User login
Survey: U.S. oncologists have high net worth, live within their means
The average annual income for oncologists surveyed was $377,000, which was 5% higher than the $359,000 reported for 2018. This put oncologists in eleventh place among 29 specialties.
However, this information was obtained prior to February 11, 2020, before the COVID-19 pandemic took hold in the United States, and the financial situation has changed for many physicians.
For example, primary care physicians have reported a 55% decrease in revenue along with a 20% to 30% reduction in patient volume. The decline has even led some to shutter their physical offices, according to the larger survey of all physicians, the Medscape Physician Debt and Net Worth Report 2020. This full survey included 17, 461 physicians and represented 30 specialties.
Physicians in specialty practices may be facing even greater reductions. “Specialists are currently having more troubles than PCPs because they’re largely dependent on elective cases, which can’t be directly addressed by telemedicine,” commented Joel Greenwald, MD, CEO of Greenwald Wealth Management, St. Louis Park, Minnesota, in the survey.
Community oncology clinics and practices have reported a substantial decline in office visits and new patients because of the COVID-19 pandemic. Even before the pandemic, clinics had been closing in recent years as a result of being acquired, merging, or because of financial struggles, although that trend has been plateauing, according to the latest report from the Community Oncology Alliance.
Oncologists’ net worth
With regard to net worth, 42% of the oncologists surveyed reported having assets totaling from $1 million to $5 million, which is about the same for physicians in general. Only 15% reported a net worth of $5 million or higher; a quarter reported a net worth of less than $500,000.
Wealth is more evenly divided when it comes to gender in comparison with other specialties. For all physicians, 56% of men and 39% of women reported a net worth of more than $1 million. For oncologists, that ratio is 59% of men and 54% of women.
Not surprisingly, net worth also increased by age. Only about a quarter (27%) of oncologists younger than age 45 reported a net worth of $1 million to $5 million, compared to 48% aged 45-54 and 56% of physicians aged 55-64. This makes sense, inasmuch as earnings generally increase over time and early-career debt is paid down. However, net worth does appear to decline somewhat after the age of 65, presumably because of a decrease in income on retirement.
Debts and expenses
For debts and expenses that are currently being paid off, mortgage on a primary residence (59%) topped the list. More than half of oncologists reported living in a home that is 3,000 sq ft or larger, and nearly half (49%) have a mortgage of $300,000 or higher. About a third of the oncologists surveyed have no mortgage or one that has been paid off.
Car loan payments (35%) and college education/medical school loans (25%) were the second and third most common sources of debt. As compared with other specialties, oncologists land right in the middle of those still paying off school loans. Only 15% reported that they had no debts or expenses to be paid off.
Savings and living within one’s means
The average American has four credit cards. About half of oncologists surveyed reported having four or fewer, although about a fifth (22%) have seven or more. But the vast majority reported living within their means (49%) or below their means (46%). Only 6% reported living above their means.
Surveyed oncologists also reported putting money aside in a tax-deferred retirement account or college savings account. Almost half (48%) are putting aside more than $2000 every month, and 28% save from $1000 to $2000. A small percentage (8%) reported not doing this on a regular basis.
A smaller percentage (40%) responded that they put more than $2000 a month into a taxable retirement or college savings account; 18% reported not doing this on a regular basis. More than two thirds also reported either having a written budget or a mental one for their personal expenses.
In 2019, most oncologists (77%) did not experience a financial loss. For those who did, bad investments on the stock market (14%) were the main cause. A smaller number reported real estate losses, problems with their practice, or job loss.
Nearly half (49%) reported that they currently work with a financial planner or have done so in the past.
This article first appeared on Medscape.com.
The average annual income for oncologists surveyed was $377,000, which was 5% higher than the $359,000 reported for 2018. This put oncologists in eleventh place among 29 specialties.
However, this information was obtained prior to February 11, 2020, before the COVID-19 pandemic took hold in the United States, and the financial situation has changed for many physicians.
For example, primary care physicians have reported a 55% decrease in revenue along with a 20% to 30% reduction in patient volume. The decline has even led some to shutter their physical offices, according to the larger survey of all physicians, the Medscape Physician Debt and Net Worth Report 2020. This full survey included 17, 461 physicians and represented 30 specialties.
Physicians in specialty practices may be facing even greater reductions. “Specialists are currently having more troubles than PCPs because they’re largely dependent on elective cases, which can’t be directly addressed by telemedicine,” commented Joel Greenwald, MD, CEO of Greenwald Wealth Management, St. Louis Park, Minnesota, in the survey.
Community oncology clinics and practices have reported a substantial decline in office visits and new patients because of the COVID-19 pandemic. Even before the pandemic, clinics had been closing in recent years as a result of being acquired, merging, or because of financial struggles, although that trend has been plateauing, according to the latest report from the Community Oncology Alliance.
Oncologists’ net worth
With regard to net worth, 42% of the oncologists surveyed reported having assets totaling from $1 million to $5 million, which is about the same for physicians in general. Only 15% reported a net worth of $5 million or higher; a quarter reported a net worth of less than $500,000.
Wealth is more evenly divided when it comes to gender in comparison with other specialties. For all physicians, 56% of men and 39% of women reported a net worth of more than $1 million. For oncologists, that ratio is 59% of men and 54% of women.
Not surprisingly, net worth also increased by age. Only about a quarter (27%) of oncologists younger than age 45 reported a net worth of $1 million to $5 million, compared to 48% aged 45-54 and 56% of physicians aged 55-64. This makes sense, inasmuch as earnings generally increase over time and early-career debt is paid down. However, net worth does appear to decline somewhat after the age of 65, presumably because of a decrease in income on retirement.
Debts and expenses
For debts and expenses that are currently being paid off, mortgage on a primary residence (59%) topped the list. More than half of oncologists reported living in a home that is 3,000 sq ft or larger, and nearly half (49%) have a mortgage of $300,000 or higher. About a third of the oncologists surveyed have no mortgage or one that has been paid off.
Car loan payments (35%) and college education/medical school loans (25%) were the second and third most common sources of debt. As compared with other specialties, oncologists land right in the middle of those still paying off school loans. Only 15% reported that they had no debts or expenses to be paid off.
Savings and living within one’s means
The average American has four credit cards. About half of oncologists surveyed reported having four or fewer, although about a fifth (22%) have seven or more. But the vast majority reported living within their means (49%) or below their means (46%). Only 6% reported living above their means.
Surveyed oncologists also reported putting money aside in a tax-deferred retirement account or college savings account. Almost half (48%) are putting aside more than $2000 every month, and 28% save from $1000 to $2000. A small percentage (8%) reported not doing this on a regular basis.
A smaller percentage (40%) responded that they put more than $2000 a month into a taxable retirement or college savings account; 18% reported not doing this on a regular basis. More than two thirds also reported either having a written budget or a mental one for their personal expenses.
In 2019, most oncologists (77%) did not experience a financial loss. For those who did, bad investments on the stock market (14%) were the main cause. A smaller number reported real estate losses, problems with their practice, or job loss.
Nearly half (49%) reported that they currently work with a financial planner or have done so in the past.
This article first appeared on Medscape.com.
The average annual income for oncologists surveyed was $377,000, which was 5% higher than the $359,000 reported for 2018. This put oncologists in eleventh place among 29 specialties.
However, this information was obtained prior to February 11, 2020, before the COVID-19 pandemic took hold in the United States, and the financial situation has changed for many physicians.
For example, primary care physicians have reported a 55% decrease in revenue along with a 20% to 30% reduction in patient volume. The decline has even led some to shutter their physical offices, according to the larger survey of all physicians, the Medscape Physician Debt and Net Worth Report 2020. This full survey included 17, 461 physicians and represented 30 specialties.
Physicians in specialty practices may be facing even greater reductions. “Specialists are currently having more troubles than PCPs because they’re largely dependent on elective cases, which can’t be directly addressed by telemedicine,” commented Joel Greenwald, MD, CEO of Greenwald Wealth Management, St. Louis Park, Minnesota, in the survey.
Community oncology clinics and practices have reported a substantial decline in office visits and new patients because of the COVID-19 pandemic. Even before the pandemic, clinics had been closing in recent years as a result of being acquired, merging, or because of financial struggles, although that trend has been plateauing, according to the latest report from the Community Oncology Alliance.
Oncologists’ net worth
With regard to net worth, 42% of the oncologists surveyed reported having assets totaling from $1 million to $5 million, which is about the same for physicians in general. Only 15% reported a net worth of $5 million or higher; a quarter reported a net worth of less than $500,000.
Wealth is more evenly divided when it comes to gender in comparison with other specialties. For all physicians, 56% of men and 39% of women reported a net worth of more than $1 million. For oncologists, that ratio is 59% of men and 54% of women.
Not surprisingly, net worth also increased by age. Only about a quarter (27%) of oncologists younger than age 45 reported a net worth of $1 million to $5 million, compared to 48% aged 45-54 and 56% of physicians aged 55-64. This makes sense, inasmuch as earnings generally increase over time and early-career debt is paid down. However, net worth does appear to decline somewhat after the age of 65, presumably because of a decrease in income on retirement.
Debts and expenses
For debts and expenses that are currently being paid off, mortgage on a primary residence (59%) topped the list. More than half of oncologists reported living in a home that is 3,000 sq ft or larger, and nearly half (49%) have a mortgage of $300,000 or higher. About a third of the oncologists surveyed have no mortgage or one that has been paid off.
Car loan payments (35%) and college education/medical school loans (25%) were the second and third most common sources of debt. As compared with other specialties, oncologists land right in the middle of those still paying off school loans. Only 15% reported that they had no debts or expenses to be paid off.
Savings and living within one’s means
The average American has four credit cards. About half of oncologists surveyed reported having four or fewer, although about a fifth (22%) have seven or more. But the vast majority reported living within their means (49%) or below their means (46%). Only 6% reported living above their means.
Surveyed oncologists also reported putting money aside in a tax-deferred retirement account or college savings account. Almost half (48%) are putting aside more than $2000 every month, and 28% save from $1000 to $2000. A small percentage (8%) reported not doing this on a regular basis.
A smaller percentage (40%) responded that they put more than $2000 a month into a taxable retirement or college savings account; 18% reported not doing this on a regular basis. More than two thirds also reported either having a written budget or a mental one for their personal expenses.
In 2019, most oncologists (77%) did not experience a financial loss. For those who did, bad investments on the stock market (14%) were the main cause. A smaller number reported real estate losses, problems with their practice, or job loss.
Nearly half (49%) reported that they currently work with a financial planner or have done so in the past.
This article first appeared on Medscape.com.
Oncologists’ income and satisfaction are up
Oncologists continue to rank above the middle range for all specialties in annual compensation for physicians, according to findings from the newly released Medscape Oncologist Compensation Report 2020.
The average earnings for oncologists who participated in the survey was $377,000, which was a 5% increase from the $359,000 reported for 2018.
Just over two-thirds (67%) of oncologists reported that they felt that they were fairly compensated, which is quite a jump from 53% last year.
In addition, oncologists appear to be very satisfied with their profession. Similar to last year’s findings, 84% said they would choose medicine again, and 96% said they would choose the specialty of oncology again.
Earning in top third of all specialties
The average annual earnings reported by oncologists put this specialty in eleventh place among 29 specialties. Orthopedic specialists remain at the head of the list, with estimated earnings of $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according to Medscape’s compensation report, which included responses from 17,461 physicians in over 30 specialties.
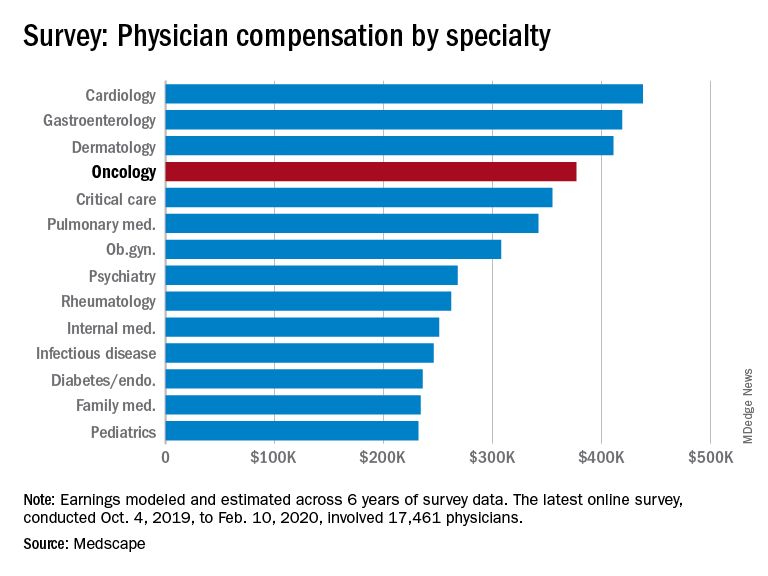
At the bottom of the estimated earnings list were public health and preventive medicine doctors and pediatricians. For both specialties, the reported annual earnings was $232,000. Family medicine specialists were only marginally higher at $234,000.
Radiologists ($427,000), gastroenterologists ($419,000), and urologists ($417,000) all reported higher earnings than oncologists, whereas neurologists, at $280,000, rheumatologists, at $262,000, and internal medicine physicians, at $251,000, earned less.
The report also found that gender disparities in income persist, with male oncologists earning 17% more than their female colleagues. The gender gap in oncology is somewhat less than that seen for all specialties combined, in which men earned 31% more than women, similar to last year’s figure of 33%.
Male oncologists reported spending 38.8 hours per week seeing patients, compared with 34.9 hours reported by female oncologists. This could be a factor contributing to the gender pay disparity. Overall, the average amount of time seeing patients was 37.9 hours per week.
Frustrations with paperwork and denied claims
Surveyed oncologists cited some of the frustrations they are facing, such as spending nearly 17 hours a week on paperwork and administrative tasks. They reported that 16% of claims are denied or have to be resubmitted. As for the most challenging part of the job, oncologists (22%), similar to physicians overall (26%), found that having so many rules and regulations takes first place, followed by working with electronic health record systems (20%), difficulties getting fair reimbursement (19%), having to work long hours (12%), and dealing with difficult patients (8%). Few oncologists were concerned about lawsuits (4%), and 4% reported that there were no challenges.
Oncologists reported that the most rewarding part of their job was gratitude/relationships with patients (31%), followed by knowing that they are making the world a better place (27%). After that, oncologists agreed with statements about being very good at what they do/finding answers/diagnoses (22%), having pride in being a doctor (9%), and making good money at a job they like (8%).
Other key findings
Other key findings from the Medscape Oncologist Compensation Report 2020 included the following:
- Regarding payment models, 80% take insurance, 41% are in fee-for-service arrangements, and 18% are in accountable care organizations (21%). Only 3% are in direct primary care, and 1% are cash-only practices or have a concierge practice.
- 65% of oncologists state that they will continue taking new and current Medicare/Medicaid patients. None said that they would not take on new Medicare/Medicaid patients, and 35% remain undecided. These numbers differed from physicians overall; 73% of all physicians surveyed said they would continue taking new/current Medicare/Medicaid patients, 6% said that will not take on new Medicare patients, and 4% said they will not take new Medicaid patients. In addition, 3% and 2% said that they would stop treating some or all of their Medicare and Medicaid patients, respectively.
- About half (51%) of oncologists use nurse practitioners, about a third (34%) use physician assistants, and 37% use neither. This was about the same as physicians overall.
- A larger percentage of oncologists (38%) expect to participate in MIPS (merit-based incentive payment system), and only 8% expect to participate in APMs (alternative payment models). This was similar to the findings for physicians overall, with more than one-third (37%) expecting to participate in MIPS and 9% planning to take part in APMs.
Impact of COVID-19 pandemic
The Medscape compensation reports also gives a glimpse of the impact the COVID-19 pandemic is having on physician compensation.
Since the beginning of the pandemic, practices have reported a 55% decrease in revenue and a 60% drop in patient volume. Physician practices and hospitals have laid off or furloughed personnel and have cut pay, and 9% of practices have closed their doors, at least for the time being.
A total of 43,000 health care workers were laid off in March, the report notes.
The findings tie in with those reported elsewhere. For example, a survey conducted by the Medical Group Management Association, which was reported by Medscape Medical News, found that 97% of physician practices have experienced negative financial effects directly or indirectly related to COVID-19.
Specialties were hard hit, especially those that rely on elective procedures, such as dermatology and cardiology. Oncology care has also been disrupted. For example, a survey conducted by the American Cancer Society Cancer Action Network found that half of the cancer patients and survivors who responded reported changes, delays, or disruptions to the care they were receiving.
This article first appeared on Medscape.com.
Oncologists continue to rank above the middle range for all specialties in annual compensation for physicians, according to findings from the newly released Medscape Oncologist Compensation Report 2020.
The average earnings for oncologists who participated in the survey was $377,000, which was a 5% increase from the $359,000 reported for 2018.
Just over two-thirds (67%) of oncologists reported that they felt that they were fairly compensated, which is quite a jump from 53% last year.
In addition, oncologists appear to be very satisfied with their profession. Similar to last year’s findings, 84% said they would choose medicine again, and 96% said they would choose the specialty of oncology again.
Earning in top third of all specialties
The average annual earnings reported by oncologists put this specialty in eleventh place among 29 specialties. Orthopedic specialists remain at the head of the list, with estimated earnings of $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according to Medscape’s compensation report, which included responses from 17,461 physicians in over 30 specialties.
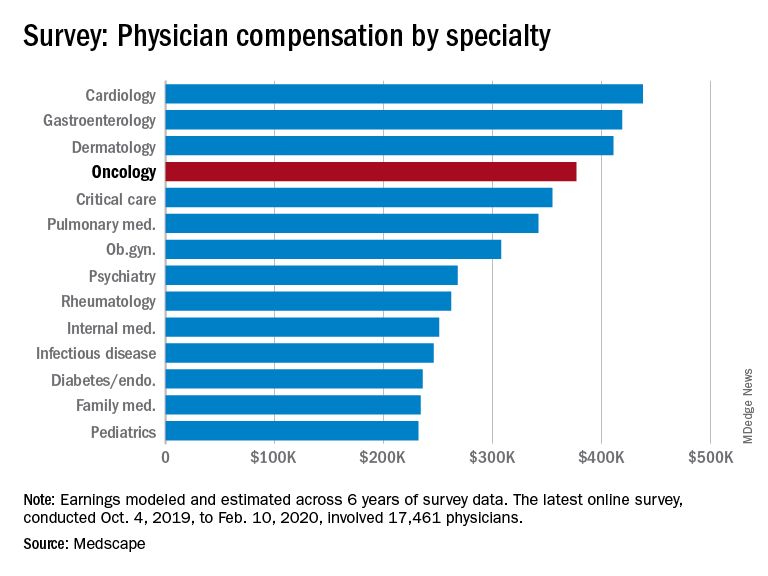
At the bottom of the estimated earnings list were public health and preventive medicine doctors and pediatricians. For both specialties, the reported annual earnings was $232,000. Family medicine specialists were only marginally higher at $234,000.
Radiologists ($427,000), gastroenterologists ($419,000), and urologists ($417,000) all reported higher earnings than oncologists, whereas neurologists, at $280,000, rheumatologists, at $262,000, and internal medicine physicians, at $251,000, earned less.
The report also found that gender disparities in income persist, with male oncologists earning 17% more than their female colleagues. The gender gap in oncology is somewhat less than that seen for all specialties combined, in which men earned 31% more than women, similar to last year’s figure of 33%.
Male oncologists reported spending 38.8 hours per week seeing patients, compared with 34.9 hours reported by female oncologists. This could be a factor contributing to the gender pay disparity. Overall, the average amount of time seeing patients was 37.9 hours per week.
Frustrations with paperwork and denied claims
Surveyed oncologists cited some of the frustrations they are facing, such as spending nearly 17 hours a week on paperwork and administrative tasks. They reported that 16% of claims are denied or have to be resubmitted. As for the most challenging part of the job, oncologists (22%), similar to physicians overall (26%), found that having so many rules and regulations takes first place, followed by working with electronic health record systems (20%), difficulties getting fair reimbursement (19%), having to work long hours (12%), and dealing with difficult patients (8%). Few oncologists were concerned about lawsuits (4%), and 4% reported that there were no challenges.
Oncologists reported that the most rewarding part of their job was gratitude/relationships with patients (31%), followed by knowing that they are making the world a better place (27%). After that, oncologists agreed with statements about being very good at what they do/finding answers/diagnoses (22%), having pride in being a doctor (9%), and making good money at a job they like (8%).
Other key findings
Other key findings from the Medscape Oncologist Compensation Report 2020 included the following:
- Regarding payment models, 80% take insurance, 41% are in fee-for-service arrangements, and 18% are in accountable care organizations (21%). Only 3% are in direct primary care, and 1% are cash-only practices or have a concierge practice.
- 65% of oncologists state that they will continue taking new and current Medicare/Medicaid patients. None said that they would not take on new Medicare/Medicaid patients, and 35% remain undecided. These numbers differed from physicians overall; 73% of all physicians surveyed said they would continue taking new/current Medicare/Medicaid patients, 6% said that will not take on new Medicare patients, and 4% said they will not take new Medicaid patients. In addition, 3% and 2% said that they would stop treating some or all of their Medicare and Medicaid patients, respectively.
- About half (51%) of oncologists use nurse practitioners, about a third (34%) use physician assistants, and 37% use neither. This was about the same as physicians overall.
- A larger percentage of oncologists (38%) expect to participate in MIPS (merit-based incentive payment system), and only 8% expect to participate in APMs (alternative payment models). This was similar to the findings for physicians overall, with more than one-third (37%) expecting to participate in MIPS and 9% planning to take part in APMs.
Impact of COVID-19 pandemic
The Medscape compensation reports also gives a glimpse of the impact the COVID-19 pandemic is having on physician compensation.
Since the beginning of the pandemic, practices have reported a 55% decrease in revenue and a 60% drop in patient volume. Physician practices and hospitals have laid off or furloughed personnel and have cut pay, and 9% of practices have closed their doors, at least for the time being.
A total of 43,000 health care workers were laid off in March, the report notes.
The findings tie in with those reported elsewhere. For example, a survey conducted by the Medical Group Management Association, which was reported by Medscape Medical News, found that 97% of physician practices have experienced negative financial effects directly or indirectly related to COVID-19.
Specialties were hard hit, especially those that rely on elective procedures, such as dermatology and cardiology. Oncology care has also been disrupted. For example, a survey conducted by the American Cancer Society Cancer Action Network found that half of the cancer patients and survivors who responded reported changes, delays, or disruptions to the care they were receiving.
This article first appeared on Medscape.com.
Oncologists continue to rank above the middle range for all specialties in annual compensation for physicians, according to findings from the newly released Medscape Oncologist Compensation Report 2020.
The average earnings for oncologists who participated in the survey was $377,000, which was a 5% increase from the $359,000 reported for 2018.
Just over two-thirds (67%) of oncologists reported that they felt that they were fairly compensated, which is quite a jump from 53% last year.
In addition, oncologists appear to be very satisfied with their profession. Similar to last year’s findings, 84% said they would choose medicine again, and 96% said they would choose the specialty of oncology again.
Earning in top third of all specialties
The average annual earnings reported by oncologists put this specialty in eleventh place among 29 specialties. Orthopedic specialists remain at the head of the list, with estimated earnings of $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according to Medscape’s compensation report, which included responses from 17,461 physicians in over 30 specialties.
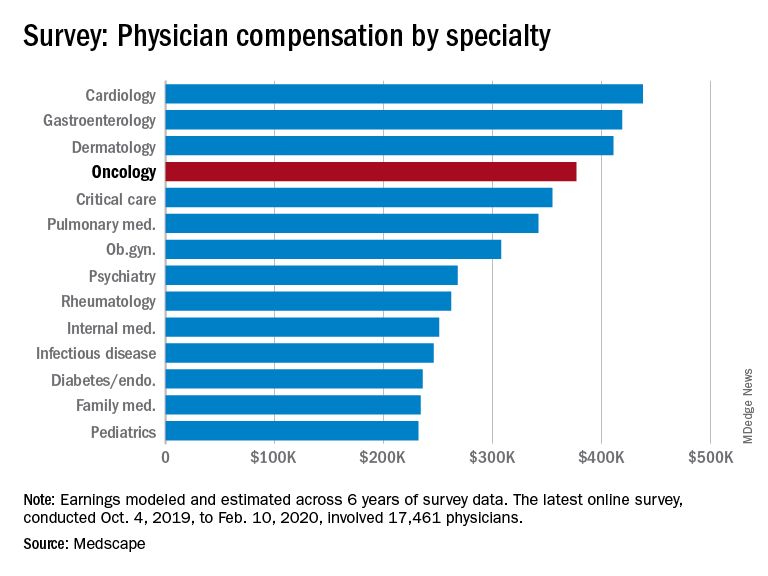
At the bottom of the estimated earnings list were public health and preventive medicine doctors and pediatricians. For both specialties, the reported annual earnings was $232,000. Family medicine specialists were only marginally higher at $234,000.
Radiologists ($427,000), gastroenterologists ($419,000), and urologists ($417,000) all reported higher earnings than oncologists, whereas neurologists, at $280,000, rheumatologists, at $262,000, and internal medicine physicians, at $251,000, earned less.
The report also found that gender disparities in income persist, with male oncologists earning 17% more than their female colleagues. The gender gap in oncology is somewhat less than that seen for all specialties combined, in which men earned 31% more than women, similar to last year’s figure of 33%.
Male oncologists reported spending 38.8 hours per week seeing patients, compared with 34.9 hours reported by female oncologists. This could be a factor contributing to the gender pay disparity. Overall, the average amount of time seeing patients was 37.9 hours per week.
Frustrations with paperwork and denied claims
Surveyed oncologists cited some of the frustrations they are facing, such as spending nearly 17 hours a week on paperwork and administrative tasks. They reported that 16% of claims are denied or have to be resubmitted. As for the most challenging part of the job, oncologists (22%), similar to physicians overall (26%), found that having so many rules and regulations takes first place, followed by working with electronic health record systems (20%), difficulties getting fair reimbursement (19%), having to work long hours (12%), and dealing with difficult patients (8%). Few oncologists were concerned about lawsuits (4%), and 4% reported that there were no challenges.
Oncologists reported that the most rewarding part of their job was gratitude/relationships with patients (31%), followed by knowing that they are making the world a better place (27%). After that, oncologists agreed with statements about being very good at what they do/finding answers/diagnoses (22%), having pride in being a doctor (9%), and making good money at a job they like (8%).
Other key findings
Other key findings from the Medscape Oncologist Compensation Report 2020 included the following:
- Regarding payment models, 80% take insurance, 41% are in fee-for-service arrangements, and 18% are in accountable care organizations (21%). Only 3% are in direct primary care, and 1% are cash-only practices or have a concierge practice.
- 65% of oncologists state that they will continue taking new and current Medicare/Medicaid patients. None said that they would not take on new Medicare/Medicaid patients, and 35% remain undecided. These numbers differed from physicians overall; 73% of all physicians surveyed said they would continue taking new/current Medicare/Medicaid patients, 6% said that will not take on new Medicare patients, and 4% said they will not take new Medicaid patients. In addition, 3% and 2% said that they would stop treating some or all of their Medicare and Medicaid patients, respectively.
- About half (51%) of oncologists use nurse practitioners, about a third (34%) use physician assistants, and 37% use neither. This was about the same as physicians overall.
- A larger percentage of oncologists (38%) expect to participate in MIPS (merit-based incentive payment system), and only 8% expect to participate in APMs (alternative payment models). This was similar to the findings for physicians overall, with more than one-third (37%) expecting to participate in MIPS and 9% planning to take part in APMs.
Impact of COVID-19 pandemic
The Medscape compensation reports also gives a glimpse of the impact the COVID-19 pandemic is having on physician compensation.
Since the beginning of the pandemic, practices have reported a 55% decrease in revenue and a 60% drop in patient volume. Physician practices and hospitals have laid off or furloughed personnel and have cut pay, and 9% of practices have closed their doors, at least for the time being.
A total of 43,000 health care workers were laid off in March, the report notes.
The findings tie in with those reported elsewhere. For example, a survey conducted by the Medical Group Management Association, which was reported by Medscape Medical News, found that 97% of physician practices have experienced negative financial effects directly or indirectly related to COVID-19.
Specialties were hard hit, especially those that rely on elective procedures, such as dermatology and cardiology. Oncology care has also been disrupted. For example, a survey conducted by the American Cancer Society Cancer Action Network found that half of the cancer patients and survivors who responded reported changes, delays, or disruptions to the care they were receiving.
This article first appeared on Medscape.com.
CSF and plasma biomarkers predict survival in sporadic Creutzfeldt-Jakob disease
, according to research published online ahead of print May 6 in JAMA Neurology. Levels of total tau in plasma and CSF are correlated, and plasma total tau is associated with survival time. These findings suggest that plasma total tau level could be a valid biomarker that guides clinical care for patients with sporadic Creutzfeldt-Jakob disease, said the investigators.
The accurate prediction of disease duration can assist clinicians and caregivers in clinical management, as well as influence the design of clinical trials. Previous studies have found that baseline protein levels in CSF and plasma are associated with disease duration in patients with sporadic Creutzfeldt-Jakob disease. To replicate these findings, Adam M. Staffaroni, PhD, of the department of neurology at the University of California, San Francisco, and colleagues conducted a longitudinal cohort study.
Evaluating fluid and nonfluid biomarkers
Dr. Staffaroni and colleagues recruited 193 participants with probable or definite sporadic Creutzfeldt-Jakob disease who had codon 129 genotyping and were referred to the UCSF Memory and Aging Center from March 2004 to January 2018. All participants underwent cognitive testing, informant measures, a neurologic examination, and CSF and blood sample collection. The researchers excluded from analysis five participants who had been placed on life-extending treatments. Participants were evaluated until death or censored at the time of statistical analysis.
Dr. Staffaroni and colleagues examined the following nonfluid biomarkers of survival: sex, age, codon 129 genotype, Barthel Index, and Medical Research Council (MRC) Prion Disease Rating Scale. In addition, they examined total tau level, phosphorylated tau level, total tau:phosphorylated tau ratio, neurofilament light (NfL) level, beta-amyloid 42 level, neuron-specific enolase level, 14-3-3 test result, and real-time quaking-induced conversion test in CSF as fluid biomarkers of survival. Finally, Dr. Staffaroni’s group analyzed total tau level, NfL level, and glial fibrillary acidic protein level in plasma as additional fluid biomarkers of survival.
The researchers fitted Cox proportional hazard models with time to event as the outcome. They log-transformed fluid biomarkers and ran models with and without nonfluid biomarkers of survival.
Plasma total tau was associated with survival
In all, 188 patients were included in the analysis. The population’s mean age was 63.8 years. Approximately 45% of participants were women. The diagnosis of sporadic Creutzfeldt-Jakob disease was pathologically confirmed for 78.2% of participants and probable for 21.8% of participants.
Dr. Staffaroni’s group observed strong correlations between plasma and CSF NfL concentrations and between plasma and CSF total tau concentrations. CSF total tau and CSF NfL concentrations were also correlated.
Among the nonfluid biomarkers, Barthel Index, MRC Scale, and codon 129 genotype were significantly associated with survival time. Lower level of function at baseline predicted a faster disease course.
Among the fluid biomarkers, greater levels of plasma total tau and NfL levels at baseline were associated with shorter survival. After the investigators controlled for Barthel Index and codon 129 genotype, the association of plasma total tau level with survival time remained significant. Plasma total tau level and Barthel Index (hazard ratio, 0.98) each independently predicted survival. Dr. Staffaroni and colleagues found that the hazard ratios for all CSF biomarkers were in the expected direction, and that those for total tau level, total tau:phosphorylated tau ratio, NfL level, and neuron-specific enolase level were statistically significant. Furthermore, positive results for 14-3-3 protein, neuron-specific enolase level, and total tau level were associated with a shorter time until death. Like the plasma biomarkers, CSF total tau level remained associated with survival after the investigators controlled for Barthel Index and codon 129 genotype. The same was true of CSF total tau:phosphorylated tau ratio, neuron-specific enolase level, and 14-3-3 result.
Plasma tau could be a diagnostic biomarker
“The hazard ratio associated with plasma total tau level was more than 40% higher than other fluid biomarkers of interest,” said the authors. “These findings further bolster the value of blood-based biomarkers, based on their minimally invasive and relatively inexpensive nature, and build on prior studies that suggested patients with sporadic Creutzfeldt-Jakob disease and controls can be discriminated with relatively high accuracy using blood-based assays.” When Dr. Staffaroni and colleagues modeled baseline functional status and plasma total tau levels together, they found that both were independent predictors of survival time. “This [finding] suggests that clinical measures and plasma total tau level could be combined to further improve prediction accuracy.”
Among the study’s limitations was its comparatively small subsample of patients for whom all plasma and CSF biomarkers were available. Disease duration and survival were longer in the study population than in the literature. “Another limitation is that the plasma biomarkers in this study, one of which showed great promise for predicting survival, were assayed using a research protocol,” said the researchers. “Widespread clinical use of these biomarkers will require well-validated commercial assays, development of which is underway.”
Before these biomarkers can be used in the clinic, these results will need to be replicated, and neurologists will need to develop consensus cutoffs for the biomarker levels. The researchers did not analyze plasma tau level as a diagnostic biomarker, but future studies should examine this potential, Dr. Staffaroni and colleagues concluded.
Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
SOURCE: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
, according to research published online ahead of print May 6 in JAMA Neurology. Levels of total tau in plasma and CSF are correlated, and plasma total tau is associated with survival time. These findings suggest that plasma total tau level could be a valid biomarker that guides clinical care for patients with sporadic Creutzfeldt-Jakob disease, said the investigators.
The accurate prediction of disease duration can assist clinicians and caregivers in clinical management, as well as influence the design of clinical trials. Previous studies have found that baseline protein levels in CSF and plasma are associated with disease duration in patients with sporadic Creutzfeldt-Jakob disease. To replicate these findings, Adam M. Staffaroni, PhD, of the department of neurology at the University of California, San Francisco, and colleagues conducted a longitudinal cohort study.
Evaluating fluid and nonfluid biomarkers
Dr. Staffaroni and colleagues recruited 193 participants with probable or definite sporadic Creutzfeldt-Jakob disease who had codon 129 genotyping and were referred to the UCSF Memory and Aging Center from March 2004 to January 2018. All participants underwent cognitive testing, informant measures, a neurologic examination, and CSF and blood sample collection. The researchers excluded from analysis five participants who had been placed on life-extending treatments. Participants were evaluated until death or censored at the time of statistical analysis.
Dr. Staffaroni and colleagues examined the following nonfluid biomarkers of survival: sex, age, codon 129 genotype, Barthel Index, and Medical Research Council (MRC) Prion Disease Rating Scale. In addition, they examined total tau level, phosphorylated tau level, total tau:phosphorylated tau ratio, neurofilament light (NfL) level, beta-amyloid 42 level, neuron-specific enolase level, 14-3-3 test result, and real-time quaking-induced conversion test in CSF as fluid biomarkers of survival. Finally, Dr. Staffaroni’s group analyzed total tau level, NfL level, and glial fibrillary acidic protein level in plasma as additional fluid biomarkers of survival.
The researchers fitted Cox proportional hazard models with time to event as the outcome. They log-transformed fluid biomarkers and ran models with and without nonfluid biomarkers of survival.
Plasma total tau was associated with survival
In all, 188 patients were included in the analysis. The population’s mean age was 63.8 years. Approximately 45% of participants were women. The diagnosis of sporadic Creutzfeldt-Jakob disease was pathologically confirmed for 78.2% of participants and probable for 21.8% of participants.
Dr. Staffaroni’s group observed strong correlations between plasma and CSF NfL concentrations and between plasma and CSF total tau concentrations. CSF total tau and CSF NfL concentrations were also correlated.
Among the nonfluid biomarkers, Barthel Index, MRC Scale, and codon 129 genotype were significantly associated with survival time. Lower level of function at baseline predicted a faster disease course.
Among the fluid biomarkers, greater levels of plasma total tau and NfL levels at baseline were associated with shorter survival. After the investigators controlled for Barthel Index and codon 129 genotype, the association of plasma total tau level with survival time remained significant. Plasma total tau level and Barthel Index (hazard ratio, 0.98) each independently predicted survival. Dr. Staffaroni and colleagues found that the hazard ratios for all CSF biomarkers were in the expected direction, and that those for total tau level, total tau:phosphorylated tau ratio, NfL level, and neuron-specific enolase level were statistically significant. Furthermore, positive results for 14-3-3 protein, neuron-specific enolase level, and total tau level were associated with a shorter time until death. Like the plasma biomarkers, CSF total tau level remained associated with survival after the investigators controlled for Barthel Index and codon 129 genotype. The same was true of CSF total tau:phosphorylated tau ratio, neuron-specific enolase level, and 14-3-3 result.
Plasma tau could be a diagnostic biomarker
“The hazard ratio associated with plasma total tau level was more than 40% higher than other fluid biomarkers of interest,” said the authors. “These findings further bolster the value of blood-based biomarkers, based on their minimally invasive and relatively inexpensive nature, and build on prior studies that suggested patients with sporadic Creutzfeldt-Jakob disease and controls can be discriminated with relatively high accuracy using blood-based assays.” When Dr. Staffaroni and colleagues modeled baseline functional status and plasma total tau levels together, they found that both were independent predictors of survival time. “This [finding] suggests that clinical measures and plasma total tau level could be combined to further improve prediction accuracy.”
Among the study’s limitations was its comparatively small subsample of patients for whom all plasma and CSF biomarkers were available. Disease duration and survival were longer in the study population than in the literature. “Another limitation is that the plasma biomarkers in this study, one of which showed great promise for predicting survival, were assayed using a research protocol,” said the researchers. “Widespread clinical use of these biomarkers will require well-validated commercial assays, development of which is underway.”
Before these biomarkers can be used in the clinic, these results will need to be replicated, and neurologists will need to develop consensus cutoffs for the biomarker levels. The researchers did not analyze plasma tau level as a diagnostic biomarker, but future studies should examine this potential, Dr. Staffaroni and colleagues concluded.
Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
SOURCE: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
, according to research published online ahead of print May 6 in JAMA Neurology. Levels of total tau in plasma and CSF are correlated, and plasma total tau is associated with survival time. These findings suggest that plasma total tau level could be a valid biomarker that guides clinical care for patients with sporadic Creutzfeldt-Jakob disease, said the investigators.
The accurate prediction of disease duration can assist clinicians and caregivers in clinical management, as well as influence the design of clinical trials. Previous studies have found that baseline protein levels in CSF and plasma are associated with disease duration in patients with sporadic Creutzfeldt-Jakob disease. To replicate these findings, Adam M. Staffaroni, PhD, of the department of neurology at the University of California, San Francisco, and colleagues conducted a longitudinal cohort study.
Evaluating fluid and nonfluid biomarkers
Dr. Staffaroni and colleagues recruited 193 participants with probable or definite sporadic Creutzfeldt-Jakob disease who had codon 129 genotyping and were referred to the UCSF Memory and Aging Center from March 2004 to January 2018. All participants underwent cognitive testing, informant measures, a neurologic examination, and CSF and blood sample collection. The researchers excluded from analysis five participants who had been placed on life-extending treatments. Participants were evaluated until death or censored at the time of statistical analysis.
Dr. Staffaroni and colleagues examined the following nonfluid biomarkers of survival: sex, age, codon 129 genotype, Barthel Index, and Medical Research Council (MRC) Prion Disease Rating Scale. In addition, they examined total tau level, phosphorylated tau level, total tau:phosphorylated tau ratio, neurofilament light (NfL) level, beta-amyloid 42 level, neuron-specific enolase level, 14-3-3 test result, and real-time quaking-induced conversion test in CSF as fluid biomarkers of survival. Finally, Dr. Staffaroni’s group analyzed total tau level, NfL level, and glial fibrillary acidic protein level in plasma as additional fluid biomarkers of survival.
The researchers fitted Cox proportional hazard models with time to event as the outcome. They log-transformed fluid biomarkers and ran models with and without nonfluid biomarkers of survival.
Plasma total tau was associated with survival
In all, 188 patients were included in the analysis. The population’s mean age was 63.8 years. Approximately 45% of participants were women. The diagnosis of sporadic Creutzfeldt-Jakob disease was pathologically confirmed for 78.2% of participants and probable for 21.8% of participants.
Dr. Staffaroni’s group observed strong correlations between plasma and CSF NfL concentrations and between plasma and CSF total tau concentrations. CSF total tau and CSF NfL concentrations were also correlated.
Among the nonfluid biomarkers, Barthel Index, MRC Scale, and codon 129 genotype were significantly associated with survival time. Lower level of function at baseline predicted a faster disease course.
Among the fluid biomarkers, greater levels of plasma total tau and NfL levels at baseline were associated with shorter survival. After the investigators controlled for Barthel Index and codon 129 genotype, the association of plasma total tau level with survival time remained significant. Plasma total tau level and Barthel Index (hazard ratio, 0.98) each independently predicted survival. Dr. Staffaroni and colleagues found that the hazard ratios for all CSF biomarkers were in the expected direction, and that those for total tau level, total tau:phosphorylated tau ratio, NfL level, and neuron-specific enolase level were statistically significant. Furthermore, positive results for 14-3-3 protein, neuron-specific enolase level, and total tau level were associated with a shorter time until death. Like the plasma biomarkers, CSF total tau level remained associated with survival after the investigators controlled for Barthel Index and codon 129 genotype. The same was true of CSF total tau:phosphorylated tau ratio, neuron-specific enolase level, and 14-3-3 result.
Plasma tau could be a diagnostic biomarker
“The hazard ratio associated with plasma total tau level was more than 40% higher than other fluid biomarkers of interest,” said the authors. “These findings further bolster the value of blood-based biomarkers, based on their minimally invasive and relatively inexpensive nature, and build on prior studies that suggested patients with sporadic Creutzfeldt-Jakob disease and controls can be discriminated with relatively high accuracy using blood-based assays.” When Dr. Staffaroni and colleagues modeled baseline functional status and plasma total tau levels together, they found that both were independent predictors of survival time. “This [finding] suggests that clinical measures and plasma total tau level could be combined to further improve prediction accuracy.”
Among the study’s limitations was its comparatively small subsample of patients for whom all plasma and CSF biomarkers were available. Disease duration and survival were longer in the study population than in the literature. “Another limitation is that the plasma biomarkers in this study, one of which showed great promise for predicting survival, were assayed using a research protocol,” said the researchers. “Widespread clinical use of these biomarkers will require well-validated commercial assays, development of which is underway.”
Before these biomarkers can be used in the clinic, these results will need to be replicated, and neurologists will need to develop consensus cutoffs for the biomarker levels. The researchers did not analyze plasma tau level as a diagnostic biomarker, but future studies should examine this potential, Dr. Staffaroni and colleagues concluded.
Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
SOURCE: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
FROM JAMA NEUROLOGY
Key clinical point: Invasive and minimally invasive biomarkers are associated with survival in sporadic Creutzfeldt-Jakob disease.
Major finding: The hazard ratio for plasma total tau level was more than 40% larger than any other biomarker.
Study details: A longitudinal study of 188 participants with sporadic Creutzfeldt-Jakob disease.
Disclosures: Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
Source: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
Geriatric assessments enhance patient care in advanced cancer
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – and boosted patient satisfaction, results of a randomized trial show.
In this video interview from the annual meeting of the American Society of Clinical Oncology, Supriya Gupta Mohile, MD, MS, from the University of Rochester, New York, discusses how a standardized written questionnaire and objective tests for physical performance and cognition can enhance the doctor-patient relationship and lead to specific recommendations for interventions, compared with usual care.
Dr. Mohile had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – and boosted patient satisfaction, results of a randomized trial show.
In this video interview from the annual meeting of the American Society of Clinical Oncology, Supriya Gupta Mohile, MD, MS, from the University of Rochester, New York, discusses how a standardized written questionnaire and objective tests for physical performance and cognition can enhance the doctor-patient relationship and lead to specific recommendations for interventions, compared with usual care.
Dr. Mohile had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – and boosted patient satisfaction, results of a randomized trial show.
In this video interview from the annual meeting of the American Society of Clinical Oncology, Supriya Gupta Mohile, MD, MS, from the University of Rochester, New York, discusses how a standardized written questionnaire and objective tests for physical performance and cognition can enhance the doctor-patient relationship and lead to specific recommendations for interventions, compared with usual care.
Dr. Mohile had no relevant financial disclosures.
REPORTING FROM ASCO 2018
Do you answer patient emails?
Recently I received a lengthy email from a woman who claimed to have once been a patient, though her name did not come up in my EHR system. She asked numerous questions about a self-diagnosed skin disorder.
I was undecided on how to reply – or even whether to reply at all – so I queried several dozen dermatology colleagues around the country, as well as a few physician friends and acquaintances in other specialties.
Responses varied all over the map – from “I never answer patient emails” to “What harm could it do, she’s better off getting correct answers from you than incorrect answers from some ‘advocacy’ web site” – and everything in between. I decided to look at what has been published on the subject.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/do-you-answer-patient-emails-take-our-poll?iframe=1"}]It turns out that as early as 1998, a group of investigators asked this same question and designed a study to address it (JAMA. 1998 Oct 21;280[15]:1333-5). Posing as a fictitious patient, they sent emails to random dermatologists describing an acute dermatological problem, tallied the responses they received, and followed up with a questionnaire to responders and nonresponders alike.
As with my informal survey, the authors found what they termed “a striking lack of consensus” on how to deal with this situation: 50% responded to the fictitious patient’s email; of those, 31% refused to give advice without seeing the patient, but 59% offered a diagnosis, and a third of that group went on to provide specific advice about therapy. In response to the questionnaire, 28% said that they tended not to answer any patient emails, 24% said they usually replied with a standard message, and 24% said they answered each request individually. The authors concluded that “standards for physician response to unsolicited patient e-mail are needed.”
Indeed. But my own unscientific survey suggests that, almost 20 years later, there is still nothing resembling a consensus on this issue. In the interim, several groups, including the American Medical Informatics Association, Medem, and the American Medical Association have proposed guidelines; but none have been generally accepted. Until such time as that happens, it seems prudent for each individual practice to adopt its own. For ideas, take a look at the proposals from the groups I mentioned, plus any others you can find. When you’re done, consider running your list past your lawyer to make sure you haven’t forgotten anything, and that there are no unique requirements in your state.
Your guidelines may be very simple (if you decide never to answer any queries) or very complex, depending on your situation and personal philosophy; but all guidelines should cover such issues as authentication of correspondents, informed consent, licensing jurisdiction (if you receive e-mails from states in which you are not licensed), and of course, confidentiality.
Contrary to popular belief, the Health Insurance Portability and Accountability Act (HIPAA) does not prohibit email communication with patients, nor does it require that it be encrypted. The HIPAA website specifically says, “Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.”
Still, if you are not comfortable with unencrypted communication, encryption software can be added to your practice’s email system. Enli, Sigaba, Tumbleweed, Zix, and many other vendors sell encryption packages. (As always, I have no financial interest in any product or enterprise mentioned in this column.)
Another option is web-based messaging: Patients enter your website and send a message using an electronic template that you design. A designated staffer will be notified by regular email when messages are received, and can post a reply on a page that can only be accessed by the patient. Besides enhancing privacy and security, you can state your guidelines in plain English to preclude any misunderstanding of what you will and will not address online.
Web-based messaging services can be freestanding or incorporated into existing secure web sites. Medfusion and RelayHealth are among the leading vendors of secure messaging services.
And now, I’m writing my guidelines.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I received a lengthy email from a woman who claimed to have once been a patient, though her name did not come up in my EHR system. She asked numerous questions about a self-diagnosed skin disorder.
I was undecided on how to reply – or even whether to reply at all – so I queried several dozen dermatology colleagues around the country, as well as a few physician friends and acquaintances in other specialties.
Responses varied all over the map – from “I never answer patient emails” to “What harm could it do, she’s better off getting correct answers from you than incorrect answers from some ‘advocacy’ web site” – and everything in between. I decided to look at what has been published on the subject.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/do-you-answer-patient-emails-take-our-poll?iframe=1"}]It turns out that as early as 1998, a group of investigators asked this same question and designed a study to address it (JAMA. 1998 Oct 21;280[15]:1333-5). Posing as a fictitious patient, they sent emails to random dermatologists describing an acute dermatological problem, tallied the responses they received, and followed up with a questionnaire to responders and nonresponders alike.
As with my informal survey, the authors found what they termed “a striking lack of consensus” on how to deal with this situation: 50% responded to the fictitious patient’s email; of those, 31% refused to give advice without seeing the patient, but 59% offered a diagnosis, and a third of that group went on to provide specific advice about therapy. In response to the questionnaire, 28% said that they tended not to answer any patient emails, 24% said they usually replied with a standard message, and 24% said they answered each request individually. The authors concluded that “standards for physician response to unsolicited patient e-mail are needed.”
Indeed. But my own unscientific survey suggests that, almost 20 years later, there is still nothing resembling a consensus on this issue. In the interim, several groups, including the American Medical Informatics Association, Medem, and the American Medical Association have proposed guidelines; but none have been generally accepted. Until such time as that happens, it seems prudent for each individual practice to adopt its own. For ideas, take a look at the proposals from the groups I mentioned, plus any others you can find. When you’re done, consider running your list past your lawyer to make sure you haven’t forgotten anything, and that there are no unique requirements in your state.
Your guidelines may be very simple (if you decide never to answer any queries) or very complex, depending on your situation and personal philosophy; but all guidelines should cover such issues as authentication of correspondents, informed consent, licensing jurisdiction (if you receive e-mails from states in which you are not licensed), and of course, confidentiality.
Contrary to popular belief, the Health Insurance Portability and Accountability Act (HIPAA) does not prohibit email communication with patients, nor does it require that it be encrypted. The HIPAA website specifically says, “Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.”
Still, if you are not comfortable with unencrypted communication, encryption software can be added to your practice’s email system. Enli, Sigaba, Tumbleweed, Zix, and many other vendors sell encryption packages. (As always, I have no financial interest in any product or enterprise mentioned in this column.)
Another option is web-based messaging: Patients enter your website and send a message using an electronic template that you design. A designated staffer will be notified by regular email when messages are received, and can post a reply on a page that can only be accessed by the patient. Besides enhancing privacy and security, you can state your guidelines in plain English to preclude any misunderstanding of what you will and will not address online.
Web-based messaging services can be freestanding or incorporated into existing secure web sites. Medfusion and RelayHealth are among the leading vendors of secure messaging services.
And now, I’m writing my guidelines.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I received a lengthy email from a woman who claimed to have once been a patient, though her name did not come up in my EHR system. She asked numerous questions about a self-diagnosed skin disorder.
I was undecided on how to reply – or even whether to reply at all – so I queried several dozen dermatology colleagues around the country, as well as a few physician friends and acquaintances in other specialties.
Responses varied all over the map – from “I never answer patient emails” to “What harm could it do, she’s better off getting correct answers from you than incorrect answers from some ‘advocacy’ web site” – and everything in between. I decided to look at what has been published on the subject.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/do-you-answer-patient-emails-take-our-poll?iframe=1"}]It turns out that as early as 1998, a group of investigators asked this same question and designed a study to address it (JAMA. 1998 Oct 21;280[15]:1333-5). Posing as a fictitious patient, they sent emails to random dermatologists describing an acute dermatological problem, tallied the responses they received, and followed up with a questionnaire to responders and nonresponders alike.
As with my informal survey, the authors found what they termed “a striking lack of consensus” on how to deal with this situation: 50% responded to the fictitious patient’s email; of those, 31% refused to give advice without seeing the patient, but 59% offered a diagnosis, and a third of that group went on to provide specific advice about therapy. In response to the questionnaire, 28% said that they tended not to answer any patient emails, 24% said they usually replied with a standard message, and 24% said they answered each request individually. The authors concluded that “standards for physician response to unsolicited patient e-mail are needed.”
Indeed. But my own unscientific survey suggests that, almost 20 years later, there is still nothing resembling a consensus on this issue. In the interim, several groups, including the American Medical Informatics Association, Medem, and the American Medical Association have proposed guidelines; but none have been generally accepted. Until such time as that happens, it seems prudent for each individual practice to adopt its own. For ideas, take a look at the proposals from the groups I mentioned, plus any others you can find. When you’re done, consider running your list past your lawyer to make sure you haven’t forgotten anything, and that there are no unique requirements in your state.
Your guidelines may be very simple (if you decide never to answer any queries) or very complex, depending on your situation and personal philosophy; but all guidelines should cover such issues as authentication of correspondents, informed consent, licensing jurisdiction (if you receive e-mails from states in which you are not licensed), and of course, confidentiality.
Contrary to popular belief, the Health Insurance Portability and Accountability Act (HIPAA) does not prohibit email communication with patients, nor does it require that it be encrypted. The HIPAA website specifically says, “Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.”
Still, if you are not comfortable with unencrypted communication, encryption software can be added to your practice’s email system. Enli, Sigaba, Tumbleweed, Zix, and many other vendors sell encryption packages. (As always, I have no financial interest in any product or enterprise mentioned in this column.)
Another option is web-based messaging: Patients enter your website and send a message using an electronic template that you design. A designated staffer will be notified by regular email when messages are received, and can post a reply on a page that can only be accessed by the patient. Besides enhancing privacy and security, you can state your guidelines in plain English to preclude any misunderstanding of what you will and will not address online.
Web-based messaging services can be freestanding or incorporated into existing secure web sites. Medfusion and RelayHealth are among the leading vendors of secure messaging services.
And now, I’m writing my guidelines.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
How to raise HPV vaccine rates: Work together
Despite widespread availability of the human papillomavirus vaccine over the last 11 years, vaccination rates continue to lag behind national targets and are far behind other vaccines routinely administered in adolescence, such as the meningococcal and tetanus vaccines.
Better collaboration among pediatricians and obstetrician-gynecologists to promote the HPV vaccine may be one answer to turning the tide, said David W. Kimberlin, MD, codirector of the division of pediatric infectious diseases at the University of Alabama at Birmingham and president of the Pediatric Infectious Diseases Society.
As of 2015, just 63% of eligible U.S. girls completed the first dose of the HPV vaccination, 52% completed two doses, and 42% finished the three-dose series, according to a recent “Call to Action” paper in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2017.02.026). Although the HPV vaccine has been recommended for boys since 2011, just half of eligible boys completed the first dose, 39% completed two doses, and 28% finished the full series. By contrast, 86% of adolescents received the tetanus, diphtheria, and acellular pertussis vaccine, and 81% received the first dose of the meningococcal vaccine. The federal government’s Office of Disease Prevention and Health Promotion aims for an 80% HPV vaccination completion rate for girls and boys aged 13-15 years by 2020.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/how-to-raise-hpv-vaccine-rates?iframe=1"}]The CDC now recommends that 11- to 12-year-olds get two doses of the HPV vaccine, rather than three, with the second dose given 6-12 months after the first (MMWR. 2016;65:1405-8).
The common ways in which the HPV vaccine is introduced to parents likely contributes to the low vaccination rates, said Beth Auslander, PhD, a clinical psychologist and associate professor in the department of pediatrics at the University of Texas Medical Branch in Galveston. Some pediatricians may tell parents about school-mandated vaccines first and then as a side note, mention the HPV vaccine.
“The way it’s presented at times is being separate from the other vaccines,” Dr. Auslander said. “Sometimes it sounds optional.”
Parents often are uncertain about the safety and efficacy of the HPV vaccine, she added, and some wrongly assume the vaccine will lead to sexual activity among their children.
“Sometimes it can take a little longer to talk about,” Dr. Yoost said in an interview. “A lot of times, parents will bring up questions or concerns about the HPV vaccine. If physicians aren’t comfortable talking about those topics, they may not give the best recommendation. Pediatricians are not dealing with cervical cancer, so they may have a harder time recommending a vaccine based on outcomes they don’t deal with.”
Ob.gyns. are in a unique position to reach out to their pediatric counterparts and discuss strategies for catching more patients eligible for the HPV vaccine, said Sarah Dilley, MD, a gynecologic oncology fellow at the University of Alabama at Birmingham and the lead author of the recent Call to Action paper.
“We offer a unique perspective in that we are treating the conditions that the HPV vaccine is preventing, so we have more of a sense of urgency and an understanding of why that is so important,” Dr. Dilley said in an interview. “Obviously, pediatricians understand this as well, but it’s not something they see every day in their practice. We, as ob.gyns., have the opportunity to talk to our pediatric colleagues about the importance and really how devastating these conditions can be and how important it is to prevent them.”
In the recent paper, Dr. Dilley and her colleagues recommend that ob.gyns. speak to pediatricians and primary care physicians in their community to promote the vaccine and encourage them to view the Centers for Disease Control and Prevention’s You Are the Key presentation. The CDC resources include tips for how to discuss the burden of HPV-related diseases and effective communication with parents, an update on state vaccination rates, and the latest HPV vaccination recommendations.
Dr. Dilley encourages ob.gyns. and pediatricians to find different opportunities and venues to discuss the HPV vaccine. Ask about the pediatrician’s current approach to the vaccine, the doctor’s communication with parents, and how such practices could be improved, she said.
“People like to hear from their colleagues,” Dr. Dilley said. “Hearing from ob.gyns. [about] their experiences could be really helpful, whether it’s doing lunch and learns, formal education, grand rounds, or even more informal talks at the hospital.”
Ob.gyns. and pediatricians also need to better coordinate their messaging so that there is more consistent emphasis during each patient encounter about the need of the HPV vaccination, Dr. Kimberlin said. There needs to be a renewed focus on the vaccine as a cancer vaccination, he said.
“The nuances of HPV and the way that HPV is acquired, namely sexually transmitted, has taken too much of a front row consideration in the conversations that parents sometimes want to have with their child’s health care providers,” Dr. Kimberlin said. “We have to stress this is a cancer vaccine. This is a vaccine that prevents the deaths of thousands of women and men. We simply need to get that message out more forcefully.”
In addition, there’s a need for joint action to debunk myths about the vaccine and work toward eliminating the stigma surrounding it, Dr. Dilley said.
“I talk to a lot parents about the HPV vaccine and there’s so much misinformation online,” she said. “But a lot of patients do look at websites of their ob.gyn. or their pediatrician, [and] if they see something reputable coming from one of those sites, they might listen. We have a lot of patients who are mothers or grandmothers of kids; that’s also an opportunity for us to say, ‘Hey while we’re screening you for cervical cancer, let’s talk about the HPV vaccine.’ That’s a really good opportunity to help our [pediatric] colleagues out.”
5 steps to increase HPV vaccination
Melissa Kottke, MD, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University offered her practice steps for increased HPV vaccination rates.
1. Be clear about your recommendation. For example, “I recommend the HPV vaccine. It can help prevent cancer.”
3. Educate the entire clinical team (front desk staff, nursing, medical assistants, etc.) about the HPV vaccine so there is consistent messaging and delivery.
4. Establish streamlined systems. The vaccine recommendation, order, and follow-up should be streamlined and automated, if possible. Systems should also ensure documentation of vaccine receipt.
5. Make time for conversations with patients who are mothers and grandmothers. Recommend the HPV vaccine for males and females aged 9-26 years old. Encourage parents/grandparents to follow-up with the child’s doctor or offer to provide the vaccine in your office.
*This story was updated 8/22/2017.
[email protected]
On Twitter @legal_med
Despite widespread availability of the human papillomavirus vaccine over the last 11 years, vaccination rates continue to lag behind national targets and are far behind other vaccines routinely administered in adolescence, such as the meningococcal and tetanus vaccines.
Better collaboration among pediatricians and obstetrician-gynecologists to promote the HPV vaccine may be one answer to turning the tide, said David W. Kimberlin, MD, codirector of the division of pediatric infectious diseases at the University of Alabama at Birmingham and president of the Pediatric Infectious Diseases Society.
As of 2015, just 63% of eligible U.S. girls completed the first dose of the HPV vaccination, 52% completed two doses, and 42% finished the three-dose series, according to a recent “Call to Action” paper in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2017.02.026). Although the HPV vaccine has been recommended for boys since 2011, just half of eligible boys completed the first dose, 39% completed two doses, and 28% finished the full series. By contrast, 86% of adolescents received the tetanus, diphtheria, and acellular pertussis vaccine, and 81% received the first dose of the meningococcal vaccine. The federal government’s Office of Disease Prevention and Health Promotion aims for an 80% HPV vaccination completion rate for girls and boys aged 13-15 years by 2020.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/how-to-raise-hpv-vaccine-rates?iframe=1"}]The CDC now recommends that 11- to 12-year-olds get two doses of the HPV vaccine, rather than three, with the second dose given 6-12 months after the first (MMWR. 2016;65:1405-8).
The common ways in which the HPV vaccine is introduced to parents likely contributes to the low vaccination rates, said Beth Auslander, PhD, a clinical psychologist and associate professor in the department of pediatrics at the University of Texas Medical Branch in Galveston. Some pediatricians may tell parents about school-mandated vaccines first and then as a side note, mention the HPV vaccine.
“The way it’s presented at times is being separate from the other vaccines,” Dr. Auslander said. “Sometimes it sounds optional.”
Parents often are uncertain about the safety and efficacy of the HPV vaccine, she added, and some wrongly assume the vaccine will lead to sexual activity among their children.
“Sometimes it can take a little longer to talk about,” Dr. Yoost said in an interview. “A lot of times, parents will bring up questions or concerns about the HPV vaccine. If physicians aren’t comfortable talking about those topics, they may not give the best recommendation. Pediatricians are not dealing with cervical cancer, so they may have a harder time recommending a vaccine based on outcomes they don’t deal with.”
Ob.gyns. are in a unique position to reach out to their pediatric counterparts and discuss strategies for catching more patients eligible for the HPV vaccine, said Sarah Dilley, MD, a gynecologic oncology fellow at the University of Alabama at Birmingham and the lead author of the recent Call to Action paper.
“We offer a unique perspective in that we are treating the conditions that the HPV vaccine is preventing, so we have more of a sense of urgency and an understanding of why that is so important,” Dr. Dilley said in an interview. “Obviously, pediatricians understand this as well, but it’s not something they see every day in their practice. We, as ob.gyns., have the opportunity to talk to our pediatric colleagues about the importance and really how devastating these conditions can be and how important it is to prevent them.”
In the recent paper, Dr. Dilley and her colleagues recommend that ob.gyns. speak to pediatricians and primary care physicians in their community to promote the vaccine and encourage them to view the Centers for Disease Control and Prevention’s You Are the Key presentation. The CDC resources include tips for how to discuss the burden of HPV-related diseases and effective communication with parents, an update on state vaccination rates, and the latest HPV vaccination recommendations.
Dr. Dilley encourages ob.gyns. and pediatricians to find different opportunities and venues to discuss the HPV vaccine. Ask about the pediatrician’s current approach to the vaccine, the doctor’s communication with parents, and how such practices could be improved, she said.
“People like to hear from their colleagues,” Dr. Dilley said. “Hearing from ob.gyns. [about] their experiences could be really helpful, whether it’s doing lunch and learns, formal education, grand rounds, or even more informal talks at the hospital.”
Ob.gyns. and pediatricians also need to better coordinate their messaging so that there is more consistent emphasis during each patient encounter about the need of the HPV vaccination, Dr. Kimberlin said. There needs to be a renewed focus on the vaccine as a cancer vaccination, he said.
“The nuances of HPV and the way that HPV is acquired, namely sexually transmitted, has taken too much of a front row consideration in the conversations that parents sometimes want to have with their child’s health care providers,” Dr. Kimberlin said. “We have to stress this is a cancer vaccine. This is a vaccine that prevents the deaths of thousands of women and men. We simply need to get that message out more forcefully.”
In addition, there’s a need for joint action to debunk myths about the vaccine and work toward eliminating the stigma surrounding it, Dr. Dilley said.
“I talk to a lot parents about the HPV vaccine and there’s so much misinformation online,” she said. “But a lot of patients do look at websites of their ob.gyn. or their pediatrician, [and] if they see something reputable coming from one of those sites, they might listen. We have a lot of patients who are mothers or grandmothers of kids; that’s also an opportunity for us to say, ‘Hey while we’re screening you for cervical cancer, let’s talk about the HPV vaccine.’ That’s a really good opportunity to help our [pediatric] colleagues out.”
5 steps to increase HPV vaccination
Melissa Kottke, MD, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University offered her practice steps for increased HPV vaccination rates.
1. Be clear about your recommendation. For example, “I recommend the HPV vaccine. It can help prevent cancer.”
3. Educate the entire clinical team (front desk staff, nursing, medical assistants, etc.) about the HPV vaccine so there is consistent messaging and delivery.
4. Establish streamlined systems. The vaccine recommendation, order, and follow-up should be streamlined and automated, if possible. Systems should also ensure documentation of vaccine receipt.
5. Make time for conversations with patients who are mothers and grandmothers. Recommend the HPV vaccine for males and females aged 9-26 years old. Encourage parents/grandparents to follow-up with the child’s doctor or offer to provide the vaccine in your office.
*This story was updated 8/22/2017.
[email protected]
On Twitter @legal_med
Despite widespread availability of the human papillomavirus vaccine over the last 11 years, vaccination rates continue to lag behind national targets and are far behind other vaccines routinely administered in adolescence, such as the meningococcal and tetanus vaccines.
Better collaboration among pediatricians and obstetrician-gynecologists to promote the HPV vaccine may be one answer to turning the tide, said David W. Kimberlin, MD, codirector of the division of pediatric infectious diseases at the University of Alabama at Birmingham and president of the Pediatric Infectious Diseases Society.
As of 2015, just 63% of eligible U.S. girls completed the first dose of the HPV vaccination, 52% completed two doses, and 42% finished the three-dose series, according to a recent “Call to Action” paper in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2017.02.026). Although the HPV vaccine has been recommended for boys since 2011, just half of eligible boys completed the first dose, 39% completed two doses, and 28% finished the full series. By contrast, 86% of adolescents received the tetanus, diphtheria, and acellular pertussis vaccine, and 81% received the first dose of the meningococcal vaccine. The federal government’s Office of Disease Prevention and Health Promotion aims for an 80% HPV vaccination completion rate for girls and boys aged 13-15 years by 2020.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/how-to-raise-hpv-vaccine-rates?iframe=1"}]The CDC now recommends that 11- to 12-year-olds get two doses of the HPV vaccine, rather than three, with the second dose given 6-12 months after the first (MMWR. 2016;65:1405-8).
The common ways in which the HPV vaccine is introduced to parents likely contributes to the low vaccination rates, said Beth Auslander, PhD, a clinical psychologist and associate professor in the department of pediatrics at the University of Texas Medical Branch in Galveston. Some pediatricians may tell parents about school-mandated vaccines first and then as a side note, mention the HPV vaccine.
“The way it’s presented at times is being separate from the other vaccines,” Dr. Auslander said. “Sometimes it sounds optional.”
Parents often are uncertain about the safety and efficacy of the HPV vaccine, she added, and some wrongly assume the vaccine will lead to sexual activity among their children.
“Sometimes it can take a little longer to talk about,” Dr. Yoost said in an interview. “A lot of times, parents will bring up questions or concerns about the HPV vaccine. If physicians aren’t comfortable talking about those topics, they may not give the best recommendation. Pediatricians are not dealing with cervical cancer, so they may have a harder time recommending a vaccine based on outcomes they don’t deal with.”
Ob.gyns. are in a unique position to reach out to their pediatric counterparts and discuss strategies for catching more patients eligible for the HPV vaccine, said Sarah Dilley, MD, a gynecologic oncology fellow at the University of Alabama at Birmingham and the lead author of the recent Call to Action paper.
“We offer a unique perspective in that we are treating the conditions that the HPV vaccine is preventing, so we have more of a sense of urgency and an understanding of why that is so important,” Dr. Dilley said in an interview. “Obviously, pediatricians understand this as well, but it’s not something they see every day in their practice. We, as ob.gyns., have the opportunity to talk to our pediatric colleagues about the importance and really how devastating these conditions can be and how important it is to prevent them.”
In the recent paper, Dr. Dilley and her colleagues recommend that ob.gyns. speak to pediatricians and primary care physicians in their community to promote the vaccine and encourage them to view the Centers for Disease Control and Prevention’s You Are the Key presentation. The CDC resources include tips for how to discuss the burden of HPV-related diseases and effective communication with parents, an update on state vaccination rates, and the latest HPV vaccination recommendations.
Dr. Dilley encourages ob.gyns. and pediatricians to find different opportunities and venues to discuss the HPV vaccine. Ask about the pediatrician’s current approach to the vaccine, the doctor’s communication with parents, and how such practices could be improved, she said.
“People like to hear from their colleagues,” Dr. Dilley said. “Hearing from ob.gyns. [about] their experiences could be really helpful, whether it’s doing lunch and learns, formal education, grand rounds, or even more informal talks at the hospital.”
Ob.gyns. and pediatricians also need to better coordinate their messaging so that there is more consistent emphasis during each patient encounter about the need of the HPV vaccination, Dr. Kimberlin said. There needs to be a renewed focus on the vaccine as a cancer vaccination, he said.
“The nuances of HPV and the way that HPV is acquired, namely sexually transmitted, has taken too much of a front row consideration in the conversations that parents sometimes want to have with their child’s health care providers,” Dr. Kimberlin said. “We have to stress this is a cancer vaccine. This is a vaccine that prevents the deaths of thousands of women and men. We simply need to get that message out more forcefully.”
In addition, there’s a need for joint action to debunk myths about the vaccine and work toward eliminating the stigma surrounding it, Dr. Dilley said.
“I talk to a lot parents about the HPV vaccine and there’s so much misinformation online,” she said. “But a lot of patients do look at websites of their ob.gyn. or their pediatrician, [and] if they see something reputable coming from one of those sites, they might listen. We have a lot of patients who are mothers or grandmothers of kids; that’s also an opportunity for us to say, ‘Hey while we’re screening you for cervical cancer, let’s talk about the HPV vaccine.’ That’s a really good opportunity to help our [pediatric] colleagues out.”
5 steps to increase HPV vaccination
Melissa Kottke, MD, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University offered her practice steps for increased HPV vaccination rates.
1. Be clear about your recommendation. For example, “I recommend the HPV vaccine. It can help prevent cancer.”
3. Educate the entire clinical team (front desk staff, nursing, medical assistants, etc.) about the HPV vaccine so there is consistent messaging and delivery.
4. Establish streamlined systems. The vaccine recommendation, order, and follow-up should be streamlined and automated, if possible. Systems should also ensure documentation of vaccine receipt.
5. Make time for conversations with patients who are mothers and grandmothers. Recommend the HPV vaccine for males and females aged 9-26 years old. Encourage parents/grandparents to follow-up with the child’s doctor or offer to provide the vaccine in your office.
*This story was updated 8/22/2017.
[email protected]
On Twitter @legal_med
Poll: How has the opioid crisis changed your practice?
[polldaddy:9772731]
[polldaddy:9772731]
[polldaddy:9772731]
Poll: How have you changed opioid prescribing in your practice?
[polldaddy:9772633]
[polldaddy:9772633]
[polldaddy:9772633]
HFrEF mortality halved when treatment matches guidelines
PARIS – Heart failure patients who received guideline-directed pharmacotherapy, at dosages that approached guideline-directed levels, had roughly half the 6-month mortality as did similar patients who did not receive this level of treatment in a real-world, observational study with more than 6,000 patients.
Adherence to pharmacologic treatment guidelines for patients with heart failure with reduced ejection fraction (HFrEF) “was strongly associated with clinical outcomes during 6-month follow-up,” Michel Komajda, MD, said at a meeting held by the Heart Failure Association of the European Society of Cardiology. The findings highlight the importance of closely following guideline recommendations in routine practice.
[polldaddy:9772629]
The analysis used data collected in the QUALIFY (Quality of Adherence to Guideline Recommendations for Life-Saving Treatment in Heart Failure: an International Survey) registry, which enrolled 7,127 HFrEF patients during September 2013–December 2014 at 547 centers in 36 countries, mostly in Europe, Asia, and Africa but also in Canada, Ecuador, and Australia. All enrolled patients had to have been hospitalized for worsening heart failure at least once during the 1-15 months before they entered QUALIFY.
Dr. Komajda and his associates assessed each enrolled patient at baseline by their treatment with each of four guideline-recommended drug classes: an ACE inhibitor or angiotensin receptor blocker; a beta-blocker; an aldosterone receptor antagonist (ARA) if the patient’s functional status was rated as New York Heart Association class II, III, or IV; and ivabradine (Corlanor) if the patient was in NYHA class II, III, or IV, in sinus rhythm, had a heart rate of at least 70 beats per minute, and if the patient was in a country where ivabradine was available. Because patient enrollment occurred in 2013 and 2014, the study couldn’t include the new formulation of sacubitril plus valsartan (Entresto) in its analysis.
For each eligible drug class a patient received 1 point if their daily prescribed dosage was at least 50% of the recommended dosage (or 100% for an ARA), 0.5 points if the patient received the recommended drug but at a lower dosage, and no points if the drug wasn’t given. A patient also received 1 point if they were appropriately not given a drug because of a documented contraindication or intolerance. The researchers then calculated each patient’s “adherence score” by dividing their point total by the potentially maximum number of points that each patient could have received (a number that ranged from 2 to 4). They defined a score of 1 (which meant the patients received at least half the recommended dosage of all recommended drugs) as good adherence, a score of 0.51-0.99 as moderate adherence, and a score of 0.5 or less as poor adherence.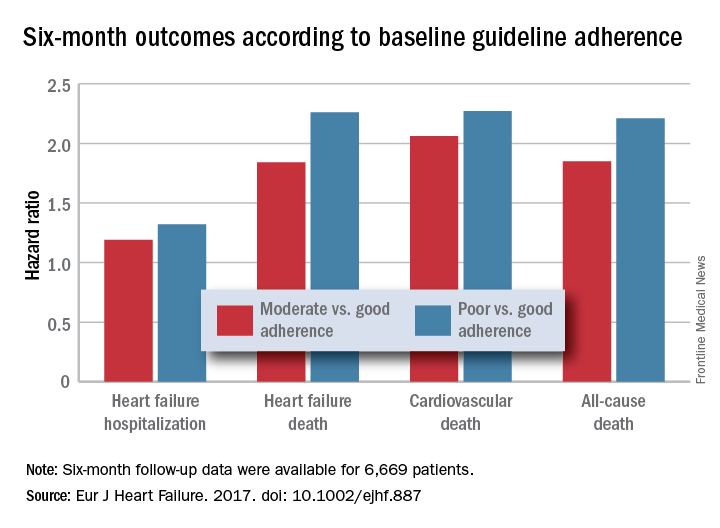
Because patient enrollment occurred during 2013 and 2014, the benchmark heart failure treatment guidelines were those issued by the European Society of Cardiology in 2012 (Eur Heart J. 2012 July;33[14]:1787-1847).
Concurrently with Dr. Komajda’s report at the meeting the results appeared in an article online (Eur J Heart Failure. 2017. doi: 10.1002/ejhf.887).
QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.
[email protected]
On Twitter @mitchelzoler
This was a wonderful and useful study. It was large, prospective, covered a wide geographic area, and showed that drug dosage matters when treating heart failure with reduced ejection fraction.
The geographic diversity was a strength, but also a potential weakness because of the resulting differences among the enrolled patients in financial resources, ethnic and genetic makeup, and their tolerance to various drugs. I hope that further research can dissect the role that each of these factors played in the results.
Another limitation is the relatively simplistic approach used for assessing drug dosages to calculate the adherence scores. While it is a very useful step forward to classify patients by the drug dosages they received, there could be some very legitimate variations in dosages based on parameters such as blood pressure. An important question to address in the future is whether it is better to use all the recommended drugs at reduced dosages if necessary, or to use fewer agents at higher dosages.
But these are just quibbles about what is a very important study.
Andrew J.S. Coats, MD , is a cardiologist, professor of medicine, and academic vice-president for the Monash Warwick Alliance of Warwick University in Coventry, England, and Monash University in Melbourne. He has received honoraria from Impulse Dynamics, Menarini, PsiOxus, ResMed, Respicardia, and Servier. He made these comments as designated discussant for Dr. Komajda’s report.
This was a wonderful and useful study. It was large, prospective, covered a wide geographic area, and showed that drug dosage matters when treating heart failure with reduced ejection fraction.
The geographic diversity was a strength, but also a potential weakness because of the resulting differences among the enrolled patients in financial resources, ethnic and genetic makeup, and their tolerance to various drugs. I hope that further research can dissect the role that each of these factors played in the results.
Another limitation is the relatively simplistic approach used for assessing drug dosages to calculate the adherence scores. While it is a very useful step forward to classify patients by the drug dosages they received, there could be some very legitimate variations in dosages based on parameters such as blood pressure. An important question to address in the future is whether it is better to use all the recommended drugs at reduced dosages if necessary, or to use fewer agents at higher dosages.
But these are just quibbles about what is a very important study.
Andrew J.S. Coats, MD , is a cardiologist, professor of medicine, and academic vice-president for the Monash Warwick Alliance of Warwick University in Coventry, England, and Monash University in Melbourne. He has received honoraria from Impulse Dynamics, Menarini, PsiOxus, ResMed, Respicardia, and Servier. He made these comments as designated discussant for Dr. Komajda’s report.
This was a wonderful and useful study. It was large, prospective, covered a wide geographic area, and showed that drug dosage matters when treating heart failure with reduced ejection fraction.
The geographic diversity was a strength, but also a potential weakness because of the resulting differences among the enrolled patients in financial resources, ethnic and genetic makeup, and their tolerance to various drugs. I hope that further research can dissect the role that each of these factors played in the results.
Another limitation is the relatively simplistic approach used for assessing drug dosages to calculate the adherence scores. While it is a very useful step forward to classify patients by the drug dosages they received, there could be some very legitimate variations in dosages based on parameters such as blood pressure. An important question to address in the future is whether it is better to use all the recommended drugs at reduced dosages if necessary, or to use fewer agents at higher dosages.
But these are just quibbles about what is a very important study.
Andrew J.S. Coats, MD , is a cardiologist, professor of medicine, and academic vice-president for the Monash Warwick Alliance of Warwick University in Coventry, England, and Monash University in Melbourne. He has received honoraria from Impulse Dynamics, Menarini, PsiOxus, ResMed, Respicardia, and Servier. He made these comments as designated discussant for Dr. Komajda’s report.
PARIS – Heart failure patients who received guideline-directed pharmacotherapy, at dosages that approached guideline-directed levels, had roughly half the 6-month mortality as did similar patients who did not receive this level of treatment in a real-world, observational study with more than 6,000 patients.
Adherence to pharmacologic treatment guidelines for patients with heart failure with reduced ejection fraction (HFrEF) “was strongly associated with clinical outcomes during 6-month follow-up,” Michel Komajda, MD, said at a meeting held by the Heart Failure Association of the European Society of Cardiology. The findings highlight the importance of closely following guideline recommendations in routine practice.
[polldaddy:9772629]
The analysis used data collected in the QUALIFY (Quality of Adherence to Guideline Recommendations for Life-Saving Treatment in Heart Failure: an International Survey) registry, which enrolled 7,127 HFrEF patients during September 2013–December 2014 at 547 centers in 36 countries, mostly in Europe, Asia, and Africa but also in Canada, Ecuador, and Australia. All enrolled patients had to have been hospitalized for worsening heart failure at least once during the 1-15 months before they entered QUALIFY.
Dr. Komajda and his associates assessed each enrolled patient at baseline by their treatment with each of four guideline-recommended drug classes: an ACE inhibitor or angiotensin receptor blocker; a beta-blocker; an aldosterone receptor antagonist (ARA) if the patient’s functional status was rated as New York Heart Association class II, III, or IV; and ivabradine (Corlanor) if the patient was in NYHA class II, III, or IV, in sinus rhythm, had a heart rate of at least 70 beats per minute, and if the patient was in a country where ivabradine was available. Because patient enrollment occurred in 2013 and 2014, the study couldn’t include the new formulation of sacubitril plus valsartan (Entresto) in its analysis.
For each eligible drug class a patient received 1 point if their daily prescribed dosage was at least 50% of the recommended dosage (or 100% for an ARA), 0.5 points if the patient received the recommended drug but at a lower dosage, and no points if the drug wasn’t given. A patient also received 1 point if they were appropriately not given a drug because of a documented contraindication or intolerance. The researchers then calculated each patient’s “adherence score” by dividing their point total by the potentially maximum number of points that each patient could have received (a number that ranged from 2 to 4). They defined a score of 1 (which meant the patients received at least half the recommended dosage of all recommended drugs) as good adherence, a score of 0.51-0.99 as moderate adherence, and a score of 0.5 or less as poor adherence.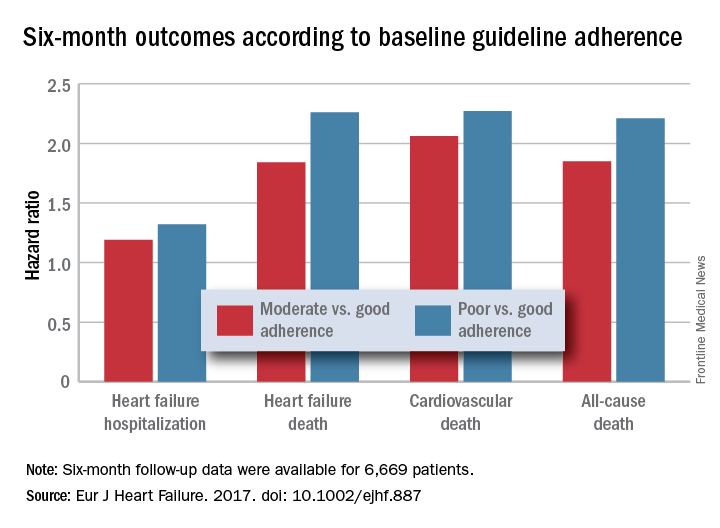
Because patient enrollment occurred during 2013 and 2014, the benchmark heart failure treatment guidelines were those issued by the European Society of Cardiology in 2012 (Eur Heart J. 2012 July;33[14]:1787-1847).
Concurrently with Dr. Komajda’s report at the meeting the results appeared in an article online (Eur J Heart Failure. 2017. doi: 10.1002/ejhf.887).
QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.
[email protected]
On Twitter @mitchelzoler
PARIS – Heart failure patients who received guideline-directed pharmacotherapy, at dosages that approached guideline-directed levels, had roughly half the 6-month mortality as did similar patients who did not receive this level of treatment in a real-world, observational study with more than 6,000 patients.
Adherence to pharmacologic treatment guidelines for patients with heart failure with reduced ejection fraction (HFrEF) “was strongly associated with clinical outcomes during 6-month follow-up,” Michel Komajda, MD, said at a meeting held by the Heart Failure Association of the European Society of Cardiology. The findings highlight the importance of closely following guideline recommendations in routine practice.
[polldaddy:9772629]
The analysis used data collected in the QUALIFY (Quality of Adherence to Guideline Recommendations for Life-Saving Treatment in Heart Failure: an International Survey) registry, which enrolled 7,127 HFrEF patients during September 2013–December 2014 at 547 centers in 36 countries, mostly in Europe, Asia, and Africa but also in Canada, Ecuador, and Australia. All enrolled patients had to have been hospitalized for worsening heart failure at least once during the 1-15 months before they entered QUALIFY.
Dr. Komajda and his associates assessed each enrolled patient at baseline by their treatment with each of four guideline-recommended drug classes: an ACE inhibitor or angiotensin receptor blocker; a beta-blocker; an aldosterone receptor antagonist (ARA) if the patient’s functional status was rated as New York Heart Association class II, III, or IV; and ivabradine (Corlanor) if the patient was in NYHA class II, III, or IV, in sinus rhythm, had a heart rate of at least 70 beats per minute, and if the patient was in a country where ivabradine was available. Because patient enrollment occurred in 2013 and 2014, the study couldn’t include the new formulation of sacubitril plus valsartan (Entresto) in its analysis.
For each eligible drug class a patient received 1 point if their daily prescribed dosage was at least 50% of the recommended dosage (or 100% for an ARA), 0.5 points if the patient received the recommended drug but at a lower dosage, and no points if the drug wasn’t given. A patient also received 1 point if they were appropriately not given a drug because of a documented contraindication or intolerance. The researchers then calculated each patient’s “adherence score” by dividing their point total by the potentially maximum number of points that each patient could have received (a number that ranged from 2 to 4). They defined a score of 1 (which meant the patients received at least half the recommended dosage of all recommended drugs) as good adherence, a score of 0.51-0.99 as moderate adherence, and a score of 0.5 or less as poor adherence.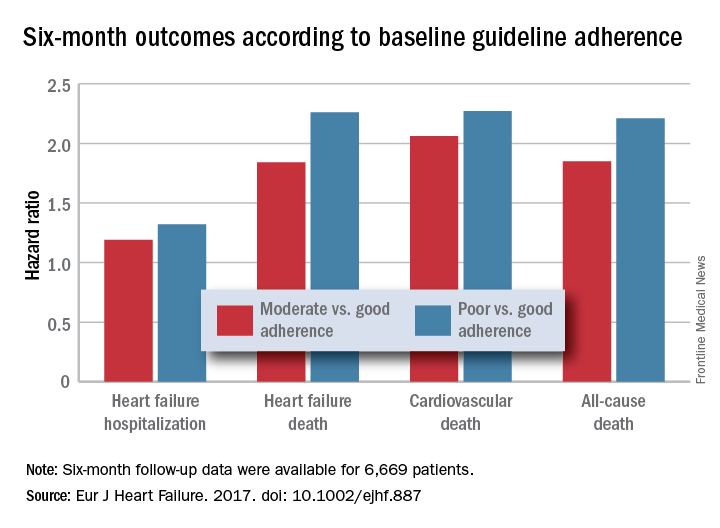
Because patient enrollment occurred during 2013 and 2014, the benchmark heart failure treatment guidelines were those issued by the European Society of Cardiology in 2012 (Eur Heart J. 2012 July;33[14]:1787-1847).
Concurrently with Dr. Komajda’s report at the meeting the results appeared in an article online (Eur J Heart Failure. 2017. doi: 10.1002/ejhf.887).
QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.
[email protected]
On Twitter @mitchelzoler
AT HEART FAILURE 2017
Key clinical point:
Major finding: Six-month all-cause, cardiovascular, and heart failure mortalities were doubled in patients not on guideline-adherent therapy and dosages.
Data source: QUANTIFY, an international registry with 6,669 HFrEF patients followed for 6 months.
Disclosures: QUANTIFY was sponsored by Servier. Dr. Komajda has received honoraria from Servier and from Amgen, AstraZeneca, Bristol-Myers Squibb, Menarini, MSD, Novartis, Novo Nordisk, and Sanofi.











