User login
Antipsychotic cuts Alzheimer’s-related agitation
results of a phase 3 study suggest.
“In this phase 3 trial of patients with agitation in Alzheimer’s dementia, treatment with brexpiprazole 2 or 3 mg/day resulted in statistically significantly greater improvements in agitation versus placebo on the primary and key secondary endpoints,” said study investigator George Grossberg, MD, professor and director of the division of geriatric psychiatry, department of psychiatry & behavioral neuroscience, Saint Louis University.
Dr. Grossberg presented the findings as part of the annual meeting of the American Association for Geriatric Psychiatry.
Agitation common, distressing
With two previous studies also showing efficacy of brexpiprazole in AD-related agitation, Dr. Grossberg speculated that brexpiprazole will become the first drug to be approved for agitation in AD.
Agitation is one of the most common AD symptoms and is arguably the most distressing for patients and caregivers alike, Dr. Grossberg noted.
The drug was approved by the Food and Drug Administration in 2015 as an adjunctive therapy to antidepressants for adults with major depressive disorder and for adults with schizophrenia.
To investigate the drug at effective doses for AD-related agitation, the researchers conducted a phase 3 multicenter trial that included 345 patients with AD who met criteria for agitation and aggression.
Study participants had a mean Mini-Mental State Examination (MMSE) score between 5 and 22 at screening and baseline and a mean Cohen-Mansfield Agitation Inventory (CMAI) total score of about 79. A score above 45 is considered clinically significant agitation. Use of AD medications were permitted.
Patients had a mean age of 74 years and were randomly assigned in a 2:1 ratio to receive treatment with brexpiprazole 2 mg (n = 75) or 3 mg (n = 153) per day, or placebo (n = 117).
The study’s primary endpoint was improvement as assessed by the CMAI. Over 12 weeks, participants in the brexpiprazole group experienced greater improvement in agitation, with a mean change of –22.6 with brexpiprazole vs. –17.3 with placebo (P = .0026).
Brexpiprazole was also associated with significantly greater improvement in the secondary outcome of change from baseline to week 12 in agitation severity, as assessed using the Clinical Global Impression-Severity of Illness (CGI-S) score (mean change, –1.20 with brexpiprazole vs. –0.93 with placebo; P = .0078).
Specifically, treatment with the drug resulted in improvements in three key subscales of agitation, including aggressive behavior, such as physically striking out (P < .01 vs. placebo); physically nonaggressive; and verbally agitated, such as screaming or cursing (both P < .05).
Treatment-emergent adverse events (TEAEs) associated with brexpiprazole vs. placebo included somnolence (3.5% vs. 0.9%), nasopharyngitis (3.1% vs. 1.7%), dizziness (2.7% vs. 1.7%), diarrhea (2.2% vs. 0.9%), urinary tract infection (2.2% vs. 0.9%), and asthenia (2.2% vs. 0.0%).
“Aside from headache, no other TEAEs had an incidence of more than 5% in the brexpiprazole (2 or 3 mg) group, or in either dose group,” Dr. Grossberg said. “Cognition also remained stable,” he added.
Boxed warnings
Adverse events commonly associated with brexpiprazole include weight change, extrapyramidal events, falls, cardiovascular events, and sedation. In the study, all occurred at an incidence of less than 2% in both study groups, he noted.
Compared with the antipsychotic aripiprazole, brexpiprazole is associated with lower weight gain and akathisia, or motor restlessness.
One death occurred in the brexpiprazole 3 mg group in a patient who had heart failure, pneumonia, and cachexia. At autopsy, it was found the patient had cerebral and coronary atherosclerosis. The death was considered to be unrelated to brexpiprazole, said Dr. Grossberg.
This finding is notable because a caveat is that brexpiprazole, like aripiprazole and other typical and atypical antipsychotics, carries an FDA boxed warning related to an increased risk for death in older patients when used for dementia-related psychosis.
Noting that a black box warning about mortality risk is not a minor issue, Dr. Grossberg added that the risks are relatively low, whereas the risks associated with agitation in dementia can be high.
“If it’s an emergency situation, you have to treat the patient because otherwise they may harm someone else, or harm the staff, or harm their loved ones or themselves, and in those cases, we want to treat the patient first, get them under control, and then we worry about the black box,” he said.
In addition, “the No. 1 reason for getting kicked out of a nursing home is agitation or severe behaviors in the context of a dementia or a major neurocognitive disorder that the facility cannot control,” Dr. Grossberg added.
In such cases, patients may wind up in an emergency department and may not be welcome back at the nursing home.
“There’s always a risk/benefit ratio, and I have that discussion with patients and their families, but I can tell you that I’ve never had a family ask me not to use a medication because of the black box warning, because they see how miserable and how out of control their loved one is and they’re miserable because they see the suffering and will ask that we do anything that we can to get this behavior under control,” Dr. Grossberg said.
Caution still warranted
Commenting on the study, Rajesh R. Tampi, MD, professor and chairman of the department of psychiatry and the Bhatia Family Endowed Chair in Psychiatry at Creighton University, Omaha, Neb., underscored that, owing to the concerns behind the FDA warnings, “nonpharmacologic management is the cornerstone of treating agitation in Alzheimer’s dementia.”
He noted that the lack of an FDA-approved drug for agitation with AD is the result of “the overall benefits of any of the drug classes or drugs trialed to treat agitation in Alzheimer’s dementia vs. their adverse effect profile,” he said.
Therefore, he continued, “any medication or medication class should be used with caution among these individuals who often have polymorbidity.”
Dr. Tampi agreed that “the use of each drug for agitation in AD should be on a case-by-case basis with a clear and documented risk/benefit discussion with the patient and their families.”
“These medications should only be used for refractory symptoms or emergency situations where the agitation is not managed adequately with nonpharmacologic techniques and with a clear and documented risk/benefit discussion with patients and their families,” Dr. Tampi said.
The study was supported by Otsuka Pharmaceutical Development & Commercialization and H. Lundbeck. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda. Dr. Tampi had no disclosures to report.
A version of this article first appeared on Medscape.com.
This article was updated 3/14/23.
results of a phase 3 study suggest.
“In this phase 3 trial of patients with agitation in Alzheimer’s dementia, treatment with brexpiprazole 2 or 3 mg/day resulted in statistically significantly greater improvements in agitation versus placebo on the primary and key secondary endpoints,” said study investigator George Grossberg, MD, professor and director of the division of geriatric psychiatry, department of psychiatry & behavioral neuroscience, Saint Louis University.
Dr. Grossberg presented the findings as part of the annual meeting of the American Association for Geriatric Psychiatry.
Agitation common, distressing
With two previous studies also showing efficacy of brexpiprazole in AD-related agitation, Dr. Grossberg speculated that brexpiprazole will become the first drug to be approved for agitation in AD.
Agitation is one of the most common AD symptoms and is arguably the most distressing for patients and caregivers alike, Dr. Grossberg noted.
The drug was approved by the Food and Drug Administration in 2015 as an adjunctive therapy to antidepressants for adults with major depressive disorder and for adults with schizophrenia.
To investigate the drug at effective doses for AD-related agitation, the researchers conducted a phase 3 multicenter trial that included 345 patients with AD who met criteria for agitation and aggression.
Study participants had a mean Mini-Mental State Examination (MMSE) score between 5 and 22 at screening and baseline and a mean Cohen-Mansfield Agitation Inventory (CMAI) total score of about 79. A score above 45 is considered clinically significant agitation. Use of AD medications were permitted.
Patients had a mean age of 74 years and were randomly assigned in a 2:1 ratio to receive treatment with brexpiprazole 2 mg (n = 75) or 3 mg (n = 153) per day, or placebo (n = 117).
The study’s primary endpoint was improvement as assessed by the CMAI. Over 12 weeks, participants in the brexpiprazole group experienced greater improvement in agitation, with a mean change of –22.6 with brexpiprazole vs. –17.3 with placebo (P = .0026).
Brexpiprazole was also associated with significantly greater improvement in the secondary outcome of change from baseline to week 12 in agitation severity, as assessed using the Clinical Global Impression-Severity of Illness (CGI-S) score (mean change, –1.20 with brexpiprazole vs. –0.93 with placebo; P = .0078).
Specifically, treatment with the drug resulted in improvements in three key subscales of agitation, including aggressive behavior, such as physically striking out (P < .01 vs. placebo); physically nonaggressive; and verbally agitated, such as screaming or cursing (both P < .05).
Treatment-emergent adverse events (TEAEs) associated with brexpiprazole vs. placebo included somnolence (3.5% vs. 0.9%), nasopharyngitis (3.1% vs. 1.7%), dizziness (2.7% vs. 1.7%), diarrhea (2.2% vs. 0.9%), urinary tract infection (2.2% vs. 0.9%), and asthenia (2.2% vs. 0.0%).
“Aside from headache, no other TEAEs had an incidence of more than 5% in the brexpiprazole (2 or 3 mg) group, or in either dose group,” Dr. Grossberg said. “Cognition also remained stable,” he added.
Boxed warnings
Adverse events commonly associated with brexpiprazole include weight change, extrapyramidal events, falls, cardiovascular events, and sedation. In the study, all occurred at an incidence of less than 2% in both study groups, he noted.
Compared with the antipsychotic aripiprazole, brexpiprazole is associated with lower weight gain and akathisia, or motor restlessness.
One death occurred in the brexpiprazole 3 mg group in a patient who had heart failure, pneumonia, and cachexia. At autopsy, it was found the patient had cerebral and coronary atherosclerosis. The death was considered to be unrelated to brexpiprazole, said Dr. Grossberg.
This finding is notable because a caveat is that brexpiprazole, like aripiprazole and other typical and atypical antipsychotics, carries an FDA boxed warning related to an increased risk for death in older patients when used for dementia-related psychosis.
Noting that a black box warning about mortality risk is not a minor issue, Dr. Grossberg added that the risks are relatively low, whereas the risks associated with agitation in dementia can be high.
“If it’s an emergency situation, you have to treat the patient because otherwise they may harm someone else, or harm the staff, or harm their loved ones or themselves, and in those cases, we want to treat the patient first, get them under control, and then we worry about the black box,” he said.
In addition, “the No. 1 reason for getting kicked out of a nursing home is agitation or severe behaviors in the context of a dementia or a major neurocognitive disorder that the facility cannot control,” Dr. Grossberg added.
In such cases, patients may wind up in an emergency department and may not be welcome back at the nursing home.
“There’s always a risk/benefit ratio, and I have that discussion with patients and their families, but I can tell you that I’ve never had a family ask me not to use a medication because of the black box warning, because they see how miserable and how out of control their loved one is and they’re miserable because they see the suffering and will ask that we do anything that we can to get this behavior under control,” Dr. Grossberg said.
Caution still warranted
Commenting on the study, Rajesh R. Tampi, MD, professor and chairman of the department of psychiatry and the Bhatia Family Endowed Chair in Psychiatry at Creighton University, Omaha, Neb., underscored that, owing to the concerns behind the FDA warnings, “nonpharmacologic management is the cornerstone of treating agitation in Alzheimer’s dementia.”
He noted that the lack of an FDA-approved drug for agitation with AD is the result of “the overall benefits of any of the drug classes or drugs trialed to treat agitation in Alzheimer’s dementia vs. their adverse effect profile,” he said.
Therefore, he continued, “any medication or medication class should be used with caution among these individuals who often have polymorbidity.”
Dr. Tampi agreed that “the use of each drug for agitation in AD should be on a case-by-case basis with a clear and documented risk/benefit discussion with the patient and their families.”
“These medications should only be used for refractory symptoms or emergency situations where the agitation is not managed adequately with nonpharmacologic techniques and with a clear and documented risk/benefit discussion with patients and their families,” Dr. Tampi said.
The study was supported by Otsuka Pharmaceutical Development & Commercialization and H. Lundbeck. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda. Dr. Tampi had no disclosures to report.
A version of this article first appeared on Medscape.com.
This article was updated 3/14/23.
results of a phase 3 study suggest.
“In this phase 3 trial of patients with agitation in Alzheimer’s dementia, treatment with brexpiprazole 2 or 3 mg/day resulted in statistically significantly greater improvements in agitation versus placebo on the primary and key secondary endpoints,” said study investigator George Grossberg, MD, professor and director of the division of geriatric psychiatry, department of psychiatry & behavioral neuroscience, Saint Louis University.
Dr. Grossberg presented the findings as part of the annual meeting of the American Association for Geriatric Psychiatry.
Agitation common, distressing
With two previous studies also showing efficacy of brexpiprazole in AD-related agitation, Dr. Grossberg speculated that brexpiprazole will become the first drug to be approved for agitation in AD.
Agitation is one of the most common AD symptoms and is arguably the most distressing for patients and caregivers alike, Dr. Grossberg noted.
The drug was approved by the Food and Drug Administration in 2015 as an adjunctive therapy to antidepressants for adults with major depressive disorder and for adults with schizophrenia.
To investigate the drug at effective doses for AD-related agitation, the researchers conducted a phase 3 multicenter trial that included 345 patients with AD who met criteria for agitation and aggression.
Study participants had a mean Mini-Mental State Examination (MMSE) score between 5 and 22 at screening and baseline and a mean Cohen-Mansfield Agitation Inventory (CMAI) total score of about 79. A score above 45 is considered clinically significant agitation. Use of AD medications were permitted.
Patients had a mean age of 74 years and were randomly assigned in a 2:1 ratio to receive treatment with brexpiprazole 2 mg (n = 75) or 3 mg (n = 153) per day, or placebo (n = 117).
The study’s primary endpoint was improvement as assessed by the CMAI. Over 12 weeks, participants in the brexpiprazole group experienced greater improvement in agitation, with a mean change of –22.6 with brexpiprazole vs. –17.3 with placebo (P = .0026).
Brexpiprazole was also associated with significantly greater improvement in the secondary outcome of change from baseline to week 12 in agitation severity, as assessed using the Clinical Global Impression-Severity of Illness (CGI-S) score (mean change, –1.20 with brexpiprazole vs. –0.93 with placebo; P = .0078).
Specifically, treatment with the drug resulted in improvements in three key subscales of agitation, including aggressive behavior, such as physically striking out (P < .01 vs. placebo); physically nonaggressive; and verbally agitated, such as screaming or cursing (both P < .05).
Treatment-emergent adverse events (TEAEs) associated with brexpiprazole vs. placebo included somnolence (3.5% vs. 0.9%), nasopharyngitis (3.1% vs. 1.7%), dizziness (2.7% vs. 1.7%), diarrhea (2.2% vs. 0.9%), urinary tract infection (2.2% vs. 0.9%), and asthenia (2.2% vs. 0.0%).
“Aside from headache, no other TEAEs had an incidence of more than 5% in the brexpiprazole (2 or 3 mg) group, or in either dose group,” Dr. Grossberg said. “Cognition also remained stable,” he added.
Boxed warnings
Adverse events commonly associated with brexpiprazole include weight change, extrapyramidal events, falls, cardiovascular events, and sedation. In the study, all occurred at an incidence of less than 2% in both study groups, he noted.
Compared with the antipsychotic aripiprazole, brexpiprazole is associated with lower weight gain and akathisia, or motor restlessness.
One death occurred in the brexpiprazole 3 mg group in a patient who had heart failure, pneumonia, and cachexia. At autopsy, it was found the patient had cerebral and coronary atherosclerosis. The death was considered to be unrelated to brexpiprazole, said Dr. Grossberg.
This finding is notable because a caveat is that brexpiprazole, like aripiprazole and other typical and atypical antipsychotics, carries an FDA boxed warning related to an increased risk for death in older patients when used for dementia-related psychosis.
Noting that a black box warning about mortality risk is not a minor issue, Dr. Grossberg added that the risks are relatively low, whereas the risks associated with agitation in dementia can be high.
“If it’s an emergency situation, you have to treat the patient because otherwise they may harm someone else, or harm the staff, or harm their loved ones or themselves, and in those cases, we want to treat the patient first, get them under control, and then we worry about the black box,” he said.
In addition, “the No. 1 reason for getting kicked out of a nursing home is agitation or severe behaviors in the context of a dementia or a major neurocognitive disorder that the facility cannot control,” Dr. Grossberg added.
In such cases, patients may wind up in an emergency department and may not be welcome back at the nursing home.
“There’s always a risk/benefit ratio, and I have that discussion with patients and their families, but I can tell you that I’ve never had a family ask me not to use a medication because of the black box warning, because they see how miserable and how out of control their loved one is and they’re miserable because they see the suffering and will ask that we do anything that we can to get this behavior under control,” Dr. Grossberg said.
Caution still warranted
Commenting on the study, Rajesh R. Tampi, MD, professor and chairman of the department of psychiatry and the Bhatia Family Endowed Chair in Psychiatry at Creighton University, Omaha, Neb., underscored that, owing to the concerns behind the FDA warnings, “nonpharmacologic management is the cornerstone of treating agitation in Alzheimer’s dementia.”
He noted that the lack of an FDA-approved drug for agitation with AD is the result of “the overall benefits of any of the drug classes or drugs trialed to treat agitation in Alzheimer’s dementia vs. their adverse effect profile,” he said.
Therefore, he continued, “any medication or medication class should be used with caution among these individuals who often have polymorbidity.”
Dr. Tampi agreed that “the use of each drug for agitation in AD should be on a case-by-case basis with a clear and documented risk/benefit discussion with the patient and their families.”
“These medications should only be used for refractory symptoms or emergency situations where the agitation is not managed adequately with nonpharmacologic techniques and with a clear and documented risk/benefit discussion with patients and their families,” Dr. Tampi said.
The study was supported by Otsuka Pharmaceutical Development & Commercialization and H. Lundbeck. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda. Dr. Tampi had no disclosures to report.
A version of this article first appeared on Medscape.com.
This article was updated 3/14/23.
AT AAGP 2023
Venetoclax shows promise for r/r hairy cell leukemia
Venetoclax is already approved for adults with chronic lymphocytic leukemia, small lymphocytic leukemia, and as part of a treatment combination in certain patients with acute myeloid leukemia.
The new findings suggest that the drug could also be a chemotherapy-free treatment option for HCL patients after the failure of multiple prior lines of therapy, including vemurafenib plus rituximab, the investigators wrote in a letter to the editor published in the New England Journal of Medicine.
Treatment options for such patients are limited, they noted.
Enrico Tiacci, MD, of the University of Perugia (Italy), and colleagues decided to explore the use of venetoclax in this patient population after reports of in vitro findings showing a possible benefit.
The investigators administered the drug off-label to six patients who had received vemurafenib plus rituximab as their most recent prior therapy; one was resistant and five relapsed after that therapy, they reported. Venetoclax was delivered in 29-day cycles.
After 6 or 12 cycles, two patients experienced complete remission with minimal residual disease (MRD), and one had partial remission, although each had incomplete platelet recovery.
Adding rituximab at a dose of 375 mg per square meter of body-surface area for three to eight cycles improved the depth of response in a patient who had a previous minor response, further reduced MRD in one who had a complete remission to venetoclax, and led to hematologic remission in one who had no response to venetoclax, they noted.
Progression-free survival ranged from 23 to 53-plus months in all five patients who did not have early progression and was similar or better than PFS seen after vemurafenib plus rituximab.
The main toxic effect of venetoclax was worsening of baseline neutropenia, which was sometimes complicated by infections or febrile neutropenia and was managed by dose reductions and granulocyte colony-stimulating factor.
“Thus, venetoclax with or without rituximab may serve as a safe and effective salvage option after failure of vemurafenib plus rituximab treatment, especially in patients who do not require a rapid recovery of blood count,” they concluded.
The study was supported by grants from Fondazione Associazione Italiana per la Ricerca sul Cancro and the Italian Ministry of Health.
A version of this article first appeared on Medscape.com.
Venetoclax is already approved for adults with chronic lymphocytic leukemia, small lymphocytic leukemia, and as part of a treatment combination in certain patients with acute myeloid leukemia.
The new findings suggest that the drug could also be a chemotherapy-free treatment option for HCL patients after the failure of multiple prior lines of therapy, including vemurafenib plus rituximab, the investigators wrote in a letter to the editor published in the New England Journal of Medicine.
Treatment options for such patients are limited, they noted.
Enrico Tiacci, MD, of the University of Perugia (Italy), and colleagues decided to explore the use of venetoclax in this patient population after reports of in vitro findings showing a possible benefit.
The investigators administered the drug off-label to six patients who had received vemurafenib plus rituximab as their most recent prior therapy; one was resistant and five relapsed after that therapy, they reported. Venetoclax was delivered in 29-day cycles.
After 6 or 12 cycles, two patients experienced complete remission with minimal residual disease (MRD), and one had partial remission, although each had incomplete platelet recovery.
Adding rituximab at a dose of 375 mg per square meter of body-surface area for three to eight cycles improved the depth of response in a patient who had a previous minor response, further reduced MRD in one who had a complete remission to venetoclax, and led to hematologic remission in one who had no response to venetoclax, they noted.
Progression-free survival ranged from 23 to 53-plus months in all five patients who did not have early progression and was similar or better than PFS seen after vemurafenib plus rituximab.
The main toxic effect of venetoclax was worsening of baseline neutropenia, which was sometimes complicated by infections or febrile neutropenia and was managed by dose reductions and granulocyte colony-stimulating factor.
“Thus, venetoclax with or without rituximab may serve as a safe and effective salvage option after failure of vemurafenib plus rituximab treatment, especially in patients who do not require a rapid recovery of blood count,” they concluded.
The study was supported by grants from Fondazione Associazione Italiana per la Ricerca sul Cancro and the Italian Ministry of Health.
A version of this article first appeared on Medscape.com.
Venetoclax is already approved for adults with chronic lymphocytic leukemia, small lymphocytic leukemia, and as part of a treatment combination in certain patients with acute myeloid leukemia.
The new findings suggest that the drug could also be a chemotherapy-free treatment option for HCL patients after the failure of multiple prior lines of therapy, including vemurafenib plus rituximab, the investigators wrote in a letter to the editor published in the New England Journal of Medicine.
Treatment options for such patients are limited, they noted.
Enrico Tiacci, MD, of the University of Perugia (Italy), and colleagues decided to explore the use of venetoclax in this patient population after reports of in vitro findings showing a possible benefit.
The investigators administered the drug off-label to six patients who had received vemurafenib plus rituximab as their most recent prior therapy; one was resistant and five relapsed after that therapy, they reported. Venetoclax was delivered in 29-day cycles.
After 6 or 12 cycles, two patients experienced complete remission with minimal residual disease (MRD), and one had partial remission, although each had incomplete platelet recovery.
Adding rituximab at a dose of 375 mg per square meter of body-surface area for three to eight cycles improved the depth of response in a patient who had a previous minor response, further reduced MRD in one who had a complete remission to venetoclax, and led to hematologic remission in one who had no response to venetoclax, they noted.
Progression-free survival ranged from 23 to 53-plus months in all five patients who did not have early progression and was similar or better than PFS seen after vemurafenib plus rituximab.
The main toxic effect of venetoclax was worsening of baseline neutropenia, which was sometimes complicated by infections or febrile neutropenia and was managed by dose reductions and granulocyte colony-stimulating factor.
“Thus, venetoclax with or without rituximab may serve as a safe and effective salvage option after failure of vemurafenib plus rituximab treatment, especially in patients who do not require a rapid recovery of blood count,” they concluded.
The study was supported by grants from Fondazione Associazione Italiana per la Ricerca sul Cancro and the Italian Ministry of Health.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Buprenorphine proves effective for fentanyl users in the ED
based on data from nearly 900 individuals.
California EDs include a facilitation program known as CA Bridge for the treatment of opioid use disorder. Guidelines for CA Bridge call for high-dose buprenorphine to treat patients in drug withdrawal, with doses starting at 8-16 mg, Hannah Snyder, MD, of the University of California, San Francisco, and colleagues wrote.
“Buprenorphine has been repeatedly shown to save lives and prevent overdoses,” Dr. Snyder said in an interview. “We know that emergency department–initiated buprenorphine is an essential tool for increasing access. In the era of fentanyl, both patients and providers have expressed concerns that buprenorphine may not work as well as it did when patients were more likely to be using heroin or opioid pills.
“This retrospective cohort study provides additional information about emergency department buprenorphine as fentanyl becomes increasingly prevalent.”
In a research letter published in JAMA Network Open, the investigators reviewed data from the electronic health records of 896 patients who presented with opioid use disorder (OUD) at 16 CA Bridge EDs between Jan. 1, 2020, and April 30, 2020. All patients with OUD were included regardless of chief concern, current treatment, treatment desires, or withdrawal. A total of 87 individuals reported fentanyl use; if no fentanyl use was reported, the patient was classified as not using fentanyl. The median age of the patients was 35 years, two thirds were male, approximately 46% were White and non-Hispanic, and 30% had unstable housing.
The primary outcome was follow-up engagement at 7-14 days and 25-37 days.
A total of 492 patients received buprenorphine, including 44 fentanyl users, and 439 initiated high doses of 8-32 mg. At a 30-day follow-up, eight patients had precipitated withdrawal, including two cases in fentanyl users; none of these cases required hospital admission.
The follow-up engagement was similar for both groups, with adjusted odds ratios of 0.60 for administered buprenorphine at the initial ED encounter, 1.09 for 7-day follow-up, and 1.33 for 30-day follow-up.
The findings were limited by the retrospective design and use of clinical documentation, which likely resulted in underreporting of fentanyl use and follow-up, the researchers noted. However, the results supported the effectiveness of buprenorphine for ED patients in withdrawal with a history of fentanyl exposure.
“We were pleased to see that precipitated withdrawal was relatively uncommon in this study, and that patients who did and did not use fentanyl followed up at similar rates,” said Dr. Snyder. “This aligns with our clinical experience and prior research showing that emergency department buprenorphine starts continue to be an essential tool.”
The message for clinicians: “If a patient presents to the emergency department in objective opioid withdrawal and desires buprenorphine, they should be offered treatment in that moment,” Dr. Snyder said. “Treatment protocols used by hospitals in this study are available online. Emergency departments can offer compassionate and evidence-based treatment initiation 24 hours a day, 7 days a week, 365 days a year.”
More data needed on dosing strategies
“We need additional research to determine best practices for patients who use fentanyl and want to start buprenorphine, but are not yet in withdrawal,” Dr. Snyder said. “Doses of buprenorphine like those in this study are only appropriate for patients who are in withdrawal with objective signs, so some patients may struggle to wait long enough after their last use to go into sufficient withdrawal.”
Precipitated withdrawal does occur in some cases, said Dr. Snyder. “If it does, the emergency department is a very good place to manage it. We need additional research to determine best practices in management to make patients as comfortable as possible, including additional high-dose buprenorphine as well as additional adjunctive agents.”
Findings support buprenorphine
“The classic approach to buprenorphine initiation, which emerged from psychiatry outpatient office visits, is to start with very small doses of buprenorphine [2-4 mg] and titrate up slowly,” Reuben J. Strayer, MD, said in an interview.
“This dose range turns out to be the ‘sour spot’ most likely to cause the most important complication around buprenorphine initiation–precipitated withdrawal,” said Dr. Strayer, the director of addiction medicine in the emergency medicine department at Maimonides Medical Center, New York.
“One of the current focus areas of OUD treatment research is determining how to initiate buprenorphine without entailing a period of spontaneous withdrawal and without causing precipitated withdrawal,” Strayer explained. “The two primary strategies are low-dose buprenorphine initiation [LDBI, less than 2 mg, sometimes called microdosing] and high-dose [HDBI, ≥ 16 mg] buprenorphine initiation. HDBI is attractive because the primary treatment of buprenorphine-precipitated withdrawal is more buprenorphine.
“Additionally, using a high dose up front immediately transitions the patient to therapeutic blood levels, which protects the patient from withdrawal, cravings, and overdose from dangerous opioids (heroin, fentanyl, oxycodone).”
However, “the contamination and now replacement of heroin with fentanyl in the street drug supply has challenged buprenorphine initiation, because fentanyl, when used chronically, accumulates in the body and leaks into the bloodstream slowly over time, preventing the opioid washout that is required to eliminate the risk of precipitated withdrawal when buprenorphine is administered,” said Dr. Strayer.
The current study demonstrates that patients who are initiated with a first dose of 8-16 mg buprenorphine are unlikely to experience precipitated withdrawal and are successfully transitioned to buprenorphine maintenance and clinic follow-up, Dr. Snyder said, but he was surprised by the low rate of precipitated withdrawal in the current study, “which is discordant with what is being anecdotally reported across the country.”
However, the take-home message for clinicians is the support for the initiation of buprenorphine in emergency department settings at a starting dose of 8-16 mg, regardless of reported fentanyl use, he said. “Given the huge impact buprenorphine therapy has on OUD-related mortality, clinicians should make every effort to initiate buprenorphine for OUD patients at every opportunity, and precipitated withdrawal is very unlikely in appropriately selected patients.
“Many clinicians remain reluctant to initiate buprenorphine in ED settings for unfamiliarity with the drug, fear of precipitated withdrawal, or concerns around the certainty of outpatient follow-up,” Dr. Snyder said. “Education, encouragement, systems programming, such as including decision support within the electronic health record, and role-modeling from local champions will promote wider adoption of this lifesaving practice.”
Looking ahead, “more research, including prospective research, is needed to refine best practices around buprenorphine administration,” said Dr. Snyder. Questions to address include which patients are most at risk for precipitated withdrawal and whether there are alternatives to standard initiation dosing that are sufficiently unlikely to cause precipitated withdrawal. “Possibly effective alternatives include buprenorphine initiation by administration of long-acting injectable depot buprenorphine, which accumulates slowly, potentially avoiding precipitated withdrawal, as well as a slow intravenous buprenorphine infusion such as 9 mg given over 12 hours.”
The study received no outside funding. Dr. Snyder disclosed grants from the Substance Abuse and Mental Health Services Administration and the California Department of Health Care Services during the study. Dr. Strayer reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
based on data from nearly 900 individuals.
California EDs include a facilitation program known as CA Bridge for the treatment of opioid use disorder. Guidelines for CA Bridge call for high-dose buprenorphine to treat patients in drug withdrawal, with doses starting at 8-16 mg, Hannah Snyder, MD, of the University of California, San Francisco, and colleagues wrote.
“Buprenorphine has been repeatedly shown to save lives and prevent overdoses,” Dr. Snyder said in an interview. “We know that emergency department–initiated buprenorphine is an essential tool for increasing access. In the era of fentanyl, both patients and providers have expressed concerns that buprenorphine may not work as well as it did when patients were more likely to be using heroin or opioid pills.
“This retrospective cohort study provides additional information about emergency department buprenorphine as fentanyl becomes increasingly prevalent.”
In a research letter published in JAMA Network Open, the investigators reviewed data from the electronic health records of 896 patients who presented with opioid use disorder (OUD) at 16 CA Bridge EDs between Jan. 1, 2020, and April 30, 2020. All patients with OUD were included regardless of chief concern, current treatment, treatment desires, or withdrawal. A total of 87 individuals reported fentanyl use; if no fentanyl use was reported, the patient was classified as not using fentanyl. The median age of the patients was 35 years, two thirds were male, approximately 46% were White and non-Hispanic, and 30% had unstable housing.
The primary outcome was follow-up engagement at 7-14 days and 25-37 days.
A total of 492 patients received buprenorphine, including 44 fentanyl users, and 439 initiated high doses of 8-32 mg. At a 30-day follow-up, eight patients had precipitated withdrawal, including two cases in fentanyl users; none of these cases required hospital admission.
The follow-up engagement was similar for both groups, with adjusted odds ratios of 0.60 for administered buprenorphine at the initial ED encounter, 1.09 for 7-day follow-up, and 1.33 for 30-day follow-up.
The findings were limited by the retrospective design and use of clinical documentation, which likely resulted in underreporting of fentanyl use and follow-up, the researchers noted. However, the results supported the effectiveness of buprenorphine for ED patients in withdrawal with a history of fentanyl exposure.
“We were pleased to see that precipitated withdrawal was relatively uncommon in this study, and that patients who did and did not use fentanyl followed up at similar rates,” said Dr. Snyder. “This aligns with our clinical experience and prior research showing that emergency department buprenorphine starts continue to be an essential tool.”
The message for clinicians: “If a patient presents to the emergency department in objective opioid withdrawal and desires buprenorphine, they should be offered treatment in that moment,” Dr. Snyder said. “Treatment protocols used by hospitals in this study are available online. Emergency departments can offer compassionate and evidence-based treatment initiation 24 hours a day, 7 days a week, 365 days a year.”
More data needed on dosing strategies
“We need additional research to determine best practices for patients who use fentanyl and want to start buprenorphine, but are not yet in withdrawal,” Dr. Snyder said. “Doses of buprenorphine like those in this study are only appropriate for patients who are in withdrawal with objective signs, so some patients may struggle to wait long enough after their last use to go into sufficient withdrawal.”
Precipitated withdrawal does occur in some cases, said Dr. Snyder. “If it does, the emergency department is a very good place to manage it. We need additional research to determine best practices in management to make patients as comfortable as possible, including additional high-dose buprenorphine as well as additional adjunctive agents.”
Findings support buprenorphine
“The classic approach to buprenorphine initiation, which emerged from psychiatry outpatient office visits, is to start with very small doses of buprenorphine [2-4 mg] and titrate up slowly,” Reuben J. Strayer, MD, said in an interview.
“This dose range turns out to be the ‘sour spot’ most likely to cause the most important complication around buprenorphine initiation–precipitated withdrawal,” said Dr. Strayer, the director of addiction medicine in the emergency medicine department at Maimonides Medical Center, New York.
“One of the current focus areas of OUD treatment research is determining how to initiate buprenorphine without entailing a period of spontaneous withdrawal and without causing precipitated withdrawal,” Strayer explained. “The two primary strategies are low-dose buprenorphine initiation [LDBI, less than 2 mg, sometimes called microdosing] and high-dose [HDBI, ≥ 16 mg] buprenorphine initiation. HDBI is attractive because the primary treatment of buprenorphine-precipitated withdrawal is more buprenorphine.
“Additionally, using a high dose up front immediately transitions the patient to therapeutic blood levels, which protects the patient from withdrawal, cravings, and overdose from dangerous opioids (heroin, fentanyl, oxycodone).”
However, “the contamination and now replacement of heroin with fentanyl in the street drug supply has challenged buprenorphine initiation, because fentanyl, when used chronically, accumulates in the body and leaks into the bloodstream slowly over time, preventing the opioid washout that is required to eliminate the risk of precipitated withdrawal when buprenorphine is administered,” said Dr. Strayer.
The current study demonstrates that patients who are initiated with a first dose of 8-16 mg buprenorphine are unlikely to experience precipitated withdrawal and are successfully transitioned to buprenorphine maintenance and clinic follow-up, Dr. Snyder said, but he was surprised by the low rate of precipitated withdrawal in the current study, “which is discordant with what is being anecdotally reported across the country.”
However, the take-home message for clinicians is the support for the initiation of buprenorphine in emergency department settings at a starting dose of 8-16 mg, regardless of reported fentanyl use, he said. “Given the huge impact buprenorphine therapy has on OUD-related mortality, clinicians should make every effort to initiate buprenorphine for OUD patients at every opportunity, and precipitated withdrawal is very unlikely in appropriately selected patients.
“Many clinicians remain reluctant to initiate buprenorphine in ED settings for unfamiliarity with the drug, fear of precipitated withdrawal, or concerns around the certainty of outpatient follow-up,” Dr. Snyder said. “Education, encouragement, systems programming, such as including decision support within the electronic health record, and role-modeling from local champions will promote wider adoption of this lifesaving practice.”
Looking ahead, “more research, including prospective research, is needed to refine best practices around buprenorphine administration,” said Dr. Snyder. Questions to address include which patients are most at risk for precipitated withdrawal and whether there are alternatives to standard initiation dosing that are sufficiently unlikely to cause precipitated withdrawal. “Possibly effective alternatives include buprenorphine initiation by administration of long-acting injectable depot buprenorphine, which accumulates slowly, potentially avoiding precipitated withdrawal, as well as a slow intravenous buprenorphine infusion such as 9 mg given over 12 hours.”
The study received no outside funding. Dr. Snyder disclosed grants from the Substance Abuse and Mental Health Services Administration and the California Department of Health Care Services during the study. Dr. Strayer reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
based on data from nearly 900 individuals.
California EDs include a facilitation program known as CA Bridge for the treatment of opioid use disorder. Guidelines for CA Bridge call for high-dose buprenorphine to treat patients in drug withdrawal, with doses starting at 8-16 mg, Hannah Snyder, MD, of the University of California, San Francisco, and colleagues wrote.
“Buprenorphine has been repeatedly shown to save lives and prevent overdoses,” Dr. Snyder said in an interview. “We know that emergency department–initiated buprenorphine is an essential tool for increasing access. In the era of fentanyl, both patients and providers have expressed concerns that buprenorphine may not work as well as it did when patients were more likely to be using heroin or opioid pills.
“This retrospective cohort study provides additional information about emergency department buprenorphine as fentanyl becomes increasingly prevalent.”
In a research letter published in JAMA Network Open, the investigators reviewed data from the electronic health records of 896 patients who presented with opioid use disorder (OUD) at 16 CA Bridge EDs between Jan. 1, 2020, and April 30, 2020. All patients with OUD were included regardless of chief concern, current treatment, treatment desires, or withdrawal. A total of 87 individuals reported fentanyl use; if no fentanyl use was reported, the patient was classified as not using fentanyl. The median age of the patients was 35 years, two thirds were male, approximately 46% were White and non-Hispanic, and 30% had unstable housing.
The primary outcome was follow-up engagement at 7-14 days and 25-37 days.
A total of 492 patients received buprenorphine, including 44 fentanyl users, and 439 initiated high doses of 8-32 mg. At a 30-day follow-up, eight patients had precipitated withdrawal, including two cases in fentanyl users; none of these cases required hospital admission.
The follow-up engagement was similar for both groups, with adjusted odds ratios of 0.60 for administered buprenorphine at the initial ED encounter, 1.09 for 7-day follow-up, and 1.33 for 30-day follow-up.
The findings were limited by the retrospective design and use of clinical documentation, which likely resulted in underreporting of fentanyl use and follow-up, the researchers noted. However, the results supported the effectiveness of buprenorphine for ED patients in withdrawal with a history of fentanyl exposure.
“We were pleased to see that precipitated withdrawal was relatively uncommon in this study, and that patients who did and did not use fentanyl followed up at similar rates,” said Dr. Snyder. “This aligns with our clinical experience and prior research showing that emergency department buprenorphine starts continue to be an essential tool.”
The message for clinicians: “If a patient presents to the emergency department in objective opioid withdrawal and desires buprenorphine, they should be offered treatment in that moment,” Dr. Snyder said. “Treatment protocols used by hospitals in this study are available online. Emergency departments can offer compassionate and evidence-based treatment initiation 24 hours a day, 7 days a week, 365 days a year.”
More data needed on dosing strategies
“We need additional research to determine best practices for patients who use fentanyl and want to start buprenorphine, but are not yet in withdrawal,” Dr. Snyder said. “Doses of buprenorphine like those in this study are only appropriate for patients who are in withdrawal with objective signs, so some patients may struggle to wait long enough after their last use to go into sufficient withdrawal.”
Precipitated withdrawal does occur in some cases, said Dr. Snyder. “If it does, the emergency department is a very good place to manage it. We need additional research to determine best practices in management to make patients as comfortable as possible, including additional high-dose buprenorphine as well as additional adjunctive agents.”
Findings support buprenorphine
“The classic approach to buprenorphine initiation, which emerged from psychiatry outpatient office visits, is to start with very small doses of buprenorphine [2-4 mg] and titrate up slowly,” Reuben J. Strayer, MD, said in an interview.
“This dose range turns out to be the ‘sour spot’ most likely to cause the most important complication around buprenorphine initiation–precipitated withdrawal,” said Dr. Strayer, the director of addiction medicine in the emergency medicine department at Maimonides Medical Center, New York.
“One of the current focus areas of OUD treatment research is determining how to initiate buprenorphine without entailing a period of spontaneous withdrawal and without causing precipitated withdrawal,” Strayer explained. “The two primary strategies are low-dose buprenorphine initiation [LDBI, less than 2 mg, sometimes called microdosing] and high-dose [HDBI, ≥ 16 mg] buprenorphine initiation. HDBI is attractive because the primary treatment of buprenorphine-precipitated withdrawal is more buprenorphine.
“Additionally, using a high dose up front immediately transitions the patient to therapeutic blood levels, which protects the patient from withdrawal, cravings, and overdose from dangerous opioids (heroin, fentanyl, oxycodone).”
However, “the contamination and now replacement of heroin with fentanyl in the street drug supply has challenged buprenorphine initiation, because fentanyl, when used chronically, accumulates in the body and leaks into the bloodstream slowly over time, preventing the opioid washout that is required to eliminate the risk of precipitated withdrawal when buprenorphine is administered,” said Dr. Strayer.
The current study demonstrates that patients who are initiated with a first dose of 8-16 mg buprenorphine are unlikely to experience precipitated withdrawal and are successfully transitioned to buprenorphine maintenance and clinic follow-up, Dr. Snyder said, but he was surprised by the low rate of precipitated withdrawal in the current study, “which is discordant with what is being anecdotally reported across the country.”
However, the take-home message for clinicians is the support for the initiation of buprenorphine in emergency department settings at a starting dose of 8-16 mg, regardless of reported fentanyl use, he said. “Given the huge impact buprenorphine therapy has on OUD-related mortality, clinicians should make every effort to initiate buprenorphine for OUD patients at every opportunity, and precipitated withdrawal is very unlikely in appropriately selected patients.
“Many clinicians remain reluctant to initiate buprenorphine in ED settings for unfamiliarity with the drug, fear of precipitated withdrawal, or concerns around the certainty of outpatient follow-up,” Dr. Snyder said. “Education, encouragement, systems programming, such as including decision support within the electronic health record, and role-modeling from local champions will promote wider adoption of this lifesaving practice.”
Looking ahead, “more research, including prospective research, is needed to refine best practices around buprenorphine administration,” said Dr. Snyder. Questions to address include which patients are most at risk for precipitated withdrawal and whether there are alternatives to standard initiation dosing that are sufficiently unlikely to cause precipitated withdrawal. “Possibly effective alternatives include buprenorphine initiation by administration of long-acting injectable depot buprenorphine, which accumulates slowly, potentially avoiding precipitated withdrawal, as well as a slow intravenous buprenorphine infusion such as 9 mg given over 12 hours.”
The study received no outside funding. Dr. Snyder disclosed grants from the Substance Abuse and Mental Health Services Administration and the California Department of Health Care Services during the study. Dr. Strayer reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Once-daily stimulant for ADHD safe, effective at 1 year
new research shows.
Results from a phase 3, multicenter, dose-optimization, open-label safety study of Azstarys (KemPharm) found that most treatment-emergent adverse events (TEAEs) were mild to moderate.
“This data show that Azstarys remains safe and effective for the treatment of ADHD when given for up to a year,” lead investigator Ann Childress, MD, president of the Center for Psychiatry and Behavioral Medicine, Las Vegas, said in an interview.
The study was published online in the Journal of Child and Adolescent Psychopharmacology.
Safety at 1 year
The drug is a combination of extended-release serdexmethylphenidate (SDX), KemPharm’s prodrug of dexmethylphenidate, coformulated with immediate-release d-MPH.
SDX is converted to d-MPH after it is absorbed in the gastrointestinal tract. The d-MPH is released gradually throughout the day, providing quick symptom control with the d-MPH and extended control with SDX.
Azstarys was approved by the Food and Drug Administration in 2021 on the basis of results from a laboratory classroom phase 3 trial, which showed significant improvement in ADHD symptoms, compared with placebo.
For this study, the second phase 3 trial of Azstarys, investigators analyzed data from 282 children aged 6-12 years in the United States, including 70 who participated in an earlier 1-month efficacy trial.
After screening and a 3-week dose-optimization phase for new participants, patients received once-daily treatment with doses of 26.1 mg/5.2 mg, 39.2 mg/7.8 mg, or 52.3 mg/10.4 mg of SDX/d-MPH.
After 1 year of treatment, 60.1% of participants reported at least one TEAE, the majority of which were moderate. Twelve patients reported severe TEAEs. Six children (2.5%) discontinued the study because of a TEAE during the treatment phase.
The investigators also measured growth and changes in sleep with the Children’s Sleep Habits Questionnaire during the 12-month study. Sleep improved on most measures and the impact on growth was mild.
There were no life-threatening TEAEs and no deaths reported during the study.
The most common TEAEs during the treatment phase were decreased appetite, upper respiratory tract infection, nasopharyngitis, decreased weight, irritability, and increased weight.
Efficacy at 1 year
ADHD symptoms improved considerably after 1 month of treatment, with responses continuing at 1 year.
At baseline, participants’ mean ADHD Rating Scale–5 score was 41.5. After 1 month of treatment, scores averaged 16.1, a decline of –25.3 (P < .001).
The mean score stabilized in the 12-15 range for the remainder of the study. After 1 year of treatment, ADHD symptoms had decreased approximately 70% from baseline.
Investigators found similar results in clinical severity. After 1 month of treatment, the average Clinical Global Impressions–Severity (CGI-S) scale score was 2.5, a decline of –2.2 (P < .0001).
CGI-S scale scores remained in the 2.2-2.4 range for the remainder of the study.
These results, combined with the results of the original classroom trial, suggest Azstarys may offer advantages over other ADHD drugs, Dr. Childress said.
“In the laboratory classroom trial, subjects taking Azstarys completed significantly more math problems than subjects taking placebo beginning at 30 minutes and up to 13 hours after dosing,” Dr. Childress said. “No other methylphenidate extended-release product currently marketed in the United States has a 13-hour duration of effect.”
‘Reassuring data’
Commenting on the findings, Aditya Pawar, MD, a child and adolescent psychiatrist with the Kennedy Krieger Institute and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, said that the study suggests the drug may be a valuable addition to ADHD treatment options for pediatric patients.
“The study provides reassuring data on the safety of stimulants in patients without significant history of cardiac events or blood pressure changes, which are usual concerns among patients and clinicians despite the evidence supporting safety, said Dr. Pawar, who was not part of the study.
“Additionally, the 1-year data on efficacy and safety of a new stimulant medication is valuable for clinicians looking for sustained relief for their patients, despite the limitations of an open-label trial,” she added.
Overall, the safety data reported in the study are fairly consistent with the safety profile of other methylphenidates used for treating ADHD, Dr. Pawar said.
However, she noted, the study does have some limitations, including its open-label design and lack of blinding. The research also excluded children with autism, disruptive mood dysregulation disorders, and other common comorbidities of ADHD, which may limit the generalizability of the results.
“These comorbidities often require stimulants as a part of treatment, and yet have a higher risk of side effects,” Dr. Pawar said. “Future studies with a broader population may be needed to better understand treatment effectiveness and potential risks.”
The study was funded by KemPharm. Dr. Childress serves as consultant for Aardvark, Arbor, Attentive, Cingulate, Ironshore, Neos Therapeutics, Neurocentria, Otsuka, Purdue, Rhodes, Sunovion, Tris Pharma, KemPharm, Supernus, Jazz, Corium, Tulex, and Lumos.
A version of this article first appeared on Medscape.com.
new research shows.
Results from a phase 3, multicenter, dose-optimization, open-label safety study of Azstarys (KemPharm) found that most treatment-emergent adverse events (TEAEs) were mild to moderate.
“This data show that Azstarys remains safe and effective for the treatment of ADHD when given for up to a year,” lead investigator Ann Childress, MD, president of the Center for Psychiatry and Behavioral Medicine, Las Vegas, said in an interview.
The study was published online in the Journal of Child and Adolescent Psychopharmacology.
Safety at 1 year
The drug is a combination of extended-release serdexmethylphenidate (SDX), KemPharm’s prodrug of dexmethylphenidate, coformulated with immediate-release d-MPH.
SDX is converted to d-MPH after it is absorbed in the gastrointestinal tract. The d-MPH is released gradually throughout the day, providing quick symptom control with the d-MPH and extended control with SDX.
Azstarys was approved by the Food and Drug Administration in 2021 on the basis of results from a laboratory classroom phase 3 trial, which showed significant improvement in ADHD symptoms, compared with placebo.
For this study, the second phase 3 trial of Azstarys, investigators analyzed data from 282 children aged 6-12 years in the United States, including 70 who participated in an earlier 1-month efficacy trial.
After screening and a 3-week dose-optimization phase for new participants, patients received once-daily treatment with doses of 26.1 mg/5.2 mg, 39.2 mg/7.8 mg, or 52.3 mg/10.4 mg of SDX/d-MPH.
After 1 year of treatment, 60.1% of participants reported at least one TEAE, the majority of which were moderate. Twelve patients reported severe TEAEs. Six children (2.5%) discontinued the study because of a TEAE during the treatment phase.
The investigators also measured growth and changes in sleep with the Children’s Sleep Habits Questionnaire during the 12-month study. Sleep improved on most measures and the impact on growth was mild.
There were no life-threatening TEAEs and no deaths reported during the study.
The most common TEAEs during the treatment phase were decreased appetite, upper respiratory tract infection, nasopharyngitis, decreased weight, irritability, and increased weight.
Efficacy at 1 year
ADHD symptoms improved considerably after 1 month of treatment, with responses continuing at 1 year.
At baseline, participants’ mean ADHD Rating Scale–5 score was 41.5. After 1 month of treatment, scores averaged 16.1, a decline of –25.3 (P < .001).
The mean score stabilized in the 12-15 range for the remainder of the study. After 1 year of treatment, ADHD symptoms had decreased approximately 70% from baseline.
Investigators found similar results in clinical severity. After 1 month of treatment, the average Clinical Global Impressions–Severity (CGI-S) scale score was 2.5, a decline of –2.2 (P < .0001).
CGI-S scale scores remained in the 2.2-2.4 range for the remainder of the study.
These results, combined with the results of the original classroom trial, suggest Azstarys may offer advantages over other ADHD drugs, Dr. Childress said.
“In the laboratory classroom trial, subjects taking Azstarys completed significantly more math problems than subjects taking placebo beginning at 30 minutes and up to 13 hours after dosing,” Dr. Childress said. “No other methylphenidate extended-release product currently marketed in the United States has a 13-hour duration of effect.”
‘Reassuring data’
Commenting on the findings, Aditya Pawar, MD, a child and adolescent psychiatrist with the Kennedy Krieger Institute and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, said that the study suggests the drug may be a valuable addition to ADHD treatment options for pediatric patients.
“The study provides reassuring data on the safety of stimulants in patients without significant history of cardiac events or blood pressure changes, which are usual concerns among patients and clinicians despite the evidence supporting safety, said Dr. Pawar, who was not part of the study.
“Additionally, the 1-year data on efficacy and safety of a new stimulant medication is valuable for clinicians looking for sustained relief for their patients, despite the limitations of an open-label trial,” she added.
Overall, the safety data reported in the study are fairly consistent with the safety profile of other methylphenidates used for treating ADHD, Dr. Pawar said.
However, she noted, the study does have some limitations, including its open-label design and lack of blinding. The research also excluded children with autism, disruptive mood dysregulation disorders, and other common comorbidities of ADHD, which may limit the generalizability of the results.
“These comorbidities often require stimulants as a part of treatment, and yet have a higher risk of side effects,” Dr. Pawar said. “Future studies with a broader population may be needed to better understand treatment effectiveness and potential risks.”
The study was funded by KemPharm. Dr. Childress serves as consultant for Aardvark, Arbor, Attentive, Cingulate, Ironshore, Neos Therapeutics, Neurocentria, Otsuka, Purdue, Rhodes, Sunovion, Tris Pharma, KemPharm, Supernus, Jazz, Corium, Tulex, and Lumos.
A version of this article first appeared on Medscape.com.
new research shows.
Results from a phase 3, multicenter, dose-optimization, open-label safety study of Azstarys (KemPharm) found that most treatment-emergent adverse events (TEAEs) were mild to moderate.
“This data show that Azstarys remains safe and effective for the treatment of ADHD when given for up to a year,” lead investigator Ann Childress, MD, president of the Center for Psychiatry and Behavioral Medicine, Las Vegas, said in an interview.
The study was published online in the Journal of Child and Adolescent Psychopharmacology.
Safety at 1 year
The drug is a combination of extended-release serdexmethylphenidate (SDX), KemPharm’s prodrug of dexmethylphenidate, coformulated with immediate-release d-MPH.
SDX is converted to d-MPH after it is absorbed in the gastrointestinal tract. The d-MPH is released gradually throughout the day, providing quick symptom control with the d-MPH and extended control with SDX.
Azstarys was approved by the Food and Drug Administration in 2021 on the basis of results from a laboratory classroom phase 3 trial, which showed significant improvement in ADHD symptoms, compared with placebo.
For this study, the second phase 3 trial of Azstarys, investigators analyzed data from 282 children aged 6-12 years in the United States, including 70 who participated in an earlier 1-month efficacy trial.
After screening and a 3-week dose-optimization phase for new participants, patients received once-daily treatment with doses of 26.1 mg/5.2 mg, 39.2 mg/7.8 mg, or 52.3 mg/10.4 mg of SDX/d-MPH.
After 1 year of treatment, 60.1% of participants reported at least one TEAE, the majority of which were moderate. Twelve patients reported severe TEAEs. Six children (2.5%) discontinued the study because of a TEAE during the treatment phase.
The investigators also measured growth and changes in sleep with the Children’s Sleep Habits Questionnaire during the 12-month study. Sleep improved on most measures and the impact on growth was mild.
There were no life-threatening TEAEs and no deaths reported during the study.
The most common TEAEs during the treatment phase were decreased appetite, upper respiratory tract infection, nasopharyngitis, decreased weight, irritability, and increased weight.
Efficacy at 1 year
ADHD symptoms improved considerably after 1 month of treatment, with responses continuing at 1 year.
At baseline, participants’ mean ADHD Rating Scale–5 score was 41.5. After 1 month of treatment, scores averaged 16.1, a decline of –25.3 (P < .001).
The mean score stabilized in the 12-15 range for the remainder of the study. After 1 year of treatment, ADHD symptoms had decreased approximately 70% from baseline.
Investigators found similar results in clinical severity. After 1 month of treatment, the average Clinical Global Impressions–Severity (CGI-S) scale score was 2.5, a decline of –2.2 (P < .0001).
CGI-S scale scores remained in the 2.2-2.4 range for the remainder of the study.
These results, combined with the results of the original classroom trial, suggest Azstarys may offer advantages over other ADHD drugs, Dr. Childress said.
“In the laboratory classroom trial, subjects taking Azstarys completed significantly more math problems than subjects taking placebo beginning at 30 minutes and up to 13 hours after dosing,” Dr. Childress said. “No other methylphenidate extended-release product currently marketed in the United States has a 13-hour duration of effect.”
‘Reassuring data’
Commenting on the findings, Aditya Pawar, MD, a child and adolescent psychiatrist with the Kennedy Krieger Institute and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, said that the study suggests the drug may be a valuable addition to ADHD treatment options for pediatric patients.
“The study provides reassuring data on the safety of stimulants in patients without significant history of cardiac events or blood pressure changes, which are usual concerns among patients and clinicians despite the evidence supporting safety, said Dr. Pawar, who was not part of the study.
“Additionally, the 1-year data on efficacy and safety of a new stimulant medication is valuable for clinicians looking for sustained relief for their patients, despite the limitations of an open-label trial,” she added.
Overall, the safety data reported in the study are fairly consistent with the safety profile of other methylphenidates used for treating ADHD, Dr. Pawar said.
However, she noted, the study does have some limitations, including its open-label design and lack of blinding. The research also excluded children with autism, disruptive mood dysregulation disorders, and other common comorbidities of ADHD, which may limit the generalizability of the results.
“These comorbidities often require stimulants as a part of treatment, and yet have a higher risk of side effects,” Dr. Pawar said. “Future studies with a broader population may be needed to better understand treatment effectiveness and potential risks.”
The study was funded by KemPharm. Dr. Childress serves as consultant for Aardvark, Arbor, Attentive, Cingulate, Ironshore, Neos Therapeutics, Neurocentria, Otsuka, Purdue, Rhodes, Sunovion, Tris Pharma, KemPharm, Supernus, Jazz, Corium, Tulex, and Lumos.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CHILD AND ADOLESCENT PSYCHOPHARMACOLOGY
Who can sue docs for wrongful death? Some states are trying to expand that group
In addition, the types of emotional damage that physicians can be sued for is expanding in pockets across the nation. The latest effort to expand the capacity to sue, a bill in New York state, failed when it was not signed by the governor – but a toned-down bill is in the works.
The impact of New York’s proposed expansion of wrongful death lawsuits would have been widespread. The New York legislation would have expanded the definition of “close family members” to include spouses, domestic partners, children, parents, stepparents, siblings, grandparents, and perhaps more. Additionally, lawsuits could have allowed juries to determine “close family members” of the deceased patient on the basis of specific circumstances of the person’s relationship with the decedent.
Currently, every state allows a wrongful death claim to be filed by immediate family members. If the patient who died was married, a surviving spouse could bring the lawsuit. If the patient had been unmarried, an adult child could bring the lawsuit in some states. A parent typically brings a lawsuit if their minor child has died from alleged wrongful death. In some states, one member of a civil union or domestic partnership may bring a wrongful death lawsuit. And if a single adult has no children or spouse/partner, more distant family members, including aunts, uncles, siblings, or grandparents, may file the suit.
The New York bill would also have expanded compensable damages to include loss of affection and companionship, and it would have expanded emotional damages, which are not currently included in New York. It would also have extended the statute of limitations of a wrongful death claim from 2 years to 3.5 years.
In general, in states that allow emotional distress to be included in wrongful death lawsuits, attorneys must demonstrate that survivors have suffered mental harm, such as depression, loss of sleep, fear, and anger, says Russ Haven, JD, general counsel for the New York Public Interest Research Group. While mental harm is not particularly easy to prove, attorneys must show that survivors have ongoing distress that is the direct result of the loss of the loved one and that the distress is significant enough to severely affect their quality of life.
Mr. Haven gives an example of emotional distress: “We worked with a woman who lost her fiancé in a motor vehicle accident,” he says. “The funeral ended up on the day she had scheduled her wedding dress fitting. A situation like that causes a good deal of lasting emotional distress.”
Expanding family members who can bring the lawsuit
The fact that a fiancé could be included in a wrongful death settlement is another aspect of the New York bill that was central to arguments both for and against the expansion of family members who can make claims. “We think a modern society includes unmarried partners, grandparents, siblings, and others,” says Mr. Haven.
“The language of who is a close family member might seem clear, but to a defense attorney, it isn’t,” says Tom Stebbins, executive director of the Lawsuit Reform Alliance of New York. “This could end up being a situation where someone has 40 grandchildren, and all could be considered close family members.”
Many states currently allow damages for claims of grief and mental anguish resulting from a wrongful death.
In her recent veto of the Grieving Families Act, New York Gov. Kathy Hochul took fire for her choices. The bill represented years of effort by the state legislature to expand the qualifiers for wrongful death lawsuits. Those supporting what ultimately became Senate Bill S74A believed they finally had the law over the finish line. Those opposed breathed a sigh of relief when the bill was vetoed.
Had Gov. Hochul signed Bill 274A, the effect on costs would have been enormous for physicians. New York already has the highest cumulative medical liability payouts in the nation, according to the Medical Society of the State of New York.
The MSSNY was among many parties that fought against the law. The Greater New York Hospital Association, insurance companies, the Defense Association of New York, and the New York Conference of Mayors all joined in lobbying against the bill.
“Gov. Hochul, in her veto message, correctly noted that the proposed New York legislation represented an extraordinary departure from New York’s wrongful death jurisprudence,” says Remi Stone, director of government relations at The Doctors Company, part of the TDC Group. “I would add that while there are some other states that allow grief damages, none are as wide-ranging as the proposed legislation.”
The NYPIRG, the AARP, and the New York Immigration Coalition supported the bill. In a statement following the veto, the New York State Trial Lawyers Association said: “By vetoing the Grieving Families Act, Gov. Hochul has sided with insurance companies, the health care industry, big corporations, and anyone else who doesn’t want to be held accountable for the negligent killing of a person. This bill passed with overwhelming bipartisan support and would rectify over a century of injustice.”
Following Gov. Hochul’s veto, the bill’s proponents and the state legislature vowed to return to the drawing board and construct a bill that the governor would eventually approve. For now, however, the controversial legislation has been put to rest.
Mr. Haven and the NYPIRG argue that New York lags behind many other states in allowing survivors to claim loss for their emotional distress. “When there is relationship loss, it has a great impact on your life,” Mr. Haven says, “and this goes beyond simply the financial impact.”
“The bill was well intended but completely vague on who could bring lawsuits and would have increased medical malpractice insurance by far too much,” says MSSNY President Parag Mehta, MD. “For safety net hospitals, one lawsuit would halt their ability to provide many programs aimed at underserved populations.”
Peter Kolbert, JD, senior vice president of claim and litigation services at Healthcare Risk Advisors (part of the TDC Group), had this to say: “The current ‘recoverable’ damages in New York in a wrongful death case include loss of guidance and support for minor children of a decedent. Those damages have been sustained at $2 million per child. It is rationally very challenging, if not impossible, to distinguish between those damages and the proposed damages that the very same people would have been entitled to under the proposed statute.”
What will happen in the future?
While the veto has stalled New York’s wrongful death expansion for now, supporters in and out of the legislature remain determined to continue their fight. “Advocates argue that the bill would have brought the state in line with wrongful death law in others,” says Brian Whitelaw, JD, a partner at Michigan’s Foley, Baron, Metzger & Juip. “But if the bill had become law as written, the economic impact would have been substantial.”
Mr. Whitelaw says that such wide-ranging lawsuits can have consequences that extend far beyond physicians’ insurance premiums. “This could impact the average person on the street’s ability to obtain the medical care they need, because doctors will go elsewhere to practice,” he says. “Beyond impacting the health care system, it can hurt small businesses as well.”
Mr. Haven says supporters of the expansion are far from finished with their efforts. “New York’s current law dates back to 1847, and it was cutting edge then,” he says. “It was designed for an agrarian society where if the husband died, his widow and children wouldn’t become destitute. Now, 175 years later, we realize that the law has biases, and tort law has evolved. The state needs to evolve as well.”
For his part, Dr. Mehta is open to a dialogue with lawmakers to revise the law in a manner agreeable to all parties. “We want to work together to make the system right,” he says. “The liability system in New York needs an overall holistic change, and we are available at any time to have discussions. The vetoed bill was a Band-Aid and didn’t address the main, underlying issues in the state.”
Mr. Stebbins, too, says he would like to continue the debate over how an expansion should look. “We hope to go through a discussion on caps to these suits,” he explains. “We have already seen the cap of $10 million broken four times in the past few years through nuclear verdicts. That’s something we need to address.”
Given the legislature’s overwhelming support for the bill, some version of it will likely make another appearance in the coming session. Whether or not it can strike the middle ground that will make all parties happy – including the governor – is yet to be seen. “Is it wrong to seek compensation for pain and suffering from a wrongful death?” asks Mr. Whitelaw. “No. But there must be limits to such laws, or where does it end?”
A version of this article first appeared on Medscape.com.
In addition, the types of emotional damage that physicians can be sued for is expanding in pockets across the nation. The latest effort to expand the capacity to sue, a bill in New York state, failed when it was not signed by the governor – but a toned-down bill is in the works.
The impact of New York’s proposed expansion of wrongful death lawsuits would have been widespread. The New York legislation would have expanded the definition of “close family members” to include spouses, domestic partners, children, parents, stepparents, siblings, grandparents, and perhaps more. Additionally, lawsuits could have allowed juries to determine “close family members” of the deceased patient on the basis of specific circumstances of the person’s relationship with the decedent.
Currently, every state allows a wrongful death claim to be filed by immediate family members. If the patient who died was married, a surviving spouse could bring the lawsuit. If the patient had been unmarried, an adult child could bring the lawsuit in some states. A parent typically brings a lawsuit if their minor child has died from alleged wrongful death. In some states, one member of a civil union or domestic partnership may bring a wrongful death lawsuit. And if a single adult has no children or spouse/partner, more distant family members, including aunts, uncles, siblings, or grandparents, may file the suit.
The New York bill would also have expanded compensable damages to include loss of affection and companionship, and it would have expanded emotional damages, which are not currently included in New York. It would also have extended the statute of limitations of a wrongful death claim from 2 years to 3.5 years.
In general, in states that allow emotional distress to be included in wrongful death lawsuits, attorneys must demonstrate that survivors have suffered mental harm, such as depression, loss of sleep, fear, and anger, says Russ Haven, JD, general counsel for the New York Public Interest Research Group. While mental harm is not particularly easy to prove, attorneys must show that survivors have ongoing distress that is the direct result of the loss of the loved one and that the distress is significant enough to severely affect their quality of life.
Mr. Haven gives an example of emotional distress: “We worked with a woman who lost her fiancé in a motor vehicle accident,” he says. “The funeral ended up on the day she had scheduled her wedding dress fitting. A situation like that causes a good deal of lasting emotional distress.”
Expanding family members who can bring the lawsuit
The fact that a fiancé could be included in a wrongful death settlement is another aspect of the New York bill that was central to arguments both for and against the expansion of family members who can make claims. “We think a modern society includes unmarried partners, grandparents, siblings, and others,” says Mr. Haven.
“The language of who is a close family member might seem clear, but to a defense attorney, it isn’t,” says Tom Stebbins, executive director of the Lawsuit Reform Alliance of New York. “This could end up being a situation where someone has 40 grandchildren, and all could be considered close family members.”
Many states currently allow damages for claims of grief and mental anguish resulting from a wrongful death.
In her recent veto of the Grieving Families Act, New York Gov. Kathy Hochul took fire for her choices. The bill represented years of effort by the state legislature to expand the qualifiers for wrongful death lawsuits. Those supporting what ultimately became Senate Bill S74A believed they finally had the law over the finish line. Those opposed breathed a sigh of relief when the bill was vetoed.
Had Gov. Hochul signed Bill 274A, the effect on costs would have been enormous for physicians. New York already has the highest cumulative medical liability payouts in the nation, according to the Medical Society of the State of New York.
The MSSNY was among many parties that fought against the law. The Greater New York Hospital Association, insurance companies, the Defense Association of New York, and the New York Conference of Mayors all joined in lobbying against the bill.
“Gov. Hochul, in her veto message, correctly noted that the proposed New York legislation represented an extraordinary departure from New York’s wrongful death jurisprudence,” says Remi Stone, director of government relations at The Doctors Company, part of the TDC Group. “I would add that while there are some other states that allow grief damages, none are as wide-ranging as the proposed legislation.”
The NYPIRG, the AARP, and the New York Immigration Coalition supported the bill. In a statement following the veto, the New York State Trial Lawyers Association said: “By vetoing the Grieving Families Act, Gov. Hochul has sided with insurance companies, the health care industry, big corporations, and anyone else who doesn’t want to be held accountable for the negligent killing of a person. This bill passed with overwhelming bipartisan support and would rectify over a century of injustice.”
Following Gov. Hochul’s veto, the bill’s proponents and the state legislature vowed to return to the drawing board and construct a bill that the governor would eventually approve. For now, however, the controversial legislation has been put to rest.
Mr. Haven and the NYPIRG argue that New York lags behind many other states in allowing survivors to claim loss for their emotional distress. “When there is relationship loss, it has a great impact on your life,” Mr. Haven says, “and this goes beyond simply the financial impact.”
“The bill was well intended but completely vague on who could bring lawsuits and would have increased medical malpractice insurance by far too much,” says MSSNY President Parag Mehta, MD. “For safety net hospitals, one lawsuit would halt their ability to provide many programs aimed at underserved populations.”
Peter Kolbert, JD, senior vice president of claim and litigation services at Healthcare Risk Advisors (part of the TDC Group), had this to say: “The current ‘recoverable’ damages in New York in a wrongful death case include loss of guidance and support for minor children of a decedent. Those damages have been sustained at $2 million per child. It is rationally very challenging, if not impossible, to distinguish between those damages and the proposed damages that the very same people would have been entitled to under the proposed statute.”
What will happen in the future?
While the veto has stalled New York’s wrongful death expansion for now, supporters in and out of the legislature remain determined to continue their fight. “Advocates argue that the bill would have brought the state in line with wrongful death law in others,” says Brian Whitelaw, JD, a partner at Michigan’s Foley, Baron, Metzger & Juip. “But if the bill had become law as written, the economic impact would have been substantial.”
Mr. Whitelaw says that such wide-ranging lawsuits can have consequences that extend far beyond physicians’ insurance premiums. “This could impact the average person on the street’s ability to obtain the medical care they need, because doctors will go elsewhere to practice,” he says. “Beyond impacting the health care system, it can hurt small businesses as well.”
Mr. Haven says supporters of the expansion are far from finished with their efforts. “New York’s current law dates back to 1847, and it was cutting edge then,” he says. “It was designed for an agrarian society where if the husband died, his widow and children wouldn’t become destitute. Now, 175 years later, we realize that the law has biases, and tort law has evolved. The state needs to evolve as well.”
For his part, Dr. Mehta is open to a dialogue with lawmakers to revise the law in a manner agreeable to all parties. “We want to work together to make the system right,” he says. “The liability system in New York needs an overall holistic change, and we are available at any time to have discussions. The vetoed bill was a Band-Aid and didn’t address the main, underlying issues in the state.”
Mr. Stebbins, too, says he would like to continue the debate over how an expansion should look. “We hope to go through a discussion on caps to these suits,” he explains. “We have already seen the cap of $10 million broken four times in the past few years through nuclear verdicts. That’s something we need to address.”
Given the legislature’s overwhelming support for the bill, some version of it will likely make another appearance in the coming session. Whether or not it can strike the middle ground that will make all parties happy – including the governor – is yet to be seen. “Is it wrong to seek compensation for pain and suffering from a wrongful death?” asks Mr. Whitelaw. “No. But there must be limits to such laws, or where does it end?”
A version of this article first appeared on Medscape.com.
In addition, the types of emotional damage that physicians can be sued for is expanding in pockets across the nation. The latest effort to expand the capacity to sue, a bill in New York state, failed when it was not signed by the governor – but a toned-down bill is in the works.
The impact of New York’s proposed expansion of wrongful death lawsuits would have been widespread. The New York legislation would have expanded the definition of “close family members” to include spouses, domestic partners, children, parents, stepparents, siblings, grandparents, and perhaps more. Additionally, lawsuits could have allowed juries to determine “close family members” of the deceased patient on the basis of specific circumstances of the person’s relationship with the decedent.
Currently, every state allows a wrongful death claim to be filed by immediate family members. If the patient who died was married, a surviving spouse could bring the lawsuit. If the patient had been unmarried, an adult child could bring the lawsuit in some states. A parent typically brings a lawsuit if their minor child has died from alleged wrongful death. In some states, one member of a civil union or domestic partnership may bring a wrongful death lawsuit. And if a single adult has no children or spouse/partner, more distant family members, including aunts, uncles, siblings, or grandparents, may file the suit.
The New York bill would also have expanded compensable damages to include loss of affection and companionship, and it would have expanded emotional damages, which are not currently included in New York. It would also have extended the statute of limitations of a wrongful death claim from 2 years to 3.5 years.
In general, in states that allow emotional distress to be included in wrongful death lawsuits, attorneys must demonstrate that survivors have suffered mental harm, such as depression, loss of sleep, fear, and anger, says Russ Haven, JD, general counsel for the New York Public Interest Research Group. While mental harm is not particularly easy to prove, attorneys must show that survivors have ongoing distress that is the direct result of the loss of the loved one and that the distress is significant enough to severely affect their quality of life.
Mr. Haven gives an example of emotional distress: “We worked with a woman who lost her fiancé in a motor vehicle accident,” he says. “The funeral ended up on the day she had scheduled her wedding dress fitting. A situation like that causes a good deal of lasting emotional distress.”
Expanding family members who can bring the lawsuit
The fact that a fiancé could be included in a wrongful death settlement is another aspect of the New York bill that was central to arguments both for and against the expansion of family members who can make claims. “We think a modern society includes unmarried partners, grandparents, siblings, and others,” says Mr. Haven.
“The language of who is a close family member might seem clear, but to a defense attorney, it isn’t,” says Tom Stebbins, executive director of the Lawsuit Reform Alliance of New York. “This could end up being a situation where someone has 40 grandchildren, and all could be considered close family members.”
Many states currently allow damages for claims of grief and mental anguish resulting from a wrongful death.
In her recent veto of the Grieving Families Act, New York Gov. Kathy Hochul took fire for her choices. The bill represented years of effort by the state legislature to expand the qualifiers for wrongful death lawsuits. Those supporting what ultimately became Senate Bill S74A believed they finally had the law over the finish line. Those opposed breathed a sigh of relief when the bill was vetoed.
Had Gov. Hochul signed Bill 274A, the effect on costs would have been enormous for physicians. New York already has the highest cumulative medical liability payouts in the nation, according to the Medical Society of the State of New York.
The MSSNY was among many parties that fought against the law. The Greater New York Hospital Association, insurance companies, the Defense Association of New York, and the New York Conference of Mayors all joined in lobbying against the bill.
“Gov. Hochul, in her veto message, correctly noted that the proposed New York legislation represented an extraordinary departure from New York’s wrongful death jurisprudence,” says Remi Stone, director of government relations at The Doctors Company, part of the TDC Group. “I would add that while there are some other states that allow grief damages, none are as wide-ranging as the proposed legislation.”
The NYPIRG, the AARP, and the New York Immigration Coalition supported the bill. In a statement following the veto, the New York State Trial Lawyers Association said: “By vetoing the Grieving Families Act, Gov. Hochul has sided with insurance companies, the health care industry, big corporations, and anyone else who doesn’t want to be held accountable for the negligent killing of a person. This bill passed with overwhelming bipartisan support and would rectify over a century of injustice.”
Following Gov. Hochul’s veto, the bill’s proponents and the state legislature vowed to return to the drawing board and construct a bill that the governor would eventually approve. For now, however, the controversial legislation has been put to rest.
Mr. Haven and the NYPIRG argue that New York lags behind many other states in allowing survivors to claim loss for their emotional distress. “When there is relationship loss, it has a great impact on your life,” Mr. Haven says, “and this goes beyond simply the financial impact.”
“The bill was well intended but completely vague on who could bring lawsuits and would have increased medical malpractice insurance by far too much,” says MSSNY President Parag Mehta, MD. “For safety net hospitals, one lawsuit would halt their ability to provide many programs aimed at underserved populations.”
Peter Kolbert, JD, senior vice president of claim and litigation services at Healthcare Risk Advisors (part of the TDC Group), had this to say: “The current ‘recoverable’ damages in New York in a wrongful death case include loss of guidance and support for minor children of a decedent. Those damages have been sustained at $2 million per child. It is rationally very challenging, if not impossible, to distinguish between those damages and the proposed damages that the very same people would have been entitled to under the proposed statute.”
What will happen in the future?
While the veto has stalled New York’s wrongful death expansion for now, supporters in and out of the legislature remain determined to continue their fight. “Advocates argue that the bill would have brought the state in line with wrongful death law in others,” says Brian Whitelaw, JD, a partner at Michigan’s Foley, Baron, Metzger & Juip. “But if the bill had become law as written, the economic impact would have been substantial.”
Mr. Whitelaw says that such wide-ranging lawsuits can have consequences that extend far beyond physicians’ insurance premiums. “This could impact the average person on the street’s ability to obtain the medical care they need, because doctors will go elsewhere to practice,” he says. “Beyond impacting the health care system, it can hurt small businesses as well.”
Mr. Haven says supporters of the expansion are far from finished with their efforts. “New York’s current law dates back to 1847, and it was cutting edge then,” he says. “It was designed for an agrarian society where if the husband died, his widow and children wouldn’t become destitute. Now, 175 years later, we realize that the law has biases, and tort law has evolved. The state needs to evolve as well.”
For his part, Dr. Mehta is open to a dialogue with lawmakers to revise the law in a manner agreeable to all parties. “We want to work together to make the system right,” he says. “The liability system in New York needs an overall holistic change, and we are available at any time to have discussions. The vetoed bill was a Band-Aid and didn’t address the main, underlying issues in the state.”
Mr. Stebbins, too, says he would like to continue the debate over how an expansion should look. “We hope to go through a discussion on caps to these suits,” he explains. “We have already seen the cap of $10 million broken four times in the past few years through nuclear verdicts. That’s something we need to address.”
Given the legislature’s overwhelming support for the bill, some version of it will likely make another appearance in the coming session. Whether or not it can strike the middle ground that will make all parties happy – including the governor – is yet to be seen. “Is it wrong to seek compensation for pain and suffering from a wrongful death?” asks Mr. Whitelaw. “No. But there must be limits to such laws, or where does it end?”
A version of this article first appeared on Medscape.com.
‘Breakthrough’ study: Diabetes drug helps prevent long COVID
with The Lancet on SSRN. The preprint hasn’t yet been peer-reviewed or published in a journal.
In particular, metformin led to a 42% drop in long COVID among people who had a mild to moderate COVID-19 infection.
“Long COVID affects millions of people, and preventing long COVID through a treatment like metformin could prevent significant disruptions in people’s lives,” said lead author Carolyn Bramante, MD, assistant professor of internal medicine and pediatrics at the University of Minnesota, Minneapolis.
Between January 2021 and February 2022, Dr. Bramante and colleagues tested three oral medications – metformin (typically used to treat type 2 diabetes), ivermectin (an antiparasitic), and fluvoxamine (an antidepressant) – in a clinical trial across the United States called COVID-OUT. The people being studied, investigators, care providers, and others involved in the study were blinded to the randomized treatments. The trial was decentralized, with no in-person contact with participants.
The researchers included patients who were aged 30-85 with overweight or obesity, had documentation of a confirmed COVID-19 infection, had fewer than 7 days of symptoms, had no known prior infection, and joined the study within 3 days of their positive test. The study included monthly follow-up for 300 days, and participants indicated whether they received a long COVID diagnosis from a medical doctor, which the researchers confirmed in medical records after participants gave consent.
The medications were prepackaged into pill boxes for fast delivery to participants and to ensure they took the correct number of each type of pill. The packages were sent via same-day courier or overnight shipping.
The metformin doses were doled out over 14 days, with 500 milligrams on the first day, 500 milligrams twice a day for the next 4 days, and then 500 milligrams in the morning and 1,000 milligrams in the evening for the remaining 9 days.
Among the 1,323 people studied, 1,125 agreed to do long-term follow-up for long COVID: 564 in the metformin group and 561 in the blinded placebo group. The average age was 45, and 56% were women, including 7% who were pregnant.
The average time from the start of symptoms to starting medication was 5 days, and 47% began taking the drug within 4 days or less. About 55% had received the primary COVID-19 vaccination series, including 5.1% who received an initial booster, before enrolling in the study.
Overall, 8.4% of participants reported that a medical provider diagnosed them with long COVID. Of those who took metformin, 6.3% developed long COVID, compared to 10.6% among those who took the identical-matched placebo.
The risk reduction for metformin was 42% versus the placebo, which was consistent across subgroups, including vaccination status and different COVID-19 variants.
When metformin was started less than 4 days after COVID-19 symptoms started, the effect was potentially even greater, with a 64% reduction, as compared with a 36% reduction among those who started metformin after 4 or more days after symptoms.
Neither ivermectin nor fluvoxamine showed any benefits for preventing long COVID.
At the same time, the study authors caution that more research is needed.
“The COVID-OUT trial does not indicate whether or not metformin would be effective at preventing long COVID if started at the time of emergency department visit or hospitalization for COVID-19, nor whether metformin would be effective as treatment in persons who already have long COVID,” they wrote. “With the burden of long COVID on society, confirmation is urgently needed in a trial that addresses our study’s limitations in order to translate these results into practice and policy.”
Several risk factors for long COVID emerged in the analysis. About 11.1% of the women had a long COVID diagnosis, compared with 4.9% of the men. Also, those who had received at least the primary vaccine series had a lower risk of developing long COVID, at 6.6%, as compared with 10.5% among the unvaccinated. Only 1 of the 57 people who received a booster shot developed long COVID.
Notably, pregnant and lactating people were included in this study, which is important given that pregnant people face higher risks for poor COVID-19 outcomes and are excluded from most nonobstetric clinical trials, the study authors wrote. In this study, they were randomized to metformin or placebo but not ivermectin or fluvoxamine due to limited research about the safety of those drugs during pregnancy and lactation.
The results are now under journal review but show findings consistent with those from other recent studies. Also, in August 2022, the authors published results from COVID-OUT that showed metformin led to a 42% reduction in hospital visits, emergency department visits, and deaths related to severe COVID-19.
“Given the lack of side effects and cost for a 2-week course, I think these data support use of metformin now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute and editor-in-chief of Medscape, WebMD’s sister site for health care professionals.
Dr. Topol, who wasn’t involved with this study, has been a leading voice on COVID-19 research throughout the pandemic. He noted the need for more studies, including a factorial design trial to test metformin and Paxlovid, which has shown promise in preventing long COVID. Dr. Topol also wrote about the preprint in Ground Truths, his online newsletter.
“As I’ve written in the past, I don’t use the term ‘breakthrough’ lightly,” he wrote. “But to see such a pronounced benefit in the current randomized trial of metformin, in the context of its being so safe and low cost, I’d give it a breakthrough categorization.”
Another way to put it, Dr. Topol wrote, is that based on this study, he would take metformin if he became infected with COVID-19.
Jeremy Faust, MD, an emergency medicine doctor at Brigham and Women’s Hospital in Boston, also wrote about the study in his newsletter, Inside Medicine. He noted that the 42% reduction in long COVID means that 23 COVID-19 patients need to be treated with metformin to prevent one long COVID diagnosis, which is an “important reduction.”
“Bottom line: If a person who meets criteria for obesity or overweight status were to ask me if they should take metformin (for 2 weeks) starting as soon as they learn they have COVID-19, I would say yes in many if not most cases, based on this new data,” he wrote. “This is starting to look like a real win.”
A version of this article first appeared on WebMD.com.
with The Lancet on SSRN. The preprint hasn’t yet been peer-reviewed or published in a journal.
In particular, metformin led to a 42% drop in long COVID among people who had a mild to moderate COVID-19 infection.
“Long COVID affects millions of people, and preventing long COVID through a treatment like metformin could prevent significant disruptions in people’s lives,” said lead author Carolyn Bramante, MD, assistant professor of internal medicine and pediatrics at the University of Minnesota, Minneapolis.
Between January 2021 and February 2022, Dr. Bramante and colleagues tested three oral medications – metformin (typically used to treat type 2 diabetes), ivermectin (an antiparasitic), and fluvoxamine (an antidepressant) – in a clinical trial across the United States called COVID-OUT. The people being studied, investigators, care providers, and others involved in the study were blinded to the randomized treatments. The trial was decentralized, with no in-person contact with participants.
The researchers included patients who were aged 30-85 with overweight or obesity, had documentation of a confirmed COVID-19 infection, had fewer than 7 days of symptoms, had no known prior infection, and joined the study within 3 days of their positive test. The study included monthly follow-up for 300 days, and participants indicated whether they received a long COVID diagnosis from a medical doctor, which the researchers confirmed in medical records after participants gave consent.
The medications were prepackaged into pill boxes for fast delivery to participants and to ensure they took the correct number of each type of pill. The packages were sent via same-day courier or overnight shipping.
The metformin doses were doled out over 14 days, with 500 milligrams on the first day, 500 milligrams twice a day for the next 4 days, and then 500 milligrams in the morning and 1,000 milligrams in the evening for the remaining 9 days.
Among the 1,323 people studied, 1,125 agreed to do long-term follow-up for long COVID: 564 in the metformin group and 561 in the blinded placebo group. The average age was 45, and 56% were women, including 7% who were pregnant.
The average time from the start of symptoms to starting medication was 5 days, and 47% began taking the drug within 4 days or less. About 55% had received the primary COVID-19 vaccination series, including 5.1% who received an initial booster, before enrolling in the study.
Overall, 8.4% of participants reported that a medical provider diagnosed them with long COVID. Of those who took metformin, 6.3% developed long COVID, compared to 10.6% among those who took the identical-matched placebo.
The risk reduction for metformin was 42% versus the placebo, which was consistent across subgroups, including vaccination status and different COVID-19 variants.
When metformin was started less than 4 days after COVID-19 symptoms started, the effect was potentially even greater, with a 64% reduction, as compared with a 36% reduction among those who started metformin after 4 or more days after symptoms.
Neither ivermectin nor fluvoxamine showed any benefits for preventing long COVID.
At the same time, the study authors caution that more research is needed.
“The COVID-OUT trial does not indicate whether or not metformin would be effective at preventing long COVID if started at the time of emergency department visit or hospitalization for COVID-19, nor whether metformin would be effective as treatment in persons who already have long COVID,” they wrote. “With the burden of long COVID on society, confirmation is urgently needed in a trial that addresses our study’s limitations in order to translate these results into practice and policy.”
Several risk factors for long COVID emerged in the analysis. About 11.1% of the women had a long COVID diagnosis, compared with 4.9% of the men. Also, those who had received at least the primary vaccine series had a lower risk of developing long COVID, at 6.6%, as compared with 10.5% among the unvaccinated. Only 1 of the 57 people who received a booster shot developed long COVID.
Notably, pregnant and lactating people were included in this study, which is important given that pregnant people face higher risks for poor COVID-19 outcomes and are excluded from most nonobstetric clinical trials, the study authors wrote. In this study, they were randomized to metformin or placebo but not ivermectin or fluvoxamine due to limited research about the safety of those drugs during pregnancy and lactation.
The results are now under journal review but show findings consistent with those from other recent studies. Also, in August 2022, the authors published results from COVID-OUT that showed metformin led to a 42% reduction in hospital visits, emergency department visits, and deaths related to severe COVID-19.
“Given the lack of side effects and cost for a 2-week course, I think these data support use of metformin now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute and editor-in-chief of Medscape, WebMD’s sister site for health care professionals.
Dr. Topol, who wasn’t involved with this study, has been a leading voice on COVID-19 research throughout the pandemic. He noted the need for more studies, including a factorial design trial to test metformin and Paxlovid, which has shown promise in preventing long COVID. Dr. Topol also wrote about the preprint in Ground Truths, his online newsletter.
“As I’ve written in the past, I don’t use the term ‘breakthrough’ lightly,” he wrote. “But to see such a pronounced benefit in the current randomized trial of metformin, in the context of its being so safe and low cost, I’d give it a breakthrough categorization.”
Another way to put it, Dr. Topol wrote, is that based on this study, he would take metformin if he became infected with COVID-19.
Jeremy Faust, MD, an emergency medicine doctor at Brigham and Women’s Hospital in Boston, also wrote about the study in his newsletter, Inside Medicine. He noted that the 42% reduction in long COVID means that 23 COVID-19 patients need to be treated with metformin to prevent one long COVID diagnosis, which is an “important reduction.”
“Bottom line: If a person who meets criteria for obesity or overweight status were to ask me if they should take metformin (for 2 weeks) starting as soon as they learn they have COVID-19, I would say yes in many if not most cases, based on this new data,” he wrote. “This is starting to look like a real win.”
A version of this article first appeared on WebMD.com.
with The Lancet on SSRN. The preprint hasn’t yet been peer-reviewed or published in a journal.
In particular, metformin led to a 42% drop in long COVID among people who had a mild to moderate COVID-19 infection.
“Long COVID affects millions of people, and preventing long COVID through a treatment like metformin could prevent significant disruptions in people’s lives,” said lead author Carolyn Bramante, MD, assistant professor of internal medicine and pediatrics at the University of Minnesota, Minneapolis.
Between January 2021 and February 2022, Dr. Bramante and colleagues tested three oral medications – metformin (typically used to treat type 2 diabetes), ivermectin (an antiparasitic), and fluvoxamine (an antidepressant) – in a clinical trial across the United States called COVID-OUT. The people being studied, investigators, care providers, and others involved in the study were blinded to the randomized treatments. The trial was decentralized, with no in-person contact with participants.
The researchers included patients who were aged 30-85 with overweight or obesity, had documentation of a confirmed COVID-19 infection, had fewer than 7 days of symptoms, had no known prior infection, and joined the study within 3 days of their positive test. The study included monthly follow-up for 300 days, and participants indicated whether they received a long COVID diagnosis from a medical doctor, which the researchers confirmed in medical records after participants gave consent.
The medications were prepackaged into pill boxes for fast delivery to participants and to ensure they took the correct number of each type of pill. The packages were sent via same-day courier or overnight shipping.
The metformin doses were doled out over 14 days, with 500 milligrams on the first day, 500 milligrams twice a day for the next 4 days, and then 500 milligrams in the morning and 1,000 milligrams in the evening for the remaining 9 days.
Among the 1,323 people studied, 1,125 agreed to do long-term follow-up for long COVID: 564 in the metformin group and 561 in the blinded placebo group. The average age was 45, and 56% were women, including 7% who were pregnant.
The average time from the start of symptoms to starting medication was 5 days, and 47% began taking the drug within 4 days or less. About 55% had received the primary COVID-19 vaccination series, including 5.1% who received an initial booster, before enrolling in the study.
Overall, 8.4% of participants reported that a medical provider diagnosed them with long COVID. Of those who took metformin, 6.3% developed long COVID, compared to 10.6% among those who took the identical-matched placebo.
The risk reduction for metformin was 42% versus the placebo, which was consistent across subgroups, including vaccination status and different COVID-19 variants.
When metformin was started less than 4 days after COVID-19 symptoms started, the effect was potentially even greater, with a 64% reduction, as compared with a 36% reduction among those who started metformin after 4 or more days after symptoms.
Neither ivermectin nor fluvoxamine showed any benefits for preventing long COVID.
At the same time, the study authors caution that more research is needed.
“The COVID-OUT trial does not indicate whether or not metformin would be effective at preventing long COVID if started at the time of emergency department visit or hospitalization for COVID-19, nor whether metformin would be effective as treatment in persons who already have long COVID,” they wrote. “With the burden of long COVID on society, confirmation is urgently needed in a trial that addresses our study’s limitations in order to translate these results into practice and policy.”
Several risk factors for long COVID emerged in the analysis. About 11.1% of the women had a long COVID diagnosis, compared with 4.9% of the men. Also, those who had received at least the primary vaccine series had a lower risk of developing long COVID, at 6.6%, as compared with 10.5% among the unvaccinated. Only 1 of the 57 people who received a booster shot developed long COVID.
Notably, pregnant and lactating people were included in this study, which is important given that pregnant people face higher risks for poor COVID-19 outcomes and are excluded from most nonobstetric clinical trials, the study authors wrote. In this study, they were randomized to metformin or placebo but not ivermectin or fluvoxamine due to limited research about the safety of those drugs during pregnancy and lactation.
The results are now under journal review but show findings consistent with those from other recent studies. Also, in August 2022, the authors published results from COVID-OUT that showed metformin led to a 42% reduction in hospital visits, emergency department visits, and deaths related to severe COVID-19.
“Given the lack of side effects and cost for a 2-week course, I think these data support use of metformin now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute and editor-in-chief of Medscape, WebMD’s sister site for health care professionals.
Dr. Topol, who wasn’t involved with this study, has been a leading voice on COVID-19 research throughout the pandemic. He noted the need for more studies, including a factorial design trial to test metformin and Paxlovid, which has shown promise in preventing long COVID. Dr. Topol also wrote about the preprint in Ground Truths, his online newsletter.
“As I’ve written in the past, I don’t use the term ‘breakthrough’ lightly,” he wrote. “But to see such a pronounced benefit in the current randomized trial of metformin, in the context of its being so safe and low cost, I’d give it a breakthrough categorization.”
Another way to put it, Dr. Topol wrote, is that based on this study, he would take metformin if he became infected with COVID-19.
Jeremy Faust, MD, an emergency medicine doctor at Brigham and Women’s Hospital in Boston, also wrote about the study in his newsletter, Inside Medicine. He noted that the 42% reduction in long COVID means that 23 COVID-19 patients need to be treated with metformin to prevent one long COVID diagnosis, which is an “important reduction.”
“Bottom line: If a person who meets criteria for obesity or overweight status were to ask me if they should take metformin (for 2 weeks) starting as soon as they learn they have COVID-19, I would say yes in many if not most cases, based on this new data,” he wrote. “This is starting to look like a real win.”
A version of this article first appeared on WebMD.com.
The triple overlap: COPD-OSA-OHS. Is it time for new definitions?
In our current society, it is likely that the “skinny patient with COPD” who walks into your clinic is less and less your “traditional” patient with COPD. We are seeing in our health care systems more of the “blue bloaters” – patients with COPD and significant obesity. This phenotype is representing what we are seeing worldwide as a consequence of the rising obesity prevalence. In the United States, the prepandemic (2017-2020) estimated percentage of adults over the age of 40 with obesity, defined as a body mass index (BMI) of at least 30 kg/m2, was over 40%. Moreover, the estimated percentage of adults with morbid obesity (BMI at least 40 kg/m2) is close to 10% (Akinbami, LJ et al. Vital Health Stat. 2022:190:1-36) and trending up. These patients with the “triple overlap” of morbid obesity, COPD, and awake daytime hypercapnia are being seen in clinics and in-hospital settings with increasing frequency, often presenting with complicating comorbidities such as acute respiratory failure, acute heart failure, kidney disease, or pulmonary hypertension. We are now faced with managing these patients with complex disease.
The obesity paradox does not seem applicable in the triple overlap phenotype. Patients with COPD who are overweight, defined as “mild obesity,” have lower mortality when compared with normal weight and underweight patients with COPD; however, this effect diminishes when BMI increases beyond 32 kg/m2. With increasing obesity severity and aging, the risk of both obstructive sleep apnea (OSA) and hypoventilation increases. It is well documented that COPD-OSA overlap is linked to worse outcomes and that continuous positive airway pressure (CPAP) as first-line therapy decreases readmission rates and mortality. The pathophysiology of hypoventilation in obesity is complex and multifactorial, and, although significant overlaps likely exist with comorbid COPD, by current definitions, to establish a diagnosis of obesity hypoventilation syndrome (OHS), one must have excluded other causes of hypoventilation, such as COPD.
These patients with the triple overlap of morbid obesity, awake daytime hypercapnia, and COPD are the subset of patients that providers struggle to fit in a diagnosis or in clinical research trials.
The triple overlap is a distinct syndrome
Different labels have been used in the medical literature: hypercapnic OSA-COPD overlap, morbid obesity and OSA-COPD overlap, hypercapnic morbidly obese COPD and OHS-COPD overlap. A better characterization of this distinctive phenotype is much needed. Patients with OSA-COPD overlap, for example, have an increased propensity to develop hypercapnia at higher FEV1 when compared with COPD without OSA – but this is thought to be a consequence of prolonged and frequent apneas and hypopneas compounded with obesity-related central hypoventilation. We found that morbidly obese patients with OSA-COPD overlap have a higher hypoxia burden, more severe OSA, and are frequently prescribed noninvasive ventilation after a failed titration polysomnogram (Htun ZM, et al. Am J Respir Crit Care Med. 2019;199:A1382), perhaps signaling a distinctive phenotype with worse outcomes, but the study had the inherent limitations of a single-center, retrospective design lacking data on awake hypercapnia. On the other side, the term OHS-COPD is contradictory and confusing based on current OHS diagnostic criteria.
In standardizing diagnostic criteria for patients with this triple overlap syndrome, challenges remain: would the patient with a BMI of 70 kg/m2 and fixed chronic airflow obstruction with FEV1 72% fall under the category of hypercapnic COPD vs OHS? Do these patients have worse outcomes regardless of their predominant feature? Would outcomes change if the apnea hypopnea index (AHI) is 10/h vs 65/h? More importantly, do patients with the triple overlap of COPD, morbid obesity, and daytime hypercapnia have worse outcomes when compared with hypercapnic COPD, or OHS with/without OSA? These questions can be better addressed once we agree on a definition. The patients with triple overlap syndrome have been traditionally excluded from clinical trials: the patient with morbid obesity has been excluded from chronic hypercapnic COPD clinical trials, and the patient with COPD has been excluded from OHS trials.
There are no specific clinical guidelines for this triple overlap phenotype. Positive airway pressure is the mainstay of treatment. CPAP is recommended as first-line therapy for patients with OSA-COPD overlap syndrome, while noninvasive ventilation (NIV) with bilevel positive airway pressure (BPAP) is recommended as first-line for the stable ambulatory hypercapnic patient with COPD. It is unclear if NIV is superior to CPAP in patients with triple overlap syndrome, although recently published data showed greater efficacy in reducing carbon dioxide (PaCO2) and improving quality of life in a small group of subjects (Zheng et al. J Clin Sleep Med. 2022;18[1]:99-107). To take a step further, the subtleties of NIV set up, such as rise time and minimum inspiratory time, are contradictory: the goal in ventilating patients with COPD is to shorten inspiratory time, prolonging expiratory time, therefore allowing a shortened inspiratory cycle. In obesity, ventilation strategies aim to prolong and sustain inspiratory time to improve ventilation and dependent atelectasis. Another area of uncertainty is device selection. Should we aim to provide a respiratory assist device (RAD): the traditional, rent to own bilevel PAP without auto-expiratory positive airway pressure (EPAP) capabilities and lower maximum inspiratory pressure delivery capacity, vs a home mechanical ventilator at a higher expense, life-time rental, and one-way only data monitoring, which limits remote prescription adjustments, but allow auto-EPAP settings for patients with comorbid OSA? More importantly, how do we get these patients, who do not fit in any of the specified insurance criteria for PAP therapy approved for treatment?
A uniform diagnostic definition and clear taxonomy allows for resource allocation, from government funded grants for clinical trials to a better-informed distribution of health care systems resources and support health care policy changes to improve patient-centric outcomes. Here, we propose that the morbidly obese patient (BMI >40 kg/m2) with chronic airflow obstruction and a forced expiratory ratio (FEV1/FVC) <0.7 with awake daytime hypercapnia (PaCO2 > 45 mm Hg) represents a different entity/phenotype and fits best under the triple overlap syndrome taxonomy.
We suspect that these patients have worse outcomes, including comorbidity burden, quality of life, exacerbation rates, longer hospital length-of-stay, and respiratory and all-cause mortality. Large, multicenter, controlled trials comparing the long-term effectiveness of NIV and CPAP: measurements of respiratory function, gas exchange, blood pressure, and health related quality of life are needed. This is a group of patients that may specifically benefit from volume-targeted pressure support mode ventilation with auto-EPAP capabilities upon discharge from the hospital after an acute exacerbation.
Inpatient (sleep medicine) and outpatient transitions
In patients hospitalized with the triple overlap syndrome, there are certain considerations that are of special interest. Given comorbid hypercapnia and limited data on NIV superiority over CPAP, a sleep study should not be needed for NIV qualification. In addition, the medical team may consider the following (Figure 1):
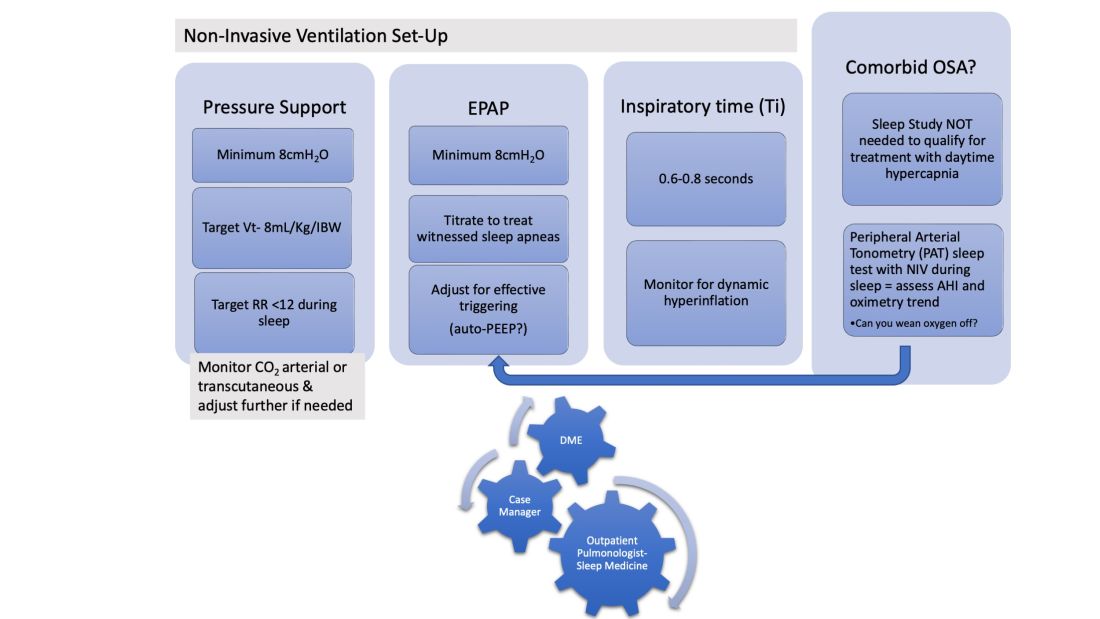
1. Noninvasive Ventilation:
a. Maintaining a high-pressure support differential between inspiratory positive airway pressure (IPAP) and EPAP. This can usually be achieved at 8-10 cm H2O, further adjusting to target a tidal volume (Vt) of 8 mL/kg of ideal body weight (IBW).
b. Higher EPAP: To overcome dependent atelectasis, improve ventilation-perfusion (VQ) matching, and better treat upper airway resistance both during wakefulness and sleep. Also, adjustments of EPAP at bedside should be considered to counteract auto-PEEP-related ineffective triggering if observed.
c. OSA screening and EPAP adjustment: for high residual obstructive apneas or hypopneas if data are available on the NIV device, or with the use of peripheral arterial tonometry sleep testing devices with NIV on overnight before discharge.
d. Does the patient meet criteria for oxygen supplementation at home? Wean oxygen off, if possible.
2. Case-managers can help establish services with a durable medical equipment provider with expertise in advanced PAP devices.3. Obesity management, Consider referral to an obesity management program for lifestyle/dietary modifications along with pharmacotherapy or bariatric surgery interventions.
4. Close follow-up, track exacerbations. Device download data are crucial to monitor adherence/tolerance and treatment effectiveness with particular interest in AHI, oximetry, and CO2 trends monitoring. Some patients may need dedicated titration polysomnograms to adjust ventilation settings, for optimization of residual OSA or for oxygen addition or discontinuation.
Conclusion
Patients with the triple overlap phenotype have not been systematically defined, studied, or included in clinical trials. We anticipate that these patients have worse outcomes: quality of life, symptom and comorbidity burden, exacerbation rates, in-hospital mortality, longer hospital stay and ICU stay, and respiratory and all-cause mortality. This is a group of patients that may specifically benefit from domiciliary NIV set-up upon discharge from the hospital with close follow-up. Properly identifying these patients will help pulmonologists and health care systems direct resources to optimally manage this complex group of patients. Funding of research trials to support clinical guidelines development should be prioritized. Triple overlap syndrome is different from COPD-OSA overlap, OHS with moderate to severe OSA, or OHS without significant OSA.
In our current society, it is likely that the “skinny patient with COPD” who walks into your clinic is less and less your “traditional” patient with COPD. We are seeing in our health care systems more of the “blue bloaters” – patients with COPD and significant obesity. This phenotype is representing what we are seeing worldwide as a consequence of the rising obesity prevalence. In the United States, the prepandemic (2017-2020) estimated percentage of adults over the age of 40 with obesity, defined as a body mass index (BMI) of at least 30 kg/m2, was over 40%. Moreover, the estimated percentage of adults with morbid obesity (BMI at least 40 kg/m2) is close to 10% (Akinbami, LJ et al. Vital Health Stat. 2022:190:1-36) and trending up. These patients with the “triple overlap” of morbid obesity, COPD, and awake daytime hypercapnia are being seen in clinics and in-hospital settings with increasing frequency, often presenting with complicating comorbidities such as acute respiratory failure, acute heart failure, kidney disease, or pulmonary hypertension. We are now faced with managing these patients with complex disease.
The obesity paradox does not seem applicable in the triple overlap phenotype. Patients with COPD who are overweight, defined as “mild obesity,” have lower mortality when compared with normal weight and underweight patients with COPD; however, this effect diminishes when BMI increases beyond 32 kg/m2. With increasing obesity severity and aging, the risk of both obstructive sleep apnea (OSA) and hypoventilation increases. It is well documented that COPD-OSA overlap is linked to worse outcomes and that continuous positive airway pressure (CPAP) as first-line therapy decreases readmission rates and mortality. The pathophysiology of hypoventilation in obesity is complex and multifactorial, and, although significant overlaps likely exist with comorbid COPD, by current definitions, to establish a diagnosis of obesity hypoventilation syndrome (OHS), one must have excluded other causes of hypoventilation, such as COPD.
These patients with the triple overlap of morbid obesity, awake daytime hypercapnia, and COPD are the subset of patients that providers struggle to fit in a diagnosis or in clinical research trials.
The triple overlap is a distinct syndrome
Different labels have been used in the medical literature: hypercapnic OSA-COPD overlap, morbid obesity and OSA-COPD overlap, hypercapnic morbidly obese COPD and OHS-COPD overlap. A better characterization of this distinctive phenotype is much needed. Patients with OSA-COPD overlap, for example, have an increased propensity to develop hypercapnia at higher FEV1 when compared with COPD without OSA – but this is thought to be a consequence of prolonged and frequent apneas and hypopneas compounded with obesity-related central hypoventilation. We found that morbidly obese patients with OSA-COPD overlap have a higher hypoxia burden, more severe OSA, and are frequently prescribed noninvasive ventilation after a failed titration polysomnogram (Htun ZM, et al. Am J Respir Crit Care Med. 2019;199:A1382), perhaps signaling a distinctive phenotype with worse outcomes, but the study had the inherent limitations of a single-center, retrospective design lacking data on awake hypercapnia. On the other side, the term OHS-COPD is contradictory and confusing based on current OHS diagnostic criteria.
In standardizing diagnostic criteria for patients with this triple overlap syndrome, challenges remain: would the patient with a BMI of 70 kg/m2 and fixed chronic airflow obstruction with FEV1 72% fall under the category of hypercapnic COPD vs OHS? Do these patients have worse outcomes regardless of their predominant feature? Would outcomes change if the apnea hypopnea index (AHI) is 10/h vs 65/h? More importantly, do patients with the triple overlap of COPD, morbid obesity, and daytime hypercapnia have worse outcomes when compared with hypercapnic COPD, or OHS with/without OSA? These questions can be better addressed once we agree on a definition. The patients with triple overlap syndrome have been traditionally excluded from clinical trials: the patient with morbid obesity has been excluded from chronic hypercapnic COPD clinical trials, and the patient with COPD has been excluded from OHS trials.
There are no specific clinical guidelines for this triple overlap phenotype. Positive airway pressure is the mainstay of treatment. CPAP is recommended as first-line therapy for patients with OSA-COPD overlap syndrome, while noninvasive ventilation (NIV) with bilevel positive airway pressure (BPAP) is recommended as first-line for the stable ambulatory hypercapnic patient with COPD. It is unclear if NIV is superior to CPAP in patients with triple overlap syndrome, although recently published data showed greater efficacy in reducing carbon dioxide (PaCO2) and improving quality of life in a small group of subjects (Zheng et al. J Clin Sleep Med. 2022;18[1]:99-107). To take a step further, the subtleties of NIV set up, such as rise time and minimum inspiratory time, are contradictory: the goal in ventilating patients with COPD is to shorten inspiratory time, prolonging expiratory time, therefore allowing a shortened inspiratory cycle. In obesity, ventilation strategies aim to prolong and sustain inspiratory time to improve ventilation and dependent atelectasis. Another area of uncertainty is device selection. Should we aim to provide a respiratory assist device (RAD): the traditional, rent to own bilevel PAP without auto-expiratory positive airway pressure (EPAP) capabilities and lower maximum inspiratory pressure delivery capacity, vs a home mechanical ventilator at a higher expense, life-time rental, and one-way only data monitoring, which limits remote prescription adjustments, but allow auto-EPAP settings for patients with comorbid OSA? More importantly, how do we get these patients, who do not fit in any of the specified insurance criteria for PAP therapy approved for treatment?
A uniform diagnostic definition and clear taxonomy allows for resource allocation, from government funded grants for clinical trials to a better-informed distribution of health care systems resources and support health care policy changes to improve patient-centric outcomes. Here, we propose that the morbidly obese patient (BMI >40 kg/m2) with chronic airflow obstruction and a forced expiratory ratio (FEV1/FVC) <0.7 with awake daytime hypercapnia (PaCO2 > 45 mm Hg) represents a different entity/phenotype and fits best under the triple overlap syndrome taxonomy.
We suspect that these patients have worse outcomes, including comorbidity burden, quality of life, exacerbation rates, longer hospital length-of-stay, and respiratory and all-cause mortality. Large, multicenter, controlled trials comparing the long-term effectiveness of NIV and CPAP: measurements of respiratory function, gas exchange, blood pressure, and health related quality of life are needed. This is a group of patients that may specifically benefit from volume-targeted pressure support mode ventilation with auto-EPAP capabilities upon discharge from the hospital after an acute exacerbation.
Inpatient (sleep medicine) and outpatient transitions
In patients hospitalized with the triple overlap syndrome, there are certain considerations that are of special interest. Given comorbid hypercapnia and limited data on NIV superiority over CPAP, a sleep study should not be needed for NIV qualification. In addition, the medical team may consider the following (Figure 1):
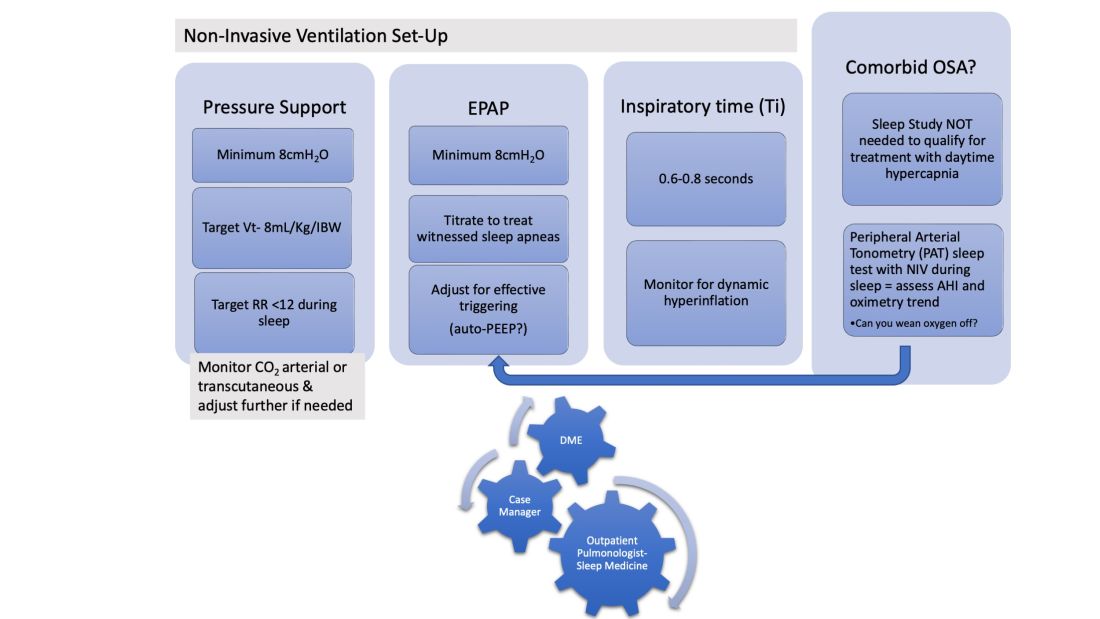
1. Noninvasive Ventilation:
a. Maintaining a high-pressure support differential between inspiratory positive airway pressure (IPAP) and EPAP. This can usually be achieved at 8-10 cm H2O, further adjusting to target a tidal volume (Vt) of 8 mL/kg of ideal body weight (IBW).
b. Higher EPAP: To overcome dependent atelectasis, improve ventilation-perfusion (VQ) matching, and better treat upper airway resistance both during wakefulness and sleep. Also, adjustments of EPAP at bedside should be considered to counteract auto-PEEP-related ineffective triggering if observed.
c. OSA screening and EPAP adjustment: for high residual obstructive apneas or hypopneas if data are available on the NIV device, or with the use of peripheral arterial tonometry sleep testing devices with NIV on overnight before discharge.
d. Does the patient meet criteria for oxygen supplementation at home? Wean oxygen off, if possible.
2. Case-managers can help establish services with a durable medical equipment provider with expertise in advanced PAP devices.3. Obesity management, Consider referral to an obesity management program for lifestyle/dietary modifications along with pharmacotherapy or bariatric surgery interventions.
4. Close follow-up, track exacerbations. Device download data are crucial to monitor adherence/tolerance and treatment effectiveness with particular interest in AHI, oximetry, and CO2 trends monitoring. Some patients may need dedicated titration polysomnograms to adjust ventilation settings, for optimization of residual OSA or for oxygen addition or discontinuation.
Conclusion
Patients with the triple overlap phenotype have not been systematically defined, studied, or included in clinical trials. We anticipate that these patients have worse outcomes: quality of life, symptom and comorbidity burden, exacerbation rates, in-hospital mortality, longer hospital stay and ICU stay, and respiratory and all-cause mortality. This is a group of patients that may specifically benefit from domiciliary NIV set-up upon discharge from the hospital with close follow-up. Properly identifying these patients will help pulmonologists and health care systems direct resources to optimally manage this complex group of patients. Funding of research trials to support clinical guidelines development should be prioritized. Triple overlap syndrome is different from COPD-OSA overlap, OHS with moderate to severe OSA, or OHS without significant OSA.
In our current society, it is likely that the “skinny patient with COPD” who walks into your clinic is less and less your “traditional” patient with COPD. We are seeing in our health care systems more of the “blue bloaters” – patients with COPD and significant obesity. This phenotype is representing what we are seeing worldwide as a consequence of the rising obesity prevalence. In the United States, the prepandemic (2017-2020) estimated percentage of adults over the age of 40 with obesity, defined as a body mass index (BMI) of at least 30 kg/m2, was over 40%. Moreover, the estimated percentage of adults with morbid obesity (BMI at least 40 kg/m2) is close to 10% (Akinbami, LJ et al. Vital Health Stat. 2022:190:1-36) and trending up. These patients with the “triple overlap” of morbid obesity, COPD, and awake daytime hypercapnia are being seen in clinics and in-hospital settings with increasing frequency, often presenting with complicating comorbidities such as acute respiratory failure, acute heart failure, kidney disease, or pulmonary hypertension. We are now faced with managing these patients with complex disease.
The obesity paradox does not seem applicable in the triple overlap phenotype. Patients with COPD who are overweight, defined as “mild obesity,” have lower mortality when compared with normal weight and underweight patients with COPD; however, this effect diminishes when BMI increases beyond 32 kg/m2. With increasing obesity severity and aging, the risk of both obstructive sleep apnea (OSA) and hypoventilation increases. It is well documented that COPD-OSA overlap is linked to worse outcomes and that continuous positive airway pressure (CPAP) as first-line therapy decreases readmission rates and mortality. The pathophysiology of hypoventilation in obesity is complex and multifactorial, and, although significant overlaps likely exist with comorbid COPD, by current definitions, to establish a diagnosis of obesity hypoventilation syndrome (OHS), one must have excluded other causes of hypoventilation, such as COPD.
These patients with the triple overlap of morbid obesity, awake daytime hypercapnia, and COPD are the subset of patients that providers struggle to fit in a diagnosis or in clinical research trials.
The triple overlap is a distinct syndrome
Different labels have been used in the medical literature: hypercapnic OSA-COPD overlap, morbid obesity and OSA-COPD overlap, hypercapnic morbidly obese COPD and OHS-COPD overlap. A better characterization of this distinctive phenotype is much needed. Patients with OSA-COPD overlap, for example, have an increased propensity to develop hypercapnia at higher FEV1 when compared with COPD without OSA – but this is thought to be a consequence of prolonged and frequent apneas and hypopneas compounded with obesity-related central hypoventilation. We found that morbidly obese patients with OSA-COPD overlap have a higher hypoxia burden, more severe OSA, and are frequently prescribed noninvasive ventilation after a failed titration polysomnogram (Htun ZM, et al. Am J Respir Crit Care Med. 2019;199:A1382), perhaps signaling a distinctive phenotype with worse outcomes, but the study had the inherent limitations of a single-center, retrospective design lacking data on awake hypercapnia. On the other side, the term OHS-COPD is contradictory and confusing based on current OHS diagnostic criteria.
In standardizing diagnostic criteria for patients with this triple overlap syndrome, challenges remain: would the patient with a BMI of 70 kg/m2 and fixed chronic airflow obstruction with FEV1 72% fall under the category of hypercapnic COPD vs OHS? Do these patients have worse outcomes regardless of their predominant feature? Would outcomes change if the apnea hypopnea index (AHI) is 10/h vs 65/h? More importantly, do patients with the triple overlap of COPD, morbid obesity, and daytime hypercapnia have worse outcomes when compared with hypercapnic COPD, or OHS with/without OSA? These questions can be better addressed once we agree on a definition. The patients with triple overlap syndrome have been traditionally excluded from clinical trials: the patient with morbid obesity has been excluded from chronic hypercapnic COPD clinical trials, and the patient with COPD has been excluded from OHS trials.
There are no specific clinical guidelines for this triple overlap phenotype. Positive airway pressure is the mainstay of treatment. CPAP is recommended as first-line therapy for patients with OSA-COPD overlap syndrome, while noninvasive ventilation (NIV) with bilevel positive airway pressure (BPAP) is recommended as first-line for the stable ambulatory hypercapnic patient with COPD. It is unclear if NIV is superior to CPAP in patients with triple overlap syndrome, although recently published data showed greater efficacy in reducing carbon dioxide (PaCO2) and improving quality of life in a small group of subjects (Zheng et al. J Clin Sleep Med. 2022;18[1]:99-107). To take a step further, the subtleties of NIV set up, such as rise time and minimum inspiratory time, are contradictory: the goal in ventilating patients with COPD is to shorten inspiratory time, prolonging expiratory time, therefore allowing a shortened inspiratory cycle. In obesity, ventilation strategies aim to prolong and sustain inspiratory time to improve ventilation and dependent atelectasis. Another area of uncertainty is device selection. Should we aim to provide a respiratory assist device (RAD): the traditional, rent to own bilevel PAP without auto-expiratory positive airway pressure (EPAP) capabilities and lower maximum inspiratory pressure delivery capacity, vs a home mechanical ventilator at a higher expense, life-time rental, and one-way only data monitoring, which limits remote prescription adjustments, but allow auto-EPAP settings for patients with comorbid OSA? More importantly, how do we get these patients, who do not fit in any of the specified insurance criteria for PAP therapy approved for treatment?
A uniform diagnostic definition and clear taxonomy allows for resource allocation, from government funded grants for clinical trials to a better-informed distribution of health care systems resources and support health care policy changes to improve patient-centric outcomes. Here, we propose that the morbidly obese patient (BMI >40 kg/m2) with chronic airflow obstruction and a forced expiratory ratio (FEV1/FVC) <0.7 with awake daytime hypercapnia (PaCO2 > 45 mm Hg) represents a different entity/phenotype and fits best under the triple overlap syndrome taxonomy.
We suspect that these patients have worse outcomes, including comorbidity burden, quality of life, exacerbation rates, longer hospital length-of-stay, and respiratory and all-cause mortality. Large, multicenter, controlled trials comparing the long-term effectiveness of NIV and CPAP: measurements of respiratory function, gas exchange, blood pressure, and health related quality of life are needed. This is a group of patients that may specifically benefit from volume-targeted pressure support mode ventilation with auto-EPAP capabilities upon discharge from the hospital after an acute exacerbation.
Inpatient (sleep medicine) and outpatient transitions
In patients hospitalized with the triple overlap syndrome, there are certain considerations that are of special interest. Given comorbid hypercapnia and limited data on NIV superiority over CPAP, a sleep study should not be needed for NIV qualification. In addition, the medical team may consider the following (Figure 1):
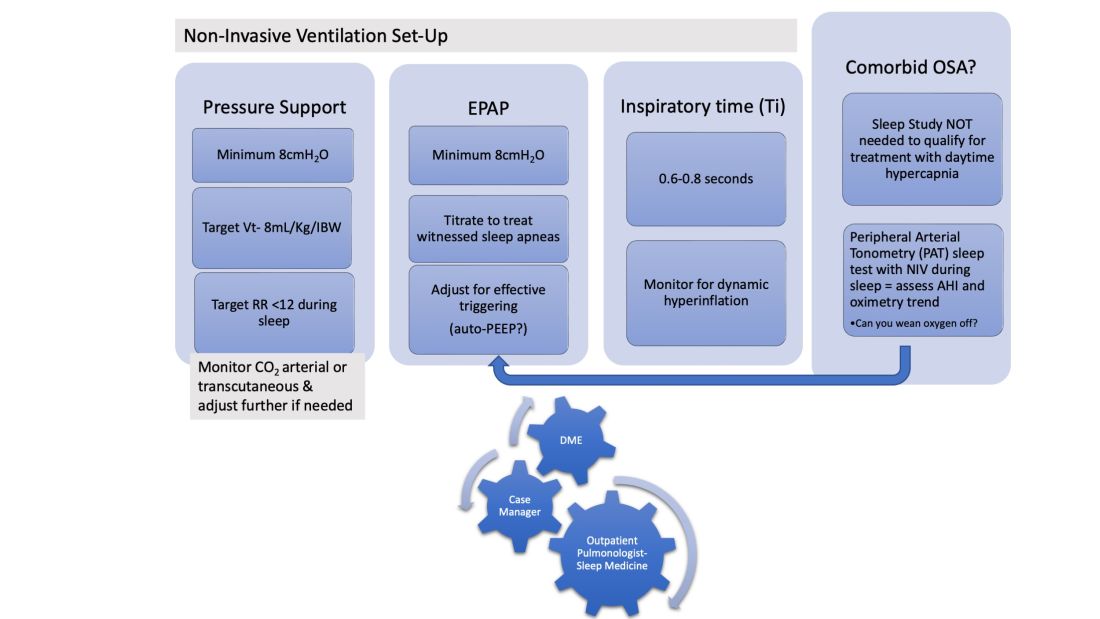
1. Noninvasive Ventilation:
a. Maintaining a high-pressure support differential between inspiratory positive airway pressure (IPAP) and EPAP. This can usually be achieved at 8-10 cm H2O, further adjusting to target a tidal volume (Vt) of 8 mL/kg of ideal body weight (IBW).
b. Higher EPAP: To overcome dependent atelectasis, improve ventilation-perfusion (VQ) matching, and better treat upper airway resistance both during wakefulness and sleep. Also, adjustments of EPAP at bedside should be considered to counteract auto-PEEP-related ineffective triggering if observed.
c. OSA screening and EPAP adjustment: for high residual obstructive apneas or hypopneas if data are available on the NIV device, or with the use of peripheral arterial tonometry sleep testing devices with NIV on overnight before discharge.
d. Does the patient meet criteria for oxygen supplementation at home? Wean oxygen off, if possible.
2. Case-managers can help establish services with a durable medical equipment provider with expertise in advanced PAP devices.3. Obesity management, Consider referral to an obesity management program for lifestyle/dietary modifications along with pharmacotherapy or bariatric surgery interventions.
4. Close follow-up, track exacerbations. Device download data are crucial to monitor adherence/tolerance and treatment effectiveness with particular interest in AHI, oximetry, and CO2 trends monitoring. Some patients may need dedicated titration polysomnograms to adjust ventilation settings, for optimization of residual OSA or for oxygen addition or discontinuation.
Conclusion
Patients with the triple overlap phenotype have not been systematically defined, studied, or included in clinical trials. We anticipate that these patients have worse outcomes: quality of life, symptom and comorbidity burden, exacerbation rates, in-hospital mortality, longer hospital stay and ICU stay, and respiratory and all-cause mortality. This is a group of patients that may specifically benefit from domiciliary NIV set-up upon discharge from the hospital with close follow-up. Properly identifying these patients will help pulmonologists and health care systems direct resources to optimally manage this complex group of patients. Funding of research trials to support clinical guidelines development should be prioritized. Triple overlap syndrome is different from COPD-OSA overlap, OHS with moderate to severe OSA, or OHS without significant OSA.
Introducing CHEST President-Designate John A. Howington, MD, MBA, FCCP
John A. Howington, MD, MBA, FCCP, is a cardiothoracic surgeon currently serving as Chief of Oncology Services and Chair of Thoracic Surgery at Ascension Saint Thomas Health and a professor at the University of Tennessee Health Sciences Center in Nashville, Tennessee.
Dr. Howington received his undergraduate degree from Tennessee Technological University and medical degree from the University of Tennessee. He completed his general surgery residency at the University of Missouri, Kansas City and thoracic surgery residency at Vanderbilt University Medical Center.
Most recently, he received his Physician Executive MBA from the University of Tennessee.
As a passionate thoracic surgeon, he has lent his knowledge to the extensive CHEST lung cancer guideline portfolio for more than a decade. He offers regular leadership in multidisciplinary and executive forums and has spearheaded a series of quality improvement initiatives at Ascension. He has served in a variety of leadership roles with CHEST and with other national thoracic surgery societies.
Dr. Howington began his CHEST leadership journey with the Networks, as a member of the Interventional Chest Medicine Steering Committee and then as the Thoracic Oncology Network Chair (2008-2010).
Other leadership positions include serving as the President of the CHEST Foundation (2014-2016), member of the Scientific Program Committee and Membership Committee, and, recently, as the Chair of the Finance Committee from 2018-2021.
Since 2017, he has served on the Board of Regents as a Member at Large. Dr. Howington will serve as the 87th CHEST President in 2025.
John A. Howington, MD, MBA, FCCP, is a cardiothoracic surgeon currently serving as Chief of Oncology Services and Chair of Thoracic Surgery at Ascension Saint Thomas Health and a professor at the University of Tennessee Health Sciences Center in Nashville, Tennessee.
Dr. Howington received his undergraduate degree from Tennessee Technological University and medical degree from the University of Tennessee. He completed his general surgery residency at the University of Missouri, Kansas City and thoracic surgery residency at Vanderbilt University Medical Center.
Most recently, he received his Physician Executive MBA from the University of Tennessee.
As a passionate thoracic surgeon, he has lent his knowledge to the extensive CHEST lung cancer guideline portfolio for more than a decade. He offers regular leadership in multidisciplinary and executive forums and has spearheaded a series of quality improvement initiatives at Ascension. He has served in a variety of leadership roles with CHEST and with other national thoracic surgery societies.
Dr. Howington began his CHEST leadership journey with the Networks, as a member of the Interventional Chest Medicine Steering Committee and then as the Thoracic Oncology Network Chair (2008-2010).
Other leadership positions include serving as the President of the CHEST Foundation (2014-2016), member of the Scientific Program Committee and Membership Committee, and, recently, as the Chair of the Finance Committee from 2018-2021.
Since 2017, he has served on the Board of Regents as a Member at Large. Dr. Howington will serve as the 87th CHEST President in 2025.
John A. Howington, MD, MBA, FCCP, is a cardiothoracic surgeon currently serving as Chief of Oncology Services and Chair of Thoracic Surgery at Ascension Saint Thomas Health and a professor at the University of Tennessee Health Sciences Center in Nashville, Tennessee.
Dr. Howington received his undergraduate degree from Tennessee Technological University and medical degree from the University of Tennessee. He completed his general surgery residency at the University of Missouri, Kansas City and thoracic surgery residency at Vanderbilt University Medical Center.
Most recently, he received his Physician Executive MBA from the University of Tennessee.
As a passionate thoracic surgeon, he has lent his knowledge to the extensive CHEST lung cancer guideline portfolio for more than a decade. He offers regular leadership in multidisciplinary and executive forums and has spearheaded a series of quality improvement initiatives at Ascension. He has served in a variety of leadership roles with CHEST and with other national thoracic surgery societies.
Dr. Howington began his CHEST leadership journey with the Networks, as a member of the Interventional Chest Medicine Steering Committee and then as the Thoracic Oncology Network Chair (2008-2010).
Other leadership positions include serving as the President of the CHEST Foundation (2014-2016), member of the Scientific Program Committee and Membership Committee, and, recently, as the Chair of the Finance Committee from 2018-2021.
Since 2017, he has served on the Board of Regents as a Member at Large. Dr. Howington will serve as the 87th CHEST President in 2025.
Three surprising studies on exercise restriction and an exercise sweet spot
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FDA strengthens mammography regulations: Final rule
A final rule, updating the regulations issued under the Mammography Quality Standards Act of 1992, requires that mammography facilities notify patients about the density of their breasts, strengthens the FDA’s oversight of facilities, and provides guidance to help physicians better categorize and assess mammograms, according to a March 9 press release.
The rule requires implementation of the changes within 18 months.
According to the final rule document, the updates are “intended to improve the delivery of mammography services” in ways that reflect changes in mammography technology, quality standards, and the way results are categorized, reported, and communicated to patients and providers.
For instance, mammography reports must include an assessment of breast density to provide greater detail on the potential limitations of the mammogram results and allow patients and physicians to make more informed decisions, such as the possibility of additional imaging for women with dense breast tissue.
“Today’s action represents the agency’s broader commitment to support innovation to prevent, detect and treat cancer,” said Hilary Marston, MD, MPH, FDA’s chief medical officer, in the agency’s press release. The FDA remains “committed to advancing efforts to improve the health of women and strengthen the fight against breast cancer.”
A version of this article first appeared on Medscape.com.
A final rule, updating the regulations issued under the Mammography Quality Standards Act of 1992, requires that mammography facilities notify patients about the density of their breasts, strengthens the FDA’s oversight of facilities, and provides guidance to help physicians better categorize and assess mammograms, according to a March 9 press release.
The rule requires implementation of the changes within 18 months.
According to the final rule document, the updates are “intended to improve the delivery of mammography services” in ways that reflect changes in mammography technology, quality standards, and the way results are categorized, reported, and communicated to patients and providers.
For instance, mammography reports must include an assessment of breast density to provide greater detail on the potential limitations of the mammogram results and allow patients and physicians to make more informed decisions, such as the possibility of additional imaging for women with dense breast tissue.
“Today’s action represents the agency’s broader commitment to support innovation to prevent, detect and treat cancer,” said Hilary Marston, MD, MPH, FDA’s chief medical officer, in the agency’s press release. The FDA remains “committed to advancing efforts to improve the health of women and strengthen the fight against breast cancer.”
A version of this article first appeared on Medscape.com.
A final rule, updating the regulations issued under the Mammography Quality Standards Act of 1992, requires that mammography facilities notify patients about the density of their breasts, strengthens the FDA’s oversight of facilities, and provides guidance to help physicians better categorize and assess mammograms, according to a March 9 press release.
The rule requires implementation of the changes within 18 months.
According to the final rule document, the updates are “intended to improve the delivery of mammography services” in ways that reflect changes in mammography technology, quality standards, and the way results are categorized, reported, and communicated to patients and providers.
For instance, mammography reports must include an assessment of breast density to provide greater detail on the potential limitations of the mammogram results and allow patients and physicians to make more informed decisions, such as the possibility of additional imaging for women with dense breast tissue.
“Today’s action represents the agency’s broader commitment to support innovation to prevent, detect and treat cancer,” said Hilary Marston, MD, MPH, FDA’s chief medical officer, in the agency’s press release. The FDA remains “committed to advancing efforts to improve the health of women and strengthen the fight against breast cancer.”
A version of this article first appeared on Medscape.com.