User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Study Helps Define Patient-Centered Definition of Atopic Dermatitis Flares
TOPLINE:
, which most agreed would help when communicating with their healthcare providers (HCPs).
METHODOLOGY:
- To develop a patient-centered definition of AD flare, researchers used a modified eDelphi method, which involved a focus group and survey to reach consensus on key aspects of an AD flare.
- The focus group included 26 US adults aged ≥ 18 years with AD who had experienced a flare within the past 12 months. The survey was conducted among 631 adults with AD to validate the identified concepts and assess their agreement with the consensus statements.
- Participants rated 98 statements on a scale from 1 to 9, with consensus defined as at least 70% rating a statement as 7-9 and less than 15% rating it as 1-3.
- In focus groups, participants identified six key concepts for a patient-centered definition of flare, including changes from baseline, mental and emotional consequences, and physical changes in skin.
TAKEAWAY:
- The focus group reached consensus on 15 statements, and survey participants reached consensus on 12 of those statements defining an AD flare, with the highest agreement on symptoms taking more attention than normal, worsening of physical symptoms associated with AD, and worsening of itching associated with AD.
- The statement “acute worsening of symptoms of AD” was ranked as the most important, while “a worsening of physical symptoms” was ranked the least important.
- Most participants (79.7%) reported that prior definitions of AD flare did not resonate with them.
- More than half (52.9%) agreed with their HCP on what constitutes an AD flare, and the majority (77.6%) indicated that a patient-centered definition would be useful for communication with their HCP and for self-management.
IN PRACTICE:
“In this consensus survey study, we identified statements that are critical to the definition of an AD flare from the patient perspective,” the authors wrote. These findings, they added, “may be useful in clinical practice to improve communication between patients and HCPs who may be using the term flare without a mutual understanding of its meaning” and “may also be applied to the development of outcome measures focused on AD flares, which is an important treatment outcome for people with AD.”
SOURCE:
The study was led by Aaron M. Drucker, MD, ScM, of the Division of Dermatology, Department of Medicine, University of Toronto, Ontario, Canada, and was published online September 11 in JAMA Dermatology.
LIMITATIONS:
Participants had higher-than-average knowledge about AD, and the study’s findings may not be generalizable to all people with AD. The study included a higher proportion of moderate to severe AD cases than the general population, which may introduce responder bias. The findings may not be applicable to children, caregivers, or individuals in other countries.
DISCLOSURES:
This work was supported by a grant to the National Eczema Association from Pfizer. Dr. Drucker disclosed received compensation from the British Journal of Dermatology, American Academy of Dermatology, and Canadian Dermatology Today, and consultant fees from the National Eczema Association and Canadian Agency for Drugs and Technologies in Health. Another author reported receiving personal fees from pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, which most agreed would help when communicating with their healthcare providers (HCPs).
METHODOLOGY:
- To develop a patient-centered definition of AD flare, researchers used a modified eDelphi method, which involved a focus group and survey to reach consensus on key aspects of an AD flare.
- The focus group included 26 US adults aged ≥ 18 years with AD who had experienced a flare within the past 12 months. The survey was conducted among 631 adults with AD to validate the identified concepts and assess their agreement with the consensus statements.
- Participants rated 98 statements on a scale from 1 to 9, with consensus defined as at least 70% rating a statement as 7-9 and less than 15% rating it as 1-3.
- In focus groups, participants identified six key concepts for a patient-centered definition of flare, including changes from baseline, mental and emotional consequences, and physical changes in skin.
TAKEAWAY:
- The focus group reached consensus on 15 statements, and survey participants reached consensus on 12 of those statements defining an AD flare, with the highest agreement on symptoms taking more attention than normal, worsening of physical symptoms associated with AD, and worsening of itching associated with AD.
- The statement “acute worsening of symptoms of AD” was ranked as the most important, while “a worsening of physical symptoms” was ranked the least important.
- Most participants (79.7%) reported that prior definitions of AD flare did not resonate with them.
- More than half (52.9%) agreed with their HCP on what constitutes an AD flare, and the majority (77.6%) indicated that a patient-centered definition would be useful for communication with their HCP and for self-management.
IN PRACTICE:
“In this consensus survey study, we identified statements that are critical to the definition of an AD flare from the patient perspective,” the authors wrote. These findings, they added, “may be useful in clinical practice to improve communication between patients and HCPs who may be using the term flare without a mutual understanding of its meaning” and “may also be applied to the development of outcome measures focused on AD flares, which is an important treatment outcome for people with AD.”
SOURCE:
The study was led by Aaron M. Drucker, MD, ScM, of the Division of Dermatology, Department of Medicine, University of Toronto, Ontario, Canada, and was published online September 11 in JAMA Dermatology.
LIMITATIONS:
Participants had higher-than-average knowledge about AD, and the study’s findings may not be generalizable to all people with AD. The study included a higher proportion of moderate to severe AD cases than the general population, which may introduce responder bias. The findings may not be applicable to children, caregivers, or individuals in other countries.
DISCLOSURES:
This work was supported by a grant to the National Eczema Association from Pfizer. Dr. Drucker disclosed received compensation from the British Journal of Dermatology, American Academy of Dermatology, and Canadian Dermatology Today, and consultant fees from the National Eczema Association and Canadian Agency for Drugs and Technologies in Health. Another author reported receiving personal fees from pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, which most agreed would help when communicating with their healthcare providers (HCPs).
METHODOLOGY:
- To develop a patient-centered definition of AD flare, researchers used a modified eDelphi method, which involved a focus group and survey to reach consensus on key aspects of an AD flare.
- The focus group included 26 US adults aged ≥ 18 years with AD who had experienced a flare within the past 12 months. The survey was conducted among 631 adults with AD to validate the identified concepts and assess their agreement with the consensus statements.
- Participants rated 98 statements on a scale from 1 to 9, with consensus defined as at least 70% rating a statement as 7-9 and less than 15% rating it as 1-3.
- In focus groups, participants identified six key concepts for a patient-centered definition of flare, including changes from baseline, mental and emotional consequences, and physical changes in skin.
TAKEAWAY:
- The focus group reached consensus on 15 statements, and survey participants reached consensus on 12 of those statements defining an AD flare, with the highest agreement on symptoms taking more attention than normal, worsening of physical symptoms associated with AD, and worsening of itching associated with AD.
- The statement “acute worsening of symptoms of AD” was ranked as the most important, while “a worsening of physical symptoms” was ranked the least important.
- Most participants (79.7%) reported that prior definitions of AD flare did not resonate with them.
- More than half (52.9%) agreed with their HCP on what constitutes an AD flare, and the majority (77.6%) indicated that a patient-centered definition would be useful for communication with their HCP and for self-management.
IN PRACTICE:
“In this consensus survey study, we identified statements that are critical to the definition of an AD flare from the patient perspective,” the authors wrote. These findings, they added, “may be useful in clinical practice to improve communication between patients and HCPs who may be using the term flare without a mutual understanding of its meaning” and “may also be applied to the development of outcome measures focused on AD flares, which is an important treatment outcome for people with AD.”
SOURCE:
The study was led by Aaron M. Drucker, MD, ScM, of the Division of Dermatology, Department of Medicine, University of Toronto, Ontario, Canada, and was published online September 11 in JAMA Dermatology.
LIMITATIONS:
Participants had higher-than-average knowledge about AD, and the study’s findings may not be generalizable to all people with AD. The study included a higher proportion of moderate to severe AD cases than the general population, which may introduce responder bias. The findings may not be applicable to children, caregivers, or individuals in other countries.
DISCLOSURES:
This work was supported by a grant to the National Eczema Association from Pfizer. Dr. Drucker disclosed received compensation from the British Journal of Dermatology, American Academy of Dermatology, and Canadian Dermatology Today, and consultant fees from the National Eczema Association and Canadian Agency for Drugs and Technologies in Health. Another author reported receiving personal fees from pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Imaging Tool Helps Identify Features of Nail Disorders
TOPLINE:
METHODOLOGY:
- The single-center, observational cross-sectional pilot study evaluated patients aged ≥ 7 years with newly diagnosed nail disorders between January 2022 and May 2023.
- A total of 128 patients (average age, 46.1 years; range, 8-84 years) with nail psoriasis, onychomycosis, idiopathic/traumatic onycholysis, brittle nail syndrome, nail lichen planus, retronychia, and other nail conditions and those with no nail findings (controls) were enrolled.
- Researchers performed nailfold capillaroscopy imaging and compared capillary features between patients with nail conditions and the controls.
TAKEAWAY:
- Patients with nail psoriasis had decreased capillary density and length (P < .001), more crossed and tortuous capillaries (P < .02), and increased abnormal capillary morphology (P = .03) compared with controls. Specific abnormalities, such as branching and meandering capillaries, were more common among those with nail psoriasis (both 26.5%).
- Patients with fingernail and toenail onychomycosis had a higher frequency of abnormal capillary morphology (P < .02), particularly meandering capillaries (75.0% for fingernails and 76.9% for toenails). However, other abnormalities were less frequently observed.
- Patients with nail lichen planus (P < .01), onychopapilloma (P = .01), and retronychia (P = .03) showed significantly shorter capillaries than controls. Retronychia was also associated with increased disorganized polymorphic capillaries (P = .02).
- Patients with brittle nail syndrome and eczema showed no significant differences compared with controls.
IN PRACTICE:
“Our findings highlight nailfold capillaroscopy as a potentially quick, cost-effective, and noninvasive imaging modality as an adjunct for diagnosis and treatment initiation for patients with onychodystrophies,” the authors wrote.
SOURCE:
This study was led by Jonathan K. Hwang, MD, Weill Cornell Medicine, New York City, and was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The study’s limitations included a small sample size for certain nail conditions and the single-center design, which limited generalizability. Additionally, the uneven surface, scaling, onycholysis, and thickening of toenails made some capillaroscopy images difficult to capture and interpret.
DISCLOSURES:
The study did not receive any funding. One author reported serving as a consultant for Eli Lilly, Ortho-Dermatologics, BelleTorus, and Moberg Pharma.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The single-center, observational cross-sectional pilot study evaluated patients aged ≥ 7 years with newly diagnosed nail disorders between January 2022 and May 2023.
- A total of 128 patients (average age, 46.1 years; range, 8-84 years) with nail psoriasis, onychomycosis, idiopathic/traumatic onycholysis, brittle nail syndrome, nail lichen planus, retronychia, and other nail conditions and those with no nail findings (controls) were enrolled.
- Researchers performed nailfold capillaroscopy imaging and compared capillary features between patients with nail conditions and the controls.
TAKEAWAY:
- Patients with nail psoriasis had decreased capillary density and length (P < .001), more crossed and tortuous capillaries (P < .02), and increased abnormal capillary morphology (P = .03) compared with controls. Specific abnormalities, such as branching and meandering capillaries, were more common among those with nail psoriasis (both 26.5%).
- Patients with fingernail and toenail onychomycosis had a higher frequency of abnormal capillary morphology (P < .02), particularly meandering capillaries (75.0% for fingernails and 76.9% for toenails). However, other abnormalities were less frequently observed.
- Patients with nail lichen planus (P < .01), onychopapilloma (P = .01), and retronychia (P = .03) showed significantly shorter capillaries than controls. Retronychia was also associated with increased disorganized polymorphic capillaries (P = .02).
- Patients with brittle nail syndrome and eczema showed no significant differences compared with controls.
IN PRACTICE:
“Our findings highlight nailfold capillaroscopy as a potentially quick, cost-effective, and noninvasive imaging modality as an adjunct for diagnosis and treatment initiation for patients with onychodystrophies,” the authors wrote.
SOURCE:
This study was led by Jonathan K. Hwang, MD, Weill Cornell Medicine, New York City, and was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The study’s limitations included a small sample size for certain nail conditions and the single-center design, which limited generalizability. Additionally, the uneven surface, scaling, onycholysis, and thickening of toenails made some capillaroscopy images difficult to capture and interpret.
DISCLOSURES:
The study did not receive any funding. One author reported serving as a consultant for Eli Lilly, Ortho-Dermatologics, BelleTorus, and Moberg Pharma.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The single-center, observational cross-sectional pilot study evaluated patients aged ≥ 7 years with newly diagnosed nail disorders between January 2022 and May 2023.
- A total of 128 patients (average age, 46.1 years; range, 8-84 years) with nail psoriasis, onychomycosis, idiopathic/traumatic onycholysis, brittle nail syndrome, nail lichen planus, retronychia, and other nail conditions and those with no nail findings (controls) were enrolled.
- Researchers performed nailfold capillaroscopy imaging and compared capillary features between patients with nail conditions and the controls.
TAKEAWAY:
- Patients with nail psoriasis had decreased capillary density and length (P < .001), more crossed and tortuous capillaries (P < .02), and increased abnormal capillary morphology (P = .03) compared with controls. Specific abnormalities, such as branching and meandering capillaries, were more common among those with nail psoriasis (both 26.5%).
- Patients with fingernail and toenail onychomycosis had a higher frequency of abnormal capillary morphology (P < .02), particularly meandering capillaries (75.0% for fingernails and 76.9% for toenails). However, other abnormalities were less frequently observed.
- Patients with nail lichen planus (P < .01), onychopapilloma (P = .01), and retronychia (P = .03) showed significantly shorter capillaries than controls. Retronychia was also associated with increased disorganized polymorphic capillaries (P = .02).
- Patients with brittle nail syndrome and eczema showed no significant differences compared with controls.
IN PRACTICE:
“Our findings highlight nailfold capillaroscopy as a potentially quick, cost-effective, and noninvasive imaging modality as an adjunct for diagnosis and treatment initiation for patients with onychodystrophies,” the authors wrote.
SOURCE:
This study was led by Jonathan K. Hwang, MD, Weill Cornell Medicine, New York City, and was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The study’s limitations included a small sample size for certain nail conditions and the single-center design, which limited generalizability. Additionally, the uneven surface, scaling, onycholysis, and thickening of toenails made some capillaroscopy images difficult to capture and interpret.
DISCLOSURES:
The study did not receive any funding. One author reported serving as a consultant for Eli Lilly, Ortho-Dermatologics, BelleTorus, and Moberg Pharma.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
When You and Your Malpractice Insurer Disagree on Your Case
You’ve been sued for medical malpractice. If you are a physician in the United States, that is not an unlikely scenario.
An analysis by the American Medical Association shows that almost half of all physicians are sued by the time they reach 54. In some specialties, such as ob.gyn., one is almost guaranteed to be sued at some point.
But that’s what medical malpractice insurance is for, right? Your medical malpractice insurer will assign an attorney to take care of you and help you through this situation. Won’t they?
Maybe so, but the attorney and the claims representative your insurer assigns to your case may have a different idea about how to proceed than you do. Though the defense attorney assigned to you represents you, he or she gets paid by the insurance carrier.
This can create a conflict when your defense counsel and your insurance claims representative aim to take your case in a direction you don’t like.
Disagreements might include:
- Choice of expert witnesses
- Tactical decisions related to trial strategy
- Public relations considerations
- Admissions of liability
- Allocation of resources
To Settle or Not?
One of the most challenging — and common — disagreements is whether to settle the case.
Sometimes a malpractice insurer wants to settle the case against the defendant doctor’s wishes. Or the doctor wants to settle but is pushed into going to trial. In the following case, one doctor had to face the consequences of a decision he didn’t even make.
The Underlying Medical Malpractice Case
Dr. D was sued by a patient who had allegedly called Dr. D’s office six times in 2 days complaining of intermittent chest pain.
Dr. D had been swamped with patients and couldn’t squeeze this patient in for an office visit, but he did call back. The patient later claimed that during the call he told the doctor he was suffering from chest pain. The doctor recalled that the patient had complained of abdominal discomfort that began after he had exercised.
The physician wrote a prescription for an ECG at the local hospital and called to ensure that the patient could just walk in. The ECG was allegedly abnormal but was not read as representing an impending or current heart attack. Later that evening, however, the patient went to the emergency department of another hospital where it was confirmed that he had suffered a heart attack. The patient underwent cardiac catheterization and stent placement to address a blockage in his left anterior descending artery.
The patient subsequently sued Dr. D and the hospital where he had the original ECG. Dr. D contacted his medical malpractice insurance company. The insurance company assigned an attorney to represent Dr. D. Discovery in the case began.
The plaintiff’s own medical expert testified in a deposition that there was no way for the heart attack to have been prevented and that the treatment would have been the same either way. But Dr. D could not find a record of the phone calls with the patient, and he had not noted his conversation the patient in their medical records.
Dr. D held a policy for $1 million, and his state had a fund that would kick in an additional $1 million. But the plaintiffs demanded $4 million to settle.
A month before trial, the plaintiff’s attorney sent a threatening letter to Dr. D’s attorney warning him that Dr. D was underinsured and suggesting that it would be in the physician’s best interests to settle.
“I want to stress to you that it is not my desire to harm your client’s reputation or to destroy his business,” wrote the plaintiff’s attorney. “However, now is the time to avoid consequences such as these by making a good faith effort to get this case resolved.”
The letter went on to note that the defense attorney should give Dr. D a copy of the letter so that everyone would be aware of the potential consequences of an award against Dr. D in excess of his limits of insurance coverage. The plaintiff’s attorney even suggested that Dr. D should retain personal counsel.
Dr. D’s defense attorney downplayed the letter and assured him that there was no reason to worry.
Meanwhile the case inched closer to trial.
The codefendant hospital settled with the plaintiff on the night before jury selection, leaving Dr. D in the uncomfortable position of being the only defendant in the case. At this point, Dr. D decided he would like to settle, and he sent his attorney an email telling him so. But the attorney instead referred him to an insurance company claims.
Just days before the trial was to start, Dr. D repeatedly told the claims representative assigned to his claim that he did not want to go to trial but rather wanted to settle. The representative told Dr. D that he had no choice in whether the action settled.
A committee at the insurance company had decided to proceed with the trial rather than settle.
The trial proved a painful debacle for Dr. D. His attorney’s idea of showing a “gotcha” video of the allegedly permanently injured plaintiff carrying a large, heavy box backfired when the jury was shown by the plaintiff that the box actually contained ice cream cones and weighed very little.
Prior to trial, the plaintiff offered to settle for $1 million. On the first day of trial, they lowered that amount to $750,000, yet the defense attorney did not settle the case, and it proceeded to a jury verdict. The jury awarded the plaintiff over $4 million — well in excess of Dr. D’s policy limits.
The Follow-up
Dr. D was horrified, but the insurance company claims representative said the insurer would promptly offer $2 million in available insurance coverage to settle the case post verdict. This did not happen. Instead, the insurer chose to appeal the verdict against Dr. D’s wishes.
Ultimately, Dr. D was forced to hire his own lawyer. He ultimately sued the insurance company for breach of contract and bad faith.
The insurance company eventually attempted to settle with the plaintiffs’ counsel, but the plaintiff refused to accept the available insurance coverage. The insurance carrier still has not posted the entire appeal bond. The case is still pending.
Protecting Yourself
The lesson from Dr. D’s experience: Understand that the insurance company is not your friend. It’s a business looking out for its own interests.
The plaintiff’s attorney was absolutely correct in suggesting that Dr. D retain his own attorney to represent his own interests. You should hire your own lawyer when:
- You disagree with your insurer on how to proceed in a case.
- You receive a demand that exceeds your available insurance coverage or for damages that may not be covered by your policy, such as punitive damages.
- Your insurance carrier attempts to deny insurance coverage for your claim or sends you a letter stating that it is “reserving its rights” not to cover or to limit coverage for your claim.
Retaining independent counsel protects your interests, not those of your insurance company.
Independent counsel can give you a second opinion on the strengths and weaknesses of your claim, help you prepare for your deposition, and attend court dates with you to ensure that you are completely protected.
Independent counsel can challenge your insurance company’s decision to deny or limit your insurance coverage and ensure that you receive all of the benefits to which you are entitled under your insurance policy. Some policies may include an independent lawyer to be paid for by your insurance carrier in case of a conflicts.
The most important takeaway? Your medical malpractice insurance carrier is not your friend, so act accordingly in times of conflict.
A version of this article first appeared on Medscape.com.
You’ve been sued for medical malpractice. If you are a physician in the United States, that is not an unlikely scenario.
An analysis by the American Medical Association shows that almost half of all physicians are sued by the time they reach 54. In some specialties, such as ob.gyn., one is almost guaranteed to be sued at some point.
But that’s what medical malpractice insurance is for, right? Your medical malpractice insurer will assign an attorney to take care of you and help you through this situation. Won’t they?
Maybe so, but the attorney and the claims representative your insurer assigns to your case may have a different idea about how to proceed than you do. Though the defense attorney assigned to you represents you, he or she gets paid by the insurance carrier.
This can create a conflict when your defense counsel and your insurance claims representative aim to take your case in a direction you don’t like.
Disagreements might include:
- Choice of expert witnesses
- Tactical decisions related to trial strategy
- Public relations considerations
- Admissions of liability
- Allocation of resources
To Settle or Not?
One of the most challenging — and common — disagreements is whether to settle the case.
Sometimes a malpractice insurer wants to settle the case against the defendant doctor’s wishes. Or the doctor wants to settle but is pushed into going to trial. In the following case, one doctor had to face the consequences of a decision he didn’t even make.
The Underlying Medical Malpractice Case
Dr. D was sued by a patient who had allegedly called Dr. D’s office six times in 2 days complaining of intermittent chest pain.
Dr. D had been swamped with patients and couldn’t squeeze this patient in for an office visit, but he did call back. The patient later claimed that during the call he told the doctor he was suffering from chest pain. The doctor recalled that the patient had complained of abdominal discomfort that began after he had exercised.
The physician wrote a prescription for an ECG at the local hospital and called to ensure that the patient could just walk in. The ECG was allegedly abnormal but was not read as representing an impending or current heart attack. Later that evening, however, the patient went to the emergency department of another hospital where it was confirmed that he had suffered a heart attack. The patient underwent cardiac catheterization and stent placement to address a blockage in his left anterior descending artery.
The patient subsequently sued Dr. D and the hospital where he had the original ECG. Dr. D contacted his medical malpractice insurance company. The insurance company assigned an attorney to represent Dr. D. Discovery in the case began.
The plaintiff’s own medical expert testified in a deposition that there was no way for the heart attack to have been prevented and that the treatment would have been the same either way. But Dr. D could not find a record of the phone calls with the patient, and he had not noted his conversation the patient in their medical records.
Dr. D held a policy for $1 million, and his state had a fund that would kick in an additional $1 million. But the plaintiffs demanded $4 million to settle.
A month before trial, the plaintiff’s attorney sent a threatening letter to Dr. D’s attorney warning him that Dr. D was underinsured and suggesting that it would be in the physician’s best interests to settle.
“I want to stress to you that it is not my desire to harm your client’s reputation or to destroy his business,” wrote the plaintiff’s attorney. “However, now is the time to avoid consequences such as these by making a good faith effort to get this case resolved.”
The letter went on to note that the defense attorney should give Dr. D a copy of the letter so that everyone would be aware of the potential consequences of an award against Dr. D in excess of his limits of insurance coverage. The plaintiff’s attorney even suggested that Dr. D should retain personal counsel.
Dr. D’s defense attorney downplayed the letter and assured him that there was no reason to worry.
Meanwhile the case inched closer to trial.
The codefendant hospital settled with the plaintiff on the night before jury selection, leaving Dr. D in the uncomfortable position of being the only defendant in the case. At this point, Dr. D decided he would like to settle, and he sent his attorney an email telling him so. But the attorney instead referred him to an insurance company claims.
Just days before the trial was to start, Dr. D repeatedly told the claims representative assigned to his claim that he did not want to go to trial but rather wanted to settle. The representative told Dr. D that he had no choice in whether the action settled.
A committee at the insurance company had decided to proceed with the trial rather than settle.
The trial proved a painful debacle for Dr. D. His attorney’s idea of showing a “gotcha” video of the allegedly permanently injured plaintiff carrying a large, heavy box backfired when the jury was shown by the plaintiff that the box actually contained ice cream cones and weighed very little.
Prior to trial, the plaintiff offered to settle for $1 million. On the first day of trial, they lowered that amount to $750,000, yet the defense attorney did not settle the case, and it proceeded to a jury verdict. The jury awarded the plaintiff over $4 million — well in excess of Dr. D’s policy limits.
The Follow-up
Dr. D was horrified, but the insurance company claims representative said the insurer would promptly offer $2 million in available insurance coverage to settle the case post verdict. This did not happen. Instead, the insurer chose to appeal the verdict against Dr. D’s wishes.
Ultimately, Dr. D was forced to hire his own lawyer. He ultimately sued the insurance company for breach of contract and bad faith.
The insurance company eventually attempted to settle with the plaintiffs’ counsel, but the plaintiff refused to accept the available insurance coverage. The insurance carrier still has not posted the entire appeal bond. The case is still pending.
Protecting Yourself
The lesson from Dr. D’s experience: Understand that the insurance company is not your friend. It’s a business looking out for its own interests.
The plaintiff’s attorney was absolutely correct in suggesting that Dr. D retain his own attorney to represent his own interests. You should hire your own lawyer when:
- You disagree with your insurer on how to proceed in a case.
- You receive a demand that exceeds your available insurance coverage or for damages that may not be covered by your policy, such as punitive damages.
- Your insurance carrier attempts to deny insurance coverage for your claim or sends you a letter stating that it is “reserving its rights” not to cover or to limit coverage for your claim.
Retaining independent counsel protects your interests, not those of your insurance company.
Independent counsel can give you a second opinion on the strengths and weaknesses of your claim, help you prepare for your deposition, and attend court dates with you to ensure that you are completely protected.
Independent counsel can challenge your insurance company’s decision to deny or limit your insurance coverage and ensure that you receive all of the benefits to which you are entitled under your insurance policy. Some policies may include an independent lawyer to be paid for by your insurance carrier in case of a conflicts.
The most important takeaway? Your medical malpractice insurance carrier is not your friend, so act accordingly in times of conflict.
A version of this article first appeared on Medscape.com.
You’ve been sued for medical malpractice. If you are a physician in the United States, that is not an unlikely scenario.
An analysis by the American Medical Association shows that almost half of all physicians are sued by the time they reach 54. In some specialties, such as ob.gyn., one is almost guaranteed to be sued at some point.
But that’s what medical malpractice insurance is for, right? Your medical malpractice insurer will assign an attorney to take care of you and help you through this situation. Won’t they?
Maybe so, but the attorney and the claims representative your insurer assigns to your case may have a different idea about how to proceed than you do. Though the defense attorney assigned to you represents you, he or she gets paid by the insurance carrier.
This can create a conflict when your defense counsel and your insurance claims representative aim to take your case in a direction you don’t like.
Disagreements might include:
- Choice of expert witnesses
- Tactical decisions related to trial strategy
- Public relations considerations
- Admissions of liability
- Allocation of resources
To Settle or Not?
One of the most challenging — and common — disagreements is whether to settle the case.
Sometimes a malpractice insurer wants to settle the case against the defendant doctor’s wishes. Or the doctor wants to settle but is pushed into going to trial. In the following case, one doctor had to face the consequences of a decision he didn’t even make.
The Underlying Medical Malpractice Case
Dr. D was sued by a patient who had allegedly called Dr. D’s office six times in 2 days complaining of intermittent chest pain.
Dr. D had been swamped with patients and couldn’t squeeze this patient in for an office visit, but he did call back. The patient later claimed that during the call he told the doctor he was suffering from chest pain. The doctor recalled that the patient had complained of abdominal discomfort that began after he had exercised.
The physician wrote a prescription for an ECG at the local hospital and called to ensure that the patient could just walk in. The ECG was allegedly abnormal but was not read as representing an impending or current heart attack. Later that evening, however, the patient went to the emergency department of another hospital where it was confirmed that he had suffered a heart attack. The patient underwent cardiac catheterization and stent placement to address a blockage in his left anterior descending artery.
The patient subsequently sued Dr. D and the hospital where he had the original ECG. Dr. D contacted his medical malpractice insurance company. The insurance company assigned an attorney to represent Dr. D. Discovery in the case began.
The plaintiff’s own medical expert testified in a deposition that there was no way for the heart attack to have been prevented and that the treatment would have been the same either way. But Dr. D could not find a record of the phone calls with the patient, and he had not noted his conversation the patient in their medical records.
Dr. D held a policy for $1 million, and his state had a fund that would kick in an additional $1 million. But the plaintiffs demanded $4 million to settle.
A month before trial, the plaintiff’s attorney sent a threatening letter to Dr. D’s attorney warning him that Dr. D was underinsured and suggesting that it would be in the physician’s best interests to settle.
“I want to stress to you that it is not my desire to harm your client’s reputation or to destroy his business,” wrote the plaintiff’s attorney. “However, now is the time to avoid consequences such as these by making a good faith effort to get this case resolved.”
The letter went on to note that the defense attorney should give Dr. D a copy of the letter so that everyone would be aware of the potential consequences of an award against Dr. D in excess of his limits of insurance coverage. The plaintiff’s attorney even suggested that Dr. D should retain personal counsel.
Dr. D’s defense attorney downplayed the letter and assured him that there was no reason to worry.
Meanwhile the case inched closer to trial.
The codefendant hospital settled with the plaintiff on the night before jury selection, leaving Dr. D in the uncomfortable position of being the only defendant in the case. At this point, Dr. D decided he would like to settle, and he sent his attorney an email telling him so. But the attorney instead referred him to an insurance company claims.
Just days before the trial was to start, Dr. D repeatedly told the claims representative assigned to his claim that he did not want to go to trial but rather wanted to settle. The representative told Dr. D that he had no choice in whether the action settled.
A committee at the insurance company had decided to proceed with the trial rather than settle.
The trial proved a painful debacle for Dr. D. His attorney’s idea of showing a “gotcha” video of the allegedly permanently injured plaintiff carrying a large, heavy box backfired when the jury was shown by the plaintiff that the box actually contained ice cream cones and weighed very little.
Prior to trial, the plaintiff offered to settle for $1 million. On the first day of trial, they lowered that amount to $750,000, yet the defense attorney did not settle the case, and it proceeded to a jury verdict. The jury awarded the plaintiff over $4 million — well in excess of Dr. D’s policy limits.
The Follow-up
Dr. D was horrified, but the insurance company claims representative said the insurer would promptly offer $2 million in available insurance coverage to settle the case post verdict. This did not happen. Instead, the insurer chose to appeal the verdict against Dr. D’s wishes.
Ultimately, Dr. D was forced to hire his own lawyer. He ultimately sued the insurance company for breach of contract and bad faith.
The insurance company eventually attempted to settle with the plaintiffs’ counsel, but the plaintiff refused to accept the available insurance coverage. The insurance carrier still has not posted the entire appeal bond. The case is still pending.
Protecting Yourself
The lesson from Dr. D’s experience: Understand that the insurance company is not your friend. It’s a business looking out for its own interests.
The plaintiff’s attorney was absolutely correct in suggesting that Dr. D retain his own attorney to represent his own interests. You should hire your own lawyer when:
- You disagree with your insurer on how to proceed in a case.
- You receive a demand that exceeds your available insurance coverage or for damages that may not be covered by your policy, such as punitive damages.
- Your insurance carrier attempts to deny insurance coverage for your claim or sends you a letter stating that it is “reserving its rights” not to cover or to limit coverage for your claim.
Retaining independent counsel protects your interests, not those of your insurance company.
Independent counsel can give you a second opinion on the strengths and weaknesses of your claim, help you prepare for your deposition, and attend court dates with you to ensure that you are completely protected.
Independent counsel can challenge your insurance company’s decision to deny or limit your insurance coverage and ensure that you receive all of the benefits to which you are entitled under your insurance policy. Some policies may include an independent lawyer to be paid for by your insurance carrier in case of a conflicts.
The most important takeaway? Your medical malpractice insurance carrier is not your friend, so act accordingly in times of conflict.
A version of this article first appeared on Medscape.com.
‘Reform School’ for Pharmacy Benefit Managers: How Might Legislation Help Patients?
The term “reform school” is a bit outdated. It used to refer to institutions where young offenders were sent instead of prison. Some argue that pharmacy benefit managers (PBMs) should bypass reform school and go straight to prison. “PBM reform” has become a ubiquitous term, encompassing any legislative or regulatory efforts aimed at curbing PBMs’ bad behavior. When discussing PBM reform, it’s crucial to understand the various segments of the healthcare system affected by PBMs. This complexity often makes it challenging to determine what these reform packages would actually achieve and who they would benefit.
Pharmacists have long been vocal critics of PBMs, and while their issues are extremely important, it is essential to remember that the ultimate victims of PBM misconduct, in terms of access to care, are patients. At some point, we will all be patients, making this issue universally relevant. It has been quite challenging to follow federal legislation on this topic as these packages attempt to address a number of bad behaviors by PBMs affecting a variety of victims. This discussion will examine those reforms that would directly improve patient’s access to available and affordable medications.
Policy Categories of PBM Reform
There are five policy categories of PBM reform legislation overall, including three that have the greatest potential to directly address patient needs. The first is patient access to medications (utilization management, copay assistance, prior authorization, etc.), followed by delinking drug list prices from PBM income and pass-through of price concessions from the manufacturer. The remaining two categories involve transparency and pharmacy-facing reform, both of which are very important. However, this discussion will revolve around the first three categories. It should be noted that many of the legislation packages addressing the categories of patient access, delinking, and pass-through also include transparency issues, particularly as they relate to pharmacy-facing issues.
Patient Access to Medications — Step Therapy Legislation
One of the major obstacles to patient access to medications is the use of PBM utilization management tools such as step therapy (“fail first”), prior authorizations, nonmedical switching, and formulary exclusions. These tools dictate when patients can obtain necessary medications and for how long patients who are stable on their current treatments can remain on them.
While many states have enacted step therapy reforms to prevent stable patients from being whip-sawed between medications that maximize PBM profits (often labeled as “savings”), these state protections apply only to state-regulated health plans. These include fully insured health plans and those offered through the Affordable Care Act’s Health Insurance Marketplace. It also includes state employees, state corrections, and, in some cases, state labor unions. State legislation does not extend to patients covered by employer self-insured health plans, called ERISA plans for the federal law that governs employee benefit plans, the Employee Retirement Income Security Act. These ERISA plans include nearly 35 million people nationwide.
This is where the Safe Step Act (S.652/H.R.2630) becomes crucial, as it allows employees to request exceptions to harmful fail-first protocols. The bill has gained significant momentum, having been reported out of the Senate HELP Committee and discussed in House markups. The Safe Step Act would mandate that an exception to a step therapy protocol must be granted if:
- The required treatment has been ineffective
- The treatment is expected to be ineffective, and delaying effective treatment would lead to irreversible consequences
- The treatment will cause or is likely to cause an adverse reaction
- The treatment is expected to prevent the individual from performing daily activities or occupational responsibilities
- The individual is stable on their current prescription drugs
- There are other circumstances as determined by the Employee Benefits Security Administration
This legislation is vital for ensuring that patients have timely access to the medications they need without unnecessary delays or disruptions.
Patient Access to Medications — Prior Authorizations
Another significant issue affecting patient access to medications is prior authorizations (PAs). According to an American Medical Association survey, nearly one in four physicians (24%) report that a PA has led to a serious adverse event for a patient in their care. In rheumatology, PAs often result in delays in care (even for those initially approved) and a significant increase in steroid usage. In particular, PAs in Medicare Advantage (MA) plans are harmful to Medicare beneficiaries.
The Improving Seniors’ Timely Access to Care Act (H.R.8702 / S.4532) aims to reform PAs used in MA plans, making the process more efficient and transparent to improve access to care for seniors. Unfortunately, it does not cover Part D drugs and may only cover Part B drugs depending on the MA plan’s benefit package. Here are the key provisions of the act:
- Electronic PA: Implementing real-time decisions for routinely approved items and services.
- Transparency: Requiring annual publication of PA information, such as the percentage of requests approved and the average response time.
- Quality and Timeliness Standards: The Centers for Medicare & Medicaid Services (CMS) will set standards for the quality and timeliness of PA determinations.
- Streamlining Approvals: Simplifying the approval process and reducing the time allowed for health plans to consider PA requests.
This bill passed the House in September 2022 but stalled in the Senate because of an unfavorable Congressional Budget Office score. CMS has since finalized portions of this bill via regulation, zeroing out the CBO score and increasing the chances of its passage.
Delinking Drug Prices from PBM Income and Pass-Through of Price Concessions
Affordability is a crucial aspect of accessibility, especially when it comes to medications. Over the years, we’ve learned that PBMs often favor placing the highest list price drugs on formularies because the rebates and various fees they receive from manufacturers are based on a percentage of the list price. In other words, the higher the medication’s price, the more money the PBM makes.
This practice is evident in both commercial and government formularies, where brand-name drugs are often preferred, while lower-priced generics are either excluded or placed on higher tiers. As a result, while major PBMs benefit from these rebates and fees, patients continue to pay their cost share based on the list price of the medication.
To improve the affordability of medications, a key aspect of PBM reform should be to disincentivize PBMs from selecting higher-priced medications and/or require the pass-through of manufacturer price concessions to patients.
Several major PBM reform bills are currently being considered that address either the delinking of price concessions from the list price of the drug or some form of pass-through of these concessions. These reforms are essential to ensure that patients can access affordable medications without being burdened by inflated costs.
The legislation includes the Pharmacy Benefit Manager Reform Act (S.1339); the Modernizing & Ensuring PBM Accountability Act (S.2973); the Better Mental Health Care, Lower Cost Drugs, and Extenders Act (S.3430); the Protecting Patients Against PBM Abuses Act (H.R. 2880); the DRUG Act (S.2474 / H.R.6283); and the Share the Savings with Seniors Act (S.2474 / H.R.5376).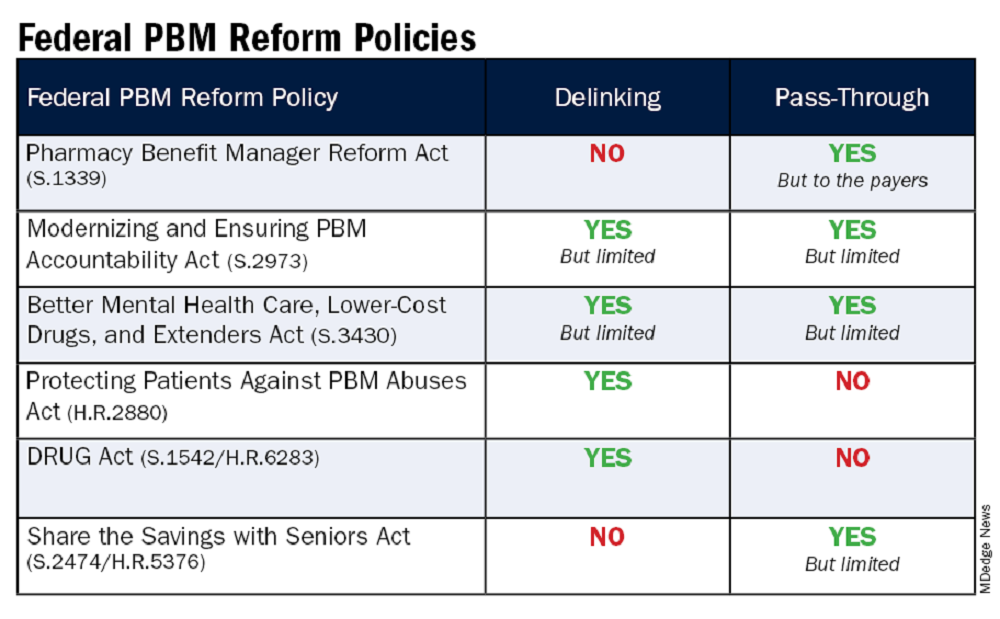
As with all legislation, there are limitations and compromises in each of these. However, these bills are a good first step in addressing PBM remuneration (rebates and fees) based on the list price of the drug and/or passing through to the patient the benefit of manufacturer price concessions. By focusing on key areas like utilization management, delinking drug prices from PBM income, and allowing patients to directly benefit from manufacturer price concessions, we can work toward a more equitable and efficient healthcare system. Reigning in PBM bad behavior is a challenge, but the potential benefits for patient care and access make it a crucial fight worth pursuing.
Please help in efforts to improve patients’ access to available and affordable medications by contacting your representatives in Congress to impart to them the importance of passing legislation. The CSRO’s legislative map tool can help to inform you of the latest information on these and other bills and assist you in engaging with your representatives on them.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of Advocacy and Government Affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. She has no relevant conflicts of interest to disclose. You can reach her at [email protected].
The term “reform school” is a bit outdated. It used to refer to institutions where young offenders were sent instead of prison. Some argue that pharmacy benefit managers (PBMs) should bypass reform school and go straight to prison. “PBM reform” has become a ubiquitous term, encompassing any legislative or regulatory efforts aimed at curbing PBMs’ bad behavior. When discussing PBM reform, it’s crucial to understand the various segments of the healthcare system affected by PBMs. This complexity often makes it challenging to determine what these reform packages would actually achieve and who they would benefit.
Pharmacists have long been vocal critics of PBMs, and while their issues are extremely important, it is essential to remember that the ultimate victims of PBM misconduct, in terms of access to care, are patients. At some point, we will all be patients, making this issue universally relevant. It has been quite challenging to follow federal legislation on this topic as these packages attempt to address a number of bad behaviors by PBMs affecting a variety of victims. This discussion will examine those reforms that would directly improve patient’s access to available and affordable medications.
Policy Categories of PBM Reform
There are five policy categories of PBM reform legislation overall, including three that have the greatest potential to directly address patient needs. The first is patient access to medications (utilization management, copay assistance, prior authorization, etc.), followed by delinking drug list prices from PBM income and pass-through of price concessions from the manufacturer. The remaining two categories involve transparency and pharmacy-facing reform, both of which are very important. However, this discussion will revolve around the first three categories. It should be noted that many of the legislation packages addressing the categories of patient access, delinking, and pass-through also include transparency issues, particularly as they relate to pharmacy-facing issues.
Patient Access to Medications — Step Therapy Legislation
One of the major obstacles to patient access to medications is the use of PBM utilization management tools such as step therapy (“fail first”), prior authorizations, nonmedical switching, and formulary exclusions. These tools dictate when patients can obtain necessary medications and for how long patients who are stable on their current treatments can remain on them.
While many states have enacted step therapy reforms to prevent stable patients from being whip-sawed between medications that maximize PBM profits (often labeled as “savings”), these state protections apply only to state-regulated health plans. These include fully insured health plans and those offered through the Affordable Care Act’s Health Insurance Marketplace. It also includes state employees, state corrections, and, in some cases, state labor unions. State legislation does not extend to patients covered by employer self-insured health plans, called ERISA plans for the federal law that governs employee benefit plans, the Employee Retirement Income Security Act. These ERISA plans include nearly 35 million people nationwide.
This is where the Safe Step Act (S.652/H.R.2630) becomes crucial, as it allows employees to request exceptions to harmful fail-first protocols. The bill has gained significant momentum, having been reported out of the Senate HELP Committee and discussed in House markups. The Safe Step Act would mandate that an exception to a step therapy protocol must be granted if:
- The required treatment has been ineffective
- The treatment is expected to be ineffective, and delaying effective treatment would lead to irreversible consequences
- The treatment will cause or is likely to cause an adverse reaction
- The treatment is expected to prevent the individual from performing daily activities or occupational responsibilities
- The individual is stable on their current prescription drugs
- There are other circumstances as determined by the Employee Benefits Security Administration
This legislation is vital for ensuring that patients have timely access to the medications they need without unnecessary delays or disruptions.
Patient Access to Medications — Prior Authorizations
Another significant issue affecting patient access to medications is prior authorizations (PAs). According to an American Medical Association survey, nearly one in four physicians (24%) report that a PA has led to a serious adverse event for a patient in their care. In rheumatology, PAs often result in delays in care (even for those initially approved) and a significant increase in steroid usage. In particular, PAs in Medicare Advantage (MA) plans are harmful to Medicare beneficiaries.
The Improving Seniors’ Timely Access to Care Act (H.R.8702 / S.4532) aims to reform PAs used in MA plans, making the process more efficient and transparent to improve access to care for seniors. Unfortunately, it does not cover Part D drugs and may only cover Part B drugs depending on the MA plan’s benefit package. Here are the key provisions of the act:
- Electronic PA: Implementing real-time decisions for routinely approved items and services.
- Transparency: Requiring annual publication of PA information, such as the percentage of requests approved and the average response time.
- Quality and Timeliness Standards: The Centers for Medicare & Medicaid Services (CMS) will set standards for the quality and timeliness of PA determinations.
- Streamlining Approvals: Simplifying the approval process and reducing the time allowed for health plans to consider PA requests.
This bill passed the House in September 2022 but stalled in the Senate because of an unfavorable Congressional Budget Office score. CMS has since finalized portions of this bill via regulation, zeroing out the CBO score and increasing the chances of its passage.
Delinking Drug Prices from PBM Income and Pass-Through of Price Concessions
Affordability is a crucial aspect of accessibility, especially when it comes to medications. Over the years, we’ve learned that PBMs often favor placing the highest list price drugs on formularies because the rebates and various fees they receive from manufacturers are based on a percentage of the list price. In other words, the higher the medication’s price, the more money the PBM makes.
This practice is evident in both commercial and government formularies, where brand-name drugs are often preferred, while lower-priced generics are either excluded or placed on higher tiers. As a result, while major PBMs benefit from these rebates and fees, patients continue to pay their cost share based on the list price of the medication.
To improve the affordability of medications, a key aspect of PBM reform should be to disincentivize PBMs from selecting higher-priced medications and/or require the pass-through of manufacturer price concessions to patients.
Several major PBM reform bills are currently being considered that address either the delinking of price concessions from the list price of the drug or some form of pass-through of these concessions. These reforms are essential to ensure that patients can access affordable medications without being burdened by inflated costs.
The legislation includes the Pharmacy Benefit Manager Reform Act (S.1339); the Modernizing & Ensuring PBM Accountability Act (S.2973); the Better Mental Health Care, Lower Cost Drugs, and Extenders Act (S.3430); the Protecting Patients Against PBM Abuses Act (H.R. 2880); the DRUG Act (S.2474 / H.R.6283); and the Share the Savings with Seniors Act (S.2474 / H.R.5376).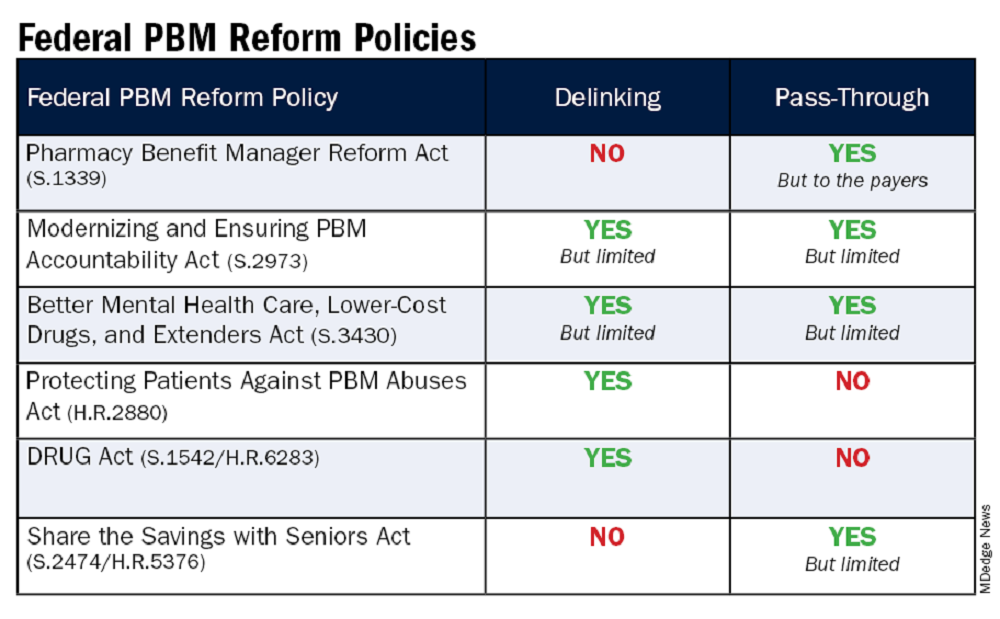
As with all legislation, there are limitations and compromises in each of these. However, these bills are a good first step in addressing PBM remuneration (rebates and fees) based on the list price of the drug and/or passing through to the patient the benefit of manufacturer price concessions. By focusing on key areas like utilization management, delinking drug prices from PBM income, and allowing patients to directly benefit from manufacturer price concessions, we can work toward a more equitable and efficient healthcare system. Reigning in PBM bad behavior is a challenge, but the potential benefits for patient care and access make it a crucial fight worth pursuing.
Please help in efforts to improve patients’ access to available and affordable medications by contacting your representatives in Congress to impart to them the importance of passing legislation. The CSRO’s legislative map tool can help to inform you of the latest information on these and other bills and assist you in engaging with your representatives on them.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of Advocacy and Government Affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. She has no relevant conflicts of interest to disclose. You can reach her at [email protected].
The term “reform school” is a bit outdated. It used to refer to institutions where young offenders were sent instead of prison. Some argue that pharmacy benefit managers (PBMs) should bypass reform school and go straight to prison. “PBM reform” has become a ubiquitous term, encompassing any legislative or regulatory efforts aimed at curbing PBMs’ bad behavior. When discussing PBM reform, it’s crucial to understand the various segments of the healthcare system affected by PBMs. This complexity often makes it challenging to determine what these reform packages would actually achieve and who they would benefit.
Pharmacists have long been vocal critics of PBMs, and while their issues are extremely important, it is essential to remember that the ultimate victims of PBM misconduct, in terms of access to care, are patients. At some point, we will all be patients, making this issue universally relevant. It has been quite challenging to follow federal legislation on this topic as these packages attempt to address a number of bad behaviors by PBMs affecting a variety of victims. This discussion will examine those reforms that would directly improve patient’s access to available and affordable medications.
Policy Categories of PBM Reform
There are five policy categories of PBM reform legislation overall, including three that have the greatest potential to directly address patient needs. The first is patient access to medications (utilization management, copay assistance, prior authorization, etc.), followed by delinking drug list prices from PBM income and pass-through of price concessions from the manufacturer. The remaining two categories involve transparency and pharmacy-facing reform, both of which are very important. However, this discussion will revolve around the first three categories. It should be noted that many of the legislation packages addressing the categories of patient access, delinking, and pass-through also include transparency issues, particularly as they relate to pharmacy-facing issues.
Patient Access to Medications — Step Therapy Legislation
One of the major obstacles to patient access to medications is the use of PBM utilization management tools such as step therapy (“fail first”), prior authorizations, nonmedical switching, and formulary exclusions. These tools dictate when patients can obtain necessary medications and for how long patients who are stable on their current treatments can remain on them.
While many states have enacted step therapy reforms to prevent stable patients from being whip-sawed between medications that maximize PBM profits (often labeled as “savings”), these state protections apply only to state-regulated health plans. These include fully insured health plans and those offered through the Affordable Care Act’s Health Insurance Marketplace. It also includes state employees, state corrections, and, in some cases, state labor unions. State legislation does not extend to patients covered by employer self-insured health plans, called ERISA plans for the federal law that governs employee benefit plans, the Employee Retirement Income Security Act. These ERISA plans include nearly 35 million people nationwide.
This is where the Safe Step Act (S.652/H.R.2630) becomes crucial, as it allows employees to request exceptions to harmful fail-first protocols. The bill has gained significant momentum, having been reported out of the Senate HELP Committee and discussed in House markups. The Safe Step Act would mandate that an exception to a step therapy protocol must be granted if:
- The required treatment has been ineffective
- The treatment is expected to be ineffective, and delaying effective treatment would lead to irreversible consequences
- The treatment will cause or is likely to cause an adverse reaction
- The treatment is expected to prevent the individual from performing daily activities or occupational responsibilities
- The individual is stable on their current prescription drugs
- There are other circumstances as determined by the Employee Benefits Security Administration
This legislation is vital for ensuring that patients have timely access to the medications they need without unnecessary delays or disruptions.
Patient Access to Medications — Prior Authorizations
Another significant issue affecting patient access to medications is prior authorizations (PAs). According to an American Medical Association survey, nearly one in four physicians (24%) report that a PA has led to a serious adverse event for a patient in their care. In rheumatology, PAs often result in delays in care (even for those initially approved) and a significant increase in steroid usage. In particular, PAs in Medicare Advantage (MA) plans are harmful to Medicare beneficiaries.
The Improving Seniors’ Timely Access to Care Act (H.R.8702 / S.4532) aims to reform PAs used in MA plans, making the process more efficient and transparent to improve access to care for seniors. Unfortunately, it does not cover Part D drugs and may only cover Part B drugs depending on the MA plan’s benefit package. Here are the key provisions of the act:
- Electronic PA: Implementing real-time decisions for routinely approved items and services.
- Transparency: Requiring annual publication of PA information, such as the percentage of requests approved and the average response time.
- Quality and Timeliness Standards: The Centers for Medicare & Medicaid Services (CMS) will set standards for the quality and timeliness of PA determinations.
- Streamlining Approvals: Simplifying the approval process and reducing the time allowed for health plans to consider PA requests.
This bill passed the House in September 2022 but stalled in the Senate because of an unfavorable Congressional Budget Office score. CMS has since finalized portions of this bill via regulation, zeroing out the CBO score and increasing the chances of its passage.
Delinking Drug Prices from PBM Income and Pass-Through of Price Concessions
Affordability is a crucial aspect of accessibility, especially when it comes to medications. Over the years, we’ve learned that PBMs often favor placing the highest list price drugs on formularies because the rebates and various fees they receive from manufacturers are based on a percentage of the list price. In other words, the higher the medication’s price, the more money the PBM makes.
This practice is evident in both commercial and government formularies, where brand-name drugs are often preferred, while lower-priced generics are either excluded or placed on higher tiers. As a result, while major PBMs benefit from these rebates and fees, patients continue to pay their cost share based on the list price of the medication.
To improve the affordability of medications, a key aspect of PBM reform should be to disincentivize PBMs from selecting higher-priced medications and/or require the pass-through of manufacturer price concessions to patients.
Several major PBM reform bills are currently being considered that address either the delinking of price concessions from the list price of the drug or some form of pass-through of these concessions. These reforms are essential to ensure that patients can access affordable medications without being burdened by inflated costs.
The legislation includes the Pharmacy Benefit Manager Reform Act (S.1339); the Modernizing & Ensuring PBM Accountability Act (S.2973); the Better Mental Health Care, Lower Cost Drugs, and Extenders Act (S.3430); the Protecting Patients Against PBM Abuses Act (H.R. 2880); the DRUG Act (S.2474 / H.R.6283); and the Share the Savings with Seniors Act (S.2474 / H.R.5376).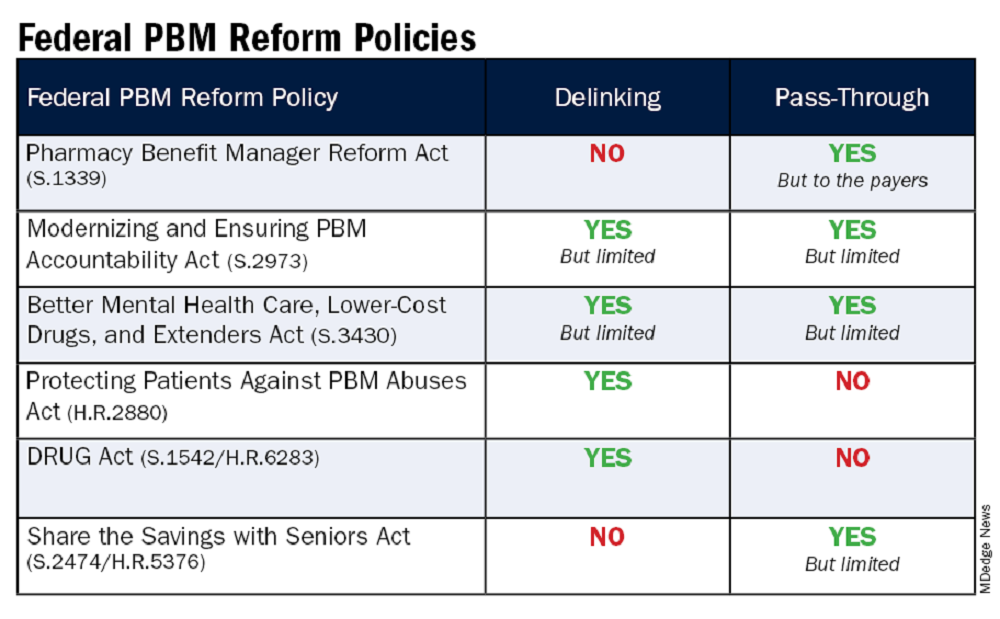
As with all legislation, there are limitations and compromises in each of these. However, these bills are a good first step in addressing PBM remuneration (rebates and fees) based on the list price of the drug and/or passing through to the patient the benefit of manufacturer price concessions. By focusing on key areas like utilization management, delinking drug prices from PBM income, and allowing patients to directly benefit from manufacturer price concessions, we can work toward a more equitable and efficient healthcare system. Reigning in PBM bad behavior is a challenge, but the potential benefits for patient care and access make it a crucial fight worth pursuing.
Please help in efforts to improve patients’ access to available and affordable medications by contacting your representatives in Congress to impart to them the importance of passing legislation. The CSRO’s legislative map tool can help to inform you of the latest information on these and other bills and assist you in engaging with your representatives on them.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of Advocacy and Government Affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. She has no relevant conflicts of interest to disclose. You can reach her at [email protected].
AI-Powered Clinical Documentation Tool Reduces EHR Time for Clinicians
TOPLINE:
An artificial intelligence (AI)-powered clinical documentation tool helped reduce time spent on electronic health records (EHR) at home for almost 48% physicians, and nearly 45% reported less weekly time spent on EHR tasks outside of normal work hours.
METHODOLOGY:
- Researchers recruited 112 clinicians from family medicine, internal medicine, and general pediatrics in North Carolina and Georgia.
- Patients were divided into an intervention group (n = 85) and control group (n = 55), with the intervention group receiving a 1-hour training program on a commercially available AI tool.
- A seven-question survey was administered to participants before and 5 weeks after the intervention to evaluate their experience.
TAKEAWAY:
- The researchers found 47.1% of clinicians in the intervention group reported spending less time on the EHR at home compared with 14.5% in the control group (P < .001); 44.7% reported decreased weekly time on the EHR outside normal work hours compared with 20% in the control group (P = .003).
- The study revealed 43.5% of physicians who used the AI instrument reported spending less time on documentation after visits compared with 18.2% in the control group (P = .002).
- Further, 44.7% reported less frustration when using the EHR compared with 14.5% in the control group (P < .001).
IN PRACTICE:
“Approximately half of clinicians using the AI-powered clinical documentation tool based on interest reported a positive outcome, potentially reducing burnout. However, a significant subset did not find time-saving benefits or improved EHR experience,” the authors of the study wrote.
SOURCE:
The study was led by Tsai-Ling Liu, PhD, Center for Health System Sciences, Atrium Health in Charlotte, North Carolina. It was published online in JAMA Network Open.
LIMITATIONS:
The researchers reported potential selection and recall bias in both groups. Additional research is needed to find areas of improvement and assess the effects on clinician groups and health systems, they said.
DISCLOSURES:
Andrew McWilliams, MD, MPH, reported receiving grants from the Agency for Healthcare Research Quality, the National Institutes of Health, and the Duke Endowment unrelated to this work. Ajay Dharod, MD, reported his role as an electronic health record consultant for the Association of American Medical College CORE program. Jeffrey Cleveland, MD, disclosed his participation on the Executive Client Council, a noncompensated advisory group, for Nuance/Microsoft.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
An artificial intelligence (AI)-powered clinical documentation tool helped reduce time spent on electronic health records (EHR) at home for almost 48% physicians, and nearly 45% reported less weekly time spent on EHR tasks outside of normal work hours.
METHODOLOGY:
- Researchers recruited 112 clinicians from family medicine, internal medicine, and general pediatrics in North Carolina and Georgia.
- Patients were divided into an intervention group (n = 85) and control group (n = 55), with the intervention group receiving a 1-hour training program on a commercially available AI tool.
- A seven-question survey was administered to participants before and 5 weeks after the intervention to evaluate their experience.
TAKEAWAY:
- The researchers found 47.1% of clinicians in the intervention group reported spending less time on the EHR at home compared with 14.5% in the control group (P < .001); 44.7% reported decreased weekly time on the EHR outside normal work hours compared with 20% in the control group (P = .003).
- The study revealed 43.5% of physicians who used the AI instrument reported spending less time on documentation after visits compared with 18.2% in the control group (P = .002).
- Further, 44.7% reported less frustration when using the EHR compared with 14.5% in the control group (P < .001).
IN PRACTICE:
“Approximately half of clinicians using the AI-powered clinical documentation tool based on interest reported a positive outcome, potentially reducing burnout. However, a significant subset did not find time-saving benefits or improved EHR experience,” the authors of the study wrote.
SOURCE:
The study was led by Tsai-Ling Liu, PhD, Center for Health System Sciences, Atrium Health in Charlotte, North Carolina. It was published online in JAMA Network Open.
LIMITATIONS:
The researchers reported potential selection and recall bias in both groups. Additional research is needed to find areas of improvement and assess the effects on clinician groups and health systems, they said.
DISCLOSURES:
Andrew McWilliams, MD, MPH, reported receiving grants from the Agency for Healthcare Research Quality, the National Institutes of Health, and the Duke Endowment unrelated to this work. Ajay Dharod, MD, reported his role as an electronic health record consultant for the Association of American Medical College CORE program. Jeffrey Cleveland, MD, disclosed his participation on the Executive Client Council, a noncompensated advisory group, for Nuance/Microsoft.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
An artificial intelligence (AI)-powered clinical documentation tool helped reduce time spent on electronic health records (EHR) at home for almost 48% physicians, and nearly 45% reported less weekly time spent on EHR tasks outside of normal work hours.
METHODOLOGY:
- Researchers recruited 112 clinicians from family medicine, internal medicine, and general pediatrics in North Carolina and Georgia.
- Patients were divided into an intervention group (n = 85) and control group (n = 55), with the intervention group receiving a 1-hour training program on a commercially available AI tool.
- A seven-question survey was administered to participants before and 5 weeks after the intervention to evaluate their experience.
TAKEAWAY:
- The researchers found 47.1% of clinicians in the intervention group reported spending less time on the EHR at home compared with 14.5% in the control group (P < .001); 44.7% reported decreased weekly time on the EHR outside normal work hours compared with 20% in the control group (P = .003).
- The study revealed 43.5% of physicians who used the AI instrument reported spending less time on documentation after visits compared with 18.2% in the control group (P = .002).
- Further, 44.7% reported less frustration when using the EHR compared with 14.5% in the control group (P < .001).
IN PRACTICE:
“Approximately half of clinicians using the AI-powered clinical documentation tool based on interest reported a positive outcome, potentially reducing burnout. However, a significant subset did not find time-saving benefits or improved EHR experience,” the authors of the study wrote.
SOURCE:
The study was led by Tsai-Ling Liu, PhD, Center for Health System Sciences, Atrium Health in Charlotte, North Carolina. It was published online in JAMA Network Open.
LIMITATIONS:
The researchers reported potential selection and recall bias in both groups. Additional research is needed to find areas of improvement and assess the effects on clinician groups and health systems, they said.
DISCLOSURES:
Andrew McWilliams, MD, MPH, reported receiving grants from the Agency for Healthcare Research Quality, the National Institutes of Health, and the Duke Endowment unrelated to this work. Ajay Dharod, MD, reported his role as an electronic health record consultant for the Association of American Medical College CORE program. Jeffrey Cleveland, MD, disclosed his participation on the Executive Client Council, a noncompensated advisory group, for Nuance/Microsoft.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Study Reports Safety Data in Children on JAK Inhibitors
TOPLINE:
which also found that acne was the most common skin-related AE in children, and serious AEs were less common.
METHODOLOGY:
- Researchers analyzed 399,649 AEs in 133,216 adult patients and 2883 AEs in 955 pediatric patients (age, < 18 years) from November 2011 to February 2023 using the US Food and Drug Administration Adverse Event Reporting System and the Canada Vigilance Adverse Reaction Online Database.
- AEs were categorized on the basis of the Medical Dictionary for Regulatory Activities system organ class.
- Five JAK inhibitors approved for use in children were included in the study: Baricitinib, upadacitinib, abrocitinib, ruxolitinib, and tofacitinib.
TAKEAWAY:
- The most frequently reported AEs in children were blood and lymphatic system disorders, including neutropenia, thrombocytopenia, and anemia (24%); viral, fungal, and bacterial infections, such as pneumonia and sepsis (17.2%); constitutional symptoms and administrative concerns, including pyrexia and fatigue (15.7%); gastrointestinal disorders, such as vomiting and abdominal pain (13.6%); and respiratory disorders, such as cough and respiratory distress (5.3%).
- In adults, the most common AEs were viral, fungal, and bacterial infections (16.8%); constitutional symptoms and administrative concerns (13.5%); musculoskeletal and connective tissue disorders (7.04%); and gastrointestinal (5.8%) and nervous system (5%) disorders.
- Acne (30.6%), atopic dermatitis (22.2%), and psoriasis (16.7%) were the most common skin and subcutaneous tissue AEs reported in children. Skin and subcutaneous AEs were more common with upadacitinib (21.1%), abrocitinib (9.1%), and tofacitinib (6.3%) in children.
- Serious AEs included in the boxed warning for JAK inhibitors — serious infection, mortality, malignancy, cardiovascular events, and thrombosis — were similar for baricitinib in children (4 of 49 patients, 8.2%) and adults (325 of 3707, 8.8%). For other JAK inhibitors, absolute numbers of these AEs in children were small and rates were lower in children than in adults.
IN PRACTICE:
“This information can support customized treatment and minimize the potential for undesired or intolerable AEs,” the authors wrote.
SOURCE:
This study was led by Sahithi Talasila, BS, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and was published online in Pediatric Dermatology.
LIMITATIONS:
Pharmacovigilance registries did not fully capture the complete range of AEs because of potential reporting bias or recall bias. Additionally, events lacking sufficient objective evidence were underreported, while common AEs associated with JAK inhibitor therapy were overreported.
DISCLOSURES:
No specific funding sources for the study were reported. One author reported being a consultant, one reported serving as a principal investigator in clinical trials, and another reported serving on data and safety monitoring boards of various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
which also found that acne was the most common skin-related AE in children, and serious AEs were less common.
METHODOLOGY:
- Researchers analyzed 399,649 AEs in 133,216 adult patients and 2883 AEs in 955 pediatric patients (age, < 18 years) from November 2011 to February 2023 using the US Food and Drug Administration Adverse Event Reporting System and the Canada Vigilance Adverse Reaction Online Database.
- AEs were categorized on the basis of the Medical Dictionary for Regulatory Activities system organ class.
- Five JAK inhibitors approved for use in children were included in the study: Baricitinib, upadacitinib, abrocitinib, ruxolitinib, and tofacitinib.
TAKEAWAY:
- The most frequently reported AEs in children were blood and lymphatic system disorders, including neutropenia, thrombocytopenia, and anemia (24%); viral, fungal, and bacterial infections, such as pneumonia and sepsis (17.2%); constitutional symptoms and administrative concerns, including pyrexia and fatigue (15.7%); gastrointestinal disorders, such as vomiting and abdominal pain (13.6%); and respiratory disorders, such as cough and respiratory distress (5.3%).
- In adults, the most common AEs were viral, fungal, and bacterial infections (16.8%); constitutional symptoms and administrative concerns (13.5%); musculoskeletal and connective tissue disorders (7.04%); and gastrointestinal (5.8%) and nervous system (5%) disorders.
- Acne (30.6%), atopic dermatitis (22.2%), and psoriasis (16.7%) were the most common skin and subcutaneous tissue AEs reported in children. Skin and subcutaneous AEs were more common with upadacitinib (21.1%), abrocitinib (9.1%), and tofacitinib (6.3%) in children.
- Serious AEs included in the boxed warning for JAK inhibitors — serious infection, mortality, malignancy, cardiovascular events, and thrombosis — were similar for baricitinib in children (4 of 49 patients, 8.2%) and adults (325 of 3707, 8.8%). For other JAK inhibitors, absolute numbers of these AEs in children were small and rates were lower in children than in adults.
IN PRACTICE:
“This information can support customized treatment and minimize the potential for undesired or intolerable AEs,” the authors wrote.
SOURCE:
This study was led by Sahithi Talasila, BS, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and was published online in Pediatric Dermatology.
LIMITATIONS:
Pharmacovigilance registries did not fully capture the complete range of AEs because of potential reporting bias or recall bias. Additionally, events lacking sufficient objective evidence were underreported, while common AEs associated with JAK inhibitor therapy were overreported.
DISCLOSURES:
No specific funding sources for the study were reported. One author reported being a consultant, one reported serving as a principal investigator in clinical trials, and another reported serving on data and safety monitoring boards of various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
which also found that acne was the most common skin-related AE in children, and serious AEs were less common.
METHODOLOGY:
- Researchers analyzed 399,649 AEs in 133,216 adult patients and 2883 AEs in 955 pediatric patients (age, < 18 years) from November 2011 to February 2023 using the US Food and Drug Administration Adverse Event Reporting System and the Canada Vigilance Adverse Reaction Online Database.
- AEs were categorized on the basis of the Medical Dictionary for Regulatory Activities system organ class.
- Five JAK inhibitors approved for use in children were included in the study: Baricitinib, upadacitinib, abrocitinib, ruxolitinib, and tofacitinib.
TAKEAWAY:
- The most frequently reported AEs in children were blood and lymphatic system disorders, including neutropenia, thrombocytopenia, and anemia (24%); viral, fungal, and bacterial infections, such as pneumonia and sepsis (17.2%); constitutional symptoms and administrative concerns, including pyrexia and fatigue (15.7%); gastrointestinal disorders, such as vomiting and abdominal pain (13.6%); and respiratory disorders, such as cough and respiratory distress (5.3%).
- In adults, the most common AEs were viral, fungal, and bacterial infections (16.8%); constitutional symptoms and administrative concerns (13.5%); musculoskeletal and connective tissue disorders (7.04%); and gastrointestinal (5.8%) and nervous system (5%) disorders.
- Acne (30.6%), atopic dermatitis (22.2%), and psoriasis (16.7%) were the most common skin and subcutaneous tissue AEs reported in children. Skin and subcutaneous AEs were more common with upadacitinib (21.1%), abrocitinib (9.1%), and tofacitinib (6.3%) in children.
- Serious AEs included in the boxed warning for JAK inhibitors — serious infection, mortality, malignancy, cardiovascular events, and thrombosis — were similar for baricitinib in children (4 of 49 patients, 8.2%) and adults (325 of 3707, 8.8%). For other JAK inhibitors, absolute numbers of these AEs in children were small and rates were lower in children than in adults.
IN PRACTICE:
“This information can support customized treatment and minimize the potential for undesired or intolerable AEs,” the authors wrote.
SOURCE:
This study was led by Sahithi Talasila, BS, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and was published online in Pediatric Dermatology.
LIMITATIONS:
Pharmacovigilance registries did not fully capture the complete range of AEs because of potential reporting bias or recall bias. Additionally, events lacking sufficient objective evidence were underreported, while common AEs associated with JAK inhibitor therapy were overreported.
DISCLOSURES:
No specific funding sources for the study were reported. One author reported being a consultant, one reported serving as a principal investigator in clinical trials, and another reported serving on data and safety monitoring boards of various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Oropouche Virus
The pediatrician’s first patient of the day was a 15-year-old boy complaining of fever, chills, and profound arthralgias. His exam, including a careful assessment of his joints, yielded no clues, and the pediatrician was ready to diagnose this as a routine viral illness. An additional bit of history provided by the patient’s mother prompted the pediatrician to pause and reconsider.
“A week ago, we returned from a visit to Cuba,” the mother reported. “Could this be Oropouche virus infection?”
Oropouche virus disease is an arboviral disease caused by the Oropouche virus (OROV). It is transmitted to humans through midge or mosquito bites. Although largely unknown to most United States clinicians until recently, this vector-borne virus is not new. The first human Oropouche virus infection was identified in Trinidad and Tobago in 1955 and since then, there have been intermittent outbreaks in the Amazon region. In recent months, though, the epidemiology of Oropouche virus infections has changed. Infections are being identified in new geographic areas, including Cuba. According to the Pan American Health Organization, 506 cases of Oropouche virus infection have been identified in Cuba since May 27, 2024.
Two deaths from Oropouche virus infection have been reported in previously healthy people. Evolving data suggests adverse outcomes associated with vertical transmission during pregnancy. One fetal death and child with congenital anomalies have been reported in Brazil. Additional fetal deaths, miscarriages, and congenital anomalies are under investigation.
Travel-associated cases have been reported in the United States. As of September 10, 2024, 52 Oropouche virus disease cases had been reported from five states in the United States. The Centers for Disease Control and Prevention confirmed that the first 31 of these cases were travelers returning from Cuba. The CDC issued a health advisory on August 16, 2024: Increased Oropouche Virus Activity and Associated Risk to Travelers.
The pediatrician quickly reviewed the signs and symptoms of Oropouche virus infection. Disease typically presents as an abrupt onset of fever, severe headache, chills, myalgia, and arthralgia 3 to 10 days after the bite of infected mosquito. Some patients develop a maculopapular rash that starts on the trunk and spreads to the extremities. Meningitis and encephalitis develop in less than 1 in 20 people. The symptoms of Oropouche virus infection overlap with those of other arboviruses such as dengue, chikungunya, and Zika viruses. The disease can also mimic malaria or rickettsial infection. Approximately 60% of people with Oropouche virus infection experience a recurrence of symptoms within days to weeks of the initial resolution of symptoms.
Testing for Oropouche virus infection is available through the CDC’s Arbovirus Diagnostic Laboratory. In people who are acutely ill, reverse transcription-polymerase chain reaction testing can be used to identify the virus in serum and cerebrospinal fluid. Serologic testing is also available for people who have been symptomatic for at least 6 days.
The pediatrician contacted his local health department to discuss the possibility of Oropouche virus infection. After reviewing the case definition, public health authorities recommended laboratory testing for Oropouche virus, dengue, and Zika virus.
Back in the exam room, the pediatrician provided anticipatory guidance to the patient and his mother. There are no antiviral medications to treat Oropouche virus infection, so the pediatrician recommended supportive care, including acetaminophen for fever and pain. He also advised avoiding aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) until dengue could be ruled out to reduce the risk of bleeding. After confirming that no one else in the home was sick with similar symptoms, he counseled about prevention strategies.
To date, transmission of Oropouche virus in the United States has not been documented, but vectors potentially capable of transmitting the virus are present in some areas of the United States. When people who are infected with Oropouche are bitten, they can spread the virus through their blood to biting midges or mosquitoes. The insects can then spread the virus to other people. To reduce to potential for local transmission, people who are sick with suspected Oropouche virus infection are advised to avoid biting-midge and mosquito bites for the first week of their illness. Any person who has recently traveled to an area where Oropouche virus transmission is occurring should also avoid insect bites for 3 weeks after returning home to account for the potential incubation period of the virus. This includes wearing an EPA-registered insect repellent.
A suspect case is a patient who has been in an area with documented or suspected OROV circulation* within 2 weeks of initial symptom onset (as patients may experience recurrent symptoms) and the following:
- Abrupt onset of reported fever, headache, and one or more of the following: myalgia, arthralgia, photophobia, retro-orbital/eye pain, or signs and symptoms of neuroinvasive disease (eg, stiff neck, altered mental status, seizures, limb weakness, or cerebrospinal fluid pleocytosis).
- Tested negative for other possible diseases, in particular dengue.†
- Absence of a more likely clinical explanation.
*If concern exists for local transmission in a nonendemic area, consider if the patient shared an exposure location with a person with confirmed OROV infection, lives in an area where travel-related cases have been identified, or has known vector exposure (eg, mosquitoes or biting midges).
†If strong suspicion of OROV disease exists based on the patient’s clinical features and history of travel to an area with virus circulation, do not wait on negative testing before sending specimens to CDC.
Adapted from: Centers for Disease Control and Prevention. Response to Oropouche Virus Disease Cases in U.S. States and Territories in the Americas. Available at: https.//www.cdc.gov/oropouche/media/pdfs/2024/09/response-to-oropouche-virus-disease.pdf
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta and Gilead. Email her at [email protected]. (Also [email protected])
The pediatrician’s first patient of the day was a 15-year-old boy complaining of fever, chills, and profound arthralgias. His exam, including a careful assessment of his joints, yielded no clues, and the pediatrician was ready to diagnose this as a routine viral illness. An additional bit of history provided by the patient’s mother prompted the pediatrician to pause and reconsider.
“A week ago, we returned from a visit to Cuba,” the mother reported. “Could this be Oropouche virus infection?”
Oropouche virus disease is an arboviral disease caused by the Oropouche virus (OROV). It is transmitted to humans through midge or mosquito bites. Although largely unknown to most United States clinicians until recently, this vector-borne virus is not new. The first human Oropouche virus infection was identified in Trinidad and Tobago in 1955 and since then, there have been intermittent outbreaks in the Amazon region. In recent months, though, the epidemiology of Oropouche virus infections has changed. Infections are being identified in new geographic areas, including Cuba. According to the Pan American Health Organization, 506 cases of Oropouche virus infection have been identified in Cuba since May 27, 2024.
Two deaths from Oropouche virus infection have been reported in previously healthy people. Evolving data suggests adverse outcomes associated with vertical transmission during pregnancy. One fetal death and child with congenital anomalies have been reported in Brazil. Additional fetal deaths, miscarriages, and congenital anomalies are under investigation.
Travel-associated cases have been reported in the United States. As of September 10, 2024, 52 Oropouche virus disease cases had been reported from five states in the United States. The Centers for Disease Control and Prevention confirmed that the first 31 of these cases were travelers returning from Cuba. The CDC issued a health advisory on August 16, 2024: Increased Oropouche Virus Activity and Associated Risk to Travelers.
The pediatrician quickly reviewed the signs and symptoms of Oropouche virus infection. Disease typically presents as an abrupt onset of fever, severe headache, chills, myalgia, and arthralgia 3 to 10 days after the bite of infected mosquito. Some patients develop a maculopapular rash that starts on the trunk and spreads to the extremities. Meningitis and encephalitis develop in less than 1 in 20 people. The symptoms of Oropouche virus infection overlap with those of other arboviruses such as dengue, chikungunya, and Zika viruses. The disease can also mimic malaria or rickettsial infection. Approximately 60% of people with Oropouche virus infection experience a recurrence of symptoms within days to weeks of the initial resolution of symptoms.
Testing for Oropouche virus infection is available through the CDC’s Arbovirus Diagnostic Laboratory. In people who are acutely ill, reverse transcription-polymerase chain reaction testing can be used to identify the virus in serum and cerebrospinal fluid. Serologic testing is also available for people who have been symptomatic for at least 6 days.
The pediatrician contacted his local health department to discuss the possibility of Oropouche virus infection. After reviewing the case definition, public health authorities recommended laboratory testing for Oropouche virus, dengue, and Zika virus.
Back in the exam room, the pediatrician provided anticipatory guidance to the patient and his mother. There are no antiviral medications to treat Oropouche virus infection, so the pediatrician recommended supportive care, including acetaminophen for fever and pain. He also advised avoiding aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) until dengue could be ruled out to reduce the risk of bleeding. After confirming that no one else in the home was sick with similar symptoms, he counseled about prevention strategies.
To date, transmission of Oropouche virus in the United States has not been documented, but vectors potentially capable of transmitting the virus are present in some areas of the United States. When people who are infected with Oropouche are bitten, they can spread the virus through their blood to biting midges or mosquitoes. The insects can then spread the virus to other people. To reduce to potential for local transmission, people who are sick with suspected Oropouche virus infection are advised to avoid biting-midge and mosquito bites for the first week of their illness. Any person who has recently traveled to an area where Oropouche virus transmission is occurring should also avoid insect bites for 3 weeks after returning home to account for the potential incubation period of the virus. This includes wearing an EPA-registered insect repellent.
A suspect case is a patient who has been in an area with documented or suspected OROV circulation* within 2 weeks of initial symptom onset (as patients may experience recurrent symptoms) and the following:
- Abrupt onset of reported fever, headache, and one or more of the following: myalgia, arthralgia, photophobia, retro-orbital/eye pain, or signs and symptoms of neuroinvasive disease (eg, stiff neck, altered mental status, seizures, limb weakness, or cerebrospinal fluid pleocytosis).
- Tested negative for other possible diseases, in particular dengue.†
- Absence of a more likely clinical explanation.
*If concern exists for local transmission in a nonendemic area, consider if the patient shared an exposure location with a person with confirmed OROV infection, lives in an area where travel-related cases have been identified, or has known vector exposure (eg, mosquitoes or biting midges).
†If strong suspicion of OROV disease exists based on the patient’s clinical features and history of travel to an area with virus circulation, do not wait on negative testing before sending specimens to CDC.
Adapted from: Centers for Disease Control and Prevention. Response to Oropouche Virus Disease Cases in U.S. States and Territories in the Americas. Available at: https.//www.cdc.gov/oropouche/media/pdfs/2024/09/response-to-oropouche-virus-disease.pdf
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta and Gilead. Email her at [email protected]. (Also [email protected])
The pediatrician’s first patient of the day was a 15-year-old boy complaining of fever, chills, and profound arthralgias. His exam, including a careful assessment of his joints, yielded no clues, and the pediatrician was ready to diagnose this as a routine viral illness. An additional bit of history provided by the patient’s mother prompted the pediatrician to pause and reconsider.
“A week ago, we returned from a visit to Cuba,” the mother reported. “Could this be Oropouche virus infection?”
Oropouche virus disease is an arboviral disease caused by the Oropouche virus (OROV). It is transmitted to humans through midge or mosquito bites. Although largely unknown to most United States clinicians until recently, this vector-borne virus is not new. The first human Oropouche virus infection was identified in Trinidad and Tobago in 1955 and since then, there have been intermittent outbreaks in the Amazon region. In recent months, though, the epidemiology of Oropouche virus infections has changed. Infections are being identified in new geographic areas, including Cuba. According to the Pan American Health Organization, 506 cases of Oropouche virus infection have been identified in Cuba since May 27, 2024.
Two deaths from Oropouche virus infection have been reported in previously healthy people. Evolving data suggests adverse outcomes associated with vertical transmission during pregnancy. One fetal death and child with congenital anomalies have been reported in Brazil. Additional fetal deaths, miscarriages, and congenital anomalies are under investigation.
Travel-associated cases have been reported in the United States. As of September 10, 2024, 52 Oropouche virus disease cases had been reported from five states in the United States. The Centers for Disease Control and Prevention confirmed that the first 31 of these cases were travelers returning from Cuba. The CDC issued a health advisory on August 16, 2024: Increased Oropouche Virus Activity and Associated Risk to Travelers.
The pediatrician quickly reviewed the signs and symptoms of Oropouche virus infection. Disease typically presents as an abrupt onset of fever, severe headache, chills, myalgia, and arthralgia 3 to 10 days after the bite of infected mosquito. Some patients develop a maculopapular rash that starts on the trunk and spreads to the extremities. Meningitis and encephalitis develop in less than 1 in 20 people. The symptoms of Oropouche virus infection overlap with those of other arboviruses such as dengue, chikungunya, and Zika viruses. The disease can also mimic malaria or rickettsial infection. Approximately 60% of people with Oropouche virus infection experience a recurrence of symptoms within days to weeks of the initial resolution of symptoms.
Testing for Oropouche virus infection is available through the CDC’s Arbovirus Diagnostic Laboratory. In people who are acutely ill, reverse transcription-polymerase chain reaction testing can be used to identify the virus in serum and cerebrospinal fluid. Serologic testing is also available for people who have been symptomatic for at least 6 days.
The pediatrician contacted his local health department to discuss the possibility of Oropouche virus infection. After reviewing the case definition, public health authorities recommended laboratory testing for Oropouche virus, dengue, and Zika virus.
Back in the exam room, the pediatrician provided anticipatory guidance to the patient and his mother. There are no antiviral medications to treat Oropouche virus infection, so the pediatrician recommended supportive care, including acetaminophen for fever and pain. He also advised avoiding aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) until dengue could be ruled out to reduce the risk of bleeding. After confirming that no one else in the home was sick with similar symptoms, he counseled about prevention strategies.
To date, transmission of Oropouche virus in the United States has not been documented, but vectors potentially capable of transmitting the virus are present in some areas of the United States. When people who are infected with Oropouche are bitten, they can spread the virus through their blood to biting midges or mosquitoes. The insects can then spread the virus to other people. To reduce to potential for local transmission, people who are sick with suspected Oropouche virus infection are advised to avoid biting-midge and mosquito bites for the first week of their illness. Any person who has recently traveled to an area where Oropouche virus transmission is occurring should also avoid insect bites for 3 weeks after returning home to account for the potential incubation period of the virus. This includes wearing an EPA-registered insect repellent.
A suspect case is a patient who has been in an area with documented or suspected OROV circulation* within 2 weeks of initial symptom onset (as patients may experience recurrent symptoms) and the following:
- Abrupt onset of reported fever, headache, and one or more of the following: myalgia, arthralgia, photophobia, retro-orbital/eye pain, or signs and symptoms of neuroinvasive disease (eg, stiff neck, altered mental status, seizures, limb weakness, or cerebrospinal fluid pleocytosis).
- Tested negative for other possible diseases, in particular dengue.†
- Absence of a more likely clinical explanation.
*If concern exists for local transmission in a nonendemic area, consider if the patient shared an exposure location with a person with confirmed OROV infection, lives in an area where travel-related cases have been identified, or has known vector exposure (eg, mosquitoes or biting midges).
†If strong suspicion of OROV disease exists based on the patient’s clinical features and history of travel to an area with virus circulation, do not wait on negative testing before sending specimens to CDC.
Adapted from: Centers for Disease Control and Prevention. Response to Oropouche Virus Disease Cases in U.S. States and Territories in the Americas. Available at: https.//www.cdc.gov/oropouche/media/pdfs/2024/09/response-to-oropouche-virus-disease.pdf
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta and Gilead. Email her at [email protected]. (Also [email protected])
Stress Management
With the changing leaves and cooling temperatures, early autumn also brings the excitement of the new school year. While returning to sports, mastering new subjects, and spending time with old and new friends is exhilarating, this season can also be a time of intense stress.
For those high school students who are especially ambitious, the school year presents the challenge of a very high stakes performance, one whose success will be measured by admission to a prized college. Not only are there classes to study for, but schedules are packed with a maximum number of subjects, a maximum number of Advanced Placement courses and a maximum number of impressive extra-curricular activities. Varsity sports practice, SAT prep, Debate Club, volunteer hours, and on and on.
What is often missing is enough time for sleep, socializing, exploring new interests, and unwinding. When you hear your patients (or parents) describing the intense stress of their overloaded schedules compounded by a sense that “I have no choice,” you have an opportunity to complicate their thinking. Introduce the idea that there are smart approaches to performing your best under stress. Pushing themselves relentlessly will inevitably lead to burnout and exhaustion. This approach will help them learn to make wise choices and will better serve their healthy development.
Start by acknowledging the stress of high-stakes performance. Telling your patients that they need to lower the temperature by not putting so much pressure on themselves is likely to be experienced as a lack of confidence in them and is unlikely to get any traction. Instead, ask your patients what matters to them the most: Is it admission to the college of their choice? Achieving a certain score or GPA? Is it their competitiveness and drive to win? There is no wrong answer, but it is helpful for them to be able to reflect on what matters to them. Are they hoping to impress someone else? Are they worried about their future financial health and convinced that getting into a certain college will secure their financial success? Do they think this matters more to their parents than to themselves? Or have they discovered an intense interest in theoretical physics and want to be able to study at Caltech? If their ambition is meaningfully connected to an authentic interest or to their emerging identity, their sense of purpose will be much deeper and able to sustain them.
Even with talent and a strong sense of purpose, performing well is very difficult and demanding. It is important to consider the cycle of performance as including preparation, performance itself, and effective rest and recovery, just as with athletic performance. Whether the performance is the SATs, an AP test, a debate or big game, there were probably hours of preparation for every hour of performance. Help them to consider the importance of this practice or preparation time, and how to use that time effectively. Are they able to work in environments where there are few distractions? Do they have the support or useful feedback they need? How are they able to know when it is time for a break or when they are ready? It can be helpful for them to appreciate whether preparation or performance is more challenging for them, as the former requires focus and patience, while the latter requires courage and tenacity. If they are aware of which is harder for them, they can be thoughtful about how to effectively handle those challenges.
What can be most valuable for your patients is hearing from their pediatricians that they need to have time protected for rest and recharging, and not only for preparation and performance. Any athlete knows that failing to do so will lead to exhaustion and injury, and performance inevitably suffers. Rest is unwinding and slowing down, and a restful activity will leave them feeling calm, relaxed, and ready for sleep. A recharging activity is one that leaves them feeling refreshed and energized. Some common restful activities are a hot bath or shower, a distracting activity such as watching a show or surfing the web, playing a simple video game or puzzle or listening to music. Some recharging activities are creative ones (making art or music), engaging in hobbies, reading, or talking with a good friend. A few activities — sleep, exercise, and mindfulness meditation, are powerful in that they pack both rest and recharge into the same activity. Your patients should be discovering and learning which activities they find restful or recharging. The college application process or preparing for a varsity tryout will both add stress and give them an opportunity to learn what rests and recharges them. They should aim to have a list of at least five effective strategies that they can turn to when it’s time to rest or to recharge. Help them turn their work ethic to building a deeper well of self-knowledge that will serve them when they face challenges in high school or when they are on their own in college. This time of stress can be a time of growth, too.
Of course, remind your patients that this is a critical time to focus on basic self-care: They need consistently adequate, restful sleep, good nutrition, and physical activity. They will benefit from regular time in nature and time spent with friends that nourish them. They can find ways to compound these activities: Go for a walk with a friend, eat dinner with family, play a relaxing game while enjoying music. Lastly, ask your patients what is the last new thing they tried. It is easy to become so focused on an ambitious project that there is no time for exploration and play. Play is important throughout life, but adolescents are actively discovering their interests, talents, tastes, and values. To do this they need to be trying things that are new and maybe less purpose-driven. I call this type of activity “senseless fun.” Splashing in the pool is senseless fun, swimming laps is purposeful exercise that my contribute to recharging, and competing in a swim meet is often more on the stressful side. As they discover new talents, deeply engaging interests, what relaxes and recharges them, they will be learning who they are. Regardless of the outcome of a test, a big game, or where they go to college, it is this emerging knowledge about themselves that will carry them into adulthood. The pediatrician’s goal: Encouraging aspiration, exploration, and self-awareness in the context of giving permission for rest, recharging, and senseless fun.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
With the changing leaves and cooling temperatures, early autumn also brings the excitement of the new school year. While returning to sports, mastering new subjects, and spending time with old and new friends is exhilarating, this season can also be a time of intense stress.
For those high school students who are especially ambitious, the school year presents the challenge of a very high stakes performance, one whose success will be measured by admission to a prized college. Not only are there classes to study for, but schedules are packed with a maximum number of subjects, a maximum number of Advanced Placement courses and a maximum number of impressive extra-curricular activities. Varsity sports practice, SAT prep, Debate Club, volunteer hours, and on and on.
What is often missing is enough time for sleep, socializing, exploring new interests, and unwinding. When you hear your patients (or parents) describing the intense stress of their overloaded schedules compounded by a sense that “I have no choice,” you have an opportunity to complicate their thinking. Introduce the idea that there are smart approaches to performing your best under stress. Pushing themselves relentlessly will inevitably lead to burnout and exhaustion. This approach will help them learn to make wise choices and will better serve their healthy development.
Start by acknowledging the stress of high-stakes performance. Telling your patients that they need to lower the temperature by not putting so much pressure on themselves is likely to be experienced as a lack of confidence in them and is unlikely to get any traction. Instead, ask your patients what matters to them the most: Is it admission to the college of their choice? Achieving a certain score or GPA? Is it their competitiveness and drive to win? There is no wrong answer, but it is helpful for them to be able to reflect on what matters to them. Are they hoping to impress someone else? Are they worried about their future financial health and convinced that getting into a certain college will secure their financial success? Do they think this matters more to their parents than to themselves? Or have they discovered an intense interest in theoretical physics and want to be able to study at Caltech? If their ambition is meaningfully connected to an authentic interest or to their emerging identity, their sense of purpose will be much deeper and able to sustain them.
Even with talent and a strong sense of purpose, performing well is very difficult and demanding. It is important to consider the cycle of performance as including preparation, performance itself, and effective rest and recovery, just as with athletic performance. Whether the performance is the SATs, an AP test, a debate or big game, there were probably hours of preparation for every hour of performance. Help them to consider the importance of this practice or preparation time, and how to use that time effectively. Are they able to work in environments where there are few distractions? Do they have the support or useful feedback they need? How are they able to know when it is time for a break or when they are ready? It can be helpful for them to appreciate whether preparation or performance is more challenging for them, as the former requires focus and patience, while the latter requires courage and tenacity. If they are aware of which is harder for them, they can be thoughtful about how to effectively handle those challenges.
What can be most valuable for your patients is hearing from their pediatricians that they need to have time protected for rest and recharging, and not only for preparation and performance. Any athlete knows that failing to do so will lead to exhaustion and injury, and performance inevitably suffers. Rest is unwinding and slowing down, and a restful activity will leave them feeling calm, relaxed, and ready for sleep. A recharging activity is one that leaves them feeling refreshed and energized. Some common restful activities are a hot bath or shower, a distracting activity such as watching a show or surfing the web, playing a simple video game or puzzle or listening to music. Some recharging activities are creative ones (making art or music), engaging in hobbies, reading, or talking with a good friend. A few activities — sleep, exercise, and mindfulness meditation, are powerful in that they pack both rest and recharge into the same activity. Your patients should be discovering and learning which activities they find restful or recharging. The college application process or preparing for a varsity tryout will both add stress and give them an opportunity to learn what rests and recharges them. They should aim to have a list of at least five effective strategies that they can turn to when it’s time to rest or to recharge. Help them turn their work ethic to building a deeper well of self-knowledge that will serve them when they face challenges in high school or when they are on their own in college. This time of stress can be a time of growth, too.
Of course, remind your patients that this is a critical time to focus on basic self-care: They need consistently adequate, restful sleep, good nutrition, and physical activity. They will benefit from regular time in nature and time spent with friends that nourish them. They can find ways to compound these activities: Go for a walk with a friend, eat dinner with family, play a relaxing game while enjoying music. Lastly, ask your patients what is the last new thing they tried. It is easy to become so focused on an ambitious project that there is no time for exploration and play. Play is important throughout life, but adolescents are actively discovering their interests, talents, tastes, and values. To do this they need to be trying things that are new and maybe less purpose-driven. I call this type of activity “senseless fun.” Splashing in the pool is senseless fun, swimming laps is purposeful exercise that my contribute to recharging, and competing in a swim meet is often more on the stressful side. As they discover new talents, deeply engaging interests, what relaxes and recharges them, they will be learning who they are. Regardless of the outcome of a test, a big game, or where they go to college, it is this emerging knowledge about themselves that will carry them into adulthood. The pediatrician’s goal: Encouraging aspiration, exploration, and self-awareness in the context of giving permission for rest, recharging, and senseless fun.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
With the changing leaves and cooling temperatures, early autumn also brings the excitement of the new school year. While returning to sports, mastering new subjects, and spending time with old and new friends is exhilarating, this season can also be a time of intense stress.
For those high school students who are especially ambitious, the school year presents the challenge of a very high stakes performance, one whose success will be measured by admission to a prized college. Not only are there classes to study for, but schedules are packed with a maximum number of subjects, a maximum number of Advanced Placement courses and a maximum number of impressive extra-curricular activities. Varsity sports practice, SAT prep, Debate Club, volunteer hours, and on and on.
What is often missing is enough time for sleep, socializing, exploring new interests, and unwinding. When you hear your patients (or parents) describing the intense stress of their overloaded schedules compounded by a sense that “I have no choice,” you have an opportunity to complicate their thinking. Introduce the idea that there are smart approaches to performing your best under stress. Pushing themselves relentlessly will inevitably lead to burnout and exhaustion. This approach will help them learn to make wise choices and will better serve their healthy development.
Start by acknowledging the stress of high-stakes performance. Telling your patients that they need to lower the temperature by not putting so much pressure on themselves is likely to be experienced as a lack of confidence in them and is unlikely to get any traction. Instead, ask your patients what matters to them the most: Is it admission to the college of their choice? Achieving a certain score or GPA? Is it their competitiveness and drive to win? There is no wrong answer, but it is helpful for them to be able to reflect on what matters to them. Are they hoping to impress someone else? Are they worried about their future financial health and convinced that getting into a certain college will secure their financial success? Do they think this matters more to their parents than to themselves? Or have they discovered an intense interest in theoretical physics and want to be able to study at Caltech? If their ambition is meaningfully connected to an authentic interest or to their emerging identity, their sense of purpose will be much deeper and able to sustain them.
Even with talent and a strong sense of purpose, performing well is very difficult and demanding. It is important to consider the cycle of performance as including preparation, performance itself, and effective rest and recovery, just as with athletic performance. Whether the performance is the SATs, an AP test, a debate or big game, there were probably hours of preparation for every hour of performance. Help them to consider the importance of this practice or preparation time, and how to use that time effectively. Are they able to work in environments where there are few distractions? Do they have the support or useful feedback they need? How are they able to know when it is time for a break or when they are ready? It can be helpful for them to appreciate whether preparation or performance is more challenging for them, as the former requires focus and patience, while the latter requires courage and tenacity. If they are aware of which is harder for them, they can be thoughtful about how to effectively handle those challenges.
What can be most valuable for your patients is hearing from their pediatricians that they need to have time protected for rest and recharging, and not only for preparation and performance. Any athlete knows that failing to do so will lead to exhaustion and injury, and performance inevitably suffers. Rest is unwinding and slowing down, and a restful activity will leave them feeling calm, relaxed, and ready for sleep. A recharging activity is one that leaves them feeling refreshed and energized. Some common restful activities are a hot bath or shower, a distracting activity such as watching a show or surfing the web, playing a simple video game or puzzle or listening to music. Some recharging activities are creative ones (making art or music), engaging in hobbies, reading, or talking with a good friend. A few activities — sleep, exercise, and mindfulness meditation, are powerful in that they pack both rest and recharge into the same activity. Your patients should be discovering and learning which activities they find restful or recharging. The college application process or preparing for a varsity tryout will both add stress and give them an opportunity to learn what rests and recharges them. They should aim to have a list of at least five effective strategies that they can turn to when it’s time to rest or to recharge. Help them turn their work ethic to building a deeper well of self-knowledge that will serve them when they face challenges in high school or when they are on their own in college. This time of stress can be a time of growth, too.
Of course, remind your patients that this is a critical time to focus on basic self-care: They need consistently adequate, restful sleep, good nutrition, and physical activity. They will benefit from regular time in nature and time spent with friends that nourish them. They can find ways to compound these activities: Go for a walk with a friend, eat dinner with family, play a relaxing game while enjoying music. Lastly, ask your patients what is the last new thing they tried. It is easy to become so focused on an ambitious project that there is no time for exploration and play. Play is important throughout life, but adolescents are actively discovering their interests, talents, tastes, and values. To do this they need to be trying things that are new and maybe less purpose-driven. I call this type of activity “senseless fun.” Splashing in the pool is senseless fun, swimming laps is purposeful exercise that my contribute to recharging, and competing in a swim meet is often more on the stressful side. As they discover new talents, deeply engaging interests, what relaxes and recharges them, they will be learning who they are. Regardless of the outcome of a test, a big game, or where they go to college, it is this emerging knowledge about themselves that will carry them into adulthood. The pediatrician’s goal: Encouraging aspiration, exploration, and self-awareness in the context of giving permission for rest, recharging, and senseless fun.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Is It Time for Universal Suicide Screening?
US suicide rates have reached alarming levels, with data from Centers for Disease Control and Prevention (CDC) showing a 37% increase from 2000 to 2022. Nearly 49,000 people died by suicide in 2022 alone, translating to one death every 11 minutes.
The increase in suicide rates has prompted calls for expansion of universal suicide screening, in which all individuals in medical or mental health care settings are screened for suicide risk, regardless of the purpose for their visit. But the psychiatric field is split on the issue, with some experts citing false positives and a lack of mental health care resources for those deemed at risk.
In 2022, when the US Preventative Services Task Force released its recommendations on suicide prevention, first in children and adolescents, and then in adults, the authors said there was insufficient evidence to support universal suicide screening.
Proponents of the practice pushed back on that finding, arguing that universal suicide screening could help identify those at high risk who might otherwise go undiagnosed, leading to earlier, potentially lifesaving, intervention.
So, what is the case for — and against — universal screening?
Sounding an Alert
The introduction of universal screening was driven by a confluence of factors that began with a 1999 report by then-US Surgeon General David Satcher, MD. This was followed by a report in 2016 from the Joint Commission on Detecting and Treating Suicidal Ideation that called for healthcare organizations to improve detection and treatment of suicidal ideation in all healthcare care settings.
Data from the alert showed that a significant number of people who died by suicide had a healthcare visit before their death. Half had seen a clinician a month before their death; nearly 30% had a medical visit just the week before — all with no detection of increased suicide risk.
It was that sort of finding that led Parkland Health and Hospital System in Dallas to become the first US hospital to implement universal suicide screening. Since the program launched in 2015, the system has screened more than 4.3 million patients in its emergency department, inpatient units, and 20 primary care clinics.
“Since the program began, we’ve completed between 40,000 to 50,000 screenings per month,” said Kimberly Roaten, PhD, associate chief quality and safety officer for behavioral health at Parkland Health.
Clinicians at Parkland use the five-item Ask Suicide-Screening Questions to assess suicidal intent, a commonly used tool that was originally developed for use in pediatric emergency rooms (ERs). The tool, which takes about 20 seconds to administer, has since been validated in both children and adults.
Based on a patient’s response, a clinical decision support system integrated into the electronic health record classifies suicide risk as none, moderate, or high.
Patients identified as moderate risk are offered a more in-depth assessment with a mental health clinician, though participation is not mandatory, said Dr. Roaten. Those at high risk receive a more thorough evaluation.
The proportion of ER patients at Parkland who screen positive for any suicidal intent has consistently remained at about 7%, and at 2% in the primary care clinics, she said.
To better understand what the program may have had on suicide prevention, Dr. Roaten is leading a National Institute of Mental Health–funded study to link a decade of mortality data from the state of Texas to patient data from Parkland Health. Investigators will analyze information about patients identified at risk for suicide, those patients’ characteristics, and who dies by suicide.
Universal Screening Expands
Other health systems have adopted universal suicide screening including the Indian Health Service and the US Veterans Health Administration. Universal suicide screening is also in place in a growing number of primary care practices and hospitals throughout the United States and will be mandatory for patients aged 12 years and older in all acute care hospitals in California beginning in 2025.
There is also a push for universal screening to be coordinated through local, state, and federal government, nonprofit, and private sectors. The National Action Alliance for Suicide Prevention is charged with advancing the White House’s 2024 National Strategy for Suicide Prevention, a 10-year plan to address gaps in suicide prevention in the United States.
Sarah Brummett, JD, director of the National Action Alliance for Suicide Prevention’s executive committee, said that universal suicide screening is part of the 2024 strategy. “We know there are barriers to universal screening, and so it’s important to recognize what they are so we can address them,” said Ms. Brummett.
Barriers may include adequate staffing, or a system in place to triage patients who screen positive.
At Parkland, cost and workload have been minimal, Dr. Roaten said. “We built a model that only dedicates our highest-value resources to the most at-risk patients.”
She also noted that relief may be on the horizon for health systems where cost is an obstacle to universal screening and subsequent intervention. “There are efforts at the federal level to increase funding for suicide assessment and crisis response,” she said.
Pushback on Universal Screening
Universal suicide screening has its detractors, including critics who say expansion is unlikely to reduce suicide rates.
“The issue with suicidal ideation is that it is very dynamic. Suicidal ideation changes very quickly — sometimes within hours,” said Craig Bryan, PsyD, professor of psychiatry and behavioral health at Ohio State University in Columbus, Ohio.
Universal screening can also lead to false positives, where a patient who screens positive for suicidal ideation has no actual intention of attempting suicide, potentially creating unnecessary concern and burden on health care resources, Dr. Bryan noted.
“What do you do with everyone who screens positive?” Dr. Bryan said. “I’ve spoken with leaders of many health systems in the United States, and there is pushback against universal screening because they don’t have enough mental health resources to handle all of the referrals.”
Suicide screening also doesn’t predict who will die by suicide, Dr. Bryan added. It only identifies those willing to disclose suicidal thoughts. There is a significant number of people without mental illness who may never seek medical care, so “the warning signs we’re teaching people to recognize — depression, anxiety, and substance abuse — might not be evident in these individuals,” he said.
“Life sideswipes them suddenly, and they go from 0 to 60 ... and they may have access to a highly lethal method [of suicide] which weaponizes that moment of despair,” said Dr. Bryan. No amount of screening could possibly predict those types of suicides, he added.
Paul Nestadt, MD, associate professor of psychiatry and behavioral sciences at Johns Hopkins School of Medicine, agrees with Dr. Bryan and noted there isn’t a strong correlation between suicidal ideation and death by suicide.
“Suicidal thoughts are very common, but suicide is a rare event,” he said.
He cited a study that showed that two thirds of individuals who died by suicide had denied experiencing suicidal thoughts when asked, and half of them died within 2 days of this denial. Other research suggests that as many as 98% of people who express suicidal ideation do not die by suicide, Dr. Nestadt said.
A Public Health Issue
If universal screening is not the answer to predicting and preventing suicide, what is? One way would be to approach suicide as a public health issue, Dr. Nestadt said.
“How did we reduce the rate of motor vehicle deaths? We didn’t test each driver’s reaction time behind the wheel,” he said. “Instead, we passed seatbelt and airbag legislation, implemented federal speed limits, and as a result, the number of motor vehicle fatalities decreased.”
Dr. Nestadt is an advocate for stronger gun safety legislation, which has proven effective in reducing suicide rates. A study published this year showed that states with child access prevention laws, negligent storage laws, and mandatory waiting periods for gun purchases reported fewer suicide deaths than those without that legislation.
Other measures might be applied in cases of extreme individual suicide risk, including extreme risk protection orders, also known as “red flag” laws, he added. This type of legislation provides a pathway for law enforcement to temporarily remove firearms from individuals who pose a risk to themselves or others.
“These have been shown to be very effective in saving lives,” Dr. Nestadt said.
Dr. Nestadt and others are also using machine learning models to predict suicide risk. Those identified as high-risk may be flagged on their electronic medical record. Ideally, when the algorithm becomes more accurate at predicting suicide, anyone treating this patient can then decide if action is needed, said Dr. Nestadt.
In his work with suicidal military personnel, Dr. Bryan and his colleagues established a brief form of cognitive behavioral therapy (BCBT) to help participants challenge cognitive distortions and build coping strategies to deal with feel with intense feelings of distress. Data show that BCBT reduced suicide attempts among active-duty soldiers by 60% compared with standard mental health treatment. It has since been shown to work in civilians as well.
Dr. Bryan is also researching fluctuations in the wish to live versus the wish to die relative to one another and mapping the trajectory of risk states along the way.
The goal is that these and other suicide prevention strategies currently under study by his team and others will help stem the rise in suicide deaths.
“Overall, we need to train mental health providers to implement suicide prevention therapies and establish suicide risk programs,” Dr. Bryan said. “But until we build one of these suicide prevention interventions to scale, we’re putting the cart before the horse.”
Dr. Roaten, Ms. Brummett, Dr. Bryan, and Dr. Nestadt reported no relevant disclosures.
A version of this article appeared on Medscape.com.
US suicide rates have reached alarming levels, with data from Centers for Disease Control and Prevention (CDC) showing a 37% increase from 2000 to 2022. Nearly 49,000 people died by suicide in 2022 alone, translating to one death every 11 minutes.
The increase in suicide rates has prompted calls for expansion of universal suicide screening, in which all individuals in medical or mental health care settings are screened for suicide risk, regardless of the purpose for their visit. But the psychiatric field is split on the issue, with some experts citing false positives and a lack of mental health care resources for those deemed at risk.
In 2022, when the US Preventative Services Task Force released its recommendations on suicide prevention, first in children and adolescents, and then in adults, the authors said there was insufficient evidence to support universal suicide screening.
Proponents of the practice pushed back on that finding, arguing that universal suicide screening could help identify those at high risk who might otherwise go undiagnosed, leading to earlier, potentially lifesaving, intervention.
So, what is the case for — and against — universal screening?
Sounding an Alert
The introduction of universal screening was driven by a confluence of factors that began with a 1999 report by then-US Surgeon General David Satcher, MD. This was followed by a report in 2016 from the Joint Commission on Detecting and Treating Suicidal Ideation that called for healthcare organizations to improve detection and treatment of suicidal ideation in all healthcare care settings.
Data from the alert showed that a significant number of people who died by suicide had a healthcare visit before their death. Half had seen a clinician a month before their death; nearly 30% had a medical visit just the week before — all with no detection of increased suicide risk.
It was that sort of finding that led Parkland Health and Hospital System in Dallas to become the first US hospital to implement universal suicide screening. Since the program launched in 2015, the system has screened more than 4.3 million patients in its emergency department, inpatient units, and 20 primary care clinics.
“Since the program began, we’ve completed between 40,000 to 50,000 screenings per month,” said Kimberly Roaten, PhD, associate chief quality and safety officer for behavioral health at Parkland Health.
Clinicians at Parkland use the five-item Ask Suicide-Screening Questions to assess suicidal intent, a commonly used tool that was originally developed for use in pediatric emergency rooms (ERs). The tool, which takes about 20 seconds to administer, has since been validated in both children and adults.
Based on a patient’s response, a clinical decision support system integrated into the electronic health record classifies suicide risk as none, moderate, or high.
Patients identified as moderate risk are offered a more in-depth assessment with a mental health clinician, though participation is not mandatory, said Dr. Roaten. Those at high risk receive a more thorough evaluation.
The proportion of ER patients at Parkland who screen positive for any suicidal intent has consistently remained at about 7%, and at 2% in the primary care clinics, she said.
To better understand what the program may have had on suicide prevention, Dr. Roaten is leading a National Institute of Mental Health–funded study to link a decade of mortality data from the state of Texas to patient data from Parkland Health. Investigators will analyze information about patients identified at risk for suicide, those patients’ characteristics, and who dies by suicide.
Universal Screening Expands
Other health systems have adopted universal suicide screening including the Indian Health Service and the US Veterans Health Administration. Universal suicide screening is also in place in a growing number of primary care practices and hospitals throughout the United States and will be mandatory for patients aged 12 years and older in all acute care hospitals in California beginning in 2025.
There is also a push for universal screening to be coordinated through local, state, and federal government, nonprofit, and private sectors. The National Action Alliance for Suicide Prevention is charged with advancing the White House’s 2024 National Strategy for Suicide Prevention, a 10-year plan to address gaps in suicide prevention in the United States.
Sarah Brummett, JD, director of the National Action Alliance for Suicide Prevention’s executive committee, said that universal suicide screening is part of the 2024 strategy. “We know there are barriers to universal screening, and so it’s important to recognize what they are so we can address them,” said Ms. Brummett.
Barriers may include adequate staffing, or a system in place to triage patients who screen positive.
At Parkland, cost and workload have been minimal, Dr. Roaten said. “We built a model that only dedicates our highest-value resources to the most at-risk patients.”
She also noted that relief may be on the horizon for health systems where cost is an obstacle to universal screening and subsequent intervention. “There are efforts at the federal level to increase funding for suicide assessment and crisis response,” she said.
Pushback on Universal Screening
Universal suicide screening has its detractors, including critics who say expansion is unlikely to reduce suicide rates.
“The issue with suicidal ideation is that it is very dynamic. Suicidal ideation changes very quickly — sometimes within hours,” said Craig Bryan, PsyD, professor of psychiatry and behavioral health at Ohio State University in Columbus, Ohio.
Universal screening can also lead to false positives, where a patient who screens positive for suicidal ideation has no actual intention of attempting suicide, potentially creating unnecessary concern and burden on health care resources, Dr. Bryan noted.
“What do you do with everyone who screens positive?” Dr. Bryan said. “I’ve spoken with leaders of many health systems in the United States, and there is pushback against universal screening because they don’t have enough mental health resources to handle all of the referrals.”
Suicide screening also doesn’t predict who will die by suicide, Dr. Bryan added. It only identifies those willing to disclose suicidal thoughts. There is a significant number of people without mental illness who may never seek medical care, so “the warning signs we’re teaching people to recognize — depression, anxiety, and substance abuse — might not be evident in these individuals,” he said.
“Life sideswipes them suddenly, and they go from 0 to 60 ... and they may have access to a highly lethal method [of suicide] which weaponizes that moment of despair,” said Dr. Bryan. No amount of screening could possibly predict those types of suicides, he added.
Paul Nestadt, MD, associate professor of psychiatry and behavioral sciences at Johns Hopkins School of Medicine, agrees with Dr. Bryan and noted there isn’t a strong correlation between suicidal ideation and death by suicide.
“Suicidal thoughts are very common, but suicide is a rare event,” he said.
He cited a study that showed that two thirds of individuals who died by suicide had denied experiencing suicidal thoughts when asked, and half of them died within 2 days of this denial. Other research suggests that as many as 98% of people who express suicidal ideation do not die by suicide, Dr. Nestadt said.
A Public Health Issue
If universal screening is not the answer to predicting and preventing suicide, what is? One way would be to approach suicide as a public health issue, Dr. Nestadt said.
“How did we reduce the rate of motor vehicle deaths? We didn’t test each driver’s reaction time behind the wheel,” he said. “Instead, we passed seatbelt and airbag legislation, implemented federal speed limits, and as a result, the number of motor vehicle fatalities decreased.”
Dr. Nestadt is an advocate for stronger gun safety legislation, which has proven effective in reducing suicide rates. A study published this year showed that states with child access prevention laws, negligent storage laws, and mandatory waiting periods for gun purchases reported fewer suicide deaths than those without that legislation.
Other measures might be applied in cases of extreme individual suicide risk, including extreme risk protection orders, also known as “red flag” laws, he added. This type of legislation provides a pathway for law enforcement to temporarily remove firearms from individuals who pose a risk to themselves or others.
“These have been shown to be very effective in saving lives,” Dr. Nestadt said.
Dr. Nestadt and others are also using machine learning models to predict suicide risk. Those identified as high-risk may be flagged on their electronic medical record. Ideally, when the algorithm becomes more accurate at predicting suicide, anyone treating this patient can then decide if action is needed, said Dr. Nestadt.
In his work with suicidal military personnel, Dr. Bryan and his colleagues established a brief form of cognitive behavioral therapy (BCBT) to help participants challenge cognitive distortions and build coping strategies to deal with feel with intense feelings of distress. Data show that BCBT reduced suicide attempts among active-duty soldiers by 60% compared with standard mental health treatment. It has since been shown to work in civilians as well.
Dr. Bryan is also researching fluctuations in the wish to live versus the wish to die relative to one another and mapping the trajectory of risk states along the way.
The goal is that these and other suicide prevention strategies currently under study by his team and others will help stem the rise in suicide deaths.
“Overall, we need to train mental health providers to implement suicide prevention therapies and establish suicide risk programs,” Dr. Bryan said. “But until we build one of these suicide prevention interventions to scale, we’re putting the cart before the horse.”
Dr. Roaten, Ms. Brummett, Dr. Bryan, and Dr. Nestadt reported no relevant disclosures.
A version of this article appeared on Medscape.com.
US suicide rates have reached alarming levels, with data from Centers for Disease Control and Prevention (CDC) showing a 37% increase from 2000 to 2022. Nearly 49,000 people died by suicide in 2022 alone, translating to one death every 11 minutes.
The increase in suicide rates has prompted calls for expansion of universal suicide screening, in which all individuals in medical or mental health care settings are screened for suicide risk, regardless of the purpose for their visit. But the psychiatric field is split on the issue, with some experts citing false positives and a lack of mental health care resources for those deemed at risk.
In 2022, when the US Preventative Services Task Force released its recommendations on suicide prevention, first in children and adolescents, and then in adults, the authors said there was insufficient evidence to support universal suicide screening.
Proponents of the practice pushed back on that finding, arguing that universal suicide screening could help identify those at high risk who might otherwise go undiagnosed, leading to earlier, potentially lifesaving, intervention.
So, what is the case for — and against — universal screening?
Sounding an Alert
The introduction of universal screening was driven by a confluence of factors that began with a 1999 report by then-US Surgeon General David Satcher, MD. This was followed by a report in 2016 from the Joint Commission on Detecting and Treating Suicidal Ideation that called for healthcare organizations to improve detection and treatment of suicidal ideation in all healthcare care settings.
Data from the alert showed that a significant number of people who died by suicide had a healthcare visit before their death. Half had seen a clinician a month before their death; nearly 30% had a medical visit just the week before — all with no detection of increased suicide risk.
It was that sort of finding that led Parkland Health and Hospital System in Dallas to become the first US hospital to implement universal suicide screening. Since the program launched in 2015, the system has screened more than 4.3 million patients in its emergency department, inpatient units, and 20 primary care clinics.
“Since the program began, we’ve completed between 40,000 to 50,000 screenings per month,” said Kimberly Roaten, PhD, associate chief quality and safety officer for behavioral health at Parkland Health.
Clinicians at Parkland use the five-item Ask Suicide-Screening Questions to assess suicidal intent, a commonly used tool that was originally developed for use in pediatric emergency rooms (ERs). The tool, which takes about 20 seconds to administer, has since been validated in both children and adults.
Based on a patient’s response, a clinical decision support system integrated into the electronic health record classifies suicide risk as none, moderate, or high.
Patients identified as moderate risk are offered a more in-depth assessment with a mental health clinician, though participation is not mandatory, said Dr. Roaten. Those at high risk receive a more thorough evaluation.
The proportion of ER patients at Parkland who screen positive for any suicidal intent has consistently remained at about 7%, and at 2% in the primary care clinics, she said.
To better understand what the program may have had on suicide prevention, Dr. Roaten is leading a National Institute of Mental Health–funded study to link a decade of mortality data from the state of Texas to patient data from Parkland Health. Investigators will analyze information about patients identified at risk for suicide, those patients’ characteristics, and who dies by suicide.
Universal Screening Expands
Other health systems have adopted universal suicide screening including the Indian Health Service and the US Veterans Health Administration. Universal suicide screening is also in place in a growing number of primary care practices and hospitals throughout the United States and will be mandatory for patients aged 12 years and older in all acute care hospitals in California beginning in 2025.
There is also a push for universal screening to be coordinated through local, state, and federal government, nonprofit, and private sectors. The National Action Alliance for Suicide Prevention is charged with advancing the White House’s 2024 National Strategy for Suicide Prevention, a 10-year plan to address gaps in suicide prevention in the United States.
Sarah Brummett, JD, director of the National Action Alliance for Suicide Prevention’s executive committee, said that universal suicide screening is part of the 2024 strategy. “We know there are barriers to universal screening, and so it’s important to recognize what they are so we can address them,” said Ms. Brummett.
Barriers may include adequate staffing, or a system in place to triage patients who screen positive.
At Parkland, cost and workload have been minimal, Dr. Roaten said. “We built a model that only dedicates our highest-value resources to the most at-risk patients.”
She also noted that relief may be on the horizon for health systems where cost is an obstacle to universal screening and subsequent intervention. “There are efforts at the federal level to increase funding for suicide assessment and crisis response,” she said.
Pushback on Universal Screening
Universal suicide screening has its detractors, including critics who say expansion is unlikely to reduce suicide rates.
“The issue with suicidal ideation is that it is very dynamic. Suicidal ideation changes very quickly — sometimes within hours,” said Craig Bryan, PsyD, professor of psychiatry and behavioral health at Ohio State University in Columbus, Ohio.
Universal screening can also lead to false positives, where a patient who screens positive for suicidal ideation has no actual intention of attempting suicide, potentially creating unnecessary concern and burden on health care resources, Dr. Bryan noted.
“What do you do with everyone who screens positive?” Dr. Bryan said. “I’ve spoken with leaders of many health systems in the United States, and there is pushback against universal screening because they don’t have enough mental health resources to handle all of the referrals.”
Suicide screening also doesn’t predict who will die by suicide, Dr. Bryan added. It only identifies those willing to disclose suicidal thoughts. There is a significant number of people without mental illness who may never seek medical care, so “the warning signs we’re teaching people to recognize — depression, anxiety, and substance abuse — might not be evident in these individuals,” he said.
“Life sideswipes them suddenly, and they go from 0 to 60 ... and they may have access to a highly lethal method [of suicide] which weaponizes that moment of despair,” said Dr. Bryan. No amount of screening could possibly predict those types of suicides, he added.
Paul Nestadt, MD, associate professor of psychiatry and behavioral sciences at Johns Hopkins School of Medicine, agrees with Dr. Bryan and noted there isn’t a strong correlation between suicidal ideation and death by suicide.
“Suicidal thoughts are very common, but suicide is a rare event,” he said.
He cited a study that showed that two thirds of individuals who died by suicide had denied experiencing suicidal thoughts when asked, and half of them died within 2 days of this denial. Other research suggests that as many as 98% of people who express suicidal ideation do not die by suicide, Dr. Nestadt said.
A Public Health Issue
If universal screening is not the answer to predicting and preventing suicide, what is? One way would be to approach suicide as a public health issue, Dr. Nestadt said.
“How did we reduce the rate of motor vehicle deaths? We didn’t test each driver’s reaction time behind the wheel,” he said. “Instead, we passed seatbelt and airbag legislation, implemented federal speed limits, and as a result, the number of motor vehicle fatalities decreased.”
Dr. Nestadt is an advocate for stronger gun safety legislation, which has proven effective in reducing suicide rates. A study published this year showed that states with child access prevention laws, negligent storage laws, and mandatory waiting periods for gun purchases reported fewer suicide deaths than those without that legislation.
Other measures might be applied in cases of extreme individual suicide risk, including extreme risk protection orders, also known as “red flag” laws, he added. This type of legislation provides a pathway for law enforcement to temporarily remove firearms from individuals who pose a risk to themselves or others.
“These have been shown to be very effective in saving lives,” Dr. Nestadt said.
Dr. Nestadt and others are also using machine learning models to predict suicide risk. Those identified as high-risk may be flagged on their electronic medical record. Ideally, when the algorithm becomes more accurate at predicting suicide, anyone treating this patient can then decide if action is needed, said Dr. Nestadt.
In his work with suicidal military personnel, Dr. Bryan and his colleagues established a brief form of cognitive behavioral therapy (BCBT) to help participants challenge cognitive distortions and build coping strategies to deal with feel with intense feelings of distress. Data show that BCBT reduced suicide attempts among active-duty soldiers by 60% compared with standard mental health treatment. It has since been shown to work in civilians as well.
Dr. Bryan is also researching fluctuations in the wish to live versus the wish to die relative to one another and mapping the trajectory of risk states along the way.
The goal is that these and other suicide prevention strategies currently under study by his team and others will help stem the rise in suicide deaths.
“Overall, we need to train mental health providers to implement suicide prevention therapies and establish suicide risk programs,” Dr. Bryan said. “But until we build one of these suicide prevention interventions to scale, we’re putting the cart before the horse.”
Dr. Roaten, Ms. Brummett, Dr. Bryan, and Dr. Nestadt reported no relevant disclosures.
A version of this article appeared on Medscape.com.
Playing the ‘Doctor’ Card: A Lesson in Three Hypotheticals
Scenario I. Let’s say you wake with a collection of symptoms. None of them is concerning, but the combination seems a bit unusual, or at least confusing. You would like to speak to your PCP, whom you have known for a long time, and ask for either reassurance or advice on whether you should make an appointment. However, your experience with the front office’s organization tells you that the quick 4-minute conversation you’re looking for is not going to happen easily.
You have that robotic phone message memorized. It begins suggesting that you think you have an emergency to call 911. Then it reminds you that if have a question about COVID to press “2,” which will take you to a recorded message and eventually link you to a triage nurse if the recording doesn’t answer your questions. If you need a prescription refill you should press “3.” If you are a doctor’s office and wish speak to the doctor press “4.” If you know you need an appointment press “5.” And finally if you have a question press “6” and leave a message and a nurse will get back to you before the end of the day.
The good news is that your PCP’s office is good to its word and will return your call the same day, but the bad news is that it is likely to be well into the afternoon. And, while you don’t consider your symptoms life-threatening, you don’t want getting an answer to be an exercise in schedule disruption.
You were a doctor before you retired and you still have an “office.” It’s really more of a combination den and studio. So, technically you are a doctor’s office wanting to speak to the doctor. And, you know that pressing “4” will get you the answer you are looking for in a matter of minutes.
Scenario II. Your spouse, or your aunt, or the elderly widow next door asks you to accompany her at an upcoming doctor’s visit because she had been having trouble understanding the physician’s plan regarding further diagnosis and possible treatment. She believes having you along as kind of an interpreter/advocate would be a big help. Do you agree and do you make any stipulations?
Scenario III. Your PCP has referred you to a specialist. You are filling out the previsit form(s). Do you list your occupation as “retired physician” or just “retired”? Or just leave it blank?
Whether you deserve it or not, graduating from medical school has conferred on you a specialness in the eyes of many people. It is assumed you are smarter than the average bear and in taking the Hippocratic oath you have joined an elite club. And, with that membership comes some special undefined privileges.
But with that specialness there are are some downsides. For example, in some states being a physician once allowed you to have a license plate with “MD” in the number sequence. Sometimes that helped you avoid the occasional parking ticket. That is until folks realized the “MD” made you a target for car thieves and drug seekers who mistakenly believe we all carry drugs in our glove compartments.
So what about that first scenario? Do you press “4” to jump yourself to the head of the queue and avoid the inconvenience of having to wait for a reasonably timely response from your PCP? After all, you are fellow physicians and you’ve known her for a decade or two. If you are retired is your time any more valuable than that of her other patients? If you are still in active practice you can argue that getting special attention will benefit your patients. But, if it’s a weekend and you are off it’s a bit harder to rationalize special treatment. Playing the doctor card in this situation is your own decision but you must be prepared to shoulder the perceptions by your PCP and her staff as well as your own sense of fairness.
The other two scenarios are much different. In neither are you risking the impression that you are asking for a favor. But, they each have their downsides. In the second scenario you are doing someone a favor to act as an interpreter. How could this have downside? Unfortunately, what happens too often in situations like this is that when the patient’s physician learns that you are a fellow physician, the rest of the visit becomes a dialogue in doctor-speak between the two physicians with the patient sitting by as an observer. In the end this discussion may benefit the patient by creating a treatment plan that the patient can understand either because they overheard it or more likely because you eventually explained it to them.
On the other the hand, this doctor-to-doctor chat has done nothing to build a doctor-patient relationship that had obviously been lacking something. In situations like this it is probably better to keep the doctor card up your sleeve to be played at the end of the visit or maybe not at all. Before agreeing to be an interpreter/advocate, ask the patient to avoid mentioning that you are a physician. Instead, ask that she introduce you as a friend or relative that she has asked to come along to serve as a memory bank. During the visit it may be helpful to occasionally interject and suggest that the patient ask a question that hasn’t been adequately addressed. While some physicians may be upset when they belatedly find you have not revealed up front that you are a physician, I find this a harmless omission that has the benefit of improving patient care.
The final scenario — in which you are the patient — is likely to occur more often as you get older. When filling out a previsit form, I often simply put retired or leave it blank. But, how I answer the question often seems to be irrelevant because I have learned that physicians and their staff read those boilerplate forms so cursorily that even when I report my status as “retired physician” everyone seems surprised if and when it later comes to light.
My rationale in keeping the doctor card close to my vest in these situations is that I want to be addressed without any assumptions regarding my medical knowledge, which in my situation is well over half a century old and spotty at best. I don’t want my physicians to say “I’m sure you understand.” Because I often don’t. I would like them to learn about who I am just as I hope they would other patients. I won’t be offended if they “talk down” to me. If this specialist is as good as I’ve heard she is, I want to hear her full performance, not one edited for fellow and former physicians.
It doesn’t arrive gold edged with a list of special privileges. If it comes with any extras, they are risks that must be avoided.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Scenario I. Let’s say you wake with a collection of symptoms. None of them is concerning, but the combination seems a bit unusual, or at least confusing. You would like to speak to your PCP, whom you have known for a long time, and ask for either reassurance or advice on whether you should make an appointment. However, your experience with the front office’s organization tells you that the quick 4-minute conversation you’re looking for is not going to happen easily.
You have that robotic phone message memorized. It begins suggesting that you think you have an emergency to call 911. Then it reminds you that if have a question about COVID to press “2,” which will take you to a recorded message and eventually link you to a triage nurse if the recording doesn’t answer your questions. If you need a prescription refill you should press “3.” If you are a doctor’s office and wish speak to the doctor press “4.” If you know you need an appointment press “5.” And finally if you have a question press “6” and leave a message and a nurse will get back to you before the end of the day.
The good news is that your PCP’s office is good to its word and will return your call the same day, but the bad news is that it is likely to be well into the afternoon. And, while you don’t consider your symptoms life-threatening, you don’t want getting an answer to be an exercise in schedule disruption.
You were a doctor before you retired and you still have an “office.” It’s really more of a combination den and studio. So, technically you are a doctor’s office wanting to speak to the doctor. And, you know that pressing “4” will get you the answer you are looking for in a matter of minutes.
Scenario II. Your spouse, or your aunt, or the elderly widow next door asks you to accompany her at an upcoming doctor’s visit because she had been having trouble understanding the physician’s plan regarding further diagnosis and possible treatment. She believes having you along as kind of an interpreter/advocate would be a big help. Do you agree and do you make any stipulations?
Scenario III. Your PCP has referred you to a specialist. You are filling out the previsit form(s). Do you list your occupation as “retired physician” or just “retired”? Or just leave it blank?
Whether you deserve it or not, graduating from medical school has conferred on you a specialness in the eyes of many people. It is assumed you are smarter than the average bear and in taking the Hippocratic oath you have joined an elite club. And, with that membership comes some special undefined privileges.
But with that specialness there are are some downsides. For example, in some states being a physician once allowed you to have a license plate with “MD” in the number sequence. Sometimes that helped you avoid the occasional parking ticket. That is until folks realized the “MD” made you a target for car thieves and drug seekers who mistakenly believe we all carry drugs in our glove compartments.
So what about that first scenario? Do you press “4” to jump yourself to the head of the queue and avoid the inconvenience of having to wait for a reasonably timely response from your PCP? After all, you are fellow physicians and you’ve known her for a decade or two. If you are retired is your time any more valuable than that of her other patients? If you are still in active practice you can argue that getting special attention will benefit your patients. But, if it’s a weekend and you are off it’s a bit harder to rationalize special treatment. Playing the doctor card in this situation is your own decision but you must be prepared to shoulder the perceptions by your PCP and her staff as well as your own sense of fairness.
The other two scenarios are much different. In neither are you risking the impression that you are asking for a favor. But, they each have their downsides. In the second scenario you are doing someone a favor to act as an interpreter. How could this have downside? Unfortunately, what happens too often in situations like this is that when the patient’s physician learns that you are a fellow physician, the rest of the visit becomes a dialogue in doctor-speak between the two physicians with the patient sitting by as an observer. In the end this discussion may benefit the patient by creating a treatment plan that the patient can understand either because they overheard it or more likely because you eventually explained it to them.
On the other the hand, this doctor-to-doctor chat has done nothing to build a doctor-patient relationship that had obviously been lacking something. In situations like this it is probably better to keep the doctor card up your sleeve to be played at the end of the visit or maybe not at all. Before agreeing to be an interpreter/advocate, ask the patient to avoid mentioning that you are a physician. Instead, ask that she introduce you as a friend or relative that she has asked to come along to serve as a memory bank. During the visit it may be helpful to occasionally interject and suggest that the patient ask a question that hasn’t been adequately addressed. While some physicians may be upset when they belatedly find you have not revealed up front that you are a physician, I find this a harmless omission that has the benefit of improving patient care.
The final scenario — in which you are the patient — is likely to occur more often as you get older. When filling out a previsit form, I often simply put retired or leave it blank. But, how I answer the question often seems to be irrelevant because I have learned that physicians and their staff read those boilerplate forms so cursorily that even when I report my status as “retired physician” everyone seems surprised if and when it later comes to light.
My rationale in keeping the doctor card close to my vest in these situations is that I want to be addressed without any assumptions regarding my medical knowledge, which in my situation is well over half a century old and spotty at best. I don’t want my physicians to say “I’m sure you understand.” Because I often don’t. I would like them to learn about who I am just as I hope they would other patients. I won’t be offended if they “talk down” to me. If this specialist is as good as I’ve heard she is, I want to hear her full performance, not one edited for fellow and former physicians.
It doesn’t arrive gold edged with a list of special privileges. If it comes with any extras, they are risks that must be avoided.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Scenario I. Let’s say you wake with a collection of symptoms. None of them is concerning, but the combination seems a bit unusual, or at least confusing. You would like to speak to your PCP, whom you have known for a long time, and ask for either reassurance or advice on whether you should make an appointment. However, your experience with the front office’s organization tells you that the quick 4-minute conversation you’re looking for is not going to happen easily.
You have that robotic phone message memorized. It begins suggesting that you think you have an emergency to call 911. Then it reminds you that if have a question about COVID to press “2,” which will take you to a recorded message and eventually link you to a triage nurse if the recording doesn’t answer your questions. If you need a prescription refill you should press “3.” If you are a doctor’s office and wish speak to the doctor press “4.” If you know you need an appointment press “5.” And finally if you have a question press “6” and leave a message and a nurse will get back to you before the end of the day.
The good news is that your PCP’s office is good to its word and will return your call the same day, but the bad news is that it is likely to be well into the afternoon. And, while you don’t consider your symptoms life-threatening, you don’t want getting an answer to be an exercise in schedule disruption.
You were a doctor before you retired and you still have an “office.” It’s really more of a combination den and studio. So, technically you are a doctor’s office wanting to speak to the doctor. And, you know that pressing “4” will get you the answer you are looking for in a matter of minutes.
Scenario II. Your spouse, or your aunt, or the elderly widow next door asks you to accompany her at an upcoming doctor’s visit because she had been having trouble understanding the physician’s plan regarding further diagnosis and possible treatment. She believes having you along as kind of an interpreter/advocate would be a big help. Do you agree and do you make any stipulations?
Scenario III. Your PCP has referred you to a specialist. You are filling out the previsit form(s). Do you list your occupation as “retired physician” or just “retired”? Or just leave it blank?
Whether you deserve it or not, graduating from medical school has conferred on you a specialness in the eyes of many people. It is assumed you are smarter than the average bear and in taking the Hippocratic oath you have joined an elite club. And, with that membership comes some special undefined privileges.
But with that specialness there are are some downsides. For example, in some states being a physician once allowed you to have a license plate with “MD” in the number sequence. Sometimes that helped you avoid the occasional parking ticket. That is until folks realized the “MD” made you a target for car thieves and drug seekers who mistakenly believe we all carry drugs in our glove compartments.
So what about that first scenario? Do you press “4” to jump yourself to the head of the queue and avoid the inconvenience of having to wait for a reasonably timely response from your PCP? After all, you are fellow physicians and you’ve known her for a decade or two. If you are retired is your time any more valuable than that of her other patients? If you are still in active practice you can argue that getting special attention will benefit your patients. But, if it’s a weekend and you are off it’s a bit harder to rationalize special treatment. Playing the doctor card in this situation is your own decision but you must be prepared to shoulder the perceptions by your PCP and her staff as well as your own sense of fairness.
The other two scenarios are much different. In neither are you risking the impression that you are asking for a favor. But, they each have their downsides. In the second scenario you are doing someone a favor to act as an interpreter. How could this have downside? Unfortunately, what happens too often in situations like this is that when the patient’s physician learns that you are a fellow physician, the rest of the visit becomes a dialogue in doctor-speak between the two physicians with the patient sitting by as an observer. In the end this discussion may benefit the patient by creating a treatment plan that the patient can understand either because they overheard it or more likely because you eventually explained it to them.
On the other the hand, this doctor-to-doctor chat has done nothing to build a doctor-patient relationship that had obviously been lacking something. In situations like this it is probably better to keep the doctor card up your sleeve to be played at the end of the visit or maybe not at all. Before agreeing to be an interpreter/advocate, ask the patient to avoid mentioning that you are a physician. Instead, ask that she introduce you as a friend or relative that she has asked to come along to serve as a memory bank. During the visit it may be helpful to occasionally interject and suggest that the patient ask a question that hasn’t been adequately addressed. While some physicians may be upset when they belatedly find you have not revealed up front that you are a physician, I find this a harmless omission that has the benefit of improving patient care.
The final scenario — in which you are the patient — is likely to occur more often as you get older. When filling out a previsit form, I often simply put retired or leave it blank. But, how I answer the question often seems to be irrelevant because I have learned that physicians and their staff read those boilerplate forms so cursorily that even when I report my status as “retired physician” everyone seems surprised if and when it later comes to light.
My rationale in keeping the doctor card close to my vest in these situations is that I want to be addressed without any assumptions regarding my medical knowledge, which in my situation is well over half a century old and spotty at best. I don’t want my physicians to say “I’m sure you understand.” Because I often don’t. I would like them to learn about who I am just as I hope they would other patients. I won’t be offended if they “talk down” to me. If this specialist is as good as I’ve heard she is, I want to hear her full performance, not one edited for fellow and former physicians.
It doesn’t arrive gold edged with a list of special privileges. If it comes with any extras, they are risks that must be avoided.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].







