover.
1) Failure to appreciate rapid growth in volume in a new practice: Unquestionably, this is the most common mistake made by new hospitalist practices. Patient volume often grows dramatically—even within the first weeks a new practice is in operation. Some institutions mistakenly plan on growth rates similar to those experienced in other types of practices. When growth proves much more rapid, the first few hospitalists in the practice can become worn out and might even quit. This has led to the collapse of some practices. There are two ways to guard against this problem. One is to continue recruiting (even with no clear need for additional staff), anticipating the length of time it can take to recruit new hospitalists. In other words, most practices should never stop recruiting.
The other, less desirable but sometimes unavoidable strategy is to have the practice start with a limited scope of work that increases as new hospitalists are added to the group. For example, the practice might accept only unassigned medical admissions from the emergency department (ED) at the outset; once a predetermined number of hospitalists has joined the group, it is ready to start accepting referrals from primary care doctors and other sources.
2) Hospitalists who have an employee mentality, rather than that of a practice owner: Hospitalist practices tend to attract doctors who simply want to see patients, leaving the management of the practice and its financial health to others. This tendency may be exacerbated in practices that compensate hospitalists in a way that is not connected to the overall financial health of the practice (e.g., a straight salary).
Unfortunately, this situation can create a culture in which a hospitalist feels that the only job that is important is to see the next patient. These hospitalists may be reluctant to participate in efforts to ensure the financial health of the practice. Examples: 1) They may not be attentive to optimal documentation and coding, and the practice may lose significant billing revenue; 2) They may not want to accept new referrals or encourage growth in the practice; or 3) They may be too quick to add doctors to the group, with the aim of working fewer hours.
Even if the doctors are employees of a hospital or other large entity, make every effort to encourage them to think of themselves as owners of their practice. One way to create this environment is to have a tight connection between the economic health of the practice and the hospitalists’ income (e.g., production-based incentive compensation). This should lead to greater autonomy in decision-making, as well as hospitalist satisfaction.
3) Poor leadership: Many hospitalist practices start with doctors who have no prior hospitalist experience. This may result in physician leaders poorly suited for their roles. For a practice that is uncertain whether it has an appropriate medical director among the initial doctors it has hired, it might be a good idea to wait a year or two to select the leader. An interim leadership model can be implemented, taking advantage of physician leaders in the hospital, perhaps including the vice president for medical affairs, respected primary care physicians, or emergency physicians. Establishing a hospitalist oversight committee that is made up of leaders among the medical staff can also provide guidance for the new program until there is an effective hospitalist leader in place.
4) Excessive or inappropriate hospitalist overhead: This can take two forms. First, excessive overhead results from securing too much office space and/or staff support. Because the majority of a hospitalist’s work is done on the hospital wards, it is usually sufficient for a hospitalist group to share a single office with enough seating and workstations, including computers, for one-third to one-half of the total number of doctors in the group. For example, a 12-hospitalist group might share an office with four to six workstations. A small group—six or fewer doctors—might function effectively with a single clerical assistant supporting the hospitalists and some other department at the same time.
Second, inappropriate overhead may occur in multispecialty groups that charge hospitalists the same overhead paid by office physicians. This high overhead rate—more than 50%—may leave insufficient funds to pay the hospitalists a competitive salary. Thus, it is important for the group to assess hospitalists’ overhead based on what they actually consume. In general, this should include the cost of billing and collections, malpractice insurance, and modest clerical support. The hospitalist collections should not ordinarily go to support office-based expenses such as support staff and building/equipment expenses.
5) Initial tolerance of inappropriate expectations of hospitalists: To gain support from the medical staff in the early stages of a program, hospitalists sometimes overcommit, assuming responsibility for the scut work that no one wants to perform. This is not a sustainable model. Eventually, it will be hard to tell physicians that they must take back responsibility for something the hospitalists have been doing. This is likely to lead to unhappiness for everyone involved.
One common example of this problem is when hospitalists assume responsibility for tuck-in admissions—those in which the hospitalist admits a physician’s patient overnight and then transfers the patient back to that physician the next day. Another example involves hospitalists who assist with paperwork on patients they did not care for; for example, the hospitalist is expected to do a discharge summary for a heart surgeon, even though the hospitalist wasn’t involved in that particular patient’s care.
The best strategy to use in avoiding this pitfall is to identify the most important services for hospitalists to provide, keeping the list relatively small initially (e.g., admit unassigned emergency medical patients, accept referrals from primary care physicians, and perform consults from other doctors). Other services, such as co-management of some surgical admissions, can be added as hospitalist staffing allows and after hospitalists have had an opportunity to participate in deciding which services are the most appropriate to add.
6) Excessive workload, leading to hospitalist dissatisfaction: A variety of factors can lead to excessive hospitalist workloads or patient volumes. The most common reason (mentioned above) is referral volume that grows faster than staff can be added. In other cases, hospitalists can make the mistake of scheduling each doctor to work relatively few annual days or shifts; this practice results in a high workload for each day worked, even though the annual patient volume may not be excessive.
Hospitalists, like other professionals, seek balance in their jobs. The biggest threat to this goal is an excessive workload, which can hinder a hospitalist’s ability to devote adequate attention to ensuring the satisfaction of the patient and the referring physician. It also limits the hospitalist’s ability to assume non-clinical responsibilities like protocol development and hospital committees. Some data suggest that, at some point, an increasing patient load begins to result in an increased length of stay. And, over time, it is likely to result in poor job satisfaction, burnout, and turnover among physicians in the group.
7) Insufficient financial support: SHM survey data from 2006 show that, in addition to collected professional fees, 97% of hospitalist practices receive financial support and/or services in kind. This money usually comes from the hospital in which the hospitalists work. The few practices that don’t receive such support usually have some combination of the following factors:
- Hospitalists who work only weekday hours;
- Hospitalists who are not responsible for emergency, unassigned patients; and
- A hospital with an excellent payer mix.
Practices that accept all the unassigned medical admissions from the ED and keep a doctor in the hospital 24 hours a day for seven days a week usually have professional fee collections that fall far short of the amount needed to pay competitive salaries. They usually need financial support from a source such as their hospital to supplement their fee collections. Without it, they must maintain high patient volumes to collect professional fee revenue that is adequate to pay reasonable salaries and benefits to the doctors. These practices are at risk of poor performance or collapse.
To Succeed, Avoid Failure
So why go to the trouble of starting over when you can get it right the first time? Setting clear and realistic expectations from the beginning gives any hospitalist practice a better chance of succeeding. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
I became a hospitalist in the 1980s, in the same year CDs outsold vinyl records for the first time. During the next eight to 10 years, I watched and participated in the growth of hospitalist practices around the country. But, by the late 1990s, a new phenomenon had begun to appear occasionally: failed hospitalist practices. I became interested in the relatively few practices that started up only to fail and dissolve. I wanted to know why they had failed and what happens at a hospital that loses its hospitalist practice?
It is worth remembering that the whole idea of hospitalist practice was more controversial in the late 1990s than it is today. Many doctors saw the concept as an invention of managed care, with the sole aim of reducing costs. When a practice collapsed, some doctors at the institution were usually delighted because, as far as they were concerned, this proved that hospitalist practice was a bad idea. Yet, to the dismay of these critics, the failure of a practice was reliably followed by an intense—sometimes even frenzied—effort to create a new and improved hospitalist practice. In fact, I’m not aware of any institution in which a hospitalist practice failed and a new one didn’t replace it. I suspect such places exist, but they’re not common.
Creating a replacement hospitalist practice is usually stressful and expensive, so of course it’s better to get it right the first time. To that end, I think every institution should be aware of the most common reasons practices fail and should work to avoid these problems. What follows are the issues I’ve seen come up regularly. While they may not cause the failure of a whole practice, they are likely to result in physician dissatisfaction and/or increased turnover.
1) Failure to appreciate rapid growth in volume in a new practice: Unquestionably, this is the most common mistake made by new hospitalist practices. Patient volume often grows dramatically—even within the first weeks a new practice is in operation. Some institutions mistakenly plan on growth rates similar to those experienced in other types of practices. When growth proves much more rapid, the first few hospitalists in the practice can become worn out and might even quit. This has led to the collapse of some practices. There are two ways to guard against this problem. One is to continue recruiting (even with no clear need for additional staff), anticipating the length of time it can take to recruit new hospitalists. In other words, most practices should never stop recruiting.
The other, less desirable but sometimes unavoidable strategy is to have the practice start with a limited scope of work that increases as new hospitalists are added to the group. For example, the practice might accept only unassigned medical admissions from the emergency department (ED) at the outset; once a predetermined number of hospitalists has joined the group, it is ready to start accepting referrals from primary care doctors and other sources.
2) Hospitalists who have an employee mentality, rather than that of a practice owner: Hospitalist practices tend to attract doctors who simply want to see patients, leaving the management of the practice and its financial health to others. This tendency may be exacerbated in practices that compensate hospitalists in a way that is not connected to the overall financial health of the practice (e.g., a straight salary).
Unfortunately, this situation can create a culture in which a hospitalist feels that the only job that is important is to see the next patient. These hospitalists may be reluctant to participate in efforts to ensure the financial health of the practice. Examples: 1) They may not be attentive to optimal documentation and coding, and the practice may lose significant billing revenue; 2) They may not want to accept new referrals or encourage growth in the practice; or 3) They may be too quick to add doctors to the group, with the aim of working fewer hours.
Even if the doctors are employees of a hospital or other large entity, make every effort to encourage them to think of themselves as owners of their practice. One way to create this environment is to have a tight connection between the economic health of the practice and the hospitalists’ income (e.g., production-based incentive compensation). This should lead to greater autonomy in decision-making, as well as hospitalist satisfaction.
3) Poor leadership: Many hospitalist practices start with doctors who have no prior hospitalist experience. This may result in physician leaders poorly suited for their roles. For a practice that is uncertain whether it has an appropriate medical director among the initial doctors it has hired, it might be a good idea to wait a year or two to select the leader. An interim leadership model can be implemented, taking advantage of physician leaders in the hospital, perhaps including the vice president for medical affairs, respected primary care physicians, or emergency physicians. Establishing a hospitalist oversight committee that is made up of leaders among the medical staff can also provide guidance for the new program until there is an effective hospitalist leader in place.
4) Excessive or inappropriate hospitalist overhead: This can take two forms. First, excessive overhead results from securing too much office space and/or staff support. Because the majority of a hospitalist’s work is done on the hospital wards, it is usually sufficient for a hospitalist group to share a single office with enough seating and workstations, including computers, for one-third to one-half of the total number of doctors in the group. For example, a 12-hospitalist group might share an office with four to six workstations. A small group—six or fewer doctors—might function effectively with a single clerical assistant supporting the hospitalists and some other department at the same time.
Second, inappropriate overhead may occur in multispecialty groups that charge hospitalists the same overhead paid by office physicians. This high overhead rate—more than 50%—may leave insufficient funds to pay the hospitalists a competitive salary. Thus, it is important for the group to assess hospitalists’ overhead based on what they actually consume. In general, this should include the cost of billing and collections, malpractice insurance, and modest clerical support. The hospitalist collections should not ordinarily go to support office-based expenses such as support staff and building/equipment expenses.
5) Initial tolerance of inappropriate expectations of hospitalists: To gain support from the medical staff in the early stages of a program, hospitalists sometimes overcommit, assuming responsibility for the scut work that no one wants to perform. This is not a sustainable model. Eventually, it will be hard to tell physicians that they must take back responsibility for something the hospitalists have been doing. This is likely to lead to unhappiness for everyone involved.
One common example of this problem is when hospitalists assume responsibility for tuck-in admissions—those in which the hospitalist admits a physician’s patient overnight and then transfers the patient back to that physician the next day. Another example involves hospitalists who assist with paperwork on patients they did not care for; for example, the hospitalist is expected to do a discharge summary for a heart surgeon, even though the hospitalist wasn’t involved in that particular patient’s care.
The best strategy to use in avoiding this pitfall is to identify the most important services for hospitalists to provide, keeping the list relatively small initially (e.g., admit unassigned emergency medical patients, accept referrals from primary care physicians, and perform consults from other doctors). Other services, such as co-management of some surgical admissions, can be added as hospitalist staffing allows and after hospitalists have had an opportunity to participate in deciding which services are the most appropriate to add.
6) Excessive workload, leading to hospitalist dissatisfaction: A variety of factors can lead to excessive hospitalist workloads or patient volumes. The most common reason (mentioned above) is referral volume that grows faster than staff can be added. In other cases, hospitalists can make the mistake of scheduling each doctor to work relatively few annual days or shifts; this practice results in a high workload for each day worked, even though the annual patient volume may not be excessive.
Hospitalists, like other professionals, seek balance in their jobs. The biggest threat to this goal is an excessive workload, which can hinder a hospitalist’s ability to devote adequate attention to ensuring the satisfaction of the patient and the referring physician. It also limits the hospitalist’s ability to assume non-clinical responsibilities like protocol development and hospital committees. Some data suggest that, at some point, an increasing patient load begins to result in an increased length of stay. And, over time, it is likely to result in poor job satisfaction, burnout, and turnover among physicians in the group.
7) Insufficient financial support: SHM survey data from 2006 show that, in addition to collected professional fees, 97% of hospitalist practices receive financial support and/or services in kind. This money usually comes from the hospital in which the hospitalists work. The few practices that don’t receive such support usually have some combination of the following factors:
- Hospitalists who work only weekday hours;
- Hospitalists who are not responsible for emergency, unassigned patients; and
- A hospital with an excellent payer mix.
Practices that accept all the unassigned medical admissions from the ED and keep a doctor in the hospital 24 hours a day for seven days a week usually have professional fee collections that fall far short of the amount needed to pay competitive salaries. They usually need financial support from a source such as their hospital to supplement their fee collections. Without it, they must maintain high patient volumes to collect professional fee revenue that is adequate to pay reasonable salaries and benefits to the doctors. These practices are at risk of poor performance or collapse.
To Succeed, Avoid Failure
So why go to the trouble of starting over when you can get it right the first time? Setting clear and realistic expectations from the beginning gives any hospitalist practice a better chance of succeeding. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
I became a hospitalist in the 1980s, in the same year CDs outsold vinyl records for the first time. During the next eight to 10 years, I watched and participated in the growth of hospitalist practices around the country. But, by the late 1990s, a new phenomenon had begun to appear occasionally: failed hospitalist practices. I became interested in the relatively few practices that started up only to fail and dissolve. I wanted to know why they had failed and what happens at a hospital that loses its hospitalist practice?
It is worth remembering that the whole idea of hospitalist practice was more controversial in the late 1990s than it is today. Many doctors saw the concept as an invention of managed care, with the sole aim of reducing costs. When a practice collapsed, some doctors at the institution were usually delighted because, as far as they were concerned, this proved that hospitalist practice was a bad idea. Yet, to the dismay of these critics, the failure of a practice was reliably followed by an intense—sometimes even frenzied—effort to create a new and improved hospitalist practice. In fact, I’m not aware of any institution in which a hospitalist practice failed and a new one didn’t replace it. I suspect such places exist, but they’re not common.
Creating a replacement hospitalist practice is usually stressful and expensive, so of course it’s better to get it right the first time. To that end, I think every institution should be aware of the most common reasons practices fail and should work to avoid these problems. What follows are the issues I’ve seen come up regularly. While they may not cause the failure of a whole practice, they are likely to result in physician dissatisfaction and/or increased turnover.
1) Failure to appreciate rapid growth in volume in a new practice: Unquestionably, this is the most common mistake made by new hospitalist practices. Patient volume often grows dramatically—even within the first weeks a new practice is in operation. Some institutions mistakenly plan on growth rates similar to those experienced in other types of practices. When growth proves much more rapid, the first few hospitalists in the practice can become worn out and might even quit. This has led to the collapse of some practices. There are two ways to guard against this problem. One is to continue recruiting (even with no clear need for additional staff), anticipating the length of time it can take to recruit new hospitalists. In other words, most practices should never stop recruiting.
The other, less desirable but sometimes unavoidable strategy is to have the practice start with a limited scope of work that increases as new hospitalists are added to the group. For example, the practice might accept only unassigned medical admissions from the emergency department (ED) at the outset; once a predetermined number of hospitalists has joined the group, it is ready to start accepting referrals from primary care doctors and other sources.
2) Hospitalists who have an employee mentality, rather than that of a practice owner: Hospitalist practices tend to attract doctors who simply want to see patients, leaving the management of the practice and its financial health to others. This tendency may be exacerbated in practices that compensate hospitalists in a way that is not connected to the overall financial health of the practice (e.g., a straight salary).
Unfortunately, this situation can create a culture in which a hospitalist feels that the only job that is important is to see the next patient. These hospitalists may be reluctant to participate in efforts to ensure the financial health of the practice. Examples: 1) They may not be attentive to optimal documentation and coding, and the practice may lose significant billing revenue; 2) They may not want to accept new referrals or encourage growth in the practice; or 3) They may be too quick to add doctors to the group, with the aim of working fewer hours.
Even if the doctors are employees of a hospital or other large entity, make every effort to encourage them to think of themselves as owners of their practice. One way to create this environment is to have a tight connection between the economic health of the practice and the hospitalists’ income (e.g., production-based incentive compensation). This should lead to greater autonomy in decision-making, as well as hospitalist satisfaction.
3) Poor leadership: Many hospitalist practices start with doctors who have no prior hospitalist experience. This may result in physician leaders poorly suited for their roles. For a practice that is uncertain whether it has an appropriate medical director among the initial doctors it has hired, it might be a good idea to wait a year or two to select the leader. An interim leadership model can be implemented, taking advantage of physician leaders in the hospital, perhaps including the vice president for medical affairs, respected primary care physicians, or emergency physicians. Establishing a hospitalist oversight committee that is made up of leaders among the medical staff can also provide guidance for the new program until there is an effective hospitalist leader in place.
4) Excessive or inappropriate hospitalist overhead: This can take two forms. First, excessive overhead results from securing too much office space and/or staff support. Because the majority of a hospitalist’s work is done on the hospital wards, it is usually sufficient for a hospitalist group to share a single office with enough seating and workstations, including computers, for one-third to one-half of the total number of doctors in the group. For example, a 12-hospitalist group might share an office with four to six workstations. A small group—six or fewer doctors—might function effectively with a single clerical assistant supporting the hospitalists and some other department at the same time.
Second, inappropriate overhead may occur in multispecialty groups that charge hospitalists the same overhead paid by office physicians. This high overhead rate—more than 50%—may leave insufficient funds to pay the hospitalists a competitive salary. Thus, it is important for the group to assess hospitalists’ overhead based on what they actually consume. In general, this should include the cost of billing and collections, malpractice insurance, and modest clerical support. The hospitalist collections should not ordinarily go to support office-based expenses such as support staff and building/equipment expenses.
5) Initial tolerance of inappropriate expectations of hospitalists: To gain support from the medical staff in the early stages of a program, hospitalists sometimes overcommit, assuming responsibility for the scut work that no one wants to perform. This is not a sustainable model. Eventually, it will be hard to tell physicians that they must take back responsibility for something the hospitalists have been doing. This is likely to lead to unhappiness for everyone involved.
One common example of this problem is when hospitalists assume responsibility for tuck-in admissions—those in which the hospitalist admits a physician’s patient overnight and then transfers the patient back to that physician the next day. Another example involves hospitalists who assist with paperwork on patients they did not care for; for example, the hospitalist is expected to do a discharge summary for a heart surgeon, even though the hospitalist wasn’t involved in that particular patient’s care.
The best strategy to use in avoiding this pitfall is to identify the most important services for hospitalists to provide, keeping the list relatively small initially (e.g., admit unassigned emergency medical patients, accept referrals from primary care physicians, and perform consults from other doctors). Other services, such as co-management of some surgical admissions, can be added as hospitalist staffing allows and after hospitalists have had an opportunity to participate in deciding which services are the most appropriate to add.
6) Excessive workload, leading to hospitalist dissatisfaction: A variety of factors can lead to excessive hospitalist workloads or patient volumes. The most common reason (mentioned above) is referral volume that grows faster than staff can be added. In other cases, hospitalists can make the mistake of scheduling each doctor to work relatively few annual days or shifts; this practice results in a high workload for each day worked, even though the annual patient volume may not be excessive.
Hospitalists, like other professionals, seek balance in their jobs. The biggest threat to this goal is an excessive workload, which can hinder a hospitalist’s ability to devote adequate attention to ensuring the satisfaction of the patient and the referring physician. It also limits the hospitalist’s ability to assume non-clinical responsibilities like protocol development and hospital committees. Some data suggest that, at some point, an increasing patient load begins to result in an increased length of stay. And, over time, it is likely to result in poor job satisfaction, burnout, and turnover among physicians in the group.
7) Insufficient financial support: SHM survey data from 2006 show that, in addition to collected professional fees, 97% of hospitalist practices receive financial support and/or services in kind. This money usually comes from the hospital in which the hospitalists work. The few practices that don’t receive such support usually have some combination of the following factors:
- Hospitalists who work only weekday hours;
- Hospitalists who are not responsible for emergency, unassigned patients; and
- A hospital with an excellent payer mix.
Practices that accept all the unassigned medical admissions from the ED and keep a doctor in the hospital 24 hours a day for seven days a week usually have professional fee collections that fall far short of the amount needed to pay competitive salaries. They usually need financial support from a source such as their hospital to supplement their fee collections. Without it, they must maintain high patient volumes to collect professional fee revenue that is adequate to pay reasonable salaries and benefits to the doctors. These practices are at risk of poor performance or collapse.
To Succeed, Avoid Failure
So why go to the trouble of starting over when you can get it right the first time? Setting clear and realistic expectations from the beginning gives any hospitalist practice a better chance of succeeding. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Big D Births an HM Program
When hospitalists stepped into Parkland Hospital (Dallas) a few months ago, they knew they were taking up a new challenge. Initially, they were known as the doctors without a team in a place where everyone was used to seeing no fewer than six to eight physicians rounding in a group.
Soon our hospitalists realized that a lot of teaching and awareness was needed among the nursing and support staff of the hospital to get them ready for this new breed of physicians.
A Case of Nerves
After four years of administrative planning and developing, the hospitalist program finally started in July 2006. Parkland started a hospitalist program due to the new restrictions on resident work hours and the number of patients a resident can admit. There used to be a considerable delay in the admission process causing patients to wait in our emergency department (ED) for hours until an admitting team could see them. This led to higher patient load in the ED. This load not only affected our patient care adversely, but it also caused considerable financial loss to the hospital because we couldn’t bill for admission until the patients were assigned a bed.
Our hospitalists help ease this overcrowding because they don’t work under these restrictions and can increase the ED throughput of the patients. Parkland also instituted a hospital medicine program to decrease length of stay.
Initially there was a lot of excitement, nervousness, and anxiety about the program. When I say nervousness and anxiety, it was primarily related to the nursing and administrative staff’s skepticism about how they would deal with full-time attending physicians. They wondered whether hospitalists would be easily approachable or not. How would they compare with medical residents?
Fortunately, during the next few months, this anxiety gave way to a new trust between the nurses and the hospitalists as the nurses realized that their concerns were answered promptly. Nursing staff also enjoyed a new benefit: the ability to communicate directly with the attending physicians and, in the process, the potential to play a greater role in the medical management of their patients.
Initially we hired eight hospitalists (actually we started with two because the others were in the process of getting credentialed). We handled the workload in the beginning by limiting the number of admissions each day for each hospitalist until everyone was on board. One hospitalist was already a Parkland doc; the rest were hired from outside.
Details
Like many new hospital medicine programs, Parkland’s hospitalists were venturing into a place where the nursing staff’s involvement in patient care was different from that of their private counterparts.
Background: Parkland Hospital is the main teaching site for the University of Texas Southwestern Medical School and Residency Training Program. The residents and medical students are involved to a great extent in patient care. They assume most patient care responsibilities, including placing PPDs (tuberculosis skin tests), caring for wounds, taking arterial blood gases (ABGs), and removing peripherally inserted central catheter (PICC) lines—to name just a few.
As a result of the residents’ involvement, our nursing staff took a back seat in these aspects of care. But once our hospitalists entered the picture they didn’t have the support of medical students or residents. Therefore, to increase the hospitalists’ efficiency in seeing more patients, the onus of doing those procedures fell on the shoulders of the nursing and paramedic staff. Educating the nursing and paramedical staff to help them regain autonomy and play a great role in patient care was a new challenge for the hospitalists.
We achieved this goal by holding a series of meetings in which physicians, including hospitalists and administrators, worked continuously on these concerns. Also, more operational issues were identified. Among them:
- Giving telephonic verbal orders to nurses for medications, laboratory studies, and radiology procedures, which was not the case with residents;
- Easing restrictions on the use of different medicines that usually require approval of attending faculty for the resident teams; and
- Setting up new dictation lines for our hospitalists (residents have to write their own patient histories and physical assessments).
We resolved to ensure that the program would run like any other private hospitalist program.
Modifications and Scheduling
Other services, including pharmacy, wound care, medical records, and pathology, were also approached by the hospitalists—including the medical director and chief of general internal medicine. The pharmacy was approached to ease restrictions on the medicine prescribed by hospitalists (as opposed to rules for residents, who have to work under different restrictions because they are training.)
Wound-care nurses were asked to implement their orders after telephone approval by the hospitalists (again, this is not the case with resident services). The Medical Records Department created a separate way to handle incomplete medical records for hospitalists—one that takes into account their week-on/week-off schedule. All these requests are now in different phases of approval and implementation.
Overall Parkland has responded well to these changes by appointing senior leadership to fast-track several of these recommendations. Many more policies are under review to complete the transformation from a resident-run model to one that is run by hospitalists.
Scheduling
Like any other new program, the hospitalist program at Parkland went through the growing pains of choosing the right kind of schedule to meet the expectations of the hospital as well as the professional expectations of its doctors. As mentioned above, we currently employ eight hospitalists. Four hospitalists work a week of 12- to 13-hour shifts; they are then off the following week. At that time the other four hospitalists take over for their counterparts. We cover nights using nocturnists.
When the program was not fully staffed there were fewer teams, depending on the number of hospitalists on shift. After the first two hospitalists were hired, we added one team to bring the total number of teams to four. Our teams worked the week-on/week-off schedule. During our initial start-up, the odd-numbered hospitalist who didn’t have a partner to work in week-on/week-off mode worked Monday through Friday each week with weekends covered by one of the main teams.
One of the most important considerations in a hospitalist’s job is the need for flexibility in working hours as compared with the schedule used in a traditional internal medicine practice. At Parkland, hospitalists see 10 to 12 patients in a week. During their week off from patient duties, they are free from all clinical duties and can handle administrative duties, conduct research projects, and accomplish any other tasks awaiting their attention.
Dual Launch Benefits Both Hospitals
At the same time the Parkland Hospital Medicine Program was launched, the Southwestern University also started a hospitalist program at St. Paul University Hospital, Dallas. The Department of Medicine of the University of Texas Southwestern oversees both the programs. All hospitalists are hired by Southwestern University and are part of the Department of General Internal medicine.
The common leadership of both of these programs in the Department of Medicine led to the implementation of a variety of policies derived from the best practices of the two groups. The interaction between these programs has been fruitful. The exchange of physicians credentialed at both hospitals has also reduced the staffing problems that tend to occur due to vacations, holidays, and illness.
Working toward the Future
As we settle down, fully staffed with eight hospitalists, we have started participating in the hospital’s administration by joining various committees. Our hospitalists participate on the pathology clinical advisory committee, the antibiotic committee, the medical reconciliation committee, and the utilization review committee.
Every day brings new challenges and continuous hard work. To make a successful program, it is not only important to grow out of the teething problems, but also to provide exceptional care so that the idea of a hospitalist program is well thought of by the hospital administration. Two of our teething issues included:
- General acceptance of our hospitalists as attending physicians by nursing, support staff, and the other physicians—not as trainees interacting with residents for patient care; and
- Recognition of the distinction between residents who traditionally work under several restrictions as a part of their training as compared with hospitalists who have already undergone training in their field.
Naturally, the hospital wants improvements in both short-term and long-term quality of care. The advantages the hospitalists provide include rendering consistent quality of care, developing new clinical pathways to provide efficient care, and ensuring greater continuity of care.
Regarding specific expectations, for example, SHM advocates 10 to 12 patient encounters per day as adequate. And so we expect our hospitalists to see that number of patients. Other expectations we have:
- That our hospitalists be involved in research projects on patient safety and quality of care; and
- That our hospitalists be involved in developing clinical pathways.
Conclusion
The future of the hospitalist program at Parkland Hospital is bright. As part of the university’s teaching faculty, our hospitalists will be progressively more involved in resident and medical student teaching. As a result, as time goes on, the schedule will have to change in order to provide both continuity of patient care and continuity in the teaching service. While our schedule now works well, we expect to get involved in a resident teaching service to a greater extent, as well as medical consult service and perioperative consult and care. These additional responsibilities may change our schedule.
The hospitalists are actively involved in developing an inpatient curriculum for the residents, along with a new set of standard orders suited to hospitalist practice. Other areas the hospitalists will become more involved in include pre- and perioperative consultations and co-management of surgical and orthopedic patients. We are also working on special hospital projects, focusing on patient safety and hospital efficiency.
The hospitalists at the University of Texas Southwestern put in nothing less than their best efforts. After all, “High achievement always takes place in a framework of high expectation” (Jack Kinder, motivational author). TH
Dr. Mohan is the medical director of the hospital medicine program at Parkland Hospital, Dallas.
When hospitalists stepped into Parkland Hospital (Dallas) a few months ago, they knew they were taking up a new challenge. Initially, they were known as the doctors without a team in a place where everyone was used to seeing no fewer than six to eight physicians rounding in a group.
Soon our hospitalists realized that a lot of teaching and awareness was needed among the nursing and support staff of the hospital to get them ready for this new breed of physicians.
A Case of Nerves
After four years of administrative planning and developing, the hospitalist program finally started in July 2006. Parkland started a hospitalist program due to the new restrictions on resident work hours and the number of patients a resident can admit. There used to be a considerable delay in the admission process causing patients to wait in our emergency department (ED) for hours until an admitting team could see them. This led to higher patient load in the ED. This load not only affected our patient care adversely, but it also caused considerable financial loss to the hospital because we couldn’t bill for admission until the patients were assigned a bed.
Our hospitalists help ease this overcrowding because they don’t work under these restrictions and can increase the ED throughput of the patients. Parkland also instituted a hospital medicine program to decrease length of stay.
Initially there was a lot of excitement, nervousness, and anxiety about the program. When I say nervousness and anxiety, it was primarily related to the nursing and administrative staff’s skepticism about how they would deal with full-time attending physicians. They wondered whether hospitalists would be easily approachable or not. How would they compare with medical residents?
Fortunately, during the next few months, this anxiety gave way to a new trust between the nurses and the hospitalists as the nurses realized that their concerns were answered promptly. Nursing staff also enjoyed a new benefit: the ability to communicate directly with the attending physicians and, in the process, the potential to play a greater role in the medical management of their patients.
Initially we hired eight hospitalists (actually we started with two because the others were in the process of getting credentialed). We handled the workload in the beginning by limiting the number of admissions each day for each hospitalist until everyone was on board. One hospitalist was already a Parkland doc; the rest were hired from outside.
Details
Like many new hospital medicine programs, Parkland’s hospitalists were venturing into a place where the nursing staff’s involvement in patient care was different from that of their private counterparts.
Background: Parkland Hospital is the main teaching site for the University of Texas Southwestern Medical School and Residency Training Program. The residents and medical students are involved to a great extent in patient care. They assume most patient care responsibilities, including placing PPDs (tuberculosis skin tests), caring for wounds, taking arterial blood gases (ABGs), and removing peripherally inserted central catheter (PICC) lines—to name just a few.
As a result of the residents’ involvement, our nursing staff took a back seat in these aspects of care. But once our hospitalists entered the picture they didn’t have the support of medical students or residents. Therefore, to increase the hospitalists’ efficiency in seeing more patients, the onus of doing those procedures fell on the shoulders of the nursing and paramedic staff. Educating the nursing and paramedical staff to help them regain autonomy and play a great role in patient care was a new challenge for the hospitalists.
We achieved this goal by holding a series of meetings in which physicians, including hospitalists and administrators, worked continuously on these concerns. Also, more operational issues were identified. Among them:
- Giving telephonic verbal orders to nurses for medications, laboratory studies, and radiology procedures, which was not the case with residents;
- Easing restrictions on the use of different medicines that usually require approval of attending faculty for the resident teams; and
- Setting up new dictation lines for our hospitalists (residents have to write their own patient histories and physical assessments).
We resolved to ensure that the program would run like any other private hospitalist program.
Modifications and Scheduling
Other services, including pharmacy, wound care, medical records, and pathology, were also approached by the hospitalists—including the medical director and chief of general internal medicine. The pharmacy was approached to ease restrictions on the medicine prescribed by hospitalists (as opposed to rules for residents, who have to work under different restrictions because they are training.)
Wound-care nurses were asked to implement their orders after telephone approval by the hospitalists (again, this is not the case with resident services). The Medical Records Department created a separate way to handle incomplete medical records for hospitalists—one that takes into account their week-on/week-off schedule. All these requests are now in different phases of approval and implementation.
Overall Parkland has responded well to these changes by appointing senior leadership to fast-track several of these recommendations. Many more policies are under review to complete the transformation from a resident-run model to one that is run by hospitalists.
Scheduling
Like any other new program, the hospitalist program at Parkland went through the growing pains of choosing the right kind of schedule to meet the expectations of the hospital as well as the professional expectations of its doctors. As mentioned above, we currently employ eight hospitalists. Four hospitalists work a week of 12- to 13-hour shifts; they are then off the following week. At that time the other four hospitalists take over for their counterparts. We cover nights using nocturnists.
When the program was not fully staffed there were fewer teams, depending on the number of hospitalists on shift. After the first two hospitalists were hired, we added one team to bring the total number of teams to four. Our teams worked the week-on/week-off schedule. During our initial start-up, the odd-numbered hospitalist who didn’t have a partner to work in week-on/week-off mode worked Monday through Friday each week with weekends covered by one of the main teams.
One of the most important considerations in a hospitalist’s job is the need for flexibility in working hours as compared with the schedule used in a traditional internal medicine practice. At Parkland, hospitalists see 10 to 12 patients in a week. During their week off from patient duties, they are free from all clinical duties and can handle administrative duties, conduct research projects, and accomplish any other tasks awaiting their attention.
Dual Launch Benefits Both Hospitals
At the same time the Parkland Hospital Medicine Program was launched, the Southwestern University also started a hospitalist program at St. Paul University Hospital, Dallas. The Department of Medicine of the University of Texas Southwestern oversees both the programs. All hospitalists are hired by Southwestern University and are part of the Department of General Internal medicine.
The common leadership of both of these programs in the Department of Medicine led to the implementation of a variety of policies derived from the best practices of the two groups. The interaction between these programs has been fruitful. The exchange of physicians credentialed at both hospitals has also reduced the staffing problems that tend to occur due to vacations, holidays, and illness.
Working toward the Future
As we settle down, fully staffed with eight hospitalists, we have started participating in the hospital’s administration by joining various committees. Our hospitalists participate on the pathology clinical advisory committee, the antibiotic committee, the medical reconciliation committee, and the utilization review committee.
Every day brings new challenges and continuous hard work. To make a successful program, it is not only important to grow out of the teething problems, but also to provide exceptional care so that the idea of a hospitalist program is well thought of by the hospital administration. Two of our teething issues included:
- General acceptance of our hospitalists as attending physicians by nursing, support staff, and the other physicians—not as trainees interacting with residents for patient care; and
- Recognition of the distinction between residents who traditionally work under several restrictions as a part of their training as compared with hospitalists who have already undergone training in their field.
Naturally, the hospital wants improvements in both short-term and long-term quality of care. The advantages the hospitalists provide include rendering consistent quality of care, developing new clinical pathways to provide efficient care, and ensuring greater continuity of care.
Regarding specific expectations, for example, SHM advocates 10 to 12 patient encounters per day as adequate. And so we expect our hospitalists to see that number of patients. Other expectations we have:
- That our hospitalists be involved in research projects on patient safety and quality of care; and
- That our hospitalists be involved in developing clinical pathways.
Conclusion
The future of the hospitalist program at Parkland Hospital is bright. As part of the university’s teaching faculty, our hospitalists will be progressively more involved in resident and medical student teaching. As a result, as time goes on, the schedule will have to change in order to provide both continuity of patient care and continuity in the teaching service. While our schedule now works well, we expect to get involved in a resident teaching service to a greater extent, as well as medical consult service and perioperative consult and care. These additional responsibilities may change our schedule.
The hospitalists are actively involved in developing an inpatient curriculum for the residents, along with a new set of standard orders suited to hospitalist practice. Other areas the hospitalists will become more involved in include pre- and perioperative consultations and co-management of surgical and orthopedic patients. We are also working on special hospital projects, focusing on patient safety and hospital efficiency.
The hospitalists at the University of Texas Southwestern put in nothing less than their best efforts. After all, “High achievement always takes place in a framework of high expectation” (Jack Kinder, motivational author). TH
Dr. Mohan is the medical director of the hospital medicine program at Parkland Hospital, Dallas.
When hospitalists stepped into Parkland Hospital (Dallas) a few months ago, they knew they were taking up a new challenge. Initially, they were known as the doctors without a team in a place where everyone was used to seeing no fewer than six to eight physicians rounding in a group.
Soon our hospitalists realized that a lot of teaching and awareness was needed among the nursing and support staff of the hospital to get them ready for this new breed of physicians.
A Case of Nerves
After four years of administrative planning and developing, the hospitalist program finally started in July 2006. Parkland started a hospitalist program due to the new restrictions on resident work hours and the number of patients a resident can admit. There used to be a considerable delay in the admission process causing patients to wait in our emergency department (ED) for hours until an admitting team could see them. This led to higher patient load in the ED. This load not only affected our patient care adversely, but it also caused considerable financial loss to the hospital because we couldn’t bill for admission until the patients were assigned a bed.
Our hospitalists help ease this overcrowding because they don’t work under these restrictions and can increase the ED throughput of the patients. Parkland also instituted a hospital medicine program to decrease length of stay.
Initially there was a lot of excitement, nervousness, and anxiety about the program. When I say nervousness and anxiety, it was primarily related to the nursing and administrative staff’s skepticism about how they would deal with full-time attending physicians. They wondered whether hospitalists would be easily approachable or not. How would they compare with medical residents?
Fortunately, during the next few months, this anxiety gave way to a new trust between the nurses and the hospitalists as the nurses realized that their concerns were answered promptly. Nursing staff also enjoyed a new benefit: the ability to communicate directly with the attending physicians and, in the process, the potential to play a greater role in the medical management of their patients.
Initially we hired eight hospitalists (actually we started with two because the others were in the process of getting credentialed). We handled the workload in the beginning by limiting the number of admissions each day for each hospitalist until everyone was on board. One hospitalist was already a Parkland doc; the rest were hired from outside.
Details
Like many new hospital medicine programs, Parkland’s hospitalists were venturing into a place where the nursing staff’s involvement in patient care was different from that of their private counterparts.
Background: Parkland Hospital is the main teaching site for the University of Texas Southwestern Medical School and Residency Training Program. The residents and medical students are involved to a great extent in patient care. They assume most patient care responsibilities, including placing PPDs (tuberculosis skin tests), caring for wounds, taking arterial blood gases (ABGs), and removing peripherally inserted central catheter (PICC) lines—to name just a few.
As a result of the residents’ involvement, our nursing staff took a back seat in these aspects of care. But once our hospitalists entered the picture they didn’t have the support of medical students or residents. Therefore, to increase the hospitalists’ efficiency in seeing more patients, the onus of doing those procedures fell on the shoulders of the nursing and paramedic staff. Educating the nursing and paramedical staff to help them regain autonomy and play a great role in patient care was a new challenge for the hospitalists.
We achieved this goal by holding a series of meetings in which physicians, including hospitalists and administrators, worked continuously on these concerns. Also, more operational issues were identified. Among them:
- Giving telephonic verbal orders to nurses for medications, laboratory studies, and radiology procedures, which was not the case with residents;
- Easing restrictions on the use of different medicines that usually require approval of attending faculty for the resident teams; and
- Setting up new dictation lines for our hospitalists (residents have to write their own patient histories and physical assessments).
We resolved to ensure that the program would run like any other private hospitalist program.
Modifications and Scheduling
Other services, including pharmacy, wound care, medical records, and pathology, were also approached by the hospitalists—including the medical director and chief of general internal medicine. The pharmacy was approached to ease restrictions on the medicine prescribed by hospitalists (as opposed to rules for residents, who have to work under different restrictions because they are training.)
Wound-care nurses were asked to implement their orders after telephone approval by the hospitalists (again, this is not the case with resident services). The Medical Records Department created a separate way to handle incomplete medical records for hospitalists—one that takes into account their week-on/week-off schedule. All these requests are now in different phases of approval and implementation.
Overall Parkland has responded well to these changes by appointing senior leadership to fast-track several of these recommendations. Many more policies are under review to complete the transformation from a resident-run model to one that is run by hospitalists.
Scheduling
Like any other new program, the hospitalist program at Parkland went through the growing pains of choosing the right kind of schedule to meet the expectations of the hospital as well as the professional expectations of its doctors. As mentioned above, we currently employ eight hospitalists. Four hospitalists work a week of 12- to 13-hour shifts; they are then off the following week. At that time the other four hospitalists take over for their counterparts. We cover nights using nocturnists.
When the program was not fully staffed there were fewer teams, depending on the number of hospitalists on shift. After the first two hospitalists were hired, we added one team to bring the total number of teams to four. Our teams worked the week-on/week-off schedule. During our initial start-up, the odd-numbered hospitalist who didn’t have a partner to work in week-on/week-off mode worked Monday through Friday each week with weekends covered by one of the main teams.
One of the most important considerations in a hospitalist’s job is the need for flexibility in working hours as compared with the schedule used in a traditional internal medicine practice. At Parkland, hospitalists see 10 to 12 patients in a week. During their week off from patient duties, they are free from all clinical duties and can handle administrative duties, conduct research projects, and accomplish any other tasks awaiting their attention.
Dual Launch Benefits Both Hospitals
At the same time the Parkland Hospital Medicine Program was launched, the Southwestern University also started a hospitalist program at St. Paul University Hospital, Dallas. The Department of Medicine of the University of Texas Southwestern oversees both the programs. All hospitalists are hired by Southwestern University and are part of the Department of General Internal medicine.
The common leadership of both of these programs in the Department of Medicine led to the implementation of a variety of policies derived from the best practices of the two groups. The interaction between these programs has been fruitful. The exchange of physicians credentialed at both hospitals has also reduced the staffing problems that tend to occur due to vacations, holidays, and illness.
Working toward the Future
As we settle down, fully staffed with eight hospitalists, we have started participating in the hospital’s administration by joining various committees. Our hospitalists participate on the pathology clinical advisory committee, the antibiotic committee, the medical reconciliation committee, and the utilization review committee.
Every day brings new challenges and continuous hard work. To make a successful program, it is not only important to grow out of the teething problems, but also to provide exceptional care so that the idea of a hospitalist program is well thought of by the hospital administration. Two of our teething issues included:
- General acceptance of our hospitalists as attending physicians by nursing, support staff, and the other physicians—not as trainees interacting with residents for patient care; and
- Recognition of the distinction between residents who traditionally work under several restrictions as a part of their training as compared with hospitalists who have already undergone training in their field.
Naturally, the hospital wants improvements in both short-term and long-term quality of care. The advantages the hospitalists provide include rendering consistent quality of care, developing new clinical pathways to provide efficient care, and ensuring greater continuity of care.
Regarding specific expectations, for example, SHM advocates 10 to 12 patient encounters per day as adequate. And so we expect our hospitalists to see that number of patients. Other expectations we have:
- That our hospitalists be involved in research projects on patient safety and quality of care; and
- That our hospitalists be involved in developing clinical pathways.
Conclusion
The future of the hospitalist program at Parkland Hospital is bright. As part of the university’s teaching faculty, our hospitalists will be progressively more involved in resident and medical student teaching. As a result, as time goes on, the schedule will have to change in order to provide both continuity of patient care and continuity in the teaching service. While our schedule now works well, we expect to get involved in a resident teaching service to a greater extent, as well as medical consult service and perioperative consult and care. These additional responsibilities may change our schedule.
The hospitalists are actively involved in developing an inpatient curriculum for the residents, along with a new set of standard orders suited to hospitalist practice. Other areas the hospitalists will become more involved in include pre- and perioperative consultations and co-management of surgical and orthopedic patients. We are also working on special hospital projects, focusing on patient safety and hospital efficiency.
The hospitalists at the University of Texas Southwestern put in nothing less than their best efforts. After all, “High achievement always takes place in a framework of high expectation” (Jack Kinder, motivational author). TH
Dr. Mohan is the medical director of the hospital medicine program at Parkland Hospital, Dallas.









