User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
COVID-19: Where doctors can get help for emotional distress
Nisha Mehta, MD, said her phone has been ringing with calls from tearful and shaken physicians who are distressed and unsettled about their work and home situation and don’t know what to do.
What’s more, many frontline physicians are living apart from family to protect them from infection. “So many physicians have called me crying. ... They can’t even come home and get a hug,” Dr. Mehta said. “What I’m hearing from a lot of people who are in New York and New Jersey is not just that they go to work all day and it’s this exhausting process throughout the entire day, not only physically but also emotionally.”
Physician burnout has held a steady spotlight since long before the COVID-19 crisis began, Dr. Mehta said. “The reason for that is multifold, but in part, it’s hard for physicians to find an appropriate way to be able to process a lot of the emotions related to their work,” she said. “A lot of that brews below the surface, but COVID-19 has really brought many of these issues above that surface.”
Frustrated that governments weren’t doing enough to support health care workers during the pandemic, Dr. Mehta, a radiologist in Charlotte, N.C., decided there needed to be change. On April 4, Dr. Mehta and two physician colleagues submitted to Congress the COVID-19 Pandemic Physician Protection Act, which ensures, among other provisions, mental health coverage for health care workers. An accompanying petition on change.org had received nearly 300,000 signatures as of May 29.
Don’t suffer in silence
A career in medicine comes with immense stress in the best of times, she notes, and managing a pandemic in an already strained system has taken those challenges to newer heights. “We need better support structures at baseline for physician mental health,” said Dr. Mehta.
“That’s something we’ve always been lacking because it’s been against the culture of medicine for so long to say, ‘I’m having a hard time.’ ”
If you’re hurting, the first thing to recognize is that you are not alone in facing these challenges. This is true with respect not only to medical care but also to all of the family, financial, and business concerns physicians are currently facing. “Having all of those things hanging over your head is a lot. We’ve got to find ways to help each other out,” Dr. Mehta said.
Where to find support
Fortunately, the medical community has created several pathways to help its own.
The following list represents a cross-section of opportunities for caregivers to receive care for themselves.
Crisis hotlines
- Physician Support Line. This free and confidential hotline was launched on March 30 by Mona Masood, DO, a Philadelphia-area psychiatrist and moderator of a Facebook forum called the COVID-19 Physicians Group. The PSL is run by more than 600 volunteer psychiatrists who take calls from U.S. physicians 7 days a week from 8:00 a.m. to 1:00 a.m., with no appointment necessary. The toll-free number is 888-409-0141.
- For the Frontlines. This 24/7 help line provides free crisis counseling for frontline workers. They can text FRONTLINE to 741741 in the United States (support is also available for residents of Canada, Ireland, and the United Kingdom).
Resources from professional groups
- Action Collaborative on Clinician Well-Being and Resilience. Created by the National Academy of Medicine in 2017, the Action Collaborative comprises more than 60 organizations committed to reversing trends in clinician burnout. In response to the pandemic, the group has compiled a list of strategies and resources to support the health and well-being of clinicians who are providing healthcare during the COVID-19 outbreak.
- American Medical Association. The AMA has created a resource center dedicated to providing care for caregivers during the COVID-19 pandemic. The website includes specific guidance for managing mental health during the pandemic.
- American College of Physicians. The professional society of internal medicine physicians has created a comprehensive guide for physicians specific to COVID-19, with a section dedicated to clinician well-being that includes information about hotlines, counseling services, grief support, and more.
- American Hospital Association. The AHA’s website now includes regularly updated resources for healthcare clinicians and staff, as well as a special section dedicated to protecting and enabling healthcare workers in the midst of the pandemic.
Virtual psychological counseling
Not unlike the way telemedicine has allowed some physicians to keep seeing their patients, many modalities enable participation in therapy through video, chat, phone call, or any combination thereof. Look for a service that is convenient, flexible, and HIPAA compliant.
Traditional in-office mental health therapy has quickly moved to telemedicine. Many if not most insurers that cover counseling visits are paying for telepsychiatry or telecounseling. If you don’t know of an appropriate therapist, check the American Psychiatric Association or its state chapters; the American Psychological Association; or look for a licensed mental health counselor.
Because financial constraints are a potential barrier to therapy, Project Parachute, in cooperation with Eleos Health, has organized a cadre of therapists willing to provide pro bono online therapy for health care workers. The amount of free therapy provided to qualified frontline workers is up to the individual therapists. Discuss these parameters with your therapists up front.
Similar services are offered from companies such as Talkspace and BetterHelp on a subscription basis. These services are typically less expensive than in-person sessions. Ask about discounts for healthcare workers. Talkspace, for example, announced in March, “Effective immediately, healthcare workers across the country can get access to a free month of our...online therapy that includes unlimited text, video, and audio messaging with a licensed therapist.”
Online support groups and social media
For more on-demand peer support, look for groups such as the COR Sharing Circle for Healthcare Workers on Facebook. The site’s search engine can point users to plenty of other groups, many of which are closed (meaning posts are visible to members only).
Dr. Mehta hosts her own Facebook group called Physician Community. “I would like to think (and genuinely feel) that we’ve been doing a great job of supporting each other there with daily threads on challenges, treatments, pick-me-ups, vent posts, advocacy, and more,” she said.
For anyone in need, PeerRxMed is a free, peer-to-peer program for physicians and other health care workers that is designed to provide support, connection, encouragement, resources, and skill-building to optimize well-being.
For those craving spiritual comfort during this crisis, a number of churches have begun offering that experience virtually, too. First Unitarian Church of Worcester, Massachusetts, for example, offers weekly services via YouTube. Similar online programming is being offered from all sorts of organizations across denominations.
Apps
For DIY or on-the-spot coping support, apps can help physicians get through the day. Apps and websites that offer guided meditations and other relaxation tools include Headspace, Calm, and Insight Timer. Before downloading, look for special discounts and promotions for healthcare workers.
Additionally, COVID Coach is a free, secure app designed by the U.S. Department of Veterans Affairs that includes tools to help you cope with stress and stay well, safe, healthy, and connected. It also offers advice on navigating parenting, care giving, and working from home while social distancing, quarantined, or sheltering in place.
For practicing daily gratitude, Delightful Journal is a free app that offers journaling prompts, themes, reminders, and unlimited private space to record one’s thoughts.
Adopt a ritual
Although self-care for physicians is more crucial now than ever, it can look different for every individual. Along the same lines as keeping a journal, wellness experts often recommend beginning a “gratitude practice” to help provide solace and perspective.
Tweak and personalize these activities to suit your own needs, but be sure to use them even when you’re feeling well, said Mohana Karlekar, MD, medical director of palliative care and assistant professor at Vanderbilt University Medical Center, Nashville, Tenn.
One exercise she recommends is known as Three Good Things. “Every day, at the end of the day, think about three good things that have happened,” she explained. “You can always find the joys. And the joys don’t have to be enormous. There is joy – there is hope – in everything,” Dr. Karlekar said.
A version of this article originally appeared on Medscape.com.
Nisha Mehta, MD, said her phone has been ringing with calls from tearful and shaken physicians who are distressed and unsettled about their work and home situation and don’t know what to do.
What’s more, many frontline physicians are living apart from family to protect them from infection. “So many physicians have called me crying. ... They can’t even come home and get a hug,” Dr. Mehta said. “What I’m hearing from a lot of people who are in New York and New Jersey is not just that they go to work all day and it’s this exhausting process throughout the entire day, not only physically but also emotionally.”
Physician burnout has held a steady spotlight since long before the COVID-19 crisis began, Dr. Mehta said. “The reason for that is multifold, but in part, it’s hard for physicians to find an appropriate way to be able to process a lot of the emotions related to their work,” she said. “A lot of that brews below the surface, but COVID-19 has really brought many of these issues above that surface.”
Frustrated that governments weren’t doing enough to support health care workers during the pandemic, Dr. Mehta, a radiologist in Charlotte, N.C., decided there needed to be change. On April 4, Dr. Mehta and two physician colleagues submitted to Congress the COVID-19 Pandemic Physician Protection Act, which ensures, among other provisions, mental health coverage for health care workers. An accompanying petition on change.org had received nearly 300,000 signatures as of May 29.
Don’t suffer in silence
A career in medicine comes with immense stress in the best of times, she notes, and managing a pandemic in an already strained system has taken those challenges to newer heights. “We need better support structures at baseline for physician mental health,” said Dr. Mehta.
“That’s something we’ve always been lacking because it’s been against the culture of medicine for so long to say, ‘I’m having a hard time.’ ”
If you’re hurting, the first thing to recognize is that you are not alone in facing these challenges. This is true with respect not only to medical care but also to all of the family, financial, and business concerns physicians are currently facing. “Having all of those things hanging over your head is a lot. We’ve got to find ways to help each other out,” Dr. Mehta said.
Where to find support
Fortunately, the medical community has created several pathways to help its own.
The following list represents a cross-section of opportunities for caregivers to receive care for themselves.
Crisis hotlines
- Physician Support Line. This free and confidential hotline was launched on March 30 by Mona Masood, DO, a Philadelphia-area psychiatrist and moderator of a Facebook forum called the COVID-19 Physicians Group. The PSL is run by more than 600 volunteer psychiatrists who take calls from U.S. physicians 7 days a week from 8:00 a.m. to 1:00 a.m., with no appointment necessary. The toll-free number is 888-409-0141.
- For the Frontlines. This 24/7 help line provides free crisis counseling for frontline workers. They can text FRONTLINE to 741741 in the United States (support is also available for residents of Canada, Ireland, and the United Kingdom).
Resources from professional groups
- Action Collaborative on Clinician Well-Being and Resilience. Created by the National Academy of Medicine in 2017, the Action Collaborative comprises more than 60 organizations committed to reversing trends in clinician burnout. In response to the pandemic, the group has compiled a list of strategies and resources to support the health and well-being of clinicians who are providing healthcare during the COVID-19 outbreak.
- American Medical Association. The AMA has created a resource center dedicated to providing care for caregivers during the COVID-19 pandemic. The website includes specific guidance for managing mental health during the pandemic.
- American College of Physicians. The professional society of internal medicine physicians has created a comprehensive guide for physicians specific to COVID-19, with a section dedicated to clinician well-being that includes information about hotlines, counseling services, grief support, and more.
- American Hospital Association. The AHA’s website now includes regularly updated resources for healthcare clinicians and staff, as well as a special section dedicated to protecting and enabling healthcare workers in the midst of the pandemic.
Virtual psychological counseling
Not unlike the way telemedicine has allowed some physicians to keep seeing their patients, many modalities enable participation in therapy through video, chat, phone call, or any combination thereof. Look for a service that is convenient, flexible, and HIPAA compliant.
Traditional in-office mental health therapy has quickly moved to telemedicine. Many if not most insurers that cover counseling visits are paying for telepsychiatry or telecounseling. If you don’t know of an appropriate therapist, check the American Psychiatric Association or its state chapters; the American Psychological Association; or look for a licensed mental health counselor.
Because financial constraints are a potential barrier to therapy, Project Parachute, in cooperation with Eleos Health, has organized a cadre of therapists willing to provide pro bono online therapy for health care workers. The amount of free therapy provided to qualified frontline workers is up to the individual therapists. Discuss these parameters with your therapists up front.
Similar services are offered from companies such as Talkspace and BetterHelp on a subscription basis. These services are typically less expensive than in-person sessions. Ask about discounts for healthcare workers. Talkspace, for example, announced in March, “Effective immediately, healthcare workers across the country can get access to a free month of our...online therapy that includes unlimited text, video, and audio messaging with a licensed therapist.”
Online support groups and social media
For more on-demand peer support, look for groups such as the COR Sharing Circle for Healthcare Workers on Facebook. The site’s search engine can point users to plenty of other groups, many of which are closed (meaning posts are visible to members only).
Dr. Mehta hosts her own Facebook group called Physician Community. “I would like to think (and genuinely feel) that we’ve been doing a great job of supporting each other there with daily threads on challenges, treatments, pick-me-ups, vent posts, advocacy, and more,” she said.
For anyone in need, PeerRxMed is a free, peer-to-peer program for physicians and other health care workers that is designed to provide support, connection, encouragement, resources, and skill-building to optimize well-being.
For those craving spiritual comfort during this crisis, a number of churches have begun offering that experience virtually, too. First Unitarian Church of Worcester, Massachusetts, for example, offers weekly services via YouTube. Similar online programming is being offered from all sorts of organizations across denominations.
Apps
For DIY or on-the-spot coping support, apps can help physicians get through the day. Apps and websites that offer guided meditations and other relaxation tools include Headspace, Calm, and Insight Timer. Before downloading, look for special discounts and promotions for healthcare workers.
Additionally, COVID Coach is a free, secure app designed by the U.S. Department of Veterans Affairs that includes tools to help you cope with stress and stay well, safe, healthy, and connected. It also offers advice on navigating parenting, care giving, and working from home while social distancing, quarantined, or sheltering in place.
For practicing daily gratitude, Delightful Journal is a free app that offers journaling prompts, themes, reminders, and unlimited private space to record one’s thoughts.
Adopt a ritual
Although self-care for physicians is more crucial now than ever, it can look different for every individual. Along the same lines as keeping a journal, wellness experts often recommend beginning a “gratitude practice” to help provide solace and perspective.
Tweak and personalize these activities to suit your own needs, but be sure to use them even when you’re feeling well, said Mohana Karlekar, MD, medical director of palliative care and assistant professor at Vanderbilt University Medical Center, Nashville, Tenn.
One exercise she recommends is known as Three Good Things. “Every day, at the end of the day, think about three good things that have happened,” she explained. “You can always find the joys. And the joys don’t have to be enormous. There is joy – there is hope – in everything,” Dr. Karlekar said.
A version of this article originally appeared on Medscape.com.
Nisha Mehta, MD, said her phone has been ringing with calls from tearful and shaken physicians who are distressed and unsettled about their work and home situation and don’t know what to do.
What’s more, many frontline physicians are living apart from family to protect them from infection. “So many physicians have called me crying. ... They can’t even come home and get a hug,” Dr. Mehta said. “What I’m hearing from a lot of people who are in New York and New Jersey is not just that they go to work all day and it’s this exhausting process throughout the entire day, not only physically but also emotionally.”
Physician burnout has held a steady spotlight since long before the COVID-19 crisis began, Dr. Mehta said. “The reason for that is multifold, but in part, it’s hard for physicians to find an appropriate way to be able to process a lot of the emotions related to their work,” she said. “A lot of that brews below the surface, but COVID-19 has really brought many of these issues above that surface.”
Frustrated that governments weren’t doing enough to support health care workers during the pandemic, Dr. Mehta, a radiologist in Charlotte, N.C., decided there needed to be change. On April 4, Dr. Mehta and two physician colleagues submitted to Congress the COVID-19 Pandemic Physician Protection Act, which ensures, among other provisions, mental health coverage for health care workers. An accompanying petition on change.org had received nearly 300,000 signatures as of May 29.
Don’t suffer in silence
A career in medicine comes with immense stress in the best of times, she notes, and managing a pandemic in an already strained system has taken those challenges to newer heights. “We need better support structures at baseline for physician mental health,” said Dr. Mehta.
“That’s something we’ve always been lacking because it’s been against the culture of medicine for so long to say, ‘I’m having a hard time.’ ”
If you’re hurting, the first thing to recognize is that you are not alone in facing these challenges. This is true with respect not only to medical care but also to all of the family, financial, and business concerns physicians are currently facing. “Having all of those things hanging over your head is a lot. We’ve got to find ways to help each other out,” Dr. Mehta said.
Where to find support
Fortunately, the medical community has created several pathways to help its own.
The following list represents a cross-section of opportunities for caregivers to receive care for themselves.
Crisis hotlines
- Physician Support Line. This free and confidential hotline was launched on March 30 by Mona Masood, DO, a Philadelphia-area psychiatrist and moderator of a Facebook forum called the COVID-19 Physicians Group. The PSL is run by more than 600 volunteer psychiatrists who take calls from U.S. physicians 7 days a week from 8:00 a.m. to 1:00 a.m., with no appointment necessary. The toll-free number is 888-409-0141.
- For the Frontlines. This 24/7 help line provides free crisis counseling for frontline workers. They can text FRONTLINE to 741741 in the United States (support is also available for residents of Canada, Ireland, and the United Kingdom).
Resources from professional groups
- Action Collaborative on Clinician Well-Being and Resilience. Created by the National Academy of Medicine in 2017, the Action Collaborative comprises more than 60 organizations committed to reversing trends in clinician burnout. In response to the pandemic, the group has compiled a list of strategies and resources to support the health and well-being of clinicians who are providing healthcare during the COVID-19 outbreak.
- American Medical Association. The AMA has created a resource center dedicated to providing care for caregivers during the COVID-19 pandemic. The website includes specific guidance for managing mental health during the pandemic.
- American College of Physicians. The professional society of internal medicine physicians has created a comprehensive guide for physicians specific to COVID-19, with a section dedicated to clinician well-being that includes information about hotlines, counseling services, grief support, and more.
- American Hospital Association. The AHA’s website now includes regularly updated resources for healthcare clinicians and staff, as well as a special section dedicated to protecting and enabling healthcare workers in the midst of the pandemic.
Virtual psychological counseling
Not unlike the way telemedicine has allowed some physicians to keep seeing their patients, many modalities enable participation in therapy through video, chat, phone call, or any combination thereof. Look for a service that is convenient, flexible, and HIPAA compliant.
Traditional in-office mental health therapy has quickly moved to telemedicine. Many if not most insurers that cover counseling visits are paying for telepsychiatry or telecounseling. If you don’t know of an appropriate therapist, check the American Psychiatric Association or its state chapters; the American Psychological Association; or look for a licensed mental health counselor.
Because financial constraints are a potential barrier to therapy, Project Parachute, in cooperation with Eleos Health, has organized a cadre of therapists willing to provide pro bono online therapy for health care workers. The amount of free therapy provided to qualified frontline workers is up to the individual therapists. Discuss these parameters with your therapists up front.
Similar services are offered from companies such as Talkspace and BetterHelp on a subscription basis. These services are typically less expensive than in-person sessions. Ask about discounts for healthcare workers. Talkspace, for example, announced in March, “Effective immediately, healthcare workers across the country can get access to a free month of our...online therapy that includes unlimited text, video, and audio messaging with a licensed therapist.”
Online support groups and social media
For more on-demand peer support, look for groups such as the COR Sharing Circle for Healthcare Workers on Facebook. The site’s search engine can point users to plenty of other groups, many of which are closed (meaning posts are visible to members only).
Dr. Mehta hosts her own Facebook group called Physician Community. “I would like to think (and genuinely feel) that we’ve been doing a great job of supporting each other there with daily threads on challenges, treatments, pick-me-ups, vent posts, advocacy, and more,” she said.
For anyone in need, PeerRxMed is a free, peer-to-peer program for physicians and other health care workers that is designed to provide support, connection, encouragement, resources, and skill-building to optimize well-being.
For those craving spiritual comfort during this crisis, a number of churches have begun offering that experience virtually, too. First Unitarian Church of Worcester, Massachusetts, for example, offers weekly services via YouTube. Similar online programming is being offered from all sorts of organizations across denominations.
Apps
For DIY or on-the-spot coping support, apps can help physicians get through the day. Apps and websites that offer guided meditations and other relaxation tools include Headspace, Calm, and Insight Timer. Before downloading, look for special discounts and promotions for healthcare workers.
Additionally, COVID Coach is a free, secure app designed by the U.S. Department of Veterans Affairs that includes tools to help you cope with stress and stay well, safe, healthy, and connected. It also offers advice on navigating parenting, care giving, and working from home while social distancing, quarantined, or sheltering in place.
For practicing daily gratitude, Delightful Journal is a free app that offers journaling prompts, themes, reminders, and unlimited private space to record one’s thoughts.
Adopt a ritual
Although self-care for physicians is more crucial now than ever, it can look different for every individual. Along the same lines as keeping a journal, wellness experts often recommend beginning a “gratitude practice” to help provide solace and perspective.
Tweak and personalize these activities to suit your own needs, but be sure to use them even when you’re feeling well, said Mohana Karlekar, MD, medical director of palliative care and assistant professor at Vanderbilt University Medical Center, Nashville, Tenn.
One exercise she recommends is known as Three Good Things. “Every day, at the end of the day, think about three good things that have happened,” she explained. “You can always find the joys. And the joys don’t have to be enormous. There is joy – there is hope – in everything,” Dr. Karlekar said.
A version of this article originally appeared on Medscape.com.
Money worries during COVID-19? Six tips to keep your finances afloat
Even before Atlanta had an official shelter-in-place order, patients at the private plastic surgery practice of Nicholas Jones, MD, began canceling and rescheduled planned procedures.
After a few weeks, Dr. Jones, aged 40 years, stopped seeing patients entirely, but as a self-employed independent contractor, that means he’d lost most of his income. Dr. Jones still makes some money via a wound care job at a local nursing home, but he’s concerned that job may also be eliminated.
“I’m not hurting yet,” he said. “But I’m preparing for the worst possible scenario.”
In preparation, he and his fiancé have cut back on extraneous expenses like Uber Eats, magazine subscriptions, and streaming music services. Even though he has a 6-month emergency fund, Jones has reached out to utility companies, mortgage lenders, and student loan servicers to find out about any programs they offer to people who’ve suffered financially from the coronavirus crisis.
He’s also considered traveling to one of the COVID-19 epicenters – he has family in New Orleans and Chicago – to work in a hospital there. Jones has trauma experience and is double-boarded in general and plastic surgery.
“I could provide relief to those in need and also float through this troubled time with some financial relief,” he said.
Whereas much of the world’s attention has been on physicians who are on the front line and working around the clock in hospitals to help COVID-19 patients, thousands of other physicians are experiencing the opposite phenomenon – a slowdown or even stoppage of work (and income) altogether.
Even among those practices that remain open, the number of patients has declined as people avoid going to the office unless they absolutely have to.
At the same time, doctors in two-income households may have a spouse experiencing a job loss or income decline. Nearly 10 million Americans applied for unemployment benefits in the last 2 weeks of March, the largest number on record.
Still, while there’s uncertainty around how long the coronavirus crisis will last, experts agree that at some point America will return to a “new normal” and business operations will begin to reopen. For physicians experiencing a reduction in income who, like Jones, have an emergency fund with a few months’ worth of expenses, now’s the time to tap into it. (Or if you still have income, now’s the time to focus on growing that emergency fund to give yourself an even bigger safety net.)
If you’re among the more than half of Americans with less than 6 months of expenses saved for a rainy day, here’s how to stay afloat in the near term:
Cut back on expenses
Some household spending has naturally tapered off for many families because social distancing restrictions reduce spending on eating out, travel, and other leisure activities. But this is also an opportunity to look for other ways to reduce spending. Look through your credit card bills to see whether there are recurring payments you can cut, such as a payment to a gym that’s temporarily closed or a monthly subscription box that you don’t need.
Some gyms are not allowing membership termination right now, but it pays to ask. If a service you’re not using won’t facilitate the cancellation, call your credit card company to dispute and stop the charges, and report them to the Better Business Bureau.
You should also stop contributing to nonemergency savings accounts such as your retirement fund or your children’s college funds.
“A lot of people are hesitant to stop their automatic savings if they’ve been maxing out their 401(k) contribution or 529 accounts,” says Andrew Musbach, a certified financial planner and cofounder of MD Wealth Management in Chelsea, Mich. “But if you’re thinking long term, the reality is that missing a couple of months won’t make or break a plan. Cutting back on the amount you’re saving in the short term will increase your cash flow and is a good way to make ends meet.”
Take advantage of regulatory changes
Although many physicians won’t qualify for direct payments via the Coronavirus Aid Relief and Economic Security (CARES) Act (the $1,200 payments to individuals start phasing out once income hits $75,000 and disappear entirely for those making more than $99,000), there are other provisions in the stimulus bill that may help physicians. The bill, for example, boosts state unemployment payments by $600 per week for the next 4 months, meaning qualified workers could receive an average of nearly $1,000 per week, depending on their state, and there are new provisions providing unemployment payments to self-employed and contract workers.
The CARES Act also includes a break for federal student loan holders. Under that rule, you can skip your payments through September without incurring additional interest. Physicians in the loan forgiveness program will still get credit for payments skipped during this program.
Separately, the IRS has extended the tax deadline from April 15 to July 15, which means not only do you not have to file your taxes until then, you also don’t have to pay any taxes you owe until mid-July. The deadline for first quarter estimated tax payments has also moved to July 15. (If you’re expecting a refund, however, you should file ASAP, since the IRS will typically issue those within a few weeks of receiving your returns.)
Tap your home equity – if you’re planning to stay put
If you have good credit and still have some income, you might consider refinancing your home mortgage or opening a home equity line of credit. Interest rates have fallen recently amid economic turbulence, so if you haven’t refinanced recently you may be able to shave your monthly payment. If you need cash, a cash-out refinance, home equity line of credit, or a reverse mortgage (available if you’re over age 62) are among the lowest-cost ways to borrow.
“With interest rates so low, there can be a lot of benefit to refinancing and leveraging your house, especially if you’re planning to stay there,” says Jamie Hopkins, a director at the Carson Group. “The challenge is if you’re planning to move in the next few years. There’s a real risk that the housing market could go down in the next couple of years, and if you’re planning to sell, there’s a risk that you might not get back what you borrowed.”
Communicate early with your bank or landlord
If you don’t have the income to refinance, and you think you’re going to run into trouble making your housing payment, you should let your bank or landlord know as soon as possible. The CARES Act allows homeowners with federally backed mortgages to obtain a 180-day postponement of mortgage payments because of COVID-19 financial hardship, with the potential to extend for another 180 days. It also bans eviction by landlords with federal mortgages for 120 days.
Even if you don’t have a federally backed mortgage, you should still get in touch with your lender. Many mortgage servicers have their own forbearance programs for borrowers who can prove a temporary financial hardship. (Some banks are also waiving fees on early withdrawals on CDs and giving cardholders a reprieve on credit card payments.) Commercial landlords are also working with struggling tenants, so you may also be able to get some relief on your office lease as well.
“All of the lenders are setting up helplines for people affected,” says Amy Guerich, a partner with Stepp & Rothwell, a Kansas City–based financial planning firm. “The best thing you can do is contact them right away if you think that you’re going to have a problem vs. just letting the bills go.”
Consider retirement account withdrawals
Standard personal finance advice holds that you should exhaust all other options before pulling money out of your retirement account because of the high penalties for early withdrawals and because money removed from retirement accounts is no longer compounding over time.
Still, the CARES act has provisions making it less financially onerous to pull money from your retirement accounts. Under the new law, you can take a distribution of up to $100,000 from your IRA or 401(k) without having to pay the 10% early withdrawal penalty. You’ll owe ordinary income taxes on the withdrawal, but you have 3 years to pay them or to return the money to your retirement account.
“That’s a great relief provision, especially for higher-income physicians who might have a higher 401(k) balance,” said Jamie Hopkins.
Be smart about credit cards
Although using credit cards that you can’t pay off every month is typically an expensive way to access money, getting a new card with a low or zero percent introductory rate is a short-term strategy to consider when you’ve exhausted other options. If you have good credit, you may be able to qualify for a credit card with a 0% introductory interest rate on new transactions. Pay close attention to the fine print, including the cap on the balance you can carry without interest and whether you’ll be required to make minimum payments.
The average 0% credit card offer is for 11 months, but there are some cards that can extend the offer for up to a year-and-a-half. If you choose to use this strategy, you’ll need a plan to pay off the entire balance before the introductory period ends. If there’s a balance remaining once the rate resets, you may end up owing deferred interest on it.
The financial ramifications of the coronavirus can feel overwhelming, but it’s important not to panic. While it remains unclear how long the current crisis will last, making some smart money moves to preserve your cash in the meantime can help you stay afloat.
A version of this article originally appeared on Medscape.com.
Even before Atlanta had an official shelter-in-place order, patients at the private plastic surgery practice of Nicholas Jones, MD, began canceling and rescheduled planned procedures.
After a few weeks, Dr. Jones, aged 40 years, stopped seeing patients entirely, but as a self-employed independent contractor, that means he’d lost most of his income. Dr. Jones still makes some money via a wound care job at a local nursing home, but he’s concerned that job may also be eliminated.
“I’m not hurting yet,” he said. “But I’m preparing for the worst possible scenario.”
In preparation, he and his fiancé have cut back on extraneous expenses like Uber Eats, magazine subscriptions, and streaming music services. Even though he has a 6-month emergency fund, Jones has reached out to utility companies, mortgage lenders, and student loan servicers to find out about any programs they offer to people who’ve suffered financially from the coronavirus crisis.
He’s also considered traveling to one of the COVID-19 epicenters – he has family in New Orleans and Chicago – to work in a hospital there. Jones has trauma experience and is double-boarded in general and plastic surgery.
“I could provide relief to those in need and also float through this troubled time with some financial relief,” he said.
Whereas much of the world’s attention has been on physicians who are on the front line and working around the clock in hospitals to help COVID-19 patients, thousands of other physicians are experiencing the opposite phenomenon – a slowdown or even stoppage of work (and income) altogether.
Even among those practices that remain open, the number of patients has declined as people avoid going to the office unless they absolutely have to.
At the same time, doctors in two-income households may have a spouse experiencing a job loss or income decline. Nearly 10 million Americans applied for unemployment benefits in the last 2 weeks of March, the largest number on record.
Still, while there’s uncertainty around how long the coronavirus crisis will last, experts agree that at some point America will return to a “new normal” and business operations will begin to reopen. For physicians experiencing a reduction in income who, like Jones, have an emergency fund with a few months’ worth of expenses, now’s the time to tap into it. (Or if you still have income, now’s the time to focus on growing that emergency fund to give yourself an even bigger safety net.)
If you’re among the more than half of Americans with less than 6 months of expenses saved for a rainy day, here’s how to stay afloat in the near term:
Cut back on expenses
Some household spending has naturally tapered off for many families because social distancing restrictions reduce spending on eating out, travel, and other leisure activities. But this is also an opportunity to look for other ways to reduce spending. Look through your credit card bills to see whether there are recurring payments you can cut, such as a payment to a gym that’s temporarily closed or a monthly subscription box that you don’t need.
Some gyms are not allowing membership termination right now, but it pays to ask. If a service you’re not using won’t facilitate the cancellation, call your credit card company to dispute and stop the charges, and report them to the Better Business Bureau.
You should also stop contributing to nonemergency savings accounts such as your retirement fund or your children’s college funds.
“A lot of people are hesitant to stop their automatic savings if they’ve been maxing out their 401(k) contribution or 529 accounts,” says Andrew Musbach, a certified financial planner and cofounder of MD Wealth Management in Chelsea, Mich. “But if you’re thinking long term, the reality is that missing a couple of months won’t make or break a plan. Cutting back on the amount you’re saving in the short term will increase your cash flow and is a good way to make ends meet.”
Take advantage of regulatory changes
Although many physicians won’t qualify for direct payments via the Coronavirus Aid Relief and Economic Security (CARES) Act (the $1,200 payments to individuals start phasing out once income hits $75,000 and disappear entirely for those making more than $99,000), there are other provisions in the stimulus bill that may help physicians. The bill, for example, boosts state unemployment payments by $600 per week for the next 4 months, meaning qualified workers could receive an average of nearly $1,000 per week, depending on their state, and there are new provisions providing unemployment payments to self-employed and contract workers.
The CARES Act also includes a break for federal student loan holders. Under that rule, you can skip your payments through September without incurring additional interest. Physicians in the loan forgiveness program will still get credit for payments skipped during this program.
Separately, the IRS has extended the tax deadline from April 15 to July 15, which means not only do you not have to file your taxes until then, you also don’t have to pay any taxes you owe until mid-July. The deadline for first quarter estimated tax payments has also moved to July 15. (If you’re expecting a refund, however, you should file ASAP, since the IRS will typically issue those within a few weeks of receiving your returns.)
Tap your home equity – if you’re planning to stay put
If you have good credit and still have some income, you might consider refinancing your home mortgage or opening a home equity line of credit. Interest rates have fallen recently amid economic turbulence, so if you haven’t refinanced recently you may be able to shave your monthly payment. If you need cash, a cash-out refinance, home equity line of credit, or a reverse mortgage (available if you’re over age 62) are among the lowest-cost ways to borrow.
“With interest rates so low, there can be a lot of benefit to refinancing and leveraging your house, especially if you’re planning to stay there,” says Jamie Hopkins, a director at the Carson Group. “The challenge is if you’re planning to move in the next few years. There’s a real risk that the housing market could go down in the next couple of years, and if you’re planning to sell, there’s a risk that you might not get back what you borrowed.”
Communicate early with your bank or landlord
If you don’t have the income to refinance, and you think you’re going to run into trouble making your housing payment, you should let your bank or landlord know as soon as possible. The CARES Act allows homeowners with federally backed mortgages to obtain a 180-day postponement of mortgage payments because of COVID-19 financial hardship, with the potential to extend for another 180 days. It also bans eviction by landlords with federal mortgages for 120 days.
Even if you don’t have a federally backed mortgage, you should still get in touch with your lender. Many mortgage servicers have their own forbearance programs for borrowers who can prove a temporary financial hardship. (Some banks are also waiving fees on early withdrawals on CDs and giving cardholders a reprieve on credit card payments.) Commercial landlords are also working with struggling tenants, so you may also be able to get some relief on your office lease as well.
“All of the lenders are setting up helplines for people affected,” says Amy Guerich, a partner with Stepp & Rothwell, a Kansas City–based financial planning firm. “The best thing you can do is contact them right away if you think that you’re going to have a problem vs. just letting the bills go.”
Consider retirement account withdrawals
Standard personal finance advice holds that you should exhaust all other options before pulling money out of your retirement account because of the high penalties for early withdrawals and because money removed from retirement accounts is no longer compounding over time.
Still, the CARES act has provisions making it less financially onerous to pull money from your retirement accounts. Under the new law, you can take a distribution of up to $100,000 from your IRA or 401(k) without having to pay the 10% early withdrawal penalty. You’ll owe ordinary income taxes on the withdrawal, but you have 3 years to pay them or to return the money to your retirement account.
“That’s a great relief provision, especially for higher-income physicians who might have a higher 401(k) balance,” said Jamie Hopkins.
Be smart about credit cards
Although using credit cards that you can’t pay off every month is typically an expensive way to access money, getting a new card with a low or zero percent introductory rate is a short-term strategy to consider when you’ve exhausted other options. If you have good credit, you may be able to qualify for a credit card with a 0% introductory interest rate on new transactions. Pay close attention to the fine print, including the cap on the balance you can carry without interest and whether you’ll be required to make minimum payments.
The average 0% credit card offer is for 11 months, but there are some cards that can extend the offer for up to a year-and-a-half. If you choose to use this strategy, you’ll need a plan to pay off the entire balance before the introductory period ends. If there’s a balance remaining once the rate resets, you may end up owing deferred interest on it.
The financial ramifications of the coronavirus can feel overwhelming, but it’s important not to panic. While it remains unclear how long the current crisis will last, making some smart money moves to preserve your cash in the meantime can help you stay afloat.
A version of this article originally appeared on Medscape.com.
Even before Atlanta had an official shelter-in-place order, patients at the private plastic surgery practice of Nicholas Jones, MD, began canceling and rescheduled planned procedures.
After a few weeks, Dr. Jones, aged 40 years, stopped seeing patients entirely, but as a self-employed independent contractor, that means he’d lost most of his income. Dr. Jones still makes some money via a wound care job at a local nursing home, but he’s concerned that job may also be eliminated.
“I’m not hurting yet,” he said. “But I’m preparing for the worst possible scenario.”
In preparation, he and his fiancé have cut back on extraneous expenses like Uber Eats, magazine subscriptions, and streaming music services. Even though he has a 6-month emergency fund, Jones has reached out to utility companies, mortgage lenders, and student loan servicers to find out about any programs they offer to people who’ve suffered financially from the coronavirus crisis.
He’s also considered traveling to one of the COVID-19 epicenters – he has family in New Orleans and Chicago – to work in a hospital there. Jones has trauma experience and is double-boarded in general and plastic surgery.
“I could provide relief to those in need and also float through this troubled time with some financial relief,” he said.
Whereas much of the world’s attention has been on physicians who are on the front line and working around the clock in hospitals to help COVID-19 patients, thousands of other physicians are experiencing the opposite phenomenon – a slowdown or even stoppage of work (and income) altogether.
Even among those practices that remain open, the number of patients has declined as people avoid going to the office unless they absolutely have to.
At the same time, doctors in two-income households may have a spouse experiencing a job loss or income decline. Nearly 10 million Americans applied for unemployment benefits in the last 2 weeks of March, the largest number on record.
Still, while there’s uncertainty around how long the coronavirus crisis will last, experts agree that at some point America will return to a “new normal” and business operations will begin to reopen. For physicians experiencing a reduction in income who, like Jones, have an emergency fund with a few months’ worth of expenses, now’s the time to tap into it. (Or if you still have income, now’s the time to focus on growing that emergency fund to give yourself an even bigger safety net.)
If you’re among the more than half of Americans with less than 6 months of expenses saved for a rainy day, here’s how to stay afloat in the near term:
Cut back on expenses
Some household spending has naturally tapered off for many families because social distancing restrictions reduce spending on eating out, travel, and other leisure activities. But this is also an opportunity to look for other ways to reduce spending. Look through your credit card bills to see whether there are recurring payments you can cut, such as a payment to a gym that’s temporarily closed or a monthly subscription box that you don’t need.
Some gyms are not allowing membership termination right now, but it pays to ask. If a service you’re not using won’t facilitate the cancellation, call your credit card company to dispute and stop the charges, and report them to the Better Business Bureau.
You should also stop contributing to nonemergency savings accounts such as your retirement fund or your children’s college funds.
“A lot of people are hesitant to stop their automatic savings if they’ve been maxing out their 401(k) contribution or 529 accounts,” says Andrew Musbach, a certified financial planner and cofounder of MD Wealth Management in Chelsea, Mich. “But if you’re thinking long term, the reality is that missing a couple of months won’t make or break a plan. Cutting back on the amount you’re saving in the short term will increase your cash flow and is a good way to make ends meet.”
Take advantage of regulatory changes
Although many physicians won’t qualify for direct payments via the Coronavirus Aid Relief and Economic Security (CARES) Act (the $1,200 payments to individuals start phasing out once income hits $75,000 and disappear entirely for those making more than $99,000), there are other provisions in the stimulus bill that may help physicians. The bill, for example, boosts state unemployment payments by $600 per week for the next 4 months, meaning qualified workers could receive an average of nearly $1,000 per week, depending on their state, and there are new provisions providing unemployment payments to self-employed and contract workers.
The CARES Act also includes a break for federal student loan holders. Under that rule, you can skip your payments through September without incurring additional interest. Physicians in the loan forgiveness program will still get credit for payments skipped during this program.
Separately, the IRS has extended the tax deadline from April 15 to July 15, which means not only do you not have to file your taxes until then, you also don’t have to pay any taxes you owe until mid-July. The deadline for first quarter estimated tax payments has also moved to July 15. (If you’re expecting a refund, however, you should file ASAP, since the IRS will typically issue those within a few weeks of receiving your returns.)
Tap your home equity – if you’re planning to stay put
If you have good credit and still have some income, you might consider refinancing your home mortgage or opening a home equity line of credit. Interest rates have fallen recently amid economic turbulence, so if you haven’t refinanced recently you may be able to shave your monthly payment. If you need cash, a cash-out refinance, home equity line of credit, or a reverse mortgage (available if you’re over age 62) are among the lowest-cost ways to borrow.
“With interest rates so low, there can be a lot of benefit to refinancing and leveraging your house, especially if you’re planning to stay there,” says Jamie Hopkins, a director at the Carson Group. “The challenge is if you’re planning to move in the next few years. There’s a real risk that the housing market could go down in the next couple of years, and if you’re planning to sell, there’s a risk that you might not get back what you borrowed.”
Communicate early with your bank or landlord
If you don’t have the income to refinance, and you think you’re going to run into trouble making your housing payment, you should let your bank or landlord know as soon as possible. The CARES Act allows homeowners with federally backed mortgages to obtain a 180-day postponement of mortgage payments because of COVID-19 financial hardship, with the potential to extend for another 180 days. It also bans eviction by landlords with federal mortgages for 120 days.
Even if you don’t have a federally backed mortgage, you should still get in touch with your lender. Many mortgage servicers have their own forbearance programs for borrowers who can prove a temporary financial hardship. (Some banks are also waiving fees on early withdrawals on CDs and giving cardholders a reprieve on credit card payments.) Commercial landlords are also working with struggling tenants, so you may also be able to get some relief on your office lease as well.
“All of the lenders are setting up helplines for people affected,” says Amy Guerich, a partner with Stepp & Rothwell, a Kansas City–based financial planning firm. “The best thing you can do is contact them right away if you think that you’re going to have a problem vs. just letting the bills go.”
Consider retirement account withdrawals
Standard personal finance advice holds that you should exhaust all other options before pulling money out of your retirement account because of the high penalties for early withdrawals and because money removed from retirement accounts is no longer compounding over time.
Still, the CARES act has provisions making it less financially onerous to pull money from your retirement accounts. Under the new law, you can take a distribution of up to $100,000 from your IRA or 401(k) without having to pay the 10% early withdrawal penalty. You’ll owe ordinary income taxes on the withdrawal, but you have 3 years to pay them or to return the money to your retirement account.
“That’s a great relief provision, especially for higher-income physicians who might have a higher 401(k) balance,” said Jamie Hopkins.
Be smart about credit cards
Although using credit cards that you can’t pay off every month is typically an expensive way to access money, getting a new card with a low or zero percent introductory rate is a short-term strategy to consider when you’ve exhausted other options. If you have good credit, you may be able to qualify for a credit card with a 0% introductory interest rate on new transactions. Pay close attention to the fine print, including the cap on the balance you can carry without interest and whether you’ll be required to make minimum payments.
The average 0% credit card offer is for 11 months, but there are some cards that can extend the offer for up to a year-and-a-half. If you choose to use this strategy, you’ll need a plan to pay off the entire balance before the introductory period ends. If there’s a balance remaining once the rate resets, you may end up owing deferred interest on it.
The financial ramifications of the coronavirus can feel overwhelming, but it’s important not to panic. While it remains unclear how long the current crisis will last, making some smart money moves to preserve your cash in the meantime can help you stay afloat.
A version of this article originally appeared on Medscape.com.
Kids with food allergies the newest victims of COVID-19?
Food insecurity is not knowing how you will get your next meal. This pandemic has led to a lot of it, especially as a result of massive unemployment. Now imagine being in that situation with a food-allergic child. It would be frightening.
There is always a level of anxiety for parents of food-allergic children, but the Food and Drug Administration–mandated labeling of food allergens has helped to allay some of those concerns. Shopping can feel safer, even if it’s not foolproof.
Now, that fear for the safety of food-allergic children is going to be compounded by the FDA’s latest announcement, made at the behest of the food industry.
Disruptions in the food supply chain caused by the COVID-19 pandemic have created some problems for the food industry. The industry sought – and received – relief from the FDA; they are now allowing some ingredient substitutions without mandating a change in labeling. These changes were made without opportunity for public comment, according to the FDA, because of the exigency of the situation. Furthermore, the changes may stay in effect for an indeterminate period of time after the pandemic is deemed under control.
Labeling of gluten and the major eight allergens (peanuts, tree nuts, milk, eggs, soy, wheat, fish, and crustacean shellfish) cannot change under the new guidelines. The FDA also advised “consideration” of major food allergens recognized in other countries (sesame, celery, lupin, buckwheat, molluscan shellfish, and mustard). Of these, lupin is known to cross-react with peanut, and sesame seed allergy is increasingly prevalent. In fact, the FDA has considered adding it to the list of major allergens.
Meanwhile, according to this temporary FDA policy, substitutions should be limited to no more than 2% of the weight of the final product unless it is a variety of the same ingredient. The example provided is substitution of one type of mushroom for another, but even that could be an issue for the rare patient. And what if this is misinterpreted – as will surely happen somewhere – and one seed is substituted for another?
A friend of mine is a pediatrician and mother of a child who is allergic to sesame, peanuts, tree nuts, and garbanzo beans. Naturally, she had grave concerns about these changes. She also wondered what the liability would be for the food manufacturing company in the current situation despite the FDA notice, which seems like a valid point. It is worth noting that, at the very top of this FDA notice, are the words “contains nonbinding recommendations,” so manufacturers may want to think twice about how they approach this. A minority of companies have pledged to relabel foods if necessary. Meanwhile, without any alert in advance, it is now up to patients and their physicians to sort out the attendant risks.
The FDA should have advised or mandated that food manufacturers give notice to online and physical retailers of ingredient changes. A simple sign in front of a display or alert online would be a very reasonable solution and pose no burden to those involved. It should be self-evident that mistakes always happen, especially under duress, and that the loosening of these regulations will have unintended consequences. To the severe problem of food insecurity, we can add one more concern for the parents of allergic children: food-allergen insecurity.
A version of this article originally appeared on Medscape.com.
Food insecurity is not knowing how you will get your next meal. This pandemic has led to a lot of it, especially as a result of massive unemployment. Now imagine being in that situation with a food-allergic child. It would be frightening.
There is always a level of anxiety for parents of food-allergic children, but the Food and Drug Administration–mandated labeling of food allergens has helped to allay some of those concerns. Shopping can feel safer, even if it’s not foolproof.
Now, that fear for the safety of food-allergic children is going to be compounded by the FDA’s latest announcement, made at the behest of the food industry.
Disruptions in the food supply chain caused by the COVID-19 pandemic have created some problems for the food industry. The industry sought – and received – relief from the FDA; they are now allowing some ingredient substitutions without mandating a change in labeling. These changes were made without opportunity for public comment, according to the FDA, because of the exigency of the situation. Furthermore, the changes may stay in effect for an indeterminate period of time after the pandemic is deemed under control.
Labeling of gluten and the major eight allergens (peanuts, tree nuts, milk, eggs, soy, wheat, fish, and crustacean shellfish) cannot change under the new guidelines. The FDA also advised “consideration” of major food allergens recognized in other countries (sesame, celery, lupin, buckwheat, molluscan shellfish, and mustard). Of these, lupin is known to cross-react with peanut, and sesame seed allergy is increasingly prevalent. In fact, the FDA has considered adding it to the list of major allergens.
Meanwhile, according to this temporary FDA policy, substitutions should be limited to no more than 2% of the weight of the final product unless it is a variety of the same ingredient. The example provided is substitution of one type of mushroom for another, but even that could be an issue for the rare patient. And what if this is misinterpreted – as will surely happen somewhere – and one seed is substituted for another?
A friend of mine is a pediatrician and mother of a child who is allergic to sesame, peanuts, tree nuts, and garbanzo beans. Naturally, she had grave concerns about these changes. She also wondered what the liability would be for the food manufacturing company in the current situation despite the FDA notice, which seems like a valid point. It is worth noting that, at the very top of this FDA notice, are the words “contains nonbinding recommendations,” so manufacturers may want to think twice about how they approach this. A minority of companies have pledged to relabel foods if necessary. Meanwhile, without any alert in advance, it is now up to patients and their physicians to sort out the attendant risks.
The FDA should have advised or mandated that food manufacturers give notice to online and physical retailers of ingredient changes. A simple sign in front of a display or alert online would be a very reasonable solution and pose no burden to those involved. It should be self-evident that mistakes always happen, especially under duress, and that the loosening of these regulations will have unintended consequences. To the severe problem of food insecurity, we can add one more concern for the parents of allergic children: food-allergen insecurity.
A version of this article originally appeared on Medscape.com.
Food insecurity is not knowing how you will get your next meal. This pandemic has led to a lot of it, especially as a result of massive unemployment. Now imagine being in that situation with a food-allergic child. It would be frightening.
There is always a level of anxiety for parents of food-allergic children, but the Food and Drug Administration–mandated labeling of food allergens has helped to allay some of those concerns. Shopping can feel safer, even if it’s not foolproof.
Now, that fear for the safety of food-allergic children is going to be compounded by the FDA’s latest announcement, made at the behest of the food industry.
Disruptions in the food supply chain caused by the COVID-19 pandemic have created some problems for the food industry. The industry sought – and received – relief from the FDA; they are now allowing some ingredient substitutions without mandating a change in labeling. These changes were made without opportunity for public comment, according to the FDA, because of the exigency of the situation. Furthermore, the changes may stay in effect for an indeterminate period of time after the pandemic is deemed under control.
Labeling of gluten and the major eight allergens (peanuts, tree nuts, milk, eggs, soy, wheat, fish, and crustacean shellfish) cannot change under the new guidelines. The FDA also advised “consideration” of major food allergens recognized in other countries (sesame, celery, lupin, buckwheat, molluscan shellfish, and mustard). Of these, lupin is known to cross-react with peanut, and sesame seed allergy is increasingly prevalent. In fact, the FDA has considered adding it to the list of major allergens.
Meanwhile, according to this temporary FDA policy, substitutions should be limited to no more than 2% of the weight of the final product unless it is a variety of the same ingredient. The example provided is substitution of one type of mushroom for another, but even that could be an issue for the rare patient. And what if this is misinterpreted – as will surely happen somewhere – and one seed is substituted for another?
A friend of mine is a pediatrician and mother of a child who is allergic to sesame, peanuts, tree nuts, and garbanzo beans. Naturally, she had grave concerns about these changes. She also wondered what the liability would be for the food manufacturing company in the current situation despite the FDA notice, which seems like a valid point. It is worth noting that, at the very top of this FDA notice, are the words “contains nonbinding recommendations,” so manufacturers may want to think twice about how they approach this. A minority of companies have pledged to relabel foods if necessary. Meanwhile, without any alert in advance, it is now up to patients and their physicians to sort out the attendant risks.
The FDA should have advised or mandated that food manufacturers give notice to online and physical retailers of ingredient changes. A simple sign in front of a display or alert online would be a very reasonable solution and pose no burden to those involved. It should be self-evident that mistakes always happen, especially under duress, and that the loosening of these regulations will have unintended consequences. To the severe problem of food insecurity, we can add one more concern for the parents of allergic children: food-allergen insecurity.
A version of this article originally appeared on Medscape.com.
No link seen between methotrexate, interstitial lung disease in RA
Patients with rheumatoid arthritis (RA) have an elevated risk of interstitial lung disease (ILD), but methotrexate does not accentuate that risk and may in fact be protective, new data show. These were among key findings of a pair of studies reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Although a guideline-recommended cornerstone in the management of RA, methotrexate has been associated with both hypersensitivity pneumonitis and diffuse lung disease. However, its involvement in the development of ILD among patients with RA is unclear.
A Danish study of more than 30,000 RA patients reported at the congress found that their risk of ILD was about three to five times that of the general population. However, risk did not differ significantly whether they had filled a methotrexate prescription or not.
In addition, a multinational case-control study of more than 1,000 RA patients also reported at the congress found that, compared with never-users of methotrexate, ever-users actually had a 59% lower likelihood of developing ILD.
However, both studies were limited by their retrospective design, Elizabeth R. Volkmann, MD, codirector of the connective tissue disease–related interstitial lung disease program at the University of California, Los Angeles, cautioned in an interview. Hence, there was likely systematic bias and confounding.
“I would interpret the conclusions of both studies with caution,” she maintained. “To understand how a particular intervention, such as methotrexate use, affects the outcome of ILD development, a prospective design is needed, which adequately adjusts for known ILD risk factors, such as male sex and smoking.”
As to whether the new findings are practice changing and how they might affect patient counseling, “the answers to these questions are not straightforward and depend on other patient-related factors,” according to Dr. Volkmann.
Danish nationwide study
René Cordtz, MD, a clinical assistant at the Center for Rheumatology and Spine Diseases, Rigshospitalet‐Gentofte, Copenhagen, and colleagues conducted a nationwide population-based cohort study using registry data from 1997 to 2015 to assess lung disease among patients with RA by prescriptions filled.
Results based on 30,512 RA patients showed that, compared with peers filling no methotrexate prescriptions, patients filling at least one did not have a significantly elevated risk of ILD at either 1 year of follow-up (hazard ratio, 1.03) or 5 years of follow-up (HR, 1.00). (Findings were similar for sulfasalazine, with respective nonsignificant HRs of 0.88 and 1.14.)
In addition, patients with RA had a similarly sharply elevated 5-year risk of ILD relative to the general population regardless of whether they had filled neither methotrexate nor sulfasalazine prescriptions (standardized incidence ratio, 3.38) or had filled prescriptions for methotrexate only (SIR, 3.63), sulfasalazine only (SIR, 4.12), or both (SIR, 5.45).
“RA patients have an increased risk of ILD, compared to the general population, which was not surprising, but very importantly, that risk was not further exacerbated in those treated with methotrexate,” Dr. Cordtz concluded. “We do acknowledge that purchasing your medicine is different from taking your medicine, which is why we found it extra reassuring that when requiring at least two methotrexate prescriptions to be considered exposed, it did not change our results.”
Multinational study
Pierre-Antoine Juge, MD, a rheumatologist at Bichat-Claude Bernard Hospital, Paris, and colleagues performed a case-control study among 482 RA patients with ILD and 741 RA patients without ILD in three cohorts: a French discovery cohort, a multinational (Brazilian, Italian, Mexican, United Kingdom, and United States) replication cohort, and a combined cohort. Those with methotrexate hypersensitivity pneumonitis were excluded.
Results showed that relative to peers without ILD, patients with ILD had a lower prevalence of ever having used methotrexate and had received a lower cumulative methotrexate dose, findings that were consistent across all three cohorts.
Methotrexate ever-use was associated with a significantly lower adjusted likelihood of ILD in the discovery cohort (odds ratio, 0.46), the replication cohort (OR, 0.38), and the combined cohort (OR, 0.41). Furthermore, ever-users were less commonly represented among patients with ILD regardless of chest high-resolution CT pattern (usual interstitial pneumonia pattern vs. not).
Finally, methotrexate use appeared to delay the adjusted time to onset of ILD by 3.5 years in the discovery cohort (P = .001), by 3.2 years in the replication cohort (P < .0001), and by 3.5 years in the combined cohort (P < .0001).
“Outside of methotrexate hypersensitivity pneumonitis, methotrexate was not a risk factor for RA-associated ILD in our study. We observed an inverse relationship that was similar whatever the high-resolution CT pattern,” Dr. Juge commented. “But this possible protective effect should be confirmed through a dedicated prospective, randomized, controlled trial.”
“Methotrexate should not be considered as a causal factor for RA-associated ILD, and its [discontinuation] should be discussed through a multidisciplinary discussion,” he recommended. In addition, “this study does not investigate the impact of methotrexate use on RA-associated ILD prognosis.”
The Danish study did not receive any specific funding, and none of its authors reported having any financial disclosures. The multinational study did not receive any specific funding. Dr. Juge disclosed that he had no relevant conflicts of interest, but many of his coauthors reported financial relationships with industry. Dr. Volkmann disclosed consulting for Boehringer Ingelheim and Forbius, and receiving grant support from Forbius and Corbus.
SOURCES: Cordtz R et al. Ann Rheum Dis. 2020;79[suppl 1]:147-8, Abstract OP0232; Juge P-A et al. Ann Rheum Dis. 2020;79[suppl 1]:25, Abstract OP0236.
Patients with rheumatoid arthritis (RA) have an elevated risk of interstitial lung disease (ILD), but methotrexate does not accentuate that risk and may in fact be protective, new data show. These were among key findings of a pair of studies reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Although a guideline-recommended cornerstone in the management of RA, methotrexate has been associated with both hypersensitivity pneumonitis and diffuse lung disease. However, its involvement in the development of ILD among patients with RA is unclear.
A Danish study of more than 30,000 RA patients reported at the congress found that their risk of ILD was about three to five times that of the general population. However, risk did not differ significantly whether they had filled a methotrexate prescription or not.
In addition, a multinational case-control study of more than 1,000 RA patients also reported at the congress found that, compared with never-users of methotrexate, ever-users actually had a 59% lower likelihood of developing ILD.
However, both studies were limited by their retrospective design, Elizabeth R. Volkmann, MD, codirector of the connective tissue disease–related interstitial lung disease program at the University of California, Los Angeles, cautioned in an interview. Hence, there was likely systematic bias and confounding.
“I would interpret the conclusions of both studies with caution,” she maintained. “To understand how a particular intervention, such as methotrexate use, affects the outcome of ILD development, a prospective design is needed, which adequately adjusts for known ILD risk factors, such as male sex and smoking.”
As to whether the new findings are practice changing and how they might affect patient counseling, “the answers to these questions are not straightforward and depend on other patient-related factors,” according to Dr. Volkmann.
Danish nationwide study
René Cordtz, MD, a clinical assistant at the Center for Rheumatology and Spine Diseases, Rigshospitalet‐Gentofte, Copenhagen, and colleagues conducted a nationwide population-based cohort study using registry data from 1997 to 2015 to assess lung disease among patients with RA by prescriptions filled.
Results based on 30,512 RA patients showed that, compared with peers filling no methotrexate prescriptions, patients filling at least one did not have a significantly elevated risk of ILD at either 1 year of follow-up (hazard ratio, 1.03) or 5 years of follow-up (HR, 1.00). (Findings were similar for sulfasalazine, with respective nonsignificant HRs of 0.88 and 1.14.)
In addition, patients with RA had a similarly sharply elevated 5-year risk of ILD relative to the general population regardless of whether they had filled neither methotrexate nor sulfasalazine prescriptions (standardized incidence ratio, 3.38) or had filled prescriptions for methotrexate only (SIR, 3.63), sulfasalazine only (SIR, 4.12), or both (SIR, 5.45).
“RA patients have an increased risk of ILD, compared to the general population, which was not surprising, but very importantly, that risk was not further exacerbated in those treated with methotrexate,” Dr. Cordtz concluded. “We do acknowledge that purchasing your medicine is different from taking your medicine, which is why we found it extra reassuring that when requiring at least two methotrexate prescriptions to be considered exposed, it did not change our results.”
Multinational study
Pierre-Antoine Juge, MD, a rheumatologist at Bichat-Claude Bernard Hospital, Paris, and colleagues performed a case-control study among 482 RA patients with ILD and 741 RA patients without ILD in three cohorts: a French discovery cohort, a multinational (Brazilian, Italian, Mexican, United Kingdom, and United States) replication cohort, and a combined cohort. Those with methotrexate hypersensitivity pneumonitis were excluded.
Results showed that relative to peers without ILD, patients with ILD had a lower prevalence of ever having used methotrexate and had received a lower cumulative methotrexate dose, findings that were consistent across all three cohorts.
Methotrexate ever-use was associated with a significantly lower adjusted likelihood of ILD in the discovery cohort (odds ratio, 0.46), the replication cohort (OR, 0.38), and the combined cohort (OR, 0.41). Furthermore, ever-users were less commonly represented among patients with ILD regardless of chest high-resolution CT pattern (usual interstitial pneumonia pattern vs. not).
Finally, methotrexate use appeared to delay the adjusted time to onset of ILD by 3.5 years in the discovery cohort (P = .001), by 3.2 years in the replication cohort (P < .0001), and by 3.5 years in the combined cohort (P < .0001).
“Outside of methotrexate hypersensitivity pneumonitis, methotrexate was not a risk factor for RA-associated ILD in our study. We observed an inverse relationship that was similar whatever the high-resolution CT pattern,” Dr. Juge commented. “But this possible protective effect should be confirmed through a dedicated prospective, randomized, controlled trial.”
“Methotrexate should not be considered as a causal factor for RA-associated ILD, and its [discontinuation] should be discussed through a multidisciplinary discussion,” he recommended. In addition, “this study does not investigate the impact of methotrexate use on RA-associated ILD prognosis.”
The Danish study did not receive any specific funding, and none of its authors reported having any financial disclosures. The multinational study did not receive any specific funding. Dr. Juge disclosed that he had no relevant conflicts of interest, but many of his coauthors reported financial relationships with industry. Dr. Volkmann disclosed consulting for Boehringer Ingelheim and Forbius, and receiving grant support from Forbius and Corbus.
SOURCES: Cordtz R et al. Ann Rheum Dis. 2020;79[suppl 1]:147-8, Abstract OP0232; Juge P-A et al. Ann Rheum Dis. 2020;79[suppl 1]:25, Abstract OP0236.
Patients with rheumatoid arthritis (RA) have an elevated risk of interstitial lung disease (ILD), but methotrexate does not accentuate that risk and may in fact be protective, new data show. These were among key findings of a pair of studies reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Although a guideline-recommended cornerstone in the management of RA, methotrexate has been associated with both hypersensitivity pneumonitis and diffuse lung disease. However, its involvement in the development of ILD among patients with RA is unclear.
A Danish study of more than 30,000 RA patients reported at the congress found that their risk of ILD was about three to five times that of the general population. However, risk did not differ significantly whether they had filled a methotrexate prescription or not.
In addition, a multinational case-control study of more than 1,000 RA patients also reported at the congress found that, compared with never-users of methotrexate, ever-users actually had a 59% lower likelihood of developing ILD.
However, both studies were limited by their retrospective design, Elizabeth R. Volkmann, MD, codirector of the connective tissue disease–related interstitial lung disease program at the University of California, Los Angeles, cautioned in an interview. Hence, there was likely systematic bias and confounding.
“I would interpret the conclusions of both studies with caution,” she maintained. “To understand how a particular intervention, such as methotrexate use, affects the outcome of ILD development, a prospective design is needed, which adequately adjusts for known ILD risk factors, such as male sex and smoking.”
As to whether the new findings are practice changing and how they might affect patient counseling, “the answers to these questions are not straightforward and depend on other patient-related factors,” according to Dr. Volkmann.
Danish nationwide study
René Cordtz, MD, a clinical assistant at the Center for Rheumatology and Spine Diseases, Rigshospitalet‐Gentofte, Copenhagen, and colleagues conducted a nationwide population-based cohort study using registry data from 1997 to 2015 to assess lung disease among patients with RA by prescriptions filled.
Results based on 30,512 RA patients showed that, compared with peers filling no methotrexate prescriptions, patients filling at least one did not have a significantly elevated risk of ILD at either 1 year of follow-up (hazard ratio, 1.03) or 5 years of follow-up (HR, 1.00). (Findings were similar for sulfasalazine, with respective nonsignificant HRs of 0.88 and 1.14.)
In addition, patients with RA had a similarly sharply elevated 5-year risk of ILD relative to the general population regardless of whether they had filled neither methotrexate nor sulfasalazine prescriptions (standardized incidence ratio, 3.38) or had filled prescriptions for methotrexate only (SIR, 3.63), sulfasalazine only (SIR, 4.12), or both (SIR, 5.45).
“RA patients have an increased risk of ILD, compared to the general population, which was not surprising, but very importantly, that risk was not further exacerbated in those treated with methotrexate,” Dr. Cordtz concluded. “We do acknowledge that purchasing your medicine is different from taking your medicine, which is why we found it extra reassuring that when requiring at least two methotrexate prescriptions to be considered exposed, it did not change our results.”
Multinational study
Pierre-Antoine Juge, MD, a rheumatologist at Bichat-Claude Bernard Hospital, Paris, and colleagues performed a case-control study among 482 RA patients with ILD and 741 RA patients without ILD in three cohorts: a French discovery cohort, a multinational (Brazilian, Italian, Mexican, United Kingdom, and United States) replication cohort, and a combined cohort. Those with methotrexate hypersensitivity pneumonitis were excluded.
Results showed that relative to peers without ILD, patients with ILD had a lower prevalence of ever having used methotrexate and had received a lower cumulative methotrexate dose, findings that were consistent across all three cohorts.
Methotrexate ever-use was associated with a significantly lower adjusted likelihood of ILD in the discovery cohort (odds ratio, 0.46), the replication cohort (OR, 0.38), and the combined cohort (OR, 0.41). Furthermore, ever-users were less commonly represented among patients with ILD regardless of chest high-resolution CT pattern (usual interstitial pneumonia pattern vs. not).
Finally, methotrexate use appeared to delay the adjusted time to onset of ILD by 3.5 years in the discovery cohort (P = .001), by 3.2 years in the replication cohort (P < .0001), and by 3.5 years in the combined cohort (P < .0001).
“Outside of methotrexate hypersensitivity pneumonitis, methotrexate was not a risk factor for RA-associated ILD in our study. We observed an inverse relationship that was similar whatever the high-resolution CT pattern,” Dr. Juge commented. “But this possible protective effect should be confirmed through a dedicated prospective, randomized, controlled trial.”
“Methotrexate should not be considered as a causal factor for RA-associated ILD, and its [discontinuation] should be discussed through a multidisciplinary discussion,” he recommended. In addition, “this study does not investigate the impact of methotrexate use on RA-associated ILD prognosis.”
The Danish study did not receive any specific funding, and none of its authors reported having any financial disclosures. The multinational study did not receive any specific funding. Dr. Juge disclosed that he had no relevant conflicts of interest, but many of his coauthors reported financial relationships with industry. Dr. Volkmann disclosed consulting for Boehringer Ingelheim and Forbius, and receiving grant support from Forbius and Corbus.
SOURCES: Cordtz R et al. Ann Rheum Dis. 2020;79[suppl 1]:147-8, Abstract OP0232; Juge P-A et al. Ann Rheum Dis. 2020;79[suppl 1]:25, Abstract OP0236.
FROM THE EULAR 2020 E-CONGRESS
Former smokers using e-cigarettes at risk for cigarette smoking relapse
The use of , results from a large longitudinal cohort study demonstrated.
“For the many clinicians treating former smokers who have successfully quit all nicotine products, the implications are that use of [electronic nicotine delivery systems] should be discouraged, just as use of all other tobacco products is discouraged,” researchers led by Colm D. Everard, PhD, reported in a study published in JAMA Network Open (2020 Jun 5. doi: 10.1001/jamanetworkopen.2020.4813).
Dr. Everard, of the National Institute on Drug Abuse, and colleagues based their comments on results from a survey of adult former smokers who participated in Waves 1-4 of the Population Assessment of Tobacco and Health (PATH) Study (2013-2018). They limited the analysis to 2,273 former cigarette smokers who self-reported reported no tobacco product use at Wave 1, and categorized them as recent former smokers (defined as having last smoked within the past 12 previous months) or as long-term former smokers (defined as having last smoked for longer ago than in the previous 12 months). The main outcome of interest was the self-reported current use of cigarettes at follow-up interviews, which was defined as every day or some days. Electronic nicotine delivery systems (ENDS) comprised e-cigarettes, e-cigars, e-pipes, and e-hookahs. Other tobacco products included cigars, pipe tobacco, hookahs, snus tobacco, other smokeless tobacco, and dissolvable tobacco.
Of the 2,273 adult former smokers, 52% were women, 60% were older than age 50, and 80% were non-Hispanic white. Adjusted hazard ratio (AHR) analysis revealed that the use of ENDS was associated with significant risk of cigarette smoking relapse among recent former smokers (AHR 1.63) and among long-term former smokers (AHR 3.79). The use of other tobacco products was associated with significant risk for cigarette smoking relapse among recent former smokers (AHR 1.97) and among long-term former smokers (AHR 3.82).
The authors acknowledged certain limitations of the study, including the fact that it did not assess different ENDS devices, different e-liquid nicotine levels, or frequency of ENDS use and their associations with cigarette smoking relapse. It also did not explore the mechanism by which ENDS use may lead to reestablishing or reinforcing nicotine-seeking behavior among former cigarette users. “Determining pharmacologic, behavioral, or some other explanation for these findings may require laboratory-based research,” they wrote.
The PATH Study is supported with federal funds from the National Institute on Drug Abuse, the National Institutes of Health, and the Food and Drug Administration and Department of Health and Human Services under a contract to Westat. One of the study authors, Wilson M. Compton, MD, reported having long-term stock holdings in General Electric, 3M, and Pfizer. The other authors reported having no financial disclosures.
The use of , results from a large longitudinal cohort study demonstrated.
“For the many clinicians treating former smokers who have successfully quit all nicotine products, the implications are that use of [electronic nicotine delivery systems] should be discouraged, just as use of all other tobacco products is discouraged,” researchers led by Colm D. Everard, PhD, reported in a study published in JAMA Network Open (2020 Jun 5. doi: 10.1001/jamanetworkopen.2020.4813).
Dr. Everard, of the National Institute on Drug Abuse, and colleagues based their comments on results from a survey of adult former smokers who participated in Waves 1-4 of the Population Assessment of Tobacco and Health (PATH) Study (2013-2018). They limited the analysis to 2,273 former cigarette smokers who self-reported reported no tobacco product use at Wave 1, and categorized them as recent former smokers (defined as having last smoked within the past 12 previous months) or as long-term former smokers (defined as having last smoked for longer ago than in the previous 12 months). The main outcome of interest was the self-reported current use of cigarettes at follow-up interviews, which was defined as every day or some days. Electronic nicotine delivery systems (ENDS) comprised e-cigarettes, e-cigars, e-pipes, and e-hookahs. Other tobacco products included cigars, pipe tobacco, hookahs, snus tobacco, other smokeless tobacco, and dissolvable tobacco.
Of the 2,273 adult former smokers, 52% were women, 60% were older than age 50, and 80% were non-Hispanic white. Adjusted hazard ratio (AHR) analysis revealed that the use of ENDS was associated with significant risk of cigarette smoking relapse among recent former smokers (AHR 1.63) and among long-term former smokers (AHR 3.79). The use of other tobacco products was associated with significant risk for cigarette smoking relapse among recent former smokers (AHR 1.97) and among long-term former smokers (AHR 3.82).
The authors acknowledged certain limitations of the study, including the fact that it did not assess different ENDS devices, different e-liquid nicotine levels, or frequency of ENDS use and their associations with cigarette smoking relapse. It also did not explore the mechanism by which ENDS use may lead to reestablishing or reinforcing nicotine-seeking behavior among former cigarette users. “Determining pharmacologic, behavioral, or some other explanation for these findings may require laboratory-based research,” they wrote.
The PATH Study is supported with federal funds from the National Institute on Drug Abuse, the National Institutes of Health, and the Food and Drug Administration and Department of Health and Human Services under a contract to Westat. One of the study authors, Wilson M. Compton, MD, reported having long-term stock holdings in General Electric, 3M, and Pfizer. The other authors reported having no financial disclosures.
The use of , results from a large longitudinal cohort study demonstrated.
“For the many clinicians treating former smokers who have successfully quit all nicotine products, the implications are that use of [electronic nicotine delivery systems] should be discouraged, just as use of all other tobacco products is discouraged,” researchers led by Colm D. Everard, PhD, reported in a study published in JAMA Network Open (2020 Jun 5. doi: 10.1001/jamanetworkopen.2020.4813).
Dr. Everard, of the National Institute on Drug Abuse, and colleagues based their comments on results from a survey of adult former smokers who participated in Waves 1-4 of the Population Assessment of Tobacco and Health (PATH) Study (2013-2018). They limited the analysis to 2,273 former cigarette smokers who self-reported reported no tobacco product use at Wave 1, and categorized them as recent former smokers (defined as having last smoked within the past 12 previous months) or as long-term former smokers (defined as having last smoked for longer ago than in the previous 12 months). The main outcome of interest was the self-reported current use of cigarettes at follow-up interviews, which was defined as every day or some days. Electronic nicotine delivery systems (ENDS) comprised e-cigarettes, e-cigars, e-pipes, and e-hookahs. Other tobacco products included cigars, pipe tobacco, hookahs, snus tobacco, other smokeless tobacco, and dissolvable tobacco.
Of the 2,273 adult former smokers, 52% were women, 60% were older than age 50, and 80% were non-Hispanic white. Adjusted hazard ratio (AHR) analysis revealed that the use of ENDS was associated with significant risk of cigarette smoking relapse among recent former smokers (AHR 1.63) and among long-term former smokers (AHR 3.79). The use of other tobacco products was associated with significant risk for cigarette smoking relapse among recent former smokers (AHR 1.97) and among long-term former smokers (AHR 3.82).
The authors acknowledged certain limitations of the study, including the fact that it did not assess different ENDS devices, different e-liquid nicotine levels, or frequency of ENDS use and their associations with cigarette smoking relapse. It also did not explore the mechanism by which ENDS use may lead to reestablishing or reinforcing nicotine-seeking behavior among former cigarette users. “Determining pharmacologic, behavioral, or some other explanation for these findings may require laboratory-based research,” they wrote.
The PATH Study is supported with federal funds from the National Institute on Drug Abuse, the National Institutes of Health, and the Food and Drug Administration and Department of Health and Human Services under a contract to Westat. One of the study authors, Wilson M. Compton, MD, reported having long-term stock holdings in General Electric, 3M, and Pfizer. The other authors reported having no financial disclosures.
FROM JAMA NETWORK OPEN
WHO clarifies comments on asymptomatic transmission of SARS-CoV-2
A World Health Organization (WHO) official is walking back her comments characterizing the spread of SARS-CoV-2 by asymptomatic individuals as “rare.”
Maria Van Kerkhove, PhD, WHO’s COVID-19 technical lead and an infectious disease epidemiologist, caused a stir June 8 when she said that countries are reporting that many of their asymptomatic cases develop into cases of mild disease. For patients with truly asymptomatic disease, countries are “not finding secondary transmission onward. It’s very rare,” she said.
Suppressing symptomatic cases, on the other hand, would result in a “drastic reduction” in transmission, she noted. “But from the data we have, it still seems to be rare that an asymptomatic person actually transmits onward to a secondary individual,” she said.
But on June 9 – following a day of confusion and criticism – Dr. Van Kerkhove sought to clarify her comments on asymptomatic transmission during a live social media Q&A. She noted that while “the majority of transmission that we know about” is through individuals with symptoms, “there are a subset of people who don’t develop symptoms, and to truly understand how many people don’t have symptoms – we don’t actually have that answer yet.”
Between 6% and 41% of individuals may be asymptomatic based on estimates, she acknowledged.“What we need to better understand is how many of the people in the population don’t have symptoms, and separately, how many of those individuals go on to transmit to others,” she said.
Dr. Van Kerkhove also emphasized that her initial comments were made in response to a question raised at the press conference, and called it a misunderstanding. “I wasn’t stating a policy of WHO or anything like that,” she said. “I was just trying to articulate what we know.”
The phrase “very rare” referred to a subset of studies and reports WHO had received from its member states following asymptomatic individuals with COVID-19. “I was referring to some detailed investigations, cluster investigations, case contact tracing, where we had reports from member states saying that, when we follow asymptomatic cases, it’s very rare – and I used the phrase very rare – that we found a secondary transmission,” she said.
Dr. Van Kerkhove’s initial comments drew criticism from medical and public health professionals, who said the statement was “confusing” and communicated poorly.
Eric J. Topol, MD, tweeted that WHO had “engendered considerable confusion” with the comments about asymptomatic individuals rarely transmitting SARS-CoV-2. Dr. Topol, the author of a recent analysis published in Annals of Internal Medicine that suggested as many as 40%-45% of COVID-19 cases may be asymptomatic, said that it was not possible to determine whether asymptomatic individuals in the cohorts he studied were capable of spread like pre-symptomatic individuals. “We only know the viral loads are similar from multiple reports. And we do know some spread occurs from [asymptomatic] people,” he said.
Andy Slavitt, former acting administrator of the Centers for Medicare and Medicaid Services, said in a tweet that he believed WHO made “an irresponsible statement even though it was based on legitimate observations.” Reports by Member States do not reach a “bar of rigor,” he said.
Natalie E. Dean, PhD, assistant professor of biostatistics at the University of Florida, tweeted that the initial comments by the WHO seemed to be trying to draw a distinction between asymptomatic individuals who never develop symptoms, and presymptomatic individuals who present as asymptomatic, but later develop symptoms. Finding that asymptomatic cases rarely transmit the virus could change how people exposed to those asymptomatic individuals are monitored, but “it seems more of scientific than practical interest,” she noted. “People without current symptoms could be infectious. Act accordingly.”
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, also weighed in on the controversial WHO comments, telling Good Morning America on June 10 that Dr. Van Kerkhove's initial statement that asymptomatic SARS-CoV-2 transmission is a rare event is "not correct."
This article was updated 6/10/20.
A World Health Organization (WHO) official is walking back her comments characterizing the spread of SARS-CoV-2 by asymptomatic individuals as “rare.”
Maria Van Kerkhove, PhD, WHO’s COVID-19 technical lead and an infectious disease epidemiologist, caused a stir June 8 when she said that countries are reporting that many of their asymptomatic cases develop into cases of mild disease. For patients with truly asymptomatic disease, countries are “not finding secondary transmission onward. It’s very rare,” she said.
Suppressing symptomatic cases, on the other hand, would result in a “drastic reduction” in transmission, she noted. “But from the data we have, it still seems to be rare that an asymptomatic person actually transmits onward to a secondary individual,” she said.
But on June 9 – following a day of confusion and criticism – Dr. Van Kerkhove sought to clarify her comments on asymptomatic transmission during a live social media Q&A. She noted that while “the majority of transmission that we know about” is through individuals with symptoms, “there are a subset of people who don’t develop symptoms, and to truly understand how many people don’t have symptoms – we don’t actually have that answer yet.”
Between 6% and 41% of individuals may be asymptomatic based on estimates, she acknowledged.“What we need to better understand is how many of the people in the population don’t have symptoms, and separately, how many of those individuals go on to transmit to others,” she said.
Dr. Van Kerkhove also emphasized that her initial comments were made in response to a question raised at the press conference, and called it a misunderstanding. “I wasn’t stating a policy of WHO or anything like that,” she said. “I was just trying to articulate what we know.”
The phrase “very rare” referred to a subset of studies and reports WHO had received from its member states following asymptomatic individuals with COVID-19. “I was referring to some detailed investigations, cluster investigations, case contact tracing, where we had reports from member states saying that, when we follow asymptomatic cases, it’s very rare – and I used the phrase very rare – that we found a secondary transmission,” she said.
Dr. Van Kerkhove’s initial comments drew criticism from medical and public health professionals, who said the statement was “confusing” and communicated poorly.
Eric J. Topol, MD, tweeted that WHO had “engendered considerable confusion” with the comments about asymptomatic individuals rarely transmitting SARS-CoV-2. Dr. Topol, the author of a recent analysis published in Annals of Internal Medicine that suggested as many as 40%-45% of COVID-19 cases may be asymptomatic, said that it was not possible to determine whether asymptomatic individuals in the cohorts he studied were capable of spread like pre-symptomatic individuals. “We only know the viral loads are similar from multiple reports. And we do know some spread occurs from [asymptomatic] people,” he said.
Andy Slavitt, former acting administrator of the Centers for Medicare and Medicaid Services, said in a tweet that he believed WHO made “an irresponsible statement even though it was based on legitimate observations.” Reports by Member States do not reach a “bar of rigor,” he said.
Natalie E. Dean, PhD, assistant professor of biostatistics at the University of Florida, tweeted that the initial comments by the WHO seemed to be trying to draw a distinction between asymptomatic individuals who never develop symptoms, and presymptomatic individuals who present as asymptomatic, but later develop symptoms. Finding that asymptomatic cases rarely transmit the virus could change how people exposed to those asymptomatic individuals are monitored, but “it seems more of scientific than practical interest,” she noted. “People without current symptoms could be infectious. Act accordingly.”
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, also weighed in on the controversial WHO comments, telling Good Morning America on June 10 that Dr. Van Kerkhove's initial statement that asymptomatic SARS-CoV-2 transmission is a rare event is "not correct."
This article was updated 6/10/20.
A World Health Organization (WHO) official is walking back her comments characterizing the spread of SARS-CoV-2 by asymptomatic individuals as “rare.”
Maria Van Kerkhove, PhD, WHO’s COVID-19 technical lead and an infectious disease epidemiologist, caused a stir June 8 when she said that countries are reporting that many of their asymptomatic cases develop into cases of mild disease. For patients with truly asymptomatic disease, countries are “not finding secondary transmission onward. It’s very rare,” she said.
Suppressing symptomatic cases, on the other hand, would result in a “drastic reduction” in transmission, she noted. “But from the data we have, it still seems to be rare that an asymptomatic person actually transmits onward to a secondary individual,” she said.
But on June 9 – following a day of confusion and criticism – Dr. Van Kerkhove sought to clarify her comments on asymptomatic transmission during a live social media Q&A. She noted that while “the majority of transmission that we know about” is through individuals with symptoms, “there are a subset of people who don’t develop symptoms, and to truly understand how many people don’t have symptoms – we don’t actually have that answer yet.”
Between 6% and 41% of individuals may be asymptomatic based on estimates, she acknowledged.“What we need to better understand is how many of the people in the population don’t have symptoms, and separately, how many of those individuals go on to transmit to others,” she said.
Dr. Van Kerkhove also emphasized that her initial comments were made in response to a question raised at the press conference, and called it a misunderstanding. “I wasn’t stating a policy of WHO or anything like that,” she said. “I was just trying to articulate what we know.”
The phrase “very rare” referred to a subset of studies and reports WHO had received from its member states following asymptomatic individuals with COVID-19. “I was referring to some detailed investigations, cluster investigations, case contact tracing, where we had reports from member states saying that, when we follow asymptomatic cases, it’s very rare – and I used the phrase very rare – that we found a secondary transmission,” she said.
Dr. Van Kerkhove’s initial comments drew criticism from medical and public health professionals, who said the statement was “confusing” and communicated poorly.
Eric J. Topol, MD, tweeted that WHO had “engendered considerable confusion” with the comments about asymptomatic individuals rarely transmitting SARS-CoV-2. Dr. Topol, the author of a recent analysis published in Annals of Internal Medicine that suggested as many as 40%-45% of COVID-19 cases may be asymptomatic, said that it was not possible to determine whether asymptomatic individuals in the cohorts he studied were capable of spread like pre-symptomatic individuals. “We only know the viral loads are similar from multiple reports. And we do know some spread occurs from [asymptomatic] people,” he said.
Andy Slavitt, former acting administrator of the Centers for Medicare and Medicaid Services, said in a tweet that he believed WHO made “an irresponsible statement even though it was based on legitimate observations.” Reports by Member States do not reach a “bar of rigor,” he said.
Natalie E. Dean, PhD, assistant professor of biostatistics at the University of Florida, tweeted that the initial comments by the WHO seemed to be trying to draw a distinction between asymptomatic individuals who never develop symptoms, and presymptomatic individuals who present as asymptomatic, but later develop symptoms. Finding that asymptomatic cases rarely transmit the virus could change how people exposed to those asymptomatic individuals are monitored, but “it seems more of scientific than practical interest,” she noted. “People without current symptoms could be infectious. Act accordingly.”
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, also weighed in on the controversial WHO comments, telling Good Morning America on June 10 that Dr. Van Kerkhove's initial statement that asymptomatic SARS-CoV-2 transmission is a rare event is "not correct."
This article was updated 6/10/20.
Age leads COVID-19 hospitalization risk factors in RMDs
Being aged older than 65 years was associated with the highest risk of people with rheumatic and musculoskeletal diseases (RMDs) needing hospital treatment for COVID-19, according to the first results to be reported from ReCoVery, the German national COVID-19 registry.
Older patients with RMDs were five times more likely than younger patients to be hospitalized if they tested positive for SARS‑CoV‑2 and developed COVID-19 (odds ratio, 5.1; 95% confidence interval, 2.3-11.4).
The likelihood of hospitalization was also significantly increased by the current or prior use of glucocorticoids (OR, 2.59; 95% CI, 1.2-5.4) and by the presence of cardiovascular disease (OR, 2.27; 95% CI, 1.2-5.4).
“The register is a joint initiative of the German Society for Rheumatology and the Justus Liebig University in Giessen,” explained Anne Regierer, MD, during a live session of the annual European Congress of Rheumatology, held online this year due to COVID-19.
“The current pandemic has changed all of our lives. For patients it brought a lot of uncertainty and fears,” said Dr. Regierer, of the German Rheumatism Research Center Berlin.
“The risk of SARS-CoV-2 infection in patients with inflammatory rheumatic diseases [IRD] is still largely unknown. We still don’t know whether they have a high risk of getting the infection or whether they have a higher risk of a severer case ... therefore there’s an urgent need to have data to generate evidence for the management of our patients.”
Launched at the end of March 2020, the German registry now includes data on 251 patients – 194 of whom have recovered – provided by more than 200 registered rheumatologists. The registry data have now been integrated into the EULAR COVID-19 Database, which is itself part of a global effort to better understand and optimally manage RMD patients during the pandemic.
“The data presented by Dr. Regierer looked at similar outcomes and found quite similar results, which is reassuring,” Kimme Hyrich, MD, PhD, professor of epidemiology at the University of Manchester (England) and a consultant rheumatologist in the Kellgren Centre for Rheumatology at Manchester University Hospitals NHS Foundation Trust, said in an interview.
“We are very grateful for this collaboration [with the German society and others]. Our first publication has looked at hospitalization, but with more data we may have the opportunity to look at less-common outcomes [e.g. death, other COVID complications] or within individual diseases or treatments. So far I don’t think we will come to a different conclusion,” observed Dr. Hyrich, who is on the steering committee for the EULAR COVID-19 Database.
“These initial data are reassuring in that the majority of cases of COVID reported to our database have recovered, including those who were hospitalized,” she said.
Current EULAR advice is to continue treatment with glucocorticoids in patients who are being chronically treated, but to use them at the lowest possible dose.
The objectives of this first analysis of the German registry was to provide a description of the patients who did and did not require hospitalization and those who needed ventilation, as well as look at possible risk factors for hospitalization.
Dr. Regierer reported that, of 192 patients they included – all with a positive lab test for SARS-CoV-2 – 128 (67%) did not require hospital admission. Of those that did (n = 64), 43 (22%) did not need ventilation and 21 (11%) did. Fifteen patients died, all of whom had been hospitalized, and all but one of them had needed ventilation.
Concerning the characteristics of the patients, those who needed hospital treatment with and without ventilation were older than those who were not admitted (70 vs. 65 vs. 54 years, respectively).
“Looking at the sexes, the gender distribution is also interesting. We see 69% females in the nonhospitalized patients, 65% of the inpatients without ventilation, but only 43% females in the ventilated patients. So in this group, the male patients are the majority,” Dr. Regierer observed.
Just over half of all patients in the nonhospitalized and the hospitalized without ventilation groups had IRD in remission, but those in the hospitalized with ventilation group less than one-fifth had their IRD under control.
“Of course we have to keep in mind the small sample sizes,” Dr. Regierer said, but the distribution of patients by disease type was “what you’d expect in clinical care.” The majority of patients in each of the three groups had RA (47%, 56%, and 57%), followed by psoriatic arthritis (19%, 7%, and 14%), axial spondyloarthritis (11%, 5%, and 0%), systemic lupus erythematosus (6%, 2%, and 0%), and vasculitis (1%, 5%, and 5%).
Patients who were hospitalized with and without ventilation were more likely to have more than one comorbidity than those who were not hospitalized with COVID-19.
“The most frequent comorbidity was cardiovascular disease with 58% and 76% in the inpatient groups,” Dr. Regierer reported. One-third of the nonhospitalized patients had a cardiovascular comorbidity.
“If we look at pulmonary disease, we see that 38% of the ventilator patients had an underlying pulmonary disease,” she added. This was in comparison with 19% of the hospitalized without ventilation and 13% of the nonhospitalized patients. Diabetes was another common comorbidity in hospitalized patients with (16%) and without (19%) ventilation versus just 2% of nonhospitalized patients. While these and other comorbidities such as chronic renal insufficiency were associated with higher odds ratios in the multivariate risk factor analysis, they did not reach statistical significance.
With regard to RMD treatments, more than 60% of patients in the hospitalized group had received treatment with glucocorticoids versus 37% of those who did not get admitted. No differences were seen for the other treatments.
Interestingly, “female sex, remission, and use of NSAIDs have an odds ratio smaller than 1. So there might be a lower risk of hospitalization associated with these factors,” Dr. Regierer said.
Dr. Regierer has received grant support and is part of speaker’s bureaus for a variety of pharmaceutical companies. Dr. Hyrich disclosed grant income from Bristol-Myers Squibb, UCB, and Pfizer, and receiving speaker fees from AbbVie.
Being aged older than 65 years was associated with the highest risk of people with rheumatic and musculoskeletal diseases (RMDs) needing hospital treatment for COVID-19, according to the first results to be reported from ReCoVery, the German national COVID-19 registry.
Older patients with RMDs were five times more likely than younger patients to be hospitalized if they tested positive for SARS‑CoV‑2 and developed COVID-19 (odds ratio, 5.1; 95% confidence interval, 2.3-11.4).
The likelihood of hospitalization was also significantly increased by the current or prior use of glucocorticoids (OR, 2.59; 95% CI, 1.2-5.4) and by the presence of cardiovascular disease (OR, 2.27; 95% CI, 1.2-5.4).
“The register is a joint initiative of the German Society for Rheumatology and the Justus Liebig University in Giessen,” explained Anne Regierer, MD, during a live session of the annual European Congress of Rheumatology, held online this year due to COVID-19.
“The current pandemic has changed all of our lives. For patients it brought a lot of uncertainty and fears,” said Dr. Regierer, of the German Rheumatism Research Center Berlin.
“The risk of SARS-CoV-2 infection in patients with inflammatory rheumatic diseases [IRD] is still largely unknown. We still don’t know whether they have a high risk of getting the infection or whether they have a higher risk of a severer case ... therefore there’s an urgent need to have data to generate evidence for the management of our patients.”
Launched at the end of March 2020, the German registry now includes data on 251 patients – 194 of whom have recovered – provided by more than 200 registered rheumatologists. The registry data have now been integrated into the EULAR COVID-19 Database, which is itself part of a global effort to better understand and optimally manage RMD patients during the pandemic.
“The data presented by Dr. Regierer looked at similar outcomes and found quite similar results, which is reassuring,” Kimme Hyrich, MD, PhD, professor of epidemiology at the University of Manchester (England) and a consultant rheumatologist in the Kellgren Centre for Rheumatology at Manchester University Hospitals NHS Foundation Trust, said in an interview.
“We are very grateful for this collaboration [with the German society and others]. Our first publication has looked at hospitalization, but with more data we may have the opportunity to look at less-common outcomes [e.g. death, other COVID complications] or within individual diseases or treatments. So far I don’t think we will come to a different conclusion,” observed Dr. Hyrich, who is on the steering committee for the EULAR COVID-19 Database.
“These initial data are reassuring in that the majority of cases of COVID reported to our database have recovered, including those who were hospitalized,” she said.
Current EULAR advice is to continue treatment with glucocorticoids in patients who are being chronically treated, but to use them at the lowest possible dose.
The objectives of this first analysis of the German registry was to provide a description of the patients who did and did not require hospitalization and those who needed ventilation, as well as look at possible risk factors for hospitalization.
Dr. Regierer reported that, of 192 patients they included – all with a positive lab test for SARS-CoV-2 – 128 (67%) did not require hospital admission. Of those that did (n = 64), 43 (22%) did not need ventilation and 21 (11%) did. Fifteen patients died, all of whom had been hospitalized, and all but one of them had needed ventilation.
Concerning the characteristics of the patients, those who needed hospital treatment with and without ventilation were older than those who were not admitted (70 vs. 65 vs. 54 years, respectively).
“Looking at the sexes, the gender distribution is also interesting. We see 69% females in the nonhospitalized patients, 65% of the inpatients without ventilation, but only 43% females in the ventilated patients. So in this group, the male patients are the majority,” Dr. Regierer observed.
Just over half of all patients in the nonhospitalized and the hospitalized without ventilation groups had IRD in remission, but those in the hospitalized with ventilation group less than one-fifth had their IRD under control.
“Of course we have to keep in mind the small sample sizes,” Dr. Regierer said, but the distribution of patients by disease type was “what you’d expect in clinical care.” The majority of patients in each of the three groups had RA (47%, 56%, and 57%), followed by psoriatic arthritis (19%, 7%, and 14%), axial spondyloarthritis (11%, 5%, and 0%), systemic lupus erythematosus (6%, 2%, and 0%), and vasculitis (1%, 5%, and 5%).
Patients who were hospitalized with and without ventilation were more likely to have more than one comorbidity than those who were not hospitalized with COVID-19.
“The most frequent comorbidity was cardiovascular disease with 58% and 76% in the inpatient groups,” Dr. Regierer reported. One-third of the nonhospitalized patients had a cardiovascular comorbidity.
“If we look at pulmonary disease, we see that 38% of the ventilator patients had an underlying pulmonary disease,” she added. This was in comparison with 19% of the hospitalized without ventilation and 13% of the nonhospitalized patients. Diabetes was another common comorbidity in hospitalized patients with (16%) and without (19%) ventilation versus just 2% of nonhospitalized patients. While these and other comorbidities such as chronic renal insufficiency were associated with higher odds ratios in the multivariate risk factor analysis, they did not reach statistical significance.
With regard to RMD treatments, more than 60% of patients in the hospitalized group had received treatment with glucocorticoids versus 37% of those who did not get admitted. No differences were seen for the other treatments.
Interestingly, “female sex, remission, and use of NSAIDs have an odds ratio smaller than 1. So there might be a lower risk of hospitalization associated with these factors,” Dr. Regierer said.
Dr. Regierer has received grant support and is part of speaker’s bureaus for a variety of pharmaceutical companies. Dr. Hyrich disclosed grant income from Bristol-Myers Squibb, UCB, and Pfizer, and receiving speaker fees from AbbVie.
Being aged older than 65 years was associated with the highest risk of people with rheumatic and musculoskeletal diseases (RMDs) needing hospital treatment for COVID-19, according to the first results to be reported from ReCoVery, the German national COVID-19 registry.
Older patients with RMDs were five times more likely than younger patients to be hospitalized if they tested positive for SARS‑CoV‑2 and developed COVID-19 (odds ratio, 5.1; 95% confidence interval, 2.3-11.4).
The likelihood of hospitalization was also significantly increased by the current or prior use of glucocorticoids (OR, 2.59; 95% CI, 1.2-5.4) and by the presence of cardiovascular disease (OR, 2.27; 95% CI, 1.2-5.4).
“The register is a joint initiative of the German Society for Rheumatology and the Justus Liebig University in Giessen,” explained Anne Regierer, MD, during a live session of the annual European Congress of Rheumatology, held online this year due to COVID-19.
“The current pandemic has changed all of our lives. For patients it brought a lot of uncertainty and fears,” said Dr. Regierer, of the German Rheumatism Research Center Berlin.
“The risk of SARS-CoV-2 infection in patients with inflammatory rheumatic diseases [IRD] is still largely unknown. We still don’t know whether they have a high risk of getting the infection or whether they have a higher risk of a severer case ... therefore there’s an urgent need to have data to generate evidence for the management of our patients.”
Launched at the end of March 2020, the German registry now includes data on 251 patients – 194 of whom have recovered – provided by more than 200 registered rheumatologists. The registry data have now been integrated into the EULAR COVID-19 Database, which is itself part of a global effort to better understand and optimally manage RMD patients during the pandemic.
“The data presented by Dr. Regierer looked at similar outcomes and found quite similar results, which is reassuring,” Kimme Hyrich, MD, PhD, professor of epidemiology at the University of Manchester (England) and a consultant rheumatologist in the Kellgren Centre for Rheumatology at Manchester University Hospitals NHS Foundation Trust, said in an interview.
“We are very grateful for this collaboration [with the German society and others]. Our first publication has looked at hospitalization, but with more data we may have the opportunity to look at less-common outcomes [e.g. death, other COVID complications] or within individual diseases or treatments. So far I don’t think we will come to a different conclusion,” observed Dr. Hyrich, who is on the steering committee for the EULAR COVID-19 Database.
“These initial data are reassuring in that the majority of cases of COVID reported to our database have recovered, including those who were hospitalized,” she said.
Current EULAR advice is to continue treatment with glucocorticoids in patients who are being chronically treated, but to use them at the lowest possible dose.
The objectives of this first analysis of the German registry was to provide a description of the patients who did and did not require hospitalization and those who needed ventilation, as well as look at possible risk factors for hospitalization.
Dr. Regierer reported that, of 192 patients they included – all with a positive lab test for SARS-CoV-2 – 128 (67%) did not require hospital admission. Of those that did (n = 64), 43 (22%) did not need ventilation and 21 (11%) did. Fifteen patients died, all of whom had been hospitalized, and all but one of them had needed ventilation.
Concerning the characteristics of the patients, those who needed hospital treatment with and without ventilation were older than those who were not admitted (70 vs. 65 vs. 54 years, respectively).
“Looking at the sexes, the gender distribution is also interesting. We see 69% females in the nonhospitalized patients, 65% of the inpatients without ventilation, but only 43% females in the ventilated patients. So in this group, the male patients are the majority,” Dr. Regierer observed.
Just over half of all patients in the nonhospitalized and the hospitalized without ventilation groups had IRD in remission, but those in the hospitalized with ventilation group less than one-fifth had their IRD under control.
“Of course we have to keep in mind the small sample sizes,” Dr. Regierer said, but the distribution of patients by disease type was “what you’d expect in clinical care.” The majority of patients in each of the three groups had RA (47%, 56%, and 57%), followed by psoriatic arthritis (19%, 7%, and 14%), axial spondyloarthritis (11%, 5%, and 0%), systemic lupus erythematosus (6%, 2%, and 0%), and vasculitis (1%, 5%, and 5%).
Patients who were hospitalized with and without ventilation were more likely to have more than one comorbidity than those who were not hospitalized with COVID-19.
“The most frequent comorbidity was cardiovascular disease with 58% and 76% in the inpatient groups,” Dr. Regierer reported. One-third of the nonhospitalized patients had a cardiovascular comorbidity.
“If we look at pulmonary disease, we see that 38% of the ventilator patients had an underlying pulmonary disease,” she added. This was in comparison with 19% of the hospitalized without ventilation and 13% of the nonhospitalized patients. Diabetes was another common comorbidity in hospitalized patients with (16%) and without (19%) ventilation versus just 2% of nonhospitalized patients. While these and other comorbidities such as chronic renal insufficiency were associated with higher odds ratios in the multivariate risk factor analysis, they did not reach statistical significance.
With regard to RMD treatments, more than 60% of patients in the hospitalized group had received treatment with glucocorticoids versus 37% of those who did not get admitted. No differences were seen for the other treatments.
Interestingly, “female sex, remission, and use of NSAIDs have an odds ratio smaller than 1. So there might be a lower risk of hospitalization associated with these factors,” Dr. Regierer said.
Dr. Regierer has received grant support and is part of speaker’s bureaus for a variety of pharmaceutical companies. Dr. Hyrich disclosed grant income from Bristol-Myers Squibb, UCB, and Pfizer, and receiving speaker fees from AbbVie.
FROM THE EULAR 2020 E-CONGRESS
COVID-19 drives nursing homes to overhaul infection control efforts
The toll that COVID-19 has taken on nursing homes and their postacute and long-term care residents has a multilayered backstory involving underresourced organizational structures, inherent susceptibilities, minimally trained infection prevention staff, variable abilities to isolate and quarantine large numbers of patients and residents, and a lack of governmental support.
“Nursing homes have been trying their best to combat this pandemic using the best infection control procedures they have, but blindfolded and with their hands tied behind their backs,” said Joseph G. Ouslander, MD, professor of geriatric medicine at Florida Atlantic University, Boca Raton, which has teaching affiliations with three senior communities.
Nursing home leaders are debating how to best use testing to guide transmission-based precautions and isolation strategies and how to keep residents safe while allowing some socialization after months of conflicting guidance from public health officials (on testing and on sites of care for patients discharged from the hospital, for instance), with a lack of adequate personal protective equipment (PPE) and testing supplies, and with nursing home resident deaths estimated to account for at least one-quarter of the total COVID-19–related mortality in the United States.
“COVID is not going away [over the next couple of years],” said Michael Wasserman, MD, medical director of the Eisenberg Village at the Los Angeles Jewish Home and president of the California Association of Long-Term Care Medicine.
Dr. Wasserman and other experts in both long-term care and infectious disease said in interviews that, through the rest of the pandemic and beyond, nursing homes need the following:
- Full-time, well-trained “infection preventionists” – infection prevention managers, in essence – who can lead improvements in emergency preparedness and infection prevention and control (IPC)
- Medical directors who are well qualified and engaged
- A survey/inspection process that is educational and not solely punitive
- More resources and attention to structural reform
“If this pandemic doesn’t create significant change in the nursing home industry, nothing ever will,” Dr. Wasserman said.
Prepandemic experience
When Ghinwa Dumyati, MD, began working with nursing homes in early March to prevent and contain COVID-19 outbreaks, her focus was on PPE.
Nursing home staff were intimately familiar with standard precautions, and many had used contact precautions to prevent transmission of infections like Clostridioides difficile and Candida auris, as well as droplet precautions for influenza. With the threat of COVID-19, nursing homes “had a brand-new requirement to do both contact and droplet precautions – with a new need for eye protection – and in some situations, respiratory precautions with N95 masks,” said Dr. Dumyati, professor of medicine and director of communicable disease surveillance and prevention at the University of Rochester (N.Y.) Medical Center. “And on top of that, [staff] had to learn to conserve and reuse PPE.”
Staff had not been fit-tested for use of N95 respirators, she noted. “The only time an N95 was used in the nursing home prior to COVID-19,” she said, “was for a suspected tuberculosis patient [before hospital admission].”
Similarly, nursing homes had experience in quarantining units to prevent transmission of illnesses like influenza or norovirus – keeping residents in their rooms with no visitations or social activity, for instance – but never did they have to arrange “massive movements of residents to completely new units or parts of a unit,” said Dr. Dumyati, who also has led hospital and nursing home collaborative programs in Rochester to beat back C. difficile, and is now helping to formulate COVID-19 recommendations and guidance for members of AMDA – The Society for Post-Acute and Long-Term Care.
As the SARS-CoV-2 virus began its spread through the United States, efforts to strengthen IPC programs in nursing homes in Rochester and elsewhere had been focused largely on multidrug resistant organisms (MDROs) and antibiotic stewardship – not on pandemic preparedness.
Reducing antibiotic use had become a national priority, and a 2016 rule by the Centers for Medicare & Medicaid Services required nursing homes to develop, over a 3-year period, an IPC program that included an antibiotic stewardship component and employment of a trained infection preventionist on at least a half-time basis. Emergency preparedness (e.g., having alternate energy sources for a facility) was also included in the rule, but it was only in 2019 when CMS updated its “Requirements for Participation” rule to stipulate that emergency preparedness include planning for “emerging infectious diseases.”
“The 2016 regulations came about because infections were so problematic in nursing homes,” especially urinary tract infections, C. difficile, and drug-resistant infections, said Patricia Stone, PhD, RN, of the Center for Health Policy at the Columbia University School of Nursing, New York, who has published widely on infection prevention and control in nursing homes.
An analysis of IPC practices in 2014 and in 2018 suggests that the IPC-focused rules were helping, mainly with antibiotic stewardship programs but also with respect to some of the practices aimed at outbreak control, such as having policies in place for grouping infected residents together, instructing infected staff to stay home, and quarantining units on which outbreaks occur, Dr. Stone said. Policies for confining residents to rooms were reported by approximately 74% of nursing homes in 2014, and by approximately 87% in 2018, for instance. Overall, nursing homes were “getting better policies in place,” she said. The analysis compared data from two cross-sectional surveys of nursing homes conducted in 2014 and 2018 (945 and 888 facilities, respectively).
Nursing homes “have a long way to go,” however, with respect to the training of infection preventionists, Dr. Stone said. In 2014, her analysis shows, almost 65% of infection preventionists had no specific infection-control training and less than 3% were Certified in Infection Control (CIC) – a credential awarded by the Certification Board of Infection Control & Epidemiology. Of the 35% who had some form of official training, most completed state or local training courses.
The numbers improved slightly in 2018, with 7% of nursing homes reporting their infection preventionists had the highest-level certification, and 44% reporting that their infection preventionists had no specific infection-control training. Research has shown that infection-control training of any kind has a “strong effect” on IPC-related outcomes. While not demonstrated in research thus far, it seems plausible that “facilities with certified [infection preventionists] will have better processes in place,” said Dr. Stone, whose research has documented the need for more monitoring of staff compliance with hand-washing and other IPC procedures.
Infection preventionists in nursing homes typically have been directors of nursing or assistant directors of nursing who fold IPC responsibilities into a multitude of other responsibilities. Before the 2016 rules, some smaller facilities hired off-site consultants to do the job.
CMS upped the ante after several months of COVID-19, recommending in mid-May that nursing homes assign at least one individual with training in infection control “to provide on-site management of the IPC program.” The infection preventionists should be a “full-time role” in facilities that have more than 100 residents, the CMS guidance said. (Prior to the pandemic, CMS issued proposed regulations in 2019 that would modify the time an infection preventionist must devote to a facility from “part time” to “sufficient time.”)
However, neither the 2016 rule nor the most recent guidance on infection preventionists define the length or content of training.
Swati Gaur, MD, chair of the Infection Advisory Committee of AMDA and a certified medical director of two skilled nursing facilities in Gainesville, Ga., said that the pandemic “has really started to crystallize some of the limitations of having a very vague role, not just in terms of what an [infection preventionists] does [in the nursing home] but also the training,”
Fortunately, Dr. Gaur said, when SARS-CoV-2 struck, she had just transitioned her facilities’ designated infection preventionist to work full-time on the role. She had worked closely with her infection preventionist on IPC issues but wishes she had arranged for more rigorous independent training. “The role of the [infection preventionist] is huge and complicated,” now involving employee health, contract tracing, cohorting, isolation, and compliance with precautions and use of PPE, in addition to surveillance, data reporting, and communication with public health officials, she said.
“Facilities are finding out now that [the infection preventionist] cannot be an afterthought. And it won’t end with COVID. We have other respiratory illnesses like flu and other viruses that we struggle with all the time,” said Dr. Gaur, who is working alongside Dr. Dumyati and two other long-term care experts on AMDA’s COVID-19 guidance. The nursing homes that Dr. Gaur directs are part of the Northeast Georgia Health Care System and together include 271 beds.
Moving forward
IPC practices often collide with facilities’ role as a home, especially to those receiving long-term care. “We always have to measure what we do [to prevent and control infections] against patient autonomy and residents’ rights,” said Dr. Gaur. “We have struggled with these issues, prior to the pandemic. If patients are positive for multidrug resistant organisms [for instance], how long can they be isolated in their own rooms? You can’t for days and months put someone in a single room and create isolation. That’s where the science of infection prevention can collide with residents’ rights.”
Over the years, the Centers for Disease Control and Prevention has acknowledged this discordance, leaving it to facilities to decide, for instance, whether to actively screen for colonization with MDROs. In 2019, to help nursing homes prevent the transmission of MDROs from residents who are colonized but not actively infected, the CDC introduced new “enhanced barrier precautions” that require the use of gowns and gloves for specific resident activities identified as having a high risk of MDRO transmission. The new category of precautions is less restrictive than traditional contact precautions, which keep residents in their rooms.
Infection control in nursing homes “isn’t where it needs to be ... but we’re always going to have in nursing homes a situation where there’s a high potential for rapid transmission of infectious disease,” said Christopher Crnich, MD, PhD, an infectious disease specialist at the University of Wisconsin–Madison who chairs the long-term care special interest group of the Society of Healthcare Epidemiology of America and has offered COVID-19 advice to his state’s department of public health.
“Anytime you have a congregative community, particularly one that involves susceptible hosts, there will be an intrinsically susceptible environment ... I’m a bit disturbed by the emphasis on saying, ‘This nursing home had a COVID-19 outbreak, therefore this nursing home did something wrong,’ ” Dr. Crnich said.
“How we mitigate the size of the outbreaks is where we need to focus our attention,” he said. The goal with SARS-CoV-2, he said, is to recognize its introduction “as rapidly as possible” and stop its spread through empiric symptom- and exposure-based isolation, multiple waves of targeted testing, widespread use of contact and droplet precautions, and isolating staff as necessary.
As awareness grew this year among long-term care leaders that relying too heavily on symptom-based strategies may not be effective to prevent introduction and transmission of SARS-CoV-2, a study published in April in the New England Journal of Medicine cemented the need for a testing strategy not limited to symptomatic individuals.
The study documented that more than half of residents in a nursing home who had positive polymerase chain reaction (PCR) test results were asymptomatic at the time of testing, and that most went on to develop symptoms. The study was conducted after one case of COVID-19 had been identified.
Some states issued calls this spring for “universal testing” of all nursing home patients and staff, and the CMS recommendations issued to state and local officials in mid-May for phased nursing home “reopening” call for baseline testing of all residents and staff, followed by retesting all residents weekly until all residents test negative and by retesting all staff continuing every week.
However, the experts contacted for this story said that, without a highly accurate and accessible point-of-care test (and even with one, considering the virus’ incubation period), a universal approach that includes all nursing home residents may have more limited value than is being touted. In many scenarios, they said, it is most meaningful to focus still-limited testing supplies on the staff, many of whom work at more than one facility and are believed to be primary vectors of SARS-CoV-2.
Dr. Ouslander, Dr. Wasserman and other long-term care leaders have been discussing testing at length, trying to reach consensus on best policies. “I don’t think there’s any uniform approach or uniform agreement,” said Dr. Ouslander. “For me, under ideal circumstances what needs to be done to protect older people in nursing homes is to get access to as many accurate viral tests as possible and test staff at least once a week or every 10 days.”
In some facilities, there may be an unspoken barrier to the frequent testing of staff: Fear that staff who test positive will need to be quarantined, with no one to take their place on the front line. Dr. Ouslander said he knows of one county health department that has discouraged nursing homes from testing asymptomatic staff. “It’s insane and truly shocking,” he said.
At the University of Rochester Medical Center, Dr. Dumyati said, staffing agencies are running short of nurse aide substitutes, and staffing issues have become the “biggest challenge” facing a regional multidisciplinary group of medical directors, hospital leaders, and health department officials who are working to troubleshoot COVID-19 issues. “Some of our nursing homes have ended up sending some of their residents to other nursing homes or to the hospital [because of the loss of staff],” she said.
Currently in the state of New York, she noted, COVID-19 patients may not be discharged to nursing homes until they test negative for the virus through PCR testing. “And some people don’t clear by PCR for 4-6 weeks.”
The barriers
Staffing shortages – real in some locales, and anticipated in others as economic reopening grows – are reflective of underlying structural and financial factors that work against optimal IPC, experts said. It’s not uncommon for certified nurse assistants (CNAs) to be assigned to 10-15 residents. And according to AMDA, 30%-46% of CNAs are reported to receive some form of public assistance. Low wages force many CNAs to work other jobs, including shifts at other nursing homes.
Turnover of nursing home leadership also creates problems. Dr. Crnich calls it “one of the biggest barriers” to effective IPC in nursing homes. “Facilities can tolerate some turnover in their front line staff,” he said, “as long as their leadership structure remains relatively stable.” Dr. Stone and her coinvestigators have documented at least yearly turnover in top positions: They found that, in 2018, approximately one-quarter of facilities reported employing three or more infection preventionists, three or more administrators, and three or more directors of nursing during the prior 3 years.
Medical directors, moreover, are not uniformly qualified, engaged with their facilities, or supported by nursing home administrators. “It’s an open secret, I think, that a lot of facilities want a medical director who is a good referral source,” said Dr. Gaur. “A medical director needs to be completely engaged in [quality improvement and] infection control practices.”
Some nursing home chains, she noted, “have realized the value of the medical director, and have changed the way they’re paying them. They’re actually holding them accountable [for quality and outcomes].”
Medical directors such as Dr. Wasserman, who previously oversaw a 74-facility nursing home chain in California as chief medical officer and then chief executive officer and has worked on nursing home quality improvement processes for his state, said there is much that can be done clinically to prevent the spread of infections, such as more frequent use of telemedicine, more attention to “deprescribing” unnecessary medications (which reduces the number of medication passes and, thus, the number of “transmission opportunities”), and the use of continuous remote monitoring. He has been trying to secure Bluetooth-enabled pulse oximetry and temperature monitoring for the Los Angeles Jewish Home and other facilities.
Dr. Wasserman and other long-term care leaders believe that a more educational inspection process would also lead to improvements in IPC. “The punitive nature of the survey process is morally deflating to frontline staff [and] penalties take money away from operations,” Dr. Wasserman said. “It’s not a productive approach to quality improvement.”
Dr. Stone agreed. Infection control is now the primary focus of CMS’s inspection process, and she said that increased regulatory scrutiny of IPC beyond COVID-19 is a “good thing.” Her research has shown that most deficiencies identified by inspectors are infection control deficiencies, and that in 2014 and 2018, approximately one-third of nursing homes had infection control citations. (CMS recently increased penalties and fines for identified deficiencies.)
“But my hope would be that the survey process would be more educational [as it is for hospitals],” she said. “We need to be supporting nursing homes to do a better job.”
A silver lining of the COVID-19 pandemic, as Dr. Stone sees it, is that nursing homes may be more engaged with data reporting and infection surveillance going forward. Nursing homes are now required to report their COVID-19 cases to the CDC through its hospital-dominant National Healthcare Safety Network, and the CDC has made technical changes that now make it “easier [than it was in the past] for nursing homes to join and participate,” she said. “Now that all nursing homes are engaged, will they be engaged post-COVID, too? I hope so. Surveillance [of infections] is a first step toward better outcomes.”
For now, said Dr. Crnich, the intensive prevention and mitigation efforts that are being required of nursing homes to minimize COVID-19’s impact is “a big deal and will tax the resources of most nursing homes and exceed the resources of many” without outside support, Dr. Crnich said. “This has been the most illuminating part of all this, and will probably require us to reconsider how we’re resourcing our nursing homes moving forward into the future.”
The toll that COVID-19 has taken on nursing homes and their postacute and long-term care residents has a multilayered backstory involving underresourced organizational structures, inherent susceptibilities, minimally trained infection prevention staff, variable abilities to isolate and quarantine large numbers of patients and residents, and a lack of governmental support.
“Nursing homes have been trying their best to combat this pandemic using the best infection control procedures they have, but blindfolded and with their hands tied behind their backs,” said Joseph G. Ouslander, MD, professor of geriatric medicine at Florida Atlantic University, Boca Raton, which has teaching affiliations with three senior communities.
Nursing home leaders are debating how to best use testing to guide transmission-based precautions and isolation strategies and how to keep residents safe while allowing some socialization after months of conflicting guidance from public health officials (on testing and on sites of care for patients discharged from the hospital, for instance), with a lack of adequate personal protective equipment (PPE) and testing supplies, and with nursing home resident deaths estimated to account for at least one-quarter of the total COVID-19–related mortality in the United States.
“COVID is not going away [over the next couple of years],” said Michael Wasserman, MD, medical director of the Eisenberg Village at the Los Angeles Jewish Home and president of the California Association of Long-Term Care Medicine.
Dr. Wasserman and other experts in both long-term care and infectious disease said in interviews that, through the rest of the pandemic and beyond, nursing homes need the following:
- Full-time, well-trained “infection preventionists” – infection prevention managers, in essence – who can lead improvements in emergency preparedness and infection prevention and control (IPC)
- Medical directors who are well qualified and engaged
- A survey/inspection process that is educational and not solely punitive
- More resources and attention to structural reform
“If this pandemic doesn’t create significant change in the nursing home industry, nothing ever will,” Dr. Wasserman said.
Prepandemic experience
When Ghinwa Dumyati, MD, began working with nursing homes in early March to prevent and contain COVID-19 outbreaks, her focus was on PPE.
Nursing home staff were intimately familiar with standard precautions, and many had used contact precautions to prevent transmission of infections like Clostridioides difficile and Candida auris, as well as droplet precautions for influenza. With the threat of COVID-19, nursing homes “had a brand-new requirement to do both contact and droplet precautions – with a new need for eye protection – and in some situations, respiratory precautions with N95 masks,” said Dr. Dumyati, professor of medicine and director of communicable disease surveillance and prevention at the University of Rochester (N.Y.) Medical Center. “And on top of that, [staff] had to learn to conserve and reuse PPE.”
Staff had not been fit-tested for use of N95 respirators, she noted. “The only time an N95 was used in the nursing home prior to COVID-19,” she said, “was for a suspected tuberculosis patient [before hospital admission].”
Similarly, nursing homes had experience in quarantining units to prevent transmission of illnesses like influenza or norovirus – keeping residents in their rooms with no visitations or social activity, for instance – but never did they have to arrange “massive movements of residents to completely new units or parts of a unit,” said Dr. Dumyati, who also has led hospital and nursing home collaborative programs in Rochester to beat back C. difficile, and is now helping to formulate COVID-19 recommendations and guidance for members of AMDA – The Society for Post-Acute and Long-Term Care.
As the SARS-CoV-2 virus began its spread through the United States, efforts to strengthen IPC programs in nursing homes in Rochester and elsewhere had been focused largely on multidrug resistant organisms (MDROs) and antibiotic stewardship – not on pandemic preparedness.
Reducing antibiotic use had become a national priority, and a 2016 rule by the Centers for Medicare & Medicaid Services required nursing homes to develop, over a 3-year period, an IPC program that included an antibiotic stewardship component and employment of a trained infection preventionist on at least a half-time basis. Emergency preparedness (e.g., having alternate energy sources for a facility) was also included in the rule, but it was only in 2019 when CMS updated its “Requirements for Participation” rule to stipulate that emergency preparedness include planning for “emerging infectious diseases.”
“The 2016 regulations came about because infections were so problematic in nursing homes,” especially urinary tract infections, C. difficile, and drug-resistant infections, said Patricia Stone, PhD, RN, of the Center for Health Policy at the Columbia University School of Nursing, New York, who has published widely on infection prevention and control in nursing homes.
An analysis of IPC practices in 2014 and in 2018 suggests that the IPC-focused rules were helping, mainly with antibiotic stewardship programs but also with respect to some of the practices aimed at outbreak control, such as having policies in place for grouping infected residents together, instructing infected staff to stay home, and quarantining units on which outbreaks occur, Dr. Stone said. Policies for confining residents to rooms were reported by approximately 74% of nursing homes in 2014, and by approximately 87% in 2018, for instance. Overall, nursing homes were “getting better policies in place,” she said. The analysis compared data from two cross-sectional surveys of nursing homes conducted in 2014 and 2018 (945 and 888 facilities, respectively).
Nursing homes “have a long way to go,” however, with respect to the training of infection preventionists, Dr. Stone said. In 2014, her analysis shows, almost 65% of infection preventionists had no specific infection-control training and less than 3% were Certified in Infection Control (CIC) – a credential awarded by the Certification Board of Infection Control & Epidemiology. Of the 35% who had some form of official training, most completed state or local training courses.
The numbers improved slightly in 2018, with 7% of nursing homes reporting their infection preventionists had the highest-level certification, and 44% reporting that their infection preventionists had no specific infection-control training. Research has shown that infection-control training of any kind has a “strong effect” on IPC-related outcomes. While not demonstrated in research thus far, it seems plausible that “facilities with certified [infection preventionists] will have better processes in place,” said Dr. Stone, whose research has documented the need for more monitoring of staff compliance with hand-washing and other IPC procedures.
Infection preventionists in nursing homes typically have been directors of nursing or assistant directors of nursing who fold IPC responsibilities into a multitude of other responsibilities. Before the 2016 rules, some smaller facilities hired off-site consultants to do the job.
CMS upped the ante after several months of COVID-19, recommending in mid-May that nursing homes assign at least one individual with training in infection control “to provide on-site management of the IPC program.” The infection preventionists should be a “full-time role” in facilities that have more than 100 residents, the CMS guidance said. (Prior to the pandemic, CMS issued proposed regulations in 2019 that would modify the time an infection preventionist must devote to a facility from “part time” to “sufficient time.”)
However, neither the 2016 rule nor the most recent guidance on infection preventionists define the length or content of training.
Swati Gaur, MD, chair of the Infection Advisory Committee of AMDA and a certified medical director of two skilled nursing facilities in Gainesville, Ga., said that the pandemic “has really started to crystallize some of the limitations of having a very vague role, not just in terms of what an [infection preventionists] does [in the nursing home] but also the training,”
Fortunately, Dr. Gaur said, when SARS-CoV-2 struck, she had just transitioned her facilities’ designated infection preventionist to work full-time on the role. She had worked closely with her infection preventionist on IPC issues but wishes she had arranged for more rigorous independent training. “The role of the [infection preventionist] is huge and complicated,” now involving employee health, contract tracing, cohorting, isolation, and compliance with precautions and use of PPE, in addition to surveillance, data reporting, and communication with public health officials, she said.
“Facilities are finding out now that [the infection preventionist] cannot be an afterthought. And it won’t end with COVID. We have other respiratory illnesses like flu and other viruses that we struggle with all the time,” said Dr. Gaur, who is working alongside Dr. Dumyati and two other long-term care experts on AMDA’s COVID-19 guidance. The nursing homes that Dr. Gaur directs are part of the Northeast Georgia Health Care System and together include 271 beds.
Moving forward
IPC practices often collide with facilities’ role as a home, especially to those receiving long-term care. “We always have to measure what we do [to prevent and control infections] against patient autonomy and residents’ rights,” said Dr. Gaur. “We have struggled with these issues, prior to the pandemic. If patients are positive for multidrug resistant organisms [for instance], how long can they be isolated in their own rooms? You can’t for days and months put someone in a single room and create isolation. That’s where the science of infection prevention can collide with residents’ rights.”
Over the years, the Centers for Disease Control and Prevention has acknowledged this discordance, leaving it to facilities to decide, for instance, whether to actively screen for colonization with MDROs. In 2019, to help nursing homes prevent the transmission of MDROs from residents who are colonized but not actively infected, the CDC introduced new “enhanced barrier precautions” that require the use of gowns and gloves for specific resident activities identified as having a high risk of MDRO transmission. The new category of precautions is less restrictive than traditional contact precautions, which keep residents in their rooms.
Infection control in nursing homes “isn’t where it needs to be ... but we’re always going to have in nursing homes a situation where there’s a high potential for rapid transmission of infectious disease,” said Christopher Crnich, MD, PhD, an infectious disease specialist at the University of Wisconsin–Madison who chairs the long-term care special interest group of the Society of Healthcare Epidemiology of America and has offered COVID-19 advice to his state’s department of public health.
“Anytime you have a congregative community, particularly one that involves susceptible hosts, there will be an intrinsically susceptible environment ... I’m a bit disturbed by the emphasis on saying, ‘This nursing home had a COVID-19 outbreak, therefore this nursing home did something wrong,’ ” Dr. Crnich said.
“How we mitigate the size of the outbreaks is where we need to focus our attention,” he said. The goal with SARS-CoV-2, he said, is to recognize its introduction “as rapidly as possible” and stop its spread through empiric symptom- and exposure-based isolation, multiple waves of targeted testing, widespread use of contact and droplet precautions, and isolating staff as necessary.
As awareness grew this year among long-term care leaders that relying too heavily on symptom-based strategies may not be effective to prevent introduction and transmission of SARS-CoV-2, a study published in April in the New England Journal of Medicine cemented the need for a testing strategy not limited to symptomatic individuals.
The study documented that more than half of residents in a nursing home who had positive polymerase chain reaction (PCR) test results were asymptomatic at the time of testing, and that most went on to develop symptoms. The study was conducted after one case of COVID-19 had been identified.
Some states issued calls this spring for “universal testing” of all nursing home patients and staff, and the CMS recommendations issued to state and local officials in mid-May for phased nursing home “reopening” call for baseline testing of all residents and staff, followed by retesting all residents weekly until all residents test negative and by retesting all staff continuing every week.
However, the experts contacted for this story said that, without a highly accurate and accessible point-of-care test (and even with one, considering the virus’ incubation period), a universal approach that includes all nursing home residents may have more limited value than is being touted. In many scenarios, they said, it is most meaningful to focus still-limited testing supplies on the staff, many of whom work at more than one facility and are believed to be primary vectors of SARS-CoV-2.
Dr. Ouslander, Dr. Wasserman and other long-term care leaders have been discussing testing at length, trying to reach consensus on best policies. “I don’t think there’s any uniform approach or uniform agreement,” said Dr. Ouslander. “For me, under ideal circumstances what needs to be done to protect older people in nursing homes is to get access to as many accurate viral tests as possible and test staff at least once a week or every 10 days.”
In some facilities, there may be an unspoken barrier to the frequent testing of staff: Fear that staff who test positive will need to be quarantined, with no one to take their place on the front line. Dr. Ouslander said he knows of one county health department that has discouraged nursing homes from testing asymptomatic staff. “It’s insane and truly shocking,” he said.
At the University of Rochester Medical Center, Dr. Dumyati said, staffing agencies are running short of nurse aide substitutes, and staffing issues have become the “biggest challenge” facing a regional multidisciplinary group of medical directors, hospital leaders, and health department officials who are working to troubleshoot COVID-19 issues. “Some of our nursing homes have ended up sending some of their residents to other nursing homes or to the hospital [because of the loss of staff],” she said.
Currently in the state of New York, she noted, COVID-19 patients may not be discharged to nursing homes until they test negative for the virus through PCR testing. “And some people don’t clear by PCR for 4-6 weeks.”
The barriers
Staffing shortages – real in some locales, and anticipated in others as economic reopening grows – are reflective of underlying structural and financial factors that work against optimal IPC, experts said. It’s not uncommon for certified nurse assistants (CNAs) to be assigned to 10-15 residents. And according to AMDA, 30%-46% of CNAs are reported to receive some form of public assistance. Low wages force many CNAs to work other jobs, including shifts at other nursing homes.
Turnover of nursing home leadership also creates problems. Dr. Crnich calls it “one of the biggest barriers” to effective IPC in nursing homes. “Facilities can tolerate some turnover in their front line staff,” he said, “as long as their leadership structure remains relatively stable.” Dr. Stone and her coinvestigators have documented at least yearly turnover in top positions: They found that, in 2018, approximately one-quarter of facilities reported employing three or more infection preventionists, three or more administrators, and three or more directors of nursing during the prior 3 years.
Medical directors, moreover, are not uniformly qualified, engaged with their facilities, or supported by nursing home administrators. “It’s an open secret, I think, that a lot of facilities want a medical director who is a good referral source,” said Dr. Gaur. “A medical director needs to be completely engaged in [quality improvement and] infection control practices.”
Some nursing home chains, she noted, “have realized the value of the medical director, and have changed the way they’re paying them. They’re actually holding them accountable [for quality and outcomes].”
Medical directors such as Dr. Wasserman, who previously oversaw a 74-facility nursing home chain in California as chief medical officer and then chief executive officer and has worked on nursing home quality improvement processes for his state, said there is much that can be done clinically to prevent the spread of infections, such as more frequent use of telemedicine, more attention to “deprescribing” unnecessary medications (which reduces the number of medication passes and, thus, the number of “transmission opportunities”), and the use of continuous remote monitoring. He has been trying to secure Bluetooth-enabled pulse oximetry and temperature monitoring for the Los Angeles Jewish Home and other facilities.
Dr. Wasserman and other long-term care leaders believe that a more educational inspection process would also lead to improvements in IPC. “The punitive nature of the survey process is morally deflating to frontline staff [and] penalties take money away from operations,” Dr. Wasserman said. “It’s not a productive approach to quality improvement.”
Dr. Stone agreed. Infection control is now the primary focus of CMS’s inspection process, and she said that increased regulatory scrutiny of IPC beyond COVID-19 is a “good thing.” Her research has shown that most deficiencies identified by inspectors are infection control deficiencies, and that in 2014 and 2018, approximately one-third of nursing homes had infection control citations. (CMS recently increased penalties and fines for identified deficiencies.)
“But my hope would be that the survey process would be more educational [as it is for hospitals],” she said. “We need to be supporting nursing homes to do a better job.”
A silver lining of the COVID-19 pandemic, as Dr. Stone sees it, is that nursing homes may be more engaged with data reporting and infection surveillance going forward. Nursing homes are now required to report their COVID-19 cases to the CDC through its hospital-dominant National Healthcare Safety Network, and the CDC has made technical changes that now make it “easier [than it was in the past] for nursing homes to join and participate,” she said. “Now that all nursing homes are engaged, will they be engaged post-COVID, too? I hope so. Surveillance [of infections] is a first step toward better outcomes.”
For now, said Dr. Crnich, the intensive prevention and mitigation efforts that are being required of nursing homes to minimize COVID-19’s impact is “a big deal and will tax the resources of most nursing homes and exceed the resources of many” without outside support, Dr. Crnich said. “This has been the most illuminating part of all this, and will probably require us to reconsider how we’re resourcing our nursing homes moving forward into the future.”
The toll that COVID-19 has taken on nursing homes and their postacute and long-term care residents has a multilayered backstory involving underresourced organizational structures, inherent susceptibilities, minimally trained infection prevention staff, variable abilities to isolate and quarantine large numbers of patients and residents, and a lack of governmental support.
“Nursing homes have been trying their best to combat this pandemic using the best infection control procedures they have, but blindfolded and with their hands tied behind their backs,” said Joseph G. Ouslander, MD, professor of geriatric medicine at Florida Atlantic University, Boca Raton, which has teaching affiliations with three senior communities.
Nursing home leaders are debating how to best use testing to guide transmission-based precautions and isolation strategies and how to keep residents safe while allowing some socialization after months of conflicting guidance from public health officials (on testing and on sites of care for patients discharged from the hospital, for instance), with a lack of adequate personal protective equipment (PPE) and testing supplies, and with nursing home resident deaths estimated to account for at least one-quarter of the total COVID-19–related mortality in the United States.
“COVID is not going away [over the next couple of years],” said Michael Wasserman, MD, medical director of the Eisenberg Village at the Los Angeles Jewish Home and president of the California Association of Long-Term Care Medicine.
Dr. Wasserman and other experts in both long-term care and infectious disease said in interviews that, through the rest of the pandemic and beyond, nursing homes need the following:
- Full-time, well-trained “infection preventionists” – infection prevention managers, in essence – who can lead improvements in emergency preparedness and infection prevention and control (IPC)
- Medical directors who are well qualified and engaged
- A survey/inspection process that is educational and not solely punitive
- More resources and attention to structural reform
“If this pandemic doesn’t create significant change in the nursing home industry, nothing ever will,” Dr. Wasserman said.
Prepandemic experience
When Ghinwa Dumyati, MD, began working with nursing homes in early March to prevent and contain COVID-19 outbreaks, her focus was on PPE.
Nursing home staff were intimately familiar with standard precautions, and many had used contact precautions to prevent transmission of infections like Clostridioides difficile and Candida auris, as well as droplet precautions for influenza. With the threat of COVID-19, nursing homes “had a brand-new requirement to do both contact and droplet precautions – with a new need for eye protection – and in some situations, respiratory precautions with N95 masks,” said Dr. Dumyati, professor of medicine and director of communicable disease surveillance and prevention at the University of Rochester (N.Y.) Medical Center. “And on top of that, [staff] had to learn to conserve and reuse PPE.”
Staff had not been fit-tested for use of N95 respirators, she noted. “The only time an N95 was used in the nursing home prior to COVID-19,” she said, “was for a suspected tuberculosis patient [before hospital admission].”
Similarly, nursing homes had experience in quarantining units to prevent transmission of illnesses like influenza or norovirus – keeping residents in their rooms with no visitations or social activity, for instance – but never did they have to arrange “massive movements of residents to completely new units or parts of a unit,” said Dr. Dumyati, who also has led hospital and nursing home collaborative programs in Rochester to beat back C. difficile, and is now helping to formulate COVID-19 recommendations and guidance for members of AMDA – The Society for Post-Acute and Long-Term Care.
As the SARS-CoV-2 virus began its spread through the United States, efforts to strengthen IPC programs in nursing homes in Rochester and elsewhere had been focused largely on multidrug resistant organisms (MDROs) and antibiotic stewardship – not on pandemic preparedness.
Reducing antibiotic use had become a national priority, and a 2016 rule by the Centers for Medicare & Medicaid Services required nursing homes to develop, over a 3-year period, an IPC program that included an antibiotic stewardship component and employment of a trained infection preventionist on at least a half-time basis. Emergency preparedness (e.g., having alternate energy sources for a facility) was also included in the rule, but it was only in 2019 when CMS updated its “Requirements for Participation” rule to stipulate that emergency preparedness include planning for “emerging infectious diseases.”
“The 2016 regulations came about because infections were so problematic in nursing homes,” especially urinary tract infections, C. difficile, and drug-resistant infections, said Patricia Stone, PhD, RN, of the Center for Health Policy at the Columbia University School of Nursing, New York, who has published widely on infection prevention and control in nursing homes.
An analysis of IPC practices in 2014 and in 2018 suggests that the IPC-focused rules were helping, mainly with antibiotic stewardship programs but also with respect to some of the practices aimed at outbreak control, such as having policies in place for grouping infected residents together, instructing infected staff to stay home, and quarantining units on which outbreaks occur, Dr. Stone said. Policies for confining residents to rooms were reported by approximately 74% of nursing homes in 2014, and by approximately 87% in 2018, for instance. Overall, nursing homes were “getting better policies in place,” she said. The analysis compared data from two cross-sectional surveys of nursing homes conducted in 2014 and 2018 (945 and 888 facilities, respectively).
Nursing homes “have a long way to go,” however, with respect to the training of infection preventionists, Dr. Stone said. In 2014, her analysis shows, almost 65% of infection preventionists had no specific infection-control training and less than 3% were Certified in Infection Control (CIC) – a credential awarded by the Certification Board of Infection Control & Epidemiology. Of the 35% who had some form of official training, most completed state or local training courses.
The numbers improved slightly in 2018, with 7% of nursing homes reporting their infection preventionists had the highest-level certification, and 44% reporting that their infection preventionists had no specific infection-control training. Research has shown that infection-control training of any kind has a “strong effect” on IPC-related outcomes. While not demonstrated in research thus far, it seems plausible that “facilities with certified [infection preventionists] will have better processes in place,” said Dr. Stone, whose research has documented the need for more monitoring of staff compliance with hand-washing and other IPC procedures.
Infection preventionists in nursing homes typically have been directors of nursing or assistant directors of nursing who fold IPC responsibilities into a multitude of other responsibilities. Before the 2016 rules, some smaller facilities hired off-site consultants to do the job.
CMS upped the ante after several months of COVID-19, recommending in mid-May that nursing homes assign at least one individual with training in infection control “to provide on-site management of the IPC program.” The infection preventionists should be a “full-time role” in facilities that have more than 100 residents, the CMS guidance said. (Prior to the pandemic, CMS issued proposed regulations in 2019 that would modify the time an infection preventionist must devote to a facility from “part time” to “sufficient time.”)
However, neither the 2016 rule nor the most recent guidance on infection preventionists define the length or content of training.
Swati Gaur, MD, chair of the Infection Advisory Committee of AMDA and a certified medical director of two skilled nursing facilities in Gainesville, Ga., said that the pandemic “has really started to crystallize some of the limitations of having a very vague role, not just in terms of what an [infection preventionists] does [in the nursing home] but also the training,”
Fortunately, Dr. Gaur said, when SARS-CoV-2 struck, she had just transitioned her facilities’ designated infection preventionist to work full-time on the role. She had worked closely with her infection preventionist on IPC issues but wishes she had arranged for more rigorous independent training. “The role of the [infection preventionist] is huge and complicated,” now involving employee health, contract tracing, cohorting, isolation, and compliance with precautions and use of PPE, in addition to surveillance, data reporting, and communication with public health officials, she said.
“Facilities are finding out now that [the infection preventionist] cannot be an afterthought. And it won’t end with COVID. We have other respiratory illnesses like flu and other viruses that we struggle with all the time,” said Dr. Gaur, who is working alongside Dr. Dumyati and two other long-term care experts on AMDA’s COVID-19 guidance. The nursing homes that Dr. Gaur directs are part of the Northeast Georgia Health Care System and together include 271 beds.
Moving forward
IPC practices often collide with facilities’ role as a home, especially to those receiving long-term care. “We always have to measure what we do [to prevent and control infections] against patient autonomy and residents’ rights,” said Dr. Gaur. “We have struggled with these issues, prior to the pandemic. If patients are positive for multidrug resistant organisms [for instance], how long can they be isolated in their own rooms? You can’t for days and months put someone in a single room and create isolation. That’s where the science of infection prevention can collide with residents’ rights.”
Over the years, the Centers for Disease Control and Prevention has acknowledged this discordance, leaving it to facilities to decide, for instance, whether to actively screen for colonization with MDROs. In 2019, to help nursing homes prevent the transmission of MDROs from residents who are colonized but not actively infected, the CDC introduced new “enhanced barrier precautions” that require the use of gowns and gloves for specific resident activities identified as having a high risk of MDRO transmission. The new category of precautions is less restrictive than traditional contact precautions, which keep residents in their rooms.
Infection control in nursing homes “isn’t where it needs to be ... but we’re always going to have in nursing homes a situation where there’s a high potential for rapid transmission of infectious disease,” said Christopher Crnich, MD, PhD, an infectious disease specialist at the University of Wisconsin–Madison who chairs the long-term care special interest group of the Society of Healthcare Epidemiology of America and has offered COVID-19 advice to his state’s department of public health.
“Anytime you have a congregative community, particularly one that involves susceptible hosts, there will be an intrinsically susceptible environment ... I’m a bit disturbed by the emphasis on saying, ‘This nursing home had a COVID-19 outbreak, therefore this nursing home did something wrong,’ ” Dr. Crnich said.
“How we mitigate the size of the outbreaks is where we need to focus our attention,” he said. The goal with SARS-CoV-2, he said, is to recognize its introduction “as rapidly as possible” and stop its spread through empiric symptom- and exposure-based isolation, multiple waves of targeted testing, widespread use of contact and droplet precautions, and isolating staff as necessary.
As awareness grew this year among long-term care leaders that relying too heavily on symptom-based strategies may not be effective to prevent introduction and transmission of SARS-CoV-2, a study published in April in the New England Journal of Medicine cemented the need for a testing strategy not limited to symptomatic individuals.
The study documented that more than half of residents in a nursing home who had positive polymerase chain reaction (PCR) test results were asymptomatic at the time of testing, and that most went on to develop symptoms. The study was conducted after one case of COVID-19 had been identified.
Some states issued calls this spring for “universal testing” of all nursing home patients and staff, and the CMS recommendations issued to state and local officials in mid-May for phased nursing home “reopening” call for baseline testing of all residents and staff, followed by retesting all residents weekly until all residents test negative and by retesting all staff continuing every week.
However, the experts contacted for this story said that, without a highly accurate and accessible point-of-care test (and even with one, considering the virus’ incubation period), a universal approach that includes all nursing home residents may have more limited value than is being touted. In many scenarios, they said, it is most meaningful to focus still-limited testing supplies on the staff, many of whom work at more than one facility and are believed to be primary vectors of SARS-CoV-2.
Dr. Ouslander, Dr. Wasserman and other long-term care leaders have been discussing testing at length, trying to reach consensus on best policies. “I don’t think there’s any uniform approach or uniform agreement,” said Dr. Ouslander. “For me, under ideal circumstances what needs to be done to protect older people in nursing homes is to get access to as many accurate viral tests as possible and test staff at least once a week or every 10 days.”
In some facilities, there may be an unspoken barrier to the frequent testing of staff: Fear that staff who test positive will need to be quarantined, with no one to take their place on the front line. Dr. Ouslander said he knows of one county health department that has discouraged nursing homes from testing asymptomatic staff. “It’s insane and truly shocking,” he said.
At the University of Rochester Medical Center, Dr. Dumyati said, staffing agencies are running short of nurse aide substitutes, and staffing issues have become the “biggest challenge” facing a regional multidisciplinary group of medical directors, hospital leaders, and health department officials who are working to troubleshoot COVID-19 issues. “Some of our nursing homes have ended up sending some of their residents to other nursing homes or to the hospital [because of the loss of staff],” she said.
Currently in the state of New York, she noted, COVID-19 patients may not be discharged to nursing homes until they test negative for the virus through PCR testing. “And some people don’t clear by PCR for 4-6 weeks.”
The barriers
Staffing shortages – real in some locales, and anticipated in others as economic reopening grows – are reflective of underlying structural and financial factors that work against optimal IPC, experts said. It’s not uncommon for certified nurse assistants (CNAs) to be assigned to 10-15 residents. And according to AMDA, 30%-46% of CNAs are reported to receive some form of public assistance. Low wages force many CNAs to work other jobs, including shifts at other nursing homes.
Turnover of nursing home leadership also creates problems. Dr. Crnich calls it “one of the biggest barriers” to effective IPC in nursing homes. “Facilities can tolerate some turnover in their front line staff,” he said, “as long as their leadership structure remains relatively stable.” Dr. Stone and her coinvestigators have documented at least yearly turnover in top positions: They found that, in 2018, approximately one-quarter of facilities reported employing three or more infection preventionists, three or more administrators, and three or more directors of nursing during the prior 3 years.
Medical directors, moreover, are not uniformly qualified, engaged with their facilities, or supported by nursing home administrators. “It’s an open secret, I think, that a lot of facilities want a medical director who is a good referral source,” said Dr. Gaur. “A medical director needs to be completely engaged in [quality improvement and] infection control practices.”
Some nursing home chains, she noted, “have realized the value of the medical director, and have changed the way they’re paying them. They’re actually holding them accountable [for quality and outcomes].”
Medical directors such as Dr. Wasserman, who previously oversaw a 74-facility nursing home chain in California as chief medical officer and then chief executive officer and has worked on nursing home quality improvement processes for his state, said there is much that can be done clinically to prevent the spread of infections, such as more frequent use of telemedicine, more attention to “deprescribing” unnecessary medications (which reduces the number of medication passes and, thus, the number of “transmission opportunities”), and the use of continuous remote monitoring. He has been trying to secure Bluetooth-enabled pulse oximetry and temperature monitoring for the Los Angeles Jewish Home and other facilities.
Dr. Wasserman and other long-term care leaders believe that a more educational inspection process would also lead to improvements in IPC. “The punitive nature of the survey process is morally deflating to frontline staff [and] penalties take money away from operations,” Dr. Wasserman said. “It’s not a productive approach to quality improvement.”
Dr. Stone agreed. Infection control is now the primary focus of CMS’s inspection process, and she said that increased regulatory scrutiny of IPC beyond COVID-19 is a “good thing.” Her research has shown that most deficiencies identified by inspectors are infection control deficiencies, and that in 2014 and 2018, approximately one-third of nursing homes had infection control citations. (CMS recently increased penalties and fines for identified deficiencies.)
“But my hope would be that the survey process would be more educational [as it is for hospitals],” she said. “We need to be supporting nursing homes to do a better job.”
A silver lining of the COVID-19 pandemic, as Dr. Stone sees it, is that nursing homes may be more engaged with data reporting and infection surveillance going forward. Nursing homes are now required to report their COVID-19 cases to the CDC through its hospital-dominant National Healthcare Safety Network, and the CDC has made technical changes that now make it “easier [than it was in the past] for nursing homes to join and participate,” she said. “Now that all nursing homes are engaged, will they be engaged post-COVID, too? I hope so. Surveillance [of infections] is a first step toward better outcomes.”
For now, said Dr. Crnich, the intensive prevention and mitigation efforts that are being required of nursing homes to minimize COVID-19’s impact is “a big deal and will tax the resources of most nursing homes and exceed the resources of many” without outside support, Dr. Crnich said. “This has been the most illuminating part of all this, and will probably require us to reconsider how we’re resourcing our nursing homes moving forward into the future.”
Elevated inflammation common in children’s severe COVID-19 disease
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
FROM JAMA PEDIATRICS
By the numbers: Asthma-COPD overlap deaths
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
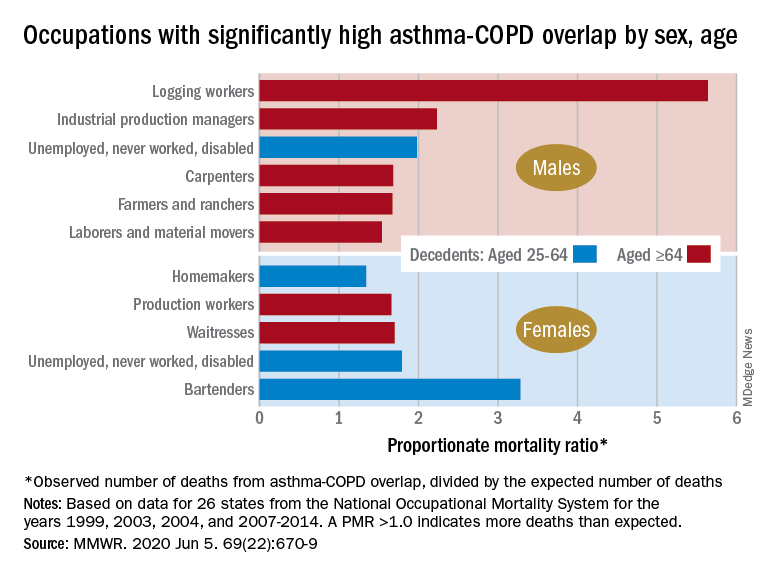
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
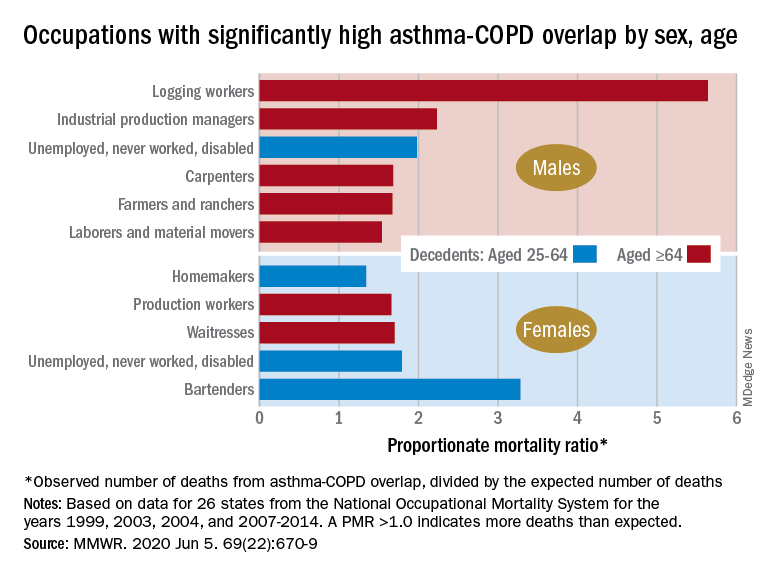
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
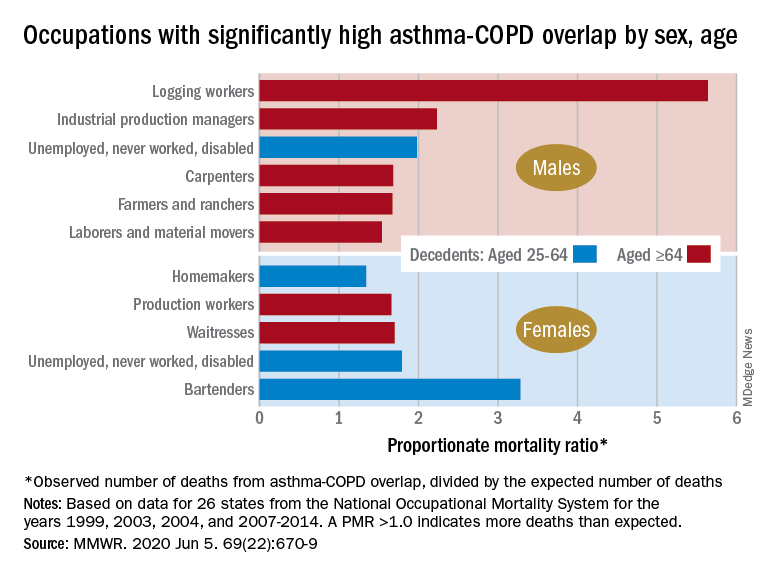
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
FROM MMWR
















