User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Medicare finalizes 2021 physician pay rule with E/M changes
Medicare officials stuck with their plan to increase payments for office visits for primary care and several other specialties that focus on helping patients manage complex conditions such as diabetes. In doing so, Medicare also finalized cuts for other fields, triggering a new wave of protests.
The final version of the 2021 Medicare physician fee schedule was unveiled on the night of Dec. 1. The Centers for Medicare & Medicaid Services posted an unofficial copy of the rule, which will later be published in the Federal Register.
CMS said it completed work on this massive annual review of payments for clinicians later than it usually does because of the demands of the federal response to the COVID-19 pandemic. The 2021 physician fee rule will take effect within a 30-day period instead of the usual 60-day time frame.
The most contentious item proposed for 2021 was a reshuffling of payments among specialties as part of an overhaul of Medicare’s approach to valuing evaluation and management (E/M) services. There was broader support for other aspects of the E/M overhaul, which are intended to cut some of the administrative hassle clinicians face.
“This finalized policy marks the most significant updates to E/M codes in 30 years, reducing burden on doctors imposed by the coding system and rewarding time spent evaluating and managing their patients’ care,” CMS Administrator Seema Verma said in a statement. “In the past, the system has rewarded interventions and procedures over time spent with patients – time taken preventing disease and managing chronic illnesses.”
In the final rule, CMS summarized these results of the E/M changes in Table 106. CMS largely stuck with the approach outlined in a draft rule released in August, with minor changes in the amounts of cuts and increases.
Specialties in line for increases under the 2021 final physician fee schedule include allergy/immunology (9%), endocrinology (16%), family practice (13%), general practice (7%), geriatrics (3%), hematology/oncology (14%), internal medicine (4%), nephrology (6%), physician assistants (8%), psychiatry (7%), rheumatology (15%), and urology (8%).
In line for cuts would be anesthesiology (–8%), cardiac surgery (–8%), emergency medicine (–6%), general surgery (–6%), infectious disease (–4%), neurosurgery (–6%), physical/occupational therapy (–9%), plastic surgery (–7%), radiology (–10%), and thoracic surgery (–8%).
CMS had initially set these changes in 2021 pay in motion in the 2020 physician fee schedule. The agency subsequently faced significant opposition to its plans. Many physician groups sought to waive a “budget-neutral” approach to the E/M overhaul, which makes the offsetting of cuts necessary. They argued this would allow increased compensation for clinicians whose practices focus on office visits without requiring offsetting cuts from other fields of medicine.
The American Medical Association is among those urging Congress to prevent or postpone the payment reductions resulting from Medicare’s budget neutrality requirement as applied to the E/M overhaul.
In a Tuesday statement, AMA President Susan R. Bailey, MD, noted that many physicians are facing “substantial economic hardships due to COVID-19.”
By AMA’s calculations, CMS’ planned 2021 E/M overhaul could result in “a shocking reduction of 10.2% to Medicare payment rates,” according to Bailey’s statement. The AMA strongly supports other aspects of the E/M changes CMS finalized, which Bailey said will result in “simpler and more flexible” coding and documentation.
The Surgical Care Coalition, which represents about a dozen medical specialty associations, is asking members of Congress to block the full implementation of the E/M overhaul.
In a Dec. 1 statement, the coalition urged the passage of a bill (HR 8702) that has been introduced in the House by a bipartisan duo of physicians, Rep. Ami Bera, MD (D-Calif.), and Rep. Larry Bucshon, MD (R-Ind.). Their bill would effectively block the cuts from going into effect on January 1, 2021. It would provide an additional Medicare payment for certain services in 2021 and 2022 if the otherwise applicable payment is less than it would have been in 2020.
The Medicare E/M overhaul “was a dangerous policy even before the pandemic, and enacting it during the worst health care crisis in a century is unconscionable. If Congress fails to act, it will further strain a health care system that’s already been pushed to the brink due to the COVID-19 pandemic and undermine patient care,” said John A. Wilson, MD, president of the American Association of Neurological Surgeons, in a statement.
Also backing the Bera-Bucshon bill is the American College of Emergency Physicians. In a statement on Tuesday, ACEP President Mark Rosenberg, DO, MBA, urged Congress to act on this measure.
“Emergency physicians and other health care providers battling on the front lines of the ongoing pandemic are already under unprecedented financial strain as they continue to bear the brunt of COVID-19,” Dr. Rosenberg said. “These cuts would have a devastating impact for the future of emergency medicine and could seriously impede patients’ access to emergency care when they need it most.”
“Long overdue”
But there also are champions for the approach CMS took in the E/M overhaul. The influential Medicare Payment Advisory Commission (MedPAC) has argued strongly for keeping the budget-neutral approach to the E/M overhaul.
In an Oct. 2 comment to CMS about the draft 2021 physician fee schedule, MedPAC Chairman Michael E. Chernew, PhD, said this approach would “help rebalance the fee schedule from services that have become overvalued to services that have become undervalued.”
This budget-neutral approach also “will go further in reducing the large gap in compensation between primary care physicians (who had a median income of $243,000 in 2018) and specialists such as surgeons (whose median income was $426,000 in 2018),” Dr. Chernew wrote.
In a Tuesday tweet, Robert B. Doherty, senior vice president of governmental affairs and public policy for the American College of Physicians, said CMS had “finalized long overdue payment increases for primary and comprehensive care including an add-in for more complex visits.”
The American Academy of Family Physicians joined ACP in a November 30 letter to congressional leaders, urging them to allow Medicare “to increase investment in primary care, benefiting millions of Medicare patients and the program itself, and reject last minute efforts to prevent these essential and long-overdue changes from going fully into effect on January 1, 2021.”
In the letter, AAFP and ACP and their cosigners argued for a need to address “underinvestment” in primary care by finalizing the E/M overhaul.
“Given that six in ten American adults have a chronic disease and four in ten have two or more chronic conditions, why would we, as a country, accept such an inadequate investment in the very care model that stands to provide maximum value to these patients?” they wrote. “Since we know that individuals with a longitudinal relationship with a primary care physician have better health outcomes and use fewer health care resources, why would we continue to direct money to higher-cost, marginal value services?”
A version of this article originally appeared on Medscape.com.
Medicare officials stuck with their plan to increase payments for office visits for primary care and several other specialties that focus on helping patients manage complex conditions such as diabetes. In doing so, Medicare also finalized cuts for other fields, triggering a new wave of protests.
The final version of the 2021 Medicare physician fee schedule was unveiled on the night of Dec. 1. The Centers for Medicare & Medicaid Services posted an unofficial copy of the rule, which will later be published in the Federal Register.
CMS said it completed work on this massive annual review of payments for clinicians later than it usually does because of the demands of the federal response to the COVID-19 pandemic. The 2021 physician fee rule will take effect within a 30-day period instead of the usual 60-day time frame.
The most contentious item proposed for 2021 was a reshuffling of payments among specialties as part of an overhaul of Medicare’s approach to valuing evaluation and management (E/M) services. There was broader support for other aspects of the E/M overhaul, which are intended to cut some of the administrative hassle clinicians face.
“This finalized policy marks the most significant updates to E/M codes in 30 years, reducing burden on doctors imposed by the coding system and rewarding time spent evaluating and managing their patients’ care,” CMS Administrator Seema Verma said in a statement. “In the past, the system has rewarded interventions and procedures over time spent with patients – time taken preventing disease and managing chronic illnesses.”
In the final rule, CMS summarized these results of the E/M changes in Table 106. CMS largely stuck with the approach outlined in a draft rule released in August, with minor changes in the amounts of cuts and increases.
Specialties in line for increases under the 2021 final physician fee schedule include allergy/immunology (9%), endocrinology (16%), family practice (13%), general practice (7%), geriatrics (3%), hematology/oncology (14%), internal medicine (4%), nephrology (6%), physician assistants (8%), psychiatry (7%), rheumatology (15%), and urology (8%).
In line for cuts would be anesthesiology (–8%), cardiac surgery (–8%), emergency medicine (–6%), general surgery (–6%), infectious disease (–4%), neurosurgery (–6%), physical/occupational therapy (–9%), plastic surgery (–7%), radiology (–10%), and thoracic surgery (–8%).
CMS had initially set these changes in 2021 pay in motion in the 2020 physician fee schedule. The agency subsequently faced significant opposition to its plans. Many physician groups sought to waive a “budget-neutral” approach to the E/M overhaul, which makes the offsetting of cuts necessary. They argued this would allow increased compensation for clinicians whose practices focus on office visits without requiring offsetting cuts from other fields of medicine.
The American Medical Association is among those urging Congress to prevent or postpone the payment reductions resulting from Medicare’s budget neutrality requirement as applied to the E/M overhaul.
In a Tuesday statement, AMA President Susan R. Bailey, MD, noted that many physicians are facing “substantial economic hardships due to COVID-19.”
By AMA’s calculations, CMS’ planned 2021 E/M overhaul could result in “a shocking reduction of 10.2% to Medicare payment rates,” according to Bailey’s statement. The AMA strongly supports other aspects of the E/M changes CMS finalized, which Bailey said will result in “simpler and more flexible” coding and documentation.
The Surgical Care Coalition, which represents about a dozen medical specialty associations, is asking members of Congress to block the full implementation of the E/M overhaul.
In a Dec. 1 statement, the coalition urged the passage of a bill (HR 8702) that has been introduced in the House by a bipartisan duo of physicians, Rep. Ami Bera, MD (D-Calif.), and Rep. Larry Bucshon, MD (R-Ind.). Their bill would effectively block the cuts from going into effect on January 1, 2021. It would provide an additional Medicare payment for certain services in 2021 and 2022 if the otherwise applicable payment is less than it would have been in 2020.
The Medicare E/M overhaul “was a dangerous policy even before the pandemic, and enacting it during the worst health care crisis in a century is unconscionable. If Congress fails to act, it will further strain a health care system that’s already been pushed to the brink due to the COVID-19 pandemic and undermine patient care,” said John A. Wilson, MD, president of the American Association of Neurological Surgeons, in a statement.
Also backing the Bera-Bucshon bill is the American College of Emergency Physicians. In a statement on Tuesday, ACEP President Mark Rosenberg, DO, MBA, urged Congress to act on this measure.
“Emergency physicians and other health care providers battling on the front lines of the ongoing pandemic are already under unprecedented financial strain as they continue to bear the brunt of COVID-19,” Dr. Rosenberg said. “These cuts would have a devastating impact for the future of emergency medicine and could seriously impede patients’ access to emergency care when they need it most.”
“Long overdue”
But there also are champions for the approach CMS took in the E/M overhaul. The influential Medicare Payment Advisory Commission (MedPAC) has argued strongly for keeping the budget-neutral approach to the E/M overhaul.
In an Oct. 2 comment to CMS about the draft 2021 physician fee schedule, MedPAC Chairman Michael E. Chernew, PhD, said this approach would “help rebalance the fee schedule from services that have become overvalued to services that have become undervalued.”
This budget-neutral approach also “will go further in reducing the large gap in compensation between primary care physicians (who had a median income of $243,000 in 2018) and specialists such as surgeons (whose median income was $426,000 in 2018),” Dr. Chernew wrote.
In a Tuesday tweet, Robert B. Doherty, senior vice president of governmental affairs and public policy for the American College of Physicians, said CMS had “finalized long overdue payment increases for primary and comprehensive care including an add-in for more complex visits.”
The American Academy of Family Physicians joined ACP in a November 30 letter to congressional leaders, urging them to allow Medicare “to increase investment in primary care, benefiting millions of Medicare patients and the program itself, and reject last minute efforts to prevent these essential and long-overdue changes from going fully into effect on January 1, 2021.”
In the letter, AAFP and ACP and their cosigners argued for a need to address “underinvestment” in primary care by finalizing the E/M overhaul.
“Given that six in ten American adults have a chronic disease and four in ten have two or more chronic conditions, why would we, as a country, accept such an inadequate investment in the very care model that stands to provide maximum value to these patients?” they wrote. “Since we know that individuals with a longitudinal relationship with a primary care physician have better health outcomes and use fewer health care resources, why would we continue to direct money to higher-cost, marginal value services?”
A version of this article originally appeared on Medscape.com.
Medicare officials stuck with their plan to increase payments for office visits for primary care and several other specialties that focus on helping patients manage complex conditions such as diabetes. In doing so, Medicare also finalized cuts for other fields, triggering a new wave of protests.
The final version of the 2021 Medicare physician fee schedule was unveiled on the night of Dec. 1. The Centers for Medicare & Medicaid Services posted an unofficial copy of the rule, which will later be published in the Federal Register.
CMS said it completed work on this massive annual review of payments for clinicians later than it usually does because of the demands of the federal response to the COVID-19 pandemic. The 2021 physician fee rule will take effect within a 30-day period instead of the usual 60-day time frame.
The most contentious item proposed for 2021 was a reshuffling of payments among specialties as part of an overhaul of Medicare’s approach to valuing evaluation and management (E/M) services. There was broader support for other aspects of the E/M overhaul, which are intended to cut some of the administrative hassle clinicians face.
“This finalized policy marks the most significant updates to E/M codes in 30 years, reducing burden on doctors imposed by the coding system and rewarding time spent evaluating and managing their patients’ care,” CMS Administrator Seema Verma said in a statement. “In the past, the system has rewarded interventions and procedures over time spent with patients – time taken preventing disease and managing chronic illnesses.”
In the final rule, CMS summarized these results of the E/M changes in Table 106. CMS largely stuck with the approach outlined in a draft rule released in August, with minor changes in the amounts of cuts and increases.
Specialties in line for increases under the 2021 final physician fee schedule include allergy/immunology (9%), endocrinology (16%), family practice (13%), general practice (7%), geriatrics (3%), hematology/oncology (14%), internal medicine (4%), nephrology (6%), physician assistants (8%), psychiatry (7%), rheumatology (15%), and urology (8%).
In line for cuts would be anesthesiology (–8%), cardiac surgery (–8%), emergency medicine (–6%), general surgery (–6%), infectious disease (–4%), neurosurgery (–6%), physical/occupational therapy (–9%), plastic surgery (–7%), radiology (–10%), and thoracic surgery (–8%).
CMS had initially set these changes in 2021 pay in motion in the 2020 physician fee schedule. The agency subsequently faced significant opposition to its plans. Many physician groups sought to waive a “budget-neutral” approach to the E/M overhaul, which makes the offsetting of cuts necessary. They argued this would allow increased compensation for clinicians whose practices focus on office visits without requiring offsetting cuts from other fields of medicine.
The American Medical Association is among those urging Congress to prevent or postpone the payment reductions resulting from Medicare’s budget neutrality requirement as applied to the E/M overhaul.
In a Tuesday statement, AMA President Susan R. Bailey, MD, noted that many physicians are facing “substantial economic hardships due to COVID-19.”
By AMA’s calculations, CMS’ planned 2021 E/M overhaul could result in “a shocking reduction of 10.2% to Medicare payment rates,” according to Bailey’s statement. The AMA strongly supports other aspects of the E/M changes CMS finalized, which Bailey said will result in “simpler and more flexible” coding and documentation.
The Surgical Care Coalition, which represents about a dozen medical specialty associations, is asking members of Congress to block the full implementation of the E/M overhaul.
In a Dec. 1 statement, the coalition urged the passage of a bill (HR 8702) that has been introduced in the House by a bipartisan duo of physicians, Rep. Ami Bera, MD (D-Calif.), and Rep. Larry Bucshon, MD (R-Ind.). Their bill would effectively block the cuts from going into effect on January 1, 2021. It would provide an additional Medicare payment for certain services in 2021 and 2022 if the otherwise applicable payment is less than it would have been in 2020.
The Medicare E/M overhaul “was a dangerous policy even before the pandemic, and enacting it during the worst health care crisis in a century is unconscionable. If Congress fails to act, it will further strain a health care system that’s already been pushed to the brink due to the COVID-19 pandemic and undermine patient care,” said John A. Wilson, MD, president of the American Association of Neurological Surgeons, in a statement.
Also backing the Bera-Bucshon bill is the American College of Emergency Physicians. In a statement on Tuesday, ACEP President Mark Rosenberg, DO, MBA, urged Congress to act on this measure.
“Emergency physicians and other health care providers battling on the front lines of the ongoing pandemic are already under unprecedented financial strain as they continue to bear the brunt of COVID-19,” Dr. Rosenberg said. “These cuts would have a devastating impact for the future of emergency medicine and could seriously impede patients’ access to emergency care when they need it most.”
“Long overdue”
But there also are champions for the approach CMS took in the E/M overhaul. The influential Medicare Payment Advisory Commission (MedPAC) has argued strongly for keeping the budget-neutral approach to the E/M overhaul.
In an Oct. 2 comment to CMS about the draft 2021 physician fee schedule, MedPAC Chairman Michael E. Chernew, PhD, said this approach would “help rebalance the fee schedule from services that have become overvalued to services that have become undervalued.”
This budget-neutral approach also “will go further in reducing the large gap in compensation between primary care physicians (who had a median income of $243,000 in 2018) and specialists such as surgeons (whose median income was $426,000 in 2018),” Dr. Chernew wrote.
In a Tuesday tweet, Robert B. Doherty, senior vice president of governmental affairs and public policy for the American College of Physicians, said CMS had “finalized long overdue payment increases for primary and comprehensive care including an add-in for more complex visits.”
The American Academy of Family Physicians joined ACP in a November 30 letter to congressional leaders, urging them to allow Medicare “to increase investment in primary care, benefiting millions of Medicare patients and the program itself, and reject last minute efforts to prevent these essential and long-overdue changes from going fully into effect on January 1, 2021.”
In the letter, AAFP and ACP and their cosigners argued for a need to address “underinvestment” in primary care by finalizing the E/M overhaul.
“Given that six in ten American adults have a chronic disease and four in ten have two or more chronic conditions, why would we, as a country, accept such an inadequate investment in the very care model that stands to provide maximum value to these patients?” they wrote. “Since we know that individuals with a longitudinal relationship with a primary care physician have better health outcomes and use fewer health care resources, why would we continue to direct money to higher-cost, marginal value services?”
A version of this article originally appeared on Medscape.com.
CDC shortens COVID-19 quarantine time to 10 or 7 days, with conditions
Citing new evidence and an “acceptable risk” of transmission, the agency hopes reducing the 14-day quarantine will increase overall compliance and improve public health and economic constraints.
The agency also suggested people postpone travel during the upcoming winter holidays and stay home because of the pandemic.
These shorter quarantine options do not replace initial CDC guidance. “CDC continues to recommend quarantining for 14 days as the best way to reduce risk for spreading COVID-19,” said Henry Walke, MD, MPH, the CDC’s COVID-19 incident manager, during a media briefing on Wednesday.
However, “after reviewing and analyzing new research and data, CDC has identified two acceptable alternative quarantine periods.”
People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.
The agency also suggests people still monitor for symptoms for a full 14 days.
Reducing the length of quarantine “may make it easier for people to take this critical public health action, by reducing the economic hardship associated with a longer period, especially if they cannot work during that time,” Dr. Walke said. “In addition, a shorter quarantine period can lessen stress on the public health system and communities, especially when new infections are rapidly rising.”
The federal guidance leaves flexibility for local jurisdictions to make their own quarantine recommendations, as warranted, he added.
An ‘acceptable risk’ calculation
Modeling by the CDC and academic and public health partners led to the new quarantine recommendations, said John Brooks, MD, chief medical officer for the CDC’s COVID-19 response. Multiple studies “point in the same direction, which is that we can safely reduce the length of quarantine but accept there is a small residual risk that a person who is leaving quarantine early could transmit to someone else.”
The residual risk is approximately 1%, with an upper limit of 10%, when people quarantine for 10 days. A 7-day quarantine carries a residual risk of about 5% and an upper limit of 12%.
“Ten days is where the risk got into a sweet spot we like, at about 1%,” Dr. Brooks said. “That is a very acceptable risk, I think, for many people.”
Although it remains unknown what proportion of people spending 14 days in quarantine leave early, “we are hearing anecdotally from our partners in public health that many people are discontinuing quarantine ahead of time because there is pressure to go back to work, to get people back into school – and it imposes a burden on the individual,” Dr. Brooks said.
“One of our hopes is that ... if we reduce the amount of time they have to spend in quarantine, people will be more compliant,” he added.
A reporter asked why the CDC is shortening quarantines when the pandemic numbers are increasing nationwide. The timing has to do with capacity, Dr. Brooks said. “We are in situation where the number of cases is rising, the number of contacts is rising and the number of people who require quarantine is rising. That is a lot of burden, not just on the people who have to quarantine, but on public health.”
Home for the holidays
Similar to its pre-Thanksgiving advisory, the CDC also recommends people avoid travel during the upcoming winter holidays. “The best way to protect yourself and others is to postpone travel and stay home,” Dr. Walke said.
If people do decide to travel, the agency recommends COVID-19 testing 1-3 days prior to travel and again 3-5 days afterward, as well as reducing nonessential activities for a full 7 days after returning home. Furthermore, if someone does not have follow-up testing, the CDC recommends reducing nonessential activities for 10 days.
Testing does not eliminate all risk, Dr. Walke said, “but when combined with reducing nonessential activities, symptom screening and continuing with precautions like wearing masks, social distancing and hand washing, it can make travel safer.”
“We are trying to reduce the number of infections by postponing travel over the winter holiday,” Cindy Friedman, MD, chief of the CDC Travelers’ Health Branch, said during the media briefing.
“Travel volume was high during Thanksgiving,” she said, “and even if only a small percentage of those travelers were asymptomatically infected, this can translate into hundreds of thousands of additional infections moving from one community to another.”
This article first appeared on Medscape.com.
Citing new evidence and an “acceptable risk” of transmission, the agency hopes reducing the 14-day quarantine will increase overall compliance and improve public health and economic constraints.
The agency also suggested people postpone travel during the upcoming winter holidays and stay home because of the pandemic.
These shorter quarantine options do not replace initial CDC guidance. “CDC continues to recommend quarantining for 14 days as the best way to reduce risk for spreading COVID-19,” said Henry Walke, MD, MPH, the CDC’s COVID-19 incident manager, during a media briefing on Wednesday.
However, “after reviewing and analyzing new research and data, CDC has identified two acceptable alternative quarantine periods.”
People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.
The agency also suggests people still monitor for symptoms for a full 14 days.
Reducing the length of quarantine “may make it easier for people to take this critical public health action, by reducing the economic hardship associated with a longer period, especially if they cannot work during that time,” Dr. Walke said. “In addition, a shorter quarantine period can lessen stress on the public health system and communities, especially when new infections are rapidly rising.”
The federal guidance leaves flexibility for local jurisdictions to make their own quarantine recommendations, as warranted, he added.
An ‘acceptable risk’ calculation
Modeling by the CDC and academic and public health partners led to the new quarantine recommendations, said John Brooks, MD, chief medical officer for the CDC’s COVID-19 response. Multiple studies “point in the same direction, which is that we can safely reduce the length of quarantine but accept there is a small residual risk that a person who is leaving quarantine early could transmit to someone else.”
The residual risk is approximately 1%, with an upper limit of 10%, when people quarantine for 10 days. A 7-day quarantine carries a residual risk of about 5% and an upper limit of 12%.
“Ten days is where the risk got into a sweet spot we like, at about 1%,” Dr. Brooks said. “That is a very acceptable risk, I think, for many people.”
Although it remains unknown what proportion of people spending 14 days in quarantine leave early, “we are hearing anecdotally from our partners in public health that many people are discontinuing quarantine ahead of time because there is pressure to go back to work, to get people back into school – and it imposes a burden on the individual,” Dr. Brooks said.
“One of our hopes is that ... if we reduce the amount of time they have to spend in quarantine, people will be more compliant,” he added.
A reporter asked why the CDC is shortening quarantines when the pandemic numbers are increasing nationwide. The timing has to do with capacity, Dr. Brooks said. “We are in situation where the number of cases is rising, the number of contacts is rising and the number of people who require quarantine is rising. That is a lot of burden, not just on the people who have to quarantine, but on public health.”
Home for the holidays
Similar to its pre-Thanksgiving advisory, the CDC also recommends people avoid travel during the upcoming winter holidays. “The best way to protect yourself and others is to postpone travel and stay home,” Dr. Walke said.
If people do decide to travel, the agency recommends COVID-19 testing 1-3 days prior to travel and again 3-5 days afterward, as well as reducing nonessential activities for a full 7 days after returning home. Furthermore, if someone does not have follow-up testing, the CDC recommends reducing nonessential activities for 10 days.
Testing does not eliminate all risk, Dr. Walke said, “but when combined with reducing nonessential activities, symptom screening and continuing with precautions like wearing masks, social distancing and hand washing, it can make travel safer.”
“We are trying to reduce the number of infections by postponing travel over the winter holiday,” Cindy Friedman, MD, chief of the CDC Travelers’ Health Branch, said during the media briefing.
“Travel volume was high during Thanksgiving,” she said, “and even if only a small percentage of those travelers were asymptomatically infected, this can translate into hundreds of thousands of additional infections moving from one community to another.”
This article first appeared on Medscape.com.
Citing new evidence and an “acceptable risk” of transmission, the agency hopes reducing the 14-day quarantine will increase overall compliance and improve public health and economic constraints.
The agency also suggested people postpone travel during the upcoming winter holidays and stay home because of the pandemic.
These shorter quarantine options do not replace initial CDC guidance. “CDC continues to recommend quarantining for 14 days as the best way to reduce risk for spreading COVID-19,” said Henry Walke, MD, MPH, the CDC’s COVID-19 incident manager, during a media briefing on Wednesday.
However, “after reviewing and analyzing new research and data, CDC has identified two acceptable alternative quarantine periods.”
People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.
The agency also suggests people still monitor for symptoms for a full 14 days.
Reducing the length of quarantine “may make it easier for people to take this critical public health action, by reducing the economic hardship associated with a longer period, especially if they cannot work during that time,” Dr. Walke said. “In addition, a shorter quarantine period can lessen stress on the public health system and communities, especially when new infections are rapidly rising.”
The federal guidance leaves flexibility for local jurisdictions to make their own quarantine recommendations, as warranted, he added.
An ‘acceptable risk’ calculation
Modeling by the CDC and academic and public health partners led to the new quarantine recommendations, said John Brooks, MD, chief medical officer for the CDC’s COVID-19 response. Multiple studies “point in the same direction, which is that we can safely reduce the length of quarantine but accept there is a small residual risk that a person who is leaving quarantine early could transmit to someone else.”
The residual risk is approximately 1%, with an upper limit of 10%, when people quarantine for 10 days. A 7-day quarantine carries a residual risk of about 5% and an upper limit of 12%.
“Ten days is where the risk got into a sweet spot we like, at about 1%,” Dr. Brooks said. “That is a very acceptable risk, I think, for many people.”
Although it remains unknown what proportion of people spending 14 days in quarantine leave early, “we are hearing anecdotally from our partners in public health that many people are discontinuing quarantine ahead of time because there is pressure to go back to work, to get people back into school – and it imposes a burden on the individual,” Dr. Brooks said.
“One of our hopes is that ... if we reduce the amount of time they have to spend in quarantine, people will be more compliant,” he added.
A reporter asked why the CDC is shortening quarantines when the pandemic numbers are increasing nationwide. The timing has to do with capacity, Dr. Brooks said. “We are in situation where the number of cases is rising, the number of contacts is rising and the number of people who require quarantine is rising. That is a lot of burden, not just on the people who have to quarantine, but on public health.”
Home for the holidays
Similar to its pre-Thanksgiving advisory, the CDC also recommends people avoid travel during the upcoming winter holidays. “The best way to protect yourself and others is to postpone travel and stay home,” Dr. Walke said.
If people do decide to travel, the agency recommends COVID-19 testing 1-3 days prior to travel and again 3-5 days afterward, as well as reducing nonessential activities for a full 7 days after returning home. Furthermore, if someone does not have follow-up testing, the CDC recommends reducing nonessential activities for 10 days.
Testing does not eliminate all risk, Dr. Walke said, “but when combined with reducing nonessential activities, symptom screening and continuing with precautions like wearing masks, social distancing and hand washing, it can make travel safer.”
“We are trying to reduce the number of infections by postponing travel over the winter holiday,” Cindy Friedman, MD, chief of the CDC Travelers’ Health Branch, said during the media briefing.
“Travel volume was high during Thanksgiving,” she said, “and even if only a small percentage of those travelers were asymptomatically infected, this can translate into hundreds of thousands of additional infections moving from one community to another.”
This article first appeared on Medscape.com.
Separating myth from reality: The role of cannabinoids in COVID-19
An intriguing pattern has emerged for cannabis enthusiasts as a result of lockdowns and statewide safety restrictions for COVID-19.
Consumers, as of late, have been shopping for larger marijuana baskets per trip to the dispensaries in various states, including California, Colorado, Nevada, and Washington, . However, they are also cutting down on the number of trips, perhaps, as a preventive measure to reduce the risk of exposure to coronavirus during this pandemic. Sales dipped considerably by the end of March only to experience a resurgence after the issuing of stimulus checks and unemployment benefits.
For the past few years, cannabis consumption remained steady while the industry continued to thrive with robust sales of the drug. It is a recession-proof phenomenon, therefore presenting a unique opportunity for clinicians with respect to patient education and individualized care.1
An unfortunate carryover of the governmental restrictions, self-isolation, and social estrangement is that consumers are now turning to the dark web as a source for continuous supply of cannabis. Prepandemic, according to the U.N. 2020 World Drug Report, there was already a 30% increase in sales of cannabis between 2009 and 2018. COVID-19 has fractured the drug’s supply chain and created an inescapable void that is being filled by drug traffickers.2 A clinical dilemma is posed when a user procures counterfeit cannabis or a drug batch with impurities.
Riding the cytokine storm
Cytokines are a host of proteins with designated regulatory and immune responses that play an instrumental role in cell signaling. The aptly named “cytokine storm” conjures up the image of an imperiled immune system spiraling out of control; it is, in fact, an extreme immune response that culminates into a massive influx of cytokines released into the bloodstream. Without the presence of an immunologic threat, cytokines are responsible for maintaining homeostasis and the functionality of immune cells. However, acute cytokine release (i.e., cytokine storm), as is the case with severe COVID-19, jeopardizes organ function (for example, interstitial lung disease) with clinical symptoms, such as fever, cough, dyspnea, and myalgia.
Benefits and drawbacks of immunosuppressive agents
To inhibit cytokine release (e.g., interleukin-6 cytokine levels), immunosuppressive agents such as tocilizumab have been leveraged to damper the body’s overactive inflammatory response to perceived immunologic stressors, in particular, COVID-19. While the aforementioned agent was remarkably effective with respect to lung consolidation clearance in most of the patients tested, a host of untoward effects prevent its general applicability and use. However, a team of researchers from the University of Nebraska, Omaha, with the Texas Biomedical Research Institute, San Antonio, might have stumbled upon a strategic workaround for mitigating the immune response.
They have proposed that cannabidiol (CBD) be used in lieu of other agents with potentially toxic effects. Animal and human trials have established that CBD confers a relatively high margin of safety coupled with favorable tolerance, providing a viable option for effectively targeting the inflammatory processes of SARS-CoV-2–based pulmonary disease. Furthermore, efficacy increased when CBD was combined with a terpene formulation, especially with respect to the more traditional steroid therapy.3
SARS-CoV-2 exhibits binding affinity for the ACE2 receptor, which is expressed in the lungs as well as other known predilection sites of infection. Ongoing studies attempt to modulate ACE2 expression, thereby eliminating its conspicuous role as “viral gateways,” perhaps even more so in patients with lung pathologies (e.g., people with chronic obstructive pulmonary disease [COPD] and smokers) as they already are prone to increased respiratory morbidity. CBD lacks tetrahydrocannabinol (THC), or the psychoactive component of cannabis sativa, rendering the agent to be particularly attractive from a therapeutic perspective. In addition to being devoid of abuse potential, CBD exhibits remarkable anti-inflammatory properties. It should be noted that considerable overlap exists between tobacco and cannabis users, and it is too early to determine the impact on COVID-19. As opposed to cannabis’s effect on ACE2 levels, smoking exhibits a proinflammatory role by up-regulating ACE2 expression.3 However, there are currently numerous conflicting reports in circulation about the positive effect of nicotine on COVID-19 outcome; confounding variables will need to be explored further in patients with a history of using nicotine and cannabis together.
From an immunologic perspective, the endocannabinoid system (ECS) plays an integral role in cell signaling by interacting with natural chemicals of the body, namely, cannabinoids with designated targets at the cannabinoid receptor 1 (CB1) and the CB2, respectively. The CB2 receptor is of particular interest as it is intimately involved in immune homeostasis; the primary goal of these COVID-19 studies is to modulate the endocannabinoid system via targeted CB2 therapies to produce an immunosuppressant effect.4 CB2 activation, be it by means of THC or CBD agonism, may prove to be beneficial by inhibiting the cytokine influx.
Unfortunately, there is a general dearth of data on COVID-19–exposed cannabis users, whether the drug is consumed for medication or recreational purposes. It has been suggested that cannabis intake might contribute toward the development of a cough, complicating the overall clinical outcome for those infected with the virus. The presence of a cough, even in an otherwise asymptomatic individual, facilitates viral spread. As for those cannabis users experiencing COVID-19 symptomatology, they can expect rapid clinical deterioration, including pronounced fatigue and a change in mental status.
According to pulmonary specialists and representatives of the American Lung Association, recreational cannabis use may be associated with a bronchitis-like inflammation (comparable with chronic bronchitis/COPD for chronic users) of the airways, along the lines of cigarette smoking.5 As far as cannabis smokers are concerned, the rationale for lung irritation is believed to stem from the relatively large portion of unburnt plant content that is inhaled in a given joint. If there is a superimposed infection, as is the case with COVID-19, the patient may experience further risk of adverse respiratory effects. This serves as a diagnostic dilemma for physicians, especially when they encounter patients who recently started dabbling with cannabis as a means of placating themselves or because they’ve heard rumors that it will somehow protect them from COVID-19. The entire assessment plan is slowed down as a result of the confounding variable (onset of a cough), which may arise independently of COVID-19 in cannabis users. Vulnerable populations include smokers and those with COPD or asthma, as they are more likely to require ventilator assistance during the course of COVID-19 therapy.5 Asthmatics and COPD patients are prone to bronchospasms because of sensitive airways.
COVID-19 safety protocols for cannabis users
Because of increased risk of respiratory morbidity, clinicians advise that consumption of recreational cannabinoids be scaled back during the course of the pandemic. In light of conflicting news from several media outlets regarding the efficacy of cannabis intake with respect to COVID-19, preexisting users might unwittingly increase their consumption as a preemptive measure against being exposed to the infection. To prevent transmission among users, clinicians should discourage patients from sharing joints. This recommendation is thematically consistent with general precautionary measures about the dangers of sharing utensils, drinking cups/glasses, and so on, amid the pandemic.
Despite promising preliminary research results, CBD cannot be wholeheartedly recommended at this time; patients already on medically administered cannabinoids are urged to discuss the risk-benefit ratio with their respective health care clinicians. Cannabinoid therapies present a massive opportunity from the perspective of immunomodulation, especially when considering the prevalence of drug use. However, to improve clinical guidelines with respect to COVID-19 outcomes, it would be prudent to increase the overall volume of preclinical knowledge by gathering retrospective data (from case-control designs) and randomized prospective trials.
A more comprehensive list of advice from physicians concerning casual or chronic cannabis users may also include: adopting a dedicated delivery or dispensing system for cannabis products, making considerations for decontamination (i.e., disinfecting mouthpieces), ensuring cleansing precautions are maintained (washing thoroughly before and after use or procurement), switching to inhalation alternates (e.g., tinctures, edibles, and/or oils) to decrease further irritation to the lungs. For bong users, it is recommended that they apply rubbing alcohol to clean their device followed with a minute of air-drying.6
Conclusion
The literature from preclinical studies appears to largely favor the use of CBD, but there remains an element of uncertainty with respect to implementing cannabinoids for the treatment of coronavirus.
COVID-19 cannabinoid intervention is a hot topic with renewed interest from the industry and the public at large, but viral-focused therapies remain a relatively underused area worth exploring with case-control designs and randomized prospective trials. As cannabis legalization is picking up momentum across five additional states, the time is ripe to systematically investigate the therapeutic applications of the drug beyond merely preclinical data. Aside from educational reform initiatives, clinicians might proactively launch a platform that integrates telemedicine as well as digital apps, directly linking the patient to the clinician and monitoring the efficacy of program initiatives in real time.
References
1. Long A. Consumers’ cannabis buying patterns change markedly in wake of COVID-19 pandemic. Marijuana Business Daily. 2020 Sep 22. https://mjbizdaily.com/consumers-cannabis-buying-patterns-change-markedly-in-wake-of-covid-pandemic/.
2. Bures B. How the coronavirus pandemic is increasing global demand for marijuana. Chicago Tribune. 2020 Jul 1. https://www.chicagotribune.com/marijuana/sns-tft-coronavirus-increases-global-marijuana-demand-20200701-oygaxryb7vhcjfeu44cgacicaa-story.html.
3. Walters J. Marijuana and COVID-19: Top studies. CannaMD. 2020 Aug 19. https://www.cannamd.com/marijuana-covid-19-top-studies/.
4. El Biali M et al. Med Cannabis Cannabinoids. 2020 Aug 19. doi: 10.1159/000510799.
5. LaMotte S. “Smoking weed and coronavirus: Even occasional use raises risk of COVID-19 complications.” CNN Health. 2020 Apr 10. https://www.cnn.com/2020/04/10/health/smoking-weed-coronavirus-wellness/index.html
6. Yafai S and Etengoff S. The case for cannabis: Advising cannabis users about COVID-19. Emergency Medicine News. 2020 May 20;42(5B).
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Mr. Choudhry is a research assistant at the IMCHF. Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. Dr. Islam, Mr. Choudhry, and Dr. Choudhry reported no relevant disclosures.
An intriguing pattern has emerged for cannabis enthusiasts as a result of lockdowns and statewide safety restrictions for COVID-19.
Consumers, as of late, have been shopping for larger marijuana baskets per trip to the dispensaries in various states, including California, Colorado, Nevada, and Washington, . However, they are also cutting down on the number of trips, perhaps, as a preventive measure to reduce the risk of exposure to coronavirus during this pandemic. Sales dipped considerably by the end of March only to experience a resurgence after the issuing of stimulus checks and unemployment benefits.
For the past few years, cannabis consumption remained steady while the industry continued to thrive with robust sales of the drug. It is a recession-proof phenomenon, therefore presenting a unique opportunity for clinicians with respect to patient education and individualized care.1
An unfortunate carryover of the governmental restrictions, self-isolation, and social estrangement is that consumers are now turning to the dark web as a source for continuous supply of cannabis. Prepandemic, according to the U.N. 2020 World Drug Report, there was already a 30% increase in sales of cannabis between 2009 and 2018. COVID-19 has fractured the drug’s supply chain and created an inescapable void that is being filled by drug traffickers.2 A clinical dilemma is posed when a user procures counterfeit cannabis or a drug batch with impurities.
Riding the cytokine storm
Cytokines are a host of proteins with designated regulatory and immune responses that play an instrumental role in cell signaling. The aptly named “cytokine storm” conjures up the image of an imperiled immune system spiraling out of control; it is, in fact, an extreme immune response that culminates into a massive influx of cytokines released into the bloodstream. Without the presence of an immunologic threat, cytokines are responsible for maintaining homeostasis and the functionality of immune cells. However, acute cytokine release (i.e., cytokine storm), as is the case with severe COVID-19, jeopardizes organ function (for example, interstitial lung disease) with clinical symptoms, such as fever, cough, dyspnea, and myalgia.
Benefits and drawbacks of immunosuppressive agents
To inhibit cytokine release (e.g., interleukin-6 cytokine levels), immunosuppressive agents such as tocilizumab have been leveraged to damper the body’s overactive inflammatory response to perceived immunologic stressors, in particular, COVID-19. While the aforementioned agent was remarkably effective with respect to lung consolidation clearance in most of the patients tested, a host of untoward effects prevent its general applicability and use. However, a team of researchers from the University of Nebraska, Omaha, with the Texas Biomedical Research Institute, San Antonio, might have stumbled upon a strategic workaround for mitigating the immune response.
They have proposed that cannabidiol (CBD) be used in lieu of other agents with potentially toxic effects. Animal and human trials have established that CBD confers a relatively high margin of safety coupled with favorable tolerance, providing a viable option for effectively targeting the inflammatory processes of SARS-CoV-2–based pulmonary disease. Furthermore, efficacy increased when CBD was combined with a terpene formulation, especially with respect to the more traditional steroid therapy.3
SARS-CoV-2 exhibits binding affinity for the ACE2 receptor, which is expressed in the lungs as well as other known predilection sites of infection. Ongoing studies attempt to modulate ACE2 expression, thereby eliminating its conspicuous role as “viral gateways,” perhaps even more so in patients with lung pathologies (e.g., people with chronic obstructive pulmonary disease [COPD] and smokers) as they already are prone to increased respiratory morbidity. CBD lacks tetrahydrocannabinol (THC), or the psychoactive component of cannabis sativa, rendering the agent to be particularly attractive from a therapeutic perspective. In addition to being devoid of abuse potential, CBD exhibits remarkable anti-inflammatory properties. It should be noted that considerable overlap exists between tobacco and cannabis users, and it is too early to determine the impact on COVID-19. As opposed to cannabis’s effect on ACE2 levels, smoking exhibits a proinflammatory role by up-regulating ACE2 expression.3 However, there are currently numerous conflicting reports in circulation about the positive effect of nicotine on COVID-19 outcome; confounding variables will need to be explored further in patients with a history of using nicotine and cannabis together.
From an immunologic perspective, the endocannabinoid system (ECS) plays an integral role in cell signaling by interacting with natural chemicals of the body, namely, cannabinoids with designated targets at the cannabinoid receptor 1 (CB1) and the CB2, respectively. The CB2 receptor is of particular interest as it is intimately involved in immune homeostasis; the primary goal of these COVID-19 studies is to modulate the endocannabinoid system via targeted CB2 therapies to produce an immunosuppressant effect.4 CB2 activation, be it by means of THC or CBD agonism, may prove to be beneficial by inhibiting the cytokine influx.
Unfortunately, there is a general dearth of data on COVID-19–exposed cannabis users, whether the drug is consumed for medication or recreational purposes. It has been suggested that cannabis intake might contribute toward the development of a cough, complicating the overall clinical outcome for those infected with the virus. The presence of a cough, even in an otherwise asymptomatic individual, facilitates viral spread. As for those cannabis users experiencing COVID-19 symptomatology, they can expect rapid clinical deterioration, including pronounced fatigue and a change in mental status.
According to pulmonary specialists and representatives of the American Lung Association, recreational cannabis use may be associated with a bronchitis-like inflammation (comparable with chronic bronchitis/COPD for chronic users) of the airways, along the lines of cigarette smoking.5 As far as cannabis smokers are concerned, the rationale for lung irritation is believed to stem from the relatively large portion of unburnt plant content that is inhaled in a given joint. If there is a superimposed infection, as is the case with COVID-19, the patient may experience further risk of adverse respiratory effects. This serves as a diagnostic dilemma for physicians, especially when they encounter patients who recently started dabbling with cannabis as a means of placating themselves or because they’ve heard rumors that it will somehow protect them from COVID-19. The entire assessment plan is slowed down as a result of the confounding variable (onset of a cough), which may arise independently of COVID-19 in cannabis users. Vulnerable populations include smokers and those with COPD or asthma, as they are more likely to require ventilator assistance during the course of COVID-19 therapy.5 Asthmatics and COPD patients are prone to bronchospasms because of sensitive airways.
COVID-19 safety protocols for cannabis users
Because of increased risk of respiratory morbidity, clinicians advise that consumption of recreational cannabinoids be scaled back during the course of the pandemic. In light of conflicting news from several media outlets regarding the efficacy of cannabis intake with respect to COVID-19, preexisting users might unwittingly increase their consumption as a preemptive measure against being exposed to the infection. To prevent transmission among users, clinicians should discourage patients from sharing joints. This recommendation is thematically consistent with general precautionary measures about the dangers of sharing utensils, drinking cups/glasses, and so on, amid the pandemic.
Despite promising preliminary research results, CBD cannot be wholeheartedly recommended at this time; patients already on medically administered cannabinoids are urged to discuss the risk-benefit ratio with their respective health care clinicians. Cannabinoid therapies present a massive opportunity from the perspective of immunomodulation, especially when considering the prevalence of drug use. However, to improve clinical guidelines with respect to COVID-19 outcomes, it would be prudent to increase the overall volume of preclinical knowledge by gathering retrospective data (from case-control designs) and randomized prospective trials.
A more comprehensive list of advice from physicians concerning casual or chronic cannabis users may also include: adopting a dedicated delivery or dispensing system for cannabis products, making considerations for decontamination (i.e., disinfecting mouthpieces), ensuring cleansing precautions are maintained (washing thoroughly before and after use or procurement), switching to inhalation alternates (e.g., tinctures, edibles, and/or oils) to decrease further irritation to the lungs. For bong users, it is recommended that they apply rubbing alcohol to clean their device followed with a minute of air-drying.6
Conclusion
The literature from preclinical studies appears to largely favor the use of CBD, but there remains an element of uncertainty with respect to implementing cannabinoids for the treatment of coronavirus.
COVID-19 cannabinoid intervention is a hot topic with renewed interest from the industry and the public at large, but viral-focused therapies remain a relatively underused area worth exploring with case-control designs and randomized prospective trials. As cannabis legalization is picking up momentum across five additional states, the time is ripe to systematically investigate the therapeutic applications of the drug beyond merely preclinical data. Aside from educational reform initiatives, clinicians might proactively launch a platform that integrates telemedicine as well as digital apps, directly linking the patient to the clinician and monitoring the efficacy of program initiatives in real time.
References
1. Long A. Consumers’ cannabis buying patterns change markedly in wake of COVID-19 pandemic. Marijuana Business Daily. 2020 Sep 22. https://mjbizdaily.com/consumers-cannabis-buying-patterns-change-markedly-in-wake-of-covid-pandemic/.
2. Bures B. How the coronavirus pandemic is increasing global demand for marijuana. Chicago Tribune. 2020 Jul 1. https://www.chicagotribune.com/marijuana/sns-tft-coronavirus-increases-global-marijuana-demand-20200701-oygaxryb7vhcjfeu44cgacicaa-story.html.
3. Walters J. Marijuana and COVID-19: Top studies. CannaMD. 2020 Aug 19. https://www.cannamd.com/marijuana-covid-19-top-studies/.
4. El Biali M et al. Med Cannabis Cannabinoids. 2020 Aug 19. doi: 10.1159/000510799.
5. LaMotte S. “Smoking weed and coronavirus: Even occasional use raises risk of COVID-19 complications.” CNN Health. 2020 Apr 10. https://www.cnn.com/2020/04/10/health/smoking-weed-coronavirus-wellness/index.html
6. Yafai S and Etengoff S. The case for cannabis: Advising cannabis users about COVID-19. Emergency Medicine News. 2020 May 20;42(5B).
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Mr. Choudhry is a research assistant at the IMCHF. Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. Dr. Islam, Mr. Choudhry, and Dr. Choudhry reported no relevant disclosures.
An intriguing pattern has emerged for cannabis enthusiasts as a result of lockdowns and statewide safety restrictions for COVID-19.
Consumers, as of late, have been shopping for larger marijuana baskets per trip to the dispensaries in various states, including California, Colorado, Nevada, and Washington, . However, they are also cutting down on the number of trips, perhaps, as a preventive measure to reduce the risk of exposure to coronavirus during this pandemic. Sales dipped considerably by the end of March only to experience a resurgence after the issuing of stimulus checks and unemployment benefits.
For the past few years, cannabis consumption remained steady while the industry continued to thrive with robust sales of the drug. It is a recession-proof phenomenon, therefore presenting a unique opportunity for clinicians with respect to patient education and individualized care.1
An unfortunate carryover of the governmental restrictions, self-isolation, and social estrangement is that consumers are now turning to the dark web as a source for continuous supply of cannabis. Prepandemic, according to the U.N. 2020 World Drug Report, there was already a 30% increase in sales of cannabis between 2009 and 2018. COVID-19 has fractured the drug’s supply chain and created an inescapable void that is being filled by drug traffickers.2 A clinical dilemma is posed when a user procures counterfeit cannabis or a drug batch with impurities.
Riding the cytokine storm
Cytokines are a host of proteins with designated regulatory and immune responses that play an instrumental role in cell signaling. The aptly named “cytokine storm” conjures up the image of an imperiled immune system spiraling out of control; it is, in fact, an extreme immune response that culminates into a massive influx of cytokines released into the bloodstream. Without the presence of an immunologic threat, cytokines are responsible for maintaining homeostasis and the functionality of immune cells. However, acute cytokine release (i.e., cytokine storm), as is the case with severe COVID-19, jeopardizes organ function (for example, interstitial lung disease) with clinical symptoms, such as fever, cough, dyspnea, and myalgia.
Benefits and drawbacks of immunosuppressive agents
To inhibit cytokine release (e.g., interleukin-6 cytokine levels), immunosuppressive agents such as tocilizumab have been leveraged to damper the body’s overactive inflammatory response to perceived immunologic stressors, in particular, COVID-19. While the aforementioned agent was remarkably effective with respect to lung consolidation clearance in most of the patients tested, a host of untoward effects prevent its general applicability and use. However, a team of researchers from the University of Nebraska, Omaha, with the Texas Biomedical Research Institute, San Antonio, might have stumbled upon a strategic workaround for mitigating the immune response.
They have proposed that cannabidiol (CBD) be used in lieu of other agents with potentially toxic effects. Animal and human trials have established that CBD confers a relatively high margin of safety coupled with favorable tolerance, providing a viable option for effectively targeting the inflammatory processes of SARS-CoV-2–based pulmonary disease. Furthermore, efficacy increased when CBD was combined with a terpene formulation, especially with respect to the more traditional steroid therapy.3
SARS-CoV-2 exhibits binding affinity for the ACE2 receptor, which is expressed in the lungs as well as other known predilection sites of infection. Ongoing studies attempt to modulate ACE2 expression, thereby eliminating its conspicuous role as “viral gateways,” perhaps even more so in patients with lung pathologies (e.g., people with chronic obstructive pulmonary disease [COPD] and smokers) as they already are prone to increased respiratory morbidity. CBD lacks tetrahydrocannabinol (THC), or the psychoactive component of cannabis sativa, rendering the agent to be particularly attractive from a therapeutic perspective. In addition to being devoid of abuse potential, CBD exhibits remarkable anti-inflammatory properties. It should be noted that considerable overlap exists between tobacco and cannabis users, and it is too early to determine the impact on COVID-19. As opposed to cannabis’s effect on ACE2 levels, smoking exhibits a proinflammatory role by up-regulating ACE2 expression.3 However, there are currently numerous conflicting reports in circulation about the positive effect of nicotine on COVID-19 outcome; confounding variables will need to be explored further in patients with a history of using nicotine and cannabis together.
From an immunologic perspective, the endocannabinoid system (ECS) plays an integral role in cell signaling by interacting with natural chemicals of the body, namely, cannabinoids with designated targets at the cannabinoid receptor 1 (CB1) and the CB2, respectively. The CB2 receptor is of particular interest as it is intimately involved in immune homeostasis; the primary goal of these COVID-19 studies is to modulate the endocannabinoid system via targeted CB2 therapies to produce an immunosuppressant effect.4 CB2 activation, be it by means of THC or CBD agonism, may prove to be beneficial by inhibiting the cytokine influx.
Unfortunately, there is a general dearth of data on COVID-19–exposed cannabis users, whether the drug is consumed for medication or recreational purposes. It has been suggested that cannabis intake might contribute toward the development of a cough, complicating the overall clinical outcome for those infected with the virus. The presence of a cough, even in an otherwise asymptomatic individual, facilitates viral spread. As for those cannabis users experiencing COVID-19 symptomatology, they can expect rapid clinical deterioration, including pronounced fatigue and a change in mental status.
According to pulmonary specialists and representatives of the American Lung Association, recreational cannabis use may be associated with a bronchitis-like inflammation (comparable with chronic bronchitis/COPD for chronic users) of the airways, along the lines of cigarette smoking.5 As far as cannabis smokers are concerned, the rationale for lung irritation is believed to stem from the relatively large portion of unburnt plant content that is inhaled in a given joint. If there is a superimposed infection, as is the case with COVID-19, the patient may experience further risk of adverse respiratory effects. This serves as a diagnostic dilemma for physicians, especially when they encounter patients who recently started dabbling with cannabis as a means of placating themselves or because they’ve heard rumors that it will somehow protect them from COVID-19. The entire assessment plan is slowed down as a result of the confounding variable (onset of a cough), which may arise independently of COVID-19 in cannabis users. Vulnerable populations include smokers and those with COPD or asthma, as they are more likely to require ventilator assistance during the course of COVID-19 therapy.5 Asthmatics and COPD patients are prone to bronchospasms because of sensitive airways.
COVID-19 safety protocols for cannabis users
Because of increased risk of respiratory morbidity, clinicians advise that consumption of recreational cannabinoids be scaled back during the course of the pandemic. In light of conflicting news from several media outlets regarding the efficacy of cannabis intake with respect to COVID-19, preexisting users might unwittingly increase their consumption as a preemptive measure against being exposed to the infection. To prevent transmission among users, clinicians should discourage patients from sharing joints. This recommendation is thematically consistent with general precautionary measures about the dangers of sharing utensils, drinking cups/glasses, and so on, amid the pandemic.
Despite promising preliminary research results, CBD cannot be wholeheartedly recommended at this time; patients already on medically administered cannabinoids are urged to discuss the risk-benefit ratio with their respective health care clinicians. Cannabinoid therapies present a massive opportunity from the perspective of immunomodulation, especially when considering the prevalence of drug use. However, to improve clinical guidelines with respect to COVID-19 outcomes, it would be prudent to increase the overall volume of preclinical knowledge by gathering retrospective data (from case-control designs) and randomized prospective trials.
A more comprehensive list of advice from physicians concerning casual or chronic cannabis users may also include: adopting a dedicated delivery or dispensing system for cannabis products, making considerations for decontamination (i.e., disinfecting mouthpieces), ensuring cleansing precautions are maintained (washing thoroughly before and after use or procurement), switching to inhalation alternates (e.g., tinctures, edibles, and/or oils) to decrease further irritation to the lungs. For bong users, it is recommended that they apply rubbing alcohol to clean their device followed with a minute of air-drying.6
Conclusion
The literature from preclinical studies appears to largely favor the use of CBD, but there remains an element of uncertainty with respect to implementing cannabinoids for the treatment of coronavirus.
COVID-19 cannabinoid intervention is a hot topic with renewed interest from the industry and the public at large, but viral-focused therapies remain a relatively underused area worth exploring with case-control designs and randomized prospective trials. As cannabis legalization is picking up momentum across five additional states, the time is ripe to systematically investigate the therapeutic applications of the drug beyond merely preclinical data. Aside from educational reform initiatives, clinicians might proactively launch a platform that integrates telemedicine as well as digital apps, directly linking the patient to the clinician and monitoring the efficacy of program initiatives in real time.
References
1. Long A. Consumers’ cannabis buying patterns change markedly in wake of COVID-19 pandemic. Marijuana Business Daily. 2020 Sep 22. https://mjbizdaily.com/consumers-cannabis-buying-patterns-change-markedly-in-wake-of-covid-pandemic/.
2. Bures B. How the coronavirus pandemic is increasing global demand for marijuana. Chicago Tribune. 2020 Jul 1. https://www.chicagotribune.com/marijuana/sns-tft-coronavirus-increases-global-marijuana-demand-20200701-oygaxryb7vhcjfeu44cgacicaa-story.html.
3. Walters J. Marijuana and COVID-19: Top studies. CannaMD. 2020 Aug 19. https://www.cannamd.com/marijuana-covid-19-top-studies/.
4. El Biali M et al. Med Cannabis Cannabinoids. 2020 Aug 19. doi: 10.1159/000510799.
5. LaMotte S. “Smoking weed and coronavirus: Even occasional use raises risk of COVID-19 complications.” CNN Health. 2020 Apr 10. https://www.cnn.com/2020/04/10/health/smoking-weed-coronavirus-wellness/index.html
6. Yafai S and Etengoff S. The case for cannabis: Advising cannabis users about COVID-19. Emergency Medicine News. 2020 May 20;42(5B).
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Mr. Choudhry is a research assistant at the IMCHF. Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. Dr. Islam, Mr. Choudhry, and Dr. Choudhry reported no relevant disclosures.
Treating alcohol withdrawal syndrome: Going beyond ‘benzos’
Alcohol withdrawal syndrome (AWS) occurs when an individual who is alcohol-dependent suddenly stops or significantly reduces his/her alcohol intake.1 Symptoms of AWS, which can be fatal, include anxiety, restlessness, seizures, confusion, and delirium.1 Because benzodiazepines have been proven effective in improving symptoms of AWS, they are considered the first-line treatment, but they also carry the risk of abuse, psychomotor sedation, cognitive impairment, and interactions with alcohol.1
Non-benzodiazepine anticonvulsants (NBACs) such as valproic acid (VPA) and carbamazepine may offer benefit as alternatives or adjuncts to benzodiazepines.1 Many NBACs affect the functioning of glutamate and gamma-aminobutyric acid (GABA) neurotransmitters,2 which are particularly dysregulated in patients with AWS. Because NBACs help stabilize this imbalance, they may be useful for managing AWS and preventing relapse without the risks associated with benzodiazepines.2
Valproic acid: A better choice than carbamazepine
Compared with other NBACs, VPA and carbamazepine have been studied more extensively for treating patients with AWS, and their clinical effectiveness has been well documented.1 For mild-to-moderate AWS, VPA and carbamazepine may be as effective as benzodiazepines in reducing the severity of symptoms, and more potent for preventing withdrawal seizures.1
Increasing data suggests that compared with VPA, adjunctive treatment with carbamazepine for AWS may be more frequently associated with intolerable adverse effects such as ataxia, orthostatic hypotension, vertigo, nausea, and vomiting.1 The rapid onset of AWS requires rapid-acting pharmacotherapy.1 In attempting to rapidly achieve the desired plasma concentrations of carbamazepine, clinicians may risk inducing adverse effects. Compared with carbamazepine, VPA is associated with faster symptom resolution, a shorter duration of pharmacologic treatment, fewer transfers to the ICU, fewer withdrawal seizures, and a more favorable adverse effect profile.1 Likely due to its shorter half-life, VPA delivers its therapeutic effects without producing significant adverse effects.1
Early and aggressive treatment of AWS is needed to block kindling,3 which is characterized by the worsening of withdrawal symptoms each time an individual attempts to quit drinking alcohol. Compared with carbamazepine, VPA may be more helpful for blocking kindling.3
More data is needed
Due to ethical concerns, few studies have compared anticonvulsant medications with placebo for treating AWS.2 Most studies examining NBACs for AWS have either used the anticonvulsant as an adjunct to a benzodiazepine to examine improvement in withdrawal symptoms, or compared the anticonvulsant with placebo or another intervention to assess the amount of a benzodiazepine required for safe detoxification.2,4 Additionally, most studies examining NBACs have been short, and few followed patients after the active medication period, which limits our knowledge of the long-term effectiveness of NBACs.2 Before NBACs can replace benzodiazepines for managing AWS, further evidence from clinical trials is needed to assess their efficiency as a stand-alone treatment.
1. Maldonado JR. Novel algorithms for the prophylaxis and management of alcohol withdrawal syndromes–beyond benzodiazepines. Crit Care Clin. 2017;33(3):559-599.
2. Hammond CJ, Niciu MJ, Drew S, et al. Anticonvulsants for the treatment of alcohol withdrawal syndrome and alcohol use disorders. CNS Drugs. 2015;29(4):293-311.
3. Eyer F, Schreckenberg M, Hecht D, et al. Carbamazepine and valproate as adjuncts in the treatment of alcohol withdrawal syndrome: a retrospective cohort study. Alcohol Alcohol. 2011;46(2):177-184.
4. Guirguis E, Richardson J, Kuhn T, et al. Treatment of severe alcohol withdrawal: a focus on adjunctive agents. J Pharm Technol. 2017;33(5):204-212.
Alcohol withdrawal syndrome (AWS) occurs when an individual who is alcohol-dependent suddenly stops or significantly reduces his/her alcohol intake.1 Symptoms of AWS, which can be fatal, include anxiety, restlessness, seizures, confusion, and delirium.1 Because benzodiazepines have been proven effective in improving symptoms of AWS, they are considered the first-line treatment, but they also carry the risk of abuse, psychomotor sedation, cognitive impairment, and interactions with alcohol.1
Non-benzodiazepine anticonvulsants (NBACs) such as valproic acid (VPA) and carbamazepine may offer benefit as alternatives or adjuncts to benzodiazepines.1 Many NBACs affect the functioning of glutamate and gamma-aminobutyric acid (GABA) neurotransmitters,2 which are particularly dysregulated in patients with AWS. Because NBACs help stabilize this imbalance, they may be useful for managing AWS and preventing relapse without the risks associated with benzodiazepines.2
Valproic acid: A better choice than carbamazepine
Compared with other NBACs, VPA and carbamazepine have been studied more extensively for treating patients with AWS, and their clinical effectiveness has been well documented.1 For mild-to-moderate AWS, VPA and carbamazepine may be as effective as benzodiazepines in reducing the severity of symptoms, and more potent for preventing withdrawal seizures.1
Increasing data suggests that compared with VPA, adjunctive treatment with carbamazepine for AWS may be more frequently associated with intolerable adverse effects such as ataxia, orthostatic hypotension, vertigo, nausea, and vomiting.1 The rapid onset of AWS requires rapid-acting pharmacotherapy.1 In attempting to rapidly achieve the desired plasma concentrations of carbamazepine, clinicians may risk inducing adverse effects. Compared with carbamazepine, VPA is associated with faster symptom resolution, a shorter duration of pharmacologic treatment, fewer transfers to the ICU, fewer withdrawal seizures, and a more favorable adverse effect profile.1 Likely due to its shorter half-life, VPA delivers its therapeutic effects without producing significant adverse effects.1
Early and aggressive treatment of AWS is needed to block kindling,3 which is characterized by the worsening of withdrawal symptoms each time an individual attempts to quit drinking alcohol. Compared with carbamazepine, VPA may be more helpful for blocking kindling.3
More data is needed
Due to ethical concerns, few studies have compared anticonvulsant medications with placebo for treating AWS.2 Most studies examining NBACs for AWS have either used the anticonvulsant as an adjunct to a benzodiazepine to examine improvement in withdrawal symptoms, or compared the anticonvulsant with placebo or another intervention to assess the amount of a benzodiazepine required for safe detoxification.2,4 Additionally, most studies examining NBACs have been short, and few followed patients after the active medication period, which limits our knowledge of the long-term effectiveness of NBACs.2 Before NBACs can replace benzodiazepines for managing AWS, further evidence from clinical trials is needed to assess their efficiency as a stand-alone treatment.
Alcohol withdrawal syndrome (AWS) occurs when an individual who is alcohol-dependent suddenly stops or significantly reduces his/her alcohol intake.1 Symptoms of AWS, which can be fatal, include anxiety, restlessness, seizures, confusion, and delirium.1 Because benzodiazepines have been proven effective in improving symptoms of AWS, they are considered the first-line treatment, but they also carry the risk of abuse, psychomotor sedation, cognitive impairment, and interactions with alcohol.1
Non-benzodiazepine anticonvulsants (NBACs) such as valproic acid (VPA) and carbamazepine may offer benefit as alternatives or adjuncts to benzodiazepines.1 Many NBACs affect the functioning of glutamate and gamma-aminobutyric acid (GABA) neurotransmitters,2 which are particularly dysregulated in patients with AWS. Because NBACs help stabilize this imbalance, they may be useful for managing AWS and preventing relapse without the risks associated with benzodiazepines.2
Valproic acid: A better choice than carbamazepine
Compared with other NBACs, VPA and carbamazepine have been studied more extensively for treating patients with AWS, and their clinical effectiveness has been well documented.1 For mild-to-moderate AWS, VPA and carbamazepine may be as effective as benzodiazepines in reducing the severity of symptoms, and more potent for preventing withdrawal seizures.1
Increasing data suggests that compared with VPA, adjunctive treatment with carbamazepine for AWS may be more frequently associated with intolerable adverse effects such as ataxia, orthostatic hypotension, vertigo, nausea, and vomiting.1 The rapid onset of AWS requires rapid-acting pharmacotherapy.1 In attempting to rapidly achieve the desired plasma concentrations of carbamazepine, clinicians may risk inducing adverse effects. Compared with carbamazepine, VPA is associated with faster symptom resolution, a shorter duration of pharmacologic treatment, fewer transfers to the ICU, fewer withdrawal seizures, and a more favorable adverse effect profile.1 Likely due to its shorter half-life, VPA delivers its therapeutic effects without producing significant adverse effects.1
Early and aggressive treatment of AWS is needed to block kindling,3 which is characterized by the worsening of withdrawal symptoms each time an individual attempts to quit drinking alcohol. Compared with carbamazepine, VPA may be more helpful for blocking kindling.3
More data is needed
Due to ethical concerns, few studies have compared anticonvulsant medications with placebo for treating AWS.2 Most studies examining NBACs for AWS have either used the anticonvulsant as an adjunct to a benzodiazepine to examine improvement in withdrawal symptoms, or compared the anticonvulsant with placebo or another intervention to assess the amount of a benzodiazepine required for safe detoxification.2,4 Additionally, most studies examining NBACs have been short, and few followed patients after the active medication period, which limits our knowledge of the long-term effectiveness of NBACs.2 Before NBACs can replace benzodiazepines for managing AWS, further evidence from clinical trials is needed to assess their efficiency as a stand-alone treatment.
1. Maldonado JR. Novel algorithms for the prophylaxis and management of alcohol withdrawal syndromes–beyond benzodiazepines. Crit Care Clin. 2017;33(3):559-599.
2. Hammond CJ, Niciu MJ, Drew S, et al. Anticonvulsants for the treatment of alcohol withdrawal syndrome and alcohol use disorders. CNS Drugs. 2015;29(4):293-311.
3. Eyer F, Schreckenberg M, Hecht D, et al. Carbamazepine and valproate as adjuncts in the treatment of alcohol withdrawal syndrome: a retrospective cohort study. Alcohol Alcohol. 2011;46(2):177-184.
4. Guirguis E, Richardson J, Kuhn T, et al. Treatment of severe alcohol withdrawal: a focus on adjunctive agents. J Pharm Technol. 2017;33(5):204-212.
1. Maldonado JR. Novel algorithms for the prophylaxis and management of alcohol withdrawal syndromes–beyond benzodiazepines. Crit Care Clin. 2017;33(3):559-599.
2. Hammond CJ, Niciu MJ, Drew S, et al. Anticonvulsants for the treatment of alcohol withdrawal syndrome and alcohol use disorders. CNS Drugs. 2015;29(4):293-311.
3. Eyer F, Schreckenberg M, Hecht D, et al. Carbamazepine and valproate as adjuncts in the treatment of alcohol withdrawal syndrome: a retrospective cohort study. Alcohol Alcohol. 2011;46(2):177-184.
4. Guirguis E, Richardson J, Kuhn T, et al. Treatment of severe alcohol withdrawal: a focus on adjunctive agents. J Pharm Technol. 2017;33(5):204-212.
ACIP: Health workers, long-term care residents first tier for COVID-19 vaccine
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices voted 13-1 that both groups be in the highest-priority group for vaccination. As such, ACIP recommends that both be included in phase 1a of the committee’s allocation plan.
The recommendation now goes to CDC director Robert Redfield, MD, for approval. State health departments are expected to rely on the recommendation, but ultimately can make their own decisions on how to allocate vaccine in their states.
“We hope that this vote gets us all one step closer to the day when we can all feel safe again and when this pandemic is over,” said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases, at today’s meeting.
Health care workers are defined as paid and unpaid individuals serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials. Long-term care residents are defined as adults who reside in facilities that provide a variety of services, including medical and personal care. Phase 1a would not include children who live in such facilities.
“Our goal in phase 1a with regard to health care personnel is to preserve the workforce and health care capacity regardless of where exposure occurs,” said ACIP panelist Grace Lee, MD, MPH, professor of paediatrics at Stanford (Calif.) University. Thus vaccination would cover clinical support staff, such as nursing assistants, environmental services staff, and food support staff.
“It is crucial to maintain our health care capacity,” said ACIP member Sharon Frey, MD, clinical director at the Center for Vaccine Development at Saint Louis University. “But it’s also important to prevent severe disease and death in the group that is at highest risk of those complications and that includes those in long-term care facilities.”
CDC staff said that staff and residents in those facilities account for 6% of COVID-19 cases and 40% of deaths.
But Helen Keipp Talbot, MD, associate professor of medicine at Vanderbilt University, Nashville, Tenn., voted against putting long-term care residents into the 1a phase. “We have traditionally tried a vaccine in a young healthy population and then hope it works in our frail older adults. So we enter this realm of ‘we hope it works and that it’s safe,’ and that concerns me on many levels particularly for this vaccine,” she said, noting that the vaccines closest to FDA authorization have not been studied in elderly adults who live in nursing homes or assisted living facilities.
She added: “I have no reservations for health care workers taking this vaccine.”
Prioritization could change
The phase 1a allocation fits within the “four ethical principles” outlined by ACIP and CDC staff Nov. 23: to maximize benefits and minimize harms, promote justice, mitigate health inequities, and promote transparency.
“My vote reflects maximum benefit, minimum harm, promoting justice and mitigating the health inequalities that exist with regard to distribution of this vaccine,” said ACIP Chair Jose Romero, MD. Romero, chief medical officer of the Arkansas Department of Health, voted in favor of the phase 1a plan.
He and other panelists noted, however, that allocation priorities could change after the FDA reviews and authorizes a vaccine.
The FDA’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) will meet December 10 to review the Pfizer/BioNTech’s messenger RNA-based vaccine (BNT162b2). The companies filed for emergency use on November 20.
A second vaccine, made by Moderna, is not far behind. The company reported on Nov. 30 that its messenger RNA vaccine was 94.1% effective and filed for emergency use the same day. The FDA’s VRBPAC will review the safety and efficacy data for the Moderna vaccine on Dec. 17.
“If individual vaccines receive emergency use authorization, we will have more data to consider, and that could lead to revision of our prioritization,” said ACIP member Robert Atmar, MD, John S. Dunn Research Foundation Clinical Professor in Infectious Diseases at Baylor College of Medicine, Houston.
ACIP will meet again after the Dec. 10 FDA advisory panel. But it won’t recommend a product until after the FDA has authorized it, said Amanda Cohn, MD, senior advisor for vaccines at the CDC’s National Center for Immunization and Respiratory Diseases.
Staggered immunization subprioritization urged
The CDC staff said that given the potential that not enough vaccine will be available immediately, it was recommending that health care organizations plan on creating a hierarchy of prioritization within institutions. And, they also urged staggering vaccination for personnel in similar units or positions, citing potential systemic or other reactions among health care workers.
“Consider planning for personnel to have time away from clinical care if health care personnel experience systemic symptoms post vaccination,” said Sarah Oliver, MD, MSPH, from the CDC.
The CDC will soon be issuing guidance on how to handle systemic symptoms with health care workers, Dr. Oliver noted.
Some 40 million doses of the Pfizer/BioNTech and Moderna vaccines are expected to be available by the end of December, with 5 million to 10 million a week coming online after that, Dr. Cohn said. That means not all health care workers will be vaccinated immediately. That may require “subprioritization, but for a limited period of time,” she said.
Dr. Messonnier said that, even with limited supplies, most of the states have told the CDC that they think they can vaccinate all of their health care workers within 3 weeks – some in less time.
The ACIP allocation plan is similar to but not exactly the same as that issued by the National Academy of Sciences, Engineering, and Medicine, which issued recommendations in October. That organization said that health care workers, first responders, older Americans living in congregate settings, and people with underlying health conditions should be the first to receive a vaccine.
ACIP has said that phase 1b would include essential workers, including police officers and firefighters, and those in education, transportation, and food and agriculture sectors. Phase 1c would include adults with high-risk medical conditions and those aged 65 years or older.
This article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices voted 13-1 that both groups be in the highest-priority group for vaccination. As such, ACIP recommends that both be included in phase 1a of the committee’s allocation plan.
The recommendation now goes to CDC director Robert Redfield, MD, for approval. State health departments are expected to rely on the recommendation, but ultimately can make their own decisions on how to allocate vaccine in their states.
“We hope that this vote gets us all one step closer to the day when we can all feel safe again and when this pandemic is over,” said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases, at today’s meeting.
Health care workers are defined as paid and unpaid individuals serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials. Long-term care residents are defined as adults who reside in facilities that provide a variety of services, including medical and personal care. Phase 1a would not include children who live in such facilities.
“Our goal in phase 1a with regard to health care personnel is to preserve the workforce and health care capacity regardless of where exposure occurs,” said ACIP panelist Grace Lee, MD, MPH, professor of paediatrics at Stanford (Calif.) University. Thus vaccination would cover clinical support staff, such as nursing assistants, environmental services staff, and food support staff.
“It is crucial to maintain our health care capacity,” said ACIP member Sharon Frey, MD, clinical director at the Center for Vaccine Development at Saint Louis University. “But it’s also important to prevent severe disease and death in the group that is at highest risk of those complications and that includes those in long-term care facilities.”
CDC staff said that staff and residents in those facilities account for 6% of COVID-19 cases and 40% of deaths.
But Helen Keipp Talbot, MD, associate professor of medicine at Vanderbilt University, Nashville, Tenn., voted against putting long-term care residents into the 1a phase. “We have traditionally tried a vaccine in a young healthy population and then hope it works in our frail older adults. So we enter this realm of ‘we hope it works and that it’s safe,’ and that concerns me on many levels particularly for this vaccine,” she said, noting that the vaccines closest to FDA authorization have not been studied in elderly adults who live in nursing homes or assisted living facilities.
She added: “I have no reservations for health care workers taking this vaccine.”
Prioritization could change
The phase 1a allocation fits within the “four ethical principles” outlined by ACIP and CDC staff Nov. 23: to maximize benefits and minimize harms, promote justice, mitigate health inequities, and promote transparency.
“My vote reflects maximum benefit, minimum harm, promoting justice and mitigating the health inequalities that exist with regard to distribution of this vaccine,” said ACIP Chair Jose Romero, MD. Romero, chief medical officer of the Arkansas Department of Health, voted in favor of the phase 1a plan.
He and other panelists noted, however, that allocation priorities could change after the FDA reviews and authorizes a vaccine.
The FDA’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) will meet December 10 to review the Pfizer/BioNTech’s messenger RNA-based vaccine (BNT162b2). The companies filed for emergency use on November 20.
A second vaccine, made by Moderna, is not far behind. The company reported on Nov. 30 that its messenger RNA vaccine was 94.1% effective and filed for emergency use the same day. The FDA’s VRBPAC will review the safety and efficacy data for the Moderna vaccine on Dec. 17.
“If individual vaccines receive emergency use authorization, we will have more data to consider, and that could lead to revision of our prioritization,” said ACIP member Robert Atmar, MD, John S. Dunn Research Foundation Clinical Professor in Infectious Diseases at Baylor College of Medicine, Houston.
ACIP will meet again after the Dec. 10 FDA advisory panel. But it won’t recommend a product until after the FDA has authorized it, said Amanda Cohn, MD, senior advisor for vaccines at the CDC’s National Center for Immunization and Respiratory Diseases.
Staggered immunization subprioritization urged
The CDC staff said that given the potential that not enough vaccine will be available immediately, it was recommending that health care organizations plan on creating a hierarchy of prioritization within institutions. And, they also urged staggering vaccination for personnel in similar units or positions, citing potential systemic or other reactions among health care workers.
“Consider planning for personnel to have time away from clinical care if health care personnel experience systemic symptoms post vaccination,” said Sarah Oliver, MD, MSPH, from the CDC.
The CDC will soon be issuing guidance on how to handle systemic symptoms with health care workers, Dr. Oliver noted.
Some 40 million doses of the Pfizer/BioNTech and Moderna vaccines are expected to be available by the end of December, with 5 million to 10 million a week coming online after that, Dr. Cohn said. That means not all health care workers will be vaccinated immediately. That may require “subprioritization, but for a limited period of time,” she said.
Dr. Messonnier said that, even with limited supplies, most of the states have told the CDC that they think they can vaccinate all of their health care workers within 3 weeks – some in less time.
The ACIP allocation plan is similar to but not exactly the same as that issued by the National Academy of Sciences, Engineering, and Medicine, which issued recommendations in October. That organization said that health care workers, first responders, older Americans living in congregate settings, and people with underlying health conditions should be the first to receive a vaccine.
ACIP has said that phase 1b would include essential workers, including police officers and firefighters, and those in education, transportation, and food and agriculture sectors. Phase 1c would include adults with high-risk medical conditions and those aged 65 years or older.
This article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices voted 13-1 that both groups be in the highest-priority group for vaccination. As such, ACIP recommends that both be included in phase 1a of the committee’s allocation plan.
The recommendation now goes to CDC director Robert Redfield, MD, for approval. State health departments are expected to rely on the recommendation, but ultimately can make their own decisions on how to allocate vaccine in their states.
“We hope that this vote gets us all one step closer to the day when we can all feel safe again and when this pandemic is over,” said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases, at today’s meeting.
Health care workers are defined as paid and unpaid individuals serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials. Long-term care residents are defined as adults who reside in facilities that provide a variety of services, including medical and personal care. Phase 1a would not include children who live in such facilities.
“Our goal in phase 1a with regard to health care personnel is to preserve the workforce and health care capacity regardless of where exposure occurs,” said ACIP panelist Grace Lee, MD, MPH, professor of paediatrics at Stanford (Calif.) University. Thus vaccination would cover clinical support staff, such as nursing assistants, environmental services staff, and food support staff.
“It is crucial to maintain our health care capacity,” said ACIP member Sharon Frey, MD, clinical director at the Center for Vaccine Development at Saint Louis University. “But it’s also important to prevent severe disease and death in the group that is at highest risk of those complications and that includes those in long-term care facilities.”
CDC staff said that staff and residents in those facilities account for 6% of COVID-19 cases and 40% of deaths.
But Helen Keipp Talbot, MD, associate professor of medicine at Vanderbilt University, Nashville, Tenn., voted against putting long-term care residents into the 1a phase. “We have traditionally tried a vaccine in a young healthy population and then hope it works in our frail older adults. So we enter this realm of ‘we hope it works and that it’s safe,’ and that concerns me on many levels particularly for this vaccine,” she said, noting that the vaccines closest to FDA authorization have not been studied in elderly adults who live in nursing homes or assisted living facilities.
She added: “I have no reservations for health care workers taking this vaccine.”
Prioritization could change
The phase 1a allocation fits within the “four ethical principles” outlined by ACIP and CDC staff Nov. 23: to maximize benefits and minimize harms, promote justice, mitigate health inequities, and promote transparency.
“My vote reflects maximum benefit, minimum harm, promoting justice and mitigating the health inequalities that exist with regard to distribution of this vaccine,” said ACIP Chair Jose Romero, MD. Romero, chief medical officer of the Arkansas Department of Health, voted in favor of the phase 1a plan.
He and other panelists noted, however, that allocation priorities could change after the FDA reviews and authorizes a vaccine.
The FDA’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) will meet December 10 to review the Pfizer/BioNTech’s messenger RNA-based vaccine (BNT162b2). The companies filed for emergency use on November 20.
A second vaccine, made by Moderna, is not far behind. The company reported on Nov. 30 that its messenger RNA vaccine was 94.1% effective and filed for emergency use the same day. The FDA’s VRBPAC will review the safety and efficacy data for the Moderna vaccine on Dec. 17.
“If individual vaccines receive emergency use authorization, we will have more data to consider, and that could lead to revision of our prioritization,” said ACIP member Robert Atmar, MD, John S. Dunn Research Foundation Clinical Professor in Infectious Diseases at Baylor College of Medicine, Houston.
ACIP will meet again after the Dec. 10 FDA advisory panel. But it won’t recommend a product until after the FDA has authorized it, said Amanda Cohn, MD, senior advisor for vaccines at the CDC’s National Center for Immunization and Respiratory Diseases.
Staggered immunization subprioritization urged
The CDC staff said that given the potential that not enough vaccine will be available immediately, it was recommending that health care organizations plan on creating a hierarchy of prioritization within institutions. And, they also urged staggering vaccination for personnel in similar units or positions, citing potential systemic or other reactions among health care workers.
“Consider planning for personnel to have time away from clinical care if health care personnel experience systemic symptoms post vaccination,” said Sarah Oliver, MD, MSPH, from the CDC.
The CDC will soon be issuing guidance on how to handle systemic symptoms with health care workers, Dr. Oliver noted.
Some 40 million doses of the Pfizer/BioNTech and Moderna vaccines are expected to be available by the end of December, with 5 million to 10 million a week coming online after that, Dr. Cohn said. That means not all health care workers will be vaccinated immediately. That may require “subprioritization, but for a limited period of time,” she said.
Dr. Messonnier said that, even with limited supplies, most of the states have told the CDC that they think they can vaccinate all of their health care workers within 3 weeks – some in less time.
The ACIP allocation plan is similar to but not exactly the same as that issued by the National Academy of Sciences, Engineering, and Medicine, which issued recommendations in October. That organization said that health care workers, first responders, older Americans living in congregate settings, and people with underlying health conditions should be the first to receive a vaccine.
ACIP has said that phase 1b would include essential workers, including police officers and firefighters, and those in education, transportation, and food and agriculture sectors. Phase 1c would include adults with high-risk medical conditions and those aged 65 years or older.
This article first appeared on Medscape.com.
Dilip V. Jeste, MD, on the state of psychiatry
Editor’s note: Psychiatry Leaders’ Perspectives is a new department in
In this first Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Dilip V. Jeste, MD. Dr. Jeste is Senior Associate Dean for Healthy Aging and Senior Care, Estelle and Edgar Levi Memorial Chair in Aging, Director of the Sam and Rose Stein Institute for Research on Aging, Distinguished Professor of Psychiatry and Neurosciences, University of California San Diego; and Co-Director of the UC San Diego-IBM Center on Artificial Intelligence for Healthy Living. His main areas of research include schizophrenia, neuropsychiatric interventions, and successful aging. He served as the 139th President of the American Psychiatric Association (APA) and also is a past president of the American Association for Geriatric Psychiatry, the West Coast College of Biological Psychiatry, and founding president of International College of Geriatric Psychoneuropharmacology.
Dr. Aftab: The focus of your term as president of the APA was on “positive psychiatry.” You are also one of the world’s foremost experts in this area. How successful have you been in your mission to promote positive psychiatry, and how has your message been received?
Dr. Jeste: Let me start with a little bit of background about why I got into positive psychiatry. As a geriatric psychiatrist, my research work has brought me face to face with the paradox of aging: although physical health declines with age, mental health and well-being improve on average. This is the case not just for individuals in the community but also for individuals with serious mental illnesses. That got me into thinking more and more about the ways in which we can bring positive change in the lives of patients. When I became the president of the APA, one of my main tasks was to finalize and publish the DSM-5, which rightly focuses on the disorders we treat, but it also provided me with an opportunity to highlight the side of psychiatry that focuses on the positive aspects of our own and our patients’ lives, such as wisdom, resilience, meaning, and social connectedness.
As is the case with any new idea, there is a lot of resistance in the beginning and this will always be the case. However, I would say that positive psychiatry has been received very well. We now have an APA Caucus and a World Psychiatric Association Section on positive psychiatry. Our book, Positive Psychiatry, turned out to be one of the best sellers for American Psychiatric Publishing! Every year, there are symposia on positive psychiatry and papers and books from other countries. Overall, the reception has been very promising.
Dr. Aftab: Thank you for this interesting background, Dr. Jeste. Now let me ask you about the current state of psychiatry. What do you see as some of the strengths of our profession?
Dr. Jeste: Psychiatry’s unique strength is our skill in promoting adaptive behavior change, with a focus on positive factors such as resilience, wisdom, optimism, social engagement, improved health, and longevity. If you look at the research literature, the effect sizes of factors such as optimism, resilience, and social engagement are equal to or greater than interventions such as statins, smoking cessation, and exercise. Cardiothoracic surgeons and radiologists can’t help people increase their resilience, optimism, and social engagement, but psychiatrists can. Behavior change is our expertise. When people are suicidal, we give them hope; we help depressed individuals become active, productive, and happy. We treat people with schizophrenia and bipolar disorder, reduce their psychopathological behaviors, and improve their everyday functioning.
Continue to: Dr. Aftab
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Jeste: Unfortunately, there are a lot of restrictions posed by the current reimbursement system. As a result, psychiatrists spend most of their time prescribing medications in clinical practice. I have nothing against psychopharmacology, but we also need to focus on important aspects of our lives, such as lifestyle, cognitive attitudes, self-care, and social engagement. We need to go beyond symptom reduction. A prominent example is loneliness, which is a major risk factor for morbidity and mortality; the treatment for loneliness is not increasing social network, it’s actually changing one’s perception of and ability to enhance appropriate socialization. Who can do that? Psychiatrists! But we don’t do that right now because the health insurance system doesn’t reimburse psychiatrists to do that.
Dr. Aftab: What is your perception of the threats that psychiatry faces? You had to fend off a variety of challenges during your year as APA president, such as issues surrounding revision of DSM-5. How has that experience shaped your assessment?
Dr. Jeste: I was honored to oversee the finalization and publication of DSM-5 as the president of the APA, even though I lost a lot of sleep working on it! What I found was that there was a lot of antagonism in the media, as well as among several advocacy groups, about the DSM. The misperception was that psychiatry and the APA were trying to expand diagnoses so that the drug companies could sell medications to more people, and psychiatry would benefit from this because of its relationship with the industry. That was actually not the case at all. What I tried to do was to understand where these groups were coming from, and to treat them as collaborators and partners, not as enemies. One thing I am particularly proud of is that we established the Summit Group for DSM-5, which brought together perspectives of the various stakeholders, and our communication both within and outside of the APA improved significantly. It’s gratifying to note that much of the controversy in the media died down after DSM-5 was published. The often-critical New York Times wrote that while DSM-5 is far from perfect, it is the best we have today clinically, and I’m very proud of the work we did on it.
Dr. Aftab: What sort of opportunities lie ahead for psychiatry? What do you envision for the future of the field?
Continue to: Dr. Jeste
Dr. Jeste: As a neuroscientist, I’m excited about the new developments in brain science. Our understanding of the neurobiologic basis of mental illnesses is slowly but surely increasing. I’m also very heartened by all the research going on with regard to the prevention of mental illnesses. I think we will be able to reduce the risk of many psychiatric disorders in the future. This is an exciting time for the field, and psychiatry is going to look very different 20 years from now!
Dr. Aftab: Some people think there’s a conflict between a neuroscientific and psychosocial understanding of psychiatry. How do you think the 2 relate to each other?
Dr. Jeste: The reality, I think, is that there is no conflict. Ultimately, the mind is a function of the brain, and the mind operates within a society. Neuroscientists are also realizing the importance of psychosocial aspects, and there is a growing social neuroscience, looking at the neurobiology of things such as loneliness, social isolation, and wisdom. The effects of psychosocial interventions such as meditation and long-term cognitive-behavioral therapy on the brain are now indisputable. I like to say that psychosocial interventions are often more biological in their effects than the drugs!
Dr. Aftab: Any words of wisdom for psychiatry trainees and early career psychiatrists?
Dr. Jeste: First of all, I congratulate them for going into psychiatry, which is rapidly advancing and is the field of the future. Looking at new developments, such as in artificial intelligence, I wish I could be a young person again just getting into psychiatry! The role of psychiatrists is also evolving, and psychiatrists will become leaders of multidisciplinary teams. I would advise trainees and early career psychiatrists not to get frustrated by issues such as insurance reimbursements; these obstacles will pass. Society is becoming far more conscious of the importance of mental health to our well-being. So I see a reason to be optimistic. I would also mention that the younger generation has a lot to teach the older generation while at the same time benefitting from the wisdom they have to offer. One of the best things we can promote is intergenerational activity, both within and outside of our profession.
Editor’s note: Psychiatry Leaders’ Perspectives is a new department in
In this first Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Dilip V. Jeste, MD. Dr. Jeste is Senior Associate Dean for Healthy Aging and Senior Care, Estelle and Edgar Levi Memorial Chair in Aging, Director of the Sam and Rose Stein Institute for Research on Aging, Distinguished Professor of Psychiatry and Neurosciences, University of California San Diego; and Co-Director of the UC San Diego-IBM Center on Artificial Intelligence for Healthy Living. His main areas of research include schizophrenia, neuropsychiatric interventions, and successful aging. He served as the 139th President of the American Psychiatric Association (APA) and also is a past president of the American Association for Geriatric Psychiatry, the West Coast College of Biological Psychiatry, and founding president of International College of Geriatric Psychoneuropharmacology.
Dr. Aftab: The focus of your term as president of the APA was on “positive psychiatry.” You are also one of the world’s foremost experts in this area. How successful have you been in your mission to promote positive psychiatry, and how has your message been received?
Dr. Jeste: Let me start with a little bit of background about why I got into positive psychiatry. As a geriatric psychiatrist, my research work has brought me face to face with the paradox of aging: although physical health declines with age, mental health and well-being improve on average. This is the case not just for individuals in the community but also for individuals with serious mental illnesses. That got me into thinking more and more about the ways in which we can bring positive change in the lives of patients. When I became the president of the APA, one of my main tasks was to finalize and publish the DSM-5, which rightly focuses on the disorders we treat, but it also provided me with an opportunity to highlight the side of psychiatry that focuses on the positive aspects of our own and our patients’ lives, such as wisdom, resilience, meaning, and social connectedness.
As is the case with any new idea, there is a lot of resistance in the beginning and this will always be the case. However, I would say that positive psychiatry has been received very well. We now have an APA Caucus and a World Psychiatric Association Section on positive psychiatry. Our book, Positive Psychiatry, turned out to be one of the best sellers for American Psychiatric Publishing! Every year, there are symposia on positive psychiatry and papers and books from other countries. Overall, the reception has been very promising.
Dr. Aftab: Thank you for this interesting background, Dr. Jeste. Now let me ask you about the current state of psychiatry. What do you see as some of the strengths of our profession?
Dr. Jeste: Psychiatry’s unique strength is our skill in promoting adaptive behavior change, with a focus on positive factors such as resilience, wisdom, optimism, social engagement, improved health, and longevity. If you look at the research literature, the effect sizes of factors such as optimism, resilience, and social engagement are equal to or greater than interventions such as statins, smoking cessation, and exercise. Cardiothoracic surgeons and radiologists can’t help people increase their resilience, optimism, and social engagement, but psychiatrists can. Behavior change is our expertise. When people are suicidal, we give them hope; we help depressed individuals become active, productive, and happy. We treat people with schizophrenia and bipolar disorder, reduce their psychopathological behaviors, and improve their everyday functioning.
Continue to: Dr. Aftab
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Jeste: Unfortunately, there are a lot of restrictions posed by the current reimbursement system. As a result, psychiatrists spend most of their time prescribing medications in clinical practice. I have nothing against psychopharmacology, but we also need to focus on important aspects of our lives, such as lifestyle, cognitive attitudes, self-care, and social engagement. We need to go beyond symptom reduction. A prominent example is loneliness, which is a major risk factor for morbidity and mortality; the treatment for loneliness is not increasing social network, it’s actually changing one’s perception of and ability to enhance appropriate socialization. Who can do that? Psychiatrists! But we don’t do that right now because the health insurance system doesn’t reimburse psychiatrists to do that.
Dr. Aftab: What is your perception of the threats that psychiatry faces? You had to fend off a variety of challenges during your year as APA president, such as issues surrounding revision of DSM-5. How has that experience shaped your assessment?
Dr. Jeste: I was honored to oversee the finalization and publication of DSM-5 as the president of the APA, even though I lost a lot of sleep working on it! What I found was that there was a lot of antagonism in the media, as well as among several advocacy groups, about the DSM. The misperception was that psychiatry and the APA were trying to expand diagnoses so that the drug companies could sell medications to more people, and psychiatry would benefit from this because of its relationship with the industry. That was actually not the case at all. What I tried to do was to understand where these groups were coming from, and to treat them as collaborators and partners, not as enemies. One thing I am particularly proud of is that we established the Summit Group for DSM-5, which brought together perspectives of the various stakeholders, and our communication both within and outside of the APA improved significantly. It’s gratifying to note that much of the controversy in the media died down after DSM-5 was published. The often-critical New York Times wrote that while DSM-5 is far from perfect, it is the best we have today clinically, and I’m very proud of the work we did on it.
Dr. Aftab: What sort of opportunities lie ahead for psychiatry? What do you envision for the future of the field?
Continue to: Dr. Jeste
Dr. Jeste: As a neuroscientist, I’m excited about the new developments in brain science. Our understanding of the neurobiologic basis of mental illnesses is slowly but surely increasing. I’m also very heartened by all the research going on with regard to the prevention of mental illnesses. I think we will be able to reduce the risk of many psychiatric disorders in the future. This is an exciting time for the field, and psychiatry is going to look very different 20 years from now!
Dr. Aftab: Some people think there’s a conflict between a neuroscientific and psychosocial understanding of psychiatry. How do you think the 2 relate to each other?
Dr. Jeste: The reality, I think, is that there is no conflict. Ultimately, the mind is a function of the brain, and the mind operates within a society. Neuroscientists are also realizing the importance of psychosocial aspects, and there is a growing social neuroscience, looking at the neurobiology of things such as loneliness, social isolation, and wisdom. The effects of psychosocial interventions such as meditation and long-term cognitive-behavioral therapy on the brain are now indisputable. I like to say that psychosocial interventions are often more biological in their effects than the drugs!
Dr. Aftab: Any words of wisdom for psychiatry trainees and early career psychiatrists?
Dr. Jeste: First of all, I congratulate them for going into psychiatry, which is rapidly advancing and is the field of the future. Looking at new developments, such as in artificial intelligence, I wish I could be a young person again just getting into psychiatry! The role of psychiatrists is also evolving, and psychiatrists will become leaders of multidisciplinary teams. I would advise trainees and early career psychiatrists not to get frustrated by issues such as insurance reimbursements; these obstacles will pass. Society is becoming far more conscious of the importance of mental health to our well-being. So I see a reason to be optimistic. I would also mention that the younger generation has a lot to teach the older generation while at the same time benefitting from the wisdom they have to offer. One of the best things we can promote is intergenerational activity, both within and outside of our profession.
Editor’s note: Psychiatry Leaders’ Perspectives is a new department in
In this first Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Dilip V. Jeste, MD. Dr. Jeste is Senior Associate Dean for Healthy Aging and Senior Care, Estelle and Edgar Levi Memorial Chair in Aging, Director of the Sam and Rose Stein Institute for Research on Aging, Distinguished Professor of Psychiatry and Neurosciences, University of California San Diego; and Co-Director of the UC San Diego-IBM Center on Artificial Intelligence for Healthy Living. His main areas of research include schizophrenia, neuropsychiatric interventions, and successful aging. He served as the 139th President of the American Psychiatric Association (APA) and also is a past president of the American Association for Geriatric Psychiatry, the West Coast College of Biological Psychiatry, and founding president of International College of Geriatric Psychoneuropharmacology.
Dr. Aftab: The focus of your term as president of the APA was on “positive psychiatry.” You are also one of the world’s foremost experts in this area. How successful have you been in your mission to promote positive psychiatry, and how has your message been received?
Dr. Jeste: Let me start with a little bit of background about why I got into positive psychiatry. As a geriatric psychiatrist, my research work has brought me face to face with the paradox of aging: although physical health declines with age, mental health and well-being improve on average. This is the case not just for individuals in the community but also for individuals with serious mental illnesses. That got me into thinking more and more about the ways in which we can bring positive change in the lives of patients. When I became the president of the APA, one of my main tasks was to finalize and publish the DSM-5, which rightly focuses on the disorders we treat, but it also provided me with an opportunity to highlight the side of psychiatry that focuses on the positive aspects of our own and our patients’ lives, such as wisdom, resilience, meaning, and social connectedness.
As is the case with any new idea, there is a lot of resistance in the beginning and this will always be the case. However, I would say that positive psychiatry has been received very well. We now have an APA Caucus and a World Psychiatric Association Section on positive psychiatry. Our book, Positive Psychiatry, turned out to be one of the best sellers for American Psychiatric Publishing! Every year, there are symposia on positive psychiatry and papers and books from other countries. Overall, the reception has been very promising.
Dr. Aftab: Thank you for this interesting background, Dr. Jeste. Now let me ask you about the current state of psychiatry. What do you see as some of the strengths of our profession?
Dr. Jeste: Psychiatry’s unique strength is our skill in promoting adaptive behavior change, with a focus on positive factors such as resilience, wisdom, optimism, social engagement, improved health, and longevity. If you look at the research literature, the effect sizes of factors such as optimism, resilience, and social engagement are equal to or greater than interventions such as statins, smoking cessation, and exercise. Cardiothoracic surgeons and radiologists can’t help people increase their resilience, optimism, and social engagement, but psychiatrists can. Behavior change is our expertise. When people are suicidal, we give them hope; we help depressed individuals become active, productive, and happy. We treat people with schizophrenia and bipolar disorder, reduce their psychopathological behaviors, and improve their everyday functioning.
Continue to: Dr. Aftab
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Jeste: Unfortunately, there are a lot of restrictions posed by the current reimbursement system. As a result, psychiatrists spend most of their time prescribing medications in clinical practice. I have nothing against psychopharmacology, but we also need to focus on important aspects of our lives, such as lifestyle, cognitive attitudes, self-care, and social engagement. We need to go beyond symptom reduction. A prominent example is loneliness, which is a major risk factor for morbidity and mortality; the treatment for loneliness is not increasing social network, it’s actually changing one’s perception of and ability to enhance appropriate socialization. Who can do that? Psychiatrists! But we don’t do that right now because the health insurance system doesn’t reimburse psychiatrists to do that.
Dr. Aftab: What is your perception of the threats that psychiatry faces? You had to fend off a variety of challenges during your year as APA president, such as issues surrounding revision of DSM-5. How has that experience shaped your assessment?
Dr. Jeste: I was honored to oversee the finalization and publication of DSM-5 as the president of the APA, even though I lost a lot of sleep working on it! What I found was that there was a lot of antagonism in the media, as well as among several advocacy groups, about the DSM. The misperception was that psychiatry and the APA were trying to expand diagnoses so that the drug companies could sell medications to more people, and psychiatry would benefit from this because of its relationship with the industry. That was actually not the case at all. What I tried to do was to understand where these groups were coming from, and to treat them as collaborators and partners, not as enemies. One thing I am particularly proud of is that we established the Summit Group for DSM-5, which brought together perspectives of the various stakeholders, and our communication both within and outside of the APA improved significantly. It’s gratifying to note that much of the controversy in the media died down after DSM-5 was published. The often-critical New York Times wrote that while DSM-5 is far from perfect, it is the best we have today clinically, and I’m very proud of the work we did on it.
Dr. Aftab: What sort of opportunities lie ahead for psychiatry? What do you envision for the future of the field?
Continue to: Dr. Jeste
Dr. Jeste: As a neuroscientist, I’m excited about the new developments in brain science. Our understanding of the neurobiologic basis of mental illnesses is slowly but surely increasing. I’m also very heartened by all the research going on with regard to the prevention of mental illnesses. I think we will be able to reduce the risk of many psychiatric disorders in the future. This is an exciting time for the field, and psychiatry is going to look very different 20 years from now!
Dr. Aftab: Some people think there’s a conflict between a neuroscientific and psychosocial understanding of psychiatry. How do you think the 2 relate to each other?
Dr. Jeste: The reality, I think, is that there is no conflict. Ultimately, the mind is a function of the brain, and the mind operates within a society. Neuroscientists are also realizing the importance of psychosocial aspects, and there is a growing social neuroscience, looking at the neurobiology of things such as loneliness, social isolation, and wisdom. The effects of psychosocial interventions such as meditation and long-term cognitive-behavioral therapy on the brain are now indisputable. I like to say that psychosocial interventions are often more biological in their effects than the drugs!
Dr. Aftab: Any words of wisdom for psychiatry trainees and early career psychiatrists?
Dr. Jeste: First of all, I congratulate them for going into psychiatry, which is rapidly advancing and is the field of the future. Looking at new developments, such as in artificial intelligence, I wish I could be a young person again just getting into psychiatry! The role of psychiatrists is also evolving, and psychiatrists will become leaders of multidisciplinary teams. I would advise trainees and early career psychiatrists not to get frustrated by issues such as insurance reimbursements; these obstacles will pass. Society is becoming far more conscious of the importance of mental health to our well-being. So I see a reason to be optimistic. I would also mention that the younger generation has a lot to teach the older generation while at the same time benefitting from the wisdom they have to offer. One of the best things we can promote is intergenerational activity, both within and outside of our profession.
2020: The year a viral asteroid collided with planet earth
Finally, 2020 is coming to an end, but the agony its viral pandemic inflicted on the entire world population will continue for a long time. And much as we would like to forget its damaging effects, it will surely be etched into our brains for the rest of our lives. The children who suffered the pain of the coronavirus disease 2019 (COVID-19) pandemic will endure its emotional scars for the rest of the 21st century.
Reading about the plagues of the past doesn’t come close to experiencing it and suffering through it. COVID-19 will continue to have ripple effects on every aspect of life on this planet, on individuals and on societies all over the world, especially on the biopsychosocial well-being of billions of humans around the globe.
Unprecedented disruptions
Think of the unprecedented disruptions inflicted by the trauma of the COVID-19 pandemic on our neural circuits. One of the wonders of the human brain is its continuous remodeling due to experiential neuroplasticity, and the formation of dendritic spines that immediately encode the memories of every experience. The turmoil of 2020 and its virulent pandemic will be forever etched into our collective brains, especially in our hippocampi and amygdalae. The impact on the developing brains of our children and grandchildren could be profound and may induce epigenetic changes that trigger psychopathology in the future.1,2
As with the dinosaurs, the 2020 pandemic is like a “viral asteroid” that left devastation on our social fabric and psychological well-being in its wake. We now have deep empathy with our 1918 ancestors and their tribulations, although so far, in the United States the proportion of people infected with COVID-19 (3% as of mid-November 20203) is dwarfed by the proportion infected with the influenza virus a century ago (30%). As of mid-November 2020, the number of global COVID-19 deaths (1.3 million3) was a tiny fraction of the 1918 influenza pandemic deaths (50 million worldwide and 675,000 in the United States4). Amazingly, researchers did not even know whether the killer germ was a virus or a bacterium until 1930, and it then took another 75 years to decode the genome of the influenza virus in 2005. In contrast, it took only a few short weeks to decode the genome of the virus that causes COVID-19 (severe acute respiratory syndrome-related coronavirus 2), and to begin developing multiple vaccines “at warp speed.” No vaccine or therapies were ever developed for victims of the 1918 pandemic.
An abundance of articles has been published about the pandemic since it ambushed us early in 2020, including many in
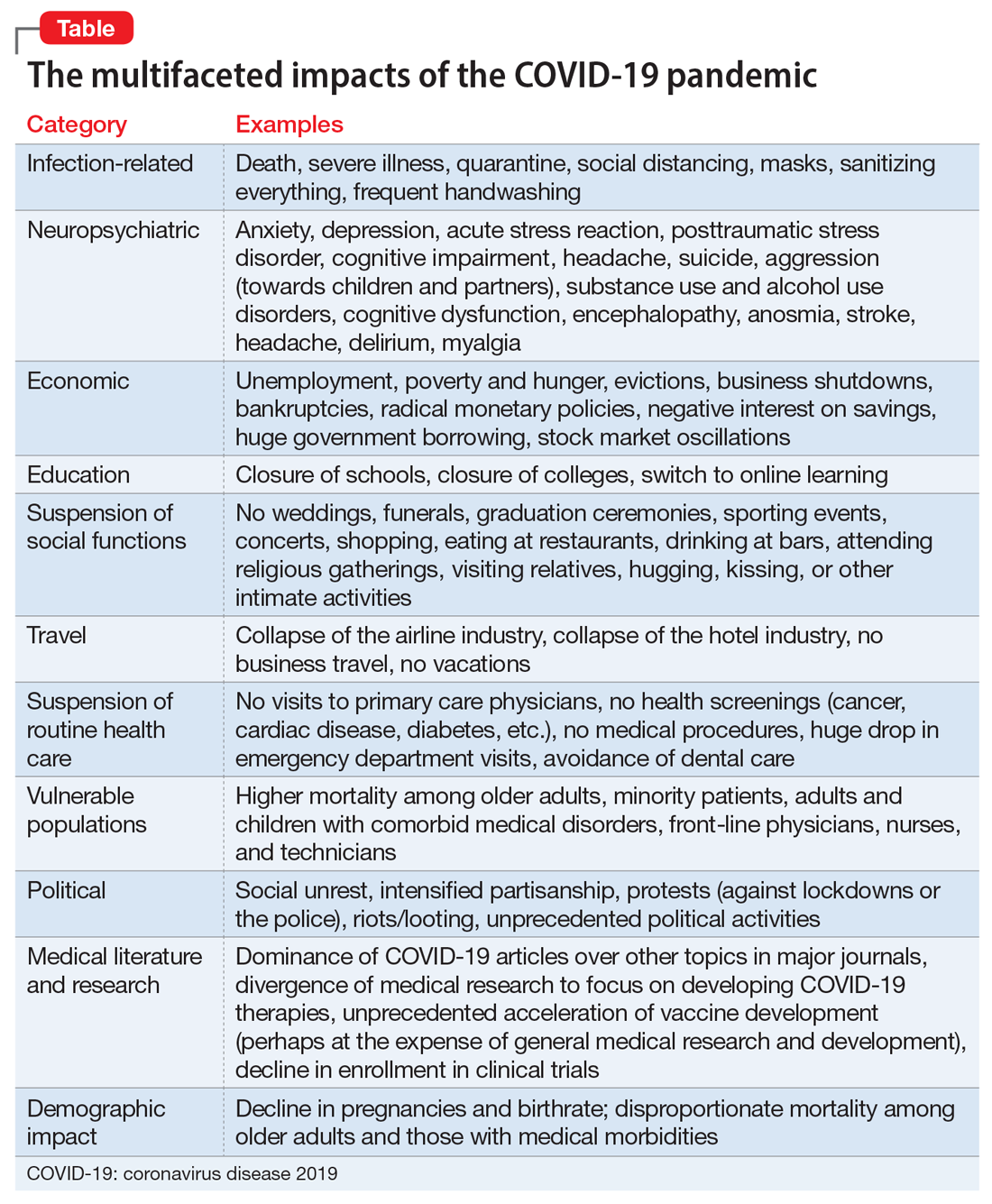
Most psychiatrists are familiar with the Holmes and Rahe Stress Scale,22 which contains 43 life events that cumulatively can progressively increase the odds of physical illness. It is likely that most of the world’s population will score very high on the Holmes and Rahe Stress Scale, which would predict an increased risk of medical illness, even after the pandemic subsides.
Exacerbating the situation is that hospitals and clinics had to shut down most of their operations to focus their resources on treating patients with COVID-19 in ICUs. This halted all routine screenings for cancer and heart, kidney, liver, lung, or brain diseases. In addition, diagnostic or therapeutic procedures such as endoscopies, colonoscopies, angiograms, or biopsies abruptly stopped, resulting in a surge of non–COVID-19 medical disorders and mortality as reported in several articles across many specialties.23 Going forward, in addition to COVID-19 morbidity and mortality, there is a significant likelihood of an increase in myriad medical disorders. The COVID-19 pandemic is obviously inflicting both direct and indirect casualties as it stretches into the next year and perhaps longer. The only hope for the community of nations is the rapid arrival of evidence-based treatments and vaccine(s).
Continue to: A progression of relentless stress
A progression of relentless stress
At the core of this pandemic is relentless stress. When it began in early 2020, the pandemic ignited an acute stress reaction due to the fear of death and the oddness of being isolated at home. Aggravating the acute stress was the realization that life as we knew it suddenly disappeared and all business or social activities had come to a screeching halt. It was almost surreal when streets usually bustling with human activity (such as Times Square in New York or Michigan Avenue in Chicago) became completely deserted and eerily silent. In addition, more stress was generated from watching television or scrolling through social media and being inundated with morbid and frightening news and updates about the number of individuals who became infected or died, and the official projections of tens of thousands or even hundreds of thousands of fatalities. Further intensifying the stress was hearing that there was a shortage of personal protective equipment (even masks), a lack of ventilators, and the absence of any medications to fight the overwhelming viral infection. Especially stressed were the front-line physicians and nurses, who heroically transcended their fears to save their patients’ lives. The sight of refrigerated trucks serving as temporary morgues outside hospital doors was chilling. The world became a macabre place where people died in hospitals without any relative to hold their hands or comfort them, and then were buried quickly without any formal funerals due to mandatory social distancing. The inability of families to grieve for their loved ones added another poignant layer of sadness and distress to the survivors who were unable to bid their loved ones goodbye. This was a jarring example of adding insult to injury.
With the protraction of the exceptional changes imposed by the pandemic, the acute stress reaction transmuted into posttraumatic stress disorder (PTSD) on a wide scale. Millions of previously healthy individuals began to succumb to the symptoms of PTSD (irritability, hypervigilance, intrusive thoughts, avoidance, insomnia, and bad dreams). The heaviest burden was inflicted on our patients, across all ages, with preexisting psychiatric conditions, who comprise approximately 25% of the population per the classic Epidemiological Catchment Area (ECA) study.24 These vulnerable patients, whom we see in our clinics and hospitals every day, had a significant exacerbation of their psychopathology, including anxiety, depression, psychosis, binge eating disorder, obsessive-compulsive disorder, alcohol and substance use disorders, child abuse, and intimate partner violence.25,26 The saving grace was the rapid adoption of telepsychiatry, which our psychiatric patients rapidly accepted. Many of them found it more convenient than dressing and driving and parking at the clinic. It also enabled psychiatrists to obtain useful collateral information from family members or partners.
If something good comes from this catastrophic social stress that emotionally hobbled the entire population, it would be the dilution of the stigma of mental illness because everyone has become more empathic due to their personal experience. Optimistically, this may also help expedite true health care parity for psychiatric brain disorders. And perhaps the government may see the need to train more psychiatrists and fund a higher number of residency stipends to all training programs.
Quo vadis COVID-19?
So, looking through the dense fog of the pandemic fatigue, what will 2021 bring us? Will waves of COVID-19 lead to pandemic exhaustion? Will the frayed public mental health care system be able to handle the surge of frayed nerves? Will social distancing intensify the widespread emotional disquietude? Will the children be able to manifest resilience and avoid disabling psychiatric disorders? Will the survivors of COVID-19 infections suffer from post–COVD-19 neuropsychiatric and other medical sequelae? Will efficacious therapies and vaccines emerge to blunt the spread of the virus? Will we all be able to gather in stadiums and arenas to enjoy sporting events, shows, and concerts? Will eating at our favorite restaurants become routine again? Will engaged couples be able to organize well-attended weddings and receptions? Will airplanes and hotels be fully booked again? Importantly, will all children and college students be able to resume their education in person and socialize ad lib? Will we be able to shed our masks and hug each other hello and goodbye? Will scientific journals and social media cover a wide array of topics again as before? Will the number of deaths dwindle to zero, and will we return to worrying mainly about the usual seasonal flu? Will everyone be able to leave home and go to work again?
I hope that the thick dust of this 2020 viral asteroid will settle in 2021, and that “normalcy” is eventually restored to our lives, allowing us to deal with other ongoing stresses such as social unrest and political hyperpartisanship.
1. Baumeister D, Akhtar R, Ciufolini S, et al. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21(5):642-649.
2. Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: a meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353-358.
3. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed November 11, 2020.
4. Centers for Disease Control and Prevention. 1918 Pandemic. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html. Accessed November 4, 2020.
5. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
6. Sharma RA, Maheshwari S, Bronsther R. COVID-19 in the era of loneliness. Current Psychiatry. 2020;19(5):31-33.
7. Joshi KG. Taking care of ourselves during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):46-47.
8. Frank B, Peterson T, Gupta S, et al. Telepsychiatry: what you need to know. Current Psychiatry. 2020;19(6):16-23.
9. Chahal K. Neuropsychiatric manifestations of COVID-19. Current Psychiatry. 2020;19(6):31-33.
10. Arbuck D. Changes in patient behavior during COVID-19: what I’ve observed. Current Psychiatry. 2020;19(6):46-47.
11. Joshi KG. Telepsychiatry during COVID-19: understanding the rules. Current Psychiatry. 2020;19(6):e12-e14.
12. Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
13. Brooks V. COVID-19’s effects on emergency psychiatry. Current Psychiatry. 2020;19(7):33-36,38-39.
14. Desarbo JR, DeSarbo L. Anorexia nervosa and COVID-19. Current Psychiatry. 2020;19(8):23-28.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-27,33-39.
16. Ryznar E. Evaluating patients’ decision-making capacity during COVID-19. Current Psychiatry. 2020;19(10):34-40.
17. Saeed SA, Hebishi K. The psychiatric consequences of COVID-19: 8 studies. Current Psychiatry. 2020;19(11):22-24,28-30,32-35.
18. Lodhi S, Marett C. Using seclusion to prevent COVID-19 transmission on inpatient psychiatry units. Current Psychiatry. 2020;19(11):37-41,53.
19. Nasrallah HA. COVID-19 and the precipitous dismantlement of societal norms. Current Psychiatry. 2020;19(7):12-14,16-17.
20. Nasrallah HA. The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING! Current Psychiatry. 2020;19(5):7-8,16.
21. Nasrallah HA. During a viral pandemic, anxiety is endemic: the psychiatric aspects of COVID-19. Current Psychiatry. 2020;19(4):e3-e5.
22. Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11(2):213-218.
23. Berkwits M, Flanagin A, Bauchner H, et al. The COVID-19 pandemic and the JAMA Network. JAMA. 2020;324(12):1159-1160.
24. Robins LN, Regier DA, eds. Psychiatric disorders in America. The Epidemiologic Catchment Area study. New York, NY: The Free Press; 1991.
25. Meninger KA. Psychosis associated with influenza. I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
26. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494.
Finally, 2020 is coming to an end, but the agony its viral pandemic inflicted on the entire world population will continue for a long time. And much as we would like to forget its damaging effects, it will surely be etched into our brains for the rest of our lives. The children who suffered the pain of the coronavirus disease 2019 (COVID-19) pandemic will endure its emotional scars for the rest of the 21st century.
Reading about the plagues of the past doesn’t come close to experiencing it and suffering through it. COVID-19 will continue to have ripple effects on every aspect of life on this planet, on individuals and on societies all over the world, especially on the biopsychosocial well-being of billions of humans around the globe.
Unprecedented disruptions
Think of the unprecedented disruptions inflicted by the trauma of the COVID-19 pandemic on our neural circuits. One of the wonders of the human brain is its continuous remodeling due to experiential neuroplasticity, and the formation of dendritic spines that immediately encode the memories of every experience. The turmoil of 2020 and its virulent pandemic will be forever etched into our collective brains, especially in our hippocampi and amygdalae. The impact on the developing brains of our children and grandchildren could be profound and may induce epigenetic changes that trigger psychopathology in the future.1,2
As with the dinosaurs, the 2020 pandemic is like a “viral asteroid” that left devastation on our social fabric and psychological well-being in its wake. We now have deep empathy with our 1918 ancestors and their tribulations, although so far, in the United States the proportion of people infected with COVID-19 (3% as of mid-November 20203) is dwarfed by the proportion infected with the influenza virus a century ago (30%). As of mid-November 2020, the number of global COVID-19 deaths (1.3 million3) was a tiny fraction of the 1918 influenza pandemic deaths (50 million worldwide and 675,000 in the United States4). Amazingly, researchers did not even know whether the killer germ was a virus or a bacterium until 1930, and it then took another 75 years to decode the genome of the influenza virus in 2005. In contrast, it took only a few short weeks to decode the genome of the virus that causes COVID-19 (severe acute respiratory syndrome-related coronavirus 2), and to begin developing multiple vaccines “at warp speed.” No vaccine or therapies were ever developed for victims of the 1918 pandemic.
An abundance of articles has been published about the pandemic since it ambushed us early in 2020, including many in
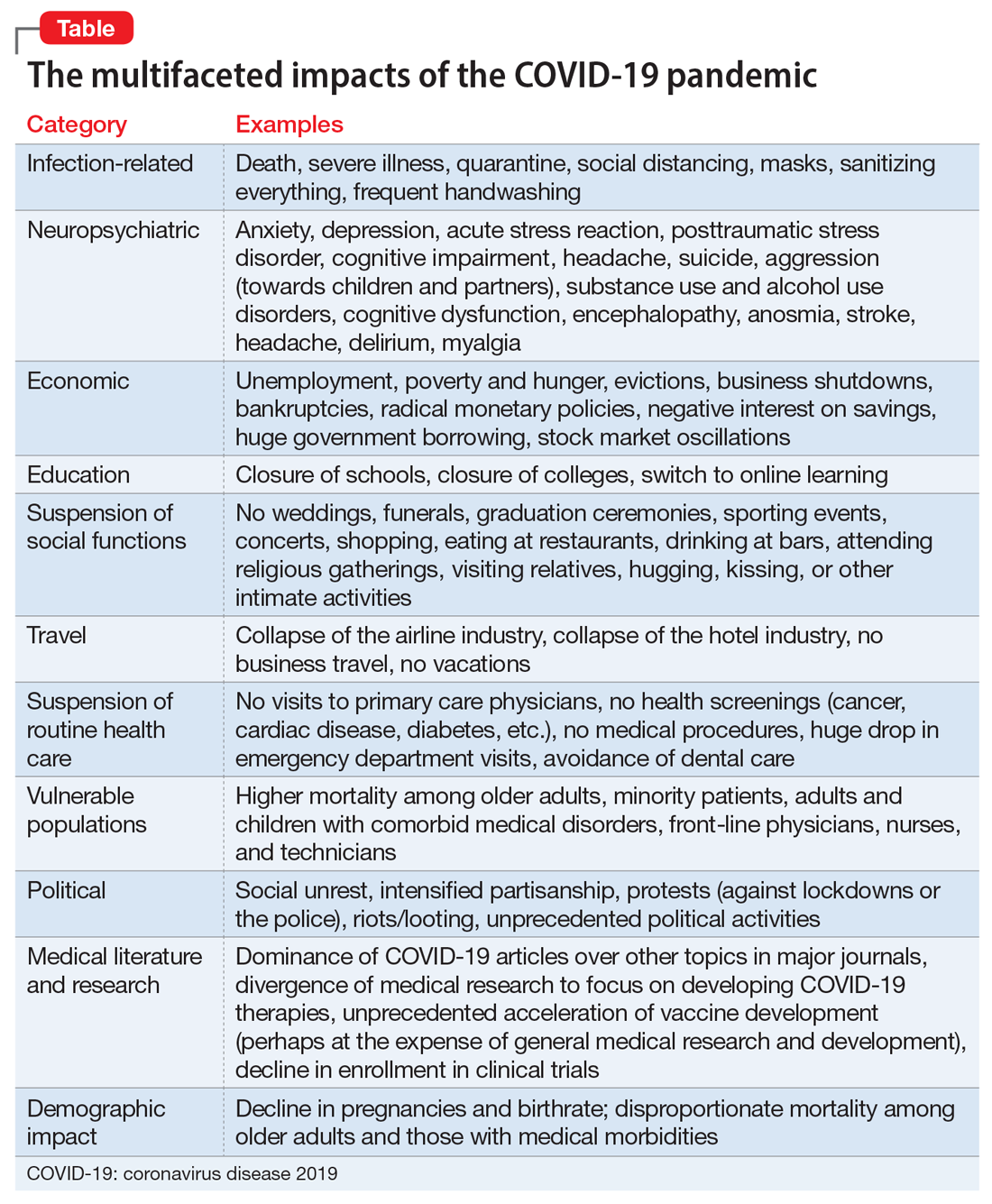
Most psychiatrists are familiar with the Holmes and Rahe Stress Scale,22 which contains 43 life events that cumulatively can progressively increase the odds of physical illness. It is likely that most of the world’s population will score very high on the Holmes and Rahe Stress Scale, which would predict an increased risk of medical illness, even after the pandemic subsides.
Exacerbating the situation is that hospitals and clinics had to shut down most of their operations to focus their resources on treating patients with COVID-19 in ICUs. This halted all routine screenings for cancer and heart, kidney, liver, lung, or brain diseases. In addition, diagnostic or therapeutic procedures such as endoscopies, colonoscopies, angiograms, or biopsies abruptly stopped, resulting in a surge of non–COVID-19 medical disorders and mortality as reported in several articles across many specialties.23 Going forward, in addition to COVID-19 morbidity and mortality, there is a significant likelihood of an increase in myriad medical disorders. The COVID-19 pandemic is obviously inflicting both direct and indirect casualties as it stretches into the next year and perhaps longer. The only hope for the community of nations is the rapid arrival of evidence-based treatments and vaccine(s).
Continue to: A progression of relentless stress
A progression of relentless stress
At the core of this pandemic is relentless stress. When it began in early 2020, the pandemic ignited an acute stress reaction due to the fear of death and the oddness of being isolated at home. Aggravating the acute stress was the realization that life as we knew it suddenly disappeared and all business or social activities had come to a screeching halt. It was almost surreal when streets usually bustling with human activity (such as Times Square in New York or Michigan Avenue in Chicago) became completely deserted and eerily silent. In addition, more stress was generated from watching television or scrolling through social media and being inundated with morbid and frightening news and updates about the number of individuals who became infected or died, and the official projections of tens of thousands or even hundreds of thousands of fatalities. Further intensifying the stress was hearing that there was a shortage of personal protective equipment (even masks), a lack of ventilators, and the absence of any medications to fight the overwhelming viral infection. Especially stressed were the front-line physicians and nurses, who heroically transcended their fears to save their patients’ lives. The sight of refrigerated trucks serving as temporary morgues outside hospital doors was chilling. The world became a macabre place where people died in hospitals without any relative to hold their hands or comfort them, and then were buried quickly without any formal funerals due to mandatory social distancing. The inability of families to grieve for their loved ones added another poignant layer of sadness and distress to the survivors who were unable to bid their loved ones goodbye. This was a jarring example of adding insult to injury.
With the protraction of the exceptional changes imposed by the pandemic, the acute stress reaction transmuted into posttraumatic stress disorder (PTSD) on a wide scale. Millions of previously healthy individuals began to succumb to the symptoms of PTSD (irritability, hypervigilance, intrusive thoughts, avoidance, insomnia, and bad dreams). The heaviest burden was inflicted on our patients, across all ages, with preexisting psychiatric conditions, who comprise approximately 25% of the population per the classic Epidemiological Catchment Area (ECA) study.24 These vulnerable patients, whom we see in our clinics and hospitals every day, had a significant exacerbation of their psychopathology, including anxiety, depression, psychosis, binge eating disorder, obsessive-compulsive disorder, alcohol and substance use disorders, child abuse, and intimate partner violence.25,26 The saving grace was the rapid adoption of telepsychiatry, which our psychiatric patients rapidly accepted. Many of them found it more convenient than dressing and driving and parking at the clinic. It also enabled psychiatrists to obtain useful collateral information from family members or partners.
If something good comes from this catastrophic social stress that emotionally hobbled the entire population, it would be the dilution of the stigma of mental illness because everyone has become more empathic due to their personal experience. Optimistically, this may also help expedite true health care parity for psychiatric brain disorders. And perhaps the government may see the need to train more psychiatrists and fund a higher number of residency stipends to all training programs.
Quo vadis COVID-19?
So, looking through the dense fog of the pandemic fatigue, what will 2021 bring us? Will waves of COVID-19 lead to pandemic exhaustion? Will the frayed public mental health care system be able to handle the surge of frayed nerves? Will social distancing intensify the widespread emotional disquietude? Will the children be able to manifest resilience and avoid disabling psychiatric disorders? Will the survivors of COVID-19 infections suffer from post–COVD-19 neuropsychiatric and other medical sequelae? Will efficacious therapies and vaccines emerge to blunt the spread of the virus? Will we all be able to gather in stadiums and arenas to enjoy sporting events, shows, and concerts? Will eating at our favorite restaurants become routine again? Will engaged couples be able to organize well-attended weddings and receptions? Will airplanes and hotels be fully booked again? Importantly, will all children and college students be able to resume their education in person and socialize ad lib? Will we be able to shed our masks and hug each other hello and goodbye? Will scientific journals and social media cover a wide array of topics again as before? Will the number of deaths dwindle to zero, and will we return to worrying mainly about the usual seasonal flu? Will everyone be able to leave home and go to work again?
I hope that the thick dust of this 2020 viral asteroid will settle in 2021, and that “normalcy” is eventually restored to our lives, allowing us to deal with other ongoing stresses such as social unrest and political hyperpartisanship.
Finally, 2020 is coming to an end, but the agony its viral pandemic inflicted on the entire world population will continue for a long time. And much as we would like to forget its damaging effects, it will surely be etched into our brains for the rest of our lives. The children who suffered the pain of the coronavirus disease 2019 (COVID-19) pandemic will endure its emotional scars for the rest of the 21st century.
Reading about the plagues of the past doesn’t come close to experiencing it and suffering through it. COVID-19 will continue to have ripple effects on every aspect of life on this planet, on individuals and on societies all over the world, especially on the biopsychosocial well-being of billions of humans around the globe.
Unprecedented disruptions
Think of the unprecedented disruptions inflicted by the trauma of the COVID-19 pandemic on our neural circuits. One of the wonders of the human brain is its continuous remodeling due to experiential neuroplasticity, and the formation of dendritic spines that immediately encode the memories of every experience. The turmoil of 2020 and its virulent pandemic will be forever etched into our collective brains, especially in our hippocampi and amygdalae. The impact on the developing brains of our children and grandchildren could be profound and may induce epigenetic changes that trigger psychopathology in the future.1,2
As with the dinosaurs, the 2020 pandemic is like a “viral asteroid” that left devastation on our social fabric and psychological well-being in its wake. We now have deep empathy with our 1918 ancestors and their tribulations, although so far, in the United States the proportion of people infected with COVID-19 (3% as of mid-November 20203) is dwarfed by the proportion infected with the influenza virus a century ago (30%). As of mid-November 2020, the number of global COVID-19 deaths (1.3 million3) was a tiny fraction of the 1918 influenza pandemic deaths (50 million worldwide and 675,000 in the United States4). Amazingly, researchers did not even know whether the killer germ was a virus or a bacterium until 1930, and it then took another 75 years to decode the genome of the influenza virus in 2005. In contrast, it took only a few short weeks to decode the genome of the virus that causes COVID-19 (severe acute respiratory syndrome-related coronavirus 2), and to begin developing multiple vaccines “at warp speed.” No vaccine or therapies were ever developed for victims of the 1918 pandemic.
An abundance of articles has been published about the pandemic since it ambushed us early in 2020, including many in
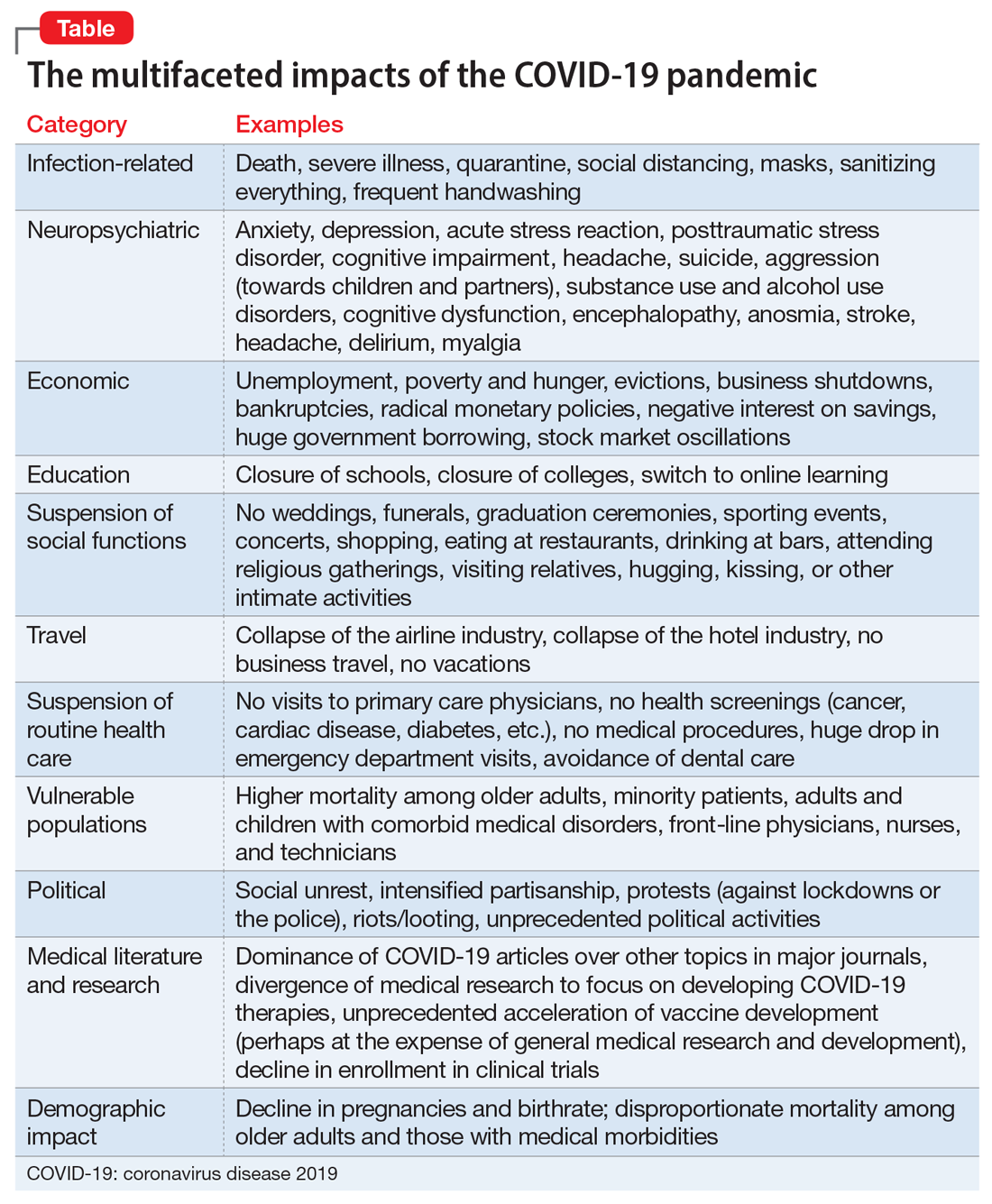
Most psychiatrists are familiar with the Holmes and Rahe Stress Scale,22 which contains 43 life events that cumulatively can progressively increase the odds of physical illness. It is likely that most of the world’s population will score very high on the Holmes and Rahe Stress Scale, which would predict an increased risk of medical illness, even after the pandemic subsides.
Exacerbating the situation is that hospitals and clinics had to shut down most of their operations to focus their resources on treating patients with COVID-19 in ICUs. This halted all routine screenings for cancer and heart, kidney, liver, lung, or brain diseases. In addition, diagnostic or therapeutic procedures such as endoscopies, colonoscopies, angiograms, or biopsies abruptly stopped, resulting in a surge of non–COVID-19 medical disorders and mortality as reported in several articles across many specialties.23 Going forward, in addition to COVID-19 morbidity and mortality, there is a significant likelihood of an increase in myriad medical disorders. The COVID-19 pandemic is obviously inflicting both direct and indirect casualties as it stretches into the next year and perhaps longer. The only hope for the community of nations is the rapid arrival of evidence-based treatments and vaccine(s).
Continue to: A progression of relentless stress
A progression of relentless stress
At the core of this pandemic is relentless stress. When it began in early 2020, the pandemic ignited an acute stress reaction due to the fear of death and the oddness of being isolated at home. Aggravating the acute stress was the realization that life as we knew it suddenly disappeared and all business or social activities had come to a screeching halt. It was almost surreal when streets usually bustling with human activity (such as Times Square in New York or Michigan Avenue in Chicago) became completely deserted and eerily silent. In addition, more stress was generated from watching television or scrolling through social media and being inundated with morbid and frightening news and updates about the number of individuals who became infected or died, and the official projections of tens of thousands or even hundreds of thousands of fatalities. Further intensifying the stress was hearing that there was a shortage of personal protective equipment (even masks), a lack of ventilators, and the absence of any medications to fight the overwhelming viral infection. Especially stressed were the front-line physicians and nurses, who heroically transcended their fears to save their patients’ lives. The sight of refrigerated trucks serving as temporary morgues outside hospital doors was chilling. The world became a macabre place where people died in hospitals without any relative to hold their hands or comfort them, and then were buried quickly without any formal funerals due to mandatory social distancing. The inability of families to grieve for their loved ones added another poignant layer of sadness and distress to the survivors who were unable to bid their loved ones goodbye. This was a jarring example of adding insult to injury.
With the protraction of the exceptional changes imposed by the pandemic, the acute stress reaction transmuted into posttraumatic stress disorder (PTSD) on a wide scale. Millions of previously healthy individuals began to succumb to the symptoms of PTSD (irritability, hypervigilance, intrusive thoughts, avoidance, insomnia, and bad dreams). The heaviest burden was inflicted on our patients, across all ages, with preexisting psychiatric conditions, who comprise approximately 25% of the population per the classic Epidemiological Catchment Area (ECA) study.24 These vulnerable patients, whom we see in our clinics and hospitals every day, had a significant exacerbation of their psychopathology, including anxiety, depression, psychosis, binge eating disorder, obsessive-compulsive disorder, alcohol and substance use disorders, child abuse, and intimate partner violence.25,26 The saving grace was the rapid adoption of telepsychiatry, which our psychiatric patients rapidly accepted. Many of them found it more convenient than dressing and driving and parking at the clinic. It also enabled psychiatrists to obtain useful collateral information from family members or partners.
If something good comes from this catastrophic social stress that emotionally hobbled the entire population, it would be the dilution of the stigma of mental illness because everyone has become more empathic due to their personal experience. Optimistically, this may also help expedite true health care parity for psychiatric brain disorders. And perhaps the government may see the need to train more psychiatrists and fund a higher number of residency stipends to all training programs.
Quo vadis COVID-19?
So, looking through the dense fog of the pandemic fatigue, what will 2021 bring us? Will waves of COVID-19 lead to pandemic exhaustion? Will the frayed public mental health care system be able to handle the surge of frayed nerves? Will social distancing intensify the widespread emotional disquietude? Will the children be able to manifest resilience and avoid disabling psychiatric disorders? Will the survivors of COVID-19 infections suffer from post–COVD-19 neuropsychiatric and other medical sequelae? Will efficacious therapies and vaccines emerge to blunt the spread of the virus? Will we all be able to gather in stadiums and arenas to enjoy sporting events, shows, and concerts? Will eating at our favorite restaurants become routine again? Will engaged couples be able to organize well-attended weddings and receptions? Will airplanes and hotels be fully booked again? Importantly, will all children and college students be able to resume their education in person and socialize ad lib? Will we be able to shed our masks and hug each other hello and goodbye? Will scientific journals and social media cover a wide array of topics again as before? Will the number of deaths dwindle to zero, and will we return to worrying mainly about the usual seasonal flu? Will everyone be able to leave home and go to work again?
I hope that the thick dust of this 2020 viral asteroid will settle in 2021, and that “normalcy” is eventually restored to our lives, allowing us to deal with other ongoing stresses such as social unrest and political hyperpartisanship.
1. Baumeister D, Akhtar R, Ciufolini S, et al. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21(5):642-649.
2. Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: a meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353-358.
3. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed November 11, 2020.
4. Centers for Disease Control and Prevention. 1918 Pandemic. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html. Accessed November 4, 2020.
5. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
6. Sharma RA, Maheshwari S, Bronsther R. COVID-19 in the era of loneliness. Current Psychiatry. 2020;19(5):31-33.
7. Joshi KG. Taking care of ourselves during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):46-47.
8. Frank B, Peterson T, Gupta S, et al. Telepsychiatry: what you need to know. Current Psychiatry. 2020;19(6):16-23.
9. Chahal K. Neuropsychiatric manifestations of COVID-19. Current Psychiatry. 2020;19(6):31-33.
10. Arbuck D. Changes in patient behavior during COVID-19: what I’ve observed. Current Psychiatry. 2020;19(6):46-47.
11. Joshi KG. Telepsychiatry during COVID-19: understanding the rules. Current Psychiatry. 2020;19(6):e12-e14.
12. Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
13. Brooks V. COVID-19’s effects on emergency psychiatry. Current Psychiatry. 2020;19(7):33-36,38-39.
14. Desarbo JR, DeSarbo L. Anorexia nervosa and COVID-19. Current Psychiatry. 2020;19(8):23-28.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-27,33-39.
16. Ryznar E. Evaluating patients’ decision-making capacity during COVID-19. Current Psychiatry. 2020;19(10):34-40.
17. Saeed SA, Hebishi K. The psychiatric consequences of COVID-19: 8 studies. Current Psychiatry. 2020;19(11):22-24,28-30,32-35.
18. Lodhi S, Marett C. Using seclusion to prevent COVID-19 transmission on inpatient psychiatry units. Current Psychiatry. 2020;19(11):37-41,53.
19. Nasrallah HA. COVID-19 and the precipitous dismantlement of societal norms. Current Psychiatry. 2020;19(7):12-14,16-17.
20. Nasrallah HA. The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING! Current Psychiatry. 2020;19(5):7-8,16.
21. Nasrallah HA. During a viral pandemic, anxiety is endemic: the psychiatric aspects of COVID-19. Current Psychiatry. 2020;19(4):e3-e5.
22. Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11(2):213-218.
23. Berkwits M, Flanagin A, Bauchner H, et al. The COVID-19 pandemic and the JAMA Network. JAMA. 2020;324(12):1159-1160.
24. Robins LN, Regier DA, eds. Psychiatric disorders in America. The Epidemiologic Catchment Area study. New York, NY: The Free Press; 1991.
25. Meninger KA. Psychosis associated with influenza. I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
26. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494.
1. Baumeister D, Akhtar R, Ciufolini S, et al. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21(5):642-649.
2. Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: a meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353-358.
3. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed November 11, 2020.
4. Centers for Disease Control and Prevention. 1918 Pandemic. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html. Accessed November 4, 2020.
5. Chepke C. Drive-up pharmacotherapy during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):29-30.
6. Sharma RA, Maheshwari S, Bronsther R. COVID-19 in the era of loneliness. Current Psychiatry. 2020;19(5):31-33.
7. Joshi KG. Taking care of ourselves during the COVID-19 pandemic. Current Psychiatry. 2020;19(5):46-47.
8. Frank B, Peterson T, Gupta S, et al. Telepsychiatry: what you need to know. Current Psychiatry. 2020;19(6):16-23.
9. Chahal K. Neuropsychiatric manifestations of COVID-19. Current Psychiatry. 2020;19(6):31-33.
10. Arbuck D. Changes in patient behavior during COVID-19: what I’ve observed. Current Psychiatry. 2020;19(6):46-47.
11. Joshi KG. Telepsychiatry during COVID-19: understanding the rules. Current Psychiatry. 2020;19(6):e12-e14.
12. Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
13. Brooks V. COVID-19’s effects on emergency psychiatry. Current Psychiatry. 2020;19(7):33-36,38-39.
14. Desarbo JR, DeSarbo L. Anorexia nervosa and COVID-19. Current Psychiatry. 2020;19(8):23-28.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-27,33-39.
16. Ryznar E. Evaluating patients’ decision-making capacity during COVID-19. Current Psychiatry. 2020;19(10):34-40.
17. Saeed SA, Hebishi K. The psychiatric consequences of COVID-19: 8 studies. Current Psychiatry. 2020;19(11):22-24,28-30,32-35.
18. Lodhi S, Marett C. Using seclusion to prevent COVID-19 transmission on inpatient psychiatry units. Current Psychiatry. 2020;19(11):37-41,53.
19. Nasrallah HA. COVID-19 and the precipitous dismantlement of societal norms. Current Psychiatry. 2020;19(7):12-14,16-17.
20. Nasrallah HA. The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING! Current Psychiatry. 2020;19(5):7-8,16.
21. Nasrallah HA. During a viral pandemic, anxiety is endemic: the psychiatric aspects of COVID-19. Current Psychiatry. 2020;19(4):e3-e5.
22. Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11(2):213-218.
23. Berkwits M, Flanagin A, Bauchner H, et al. The COVID-19 pandemic and the JAMA Network. JAMA. 2020;324(12):1159-1160.
24. Robins LN, Regier DA, eds. Psychiatric disorders in America. The Epidemiologic Catchment Area study. New York, NY: The Free Press; 1991.
25. Meninger KA. Psychosis associated with influenza. I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
26. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494.
My journey with mental illness
I am a retired advanced practice psychiatric nurse who has lived and worked on “both sides of the door.” This wording is paraphrased from psychologist and therapist Lauren Slater, PhD, who wrote about a time she went to McLean Hospital in Belmont, Massachusetts, as a therapist after staying there as a patient years earlier: “And now I am standing on the other—the wrong, I mean the right side of the door and I ring the buzzer.”1 Here I tell my story of the physical and emotional effects of my mental illness and treatment.
Onset of bipolar disorder. My bipolar illness started with a bout of depression in 1963 at age 13, which resulted in a low-key summer of often staying inside. I received no medication, and no one sent me for evaluation. In the fall, I went back to school and finished the year without incident. I continued as a quiet, shy kid through high school in the late 1960s. In my senior year, I decided to take an overload of difficult courses and run on the varsity cross-country team. The amount and intensity of these activities were too much. This resulted in my first manic episode, which started during a weekend visit to a college I hoped to attend. I became excitable, grandiose, and had delusions. A day later, I returned home, and my parents had me admitted to a psychiatric hospital, where I remained for 3 months.
At first, my diagnosis was unclear, and initially no one considered what at the time was called manic depression. At that point, I was unaware of my extensive family psychiatric history. My pharmacologic treatment consisted of chlorpromazine, trifluoperazine, and procyclidine. I returned home just before Christmas and barely finished my senior year of high school. A good college accepted me. But during the orientation, I was asked to leave because I experienced a second manic episode. After 4 more psychiatric hospitalizations, I finally stabilized.
During one of my hospitalizations, I had the good fortune to be interviewed by Dr. Thomas Detre. During this interview, I talked expansively about Don Quixote, Aldonza, and Sancho Panza. Dr. Detre diagnosed me with manic depression, and suggested that I see Dr. Christiaan van der Velde, who was researching lithium carbonate.2 In 1970, I was hospitalized at Norwich State Hospital in Preston, Connecticut and was started on lithium, even though it had not yet been FDA-approved. I responded well to lithium monotherapy.
An extensive family history. Having bipolar disorder was not something I would discuss with others because I felt ashamed. I commonly hid my medication during college, especially from my roommates or other friends. By then, I had learned a little about my family’s psychiatric history, but I knew few specifics. Over time, I became aware of a dense familial cluster of affective illness going back several generations. My maternal grandmother was hospitalized for depression in 1921 after her husband suddenly died during her fourth pregnancy. She became bereft and suicidal because she had no one to support her 4 children. During my grandmother’s hospitalization, her sister and sister’s husband took care of her children. My grandmother remained hospitalized until she died in 1943. At that time, no medications were available to treat her illness. Over the next 2 generations, 2 of her 4 children and 6 of her 12 grandchildren (including me) developed bipolar disorder.
A career and family. In 1970, I started to work as a nursing assistant, then as a nursing technician for 1.5 years in a specialty hospital in New England. In 1973, I began nursing school at a junior college. I received my RN in 1975, a BS in nursing in 1979, and an MS in psychiatric nursing in 1982. I worked steadily as a psychiatric nurse in both inpatient and outpatient settings from 1975 until I retired in 2019.
In the early 1980s, I married my first wife and had 2 wonderful children. During our courtship in 1981 and 1982, I became hypomanic, which perhaps made me more outgoing and sociable. In 1985, after my father required open heart surgery, I had a manic episode that lasted 1 week. Over the next 20 years, although I was not happy with my marriage, I remained euthymic and productive at work. My marriage ended in 2012.
Continue to: By the end of 2012...
By the end of 2012, I had been taking lithium continuously for 42 years. My laboratory tests showed peak lithium levels between 0.6 and 1.2 mmol/L. I remained otherwise healthy, as demonstrated by annual physical exams and laboratory test results. In 2015, I developed an increase in my blood pressure and my primary care physician (PCP) prescribed oral lisinopril, initially 10 mg/d, and later 10 mg twice daily. My blood pressure improved and ranged from 120/74 to 130/82 mm Hg.
Hyperparathyroidism. By 2016, my psychiatrist, PCP, and nephrologist all urged me to consider parathyroid surgery.3-5 Hypercalcemia and hyperparathyroidism caused the most worry. Laboratory tests indicated calcium 11.2 mg/dL, parathyroid hormone (PTH) 88 pg/mL, estimated glomerular filtration rate (eGFR) 59 mL/min, and thyroid-stimulating hormone (TSH) 0.78 mIU/L. Electrocardiographysometimes showed a slight QT elongation. A right bundle branch block, which was first noted in 2015, continued. Due to my elevated calcium levels, I eliminated most calcium from my diet. My psychiatrist began to speak more strongly of parathyroid surgery. I then consulted a senior endocrinologist and a senior nephrologist, who each recommended parathyroid surgery.
I remarried in July 2016, and we moved to a different area of the country. My second wife became a stabilizing force for me. My new PCP, however, found elevated high-density lipoproteins during a routine physical examination, and started me on simvastatin, 10 mg/d. My calcium and PTH levels continued to be elevated. My PCP, nephrologist, therapist, and wife urged me to proceed with the parathyroidectomy. After a short period of watchful waiting and a second consultation with a nephrologist, I agreed to schedule a subtotal parathyroidectomy.
Surgery. In spring 2017, I began preparation for parathyroidectomy. At the time, my lithium carbonate dose was 600 mg/d, alternating with 900 mg/d. My peak level of lithium was 0.6 mmol/L. Lisinopril is synergistic, which allowed me to take a smaller effective dose of lithium.
My parathyroid surgery occurred on June 28, 2017 at Norman Parathyroid Center in Tampa, Florida.6 The surgeon recorded my parathyroid glands as 136, 602, and 348 units using a measure developed at Norman Parathyroid Center. No reading was given for my fourth parathyroid gland, which they did not remove. Following the surgery, I resumed my previous functions, including employment as a visiting nurse. I initially took calcium supplements after surgery, and my lithium dose was reduced to 300 mg orally, twice daily, which I have continued. I have remained euthymic. On August 3, 2017 my laboratory workup showed an eGFR of 64 mL/min, calcium 10.0 mg/dL, and PTH 17 pg/mL. Vitamin D25 OH 33, glucose, BUN/Cr, electrolytes, complete blood count, and albumin were all within normal limits. Repeat bloodwork on September 19, 2017 showed Ca++ 10.1 mg/dL and PTH 18 pg/mL. Nine months after the surgery, I showed an incredibly positive physical and mental response, which has continued to this day.
Continue to: Clinical implications
Clinical implications. This is a single case study. However, it is important for clinicians treating patients with lithium carbonate to regularly order laboratory testing, including for lithium levels, PTH, and calcium, to detect early signs of complications from treatment, including hyperparathyroidism and hypercalcemia.7 These levels could be obtained every 6 months. If a patient’s PTH levels are >70 pg/mL and calcium levels are >11.0 mg/dL, it would be prudent to refer him/her for further medical evaluation. Additionally, it would be helpful to counsel the patient about considering alternative medication and adjunct mental health treatment. At some future point, it could be useful for the clinician and his/her patient to explore the idea of parathyroid surgery.
In addition to chronic lithium use, other causes of hyperparathyroidism include an adenoma on a gland, hyperplasia of ≥2 parathyroid glands, a malignant tumor, severe calcium deficiency, severe vitamin D deficiency, chronic renal failure, and (rarely) an inherited gene that causes hyperparathyroidism.
How I’m doing today. Currently, I am euthymic and in a happy marriage. My laboratory workup in May 2020 included glucose 107 mg/dL, Ca++ 9.5 mg/dL, eGFR 61 mL/min, PTH 32 pg/mL, lithium 0.3 mmol/L (300 mg twice daily), and TSH 1.79 mIU/L. A comprehensive metabolic panel, complete blood count, and lipid panel were all within normal limits.
I am fortunate to continue having excellent care provided by my PCP, nephrologist, urologist, and psychiatric APRN. Together with these wonderful professionals, I have been able to maintain my physical and mental health.
Acknowledgment: I gratefully acknowledge the help and skills of Robin Scharak and Gary Blake for providing some of the editing on this article.
Bill Greenberg MS, RN, APRN
Delray Beach, Florida
1. Slater L. Welcome to my country. New York, NY: Random House; 1996:187.
2. Van der Velde CD. Effectiveness of lithium in the treatment of manic-depressive illness. Am J Psychiatry. 1970;127(3):345-351.
3. Norman Parathyroid Center. Parathyroid glands, high calcium and hyperparathyroidism. www.parathyroid.com. Updated October 21, 2020. Accessed November 11, 2020.
4. Meehan AD, Udumyan R, Kardell M, et al. Lithium-associated hypercalcemia: pathophysiology, prevalence, management. World J Surg. 2018;42(2):415-424.
5. Lally J, Lee B, McDonald C. Prevalence of hypercalcaemia in patients on maintenance lithium therapy monitored in primary care. Ir Med J. 2013;106(1):15-17.
6. Norman Parathyroid Center. Parathyroid surgery: minimally invasive 4-gland parathyroid surgery video. (4-Gland MIRP Parathyroid Operation). https://www.parathyroid.com/parathyroid-surgery.htm. Updated October 1, 2020. Accessed November 5, 2020.
7. MEDSAFE. Hyperparathyroidism and hypercalcaemia with lithium treatment. New Zealand Medicines and Medical Devices Safety Authority. 2014;35(3):37-38.
I am a retired advanced practice psychiatric nurse who has lived and worked on “both sides of the door.” This wording is paraphrased from psychologist and therapist Lauren Slater, PhD, who wrote about a time she went to McLean Hospital in Belmont, Massachusetts, as a therapist after staying there as a patient years earlier: “And now I am standing on the other—the wrong, I mean the right side of the door and I ring the buzzer.”1 Here I tell my story of the physical and emotional effects of my mental illness and treatment.
Onset of bipolar disorder. My bipolar illness started with a bout of depression in 1963 at age 13, which resulted in a low-key summer of often staying inside. I received no medication, and no one sent me for evaluation. In the fall, I went back to school and finished the year without incident. I continued as a quiet, shy kid through high school in the late 1960s. In my senior year, I decided to take an overload of difficult courses and run on the varsity cross-country team. The amount and intensity of these activities were too much. This resulted in my first manic episode, which started during a weekend visit to a college I hoped to attend. I became excitable, grandiose, and had delusions. A day later, I returned home, and my parents had me admitted to a psychiatric hospital, where I remained for 3 months.
At first, my diagnosis was unclear, and initially no one considered what at the time was called manic depression. At that point, I was unaware of my extensive family psychiatric history. My pharmacologic treatment consisted of chlorpromazine, trifluoperazine, and procyclidine. I returned home just before Christmas and barely finished my senior year of high school. A good college accepted me. But during the orientation, I was asked to leave because I experienced a second manic episode. After 4 more psychiatric hospitalizations, I finally stabilized.
During one of my hospitalizations, I had the good fortune to be interviewed by Dr. Thomas Detre. During this interview, I talked expansively about Don Quixote, Aldonza, and Sancho Panza. Dr. Detre diagnosed me with manic depression, and suggested that I see Dr. Christiaan van der Velde, who was researching lithium carbonate.2 In 1970, I was hospitalized at Norwich State Hospital in Preston, Connecticut and was started on lithium, even though it had not yet been FDA-approved. I responded well to lithium monotherapy.
An extensive family history. Having bipolar disorder was not something I would discuss with others because I felt ashamed. I commonly hid my medication during college, especially from my roommates or other friends. By then, I had learned a little about my family’s psychiatric history, but I knew few specifics. Over time, I became aware of a dense familial cluster of affective illness going back several generations. My maternal grandmother was hospitalized for depression in 1921 after her husband suddenly died during her fourth pregnancy. She became bereft and suicidal because she had no one to support her 4 children. During my grandmother’s hospitalization, her sister and sister’s husband took care of her children. My grandmother remained hospitalized until she died in 1943. At that time, no medications were available to treat her illness. Over the next 2 generations, 2 of her 4 children and 6 of her 12 grandchildren (including me) developed bipolar disorder.
A career and family. In 1970, I started to work as a nursing assistant, then as a nursing technician for 1.5 years in a specialty hospital in New England. In 1973, I began nursing school at a junior college. I received my RN in 1975, a BS in nursing in 1979, and an MS in psychiatric nursing in 1982. I worked steadily as a psychiatric nurse in both inpatient and outpatient settings from 1975 until I retired in 2019.
In the early 1980s, I married my first wife and had 2 wonderful children. During our courtship in 1981 and 1982, I became hypomanic, which perhaps made me more outgoing and sociable. In 1985, after my father required open heart surgery, I had a manic episode that lasted 1 week. Over the next 20 years, although I was not happy with my marriage, I remained euthymic and productive at work. My marriage ended in 2012.
Continue to: By the end of 2012...
By the end of 2012, I had been taking lithium continuously for 42 years. My laboratory tests showed peak lithium levels between 0.6 and 1.2 mmol/L. I remained otherwise healthy, as demonstrated by annual physical exams and laboratory test results. In 2015, I developed an increase in my blood pressure and my primary care physician (PCP) prescribed oral lisinopril, initially 10 mg/d, and later 10 mg twice daily. My blood pressure improved and ranged from 120/74 to 130/82 mm Hg.
Hyperparathyroidism. By 2016, my psychiatrist, PCP, and nephrologist all urged me to consider parathyroid surgery.3-5 Hypercalcemia and hyperparathyroidism caused the most worry. Laboratory tests indicated calcium 11.2 mg/dL, parathyroid hormone (PTH) 88 pg/mL, estimated glomerular filtration rate (eGFR) 59 mL/min, and thyroid-stimulating hormone (TSH) 0.78 mIU/L. Electrocardiographysometimes showed a slight QT elongation. A right bundle branch block, which was first noted in 2015, continued. Due to my elevated calcium levels, I eliminated most calcium from my diet. My psychiatrist began to speak more strongly of parathyroid surgery. I then consulted a senior endocrinologist and a senior nephrologist, who each recommended parathyroid surgery.
I remarried in July 2016, and we moved to a different area of the country. My second wife became a stabilizing force for me. My new PCP, however, found elevated high-density lipoproteins during a routine physical examination, and started me on simvastatin, 10 mg/d. My calcium and PTH levels continued to be elevated. My PCP, nephrologist, therapist, and wife urged me to proceed with the parathyroidectomy. After a short period of watchful waiting and a second consultation with a nephrologist, I agreed to schedule a subtotal parathyroidectomy.
Surgery. In spring 2017, I began preparation for parathyroidectomy. At the time, my lithium carbonate dose was 600 mg/d, alternating with 900 mg/d. My peak level of lithium was 0.6 mmol/L. Lisinopril is synergistic, which allowed me to take a smaller effective dose of lithium.
My parathyroid surgery occurred on June 28, 2017 at Norman Parathyroid Center in Tampa, Florida.6 The surgeon recorded my parathyroid glands as 136, 602, and 348 units using a measure developed at Norman Parathyroid Center. No reading was given for my fourth parathyroid gland, which they did not remove. Following the surgery, I resumed my previous functions, including employment as a visiting nurse. I initially took calcium supplements after surgery, and my lithium dose was reduced to 300 mg orally, twice daily, which I have continued. I have remained euthymic. On August 3, 2017 my laboratory workup showed an eGFR of 64 mL/min, calcium 10.0 mg/dL, and PTH 17 pg/mL. Vitamin D25 OH 33, glucose, BUN/Cr, electrolytes, complete blood count, and albumin were all within normal limits. Repeat bloodwork on September 19, 2017 showed Ca++ 10.1 mg/dL and PTH 18 pg/mL. Nine months after the surgery, I showed an incredibly positive physical and mental response, which has continued to this day.
Continue to: Clinical implications
Clinical implications. This is a single case study. However, it is important for clinicians treating patients with lithium carbonate to regularly order laboratory testing, including for lithium levels, PTH, and calcium, to detect early signs of complications from treatment, including hyperparathyroidism and hypercalcemia.7 These levels could be obtained every 6 months. If a patient’s PTH levels are >70 pg/mL and calcium levels are >11.0 mg/dL, it would be prudent to refer him/her for further medical evaluation. Additionally, it would be helpful to counsel the patient about considering alternative medication and adjunct mental health treatment. At some future point, it could be useful for the clinician and his/her patient to explore the idea of parathyroid surgery.
In addition to chronic lithium use, other causes of hyperparathyroidism include an adenoma on a gland, hyperplasia of ≥2 parathyroid glands, a malignant tumor, severe calcium deficiency, severe vitamin D deficiency, chronic renal failure, and (rarely) an inherited gene that causes hyperparathyroidism.
How I’m doing today. Currently, I am euthymic and in a happy marriage. My laboratory workup in May 2020 included glucose 107 mg/dL, Ca++ 9.5 mg/dL, eGFR 61 mL/min, PTH 32 pg/mL, lithium 0.3 mmol/L (300 mg twice daily), and TSH 1.79 mIU/L. A comprehensive metabolic panel, complete blood count, and lipid panel were all within normal limits.
I am fortunate to continue having excellent care provided by my PCP, nephrologist, urologist, and psychiatric APRN. Together with these wonderful professionals, I have been able to maintain my physical and mental health.
Acknowledgment: I gratefully acknowledge the help and skills of Robin Scharak and Gary Blake for providing some of the editing on this article.
Bill Greenberg MS, RN, APRN
Delray Beach, Florida
I am a retired advanced practice psychiatric nurse who has lived and worked on “both sides of the door.” This wording is paraphrased from psychologist and therapist Lauren Slater, PhD, who wrote about a time she went to McLean Hospital in Belmont, Massachusetts, as a therapist after staying there as a patient years earlier: “And now I am standing on the other—the wrong, I mean the right side of the door and I ring the buzzer.”1 Here I tell my story of the physical and emotional effects of my mental illness and treatment.
Onset of bipolar disorder. My bipolar illness started with a bout of depression in 1963 at age 13, which resulted in a low-key summer of often staying inside. I received no medication, and no one sent me for evaluation. In the fall, I went back to school and finished the year without incident. I continued as a quiet, shy kid through high school in the late 1960s. In my senior year, I decided to take an overload of difficult courses and run on the varsity cross-country team. The amount and intensity of these activities were too much. This resulted in my first manic episode, which started during a weekend visit to a college I hoped to attend. I became excitable, grandiose, and had delusions. A day later, I returned home, and my parents had me admitted to a psychiatric hospital, where I remained for 3 months.
At first, my diagnosis was unclear, and initially no one considered what at the time was called manic depression. At that point, I was unaware of my extensive family psychiatric history. My pharmacologic treatment consisted of chlorpromazine, trifluoperazine, and procyclidine. I returned home just before Christmas and barely finished my senior year of high school. A good college accepted me. But during the orientation, I was asked to leave because I experienced a second manic episode. After 4 more psychiatric hospitalizations, I finally stabilized.
During one of my hospitalizations, I had the good fortune to be interviewed by Dr. Thomas Detre. During this interview, I talked expansively about Don Quixote, Aldonza, and Sancho Panza. Dr. Detre diagnosed me with manic depression, and suggested that I see Dr. Christiaan van der Velde, who was researching lithium carbonate.2 In 1970, I was hospitalized at Norwich State Hospital in Preston, Connecticut and was started on lithium, even though it had not yet been FDA-approved. I responded well to lithium monotherapy.
An extensive family history. Having bipolar disorder was not something I would discuss with others because I felt ashamed. I commonly hid my medication during college, especially from my roommates or other friends. By then, I had learned a little about my family’s psychiatric history, but I knew few specifics. Over time, I became aware of a dense familial cluster of affective illness going back several generations. My maternal grandmother was hospitalized for depression in 1921 after her husband suddenly died during her fourth pregnancy. She became bereft and suicidal because she had no one to support her 4 children. During my grandmother’s hospitalization, her sister and sister’s husband took care of her children. My grandmother remained hospitalized until she died in 1943. At that time, no medications were available to treat her illness. Over the next 2 generations, 2 of her 4 children and 6 of her 12 grandchildren (including me) developed bipolar disorder.
A career and family. In 1970, I started to work as a nursing assistant, then as a nursing technician for 1.5 years in a specialty hospital in New England. In 1973, I began nursing school at a junior college. I received my RN in 1975, a BS in nursing in 1979, and an MS in psychiatric nursing in 1982. I worked steadily as a psychiatric nurse in both inpatient and outpatient settings from 1975 until I retired in 2019.
In the early 1980s, I married my first wife and had 2 wonderful children. During our courtship in 1981 and 1982, I became hypomanic, which perhaps made me more outgoing and sociable. In 1985, after my father required open heart surgery, I had a manic episode that lasted 1 week. Over the next 20 years, although I was not happy with my marriage, I remained euthymic and productive at work. My marriage ended in 2012.
Continue to: By the end of 2012...
By the end of 2012, I had been taking lithium continuously for 42 years. My laboratory tests showed peak lithium levels between 0.6 and 1.2 mmol/L. I remained otherwise healthy, as demonstrated by annual physical exams and laboratory test results. In 2015, I developed an increase in my blood pressure and my primary care physician (PCP) prescribed oral lisinopril, initially 10 mg/d, and later 10 mg twice daily. My blood pressure improved and ranged from 120/74 to 130/82 mm Hg.
Hyperparathyroidism. By 2016, my psychiatrist, PCP, and nephrologist all urged me to consider parathyroid surgery.3-5 Hypercalcemia and hyperparathyroidism caused the most worry. Laboratory tests indicated calcium 11.2 mg/dL, parathyroid hormone (PTH) 88 pg/mL, estimated glomerular filtration rate (eGFR) 59 mL/min, and thyroid-stimulating hormone (TSH) 0.78 mIU/L. Electrocardiographysometimes showed a slight QT elongation. A right bundle branch block, which was first noted in 2015, continued. Due to my elevated calcium levels, I eliminated most calcium from my diet. My psychiatrist began to speak more strongly of parathyroid surgery. I then consulted a senior endocrinologist and a senior nephrologist, who each recommended parathyroid surgery.
I remarried in July 2016, and we moved to a different area of the country. My second wife became a stabilizing force for me. My new PCP, however, found elevated high-density lipoproteins during a routine physical examination, and started me on simvastatin, 10 mg/d. My calcium and PTH levels continued to be elevated. My PCP, nephrologist, therapist, and wife urged me to proceed with the parathyroidectomy. After a short period of watchful waiting and a second consultation with a nephrologist, I agreed to schedule a subtotal parathyroidectomy.
Surgery. In spring 2017, I began preparation for parathyroidectomy. At the time, my lithium carbonate dose was 600 mg/d, alternating with 900 mg/d. My peak level of lithium was 0.6 mmol/L. Lisinopril is synergistic, which allowed me to take a smaller effective dose of lithium.
My parathyroid surgery occurred on June 28, 2017 at Norman Parathyroid Center in Tampa, Florida.6 The surgeon recorded my parathyroid glands as 136, 602, and 348 units using a measure developed at Norman Parathyroid Center. No reading was given for my fourth parathyroid gland, which they did not remove. Following the surgery, I resumed my previous functions, including employment as a visiting nurse. I initially took calcium supplements after surgery, and my lithium dose was reduced to 300 mg orally, twice daily, which I have continued. I have remained euthymic. On August 3, 2017 my laboratory workup showed an eGFR of 64 mL/min, calcium 10.0 mg/dL, and PTH 17 pg/mL. Vitamin D25 OH 33, glucose, BUN/Cr, electrolytes, complete blood count, and albumin were all within normal limits. Repeat bloodwork on September 19, 2017 showed Ca++ 10.1 mg/dL and PTH 18 pg/mL. Nine months after the surgery, I showed an incredibly positive physical and mental response, which has continued to this day.
Continue to: Clinical implications
Clinical implications. This is a single case study. However, it is important for clinicians treating patients with lithium carbonate to regularly order laboratory testing, including for lithium levels, PTH, and calcium, to detect early signs of complications from treatment, including hyperparathyroidism and hypercalcemia.7 These levels could be obtained every 6 months. If a patient’s PTH levels are >70 pg/mL and calcium levels are >11.0 mg/dL, it would be prudent to refer him/her for further medical evaluation. Additionally, it would be helpful to counsel the patient about considering alternative medication and adjunct mental health treatment. At some future point, it could be useful for the clinician and his/her patient to explore the idea of parathyroid surgery.
In addition to chronic lithium use, other causes of hyperparathyroidism include an adenoma on a gland, hyperplasia of ≥2 parathyroid glands, a malignant tumor, severe calcium deficiency, severe vitamin D deficiency, chronic renal failure, and (rarely) an inherited gene that causes hyperparathyroidism.
How I’m doing today. Currently, I am euthymic and in a happy marriage. My laboratory workup in May 2020 included glucose 107 mg/dL, Ca++ 9.5 mg/dL, eGFR 61 mL/min, PTH 32 pg/mL, lithium 0.3 mmol/L (300 mg twice daily), and TSH 1.79 mIU/L. A comprehensive metabolic panel, complete blood count, and lipid panel were all within normal limits.
I am fortunate to continue having excellent care provided by my PCP, nephrologist, urologist, and psychiatric APRN. Together with these wonderful professionals, I have been able to maintain my physical and mental health.
Acknowledgment: I gratefully acknowledge the help and skills of Robin Scharak and Gary Blake for providing some of the editing on this article.
Bill Greenberg MS, RN, APRN
Delray Beach, Florida
1. Slater L. Welcome to my country. New York, NY: Random House; 1996:187.
2. Van der Velde CD. Effectiveness of lithium in the treatment of manic-depressive illness. Am J Psychiatry. 1970;127(3):345-351.
3. Norman Parathyroid Center. Parathyroid glands, high calcium and hyperparathyroidism. www.parathyroid.com. Updated October 21, 2020. Accessed November 11, 2020.
4. Meehan AD, Udumyan R, Kardell M, et al. Lithium-associated hypercalcemia: pathophysiology, prevalence, management. World J Surg. 2018;42(2):415-424.
5. Lally J, Lee B, McDonald C. Prevalence of hypercalcaemia in patients on maintenance lithium therapy monitored in primary care. Ir Med J. 2013;106(1):15-17.
6. Norman Parathyroid Center. Parathyroid surgery: minimally invasive 4-gland parathyroid surgery video. (4-Gland MIRP Parathyroid Operation). https://www.parathyroid.com/parathyroid-surgery.htm. Updated October 1, 2020. Accessed November 5, 2020.
7. MEDSAFE. Hyperparathyroidism and hypercalcaemia with lithium treatment. New Zealand Medicines and Medical Devices Safety Authority. 2014;35(3):37-38.
1. Slater L. Welcome to my country. New York, NY: Random House; 1996:187.
2. Van der Velde CD. Effectiveness of lithium in the treatment of manic-depressive illness. Am J Psychiatry. 1970;127(3):345-351.
3. Norman Parathyroid Center. Parathyroid glands, high calcium and hyperparathyroidism. www.parathyroid.com. Updated October 21, 2020. Accessed November 11, 2020.
4. Meehan AD, Udumyan R, Kardell M, et al. Lithium-associated hypercalcemia: pathophysiology, prevalence, management. World J Surg. 2018;42(2):415-424.
5. Lally J, Lee B, McDonald C. Prevalence of hypercalcaemia in patients on maintenance lithium therapy monitored in primary care. Ir Med J. 2013;106(1):15-17.
6. Norman Parathyroid Center. Parathyroid surgery: minimally invasive 4-gland parathyroid surgery video. (4-Gland MIRP Parathyroid Operation). https://www.parathyroid.com/parathyroid-surgery.htm. Updated October 1, 2020. Accessed November 5, 2020.
7. MEDSAFE. Hyperparathyroidism and hypercalcaemia with lithium treatment. New Zealand Medicines and Medical Devices Safety Authority. 2014;35(3):37-38.
Death anxiety among psychiatry trainees during COVID-19
The coronavirus disease 2019 (COVID-19) pandemic
The far-reaching effects of death anxiety
Postgraduate psychiatry training may expose one to stressful situations with adverse psychologic consequences.1 Furthermore, when caring for patients, psychiatry trainees frequently need to face issues of death and dying in the form of suicide risk assessments, grief and bereavement processes, near-death experiences, posttraumatic stress disorder, and psycho-oncology rotations. Because these interactions are incredibly personal, the emotions they provoke inevitably affect every interaction, theoretical discussion, diagnostic work-up, and treatment plan.
How each of us experiences death anxiety is unique. For some, it could be a fear of nonexistence, ultimate loss, disruption of the flow of life, worry about leaving loved ones behind, or fear of pain or loneliness in dying. Some might fear an untimely or violent death and subsequent judgment and retributions. The literature suggests that fear of death may be at the root of various mental health problems and, if left unaddressed, may adversely impact long-term treatment outcomes.2 Despite this, many standard treatment approaches typically do not target death anxiety, which potentially contributes to a “revolving door” of mental health problems.3
American existential psychiatrist Irvin Yalom, MD, cautioned psychiatrists not to “scratch where it does not itch.”4 Yet death, according to Dr. Yalom, does itch. Violent death is that caused by human intent or negligence, and is characterized by feeling helpless and terrorized at the time of dying. It may occur as an acute incident that denies the dying individual and his/her family members the time and space to prepare for the death.5 For survivors, accommodating the mental, emotional, psychological, and spiritual effects of violent death is a complex process that rarely has a conclusion. It often is accompanied by survivors’ guilt, which is replayed in the form of flashbacks and nightmares.6 With this understanding, I view COVID-19 deaths as violent deaths.
Pay close attention to countertransference
As much as we influence our patients and their families, we also are profoundly influenced by them. We need to pay attention to any feelings our clinical encounters generate within us, and to carefully use these feelings in our clinical judgment, and not just make causal inferences. For instance, if a clinician thinks that a patient with suicidal ideation would be better off dead, these feelings are a reliable indicator that the patient is, indeed, at a high risk of completing suicide.7 It is our ethical and moral responsibility towards our patients to listen to our countertransference responses. The aim is to identify countertransference and use it to inform us, not to rule us. By taking an active role in managing our emotional responses in the face of loss, we can harness the spirit of resilience. This is not always as easy as it seems. We need our peers, experienced clinicians, and supervisors to help us explore our feelings, resistances, and countertransference reactions.
Strategies to combat burnout
Psychiatric trainees must be encouraged to establish and maintain rigorous plans of self-care to prevent compassion fatigue and burnout. Most importantly, training programs must diversify residents’ clinical exposure by providing activities that promote mental health promotion activities, scholarly endeavors, and peer support groups. This will help trainees to restore meaning and purpose in life beyond.
1. Coverdale J, Balon R, Beresin EV, et al. What are some stressful adversities in psychiatry residency training, and how should they be managed professionally? Acad Psychiatry. 2019;43(2):145-150.
2. Russac RJ, Gatliff C, Reece M, et al. Death anxiety across the adult years: an examination of age and gender effects. Death Stud. 2007;31(6):549-561.
3. Lisa I, Menzies RG, Menzies RE. Death anxiety and its role in psychopathology: reviewing the status of a transdiagnostic construct. Clinical Psychology Review. 2014;34(7):580-593.
4. Yalom ID. Staring at the sun: being at peace with your own mortality. London, UK: Piatkus; 2011.
5. Rynearson EK, Johnson TA, Correa F. The horror and helplessness of violent death. In: Katz RS, Johnson TA (eds). When professionals weep: emotional and countertransference responses in palliative and end-of-life care. Abingdon, UK: Routledge; 2016:91-103.
6. Breggin PR. Guilt, shame, and anxiety: understanding and overcoming negative emotions. Buffalo, NY: Prometheus Books; 2014.
7. Katz RS, Johnson TA, (eds). When professionals weep: Emotional and countertransference responses in palliative and end-of-life care. Abingdon, UK: Routledge; 2016.
The coronavirus disease 2019 (COVID-19) pandemic
The far-reaching effects of death anxiety
Postgraduate psychiatry training may expose one to stressful situations with adverse psychologic consequences.1 Furthermore, when caring for patients, psychiatry trainees frequently need to face issues of death and dying in the form of suicide risk assessments, grief and bereavement processes, near-death experiences, posttraumatic stress disorder, and psycho-oncology rotations. Because these interactions are incredibly personal, the emotions they provoke inevitably affect every interaction, theoretical discussion, diagnostic work-up, and treatment plan.
How each of us experiences death anxiety is unique. For some, it could be a fear of nonexistence, ultimate loss, disruption of the flow of life, worry about leaving loved ones behind, or fear of pain or loneliness in dying. Some might fear an untimely or violent death and subsequent judgment and retributions. The literature suggests that fear of death may be at the root of various mental health problems and, if left unaddressed, may adversely impact long-term treatment outcomes.2 Despite this, many standard treatment approaches typically do not target death anxiety, which potentially contributes to a “revolving door” of mental health problems.3
American existential psychiatrist Irvin Yalom, MD, cautioned psychiatrists not to “scratch where it does not itch.”4 Yet death, according to Dr. Yalom, does itch. Violent death is that caused by human intent or negligence, and is characterized by feeling helpless and terrorized at the time of dying. It may occur as an acute incident that denies the dying individual and his/her family members the time and space to prepare for the death.5 For survivors, accommodating the mental, emotional, psychological, and spiritual effects of violent death is a complex process that rarely has a conclusion. It often is accompanied by survivors’ guilt, which is replayed in the form of flashbacks and nightmares.6 With this understanding, I view COVID-19 deaths as violent deaths.
Pay close attention to countertransference
As much as we influence our patients and their families, we also are profoundly influenced by them. We need to pay attention to any feelings our clinical encounters generate within us, and to carefully use these feelings in our clinical judgment, and not just make causal inferences. For instance, if a clinician thinks that a patient with suicidal ideation would be better off dead, these feelings are a reliable indicator that the patient is, indeed, at a high risk of completing suicide.7 It is our ethical and moral responsibility towards our patients to listen to our countertransference responses. The aim is to identify countertransference and use it to inform us, not to rule us. By taking an active role in managing our emotional responses in the face of loss, we can harness the spirit of resilience. This is not always as easy as it seems. We need our peers, experienced clinicians, and supervisors to help us explore our feelings, resistances, and countertransference reactions.
Strategies to combat burnout
Psychiatric trainees must be encouraged to establish and maintain rigorous plans of self-care to prevent compassion fatigue and burnout. Most importantly, training programs must diversify residents’ clinical exposure by providing activities that promote mental health promotion activities, scholarly endeavors, and peer support groups. This will help trainees to restore meaning and purpose in life beyond.
The coronavirus disease 2019 (COVID-19) pandemic
The far-reaching effects of death anxiety
Postgraduate psychiatry training may expose one to stressful situations with adverse psychologic consequences.1 Furthermore, when caring for patients, psychiatry trainees frequently need to face issues of death and dying in the form of suicide risk assessments, grief and bereavement processes, near-death experiences, posttraumatic stress disorder, and psycho-oncology rotations. Because these interactions are incredibly personal, the emotions they provoke inevitably affect every interaction, theoretical discussion, diagnostic work-up, and treatment plan.
How each of us experiences death anxiety is unique. For some, it could be a fear of nonexistence, ultimate loss, disruption of the flow of life, worry about leaving loved ones behind, or fear of pain or loneliness in dying. Some might fear an untimely or violent death and subsequent judgment and retributions. The literature suggests that fear of death may be at the root of various mental health problems and, if left unaddressed, may adversely impact long-term treatment outcomes.2 Despite this, many standard treatment approaches typically do not target death anxiety, which potentially contributes to a “revolving door” of mental health problems.3
American existential psychiatrist Irvin Yalom, MD, cautioned psychiatrists not to “scratch where it does not itch.”4 Yet death, according to Dr. Yalom, does itch. Violent death is that caused by human intent or negligence, and is characterized by feeling helpless and terrorized at the time of dying. It may occur as an acute incident that denies the dying individual and his/her family members the time and space to prepare for the death.5 For survivors, accommodating the mental, emotional, psychological, and spiritual effects of violent death is a complex process that rarely has a conclusion. It often is accompanied by survivors’ guilt, which is replayed in the form of flashbacks and nightmares.6 With this understanding, I view COVID-19 deaths as violent deaths.
Pay close attention to countertransference
As much as we influence our patients and their families, we also are profoundly influenced by them. We need to pay attention to any feelings our clinical encounters generate within us, and to carefully use these feelings in our clinical judgment, and not just make causal inferences. For instance, if a clinician thinks that a patient with suicidal ideation would be better off dead, these feelings are a reliable indicator that the patient is, indeed, at a high risk of completing suicide.7 It is our ethical and moral responsibility towards our patients to listen to our countertransference responses. The aim is to identify countertransference and use it to inform us, not to rule us. By taking an active role in managing our emotional responses in the face of loss, we can harness the spirit of resilience. This is not always as easy as it seems. We need our peers, experienced clinicians, and supervisors to help us explore our feelings, resistances, and countertransference reactions.
Strategies to combat burnout
Psychiatric trainees must be encouraged to establish and maintain rigorous plans of self-care to prevent compassion fatigue and burnout. Most importantly, training programs must diversify residents’ clinical exposure by providing activities that promote mental health promotion activities, scholarly endeavors, and peer support groups. This will help trainees to restore meaning and purpose in life beyond.
1. Coverdale J, Balon R, Beresin EV, et al. What are some stressful adversities in psychiatry residency training, and how should they be managed professionally? Acad Psychiatry. 2019;43(2):145-150.
2. Russac RJ, Gatliff C, Reece M, et al. Death anxiety across the adult years: an examination of age and gender effects. Death Stud. 2007;31(6):549-561.
3. Lisa I, Menzies RG, Menzies RE. Death anxiety and its role in psychopathology: reviewing the status of a transdiagnostic construct. Clinical Psychology Review. 2014;34(7):580-593.
4. Yalom ID. Staring at the sun: being at peace with your own mortality. London, UK: Piatkus; 2011.
5. Rynearson EK, Johnson TA, Correa F. The horror and helplessness of violent death. In: Katz RS, Johnson TA (eds). When professionals weep: emotional and countertransference responses in palliative and end-of-life care. Abingdon, UK: Routledge; 2016:91-103.
6. Breggin PR. Guilt, shame, and anxiety: understanding and overcoming negative emotions. Buffalo, NY: Prometheus Books; 2014.
7. Katz RS, Johnson TA, (eds). When professionals weep: Emotional and countertransference responses in palliative and end-of-life care. Abingdon, UK: Routledge; 2016.
1. Coverdale J, Balon R, Beresin EV, et al. What are some stressful adversities in psychiatry residency training, and how should they be managed professionally? Acad Psychiatry. 2019;43(2):145-150.
2. Russac RJ, Gatliff C, Reece M, et al. Death anxiety across the adult years: an examination of age and gender effects. Death Stud. 2007;31(6):549-561.
3. Lisa I, Menzies RG, Menzies RE. Death anxiety and its role in psychopathology: reviewing the status of a transdiagnostic construct. Clinical Psychology Review. 2014;34(7):580-593.
4. Yalom ID. Staring at the sun: being at peace with your own mortality. London, UK: Piatkus; 2011.
5. Rynearson EK, Johnson TA, Correa F. The horror and helplessness of violent death. In: Katz RS, Johnson TA (eds). When professionals weep: emotional and countertransference responses in palliative and end-of-life care. Abingdon, UK: Routledge; 2016:91-103.
6. Breggin PR. Guilt, shame, and anxiety: understanding and overcoming negative emotions. Buffalo, NY: Prometheus Books; 2014.
7. Katz RS, Johnson TA, (eds). When professionals weep: Emotional and countertransference responses in palliative and end-of-life care. Abingdon, UK: Routledge; 2016.







