User login
Follow five tips to mitigate opioid prescribing risks
CHICAGO – As the epidemic of opioid addiction and overdose deaths continues to surge, state and federal authorities are keeping a close eye on physicians who prescribe controlled substances.
Experts offer the following guidance on how well-meaning doctors can avoid coming under scrutiny for prescribing opioids and successfully manage investigations and audits.
1. Know who’s on the radar: The Drug Enforcement Agency (DEA) compiles a “black list” yearly of physicians and health care providers they plan to target for audits, said Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law. For 2017, the list includes physicians who have prior noncompliance records, providers who specialize in pain management, and those who dispense or administer large quantities of controlled substances.
In addition, family physicians, psychiatrists, and other specialists who come under investigation by a state medical board because of suspected inappropriate prescribing or reporting violations may also come under the purview of federal authorities, Ms. Mazina said.
“If they come on the medical board radar, they may come on the [DEA’s] radar as well,” she said during the interview. “They just have to watch how many prescriptions they write for controlled substances and make sure they are legitimate prescriptions.”
2. Maintain proper records: Poor record keeping is a top reason that the DEA investigates health care providers for potential prescribing violations, said Dennis A. Wichern, a DEA agent with the Chicago Field Division. Federal law requires that registered practitioners who store or dispense controlled substances keep records of controlled substances coming in and out of the practice. That includes physicians who hand out samples of controlled substances to patients and also pertains to samples provided to doctors by pharmaceutical companies.
Records should include whether the inventory was taken at the beginning or close of business, names of controlled substances, each finished form of the substances, the number of dosage units of each finished form in the commercial container, the number of commercial containers of each finished form, and disposition of the controlled substances.
Law requires that physicians take a new inventory of all controlled substances on hand every 2 years. Doctors are not required to keep records of controlled substances that are merely prescribed, unless such substances are prescribed in the course of maintenance or detoxification treatment.
Ms. Mazina notes that there are many software platforms that can assist practices with proper inventory and record keeping for opioids and other drugs.
3. Check the state database: Before prescribing opioids, check your state’s prescription drug monitoring program (PDMP) database, advises Ms. Mazina. At least 37 states have operational PDMPs that receive and distribute controlled substance prescription information to authorized users. About 11 states have enacted legislation to establish a PDMP, but some databases are not fully operational.
A state’s PDMP can reveal whether patients may be obtaining multiple controlled substance prescriptions from different doctors or doctor-shopping, Ms. Mazina said. Such due diligence helps inform treatment decisions and can assist a doctor’s case if a medical board or DEA investigation later arises.
“Even if your state law does not require you to check a patient’s history prior to prescribing, you have to check it to protect yourself,” she said. “If you want to avoid controlled substances problems, PDMP is the way to go.”
4. Establish an audit response plan: Have an audit response plan ready to roll should an inquiry arise, experts advise. The policies ensure that only approved information is released to authorities, and that all staff members are on the same page about how to react to audits, Ms. Mazina said.
Plans should clearly state what information can be collected and what data should be kept confidential. Financial information, for example, should be off limits, she said. Government agents are entitled to inventory, dispensary data, and records of receipts.
“Agents very often do the mirror image of the database, and they get too much information,” she said. “You don’t want to [allow] that.”
Train staff members how to respond to government authorities seeking audit information, and explain they have the right to refuse being interviewed, Ms. Mazina said.
“Train your employees on what’s going to happen if the DEA comes in,” she said. “If I don’t have clear policies and procedures, and I’m not trained, I might disclose everything and blame someone. That puts everyone in a [bad] position, because [authorities] will record everything and use it against [the practice].”
5. Confer with the experts: It doesn’t hurt to consult with other medical professionals, such as emergency physicians or pain management specialists, for practical advice on inventory policies or software suggestions. But when it comes to staying updated on new drug laws and regulations, confer with a health law attorney or compliance officer, Ms. Mazina said. The DEA website also includes useful information about recent laws and rules pertaining to prescription drugs, as does the Centers for Disease Control and Prevention website.
If an investigation or audit emerges, work with an attorney as early as possible. Often, practices wait until too late after an investigation begins to contact legal counsel, Ms. Mazina noted. The earlier an attorney gets involved, the sooner that person can build a strong case for the practice and work toward the best resolution.
“Very often, the physician thinks they are right, and there’s nothing for them to fear,” she said. “There is something for you to fear. There’s a lot at stake.”
[email protected]
On Twitter @legal_med
CHICAGO – As the epidemic of opioid addiction and overdose deaths continues to surge, state and federal authorities are keeping a close eye on physicians who prescribe controlled substances.
Experts offer the following guidance on how well-meaning doctors can avoid coming under scrutiny for prescribing opioids and successfully manage investigations and audits.
1. Know who’s on the radar: The Drug Enforcement Agency (DEA) compiles a “black list” yearly of physicians and health care providers they plan to target for audits, said Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law. For 2017, the list includes physicians who have prior noncompliance records, providers who specialize in pain management, and those who dispense or administer large quantities of controlled substances.
In addition, family physicians, psychiatrists, and other specialists who come under investigation by a state medical board because of suspected inappropriate prescribing or reporting violations may also come under the purview of federal authorities, Ms. Mazina said.
“If they come on the medical board radar, they may come on the [DEA’s] radar as well,” she said during the interview. “They just have to watch how many prescriptions they write for controlled substances and make sure they are legitimate prescriptions.”
2. Maintain proper records: Poor record keeping is a top reason that the DEA investigates health care providers for potential prescribing violations, said Dennis A. Wichern, a DEA agent with the Chicago Field Division. Federal law requires that registered practitioners who store or dispense controlled substances keep records of controlled substances coming in and out of the practice. That includes physicians who hand out samples of controlled substances to patients and also pertains to samples provided to doctors by pharmaceutical companies.
Records should include whether the inventory was taken at the beginning or close of business, names of controlled substances, each finished form of the substances, the number of dosage units of each finished form in the commercial container, the number of commercial containers of each finished form, and disposition of the controlled substances.
Law requires that physicians take a new inventory of all controlled substances on hand every 2 years. Doctors are not required to keep records of controlled substances that are merely prescribed, unless such substances are prescribed in the course of maintenance or detoxification treatment.
Ms. Mazina notes that there are many software platforms that can assist practices with proper inventory and record keeping for opioids and other drugs.
3. Check the state database: Before prescribing opioids, check your state’s prescription drug monitoring program (PDMP) database, advises Ms. Mazina. At least 37 states have operational PDMPs that receive and distribute controlled substance prescription information to authorized users. About 11 states have enacted legislation to establish a PDMP, but some databases are not fully operational.
A state’s PDMP can reveal whether patients may be obtaining multiple controlled substance prescriptions from different doctors or doctor-shopping, Ms. Mazina said. Such due diligence helps inform treatment decisions and can assist a doctor’s case if a medical board or DEA investigation later arises.
“Even if your state law does not require you to check a patient’s history prior to prescribing, you have to check it to protect yourself,” she said. “If you want to avoid controlled substances problems, PDMP is the way to go.”
4. Establish an audit response plan: Have an audit response plan ready to roll should an inquiry arise, experts advise. The policies ensure that only approved information is released to authorities, and that all staff members are on the same page about how to react to audits, Ms. Mazina said.
Plans should clearly state what information can be collected and what data should be kept confidential. Financial information, for example, should be off limits, she said. Government agents are entitled to inventory, dispensary data, and records of receipts.
“Agents very often do the mirror image of the database, and they get too much information,” she said. “You don’t want to [allow] that.”
Train staff members how to respond to government authorities seeking audit information, and explain they have the right to refuse being interviewed, Ms. Mazina said.
“Train your employees on what’s going to happen if the DEA comes in,” she said. “If I don’t have clear policies and procedures, and I’m not trained, I might disclose everything and blame someone. That puts everyone in a [bad] position, because [authorities] will record everything and use it against [the practice].”
5. Confer with the experts: It doesn’t hurt to consult with other medical professionals, such as emergency physicians or pain management specialists, for practical advice on inventory policies or software suggestions. But when it comes to staying updated on new drug laws and regulations, confer with a health law attorney or compliance officer, Ms. Mazina said. The DEA website also includes useful information about recent laws and rules pertaining to prescription drugs, as does the Centers for Disease Control and Prevention website.
If an investigation or audit emerges, work with an attorney as early as possible. Often, practices wait until too late after an investigation begins to contact legal counsel, Ms. Mazina noted. The earlier an attorney gets involved, the sooner that person can build a strong case for the practice and work toward the best resolution.
“Very often, the physician thinks they are right, and there’s nothing for them to fear,” she said. “There is something for you to fear. There’s a lot at stake.”
[email protected]
On Twitter @legal_med
CHICAGO – As the epidemic of opioid addiction and overdose deaths continues to surge, state and federal authorities are keeping a close eye on physicians who prescribe controlled substances.
Experts offer the following guidance on how well-meaning doctors can avoid coming under scrutiny for prescribing opioids and successfully manage investigations and audits.
1. Know who’s on the radar: The Drug Enforcement Agency (DEA) compiles a “black list” yearly of physicians and health care providers they plan to target for audits, said Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law. For 2017, the list includes physicians who have prior noncompliance records, providers who specialize in pain management, and those who dispense or administer large quantities of controlled substances.
In addition, family physicians, psychiatrists, and other specialists who come under investigation by a state medical board because of suspected inappropriate prescribing or reporting violations may also come under the purview of federal authorities, Ms. Mazina said.
“If they come on the medical board radar, they may come on the [DEA’s] radar as well,” she said during the interview. “They just have to watch how many prescriptions they write for controlled substances and make sure they are legitimate prescriptions.”
2. Maintain proper records: Poor record keeping is a top reason that the DEA investigates health care providers for potential prescribing violations, said Dennis A. Wichern, a DEA agent with the Chicago Field Division. Federal law requires that registered practitioners who store or dispense controlled substances keep records of controlled substances coming in and out of the practice. That includes physicians who hand out samples of controlled substances to patients and also pertains to samples provided to doctors by pharmaceutical companies.
Records should include whether the inventory was taken at the beginning or close of business, names of controlled substances, each finished form of the substances, the number of dosage units of each finished form in the commercial container, the number of commercial containers of each finished form, and disposition of the controlled substances.
Law requires that physicians take a new inventory of all controlled substances on hand every 2 years. Doctors are not required to keep records of controlled substances that are merely prescribed, unless such substances are prescribed in the course of maintenance or detoxification treatment.
Ms. Mazina notes that there are many software platforms that can assist practices with proper inventory and record keeping for opioids and other drugs.
3. Check the state database: Before prescribing opioids, check your state’s prescription drug monitoring program (PDMP) database, advises Ms. Mazina. At least 37 states have operational PDMPs that receive and distribute controlled substance prescription information to authorized users. About 11 states have enacted legislation to establish a PDMP, but some databases are not fully operational.
A state’s PDMP can reveal whether patients may be obtaining multiple controlled substance prescriptions from different doctors or doctor-shopping, Ms. Mazina said. Such due diligence helps inform treatment decisions and can assist a doctor’s case if a medical board or DEA investigation later arises.
“Even if your state law does not require you to check a patient’s history prior to prescribing, you have to check it to protect yourself,” she said. “If you want to avoid controlled substances problems, PDMP is the way to go.”
4. Establish an audit response plan: Have an audit response plan ready to roll should an inquiry arise, experts advise. The policies ensure that only approved information is released to authorities, and that all staff members are on the same page about how to react to audits, Ms. Mazina said.
Plans should clearly state what information can be collected and what data should be kept confidential. Financial information, for example, should be off limits, she said. Government agents are entitled to inventory, dispensary data, and records of receipts.
“Agents very often do the mirror image of the database, and they get too much information,” she said. “You don’t want to [allow] that.”
Train staff members how to respond to government authorities seeking audit information, and explain they have the right to refuse being interviewed, Ms. Mazina said.
“Train your employees on what’s going to happen if the DEA comes in,” she said. “If I don’t have clear policies and procedures, and I’m not trained, I might disclose everything and blame someone. That puts everyone in a [bad] position, because [authorities] will record everything and use it against [the practice].”
5. Confer with the experts: It doesn’t hurt to consult with other medical professionals, such as emergency physicians or pain management specialists, for practical advice on inventory policies or software suggestions. But when it comes to staying updated on new drug laws and regulations, confer with a health law attorney or compliance officer, Ms. Mazina said. The DEA website also includes useful information about recent laws and rules pertaining to prescription drugs, as does the Centers for Disease Control and Prevention website.
If an investigation or audit emerges, work with an attorney as early as possible. Often, practices wait until too late after an investigation begins to contact legal counsel, Ms. Mazina noted. The earlier an attorney gets involved, the sooner that person can build a strong case for the practice and work toward the best resolution.
“Very often, the physician thinks they are right, and there’s nothing for them to fear,” she said. “There is something for you to fear. There’s a lot at stake.”
[email protected]
On Twitter @legal_med
AT THE PHYSICIANS LEGAL ISSUES CONFERENCE
For opioid-related hospitalizations, men and women are equal
Equality is not always a good thing, particularly with opioids.
In 2005, the rate of opioid-related inpatient hospital stays was 145.6 per 100,000 population for males of all ages and 127.8 for females of all ages. By 2014, however, equality had arrived: Females had a rate of 224.1 per 100,000, compared with 225 for males, according to the Agency for Healthcare Research and Quality. Those increases in hospital admissions work out to 75% for females and 55% for males.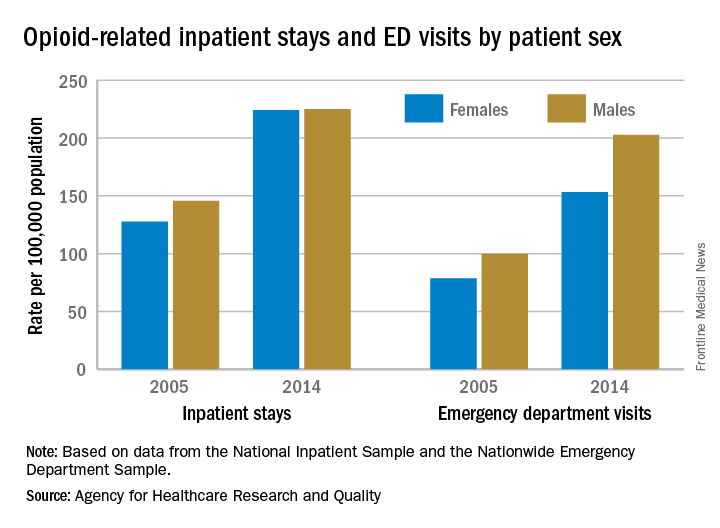
The states tell a similarly unequal story for opioid-related ED visits. In 2014, males had the higher rate in 23 states, and females had the higher rate in 7 states. (Washington, D.C., and 20 states do not participate in the State Emergency Department Databases and were not included in this analysis.)
Among the 30 participating states, Massachusetts had the highest visit rates for both males (598.8) and females (310.4), and Iowa had the lowest at 37 for males and 53.1 for females, AHRQ said.
The roles were reversed for opioid-related hospital admissions in the states in 2014: Females had the higher rate in 33 of the states participating in the State Inpatient Databases, compared with 11 states and the District of Columbia for males.
West Virginia had the highest rate for females at 371.2, and Washington, D.C., had the highest rate for males at 472. The lowest rates for both females (82.3) and males (63) were found in Iowa, according to the report.
Equality is not always a good thing, particularly with opioids.
In 2005, the rate of opioid-related inpatient hospital stays was 145.6 per 100,000 population for males of all ages and 127.8 for females of all ages. By 2014, however, equality had arrived: Females had a rate of 224.1 per 100,000, compared with 225 for males, according to the Agency for Healthcare Research and Quality. Those increases in hospital admissions work out to 75% for females and 55% for males.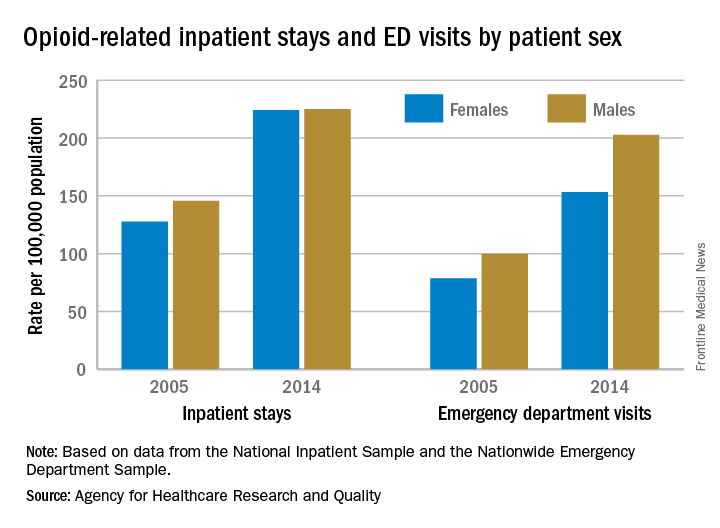
The states tell a similarly unequal story for opioid-related ED visits. In 2014, males had the higher rate in 23 states, and females had the higher rate in 7 states. (Washington, D.C., and 20 states do not participate in the State Emergency Department Databases and were not included in this analysis.)
Among the 30 participating states, Massachusetts had the highest visit rates for both males (598.8) and females (310.4), and Iowa had the lowest at 37 for males and 53.1 for females, AHRQ said.
The roles were reversed for opioid-related hospital admissions in the states in 2014: Females had the higher rate in 33 of the states participating in the State Inpatient Databases, compared with 11 states and the District of Columbia for males.
West Virginia had the highest rate for females at 371.2, and Washington, D.C., had the highest rate for males at 472. The lowest rates for both females (82.3) and males (63) were found in Iowa, according to the report.
Equality is not always a good thing, particularly with opioids.
In 2005, the rate of opioid-related inpatient hospital stays was 145.6 per 100,000 population for males of all ages and 127.8 for females of all ages. By 2014, however, equality had arrived: Females had a rate of 224.1 per 100,000, compared with 225 for males, according to the Agency for Healthcare Research and Quality. Those increases in hospital admissions work out to 75% for females and 55% for males.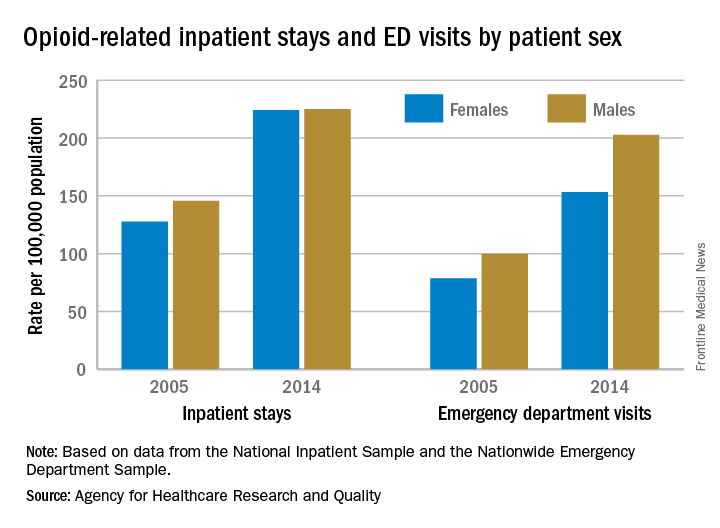
The states tell a similarly unequal story for opioid-related ED visits. In 2014, males had the higher rate in 23 states, and females had the higher rate in 7 states. (Washington, D.C., and 20 states do not participate in the State Emergency Department Databases and were not included in this analysis.)
Among the 30 participating states, Massachusetts had the highest visit rates for both males (598.8) and females (310.4), and Iowa had the lowest at 37 for males and 53.1 for females, AHRQ said.
The roles were reversed for opioid-related hospital admissions in the states in 2014: Females had the higher rate in 33 of the states participating in the State Inpatient Databases, compared with 11 states and the District of Columbia for males.
West Virginia had the highest rate for females at 371.2, and Washington, D.C., had the highest rate for males at 472. The lowest rates for both females (82.3) and males (63) were found in Iowa, according to the report.
Hospitalist meta-leader: Your new mission has arrived
If you are a hospitalist and leader in your health care organization, the ongoing controversies surrounding the Affordable Care Act repeal and replace campaign are unsettling. No matter your politics, Washington’s political drama and gamesmanship pose a genuine threat to the solvency of your hospital’s budget, services, workforce, and patients.
Health care has devolved into a political football, tossed from skirmish to skirmish. Political leaders warn of the implosion of the health care system as a political tactic, not an outcome that could cost and ruin lives. Both Democrats and Republicans hope that if or when that happens, it does so in ways that allow them to blame the other side. For them, this is a game of partisan advantage that wagers the well-being of your health care system.
For you, the situation remains predictably unpredictable. The future directives from Washington are unknowable. This makes your strategic planning – and health care leadership itself – a complex and puzzling task. Your job now is not simply leading your organization for today. Your more important mission is preparing your organization to perform in this unpredictable and perplexing future.
Forecasting is the life blood of leadership: Craft a vision and the work to achieve it; be mindful of the range of obstacles and opportunities; and know and coalesce your followers. The problem is that today’s prospects are loaded with puzzling twists and turns. The viability of both the private insurance market and public dollars are – maybe! – in future jeopardy. Patients and the workforce are understandably jittery. What is a hospitalist leader to do?
It is time to refresh your thinking, to take a big picture view of what is happening and to assess what can be done about it. There is a tendency for leaders to look at problems and then wonder how to fit solutions into their established organizational framework. In other words, solutions are cast into the mold of retaining what you have, ignoring larger options and innovative possibilities. Solutions are expected to adapt to the organization rather than the organization adapting to the solutions.
The hospitalist movement grew as early leaders – true innovators – recognized the problems of costly, inefficient and uncoordinated care. Rather than tinkering with what was, hospitalist leaders introduced a new and proactive model to provide care. It had to first prove itself and once it did, a once revolutionary idea evolved into an institutionalized solution.
No matter what emerges from the current policy debate, the national pressures on the health care system persist: rising expectations for access; decreasing patience for spending; increasing appetite for breakthrough technology; shifting workforce requirements; all combined with a population that is aging and more in need of care. These are meta-trends that will redefine how the health system operates and what it will achieve. What is a health care leader to do?
Think and act like a “meta-leader.” This framework, developed at the Harvard T.H. Chan School of Public Health, guides leaders facing complex and transformational problem solving. The prefix “meta-” encourages expansive analysis directed toward a wide range of options and opportunities. In keeping with the strategies employed by hospitalist pioneers, rather than building solutions around “what already is,” meta-leaders pursue “what could be.” In this way, solutions are designed and constructed to fit the problems they are intended to overcome.
There are three critical dimensions to the thinking and practices of meta-leadership.
The first is the Person of the meta-leader. This is who you are, your priorities and values. This is how other people regard your leadership, translated into the respect, trust, and “followership” you garner. Be a role model. This involves building your own confidence for the task at hand so that you gain and then foster the confidence of those you lead. As a meta-leader, you shape your mindset and that of others for innovation, sharpening the curiosity necessary for fostering discovery and exploration of new ideas. Be ready to take appropriate risks.
The second dimension of meta-leadership practice is the Situation. This is what is happening and what can be done about it. You did not create the complex circumstances that derive from the political showdown in Washington. However, it is your job to understand them and to develop effective strategies and operations in response. This is where the “think big” of meta-leadership comes into play. You distinguish the chasm between the adversarial policy confrontation in Washington and the collaborative solution building needed in your home institution. You want to set the stage to meaningfully coalesce the thinking, resources, and people in your organization. The invigorated shared mission is a health care system that leads into the future.
The third dimension of meta-leadership practice is about building the Connectivity needed to make that happen. This involves developing the communication, coordination, and cooperation necessary for constructing something new. Many of your answers lie within the walls of your organization, even the most innovative among them. This is where you sow adaptability and flexibility. It translates into necessary change and transformation. This is reorienting what you and others do and how you go about doing it, from shifts and adjustments to, when necessary, disruptive innovation.
A recent Harvard Business School and Harvard Medical School forum on health care innovation identified five imperatives for meeting innovation challenges in health care: 1) Creating value is the key aim for innovation and it requires a combination of care coordination along with communication; 2) Seek opportunities for process improvement that allows new ideas to be tested, accepting that failure is a step on the road to discovery; 3) Adopt a consumerism strategy for service organization that engages and involves active patients; 4) Decentralize problem solving to encourage field innovation and collaboration; and 5) Integrate new models into established institutions, introducing fresh thinking to replace outdated practices.
Meta-leadership is not a formula for an easy fix. While much remains unpredictable, an impending economic squeeze is a likely scenario. There is nothing easy about a shortage of dollars to serve more and more people in need of clinical care. This may very well be the prompt – today – that encourages the sort of innovative thinking and disruptive solution development that the future requires. Will you and your organization get ahead of this curve?
Your mission as a hospitalist meta-leader is in forging this process of discovery. Perceive what is going on through a wide lens. Orient yourself to emerging trends. Predict what is likely to emerge from this unpredictable policy environment. Take decisions and operationalize them in ways responsive to the circumstances at hand. And then communicate with your constituencies, not only to inform them of direction but also to learn from them what is working and what not. And then you start the process again, trying on ideas and practices, learning from them and through this continuous process, finding solutions that fit your situation at hand.
Health care meta-leaders today must keep both eyes firmly on their feet, to know that current operations are achieving necessary success. At the same time, they must also keep both eyes focused on the horizon, to ensure that when conditions change, their organizations are ready to adaptively innovate and transform.
Leonard J. Marcus, Ph.D. is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected]
If you are a hospitalist and leader in your health care organization, the ongoing controversies surrounding the Affordable Care Act repeal and replace campaign are unsettling. No matter your politics, Washington’s political drama and gamesmanship pose a genuine threat to the solvency of your hospital’s budget, services, workforce, and patients.
Health care has devolved into a political football, tossed from skirmish to skirmish. Political leaders warn of the implosion of the health care system as a political tactic, not an outcome that could cost and ruin lives. Both Democrats and Republicans hope that if or when that happens, it does so in ways that allow them to blame the other side. For them, this is a game of partisan advantage that wagers the well-being of your health care system.
For you, the situation remains predictably unpredictable. The future directives from Washington are unknowable. This makes your strategic planning – and health care leadership itself – a complex and puzzling task. Your job now is not simply leading your organization for today. Your more important mission is preparing your organization to perform in this unpredictable and perplexing future.
Forecasting is the life blood of leadership: Craft a vision and the work to achieve it; be mindful of the range of obstacles and opportunities; and know and coalesce your followers. The problem is that today’s prospects are loaded with puzzling twists and turns. The viability of both the private insurance market and public dollars are – maybe! – in future jeopardy. Patients and the workforce are understandably jittery. What is a hospitalist leader to do?
It is time to refresh your thinking, to take a big picture view of what is happening and to assess what can be done about it. There is a tendency for leaders to look at problems and then wonder how to fit solutions into their established organizational framework. In other words, solutions are cast into the mold of retaining what you have, ignoring larger options and innovative possibilities. Solutions are expected to adapt to the organization rather than the organization adapting to the solutions.
The hospitalist movement grew as early leaders – true innovators – recognized the problems of costly, inefficient and uncoordinated care. Rather than tinkering with what was, hospitalist leaders introduced a new and proactive model to provide care. It had to first prove itself and once it did, a once revolutionary idea evolved into an institutionalized solution.
No matter what emerges from the current policy debate, the national pressures on the health care system persist: rising expectations for access; decreasing patience for spending; increasing appetite for breakthrough technology; shifting workforce requirements; all combined with a population that is aging and more in need of care. These are meta-trends that will redefine how the health system operates and what it will achieve. What is a health care leader to do?
Think and act like a “meta-leader.” This framework, developed at the Harvard T.H. Chan School of Public Health, guides leaders facing complex and transformational problem solving. The prefix “meta-” encourages expansive analysis directed toward a wide range of options and opportunities. In keeping with the strategies employed by hospitalist pioneers, rather than building solutions around “what already is,” meta-leaders pursue “what could be.” In this way, solutions are designed and constructed to fit the problems they are intended to overcome.
There are three critical dimensions to the thinking and practices of meta-leadership.
The first is the Person of the meta-leader. This is who you are, your priorities and values. This is how other people regard your leadership, translated into the respect, trust, and “followership” you garner. Be a role model. This involves building your own confidence for the task at hand so that you gain and then foster the confidence of those you lead. As a meta-leader, you shape your mindset and that of others for innovation, sharpening the curiosity necessary for fostering discovery and exploration of new ideas. Be ready to take appropriate risks.
The second dimension of meta-leadership practice is the Situation. This is what is happening and what can be done about it. You did not create the complex circumstances that derive from the political showdown in Washington. However, it is your job to understand them and to develop effective strategies and operations in response. This is where the “think big” of meta-leadership comes into play. You distinguish the chasm between the adversarial policy confrontation in Washington and the collaborative solution building needed in your home institution. You want to set the stage to meaningfully coalesce the thinking, resources, and people in your organization. The invigorated shared mission is a health care system that leads into the future.
The third dimension of meta-leadership practice is about building the Connectivity needed to make that happen. This involves developing the communication, coordination, and cooperation necessary for constructing something new. Many of your answers lie within the walls of your organization, even the most innovative among them. This is where you sow adaptability and flexibility. It translates into necessary change and transformation. This is reorienting what you and others do and how you go about doing it, from shifts and adjustments to, when necessary, disruptive innovation.
A recent Harvard Business School and Harvard Medical School forum on health care innovation identified five imperatives for meeting innovation challenges in health care: 1) Creating value is the key aim for innovation and it requires a combination of care coordination along with communication; 2) Seek opportunities for process improvement that allows new ideas to be tested, accepting that failure is a step on the road to discovery; 3) Adopt a consumerism strategy for service organization that engages and involves active patients; 4) Decentralize problem solving to encourage field innovation and collaboration; and 5) Integrate new models into established institutions, introducing fresh thinking to replace outdated practices.
Meta-leadership is not a formula for an easy fix. While much remains unpredictable, an impending economic squeeze is a likely scenario. There is nothing easy about a shortage of dollars to serve more and more people in need of clinical care. This may very well be the prompt – today – that encourages the sort of innovative thinking and disruptive solution development that the future requires. Will you and your organization get ahead of this curve?
Your mission as a hospitalist meta-leader is in forging this process of discovery. Perceive what is going on through a wide lens. Orient yourself to emerging trends. Predict what is likely to emerge from this unpredictable policy environment. Take decisions and operationalize them in ways responsive to the circumstances at hand. And then communicate with your constituencies, not only to inform them of direction but also to learn from them what is working and what not. And then you start the process again, trying on ideas and practices, learning from them and through this continuous process, finding solutions that fit your situation at hand.
Health care meta-leaders today must keep both eyes firmly on their feet, to know that current operations are achieving necessary success. At the same time, they must also keep both eyes focused on the horizon, to ensure that when conditions change, their organizations are ready to adaptively innovate and transform.
Leonard J. Marcus, Ph.D. is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected]
If you are a hospitalist and leader in your health care organization, the ongoing controversies surrounding the Affordable Care Act repeal and replace campaign are unsettling. No matter your politics, Washington’s political drama and gamesmanship pose a genuine threat to the solvency of your hospital’s budget, services, workforce, and patients.
Health care has devolved into a political football, tossed from skirmish to skirmish. Political leaders warn of the implosion of the health care system as a political tactic, not an outcome that could cost and ruin lives. Both Democrats and Republicans hope that if or when that happens, it does so in ways that allow them to blame the other side. For them, this is a game of partisan advantage that wagers the well-being of your health care system.
For you, the situation remains predictably unpredictable. The future directives from Washington are unknowable. This makes your strategic planning – and health care leadership itself – a complex and puzzling task. Your job now is not simply leading your organization for today. Your more important mission is preparing your organization to perform in this unpredictable and perplexing future.
Forecasting is the life blood of leadership: Craft a vision and the work to achieve it; be mindful of the range of obstacles and opportunities; and know and coalesce your followers. The problem is that today’s prospects are loaded with puzzling twists and turns. The viability of both the private insurance market and public dollars are – maybe! – in future jeopardy. Patients and the workforce are understandably jittery. What is a hospitalist leader to do?
It is time to refresh your thinking, to take a big picture view of what is happening and to assess what can be done about it. There is a tendency for leaders to look at problems and then wonder how to fit solutions into their established organizational framework. In other words, solutions are cast into the mold of retaining what you have, ignoring larger options and innovative possibilities. Solutions are expected to adapt to the organization rather than the organization adapting to the solutions.
The hospitalist movement grew as early leaders – true innovators – recognized the problems of costly, inefficient and uncoordinated care. Rather than tinkering with what was, hospitalist leaders introduced a new and proactive model to provide care. It had to first prove itself and once it did, a once revolutionary idea evolved into an institutionalized solution.
No matter what emerges from the current policy debate, the national pressures on the health care system persist: rising expectations for access; decreasing patience for spending; increasing appetite for breakthrough technology; shifting workforce requirements; all combined with a population that is aging and more in need of care. These are meta-trends that will redefine how the health system operates and what it will achieve. What is a health care leader to do?
Think and act like a “meta-leader.” This framework, developed at the Harvard T.H. Chan School of Public Health, guides leaders facing complex and transformational problem solving. The prefix “meta-” encourages expansive analysis directed toward a wide range of options and opportunities. In keeping with the strategies employed by hospitalist pioneers, rather than building solutions around “what already is,” meta-leaders pursue “what could be.” In this way, solutions are designed and constructed to fit the problems they are intended to overcome.
There are three critical dimensions to the thinking and practices of meta-leadership.
The first is the Person of the meta-leader. This is who you are, your priorities and values. This is how other people regard your leadership, translated into the respect, trust, and “followership” you garner. Be a role model. This involves building your own confidence for the task at hand so that you gain and then foster the confidence of those you lead. As a meta-leader, you shape your mindset and that of others for innovation, sharpening the curiosity necessary for fostering discovery and exploration of new ideas. Be ready to take appropriate risks.
The second dimension of meta-leadership practice is the Situation. This is what is happening and what can be done about it. You did not create the complex circumstances that derive from the political showdown in Washington. However, it is your job to understand them and to develop effective strategies and operations in response. This is where the “think big” of meta-leadership comes into play. You distinguish the chasm between the adversarial policy confrontation in Washington and the collaborative solution building needed in your home institution. You want to set the stage to meaningfully coalesce the thinking, resources, and people in your organization. The invigorated shared mission is a health care system that leads into the future.
The third dimension of meta-leadership practice is about building the Connectivity needed to make that happen. This involves developing the communication, coordination, and cooperation necessary for constructing something new. Many of your answers lie within the walls of your organization, even the most innovative among them. This is where you sow adaptability and flexibility. It translates into necessary change and transformation. This is reorienting what you and others do and how you go about doing it, from shifts and adjustments to, when necessary, disruptive innovation.
A recent Harvard Business School and Harvard Medical School forum on health care innovation identified five imperatives for meeting innovation challenges in health care: 1) Creating value is the key aim for innovation and it requires a combination of care coordination along with communication; 2) Seek opportunities for process improvement that allows new ideas to be tested, accepting that failure is a step on the road to discovery; 3) Adopt a consumerism strategy for service organization that engages and involves active patients; 4) Decentralize problem solving to encourage field innovation and collaboration; and 5) Integrate new models into established institutions, introducing fresh thinking to replace outdated practices.
Meta-leadership is not a formula for an easy fix. While much remains unpredictable, an impending economic squeeze is a likely scenario. There is nothing easy about a shortage of dollars to serve more and more people in need of clinical care. This may very well be the prompt – today – that encourages the sort of innovative thinking and disruptive solution development that the future requires. Will you and your organization get ahead of this curve?
Your mission as a hospitalist meta-leader is in forging this process of discovery. Perceive what is going on through a wide lens. Orient yourself to emerging trends. Predict what is likely to emerge from this unpredictable policy environment. Take decisions and operationalize them in ways responsive to the circumstances at hand. And then communicate with your constituencies, not only to inform them of direction but also to learn from them what is working and what not. And then you start the process again, trying on ideas and practices, learning from them and through this continuous process, finding solutions that fit your situation at hand.
Health care meta-leaders today must keep both eyes firmly on their feet, to know that current operations are achieving necessary success. At the same time, they must also keep both eyes focused on the horizon, to ensure that when conditions change, their organizations are ready to adaptively innovate and transform.
Leonard J. Marcus, Ph.D. is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected]
Hospitalist movers and shakers - June/July 2017
Three members of the hospital medicine community – Thiruvoipati Nanda Kumar, MD; Anthony Aghenta, MD, MS, FACP; and Angela Aboutalib, MD – recently were honored for their work by the International Association of HealthCare Professionals, earning spots in its publication, The Leading Physicians of the World.
Hospitalist and internist Dr. Nanda Kumar serves patients at Vibra Hospital in Redding, Calif., where he is also a clinical associate professor at the University of California at Davis. He is a member of both the Society of Hospital Medicine and the American Diabetes Association.
Dr. Aghenta is a 17-year veteran internist who currently serves as medical director for Coronado Healthcare Center in Phoenix. There, he also is affiliated with St. Joseph’s Hospital and Medical Center. A member of SHM, Dr. Aghenta also has the title of Fellow of the American College of Physicians.
Dr. Aboutalib, whose experience as an internist includes expertise in hospital medicine, serves as hospitalist and medical director of clinical operations at U.S. Acute Care Solutions, Canton, Ohio. Previously, this member of the American College of Physicians served South Physicians as a hospitalist at Mercy Hospital in Chicago.
Andrew Dunn, MD, MPH, FACP, SFHM, recently was named chair-elect of the Board of Regents of the American College of Physicians (ACP), the national organization of internists. He assumed the role at the start of the ACP’s annual scientific meeting held in San Diego, March 30–April 1.
Susan Herson, MD, has been named the new chief of staff at the Bath, N.Y., Veterans Affairs Medical Center. Dr. Herson comes to Bath from the Sioux Falls (S.D.) VA, where she was a hospitalist, a hospitalist-clinician educator, and medical director of clinical documentation improvement, while also serving as clinical assistant professor for New York Medical College and medical director at Norwalk (Conn.) Hospital.
Dr. Herson served in the U.S. Navy, doing her training at Walter Reed Medical Center, Bethesda, Md. She was a general medical officer while stationed at U.S. Marine Corps Base Camp Lejeune in Jacksonville, N.C.
Chad Whelan, MD, has been elevated to president of the Loyola (Ill.) University Medical Center, moving up from his chair as senior vice president and chief medical officer. This longtime hospitalist also serves as a professor of medicine in the Loyola Chicago Stritch School of Medicine.
Kevin Tulipana, DO, recently was promoted to medical director of hospital medicine at Cancer Treatment Centers of America’s Southwest Regional Medical Center in Tulsa, Okla. Previously, Dr. Tulipana was a hospitalist in the special care unit at CTCA Tulsa.
Mustafa Sardini, MD, has been named Envision Physician Services’ 2017 Hospital Medicine Physician of the Year. Dr. Sardini is the site medical director as Baylor Scott & White Medical Center, Sunnyvale, Texas. EPS presents the award to a hospitalist who peers deem as a leader in the industry.
Business moves
Physicians’ Alliance, (PAL) recently announced plans to partner with Penn State Health. As the largest independent physician group in Lancaster County, Pa., they will bring its more than 120 physicians, hospitalists, and dieticians to central Pennsylvania giant Penn State.
The alliance will allow patients of PAL physicians access to advanced care at Milton S. Hershey Medical Center and Penn State Children’s Hospital in Hershey.
Envision Healthcare, Greenwood Village, Colo. has created the Envision Physical Services (EPS) as a result of a merger with AmSurg ambulatory surgical center in December 2016. EPS combines EmCare and Sheridan Healthcare’s physician services divisions.
EPS specializes in hospital medicine, anesthesia, emergency medicine, radiology, and surgical services.
Three members of the hospital medicine community – Thiruvoipati Nanda Kumar, MD; Anthony Aghenta, MD, MS, FACP; and Angela Aboutalib, MD – recently were honored for their work by the International Association of HealthCare Professionals, earning spots in its publication, The Leading Physicians of the World.
Hospitalist and internist Dr. Nanda Kumar serves patients at Vibra Hospital in Redding, Calif., where he is also a clinical associate professor at the University of California at Davis. He is a member of both the Society of Hospital Medicine and the American Diabetes Association.
Dr. Aghenta is a 17-year veteran internist who currently serves as medical director for Coronado Healthcare Center in Phoenix. There, he also is affiliated with St. Joseph’s Hospital and Medical Center. A member of SHM, Dr. Aghenta also has the title of Fellow of the American College of Physicians.
Dr. Aboutalib, whose experience as an internist includes expertise in hospital medicine, serves as hospitalist and medical director of clinical operations at U.S. Acute Care Solutions, Canton, Ohio. Previously, this member of the American College of Physicians served South Physicians as a hospitalist at Mercy Hospital in Chicago.
Andrew Dunn, MD, MPH, FACP, SFHM, recently was named chair-elect of the Board of Regents of the American College of Physicians (ACP), the national organization of internists. He assumed the role at the start of the ACP’s annual scientific meeting held in San Diego, March 30–April 1.
Susan Herson, MD, has been named the new chief of staff at the Bath, N.Y., Veterans Affairs Medical Center. Dr. Herson comes to Bath from the Sioux Falls (S.D.) VA, where she was a hospitalist, a hospitalist-clinician educator, and medical director of clinical documentation improvement, while also serving as clinical assistant professor for New York Medical College and medical director at Norwalk (Conn.) Hospital.
Dr. Herson served in the U.S. Navy, doing her training at Walter Reed Medical Center, Bethesda, Md. She was a general medical officer while stationed at U.S. Marine Corps Base Camp Lejeune in Jacksonville, N.C.
Chad Whelan, MD, has been elevated to president of the Loyola (Ill.) University Medical Center, moving up from his chair as senior vice president and chief medical officer. This longtime hospitalist also serves as a professor of medicine in the Loyola Chicago Stritch School of Medicine.
Kevin Tulipana, DO, recently was promoted to medical director of hospital medicine at Cancer Treatment Centers of America’s Southwest Regional Medical Center in Tulsa, Okla. Previously, Dr. Tulipana was a hospitalist in the special care unit at CTCA Tulsa.
Mustafa Sardini, MD, has been named Envision Physician Services’ 2017 Hospital Medicine Physician of the Year. Dr. Sardini is the site medical director as Baylor Scott & White Medical Center, Sunnyvale, Texas. EPS presents the award to a hospitalist who peers deem as a leader in the industry.
Business moves
Physicians’ Alliance, (PAL) recently announced plans to partner with Penn State Health. As the largest independent physician group in Lancaster County, Pa., they will bring its more than 120 physicians, hospitalists, and dieticians to central Pennsylvania giant Penn State.
The alliance will allow patients of PAL physicians access to advanced care at Milton S. Hershey Medical Center and Penn State Children’s Hospital in Hershey.
Envision Healthcare, Greenwood Village, Colo. has created the Envision Physical Services (EPS) as a result of a merger with AmSurg ambulatory surgical center in December 2016. EPS combines EmCare and Sheridan Healthcare’s physician services divisions.
EPS specializes in hospital medicine, anesthesia, emergency medicine, radiology, and surgical services.
Three members of the hospital medicine community – Thiruvoipati Nanda Kumar, MD; Anthony Aghenta, MD, MS, FACP; and Angela Aboutalib, MD – recently were honored for their work by the International Association of HealthCare Professionals, earning spots in its publication, The Leading Physicians of the World.
Hospitalist and internist Dr. Nanda Kumar serves patients at Vibra Hospital in Redding, Calif., where he is also a clinical associate professor at the University of California at Davis. He is a member of both the Society of Hospital Medicine and the American Diabetes Association.
Dr. Aghenta is a 17-year veteran internist who currently serves as medical director for Coronado Healthcare Center in Phoenix. There, he also is affiliated with St. Joseph’s Hospital and Medical Center. A member of SHM, Dr. Aghenta also has the title of Fellow of the American College of Physicians.
Dr. Aboutalib, whose experience as an internist includes expertise in hospital medicine, serves as hospitalist and medical director of clinical operations at U.S. Acute Care Solutions, Canton, Ohio. Previously, this member of the American College of Physicians served South Physicians as a hospitalist at Mercy Hospital in Chicago.
Andrew Dunn, MD, MPH, FACP, SFHM, recently was named chair-elect of the Board of Regents of the American College of Physicians (ACP), the national organization of internists. He assumed the role at the start of the ACP’s annual scientific meeting held in San Diego, March 30–April 1.
Susan Herson, MD, has been named the new chief of staff at the Bath, N.Y., Veterans Affairs Medical Center. Dr. Herson comes to Bath from the Sioux Falls (S.D.) VA, where she was a hospitalist, a hospitalist-clinician educator, and medical director of clinical documentation improvement, while also serving as clinical assistant professor for New York Medical College and medical director at Norwalk (Conn.) Hospital.
Dr. Herson served in the U.S. Navy, doing her training at Walter Reed Medical Center, Bethesda, Md. She was a general medical officer while stationed at U.S. Marine Corps Base Camp Lejeune in Jacksonville, N.C.
Chad Whelan, MD, has been elevated to president of the Loyola (Ill.) University Medical Center, moving up from his chair as senior vice president and chief medical officer. This longtime hospitalist also serves as a professor of medicine in the Loyola Chicago Stritch School of Medicine.
Kevin Tulipana, DO, recently was promoted to medical director of hospital medicine at Cancer Treatment Centers of America’s Southwest Regional Medical Center in Tulsa, Okla. Previously, Dr. Tulipana was a hospitalist in the special care unit at CTCA Tulsa.
Mustafa Sardini, MD, has been named Envision Physician Services’ 2017 Hospital Medicine Physician of the Year. Dr. Sardini is the site medical director as Baylor Scott & White Medical Center, Sunnyvale, Texas. EPS presents the award to a hospitalist who peers deem as a leader in the industry.
Business moves
Physicians’ Alliance, (PAL) recently announced plans to partner with Penn State Health. As the largest independent physician group in Lancaster County, Pa., they will bring its more than 120 physicians, hospitalists, and dieticians to central Pennsylvania giant Penn State.
The alliance will allow patients of PAL physicians access to advanced care at Milton S. Hershey Medical Center and Penn State Children’s Hospital in Hershey.
Envision Healthcare, Greenwood Village, Colo. has created the Envision Physical Services (EPS) as a result of a merger with AmSurg ambulatory surgical center in December 2016. EPS combines EmCare and Sheridan Healthcare’s physician services divisions.
EPS specializes in hospital medicine, anesthesia, emergency medicine, radiology, and surgical services.
Tipoffs that an infant hospitalized with pertussis may require ICU
MADRID – Infants hospitalized for pertussis are more likely to develop severe disease requiring pediatric ICU admission if they are experiencing apnea, are unvaccinated against pertussis, or are less than 2 months old, Maria Arranz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“The presence of these parameters on admission should warn us of possible severe disease,” said Dr. Arranz of Gregorio Maranon Hospital in Madrid.
Dr. Arranz presented a retrospective observational study of 101 children under 1 year of age who were hospitalized for pertussis at the Madrid tertiary center prior to the hospital’s 2016 shift to a strategy of maternal immunization during pregnancy as a means of preventing pertussis in infancy. Thirteen percent of the children required admission to the pediatric ICU and thus by definition had severe disease.
Half of infants in the study were not vaccinated against pertussis. That proved to be a powerful risk factor for severe disease requiring an ICU stay. Only 8% of children with severe pertussis were vaccinated, compared with a 58% vaccination rate among those who avoided the ICU.
Apneic pauses were noted in 67% of the severe disease group, compared with 28% of the infants who didn’t need the ICU.
The pertussis patients admitted to the pediatric ICU averaged 1 month of age, compared with age 2 months in the nonsevere group.
The maximum leukocyte, lymphocyte, and neutrophil counts during the hospital stay of the severe disease group averaged 23,600 cells/mm3, 18,000/mm3, and 5,000/mm3, respectively, significantly greater than the 15,300, 10,700, and 3,900 cells/mm3 in infants who did not require the ICU. Levels of all three cells also were higher at admission in the severe pertussis group than in those who didn’t make it to the ICU, albeit not statistically significantly so.
Dr. Arranz reported having no financial conflicts of interest regarding her study.
MADRID – Infants hospitalized for pertussis are more likely to develop severe disease requiring pediatric ICU admission if they are experiencing apnea, are unvaccinated against pertussis, or are less than 2 months old, Maria Arranz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“The presence of these parameters on admission should warn us of possible severe disease,” said Dr. Arranz of Gregorio Maranon Hospital in Madrid.
Dr. Arranz presented a retrospective observational study of 101 children under 1 year of age who were hospitalized for pertussis at the Madrid tertiary center prior to the hospital’s 2016 shift to a strategy of maternal immunization during pregnancy as a means of preventing pertussis in infancy. Thirteen percent of the children required admission to the pediatric ICU and thus by definition had severe disease.
Half of infants in the study were not vaccinated against pertussis. That proved to be a powerful risk factor for severe disease requiring an ICU stay. Only 8% of children with severe pertussis were vaccinated, compared with a 58% vaccination rate among those who avoided the ICU.
Apneic pauses were noted in 67% of the severe disease group, compared with 28% of the infants who didn’t need the ICU.
The pertussis patients admitted to the pediatric ICU averaged 1 month of age, compared with age 2 months in the nonsevere group.
The maximum leukocyte, lymphocyte, and neutrophil counts during the hospital stay of the severe disease group averaged 23,600 cells/mm3, 18,000/mm3, and 5,000/mm3, respectively, significantly greater than the 15,300, 10,700, and 3,900 cells/mm3 in infants who did not require the ICU. Levels of all three cells also were higher at admission in the severe pertussis group than in those who didn’t make it to the ICU, albeit not statistically significantly so.
Dr. Arranz reported having no financial conflicts of interest regarding her study.
MADRID – Infants hospitalized for pertussis are more likely to develop severe disease requiring pediatric ICU admission if they are experiencing apnea, are unvaccinated against pertussis, or are less than 2 months old, Maria Arranz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“The presence of these parameters on admission should warn us of possible severe disease,” said Dr. Arranz of Gregorio Maranon Hospital in Madrid.
Dr. Arranz presented a retrospective observational study of 101 children under 1 year of age who were hospitalized for pertussis at the Madrid tertiary center prior to the hospital’s 2016 shift to a strategy of maternal immunization during pregnancy as a means of preventing pertussis in infancy. Thirteen percent of the children required admission to the pediatric ICU and thus by definition had severe disease.
Half of infants in the study were not vaccinated against pertussis. That proved to be a powerful risk factor for severe disease requiring an ICU stay. Only 8% of children with severe pertussis were vaccinated, compared with a 58% vaccination rate among those who avoided the ICU.
Apneic pauses were noted in 67% of the severe disease group, compared with 28% of the infants who didn’t need the ICU.
The pertussis patients admitted to the pediatric ICU averaged 1 month of age, compared with age 2 months in the nonsevere group.
The maximum leukocyte, lymphocyte, and neutrophil counts during the hospital stay of the severe disease group averaged 23,600 cells/mm3, 18,000/mm3, and 5,000/mm3, respectively, significantly greater than the 15,300, 10,700, and 3,900 cells/mm3 in infants who did not require the ICU. Levels of all three cells also were higher at admission in the severe pertussis group than in those who didn’t make it to the ICU, albeit not statistically significantly so.
Dr. Arranz reported having no financial conflicts of interest regarding her study.
AT ESPID 2017
Key clinical point:
Major finding: Among infants hospitalized for pertussis, apneic pauses were present in two-thirds of those with severe disease, ultimately resulting in admission to the pediatric ICU, compared with 28% of those who didn’t require an ICU stay.
Data source: This retrospective observational study sought to identify factors associated with severe pertussis requiring an ICU stay in a group of 101 Spanish infants hospitalized with the disease.
Disclosures: The presenter reported having no financial conflicts of interest regarding her study.
Sneak Peek: Journal of Hospital Medicine – July 2017
BACKGROUND: Medicare patients account for approximately 50% of hospital days. Hospitalization in older adults often results in poor outcomes.
OBJECTIVE: To test the feasibility and impact of using Assessing Care of Vulnerable Elders (ACOVE) quality indicators (QIs) as a therapeutic intervention to improve care of hospitalized older adults.
SETTING: Large tertiary hospital in the greater New York Metropolitan area.
PATIENTS: Hospitalized patients, 75 and over, admitted to medical units.
INTERVENTION: A checklist, comprised of four ACOVE QIs, administered during daily interdisciplinary rounds: venous thrombosis prophylaxis (VTE) (QI 1), indwelling bladder catheters (QI 2), mobilization (QI 3), and delirium evaluation (QI 4).
MEASUREMENTS: Variables were extracted from electronic medical records with QI compliance as the primary outcome, and length of stay (LOS), discharge disposition, and readmissions as secondary outcomes. Generalized linear mixed models for binary clustered data were used to estimate compliance rates for each group (intervention group or control group) in the postintervention period, along with their corresponding 95% confidence intervals.
RESULTS: Of the 2,396 patients, 530 were on an intervention unit. In those patients not already compliant with VTE, the compliance rate was 57% in intervention vs. 39% in control (P less than .0056). For indwelling catheters, mobilization, and delirium evaluation, overall compliance was significantly higher in the intervention group 72.2% vs. 54.4% (P = .1061), 62.9% vs. 48.2% (P less than .0001), and 27.9% vs. 21.7% (P = .0027), respectively.
CONCLUSIONS: The study demonstrates the feasibility and effectiveness of integrating ACOVE QIs to improve the quality of care in hospitalized older adults.
Also in JHM
Use of simulation to assess incoming interns’ recognition of opportunities to choose wisely
AUTHORS: Kathleen M. Wiest, Jeanne M. Farnan, MD, MHPE, Ellen Byrne, Lukas Matern, Melissa Cappaert, MA, Kristen Hirsch, Vineet M. Arora, MD, MAPP
Clinician attitudes regarding ICD deactivation in DNR/DNI patients
AUTHORS: Andrew J. Bradley, MD, Adam D. Marks, MD, MPH
Using standardized patients to assess hospitalist communication skills
AUTHORS: Dennis T. Chang, MD, Micah Mann, MD, Terry Sommer, BFA, Robert Fallar, PhD, Alan Weinberg, MS, Erica Friedman, MD
Techniques and behaviors associated with exemplary inpatient general medicine teaching: An exploratory qualitative study
AUTHORS: Nathan Houchens, MD, Molly Harrod, PhD, Stephanie Moody, PhD, Karen E. Fowler, MPH, Sanjay Saint, MD, MPH
A simple algorithm for predicting bacteremia using food consumption and shaking chills: A prospective observational study
AUTHORS: Takayuki Komatsu, MD, PhD, Erika Takahashi, MD, Kentaro Mishima, MD, Takeo Toyoda, MD, Fumihiro Saitoh, MD, Akari Yasuda, RN, Joe Matsuoka, PhD, Manabu Sugita, MD, PhD, Joel Branch, MD, Makoto Aoki, MD, Lawrence M. Tierney Jr., MD, Kenji Inoue, MD, PhD
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
BACKGROUND: Medicare patients account for approximately 50% of hospital days. Hospitalization in older adults often results in poor outcomes.
OBJECTIVE: To test the feasibility and impact of using Assessing Care of Vulnerable Elders (ACOVE) quality indicators (QIs) as a therapeutic intervention to improve care of hospitalized older adults.
SETTING: Large tertiary hospital in the greater New York Metropolitan area.
PATIENTS: Hospitalized patients, 75 and over, admitted to medical units.
INTERVENTION: A checklist, comprised of four ACOVE QIs, administered during daily interdisciplinary rounds: venous thrombosis prophylaxis (VTE) (QI 1), indwelling bladder catheters (QI 2), mobilization (QI 3), and delirium evaluation (QI 4).
MEASUREMENTS: Variables were extracted from electronic medical records with QI compliance as the primary outcome, and length of stay (LOS), discharge disposition, and readmissions as secondary outcomes. Generalized linear mixed models for binary clustered data were used to estimate compliance rates for each group (intervention group or control group) in the postintervention period, along with their corresponding 95% confidence intervals.
RESULTS: Of the 2,396 patients, 530 were on an intervention unit. In those patients not already compliant with VTE, the compliance rate was 57% in intervention vs. 39% in control (P less than .0056). For indwelling catheters, mobilization, and delirium evaluation, overall compliance was significantly higher in the intervention group 72.2% vs. 54.4% (P = .1061), 62.9% vs. 48.2% (P less than .0001), and 27.9% vs. 21.7% (P = .0027), respectively.
CONCLUSIONS: The study demonstrates the feasibility and effectiveness of integrating ACOVE QIs to improve the quality of care in hospitalized older adults.
Also in JHM
Use of simulation to assess incoming interns’ recognition of opportunities to choose wisely
AUTHORS: Kathleen M. Wiest, Jeanne M. Farnan, MD, MHPE, Ellen Byrne, Lukas Matern, Melissa Cappaert, MA, Kristen Hirsch, Vineet M. Arora, MD, MAPP
Clinician attitudes regarding ICD deactivation in DNR/DNI patients
AUTHORS: Andrew J. Bradley, MD, Adam D. Marks, MD, MPH
Using standardized patients to assess hospitalist communication skills
AUTHORS: Dennis T. Chang, MD, Micah Mann, MD, Terry Sommer, BFA, Robert Fallar, PhD, Alan Weinberg, MS, Erica Friedman, MD
Techniques and behaviors associated with exemplary inpatient general medicine teaching: An exploratory qualitative study
AUTHORS: Nathan Houchens, MD, Molly Harrod, PhD, Stephanie Moody, PhD, Karen E. Fowler, MPH, Sanjay Saint, MD, MPH
A simple algorithm for predicting bacteremia using food consumption and shaking chills: A prospective observational study
AUTHORS: Takayuki Komatsu, MD, PhD, Erika Takahashi, MD, Kentaro Mishima, MD, Takeo Toyoda, MD, Fumihiro Saitoh, MD, Akari Yasuda, RN, Joe Matsuoka, PhD, Manabu Sugita, MD, PhD, Joel Branch, MD, Makoto Aoki, MD, Lawrence M. Tierney Jr., MD, Kenji Inoue, MD, PhD
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
BACKGROUND: Medicare patients account for approximately 50% of hospital days. Hospitalization in older adults often results in poor outcomes.
OBJECTIVE: To test the feasibility and impact of using Assessing Care of Vulnerable Elders (ACOVE) quality indicators (QIs) as a therapeutic intervention to improve care of hospitalized older adults.
SETTING: Large tertiary hospital in the greater New York Metropolitan area.
PATIENTS: Hospitalized patients, 75 and over, admitted to medical units.
INTERVENTION: A checklist, comprised of four ACOVE QIs, administered during daily interdisciplinary rounds: venous thrombosis prophylaxis (VTE) (QI 1), indwelling bladder catheters (QI 2), mobilization (QI 3), and delirium evaluation (QI 4).
MEASUREMENTS: Variables were extracted from electronic medical records with QI compliance as the primary outcome, and length of stay (LOS), discharge disposition, and readmissions as secondary outcomes. Generalized linear mixed models for binary clustered data were used to estimate compliance rates for each group (intervention group or control group) in the postintervention period, along with their corresponding 95% confidence intervals.
RESULTS: Of the 2,396 patients, 530 were on an intervention unit. In those patients not already compliant with VTE, the compliance rate was 57% in intervention vs. 39% in control (P less than .0056). For indwelling catheters, mobilization, and delirium evaluation, overall compliance was significantly higher in the intervention group 72.2% vs. 54.4% (P = .1061), 62.9% vs. 48.2% (P less than .0001), and 27.9% vs. 21.7% (P = .0027), respectively.
CONCLUSIONS: The study demonstrates the feasibility and effectiveness of integrating ACOVE QIs to improve the quality of care in hospitalized older adults.
Also in JHM
Use of simulation to assess incoming interns’ recognition of opportunities to choose wisely
AUTHORS: Kathleen M. Wiest, Jeanne M. Farnan, MD, MHPE, Ellen Byrne, Lukas Matern, Melissa Cappaert, MA, Kristen Hirsch, Vineet M. Arora, MD, MAPP
Clinician attitudes regarding ICD deactivation in DNR/DNI patients
AUTHORS: Andrew J. Bradley, MD, Adam D. Marks, MD, MPH
Using standardized patients to assess hospitalist communication skills
AUTHORS: Dennis T. Chang, MD, Micah Mann, MD, Terry Sommer, BFA, Robert Fallar, PhD, Alan Weinberg, MS, Erica Friedman, MD
Techniques and behaviors associated with exemplary inpatient general medicine teaching: An exploratory qualitative study
AUTHORS: Nathan Houchens, MD, Molly Harrod, PhD, Stephanie Moody, PhD, Karen E. Fowler, MPH, Sanjay Saint, MD, MPH
A simple algorithm for predicting bacteremia using food consumption and shaking chills: A prospective observational study
AUTHORS: Takayuki Komatsu, MD, PhD, Erika Takahashi, MD, Kentaro Mishima, MD, Takeo Toyoda, MD, Fumihiro Saitoh, MD, Akari Yasuda, RN, Joe Matsuoka, PhD, Manabu Sugita, MD, PhD, Joel Branch, MD, Makoto Aoki, MD, Lawrence M. Tierney Jr., MD, Kenji Inoue, MD, PhD
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
Rest dyspnea dims as acute heart failure treatment target
PARIS – During the most recent pharmaceutical generation, drug development for heart failure largely focused on acute heart failure, and specifically on patients with rest dyspnea as the primary manifestation of their acute heart failure decompensation events.
That has now changed, agreed heart failure experts as they debated the upshot of sobering results from two neutral trials that failed to show a midterm mortality benefit in patients hospitalized for acute heart failure who underwent aggressive management of their congestion using 2 days of intravenous treatment with either of two potent vasodilating drugs. Results first reported in November 2016 failed to show a survival benefit from ularitide in the 2,100-patient TRUE-AHF (Efficacy and Safety of Ularitide for the Treatment of Acute Decompensated Heart Failure) trial (N Engl J Med. 2017 May 18;376[20]:1956-64). And results reported at a meeting of the Heart Failure Association of the ESC failed to show a survival benefit from serelaxin in more than 6,500 acute heart failure patients in the RELAX-AHF-2 (Efficacy, Safety and Tolerability of Serelaxin When Added to Standard Therapy in AHF) trial.
The failure of a 2-day infusion of serelaxin to produce a significant reduction in cardiovascular death in RELAX-AHF-2 was especially surprising because the predecessor trial, RELAX-AHF, which randomized only 1,160 patients and used a surrogate endpoint of dyspnea improvement, had shown significant benefit that hinted more clinically meaningful benefits might also result from serelaxin treatment (Lancet. 2013 Jan 5;381[9860]:29-39). The disappointing serelaxin and ularitide results also culminate a series of studies using several different agents or procedures to treat acute decompensated heart failure patients that all failed to produce a reduction in deaths.
“This is a sea change; make no mistake. We will need a more targeted, selective approach. It was always a daunting proposition to believe that short-term infusion could have an effect 6 months later. We were misled by the analogy [of acute heart failure] to acute coronary syndrome,” said Dr. Ruschitzka, professor of medicine at the University of Zürich.
The right time to intervene
Meeting attendees offered several hypotheses to explain why the acute ularitide and serelaxin trials both failed to show a mortality benefit, with timing of treatment the most common denominator.
Acute heart failure “is an event, not a disease,” declared Milton Packer, MD, lead investigator of TRUE-AHF, during a session devoted to vasodilator treatment of acute heart failure. Acute heart failure decompensations “are fluctuations in a chronic disease. It doesn’t matter what you do during the episode – it matters what you do between acute episodes. We focus all our attention on which vasodilator and which dose of Lasix [furosemide], but we send patients home on inadequate chronic therapy. It doesn’t matter what you do to the dyspnea, the shortness of breath will get better. Do we need a new drug that makes dyspnea go away an hour sooner and doesn’t cost a fortune? What really matters is what patients do between acute episodes and how to prevent them, ” said Dr. Packer, distinguished scholar in cardiovascular science at Baylor University Medical Center in Dallas.
Dr. Packer strongly urged clinicians to put heart failure patients on the full regimen of guideline-directed drugs and at full dosages, a step he thinks would go a long way toward preventing a majority of decompensation episodes. “Chronic heart failure treatment has improved dramatically, but implementation is abysmal,” he said.
Of course, at this phase of their disease heart failure patients are usually at home, which more or less demands that the treatments they take are oral or at least delivered by subcutaneous injection.
“We’ve had a mismatch of candidate drugs, which have mostly been IV infusions, with a clinical setting where an IV infusion is challenging to use.”
“We are killing good drugs by the way we’re testing them,” commented Javed Butler, MD, who bemoaned the ignominious outcome of serelaxin treatment in RELAX-AHF-2. “The available data show it makes no sense to treat for just 2 days. We should take true worsening heart failure patients, those who are truly failing standard treatment, and look at new chronic oral therapies to try on them.” Oral drugs similar to serelaxin and ularitide could be used chronically, suggested Dr. Butler, professor of medicine and chief of cardiology at Stony Brook (N.Y.) School of Medicine.
Wrong patients with the wrong presentation
Perhaps just as big a flaw of the acute heart failure trials has been their target patient population, patients with rest dyspnea at the time of admission. “Why do we think that dyspnea is a clinically relevant symptom for acute heart failure?” Dr. Packer asked.
Dr. Cleland and his associates analyzed data on 116,752 hospitalizations for acute heart failure in England and Wales during April 2007–March 2013, a database that included more than 90% of hospitals for these regions. “We found that a large proportion of admitted patients did not have breathlessness at rest as their primary reason for seeking hospitalization. For about half the patients, moderate or severe peripheral edema was the main problem,” he reported. Roughly a third of patients had rest dyspnea as their main symptom.
An unadjusted analysis also showed a stronger link between peripheral edema and the rate of mortality during a median follow-up of about a year following hospitalization, compared with rest dyspnea. Compared with the lowest-risk subgroup, the patients with severe peripheral edema (18% of the population) had more than twice the mortality. In contrast, the patients with the most severe rest dyspnea and no evidence at all of peripheral edema, just 6% of the population, had a 50% higher mortality rate than the lowest-risk patients.
”It’s peripheral edema rather than breathlessness that is the important determinant of length of stay and prognosis. The disastrous neutral trials for acute heart failure have all targeted the breathless subset of patients. Maybe a reason for the failures has been that they’ve been treating a problem that does not exist. The trials have looked at the wrong patients,” Dr. Cleland said.
‘We’ve told the wrong story to industry” about the importance of rest dyspnea to acute heart failure patients. “When we say acute heart failure, we mean an ambulance and oxygen and the emergency department and rapid IV treatment. That’s breathlessness. Patients with peripheral edema usually get driven in and walk from the car to a wheelchair and they wait 4 hours to be seen. I think that, following the TRUE-AHF and RELAX-AHF-2 results, we’ll see a radical change.”
But just because the focus should be on peripheral edema rather than dyspnea, that doesn’t mean better drugs aren’t needed, Dr. Cleland added.
“We need better treatments to deal with congestion. Once a patient is congested, we are not very good at getting rid of it. We depend on diuretics, which we don’t use properly. Ultimately I’d like to see agents as adjuncts to diuretics, to produce better kidney function.” But treatments for breathlessness are decent as they now exist: furosemide plus oxygen. When a simple, cheap drug works 80% of the time, it is really hard to improve on that.” The real unmet needs for treating acute decompensated heart failure are patients with rest dyspnea who don’t respond to conventional treatment, and especially patients with gross peripheral edema plus low blood pressure and renal dysfunction for whom no good treatments have been developed, Dr. Cleland said.
Another flaw in the patient selection criteria for the acute heart failure studies has been the focus on patients with elevated blood pressures, the logical target for vasodilator drugs that lower blood pressure, noted Dr. Felker. “But these are the patients at lowest risk. We’ve had a mismatch between the patients with the biggest need and the patients we actually study, which relates to the types of drugs we’ve developed.”
Acute heart failure remains a target
Despite all the talk of refocusing attention on chronic heart failure and peripheral edema, at least one expert remained steadfast in talking up the importance of new acute interventions.
Part of the problem in believing that existing treatments can adequately manage heart failure and prevent acute decompensations is that about 75% of acute heart failure episodes either occur as the first presentation of heart failure, or occur in patients with heart failure with preserved ejection fraction (HFpEF), a type of heart failure that, until recently, had no chronic drug regimens with widely acknowledged efficacy for HFpEF. (The 2017 U.S. heart failure management guidelines update listed aldosterone receptor antagonists as a class IIb recommendation for treating HFpEF, the first time guidelines have sanctioned a drug class for treating HFpEF [Circulation. 2017 Apr 28. doi: 10.1161/CIR.0000000000000509].)
“For patients with heart failure with reduced ejection fraction, you can give optimal treatments and [decompensations] are prevented,” noted Dr. Mebazaa, a professor of anesthesiology and resuscitation at Lariboisière Hospital in Paris. “But for the huge number of HFpEF patients we have nothing. Acute heart failure will remain prevalent, and we still don’t have the right drugs to use on these patients.”
The TRUE-AHF trial was sponsored by Cardiorentis. RELAX-AHF-2 was sponsored by Novartis. Dr. Ruschitzka has been a speaker on behalf of Novartis, and has been a speaker for or consultant to several companies and was a coinvestigator for TRUE-AHF and received fees from Cardiorentis for his participation. Dr. Packer is a consultant to and stockholder in Cardiorentis and has been a consultant to several other companies. Dr. Felker has been a consultant to Novartis and several other companies and was a coinvestigator on RELAX-AHF-2. Dr. Butler has been a consultant to several companies. Dr. Cleland has received research support from Novartis, and he has been a consultant to and received research support from several other companies. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis as well as from several other companies and was a coinvestigator on TRUE-AHF.
[email protected]
On Twitter @mitchelzoler
PARIS – During the most recent pharmaceutical generation, drug development for heart failure largely focused on acute heart failure, and specifically on patients with rest dyspnea as the primary manifestation of their acute heart failure decompensation events.
That has now changed, agreed heart failure experts as they debated the upshot of sobering results from two neutral trials that failed to show a midterm mortality benefit in patients hospitalized for acute heart failure who underwent aggressive management of their congestion using 2 days of intravenous treatment with either of two potent vasodilating drugs. Results first reported in November 2016 failed to show a survival benefit from ularitide in the 2,100-patient TRUE-AHF (Efficacy and Safety of Ularitide for the Treatment of Acute Decompensated Heart Failure) trial (N Engl J Med. 2017 May 18;376[20]:1956-64). And results reported at a meeting of the Heart Failure Association of the ESC failed to show a survival benefit from serelaxin in more than 6,500 acute heart failure patients in the RELAX-AHF-2 (Efficacy, Safety and Tolerability of Serelaxin When Added to Standard Therapy in AHF) trial.
The failure of a 2-day infusion of serelaxin to produce a significant reduction in cardiovascular death in RELAX-AHF-2 was especially surprising because the predecessor trial, RELAX-AHF, which randomized only 1,160 patients and used a surrogate endpoint of dyspnea improvement, had shown significant benefit that hinted more clinically meaningful benefits might also result from serelaxin treatment (Lancet. 2013 Jan 5;381[9860]:29-39). The disappointing serelaxin and ularitide results also culminate a series of studies using several different agents or procedures to treat acute decompensated heart failure patients that all failed to produce a reduction in deaths.
“This is a sea change; make no mistake. We will need a more targeted, selective approach. It was always a daunting proposition to believe that short-term infusion could have an effect 6 months later. We were misled by the analogy [of acute heart failure] to acute coronary syndrome,” said Dr. Ruschitzka, professor of medicine at the University of Zürich.
The right time to intervene
Meeting attendees offered several hypotheses to explain why the acute ularitide and serelaxin trials both failed to show a mortality benefit, with timing of treatment the most common denominator.
Acute heart failure “is an event, not a disease,” declared Milton Packer, MD, lead investigator of TRUE-AHF, during a session devoted to vasodilator treatment of acute heart failure. Acute heart failure decompensations “are fluctuations in a chronic disease. It doesn’t matter what you do during the episode – it matters what you do between acute episodes. We focus all our attention on which vasodilator and which dose of Lasix [furosemide], but we send patients home on inadequate chronic therapy. It doesn’t matter what you do to the dyspnea, the shortness of breath will get better. Do we need a new drug that makes dyspnea go away an hour sooner and doesn’t cost a fortune? What really matters is what patients do between acute episodes and how to prevent them, ” said Dr. Packer, distinguished scholar in cardiovascular science at Baylor University Medical Center in Dallas.
Dr. Packer strongly urged clinicians to put heart failure patients on the full regimen of guideline-directed drugs and at full dosages, a step he thinks would go a long way toward preventing a majority of decompensation episodes. “Chronic heart failure treatment has improved dramatically, but implementation is abysmal,” he said.
Of course, at this phase of their disease heart failure patients are usually at home, which more or less demands that the treatments they take are oral or at least delivered by subcutaneous injection.
“We’ve had a mismatch of candidate drugs, which have mostly been IV infusions, with a clinical setting where an IV infusion is challenging to use.”
“We are killing good drugs by the way we’re testing them,” commented Javed Butler, MD, who bemoaned the ignominious outcome of serelaxin treatment in RELAX-AHF-2. “The available data show it makes no sense to treat for just 2 days. We should take true worsening heart failure patients, those who are truly failing standard treatment, and look at new chronic oral therapies to try on them.” Oral drugs similar to serelaxin and ularitide could be used chronically, suggested Dr. Butler, professor of medicine and chief of cardiology at Stony Brook (N.Y.) School of Medicine.
Wrong patients with the wrong presentation
Perhaps just as big a flaw of the acute heart failure trials has been their target patient population, patients with rest dyspnea at the time of admission. “Why do we think that dyspnea is a clinically relevant symptom for acute heart failure?” Dr. Packer asked.
Dr. Cleland and his associates analyzed data on 116,752 hospitalizations for acute heart failure in England and Wales during April 2007–March 2013, a database that included more than 90% of hospitals for these regions. “We found that a large proportion of admitted patients did not have breathlessness at rest as their primary reason for seeking hospitalization. For about half the patients, moderate or severe peripheral edema was the main problem,” he reported. Roughly a third of patients had rest dyspnea as their main symptom.
An unadjusted analysis also showed a stronger link between peripheral edema and the rate of mortality during a median follow-up of about a year following hospitalization, compared with rest dyspnea. Compared with the lowest-risk subgroup, the patients with severe peripheral edema (18% of the population) had more than twice the mortality. In contrast, the patients with the most severe rest dyspnea and no evidence at all of peripheral edema, just 6% of the population, had a 50% higher mortality rate than the lowest-risk patients.
”It’s peripheral edema rather than breathlessness that is the important determinant of length of stay and prognosis. The disastrous neutral trials for acute heart failure have all targeted the breathless subset of patients. Maybe a reason for the failures has been that they’ve been treating a problem that does not exist. The trials have looked at the wrong patients,” Dr. Cleland said.
‘We’ve told the wrong story to industry” about the importance of rest dyspnea to acute heart failure patients. “When we say acute heart failure, we mean an ambulance and oxygen and the emergency department and rapid IV treatment. That’s breathlessness. Patients with peripheral edema usually get driven in and walk from the car to a wheelchair and they wait 4 hours to be seen. I think that, following the TRUE-AHF and RELAX-AHF-2 results, we’ll see a radical change.”
But just because the focus should be on peripheral edema rather than dyspnea, that doesn’t mean better drugs aren’t needed, Dr. Cleland added.
“We need better treatments to deal with congestion. Once a patient is congested, we are not very good at getting rid of it. We depend on diuretics, which we don’t use properly. Ultimately I’d like to see agents as adjuncts to diuretics, to produce better kidney function.” But treatments for breathlessness are decent as they now exist: furosemide plus oxygen. When a simple, cheap drug works 80% of the time, it is really hard to improve on that.” The real unmet needs for treating acute decompensated heart failure are patients with rest dyspnea who don’t respond to conventional treatment, and especially patients with gross peripheral edema plus low blood pressure and renal dysfunction for whom no good treatments have been developed, Dr. Cleland said.
Another flaw in the patient selection criteria for the acute heart failure studies has been the focus on patients with elevated blood pressures, the logical target for vasodilator drugs that lower blood pressure, noted Dr. Felker. “But these are the patients at lowest risk. We’ve had a mismatch between the patients with the biggest need and the patients we actually study, which relates to the types of drugs we’ve developed.”
Acute heart failure remains a target
Despite all the talk of refocusing attention on chronic heart failure and peripheral edema, at least one expert remained steadfast in talking up the importance of new acute interventions.
Part of the problem in believing that existing treatments can adequately manage heart failure and prevent acute decompensations is that about 75% of acute heart failure episodes either occur as the first presentation of heart failure, or occur in patients with heart failure with preserved ejection fraction (HFpEF), a type of heart failure that, until recently, had no chronic drug regimens with widely acknowledged efficacy for HFpEF. (The 2017 U.S. heart failure management guidelines update listed aldosterone receptor antagonists as a class IIb recommendation for treating HFpEF, the first time guidelines have sanctioned a drug class for treating HFpEF [Circulation. 2017 Apr 28. doi: 10.1161/CIR.0000000000000509].)
“For patients with heart failure with reduced ejection fraction, you can give optimal treatments and [decompensations] are prevented,” noted Dr. Mebazaa, a professor of anesthesiology and resuscitation at Lariboisière Hospital in Paris. “But for the huge number of HFpEF patients we have nothing. Acute heart failure will remain prevalent, and we still don’t have the right drugs to use on these patients.”
The TRUE-AHF trial was sponsored by Cardiorentis. RELAX-AHF-2 was sponsored by Novartis. Dr. Ruschitzka has been a speaker on behalf of Novartis, and has been a speaker for or consultant to several companies and was a coinvestigator for TRUE-AHF and received fees from Cardiorentis for his participation. Dr. Packer is a consultant to and stockholder in Cardiorentis and has been a consultant to several other companies. Dr. Felker has been a consultant to Novartis and several other companies and was a coinvestigator on RELAX-AHF-2. Dr. Butler has been a consultant to several companies. Dr. Cleland has received research support from Novartis, and he has been a consultant to and received research support from several other companies. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis as well as from several other companies and was a coinvestigator on TRUE-AHF.
[email protected]
On Twitter @mitchelzoler
PARIS – During the most recent pharmaceutical generation, drug development for heart failure largely focused on acute heart failure, and specifically on patients with rest dyspnea as the primary manifestation of their acute heart failure decompensation events.
That has now changed, agreed heart failure experts as they debated the upshot of sobering results from two neutral trials that failed to show a midterm mortality benefit in patients hospitalized for acute heart failure who underwent aggressive management of their congestion using 2 days of intravenous treatment with either of two potent vasodilating drugs. Results first reported in November 2016 failed to show a survival benefit from ularitide in the 2,100-patient TRUE-AHF (Efficacy and Safety of Ularitide for the Treatment of Acute Decompensated Heart Failure) trial (N Engl J Med. 2017 May 18;376[20]:1956-64). And results reported at a meeting of the Heart Failure Association of the ESC failed to show a survival benefit from serelaxin in more than 6,500 acute heart failure patients in the RELAX-AHF-2 (Efficacy, Safety and Tolerability of Serelaxin When Added to Standard Therapy in AHF) trial.
The failure of a 2-day infusion of serelaxin to produce a significant reduction in cardiovascular death in RELAX-AHF-2 was especially surprising because the predecessor trial, RELAX-AHF, which randomized only 1,160 patients and used a surrogate endpoint of dyspnea improvement, had shown significant benefit that hinted more clinically meaningful benefits might also result from serelaxin treatment (Lancet. 2013 Jan 5;381[9860]:29-39). The disappointing serelaxin and ularitide results also culminate a series of studies using several different agents or procedures to treat acute decompensated heart failure patients that all failed to produce a reduction in deaths.
“This is a sea change; make no mistake. We will need a more targeted, selective approach. It was always a daunting proposition to believe that short-term infusion could have an effect 6 months later. We were misled by the analogy [of acute heart failure] to acute coronary syndrome,” said Dr. Ruschitzka, professor of medicine at the University of Zürich.
The right time to intervene
Meeting attendees offered several hypotheses to explain why the acute ularitide and serelaxin trials both failed to show a mortality benefit, with timing of treatment the most common denominator.
Acute heart failure “is an event, not a disease,” declared Milton Packer, MD, lead investigator of TRUE-AHF, during a session devoted to vasodilator treatment of acute heart failure. Acute heart failure decompensations “are fluctuations in a chronic disease. It doesn’t matter what you do during the episode – it matters what you do between acute episodes. We focus all our attention on which vasodilator and which dose of Lasix [furosemide], but we send patients home on inadequate chronic therapy. It doesn’t matter what you do to the dyspnea, the shortness of breath will get better. Do we need a new drug that makes dyspnea go away an hour sooner and doesn’t cost a fortune? What really matters is what patients do between acute episodes and how to prevent them, ” said Dr. Packer, distinguished scholar in cardiovascular science at Baylor University Medical Center in Dallas.
Dr. Packer strongly urged clinicians to put heart failure patients on the full regimen of guideline-directed drugs and at full dosages, a step he thinks would go a long way toward preventing a majority of decompensation episodes. “Chronic heart failure treatment has improved dramatically, but implementation is abysmal,” he said.
Of course, at this phase of their disease heart failure patients are usually at home, which more or less demands that the treatments they take are oral or at least delivered by subcutaneous injection.
“We’ve had a mismatch of candidate drugs, which have mostly been IV infusions, with a clinical setting where an IV infusion is challenging to use.”
“We are killing good drugs by the way we’re testing them,” commented Javed Butler, MD, who bemoaned the ignominious outcome of serelaxin treatment in RELAX-AHF-2. “The available data show it makes no sense to treat for just 2 days. We should take true worsening heart failure patients, those who are truly failing standard treatment, and look at new chronic oral therapies to try on them.” Oral drugs similar to serelaxin and ularitide could be used chronically, suggested Dr. Butler, professor of medicine and chief of cardiology at Stony Brook (N.Y.) School of Medicine.
Wrong patients with the wrong presentation
Perhaps just as big a flaw of the acute heart failure trials has been their target patient population, patients with rest dyspnea at the time of admission. “Why do we think that dyspnea is a clinically relevant symptom for acute heart failure?” Dr. Packer asked.
Dr. Cleland and his associates analyzed data on 116,752 hospitalizations for acute heart failure in England and Wales during April 2007–March 2013, a database that included more than 90% of hospitals for these regions. “We found that a large proportion of admitted patients did not have breathlessness at rest as their primary reason for seeking hospitalization. For about half the patients, moderate or severe peripheral edema was the main problem,” he reported. Roughly a third of patients had rest dyspnea as their main symptom.
An unadjusted analysis also showed a stronger link between peripheral edema and the rate of mortality during a median follow-up of about a year following hospitalization, compared with rest dyspnea. Compared with the lowest-risk subgroup, the patients with severe peripheral edema (18% of the population) had more than twice the mortality. In contrast, the patients with the most severe rest dyspnea and no evidence at all of peripheral edema, just 6% of the population, had a 50% higher mortality rate than the lowest-risk patients.
”It’s peripheral edema rather than breathlessness that is the important determinant of length of stay and prognosis. The disastrous neutral trials for acute heart failure have all targeted the breathless subset of patients. Maybe a reason for the failures has been that they’ve been treating a problem that does not exist. The trials have looked at the wrong patients,” Dr. Cleland said.
‘We’ve told the wrong story to industry” about the importance of rest dyspnea to acute heart failure patients. “When we say acute heart failure, we mean an ambulance and oxygen and the emergency department and rapid IV treatment. That’s breathlessness. Patients with peripheral edema usually get driven in and walk from the car to a wheelchair and they wait 4 hours to be seen. I think that, following the TRUE-AHF and RELAX-AHF-2 results, we’ll see a radical change.”
But just because the focus should be on peripheral edema rather than dyspnea, that doesn’t mean better drugs aren’t needed, Dr. Cleland added.
“We need better treatments to deal with congestion. Once a patient is congested, we are not very good at getting rid of it. We depend on diuretics, which we don’t use properly. Ultimately I’d like to see agents as adjuncts to diuretics, to produce better kidney function.” But treatments for breathlessness are decent as they now exist: furosemide plus oxygen. When a simple, cheap drug works 80% of the time, it is really hard to improve on that.” The real unmet needs for treating acute decompensated heart failure are patients with rest dyspnea who don’t respond to conventional treatment, and especially patients with gross peripheral edema plus low blood pressure and renal dysfunction for whom no good treatments have been developed, Dr. Cleland said.
Another flaw in the patient selection criteria for the acute heart failure studies has been the focus on patients with elevated blood pressures, the logical target for vasodilator drugs that lower blood pressure, noted Dr. Felker. “But these are the patients at lowest risk. We’ve had a mismatch between the patients with the biggest need and the patients we actually study, which relates to the types of drugs we’ve developed.”
Acute heart failure remains a target
Despite all the talk of refocusing attention on chronic heart failure and peripheral edema, at least one expert remained steadfast in talking up the importance of new acute interventions.
Part of the problem in believing that existing treatments can adequately manage heart failure and prevent acute decompensations is that about 75% of acute heart failure episodes either occur as the first presentation of heart failure, or occur in patients with heart failure with preserved ejection fraction (HFpEF), a type of heart failure that, until recently, had no chronic drug regimens with widely acknowledged efficacy for HFpEF. (The 2017 U.S. heart failure management guidelines update listed aldosterone receptor antagonists as a class IIb recommendation for treating HFpEF, the first time guidelines have sanctioned a drug class for treating HFpEF [Circulation. 2017 Apr 28. doi: 10.1161/CIR.0000000000000509].)
“For patients with heart failure with reduced ejection fraction, you can give optimal treatments and [decompensations] are prevented,” noted Dr. Mebazaa, a professor of anesthesiology and resuscitation at Lariboisière Hospital in Paris. “But for the huge number of HFpEF patients we have nothing. Acute heart failure will remain prevalent, and we still don’t have the right drugs to use on these patients.”
The TRUE-AHF trial was sponsored by Cardiorentis. RELAX-AHF-2 was sponsored by Novartis. Dr. Ruschitzka has been a speaker on behalf of Novartis, and has been a speaker for or consultant to several companies and was a coinvestigator for TRUE-AHF and received fees from Cardiorentis for his participation. Dr. Packer is a consultant to and stockholder in Cardiorentis and has been a consultant to several other companies. Dr. Felker has been a consultant to Novartis and several other companies and was a coinvestigator on RELAX-AHF-2. Dr. Butler has been a consultant to several companies. Dr. Cleland has received research support from Novartis, and he has been a consultant to and received research support from several other companies. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis as well as from several other companies and was a coinvestigator on TRUE-AHF.
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM HEART FAILURE 2017
HM17 session summary: Rheumatology pearls for the inpatient provider
Presenter
Neal Birnbaum, MD
Session Summary
Dr. Birnbaum began with the differential diagnosis of acute monoarthritis, which is one of the more common reasons for inpatient rheumatology consultation and includes crystalline (e.g., gout), septic, autoimmune (psoriasis), traumatic, and hemorrhagic.
The synovial fluid will give an idea as to whether one is more likely than the other, he said. Normal synovial fluid is transparent, clear, has a low cell count, and is very viscous in nature. Noninflammatory etiologies (osteoarthritis) will have some cells but will largely be similar to normal synovial fluid. Inflammatory causes will have higher cell counts (2-10K WBC) but will have much lower viscosity. Septic joints will look pustular with very high cell counts (sometimes too high to be recorded) and will be positive on fluid culture (unless the patient has already received antimicrobial therapy). Hemorrhagic fluid will look like blood, and the history will give clues as to whether that is the case (recent trauma, history of hemophilia).
Pseudogout (CPPD) is more likely to manifest in different joints (knees more so than wrist more so than shoulders/hips). One should suspect pseudogout in patients with acute arthritis in patients more than 70 years old. Crystals will be positively bifringent and more rectangular or square shaped, compared with gout crystals. Finding chondrocalcinosis on x-ray on a symptomatic patient can make the diagnosis much more likely. However, a patient can have chondrocalcinosis on an x-ray and not have CPPD. A patient can also have no chondrocalcinosis and have CPPD. It is the combination of the x-ray sign and symptoms that creates the high accuracy of the test.
The treatment for both in the acute setting includes colchicine (2 tabs x 1, then 1 more 1 hour later), NSAIDS (although may not be ideal inpatient because of potential toxicities), and corticosteroids (this can be either oral [prednisone 40 mg q24 with rapid taper], intraarticular [triamcinolone 10 mg-40 mg depending on the joint size], or IV [solumedrol or solucortef equivalent to prednisone 40 q24]).
For management of gout chronically, one should strive for a uric acid level of less than 6.0. Contrary to what is commonly believed, one can start urate lowering agents like allopurinol acutely (start with 100 mg for 2 weeks, then titrate up every 2 weeks until one hits the target uric acid level). Clinicians can consider using febuxostat for those patients who have renal insufficiency. While on the urate lowering agent, use low dose colchicine or NSAIDS for the first few months. Unfortunately, there is no long-term chronic strategy to prevent pseudogout flares. If there is an underlying cause for the pseudogout, then try to address it.
Consults for positive antinuclear antibodies (ANA) are common reasons for rheumatology referrals. The patterns of the ANA and the titer are important to the differential diagnosis. Up to 30% of healthy individuals have a positive ANA. ANA can be helpful as a rule out test for systemic lupus erythematosus (SLE), as it has a high sensitivity and a low specificity. However, because SLE is a clinical diagnosis and because of the high ANA positivity in the population, a high ANA alone does not prove a patient has SLE.
Concerning vasculitis, Dr. Birnbaum recommended thinking about it in terms of small versus large vessel disease. For initial evaluation, one should draw a CBC, erythrocyte sedimentation rate/C-reactive protein, urinalysis, chemistry panel, ANA, antineutrophil cytoplasmic antibodies, rheumatoid factor, hepatitis C antibody, and complement levels (C3, C4, CH50). One can also think of drawing cryoglobulins, especially in settings where one is suspicious that hepatitis C may be present. The differential diagnosis for vasculitis includes drug reactions, infections (mostly viral), malignancy, collagen vascular disease, and idiopathic causes (33%-50% of cases). The treatment is to remove offending agents (i.e., drug-induced vasculitis), treat infections (if applicable), and use steroids (the dosing depends on the situation).
Dr. Birnbaum finished with two relatively new illnesses that should be on clinicians’ radars. Chikungunya virus is transmitted by mosquitoes in the same distribution that one may see Zika virus. The symptoms include headaches, fevers, extreme joint pain, and joint swelling (this aspect is different from many other viral illnesses). The illness is usually acute. However, some patients will continue to have symptoms for up to a year. There is no specific treatment other than symptom relief (pain medications, NSAIDs).
Finally, immunoglobulin G4–related disease can affect virtually any organ system, but seems to manifest frequently as pancreatitis in the hospital setting. Think about this in patients with pancreatitis not secondary to the usual alcoholic or gallstone variety. The gold standard for diagnosis is biopsy with histologic findings of IgG4 in plasma cells. Most patients will be noted to have elevated IgG4 levels. The treatment is prednisone 40mg q24 with a taper over 2 months. For those who cannot be weaned or for those with recurrent disease, rituximab (1000mg IV x 1 then approximately 2 weeks later) can be used.
Key takeaways for HM
- Know the differential diagnosis of acute monoarticular arthritis and how the synovial fluid will vary depending on the diagnosis.
- Gout can manifest in other joints besides the first toe. One can use allopurinol even in the acute setting. The goal is to attain a uric acid level of less than 6.0.
- Pseudogout should be considered in patients older than 70 years with acute arthritis. There is no allopurinol equivalent for chronic management.
- Positive ANAs are common, but they do not make the diagnosis of SLE (although a negative ANA generally does rule out SLE).
- SLE is a clinical diagnosis that requires multiple symptoms and findings to make the diagnosis. Please refer to the ACR classification criteria.
- Think of vasculitis in terms of small versus large vessel disease and think of the differential diagnosis as to the etiology (realizing that 33%-50% will end up being idiopathic).
- Chikungunya is mosquito-borne and associated with severe joint pains, headaches, and fevers but can also have joint swelling. While often acute, the symptoms can last for up to a year. Treatment is symptomatic management.
- Think of IgG4-related disease in patients with pancreatitis without the usual causes (alcohol, gallstones). Diagnosis is based on pathology and IgG4 levels. Treatment is with steroids and/or rituximab.
Dr. Kim is a hospitalist who works at Emory University Hospital in Atlanta and is an editorial board member of The Hospitalist.
Presenter
Neal Birnbaum, MD
Session Summary
Dr. Birnbaum began with the differential diagnosis of acute monoarthritis, which is one of the more common reasons for inpatient rheumatology consultation and includes crystalline (e.g., gout), septic, autoimmune (psoriasis), traumatic, and hemorrhagic.
The synovial fluid will give an idea as to whether one is more likely than the other, he said. Normal synovial fluid is transparent, clear, has a low cell count, and is very viscous in nature. Noninflammatory etiologies (osteoarthritis) will have some cells but will largely be similar to normal synovial fluid. Inflammatory causes will have higher cell counts (2-10K WBC) but will have much lower viscosity. Septic joints will look pustular with very high cell counts (sometimes too high to be recorded) and will be positive on fluid culture (unless the patient has already received antimicrobial therapy). Hemorrhagic fluid will look like blood, and the history will give clues as to whether that is the case (recent trauma, history of hemophilia).
Pseudogout (CPPD) is more likely to manifest in different joints (knees more so than wrist more so than shoulders/hips). One should suspect pseudogout in patients with acute arthritis in patients more than 70 years old. Crystals will be positively bifringent and more rectangular or square shaped, compared with gout crystals. Finding chondrocalcinosis on x-ray on a symptomatic patient can make the diagnosis much more likely. However, a patient can have chondrocalcinosis on an x-ray and not have CPPD. A patient can also have no chondrocalcinosis and have CPPD. It is the combination of the x-ray sign and symptoms that creates the high accuracy of the test.
The treatment for both in the acute setting includes colchicine (2 tabs x 1, then 1 more 1 hour later), NSAIDS (although may not be ideal inpatient because of potential toxicities), and corticosteroids (this can be either oral [prednisone 40 mg q24 with rapid taper], intraarticular [triamcinolone 10 mg-40 mg depending on the joint size], or IV [solumedrol or solucortef equivalent to prednisone 40 q24]).
For management of gout chronically, one should strive for a uric acid level of less than 6.0. Contrary to what is commonly believed, one can start urate lowering agents like allopurinol acutely (start with 100 mg for 2 weeks, then titrate up every 2 weeks until one hits the target uric acid level). Clinicians can consider using febuxostat for those patients who have renal insufficiency. While on the urate lowering agent, use low dose colchicine or NSAIDS for the first few months. Unfortunately, there is no long-term chronic strategy to prevent pseudogout flares. If there is an underlying cause for the pseudogout, then try to address it.
Consults for positive antinuclear antibodies (ANA) are common reasons for rheumatology referrals. The patterns of the ANA and the titer are important to the differential diagnosis. Up to 30% of healthy individuals have a positive ANA. ANA can be helpful as a rule out test for systemic lupus erythematosus (SLE), as it has a high sensitivity and a low specificity. However, because SLE is a clinical diagnosis and because of the high ANA positivity in the population, a high ANA alone does not prove a patient has SLE.
Concerning vasculitis, Dr. Birnbaum recommended thinking about it in terms of small versus large vessel disease. For initial evaluation, one should draw a CBC, erythrocyte sedimentation rate/C-reactive protein, urinalysis, chemistry panel, ANA, antineutrophil cytoplasmic antibodies, rheumatoid factor, hepatitis C antibody, and complement levels (C3, C4, CH50). One can also think of drawing cryoglobulins, especially in settings where one is suspicious that hepatitis C may be present. The differential diagnosis for vasculitis includes drug reactions, infections (mostly viral), malignancy, collagen vascular disease, and idiopathic causes (33%-50% of cases). The treatment is to remove offending agents (i.e., drug-induced vasculitis), treat infections (if applicable), and use steroids (the dosing depends on the situation).
Dr. Birnbaum finished with two relatively new illnesses that should be on clinicians’ radars. Chikungunya virus is transmitted by mosquitoes in the same distribution that one may see Zika virus. The symptoms include headaches, fevers, extreme joint pain, and joint swelling (this aspect is different from many other viral illnesses). The illness is usually acute. However, some patients will continue to have symptoms for up to a year. There is no specific treatment other than symptom relief (pain medications, NSAIDs).
Finally, immunoglobulin G4–related disease can affect virtually any organ system, but seems to manifest frequently as pancreatitis in the hospital setting. Think about this in patients with pancreatitis not secondary to the usual alcoholic or gallstone variety. The gold standard for diagnosis is biopsy with histologic findings of IgG4 in plasma cells. Most patients will be noted to have elevated IgG4 levels. The treatment is prednisone 40mg q24 with a taper over 2 months. For those who cannot be weaned or for those with recurrent disease, rituximab (1000mg IV x 1 then approximately 2 weeks later) can be used.
Key takeaways for HM
- Know the differential diagnosis of acute monoarticular arthritis and how the synovial fluid will vary depending on the diagnosis.
- Gout can manifest in other joints besides the first toe. One can use allopurinol even in the acute setting. The goal is to attain a uric acid level of less than 6.0.
- Pseudogout should be considered in patients older than 70 years with acute arthritis. There is no allopurinol equivalent for chronic management.
- Positive ANAs are common, but they do not make the diagnosis of SLE (although a negative ANA generally does rule out SLE).
- SLE is a clinical diagnosis that requires multiple symptoms and findings to make the diagnosis. Please refer to the ACR classification criteria.
- Think of vasculitis in terms of small versus large vessel disease and think of the differential diagnosis as to the etiology (realizing that 33%-50% will end up being idiopathic).
- Chikungunya is mosquito-borne and associated with severe joint pains, headaches, and fevers but can also have joint swelling. While often acute, the symptoms can last for up to a year. Treatment is symptomatic management.
- Think of IgG4-related disease in patients with pancreatitis without the usual causes (alcohol, gallstones). Diagnosis is based on pathology and IgG4 levels. Treatment is with steroids and/or rituximab.
Dr. Kim is a hospitalist who works at Emory University Hospital in Atlanta and is an editorial board member of The Hospitalist.
Presenter
Neal Birnbaum, MD
Session Summary
Dr. Birnbaum began with the differential diagnosis of acute monoarthritis, which is one of the more common reasons for inpatient rheumatology consultation and includes crystalline (e.g., gout), septic, autoimmune (psoriasis), traumatic, and hemorrhagic.
The synovial fluid will give an idea as to whether one is more likely than the other, he said. Normal synovial fluid is transparent, clear, has a low cell count, and is very viscous in nature. Noninflammatory etiologies (osteoarthritis) will have some cells but will largely be similar to normal synovial fluid. Inflammatory causes will have higher cell counts (2-10K WBC) but will have much lower viscosity. Septic joints will look pustular with very high cell counts (sometimes too high to be recorded) and will be positive on fluid culture (unless the patient has already received antimicrobial therapy). Hemorrhagic fluid will look like blood, and the history will give clues as to whether that is the case (recent trauma, history of hemophilia).
Pseudogout (CPPD) is more likely to manifest in different joints (knees more so than wrist more so than shoulders/hips). One should suspect pseudogout in patients with acute arthritis in patients more than 70 years old. Crystals will be positively bifringent and more rectangular or square shaped, compared with gout crystals. Finding chondrocalcinosis on x-ray on a symptomatic patient can make the diagnosis much more likely. However, a patient can have chondrocalcinosis on an x-ray and not have CPPD. A patient can also have no chondrocalcinosis and have CPPD. It is the combination of the x-ray sign and symptoms that creates the high accuracy of the test.
The treatment for both in the acute setting includes colchicine (2 tabs x 1, then 1 more 1 hour later), NSAIDS (although may not be ideal inpatient because of potential toxicities), and corticosteroids (this can be either oral [prednisone 40 mg q24 with rapid taper], intraarticular [triamcinolone 10 mg-40 mg depending on the joint size], or IV [solumedrol or solucortef equivalent to prednisone 40 q24]).
For management of gout chronically, one should strive for a uric acid level of less than 6.0. Contrary to what is commonly believed, one can start urate lowering agents like allopurinol acutely (start with 100 mg for 2 weeks, then titrate up every 2 weeks until one hits the target uric acid level). Clinicians can consider using febuxostat for those patients who have renal insufficiency. While on the urate lowering agent, use low dose colchicine or NSAIDS for the first few months. Unfortunately, there is no long-term chronic strategy to prevent pseudogout flares. If there is an underlying cause for the pseudogout, then try to address it.
Consults for positive antinuclear antibodies (ANA) are common reasons for rheumatology referrals. The patterns of the ANA and the titer are important to the differential diagnosis. Up to 30% of healthy individuals have a positive ANA. ANA can be helpful as a rule out test for systemic lupus erythematosus (SLE), as it has a high sensitivity and a low specificity. However, because SLE is a clinical diagnosis and because of the high ANA positivity in the population, a high ANA alone does not prove a patient has SLE.
Concerning vasculitis, Dr. Birnbaum recommended thinking about it in terms of small versus large vessel disease. For initial evaluation, one should draw a CBC, erythrocyte sedimentation rate/C-reactive protein, urinalysis, chemistry panel, ANA, antineutrophil cytoplasmic antibodies, rheumatoid factor, hepatitis C antibody, and complement levels (C3, C4, CH50). One can also think of drawing cryoglobulins, especially in settings where one is suspicious that hepatitis C may be present. The differential diagnosis for vasculitis includes drug reactions, infections (mostly viral), malignancy, collagen vascular disease, and idiopathic causes (33%-50% of cases). The treatment is to remove offending agents (i.e., drug-induced vasculitis), treat infections (if applicable), and use steroids (the dosing depends on the situation).
Dr. Birnbaum finished with two relatively new illnesses that should be on clinicians’ radars. Chikungunya virus is transmitted by mosquitoes in the same distribution that one may see Zika virus. The symptoms include headaches, fevers, extreme joint pain, and joint swelling (this aspect is different from many other viral illnesses). The illness is usually acute. However, some patients will continue to have symptoms for up to a year. There is no specific treatment other than symptom relief (pain medications, NSAIDs).
Finally, immunoglobulin G4–related disease can affect virtually any organ system, but seems to manifest frequently as pancreatitis in the hospital setting. Think about this in patients with pancreatitis not secondary to the usual alcoholic or gallstone variety. The gold standard for diagnosis is biopsy with histologic findings of IgG4 in plasma cells. Most patients will be noted to have elevated IgG4 levels. The treatment is prednisone 40mg q24 with a taper over 2 months. For those who cannot be weaned or for those with recurrent disease, rituximab (1000mg IV x 1 then approximately 2 weeks later) can be used.
Key takeaways for HM
- Know the differential diagnosis of acute monoarticular arthritis and how the synovial fluid will vary depending on the diagnosis.
- Gout can manifest in other joints besides the first toe. One can use allopurinol even in the acute setting. The goal is to attain a uric acid level of less than 6.0.
- Pseudogout should be considered in patients older than 70 years with acute arthritis. There is no allopurinol equivalent for chronic management.
- Positive ANAs are common, but they do not make the diagnosis of SLE (although a negative ANA generally does rule out SLE).
- SLE is a clinical diagnosis that requires multiple symptoms and findings to make the diagnosis. Please refer to the ACR classification criteria.
- Think of vasculitis in terms of small versus large vessel disease and think of the differential diagnosis as to the etiology (realizing that 33%-50% will end up being idiopathic).
- Chikungunya is mosquito-borne and associated with severe joint pains, headaches, and fevers but can also have joint swelling. While often acute, the symptoms can last for up to a year. Treatment is symptomatic management.
- Think of IgG4-related disease in patients with pancreatitis without the usual causes (alcohol, gallstones). Diagnosis is based on pathology and IgG4 levels. Treatment is with steroids and/or rituximab.
Dr. Kim is a hospitalist who works at Emory University Hospital in Atlanta and is an editorial board member of The Hospitalist.
HFrEF mortality halved when treatment matches guidelines
PARIS – Heart failure patients who received guideline-directed pharmacotherapy, at dosages that approached guideline-directed levels, had roughly half the 6-month mortality as did similar patients who did not receive this level of treatment in a real-world, observational study with more than 6,000 patients.
Adherence to pharmacologic treatment guidelines for patients with heart failure with reduced ejection fraction (HFrEF) “was strongly associated with clinical outcomes during 6-month follow-up,” Michel Komajda, MD, said at a meeting held by the Heart Failure Association of the European Society of Cardiology. The findings highlight the importance of closely following guideline recommendations in routine practice.
[polldaddy:9772629]
The analysis used data collected in the QUALIFY (Quality of Adherence to Guideline Recommendations for Life-Saving Treatment in Heart Failure: an International Survey) registry, which enrolled 7,127 HFrEF patients during September 2013–December 2014 at 547 centers in 36 countries, mostly in Europe, Asia, and Africa but also in Canada, Ecuador, and Australia. All enrolled patients had to have been hospitalized for worsening heart failure at least once during the 1-15 months before they entered QUALIFY.
Dr. Komajda and his associates assessed each enrolled patient at baseline by their treatment with each of four guideline-recommended drug classes: an ACE inhibitor or angiotensin receptor blocker; a beta-blocker; an aldosterone receptor antagonist (ARA) if the patient’s functional status was rated as New York Heart Association class II, III, or IV; and ivabradine (Corlanor) if the patient was in NYHA class II, III, or IV, in sinus rhythm, had a heart rate of at least 70 beats per minute, and if the patient was in a country where ivabradine was available. Because patient enrollment occurred in 2013 and 2014, the study couldn’t include the new formulation of sacubitril plus valsartan (Entresto) in its analysis.
For each eligible drug class a patient received 1 point if their daily prescribed dosage was at least 50% of the recommended dosage (or 100% for an ARA), 0.5 points if the patient received the recommended drug but at a lower dosage, and no points if the drug wasn’t given. A patient also received 1 point if they were appropriately not given a drug because of a documented contraindication or intolerance. The researchers then calculated each patient’s “adherence score” by dividing their point total by the potentially maximum number of points that each patient could have received (a number that ranged from 2 to 4). They defined a score of 1 (which meant the patients received at least half the recommended dosage of all recommended drugs) as good adherence, a score of 0.51-0.99 as moderate adherence, and a score of 0.5 or less as poor adherence.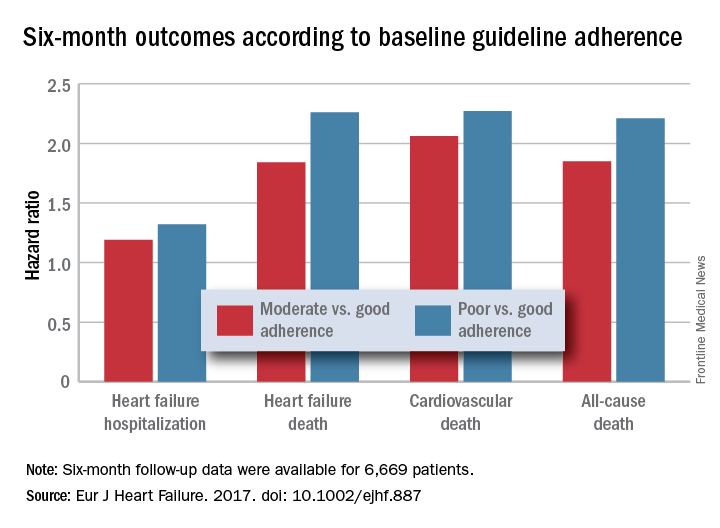
Because patient enrollment occurred during 2013 and 2014, the benchmark heart failure treatment guidelines were those issued by the European Society of Cardiology in 2012 (Eur Heart J. 2012 July;33[14]:1787-1847).
Concurrently with Dr. Komajda’s report at the meeting the results appeared in an article online (Eur J Heart Failure. 2017. doi: 10.1002/ejhf.887).
QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.
[email protected]
On Twitter @mitchelzoler
This was a wonderful and useful study. It was large, prospective, covered a wide geographic area, and showed that drug dosage matters when treating heart failure with reduced ejection fraction.
The geographic diversity was a strength, but also a potential weakness because of the resulting differences among the enrolled patients in financial resources, ethnic and genetic makeup, and their tolerance to various drugs. I hope that further research can dissect the role that each of these factors played in the results.
Another limitation is the relatively simplistic approach used for assessing drug dosages to calculate the adherence scores. While it is a very useful step forward to classify patients by the drug dosages they received, there could be some very legitimate variations in dosages based on parameters such as blood pressure. An important question to address in the future is whether it is better to use all the recommended drugs at reduced dosages if necessary, or to use fewer agents at higher dosages.
But these are just quibbles about what is a very important study.
Andrew J.S. Coats, MD , is a cardiologist, professor of medicine, and academic vice-president for the Monash Warwick Alliance of Warwick University in Coventry, England, and Monash University in Melbourne. He has received honoraria from Impulse Dynamics, Menarini, PsiOxus, ResMed, Respicardia, and Servier. He made these comments as designated discussant for Dr. Komajda’s report.
This was a wonderful and useful study. It was large, prospective, covered a wide geographic area, and showed that drug dosage matters when treating heart failure with reduced ejection fraction.
The geographic diversity was a strength, but also a potential weakness because of the resulting differences among the enrolled patients in financial resources, ethnic and genetic makeup, and their tolerance to various drugs. I hope that further research can dissect the role that each of these factors played in the results.
Another limitation is the relatively simplistic approach used for assessing drug dosages to calculate the adherence scores. While it is a very useful step forward to classify patients by the drug dosages they received, there could be some very legitimate variations in dosages based on parameters such as blood pressure. An important question to address in the future is whether it is better to use all the recommended drugs at reduced dosages if necessary, or to use fewer agents at higher dosages.
But these are just quibbles about what is a very important study.
Andrew J.S. Coats, MD , is a cardiologist, professor of medicine, and academic vice-president for the Monash Warwick Alliance of Warwick University in Coventry, England, and Monash University in Melbourne. He has received honoraria from Impulse Dynamics, Menarini, PsiOxus, ResMed, Respicardia, and Servier. He made these comments as designated discussant for Dr. Komajda’s report.
This was a wonderful and useful study. It was large, prospective, covered a wide geographic area, and showed that drug dosage matters when treating heart failure with reduced ejection fraction.
The geographic diversity was a strength, but also a potential weakness because of the resulting differences among the enrolled patients in financial resources, ethnic and genetic makeup, and their tolerance to various drugs. I hope that further research can dissect the role that each of these factors played in the results.
Another limitation is the relatively simplistic approach used for assessing drug dosages to calculate the adherence scores. While it is a very useful step forward to classify patients by the drug dosages they received, there could be some very legitimate variations in dosages based on parameters such as blood pressure. An important question to address in the future is whether it is better to use all the recommended drugs at reduced dosages if necessary, or to use fewer agents at higher dosages.
But these are just quibbles about what is a very important study.
Andrew J.S. Coats, MD , is a cardiologist, professor of medicine, and academic vice-president for the Monash Warwick Alliance of Warwick University in Coventry, England, and Monash University in Melbourne. He has received honoraria from Impulse Dynamics, Menarini, PsiOxus, ResMed, Respicardia, and Servier. He made these comments as designated discussant for Dr. Komajda’s report.
PARIS – Heart failure patients who received guideline-directed pharmacotherapy, at dosages that approached guideline-directed levels, had roughly half the 6-month mortality as did similar patients who did not receive this level of treatment in a real-world, observational study with more than 6,000 patients.
Adherence to pharmacologic treatment guidelines for patients with heart failure with reduced ejection fraction (HFrEF) “was strongly associated with clinical outcomes during 6-month follow-up,” Michel Komajda, MD, said at a meeting held by the Heart Failure Association of the European Society of Cardiology. The findings highlight the importance of closely following guideline recommendations in routine practice.
[polldaddy:9772629]
The analysis used data collected in the QUALIFY (Quality of Adherence to Guideline Recommendations for Life-Saving Treatment in Heart Failure: an International Survey) registry, which enrolled 7,127 HFrEF patients during September 2013–December 2014 at 547 centers in 36 countries, mostly in Europe, Asia, and Africa but also in Canada, Ecuador, and Australia. All enrolled patients had to have been hospitalized for worsening heart failure at least once during the 1-15 months before they entered QUALIFY.
Dr. Komajda and his associates assessed each enrolled patient at baseline by their treatment with each of four guideline-recommended drug classes: an ACE inhibitor or angiotensin receptor blocker; a beta-blocker; an aldosterone receptor antagonist (ARA) if the patient’s functional status was rated as New York Heart Association class II, III, or IV; and ivabradine (Corlanor) if the patient was in NYHA class II, III, or IV, in sinus rhythm, had a heart rate of at least 70 beats per minute, and if the patient was in a country where ivabradine was available. Because patient enrollment occurred in 2013 and 2014, the study couldn’t include the new formulation of sacubitril plus valsartan (Entresto) in its analysis.
For each eligible drug class a patient received 1 point if their daily prescribed dosage was at least 50% of the recommended dosage (or 100% for an ARA), 0.5 points if the patient received the recommended drug but at a lower dosage, and no points if the drug wasn’t given. A patient also received 1 point if they were appropriately not given a drug because of a documented contraindication or intolerance. The researchers then calculated each patient’s “adherence score” by dividing their point total by the potentially maximum number of points that each patient could have received (a number that ranged from 2 to 4). They defined a score of 1 (which meant the patients received at least half the recommended dosage of all recommended drugs) as good adherence, a score of 0.51-0.99 as moderate adherence, and a score of 0.5 or less as poor adherence.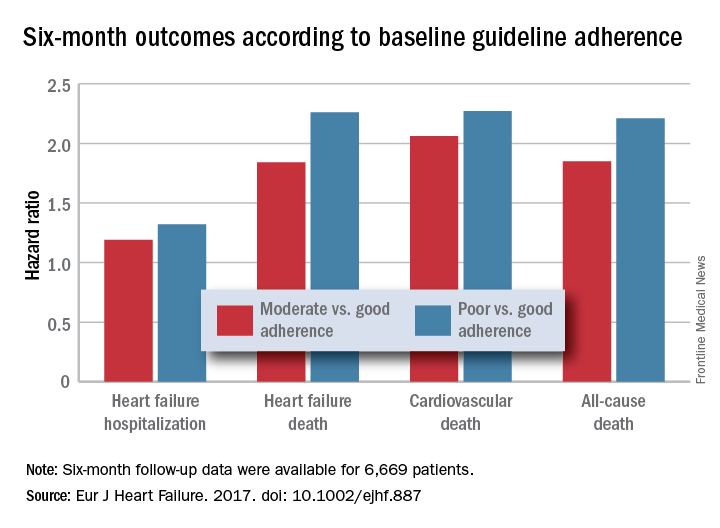
Because patient enrollment occurred during 2013 and 2014, the benchmark heart failure treatment guidelines were those issued by the European Society of Cardiology in 2012 (Eur Heart J. 2012 July;33[14]:1787-1847).
Concurrently with Dr. Komajda’s report at the meeting the results appeared in an article online (Eur J Heart Failure. 2017. doi: 10.1002/ejhf.887).
QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.
[email protected]
On Twitter @mitchelzoler
PARIS – Heart failure patients who received guideline-directed pharmacotherapy, at dosages that approached guideline-directed levels, had roughly half the 6-month mortality as did similar patients who did not receive this level of treatment in a real-world, observational study with more than 6,000 patients.
Adherence to pharmacologic treatment guidelines for patients with heart failure with reduced ejection fraction (HFrEF) “was strongly associated with clinical outcomes during 6-month follow-up,” Michel Komajda, MD, said at a meeting held by the Heart Failure Association of the European Society of Cardiology. The findings highlight the importance of closely following guideline recommendations in routine practice.
[polldaddy:9772629]
The analysis used data collected in the QUALIFY (Quality of Adherence to Guideline Recommendations for Life-Saving Treatment in Heart Failure: an International Survey) registry, which enrolled 7,127 HFrEF patients during September 2013–December 2014 at 547 centers in 36 countries, mostly in Europe, Asia, and Africa but also in Canada, Ecuador, and Australia. All enrolled patients had to have been hospitalized for worsening heart failure at least once during the 1-15 months before they entered QUALIFY.
Dr. Komajda and his associates assessed each enrolled patient at baseline by their treatment with each of four guideline-recommended drug classes: an ACE inhibitor or angiotensin receptor blocker; a beta-blocker; an aldosterone receptor antagonist (ARA) if the patient’s functional status was rated as New York Heart Association class II, III, or IV; and ivabradine (Corlanor) if the patient was in NYHA class II, III, or IV, in sinus rhythm, had a heart rate of at least 70 beats per minute, and if the patient was in a country where ivabradine was available. Because patient enrollment occurred in 2013 and 2014, the study couldn’t include the new formulation of sacubitril plus valsartan (Entresto) in its analysis.
For each eligible drug class a patient received 1 point if their daily prescribed dosage was at least 50% of the recommended dosage (or 100% for an ARA), 0.5 points if the patient received the recommended drug but at a lower dosage, and no points if the drug wasn’t given. A patient also received 1 point if they were appropriately not given a drug because of a documented contraindication or intolerance. The researchers then calculated each patient’s “adherence score” by dividing their point total by the potentially maximum number of points that each patient could have received (a number that ranged from 2 to 4). They defined a score of 1 (which meant the patients received at least half the recommended dosage of all recommended drugs) as good adherence, a score of 0.51-0.99 as moderate adherence, and a score of 0.5 or less as poor adherence.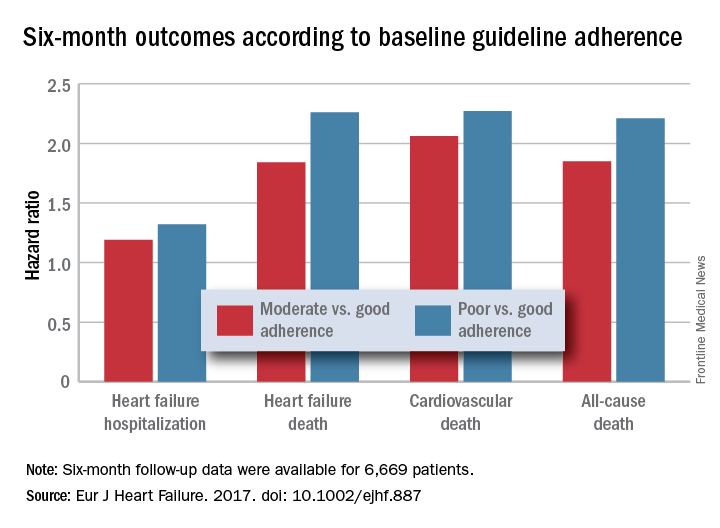
Because patient enrollment occurred during 2013 and 2014, the benchmark heart failure treatment guidelines were those issued by the European Society of Cardiology in 2012 (Eur Heart J. 2012 July;33[14]:1787-1847).
Concurrently with Dr. Komajda’s report at the meeting the results appeared in an article online (Eur J Heart Failure. 2017. doi: 10.1002/ejhf.887).
QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.
[email protected]
On Twitter @mitchelzoler
AT HEART FAILURE 2017
Key clinical point:
Major finding: Six-month all-cause, cardiovascular, and heart failure mortalities were doubled in patients not on guideline-adherent therapy and dosages.
Data source: QUANTIFY, an international registry with 6,669 HFrEF patients followed for 6 months.
Disclosures: QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.
Use of probiotics in hospitalized adults to prevent Clostridium difficile infection
Clinical Question: Does the use and timing of probiotics in hospitalized adult patients with Clostridium difficile infection (CDI) improve clinical outcomes?
Background: The incidence of CDI in hospitalized patients has increased significantly over the past years, resulting in significant morbidity and mortality. Improved prevention of CDI could have substantial public health benefits.
Study design: Systematic review and metaregression analysis.
Setting: 19 studies meeting inclusion criteria.
Synopsis: Computerized bibliography databases were searched for randomized controlled trials (RCTs) evaluating probiotic effects on CDI in hospitalized adults taking antibiotics.
Comprising 6261 subjects, 19 RCTs were analyzed. The incidence of CDI was lower in the probiotic cohort than in the control group (1.6% vs. 3.9%; P less than 0.001). The pooled relative risk of CDI in probiotic users was 0.42 (95% CI, 0.30-0.57). Metaregression analysis demonstrated that probiotics were significantly more effective if given closer to the first antibiotic dose, with a decrease in efficacy for every day of delay in starting probiotics (P = .04). Probiotics given within 2 days of antibiotic initiation produced a greater reduction of risk for CDI (RR, 0.32; 95% CI, 0.22-0.48) than later administration (RR, 0.70; 95% CI, 0.40-1.23; P = .02). There was no increased risk for adverse events among patients receiving probiotics.
Limitations included high risk of bias because of missing data, attrition, restricted patient population, lack of placebo, and conflict of interest.
Bottom Line: Administration of probiotics soon after the first dose of antibiotic reduces the risk of CDI by more than 50% in hospitalized adults without any increased risk of adverse events.
Reference: Shen NT, Maw A, Tmanova LL et al. Timely use of Probiotics in Hospitalized Adults Prevents Clostridium difficile Infection: A Systematic Review with Meta-Regression Analysis. Gastroenterology. Published on 9 Feb 2017. doi: 10.1053/j.gastro.2017.02.003.
Dr. Martin is clinical professor in the division of hospital medicine, department of medicine, University of California, San Diego.
Clinical Question: Does the use and timing of probiotics in hospitalized adult patients with Clostridium difficile infection (CDI) improve clinical outcomes?
Background: The incidence of CDI in hospitalized patients has increased significantly over the past years, resulting in significant morbidity and mortality. Improved prevention of CDI could have substantial public health benefits.
Study design: Systematic review and metaregression analysis.
Setting: 19 studies meeting inclusion criteria.
Synopsis: Computerized bibliography databases were searched for randomized controlled trials (RCTs) evaluating probiotic effects on CDI in hospitalized adults taking antibiotics.
Comprising 6261 subjects, 19 RCTs were analyzed. The incidence of CDI was lower in the probiotic cohort than in the control group (1.6% vs. 3.9%; P less than 0.001). The pooled relative risk of CDI in probiotic users was 0.42 (95% CI, 0.30-0.57). Metaregression analysis demonstrated that probiotics were significantly more effective if given closer to the first antibiotic dose, with a decrease in efficacy for every day of delay in starting probiotics (P = .04). Probiotics given within 2 days of antibiotic initiation produced a greater reduction of risk for CDI (RR, 0.32; 95% CI, 0.22-0.48) than later administration (RR, 0.70; 95% CI, 0.40-1.23; P = .02). There was no increased risk for adverse events among patients receiving probiotics.
Limitations included high risk of bias because of missing data, attrition, restricted patient population, lack of placebo, and conflict of interest.
Bottom Line: Administration of probiotics soon after the first dose of antibiotic reduces the risk of CDI by more than 50% in hospitalized adults without any increased risk of adverse events.
Reference: Shen NT, Maw A, Tmanova LL et al. Timely use of Probiotics in Hospitalized Adults Prevents Clostridium difficile Infection: A Systematic Review with Meta-Regression Analysis. Gastroenterology. Published on 9 Feb 2017. doi: 10.1053/j.gastro.2017.02.003.
Dr. Martin is clinical professor in the division of hospital medicine, department of medicine, University of California, San Diego.
Clinical Question: Does the use and timing of probiotics in hospitalized adult patients with Clostridium difficile infection (CDI) improve clinical outcomes?
Background: The incidence of CDI in hospitalized patients has increased significantly over the past years, resulting in significant morbidity and mortality. Improved prevention of CDI could have substantial public health benefits.
Study design: Systematic review and metaregression analysis.
Setting: 19 studies meeting inclusion criteria.
Synopsis: Computerized bibliography databases were searched for randomized controlled trials (RCTs) evaluating probiotic effects on CDI in hospitalized adults taking antibiotics.
Comprising 6261 subjects, 19 RCTs were analyzed. The incidence of CDI was lower in the probiotic cohort than in the control group (1.6% vs. 3.9%; P less than 0.001). The pooled relative risk of CDI in probiotic users was 0.42 (95% CI, 0.30-0.57). Metaregression analysis demonstrated that probiotics were significantly more effective if given closer to the first antibiotic dose, with a decrease in efficacy for every day of delay in starting probiotics (P = .04). Probiotics given within 2 days of antibiotic initiation produced a greater reduction of risk for CDI (RR, 0.32; 95% CI, 0.22-0.48) than later administration (RR, 0.70; 95% CI, 0.40-1.23; P = .02). There was no increased risk for adverse events among patients receiving probiotics.
Limitations included high risk of bias because of missing data, attrition, restricted patient population, lack of placebo, and conflict of interest.
Bottom Line: Administration of probiotics soon after the first dose of antibiotic reduces the risk of CDI by more than 50% in hospitalized adults without any increased risk of adverse events.
Reference: Shen NT, Maw A, Tmanova LL et al. Timely use of Probiotics in Hospitalized Adults Prevents Clostridium difficile Infection: A Systematic Review with Meta-Regression Analysis. Gastroenterology. Published on 9 Feb 2017. doi: 10.1053/j.gastro.2017.02.003.
Dr. Martin is clinical professor in the division of hospital medicine, department of medicine, University of California, San Diego.