User login
Fentanyl-related deaths show strong regional pattern
Fentanyl was involved in more overdose deaths than any other drug in 2017, and the death rate in New England was 15 times higher than in regions of the Midwest and West, according to the National Center for Health Statistics.
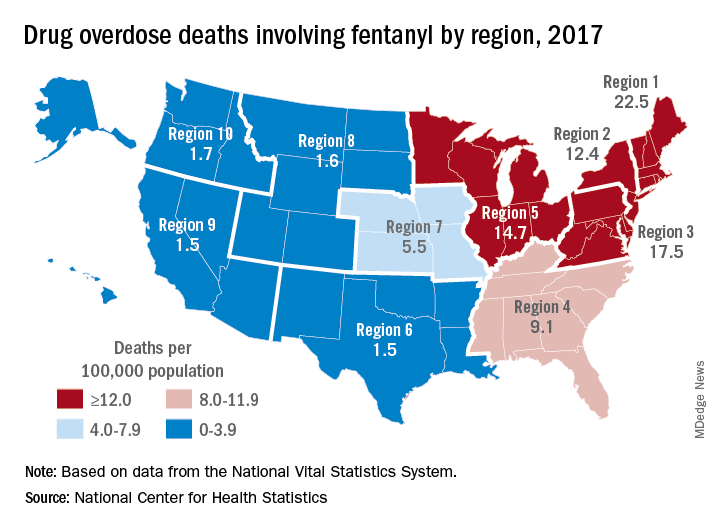
Nationally, fentanyl was involved in 39% of all drug overdose deaths and had an age-adjusted death rate of 8.7/100,000 standard population in 2017. In 2016, when fentanyl also was the most involved drug in the United States, the corresponding figures were 29% and 5.9/100,000, the agency said in a recent report.
Fentanyl was the most involved drug in overdose deaths for 6 of the country’s 10 public health regions in 2017, with a clear pattern of decreasing use from east to west. The highest death rate (22.5/100,000) occurred in Region 1 (New England) and the lowest rates (1.5/100,000) came in Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) and Region 9 (Arizona, California, Hawaii, and Nevada), the researchers said.
A somewhat similar pattern was seen for heroin, which was second nationally on the list of drugs most frequently involved in overdose deaths (23%), except that New England was somewhat below three other regions in the East and upper Midwest. The highest heroin death rate (8.6/100,000) was seen in Region 2 (New Jersey and New York) and the lowest (2.2) occurred in Region 9, they said, based on data from the National Vital Statistics System’s mortality files.
The fentanyl pattern was even more closely repeated with cocaine, third in involvement nationally at 21% of overdose deaths in 2017. The high in overdose deaths (9.5/100,000) came in Region 1 again, and the low in Region 9 (1.3), along with Region 7 (Iowa, Kansas, Missouri, and Nebraska) and Region 10 (Alaska, Idaho, Oregon, and Washington), the report showed.
The regional pattern of overdose deaths for methamphetamine, which was fourth nationally in involvement (13.3%), basically reversed the other three drugs: highest in the West and lowest in the Northeast. Region 9 had the highest death rate (5.2/100,000) and Region 2 the lowest (0.4), with Region 1 just ahead at 0.6.
Fentanyl was involved in more overdose deaths than any other drug in 2017, and the death rate in New England was 15 times higher than in regions of the Midwest and West, according to the National Center for Health Statistics.
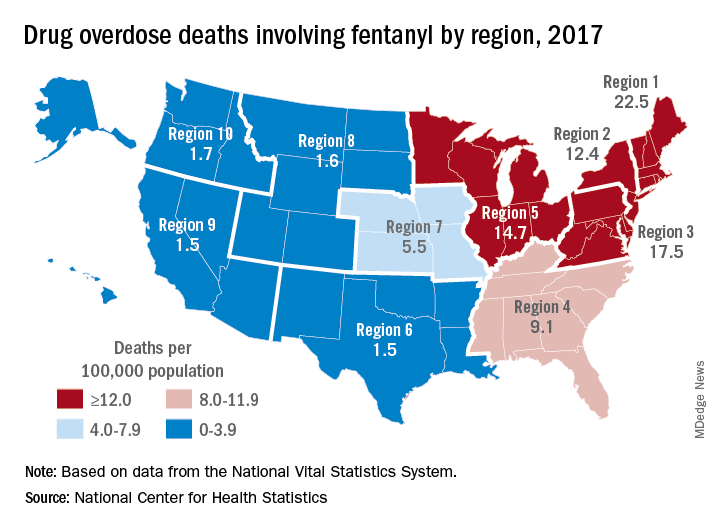
Nationally, fentanyl was involved in 39% of all drug overdose deaths and had an age-adjusted death rate of 8.7/100,000 standard population in 2017. In 2016, when fentanyl also was the most involved drug in the United States, the corresponding figures were 29% and 5.9/100,000, the agency said in a recent report.
Fentanyl was the most involved drug in overdose deaths for 6 of the country’s 10 public health regions in 2017, with a clear pattern of decreasing use from east to west. The highest death rate (22.5/100,000) occurred in Region 1 (New England) and the lowest rates (1.5/100,000) came in Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) and Region 9 (Arizona, California, Hawaii, and Nevada), the researchers said.
A somewhat similar pattern was seen for heroin, which was second nationally on the list of drugs most frequently involved in overdose deaths (23%), except that New England was somewhat below three other regions in the East and upper Midwest. The highest heroin death rate (8.6/100,000) was seen in Region 2 (New Jersey and New York) and the lowest (2.2) occurred in Region 9, they said, based on data from the National Vital Statistics System’s mortality files.
The fentanyl pattern was even more closely repeated with cocaine, third in involvement nationally at 21% of overdose deaths in 2017. The high in overdose deaths (9.5/100,000) came in Region 1 again, and the low in Region 9 (1.3), along with Region 7 (Iowa, Kansas, Missouri, and Nebraska) and Region 10 (Alaska, Idaho, Oregon, and Washington), the report showed.
The regional pattern of overdose deaths for methamphetamine, which was fourth nationally in involvement (13.3%), basically reversed the other three drugs: highest in the West and lowest in the Northeast. Region 9 had the highest death rate (5.2/100,000) and Region 2 the lowest (0.4), with Region 1 just ahead at 0.6.
Fentanyl was involved in more overdose deaths than any other drug in 2017, and the death rate in New England was 15 times higher than in regions of the Midwest and West, according to the National Center for Health Statistics.
Nationally, fentanyl was involved in 39% of all drug overdose deaths and had an age-adjusted death rate of 8.7/100,000 standard population in 2017. In 2016, when fentanyl also was the most involved drug in the United States, the corresponding figures were 29% and 5.9/100,000, the agency said in a recent report.
Fentanyl was the most involved drug in overdose deaths for 6 of the country’s 10 public health regions in 2017, with a clear pattern of decreasing use from east to west. The highest death rate (22.5/100,000) occurred in Region 1 (New England) and the lowest rates (1.5/100,000) came in Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) and Region 9 (Arizona, California, Hawaii, and Nevada), the researchers said.
A somewhat similar pattern was seen for heroin, which was second nationally on the list of drugs most frequently involved in overdose deaths (23%), except that New England was somewhat below three other regions in the East and upper Midwest. The highest heroin death rate (8.6/100,000) was seen in Region 2 (New Jersey and New York) and the lowest (2.2) occurred in Region 9, they said, based on data from the National Vital Statistics System’s mortality files.
The fentanyl pattern was even more closely repeated with cocaine, third in involvement nationally at 21% of overdose deaths in 2017. The high in overdose deaths (9.5/100,000) came in Region 1 again, and the low in Region 9 (1.3), along with Region 7 (Iowa, Kansas, Missouri, and Nebraska) and Region 10 (Alaska, Idaho, Oregon, and Washington), the report showed.
The regional pattern of overdose deaths for methamphetamine, which was fourth nationally in involvement (13.3%), basically reversed the other three drugs: highest in the West and lowest in the Northeast. Region 9 had the highest death rate (5.2/100,000) and Region 2 the lowest (0.4), with Region 1 just ahead at 0.6.
Smokers with PE have higher rate of hospital readmission
NEW ORLEANS – , according to a retrospective study.
The rate of readmission was significantly higher among patients with tobacco dependence, and tobacco dependence was independently associated with an increased risk of readmission.
“This is the first study to quantify the increased rate of hospital readmission due to smoking,” said study investigator Kam Sing Ho, MD, of Mount Sinai St. Luke’s and Mount Sinai West, New York.
Dr. Ho and colleagues described this study and its results in a poster presented at the annual meeting of the American College of Chest Physicians.
The researchers analyzed data on 168,891 hospital admissions of adults with PE, 34.2% of whom had tobacco dependence. Patients with and without tobacco dependence were propensity matched for baseline characteristics (n = 24,262 in each group).
The 30-day readmission rate was significantly higher in patients with tobacco dependence than in those without it – 11.0% and 8.9%, respectively (P less than .001). The most common reason for readmission in both groups was PE.
Dr. Ho said the higher readmission rate among patients with tobacco dependence might be explained by the fact that smokers have a higher level of fibrinogen, which may affect blood viscosity and contribute to thrombus formation (Proc Am Thorac Soc. 2005;2[1]:71-7).
The investigators also found that tobacco dependence was an independent predictor of readmission (hazard ratio, 1.43; P less than .001). And the mortality rate was significantly higher after readmission than after index admission – 6.27% and 3.15%, respectively (P less than .001).
The increased risk of readmission and death among smokers highlights the importance of smoking cessation services. Dr. Ho cited previous research suggesting these services are underused in the hospital setting (BMJ Qual Improv Rep. 2014;3[1]:u204964.w2110).
“Given that smoking is a common phenomenon among patients admitted with pulmonary embolism, we suggest that more rigorous smoking cessation services are implemented prior to discharge for all active smokers,” Dr. Ho said. “[P]atients have the right to be informed on the benefits of smoking cessation and the autonomy to choose. Future research will focus on implementing inpatient smoking cessation at our hospital and its effect on local readmission rate, health resources utilization, and mortality.”
Dr. Ho has no relevant relationships to disclose.
SOURCE: Ho KS et al. CHEST 2019 October. doi: 10.1016/j.chest.2019.08.1551.
NEW ORLEANS – , according to a retrospective study.
The rate of readmission was significantly higher among patients with tobacco dependence, and tobacco dependence was independently associated with an increased risk of readmission.
“This is the first study to quantify the increased rate of hospital readmission due to smoking,” said study investigator Kam Sing Ho, MD, of Mount Sinai St. Luke’s and Mount Sinai West, New York.
Dr. Ho and colleagues described this study and its results in a poster presented at the annual meeting of the American College of Chest Physicians.
The researchers analyzed data on 168,891 hospital admissions of adults with PE, 34.2% of whom had tobacco dependence. Patients with and without tobacco dependence were propensity matched for baseline characteristics (n = 24,262 in each group).
The 30-day readmission rate was significantly higher in patients with tobacco dependence than in those without it – 11.0% and 8.9%, respectively (P less than .001). The most common reason for readmission in both groups was PE.
Dr. Ho said the higher readmission rate among patients with tobacco dependence might be explained by the fact that smokers have a higher level of fibrinogen, which may affect blood viscosity and contribute to thrombus formation (Proc Am Thorac Soc. 2005;2[1]:71-7).
The investigators also found that tobacco dependence was an independent predictor of readmission (hazard ratio, 1.43; P less than .001). And the mortality rate was significantly higher after readmission than after index admission – 6.27% and 3.15%, respectively (P less than .001).
The increased risk of readmission and death among smokers highlights the importance of smoking cessation services. Dr. Ho cited previous research suggesting these services are underused in the hospital setting (BMJ Qual Improv Rep. 2014;3[1]:u204964.w2110).
“Given that smoking is a common phenomenon among patients admitted with pulmonary embolism, we suggest that more rigorous smoking cessation services are implemented prior to discharge for all active smokers,” Dr. Ho said. “[P]atients have the right to be informed on the benefits of smoking cessation and the autonomy to choose. Future research will focus on implementing inpatient smoking cessation at our hospital and its effect on local readmission rate, health resources utilization, and mortality.”
Dr. Ho has no relevant relationships to disclose.
SOURCE: Ho KS et al. CHEST 2019 October. doi: 10.1016/j.chest.2019.08.1551.
NEW ORLEANS – , according to a retrospective study.
The rate of readmission was significantly higher among patients with tobacco dependence, and tobacco dependence was independently associated with an increased risk of readmission.
“This is the first study to quantify the increased rate of hospital readmission due to smoking,” said study investigator Kam Sing Ho, MD, of Mount Sinai St. Luke’s and Mount Sinai West, New York.
Dr. Ho and colleagues described this study and its results in a poster presented at the annual meeting of the American College of Chest Physicians.
The researchers analyzed data on 168,891 hospital admissions of adults with PE, 34.2% of whom had tobacco dependence. Patients with and without tobacco dependence were propensity matched for baseline characteristics (n = 24,262 in each group).
The 30-day readmission rate was significantly higher in patients with tobacco dependence than in those without it – 11.0% and 8.9%, respectively (P less than .001). The most common reason for readmission in both groups was PE.
Dr. Ho said the higher readmission rate among patients with tobacco dependence might be explained by the fact that smokers have a higher level of fibrinogen, which may affect blood viscosity and contribute to thrombus formation (Proc Am Thorac Soc. 2005;2[1]:71-7).
The investigators also found that tobacco dependence was an independent predictor of readmission (hazard ratio, 1.43; P less than .001). And the mortality rate was significantly higher after readmission than after index admission – 6.27% and 3.15%, respectively (P less than .001).
The increased risk of readmission and death among smokers highlights the importance of smoking cessation services. Dr. Ho cited previous research suggesting these services are underused in the hospital setting (BMJ Qual Improv Rep. 2014;3[1]:u204964.w2110).
“Given that smoking is a common phenomenon among patients admitted with pulmonary embolism, we suggest that more rigorous smoking cessation services are implemented prior to discharge for all active smokers,” Dr. Ho said. “[P]atients have the right to be informed on the benefits of smoking cessation and the autonomy to choose. Future research will focus on implementing inpatient smoking cessation at our hospital and its effect on local readmission rate, health resources utilization, and mortality.”
Dr. Ho has no relevant relationships to disclose.
SOURCE: Ho KS et al. CHEST 2019 October. doi: 10.1016/j.chest.2019.08.1551.
REPORTING FROM CHEST 2019
Oral vs. IV antibiotic therapy in early treatment of complex bone and joint infections
Background: The standard of care for complex bone and joint infections includes the use of IV antibiotics. A prior meta-analysis suggested that the outcomes for bone and joint infections treated with oral and IV antibiotics are similar.
Study design: Randomized, controlled trial.
Setting: Twenty-six U.K. sites during June 2010–October 2015.
Synopsis: The study enrolled 1,054 adults with bone or joint infections who would have been treated with 6 weeks of IV antibiotics; they were then randomized to receive either IV or oral antibiotics. Treatment regimens were selected by infectious disease specialists. The rate of the primary endpoint, definite treatment failure at 1 year after randomization, was 14.6% in the intravenous group and 13.2% in the oral group. The difference in the risk of definite treatment failure between the two groups was –1.4% (95% confidence interval, –5.6 to 2.9), which met the predefined noninferiority criteria. The use of oral antibiotics also was associated with a shorter hospital stay and fewer complications. The conclusions of the trial are limited by the open-label design. An associated editorial advocated for additional research before widespread change to current treatment recommendations.
Bottom line: Bone and joint infections treated with oral versus IV antibiotics may have similar treatment failure rates.
Citation: Li HK et al. Oral versus intravenous antibiotics for bone and joint infection. N Eng J Med. 2019 Jan 31;380(5):425-36.
Dr. Roy is a hospitalist at Beth Israel Deaconess Medical Center and instructor in medicine at Harvard Medical School.
Background: The standard of care for complex bone and joint infections includes the use of IV antibiotics. A prior meta-analysis suggested that the outcomes for bone and joint infections treated with oral and IV antibiotics are similar.
Study design: Randomized, controlled trial.
Setting: Twenty-six U.K. sites during June 2010–October 2015.
Synopsis: The study enrolled 1,054 adults with bone or joint infections who would have been treated with 6 weeks of IV antibiotics; they were then randomized to receive either IV or oral antibiotics. Treatment regimens were selected by infectious disease specialists. The rate of the primary endpoint, definite treatment failure at 1 year after randomization, was 14.6% in the intravenous group and 13.2% in the oral group. The difference in the risk of definite treatment failure between the two groups was –1.4% (95% confidence interval, –5.6 to 2.9), which met the predefined noninferiority criteria. The use of oral antibiotics also was associated with a shorter hospital stay and fewer complications. The conclusions of the trial are limited by the open-label design. An associated editorial advocated for additional research before widespread change to current treatment recommendations.
Bottom line: Bone and joint infections treated with oral versus IV antibiotics may have similar treatment failure rates.
Citation: Li HK et al. Oral versus intravenous antibiotics for bone and joint infection. N Eng J Med. 2019 Jan 31;380(5):425-36.
Dr. Roy is a hospitalist at Beth Israel Deaconess Medical Center and instructor in medicine at Harvard Medical School.
Background: The standard of care for complex bone and joint infections includes the use of IV antibiotics. A prior meta-analysis suggested that the outcomes for bone and joint infections treated with oral and IV antibiotics are similar.
Study design: Randomized, controlled trial.
Setting: Twenty-six U.K. sites during June 2010–October 2015.
Synopsis: The study enrolled 1,054 adults with bone or joint infections who would have been treated with 6 weeks of IV antibiotics; they were then randomized to receive either IV or oral antibiotics. Treatment regimens were selected by infectious disease specialists. The rate of the primary endpoint, definite treatment failure at 1 year after randomization, was 14.6% in the intravenous group and 13.2% in the oral group. The difference in the risk of definite treatment failure between the two groups was –1.4% (95% confidence interval, –5.6 to 2.9), which met the predefined noninferiority criteria. The use of oral antibiotics also was associated with a shorter hospital stay and fewer complications. The conclusions of the trial are limited by the open-label design. An associated editorial advocated for additional research before widespread change to current treatment recommendations.
Bottom line: Bone and joint infections treated with oral versus IV antibiotics may have similar treatment failure rates.
Citation: Li HK et al. Oral versus intravenous antibiotics for bone and joint infection. N Eng J Med. 2019 Jan 31;380(5):425-36.
Dr. Roy is a hospitalist at Beth Israel Deaconess Medical Center and instructor in medicine at Harvard Medical School.
Glycemic Control eQUIPS yields success at Dignity Health Sequoia Hospital
Glucometrics database aids tracking, trending
In honor of Diabetes Awareness Month, The Hospitalist spoke recently with Stephanie Dizon, PharmD, BCPS, director of pharmacy at Dignity Health Sequoia Hospital in Redwood City, Calif. Dr. Dizon was the project lead for Dignity Health Sequoia’s participation in the Society of Hospital Medicine’s Glycemic Control eQUIPS program. The Northern California hospital was recognized as a top performer in the program.
SHM’s eQUIPS offers a virtual library of resources, including a step-by-step implementation guide, that addresses various issues that range from subcutaneous insulin protocols to care coordination and good hypoglycemia management. In addition, the program offers access to a data center for performance tracking and benchmarking.
Dr. Dizon shared her experience as a participant in the program, and explained its impact on glycemic control at Dignity Health Sequoia Hospital.
Could you tell us about your personal involvement with SHM?
I started as the quality lead for glycemic control for Sequoia Hospital in 2017 while serving in the role as the clinical pharmacy manager. Currently, I am the director of pharmacy.
What inspired your institution to enroll in the GC eQUIPS program? What were the challenges it helped you address?
Sequoia Hospital started in this journey to improve overall glycemic control in a collaborative with eight other Dignity Health hospitals in 2011. At Sequoia Hospital, this effort was led by Karen Harrison, RN, MSN, CCRN. At the time, Dignity Health saw variations in insulin management and adverse events, and it inspired this group to review their practices and try to find a better way to standardize them. The hope was that sharing information and making efforts to standardize practices would lead to better glycemic control.
Enrollment in the GC eQUIPS program helped Sequoia Hospital efficiently analyze data that would otherwise be too large to manage. In addition, by tracking and trending these large data sets, it helped us not only to see where the hospital’s greatest challenges are in glycemic control but also observe what the impact is when making changes. We were part of a nine-site study that proved the effectiveness of GC eQUIPS and highlighted the collective success across the health system.
What did you find most useful in the suite of resources included in eQUIPS?
The benchmarking webinars and informational webinars that have been provided by Greg Maynard, MD, over the years have been especially helpful. They have broadened my understanding of glycemic control. The glucometrics database is especially helpful for tracking and trending – we share these reports on a monthly basis with nursing and provider leadership. In addition, being able to benchmark ourselves with other hospitals pushes us to improve and keep an eye on glycemic control.
Are there any other highlights from your participation– and your institution’s – in the program that you feel would be beneficial to others who may be considering enrollment?
Having access to the tools available in the GC eQUIPS program is very powerful for data analysis and benchmarking. As a result, it allows the people at an institution to focus on the day-to-day tasks, clinical initiatives, and building a culture that can make a program successful instead of focusing on data collection.
For more information on SHM’s Glycemic Control resources or to enroll in eQUIPS, visit hospitalmedicine.org/gc.
Glucometrics database aids tracking, trending
Glucometrics database aids tracking, trending
In honor of Diabetes Awareness Month, The Hospitalist spoke recently with Stephanie Dizon, PharmD, BCPS, director of pharmacy at Dignity Health Sequoia Hospital in Redwood City, Calif. Dr. Dizon was the project lead for Dignity Health Sequoia’s participation in the Society of Hospital Medicine’s Glycemic Control eQUIPS program. The Northern California hospital was recognized as a top performer in the program.
SHM’s eQUIPS offers a virtual library of resources, including a step-by-step implementation guide, that addresses various issues that range from subcutaneous insulin protocols to care coordination and good hypoglycemia management. In addition, the program offers access to a data center for performance tracking and benchmarking.
Dr. Dizon shared her experience as a participant in the program, and explained its impact on glycemic control at Dignity Health Sequoia Hospital.
Could you tell us about your personal involvement with SHM?
I started as the quality lead for glycemic control for Sequoia Hospital in 2017 while serving in the role as the clinical pharmacy manager. Currently, I am the director of pharmacy.
What inspired your institution to enroll in the GC eQUIPS program? What were the challenges it helped you address?
Sequoia Hospital started in this journey to improve overall glycemic control in a collaborative with eight other Dignity Health hospitals in 2011. At Sequoia Hospital, this effort was led by Karen Harrison, RN, MSN, CCRN. At the time, Dignity Health saw variations in insulin management and adverse events, and it inspired this group to review their practices and try to find a better way to standardize them. The hope was that sharing information and making efforts to standardize practices would lead to better glycemic control.
Enrollment in the GC eQUIPS program helped Sequoia Hospital efficiently analyze data that would otherwise be too large to manage. In addition, by tracking and trending these large data sets, it helped us not only to see where the hospital’s greatest challenges are in glycemic control but also observe what the impact is when making changes. We were part of a nine-site study that proved the effectiveness of GC eQUIPS and highlighted the collective success across the health system.
What did you find most useful in the suite of resources included in eQUIPS?
The benchmarking webinars and informational webinars that have been provided by Greg Maynard, MD, over the years have been especially helpful. They have broadened my understanding of glycemic control. The glucometrics database is especially helpful for tracking and trending – we share these reports on a monthly basis with nursing and provider leadership. In addition, being able to benchmark ourselves with other hospitals pushes us to improve and keep an eye on glycemic control.
Are there any other highlights from your participation– and your institution’s – in the program that you feel would be beneficial to others who may be considering enrollment?
Having access to the tools available in the GC eQUIPS program is very powerful for data analysis and benchmarking. As a result, it allows the people at an institution to focus on the day-to-day tasks, clinical initiatives, and building a culture that can make a program successful instead of focusing on data collection.
For more information on SHM’s Glycemic Control resources or to enroll in eQUIPS, visit hospitalmedicine.org/gc.
In honor of Diabetes Awareness Month, The Hospitalist spoke recently with Stephanie Dizon, PharmD, BCPS, director of pharmacy at Dignity Health Sequoia Hospital in Redwood City, Calif. Dr. Dizon was the project lead for Dignity Health Sequoia’s participation in the Society of Hospital Medicine’s Glycemic Control eQUIPS program. The Northern California hospital was recognized as a top performer in the program.
SHM’s eQUIPS offers a virtual library of resources, including a step-by-step implementation guide, that addresses various issues that range from subcutaneous insulin protocols to care coordination and good hypoglycemia management. In addition, the program offers access to a data center for performance tracking and benchmarking.
Dr. Dizon shared her experience as a participant in the program, and explained its impact on glycemic control at Dignity Health Sequoia Hospital.
Could you tell us about your personal involvement with SHM?
I started as the quality lead for glycemic control for Sequoia Hospital in 2017 while serving in the role as the clinical pharmacy manager. Currently, I am the director of pharmacy.
What inspired your institution to enroll in the GC eQUIPS program? What were the challenges it helped you address?
Sequoia Hospital started in this journey to improve overall glycemic control in a collaborative with eight other Dignity Health hospitals in 2011. At Sequoia Hospital, this effort was led by Karen Harrison, RN, MSN, CCRN. At the time, Dignity Health saw variations in insulin management and adverse events, and it inspired this group to review their practices and try to find a better way to standardize them. The hope was that sharing information and making efforts to standardize practices would lead to better glycemic control.
Enrollment in the GC eQUIPS program helped Sequoia Hospital efficiently analyze data that would otherwise be too large to manage. In addition, by tracking and trending these large data sets, it helped us not only to see where the hospital’s greatest challenges are in glycemic control but also observe what the impact is when making changes. We were part of a nine-site study that proved the effectiveness of GC eQUIPS and highlighted the collective success across the health system.
What did you find most useful in the suite of resources included in eQUIPS?
The benchmarking webinars and informational webinars that have been provided by Greg Maynard, MD, over the years have been especially helpful. They have broadened my understanding of glycemic control. The glucometrics database is especially helpful for tracking and trending – we share these reports on a monthly basis with nursing and provider leadership. In addition, being able to benchmark ourselves with other hospitals pushes us to improve and keep an eye on glycemic control.
Are there any other highlights from your participation– and your institution’s – in the program that you feel would be beneficial to others who may be considering enrollment?
Having access to the tools available in the GC eQUIPS program is very powerful for data analysis and benchmarking. As a result, it allows the people at an institution to focus on the day-to-day tasks, clinical initiatives, and building a culture that can make a program successful instead of focusing on data collection.
For more information on SHM’s Glycemic Control resources or to enroll in eQUIPS, visit hospitalmedicine.org/gc.
Better time data from in-hospital resuscitations
Benefits of an undocumented defibrillator feature
Research and quality improvement (QI) related to in-hospital cardiopulmonary resuscitation attempts (“codes” from here forward) are hampered significantly by the poor quality of data on time intervals from arrest onset to clinical interventions.1
In 2000, the American Heart Association’s (AHA) Emergency Cardiac Care Guidelines said that current data were inaccurate and that greater accuracy was “the key to future high-quality research”2 – but since then, the general situation has not improved: Time intervals reported by the national AHA-supported registry Get With the Guidelines–Resuscitation (GWTG-R, 200+ hospitals enrolled) include a figure from all hospitals for times to first defibrillation of 1 minute median and 0 minutes first interquartile.3 Such numbers are typical – when they are tracked at all – but they strain credulity, and prima facie evidence is available at most clinical simulation centers simply by timing simulated defibrillation attempts under realistic conditions, as in “mock codes.”4,5
Taking artificially short time-interval data from GWTG-R or other sources at face value can hide serious delays in response to in-hospital arrests. It can also lead to flawed studies and highly questionable conclusions.6
The key to accuracy of critical time intervals – the intervals from arrest to key interventions – is an accurate time of arrest.7 Codes are typically recorded in handwritten form, though they may later be transcribed or scanned into electronic records. The “start” of the code for unmonitored arrests and most monitored arrests is typically taken to be the time that a human bedside recorder, arriving at an unknown interval after the arrest, writes down the first intervention. Researchers acknowledged the problem of artificially short time intervals in 2005, but they did not propose a remedy.1 Since then, the problem of in-hospital resuscitation delays has received little to no attention in the professional literature.
Description of feature
To get better time data from unmonitored resuscitation attempts, it is necessary to use a “surrogate marker” – a stand-in or substitute event – for the time of arrest. This event should occur reliably for each code, and as near as possible to the actual time of arrest. The main early events in a code are starting basic CPR, paging the code, and moving the defibrillator (usually on a code cart) to the scene. Ideally these events occur almost simultaneously, but that is not consistently achieved.
There are significant problems with use of the first two events as surrogate markers: the time of starting CPR cannot be determined accurately, and paging the code is dependent on several intermediate steps that lead to inaccuracy. Furthermore, the times of both markers are recorded using clocks that are typically not synchronized with the clock used for recording the code (defibrillator clock or the human recorder’s timepiece). Reconciliation of these times with the code record, while not particularly difficult,8 is rarely if ever done.
Defibrillator Power On is recorded on the defibrillator timeline and thus does not need to be reconciled with the defibrillator clock, but it is not suitable as a surrogate marker because this time is highly variable: It often does not occur until the time that monitoring pads are placed. Moving the code cart to the scene, which must occur early in the code, is a much more valid surrogate marker, with the added benefit that it can be marked on the defibrillator timeline.
The undocumented feature described here provides that marker. This feature has been a part of the LIFEPAK 20/20e’s design since it was launched in 2002, but it has not been publicized until now and is not documented in the user manual.
Hospital defibrillators are connected to alternating-current (AC) power when not in use. When the defibrillator is moved to the scene of the code, it is obviously necessary to disconnect the defibrillator from the wall outlet, at which time “AC Power Loss” is recorded on the event record generated by the LIFEPAK 20/20e defibrillators. The defibrillator may be powered on up to 10 minutes later while retaining the AC Power Loss marker in the event record. This surrogate marker for the start time will be on the same timeline as other events recorded by the defibrillator, including times of first monitoring and shocks.
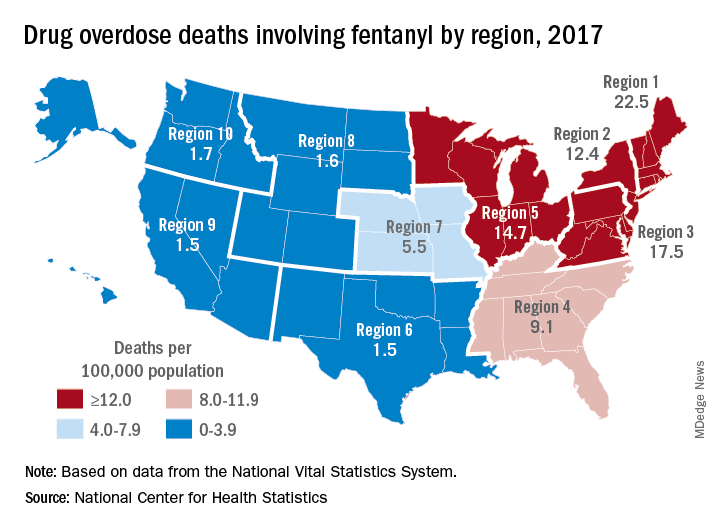
Once the event record is acquired, determining time intervals is accomplished by subtracting clock times (see example, Figure 1).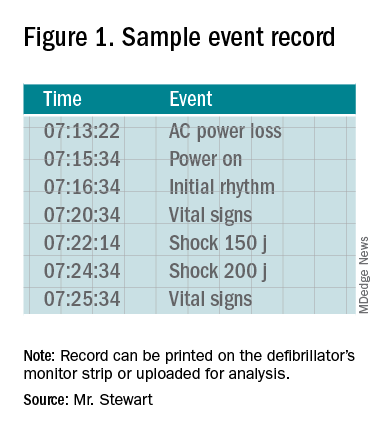
In the example, using AC Power Loss as the start time, time intervals from arrest to first monitoring (Initial Rhythm on the Event Record) and first shock were 3:12 (07:16:34 minus 07:13:22) and 8:42 (07:22:14 minus 07:13:22). Note that if Power On were used as the surrogate time of arrest in the example, the calculated intervals would be artificially shorter, by 2 min 12 sec.
Using this undocumented feature, any facility using LIFEPAK 20/20e defibrillators can easily measure critical time intervals during resuscitation attempts with much greater accuracy, including times to first monitoring and first defibrillation. Each defibrillator stores code summaries sufficient for dozens of events and accessing past data is simple. Analysis of the data can provide a much-improved measure of the facility’s speed of response as a baseline for QI.
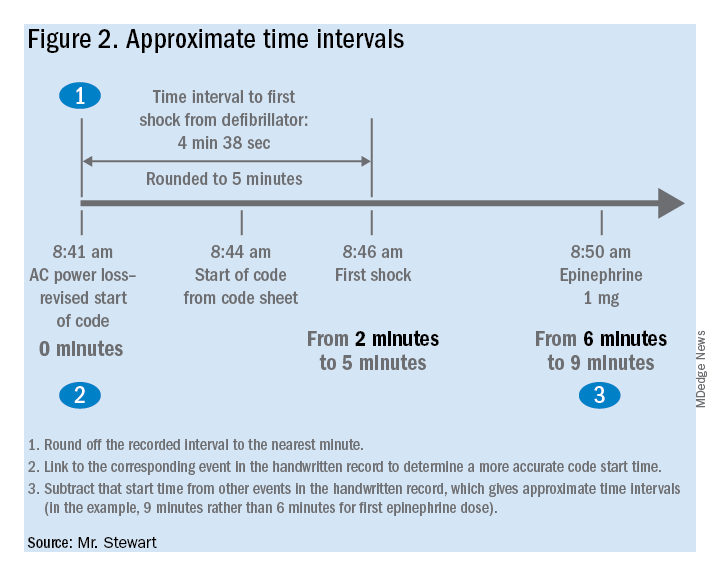
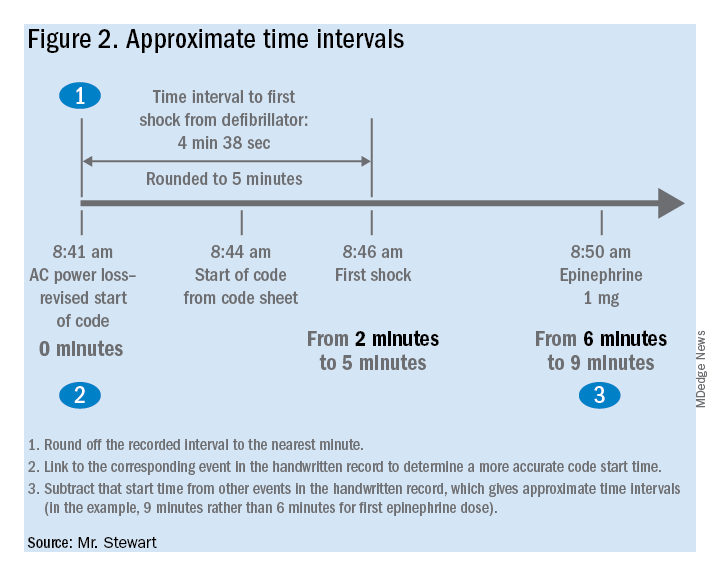
If desired, the time-interval data thus obtained can also be integrated with the handwritten record. The usual handwritten code sheet records times only in whole minutes, but with one of the more accurate intervals from the defibrillator – to first monitoring or first defibrillation – an adjusted time of arrest can be added to any code record to get other intervals that better approximate real-world response times.9
Research prospects
The feature opens multiple avenues for future research. Acquiring data by this method should be simple for any facility using LIFEPAK 20/20e defibrillators as its standard devices. Matching the existing handwritten code records with the time intervals obtained using this surrogate time marker will show how inaccurate the commonly reported data are. This can be done with a retrospective study comparing the time intervals from the archived event records with those from the handwritten records, to provide an example of the inaccuracy of data reported in the medical literature. The more accurate picture of time intervals can provide a much-needed yardstick for future research aimed at shortening response times.
The feature can facilitate aggregation of data across multiple facilities that use the LIFEPAK 20/20e as their standard defibrillator. Also, it is possible that other defibrillator manufacturers will duplicate this feature with their devices – it should produce valid data with any defibrillator – although there may be legal and technical obstacles to adopting it.
Combining data from multiple sites might lead to an important contribution to resuscitation research: a reasonably accurate overall survival curve for in-hospital tachyarrhythmic arrests. A commonly cited but crude guideline is that survival from tachyarrhythmic arrests decreases by 10%-15% per minute as defibrillation is delayed,10 but it seems unlikely that the relationship would be linear: Experience and the literature suggest that survival drops very quickly in the first few minutes, flattening out as elapsed time after arrest increases. Aggregating the much more accurate time-interval data from multiple facilities should produce a survival curve for in-hospital tachyarrhythmic arrests that comes much closer to reality.
Conclusion
It is unknown whether this feature will be used to improve the accuracy of reported code response times. It greatly facilitates acquiring more accurate times, but the task has never been especially difficult – particularly when balanced with the importance of better time data for QI and research.8 One possible impediment may be institutional obstacles to publishing studies with accurate response times due to concerns about public relations or legal exposure: The more accurate times will almost certainly be longer than those generally reported.
As was stated almost 2 decades ago and remains true today, acquiring accurate time-interval data is “the key to future high-quality research.”2 It is also key to improving any hospital’s quality of code response. As described in this article, better time data can easily be acquired. It is time for this important problem to be recognized and remedied.
Mr. Stewart has worked as a hospital nurse in Seattle for many years, and has numerous publications to his credit related to resuscitation issues. You can contact him at [email protected].
References
1. Kaye W et al. When minutes count – the fallacy of accurate time documentation during in-hospital resuscitation. Resuscitation. 2005;65(3):285-90.
2. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 4: the automated external defibrillator: key link in the chain of survival. Circulation. 2000;102(8 Suppl):I-60-76.
3. Chan PS et al. American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008 Jan 3;358(1):9-17. doi: 10.1056/NEJMoa0706467.
4. Hunt EA et al. Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: Highlighting the importance of the first 5 minutes. Pediatrics. 2008;121(1):e34-e43. doi: 10.1542/peds.2007-0029.
5. Reeson M et al. Defibrillator design and usability may be impeding timely defibrillation. Comm J Qual Patient Saf. 2018 Sep;44(9):536-544. doi: 10.1016/j.jcjq.2018.01.005.
6. Hunt EA et al. American Heart Association’s Get With The Guidelines – Resuscitation Investigators. Association between time to defibrillation and survival in pediatric in-hospital cardiac arrest with a first documented shockable rhythm JAMA Netw Open. 2018;1(5):e182643. doi: 10.1001/jamanetworkopen.2018.2643.
7. Cummins RO et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital “Utstein” style. Circulation. 1997;95:2213-39.
8. Stewart JA. Determining accurate call-to-shock times is easy. Resuscitation. 2005 Oct;67(1):150-1.
9. In infrequent cases, the code cart and defibrillator may be moved to a deteriorating patient before a full arrest. Such occurrences should be analyzed separately or excluded from analysis.
10. Valenzuela TD et al. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96(10):3308-13. doi: 10.1161/01.cir.96.10.3308.
Benefits of an undocumented defibrillator feature
Benefits of an undocumented defibrillator feature
Research and quality improvement (QI) related to in-hospital cardiopulmonary resuscitation attempts (“codes” from here forward) are hampered significantly by the poor quality of data on time intervals from arrest onset to clinical interventions.1
In 2000, the American Heart Association’s (AHA) Emergency Cardiac Care Guidelines said that current data were inaccurate and that greater accuracy was “the key to future high-quality research”2 – but since then, the general situation has not improved: Time intervals reported by the national AHA-supported registry Get With the Guidelines–Resuscitation (GWTG-R, 200+ hospitals enrolled) include a figure from all hospitals for times to first defibrillation of 1 minute median and 0 minutes first interquartile.3 Such numbers are typical – when they are tracked at all – but they strain credulity, and prima facie evidence is available at most clinical simulation centers simply by timing simulated defibrillation attempts under realistic conditions, as in “mock codes.”4,5
Taking artificially short time-interval data from GWTG-R or other sources at face value can hide serious delays in response to in-hospital arrests. It can also lead to flawed studies and highly questionable conclusions.6
The key to accuracy of critical time intervals – the intervals from arrest to key interventions – is an accurate time of arrest.7 Codes are typically recorded in handwritten form, though they may later be transcribed or scanned into electronic records. The “start” of the code for unmonitored arrests and most monitored arrests is typically taken to be the time that a human bedside recorder, arriving at an unknown interval after the arrest, writes down the first intervention. Researchers acknowledged the problem of artificially short time intervals in 2005, but they did not propose a remedy.1 Since then, the problem of in-hospital resuscitation delays has received little to no attention in the professional literature.
Description of feature
To get better time data from unmonitored resuscitation attempts, it is necessary to use a “surrogate marker” – a stand-in or substitute event – for the time of arrest. This event should occur reliably for each code, and as near as possible to the actual time of arrest. The main early events in a code are starting basic CPR, paging the code, and moving the defibrillator (usually on a code cart) to the scene. Ideally these events occur almost simultaneously, but that is not consistently achieved.
There are significant problems with use of the first two events as surrogate markers: the time of starting CPR cannot be determined accurately, and paging the code is dependent on several intermediate steps that lead to inaccuracy. Furthermore, the times of both markers are recorded using clocks that are typically not synchronized with the clock used for recording the code (defibrillator clock or the human recorder’s timepiece). Reconciliation of these times with the code record, while not particularly difficult,8 is rarely if ever done.
Defibrillator Power On is recorded on the defibrillator timeline and thus does not need to be reconciled with the defibrillator clock, but it is not suitable as a surrogate marker because this time is highly variable: It often does not occur until the time that monitoring pads are placed. Moving the code cart to the scene, which must occur early in the code, is a much more valid surrogate marker, with the added benefit that it can be marked on the defibrillator timeline.
The undocumented feature described here provides that marker. This feature has been a part of the LIFEPAK 20/20e’s design since it was launched in 2002, but it has not been publicized until now and is not documented in the user manual.
Hospital defibrillators are connected to alternating-current (AC) power when not in use. When the defibrillator is moved to the scene of the code, it is obviously necessary to disconnect the defibrillator from the wall outlet, at which time “AC Power Loss” is recorded on the event record generated by the LIFEPAK 20/20e defibrillators. The defibrillator may be powered on up to 10 minutes later while retaining the AC Power Loss marker in the event record. This surrogate marker for the start time will be on the same timeline as other events recorded by the defibrillator, including times of first monitoring and shocks.
Once the event record is acquired, determining time intervals is accomplished by subtracting clock times (see example, Figure 1).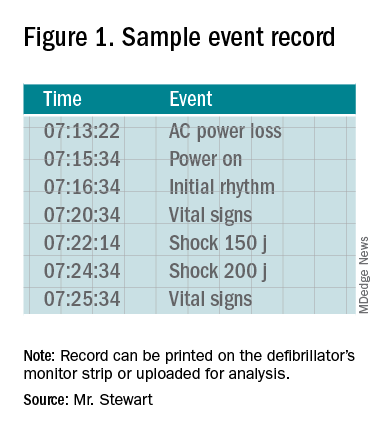
In the example, using AC Power Loss as the start time, time intervals from arrest to first monitoring (Initial Rhythm on the Event Record) and first shock were 3:12 (07:16:34 minus 07:13:22) and 8:42 (07:22:14 minus 07:13:22). Note that if Power On were used as the surrogate time of arrest in the example, the calculated intervals would be artificially shorter, by 2 min 12 sec.
Using this undocumented feature, any facility using LIFEPAK 20/20e defibrillators can easily measure critical time intervals during resuscitation attempts with much greater accuracy, including times to first monitoring and first defibrillation. Each defibrillator stores code summaries sufficient for dozens of events and accessing past data is simple. Analysis of the data can provide a much-improved measure of the facility’s speed of response as a baseline for QI.
If desired, the time-interval data thus obtained can also be integrated with the handwritten record. The usual handwritten code sheet records times only in whole minutes, but with one of the more accurate intervals from the defibrillator – to first monitoring or first defibrillation – an adjusted time of arrest can be added to any code record to get other intervals that better approximate real-world response times.9
Research prospects
The feature opens multiple avenues for future research. Acquiring data by this method should be simple for any facility using LIFEPAK 20/20e defibrillators as its standard devices. Matching the existing handwritten code records with the time intervals obtained using this surrogate time marker will show how inaccurate the commonly reported data are. This can be done with a retrospective study comparing the time intervals from the archived event records with those from the handwritten records, to provide an example of the inaccuracy of data reported in the medical literature. The more accurate picture of time intervals can provide a much-needed yardstick for future research aimed at shortening response times.
The feature can facilitate aggregation of data across multiple facilities that use the LIFEPAK 20/20e as their standard defibrillator. Also, it is possible that other defibrillator manufacturers will duplicate this feature with their devices – it should produce valid data with any defibrillator – although there may be legal and technical obstacles to adopting it.
Combining data from multiple sites might lead to an important contribution to resuscitation research: a reasonably accurate overall survival curve for in-hospital tachyarrhythmic arrests. A commonly cited but crude guideline is that survival from tachyarrhythmic arrests decreases by 10%-15% per minute as defibrillation is delayed,10 but it seems unlikely that the relationship would be linear: Experience and the literature suggest that survival drops very quickly in the first few minutes, flattening out as elapsed time after arrest increases. Aggregating the much more accurate time-interval data from multiple facilities should produce a survival curve for in-hospital tachyarrhythmic arrests that comes much closer to reality.
Conclusion
It is unknown whether this feature will be used to improve the accuracy of reported code response times. It greatly facilitates acquiring more accurate times, but the task has never been especially difficult – particularly when balanced with the importance of better time data for QI and research.8 One possible impediment may be institutional obstacles to publishing studies with accurate response times due to concerns about public relations or legal exposure: The more accurate times will almost certainly be longer than those generally reported.
As was stated almost 2 decades ago and remains true today, acquiring accurate time-interval data is “the key to future high-quality research.”2 It is also key to improving any hospital’s quality of code response. As described in this article, better time data can easily be acquired. It is time for this important problem to be recognized and remedied.
Mr. Stewart has worked as a hospital nurse in Seattle for many years, and has numerous publications to his credit related to resuscitation issues. You can contact him at [email protected].
References
1. Kaye W et al. When minutes count – the fallacy of accurate time documentation during in-hospital resuscitation. Resuscitation. 2005;65(3):285-90.
2. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 4: the automated external defibrillator: key link in the chain of survival. Circulation. 2000;102(8 Suppl):I-60-76.
3. Chan PS et al. American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008 Jan 3;358(1):9-17. doi: 10.1056/NEJMoa0706467.
4. Hunt EA et al. Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: Highlighting the importance of the first 5 minutes. Pediatrics. 2008;121(1):e34-e43. doi: 10.1542/peds.2007-0029.
5. Reeson M et al. Defibrillator design and usability may be impeding timely defibrillation. Comm J Qual Patient Saf. 2018 Sep;44(9):536-544. doi: 10.1016/j.jcjq.2018.01.005.
6. Hunt EA et al. American Heart Association’s Get With The Guidelines – Resuscitation Investigators. Association between time to defibrillation and survival in pediatric in-hospital cardiac arrest with a first documented shockable rhythm JAMA Netw Open. 2018;1(5):e182643. doi: 10.1001/jamanetworkopen.2018.2643.
7. Cummins RO et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital “Utstein” style. Circulation. 1997;95:2213-39.
8. Stewart JA. Determining accurate call-to-shock times is easy. Resuscitation. 2005 Oct;67(1):150-1.
9. In infrequent cases, the code cart and defibrillator may be moved to a deteriorating patient before a full arrest. Such occurrences should be analyzed separately or excluded from analysis.
10. Valenzuela TD et al. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96(10):3308-13. doi: 10.1161/01.cir.96.10.3308.
Research and quality improvement (QI) related to in-hospital cardiopulmonary resuscitation attempts (“codes” from here forward) are hampered significantly by the poor quality of data on time intervals from arrest onset to clinical interventions.1
In 2000, the American Heart Association’s (AHA) Emergency Cardiac Care Guidelines said that current data were inaccurate and that greater accuracy was “the key to future high-quality research”2 – but since then, the general situation has not improved: Time intervals reported by the national AHA-supported registry Get With the Guidelines–Resuscitation (GWTG-R, 200+ hospitals enrolled) include a figure from all hospitals for times to first defibrillation of 1 minute median and 0 minutes first interquartile.3 Such numbers are typical – when they are tracked at all – but they strain credulity, and prima facie evidence is available at most clinical simulation centers simply by timing simulated defibrillation attempts under realistic conditions, as in “mock codes.”4,5
Taking artificially short time-interval data from GWTG-R or other sources at face value can hide serious delays in response to in-hospital arrests. It can also lead to flawed studies and highly questionable conclusions.6
The key to accuracy of critical time intervals – the intervals from arrest to key interventions – is an accurate time of arrest.7 Codes are typically recorded in handwritten form, though they may later be transcribed or scanned into electronic records. The “start” of the code for unmonitored arrests and most monitored arrests is typically taken to be the time that a human bedside recorder, arriving at an unknown interval after the arrest, writes down the first intervention. Researchers acknowledged the problem of artificially short time intervals in 2005, but they did not propose a remedy.1 Since then, the problem of in-hospital resuscitation delays has received little to no attention in the professional literature.
Description of feature
To get better time data from unmonitored resuscitation attempts, it is necessary to use a “surrogate marker” – a stand-in or substitute event – for the time of arrest. This event should occur reliably for each code, and as near as possible to the actual time of arrest. The main early events in a code are starting basic CPR, paging the code, and moving the defibrillator (usually on a code cart) to the scene. Ideally these events occur almost simultaneously, but that is not consistently achieved.
There are significant problems with use of the first two events as surrogate markers: the time of starting CPR cannot be determined accurately, and paging the code is dependent on several intermediate steps that lead to inaccuracy. Furthermore, the times of both markers are recorded using clocks that are typically not synchronized with the clock used for recording the code (defibrillator clock or the human recorder’s timepiece). Reconciliation of these times with the code record, while not particularly difficult,8 is rarely if ever done.
Defibrillator Power On is recorded on the defibrillator timeline and thus does not need to be reconciled with the defibrillator clock, but it is not suitable as a surrogate marker because this time is highly variable: It often does not occur until the time that monitoring pads are placed. Moving the code cart to the scene, which must occur early in the code, is a much more valid surrogate marker, with the added benefit that it can be marked on the defibrillator timeline.
The undocumented feature described here provides that marker. This feature has been a part of the LIFEPAK 20/20e’s design since it was launched in 2002, but it has not been publicized until now and is not documented in the user manual.
Hospital defibrillators are connected to alternating-current (AC) power when not in use. When the defibrillator is moved to the scene of the code, it is obviously necessary to disconnect the defibrillator from the wall outlet, at which time “AC Power Loss” is recorded on the event record generated by the LIFEPAK 20/20e defibrillators. The defibrillator may be powered on up to 10 minutes later while retaining the AC Power Loss marker in the event record. This surrogate marker for the start time will be on the same timeline as other events recorded by the defibrillator, including times of first monitoring and shocks.
Once the event record is acquired, determining time intervals is accomplished by subtracting clock times (see example, Figure 1).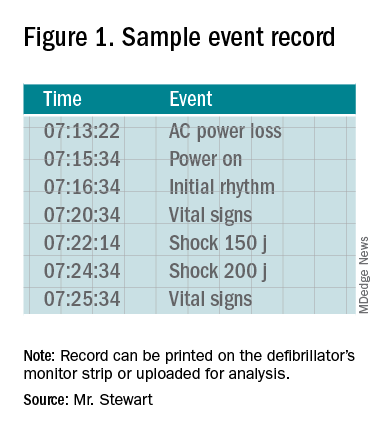
In the example, using AC Power Loss as the start time, time intervals from arrest to first monitoring (Initial Rhythm on the Event Record) and first shock were 3:12 (07:16:34 minus 07:13:22) and 8:42 (07:22:14 minus 07:13:22). Note that if Power On were used as the surrogate time of arrest in the example, the calculated intervals would be artificially shorter, by 2 min 12 sec.
Using this undocumented feature, any facility using LIFEPAK 20/20e defibrillators can easily measure critical time intervals during resuscitation attempts with much greater accuracy, including times to first monitoring and first defibrillation. Each defibrillator stores code summaries sufficient for dozens of events and accessing past data is simple. Analysis of the data can provide a much-improved measure of the facility’s speed of response as a baseline for QI.
If desired, the time-interval data thus obtained can also be integrated with the handwritten record. The usual handwritten code sheet records times only in whole minutes, but with one of the more accurate intervals from the defibrillator – to first monitoring or first defibrillation – an adjusted time of arrest can be added to any code record to get other intervals that better approximate real-world response times.9
Research prospects
The feature opens multiple avenues for future research. Acquiring data by this method should be simple for any facility using LIFEPAK 20/20e defibrillators as its standard devices. Matching the existing handwritten code records with the time intervals obtained using this surrogate time marker will show how inaccurate the commonly reported data are. This can be done with a retrospective study comparing the time intervals from the archived event records with those from the handwritten records, to provide an example of the inaccuracy of data reported in the medical literature. The more accurate picture of time intervals can provide a much-needed yardstick for future research aimed at shortening response times.
The feature can facilitate aggregation of data across multiple facilities that use the LIFEPAK 20/20e as their standard defibrillator. Also, it is possible that other defibrillator manufacturers will duplicate this feature with their devices – it should produce valid data with any defibrillator – although there may be legal and technical obstacles to adopting it.
Combining data from multiple sites might lead to an important contribution to resuscitation research: a reasonably accurate overall survival curve for in-hospital tachyarrhythmic arrests. A commonly cited but crude guideline is that survival from tachyarrhythmic arrests decreases by 10%-15% per minute as defibrillation is delayed,10 but it seems unlikely that the relationship would be linear: Experience and the literature suggest that survival drops very quickly in the first few minutes, flattening out as elapsed time after arrest increases. Aggregating the much more accurate time-interval data from multiple facilities should produce a survival curve for in-hospital tachyarrhythmic arrests that comes much closer to reality.
Conclusion
It is unknown whether this feature will be used to improve the accuracy of reported code response times. It greatly facilitates acquiring more accurate times, but the task has never been especially difficult – particularly when balanced with the importance of better time data for QI and research.8 One possible impediment may be institutional obstacles to publishing studies with accurate response times due to concerns about public relations or legal exposure: The more accurate times will almost certainly be longer than those generally reported.
As was stated almost 2 decades ago and remains true today, acquiring accurate time-interval data is “the key to future high-quality research.”2 It is also key to improving any hospital’s quality of code response. As described in this article, better time data can easily be acquired. It is time for this important problem to be recognized and remedied.
Mr. Stewart has worked as a hospital nurse in Seattle for many years, and has numerous publications to his credit related to resuscitation issues. You can contact him at [email protected].
References
1. Kaye W et al. When minutes count – the fallacy of accurate time documentation during in-hospital resuscitation. Resuscitation. 2005;65(3):285-90.
2. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 4: the automated external defibrillator: key link in the chain of survival. Circulation. 2000;102(8 Suppl):I-60-76.
3. Chan PS et al. American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008 Jan 3;358(1):9-17. doi: 10.1056/NEJMoa0706467.
4. Hunt EA et al. Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: Highlighting the importance of the first 5 minutes. Pediatrics. 2008;121(1):e34-e43. doi: 10.1542/peds.2007-0029.
5. Reeson M et al. Defibrillator design and usability may be impeding timely defibrillation. Comm J Qual Patient Saf. 2018 Sep;44(9):536-544. doi: 10.1016/j.jcjq.2018.01.005.
6. Hunt EA et al. American Heart Association’s Get With The Guidelines – Resuscitation Investigators. Association between time to defibrillation and survival in pediatric in-hospital cardiac arrest with a first documented shockable rhythm JAMA Netw Open. 2018;1(5):e182643. doi: 10.1001/jamanetworkopen.2018.2643.
7. Cummins RO et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital “Utstein” style. Circulation. 1997;95:2213-39.
8. Stewart JA. Determining accurate call-to-shock times is easy. Resuscitation. 2005 Oct;67(1):150-1.
9. In infrequent cases, the code cart and defibrillator may be moved to a deteriorating patient before a full arrest. Such occurrences should be analyzed separately or excluded from analysis.
10. Valenzuela TD et al. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96(10):3308-13. doi: 10.1161/01.cir.96.10.3308.
CDC identifies probable culprit in vaping lung injuries
found in lung fluid of victims.
In a telebriefing on Friday, Anne Schuchat, MD, the CDC’s principal deputy director, provided an update on recent lab findings and on case and death numbers reported so far to the CDC. The findings and more case information were published in the Mortality and Morbidity Weekly Report.
At the telebriefing, Dr. Schuchat stated that CDC has received 29 samples of bronchoalveolar lavage (BAL) fluid from EVALI patients from 10 states and that vitamin E acetate was identified in all samples. Vitamin E acetate has already been found in some vaping devices and the discovery of the chemical in the lungs of patients increases the likelihood that this toxin is at least one source of EVALI. These findings are the first to link substances found in vaping products with biological samples from patients hospitalized with EVALI.
Tetrahydrocannabinol (THC) was found in 23 of 28 samples tested and nicotine was found in 16 of 26 samples tested. Other diluents and additives of concern (such as plant oils, medium chain triglyceride oil, petroleum distillates, and diluent terpenes) were not detected in BAL fluid specimens from EVALI patients.
BAL fluid specimens were collected from hospitalized EVALI patients in the course of their treatment, although not for the specific purpose of the CDC investigation, and sent to the CDC by public health laboratories and health departments in California, Connecticut, Hawaii, Illinois, Maryland, Michigan, Minnesota, Texas, Utah, and Wisconsin for analysis.
Dr. Schuchat stated that, as of Nov. 5, there have been 2,051 cases of EVALI reported to the CDC and 39 EVALI patients have died, with other deaths still under investigation as possibly related to EVALI. She said that the trend in new EVALI cases reported appears to be decreasing, but some states continue to see new cases. She cautioned that the lab findings of vitamin E acetate in BAL fluid do not rule out other possible compounds or ingredients that may contribute to EVALI and said the investigation will continue.
E-cigarette user survey
During the telebriefing, Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist with the Illinois Department of Public Health (IDPH), gave an update on her department’s efforts to investigate vaping behaviors that might have led to EVALI in e-cigarette users and also to obtain more information on sources of vaping devices that could be linked to EVALI. The data were also reported in a MMWR.
The IDPH conducted an online public survey during September 2019 to October 2019 targeting e-cigarette, or vaping, product users in Illinois. The survey was promoted via social media on the IDPH website, local health departments, and other outlets. The survey yielded 4,631 respondents who answered questions about the frequency of vaping, sources of supply, and types of substances used. The investigators were then able to compare vaping-use habits and behaviors with similar information gleaned from EVALI patients.
Among survey respondents, 94% reported using any nicotine-containing e-cigarette, or vaping, products in the past 3 months; 21% used any THC-containing products; and 11% used both THC-containing products and nicotine-containing products. THC-containing product use was highest among survey respondents aged 18-24 years (36%) and decreased with increasing age. Compared with these survey respondents, EVALI patients were more likely to report exclusive use of THC-containing products (adjusted odds ratio, 2.0; 95% confidence interval, 1.1-3.6), frequent use (more than five times per day) of these products (aOR, 3.1; 95% CI, 1.6-6.0), and obtaining these products from informal sources, such as from a dealer, off the street, or from a friend (aOR, 9.2; 95% CI, 2.2-39.4). In addition, “the odds of using Dank Vapes, a class of largely counterfeit THC-containing products, was also higher among EVALI patients” (aOR, 8.5; 95% CI, 3.8-19.0), according to the MMWR.
Recommendations
CDC recommends that people should not buy any type of e-cigarette, or vaping, products, particularly those containing THC, off the street. They should also refrain from modifying or adding any substances to e-cigarette, or vaping, products that are not intended by the manufacturer, including products purchased through retail establishments.
Dr. Layden concluded, “we are in a better place today than we were a few weeks ago in terms of having one very strong culprit of concern based on the lung fluid testing,” but since the specific substances causing lung injury are not yet known, the only way to assure that individuals are not at risk while the investigation continues is to consider refraining from use of all vaping products.
For more information and resources visit For the Public, For Healthcare Providers, and For Health Departments pages, as well as the CDC’s Publications and Resources page.
found in lung fluid of victims.
In a telebriefing on Friday, Anne Schuchat, MD, the CDC’s principal deputy director, provided an update on recent lab findings and on case and death numbers reported so far to the CDC. The findings and more case information were published in the Mortality and Morbidity Weekly Report.
At the telebriefing, Dr. Schuchat stated that CDC has received 29 samples of bronchoalveolar lavage (BAL) fluid from EVALI patients from 10 states and that vitamin E acetate was identified in all samples. Vitamin E acetate has already been found in some vaping devices and the discovery of the chemical in the lungs of patients increases the likelihood that this toxin is at least one source of EVALI. These findings are the first to link substances found in vaping products with biological samples from patients hospitalized with EVALI.
Tetrahydrocannabinol (THC) was found in 23 of 28 samples tested and nicotine was found in 16 of 26 samples tested. Other diluents and additives of concern (such as plant oils, medium chain triglyceride oil, petroleum distillates, and diluent terpenes) were not detected in BAL fluid specimens from EVALI patients.
BAL fluid specimens were collected from hospitalized EVALI patients in the course of their treatment, although not for the specific purpose of the CDC investigation, and sent to the CDC by public health laboratories and health departments in California, Connecticut, Hawaii, Illinois, Maryland, Michigan, Minnesota, Texas, Utah, and Wisconsin for analysis.
Dr. Schuchat stated that, as of Nov. 5, there have been 2,051 cases of EVALI reported to the CDC and 39 EVALI patients have died, with other deaths still under investigation as possibly related to EVALI. She said that the trend in new EVALI cases reported appears to be decreasing, but some states continue to see new cases. She cautioned that the lab findings of vitamin E acetate in BAL fluid do not rule out other possible compounds or ingredients that may contribute to EVALI and said the investigation will continue.
E-cigarette user survey
During the telebriefing, Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist with the Illinois Department of Public Health (IDPH), gave an update on her department’s efforts to investigate vaping behaviors that might have led to EVALI in e-cigarette users and also to obtain more information on sources of vaping devices that could be linked to EVALI. The data were also reported in a MMWR.
The IDPH conducted an online public survey during September 2019 to October 2019 targeting e-cigarette, or vaping, product users in Illinois. The survey was promoted via social media on the IDPH website, local health departments, and other outlets. The survey yielded 4,631 respondents who answered questions about the frequency of vaping, sources of supply, and types of substances used. The investigators were then able to compare vaping-use habits and behaviors with similar information gleaned from EVALI patients.
Among survey respondents, 94% reported using any nicotine-containing e-cigarette, or vaping, products in the past 3 months; 21% used any THC-containing products; and 11% used both THC-containing products and nicotine-containing products. THC-containing product use was highest among survey respondents aged 18-24 years (36%) and decreased with increasing age. Compared with these survey respondents, EVALI patients were more likely to report exclusive use of THC-containing products (adjusted odds ratio, 2.0; 95% confidence interval, 1.1-3.6), frequent use (more than five times per day) of these products (aOR, 3.1; 95% CI, 1.6-6.0), and obtaining these products from informal sources, such as from a dealer, off the street, or from a friend (aOR, 9.2; 95% CI, 2.2-39.4). In addition, “the odds of using Dank Vapes, a class of largely counterfeit THC-containing products, was also higher among EVALI patients” (aOR, 8.5; 95% CI, 3.8-19.0), according to the MMWR.
Recommendations
CDC recommends that people should not buy any type of e-cigarette, or vaping, products, particularly those containing THC, off the street. They should also refrain from modifying or adding any substances to e-cigarette, or vaping, products that are not intended by the manufacturer, including products purchased through retail establishments.
Dr. Layden concluded, “we are in a better place today than we were a few weeks ago in terms of having one very strong culprit of concern based on the lung fluid testing,” but since the specific substances causing lung injury are not yet known, the only way to assure that individuals are not at risk while the investigation continues is to consider refraining from use of all vaping products.
For more information and resources visit For the Public, For Healthcare Providers, and For Health Departments pages, as well as the CDC’s Publications and Resources page.
found in lung fluid of victims.
In a telebriefing on Friday, Anne Schuchat, MD, the CDC’s principal deputy director, provided an update on recent lab findings and on case and death numbers reported so far to the CDC. The findings and more case information were published in the Mortality and Morbidity Weekly Report.
At the telebriefing, Dr. Schuchat stated that CDC has received 29 samples of bronchoalveolar lavage (BAL) fluid from EVALI patients from 10 states and that vitamin E acetate was identified in all samples. Vitamin E acetate has already been found in some vaping devices and the discovery of the chemical in the lungs of patients increases the likelihood that this toxin is at least one source of EVALI. These findings are the first to link substances found in vaping products with biological samples from patients hospitalized with EVALI.
Tetrahydrocannabinol (THC) was found in 23 of 28 samples tested and nicotine was found in 16 of 26 samples tested. Other diluents and additives of concern (such as plant oils, medium chain triglyceride oil, petroleum distillates, and diluent terpenes) were not detected in BAL fluid specimens from EVALI patients.
BAL fluid specimens were collected from hospitalized EVALI patients in the course of their treatment, although not for the specific purpose of the CDC investigation, and sent to the CDC by public health laboratories and health departments in California, Connecticut, Hawaii, Illinois, Maryland, Michigan, Minnesota, Texas, Utah, and Wisconsin for analysis.
Dr. Schuchat stated that, as of Nov. 5, there have been 2,051 cases of EVALI reported to the CDC and 39 EVALI patients have died, with other deaths still under investigation as possibly related to EVALI. She said that the trend in new EVALI cases reported appears to be decreasing, but some states continue to see new cases. She cautioned that the lab findings of vitamin E acetate in BAL fluid do not rule out other possible compounds or ingredients that may contribute to EVALI and said the investigation will continue.
E-cigarette user survey
During the telebriefing, Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist with the Illinois Department of Public Health (IDPH), gave an update on her department’s efforts to investigate vaping behaviors that might have led to EVALI in e-cigarette users and also to obtain more information on sources of vaping devices that could be linked to EVALI. The data were also reported in a MMWR.
The IDPH conducted an online public survey during September 2019 to October 2019 targeting e-cigarette, or vaping, product users in Illinois. The survey was promoted via social media on the IDPH website, local health departments, and other outlets. The survey yielded 4,631 respondents who answered questions about the frequency of vaping, sources of supply, and types of substances used. The investigators were then able to compare vaping-use habits and behaviors with similar information gleaned from EVALI patients.
Among survey respondents, 94% reported using any nicotine-containing e-cigarette, or vaping, products in the past 3 months; 21% used any THC-containing products; and 11% used both THC-containing products and nicotine-containing products. THC-containing product use was highest among survey respondents aged 18-24 years (36%) and decreased with increasing age. Compared with these survey respondents, EVALI patients were more likely to report exclusive use of THC-containing products (adjusted odds ratio, 2.0; 95% confidence interval, 1.1-3.6), frequent use (more than five times per day) of these products (aOR, 3.1; 95% CI, 1.6-6.0), and obtaining these products from informal sources, such as from a dealer, off the street, or from a friend (aOR, 9.2; 95% CI, 2.2-39.4). In addition, “the odds of using Dank Vapes, a class of largely counterfeit THC-containing products, was also higher among EVALI patients” (aOR, 8.5; 95% CI, 3.8-19.0), according to the MMWR.
Recommendations
CDC recommends that people should not buy any type of e-cigarette, or vaping, products, particularly those containing THC, off the street. They should also refrain from modifying or adding any substances to e-cigarette, or vaping, products that are not intended by the manufacturer, including products purchased through retail establishments.
Dr. Layden concluded, “we are in a better place today than we were a few weeks ago in terms of having one very strong culprit of concern based on the lung fluid testing,” but since the specific substances causing lung injury are not yet known, the only way to assure that individuals are not at risk while the investigation continues is to consider refraining from use of all vaping products.
For more information and resources visit For the Public, For Healthcare Providers, and For Health Departments pages, as well as the CDC’s Publications and Resources page.
Was the success of hospital medicine inevitable?
Early on, SHM defined the specialty
When I started at the Society of Hospital Medicine – known then as the National Association of Inpatient Physicians (NAIP) – in January 2000, Bill Clinton was still president. There were probably 500 hospitalists in the United States, and SHM had about 200-250 members.
It was so long ago that the iPhone hadn’t been invented, Twitter wasn’t even an idea, and Amazon was an online book store. SHM’s national offices were a cubicle at the American College of Physicians headquarters in Philadelphia, and our entire staff was me and a part-time assistant.
We have certainly come a long way in my 20 years as CEO of SHM.
When I first became involved with NAIP, it was to help the board with their strategic planning in 1998. At that time, the national thought leaders for the hospitalist movement (the term hospital medicine had not been invented yet) predicted that hospitalists would eventually do the inpatient work for about 25% of family doctors and for 15% of internists. Hospitalists were considered to be a form of “general medicine” without an office-based practice.
One of the first things we set about doing was to define the new specialty of hospital medicine before anyone else (e.g., American Medical Association, ACP, American Academy of Family Physicians, American Academy of Pediatrics, the government) defined us.
Most specialties were defined by a body organ (e.g., cardiology, renal), a population (e.g., pediatrics, geriatrics), or a disease (e.g., oncology), and there were a few other site-specific specialties (e.g., ED medicine, critical care). We felt that, to be a specialty, we needed certain key elements:
- Separate group consciousness
- Professional society
- Distinct residency and fellowship programs
- Separate CME
- Distinct educational materials (e.g., textbooks)
- Definable and distinct competencies
- Separate credentials – certification and/or hospital insurance driven
Early on, SHM defined the Core Competencies for Hospital Medicine for adults in patient care and, eventually, for pediatric patients. We rebranded our specialty as hospital medicine to be more than just inpatient physicians, and to broadly encompass the growing “big tent” of SHM that included those trained in internal medicine, family medicine, pediatrics, med-peds, as well as nurse practitioners, physician assistants, pharmacists, and others.
We were the first and only specialty society to set the standard for hospitalist compensation (how much you are paid) and productivity (what you are expected to do) with our unique State of Hospital Medicine (SOHM) Report. Other specialties left this work to the Medical Group Management Association, the AMA, or commercial companies.
Our specialty was soon being asked to do things that no other group of clinicians was ever asked to do.
Hospitalists were expected to Save Money by reducing length of stay and the use of resources on the sickest patients. Hospitalists were asked to Improve Measurable Quality at a time when most other physicians or even hospitals weren’t even being measured.
We were expected to form and Lead Teams of other clinicians when health care was still seen as a solo enterprise. Hospitalists were expected to Improve Efficiency and to create a Seamless Continuity, both during the hospital stay and in the transitions out of the hospital.
Hospitalists were asked to do things no one else wanted to do, such as taking on the uncompensated patients and extra hospital committee work and just about any new project their hospital wanted to be involved in. Along the way, we were expected to Make Other Physicians’ Lives Better by taking on their inpatients, inpatient calls, comanagement with specialists, and unloading the ED.
And both at medical schools and in the community, hospitalists became the Major Educators of medical students, residents, nurses, and other hospital staff.
At the same time, SHM was focusing on becoming a very unique medical professional society.
SHM built on the energy of our young and innovative hospitalists to forge a different path. We had no reputation to protect. We were not bound like most other specialty societies to over 100 years of “the way it’s always been done.”
While other professional societies thought their role in quality improvement was to pontificate and publish clinical guidelines that often were little used, SHM embarked on an aggressive, hands-on, frontline approach by starting SHM’s Center for Quality Improvement. Over the last 15 years, the center has raised millions of dollars to deliver real change and improvement at hundreds of hospitals nationwide, many times bringing work plans and mentors to support and train local clinicians in quality improvement skills and data collection. This approach was recognized by the National Quality Forum and the Joint Commission with their prestigious John Eisenberg Award for Quality Improvement.
When we went to Washington to help shape the future of health care, we did not ask for more money for hospitalists. We did not ask for more power or to use regulations to protect our new specialty. Instead, we went with ideas of how to make acute medical care more effective and efficient. We could show the politicians and the regulators how we could reduce incidence of deep vein thrombosis and pulmonary emboli, how we could make the hospital discharge process work better, how we could help chart a smoother medication reconciliation process, and so many other ways the system could be improved.
And even the way SHM generated our new ideas was uniquely different than other specialties. Way back in 2000 – long before Twitter and other social media were able to crowdsource and use the Internet to percolate new ideas – SHM relied on our members’ conversations on the SHM electronic mail discussion list to see what hospitalists were worried about, and what everyone was being asked to do, and SHM provided the resources and initiatives to support our nation’s hospitalists.
From these early conversations, SHM heard that hospitalists were being asked to Lead Change without much of an idea of the skills they would need. And so, the SHM leadership academies were born, which have now educated more than 2,700 hospitalist leaders.
Early on, we learned that hospitalists and even their bosses had no idea of how to start or run a successful hospital medicine group. SHM started our practice management courses and webinars and we developed the groundbreaking document, Key Characteristics of Effective Hospital Medicine Groups. In a typical SHM manner, we challenged most of our members to improve and get better rather trying to defend the status quo. At SHM, we have constantly felt that hospital medicine was a “work in progress.” We may not be perfect today, but we will be better in 90 days and even better in a year.
I have more to say about how we got this far and even more to say about where we might go. So, stay tuned and keep contributing to the future and success of SHM and hospital medicine.
Dr. Wellikson is the CEO of SHM. He has announced his plan to retire from SHM in late 2020. This article is the first in a series celebrating Dr. Wellikson’s tenure as CEO.
Early on, SHM defined the specialty
Early on, SHM defined the specialty
When I started at the Society of Hospital Medicine – known then as the National Association of Inpatient Physicians (NAIP) – in January 2000, Bill Clinton was still president. There were probably 500 hospitalists in the United States, and SHM had about 200-250 members.
It was so long ago that the iPhone hadn’t been invented, Twitter wasn’t even an idea, and Amazon was an online book store. SHM’s national offices were a cubicle at the American College of Physicians headquarters in Philadelphia, and our entire staff was me and a part-time assistant.
We have certainly come a long way in my 20 years as CEO of SHM.
When I first became involved with NAIP, it was to help the board with their strategic planning in 1998. At that time, the national thought leaders for the hospitalist movement (the term hospital medicine had not been invented yet) predicted that hospitalists would eventually do the inpatient work for about 25% of family doctors and for 15% of internists. Hospitalists were considered to be a form of “general medicine” without an office-based practice.
One of the first things we set about doing was to define the new specialty of hospital medicine before anyone else (e.g., American Medical Association, ACP, American Academy of Family Physicians, American Academy of Pediatrics, the government) defined us.
Most specialties were defined by a body organ (e.g., cardiology, renal), a population (e.g., pediatrics, geriatrics), or a disease (e.g., oncology), and there were a few other site-specific specialties (e.g., ED medicine, critical care). We felt that, to be a specialty, we needed certain key elements:
- Separate group consciousness
- Professional society
- Distinct residency and fellowship programs
- Separate CME
- Distinct educational materials (e.g., textbooks)
- Definable and distinct competencies
- Separate credentials – certification and/or hospital insurance driven
Early on, SHM defined the Core Competencies for Hospital Medicine for adults in patient care and, eventually, for pediatric patients. We rebranded our specialty as hospital medicine to be more than just inpatient physicians, and to broadly encompass the growing “big tent” of SHM that included those trained in internal medicine, family medicine, pediatrics, med-peds, as well as nurse practitioners, physician assistants, pharmacists, and others.
We were the first and only specialty society to set the standard for hospitalist compensation (how much you are paid) and productivity (what you are expected to do) with our unique State of Hospital Medicine (SOHM) Report. Other specialties left this work to the Medical Group Management Association, the AMA, or commercial companies.
Our specialty was soon being asked to do things that no other group of clinicians was ever asked to do.
Hospitalists were expected to Save Money by reducing length of stay and the use of resources on the sickest patients. Hospitalists were asked to Improve Measurable Quality at a time when most other physicians or even hospitals weren’t even being measured.
We were expected to form and Lead Teams of other clinicians when health care was still seen as a solo enterprise. Hospitalists were expected to Improve Efficiency and to create a Seamless Continuity, both during the hospital stay and in the transitions out of the hospital.
Hospitalists were asked to do things no one else wanted to do, such as taking on the uncompensated patients and extra hospital committee work and just about any new project their hospital wanted to be involved in. Along the way, we were expected to Make Other Physicians’ Lives Better by taking on their inpatients, inpatient calls, comanagement with specialists, and unloading the ED.
And both at medical schools and in the community, hospitalists became the Major Educators of medical students, residents, nurses, and other hospital staff.
At the same time, SHM was focusing on becoming a very unique medical professional society.
SHM built on the energy of our young and innovative hospitalists to forge a different path. We had no reputation to protect. We were not bound like most other specialty societies to over 100 years of “the way it’s always been done.”
While other professional societies thought their role in quality improvement was to pontificate and publish clinical guidelines that often were little used, SHM embarked on an aggressive, hands-on, frontline approach by starting SHM’s Center for Quality Improvement. Over the last 15 years, the center has raised millions of dollars to deliver real change and improvement at hundreds of hospitals nationwide, many times bringing work plans and mentors to support and train local clinicians in quality improvement skills and data collection. This approach was recognized by the National Quality Forum and the Joint Commission with their prestigious John Eisenberg Award for Quality Improvement.
When we went to Washington to help shape the future of health care, we did not ask for more money for hospitalists. We did not ask for more power or to use regulations to protect our new specialty. Instead, we went with ideas of how to make acute medical care more effective and efficient. We could show the politicians and the regulators how we could reduce incidence of deep vein thrombosis and pulmonary emboli, how we could make the hospital discharge process work better, how we could help chart a smoother medication reconciliation process, and so many other ways the system could be improved.
And even the way SHM generated our new ideas was uniquely different than other specialties. Way back in 2000 – long before Twitter and other social media were able to crowdsource and use the Internet to percolate new ideas – SHM relied on our members’ conversations on the SHM electronic mail discussion list to see what hospitalists were worried about, and what everyone was being asked to do, and SHM provided the resources and initiatives to support our nation’s hospitalists.
From these early conversations, SHM heard that hospitalists were being asked to Lead Change without much of an idea of the skills they would need. And so, the SHM leadership academies were born, which have now educated more than 2,700 hospitalist leaders.
Early on, we learned that hospitalists and even their bosses had no idea of how to start or run a successful hospital medicine group. SHM started our practice management courses and webinars and we developed the groundbreaking document, Key Characteristics of Effective Hospital Medicine Groups. In a typical SHM manner, we challenged most of our members to improve and get better rather trying to defend the status quo. At SHM, we have constantly felt that hospital medicine was a “work in progress.” We may not be perfect today, but we will be better in 90 days and even better in a year.
I have more to say about how we got this far and even more to say about where we might go. So, stay tuned and keep contributing to the future and success of SHM and hospital medicine.
Dr. Wellikson is the CEO of SHM. He has announced his plan to retire from SHM in late 2020. This article is the first in a series celebrating Dr. Wellikson’s tenure as CEO.
When I started at the Society of Hospital Medicine – known then as the National Association of Inpatient Physicians (NAIP) – in January 2000, Bill Clinton was still president. There were probably 500 hospitalists in the United States, and SHM had about 200-250 members.
It was so long ago that the iPhone hadn’t been invented, Twitter wasn’t even an idea, and Amazon was an online book store. SHM’s national offices were a cubicle at the American College of Physicians headquarters in Philadelphia, and our entire staff was me and a part-time assistant.
We have certainly come a long way in my 20 years as CEO of SHM.
When I first became involved with NAIP, it was to help the board with their strategic planning in 1998. At that time, the national thought leaders for the hospitalist movement (the term hospital medicine had not been invented yet) predicted that hospitalists would eventually do the inpatient work for about 25% of family doctors and for 15% of internists. Hospitalists were considered to be a form of “general medicine” without an office-based practice.
One of the first things we set about doing was to define the new specialty of hospital medicine before anyone else (e.g., American Medical Association, ACP, American Academy of Family Physicians, American Academy of Pediatrics, the government) defined us.
Most specialties were defined by a body organ (e.g., cardiology, renal), a population (e.g., pediatrics, geriatrics), or a disease (e.g., oncology), and there were a few other site-specific specialties (e.g., ED medicine, critical care). We felt that, to be a specialty, we needed certain key elements:
- Separate group consciousness
- Professional society
- Distinct residency and fellowship programs
- Separate CME
- Distinct educational materials (e.g., textbooks)
- Definable and distinct competencies
- Separate credentials – certification and/or hospital insurance driven
Early on, SHM defined the Core Competencies for Hospital Medicine for adults in patient care and, eventually, for pediatric patients. We rebranded our specialty as hospital medicine to be more than just inpatient physicians, and to broadly encompass the growing “big tent” of SHM that included those trained in internal medicine, family medicine, pediatrics, med-peds, as well as nurse practitioners, physician assistants, pharmacists, and others.
We were the first and only specialty society to set the standard for hospitalist compensation (how much you are paid) and productivity (what you are expected to do) with our unique State of Hospital Medicine (SOHM) Report. Other specialties left this work to the Medical Group Management Association, the AMA, or commercial companies.
Our specialty was soon being asked to do things that no other group of clinicians was ever asked to do.
Hospitalists were expected to Save Money by reducing length of stay and the use of resources on the sickest patients. Hospitalists were asked to Improve Measurable Quality at a time when most other physicians or even hospitals weren’t even being measured.
We were expected to form and Lead Teams of other clinicians when health care was still seen as a solo enterprise. Hospitalists were expected to Improve Efficiency and to create a Seamless Continuity, both during the hospital stay and in the transitions out of the hospital.
Hospitalists were asked to do things no one else wanted to do, such as taking on the uncompensated patients and extra hospital committee work and just about any new project their hospital wanted to be involved in. Along the way, we were expected to Make Other Physicians’ Lives Better by taking on their inpatients, inpatient calls, comanagement with specialists, and unloading the ED.
And both at medical schools and in the community, hospitalists became the Major Educators of medical students, residents, nurses, and other hospital staff.
At the same time, SHM was focusing on becoming a very unique medical professional society.
SHM built on the energy of our young and innovative hospitalists to forge a different path. We had no reputation to protect. We were not bound like most other specialty societies to over 100 years of “the way it’s always been done.”
While other professional societies thought their role in quality improvement was to pontificate and publish clinical guidelines that often were little used, SHM embarked on an aggressive, hands-on, frontline approach by starting SHM’s Center for Quality Improvement. Over the last 15 years, the center has raised millions of dollars to deliver real change and improvement at hundreds of hospitals nationwide, many times bringing work plans and mentors to support and train local clinicians in quality improvement skills and data collection. This approach was recognized by the National Quality Forum and the Joint Commission with their prestigious John Eisenberg Award for Quality Improvement.
When we went to Washington to help shape the future of health care, we did not ask for more money for hospitalists. We did not ask for more power or to use regulations to protect our new specialty. Instead, we went with ideas of how to make acute medical care more effective and efficient. We could show the politicians and the regulators how we could reduce incidence of deep vein thrombosis and pulmonary emboli, how we could make the hospital discharge process work better, how we could help chart a smoother medication reconciliation process, and so many other ways the system could be improved.
And even the way SHM generated our new ideas was uniquely different than other specialties. Way back in 2000 – long before Twitter and other social media were able to crowdsource and use the Internet to percolate new ideas – SHM relied on our members’ conversations on the SHM electronic mail discussion list to see what hospitalists were worried about, and what everyone was being asked to do, and SHM provided the resources and initiatives to support our nation’s hospitalists.
From these early conversations, SHM heard that hospitalists were being asked to Lead Change without much of an idea of the skills they would need. And so, the SHM leadership academies were born, which have now educated more than 2,700 hospitalist leaders.
Early on, we learned that hospitalists and even their bosses had no idea of how to start or run a successful hospital medicine group. SHM started our practice management courses and webinars and we developed the groundbreaking document, Key Characteristics of Effective Hospital Medicine Groups. In a typical SHM manner, we challenged most of our members to improve and get better rather trying to defend the status quo. At SHM, we have constantly felt that hospital medicine was a “work in progress.” We may not be perfect today, but we will be better in 90 days and even better in a year.
I have more to say about how we got this far and even more to say about where we might go. So, stay tuned and keep contributing to the future and success of SHM and hospital medicine.
Dr. Wellikson is the CEO of SHM. He has announced his plan to retire from SHM in late 2020. This article is the first in a series celebrating Dr. Wellikson’s tenure as CEO.
New model for CKD risk draws on clinical, demographic factors
Data from more than 5 million individuals has been used to develop an equation for predicting the risk of incident chronic kidney disease (CKD) in people with or without diabetes, according to a presentation at Kidney Week 2019, sponsored by the American Society of Nephrology.
In a paper published simultaneously online in JAMA, researchers reported the outcome of an individual-level data analysis of 34 multinational cohorts involving 5,222,711 individuals – including 781,627 with diabetes – from 28 countries as part of the Chronic Kidney Disease Prognosis Consortium.
“An equation for kidney failure risk may help improve care for patients with established CKD, but relatively little work has been performed to develop predictive tools to identify those at increased risk of developing CKD – defined by reduced eGFR [estimated glomerular filtration rate], despite the high lifetime risk of CKD – which is estimated to be 59.1% in the United States,” wrote Robert G. Nelson, MD, PhD, from the National Institute of Diabetes and Digestive and Kidney Diseases in Phoenix and colleagues.
Over a mean follow-up of 4 years, 15% of individuals without diabetes and 40% of individuals with diabetes developed incident chronic kidney disease, defined as an eGFR below 60 mL/min per 1.73m2.
The key risk factors were older age, female sex, black race, hypertension, history of cardiovascular disease, lower eGFR values, and higher urine albumin to creatinine ratio. Smoking was also significantly associated with reduced eGFR but only in cohorts without diabetes. In cohorts with diabetes, elevated hemoglobin A1c and the presence and type of diabetes medication were also significantly associated with reduced eGFR.
Using this information, the researchers developed a prediction model built from weighted-average hazard ratios and validated it in nine external validation cohorts of 18 study populations involving a total of 2,253,540 individuals. They found that in 16 of the 18 study populations, the slope of observed to predicted risk ranged from 0.80 to 1.25.
Moreover, in the cohorts without diabetes, the risk equations had a median C-statistic for the 5-year predicted probability of 0.845 (interquartile range, 0.789-0.890) and of 0.801 (IQR, 0.750-0.819) in the cohorts with diabetes, the investigators reported.
“Several models have been developed for estimating the risk of prevalent and incident CKD and end-stage kidney disease, but even those with good discriminative performance have not always performed well for cohorts of people outside the original derivation cohort,” the authors wrote. They argued that their model “demonstrated high discrimination and variable calibration in diverse populations.”
However, they stressed that further study was needed to determine if use of the equations would actually lead to improvements in clinical care and patient outcomes. In an accompanying editorial, Sri Lekha Tummalapalli, MD, and Michelle M. Estrella, MD, of the Kidney Health Research Collaborative at the University of California, San Francisco, said the study and its focus on primary, rather than secondary, prevention of kidney disease is a critical step toward reducing the burden of that disease, especially given that an estimated 37 million people in the United States have chronic kidney disease.
It is also important, they added, that primary prevention of kidney disease is tailored to the individual patient’s risk because risk prediction and screening strategies are unlikely to improve outcomes if they are not paired with effective individualized interventions, such as lifestyle modification or management of blood pressure.
These risk equations could be more holistic by integrating the prediction of both elevated albuminuria and reduced eGFR because more than 40% of individuals with chronic kidney disease have increased albuminuria without reduced eGFR, they noted (JAMA. 2019 Nov 8. doi: 10.1001/jama.2019.17378).
The study and CKD Prognosis Consortium were supported by the U.S. National Kidney Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases. One author was supported by a grant from the German Research Foundation. Nine authors declared grants, consultancies, and other support from the private sector and research organizations. No other conflicts of interest were declared. Dr. Tummalapalli and Dr. Estrella reported no conflicts of interest.
SOURCE: Nelson R et al. JAMA. 2019 Nov 8. doi: 10.1001/jama.2019.17379.
Data from more than 5 million individuals has been used to develop an equation for predicting the risk of incident chronic kidney disease (CKD) in people with or without diabetes, according to a presentation at Kidney Week 2019, sponsored by the American Society of Nephrology.
In a paper published simultaneously online in JAMA, researchers reported the outcome of an individual-level data analysis of 34 multinational cohorts involving 5,222,711 individuals – including 781,627 with diabetes – from 28 countries as part of the Chronic Kidney Disease Prognosis Consortium.
“An equation for kidney failure risk may help improve care for patients with established CKD, but relatively little work has been performed to develop predictive tools to identify those at increased risk of developing CKD – defined by reduced eGFR [estimated glomerular filtration rate], despite the high lifetime risk of CKD – which is estimated to be 59.1% in the United States,” wrote Robert G. Nelson, MD, PhD, from the National Institute of Diabetes and Digestive and Kidney Diseases in Phoenix and colleagues.
Over a mean follow-up of 4 years, 15% of individuals without diabetes and 40% of individuals with diabetes developed incident chronic kidney disease, defined as an eGFR below 60 mL/min per 1.73m2.
The key risk factors were older age, female sex, black race, hypertension, history of cardiovascular disease, lower eGFR values, and higher urine albumin to creatinine ratio. Smoking was also significantly associated with reduced eGFR but only in cohorts without diabetes. In cohorts with diabetes, elevated hemoglobin A1c and the presence and type of diabetes medication were also significantly associated with reduced eGFR.
Using this information, the researchers developed a prediction model built from weighted-average hazard ratios and validated it in nine external validation cohorts of 18 study populations involving a total of 2,253,540 individuals. They found that in 16 of the 18 study populations, the slope of observed to predicted risk ranged from 0.80 to 1.25.
Moreover, in the cohorts without diabetes, the risk equations had a median C-statistic for the 5-year predicted probability of 0.845 (interquartile range, 0.789-0.890) and of 0.801 (IQR, 0.750-0.819) in the cohorts with diabetes, the investigators reported.
“Several models have been developed for estimating the risk of prevalent and incident CKD and end-stage kidney disease, but even those with good discriminative performance have not always performed well for cohorts of people outside the original derivation cohort,” the authors wrote. They argued that their model “demonstrated high discrimination and variable calibration in diverse populations.”
However, they stressed that further study was needed to determine if use of the equations would actually lead to improvements in clinical care and patient outcomes. In an accompanying editorial, Sri Lekha Tummalapalli, MD, and Michelle M. Estrella, MD, of the Kidney Health Research Collaborative at the University of California, San Francisco, said the study and its focus on primary, rather than secondary, prevention of kidney disease is a critical step toward reducing the burden of that disease, especially given that an estimated 37 million people in the United States have chronic kidney disease.
It is also important, they added, that primary prevention of kidney disease is tailored to the individual patient’s risk because risk prediction and screening strategies are unlikely to improve outcomes if they are not paired with effective individualized interventions, such as lifestyle modification or management of blood pressure.
These risk equations could be more holistic by integrating the prediction of both elevated albuminuria and reduced eGFR because more than 40% of individuals with chronic kidney disease have increased albuminuria without reduced eGFR, they noted (JAMA. 2019 Nov 8. doi: 10.1001/jama.2019.17378).
The study and CKD Prognosis Consortium were supported by the U.S. National Kidney Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases. One author was supported by a grant from the German Research Foundation. Nine authors declared grants, consultancies, and other support from the private sector and research organizations. No other conflicts of interest were declared. Dr. Tummalapalli and Dr. Estrella reported no conflicts of interest.
SOURCE: Nelson R et al. JAMA. 2019 Nov 8. doi: 10.1001/jama.2019.17379.
Data from more than 5 million individuals has been used to develop an equation for predicting the risk of incident chronic kidney disease (CKD) in people with or without diabetes, according to a presentation at Kidney Week 2019, sponsored by the American Society of Nephrology.
In a paper published simultaneously online in JAMA, researchers reported the outcome of an individual-level data analysis of 34 multinational cohorts involving 5,222,711 individuals – including 781,627 with diabetes – from 28 countries as part of the Chronic Kidney Disease Prognosis Consortium.
“An equation for kidney failure risk may help improve care for patients with established CKD, but relatively little work has been performed to develop predictive tools to identify those at increased risk of developing CKD – defined by reduced eGFR [estimated glomerular filtration rate], despite the high lifetime risk of CKD – which is estimated to be 59.1% in the United States,” wrote Robert G. Nelson, MD, PhD, from the National Institute of Diabetes and Digestive and Kidney Diseases in Phoenix and colleagues.
Over a mean follow-up of 4 years, 15% of individuals without diabetes and 40% of individuals with diabetes developed incident chronic kidney disease, defined as an eGFR below 60 mL/min per 1.73m2.
The key risk factors were older age, female sex, black race, hypertension, history of cardiovascular disease, lower eGFR values, and higher urine albumin to creatinine ratio. Smoking was also significantly associated with reduced eGFR but only in cohorts without diabetes. In cohorts with diabetes, elevated hemoglobin A1c and the presence and type of diabetes medication were also significantly associated with reduced eGFR.
Using this information, the researchers developed a prediction model built from weighted-average hazard ratios and validated it in nine external validation cohorts of 18 study populations involving a total of 2,253,540 individuals. They found that in 16 of the 18 study populations, the slope of observed to predicted risk ranged from 0.80 to 1.25.
Moreover, in the cohorts without diabetes, the risk equations had a median C-statistic for the 5-year predicted probability of 0.845 (interquartile range, 0.789-0.890) and of 0.801 (IQR, 0.750-0.819) in the cohorts with diabetes, the investigators reported.
“Several models have been developed for estimating the risk of prevalent and incident CKD and end-stage kidney disease, but even those with good discriminative performance have not always performed well for cohorts of people outside the original derivation cohort,” the authors wrote. They argued that their model “demonstrated high discrimination and variable calibration in diverse populations.”
However, they stressed that further study was needed to determine if use of the equations would actually lead to improvements in clinical care and patient outcomes. In an accompanying editorial, Sri Lekha Tummalapalli, MD, and Michelle M. Estrella, MD, of the Kidney Health Research Collaborative at the University of California, San Francisco, said the study and its focus on primary, rather than secondary, prevention of kidney disease is a critical step toward reducing the burden of that disease, especially given that an estimated 37 million people in the United States have chronic kidney disease.
It is also important, they added, that primary prevention of kidney disease is tailored to the individual patient’s risk because risk prediction and screening strategies are unlikely to improve outcomes if they are not paired with effective individualized interventions, such as lifestyle modification or management of blood pressure.
These risk equations could be more holistic by integrating the prediction of both elevated albuminuria and reduced eGFR because more than 40% of individuals with chronic kidney disease have increased albuminuria without reduced eGFR, they noted (JAMA. 2019 Nov 8. doi: 10.1001/jama.2019.17378).
The study and CKD Prognosis Consortium were supported by the U.S. National Kidney Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases. One author was supported by a grant from the German Research Foundation. Nine authors declared grants, consultancies, and other support from the private sector and research organizations. No other conflicts of interest were declared. Dr. Tummalapalli and Dr. Estrella reported no conflicts of interest.
SOURCE: Nelson R et al. JAMA. 2019 Nov 8. doi: 10.1001/jama.2019.17379.
REPORTING FROM KIDNEY WEEK 2019
Key clinical point:
Major finding: In the cohorts without diabetes, the risk equations had a median C-statistic for the 5-year predicted probability of 0.845 (interquartile range, 0.789-0.890), and of 0.801 (IQR, 0.750-0.819) in the cohorts with diabetes,
Study details: Analysis of cohort data from 5,222,711 individuals, including 781,627 with diabetes.
Disclosures: The study and CKD Prognosis Consortium were supported by the U.S. National Kidney Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases. One author was supported by a grant from the German Research Foundation. Nine authors declared grants, consultancies, and other support from the private sector and research organizations. No other conflicts of interest were declared. Dr. Tummalapalli and Dr. Estrella reported no conflicts of interest.
Source: Nelson R et al. JAMA. 2019 Nov 8. doi: 10.1001/jama.2019.17379.
Aspirin for primary prevention reduces risk of CV events, increases bleeding
Background: Aspirin is beneficial in secondary prevention of stroke and MI. There is no consensus on its role in primary prevention of the same.
Study design: Systematic review and meta-analysis.
Setting: PubMed and Embase search on Cochrane from the earliest publication available through Nov. 1, 2018.
Synopsis: This meta-analysis included randomized, controlled trials that compared aspirin use versus no aspirin use in more than 1,000 participants without known cardiovascular (CV) disease. The primary CV outcome was a composite of CV mortality, nonfatal MI, and nonfatal stroke. The primary bleeding outcome was major bleeding (defined by individual studies). Thirteen studies enrolling 164,225 participants and including 1,050,511 participant-years were included. Compared with no aspirin use, aspirin use showed a reduction in composite CV outcomes (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95; number needed to treat, 265) and an increased risk of major bleeding (HR, 1.43; 95% CI, 1.30-1.56; number needed to harm, 210). Limitations of the study include variations in data quality, outcome definitions, and aspirin doses among trials. The study authors advocate for including the lower risk of CV events and increased risk of major bleeding as part of discussions with patients about the use of aspirin for primary prevention.
Bottom line: Aspirin for primary prevention lowers risk of CV events and increases risk of major bleeding. Health care providers should include this as part of informed decision-making discussions with patients about the use of aspirin for primary prevention.
Citation: Zheng S et al. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: A systematic review and meta-analysis. JAMA. 2019 Jan 22;321(3):277-87.
Dr. Radhakrishnan is a hospitalist at Beth Israel Deaconess Medical Center.
Background: Aspirin is beneficial in secondary prevention of stroke and MI. There is no consensus on its role in primary prevention of the same.
Study design: Systematic review and meta-analysis.
Setting: PubMed and Embase search on Cochrane from the earliest publication available through Nov. 1, 2018.
Synopsis: This meta-analysis included randomized, controlled trials that compared aspirin use versus no aspirin use in more than 1,000 participants without known cardiovascular (CV) disease. The primary CV outcome was a composite of CV mortality, nonfatal MI, and nonfatal stroke. The primary bleeding outcome was major bleeding (defined by individual studies). Thirteen studies enrolling 164,225 participants and including 1,050,511 participant-years were included. Compared with no aspirin use, aspirin use showed a reduction in composite CV outcomes (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95; number needed to treat, 265) and an increased risk of major bleeding (HR, 1.43; 95% CI, 1.30-1.56; number needed to harm, 210). Limitations of the study include variations in data quality, outcome definitions, and aspirin doses among trials. The study authors advocate for including the lower risk of CV events and increased risk of major bleeding as part of discussions with patients about the use of aspirin for primary prevention.
Bottom line: Aspirin for primary prevention lowers risk of CV events and increases risk of major bleeding. Health care providers should include this as part of informed decision-making discussions with patients about the use of aspirin for primary prevention.
Citation: Zheng S et al. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: A systematic review and meta-analysis. JAMA. 2019 Jan 22;321(3):277-87.
Dr. Radhakrishnan is a hospitalist at Beth Israel Deaconess Medical Center.
Background: Aspirin is beneficial in secondary prevention of stroke and MI. There is no consensus on its role in primary prevention of the same.
Study design: Systematic review and meta-analysis.
Setting: PubMed and Embase search on Cochrane from the earliest publication available through Nov. 1, 2018.
Synopsis: This meta-analysis included randomized, controlled trials that compared aspirin use versus no aspirin use in more than 1,000 participants without known cardiovascular (CV) disease. The primary CV outcome was a composite of CV mortality, nonfatal MI, and nonfatal stroke. The primary bleeding outcome was major bleeding (defined by individual studies). Thirteen studies enrolling 164,225 participants and including 1,050,511 participant-years were included. Compared with no aspirin use, aspirin use showed a reduction in composite CV outcomes (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95; number needed to treat, 265) and an increased risk of major bleeding (HR, 1.43; 95% CI, 1.30-1.56; number needed to harm, 210). Limitations of the study include variations in data quality, outcome definitions, and aspirin doses among trials. The study authors advocate for including the lower risk of CV events and increased risk of major bleeding as part of discussions with patients about the use of aspirin for primary prevention.
Bottom line: Aspirin for primary prevention lowers risk of CV events and increases risk of major bleeding. Health care providers should include this as part of informed decision-making discussions with patients about the use of aspirin for primary prevention.
Citation: Zheng S et al. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: A systematic review and meta-analysis. JAMA. 2019 Jan 22;321(3):277-87.
Dr. Radhakrishnan is a hospitalist at Beth Israel Deaconess Medical Center.
Spanish risk score predicts 30-day mortality in acute HF in ED patients
Background: The MEESSI-AHF (Multiple Estimation of Risk based on the Emergency Department Spanish Score In patients with Acute Heart Failure) score is a risk-stratification tool that includes systolic blood pressure, age, NT-proBNP, potassium, cardiac troponin T, New York Heart Association class 4 disease, respiratory rate, low-output symptoms, oxygen saturation, episode associated with acute coronary syndrome, signs of left ventricular hypertrophy on EKG, creatinine, and Barthel Index Score. Prior research has shown that it accurately risk-stratified ED patients with AHF in Spain. It has not been studied in other populations.
Study design: Prospective multicenter cohort study.
Setting: Adult ED patients with acute dyspnea in four hospitals in Switzerland.
Synopsis: The study included 1,247 nonhemodialysis patients who presented to the ED with acute dyspnea, were found to have all the necessary variables to calculate the MEESSI-AHF score, and were adjudicated to have acute heart failure. The authors calculated a modified MEESSI-AHF score, excluding the Barthel Index for all patients. The authors found that a six-group modified MEESSI-AHF risk-stratification model could predict 30-day mortality with excellent discrimination (C-Statistic, 0.80). Limitations of the study include the exclusion of all hemodynamically unstable patients and those on hemodialysis.
Bottom line: The MEESSI-AHF score effectively predicts 30-day mortality in AHF in Swiss and Spanish ED patients.
Citation: Wussler D et al. External validation of the MEESSI acute heart failure risk score: A cohort study. Ann Intern Med. 2019;170:248-56.
Dr. Radhakrishnan is a hospitalist at Beth Israel Deaconess Medical Center.
Background: The MEESSI-AHF (Multiple Estimation of Risk based on the Emergency Department Spanish Score In patients with Acute Heart Failure) score is a risk-stratification tool that includes systolic blood pressure, age, NT-proBNP, potassium, cardiac troponin T, New York Heart Association class 4 disease, respiratory rate, low-output symptoms, oxygen saturation, episode associated with acute coronary syndrome, signs of left ventricular hypertrophy on EKG, creatinine, and Barthel Index Score. Prior research has shown that it accurately risk-stratified ED patients with AHF in Spain. It has not been studied in other populations.
Study design: Prospective multicenter cohort study.
Setting: Adult ED patients with acute dyspnea in four hospitals in Switzerland.
Synopsis: The study included 1,247 nonhemodialysis patients who presented to the ED with acute dyspnea, were found to have all the necessary variables to calculate the MEESSI-AHF score, and were adjudicated to have acute heart failure. The authors calculated a modified MEESSI-AHF score, excluding the Barthel Index for all patients. The authors found that a six-group modified MEESSI-AHF risk-stratification model could predict 30-day mortality with excellent discrimination (C-Statistic, 0.80). Limitations of the study include the exclusion of all hemodynamically unstable patients and those on hemodialysis.
Bottom line: The MEESSI-AHF score effectively predicts 30-day mortality in AHF in Swiss and Spanish ED patients.
Citation: Wussler D et al. External validation of the MEESSI acute heart failure risk score: A cohort study. Ann Intern Med. 2019;170:248-56.
Dr. Radhakrishnan is a hospitalist at Beth Israel Deaconess Medical Center.
Background: The MEESSI-AHF (Multiple Estimation of Risk based on the Emergency Department Spanish Score In patients with Acute Heart Failure) score is a risk-stratification tool that includes systolic blood pressure, age, NT-proBNP, potassium, cardiac troponin T, New York Heart Association class 4 disease, respiratory rate, low-output symptoms, oxygen saturation, episode associated with acute coronary syndrome, signs of left ventricular hypertrophy on EKG, creatinine, and Barthel Index Score. Prior research has shown that it accurately risk-stratified ED patients with AHF in Spain. It has not been studied in other populations.
Study design: Prospective multicenter cohort study.
Setting: Adult ED patients with acute dyspnea in four hospitals in Switzerland.
Synopsis: The study included 1,247 nonhemodialysis patients who presented to the ED with acute dyspnea, were found to have all the necessary variables to calculate the MEESSI-AHF score, and were adjudicated to have acute heart failure. The authors calculated a modified MEESSI-AHF score, excluding the Barthel Index for all patients. The authors found that a six-group modified MEESSI-AHF risk-stratification model could predict 30-day mortality with excellent discrimination (C-Statistic, 0.80). Limitations of the study include the exclusion of all hemodynamically unstable patients and those on hemodialysis.
Bottom line: The MEESSI-AHF score effectively predicts 30-day mortality in AHF in Swiss and Spanish ED patients.
Citation: Wussler D et al. External validation of the MEESSI acute heart failure risk score: A cohort study. Ann Intern Med. 2019;170:248-56.
Dr. Radhakrishnan is a hospitalist at Beth Israel Deaconess Medical Center.