User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Docs fight back after losing hospital privileges, patients, and income
In April, a group of more than a dozen cardiologists at St. Louis Heart and Vascular (SLHV) lost their privileges at SSM Health, an eight-hospital system in St. Louis.
The physicians did not lose their privileges because of a clinical failure. Rather, it was because of SSM’s decision to enter into an exclusive contract with another set of cardiologists.
“The current situation is economically untenable for us,” said Harvey Serota, MD, founder and medical director of SLHV. “This is an existential threat to the practice.”
Because of the exclusive contract, many of SLHV’s patients are now being redirected to SSM-contracted cardiologists. Volume for the group’s new $15 million catheterization lab has plummeted. SLHV is suing SSM to restore its privileges, claiming lack of due process, restraint of trade, interference with its business, and breach of contract.
Losing privileges because a hospital seeks to increase their profits is becoming all too familiar for many independent specialists in fields such as cardiology, orthopedic surgery, and urology, as the hospitals that hosted them become their competitors and forge exclusive contracts with opposing groups.
What can these doctors do if they’re shut out? File a lawsuit, as SLHV has done? Demand a hearing before the medical staff and try to resolve the problem? Or simply give up their privileges and move on?
Unfortunately, none of these approaches offer a quick or certain solution, and each comes with risks.
Generally, courts have upheld hospitals’ use of exclusive contracts, which is also known as economic credentialing, says Barry F. Rosen, a health law attorney at Gordon Feinblatt, in Baltimore.
“Courts have long recognized exclusive contracts, and challenges by excluded doctors usually fail,” he says.
However, Mr. Rosen can cite several examples in which excluded doctors launched legal challenges that prevailed, owing to nuances in the law. The legal field in this area is tangled, and it varies by state.
Can hospitals make exclusive deals?
Hospitals have long used exclusive contracts for hospital-based specialists – anesthesiologists, radiologists, pathologists, emergency physicians, and hospitalists. They say that restricting patients to one group of anesthesiologists or radiologists enhances operational efficiency and that these contracts do not disrupt patients, because patients have no ties to hospital-based physicians. Such contracts are often more profitable for the hospital because of the negotiated rates.
Exclusive contracts in other specialties, however, are less accepted because they involve markedly different strategies and have different effects. In such cases, the hospital is no longer simply enhancing operational efficiency but is competing with physicians on staff, and the arrangement can disrupt the care of patients of the excluded doctors.
In the courts, these concerns might form the basis of an antitrust action or a claim of tortious interference with physicians’ ability to provide care for their patients, but neither claim is easy to win, Mr. Rosen says.
In antitrust cases, “the issue is not whether the excluded doctor was injured but whether the action harmed competition,” Mr. Rosen says. “Will the exclusion lead to higher prices?”
In the case of interference with patient care, “you will always find interference by one entity in the affairs of another,” he says, “but tortious interference applies to situations where something nefarious is going on, such as the other side was out to destroy your business and create a monopoly.”
Hospitals may try to restrict the privileges of physicians who invest in competing facilities such as cath labs and ambulatory surgery centers (ASCs), says Gregory Mertz, managing director of Physician Strategies Group, a consultancy in Virginia Beach.
“However, any revenge that a hospital might take against the doctors who started an ASC would usually not be publicly admitted,” Mr. Mertz says. “Revenge would be exacted in subtle ways.”
In the St. Louis situation, SSM did not cite SLHV’s cath lab as a reason for its exclusive contract. SSM stated in court documents that the decision was based on the recommendations of an expert panel. Furthermore, SSM said the board created the panel in response to a state report that cited the limited experience of some SLHV cardiologists in treating a rare type of heart attack.
Mr. Mertz says the board’s interest in the state’s concern and then its forming the special panel lent a great deal of legitimacy to SSM’s decision to start an exclusive contract. “SSM can show evidence that the board’s decision was based on a clinical matter and not on trying to squeeze out the cardiologists,” he says.
In SLHV’s defense, Dr. Serota says the practice offered to stop taking calls for the type of heart attack that was cited, but the hospital did not respond to its offer. He says SSM should have consulted the hospital’s medical staff to address the state’s concern and to create the exclusive contract, because these decisions involved clinical issues that the medical staff understands better than the board.
The law, however, does not require a hospital board to consult with its medical staff, says Alice G. Gosfield, a health care attorney in Philadelphia. “The board has ultimate legal control of everything in the hospital,” she says. However, the board often delegates certain functions to the medical staff in the hospital bylaws, and depending on the wording of the bylaws, it is still possible that the board violated the bylaws, Ms. Gosfield adds.
Can excluded physicians get peer review?
Can the hospital medical staff help restore the privileges of excluded physicians? Don’t these physicians have the right to peer review – a hearing before the medical staff?
Indeed, the Joint Commission, which accredits hospitals, states that the hospital must have “mechanisms, including a fair hearing and appeal process, for addressing adverse decisions for existing medical staff members and other individuals holding clinical privileges for renewal, revocation, or revision of clinical privileges.”
However, excluded physicians may not have a right to a hearing if they have not been fully stripped of privileges. SSM discontinued adult cardiology privileges for SLHV doctors but retained some doctors’ internal medicine privileges. Dr. Serota says internal medicine privileges are useless to cardiologists, but because the doctors’ privileges had not been fully removed, they cannot ask for a hearing.
More fundamentally, exclusive contracts are not a good fit for peer review. Mr. Rosen says the hearings were designed to review the physicians’ clinical competence or behavior, but excluded physicians do not have these problems. About all the hearing could focus on is the hospital’s policy, which the board would not want to allow. To avoid this, “the hospital might rule out a hearing as contrary to the intent of the bylaws,” Mr. Rosen says.
Furthermore, even if peer review goes forward, “what the medical staff decides is only advisory, and the hospital board makes the final decision,” Mr. Rosen says. He notes that the doctor could challenge the decision in court, but the hospital might still prevail.
Excluded physicians sometimes prevail
Although it is rare for excluded physicians to win a lawsuit against their hospital, it does happen, says Michael R. Callahan, health lawyer at Katten Muchin Rosenman, in Chicago.
Mr. Callahan cites a 2010 decision by the Arkansas Supreme Court that stopped the state’s largest health system from denying physicians’ privileges. Among other things, the hospital was found to have tortiously interfered with the physicians’ contracts with patients.
In a 2007 decision, a West Virginia court ruled that hospitals that have a mission to serve the public cannot exclude physicians for nonquality issues. In addition, some states, such as Texas, limit the economic factors that can be considered when credentialing decisions are made. Other states, such as Ohio, give hospitals a great deal of leeway to alter credentialing.
Dr. Serota is optimistic about his Missouri lawsuit. Although the judge in the case did not immediately grant SLHV’s request for restoration of privileges while the case proceeds, she did grant expedited discovery – allowing SLHV to obtain documents from SSM that could strengthen the doctors’ case – and she agreed to a hearing on SLHV’s request for a temporary restoration of privileges.
Ms. Gosfield says Dr. Serota’s optimism seems justified, but she adds that such cases cost a lot of money and that they may still not be winnable.
Often plaintiffs can settle lawsuits before they go to trial, but Mr. Callahan says hospitals are loath to restore privileges in a settlement because they don’t want to undermine an exclusivity deal. “The exclusive group expects a certain volume, which can’t be reached if the competing doctors are allowed back in,” he says.
Many physicians don’t challenge the exclusion
Quite often, excluded doctors decide not to challenge the decision. For example, Dr. Serota says groups of orthopedic surgeons and urologists have decided not to challenge similar decisions by SSM. “They wanted to move on,” he says.
Mr. Callahan says many excluded doctors also don’t even ask for a hearing. “They expect that the hospital’s decision will be upheld,” he says.
This was the case for Devendra K. Amin, MD, an independent cardiologist in Easton, Pa. Dr. Amin has not had any hospital privileges since July 2020. Even though he is board certified in interventional cardiology, which involves catheterization, Dr. Amin says he cannot perform these procedures because they can only be performed in a hospital in the area.
In the 1990s, Dr. Amin says, he had invasive cardiology privileges at five hospitals, but then those hospitals consolidated, and the remaining ones started constricting his privileges. First he could no longer work in the emergency department, then he could no longer read echocardiograms and interpret stress test results, because that work was assigned exclusively to employed doctors, he says.
Then the one remaining hospital announced that privileges would only be available to physicians by invitation, and he was not invited. Dr. Amin says he could have regained general cardiology privileges if he had accepted employment at the hospital, but he did not want to do this. A recruiter and the head of the cardiology section at the hospital even took him out to dinner 2 years ago to discuss employment, but there was a stipulation that the hospital would not agree to.
“I wanted to get back my interventional privileges back,” Dr. Amin says, “but they told me that would not be possible because they had an exclusive contract with a group.”
Dr. Amin says that now, he can only work as a general cardiologist with reduced volume. He says primary care physicians in the local hospital systems only refer to cardiologists within their systems. “When these patients do come to me, it is only because they specifically requested to see me,” Dr. Amin says.
He does not want to challenge the decisions regarding privileging. “Look, I am 68 years old,” Dr. Amin says. “I’m not retiring yet, but I don’t want to get into a battle with a hospital that has very deep pockets. I’m not a confrontational person to begin with, and I don’t want to spend the next 10 years of my life in litigation.”
Diverging expectations
The law on exclusive contracts does not provide easy answers for excluded doctors, and often it defies physicians’ conception of their own role in the hospital.
Many physicians expect the hospital to be a haven where they can do their work without being cut out by a competitor. This view is reinforced by organizations such as the American Medical Association.
The AMA Council on Medical Service states that privileges “can only be abridged upon recommendation of the medical staff and only for reason related to professional competence, adherence to standards of care, and other parameters agreed to by the medical staff.”
But the courts don’t tend to agree with that position. “Hospitals have a fiduciary duty to protect their own financial interests,” Mr. Callahan says. “This may involve anything that furthers the hospital’s mission to provide high-quality health care services to its patient community.”
At the same time, however, there are plenty of instances in which courts have ruled that exclusive contracts had gone too far. But usually it takes a lawyer experienced in these cases to know what those exceptions are.
A version of this article first appeared on Medscape.com.
In April, a group of more than a dozen cardiologists at St. Louis Heart and Vascular (SLHV) lost their privileges at SSM Health, an eight-hospital system in St. Louis.
The physicians did not lose their privileges because of a clinical failure. Rather, it was because of SSM’s decision to enter into an exclusive contract with another set of cardiologists.
“The current situation is economically untenable for us,” said Harvey Serota, MD, founder and medical director of SLHV. “This is an existential threat to the practice.”
Because of the exclusive contract, many of SLHV’s patients are now being redirected to SSM-contracted cardiologists. Volume for the group’s new $15 million catheterization lab has plummeted. SLHV is suing SSM to restore its privileges, claiming lack of due process, restraint of trade, interference with its business, and breach of contract.
Losing privileges because a hospital seeks to increase their profits is becoming all too familiar for many independent specialists in fields such as cardiology, orthopedic surgery, and urology, as the hospitals that hosted them become their competitors and forge exclusive contracts with opposing groups.
What can these doctors do if they’re shut out? File a lawsuit, as SLHV has done? Demand a hearing before the medical staff and try to resolve the problem? Or simply give up their privileges and move on?
Unfortunately, none of these approaches offer a quick or certain solution, and each comes with risks.
Generally, courts have upheld hospitals’ use of exclusive contracts, which is also known as economic credentialing, says Barry F. Rosen, a health law attorney at Gordon Feinblatt, in Baltimore.
“Courts have long recognized exclusive contracts, and challenges by excluded doctors usually fail,” he says.
However, Mr. Rosen can cite several examples in which excluded doctors launched legal challenges that prevailed, owing to nuances in the law. The legal field in this area is tangled, and it varies by state.
Can hospitals make exclusive deals?
Hospitals have long used exclusive contracts for hospital-based specialists – anesthesiologists, radiologists, pathologists, emergency physicians, and hospitalists. They say that restricting patients to one group of anesthesiologists or radiologists enhances operational efficiency and that these contracts do not disrupt patients, because patients have no ties to hospital-based physicians. Such contracts are often more profitable for the hospital because of the negotiated rates.
Exclusive contracts in other specialties, however, are less accepted because they involve markedly different strategies and have different effects. In such cases, the hospital is no longer simply enhancing operational efficiency but is competing with physicians on staff, and the arrangement can disrupt the care of patients of the excluded doctors.
In the courts, these concerns might form the basis of an antitrust action or a claim of tortious interference with physicians’ ability to provide care for their patients, but neither claim is easy to win, Mr. Rosen says.
In antitrust cases, “the issue is not whether the excluded doctor was injured but whether the action harmed competition,” Mr. Rosen says. “Will the exclusion lead to higher prices?”
In the case of interference with patient care, “you will always find interference by one entity in the affairs of another,” he says, “but tortious interference applies to situations where something nefarious is going on, such as the other side was out to destroy your business and create a monopoly.”
Hospitals may try to restrict the privileges of physicians who invest in competing facilities such as cath labs and ambulatory surgery centers (ASCs), says Gregory Mertz, managing director of Physician Strategies Group, a consultancy in Virginia Beach.
“However, any revenge that a hospital might take against the doctors who started an ASC would usually not be publicly admitted,” Mr. Mertz says. “Revenge would be exacted in subtle ways.”
In the St. Louis situation, SSM did not cite SLHV’s cath lab as a reason for its exclusive contract. SSM stated in court documents that the decision was based on the recommendations of an expert panel. Furthermore, SSM said the board created the panel in response to a state report that cited the limited experience of some SLHV cardiologists in treating a rare type of heart attack.
Mr. Mertz says the board’s interest in the state’s concern and then its forming the special panel lent a great deal of legitimacy to SSM’s decision to start an exclusive contract. “SSM can show evidence that the board’s decision was based on a clinical matter and not on trying to squeeze out the cardiologists,” he says.
In SLHV’s defense, Dr. Serota says the practice offered to stop taking calls for the type of heart attack that was cited, but the hospital did not respond to its offer. He says SSM should have consulted the hospital’s medical staff to address the state’s concern and to create the exclusive contract, because these decisions involved clinical issues that the medical staff understands better than the board.
The law, however, does not require a hospital board to consult with its medical staff, says Alice G. Gosfield, a health care attorney in Philadelphia. “The board has ultimate legal control of everything in the hospital,” she says. However, the board often delegates certain functions to the medical staff in the hospital bylaws, and depending on the wording of the bylaws, it is still possible that the board violated the bylaws, Ms. Gosfield adds.
Can excluded physicians get peer review?
Can the hospital medical staff help restore the privileges of excluded physicians? Don’t these physicians have the right to peer review – a hearing before the medical staff?
Indeed, the Joint Commission, which accredits hospitals, states that the hospital must have “mechanisms, including a fair hearing and appeal process, for addressing adverse decisions for existing medical staff members and other individuals holding clinical privileges for renewal, revocation, or revision of clinical privileges.”
However, excluded physicians may not have a right to a hearing if they have not been fully stripped of privileges. SSM discontinued adult cardiology privileges for SLHV doctors but retained some doctors’ internal medicine privileges. Dr. Serota says internal medicine privileges are useless to cardiologists, but because the doctors’ privileges had not been fully removed, they cannot ask for a hearing.
More fundamentally, exclusive contracts are not a good fit for peer review. Mr. Rosen says the hearings were designed to review the physicians’ clinical competence or behavior, but excluded physicians do not have these problems. About all the hearing could focus on is the hospital’s policy, which the board would not want to allow. To avoid this, “the hospital might rule out a hearing as contrary to the intent of the bylaws,” Mr. Rosen says.
Furthermore, even if peer review goes forward, “what the medical staff decides is only advisory, and the hospital board makes the final decision,” Mr. Rosen says. He notes that the doctor could challenge the decision in court, but the hospital might still prevail.
Excluded physicians sometimes prevail
Although it is rare for excluded physicians to win a lawsuit against their hospital, it does happen, says Michael R. Callahan, health lawyer at Katten Muchin Rosenman, in Chicago.
Mr. Callahan cites a 2010 decision by the Arkansas Supreme Court that stopped the state’s largest health system from denying physicians’ privileges. Among other things, the hospital was found to have tortiously interfered with the physicians’ contracts with patients.
In a 2007 decision, a West Virginia court ruled that hospitals that have a mission to serve the public cannot exclude physicians for nonquality issues. In addition, some states, such as Texas, limit the economic factors that can be considered when credentialing decisions are made. Other states, such as Ohio, give hospitals a great deal of leeway to alter credentialing.
Dr. Serota is optimistic about his Missouri lawsuit. Although the judge in the case did not immediately grant SLHV’s request for restoration of privileges while the case proceeds, she did grant expedited discovery – allowing SLHV to obtain documents from SSM that could strengthen the doctors’ case – and she agreed to a hearing on SLHV’s request for a temporary restoration of privileges.
Ms. Gosfield says Dr. Serota’s optimism seems justified, but she adds that such cases cost a lot of money and that they may still not be winnable.
Often plaintiffs can settle lawsuits before they go to trial, but Mr. Callahan says hospitals are loath to restore privileges in a settlement because they don’t want to undermine an exclusivity deal. “The exclusive group expects a certain volume, which can’t be reached if the competing doctors are allowed back in,” he says.
Many physicians don’t challenge the exclusion
Quite often, excluded doctors decide not to challenge the decision. For example, Dr. Serota says groups of orthopedic surgeons and urologists have decided not to challenge similar decisions by SSM. “They wanted to move on,” he says.
Mr. Callahan says many excluded doctors also don’t even ask for a hearing. “They expect that the hospital’s decision will be upheld,” he says.
This was the case for Devendra K. Amin, MD, an independent cardiologist in Easton, Pa. Dr. Amin has not had any hospital privileges since July 2020. Even though he is board certified in interventional cardiology, which involves catheterization, Dr. Amin says he cannot perform these procedures because they can only be performed in a hospital in the area.
In the 1990s, Dr. Amin says, he had invasive cardiology privileges at five hospitals, but then those hospitals consolidated, and the remaining ones started constricting his privileges. First he could no longer work in the emergency department, then he could no longer read echocardiograms and interpret stress test results, because that work was assigned exclusively to employed doctors, he says.
Then the one remaining hospital announced that privileges would only be available to physicians by invitation, and he was not invited. Dr. Amin says he could have regained general cardiology privileges if he had accepted employment at the hospital, but he did not want to do this. A recruiter and the head of the cardiology section at the hospital even took him out to dinner 2 years ago to discuss employment, but there was a stipulation that the hospital would not agree to.
“I wanted to get back my interventional privileges back,” Dr. Amin says, “but they told me that would not be possible because they had an exclusive contract with a group.”
Dr. Amin says that now, he can only work as a general cardiologist with reduced volume. He says primary care physicians in the local hospital systems only refer to cardiologists within their systems. “When these patients do come to me, it is only because they specifically requested to see me,” Dr. Amin says.
He does not want to challenge the decisions regarding privileging. “Look, I am 68 years old,” Dr. Amin says. “I’m not retiring yet, but I don’t want to get into a battle with a hospital that has very deep pockets. I’m not a confrontational person to begin with, and I don’t want to spend the next 10 years of my life in litigation.”
Diverging expectations
The law on exclusive contracts does not provide easy answers for excluded doctors, and often it defies physicians’ conception of their own role in the hospital.
Many physicians expect the hospital to be a haven where they can do their work without being cut out by a competitor. This view is reinforced by organizations such as the American Medical Association.
The AMA Council on Medical Service states that privileges “can only be abridged upon recommendation of the medical staff and only for reason related to professional competence, adherence to standards of care, and other parameters agreed to by the medical staff.”
But the courts don’t tend to agree with that position. “Hospitals have a fiduciary duty to protect their own financial interests,” Mr. Callahan says. “This may involve anything that furthers the hospital’s mission to provide high-quality health care services to its patient community.”
At the same time, however, there are plenty of instances in which courts have ruled that exclusive contracts had gone too far. But usually it takes a lawyer experienced in these cases to know what those exceptions are.
A version of this article first appeared on Medscape.com.
In April, a group of more than a dozen cardiologists at St. Louis Heart and Vascular (SLHV) lost their privileges at SSM Health, an eight-hospital system in St. Louis.
The physicians did not lose their privileges because of a clinical failure. Rather, it was because of SSM’s decision to enter into an exclusive contract with another set of cardiologists.
“The current situation is economically untenable for us,” said Harvey Serota, MD, founder and medical director of SLHV. “This is an existential threat to the practice.”
Because of the exclusive contract, many of SLHV’s patients are now being redirected to SSM-contracted cardiologists. Volume for the group’s new $15 million catheterization lab has plummeted. SLHV is suing SSM to restore its privileges, claiming lack of due process, restraint of trade, interference with its business, and breach of contract.
Losing privileges because a hospital seeks to increase their profits is becoming all too familiar for many independent specialists in fields such as cardiology, orthopedic surgery, and urology, as the hospitals that hosted them become their competitors and forge exclusive contracts with opposing groups.
What can these doctors do if they’re shut out? File a lawsuit, as SLHV has done? Demand a hearing before the medical staff and try to resolve the problem? Or simply give up their privileges and move on?
Unfortunately, none of these approaches offer a quick or certain solution, and each comes with risks.
Generally, courts have upheld hospitals’ use of exclusive contracts, which is also known as economic credentialing, says Barry F. Rosen, a health law attorney at Gordon Feinblatt, in Baltimore.
“Courts have long recognized exclusive contracts, and challenges by excluded doctors usually fail,” he says.
However, Mr. Rosen can cite several examples in which excluded doctors launched legal challenges that prevailed, owing to nuances in the law. The legal field in this area is tangled, and it varies by state.
Can hospitals make exclusive deals?
Hospitals have long used exclusive contracts for hospital-based specialists – anesthesiologists, radiologists, pathologists, emergency physicians, and hospitalists. They say that restricting patients to one group of anesthesiologists or radiologists enhances operational efficiency and that these contracts do not disrupt patients, because patients have no ties to hospital-based physicians. Such contracts are often more profitable for the hospital because of the negotiated rates.
Exclusive contracts in other specialties, however, are less accepted because they involve markedly different strategies and have different effects. In such cases, the hospital is no longer simply enhancing operational efficiency but is competing with physicians on staff, and the arrangement can disrupt the care of patients of the excluded doctors.
In the courts, these concerns might form the basis of an antitrust action or a claim of tortious interference with physicians’ ability to provide care for their patients, but neither claim is easy to win, Mr. Rosen says.
In antitrust cases, “the issue is not whether the excluded doctor was injured but whether the action harmed competition,” Mr. Rosen says. “Will the exclusion lead to higher prices?”
In the case of interference with patient care, “you will always find interference by one entity in the affairs of another,” he says, “but tortious interference applies to situations where something nefarious is going on, such as the other side was out to destroy your business and create a monopoly.”
Hospitals may try to restrict the privileges of physicians who invest in competing facilities such as cath labs and ambulatory surgery centers (ASCs), says Gregory Mertz, managing director of Physician Strategies Group, a consultancy in Virginia Beach.
“However, any revenge that a hospital might take against the doctors who started an ASC would usually not be publicly admitted,” Mr. Mertz says. “Revenge would be exacted in subtle ways.”
In the St. Louis situation, SSM did not cite SLHV’s cath lab as a reason for its exclusive contract. SSM stated in court documents that the decision was based on the recommendations of an expert panel. Furthermore, SSM said the board created the panel in response to a state report that cited the limited experience of some SLHV cardiologists in treating a rare type of heart attack.
Mr. Mertz says the board’s interest in the state’s concern and then its forming the special panel lent a great deal of legitimacy to SSM’s decision to start an exclusive contract. “SSM can show evidence that the board’s decision was based on a clinical matter and not on trying to squeeze out the cardiologists,” he says.
In SLHV’s defense, Dr. Serota says the practice offered to stop taking calls for the type of heart attack that was cited, but the hospital did not respond to its offer. He says SSM should have consulted the hospital’s medical staff to address the state’s concern and to create the exclusive contract, because these decisions involved clinical issues that the medical staff understands better than the board.
The law, however, does not require a hospital board to consult with its medical staff, says Alice G. Gosfield, a health care attorney in Philadelphia. “The board has ultimate legal control of everything in the hospital,” she says. However, the board often delegates certain functions to the medical staff in the hospital bylaws, and depending on the wording of the bylaws, it is still possible that the board violated the bylaws, Ms. Gosfield adds.
Can excluded physicians get peer review?
Can the hospital medical staff help restore the privileges of excluded physicians? Don’t these physicians have the right to peer review – a hearing before the medical staff?
Indeed, the Joint Commission, which accredits hospitals, states that the hospital must have “mechanisms, including a fair hearing and appeal process, for addressing adverse decisions for existing medical staff members and other individuals holding clinical privileges for renewal, revocation, or revision of clinical privileges.”
However, excluded physicians may not have a right to a hearing if they have not been fully stripped of privileges. SSM discontinued adult cardiology privileges for SLHV doctors but retained some doctors’ internal medicine privileges. Dr. Serota says internal medicine privileges are useless to cardiologists, but because the doctors’ privileges had not been fully removed, they cannot ask for a hearing.
More fundamentally, exclusive contracts are not a good fit for peer review. Mr. Rosen says the hearings were designed to review the physicians’ clinical competence or behavior, but excluded physicians do not have these problems. About all the hearing could focus on is the hospital’s policy, which the board would not want to allow. To avoid this, “the hospital might rule out a hearing as contrary to the intent of the bylaws,” Mr. Rosen says.
Furthermore, even if peer review goes forward, “what the medical staff decides is only advisory, and the hospital board makes the final decision,” Mr. Rosen says. He notes that the doctor could challenge the decision in court, but the hospital might still prevail.
Excluded physicians sometimes prevail
Although it is rare for excluded physicians to win a lawsuit against their hospital, it does happen, says Michael R. Callahan, health lawyer at Katten Muchin Rosenman, in Chicago.
Mr. Callahan cites a 2010 decision by the Arkansas Supreme Court that stopped the state’s largest health system from denying physicians’ privileges. Among other things, the hospital was found to have tortiously interfered with the physicians’ contracts with patients.
In a 2007 decision, a West Virginia court ruled that hospitals that have a mission to serve the public cannot exclude physicians for nonquality issues. In addition, some states, such as Texas, limit the economic factors that can be considered when credentialing decisions are made. Other states, such as Ohio, give hospitals a great deal of leeway to alter credentialing.
Dr. Serota is optimistic about his Missouri lawsuit. Although the judge in the case did not immediately grant SLHV’s request for restoration of privileges while the case proceeds, she did grant expedited discovery – allowing SLHV to obtain documents from SSM that could strengthen the doctors’ case – and she agreed to a hearing on SLHV’s request for a temporary restoration of privileges.
Ms. Gosfield says Dr. Serota’s optimism seems justified, but she adds that such cases cost a lot of money and that they may still not be winnable.
Often plaintiffs can settle lawsuits before they go to trial, but Mr. Callahan says hospitals are loath to restore privileges in a settlement because they don’t want to undermine an exclusivity deal. “The exclusive group expects a certain volume, which can’t be reached if the competing doctors are allowed back in,” he says.
Many physicians don’t challenge the exclusion
Quite often, excluded doctors decide not to challenge the decision. For example, Dr. Serota says groups of orthopedic surgeons and urologists have decided not to challenge similar decisions by SSM. “They wanted to move on,” he says.
Mr. Callahan says many excluded doctors also don’t even ask for a hearing. “They expect that the hospital’s decision will be upheld,” he says.
This was the case for Devendra K. Amin, MD, an independent cardiologist in Easton, Pa. Dr. Amin has not had any hospital privileges since July 2020. Even though he is board certified in interventional cardiology, which involves catheterization, Dr. Amin says he cannot perform these procedures because they can only be performed in a hospital in the area.
In the 1990s, Dr. Amin says, he had invasive cardiology privileges at five hospitals, but then those hospitals consolidated, and the remaining ones started constricting his privileges. First he could no longer work in the emergency department, then he could no longer read echocardiograms and interpret stress test results, because that work was assigned exclusively to employed doctors, he says.
Then the one remaining hospital announced that privileges would only be available to physicians by invitation, and he was not invited. Dr. Amin says he could have regained general cardiology privileges if he had accepted employment at the hospital, but he did not want to do this. A recruiter and the head of the cardiology section at the hospital even took him out to dinner 2 years ago to discuss employment, but there was a stipulation that the hospital would not agree to.
“I wanted to get back my interventional privileges back,” Dr. Amin says, “but they told me that would not be possible because they had an exclusive contract with a group.”
Dr. Amin says that now, he can only work as a general cardiologist with reduced volume. He says primary care physicians in the local hospital systems only refer to cardiologists within their systems. “When these patients do come to me, it is only because they specifically requested to see me,” Dr. Amin says.
He does not want to challenge the decisions regarding privileging. “Look, I am 68 years old,” Dr. Amin says. “I’m not retiring yet, but I don’t want to get into a battle with a hospital that has very deep pockets. I’m not a confrontational person to begin with, and I don’t want to spend the next 10 years of my life in litigation.”
Diverging expectations
The law on exclusive contracts does not provide easy answers for excluded doctors, and often it defies physicians’ conception of their own role in the hospital.
Many physicians expect the hospital to be a haven where they can do their work without being cut out by a competitor. This view is reinforced by organizations such as the American Medical Association.
The AMA Council on Medical Service states that privileges “can only be abridged upon recommendation of the medical staff and only for reason related to professional competence, adherence to standards of care, and other parameters agreed to by the medical staff.”
But the courts don’t tend to agree with that position. “Hospitals have a fiduciary duty to protect their own financial interests,” Mr. Callahan says. “This may involve anything that furthers the hospital’s mission to provide high-quality health care services to its patient community.”
At the same time, however, there are plenty of instances in which courts have ruled that exclusive contracts had gone too far. But usually it takes a lawyer experienced in these cases to know what those exceptions are.
A version of this article first appeared on Medscape.com.
Task force affirms routine gestational diabetes testing
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
FROM JAMA
Heart doc offering ‘fountain of youth’ jailed for 6 1/2 years
Cardiologist Samirkumar J. Shah, MD, was sentenced to 78 months in prison after his conviction on two counts of federal health care fraud involving more than $13 million.
As part of his sentence, Dr. Shah, 58, of Fox Chapel, Pa., must pay $1.7 million in restitution and other penalties and undergo 3 years of supervised release after prison.
“Dr. Shah risked the health of his patients so he could make millions of dollars through unnecessary procedures, and lied and fabricated records for years to perpetuate his fraud scheme,” acting U.S. Attorney Stephen R. Kaufman said in an Aug. 5 statement from the Department of Justice.
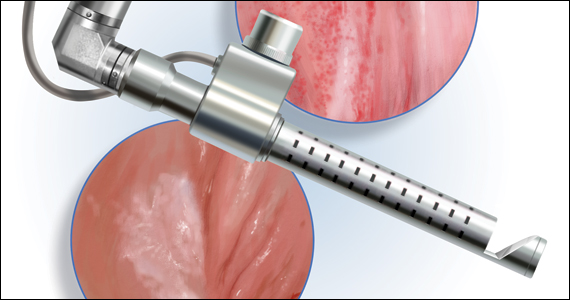
As previously reported, Dr. Shah was convicted June 14, 2019, of submitting fraudulent claims to private and federal insurance programs between 2008 and 2013 for external counterpulsation (ECP) therapy, a lower limb compression treatment approved for patients with coronary artery disease and refractory angina.
Dr. Shah, however, advertised ECP as the “fountain of youth,” claimed it made patients “younger and smarter,” and offered the treatment for conditions such as obesity, hypertension, hypotension, diabetes, and erectile dysfunction.
Patients were required to undergo diagnostic ultrasounds as a precautionary measure prior to starting ECP, but witness testimony established that Dr. Shah did not review any of the imaging before approving new patients for ECP, placing his patients at risk for serious injury or even death, the DOJ stated.
The evidence also showed that Dr. Shah double-billed insurers, routinely submitted fabricated patient files, and made false statements concerning his practice, patient population, recording keeping, and compliance with coverage guidelines, the government said.
During the scheme, Dr. Shah submitted ECP-related claims for Medicare Part B, UPMC Health Plan, Highmark Blue Cross Blue Shield, and Gateway Health Plan beneficiaries totalling more than $13 million and received reimbursement payments in excess of $3.5 million.
“Rather than upholding the oath he swore and providing care for patients who trusted him, this defendant misled patients and drained critical Medicaid funds from families who needed it,” said Attorney General Josh Shapiro. “We will not let anyone put their patients’ lives at risk for a profit.”
“Today’s sentence holds Mr. Shah accountable for his appalling actions,” said FBI Pittsburgh Special Agent in Charge Mike Nordwall. “Mr. Shah used his position as a doctor to illegally profit from a health care program paid for by taxpayers. Fraud of this magnitude will not be tolerated.”
Dr. Shah has been in custody since July 15, 2021, after skipping out on his original July 14 sentencing date. The Tribune-Review reported that Dr. Shah filed a last-minute request for a continuance, claiming he had an adverse reaction to the Pfizer COVID-19 vaccination and was advised by his doctor that he needed “strict bedrest for at least 6 weeks.”
Dr. Shah reportedly turned himself after presiding U.S. District Judge David S. Cercone denied the motion and issued an arrest warrant.
A version of this article first appeared on Medscape.com.
Cardiologist Samirkumar J. Shah, MD, was sentenced to 78 months in prison after his conviction on two counts of federal health care fraud involving more than $13 million.
As part of his sentence, Dr. Shah, 58, of Fox Chapel, Pa., must pay $1.7 million in restitution and other penalties and undergo 3 years of supervised release after prison.
“Dr. Shah risked the health of his patients so he could make millions of dollars through unnecessary procedures, and lied and fabricated records for years to perpetuate his fraud scheme,” acting U.S. Attorney Stephen R. Kaufman said in an Aug. 5 statement from the Department of Justice.
As previously reported, Dr. Shah was convicted June 14, 2019, of submitting fraudulent claims to private and federal insurance programs between 2008 and 2013 for external counterpulsation (ECP) therapy, a lower limb compression treatment approved for patients with coronary artery disease and refractory angina.
Dr. Shah, however, advertised ECP as the “fountain of youth,” claimed it made patients “younger and smarter,” and offered the treatment for conditions such as obesity, hypertension, hypotension, diabetes, and erectile dysfunction.
Patients were required to undergo diagnostic ultrasounds as a precautionary measure prior to starting ECP, but witness testimony established that Dr. Shah did not review any of the imaging before approving new patients for ECP, placing his patients at risk for serious injury or even death, the DOJ stated.
The evidence also showed that Dr. Shah double-billed insurers, routinely submitted fabricated patient files, and made false statements concerning his practice, patient population, recording keeping, and compliance with coverage guidelines, the government said.
During the scheme, Dr. Shah submitted ECP-related claims for Medicare Part B, UPMC Health Plan, Highmark Blue Cross Blue Shield, and Gateway Health Plan beneficiaries totalling more than $13 million and received reimbursement payments in excess of $3.5 million.
“Rather than upholding the oath he swore and providing care for patients who trusted him, this defendant misled patients and drained critical Medicaid funds from families who needed it,” said Attorney General Josh Shapiro. “We will not let anyone put their patients’ lives at risk for a profit.”
“Today’s sentence holds Mr. Shah accountable for his appalling actions,” said FBI Pittsburgh Special Agent in Charge Mike Nordwall. “Mr. Shah used his position as a doctor to illegally profit from a health care program paid for by taxpayers. Fraud of this magnitude will not be tolerated.”
Dr. Shah has been in custody since July 15, 2021, after skipping out on his original July 14 sentencing date. The Tribune-Review reported that Dr. Shah filed a last-minute request for a continuance, claiming he had an adverse reaction to the Pfizer COVID-19 vaccination and was advised by his doctor that he needed “strict bedrest for at least 6 weeks.”
Dr. Shah reportedly turned himself after presiding U.S. District Judge David S. Cercone denied the motion and issued an arrest warrant.
A version of this article first appeared on Medscape.com.
Cardiologist Samirkumar J. Shah, MD, was sentenced to 78 months in prison after his conviction on two counts of federal health care fraud involving more than $13 million.
As part of his sentence, Dr. Shah, 58, of Fox Chapel, Pa., must pay $1.7 million in restitution and other penalties and undergo 3 years of supervised release after prison.
“Dr. Shah risked the health of his patients so he could make millions of dollars through unnecessary procedures, and lied and fabricated records for years to perpetuate his fraud scheme,” acting U.S. Attorney Stephen R. Kaufman said in an Aug. 5 statement from the Department of Justice.
As previously reported, Dr. Shah was convicted June 14, 2019, of submitting fraudulent claims to private and federal insurance programs between 2008 and 2013 for external counterpulsation (ECP) therapy, a lower limb compression treatment approved for patients with coronary artery disease and refractory angina.
Dr. Shah, however, advertised ECP as the “fountain of youth,” claimed it made patients “younger and smarter,” and offered the treatment for conditions such as obesity, hypertension, hypotension, diabetes, and erectile dysfunction.
Patients were required to undergo diagnostic ultrasounds as a precautionary measure prior to starting ECP, but witness testimony established that Dr. Shah did not review any of the imaging before approving new patients for ECP, placing his patients at risk for serious injury or even death, the DOJ stated.
The evidence also showed that Dr. Shah double-billed insurers, routinely submitted fabricated patient files, and made false statements concerning his practice, patient population, recording keeping, and compliance with coverage guidelines, the government said.
During the scheme, Dr. Shah submitted ECP-related claims for Medicare Part B, UPMC Health Plan, Highmark Blue Cross Blue Shield, and Gateway Health Plan beneficiaries totalling more than $13 million and received reimbursement payments in excess of $3.5 million.
“Rather than upholding the oath he swore and providing care for patients who trusted him, this defendant misled patients and drained critical Medicaid funds from families who needed it,” said Attorney General Josh Shapiro. “We will not let anyone put their patients’ lives at risk for a profit.”
“Today’s sentence holds Mr. Shah accountable for his appalling actions,” said FBI Pittsburgh Special Agent in Charge Mike Nordwall. “Mr. Shah used his position as a doctor to illegally profit from a health care program paid for by taxpayers. Fraud of this magnitude will not be tolerated.”
Dr. Shah has been in custody since July 15, 2021, after skipping out on his original July 14 sentencing date. The Tribune-Review reported that Dr. Shah filed a last-minute request for a continuance, claiming he had an adverse reaction to the Pfizer COVID-19 vaccination and was advised by his doctor that he needed “strict bedrest for at least 6 weeks.”
Dr. Shah reportedly turned himself after presiding U.S. District Judge David S. Cercone denied the motion and issued an arrest warrant.
A version of this article first appeared on Medscape.com.
Medical residents need breastfeeding support too
As working mothers with babies in tow when the COVID-19 crisis struck, countless uncertainties threatened our already precarious work-life balance. We suddenly had many questions:
“If my daycare closes, what will I do for childcare?”
“How do I navigate diaper changes, feedings, and naps with my hectic remote work schedule?”
“If I’m constantly interrupted during the day, should I skip sleep to catch up on work and not let my colleagues down?”
As professionals who work closely with medical trainees, we knew our parenting dilemmas were being experienced even more acutely by our frontline worker colleagues.
Medical training is an increasingly common time to start a family. In a recent study, 34% of trainees in Harvard-affiliated residency programs became parents during training, and another 52% planned to do so. Trainees have higher breastfeeding initiation rates but lower continuation rates than the general population. Early nursing cessation among trainees is well documented nationally and is most often attributed to work-related barriers. These barriers range from insufficient time and limited access to facilities to a lack of support and discrimination by supervisors and peers.
This trend does not discriminate by specialty. Even among training programs known to be “family friendly,” the average duration of nursing is just 4.5 months. Residents of color are disproportionately affected by inadequate support. Studies show that Black parents breastfeed at lower rates than White parents. This has been largely attributed to structural racism and implicit bias, such as Black parents receiving less assistance initiating nursing after delivery. Adequate lactation support and inclusivity are also lacking for transgender parents who choose to breastfeed or chestfeed.
The very nature of residency training, which includes shifts that can span more than 24 hours, conflicts with many health-promoting behaviors like sleeping and eating well. However, its interference with lactation is correlated with gender. Women are disproportionately affected by the negative outcomes of unmet lactation goals. These include work-life imbalance, career dissatisfaction, and negative emotions. In a study of pediatric residents, one in four did not achieve their breastfeeding goals. Respondents reported feeling “sad, devastated, defeated, disappointed, guilty, embarrassed, frustrated, angry, like a failure, and inadequate.” Among physician mothers more broadly, discrimination related to pregnancy, parental leave, and nursing is associated with higher self-reported burnout.
Navigating nursing during residency training has more than just emotional and psychological consequences – it also has professional ones. Pursuing personal lactation goals can delay residency program completion and board certification, influence specialty selection, negatively impact research productivity, impede career advancement, and lead to misgivings about career choice.
Trainees and their families are not the only ones harmed by inadequate support in residency programs. Patients and their families are affected, too. Research suggests that physicians’ personal breastfeeding practices affect the advice they give to patients. Those who receive lactation support are more likely to help patients meet their own goals. In the previously mentioned study of pediatric residents, more than 90% of the 400 respondents said their own or their partner’s nursing experience affected their interaction with lactating patients in their clinic or hospital.
Increased lactation support is a straightforward, low-cost, high-impact intervention. It benefits trainee well-being, satisfaction, workflow, and future patient care. The Accreditation Council for Graduate Medical Education mandated in July 2019 that all residency programs provide adequate lactation facilities – including refrigeration capabilities and proximity for safe patient care. However, to our knowledge, rates of compliance with this new policy and citation for noncompliance have yet to be seen. Regardless, facilities alone are not enough. Residency programs should develop and enforce formal lactation policies.
Several institutions have successfully piloted such policies in recent years. One in particular from the University of Michigan’s surgery residency program inspired the development of a lactation policy within the internal medicine residency at our institution. These policies designate appropriate spaces at each clinical rotation site, clarify that residents are encouraged to take pumping breaks as needed – in coordination with clinical teams so as not to compromise patient care – and communicate support from supervisors.
Our program also established an informal peer mentoring program. Residents with experience pumping at work pair up with newer trainees. The policy benefits residents who wish to chestfeed or breastfeed, normalizes lactation, and empowers trainees by diminishing the need to ask for individual accommodations. It also costs the program nothing.
As more women enter medicine and more trainees become parents during residency, the need for support in this area will only continue to grow. The widespread lack of such resources, and the fact that clean and private facilities are only now being mandated, is symbolic. If even this basic need is rarely acknowledged or met, what other resident needs are being neglected?
A version of this article first appeared on Medscape.com.
As working mothers with babies in tow when the COVID-19 crisis struck, countless uncertainties threatened our already precarious work-life balance. We suddenly had many questions:
“If my daycare closes, what will I do for childcare?”
“How do I navigate diaper changes, feedings, and naps with my hectic remote work schedule?”
“If I’m constantly interrupted during the day, should I skip sleep to catch up on work and not let my colleagues down?”
As professionals who work closely with medical trainees, we knew our parenting dilemmas were being experienced even more acutely by our frontline worker colleagues.
Medical training is an increasingly common time to start a family. In a recent study, 34% of trainees in Harvard-affiliated residency programs became parents during training, and another 52% planned to do so. Trainees have higher breastfeeding initiation rates but lower continuation rates than the general population. Early nursing cessation among trainees is well documented nationally and is most often attributed to work-related barriers. These barriers range from insufficient time and limited access to facilities to a lack of support and discrimination by supervisors and peers.
This trend does not discriminate by specialty. Even among training programs known to be “family friendly,” the average duration of nursing is just 4.5 months. Residents of color are disproportionately affected by inadequate support. Studies show that Black parents breastfeed at lower rates than White parents. This has been largely attributed to structural racism and implicit bias, such as Black parents receiving less assistance initiating nursing after delivery. Adequate lactation support and inclusivity are also lacking for transgender parents who choose to breastfeed or chestfeed.
The very nature of residency training, which includes shifts that can span more than 24 hours, conflicts with many health-promoting behaviors like sleeping and eating well. However, its interference with lactation is correlated with gender. Women are disproportionately affected by the negative outcomes of unmet lactation goals. These include work-life imbalance, career dissatisfaction, and negative emotions. In a study of pediatric residents, one in four did not achieve their breastfeeding goals. Respondents reported feeling “sad, devastated, defeated, disappointed, guilty, embarrassed, frustrated, angry, like a failure, and inadequate.” Among physician mothers more broadly, discrimination related to pregnancy, parental leave, and nursing is associated with higher self-reported burnout.
Navigating nursing during residency training has more than just emotional and psychological consequences – it also has professional ones. Pursuing personal lactation goals can delay residency program completion and board certification, influence specialty selection, negatively impact research productivity, impede career advancement, and lead to misgivings about career choice.
Trainees and their families are not the only ones harmed by inadequate support in residency programs. Patients and their families are affected, too. Research suggests that physicians’ personal breastfeeding practices affect the advice they give to patients. Those who receive lactation support are more likely to help patients meet their own goals. In the previously mentioned study of pediatric residents, more than 90% of the 400 respondents said their own or their partner’s nursing experience affected their interaction with lactating patients in their clinic or hospital.
Increased lactation support is a straightforward, low-cost, high-impact intervention. It benefits trainee well-being, satisfaction, workflow, and future patient care. The Accreditation Council for Graduate Medical Education mandated in July 2019 that all residency programs provide adequate lactation facilities – including refrigeration capabilities and proximity for safe patient care. However, to our knowledge, rates of compliance with this new policy and citation for noncompliance have yet to be seen. Regardless, facilities alone are not enough. Residency programs should develop and enforce formal lactation policies.
Several institutions have successfully piloted such policies in recent years. One in particular from the University of Michigan’s surgery residency program inspired the development of a lactation policy within the internal medicine residency at our institution. These policies designate appropriate spaces at each clinical rotation site, clarify that residents are encouraged to take pumping breaks as needed – in coordination with clinical teams so as not to compromise patient care – and communicate support from supervisors.
Our program also established an informal peer mentoring program. Residents with experience pumping at work pair up with newer trainees. The policy benefits residents who wish to chestfeed or breastfeed, normalizes lactation, and empowers trainees by diminishing the need to ask for individual accommodations. It also costs the program nothing.
As more women enter medicine and more trainees become parents during residency, the need for support in this area will only continue to grow. The widespread lack of such resources, and the fact that clean and private facilities are only now being mandated, is symbolic. If even this basic need is rarely acknowledged or met, what other resident needs are being neglected?
A version of this article first appeared on Medscape.com.
As working mothers with babies in tow when the COVID-19 crisis struck, countless uncertainties threatened our already precarious work-life balance. We suddenly had many questions:
“If my daycare closes, what will I do for childcare?”
“How do I navigate diaper changes, feedings, and naps with my hectic remote work schedule?”
“If I’m constantly interrupted during the day, should I skip sleep to catch up on work and not let my colleagues down?”
As professionals who work closely with medical trainees, we knew our parenting dilemmas were being experienced even more acutely by our frontline worker colleagues.
Medical training is an increasingly common time to start a family. In a recent study, 34% of trainees in Harvard-affiliated residency programs became parents during training, and another 52% planned to do so. Trainees have higher breastfeeding initiation rates but lower continuation rates than the general population. Early nursing cessation among trainees is well documented nationally and is most often attributed to work-related barriers. These barriers range from insufficient time and limited access to facilities to a lack of support and discrimination by supervisors and peers.
This trend does not discriminate by specialty. Even among training programs known to be “family friendly,” the average duration of nursing is just 4.5 months. Residents of color are disproportionately affected by inadequate support. Studies show that Black parents breastfeed at lower rates than White parents. This has been largely attributed to structural racism and implicit bias, such as Black parents receiving less assistance initiating nursing after delivery. Adequate lactation support and inclusivity are also lacking for transgender parents who choose to breastfeed or chestfeed.
The very nature of residency training, which includes shifts that can span more than 24 hours, conflicts with many health-promoting behaviors like sleeping and eating well. However, its interference with lactation is correlated with gender. Women are disproportionately affected by the negative outcomes of unmet lactation goals. These include work-life imbalance, career dissatisfaction, and negative emotions. In a study of pediatric residents, one in four did not achieve their breastfeeding goals. Respondents reported feeling “sad, devastated, defeated, disappointed, guilty, embarrassed, frustrated, angry, like a failure, and inadequate.” Among physician mothers more broadly, discrimination related to pregnancy, parental leave, and nursing is associated with higher self-reported burnout.
Navigating nursing during residency training has more than just emotional and psychological consequences – it also has professional ones. Pursuing personal lactation goals can delay residency program completion and board certification, influence specialty selection, negatively impact research productivity, impede career advancement, and lead to misgivings about career choice.
Trainees and their families are not the only ones harmed by inadequate support in residency programs. Patients and their families are affected, too. Research suggests that physicians’ personal breastfeeding practices affect the advice they give to patients. Those who receive lactation support are more likely to help patients meet their own goals. In the previously mentioned study of pediatric residents, more than 90% of the 400 respondents said their own or their partner’s nursing experience affected their interaction with lactating patients in their clinic or hospital.
Increased lactation support is a straightforward, low-cost, high-impact intervention. It benefits trainee well-being, satisfaction, workflow, and future patient care. The Accreditation Council for Graduate Medical Education mandated in July 2019 that all residency programs provide adequate lactation facilities – including refrigeration capabilities and proximity for safe patient care. However, to our knowledge, rates of compliance with this new policy and citation for noncompliance have yet to be seen. Regardless, facilities alone are not enough. Residency programs should develop and enforce formal lactation policies.
Several institutions have successfully piloted such policies in recent years. One in particular from the University of Michigan’s surgery residency program inspired the development of a lactation policy within the internal medicine residency at our institution. These policies designate appropriate spaces at each clinical rotation site, clarify that residents are encouraged to take pumping breaks as needed – in coordination with clinical teams so as not to compromise patient care – and communicate support from supervisors.
Our program also established an informal peer mentoring program. Residents with experience pumping at work pair up with newer trainees. The policy benefits residents who wish to chestfeed or breastfeed, normalizes lactation, and empowers trainees by diminishing the need to ask for individual accommodations. It also costs the program nothing.
As more women enter medicine and more trainees become parents during residency, the need for support in this area will only continue to grow. The widespread lack of such resources, and the fact that clean and private facilities are only now being mandated, is symbolic. If even this basic need is rarely acknowledged or met, what other resident needs are being neglected?
A version of this article first appeared on Medscape.com.
Achieving a ‘new sexual-health paradigm’ means expanding STI care
A vital aspect of expanding access and care for sexually transmitted infections (STIs) in the United States is broadening responsibility for this care across the health care system and other community resources, according to an article published online July 6 in Clinical Infectious Diseases. This expansion and decentralization of care are central to adopting the “new sexual health paradigm” recommended by a National Academies report that was published in March.
“STIs represent a sizable, longstanding, and growing public health challenge,” write Vincent Guilamo-Ramos, PhD, MPH, dean and professor at the Duke University School of Nursing and director of the Center for Latino Adolescent and Family Health (CLAFH) at Duke University, both in Durham, N.C., and his colleagues. Yet the limitations on the current STI workforce and limited federal funding and support for STI prevention and care mean it will take clinicians of all types from across the health care spectrum to meet the challenge, they explain.
“For too long, STI prevention and treatment has been perceived as the sole responsibility of a narrow workforce of specialized STI and HIV service providers,” Dr. Guilamo-Ramos and his coauthor, Marco Thimm-Kaiser, MPH, associate in research at Duke University and epidemiologist at CLAFH, wrote in an email.
“However, the resources allocated to this STI specialty workforce have diminished over time, along with decreasing investments in the broader U.S. public health infrastructure,” they continued. “At the same time – and in part due to this underinvestment – STI rates have soared, reaching a record high for the sixth year in a row in 2019.”
Those factors led to the National Academies report, which recommends moving “away from the traditional, disease-focused perspective on STIs in favor of a holistic perspective of sexual health as an integral component of overall health and well-being,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote to this news organization.
In their article, the authors review the limitations in the STI workforce, the implications of those limitations for the broader health care industry, and what it will take for STI and HIV specialists as well as regulators to ensure it’s possible to achieve the paradigm shift recommended by the National Academies.
Currently, the biggest limitation is access to care, said Laura Mercer, MD, MBA, of the department of obstetrics and gynecology and the ob.gyn. clerkship director at the University of Arizona, Phoenix. Dr. Mercer, who was not involved with the National Academies report or the analysis of it, said in an interview that it’s essential to emphasize “sexual health as a core element of routine primary and preventative care” to ensure it becomes more accessible to patients without the need to seek out specialty care.
Dr. Guilamo-Ramos and his colleagues drive home the importance of such a shift by noting that more than 200 million Americans live in counties with no practicing infectious disease physicians. The disparities are greatest in Southern states, which account for 40% of all reported STIs. The workforce shortage has continued to worsen alongside the deterioration of the clinical infrastructure supporting STI specialty services, the authors write.
Hence the need to expand accountability for care not only to primary-care physicians but also to nurses, pharmacists, physician assistants, nurse practitioners, and behavioral health practitioners. Doing so also requires normalizing sexual health services across health care professions.
“Prevention is a crucial first step” to this, Dr. Mercer said. “This is particularly important as we recall that almost half of new sexually transmitted infections occur in teenagers. Destigmatizing sexual health and sexual health education will also help encourage patients of all ages to request and accept testing.”
Further, with primary care practitioners managing most STI testing and treatment, subspecialists can focus primarily on complex or refractory cases, she added. Ways to help broaden care include developing point-of-care testing for STIs and improving the accuracy of existing testing, she said.
“The goal is to make routine sexual health services accessible in a wide range of settings, such as in primary care, at pharmacies, and in community-based settings, and to draw on a broader workforce for delivery of sexual health services,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser said in an interview.
Kevin Ault, MD, professor of obstetrics and gynecology and director of clinical and translational research at the University of Kansas Medical Center in Kansas City, said that many medical organizations, such as the American College of Obstetricians and Gynecologists, have long advocated incorporating sexual health into routine preventive care. He also noted that pharmacists have already become proactive in preventing STIs and could continue to do so.
“Vaccines for hepatitis and human papillomavirus are commonly available at pharmacies,” Dr. Ault said. He was not involved in the article by Dr. Guilamo-Ramos and colleagues or the original report. “Pharmacists could also fill a gap by administering injectable medications such as penicillin. States would have to approve changes in policy, but many states have already done this for expedited partner therapy.”
Dr. Guilamo-Ramos and Mr. Thimm-Kaiser noted similar barriers that must be removed to broaden delivery of STI services.
“Unfortunately, too many highly trained health care providers who are well-positioned for the delivery of sexual health services face regulatory or administrative barriers to practice to the full scope of their training,” they wrote. “These barriers can have a particularly negative impact in medically underserved communities, where physician shortages are common and where novel, decentralized health care service delivery models that draw on nonphysician providers may hold the greatest promise.”
As more diverse health care practitioners take on these roles, ID and HIV specialists can provide their expertise in developing training and technical assistance to support generalists, Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote. They can also aid in aligning “clinical training curricula, licensing criteria, and practice guidelines with routine delivery of sexual health services.”
Dr. Guilamo-Ramos and his coauthors offer specific recommendations for professional training, licensing, and practice guidelines to help overcome the “insufficient knowledge, inadequate training, and absence of explicit protocols” that currently impede delivery of STI services in general practice settings.
Although the paradigm shift recommended by the National Academies is ambitious, it’s also necessary, and “none of the recommendations are out of reach,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser said in an interview. They pointed out how the COVID-19 pandemic has highlighted how underresourced the health care workforce and infrastructure are and how great health care disparities are.
“There is momentum toward rebuilding the nation’s health and public health system in a more effective and efficient way,” they said, and many of the STI report’s recommendations “overlap with priorities for the broader health and public health system moving forward.”
Dr. Mercer also believes the recommendations are realistic, “but only the beginning,” she told this news organization. “Comprehensive sexual education to expand knowledge about STI prevention and public health campaigns to help destigmatize sexual health care in general will remain crucial,” she said.
Sexual education, expanded access, and destigmatizing sexual care are particularly important for reaching the populations most in need of care, such as adolescents and young adults, as well as ethnic, racial, sexual, and gender-minority youth.
“It cannot be overstated how important of a priority population adolescents and young adults are,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote. They noted that those aged 15-24 account for half of all STIs each year but represent only a quarter of the sexually active population. “Targeted efforts for STI prevention and treatment among adolescents and young adults are therefore essential for an overall successful strategy to address STIs and sexual health in the United States.”
The National Academies report was supported by the Centers for Disease Control and Prevention and the National Association of County and City Health Officials. Dr. Mercer, Dr. Ault, and Mr. Thimm-Kaiser have disclosed no relevant financial relationships. Dr. Guilamo-Ramos has received grants and personal fees from ViiV Health care.
A version of this article first appeared on Medscape.com.
A vital aspect of expanding access and care for sexually transmitted infections (STIs) in the United States is broadening responsibility for this care across the health care system and other community resources, according to an article published online July 6 in Clinical Infectious Diseases. This expansion and decentralization of care are central to adopting the “new sexual health paradigm” recommended by a National Academies report that was published in March.
“STIs represent a sizable, longstanding, and growing public health challenge,” write Vincent Guilamo-Ramos, PhD, MPH, dean and professor at the Duke University School of Nursing and director of the Center for Latino Adolescent and Family Health (CLAFH) at Duke University, both in Durham, N.C., and his colleagues. Yet the limitations on the current STI workforce and limited federal funding and support for STI prevention and care mean it will take clinicians of all types from across the health care spectrum to meet the challenge, they explain.
“For too long, STI prevention and treatment has been perceived as the sole responsibility of a narrow workforce of specialized STI and HIV service providers,” Dr. Guilamo-Ramos and his coauthor, Marco Thimm-Kaiser, MPH, associate in research at Duke University and epidemiologist at CLAFH, wrote in an email.
“However, the resources allocated to this STI specialty workforce have diminished over time, along with decreasing investments in the broader U.S. public health infrastructure,” they continued. “At the same time – and in part due to this underinvestment – STI rates have soared, reaching a record high for the sixth year in a row in 2019.”
Those factors led to the National Academies report, which recommends moving “away from the traditional, disease-focused perspective on STIs in favor of a holistic perspective of sexual health as an integral component of overall health and well-being,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote to this news organization.
In their article, the authors review the limitations in the STI workforce, the implications of those limitations for the broader health care industry, and what it will take for STI and HIV specialists as well as regulators to ensure it’s possible to achieve the paradigm shift recommended by the National Academies.
Currently, the biggest limitation is access to care, said Laura Mercer, MD, MBA, of the department of obstetrics and gynecology and the ob.gyn. clerkship director at the University of Arizona, Phoenix. Dr. Mercer, who was not involved with the National Academies report or the analysis of it, said in an interview that it’s essential to emphasize “sexual health as a core element of routine primary and preventative care” to ensure it becomes more accessible to patients without the need to seek out specialty care.
Dr. Guilamo-Ramos and his colleagues drive home the importance of such a shift by noting that more than 200 million Americans live in counties with no practicing infectious disease physicians. The disparities are greatest in Southern states, which account for 40% of all reported STIs. The workforce shortage has continued to worsen alongside the deterioration of the clinical infrastructure supporting STI specialty services, the authors write.
Hence the need to expand accountability for care not only to primary-care physicians but also to nurses, pharmacists, physician assistants, nurse practitioners, and behavioral health practitioners. Doing so also requires normalizing sexual health services across health care professions.
“Prevention is a crucial first step” to this, Dr. Mercer said. “This is particularly important as we recall that almost half of new sexually transmitted infections occur in teenagers. Destigmatizing sexual health and sexual health education will also help encourage patients of all ages to request and accept testing.”
Further, with primary care practitioners managing most STI testing and treatment, subspecialists can focus primarily on complex or refractory cases, she added. Ways to help broaden care include developing point-of-care testing for STIs and improving the accuracy of existing testing, she said.
“The goal is to make routine sexual health services accessible in a wide range of settings, such as in primary care, at pharmacies, and in community-based settings, and to draw on a broader workforce for delivery of sexual health services,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser said in an interview.
Kevin Ault, MD, professor of obstetrics and gynecology and director of clinical and translational research at the University of Kansas Medical Center in Kansas City, said that many medical organizations, such as the American College of Obstetricians and Gynecologists, have long advocated incorporating sexual health into routine preventive care. He also noted that pharmacists have already become proactive in preventing STIs and could continue to do so.
“Vaccines for hepatitis and human papillomavirus are commonly available at pharmacies,” Dr. Ault said. He was not involved in the article by Dr. Guilamo-Ramos and colleagues or the original report. “Pharmacists could also fill a gap by administering injectable medications such as penicillin. States would have to approve changes in policy, but many states have already done this for expedited partner therapy.”
Dr. Guilamo-Ramos and Mr. Thimm-Kaiser noted similar barriers that must be removed to broaden delivery of STI services.
“Unfortunately, too many highly trained health care providers who are well-positioned for the delivery of sexual health services face regulatory or administrative barriers to practice to the full scope of their training,” they wrote. “These barriers can have a particularly negative impact in medically underserved communities, where physician shortages are common and where novel, decentralized health care service delivery models that draw on nonphysician providers may hold the greatest promise.”
As more diverse health care practitioners take on these roles, ID and HIV specialists can provide their expertise in developing training and technical assistance to support generalists, Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote. They can also aid in aligning “clinical training curricula, licensing criteria, and practice guidelines with routine delivery of sexual health services.”
Dr. Guilamo-Ramos and his coauthors offer specific recommendations for professional training, licensing, and practice guidelines to help overcome the “insufficient knowledge, inadequate training, and absence of explicit protocols” that currently impede delivery of STI services in general practice settings.
Although the paradigm shift recommended by the National Academies is ambitious, it’s also necessary, and “none of the recommendations are out of reach,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser said in an interview. They pointed out how the COVID-19 pandemic has highlighted how underresourced the health care workforce and infrastructure are and how great health care disparities are.
“There is momentum toward rebuilding the nation’s health and public health system in a more effective and efficient way,” they said, and many of the STI report’s recommendations “overlap with priorities for the broader health and public health system moving forward.”
Dr. Mercer also believes the recommendations are realistic, “but only the beginning,” she told this news organization. “Comprehensive sexual education to expand knowledge about STI prevention and public health campaigns to help destigmatize sexual health care in general will remain crucial,” she said.
Sexual education, expanded access, and destigmatizing sexual care are particularly important for reaching the populations most in need of care, such as adolescents and young adults, as well as ethnic, racial, sexual, and gender-minority youth.
“It cannot be overstated how important of a priority population adolescents and young adults are,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote. They noted that those aged 15-24 account for half of all STIs each year but represent only a quarter of the sexually active population. “Targeted efforts for STI prevention and treatment among adolescents and young adults are therefore essential for an overall successful strategy to address STIs and sexual health in the United States.”
The National Academies report was supported by the Centers for Disease Control and Prevention and the National Association of County and City Health Officials. Dr. Mercer, Dr. Ault, and Mr. Thimm-Kaiser have disclosed no relevant financial relationships. Dr. Guilamo-Ramos has received grants and personal fees from ViiV Health care.
A version of this article first appeared on Medscape.com.
A vital aspect of expanding access and care for sexually transmitted infections (STIs) in the United States is broadening responsibility for this care across the health care system and other community resources, according to an article published online July 6 in Clinical Infectious Diseases. This expansion and decentralization of care are central to adopting the “new sexual health paradigm” recommended by a National Academies report that was published in March.
“STIs represent a sizable, longstanding, and growing public health challenge,” write Vincent Guilamo-Ramos, PhD, MPH, dean and professor at the Duke University School of Nursing and director of the Center for Latino Adolescent and Family Health (CLAFH) at Duke University, both in Durham, N.C., and his colleagues. Yet the limitations on the current STI workforce and limited federal funding and support for STI prevention and care mean it will take clinicians of all types from across the health care spectrum to meet the challenge, they explain.
“For too long, STI prevention and treatment has been perceived as the sole responsibility of a narrow workforce of specialized STI and HIV service providers,” Dr. Guilamo-Ramos and his coauthor, Marco Thimm-Kaiser, MPH, associate in research at Duke University and epidemiologist at CLAFH, wrote in an email.
“However, the resources allocated to this STI specialty workforce have diminished over time, along with decreasing investments in the broader U.S. public health infrastructure,” they continued. “At the same time – and in part due to this underinvestment – STI rates have soared, reaching a record high for the sixth year in a row in 2019.”
Those factors led to the National Academies report, which recommends moving “away from the traditional, disease-focused perspective on STIs in favor of a holistic perspective of sexual health as an integral component of overall health and well-being,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote to this news organization.
In their article, the authors review the limitations in the STI workforce, the implications of those limitations for the broader health care industry, and what it will take for STI and HIV specialists as well as regulators to ensure it’s possible to achieve the paradigm shift recommended by the National Academies.
Currently, the biggest limitation is access to care, said Laura Mercer, MD, MBA, of the department of obstetrics and gynecology and the ob.gyn. clerkship director at the University of Arizona, Phoenix. Dr. Mercer, who was not involved with the National Academies report or the analysis of it, said in an interview that it’s essential to emphasize “sexual health as a core element of routine primary and preventative care” to ensure it becomes more accessible to patients without the need to seek out specialty care.
Dr. Guilamo-Ramos and his colleagues drive home the importance of such a shift by noting that more than 200 million Americans live in counties with no practicing infectious disease physicians. The disparities are greatest in Southern states, which account for 40% of all reported STIs. The workforce shortage has continued to worsen alongside the deterioration of the clinical infrastructure supporting STI specialty services, the authors write.
Hence the need to expand accountability for care not only to primary-care physicians but also to nurses, pharmacists, physician assistants, nurse practitioners, and behavioral health practitioners. Doing so also requires normalizing sexual health services across health care professions.
“Prevention is a crucial first step” to this, Dr. Mercer said. “This is particularly important as we recall that almost half of new sexually transmitted infections occur in teenagers. Destigmatizing sexual health and sexual health education will also help encourage patients of all ages to request and accept testing.”
Further, with primary care practitioners managing most STI testing and treatment, subspecialists can focus primarily on complex or refractory cases, she added. Ways to help broaden care include developing point-of-care testing for STIs and improving the accuracy of existing testing, she said.
“The goal is to make routine sexual health services accessible in a wide range of settings, such as in primary care, at pharmacies, and in community-based settings, and to draw on a broader workforce for delivery of sexual health services,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser said in an interview.
Kevin Ault, MD, professor of obstetrics and gynecology and director of clinical and translational research at the University of Kansas Medical Center in Kansas City, said that many medical organizations, such as the American College of Obstetricians and Gynecologists, have long advocated incorporating sexual health into routine preventive care. He also noted that pharmacists have already become proactive in preventing STIs and could continue to do so.
“Vaccines for hepatitis and human papillomavirus are commonly available at pharmacies,” Dr. Ault said. He was not involved in the article by Dr. Guilamo-Ramos and colleagues or the original report. “Pharmacists could also fill a gap by administering injectable medications such as penicillin. States would have to approve changes in policy, but many states have already done this for expedited partner therapy.”
Dr. Guilamo-Ramos and Mr. Thimm-Kaiser noted similar barriers that must be removed to broaden delivery of STI services.
“Unfortunately, too many highly trained health care providers who are well-positioned for the delivery of sexual health services face regulatory or administrative barriers to practice to the full scope of their training,” they wrote. “These barriers can have a particularly negative impact in medically underserved communities, where physician shortages are common and where novel, decentralized health care service delivery models that draw on nonphysician providers may hold the greatest promise.”
As more diverse health care practitioners take on these roles, ID and HIV specialists can provide their expertise in developing training and technical assistance to support generalists, Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote. They can also aid in aligning “clinical training curricula, licensing criteria, and practice guidelines with routine delivery of sexual health services.”
Dr. Guilamo-Ramos and his coauthors offer specific recommendations for professional training, licensing, and practice guidelines to help overcome the “insufficient knowledge, inadequate training, and absence of explicit protocols” that currently impede delivery of STI services in general practice settings.
Although the paradigm shift recommended by the National Academies is ambitious, it’s also necessary, and “none of the recommendations are out of reach,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser said in an interview. They pointed out how the COVID-19 pandemic has highlighted how underresourced the health care workforce and infrastructure are and how great health care disparities are.
“There is momentum toward rebuilding the nation’s health and public health system in a more effective and efficient way,” they said, and many of the STI report’s recommendations “overlap with priorities for the broader health and public health system moving forward.”
Dr. Mercer also believes the recommendations are realistic, “but only the beginning,” she told this news organization. “Comprehensive sexual education to expand knowledge about STI prevention and public health campaigns to help destigmatize sexual health care in general will remain crucial,” she said.
Sexual education, expanded access, and destigmatizing sexual care are particularly important for reaching the populations most in need of care, such as adolescents and young adults, as well as ethnic, racial, sexual, and gender-minority youth.
“It cannot be overstated how important of a priority population adolescents and young adults are,” Dr. Guilamo-Ramos and Mr. Thimm-Kaiser wrote. They noted that those aged 15-24 account for half of all STIs each year but represent only a quarter of the sexually active population. “Targeted efforts for STI prevention and treatment among adolescents and young adults are therefore essential for an overall successful strategy to address STIs and sexual health in the United States.”
The National Academies report was supported by the Centers for Disease Control and Prevention and the National Association of County and City Health Officials. Dr. Mercer, Dr. Ault, and Mr. Thimm-Kaiser have disclosed no relevant financial relationships. Dr. Guilamo-Ramos has received grants and personal fees from ViiV Health care.
A version of this article first appeared on Medscape.com.
A sizzling hybrid meeting of the Society of Gynecologic Surgeons
The 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS), like so many things in our modern world, endured many changes and had to stay nimble and evolve to changing times. In the end, however, SGS was able to adapt and succeed, just like a skilled gynecologic surgeon in the operating room, to deliver a fresh new type of meeting.
When we chose the meeting theme, “Working together: How collaboration enables us to better help our patients,” we anticipated a meeting discussing medical colleagues and consultants. In our forever-changed world, we knew we needed to reinterpret this to a broader social context. Our special lectures and panel discussions sought to open attendees’ eyes to disparities in health care for people of color and women.
While we highlighted the realities faced by colleagues in medicine, the topics addressed also were designed to grow awareness about struggles our patients encounter as well. Social disparities are sobering, long-standing, and sometimes require creative collaborations to achieve successful outcomes for all patients. The faculty of one of our postgraduate courses reviews in this special 2-part section to
The meeting also kicked off with a postgraduate course on fibroid management, with workshops on harnessing the power of social media and lessons on leadership from a female Fortune 500 CEO, Lori Ryerkerk, offered as well. As the scientific program launched, we were once again treated to strong science on gynecologic surgery, with only a small dip in abstract submissions, despite the challenges of research during a pandemic. Mark Walters, MD, gave the inaugural lecture in his name on the crucial topic of surgical education and teaching. We also heard a special report from the SGS SOCOVID research group, led by Dr. Rosanne Kho, on gynecologic surgery during the pandemic. We also convened a virtual panel for our hybrid attendees on the benefits to patients of a multidisciplinary approach to gynecologic surgery, presented here by Cecile Ferrando, MD.
As our practices continue to grow and evolve, the introduction of innovative technologies can pose a new challenge, as Miles Murphy, MD, and members of the panel on novel gynecologic office procedures will present in this series next month.
The TeLinde keynote speaker was Janet Dombrowski, who works as a coach for many surgeons in various disciplines across the country. She spoke to the resilience gained through community and collaboration.
While our meeting theme dated to the “before” pandemic era, those who were able to be in attendance in person can attest to the value we can all place now on community and personal interactions. With experience strengthened by science, I hope this meeting summary serves to highlight the many ways in which we can collaborate to improve outcomes for ourselves in medicine and for patients.
The 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS), like so many things in our modern world, endured many changes and had to stay nimble and evolve to changing times. In the end, however, SGS was able to adapt and succeed, just like a skilled gynecologic surgeon in the operating room, to deliver a fresh new type of meeting.
When we chose the meeting theme, “Working together: How collaboration enables us to better help our patients,” we anticipated a meeting discussing medical colleagues and consultants. In our forever-changed world, we knew we needed to reinterpret this to a broader social context. Our special lectures and panel discussions sought to open attendees’ eyes to disparities in health care for people of color and women.
While we highlighted the realities faced by colleagues in medicine, the topics addressed also were designed to grow awareness about struggles our patients encounter as well. Social disparities are sobering, long-standing, and sometimes require creative collaborations to achieve successful outcomes for all patients. The faculty of one of our postgraduate courses reviews in this special 2-part section to
The meeting also kicked off with a postgraduate course on fibroid management, with workshops on harnessing the power of social media and lessons on leadership from a female Fortune 500 CEO, Lori Ryerkerk, offered as well. As the scientific program launched, we were once again treated to strong science on gynecologic surgery, with only a small dip in abstract submissions, despite the challenges of research during a pandemic. Mark Walters, MD, gave the inaugural lecture in his name on the crucial topic of surgical education and teaching. We also heard a special report from the SGS SOCOVID research group, led by Dr. Rosanne Kho, on gynecologic surgery during the pandemic. We also convened a virtual panel for our hybrid attendees on the benefits to patients of a multidisciplinary approach to gynecologic surgery, presented here by Cecile Ferrando, MD.
As our practices continue to grow and evolve, the introduction of innovative technologies can pose a new challenge, as Miles Murphy, MD, and members of the panel on novel gynecologic office procedures will present in this series next month.
The TeLinde keynote speaker was Janet Dombrowski, who works as a coach for many surgeons in various disciplines across the country. She spoke to the resilience gained through community and collaboration.
While our meeting theme dated to the “before” pandemic era, those who were able to be in attendance in person can attest to the value we can all place now on community and personal interactions. With experience strengthened by science, I hope this meeting summary serves to highlight the many ways in which we can collaborate to improve outcomes for ourselves in medicine and for patients.
The 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS), like so many things in our modern world, endured many changes and had to stay nimble and evolve to changing times. In the end, however, SGS was able to adapt and succeed, just like a skilled gynecologic surgeon in the operating room, to deliver a fresh new type of meeting.
When we chose the meeting theme, “Working together: How collaboration enables us to better help our patients,” we anticipated a meeting discussing medical colleagues and consultants. In our forever-changed world, we knew we needed to reinterpret this to a broader social context. Our special lectures and panel discussions sought to open attendees’ eyes to disparities in health care for people of color and women.
While we highlighted the realities faced by colleagues in medicine, the topics addressed also were designed to grow awareness about struggles our patients encounter as well. Social disparities are sobering, long-standing, and sometimes require creative collaborations to achieve successful outcomes for all patients. The faculty of one of our postgraduate courses reviews in this special 2-part section to
The meeting also kicked off with a postgraduate course on fibroid management, with workshops on harnessing the power of social media and lessons on leadership from a female Fortune 500 CEO, Lori Ryerkerk, offered as well. As the scientific program launched, we were once again treated to strong science on gynecologic surgery, with only a small dip in abstract submissions, despite the challenges of research during a pandemic. Mark Walters, MD, gave the inaugural lecture in his name on the crucial topic of surgical education and teaching. We also heard a special report from the SGS SOCOVID research group, led by Dr. Rosanne Kho, on gynecologic surgery during the pandemic. We also convened a virtual panel for our hybrid attendees on the benefits to patients of a multidisciplinary approach to gynecologic surgery, presented here by Cecile Ferrando, MD.
As our practices continue to grow and evolve, the introduction of innovative technologies can pose a new challenge, as Miles Murphy, MD, and members of the panel on novel gynecologic office procedures will present in this series next month.
The TeLinde keynote speaker was Janet Dombrowski, who works as a coach for many surgeons in various disciplines across the country. She spoke to the resilience gained through community and collaboration.
While our meeting theme dated to the “before” pandemic era, those who were able to be in attendance in person can attest to the value we can all place now on community and personal interactions. With experience strengthened by science, I hope this meeting summary serves to highlight the many ways in which we can collaborate to improve outcomes for ourselves in medicine and for patients.
2021 Update on female sexual health
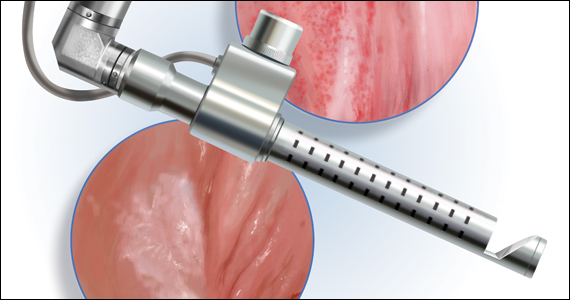
The approach to diagnosis and treatment of female sexual function continues to be a challenge for women’s health professionals. The search for a female “little blue pill” remains elusive as researchers struggle to understand the mechanisms that underlie the complex aspects of female sexual health. This Update will review the recent literature on the use of fractional CO2 laser for treatment of female sexual dysfunction and vulvovaginal symptoms. Bottom line: While the quality of the studies is poor overall, fractional CO2 laser treatment seems to temporarily improve symptoms of genitourinary syndrome of menopause (GSM). The duration of response, cost, and the overall long-term impact on sexual health remain in question.
A retrospective look at CO2 laser and postmenopausal GSM
Filippini M, Luvero D, Salvatore S, et al. Efficacy of fractional CO2 laser treatment in postmenopausal women with genitourinary syndrome: a multicenter study. Menopause. 2019;27:43-49. doi: 10.1097/GME. 0000000000001428.
Researchers conducted a retrospective, multicenter study of postmenopausal women with at least one symptom of GSM, including itching, burning, dyspareunia with penetration, and dryness.
Study details
A total of 171 of the 645 women (26.5%) were oncology patients. Women were excluded from analysis if they used any form of topical therapy within 15 days; had prolapse stage 2 or greater; or had any infection, abscess, or anatomical deformity precluding treatment with the laser.
Patients underwent gynecologic examination and were given a questionnaire to assess vulvovaginal symptoms. Exams occurred monthly during treatment (average, 6.5 months), at 6- and 12-months posttreatment, and then annually. No topical therapy was advised during or after treatment.
Patients received either 3 or 4 fractional CO2 laser treatments to the vulva and/or vagina depending on symptom location and type. Higher power settings of the same laser were used to treat vaginal symptoms (40W; 1,000 microseconds) versus vulvar symptoms (25W; 500 microseconds). Treatment sessions were 5 to 6 minutes. The study authors used a visual analog rating scale (VAS) for “atrophy and related symptoms,” tested vaginal pH, and completed the Vaginal Health Index Score. VAS scores were obtained from the patients prior to the initial laser intervention and 1 month after the final treatment.
Results
There were statistically significant improvements in dryness, vaginal orifice pain, dyspareunia, itching, and burning for both the 3-treatment and 4-treatment cohorts. The delta of improvement was then compared for the 2 subgroups; curiously, there was greater improvement of symptoms such as dryness (65% vs 61%), itching (78% vs 72%), burning (72% vs 67%), and vaginal orifice pain (67% vs 60%) in the group that received 3 cycles than in the group that received 4 cycles.
With regard to vaginal pH improvement, the 4-cycle group performed better than the 3-cycle group (1% improvement in the 4-cycle group vs 6% in the 3-cycle group). Although vaginal pH reduction was somewhat better in the group that received 4 treatments, and the pre versus posttreatment percentages were statistically significantly different, the clinical significance of a pH difference between 5.72 and 5.53 is questionable, especially since there was a greater difference in baseline pH between the two cohorts (6.08 in the 4-cycle group vs 5.59 in the 3-cycle group).
There were no reported adverse events related to the fractional laser treatments, and 6% of the patients underwent additional laser treatments during the followup timeframe of 8 to 20 months.
This was a retrospective study with no control or comparison group and short-term follow-up. The VAS scores were obtained 1 month after the final treatment. Failure to request additional treatment at 8 to 20 months cannot be used to infer that the therapeutic improvements recorded at 1 month were enduring. In addition, although the large number of patients in this study may lead to statistical significance, clinical significance is still questionable. Given the lack of a comparison group and the very short follow-up, it is hard to draw any scientifically valid conclusions from this study.
Continue to: Randomized data on CO2 laser vs Kegels for sexual dysfunction...
Randomized data on CO2 laser vs Kegels for sexual dysfunction
Lou W, Chen F, Xu T, et al. A randomized controlled study of vaginal fractional CO2 laser therapy for female sexual dysfunction. Lasers Med Sci. March 15, 2021. doi: 10.1007/s10103-021-03260-x.
In a small randomized controlled trial (RCT) conducted in China, Lou and colleagues identified premenopausal women at “high risk” for sexual dysfunction as determined by the Chinese version of the Female Sexual Function Index (CFSFI).
Details of the study
A total of 84 women (mean age, 36.5 years) were included in the study. All the participants were heterosexual and married or with a long-term partner. The domain of sexual dysfunction was not considered. Women were excluded if they had no current heterosexual partner; had genital malformation, urinary incontinence, or prolapse stage 2 or higher; a history of pelvic floor mesh treatment; current gynecologic malignancy; abnormal cervical cytology; or were currently pregnant or postpartum. In addition, women were excluded if they had been treated previously for sexual dysfunction or mental “disease.” The cohort was randomized to receive fractional CO2 laser treatments (three 15-minute treatments 1 month apart at 60W, 1,000 microseconds) or coached Kegel exercises (10 exercises repeated twice daily at least 3 times/week and monitored by physical therapists at biweekly clinic visits). Sexual distress was evaluated by using the Female Sexual Distress Scale-Revised (FSDSR). Outcomes measured were pelvic floor muscle strength and scores on the CFSFI and FSDSR. Data were obtained at 3, 6, 9, and 12 months after initiation of therapy.
Both groups showed improvement
The laser cohort showed slightly more improvement in scale scores at 6 and 12 months. Specifically, the laser group had better scores on lubrication and overall satisfaction, with moderate effect size; neither group had improvements in arousal, desire, or orgasm. The Kegel group showed a significant improvement in pelvic floor strength and orgasm at 12 months, an improvement not seen in the laser cohort. Both groups showed gradual improvement in the FSDSR, with the laser group reporting a lower score (10.0) at 12 months posttreatment relative to the Kegel group (11.1). Again, these were modest effects as baseline scores for both cohorts were around 12.5. There were minimal safety signals in the laser group, with 22.5% of women reporting scant bloody discharge posttreatment and 72.5% describing mild discomfort (1 on a 1–10 VAS scale) during the procedure.
This study is problematic in several areas. Although it was a prospective, randomized trial, it was not blinded, and the therapeutic interventions were markedly different in nature and requirement for individual patient motivation. The experiences of sexual dysfunction among the participants were not stratified by type—arousal, desire, lubrication, orgasm, or pain. All patients had regular cyclic menses; however, the authors do not report on contraceptive methods, hormonal therapy, or other comorbid conditions that could impact sexual health. The cohorts may or may not have been similar in baseline types of sexual dissatisfaction.
CO2 laser for lichen sclerosus: Is it effective?
Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422. doi: 10.1097 /GME.0000000000001482.
Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi: 10.1097 /AOG.0000000000004332.
Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi: 10.1097 /AOG.0000000000004409.
High potency corticosteroid ointment is the current standard treatment for lichen sclerosus. Alternative options for disease that is refractory to steroids are limited. Three studies published in the past year explored the CO2 laser’s ability to treat lichen sclerosus symptoms and resultant sexual dysfunction—Pagano and colleagues conducted a small prospective study and Burkett and colleagues and Mitchell et al conducted small RCTs.
Details of the Pagano study
Three premenopausal and 37 postmenopausal women with refractory lichen sclerosus (defined as no improvement after 4 cycles of ultra-high potency steroids) were included in the study. Lichen sclerosus was uniformly biopsy confirmed. Women using topical or systemic hormones were excluded. VAS was administered prior to initial treatment and after each of 2 fractional CO2 treatments (25–30 W; 1,000 microseconds) 30 to 40 days apart to determine severity of vulvar itching, dyspareunia with penetration, vulvar dryness, sexual dysfunction, and procedure discomfort. Follow-up was conducted at 1 month after the final treatment. VAS score for the primary outcome of vulvar itching declined from 8 pretreatment to 6 after the first treatment and to 3 after the second. There was no significant treatment-related pain reported.
The authors acknowledged the limitations of their study; it was a relatively small sample size, nonrandomized and had short-term follow-up of a mixed patient population and no sham or control group. The short-term improvements reported in the study patients may not be sustained without ongoing treatment for a lifelong chronic disease, and the long-term potential for development of squamous cell carcinoma may or may not be ameliorated.
Continue to: Burkett et al: RCT study 1...
Burkett et al: RCT study 1
A total of 52 postmenopausal patients with biopsy-proven lichen sclerosus were randomly assigned to clobetasol or CO2 laser; 51 women completed 6-month follow-up. The outcomes were stratified by prior high-potency steroid use. The steroid cohort used clobetasol 0.05% nightly for 1 month, 3 times per week for 2 months, then as needed. The laser cohort received 3 treatments (26 W; 800 microseconds) 4 to 6 weeks apart. Overall adherence was only 75% in the clobetasol group, compared with 96% in the laser group. The authors found treatment efficacy of CO2 laser therapy only in the group of patients who had prior treatment with high potency topical corticosteroids. They conclude that, …“Despite previously optimistic results in well designed clinical trials of fractionated CO2 for genitourinary syndrome of menopause, and in noncontrolled case series for vulvar lichen sclerosus, our study failed to show any significant benefit of monotherapy of fractionated CO2 for vulvar lichen sclerosus. There may be a role for fractionated CO2 as an adjuvant therapy along with topical ultrapotent corticosteroids in vulvar lichen sclerosus.”
Mitchell et al: RCT study 2
This was a double blind, placebo-controlled, and histologically validated study of fractional CO2 for treatment of lichen sclerosus in 35 women; 17 in the treatment arm and 18 in the sham laser encounters. At least a 4-week no treatment period of topical steroids was required before monotherapy with CO2 laser was initiated.
The authors found no difference in their primary outcome—histopathology scale scores—after 5 treatments over 24 weeks. Secondary endpoints were changes in the CSS (Clinical Scoring System for Vulvar Lichen Sclerosus), a validated instrument that includes both a clinician’s examination of the severity of disease and a patient’s report of the severity of her symptoms. The patient score is the total of 4 domains: itching, soreness, burning, and dyspareunia. The clinician objective examination documents fissures, erosions, hyperkeratosis, agglutination, stenosis, and atrophy. At the conclusion of treatment there were no significant differences in the patient reported symptoms or the clinical findings between the active treatment and sham groups.
As a monotherapy, CO2 laser therapy is not effective in treating lichen sclerosus, although it may help improve symptoms as an adjunct to high potency steroid therapy when topical treatment alone has failed to provide adequate response.
Conclusion
The quality of evidence to support the use of the CO2 laser for improvement in sexual dysfunction is poor. Although patient satisfaction scores improved overall, and most specifically for symptoms related to GSM, the lack of blinding; inappropriate or no control groups; the very short-term outcomes; and for one of the studies, the lack of a clear definition of sexual dysfunction, make it difficult to draw meaningful conclusions for clinical care.
For GSM, we know that topical estrogen therapy works—and with little to no systemic absorption. The CO2 laser should be studied in comparison to this gold standard, with consideration of costs and potential long-term harms in addition to patient satisfaction and short-term measures of improvement. In addition, and very importantly, it is our professional responsibility to present the evidence for safety of topical estrogens to our professional colleagues as well as to our patients with estrogen-dependent cancers so that they understand the value of estrogen as a safe and appropriate alternative to expensive and potentially short-term interventions such as CO2 laser treatment. ●

Cheryl Iglesia, MD
Dr. Iglesia is Director, Section of Female Pelvic Medicine and Reconstructive Surgery, MedStar Washington Hospital Center, and Professor, Departments of ObGyn and Urology, Georgetown University School of Medicine, Washington, DC. She is a member of the OBG Management Board of Editors.
Barbara Levy, MD: Cheryl, you have more experience with use of the energy-based cosmetic laser than most ObGyns, and I thought that speaking with you about this technology would be of benefit, not only to me in learning more about the hands-on experience of a lead researcher and practitioner but also readers who are hearing more and more about the growth of cosmetic gynecology in general. Thank you for taking the time today.
Cheryl Iglesia, MD: I’m happy to speak about this with you, Barbara.
Dr. Levy: Specifically, I would like to talk about use of these technologies for sexual dysfunction. In the last few years some of the available data have been on the CO2 laser versus physical therapy, which is not an appropriate comparison.1
Dr. Iglesia: There have been limited data, and less randomized, controlled data, on laser and radiofrequency energies for cosmetic gynecology, and in fact these devices remain unapproved for any gynecologic indication. In 2018 the US Food and Drug Administration (FDA) issued a Safety Communication about the use of energy-based devices to perform vaginal rejuvenation or cosmetic procedures. The International Urogynecological Association (IUGA) issued a consensus statement echoing concerns about the devices, and an International Continence Society/International Society for the Study of Vulvovaginal Disease Best Practice Consensus Statement did not recommend the laser for “routine treatment of vaginal atrophy or urinary incontinence unless treatment is part of a well-designed trial or with special arrangements for clinical governance, consent, and audit.”2
In May 2020, as evidence remains limited (although 522 studies are ongoing in coordination with the FDA), the American Urogynecologic Society (AUGS) published a clinical consensus statement from a panel of experts in female pelvic medicine and reconstructive surgery. The panel had about 90% consensus that there is short-term efficacy for the laser with GSM and dyspareunia. But we only have outcomes data that lasts a maximum of 1 year.2
A problem with our VeLVET trial,3 which was published in Menopause, and the Cruz and colleagues’ trial from South America,4 both of which compared the CO2 laser to estrogen and had randomized groups, was that they were limited by the outcome measures used, none of which were consistently validated. But these studies also had small numbers of participants and short-term follow-up. So I don’t think there are much existing data that are promising for supporting energy-based treatment for GSM.
We also have just-published data on the laser for lichen sclerosus.5 For the AUGS panel, there was about 80% consensus for energy-based-device use and lichen sclerosus.2 According to Mitchell et al, who conducted a small, randomized, sham-controlled trial, CO2 laser resulted in no significant difference in histopathology scale score between active and sham arms.5
Future trials may want to assess laser as a mechanism for improved local drug delivery (eg, use of combined laser plus local estrogen for GSM or combined laser plus topical steroid for lichen sclerosus). I am also aware that properly designed laser versus sham studies are underway.
Dr. Levy: What about for stress urinary incontinence (SUI)? I don’t think these technologies are going to work.
Dr. Iglesia: For the AUGS panel, there was only about 70% consensus for energy-based-device use and SUI,2 and I’m one of the naysayers. The pathophysiology of SUI is so multifactorial that it’s hard to believe that laser or radiofrequency wand therapy could have sustained improvements, especially since prior radiofrequency therapy from the last decade (for instance, Renessa, Novasys Medical) did not show long-term efficacy.
Understanding lasers and coordinating care
Dr. Levy: We don’t know what the long-term outcomes are for the CO2 laser and GSM.
Dr. Iglesia: I agree with you, and I think there needs to be an understanding of the mechanism of how lasers work, whether it be erbium (Er:YAG), which is the most common, or CO2. Erbium and CO2 lasers, which are on the far-infrared spectrum, target the chromophore, water. My feeling is that, when you look at results from the Cruz trial,4 or even our trial that compared vaginal estrogen with laser,3 when there is severe GSM and high pH with virtually no water present in the tissues, that laser is not going to properly function. But I don’t think we know exactly what optimal pretreatment is necessary, and that is one of the problems. Furthermore, when intravaginal lasers are done and no adequate speculum exam is conducted prior to introducing the laser, there could be discharge or old creams present that block the mirrors necessary to adequately fire the fractionated laser beams.
Unfortunately, oftentimes these devices are marketed to women with breast cancer, who may be taking aromatase inhibitors, which cause the no-water problem; they dry out everything. They are effective for preventing breast cancer recurrence, but they cause severe atrophy (perhaps worse than many of the other selective estrogen-receptor modulators), with a resultant high vaginal pH. If we can bring that pH level down, closer to the normal 4.5 range so that we could have some level of moisture, and add estrogen first, the overall treatment approach will probably be more effective. We still do not know what happens after 1 year, though, and how often touch-ups need to be performed.
In fact, when working with a patient with breast cancer, I will speak with her oncologist; I will collaborate to put in place a treatment plan that may include initial pretreatment with low-dose vaginal estrogen followed by laser treatment for vaginal atrophy. But I will make sure I use the lowest dose. Sometimes when the patient comes back, the estrogen’s worked so well she’ll say, “Oh, I’m happy, so I don’t need the laser anymore.” A balanced conversation is necessary, especially with cancer survivors.
Informing patients and colleagues
Dr. Levy: I completely agree, and I think one of the key points here is that our purpose is to serve our patients. The data demonstrate that low doses of vaginal estrogen are not harmful for women who are being treated for or who have recovered from breast cancer. It is our ethical obligation to convince these women and their oncologists that ongoing treatment with vaginal estrogen not only will help their GSM but also their overactive bladder and their risk of urinary tract infections and other things. We could be exploiting patients who are really fearful of using any estrogen because of a perceived cancer risk. We could actually be validating their fear by telling them we have an alternative treatment for which they have to pay cash.
Treatment access
Dr. Iglesia: Yes, these are not cosmetic conditions that we are treating. So my goal when evaluating treatment for refractory GSM or lichen sclerosus is to find optimal energy-based therapies with the hope that one day these will be approved gynecologic conditions by the US FDA for laser and wand therapies and that they will ultimately not be out-of-pocket expenses but rather therapies covered by insurance.
Dr. Levy: Great. I understand that AUGS/IUGA have been working on a terminology algorithm to help distinguish between procedures being performed to resolve a medical problem such as prolapse or incontinence versus those designed to be cosmetic.
Dr. Iglesia: Yes, there is a big document from experts in both societies out for public comment right now. It will hopefully be published soon.
Outstanding questions remain
Dr. Levy: Really, we as ObGyns shouldn’t be quick to incorporate these things into our practices without high-quality studies demonstrating value. I have a major concern about these devices in the long term. When you look at fractional CO2 use on the face, for instance, which is a much different type of skin than the vagina, the laser builds collagen—but we don’t have long-term outcome results. The vagina is supposed to be an elastic tissue, so what is the risk of long-term scarring there? Yes, the laser builds collagen in the vaginal epithelium, but what does it do to scarring in the rest of the tissue? We don’t have answers to that.
Dr. Iglesia: And that is the question—how does histology equate with function? Well, I would go with what the patients are reporting.
Dr. Levy: Absolutely. But the thing about vaginal low-dose estrogen is that it is something that the oncologists or the ObGyns could be implementing with patients while they are undergoing cancer therapy, while in their menopausal transition, to preserve vulvovaginal function as opposed to trying to regain it.
Dr. Iglesia: Certainly, although it still needs to be determined when that type of approach would actually be contraindicated.
Dr. Levy: Thank you, Cheryl, for your valuable insights.
Dr. Iglesia: Of course. Thank you. ●
References
1. Lou W, Chen F, Xu T, et al. A randomized controlled study of vaginal fractional CO2 laser therapy for female sexual dysfunction. Lasers Med Sci. March 15, 2021. doi: 10.1007/s10103-021-03260-x.
2. Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices. Female Pelvic Med Reconstr Surg. 2020;26:287-298. doi: 10.1097 /SPV.0000000000000872.
3. Paraiso MF, Ferrando CA, et al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET Trial. Menopause. 2020;27:50-56. doi: 10.1097/GME.0000000000001416.
4. Cruz VL, Steiner ML, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25:21-28. doi: 10.1097 /GME.0000000000000955.
5. Mitchell L, Goldstein A, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi: 10.1097/AOG.0000000000004409.
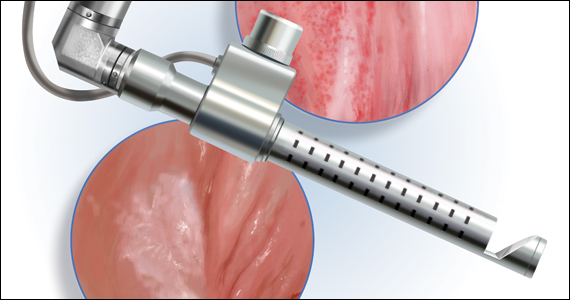
The approach to diagnosis and treatment of female sexual function continues to be a challenge for women’s health professionals. The search for a female “little blue pill” remains elusive as researchers struggle to understand the mechanisms that underlie the complex aspects of female sexual health. This Update will review the recent literature on the use of fractional CO2 laser for treatment of female sexual dysfunction and vulvovaginal symptoms. Bottom line: While the quality of the studies is poor overall, fractional CO2 laser treatment seems to temporarily improve symptoms of genitourinary syndrome of menopause (GSM). The duration of response, cost, and the overall long-term impact on sexual health remain in question.
A retrospective look at CO2 laser and postmenopausal GSM
Filippini M, Luvero D, Salvatore S, et al. Efficacy of fractional CO2 laser treatment in postmenopausal women with genitourinary syndrome: a multicenter study. Menopause. 2019;27:43-49. doi: 10.1097/GME. 0000000000001428.
Researchers conducted a retrospective, multicenter study of postmenopausal women with at least one symptom of GSM, including itching, burning, dyspareunia with penetration, and dryness.
Study details
A total of 171 of the 645 women (26.5%) were oncology patients. Women were excluded from analysis if they used any form of topical therapy within 15 days; had prolapse stage 2 or greater; or had any infection, abscess, or anatomical deformity precluding treatment with the laser.
Patients underwent gynecologic examination and were given a questionnaire to assess vulvovaginal symptoms. Exams occurred monthly during treatment (average, 6.5 months), at 6- and 12-months posttreatment, and then annually. No topical therapy was advised during or after treatment.
Patients received either 3 or 4 fractional CO2 laser treatments to the vulva and/or vagina depending on symptom location and type. Higher power settings of the same laser were used to treat vaginal symptoms (40W; 1,000 microseconds) versus vulvar symptoms (25W; 500 microseconds). Treatment sessions were 5 to 6 minutes. The study authors used a visual analog rating scale (VAS) for “atrophy and related symptoms,” tested vaginal pH, and completed the Vaginal Health Index Score. VAS scores were obtained from the patients prior to the initial laser intervention and 1 month after the final treatment.
Results
There were statistically significant improvements in dryness, vaginal orifice pain, dyspareunia, itching, and burning for both the 3-treatment and 4-treatment cohorts. The delta of improvement was then compared for the 2 subgroups; curiously, there was greater improvement of symptoms such as dryness (65% vs 61%), itching (78% vs 72%), burning (72% vs 67%), and vaginal orifice pain (67% vs 60%) in the group that received 3 cycles than in the group that received 4 cycles.
With regard to vaginal pH improvement, the 4-cycle group performed better than the 3-cycle group (1% improvement in the 4-cycle group vs 6% in the 3-cycle group). Although vaginal pH reduction was somewhat better in the group that received 4 treatments, and the pre versus posttreatment percentages were statistically significantly different, the clinical significance of a pH difference between 5.72 and 5.53 is questionable, especially since there was a greater difference in baseline pH between the two cohorts (6.08 in the 4-cycle group vs 5.59 in the 3-cycle group).
There were no reported adverse events related to the fractional laser treatments, and 6% of the patients underwent additional laser treatments during the followup timeframe of 8 to 20 months.
This was a retrospective study with no control or comparison group and short-term follow-up. The VAS scores were obtained 1 month after the final treatment. Failure to request additional treatment at 8 to 20 months cannot be used to infer that the therapeutic improvements recorded at 1 month were enduring. In addition, although the large number of patients in this study may lead to statistical significance, clinical significance is still questionable. Given the lack of a comparison group and the very short follow-up, it is hard to draw any scientifically valid conclusions from this study.
Continue to: Randomized data on CO2 laser vs Kegels for sexual dysfunction...
Randomized data on CO2 laser vs Kegels for sexual dysfunction
Lou W, Chen F, Xu T, et al. A randomized controlled study of vaginal fractional CO2 laser therapy for female sexual dysfunction. Lasers Med Sci. March 15, 2021. doi: 10.1007/s10103-021-03260-x.
In a small randomized controlled trial (RCT) conducted in China, Lou and colleagues identified premenopausal women at “high risk” for sexual dysfunction as determined by the Chinese version of the Female Sexual Function Index (CFSFI).
Details of the study
A total of 84 women (mean age, 36.5 years) were included in the study. All the participants were heterosexual and married or with a long-term partner. The domain of sexual dysfunction was not considered. Women were excluded if they had no current heterosexual partner; had genital malformation, urinary incontinence, or prolapse stage 2 or higher; a history of pelvic floor mesh treatment; current gynecologic malignancy; abnormal cervical cytology; or were currently pregnant or postpartum. In addition, women were excluded if they had been treated previously for sexual dysfunction or mental “disease.” The cohort was randomized to receive fractional CO2 laser treatments (three 15-minute treatments 1 month apart at 60W, 1,000 microseconds) or coached Kegel exercises (10 exercises repeated twice daily at least 3 times/week and monitored by physical therapists at biweekly clinic visits). Sexual distress was evaluated by using the Female Sexual Distress Scale-Revised (FSDSR). Outcomes measured were pelvic floor muscle strength and scores on the CFSFI and FSDSR. Data were obtained at 3, 6, 9, and 12 months after initiation of therapy.
Both groups showed improvement
The laser cohort showed slightly more improvement in scale scores at 6 and 12 months. Specifically, the laser group had better scores on lubrication and overall satisfaction, with moderate effect size; neither group had improvements in arousal, desire, or orgasm. The Kegel group showed a significant improvement in pelvic floor strength and orgasm at 12 months, an improvement not seen in the laser cohort. Both groups showed gradual improvement in the FSDSR, with the laser group reporting a lower score (10.0) at 12 months posttreatment relative to the Kegel group (11.1). Again, these were modest effects as baseline scores for both cohorts were around 12.5. There were minimal safety signals in the laser group, with 22.5% of women reporting scant bloody discharge posttreatment and 72.5% describing mild discomfort (1 on a 1–10 VAS scale) during the procedure.
This study is problematic in several areas. Although it was a prospective, randomized trial, it was not blinded, and the therapeutic interventions were markedly different in nature and requirement for individual patient motivation. The experiences of sexual dysfunction among the participants were not stratified by type—arousal, desire, lubrication, orgasm, or pain. All patients had regular cyclic menses; however, the authors do not report on contraceptive methods, hormonal therapy, or other comorbid conditions that could impact sexual health. The cohorts may or may not have been similar in baseline types of sexual dissatisfaction.
CO2 laser for lichen sclerosus: Is it effective?
Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422. doi: 10.1097 /GME.0000000000001482.
Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi: 10.1097 /AOG.0000000000004332.
Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi: 10.1097 /AOG.0000000000004409.
High potency corticosteroid ointment is the current standard treatment for lichen sclerosus. Alternative options for disease that is refractory to steroids are limited. Three studies published in the past year explored the CO2 laser’s ability to treat lichen sclerosus symptoms and resultant sexual dysfunction—Pagano and colleagues conducted a small prospective study and Burkett and colleagues and Mitchell et al conducted small RCTs.
Details of the Pagano study
Three premenopausal and 37 postmenopausal women with refractory lichen sclerosus (defined as no improvement after 4 cycles of ultra-high potency steroids) were included in the study. Lichen sclerosus was uniformly biopsy confirmed. Women using topical or systemic hormones were excluded. VAS was administered prior to initial treatment and after each of 2 fractional CO2 treatments (25–30 W; 1,000 microseconds) 30 to 40 days apart to determine severity of vulvar itching, dyspareunia with penetration, vulvar dryness, sexual dysfunction, and procedure discomfort. Follow-up was conducted at 1 month after the final treatment. VAS score for the primary outcome of vulvar itching declined from 8 pretreatment to 6 after the first treatment and to 3 after the second. There was no significant treatment-related pain reported.
The authors acknowledged the limitations of their study; it was a relatively small sample size, nonrandomized and had short-term follow-up of a mixed patient population and no sham or control group. The short-term improvements reported in the study patients may not be sustained without ongoing treatment for a lifelong chronic disease, and the long-term potential for development of squamous cell carcinoma may or may not be ameliorated.
Continue to: Burkett et al: RCT study 1...
Burkett et al: RCT study 1
A total of 52 postmenopausal patients with biopsy-proven lichen sclerosus were randomly assigned to clobetasol or CO2 laser; 51 women completed 6-month follow-up. The outcomes were stratified by prior high-potency steroid use. The steroid cohort used clobetasol 0.05% nightly for 1 month, 3 times per week for 2 months, then as needed. The laser cohort received 3 treatments (26 W; 800 microseconds) 4 to 6 weeks apart. Overall adherence was only 75% in the clobetasol group, compared with 96% in the laser group. The authors found treatment efficacy of CO2 laser therapy only in the group of patients who had prior treatment with high potency topical corticosteroids. They conclude that, …“Despite previously optimistic results in well designed clinical trials of fractionated CO2 for genitourinary syndrome of menopause, and in noncontrolled case series for vulvar lichen sclerosus, our study failed to show any significant benefit of monotherapy of fractionated CO2 for vulvar lichen sclerosus. There may be a role for fractionated CO2 as an adjuvant therapy along with topical ultrapotent corticosteroids in vulvar lichen sclerosus.”
Mitchell et al: RCT study 2
This was a double blind, placebo-controlled, and histologically validated study of fractional CO2 for treatment of lichen sclerosus in 35 women; 17 in the treatment arm and 18 in the sham laser encounters. At least a 4-week no treatment period of topical steroids was required before monotherapy with CO2 laser was initiated.
The authors found no difference in their primary outcome—histopathology scale scores—after 5 treatments over 24 weeks. Secondary endpoints were changes in the CSS (Clinical Scoring System for Vulvar Lichen Sclerosus), a validated instrument that includes both a clinician’s examination of the severity of disease and a patient’s report of the severity of her symptoms. The patient score is the total of 4 domains: itching, soreness, burning, and dyspareunia. The clinician objective examination documents fissures, erosions, hyperkeratosis, agglutination, stenosis, and atrophy. At the conclusion of treatment there were no significant differences in the patient reported symptoms or the clinical findings between the active treatment and sham groups.
As a monotherapy, CO2 laser therapy is not effective in treating lichen sclerosus, although it may help improve symptoms as an adjunct to high potency steroid therapy when topical treatment alone has failed to provide adequate response.
Conclusion
The quality of evidence to support the use of the CO2 laser for improvement in sexual dysfunction is poor. Although patient satisfaction scores improved overall, and most specifically for symptoms related to GSM, the lack of blinding; inappropriate or no control groups; the very short-term outcomes; and for one of the studies, the lack of a clear definition of sexual dysfunction, make it difficult to draw meaningful conclusions for clinical care.
For GSM, we know that topical estrogen therapy works—and with little to no systemic absorption. The CO2 laser should be studied in comparison to this gold standard, with consideration of costs and potential long-term harms in addition to patient satisfaction and short-term measures of improvement. In addition, and very importantly, it is our professional responsibility to present the evidence for safety of topical estrogens to our professional colleagues as well as to our patients with estrogen-dependent cancers so that they understand the value of estrogen as a safe and appropriate alternative to expensive and potentially short-term interventions such as CO2 laser treatment. ●

Cheryl Iglesia, MD
Dr. Iglesia is Director, Section of Female Pelvic Medicine and Reconstructive Surgery, MedStar Washington Hospital Center, and Professor, Departments of ObGyn and Urology, Georgetown University School of Medicine, Washington, DC. She is a member of the OBG Management Board of Editors.
Barbara Levy, MD: Cheryl, you have more experience with use of the energy-based cosmetic laser than most ObGyns, and I thought that speaking with you about this technology would be of benefit, not only to me in learning more about the hands-on experience of a lead researcher and practitioner but also readers who are hearing more and more about the growth of cosmetic gynecology in general. Thank you for taking the time today.
Cheryl Iglesia, MD: I’m happy to speak about this with you, Barbara.
Dr. Levy: Specifically, I would like to talk about use of these technologies for sexual dysfunction. In the last few years some of the available data have been on the CO2 laser versus physical therapy, which is not an appropriate comparison.1
Dr. Iglesia: There have been limited data, and less randomized, controlled data, on laser and radiofrequency energies for cosmetic gynecology, and in fact these devices remain unapproved for any gynecologic indication. In 2018 the US Food and Drug Administration (FDA) issued a Safety Communication about the use of energy-based devices to perform vaginal rejuvenation or cosmetic procedures. The International Urogynecological Association (IUGA) issued a consensus statement echoing concerns about the devices, and an International Continence Society/International Society for the Study of Vulvovaginal Disease Best Practice Consensus Statement did not recommend the laser for “routine treatment of vaginal atrophy or urinary incontinence unless treatment is part of a well-designed trial or with special arrangements for clinical governance, consent, and audit.”2
In May 2020, as evidence remains limited (although 522 studies are ongoing in coordination with the FDA), the American Urogynecologic Society (AUGS) published a clinical consensus statement from a panel of experts in female pelvic medicine and reconstructive surgery. The panel had about 90% consensus that there is short-term efficacy for the laser with GSM and dyspareunia. But we only have outcomes data that lasts a maximum of 1 year.2
A problem with our VeLVET trial,3 which was published in Menopause, and the Cruz and colleagues’ trial from South America,4 both of which compared the CO2 laser to estrogen and had randomized groups, was that they were limited by the outcome measures used, none of which were consistently validated. But these studies also had small numbers of participants and short-term follow-up. So I don’t think there are much existing data that are promising for supporting energy-based treatment for GSM.
We also have just-published data on the laser for lichen sclerosus.5 For the AUGS panel, there was about 80% consensus for energy-based-device use and lichen sclerosus.2 According to Mitchell et al, who conducted a small, randomized, sham-controlled trial, CO2 laser resulted in no significant difference in histopathology scale score between active and sham arms.5
Future trials may want to assess laser as a mechanism for improved local drug delivery (eg, use of combined laser plus local estrogen for GSM or combined laser plus topical steroid for lichen sclerosus). I am also aware that properly designed laser versus sham studies are underway.
Dr. Levy: What about for stress urinary incontinence (SUI)? I don’t think these technologies are going to work.
Dr. Iglesia: For the AUGS panel, there was only about 70% consensus for energy-based-device use and SUI,2 and I’m one of the naysayers. The pathophysiology of SUI is so multifactorial that it’s hard to believe that laser or radiofrequency wand therapy could have sustained improvements, especially since prior radiofrequency therapy from the last decade (for instance, Renessa, Novasys Medical) did not show long-term efficacy.
Understanding lasers and coordinating care
Dr. Levy: We don’t know what the long-term outcomes are for the CO2 laser and GSM.
Dr. Iglesia: I agree with you, and I think there needs to be an understanding of the mechanism of how lasers work, whether it be erbium (Er:YAG), which is the most common, or CO2. Erbium and CO2 lasers, which are on the far-infrared spectrum, target the chromophore, water. My feeling is that, when you look at results from the Cruz trial,4 or even our trial that compared vaginal estrogen with laser,3 when there is severe GSM and high pH with virtually no water present in the tissues, that laser is not going to properly function. But I don’t think we know exactly what optimal pretreatment is necessary, and that is one of the problems. Furthermore, when intravaginal lasers are done and no adequate speculum exam is conducted prior to introducing the laser, there could be discharge or old creams present that block the mirrors necessary to adequately fire the fractionated laser beams.
Unfortunately, oftentimes these devices are marketed to women with breast cancer, who may be taking aromatase inhibitors, which cause the no-water problem; they dry out everything. They are effective for preventing breast cancer recurrence, but they cause severe atrophy (perhaps worse than many of the other selective estrogen-receptor modulators), with a resultant high vaginal pH. If we can bring that pH level down, closer to the normal 4.5 range so that we could have some level of moisture, and add estrogen first, the overall treatment approach will probably be more effective. We still do not know what happens after 1 year, though, and how often touch-ups need to be performed.
In fact, when working with a patient with breast cancer, I will speak with her oncologist; I will collaborate to put in place a treatment plan that may include initial pretreatment with low-dose vaginal estrogen followed by laser treatment for vaginal atrophy. But I will make sure I use the lowest dose. Sometimes when the patient comes back, the estrogen’s worked so well she’ll say, “Oh, I’m happy, so I don’t need the laser anymore.” A balanced conversation is necessary, especially with cancer survivors.
Informing patients and colleagues
Dr. Levy: I completely agree, and I think one of the key points here is that our purpose is to serve our patients. The data demonstrate that low doses of vaginal estrogen are not harmful for women who are being treated for or who have recovered from breast cancer. It is our ethical obligation to convince these women and their oncologists that ongoing treatment with vaginal estrogen not only will help their GSM but also their overactive bladder and their risk of urinary tract infections and other things. We could be exploiting patients who are really fearful of using any estrogen because of a perceived cancer risk. We could actually be validating their fear by telling them we have an alternative treatment for which they have to pay cash.
Treatment access
Dr. Iglesia: Yes, these are not cosmetic conditions that we are treating. So my goal when evaluating treatment for refractory GSM or lichen sclerosus is to find optimal energy-based therapies with the hope that one day these will be approved gynecologic conditions by the US FDA for laser and wand therapies and that they will ultimately not be out-of-pocket expenses but rather therapies covered by insurance.
Dr. Levy: Great. I understand that AUGS/IUGA have been working on a terminology algorithm to help distinguish between procedures being performed to resolve a medical problem such as prolapse or incontinence versus those designed to be cosmetic.
Dr. Iglesia: Yes, there is a big document from experts in both societies out for public comment right now. It will hopefully be published soon.
Outstanding questions remain
Dr. Levy: Really, we as ObGyns shouldn’t be quick to incorporate these things into our practices without high-quality studies demonstrating value. I have a major concern about these devices in the long term. When you look at fractional CO2 use on the face, for instance, which is a much different type of skin than the vagina, the laser builds collagen—but we don’t have long-term outcome results. The vagina is supposed to be an elastic tissue, so what is the risk of long-term scarring there? Yes, the laser builds collagen in the vaginal epithelium, but what does it do to scarring in the rest of the tissue? We don’t have answers to that.
Dr. Iglesia: And that is the question—how does histology equate with function? Well, I would go with what the patients are reporting.
Dr. Levy: Absolutely. But the thing about vaginal low-dose estrogen is that it is something that the oncologists or the ObGyns could be implementing with patients while they are undergoing cancer therapy, while in their menopausal transition, to preserve vulvovaginal function as opposed to trying to regain it.
Dr. Iglesia: Certainly, although it still needs to be determined when that type of approach would actually be contraindicated.
Dr. Levy: Thank you, Cheryl, for your valuable insights.
Dr. Iglesia: Of course. Thank you. ●
References
1. Lou W, Chen F, Xu T, et al. A randomized controlled study of vaginal fractional CO2 laser therapy for female sexual dysfunction. Lasers Med Sci. March 15, 2021. doi: 10.1007/s10103-021-03260-x.
2. Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices. Female Pelvic Med Reconstr Surg. 2020;26:287-298. doi: 10.1097 /SPV.0000000000000872.
3. Paraiso MF, Ferrando CA, et al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET Trial. Menopause. 2020;27:50-56. doi: 10.1097/GME.0000000000001416.
4. Cruz VL, Steiner ML, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25:21-28. doi: 10.1097 /GME.0000000000000955.
5. Mitchell L, Goldstein A, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi: 10.1097/AOG.0000000000004409.
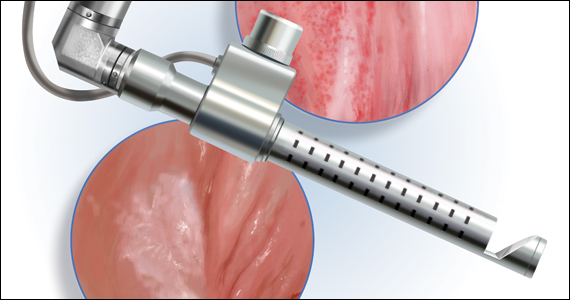
The approach to diagnosis and treatment of female sexual function continues to be a challenge for women’s health professionals. The search for a female “little blue pill” remains elusive as researchers struggle to understand the mechanisms that underlie the complex aspects of female sexual health. This Update will review the recent literature on the use of fractional CO2 laser for treatment of female sexual dysfunction and vulvovaginal symptoms. Bottom line: While the quality of the studies is poor overall, fractional CO2 laser treatment seems to temporarily improve symptoms of genitourinary syndrome of menopause (GSM). The duration of response, cost, and the overall long-term impact on sexual health remain in question.
A retrospective look at CO2 laser and postmenopausal GSM
Filippini M, Luvero D, Salvatore S, et al. Efficacy of fractional CO2 laser treatment in postmenopausal women with genitourinary syndrome: a multicenter study. Menopause. 2019;27:43-49. doi: 10.1097/GME. 0000000000001428.
Researchers conducted a retrospective, multicenter study of postmenopausal women with at least one symptom of GSM, including itching, burning, dyspareunia with penetration, and dryness.
Study details
A total of 171 of the 645 women (26.5%) were oncology patients. Women were excluded from analysis if they used any form of topical therapy within 15 days; had prolapse stage 2 or greater; or had any infection, abscess, or anatomical deformity precluding treatment with the laser.
Patients underwent gynecologic examination and were given a questionnaire to assess vulvovaginal symptoms. Exams occurred monthly during treatment (average, 6.5 months), at 6- and 12-months posttreatment, and then annually. No topical therapy was advised during or after treatment.
Patients received either 3 or 4 fractional CO2 laser treatments to the vulva and/or vagina depending on symptom location and type. Higher power settings of the same laser were used to treat vaginal symptoms (40W; 1,000 microseconds) versus vulvar symptoms (25W; 500 microseconds). Treatment sessions were 5 to 6 minutes. The study authors used a visual analog rating scale (VAS) for “atrophy and related symptoms,” tested vaginal pH, and completed the Vaginal Health Index Score. VAS scores were obtained from the patients prior to the initial laser intervention and 1 month after the final treatment.
Results
There were statistically significant improvements in dryness, vaginal orifice pain, dyspareunia, itching, and burning for both the 3-treatment and 4-treatment cohorts. The delta of improvement was then compared for the 2 subgroups; curiously, there was greater improvement of symptoms such as dryness (65% vs 61%), itching (78% vs 72%), burning (72% vs 67%), and vaginal orifice pain (67% vs 60%) in the group that received 3 cycles than in the group that received 4 cycles.
With regard to vaginal pH improvement, the 4-cycle group performed better than the 3-cycle group (1% improvement in the 4-cycle group vs 6% in the 3-cycle group). Although vaginal pH reduction was somewhat better in the group that received 4 treatments, and the pre versus posttreatment percentages were statistically significantly different, the clinical significance of a pH difference between 5.72 and 5.53 is questionable, especially since there was a greater difference in baseline pH between the two cohorts (6.08 in the 4-cycle group vs 5.59 in the 3-cycle group).
There were no reported adverse events related to the fractional laser treatments, and 6% of the patients underwent additional laser treatments during the followup timeframe of 8 to 20 months.
This was a retrospective study with no control or comparison group and short-term follow-up. The VAS scores were obtained 1 month after the final treatment. Failure to request additional treatment at 8 to 20 months cannot be used to infer that the therapeutic improvements recorded at 1 month were enduring. In addition, although the large number of patients in this study may lead to statistical significance, clinical significance is still questionable. Given the lack of a comparison group and the very short follow-up, it is hard to draw any scientifically valid conclusions from this study.
Continue to: Randomized data on CO2 laser vs Kegels for sexual dysfunction...
Randomized data on CO2 laser vs Kegels for sexual dysfunction
Lou W, Chen F, Xu T, et al. A randomized controlled study of vaginal fractional CO2 laser therapy for female sexual dysfunction. Lasers Med Sci. March 15, 2021. doi: 10.1007/s10103-021-03260-x.
In a small randomized controlled trial (RCT) conducted in China, Lou and colleagues identified premenopausal women at “high risk” for sexual dysfunction as determined by the Chinese version of the Female Sexual Function Index (CFSFI).
Details of the study
A total of 84 women (mean age, 36.5 years) were included in the study. All the participants were heterosexual and married or with a long-term partner. The domain of sexual dysfunction was not considered. Women were excluded if they had no current heterosexual partner; had genital malformation, urinary incontinence, or prolapse stage 2 or higher; a history of pelvic floor mesh treatment; current gynecologic malignancy; abnormal cervical cytology; or were currently pregnant or postpartum. In addition, women were excluded if they had been treated previously for sexual dysfunction or mental “disease.” The cohort was randomized to receive fractional CO2 laser treatments (three 15-minute treatments 1 month apart at 60W, 1,000 microseconds) or coached Kegel exercises (10 exercises repeated twice daily at least 3 times/week and monitored by physical therapists at biweekly clinic visits). Sexual distress was evaluated by using the Female Sexual Distress Scale-Revised (FSDSR). Outcomes measured were pelvic floor muscle strength and scores on the CFSFI and FSDSR. Data were obtained at 3, 6, 9, and 12 months after initiation of therapy.
Both groups showed improvement
The laser cohort showed slightly more improvement in scale scores at 6 and 12 months. Specifically, the laser group had better scores on lubrication and overall satisfaction, with moderate effect size; neither group had improvements in arousal, desire, or orgasm. The Kegel group showed a significant improvement in pelvic floor strength and orgasm at 12 months, an improvement not seen in the laser cohort. Both groups showed gradual improvement in the FSDSR, with the laser group reporting a lower score (10.0) at 12 months posttreatment relative to the Kegel group (11.1). Again, these were modest effects as baseline scores for both cohorts were around 12.5. There were minimal safety signals in the laser group, with 22.5% of women reporting scant bloody discharge posttreatment and 72.5% describing mild discomfort (1 on a 1–10 VAS scale) during the procedure.
This study is problematic in several areas. Although it was a prospective, randomized trial, it was not blinded, and the therapeutic interventions were markedly different in nature and requirement for individual patient motivation. The experiences of sexual dysfunction among the participants were not stratified by type—arousal, desire, lubrication, orgasm, or pain. All patients had regular cyclic menses; however, the authors do not report on contraceptive methods, hormonal therapy, or other comorbid conditions that could impact sexual health. The cohorts may or may not have been similar in baseline types of sexual dissatisfaction.
CO2 laser for lichen sclerosus: Is it effective?
Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422. doi: 10.1097 /GME.0000000000001482.
Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi: 10.1097 /AOG.0000000000004332.
Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi: 10.1097 /AOG.0000000000004409.
High potency corticosteroid ointment is the current standard treatment for lichen sclerosus. Alternative options for disease that is refractory to steroids are limited. Three studies published in the past year explored the CO2 laser’s ability to treat lichen sclerosus symptoms and resultant sexual dysfunction—Pagano and colleagues conducted a small prospective study and Burkett and colleagues and Mitchell et al conducted small RCTs.
Details of the Pagano study
Three premenopausal and 37 postmenopausal women with refractory lichen sclerosus (defined as no improvement after 4 cycles of ultra-high potency steroids) were included in the study. Lichen sclerosus was uniformly biopsy confirmed. Women using topical or systemic hormones were excluded. VAS was administered prior to initial treatment and after each of 2 fractional CO2 treatments (25–30 W; 1,000 microseconds) 30 to 40 days apart to determine severity of vulvar itching, dyspareunia with penetration, vulvar dryness, sexual dysfunction, and procedure discomfort. Follow-up was conducted at 1 month after the final treatment. VAS score for the primary outcome of vulvar itching declined from 8 pretreatment to 6 after the first treatment and to 3 after the second. There was no significant treatment-related pain reported.
The authors acknowledged the limitations of their study; it was a relatively small sample size, nonrandomized and had short-term follow-up of a mixed patient population and no sham or control group. The short-term improvements reported in the study patients may not be sustained without ongoing treatment for a lifelong chronic disease, and the long-term potential for development of squamous cell carcinoma may or may not be ameliorated.
Continue to: Burkett et al: RCT study 1...
Burkett et al: RCT study 1
A total of 52 postmenopausal patients with biopsy-proven lichen sclerosus were randomly assigned to clobetasol or CO2 laser; 51 women completed 6-month follow-up. The outcomes were stratified by prior high-potency steroid use. The steroid cohort used clobetasol 0.05% nightly for 1 month, 3 times per week for 2 months, then as needed. The laser cohort received 3 treatments (26 W; 800 microseconds) 4 to 6 weeks apart. Overall adherence was only 75% in the clobetasol group, compared with 96% in the laser group. The authors found treatment efficacy of CO2 laser therapy only in the group of patients who had prior treatment with high potency topical corticosteroids. They conclude that, …“Despite previously optimistic results in well designed clinical trials of fractionated CO2 for genitourinary syndrome of menopause, and in noncontrolled case series for vulvar lichen sclerosus, our study failed to show any significant benefit of monotherapy of fractionated CO2 for vulvar lichen sclerosus. There may be a role for fractionated CO2 as an adjuvant therapy along with topical ultrapotent corticosteroids in vulvar lichen sclerosus.”
Mitchell et al: RCT study 2
This was a double blind, placebo-controlled, and histologically validated study of fractional CO2 for treatment of lichen sclerosus in 35 women; 17 in the treatment arm and 18 in the sham laser encounters. At least a 4-week no treatment period of topical steroids was required before monotherapy with CO2 laser was initiated.
The authors found no difference in their primary outcome—histopathology scale scores—after 5 treatments over 24 weeks. Secondary endpoints were changes in the CSS (Clinical Scoring System for Vulvar Lichen Sclerosus), a validated instrument that includes both a clinician’s examination of the severity of disease and a patient’s report of the severity of her symptoms. The patient score is the total of 4 domains: itching, soreness, burning, and dyspareunia. The clinician objective examination documents fissures, erosions, hyperkeratosis, agglutination, stenosis, and atrophy. At the conclusion of treatment there were no significant differences in the patient reported symptoms or the clinical findings between the active treatment and sham groups.
As a monotherapy, CO2 laser therapy is not effective in treating lichen sclerosus, although it may help improve symptoms as an adjunct to high potency steroid therapy when topical treatment alone has failed to provide adequate response.
Conclusion
The quality of evidence to support the use of the CO2 laser for improvement in sexual dysfunction is poor. Although patient satisfaction scores improved overall, and most specifically for symptoms related to GSM, the lack of blinding; inappropriate or no control groups; the very short-term outcomes; and for one of the studies, the lack of a clear definition of sexual dysfunction, make it difficult to draw meaningful conclusions for clinical care.
For GSM, we know that topical estrogen therapy works—and with little to no systemic absorption. The CO2 laser should be studied in comparison to this gold standard, with consideration of costs and potential long-term harms in addition to patient satisfaction and short-term measures of improvement. In addition, and very importantly, it is our professional responsibility to present the evidence for safety of topical estrogens to our professional colleagues as well as to our patients with estrogen-dependent cancers so that they understand the value of estrogen as a safe and appropriate alternative to expensive and potentially short-term interventions such as CO2 laser treatment. ●

Cheryl Iglesia, MD
Dr. Iglesia is Director, Section of Female Pelvic Medicine and Reconstructive Surgery, MedStar Washington Hospital Center, and Professor, Departments of ObGyn and Urology, Georgetown University School of Medicine, Washington, DC. She is a member of the OBG Management Board of Editors.
Barbara Levy, MD: Cheryl, you have more experience with use of the energy-based cosmetic laser than most ObGyns, and I thought that speaking with you about this technology would be of benefit, not only to me in learning more about the hands-on experience of a lead researcher and practitioner but also readers who are hearing more and more about the growth of cosmetic gynecology in general. Thank you for taking the time today.
Cheryl Iglesia, MD: I’m happy to speak about this with you, Barbara.
Dr. Levy: Specifically, I would like to talk about use of these technologies for sexual dysfunction. In the last few years some of the available data have been on the CO2 laser versus physical therapy, which is not an appropriate comparison.1
Dr. Iglesia: There have been limited data, and less randomized, controlled data, on laser and radiofrequency energies for cosmetic gynecology, and in fact these devices remain unapproved for any gynecologic indication. In 2018 the US Food and Drug Administration (FDA) issued a Safety Communication about the use of energy-based devices to perform vaginal rejuvenation or cosmetic procedures. The International Urogynecological Association (IUGA) issued a consensus statement echoing concerns about the devices, and an International Continence Society/International Society for the Study of Vulvovaginal Disease Best Practice Consensus Statement did not recommend the laser for “routine treatment of vaginal atrophy or urinary incontinence unless treatment is part of a well-designed trial or with special arrangements for clinical governance, consent, and audit.”2
In May 2020, as evidence remains limited (although 522 studies are ongoing in coordination with the FDA), the American Urogynecologic Society (AUGS) published a clinical consensus statement from a panel of experts in female pelvic medicine and reconstructive surgery. The panel had about 90% consensus that there is short-term efficacy for the laser with GSM and dyspareunia. But we only have outcomes data that lasts a maximum of 1 year.2
A problem with our VeLVET trial,3 which was published in Menopause, and the Cruz and colleagues’ trial from South America,4 both of which compared the CO2 laser to estrogen and had randomized groups, was that they were limited by the outcome measures used, none of which were consistently validated. But these studies also had small numbers of participants and short-term follow-up. So I don’t think there are much existing data that are promising for supporting energy-based treatment for GSM.
We also have just-published data on the laser for lichen sclerosus.5 For the AUGS panel, there was about 80% consensus for energy-based-device use and lichen sclerosus.2 According to Mitchell et al, who conducted a small, randomized, sham-controlled trial, CO2 laser resulted in no significant difference in histopathology scale score between active and sham arms.5
Future trials may want to assess laser as a mechanism for improved local drug delivery (eg, use of combined laser plus local estrogen for GSM or combined laser plus topical steroid for lichen sclerosus). I am also aware that properly designed laser versus sham studies are underway.
Dr. Levy: What about for stress urinary incontinence (SUI)? I don’t think these technologies are going to work.
Dr. Iglesia: For the AUGS panel, there was only about 70% consensus for energy-based-device use and SUI,2 and I’m one of the naysayers. The pathophysiology of SUI is so multifactorial that it’s hard to believe that laser or radiofrequency wand therapy could have sustained improvements, especially since prior radiofrequency therapy from the last decade (for instance, Renessa, Novasys Medical) did not show long-term efficacy.
Understanding lasers and coordinating care
Dr. Levy: We don’t know what the long-term outcomes are for the CO2 laser and GSM.
Dr. Iglesia: I agree with you, and I think there needs to be an understanding of the mechanism of how lasers work, whether it be erbium (Er:YAG), which is the most common, or CO2. Erbium and CO2 lasers, which are on the far-infrared spectrum, target the chromophore, water. My feeling is that, when you look at results from the Cruz trial,4 or even our trial that compared vaginal estrogen with laser,3 when there is severe GSM and high pH with virtually no water present in the tissues, that laser is not going to properly function. But I don’t think we know exactly what optimal pretreatment is necessary, and that is one of the problems. Furthermore, when intravaginal lasers are done and no adequate speculum exam is conducted prior to introducing the laser, there could be discharge or old creams present that block the mirrors necessary to adequately fire the fractionated laser beams.
Unfortunately, oftentimes these devices are marketed to women with breast cancer, who may be taking aromatase inhibitors, which cause the no-water problem; they dry out everything. They are effective for preventing breast cancer recurrence, but they cause severe atrophy (perhaps worse than many of the other selective estrogen-receptor modulators), with a resultant high vaginal pH. If we can bring that pH level down, closer to the normal 4.5 range so that we could have some level of moisture, and add estrogen first, the overall treatment approach will probably be more effective. We still do not know what happens after 1 year, though, and how often touch-ups need to be performed.
In fact, when working with a patient with breast cancer, I will speak with her oncologist; I will collaborate to put in place a treatment plan that may include initial pretreatment with low-dose vaginal estrogen followed by laser treatment for vaginal atrophy. But I will make sure I use the lowest dose. Sometimes when the patient comes back, the estrogen’s worked so well she’ll say, “Oh, I’m happy, so I don’t need the laser anymore.” A balanced conversation is necessary, especially with cancer survivors.
Informing patients and colleagues
Dr. Levy: I completely agree, and I think one of the key points here is that our purpose is to serve our patients. The data demonstrate that low doses of vaginal estrogen are not harmful for women who are being treated for or who have recovered from breast cancer. It is our ethical obligation to convince these women and their oncologists that ongoing treatment with vaginal estrogen not only will help their GSM but also their overactive bladder and their risk of urinary tract infections and other things. We could be exploiting patients who are really fearful of using any estrogen because of a perceived cancer risk. We could actually be validating their fear by telling them we have an alternative treatment for which they have to pay cash.
Treatment access
Dr. Iglesia: Yes, these are not cosmetic conditions that we are treating. So my goal when evaluating treatment for refractory GSM or lichen sclerosus is to find optimal energy-based therapies with the hope that one day these will be approved gynecologic conditions by the US FDA for laser and wand therapies and that they will ultimately not be out-of-pocket expenses but rather therapies covered by insurance.
Dr. Levy: Great. I understand that AUGS/IUGA have been working on a terminology algorithm to help distinguish between procedures being performed to resolve a medical problem such as prolapse or incontinence versus those designed to be cosmetic.
Dr. Iglesia: Yes, there is a big document from experts in both societies out for public comment right now. It will hopefully be published soon.
Outstanding questions remain
Dr. Levy: Really, we as ObGyns shouldn’t be quick to incorporate these things into our practices without high-quality studies demonstrating value. I have a major concern about these devices in the long term. When you look at fractional CO2 use on the face, for instance, which is a much different type of skin than the vagina, the laser builds collagen—but we don’t have long-term outcome results. The vagina is supposed to be an elastic tissue, so what is the risk of long-term scarring there? Yes, the laser builds collagen in the vaginal epithelium, but what does it do to scarring in the rest of the tissue? We don’t have answers to that.
Dr. Iglesia: And that is the question—how does histology equate with function? Well, I would go with what the patients are reporting.
Dr. Levy: Absolutely. But the thing about vaginal low-dose estrogen is that it is something that the oncologists or the ObGyns could be implementing with patients while they are undergoing cancer therapy, while in their menopausal transition, to preserve vulvovaginal function as opposed to trying to regain it.
Dr. Iglesia: Certainly, although it still needs to be determined when that type of approach would actually be contraindicated.
Dr. Levy: Thank you, Cheryl, for your valuable insights.
Dr. Iglesia: Of course. Thank you. ●
References
1. Lou W, Chen F, Xu T, et al. A randomized controlled study of vaginal fractional CO2 laser therapy for female sexual dysfunction. Lasers Med Sci. March 15, 2021. doi: 10.1007/s10103-021-03260-x.
2. Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices. Female Pelvic Med Reconstr Surg. 2020;26:287-298. doi: 10.1097 /SPV.0000000000000872.
3. Paraiso MF, Ferrando CA, et al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET Trial. Menopause. 2020;27:50-56. doi: 10.1097/GME.0000000000001416.
4. Cruz VL, Steiner ML, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25:21-28. doi: 10.1097 /GME.0000000000000955.
5. Mitchell L, Goldstein A, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi: 10.1097/AOG.0000000000004409.
A multidisciplinary approach to gyn care: A single center’s experience
In her book The Silo Effect: The Peril of Expertise and the Promise of Breaking Down Barriers, Gillian Tett wrote that “the word ‘silo’ does not just refer to a physical structure or organization (such as a department). It can also be a state of mind. Silos exist in structures. But they exist in our minds and social groups too. Silos breed tribalism. But they can also go hand in hand with tunnel vision.”
Tertiary care referral centers seem to be trending toward being more and more “un-siloed” and collaborative within their own departments and between departments in order to care for patients. The terms multidisciplinary and intradisciplinary have become popular in medicine, and teams are joining forces to create care paths for patients that are intended to improve the efficiency of and the quality of care that is rendered. There is no better example of the move to improve collaboration in medicine than the theme of the 2021 Society of Gynecologic Surgeons annual meeting, “Working Together: How Collaboration Enables Us to Better Help Our Patients.”
In this article, we provide examples of how collaborating with other specialties—within and outside of an ObGyn department—should become the standard of care. We discuss how to make this team approach easier and provide evidence that patients experience favorable outcomes. While data on combined care remain sparse, the existing literature on this topic helps us to guide and counsel patients about what to expect when a combined approach is taken.
Addressing pelvic floor disorders in women with gynecologic malignancy
In 2018, authors of a systematic review that looked at concurrent pelvic floor disorders in gynecologic oncologic survivors found that the prevalence of these disorders was high enough to warrant evaluation and management of these conditions to help improve quality of life for patients.1 Furthermore, it is possible that the prevalence of urinary incontinence is higher in patients who have undergone surgery for a gynecologic malignancy compared with controls, which has been reported in previous studies.2,3 At Cleveland Clinic, we recognize the need to evaluate our patients receiving oncologic care for urinary, fecal, and pelvic organ prolapse symptoms. Our oncologists routinely inquire about these symptoms once their patients have undergone surgery with them, and they make referrals for all their symptomatic patients. They have even learned about our own counseling, and they pre-emptively let patients know what our counseling may encompass.
For instance, many patients who received radiation therapy have stress urinary incontinence that is likely related to a hypomobile urethra, and they may benefit more from transurethral bulking than an anti-incontinence procedure in the operating room. Reassuring patients ahead of time that they do not need major interventions for their symptoms is helpful, as these patients are already experiencing tremendous burden from their oncologic conditions. We have made our referral patterns easy for these patients, and most patients are seen within days to weeks of the referral placed, depending on the urgency of the consult and the need to proceed with their oncologic treatment plan.
Gynecologic oncology patients who present with preoperative stress urinary incontinence and pelvic organ prolapse also are referred to a urogynecology specialist for concurrent care. Care paths have been created to help inform both the urogynecologists and the oncologists about options for patients depending on their respective conditions, as both their malignancy and their pelvic floor disorder(s) are considered in treatment planning. There is agreement in this planning that the oncologic surgery takes priority, and the urogynecologic approach is based on the oncologic plan.
Our urogynecologists routinely ask if future radiation is in the treatment plan, as this usually precludes us from placing a midurethral sling at the time of any surgery. Surgical approach (vaginal versus abdominal; open or minimally invasive) also is determined by the oncologic team. At the time of surgery, patient positioning is considered to optimize access for all of the surgeons. For instance, having the oncologist know that the patient needs to be far down on the bed as their steep Trendelenburg positioning during laparoscopy or robotic surgery may cause the patient to slide cephalad during the case may make a vaginal repair or sling placement at the end of the case challenging. All these small nuances are important, and a collaborative team develops the right plan for each patient in advance.
Data on the outcomes of combined surgery are sparse. In a retrospective matched cohort study, our group compared outcomes in women who underwent concurrent surgery with those who underwent urogynecologic surgery alone.4 We found that concurrent surgeries had an increased incidence of minor but not serious perioperative adverse events. Importantly, we determined that 1 in 10 planned urogynecologic procedures needed to be either modified or abandoned as a result of the oncologic plan. These data help guide our counseling, and both the oncologist and urogynecologist contributing to the combined case counsel patients according to these data.
Continue to: Concurrent colorectal and gynecologic surgery...
Concurrent colorectal and gynecologic surgery
Many women have pelvic floor disorders. As gynecologists, we often compartmentalize these conditions as gynecologic problems; frequently, however, colorectal conditions are at play as well and should be addressed concurrently. For instance, a high incidence of anorectal dysfunction occurs in women who present with pelvic organ prolapse.5 Furthermore, outlet defecation disorders are not always a result of a straightforward rectocele that can be fixed vaginally. Sometimes, a more thorough evaluation is warranted depending on the patient’s concurrent symptoms and history. Outlet symptoms may be attributed to large enteroceles, sigmoidoceles, perineal descent, rectal intussusception, and rectal prolapse.6
As a result, a combined approach to caring for patients with complex pelvic floor disorders is optimal. Several studies describe this type of combined and coordinated patient care.7,8 Ideally, patients are seen by both surgeons in the office so that the surgeons may make a combined plan for their care, especially if the decision is made to proceed with surgery. Urogynecology specialists and colorectal surgeons must decide together whether to approach combined prolapse procedures via a perineal and vaginal approach versus an abdominal approach. Several factors can determine this, including surgeon experience and preference, which is why it is important for surgeons working together to have either well-designed care paths or simply open communication and experience working together for the conditions they are treating.
In an ideal coordinated care approach, both surgeons review the patient records in advance. Any needed imaging or testing is done before the official patient consult; the patient is then seen by both clinicians in the same visit and counseled about the options. This is the most efficient and effective way to see patients, and we have had significant success using this approach.
Complications of combined surgery
The safety of combining procedures such as laparoscopic sacrocolpopexy and concurrent rectopexy has been studied, and intraoperative complications have been reported to be low.9,10 In a cohort study, Wallace and colleagues looked at postoperative outcomes and complications following combined surgery and reported that reoperation for the rectal prolapse component of the surgery was more common than the pelvic organ prolapse component, and that 1 in 5 of their patients experienced a surgical complication within 30 days of their surgery.11 This incidence is higher than that seen with isolated pelvic organ prolapse surgery. These data help us understand that a combined approach requires good patient counseling in the office about both the need for repeat surgery in certain circumstances and the increased risk of complications. Further, combined perineal and vaginal approaches have been compared with abdominal approaches and also have shown no age-adjusted differences in outcomes and complications.12
These data point to the need for surgeons to choose the approach to surgery that best fits their own experiences and to discuss this together before counseling the patient in the office, thus streamlining the effort so that the patient feels comfortable under the care of 2 surgeons.
Patients presenting with urogynecologic and gynecologic conditions also report symptomatic hemorrhoids, and colorectal referral is often made by the gynecologist. Sparse data are available regarding combined approaches to managing hemorrhoids and gynecologic conditions. Our group was the first to publish on outcomes and complications in patients undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery.13 In that retrospective cohort, we found that minor complications, such as postoperative urinary tract infection and transient voiding dysfunction, was more common in patients who underwent combined surgery. From this, we gathered that there is a need to counsel patients appropriately about the risk of combined surgery. That said, for some patients, coordinated care is desirable, and surgeons should make the effort to work together in combining their procedures.
Continue to: Integrating plastic and reconstructive surgery in gynecology...
Integrating plastic and reconstructive surgery in gynecology
Reconstructive gynecologic procedures often require a multidisciplinary approach to what can be very complex reconstructive surgery. The intended goal usually is to achieve a good cosmetic result in the genital area, as well as to restore sexual, defecatory, and/or genitourinary functionality. As a result, surgeons must work together to develop a feasible reconstructive plan for these patients.
Women experience vaginal stenosis or foreshortening for a number of reasons. Women with congenital anomalies often are cared for by specialists in pediatric and adolescent gynecology. Other women, such as those who have undergone vaginectomy and/or pelvic or vaginal radiation for cancer treatment, complications from vaginal mesh placement, and severe vaginal scarring from dermatologic conditions like lichen planus, are cared for by other gynecologic specialists, often general gynecologists or urogynecologists. In some of these cases, a gynecologic surgeon can perform vaginal adhesiolysis followed by vaginal estrogen treatment (when appropriate) and aggressive postoperative vaginal dilation with adjunctive pelvic floor physical therapy as well as sex therapy or counseling. A simple reconstructive approach may be necessary if lysis of adhesions alone is not sufficient. Sometimes, the vaginal apex must be opened vaginally or abdominally, or releasing incisions need to be made to improve the caliber of the vagina in addition to its length. Under these circumstances, the use of additional local skin grafts, local peritoneal flaps, or biologic grafts or xenografts can help achieve a satisfying result. While not all gynecologists are trained to perform these procedures, some are, and certainly gynecologic subspecialists have the skill sets to care for these patients.
Under other circumstances, when the vagina is truly foreshortened, more aggressive reconstructive surgery is necessary and consultation and collaboration with plastic surgery specialists often is helpful. At our center, these patients’ care is initially managed by gynecologists and, when simple approaches to their reconstructive needs are exhausted, collaboration is warranted. As with the other team approaches discussed in this article, the recommendation is for a consistent referral team that has established care paths for patients. Not all plastic surgeons are familiar with neovaginal reconstruction and understand the functional aspects that gynecologists are hoping to achieve for their patients. Therefore, it is important to form cohesive teams that have the same goals for the patient.
The literature on neovaginal reconstruction is sparse. There are no true agreed on approaches or techniques for vaginal reconstruction because there is no “one size fits all” for these repairs. Defects also vary depending on whether they are due to resections or radiation for oncologic treatment, reconstruction as part of the repair of a genitourinary or rectovaginal fistula, or stenosis from other etiologies.
In 2002, Cordeiro and colleagues published a classification system and reconstructive algorithm for acquired vaginal defects.14 Not all reconstructive surgeons subscribe to this algorithm, but it is the only rubric that currently exists. The authors differentiate between “partial” and “circumferential” defects and recommend different types of fasciocutaneous and myocutaneous flaps for reconstruction.
In our experience at our center, we believe that the choice of flap should also depend on whether or not perineal reconstruction is needed. This decision is made by both the gynecologic specialist and the plastic surgeon. Common flap choices include the Singapore flap, a fasciocutaneous flap based on perforators from the pudendal vessels; the gracilis flap, a myocutaneous flap based off the medial circumflex femoral vessels; and the rectus abdominis flap (transverse or vertical), which is also a myocutaneous flap that relies on the blood supply from the deep inferior epigastric vessels.
One of the most important parts of the coordinated effort of neovaginal surgery is postoperative care. Plastic surgeons play a key role in ensuring that the flap survives in the immediate postoperative period. The gynecology team should be responsible for postoperative vaginal dilation teaching and follow-up to ensure that the patient dilates properly and upsizes her dilator appropriately over the postoperative period. In our practice, our advanced practice clinicians often care for these patients and are responsible for continuity and dilation teaching. Patients have easy access to these clinicians, and this enhances the postoperative experience. Referral to a pelvic floor physical therapist knowledgeable about neovaginal surgery also helps to ensure that the dilation process goes successfully. It also helps to have office days on the same days as the plastic surgery team that is following the patient. This way, the patient may be seen by both teams on the same day. This allows for good patient communication with regard to aftercare, as well as a combined approach to teaching the trainees involved in the case. Coordination with pelvic floor physical therapists on those days also enhances the patient experience and is highly recommended.
Continue to: Combining gyn and urogyn procedures with plastic surgery...
Combining gyn and urogyn procedures with plastic surgery
While there are no data on combining gynecologic and urogynecologic procedures with plastic reconstructive surgeries, a team approach to combining surgeries is possible. At our center, we have performed tubal ligation, ovarian surgery, hysterectomy, and sling and prolapse surgery in patients who were undergoing cosmetic procedures, such as breast augmentation and abdominoplasty.
Gender affirmation surgery also can be performed through a combined approach between gynecologists and plastic surgeons. Our gynecologists perform hysterectomy for transmasculine men, and this procedure is sometimes safely and effectively performed in combination with masculinizing chest surgery (mastectomy) performed by our plastic surgeons. Vaginoplasty surgery (feminizing genital surgery) also is performed by urogynecology specialists at our center, and it is sometimes done concurrently at the time of breast augmentation and/or facial feminization surgery.
Case order. Some plastic surgeons vocalize concerns about combining clean procedures with clean contaminated cases, especially in situations in which implants are being placed in the body. During these cases, communication and organization between surgeons is important. For instance, there should be a discussion about case order. In general, the clean procedures should be performed first. In addition, separate operating tables and instruments should be used. Simultaneous operating also should be avoided. Fresh incisions should be dressed and covered before subsequent procedures are performed.
Incision placement. Last, planning around incision placement should be discussed before each case. Laparoscopic and abdominal incisions may interfere with plastic surgery procedures and alter the end cosmesis. These incisions often can be incorporated into the reconstructive procedure. The most important part of the coordinated surgical effort is ensuring that both surgical teams understand each other’s respective surgeries and the approach needed to complete them. When this is achieved, the cases are usually very successful.
Creating collaboration between obstetricians and gynecologic specialists
The impacts of pregnancy and vaginal delivery on the pelvic floor are well established. Urinary and fecal incontinence, pelvic organ prolapse, perineal pain, and dyspareunia are not uncommon in the postpartum period and may persist long term. The effects of obstetric anal sphincter injury (OASI) are significant, with up to 25% of women experiencing wound complications and 17% experiencing fecal incontinence at 6 months postpartum.15,16 Care of women with peripartum pelvic floor disorders and OASIs present an ideal opportunity for collaboration between urogynecologists and obstetricians. The Cleveland Clinic has a multidisciplinary Postpartum Care Clinic (PPCC) where we provide specialized, collaborative care for women with peripartum pelvic floor disorders and complex obstetric lacerations.
Our PPCC accepts referrals up to 1 year postpartum for women who experience OASI, urinary or fecal incontinence, perineal pain or dyspareunia, voiding dysfunction or urinary retention, and wound healing complications. When a woman is diagnosed with an OASI at the time of delivery, a “best practice alert” is released in the medical record recommending a referral to the PPCC to encourage referral of all women with OASI. We strive to see all referrals within 2 weeks of delivery.
At the time of the initial consultation, we collect validated questionnaires on bowel and bladder function, assess pain and healing, and discuss future delivery planning. The success of the PPCC is rooted in communication. When the clinic first opened, we provided education to our obstetrics colleagues on the purpose of the clinic, when and how to refer, and what to expect from our consultations. Open communication between referring obstetric clinicians and the urogynecologists that run the PPCC is key in providing collaborative care where patients know that their clinicians are working as a team. All recommendations are communicated to referring clinicians, and all women are ultimately referred back to their primary clinician for long-term care. Evidence demonstrates that this type of clinic leads to high obstetric clinician satisfaction and increased awareness of OASIs and their impact on maternal health.17
Combined team approach fosters innovation in patient care
A combined approach to the care of the patient who presents with gynecologic conditions is optimal. In this article, we presented examples of care that integrates gynecology, urogynecology, gynecologic oncology, colorectal surgery, plastic surgery, and obstetrics. There are, however, many more existing examples as well as opportunities to create teams that really make a difference in the way patients receive—and perceive—their care. This is a good starting point, and we should strive to use this model to continue to innovate our approach to patient care.
- Ramaseshan AS, Felton J, Roque D, et al. Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J. 2018;29:459-476.
- Nakayama N, Tsuji T, Aoyama M, et al. Quality of life and the prevalence of urinary incontinence after surgical treatment for gynecologic cancer: a questionnaire survey. BMC Womens Health. 2020;20:148-157.
- Cascales-Campos PA, Gonzalez-Gil A, Fernandez-Luna E, et al. Urinary and fecal incontinence in patients with advanced ovarian cancer treated with CRS + HIPEC. Surg Oncol. 2021;36:115-119.
- Davidson ER, Woodburn K, AlHilli M, et al. Perioperative adverse events in women undergoing concurrent urogynecologic and gynecologic oncology surgeries for suspected malignancy. Int Urogynecol J. 2019;30:1195-1201.
- Spence-Jones C, Kamm MA, Henry MM, et al. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and stress urinary incontinence. Br J Obstet Gynaecol. 1994;101:147-152.
- Thompson JR, Chen AH, Pettit PD, et al. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187:1494-1500.
- Jallad K, Gurland B. Multidisciplinary approach to the treatment of concomitant rectal and vaginal prolapse. Clin Colon Rectal Surg. 2016;29:101-105.
- Kapoor DS, Sultan AH, Thakar R, et al. Management of complex pelvic floor disorders in a multidisciplinary pelvic floor clinic. Colorectal Dis. 2008;10:118-123.
- Weinberg D, Qeadan F, McKee R, et al. Safety of laparoscopic sacrocolpopexy with concurrent rectopexy: peri-operative morbidity in a nationwide cohort. Int Urogynecol J. 2019;30:385-392.
- Geltzeiler CB, Birnbaum EH, Silviera ML, et al. Combined rectopexy and sacrocolpopexy is safe for correction of pelvic organ prolapse. Int J Colorectal Dis. 2018;33:1453-1459.
- Wallace SL, Syan R, Enemchukwu EA, et al. Surgical approach, complications, and reoperation rates of combined rectal and pelvic organ prolapse surgery. Int Urogynecol J. 2020;31:2101-2108.
- Smith PE, Hade EM, Pandya LK, et al. Perioperative outcomes for combined ventral rectopexy with sacrocolpopexy compared to perineal rectopexy with vaginal apical suspension. Female Pelvic Med Reconstr Surg. 2020;26:376-381.
- Casas-Puig V, Bretschneider CE, Ferrando CA. Perioperative adverse events in women undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2019;25:88-92.
- Cordeiro PG, Pusic AL, Disa JJ. A classification system and reconstructive algorithm for acquired vaginal defects. Plast Reconstr Surg. 2002;110:1058-1065.
- Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, et al. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125:1088-1093.
- Borello-France D, Burgio KL, Richter HE, et al; Pelvic Floor Disorders Network. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108:863-872.
- Propst K, Hickman LC. Peripartum pelvic floor disorder clinics inform obstetric provider practices. Int Urogynecol J. 2021;32:1793-1799.
In her book The Silo Effect: The Peril of Expertise and the Promise of Breaking Down Barriers, Gillian Tett wrote that “the word ‘silo’ does not just refer to a physical structure or organization (such as a department). It can also be a state of mind. Silos exist in structures. But they exist in our minds and social groups too. Silos breed tribalism. But they can also go hand in hand with tunnel vision.”
Tertiary care referral centers seem to be trending toward being more and more “un-siloed” and collaborative within their own departments and between departments in order to care for patients. The terms multidisciplinary and intradisciplinary have become popular in medicine, and teams are joining forces to create care paths for patients that are intended to improve the efficiency of and the quality of care that is rendered. There is no better example of the move to improve collaboration in medicine than the theme of the 2021 Society of Gynecologic Surgeons annual meeting, “Working Together: How Collaboration Enables Us to Better Help Our Patients.”
In this article, we provide examples of how collaborating with other specialties—within and outside of an ObGyn department—should become the standard of care. We discuss how to make this team approach easier and provide evidence that patients experience favorable outcomes. While data on combined care remain sparse, the existing literature on this topic helps us to guide and counsel patients about what to expect when a combined approach is taken.
Addressing pelvic floor disorders in women with gynecologic malignancy
In 2018, authors of a systematic review that looked at concurrent pelvic floor disorders in gynecologic oncologic survivors found that the prevalence of these disorders was high enough to warrant evaluation and management of these conditions to help improve quality of life for patients.1 Furthermore, it is possible that the prevalence of urinary incontinence is higher in patients who have undergone surgery for a gynecologic malignancy compared with controls, which has been reported in previous studies.2,3 At Cleveland Clinic, we recognize the need to evaluate our patients receiving oncologic care for urinary, fecal, and pelvic organ prolapse symptoms. Our oncologists routinely inquire about these symptoms once their patients have undergone surgery with them, and they make referrals for all their symptomatic patients. They have even learned about our own counseling, and they pre-emptively let patients know what our counseling may encompass.
For instance, many patients who received radiation therapy have stress urinary incontinence that is likely related to a hypomobile urethra, and they may benefit more from transurethral bulking than an anti-incontinence procedure in the operating room. Reassuring patients ahead of time that they do not need major interventions for their symptoms is helpful, as these patients are already experiencing tremendous burden from their oncologic conditions. We have made our referral patterns easy for these patients, and most patients are seen within days to weeks of the referral placed, depending on the urgency of the consult and the need to proceed with their oncologic treatment plan.
Gynecologic oncology patients who present with preoperative stress urinary incontinence and pelvic organ prolapse also are referred to a urogynecology specialist for concurrent care. Care paths have been created to help inform both the urogynecologists and the oncologists about options for patients depending on their respective conditions, as both their malignancy and their pelvic floor disorder(s) are considered in treatment planning. There is agreement in this planning that the oncologic surgery takes priority, and the urogynecologic approach is based on the oncologic plan.
Our urogynecologists routinely ask if future radiation is in the treatment plan, as this usually precludes us from placing a midurethral sling at the time of any surgery. Surgical approach (vaginal versus abdominal; open or minimally invasive) also is determined by the oncologic team. At the time of surgery, patient positioning is considered to optimize access for all of the surgeons. For instance, having the oncologist know that the patient needs to be far down on the bed as their steep Trendelenburg positioning during laparoscopy or robotic surgery may cause the patient to slide cephalad during the case may make a vaginal repair or sling placement at the end of the case challenging. All these small nuances are important, and a collaborative team develops the right plan for each patient in advance.
Data on the outcomes of combined surgery are sparse. In a retrospective matched cohort study, our group compared outcomes in women who underwent concurrent surgery with those who underwent urogynecologic surgery alone.4 We found that concurrent surgeries had an increased incidence of minor but not serious perioperative adverse events. Importantly, we determined that 1 in 10 planned urogynecologic procedures needed to be either modified or abandoned as a result of the oncologic plan. These data help guide our counseling, and both the oncologist and urogynecologist contributing to the combined case counsel patients according to these data.
Continue to: Concurrent colorectal and gynecologic surgery...
Concurrent colorectal and gynecologic surgery
Many women have pelvic floor disorders. As gynecologists, we often compartmentalize these conditions as gynecologic problems; frequently, however, colorectal conditions are at play as well and should be addressed concurrently. For instance, a high incidence of anorectal dysfunction occurs in women who present with pelvic organ prolapse.5 Furthermore, outlet defecation disorders are not always a result of a straightforward rectocele that can be fixed vaginally. Sometimes, a more thorough evaluation is warranted depending on the patient’s concurrent symptoms and history. Outlet symptoms may be attributed to large enteroceles, sigmoidoceles, perineal descent, rectal intussusception, and rectal prolapse.6
As a result, a combined approach to caring for patients with complex pelvic floor disorders is optimal. Several studies describe this type of combined and coordinated patient care.7,8 Ideally, patients are seen by both surgeons in the office so that the surgeons may make a combined plan for their care, especially if the decision is made to proceed with surgery. Urogynecology specialists and colorectal surgeons must decide together whether to approach combined prolapse procedures via a perineal and vaginal approach versus an abdominal approach. Several factors can determine this, including surgeon experience and preference, which is why it is important for surgeons working together to have either well-designed care paths or simply open communication and experience working together for the conditions they are treating.
In an ideal coordinated care approach, both surgeons review the patient records in advance. Any needed imaging or testing is done before the official patient consult; the patient is then seen by both clinicians in the same visit and counseled about the options. This is the most efficient and effective way to see patients, and we have had significant success using this approach.
Complications of combined surgery
The safety of combining procedures such as laparoscopic sacrocolpopexy and concurrent rectopexy has been studied, and intraoperative complications have been reported to be low.9,10 In a cohort study, Wallace and colleagues looked at postoperative outcomes and complications following combined surgery and reported that reoperation for the rectal prolapse component of the surgery was more common than the pelvic organ prolapse component, and that 1 in 5 of their patients experienced a surgical complication within 30 days of their surgery.11 This incidence is higher than that seen with isolated pelvic organ prolapse surgery. These data help us understand that a combined approach requires good patient counseling in the office about both the need for repeat surgery in certain circumstances and the increased risk of complications. Further, combined perineal and vaginal approaches have been compared with abdominal approaches and also have shown no age-adjusted differences in outcomes and complications.12
These data point to the need for surgeons to choose the approach to surgery that best fits their own experiences and to discuss this together before counseling the patient in the office, thus streamlining the effort so that the patient feels comfortable under the care of 2 surgeons.
Patients presenting with urogynecologic and gynecologic conditions also report symptomatic hemorrhoids, and colorectal referral is often made by the gynecologist. Sparse data are available regarding combined approaches to managing hemorrhoids and gynecologic conditions. Our group was the first to publish on outcomes and complications in patients undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery.13 In that retrospective cohort, we found that minor complications, such as postoperative urinary tract infection and transient voiding dysfunction, was more common in patients who underwent combined surgery. From this, we gathered that there is a need to counsel patients appropriately about the risk of combined surgery. That said, for some patients, coordinated care is desirable, and surgeons should make the effort to work together in combining their procedures.
Continue to: Integrating plastic and reconstructive surgery in gynecology...
Integrating plastic and reconstructive surgery in gynecology
Reconstructive gynecologic procedures often require a multidisciplinary approach to what can be very complex reconstructive surgery. The intended goal usually is to achieve a good cosmetic result in the genital area, as well as to restore sexual, defecatory, and/or genitourinary functionality. As a result, surgeons must work together to develop a feasible reconstructive plan for these patients.
Women experience vaginal stenosis or foreshortening for a number of reasons. Women with congenital anomalies often are cared for by specialists in pediatric and adolescent gynecology. Other women, such as those who have undergone vaginectomy and/or pelvic or vaginal radiation for cancer treatment, complications from vaginal mesh placement, and severe vaginal scarring from dermatologic conditions like lichen planus, are cared for by other gynecologic specialists, often general gynecologists or urogynecologists. In some of these cases, a gynecologic surgeon can perform vaginal adhesiolysis followed by vaginal estrogen treatment (when appropriate) and aggressive postoperative vaginal dilation with adjunctive pelvic floor physical therapy as well as sex therapy or counseling. A simple reconstructive approach may be necessary if lysis of adhesions alone is not sufficient. Sometimes, the vaginal apex must be opened vaginally or abdominally, or releasing incisions need to be made to improve the caliber of the vagina in addition to its length. Under these circumstances, the use of additional local skin grafts, local peritoneal flaps, or biologic grafts or xenografts can help achieve a satisfying result. While not all gynecologists are trained to perform these procedures, some are, and certainly gynecologic subspecialists have the skill sets to care for these patients.
Under other circumstances, when the vagina is truly foreshortened, more aggressive reconstructive surgery is necessary and consultation and collaboration with plastic surgery specialists often is helpful. At our center, these patients’ care is initially managed by gynecologists and, when simple approaches to their reconstructive needs are exhausted, collaboration is warranted. As with the other team approaches discussed in this article, the recommendation is for a consistent referral team that has established care paths for patients. Not all plastic surgeons are familiar with neovaginal reconstruction and understand the functional aspects that gynecologists are hoping to achieve for their patients. Therefore, it is important to form cohesive teams that have the same goals for the patient.
The literature on neovaginal reconstruction is sparse. There are no true agreed on approaches or techniques for vaginal reconstruction because there is no “one size fits all” for these repairs. Defects also vary depending on whether they are due to resections or radiation for oncologic treatment, reconstruction as part of the repair of a genitourinary or rectovaginal fistula, or stenosis from other etiologies.
In 2002, Cordeiro and colleagues published a classification system and reconstructive algorithm for acquired vaginal defects.14 Not all reconstructive surgeons subscribe to this algorithm, but it is the only rubric that currently exists. The authors differentiate between “partial” and “circumferential” defects and recommend different types of fasciocutaneous and myocutaneous flaps for reconstruction.
In our experience at our center, we believe that the choice of flap should also depend on whether or not perineal reconstruction is needed. This decision is made by both the gynecologic specialist and the plastic surgeon. Common flap choices include the Singapore flap, a fasciocutaneous flap based on perforators from the pudendal vessels; the gracilis flap, a myocutaneous flap based off the medial circumflex femoral vessels; and the rectus abdominis flap (transverse or vertical), which is also a myocutaneous flap that relies on the blood supply from the deep inferior epigastric vessels.
One of the most important parts of the coordinated effort of neovaginal surgery is postoperative care. Plastic surgeons play a key role in ensuring that the flap survives in the immediate postoperative period. The gynecology team should be responsible for postoperative vaginal dilation teaching and follow-up to ensure that the patient dilates properly and upsizes her dilator appropriately over the postoperative period. In our practice, our advanced practice clinicians often care for these patients and are responsible for continuity and dilation teaching. Patients have easy access to these clinicians, and this enhances the postoperative experience. Referral to a pelvic floor physical therapist knowledgeable about neovaginal surgery also helps to ensure that the dilation process goes successfully. It also helps to have office days on the same days as the plastic surgery team that is following the patient. This way, the patient may be seen by both teams on the same day. This allows for good patient communication with regard to aftercare, as well as a combined approach to teaching the trainees involved in the case. Coordination with pelvic floor physical therapists on those days also enhances the patient experience and is highly recommended.
Continue to: Combining gyn and urogyn procedures with plastic surgery...
Combining gyn and urogyn procedures with plastic surgery
While there are no data on combining gynecologic and urogynecologic procedures with plastic reconstructive surgeries, a team approach to combining surgeries is possible. At our center, we have performed tubal ligation, ovarian surgery, hysterectomy, and sling and prolapse surgery in patients who were undergoing cosmetic procedures, such as breast augmentation and abdominoplasty.
Gender affirmation surgery also can be performed through a combined approach between gynecologists and plastic surgeons. Our gynecologists perform hysterectomy for transmasculine men, and this procedure is sometimes safely and effectively performed in combination with masculinizing chest surgery (mastectomy) performed by our plastic surgeons. Vaginoplasty surgery (feminizing genital surgery) also is performed by urogynecology specialists at our center, and it is sometimes done concurrently at the time of breast augmentation and/or facial feminization surgery.
Case order. Some plastic surgeons vocalize concerns about combining clean procedures with clean contaminated cases, especially in situations in which implants are being placed in the body. During these cases, communication and organization between surgeons is important. For instance, there should be a discussion about case order. In general, the clean procedures should be performed first. In addition, separate operating tables and instruments should be used. Simultaneous operating also should be avoided. Fresh incisions should be dressed and covered before subsequent procedures are performed.
Incision placement. Last, planning around incision placement should be discussed before each case. Laparoscopic and abdominal incisions may interfere with plastic surgery procedures and alter the end cosmesis. These incisions often can be incorporated into the reconstructive procedure. The most important part of the coordinated surgical effort is ensuring that both surgical teams understand each other’s respective surgeries and the approach needed to complete them. When this is achieved, the cases are usually very successful.
Creating collaboration between obstetricians and gynecologic specialists
The impacts of pregnancy and vaginal delivery on the pelvic floor are well established. Urinary and fecal incontinence, pelvic organ prolapse, perineal pain, and dyspareunia are not uncommon in the postpartum period and may persist long term. The effects of obstetric anal sphincter injury (OASI) are significant, with up to 25% of women experiencing wound complications and 17% experiencing fecal incontinence at 6 months postpartum.15,16 Care of women with peripartum pelvic floor disorders and OASIs present an ideal opportunity for collaboration between urogynecologists and obstetricians. The Cleveland Clinic has a multidisciplinary Postpartum Care Clinic (PPCC) where we provide specialized, collaborative care for women with peripartum pelvic floor disorders and complex obstetric lacerations.
Our PPCC accepts referrals up to 1 year postpartum for women who experience OASI, urinary or fecal incontinence, perineal pain or dyspareunia, voiding dysfunction or urinary retention, and wound healing complications. When a woman is diagnosed with an OASI at the time of delivery, a “best practice alert” is released in the medical record recommending a referral to the PPCC to encourage referral of all women with OASI. We strive to see all referrals within 2 weeks of delivery.
At the time of the initial consultation, we collect validated questionnaires on bowel and bladder function, assess pain and healing, and discuss future delivery planning. The success of the PPCC is rooted in communication. When the clinic first opened, we provided education to our obstetrics colleagues on the purpose of the clinic, when and how to refer, and what to expect from our consultations. Open communication between referring obstetric clinicians and the urogynecologists that run the PPCC is key in providing collaborative care where patients know that their clinicians are working as a team. All recommendations are communicated to referring clinicians, and all women are ultimately referred back to their primary clinician for long-term care. Evidence demonstrates that this type of clinic leads to high obstetric clinician satisfaction and increased awareness of OASIs and their impact on maternal health.17
Combined team approach fosters innovation in patient care
A combined approach to the care of the patient who presents with gynecologic conditions is optimal. In this article, we presented examples of care that integrates gynecology, urogynecology, gynecologic oncology, colorectal surgery, plastic surgery, and obstetrics. There are, however, many more existing examples as well as opportunities to create teams that really make a difference in the way patients receive—and perceive—their care. This is a good starting point, and we should strive to use this model to continue to innovate our approach to patient care.
In her book The Silo Effect: The Peril of Expertise and the Promise of Breaking Down Barriers, Gillian Tett wrote that “the word ‘silo’ does not just refer to a physical structure or organization (such as a department). It can also be a state of mind. Silos exist in structures. But they exist in our minds and social groups too. Silos breed tribalism. But they can also go hand in hand with tunnel vision.”
Tertiary care referral centers seem to be trending toward being more and more “un-siloed” and collaborative within their own departments and between departments in order to care for patients. The terms multidisciplinary and intradisciplinary have become popular in medicine, and teams are joining forces to create care paths for patients that are intended to improve the efficiency of and the quality of care that is rendered. There is no better example of the move to improve collaboration in medicine than the theme of the 2021 Society of Gynecologic Surgeons annual meeting, “Working Together: How Collaboration Enables Us to Better Help Our Patients.”
In this article, we provide examples of how collaborating with other specialties—within and outside of an ObGyn department—should become the standard of care. We discuss how to make this team approach easier and provide evidence that patients experience favorable outcomes. While data on combined care remain sparse, the existing literature on this topic helps us to guide and counsel patients about what to expect when a combined approach is taken.
Addressing pelvic floor disorders in women with gynecologic malignancy
In 2018, authors of a systematic review that looked at concurrent pelvic floor disorders in gynecologic oncologic survivors found that the prevalence of these disorders was high enough to warrant evaluation and management of these conditions to help improve quality of life for patients.1 Furthermore, it is possible that the prevalence of urinary incontinence is higher in patients who have undergone surgery for a gynecologic malignancy compared with controls, which has been reported in previous studies.2,3 At Cleveland Clinic, we recognize the need to evaluate our patients receiving oncologic care for urinary, fecal, and pelvic organ prolapse symptoms. Our oncologists routinely inquire about these symptoms once their patients have undergone surgery with them, and they make referrals for all their symptomatic patients. They have even learned about our own counseling, and they pre-emptively let patients know what our counseling may encompass.
For instance, many patients who received radiation therapy have stress urinary incontinence that is likely related to a hypomobile urethra, and they may benefit more from transurethral bulking than an anti-incontinence procedure in the operating room. Reassuring patients ahead of time that they do not need major interventions for their symptoms is helpful, as these patients are already experiencing tremendous burden from their oncologic conditions. We have made our referral patterns easy for these patients, and most patients are seen within days to weeks of the referral placed, depending on the urgency of the consult and the need to proceed with their oncologic treatment plan.
Gynecologic oncology patients who present with preoperative stress urinary incontinence and pelvic organ prolapse also are referred to a urogynecology specialist for concurrent care. Care paths have been created to help inform both the urogynecologists and the oncologists about options for patients depending on their respective conditions, as both their malignancy and their pelvic floor disorder(s) are considered in treatment planning. There is agreement in this planning that the oncologic surgery takes priority, and the urogynecologic approach is based on the oncologic plan.
Our urogynecologists routinely ask if future radiation is in the treatment plan, as this usually precludes us from placing a midurethral sling at the time of any surgery. Surgical approach (vaginal versus abdominal; open or minimally invasive) also is determined by the oncologic team. At the time of surgery, patient positioning is considered to optimize access for all of the surgeons. For instance, having the oncologist know that the patient needs to be far down on the bed as their steep Trendelenburg positioning during laparoscopy or robotic surgery may cause the patient to slide cephalad during the case may make a vaginal repair or sling placement at the end of the case challenging. All these small nuances are important, and a collaborative team develops the right plan for each patient in advance.
Data on the outcomes of combined surgery are sparse. In a retrospective matched cohort study, our group compared outcomes in women who underwent concurrent surgery with those who underwent urogynecologic surgery alone.4 We found that concurrent surgeries had an increased incidence of minor but not serious perioperative adverse events. Importantly, we determined that 1 in 10 planned urogynecologic procedures needed to be either modified or abandoned as a result of the oncologic plan. These data help guide our counseling, and both the oncologist and urogynecologist contributing to the combined case counsel patients according to these data.
Continue to: Concurrent colorectal and gynecologic surgery...
Concurrent colorectal and gynecologic surgery
Many women have pelvic floor disorders. As gynecologists, we often compartmentalize these conditions as gynecologic problems; frequently, however, colorectal conditions are at play as well and should be addressed concurrently. For instance, a high incidence of anorectal dysfunction occurs in women who present with pelvic organ prolapse.5 Furthermore, outlet defecation disorders are not always a result of a straightforward rectocele that can be fixed vaginally. Sometimes, a more thorough evaluation is warranted depending on the patient’s concurrent symptoms and history. Outlet symptoms may be attributed to large enteroceles, sigmoidoceles, perineal descent, rectal intussusception, and rectal prolapse.6
As a result, a combined approach to caring for patients with complex pelvic floor disorders is optimal. Several studies describe this type of combined and coordinated patient care.7,8 Ideally, patients are seen by both surgeons in the office so that the surgeons may make a combined plan for their care, especially if the decision is made to proceed with surgery. Urogynecology specialists and colorectal surgeons must decide together whether to approach combined prolapse procedures via a perineal and vaginal approach versus an abdominal approach. Several factors can determine this, including surgeon experience and preference, which is why it is important for surgeons working together to have either well-designed care paths or simply open communication and experience working together for the conditions they are treating.
In an ideal coordinated care approach, both surgeons review the patient records in advance. Any needed imaging or testing is done before the official patient consult; the patient is then seen by both clinicians in the same visit and counseled about the options. This is the most efficient and effective way to see patients, and we have had significant success using this approach.
Complications of combined surgery
The safety of combining procedures such as laparoscopic sacrocolpopexy and concurrent rectopexy has been studied, and intraoperative complications have been reported to be low.9,10 In a cohort study, Wallace and colleagues looked at postoperative outcomes and complications following combined surgery and reported that reoperation for the rectal prolapse component of the surgery was more common than the pelvic organ prolapse component, and that 1 in 5 of their patients experienced a surgical complication within 30 days of their surgery.11 This incidence is higher than that seen with isolated pelvic organ prolapse surgery. These data help us understand that a combined approach requires good patient counseling in the office about both the need for repeat surgery in certain circumstances and the increased risk of complications. Further, combined perineal and vaginal approaches have been compared with abdominal approaches and also have shown no age-adjusted differences in outcomes and complications.12
These data point to the need for surgeons to choose the approach to surgery that best fits their own experiences and to discuss this together before counseling the patient in the office, thus streamlining the effort so that the patient feels comfortable under the care of 2 surgeons.
Patients presenting with urogynecologic and gynecologic conditions also report symptomatic hemorrhoids, and colorectal referral is often made by the gynecologist. Sparse data are available regarding combined approaches to managing hemorrhoids and gynecologic conditions. Our group was the first to publish on outcomes and complications in patients undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery.13 In that retrospective cohort, we found that minor complications, such as postoperative urinary tract infection and transient voiding dysfunction, was more common in patients who underwent combined surgery. From this, we gathered that there is a need to counsel patients appropriately about the risk of combined surgery. That said, for some patients, coordinated care is desirable, and surgeons should make the effort to work together in combining their procedures.
Continue to: Integrating plastic and reconstructive surgery in gynecology...
Integrating plastic and reconstructive surgery in gynecology
Reconstructive gynecologic procedures often require a multidisciplinary approach to what can be very complex reconstructive surgery. The intended goal usually is to achieve a good cosmetic result in the genital area, as well as to restore sexual, defecatory, and/or genitourinary functionality. As a result, surgeons must work together to develop a feasible reconstructive plan for these patients.
Women experience vaginal stenosis or foreshortening for a number of reasons. Women with congenital anomalies often are cared for by specialists in pediatric and adolescent gynecology. Other women, such as those who have undergone vaginectomy and/or pelvic or vaginal radiation for cancer treatment, complications from vaginal mesh placement, and severe vaginal scarring from dermatologic conditions like lichen planus, are cared for by other gynecologic specialists, often general gynecologists or urogynecologists. In some of these cases, a gynecologic surgeon can perform vaginal adhesiolysis followed by vaginal estrogen treatment (when appropriate) and aggressive postoperative vaginal dilation with adjunctive pelvic floor physical therapy as well as sex therapy or counseling. A simple reconstructive approach may be necessary if lysis of adhesions alone is not sufficient. Sometimes, the vaginal apex must be opened vaginally or abdominally, or releasing incisions need to be made to improve the caliber of the vagina in addition to its length. Under these circumstances, the use of additional local skin grafts, local peritoneal flaps, or biologic grafts or xenografts can help achieve a satisfying result. While not all gynecologists are trained to perform these procedures, some are, and certainly gynecologic subspecialists have the skill sets to care for these patients.
Under other circumstances, when the vagina is truly foreshortened, more aggressive reconstructive surgery is necessary and consultation and collaboration with plastic surgery specialists often is helpful. At our center, these patients’ care is initially managed by gynecologists and, when simple approaches to their reconstructive needs are exhausted, collaboration is warranted. As with the other team approaches discussed in this article, the recommendation is for a consistent referral team that has established care paths for patients. Not all plastic surgeons are familiar with neovaginal reconstruction and understand the functional aspects that gynecologists are hoping to achieve for their patients. Therefore, it is important to form cohesive teams that have the same goals for the patient.
The literature on neovaginal reconstruction is sparse. There are no true agreed on approaches or techniques for vaginal reconstruction because there is no “one size fits all” for these repairs. Defects also vary depending on whether they are due to resections or radiation for oncologic treatment, reconstruction as part of the repair of a genitourinary or rectovaginal fistula, or stenosis from other etiologies.
In 2002, Cordeiro and colleagues published a classification system and reconstructive algorithm for acquired vaginal defects.14 Not all reconstructive surgeons subscribe to this algorithm, but it is the only rubric that currently exists. The authors differentiate between “partial” and “circumferential” defects and recommend different types of fasciocutaneous and myocutaneous flaps for reconstruction.
In our experience at our center, we believe that the choice of flap should also depend on whether or not perineal reconstruction is needed. This decision is made by both the gynecologic specialist and the plastic surgeon. Common flap choices include the Singapore flap, a fasciocutaneous flap based on perforators from the pudendal vessels; the gracilis flap, a myocutaneous flap based off the medial circumflex femoral vessels; and the rectus abdominis flap (transverse or vertical), which is also a myocutaneous flap that relies on the blood supply from the deep inferior epigastric vessels.
One of the most important parts of the coordinated effort of neovaginal surgery is postoperative care. Plastic surgeons play a key role in ensuring that the flap survives in the immediate postoperative period. The gynecology team should be responsible for postoperative vaginal dilation teaching and follow-up to ensure that the patient dilates properly and upsizes her dilator appropriately over the postoperative period. In our practice, our advanced practice clinicians often care for these patients and are responsible for continuity and dilation teaching. Patients have easy access to these clinicians, and this enhances the postoperative experience. Referral to a pelvic floor physical therapist knowledgeable about neovaginal surgery also helps to ensure that the dilation process goes successfully. It also helps to have office days on the same days as the plastic surgery team that is following the patient. This way, the patient may be seen by both teams on the same day. This allows for good patient communication with regard to aftercare, as well as a combined approach to teaching the trainees involved in the case. Coordination with pelvic floor physical therapists on those days also enhances the patient experience and is highly recommended.
Continue to: Combining gyn and urogyn procedures with plastic surgery...
Combining gyn and urogyn procedures with plastic surgery
While there are no data on combining gynecologic and urogynecologic procedures with plastic reconstructive surgeries, a team approach to combining surgeries is possible. At our center, we have performed tubal ligation, ovarian surgery, hysterectomy, and sling and prolapse surgery in patients who were undergoing cosmetic procedures, such as breast augmentation and abdominoplasty.
Gender affirmation surgery also can be performed through a combined approach between gynecologists and plastic surgeons. Our gynecologists perform hysterectomy for transmasculine men, and this procedure is sometimes safely and effectively performed in combination with masculinizing chest surgery (mastectomy) performed by our plastic surgeons. Vaginoplasty surgery (feminizing genital surgery) also is performed by urogynecology specialists at our center, and it is sometimes done concurrently at the time of breast augmentation and/or facial feminization surgery.
Case order. Some plastic surgeons vocalize concerns about combining clean procedures with clean contaminated cases, especially in situations in which implants are being placed in the body. During these cases, communication and organization between surgeons is important. For instance, there should be a discussion about case order. In general, the clean procedures should be performed first. In addition, separate operating tables and instruments should be used. Simultaneous operating also should be avoided. Fresh incisions should be dressed and covered before subsequent procedures are performed.
Incision placement. Last, planning around incision placement should be discussed before each case. Laparoscopic and abdominal incisions may interfere with plastic surgery procedures and alter the end cosmesis. These incisions often can be incorporated into the reconstructive procedure. The most important part of the coordinated surgical effort is ensuring that both surgical teams understand each other’s respective surgeries and the approach needed to complete them. When this is achieved, the cases are usually very successful.
Creating collaboration between obstetricians and gynecologic specialists
The impacts of pregnancy and vaginal delivery on the pelvic floor are well established. Urinary and fecal incontinence, pelvic organ prolapse, perineal pain, and dyspareunia are not uncommon in the postpartum period and may persist long term. The effects of obstetric anal sphincter injury (OASI) are significant, with up to 25% of women experiencing wound complications and 17% experiencing fecal incontinence at 6 months postpartum.15,16 Care of women with peripartum pelvic floor disorders and OASIs present an ideal opportunity for collaboration between urogynecologists and obstetricians. The Cleveland Clinic has a multidisciplinary Postpartum Care Clinic (PPCC) where we provide specialized, collaborative care for women with peripartum pelvic floor disorders and complex obstetric lacerations.
Our PPCC accepts referrals up to 1 year postpartum for women who experience OASI, urinary or fecal incontinence, perineal pain or dyspareunia, voiding dysfunction or urinary retention, and wound healing complications. When a woman is diagnosed with an OASI at the time of delivery, a “best practice alert” is released in the medical record recommending a referral to the PPCC to encourage referral of all women with OASI. We strive to see all referrals within 2 weeks of delivery.
At the time of the initial consultation, we collect validated questionnaires on bowel and bladder function, assess pain and healing, and discuss future delivery planning. The success of the PPCC is rooted in communication. When the clinic first opened, we provided education to our obstetrics colleagues on the purpose of the clinic, when and how to refer, and what to expect from our consultations. Open communication between referring obstetric clinicians and the urogynecologists that run the PPCC is key in providing collaborative care where patients know that their clinicians are working as a team. All recommendations are communicated to referring clinicians, and all women are ultimately referred back to their primary clinician for long-term care. Evidence demonstrates that this type of clinic leads to high obstetric clinician satisfaction and increased awareness of OASIs and their impact on maternal health.17
Combined team approach fosters innovation in patient care
A combined approach to the care of the patient who presents with gynecologic conditions is optimal. In this article, we presented examples of care that integrates gynecology, urogynecology, gynecologic oncology, colorectal surgery, plastic surgery, and obstetrics. There are, however, many more existing examples as well as opportunities to create teams that really make a difference in the way patients receive—and perceive—their care. This is a good starting point, and we should strive to use this model to continue to innovate our approach to patient care.
- Ramaseshan AS, Felton J, Roque D, et al. Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J. 2018;29:459-476.
- Nakayama N, Tsuji T, Aoyama M, et al. Quality of life and the prevalence of urinary incontinence after surgical treatment for gynecologic cancer: a questionnaire survey. BMC Womens Health. 2020;20:148-157.
- Cascales-Campos PA, Gonzalez-Gil A, Fernandez-Luna E, et al. Urinary and fecal incontinence in patients with advanced ovarian cancer treated with CRS + HIPEC. Surg Oncol. 2021;36:115-119.
- Davidson ER, Woodburn K, AlHilli M, et al. Perioperative adverse events in women undergoing concurrent urogynecologic and gynecologic oncology surgeries for suspected malignancy. Int Urogynecol J. 2019;30:1195-1201.
- Spence-Jones C, Kamm MA, Henry MM, et al. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and stress urinary incontinence. Br J Obstet Gynaecol. 1994;101:147-152.
- Thompson JR, Chen AH, Pettit PD, et al. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187:1494-1500.
- Jallad K, Gurland B. Multidisciplinary approach to the treatment of concomitant rectal and vaginal prolapse. Clin Colon Rectal Surg. 2016;29:101-105.
- Kapoor DS, Sultan AH, Thakar R, et al. Management of complex pelvic floor disorders in a multidisciplinary pelvic floor clinic. Colorectal Dis. 2008;10:118-123.
- Weinberg D, Qeadan F, McKee R, et al. Safety of laparoscopic sacrocolpopexy with concurrent rectopexy: peri-operative morbidity in a nationwide cohort. Int Urogynecol J. 2019;30:385-392.
- Geltzeiler CB, Birnbaum EH, Silviera ML, et al. Combined rectopexy and sacrocolpopexy is safe for correction of pelvic organ prolapse. Int J Colorectal Dis. 2018;33:1453-1459.
- Wallace SL, Syan R, Enemchukwu EA, et al. Surgical approach, complications, and reoperation rates of combined rectal and pelvic organ prolapse surgery. Int Urogynecol J. 2020;31:2101-2108.
- Smith PE, Hade EM, Pandya LK, et al. Perioperative outcomes for combined ventral rectopexy with sacrocolpopexy compared to perineal rectopexy with vaginal apical suspension. Female Pelvic Med Reconstr Surg. 2020;26:376-381.
- Casas-Puig V, Bretschneider CE, Ferrando CA. Perioperative adverse events in women undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2019;25:88-92.
- Cordeiro PG, Pusic AL, Disa JJ. A classification system and reconstructive algorithm for acquired vaginal defects. Plast Reconstr Surg. 2002;110:1058-1065.
- Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, et al. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125:1088-1093.
- Borello-France D, Burgio KL, Richter HE, et al; Pelvic Floor Disorders Network. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108:863-872.
- Propst K, Hickman LC. Peripartum pelvic floor disorder clinics inform obstetric provider practices. Int Urogynecol J. 2021;32:1793-1799.
- Ramaseshan AS, Felton J, Roque D, et al. Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J. 2018;29:459-476.
- Nakayama N, Tsuji T, Aoyama M, et al. Quality of life and the prevalence of urinary incontinence after surgical treatment for gynecologic cancer: a questionnaire survey. BMC Womens Health. 2020;20:148-157.
- Cascales-Campos PA, Gonzalez-Gil A, Fernandez-Luna E, et al. Urinary and fecal incontinence in patients with advanced ovarian cancer treated with CRS + HIPEC. Surg Oncol. 2021;36:115-119.
- Davidson ER, Woodburn K, AlHilli M, et al. Perioperative adverse events in women undergoing concurrent urogynecologic and gynecologic oncology surgeries for suspected malignancy. Int Urogynecol J. 2019;30:1195-1201.
- Spence-Jones C, Kamm MA, Henry MM, et al. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and stress urinary incontinence. Br J Obstet Gynaecol. 1994;101:147-152.
- Thompson JR, Chen AH, Pettit PD, et al. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187:1494-1500.
- Jallad K, Gurland B. Multidisciplinary approach to the treatment of concomitant rectal and vaginal prolapse. Clin Colon Rectal Surg. 2016;29:101-105.
- Kapoor DS, Sultan AH, Thakar R, et al. Management of complex pelvic floor disorders in a multidisciplinary pelvic floor clinic. Colorectal Dis. 2008;10:118-123.
- Weinberg D, Qeadan F, McKee R, et al. Safety of laparoscopic sacrocolpopexy with concurrent rectopexy: peri-operative morbidity in a nationwide cohort. Int Urogynecol J. 2019;30:385-392.
- Geltzeiler CB, Birnbaum EH, Silviera ML, et al. Combined rectopexy and sacrocolpopexy is safe for correction of pelvic organ prolapse. Int J Colorectal Dis. 2018;33:1453-1459.
- Wallace SL, Syan R, Enemchukwu EA, et al. Surgical approach, complications, and reoperation rates of combined rectal and pelvic organ prolapse surgery. Int Urogynecol J. 2020;31:2101-2108.
- Smith PE, Hade EM, Pandya LK, et al. Perioperative outcomes for combined ventral rectopexy with sacrocolpopexy compared to perineal rectopexy with vaginal apical suspension. Female Pelvic Med Reconstr Surg. 2020;26:376-381.
- Casas-Puig V, Bretschneider CE, Ferrando CA. Perioperative adverse events in women undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2019;25:88-92.
- Cordeiro PG, Pusic AL, Disa JJ. A classification system and reconstructive algorithm for acquired vaginal defects. Plast Reconstr Surg. 2002;110:1058-1065.
- Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, et al. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125:1088-1093.
- Borello-France D, Burgio KL, Richter HE, et al; Pelvic Floor Disorders Network. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108:863-872.
- Propst K, Hickman LC. Peripartum pelvic floor disorder clinics inform obstetric provider practices. Int Urogynecol J. 2021;32:1793-1799.
Dismantling racism in your personal and professional spheres
On May 25, 2020, George Floyd was murdered by a White police officer who held his knee on Floyd’s neck for nine and a half minutes. Nine and a half minutes. George Floyd was not the first Black person killed by law enforcement. He has not been the last. Much has been written about why Floyd’s murder sparked unprecedented worldwide outrage despite being far from unprecedented itself. We cannot be so naive as to think what happened was new, and we should not ignore the tireless work that so many have been doing to fight racism up to this point. But for many who have been stirred to do something for the first time, especially White people, the question has been,
“What do I do?” The answer is, do the work.
This article is centered on anti-Black racism with a focus on medicine. We recognize that there is racism against other minoritized groups. Each group deserves attention and to have their stories told. We recognize intersectionality and that an individual has multiple identities and that these may compound the marginalization they experience. This too deserves attention.
However, we cannot satisfactorily explore any of these concepts within the confines of a single article. Our intention is to use this forum to promote further conversation, specifically about anti-Black racism in medicine. We hope it compels you to begin learning to recognize and dismantle racism in yourself and your surroundings, both at home and at work.
Being a health care provider requires lifelong learning. If we practiced only what we learned in training, our patients could suffer. So we continually seek out updated research and guidelines to best treat our patients. Understanding how racism impacts your patients, colleagues, family, and friends is your responsibility as much as understanding guidelines for standards of care. We must resist the urge to feel this is someone else’s duty. It is the job of each and every one of us. We must do the work.
Race is real but it’s not biologic
It is imperative to understand that race is not a biologic category. Phenotypic differences between humans do not reliably map to racial categories. Racial categories themselves have morphed over the centuries, and interpretation of race has been litigated in this country since its founding.1 People who identify as a given race do not have inherent biology that is different from those who identify as another race. It may then be tempting to try to erase race from our thinking, and, indeed, the idea of being “color blind” was long worn as a badge of honor signifying a commitment to equality. So this is the tension: if race exists, it must be a biologic trait and with it must go other inherent traits. But if race is not a biologic entity, perhaps it is not real and, therefore, should be ignored. In fact, neither is true. Race is not based on genetic or biologic inheritance, but it is a social and political categorization that is real and has very real ramifications. As we will discuss further, race does have a biologic impact on individuals. The mechanism by which that happens is racism.
Continue to: What is racism, and who is racist?...
What is racism, and who is racist?
Various definitions of racism have been offered:
- prejudice, discrimination, or antagonism directed against a person or people on the basis of their membership in a particular racial or ethnic group, typically one that is minoritized or marginalized2
- a belief that race is a fundamental determinant of human traits and capacities and that racial differences produce an inherent superiority of a particular race3
- the systemic oppression of a racial group to the social, economic, and political advantage of another; a political or social system founded on racism and designed to execute its principles.3
The common themes in these definitions are power, hierarchy, and oppression. Racism is a fabricated system to justify and reinforce power for some and disenfranchisement for others based on race. The system is pervasive and beneficial to the group that it serves.
Ibram X. Kendi posits that all racism is structural racism: “‘Institutional racism’ and ‘structural racism’ and ‘systemic racism’ are redundant. Racism itself is institutional, structural, and systemic.”4 This is not saying that individuals don’t enact racism, but it emphasizes that racism is not the action of a “few bad apples.” Furthermore, it underscores that race was created to bolster power structures ensuring White dominance. The racism that has followed, in all of its forms, is both because these ideas were created in the first place and to perpetuate that ongoing power structure.4
Dorothy Roberts, JD, writes in her book Fatal Invention that, while grouping people and creating hierarchy has always happened amongst humans, there is a specific history in our country of using race to create and perpetuate the dominance of White people and the subjugation of Black people.
Kendi also asserts that there is no neutrality with regard to racism—there is racist and antiracist: “A racist: one who is supporting a racist policy through their actions or inaction or expressing a racist idea. An antiracist: one who is supporting an antiracist policy through their actions or expressing an antiracist idea.”4 He describes all people as moving in and out of being racist and antiracist, and states “being an antiracist requires persistent self-awareness, constant self-criticism, and regular self-examination.”4 In thinking about race and racism in this way, we all must grapple with our own racism, but in so doing are taking a step toward antiracism.
History is important
Among the most important things one can do in a journey to dismantle racism is learn the history of racism.
The infrastructure and institutions of our nation were created on a foundation of slavery, including the origins of American medicine and gynecology. Physicians in the antebellum South performed inspections of enslaved people’s bodies to certify them for sale.5 The ability to assign market value to a Black person’s body was published as an essential physician competency.5
Gynecology has a particularly painful history with regard to slavery. By 1808, transatlantic slave trade was banned in the United States and, as Dr. Cooper Owens describes in her book Medical Bondage: Race, Gender, and the Origins of American Gynecology, this made reproduction of enslaved people within the United States a priority for slave owners and those invested in an economy that depended on slavery.6 Gynecologists were permitted unrestricted access to enslaved women for experiments to optimize reproduction. Many of these physicians became prominent voices adding to the canon of racialized medicine. Medical journals themselves gained reverence because of heightened interest in keeping enslaved people alive and just well enough to work and reproduce.6 Today, we hold sacred the relationship between a patient and their physician. We must understand that there was no such relationship between a doctor and an enslaved person. The relationship was between the doctor and slave owner.6,7 Slavery does not allow for the autonomy of the enslaved. This is the context in which we must understand the discoveries of gynecologists during that time.
Despite the abolition of slavery with the passage of the 13th amendment, racist policies remained ubiquitous in the United States. Segregation of Black people was codified not only in the Jim Crow South but also in the North. Interracial marriage was outlawed by all but 9 states.
While there are numerous federal policies that led to cumulative and egregious disadvantage for Black Americans, one powerful example is redlining. In 1934 the Federal Housing Administration was created, and by insuring private mortgages, the FHA made it easier for eligible home buyers to obtain financing. The FHA used a system of maps that graded neighborhoods. Racial composition of neighborhoods was overtly used as a component of grading, and the presence of Black people led a neighborhood to be downgraded or redlined.8,9 This meant Black people were largely ineligible for FHA-backed loans. In The Color of Law, Richard Rothstein writes, “Today’s residential segregation in the North, South, Midwest, and West is not the unintended consequence of individual choices and of otherwise well-meaning law or regulation but of unhidden public policy that explicitly segregated every metropolitan area in the United States.The policy was so systematic and forceful that its effects endure to the present time.”9
Though these specific policies are no longer in place, many correlations have been found between historically redlined neighborhoods and higher rates of diseases today, including diabetes, hypertension, asthma, and preterm deliveries.10 These policies also have played a role in creating the wealth gap—directly by limiting the opportunity for home ownership, which translates to intergenerational wealth, and indirectly by the disinvestment in neighborhoods where Black people live, leading to reduced access to quality education, decreased employment opportunities, and increased environmental hazards.8,11
Continue to: Health disparities...
Health disparities
The numerous health disparities, more accurately termed health inequities, suffered by racial minority groups is well documented.12
COVID-19 death and vaccination-rate inequities. Early in the COVID-19 pandemic, data emerged that racial minorities were being disparately affected.13 In December 2020, the Centers for Disease Control and Prevention (CDC) reported that Hispanic or Latino, non-Hispanic Black, and non-Hispanic American Indian or Alaska Native people had all died at higher rates than White Americans.14 These racial groups had higher hospitalization rates across age groups and, after adjusting for age, rates of hospitalization were 2.8 to 3.4 times higher.15 We are continuing to learn what factors contribute to these inequities, but it has highlighted how racist policies have led to disparate access to health care, or even clean air, clean water, and nutritious food, and left communities of color more vulnerable to severe illness and death from COVID-19. With the advent of vaccines for COVID-19, we continue to see racial disparities as Black Americans have the lowest rates of vaccination.16 All of these inequities have to be understood in the context of the racist structures that exist in our society. As medical providers, we must understand and help to dismantle these structures.
Pregnancy-related mortality (PRM) inequities. A powerful example of a persistent health inequity in our field is the well-known disparity in pregnancy-related mortality when examining this outcome by race. Per CDC analysis of data on PRM from 2007–2016, Black women died at a rate 3.2 times higher than White women. This disparity was even greater in patients older than 30 years of age. When they compared rates while controlling for the highest level of education, the disparity is even more pronounced: PRM rate for those with a college degree or higher was 5.2 times greater for Black people compared with White people.16The CDC also reported that, in 2018, the infant mortality for non-Hispanic Black infants was 10.8 per 1,000 live births, compared with 4.6 per 1,000 live births for White infants. This is a rate 2.4-times higher for Black infants.17 Dr. Cooper Owens and Dr. Fett note in their article, “Black maternal and infant health: Historical legacies of slavery,” that in 1850 this rate was 1.6-times higher for Black infants, which means the inequity was worse in 2018 America than in the antebellum South.5
The role of patient experience
As discussed, governmental policies have created persistent inequities in wealth, access to health care, and exposure to environmental toxins, among many other disparities. However, the data finding that highly educated Black pregnant patients suffer markedly increased risk of maternal death, indicate that inequities cannot be attributed only to education or lack of access to health care. This is where some will once again lean on the idea that there is something inherently different about Black people. But if we know that race was created and is not an empiric category, we must consider the social variables impacting Black patients’ experience.
As Linda Blount, President and CEO of the Black Women’s Health Imperative, put it, “Race is not a risk factor. It is the lived experience of being a Black woman in this society that is the risk factor.”18 So how much of these inequities can be accounted for by differential treatment of Black patients? There is, for example, data on the disproportionately lower rates of Black renal transplant recipients and inordinately higher rates of amputations among Black patients.19,20 None of us wants to think we are treating our Black patients differently, but the data demand that we ask ourselves if we are. Some of this is built into the system. For example, in their article “Hidden in plain sight—Reconsidering the use of race correction in clinical algorithms,” Vyas and colleagues outline a list of calculators and algorithms that include race.21 This means we may be using these calculators and changing outcomes for our patients based on their race. This is only one example of racism hidden within guidelines and standards of care.
The existence of racism on an interpersonal level also cannot be denied. This could lead to differential care specifically, but also can manifest by way of the toll it takes on a patient generally. This is the concept of allostatic load or weathering: the chronic stress of experiencing racism creates detrimental physiologic change. There is ongoing research into epigenetic modifications from stress that could be impacting health outcomes in Black populations.
Continue to: What is the work we need to do?...
What is the work we need to do?
Become educated. We have discussed taking the initiative to learn about the history of racism, including the legacies of slavery and the ongoing impact of racism on health. This knowledge is foundational and sometimes transformative. It allows us to see opportunities for antiracism and gives us the knowledge to begin meaningful conversations.
Take action. We must take inventory within our lives. What are our spheres of influence? What are our resources? Where can we make an impact? Right now, you can take out a pen and paper and write down all the roles you play. Look for opportunities in personal interactions and daily routines. Unfortunately, there will be many opportunities to speak up against racism—although this is rarely easy. Find articles, podcasts, and workshops on upstander training. One framework to respond to microaggressions has been proposed by faculty at Boston University Medical Center using the acronym LIFT (Lights on, Impact vs Intent, Full stop, Teach).22 It advises highlighting, clarifying, and directly addressing problematic comments with such statements as “I heard you say…” or “What did you mean by that comment?”, or a more direct “Statements like that are not OK with me,” or a teaching statement of “I read an article that made me think differently about comments like the one you made...”22 How and when to employ these strategies takes deliberate practice and will be uncomfortable. But we must do the work.
Practice empathetic listening. In a podcast discussion with Brené Brown on creating transformative cultures, Aiko Bethea, a leader in diversity and equity innovation, implores listeners to believe people of color.23,24 Draw on the history you’ve learned and understand the context in which Black people live in our society. Don’t brush off your Black friend who is upset about being stopped by security. That wasn’t the first time she was in that situation. Take seriously your patient’s concern that they are not being treated appropriately because of being Black. At the same time, do not think of Black people as a monolith or a stereotype. Respect people’s individuality.
Teach our kids all of this. We must also find ways to make change on a larger scale—within our practices, hospitals, medical schools, places of worship, town councils, school boards, state legislatures, and so on. If you are in a faculty position, you can reach out to leadership to scrutinize the curriculum while also ensuring that what and how you are teaching aligns with your antiracist principles. Question the theories, calculators, and algorithms being used and taught. Inquire about policies around recruitment of trainees and faculty as well as promotion, and implement strategies to make this inclusive and equitable. If you run a practice, you can ensure hiring and compensation policies are equitable. Examine patient access and barriers that your minoritized patients are facing, and address those barriers. Share resources and tools that you find helpful and develop a community of colleagues to develop with and hold one another accountable.
In her June 2020 article, An Open Letter to Corporate America, Philanthropy, Academia, etc: What now?, Bethea lays out an extensive framework for approaching antiracism at a high level.25 Among the principles she emphasizes is that the work of diversity, equity, and inclusion should not be siloed and cannot continue to be undervalued. It must be viewed as leadership and engaged in by leadership. The work of diversity, equity, and inclusion for any given institution must be explicit, intentional, measured, and transparent. Within that work, antiracism deserves individual attention. This work must center the people of color for whom you are pursuing equity. White people must resist the urge to make this about them.25
Drs. Esther Choo and J. Nwando Olayiwola present their proposals for combating racism in two 2020 Lancet articles.26,27 They discuss anticipating failure and backlash and learning from them but not being derailed by them. They emphasize the need for ongoing, serious financial investment and transformation in leadership. They also point out the need for data, discouraging more research on well-established inequities while recommending investigating interventions.26,27 If you are in leadership positions, read these articles and many more. Enact these principles. Make the investment. If you are not in such a position, find ways to hold your organization’s leadership accountable. Find ways to get a seat at the table and steer the conversation. In medicine, we have to make change at every level of our organizations. That will include the very difficult work of changing climate and culture. In addition, we have to look not only within our organizations but also to the communities we serve. Those voices must be valued in this conversation.
Will this take time? Yes. Will this be hard? Yes. Can you do everything? No. Can you do your part? Yes! Do the work.
- Roberts D. Fatal Invention: How Science, Politics and Big Business Re-create Race in the Twenty-First Century. The New Press: New York, New York; 2012.
- Definition of racism in English. Lexico web site. https://www.lexico. com/en/definition/racism. Accessed July 30, 2021.
- Definition of racism. Merriam-Webster web site. https://www .merriam-webster.com/dictionary/racism. Accessed July 30, 2021.
- Kendi IX. How To Be an Antiracist. One World: New York, NY; 2019.
- Cooper Owens D, Fett SM. Black maternal and infant health: historical legacies of slavery. Am J Public Health. 2019;109:1342-1345. doi: 10.2105/AJPH.2019.305243.
- Cooper Owens D. Medical Bondage: Race, Gender, and the Origins of American Gynecology. University of Georgia Press: Athens, GA; 2017.
- Washington H. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. Anchor Books: New York, NY; 2006.
- Coates T. The case for reparations. The Atlantic. 2014;313.5:54-71.
- Rothstein R. The Color of the Law: A Forgotten History of How our Government Segregated America. Liveright Publishing Corporation: New York, NY; 2017.
- Nelson RK, Ayers EL; The Digital Scholarship Lab and the National Community Reinvestment Coalition. American Panorama, ed. Not Even Past: Social Vulnerability and the Legacy of Redlining. https://dsl.richmond.edu/socialvulnerability. Accessed July 30, 2021.
- Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105-125. doi: 10.1146 /annurev-publhealth-040218-043750.
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press: Washington, DC; 2003.
- Artiga S, Corallo B, Pham O. Racial disparities in COVID-19: key findings from available data and analysis. KFF web site. August 17, 2020. https://www.kff.org/racial-equity-and-health-policy/issue-brief /racial-disparities-covid-19-key-findings-available-data-analysis/. Accessed July 30, 2021.
- Disparities in deaths from COVID-19. Centers for Disease Control and Prevention web site. https://www.cdc.gov/coronavirus/2019-ncov /community/health-equity/racial-ethnic-disparities/disparities -deaths.html. Updated December 10, 2020. Accessed July 30, 2021.
- Disparities in COVID-19 hospitalizations. Centers for Disease Control and Prevention web site. https://www.cdc.gov/coronavirus/2019 -ncov/community/health-equity/racial-ethnic-disparities/disparities -hospitalization.html. Updated July 28, 2021. Accessed July 30, 2021.
- COVID data tracker. Centers for Disease Control and Prevention web site. https://covid.cdc.gov/covid-data-tracker/#vaccination -demographics-trends. Accessed July 30, 2021.
- Infant mortality. Centers for Disease Control and Prevention web site. https://www.cdc.gov/reproductivehealth/maternalinfanthealth /infantmortality.htm. Last reviewed September 2020. Accessed July 30, 2021.
- Roeder A. America is failing its Black mothers. Harvard Public Health. Winter 2019. https://www.hsph.harvard.edu/magazine/magazine _article/america-is-failing-its-black-mothers/. Accessed July 30, 2021.
- Ku E, Lee BK, McCulloch CE, et al. Racial and ethnic disparities in kidney transplant access within a theoretical context of medical eligibility. Transplantation. 2020;104:1437-1444. doi: 10.1097/TP .0000000000002962.
- Arya S, Binney Z, Khakharia A, et al. Race and socioeconomic status independently affect risk of major amputation in peripheral artery disease. J Am Heart Assoc. 2018;7:e007425. doi: 10.1161 /JAHA.117.007425.
- Vyas DA, Eisenstein LG, Jones DS, et al. Hidden in plain sight— reconsidering the use of race correction in clinical algorithms. N Engl J Med. 2020;383:874-882. doi: 10.1056/NEJMms2004740.
- A Curriculum to Increase Faculty Engagement in the CLER Program. Boston University Medical Center web site. https://www.bumc .bu.edu/facdev-medicine/files/2020/05/Bystander-Training-for -Microaggressions-Executive-Summary.pdf. Accessed July 30, 2021.
- Brenè with Aiko Bethea on inclusivity at work: the heart of hard conversations. Spotify web site. https://open.spotify.com/episod e/3IODQ37EurkFf0zMNhazqI?si=wJIZgzpWTDCF1QVhwAdhiw. Accessed July 30, 2021.
- Brenè with Aiko Bethea on creating transformative cultures. Spotify web site. https://open.spotify.com/episode/7K47gQF5Ruc7MAXxEN q6jI?si=X0pzd2NnRAGwMD-bkyg-VQ. Accessed July 30, 2021.
- Bethea A. An open letter to corporate America, philanthropy, academia, etc.: What now? June 1, 2020. https://aikobethea.medium. com/an-open-letter-to-corporate-america-philanthropy-academiaetc-what-now-8b2d3a310f22. Accessed July 30, 2021.
- Choo E. Seven things organisations should be doing to combat racism. Lancet. 2020;396:157. doi:10.1016/S0140-6736(20)31565-8.
- Olayiwola JN, Choo E. Seven more things organisations should be doing to combat racism. Lancet. 2020;396:593. doi: 10.1016/S0140 -6736(20)31718-9.
On May 25, 2020, George Floyd was murdered by a White police officer who held his knee on Floyd’s neck for nine and a half minutes. Nine and a half minutes. George Floyd was not the first Black person killed by law enforcement. He has not been the last. Much has been written about why Floyd’s murder sparked unprecedented worldwide outrage despite being far from unprecedented itself. We cannot be so naive as to think what happened was new, and we should not ignore the tireless work that so many have been doing to fight racism up to this point. But for many who have been stirred to do something for the first time, especially White people, the question has been,
“What do I do?” The answer is, do the work.
This article is centered on anti-Black racism with a focus on medicine. We recognize that there is racism against other minoritized groups. Each group deserves attention and to have their stories told. We recognize intersectionality and that an individual has multiple identities and that these may compound the marginalization they experience. This too deserves attention.
However, we cannot satisfactorily explore any of these concepts within the confines of a single article. Our intention is to use this forum to promote further conversation, specifically about anti-Black racism in medicine. We hope it compels you to begin learning to recognize and dismantle racism in yourself and your surroundings, both at home and at work.
Being a health care provider requires lifelong learning. If we practiced only what we learned in training, our patients could suffer. So we continually seek out updated research and guidelines to best treat our patients. Understanding how racism impacts your patients, colleagues, family, and friends is your responsibility as much as understanding guidelines for standards of care. We must resist the urge to feel this is someone else’s duty. It is the job of each and every one of us. We must do the work.
Race is real but it’s not biologic
It is imperative to understand that race is not a biologic category. Phenotypic differences between humans do not reliably map to racial categories. Racial categories themselves have morphed over the centuries, and interpretation of race has been litigated in this country since its founding.1 People who identify as a given race do not have inherent biology that is different from those who identify as another race. It may then be tempting to try to erase race from our thinking, and, indeed, the idea of being “color blind” was long worn as a badge of honor signifying a commitment to equality. So this is the tension: if race exists, it must be a biologic trait and with it must go other inherent traits. But if race is not a biologic entity, perhaps it is not real and, therefore, should be ignored. In fact, neither is true. Race is not based on genetic or biologic inheritance, but it is a social and political categorization that is real and has very real ramifications. As we will discuss further, race does have a biologic impact on individuals. The mechanism by which that happens is racism.
Continue to: What is racism, and who is racist?...
What is racism, and who is racist?
Various definitions of racism have been offered:
- prejudice, discrimination, or antagonism directed against a person or people on the basis of their membership in a particular racial or ethnic group, typically one that is minoritized or marginalized2
- a belief that race is a fundamental determinant of human traits and capacities and that racial differences produce an inherent superiority of a particular race3
- the systemic oppression of a racial group to the social, economic, and political advantage of another; a political or social system founded on racism and designed to execute its principles.3
The common themes in these definitions are power, hierarchy, and oppression. Racism is a fabricated system to justify and reinforce power for some and disenfranchisement for others based on race. The system is pervasive and beneficial to the group that it serves.
Ibram X. Kendi posits that all racism is structural racism: “‘Institutional racism’ and ‘structural racism’ and ‘systemic racism’ are redundant. Racism itself is institutional, structural, and systemic.”4 This is not saying that individuals don’t enact racism, but it emphasizes that racism is not the action of a “few bad apples.” Furthermore, it underscores that race was created to bolster power structures ensuring White dominance. The racism that has followed, in all of its forms, is both because these ideas were created in the first place and to perpetuate that ongoing power structure.4
Dorothy Roberts, JD, writes in her book Fatal Invention that, while grouping people and creating hierarchy has always happened amongst humans, there is a specific history in our country of using race to create and perpetuate the dominance of White people and the subjugation of Black people.
Kendi also asserts that there is no neutrality with regard to racism—there is racist and antiracist: “A racist: one who is supporting a racist policy through their actions or inaction or expressing a racist idea. An antiracist: one who is supporting an antiracist policy through their actions or expressing an antiracist idea.”4 He describes all people as moving in and out of being racist and antiracist, and states “being an antiracist requires persistent self-awareness, constant self-criticism, and regular self-examination.”4 In thinking about race and racism in this way, we all must grapple with our own racism, but in so doing are taking a step toward antiracism.
History is important
Among the most important things one can do in a journey to dismantle racism is learn the history of racism.
The infrastructure and institutions of our nation were created on a foundation of slavery, including the origins of American medicine and gynecology. Physicians in the antebellum South performed inspections of enslaved people’s bodies to certify them for sale.5 The ability to assign market value to a Black person’s body was published as an essential physician competency.5
Gynecology has a particularly painful history with regard to slavery. By 1808, transatlantic slave trade was banned in the United States and, as Dr. Cooper Owens describes in her book Medical Bondage: Race, Gender, and the Origins of American Gynecology, this made reproduction of enslaved people within the United States a priority for slave owners and those invested in an economy that depended on slavery.6 Gynecologists were permitted unrestricted access to enslaved women for experiments to optimize reproduction. Many of these physicians became prominent voices adding to the canon of racialized medicine. Medical journals themselves gained reverence because of heightened interest in keeping enslaved people alive and just well enough to work and reproduce.6 Today, we hold sacred the relationship between a patient and their physician. We must understand that there was no such relationship between a doctor and an enslaved person. The relationship was between the doctor and slave owner.6,7 Slavery does not allow for the autonomy of the enslaved. This is the context in which we must understand the discoveries of gynecologists during that time.
Despite the abolition of slavery with the passage of the 13th amendment, racist policies remained ubiquitous in the United States. Segregation of Black people was codified not only in the Jim Crow South but also in the North. Interracial marriage was outlawed by all but 9 states.
While there are numerous federal policies that led to cumulative and egregious disadvantage for Black Americans, one powerful example is redlining. In 1934 the Federal Housing Administration was created, and by insuring private mortgages, the FHA made it easier for eligible home buyers to obtain financing. The FHA used a system of maps that graded neighborhoods. Racial composition of neighborhoods was overtly used as a component of grading, and the presence of Black people led a neighborhood to be downgraded or redlined.8,9 This meant Black people were largely ineligible for FHA-backed loans. In The Color of Law, Richard Rothstein writes, “Today’s residential segregation in the North, South, Midwest, and West is not the unintended consequence of individual choices and of otherwise well-meaning law or regulation but of unhidden public policy that explicitly segregated every metropolitan area in the United States.The policy was so systematic and forceful that its effects endure to the present time.”9
Though these specific policies are no longer in place, many correlations have been found between historically redlined neighborhoods and higher rates of diseases today, including diabetes, hypertension, asthma, and preterm deliveries.10 These policies also have played a role in creating the wealth gap—directly by limiting the opportunity for home ownership, which translates to intergenerational wealth, and indirectly by the disinvestment in neighborhoods where Black people live, leading to reduced access to quality education, decreased employment opportunities, and increased environmental hazards.8,11
Continue to: Health disparities...
Health disparities
The numerous health disparities, more accurately termed health inequities, suffered by racial minority groups is well documented.12
COVID-19 death and vaccination-rate inequities. Early in the COVID-19 pandemic, data emerged that racial minorities were being disparately affected.13 In December 2020, the Centers for Disease Control and Prevention (CDC) reported that Hispanic or Latino, non-Hispanic Black, and non-Hispanic American Indian or Alaska Native people had all died at higher rates than White Americans.14 These racial groups had higher hospitalization rates across age groups and, after adjusting for age, rates of hospitalization were 2.8 to 3.4 times higher.15 We are continuing to learn what factors contribute to these inequities, but it has highlighted how racist policies have led to disparate access to health care, or even clean air, clean water, and nutritious food, and left communities of color more vulnerable to severe illness and death from COVID-19. With the advent of vaccines for COVID-19, we continue to see racial disparities as Black Americans have the lowest rates of vaccination.16 All of these inequities have to be understood in the context of the racist structures that exist in our society. As medical providers, we must understand and help to dismantle these structures.
Pregnancy-related mortality (PRM) inequities. A powerful example of a persistent health inequity in our field is the well-known disparity in pregnancy-related mortality when examining this outcome by race. Per CDC analysis of data on PRM from 2007–2016, Black women died at a rate 3.2 times higher than White women. This disparity was even greater in patients older than 30 years of age. When they compared rates while controlling for the highest level of education, the disparity is even more pronounced: PRM rate for those with a college degree or higher was 5.2 times greater for Black people compared with White people.16The CDC also reported that, in 2018, the infant mortality for non-Hispanic Black infants was 10.8 per 1,000 live births, compared with 4.6 per 1,000 live births for White infants. This is a rate 2.4-times higher for Black infants.17 Dr. Cooper Owens and Dr. Fett note in their article, “Black maternal and infant health: Historical legacies of slavery,” that in 1850 this rate was 1.6-times higher for Black infants, which means the inequity was worse in 2018 America than in the antebellum South.5
The role of patient experience
As discussed, governmental policies have created persistent inequities in wealth, access to health care, and exposure to environmental toxins, among many other disparities. However, the data finding that highly educated Black pregnant patients suffer markedly increased risk of maternal death, indicate that inequities cannot be attributed only to education or lack of access to health care. This is where some will once again lean on the idea that there is something inherently different about Black people. But if we know that race was created and is not an empiric category, we must consider the social variables impacting Black patients’ experience.
As Linda Blount, President and CEO of the Black Women’s Health Imperative, put it, “Race is not a risk factor. It is the lived experience of being a Black woman in this society that is the risk factor.”18 So how much of these inequities can be accounted for by differential treatment of Black patients? There is, for example, data on the disproportionately lower rates of Black renal transplant recipients and inordinately higher rates of amputations among Black patients.19,20 None of us wants to think we are treating our Black patients differently, but the data demand that we ask ourselves if we are. Some of this is built into the system. For example, in their article “Hidden in plain sight—Reconsidering the use of race correction in clinical algorithms,” Vyas and colleagues outline a list of calculators and algorithms that include race.21 This means we may be using these calculators and changing outcomes for our patients based on their race. This is only one example of racism hidden within guidelines and standards of care.
The existence of racism on an interpersonal level also cannot be denied. This could lead to differential care specifically, but also can manifest by way of the toll it takes on a patient generally. This is the concept of allostatic load or weathering: the chronic stress of experiencing racism creates detrimental physiologic change. There is ongoing research into epigenetic modifications from stress that could be impacting health outcomes in Black populations.
Continue to: What is the work we need to do?...
What is the work we need to do?
Become educated. We have discussed taking the initiative to learn about the history of racism, including the legacies of slavery and the ongoing impact of racism on health. This knowledge is foundational and sometimes transformative. It allows us to see opportunities for antiracism and gives us the knowledge to begin meaningful conversations.
Take action. We must take inventory within our lives. What are our spheres of influence? What are our resources? Where can we make an impact? Right now, you can take out a pen and paper and write down all the roles you play. Look for opportunities in personal interactions and daily routines. Unfortunately, there will be many opportunities to speak up against racism—although this is rarely easy. Find articles, podcasts, and workshops on upstander training. One framework to respond to microaggressions has been proposed by faculty at Boston University Medical Center using the acronym LIFT (Lights on, Impact vs Intent, Full stop, Teach).22 It advises highlighting, clarifying, and directly addressing problematic comments with such statements as “I heard you say…” or “What did you mean by that comment?”, or a more direct “Statements like that are not OK with me,” or a teaching statement of “I read an article that made me think differently about comments like the one you made...”22 How and when to employ these strategies takes deliberate practice and will be uncomfortable. But we must do the work.
Practice empathetic listening. In a podcast discussion with Brené Brown on creating transformative cultures, Aiko Bethea, a leader in diversity and equity innovation, implores listeners to believe people of color.23,24 Draw on the history you’ve learned and understand the context in which Black people live in our society. Don’t brush off your Black friend who is upset about being stopped by security. That wasn’t the first time she was in that situation. Take seriously your patient’s concern that they are not being treated appropriately because of being Black. At the same time, do not think of Black people as a monolith or a stereotype. Respect people’s individuality.
Teach our kids all of this. We must also find ways to make change on a larger scale—within our practices, hospitals, medical schools, places of worship, town councils, school boards, state legislatures, and so on. If you are in a faculty position, you can reach out to leadership to scrutinize the curriculum while also ensuring that what and how you are teaching aligns with your antiracist principles. Question the theories, calculators, and algorithms being used and taught. Inquire about policies around recruitment of trainees and faculty as well as promotion, and implement strategies to make this inclusive and equitable. If you run a practice, you can ensure hiring and compensation policies are equitable. Examine patient access and barriers that your minoritized patients are facing, and address those barriers. Share resources and tools that you find helpful and develop a community of colleagues to develop with and hold one another accountable.
In her June 2020 article, An Open Letter to Corporate America, Philanthropy, Academia, etc: What now?, Bethea lays out an extensive framework for approaching antiracism at a high level.25 Among the principles she emphasizes is that the work of diversity, equity, and inclusion should not be siloed and cannot continue to be undervalued. It must be viewed as leadership and engaged in by leadership. The work of diversity, equity, and inclusion for any given institution must be explicit, intentional, measured, and transparent. Within that work, antiracism deserves individual attention. This work must center the people of color for whom you are pursuing equity. White people must resist the urge to make this about them.25
Drs. Esther Choo and J. Nwando Olayiwola present their proposals for combating racism in two 2020 Lancet articles.26,27 They discuss anticipating failure and backlash and learning from them but not being derailed by them. They emphasize the need for ongoing, serious financial investment and transformation in leadership. They also point out the need for data, discouraging more research on well-established inequities while recommending investigating interventions.26,27 If you are in leadership positions, read these articles and many more. Enact these principles. Make the investment. If you are not in such a position, find ways to hold your organization’s leadership accountable. Find ways to get a seat at the table and steer the conversation. In medicine, we have to make change at every level of our organizations. That will include the very difficult work of changing climate and culture. In addition, we have to look not only within our organizations but also to the communities we serve. Those voices must be valued in this conversation.
Will this take time? Yes. Will this be hard? Yes. Can you do everything? No. Can you do your part? Yes! Do the work.
On May 25, 2020, George Floyd was murdered by a White police officer who held his knee on Floyd’s neck for nine and a half minutes. Nine and a half minutes. George Floyd was not the first Black person killed by law enforcement. He has not been the last. Much has been written about why Floyd’s murder sparked unprecedented worldwide outrage despite being far from unprecedented itself. We cannot be so naive as to think what happened was new, and we should not ignore the tireless work that so many have been doing to fight racism up to this point. But for many who have been stirred to do something for the first time, especially White people, the question has been,
“What do I do?” The answer is, do the work.
This article is centered on anti-Black racism with a focus on medicine. We recognize that there is racism against other minoritized groups. Each group deserves attention and to have their stories told. We recognize intersectionality and that an individual has multiple identities and that these may compound the marginalization they experience. This too deserves attention.
However, we cannot satisfactorily explore any of these concepts within the confines of a single article. Our intention is to use this forum to promote further conversation, specifically about anti-Black racism in medicine. We hope it compels you to begin learning to recognize and dismantle racism in yourself and your surroundings, both at home and at work.
Being a health care provider requires lifelong learning. If we practiced only what we learned in training, our patients could suffer. So we continually seek out updated research and guidelines to best treat our patients. Understanding how racism impacts your patients, colleagues, family, and friends is your responsibility as much as understanding guidelines for standards of care. We must resist the urge to feel this is someone else’s duty. It is the job of each and every one of us. We must do the work.
Race is real but it’s not biologic
It is imperative to understand that race is not a biologic category. Phenotypic differences between humans do not reliably map to racial categories. Racial categories themselves have morphed over the centuries, and interpretation of race has been litigated in this country since its founding.1 People who identify as a given race do not have inherent biology that is different from those who identify as another race. It may then be tempting to try to erase race from our thinking, and, indeed, the idea of being “color blind” was long worn as a badge of honor signifying a commitment to equality. So this is the tension: if race exists, it must be a biologic trait and with it must go other inherent traits. But if race is not a biologic entity, perhaps it is not real and, therefore, should be ignored. In fact, neither is true. Race is not based on genetic or biologic inheritance, but it is a social and political categorization that is real and has very real ramifications. As we will discuss further, race does have a biologic impact on individuals. The mechanism by which that happens is racism.
Continue to: What is racism, and who is racist?...
What is racism, and who is racist?
Various definitions of racism have been offered:
- prejudice, discrimination, or antagonism directed against a person or people on the basis of their membership in a particular racial or ethnic group, typically one that is minoritized or marginalized2
- a belief that race is a fundamental determinant of human traits and capacities and that racial differences produce an inherent superiority of a particular race3
- the systemic oppression of a racial group to the social, economic, and political advantage of another; a political or social system founded on racism and designed to execute its principles.3
The common themes in these definitions are power, hierarchy, and oppression. Racism is a fabricated system to justify and reinforce power for some and disenfranchisement for others based on race. The system is pervasive and beneficial to the group that it serves.
Ibram X. Kendi posits that all racism is structural racism: “‘Institutional racism’ and ‘structural racism’ and ‘systemic racism’ are redundant. Racism itself is institutional, structural, and systemic.”4 This is not saying that individuals don’t enact racism, but it emphasizes that racism is not the action of a “few bad apples.” Furthermore, it underscores that race was created to bolster power structures ensuring White dominance. The racism that has followed, in all of its forms, is both because these ideas were created in the first place and to perpetuate that ongoing power structure.4
Dorothy Roberts, JD, writes in her book Fatal Invention that, while grouping people and creating hierarchy has always happened amongst humans, there is a specific history in our country of using race to create and perpetuate the dominance of White people and the subjugation of Black people.
Kendi also asserts that there is no neutrality with regard to racism—there is racist and antiracist: “A racist: one who is supporting a racist policy through their actions or inaction or expressing a racist idea. An antiracist: one who is supporting an antiracist policy through their actions or expressing an antiracist idea.”4 He describes all people as moving in and out of being racist and antiracist, and states “being an antiracist requires persistent self-awareness, constant self-criticism, and regular self-examination.”4 In thinking about race and racism in this way, we all must grapple with our own racism, but in so doing are taking a step toward antiracism.
History is important
Among the most important things one can do in a journey to dismantle racism is learn the history of racism.
The infrastructure and institutions of our nation were created on a foundation of slavery, including the origins of American medicine and gynecology. Physicians in the antebellum South performed inspections of enslaved people’s bodies to certify them for sale.5 The ability to assign market value to a Black person’s body was published as an essential physician competency.5
Gynecology has a particularly painful history with regard to slavery. By 1808, transatlantic slave trade was banned in the United States and, as Dr. Cooper Owens describes in her book Medical Bondage: Race, Gender, and the Origins of American Gynecology, this made reproduction of enslaved people within the United States a priority for slave owners and those invested in an economy that depended on slavery.6 Gynecologists were permitted unrestricted access to enslaved women for experiments to optimize reproduction. Many of these physicians became prominent voices adding to the canon of racialized medicine. Medical journals themselves gained reverence because of heightened interest in keeping enslaved people alive and just well enough to work and reproduce.6 Today, we hold sacred the relationship between a patient and their physician. We must understand that there was no such relationship between a doctor and an enslaved person. The relationship was between the doctor and slave owner.6,7 Slavery does not allow for the autonomy of the enslaved. This is the context in which we must understand the discoveries of gynecologists during that time.
Despite the abolition of slavery with the passage of the 13th amendment, racist policies remained ubiquitous in the United States. Segregation of Black people was codified not only in the Jim Crow South but also in the North. Interracial marriage was outlawed by all but 9 states.
While there are numerous federal policies that led to cumulative and egregious disadvantage for Black Americans, one powerful example is redlining. In 1934 the Federal Housing Administration was created, and by insuring private mortgages, the FHA made it easier for eligible home buyers to obtain financing. The FHA used a system of maps that graded neighborhoods. Racial composition of neighborhoods was overtly used as a component of grading, and the presence of Black people led a neighborhood to be downgraded or redlined.8,9 This meant Black people were largely ineligible for FHA-backed loans. In The Color of Law, Richard Rothstein writes, “Today’s residential segregation in the North, South, Midwest, and West is not the unintended consequence of individual choices and of otherwise well-meaning law or regulation but of unhidden public policy that explicitly segregated every metropolitan area in the United States.The policy was so systematic and forceful that its effects endure to the present time.”9
Though these specific policies are no longer in place, many correlations have been found between historically redlined neighborhoods and higher rates of diseases today, including diabetes, hypertension, asthma, and preterm deliveries.10 These policies also have played a role in creating the wealth gap—directly by limiting the opportunity for home ownership, which translates to intergenerational wealth, and indirectly by the disinvestment in neighborhoods where Black people live, leading to reduced access to quality education, decreased employment opportunities, and increased environmental hazards.8,11
Continue to: Health disparities...
Health disparities
The numerous health disparities, more accurately termed health inequities, suffered by racial minority groups is well documented.12
COVID-19 death and vaccination-rate inequities. Early in the COVID-19 pandemic, data emerged that racial minorities were being disparately affected.13 In December 2020, the Centers for Disease Control and Prevention (CDC) reported that Hispanic or Latino, non-Hispanic Black, and non-Hispanic American Indian or Alaska Native people had all died at higher rates than White Americans.14 These racial groups had higher hospitalization rates across age groups and, after adjusting for age, rates of hospitalization were 2.8 to 3.4 times higher.15 We are continuing to learn what factors contribute to these inequities, but it has highlighted how racist policies have led to disparate access to health care, or even clean air, clean water, and nutritious food, and left communities of color more vulnerable to severe illness and death from COVID-19. With the advent of vaccines for COVID-19, we continue to see racial disparities as Black Americans have the lowest rates of vaccination.16 All of these inequities have to be understood in the context of the racist structures that exist in our society. As medical providers, we must understand and help to dismantle these structures.
Pregnancy-related mortality (PRM) inequities. A powerful example of a persistent health inequity in our field is the well-known disparity in pregnancy-related mortality when examining this outcome by race. Per CDC analysis of data on PRM from 2007–2016, Black women died at a rate 3.2 times higher than White women. This disparity was even greater in patients older than 30 years of age. When they compared rates while controlling for the highest level of education, the disparity is even more pronounced: PRM rate for those with a college degree or higher was 5.2 times greater for Black people compared with White people.16The CDC also reported that, in 2018, the infant mortality for non-Hispanic Black infants was 10.8 per 1,000 live births, compared with 4.6 per 1,000 live births for White infants. This is a rate 2.4-times higher for Black infants.17 Dr. Cooper Owens and Dr. Fett note in their article, “Black maternal and infant health: Historical legacies of slavery,” that in 1850 this rate was 1.6-times higher for Black infants, which means the inequity was worse in 2018 America than in the antebellum South.5
The role of patient experience
As discussed, governmental policies have created persistent inequities in wealth, access to health care, and exposure to environmental toxins, among many other disparities. However, the data finding that highly educated Black pregnant patients suffer markedly increased risk of maternal death, indicate that inequities cannot be attributed only to education or lack of access to health care. This is where some will once again lean on the idea that there is something inherently different about Black people. But if we know that race was created and is not an empiric category, we must consider the social variables impacting Black patients’ experience.
As Linda Blount, President and CEO of the Black Women’s Health Imperative, put it, “Race is not a risk factor. It is the lived experience of being a Black woman in this society that is the risk factor.”18 So how much of these inequities can be accounted for by differential treatment of Black patients? There is, for example, data on the disproportionately lower rates of Black renal transplant recipients and inordinately higher rates of amputations among Black patients.19,20 None of us wants to think we are treating our Black patients differently, but the data demand that we ask ourselves if we are. Some of this is built into the system. For example, in their article “Hidden in plain sight—Reconsidering the use of race correction in clinical algorithms,” Vyas and colleagues outline a list of calculators and algorithms that include race.21 This means we may be using these calculators and changing outcomes for our patients based on their race. This is only one example of racism hidden within guidelines and standards of care.
The existence of racism on an interpersonal level also cannot be denied. This could lead to differential care specifically, but also can manifest by way of the toll it takes on a patient generally. This is the concept of allostatic load or weathering: the chronic stress of experiencing racism creates detrimental physiologic change. There is ongoing research into epigenetic modifications from stress that could be impacting health outcomes in Black populations.
Continue to: What is the work we need to do?...
What is the work we need to do?
Become educated. We have discussed taking the initiative to learn about the history of racism, including the legacies of slavery and the ongoing impact of racism on health. This knowledge is foundational and sometimes transformative. It allows us to see opportunities for antiracism and gives us the knowledge to begin meaningful conversations.
Take action. We must take inventory within our lives. What are our spheres of influence? What are our resources? Where can we make an impact? Right now, you can take out a pen and paper and write down all the roles you play. Look for opportunities in personal interactions and daily routines. Unfortunately, there will be many opportunities to speak up against racism—although this is rarely easy. Find articles, podcasts, and workshops on upstander training. One framework to respond to microaggressions has been proposed by faculty at Boston University Medical Center using the acronym LIFT (Lights on, Impact vs Intent, Full stop, Teach).22 It advises highlighting, clarifying, and directly addressing problematic comments with such statements as “I heard you say…” or “What did you mean by that comment?”, or a more direct “Statements like that are not OK with me,” or a teaching statement of “I read an article that made me think differently about comments like the one you made...”22 How and when to employ these strategies takes deliberate practice and will be uncomfortable. But we must do the work.
Practice empathetic listening. In a podcast discussion with Brené Brown on creating transformative cultures, Aiko Bethea, a leader in diversity and equity innovation, implores listeners to believe people of color.23,24 Draw on the history you’ve learned and understand the context in which Black people live in our society. Don’t brush off your Black friend who is upset about being stopped by security. That wasn’t the first time she was in that situation. Take seriously your patient’s concern that they are not being treated appropriately because of being Black. At the same time, do not think of Black people as a monolith or a stereotype. Respect people’s individuality.
Teach our kids all of this. We must also find ways to make change on a larger scale—within our practices, hospitals, medical schools, places of worship, town councils, school boards, state legislatures, and so on. If you are in a faculty position, you can reach out to leadership to scrutinize the curriculum while also ensuring that what and how you are teaching aligns with your antiracist principles. Question the theories, calculators, and algorithms being used and taught. Inquire about policies around recruitment of trainees and faculty as well as promotion, and implement strategies to make this inclusive and equitable. If you run a practice, you can ensure hiring and compensation policies are equitable. Examine patient access and barriers that your minoritized patients are facing, and address those barriers. Share resources and tools that you find helpful and develop a community of colleagues to develop with and hold one another accountable.
In her June 2020 article, An Open Letter to Corporate America, Philanthropy, Academia, etc: What now?, Bethea lays out an extensive framework for approaching antiracism at a high level.25 Among the principles she emphasizes is that the work of diversity, equity, and inclusion should not be siloed and cannot continue to be undervalued. It must be viewed as leadership and engaged in by leadership. The work of diversity, equity, and inclusion for any given institution must be explicit, intentional, measured, and transparent. Within that work, antiracism deserves individual attention. This work must center the people of color for whom you are pursuing equity. White people must resist the urge to make this about them.25
Drs. Esther Choo and J. Nwando Olayiwola present their proposals for combating racism in two 2020 Lancet articles.26,27 They discuss anticipating failure and backlash and learning from them but not being derailed by them. They emphasize the need for ongoing, serious financial investment and transformation in leadership. They also point out the need for data, discouraging more research on well-established inequities while recommending investigating interventions.26,27 If you are in leadership positions, read these articles and many more. Enact these principles. Make the investment. If you are not in such a position, find ways to hold your organization’s leadership accountable. Find ways to get a seat at the table and steer the conversation. In medicine, we have to make change at every level of our organizations. That will include the very difficult work of changing climate and culture. In addition, we have to look not only within our organizations but also to the communities we serve. Those voices must be valued in this conversation.
Will this take time? Yes. Will this be hard? Yes. Can you do everything? No. Can you do your part? Yes! Do the work.
- Roberts D. Fatal Invention: How Science, Politics and Big Business Re-create Race in the Twenty-First Century. The New Press: New York, New York; 2012.
- Definition of racism in English. Lexico web site. https://www.lexico. com/en/definition/racism. Accessed July 30, 2021.
- Definition of racism. Merriam-Webster web site. https://www .merriam-webster.com/dictionary/racism. Accessed July 30, 2021.
- Kendi IX. How To Be an Antiracist. One World: New York, NY; 2019.
- Cooper Owens D, Fett SM. Black maternal and infant health: historical legacies of slavery. Am J Public Health. 2019;109:1342-1345. doi: 10.2105/AJPH.2019.305243.
- Cooper Owens D. Medical Bondage: Race, Gender, and the Origins of American Gynecology. University of Georgia Press: Athens, GA; 2017.
- Washington H. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. Anchor Books: New York, NY; 2006.
- Coates T. The case for reparations. The Atlantic. 2014;313.5:54-71.
- Rothstein R. The Color of the Law: A Forgotten History of How our Government Segregated America. Liveright Publishing Corporation: New York, NY; 2017.
- Nelson RK, Ayers EL; The Digital Scholarship Lab and the National Community Reinvestment Coalition. American Panorama, ed. Not Even Past: Social Vulnerability and the Legacy of Redlining. https://dsl.richmond.edu/socialvulnerability. Accessed July 30, 2021.
- Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105-125. doi: 10.1146 /annurev-publhealth-040218-043750.
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press: Washington, DC; 2003.
- Artiga S, Corallo B, Pham O. Racial disparities in COVID-19: key findings from available data and analysis. KFF web site. August 17, 2020. https://www.kff.org/racial-equity-and-health-policy/issue-brief /racial-disparities-covid-19-key-findings-available-data-analysis/. Accessed July 30, 2021.
- Disparities in deaths from COVID-19. Centers for Disease Control and Prevention web site. https://www.cdc.gov/coronavirus/2019-ncov /community/health-equity/racial-ethnic-disparities/disparities -deaths.html. Updated December 10, 2020. Accessed July 30, 2021.
- Disparities in COVID-19 hospitalizations. Centers for Disease Control and Prevention web site. https://www.cdc.gov/coronavirus/2019 -ncov/community/health-equity/racial-ethnic-disparities/disparities -hospitalization.html. Updated July 28, 2021. Accessed July 30, 2021.
- COVID data tracker. Centers for Disease Control and Prevention web site. https://covid.cdc.gov/covid-data-tracker/#vaccination -demographics-trends. Accessed July 30, 2021.
- Infant mortality. Centers for Disease Control and Prevention web site. https://www.cdc.gov/reproductivehealth/maternalinfanthealth /infantmortality.htm. Last reviewed September 2020. Accessed July 30, 2021.
- Roeder A. America is failing its Black mothers. Harvard Public Health. Winter 2019. https://www.hsph.harvard.edu/magazine/magazine _article/america-is-failing-its-black-mothers/. Accessed July 30, 2021.
- Ku E, Lee BK, McCulloch CE, et al. Racial and ethnic disparities in kidney transplant access within a theoretical context of medical eligibility. Transplantation. 2020;104:1437-1444. doi: 10.1097/TP .0000000000002962.
- Arya S, Binney Z, Khakharia A, et al. Race and socioeconomic status independently affect risk of major amputation in peripheral artery disease. J Am Heart Assoc. 2018;7:e007425. doi: 10.1161 /JAHA.117.007425.
- Vyas DA, Eisenstein LG, Jones DS, et al. Hidden in plain sight— reconsidering the use of race correction in clinical algorithms. N Engl J Med. 2020;383:874-882. doi: 10.1056/NEJMms2004740.
- A Curriculum to Increase Faculty Engagement in the CLER Program. Boston University Medical Center web site. https://www.bumc .bu.edu/facdev-medicine/files/2020/05/Bystander-Training-for -Microaggressions-Executive-Summary.pdf. Accessed July 30, 2021.
- Brenè with Aiko Bethea on inclusivity at work: the heart of hard conversations. Spotify web site. https://open.spotify.com/episod e/3IODQ37EurkFf0zMNhazqI?si=wJIZgzpWTDCF1QVhwAdhiw. Accessed July 30, 2021.
- Brenè with Aiko Bethea on creating transformative cultures. Spotify web site. https://open.spotify.com/episode/7K47gQF5Ruc7MAXxEN q6jI?si=X0pzd2NnRAGwMD-bkyg-VQ. Accessed July 30, 2021.
- Bethea A. An open letter to corporate America, philanthropy, academia, etc.: What now? June 1, 2020. https://aikobethea.medium. com/an-open-letter-to-corporate-america-philanthropy-academiaetc-what-now-8b2d3a310f22. Accessed July 30, 2021.
- Choo E. Seven things organisations should be doing to combat racism. Lancet. 2020;396:157. doi:10.1016/S0140-6736(20)31565-8.
- Olayiwola JN, Choo E. Seven more things organisations should be doing to combat racism. Lancet. 2020;396:593. doi: 10.1016/S0140 -6736(20)31718-9.
- Roberts D. Fatal Invention: How Science, Politics and Big Business Re-create Race in the Twenty-First Century. The New Press: New York, New York; 2012.
- Definition of racism in English. Lexico web site. https://www.lexico. com/en/definition/racism. Accessed July 30, 2021.
- Definition of racism. Merriam-Webster web site. https://www .merriam-webster.com/dictionary/racism. Accessed July 30, 2021.
- Kendi IX. How To Be an Antiracist. One World: New York, NY; 2019.
- Cooper Owens D, Fett SM. Black maternal and infant health: historical legacies of slavery. Am J Public Health. 2019;109:1342-1345. doi: 10.2105/AJPH.2019.305243.
- Cooper Owens D. Medical Bondage: Race, Gender, and the Origins of American Gynecology. University of Georgia Press: Athens, GA; 2017.
- Washington H. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. Anchor Books: New York, NY; 2006.
- Coates T. The case for reparations. The Atlantic. 2014;313.5:54-71.
- Rothstein R. The Color of the Law: A Forgotten History of How our Government Segregated America. Liveright Publishing Corporation: New York, NY; 2017.
- Nelson RK, Ayers EL; The Digital Scholarship Lab and the National Community Reinvestment Coalition. American Panorama, ed. Not Even Past: Social Vulnerability and the Legacy of Redlining. https://dsl.richmond.edu/socialvulnerability. Accessed July 30, 2021.
- Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105-125. doi: 10.1146 /annurev-publhealth-040218-043750.
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press: Washington, DC; 2003.
- Artiga S, Corallo B, Pham O. Racial disparities in COVID-19: key findings from available data and analysis. KFF web site. August 17, 2020. https://www.kff.org/racial-equity-and-health-policy/issue-brief /racial-disparities-covid-19-key-findings-available-data-analysis/. Accessed July 30, 2021.
- Disparities in deaths from COVID-19. Centers for Disease Control and Prevention web site. https://www.cdc.gov/coronavirus/2019-ncov /community/health-equity/racial-ethnic-disparities/disparities -deaths.html. Updated December 10, 2020. Accessed July 30, 2021.
- Disparities in COVID-19 hospitalizations. Centers for Disease Control and Prevention web site. https://www.cdc.gov/coronavirus/2019 -ncov/community/health-equity/racial-ethnic-disparities/disparities -hospitalization.html. Updated July 28, 2021. Accessed July 30, 2021.
- COVID data tracker. Centers for Disease Control and Prevention web site. https://covid.cdc.gov/covid-data-tracker/#vaccination -demographics-trends. Accessed July 30, 2021.
- Infant mortality. Centers for Disease Control and Prevention web site. https://www.cdc.gov/reproductivehealth/maternalinfanthealth /infantmortality.htm. Last reviewed September 2020. Accessed July 30, 2021.
- Roeder A. America is failing its Black mothers. Harvard Public Health. Winter 2019. https://www.hsph.harvard.edu/magazine/magazine _article/america-is-failing-its-black-mothers/. Accessed July 30, 2021.
- Ku E, Lee BK, McCulloch CE, et al. Racial and ethnic disparities in kidney transplant access within a theoretical context of medical eligibility. Transplantation. 2020;104:1437-1444. doi: 10.1097/TP .0000000000002962.
- Arya S, Binney Z, Khakharia A, et al. Race and socioeconomic status independently affect risk of major amputation in peripheral artery disease. J Am Heart Assoc. 2018;7:e007425. doi: 10.1161 /JAHA.117.007425.
- Vyas DA, Eisenstein LG, Jones DS, et al. Hidden in plain sight— reconsidering the use of race correction in clinical algorithms. N Engl J Med. 2020;383:874-882. doi: 10.1056/NEJMms2004740.
- A Curriculum to Increase Faculty Engagement in the CLER Program. Boston University Medical Center web site. https://www.bumc .bu.edu/facdev-medicine/files/2020/05/Bystander-Training-for -Microaggressions-Executive-Summary.pdf. Accessed July 30, 2021.
- Brenè with Aiko Bethea on inclusivity at work: the heart of hard conversations. Spotify web site. https://open.spotify.com/episod e/3IODQ37EurkFf0zMNhazqI?si=wJIZgzpWTDCF1QVhwAdhiw. Accessed July 30, 2021.
- Brenè with Aiko Bethea on creating transformative cultures. Spotify web site. https://open.spotify.com/episode/7K47gQF5Ruc7MAXxEN q6jI?si=X0pzd2NnRAGwMD-bkyg-VQ. Accessed July 30, 2021.
- Bethea A. An open letter to corporate America, philanthropy, academia, etc.: What now? June 1, 2020. https://aikobethea.medium. com/an-open-letter-to-corporate-america-philanthropy-academiaetc-what-now-8b2d3a310f22. Accessed July 30, 2021.
- Choo E. Seven things organisations should be doing to combat racism. Lancet. 2020;396:157. doi:10.1016/S0140-6736(20)31565-8.
- Olayiwola JN, Choo E. Seven more things organisations should be doing to combat racism. Lancet. 2020;396:593. doi: 10.1016/S0140 -6736(20)31718-9.
CDC: Vaccination may cut risk of COVID reinfection in half
The Centers for Disease Control and Prevention has recommended that everyone get a COVID-19 vaccine, even if they’ve had the virus before. Yet many skeptics have held off getting the shots, believing that immunity generated by their previous infection will protect them if they should encounter the virus again.
A new study published in the CDC’s Morbidity and Mortality Weekly Report pokes holes in this notion. It shows people who have recovered from COVID-19 but haven’t been vaccinated have more than double the risk of testing positive for the virus again, compared with someone who was vaccinated after an initial infection.
The study looked at 738 Kentucky residents who had an initial bout of COVID-19 in 2020. About 250 of them tested positive for COVID-19 a second time between May and July of 2021, when the Delta variant became dominant in the United States.
The study matched each person who’d been reinfected with two people of the same sex and roughly the same age who had caught their initial COVID infection within the same week. The researchers then cross-matched those cases with data from Kentucky’s Immunization Registry.
They found that those who were unvaccinated had more than double the risk of being reinfected during the Delta wave. Partial vaccination appeared to have no significant impact on the risk of reinfection.
Among those who were reinfected, 20% were fully vaccinated, while 34% of those who did not get reinfected were fully vaccinated.
The study is observational, meaning it can’t show cause and effect; and the researchers had no information on the severity of the infections. Alyson Cavanaugh, PhD, a member of the CDC’s Epidemic Intelligence Service who led the study, said it is possible that some of the people who tested positive a second time had asymptomatic infections that were picked up through routine screening.
Still, the study backs up previous research and suggests that vaccination offers important additional protection.
“Our laboratory studies have shown that there’s an added benefit of vaccine for people who’ve had previous COVID-19. This is a real-world, epidemiologic study that found that among people who’d previously already had COVID-19, those who were vaccinated had lower odds of being reinfected,” Dr. Cavanaugh said.
“If you have had COVID-19 before, please still get vaccinated,” said CDC Director Rochelle Walensky, MD, in a written media statement. “This study shows you are twice as likely to get infected again if you are unvaccinated. Getting the vaccine is the best way to protect yourself and others around you, especially as the more contagious Delta variant spreads around the country.”
In a White House COVID-19 Response Team briefing in May, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease, explained why vaccines create stronger immunity than infection. He highlighted new research showing that two doses of an mRNA vaccine produce levels of neutralizing antibodies that are up to 10 times higher than the levels found in the blood of people who’ve recovered from COVID-19. Vaccines also enhance B cells and T cells in people who’ve recovered from COVID-19, which broadens the spectrum of protection and helps to fend off variants.
The study has some important limitations, which the authors acknowledged. The first is that second infections weren’t confirmed with genetic sequencing, so the researchers couldn’t definitively tell if a person tested positive a second time because they caught a new virus, or if they were somehow still shedding virus from their first infection. Given that the tests were at least 5 months apart, though, the researchers think reinfection is the most likely explanation.
Another bias in the study could have something to do with vaccination. Vaccinated people may have been less likely to be tested for COVID-19 after their vaccines, so the association or reinfection with a lack of vaccination may be overestimated.
Also, people who were vaccinated at federal sites or in another state were not logged in the state’s immunization registry, which may have skewed the data.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention has recommended that everyone get a COVID-19 vaccine, even if they’ve had the virus before. Yet many skeptics have held off getting the shots, believing that immunity generated by their previous infection will protect them if they should encounter the virus again.
A new study published in the CDC’s Morbidity and Mortality Weekly Report pokes holes in this notion. It shows people who have recovered from COVID-19 but haven’t been vaccinated have more than double the risk of testing positive for the virus again, compared with someone who was vaccinated after an initial infection.
The study looked at 738 Kentucky residents who had an initial bout of COVID-19 in 2020. About 250 of them tested positive for COVID-19 a second time between May and July of 2021, when the Delta variant became dominant in the United States.
The study matched each person who’d been reinfected with two people of the same sex and roughly the same age who had caught their initial COVID infection within the same week. The researchers then cross-matched those cases with data from Kentucky’s Immunization Registry.
They found that those who were unvaccinated had more than double the risk of being reinfected during the Delta wave. Partial vaccination appeared to have no significant impact on the risk of reinfection.
Among those who were reinfected, 20% were fully vaccinated, while 34% of those who did not get reinfected were fully vaccinated.
The study is observational, meaning it can’t show cause and effect; and the researchers had no information on the severity of the infections. Alyson Cavanaugh, PhD, a member of the CDC’s Epidemic Intelligence Service who led the study, said it is possible that some of the people who tested positive a second time had asymptomatic infections that were picked up through routine screening.
Still, the study backs up previous research and suggests that vaccination offers important additional protection.
“Our laboratory studies have shown that there’s an added benefit of vaccine for people who’ve had previous COVID-19. This is a real-world, epidemiologic study that found that among people who’d previously already had COVID-19, those who were vaccinated had lower odds of being reinfected,” Dr. Cavanaugh said.
“If you have had COVID-19 before, please still get vaccinated,” said CDC Director Rochelle Walensky, MD, in a written media statement. “This study shows you are twice as likely to get infected again if you are unvaccinated. Getting the vaccine is the best way to protect yourself and others around you, especially as the more contagious Delta variant spreads around the country.”
In a White House COVID-19 Response Team briefing in May, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease, explained why vaccines create stronger immunity than infection. He highlighted new research showing that two doses of an mRNA vaccine produce levels of neutralizing antibodies that are up to 10 times higher than the levels found in the blood of people who’ve recovered from COVID-19. Vaccines also enhance B cells and T cells in people who’ve recovered from COVID-19, which broadens the spectrum of protection and helps to fend off variants.
The study has some important limitations, which the authors acknowledged. The first is that second infections weren’t confirmed with genetic sequencing, so the researchers couldn’t definitively tell if a person tested positive a second time because they caught a new virus, or if they were somehow still shedding virus from their first infection. Given that the tests were at least 5 months apart, though, the researchers think reinfection is the most likely explanation.
Another bias in the study could have something to do with vaccination. Vaccinated people may have been less likely to be tested for COVID-19 after their vaccines, so the association or reinfection with a lack of vaccination may be overestimated.
Also, people who were vaccinated at federal sites or in another state were not logged in the state’s immunization registry, which may have skewed the data.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention has recommended that everyone get a COVID-19 vaccine, even if they’ve had the virus before. Yet many skeptics have held off getting the shots, believing that immunity generated by their previous infection will protect them if they should encounter the virus again.
A new study published in the CDC’s Morbidity and Mortality Weekly Report pokes holes in this notion. It shows people who have recovered from COVID-19 but haven’t been vaccinated have more than double the risk of testing positive for the virus again, compared with someone who was vaccinated after an initial infection.
The study looked at 738 Kentucky residents who had an initial bout of COVID-19 in 2020. About 250 of them tested positive for COVID-19 a second time between May and July of 2021, when the Delta variant became dominant in the United States.
The study matched each person who’d been reinfected with two people of the same sex and roughly the same age who had caught their initial COVID infection within the same week. The researchers then cross-matched those cases with data from Kentucky’s Immunization Registry.
They found that those who were unvaccinated had more than double the risk of being reinfected during the Delta wave. Partial vaccination appeared to have no significant impact on the risk of reinfection.
Among those who were reinfected, 20% were fully vaccinated, while 34% of those who did not get reinfected were fully vaccinated.
The study is observational, meaning it can’t show cause and effect; and the researchers had no information on the severity of the infections. Alyson Cavanaugh, PhD, a member of the CDC’s Epidemic Intelligence Service who led the study, said it is possible that some of the people who tested positive a second time had asymptomatic infections that were picked up through routine screening.
Still, the study backs up previous research and suggests that vaccination offers important additional protection.
“Our laboratory studies have shown that there’s an added benefit of vaccine for people who’ve had previous COVID-19. This is a real-world, epidemiologic study that found that among people who’d previously already had COVID-19, those who were vaccinated had lower odds of being reinfected,” Dr. Cavanaugh said.
“If you have had COVID-19 before, please still get vaccinated,” said CDC Director Rochelle Walensky, MD, in a written media statement. “This study shows you are twice as likely to get infected again if you are unvaccinated. Getting the vaccine is the best way to protect yourself and others around you, especially as the more contagious Delta variant spreads around the country.”
In a White House COVID-19 Response Team briefing in May, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease, explained why vaccines create stronger immunity than infection. He highlighted new research showing that two doses of an mRNA vaccine produce levels of neutralizing antibodies that are up to 10 times higher than the levels found in the blood of people who’ve recovered from COVID-19. Vaccines also enhance B cells and T cells in people who’ve recovered from COVID-19, which broadens the spectrum of protection and helps to fend off variants.
The study has some important limitations, which the authors acknowledged. The first is that second infections weren’t confirmed with genetic sequencing, so the researchers couldn’t definitively tell if a person tested positive a second time because they caught a new virus, or if they were somehow still shedding virus from their first infection. Given that the tests were at least 5 months apart, though, the researchers think reinfection is the most likely explanation.
Another bias in the study could have something to do with vaccination. Vaccinated people may have been less likely to be tested for COVID-19 after their vaccines, so the association or reinfection with a lack of vaccination may be overestimated.
Also, people who were vaccinated at federal sites or in another state were not logged in the state’s immunization registry, which may have skewed the data.
A version of this article first appeared on Medscape.com.