User login
Is your practice really that predictable? Nonlinearity principles in family medicine
- Heighten your awareness of nonlinear patient behaviors including sensitivity to minor changes, resistance to change, sudden dramatic change in behavior, and intermittent catastrophes.
- Nonlinearity means we should expect the unexpected but limit unpredictability through in-depth knowledge of patients and context.
- Reinforce positive attractors, use small well-timed interventions, and encourage healthy variability and nonlinearity.
Had Sir Isaac Newton attempted family medicine, he likely would have been uncomfortable with its nonlinear aspect typified by unpredictable disease courses and treatment responses.
Linearity forms the basis of our knowledge… Life in a Newtonian world is ordered and predictable, where causes are directly linked to effects and behavior is linear or cyclic (periodic). In this world, stability and predictability define a healthy system. Furthermore, by understanding the parts of a system, we understand the system. As physicians, we are trained to expect this linear, predictable, reductionistic view of health.
…but it does not reflect the human system. However, humans are complex adaptive systems, characterized by multiple interconnected and interdependent parts at levels from the microscopic to the community. Interactions change over time, producing synergistic nonlinear behavior as components periodically self-organize into functional groups.
TABLE 1 compares the Newtonian world view with that of complexity science. Although all of the characteristics of complexity science are relevant to family physicians, this article will focus on the nonlinear behavior of patients as the visible, unpredictable, and often frustrating manifestation of the complexity characteristics. TABLE 2 defines specific characteristics of nonlinearity.
In understanding nonlinearity—as depicted in 4 patient cases presented here—family physicians can learn to
- expect the unexpected
- reduce unpredictability by learning about patients and their context
- attack patient resistance by seeking epiphanies or using positive attractors
- recognize the sensitivity of our patients’ trajectories and use or anticipate it
- promote the healthy benefits of nonlinearity.
TABLE 1
Basic tenets of Newtonian and complexity world views
| CHARACTERISTIC | NEWTONIAN | COMPLEXITY |
|---|---|---|
| Cause-and-effect | Every effect has a clear cause | Events not always linked to a cause |
| Predictability | Predictable | Not predictable |
| Dynamics | Linear | Nonlinear |
| Whole vs parts | Whole equals sum of parts | Whole is not the sum of its parts |
| Adaptation to stress | Predictable, logical stress-reducing behaviors | Unpredictable, sometimes detrimental responses |
| Leveraging change | Predictable response to intervention | Multiple, well-timed interventions may be necessary |
TABLE 2
Nonlinear characteristics relevant to family practice
| CHARACTERISTIC | DEFINITION | CLINICAL EXAMPLE |
|---|---|---|
| Sensitivity to initial conditions | The phenomenon wherein a small change initially can send the system on a new trajectory, drastically changing the system’s subsequent performance | Panic attack experienced without a perceived reason can lead to agoraphobia, whereas a similar but “explainable” attack may be perceived by the patient as merely annoying |
| Attractor | Set of values to which a system migrates over time. An attractor limits the range of possible behaviors of a system and prevents random activity, but does not dictate the specific path the system follows | Self-destructive behavior—eg, alcoholism—is governed partly by a learned set of beliefs and expectations (negative attractor) that limit a person’s ability to make healthy choices. Treatment may be aided by substitution of a positive attractor—eg, well-being of family |
| Bifurcation | Sudden qualitative change in the behavior of a system as the system reaches a “tipping point” | Epiphanies, such as those realized in the decline of a relative who shares a disease, can provide leverage for change in behavior |
| Self-organized systems | System of tenuously linked parts at the edge of stability. Complex interrelationships among components produce a system in which a single event can result in a cascading effect due to the coupling of components | Detrimental self-organized behavior may manifest in a person’s over-reaction to a minor stressor. Using multiple stress reducing techniques and encouraging connectedness with others can introduce healthy, chaotic variability |
Nonlinearity as a truer model of health
Although our basic medical knowledge is built on a reductionistic approach that assumes linear dynamics, our models rarely account for more than 30% of whatever outcome we are investigating. Clinical providers are often faced with the unexpected.
Although linearity suggests that illness should respond in predictable ways regardless of the environment, family physicians know that context is critical. In addition, the human condition is often nonlinear; nonlinear dynamics (chaotic or random dynamics) have been documented in physiology,1 psychology,2,3 sociology,4 business,5-7 and economics.8
In fact, nonlinear dynamics are often a sign of health. For example, mood may vary in linear patterns among patients with affective disorders; therapy for mood disorders may work by changing the pathological linear dynamics in mood into more healthy nonlinear dynamics.9 Linear (or periodic) dynamics often indicate a pathological condition.10,11
As science and medicine begin to embrace the nonlinearity of complexity science, we must anticipate, recognize, and apply nonlinearity to the care of our patients. This is particularly important for family physicians.
Applying nonlinearity to patient cases
The following cases demonstrate characteristics of nonlinear dynamics (TABLE 2).
Case 1: Sensitivity to initial conditions
I.C. is a 25-year-old teacher who is 6 weeks postpartum. Recently, while at a local shopping mall, she experienced a sudden onset of chest discomfort, palpitations, dizziness, trembling, and a sense of impending doom. The episode peaked in intensity within 3 minutes and lasted 20 minutes after leaving the mall. Although she has not experienced another attack, she has progressively limited her activities since, until now, she has not been able to bring herself to re-enter the mall for fear of another attack. In fact, she reports intense anxiety in anticipation of possibly visiting the mall and has begun limiting her driving in general.
Agoraphobia is linked to the location and interpretation of the first panic attack.12 This demonstrates the concept of sensitivity to initial conditions whereby small differences in starting values result in very different behaviors later. In other words, apparently minor differences in a patient’s initial physical and emotional state can translate into drastically different outcomes over time.
This emphasizes the need for physicians to pay attention to detail during stressful events that patients experience. For example, if a patient experiences the first panic attack in a self-perceived “safe” environment or interprets the attack as a normal response, she may avoid the disabling consequence of agoraphobia and remain functional. There are other examples of this sensitivity to small changes, such as siblings of similar genetic make-up and environment who exhibit markedly different health as adults may do so because of “minor” life events each experienced.
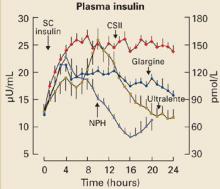
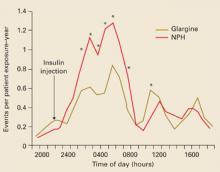
Similarly, patients with chronic stable disease who, after a minor event, suddenly change their disease trajectory may be demonstrating sensitivity to initial conditions. This sensitivity has been proposed as an explanation for sudden infant death syndrome13 (SIDS) and “brittle” diabetes.14 Treatment response may depend on sensitivity to initial conditions; cases documenting placebo effects or unpredictable potassium excretion on re-administration of potassium-sparing diuretics are examples.15
Implications for management. Sensitivity to initial conditions has several implications for patient management.
First, we need to recognize the impact it has on patients. Minor life changes can alter the trajectories of patients, so we need to seek the patient’s perspective on stressors they experience. This inherent instability means that “watchful waiting” is a viable approach in some patients because illness may resolve without intervention. It also means that we need to be watchful for signs of an unhealthy trajectory developing in patients even after minor stressors.
Second, sensitivity to initial conditions implies that nonlinear behaviors can change with minor but well-timed interventions. The importance of chronotherapy (timed dosing based on biological rhythms) is receiving increasing attention. Drug efficacy often varies with the time of day.16,17 Though focused on matching circadian rhythms, chronotherapy may be valuable in nonlinear systems if, through our in-depth knowledge of the patient and context, we can identify a point of leverage when an otherwise “ineffective” treatment may be effective for the patient at a specific point in time. There may be justification for re-administering a previously ineffective treatment if you believe the responsiveness of the patient may have changed. Sensitivity to initial conditions may also explain the effectiveness of placebos.
- For the patient above, minimizing the impact of sensitivity to initial conditions requires immediate access to the patient during a subsequent sensitive time. If the patient has a family history of panic disorder or has had panic attacks in the past, you could anticipate that the patient may experience a panic attack in the future and prepare her for it by discussing the chemical basis for panic (and its lack of serious physical consequences) and by encouraging her to contact you day-or-night immediately after experiencing one so that you can help her to identify a nonthreatening (even if illogical) cause for it, thus preventing the fears that lead to agoraphobia.
- For the practitioner, sensitivity to initial conditions emphasizes the need to understand the details surrounding a stressor by asking patients about their perceptions of the events, the circumstances, and how they are being affected by the stressor. Using this sensitivity for treatment implies focusing on the timing of interventions, and considering re-administration of treatments or even the use of placebos.
Case 2: Effects of attractors
A.T. is a 47-year-old factory worker with a 30-year history of alcohol consumption. His daily intake consisted of a case of beer until he quit 3 years ago. He has periodically suffered relapses consisting of 3 or 4 days of binge drinking followed by prolonged abstinence. Although his wife and 2 children are supportive of his efforts at abstinence, his son dramatically increased his alcohol consumption when his father stopped his daily consumption. In addition, his teenage daughter began experimenting with drugs 2 years ago.
Alcoholism serves as an attractor, controlling not only the patient’s behavior, but the behavior of the family.18 Attractors limit the range of possible behaviors and thereby resist or limit changes in a patient’s course. Attractors may be internalized models or belief systems that lead to recurring patterns of behavior, even though sensitivity to initial conditions prevents one from predicting the specific path the system will follow; patterns are predictable, the path followed is not. The combination of attractors and sensitivity to initial conditions ensures nonlinearity.
Alcoholism is not the only example of a factor that molds behavior and resists change. Our lives are governed by repeating patterns of behavior. Lifestyle routines are deeply ingrained and resist change even for medically important reasons. These lifestyle patterns may be due to attractors and may explain the resistance to change that many of our diabetic patients exhibit. Similarly, dysfunctional families often display counterproductive patterns of behavior that are resistant to even the best counseling.
Implications for management. The presence of attractors suggests several implications for patient management.
First, we should anticipate resistance and not be frustrated when it occurs.
Second, we can attack the attractor itself,19 by identifying another, more positive attractor in the patient’s life and reinforcing it to diminish the negative attractor’s impact. For example, instead of simply criticizing the inactive lifestyle ingrained in a hypercholesterolemic patient, we reinforce the positive attractor of the patient’s affection for his grandchildren and use that attractor to get the patient to exercise.
For strongly negative attractors (eg, alcohol use), we could simply attack the attractor itself without providing an alternate attractor. Though this approach is more risky because of the unpredictability of what the patient will substitute, if the attractor is bad enough, we may be willing to allow the patient to choose any other attractor, assuming that it must be more positive than the original.
- For the patient above, simply attacking the negative attractor may lead to other negative behaviors (eg, smoking). The best approach may be to focus on positive attractors (ie, wife, children, social relationships, hobbies), perhaps even positive attractors for the entire family, to move him or them away from the negative attractor.
- For the practitioner, it is imperative to identify the attractors producing recurrent detrimental behaviors that need to be changed. Using attractors for management means that potential positive attractors need to be identified through exploration with patients and reinforced while attacking the negative attractors currently producing the unhealthy behavior.
Case 3: Bifurcation effects
B.I. is a 50-year-old plumber who has had type 2 diabetes for more than 10 years. Though he has regularly seen his physician and taken his medications, his diabetes control has been poor (hemoglobin A1c=10.2). He admits that compliance with his diet and exercise has been “spotty” at best. Six months ago, his older brother began dialysis for end-stage renal disease secondary to diabetes. Within 1 week of his brother’s first dialysis session, B.I. began walking 30 minutes each night and eliminated evening snacks. Consequently, he has lost 22 pounds, and his hemoglobin A1c has dropped to 8.1.
Sudden dramatic changes (bifurcations) can occur in nonlinear systems as the system reaches a “tipping point.” In this case, chronic noncompliance suddenly changed to compliance after a meaningful event.20 These bifurcations represent a qualitative change in behavior linked to a change in an attractor. Hence, epiphanies may represent behavioral bifurcations.21 Such epiphanies are important in premature menopause22 and initial family decisions to hospitalize a mentally ill relative.23
Bifurcations have been best documented in cardiovascular disease. Pulsus paradoxicus, pulsus alternans in congestive heart failure (CHF), and cardiac movement in tamponade reflect bifurcations in the system as minor changes cause the system to cross a “tipping point” and produce sudden drastic effects.10 Similarly, bifurcations in heart rhythm are seen in sick sinus syndrome and ST-T alternans in ventricular tachycardia.24 Paradoxical behavior of the PR interval25 and the disastrous effect of the R-on-T phenomenon are other examples. However, bifurcation dynamics are also important in psychosocial behavior. Sudden drastic changes in mood have been documented in patients with generalized anxiety disorder.26
Implications for management.
- For the patient above, we can first look for events that could serve as epiphanies (eg, development of lung cancer in a relative of our tobacco-dependent patient) and use them to alter behavior. Many physicians already look for consequences of diabetes in friends and relatives to motivate their patients.
- For the practitioner, the existence of bifurcations implies that sudden unforeseen behavior should be expected and should not be a source of frustration. From a management perspective, drastic changes in patient behavior can be achieved by exploring patients’ lives and recognizing and reinforcing epiphanies.
Case 4: Self-organized behavior
S.O. is a 40-year-old housewife with a long history of intermittent anxiety, usually in response to a family stressor. She presents with extreme apprehension and insomnia. On examination, she is restless and mildly tachycardic. Upon further questioning, she denies any recent adverse events but, in fact, reports that her husband recently received a promotion including a significant increase in salary. In reviewing her chart, you notice that you have diagnosed her with adjustment disorder with anxious mood on 3 previous occasions after adverse family stressors. However, her reactions have often been out-of-proportion to the level of stress and she has occasionally reported significant stressors (eg, death of a sister) without subsequent anxiety.
Neurologic systems tend to organize themselves in response to external events and internal models. These self-organized systems consist of tenuously linked parts at the edge of stability balanced between periodic and chaotic behavior. They react to stressors in patterned ways, but the magnitude of the reaction can vary from little or no response to a catastrophic reaction. Because such self-organization can be temporary, with groups periodically forming and dissolving, behavior over time is random without recurrent patterns.
With this patient, varying degrees of stress (even positive events) result in varying degrees of dysfunction with little relationship between the magnitude of stress and the magnitude of dysfunction. The periodic collapse in response to cumulative stress is not the only example of self-organized behavior.
Self-organization is believed to be critical in a variety of neuropsychiatric conditions from personality disorders2 and conversion reactions to adult consequences of childhood adversity.27 Patterns of detoxification in groups of alcoholics demonstrate self-organized behavior.28 Self-organization is important to understanding self-regulation and behavior in families.29,30 Even social interaction patterns among groups of patients on psychiatric wards show self-organized behavior as unstable groups form, dissolve, and reform.31
Implications for management. If non-linearity indeed reflects health and helps to keep patients in good health, we should be promoting nonlinear behavior. Studies have shown that frequent small interventions can keep a system that is prone to periodic behavior in nonlinearity.32,33 Similarly, because nonlinear systems can display a spectrum of behaviors from periodic-to-self-organized behavior-to-chaotic dynamics depending upon their resources and interconnectedness, social systems exhibiting periodic behavior may move into nonlinearity in response to increased resources and decreased restraints,5 or to increased interconnectedness.34
Perhaps we can train systems to maximize their variability. For example, exercise programs that used variable intensities and durations may promote a cardiovascular system capable of responding to whatever stressor comes along.
- For the patient above, the self-organized behavior is detrimental, producing over-reaction to stressors; a more chaotic mood pattern would minimize the impact of stressors. The best approach to achieve this may be to increase resources and decrease restraints. Thus, providing the patient with several ways of dealing with stress (ie, multiple treatment modalities including relaxation techniques, self-hypnosis, meditation, PRN anxiolytics) while promoting connectedness with others (ie, support groups, internet, church contacts, meditation) may increase chaotic variability.
- For the practitioner, self-organized behavior may explain the apparent random response to stress in patients. Such unstable behavior can be managed by providing multiple interventions simultaneously (ie, behavioral, pharmacological, social) or temporally (eg, frequent reinforcements of desired behavior) to encourage healthy nonlinearity.
Nonlinearity of primary versus specialty care
Do patients in primary care exhibit a different degree of nonlinearity than those seen in specialty care settings? Generally, yes. Mental illness, for instance, tends to be more severe among psychiatric patients than among primary care patients,35-37 and CHF is more severe among cardiology patients.38
Differences in severity of illness are important because, in some cases, the more severe the illness, the more periodic the dynamics.9,39,40 Thus, the nonlinearity decreases as the severity increases. Because diseases exhibiting periodic dynamics should have a more predictable response to therapy, we would expect more severe illnesses to respond more predictably.41 This pattern has indeed been observed. Prognosis and predictability of treatment response is related to severity of illness in CHF, acute myocardial infarction, depression, and agoraphobia.38,42-47
Thus, for both biomedical and psychosocial problems, predictability of treatment response correlates with the severity of illness. If patients seen in specialty settings have more severe disease, then we should expect that primary care patients exhibit more nonlinear behavior and are thus less predictable in their response.
Learning to see differently
Though trained to approach medical problems looking through “linear lenses,” we see nonlinear behavior all the time in our patients. If nonlinear processes represent health, then when systems are using healthy, nonlinear dynamics, they are resistant to disruptive external stressors. However, when such systems transition into periodicity due to illness, they may become predictable and more amenable to intervention, permitting physicians to treat them and hopefully restore the healthy, nonlinear dynamics.
Sensitivity to minor changes in their environment, resistance to change, sudden dramatic change in behavior, and intermittent collapses characterize behaviors in many patients. If we understand the nonlinear nature of these behaviors, we will be better able to help our patients.
Expect the unexpected, reduce unpredictability by learning about patients and their contexts, attack resistance by seeking epiphanies or using positive attractors, recognize the sensitivity of our patients’ trajectories and use or anticipate it when possible, and promote the healthy benefits of nonlinearity.
CORRESPONDENCE
David A. Katerndahl, MD, MA, Department of Family and Community Medicine, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Dr. MC 7795, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Freeman W. Physiology of perception. Sci Am 1991;264:78-85.
2. Barton S. Chaos, self-organization, and psychology. Am Psychol 1994;49:5-14.
3. Guastello S. Chaos, Catastrophe, and Human Affairs. Mahwah, NJ: Erlbaum, 1995.
4. Dendrinos D, Sonis M. Chaos and Socio-Spatial Dynamics. New York: Springer Verlag, 1990.
5. Cheng Y, Van de Ven AH. Learning the innovation journey. Organization Sci 1996;7:593-614.
6. Dooley K, Johnson T, Bush D. TQM, chaos, and complexity. Hum Syst Mgmt 1995;14:1-16.
7. Dooley K. Complex adaptive systems model of organizational change. Nonlinear Dynamics, Psychology, and the Life Sciences 1997;1:69-97.
8. Arthur WB. Economy and complexity. In: Stein DL, ed. Lectures in the Sciences of Complexity. Redwood City, Calif: Addison-Wesley, 1989;713-740.
9. Gottschalk A, Bauer MS, Whybrow PC. Evidence of chaotic mood variation in bipolar disorder. Arch Gen Psychiatry 1995;52:947-959.
10. Goldberger AL. Nonlinear dynamics for clinicians. Lancet 1996;347:1312-1314.
11. Hull RL. Chronobiology and chronotherapeutics in disease states. Drug Benefit Trends 2002;14:31-42.
12. Breier A, Charney DS, Heninger GR. Agoraphobia with panic attacks. Arch Gen Psychiatry 1986;43:1029-1036.
13. Sheridan MS, Kostlany F. SIDS and chaos. Med Hypotheses 1994;42:11-12.
14. Wilson T, Holt T. Complexity and clinical care. BMJ 2001;323:685-688.
15. Rado JP. Change in antikaliuretic response to potassium-sparing diuretics in patients with cirrhotic ascites. J Am Geriatr Soc 1976;24:340-343.
16. Kraft M, Martin RJ. Chronobiology and chronotherapy in medicine. Dis Mon 1995;41:503-575.
17. Nagayama H. Influences of biological rhythms on the effects of psychotropic drugs. Psychosom Med 1999;6:618-629.
18. Pruessner HT, Hensel WA, Rasco TL. Scientific basis of generalist medicine. Acad Med 1992;67:232-235.
19. Miller WL, Crabtree BF, McDaniel R, Stange KC. Understanding change in primary care practice using complexity theory. J Fam Pract 1998;46:369-376.
20. O’Connor PJ, Crabtree BF, Yanoshik MK. Differences between diabetic patients who do and do not respond to a diabetic care intervention. Fam Med 1997;29:424-428.
21. Jarvis AN. Taking a break. Dissert Abstr Intl 1997;57(10-B):6605.-
22. Boughton MA. Premature menopause. J Adv Nurs 2002;37:423-430.
23. Forsyth DM. Families and the life transition of first time mental illness. Dissert Abstr Intl 1995;56(4-B):1935.-
24. Goldberger AL, Bhargava V, West BJ, Mandell AJ. Nonlinear dynamics of the heart beat. Physica 1985;17D:207-214.
25. Moleiro F, Misticchio F, Mendoza I, Rodriguez A, Costellanos A, Myerburg RJ. Paradoxical behavior of PR interval dynamics during exercise and recovery and its relationship to cardiac memory at the atrioventricular node. J Electrocardiol 2001;34:31-34.
26. Warren K, Sprott JC, Hawkins RC. Spirit is willing. Nonlinear Dynamics Psychol Life Sci 2002;6:55-70.
27. Weiss MJS, Wagner SH. What explains the negative consequences of adverse childhood experiences on adult health? Am J Prev Med 1998;14:356-360.
28. Campbell WG. Is self-organized criticality relevant to alcoholism? J Addict Dis 1997;16:41-50.
29. Pincus D. Framework and methodology for the study of nonlinear, self-organizing family dynamics. Nonlinear Dynamics Psychol Life Sci 2001;5:139-173.
30. Koopmans M. Chaos theory and the problem of change in family systems. Nonlinear Dynamics Psychol Life Sci 1998;2:133-148.
31. Piqueira JRC, Monteiro LHA, De Magalhaes TMC, Ramos RT, Sassi RB, Cruz EG. Zipf’s law organizes a psychiatric ward. J Theor Biol 1999;198:439-443.
32. Christini D, Collins J, Linsay P. Experimental control of high dimensional chaos. Physical Rev E Stat Nonlin Soft Matter Phys 1996;54:4824-4827.
33. Regalado A. Gentle scheme for unleashing chaos. Science 1995;268:1848.-
34. Kauffman SA. Origins Of Order. New York: Oxford University Press; 1993.
35. Klinkman MS, Schwenk TL, Coyne JC. Depression in primary care-more like asthma than appendicitis. Can J Psychiatry 1997;42:966-973.
36. Wells KB, Burnam A, Camp P. Severity of depression in prepaid and fee-for-service general medical and mental health specialty practices. Med Care 1995;33:350-364.
37. Katerndahl D, Realini JP. Patients with panic attacks seeking care from family physicians compared with those seeking care from psychiatrists. J Nerv Ment Dis 1998;186:249-250.
38. Reis SE, Holubkov R, Edmundowicz D, et al. Treatment of patients admitted to the hospital with congestive heart failure. J Am Coll Cardiol 1997;30:733-738.
39. Schulberg D, Gottlieb J. Dynamics and correlates of microscopic changes in affect. Nonlinear Dynamics Psychol Life Sci 2002;6:231-257.
40. Ehlers CL. Chaos and complexity: can it help us to understand mood and behavior? Arch Gen Psychiatry 1995;2:960-964.
41. Wilder J. Modern psychophysiology and the law of initial value. Am J Psychother 1958;12:199-221.
42. Uhlenhuth EH, Matuzas W, Warner TD, Paine S, Lydiard RB, Pollack MH. Do antidepressants selectively suppress spontaneous (unexpected) panic attacks? J Clin Psychopharmacol 2000;20:622-627.
43. Nash JS, Carrato RR, Dlutowski MJ, O’Connor JP, Nash DB. Generalist versus specialist care for acute myocardial infarction. Am J Cardiol 1999;83:650-654.
44. Chen J, Redford MJ, Wang Y, Krumholz HM. Care and outcomes of elderly patients with acute myocardial infarction by physician specialty. Am J Med 2000;108:460-469.
45. Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines. JAMA 1995;273:1026-1031.
46. Lyketsus CG, Taragano F, Triesman GJ, Paz J. Major depression and its response to sertraline in primary care versus psychiatric office practice patients. Psychosomatics 1999;40:70-75.
47. Thomas L, Mulsant BH, Solano FX, et al. Response speed and rate of remission in primary and specialty care patients with depression. Am J Geriatr Psychiatry 2002;10:583-591.
- Heighten your awareness of nonlinear patient behaviors including sensitivity to minor changes, resistance to change, sudden dramatic change in behavior, and intermittent catastrophes.
- Nonlinearity means we should expect the unexpected but limit unpredictability through in-depth knowledge of patients and context.
- Reinforce positive attractors, use small well-timed interventions, and encourage healthy variability and nonlinearity.
Had Sir Isaac Newton attempted family medicine, he likely would have been uncomfortable with its nonlinear aspect typified by unpredictable disease courses and treatment responses.
Linearity forms the basis of our knowledge… Life in a Newtonian world is ordered and predictable, where causes are directly linked to effects and behavior is linear or cyclic (periodic). In this world, stability and predictability define a healthy system. Furthermore, by understanding the parts of a system, we understand the system. As physicians, we are trained to expect this linear, predictable, reductionistic view of health.
…but it does not reflect the human system. However, humans are complex adaptive systems, characterized by multiple interconnected and interdependent parts at levels from the microscopic to the community. Interactions change over time, producing synergistic nonlinear behavior as components periodically self-organize into functional groups.
TABLE 1 compares the Newtonian world view with that of complexity science. Although all of the characteristics of complexity science are relevant to family physicians, this article will focus on the nonlinear behavior of patients as the visible, unpredictable, and often frustrating manifestation of the complexity characteristics. TABLE 2 defines specific characteristics of nonlinearity.
In understanding nonlinearity—as depicted in 4 patient cases presented here—family physicians can learn to
- expect the unexpected
- reduce unpredictability by learning about patients and their context
- attack patient resistance by seeking epiphanies or using positive attractors
- recognize the sensitivity of our patients’ trajectories and use or anticipate it
- promote the healthy benefits of nonlinearity.
TABLE 1
Basic tenets of Newtonian and complexity world views
| CHARACTERISTIC | NEWTONIAN | COMPLEXITY |
|---|---|---|
| Cause-and-effect | Every effect has a clear cause | Events not always linked to a cause |
| Predictability | Predictable | Not predictable |
| Dynamics | Linear | Nonlinear |
| Whole vs parts | Whole equals sum of parts | Whole is not the sum of its parts |
| Adaptation to stress | Predictable, logical stress-reducing behaviors | Unpredictable, sometimes detrimental responses |
| Leveraging change | Predictable response to intervention | Multiple, well-timed interventions may be necessary |
TABLE 2
Nonlinear characteristics relevant to family practice
| CHARACTERISTIC | DEFINITION | CLINICAL EXAMPLE |
|---|---|---|
| Sensitivity to initial conditions | The phenomenon wherein a small change initially can send the system on a new trajectory, drastically changing the system’s subsequent performance | Panic attack experienced without a perceived reason can lead to agoraphobia, whereas a similar but “explainable” attack may be perceived by the patient as merely annoying |
| Attractor | Set of values to which a system migrates over time. An attractor limits the range of possible behaviors of a system and prevents random activity, but does not dictate the specific path the system follows | Self-destructive behavior—eg, alcoholism—is governed partly by a learned set of beliefs and expectations (negative attractor) that limit a person’s ability to make healthy choices. Treatment may be aided by substitution of a positive attractor—eg, well-being of family |
| Bifurcation | Sudden qualitative change in the behavior of a system as the system reaches a “tipping point” | Epiphanies, such as those realized in the decline of a relative who shares a disease, can provide leverage for change in behavior |
| Self-organized systems | System of tenuously linked parts at the edge of stability. Complex interrelationships among components produce a system in which a single event can result in a cascading effect due to the coupling of components | Detrimental self-organized behavior may manifest in a person’s over-reaction to a minor stressor. Using multiple stress reducing techniques and encouraging connectedness with others can introduce healthy, chaotic variability |
Nonlinearity as a truer model of health
Although our basic medical knowledge is built on a reductionistic approach that assumes linear dynamics, our models rarely account for more than 30% of whatever outcome we are investigating. Clinical providers are often faced with the unexpected.
Although linearity suggests that illness should respond in predictable ways regardless of the environment, family physicians know that context is critical. In addition, the human condition is often nonlinear; nonlinear dynamics (chaotic or random dynamics) have been documented in physiology,1 psychology,2,3 sociology,4 business,5-7 and economics.8
In fact, nonlinear dynamics are often a sign of health. For example, mood may vary in linear patterns among patients with affective disorders; therapy for mood disorders may work by changing the pathological linear dynamics in mood into more healthy nonlinear dynamics.9 Linear (or periodic) dynamics often indicate a pathological condition.10,11
As science and medicine begin to embrace the nonlinearity of complexity science, we must anticipate, recognize, and apply nonlinearity to the care of our patients. This is particularly important for family physicians.
Applying nonlinearity to patient cases
The following cases demonstrate characteristics of nonlinear dynamics (TABLE 2).
Case 1: Sensitivity to initial conditions
I.C. is a 25-year-old teacher who is 6 weeks postpartum. Recently, while at a local shopping mall, she experienced a sudden onset of chest discomfort, palpitations, dizziness, trembling, and a sense of impending doom. The episode peaked in intensity within 3 minutes and lasted 20 minutes after leaving the mall. Although she has not experienced another attack, she has progressively limited her activities since, until now, she has not been able to bring herself to re-enter the mall for fear of another attack. In fact, she reports intense anxiety in anticipation of possibly visiting the mall and has begun limiting her driving in general.
Agoraphobia is linked to the location and interpretation of the first panic attack.12 This demonstrates the concept of sensitivity to initial conditions whereby small differences in starting values result in very different behaviors later. In other words, apparently minor differences in a patient’s initial physical and emotional state can translate into drastically different outcomes over time.
This emphasizes the need for physicians to pay attention to detail during stressful events that patients experience. For example, if a patient experiences the first panic attack in a self-perceived “safe” environment or interprets the attack as a normal response, she may avoid the disabling consequence of agoraphobia and remain functional. There are other examples of this sensitivity to small changes, such as siblings of similar genetic make-up and environment who exhibit markedly different health as adults may do so because of “minor” life events each experienced.
Similarly, patients with chronic stable disease who, after a minor event, suddenly change their disease trajectory may be demonstrating sensitivity to initial conditions. This sensitivity has been proposed as an explanation for sudden infant death syndrome13 (SIDS) and “brittle” diabetes.14 Treatment response may depend on sensitivity to initial conditions; cases documenting placebo effects or unpredictable potassium excretion on re-administration of potassium-sparing diuretics are examples.15
Implications for management. Sensitivity to initial conditions has several implications for patient management.
First, we need to recognize the impact it has on patients. Minor life changes can alter the trajectories of patients, so we need to seek the patient’s perspective on stressors they experience. This inherent instability means that “watchful waiting” is a viable approach in some patients because illness may resolve without intervention. It also means that we need to be watchful for signs of an unhealthy trajectory developing in patients even after minor stressors.
Second, sensitivity to initial conditions implies that nonlinear behaviors can change with minor but well-timed interventions. The importance of chronotherapy (timed dosing based on biological rhythms) is receiving increasing attention. Drug efficacy often varies with the time of day.16,17 Though focused on matching circadian rhythms, chronotherapy may be valuable in nonlinear systems if, through our in-depth knowledge of the patient and context, we can identify a point of leverage when an otherwise “ineffective” treatment may be effective for the patient at a specific point in time. There may be justification for re-administering a previously ineffective treatment if you believe the responsiveness of the patient may have changed. Sensitivity to initial conditions may also explain the effectiveness of placebos.
- For the patient above, minimizing the impact of sensitivity to initial conditions requires immediate access to the patient during a subsequent sensitive time. If the patient has a family history of panic disorder or has had panic attacks in the past, you could anticipate that the patient may experience a panic attack in the future and prepare her for it by discussing the chemical basis for panic (and its lack of serious physical consequences) and by encouraging her to contact you day-or-night immediately after experiencing one so that you can help her to identify a nonthreatening (even if illogical) cause for it, thus preventing the fears that lead to agoraphobia.
- For the practitioner, sensitivity to initial conditions emphasizes the need to understand the details surrounding a stressor by asking patients about their perceptions of the events, the circumstances, and how they are being affected by the stressor. Using this sensitivity for treatment implies focusing on the timing of interventions, and considering re-administration of treatments or even the use of placebos.
Case 2: Effects of attractors
A.T. is a 47-year-old factory worker with a 30-year history of alcohol consumption. His daily intake consisted of a case of beer until he quit 3 years ago. He has periodically suffered relapses consisting of 3 or 4 days of binge drinking followed by prolonged abstinence. Although his wife and 2 children are supportive of his efforts at abstinence, his son dramatically increased his alcohol consumption when his father stopped his daily consumption. In addition, his teenage daughter began experimenting with drugs 2 years ago.
Alcoholism serves as an attractor, controlling not only the patient’s behavior, but the behavior of the family.18 Attractors limit the range of possible behaviors and thereby resist or limit changes in a patient’s course. Attractors may be internalized models or belief systems that lead to recurring patterns of behavior, even though sensitivity to initial conditions prevents one from predicting the specific path the system will follow; patterns are predictable, the path followed is not. The combination of attractors and sensitivity to initial conditions ensures nonlinearity.
Alcoholism is not the only example of a factor that molds behavior and resists change. Our lives are governed by repeating patterns of behavior. Lifestyle routines are deeply ingrained and resist change even for medically important reasons. These lifestyle patterns may be due to attractors and may explain the resistance to change that many of our diabetic patients exhibit. Similarly, dysfunctional families often display counterproductive patterns of behavior that are resistant to even the best counseling.
Implications for management. The presence of attractors suggests several implications for patient management.
First, we should anticipate resistance and not be frustrated when it occurs.
Second, we can attack the attractor itself,19 by identifying another, more positive attractor in the patient’s life and reinforcing it to diminish the negative attractor’s impact. For example, instead of simply criticizing the inactive lifestyle ingrained in a hypercholesterolemic patient, we reinforce the positive attractor of the patient’s affection for his grandchildren and use that attractor to get the patient to exercise.
For strongly negative attractors (eg, alcohol use), we could simply attack the attractor itself without providing an alternate attractor. Though this approach is more risky because of the unpredictability of what the patient will substitute, if the attractor is bad enough, we may be willing to allow the patient to choose any other attractor, assuming that it must be more positive than the original.
- For the patient above, simply attacking the negative attractor may lead to other negative behaviors (eg, smoking). The best approach may be to focus on positive attractors (ie, wife, children, social relationships, hobbies), perhaps even positive attractors for the entire family, to move him or them away from the negative attractor.
- For the practitioner, it is imperative to identify the attractors producing recurrent detrimental behaviors that need to be changed. Using attractors for management means that potential positive attractors need to be identified through exploration with patients and reinforced while attacking the negative attractors currently producing the unhealthy behavior.
Case 3: Bifurcation effects
B.I. is a 50-year-old plumber who has had type 2 diabetes for more than 10 years. Though he has regularly seen his physician and taken his medications, his diabetes control has been poor (hemoglobin A1c=10.2). He admits that compliance with his diet and exercise has been “spotty” at best. Six months ago, his older brother began dialysis for end-stage renal disease secondary to diabetes. Within 1 week of his brother’s first dialysis session, B.I. began walking 30 minutes each night and eliminated evening snacks. Consequently, he has lost 22 pounds, and his hemoglobin A1c has dropped to 8.1.
Sudden dramatic changes (bifurcations) can occur in nonlinear systems as the system reaches a “tipping point.” In this case, chronic noncompliance suddenly changed to compliance after a meaningful event.20 These bifurcations represent a qualitative change in behavior linked to a change in an attractor. Hence, epiphanies may represent behavioral bifurcations.21 Such epiphanies are important in premature menopause22 and initial family decisions to hospitalize a mentally ill relative.23
Bifurcations have been best documented in cardiovascular disease. Pulsus paradoxicus, pulsus alternans in congestive heart failure (CHF), and cardiac movement in tamponade reflect bifurcations in the system as minor changes cause the system to cross a “tipping point” and produce sudden drastic effects.10 Similarly, bifurcations in heart rhythm are seen in sick sinus syndrome and ST-T alternans in ventricular tachycardia.24 Paradoxical behavior of the PR interval25 and the disastrous effect of the R-on-T phenomenon are other examples. However, bifurcation dynamics are also important in psychosocial behavior. Sudden drastic changes in mood have been documented in patients with generalized anxiety disorder.26
Implications for management.
- For the patient above, we can first look for events that could serve as epiphanies (eg, development of lung cancer in a relative of our tobacco-dependent patient) and use them to alter behavior. Many physicians already look for consequences of diabetes in friends and relatives to motivate their patients.
- For the practitioner, the existence of bifurcations implies that sudden unforeseen behavior should be expected and should not be a source of frustration. From a management perspective, drastic changes in patient behavior can be achieved by exploring patients’ lives and recognizing and reinforcing epiphanies.
Case 4: Self-organized behavior
S.O. is a 40-year-old housewife with a long history of intermittent anxiety, usually in response to a family stressor. She presents with extreme apprehension and insomnia. On examination, she is restless and mildly tachycardic. Upon further questioning, she denies any recent adverse events but, in fact, reports that her husband recently received a promotion including a significant increase in salary. In reviewing her chart, you notice that you have diagnosed her with adjustment disorder with anxious mood on 3 previous occasions after adverse family stressors. However, her reactions have often been out-of-proportion to the level of stress and she has occasionally reported significant stressors (eg, death of a sister) without subsequent anxiety.
Neurologic systems tend to organize themselves in response to external events and internal models. These self-organized systems consist of tenuously linked parts at the edge of stability balanced between periodic and chaotic behavior. They react to stressors in patterned ways, but the magnitude of the reaction can vary from little or no response to a catastrophic reaction. Because such self-organization can be temporary, with groups periodically forming and dissolving, behavior over time is random without recurrent patterns.
With this patient, varying degrees of stress (even positive events) result in varying degrees of dysfunction with little relationship between the magnitude of stress and the magnitude of dysfunction. The periodic collapse in response to cumulative stress is not the only example of self-organized behavior.
Self-organization is believed to be critical in a variety of neuropsychiatric conditions from personality disorders2 and conversion reactions to adult consequences of childhood adversity.27 Patterns of detoxification in groups of alcoholics demonstrate self-organized behavior.28 Self-organization is important to understanding self-regulation and behavior in families.29,30 Even social interaction patterns among groups of patients on psychiatric wards show self-organized behavior as unstable groups form, dissolve, and reform.31
Implications for management. If non-linearity indeed reflects health and helps to keep patients in good health, we should be promoting nonlinear behavior. Studies have shown that frequent small interventions can keep a system that is prone to periodic behavior in nonlinearity.32,33 Similarly, because nonlinear systems can display a spectrum of behaviors from periodic-to-self-organized behavior-to-chaotic dynamics depending upon their resources and interconnectedness, social systems exhibiting periodic behavior may move into nonlinearity in response to increased resources and decreased restraints,5 or to increased interconnectedness.34
Perhaps we can train systems to maximize their variability. For example, exercise programs that used variable intensities and durations may promote a cardiovascular system capable of responding to whatever stressor comes along.
- For the patient above, the self-organized behavior is detrimental, producing over-reaction to stressors; a more chaotic mood pattern would minimize the impact of stressors. The best approach to achieve this may be to increase resources and decrease restraints. Thus, providing the patient with several ways of dealing with stress (ie, multiple treatment modalities including relaxation techniques, self-hypnosis, meditation, PRN anxiolytics) while promoting connectedness with others (ie, support groups, internet, church contacts, meditation) may increase chaotic variability.
- For the practitioner, self-organized behavior may explain the apparent random response to stress in patients. Such unstable behavior can be managed by providing multiple interventions simultaneously (ie, behavioral, pharmacological, social) or temporally (eg, frequent reinforcements of desired behavior) to encourage healthy nonlinearity.
Nonlinearity of primary versus specialty care
Do patients in primary care exhibit a different degree of nonlinearity than those seen in specialty care settings? Generally, yes. Mental illness, for instance, tends to be more severe among psychiatric patients than among primary care patients,35-37 and CHF is more severe among cardiology patients.38
Differences in severity of illness are important because, in some cases, the more severe the illness, the more periodic the dynamics.9,39,40 Thus, the nonlinearity decreases as the severity increases. Because diseases exhibiting periodic dynamics should have a more predictable response to therapy, we would expect more severe illnesses to respond more predictably.41 This pattern has indeed been observed. Prognosis and predictability of treatment response is related to severity of illness in CHF, acute myocardial infarction, depression, and agoraphobia.38,42-47
Thus, for both biomedical and psychosocial problems, predictability of treatment response correlates with the severity of illness. If patients seen in specialty settings have more severe disease, then we should expect that primary care patients exhibit more nonlinear behavior and are thus less predictable in their response.
Learning to see differently
Though trained to approach medical problems looking through “linear lenses,” we see nonlinear behavior all the time in our patients. If nonlinear processes represent health, then when systems are using healthy, nonlinear dynamics, they are resistant to disruptive external stressors. However, when such systems transition into periodicity due to illness, they may become predictable and more amenable to intervention, permitting physicians to treat them and hopefully restore the healthy, nonlinear dynamics.
Sensitivity to minor changes in their environment, resistance to change, sudden dramatic change in behavior, and intermittent collapses characterize behaviors in many patients. If we understand the nonlinear nature of these behaviors, we will be better able to help our patients.
Expect the unexpected, reduce unpredictability by learning about patients and their contexts, attack resistance by seeking epiphanies or using positive attractors, recognize the sensitivity of our patients’ trajectories and use or anticipate it when possible, and promote the healthy benefits of nonlinearity.
CORRESPONDENCE
David A. Katerndahl, MD, MA, Department of Family and Community Medicine, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Dr. MC 7795, San Antonio, TX 78229-3900. E-mail: [email protected].
- Heighten your awareness of nonlinear patient behaviors including sensitivity to minor changes, resistance to change, sudden dramatic change in behavior, and intermittent catastrophes.
- Nonlinearity means we should expect the unexpected but limit unpredictability through in-depth knowledge of patients and context.
- Reinforce positive attractors, use small well-timed interventions, and encourage healthy variability and nonlinearity.
Had Sir Isaac Newton attempted family medicine, he likely would have been uncomfortable with its nonlinear aspect typified by unpredictable disease courses and treatment responses.
Linearity forms the basis of our knowledge… Life in a Newtonian world is ordered and predictable, where causes are directly linked to effects and behavior is linear or cyclic (periodic). In this world, stability and predictability define a healthy system. Furthermore, by understanding the parts of a system, we understand the system. As physicians, we are trained to expect this linear, predictable, reductionistic view of health.
…but it does not reflect the human system. However, humans are complex adaptive systems, characterized by multiple interconnected and interdependent parts at levels from the microscopic to the community. Interactions change over time, producing synergistic nonlinear behavior as components periodically self-organize into functional groups.
TABLE 1 compares the Newtonian world view with that of complexity science. Although all of the characteristics of complexity science are relevant to family physicians, this article will focus on the nonlinear behavior of patients as the visible, unpredictable, and often frustrating manifestation of the complexity characteristics. TABLE 2 defines specific characteristics of nonlinearity.
In understanding nonlinearity—as depicted in 4 patient cases presented here—family physicians can learn to
- expect the unexpected
- reduce unpredictability by learning about patients and their context
- attack patient resistance by seeking epiphanies or using positive attractors
- recognize the sensitivity of our patients’ trajectories and use or anticipate it
- promote the healthy benefits of nonlinearity.
TABLE 1
Basic tenets of Newtonian and complexity world views
| CHARACTERISTIC | NEWTONIAN | COMPLEXITY |
|---|---|---|
| Cause-and-effect | Every effect has a clear cause | Events not always linked to a cause |
| Predictability | Predictable | Not predictable |
| Dynamics | Linear | Nonlinear |
| Whole vs parts | Whole equals sum of parts | Whole is not the sum of its parts |
| Adaptation to stress | Predictable, logical stress-reducing behaviors | Unpredictable, sometimes detrimental responses |
| Leveraging change | Predictable response to intervention | Multiple, well-timed interventions may be necessary |
TABLE 2
Nonlinear characteristics relevant to family practice
| CHARACTERISTIC | DEFINITION | CLINICAL EXAMPLE |
|---|---|---|
| Sensitivity to initial conditions | The phenomenon wherein a small change initially can send the system on a new trajectory, drastically changing the system’s subsequent performance | Panic attack experienced without a perceived reason can lead to agoraphobia, whereas a similar but “explainable” attack may be perceived by the patient as merely annoying |
| Attractor | Set of values to which a system migrates over time. An attractor limits the range of possible behaviors of a system and prevents random activity, but does not dictate the specific path the system follows | Self-destructive behavior—eg, alcoholism—is governed partly by a learned set of beliefs and expectations (negative attractor) that limit a person’s ability to make healthy choices. Treatment may be aided by substitution of a positive attractor—eg, well-being of family |
| Bifurcation | Sudden qualitative change in the behavior of a system as the system reaches a “tipping point” | Epiphanies, such as those realized in the decline of a relative who shares a disease, can provide leverage for change in behavior |
| Self-organized systems | System of tenuously linked parts at the edge of stability. Complex interrelationships among components produce a system in which a single event can result in a cascading effect due to the coupling of components | Detrimental self-organized behavior may manifest in a person’s over-reaction to a minor stressor. Using multiple stress reducing techniques and encouraging connectedness with others can introduce healthy, chaotic variability |
Nonlinearity as a truer model of health
Although our basic medical knowledge is built on a reductionistic approach that assumes linear dynamics, our models rarely account for more than 30% of whatever outcome we are investigating. Clinical providers are often faced with the unexpected.
Although linearity suggests that illness should respond in predictable ways regardless of the environment, family physicians know that context is critical. In addition, the human condition is often nonlinear; nonlinear dynamics (chaotic or random dynamics) have been documented in physiology,1 psychology,2,3 sociology,4 business,5-7 and economics.8
In fact, nonlinear dynamics are often a sign of health. For example, mood may vary in linear patterns among patients with affective disorders; therapy for mood disorders may work by changing the pathological linear dynamics in mood into more healthy nonlinear dynamics.9 Linear (or periodic) dynamics often indicate a pathological condition.10,11
As science and medicine begin to embrace the nonlinearity of complexity science, we must anticipate, recognize, and apply nonlinearity to the care of our patients. This is particularly important for family physicians.
Applying nonlinearity to patient cases
The following cases demonstrate characteristics of nonlinear dynamics (TABLE 2).
Case 1: Sensitivity to initial conditions
I.C. is a 25-year-old teacher who is 6 weeks postpartum. Recently, while at a local shopping mall, she experienced a sudden onset of chest discomfort, palpitations, dizziness, trembling, and a sense of impending doom. The episode peaked in intensity within 3 minutes and lasted 20 minutes after leaving the mall. Although she has not experienced another attack, she has progressively limited her activities since, until now, she has not been able to bring herself to re-enter the mall for fear of another attack. In fact, she reports intense anxiety in anticipation of possibly visiting the mall and has begun limiting her driving in general.
Agoraphobia is linked to the location and interpretation of the first panic attack.12 This demonstrates the concept of sensitivity to initial conditions whereby small differences in starting values result in very different behaviors later. In other words, apparently minor differences in a patient’s initial physical and emotional state can translate into drastically different outcomes over time.
This emphasizes the need for physicians to pay attention to detail during stressful events that patients experience. For example, if a patient experiences the first panic attack in a self-perceived “safe” environment or interprets the attack as a normal response, she may avoid the disabling consequence of agoraphobia and remain functional. There are other examples of this sensitivity to small changes, such as siblings of similar genetic make-up and environment who exhibit markedly different health as adults may do so because of “minor” life events each experienced.
Similarly, patients with chronic stable disease who, after a minor event, suddenly change their disease trajectory may be demonstrating sensitivity to initial conditions. This sensitivity has been proposed as an explanation for sudden infant death syndrome13 (SIDS) and “brittle” diabetes.14 Treatment response may depend on sensitivity to initial conditions; cases documenting placebo effects or unpredictable potassium excretion on re-administration of potassium-sparing diuretics are examples.15
Implications for management. Sensitivity to initial conditions has several implications for patient management.
First, we need to recognize the impact it has on patients. Minor life changes can alter the trajectories of patients, so we need to seek the patient’s perspective on stressors they experience. This inherent instability means that “watchful waiting” is a viable approach in some patients because illness may resolve without intervention. It also means that we need to be watchful for signs of an unhealthy trajectory developing in patients even after minor stressors.
Second, sensitivity to initial conditions implies that nonlinear behaviors can change with minor but well-timed interventions. The importance of chronotherapy (timed dosing based on biological rhythms) is receiving increasing attention. Drug efficacy often varies with the time of day.16,17 Though focused on matching circadian rhythms, chronotherapy may be valuable in nonlinear systems if, through our in-depth knowledge of the patient and context, we can identify a point of leverage when an otherwise “ineffective” treatment may be effective for the patient at a specific point in time. There may be justification for re-administering a previously ineffective treatment if you believe the responsiveness of the patient may have changed. Sensitivity to initial conditions may also explain the effectiveness of placebos.
- For the patient above, minimizing the impact of sensitivity to initial conditions requires immediate access to the patient during a subsequent sensitive time. If the patient has a family history of panic disorder or has had panic attacks in the past, you could anticipate that the patient may experience a panic attack in the future and prepare her for it by discussing the chemical basis for panic (and its lack of serious physical consequences) and by encouraging her to contact you day-or-night immediately after experiencing one so that you can help her to identify a nonthreatening (even if illogical) cause for it, thus preventing the fears that lead to agoraphobia.
- For the practitioner, sensitivity to initial conditions emphasizes the need to understand the details surrounding a stressor by asking patients about their perceptions of the events, the circumstances, and how they are being affected by the stressor. Using this sensitivity for treatment implies focusing on the timing of interventions, and considering re-administration of treatments or even the use of placebos.
Case 2: Effects of attractors
A.T. is a 47-year-old factory worker with a 30-year history of alcohol consumption. His daily intake consisted of a case of beer until he quit 3 years ago. He has periodically suffered relapses consisting of 3 or 4 days of binge drinking followed by prolonged abstinence. Although his wife and 2 children are supportive of his efforts at abstinence, his son dramatically increased his alcohol consumption when his father stopped his daily consumption. In addition, his teenage daughter began experimenting with drugs 2 years ago.
Alcoholism serves as an attractor, controlling not only the patient’s behavior, but the behavior of the family.18 Attractors limit the range of possible behaviors and thereby resist or limit changes in a patient’s course. Attractors may be internalized models or belief systems that lead to recurring patterns of behavior, even though sensitivity to initial conditions prevents one from predicting the specific path the system will follow; patterns are predictable, the path followed is not. The combination of attractors and sensitivity to initial conditions ensures nonlinearity.
Alcoholism is not the only example of a factor that molds behavior and resists change. Our lives are governed by repeating patterns of behavior. Lifestyle routines are deeply ingrained and resist change even for medically important reasons. These lifestyle patterns may be due to attractors and may explain the resistance to change that many of our diabetic patients exhibit. Similarly, dysfunctional families often display counterproductive patterns of behavior that are resistant to even the best counseling.
Implications for management. The presence of attractors suggests several implications for patient management.
First, we should anticipate resistance and not be frustrated when it occurs.
Second, we can attack the attractor itself,19 by identifying another, more positive attractor in the patient’s life and reinforcing it to diminish the negative attractor’s impact. For example, instead of simply criticizing the inactive lifestyle ingrained in a hypercholesterolemic patient, we reinforce the positive attractor of the patient’s affection for his grandchildren and use that attractor to get the patient to exercise.
For strongly negative attractors (eg, alcohol use), we could simply attack the attractor itself without providing an alternate attractor. Though this approach is more risky because of the unpredictability of what the patient will substitute, if the attractor is bad enough, we may be willing to allow the patient to choose any other attractor, assuming that it must be more positive than the original.
- For the patient above, simply attacking the negative attractor may lead to other negative behaviors (eg, smoking). The best approach may be to focus on positive attractors (ie, wife, children, social relationships, hobbies), perhaps even positive attractors for the entire family, to move him or them away from the negative attractor.
- For the practitioner, it is imperative to identify the attractors producing recurrent detrimental behaviors that need to be changed. Using attractors for management means that potential positive attractors need to be identified through exploration with patients and reinforced while attacking the negative attractors currently producing the unhealthy behavior.
Case 3: Bifurcation effects
B.I. is a 50-year-old plumber who has had type 2 diabetes for more than 10 years. Though he has regularly seen his physician and taken his medications, his diabetes control has been poor (hemoglobin A1c=10.2). He admits that compliance with his diet and exercise has been “spotty” at best. Six months ago, his older brother began dialysis for end-stage renal disease secondary to diabetes. Within 1 week of his brother’s first dialysis session, B.I. began walking 30 minutes each night and eliminated evening snacks. Consequently, he has lost 22 pounds, and his hemoglobin A1c has dropped to 8.1.
Sudden dramatic changes (bifurcations) can occur in nonlinear systems as the system reaches a “tipping point.” In this case, chronic noncompliance suddenly changed to compliance after a meaningful event.20 These bifurcations represent a qualitative change in behavior linked to a change in an attractor. Hence, epiphanies may represent behavioral bifurcations.21 Such epiphanies are important in premature menopause22 and initial family decisions to hospitalize a mentally ill relative.23
Bifurcations have been best documented in cardiovascular disease. Pulsus paradoxicus, pulsus alternans in congestive heart failure (CHF), and cardiac movement in tamponade reflect bifurcations in the system as minor changes cause the system to cross a “tipping point” and produce sudden drastic effects.10 Similarly, bifurcations in heart rhythm are seen in sick sinus syndrome and ST-T alternans in ventricular tachycardia.24 Paradoxical behavior of the PR interval25 and the disastrous effect of the R-on-T phenomenon are other examples. However, bifurcation dynamics are also important in psychosocial behavior. Sudden drastic changes in mood have been documented in patients with generalized anxiety disorder.26
Implications for management.
- For the patient above, we can first look for events that could serve as epiphanies (eg, development of lung cancer in a relative of our tobacco-dependent patient) and use them to alter behavior. Many physicians already look for consequences of diabetes in friends and relatives to motivate their patients.
- For the practitioner, the existence of bifurcations implies that sudden unforeseen behavior should be expected and should not be a source of frustration. From a management perspective, drastic changes in patient behavior can be achieved by exploring patients’ lives and recognizing and reinforcing epiphanies.
Case 4: Self-organized behavior
S.O. is a 40-year-old housewife with a long history of intermittent anxiety, usually in response to a family stressor. She presents with extreme apprehension and insomnia. On examination, she is restless and mildly tachycardic. Upon further questioning, she denies any recent adverse events but, in fact, reports that her husband recently received a promotion including a significant increase in salary. In reviewing her chart, you notice that you have diagnosed her with adjustment disorder with anxious mood on 3 previous occasions after adverse family stressors. However, her reactions have often been out-of-proportion to the level of stress and she has occasionally reported significant stressors (eg, death of a sister) without subsequent anxiety.
Neurologic systems tend to organize themselves in response to external events and internal models. These self-organized systems consist of tenuously linked parts at the edge of stability balanced between periodic and chaotic behavior. They react to stressors in patterned ways, but the magnitude of the reaction can vary from little or no response to a catastrophic reaction. Because such self-organization can be temporary, with groups periodically forming and dissolving, behavior over time is random without recurrent patterns.
With this patient, varying degrees of stress (even positive events) result in varying degrees of dysfunction with little relationship between the magnitude of stress and the magnitude of dysfunction. The periodic collapse in response to cumulative stress is not the only example of self-organized behavior.
Self-organization is believed to be critical in a variety of neuropsychiatric conditions from personality disorders2 and conversion reactions to adult consequences of childhood adversity.27 Patterns of detoxification in groups of alcoholics demonstrate self-organized behavior.28 Self-organization is important to understanding self-regulation and behavior in families.29,30 Even social interaction patterns among groups of patients on psychiatric wards show self-organized behavior as unstable groups form, dissolve, and reform.31
Implications for management. If non-linearity indeed reflects health and helps to keep patients in good health, we should be promoting nonlinear behavior. Studies have shown that frequent small interventions can keep a system that is prone to periodic behavior in nonlinearity.32,33 Similarly, because nonlinear systems can display a spectrum of behaviors from periodic-to-self-organized behavior-to-chaotic dynamics depending upon their resources and interconnectedness, social systems exhibiting periodic behavior may move into nonlinearity in response to increased resources and decreased restraints,5 or to increased interconnectedness.34
Perhaps we can train systems to maximize their variability. For example, exercise programs that used variable intensities and durations may promote a cardiovascular system capable of responding to whatever stressor comes along.
- For the patient above, the self-organized behavior is detrimental, producing over-reaction to stressors; a more chaotic mood pattern would minimize the impact of stressors. The best approach to achieve this may be to increase resources and decrease restraints. Thus, providing the patient with several ways of dealing with stress (ie, multiple treatment modalities including relaxation techniques, self-hypnosis, meditation, PRN anxiolytics) while promoting connectedness with others (ie, support groups, internet, church contacts, meditation) may increase chaotic variability.
- For the practitioner, self-organized behavior may explain the apparent random response to stress in patients. Such unstable behavior can be managed by providing multiple interventions simultaneously (ie, behavioral, pharmacological, social) or temporally (eg, frequent reinforcements of desired behavior) to encourage healthy nonlinearity.
Nonlinearity of primary versus specialty care
Do patients in primary care exhibit a different degree of nonlinearity than those seen in specialty care settings? Generally, yes. Mental illness, for instance, tends to be more severe among psychiatric patients than among primary care patients,35-37 and CHF is more severe among cardiology patients.38
Differences in severity of illness are important because, in some cases, the more severe the illness, the more periodic the dynamics.9,39,40 Thus, the nonlinearity decreases as the severity increases. Because diseases exhibiting periodic dynamics should have a more predictable response to therapy, we would expect more severe illnesses to respond more predictably.41 This pattern has indeed been observed. Prognosis and predictability of treatment response is related to severity of illness in CHF, acute myocardial infarction, depression, and agoraphobia.38,42-47
Thus, for both biomedical and psychosocial problems, predictability of treatment response correlates with the severity of illness. If patients seen in specialty settings have more severe disease, then we should expect that primary care patients exhibit more nonlinear behavior and are thus less predictable in their response.
Learning to see differently
Though trained to approach medical problems looking through “linear lenses,” we see nonlinear behavior all the time in our patients. If nonlinear processes represent health, then when systems are using healthy, nonlinear dynamics, they are resistant to disruptive external stressors. However, when such systems transition into periodicity due to illness, they may become predictable and more amenable to intervention, permitting physicians to treat them and hopefully restore the healthy, nonlinear dynamics.
Sensitivity to minor changes in their environment, resistance to change, sudden dramatic change in behavior, and intermittent collapses characterize behaviors in many patients. If we understand the nonlinear nature of these behaviors, we will be better able to help our patients.
Expect the unexpected, reduce unpredictability by learning about patients and their contexts, attack resistance by seeking epiphanies or using positive attractors, recognize the sensitivity of our patients’ trajectories and use or anticipate it when possible, and promote the healthy benefits of nonlinearity.
CORRESPONDENCE
David A. Katerndahl, MD, MA, Department of Family and Community Medicine, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Dr. MC 7795, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Freeman W. Physiology of perception. Sci Am 1991;264:78-85.
2. Barton S. Chaos, self-organization, and psychology. Am Psychol 1994;49:5-14.
3. Guastello S. Chaos, Catastrophe, and Human Affairs. Mahwah, NJ: Erlbaum, 1995.
4. Dendrinos D, Sonis M. Chaos and Socio-Spatial Dynamics. New York: Springer Verlag, 1990.
5. Cheng Y, Van de Ven AH. Learning the innovation journey. Organization Sci 1996;7:593-614.
6. Dooley K, Johnson T, Bush D. TQM, chaos, and complexity. Hum Syst Mgmt 1995;14:1-16.
7. Dooley K. Complex adaptive systems model of organizational change. Nonlinear Dynamics, Psychology, and the Life Sciences 1997;1:69-97.
8. Arthur WB. Economy and complexity. In: Stein DL, ed. Lectures in the Sciences of Complexity. Redwood City, Calif: Addison-Wesley, 1989;713-740.
9. Gottschalk A, Bauer MS, Whybrow PC. Evidence of chaotic mood variation in bipolar disorder. Arch Gen Psychiatry 1995;52:947-959.
10. Goldberger AL. Nonlinear dynamics for clinicians. Lancet 1996;347:1312-1314.
11. Hull RL. Chronobiology and chronotherapeutics in disease states. Drug Benefit Trends 2002;14:31-42.
12. Breier A, Charney DS, Heninger GR. Agoraphobia with panic attacks. Arch Gen Psychiatry 1986;43:1029-1036.
13. Sheridan MS, Kostlany F. SIDS and chaos. Med Hypotheses 1994;42:11-12.
14. Wilson T, Holt T. Complexity and clinical care. BMJ 2001;323:685-688.
15. Rado JP. Change in antikaliuretic response to potassium-sparing diuretics in patients with cirrhotic ascites. J Am Geriatr Soc 1976;24:340-343.
16. Kraft M, Martin RJ. Chronobiology and chronotherapy in medicine. Dis Mon 1995;41:503-575.
17. Nagayama H. Influences of biological rhythms on the effects of psychotropic drugs. Psychosom Med 1999;6:618-629.
18. Pruessner HT, Hensel WA, Rasco TL. Scientific basis of generalist medicine. Acad Med 1992;67:232-235.
19. Miller WL, Crabtree BF, McDaniel R, Stange KC. Understanding change in primary care practice using complexity theory. J Fam Pract 1998;46:369-376.
20. O’Connor PJ, Crabtree BF, Yanoshik MK. Differences between diabetic patients who do and do not respond to a diabetic care intervention. Fam Med 1997;29:424-428.
21. Jarvis AN. Taking a break. Dissert Abstr Intl 1997;57(10-B):6605.-
22. Boughton MA. Premature menopause. J Adv Nurs 2002;37:423-430.
23. Forsyth DM. Families and the life transition of first time mental illness. Dissert Abstr Intl 1995;56(4-B):1935.-
24. Goldberger AL, Bhargava V, West BJ, Mandell AJ. Nonlinear dynamics of the heart beat. Physica 1985;17D:207-214.
25. Moleiro F, Misticchio F, Mendoza I, Rodriguez A, Costellanos A, Myerburg RJ. Paradoxical behavior of PR interval dynamics during exercise and recovery and its relationship to cardiac memory at the atrioventricular node. J Electrocardiol 2001;34:31-34.
26. Warren K, Sprott JC, Hawkins RC. Spirit is willing. Nonlinear Dynamics Psychol Life Sci 2002;6:55-70.
27. Weiss MJS, Wagner SH. What explains the negative consequences of adverse childhood experiences on adult health? Am J Prev Med 1998;14:356-360.
28. Campbell WG. Is self-organized criticality relevant to alcoholism? J Addict Dis 1997;16:41-50.
29. Pincus D. Framework and methodology for the study of nonlinear, self-organizing family dynamics. Nonlinear Dynamics Psychol Life Sci 2001;5:139-173.
30. Koopmans M. Chaos theory and the problem of change in family systems. Nonlinear Dynamics Psychol Life Sci 1998;2:133-148.
31. Piqueira JRC, Monteiro LHA, De Magalhaes TMC, Ramos RT, Sassi RB, Cruz EG. Zipf’s law organizes a psychiatric ward. J Theor Biol 1999;198:439-443.
32. Christini D, Collins J, Linsay P. Experimental control of high dimensional chaos. Physical Rev E Stat Nonlin Soft Matter Phys 1996;54:4824-4827.
33. Regalado A. Gentle scheme for unleashing chaos. Science 1995;268:1848.-
34. Kauffman SA. Origins Of Order. New York: Oxford University Press; 1993.
35. Klinkman MS, Schwenk TL, Coyne JC. Depression in primary care-more like asthma than appendicitis. Can J Psychiatry 1997;42:966-973.
36. Wells KB, Burnam A, Camp P. Severity of depression in prepaid and fee-for-service general medical and mental health specialty practices. Med Care 1995;33:350-364.
37. Katerndahl D, Realini JP. Patients with panic attacks seeking care from family physicians compared with those seeking care from psychiatrists. J Nerv Ment Dis 1998;186:249-250.
38. Reis SE, Holubkov R, Edmundowicz D, et al. Treatment of patients admitted to the hospital with congestive heart failure. J Am Coll Cardiol 1997;30:733-738.
39. Schulberg D, Gottlieb J. Dynamics and correlates of microscopic changes in affect. Nonlinear Dynamics Psychol Life Sci 2002;6:231-257.
40. Ehlers CL. Chaos and complexity: can it help us to understand mood and behavior? Arch Gen Psychiatry 1995;2:960-964.
41. Wilder J. Modern psychophysiology and the law of initial value. Am J Psychother 1958;12:199-221.
42. Uhlenhuth EH, Matuzas W, Warner TD, Paine S, Lydiard RB, Pollack MH. Do antidepressants selectively suppress spontaneous (unexpected) panic attacks? J Clin Psychopharmacol 2000;20:622-627.
43. Nash JS, Carrato RR, Dlutowski MJ, O’Connor JP, Nash DB. Generalist versus specialist care for acute myocardial infarction. Am J Cardiol 1999;83:650-654.
44. Chen J, Redford MJ, Wang Y, Krumholz HM. Care and outcomes of elderly patients with acute myocardial infarction by physician specialty. Am J Med 2000;108:460-469.
45. Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines. JAMA 1995;273:1026-1031.
46. Lyketsus CG, Taragano F, Triesman GJ, Paz J. Major depression and its response to sertraline in primary care versus psychiatric office practice patients. Psychosomatics 1999;40:70-75.
47. Thomas L, Mulsant BH, Solano FX, et al. Response speed and rate of remission in primary and specialty care patients with depression. Am J Geriatr Psychiatry 2002;10:583-591.
1. Freeman W. Physiology of perception. Sci Am 1991;264:78-85.
2. Barton S. Chaos, self-organization, and psychology. Am Psychol 1994;49:5-14.
3. Guastello S. Chaos, Catastrophe, and Human Affairs. Mahwah, NJ: Erlbaum, 1995.
4. Dendrinos D, Sonis M. Chaos and Socio-Spatial Dynamics. New York: Springer Verlag, 1990.
5. Cheng Y, Van de Ven AH. Learning the innovation journey. Organization Sci 1996;7:593-614.
6. Dooley K, Johnson T, Bush D. TQM, chaos, and complexity. Hum Syst Mgmt 1995;14:1-16.
7. Dooley K. Complex adaptive systems model of organizational change. Nonlinear Dynamics, Psychology, and the Life Sciences 1997;1:69-97.
8. Arthur WB. Economy and complexity. In: Stein DL, ed. Lectures in the Sciences of Complexity. Redwood City, Calif: Addison-Wesley, 1989;713-740.
9. Gottschalk A, Bauer MS, Whybrow PC. Evidence of chaotic mood variation in bipolar disorder. Arch Gen Psychiatry 1995;52:947-959.
10. Goldberger AL. Nonlinear dynamics for clinicians. Lancet 1996;347:1312-1314.
11. Hull RL. Chronobiology and chronotherapeutics in disease states. Drug Benefit Trends 2002;14:31-42.
12. Breier A, Charney DS, Heninger GR. Agoraphobia with panic attacks. Arch Gen Psychiatry 1986;43:1029-1036.
13. Sheridan MS, Kostlany F. SIDS and chaos. Med Hypotheses 1994;42:11-12.
14. Wilson T, Holt T. Complexity and clinical care. BMJ 2001;323:685-688.
15. Rado JP. Change in antikaliuretic response to potassium-sparing diuretics in patients with cirrhotic ascites. J Am Geriatr Soc 1976;24:340-343.
16. Kraft M, Martin RJ. Chronobiology and chronotherapy in medicine. Dis Mon 1995;41:503-575.
17. Nagayama H. Influences of biological rhythms on the effects of psychotropic drugs. Psychosom Med 1999;6:618-629.
18. Pruessner HT, Hensel WA, Rasco TL. Scientific basis of generalist medicine. Acad Med 1992;67:232-235.
19. Miller WL, Crabtree BF, McDaniel R, Stange KC. Understanding change in primary care practice using complexity theory. J Fam Pract 1998;46:369-376.
20. O’Connor PJ, Crabtree BF, Yanoshik MK. Differences between diabetic patients who do and do not respond to a diabetic care intervention. Fam Med 1997;29:424-428.
21. Jarvis AN. Taking a break. Dissert Abstr Intl 1997;57(10-B):6605.-
22. Boughton MA. Premature menopause. J Adv Nurs 2002;37:423-430.
23. Forsyth DM. Families and the life transition of first time mental illness. Dissert Abstr Intl 1995;56(4-B):1935.-
24. Goldberger AL, Bhargava V, West BJ, Mandell AJ. Nonlinear dynamics of the heart beat. Physica 1985;17D:207-214.
25. Moleiro F, Misticchio F, Mendoza I, Rodriguez A, Costellanos A, Myerburg RJ. Paradoxical behavior of PR interval dynamics during exercise and recovery and its relationship to cardiac memory at the atrioventricular node. J Electrocardiol 2001;34:31-34.
26. Warren K, Sprott JC, Hawkins RC. Spirit is willing. Nonlinear Dynamics Psychol Life Sci 2002;6:55-70.
27. Weiss MJS, Wagner SH. What explains the negative consequences of adverse childhood experiences on adult health? Am J Prev Med 1998;14:356-360.
28. Campbell WG. Is self-organized criticality relevant to alcoholism? J Addict Dis 1997;16:41-50.
29. Pincus D. Framework and methodology for the study of nonlinear, self-organizing family dynamics. Nonlinear Dynamics Psychol Life Sci 2001;5:139-173.
30. Koopmans M. Chaos theory and the problem of change in family systems. Nonlinear Dynamics Psychol Life Sci 1998;2:133-148.
31. Piqueira JRC, Monteiro LHA, De Magalhaes TMC, Ramos RT, Sassi RB, Cruz EG. Zipf’s law organizes a psychiatric ward. J Theor Biol 1999;198:439-443.
32. Christini D, Collins J, Linsay P. Experimental control of high dimensional chaos. Physical Rev E Stat Nonlin Soft Matter Phys 1996;54:4824-4827.
33. Regalado A. Gentle scheme for unleashing chaos. Science 1995;268:1848.-
34. Kauffman SA. Origins Of Order. New York: Oxford University Press; 1993.
35. Klinkman MS, Schwenk TL, Coyne JC. Depression in primary care-more like asthma than appendicitis. Can J Psychiatry 1997;42:966-973.
36. Wells KB, Burnam A, Camp P. Severity of depression in prepaid and fee-for-service general medical and mental health specialty practices. Med Care 1995;33:350-364.
37. Katerndahl D, Realini JP. Patients with panic attacks seeking care from family physicians compared with those seeking care from psychiatrists. J Nerv Ment Dis 1998;186:249-250.
38. Reis SE, Holubkov R, Edmundowicz D, et al. Treatment of patients admitted to the hospital with congestive heart failure. J Am Coll Cardiol 1997;30:733-738.
39. Schulberg D, Gottlieb J. Dynamics and correlates of microscopic changes in affect. Nonlinear Dynamics Psychol Life Sci 2002;6:231-257.
40. Ehlers CL. Chaos and complexity: can it help us to understand mood and behavior? Arch Gen Psychiatry 1995;2:960-964.
41. Wilder J. Modern psychophysiology and the law of initial value. Am J Psychother 1958;12:199-221.
42. Uhlenhuth EH, Matuzas W, Warner TD, Paine S, Lydiard RB, Pollack MH. Do antidepressants selectively suppress spontaneous (unexpected) panic attacks? J Clin Psychopharmacol 2000;20:622-627.
43. Nash JS, Carrato RR, Dlutowski MJ, O’Connor JP, Nash DB. Generalist versus specialist care for acute myocardial infarction. Am J Cardiol 1999;83:650-654.
44. Chen J, Redford MJ, Wang Y, Krumholz HM. Care and outcomes of elderly patients with acute myocardial infarction by physician specialty. Am J Med 2000;108:460-469.
45. Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines. JAMA 1995;273:1026-1031.
46. Lyketsus CG, Taragano F, Triesman GJ, Paz J. Major depression and its response to sertraline in primary care versus psychiatric office practice patients. Psychosomatics 1999;40:70-75.
47. Thomas L, Mulsant BH, Solano FX, et al. Response speed and rate of remission in primary and specialty care patients with depression. Am J Geriatr Psychiatry 2002;10:583-591.
Chronic compartment syndrome: Tips on recognizing and treating
- A patient’s description of symptoms and pattern of occurrence is the most reliable clinical guide. Confirm suspicion of chronic compartment syndrome by documenting intracompartmental pressures. Other diagnostic modalities, though promising, have no place in the work up currently (C).
- Study data are sparse for conservative treatments, which seem largely unsuccessful in common clinical experience. Base any decision to offer conservative therapy on an individual’s circumstances. It is usually impractical to ask competitive athletes to change sports or reduce intensity (C).
- Fasciotomy is an effective treatment for chronic compartment syndrome. Fasciectomy is preferred by some practitioners (C).
Shin splints and stress fractures are injuries we are accustomed to seeing among younger athletes. A less wellknown painful injury becoming more prevalent—perhaps especially among young female athletes—is chronic compartment syndrome (CCS).
The patient’s history offers more important clues to CCS than does the physical exam. Direct measurement of intracompartmental pressure—as described in this article—is the best means of confirming the diagnosis. Because it’s an invasive procedure, first rule out shin splints and other more common disorders. In older, even nonathletic persons, who can also suffer from CCS, the list of disorders to rule out grows longer.
Outpatient surgical treatment relieves the pain of CCS and most often prevents recurrences.
Clinical presentation
The classic presentation of CCS is a young athlete who complains of an aching pain or a crampy ache in the lower leg during exercise, in an area of the leg corresponding to 1 of its 4 compartments (FIGURE 1). Symptoms are bilateral in 70% to 80% of athletes who develop compartment syndrome.1,2,3
Symptom traits vary. Other patients describe a sensation of tightness, and some even notice a swelling or bulge over the affected compartment. Many patients describe a numbness or tingling at the affected site that occasionally radiates to the foot. They also often report a feeling of weakness and, in severe cases, may develop true muscle weakness such as drop foot (slap sign). Less often, patients with CCS report a severe shooting pain.
Symptoms usually resolve within minutes to hours following the cessation of activity. However, they can linger for 1 to 2 days following intense activity, especially when the athlete continues to participate despite symptoms.3
Symptoms follow regular pattern. While the onset of symptoms can vary among CCS sufferers, patients often note that symptoms recur consistently at a specific distance (if running or cycling) or duration of exercise.7 Temporary rest from or complete cessation of the associated activity may relieve symptoms, but a return to full participation inevitably leads to more severe symptoms. Those who ignore symptoms and continue their activity may over weeks or months experience a worsening in severity and an earlier onset of symptoms.2
Clinical exam much less helpful than the history. With most patients who have CCS, the exam is completely normal. In fact, the real value of the exam may be to detect signs associated with other disorders in the differential (TABLE).
However, occasionally positive findings support the diagnosis of CCS. The finding most commonly encountered is muscle herniation, seen in 40% to 50% of patients.7,8 These hernias result from a defect in the overlying fascia and are evidenced by a soft tissue bulge that becomes more prominent with muscle contraction. Hernias can be tender to palpation or asymptomatic.2
Another finding, in the absence of herniation, is tenderness of the affected area when palpated. Less frequently, the examiner may note swelling or tightness over the affected compartment.
A few patients with anterior or lateral compartment syndromes have significant weakness on dorsiflexion.2,8
Examining the patient immediately after exercise may increase the sensitivity of all tests for abnormal sensations and weakness.
TABLE 1
Differential diagnosis for chronic compartment syndrome
| Shin splints |
| Stress fracture |
| Gastrocnemius/Soleus strain |
| Claudication |
| Disk herniation |
| Spinal stenosis |
| Peripheral neuropathy |
| Popliteal artery entrapment syndrome |
| Peroneal nerve entrapments |
| Osteomyelitis |
| Tumor |
Rule out other disorders early
Since confirmatory testing for CCS is invasive, rule out alternative diagnoses before proceeding with the workup. Two much more common diagnoses in young athletes are shin splints and stress fractures. Diffuse tenderness along the posteromedial aspect of the tibia suggests shin splints. Point tenderness along the anterior or posteromedial tibia suggests a stress fracture.
Another common diagnosis to consider in all age groups is disk herniation. Concomitant low back pain or pain that radiates from above the knee in a dermatomal distribution makes this diagnosis more likely. In older patients, spinal stenosis can cause radicular pain that must be distinguished from CCS. A thorough neurologic examination is imperative to rule out these conditions.
Also consider claudication with older patients, particularly those who have risk factors for peripheral vascular disease.
Peripheral neuropathy and gastrocnemius/soleus strain are other common diagnoses that are part of the differential. Uncommon yet important diagnoses to consider include osteomyelitis and tumor.
Rare disorders
Though much less common than the above diagnoses, popliteal artery entrapment syndrome (PAES) and peroneal nerve entrapments are important to discuss since their presentations can be almost identical to CCS.
PAES can mimic posterior CCS in presentation and should be part of the differential for any young patient complaining of exertional calf pain. PAES is a rare condition in which the popliteal artery becomes compressed from strenuous exercise, resulting in ischemia. The underlying anatomic anomaly is the relationship of the popliteal artery to the adjacent musculotendinous structures.9 If you suspect PAES, evaluate for a diminished dorsalis pedis pulse with either passive plantar flexion or active dorsiflexion. Patients with exertional calf pain and a positive test result require imaging. These patients should undergo Doppler imaging at rest, with passive plantar flexion, and with active dorsiflexion. Equivocal or incomplete studies require arteriography.10
Similarly, peroneal nerve entrapments can masquerade as anterior/lateral compartment syndromes. While the common, deep, and superficial peroneal nerves can all be entrapped, the superficial branch is most frequently involved.11 The superficial branch exits the lateral compartment approximately 10 cm proximal to the lateral malleolus. Tenderness at this site upon active dorsiflexion, a positive tinel sign at this site, or lateral leg pain upon plantar flexion and inversion all suggest superficial peroneal entrapment.11 Electromyography, oftentimes performed after compartment pressures are found to be normal, is necessary to confirm the diagnosis.
Chronic compartment syndrome was first identified by Mavor in 1956,12 but it was not until 1975 that the disorder’s clinical manifestations and basic pathophysiology were described.13 CCS is an uncommon condition and no published data exist regarding its incidence or prevalence. However, because more physicians are becoming aware of it, CCS is being increasingly recognized. At the University of Wisconsin, the number of patients diagnosed with CCS has more than tripled in each of the last 2 decades.1,2
Athletes most affected. CCS, also known as exertional compartment syndrome or effort-related compartment syndrome, affects primarily young athletes. The mean age of afflicted persons at the time of diagnosis is mid to late twenties. The average duration of symptoms before diagnosis is 2 years.1 The syndrome most commonly affects runners and soccer players, but other sports linked to the development of CCS are cycling, football, gymnastics, and tennis.1,2,3,7 Although the syndrome most commonly affects the lower extremities, many reported cases of CCS have occurred in the forearms and hands.
Young women may be most at risk. Early studies from the United States in the mid-1980s showed that the male to female ratio of affected patients was approximately 1:1.2,8 However, a large, more recent study showed a female-to-male ratio greater than 2:1.1 This likely reflects the increase in female sports participation over the last 2 decades and suggests that females may be at a greater risk of developing the syndrome.
Direct pressure measurement best evaluation
Despite attempts to develop noninvasive testing for CCS, the gold standard remains the direct measurement of intracompartmental pressures. There is some controversy regarding the upper limit of normal, but most authors agree that a resting pressure >15 mm Hg is abnormally elevated.1,2,5 Other cutoffs cited in the literature include a 1-minute post-exercise value greater than 30 mm Hg, and a 5-minute post-exercise reading >25 mm Hg.5 Turnipseed and colleagues recommend checking post-exercise values in patients with modestly elevated resting pressures of 16 to 24 mm Hg to confirm the diagnosis. Because of the pathophysiology of the syndrome, it seems appropriate to also check 5- or 10-minute post-exercise pressures in patients with typical clinical presentations and normal resting pressures.
Orthopedic, vascular, and general surgeons receive training in compartmental pressure measurement. There are 4 techniques for measurement: the simple needle, the Whitesides infusion, the wick catheter, and the slit catheter. Simple needle devices (such as the Stryker stic, FIGURE 2) have increased in popularity because they are handheld, portable, contain a scale within the device for direct measurement, and are easily operated in a clinic setting.14
Diagnostic tools that may yet prove useful
Many other diagnostic modalities have been studied in the last 10 years and may eventually prove helpful. Near infrared spectroscopy has demonstrated a relative deoxygenation during exercise in CCS patients and a delayed reoxygenation in the immediate post-exercise period.15
MIBI scintigraphy has shown decreased muscle perfusion at peak exercise when compared with next-day imaging.16,17
Laser Doppler flow studies conducted in the post-exercise period have demonstrated a delayed peak hyperemia in CCS patients, different from the gradual decrease in blood flow seen in controls.18
Finally, multiple studies have been conducted done with magnetic resonance imaging. Comparisons of pre- and postexercise imaging have shown a greater increase in signal intensity in patients with CCS.19 Despite these findings, though, no clear clinical indications for these tools exist.
FIGURE 2
Measurement with Stryker stic
Measurement of lateral superficial posterior compartment pressure with the Stryker stic on a 16-year-old girl with 4-month history of exertional calf pain.
Treatment options
Conservative measures unconvincing
A few studies have addressed the efficacy of conservative treatment of CCS, but most physicians have found such therapy unsuccessful. Modalities tried include nonsteroidal anti-inflammatory drugs (NSAIDs), diuretics, compression, stretching, orthoses, massage, prolonged rest, change in training surface, change in footwear, change in sport, heat, electrostimulation, and whirlpool.20
One small study showed that compartment pressures in middle-aged men with CCS decreased following treatment with diuretics.21 Another small study showed that athletes receiving compartmental massage increased the duration of time they were able to exercise before developing symptoms.22 A third trial found competitive runners to have significantly higher pressures than competitive cyclists, suggesting runners with CCS may be able to bike as an alternative form of exercise.23
The few data regarding other modalities suggests that only prolonged rest or cessation of sport is effective.24,25 These options, however, may be impractical for competitive athletes who often have no desire to modify their sports participation. With little available evidence, the decision to offer conservative treatment and the type of conservative therapy to recommend remain controversial.
Fasciotomy track record good
Fasciotomy is the most widely used surgical treatment for CCS. The surgeon makes 1 to 3 small skin incisions, exposes the underlying fascia of the affected compartment, and incises the fascia (FIGURES 3 AND 4). Most of these operations are performed under local anesthesia and last less than an hour. Complications are rare, but can include seroma, hemorrhage, cellulitis, peripheral nerve injury, popliteal injury, tibial artery injury, and deep vein thrombosis (DVT).1,2
Patient satisfaction with the operation ranges from 80% to 95% in most published series.1,2,3,5,26 The typical postoperative course involves crutches for the first few days, followed by nonimpact aerobic training for 2 to 4 weeks. Impact aerobic training is next, with gradual return to sport by 2 to 3 months depending on the intensity of sports participation and type of sport practiced.1,4
Faciectomy preferred by some. Though published long-term follow-up data are few, Turnipseed et al found an 11% CCS recurrence rate among patients undergoing fasciotomies before 1985, compared with a 6% recurrence among patients who received fasciectomies between 1991 and 2001.1 The latter procedure involves excision of strips of fascia, which theoretically should decrease the risk of scarring over the compartment and subsequent recurrence of symptoms. This is one reason fasciectomy has become the procedure of choice for some physicians, while others reserved it for patients with recurrent CCS. Until a randomized study is performed, it will be difficult to compare the efficacy of fasciotomy and faciectomy.
FIGURE 3
5 days postsurgery
21-year-old female collegiate track athlete 5 days after anterior, lateral, and lateral superficial posterior compartment release.
FIGURE 4
6 months later
16-year-old female hockey and soccer player 6 months after anterior and lateral fasciectomy.
Acknowledgments
The author would like to thank Dr. William Turnipseed, MD, Department of Vascular Surgery, University of Wisconsin, for his assistance in the preparation of this review article.
CORRESPONDING AUTHOR
Jon Englund, MD, Memorial Healthplex Sports Medicine Institute, 111 West Jefferson, South Bend, IN 46601. E-mail: [email protected]
1. Turnipseed WD. Diagnosis and management of chronic compartment syndrome. Surgery 2002;132:613-619.
2. Detmer DE, Sharpe K, Sufit RL, Girdley FM. Chronic compartment syndrome: diagnosis, management, and outcomes. Am J Sports Med 1985;13:162-170.
3. Moeyersoons JP, Martens M. Chronic compartment syndrome: diagnosis and management. Acta Orthop Belg 1992;58:23-27.
4. Hargens AR, Muburak SJ. Current concepts in the pathophysiology, evaluation, and diagnosis of compartment syndrome. Hand Clin 1998;14:371-383.
5. Tubb CC, Vermillion D. Chronic exertional compartment syndrome after minor injury to the lower extremity. Mil Med 2001;166:366-368.
6. Jerosch J, Castro WHM, Hoffstetter R, Reer R. Secondary effects of knee braces on the intracompartmental pressure in the anterior tibial compartment. Acta Orthop Belg 1995;61:37-42.
7. Martens MA, Moeyersoons JP. Acute and recurrent effort-related compartment syndrome in sports. Sports Med 1990;9:62-68.
8. Pedowitz RA, Hargens AR, Murbarak SJ, Gershuni DN. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 1990;18:35-40.
9. Adams MT, Wixon CL. Popliteal artery entrapment syndrome. J Am Coll Surg 2003;196:152-153.
10. Allen MJ, Barnes MR, Bell PR, Bolia A, Hartshorne TC. Popliteal entrapment syndrome: misdiagnosed as a compartment syndrome. Eur J Vasc Surg 1993;7:342-345.
11. DeLee J, Drez D, Miller MD. DeLee and Drez’s Orthopaedic Sports Medicine. 2nd ed. Philadelphia, Pa: WB Saunders 2003;2177-2178.
12. Mavor GE. The anterior tibial syndrome: a chronic form. J Bone Joint Surg Br 1956;38:513-517.
13. Reneman RS. The anterior and lateral compartment syndrome of the leg due to intensive use of muscles. Clinic Orthop Relat Res 1975;113:69-80.
14. Heppenstall RB. An update in compartment syndrome investigation and treatment. Univ Penn Ortho J 1997;10:49-57.
15. Mohler LR, Styf JR, Pedowitz RA, Hargens AR, Gershuni DH. Intramuscular deoxygenation during exercise in patients who have chronic anterior compartment syndrome of the leg. J Bone Joint Surg Am 1997;79:844-849.
16. Edwards PD, Miles KA, Owens SJ, Kemp PM, Jenner JR. A new non-invasive test for the detection of compartment syndromes. Nuc Med Commun 1999;20:215-218.
17. Owens S, Edwards P, Miles K, Jenner J, Allen M. Chronic compartment syndrome affecting lower limb: MIBI perfusion imaging as an alternative to pressure monitoring: two case reports. Br J Sports Med 1999;33:49-53.
18. Abraham P, Leftheriotis G, Saumet JL. Laser Doppler flowmetry in the diagnosis of chronic compartment syndrome. J Bone Joint Surg Br 1998;80:365-369.
19. Verleisdonk EJ, van Gils A, van der Werken C. The diagnostic value of MRI scans for the diagnosis of chronic exertional compartment syndrome of the lower leg. Skeletal Radiol 2001;30:321-325.
20. Micheli LJ, Solomon R, Solomon J, Plasschaert VF, Mitchell R. Surgical treatment for lower-leg compartment syndrome in young female athletes. Am J Sports Med 1999;27:197-201.
21. Christensen JT, Eklof B, Wulff K. The chronic compartment syndrome and response to diuretic treatment. Acta Chir Scand 1983;149:249-252.
22. Blackman PG, Simmons LR, Crossley KM. Treatment of chronic exertional anterior compartment syndrome with massage: a pilot study. Clin J Sport Med 1998;8:14-17.
23. Beckham SG, Grana WA, Buckley P, Breazile JL, Claypool PL. A comparison of anterior compartment pressures in competitive runners and cyclists. Am J Sports Med 1993;21,1:36-40.
24. Shah S, Miller B, Kuhn J. Chronic exertional compartment syndrome. Am J Orthop 2004;33:335-341.
25. Martens MA, Backaert M, Vermaut G, Mulier JC. Chronic leg pain in athletes due to recurrent compartment syndrome. Am J Sports Med 1984;12:148-151.
26. Styf J, Korner L. Chronic anterior-compartment syndrome of the leg. Results of treatment by fasciotomy J Bone Joint Surg Am 1986;68:1338-1347.
- A patient’s description of symptoms and pattern of occurrence is the most reliable clinical guide. Confirm suspicion of chronic compartment syndrome by documenting intracompartmental pressures. Other diagnostic modalities, though promising, have no place in the work up currently (C).
- Study data are sparse for conservative treatments, which seem largely unsuccessful in common clinical experience. Base any decision to offer conservative therapy on an individual’s circumstances. It is usually impractical to ask competitive athletes to change sports or reduce intensity (C).
- Fasciotomy is an effective treatment for chronic compartment syndrome. Fasciectomy is preferred by some practitioners (C).
Shin splints and stress fractures are injuries we are accustomed to seeing among younger athletes. A less wellknown painful injury becoming more prevalent—perhaps especially among young female athletes—is chronic compartment syndrome (CCS).
The patient’s history offers more important clues to CCS than does the physical exam. Direct measurement of intracompartmental pressure—as described in this article—is the best means of confirming the diagnosis. Because it’s an invasive procedure, first rule out shin splints and other more common disorders. In older, even nonathletic persons, who can also suffer from CCS, the list of disorders to rule out grows longer.
Outpatient surgical treatment relieves the pain of CCS and most often prevents recurrences.
Clinical presentation
The classic presentation of CCS is a young athlete who complains of an aching pain or a crampy ache in the lower leg during exercise, in an area of the leg corresponding to 1 of its 4 compartments (FIGURE 1). Symptoms are bilateral in 70% to 80% of athletes who develop compartment syndrome.1,2,3
Symptom traits vary. Other patients describe a sensation of tightness, and some even notice a swelling or bulge over the affected compartment. Many patients describe a numbness or tingling at the affected site that occasionally radiates to the foot. They also often report a feeling of weakness and, in severe cases, may develop true muscle weakness such as drop foot (slap sign). Less often, patients with CCS report a severe shooting pain.
Symptoms usually resolve within minutes to hours following the cessation of activity. However, they can linger for 1 to 2 days following intense activity, especially when the athlete continues to participate despite symptoms.3
Symptoms follow regular pattern. While the onset of symptoms can vary among CCS sufferers, patients often note that symptoms recur consistently at a specific distance (if running or cycling) or duration of exercise.7 Temporary rest from or complete cessation of the associated activity may relieve symptoms, but a return to full participation inevitably leads to more severe symptoms. Those who ignore symptoms and continue their activity may over weeks or months experience a worsening in severity and an earlier onset of symptoms.2
Clinical exam much less helpful than the history. With most patients who have CCS, the exam is completely normal. In fact, the real value of the exam may be to detect signs associated with other disorders in the differential (TABLE).
However, occasionally positive findings support the diagnosis of CCS. The finding most commonly encountered is muscle herniation, seen in 40% to 50% of patients.7,8 These hernias result from a defect in the overlying fascia and are evidenced by a soft tissue bulge that becomes more prominent with muscle contraction. Hernias can be tender to palpation or asymptomatic.2
Another finding, in the absence of herniation, is tenderness of the affected area when palpated. Less frequently, the examiner may note swelling or tightness over the affected compartment.
A few patients with anterior or lateral compartment syndromes have significant weakness on dorsiflexion.2,8
Examining the patient immediately after exercise may increase the sensitivity of all tests for abnormal sensations and weakness.
TABLE 1
Differential diagnosis for chronic compartment syndrome
| Shin splints |
| Stress fracture |
| Gastrocnemius/Soleus strain |
| Claudication |
| Disk herniation |
| Spinal stenosis |
| Peripheral neuropathy |
| Popliteal artery entrapment syndrome |
| Peroneal nerve entrapments |
| Osteomyelitis |
| Tumor |
Rule out other disorders early
Since confirmatory testing for CCS is invasive, rule out alternative diagnoses before proceeding with the workup. Two much more common diagnoses in young athletes are shin splints and stress fractures. Diffuse tenderness along the posteromedial aspect of the tibia suggests shin splints. Point tenderness along the anterior or posteromedial tibia suggests a stress fracture.
Another common diagnosis to consider in all age groups is disk herniation. Concomitant low back pain or pain that radiates from above the knee in a dermatomal distribution makes this diagnosis more likely. In older patients, spinal stenosis can cause radicular pain that must be distinguished from CCS. A thorough neurologic examination is imperative to rule out these conditions.
Also consider claudication with older patients, particularly those who have risk factors for peripheral vascular disease.
Peripheral neuropathy and gastrocnemius/soleus strain are other common diagnoses that are part of the differential. Uncommon yet important diagnoses to consider include osteomyelitis and tumor.
Rare disorders
Though much less common than the above diagnoses, popliteal artery entrapment syndrome (PAES) and peroneal nerve entrapments are important to discuss since their presentations can be almost identical to CCS.
PAES can mimic posterior CCS in presentation and should be part of the differential for any young patient complaining of exertional calf pain. PAES is a rare condition in which the popliteal artery becomes compressed from strenuous exercise, resulting in ischemia. The underlying anatomic anomaly is the relationship of the popliteal artery to the adjacent musculotendinous structures.9 If you suspect PAES, evaluate for a diminished dorsalis pedis pulse with either passive plantar flexion or active dorsiflexion. Patients with exertional calf pain and a positive test result require imaging. These patients should undergo Doppler imaging at rest, with passive plantar flexion, and with active dorsiflexion. Equivocal or incomplete studies require arteriography.10
Similarly, peroneal nerve entrapments can masquerade as anterior/lateral compartment syndromes. While the common, deep, and superficial peroneal nerves can all be entrapped, the superficial branch is most frequently involved.11 The superficial branch exits the lateral compartment approximately 10 cm proximal to the lateral malleolus. Tenderness at this site upon active dorsiflexion, a positive tinel sign at this site, or lateral leg pain upon plantar flexion and inversion all suggest superficial peroneal entrapment.11 Electromyography, oftentimes performed after compartment pressures are found to be normal, is necessary to confirm the diagnosis.
Chronic compartment syndrome was first identified by Mavor in 1956,12 but it was not until 1975 that the disorder’s clinical manifestations and basic pathophysiology were described.13 CCS is an uncommon condition and no published data exist regarding its incidence or prevalence. However, because more physicians are becoming aware of it, CCS is being increasingly recognized. At the University of Wisconsin, the number of patients diagnosed with CCS has more than tripled in each of the last 2 decades.1,2
Athletes most affected. CCS, also known as exertional compartment syndrome or effort-related compartment syndrome, affects primarily young athletes. The mean age of afflicted persons at the time of diagnosis is mid to late twenties. The average duration of symptoms before diagnosis is 2 years.1 The syndrome most commonly affects runners and soccer players, but other sports linked to the development of CCS are cycling, football, gymnastics, and tennis.1,2,3,7 Although the syndrome most commonly affects the lower extremities, many reported cases of CCS have occurred in the forearms and hands.
Young women may be most at risk. Early studies from the United States in the mid-1980s showed that the male to female ratio of affected patients was approximately 1:1.2,8 However, a large, more recent study showed a female-to-male ratio greater than 2:1.1 This likely reflects the increase in female sports participation over the last 2 decades and suggests that females may be at a greater risk of developing the syndrome.
Direct pressure measurement best evaluation
Despite attempts to develop noninvasive testing for CCS, the gold standard remains the direct measurement of intracompartmental pressures. There is some controversy regarding the upper limit of normal, but most authors agree that a resting pressure >15 mm Hg is abnormally elevated.1,2,5 Other cutoffs cited in the literature include a 1-minute post-exercise value greater than 30 mm Hg, and a 5-minute post-exercise reading >25 mm Hg.5 Turnipseed and colleagues recommend checking post-exercise values in patients with modestly elevated resting pressures of 16 to 24 mm Hg to confirm the diagnosis. Because of the pathophysiology of the syndrome, it seems appropriate to also check 5- or 10-minute post-exercise pressures in patients with typical clinical presentations and normal resting pressures.
Orthopedic, vascular, and general surgeons receive training in compartmental pressure measurement. There are 4 techniques for measurement: the simple needle, the Whitesides infusion, the wick catheter, and the slit catheter. Simple needle devices (such as the Stryker stic, FIGURE 2) have increased in popularity because they are handheld, portable, contain a scale within the device for direct measurement, and are easily operated in a clinic setting.14
Diagnostic tools that may yet prove useful
Many other diagnostic modalities have been studied in the last 10 years and may eventually prove helpful. Near infrared spectroscopy has demonstrated a relative deoxygenation during exercise in CCS patients and a delayed reoxygenation in the immediate post-exercise period.15
MIBI scintigraphy has shown decreased muscle perfusion at peak exercise when compared with next-day imaging.16,17
Laser Doppler flow studies conducted in the post-exercise period have demonstrated a delayed peak hyperemia in CCS patients, different from the gradual decrease in blood flow seen in controls.18
Finally, multiple studies have been conducted done with magnetic resonance imaging. Comparisons of pre- and postexercise imaging have shown a greater increase in signal intensity in patients with CCS.19 Despite these findings, though, no clear clinical indications for these tools exist.
FIGURE 2
Measurement with Stryker stic
Measurement of lateral superficial posterior compartment pressure with the Stryker stic on a 16-year-old girl with 4-month history of exertional calf pain.
Treatment options
Conservative measures unconvincing
A few studies have addressed the efficacy of conservative treatment of CCS, but most physicians have found such therapy unsuccessful. Modalities tried include nonsteroidal anti-inflammatory drugs (NSAIDs), diuretics, compression, stretching, orthoses, massage, prolonged rest, change in training surface, change in footwear, change in sport, heat, electrostimulation, and whirlpool.20
One small study showed that compartment pressures in middle-aged men with CCS decreased following treatment with diuretics.21 Another small study showed that athletes receiving compartmental massage increased the duration of time they were able to exercise before developing symptoms.22 A third trial found competitive runners to have significantly higher pressures than competitive cyclists, suggesting runners with CCS may be able to bike as an alternative form of exercise.23
The few data regarding other modalities suggests that only prolonged rest or cessation of sport is effective.24,25 These options, however, may be impractical for competitive athletes who often have no desire to modify their sports participation. With little available evidence, the decision to offer conservative treatment and the type of conservative therapy to recommend remain controversial.
Fasciotomy track record good
Fasciotomy is the most widely used surgical treatment for CCS. The surgeon makes 1 to 3 small skin incisions, exposes the underlying fascia of the affected compartment, and incises the fascia (FIGURES 3 AND 4). Most of these operations are performed under local anesthesia and last less than an hour. Complications are rare, but can include seroma, hemorrhage, cellulitis, peripheral nerve injury, popliteal injury, tibial artery injury, and deep vein thrombosis (DVT).1,2
Patient satisfaction with the operation ranges from 80% to 95% in most published series.1,2,3,5,26 The typical postoperative course involves crutches for the first few days, followed by nonimpact aerobic training for 2 to 4 weeks. Impact aerobic training is next, with gradual return to sport by 2 to 3 months depending on the intensity of sports participation and type of sport practiced.1,4
Faciectomy preferred by some. Though published long-term follow-up data are few, Turnipseed et al found an 11% CCS recurrence rate among patients undergoing fasciotomies before 1985, compared with a 6% recurrence among patients who received fasciectomies between 1991 and 2001.1 The latter procedure involves excision of strips of fascia, which theoretically should decrease the risk of scarring over the compartment and subsequent recurrence of symptoms. This is one reason fasciectomy has become the procedure of choice for some physicians, while others reserved it for patients with recurrent CCS. Until a randomized study is performed, it will be difficult to compare the efficacy of fasciotomy and faciectomy.
FIGURE 3
5 days postsurgery
21-year-old female collegiate track athlete 5 days after anterior, lateral, and lateral superficial posterior compartment release.
FIGURE 4
6 months later
16-year-old female hockey and soccer player 6 months after anterior and lateral fasciectomy.
Acknowledgments
The author would like to thank Dr. William Turnipseed, MD, Department of Vascular Surgery, University of Wisconsin, for his assistance in the preparation of this review article.
CORRESPONDING AUTHOR
Jon Englund, MD, Memorial Healthplex Sports Medicine Institute, 111 West Jefferson, South Bend, IN 46601. E-mail: [email protected]
- A patient’s description of symptoms and pattern of occurrence is the most reliable clinical guide. Confirm suspicion of chronic compartment syndrome by documenting intracompartmental pressures. Other diagnostic modalities, though promising, have no place in the work up currently (C).
- Study data are sparse for conservative treatments, which seem largely unsuccessful in common clinical experience. Base any decision to offer conservative therapy on an individual’s circumstances. It is usually impractical to ask competitive athletes to change sports or reduce intensity (C).
- Fasciotomy is an effective treatment for chronic compartment syndrome. Fasciectomy is preferred by some practitioners (C).
Shin splints and stress fractures are injuries we are accustomed to seeing among younger athletes. A less wellknown painful injury becoming more prevalent—perhaps especially among young female athletes—is chronic compartment syndrome (CCS).
The patient’s history offers more important clues to CCS than does the physical exam. Direct measurement of intracompartmental pressure—as described in this article—is the best means of confirming the diagnosis. Because it’s an invasive procedure, first rule out shin splints and other more common disorders. In older, even nonathletic persons, who can also suffer from CCS, the list of disorders to rule out grows longer.
Outpatient surgical treatment relieves the pain of CCS and most often prevents recurrences.
Clinical presentation
The classic presentation of CCS is a young athlete who complains of an aching pain or a crampy ache in the lower leg during exercise, in an area of the leg corresponding to 1 of its 4 compartments (FIGURE 1). Symptoms are bilateral in 70% to 80% of athletes who develop compartment syndrome.1,2,3
Symptom traits vary. Other patients describe a sensation of tightness, and some even notice a swelling or bulge over the affected compartment. Many patients describe a numbness or tingling at the affected site that occasionally radiates to the foot. They also often report a feeling of weakness and, in severe cases, may develop true muscle weakness such as drop foot (slap sign). Less often, patients with CCS report a severe shooting pain.
Symptoms usually resolve within minutes to hours following the cessation of activity. However, they can linger for 1 to 2 days following intense activity, especially when the athlete continues to participate despite symptoms.3
Symptoms follow regular pattern. While the onset of symptoms can vary among CCS sufferers, patients often note that symptoms recur consistently at a specific distance (if running or cycling) or duration of exercise.7 Temporary rest from or complete cessation of the associated activity may relieve symptoms, but a return to full participation inevitably leads to more severe symptoms. Those who ignore symptoms and continue their activity may over weeks or months experience a worsening in severity and an earlier onset of symptoms.2
Clinical exam much less helpful than the history. With most patients who have CCS, the exam is completely normal. In fact, the real value of the exam may be to detect signs associated with other disorders in the differential (TABLE).
However, occasionally positive findings support the diagnosis of CCS. The finding most commonly encountered is muscle herniation, seen in 40% to 50% of patients.7,8 These hernias result from a defect in the overlying fascia and are evidenced by a soft tissue bulge that becomes more prominent with muscle contraction. Hernias can be tender to palpation or asymptomatic.2
Another finding, in the absence of herniation, is tenderness of the affected area when palpated. Less frequently, the examiner may note swelling or tightness over the affected compartment.
A few patients with anterior or lateral compartment syndromes have significant weakness on dorsiflexion.2,8
Examining the patient immediately after exercise may increase the sensitivity of all tests for abnormal sensations and weakness.
TABLE 1
Differential diagnosis for chronic compartment syndrome
| Shin splints |
| Stress fracture |
| Gastrocnemius/Soleus strain |
| Claudication |
| Disk herniation |
| Spinal stenosis |
| Peripheral neuropathy |
| Popliteal artery entrapment syndrome |
| Peroneal nerve entrapments |
| Osteomyelitis |
| Tumor |
Rule out other disorders early
Since confirmatory testing for CCS is invasive, rule out alternative diagnoses before proceeding with the workup. Two much more common diagnoses in young athletes are shin splints and stress fractures. Diffuse tenderness along the posteromedial aspect of the tibia suggests shin splints. Point tenderness along the anterior or posteromedial tibia suggests a stress fracture.
Another common diagnosis to consider in all age groups is disk herniation. Concomitant low back pain or pain that radiates from above the knee in a dermatomal distribution makes this diagnosis more likely. In older patients, spinal stenosis can cause radicular pain that must be distinguished from CCS. A thorough neurologic examination is imperative to rule out these conditions.
Also consider claudication with older patients, particularly those who have risk factors for peripheral vascular disease.
Peripheral neuropathy and gastrocnemius/soleus strain are other common diagnoses that are part of the differential. Uncommon yet important diagnoses to consider include osteomyelitis and tumor.
Rare disorders
Though much less common than the above diagnoses, popliteal artery entrapment syndrome (PAES) and peroneal nerve entrapments are important to discuss since their presentations can be almost identical to CCS.
PAES can mimic posterior CCS in presentation and should be part of the differential for any young patient complaining of exertional calf pain. PAES is a rare condition in which the popliteal artery becomes compressed from strenuous exercise, resulting in ischemia. The underlying anatomic anomaly is the relationship of the popliteal artery to the adjacent musculotendinous structures.9 If you suspect PAES, evaluate for a diminished dorsalis pedis pulse with either passive plantar flexion or active dorsiflexion. Patients with exertional calf pain and a positive test result require imaging. These patients should undergo Doppler imaging at rest, with passive plantar flexion, and with active dorsiflexion. Equivocal or incomplete studies require arteriography.10
Similarly, peroneal nerve entrapments can masquerade as anterior/lateral compartment syndromes. While the common, deep, and superficial peroneal nerves can all be entrapped, the superficial branch is most frequently involved.11 The superficial branch exits the lateral compartment approximately 10 cm proximal to the lateral malleolus. Tenderness at this site upon active dorsiflexion, a positive tinel sign at this site, or lateral leg pain upon plantar flexion and inversion all suggest superficial peroneal entrapment.11 Electromyography, oftentimes performed after compartment pressures are found to be normal, is necessary to confirm the diagnosis.
Chronic compartment syndrome was first identified by Mavor in 1956,12 but it was not until 1975 that the disorder’s clinical manifestations and basic pathophysiology were described.13 CCS is an uncommon condition and no published data exist regarding its incidence or prevalence. However, because more physicians are becoming aware of it, CCS is being increasingly recognized. At the University of Wisconsin, the number of patients diagnosed with CCS has more than tripled in each of the last 2 decades.1,2
Athletes most affected. CCS, also known as exertional compartment syndrome or effort-related compartment syndrome, affects primarily young athletes. The mean age of afflicted persons at the time of diagnosis is mid to late twenties. The average duration of symptoms before diagnosis is 2 years.1 The syndrome most commonly affects runners and soccer players, but other sports linked to the development of CCS are cycling, football, gymnastics, and tennis.1,2,3,7 Although the syndrome most commonly affects the lower extremities, many reported cases of CCS have occurred in the forearms and hands.
Young women may be most at risk. Early studies from the United States in the mid-1980s showed that the male to female ratio of affected patients was approximately 1:1.2,8 However, a large, more recent study showed a female-to-male ratio greater than 2:1.1 This likely reflects the increase in female sports participation over the last 2 decades and suggests that females may be at a greater risk of developing the syndrome.
Direct pressure measurement best evaluation
Despite attempts to develop noninvasive testing for CCS, the gold standard remains the direct measurement of intracompartmental pressures. There is some controversy regarding the upper limit of normal, but most authors agree that a resting pressure >15 mm Hg is abnormally elevated.1,2,5 Other cutoffs cited in the literature include a 1-minute post-exercise value greater than 30 mm Hg, and a 5-minute post-exercise reading >25 mm Hg.5 Turnipseed and colleagues recommend checking post-exercise values in patients with modestly elevated resting pressures of 16 to 24 mm Hg to confirm the diagnosis. Because of the pathophysiology of the syndrome, it seems appropriate to also check 5- or 10-minute post-exercise pressures in patients with typical clinical presentations and normal resting pressures.
Orthopedic, vascular, and general surgeons receive training in compartmental pressure measurement. There are 4 techniques for measurement: the simple needle, the Whitesides infusion, the wick catheter, and the slit catheter. Simple needle devices (such as the Stryker stic, FIGURE 2) have increased in popularity because they are handheld, portable, contain a scale within the device for direct measurement, and are easily operated in a clinic setting.14
Diagnostic tools that may yet prove useful
Many other diagnostic modalities have been studied in the last 10 years and may eventually prove helpful. Near infrared spectroscopy has demonstrated a relative deoxygenation during exercise in CCS patients and a delayed reoxygenation in the immediate post-exercise period.15
MIBI scintigraphy has shown decreased muscle perfusion at peak exercise when compared with next-day imaging.16,17
Laser Doppler flow studies conducted in the post-exercise period have demonstrated a delayed peak hyperemia in CCS patients, different from the gradual decrease in blood flow seen in controls.18
Finally, multiple studies have been conducted done with magnetic resonance imaging. Comparisons of pre- and postexercise imaging have shown a greater increase in signal intensity in patients with CCS.19 Despite these findings, though, no clear clinical indications for these tools exist.
FIGURE 2
Measurement with Stryker stic
Measurement of lateral superficial posterior compartment pressure with the Stryker stic on a 16-year-old girl with 4-month history of exertional calf pain.
Treatment options
Conservative measures unconvincing
A few studies have addressed the efficacy of conservative treatment of CCS, but most physicians have found such therapy unsuccessful. Modalities tried include nonsteroidal anti-inflammatory drugs (NSAIDs), diuretics, compression, stretching, orthoses, massage, prolonged rest, change in training surface, change in footwear, change in sport, heat, electrostimulation, and whirlpool.20
One small study showed that compartment pressures in middle-aged men with CCS decreased following treatment with diuretics.21 Another small study showed that athletes receiving compartmental massage increased the duration of time they were able to exercise before developing symptoms.22 A third trial found competitive runners to have significantly higher pressures than competitive cyclists, suggesting runners with CCS may be able to bike as an alternative form of exercise.23
The few data regarding other modalities suggests that only prolonged rest or cessation of sport is effective.24,25 These options, however, may be impractical for competitive athletes who often have no desire to modify their sports participation. With little available evidence, the decision to offer conservative treatment and the type of conservative therapy to recommend remain controversial.
Fasciotomy track record good
Fasciotomy is the most widely used surgical treatment for CCS. The surgeon makes 1 to 3 small skin incisions, exposes the underlying fascia of the affected compartment, and incises the fascia (FIGURES 3 AND 4). Most of these operations are performed under local anesthesia and last less than an hour. Complications are rare, but can include seroma, hemorrhage, cellulitis, peripheral nerve injury, popliteal injury, tibial artery injury, and deep vein thrombosis (DVT).1,2
Patient satisfaction with the operation ranges from 80% to 95% in most published series.1,2,3,5,26 The typical postoperative course involves crutches for the first few days, followed by nonimpact aerobic training for 2 to 4 weeks. Impact aerobic training is next, with gradual return to sport by 2 to 3 months depending on the intensity of sports participation and type of sport practiced.1,4
Faciectomy preferred by some. Though published long-term follow-up data are few, Turnipseed et al found an 11% CCS recurrence rate among patients undergoing fasciotomies before 1985, compared with a 6% recurrence among patients who received fasciectomies between 1991 and 2001.1 The latter procedure involves excision of strips of fascia, which theoretically should decrease the risk of scarring over the compartment and subsequent recurrence of symptoms. This is one reason fasciectomy has become the procedure of choice for some physicians, while others reserved it for patients with recurrent CCS. Until a randomized study is performed, it will be difficult to compare the efficacy of fasciotomy and faciectomy.
FIGURE 3
5 days postsurgery
21-year-old female collegiate track athlete 5 days after anterior, lateral, and lateral superficial posterior compartment release.
FIGURE 4
6 months later
16-year-old female hockey and soccer player 6 months after anterior and lateral fasciectomy.
Acknowledgments
The author would like to thank Dr. William Turnipseed, MD, Department of Vascular Surgery, University of Wisconsin, for his assistance in the preparation of this review article.
CORRESPONDING AUTHOR
Jon Englund, MD, Memorial Healthplex Sports Medicine Institute, 111 West Jefferson, South Bend, IN 46601. E-mail: [email protected]
1. Turnipseed WD. Diagnosis and management of chronic compartment syndrome. Surgery 2002;132:613-619.
2. Detmer DE, Sharpe K, Sufit RL, Girdley FM. Chronic compartment syndrome: diagnosis, management, and outcomes. Am J Sports Med 1985;13:162-170.
3. Moeyersoons JP, Martens M. Chronic compartment syndrome: diagnosis and management. Acta Orthop Belg 1992;58:23-27.
4. Hargens AR, Muburak SJ. Current concepts in the pathophysiology, evaluation, and diagnosis of compartment syndrome. Hand Clin 1998;14:371-383.
5. Tubb CC, Vermillion D. Chronic exertional compartment syndrome after minor injury to the lower extremity. Mil Med 2001;166:366-368.
6. Jerosch J, Castro WHM, Hoffstetter R, Reer R. Secondary effects of knee braces on the intracompartmental pressure in the anterior tibial compartment. Acta Orthop Belg 1995;61:37-42.
7. Martens MA, Moeyersoons JP. Acute and recurrent effort-related compartment syndrome in sports. Sports Med 1990;9:62-68.
8. Pedowitz RA, Hargens AR, Murbarak SJ, Gershuni DN. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 1990;18:35-40.
9. Adams MT, Wixon CL. Popliteal artery entrapment syndrome. J Am Coll Surg 2003;196:152-153.
10. Allen MJ, Barnes MR, Bell PR, Bolia A, Hartshorne TC. Popliteal entrapment syndrome: misdiagnosed as a compartment syndrome. Eur J Vasc Surg 1993;7:342-345.
11. DeLee J, Drez D, Miller MD. DeLee and Drez’s Orthopaedic Sports Medicine. 2nd ed. Philadelphia, Pa: WB Saunders 2003;2177-2178.
12. Mavor GE. The anterior tibial syndrome: a chronic form. J Bone Joint Surg Br 1956;38:513-517.
13. Reneman RS. The anterior and lateral compartment syndrome of the leg due to intensive use of muscles. Clinic Orthop Relat Res 1975;113:69-80.
14. Heppenstall RB. An update in compartment syndrome investigation and treatment. Univ Penn Ortho J 1997;10:49-57.
15. Mohler LR, Styf JR, Pedowitz RA, Hargens AR, Gershuni DH. Intramuscular deoxygenation during exercise in patients who have chronic anterior compartment syndrome of the leg. J Bone Joint Surg Am 1997;79:844-849.
16. Edwards PD, Miles KA, Owens SJ, Kemp PM, Jenner JR. A new non-invasive test for the detection of compartment syndromes. Nuc Med Commun 1999;20:215-218.
17. Owens S, Edwards P, Miles K, Jenner J, Allen M. Chronic compartment syndrome affecting lower limb: MIBI perfusion imaging as an alternative to pressure monitoring: two case reports. Br J Sports Med 1999;33:49-53.
18. Abraham P, Leftheriotis G, Saumet JL. Laser Doppler flowmetry in the diagnosis of chronic compartment syndrome. J Bone Joint Surg Br 1998;80:365-369.
19. Verleisdonk EJ, van Gils A, van der Werken C. The diagnostic value of MRI scans for the diagnosis of chronic exertional compartment syndrome of the lower leg. Skeletal Radiol 2001;30:321-325.
20. Micheli LJ, Solomon R, Solomon J, Plasschaert VF, Mitchell R. Surgical treatment for lower-leg compartment syndrome in young female athletes. Am J Sports Med 1999;27:197-201.
21. Christensen JT, Eklof B, Wulff K. The chronic compartment syndrome and response to diuretic treatment. Acta Chir Scand 1983;149:249-252.
22. Blackman PG, Simmons LR, Crossley KM. Treatment of chronic exertional anterior compartment syndrome with massage: a pilot study. Clin J Sport Med 1998;8:14-17.
23. Beckham SG, Grana WA, Buckley P, Breazile JL, Claypool PL. A comparison of anterior compartment pressures in competitive runners and cyclists. Am J Sports Med 1993;21,1:36-40.
24. Shah S, Miller B, Kuhn J. Chronic exertional compartment syndrome. Am J Orthop 2004;33:335-341.
25. Martens MA, Backaert M, Vermaut G, Mulier JC. Chronic leg pain in athletes due to recurrent compartment syndrome. Am J Sports Med 1984;12:148-151.
26. Styf J, Korner L. Chronic anterior-compartment syndrome of the leg. Results of treatment by fasciotomy J Bone Joint Surg Am 1986;68:1338-1347.
1. Turnipseed WD. Diagnosis and management of chronic compartment syndrome. Surgery 2002;132:613-619.
2. Detmer DE, Sharpe K, Sufit RL, Girdley FM. Chronic compartment syndrome: diagnosis, management, and outcomes. Am J Sports Med 1985;13:162-170.
3. Moeyersoons JP, Martens M. Chronic compartment syndrome: diagnosis and management. Acta Orthop Belg 1992;58:23-27.
4. Hargens AR, Muburak SJ. Current concepts in the pathophysiology, evaluation, and diagnosis of compartment syndrome. Hand Clin 1998;14:371-383.
5. Tubb CC, Vermillion D. Chronic exertional compartment syndrome after minor injury to the lower extremity. Mil Med 2001;166:366-368.
6. Jerosch J, Castro WHM, Hoffstetter R, Reer R. Secondary effects of knee braces on the intracompartmental pressure in the anterior tibial compartment. Acta Orthop Belg 1995;61:37-42.
7. Martens MA, Moeyersoons JP. Acute and recurrent effort-related compartment syndrome in sports. Sports Med 1990;9:62-68.
8. Pedowitz RA, Hargens AR, Murbarak SJ, Gershuni DN. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 1990;18:35-40.
9. Adams MT, Wixon CL. Popliteal artery entrapment syndrome. J Am Coll Surg 2003;196:152-153.
10. Allen MJ, Barnes MR, Bell PR, Bolia A, Hartshorne TC. Popliteal entrapment syndrome: misdiagnosed as a compartment syndrome. Eur J Vasc Surg 1993;7:342-345.
11. DeLee J, Drez D, Miller MD. DeLee and Drez’s Orthopaedic Sports Medicine. 2nd ed. Philadelphia, Pa: WB Saunders 2003;2177-2178.
12. Mavor GE. The anterior tibial syndrome: a chronic form. J Bone Joint Surg Br 1956;38:513-517.
13. Reneman RS. The anterior and lateral compartment syndrome of the leg due to intensive use of muscles. Clinic Orthop Relat Res 1975;113:69-80.
14. Heppenstall RB. An update in compartment syndrome investigation and treatment. Univ Penn Ortho J 1997;10:49-57.
15. Mohler LR, Styf JR, Pedowitz RA, Hargens AR, Gershuni DH. Intramuscular deoxygenation during exercise in patients who have chronic anterior compartment syndrome of the leg. J Bone Joint Surg Am 1997;79:844-849.
16. Edwards PD, Miles KA, Owens SJ, Kemp PM, Jenner JR. A new non-invasive test for the detection of compartment syndromes. Nuc Med Commun 1999;20:215-218.
17. Owens S, Edwards P, Miles K, Jenner J, Allen M. Chronic compartment syndrome affecting lower limb: MIBI perfusion imaging as an alternative to pressure monitoring: two case reports. Br J Sports Med 1999;33:49-53.
18. Abraham P, Leftheriotis G, Saumet JL. Laser Doppler flowmetry in the diagnosis of chronic compartment syndrome. J Bone Joint Surg Br 1998;80:365-369.
19. Verleisdonk EJ, van Gils A, van der Werken C. The diagnostic value of MRI scans for the diagnosis of chronic exertional compartment syndrome of the lower leg. Skeletal Radiol 2001;30:321-325.
20. Micheli LJ, Solomon R, Solomon J, Plasschaert VF, Mitchell R. Surgical treatment for lower-leg compartment syndrome in young female athletes. Am J Sports Med 1999;27:197-201.
21. Christensen JT, Eklof B, Wulff K. The chronic compartment syndrome and response to diuretic treatment. Acta Chir Scand 1983;149:249-252.
22. Blackman PG, Simmons LR, Crossley KM. Treatment of chronic exertional anterior compartment syndrome with massage: a pilot study. Clin J Sport Med 1998;8:14-17.
23. Beckham SG, Grana WA, Buckley P, Breazile JL, Claypool PL. A comparison of anterior compartment pressures in competitive runners and cyclists. Am J Sports Med 1993;21,1:36-40.
24. Shah S, Miller B, Kuhn J. Chronic exertional compartment syndrome. Am J Orthop 2004;33:335-341.
25. Martens MA, Backaert M, Vermaut G, Mulier JC. Chronic leg pain in athletes due to recurrent compartment syndrome. Am J Sports Med 1984;12:148-151.
26. Styf J, Korner L. Chronic anterior-compartment syndrome of the leg. Results of treatment by fasciotomy J Bone Joint Surg Am 1986;68:1338-1347.
Are Ayurvedic herbs for diabetes effective?
- Limited randomized control trial data and observational studies show that the herbs Coccinia indica, holy basil, fenugreek, Gymnema sylvestre, and the herbal formulas Ayush-82 and D-400 have glucose-lowering effects. But these herbs are not as well studied as others more familiar to Western medicine. (B)
- Inform patients who ask about Ayurveda that traditional practitioners rely on the interaction of several components, of which herbs are just one, and that no formal studies have looked at Ayurveda as a whole system. (B)
- Objective: To evaluate and synthesize the evidence on the effect of Ayurvedic therapies for diabetes mellitus.
- Design: Systematic review of trials.
- Measurements and main results: We found no study that assessed Ayurvedic as a system of care. Botanical therapy was by far the most commonly studied Ayurvedic treatment. Herbs were studied either singly or as formulas. In all, 993 titles in Western computerized databases and 318 titles identified by hand-searching journals in India were examined, yielding 54 articles reporting the results of 62 studies. The most-studied herbs were G sylvestre, C indica, fenugreek, and Eugenia jambolana. A number of herbal formulas were tested, but Ayush-82 and D-400 were most often studied. Thirty-five of the studies included came from the Western literature, 27 from the Indian. Seven were randomized controlled trials (RCTs) and 10 controlled clinical trials (CCTs) or natural experiments. Twenty-two studies went on to further analysis based on a set of criteria. Of these, 10 were RCTs, CCTs, or natural experiments, 12 were case series or cohort studies. There is evidence to suggest that the herbs C indica, holy basil, fenugreek, and G sylvestre, and the herbal formulas Ayush-82 and D-400 have a glucose-lowering effect and deserve further study. Evidence of effectiveness of several other herbs is less extensive (C tamala, E jambolana, and Momordica charantia).
- Conclusions: There is heterogeneity in the available literature on Ayurvedic treatment for diabetes. Most studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested (more than 44 different interventions identified) and in the method of their preparation. Despite these limitations, there are sufficient data for several herbs or herbal formulas to warrant further studies.
Given the US population’s increasing interest in herbal and alternative therapies, it is just a matter of time before you will be fielding questions from patients about Ayurveda—a comprehensive system of health care that originated in India roughly 3000 years ago, emphasizing the relationships among body, mind, and spirit. Diabetes has been a particular focus of this medical system, and a few Ayurvedic herbs do indeed appear to exert glucose lowering mechanisms.
But how strong is the evidence? Though Ayurveda involves the interaction of many kinds of therapy, this review examines only the literature pertaining to herbal remedies your patients with diabetes are likely to ask about.
Ayurveda more than herbs
Ayurveda (Sanskrit for “knowledge of life” or “knowledge of longevity”) has now spread beyond India’s borders to include the rest of the Indian subcontinent, Sri Lanka, Malaysia, Mauritius, South Africa, Japan, Russia, Europe, and North America. At its root, Ayurveda seeks to restore an individual’s innate harmony. Primary Ayurvedic treatments include diet, exercise, meditation, herbs, massage, exposure to sunlight, controlled breathing, and detoxification treatments.
Dosha imbalance. Ayurveda considers human beings a microcosm of nature. All living and nonliving things are believed to consist of 5 basic elements: ether (space), air, fire, water, and earth. In humans these elements combine and manifest in the human body as 3 humors, or doshas, known as vata, pitta, and kapha.
The doshas govern all biological, psychological, and pathophysiological functions. They are fundamental to human health, and an imbalance of the doshas brings on illness. Consequently, Ayurveda seeks to bring the doshas back into harmony. Balanced doshas, as well as good-quality tissues (dhatus), proper digestion, and elimination of excretions (malas), are considered essential in Ayurveda for maintaining health.
Dosha body type influences treatment. In addition, humans are endowed at birth with 1 of 7 body types, depending on which dosha or combination of the 3 basic doshas dominates. Body types can be dominated by a single humor (vata, pitta, or kapha), or they can be dominated by combinations: vata-kapha (when vata and kapha are present in almost equal amounts); vata-pitta; pitta-kapha; or vata-pitta-kapha. A person’s dosha body type is expressed physically and emotionally; for example, a person with a vata-dominant body type will have a thin frame and an insecure temperament. The Ayurvedic physician takes body type and imbalances among the doshas into consideration when treating a patient.
Application to diabetes. The Indian word for diabetes is madhumeha, from madhu, meaning “sweet/sweetness,” and meha, meaning excessive urination. Classical Ayurvedic therapy for madhumeha (diabetes) begins with an assessment of the dosha imbalance. In all types of pramehas (urinary disorders), kapha is vitiated, but in madhumeha, vata is often aggravated as well. Therefore, therapies will be directed at both vata and kapha simultaneously to restore the balance of the doshas.1,2
Herbs are a commonly used treatment in Ayurveda. Ethnobotanical studies of traditional herbal remedies used for diabetes around the world have identified more than 1200 species of plants with hypoglycemic activity. These plants are broadly distributed throughout 725 different genera. The pharmacopoeia of India is especially rich in herbal treatments for diabetes. Eighty-five percent of the 20 antidiabetes plants most widely used around the world are prescribed in India.3 A few of the herbs commonly used by Ayurveda practitioners to treat diabetes are summarized in the TABLE.
In response to the increasing interest in Ayurveda and herbal treatments for diabetes in this country, the National Center for Complimentary and Alternative Medicine (NCCAM) requested we conduct a systematic review of Ayurvedic therapy for diabetes. This paper reports the results of that review, and is a condensation of an evidence report available at www.ahrq.gov/clinic/epcsums/ayurvsum.htm.
TABLE
Ayurvedic characteristics of herbs commonly used to treat diabetes
| HERB | TASTE (RASA) | INCREASES (AGGRAVATES) | DECREASES (PACIFIES) |
|---|---|---|---|
| Gymnema | Kasaya (astringent) | Kapha, Pitta | |
| Momordica | Tikta (bitter) | Kapha, Pitta | |
| Trigonella (fenugreek) | Tikta (bitter); Madhura (sweet) | Pitta | Kapha, Vata |
| Coccinia indica | Kasaya (astringent); Tikta (bitter) | Vata, Pitta | |
| Pterocarpus | Kasaya (astringent) | Vata | |
| Source: Kapoor, 1990;32 Dash, 198733 Mishra, Singh, and Dagenais, 2001.34 | |||
Methods
Identification of literature
We used the search term “Ayurveda” plus the names of 16 major botanicals characteristically used in Ayurveda for an initial search of the Western literature. The herbal terms were added to the search to increase its sensitivity, making it possible to find studies that used Ayurvedic herbal therapy without necessarily being directly identified as Ayurvedic studies.
We were concerned that a large body of literature existed in India that could not be obtained through the conventional search strategy outlined above. Hence, we decided to conduct a search for Ayurvedic literature from the Indian subcontinent. A physician member of the research team, fluent in English and Hindi and who had trained in India, went to India to identify Ayurvedic literature available there.
We therefore used several sources for our search:
- An initial “waterfront” search, which already had identified 120 articles on diabetes and Ayurveda (which was used by NCCAM to establish the rationale for selecting diabetes as the focus of this review).4 This search is detailed in our Evidence Report (available at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372) and included Medline, HealthSTAR, Allied and Complementary Medicine, MANTIS, CAB HEALTH, BIOSIS Previews, and EMBASE.
- The in-person literature search in India—we obtained 16 volumes of abstracts from various Indian Ayurvedic journals, as compiled by the Central Council for Research in Ayurveda and Siddha (CCRAS) library. This yielded 318 titles.
- An additional online search of the previously mentioned databases for common botanicals used in the treatment of diabetes. This search yielded 773 additional articles.
- A search of the online CINAHL database, which yielded 70 articles.
- The reference lists of important articles in the Ayurveda/diabetes literature. We identified review articles of herbal treatment of diabetes and checked to see if they focused on any of the Ayurvedic herbal therapies we had identified for diabetes. Checking the bibliographies of all the articles we identified from any source, we found an additional 30 titles that were potentially relevant to our search.
- An RCT or a CCT or a natural experiment with a comparison arm that did not receive an herb or Ayurvedic therapy. RCTs of any size were included. For CCTs or natural experiments, the study had to have at least 1 treatment arm that contained at least 10 patients.
- Because of a paucity of studies meeting these design criteria, we also assessed cohort or case series data that used a “pre/post” method of analysis, if their sample included at least 10 subjects.
- The study had to test Ayurveda as a method or herbs used as a single agent, a formula acting as a single agent, or a limited combination of products (no more than 3) acting as a single agent. The agent had to be dispensed more than 1 time to the study patients (in other words, no single-dose studies).
- The study had to report on at least 1 of 3 outcome measures at 30 days minimum following the start of the study: glycosylated hemoglobin (Hb A1c), fasting blood glucose, or postprandial blood glucose at either 2 hours (preferred) or 1 hour (acceptable).
Data extraction
Detailed information from each study was extracted using a specialized form. The physician reviewers, working independently, extracted data in duplicate and resolved disagreements by consensus. A senior physician resolved any remaining disagreements. Information extracted from articles included the diagnostic criteria used to make the diagnosis (Ayurvedic or Western or both); the location in which the study was done; the subject population (age, gender, other demographics); the sample size in each arm of the study; the interventions used (primarily the names of the individual herbs or mineral and the manner of their preparation); the length of the study; and the outcomes. To evaluate the quality of the design and execution of trials, we collected information on the study design, appropriateness of randomization, blinding, description of withdrawals and dropouts, and concealment of allocation.5,6 A quality score was calculated for each trial using a system developed by Jadad.5 Empirical evidence has shown that studies scoring 2 or less on the Jadad scale report exaggerated results compared with studies scoring 3 or more.7 While other elements of the design and execution of controlled trials have been proposed as quality measures, empirical evidence supporting their use as generic quality measures is lacking.8
Data synthesis
The studies we reviewed were judged clinically to be too heterogeneous to support a quantitative synthesis; therefore, our review is narrative. However, to promote the comparison of results across studies we extracted outcome data in a common format and present it in graphs for visual comparison. For studies that reported on both 1-hour and 2-hour postprandial blood glucose levels, we chose the 2-hour measurement for the analysis. For studies that reported more than 1 follow-up time, we selected the follow-up time that was closest to 3 months.
Twenty-two studies were selected for further analysis based on the criteria described above. These studies represented either RCTs (2) or CCTs/natural experiments (5) with a comparison arm that did not receive an herb, or studies that had pre/post comparison data available (8).
We considered 2 subgroups of eligible studies separately: the RCTs and CCTs or natural experiments that had nonherbal/Ayurvedic comparison arm(s) were considered 1 subgroup, and all other eligible (pre/post data available) studies made up the second subgroup. The RCT/CCT/natural experiments subgroup allowed us to do a comparison between herbal and nonherbal arms within a study, providing a stronger level of evidence than pre/post comparisons. For these studies, we were able to compare the effects of different treatments after the placebo or nonherbal arm results were taken into account by estimating a difference of differences statistic and its 95% confidence interval. This statistic is equal to the difference between the pre- and post-treatment means in the Ayurvedic arm minus the analogous difference in the nonherbal/Ayurvedic arm. The pre/post studies subgroup did not allow a concurrent comparison, but the difference between pre- and post-treatment means could be estimated along with a 95% confidence interval.4 Further details are given in our Evidence Report (available online at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372).
For each study subgroup, we assessed the possibility of publication bias graphically by evaluating a funnel plot of the study summary statistics for asymmetry, which would result from the nonpublication of small trials with negative outcomes. Because graphical evaluation can be subjective, we also conducted an adjusted rank-correlation test9 and a regression asymmetry test10 as formal statistical tests for publication bias.
Results
Description of the evidence
As a result of our search, we considered a total of 1311 articles (FIGURE 1). We reviewed in depth 62 studies, of which 22 were analyzed statistically. Ten studies came from the Western literature, and 12 came from the Indian literature. There were 7 randomized controlled trials, controlled clinical trials, or natural experiments with a treatment/no treatment comparison. There were 15 case series or cohort studies using a “pre/post” analysis. TABLE W2 (available online at www.jfponline.com) summarizes the characteristics of studies.
In terms of interventions, there was no study that tested Ayurveda as a system of care; all tested herbs. Of the 22 studies described narratively in this article, the 2 most commonly tested single herbs were Coccinia indica and fenugreek. The Ayurvedic formula Ayush-82 was the most commonly tested herbal formula. Diet was used as an intervention or co-intervention in 15 of the 22 studies.
FIGURE 1
Ayurveda literature review strategy of focused search for human diabetes articles
Quality of the evidence
Only the RCTs, CCTs, and natural experiments were given a Jadad score, which rates studies on a 0 to 5 scale.5 Of the 7 such studies, 3 received a Jadad score of zero, 3 studies scored a 1, and only 1 study received a 4 on this scale. This is the only high quality study in our analysis.
Controlled trials/natural experiments with nonherbal comparison arm(s)
There were 7 RCTs, CCTs or natural experiments that met the inclusion criteria. The data for these 7 studies are reported in FIGURE 2.
Coccinia indica. Azad Khan, Akhtar, and Mahtab (1979) performed a randomized controlled trial to assess the hypoglycemic properties of a preparation of the herb C indica on uncontrolled and untreated type 2 diabetes patients.11 Thirty-eight patients with type 2 diabetes who were attending the outpatient department of the Bangladesh Institute of Research and Rehabilitation in Diabetes in Dhaka, Bangladesh, were recruited for the study. Only uncontrolled or newly diagnosed patients were enlisted. The intervention consisted of a freeze-dried powder of crushed leaves of C indica, given in a dose of 900 mg twice a day for 6 weeks. Control patients received placebo twice a day for the same period. Of the 16 patients receiving C indica, 10 patients showed a marked improvement in the glucose tolerance tests to values closer to normal, while none in the placebo arm showed marked improvement. The Jadad score for the trial was 4. This study was identified from the Eastern literature search.
Holy basil. Agrawal, Rai, and Singh (1996) reported the results of a randomized, placebo controlled crossover trial of the effects of a leaf extract of holy basil (Ocimum sanctum) on patients with type 2 diabetes.12 Forty patients were recruited from community advertisements in Kanpur, India, and through visits to the offices of local dieticians. All subjects had a 5-day run-in period during which they all consumed a tea made from holy basil leaves. This was followed by an 8-week experimental period. The patients were randomly assigned to drink the holy basil leaf tea for 4 weeks followed by placebo leaves for 4 weeks, or the reverse (the placebo leaves first, followed by the holy basil leaf tea). The authors concluded that holy basil leaf powder caused significant reduction in the level of fasting blood sugar and postprandial blood sugar, and a moderate reduction in cholesterol. The Jadad score for this trial is 1. This study was identified from the Western literature search.
Cinnamonum tamala. Chandola, Tripathi, and Udupa (1980) assessed the hypoglycemic effects of C tamala in type 2 diabetes patients.13 Thirty-two patients were recruited from the outpatient departments of the Institute of Medical Sciences, Varanasi, India, and received the intervention and 8 patients with type 2 diabetes served as controls. The socioeconomic characteristics of the patients were not noted, and the authors did not report if the 2 arms of patients were statistically equivalent on important prognostic variables at the start of the trial. The intervention consisted of leaves of C tamala (tejpatra) that were dried, pulverized, and filtered through a fine mesh, and given as 2 heaped teaspoons 4 times a day before meals and tea for a total of 1 month. All patients were advised to follow a 1800-calorie diet with restriction of sugar, potato, and rice. The control patients were only instructed to follow the above diet with no other medications. Fasting blood sugars were assessed in both arms of patients before the trial and at the end of 1 month. The authors reported the mean fasting blood sugar improved from 153 mg/dL to 113 mg/dL (P<.001) at the end of 1 month in patients treated with C tamala, while there was no improvement in control patients. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Coccina indica. Kamble, Jyotishi, Kamalakar, et al (1996) studied the effect of fresh leaves of C indica on blood sugar levels and on hyperlipidemia in noninsulin-dependent diabetes mellitus (NIDDM, type 2) patients at an Ayurvedic clinic in Nagpur, India.14 Patients were classified into 4 arms: a healthy comparison arm (arm I, 15 patients); a NIDDM comparison arm (arm II, 30 patients); NIDDM patients treated with Coccinia (arm III, 25 patients); and a NIDDM arm treated with chlorpropamide (arm IV, 15 patients). Patients were given the Coccinia (decocted from fresh leaves, dried into a paste, and made into a 3-g tablet) twice a day for 12 weeks, although control group data only exist at 6 weeks. For patients in arm III, the study showed a statistically significant reduction in mean fasting blood sugar, from 160 to 118 mg/dL (P<.001) at 12 weeks, and a significant decrease in blood sugar levels after glucose tolerance tests: the 2-hour level dropped from 308 mg/dL to 142 mg/dL (P<.001). These results were roughly equivalent to those found in the chlorpropamide arm at 6 weeks, with any differences being not statistically significant. Additionally, after 12 weeks of treatment, the Coccinia treated patients showed significant within group reductions in levels of cholesterol (P<.001), phospholipid (P<.05), triglyceride (P<.001), and free fatty acid (P<.001) compared with untreated patients with diabetes. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Jamun beej. Kohli and Singh (1993) studied the effects of Jamun beej (Eugenia jambolana) on fasting blood sugar, glucose tolerance test, and symptomatic relief of symptoms associated with diabetes.15 Thirty patients identified from the outpatient unit of the Sunderlal Hospital in Varanasi, India, who had NIDDM confirmed by glucose tolerance test, were given E jambolana crushed into a fine powder at a dose of 4 g 3 times a day for 3 months. No dietary restrictions were included in the study. A second arm of 6 patients with confirmed NIDDM was given chlorpropamide (250 mg/d). No demographic information was provided on these patients. The authors reported a statistically significant reduction in mean fasting blood sugar of 51.86 mg/dL at 2 months (P<.001) but not at 3 months. The study also demonstrated a significant reduction in the response to the glucose tolerance test at both 2 months (P<.001) and at 3 months (P<.01), but comparisons with the patients receiving chlorpropamide were not statistically significant. The Jadad score total is 1. This study was identified from the Eastern literature search.
Gymnema sylvestre. Baskaran, Ahamath, Shanmugasundaram, et al (1990) studied the effects of GS4, a specific isolate of G sylvestre, on the blood sugar of 47 type 2 diabetes patients.16 The intervention group consisted of 22 patients with diabetes on oral hypoglycemic therapy (continued during the trial), plus herbal therapy with Gymnema at a dose of 400 mg/d. The control group consisted of 25 patients with type 2 diabetes on conventional medications alone. Although the arms were reasonably matched for age and Broca index (percent of ideal body weight) based on our analysis of individual patient data in the study, the 2 arms were statistically different at baseline with respect to fasting blood sugar. The authors reported that in the intervention group at 12 months of follow-up, mean fasting blood sugar improved from 174 mg/dL to 124 mg/dL (P<.001) and Hb A1c improved from 11.9% to 8.48% (P<.001). Changes in the control group over this time were not significant. Virtually all patients in arm I developed hypoglycemic symptoms, and the dose of their normal oral hypoglycemic agent needed to be changed or stopped. The Jadad score is 0. This study was identified from the Western literature search.
GS4. Shanmugasundaram, Rajeswari, Baskaran, et al (1990b) reported the effect of an herbal compound GS4 on blood glucose, insulin requirements, and cholesterol in patients with type 1 and type 2 diabetes.17 The intervention group consisted of 23 type 1 patients and 4 type 2 patients (ages 44–50 years, 25% female) who continued their insulin in addition to taking the herbal intervention, and the control group consisted of 37 type 1 patients who were on insulin therapy. The clinical equivalence of the 2 arms at baseline was not mentioned. The intervention drug was GS4, a recrystallized precipitate of the alcoholic extract of the acidic fraction of G sylvestre; at dose of 400 mg/d. At 6 to 8 months of follow-up, all patients in the intervention group developed hypoglycemic episodes, and their insulin doses were reduced by 10 units at a time; differences compared to controls were statistically significant. The Jadad score was 1. This study was identified from the Western literature search.
Summary. In summary, comparisons of the studied herbs with either placebo, diet, or as an adjunct to medical hypoglycemic therapy consistently reported statistically significant benefits in glucose control. Studies comparing herbs to the oral hypoglycemic chlorpropamide did not report differences between groups.
FIGURE 2
Glucose-lowering effects of Ayurvedic herbs compared with nonherbal treatments
Case series or cohort studies without a concurrent comparison group
Fifteen studies had treatment arms that reported blood glucose or Hb A1c values before and after herbal interventions—ie, that made available pre/post data.13,18-31 Herbs were tested singly (7 studies), in combination (7 studies), or both singly and in combination (1 study). All of these studies are limited by the lack of randomization. Many are also limited by small sample size and short study duration.
The data are presented in FIGURE 3 in the following order: studies or arms of studies using a single herbal preparation first, followed by studies that use a formula or a group of herbs and minerals. Some studies with multiple arms will have listings in more than one place. As FIGURE 3 shows, most pre/post comparison studies using single herbs and formulas favor treatment. Hb A1c is measured in only 5 of the studies. Two of those studies seem to strongly favor treatment; 2 are almost equivocal; and 1 does not favor treatment.
The small number of RCTs/CCTs/natural experiments measuring postprandial blood glucose and Hb A1c, and the small number of case series and cohorts measuring Hb A1c, make the assessment of publication bias for these outcomes problematic. For the remaining outcomes, only slight evidence of publication bias was evident among the case series and cohort studies for the fasting blood glucose outcome (adjusted rank correlation test P=.97; regression asymmetry test P=.06). For this outcome, we have trial data available, a setting in which no evidence of publication bias is seen.
FIGURE 3
Effect of Ayurvedic herbs on blood glucose and Hb A1c
Discussion
No controlled trials have assessed Ayurveda as a system of care. Furthermore, among studies of herbal preparations, controlled trials are rare and mostly of poor quality. Still, we found evidence suggesting that some Ayurvedic herbs have clinically important hypoglycemic effects.
The best-quality RCT reported beneficial results for C indica. Other studies have generally reported benefits of C indica; however, results have been inconsistent.
A single trial of holy basil reported a benefit in controlling fasting blood glucose only. G sylvestre was used in a number of studies, again with generally beneficial results. Gymnema was also a constituent in 2 of the formulas that reported beneficial results: D-400 and Ayush-82.
Methodological shortcomings. The evidence we found falls short of proof. As noted, the individual studies we assessed had significant methodological shortcomings. Few used a randomized, placebo-controlled design, despite the feasibility of such methods. Studies generally were underpowered to determine even large effect sizes. Many studies involved an extremely small number of subjects (fewer than 10). A number of studies failed to use appropriate statistical methods in reporting the results. Furthermore, the duration of most studies was short, and only intermediate outcomes (measure of blood sugar control) were reported. Longer term studies that assess clinical outcomes are required. Lastly, there is great heterogeneity in the available literature on Ayurvedic treatment for diabetes, despite the fact that the overwhelming majority of studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested and in the method of their preparation.
No true studies of Ayurveda. None of the identified studies assessed Ayurveda as a system of diagnosis and care. The literature reported mainly studies of single herbs; however, in clinical Ayurvedic practice, herbs are usually given in combination. Formulas can include minerals and metals in addition to multiple plants.
Ayurvedic practitioners assert that the sum of a formula is more potent than the constituents taken individually and, further, that the mineral and metal components boost the formula’s potency. Additional Ayurvedic therapies such as diet, yoga, or special purification routines, should be controlled for when recruiting and assessing patients. It is unclear, perhaps doubtful, that taking a single component of Ayurvedic is sufficient to represent the holistic effect of Ayurvedic interventions.
Limitations of our review. Our searches showed that herbal therapies were emphasized in published studies of Ayurveda. However, no conclusions can be drawn about the use of Ayurveda as a whole system for the treatment of diabetes. Although extensive efforts were made to obtain the relevant literature from India, studies not published in English were excluded, as were MD thesis reports. A handful of studies could not be obtained. Therefore we may not have included in this review all clinical trials. By specifically hand searching documents published in India, we identified that an important body of Ayurvedic literature is not identifiable using traditional systematic review methods.
In summary, we found preliminary evidence suggesting that some herbs and herbal formulas used in Ayurvedic therapy can have clinically important glucose-lowering effects. C indica, holy basil, and Gymnema are particularly worthy of additional study.
Acknowledgments
This research was performed by the Southern California Evidence-Based Practice Center based at RAND, Santa Monica, CA under contract with the Agency for Healthcare Research and Quality (Contract No. 290-97-0001) with support from the National Center for Complementary and Alternative Medicine. The authors of this article are responsible for its contents. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality, the National Center for Complementary and Alternative Medicine, National Institutes of Health, or the US Department of Health and Human Services.
CORRESPONDING AUTHOR
Paul G. Shekelle, MD, PhD, West Los Angeles VA Medical Center, 111G, 11301 Wilshire Blvd, Los Angeles, CA 90073. E-mail: [email protected]. At the time of this study, Dr. Shekelle was a Senior Research Associate of the Veterans Affairs Health Services Research and Development Service.
1. Lad V. An introduction to Ayurveda. Altern Ther Health Med 1995;1:57-63.
2. Chopra A, Doiphode VV. Ayurvedic medicine. Core concept, therapeutic principles and current relevance. Med Clin North Am 2002;86:75-89.
3. Marles RJ, Farnsworth NR. Antidiabetic plants and their active constituents. Phytomedicine 1995;2:137-189.
4. Hardy M, Coulter I, Venuturupalli S, et al. Ayurvedic interventions for diabetes mellitus: a systematic review. Evidence Report/Technology Assessment No. 41. AHRQ Publication No. 01-E040; 2001.
5. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12.
6. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-412.
7. Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-613.
8. Balk EM, Bonis PA, Moskowitz H, et al. Correlation of quality measures with estimates of treatment effect in meta-analyses of randomized controlled trials. JAMA 2002;287:2973-2982.
9. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-1101.
10. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
11. Azad Khan A, Akhtar S, Mahtab H. Coccinia indica in the treatment of patients with diabetes mellitus. Bangladesh Med Res Counc Bull 1979;5:60-66.
12. Agrawal P, Rai V, Singh RB. Randomized placebo-controlled single-blind trial of holy basil leaves in patients with non-insulin-dependent diabetes mellitus. Int J Clin Pharmacol Ther 1996;34:406-409.
13. Chandola HM, Tripathi SN, Udupa KH. Hypoglycaemic response of c. tamala in patients of maturity onset (insulin independent) diabetes. J Res Ayurveda Sidda 1980;1:275-290.
14. Kamble SM, Jyotishi GS, Kamalakar PL, Vaidya SM. Efficacy of coccinia indica w. & a. in diabetes mellitus. J Res Ayurveda and Sidda 1996;17(1–2):77-84.
15. Kohli KR, Singh RH. A clinical trial of jambu (eugenia jambolana) in non-insulin dependant diabetes mellitus. J Res Ayurveda Sidda 1993;14(3–4):89-97.
16. Baskaran K, Kizar Ahamath B, Radha Shanmugasundaram K, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol 1990;30:295-300.
17. Shanmugasundaram E, Rajeswari G, Baskaran K, Rajesh Kumar BR, Radha Shanmugasundaram K, Kizar Ahmath B. Use of gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J Ethnopharmacol 1990;30:281-294.
18. Kuppurajan K, Seshadri C, Revathi R. Hypoglycaemic effect of coccinia indica in diabetes mellitus. Nagarjun 1986;29:1-4.
19. Kuppurajan K, Srivatsa A, Krishnaswami CV. Hypoglycemic and hypotriglyceridemic effects of methika churna (fenugreek). Antiseptic 1998;95:78-79.
20. Kumar N, Kumar A, Sharma ML. Clinical evaluation of single and herbo-mineral compound drugs in the management of madhumeha. J Res Ayurveda Sidda 1999;20(1–2):1-9.
21. Sharma RD, et al. Use of fenugreek seed powder in the management of non-insulin dependent diabetes mellitus. Nutr Res 1996;16:1331-1339.
22. Flexible dose open trial of Vijayasar in cases of newly-diagnosed non-insulin-dependent diabetes mellitus. Indian Council of Medical Research (ICMR), Collaborating Centres, New Delhi. Indian J Med Res 1998;108:24-29.
23. Goyal DK, Tiwari SK. Study on sadabahar (vinca rosea linn.) In madhumeha (diabetes mellitus). J Res Ayurveda Sidda 1999;20(1–2):93-100.
24. Chowdhary DP, Dua M, Bharti, Kishore P. Hypoglycaemic effect of a coded formulation: aysuh-82. J Res Ayurveda Sidda 1998;19(3–4):107-115.
25. Pandey VN, Rajagopalan SS, Chowdhary DP. An effective ayurvedic hypoglycemic formulation. J Res Ayurveda Sidda 1995;16(1–2):1-14.
26. Shankar R, Singhal R. Clinical studies of the effect of abraga (mica) chendooram in the treatment of diabetes mellitus (neerazhivu). J Res Ayurveda Sidda 1995;16(3–4):108-117.
27. Maji D, Singh AK. Clinical trial of D-400, a herbomineral preparation in diabetes mellitus. J Diabetic Assoc India 1995;35:1-4.
28. Sircar AR, Ahuja RC, Natu SM, Roy B, Sharma HM. Hypoglycemic, hypolipidemic and general beneficial effects of an herbal mixture MA-471. Alternat Ther Clin Pract 1996;3:26-31.
29. Shankar R, Sighal R. Clinical assessment of the effects of sandana (sandal) podi-a in the treatment of diabetes mellitus (neerazhiv). J Res Ayurveda Sidda 1994;15(3–4):89-97.
30. Sivaprakasam K, Rao KK, Yasodha R, Veluchamy G. Siddha remedy for diabetes mellitus. J Res Ayurveda Sidda 1984;5(1–4):25-32.
31. Kamble SM, Kamlakar PL, Vaidya S, Bambole VD. Influence of coccinia indica on certain enzymes in glycolytic and lipolytic pathway in human diabetes. Indian J Med Sci 1998;52:143-146.
32. Kapoor LD. CRC Handbook of Ayurvedic Medicinal Plants. Boca Raton, Fla: CRC Press; 1990.
33. Dash VB. Materia Medica of Indo-Tibetan Medicine. Delhi, India: MDIA Classics India; 1987;10-11.
34. Mishra L, Singh B, Dagenais S. Ayurveda: a historical perspective and principles of the traditional healthcare system in India. Altern Ther Health Med 2001;7:36-42.
- Limited randomized control trial data and observational studies show that the herbs Coccinia indica, holy basil, fenugreek, Gymnema sylvestre, and the herbal formulas Ayush-82 and D-400 have glucose-lowering effects. But these herbs are not as well studied as others more familiar to Western medicine. (B)
- Inform patients who ask about Ayurveda that traditional practitioners rely on the interaction of several components, of which herbs are just one, and that no formal studies have looked at Ayurveda as a whole system. (B)
- Objective: To evaluate and synthesize the evidence on the effect of Ayurvedic therapies for diabetes mellitus.
- Design: Systematic review of trials.
- Measurements and main results: We found no study that assessed Ayurvedic as a system of care. Botanical therapy was by far the most commonly studied Ayurvedic treatment. Herbs were studied either singly or as formulas. In all, 993 titles in Western computerized databases and 318 titles identified by hand-searching journals in India were examined, yielding 54 articles reporting the results of 62 studies. The most-studied herbs were G sylvestre, C indica, fenugreek, and Eugenia jambolana. A number of herbal formulas were tested, but Ayush-82 and D-400 were most often studied. Thirty-five of the studies included came from the Western literature, 27 from the Indian. Seven were randomized controlled trials (RCTs) and 10 controlled clinical trials (CCTs) or natural experiments. Twenty-two studies went on to further analysis based on a set of criteria. Of these, 10 were RCTs, CCTs, or natural experiments, 12 were case series or cohort studies. There is evidence to suggest that the herbs C indica, holy basil, fenugreek, and G sylvestre, and the herbal formulas Ayush-82 and D-400 have a glucose-lowering effect and deserve further study. Evidence of effectiveness of several other herbs is less extensive (C tamala, E jambolana, and Momordica charantia).
- Conclusions: There is heterogeneity in the available literature on Ayurvedic treatment for diabetes. Most studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested (more than 44 different interventions identified) and in the method of their preparation. Despite these limitations, there are sufficient data for several herbs or herbal formulas to warrant further studies.
Given the US population’s increasing interest in herbal and alternative therapies, it is just a matter of time before you will be fielding questions from patients about Ayurveda—a comprehensive system of health care that originated in India roughly 3000 years ago, emphasizing the relationships among body, mind, and spirit. Diabetes has been a particular focus of this medical system, and a few Ayurvedic herbs do indeed appear to exert glucose lowering mechanisms.
But how strong is the evidence? Though Ayurveda involves the interaction of many kinds of therapy, this review examines only the literature pertaining to herbal remedies your patients with diabetes are likely to ask about.
Ayurveda more than herbs
Ayurveda (Sanskrit for “knowledge of life” or “knowledge of longevity”) has now spread beyond India’s borders to include the rest of the Indian subcontinent, Sri Lanka, Malaysia, Mauritius, South Africa, Japan, Russia, Europe, and North America. At its root, Ayurveda seeks to restore an individual’s innate harmony. Primary Ayurvedic treatments include diet, exercise, meditation, herbs, massage, exposure to sunlight, controlled breathing, and detoxification treatments.
Dosha imbalance. Ayurveda considers human beings a microcosm of nature. All living and nonliving things are believed to consist of 5 basic elements: ether (space), air, fire, water, and earth. In humans these elements combine and manifest in the human body as 3 humors, or doshas, known as vata, pitta, and kapha.
The doshas govern all biological, psychological, and pathophysiological functions. They are fundamental to human health, and an imbalance of the doshas brings on illness. Consequently, Ayurveda seeks to bring the doshas back into harmony. Balanced doshas, as well as good-quality tissues (dhatus), proper digestion, and elimination of excretions (malas), are considered essential in Ayurveda for maintaining health.
Dosha body type influences treatment. In addition, humans are endowed at birth with 1 of 7 body types, depending on which dosha or combination of the 3 basic doshas dominates. Body types can be dominated by a single humor (vata, pitta, or kapha), or they can be dominated by combinations: vata-kapha (when vata and kapha are present in almost equal amounts); vata-pitta; pitta-kapha; or vata-pitta-kapha. A person’s dosha body type is expressed physically and emotionally; for example, a person with a vata-dominant body type will have a thin frame and an insecure temperament. The Ayurvedic physician takes body type and imbalances among the doshas into consideration when treating a patient.
Application to diabetes. The Indian word for diabetes is madhumeha, from madhu, meaning “sweet/sweetness,” and meha, meaning excessive urination. Classical Ayurvedic therapy for madhumeha (diabetes) begins with an assessment of the dosha imbalance. In all types of pramehas (urinary disorders), kapha is vitiated, but in madhumeha, vata is often aggravated as well. Therefore, therapies will be directed at both vata and kapha simultaneously to restore the balance of the doshas.1,2
Herbs are a commonly used treatment in Ayurveda. Ethnobotanical studies of traditional herbal remedies used for diabetes around the world have identified more than 1200 species of plants with hypoglycemic activity. These plants are broadly distributed throughout 725 different genera. The pharmacopoeia of India is especially rich in herbal treatments for diabetes. Eighty-five percent of the 20 antidiabetes plants most widely used around the world are prescribed in India.3 A few of the herbs commonly used by Ayurveda practitioners to treat diabetes are summarized in the TABLE.
In response to the increasing interest in Ayurveda and herbal treatments for diabetes in this country, the National Center for Complimentary and Alternative Medicine (NCCAM) requested we conduct a systematic review of Ayurvedic therapy for diabetes. This paper reports the results of that review, and is a condensation of an evidence report available at www.ahrq.gov/clinic/epcsums/ayurvsum.htm.
TABLE
Ayurvedic characteristics of herbs commonly used to treat diabetes
| HERB | TASTE (RASA) | INCREASES (AGGRAVATES) | DECREASES (PACIFIES) |
|---|---|---|---|
| Gymnema | Kasaya (astringent) | Kapha, Pitta | |
| Momordica | Tikta (bitter) | Kapha, Pitta | |
| Trigonella (fenugreek) | Tikta (bitter); Madhura (sweet) | Pitta | Kapha, Vata |
| Coccinia indica | Kasaya (astringent); Tikta (bitter) | Vata, Pitta | |
| Pterocarpus | Kasaya (astringent) | Vata | |
| Source: Kapoor, 1990;32 Dash, 198733 Mishra, Singh, and Dagenais, 2001.34 | |||
Methods
Identification of literature
We used the search term “Ayurveda” plus the names of 16 major botanicals characteristically used in Ayurveda for an initial search of the Western literature. The herbal terms were added to the search to increase its sensitivity, making it possible to find studies that used Ayurvedic herbal therapy without necessarily being directly identified as Ayurvedic studies.
We were concerned that a large body of literature existed in India that could not be obtained through the conventional search strategy outlined above. Hence, we decided to conduct a search for Ayurvedic literature from the Indian subcontinent. A physician member of the research team, fluent in English and Hindi and who had trained in India, went to India to identify Ayurvedic literature available there.
We therefore used several sources for our search:
- An initial “waterfront” search, which already had identified 120 articles on diabetes and Ayurveda (which was used by NCCAM to establish the rationale for selecting diabetes as the focus of this review).4 This search is detailed in our Evidence Report (available at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372) and included Medline, HealthSTAR, Allied and Complementary Medicine, MANTIS, CAB HEALTH, BIOSIS Previews, and EMBASE.
- The in-person literature search in India—we obtained 16 volumes of abstracts from various Indian Ayurvedic journals, as compiled by the Central Council for Research in Ayurveda and Siddha (CCRAS) library. This yielded 318 titles.
- An additional online search of the previously mentioned databases for common botanicals used in the treatment of diabetes. This search yielded 773 additional articles.
- A search of the online CINAHL database, which yielded 70 articles.
- The reference lists of important articles in the Ayurveda/diabetes literature. We identified review articles of herbal treatment of diabetes and checked to see if they focused on any of the Ayurvedic herbal therapies we had identified for diabetes. Checking the bibliographies of all the articles we identified from any source, we found an additional 30 titles that were potentially relevant to our search.
- An RCT or a CCT or a natural experiment with a comparison arm that did not receive an herb or Ayurvedic therapy. RCTs of any size were included. For CCTs or natural experiments, the study had to have at least 1 treatment arm that contained at least 10 patients.
- Because of a paucity of studies meeting these design criteria, we also assessed cohort or case series data that used a “pre/post” method of analysis, if their sample included at least 10 subjects.
- The study had to test Ayurveda as a method or herbs used as a single agent, a formula acting as a single agent, or a limited combination of products (no more than 3) acting as a single agent. The agent had to be dispensed more than 1 time to the study patients (in other words, no single-dose studies).
- The study had to report on at least 1 of 3 outcome measures at 30 days minimum following the start of the study: glycosylated hemoglobin (Hb A1c), fasting blood glucose, or postprandial blood glucose at either 2 hours (preferred) or 1 hour (acceptable).
Data extraction
Detailed information from each study was extracted using a specialized form. The physician reviewers, working independently, extracted data in duplicate and resolved disagreements by consensus. A senior physician resolved any remaining disagreements. Information extracted from articles included the diagnostic criteria used to make the diagnosis (Ayurvedic or Western or both); the location in which the study was done; the subject population (age, gender, other demographics); the sample size in each arm of the study; the interventions used (primarily the names of the individual herbs or mineral and the manner of their preparation); the length of the study; and the outcomes. To evaluate the quality of the design and execution of trials, we collected information on the study design, appropriateness of randomization, blinding, description of withdrawals and dropouts, and concealment of allocation.5,6 A quality score was calculated for each trial using a system developed by Jadad.5 Empirical evidence has shown that studies scoring 2 or less on the Jadad scale report exaggerated results compared with studies scoring 3 or more.7 While other elements of the design and execution of controlled trials have been proposed as quality measures, empirical evidence supporting their use as generic quality measures is lacking.8
Data synthesis
The studies we reviewed were judged clinically to be too heterogeneous to support a quantitative synthesis; therefore, our review is narrative. However, to promote the comparison of results across studies we extracted outcome data in a common format and present it in graphs for visual comparison. For studies that reported on both 1-hour and 2-hour postprandial blood glucose levels, we chose the 2-hour measurement for the analysis. For studies that reported more than 1 follow-up time, we selected the follow-up time that was closest to 3 months.
Twenty-two studies were selected for further analysis based on the criteria described above. These studies represented either RCTs (2) or CCTs/natural experiments (5) with a comparison arm that did not receive an herb, or studies that had pre/post comparison data available (8).
We considered 2 subgroups of eligible studies separately: the RCTs and CCTs or natural experiments that had nonherbal/Ayurvedic comparison arm(s) were considered 1 subgroup, and all other eligible (pre/post data available) studies made up the second subgroup. The RCT/CCT/natural experiments subgroup allowed us to do a comparison between herbal and nonherbal arms within a study, providing a stronger level of evidence than pre/post comparisons. For these studies, we were able to compare the effects of different treatments after the placebo or nonherbal arm results were taken into account by estimating a difference of differences statistic and its 95% confidence interval. This statistic is equal to the difference between the pre- and post-treatment means in the Ayurvedic arm minus the analogous difference in the nonherbal/Ayurvedic arm. The pre/post studies subgroup did not allow a concurrent comparison, but the difference between pre- and post-treatment means could be estimated along with a 95% confidence interval.4 Further details are given in our Evidence Report (available online at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372).
For each study subgroup, we assessed the possibility of publication bias graphically by evaluating a funnel plot of the study summary statistics for asymmetry, which would result from the nonpublication of small trials with negative outcomes. Because graphical evaluation can be subjective, we also conducted an adjusted rank-correlation test9 and a regression asymmetry test10 as formal statistical tests for publication bias.
Results
Description of the evidence
As a result of our search, we considered a total of 1311 articles (FIGURE 1). We reviewed in depth 62 studies, of which 22 were analyzed statistically. Ten studies came from the Western literature, and 12 came from the Indian literature. There were 7 randomized controlled trials, controlled clinical trials, or natural experiments with a treatment/no treatment comparison. There were 15 case series or cohort studies using a “pre/post” analysis. TABLE W2 (available online at www.jfponline.com) summarizes the characteristics of studies.
In terms of interventions, there was no study that tested Ayurveda as a system of care; all tested herbs. Of the 22 studies described narratively in this article, the 2 most commonly tested single herbs were Coccinia indica and fenugreek. The Ayurvedic formula Ayush-82 was the most commonly tested herbal formula. Diet was used as an intervention or co-intervention in 15 of the 22 studies.
FIGURE 1
Ayurveda literature review strategy of focused search for human diabetes articles
Quality of the evidence
Only the RCTs, CCTs, and natural experiments were given a Jadad score, which rates studies on a 0 to 5 scale.5 Of the 7 such studies, 3 received a Jadad score of zero, 3 studies scored a 1, and only 1 study received a 4 on this scale. This is the only high quality study in our analysis.
Controlled trials/natural experiments with nonherbal comparison arm(s)
There were 7 RCTs, CCTs or natural experiments that met the inclusion criteria. The data for these 7 studies are reported in FIGURE 2.
Coccinia indica. Azad Khan, Akhtar, and Mahtab (1979) performed a randomized controlled trial to assess the hypoglycemic properties of a preparation of the herb C indica on uncontrolled and untreated type 2 diabetes patients.11 Thirty-eight patients with type 2 diabetes who were attending the outpatient department of the Bangladesh Institute of Research and Rehabilitation in Diabetes in Dhaka, Bangladesh, were recruited for the study. Only uncontrolled or newly diagnosed patients were enlisted. The intervention consisted of a freeze-dried powder of crushed leaves of C indica, given in a dose of 900 mg twice a day for 6 weeks. Control patients received placebo twice a day for the same period. Of the 16 patients receiving C indica, 10 patients showed a marked improvement in the glucose tolerance tests to values closer to normal, while none in the placebo arm showed marked improvement. The Jadad score for the trial was 4. This study was identified from the Eastern literature search.
Holy basil. Agrawal, Rai, and Singh (1996) reported the results of a randomized, placebo controlled crossover trial of the effects of a leaf extract of holy basil (Ocimum sanctum) on patients with type 2 diabetes.12 Forty patients were recruited from community advertisements in Kanpur, India, and through visits to the offices of local dieticians. All subjects had a 5-day run-in period during which they all consumed a tea made from holy basil leaves. This was followed by an 8-week experimental period. The patients were randomly assigned to drink the holy basil leaf tea for 4 weeks followed by placebo leaves for 4 weeks, or the reverse (the placebo leaves first, followed by the holy basil leaf tea). The authors concluded that holy basil leaf powder caused significant reduction in the level of fasting blood sugar and postprandial blood sugar, and a moderate reduction in cholesterol. The Jadad score for this trial is 1. This study was identified from the Western literature search.
Cinnamonum tamala. Chandola, Tripathi, and Udupa (1980) assessed the hypoglycemic effects of C tamala in type 2 diabetes patients.13 Thirty-two patients were recruited from the outpatient departments of the Institute of Medical Sciences, Varanasi, India, and received the intervention and 8 patients with type 2 diabetes served as controls. The socioeconomic characteristics of the patients were not noted, and the authors did not report if the 2 arms of patients were statistically equivalent on important prognostic variables at the start of the trial. The intervention consisted of leaves of C tamala (tejpatra) that were dried, pulverized, and filtered through a fine mesh, and given as 2 heaped teaspoons 4 times a day before meals and tea for a total of 1 month. All patients were advised to follow a 1800-calorie diet with restriction of sugar, potato, and rice. The control patients were only instructed to follow the above diet with no other medications. Fasting blood sugars were assessed in both arms of patients before the trial and at the end of 1 month. The authors reported the mean fasting blood sugar improved from 153 mg/dL to 113 mg/dL (P<.001) at the end of 1 month in patients treated with C tamala, while there was no improvement in control patients. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Coccina indica. Kamble, Jyotishi, Kamalakar, et al (1996) studied the effect of fresh leaves of C indica on blood sugar levels and on hyperlipidemia in noninsulin-dependent diabetes mellitus (NIDDM, type 2) patients at an Ayurvedic clinic in Nagpur, India.14 Patients were classified into 4 arms: a healthy comparison arm (arm I, 15 patients); a NIDDM comparison arm (arm II, 30 patients); NIDDM patients treated with Coccinia (arm III, 25 patients); and a NIDDM arm treated with chlorpropamide (arm IV, 15 patients). Patients were given the Coccinia (decocted from fresh leaves, dried into a paste, and made into a 3-g tablet) twice a day for 12 weeks, although control group data only exist at 6 weeks. For patients in arm III, the study showed a statistically significant reduction in mean fasting blood sugar, from 160 to 118 mg/dL (P<.001) at 12 weeks, and a significant decrease in blood sugar levels after glucose tolerance tests: the 2-hour level dropped from 308 mg/dL to 142 mg/dL (P<.001). These results were roughly equivalent to those found in the chlorpropamide arm at 6 weeks, with any differences being not statistically significant. Additionally, after 12 weeks of treatment, the Coccinia treated patients showed significant within group reductions in levels of cholesterol (P<.001), phospholipid (P<.05), triglyceride (P<.001), and free fatty acid (P<.001) compared with untreated patients with diabetes. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Jamun beej. Kohli and Singh (1993) studied the effects of Jamun beej (Eugenia jambolana) on fasting blood sugar, glucose tolerance test, and symptomatic relief of symptoms associated with diabetes.15 Thirty patients identified from the outpatient unit of the Sunderlal Hospital in Varanasi, India, who had NIDDM confirmed by glucose tolerance test, were given E jambolana crushed into a fine powder at a dose of 4 g 3 times a day for 3 months. No dietary restrictions were included in the study. A second arm of 6 patients with confirmed NIDDM was given chlorpropamide (250 mg/d). No demographic information was provided on these patients. The authors reported a statistically significant reduction in mean fasting blood sugar of 51.86 mg/dL at 2 months (P<.001) but not at 3 months. The study also demonstrated a significant reduction in the response to the glucose tolerance test at both 2 months (P<.001) and at 3 months (P<.01), but comparisons with the patients receiving chlorpropamide were not statistically significant. The Jadad score total is 1. This study was identified from the Eastern literature search.
Gymnema sylvestre. Baskaran, Ahamath, Shanmugasundaram, et al (1990) studied the effects of GS4, a specific isolate of G sylvestre, on the blood sugar of 47 type 2 diabetes patients.16 The intervention group consisted of 22 patients with diabetes on oral hypoglycemic therapy (continued during the trial), plus herbal therapy with Gymnema at a dose of 400 mg/d. The control group consisted of 25 patients with type 2 diabetes on conventional medications alone. Although the arms were reasonably matched for age and Broca index (percent of ideal body weight) based on our analysis of individual patient data in the study, the 2 arms were statistically different at baseline with respect to fasting blood sugar. The authors reported that in the intervention group at 12 months of follow-up, mean fasting blood sugar improved from 174 mg/dL to 124 mg/dL (P<.001) and Hb A1c improved from 11.9% to 8.48% (P<.001). Changes in the control group over this time were not significant. Virtually all patients in arm I developed hypoglycemic symptoms, and the dose of their normal oral hypoglycemic agent needed to be changed or stopped. The Jadad score is 0. This study was identified from the Western literature search.
GS4. Shanmugasundaram, Rajeswari, Baskaran, et al (1990b) reported the effect of an herbal compound GS4 on blood glucose, insulin requirements, and cholesterol in patients with type 1 and type 2 diabetes.17 The intervention group consisted of 23 type 1 patients and 4 type 2 patients (ages 44–50 years, 25% female) who continued their insulin in addition to taking the herbal intervention, and the control group consisted of 37 type 1 patients who were on insulin therapy. The clinical equivalence of the 2 arms at baseline was not mentioned. The intervention drug was GS4, a recrystallized precipitate of the alcoholic extract of the acidic fraction of G sylvestre; at dose of 400 mg/d. At 6 to 8 months of follow-up, all patients in the intervention group developed hypoglycemic episodes, and their insulin doses were reduced by 10 units at a time; differences compared to controls were statistically significant. The Jadad score was 1. This study was identified from the Western literature search.
Summary. In summary, comparisons of the studied herbs with either placebo, diet, or as an adjunct to medical hypoglycemic therapy consistently reported statistically significant benefits in glucose control. Studies comparing herbs to the oral hypoglycemic chlorpropamide did not report differences between groups.
FIGURE 2
Glucose-lowering effects of Ayurvedic herbs compared with nonherbal treatments
Case series or cohort studies without a concurrent comparison group
Fifteen studies had treatment arms that reported blood glucose or Hb A1c values before and after herbal interventions—ie, that made available pre/post data.13,18-31 Herbs were tested singly (7 studies), in combination (7 studies), or both singly and in combination (1 study). All of these studies are limited by the lack of randomization. Many are also limited by small sample size and short study duration.
The data are presented in FIGURE 3 in the following order: studies or arms of studies using a single herbal preparation first, followed by studies that use a formula or a group of herbs and minerals. Some studies with multiple arms will have listings in more than one place. As FIGURE 3 shows, most pre/post comparison studies using single herbs and formulas favor treatment. Hb A1c is measured in only 5 of the studies. Two of those studies seem to strongly favor treatment; 2 are almost equivocal; and 1 does not favor treatment.
The small number of RCTs/CCTs/natural experiments measuring postprandial blood glucose and Hb A1c, and the small number of case series and cohorts measuring Hb A1c, make the assessment of publication bias for these outcomes problematic. For the remaining outcomes, only slight evidence of publication bias was evident among the case series and cohort studies for the fasting blood glucose outcome (adjusted rank correlation test P=.97; regression asymmetry test P=.06). For this outcome, we have trial data available, a setting in which no evidence of publication bias is seen.
FIGURE 3
Effect of Ayurvedic herbs on blood glucose and Hb A1c
Discussion
No controlled trials have assessed Ayurveda as a system of care. Furthermore, among studies of herbal preparations, controlled trials are rare and mostly of poor quality. Still, we found evidence suggesting that some Ayurvedic herbs have clinically important hypoglycemic effects.
The best-quality RCT reported beneficial results for C indica. Other studies have generally reported benefits of C indica; however, results have been inconsistent.
A single trial of holy basil reported a benefit in controlling fasting blood glucose only. G sylvestre was used in a number of studies, again with generally beneficial results. Gymnema was also a constituent in 2 of the formulas that reported beneficial results: D-400 and Ayush-82.
Methodological shortcomings. The evidence we found falls short of proof. As noted, the individual studies we assessed had significant methodological shortcomings. Few used a randomized, placebo-controlled design, despite the feasibility of such methods. Studies generally were underpowered to determine even large effect sizes. Many studies involved an extremely small number of subjects (fewer than 10). A number of studies failed to use appropriate statistical methods in reporting the results. Furthermore, the duration of most studies was short, and only intermediate outcomes (measure of blood sugar control) were reported. Longer term studies that assess clinical outcomes are required. Lastly, there is great heterogeneity in the available literature on Ayurvedic treatment for diabetes, despite the fact that the overwhelming majority of studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested and in the method of their preparation.
No true studies of Ayurveda. None of the identified studies assessed Ayurveda as a system of diagnosis and care. The literature reported mainly studies of single herbs; however, in clinical Ayurvedic practice, herbs are usually given in combination. Formulas can include minerals and metals in addition to multiple plants.
Ayurvedic practitioners assert that the sum of a formula is more potent than the constituents taken individually and, further, that the mineral and metal components boost the formula’s potency. Additional Ayurvedic therapies such as diet, yoga, or special purification routines, should be controlled for when recruiting and assessing patients. It is unclear, perhaps doubtful, that taking a single component of Ayurvedic is sufficient to represent the holistic effect of Ayurvedic interventions.
Limitations of our review. Our searches showed that herbal therapies were emphasized in published studies of Ayurveda. However, no conclusions can be drawn about the use of Ayurveda as a whole system for the treatment of diabetes. Although extensive efforts were made to obtain the relevant literature from India, studies not published in English were excluded, as were MD thesis reports. A handful of studies could not be obtained. Therefore we may not have included in this review all clinical trials. By specifically hand searching documents published in India, we identified that an important body of Ayurvedic literature is not identifiable using traditional systematic review methods.
In summary, we found preliminary evidence suggesting that some herbs and herbal formulas used in Ayurvedic therapy can have clinically important glucose-lowering effects. C indica, holy basil, and Gymnema are particularly worthy of additional study.
Acknowledgments
This research was performed by the Southern California Evidence-Based Practice Center based at RAND, Santa Monica, CA under contract with the Agency for Healthcare Research and Quality (Contract No. 290-97-0001) with support from the National Center for Complementary and Alternative Medicine. The authors of this article are responsible for its contents. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality, the National Center for Complementary and Alternative Medicine, National Institutes of Health, or the US Department of Health and Human Services.
CORRESPONDING AUTHOR
Paul G. Shekelle, MD, PhD, West Los Angeles VA Medical Center, 111G, 11301 Wilshire Blvd, Los Angeles, CA 90073. E-mail: [email protected]. At the time of this study, Dr. Shekelle was a Senior Research Associate of the Veterans Affairs Health Services Research and Development Service.
- Limited randomized control trial data and observational studies show that the herbs Coccinia indica, holy basil, fenugreek, Gymnema sylvestre, and the herbal formulas Ayush-82 and D-400 have glucose-lowering effects. But these herbs are not as well studied as others more familiar to Western medicine. (B)
- Inform patients who ask about Ayurveda that traditional practitioners rely on the interaction of several components, of which herbs are just one, and that no formal studies have looked at Ayurveda as a whole system. (B)
- Objective: To evaluate and synthesize the evidence on the effect of Ayurvedic therapies for diabetes mellitus.
- Design: Systematic review of trials.
- Measurements and main results: We found no study that assessed Ayurvedic as a system of care. Botanical therapy was by far the most commonly studied Ayurvedic treatment. Herbs were studied either singly or as formulas. In all, 993 titles in Western computerized databases and 318 titles identified by hand-searching journals in India were examined, yielding 54 articles reporting the results of 62 studies. The most-studied herbs were G sylvestre, C indica, fenugreek, and Eugenia jambolana. A number of herbal formulas were tested, but Ayush-82 and D-400 were most often studied. Thirty-five of the studies included came from the Western literature, 27 from the Indian. Seven were randomized controlled trials (RCTs) and 10 controlled clinical trials (CCTs) or natural experiments. Twenty-two studies went on to further analysis based on a set of criteria. Of these, 10 were RCTs, CCTs, or natural experiments, 12 were case series or cohort studies. There is evidence to suggest that the herbs C indica, holy basil, fenugreek, and G sylvestre, and the herbal formulas Ayush-82 and D-400 have a glucose-lowering effect and deserve further study. Evidence of effectiveness of several other herbs is less extensive (C tamala, E jambolana, and Momordica charantia).
- Conclusions: There is heterogeneity in the available literature on Ayurvedic treatment for diabetes. Most studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested (more than 44 different interventions identified) and in the method of their preparation. Despite these limitations, there are sufficient data for several herbs or herbal formulas to warrant further studies.
Given the US population’s increasing interest in herbal and alternative therapies, it is just a matter of time before you will be fielding questions from patients about Ayurveda—a comprehensive system of health care that originated in India roughly 3000 years ago, emphasizing the relationships among body, mind, and spirit. Diabetes has been a particular focus of this medical system, and a few Ayurvedic herbs do indeed appear to exert glucose lowering mechanisms.
But how strong is the evidence? Though Ayurveda involves the interaction of many kinds of therapy, this review examines only the literature pertaining to herbal remedies your patients with diabetes are likely to ask about.
Ayurveda more than herbs
Ayurveda (Sanskrit for “knowledge of life” or “knowledge of longevity”) has now spread beyond India’s borders to include the rest of the Indian subcontinent, Sri Lanka, Malaysia, Mauritius, South Africa, Japan, Russia, Europe, and North America. At its root, Ayurveda seeks to restore an individual’s innate harmony. Primary Ayurvedic treatments include diet, exercise, meditation, herbs, massage, exposure to sunlight, controlled breathing, and detoxification treatments.
Dosha imbalance. Ayurveda considers human beings a microcosm of nature. All living and nonliving things are believed to consist of 5 basic elements: ether (space), air, fire, water, and earth. In humans these elements combine and manifest in the human body as 3 humors, or doshas, known as vata, pitta, and kapha.
The doshas govern all biological, psychological, and pathophysiological functions. They are fundamental to human health, and an imbalance of the doshas brings on illness. Consequently, Ayurveda seeks to bring the doshas back into harmony. Balanced doshas, as well as good-quality tissues (dhatus), proper digestion, and elimination of excretions (malas), are considered essential in Ayurveda for maintaining health.
Dosha body type influences treatment. In addition, humans are endowed at birth with 1 of 7 body types, depending on which dosha or combination of the 3 basic doshas dominates. Body types can be dominated by a single humor (vata, pitta, or kapha), or they can be dominated by combinations: vata-kapha (when vata and kapha are present in almost equal amounts); vata-pitta; pitta-kapha; or vata-pitta-kapha. A person’s dosha body type is expressed physically and emotionally; for example, a person with a vata-dominant body type will have a thin frame and an insecure temperament. The Ayurvedic physician takes body type and imbalances among the doshas into consideration when treating a patient.
Application to diabetes. The Indian word for diabetes is madhumeha, from madhu, meaning “sweet/sweetness,” and meha, meaning excessive urination. Classical Ayurvedic therapy for madhumeha (diabetes) begins with an assessment of the dosha imbalance. In all types of pramehas (urinary disorders), kapha is vitiated, but in madhumeha, vata is often aggravated as well. Therefore, therapies will be directed at both vata and kapha simultaneously to restore the balance of the doshas.1,2
Herbs are a commonly used treatment in Ayurveda. Ethnobotanical studies of traditional herbal remedies used for diabetes around the world have identified more than 1200 species of plants with hypoglycemic activity. These plants are broadly distributed throughout 725 different genera. The pharmacopoeia of India is especially rich in herbal treatments for diabetes. Eighty-five percent of the 20 antidiabetes plants most widely used around the world are prescribed in India.3 A few of the herbs commonly used by Ayurveda practitioners to treat diabetes are summarized in the TABLE.
In response to the increasing interest in Ayurveda and herbal treatments for diabetes in this country, the National Center for Complimentary and Alternative Medicine (NCCAM) requested we conduct a systematic review of Ayurvedic therapy for diabetes. This paper reports the results of that review, and is a condensation of an evidence report available at www.ahrq.gov/clinic/epcsums/ayurvsum.htm.
TABLE
Ayurvedic characteristics of herbs commonly used to treat diabetes
| HERB | TASTE (RASA) | INCREASES (AGGRAVATES) | DECREASES (PACIFIES) |
|---|---|---|---|
| Gymnema | Kasaya (astringent) | Kapha, Pitta | |
| Momordica | Tikta (bitter) | Kapha, Pitta | |
| Trigonella (fenugreek) | Tikta (bitter); Madhura (sweet) | Pitta | Kapha, Vata |
| Coccinia indica | Kasaya (astringent); Tikta (bitter) | Vata, Pitta | |
| Pterocarpus | Kasaya (astringent) | Vata | |
| Source: Kapoor, 1990;32 Dash, 198733 Mishra, Singh, and Dagenais, 2001.34 | |||
Methods
Identification of literature
We used the search term “Ayurveda” plus the names of 16 major botanicals characteristically used in Ayurveda for an initial search of the Western literature. The herbal terms were added to the search to increase its sensitivity, making it possible to find studies that used Ayurvedic herbal therapy without necessarily being directly identified as Ayurvedic studies.
We were concerned that a large body of literature existed in India that could not be obtained through the conventional search strategy outlined above. Hence, we decided to conduct a search for Ayurvedic literature from the Indian subcontinent. A physician member of the research team, fluent in English and Hindi and who had trained in India, went to India to identify Ayurvedic literature available there.
We therefore used several sources for our search:
- An initial “waterfront” search, which already had identified 120 articles on diabetes and Ayurveda (which was used by NCCAM to establish the rationale for selecting diabetes as the focus of this review).4 This search is detailed in our Evidence Report (available at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372) and included Medline, HealthSTAR, Allied and Complementary Medicine, MANTIS, CAB HEALTH, BIOSIS Previews, and EMBASE.
- The in-person literature search in India—we obtained 16 volumes of abstracts from various Indian Ayurvedic journals, as compiled by the Central Council for Research in Ayurveda and Siddha (CCRAS) library. This yielded 318 titles.
- An additional online search of the previously mentioned databases for common botanicals used in the treatment of diabetes. This search yielded 773 additional articles.
- A search of the online CINAHL database, which yielded 70 articles.
- The reference lists of important articles in the Ayurveda/diabetes literature. We identified review articles of herbal treatment of diabetes and checked to see if they focused on any of the Ayurvedic herbal therapies we had identified for diabetes. Checking the bibliographies of all the articles we identified from any source, we found an additional 30 titles that were potentially relevant to our search.
- An RCT or a CCT or a natural experiment with a comparison arm that did not receive an herb or Ayurvedic therapy. RCTs of any size were included. For CCTs or natural experiments, the study had to have at least 1 treatment arm that contained at least 10 patients.
- Because of a paucity of studies meeting these design criteria, we also assessed cohort or case series data that used a “pre/post” method of analysis, if their sample included at least 10 subjects.
- The study had to test Ayurveda as a method or herbs used as a single agent, a formula acting as a single agent, or a limited combination of products (no more than 3) acting as a single agent. The agent had to be dispensed more than 1 time to the study patients (in other words, no single-dose studies).
- The study had to report on at least 1 of 3 outcome measures at 30 days minimum following the start of the study: glycosylated hemoglobin (Hb A1c), fasting blood glucose, or postprandial blood glucose at either 2 hours (preferred) or 1 hour (acceptable).
Data extraction
Detailed information from each study was extracted using a specialized form. The physician reviewers, working independently, extracted data in duplicate and resolved disagreements by consensus. A senior physician resolved any remaining disagreements. Information extracted from articles included the diagnostic criteria used to make the diagnosis (Ayurvedic or Western or both); the location in which the study was done; the subject population (age, gender, other demographics); the sample size in each arm of the study; the interventions used (primarily the names of the individual herbs or mineral and the manner of their preparation); the length of the study; and the outcomes. To evaluate the quality of the design and execution of trials, we collected information on the study design, appropriateness of randomization, blinding, description of withdrawals and dropouts, and concealment of allocation.5,6 A quality score was calculated for each trial using a system developed by Jadad.5 Empirical evidence has shown that studies scoring 2 or less on the Jadad scale report exaggerated results compared with studies scoring 3 or more.7 While other elements of the design and execution of controlled trials have been proposed as quality measures, empirical evidence supporting their use as generic quality measures is lacking.8
Data synthesis
The studies we reviewed were judged clinically to be too heterogeneous to support a quantitative synthesis; therefore, our review is narrative. However, to promote the comparison of results across studies we extracted outcome data in a common format and present it in graphs for visual comparison. For studies that reported on both 1-hour and 2-hour postprandial blood glucose levels, we chose the 2-hour measurement for the analysis. For studies that reported more than 1 follow-up time, we selected the follow-up time that was closest to 3 months.
Twenty-two studies were selected for further analysis based on the criteria described above. These studies represented either RCTs (2) or CCTs/natural experiments (5) with a comparison arm that did not receive an herb, or studies that had pre/post comparison data available (8).
We considered 2 subgroups of eligible studies separately: the RCTs and CCTs or natural experiments that had nonherbal/Ayurvedic comparison arm(s) were considered 1 subgroup, and all other eligible (pre/post data available) studies made up the second subgroup. The RCT/CCT/natural experiments subgroup allowed us to do a comparison between herbal and nonherbal arms within a study, providing a stronger level of evidence than pre/post comparisons. For these studies, we were able to compare the effects of different treatments after the placebo or nonherbal arm results were taken into account by estimating a difference of differences statistic and its 95% confidence interval. This statistic is equal to the difference between the pre- and post-treatment means in the Ayurvedic arm minus the analogous difference in the nonherbal/Ayurvedic arm. The pre/post studies subgroup did not allow a concurrent comparison, but the difference between pre- and post-treatment means could be estimated along with a 95% confidence interval.4 Further details are given in our Evidence Report (available online at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372).
For each study subgroup, we assessed the possibility of publication bias graphically by evaluating a funnel plot of the study summary statistics for asymmetry, which would result from the nonpublication of small trials with negative outcomes. Because graphical evaluation can be subjective, we also conducted an adjusted rank-correlation test9 and a regression asymmetry test10 as formal statistical tests for publication bias.
Results
Description of the evidence
As a result of our search, we considered a total of 1311 articles (FIGURE 1). We reviewed in depth 62 studies, of which 22 were analyzed statistically. Ten studies came from the Western literature, and 12 came from the Indian literature. There were 7 randomized controlled trials, controlled clinical trials, or natural experiments with a treatment/no treatment comparison. There were 15 case series or cohort studies using a “pre/post” analysis. TABLE W2 (available online at www.jfponline.com) summarizes the characteristics of studies.
In terms of interventions, there was no study that tested Ayurveda as a system of care; all tested herbs. Of the 22 studies described narratively in this article, the 2 most commonly tested single herbs were Coccinia indica and fenugreek. The Ayurvedic formula Ayush-82 was the most commonly tested herbal formula. Diet was used as an intervention or co-intervention in 15 of the 22 studies.
FIGURE 1
Ayurveda literature review strategy of focused search for human diabetes articles
Quality of the evidence
Only the RCTs, CCTs, and natural experiments were given a Jadad score, which rates studies on a 0 to 5 scale.5 Of the 7 such studies, 3 received a Jadad score of zero, 3 studies scored a 1, and only 1 study received a 4 on this scale. This is the only high quality study in our analysis.
Controlled trials/natural experiments with nonherbal comparison arm(s)
There were 7 RCTs, CCTs or natural experiments that met the inclusion criteria. The data for these 7 studies are reported in FIGURE 2.
Coccinia indica. Azad Khan, Akhtar, and Mahtab (1979) performed a randomized controlled trial to assess the hypoglycemic properties of a preparation of the herb C indica on uncontrolled and untreated type 2 diabetes patients.11 Thirty-eight patients with type 2 diabetes who were attending the outpatient department of the Bangladesh Institute of Research and Rehabilitation in Diabetes in Dhaka, Bangladesh, were recruited for the study. Only uncontrolled or newly diagnosed patients were enlisted. The intervention consisted of a freeze-dried powder of crushed leaves of C indica, given in a dose of 900 mg twice a day for 6 weeks. Control patients received placebo twice a day for the same period. Of the 16 patients receiving C indica, 10 patients showed a marked improvement in the glucose tolerance tests to values closer to normal, while none in the placebo arm showed marked improvement. The Jadad score for the trial was 4. This study was identified from the Eastern literature search.
Holy basil. Agrawal, Rai, and Singh (1996) reported the results of a randomized, placebo controlled crossover trial of the effects of a leaf extract of holy basil (Ocimum sanctum) on patients with type 2 diabetes.12 Forty patients were recruited from community advertisements in Kanpur, India, and through visits to the offices of local dieticians. All subjects had a 5-day run-in period during which they all consumed a tea made from holy basil leaves. This was followed by an 8-week experimental period. The patients were randomly assigned to drink the holy basil leaf tea for 4 weeks followed by placebo leaves for 4 weeks, or the reverse (the placebo leaves first, followed by the holy basil leaf tea). The authors concluded that holy basil leaf powder caused significant reduction in the level of fasting blood sugar and postprandial blood sugar, and a moderate reduction in cholesterol. The Jadad score for this trial is 1. This study was identified from the Western literature search.
Cinnamonum tamala. Chandola, Tripathi, and Udupa (1980) assessed the hypoglycemic effects of C tamala in type 2 diabetes patients.13 Thirty-two patients were recruited from the outpatient departments of the Institute of Medical Sciences, Varanasi, India, and received the intervention and 8 patients with type 2 diabetes served as controls. The socioeconomic characteristics of the patients were not noted, and the authors did not report if the 2 arms of patients were statistically equivalent on important prognostic variables at the start of the trial. The intervention consisted of leaves of C tamala (tejpatra) that were dried, pulverized, and filtered through a fine mesh, and given as 2 heaped teaspoons 4 times a day before meals and tea for a total of 1 month. All patients were advised to follow a 1800-calorie diet with restriction of sugar, potato, and rice. The control patients were only instructed to follow the above diet with no other medications. Fasting blood sugars were assessed in both arms of patients before the trial and at the end of 1 month. The authors reported the mean fasting blood sugar improved from 153 mg/dL to 113 mg/dL (P<.001) at the end of 1 month in patients treated with C tamala, while there was no improvement in control patients. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Coccina indica. Kamble, Jyotishi, Kamalakar, et al (1996) studied the effect of fresh leaves of C indica on blood sugar levels and on hyperlipidemia in noninsulin-dependent diabetes mellitus (NIDDM, type 2) patients at an Ayurvedic clinic in Nagpur, India.14 Patients were classified into 4 arms: a healthy comparison arm (arm I, 15 patients); a NIDDM comparison arm (arm II, 30 patients); NIDDM patients treated with Coccinia (arm III, 25 patients); and a NIDDM arm treated with chlorpropamide (arm IV, 15 patients). Patients were given the Coccinia (decocted from fresh leaves, dried into a paste, and made into a 3-g tablet) twice a day for 12 weeks, although control group data only exist at 6 weeks. For patients in arm III, the study showed a statistically significant reduction in mean fasting blood sugar, from 160 to 118 mg/dL (P<.001) at 12 weeks, and a significant decrease in blood sugar levels after glucose tolerance tests: the 2-hour level dropped from 308 mg/dL to 142 mg/dL (P<.001). These results were roughly equivalent to those found in the chlorpropamide arm at 6 weeks, with any differences being not statistically significant. Additionally, after 12 weeks of treatment, the Coccinia treated patients showed significant within group reductions in levels of cholesterol (P<.001), phospholipid (P<.05), triglyceride (P<.001), and free fatty acid (P<.001) compared with untreated patients with diabetes. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Jamun beej. Kohli and Singh (1993) studied the effects of Jamun beej (Eugenia jambolana) on fasting blood sugar, glucose tolerance test, and symptomatic relief of symptoms associated with diabetes.15 Thirty patients identified from the outpatient unit of the Sunderlal Hospital in Varanasi, India, who had NIDDM confirmed by glucose tolerance test, were given E jambolana crushed into a fine powder at a dose of 4 g 3 times a day for 3 months. No dietary restrictions were included in the study. A second arm of 6 patients with confirmed NIDDM was given chlorpropamide (250 mg/d). No demographic information was provided on these patients. The authors reported a statistically significant reduction in mean fasting blood sugar of 51.86 mg/dL at 2 months (P<.001) but not at 3 months. The study also demonstrated a significant reduction in the response to the glucose tolerance test at both 2 months (P<.001) and at 3 months (P<.01), but comparisons with the patients receiving chlorpropamide were not statistically significant. The Jadad score total is 1. This study was identified from the Eastern literature search.
Gymnema sylvestre. Baskaran, Ahamath, Shanmugasundaram, et al (1990) studied the effects of GS4, a specific isolate of G sylvestre, on the blood sugar of 47 type 2 diabetes patients.16 The intervention group consisted of 22 patients with diabetes on oral hypoglycemic therapy (continued during the trial), plus herbal therapy with Gymnema at a dose of 400 mg/d. The control group consisted of 25 patients with type 2 diabetes on conventional medications alone. Although the arms were reasonably matched for age and Broca index (percent of ideal body weight) based on our analysis of individual patient data in the study, the 2 arms were statistically different at baseline with respect to fasting blood sugar. The authors reported that in the intervention group at 12 months of follow-up, mean fasting blood sugar improved from 174 mg/dL to 124 mg/dL (P<.001) and Hb A1c improved from 11.9% to 8.48% (P<.001). Changes in the control group over this time were not significant. Virtually all patients in arm I developed hypoglycemic symptoms, and the dose of their normal oral hypoglycemic agent needed to be changed or stopped. The Jadad score is 0. This study was identified from the Western literature search.
GS4. Shanmugasundaram, Rajeswari, Baskaran, et al (1990b) reported the effect of an herbal compound GS4 on blood glucose, insulin requirements, and cholesterol in patients with type 1 and type 2 diabetes.17 The intervention group consisted of 23 type 1 patients and 4 type 2 patients (ages 44–50 years, 25% female) who continued their insulin in addition to taking the herbal intervention, and the control group consisted of 37 type 1 patients who were on insulin therapy. The clinical equivalence of the 2 arms at baseline was not mentioned. The intervention drug was GS4, a recrystallized precipitate of the alcoholic extract of the acidic fraction of G sylvestre; at dose of 400 mg/d. At 6 to 8 months of follow-up, all patients in the intervention group developed hypoglycemic episodes, and their insulin doses were reduced by 10 units at a time; differences compared to controls were statistically significant. The Jadad score was 1. This study was identified from the Western literature search.
Summary. In summary, comparisons of the studied herbs with either placebo, diet, or as an adjunct to medical hypoglycemic therapy consistently reported statistically significant benefits in glucose control. Studies comparing herbs to the oral hypoglycemic chlorpropamide did not report differences between groups.
FIGURE 2
Glucose-lowering effects of Ayurvedic herbs compared with nonherbal treatments
Case series or cohort studies without a concurrent comparison group
Fifteen studies had treatment arms that reported blood glucose or Hb A1c values before and after herbal interventions—ie, that made available pre/post data.13,18-31 Herbs were tested singly (7 studies), in combination (7 studies), or both singly and in combination (1 study). All of these studies are limited by the lack of randomization. Many are also limited by small sample size and short study duration.
The data are presented in FIGURE 3 in the following order: studies or arms of studies using a single herbal preparation first, followed by studies that use a formula or a group of herbs and minerals. Some studies with multiple arms will have listings in more than one place. As FIGURE 3 shows, most pre/post comparison studies using single herbs and formulas favor treatment. Hb A1c is measured in only 5 of the studies. Two of those studies seem to strongly favor treatment; 2 are almost equivocal; and 1 does not favor treatment.
The small number of RCTs/CCTs/natural experiments measuring postprandial blood glucose and Hb A1c, and the small number of case series and cohorts measuring Hb A1c, make the assessment of publication bias for these outcomes problematic. For the remaining outcomes, only slight evidence of publication bias was evident among the case series and cohort studies for the fasting blood glucose outcome (adjusted rank correlation test P=.97; regression asymmetry test P=.06). For this outcome, we have trial data available, a setting in which no evidence of publication bias is seen.
FIGURE 3
Effect of Ayurvedic herbs on blood glucose and Hb A1c
Discussion
No controlled trials have assessed Ayurveda as a system of care. Furthermore, among studies of herbal preparations, controlled trials are rare and mostly of poor quality. Still, we found evidence suggesting that some Ayurvedic herbs have clinically important hypoglycemic effects.
The best-quality RCT reported beneficial results for C indica. Other studies have generally reported benefits of C indica; however, results have been inconsistent.
A single trial of holy basil reported a benefit in controlling fasting blood glucose only. G sylvestre was used in a number of studies, again with generally beneficial results. Gymnema was also a constituent in 2 of the formulas that reported beneficial results: D-400 and Ayush-82.
Methodological shortcomings. The evidence we found falls short of proof. As noted, the individual studies we assessed had significant methodological shortcomings. Few used a randomized, placebo-controlled design, despite the feasibility of such methods. Studies generally were underpowered to determine even large effect sizes. Many studies involved an extremely small number of subjects (fewer than 10). A number of studies failed to use appropriate statistical methods in reporting the results. Furthermore, the duration of most studies was short, and only intermediate outcomes (measure of blood sugar control) were reported. Longer term studies that assess clinical outcomes are required. Lastly, there is great heterogeneity in the available literature on Ayurvedic treatment for diabetes, despite the fact that the overwhelming majority of studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested and in the method of their preparation.
No true studies of Ayurveda. None of the identified studies assessed Ayurveda as a system of diagnosis and care. The literature reported mainly studies of single herbs; however, in clinical Ayurvedic practice, herbs are usually given in combination. Formulas can include minerals and metals in addition to multiple plants.
Ayurvedic practitioners assert that the sum of a formula is more potent than the constituents taken individually and, further, that the mineral and metal components boost the formula’s potency. Additional Ayurvedic therapies such as diet, yoga, or special purification routines, should be controlled for when recruiting and assessing patients. It is unclear, perhaps doubtful, that taking a single component of Ayurvedic is sufficient to represent the holistic effect of Ayurvedic interventions.
Limitations of our review. Our searches showed that herbal therapies were emphasized in published studies of Ayurveda. However, no conclusions can be drawn about the use of Ayurveda as a whole system for the treatment of diabetes. Although extensive efforts were made to obtain the relevant literature from India, studies not published in English were excluded, as were MD thesis reports. A handful of studies could not be obtained. Therefore we may not have included in this review all clinical trials. By specifically hand searching documents published in India, we identified that an important body of Ayurvedic literature is not identifiable using traditional systematic review methods.
In summary, we found preliminary evidence suggesting that some herbs and herbal formulas used in Ayurvedic therapy can have clinically important glucose-lowering effects. C indica, holy basil, and Gymnema are particularly worthy of additional study.
Acknowledgments
This research was performed by the Southern California Evidence-Based Practice Center based at RAND, Santa Monica, CA under contract with the Agency for Healthcare Research and Quality (Contract No. 290-97-0001) with support from the National Center for Complementary and Alternative Medicine. The authors of this article are responsible for its contents. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality, the National Center for Complementary and Alternative Medicine, National Institutes of Health, or the US Department of Health and Human Services.
CORRESPONDING AUTHOR
Paul G. Shekelle, MD, PhD, West Los Angeles VA Medical Center, 111G, 11301 Wilshire Blvd, Los Angeles, CA 90073. E-mail: [email protected]. At the time of this study, Dr. Shekelle was a Senior Research Associate of the Veterans Affairs Health Services Research and Development Service.
1. Lad V. An introduction to Ayurveda. Altern Ther Health Med 1995;1:57-63.
2. Chopra A, Doiphode VV. Ayurvedic medicine. Core concept, therapeutic principles and current relevance. Med Clin North Am 2002;86:75-89.
3. Marles RJ, Farnsworth NR. Antidiabetic plants and their active constituents. Phytomedicine 1995;2:137-189.
4. Hardy M, Coulter I, Venuturupalli S, et al. Ayurvedic interventions for diabetes mellitus: a systematic review. Evidence Report/Technology Assessment No. 41. AHRQ Publication No. 01-E040; 2001.
5. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12.
6. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-412.
7. Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-613.
8. Balk EM, Bonis PA, Moskowitz H, et al. Correlation of quality measures with estimates of treatment effect in meta-analyses of randomized controlled trials. JAMA 2002;287:2973-2982.
9. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-1101.
10. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
11. Azad Khan A, Akhtar S, Mahtab H. Coccinia indica in the treatment of patients with diabetes mellitus. Bangladesh Med Res Counc Bull 1979;5:60-66.
12. Agrawal P, Rai V, Singh RB. Randomized placebo-controlled single-blind trial of holy basil leaves in patients with non-insulin-dependent diabetes mellitus. Int J Clin Pharmacol Ther 1996;34:406-409.
13. Chandola HM, Tripathi SN, Udupa KH. Hypoglycaemic response of c. tamala in patients of maturity onset (insulin independent) diabetes. J Res Ayurveda Sidda 1980;1:275-290.
14. Kamble SM, Jyotishi GS, Kamalakar PL, Vaidya SM. Efficacy of coccinia indica w. & a. in diabetes mellitus. J Res Ayurveda and Sidda 1996;17(1–2):77-84.
15. Kohli KR, Singh RH. A clinical trial of jambu (eugenia jambolana) in non-insulin dependant diabetes mellitus. J Res Ayurveda Sidda 1993;14(3–4):89-97.
16. Baskaran K, Kizar Ahamath B, Radha Shanmugasundaram K, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol 1990;30:295-300.
17. Shanmugasundaram E, Rajeswari G, Baskaran K, Rajesh Kumar BR, Radha Shanmugasundaram K, Kizar Ahmath B. Use of gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J Ethnopharmacol 1990;30:281-294.
18. Kuppurajan K, Seshadri C, Revathi R. Hypoglycaemic effect of coccinia indica in diabetes mellitus. Nagarjun 1986;29:1-4.
19. Kuppurajan K, Srivatsa A, Krishnaswami CV. Hypoglycemic and hypotriglyceridemic effects of methika churna (fenugreek). Antiseptic 1998;95:78-79.
20. Kumar N, Kumar A, Sharma ML. Clinical evaluation of single and herbo-mineral compound drugs in the management of madhumeha. J Res Ayurveda Sidda 1999;20(1–2):1-9.
21. Sharma RD, et al. Use of fenugreek seed powder in the management of non-insulin dependent diabetes mellitus. Nutr Res 1996;16:1331-1339.
22. Flexible dose open trial of Vijayasar in cases of newly-diagnosed non-insulin-dependent diabetes mellitus. Indian Council of Medical Research (ICMR), Collaborating Centres, New Delhi. Indian J Med Res 1998;108:24-29.
23. Goyal DK, Tiwari SK. Study on sadabahar (vinca rosea linn.) In madhumeha (diabetes mellitus). J Res Ayurveda Sidda 1999;20(1–2):93-100.
24. Chowdhary DP, Dua M, Bharti, Kishore P. Hypoglycaemic effect of a coded formulation: aysuh-82. J Res Ayurveda Sidda 1998;19(3–4):107-115.
25. Pandey VN, Rajagopalan SS, Chowdhary DP. An effective ayurvedic hypoglycemic formulation. J Res Ayurveda Sidda 1995;16(1–2):1-14.
26. Shankar R, Singhal R. Clinical studies of the effect of abraga (mica) chendooram in the treatment of diabetes mellitus (neerazhivu). J Res Ayurveda Sidda 1995;16(3–4):108-117.
27. Maji D, Singh AK. Clinical trial of D-400, a herbomineral preparation in diabetes mellitus. J Diabetic Assoc India 1995;35:1-4.
28. Sircar AR, Ahuja RC, Natu SM, Roy B, Sharma HM. Hypoglycemic, hypolipidemic and general beneficial effects of an herbal mixture MA-471. Alternat Ther Clin Pract 1996;3:26-31.
29. Shankar R, Sighal R. Clinical assessment of the effects of sandana (sandal) podi-a in the treatment of diabetes mellitus (neerazhiv). J Res Ayurveda Sidda 1994;15(3–4):89-97.
30. Sivaprakasam K, Rao KK, Yasodha R, Veluchamy G. Siddha remedy for diabetes mellitus. J Res Ayurveda Sidda 1984;5(1–4):25-32.
31. Kamble SM, Kamlakar PL, Vaidya S, Bambole VD. Influence of coccinia indica on certain enzymes in glycolytic and lipolytic pathway in human diabetes. Indian J Med Sci 1998;52:143-146.
32. Kapoor LD. CRC Handbook of Ayurvedic Medicinal Plants. Boca Raton, Fla: CRC Press; 1990.
33. Dash VB. Materia Medica of Indo-Tibetan Medicine. Delhi, India: MDIA Classics India; 1987;10-11.
34. Mishra L, Singh B, Dagenais S. Ayurveda: a historical perspective and principles of the traditional healthcare system in India. Altern Ther Health Med 2001;7:36-42.
1. Lad V. An introduction to Ayurveda. Altern Ther Health Med 1995;1:57-63.
2. Chopra A, Doiphode VV. Ayurvedic medicine. Core concept, therapeutic principles and current relevance. Med Clin North Am 2002;86:75-89.
3. Marles RJ, Farnsworth NR. Antidiabetic plants and their active constituents. Phytomedicine 1995;2:137-189.
4. Hardy M, Coulter I, Venuturupalli S, et al. Ayurvedic interventions for diabetes mellitus: a systematic review. Evidence Report/Technology Assessment No. 41. AHRQ Publication No. 01-E040; 2001.
5. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12.
6. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-412.
7. Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-613.
8. Balk EM, Bonis PA, Moskowitz H, et al. Correlation of quality measures with estimates of treatment effect in meta-analyses of randomized controlled trials. JAMA 2002;287:2973-2982.
9. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-1101.
10. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
11. Azad Khan A, Akhtar S, Mahtab H. Coccinia indica in the treatment of patients with diabetes mellitus. Bangladesh Med Res Counc Bull 1979;5:60-66.
12. Agrawal P, Rai V, Singh RB. Randomized placebo-controlled single-blind trial of holy basil leaves in patients with non-insulin-dependent diabetes mellitus. Int J Clin Pharmacol Ther 1996;34:406-409.
13. Chandola HM, Tripathi SN, Udupa KH. Hypoglycaemic response of c. tamala in patients of maturity onset (insulin independent) diabetes. J Res Ayurveda Sidda 1980;1:275-290.
14. Kamble SM, Jyotishi GS, Kamalakar PL, Vaidya SM. Efficacy of coccinia indica w. & a. in diabetes mellitus. J Res Ayurveda and Sidda 1996;17(1–2):77-84.
15. Kohli KR, Singh RH. A clinical trial of jambu (eugenia jambolana) in non-insulin dependant diabetes mellitus. J Res Ayurveda Sidda 1993;14(3–4):89-97.
16. Baskaran K, Kizar Ahamath B, Radha Shanmugasundaram K, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol 1990;30:295-300.
17. Shanmugasundaram E, Rajeswari G, Baskaran K, Rajesh Kumar BR, Radha Shanmugasundaram K, Kizar Ahmath B. Use of gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J Ethnopharmacol 1990;30:281-294.
18. Kuppurajan K, Seshadri C, Revathi R. Hypoglycaemic effect of coccinia indica in diabetes mellitus. Nagarjun 1986;29:1-4.
19. Kuppurajan K, Srivatsa A, Krishnaswami CV. Hypoglycemic and hypotriglyceridemic effects of methika churna (fenugreek). Antiseptic 1998;95:78-79.
20. Kumar N, Kumar A, Sharma ML. Clinical evaluation of single and herbo-mineral compound drugs in the management of madhumeha. J Res Ayurveda Sidda 1999;20(1–2):1-9.
21. Sharma RD, et al. Use of fenugreek seed powder in the management of non-insulin dependent diabetes mellitus. Nutr Res 1996;16:1331-1339.
22. Flexible dose open trial of Vijayasar in cases of newly-diagnosed non-insulin-dependent diabetes mellitus. Indian Council of Medical Research (ICMR), Collaborating Centres, New Delhi. Indian J Med Res 1998;108:24-29.
23. Goyal DK, Tiwari SK. Study on sadabahar (vinca rosea linn.) In madhumeha (diabetes mellitus). J Res Ayurveda Sidda 1999;20(1–2):93-100.
24. Chowdhary DP, Dua M, Bharti, Kishore P. Hypoglycaemic effect of a coded formulation: aysuh-82. J Res Ayurveda Sidda 1998;19(3–4):107-115.
25. Pandey VN, Rajagopalan SS, Chowdhary DP. An effective ayurvedic hypoglycemic formulation. J Res Ayurveda Sidda 1995;16(1–2):1-14.
26. Shankar R, Singhal R. Clinical studies of the effect of abraga (mica) chendooram in the treatment of diabetes mellitus (neerazhivu). J Res Ayurveda Sidda 1995;16(3–4):108-117.
27. Maji D, Singh AK. Clinical trial of D-400, a herbomineral preparation in diabetes mellitus. J Diabetic Assoc India 1995;35:1-4.
28. Sircar AR, Ahuja RC, Natu SM, Roy B, Sharma HM. Hypoglycemic, hypolipidemic and general beneficial effects of an herbal mixture MA-471. Alternat Ther Clin Pract 1996;3:26-31.
29. Shankar R, Sighal R. Clinical assessment of the effects of sandana (sandal) podi-a in the treatment of diabetes mellitus (neerazhiv). J Res Ayurveda Sidda 1994;15(3–4):89-97.
30. Sivaprakasam K, Rao KK, Yasodha R, Veluchamy G. Siddha remedy for diabetes mellitus. J Res Ayurveda Sidda 1984;5(1–4):25-32.
31. Kamble SM, Kamlakar PL, Vaidya S, Bambole VD. Influence of coccinia indica on certain enzymes in glycolytic and lipolytic pathway in human diabetes. Indian J Med Sci 1998;52:143-146.
32. Kapoor LD. CRC Handbook of Ayurvedic Medicinal Plants. Boca Raton, Fla: CRC Press; 1990.
33. Dash VB. Materia Medica of Indo-Tibetan Medicine. Delhi, India: MDIA Classics India; 1987;10-11.
34. Mishra L, Singh B, Dagenais S. Ayurveda: a historical perspective and principles of the traditional healthcare system in India. Altern Ther Health Med 2001;7:36-42.
Controlling hypoglycemia in type 2 diabetes: Which agent for which patient?
- Advise patients to monitor blood glucose levels frequently and learn to correlate drops in glucose to symptoms, which vary among patients.
- Ask patients at each visit about awareness of hypoglycemic episodes, their severity and timing, and how events relate to dosing, meals, and activities.
- When using oral agents, consider insulin sensitizers or newer sulfonylureas or meglitinides to reduce risk of hypoglycemia.
- If adding basal insulin to an oral regimen, the analog glargine has proven superior to NPH insulin in avoiding hypoglycemia.
Signs and symptoms of hypoglycemia vary considerably among patients with type 2 diabetes, making the condition easy to miss. Moreover, the most common symptoms are not necessarily the first symptoms.
If hypoglycemia occurs repeatedly, it can start a vicious cycle of physiologic reactions that mask or diminish the symptoms that warn patients of an impending episode. This may lead to hypoglycemia unawareness and hypoglycemic episodes of increasing severity. Fear of hypoglycemia, particularly of nocturnal events, may discourage patients from more intensive glycemic control, particularly using insulin. Such fear may even lead them to reduce their antidiabetic medication dosage, resulting in poor glycemic control.1
Breaking this cycle and restoring normal physiologic responses is one focus of this article, as is teaching patients how to monitor their blood glucose levels and how to correlate low blood glucose with the signs and symptoms of hypoglycemia.
Other therapies and strategies that we discuss in this article:
- Newer insulin analogs and the associated risk of hypoglycemia with each
- Appropriate combination of insulin with oral antidiabetic medications
- The long-acting analog insulin glargine used as basal insulin to lower the incidence of hypoglycemia, including nocturnal and severe hypoglycemia
- Rapid-acting insulin analogs (aspart, glulisine, and lispro) used in basalprandial insulin regimens.
First symptoms vary among individuals
Symptoms of hypoglycemia result primarily from a lowered glucose level in the brain and its effects on the central and autonomic nervous systems (FIGURE 1). A decrease in glucose below physiologic levels has acute consequences for brain function because the brain has an immediate requirement for glucose and little capacity for storage.
Two types of symptoms
Neuroglycopenia and the inhibition of neuronal metabolism causes sensations of warmth, weakness, fatigue, difficulty concentrating, confusion, behavioral changes, and in the most severe cases, a loss of consciousness, seizures, brain damage, and even death.2-4
Neurogenic symptoms are mediated by the hormones and neurotransmitters secreted in response to low brain glucose levels (FIGURE 1). The gluconeogenic actions of the autonomic nervous system produce the classic warning symptoms—tremulousness, pounding heart, anxiety, sweating, hunger, and tingling sensations—that usually precede the symptoms of hypoglycemia.2-4 This is particularly so in iatrogenic hypoglycemia.
These direct symptoms of neuroglycopenia are the ones patients typically identify with hypoglycemia. The most common symptoms of hypoglycemia are therefore not necessarily the first symptoms of hypoglycemia (TABLE 1).5 For example, though most patients experience sweating as a symptom of hypoglycemia, the first symptom might be trembling or anxiety, depending on the individual.5
TABLE 1
Signs and symptoms most commonly associated with hypoglycemia are not always the first to appear
| SYMPTOM | FREQUENCY (%) | FIRST SYMPTOM (%) |
|---|---|---|
| Sweating | 78 | 25 |
| Trembling | 62 | 6 |
| Inability to concentrate | 49 | 6 |
| Confusion | 40 | 3 |
| Weakness | 36 | 4 |
| Dry mouth | 35 | 0 |
| Blurred vision | 34 | 3 |
| Hunger | 33 | 3 |
| Anxiety | 26 | 1 |
| Headache | 21 | 0 |
| Difficulty walking | 21 | 3 |
| Pounding heart | 20 | 0 |
| Tingling around mouth | 20 | 6 |
| Difficulty speaking | 17 | 0 |
| Drowsiness | 15 | 0 |
| Odd behavior | 13 | 1 |
| Nausea | 13 | 0 |
| Adapted from Hepburn DA, MacLeod KM, Pell AC, et al. Diabet Med 1993;10:231–237.5 | ||
Factors influencing frequency and severity of hypoglycemia
Aggressive diabetes management commonly causes mild-to-moderate hypoglycemia, defined as a blood glucose value <60 mg/dL, that can be managed by the patient without assistance.
Severe hypoglycemia—a blood glucose value <50 mg/dL—is relatively uncommon in type 2 diabetes and requires the assistance of another person to manage, since neurological impairment may render patients unable to treat themselves.2,6 Severe hypoglycemia, whether in patients with type 1 or type 2 diabetes, can have debilitating consequences, including seizures or coma or even death.7
Long-standing type 2 disease. Hypoglycemia is more common in patients with type 1 diabetes than in those with type 2, but it can occur in type 2 diabetes patients who require insulin or are treated intensively with combinations of oral agents.6 As type 2 diabetes progresses,8 the incidence of hypoglycemic events increases, as endogenously produced insulin declines and is replaced by exogenous insulin.5,9 In fact, the prevalence of severe episodes (eg, requiring assistance of another person to administer glucose or glucagon) in patients with type 2 diabetes was comparable to that exhibited among patients with type 1 diabetes if they had been on insulin therapy for the same length of time.5,10
Nocturnal hypoglycemia. This event poses a special concern because the warning signs of hypoglycemia may be blunted during sleep. It has been reported that as many as 29% to 56% of all adult patients treated with insulin have an overnight glucose profile that indicates hypoglycemia occurs at night.11-13 However, it is important to note that the extent of the problem of nocturnal hypoglycemia is difficult to assess since overnight monitoring of glucose levels is required.
Additional insights from the UKPDS
Hypoglycemia in type 2 diabetes has not received rigorous attention in clinical trials. However, the United Kingdom Prospective Diabetes Study (UKPDS) was a large longitudinal trial in type 2 diabetes that included hypoglycemia as an outcome measure and thus provides some helpful information.
Events with insulin>sulfonylureas>diet. The 6-year follow-up revealed that the cumulative proportion of patients reporting 1 or more hypoglycemic events (of any type) was 76% for those using insulin, 45% among those taking sulfonylureas, and 3% for those on diet alone. Expressed as events per patient year, this was 37%, 17%, and 0.9%, respectively. When only “major” events (those requiring third-party assistance or hospital admission) were considered, the proportion of patients per year reporting 1 or more such events, was 2.3% for insulin, 0.7% for sulfonylureas, and 0.03% for diet alone. The cumulative proportion over 6 years was 3.3% of participants using sulfonylureas, 11.2% of those using insulin, and 0.15% of those on diet therapy.8
Metformin increases risk. The cumulative proportion of obese patients reporting any hypoglycemic event was 17.6% for those taking metformin vs 2.8% for those on diet. Severe hypoglycemia (as defined earlier) occurred in 2.4% of participants using metformin compared with 0.4% of those on diet therapy.8
Findings from other studies
Interestingly, in a recent systematic review of randomized controlled trials comparing insulin monotherapy with insulin plus oral antidiabetic agents, 13 of 14 studies reporting hypoglycemia demonstrated no difference in events.14
The occurrence of hypoglycemia among patients on metformin monotherapy in the UKPDS study is notable since, theoretically, hypoglycemia should not occur with agents whose mechanisms of action do not increase insulin secretion (biguanides, thiazolidinediones [TZDs], or α-glucosidase inhibitors),1 Since newer classes such as TZDs, α-glucosidase inhibitors, and meglitinides were not available when UKPDS was initiated, the trial does not provide data on these classes.
In a small comparative study of insulin combined with either metformin or a TZD, it appeared that metformin combination was associated with fewer occurrences of hypoglycemia; however, the small patient sample limits generalizability of the finding.15
How hypoglycemia occurs
Normally, as blood glucose levels (red) rise, insulin secretion increases, circulating insulin levels (blue) rise, and hepatic glucose production is inhibited. As glucose is disposed and circulating levels decrease due to insulin action, insulin levels then drop and hepatic glucose production begins again.
Hypoglycemia in diabetes can result from an excess of endogenous or exogenous insulin (iatrogenic hypoglycemia). In healthy patients, high insulin and falling glucose levels suppress insulin production and stimulate a hormone-mediated burst of glucose production. In patients with diabetes, the loss of physiologic control of insulin secretion coupled with exogenous administration of insulin or insulin secretagogues can interfere with the normal physiologic response to low blood glucose levels, resulting in hypoglycemia.1
With intense insulin regimens, the incidence of hypoglycemia can be as high as 30%, in contrast to 12% for patients treated with diet alone and 16% for those taking oral agents.6
With secretagogues, it has been suggested that the incidence of hypoglycemia is higher with the older, longer acting sulfonylurea agents.1,6,16-19 Although populationbased data on hypoglycemic rates associated with combination therapy with oral antidiabetic agents are not available, numerous clinical studies have reported rates of 10% to 20% for any hypoglycemic event.20-23
Heightening patient awareness, and yours
Because the signs of hypoglycemia vary considerably among individuals, they can easily be missed.3 In addition, repeated episodes of hypoglycemia can alter the normal regulatory responses and diminish the most important signs of a drop in glucose levels.1,2,24,25 The loss of the physiologic warning signs is thought to stem from dampening and eventual loss of the neuroadrenal response to low glucose levels in the brain (FIGURE 1). A vicious cycle is set up, whereby reduction in the neurogenic response attenuates hypoglycemic symptoms, causing more episodes to occur and become more severe as they are repeated. This cycle can be broken, and the normal physiologic response restored, if hypoglycemic events can be avoided for just a few weeks.2,26
Key points for patients. The main strategy for managing hypoglycemia is educating patients about the early symptoms of hypoglycemia and how to self-treat when they occur. Reinforce the need to time meals consistently and to limit the amount of carbohydrate ingested.
Advise patients to monitor blood glucose levels frequently, and to learn to relate a drop in glucose levels to hypoglycemic symptoms.2
Counsel patients to eat a snack or, preferably, drink fruit juice to counteract hypoglycemia. Patients may also carry glucose tablets, which are convenient and less tempting than candy.27
Glucagon is indicated for severe cases.
Whenever possible, a patient’s family members (particularly in the case of children) should be educated too.
Ask regularly about episodes. Finally, act to identify problems by querying patients and family members at every visit about hypoglycemia episodes, probing for information about awareness, severity and timing of the episodes, and how these events relate to dosing, meals, and activities.27 If hypoglycemia recurs, analyze the dosing regimen and consider flexible insulin dosing.1
Anti-hypoglycemia strategies for each new phase of therapy
As the course of diabetes therapy moves, typically, from oral medications to insulin to combination regimens, drug selections can be made in part to reduce the risk of hypoglycemia.
Oral agents: Insulin sensitizers, newer agents generally better
As noted earlier, among oral agents, insulin sensitizers are generally thought to have lower rates of hypoglycemia.
Newer sulfonylureas such as glimepiride and the rapid-acting meglitinides may also cause fewer hypoglycemic events.
Given the progressive decline of endogenous insulin secretion, combination therapy with secretagogues or insulin is eventually required for most patients.
Insulin analogs
A number of rapid-, short-, intermediateand long-acting insulin analogs have been introduced, and many of them make it possible to mimic different phases of physiologic insulin secretion (FIGURE 2). One of the newer analogs less likely to cause hypoglycemia is glargine, a long-acting insulin with a steady, relatively consistent action profile over a 24-hour period, closely mimicking normal basal pancreatic insulin secretion.28
FIGURE 2
Plasma insulin levels with newer analogs
N=20 type 1 diabetic patients; mean±SE
CSII, continuous subcutaneous insulin infusion; NPH, neutral protamine Hagedorn.
Copyright © 2000 American Diabetes Association. From Diabetes 2000; 49:2142–2148.28 Reprinted with permission from American Diabetes Association.
TABLE 2
Strategies for avoiding and addressing hypoglycemia
|
Insulin mixtures helpful when meal times guaranteed
Other insulins include mixtures of regular insulin and long-acting insulin available in split mixed or premixed formulations. These mixtures are intended to cover insulin peaks at mealtimes with twice-daily administration.
Mixed insulin formulations are often perceived as relatively convenient and simple to use, but they require meals to be taken within set time frames, without a great deal of flexibility. Since the ratios of the insulin components are fixed, and designed to work with meals consumed on a fixed schedule, hypoglycemia can occur if patients miss a meal. In addition, the time-activity profile of the insulin may not match the postprandial glucose peak even if the meal is consumed, and will increase the chance of postprandial hypoglycemia.
Basal insulin plus oral regimens
For patients with type 2 diabetes, adding basal insulin to oral regimens can significantly improve glycemic control. Ideally, basal insulin therapy provides a sustained and relatively constant concentration of insulin throughout the day. In the past, neutral protamine Hagedorn (NPH) insulin, a longer-acting insulin, was used for basal insulin therapy, and regular insulin was used to cover prandial insulin needs. Ultralente, also used as a basal insulin, has a relatively unpredictable timeactivity profile.28
Insulin glargine superior to NPH. In a recent clinical trial, patients with type 2 diabetes whose glucose levels were inadequately controlled on oral antidiabetic medications were given bedtime insulin glargine or NPH insulin.29 The insulin doses were titrated using a simple algorithm targeting a fasting plasma glucose (FPG) of ≤100 mg/dL to reach recommended glycosylated hemoglobin (Hb A1c) levels. Though no significant difference in glycemic control was found between insulin glargine and NPH insulin, significantly fewer hypoglycemic episodes occurred with insulin glargine therapy. The 24-hour distribution per patient-year of hypoglycemia for glargine vs NPH is shown in FIGURE 3.
Specifically, nearly 25% more patients treated with insulin glargine than with NPH insulin reached target Hb A1c levels of ≤7.0% without nocturnal hypoglycemia. Moreover, the overall incidence of any hypoglycemic event (eg, plasma-referenced glucose ≤72 mg/dL) and severe hypoglycemia (eg, patient required assistance of another person, and had a glucose level <56 mg/dL or prompt recovery after glucose or glucagons) was lower with insulin glargine than with NPH insulin. Results from other studies and a recent metaanalysis have been similar.30-32
Thus, using insulin glargine as basal insulin allows patients to reach recommended targets with fewer episodes of hypoglycemia, and can help address patients’ fear that can be a barrier to initiating insulin therapy in type 2 diabetes. Two recent studies have reported that dosing of insulin glargine can be flexible—morning or bedtime administration yields comparable low rates of hypoglycemia.30,31
FIGURE 3
Hourly hypoglycemia rate with glargine much less than with NPH
*P<.05 (between treatment).
Copyright © 2003 American Diabetes Association. From Diabetes Care 2003; 26:3080–3086.29 Reprinted with permission from American Diabetes Association.
Basal insulin plus prandial insulin
For patients who cannot otherwise reach Hb A1c goals, basal insulin therapy may be supplemented with prandial insulin. Newer, rapid-acting analogs used for the prandial component are insulin lispro, insulin glulisine, or insulin aspart. Although this approach is physiologically more rational than regimens using conventional insulins, data are limited for use in type 2 diabetes.
The incidence of nocturnal hypoglycemia was evaluated in a study of patients with type 1 diabetes and impaired hypoglycemic awareness who were treated with 1 of 2 regimens: insulin lispro in a basal-prandial combination with NPH insulin, or twice-daily, premixed NPH/regular insulin.33 Results showed that the incidence of nocturnal hypoglycemia was lower in patients receiving the insulin lispro regimen.
Another study, comparing insulin aspart and regular insulin as the prandial component in a basal-prandial regimen with NPH, showed that postprandial glucose control and Hb A1c levels were significantly better after 1 year of treatment in the insulin aspart group than in the group receiving regular insulin, without an increased risk for hypoglycemia.34 These results suggest that treatment with rapidacting insulin analogs could be helpful in avoiding hypoglycemia in patients with type 2 diabetes when a basal-prandial insulin regimen is indicated.
Avoiding hypoglycemia in the elderly
Elderly patients may be at increased risk for iatrogenic hypoglycemia. A populationbased study of patients presenting to an emergency room with severe hypoglycemic symptoms reported that rates of such events among elderly patients with type 2 diabetes and multiple comorbidities approached the rates among patients with type 1 diabetes.35
Creatinine clearance is often decreased in elderly patients, slowing elimination of oral agents and insulin and potentially resulting in sustained pharmacological action and creating a greater risk for hypoglycemia.
Furthermore, there is evidence that the neurogenic symptoms of hypoglycemia are reduced in elderly patients, diminishing awareness of hypoglycemia.36
In the demented elderly, malnutrition, weight loss, and anorexia may exacerbate the risk for hypoglycemia. For elderly patients with tertiary disease (eg, cerebrovascular accident, myocardial infarction, congestive heart failure, blindness, chronic renal failure), the risk for hypoglycemia and subsequent comorbidity may outweigh the benefits of strict glycemic control.3,37 Elderly patients may have comorbid conditions that increase risk of falls (eg, poor vision, neurologic conditions), and hypoglycemic episodes may further increase the risk of falls and lead to morbidity (eg, fragility fracture in patients with osteopenia or osteoporosis).
Because the elderly are at a greater risk for hypoglycemia, a switch to a less restrictive diet, such as a “no concentrated sweets” diet, is an option, with control of glucose levels through the administration of oral agents or insulin.36 This may also promote a better quality of life, considering that many of these patients already have secondary and tertiary complications of diabetes, prevention of which is not a realistic goal.
CORRESPONDING AUTHOR
William Cefalu, MD, Professor and Chief, Division of Nutrition and Chronic Diseases, Pennington Biomedical Research Center, Louisiana State University, 6400 Perkins Road, Baton Rouge, LA 70808. Email: [email protected]
1. Cryer PE, Childs BP. Negotiating the barrier of hypoglycemia in diabetes. Diabetes Spectrum 2002;15:20-27.
2. Cryer PE, ed. Hypoglycemia: Pathophysiology, Diagnosis, and Treatment. New York, NY: Oxford University Press; 1997.
3. McAulay V, Deary IJ, Frier BM. Symptoms of hypoglycaemia in people with diabetes. Diabet Med 2001;18:690-705.
4. Towler DA, Havlin CE, Craft S, Cryer P. Mechanism of awareness of hypoglycemia. Perception of neurogenic (predominantly cholinergic) rather than neuroglycopenic symptoms. Diabetes 1993;42:1791-1798.
5. Hepburn DA, MacLeod KM, Pell AC, Scougal IJ, Frier BM. Frequency and symptoms of hypoglycaemia experienced by patients with type 2 diabetes treated with insulin. Diabet Med 1993;10:231-237.
6. Miller CD, Phillips LS, Ziemer DC, Gallina DL, Cook CB, El-Kebbi IM. Hypoglycemia in patients with type 2 diabetes mellitus. Arch Intern Med 2001;161:1653-1659.
7. The DCCT Research Group. Epidemiology of severe hypoglycemia in the diabetes control and complications trial. Am J Med 1991;90:450-459.
8. UK Prospective Diabetes Study Group. Perspectives in diabetes. UK Prospective Diabetes Study 16: overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes 1995;44:1249-1258.
9. United Kingdom Prospective Diabetes Study Group. UKPDS 24: a 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy. Ann Intern Med 1998;128:165-175.
10. MacLeod KM, Hepburn DA, Frier BM. Frequency and morbidity of severe hypoglycaemia in insulin-treated diabetic patients. Diabet Med 1993;10:238-245.
11. Vervoort G, Goldschmidt HM, van Doorn LG. Nocturnal blood glucose profiles in patients with type 1 diabetes mellitus on multiple (>or=4) daily insulin injection regimens. Diabet Med 1996;13:794-799.
12. Gale EA, Tattersall RB. Unrecognised nocturnal hypoglycaemia in insulin-treated diabetics. Lancet 1979;1:1049-1052.
13. Pramming S, Thorsteinsson B, Bendtson I, Ronn B, Binder C. Nocturnal hypoglycaemia in patients receiving conventional treatment with insulin. Br Med J (Clin Res Ed) 1985;291:376-379.
14. Goudswaard AN, Furlong NJ, Valk GD, Stolk RP, Rutten GEHM. Insulin monotherapy versus combinations of insulin with oral hypoglycaemic agents in patients with type 2 diabetes mellitus. Cochrane Database Syst Rev 2004;4:1-51.
15. Strowig SM, Avilés-Santa ML, Raskin P. Comparison of insulin monotherapy and combination therapy with insulin and metformin or insulin and troglitazone in type 2 diabetes. Diabetes Care 2002;25:1691-1698.
16. Campbell IW. Hypoglycaemia and type 2 diabetes: sulphonylureas. In: Frier BM, Fisher BM, eds. Hypoglycaemia and Diabetes: Clinical and Physiological Aspects. London, UK: Edward Arnold, 1993;387-392.
17. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Individual sulfonylureas and serious hypoglycemia in older people. J Am Geriatr Soc 1996;44:751-755.
18. Holstein A, Egberts EH. Risk of hypoglycaemia with oral antidiabetic agents in patients with Type 2 diabetes. Exp Clin Endocrinol Diabetes 2003;111:405-414.
19. Holstein A, Plaschke A, Egberts E-H. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev 2001;17:467-473.
20. Aljabri K, Kozak SE, Thompson DM. Addition of pioglitazone or bedtime insulin to maximal doses of sulfonylurea and metformin in type 2 diabetes patients with poor glucose control: a prospective, randomized trial. Am J Med 2004;116:230-235.
21. Wolffenbuttel BHR, Landgraf R. A 1-year multicenter randomized double-blind comparison of repaglinide and glyburide for the treatment of type 2 diabetes. Dutch and German Repaglinide Study Group. Diabetes Care 1999;22:463-467.
22. Raskin P, McGill J, Saad MF, et al. Combination therapy for type 2 diabetes: repaglinide plus rosiglitazone. Diabetes Med 2004;21:329-335.
23. Dailey GE, III, Noor MA, Park JS, Bruce S, Fiedorek FT. Glycemic control with glyburide/metformin tablets in combination with rosiglitazone in patients with type 2 diabetes: a randomized, double-blind trial. Am J Med 2004;116:223-229.
24. Korytkowski MT, Mokan M, Veneman TF, Mitrakou A, Cryer PE, Gerich JE. Reduced beta-adrenergic sensitivity in patients with type 1 diabetes and hypoglycemia unawareness. Diabetes Care 1998;21:1939-1943.
25. Fritsche A, Stumvoll M, Grub M, et al. Effect of hypoglycemia on beta-adrenergic sensitivity in normal and type 1 diabetic subjects. Diabetes Care 1998;21:1505-1510.
26. Fritsche A, Stefan N, Haring H, Gerich J, Stumvoll M. Avoidance of hypoglycemia restores hypoglycemia awareness by increasing beta-adrenergic sensitivity in type 1 diabetes. Ann Intern Med 2001;134:729-736.
27. Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003;26:1902-1912.
28. Lepore M, Pampanelli S, Fanelli C, et al. Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes 2000;49:2142-2148.
29. Riddle MC, Rosenstock J, Gerich J. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003;26:3080-3086.
30. Fritsche A, Schweitzer MA, Häring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine Hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes: a randomized, controlled trial. Ann Intern Med 2003;138:952-959.
31. Standl E, Maxeiner S, Raptis S, Karimi-Anderesi Z, Schweitzer MA. Good glycemic control with flexibility in timing of basal insulin supply: a 24-week comparison of insulin glargine given once daily in the morning or at bedtime in combination with morning glimepiride. Diabetes Care 2005;28:419-420.
32. Rosenstock J, Dailey G, Massi Benedetti M, Fritsche A, Lin Z, Salzman A. Reduced hypoglycemia risk with insulin glargine. A meta-analysis comparing insulin glargine with human NPH insulin in type 2 diabetes. Diabetes Care 2005;28:950-955.
33. Ferguson SC, Strachan MW, Janes JM, Frier BM. Severe hypoglycaemia in patients with type 1 diabetes and impaired awareness of hypoglycaemia: a comparative study of insulin lispro and regular human insulin. Diabetes Metab Res Rev 2001;17:285-291.
34. Raskin P, Guthrie RA, Leiter L, Riis A, Jovanovic L. Use of insulin aspart, a fast-acting insulin analog, as the mealtime insulin in the management of patients with type 1 diabetes. Diabetes Care 2000;23:583-558.
35. Holstein A, Plaschke A, Egberts EH. Clinical characterisation of severe hypoglycaemia-a prospective population-based study. Exp Clin Endocrinol Diabetes 2003;111:364-369.
36. Meneilly GS, Cheung E, Tuokko H. Counterregulatory hormone responses to hypoglycemia in the elderly patient with diabetes. Diabetes 1994;43:403-410.
37. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2003;26(suppl 1):S33-S50.
- Advise patients to monitor blood glucose levels frequently and learn to correlate drops in glucose to symptoms, which vary among patients.
- Ask patients at each visit about awareness of hypoglycemic episodes, their severity and timing, and how events relate to dosing, meals, and activities.
- When using oral agents, consider insulin sensitizers or newer sulfonylureas or meglitinides to reduce risk of hypoglycemia.
- If adding basal insulin to an oral regimen, the analog glargine has proven superior to NPH insulin in avoiding hypoglycemia.
Signs and symptoms of hypoglycemia vary considerably among patients with type 2 diabetes, making the condition easy to miss. Moreover, the most common symptoms are not necessarily the first symptoms.
If hypoglycemia occurs repeatedly, it can start a vicious cycle of physiologic reactions that mask or diminish the symptoms that warn patients of an impending episode. This may lead to hypoglycemia unawareness and hypoglycemic episodes of increasing severity. Fear of hypoglycemia, particularly of nocturnal events, may discourage patients from more intensive glycemic control, particularly using insulin. Such fear may even lead them to reduce their antidiabetic medication dosage, resulting in poor glycemic control.1
Breaking this cycle and restoring normal physiologic responses is one focus of this article, as is teaching patients how to monitor their blood glucose levels and how to correlate low blood glucose with the signs and symptoms of hypoglycemia.
Other therapies and strategies that we discuss in this article:
- Newer insulin analogs and the associated risk of hypoglycemia with each
- Appropriate combination of insulin with oral antidiabetic medications
- The long-acting analog insulin glargine used as basal insulin to lower the incidence of hypoglycemia, including nocturnal and severe hypoglycemia
- Rapid-acting insulin analogs (aspart, glulisine, and lispro) used in basalprandial insulin regimens.
First symptoms vary among individuals
Symptoms of hypoglycemia result primarily from a lowered glucose level in the brain and its effects on the central and autonomic nervous systems (FIGURE 1). A decrease in glucose below physiologic levels has acute consequences for brain function because the brain has an immediate requirement for glucose and little capacity for storage.
Two types of symptoms
Neuroglycopenia and the inhibition of neuronal metabolism causes sensations of warmth, weakness, fatigue, difficulty concentrating, confusion, behavioral changes, and in the most severe cases, a loss of consciousness, seizures, brain damage, and even death.2-4
Neurogenic symptoms are mediated by the hormones and neurotransmitters secreted in response to low brain glucose levels (FIGURE 1). The gluconeogenic actions of the autonomic nervous system produce the classic warning symptoms—tremulousness, pounding heart, anxiety, sweating, hunger, and tingling sensations—that usually precede the symptoms of hypoglycemia.2-4 This is particularly so in iatrogenic hypoglycemia.
These direct symptoms of neuroglycopenia are the ones patients typically identify with hypoglycemia. The most common symptoms of hypoglycemia are therefore not necessarily the first symptoms of hypoglycemia (TABLE 1).5 For example, though most patients experience sweating as a symptom of hypoglycemia, the first symptom might be trembling or anxiety, depending on the individual.5
TABLE 1
Signs and symptoms most commonly associated with hypoglycemia are not always the first to appear
| SYMPTOM | FREQUENCY (%) | FIRST SYMPTOM (%) |
|---|---|---|
| Sweating | 78 | 25 |
| Trembling | 62 | 6 |
| Inability to concentrate | 49 | 6 |
| Confusion | 40 | 3 |
| Weakness | 36 | 4 |
| Dry mouth | 35 | 0 |
| Blurred vision | 34 | 3 |
| Hunger | 33 | 3 |
| Anxiety | 26 | 1 |
| Headache | 21 | 0 |
| Difficulty walking | 21 | 3 |
| Pounding heart | 20 | 0 |
| Tingling around mouth | 20 | 6 |
| Difficulty speaking | 17 | 0 |
| Drowsiness | 15 | 0 |
| Odd behavior | 13 | 1 |
| Nausea | 13 | 0 |
| Adapted from Hepburn DA, MacLeod KM, Pell AC, et al. Diabet Med 1993;10:231–237.5 | ||
Factors influencing frequency and severity of hypoglycemia
Aggressive diabetes management commonly causes mild-to-moderate hypoglycemia, defined as a blood glucose value <60 mg/dL, that can be managed by the patient without assistance.
Severe hypoglycemia—a blood glucose value <50 mg/dL—is relatively uncommon in type 2 diabetes and requires the assistance of another person to manage, since neurological impairment may render patients unable to treat themselves.2,6 Severe hypoglycemia, whether in patients with type 1 or type 2 diabetes, can have debilitating consequences, including seizures or coma or even death.7
Long-standing type 2 disease. Hypoglycemia is more common in patients with type 1 diabetes than in those with type 2, but it can occur in type 2 diabetes patients who require insulin or are treated intensively with combinations of oral agents.6 As type 2 diabetes progresses,8 the incidence of hypoglycemic events increases, as endogenously produced insulin declines and is replaced by exogenous insulin.5,9 In fact, the prevalence of severe episodes (eg, requiring assistance of another person to administer glucose or glucagon) in patients with type 2 diabetes was comparable to that exhibited among patients with type 1 diabetes if they had been on insulin therapy for the same length of time.5,10
Nocturnal hypoglycemia. This event poses a special concern because the warning signs of hypoglycemia may be blunted during sleep. It has been reported that as many as 29% to 56% of all adult patients treated with insulin have an overnight glucose profile that indicates hypoglycemia occurs at night.11-13 However, it is important to note that the extent of the problem of nocturnal hypoglycemia is difficult to assess since overnight monitoring of glucose levels is required.
Additional insights from the UKPDS
Hypoglycemia in type 2 diabetes has not received rigorous attention in clinical trials. However, the United Kingdom Prospective Diabetes Study (UKPDS) was a large longitudinal trial in type 2 diabetes that included hypoglycemia as an outcome measure and thus provides some helpful information.
Events with insulin>sulfonylureas>diet. The 6-year follow-up revealed that the cumulative proportion of patients reporting 1 or more hypoglycemic events (of any type) was 76% for those using insulin, 45% among those taking sulfonylureas, and 3% for those on diet alone. Expressed as events per patient year, this was 37%, 17%, and 0.9%, respectively. When only “major” events (those requiring third-party assistance or hospital admission) were considered, the proportion of patients per year reporting 1 or more such events, was 2.3% for insulin, 0.7% for sulfonylureas, and 0.03% for diet alone. The cumulative proportion over 6 years was 3.3% of participants using sulfonylureas, 11.2% of those using insulin, and 0.15% of those on diet therapy.8
Metformin increases risk. The cumulative proportion of obese patients reporting any hypoglycemic event was 17.6% for those taking metformin vs 2.8% for those on diet. Severe hypoglycemia (as defined earlier) occurred in 2.4% of participants using metformin compared with 0.4% of those on diet therapy.8
Findings from other studies
Interestingly, in a recent systematic review of randomized controlled trials comparing insulin monotherapy with insulin plus oral antidiabetic agents, 13 of 14 studies reporting hypoglycemia demonstrated no difference in events.14
The occurrence of hypoglycemia among patients on metformin monotherapy in the UKPDS study is notable since, theoretically, hypoglycemia should not occur with agents whose mechanisms of action do not increase insulin secretion (biguanides, thiazolidinediones [TZDs], or α-glucosidase inhibitors),1 Since newer classes such as TZDs, α-glucosidase inhibitors, and meglitinides were not available when UKPDS was initiated, the trial does not provide data on these classes.
In a small comparative study of insulin combined with either metformin or a TZD, it appeared that metformin combination was associated with fewer occurrences of hypoglycemia; however, the small patient sample limits generalizability of the finding.15
How hypoglycemia occurs
Normally, as blood glucose levels (red) rise, insulin secretion increases, circulating insulin levels (blue) rise, and hepatic glucose production is inhibited. As glucose is disposed and circulating levels decrease due to insulin action, insulin levels then drop and hepatic glucose production begins again.
Hypoglycemia in diabetes can result from an excess of endogenous or exogenous insulin (iatrogenic hypoglycemia). In healthy patients, high insulin and falling glucose levels suppress insulin production and stimulate a hormone-mediated burst of glucose production. In patients with diabetes, the loss of physiologic control of insulin secretion coupled with exogenous administration of insulin or insulin secretagogues can interfere with the normal physiologic response to low blood glucose levels, resulting in hypoglycemia.1
With intense insulin regimens, the incidence of hypoglycemia can be as high as 30%, in contrast to 12% for patients treated with diet alone and 16% for those taking oral agents.6
With secretagogues, it has been suggested that the incidence of hypoglycemia is higher with the older, longer acting sulfonylurea agents.1,6,16-19 Although populationbased data on hypoglycemic rates associated with combination therapy with oral antidiabetic agents are not available, numerous clinical studies have reported rates of 10% to 20% for any hypoglycemic event.20-23
Heightening patient awareness, and yours
Because the signs of hypoglycemia vary considerably among individuals, they can easily be missed.3 In addition, repeated episodes of hypoglycemia can alter the normal regulatory responses and diminish the most important signs of a drop in glucose levels.1,2,24,25 The loss of the physiologic warning signs is thought to stem from dampening and eventual loss of the neuroadrenal response to low glucose levels in the brain (FIGURE 1). A vicious cycle is set up, whereby reduction in the neurogenic response attenuates hypoglycemic symptoms, causing more episodes to occur and become more severe as they are repeated. This cycle can be broken, and the normal physiologic response restored, if hypoglycemic events can be avoided for just a few weeks.2,26
Key points for patients. The main strategy for managing hypoglycemia is educating patients about the early symptoms of hypoglycemia and how to self-treat when they occur. Reinforce the need to time meals consistently and to limit the amount of carbohydrate ingested.
Advise patients to monitor blood glucose levels frequently, and to learn to relate a drop in glucose levels to hypoglycemic symptoms.2
Counsel patients to eat a snack or, preferably, drink fruit juice to counteract hypoglycemia. Patients may also carry glucose tablets, which are convenient and less tempting than candy.27
Glucagon is indicated for severe cases.
Whenever possible, a patient’s family members (particularly in the case of children) should be educated too.
Ask regularly about episodes. Finally, act to identify problems by querying patients and family members at every visit about hypoglycemia episodes, probing for information about awareness, severity and timing of the episodes, and how these events relate to dosing, meals, and activities.27 If hypoglycemia recurs, analyze the dosing regimen and consider flexible insulin dosing.1
Anti-hypoglycemia strategies for each new phase of therapy
As the course of diabetes therapy moves, typically, from oral medications to insulin to combination regimens, drug selections can be made in part to reduce the risk of hypoglycemia.
Oral agents: Insulin sensitizers, newer agents generally better
As noted earlier, among oral agents, insulin sensitizers are generally thought to have lower rates of hypoglycemia.
Newer sulfonylureas such as glimepiride and the rapid-acting meglitinides may also cause fewer hypoglycemic events.
Given the progressive decline of endogenous insulin secretion, combination therapy with secretagogues or insulin is eventually required for most patients.
Insulin analogs
A number of rapid-, short-, intermediateand long-acting insulin analogs have been introduced, and many of them make it possible to mimic different phases of physiologic insulin secretion (FIGURE 2). One of the newer analogs less likely to cause hypoglycemia is glargine, a long-acting insulin with a steady, relatively consistent action profile over a 24-hour period, closely mimicking normal basal pancreatic insulin secretion.28
FIGURE 2
Plasma insulin levels with newer analogs
N=20 type 1 diabetic patients; mean±SE
CSII, continuous subcutaneous insulin infusion; NPH, neutral protamine Hagedorn.
Copyright © 2000 American Diabetes Association. From Diabetes 2000; 49:2142–2148.28 Reprinted with permission from American Diabetes Association.
TABLE 2
Strategies for avoiding and addressing hypoglycemia
|
Insulin mixtures helpful when meal times guaranteed
Other insulins include mixtures of regular insulin and long-acting insulin available in split mixed or premixed formulations. These mixtures are intended to cover insulin peaks at mealtimes with twice-daily administration.
Mixed insulin formulations are often perceived as relatively convenient and simple to use, but they require meals to be taken within set time frames, without a great deal of flexibility. Since the ratios of the insulin components are fixed, and designed to work with meals consumed on a fixed schedule, hypoglycemia can occur if patients miss a meal. In addition, the time-activity profile of the insulin may not match the postprandial glucose peak even if the meal is consumed, and will increase the chance of postprandial hypoglycemia.
Basal insulin plus oral regimens
For patients with type 2 diabetes, adding basal insulin to oral regimens can significantly improve glycemic control. Ideally, basal insulin therapy provides a sustained and relatively constant concentration of insulin throughout the day. In the past, neutral protamine Hagedorn (NPH) insulin, a longer-acting insulin, was used for basal insulin therapy, and regular insulin was used to cover prandial insulin needs. Ultralente, also used as a basal insulin, has a relatively unpredictable timeactivity profile.28
Insulin glargine superior to NPH. In a recent clinical trial, patients with type 2 diabetes whose glucose levels were inadequately controlled on oral antidiabetic medications were given bedtime insulin glargine or NPH insulin.29 The insulin doses were titrated using a simple algorithm targeting a fasting plasma glucose (FPG) of ≤100 mg/dL to reach recommended glycosylated hemoglobin (Hb A1c) levels. Though no significant difference in glycemic control was found between insulin glargine and NPH insulin, significantly fewer hypoglycemic episodes occurred with insulin glargine therapy. The 24-hour distribution per patient-year of hypoglycemia for glargine vs NPH is shown in FIGURE 3.
Specifically, nearly 25% more patients treated with insulin glargine than with NPH insulin reached target Hb A1c levels of ≤7.0% without nocturnal hypoglycemia. Moreover, the overall incidence of any hypoglycemic event (eg, plasma-referenced glucose ≤72 mg/dL) and severe hypoglycemia (eg, patient required assistance of another person, and had a glucose level <56 mg/dL or prompt recovery after glucose or glucagons) was lower with insulin glargine than with NPH insulin. Results from other studies and a recent metaanalysis have been similar.30-32
Thus, using insulin glargine as basal insulin allows patients to reach recommended targets with fewer episodes of hypoglycemia, and can help address patients’ fear that can be a barrier to initiating insulin therapy in type 2 diabetes. Two recent studies have reported that dosing of insulin glargine can be flexible—morning or bedtime administration yields comparable low rates of hypoglycemia.30,31
FIGURE 3
Hourly hypoglycemia rate with glargine much less than with NPH
*P<.05 (between treatment).
Copyright © 2003 American Diabetes Association. From Diabetes Care 2003; 26:3080–3086.29 Reprinted with permission from American Diabetes Association.
Basal insulin plus prandial insulin
For patients who cannot otherwise reach Hb A1c goals, basal insulin therapy may be supplemented with prandial insulin. Newer, rapid-acting analogs used for the prandial component are insulin lispro, insulin glulisine, or insulin aspart. Although this approach is physiologically more rational than regimens using conventional insulins, data are limited for use in type 2 diabetes.
The incidence of nocturnal hypoglycemia was evaluated in a study of patients with type 1 diabetes and impaired hypoglycemic awareness who were treated with 1 of 2 regimens: insulin lispro in a basal-prandial combination with NPH insulin, or twice-daily, premixed NPH/regular insulin.33 Results showed that the incidence of nocturnal hypoglycemia was lower in patients receiving the insulin lispro regimen.
Another study, comparing insulin aspart and regular insulin as the prandial component in a basal-prandial regimen with NPH, showed that postprandial glucose control and Hb A1c levels were significantly better after 1 year of treatment in the insulin aspart group than in the group receiving regular insulin, without an increased risk for hypoglycemia.34 These results suggest that treatment with rapidacting insulin analogs could be helpful in avoiding hypoglycemia in patients with type 2 diabetes when a basal-prandial insulin regimen is indicated.
Avoiding hypoglycemia in the elderly
Elderly patients may be at increased risk for iatrogenic hypoglycemia. A populationbased study of patients presenting to an emergency room with severe hypoglycemic symptoms reported that rates of such events among elderly patients with type 2 diabetes and multiple comorbidities approached the rates among patients with type 1 diabetes.35
Creatinine clearance is often decreased in elderly patients, slowing elimination of oral agents and insulin and potentially resulting in sustained pharmacological action and creating a greater risk for hypoglycemia.
Furthermore, there is evidence that the neurogenic symptoms of hypoglycemia are reduced in elderly patients, diminishing awareness of hypoglycemia.36
In the demented elderly, malnutrition, weight loss, and anorexia may exacerbate the risk for hypoglycemia. For elderly patients with tertiary disease (eg, cerebrovascular accident, myocardial infarction, congestive heart failure, blindness, chronic renal failure), the risk for hypoglycemia and subsequent comorbidity may outweigh the benefits of strict glycemic control.3,37 Elderly patients may have comorbid conditions that increase risk of falls (eg, poor vision, neurologic conditions), and hypoglycemic episodes may further increase the risk of falls and lead to morbidity (eg, fragility fracture in patients with osteopenia or osteoporosis).
Because the elderly are at a greater risk for hypoglycemia, a switch to a less restrictive diet, such as a “no concentrated sweets” diet, is an option, with control of glucose levels through the administration of oral agents or insulin.36 This may also promote a better quality of life, considering that many of these patients already have secondary and tertiary complications of diabetes, prevention of which is not a realistic goal.
CORRESPONDING AUTHOR
William Cefalu, MD, Professor and Chief, Division of Nutrition and Chronic Diseases, Pennington Biomedical Research Center, Louisiana State University, 6400 Perkins Road, Baton Rouge, LA 70808. Email: [email protected]
- Advise patients to monitor blood glucose levels frequently and learn to correlate drops in glucose to symptoms, which vary among patients.
- Ask patients at each visit about awareness of hypoglycemic episodes, their severity and timing, and how events relate to dosing, meals, and activities.
- When using oral agents, consider insulin sensitizers or newer sulfonylureas or meglitinides to reduce risk of hypoglycemia.
- If adding basal insulin to an oral regimen, the analog glargine has proven superior to NPH insulin in avoiding hypoglycemia.
Signs and symptoms of hypoglycemia vary considerably among patients with type 2 diabetes, making the condition easy to miss. Moreover, the most common symptoms are not necessarily the first symptoms.
If hypoglycemia occurs repeatedly, it can start a vicious cycle of physiologic reactions that mask or diminish the symptoms that warn patients of an impending episode. This may lead to hypoglycemia unawareness and hypoglycemic episodes of increasing severity. Fear of hypoglycemia, particularly of nocturnal events, may discourage patients from more intensive glycemic control, particularly using insulin. Such fear may even lead them to reduce their antidiabetic medication dosage, resulting in poor glycemic control.1
Breaking this cycle and restoring normal physiologic responses is one focus of this article, as is teaching patients how to monitor their blood glucose levels and how to correlate low blood glucose with the signs and symptoms of hypoglycemia.
Other therapies and strategies that we discuss in this article:
- Newer insulin analogs and the associated risk of hypoglycemia with each
- Appropriate combination of insulin with oral antidiabetic medications
- The long-acting analog insulin glargine used as basal insulin to lower the incidence of hypoglycemia, including nocturnal and severe hypoglycemia
- Rapid-acting insulin analogs (aspart, glulisine, and lispro) used in basalprandial insulin regimens.
First symptoms vary among individuals
Symptoms of hypoglycemia result primarily from a lowered glucose level in the brain and its effects on the central and autonomic nervous systems (FIGURE 1). A decrease in glucose below physiologic levels has acute consequences for brain function because the brain has an immediate requirement for glucose and little capacity for storage.
Two types of symptoms
Neuroglycopenia and the inhibition of neuronal metabolism causes sensations of warmth, weakness, fatigue, difficulty concentrating, confusion, behavioral changes, and in the most severe cases, a loss of consciousness, seizures, brain damage, and even death.2-4
Neurogenic symptoms are mediated by the hormones and neurotransmitters secreted in response to low brain glucose levels (FIGURE 1). The gluconeogenic actions of the autonomic nervous system produce the classic warning symptoms—tremulousness, pounding heart, anxiety, sweating, hunger, and tingling sensations—that usually precede the symptoms of hypoglycemia.2-4 This is particularly so in iatrogenic hypoglycemia.
These direct symptoms of neuroglycopenia are the ones patients typically identify with hypoglycemia. The most common symptoms of hypoglycemia are therefore not necessarily the first symptoms of hypoglycemia (TABLE 1).5 For example, though most patients experience sweating as a symptom of hypoglycemia, the first symptom might be trembling or anxiety, depending on the individual.5
TABLE 1
Signs and symptoms most commonly associated with hypoglycemia are not always the first to appear
| SYMPTOM | FREQUENCY (%) | FIRST SYMPTOM (%) |
|---|---|---|
| Sweating | 78 | 25 |
| Trembling | 62 | 6 |
| Inability to concentrate | 49 | 6 |
| Confusion | 40 | 3 |
| Weakness | 36 | 4 |
| Dry mouth | 35 | 0 |
| Blurred vision | 34 | 3 |
| Hunger | 33 | 3 |
| Anxiety | 26 | 1 |
| Headache | 21 | 0 |
| Difficulty walking | 21 | 3 |
| Pounding heart | 20 | 0 |
| Tingling around mouth | 20 | 6 |
| Difficulty speaking | 17 | 0 |
| Drowsiness | 15 | 0 |
| Odd behavior | 13 | 1 |
| Nausea | 13 | 0 |
| Adapted from Hepburn DA, MacLeod KM, Pell AC, et al. Diabet Med 1993;10:231–237.5 | ||
Factors influencing frequency and severity of hypoglycemia
Aggressive diabetes management commonly causes mild-to-moderate hypoglycemia, defined as a blood glucose value <60 mg/dL, that can be managed by the patient without assistance.
Severe hypoglycemia—a blood glucose value <50 mg/dL—is relatively uncommon in type 2 diabetes and requires the assistance of another person to manage, since neurological impairment may render patients unable to treat themselves.2,6 Severe hypoglycemia, whether in patients with type 1 or type 2 diabetes, can have debilitating consequences, including seizures or coma or even death.7
Long-standing type 2 disease. Hypoglycemia is more common in patients with type 1 diabetes than in those with type 2, but it can occur in type 2 diabetes patients who require insulin or are treated intensively with combinations of oral agents.6 As type 2 diabetes progresses,8 the incidence of hypoglycemic events increases, as endogenously produced insulin declines and is replaced by exogenous insulin.5,9 In fact, the prevalence of severe episodes (eg, requiring assistance of another person to administer glucose or glucagon) in patients with type 2 diabetes was comparable to that exhibited among patients with type 1 diabetes if they had been on insulin therapy for the same length of time.5,10
Nocturnal hypoglycemia. This event poses a special concern because the warning signs of hypoglycemia may be blunted during sleep. It has been reported that as many as 29% to 56% of all adult patients treated with insulin have an overnight glucose profile that indicates hypoglycemia occurs at night.11-13 However, it is important to note that the extent of the problem of nocturnal hypoglycemia is difficult to assess since overnight monitoring of glucose levels is required.
Additional insights from the UKPDS
Hypoglycemia in type 2 diabetes has not received rigorous attention in clinical trials. However, the United Kingdom Prospective Diabetes Study (UKPDS) was a large longitudinal trial in type 2 diabetes that included hypoglycemia as an outcome measure and thus provides some helpful information.
Events with insulin>sulfonylureas>diet. The 6-year follow-up revealed that the cumulative proportion of patients reporting 1 or more hypoglycemic events (of any type) was 76% for those using insulin, 45% among those taking sulfonylureas, and 3% for those on diet alone. Expressed as events per patient year, this was 37%, 17%, and 0.9%, respectively. When only “major” events (those requiring third-party assistance or hospital admission) were considered, the proportion of patients per year reporting 1 or more such events, was 2.3% for insulin, 0.7% for sulfonylureas, and 0.03% for diet alone. The cumulative proportion over 6 years was 3.3% of participants using sulfonylureas, 11.2% of those using insulin, and 0.15% of those on diet therapy.8
Metformin increases risk. The cumulative proportion of obese patients reporting any hypoglycemic event was 17.6% for those taking metformin vs 2.8% for those on diet. Severe hypoglycemia (as defined earlier) occurred in 2.4% of participants using metformin compared with 0.4% of those on diet therapy.8
Findings from other studies
Interestingly, in a recent systematic review of randomized controlled trials comparing insulin monotherapy with insulin plus oral antidiabetic agents, 13 of 14 studies reporting hypoglycemia demonstrated no difference in events.14
The occurrence of hypoglycemia among patients on metformin monotherapy in the UKPDS study is notable since, theoretically, hypoglycemia should not occur with agents whose mechanisms of action do not increase insulin secretion (biguanides, thiazolidinediones [TZDs], or α-glucosidase inhibitors),1 Since newer classes such as TZDs, α-glucosidase inhibitors, and meglitinides were not available when UKPDS was initiated, the trial does not provide data on these classes.
In a small comparative study of insulin combined with either metformin or a TZD, it appeared that metformin combination was associated with fewer occurrences of hypoglycemia; however, the small patient sample limits generalizability of the finding.15
How hypoglycemia occurs
Normally, as blood glucose levels (red) rise, insulin secretion increases, circulating insulin levels (blue) rise, and hepatic glucose production is inhibited. As glucose is disposed and circulating levels decrease due to insulin action, insulin levels then drop and hepatic glucose production begins again.
Hypoglycemia in diabetes can result from an excess of endogenous or exogenous insulin (iatrogenic hypoglycemia). In healthy patients, high insulin and falling glucose levels suppress insulin production and stimulate a hormone-mediated burst of glucose production. In patients with diabetes, the loss of physiologic control of insulin secretion coupled with exogenous administration of insulin or insulin secretagogues can interfere with the normal physiologic response to low blood glucose levels, resulting in hypoglycemia.1
With intense insulin regimens, the incidence of hypoglycemia can be as high as 30%, in contrast to 12% for patients treated with diet alone and 16% for those taking oral agents.6
With secretagogues, it has been suggested that the incidence of hypoglycemia is higher with the older, longer acting sulfonylurea agents.1,6,16-19 Although populationbased data on hypoglycemic rates associated with combination therapy with oral antidiabetic agents are not available, numerous clinical studies have reported rates of 10% to 20% for any hypoglycemic event.20-23
Heightening patient awareness, and yours
Because the signs of hypoglycemia vary considerably among individuals, they can easily be missed.3 In addition, repeated episodes of hypoglycemia can alter the normal regulatory responses and diminish the most important signs of a drop in glucose levels.1,2,24,25 The loss of the physiologic warning signs is thought to stem from dampening and eventual loss of the neuroadrenal response to low glucose levels in the brain (FIGURE 1). A vicious cycle is set up, whereby reduction in the neurogenic response attenuates hypoglycemic symptoms, causing more episodes to occur and become more severe as they are repeated. This cycle can be broken, and the normal physiologic response restored, if hypoglycemic events can be avoided for just a few weeks.2,26
Key points for patients. The main strategy for managing hypoglycemia is educating patients about the early symptoms of hypoglycemia and how to self-treat when they occur. Reinforce the need to time meals consistently and to limit the amount of carbohydrate ingested.
Advise patients to monitor blood glucose levels frequently, and to learn to relate a drop in glucose levels to hypoglycemic symptoms.2
Counsel patients to eat a snack or, preferably, drink fruit juice to counteract hypoglycemia. Patients may also carry glucose tablets, which are convenient and less tempting than candy.27
Glucagon is indicated for severe cases.
Whenever possible, a patient’s family members (particularly in the case of children) should be educated too.
Ask regularly about episodes. Finally, act to identify problems by querying patients and family members at every visit about hypoglycemia episodes, probing for information about awareness, severity and timing of the episodes, and how these events relate to dosing, meals, and activities.27 If hypoglycemia recurs, analyze the dosing regimen and consider flexible insulin dosing.1
Anti-hypoglycemia strategies for each new phase of therapy
As the course of diabetes therapy moves, typically, from oral medications to insulin to combination regimens, drug selections can be made in part to reduce the risk of hypoglycemia.
Oral agents: Insulin sensitizers, newer agents generally better
As noted earlier, among oral agents, insulin sensitizers are generally thought to have lower rates of hypoglycemia.
Newer sulfonylureas such as glimepiride and the rapid-acting meglitinides may also cause fewer hypoglycemic events.
Given the progressive decline of endogenous insulin secretion, combination therapy with secretagogues or insulin is eventually required for most patients.
Insulin analogs
A number of rapid-, short-, intermediateand long-acting insulin analogs have been introduced, and many of them make it possible to mimic different phases of physiologic insulin secretion (FIGURE 2). One of the newer analogs less likely to cause hypoglycemia is glargine, a long-acting insulin with a steady, relatively consistent action profile over a 24-hour period, closely mimicking normal basal pancreatic insulin secretion.28
FIGURE 2
Plasma insulin levels with newer analogs
N=20 type 1 diabetic patients; mean±SE
CSII, continuous subcutaneous insulin infusion; NPH, neutral protamine Hagedorn.
Copyright © 2000 American Diabetes Association. From Diabetes 2000; 49:2142–2148.28 Reprinted with permission from American Diabetes Association.
TABLE 2
Strategies for avoiding and addressing hypoglycemia
|
Insulin mixtures helpful when meal times guaranteed
Other insulins include mixtures of regular insulin and long-acting insulin available in split mixed or premixed formulations. These mixtures are intended to cover insulin peaks at mealtimes with twice-daily administration.
Mixed insulin formulations are often perceived as relatively convenient and simple to use, but they require meals to be taken within set time frames, without a great deal of flexibility. Since the ratios of the insulin components are fixed, and designed to work with meals consumed on a fixed schedule, hypoglycemia can occur if patients miss a meal. In addition, the time-activity profile of the insulin may not match the postprandial glucose peak even if the meal is consumed, and will increase the chance of postprandial hypoglycemia.
Basal insulin plus oral regimens
For patients with type 2 diabetes, adding basal insulin to oral regimens can significantly improve glycemic control. Ideally, basal insulin therapy provides a sustained and relatively constant concentration of insulin throughout the day. In the past, neutral protamine Hagedorn (NPH) insulin, a longer-acting insulin, was used for basal insulin therapy, and regular insulin was used to cover prandial insulin needs. Ultralente, also used as a basal insulin, has a relatively unpredictable timeactivity profile.28
Insulin glargine superior to NPH. In a recent clinical trial, patients with type 2 diabetes whose glucose levels were inadequately controlled on oral antidiabetic medications were given bedtime insulin glargine or NPH insulin.29 The insulin doses were titrated using a simple algorithm targeting a fasting plasma glucose (FPG) of ≤100 mg/dL to reach recommended glycosylated hemoglobin (Hb A1c) levels. Though no significant difference in glycemic control was found between insulin glargine and NPH insulin, significantly fewer hypoglycemic episodes occurred with insulin glargine therapy. The 24-hour distribution per patient-year of hypoglycemia for glargine vs NPH is shown in FIGURE 3.
Specifically, nearly 25% more patients treated with insulin glargine than with NPH insulin reached target Hb A1c levels of ≤7.0% without nocturnal hypoglycemia. Moreover, the overall incidence of any hypoglycemic event (eg, plasma-referenced glucose ≤72 mg/dL) and severe hypoglycemia (eg, patient required assistance of another person, and had a glucose level <56 mg/dL or prompt recovery after glucose or glucagons) was lower with insulin glargine than with NPH insulin. Results from other studies and a recent metaanalysis have been similar.30-32
Thus, using insulin glargine as basal insulin allows patients to reach recommended targets with fewer episodes of hypoglycemia, and can help address patients’ fear that can be a barrier to initiating insulin therapy in type 2 diabetes. Two recent studies have reported that dosing of insulin glargine can be flexible—morning or bedtime administration yields comparable low rates of hypoglycemia.30,31
FIGURE 3
Hourly hypoglycemia rate with glargine much less than with NPH
*P<.05 (between treatment).
Copyright © 2003 American Diabetes Association. From Diabetes Care 2003; 26:3080–3086.29 Reprinted with permission from American Diabetes Association.
Basal insulin plus prandial insulin
For patients who cannot otherwise reach Hb A1c goals, basal insulin therapy may be supplemented with prandial insulin. Newer, rapid-acting analogs used for the prandial component are insulin lispro, insulin glulisine, or insulin aspart. Although this approach is physiologically more rational than regimens using conventional insulins, data are limited for use in type 2 diabetes.
The incidence of nocturnal hypoglycemia was evaluated in a study of patients with type 1 diabetes and impaired hypoglycemic awareness who were treated with 1 of 2 regimens: insulin lispro in a basal-prandial combination with NPH insulin, or twice-daily, premixed NPH/regular insulin.33 Results showed that the incidence of nocturnal hypoglycemia was lower in patients receiving the insulin lispro regimen.
Another study, comparing insulin aspart and regular insulin as the prandial component in a basal-prandial regimen with NPH, showed that postprandial glucose control and Hb A1c levels were significantly better after 1 year of treatment in the insulin aspart group than in the group receiving regular insulin, without an increased risk for hypoglycemia.34 These results suggest that treatment with rapidacting insulin analogs could be helpful in avoiding hypoglycemia in patients with type 2 diabetes when a basal-prandial insulin regimen is indicated.
Avoiding hypoglycemia in the elderly
Elderly patients may be at increased risk for iatrogenic hypoglycemia. A populationbased study of patients presenting to an emergency room with severe hypoglycemic symptoms reported that rates of such events among elderly patients with type 2 diabetes and multiple comorbidities approached the rates among patients with type 1 diabetes.35
Creatinine clearance is often decreased in elderly patients, slowing elimination of oral agents and insulin and potentially resulting in sustained pharmacological action and creating a greater risk for hypoglycemia.
Furthermore, there is evidence that the neurogenic symptoms of hypoglycemia are reduced in elderly patients, diminishing awareness of hypoglycemia.36
In the demented elderly, malnutrition, weight loss, and anorexia may exacerbate the risk for hypoglycemia. For elderly patients with tertiary disease (eg, cerebrovascular accident, myocardial infarction, congestive heart failure, blindness, chronic renal failure), the risk for hypoglycemia and subsequent comorbidity may outweigh the benefits of strict glycemic control.3,37 Elderly patients may have comorbid conditions that increase risk of falls (eg, poor vision, neurologic conditions), and hypoglycemic episodes may further increase the risk of falls and lead to morbidity (eg, fragility fracture in patients with osteopenia or osteoporosis).
Because the elderly are at a greater risk for hypoglycemia, a switch to a less restrictive diet, such as a “no concentrated sweets” diet, is an option, with control of glucose levels through the administration of oral agents or insulin.36 This may also promote a better quality of life, considering that many of these patients already have secondary and tertiary complications of diabetes, prevention of which is not a realistic goal.
CORRESPONDING AUTHOR
William Cefalu, MD, Professor and Chief, Division of Nutrition and Chronic Diseases, Pennington Biomedical Research Center, Louisiana State University, 6400 Perkins Road, Baton Rouge, LA 70808. Email: [email protected]
1. Cryer PE, Childs BP. Negotiating the barrier of hypoglycemia in diabetes. Diabetes Spectrum 2002;15:20-27.
2. Cryer PE, ed. Hypoglycemia: Pathophysiology, Diagnosis, and Treatment. New York, NY: Oxford University Press; 1997.
3. McAulay V, Deary IJ, Frier BM. Symptoms of hypoglycaemia in people with diabetes. Diabet Med 2001;18:690-705.
4. Towler DA, Havlin CE, Craft S, Cryer P. Mechanism of awareness of hypoglycemia. Perception of neurogenic (predominantly cholinergic) rather than neuroglycopenic symptoms. Diabetes 1993;42:1791-1798.
5. Hepburn DA, MacLeod KM, Pell AC, Scougal IJ, Frier BM. Frequency and symptoms of hypoglycaemia experienced by patients with type 2 diabetes treated with insulin. Diabet Med 1993;10:231-237.
6. Miller CD, Phillips LS, Ziemer DC, Gallina DL, Cook CB, El-Kebbi IM. Hypoglycemia in patients with type 2 diabetes mellitus. Arch Intern Med 2001;161:1653-1659.
7. The DCCT Research Group. Epidemiology of severe hypoglycemia in the diabetes control and complications trial. Am J Med 1991;90:450-459.
8. UK Prospective Diabetes Study Group. Perspectives in diabetes. UK Prospective Diabetes Study 16: overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes 1995;44:1249-1258.
9. United Kingdom Prospective Diabetes Study Group. UKPDS 24: a 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy. Ann Intern Med 1998;128:165-175.
10. MacLeod KM, Hepburn DA, Frier BM. Frequency and morbidity of severe hypoglycaemia in insulin-treated diabetic patients. Diabet Med 1993;10:238-245.
11. Vervoort G, Goldschmidt HM, van Doorn LG. Nocturnal blood glucose profiles in patients with type 1 diabetes mellitus on multiple (>or=4) daily insulin injection regimens. Diabet Med 1996;13:794-799.
12. Gale EA, Tattersall RB. Unrecognised nocturnal hypoglycaemia in insulin-treated diabetics. Lancet 1979;1:1049-1052.
13. Pramming S, Thorsteinsson B, Bendtson I, Ronn B, Binder C. Nocturnal hypoglycaemia in patients receiving conventional treatment with insulin. Br Med J (Clin Res Ed) 1985;291:376-379.
14. Goudswaard AN, Furlong NJ, Valk GD, Stolk RP, Rutten GEHM. Insulin monotherapy versus combinations of insulin with oral hypoglycaemic agents in patients with type 2 diabetes mellitus. Cochrane Database Syst Rev 2004;4:1-51.
15. Strowig SM, Avilés-Santa ML, Raskin P. Comparison of insulin monotherapy and combination therapy with insulin and metformin or insulin and troglitazone in type 2 diabetes. Diabetes Care 2002;25:1691-1698.
16. Campbell IW. Hypoglycaemia and type 2 diabetes: sulphonylureas. In: Frier BM, Fisher BM, eds. Hypoglycaemia and Diabetes: Clinical and Physiological Aspects. London, UK: Edward Arnold, 1993;387-392.
17. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Individual sulfonylureas and serious hypoglycemia in older people. J Am Geriatr Soc 1996;44:751-755.
18. Holstein A, Egberts EH. Risk of hypoglycaemia with oral antidiabetic agents in patients with Type 2 diabetes. Exp Clin Endocrinol Diabetes 2003;111:405-414.
19. Holstein A, Plaschke A, Egberts E-H. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev 2001;17:467-473.
20. Aljabri K, Kozak SE, Thompson DM. Addition of pioglitazone or bedtime insulin to maximal doses of sulfonylurea and metformin in type 2 diabetes patients with poor glucose control: a prospective, randomized trial. Am J Med 2004;116:230-235.
21. Wolffenbuttel BHR, Landgraf R. A 1-year multicenter randomized double-blind comparison of repaglinide and glyburide for the treatment of type 2 diabetes. Dutch and German Repaglinide Study Group. Diabetes Care 1999;22:463-467.
22. Raskin P, McGill J, Saad MF, et al. Combination therapy for type 2 diabetes: repaglinide plus rosiglitazone. Diabetes Med 2004;21:329-335.
23. Dailey GE, III, Noor MA, Park JS, Bruce S, Fiedorek FT. Glycemic control with glyburide/metformin tablets in combination with rosiglitazone in patients with type 2 diabetes: a randomized, double-blind trial. Am J Med 2004;116:223-229.
24. Korytkowski MT, Mokan M, Veneman TF, Mitrakou A, Cryer PE, Gerich JE. Reduced beta-adrenergic sensitivity in patients with type 1 diabetes and hypoglycemia unawareness. Diabetes Care 1998;21:1939-1943.
25. Fritsche A, Stumvoll M, Grub M, et al. Effect of hypoglycemia on beta-adrenergic sensitivity in normal and type 1 diabetic subjects. Diabetes Care 1998;21:1505-1510.
26. Fritsche A, Stefan N, Haring H, Gerich J, Stumvoll M. Avoidance of hypoglycemia restores hypoglycemia awareness by increasing beta-adrenergic sensitivity in type 1 diabetes. Ann Intern Med 2001;134:729-736.
27. Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003;26:1902-1912.
28. Lepore M, Pampanelli S, Fanelli C, et al. Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes 2000;49:2142-2148.
29. Riddle MC, Rosenstock J, Gerich J. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003;26:3080-3086.
30. Fritsche A, Schweitzer MA, Häring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine Hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes: a randomized, controlled trial. Ann Intern Med 2003;138:952-959.
31. Standl E, Maxeiner S, Raptis S, Karimi-Anderesi Z, Schweitzer MA. Good glycemic control with flexibility in timing of basal insulin supply: a 24-week comparison of insulin glargine given once daily in the morning or at bedtime in combination with morning glimepiride. Diabetes Care 2005;28:419-420.
32. Rosenstock J, Dailey G, Massi Benedetti M, Fritsche A, Lin Z, Salzman A. Reduced hypoglycemia risk with insulin glargine. A meta-analysis comparing insulin glargine with human NPH insulin in type 2 diabetes. Diabetes Care 2005;28:950-955.
33. Ferguson SC, Strachan MW, Janes JM, Frier BM. Severe hypoglycaemia in patients with type 1 diabetes and impaired awareness of hypoglycaemia: a comparative study of insulin lispro and regular human insulin. Diabetes Metab Res Rev 2001;17:285-291.
34. Raskin P, Guthrie RA, Leiter L, Riis A, Jovanovic L. Use of insulin aspart, a fast-acting insulin analog, as the mealtime insulin in the management of patients with type 1 diabetes. Diabetes Care 2000;23:583-558.
35. Holstein A, Plaschke A, Egberts EH. Clinical characterisation of severe hypoglycaemia-a prospective population-based study. Exp Clin Endocrinol Diabetes 2003;111:364-369.
36. Meneilly GS, Cheung E, Tuokko H. Counterregulatory hormone responses to hypoglycemia in the elderly patient with diabetes. Diabetes 1994;43:403-410.
37. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2003;26(suppl 1):S33-S50.
1. Cryer PE, Childs BP. Negotiating the barrier of hypoglycemia in diabetes. Diabetes Spectrum 2002;15:20-27.
2. Cryer PE, ed. Hypoglycemia: Pathophysiology, Diagnosis, and Treatment. New York, NY: Oxford University Press; 1997.
3. McAulay V, Deary IJ, Frier BM. Symptoms of hypoglycaemia in people with diabetes. Diabet Med 2001;18:690-705.
4. Towler DA, Havlin CE, Craft S, Cryer P. Mechanism of awareness of hypoglycemia. Perception of neurogenic (predominantly cholinergic) rather than neuroglycopenic symptoms. Diabetes 1993;42:1791-1798.
5. Hepburn DA, MacLeod KM, Pell AC, Scougal IJ, Frier BM. Frequency and symptoms of hypoglycaemia experienced by patients with type 2 diabetes treated with insulin. Diabet Med 1993;10:231-237.
6. Miller CD, Phillips LS, Ziemer DC, Gallina DL, Cook CB, El-Kebbi IM. Hypoglycemia in patients with type 2 diabetes mellitus. Arch Intern Med 2001;161:1653-1659.
7. The DCCT Research Group. Epidemiology of severe hypoglycemia in the diabetes control and complications trial. Am J Med 1991;90:450-459.
8. UK Prospective Diabetes Study Group. Perspectives in diabetes. UK Prospective Diabetes Study 16: overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes 1995;44:1249-1258.
9. United Kingdom Prospective Diabetes Study Group. UKPDS 24: a 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy. Ann Intern Med 1998;128:165-175.
10. MacLeod KM, Hepburn DA, Frier BM. Frequency and morbidity of severe hypoglycaemia in insulin-treated diabetic patients. Diabet Med 1993;10:238-245.
11. Vervoort G, Goldschmidt HM, van Doorn LG. Nocturnal blood glucose profiles in patients with type 1 diabetes mellitus on multiple (>or=4) daily insulin injection regimens. Diabet Med 1996;13:794-799.
12. Gale EA, Tattersall RB. Unrecognised nocturnal hypoglycaemia in insulin-treated diabetics. Lancet 1979;1:1049-1052.
13. Pramming S, Thorsteinsson B, Bendtson I, Ronn B, Binder C. Nocturnal hypoglycaemia in patients receiving conventional treatment with insulin. Br Med J (Clin Res Ed) 1985;291:376-379.
14. Goudswaard AN, Furlong NJ, Valk GD, Stolk RP, Rutten GEHM. Insulin monotherapy versus combinations of insulin with oral hypoglycaemic agents in patients with type 2 diabetes mellitus. Cochrane Database Syst Rev 2004;4:1-51.
15. Strowig SM, Avilés-Santa ML, Raskin P. Comparison of insulin monotherapy and combination therapy with insulin and metformin or insulin and troglitazone in type 2 diabetes. Diabetes Care 2002;25:1691-1698.
16. Campbell IW. Hypoglycaemia and type 2 diabetes: sulphonylureas. In: Frier BM, Fisher BM, eds. Hypoglycaemia and Diabetes: Clinical and Physiological Aspects. London, UK: Edward Arnold, 1993;387-392.
17. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Individual sulfonylureas and serious hypoglycemia in older people. J Am Geriatr Soc 1996;44:751-755.
18. Holstein A, Egberts EH. Risk of hypoglycaemia with oral antidiabetic agents in patients with Type 2 diabetes. Exp Clin Endocrinol Diabetes 2003;111:405-414.
19. Holstein A, Plaschke A, Egberts E-H. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev 2001;17:467-473.
20. Aljabri K, Kozak SE, Thompson DM. Addition of pioglitazone or bedtime insulin to maximal doses of sulfonylurea and metformin in type 2 diabetes patients with poor glucose control: a prospective, randomized trial. Am J Med 2004;116:230-235.
21. Wolffenbuttel BHR, Landgraf R. A 1-year multicenter randomized double-blind comparison of repaglinide and glyburide for the treatment of type 2 diabetes. Dutch and German Repaglinide Study Group. Diabetes Care 1999;22:463-467.
22. Raskin P, McGill J, Saad MF, et al. Combination therapy for type 2 diabetes: repaglinide plus rosiglitazone. Diabetes Med 2004;21:329-335.
23. Dailey GE, III, Noor MA, Park JS, Bruce S, Fiedorek FT. Glycemic control with glyburide/metformin tablets in combination with rosiglitazone in patients with type 2 diabetes: a randomized, double-blind trial. Am J Med 2004;116:223-229.
24. Korytkowski MT, Mokan M, Veneman TF, Mitrakou A, Cryer PE, Gerich JE. Reduced beta-adrenergic sensitivity in patients with type 1 diabetes and hypoglycemia unawareness. Diabetes Care 1998;21:1939-1943.
25. Fritsche A, Stumvoll M, Grub M, et al. Effect of hypoglycemia on beta-adrenergic sensitivity in normal and type 1 diabetic subjects. Diabetes Care 1998;21:1505-1510.
26. Fritsche A, Stefan N, Haring H, Gerich J, Stumvoll M. Avoidance of hypoglycemia restores hypoglycemia awareness by increasing beta-adrenergic sensitivity in type 1 diabetes. Ann Intern Med 2001;134:729-736.
27. Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003;26:1902-1912.
28. Lepore M, Pampanelli S, Fanelli C, et al. Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes 2000;49:2142-2148.
29. Riddle MC, Rosenstock J, Gerich J. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003;26:3080-3086.
30. Fritsche A, Schweitzer MA, Häring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine Hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes: a randomized, controlled trial. Ann Intern Med 2003;138:952-959.
31. Standl E, Maxeiner S, Raptis S, Karimi-Anderesi Z, Schweitzer MA. Good glycemic control with flexibility in timing of basal insulin supply: a 24-week comparison of insulin glargine given once daily in the morning or at bedtime in combination with morning glimepiride. Diabetes Care 2005;28:419-420.
32. Rosenstock J, Dailey G, Massi Benedetti M, Fritsche A, Lin Z, Salzman A. Reduced hypoglycemia risk with insulin glargine. A meta-analysis comparing insulin glargine with human NPH insulin in type 2 diabetes. Diabetes Care 2005;28:950-955.
33. Ferguson SC, Strachan MW, Janes JM, Frier BM. Severe hypoglycaemia in patients with type 1 diabetes and impaired awareness of hypoglycaemia: a comparative study of insulin lispro and regular human insulin. Diabetes Metab Res Rev 2001;17:285-291.
34. Raskin P, Guthrie RA, Leiter L, Riis A, Jovanovic L. Use of insulin aspart, a fast-acting insulin analog, as the mealtime insulin in the management of patients with type 1 diabetes. Diabetes Care 2000;23:583-558.
35. Holstein A, Plaschke A, Egberts EH. Clinical characterisation of severe hypoglycaemia-a prospective population-based study. Exp Clin Endocrinol Diabetes 2003;111:364-369.
36. Meneilly GS, Cheung E, Tuokko H. Counterregulatory hormone responses to hypoglycemia in the elderly patient with diabetes. Diabetes 1994;43:403-410.
37. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2003;26(suppl 1):S33-S50.
Hyaluronic acid injections relieve knee pain
- Consider injections of hyaluronic acid only after conservative therapy has been tried for at least 3 months or the patient is unable to tolerate NSAIDs.
- Stress to patients that pain relief may not be fully experienced until 5 to 7 weeks following the last injection.
Hyaluronic acid injections can help relieve pain for carefully selected patients with knee osteoarthritis. But this option should be reserved for those whose pain has not responded to adequate trials of systemic therapeutic agents (acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs], cyclooxygenase-2 [COX-2] inhibitors), topical agents, or to lifestyle modifications such as weight reduction and exercise.
Hyaluronic acid injections may also be indicated when knee surgery must be delayed for middle-aged persons.1
In spite of the Food and Drug Administration’s approval of this therapy, uncertainty about its efficacy exists among the medical community. A recent meta-analysis of the effectiveness of intra-articular hyaluronic acid for knee osteoarthritis that included 22 published and unpublished, English and non-English, single or double-blinded, randomized controlled trials in humans showed that hyaluronic acid has only a small effect on pain relief when compared with placebo.2
We provide here a stringent test of the efficacy of viscosupplementation for relieving knee pain from osteoarthritis with a meta-analysis that includes only data from randomized, double-blinded, controlled trials of hyaluronic acid that measured pain using a visual analogue scale (VAS), the most widely accepted method for pain evaluation.
Long time coming
Balazs first proposed hyaluronic acid as a treatment for patients with arthritic diseases in 1942. In the early 1970s, therapeutic studies were begun to test the efficacy of hyaluronic acid on knee osteoarthritis. The results were encouraging and side effects were few.28 With the FDA’s approval in 1998, intra-articular “viscosupplementation” with hyaluronic acid—also called hyaluronan or hyaluronate, and the hylan derivatives of hyaluronic acid—is a welcome option for many of the 16 million older Americans with osteoarthritis of the knee.1
Methods
Selection of studies
We identified clinical trials of viscosupplementation with hyaluronic acid in humans published in English from 1965 through August 2004 through a computerized literature search of Medline. The keyword used was “hyaluronic acid,” which was combined with “trial” or “osteoarthritis knee” or “viscosupplementation.” We conducted an additional manual search of the reference lists of included articles and review articles. We also searched the Cochrane Library and websites of the Agency for Healthcare Research and Quality (AHRQ) for information on hyaluronic acid in knee osteoarthritis. We identified 1872 articles with this search process.
Of the 1872 articles, we identified by title and abstract 33 that might be pertinent to this study, including 17 randomized trials. We excluded reviews, meta-analyses, comparison trials, and trials reporting VAS as part of the WOMAC (Western Ontario McMaster Universities Index) scale. We attempted to contact authors of the studies that used a double-blind, randomized controlled design, to obtain any data that may not have been included in the publications. Three authors provided the details requested; the others did not respond or stated that additional data were not available. Of the 17 randomized trials we identified, 8 were excluded because they were open, single-blinded, or did not use the VAS to measure pain outcomes.3-10 The remaining 9 double-blinded, placebo controlled, randomized clinical trials of viscosupplementation with hyaluronic acid for knee osteoarthritis that did use a VAS to measure pain were included in this meta-analysis (TABLE 1). Because one of the studies (by Henderson) included 2 subgroups of pain severity, these were considered as 2 separate trials. The trial by Petrella had 2 treatment groups, one with only hyaluronic acid and the other with hyaluronic acid and NSAIDs. We considered them separately in the analysis, resulting in a total of 11 clinical trials for the meta-analysis.19 Henceforth in this report, we will refer to 11 rather than 9 clinical trials.
Extraction of data
Two investigators independently extracted the following data for each study: year of publication, study design, mean age, number of patients enrolled in each treatment group, number of doses of treatment used, and outcomes measured. When disagreements between investigators occurred, the point of disagreement was discussed until a consensus was reached. Since the treatment duration and the time post-treatment when pain was assessed varied among the trials, we grouped outcomes into four time intervals: at 1 week, 5 to 7 weeks, 8 to 12 weeks, and 15 to 22 weeks after the last hyaluronic acid injection.
Statistical analysis
The outcome was knee pain reported by patients on activity or at rest, measured using a VAS of 100 mm. The results of the clinical trials were recorded as the mean differences of change from baseline between the treatment and placebo groups. If not reported in the publication or provided by the authors, standard error was imputed using the method of Follman et al.20 We used the method of Chalmers for measuring the quality of randomized trials, with 2 of the authors rating the studies independently.21
This clinical trial grading system takes into account the following aspects of the trial to determine a quality score: evaluation of recruitment of subjects, rejection log, therapeutic regimen definition, randomization, blinding, prior estimates of numbers, testing compliance, statistical inference, use of appropriate statistical analysis, handling of withdrawal and side effects, dates of starting and ending, timing and tabulation of events. Because 4 of the trials had poor quality scores, an additional analysis excluding these 4 was performed. The DerSimonian and Laird random-effects model was used to obtain the summary estimates.22,23
An important element of meta-analysis is exploration of the heterogeneity of the outcomes and the possible causes of heterogeneity if it exists. Heterogeneity is the degree to which results vary from study to study. If a test for heterogeneity is statistically significant, there is significant variability among the treatment effects observed in the trials. We explored heterogeneity using Galbraith plots (FIGURE 1).24 In the absence of heterogeneity, all points fall within the confidence limits. Because we did find heterogeneity among these trials, we developed random-effect regression models to explore 3 possible sources of heterogeneity in the efficacy of hyaluronic acid; pain (measured at rest or on activity), the form used (hyaluronan or hylan G-F20), and the quality of the study method (good or poor).
Publication bias was assessed by the Egger et al regression asymmetry test.25 Analyses were performed using the meta-analytic software program of STATA, Inc (College Station, Tex; available at www.stata.com).
FIGURE 1
Evidence of heterogeneity for the studies evaluated at outcome measurement time (week 1)
This Galbraith plot shows standardized effects (b/se=mean difference/standard error) as a function of study precision (1/standard error), slope of the line shows average effect over all the studies with upper and lower lines denoting an approximate 95% confidence interval for this common effect. Under the hypothesis of study heterogeneity, the common slope intersect zero at 1/se=0, and 95% of all study estimates (authors initials) will fall within the confidence interval of the regression line. Gr: Grecomoro; Pu: Puhl; H1: Henderson 1; H2: Henderson 2; Sc: Scale; Lo: Lohmander; Al: Altman; Wo: Wobig; Hu: Huskisson; P1: Petrella 1; P2: Petrella 2.
Results
The 11 randomized, placebo-controlled, double-blinded clinical trials that met our inclusion criteria are summarized in TABLE 1. Nine trials used hyaluronic acid, hyaluronan, or hyaluronate (all types will be referred to as hyaluronan in the text), and 2 studies used hylan GF-20. Only 3 hyaluronan trials have published outcome data at 15 to 22 weeks follow-up. Treatment was administered to patients as 3 to 5 weekly injections, with the exception of the Grecomoro study in which treatment was administered twice weekly. The control group in 10 trials received intra-articular saline injections as placebo. In the Puhl study the investigators added 0.25 mg of hyaluronic acid to the saline injections to impart viscosity to the solution. The mean age of the subjects for the 11 trials was 63 years.
Eight trials received support from pharmaceutical companies and 3 (the 2 by Henderson and the Grecomoro study) did not disclose any pharmaceutical support. One study was conducted in the United States, 3 in the UK, 3 in Germany, 1 in Sweden, 1 in Italy, and 2 in Canada. Five of the studies had scores over a cutoff quality score of >0.75,12,13,15,16,19 indicating they were good-quality randomized controlled trials; the remaining 4 had scores below 0.75.11,14,16,17
The outcomes of the 11 trials are summarized in TABLE 2. Patients’ pain ratings in both the active treatment and placebo groups improved in all the trials. Mean difference between improvements in treatment and placebo groups are shown in FIGURES 2A-2D for pain assessed at weeks 1, 5 to 7, 8 to 12 and 15 to 22, respectively. In each figure, we show the summary estimate of effect size with all the trials included and after excluding the 4 trials considered of poor quality, shown as “good quality studies.”
The mean difference in pain scores between treatment and placebo at week 1 was 4.4 (95% CI, +1.1, +7.2) and –1.0 (95% CI, -3.2, +1.2) for analysis restricted to the 7 good quality trials. The mean difference in pain scores at 5 to 7 weeks was 17.6 (95% CI, +7.5, +28.0) and 7.2 (95% CI, +2.4, +12.0) for the analysis restricted to the 2 good quality studies. At weeks 8 to 12 the mean difference in VAS between treatment and control was 18.1 (95% CI, +6.3, +29.9), and 7.1 (95% CI, +3.0, +11.3) in the analysis restricted to good quality trials. At weeks 15 to 22, the mean difference was 4.4 (95% CI, –15.3, +24.1). The Egger test was not statistically significant (2.3; P=.096; 95% CI, –0.5, +5.2) suggesting that there is no publication bias.
High heterogeneity was observed at all time intervals except 1 week (FIGURE 1). Of the 5 trials outside the confidence bounds (positioned 2 units above and below the regression line), 4 were poor-quality studies.
TABLE 3 shows the random-effect regression models we used to test the influence on the outcome of type of pain measured (pain with activity or pain at rest), type of medication (hyaluronan or hylan G-F 20), and study quality (good or poor). No significant association between treatment efficacy and type of pain used as outcome variable was observed. Clinical trials using hylan GF-20 showed statistically significant better results than those using hyaluronan at weeks 5 to 7 and 8 to 12. Poor-quality studies showed a larger treatment effect, but the difference was statistically significant only at week 1.
TABLE 3
Regression models to assess the sources of heterogeneity in the meta-analysis
| WEEK 1 | WEEKS 5–7 | WEEKS 8–12 | ||||
|---|---|---|---|---|---|---|
| Coef. (SE) [95% CI] | P value | Coef. (SE) [95% CI] | P value | Coef. (SE) [95% CI] | P value | |
| Pain | ||||||
| With activity | 1.7 (3.8) | 1.8 (4.3) | –0.5 (4.6) | |||
| At rest | [–5.8, +9.2] | 0.657 | [–6.6, +10.2] | 0.671 | [–9.5, +8.6] | 0.916 |
| Medication | ||||||
| Hyaluronan** | –3.4 (6.8) | 0.614 | 17.5 (4.9) | <0.001 | 14.8 (6.1) | 0.016 |
| Hylan G-F 20 | –16.7, +9.9] | [+7.8, +27.1] | [+2.8, +26.8] | |||
| Quality* | ||||||
| Poor (<0.75) | –19.9 (5.7) | 0.001 | –7.4 (4.9) | 0.131 | –11.7 (7.0) | 0.092 |
| Good (≥0.75) | [–31.1, –8.7] | [–17.0, +2.2] | [–25.3, +1.9] | |||
| Constant | 18.4 (5.6) | 0.001 | 13.5 (4.5) | 0.003 | 19.2 (5.8) | 0.001 |
| [+7.5, +29.3] | [+4.6, +22.3] | [+7.9, +30.5] | ||||
| *<.75 quality score: Grecomoro .439, Scale .570, Wobig .731, Huskisson .718. | ||||||
| ** 9 trials for hyaluronan (3 for Hyalgan®) and 2 trials for hylan G-F20 (Synvisc®). | ||||||
Discussion
This meta-analysis synthesized data from 9 randomized, double-blinded, placebo-controlled trials that evaluated the efficacy of intra-articular hyaluronic acid. Our findings show significantly decreased pain as measured by VAS at 5 to 7 weeks and at 8 to 12 weeks after the last injection. Intra-articular hyaluronic acid was not more effective than placebo in relieving pain at 1 week or at 15 to 22 weeks after the last injection. Because only 3 of the trials assessed patients after 12 weeks, however, the sample size is too small to definitively rule out a significant therapeutic effect after 12 weeks.
Reasons for the differences in efficacy among trials of hyaluronic acid in the treatment of knee osteoarthritis include dose, type, and frequency of administration, genetic or age differences among the study subjects, severity of osteoarthritis, time of follow-up, and quality of the studies. We confirmed that the treatment effect is time dependent. Although our meta-regression analysis (TABLE 2) suggests that hylan GF-20 is more effective than hyaluronan at 5 to 12 weeks, the number of clinical trials is relatively small and both of the hylan G-F20 studies were of poor quality. Therefore, we cannot say with confidence that one form is better than the other. Data in these trials were insufficient to assess the impact of body mass index, genetics, or severity of osteoarthritis.
We did not evaluate functional improvement in this meta-analysis because functional status was not measured in some trials and the assessment methods were too variable in the trials that did assess functional status. Publication bias, or the possibility that unpublished data would contradict the results of published studies, is always a potential source of bias in meta-analysis. However, the Egger test was not statistically significant (6.5; 95% CI, –0.5, +13.5) suggesting that there is no publication bias.25
Finally, the presence of heterogeneity of results indicates there were important differences among the studies. Exclusion of clinical trials considered of poor quality diminished this heterogeneity substantially. Subanalysis restricted to good-quality studies supports the efficacy of intra-articular hyaluronic acid in the treatment of knee osteoarthritis pain, although the effect size is smaller when one considers only the good quality studies.
There are 2 other potential limitations of this meta-analysis. Five studies allowed pain to be treated with analgesics such as acetaminophen or NSAIDs,12,13,16-18 and use of acetaminophen or NSAIDs may have altered the response to hyaluronic acid treatment. An intention-to-treat analysis was performed in only 2 studies (by Altman and Huskisson),16,18 wherein a post-hoc and “last observation carried forward” analysis showed a trend favoring hyaluronic acid. The treatment effects may have been smaller had the other trials used an intention to treat analysis.
This meta-analysis confirms that viscosupplementation with hyaluronic acid is modestly effective in short term relief of pain in knee osteoarthritis. Our meta-analysis included only double-blinded, randomized trials published in English language in humans using VAS as the pain outcome measure, and our conclusions are very similar to those of Lo.2
Indications for use. Hyaluronic acid is helpful in relieving pain for carefully selected patients with knee osteoarthritis who have not responded to adequate use of systemic therapeutic agents, including acetaminophen, NSAIDs and COX-2 inhibitors and topical agents, along with lifestyle modification such as weight reduction and exercise.
Patients should have a trial for at least three months of conservative therapy or be unable to tolerate NSAIDs before a decision to give 3- to 5-injection course with hyaluronic acid is made.
Hyaluronic acid may be an option when there is a need to delay knee surgery in middle-aged persons1 or for patients who have failed other treatments.
Time to pain relief. To improve adherence to treatment, tell patients receiving intra-articular hyaluronic acid that the benefits in pain reduction may not be noticeable until 5 to 10 weeks after the last injection.
Cost. Although the cost of hyaluronic acid treatment is covered by Medicare and most insurance plans for symptomatic osteoarthritis of knee, documentation in patient medical records should indicate the signs and symptoms supporting the diagnosis and functional impairment. Objective data to support a diagnosis of osteoarthritis such as x-ray, arthroscopy report, computed tomography scan, or magnetic resonance imaging should be available in the event of a review.
The cost of 1 hyaluronic acid (30 mg/mL) injection is approximately $230. Considering a course of 3 to 5 weekly knee injections, and adding other pharmacy, hospital, or clinic charges, the cost per treatment may exceed $1000 per knee.26,27 The cost-benefit of pain control with viscosupplementation must be carefully compared with other therapeutic agents and regimens currently available for knee osteoarthritis management.
FIGURE 3
Studies evaluated at outcome measurement time (week 1)
Egger’s publication bias plot for the studies evaluated at outcome measurement time (week 1) not significant (+2.3, P=0.096, 95% CI: –0.5, +5.2).
Acknowledgments
Jeff Welge, PhD, University of Cincinnati Medical Center, Center for Bio-statistical Services, for comments on final data analysis and presentation, Marie Marley, PhD for editing the manuscript, and Charity Noble for help in preparation of this manuscript.
CORRESPONDING AUTHOR
Arvind Modawal, MD, MPH, MRCGP, University of Cincinnati Department of Family Medicine/Geriatrics, PO Box 670582, Cincinnati, OH 45267-0582. E-mail: [email protected]
1. Cefalu CA, Waddell DS. Viscosupplementation: Treatment alternative for osteoarthritis of the knee. Geriatrics 1999;54:51-57.
2. Lo GH, LaValley M, McAlindon T, Felson DT. Intra-articular hyaluronic acid in treatment of knee osteoarthritis. JAMA 2003;290:3115-3121.
3. Jones AC, Pattrick M, Doherty S, Doherty M. Intra-articular hyaluronic acid compared to intra-articular triamcinolone hexacetonide in inflammatory knee osteoarthritis. Osteoarthritis Cartilage 1995;3:269-273.
4. Graf J, Neusel E, Schneider E, Niethard FU. Intra-articular treatment with hyaluronic acid in osteoarthritis of the knee joint: a controlled clinical trial versus mucopolysaccharide polysulfuric acid ester. Clin Exp Rheumatol 1993;11:367-72.
5. Dougados M, Nguyen M, Listrat V, Amor B. High molecular weight sodium hyaluronate (hyalectin) in osteoarthritis of the knee: A one year placebo-controlled trial. Osteoarthritis Cartilage 1993;1:97-103.
6. Adams ME. An analysis of clinical studies of the use of cross-linked hyaluronan, hylan, in the treatment of osteoarthritis. J Rheumatol Supp 1993;39:16-18.
7. Grecomoro G, Piccione F, Letizia G. Therapeutic synergism between hyaluronic acid and dexamethasone in the intra-articular treatment of osteoarthritis of the knee: a preliminary open study. Curr Med Res Opin 1992;13:49-55.
8. Leardini G, Mattara L, Franceschini M, Perbellini A. Intra-articular treatment of knee osteoarthritis. A comparative study between hyaluronic acid and 6-methyl prednisolone acetate. Clin Exp Rheumatol 1991;9:375-381.
9. Wu J, Shih L, Hsu H, Chen T. The double-blind test of sodium hyaluronate (ARTZ) on osteoarthritis knee. Chin Med J (Taipei) 1997;59:99-106.
10. Dixon AS, Jacoby RK, Berry H, Hamilton EB. Clinical trial of intra-articular injection of sodium hyaluronate in patients with osteoarthritis of the knee. Curr Med Res Opin 1988;11:205-213.
11. Grecomoro G, Martorana U, Di Marco C. Intra-articular treatment with sodium hyaluronate in gonarthrosis: a controlled clinical trial versus placebo. Pharmather 1987;5:137-141.
12. Puhl W, Bernau A, Greiling H, Kopcke W, Pforringer W, Steck KJ. Intra-articular sodium hyaluronate in osteoarthritis of the knee: a multicenter, double-blind study. Osteoarthritis Cartilage 1993;1:233-241.
13. Henderson EB, Smith EC, Pegley F, Blake DR. Intra-articular injections of 750 kD hyaluronan in the treatment of osteoarthritis: a randomized single centre double-blind placebo-controlled trial of 91 patients demonstrating lack of efficacy. Ann Rheum Dis 1994;53:529-554.
14. Scale D, Wobig M, Wolpert W. Viscosupplementation of osteoarthritic knees with Hylan: A treatment schedule study. Curr Ther Res 1994;55:220-232.
15. Lohmander LS, Dalen N, Englund G, et al. Intra-articular hyaluronan injections in the treatment of osteoarthritis of the knee: a randomized, double blind, placebo controlled multicentre trial. Hyaluronan Multicentre Trial Group [see comments]. Ann Rheum Dis 1996;55:424-431.
16. Altman RD, Moskowitz R. Intra-articular sodium hyaluronate (Hyalgan®) in the treatment of patients with osteoarthritis of the knee: A randomized clinical trial. J Rheumatol 1998;25:2203-2212.
17. Wobig M, Dickhut A, Maier R, Vetter G. Viscosupplementation with Hylan G-F-20: A 26-week controlled trial of efficacy and safety in the osteoarthritic knee. Clin Ther 1998;20:410-423.
18. Huskisson EC, Donnelly S. Hyaluronic acid in the treatment of osteoarthritis of the knee. Rheumatology 1999;38:602-607.
19. Petrella RJ, DiSilvestro MD, Hildebrand C. Effects of hyaluronate sodium on pain and physical functioning in osteoarthritis of the knee. Arch Intern Med 2002;162:292-298.
20. Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol 1992;45:769-773.
21. Chalmers TC, Smith H, Jr, Blackburn B, et al. A Method for Assessing the quality of a randomized control trial. Control Clin Trials 1981;2:31-49.
22. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-188.
23. Sacks HS, Berrier J, Reitman D, Ancona-Berk VA, Chalmers TC. Meta-analyses of randomized controlled trials. N Engl J Med 1987;316:450-455.
24. Galbraith R. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 1988;7:889-894.
25. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
26. CIGNA Government Services. Not otherwise classified drug fee schedule. Available at: www.cignamedicare.com/partb/fsch/2004/q2/noc.html. Accessed on June 20, 2005.
27. Empire Medicare Services. Local coverage determination. Hyaluronate polymers (Synvisc, Hyalgan) (A02-0011-R3). Available at: www.empiremedicare.com/Nyorkpolicya/policy/A02-0011-R_FINAL.htm.
28. Peyron JG, Balazs EA. Preliminary clinical assessment of Na-hyaluronate injection into human arthritic joints. Pathol Biol 1974;22:731-736.
- Consider injections of hyaluronic acid only after conservative therapy has been tried for at least 3 months or the patient is unable to tolerate NSAIDs.
- Stress to patients that pain relief may not be fully experienced until 5 to 7 weeks following the last injection.
Hyaluronic acid injections can help relieve pain for carefully selected patients with knee osteoarthritis. But this option should be reserved for those whose pain has not responded to adequate trials of systemic therapeutic agents (acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs], cyclooxygenase-2 [COX-2] inhibitors), topical agents, or to lifestyle modifications such as weight reduction and exercise.
Hyaluronic acid injections may also be indicated when knee surgery must be delayed for middle-aged persons.1
In spite of the Food and Drug Administration’s approval of this therapy, uncertainty about its efficacy exists among the medical community. A recent meta-analysis of the effectiveness of intra-articular hyaluronic acid for knee osteoarthritis that included 22 published and unpublished, English and non-English, single or double-blinded, randomized controlled trials in humans showed that hyaluronic acid has only a small effect on pain relief when compared with placebo.2
We provide here a stringent test of the efficacy of viscosupplementation for relieving knee pain from osteoarthritis with a meta-analysis that includes only data from randomized, double-blinded, controlled trials of hyaluronic acid that measured pain using a visual analogue scale (VAS), the most widely accepted method for pain evaluation.
Long time coming
Balazs first proposed hyaluronic acid as a treatment for patients with arthritic diseases in 1942. In the early 1970s, therapeutic studies were begun to test the efficacy of hyaluronic acid on knee osteoarthritis. The results were encouraging and side effects were few.28 With the FDA’s approval in 1998, intra-articular “viscosupplementation” with hyaluronic acid—also called hyaluronan or hyaluronate, and the hylan derivatives of hyaluronic acid—is a welcome option for many of the 16 million older Americans with osteoarthritis of the knee.1
Methods
Selection of studies
We identified clinical trials of viscosupplementation with hyaluronic acid in humans published in English from 1965 through August 2004 through a computerized literature search of Medline. The keyword used was “hyaluronic acid,” which was combined with “trial” or “osteoarthritis knee” or “viscosupplementation.” We conducted an additional manual search of the reference lists of included articles and review articles. We also searched the Cochrane Library and websites of the Agency for Healthcare Research and Quality (AHRQ) for information on hyaluronic acid in knee osteoarthritis. We identified 1872 articles with this search process.
Of the 1872 articles, we identified by title and abstract 33 that might be pertinent to this study, including 17 randomized trials. We excluded reviews, meta-analyses, comparison trials, and trials reporting VAS as part of the WOMAC (Western Ontario McMaster Universities Index) scale. We attempted to contact authors of the studies that used a double-blind, randomized controlled design, to obtain any data that may not have been included in the publications. Three authors provided the details requested; the others did not respond or stated that additional data were not available. Of the 17 randomized trials we identified, 8 were excluded because they were open, single-blinded, or did not use the VAS to measure pain outcomes.3-10 The remaining 9 double-blinded, placebo controlled, randomized clinical trials of viscosupplementation with hyaluronic acid for knee osteoarthritis that did use a VAS to measure pain were included in this meta-analysis (TABLE 1). Because one of the studies (by Henderson) included 2 subgroups of pain severity, these were considered as 2 separate trials. The trial by Petrella had 2 treatment groups, one with only hyaluronic acid and the other with hyaluronic acid and NSAIDs. We considered them separately in the analysis, resulting in a total of 11 clinical trials for the meta-analysis.19 Henceforth in this report, we will refer to 11 rather than 9 clinical trials.
Extraction of data
Two investigators independently extracted the following data for each study: year of publication, study design, mean age, number of patients enrolled in each treatment group, number of doses of treatment used, and outcomes measured. When disagreements between investigators occurred, the point of disagreement was discussed until a consensus was reached. Since the treatment duration and the time post-treatment when pain was assessed varied among the trials, we grouped outcomes into four time intervals: at 1 week, 5 to 7 weeks, 8 to 12 weeks, and 15 to 22 weeks after the last hyaluronic acid injection.
Statistical analysis
The outcome was knee pain reported by patients on activity or at rest, measured using a VAS of 100 mm. The results of the clinical trials were recorded as the mean differences of change from baseline between the treatment and placebo groups. If not reported in the publication or provided by the authors, standard error was imputed using the method of Follman et al.20 We used the method of Chalmers for measuring the quality of randomized trials, with 2 of the authors rating the studies independently.21
This clinical trial grading system takes into account the following aspects of the trial to determine a quality score: evaluation of recruitment of subjects, rejection log, therapeutic regimen definition, randomization, blinding, prior estimates of numbers, testing compliance, statistical inference, use of appropriate statistical analysis, handling of withdrawal and side effects, dates of starting and ending, timing and tabulation of events. Because 4 of the trials had poor quality scores, an additional analysis excluding these 4 was performed. The DerSimonian and Laird random-effects model was used to obtain the summary estimates.22,23
An important element of meta-analysis is exploration of the heterogeneity of the outcomes and the possible causes of heterogeneity if it exists. Heterogeneity is the degree to which results vary from study to study. If a test for heterogeneity is statistically significant, there is significant variability among the treatment effects observed in the trials. We explored heterogeneity using Galbraith plots (FIGURE 1).24 In the absence of heterogeneity, all points fall within the confidence limits. Because we did find heterogeneity among these trials, we developed random-effect regression models to explore 3 possible sources of heterogeneity in the efficacy of hyaluronic acid; pain (measured at rest or on activity), the form used (hyaluronan or hylan G-F20), and the quality of the study method (good or poor).
Publication bias was assessed by the Egger et al regression asymmetry test.25 Analyses were performed using the meta-analytic software program of STATA, Inc (College Station, Tex; available at www.stata.com).
FIGURE 1
Evidence of heterogeneity for the studies evaluated at outcome measurement time (week 1)
This Galbraith plot shows standardized effects (b/se=mean difference/standard error) as a function of study precision (1/standard error), slope of the line shows average effect over all the studies with upper and lower lines denoting an approximate 95% confidence interval for this common effect. Under the hypothesis of study heterogeneity, the common slope intersect zero at 1/se=0, and 95% of all study estimates (authors initials) will fall within the confidence interval of the regression line. Gr: Grecomoro; Pu: Puhl; H1: Henderson 1; H2: Henderson 2; Sc: Scale; Lo: Lohmander; Al: Altman; Wo: Wobig; Hu: Huskisson; P1: Petrella 1; P2: Petrella 2.
Results
The 11 randomized, placebo-controlled, double-blinded clinical trials that met our inclusion criteria are summarized in TABLE 1. Nine trials used hyaluronic acid, hyaluronan, or hyaluronate (all types will be referred to as hyaluronan in the text), and 2 studies used hylan GF-20. Only 3 hyaluronan trials have published outcome data at 15 to 22 weeks follow-up. Treatment was administered to patients as 3 to 5 weekly injections, with the exception of the Grecomoro study in which treatment was administered twice weekly. The control group in 10 trials received intra-articular saline injections as placebo. In the Puhl study the investigators added 0.25 mg of hyaluronic acid to the saline injections to impart viscosity to the solution. The mean age of the subjects for the 11 trials was 63 years.
Eight trials received support from pharmaceutical companies and 3 (the 2 by Henderson and the Grecomoro study) did not disclose any pharmaceutical support. One study was conducted in the United States, 3 in the UK, 3 in Germany, 1 in Sweden, 1 in Italy, and 2 in Canada. Five of the studies had scores over a cutoff quality score of >0.75,12,13,15,16,19 indicating they were good-quality randomized controlled trials; the remaining 4 had scores below 0.75.11,14,16,17
The outcomes of the 11 trials are summarized in TABLE 2. Patients’ pain ratings in both the active treatment and placebo groups improved in all the trials. Mean difference between improvements in treatment and placebo groups are shown in FIGURES 2A-2D for pain assessed at weeks 1, 5 to 7, 8 to 12 and 15 to 22, respectively. In each figure, we show the summary estimate of effect size with all the trials included and after excluding the 4 trials considered of poor quality, shown as “good quality studies.”
The mean difference in pain scores between treatment and placebo at week 1 was 4.4 (95% CI, +1.1, +7.2) and –1.0 (95% CI, -3.2, +1.2) for analysis restricted to the 7 good quality trials. The mean difference in pain scores at 5 to 7 weeks was 17.6 (95% CI, +7.5, +28.0) and 7.2 (95% CI, +2.4, +12.0) for the analysis restricted to the 2 good quality studies. At weeks 8 to 12 the mean difference in VAS between treatment and control was 18.1 (95% CI, +6.3, +29.9), and 7.1 (95% CI, +3.0, +11.3) in the analysis restricted to good quality trials. At weeks 15 to 22, the mean difference was 4.4 (95% CI, –15.3, +24.1). The Egger test was not statistically significant (2.3; P=.096; 95% CI, –0.5, +5.2) suggesting that there is no publication bias.
High heterogeneity was observed at all time intervals except 1 week (FIGURE 1). Of the 5 trials outside the confidence bounds (positioned 2 units above and below the regression line), 4 were poor-quality studies.
TABLE 3 shows the random-effect regression models we used to test the influence on the outcome of type of pain measured (pain with activity or pain at rest), type of medication (hyaluronan or hylan G-F 20), and study quality (good or poor). No significant association between treatment efficacy and type of pain used as outcome variable was observed. Clinical trials using hylan GF-20 showed statistically significant better results than those using hyaluronan at weeks 5 to 7 and 8 to 12. Poor-quality studies showed a larger treatment effect, but the difference was statistically significant only at week 1.
TABLE 3
Regression models to assess the sources of heterogeneity in the meta-analysis
| WEEK 1 | WEEKS 5–7 | WEEKS 8–12 | ||||
|---|---|---|---|---|---|---|
| Coef. (SE) [95% CI] | P value | Coef. (SE) [95% CI] | P value | Coef. (SE) [95% CI] | P value | |
| Pain | ||||||
| With activity | 1.7 (3.8) | 1.8 (4.3) | –0.5 (4.6) | |||
| At rest | [–5.8, +9.2] | 0.657 | [–6.6, +10.2] | 0.671 | [–9.5, +8.6] | 0.916 |
| Medication | ||||||
| Hyaluronan** | –3.4 (6.8) | 0.614 | 17.5 (4.9) | <0.001 | 14.8 (6.1) | 0.016 |
| Hylan G-F 20 | –16.7, +9.9] | [+7.8, +27.1] | [+2.8, +26.8] | |||
| Quality* | ||||||
| Poor (<0.75) | –19.9 (5.7) | 0.001 | –7.4 (4.9) | 0.131 | –11.7 (7.0) | 0.092 |
| Good (≥0.75) | [–31.1, –8.7] | [–17.0, +2.2] | [–25.3, +1.9] | |||
| Constant | 18.4 (5.6) | 0.001 | 13.5 (4.5) | 0.003 | 19.2 (5.8) | 0.001 |
| [+7.5, +29.3] | [+4.6, +22.3] | [+7.9, +30.5] | ||||
| *<.75 quality score: Grecomoro .439, Scale .570, Wobig .731, Huskisson .718. | ||||||
| ** 9 trials for hyaluronan (3 for Hyalgan®) and 2 trials for hylan G-F20 (Synvisc®). | ||||||
Discussion
This meta-analysis synthesized data from 9 randomized, double-blinded, placebo-controlled trials that evaluated the efficacy of intra-articular hyaluronic acid. Our findings show significantly decreased pain as measured by VAS at 5 to 7 weeks and at 8 to 12 weeks after the last injection. Intra-articular hyaluronic acid was not more effective than placebo in relieving pain at 1 week or at 15 to 22 weeks after the last injection. Because only 3 of the trials assessed patients after 12 weeks, however, the sample size is too small to definitively rule out a significant therapeutic effect after 12 weeks.
Reasons for the differences in efficacy among trials of hyaluronic acid in the treatment of knee osteoarthritis include dose, type, and frequency of administration, genetic or age differences among the study subjects, severity of osteoarthritis, time of follow-up, and quality of the studies. We confirmed that the treatment effect is time dependent. Although our meta-regression analysis (TABLE 2) suggests that hylan GF-20 is more effective than hyaluronan at 5 to 12 weeks, the number of clinical trials is relatively small and both of the hylan G-F20 studies were of poor quality. Therefore, we cannot say with confidence that one form is better than the other. Data in these trials were insufficient to assess the impact of body mass index, genetics, or severity of osteoarthritis.
We did not evaluate functional improvement in this meta-analysis because functional status was not measured in some trials and the assessment methods were too variable in the trials that did assess functional status. Publication bias, or the possibility that unpublished data would contradict the results of published studies, is always a potential source of bias in meta-analysis. However, the Egger test was not statistically significant (6.5; 95% CI, –0.5, +13.5) suggesting that there is no publication bias.25
Finally, the presence of heterogeneity of results indicates there were important differences among the studies. Exclusion of clinical trials considered of poor quality diminished this heterogeneity substantially. Subanalysis restricted to good-quality studies supports the efficacy of intra-articular hyaluronic acid in the treatment of knee osteoarthritis pain, although the effect size is smaller when one considers only the good quality studies.
There are 2 other potential limitations of this meta-analysis. Five studies allowed pain to be treated with analgesics such as acetaminophen or NSAIDs,12,13,16-18 and use of acetaminophen or NSAIDs may have altered the response to hyaluronic acid treatment. An intention-to-treat analysis was performed in only 2 studies (by Altman and Huskisson),16,18 wherein a post-hoc and “last observation carried forward” analysis showed a trend favoring hyaluronic acid. The treatment effects may have been smaller had the other trials used an intention to treat analysis.
This meta-analysis confirms that viscosupplementation with hyaluronic acid is modestly effective in short term relief of pain in knee osteoarthritis. Our meta-analysis included only double-blinded, randomized trials published in English language in humans using VAS as the pain outcome measure, and our conclusions are very similar to those of Lo.2
Indications for use. Hyaluronic acid is helpful in relieving pain for carefully selected patients with knee osteoarthritis who have not responded to adequate use of systemic therapeutic agents, including acetaminophen, NSAIDs and COX-2 inhibitors and topical agents, along with lifestyle modification such as weight reduction and exercise.
Patients should have a trial for at least three months of conservative therapy or be unable to tolerate NSAIDs before a decision to give 3- to 5-injection course with hyaluronic acid is made.
Hyaluronic acid may be an option when there is a need to delay knee surgery in middle-aged persons1 or for patients who have failed other treatments.
Time to pain relief. To improve adherence to treatment, tell patients receiving intra-articular hyaluronic acid that the benefits in pain reduction may not be noticeable until 5 to 10 weeks after the last injection.
Cost. Although the cost of hyaluronic acid treatment is covered by Medicare and most insurance plans for symptomatic osteoarthritis of knee, documentation in patient medical records should indicate the signs and symptoms supporting the diagnosis and functional impairment. Objective data to support a diagnosis of osteoarthritis such as x-ray, arthroscopy report, computed tomography scan, or magnetic resonance imaging should be available in the event of a review.
The cost of 1 hyaluronic acid (30 mg/mL) injection is approximately $230. Considering a course of 3 to 5 weekly knee injections, and adding other pharmacy, hospital, or clinic charges, the cost per treatment may exceed $1000 per knee.26,27 The cost-benefit of pain control with viscosupplementation must be carefully compared with other therapeutic agents and regimens currently available for knee osteoarthritis management.
FIGURE 3
Studies evaluated at outcome measurement time (week 1)
Egger’s publication bias plot for the studies evaluated at outcome measurement time (week 1) not significant (+2.3, P=0.096, 95% CI: –0.5, +5.2).
Acknowledgments
Jeff Welge, PhD, University of Cincinnati Medical Center, Center for Bio-statistical Services, for comments on final data analysis and presentation, Marie Marley, PhD for editing the manuscript, and Charity Noble for help in preparation of this manuscript.
CORRESPONDING AUTHOR
Arvind Modawal, MD, MPH, MRCGP, University of Cincinnati Department of Family Medicine/Geriatrics, PO Box 670582, Cincinnati, OH 45267-0582. E-mail: [email protected]
- Consider injections of hyaluronic acid only after conservative therapy has been tried for at least 3 months or the patient is unable to tolerate NSAIDs.
- Stress to patients that pain relief may not be fully experienced until 5 to 7 weeks following the last injection.
Hyaluronic acid injections can help relieve pain for carefully selected patients with knee osteoarthritis. But this option should be reserved for those whose pain has not responded to adequate trials of systemic therapeutic agents (acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs], cyclooxygenase-2 [COX-2] inhibitors), topical agents, or to lifestyle modifications such as weight reduction and exercise.
Hyaluronic acid injections may also be indicated when knee surgery must be delayed for middle-aged persons.1
In spite of the Food and Drug Administration’s approval of this therapy, uncertainty about its efficacy exists among the medical community. A recent meta-analysis of the effectiveness of intra-articular hyaluronic acid for knee osteoarthritis that included 22 published and unpublished, English and non-English, single or double-blinded, randomized controlled trials in humans showed that hyaluronic acid has only a small effect on pain relief when compared with placebo.2
We provide here a stringent test of the efficacy of viscosupplementation for relieving knee pain from osteoarthritis with a meta-analysis that includes only data from randomized, double-blinded, controlled trials of hyaluronic acid that measured pain using a visual analogue scale (VAS), the most widely accepted method for pain evaluation.
Long time coming
Balazs first proposed hyaluronic acid as a treatment for patients with arthritic diseases in 1942. In the early 1970s, therapeutic studies were begun to test the efficacy of hyaluronic acid on knee osteoarthritis. The results were encouraging and side effects were few.28 With the FDA’s approval in 1998, intra-articular “viscosupplementation” with hyaluronic acid—also called hyaluronan or hyaluronate, and the hylan derivatives of hyaluronic acid—is a welcome option for many of the 16 million older Americans with osteoarthritis of the knee.1
Methods
Selection of studies
We identified clinical trials of viscosupplementation with hyaluronic acid in humans published in English from 1965 through August 2004 through a computerized literature search of Medline. The keyword used was “hyaluronic acid,” which was combined with “trial” or “osteoarthritis knee” or “viscosupplementation.” We conducted an additional manual search of the reference lists of included articles and review articles. We also searched the Cochrane Library and websites of the Agency for Healthcare Research and Quality (AHRQ) for information on hyaluronic acid in knee osteoarthritis. We identified 1872 articles with this search process.
Of the 1872 articles, we identified by title and abstract 33 that might be pertinent to this study, including 17 randomized trials. We excluded reviews, meta-analyses, comparison trials, and trials reporting VAS as part of the WOMAC (Western Ontario McMaster Universities Index) scale. We attempted to contact authors of the studies that used a double-blind, randomized controlled design, to obtain any data that may not have been included in the publications. Three authors provided the details requested; the others did not respond or stated that additional data were not available. Of the 17 randomized trials we identified, 8 were excluded because they were open, single-blinded, or did not use the VAS to measure pain outcomes.3-10 The remaining 9 double-blinded, placebo controlled, randomized clinical trials of viscosupplementation with hyaluronic acid for knee osteoarthritis that did use a VAS to measure pain were included in this meta-analysis (TABLE 1). Because one of the studies (by Henderson) included 2 subgroups of pain severity, these were considered as 2 separate trials. The trial by Petrella had 2 treatment groups, one with only hyaluronic acid and the other with hyaluronic acid and NSAIDs. We considered them separately in the analysis, resulting in a total of 11 clinical trials for the meta-analysis.19 Henceforth in this report, we will refer to 11 rather than 9 clinical trials.
Extraction of data
Two investigators independently extracted the following data for each study: year of publication, study design, mean age, number of patients enrolled in each treatment group, number of doses of treatment used, and outcomes measured. When disagreements between investigators occurred, the point of disagreement was discussed until a consensus was reached. Since the treatment duration and the time post-treatment when pain was assessed varied among the trials, we grouped outcomes into four time intervals: at 1 week, 5 to 7 weeks, 8 to 12 weeks, and 15 to 22 weeks after the last hyaluronic acid injection.
Statistical analysis
The outcome was knee pain reported by patients on activity or at rest, measured using a VAS of 100 mm. The results of the clinical trials were recorded as the mean differences of change from baseline between the treatment and placebo groups. If not reported in the publication or provided by the authors, standard error was imputed using the method of Follman et al.20 We used the method of Chalmers for measuring the quality of randomized trials, with 2 of the authors rating the studies independently.21
This clinical trial grading system takes into account the following aspects of the trial to determine a quality score: evaluation of recruitment of subjects, rejection log, therapeutic regimen definition, randomization, blinding, prior estimates of numbers, testing compliance, statistical inference, use of appropriate statistical analysis, handling of withdrawal and side effects, dates of starting and ending, timing and tabulation of events. Because 4 of the trials had poor quality scores, an additional analysis excluding these 4 was performed. The DerSimonian and Laird random-effects model was used to obtain the summary estimates.22,23
An important element of meta-analysis is exploration of the heterogeneity of the outcomes and the possible causes of heterogeneity if it exists. Heterogeneity is the degree to which results vary from study to study. If a test for heterogeneity is statistically significant, there is significant variability among the treatment effects observed in the trials. We explored heterogeneity using Galbraith plots (FIGURE 1).24 In the absence of heterogeneity, all points fall within the confidence limits. Because we did find heterogeneity among these trials, we developed random-effect regression models to explore 3 possible sources of heterogeneity in the efficacy of hyaluronic acid; pain (measured at rest or on activity), the form used (hyaluronan or hylan G-F20), and the quality of the study method (good or poor).
Publication bias was assessed by the Egger et al regression asymmetry test.25 Analyses were performed using the meta-analytic software program of STATA, Inc (College Station, Tex; available at www.stata.com).
FIGURE 1
Evidence of heterogeneity for the studies evaluated at outcome measurement time (week 1)
This Galbraith plot shows standardized effects (b/se=mean difference/standard error) as a function of study precision (1/standard error), slope of the line shows average effect over all the studies with upper and lower lines denoting an approximate 95% confidence interval for this common effect. Under the hypothesis of study heterogeneity, the common slope intersect zero at 1/se=0, and 95% of all study estimates (authors initials) will fall within the confidence interval of the regression line. Gr: Grecomoro; Pu: Puhl; H1: Henderson 1; H2: Henderson 2; Sc: Scale; Lo: Lohmander; Al: Altman; Wo: Wobig; Hu: Huskisson; P1: Petrella 1; P2: Petrella 2.
Results
The 11 randomized, placebo-controlled, double-blinded clinical trials that met our inclusion criteria are summarized in TABLE 1. Nine trials used hyaluronic acid, hyaluronan, or hyaluronate (all types will be referred to as hyaluronan in the text), and 2 studies used hylan GF-20. Only 3 hyaluronan trials have published outcome data at 15 to 22 weeks follow-up. Treatment was administered to patients as 3 to 5 weekly injections, with the exception of the Grecomoro study in which treatment was administered twice weekly. The control group in 10 trials received intra-articular saline injections as placebo. In the Puhl study the investigators added 0.25 mg of hyaluronic acid to the saline injections to impart viscosity to the solution. The mean age of the subjects for the 11 trials was 63 years.
Eight trials received support from pharmaceutical companies and 3 (the 2 by Henderson and the Grecomoro study) did not disclose any pharmaceutical support. One study was conducted in the United States, 3 in the UK, 3 in Germany, 1 in Sweden, 1 in Italy, and 2 in Canada. Five of the studies had scores over a cutoff quality score of >0.75,12,13,15,16,19 indicating they were good-quality randomized controlled trials; the remaining 4 had scores below 0.75.11,14,16,17
The outcomes of the 11 trials are summarized in TABLE 2. Patients’ pain ratings in both the active treatment and placebo groups improved in all the trials. Mean difference between improvements in treatment and placebo groups are shown in FIGURES 2A-2D for pain assessed at weeks 1, 5 to 7, 8 to 12 and 15 to 22, respectively. In each figure, we show the summary estimate of effect size with all the trials included and after excluding the 4 trials considered of poor quality, shown as “good quality studies.”
The mean difference in pain scores between treatment and placebo at week 1 was 4.4 (95% CI, +1.1, +7.2) and –1.0 (95% CI, -3.2, +1.2) for analysis restricted to the 7 good quality trials. The mean difference in pain scores at 5 to 7 weeks was 17.6 (95% CI, +7.5, +28.0) and 7.2 (95% CI, +2.4, +12.0) for the analysis restricted to the 2 good quality studies. At weeks 8 to 12 the mean difference in VAS between treatment and control was 18.1 (95% CI, +6.3, +29.9), and 7.1 (95% CI, +3.0, +11.3) in the analysis restricted to good quality trials. At weeks 15 to 22, the mean difference was 4.4 (95% CI, –15.3, +24.1). The Egger test was not statistically significant (2.3; P=.096; 95% CI, –0.5, +5.2) suggesting that there is no publication bias.
High heterogeneity was observed at all time intervals except 1 week (FIGURE 1). Of the 5 trials outside the confidence bounds (positioned 2 units above and below the regression line), 4 were poor-quality studies.
TABLE 3 shows the random-effect regression models we used to test the influence on the outcome of type of pain measured (pain with activity or pain at rest), type of medication (hyaluronan or hylan G-F 20), and study quality (good or poor). No significant association between treatment efficacy and type of pain used as outcome variable was observed. Clinical trials using hylan GF-20 showed statistically significant better results than those using hyaluronan at weeks 5 to 7 and 8 to 12. Poor-quality studies showed a larger treatment effect, but the difference was statistically significant only at week 1.
TABLE 3
Regression models to assess the sources of heterogeneity in the meta-analysis
| WEEK 1 | WEEKS 5–7 | WEEKS 8–12 | ||||
|---|---|---|---|---|---|---|
| Coef. (SE) [95% CI] | P value | Coef. (SE) [95% CI] | P value | Coef. (SE) [95% CI] | P value | |
| Pain | ||||||
| With activity | 1.7 (3.8) | 1.8 (4.3) | –0.5 (4.6) | |||
| At rest | [–5.8, +9.2] | 0.657 | [–6.6, +10.2] | 0.671 | [–9.5, +8.6] | 0.916 |
| Medication | ||||||
| Hyaluronan** | –3.4 (6.8) | 0.614 | 17.5 (4.9) | <0.001 | 14.8 (6.1) | 0.016 |
| Hylan G-F 20 | –16.7, +9.9] | [+7.8, +27.1] | [+2.8, +26.8] | |||
| Quality* | ||||||
| Poor (<0.75) | –19.9 (5.7) | 0.001 | –7.4 (4.9) | 0.131 | –11.7 (7.0) | 0.092 |
| Good (≥0.75) | [–31.1, –8.7] | [–17.0, +2.2] | [–25.3, +1.9] | |||
| Constant | 18.4 (5.6) | 0.001 | 13.5 (4.5) | 0.003 | 19.2 (5.8) | 0.001 |
| [+7.5, +29.3] | [+4.6, +22.3] | [+7.9, +30.5] | ||||
| *<.75 quality score: Grecomoro .439, Scale .570, Wobig .731, Huskisson .718. | ||||||
| ** 9 trials for hyaluronan (3 for Hyalgan®) and 2 trials for hylan G-F20 (Synvisc®). | ||||||
Discussion
This meta-analysis synthesized data from 9 randomized, double-blinded, placebo-controlled trials that evaluated the efficacy of intra-articular hyaluronic acid. Our findings show significantly decreased pain as measured by VAS at 5 to 7 weeks and at 8 to 12 weeks after the last injection. Intra-articular hyaluronic acid was not more effective than placebo in relieving pain at 1 week or at 15 to 22 weeks after the last injection. Because only 3 of the trials assessed patients after 12 weeks, however, the sample size is too small to definitively rule out a significant therapeutic effect after 12 weeks.
Reasons for the differences in efficacy among trials of hyaluronic acid in the treatment of knee osteoarthritis include dose, type, and frequency of administration, genetic or age differences among the study subjects, severity of osteoarthritis, time of follow-up, and quality of the studies. We confirmed that the treatment effect is time dependent. Although our meta-regression analysis (TABLE 2) suggests that hylan GF-20 is more effective than hyaluronan at 5 to 12 weeks, the number of clinical trials is relatively small and both of the hylan G-F20 studies were of poor quality. Therefore, we cannot say with confidence that one form is better than the other. Data in these trials were insufficient to assess the impact of body mass index, genetics, or severity of osteoarthritis.
We did not evaluate functional improvement in this meta-analysis because functional status was not measured in some trials and the assessment methods were too variable in the trials that did assess functional status. Publication bias, or the possibility that unpublished data would contradict the results of published studies, is always a potential source of bias in meta-analysis. However, the Egger test was not statistically significant (6.5; 95% CI, –0.5, +13.5) suggesting that there is no publication bias.25
Finally, the presence of heterogeneity of results indicates there were important differences among the studies. Exclusion of clinical trials considered of poor quality diminished this heterogeneity substantially. Subanalysis restricted to good-quality studies supports the efficacy of intra-articular hyaluronic acid in the treatment of knee osteoarthritis pain, although the effect size is smaller when one considers only the good quality studies.
There are 2 other potential limitations of this meta-analysis. Five studies allowed pain to be treated with analgesics such as acetaminophen or NSAIDs,12,13,16-18 and use of acetaminophen or NSAIDs may have altered the response to hyaluronic acid treatment. An intention-to-treat analysis was performed in only 2 studies (by Altman and Huskisson),16,18 wherein a post-hoc and “last observation carried forward” analysis showed a trend favoring hyaluronic acid. The treatment effects may have been smaller had the other trials used an intention to treat analysis.
This meta-analysis confirms that viscosupplementation with hyaluronic acid is modestly effective in short term relief of pain in knee osteoarthritis. Our meta-analysis included only double-blinded, randomized trials published in English language in humans using VAS as the pain outcome measure, and our conclusions are very similar to those of Lo.2
Indications for use. Hyaluronic acid is helpful in relieving pain for carefully selected patients with knee osteoarthritis who have not responded to adequate use of systemic therapeutic agents, including acetaminophen, NSAIDs and COX-2 inhibitors and topical agents, along with lifestyle modification such as weight reduction and exercise.
Patients should have a trial for at least three months of conservative therapy or be unable to tolerate NSAIDs before a decision to give 3- to 5-injection course with hyaluronic acid is made.
Hyaluronic acid may be an option when there is a need to delay knee surgery in middle-aged persons1 or for patients who have failed other treatments.
Time to pain relief. To improve adherence to treatment, tell patients receiving intra-articular hyaluronic acid that the benefits in pain reduction may not be noticeable until 5 to 10 weeks after the last injection.
Cost. Although the cost of hyaluronic acid treatment is covered by Medicare and most insurance plans for symptomatic osteoarthritis of knee, documentation in patient medical records should indicate the signs and symptoms supporting the diagnosis and functional impairment. Objective data to support a diagnosis of osteoarthritis such as x-ray, arthroscopy report, computed tomography scan, or magnetic resonance imaging should be available in the event of a review.
The cost of 1 hyaluronic acid (30 mg/mL) injection is approximately $230. Considering a course of 3 to 5 weekly knee injections, and adding other pharmacy, hospital, or clinic charges, the cost per treatment may exceed $1000 per knee.26,27 The cost-benefit of pain control with viscosupplementation must be carefully compared with other therapeutic agents and regimens currently available for knee osteoarthritis management.
FIGURE 3
Studies evaluated at outcome measurement time (week 1)
Egger’s publication bias plot for the studies evaluated at outcome measurement time (week 1) not significant (+2.3, P=0.096, 95% CI: –0.5, +5.2).
Acknowledgments
Jeff Welge, PhD, University of Cincinnati Medical Center, Center for Bio-statistical Services, for comments on final data analysis and presentation, Marie Marley, PhD for editing the manuscript, and Charity Noble for help in preparation of this manuscript.
CORRESPONDING AUTHOR
Arvind Modawal, MD, MPH, MRCGP, University of Cincinnati Department of Family Medicine/Geriatrics, PO Box 670582, Cincinnati, OH 45267-0582. E-mail: [email protected]
1. Cefalu CA, Waddell DS. Viscosupplementation: Treatment alternative for osteoarthritis of the knee. Geriatrics 1999;54:51-57.
2. Lo GH, LaValley M, McAlindon T, Felson DT. Intra-articular hyaluronic acid in treatment of knee osteoarthritis. JAMA 2003;290:3115-3121.
3. Jones AC, Pattrick M, Doherty S, Doherty M. Intra-articular hyaluronic acid compared to intra-articular triamcinolone hexacetonide in inflammatory knee osteoarthritis. Osteoarthritis Cartilage 1995;3:269-273.
4. Graf J, Neusel E, Schneider E, Niethard FU. Intra-articular treatment with hyaluronic acid in osteoarthritis of the knee joint: a controlled clinical trial versus mucopolysaccharide polysulfuric acid ester. Clin Exp Rheumatol 1993;11:367-72.
5. Dougados M, Nguyen M, Listrat V, Amor B. High molecular weight sodium hyaluronate (hyalectin) in osteoarthritis of the knee: A one year placebo-controlled trial. Osteoarthritis Cartilage 1993;1:97-103.
6. Adams ME. An analysis of clinical studies of the use of cross-linked hyaluronan, hylan, in the treatment of osteoarthritis. J Rheumatol Supp 1993;39:16-18.
7. Grecomoro G, Piccione F, Letizia G. Therapeutic synergism between hyaluronic acid and dexamethasone in the intra-articular treatment of osteoarthritis of the knee: a preliminary open study. Curr Med Res Opin 1992;13:49-55.
8. Leardini G, Mattara L, Franceschini M, Perbellini A. Intra-articular treatment of knee osteoarthritis. A comparative study between hyaluronic acid and 6-methyl prednisolone acetate. Clin Exp Rheumatol 1991;9:375-381.
9. Wu J, Shih L, Hsu H, Chen T. The double-blind test of sodium hyaluronate (ARTZ) on osteoarthritis knee. Chin Med J (Taipei) 1997;59:99-106.
10. Dixon AS, Jacoby RK, Berry H, Hamilton EB. Clinical trial of intra-articular injection of sodium hyaluronate in patients with osteoarthritis of the knee. Curr Med Res Opin 1988;11:205-213.
11. Grecomoro G, Martorana U, Di Marco C. Intra-articular treatment with sodium hyaluronate in gonarthrosis: a controlled clinical trial versus placebo. Pharmather 1987;5:137-141.
12. Puhl W, Bernau A, Greiling H, Kopcke W, Pforringer W, Steck KJ. Intra-articular sodium hyaluronate in osteoarthritis of the knee: a multicenter, double-blind study. Osteoarthritis Cartilage 1993;1:233-241.
13. Henderson EB, Smith EC, Pegley F, Blake DR. Intra-articular injections of 750 kD hyaluronan in the treatment of osteoarthritis: a randomized single centre double-blind placebo-controlled trial of 91 patients demonstrating lack of efficacy. Ann Rheum Dis 1994;53:529-554.
14. Scale D, Wobig M, Wolpert W. Viscosupplementation of osteoarthritic knees with Hylan: A treatment schedule study. Curr Ther Res 1994;55:220-232.
15. Lohmander LS, Dalen N, Englund G, et al. Intra-articular hyaluronan injections in the treatment of osteoarthritis of the knee: a randomized, double blind, placebo controlled multicentre trial. Hyaluronan Multicentre Trial Group [see comments]. Ann Rheum Dis 1996;55:424-431.
16. Altman RD, Moskowitz R. Intra-articular sodium hyaluronate (Hyalgan®) in the treatment of patients with osteoarthritis of the knee: A randomized clinical trial. J Rheumatol 1998;25:2203-2212.
17. Wobig M, Dickhut A, Maier R, Vetter G. Viscosupplementation with Hylan G-F-20: A 26-week controlled trial of efficacy and safety in the osteoarthritic knee. Clin Ther 1998;20:410-423.
18. Huskisson EC, Donnelly S. Hyaluronic acid in the treatment of osteoarthritis of the knee. Rheumatology 1999;38:602-607.
19. Petrella RJ, DiSilvestro MD, Hildebrand C. Effects of hyaluronate sodium on pain and physical functioning in osteoarthritis of the knee. Arch Intern Med 2002;162:292-298.
20. Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol 1992;45:769-773.
21. Chalmers TC, Smith H, Jr, Blackburn B, et al. A Method for Assessing the quality of a randomized control trial. Control Clin Trials 1981;2:31-49.
22. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-188.
23. Sacks HS, Berrier J, Reitman D, Ancona-Berk VA, Chalmers TC. Meta-analyses of randomized controlled trials. N Engl J Med 1987;316:450-455.
24. Galbraith R. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 1988;7:889-894.
25. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
26. CIGNA Government Services. Not otherwise classified drug fee schedule. Available at: www.cignamedicare.com/partb/fsch/2004/q2/noc.html. Accessed on June 20, 2005.
27. Empire Medicare Services. Local coverage determination. Hyaluronate polymers (Synvisc, Hyalgan) (A02-0011-R3). Available at: www.empiremedicare.com/Nyorkpolicya/policy/A02-0011-R_FINAL.htm.
28. Peyron JG, Balazs EA. Preliminary clinical assessment of Na-hyaluronate injection into human arthritic joints. Pathol Biol 1974;22:731-736.
1. Cefalu CA, Waddell DS. Viscosupplementation: Treatment alternative for osteoarthritis of the knee. Geriatrics 1999;54:51-57.
2. Lo GH, LaValley M, McAlindon T, Felson DT. Intra-articular hyaluronic acid in treatment of knee osteoarthritis. JAMA 2003;290:3115-3121.
3. Jones AC, Pattrick M, Doherty S, Doherty M. Intra-articular hyaluronic acid compared to intra-articular triamcinolone hexacetonide in inflammatory knee osteoarthritis. Osteoarthritis Cartilage 1995;3:269-273.
4. Graf J, Neusel E, Schneider E, Niethard FU. Intra-articular treatment with hyaluronic acid in osteoarthritis of the knee joint: a controlled clinical trial versus mucopolysaccharide polysulfuric acid ester. Clin Exp Rheumatol 1993;11:367-72.
5. Dougados M, Nguyen M, Listrat V, Amor B. High molecular weight sodium hyaluronate (hyalectin) in osteoarthritis of the knee: A one year placebo-controlled trial. Osteoarthritis Cartilage 1993;1:97-103.
6. Adams ME. An analysis of clinical studies of the use of cross-linked hyaluronan, hylan, in the treatment of osteoarthritis. J Rheumatol Supp 1993;39:16-18.
7. Grecomoro G, Piccione F, Letizia G. Therapeutic synergism between hyaluronic acid and dexamethasone in the intra-articular treatment of osteoarthritis of the knee: a preliminary open study. Curr Med Res Opin 1992;13:49-55.
8. Leardini G, Mattara L, Franceschini M, Perbellini A. Intra-articular treatment of knee osteoarthritis. A comparative study between hyaluronic acid and 6-methyl prednisolone acetate. Clin Exp Rheumatol 1991;9:375-381.
9. Wu J, Shih L, Hsu H, Chen T. The double-blind test of sodium hyaluronate (ARTZ) on osteoarthritis knee. Chin Med J (Taipei) 1997;59:99-106.
10. Dixon AS, Jacoby RK, Berry H, Hamilton EB. Clinical trial of intra-articular injection of sodium hyaluronate in patients with osteoarthritis of the knee. Curr Med Res Opin 1988;11:205-213.
11. Grecomoro G, Martorana U, Di Marco C. Intra-articular treatment with sodium hyaluronate in gonarthrosis: a controlled clinical trial versus placebo. Pharmather 1987;5:137-141.
12. Puhl W, Bernau A, Greiling H, Kopcke W, Pforringer W, Steck KJ. Intra-articular sodium hyaluronate in osteoarthritis of the knee: a multicenter, double-blind study. Osteoarthritis Cartilage 1993;1:233-241.
13. Henderson EB, Smith EC, Pegley F, Blake DR. Intra-articular injections of 750 kD hyaluronan in the treatment of osteoarthritis: a randomized single centre double-blind placebo-controlled trial of 91 patients demonstrating lack of efficacy. Ann Rheum Dis 1994;53:529-554.
14. Scale D, Wobig M, Wolpert W. Viscosupplementation of osteoarthritic knees with Hylan: A treatment schedule study. Curr Ther Res 1994;55:220-232.
15. Lohmander LS, Dalen N, Englund G, et al. Intra-articular hyaluronan injections in the treatment of osteoarthritis of the knee: a randomized, double blind, placebo controlled multicentre trial. Hyaluronan Multicentre Trial Group [see comments]. Ann Rheum Dis 1996;55:424-431.
16. Altman RD, Moskowitz R. Intra-articular sodium hyaluronate (Hyalgan®) in the treatment of patients with osteoarthritis of the knee: A randomized clinical trial. J Rheumatol 1998;25:2203-2212.
17. Wobig M, Dickhut A, Maier R, Vetter G. Viscosupplementation with Hylan G-F-20: A 26-week controlled trial of efficacy and safety in the osteoarthritic knee. Clin Ther 1998;20:410-423.
18. Huskisson EC, Donnelly S. Hyaluronic acid in the treatment of osteoarthritis of the knee. Rheumatology 1999;38:602-607.
19. Petrella RJ, DiSilvestro MD, Hildebrand C. Effects of hyaluronate sodium on pain and physical functioning in osteoarthritis of the knee. Arch Intern Med 2002;162:292-298.
20. Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol 1992;45:769-773.
21. Chalmers TC, Smith H, Jr, Blackburn B, et al. A Method for Assessing the quality of a randomized control trial. Control Clin Trials 1981;2:31-49.
22. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-188.
23. Sacks HS, Berrier J, Reitman D, Ancona-Berk VA, Chalmers TC. Meta-analyses of randomized controlled trials. N Engl J Med 1987;316:450-455.
24. Galbraith R. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 1988;7:889-894.
25. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
26. CIGNA Government Services. Not otherwise classified drug fee schedule. Available at: www.cignamedicare.com/partb/fsch/2004/q2/noc.html. Accessed on June 20, 2005.
27. Empire Medicare Services. Local coverage determination. Hyaluronate polymers (Synvisc, Hyalgan) (A02-0011-R3). Available at: www.empiremedicare.com/Nyorkpolicya/policy/A02-0011-R_FINAL.htm.
28. Peyron JG, Balazs EA. Preliminary clinical assessment of Na-hyaluronate injection into human arthritic joints. Pathol Biol 1974;22:731-736.
Herbs for mental illness: Effectiveness and interaction with conventional medicines
- Many of your patients may be self-treating with herbal preparations. Ask candidly about this possibility, and become familiar with the increasing evidence on efficacy and safety of alternative treatments
- A large meta-analysis and a Cochrane Review both suggest St. John’s Wort (A) is as effective as conventional antidepressants and more effective than placebo for mild to moderate depression. With patients taking St. John’s Wort and a conventional antidepressant, remain alert for a potentiating effect, “serotonin syndrome.” Use with caution if the patient must also receive anticoagulants, oral contraceptives, or antiviral agents.
- The efficacy and safety of ginseng (B, in terms of psychological well-being) and evening primrose (C) for depression are not well established.
- Kava-kava (A, for short-term treatment for anxiety treatment) has well-known anxiolytic properties, but its potential adverse effects, particularly liver toxicity, dramatically reduce its usefulness. Valerian, though commonly used for anxiety (C, for insomnia and anxiety), is not well supported by good data.
- Ginkgo has shown promise in improving cognitive function in dementia, and its side effects are few and uncommon (A, for cognitive function in dementia). Monitor carefully if there is concomitant anticoagulant therapy.
Based on epidemiologic estimates, it may be that 20% to 30% of your patient population is using alternative/complementary medicines.1 Twenty percent of adults who take prescription medicine also rely on herbal products,2 and patients who use herbal products the most are those with chronic conditions.3
Included in this group are persons with mental health problems, who, compared with the general population, report a much greater use of alternative treatments, including herbal and homeopathic remedies.4 These remedies, when used to treat psychiatric symptoms, may produce changes in mood, thinking, or behavior, and they may interact with a number of conventional medications.3
Largely uncharted territory. With the exception of St. John’s Wort for depression and ginkgo for dementia, minimal evidence is currently available to recommend the use of herbal medicines as the primary treatment for mental illness. Although some herbs have been found to be effective at specific doses for specific conditions, there is no evidence to show their superiority to conventional drug treatments, nor has their safety been established for use during pregnancy and lactation.8
Helping patients navigate. Nevertheless, our patients are increasingly turning to alternative therapies, and it is therefore critical that we clinicians avail ourselves of current knowledge and that investigators pursue intensive clinical research to establish safety (TABLE 1) and efficacy. Additionally, greater understanding of the biochemical and pharmacological effects of these herbs may uncover novel treatments or yield fresh insights into basic disease mechanisms.9
The herbal remedies discussed in this article are those commonly used for psychiatric conditions. Their effectiveness and potential for adverse side effects and interactions are assessed.
Depression
St. John’s Wort
St. John’s Wort (Hypericum perforatum L) is a popular herbal treatment readily used by the public in various forms, such as tablets and teas. Efficacy of hypericum—one of the hypothesized active ingredients in St. John’s Wort—in the treatment of depression was reported in the texts of the ancient Greek physicians Hippocrates, Pliny, and Galen, and it continued to be cited throughout the Classical, Renaissance, and Victorian eras. Its contemporary usage as an antidepressant has been supported by more rigorous evidence than any other herbal remedy.9
Efficacy. Evidence of efficacy in mild to moderate depression has been reported in a meta-analysis of 23 randomized trials with a total of 1757 outpatients, in which extracts of St. John’s Wort alone (20 of 23 trials) or in combination with other herbs (3 of 23) were tested against placebo (15 trials) or antidepressant drugs (8 trials).10 St. John’s Wort was reported to be clearly superior to placebo and comparable with conventional drug treatment, with lower side-effect and dropout rates. Similarly, a recent Cochrane Review of 27 trials and 2291 patients concluded that St. John’s Wort was more effective than placebo in treating mild to moderately severe depression; however, there was inadequate evidence to determine whether the herb was as effective as traditional antidepressants.11
The superiority of hypericum to placebo has been called into question, however, by a large-scale, multicenter, double-blind case report tabulation. The study, conducted with 200 patients across 11 academic medical centers in the United States, found no evidence that St. John’s Wort was more efficacious than placebo.12 Another such trial also concluded that St. John’s Wort was not an effective treatment for major depression. In addition, the herb was found to be no different than sertraline, which was also indistinguishable from the placebo, further confusing the issue.13 Strength of recommendation (SOR) is level A for the evidence in support of St. John’s Wort as an antidepressant.
Because many alternative options do not require the approval of the US Food and Drug Administration (FDA), products sold in health food stores can be purchased without a prescription or the provision of any clinical advice or professional review. The quality of many herbal preparations is thus unpredictable, with the content varying not only from brand to brand but also from batch to batch.5
A working knowledge of the pharmacologic data and clinical literature is necessary to properly counsel, diagnose, and treat patients who may be using herbal products. However, 1 study reported that only 5% of British doctors claimed more than a poor knowledge of herbal medicine,6 and another survey revealed that most psychiatrists who do not recommend herbal products avoid doing so because they feel uncomfortable with their current knowledge of alternative therapies.7 Alarmingly, the latter study reported that among psychiatrists who do not recommend herbal treatments, the safety of such treatments is not an issue in their decision-making process.
Mechanisms of action. The mechanisms for the antidepressant effects of St. John’s Wort are not fully understood, although monoamine oxidase (MAO) inhibition, inhibition of serotonin receptor expression, serotonin reuptake inhibition, and reduction of cytokine expression have all been suggested as means of its activity.9
Herb-drug interactions. Evidence suggests St. John’s Wort contains both inhibitory and inducing constituents for the cytochrome P-450 (CYP) system, resulting in both inhibition and induction on the CYP system.14 Consequently, it’s difficult to predict which drugs St. John’s Wort will interact with in a significant way.15 Best estimates of its activity suggest it has minimal short-term activity; when used for a longer period, it will inhibit the CytP450-3A4, 2C19, and 2D6 systems (TABLE 2). Therefore, St. John’s Wort may alter the blood levels of such medications as anticoagulants,16 oral contraceptives,18 and antiviral agents,19 possibly resulting in serious consequences.16,17 Exercise caution when initiating treatment for patients already taking St. John’s Wort.
The potential of St. John’s Wort to interact with standard prescribed antidepressants, possibly to produce a “serotonin syndrome,” is also a concern. Gordon20 reported a case in which a woman taking St. John’s Wort became groggy, weak, and lethargic shortly after taking a single 20-mg dose of paroxetine. This patient had tolerated St. John’s Wort and paroxetine separately, suggesting a drug-herb interaction.3 St. John’s Wort has also been implicated in reducing blood levels of digoxin when the two are taken together,21 and 1 study documented that 8% of psychiatrists treating patients who had used St. John’s Wort reported drug interactions between the herb and another agent.22
Adverse effects. In general, fewer adverse effects are seen with hypericum than with conventional antidepressants but they may include photodermatitis, delayed hypersensitivity, gastrointestinal tract upset, dizziness, dry mouth, sedation, restlessness, and constipation. Use of St. John’s Wort is contraindicated during pregnancy and lactation, for patients who experience intense exposure to strong sunlight, and for patients with a pheochromocytoma.23
There are several anecdotal reports of mania or hypomania associated with the herb. For example, O’Breasail and Argouarch24 reported 2 cases of persons with no history of bipolar disorder who developed hypomanic episodes after taking St. John’s Wort. Likewise, Moses and Mallinger25 reported 3 cases of possible mania induction associated with the herb.
TABLE 2
Effects of common herbs on cytochrome P-450 enzymes
| CYTOCHROME P-450 | |||
|---|---|---|---|
| CYTP450-3A4 | CYTP450-2C19 | CYP450-2D6 | |
| St. John’s Wort | ++++ inhibition (short-term?) | +++ inhibition | ++ inhibition |
| Long-term induction in intestinal wall99 | |||
| Kava-kava100 | ++ inhibition | ++ inhibition | ++ inhibition |
| Valerian | + inhibition | + inhibition | 0 |
| Fish oil, omega-3 fatty acids | +++ inhibition | ++++ inhibition | + inhibition |
| Key: ++++ = very potent; ++ = potent (detectable); + = mildly potent; 0 = does not inhibit | |||
| Note: Caution should be undertaken when developing tables such as these, as the data came from a variety of in vivo and in vitro animal and human studies using simplified models (eg, cDNA-expressed CYP enzymes) of which there are significant interspecies variations in the activity of these systems. As well, in the presence of some pathological inflammatory states such as during an infection, the enzyme activity of the CYP can be modulated through cytokines and other mediators of inflammation.101 | |||
Ginseng
This herb is derived from the root of Panax ginseng and has been used as a cure-all in Eastern folk medicine for thousands of years.26 Today, both Chinese ginseng (P ginseng CA Meyer) and North American ginseng (P quinquefolius L) are associated with the treatment of mood and anxiety disorders and are used to reduce stress and fatigue and to improve endurance.
Efficacy. A systematic review of 16 double-blind randomized controlled trials found that ginseng did not improve cognitive function or psychomotor and physical performance.27 Another review reported conflicting results from several studies.28 For example, 1 double-blind randomized controlled trial of postmenopausal women who received either a placebo or ginseng for 16 weeks revealed the superiority of ginseng on measures of psychological well-being.29 Another double-blind randomized controlled trial, however, failed to find an effect of ginseng on positive affect, negative affect, or total mood disturbance in 83 healthy adults who took the herb for 8 weeks.30 Thus, at best, SOR=B for the evidence in support of ginseng, but only at best in relation to psychological well-being.
Mechanisms of action. The key active components of Panax ginseng are ginsenosides, a group of steroidal saponins that target a multitude of tissues to produce pharmacologic responses. The overall pharmacology of ginseng is complex due to the ability of ginsenosides to initiate multiple actions in the same tissue. Attele and colleagues31 provide an in-depth review of these mechanisms.
Herb-drug interactions. Ginseng may potentiate the effect of MAO inhibitors,32 stimulants (including caffeine), and haloperidol.33 In addition, a case study suggests a probable interaction with warfarin.34
Adverse effects. Reported side effects include insomnia, hypertension, diarrhea, restlessness, anxiety, and euphoria.35 There is at least 1 report of ginseng-induced mania, which occurred within 4 to 10 days of a patient’s interrupting a lithium and amitriptyline treatment.26
Evening primrose
Evening primrose (Oenothera biennis L) is a plant native to North America. The oil pressed from its seed is marketed as a nutritional supplement, and it has been used to treat many disorders, including premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD), both which are marked by affective disturbances.36,37
Efficacy. A systematic review38 of the efficacy of evening primrose oil in the treatment of PMS revealed few clinical trials of adequate methodology. The authors found only 2 well-controlled studies, both which failed to show beneficial effects for the herb. Thus, at best, SOR=C for the evidence in support of evening primrose.
Literature searches were conducted using Medline, PsycInfo, and the Cochrane Library electronic databases, and by consulting bibliographies of pertinent publications. We focused primarily on meta-analyses and large-scale case report tabulations at an evidence level of 1b. Additionally, articles selected included those that discussed the use of herbal treatments for mental illness, as well as those that addressed drug-herb interactions between herbal and traditional psychiatric drug treatments.
Mechanisms of action. Gamma linolenic acid, a precursor of prostaglandin E and several other active substances, is the main constituent responsible for the therapeutic effects of evening primrose.37
Herb-drug interactions. This herb has the potential to interact with phenothiazines, nonsteroidal anti-inflammatory drugs, corticosteroids, beta-blockers, and anticoagulants.9
Adverse effects. Although it is generally safe, evening primrose oil has occasionally exacerbated the symptoms of epilepsy.39 Other adverse effects are nausea, softening of the stool, and headache.37
Ephedra
Ephedra (Ephedra sinica) is an evergreen shrub native to Asia used in traditional Chinese medicine for thousands of years. In recent decades, ma-huang, the extract derived from this herb, has been a common ingredient in many natural supplements that promote increased energy, mood enhancement, and weight loss.40,41 In early 2004, the FDA banned the sale of dietary products containing ephedra due to concerns over its adverse effects.42
Efficacy. Research on ephedra’s efficacy is largely focused on its role in weight loss, and there is little evidence that evaluates it as a mood enhancer. A comprehensive meta-analysis43 assessed 20 controlled trials with a treatment duration of at least 8 weeks and concluded that ephedra, when administered alone or with caffeine, promotes modest short-term weight loss (0.9 kg/month more than placebo). However, not all of the included studies were randomized or double-blind, and no data were available on long-term effects. A smaller systematic review44 of 5 double-blind studies also found the combination of ephedra and caffeine stimulated weight loss, but it was unclear whether 2 of the trials were randomized. Thus, SOR=A for the evidence in support of weight loss in the short term. There is no evidence in support of it as a mood-enhancing treatment.
Mechanisms of action. The primary constituents of ephedra are ephedrine-type alkaloids. As a sympathomimetic agonist at both α- and β-adrenergic receptors, ephedrine enhances cardiac rate and contractibility, peripheral vasoconstriction, bronchodilation, and central nervous system stimulation.41
Herb-drug interactions. Ephedra should not be used with anesthetic agents,45 MAO inhibitors,46,47 antihypertensives, or antidepressants.41
Adverse effects. The relative risk of adverse reactions to ephedra is more than 100 times greater than that of all other herbs.40 As noted by Jacobs and Hirsch,48 between 1993 and 1997 the FDA had received 34 notices of death and reports of approximately 800 medical and psychiatric complications all directly linked to ephedra. A more recent review49 indicated that hypertension, palpitations, tachycardia, stroke, seizures, and death are related to ephedra use. The herb has also been noted to induce symptoms of psychosis and affective disturbances.50,51
Anxiety
Kava-kava
Kava-kava is derived from the dried rhizome of the oceanic kava plant (Piper methysticum), and it has been cultivated for thousands of years throughout the South Pacific, where it is consumed as a psychotropic drink for recreational and medicinal purposes.52 Kava has been shown to alleviate anxiety symptoms,53 and it has euphoric and muscle relaxant properties, although its effect on arousal and alertness appears to be minimal.9 It is commonly used in Europe and North America for its anxiolytic effects.
Efficacy. A Cochrane review54 of 6 double-blind randomized controlled trials that used a common outcome measure (Hamilton Anxiety Scale) concluded that kava is significantly superior to placebo as a short-term treatment for anxiety. The authors note, however, that further investigation is required to determine long-term efficacy and safety. Another meta-analysis55 of 7 double-blind randomized controlled trials also suggests that, relative to a placebo, kava is an efficacious treatment for anxiety. Thus, SOR=A for the evidence in support of short-term efficacy in kava in anxiety. However, long-term data in terms of safety and efficacy has not been shown.
Mechanisms of action. Kavapyrones are the major constituents of this herb and are responsible for its pharmacologic activity. The mechanisms of their anxiolytic effect are still unclear. One line of research suggests that kavapyrones might mediate sedative effects by influencing gamma-aminobutyric acid (GABA)(A) receptor binding,56-58 whereas another theory posits that kavapyrones are a reversible inhibitor of human platelet MAO-B.52 Others have suggested the inhibition of voltage-gated ion channels as a potential mechanism of action.59,60
Herb-drug interactions. This herb has the potential to interact with benzodiazepines,61 and the combination with central nervous system depressants like ethanol and barbiturates can produce synergistic effects.56,62
Adverse effects. Liver damage has been reported in patients who use kava.63-65 A recent study66 analyzed 29 cases of purported liver dysfunction in addition to 7 cases that have already been published; the authors concluded that kava ingestion was the direct cause of liver injury in 3 cases, a probable cause in 21 cases, and a possible cause in 12 cases. The most frequent liver injury was necrosis. Other adverse effects of this herb include dizziness, mild gastrointestinal disturbance, and a temporary yellow discoloration of skin, hair, and nails.67 In addition, long-term administration of kava at higher doses my cause scaling of the skin on the extremities, also known as kava dermopathy.68
Valerian
Valerian (Valerian officinalis) is a root extract, with purported healing properties that can be traced to ancient Greece and Rome. Today, valerian root preparations are used for their sedative, anxiolytic, and antidepressant properties. The herb, a GABA agonist,9 is commonly used in the treatment of sleeplessness and the management of anxiety associated with muscle tension.10
Efficacy. A recent systematic review of randomized clinical trials (including reports in all languages) assessed the efficacy of valerian in patients with insomnia.69 Nine randomized, double-blind, placebo-controlled trials satisfied the inclusion criteria; however, even in these studies questionable methods in randomization, blinding, compliance, withdrawal, confounding variables, diagnostic criteria, and statistical analysis rendered contradictory results, and the authors concluded that evidence for valerian in the treatment of insomnia is inconclusive.
Data to confirm valerian’s effectiveness as an anxiolytic are also minimal. One randomized placebo-controlled pilot study examined the effects of valerian on generalized anxiety disorder; 36 patients were treated with placebo, diazepam, or valerian extract for 4 weeks.70 The authors found a significant reduction in the psychic factors of anxiety with diazepam and valerian. However, the study was limited by the small number of patients in each group, relatively low dosages of the active agents, and a short duration of treatment. Similar studies71 suffer from the same shortcomings, and thus further research is necessary to assess the effect of valerian on anxiety. Thus, SOR=C for the evidence in support of valerian as a somnolent and as a anxiolytic, and further research is necessary to assess the effect of valerian in insomnia and anxiety
Mechanisms of action. Valerian’s constituents include sesquiterpenes of the volatile oil (including valeric acid), iridoids (valepotriates), alkaloids, furanofuran lignans, and free amino acids such as GABA, tyrosine, arginine, and glutamine.72 The precise mechanisms of action are still unclear, though it has been suggested that all of the active constituents act synergistically to produce a clinical response. Research has also demonstrated modulation of GABA neurotransmission and receptor function (see Houghton73 for a comprehensive review of valerian’s pharmacology).
Herb-drug interactions. Valerian has the potential to prolong thio-, pental-, and pentobarbital-induced sleep and should, therefore, not be combined with barbiturates.74,75 It may also potentiate the sedative effects of anesthetics and other central nervous system depressants.45
Adverse effects. Adverse affects with this product are rare, but when they occur they may include headaches, excitability, uneasiness, gastrointestinal effects, dizziness, and cardiac disturbances.76-78
Dementia
Ginkgo
Ginkgo extracts are derived from one of the oldest known tree species (Ginkgo biloba L). They have been used in traditional Chinese medicine for 5000 years for a variety of purposes and are believed to be helpful in the treatment of memory impairment caused by dementia.79 The herb is also used to treat stress, fatigue, chronic cerebrovascular insufficiency, and cerebral trauma, and to improve endurance.9
Efficacy. Evidence for ginkgo’s efficacy is encouraging, but more rigorous research is needed. Kleijnen and Knipschild80 reviewed 40 controlled trials on the use of ginkgo to treat “chronic cerebral insufficiency.” Only 8 of the studies were deemed to be of good quality, although all but 1 found clinically significant improvement in symptoms including memory loss, concentration difficulties, fatigue, anxiety, and depressed mood.
Another meta-analysis79 identified more than 50 articles on the effect of ginkgo on the cognitive function in Alzheimer patients, but only 4 studies were found to be properly blinded and placebo-controlled with well-characterized subjects. The authors concluded that gingko appears to have a modest effect on cognitive function in Alzheimer’s but note that further research is necessary.
A systematic review by Ernst and colleagues81 concluded that ginkgo was superior to a placebo in delaying the clinical course of dementia. The authors reported on 9 placebo controlled, double-blind randomized trials including 1497 patients in their analysis.
Ginkgo has also been used to treat impotence, including antidepressant-induced sexual dysfunction. In 1 trial, 60 patients with proven arterial erectile dysfunction who had not previously responded to papaverine showed improvement with a daily dose of 60 mg of ginkgo over 12 to 18 months.9 However, further research must be undertaken in this domain, in part because this trial was not blinded, with both doctors and patients aware of who was receiving the ginkgo treatment.
Thus, SOR=A for the evidence in support of ginkgo as a cognitive enhancer in mild to moderate dementia, and B for the evidence in support of ginkgo as a treatment for erectile dysfunction.
Mechanisms of action. Ginkgo leaves contain several bioactive compounds, including flavonoids, terpenoids (ginkgolide, bilbobide), and organic acids. Although the mechanisms of action are only partially understood, the main effects appear to be related to its antioxidant properties, which require the synergistic action of the principal constituents.82 These compounds act as free radical scavengers.83 Other pharmacologic actions involve antihypoxic and antiplatelet effects.84
Herb-drug interactions. Researchers have suggested that ginkgo may potentiate other anticoagulants or increase bleeding over time,85,86 which can be attributed to ginkgolide B, a potent inhibitor of platelet-activating factor needed for inducing arachidonate-independent platelet aggregation.87 Caution should be exercised when ginkgo is taken in conjunction with anticoagulant treatment (including aspirin) or when there is a risk of bleeding (eg, peptic ulcer disease and subdural hematoma).9,86
Adverse effects. Side effects from ginkgo appear to be relatively uncommon; however, they may include headaches, gastrointestinal tract upset, nausea, vomiting, and a skin allergy to the ginkgo fruit.17,88
Sexual dysfunction
Yohimbine
Yohimbine is an alkaloid derived from the cortex of the Central African tree Corianthe yohimbe.89 The bark of the tree was used traditionally to enhance virility. Today, yohimbine is still reputed as an aphrodisiac and used as a remedy for erectile problems.90
Efficacy. Overall, the efficacy of yohimbine in the treatment of erectile dysfunction appears promising, although, as with studies of other herbal products, clinical trials often suffer from methodological flaws. Carey and Johnson91 conducted 4 independent meta-analyses to examine the effects of yohimbine alone or in combination with other drugs in controlled and uncontrolled trials. The authors found positive results for yohimbine across all 4 analyses, but they note that the highest-quality data were derived from controlled clinical trials when yohimbine was administered on its own. In their analysis, this included 242 patients across 4 studies. Another systematic review yielded similar results: a meta-analysis of 7 randomized, placebo-controlled trials including 419 patients demonstrated that yohimbine is superior to placebo as a treatment for erectile dysfunction.89 Thus, SOR=A for the evidence in support of yohimbine as a treatment for erectile dysfunction.
Mechanisms of action. Yohimbine is an alpha2-adrenergic antagonist. Its blocking activity increases the release of noradrenaline and the firing rate of noradrenergic neurons in the central nervous system.92
Herb-drug interactions. Yohimbine should not be taken with sibutramine, a serotonin and norepinephrine reuptake inhibitor. The concomitant use of the 2 products could unmask the peripheral effect of sibutramine and produce negative cardiovascular effects.93 Potential interactions also exist with heart or blood pressure medications,94 lithium,95 morphine,96 and alcohol.97
Adverse effects. Adverse effects are not common with yohimbine; however, they may include headaches, sweating, agitation, hypertension, and restlessness.98 Yohimbine has also been reported to contribute to psychotic symptoms, mania, and seizures, though such occurrences are not well documented.9
Growing need for the 2 worlds to merge
One of the most frequent scenarios encountered by the naturopath is the patient who is taking a psychotropic medication and wants to explore natural solutions to reduce the drug’s unpleasant side effects or to enhance general well being. Sharing information is the key to a healthy treatment regimen for such individuals (TABLES 3 AND 4). The patient should inform both the physician and naturopath about health care decisions, the naturopath must encourage the patient to be candid with the physician about proposed treatments, and the physician can be helpful by communicating to the naturopath the extent of the patient’s disorder.
Professionally, one must consider before asking a patient to discontinue one agent or the other whether the alternative treatment might be improving the patient’s condition or reducing negative side effects caused by the psychotropic medication. On one hand, withdrawing the drug can destabilize the patient’s condition, which may not be rapidly amenable to a botanical or nutritional treatment. Alternatively, to supplement an antidepressant, benzodiazepine, or antipsychotic regimen by adding an herbal preparation could lead to unpredictable interactions and unpleasant or even dangerous symptoms. For many cases of mild depression or mild anxiety disorder, natural therapies can be sufficient treatment. However, for more complicated cases, where little is known about the consequences of using alternative treatments, involvement by a clinician with more specialized training is recommended.
TABLE 3
Recommendations for clinicians
| Ask your patients if they are using natural health products or seeing a natural health practitioner. Recognize that they may be covertly self-medicating with herbal or alternative treatments. Better-studied alternative treatments should be substituted. |
| Create an environment where patients are not reluctant to disclose the use of natural health care. |
| If the patient is seeing a naturopathic doctor, obtain contact information so that the specifics of the therapy can be requested. |
| Communicate directly with the naturopathic clinician about changes in treatment choices that are taking place in the ongoing care of the patient. This may often include sending consultation letters and other information to all individuals involved in the treatment of the patient. |
| Acquire good reference materials on natural health products. Suggestions: Natural Alternatives to Prozac by Michael T. Murray, ND, and The Textbook of Natural Medicine by Joseph Pizzorno, ND and Michael T. Murray, ND. |
| Never underestimate the potential risk of possible chemical interactions between medications. |
| Make contact with a community naturopathic doctor who can answer questions about specific natural health products. |
TABLE 4
Internet resources about herbal products
| The Natural Pharmacist ($) www.tnp.com |
| Evidence-based content developed and reviewed byphysicians and pharmacologists; sections on herbs and supplements, health conditions, and drug interactions; information referenced |
| Natural Medicines Comprehensive Database ($) www.naturaldatabase.com |
| Well-referenced, comprehensive database |
| Complementary and Alternative Therapies (Bandolier) www.jr2.ox.ac.uk/bandolier/booth/booths/altmed.html Evidence-based content; abstracts of systematic reviews, meta-analyses, or other studies about herbal therapies |
| National Center for Complementary and Alternative Medicine www.nlm.nih.gov/nccam/camonpubmed.html |
| Access to PubMed’s CAM database |
| HerbMed www.herbmed.org |
| Access to scientific evidence about the use of herbs for health $ = paid subscription required; all websites accessed April 5, 2005. Table adapted from Gardener.102 |
CORRESPONDING AUTHOR
Martin A. Katzman, BSc, MD, FRCPC, Stress, Trauma, Anxiety, Rehabilitation Treatment (S.T.A.R.T.) Clinic for Mood & Anxiety Disorders, 790 Bay Street, Toronto, Ontario, Canada M5G 1N8. E-mail: [email protected]
1. Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States—prevalence, costs and patterns of use. N Engl J Med 1993;328:246-252.
2. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in Alternative Medicine Use in the United States, 1990-1997: Results of a Follow-up National Survey. JAMA 1998;280:1569-1575.
3. Pies R. Adverse neuropsychiatric reactions to herbal and over-the counter “antidepressants.” J Clin Psychiatry 2000;61:815-820.
4. Knaudt PR, Connor KM, Weisler RH, Churchill LE, Davidson JRT. Alternative therapy use by psychiatric outpatients. J Nerv Ment Dis 1999;187:692-695.
5. Mamtani R, Cimino A. A primer of complementary and alternative medicine and its relevance in the treatment of mental health problems. Psychiatr Quart 2002;73:367-381.
6. Wharton R, Lewith G. Complementary medicine and the general practitioner. BMJ 1986;292:1498-1500.
7. Scimone A, Scimone AA. Recommendation of herbal remedies by psychiatrists. J Orthomol Med 2001;16:155-156.
8. Wong AHC, Smith M, Boon HS. Botanical medicine in psychiatry. Psychiatry Rounds 1999;3(2):1-5.
9. Wong AHC, Smith M, Boon HS. Herbal remedies in psychiatric practice. Arch Gen Psychiatry 1998;55:1033-1044.
10. Linde K, Ramirez G, Mulrow CD, Pauls A, Weidenhammer W, Melchart D. St. John’s wort for depression: An overview and meta-analysis of randomized clinical trials. BMJ 1996;313:253-258.
11. Linde K, Mulrow CD. St. John’s wort for depression (Cochrane Review). In: The Cochrane Library, Issue 4, 2003. Chinchester, UK: John Wiley & Sons, Ltd.
12. Shelton RC, Keller MB, Gelenberg A, et al. Effectiveness of St. John’s wort in major depression. JAMA 2001;285:1978-1986.
13. Davidson JRT. Effect of Hypericum perforatum (St John’s wort) in major depressive disorder. JAMA 2002;287:1807-1814.
14. Strandell J, Neil A, Carlin G. An approach to the in vitro evaluation of potential for cytochrome P450 enzyme inhibition from herbals and other natural remedies. Phytomedicine 2004;11:98-104.
15. Zhou S, Gao Y, Jiang W, Huang M, Xu A, Paxton JW. Interactions of herbs with cytochrome P450. Drug Metab Rev 2003;35:35-98.
16. Ernst E. Second thoughts about safety of St John’s wort. Lancet 1999;354:2014-2016.
17. Ernst E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John’s Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann Intern Med 2002;136:42-53.
18. Hall S, Wang Z, Huang S, et al. The interaction between St John’s wort and an oral contraceptive. Clin Pharmacol Ther 2003;74:525-535.
19. Piscitelli SC, Burstein AH, Chaitt D, Alfaro RM, Falloon J. Indinavir concentrations and St John’s wort. Lancet 2000;355:547-548.
20. Gordon JB. SSRIs and St. John’s wort: Possible toxicity? Am Fam Physician 1998;57:950-953.
21. Johne A, Brockmoller J, Bauer S. Pharmacokinetic interaction of digoxin with an herbal extract from St. John’s wort (Hypericum perforatum). Clin Pharmacol Ther 1999;66:338-345.
22. Walter G, Rey JM, Harding M. Psychiatrists’ experience and views regarding St. John’s wort and ‘alternative’ treatments. Aust NZ J Psychiatry 2000;34:992-996.
23. Newall C, Anderson LA, Phillipson JD. Herbal Medicines: A Guide for Health-Care Professionals. London, England: Pharmaceutical Press; 1996.
24. O’Breasail AM, Argouarch S. Hypomania and St. John’s wort. Can J Psychiatry 1998;43:747.-
25. Moses EL, Mallinger AG. St. John’s wort: Three cases of possible mania induction. J Clin Psychopharmacol 2000;20:115-117.
26. Gonzalez-Seijo JC, Ramos YM, Lastra I. Manic episode and ginseng: Report of a possible case. J Clin Psychopharmacol 1995;15:447-448.
27. Vogler BK, Pittler MH, Ernst E. The efficacy of ginseng. A systematic review of randomised clinical trials. Eur J Clin Pharmacol 1999;55:567-575.
28. Kieffer D, Pantuso T. Panax ginseng. Am Fam Physician 2003;68:1539-1542.
29. Wiklund IK, Mattsson LA, Lindgren R, Limoni C. Effects of a standardized ginseng extract on quality of life and physiological parameters in symptomatic postmenopausal women: a double-blind, placebo-controlled trial. Swedish Alternative Medicine Group. Int J Clin Pharmacol Res 1999;19:89-99.
30. Cardinal BJ, Engels HJ. Ginseng does not enhance psychological well-being in healthy, young adults: results of a double-blind, placebo-controlled, randomized clinical trial. J Am Diet Assoc 2001;101:655-660.
31. Attele AS, Wua JA, Yuan CS. Ginseng pharmacology: Multiple constituents and multiple actions. Biochem Pharmacol 1999;58:1685-1693.
32. Stockley I. Drug Interactions: A Sourcebook of Adverse Interactions, Their Mechanisms, Clinical Importance, and Management. 3rd ed. Cambridge, England: Blackwell Scientific Press; 1994.
33. Mitra SK, Chakraborti A, Bhattacharya SK. Neuropharmacological studies on Panax ginseng. Indian J Exp Biol 1996;34:41-47.
34. Janetzky K, Morreale AP. Probable interaction between warfarin and ginseng. Am J Health Syst Pharm 1997;54:692-693.
35. Siegel RK. Ginseng abuse syndrome. JAMA 1979;241:1614-1615.
36. Girman A, Lee R, Kligler B. An integrative medicine approach to premenstrual syndrome. Am J Obstet Gynecol 2003;188(5 Suppl):S56-S65.
37. Kleijnen J. Evening primrose oil. BMJ 1994;309:824-825.
38. Budeiri D, Li Wan Po A, Dornan JC. Is evening primrose oil of value in the treatment of premenstrual syndrome? Controlled Clinical Trials 1996;17:60-68.
39. Barber HJ. Evening primrose oil: A panacea? Pharm J 1988;240:723-725.
40. Bent S, Tiedt TN, Odden MC, Shlipak MG. The relative safety of ephedra compared with other herbal products. Ann Intern Med 2003;138:468-471.
41. Abourashed EA, El-Alfy AT, Khan IA, Walker L. Ephedra in perspective—a current review. Phytother Res 2003;17:703-712.
42. Rados C. Ephedra ban: no shortage of reasons. FDA Consum 2004;38:6-7.
43. Shekelle PG, Hardy ML, Morton SC, et al. Efficacy and safety of ephedra and ephedrine for weight loss and athletic performance: a meta-analysis. JAMA 2003;289:1537-1545.
44. Greenway FL. The safety and efficacy of pharmaceutical and herbal caffeine and ephedrine use as a weight loss agent. Obes Rev 2001;2:199-211.
45. Ang-Lee M, Moss J, Yuan C. Herbal medicines and perioperative care. JAMA 2001;286:208-216.
46. Dawson JK, Earnshaw SM, Graham CS. Dangerous monoamine oxidase inhibitor interactions are still occurring in the 1990s. J Accid Emerg Med 1995;12:49-51.
47. Brinker F. Interactions of pharmaceutical and botanical medicines. J Naturopathic Med 1997;7:14-20.
48. Jacobs KM, Hirsch KA. Psychiatric complications of ma-huang. Psychosomatics 2000;41:58-62.
49. Haller CA, Benowitz NL. Adverse cardiovascular and central nervous system events associated with dietary supplements containing ephedra alkaloids. N Engl J Med 2000;343:833-838.
50. Doyle H, Kargin M. Herbal stimulant containing ephedrine has also caused psychosis. BMJ 1996;313:756.-
51. Capwell RR. Ephedrine-induced mania from an herbal diet supplement. Am J Psychiatry 1995;152:647.-
52. Uebelhack R, Franke L, Schewe HJ. Inhibition of platelet MAO-B by kava pyrone-enriched extract from piper methysticum forster (kava-kava). Pharmacopsychiat 1998;31:187-192.
53. Volz HP, Kieser M. Kava-kava extract WS 1490 verses placebo in anxiety disorders: A randomized placebo-controlled 25-week outpatient trial. Pharmacopsychiat 1997;30:1-5.
54. Pittler MH, Ehret V. Kava extract for treating anxiety (Cochrane Review). In: The Cochrane Library, Issue 4, 2003. Chichester, UK: John Wiley & Sons, Ltd.
55. Pittler MH, Ernst E. Efficacy of kava extract for treating anxiety: systematic review and meta-analysis. J Clin Psychopharmacol 2000;20:84-90.
56. Jussofie A, Schmiz A, Himke C. Kava-pyrone enriched extract from Piper methysticum as modulator of the GABA binding site in different regions of rat brain. Psychopharmacology (Berl) 1994;116:469-474.
57. Boonen G, Haberlein H. Influence of genuine kavapyrone enantiomers on the GABAA binding site. Planta Med 1998;64:504-506.
58. Davies LP, Drew CA, Duffield P, Johnston GA, Jamieson DD. Kava pyrones and resin: studies on GABA-A, GABA-B, and benzodiazepine binding sites in rodent brain. Pharmacol Toxicol 1992;712:120-126.
59. Gleitz J, Beile A, Peters T. (±)-Kavain inhibits veratridine-activated voltage- dependent Na+-channels in synaptosomes prepared from rat cerebral cortex. Neuropharmacology 1995;34:1133-1138.
60. Magura EI, Kopanitsa MV, Gleitz J, Peters T, Krishtal OA. Kava extract ingredients, (+)-methysticin and (+/-)-kavain inhibit voltage-operated Na+-channels in rat CA1 hippocampal neurons. Neuroscience 1997;91:345-351.
61. Almeida JC, Grimsley EW. Coma from the health food store: Interaction between kava kava and alprazolam. Annu Int Med 1996;125:940-941.
62. Foo H, Lemon J. Acute effects of kava, alone or in combination with alcohol, on subjective measures of impairment and intoxication and on cognitive performance. Drug Alcohol Rev 1997;16:147-155.
63. Kraft M, Spahn TW, Menzel J, et al. Fulminant liver failure after administration of the herbal antidepressant kava-kava. Dtsch Med Wochenschr 2001;126:970-972.
64. Strahl S, Ehret V, Dahm HH, Maier KP. Necrotizing hepatitis after taking herbal remedies. Dtsch Med Wochenschr 1998;23:1410-1414.
65. Escher M, Desmeules J, Giostra E, Mentha G. Hepatitis associated with kava, a herbal remedy for anxiety. BMJ 2001;322:7279.-
66. Stickel F, Baumuller HM, Seitz K, et al. Hepatitis induced by Kava (Piper methysticum rhizoma). J Hepatol 2003;39:62-67.
67. Blumenthal M, Busse W, Goldberg A, et al, eds. The Complete German Commission E Monographs-Therapeutic Guide to Herbal Medicines. Austin: American Botanical Council; Boston: Integrative Medicine Communications; 1998.
68. Norton SA, Ruze P. Kava dermopathy. J Am Acad Dermatol 1994;31:89-97.
69. Stevinson C, Ernst E. Valerian for insomnia: A systematic review of randomized clinical trials. Sleep Medicine 2000;1:91-99.
70. Andreatini R, Sartori V, Seabra M, Leite J. Effect of valepotriates (valerian extract) in generalized anxiety disorder: a randomized placebo-controlled pilot study. Phytother Res 2002;16:650-654.
71. Cropley M, Cave Z, Ellis J, Middleton R. Effect of kava and valerian on human physiological and psychological responses to mental stress assessed under laboratory conditions. Phytother Res 2002;16:23-27.
72. Hadley S, Petry J. Valerian. Am Fam Physician 2003;67:1755-1758.
73. Houghton P. The scientific basis for the reputed activity of Valerian. J Pharm Pharmacol 1999;51:505-512.
74. Hiller K, Zetler G. Neuropharmacological studies on ethanol extracts of Valeriana officinalis L: Behavioural and anticonvulsant properties. Physiother Res Int 1996;10:145-151.
75. Capasso A, DeFeo V, DeSimon F, Sorrentino L. Pharmacological effects of aqueous extracts from Valeriana adscendens. Physiother Res Int 1996;10:309-312.
76. McGuffin M, Hobbs C, Upton R, Goldberg A, eds. American Herbal Products Association’s Botanical Safety Handbook. Boca Raton, Fla: CRC Press; 1997.
77. Donath F, Quispe S, Diefenbach K, Maurer A, Fietze I, Roots I. Critical evaluation of the effect of valerian extract on sleep structure and sleep quality. Pharmacopsychiatry 2000;33:47-53.
78. Kuhlmann J, Berger W, Podzuweit H, Schmidt U. The influence of valerian treatment on “reaction time, alertness and concentration” in volunteers. Pharmacopsychiatry 1999;32:235-241.
79. Oken B, Storzbach D, Kaye J. The efficacy of Ginkgo biloba on cognitive function in Alzheimer disease. Arch Neurol 1998;55:1409-1415.
80. Kleijnen J, Knipschild P. Ginkgo biloba for cerebral insufficiency. Br J Clin Pharmacol 1992;34:352-358.
81. Ernst E, Pittler M. Ginkgo biloba for dementia: a systematic review of double-blind, placebo-controlled trials. Clin Drug Invest 1999;17:301-308.
82. Le Bars PL, Katz MM, Berman N, Itil TM, Freedman AM, Schatzberg AF. A placebo-controlled, double-blind, randomized trial of an extract of Ginkgo biloba for dementia. JAMA 1997;278:1327-1332.
83. Oyama Y, Fuchs P, Katayama N, Noda K. Myricetin and quercetin, the flavonoid constituents of Ginkgo biloba extract, greatly reduce oxidative metabolism in both resting and Ca(2+)-loaded brain neurons. Brain Res 1994;635:125-129.
84. Cupp M, ed. Toxicology and Clinical Pharmacology of Herbal Products. Totowa, NJ: Humana Press; 2000.
85. Rowin J, Lewis SL. Spontaneous bilateral subdural hematomas associated with chronic Ginkgo. Neurol 1996;46:1775-1776.
86. Rosenblatt M, Mindel J. Spontaneous hyphema associated with ingestion of Ginkgo biloba extract. N Engl J Med 1997;336:1108.-
87. Miller LG. Herbal medicinals: Selected clinical considerations focusing on known or potential drug-herb interactions. Arch Intern Med 1998;158:2200-2211.
88. Houghton P. Ginkgo. Pharm J 1994;253:121-122.
89. Ernst E, Pittler M. Yohimbine for erectile dysfunction: A systematic review and meta-analysis of randomized clinical trials. J Urol 1998;159:433-436.
90. Morales A. Yohimbine in erectile dysfunction: The facts. Int J Impot Res 2000;Suppl 1:S70-S74.
91. Carey M, Johnson B. Effectiveness of yohimbine in the treatment of erectile disorder: Four meta-analytic integrations. Arch Sex Behav 1996;25:341-360.
92. Charney DS, Woods SW, Goodman WK, Heninger GR. Neurobiological mechanisms of panic anxiety: Biochemical and behavioural correlates of yohimbine-induced panic attacks. Am J Psychiatry 1987;144:1030-1036.
93. Jordan J, Sharma A. Potential for sibutramine-yohimbine interaction? Lancet 2003;361:1826.-
94. Goldstein D, Grossman E, Listwak S, Folio C. Sympathetic reactivity during a yohimbine challenge test in essential hypertension. Hypertension 1991;18 (Suppl 3):40-48.
95. Price L, Charney D, Heninger G. Three cases of manic symptoms following yohimbine administration. Am J Psychiatry 1984;141:1267-1268.
96. Gear R, Gordon N, Heller P, Levine J. Enhancement of morphine analgesia by the alpha2-adrenergic antagonist yohimbine. Neuroscience 1995;66:5-8.
97. McDougle C, Krystal J, Price L, Heninger G, Charney D. Noradrenergic response to acute ethanol administration in healthy subjects: comparison with intravenous yohimbine. Psychopharmacology (Berl) 1995;118:127-135.
98. Rowland D, Tai W. A review of plant-derived and herbal approaches to the treatment of sexual dysfunctions. J Sex Marital Ther 2003;29:185-205.
99. Wang Z, Gorski JC, Hamman MA, Huang SM, Lesko LJ, Hall SD. The effects of St John’s wort (Hypericum perforatum) on human cytochrome P450 activity. Clin Pharmacol Ther 2001;70:317-326.
100. Mathews JM, Etheridge AS, Black SR. Inhibition of human cytochrome P450 activities by kava extract and kavalactones. Drug Metab Dispos 2002;30:1153-1157.
101. Renton KW. Alteration of drug biotransformation and elimination during infection and inflammation. Pharmacol Ther 2001;92:147-163.
102. Gardener D. Evidence-based decisions about herbal products for treating mental disorders. J Psychiatry Neurosci 2002;27:324-333.
- Many of your patients may be self-treating with herbal preparations. Ask candidly about this possibility, and become familiar with the increasing evidence on efficacy and safety of alternative treatments
- A large meta-analysis and a Cochrane Review both suggest St. John’s Wort (A) is as effective as conventional antidepressants and more effective than placebo for mild to moderate depression. With patients taking St. John’s Wort and a conventional antidepressant, remain alert for a potentiating effect, “serotonin syndrome.” Use with caution if the patient must also receive anticoagulants, oral contraceptives, or antiviral agents.
- The efficacy and safety of ginseng (B, in terms of psychological well-being) and evening primrose (C) for depression are not well established.
- Kava-kava (A, for short-term treatment for anxiety treatment) has well-known anxiolytic properties, but its potential adverse effects, particularly liver toxicity, dramatically reduce its usefulness. Valerian, though commonly used for anxiety (C, for insomnia and anxiety), is not well supported by good data.
- Ginkgo has shown promise in improving cognitive function in dementia, and its side effects are few and uncommon (A, for cognitive function in dementia). Monitor carefully if there is concomitant anticoagulant therapy.
Based on epidemiologic estimates, it may be that 20% to 30% of your patient population is using alternative/complementary medicines.1 Twenty percent of adults who take prescription medicine also rely on herbal products,2 and patients who use herbal products the most are those with chronic conditions.3
Included in this group are persons with mental health problems, who, compared with the general population, report a much greater use of alternative treatments, including herbal and homeopathic remedies.4 These remedies, when used to treat psychiatric symptoms, may produce changes in mood, thinking, or behavior, and they may interact with a number of conventional medications.3
Largely uncharted territory. With the exception of St. John’s Wort for depression and ginkgo for dementia, minimal evidence is currently available to recommend the use of herbal medicines as the primary treatment for mental illness. Although some herbs have been found to be effective at specific doses for specific conditions, there is no evidence to show their superiority to conventional drug treatments, nor has their safety been established for use during pregnancy and lactation.8
Helping patients navigate. Nevertheless, our patients are increasingly turning to alternative therapies, and it is therefore critical that we clinicians avail ourselves of current knowledge and that investigators pursue intensive clinical research to establish safety (TABLE 1) and efficacy. Additionally, greater understanding of the biochemical and pharmacological effects of these herbs may uncover novel treatments or yield fresh insights into basic disease mechanisms.9
The herbal remedies discussed in this article are those commonly used for psychiatric conditions. Their effectiveness and potential for adverse side effects and interactions are assessed.
Depression
St. John’s Wort
St. John’s Wort (Hypericum perforatum L) is a popular herbal treatment readily used by the public in various forms, such as tablets and teas. Efficacy of hypericum—one of the hypothesized active ingredients in St. John’s Wort—in the treatment of depression was reported in the texts of the ancient Greek physicians Hippocrates, Pliny, and Galen, and it continued to be cited throughout the Classical, Renaissance, and Victorian eras. Its contemporary usage as an antidepressant has been supported by more rigorous evidence than any other herbal remedy.9
Efficacy. Evidence of efficacy in mild to moderate depression has been reported in a meta-analysis of 23 randomized trials with a total of 1757 outpatients, in which extracts of St. John’s Wort alone (20 of 23 trials) or in combination with other herbs (3 of 23) were tested against placebo (15 trials) or antidepressant drugs (8 trials).10 St. John’s Wort was reported to be clearly superior to placebo and comparable with conventional drug treatment, with lower side-effect and dropout rates. Similarly, a recent Cochrane Review of 27 trials and 2291 patients concluded that St. John’s Wort was more effective than placebo in treating mild to moderately severe depression; however, there was inadequate evidence to determine whether the herb was as effective as traditional antidepressants.11
The superiority of hypericum to placebo has been called into question, however, by a large-scale, multicenter, double-blind case report tabulation. The study, conducted with 200 patients across 11 academic medical centers in the United States, found no evidence that St. John’s Wort was more efficacious than placebo.12 Another such trial also concluded that St. John’s Wort was not an effective treatment for major depression. In addition, the herb was found to be no different than sertraline, which was also indistinguishable from the placebo, further confusing the issue.13 Strength of recommendation (SOR) is level A for the evidence in support of St. John’s Wort as an antidepressant.
Because many alternative options do not require the approval of the US Food and Drug Administration (FDA), products sold in health food stores can be purchased without a prescription or the provision of any clinical advice or professional review. The quality of many herbal preparations is thus unpredictable, with the content varying not only from brand to brand but also from batch to batch.5
A working knowledge of the pharmacologic data and clinical literature is necessary to properly counsel, diagnose, and treat patients who may be using herbal products. However, 1 study reported that only 5% of British doctors claimed more than a poor knowledge of herbal medicine,6 and another survey revealed that most psychiatrists who do not recommend herbal products avoid doing so because they feel uncomfortable with their current knowledge of alternative therapies.7 Alarmingly, the latter study reported that among psychiatrists who do not recommend herbal treatments, the safety of such treatments is not an issue in their decision-making process.
Mechanisms of action. The mechanisms for the antidepressant effects of St. John’s Wort are not fully understood, although monoamine oxidase (MAO) inhibition, inhibition of serotonin receptor expression, serotonin reuptake inhibition, and reduction of cytokine expression have all been suggested as means of its activity.9
Herb-drug interactions. Evidence suggests St. John’s Wort contains both inhibitory and inducing constituents for the cytochrome P-450 (CYP) system, resulting in both inhibition and induction on the CYP system.14 Consequently, it’s difficult to predict which drugs St. John’s Wort will interact with in a significant way.15 Best estimates of its activity suggest it has minimal short-term activity; when used for a longer period, it will inhibit the CytP450-3A4, 2C19, and 2D6 systems (TABLE 2). Therefore, St. John’s Wort may alter the blood levels of such medications as anticoagulants,16 oral contraceptives,18 and antiviral agents,19 possibly resulting in serious consequences.16,17 Exercise caution when initiating treatment for patients already taking St. John’s Wort.
The potential of St. John’s Wort to interact with standard prescribed antidepressants, possibly to produce a “serotonin syndrome,” is also a concern. Gordon20 reported a case in which a woman taking St. John’s Wort became groggy, weak, and lethargic shortly after taking a single 20-mg dose of paroxetine. This patient had tolerated St. John’s Wort and paroxetine separately, suggesting a drug-herb interaction.3 St. John’s Wort has also been implicated in reducing blood levels of digoxin when the two are taken together,21 and 1 study documented that 8% of psychiatrists treating patients who had used St. John’s Wort reported drug interactions between the herb and another agent.22
Adverse effects. In general, fewer adverse effects are seen with hypericum than with conventional antidepressants but they may include photodermatitis, delayed hypersensitivity, gastrointestinal tract upset, dizziness, dry mouth, sedation, restlessness, and constipation. Use of St. John’s Wort is contraindicated during pregnancy and lactation, for patients who experience intense exposure to strong sunlight, and for patients with a pheochromocytoma.23
There are several anecdotal reports of mania or hypomania associated with the herb. For example, O’Breasail and Argouarch24 reported 2 cases of persons with no history of bipolar disorder who developed hypomanic episodes after taking St. John’s Wort. Likewise, Moses and Mallinger25 reported 3 cases of possible mania induction associated with the herb.
TABLE 2
Effects of common herbs on cytochrome P-450 enzymes
| CYTOCHROME P-450 | |||
|---|---|---|---|
| CYTP450-3A4 | CYTP450-2C19 | CYP450-2D6 | |
| St. John’s Wort | ++++ inhibition (short-term?) | +++ inhibition | ++ inhibition |
| Long-term induction in intestinal wall99 | |||
| Kava-kava100 | ++ inhibition | ++ inhibition | ++ inhibition |
| Valerian | + inhibition | + inhibition | 0 |
| Fish oil, omega-3 fatty acids | +++ inhibition | ++++ inhibition | + inhibition |
| Key: ++++ = very potent; ++ = potent (detectable); + = mildly potent; 0 = does not inhibit | |||
| Note: Caution should be undertaken when developing tables such as these, as the data came from a variety of in vivo and in vitro animal and human studies using simplified models (eg, cDNA-expressed CYP enzymes) of which there are significant interspecies variations in the activity of these systems. As well, in the presence of some pathological inflammatory states such as during an infection, the enzyme activity of the CYP can be modulated through cytokines and other mediators of inflammation.101 | |||
Ginseng
This herb is derived from the root of Panax ginseng and has been used as a cure-all in Eastern folk medicine for thousands of years.26 Today, both Chinese ginseng (P ginseng CA Meyer) and North American ginseng (P quinquefolius L) are associated with the treatment of mood and anxiety disorders and are used to reduce stress and fatigue and to improve endurance.
Efficacy. A systematic review of 16 double-blind randomized controlled trials found that ginseng did not improve cognitive function or psychomotor and physical performance.27 Another review reported conflicting results from several studies.28 For example, 1 double-blind randomized controlled trial of postmenopausal women who received either a placebo or ginseng for 16 weeks revealed the superiority of ginseng on measures of psychological well-being.29 Another double-blind randomized controlled trial, however, failed to find an effect of ginseng on positive affect, negative affect, or total mood disturbance in 83 healthy adults who took the herb for 8 weeks.30 Thus, at best, SOR=B for the evidence in support of ginseng, but only at best in relation to psychological well-being.
Mechanisms of action. The key active components of Panax ginseng are ginsenosides, a group of steroidal saponins that target a multitude of tissues to produce pharmacologic responses. The overall pharmacology of ginseng is complex due to the ability of ginsenosides to initiate multiple actions in the same tissue. Attele and colleagues31 provide an in-depth review of these mechanisms.
Herb-drug interactions. Ginseng may potentiate the effect of MAO inhibitors,32 stimulants (including caffeine), and haloperidol.33 In addition, a case study suggests a probable interaction with warfarin.34
Adverse effects. Reported side effects include insomnia, hypertension, diarrhea, restlessness, anxiety, and euphoria.35 There is at least 1 report of ginseng-induced mania, which occurred within 4 to 10 days of a patient’s interrupting a lithium and amitriptyline treatment.26
Evening primrose
Evening primrose (Oenothera biennis L) is a plant native to North America. The oil pressed from its seed is marketed as a nutritional supplement, and it has been used to treat many disorders, including premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD), both which are marked by affective disturbances.36,37
Efficacy. A systematic review38 of the efficacy of evening primrose oil in the treatment of PMS revealed few clinical trials of adequate methodology. The authors found only 2 well-controlled studies, both which failed to show beneficial effects for the herb. Thus, at best, SOR=C for the evidence in support of evening primrose.
Literature searches were conducted using Medline, PsycInfo, and the Cochrane Library electronic databases, and by consulting bibliographies of pertinent publications. We focused primarily on meta-analyses and large-scale case report tabulations at an evidence level of 1b. Additionally, articles selected included those that discussed the use of herbal treatments for mental illness, as well as those that addressed drug-herb interactions between herbal and traditional psychiatric drug treatments.
Mechanisms of action. Gamma linolenic acid, a precursor of prostaglandin E and several other active substances, is the main constituent responsible for the therapeutic effects of evening primrose.37
Herb-drug interactions. This herb has the potential to interact with phenothiazines, nonsteroidal anti-inflammatory drugs, corticosteroids, beta-blockers, and anticoagulants.9
Adverse effects. Although it is generally safe, evening primrose oil has occasionally exacerbated the symptoms of epilepsy.39 Other adverse effects are nausea, softening of the stool, and headache.37
Ephedra
Ephedra (Ephedra sinica) is an evergreen shrub native to Asia used in traditional Chinese medicine for thousands of years. In recent decades, ma-huang, the extract derived from this herb, has been a common ingredient in many natural supplements that promote increased energy, mood enhancement, and weight loss.40,41 In early 2004, the FDA banned the sale of dietary products containing ephedra due to concerns over its adverse effects.42
Efficacy. Research on ephedra’s efficacy is largely focused on its role in weight loss, and there is little evidence that evaluates it as a mood enhancer. A comprehensive meta-analysis43 assessed 20 controlled trials with a treatment duration of at least 8 weeks and concluded that ephedra, when administered alone or with caffeine, promotes modest short-term weight loss (0.9 kg/month more than placebo). However, not all of the included studies were randomized or double-blind, and no data were available on long-term effects. A smaller systematic review44 of 5 double-blind studies also found the combination of ephedra and caffeine stimulated weight loss, but it was unclear whether 2 of the trials were randomized. Thus, SOR=A for the evidence in support of weight loss in the short term. There is no evidence in support of it as a mood-enhancing treatment.
Mechanisms of action. The primary constituents of ephedra are ephedrine-type alkaloids. As a sympathomimetic agonist at both α- and β-adrenergic receptors, ephedrine enhances cardiac rate and contractibility, peripheral vasoconstriction, bronchodilation, and central nervous system stimulation.41
Herb-drug interactions. Ephedra should not be used with anesthetic agents,45 MAO inhibitors,46,47 antihypertensives, or antidepressants.41
Adverse effects. The relative risk of adverse reactions to ephedra is more than 100 times greater than that of all other herbs.40 As noted by Jacobs and Hirsch,48 between 1993 and 1997 the FDA had received 34 notices of death and reports of approximately 800 medical and psychiatric complications all directly linked to ephedra. A more recent review49 indicated that hypertension, palpitations, tachycardia, stroke, seizures, and death are related to ephedra use. The herb has also been noted to induce symptoms of psychosis and affective disturbances.50,51
Anxiety
Kava-kava
Kava-kava is derived from the dried rhizome of the oceanic kava plant (Piper methysticum), and it has been cultivated for thousands of years throughout the South Pacific, where it is consumed as a psychotropic drink for recreational and medicinal purposes.52 Kava has been shown to alleviate anxiety symptoms,53 and it has euphoric and muscle relaxant properties, although its effect on arousal and alertness appears to be minimal.9 It is commonly used in Europe and North America for its anxiolytic effects.
Efficacy. A Cochrane review54 of 6 double-blind randomized controlled trials that used a common outcome measure (Hamilton Anxiety Scale) concluded that kava is significantly superior to placebo as a short-term treatment for anxiety. The authors note, however, that further investigation is required to determine long-term efficacy and safety. Another meta-analysis55 of 7 double-blind randomized controlled trials also suggests that, relative to a placebo, kava is an efficacious treatment for anxiety. Thus, SOR=A for the evidence in support of short-term efficacy in kava in anxiety. However, long-term data in terms of safety and efficacy has not been shown.
Mechanisms of action. Kavapyrones are the major constituents of this herb and are responsible for its pharmacologic activity. The mechanisms of their anxiolytic effect are still unclear. One line of research suggests that kavapyrones might mediate sedative effects by influencing gamma-aminobutyric acid (GABA)(A) receptor binding,56-58 whereas another theory posits that kavapyrones are a reversible inhibitor of human platelet MAO-B.52 Others have suggested the inhibition of voltage-gated ion channels as a potential mechanism of action.59,60
Herb-drug interactions. This herb has the potential to interact with benzodiazepines,61 and the combination with central nervous system depressants like ethanol and barbiturates can produce synergistic effects.56,62
Adverse effects. Liver damage has been reported in patients who use kava.63-65 A recent study66 analyzed 29 cases of purported liver dysfunction in addition to 7 cases that have already been published; the authors concluded that kava ingestion was the direct cause of liver injury in 3 cases, a probable cause in 21 cases, and a possible cause in 12 cases. The most frequent liver injury was necrosis. Other adverse effects of this herb include dizziness, mild gastrointestinal disturbance, and a temporary yellow discoloration of skin, hair, and nails.67 In addition, long-term administration of kava at higher doses my cause scaling of the skin on the extremities, also known as kava dermopathy.68
Valerian
Valerian (Valerian officinalis) is a root extract, with purported healing properties that can be traced to ancient Greece and Rome. Today, valerian root preparations are used for their sedative, anxiolytic, and antidepressant properties. The herb, a GABA agonist,9 is commonly used in the treatment of sleeplessness and the management of anxiety associated with muscle tension.10
Efficacy. A recent systematic review of randomized clinical trials (including reports in all languages) assessed the efficacy of valerian in patients with insomnia.69 Nine randomized, double-blind, placebo-controlled trials satisfied the inclusion criteria; however, even in these studies questionable methods in randomization, blinding, compliance, withdrawal, confounding variables, diagnostic criteria, and statistical analysis rendered contradictory results, and the authors concluded that evidence for valerian in the treatment of insomnia is inconclusive.
Data to confirm valerian’s effectiveness as an anxiolytic are also minimal. One randomized placebo-controlled pilot study examined the effects of valerian on generalized anxiety disorder; 36 patients were treated with placebo, diazepam, or valerian extract for 4 weeks.70 The authors found a significant reduction in the psychic factors of anxiety with diazepam and valerian. However, the study was limited by the small number of patients in each group, relatively low dosages of the active agents, and a short duration of treatment. Similar studies71 suffer from the same shortcomings, and thus further research is necessary to assess the effect of valerian on anxiety. Thus, SOR=C for the evidence in support of valerian as a somnolent and as a anxiolytic, and further research is necessary to assess the effect of valerian in insomnia and anxiety
Mechanisms of action. Valerian’s constituents include sesquiterpenes of the volatile oil (including valeric acid), iridoids (valepotriates), alkaloids, furanofuran lignans, and free amino acids such as GABA, tyrosine, arginine, and glutamine.72 The precise mechanisms of action are still unclear, though it has been suggested that all of the active constituents act synergistically to produce a clinical response. Research has also demonstrated modulation of GABA neurotransmission and receptor function (see Houghton73 for a comprehensive review of valerian’s pharmacology).
Herb-drug interactions. Valerian has the potential to prolong thio-, pental-, and pentobarbital-induced sleep and should, therefore, not be combined with barbiturates.74,75 It may also potentiate the sedative effects of anesthetics and other central nervous system depressants.45
Adverse effects. Adverse affects with this product are rare, but when they occur they may include headaches, excitability, uneasiness, gastrointestinal effects, dizziness, and cardiac disturbances.76-78
Dementia
Ginkgo
Ginkgo extracts are derived from one of the oldest known tree species (Ginkgo biloba L). They have been used in traditional Chinese medicine for 5000 years for a variety of purposes and are believed to be helpful in the treatment of memory impairment caused by dementia.79 The herb is also used to treat stress, fatigue, chronic cerebrovascular insufficiency, and cerebral trauma, and to improve endurance.9
Efficacy. Evidence for ginkgo’s efficacy is encouraging, but more rigorous research is needed. Kleijnen and Knipschild80 reviewed 40 controlled trials on the use of ginkgo to treat “chronic cerebral insufficiency.” Only 8 of the studies were deemed to be of good quality, although all but 1 found clinically significant improvement in symptoms including memory loss, concentration difficulties, fatigue, anxiety, and depressed mood.
Another meta-analysis79 identified more than 50 articles on the effect of ginkgo on the cognitive function in Alzheimer patients, but only 4 studies were found to be properly blinded and placebo-controlled with well-characterized subjects. The authors concluded that gingko appears to have a modest effect on cognitive function in Alzheimer’s but note that further research is necessary.
A systematic review by Ernst and colleagues81 concluded that ginkgo was superior to a placebo in delaying the clinical course of dementia. The authors reported on 9 placebo controlled, double-blind randomized trials including 1497 patients in their analysis.
Ginkgo has also been used to treat impotence, including antidepressant-induced sexual dysfunction. In 1 trial, 60 patients with proven arterial erectile dysfunction who had not previously responded to papaverine showed improvement with a daily dose of 60 mg of ginkgo over 12 to 18 months.9 However, further research must be undertaken in this domain, in part because this trial was not blinded, with both doctors and patients aware of who was receiving the ginkgo treatment.
Thus, SOR=A for the evidence in support of ginkgo as a cognitive enhancer in mild to moderate dementia, and B for the evidence in support of ginkgo as a treatment for erectile dysfunction.
Mechanisms of action. Ginkgo leaves contain several bioactive compounds, including flavonoids, terpenoids (ginkgolide, bilbobide), and organic acids. Although the mechanisms of action are only partially understood, the main effects appear to be related to its antioxidant properties, which require the synergistic action of the principal constituents.82 These compounds act as free radical scavengers.83 Other pharmacologic actions involve antihypoxic and antiplatelet effects.84
Herb-drug interactions. Researchers have suggested that ginkgo may potentiate other anticoagulants or increase bleeding over time,85,86 which can be attributed to ginkgolide B, a potent inhibitor of platelet-activating factor needed for inducing arachidonate-independent platelet aggregation.87 Caution should be exercised when ginkgo is taken in conjunction with anticoagulant treatment (including aspirin) or when there is a risk of bleeding (eg, peptic ulcer disease and subdural hematoma).9,86
Adverse effects. Side effects from ginkgo appear to be relatively uncommon; however, they may include headaches, gastrointestinal tract upset, nausea, vomiting, and a skin allergy to the ginkgo fruit.17,88
Sexual dysfunction
Yohimbine
Yohimbine is an alkaloid derived from the cortex of the Central African tree Corianthe yohimbe.89 The bark of the tree was used traditionally to enhance virility. Today, yohimbine is still reputed as an aphrodisiac and used as a remedy for erectile problems.90
Efficacy. Overall, the efficacy of yohimbine in the treatment of erectile dysfunction appears promising, although, as with studies of other herbal products, clinical trials often suffer from methodological flaws. Carey and Johnson91 conducted 4 independent meta-analyses to examine the effects of yohimbine alone or in combination with other drugs in controlled and uncontrolled trials. The authors found positive results for yohimbine across all 4 analyses, but they note that the highest-quality data were derived from controlled clinical trials when yohimbine was administered on its own. In their analysis, this included 242 patients across 4 studies. Another systematic review yielded similar results: a meta-analysis of 7 randomized, placebo-controlled trials including 419 patients demonstrated that yohimbine is superior to placebo as a treatment for erectile dysfunction.89 Thus, SOR=A for the evidence in support of yohimbine as a treatment for erectile dysfunction.
Mechanisms of action. Yohimbine is an alpha2-adrenergic antagonist. Its blocking activity increases the release of noradrenaline and the firing rate of noradrenergic neurons in the central nervous system.92
Herb-drug interactions. Yohimbine should not be taken with sibutramine, a serotonin and norepinephrine reuptake inhibitor. The concomitant use of the 2 products could unmask the peripheral effect of sibutramine and produce negative cardiovascular effects.93 Potential interactions also exist with heart or blood pressure medications,94 lithium,95 morphine,96 and alcohol.97
Adverse effects. Adverse effects are not common with yohimbine; however, they may include headaches, sweating, agitation, hypertension, and restlessness.98 Yohimbine has also been reported to contribute to psychotic symptoms, mania, and seizures, though such occurrences are not well documented.9
Growing need for the 2 worlds to merge
One of the most frequent scenarios encountered by the naturopath is the patient who is taking a psychotropic medication and wants to explore natural solutions to reduce the drug’s unpleasant side effects or to enhance general well being. Sharing information is the key to a healthy treatment regimen for such individuals (TABLES 3 AND 4). The patient should inform both the physician and naturopath about health care decisions, the naturopath must encourage the patient to be candid with the physician about proposed treatments, and the physician can be helpful by communicating to the naturopath the extent of the patient’s disorder.
Professionally, one must consider before asking a patient to discontinue one agent or the other whether the alternative treatment might be improving the patient’s condition or reducing negative side effects caused by the psychotropic medication. On one hand, withdrawing the drug can destabilize the patient’s condition, which may not be rapidly amenable to a botanical or nutritional treatment. Alternatively, to supplement an antidepressant, benzodiazepine, or antipsychotic regimen by adding an herbal preparation could lead to unpredictable interactions and unpleasant or even dangerous symptoms. For many cases of mild depression or mild anxiety disorder, natural therapies can be sufficient treatment. However, for more complicated cases, where little is known about the consequences of using alternative treatments, involvement by a clinician with more specialized training is recommended.
TABLE 3
Recommendations for clinicians
| Ask your patients if they are using natural health products or seeing a natural health practitioner. Recognize that they may be covertly self-medicating with herbal or alternative treatments. Better-studied alternative treatments should be substituted. |
| Create an environment where patients are not reluctant to disclose the use of natural health care. |
| If the patient is seeing a naturopathic doctor, obtain contact information so that the specifics of the therapy can be requested. |
| Communicate directly with the naturopathic clinician about changes in treatment choices that are taking place in the ongoing care of the patient. This may often include sending consultation letters and other information to all individuals involved in the treatment of the patient. |
| Acquire good reference materials on natural health products. Suggestions: Natural Alternatives to Prozac by Michael T. Murray, ND, and The Textbook of Natural Medicine by Joseph Pizzorno, ND and Michael T. Murray, ND. |
| Never underestimate the potential risk of possible chemical interactions between medications. |
| Make contact with a community naturopathic doctor who can answer questions about specific natural health products. |
TABLE 4
Internet resources about herbal products
| The Natural Pharmacist ($) www.tnp.com |
| Evidence-based content developed and reviewed byphysicians and pharmacologists; sections on herbs and supplements, health conditions, and drug interactions; information referenced |
| Natural Medicines Comprehensive Database ($) www.naturaldatabase.com |
| Well-referenced, comprehensive database |
| Complementary and Alternative Therapies (Bandolier) www.jr2.ox.ac.uk/bandolier/booth/booths/altmed.html Evidence-based content; abstracts of systematic reviews, meta-analyses, or other studies about herbal therapies |
| National Center for Complementary and Alternative Medicine www.nlm.nih.gov/nccam/camonpubmed.html |
| Access to PubMed’s CAM database |
| HerbMed www.herbmed.org |
| Access to scientific evidence about the use of herbs for health $ = paid subscription required; all websites accessed April 5, 2005. Table adapted from Gardener.102 |
CORRESPONDING AUTHOR
Martin A. Katzman, BSc, MD, FRCPC, Stress, Trauma, Anxiety, Rehabilitation Treatment (S.T.A.R.T.) Clinic for Mood & Anxiety Disorders, 790 Bay Street, Toronto, Ontario, Canada M5G 1N8. E-mail: [email protected]
- Many of your patients may be self-treating with herbal preparations. Ask candidly about this possibility, and become familiar with the increasing evidence on efficacy and safety of alternative treatments
- A large meta-analysis and a Cochrane Review both suggest St. John’s Wort (A) is as effective as conventional antidepressants and more effective than placebo for mild to moderate depression. With patients taking St. John’s Wort and a conventional antidepressant, remain alert for a potentiating effect, “serotonin syndrome.” Use with caution if the patient must also receive anticoagulants, oral contraceptives, or antiviral agents.
- The efficacy and safety of ginseng (B, in terms of psychological well-being) and evening primrose (C) for depression are not well established.
- Kava-kava (A, for short-term treatment for anxiety treatment) has well-known anxiolytic properties, but its potential adverse effects, particularly liver toxicity, dramatically reduce its usefulness. Valerian, though commonly used for anxiety (C, for insomnia and anxiety), is not well supported by good data.
- Ginkgo has shown promise in improving cognitive function in dementia, and its side effects are few and uncommon (A, for cognitive function in dementia). Monitor carefully if there is concomitant anticoagulant therapy.
Based on epidemiologic estimates, it may be that 20% to 30% of your patient population is using alternative/complementary medicines.1 Twenty percent of adults who take prescription medicine also rely on herbal products,2 and patients who use herbal products the most are those with chronic conditions.3
Included in this group are persons with mental health problems, who, compared with the general population, report a much greater use of alternative treatments, including herbal and homeopathic remedies.4 These remedies, when used to treat psychiatric symptoms, may produce changes in mood, thinking, or behavior, and they may interact with a number of conventional medications.3
Largely uncharted territory. With the exception of St. John’s Wort for depression and ginkgo for dementia, minimal evidence is currently available to recommend the use of herbal medicines as the primary treatment for mental illness. Although some herbs have been found to be effective at specific doses for specific conditions, there is no evidence to show their superiority to conventional drug treatments, nor has their safety been established for use during pregnancy and lactation.8
Helping patients navigate. Nevertheless, our patients are increasingly turning to alternative therapies, and it is therefore critical that we clinicians avail ourselves of current knowledge and that investigators pursue intensive clinical research to establish safety (TABLE 1) and efficacy. Additionally, greater understanding of the biochemical and pharmacological effects of these herbs may uncover novel treatments or yield fresh insights into basic disease mechanisms.9
The herbal remedies discussed in this article are those commonly used for psychiatric conditions. Their effectiveness and potential for adverse side effects and interactions are assessed.
Depression
St. John’s Wort
St. John’s Wort (Hypericum perforatum L) is a popular herbal treatment readily used by the public in various forms, such as tablets and teas. Efficacy of hypericum—one of the hypothesized active ingredients in St. John’s Wort—in the treatment of depression was reported in the texts of the ancient Greek physicians Hippocrates, Pliny, and Galen, and it continued to be cited throughout the Classical, Renaissance, and Victorian eras. Its contemporary usage as an antidepressant has been supported by more rigorous evidence than any other herbal remedy.9
Efficacy. Evidence of efficacy in mild to moderate depression has been reported in a meta-analysis of 23 randomized trials with a total of 1757 outpatients, in which extracts of St. John’s Wort alone (20 of 23 trials) or in combination with other herbs (3 of 23) were tested against placebo (15 trials) or antidepressant drugs (8 trials).10 St. John’s Wort was reported to be clearly superior to placebo and comparable with conventional drug treatment, with lower side-effect and dropout rates. Similarly, a recent Cochrane Review of 27 trials and 2291 patients concluded that St. John’s Wort was more effective than placebo in treating mild to moderately severe depression; however, there was inadequate evidence to determine whether the herb was as effective as traditional antidepressants.11
The superiority of hypericum to placebo has been called into question, however, by a large-scale, multicenter, double-blind case report tabulation. The study, conducted with 200 patients across 11 academic medical centers in the United States, found no evidence that St. John’s Wort was more efficacious than placebo.12 Another such trial also concluded that St. John’s Wort was not an effective treatment for major depression. In addition, the herb was found to be no different than sertraline, which was also indistinguishable from the placebo, further confusing the issue.13 Strength of recommendation (SOR) is level A for the evidence in support of St. John’s Wort as an antidepressant.
Because many alternative options do not require the approval of the US Food and Drug Administration (FDA), products sold in health food stores can be purchased without a prescription or the provision of any clinical advice or professional review. The quality of many herbal preparations is thus unpredictable, with the content varying not only from brand to brand but also from batch to batch.5
A working knowledge of the pharmacologic data and clinical literature is necessary to properly counsel, diagnose, and treat patients who may be using herbal products. However, 1 study reported that only 5% of British doctors claimed more than a poor knowledge of herbal medicine,6 and another survey revealed that most psychiatrists who do not recommend herbal products avoid doing so because they feel uncomfortable with their current knowledge of alternative therapies.7 Alarmingly, the latter study reported that among psychiatrists who do not recommend herbal treatments, the safety of such treatments is not an issue in their decision-making process.
Mechanisms of action. The mechanisms for the antidepressant effects of St. John’s Wort are not fully understood, although monoamine oxidase (MAO) inhibition, inhibition of serotonin receptor expression, serotonin reuptake inhibition, and reduction of cytokine expression have all been suggested as means of its activity.9
Herb-drug interactions. Evidence suggests St. John’s Wort contains both inhibitory and inducing constituents for the cytochrome P-450 (CYP) system, resulting in both inhibition and induction on the CYP system.14 Consequently, it’s difficult to predict which drugs St. John’s Wort will interact with in a significant way.15 Best estimates of its activity suggest it has minimal short-term activity; when used for a longer period, it will inhibit the CytP450-3A4, 2C19, and 2D6 systems (TABLE 2). Therefore, St. John’s Wort may alter the blood levels of such medications as anticoagulants,16 oral contraceptives,18 and antiviral agents,19 possibly resulting in serious consequences.16,17 Exercise caution when initiating treatment for patients already taking St. John’s Wort.
The potential of St. John’s Wort to interact with standard prescribed antidepressants, possibly to produce a “serotonin syndrome,” is also a concern. Gordon20 reported a case in which a woman taking St. John’s Wort became groggy, weak, and lethargic shortly after taking a single 20-mg dose of paroxetine. This patient had tolerated St. John’s Wort and paroxetine separately, suggesting a drug-herb interaction.3 St. John’s Wort has also been implicated in reducing blood levels of digoxin when the two are taken together,21 and 1 study documented that 8% of psychiatrists treating patients who had used St. John’s Wort reported drug interactions between the herb and another agent.22
Adverse effects. In general, fewer adverse effects are seen with hypericum than with conventional antidepressants but they may include photodermatitis, delayed hypersensitivity, gastrointestinal tract upset, dizziness, dry mouth, sedation, restlessness, and constipation. Use of St. John’s Wort is contraindicated during pregnancy and lactation, for patients who experience intense exposure to strong sunlight, and for patients with a pheochromocytoma.23
There are several anecdotal reports of mania or hypomania associated with the herb. For example, O’Breasail and Argouarch24 reported 2 cases of persons with no history of bipolar disorder who developed hypomanic episodes after taking St. John’s Wort. Likewise, Moses and Mallinger25 reported 3 cases of possible mania induction associated with the herb.
TABLE 2
Effects of common herbs on cytochrome P-450 enzymes
| CYTOCHROME P-450 | |||
|---|---|---|---|
| CYTP450-3A4 | CYTP450-2C19 | CYP450-2D6 | |
| St. John’s Wort | ++++ inhibition (short-term?) | +++ inhibition | ++ inhibition |
| Long-term induction in intestinal wall99 | |||
| Kava-kava100 | ++ inhibition | ++ inhibition | ++ inhibition |
| Valerian | + inhibition | + inhibition | 0 |
| Fish oil, omega-3 fatty acids | +++ inhibition | ++++ inhibition | + inhibition |
| Key: ++++ = very potent; ++ = potent (detectable); + = mildly potent; 0 = does not inhibit | |||
| Note: Caution should be undertaken when developing tables such as these, as the data came from a variety of in vivo and in vitro animal and human studies using simplified models (eg, cDNA-expressed CYP enzymes) of which there are significant interspecies variations in the activity of these systems. As well, in the presence of some pathological inflammatory states such as during an infection, the enzyme activity of the CYP can be modulated through cytokines and other mediators of inflammation.101 | |||
Ginseng
This herb is derived from the root of Panax ginseng and has been used as a cure-all in Eastern folk medicine for thousands of years.26 Today, both Chinese ginseng (P ginseng CA Meyer) and North American ginseng (P quinquefolius L) are associated with the treatment of mood and anxiety disorders and are used to reduce stress and fatigue and to improve endurance.
Efficacy. A systematic review of 16 double-blind randomized controlled trials found that ginseng did not improve cognitive function or psychomotor and physical performance.27 Another review reported conflicting results from several studies.28 For example, 1 double-blind randomized controlled trial of postmenopausal women who received either a placebo or ginseng for 16 weeks revealed the superiority of ginseng on measures of psychological well-being.29 Another double-blind randomized controlled trial, however, failed to find an effect of ginseng on positive affect, negative affect, or total mood disturbance in 83 healthy adults who took the herb for 8 weeks.30 Thus, at best, SOR=B for the evidence in support of ginseng, but only at best in relation to psychological well-being.
Mechanisms of action. The key active components of Panax ginseng are ginsenosides, a group of steroidal saponins that target a multitude of tissues to produce pharmacologic responses. The overall pharmacology of ginseng is complex due to the ability of ginsenosides to initiate multiple actions in the same tissue. Attele and colleagues31 provide an in-depth review of these mechanisms.
Herb-drug interactions. Ginseng may potentiate the effect of MAO inhibitors,32 stimulants (including caffeine), and haloperidol.33 In addition, a case study suggests a probable interaction with warfarin.34
Adverse effects. Reported side effects include insomnia, hypertension, diarrhea, restlessness, anxiety, and euphoria.35 There is at least 1 report of ginseng-induced mania, which occurred within 4 to 10 days of a patient’s interrupting a lithium and amitriptyline treatment.26
Evening primrose
Evening primrose (Oenothera biennis L) is a plant native to North America. The oil pressed from its seed is marketed as a nutritional supplement, and it has been used to treat many disorders, including premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD), both which are marked by affective disturbances.36,37
Efficacy. A systematic review38 of the efficacy of evening primrose oil in the treatment of PMS revealed few clinical trials of adequate methodology. The authors found only 2 well-controlled studies, both which failed to show beneficial effects for the herb. Thus, at best, SOR=C for the evidence in support of evening primrose.
Literature searches were conducted using Medline, PsycInfo, and the Cochrane Library electronic databases, and by consulting bibliographies of pertinent publications. We focused primarily on meta-analyses and large-scale case report tabulations at an evidence level of 1b. Additionally, articles selected included those that discussed the use of herbal treatments for mental illness, as well as those that addressed drug-herb interactions between herbal and traditional psychiatric drug treatments.
Mechanisms of action. Gamma linolenic acid, a precursor of prostaglandin E and several other active substances, is the main constituent responsible for the therapeutic effects of evening primrose.37
Herb-drug interactions. This herb has the potential to interact with phenothiazines, nonsteroidal anti-inflammatory drugs, corticosteroids, beta-blockers, and anticoagulants.9
Adverse effects. Although it is generally safe, evening primrose oil has occasionally exacerbated the symptoms of epilepsy.39 Other adverse effects are nausea, softening of the stool, and headache.37
Ephedra
Ephedra (Ephedra sinica) is an evergreen shrub native to Asia used in traditional Chinese medicine for thousands of years. In recent decades, ma-huang, the extract derived from this herb, has been a common ingredient in many natural supplements that promote increased energy, mood enhancement, and weight loss.40,41 In early 2004, the FDA banned the sale of dietary products containing ephedra due to concerns over its adverse effects.42
Efficacy. Research on ephedra’s efficacy is largely focused on its role in weight loss, and there is little evidence that evaluates it as a mood enhancer. A comprehensive meta-analysis43 assessed 20 controlled trials with a treatment duration of at least 8 weeks and concluded that ephedra, when administered alone or with caffeine, promotes modest short-term weight loss (0.9 kg/month more than placebo). However, not all of the included studies were randomized or double-blind, and no data were available on long-term effects. A smaller systematic review44 of 5 double-blind studies also found the combination of ephedra and caffeine stimulated weight loss, but it was unclear whether 2 of the trials were randomized. Thus, SOR=A for the evidence in support of weight loss in the short term. There is no evidence in support of it as a mood-enhancing treatment.
Mechanisms of action. The primary constituents of ephedra are ephedrine-type alkaloids. As a sympathomimetic agonist at both α- and β-adrenergic receptors, ephedrine enhances cardiac rate and contractibility, peripheral vasoconstriction, bronchodilation, and central nervous system stimulation.41
Herb-drug interactions. Ephedra should not be used with anesthetic agents,45 MAO inhibitors,46,47 antihypertensives, or antidepressants.41
Adverse effects. The relative risk of adverse reactions to ephedra is more than 100 times greater than that of all other herbs.40 As noted by Jacobs and Hirsch,48 between 1993 and 1997 the FDA had received 34 notices of death and reports of approximately 800 medical and psychiatric complications all directly linked to ephedra. A more recent review49 indicated that hypertension, palpitations, tachycardia, stroke, seizures, and death are related to ephedra use. The herb has also been noted to induce symptoms of psychosis and affective disturbances.50,51
Anxiety
Kava-kava
Kava-kava is derived from the dried rhizome of the oceanic kava plant (Piper methysticum), and it has been cultivated for thousands of years throughout the South Pacific, where it is consumed as a psychotropic drink for recreational and medicinal purposes.52 Kava has been shown to alleviate anxiety symptoms,53 and it has euphoric and muscle relaxant properties, although its effect on arousal and alertness appears to be minimal.9 It is commonly used in Europe and North America for its anxiolytic effects.
Efficacy. A Cochrane review54 of 6 double-blind randomized controlled trials that used a common outcome measure (Hamilton Anxiety Scale) concluded that kava is significantly superior to placebo as a short-term treatment for anxiety. The authors note, however, that further investigation is required to determine long-term efficacy and safety. Another meta-analysis55 of 7 double-blind randomized controlled trials also suggests that, relative to a placebo, kava is an efficacious treatment for anxiety. Thus, SOR=A for the evidence in support of short-term efficacy in kava in anxiety. However, long-term data in terms of safety and efficacy has not been shown.
Mechanisms of action. Kavapyrones are the major constituents of this herb and are responsible for its pharmacologic activity. The mechanisms of their anxiolytic effect are still unclear. One line of research suggests that kavapyrones might mediate sedative effects by influencing gamma-aminobutyric acid (GABA)(A) receptor binding,56-58 whereas another theory posits that kavapyrones are a reversible inhibitor of human platelet MAO-B.52 Others have suggested the inhibition of voltage-gated ion channels as a potential mechanism of action.59,60
Herb-drug interactions. This herb has the potential to interact with benzodiazepines,61 and the combination with central nervous system depressants like ethanol and barbiturates can produce synergistic effects.56,62
Adverse effects. Liver damage has been reported in patients who use kava.63-65 A recent study66 analyzed 29 cases of purported liver dysfunction in addition to 7 cases that have already been published; the authors concluded that kava ingestion was the direct cause of liver injury in 3 cases, a probable cause in 21 cases, and a possible cause in 12 cases. The most frequent liver injury was necrosis. Other adverse effects of this herb include dizziness, mild gastrointestinal disturbance, and a temporary yellow discoloration of skin, hair, and nails.67 In addition, long-term administration of kava at higher doses my cause scaling of the skin on the extremities, also known as kava dermopathy.68
Valerian
Valerian (Valerian officinalis) is a root extract, with purported healing properties that can be traced to ancient Greece and Rome. Today, valerian root preparations are used for their sedative, anxiolytic, and antidepressant properties. The herb, a GABA agonist,9 is commonly used in the treatment of sleeplessness and the management of anxiety associated with muscle tension.10
Efficacy. A recent systematic review of randomized clinical trials (including reports in all languages) assessed the efficacy of valerian in patients with insomnia.69 Nine randomized, double-blind, placebo-controlled trials satisfied the inclusion criteria; however, even in these studies questionable methods in randomization, blinding, compliance, withdrawal, confounding variables, diagnostic criteria, and statistical analysis rendered contradictory results, and the authors concluded that evidence for valerian in the treatment of insomnia is inconclusive.
Data to confirm valerian’s effectiveness as an anxiolytic are also minimal. One randomized placebo-controlled pilot study examined the effects of valerian on generalized anxiety disorder; 36 patients were treated with placebo, diazepam, or valerian extract for 4 weeks.70 The authors found a significant reduction in the psychic factors of anxiety with diazepam and valerian. However, the study was limited by the small number of patients in each group, relatively low dosages of the active agents, and a short duration of treatment. Similar studies71 suffer from the same shortcomings, and thus further research is necessary to assess the effect of valerian on anxiety. Thus, SOR=C for the evidence in support of valerian as a somnolent and as a anxiolytic, and further research is necessary to assess the effect of valerian in insomnia and anxiety
Mechanisms of action. Valerian’s constituents include sesquiterpenes of the volatile oil (including valeric acid), iridoids (valepotriates), alkaloids, furanofuran lignans, and free amino acids such as GABA, tyrosine, arginine, and glutamine.72 The precise mechanisms of action are still unclear, though it has been suggested that all of the active constituents act synergistically to produce a clinical response. Research has also demonstrated modulation of GABA neurotransmission and receptor function (see Houghton73 for a comprehensive review of valerian’s pharmacology).
Herb-drug interactions. Valerian has the potential to prolong thio-, pental-, and pentobarbital-induced sleep and should, therefore, not be combined with barbiturates.74,75 It may also potentiate the sedative effects of anesthetics and other central nervous system depressants.45
Adverse effects. Adverse affects with this product are rare, but when they occur they may include headaches, excitability, uneasiness, gastrointestinal effects, dizziness, and cardiac disturbances.76-78
Dementia
Ginkgo
Ginkgo extracts are derived from one of the oldest known tree species (Ginkgo biloba L). They have been used in traditional Chinese medicine for 5000 years for a variety of purposes and are believed to be helpful in the treatment of memory impairment caused by dementia.79 The herb is also used to treat stress, fatigue, chronic cerebrovascular insufficiency, and cerebral trauma, and to improve endurance.9
Efficacy. Evidence for ginkgo’s efficacy is encouraging, but more rigorous research is needed. Kleijnen and Knipschild80 reviewed 40 controlled trials on the use of ginkgo to treat “chronic cerebral insufficiency.” Only 8 of the studies were deemed to be of good quality, although all but 1 found clinically significant improvement in symptoms including memory loss, concentration difficulties, fatigue, anxiety, and depressed mood.
Another meta-analysis79 identified more than 50 articles on the effect of ginkgo on the cognitive function in Alzheimer patients, but only 4 studies were found to be properly blinded and placebo-controlled with well-characterized subjects. The authors concluded that gingko appears to have a modest effect on cognitive function in Alzheimer’s but note that further research is necessary.
A systematic review by Ernst and colleagues81 concluded that ginkgo was superior to a placebo in delaying the clinical course of dementia. The authors reported on 9 placebo controlled, double-blind randomized trials including 1497 patients in their analysis.
Ginkgo has also been used to treat impotence, including antidepressant-induced sexual dysfunction. In 1 trial, 60 patients with proven arterial erectile dysfunction who had not previously responded to papaverine showed improvement with a daily dose of 60 mg of ginkgo over 12 to 18 months.9 However, further research must be undertaken in this domain, in part because this trial was not blinded, with both doctors and patients aware of who was receiving the ginkgo treatment.
Thus, SOR=A for the evidence in support of ginkgo as a cognitive enhancer in mild to moderate dementia, and B for the evidence in support of ginkgo as a treatment for erectile dysfunction.
Mechanisms of action. Ginkgo leaves contain several bioactive compounds, including flavonoids, terpenoids (ginkgolide, bilbobide), and organic acids. Although the mechanisms of action are only partially understood, the main effects appear to be related to its antioxidant properties, which require the synergistic action of the principal constituents.82 These compounds act as free radical scavengers.83 Other pharmacologic actions involve antihypoxic and antiplatelet effects.84
Herb-drug interactions. Researchers have suggested that ginkgo may potentiate other anticoagulants or increase bleeding over time,85,86 which can be attributed to ginkgolide B, a potent inhibitor of platelet-activating factor needed for inducing arachidonate-independent platelet aggregation.87 Caution should be exercised when ginkgo is taken in conjunction with anticoagulant treatment (including aspirin) or when there is a risk of bleeding (eg, peptic ulcer disease and subdural hematoma).9,86
Adverse effects. Side effects from ginkgo appear to be relatively uncommon; however, they may include headaches, gastrointestinal tract upset, nausea, vomiting, and a skin allergy to the ginkgo fruit.17,88
Sexual dysfunction
Yohimbine
Yohimbine is an alkaloid derived from the cortex of the Central African tree Corianthe yohimbe.89 The bark of the tree was used traditionally to enhance virility. Today, yohimbine is still reputed as an aphrodisiac and used as a remedy for erectile problems.90
Efficacy. Overall, the efficacy of yohimbine in the treatment of erectile dysfunction appears promising, although, as with studies of other herbal products, clinical trials often suffer from methodological flaws. Carey and Johnson91 conducted 4 independent meta-analyses to examine the effects of yohimbine alone or in combination with other drugs in controlled and uncontrolled trials. The authors found positive results for yohimbine across all 4 analyses, but they note that the highest-quality data were derived from controlled clinical trials when yohimbine was administered on its own. In their analysis, this included 242 patients across 4 studies. Another systematic review yielded similar results: a meta-analysis of 7 randomized, placebo-controlled trials including 419 patients demonstrated that yohimbine is superior to placebo as a treatment for erectile dysfunction.89 Thus, SOR=A for the evidence in support of yohimbine as a treatment for erectile dysfunction.
Mechanisms of action. Yohimbine is an alpha2-adrenergic antagonist. Its blocking activity increases the release of noradrenaline and the firing rate of noradrenergic neurons in the central nervous system.92
Herb-drug interactions. Yohimbine should not be taken with sibutramine, a serotonin and norepinephrine reuptake inhibitor. The concomitant use of the 2 products could unmask the peripheral effect of sibutramine and produce negative cardiovascular effects.93 Potential interactions also exist with heart or blood pressure medications,94 lithium,95 morphine,96 and alcohol.97
Adverse effects. Adverse effects are not common with yohimbine; however, they may include headaches, sweating, agitation, hypertension, and restlessness.98 Yohimbine has also been reported to contribute to psychotic symptoms, mania, and seizures, though such occurrences are not well documented.9
Growing need for the 2 worlds to merge
One of the most frequent scenarios encountered by the naturopath is the patient who is taking a psychotropic medication and wants to explore natural solutions to reduce the drug’s unpleasant side effects or to enhance general well being. Sharing information is the key to a healthy treatment regimen for such individuals (TABLES 3 AND 4). The patient should inform both the physician and naturopath about health care decisions, the naturopath must encourage the patient to be candid with the physician about proposed treatments, and the physician can be helpful by communicating to the naturopath the extent of the patient’s disorder.
Professionally, one must consider before asking a patient to discontinue one agent or the other whether the alternative treatment might be improving the patient’s condition or reducing negative side effects caused by the psychotropic medication. On one hand, withdrawing the drug can destabilize the patient’s condition, which may not be rapidly amenable to a botanical or nutritional treatment. Alternatively, to supplement an antidepressant, benzodiazepine, or antipsychotic regimen by adding an herbal preparation could lead to unpredictable interactions and unpleasant or even dangerous symptoms. For many cases of mild depression or mild anxiety disorder, natural therapies can be sufficient treatment. However, for more complicated cases, where little is known about the consequences of using alternative treatments, involvement by a clinician with more specialized training is recommended.
TABLE 3
Recommendations for clinicians
| Ask your patients if they are using natural health products or seeing a natural health practitioner. Recognize that they may be covertly self-medicating with herbal or alternative treatments. Better-studied alternative treatments should be substituted. |
| Create an environment where patients are not reluctant to disclose the use of natural health care. |
| If the patient is seeing a naturopathic doctor, obtain contact information so that the specifics of the therapy can be requested. |
| Communicate directly with the naturopathic clinician about changes in treatment choices that are taking place in the ongoing care of the patient. This may often include sending consultation letters and other information to all individuals involved in the treatment of the patient. |
| Acquire good reference materials on natural health products. Suggestions: Natural Alternatives to Prozac by Michael T. Murray, ND, and The Textbook of Natural Medicine by Joseph Pizzorno, ND and Michael T. Murray, ND. |
| Never underestimate the potential risk of possible chemical interactions between medications. |
| Make contact with a community naturopathic doctor who can answer questions about specific natural health products. |
TABLE 4
Internet resources about herbal products
| The Natural Pharmacist ($) www.tnp.com |
| Evidence-based content developed and reviewed byphysicians and pharmacologists; sections on herbs and supplements, health conditions, and drug interactions; information referenced |
| Natural Medicines Comprehensive Database ($) www.naturaldatabase.com |
| Well-referenced, comprehensive database |
| Complementary and Alternative Therapies (Bandolier) www.jr2.ox.ac.uk/bandolier/booth/booths/altmed.html Evidence-based content; abstracts of systematic reviews, meta-analyses, or other studies about herbal therapies |
| National Center for Complementary and Alternative Medicine www.nlm.nih.gov/nccam/camonpubmed.html |
| Access to PubMed’s CAM database |
| HerbMed www.herbmed.org |
| Access to scientific evidence about the use of herbs for health $ = paid subscription required; all websites accessed April 5, 2005. Table adapted from Gardener.102 |
CORRESPONDING AUTHOR
Martin A. Katzman, BSc, MD, FRCPC, Stress, Trauma, Anxiety, Rehabilitation Treatment (S.T.A.R.T.) Clinic for Mood & Anxiety Disorders, 790 Bay Street, Toronto, Ontario, Canada M5G 1N8. E-mail: [email protected]
1. Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States—prevalence, costs and patterns of use. N Engl J Med 1993;328:246-252.
2. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in Alternative Medicine Use in the United States, 1990-1997: Results of a Follow-up National Survey. JAMA 1998;280:1569-1575.
3. Pies R. Adverse neuropsychiatric reactions to herbal and over-the counter “antidepressants.” J Clin Psychiatry 2000;61:815-820.
4. Knaudt PR, Connor KM, Weisler RH, Churchill LE, Davidson JRT. Alternative therapy use by psychiatric outpatients. J Nerv Ment Dis 1999;187:692-695.
5. Mamtani R, Cimino A. A primer of complementary and alternative medicine and its relevance in the treatment of mental health problems. Psychiatr Quart 2002;73:367-381.
6. Wharton R, Lewith G. Complementary medicine and the general practitioner. BMJ 1986;292:1498-1500.
7. Scimone A, Scimone AA. Recommendation of herbal remedies by psychiatrists. J Orthomol Med 2001;16:155-156.
8. Wong AHC, Smith M, Boon HS. Botanical medicine in psychiatry. Psychiatry Rounds 1999;3(2):1-5.
9. Wong AHC, Smith M, Boon HS. Herbal remedies in psychiatric practice. Arch Gen Psychiatry 1998;55:1033-1044.
10. Linde K, Ramirez G, Mulrow CD, Pauls A, Weidenhammer W, Melchart D. St. John’s wort for depression: An overview and meta-analysis of randomized clinical trials. BMJ 1996;313:253-258.
11. Linde K, Mulrow CD. St. John’s wort for depression (Cochrane Review). In: The Cochrane Library, Issue 4, 2003. Chinchester, UK: John Wiley & Sons, Ltd.
12. Shelton RC, Keller MB, Gelenberg A, et al. Effectiveness of St. John’s wort in major depression. JAMA 2001;285:1978-1986.
13. Davidson JRT. Effect of Hypericum perforatum (St John’s wort) in major depressive disorder. JAMA 2002;287:1807-1814.
14. Strandell J, Neil A, Carlin G. An approach to the in vitro evaluation of potential for cytochrome P450 enzyme inhibition from herbals and other natural remedies. Phytomedicine 2004;11:98-104.
15. Zhou S, Gao Y, Jiang W, Huang M, Xu A, Paxton JW. Interactions of herbs with cytochrome P450. Drug Metab Rev 2003;35:35-98.
16. Ernst E. Second thoughts about safety of St John’s wort. Lancet 1999;354:2014-2016.
17. Ernst E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John’s Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann Intern Med 2002;136:42-53.
18. Hall S, Wang Z, Huang S, et al. The interaction between St John’s wort and an oral contraceptive. Clin Pharmacol Ther 2003;74:525-535.
19. Piscitelli SC, Burstein AH, Chaitt D, Alfaro RM, Falloon J. Indinavir concentrations and St John’s wort. Lancet 2000;355:547-548.
20. Gordon JB. SSRIs and St. John’s wort: Possible toxicity? Am Fam Physician 1998;57:950-953.
21. Johne A, Brockmoller J, Bauer S. Pharmacokinetic interaction of digoxin with an herbal extract from St. John’s wort (Hypericum perforatum). Clin Pharmacol Ther 1999;66:338-345.
22. Walter G, Rey JM, Harding M. Psychiatrists’ experience and views regarding St. John’s wort and ‘alternative’ treatments. Aust NZ J Psychiatry 2000;34:992-996.
23. Newall C, Anderson LA, Phillipson JD. Herbal Medicines: A Guide for Health-Care Professionals. London, England: Pharmaceutical Press; 1996.
24. O’Breasail AM, Argouarch S. Hypomania and St. John’s wort. Can J Psychiatry 1998;43:747.-
25. Moses EL, Mallinger AG. St. John’s wort: Three cases of possible mania induction. J Clin Psychopharmacol 2000;20:115-117.
26. Gonzalez-Seijo JC, Ramos YM, Lastra I. Manic episode and ginseng: Report of a possible case. J Clin Psychopharmacol 1995;15:447-448.
27. Vogler BK, Pittler MH, Ernst E. The efficacy of ginseng. A systematic review of randomised clinical trials. Eur J Clin Pharmacol 1999;55:567-575.
28. Kieffer D, Pantuso T. Panax ginseng. Am Fam Physician 2003;68:1539-1542.
29. Wiklund IK, Mattsson LA, Lindgren R, Limoni C. Effects of a standardized ginseng extract on quality of life and physiological parameters in symptomatic postmenopausal women: a double-blind, placebo-controlled trial. Swedish Alternative Medicine Group. Int J Clin Pharmacol Res 1999;19:89-99.
30. Cardinal BJ, Engels HJ. Ginseng does not enhance psychological well-being in healthy, young adults: results of a double-blind, placebo-controlled, randomized clinical trial. J Am Diet Assoc 2001;101:655-660.
31. Attele AS, Wua JA, Yuan CS. Ginseng pharmacology: Multiple constituents and multiple actions. Biochem Pharmacol 1999;58:1685-1693.
32. Stockley I. Drug Interactions: A Sourcebook of Adverse Interactions, Their Mechanisms, Clinical Importance, and Management. 3rd ed. Cambridge, England: Blackwell Scientific Press; 1994.
33. Mitra SK, Chakraborti A, Bhattacharya SK. Neuropharmacological studies on Panax ginseng. Indian J Exp Biol 1996;34:41-47.
34. Janetzky K, Morreale AP. Probable interaction between warfarin and ginseng. Am J Health Syst Pharm 1997;54:692-693.
35. Siegel RK. Ginseng abuse syndrome. JAMA 1979;241:1614-1615.
36. Girman A, Lee R, Kligler B. An integrative medicine approach to premenstrual syndrome. Am J Obstet Gynecol 2003;188(5 Suppl):S56-S65.
37. Kleijnen J. Evening primrose oil. BMJ 1994;309:824-825.
38. Budeiri D, Li Wan Po A, Dornan JC. Is evening primrose oil of value in the treatment of premenstrual syndrome? Controlled Clinical Trials 1996;17:60-68.
39. Barber HJ. Evening primrose oil: A panacea? Pharm J 1988;240:723-725.
40. Bent S, Tiedt TN, Odden MC, Shlipak MG. The relative safety of ephedra compared with other herbal products. Ann Intern Med 2003;138:468-471.
41. Abourashed EA, El-Alfy AT, Khan IA, Walker L. Ephedra in perspective—a current review. Phytother Res 2003;17:703-712.
42. Rados C. Ephedra ban: no shortage of reasons. FDA Consum 2004;38:6-7.
43. Shekelle PG, Hardy ML, Morton SC, et al. Efficacy and safety of ephedra and ephedrine for weight loss and athletic performance: a meta-analysis. JAMA 2003;289:1537-1545.
44. Greenway FL. The safety and efficacy of pharmaceutical and herbal caffeine and ephedrine use as a weight loss agent. Obes Rev 2001;2:199-211.
45. Ang-Lee M, Moss J, Yuan C. Herbal medicines and perioperative care. JAMA 2001;286:208-216.
46. Dawson JK, Earnshaw SM, Graham CS. Dangerous monoamine oxidase inhibitor interactions are still occurring in the 1990s. J Accid Emerg Med 1995;12:49-51.
47. Brinker F. Interactions of pharmaceutical and botanical medicines. J Naturopathic Med 1997;7:14-20.
48. Jacobs KM, Hirsch KA. Psychiatric complications of ma-huang. Psychosomatics 2000;41:58-62.
49. Haller CA, Benowitz NL. Adverse cardiovascular and central nervous system events associated with dietary supplements containing ephedra alkaloids. N Engl J Med 2000;343:833-838.
50. Doyle H, Kargin M. Herbal stimulant containing ephedrine has also caused psychosis. BMJ 1996;313:756.-
51. Capwell RR. Ephedrine-induced mania from an herbal diet supplement. Am J Psychiatry 1995;152:647.-
52. Uebelhack R, Franke L, Schewe HJ. Inhibition of platelet MAO-B by kava pyrone-enriched extract from piper methysticum forster (kava-kava). Pharmacopsychiat 1998;31:187-192.
53. Volz HP, Kieser M. Kava-kava extract WS 1490 verses placebo in anxiety disorders: A randomized placebo-controlled 25-week outpatient trial. Pharmacopsychiat 1997;30:1-5.
54. Pittler MH, Ehret V. Kava extract for treating anxiety (Cochrane Review). In: The Cochrane Library, Issue 4, 2003. Chichester, UK: John Wiley & Sons, Ltd.
55. Pittler MH, Ernst E. Efficacy of kava extract for treating anxiety: systematic review and meta-analysis. J Clin Psychopharmacol 2000;20:84-90.
56. Jussofie A, Schmiz A, Himke C. Kava-pyrone enriched extract from Piper methysticum as modulator of the GABA binding site in different regions of rat brain. Psychopharmacology (Berl) 1994;116:469-474.
57. Boonen G, Haberlein H. Influence of genuine kavapyrone enantiomers on the GABAA binding site. Planta Med 1998;64:504-506.
58. Davies LP, Drew CA, Duffield P, Johnston GA, Jamieson DD. Kava pyrones and resin: studies on GABA-A, GABA-B, and benzodiazepine binding sites in rodent brain. Pharmacol Toxicol 1992;712:120-126.
59. Gleitz J, Beile A, Peters T. (±)-Kavain inhibits veratridine-activated voltage- dependent Na+-channels in synaptosomes prepared from rat cerebral cortex. Neuropharmacology 1995;34:1133-1138.
60. Magura EI, Kopanitsa MV, Gleitz J, Peters T, Krishtal OA. Kava extract ingredients, (+)-methysticin and (+/-)-kavain inhibit voltage-operated Na+-channels in rat CA1 hippocampal neurons. Neuroscience 1997;91:345-351.
61. Almeida JC, Grimsley EW. Coma from the health food store: Interaction between kava kava and alprazolam. Annu Int Med 1996;125:940-941.
62. Foo H, Lemon J. Acute effects of kava, alone or in combination with alcohol, on subjective measures of impairment and intoxication and on cognitive performance. Drug Alcohol Rev 1997;16:147-155.
63. Kraft M, Spahn TW, Menzel J, et al. Fulminant liver failure after administration of the herbal antidepressant kava-kava. Dtsch Med Wochenschr 2001;126:970-972.
64. Strahl S, Ehret V, Dahm HH, Maier KP. Necrotizing hepatitis after taking herbal remedies. Dtsch Med Wochenschr 1998;23:1410-1414.
65. Escher M, Desmeules J, Giostra E, Mentha G. Hepatitis associated with kava, a herbal remedy for anxiety. BMJ 2001;322:7279.-
66. Stickel F, Baumuller HM, Seitz K, et al. Hepatitis induced by Kava (Piper methysticum rhizoma). J Hepatol 2003;39:62-67.
67. Blumenthal M, Busse W, Goldberg A, et al, eds. The Complete German Commission E Monographs-Therapeutic Guide to Herbal Medicines. Austin: American Botanical Council; Boston: Integrative Medicine Communications; 1998.
68. Norton SA, Ruze P. Kava dermopathy. J Am Acad Dermatol 1994;31:89-97.
69. Stevinson C, Ernst E. Valerian for insomnia: A systematic review of randomized clinical trials. Sleep Medicine 2000;1:91-99.
70. Andreatini R, Sartori V, Seabra M, Leite J. Effect of valepotriates (valerian extract) in generalized anxiety disorder: a randomized placebo-controlled pilot study. Phytother Res 2002;16:650-654.
71. Cropley M, Cave Z, Ellis J, Middleton R. Effect of kava and valerian on human physiological and psychological responses to mental stress assessed under laboratory conditions. Phytother Res 2002;16:23-27.
72. Hadley S, Petry J. Valerian. Am Fam Physician 2003;67:1755-1758.
73. Houghton P. The scientific basis for the reputed activity of Valerian. J Pharm Pharmacol 1999;51:505-512.
74. Hiller K, Zetler G. Neuropharmacological studies on ethanol extracts of Valeriana officinalis L: Behavioural and anticonvulsant properties. Physiother Res Int 1996;10:145-151.
75. Capasso A, DeFeo V, DeSimon F, Sorrentino L. Pharmacological effects of aqueous extracts from Valeriana adscendens. Physiother Res Int 1996;10:309-312.
76. McGuffin M, Hobbs C, Upton R, Goldberg A, eds. American Herbal Products Association’s Botanical Safety Handbook. Boca Raton, Fla: CRC Press; 1997.
77. Donath F, Quispe S, Diefenbach K, Maurer A, Fietze I, Roots I. Critical evaluation of the effect of valerian extract on sleep structure and sleep quality. Pharmacopsychiatry 2000;33:47-53.
78. Kuhlmann J, Berger W, Podzuweit H, Schmidt U. The influence of valerian treatment on “reaction time, alertness and concentration” in volunteers. Pharmacopsychiatry 1999;32:235-241.
79. Oken B, Storzbach D, Kaye J. The efficacy of Ginkgo biloba on cognitive function in Alzheimer disease. Arch Neurol 1998;55:1409-1415.
80. Kleijnen J, Knipschild P. Ginkgo biloba for cerebral insufficiency. Br J Clin Pharmacol 1992;34:352-358.
81. Ernst E, Pittler M. Ginkgo biloba for dementia: a systematic review of double-blind, placebo-controlled trials. Clin Drug Invest 1999;17:301-308.
82. Le Bars PL, Katz MM, Berman N, Itil TM, Freedman AM, Schatzberg AF. A placebo-controlled, double-blind, randomized trial of an extract of Ginkgo biloba for dementia. JAMA 1997;278:1327-1332.
83. Oyama Y, Fuchs P, Katayama N, Noda K. Myricetin and quercetin, the flavonoid constituents of Ginkgo biloba extract, greatly reduce oxidative metabolism in both resting and Ca(2+)-loaded brain neurons. Brain Res 1994;635:125-129.
84. Cupp M, ed. Toxicology and Clinical Pharmacology of Herbal Products. Totowa, NJ: Humana Press; 2000.
85. Rowin J, Lewis SL. Spontaneous bilateral subdural hematomas associated with chronic Ginkgo. Neurol 1996;46:1775-1776.
86. Rosenblatt M, Mindel J. Spontaneous hyphema associated with ingestion of Ginkgo biloba extract. N Engl J Med 1997;336:1108.-
87. Miller LG. Herbal medicinals: Selected clinical considerations focusing on known or potential drug-herb interactions. Arch Intern Med 1998;158:2200-2211.
88. Houghton P. Ginkgo. Pharm J 1994;253:121-122.
89. Ernst E, Pittler M. Yohimbine for erectile dysfunction: A systematic review and meta-analysis of randomized clinical trials. J Urol 1998;159:433-436.
90. Morales A. Yohimbine in erectile dysfunction: The facts. Int J Impot Res 2000;Suppl 1:S70-S74.
91. Carey M, Johnson B. Effectiveness of yohimbine in the treatment of erectile disorder: Four meta-analytic integrations. Arch Sex Behav 1996;25:341-360.
92. Charney DS, Woods SW, Goodman WK, Heninger GR. Neurobiological mechanisms of panic anxiety: Biochemical and behavioural correlates of yohimbine-induced panic attacks. Am J Psychiatry 1987;144:1030-1036.
93. Jordan J, Sharma A. Potential for sibutramine-yohimbine interaction? Lancet 2003;361:1826.-
94. Goldstein D, Grossman E, Listwak S, Folio C. Sympathetic reactivity during a yohimbine challenge test in essential hypertension. Hypertension 1991;18 (Suppl 3):40-48.
95. Price L, Charney D, Heninger G. Three cases of manic symptoms following yohimbine administration. Am J Psychiatry 1984;141:1267-1268.
96. Gear R, Gordon N, Heller P, Levine J. Enhancement of morphine analgesia by the alpha2-adrenergic antagonist yohimbine. Neuroscience 1995;66:5-8.
97. McDougle C, Krystal J, Price L, Heninger G, Charney D. Noradrenergic response to acute ethanol administration in healthy subjects: comparison with intravenous yohimbine. Psychopharmacology (Berl) 1995;118:127-135.
98. Rowland D, Tai W. A review of plant-derived and herbal approaches to the treatment of sexual dysfunctions. J Sex Marital Ther 2003;29:185-205.
99. Wang Z, Gorski JC, Hamman MA, Huang SM, Lesko LJ, Hall SD. The effects of St John’s wort (Hypericum perforatum) on human cytochrome P450 activity. Clin Pharmacol Ther 2001;70:317-326.
100. Mathews JM, Etheridge AS, Black SR. Inhibition of human cytochrome P450 activities by kava extract and kavalactones. Drug Metab Dispos 2002;30:1153-1157.
101. Renton KW. Alteration of drug biotransformation and elimination during infection and inflammation. Pharmacol Ther 2001;92:147-163.
102. Gardener D. Evidence-based decisions about herbal products for treating mental disorders. J Psychiatry Neurosci 2002;27:324-333.
1. Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States—prevalence, costs and patterns of use. N Engl J Med 1993;328:246-252.
2. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in Alternative Medicine Use in the United States, 1990-1997: Results of a Follow-up National Survey. JAMA 1998;280:1569-1575.
3. Pies R. Adverse neuropsychiatric reactions to herbal and over-the counter “antidepressants.” J Clin Psychiatry 2000;61:815-820.
4. Knaudt PR, Connor KM, Weisler RH, Churchill LE, Davidson JRT. Alternative therapy use by psychiatric outpatients. J Nerv Ment Dis 1999;187:692-695.
5. Mamtani R, Cimino A. A primer of complementary and alternative medicine and its relevance in the treatment of mental health problems. Psychiatr Quart 2002;73:367-381.
6. Wharton R, Lewith G. Complementary medicine and the general practitioner. BMJ 1986;292:1498-1500.
7. Scimone A, Scimone AA. Recommendation of herbal remedies by psychiatrists. J Orthomol Med 2001;16:155-156.
8. Wong AHC, Smith M, Boon HS. Botanical medicine in psychiatry. Psychiatry Rounds 1999;3(2):1-5.
9. Wong AHC, Smith M, Boon HS. Herbal remedies in psychiatric practice. Arch Gen Psychiatry 1998;55:1033-1044.
10. Linde K, Ramirez G, Mulrow CD, Pauls A, Weidenhammer W, Melchart D. St. John’s wort for depression: An overview and meta-analysis of randomized clinical trials. BMJ 1996;313:253-258.
11. Linde K, Mulrow CD. St. John’s wort for depression (Cochrane Review). In: The Cochrane Library, Issue 4, 2003. Chinchester, UK: John Wiley & Sons, Ltd.
12. Shelton RC, Keller MB, Gelenberg A, et al. Effectiveness of St. John’s wort in major depression. JAMA 2001;285:1978-1986.
13. Davidson JRT. Effect of Hypericum perforatum (St John’s wort) in major depressive disorder. JAMA 2002;287:1807-1814.
14. Strandell J, Neil A, Carlin G. An approach to the in vitro evaluation of potential for cytochrome P450 enzyme inhibition from herbals and other natural remedies. Phytomedicine 2004;11:98-104.
15. Zhou S, Gao Y, Jiang W, Huang M, Xu A, Paxton JW. Interactions of herbs with cytochrome P450. Drug Metab Rev 2003;35:35-98.
16. Ernst E. Second thoughts about safety of St John’s wort. Lancet 1999;354:2014-2016.
17. Ernst E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John’s Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann Intern Med 2002;136:42-53.
18. Hall S, Wang Z, Huang S, et al. The interaction between St John’s wort and an oral contraceptive. Clin Pharmacol Ther 2003;74:525-535.
19. Piscitelli SC, Burstein AH, Chaitt D, Alfaro RM, Falloon J. Indinavir concentrations and St John’s wort. Lancet 2000;355:547-548.
20. Gordon JB. SSRIs and St. John’s wort: Possible toxicity? Am Fam Physician 1998;57:950-953.
21. Johne A, Brockmoller J, Bauer S. Pharmacokinetic interaction of digoxin with an herbal extract from St. John’s wort (Hypericum perforatum). Clin Pharmacol Ther 1999;66:338-345.
22. Walter G, Rey JM, Harding M. Psychiatrists’ experience and views regarding St. John’s wort and ‘alternative’ treatments. Aust NZ J Psychiatry 2000;34:992-996.
23. Newall C, Anderson LA, Phillipson JD. Herbal Medicines: A Guide for Health-Care Professionals. London, England: Pharmaceutical Press; 1996.
24. O’Breasail AM, Argouarch S. Hypomania and St. John’s wort. Can J Psychiatry 1998;43:747.-
25. Moses EL, Mallinger AG. St. John’s wort: Three cases of possible mania induction. J Clin Psychopharmacol 2000;20:115-117.
26. Gonzalez-Seijo JC, Ramos YM, Lastra I. Manic episode and ginseng: Report of a possible case. J Clin Psychopharmacol 1995;15:447-448.
27. Vogler BK, Pittler MH, Ernst E. The efficacy of ginseng. A systematic review of randomised clinical trials. Eur J Clin Pharmacol 1999;55:567-575.
28. Kieffer D, Pantuso T. Panax ginseng. Am Fam Physician 2003;68:1539-1542.
29. Wiklund IK, Mattsson LA, Lindgren R, Limoni C. Effects of a standardized ginseng extract on quality of life and physiological parameters in symptomatic postmenopausal women: a double-blind, placebo-controlled trial. Swedish Alternative Medicine Group. Int J Clin Pharmacol Res 1999;19:89-99.
30. Cardinal BJ, Engels HJ. Ginseng does not enhance psychological well-being in healthy, young adults: results of a double-blind, placebo-controlled, randomized clinical trial. J Am Diet Assoc 2001;101:655-660.
31. Attele AS, Wua JA, Yuan CS. Ginseng pharmacology: Multiple constituents and multiple actions. Biochem Pharmacol 1999;58:1685-1693.
32. Stockley I. Drug Interactions: A Sourcebook of Adverse Interactions, Their Mechanisms, Clinical Importance, and Management. 3rd ed. Cambridge, England: Blackwell Scientific Press; 1994.
33. Mitra SK, Chakraborti A, Bhattacharya SK. Neuropharmacological studies on Panax ginseng. Indian J Exp Biol 1996;34:41-47.
34. Janetzky K, Morreale AP. Probable interaction between warfarin and ginseng. Am J Health Syst Pharm 1997;54:692-693.
35. Siegel RK. Ginseng abuse syndrome. JAMA 1979;241:1614-1615.
36. Girman A, Lee R, Kligler B. An integrative medicine approach to premenstrual syndrome. Am J Obstet Gynecol 2003;188(5 Suppl):S56-S65.
37. Kleijnen J. Evening primrose oil. BMJ 1994;309:824-825.
38. Budeiri D, Li Wan Po A, Dornan JC. Is evening primrose oil of value in the treatment of premenstrual syndrome? Controlled Clinical Trials 1996;17:60-68.
39. Barber HJ. Evening primrose oil: A panacea? Pharm J 1988;240:723-725.
40. Bent S, Tiedt TN, Odden MC, Shlipak MG. The relative safety of ephedra compared with other herbal products. Ann Intern Med 2003;138:468-471.
41. Abourashed EA, El-Alfy AT, Khan IA, Walker L. Ephedra in perspective—a current review. Phytother Res 2003;17:703-712.
42. Rados C. Ephedra ban: no shortage of reasons. FDA Consum 2004;38:6-7.
43. Shekelle PG, Hardy ML, Morton SC, et al. Efficacy and safety of ephedra and ephedrine for weight loss and athletic performance: a meta-analysis. JAMA 2003;289:1537-1545.
44. Greenway FL. The safety and efficacy of pharmaceutical and herbal caffeine and ephedrine use as a weight loss agent. Obes Rev 2001;2:199-211.
45. Ang-Lee M, Moss J, Yuan C. Herbal medicines and perioperative care. JAMA 2001;286:208-216.
46. Dawson JK, Earnshaw SM, Graham CS. Dangerous monoamine oxidase inhibitor interactions are still occurring in the 1990s. J Accid Emerg Med 1995;12:49-51.
47. Brinker F. Interactions of pharmaceutical and botanical medicines. J Naturopathic Med 1997;7:14-20.
48. Jacobs KM, Hirsch KA. Psychiatric complications of ma-huang. Psychosomatics 2000;41:58-62.
49. Haller CA, Benowitz NL. Adverse cardiovascular and central nervous system events associated with dietary supplements containing ephedra alkaloids. N Engl J Med 2000;343:833-838.
50. Doyle H, Kargin M. Herbal stimulant containing ephedrine has also caused psychosis. BMJ 1996;313:756.-
51. Capwell RR. Ephedrine-induced mania from an herbal diet supplement. Am J Psychiatry 1995;152:647.-
52. Uebelhack R, Franke L, Schewe HJ. Inhibition of platelet MAO-B by kava pyrone-enriched extract from piper methysticum forster (kava-kava). Pharmacopsychiat 1998;31:187-192.
53. Volz HP, Kieser M. Kava-kava extract WS 1490 verses placebo in anxiety disorders: A randomized placebo-controlled 25-week outpatient trial. Pharmacopsychiat 1997;30:1-5.
54. Pittler MH, Ehret V. Kava extract for treating anxiety (Cochrane Review). In: The Cochrane Library, Issue 4, 2003. Chichester, UK: John Wiley & Sons, Ltd.
55. Pittler MH, Ernst E. Efficacy of kava extract for treating anxiety: systematic review and meta-analysis. J Clin Psychopharmacol 2000;20:84-90.
56. Jussofie A, Schmiz A, Himke C. Kava-pyrone enriched extract from Piper methysticum as modulator of the GABA binding site in different regions of rat brain. Psychopharmacology (Berl) 1994;116:469-474.
57. Boonen G, Haberlein H. Influence of genuine kavapyrone enantiomers on the GABAA binding site. Planta Med 1998;64:504-506.
58. Davies LP, Drew CA, Duffield P, Johnston GA, Jamieson DD. Kava pyrones and resin: studies on GABA-A, GABA-B, and benzodiazepine binding sites in rodent brain. Pharmacol Toxicol 1992;712:120-126.
59. Gleitz J, Beile A, Peters T. (±)-Kavain inhibits veratridine-activated voltage- dependent Na+-channels in synaptosomes prepared from rat cerebral cortex. Neuropharmacology 1995;34:1133-1138.
60. Magura EI, Kopanitsa MV, Gleitz J, Peters T, Krishtal OA. Kava extract ingredients, (+)-methysticin and (+/-)-kavain inhibit voltage-operated Na+-channels in rat CA1 hippocampal neurons. Neuroscience 1997;91:345-351.
61. Almeida JC, Grimsley EW. Coma from the health food store: Interaction between kava kava and alprazolam. Annu Int Med 1996;125:940-941.
62. Foo H, Lemon J. Acute effects of kava, alone or in combination with alcohol, on subjective measures of impairment and intoxication and on cognitive performance. Drug Alcohol Rev 1997;16:147-155.
63. Kraft M, Spahn TW, Menzel J, et al. Fulminant liver failure after administration of the herbal antidepressant kava-kava. Dtsch Med Wochenschr 2001;126:970-972.
64. Strahl S, Ehret V, Dahm HH, Maier KP. Necrotizing hepatitis after taking herbal remedies. Dtsch Med Wochenschr 1998;23:1410-1414.
65. Escher M, Desmeules J, Giostra E, Mentha G. Hepatitis associated with kava, a herbal remedy for anxiety. BMJ 2001;322:7279.-
66. Stickel F, Baumuller HM, Seitz K, et al. Hepatitis induced by Kava (Piper methysticum rhizoma). J Hepatol 2003;39:62-67.
67. Blumenthal M, Busse W, Goldberg A, et al, eds. The Complete German Commission E Monographs-Therapeutic Guide to Herbal Medicines. Austin: American Botanical Council; Boston: Integrative Medicine Communications; 1998.
68. Norton SA, Ruze P. Kava dermopathy. J Am Acad Dermatol 1994;31:89-97.
69. Stevinson C, Ernst E. Valerian for insomnia: A systematic review of randomized clinical trials. Sleep Medicine 2000;1:91-99.
70. Andreatini R, Sartori V, Seabra M, Leite J. Effect of valepotriates (valerian extract) in generalized anxiety disorder: a randomized placebo-controlled pilot study. Phytother Res 2002;16:650-654.
71. Cropley M, Cave Z, Ellis J, Middleton R. Effect of kava and valerian on human physiological and psychological responses to mental stress assessed under laboratory conditions. Phytother Res 2002;16:23-27.
72. Hadley S, Petry J. Valerian. Am Fam Physician 2003;67:1755-1758.
73. Houghton P. The scientific basis for the reputed activity of Valerian. J Pharm Pharmacol 1999;51:505-512.
74. Hiller K, Zetler G. Neuropharmacological studies on ethanol extracts of Valeriana officinalis L: Behavioural and anticonvulsant properties. Physiother Res Int 1996;10:145-151.
75. Capasso A, DeFeo V, DeSimon F, Sorrentino L. Pharmacological effects of aqueous extracts from Valeriana adscendens. Physiother Res Int 1996;10:309-312.
76. McGuffin M, Hobbs C, Upton R, Goldberg A, eds. American Herbal Products Association’s Botanical Safety Handbook. Boca Raton, Fla: CRC Press; 1997.
77. Donath F, Quispe S, Diefenbach K, Maurer A, Fietze I, Roots I. Critical evaluation of the effect of valerian extract on sleep structure and sleep quality. Pharmacopsychiatry 2000;33:47-53.
78. Kuhlmann J, Berger W, Podzuweit H, Schmidt U. The influence of valerian treatment on “reaction time, alertness and concentration” in volunteers. Pharmacopsychiatry 1999;32:235-241.
79. Oken B, Storzbach D, Kaye J. The efficacy of Ginkgo biloba on cognitive function in Alzheimer disease. Arch Neurol 1998;55:1409-1415.
80. Kleijnen J, Knipschild P. Ginkgo biloba for cerebral insufficiency. Br J Clin Pharmacol 1992;34:352-358.
81. Ernst E, Pittler M. Ginkgo biloba for dementia: a systematic review of double-blind, placebo-controlled trials. Clin Drug Invest 1999;17:301-308.
82. Le Bars PL, Katz MM, Berman N, Itil TM, Freedman AM, Schatzberg AF. A placebo-controlled, double-blind, randomized trial of an extract of Ginkgo biloba for dementia. JAMA 1997;278:1327-1332.
83. Oyama Y, Fuchs P, Katayama N, Noda K. Myricetin and quercetin, the flavonoid constituents of Ginkgo biloba extract, greatly reduce oxidative metabolism in both resting and Ca(2+)-loaded brain neurons. Brain Res 1994;635:125-129.
84. Cupp M, ed. Toxicology and Clinical Pharmacology of Herbal Products. Totowa, NJ: Humana Press; 2000.
85. Rowin J, Lewis SL. Spontaneous bilateral subdural hematomas associated with chronic Ginkgo. Neurol 1996;46:1775-1776.
86. Rosenblatt M, Mindel J. Spontaneous hyphema associated with ingestion of Ginkgo biloba extract. N Engl J Med 1997;336:1108.-
87. Miller LG. Herbal medicinals: Selected clinical considerations focusing on known or potential drug-herb interactions. Arch Intern Med 1998;158:2200-2211.
88. Houghton P. Ginkgo. Pharm J 1994;253:121-122.
89. Ernst E, Pittler M. Yohimbine for erectile dysfunction: A systematic review and meta-analysis of randomized clinical trials. J Urol 1998;159:433-436.
90. Morales A. Yohimbine in erectile dysfunction: The facts. Int J Impot Res 2000;Suppl 1:S70-S74.
91. Carey M, Johnson B. Effectiveness of yohimbine in the treatment of erectile disorder: Four meta-analytic integrations. Arch Sex Behav 1996;25:341-360.
92. Charney DS, Woods SW, Goodman WK, Heninger GR. Neurobiological mechanisms of panic anxiety: Biochemical and behavioural correlates of yohimbine-induced panic attacks. Am J Psychiatry 1987;144:1030-1036.
93. Jordan J, Sharma A. Potential for sibutramine-yohimbine interaction? Lancet 2003;361:1826.-
94. Goldstein D, Grossman E, Listwak S, Folio C. Sympathetic reactivity during a yohimbine challenge test in essential hypertension. Hypertension 1991;18 (Suppl 3):40-48.
95. Price L, Charney D, Heninger G. Three cases of manic symptoms following yohimbine administration. Am J Psychiatry 1984;141:1267-1268.
96. Gear R, Gordon N, Heller P, Levine J. Enhancement of morphine analgesia by the alpha2-adrenergic antagonist yohimbine. Neuroscience 1995;66:5-8.
97. McDougle C, Krystal J, Price L, Heninger G, Charney D. Noradrenergic response to acute ethanol administration in healthy subjects: comparison with intravenous yohimbine. Psychopharmacology (Berl) 1995;118:127-135.
98. Rowland D, Tai W. A review of plant-derived and herbal approaches to the treatment of sexual dysfunctions. J Sex Marital Ther 2003;29:185-205.
99. Wang Z, Gorski JC, Hamman MA, Huang SM, Lesko LJ, Hall SD. The effects of St John’s wort (Hypericum perforatum) on human cytochrome P450 activity. Clin Pharmacol Ther 2001;70:317-326.
100. Mathews JM, Etheridge AS, Black SR. Inhibition of human cytochrome P450 activities by kava extract and kavalactones. Drug Metab Dispos 2002;30:1153-1157.
101. Renton KW. Alteration of drug biotransformation and elimination during infection and inflammation. Pharmacol Ther 2001;92:147-163.
102. Gardener D. Evidence-based decisions about herbal products for treating mental disorders. J Psychiatry Neurosci 2002;27:324-333.
How should we evaluate and treat constipation in infants and children?
- What are the indications for laboratory studies and imaging?
- What dietary adjustments are most effective?
- What medications are helpful?
- When can enemas be used?
- How effective is behavior modification?
These questions are answered in the recommendations at right, derived from a guideline developed and funded by the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. The target populations are infants and children with constipation who have no preexisting medical diagnosis.
The evidence categories for this guideline are diagnosis, evaluation, management, and treatment. Outcomes considered are 1) sensitivity and specificity of diagnostic tests; 2) rate of symptomatic relief; 3) prevention and control of symptoms; 4) medication and treatment side effects; 5) quality of life; and 6) bowel movement frequency. Recommendations were grouped by patient age: infants (age <1 year), children (age 1 year and older), and in general for all ages. Functional constipation was defined as fecal retention, unrelated to a medical or anatomic abnormality. Potential benefits and harms of implementing the guidelines were considered in the development. The rating scheme is updated to comply with the SORT taxonomy.1
Guideline relevance and limitations
Constipation is common among infants and children, accounting for 3% to 5% of visits to pediatric outpatient clinics. Males and females are equally affected.2 In one study,3 16% of parents reported constipation in their 2-year-olds.
A long bibliography accompanies this guideline, along with 77 references. The guideline is strengthened by inclusion of 2 algorithms for management of constipation in children aged <1 and >1 year, and consideration of potential harm. It was weakened by lack of a cost-effectiveness analysis.
Guideline development and evidence review
The constipation guideline committee first determined the scope of the guideline. A literature search in Medline from 1966 through 1997 was performed. These were filtered to include only randomized control trials. A second search strategy identified articles on treatment, including drug therapy, surgery, and “therapy.” In total, 160 articles were reviewed for development of the guideline. A systematic review of the literature was performed. Quality and strength of evidence were weighted according to a rating scheme.
The initial guideline was published in 1999. It was reviewed in 2004 and deemed current, after a new literature review and expert committee review.
Source for this guideline
Baker BB, Liptak GS, Colletti RB, et al. Constipation in infants and children: evaluation and treatment. A medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr 1999; 29:612–626.
Another similar guideline
Functional constipation and soiling in children
This 2003 guideline presents methods for diagnosis and treatment of functional constipation, associated with soiling in children. It is only pertinent for children with encopresis: voluntary or involuntary passage of formed, semiformed, or liquid stool in places other than the toilet.
Source. University of Michigan Health System. Functional constipation and soiling in children. Ann Arbor: University of Michigan Health System; 2003. 10 pp. [8 references]
GRADE A RECOMMENDATIONS
- Mineral oil and osmotic laxatives are safe and effective for children.
- Medications combined with behavioral management can reduce time to remission in children with functional constipation.
GRADE B RECOMMENDATIONS
- An abdominal radiograph can be useful to diagnose fecal impaction.
- Rectal biopsy and rectal manometry are the only studies to reliably diagnose Hirschsprung disease.
- In infants, rectal disimpaction may be carried out with glycerin suppositories. Enemas should be avoided.
- In children, rectal disimpaction may be carried out with either oral or rectal medications, including enemas.
- In infants, juices that contain sorbitol, such as prune, pear, and apple juice, can decrease constipation.
- Osmotic laxatives (barley malt extract, corn syrup, lactulose, and sorbitol) can be used as stool softeners.
- Stimulant laxatives (senna and bisacodyl) can be useful in more difficult-to-treat cases.
GRADE C RECOMMENDATIONS
- A thorough history and physical is adequate to diagnose functional constipation.
- Stool exam for occult blood should be performed in constipated infants and in children with abdominal pain, failure to thrive, diarrhea, or family history of colon polyps/cancers.
- Mineral oil and stimulant laxatives should not be used in infants.
- In children, a balanced diet, containing whole grains, fruits, and vegetables is recommended.
- Polyethylene glycol electrolyte solution, in low doses, can be effective for difficult to treat patients.
Correspondence
Keith B. Holten, MD, 825 Locust Street, Wilmington, OH 45177. E-mail: [email protected]
1. Ebell M, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-120.
2. Borowitz S. Constipation. eMedicine June 2004. Available at: www.emedicine.com/ped/topic471.htm. Accessed on June 27, 2005.
3. Issenman RM, Hewson S, Pirhonen D, et al. Are chronic digestive complaints the result of abnormal dietary patterns? Diet and digestive complaints in children at 22 and 40 months of age. Am J Dis Child 1987;141:679-682.
- What are the indications for laboratory studies and imaging?
- What dietary adjustments are most effective?
- What medications are helpful?
- When can enemas be used?
- How effective is behavior modification?
These questions are answered in the recommendations at right, derived from a guideline developed and funded by the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. The target populations are infants and children with constipation who have no preexisting medical diagnosis.
The evidence categories for this guideline are diagnosis, evaluation, management, and treatment. Outcomes considered are 1) sensitivity and specificity of diagnostic tests; 2) rate of symptomatic relief; 3) prevention and control of symptoms; 4) medication and treatment side effects; 5) quality of life; and 6) bowel movement frequency. Recommendations were grouped by patient age: infants (age <1 year), children (age 1 year and older), and in general for all ages. Functional constipation was defined as fecal retention, unrelated to a medical or anatomic abnormality. Potential benefits and harms of implementing the guidelines were considered in the development. The rating scheme is updated to comply with the SORT taxonomy.1
Guideline relevance and limitations
Constipation is common among infants and children, accounting for 3% to 5% of visits to pediatric outpatient clinics. Males and females are equally affected.2 In one study,3 16% of parents reported constipation in their 2-year-olds.
A long bibliography accompanies this guideline, along with 77 references. The guideline is strengthened by inclusion of 2 algorithms for management of constipation in children aged <1 and >1 year, and consideration of potential harm. It was weakened by lack of a cost-effectiveness analysis.
Guideline development and evidence review
The constipation guideline committee first determined the scope of the guideline. A literature search in Medline from 1966 through 1997 was performed. These were filtered to include only randomized control trials. A second search strategy identified articles on treatment, including drug therapy, surgery, and “therapy.” In total, 160 articles were reviewed for development of the guideline. A systematic review of the literature was performed. Quality and strength of evidence were weighted according to a rating scheme.
The initial guideline was published in 1999. It was reviewed in 2004 and deemed current, after a new literature review and expert committee review.
Source for this guideline
Baker BB, Liptak GS, Colletti RB, et al. Constipation in infants and children: evaluation and treatment. A medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr 1999; 29:612–626.
Another similar guideline
Functional constipation and soiling in children
This 2003 guideline presents methods for diagnosis and treatment of functional constipation, associated with soiling in children. It is only pertinent for children with encopresis: voluntary or involuntary passage of formed, semiformed, or liquid stool in places other than the toilet.
Source. University of Michigan Health System. Functional constipation and soiling in children. Ann Arbor: University of Michigan Health System; 2003. 10 pp. [8 references]
GRADE A RECOMMENDATIONS
- Mineral oil and osmotic laxatives are safe and effective for children.
- Medications combined with behavioral management can reduce time to remission in children with functional constipation.
GRADE B RECOMMENDATIONS
- An abdominal radiograph can be useful to diagnose fecal impaction.
- Rectal biopsy and rectal manometry are the only studies to reliably diagnose Hirschsprung disease.
- In infants, rectal disimpaction may be carried out with glycerin suppositories. Enemas should be avoided.
- In children, rectal disimpaction may be carried out with either oral or rectal medications, including enemas.
- In infants, juices that contain sorbitol, such as prune, pear, and apple juice, can decrease constipation.
- Osmotic laxatives (barley malt extract, corn syrup, lactulose, and sorbitol) can be used as stool softeners.
- Stimulant laxatives (senna and bisacodyl) can be useful in more difficult-to-treat cases.
GRADE C RECOMMENDATIONS
- A thorough history and physical is adequate to diagnose functional constipation.
- Stool exam for occult blood should be performed in constipated infants and in children with abdominal pain, failure to thrive, diarrhea, or family history of colon polyps/cancers.
- Mineral oil and stimulant laxatives should not be used in infants.
- In children, a balanced diet, containing whole grains, fruits, and vegetables is recommended.
- Polyethylene glycol electrolyte solution, in low doses, can be effective for difficult to treat patients.
Correspondence
Keith B. Holten, MD, 825 Locust Street, Wilmington, OH 45177. E-mail: [email protected]
- What are the indications for laboratory studies and imaging?
- What dietary adjustments are most effective?
- What medications are helpful?
- When can enemas be used?
- How effective is behavior modification?
These questions are answered in the recommendations at right, derived from a guideline developed and funded by the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. The target populations are infants and children with constipation who have no preexisting medical diagnosis.
The evidence categories for this guideline are diagnosis, evaluation, management, and treatment. Outcomes considered are 1) sensitivity and specificity of diagnostic tests; 2) rate of symptomatic relief; 3) prevention and control of symptoms; 4) medication and treatment side effects; 5) quality of life; and 6) bowel movement frequency. Recommendations were grouped by patient age: infants (age <1 year), children (age 1 year and older), and in general for all ages. Functional constipation was defined as fecal retention, unrelated to a medical or anatomic abnormality. Potential benefits and harms of implementing the guidelines were considered in the development. The rating scheme is updated to comply with the SORT taxonomy.1
Guideline relevance and limitations
Constipation is common among infants and children, accounting for 3% to 5% of visits to pediatric outpatient clinics. Males and females are equally affected.2 In one study,3 16% of parents reported constipation in their 2-year-olds.
A long bibliography accompanies this guideline, along with 77 references. The guideline is strengthened by inclusion of 2 algorithms for management of constipation in children aged <1 and >1 year, and consideration of potential harm. It was weakened by lack of a cost-effectiveness analysis.
Guideline development and evidence review
The constipation guideline committee first determined the scope of the guideline. A literature search in Medline from 1966 through 1997 was performed. These were filtered to include only randomized control trials. A second search strategy identified articles on treatment, including drug therapy, surgery, and “therapy.” In total, 160 articles were reviewed for development of the guideline. A systematic review of the literature was performed. Quality and strength of evidence were weighted according to a rating scheme.
The initial guideline was published in 1999. It was reviewed in 2004 and deemed current, after a new literature review and expert committee review.
Source for this guideline
Baker BB, Liptak GS, Colletti RB, et al. Constipation in infants and children: evaluation and treatment. A medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr 1999; 29:612–626.
Another similar guideline
Functional constipation and soiling in children
This 2003 guideline presents methods for diagnosis and treatment of functional constipation, associated with soiling in children. It is only pertinent for children with encopresis: voluntary or involuntary passage of formed, semiformed, or liquid stool in places other than the toilet.
Source. University of Michigan Health System. Functional constipation and soiling in children. Ann Arbor: University of Michigan Health System; 2003. 10 pp. [8 references]
GRADE A RECOMMENDATIONS
- Mineral oil and osmotic laxatives are safe and effective for children.
- Medications combined with behavioral management can reduce time to remission in children with functional constipation.
GRADE B RECOMMENDATIONS
- An abdominal radiograph can be useful to diagnose fecal impaction.
- Rectal biopsy and rectal manometry are the only studies to reliably diagnose Hirschsprung disease.
- In infants, rectal disimpaction may be carried out with glycerin suppositories. Enemas should be avoided.
- In children, rectal disimpaction may be carried out with either oral or rectal medications, including enemas.
- In infants, juices that contain sorbitol, such as prune, pear, and apple juice, can decrease constipation.
- Osmotic laxatives (barley malt extract, corn syrup, lactulose, and sorbitol) can be used as stool softeners.
- Stimulant laxatives (senna and bisacodyl) can be useful in more difficult-to-treat cases.
GRADE C RECOMMENDATIONS
- A thorough history and physical is adequate to diagnose functional constipation.
- Stool exam for occult blood should be performed in constipated infants and in children with abdominal pain, failure to thrive, diarrhea, or family history of colon polyps/cancers.
- Mineral oil and stimulant laxatives should not be used in infants.
- In children, a balanced diet, containing whole grains, fruits, and vegetables is recommended.
- Polyethylene glycol electrolyte solution, in low doses, can be effective for difficult to treat patients.
Correspondence
Keith B. Holten, MD, 825 Locust Street, Wilmington, OH 45177. E-mail: [email protected]
1. Ebell M, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-120.
2. Borowitz S. Constipation. eMedicine June 2004. Available at: www.emedicine.com/ped/topic471.htm. Accessed on June 27, 2005.
3. Issenman RM, Hewson S, Pirhonen D, et al. Are chronic digestive complaints the result of abnormal dietary patterns? Diet and digestive complaints in children at 22 and 40 months of age. Am J Dis Child 1987;141:679-682.
1. Ebell M, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-120.
2. Borowitz S. Constipation. eMedicine June 2004. Available at: www.emedicine.com/ped/topic471.htm. Accessed on June 27, 2005.
3. Issenman RM, Hewson S, Pirhonen D, et al. Are chronic digestive complaints the result of abnormal dietary patterns? Diet and digestive complaints in children at 22 and 40 months of age. Am J Dis Child 1987;141:679-682.
Earning trust and losing it: Adolescents’ views on trusting physicians
Objective: To explore how adolescents with and without chronic illness perceive patient-physician trust and to identify physician behaviors related to these perceptions that might be modified to promote adolescent health care.
Methods: Fifty-four adolescents recruited from the community (healthy subjects) and from hospital-based clinics (subjects with chronic illnesses) participated in 12 focus groups divided by age (11–14 or 15–19 years old), gender, and health status. Major themes related to preferred physician characteristics and trusting one’s doctor were derived through a multistep, team-based qualitative analytic process.
Results: Adolescents hold varied perspectives of trust in their physicians. They describe elements of patient-physician trust similarly to the comprehensive model developed with adults, including fidelity, confidentiality, competency, honesty, and a global perspective intersecting several of the more specific domains. However, adolescents differ in the relative importance of these dimensions. Younger adolescents express more concern about confidentiality of their health information, and adolescents with chronic illnesses are more interested in involving parents in their care than are adolescents without chronic illnesses. Examples of specific behaviors to improve trust include asking for adolescent’s opinion, keeping private information confidential, not withholding information, and engaging in small talk to show concern.
Conclusion: Understanding the importance of trust and listening to recommendations about behaviors to improve it, in the words of the adolescents, may help physicians build positive relationships with their adolescent patients.
- Keep in mind that adolescents are generally more concerned than adults about confidentiality when deciding on a physician’s trustworthiness.
- Approach adolescents who have chronic illnesses with the expectation that they will be more comfortable involving parents in their care than will healthy adolescents.
In the primary care setting, a patient’s trust of the physician is more strongly associated with self-reports of improved health than is any other characteristic of the patient-physician relationship.1 Trust has been shown to affect a patient’s satisfaction with health care services and willingness to disclose sensitive information, adhere to treatment, continue with a physician, and recommend that physician to others.1,2
Increasing age of a patient has a modestly positive correlation with trust, possibly due to greater contact with physicians; other demographic characteristics have not been consistently found to relate to trust.3,4
Studies examining health status and trust have shown a weak and inconsistent relationship.1,3 Persons with poor health, such as a chronic illness, may be more vulnerable and thus have a greater need to trust. Poor health may also cause negative feelings that may influence how patients trust their physicians.
Physician behavior and patient trust
The importance of patient trust to the process and outcome of health care has prompted the study of how specific physician behaviors may help to build trust. Among adults with and without chronic conditions, trust is associated with perceived physician caring, competence, and communication.1,5,6 Among adolescents, trust seems more strongly influenced by a physician’s confidentiality, competence, honesty, and respect, than by any other set of characteristics pertaining to health care professionals, health care sites, or incentives to use primary care services.7,8 Distrust that physicians will protect confidentiality has been cited as a barrier to health care use and compliance among adolescents.9
However, unlike the adult literature on patient-physician trust, no study of adolescents has defined trust from the patient’s perspective or identified physician behaviors that promote trust among adolescent patients. Directly asking adolescents about trust in their doctor may identify specific physician behaviors that encourage building trust. Understanding the importance of trust to adolescents and listening to their recommendations about behaviors to improve it, in the words of the adolescents, may help physicians build positive relationships with their adolescent patients.
This study addresses the call by Rosser and Kasperski for more research pertaining to the development of trust between doctors and patients.10 A model of trust between adult patients and their physicians, developed by Hall et al,3 was used as a framework to understand adolescents’ perceptions of patient-physician trust. The 5 specific domains of this model include patient perceptions of physician fidelity, protection of confidential information, competence, honesty, and a global perspective that intersects several of the more specific domains and captures the holistic aspect of trust. This study’s objective was to explore how adolescents with and without chronic illness perceive patient-physician trust and to identify physician behaviors related to these perceptions that might be modified to promote adolescent health care.
Methods
Participants
This study was part of a larger qualitative and quantitative research project examining health care preferences of adolescents with chronic health conditions.11 The protocol for the research project on adolescent health care preferences and the analyses performed for the current study on trust were approved by the Institutional Review Board of the Cincinnati Children’s Hospital Medical Center.
Adolescents aged 11 to 19 years with cystic fibrosis, sickle-cell disease, juvenile rheumatoid arthritis, or inflammatory bowel disease diagnosed at least 2 years previously were recruited from hospital-based clinics. We attempted to contact all patients aged 11 to 19 years in these sub-specialty clinics for their participation. Introductory letters were sent, followed by phone calls, to these adolescents and their guardians to explain the study and to invite participation in a focus group. For comparison, a convenience sample of adolescents aged 11 to 19 years without chronic conditions were recruited from local summer recreation programs, a church, and a school using flyers and personal contacts.
Written informed consent was obtained from participants who were age 18 years and older and from the legal guardians of participants who were younger than age 18 years. Participants were reimbursed 10 dollars for their time and travel expenses. The study sample consisted of 54 participants divided by age (11 to 14 years and 15 to 19 years), gender, and the presence or absence of chronic disease into 12 focus groups ranging in size from 2 to 10 individuals (mean=5) (TABLE).
Following focus group protocol recommendations for homogenous groups12 and other similar studies,7,8 groups were divided by age due to differing developmental levels (early vs later adolescence) and gender, since same-sex groups are preferred for young adolescents. Participants were divided based on the presence or absence of chronic disease due to different health care experiences. For the groups of participants with a chronic disease, 17 were 11 to 14 years old (6 male; 11 female) and 12 were 15 to 19 years old (7 male; 5 female). For the groups of healthy participants, 13 were 11 to 14 years old (8 male; 5 female) and 12 were 15 to 19 years old (4 male; 8 female).
TABLE
Demographics of sample (N=54)
| N | % | |
|---|---|---|
| Gender | ||
| Female | 30 | 56 |
| Health status | ||
| Healthy | 25 | 46 |
| Chronic Illness | 29 | 54 |
| Cystic fibrosis | 7 | 24 |
| Inflammatory bowel disease | 10 | 35 |
| Juvenile rheumatoid arthritis | 5 | 17 |
| Sickle-cell disease | 7 | 24 |
| Age | ||
| Range: 11–20 | ||
| Mean: 14 | ||
Data collection
Focus groups were conducted as part of the larger research project to explore adolescents’ preferences on various aspects of their health care (eg, doctor-patient relationship, doctors’ characteristics, physical environment, doctor-patient communication).11 The current analysis examined one aspect of the doctor-patient relationship identified by participants: trust.
One professional facilitator led the 12 groups through 2-hour discussions about health concerns, preferred physician characteristics, and preferred visit characteristics. New topics raised by a given group were highlighted by the facilitator for discussion by subsequent groups, and discussions were directed away from topics that had reached saturation in previous groups.13
In general, adolescents discussed the dimensions of trust in response to 2 questions: “What makes a good doctor?” and “How do you know you can trust your doctor?” Audiotapes of all discussions were transcribed verbatim, edited for accuracy, and supplemented by field notes taken by co-investigators who attended the group discussions as observers. The presence of the co-investigators enhanced understanding of the transcripts, without apparent discomfort or inhibition of the participants.
Data analysis
The analyses occurred in multiple stages. During the first phase of analyses, 4 coinvestigators independently prepared summaries of each group transcript and initial lists of the themes discussed by the participants, using Crabtree and Miller’s editing-organizing style.14 They then met as a team to discuss their observations and to begin preliminary interpretation of that focus group. Consensus on the themes was reached for each group.
After the groups’ results were analyzed separately, the research team compared and contrasted the group themes and generated a comprehensive coding scheme for all of the focus groups combined. Emphasis was placed on a comprehensive coding scheme (ie, topics discussed less often were included along with topics discussed more often). Trust was identified as a major theme discussed in all 12 focus groups.
In the next stage of analysis, the edited transcripts and the coding scheme were imported into the qualitative text analysis software package N5 NUD*IST.15 Two authors (TT and MB) independently coded the first 2 transcripts using the comprehensive coding scheme. Discrepancies in coding were resolved by negotiation. The remaining transcripts were then coded by one of the authors (TT). Unclear or confusing statements were discussed with other team members for coding clarification.
Trust emerged as an important concept and was selected for more detailed, theoretical analysis. For this analysis, a team member (BK) reviewed the transcripts and used the N5 NUD*IST search feature to identify comments in the transcripts related to trust. Then, the research literature was surveyed for frameworks to help us further understand and analyze the data pertaining to physician-patient trust in adolescents. Hall et al’s model of trust between adult patients and their physicians was selected as a framework for categorizing the comments into 5 specific domains.3 One team member (BK) assigned each comment to a category using the data matrix method of Miles and Huberman16 and noted in which gender-age-health groups it had been discussed. Although the analytic plan called for no categorization of comments that did not fit the schema of Hall et al, all comments discussed by all groups were readily assigned to categories.
To ensure trustworthiness of the data, another team member (MB) reread the transcripts to identify and categorize statements related to trust that might have been missed by the software search and to confirm the assignments made by the first reviewer. The reviewers looked for patterns of similarities and differences in responses from the participants. Specifically, groups were compared by gender, age, and health condition for the dimensions of trust and the specific topics within each dimension that were discussed. Once the 2 reviewers agreed on the categorization of the comments, their interpretations were reviewed, discussed, and finalized by 2 other team members for further verification and to look for disconfirming data.
Results
All groups discussed topics related to at least 2 of the 5 dimensions of trust. Nine of the 12 groups discussed topics in at least 4 of the 5 dimensions.
Fidelity
Fidelity—the physician’s pursuit of the patient’s best interest, not taking advantage of the patient’s vulnerability—was discussed by 9 of the 12 groups. The words used by the adolescent participants to describe fidelity included caring, respect, and advocacy, as demonstrated below.
- 13-year-old male without chronic illness: “Doctors show they care by trying to understand how you’re feeling rather than just coming in to try to fix things.”
- 15-year-old male with Crohn’s disease: “If he asks for my opinion or if he takes my advice seriously…or how he talks to me. I know if he either respects me or not…if he doesn’t talk down to me, like, still doesn’t think I’m a little kid.”
- 13-year-old female with cystic fibrosis: “[A good doctor is] someone that you can trust to take care of you and do what’s right for you.”
When asked about behaviors that would diminish trust, several participants gave examples of how a physician might take advantage of an adolescent’s vulnerability. For example, a 15-year-old female without chronic illness mentioned she would lose trust if her doctor “touched her in the wrong way.” A 13-year-old male without chronic illness stated: “This never happened, but I just feel like it would happen like, as soon as my mom walks out of the door, the doctor would pull out that clipboard [and say] ‘Oh, I’m trying to ask these questions [about sensitive topics].’”
Confidentiality
Confidentiality (ie, keeping sensitive or private patient information from others) was discussed by nearly all of the groups. Although there was consensus about the overall importance of the dimension, adolescents varied in their beliefs about specific definitions, such as the types of information that should be kept confidential or from whom information should be withheld.
The general concept of confidentiality, however, was incorporated by many adolescents into descriptions of a good doctor and a trusted doctor. For example:
- 13-year-old male without chronic illness: “[A good doctor is] somebody who protects what you say and keeps things in a closed record to where nobody else can get to ’em.”
- 16-year-old female with cystic fibrosis: “He needs to keep that [conversation during doctor visit] zipped, especially when they talk to your parents afterwards. You may tell him something that you don’t want your parents to know about, and he should respect that if you tell him something.”
The following comment conveys how quickly an adolescent might lose trust in a doctor if confidentiality is broken:
- 19-year-old male with sickle-cell disease: “If I told my doctor something really personal that nobody else needed to know, and then he went and told everybody, I don’t care if it’s people on the hospital staff, sometimes I’ll be like ‘Uhhh, could you just keep this between us’ and if they go and tell everybody, that would make you lose trust in the doctor.”
Several younger males in one focus group expressed concern about information that might have been shared years earlier, when they were children:
- SUBJECT #1 (13-year-old male without chronic illness): “Because, some doctor, a doctor a long time ago when I was about 6, he sent my records all the way down to Children’s and it was not like what a normal doctor would do.”
- MODERATOR: “And that made you feel uncomfortable?”
- SUBJECT #1: “Yeah.”
- SUBJECT #2 (13-year-old male without chronic illness): “Like they were telling them everything.”
- SUBJECT #3 (11-year-old male without chronic illness): “And then next time you come: ‘Oh there’s the sick boy’.”
- SUBJECT #4 (13-year-old male without chronic illness): “Yeah.”
Competency
Six of the 12 groups, particularly the older female groups, discussed competency in terms of trusting their doctors and identifying what makes a good doctor. As with other dimensions, the discussions explored both the presence and absence of competency:
- 17-year-old female without chronic illness: “Like a doctor that gave you the wrong like…gave you a bad diagnosis or something and was, you know, had made a mistake, and they knew that they had made a mistake. You would naturally not go back to them.”
- 17-year-old female without chronic illness: “I think that you can get people to trust you and respect you and stuff by being efficient, professional, doing a job well and making it as painless as possible. Not necessarily, you know, talking to them about this that and the other thing.”
Honesty
Eight of the 12 groups identified honesty as an attribute of a good doctor and a trusted doctor. Adolescents defined an honest doctor as one who is realistic, accurate, and does not withhold information. For example,
- 15-year-old female with sickle-cell: “But I would like to know if I have bad news so I can, like, pump myself up to feel better. I don’t want them to come in to say ‘you’re feeling better, you’ll probably be out soon’, and then [find out I have something bad].”
- 12-year-old female with cystic fibrosis: “Yeah, if they lie to you, you kind of feel like you cannot trust them anymore.”
- 15-year-old female without chronic illness: “If there’s something’s wrong with you, you trust ’em to tell you.”
When asked if there were times when a doctor should not share bad news, all participants responded that the doctor should either share the news directly with the adolescent or with a parent, who would then discuss it with the adolescent. Access to all information was particularly important to participants with chronic illnesses, as demonstrated by this comment:
- 16-year-old female with cystic fibrosis: “I think it’s very important and if he didn’t, if my doctor didn’t [tell me the bad news], it could result in weeks of hospitalization. But my doctor does tell me the truth. I mean there’s hardly any time where he keeps something from me. I think the only way he’d keep something from me is if I wasn’t ready to hear it or if it really didn’t concern what I did just as long as my parents know about it.”
Global
Hall et al describe the global dimension of trust as serving 2 functions. The first is for comments that intersect 2 or more of the other areas but do not fit exclusively in one. The second is to capture the holistic quality of trust.
Group discussions about this global dimension involved a “friend-like” relationship with the doctor, comfort with the doctor, and an overall sense that the doctor could be trusted. The comments noted below are organized into these content areas:
- Friend-like.
- 14-year-old male with Crohn’s disease: “[The doctors] know their patient as a friend and not as a patient…they know them like a friendship and everything.”
- 16-year-old female without chronic illness: “[A good doctor] would be a friend with the patient, not just be an authority [figure].”
When asked how a doctor should relate to an adolescent patient as a friend, several adolescents suggested the doctor telling about his personal life (eg, family, children) and asking about the adolescent’s personal life (eg, sports, school). A 14-year-old male with Crohn’s disease suggested, “Have a conversation with them, not like question-answer, question-answer, having a conversation so it all flows.”
Comfort. Participants described physician use of introductory small talk as a means of building comfort, and the premature introduction of sensitive topics (eg, drug use, sexual behavior, family issues) as a barrier to comfort.
- 16-year-old female without chronic illness: “It’s sort of like an introductory question, like they’ll get you in there, try to make you feel comfortable, and they’re like,’ how’s school going’…I think they try to strike up a conversation to make you feel more comfortable.”
- 11-year-old female without chronic illness: “But if the doctor is a guy, then you probably won’t feel comfortable talking about that [peer pressure and menstrual cycles].”
Comfort was a prerequisite for trust for some adolescents. Participants described feeling comfortable telling their doctor and then trusting them with the information. The following comment illustrates the relationship:
- 15-year-old female without chronic illness: “If you’re comfortable, you have more trust in the person.”
Overall sense of trust. The older, healthy female group was the only group that described trust from a holistic perspective:
- MODERATOR: “I mean, what is it that makes them trustworthy? (Pause.) Just ‘cuz they’re doctors? Ok.”
- 17-year-old female without chronic illness: “I mean, you kinda want to trust your doctor and you don’t want to believe that they’re trying to get you…there’s nothing behind their back. You do want to be able to trust them.”
Discussion
Adolescents in our study defined a good doctor as one they can trust and, similar to other studies of adolescent populations, said trustworthiness is a core attribute they seek in a physician.7-9 The comprehensive model of patient-physician trust developed by Hall et al in adults depicts trust as perceived by the adolescent participants in our study.3 The dimensions of caring, confidentiality, competency, honesty, and holistic trust captured the beliefs expressed by the adolescents, suggesting that adolescent and adult models of physician trust may be similar.
Confidentiality is the one dimension in which the specifics may differ for adolescents and adults. Similar to other research with adolescents,7,9 adolescents in our study indicated that confidentiality (ie, keeping health and personal information private) is an important characteristic of a good doctor and a trusted doctor. Adults, on the other hand, are less concerned about confidentiality as it relates to trusting their physicians.2,3,6,17
Adolescents may be uncertain about a physician’s obligation to inform or not inform parents about private information, which, in turn, may increase their sensitivity to confidentiality. Because adolescents, unlike adults, are accountable to an adult who controls access to activities and friends, they may be more likely to conceal sensitive activities for fear of losing privileges. Chronically ill teens may conceal certain symptoms or lack of compliance with treatment for similar reasons.
Developmental differences may help explain the reason younger adolescents in our study expressed more concern and uncertainty about how health information is protected than did older adolescents. The capacity for formal operational thinking that develops during adolescence enables abstraction and leads to an increasing interest in how the outside world views personal attitudes and behaviors.18 Until adolescents test the responses of the outside world, they may feel center-stage, as though “everyone” is judging them. Keeping personal information private thus becomes extremely important to maturing adolescents.
Adults who have tested the views of others’ responses are better able than adolescents to keep in perspective the interests of the outside world and, therefore, may have fewer concerns about how their personal information is managed. In addition, adults are more likely to have a better understanding of confidentiality policies within a healthcare system and thus realize their private information is safeguarded.
Given that this analysis was part of a larger study and issues surrounding confidentiality were not studied in-depth, future research involving both adolescents and adults focusing on confidentiality and the uncertainty about parental involvement that often accompanies adolescent health care could shed light on this topic.
Although adolescents with and without chronic illnesses discussed the same dimensions of trust, honesty and advocacy were noted more often by the former. This resembles findings reported in studies of adults with serious illnesses.6 Adolescents with chronic illnesses tend to consider parents acceptable recipients of bad news. In addition, adolescents with chronic illnesses expect physicians to reveal bad news to either the adolescent or their parent, given the potential dire health consequences of withholding important medical information.
The issue of honesty may have been mentioned less frequently by healthy adolescents since they have not had to contend with major health issues and receiving bad news. Adolescents with chronic illnesses expect good doctors to “go the extra mile,” a task that is increasingly difficult in a health care environment that seeks to limit reimbursement and expenditure.19
Keeping in mind the qualitative nature of our study and size of our sample, the findings from our focus groups suggest that physicians working with adolescents with a chronic illness be cognizant of their increased need for complete and accurate information, as well as the higher expectation that the doctor will act on their behalf. Additional studies are needed to investigate whether adolescents with a chronic illness have a higher need for honesty and advocacy than healthy adolescents.
Although identified as a predictor, rather than a dimension, of trust,3 duration of the patient-physician relationship was discussed by adolescents with and without chronic illnesses in our study. Comments similar to “he’s been taking care of me for a long time” or “because I’ve known her all my life” were repeated often. Studies in both adolescent7,20 and adult populations,2,4,17 have reported similar findings. Adolescents in our study varied in their estimations of sufficient duration, from 4 to 5 visits to knowing the doctor “forever.”
Unlike the many comments pertaining to duration of acquaintance, there was no discussion of the frequency or intensity of visits. Comfort appears to be a prerequisite for trust for adolescents in our study and may perhaps be a moderating factor when examining how the duration of the patient-physician relationship influences trust. The length of time necessary to feel comfortable may vary among individuals and may be influenced by other factors (eg, experience with doctors or the health care system, friendliness of the physician). Thus, it may not be possible to determine a standard time period (eg, 6 months) in which adolescents feel comfortable to trust their doctor. Future studies examining what influences adolescents’ comfort level (eg, length of relationship, intensity of health care experience) with their physician may provide additional insight for improving adolescents’ trust in their physicians.
When asked how doctors could gain the trust of adolescent patients, participants in our study responded “be truthful,” “be friendly,” and “be there.” More specific behaviors included asking for the adolescent’s opinion, keeping private information confidential, not withholding clinical information from the patient, and engaging in small talk to show concern.
Participants were quick to point out that physician violation of gained trust is viewed as serious behavior that leads to rapid deterioration in the doctor-patient relationship.3,19 They identified examples of violated trust as medical mistakes, breaks in confidentiality, and taking advantage of patients when vulnerable (eg, during the physical examination). These descriptions highlight the importance of proactive discussions early in the doctor-patient relationship, clarifying the legal and ethical limitations of issues such as confidentiality.
There are several limitations to this study. First, these analyses were part of a larger study examining health care preferences of adolescents with a chronic illness. Because the issue of physician-patient trust was not the focal point of the original study, there may be issues relating to trust that our study did not address. Further research with additional samples is needed to confirm if all aspects of trust were explored.
Second, while our findings support those of earlier studies in both adolescents and adults, our sample was drawn from the patient population of only one mid-western city in the US.7-9,20
Third, adolescents who declined participation in the study may differ in their attitudes or beliefs about health care providers than adolescents who agreed to participate, thus introducing a potential selection bias.
Fourth, we were unable to perform member checking or reactor panels to examine “external validity” due to the participants’ cognitive level (ie, difficulty discussing abstract concepts). However, corroborating evidence from earlier studies supported our findings.
Fifth, our study was designed to collect qualitative data and to use analytic methods that are appropriate for such data. The data and statistical methods were not intended to be quantitative, and the interpretations of the reported findings therefore were appropriate for those of a qualitative, not quantitative study design.
In conclusion, our study provides the first steps in suggesting that adolescents and adults agree on the major dimensions of trust but differ in the relative importance of these dimensions to the overall definition of trust. Adolescents in our study expressed the broadest range of beliefs within the dimension of confidentiality. Younger adolescents expressed more concern and uncertainty about how health information is protected than did older adolescents.
Adolescents with chronic illnesses seemed more comfortable involving parents in their care than did adolescents without chronic illnesses. Since adolescents with chronic illness have more experience involving their parents in their care, future studies could examine whether having a chronic illness makes a difference in whether an adolescent would involve their parent more when faced with the same health concerns typical of healthy adolescents (eg, sexual health, psychological issues).
Additional studies focusing specifically on physician-patient trust are needed to further explore similarities and differences between adults and adolescents’ perceptions. Understanding the importance of trust to adolescents and listening to their recommendations about behaviors that promote it may help physicians build positive relationships with patients that will continue into and beyond young adulthood.
Acknowledgments
Supported by a Robert Wood Johnson Generalist Physician Faculty Scholar Award to the senior author.
CORRESPONDING AUTHOR
Brenda K. Klostermann, PhD, Illinois Education Research Council, Southern Illinois University Edwardsville, Box 1064, Edwardsville, IL 62026-1064. E-mail: [email protected]
1. Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract 1998;47:213-220.
2. Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev 2002;59:293-318.
3. Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: What is it, can it be measure, and does it matter? Milbank Q 2001;79:613-639.
4. Thom DH, Ribisl KM, Stewart AL, Luke DA. The Stanford Trust Study Physicians. Further validation and reliability testing of the Trust in Physician scale. Med Care 1999;37:510-517.
5. Thom DH. Stanford Trust Study Physicians. Physician behaviors that predict patient trust. J Fam Pract 2001;50:323-328.
6. Mechanic D, Meyer S. Concepts of trust among patients with serious illness. Soc Sci Med 2000;51:657-668.
7. Ginsburg KR, Menapace AS, Slap GB. Factors affecting the decision to seek health care: The voice of adolescents. Pediatrics 1997;100:922-930.
8. Ginsburg KR, Slap GB, Cnaan A, Forke CM, Balsley CM, Rouselle DM. Adolescents’ perceptions of factors affecting their decisions to seek health care. JAMA 1995;273:1913-1918.
9. Cogswell BE. Cultivating the trust of adolescent patients. Fam Med 1985;17:254-258.
10. Rosser WW, Kasperski J. The benefits of a trusting physician-patient relationship. J Fam Pract 2001;50:329-330.
11. Britto MT, DeVellis RF, Hornung RW, DeFriese GH, Atherton HD, Slap GB. Health care p and priorities of adolescents with chronic illness. Pediatrics 2004;114:1272-1280.
12. Krueger RA. Focus Groups: A Practical Guide for Applied Research. Newbury Park, Calif: Sage Publications; 1998.
13. Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, Calif: Sage Publications; 1998.
14. Crabtree BF, Miller WL. Doing Qualitative Research. 2nd ed.Thousand Oaks, Calif: Sage Publications; 1999.
15. Qualitative Solutions and Research International Pty Ltd., N5 NUD*IST for Windows [Computer Software]. Victoria, Australia: Qualitative Solutions; 2000.
16. Miles MB, Huberman AM. Qualitative Data Analysis. 2nd ed. Thousand Oaks, Calif: Sage Publications; 1994.
17. Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: Effects of choice, continuity, and payment method. J Gen Intern Med 1998;13:681-686.
18. Elkind D. Teenage thinking: Implications for health care. Pediatric Nursing 1984;10:383-385.
19. Davies HTO, Rundall TG. Managing patient trust in managed care. Milbank Q 2000;78:609-624.
20. Ginsburg KR, Forke CM, Cnaan A, Slap GB. Important health provider characteristics: The perspective of urban ninth graders. Dev Behav Ped 2002;23:237-243.
Objective: To explore how adolescents with and without chronic illness perceive patient-physician trust and to identify physician behaviors related to these perceptions that might be modified to promote adolescent health care.
Methods: Fifty-four adolescents recruited from the community (healthy subjects) and from hospital-based clinics (subjects with chronic illnesses) participated in 12 focus groups divided by age (11–14 or 15–19 years old), gender, and health status. Major themes related to preferred physician characteristics and trusting one’s doctor were derived through a multistep, team-based qualitative analytic process.
Results: Adolescents hold varied perspectives of trust in their physicians. They describe elements of patient-physician trust similarly to the comprehensive model developed with adults, including fidelity, confidentiality, competency, honesty, and a global perspective intersecting several of the more specific domains. However, adolescents differ in the relative importance of these dimensions. Younger adolescents express more concern about confidentiality of their health information, and adolescents with chronic illnesses are more interested in involving parents in their care than are adolescents without chronic illnesses. Examples of specific behaviors to improve trust include asking for adolescent’s opinion, keeping private information confidential, not withholding information, and engaging in small talk to show concern.
Conclusion: Understanding the importance of trust and listening to recommendations about behaviors to improve it, in the words of the adolescents, may help physicians build positive relationships with their adolescent patients.
- Keep in mind that adolescents are generally more concerned than adults about confidentiality when deciding on a physician’s trustworthiness.
- Approach adolescents who have chronic illnesses with the expectation that they will be more comfortable involving parents in their care than will healthy adolescents.
In the primary care setting, a patient’s trust of the physician is more strongly associated with self-reports of improved health than is any other characteristic of the patient-physician relationship.1 Trust has been shown to affect a patient’s satisfaction with health care services and willingness to disclose sensitive information, adhere to treatment, continue with a physician, and recommend that physician to others.1,2
Increasing age of a patient has a modestly positive correlation with trust, possibly due to greater contact with physicians; other demographic characteristics have not been consistently found to relate to trust.3,4
Studies examining health status and trust have shown a weak and inconsistent relationship.1,3 Persons with poor health, such as a chronic illness, may be more vulnerable and thus have a greater need to trust. Poor health may also cause negative feelings that may influence how patients trust their physicians.
Physician behavior and patient trust
The importance of patient trust to the process and outcome of health care has prompted the study of how specific physician behaviors may help to build trust. Among adults with and without chronic conditions, trust is associated with perceived physician caring, competence, and communication.1,5,6 Among adolescents, trust seems more strongly influenced by a physician’s confidentiality, competence, honesty, and respect, than by any other set of characteristics pertaining to health care professionals, health care sites, or incentives to use primary care services.7,8 Distrust that physicians will protect confidentiality has been cited as a barrier to health care use and compliance among adolescents.9
However, unlike the adult literature on patient-physician trust, no study of adolescents has defined trust from the patient’s perspective or identified physician behaviors that promote trust among adolescent patients. Directly asking adolescents about trust in their doctor may identify specific physician behaviors that encourage building trust. Understanding the importance of trust to adolescents and listening to their recommendations about behaviors to improve it, in the words of the adolescents, may help physicians build positive relationships with their adolescent patients.
This study addresses the call by Rosser and Kasperski for more research pertaining to the development of trust between doctors and patients.10 A model of trust between adult patients and their physicians, developed by Hall et al,3 was used as a framework to understand adolescents’ perceptions of patient-physician trust. The 5 specific domains of this model include patient perceptions of physician fidelity, protection of confidential information, competence, honesty, and a global perspective that intersects several of the more specific domains and captures the holistic aspect of trust. This study’s objective was to explore how adolescents with and without chronic illness perceive patient-physician trust and to identify physician behaviors related to these perceptions that might be modified to promote adolescent health care.
Methods
Participants
This study was part of a larger qualitative and quantitative research project examining health care preferences of adolescents with chronic health conditions.11 The protocol for the research project on adolescent health care preferences and the analyses performed for the current study on trust were approved by the Institutional Review Board of the Cincinnati Children’s Hospital Medical Center.
Adolescents aged 11 to 19 years with cystic fibrosis, sickle-cell disease, juvenile rheumatoid arthritis, or inflammatory bowel disease diagnosed at least 2 years previously were recruited from hospital-based clinics. We attempted to contact all patients aged 11 to 19 years in these sub-specialty clinics for their participation. Introductory letters were sent, followed by phone calls, to these adolescents and their guardians to explain the study and to invite participation in a focus group. For comparison, a convenience sample of adolescents aged 11 to 19 years without chronic conditions were recruited from local summer recreation programs, a church, and a school using flyers and personal contacts.
Written informed consent was obtained from participants who were age 18 years and older and from the legal guardians of participants who were younger than age 18 years. Participants were reimbursed 10 dollars for their time and travel expenses. The study sample consisted of 54 participants divided by age (11 to 14 years and 15 to 19 years), gender, and the presence or absence of chronic disease into 12 focus groups ranging in size from 2 to 10 individuals (mean=5) (TABLE).
Following focus group protocol recommendations for homogenous groups12 and other similar studies,7,8 groups were divided by age due to differing developmental levels (early vs later adolescence) and gender, since same-sex groups are preferred for young adolescents. Participants were divided based on the presence or absence of chronic disease due to different health care experiences. For the groups of participants with a chronic disease, 17 were 11 to 14 years old (6 male; 11 female) and 12 were 15 to 19 years old (7 male; 5 female). For the groups of healthy participants, 13 were 11 to 14 years old (8 male; 5 female) and 12 were 15 to 19 years old (4 male; 8 female).
TABLE
Demographics of sample (N=54)
| N | % | |
|---|---|---|
| Gender | ||
| Female | 30 | 56 |
| Health status | ||
| Healthy | 25 | 46 |
| Chronic Illness | 29 | 54 |
| Cystic fibrosis | 7 | 24 |
| Inflammatory bowel disease | 10 | 35 |
| Juvenile rheumatoid arthritis | 5 | 17 |
| Sickle-cell disease | 7 | 24 |
| Age | ||
| Range: 11–20 | ||
| Mean: 14 | ||
Data collection
Focus groups were conducted as part of the larger research project to explore adolescents’ preferences on various aspects of their health care (eg, doctor-patient relationship, doctors’ characteristics, physical environment, doctor-patient communication).11 The current analysis examined one aspect of the doctor-patient relationship identified by participants: trust.
One professional facilitator led the 12 groups through 2-hour discussions about health concerns, preferred physician characteristics, and preferred visit characteristics. New topics raised by a given group were highlighted by the facilitator for discussion by subsequent groups, and discussions were directed away from topics that had reached saturation in previous groups.13
In general, adolescents discussed the dimensions of trust in response to 2 questions: “What makes a good doctor?” and “How do you know you can trust your doctor?” Audiotapes of all discussions were transcribed verbatim, edited for accuracy, and supplemented by field notes taken by co-investigators who attended the group discussions as observers. The presence of the co-investigators enhanced understanding of the transcripts, without apparent discomfort or inhibition of the participants.
Data analysis
The analyses occurred in multiple stages. During the first phase of analyses, 4 coinvestigators independently prepared summaries of each group transcript and initial lists of the themes discussed by the participants, using Crabtree and Miller’s editing-organizing style.14 They then met as a team to discuss their observations and to begin preliminary interpretation of that focus group. Consensus on the themes was reached for each group.
After the groups’ results were analyzed separately, the research team compared and contrasted the group themes and generated a comprehensive coding scheme for all of the focus groups combined. Emphasis was placed on a comprehensive coding scheme (ie, topics discussed less often were included along with topics discussed more often). Trust was identified as a major theme discussed in all 12 focus groups.
In the next stage of analysis, the edited transcripts and the coding scheme were imported into the qualitative text analysis software package N5 NUD*IST.15 Two authors (TT and MB) independently coded the first 2 transcripts using the comprehensive coding scheme. Discrepancies in coding were resolved by negotiation. The remaining transcripts were then coded by one of the authors (TT). Unclear or confusing statements were discussed with other team members for coding clarification.
Trust emerged as an important concept and was selected for more detailed, theoretical analysis. For this analysis, a team member (BK) reviewed the transcripts and used the N5 NUD*IST search feature to identify comments in the transcripts related to trust. Then, the research literature was surveyed for frameworks to help us further understand and analyze the data pertaining to physician-patient trust in adolescents. Hall et al’s model of trust between adult patients and their physicians was selected as a framework for categorizing the comments into 5 specific domains.3 One team member (BK) assigned each comment to a category using the data matrix method of Miles and Huberman16 and noted in which gender-age-health groups it had been discussed. Although the analytic plan called for no categorization of comments that did not fit the schema of Hall et al, all comments discussed by all groups were readily assigned to categories.
To ensure trustworthiness of the data, another team member (MB) reread the transcripts to identify and categorize statements related to trust that might have been missed by the software search and to confirm the assignments made by the first reviewer. The reviewers looked for patterns of similarities and differences in responses from the participants. Specifically, groups were compared by gender, age, and health condition for the dimensions of trust and the specific topics within each dimension that were discussed. Once the 2 reviewers agreed on the categorization of the comments, their interpretations were reviewed, discussed, and finalized by 2 other team members for further verification and to look for disconfirming data.
Results
All groups discussed topics related to at least 2 of the 5 dimensions of trust. Nine of the 12 groups discussed topics in at least 4 of the 5 dimensions.
Fidelity
Fidelity—the physician’s pursuit of the patient’s best interest, not taking advantage of the patient’s vulnerability—was discussed by 9 of the 12 groups. The words used by the adolescent participants to describe fidelity included caring, respect, and advocacy, as demonstrated below.
- 13-year-old male without chronic illness: “Doctors show they care by trying to understand how you’re feeling rather than just coming in to try to fix things.”
- 15-year-old male with Crohn’s disease: “If he asks for my opinion or if he takes my advice seriously…or how he talks to me. I know if he either respects me or not…if he doesn’t talk down to me, like, still doesn’t think I’m a little kid.”
- 13-year-old female with cystic fibrosis: “[A good doctor is] someone that you can trust to take care of you and do what’s right for you.”
When asked about behaviors that would diminish trust, several participants gave examples of how a physician might take advantage of an adolescent’s vulnerability. For example, a 15-year-old female without chronic illness mentioned she would lose trust if her doctor “touched her in the wrong way.” A 13-year-old male without chronic illness stated: “This never happened, but I just feel like it would happen like, as soon as my mom walks out of the door, the doctor would pull out that clipboard [and say] ‘Oh, I’m trying to ask these questions [about sensitive topics].’”
Confidentiality
Confidentiality (ie, keeping sensitive or private patient information from others) was discussed by nearly all of the groups. Although there was consensus about the overall importance of the dimension, adolescents varied in their beliefs about specific definitions, such as the types of information that should be kept confidential or from whom information should be withheld.
The general concept of confidentiality, however, was incorporated by many adolescents into descriptions of a good doctor and a trusted doctor. For example:
- 13-year-old male without chronic illness: “[A good doctor is] somebody who protects what you say and keeps things in a closed record to where nobody else can get to ’em.”
- 16-year-old female with cystic fibrosis: “He needs to keep that [conversation during doctor visit] zipped, especially when they talk to your parents afterwards. You may tell him something that you don’t want your parents to know about, and he should respect that if you tell him something.”
The following comment conveys how quickly an adolescent might lose trust in a doctor if confidentiality is broken:
- 19-year-old male with sickle-cell disease: “If I told my doctor something really personal that nobody else needed to know, and then he went and told everybody, I don’t care if it’s people on the hospital staff, sometimes I’ll be like ‘Uhhh, could you just keep this between us’ and if they go and tell everybody, that would make you lose trust in the doctor.”
Several younger males in one focus group expressed concern about information that might have been shared years earlier, when they were children:
- SUBJECT #1 (13-year-old male without chronic illness): “Because, some doctor, a doctor a long time ago when I was about 6, he sent my records all the way down to Children’s and it was not like what a normal doctor would do.”
- MODERATOR: “And that made you feel uncomfortable?”
- SUBJECT #1: “Yeah.”
- SUBJECT #2 (13-year-old male without chronic illness): “Like they were telling them everything.”
- SUBJECT #3 (11-year-old male without chronic illness): “And then next time you come: ‘Oh there’s the sick boy’.”
- SUBJECT #4 (13-year-old male without chronic illness): “Yeah.”
Competency
Six of the 12 groups, particularly the older female groups, discussed competency in terms of trusting their doctors and identifying what makes a good doctor. As with other dimensions, the discussions explored both the presence and absence of competency:
- 17-year-old female without chronic illness: “Like a doctor that gave you the wrong like…gave you a bad diagnosis or something and was, you know, had made a mistake, and they knew that they had made a mistake. You would naturally not go back to them.”
- 17-year-old female without chronic illness: “I think that you can get people to trust you and respect you and stuff by being efficient, professional, doing a job well and making it as painless as possible. Not necessarily, you know, talking to them about this that and the other thing.”
Honesty
Eight of the 12 groups identified honesty as an attribute of a good doctor and a trusted doctor. Adolescents defined an honest doctor as one who is realistic, accurate, and does not withhold information. For example,
- 15-year-old female with sickle-cell: “But I would like to know if I have bad news so I can, like, pump myself up to feel better. I don’t want them to come in to say ‘you’re feeling better, you’ll probably be out soon’, and then [find out I have something bad].”
- 12-year-old female with cystic fibrosis: “Yeah, if they lie to you, you kind of feel like you cannot trust them anymore.”
- 15-year-old female without chronic illness: “If there’s something’s wrong with you, you trust ’em to tell you.”
When asked if there were times when a doctor should not share bad news, all participants responded that the doctor should either share the news directly with the adolescent or with a parent, who would then discuss it with the adolescent. Access to all information was particularly important to participants with chronic illnesses, as demonstrated by this comment:
- 16-year-old female with cystic fibrosis: “I think it’s very important and if he didn’t, if my doctor didn’t [tell me the bad news], it could result in weeks of hospitalization. But my doctor does tell me the truth. I mean there’s hardly any time where he keeps something from me. I think the only way he’d keep something from me is if I wasn’t ready to hear it or if it really didn’t concern what I did just as long as my parents know about it.”
Global
Hall et al describe the global dimension of trust as serving 2 functions. The first is for comments that intersect 2 or more of the other areas but do not fit exclusively in one. The second is to capture the holistic quality of trust.
Group discussions about this global dimension involved a “friend-like” relationship with the doctor, comfort with the doctor, and an overall sense that the doctor could be trusted. The comments noted below are organized into these content areas:
- Friend-like.
- 14-year-old male with Crohn’s disease: “[The doctors] know their patient as a friend and not as a patient…they know them like a friendship and everything.”
- 16-year-old female without chronic illness: “[A good doctor] would be a friend with the patient, not just be an authority [figure].”
When asked how a doctor should relate to an adolescent patient as a friend, several adolescents suggested the doctor telling about his personal life (eg, family, children) and asking about the adolescent’s personal life (eg, sports, school). A 14-year-old male with Crohn’s disease suggested, “Have a conversation with them, not like question-answer, question-answer, having a conversation so it all flows.”
Comfort. Participants described physician use of introductory small talk as a means of building comfort, and the premature introduction of sensitive topics (eg, drug use, sexual behavior, family issues) as a barrier to comfort.
- 16-year-old female without chronic illness: “It’s sort of like an introductory question, like they’ll get you in there, try to make you feel comfortable, and they’re like,’ how’s school going’…I think they try to strike up a conversation to make you feel more comfortable.”
- 11-year-old female without chronic illness: “But if the doctor is a guy, then you probably won’t feel comfortable talking about that [peer pressure and menstrual cycles].”
Comfort was a prerequisite for trust for some adolescents. Participants described feeling comfortable telling their doctor and then trusting them with the information. The following comment illustrates the relationship:
- 15-year-old female without chronic illness: “If you’re comfortable, you have more trust in the person.”
Overall sense of trust. The older, healthy female group was the only group that described trust from a holistic perspective:
- MODERATOR: “I mean, what is it that makes them trustworthy? (Pause.) Just ‘cuz they’re doctors? Ok.”
- 17-year-old female without chronic illness: “I mean, you kinda want to trust your doctor and you don’t want to believe that they’re trying to get you…there’s nothing behind their back. You do want to be able to trust them.”
Discussion
Adolescents in our study defined a good doctor as one they can trust and, similar to other studies of adolescent populations, said trustworthiness is a core attribute they seek in a physician.7-9 The comprehensive model of patient-physician trust developed by Hall et al in adults depicts trust as perceived by the adolescent participants in our study.3 The dimensions of caring, confidentiality, competency, honesty, and holistic trust captured the beliefs expressed by the adolescents, suggesting that adolescent and adult models of physician trust may be similar.
Confidentiality is the one dimension in which the specifics may differ for adolescents and adults. Similar to other research with adolescents,7,9 adolescents in our study indicated that confidentiality (ie, keeping health and personal information private) is an important characteristic of a good doctor and a trusted doctor. Adults, on the other hand, are less concerned about confidentiality as it relates to trusting their physicians.2,3,6,17
Adolescents may be uncertain about a physician’s obligation to inform or not inform parents about private information, which, in turn, may increase their sensitivity to confidentiality. Because adolescents, unlike adults, are accountable to an adult who controls access to activities and friends, they may be more likely to conceal sensitive activities for fear of losing privileges. Chronically ill teens may conceal certain symptoms or lack of compliance with treatment for similar reasons.
Developmental differences may help explain the reason younger adolescents in our study expressed more concern and uncertainty about how health information is protected than did older adolescents. The capacity for formal operational thinking that develops during adolescence enables abstraction and leads to an increasing interest in how the outside world views personal attitudes and behaviors.18 Until adolescents test the responses of the outside world, they may feel center-stage, as though “everyone” is judging them. Keeping personal information private thus becomes extremely important to maturing adolescents.
Adults who have tested the views of others’ responses are better able than adolescents to keep in perspective the interests of the outside world and, therefore, may have fewer concerns about how their personal information is managed. In addition, adults are more likely to have a better understanding of confidentiality policies within a healthcare system and thus realize their private information is safeguarded.
Given that this analysis was part of a larger study and issues surrounding confidentiality were not studied in-depth, future research involving both adolescents and adults focusing on confidentiality and the uncertainty about parental involvement that often accompanies adolescent health care could shed light on this topic.
Although adolescents with and without chronic illnesses discussed the same dimensions of trust, honesty and advocacy were noted more often by the former. This resembles findings reported in studies of adults with serious illnesses.6 Adolescents with chronic illnesses tend to consider parents acceptable recipients of bad news. In addition, adolescents with chronic illnesses expect physicians to reveal bad news to either the adolescent or their parent, given the potential dire health consequences of withholding important medical information.
The issue of honesty may have been mentioned less frequently by healthy adolescents since they have not had to contend with major health issues and receiving bad news. Adolescents with chronic illnesses expect good doctors to “go the extra mile,” a task that is increasingly difficult in a health care environment that seeks to limit reimbursement and expenditure.19
Keeping in mind the qualitative nature of our study and size of our sample, the findings from our focus groups suggest that physicians working with adolescents with a chronic illness be cognizant of their increased need for complete and accurate information, as well as the higher expectation that the doctor will act on their behalf. Additional studies are needed to investigate whether adolescents with a chronic illness have a higher need for honesty and advocacy than healthy adolescents.
Although identified as a predictor, rather than a dimension, of trust,3 duration of the patient-physician relationship was discussed by adolescents with and without chronic illnesses in our study. Comments similar to “he’s been taking care of me for a long time” or “because I’ve known her all my life” were repeated often. Studies in both adolescent7,20 and adult populations,2,4,17 have reported similar findings. Adolescents in our study varied in their estimations of sufficient duration, from 4 to 5 visits to knowing the doctor “forever.”
Unlike the many comments pertaining to duration of acquaintance, there was no discussion of the frequency or intensity of visits. Comfort appears to be a prerequisite for trust for adolescents in our study and may perhaps be a moderating factor when examining how the duration of the patient-physician relationship influences trust. The length of time necessary to feel comfortable may vary among individuals and may be influenced by other factors (eg, experience with doctors or the health care system, friendliness of the physician). Thus, it may not be possible to determine a standard time period (eg, 6 months) in which adolescents feel comfortable to trust their doctor. Future studies examining what influences adolescents’ comfort level (eg, length of relationship, intensity of health care experience) with their physician may provide additional insight for improving adolescents’ trust in their physicians.
When asked how doctors could gain the trust of adolescent patients, participants in our study responded “be truthful,” “be friendly,” and “be there.” More specific behaviors included asking for the adolescent’s opinion, keeping private information confidential, not withholding clinical information from the patient, and engaging in small talk to show concern.
Participants were quick to point out that physician violation of gained trust is viewed as serious behavior that leads to rapid deterioration in the doctor-patient relationship.3,19 They identified examples of violated trust as medical mistakes, breaks in confidentiality, and taking advantage of patients when vulnerable (eg, during the physical examination). These descriptions highlight the importance of proactive discussions early in the doctor-patient relationship, clarifying the legal and ethical limitations of issues such as confidentiality.
There are several limitations to this study. First, these analyses were part of a larger study examining health care preferences of adolescents with a chronic illness. Because the issue of physician-patient trust was not the focal point of the original study, there may be issues relating to trust that our study did not address. Further research with additional samples is needed to confirm if all aspects of trust were explored.
Second, while our findings support those of earlier studies in both adolescents and adults, our sample was drawn from the patient population of only one mid-western city in the US.7-9,20
Third, adolescents who declined participation in the study may differ in their attitudes or beliefs about health care providers than adolescents who agreed to participate, thus introducing a potential selection bias.
Fourth, we were unable to perform member checking or reactor panels to examine “external validity” due to the participants’ cognitive level (ie, difficulty discussing abstract concepts). However, corroborating evidence from earlier studies supported our findings.
Fifth, our study was designed to collect qualitative data and to use analytic methods that are appropriate for such data. The data and statistical methods were not intended to be quantitative, and the interpretations of the reported findings therefore were appropriate for those of a qualitative, not quantitative study design.
In conclusion, our study provides the first steps in suggesting that adolescents and adults agree on the major dimensions of trust but differ in the relative importance of these dimensions to the overall definition of trust. Adolescents in our study expressed the broadest range of beliefs within the dimension of confidentiality. Younger adolescents expressed more concern and uncertainty about how health information is protected than did older adolescents.
Adolescents with chronic illnesses seemed more comfortable involving parents in their care than did adolescents without chronic illnesses. Since adolescents with chronic illness have more experience involving their parents in their care, future studies could examine whether having a chronic illness makes a difference in whether an adolescent would involve their parent more when faced with the same health concerns typical of healthy adolescents (eg, sexual health, psychological issues).
Additional studies focusing specifically on physician-patient trust are needed to further explore similarities and differences between adults and adolescents’ perceptions. Understanding the importance of trust to adolescents and listening to their recommendations about behaviors that promote it may help physicians build positive relationships with patients that will continue into and beyond young adulthood.
Acknowledgments
Supported by a Robert Wood Johnson Generalist Physician Faculty Scholar Award to the senior author.
CORRESPONDING AUTHOR
Brenda K. Klostermann, PhD, Illinois Education Research Council, Southern Illinois University Edwardsville, Box 1064, Edwardsville, IL 62026-1064. E-mail: [email protected]
Objective: To explore how adolescents with and without chronic illness perceive patient-physician trust and to identify physician behaviors related to these perceptions that might be modified to promote adolescent health care.
Methods: Fifty-four adolescents recruited from the community (healthy subjects) and from hospital-based clinics (subjects with chronic illnesses) participated in 12 focus groups divided by age (11–14 or 15–19 years old), gender, and health status. Major themes related to preferred physician characteristics and trusting one’s doctor were derived through a multistep, team-based qualitative analytic process.
Results: Adolescents hold varied perspectives of trust in their physicians. They describe elements of patient-physician trust similarly to the comprehensive model developed with adults, including fidelity, confidentiality, competency, honesty, and a global perspective intersecting several of the more specific domains. However, adolescents differ in the relative importance of these dimensions. Younger adolescents express more concern about confidentiality of their health information, and adolescents with chronic illnesses are more interested in involving parents in their care than are adolescents without chronic illnesses. Examples of specific behaviors to improve trust include asking for adolescent’s opinion, keeping private information confidential, not withholding information, and engaging in small talk to show concern.
Conclusion: Understanding the importance of trust and listening to recommendations about behaviors to improve it, in the words of the adolescents, may help physicians build positive relationships with their adolescent patients.
- Keep in mind that adolescents are generally more concerned than adults about confidentiality when deciding on a physician’s trustworthiness.
- Approach adolescents who have chronic illnesses with the expectation that they will be more comfortable involving parents in their care than will healthy adolescents.
In the primary care setting, a patient’s trust of the physician is more strongly associated with self-reports of improved health than is any other characteristic of the patient-physician relationship.1 Trust has been shown to affect a patient’s satisfaction with health care services and willingness to disclose sensitive information, adhere to treatment, continue with a physician, and recommend that physician to others.1,2
Increasing age of a patient has a modestly positive correlation with trust, possibly due to greater contact with physicians; other demographic characteristics have not been consistently found to relate to trust.3,4
Studies examining health status and trust have shown a weak and inconsistent relationship.1,3 Persons with poor health, such as a chronic illness, may be more vulnerable and thus have a greater need to trust. Poor health may also cause negative feelings that may influence how patients trust their physicians.
Physician behavior and patient trust
The importance of patient trust to the process and outcome of health care has prompted the study of how specific physician behaviors may help to build trust. Among adults with and without chronic conditions, trust is associated with perceived physician caring, competence, and communication.1,5,6 Among adolescents, trust seems more strongly influenced by a physician’s confidentiality, competence, honesty, and respect, than by any other set of characteristics pertaining to health care professionals, health care sites, or incentives to use primary care services.7,8 Distrust that physicians will protect confidentiality has been cited as a barrier to health care use and compliance among adolescents.9
However, unlike the adult literature on patient-physician trust, no study of adolescents has defined trust from the patient’s perspective or identified physician behaviors that promote trust among adolescent patients. Directly asking adolescents about trust in their doctor may identify specific physician behaviors that encourage building trust. Understanding the importance of trust to adolescents and listening to their recommendations about behaviors to improve it, in the words of the adolescents, may help physicians build positive relationships with their adolescent patients.
This study addresses the call by Rosser and Kasperski for more research pertaining to the development of trust between doctors and patients.10 A model of trust between adult patients and their physicians, developed by Hall et al,3 was used as a framework to understand adolescents’ perceptions of patient-physician trust. The 5 specific domains of this model include patient perceptions of physician fidelity, protection of confidential information, competence, honesty, and a global perspective that intersects several of the more specific domains and captures the holistic aspect of trust. This study’s objective was to explore how adolescents with and without chronic illness perceive patient-physician trust and to identify physician behaviors related to these perceptions that might be modified to promote adolescent health care.
Methods
Participants
This study was part of a larger qualitative and quantitative research project examining health care preferences of adolescents with chronic health conditions.11 The protocol for the research project on adolescent health care preferences and the analyses performed for the current study on trust were approved by the Institutional Review Board of the Cincinnati Children’s Hospital Medical Center.
Adolescents aged 11 to 19 years with cystic fibrosis, sickle-cell disease, juvenile rheumatoid arthritis, or inflammatory bowel disease diagnosed at least 2 years previously were recruited from hospital-based clinics. We attempted to contact all patients aged 11 to 19 years in these sub-specialty clinics for their participation. Introductory letters were sent, followed by phone calls, to these adolescents and their guardians to explain the study and to invite participation in a focus group. For comparison, a convenience sample of adolescents aged 11 to 19 years without chronic conditions were recruited from local summer recreation programs, a church, and a school using flyers and personal contacts.
Written informed consent was obtained from participants who were age 18 years and older and from the legal guardians of participants who were younger than age 18 years. Participants were reimbursed 10 dollars for their time and travel expenses. The study sample consisted of 54 participants divided by age (11 to 14 years and 15 to 19 years), gender, and the presence or absence of chronic disease into 12 focus groups ranging in size from 2 to 10 individuals (mean=5) (TABLE).
Following focus group protocol recommendations for homogenous groups12 and other similar studies,7,8 groups were divided by age due to differing developmental levels (early vs later adolescence) and gender, since same-sex groups are preferred for young adolescents. Participants were divided based on the presence or absence of chronic disease due to different health care experiences. For the groups of participants with a chronic disease, 17 were 11 to 14 years old (6 male; 11 female) and 12 were 15 to 19 years old (7 male; 5 female). For the groups of healthy participants, 13 were 11 to 14 years old (8 male; 5 female) and 12 were 15 to 19 years old (4 male; 8 female).
TABLE
Demographics of sample (N=54)
| N | % | |
|---|---|---|
| Gender | ||
| Female | 30 | 56 |
| Health status | ||
| Healthy | 25 | 46 |
| Chronic Illness | 29 | 54 |
| Cystic fibrosis | 7 | 24 |
| Inflammatory bowel disease | 10 | 35 |
| Juvenile rheumatoid arthritis | 5 | 17 |
| Sickle-cell disease | 7 | 24 |
| Age | ||
| Range: 11–20 | ||
| Mean: 14 | ||
Data collection
Focus groups were conducted as part of the larger research project to explore adolescents’ preferences on various aspects of their health care (eg, doctor-patient relationship, doctors’ characteristics, physical environment, doctor-patient communication).11 The current analysis examined one aspect of the doctor-patient relationship identified by participants: trust.
One professional facilitator led the 12 groups through 2-hour discussions about health concerns, preferred physician characteristics, and preferred visit characteristics. New topics raised by a given group were highlighted by the facilitator for discussion by subsequent groups, and discussions were directed away from topics that had reached saturation in previous groups.13
In general, adolescents discussed the dimensions of trust in response to 2 questions: “What makes a good doctor?” and “How do you know you can trust your doctor?” Audiotapes of all discussions were transcribed verbatim, edited for accuracy, and supplemented by field notes taken by co-investigators who attended the group discussions as observers. The presence of the co-investigators enhanced understanding of the transcripts, without apparent discomfort or inhibition of the participants.
Data analysis
The analyses occurred in multiple stages. During the first phase of analyses, 4 coinvestigators independently prepared summaries of each group transcript and initial lists of the themes discussed by the participants, using Crabtree and Miller’s editing-organizing style.14 They then met as a team to discuss their observations and to begin preliminary interpretation of that focus group. Consensus on the themes was reached for each group.
After the groups’ results were analyzed separately, the research team compared and contrasted the group themes and generated a comprehensive coding scheme for all of the focus groups combined. Emphasis was placed on a comprehensive coding scheme (ie, topics discussed less often were included along with topics discussed more often). Trust was identified as a major theme discussed in all 12 focus groups.
In the next stage of analysis, the edited transcripts and the coding scheme were imported into the qualitative text analysis software package N5 NUD*IST.15 Two authors (TT and MB) independently coded the first 2 transcripts using the comprehensive coding scheme. Discrepancies in coding were resolved by negotiation. The remaining transcripts were then coded by one of the authors (TT). Unclear or confusing statements were discussed with other team members for coding clarification.
Trust emerged as an important concept and was selected for more detailed, theoretical analysis. For this analysis, a team member (BK) reviewed the transcripts and used the N5 NUD*IST search feature to identify comments in the transcripts related to trust. Then, the research literature was surveyed for frameworks to help us further understand and analyze the data pertaining to physician-patient trust in adolescents. Hall et al’s model of trust between adult patients and their physicians was selected as a framework for categorizing the comments into 5 specific domains.3 One team member (BK) assigned each comment to a category using the data matrix method of Miles and Huberman16 and noted in which gender-age-health groups it had been discussed. Although the analytic plan called for no categorization of comments that did not fit the schema of Hall et al, all comments discussed by all groups were readily assigned to categories.
To ensure trustworthiness of the data, another team member (MB) reread the transcripts to identify and categorize statements related to trust that might have been missed by the software search and to confirm the assignments made by the first reviewer. The reviewers looked for patterns of similarities and differences in responses from the participants. Specifically, groups were compared by gender, age, and health condition for the dimensions of trust and the specific topics within each dimension that were discussed. Once the 2 reviewers agreed on the categorization of the comments, their interpretations were reviewed, discussed, and finalized by 2 other team members for further verification and to look for disconfirming data.
Results
All groups discussed topics related to at least 2 of the 5 dimensions of trust. Nine of the 12 groups discussed topics in at least 4 of the 5 dimensions.
Fidelity
Fidelity—the physician’s pursuit of the patient’s best interest, not taking advantage of the patient’s vulnerability—was discussed by 9 of the 12 groups. The words used by the adolescent participants to describe fidelity included caring, respect, and advocacy, as demonstrated below.
- 13-year-old male without chronic illness: “Doctors show they care by trying to understand how you’re feeling rather than just coming in to try to fix things.”
- 15-year-old male with Crohn’s disease: “If he asks for my opinion or if he takes my advice seriously…or how he talks to me. I know if he either respects me or not…if he doesn’t talk down to me, like, still doesn’t think I’m a little kid.”
- 13-year-old female with cystic fibrosis: “[A good doctor is] someone that you can trust to take care of you and do what’s right for you.”
When asked about behaviors that would diminish trust, several participants gave examples of how a physician might take advantage of an adolescent’s vulnerability. For example, a 15-year-old female without chronic illness mentioned she would lose trust if her doctor “touched her in the wrong way.” A 13-year-old male without chronic illness stated: “This never happened, but I just feel like it would happen like, as soon as my mom walks out of the door, the doctor would pull out that clipboard [and say] ‘Oh, I’m trying to ask these questions [about sensitive topics].’”
Confidentiality
Confidentiality (ie, keeping sensitive or private patient information from others) was discussed by nearly all of the groups. Although there was consensus about the overall importance of the dimension, adolescents varied in their beliefs about specific definitions, such as the types of information that should be kept confidential or from whom information should be withheld.
The general concept of confidentiality, however, was incorporated by many adolescents into descriptions of a good doctor and a trusted doctor. For example:
- 13-year-old male without chronic illness: “[A good doctor is] somebody who protects what you say and keeps things in a closed record to where nobody else can get to ’em.”
- 16-year-old female with cystic fibrosis: “He needs to keep that [conversation during doctor visit] zipped, especially when they talk to your parents afterwards. You may tell him something that you don’t want your parents to know about, and he should respect that if you tell him something.”
The following comment conveys how quickly an adolescent might lose trust in a doctor if confidentiality is broken:
- 19-year-old male with sickle-cell disease: “If I told my doctor something really personal that nobody else needed to know, and then he went and told everybody, I don’t care if it’s people on the hospital staff, sometimes I’ll be like ‘Uhhh, could you just keep this between us’ and if they go and tell everybody, that would make you lose trust in the doctor.”
Several younger males in one focus group expressed concern about information that might have been shared years earlier, when they were children:
- SUBJECT #1 (13-year-old male without chronic illness): “Because, some doctor, a doctor a long time ago when I was about 6, he sent my records all the way down to Children’s and it was not like what a normal doctor would do.”
- MODERATOR: “And that made you feel uncomfortable?”
- SUBJECT #1: “Yeah.”
- SUBJECT #2 (13-year-old male without chronic illness): “Like they were telling them everything.”
- SUBJECT #3 (11-year-old male without chronic illness): “And then next time you come: ‘Oh there’s the sick boy’.”
- SUBJECT #4 (13-year-old male without chronic illness): “Yeah.”
Competency
Six of the 12 groups, particularly the older female groups, discussed competency in terms of trusting their doctors and identifying what makes a good doctor. As with other dimensions, the discussions explored both the presence and absence of competency:
- 17-year-old female without chronic illness: “Like a doctor that gave you the wrong like…gave you a bad diagnosis or something and was, you know, had made a mistake, and they knew that they had made a mistake. You would naturally not go back to them.”
- 17-year-old female without chronic illness: “I think that you can get people to trust you and respect you and stuff by being efficient, professional, doing a job well and making it as painless as possible. Not necessarily, you know, talking to them about this that and the other thing.”
Honesty
Eight of the 12 groups identified honesty as an attribute of a good doctor and a trusted doctor. Adolescents defined an honest doctor as one who is realistic, accurate, and does not withhold information. For example,
- 15-year-old female with sickle-cell: “But I would like to know if I have bad news so I can, like, pump myself up to feel better. I don’t want them to come in to say ‘you’re feeling better, you’ll probably be out soon’, and then [find out I have something bad].”
- 12-year-old female with cystic fibrosis: “Yeah, if they lie to you, you kind of feel like you cannot trust them anymore.”
- 15-year-old female without chronic illness: “If there’s something’s wrong with you, you trust ’em to tell you.”
When asked if there were times when a doctor should not share bad news, all participants responded that the doctor should either share the news directly with the adolescent or with a parent, who would then discuss it with the adolescent. Access to all information was particularly important to participants with chronic illnesses, as demonstrated by this comment:
- 16-year-old female with cystic fibrosis: “I think it’s very important and if he didn’t, if my doctor didn’t [tell me the bad news], it could result in weeks of hospitalization. But my doctor does tell me the truth. I mean there’s hardly any time where he keeps something from me. I think the only way he’d keep something from me is if I wasn’t ready to hear it or if it really didn’t concern what I did just as long as my parents know about it.”
Global
Hall et al describe the global dimension of trust as serving 2 functions. The first is for comments that intersect 2 or more of the other areas but do not fit exclusively in one. The second is to capture the holistic quality of trust.
Group discussions about this global dimension involved a “friend-like” relationship with the doctor, comfort with the doctor, and an overall sense that the doctor could be trusted. The comments noted below are organized into these content areas:
- Friend-like.
- 14-year-old male with Crohn’s disease: “[The doctors] know their patient as a friend and not as a patient…they know them like a friendship and everything.”
- 16-year-old female without chronic illness: “[A good doctor] would be a friend with the patient, not just be an authority [figure].”
When asked how a doctor should relate to an adolescent patient as a friend, several adolescents suggested the doctor telling about his personal life (eg, family, children) and asking about the adolescent’s personal life (eg, sports, school). A 14-year-old male with Crohn’s disease suggested, “Have a conversation with them, not like question-answer, question-answer, having a conversation so it all flows.”
Comfort. Participants described physician use of introductory small talk as a means of building comfort, and the premature introduction of sensitive topics (eg, drug use, sexual behavior, family issues) as a barrier to comfort.
- 16-year-old female without chronic illness: “It’s sort of like an introductory question, like they’ll get you in there, try to make you feel comfortable, and they’re like,’ how’s school going’…I think they try to strike up a conversation to make you feel more comfortable.”
- 11-year-old female without chronic illness: “But if the doctor is a guy, then you probably won’t feel comfortable talking about that [peer pressure and menstrual cycles].”
Comfort was a prerequisite for trust for some adolescents. Participants described feeling comfortable telling their doctor and then trusting them with the information. The following comment illustrates the relationship:
- 15-year-old female without chronic illness: “If you’re comfortable, you have more trust in the person.”
Overall sense of trust. The older, healthy female group was the only group that described trust from a holistic perspective:
- MODERATOR: “I mean, what is it that makes them trustworthy? (Pause.) Just ‘cuz they’re doctors? Ok.”
- 17-year-old female without chronic illness: “I mean, you kinda want to trust your doctor and you don’t want to believe that they’re trying to get you…there’s nothing behind their back. You do want to be able to trust them.”
Discussion
Adolescents in our study defined a good doctor as one they can trust and, similar to other studies of adolescent populations, said trustworthiness is a core attribute they seek in a physician.7-9 The comprehensive model of patient-physician trust developed by Hall et al in adults depicts trust as perceived by the adolescent participants in our study.3 The dimensions of caring, confidentiality, competency, honesty, and holistic trust captured the beliefs expressed by the adolescents, suggesting that adolescent and adult models of physician trust may be similar.
Confidentiality is the one dimension in which the specifics may differ for adolescents and adults. Similar to other research with adolescents,7,9 adolescents in our study indicated that confidentiality (ie, keeping health and personal information private) is an important characteristic of a good doctor and a trusted doctor. Adults, on the other hand, are less concerned about confidentiality as it relates to trusting their physicians.2,3,6,17
Adolescents may be uncertain about a physician’s obligation to inform or not inform parents about private information, which, in turn, may increase their sensitivity to confidentiality. Because adolescents, unlike adults, are accountable to an adult who controls access to activities and friends, they may be more likely to conceal sensitive activities for fear of losing privileges. Chronically ill teens may conceal certain symptoms or lack of compliance with treatment for similar reasons.
Developmental differences may help explain the reason younger adolescents in our study expressed more concern and uncertainty about how health information is protected than did older adolescents. The capacity for formal operational thinking that develops during adolescence enables abstraction and leads to an increasing interest in how the outside world views personal attitudes and behaviors.18 Until adolescents test the responses of the outside world, they may feel center-stage, as though “everyone” is judging them. Keeping personal information private thus becomes extremely important to maturing adolescents.
Adults who have tested the views of others’ responses are better able than adolescents to keep in perspective the interests of the outside world and, therefore, may have fewer concerns about how their personal information is managed. In addition, adults are more likely to have a better understanding of confidentiality policies within a healthcare system and thus realize their private information is safeguarded.
Given that this analysis was part of a larger study and issues surrounding confidentiality were not studied in-depth, future research involving both adolescents and adults focusing on confidentiality and the uncertainty about parental involvement that often accompanies adolescent health care could shed light on this topic.
Although adolescents with and without chronic illnesses discussed the same dimensions of trust, honesty and advocacy were noted more often by the former. This resembles findings reported in studies of adults with serious illnesses.6 Adolescents with chronic illnesses tend to consider parents acceptable recipients of bad news. In addition, adolescents with chronic illnesses expect physicians to reveal bad news to either the adolescent or their parent, given the potential dire health consequences of withholding important medical information.
The issue of honesty may have been mentioned less frequently by healthy adolescents since they have not had to contend with major health issues and receiving bad news. Adolescents with chronic illnesses expect good doctors to “go the extra mile,” a task that is increasingly difficult in a health care environment that seeks to limit reimbursement and expenditure.19
Keeping in mind the qualitative nature of our study and size of our sample, the findings from our focus groups suggest that physicians working with adolescents with a chronic illness be cognizant of their increased need for complete and accurate information, as well as the higher expectation that the doctor will act on their behalf. Additional studies are needed to investigate whether adolescents with a chronic illness have a higher need for honesty and advocacy than healthy adolescents.
Although identified as a predictor, rather than a dimension, of trust,3 duration of the patient-physician relationship was discussed by adolescents with and without chronic illnesses in our study. Comments similar to “he’s been taking care of me for a long time” or “because I’ve known her all my life” were repeated often. Studies in both adolescent7,20 and adult populations,2,4,17 have reported similar findings. Adolescents in our study varied in their estimations of sufficient duration, from 4 to 5 visits to knowing the doctor “forever.”
Unlike the many comments pertaining to duration of acquaintance, there was no discussion of the frequency or intensity of visits. Comfort appears to be a prerequisite for trust for adolescents in our study and may perhaps be a moderating factor when examining how the duration of the patient-physician relationship influences trust. The length of time necessary to feel comfortable may vary among individuals and may be influenced by other factors (eg, experience with doctors or the health care system, friendliness of the physician). Thus, it may not be possible to determine a standard time period (eg, 6 months) in which adolescents feel comfortable to trust their doctor. Future studies examining what influences adolescents’ comfort level (eg, length of relationship, intensity of health care experience) with their physician may provide additional insight for improving adolescents’ trust in their physicians.
When asked how doctors could gain the trust of adolescent patients, participants in our study responded “be truthful,” “be friendly,” and “be there.” More specific behaviors included asking for the adolescent’s opinion, keeping private information confidential, not withholding clinical information from the patient, and engaging in small talk to show concern.
Participants were quick to point out that physician violation of gained trust is viewed as serious behavior that leads to rapid deterioration in the doctor-patient relationship.3,19 They identified examples of violated trust as medical mistakes, breaks in confidentiality, and taking advantage of patients when vulnerable (eg, during the physical examination). These descriptions highlight the importance of proactive discussions early in the doctor-patient relationship, clarifying the legal and ethical limitations of issues such as confidentiality.
There are several limitations to this study. First, these analyses were part of a larger study examining health care preferences of adolescents with a chronic illness. Because the issue of physician-patient trust was not the focal point of the original study, there may be issues relating to trust that our study did not address. Further research with additional samples is needed to confirm if all aspects of trust were explored.
Second, while our findings support those of earlier studies in both adolescents and adults, our sample was drawn from the patient population of only one mid-western city in the US.7-9,20
Third, adolescents who declined participation in the study may differ in their attitudes or beliefs about health care providers than adolescents who agreed to participate, thus introducing a potential selection bias.
Fourth, we were unable to perform member checking or reactor panels to examine “external validity” due to the participants’ cognitive level (ie, difficulty discussing abstract concepts). However, corroborating evidence from earlier studies supported our findings.
Fifth, our study was designed to collect qualitative data and to use analytic methods that are appropriate for such data. The data and statistical methods were not intended to be quantitative, and the interpretations of the reported findings therefore were appropriate for those of a qualitative, not quantitative study design.
In conclusion, our study provides the first steps in suggesting that adolescents and adults agree on the major dimensions of trust but differ in the relative importance of these dimensions to the overall definition of trust. Adolescents in our study expressed the broadest range of beliefs within the dimension of confidentiality. Younger adolescents expressed more concern and uncertainty about how health information is protected than did older adolescents.
Adolescents with chronic illnesses seemed more comfortable involving parents in their care than did adolescents without chronic illnesses. Since adolescents with chronic illness have more experience involving their parents in their care, future studies could examine whether having a chronic illness makes a difference in whether an adolescent would involve their parent more when faced with the same health concerns typical of healthy adolescents (eg, sexual health, psychological issues).
Additional studies focusing specifically on physician-patient trust are needed to further explore similarities and differences between adults and adolescents’ perceptions. Understanding the importance of trust to adolescents and listening to their recommendations about behaviors that promote it may help physicians build positive relationships with patients that will continue into and beyond young adulthood.
Acknowledgments
Supported by a Robert Wood Johnson Generalist Physician Faculty Scholar Award to the senior author.
CORRESPONDING AUTHOR
Brenda K. Klostermann, PhD, Illinois Education Research Council, Southern Illinois University Edwardsville, Box 1064, Edwardsville, IL 62026-1064. E-mail: [email protected]
1. Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract 1998;47:213-220.
2. Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev 2002;59:293-318.
3. Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: What is it, can it be measure, and does it matter? Milbank Q 2001;79:613-639.
4. Thom DH, Ribisl KM, Stewart AL, Luke DA. The Stanford Trust Study Physicians. Further validation and reliability testing of the Trust in Physician scale. Med Care 1999;37:510-517.
5. Thom DH. Stanford Trust Study Physicians. Physician behaviors that predict patient trust. J Fam Pract 2001;50:323-328.
6. Mechanic D, Meyer S. Concepts of trust among patients with serious illness. Soc Sci Med 2000;51:657-668.
7. Ginsburg KR, Menapace AS, Slap GB. Factors affecting the decision to seek health care: The voice of adolescents. Pediatrics 1997;100:922-930.
8. Ginsburg KR, Slap GB, Cnaan A, Forke CM, Balsley CM, Rouselle DM. Adolescents’ perceptions of factors affecting their decisions to seek health care. JAMA 1995;273:1913-1918.
9. Cogswell BE. Cultivating the trust of adolescent patients. Fam Med 1985;17:254-258.
10. Rosser WW, Kasperski J. The benefits of a trusting physician-patient relationship. J Fam Pract 2001;50:329-330.
11. Britto MT, DeVellis RF, Hornung RW, DeFriese GH, Atherton HD, Slap GB. Health care p and priorities of adolescents with chronic illness. Pediatrics 2004;114:1272-1280.
12. Krueger RA. Focus Groups: A Practical Guide for Applied Research. Newbury Park, Calif: Sage Publications; 1998.
13. Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, Calif: Sage Publications; 1998.
14. Crabtree BF, Miller WL. Doing Qualitative Research. 2nd ed.Thousand Oaks, Calif: Sage Publications; 1999.
15. Qualitative Solutions and Research International Pty Ltd., N5 NUD*IST for Windows [Computer Software]. Victoria, Australia: Qualitative Solutions; 2000.
16. Miles MB, Huberman AM. Qualitative Data Analysis. 2nd ed. Thousand Oaks, Calif: Sage Publications; 1994.
17. Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: Effects of choice, continuity, and payment method. J Gen Intern Med 1998;13:681-686.
18. Elkind D. Teenage thinking: Implications for health care. Pediatric Nursing 1984;10:383-385.
19. Davies HTO, Rundall TG. Managing patient trust in managed care. Milbank Q 2000;78:609-624.
20. Ginsburg KR, Forke CM, Cnaan A, Slap GB. Important health provider characteristics: The perspective of urban ninth graders. Dev Behav Ped 2002;23:237-243.
1. Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract 1998;47:213-220.
2. Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev 2002;59:293-318.
3. Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: What is it, can it be measure, and does it matter? Milbank Q 2001;79:613-639.
4. Thom DH, Ribisl KM, Stewart AL, Luke DA. The Stanford Trust Study Physicians. Further validation and reliability testing of the Trust in Physician scale. Med Care 1999;37:510-517.
5. Thom DH. Stanford Trust Study Physicians. Physician behaviors that predict patient trust. J Fam Pract 2001;50:323-328.
6. Mechanic D, Meyer S. Concepts of trust among patients with serious illness. Soc Sci Med 2000;51:657-668.
7. Ginsburg KR, Menapace AS, Slap GB. Factors affecting the decision to seek health care: The voice of adolescents. Pediatrics 1997;100:922-930.
8. Ginsburg KR, Slap GB, Cnaan A, Forke CM, Balsley CM, Rouselle DM. Adolescents’ perceptions of factors affecting their decisions to seek health care. JAMA 1995;273:1913-1918.
9. Cogswell BE. Cultivating the trust of adolescent patients. Fam Med 1985;17:254-258.
10. Rosser WW, Kasperski J. The benefits of a trusting physician-patient relationship. J Fam Pract 2001;50:329-330.
11. Britto MT, DeVellis RF, Hornung RW, DeFriese GH, Atherton HD, Slap GB. Health care p and priorities of adolescents with chronic illness. Pediatrics 2004;114:1272-1280.
12. Krueger RA. Focus Groups: A Practical Guide for Applied Research. Newbury Park, Calif: Sage Publications; 1998.
13. Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, Calif: Sage Publications; 1998.
14. Crabtree BF, Miller WL. Doing Qualitative Research. 2nd ed.Thousand Oaks, Calif: Sage Publications; 1999.
15. Qualitative Solutions and Research International Pty Ltd., N5 NUD*IST for Windows [Computer Software]. Victoria, Australia: Qualitative Solutions; 2000.
16. Miles MB, Huberman AM. Qualitative Data Analysis. 2nd ed. Thousand Oaks, Calif: Sage Publications; 1994.
17. Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: Effects of choice, continuity, and payment method. J Gen Intern Med 1998;13:681-686.
18. Elkind D. Teenage thinking: Implications for health care. Pediatric Nursing 1984;10:383-385.
19. Davies HTO, Rundall TG. Managing patient trust in managed care. Milbank Q 2000;78:609-624.
20. Ginsburg KR, Forke CM, Cnaan A, Slap GB. Important health provider characteristics: The perspective of urban ninth graders. Dev Behav Ped 2002;23:237-243.
Otitis externa: Providing relief while avoiding complications
- Topical antimicrobial otic drops, supplemented by oral analgesics, provide prompt and effective therapy (B).
- Fluoroquinolones and neomycinpolymyxin B combinations have shown equal efficacy (A), but the former are preferred when trying to guard against ototoxicity or hypersensitivity (C).
- For severely painful otitis externa, consider inserting an ear wick and giving oral narcotics (C).
- Localized cellulitis requires systemic antimicrobial therapy (C).
- No compelling evidence exists on the effectiveness of astringent topical treatments for otitis externa. Also, topical astringents are often painful, which may impede adherence (B).
Widespread use of neomycin combinations may have led to an increase in the incidence of patient hypersensitivity and promoted antibiotic resistance in Staphylococcus aureus and Pseudomonas aeruginosa, the 2 most common pathogens of otitis externa (see Pathogens of otitis externa).
Recent controlled clinical trials have shown the effectiveness of otic fluoroquinolones, ofloxacin (Floxin Otic) and ciprofloxacin (Ciprodex), which have several clinical, microbiologic, and dosing advantages over older topical antibiotics. Fluoroquinolones are not ototoxic and are effective against S aureus and P aeruginosa.
The incidence of fluoroquinolone-resistant Pseudomonas in otitis externa is low, and hypersensitivity is quite rare. Although they are slightly more expensive than neomycin combinations, fluoroquinolones require only 1 or 2 daily doses, possess superior in vitro activity, and provide a better safety profile that favor their use in moderate to severe otitis externa.
Symptoms and complications to watch for
Pain, which may be incapacitating, is the predominant complaint and the only symptom directly related to disease severity.1,6 Patients may also experience discharge, itchiness, and, in some cases, temporary hearing loss.1,5 A fluffy white exudate may signal a rare fungal infection, perhaps complicating an underlying bacterial infection.
Bone involvement. A rare, extremely severe form of otitis externa, known as malignant (or necrotizing) otitis externa, is caused by a Pseudomonas infection that invades the posterior cranial bone. This life-threatening form of otitis externa affects primarily elderly patients with diabetes who live in hot, humid environments. Malignant otitis externa usually requires hospitalization and parenteral antibiotic therapy.7
Secondary cellulitis. Summer often ushers in several cases of another severe form of otitis externa in children, involving a secondary cellulitis of the pre- and postauricular skin structures. If an underlying mastoiditis is uncertain, consider ordering a computerized tomography scan and referring for an otolaryngologic exam. This cellulitis infection also requires aggressive broad-spectrum oral or parenteral therapy.
Elements of successful treatment
Most treated cases of otitis externa resolve completely within 5 days. In a study conducted in the Netherlands, 35 out of 98 adult patients discontinued daily activities for a median of 4 days, and the median duration of bed rest was 3 days.3
However, secondary skin and soft tissue infections can slow resolution. They may also develop if treatment is delayed or ineffective. For uncomplicated otitis externa, treatment with an appropriate topical antibiotic, plus potent analgesics to relieve pain, is the preferred therapeutic approach.4,8 Choosing the optimal topical treatment, however, requires knowledge of evolving resistance among pathogens, possible hypersensitivity to neomycin, adherence factors, and cost issues.
Topical antibiotics usually sufficient. Most cases of otitis externa without significant complications9 are effectively treated with just topical antibiotics; though, for more severe cases, I prefer to insert an ear wick and to use oral narcotics.7
In the 1970s to 1990s, topical combination preparations containing hydrocortisone and the antibiotics neomycin sulfate and polymyxin B were the mainstay of therapy for otitis externa.6,9 Approximately 5 years ago, topical fluoroquinolones became available for otitis externa. Given this range of antibiotic choices, physicians need to know the various treatment options and other modalities available.
Oral antibiotics. Additional oral or parenteral antibiotics are usually necessary for severe cases of otitis externa with secondary cellulitis or lymphadenitis.10,11 Oral antibiotics may also be necessary with concomitant disease at other sites (sinus, middle ear) or complications.
Pain relief. Nonsteroidal anti-inflammatory drugs (NSAIDs—eg, ibuprofen), acetaminophen, and narcotics (eg, codeine) are adjunctive measures for reducing ear pain.
Enabling compliance. Patient compliance, according to one systematic review, is inversely proportional to the prescribed number of doses per day.12 Adherence with twice-daily dosing was significantly better than with 4-times-daily dosing for oral and topical medications.12 Twice-daily dosing is accepted as readily as once-daily dosing12 and may maintain continuity of drug action better than a once-daily regimen in the event a dose is forgotten.13
Acute inflammation of the external auditory canal most often is caused by bacterial infection. Infrequently, a fungal infection may be the cause.
Pseudomonas aeruginosa and Staphylococcus aureus are the predominant bacterial pathogens associated with otitis externa.1,2 The pathogenesis involves modification of the natural antimicrobial defense mechanisms of the external ear canal. Under healthy conditions, cerumen (ear wax), which is secreted by sebaceous and apocrine glands in the external ear canal, is acidic and contains lysozyme, an antimicrobial substance. The ear canal becomes vulnerable to bacterial infection when the cerumen barrier is disrupted by scratching or scraping, or macerated by prolonged exposure to water. Disruption of the external ear’s epithelium, caused by seborrhea, eczema, or trauma, can also increase the risk of otitis externa. Because frequent swimming is the most common predisposing factor for the disease, otitis externa is commonly referred to as “swimmer’s ear.”1,3 As may be expected, the number of cases of otitis externa increases markedly during the summer months in temperate climates.4 The infection is uncommon in children aged less than 2 years.
Rarely, otitis externa appears to be caused by fungal infection.5 Such cases are not usually differentiated on clinical grounds, except when there is appearance of a fluffy white exudate. In most cases of fungal otitis externa, the fungus appears to be a superinfection after the bacterial infection. Thus, persistent otitis externa is typically treated with 2 or 3 courses of topical antibiotics before the clinician begins to investigate more specifically for fungal superinfection.
Is there a place for astringents?
Before antibiotic availability, the mainstay of treatment was topical compounds containing astringents such as aluminum acetate solution (Burow’s Solution USP, Domeboro, and others) and acetic acid solutions (Vosol Otic).14-16 These preparations are still widely used but principally to prevent otitis externa.
Topical 8% aluminum acetate solution was as effective as a commonly used antimicrobial-corticosteroid topical mixture (polymyxin-neomycin-hydrocortisone) for 25 adult patients with otitis externa (72% vs 76%, respectively).17 In a doubleblind, randomized study involving 65 adults and children, the effectiveness of aluminum acetate equaled that of gentamicin otic solution.18
In a Dutch study evaluating otitis externa in 213 adults, topical antibiotics were more effective than topical acetic acid alone and alleviated symptoms faster than acetic acid plus steroids.
The lack of a large, well-structured, placebo-controlled study or other compelling evidence casts doubt on the relative effectiveness of astringent topical treatments for otitis externa. Also, topical astringents are often painful, which may impede adherence.19
Practitioners usually reserve nonspecific therapy such as acetic acid and Burow’s solution for prevention and self-medication for mild symptoms. Studies that include measures of clinical goals, such as pain relief, cessation of symptoms, and eradication of infection, are needed before astringent agents can be recommended for routine therapy of moderate to severe otitis externa. Most treatment data concerning otitis externa have centered on therapy with antimicrobial otic drops.20
Preparing the ear for antibiotic administration
Topical antibiotics are presumed to eradicate pathogens most effectively through direct contact at concentrations exceeding the minimum inhibitory concentration (MIC90).21-23
Debride if possible. Though the severity of pain may preclude debridement, removing debris from the external ear canal during the office visit will maximize delivery of the medication. This can be performed with a dry cotton swab or small Calgiswab or by suctioning with a metal or plastic catheter. Cleansing by irrigation or flushing of the ear canal with a syringe or pulsatile irrigator (Water-Pik) may be more tolerable for some patients, but probably should be performed only when the tympanic membrane can be visualized due to the risk that the debris overlies an unseen perforation of the tympanic membrane.24
Ear wick helpful. After the ear canal has been debrided, consider the benefit of inserting an ear wick. Particularly if the ear canal is swollen, medication may not penetrate deep enough into the canal. In this situation, an ear wick, such as a Pope Oto-wick or Merocel XL (Medtronic Xomed, Inc, Jacksonville, Fla) hydrogel polymer, can enhance medication delivery directly to the entire ear canal.
The medication is absorbed into the ear wick, which delivers the drug to the infected skin (FIGURE). As swelling subsides, most ear wicks extrude spontaneously, usually within 12 to 36 hours. Once the edema subsides and much of the debris in the external ear canal has been cleared, topical antibiotics can be instilled.
FIGURE 1
Ear wick within the external ear canal
The ear wick is inserted into the external auditory canal until the remaining edge is flush with the external ear. In smaller children, one fourth to one third of the wick may be cut to prevent it from falling out prematurely. Several drops of topical antibiotics are instilled onto the wick until it has fully expanded. At home, a few drops of topical antibiotic should be applied to the wick every few hours for the first 24 hours to keep the wick moist. The wick should be removed with tweezers within 24 to 48 hours if it has not already fallen out.
Common topical therapies
Topical antibiotics commonly used for otitis externa are listed in the TABLE.
TABLE
Common topical antibiotic treatments for otitis externa
| TREATMENT (FORMULATION) | DOSING REGIMEN | ADVANTAGES/DISADVANTAGES |
|---|---|---|
| Neomycin sulfate/polymyxin B/hydrocortisone (suspension/acidic) | 4 times daily | Efficacious, extensively used; moderately expensive (AWP $65) |
| Resistance and hypersensitivity increasing; potentially ototoxic; discourages compliance | ||
| Ofloxacin otic (solution/neutral) | Once or twice daily | Efficacious; no ototoxicity or hypersensitivity; favors compliance |
| Resistance increasing; moderately expensive (AWP 5 cc $44.45; 10 cc $82.25) | ||
| Ciprofloxacin otic, with dexamethasone (suspension/acidic) | Twice daily | Efficacious; no ototoxicity with ciprofloxacin; favors compliance |
| Resistance increasing; expensive (AWP $85) | ||
| AWP, average wholesale price | ||
Combination drugs containing aminoglycosides
Combination topical drugs containing an aminoglycoside (neomycin), polymyxin B, and a corticosteroid were once the only antibiotic treatments for otitis externa approved by the US Food and Drug Administration.9 Neomycin is a bactericidal inhibitor of protein synthesis that is modestly active against S aureus but has minimal activity against P aeruginosa.25
In 1999, a prevalence study of aminoglycoside resistance in Europe found that 25% of the S aureus isolates tested were resistant to gentamicin.26 This study also found a high incidence (20%–38%) of gentamicin-resistant P aeruginosa isolates from Belgium, France, Italy, and Poland.26 Furthermore, in a prospective study of aural isolates of P aeruginosa, only 17.8% were susceptible to neomycin.27
Polymyxin B is active against P aeruginosa but not against S aureus.28
Combining neomycin and polymyxin B broadens the spectrum of antimicrobial activity. Hydrocortisone, a low-potency steroid, purportedly helps reduce associated inflammation. Several ophthalmic preparations that contain a corticosteroid or an aminoglycoside, such as gentamicin or tobramycin, have been used off-label for otitis externa.3,29
Neomycin/polymyxin B/hydrocortisone has been shown in earlier clinical trials to be efficacious in up to 97% of cases of otitis externa.16 However, S aureus has been increasingly resistant to aminoglycosides.30,31 More than 10% of S aureus strains were resistant to gentamicin between 1987 and 1999.26,32
Possible ototoxicity. Aminoglycoside drops may cause vestibular ototoxicity when the tympanic membrane is perforated. Aminoglycosides instilled into the inner ear of test animals have been shown to damage cochlear inner and outer hair cells.33-35 Only a few similar case studies in humans have been published.36-38 Assessment of the tympanic membrane is often difficult because of excessive swelling of the external ear canal1 or patient noncooperation due to pain. In such cases—though tympanic membrane perforation is uncommon in otitis externa—physicians may want to avoid aminoglycosides.
Beware hypersensitivity. Drug hypersensitivity is another concern with topical aminoglycosides. Neomycin and thimerosal are among the antibiotic allergens most commonly detected on patch testing.39,40 Thimerosal is a preservative added to common otic formulations of neomycin/polymyxin B/hydrocortisone.41 In a retrospective review of patch testing reactions from 587 adult patients, neomycin sulfate and thimerosal elicited a hypersensitivity reaction in 53% and 18% of the patients, respectively.40
Hypersensitivity to these agents has also been shown in children by skin testing, although it is apparently rare clinically.42,43 A patch testing study involving 562 healthy schoolchildren found that 18.4% and 14.9% of the children had hypersensitivity on skin testing to neomycin sulfate and thimerosal, respectively.43 The high incidence of sensitization to neomycin and thimerosal may be related to the common use of neomycin as a topical ointment on skin abrasions and of thimerosal as a bacteriostatic preservative in immunizations in the past.
Fluoroquinolones
Oral fluoroquinolone antibiotics have been available for adults since 1990. The fluoroquinolones ofloxacin and ciprofloxacin were approved as topical therapy for otitis externa in 1997 and 1998, respectively. In addition, ofloxacin is indicated for otorrhea from the middle ear through an implanted tympanostomy tube (tube otorrhea).
Fluoroquinolones inhibit DNA gyrase and topoisomerase, which are required for bacterial DNA synthesis.23 These are broad-spectrum antibiotics that have good in vitro activity against both S aureus and P aeruginosa.23 An in vitro analysis of antimicrobial activity against clinical isolates ofS aureus and P aeruginosa indicated that ofloxacin and ciprofloxacin were more active against these pathogens than was neomycin.44 The MIC90 values of ofloxacin and ciprofloxacin, respectively, were 1.0 μg/mL and 2.0 μg/mL for S aureus and 2.0 μg/mL and 0.25 μg/mL for P aeruginosa. In contrast, the MIC90 values of neomycin were 4.0 μg/mL forS aureus and 16.0 μg/mL for P aeruginosa. The MIC90 for polymyxin B against P aeruginosa was 2.0 g/mL.45
Clinically equivalent to neomycin compound. Recent clinical studies have shown that ofloxacin and ciprofloxacin are as efficacious as neomycin/polymyxin B/hydrocortisone in the treatment of otitis externa.21,22,46 In one study, the overall cure rate was 89% in patients treated with either ofloxacin (N=301) or neomycin/polymyxin B/hydrocortisone (N=300).21 In another study, ciprofloxacin was comparably effective as neomycin/polymyxin B/hydrocortisone therapy (93% [N=239] vs 87% [N=228]; 95% confidence interval, 0.0–10.5).22
S aureus resistance has increased. Fluoroquinolone use has been reported to lead to resistance in topical infections other than otitis externa. For example, the incidence of fluoroquinolone-resistant keratitis isolates of S aureus increased from 11% in 1990 to 28% in 1998.47 In another 5-year review of bacterial keratitis cases,48 the incidence of ciprofloxacin-resistant isolates of S aureus increased annually from 5.8% in 1993 to 35.0% in 1997, and the incidence of resistant isolates to ofloxacin increased from 4.7% to 35.0% over the same period.48 In contrast, P aeruginosa isolates remained susceptible to fluoroquinolones during the study periods.48 Resistance ofP aeruginosa to fluoroquinolones has increased only slightly.49 Between 1991 and 1994, 0.44% of ocular isolates of P aeruginosa were resistant to ciprofloxacin, while 4.1% showed in vitro resistance between 1995 and 1998.49
Fluoroquinolone has advantages over combination therapy. Ofloxacin and ciprofloxacin do not cause ototoxicity in humans and do not damage isolated cochlear cells, as can neomycin/polymyxin B/hydrocortisone combinations.34,50 In fact, both ofloxacin and ciprofloxacin/dexamethasone have been approved for use in patients with patent tympanostomy tube otorrhea.29
Topical use of ofloxacin and ciprofloxacin is not associated with hypersensitivity, and hypersensitivity after the oral administration of these drugs is rare.51,52
Finally, the once- or twice-daily dosage regimen of the topical fluoroquinolones markedly improves therapeutic adherence when compared with the 4-timesdaily regimen of neomycin/polymyxin B/hydrocortisone.21,22,46
Preparations containing corticosteroids
The benefit of corticosteroids for otitis externa is not well established, though they are added to many topical antibiotic preparations. In one study, the addition of hydrocortisone to neomycin and polymyx in B reduced pain by approximately 1 day for patients with otitis externa.22 A combination of ciprofloxacin 0.3% and dexamethasone 0.1% administered twice daily is indicated for acute otitis externa,53 as was supported by an efficacy rate of 90.9% in a recent randomized, observer-masked, parallel-group, multicenter study in 468 children and adults.54 Although hypersensitivity to topical corticosteroids is well documented in published clinical studies, it seems to be rare in clinical practice.55-57
Special circumstances
Severe pain. Inserting an ear wick and prescribing a topical fluoroquinolone plus an oral narcotic, such as acetaminophen with codeine, may be the optimal approach to resolving the infection and managing pain. Compared with neomycin combinations, ofloxacin and ciprofloxacin are somewhat more active in vitro against likely pathogens.
Otitis externa with concomitant acute otitis media. Antibiotics such as amoxicillin/clavulanate or cefdinir for acute otitis media should be used in addition to topical antibiotics.
Otitis externa with mild localized cellulitis. A standard oral antibiotic that covers staphylococci is recommended. Oral fluoroquinolones, for patients over 17 years of age, or intravenous ceftazidime may also be considered for more severe cases associated with aural cellulitis.
For younger children, I have prescribed oral ciprofloxacin (off-label), which has been recently approved for children older than 12 months with complicated urinary tract infection. Outpatient parenteral ceftriaxone may alternatively be used for some cases of cellulitis if the patient is only moderately ill. If rates of communityacquired methicillin-resistant S aureus exceed 15% to 20% in the community, clinicians should consider empiric therapy initially with trimethoprim-sulfamethoxazole or clindamycin.
Fungal infection. If a patient develops (1) otitis externa refractory to 2 consecutive courses of topical antibiotics, or (2) exhibits a discharge that looks like a white, fluffy exudate, suspect a fungal infection and obtain a culture of the exudate. Empiric therapy with either oral fluconazole (Diflucan) or topical ciclopirox (Loprox) solution should be considered.
CORRESPONDING AUTHOR
Stan L. Block, MD 201 South Fifth Street, Suite 102, Bardstown, KY 40004. E-mail: [email protected]
1. Agius AM, Pickles JM, Burch KL. A prospective study of otitis externa. Clin Otolaryngol 1992;17:150-154.
2. Clark WB, Brook I, Bianki D, Thompson DH. Microbiology of otitis externa. Otolaryngol Head Neck Surg 1997;116:23-25.
3. van Asperen I, de Rover CM, Schijven JF, Oetomo SB, Schellekens JF, van Leeuwen NJ, et al. Risk of otitis externa after swimming in recreational fresh water lakes containing Pseudomonas aeruginosa. BMJ 1995;311:1407-1410.
4. Rowlands S, Devalia H, Smith C, Hubbard R, Dean A. Otitis externa in UK general practice: a survey using the UK General Practice Research Database. Br J Gen Pract 2001;51:533-538.
5. Hawke M, Wong J, Krajden S. Clinical and microbiological features of otitis externa. J Otolaryngol 1984;13:289-295.
6. Halpern MT, Palmer CS, Seidlin M. Treatment patterns for otitis externa. J Am Board Fam Pract 1999;12:1-7.
7. Lang R, Palmer S, Kitzes-Cohen R, Sade J. Successful treatment of malignant external otitis with oral ciprofloxacin: report of experience with 23 patients. J Infect Dis 1990;161:537-540.
8. Hannley MT, Denneny JC, Holzer SS. Use of ototopical antibiotics in treating 3 common ear diseases. Otolaryngol Head Neck Surg 2000;122:934-940.
9. Cassisi N, Cohn A, Davidson T, Witten BR. Diffuse otitis externa: clinical and microbiologic findings in the course of a multicenter study on a new otic solution. Ann Otol Rhinol Laryngol Suppl 1977;86:1-16.
10. Zikk D, Rapoport Y, Redianu C, Shalit I, Himmelfarb MZ. Oral ofloxacin therapy for invasive external otitis. Ann Otol Rhinol Laryngol 1991;100:632-637.
11. Kimura AC, Pien FD. Head and neck cellulitis in hospitalized adults. Am J Otolaryngol 1993;14:343-349.
12. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther 2001;23:1296-1310.
13. Urquhart J. Ascertaining how much compliance is enough with outpatient antibiotic regimens. Postgrad Med J 1992;68(suppl 3):S49-S59.
15. Garrity JD, Halliday TC, Glassman JM. Prevention of swimmer’s ear by simple prophylactic regimen. Curr Ther Res Clin Exp 1974;16:437-441.
16. Dadagian AJ, Hicks JJ, Ordonez GE, Glassman JM. Treatment of otitis externa: a controlled bacteriological-clinical evaluation. Curr Ther Res Clin Exp 1974;16:431-436.
17. Lambert IJ. A comparison of the treatment of otitis externa with ‘Otosporin’ and aluminium acetate: a report from a services practice in Cyprus. J R Coll Gen Pract 1981;31:291-294.
18. Clayton MI, Osborne JE, Rutherford D, Rivron RP. A double-blind, randomized, prospective trial of a topical antiseptic versus a topical antibiotic in the treatment of otorrhoea. Clin Otolaryngol 1990;15:7-10.
19. Kleinerman ES, Knowles RD, Lachman LB, Gutterman JU. Effect of recombinant granulocyte/macrophage colony-stimulating factor on human monocyte activity in vitro and following intravenous administration. Cancer Res 1988;48:2604-2609.
20. van Balen FA, Smit WM, Zuithoff NP, Verheij TJ. Clinical efficacy of three common treatments in acute otitis externa in primary care: randomised controlled trial. BMJ 2003;327:1201-1205.
21. Jones RN, Milazzo J, Seidlin M. Ofloxacin otic solution for treatment of otitis externa in children and adults. Arch Otolaryngol Head Neck Surg 1997;123:1193-1200.
22. Pistorius B, Westberry K, Drehobl M. Prospective, randomized, comparative trial of ciprofloxacin otic drops, with or without hydrocortisone, vs.polymyxin Bneomycin-hydrocortisone otic suspension in the treatment of acute diffuse otitis externa. Infect Dis Clin Pract 1999;8:387-395.
23. Hooper DC. Quinolones. In: Mandell G, Bennett J, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Philadelphia, Pa: Churchill Livingstone, 2000;404-413.
24. Blake P, Matthews R, Hornibrook J. When not to syringe an ear. N Z Med J 1998;111:422-424.
25. Chambers H. Antimicrobial agents: the aminoglycosides. In: Hardman J, Limbird L, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. New York: McGraw-Hill, 2001;1219-1238.
26. Schmitz F-J, Verhoef J, Fluit AC. Prevalence of aminoglycoside resistance in 20 European university hospitals participating in the European SENTRY Antimicrobial Surveillance Programme. Eur J Clin Microbiol Infect Dis 1999;18:414-421.
27. Dohar JE, Kenna MA, Wadowsky RM. In vitro susceptibility of aural isolates of Pseudomonas aeruginosa to commonly used ototopical antibiotics. Am J Otol 1996;17:207-209.
28. Chambers H. Antimicrobial agents: protein synthesis inhibitors and miscellaneous antibacterial agents. In: Hardman J, Limbird L, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. New York: McGraw-Hill, 2001;1239-1271.
29. Goldblatt EL. Efficacy of ofloxacin and other otic preparations for acute otitis media in patients with tympanostomy tubes. Pediatr Infect Dis J 2001;20:116-119.
30. Bovelacci A, Montini G, Ramacciotti PG. Changes in resistance to aminoglycoside antibiotics of different bacterial strains isolated during the period 1978 to 1983. Netilmicin as alternative therapy. Chemioterapia 1985;4:439-444.
31. Courcol RJ, Pinkas M, Martin GR. A seven year survey of antibiotic susceptibility and its relationship with usage. J Antimicrob Chemother 1989;23:441-451.
32. Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 2001;7:178-182.
33. Wright CG, Meyerhoff WL. Ototoxicity of otic drops applied to the middle ear in the chinchilla. Am J Otolaryngol 1984;5:166-176.
34. Barlow DW, Duckert LG, Kreig CS, Gates GA. Ototoxicity of topical otomicrobial agents. Acta Otolaryngol 1995;115:231-235.
35. Jinn TH, Kim PD, Russell PT, Church CA, John EO, Jung TT. Determination of ototoxicity of common otic drops using isolated cochlear outer hair cells. Laryngoscope 2001;111:2105-2108.
36. Wong DL, Rutka JA. Do aminoglycoside otic preparations cause ototoxicity in the presence of tympanic membrane perforations? Otolaryngol Head Neck Surg 1997;116:404-410.
37. Marais J, Rutka JA. Ototoxicity and topical eardrops. Clin Otolaryngol 1998;23:360-367.
38. Bath AP, Walsh RM, Bance ML, Rutka JA. Ototoxicity of topical gentamicin preparations. Laryngoscope 1999;109:1088-1093.
39. Van Ginkel CJ, Bruintjes TD, Huizing EH. Allergy due to topical medications in chronic otitis externa and chronic otitis media. Clin Otolaryngol 1995;20:326-328.
40. Dickel H, Taylor JS, Evey P, Merk HF. Delayed readings of a standard screening patch test tray: frequency of “lost,” “found,” and “persistent” reactions. Am J Contact Dermat 2000;11:213-217.
41. Suneja T, Belsito DV. Thimerosal in the detection of clinically relevant allergic contact reactions. J Am Acad Dermatol 2001;45:23-27.
42. Manzini BM, Ferdani G, Simonetti V, Donini M, Seidenari S. Contact sensitization in children. Pediatr Dermatol 1998;15:12-17.
43. Barros MA, Baptista A, Correia TM, Azevedo F. Patch. testing in children: a study of 562 schoolchildren. Contact Dermatitis 1991;25:156-159.
44. Roland PS, Stroman DW. Microbiology of acute otitis externa. Laryngoscope 2002;112:1166-1177.
45. Gales AC, Reis AO, Jones RN. Contemporary assessment of antimicrobial susceptibility testing methods for polymyxin B and colistin: review of available interpretative criteria and quality control guidelines. J Clin Microbiol 2001;39:183-190.
46. Torum B, Block SL, Avila H, Montiel F, Oliva A, Quintanilla W, et al. Efficacy of ofloxacin otic solution once daily for 7 days in the treatment of otitis externa: a multicenter, open-label, phase III trial. Clin Ther 2004;26:1046-1054.
47. Alexandrakis G, Alfonso EC, Miller D. Shifting trends in bacterial keratitis in south Florida and emerging resistance to fluoroquinolones. Ophthalmology 2000;107:1497-1502.
48. Goldstein MH, Kowalski RP, Gordon YJ. Emerging fluoroquinolone resistance in bacterial keratitis: a 5-year review. Ophthalmology 1999;106:1313-1318.
49. Chaudhry NA, Flynn HW, Jr, Murray TG, Tabandeh H, Mello MO, Jr, Miller D. Emerging ciprofloxacin-resistant Pseudomonas aeruginosa. Am J Ophthalmol 1999;128:509-510.
50. Russell PT, Church CA, Jinn TH, Kim DJ, John EO, Jung TT. Effects of common topical otic preparations on the morphology of isolated cochlear outer hair cells. Acta Otolaryngol 2001;121:135-139.
51. Pipek R, Vulfsons S, Wolfovitz E, Har-Shai Y, Taran A, Peled IJ. Case report: ofloxacin-induced hypersensitivity vasculitis. Am J Med Sci 1996;311:82-83.
52. Reaño M, Vives R, Rodriguez J, Daroca P, Canto G, Fernandez J. Ciprofloxacin-induced vasculitis. Allergy 1997;52:599-600.
53. Ciprodex® [manufacturer’s prescribing information]. Fort Worth, Tex: Alcon Laboratories, Inc, 2003.
54. Roland PS, Pien FD, Schultz CC, Henry DC, Conroy PJ, Wall GM, et al. Efficacy and safety of topical ciprofloxacin/dexamethasone versus neomycin/polymyxin B/hydrocortisone for otitis externa. Curr Med Res Opin 2004;20:1175-1183.
55. Burden AD, Beck MH. Contact hypersensitivity to topical corticosteroids. Br J Dermatol 1992;127:497-500.
56. Dooms-Goossens A, Morren M. Results of routine patch testing with corticosteroid series in 2073 patients. Contact Dermatitis 1992;26:182-191.
57. Bircher AJ, Thurlimann W, Hunziker T, et al. Contact hypersensitivity to corticosteroids in routine patch test patients.A multi-centre study of the Swiss Contact Dermatitis Research Group. Dermatology 1995;191:109-114.
- Topical antimicrobial otic drops, supplemented by oral analgesics, provide prompt and effective therapy (B).
- Fluoroquinolones and neomycinpolymyxin B combinations have shown equal efficacy (A), but the former are preferred when trying to guard against ototoxicity or hypersensitivity (C).
- For severely painful otitis externa, consider inserting an ear wick and giving oral narcotics (C).
- Localized cellulitis requires systemic antimicrobial therapy (C).
- No compelling evidence exists on the effectiveness of astringent topical treatments for otitis externa. Also, topical astringents are often painful, which may impede adherence (B).
Widespread use of neomycin combinations may have led to an increase in the incidence of patient hypersensitivity and promoted antibiotic resistance in Staphylococcus aureus and Pseudomonas aeruginosa, the 2 most common pathogens of otitis externa (see Pathogens of otitis externa).
Recent controlled clinical trials have shown the effectiveness of otic fluoroquinolones, ofloxacin (Floxin Otic) and ciprofloxacin (Ciprodex), which have several clinical, microbiologic, and dosing advantages over older topical antibiotics. Fluoroquinolones are not ototoxic and are effective against S aureus and P aeruginosa.
The incidence of fluoroquinolone-resistant Pseudomonas in otitis externa is low, and hypersensitivity is quite rare. Although they are slightly more expensive than neomycin combinations, fluoroquinolones require only 1 or 2 daily doses, possess superior in vitro activity, and provide a better safety profile that favor their use in moderate to severe otitis externa.
Symptoms and complications to watch for
Pain, which may be incapacitating, is the predominant complaint and the only symptom directly related to disease severity.1,6 Patients may also experience discharge, itchiness, and, in some cases, temporary hearing loss.1,5 A fluffy white exudate may signal a rare fungal infection, perhaps complicating an underlying bacterial infection.
Bone involvement. A rare, extremely severe form of otitis externa, known as malignant (or necrotizing) otitis externa, is caused by a Pseudomonas infection that invades the posterior cranial bone. This life-threatening form of otitis externa affects primarily elderly patients with diabetes who live in hot, humid environments. Malignant otitis externa usually requires hospitalization and parenteral antibiotic therapy.7
Secondary cellulitis. Summer often ushers in several cases of another severe form of otitis externa in children, involving a secondary cellulitis of the pre- and postauricular skin structures. If an underlying mastoiditis is uncertain, consider ordering a computerized tomography scan and referring for an otolaryngologic exam. This cellulitis infection also requires aggressive broad-spectrum oral or parenteral therapy.
Elements of successful treatment
Most treated cases of otitis externa resolve completely within 5 days. In a study conducted in the Netherlands, 35 out of 98 adult patients discontinued daily activities for a median of 4 days, and the median duration of bed rest was 3 days.3
However, secondary skin and soft tissue infections can slow resolution. They may also develop if treatment is delayed or ineffective. For uncomplicated otitis externa, treatment with an appropriate topical antibiotic, plus potent analgesics to relieve pain, is the preferred therapeutic approach.4,8 Choosing the optimal topical treatment, however, requires knowledge of evolving resistance among pathogens, possible hypersensitivity to neomycin, adherence factors, and cost issues.
Topical antibiotics usually sufficient. Most cases of otitis externa without significant complications9 are effectively treated with just topical antibiotics; though, for more severe cases, I prefer to insert an ear wick and to use oral narcotics.7
In the 1970s to 1990s, topical combination preparations containing hydrocortisone and the antibiotics neomycin sulfate and polymyxin B were the mainstay of therapy for otitis externa.6,9 Approximately 5 years ago, topical fluoroquinolones became available for otitis externa. Given this range of antibiotic choices, physicians need to know the various treatment options and other modalities available.
Oral antibiotics. Additional oral or parenteral antibiotics are usually necessary for severe cases of otitis externa with secondary cellulitis or lymphadenitis.10,11 Oral antibiotics may also be necessary with concomitant disease at other sites (sinus, middle ear) or complications.
Pain relief. Nonsteroidal anti-inflammatory drugs (NSAIDs—eg, ibuprofen), acetaminophen, and narcotics (eg, codeine) are adjunctive measures for reducing ear pain.
Enabling compliance. Patient compliance, according to one systematic review, is inversely proportional to the prescribed number of doses per day.12 Adherence with twice-daily dosing was significantly better than with 4-times-daily dosing for oral and topical medications.12 Twice-daily dosing is accepted as readily as once-daily dosing12 and may maintain continuity of drug action better than a once-daily regimen in the event a dose is forgotten.13
Acute inflammation of the external auditory canal most often is caused by bacterial infection. Infrequently, a fungal infection may be the cause.
Pseudomonas aeruginosa and Staphylococcus aureus are the predominant bacterial pathogens associated with otitis externa.1,2 The pathogenesis involves modification of the natural antimicrobial defense mechanisms of the external ear canal. Under healthy conditions, cerumen (ear wax), which is secreted by sebaceous and apocrine glands in the external ear canal, is acidic and contains lysozyme, an antimicrobial substance. The ear canal becomes vulnerable to bacterial infection when the cerumen barrier is disrupted by scratching or scraping, or macerated by prolonged exposure to water. Disruption of the external ear’s epithelium, caused by seborrhea, eczema, or trauma, can also increase the risk of otitis externa. Because frequent swimming is the most common predisposing factor for the disease, otitis externa is commonly referred to as “swimmer’s ear.”1,3 As may be expected, the number of cases of otitis externa increases markedly during the summer months in temperate climates.4 The infection is uncommon in children aged less than 2 years.
Rarely, otitis externa appears to be caused by fungal infection.5 Such cases are not usually differentiated on clinical grounds, except when there is appearance of a fluffy white exudate. In most cases of fungal otitis externa, the fungus appears to be a superinfection after the bacterial infection. Thus, persistent otitis externa is typically treated with 2 or 3 courses of topical antibiotics before the clinician begins to investigate more specifically for fungal superinfection.
Is there a place for astringents?
Before antibiotic availability, the mainstay of treatment was topical compounds containing astringents such as aluminum acetate solution (Burow’s Solution USP, Domeboro, and others) and acetic acid solutions (Vosol Otic).14-16 These preparations are still widely used but principally to prevent otitis externa.
Topical 8% aluminum acetate solution was as effective as a commonly used antimicrobial-corticosteroid topical mixture (polymyxin-neomycin-hydrocortisone) for 25 adult patients with otitis externa (72% vs 76%, respectively).17 In a doubleblind, randomized study involving 65 adults and children, the effectiveness of aluminum acetate equaled that of gentamicin otic solution.18
In a Dutch study evaluating otitis externa in 213 adults, topical antibiotics were more effective than topical acetic acid alone and alleviated symptoms faster than acetic acid plus steroids.
The lack of a large, well-structured, placebo-controlled study or other compelling evidence casts doubt on the relative effectiveness of astringent topical treatments for otitis externa. Also, topical astringents are often painful, which may impede adherence.19
Practitioners usually reserve nonspecific therapy such as acetic acid and Burow’s solution for prevention and self-medication for mild symptoms. Studies that include measures of clinical goals, such as pain relief, cessation of symptoms, and eradication of infection, are needed before astringent agents can be recommended for routine therapy of moderate to severe otitis externa. Most treatment data concerning otitis externa have centered on therapy with antimicrobial otic drops.20
Preparing the ear for antibiotic administration
Topical antibiotics are presumed to eradicate pathogens most effectively through direct contact at concentrations exceeding the minimum inhibitory concentration (MIC90).21-23
Debride if possible. Though the severity of pain may preclude debridement, removing debris from the external ear canal during the office visit will maximize delivery of the medication. This can be performed with a dry cotton swab or small Calgiswab or by suctioning with a metal or plastic catheter. Cleansing by irrigation or flushing of the ear canal with a syringe or pulsatile irrigator (Water-Pik) may be more tolerable for some patients, but probably should be performed only when the tympanic membrane can be visualized due to the risk that the debris overlies an unseen perforation of the tympanic membrane.24
Ear wick helpful. After the ear canal has been debrided, consider the benefit of inserting an ear wick. Particularly if the ear canal is swollen, medication may not penetrate deep enough into the canal. In this situation, an ear wick, such as a Pope Oto-wick or Merocel XL (Medtronic Xomed, Inc, Jacksonville, Fla) hydrogel polymer, can enhance medication delivery directly to the entire ear canal.
The medication is absorbed into the ear wick, which delivers the drug to the infected skin (FIGURE). As swelling subsides, most ear wicks extrude spontaneously, usually within 12 to 36 hours. Once the edema subsides and much of the debris in the external ear canal has been cleared, topical antibiotics can be instilled.
FIGURE 1
Ear wick within the external ear canal
The ear wick is inserted into the external auditory canal until the remaining edge is flush with the external ear. In smaller children, one fourth to one third of the wick may be cut to prevent it from falling out prematurely. Several drops of topical antibiotics are instilled onto the wick until it has fully expanded. At home, a few drops of topical antibiotic should be applied to the wick every few hours for the first 24 hours to keep the wick moist. The wick should be removed with tweezers within 24 to 48 hours if it has not already fallen out.
Common topical therapies
Topical antibiotics commonly used for otitis externa are listed in the TABLE.
TABLE
Common topical antibiotic treatments for otitis externa
| TREATMENT (FORMULATION) | DOSING REGIMEN | ADVANTAGES/DISADVANTAGES |
|---|---|---|
| Neomycin sulfate/polymyxin B/hydrocortisone (suspension/acidic) | 4 times daily | Efficacious, extensively used; moderately expensive (AWP $65) |
| Resistance and hypersensitivity increasing; potentially ototoxic; discourages compliance | ||
| Ofloxacin otic (solution/neutral) | Once or twice daily | Efficacious; no ototoxicity or hypersensitivity; favors compliance |
| Resistance increasing; moderately expensive (AWP 5 cc $44.45; 10 cc $82.25) | ||
| Ciprofloxacin otic, with dexamethasone (suspension/acidic) | Twice daily | Efficacious; no ototoxicity with ciprofloxacin; favors compliance |
| Resistance increasing; expensive (AWP $85) | ||
| AWP, average wholesale price | ||
Combination drugs containing aminoglycosides
Combination topical drugs containing an aminoglycoside (neomycin), polymyxin B, and a corticosteroid were once the only antibiotic treatments for otitis externa approved by the US Food and Drug Administration.9 Neomycin is a bactericidal inhibitor of protein synthesis that is modestly active against S aureus but has minimal activity against P aeruginosa.25
In 1999, a prevalence study of aminoglycoside resistance in Europe found that 25% of the S aureus isolates tested were resistant to gentamicin.26 This study also found a high incidence (20%–38%) of gentamicin-resistant P aeruginosa isolates from Belgium, France, Italy, and Poland.26 Furthermore, in a prospective study of aural isolates of P aeruginosa, only 17.8% were susceptible to neomycin.27
Polymyxin B is active against P aeruginosa but not against S aureus.28
Combining neomycin and polymyxin B broadens the spectrum of antimicrobial activity. Hydrocortisone, a low-potency steroid, purportedly helps reduce associated inflammation. Several ophthalmic preparations that contain a corticosteroid or an aminoglycoside, such as gentamicin or tobramycin, have been used off-label for otitis externa.3,29
Neomycin/polymyxin B/hydrocortisone has been shown in earlier clinical trials to be efficacious in up to 97% of cases of otitis externa.16 However, S aureus has been increasingly resistant to aminoglycosides.30,31 More than 10% of S aureus strains were resistant to gentamicin between 1987 and 1999.26,32
Possible ototoxicity. Aminoglycoside drops may cause vestibular ototoxicity when the tympanic membrane is perforated. Aminoglycosides instilled into the inner ear of test animals have been shown to damage cochlear inner and outer hair cells.33-35 Only a few similar case studies in humans have been published.36-38 Assessment of the tympanic membrane is often difficult because of excessive swelling of the external ear canal1 or patient noncooperation due to pain. In such cases—though tympanic membrane perforation is uncommon in otitis externa—physicians may want to avoid aminoglycosides.
Beware hypersensitivity. Drug hypersensitivity is another concern with topical aminoglycosides. Neomycin and thimerosal are among the antibiotic allergens most commonly detected on patch testing.39,40 Thimerosal is a preservative added to common otic formulations of neomycin/polymyxin B/hydrocortisone.41 In a retrospective review of patch testing reactions from 587 adult patients, neomycin sulfate and thimerosal elicited a hypersensitivity reaction in 53% and 18% of the patients, respectively.40
Hypersensitivity to these agents has also been shown in children by skin testing, although it is apparently rare clinically.42,43 A patch testing study involving 562 healthy schoolchildren found that 18.4% and 14.9% of the children had hypersensitivity on skin testing to neomycin sulfate and thimerosal, respectively.43 The high incidence of sensitization to neomycin and thimerosal may be related to the common use of neomycin as a topical ointment on skin abrasions and of thimerosal as a bacteriostatic preservative in immunizations in the past.
Fluoroquinolones
Oral fluoroquinolone antibiotics have been available for adults since 1990. The fluoroquinolones ofloxacin and ciprofloxacin were approved as topical therapy for otitis externa in 1997 and 1998, respectively. In addition, ofloxacin is indicated for otorrhea from the middle ear through an implanted tympanostomy tube (tube otorrhea).
Fluoroquinolones inhibit DNA gyrase and topoisomerase, which are required for bacterial DNA synthesis.23 These are broad-spectrum antibiotics that have good in vitro activity against both S aureus and P aeruginosa.23 An in vitro analysis of antimicrobial activity against clinical isolates ofS aureus and P aeruginosa indicated that ofloxacin and ciprofloxacin were more active against these pathogens than was neomycin.44 The MIC90 values of ofloxacin and ciprofloxacin, respectively, were 1.0 μg/mL and 2.0 μg/mL for S aureus and 2.0 μg/mL and 0.25 μg/mL for P aeruginosa. In contrast, the MIC90 values of neomycin were 4.0 μg/mL forS aureus and 16.0 μg/mL for P aeruginosa. The MIC90 for polymyxin B against P aeruginosa was 2.0 g/mL.45
Clinically equivalent to neomycin compound. Recent clinical studies have shown that ofloxacin and ciprofloxacin are as efficacious as neomycin/polymyxin B/hydrocortisone in the treatment of otitis externa.21,22,46 In one study, the overall cure rate was 89% in patients treated with either ofloxacin (N=301) or neomycin/polymyxin B/hydrocortisone (N=300).21 In another study, ciprofloxacin was comparably effective as neomycin/polymyxin B/hydrocortisone therapy (93% [N=239] vs 87% [N=228]; 95% confidence interval, 0.0–10.5).22
S aureus resistance has increased. Fluoroquinolone use has been reported to lead to resistance in topical infections other than otitis externa. For example, the incidence of fluoroquinolone-resistant keratitis isolates of S aureus increased from 11% in 1990 to 28% in 1998.47 In another 5-year review of bacterial keratitis cases,48 the incidence of ciprofloxacin-resistant isolates of S aureus increased annually from 5.8% in 1993 to 35.0% in 1997, and the incidence of resistant isolates to ofloxacin increased from 4.7% to 35.0% over the same period.48 In contrast, P aeruginosa isolates remained susceptible to fluoroquinolones during the study periods.48 Resistance ofP aeruginosa to fluoroquinolones has increased only slightly.49 Between 1991 and 1994, 0.44% of ocular isolates of P aeruginosa were resistant to ciprofloxacin, while 4.1% showed in vitro resistance between 1995 and 1998.49
Fluoroquinolone has advantages over combination therapy. Ofloxacin and ciprofloxacin do not cause ototoxicity in humans and do not damage isolated cochlear cells, as can neomycin/polymyxin B/hydrocortisone combinations.34,50 In fact, both ofloxacin and ciprofloxacin/dexamethasone have been approved for use in patients with patent tympanostomy tube otorrhea.29
Topical use of ofloxacin and ciprofloxacin is not associated with hypersensitivity, and hypersensitivity after the oral administration of these drugs is rare.51,52
Finally, the once- or twice-daily dosage regimen of the topical fluoroquinolones markedly improves therapeutic adherence when compared with the 4-timesdaily regimen of neomycin/polymyxin B/hydrocortisone.21,22,46
Preparations containing corticosteroids
The benefit of corticosteroids for otitis externa is not well established, though they are added to many topical antibiotic preparations. In one study, the addition of hydrocortisone to neomycin and polymyx in B reduced pain by approximately 1 day for patients with otitis externa.22 A combination of ciprofloxacin 0.3% and dexamethasone 0.1% administered twice daily is indicated for acute otitis externa,53 as was supported by an efficacy rate of 90.9% in a recent randomized, observer-masked, parallel-group, multicenter study in 468 children and adults.54 Although hypersensitivity to topical corticosteroids is well documented in published clinical studies, it seems to be rare in clinical practice.55-57
Special circumstances
Severe pain. Inserting an ear wick and prescribing a topical fluoroquinolone plus an oral narcotic, such as acetaminophen with codeine, may be the optimal approach to resolving the infection and managing pain. Compared with neomycin combinations, ofloxacin and ciprofloxacin are somewhat more active in vitro against likely pathogens.
Otitis externa with concomitant acute otitis media. Antibiotics such as amoxicillin/clavulanate or cefdinir for acute otitis media should be used in addition to topical antibiotics.
Otitis externa with mild localized cellulitis. A standard oral antibiotic that covers staphylococci is recommended. Oral fluoroquinolones, for patients over 17 years of age, or intravenous ceftazidime may also be considered for more severe cases associated with aural cellulitis.
For younger children, I have prescribed oral ciprofloxacin (off-label), which has been recently approved for children older than 12 months with complicated urinary tract infection. Outpatient parenteral ceftriaxone may alternatively be used for some cases of cellulitis if the patient is only moderately ill. If rates of communityacquired methicillin-resistant S aureus exceed 15% to 20% in the community, clinicians should consider empiric therapy initially with trimethoprim-sulfamethoxazole or clindamycin.
Fungal infection. If a patient develops (1) otitis externa refractory to 2 consecutive courses of topical antibiotics, or (2) exhibits a discharge that looks like a white, fluffy exudate, suspect a fungal infection and obtain a culture of the exudate. Empiric therapy with either oral fluconazole (Diflucan) or topical ciclopirox (Loprox) solution should be considered.
CORRESPONDING AUTHOR
Stan L. Block, MD 201 South Fifth Street, Suite 102, Bardstown, KY 40004. E-mail: [email protected]
- Topical antimicrobial otic drops, supplemented by oral analgesics, provide prompt and effective therapy (B).
- Fluoroquinolones and neomycinpolymyxin B combinations have shown equal efficacy (A), but the former are preferred when trying to guard against ototoxicity or hypersensitivity (C).
- For severely painful otitis externa, consider inserting an ear wick and giving oral narcotics (C).
- Localized cellulitis requires systemic antimicrobial therapy (C).
- No compelling evidence exists on the effectiveness of astringent topical treatments for otitis externa. Also, topical astringents are often painful, which may impede adherence (B).
Widespread use of neomycin combinations may have led to an increase in the incidence of patient hypersensitivity and promoted antibiotic resistance in Staphylococcus aureus and Pseudomonas aeruginosa, the 2 most common pathogens of otitis externa (see Pathogens of otitis externa).
Recent controlled clinical trials have shown the effectiveness of otic fluoroquinolones, ofloxacin (Floxin Otic) and ciprofloxacin (Ciprodex), which have several clinical, microbiologic, and dosing advantages over older topical antibiotics. Fluoroquinolones are not ototoxic and are effective against S aureus and P aeruginosa.
The incidence of fluoroquinolone-resistant Pseudomonas in otitis externa is low, and hypersensitivity is quite rare. Although they are slightly more expensive than neomycin combinations, fluoroquinolones require only 1 or 2 daily doses, possess superior in vitro activity, and provide a better safety profile that favor their use in moderate to severe otitis externa.
Symptoms and complications to watch for
Pain, which may be incapacitating, is the predominant complaint and the only symptom directly related to disease severity.1,6 Patients may also experience discharge, itchiness, and, in some cases, temporary hearing loss.1,5 A fluffy white exudate may signal a rare fungal infection, perhaps complicating an underlying bacterial infection.
Bone involvement. A rare, extremely severe form of otitis externa, known as malignant (or necrotizing) otitis externa, is caused by a Pseudomonas infection that invades the posterior cranial bone. This life-threatening form of otitis externa affects primarily elderly patients with diabetes who live in hot, humid environments. Malignant otitis externa usually requires hospitalization and parenteral antibiotic therapy.7
Secondary cellulitis. Summer often ushers in several cases of another severe form of otitis externa in children, involving a secondary cellulitis of the pre- and postauricular skin structures. If an underlying mastoiditis is uncertain, consider ordering a computerized tomography scan and referring for an otolaryngologic exam. This cellulitis infection also requires aggressive broad-spectrum oral or parenteral therapy.
Elements of successful treatment
Most treated cases of otitis externa resolve completely within 5 days. In a study conducted in the Netherlands, 35 out of 98 adult patients discontinued daily activities for a median of 4 days, and the median duration of bed rest was 3 days.3
However, secondary skin and soft tissue infections can slow resolution. They may also develop if treatment is delayed or ineffective. For uncomplicated otitis externa, treatment with an appropriate topical antibiotic, plus potent analgesics to relieve pain, is the preferred therapeutic approach.4,8 Choosing the optimal topical treatment, however, requires knowledge of evolving resistance among pathogens, possible hypersensitivity to neomycin, adherence factors, and cost issues.
Topical antibiotics usually sufficient. Most cases of otitis externa without significant complications9 are effectively treated with just topical antibiotics; though, for more severe cases, I prefer to insert an ear wick and to use oral narcotics.7
In the 1970s to 1990s, topical combination preparations containing hydrocortisone and the antibiotics neomycin sulfate and polymyxin B were the mainstay of therapy for otitis externa.6,9 Approximately 5 years ago, topical fluoroquinolones became available for otitis externa. Given this range of antibiotic choices, physicians need to know the various treatment options and other modalities available.
Oral antibiotics. Additional oral or parenteral antibiotics are usually necessary for severe cases of otitis externa with secondary cellulitis or lymphadenitis.10,11 Oral antibiotics may also be necessary with concomitant disease at other sites (sinus, middle ear) or complications.
Pain relief. Nonsteroidal anti-inflammatory drugs (NSAIDs—eg, ibuprofen), acetaminophen, and narcotics (eg, codeine) are adjunctive measures for reducing ear pain.
Enabling compliance. Patient compliance, according to one systematic review, is inversely proportional to the prescribed number of doses per day.12 Adherence with twice-daily dosing was significantly better than with 4-times-daily dosing for oral and topical medications.12 Twice-daily dosing is accepted as readily as once-daily dosing12 and may maintain continuity of drug action better than a once-daily regimen in the event a dose is forgotten.13
Acute inflammation of the external auditory canal most often is caused by bacterial infection. Infrequently, a fungal infection may be the cause.
Pseudomonas aeruginosa and Staphylococcus aureus are the predominant bacterial pathogens associated with otitis externa.1,2 The pathogenesis involves modification of the natural antimicrobial defense mechanisms of the external ear canal. Under healthy conditions, cerumen (ear wax), which is secreted by sebaceous and apocrine glands in the external ear canal, is acidic and contains lysozyme, an antimicrobial substance. The ear canal becomes vulnerable to bacterial infection when the cerumen barrier is disrupted by scratching or scraping, or macerated by prolonged exposure to water. Disruption of the external ear’s epithelium, caused by seborrhea, eczema, or trauma, can also increase the risk of otitis externa. Because frequent swimming is the most common predisposing factor for the disease, otitis externa is commonly referred to as “swimmer’s ear.”1,3 As may be expected, the number of cases of otitis externa increases markedly during the summer months in temperate climates.4 The infection is uncommon in children aged less than 2 years.
Rarely, otitis externa appears to be caused by fungal infection.5 Such cases are not usually differentiated on clinical grounds, except when there is appearance of a fluffy white exudate. In most cases of fungal otitis externa, the fungus appears to be a superinfection after the bacterial infection. Thus, persistent otitis externa is typically treated with 2 or 3 courses of topical antibiotics before the clinician begins to investigate more specifically for fungal superinfection.
Is there a place for astringents?
Before antibiotic availability, the mainstay of treatment was topical compounds containing astringents such as aluminum acetate solution (Burow’s Solution USP, Domeboro, and others) and acetic acid solutions (Vosol Otic).14-16 These preparations are still widely used but principally to prevent otitis externa.
Topical 8% aluminum acetate solution was as effective as a commonly used antimicrobial-corticosteroid topical mixture (polymyxin-neomycin-hydrocortisone) for 25 adult patients with otitis externa (72% vs 76%, respectively).17 In a doubleblind, randomized study involving 65 adults and children, the effectiveness of aluminum acetate equaled that of gentamicin otic solution.18
In a Dutch study evaluating otitis externa in 213 adults, topical antibiotics were more effective than topical acetic acid alone and alleviated symptoms faster than acetic acid plus steroids.
The lack of a large, well-structured, placebo-controlled study or other compelling evidence casts doubt on the relative effectiveness of astringent topical treatments for otitis externa. Also, topical astringents are often painful, which may impede adherence.19
Practitioners usually reserve nonspecific therapy such as acetic acid and Burow’s solution for prevention and self-medication for mild symptoms. Studies that include measures of clinical goals, such as pain relief, cessation of symptoms, and eradication of infection, are needed before astringent agents can be recommended for routine therapy of moderate to severe otitis externa. Most treatment data concerning otitis externa have centered on therapy with antimicrobial otic drops.20
Preparing the ear for antibiotic administration
Topical antibiotics are presumed to eradicate pathogens most effectively through direct contact at concentrations exceeding the minimum inhibitory concentration (MIC90).21-23
Debride if possible. Though the severity of pain may preclude debridement, removing debris from the external ear canal during the office visit will maximize delivery of the medication. This can be performed with a dry cotton swab or small Calgiswab or by suctioning with a metal or plastic catheter. Cleansing by irrigation or flushing of the ear canal with a syringe or pulsatile irrigator (Water-Pik) may be more tolerable for some patients, but probably should be performed only when the tympanic membrane can be visualized due to the risk that the debris overlies an unseen perforation of the tympanic membrane.24
Ear wick helpful. After the ear canal has been debrided, consider the benefit of inserting an ear wick. Particularly if the ear canal is swollen, medication may not penetrate deep enough into the canal. In this situation, an ear wick, such as a Pope Oto-wick or Merocel XL (Medtronic Xomed, Inc, Jacksonville, Fla) hydrogel polymer, can enhance medication delivery directly to the entire ear canal.
The medication is absorbed into the ear wick, which delivers the drug to the infected skin (FIGURE). As swelling subsides, most ear wicks extrude spontaneously, usually within 12 to 36 hours. Once the edema subsides and much of the debris in the external ear canal has been cleared, topical antibiotics can be instilled.
FIGURE 1
Ear wick within the external ear canal
The ear wick is inserted into the external auditory canal until the remaining edge is flush with the external ear. In smaller children, one fourth to one third of the wick may be cut to prevent it from falling out prematurely. Several drops of topical antibiotics are instilled onto the wick until it has fully expanded. At home, a few drops of topical antibiotic should be applied to the wick every few hours for the first 24 hours to keep the wick moist. The wick should be removed with tweezers within 24 to 48 hours if it has not already fallen out.
Common topical therapies
Topical antibiotics commonly used for otitis externa are listed in the TABLE.
TABLE
Common topical antibiotic treatments for otitis externa
| TREATMENT (FORMULATION) | DOSING REGIMEN | ADVANTAGES/DISADVANTAGES |
|---|---|---|
| Neomycin sulfate/polymyxin B/hydrocortisone (suspension/acidic) | 4 times daily | Efficacious, extensively used; moderately expensive (AWP $65) |
| Resistance and hypersensitivity increasing; potentially ototoxic; discourages compliance | ||
| Ofloxacin otic (solution/neutral) | Once or twice daily | Efficacious; no ototoxicity or hypersensitivity; favors compliance |
| Resistance increasing; moderately expensive (AWP 5 cc $44.45; 10 cc $82.25) | ||
| Ciprofloxacin otic, with dexamethasone (suspension/acidic) | Twice daily | Efficacious; no ototoxicity with ciprofloxacin; favors compliance |
| Resistance increasing; expensive (AWP $85) | ||
| AWP, average wholesale price | ||
Combination drugs containing aminoglycosides
Combination topical drugs containing an aminoglycoside (neomycin), polymyxin B, and a corticosteroid were once the only antibiotic treatments for otitis externa approved by the US Food and Drug Administration.9 Neomycin is a bactericidal inhibitor of protein synthesis that is modestly active against S aureus but has minimal activity against P aeruginosa.25
In 1999, a prevalence study of aminoglycoside resistance in Europe found that 25% of the S aureus isolates tested were resistant to gentamicin.26 This study also found a high incidence (20%–38%) of gentamicin-resistant P aeruginosa isolates from Belgium, France, Italy, and Poland.26 Furthermore, in a prospective study of aural isolates of P aeruginosa, only 17.8% were susceptible to neomycin.27
Polymyxin B is active against P aeruginosa but not against S aureus.28
Combining neomycin and polymyxin B broadens the spectrum of antimicrobial activity. Hydrocortisone, a low-potency steroid, purportedly helps reduce associated inflammation. Several ophthalmic preparations that contain a corticosteroid or an aminoglycoside, such as gentamicin or tobramycin, have been used off-label for otitis externa.3,29
Neomycin/polymyxin B/hydrocortisone has been shown in earlier clinical trials to be efficacious in up to 97% of cases of otitis externa.16 However, S aureus has been increasingly resistant to aminoglycosides.30,31 More than 10% of S aureus strains were resistant to gentamicin between 1987 and 1999.26,32
Possible ototoxicity. Aminoglycoside drops may cause vestibular ototoxicity when the tympanic membrane is perforated. Aminoglycosides instilled into the inner ear of test animals have been shown to damage cochlear inner and outer hair cells.33-35 Only a few similar case studies in humans have been published.36-38 Assessment of the tympanic membrane is often difficult because of excessive swelling of the external ear canal1 or patient noncooperation due to pain. In such cases—though tympanic membrane perforation is uncommon in otitis externa—physicians may want to avoid aminoglycosides.
Beware hypersensitivity. Drug hypersensitivity is another concern with topical aminoglycosides. Neomycin and thimerosal are among the antibiotic allergens most commonly detected on patch testing.39,40 Thimerosal is a preservative added to common otic formulations of neomycin/polymyxin B/hydrocortisone.41 In a retrospective review of patch testing reactions from 587 adult patients, neomycin sulfate and thimerosal elicited a hypersensitivity reaction in 53% and 18% of the patients, respectively.40
Hypersensitivity to these agents has also been shown in children by skin testing, although it is apparently rare clinically.42,43 A patch testing study involving 562 healthy schoolchildren found that 18.4% and 14.9% of the children had hypersensitivity on skin testing to neomycin sulfate and thimerosal, respectively.43 The high incidence of sensitization to neomycin and thimerosal may be related to the common use of neomycin as a topical ointment on skin abrasions and of thimerosal as a bacteriostatic preservative in immunizations in the past.
Fluoroquinolones
Oral fluoroquinolone antibiotics have been available for adults since 1990. The fluoroquinolones ofloxacin and ciprofloxacin were approved as topical therapy for otitis externa in 1997 and 1998, respectively. In addition, ofloxacin is indicated for otorrhea from the middle ear through an implanted tympanostomy tube (tube otorrhea).
Fluoroquinolones inhibit DNA gyrase and topoisomerase, which are required for bacterial DNA synthesis.23 These are broad-spectrum antibiotics that have good in vitro activity against both S aureus and P aeruginosa.23 An in vitro analysis of antimicrobial activity against clinical isolates ofS aureus and P aeruginosa indicated that ofloxacin and ciprofloxacin were more active against these pathogens than was neomycin.44 The MIC90 values of ofloxacin and ciprofloxacin, respectively, were 1.0 μg/mL and 2.0 μg/mL for S aureus and 2.0 μg/mL and 0.25 μg/mL for P aeruginosa. In contrast, the MIC90 values of neomycin were 4.0 μg/mL forS aureus and 16.0 μg/mL for P aeruginosa. The MIC90 for polymyxin B against P aeruginosa was 2.0 g/mL.45
Clinically equivalent to neomycin compound. Recent clinical studies have shown that ofloxacin and ciprofloxacin are as efficacious as neomycin/polymyxin B/hydrocortisone in the treatment of otitis externa.21,22,46 In one study, the overall cure rate was 89% in patients treated with either ofloxacin (N=301) or neomycin/polymyxin B/hydrocortisone (N=300).21 In another study, ciprofloxacin was comparably effective as neomycin/polymyxin B/hydrocortisone therapy (93% [N=239] vs 87% [N=228]; 95% confidence interval, 0.0–10.5).22
S aureus resistance has increased. Fluoroquinolone use has been reported to lead to resistance in topical infections other than otitis externa. For example, the incidence of fluoroquinolone-resistant keratitis isolates of S aureus increased from 11% in 1990 to 28% in 1998.47 In another 5-year review of bacterial keratitis cases,48 the incidence of ciprofloxacin-resistant isolates of S aureus increased annually from 5.8% in 1993 to 35.0% in 1997, and the incidence of resistant isolates to ofloxacin increased from 4.7% to 35.0% over the same period.48 In contrast, P aeruginosa isolates remained susceptible to fluoroquinolones during the study periods.48 Resistance ofP aeruginosa to fluoroquinolones has increased only slightly.49 Between 1991 and 1994, 0.44% of ocular isolates of P aeruginosa were resistant to ciprofloxacin, while 4.1% showed in vitro resistance between 1995 and 1998.49
Fluoroquinolone has advantages over combination therapy. Ofloxacin and ciprofloxacin do not cause ototoxicity in humans and do not damage isolated cochlear cells, as can neomycin/polymyxin B/hydrocortisone combinations.34,50 In fact, both ofloxacin and ciprofloxacin/dexamethasone have been approved for use in patients with patent tympanostomy tube otorrhea.29
Topical use of ofloxacin and ciprofloxacin is not associated with hypersensitivity, and hypersensitivity after the oral administration of these drugs is rare.51,52
Finally, the once- or twice-daily dosage regimen of the topical fluoroquinolones markedly improves therapeutic adherence when compared with the 4-timesdaily regimen of neomycin/polymyxin B/hydrocortisone.21,22,46
Preparations containing corticosteroids
The benefit of corticosteroids for otitis externa is not well established, though they are added to many topical antibiotic preparations. In one study, the addition of hydrocortisone to neomycin and polymyx in B reduced pain by approximately 1 day for patients with otitis externa.22 A combination of ciprofloxacin 0.3% and dexamethasone 0.1% administered twice daily is indicated for acute otitis externa,53 as was supported by an efficacy rate of 90.9% in a recent randomized, observer-masked, parallel-group, multicenter study in 468 children and adults.54 Although hypersensitivity to topical corticosteroids is well documented in published clinical studies, it seems to be rare in clinical practice.55-57
Special circumstances
Severe pain. Inserting an ear wick and prescribing a topical fluoroquinolone plus an oral narcotic, such as acetaminophen with codeine, may be the optimal approach to resolving the infection and managing pain. Compared with neomycin combinations, ofloxacin and ciprofloxacin are somewhat more active in vitro against likely pathogens.
Otitis externa with concomitant acute otitis media. Antibiotics such as amoxicillin/clavulanate or cefdinir for acute otitis media should be used in addition to topical antibiotics.
Otitis externa with mild localized cellulitis. A standard oral antibiotic that covers staphylococci is recommended. Oral fluoroquinolones, for patients over 17 years of age, or intravenous ceftazidime may also be considered for more severe cases associated with aural cellulitis.
For younger children, I have prescribed oral ciprofloxacin (off-label), which has been recently approved for children older than 12 months with complicated urinary tract infection. Outpatient parenteral ceftriaxone may alternatively be used for some cases of cellulitis if the patient is only moderately ill. If rates of communityacquired methicillin-resistant S aureus exceed 15% to 20% in the community, clinicians should consider empiric therapy initially with trimethoprim-sulfamethoxazole or clindamycin.
Fungal infection. If a patient develops (1) otitis externa refractory to 2 consecutive courses of topical antibiotics, or (2) exhibits a discharge that looks like a white, fluffy exudate, suspect a fungal infection and obtain a culture of the exudate. Empiric therapy with either oral fluconazole (Diflucan) or topical ciclopirox (Loprox) solution should be considered.
CORRESPONDING AUTHOR
Stan L. Block, MD 201 South Fifth Street, Suite 102, Bardstown, KY 40004. E-mail: [email protected]
1. Agius AM, Pickles JM, Burch KL. A prospective study of otitis externa. Clin Otolaryngol 1992;17:150-154.
2. Clark WB, Brook I, Bianki D, Thompson DH. Microbiology of otitis externa. Otolaryngol Head Neck Surg 1997;116:23-25.
3. van Asperen I, de Rover CM, Schijven JF, Oetomo SB, Schellekens JF, van Leeuwen NJ, et al. Risk of otitis externa after swimming in recreational fresh water lakes containing Pseudomonas aeruginosa. BMJ 1995;311:1407-1410.
4. Rowlands S, Devalia H, Smith C, Hubbard R, Dean A. Otitis externa in UK general practice: a survey using the UK General Practice Research Database. Br J Gen Pract 2001;51:533-538.
5. Hawke M, Wong J, Krajden S. Clinical and microbiological features of otitis externa. J Otolaryngol 1984;13:289-295.
6. Halpern MT, Palmer CS, Seidlin M. Treatment patterns for otitis externa. J Am Board Fam Pract 1999;12:1-7.
7. Lang R, Palmer S, Kitzes-Cohen R, Sade J. Successful treatment of malignant external otitis with oral ciprofloxacin: report of experience with 23 patients. J Infect Dis 1990;161:537-540.
8. Hannley MT, Denneny JC, Holzer SS. Use of ototopical antibiotics in treating 3 common ear diseases. Otolaryngol Head Neck Surg 2000;122:934-940.
9. Cassisi N, Cohn A, Davidson T, Witten BR. Diffuse otitis externa: clinical and microbiologic findings in the course of a multicenter study on a new otic solution. Ann Otol Rhinol Laryngol Suppl 1977;86:1-16.
10. Zikk D, Rapoport Y, Redianu C, Shalit I, Himmelfarb MZ. Oral ofloxacin therapy for invasive external otitis. Ann Otol Rhinol Laryngol 1991;100:632-637.
11. Kimura AC, Pien FD. Head and neck cellulitis in hospitalized adults. Am J Otolaryngol 1993;14:343-349.
12. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther 2001;23:1296-1310.
13. Urquhart J. Ascertaining how much compliance is enough with outpatient antibiotic regimens. Postgrad Med J 1992;68(suppl 3):S49-S59.
15. Garrity JD, Halliday TC, Glassman JM. Prevention of swimmer’s ear by simple prophylactic regimen. Curr Ther Res Clin Exp 1974;16:437-441.
16. Dadagian AJ, Hicks JJ, Ordonez GE, Glassman JM. Treatment of otitis externa: a controlled bacteriological-clinical evaluation. Curr Ther Res Clin Exp 1974;16:431-436.
17. Lambert IJ. A comparison of the treatment of otitis externa with ‘Otosporin’ and aluminium acetate: a report from a services practice in Cyprus. J R Coll Gen Pract 1981;31:291-294.
18. Clayton MI, Osborne JE, Rutherford D, Rivron RP. A double-blind, randomized, prospective trial of a topical antiseptic versus a topical antibiotic in the treatment of otorrhoea. Clin Otolaryngol 1990;15:7-10.
19. Kleinerman ES, Knowles RD, Lachman LB, Gutterman JU. Effect of recombinant granulocyte/macrophage colony-stimulating factor on human monocyte activity in vitro and following intravenous administration. Cancer Res 1988;48:2604-2609.
20. van Balen FA, Smit WM, Zuithoff NP, Verheij TJ. Clinical efficacy of three common treatments in acute otitis externa in primary care: randomised controlled trial. BMJ 2003;327:1201-1205.
21. Jones RN, Milazzo J, Seidlin M. Ofloxacin otic solution for treatment of otitis externa in children and adults. Arch Otolaryngol Head Neck Surg 1997;123:1193-1200.
22. Pistorius B, Westberry K, Drehobl M. Prospective, randomized, comparative trial of ciprofloxacin otic drops, with or without hydrocortisone, vs.polymyxin Bneomycin-hydrocortisone otic suspension in the treatment of acute diffuse otitis externa. Infect Dis Clin Pract 1999;8:387-395.
23. Hooper DC. Quinolones. In: Mandell G, Bennett J, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Philadelphia, Pa: Churchill Livingstone, 2000;404-413.
24. Blake P, Matthews R, Hornibrook J. When not to syringe an ear. N Z Med J 1998;111:422-424.
25. Chambers H. Antimicrobial agents: the aminoglycosides. In: Hardman J, Limbird L, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. New York: McGraw-Hill, 2001;1219-1238.
26. Schmitz F-J, Verhoef J, Fluit AC. Prevalence of aminoglycoside resistance in 20 European university hospitals participating in the European SENTRY Antimicrobial Surveillance Programme. Eur J Clin Microbiol Infect Dis 1999;18:414-421.
27. Dohar JE, Kenna MA, Wadowsky RM. In vitro susceptibility of aural isolates of Pseudomonas aeruginosa to commonly used ototopical antibiotics. Am J Otol 1996;17:207-209.
28. Chambers H. Antimicrobial agents: protein synthesis inhibitors and miscellaneous antibacterial agents. In: Hardman J, Limbird L, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. New York: McGraw-Hill, 2001;1239-1271.
29. Goldblatt EL. Efficacy of ofloxacin and other otic preparations for acute otitis media in patients with tympanostomy tubes. Pediatr Infect Dis J 2001;20:116-119.
30. Bovelacci A, Montini G, Ramacciotti PG. Changes in resistance to aminoglycoside antibiotics of different bacterial strains isolated during the period 1978 to 1983. Netilmicin as alternative therapy. Chemioterapia 1985;4:439-444.
31. Courcol RJ, Pinkas M, Martin GR. A seven year survey of antibiotic susceptibility and its relationship with usage. J Antimicrob Chemother 1989;23:441-451.
32. Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 2001;7:178-182.
33. Wright CG, Meyerhoff WL. Ototoxicity of otic drops applied to the middle ear in the chinchilla. Am J Otolaryngol 1984;5:166-176.
34. Barlow DW, Duckert LG, Kreig CS, Gates GA. Ototoxicity of topical otomicrobial agents. Acta Otolaryngol 1995;115:231-235.
35. Jinn TH, Kim PD, Russell PT, Church CA, John EO, Jung TT. Determination of ototoxicity of common otic drops using isolated cochlear outer hair cells. Laryngoscope 2001;111:2105-2108.
36. Wong DL, Rutka JA. Do aminoglycoside otic preparations cause ototoxicity in the presence of tympanic membrane perforations? Otolaryngol Head Neck Surg 1997;116:404-410.
37. Marais J, Rutka JA. Ototoxicity and topical eardrops. Clin Otolaryngol 1998;23:360-367.
38. Bath AP, Walsh RM, Bance ML, Rutka JA. Ototoxicity of topical gentamicin preparations. Laryngoscope 1999;109:1088-1093.
39. Van Ginkel CJ, Bruintjes TD, Huizing EH. Allergy due to topical medications in chronic otitis externa and chronic otitis media. Clin Otolaryngol 1995;20:326-328.
40. Dickel H, Taylor JS, Evey P, Merk HF. Delayed readings of a standard screening patch test tray: frequency of “lost,” “found,” and “persistent” reactions. Am J Contact Dermat 2000;11:213-217.
41. Suneja T, Belsito DV. Thimerosal in the detection of clinically relevant allergic contact reactions. J Am Acad Dermatol 2001;45:23-27.
42. Manzini BM, Ferdani G, Simonetti V, Donini M, Seidenari S. Contact sensitization in children. Pediatr Dermatol 1998;15:12-17.
43. Barros MA, Baptista A, Correia TM, Azevedo F. Patch. testing in children: a study of 562 schoolchildren. Contact Dermatitis 1991;25:156-159.
44. Roland PS, Stroman DW. Microbiology of acute otitis externa. Laryngoscope 2002;112:1166-1177.
45. Gales AC, Reis AO, Jones RN. Contemporary assessment of antimicrobial susceptibility testing methods for polymyxin B and colistin: review of available interpretative criteria and quality control guidelines. J Clin Microbiol 2001;39:183-190.
46. Torum B, Block SL, Avila H, Montiel F, Oliva A, Quintanilla W, et al. Efficacy of ofloxacin otic solution once daily for 7 days in the treatment of otitis externa: a multicenter, open-label, phase III trial. Clin Ther 2004;26:1046-1054.
47. Alexandrakis G, Alfonso EC, Miller D. Shifting trends in bacterial keratitis in south Florida and emerging resistance to fluoroquinolones. Ophthalmology 2000;107:1497-1502.
48. Goldstein MH, Kowalski RP, Gordon YJ. Emerging fluoroquinolone resistance in bacterial keratitis: a 5-year review. Ophthalmology 1999;106:1313-1318.
49. Chaudhry NA, Flynn HW, Jr, Murray TG, Tabandeh H, Mello MO, Jr, Miller D. Emerging ciprofloxacin-resistant Pseudomonas aeruginosa. Am J Ophthalmol 1999;128:509-510.
50. Russell PT, Church CA, Jinn TH, Kim DJ, John EO, Jung TT. Effects of common topical otic preparations on the morphology of isolated cochlear outer hair cells. Acta Otolaryngol 2001;121:135-139.
51. Pipek R, Vulfsons S, Wolfovitz E, Har-Shai Y, Taran A, Peled IJ. Case report: ofloxacin-induced hypersensitivity vasculitis. Am J Med Sci 1996;311:82-83.
52. Reaño M, Vives R, Rodriguez J, Daroca P, Canto G, Fernandez J. Ciprofloxacin-induced vasculitis. Allergy 1997;52:599-600.
53. Ciprodex® [manufacturer’s prescribing information]. Fort Worth, Tex: Alcon Laboratories, Inc, 2003.
54. Roland PS, Pien FD, Schultz CC, Henry DC, Conroy PJ, Wall GM, et al. Efficacy and safety of topical ciprofloxacin/dexamethasone versus neomycin/polymyxin B/hydrocortisone for otitis externa. Curr Med Res Opin 2004;20:1175-1183.
55. Burden AD, Beck MH. Contact hypersensitivity to topical corticosteroids. Br J Dermatol 1992;127:497-500.
56. Dooms-Goossens A, Morren M. Results of routine patch testing with corticosteroid series in 2073 patients. Contact Dermatitis 1992;26:182-191.
57. Bircher AJ, Thurlimann W, Hunziker T, et al. Contact hypersensitivity to corticosteroids in routine patch test patients.A multi-centre study of the Swiss Contact Dermatitis Research Group. Dermatology 1995;191:109-114.
1. Agius AM, Pickles JM, Burch KL. A prospective study of otitis externa. Clin Otolaryngol 1992;17:150-154.
2. Clark WB, Brook I, Bianki D, Thompson DH. Microbiology of otitis externa. Otolaryngol Head Neck Surg 1997;116:23-25.
3. van Asperen I, de Rover CM, Schijven JF, Oetomo SB, Schellekens JF, van Leeuwen NJ, et al. Risk of otitis externa after swimming in recreational fresh water lakes containing Pseudomonas aeruginosa. BMJ 1995;311:1407-1410.
4. Rowlands S, Devalia H, Smith C, Hubbard R, Dean A. Otitis externa in UK general practice: a survey using the UK General Practice Research Database. Br J Gen Pract 2001;51:533-538.
5. Hawke M, Wong J, Krajden S. Clinical and microbiological features of otitis externa. J Otolaryngol 1984;13:289-295.
6. Halpern MT, Palmer CS, Seidlin M. Treatment patterns for otitis externa. J Am Board Fam Pract 1999;12:1-7.
7. Lang R, Palmer S, Kitzes-Cohen R, Sade J. Successful treatment of malignant external otitis with oral ciprofloxacin: report of experience with 23 patients. J Infect Dis 1990;161:537-540.
8. Hannley MT, Denneny JC, Holzer SS. Use of ototopical antibiotics in treating 3 common ear diseases. Otolaryngol Head Neck Surg 2000;122:934-940.
9. Cassisi N, Cohn A, Davidson T, Witten BR. Diffuse otitis externa: clinical and microbiologic findings in the course of a multicenter study on a new otic solution. Ann Otol Rhinol Laryngol Suppl 1977;86:1-16.
10. Zikk D, Rapoport Y, Redianu C, Shalit I, Himmelfarb MZ. Oral ofloxacin therapy for invasive external otitis. Ann Otol Rhinol Laryngol 1991;100:632-637.
11. Kimura AC, Pien FD. Head and neck cellulitis in hospitalized adults. Am J Otolaryngol 1993;14:343-349.
12. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther 2001;23:1296-1310.
13. Urquhart J. Ascertaining how much compliance is enough with outpatient antibiotic regimens. Postgrad Med J 1992;68(suppl 3):S49-S59.
15. Garrity JD, Halliday TC, Glassman JM. Prevention of swimmer’s ear by simple prophylactic regimen. Curr Ther Res Clin Exp 1974;16:437-441.
16. Dadagian AJ, Hicks JJ, Ordonez GE, Glassman JM. Treatment of otitis externa: a controlled bacteriological-clinical evaluation. Curr Ther Res Clin Exp 1974;16:431-436.
17. Lambert IJ. A comparison of the treatment of otitis externa with ‘Otosporin’ and aluminium acetate: a report from a services practice in Cyprus. J R Coll Gen Pract 1981;31:291-294.
18. Clayton MI, Osborne JE, Rutherford D, Rivron RP. A double-blind, randomized, prospective trial of a topical antiseptic versus a topical antibiotic in the treatment of otorrhoea. Clin Otolaryngol 1990;15:7-10.
19. Kleinerman ES, Knowles RD, Lachman LB, Gutterman JU. Effect of recombinant granulocyte/macrophage colony-stimulating factor on human monocyte activity in vitro and following intravenous administration. Cancer Res 1988;48:2604-2609.
20. van Balen FA, Smit WM, Zuithoff NP, Verheij TJ. Clinical efficacy of three common treatments in acute otitis externa in primary care: randomised controlled trial. BMJ 2003;327:1201-1205.
21. Jones RN, Milazzo J, Seidlin M. Ofloxacin otic solution for treatment of otitis externa in children and adults. Arch Otolaryngol Head Neck Surg 1997;123:1193-1200.
22. Pistorius B, Westberry K, Drehobl M. Prospective, randomized, comparative trial of ciprofloxacin otic drops, with or without hydrocortisone, vs.polymyxin Bneomycin-hydrocortisone otic suspension in the treatment of acute diffuse otitis externa. Infect Dis Clin Pract 1999;8:387-395.
23. Hooper DC. Quinolones. In: Mandell G, Bennett J, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Philadelphia, Pa: Churchill Livingstone, 2000;404-413.
24. Blake P, Matthews R, Hornibrook J. When not to syringe an ear. N Z Med J 1998;111:422-424.
25. Chambers H. Antimicrobial agents: the aminoglycosides. In: Hardman J, Limbird L, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. New York: McGraw-Hill, 2001;1219-1238.
26. Schmitz F-J, Verhoef J, Fluit AC. Prevalence of aminoglycoside resistance in 20 European university hospitals participating in the European SENTRY Antimicrobial Surveillance Programme. Eur J Clin Microbiol Infect Dis 1999;18:414-421.
27. Dohar JE, Kenna MA, Wadowsky RM. In vitro susceptibility of aural isolates of Pseudomonas aeruginosa to commonly used ototopical antibiotics. Am J Otol 1996;17:207-209.
28. Chambers H. Antimicrobial agents: protein synthesis inhibitors and miscellaneous antibacterial agents. In: Hardman J, Limbird L, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. New York: McGraw-Hill, 2001;1239-1271.
29. Goldblatt EL. Efficacy of ofloxacin and other otic preparations for acute otitis media in patients with tympanostomy tubes. Pediatr Infect Dis J 2001;20:116-119.
30. Bovelacci A, Montini G, Ramacciotti PG. Changes in resistance to aminoglycoside antibiotics of different bacterial strains isolated during the period 1978 to 1983. Netilmicin as alternative therapy. Chemioterapia 1985;4:439-444.
31. Courcol RJ, Pinkas M, Martin GR. A seven year survey of antibiotic susceptibility and its relationship with usage. J Antimicrob Chemother 1989;23:441-451.
32. Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 2001;7:178-182.
33. Wright CG, Meyerhoff WL. Ototoxicity of otic drops applied to the middle ear in the chinchilla. Am J Otolaryngol 1984;5:166-176.
34. Barlow DW, Duckert LG, Kreig CS, Gates GA. Ototoxicity of topical otomicrobial agents. Acta Otolaryngol 1995;115:231-235.
35. Jinn TH, Kim PD, Russell PT, Church CA, John EO, Jung TT. Determination of ototoxicity of common otic drops using isolated cochlear outer hair cells. Laryngoscope 2001;111:2105-2108.
36. Wong DL, Rutka JA. Do aminoglycoside otic preparations cause ototoxicity in the presence of tympanic membrane perforations? Otolaryngol Head Neck Surg 1997;116:404-410.
37. Marais J, Rutka JA. Ototoxicity and topical eardrops. Clin Otolaryngol 1998;23:360-367.
38. Bath AP, Walsh RM, Bance ML, Rutka JA. Ototoxicity of topical gentamicin preparations. Laryngoscope 1999;109:1088-1093.
39. Van Ginkel CJ, Bruintjes TD, Huizing EH. Allergy due to topical medications in chronic otitis externa and chronic otitis media. Clin Otolaryngol 1995;20:326-328.
40. Dickel H, Taylor JS, Evey P, Merk HF. Delayed readings of a standard screening patch test tray: frequency of “lost,” “found,” and “persistent” reactions. Am J Contact Dermat 2000;11:213-217.
41. Suneja T, Belsito DV. Thimerosal in the detection of clinically relevant allergic contact reactions. J Am Acad Dermatol 2001;45:23-27.
42. Manzini BM, Ferdani G, Simonetti V, Donini M, Seidenari S. Contact sensitization in children. Pediatr Dermatol 1998;15:12-17.
43. Barros MA, Baptista A, Correia TM, Azevedo F. Patch. testing in children: a study of 562 schoolchildren. Contact Dermatitis 1991;25:156-159.
44. Roland PS, Stroman DW. Microbiology of acute otitis externa. Laryngoscope 2002;112:1166-1177.
45. Gales AC, Reis AO, Jones RN. Contemporary assessment of antimicrobial susceptibility testing methods for polymyxin B and colistin: review of available interpretative criteria and quality control guidelines. J Clin Microbiol 2001;39:183-190.
46. Torum B, Block SL, Avila H, Montiel F, Oliva A, Quintanilla W, et al. Efficacy of ofloxacin otic solution once daily for 7 days in the treatment of otitis externa: a multicenter, open-label, phase III trial. Clin Ther 2004;26:1046-1054.
47. Alexandrakis G, Alfonso EC, Miller D. Shifting trends in bacterial keratitis in south Florida and emerging resistance to fluoroquinolones. Ophthalmology 2000;107:1497-1502.
48. Goldstein MH, Kowalski RP, Gordon YJ. Emerging fluoroquinolone resistance in bacterial keratitis: a 5-year review. Ophthalmology 1999;106:1313-1318.
49. Chaudhry NA, Flynn HW, Jr, Murray TG, Tabandeh H, Mello MO, Jr, Miller D. Emerging ciprofloxacin-resistant Pseudomonas aeruginosa. Am J Ophthalmol 1999;128:509-510.
50. Russell PT, Church CA, Jinn TH, Kim DJ, John EO, Jung TT. Effects of common topical otic preparations on the morphology of isolated cochlear outer hair cells. Acta Otolaryngol 2001;121:135-139.
51. Pipek R, Vulfsons S, Wolfovitz E, Har-Shai Y, Taran A, Peled IJ. Case report: ofloxacin-induced hypersensitivity vasculitis. Am J Med Sci 1996;311:82-83.
52. Reaño M, Vives R, Rodriguez J, Daroca P, Canto G, Fernandez J. Ciprofloxacin-induced vasculitis. Allergy 1997;52:599-600.
53. Ciprodex® [manufacturer’s prescribing information]. Fort Worth, Tex: Alcon Laboratories, Inc, 2003.
54. Roland PS, Pien FD, Schultz CC, Henry DC, Conroy PJ, Wall GM, et al. Efficacy and safety of topical ciprofloxacin/dexamethasone versus neomycin/polymyxin B/hydrocortisone for otitis externa. Curr Med Res Opin 2004;20:1175-1183.
55. Burden AD, Beck MH. Contact hypersensitivity to topical corticosteroids. Br J Dermatol 1992;127:497-500.
56. Dooms-Goossens A, Morren M. Results of routine patch testing with corticosteroid series in 2073 patients. Contact Dermatitis 1992;26:182-191.
57. Bircher AJ, Thurlimann W, Hunziker T, et al. Contact hypersensitivity to corticosteroids in routine patch test patients.A multi-centre study of the Swiss Contact Dermatitis Research Group. Dermatology 1995;191:109-114.
Complex regional pain syndrome: Which treatments show promise?
- Treatments for CRPS type 1 supported by evidence of efficacy and little likelihood for harm are: topical DMSO cream (B), IV bisphosphonates (A) and limited courses of oral corticosteroids (B). Despite some contradictory evidence, physical therapy and calcitonin (intranasal or intramuscular) are likely to benefit patients with CRPS type 1 (B).
- Due to modest benefits and the invasiveness of the therapies, epidural clonidine injection, intravenous regional sympathetic block with bretylium and spinal cord stimulation should be offered only after careful counseling (B).
- Therapies to avoid due to lack of efficacy, lack of evidence, or a high likelihood of adverse outcomes are IV regional sympathetic blocks with anything but bretylium, sympathetic ganglion blocks with local anesthetics, systemic IV sympathetic inhibition, acupuncture, and sympathectomy (B).
In last issue of the Journal of Family Practice, we discussed diagnosis of CRPS type 1 (“Complex regional pain syndrome underdiagnosed,” 2005; 54: 524–532). Once other conditions have been ruled out, a primary care practitioner can diagnose CRPS type 1 right in the office using clinical findings and the patient’s report of symptoms. Similarly, primary care practitioners can provide most of the best treatments for CRPS type 1. In fact, evidence indicates that no benefit has been proven from more invasive treatments such as sympathectomy which continue to be included in recommendations by experts.1
Evidence for intervention less than compelling
A review of the literature on treating CRPS type 1 raises a question: is there any evidence that treatment makes a difference in outcomes that matter to patients, such as returning to work, regaining functionality of the affected limb, or resolution of pain? The large discrepancy between the high rates of CRPS type 1 documented in prospective studies of post-traumatic patients and the low rates of diagnosis of CRPS type 1 in actual practice suggests that most cases of CRPS type 1 resolve without being diagnosed and treated. This is not proven because, unfortunately, the natural history of persons diagnosed in the first 9 weeks after injury is not known.2
Are there benefits to early treatment?
From the clinician’s perspective, persons diagnosed with CRPS type 1 early appear more likely to respond to treatment. There is an “oft-quoted contention that results of early treatment will be better than those when the pain is treated late.”2 Yet, the great majority of these patients may have improved just as readily without treatment. For the few cases of undiagnosed CRPS type 1 that will persist to become chronic and treatment resistant, it is unknown whether early treatment would have been preventive2 or how clinicians could distinguish these cases early enough to target them for treatment.
Intriguing but limited data exist for using preventive therapies in all at-risk patients. One prospective cohort study documented a lower rate of CRPS type 1 in stroke patients who underwent early inpatient rehabilitation, compared with patients in earlier studies who rarely received early rehabilitation. This finding indirectly suggests a possible preventive effect of physical/occupational therapy (LOE: 3, cross-study comparison).3 Luckily, early inpatient rehabilitation in stroke patients has become the standard of care, which may prevent many cases of CRPS type 1 as a side effect.
It also appears that injury to a newly hemiplegic arm may contribute to the shoulder-hand syndrome; a study that alerted patients and care-takers to the risk of injury reduced the rate of shoulder hand syndrome from 27 to 8% (LOE: 2, lowerquality RCT).4 Among post-traumatic patients with wrist fracture, a double-blind randomized placebo controlled trial (n=115) of vitamin C 500 mg tabs initiated upon diagnosis of fracture and continued for 50 days resulted in a marked decrease of CRPS type 1 from 22% in the placebo group to 7% in the vitamin C group (relative risk=0.17) (LOE: 1, high-quality RCT).5 These results have not been tested in subsequent trials, however.
Guideline recommendations: Physical and psychological therapy, pain management
Many treatments for CRPS have been tried and are summarized without a systematic or evidence-based approach to the literature in a consensus statement released in 2002 by an interdisciplinary expert panel (LOE: 3, consensus guideline).1 These guidelines suggest rapid initiation of multidisciplinary treatment with advancement to higher levels of intervention if no benefit from initial therapy occurs in 2 weeks. Simultaneous physical rehabilitation, psychological therapy, and pain management are recommended.
Rehabilitation through physical therapy and occupational therapy starts with desensitization and stress loading, progresses to increasing flexibility with gentle active range of motion and stretching, and eventually to normalization of use.
Psychological therapy starts with teaching patients that 1) pain sensations in CRPS type 1 do not indicate tissue damage, and 2) reactivation of the affected limb is important. With persistent symptoms, clinical psychological assessment is recommended, eventually followed by cognitive behavioral therapy.
Pain management starts with oral or topical medications typically used for other neuropathic pain conditions (eg, amitriptyline (Elavil), gabapentin (Neurontin), opioids, and nonsteroidal antidepressants). The guideline also recommends steroids, calcitonin, and alpha-1 adrenoceptor antagonists (terazosin [Hytrin] or phenoxybenzamine [Dibenzylene]). With persistent symptoms, intravenous regional sympathetic blocks (IRSBs) and somatic nerve blocks are recommended. According to the guideline, treatment for resistant cases may progress to epidural catheters for sympathetic blockade, spinal cord stimulation, intrathecal baclofen (Lioresal), or sympathectomy.1
Reviews of medication trials show minimal effectiveness
Meta-analyses and systematic reviews of the literature reveal that many of the treatments recommended in the guidelines are minimally if at all effective, or have been inadequately researched.6-12 This is particularly so concerning invasive therapies such as sympathetic ganglion block,13 sympathectomy,12 and spinal cord stimulation9,10 that introduce the possibility of adverse effects. Yet, evidence is equally sparse for common pain therapies in CRPS type 1, such as nonsteroidal anti-inflammatory drugs, antidepressants, opiates, or antiseizure medications.
Systematic review and meta-analysis of medication trials for CRPS only partially agree.6-8,11 A 1999 systematic review concluded that oral corticosteroids demonstrated a consistent and long-term analgesic effect in CRPS.6 This review identified only limited data to suggest an analgesic effect from topical dimethylsulfoxide (DMSO), epidural clonidine and IRSB with ketanserin (not available in the US), and bretylium. The review concluded there was contradictory evidence of an analgesic effect from calcitonin or intravenous phentolamine and most likely no effect, and evidence against the effectiveness of guanethidine and reserpine IRSBs, and droperidol and atropine IRSBs.6
A 1995 systematic review of IRSBs concluded as well that overall there was no effect on pain, but a single RCT of each bretylium and ketanserin showed an analgesic effect.8 In a systematic review focused on upper extremity post-stroke CRPS (also known as shoulder-hand syndrome), 1 RCT was identified, and indicated that corticosteroids had an analgesic effect.11 High-quality evidence for the use of intramuscular calcitonin was lacking.11
Calcitonin may be one exception. A systematic review of medical treatment for CRPS type 1 identified 21 randomized trials, enough to undertake a statistical analysis of the analgesic effect of 4 types of treatment: sympathetic suppressors, guanethidine, intravenous regional blocks, and calcitonin.7 Of the 4, only calcitonin appeared to have a significant beneficial effect on pain.7
IV bisphosphonates show promise. More recently, intravenous bisphosphonates have demonstrated clinical and analgesic benefits in 2 small but high-quality RCTs.14,15 Strikingly, short-term therapy of 3 to 10 days of IV alendronate (Fosamax) or clodronate (Bonefos) without adverse effects resulted in significant overall improvements for the duration of the 2 trials, 4 weeks14 and 180 days.15
Nonpharmacologic treatments
Nonmedical treatments that have been studied include spinal cord stimulation, physical therapy, occupational therapy, and acupuncture. Spinal cord stimulation demonstrated a modest long-term (2-year) reduction in pain and improvement in health related quality of life in 1 RCT,16 but with no improvement in patient functioning and a 34% rate of adverse occurrences.9 Similarly, physical therapy and occupational therapy have been studied only in 1 large RCT (n=135).
Treatment with physical therapy did decrease pain compared with occupational therapy and control therapy,17 but revealed no improvement in active range of motion with physical or occupational therapy compared with control therapy.17 Furthermore, physical therapy led only to uncertain diminishment of impairment when data were analyzed in 2 different ways, 1 of which showed a benefit of physical and occupational therapy over control treatment,18 1 of which did not.19
Acupuncture demonstrated no improvement over sham treatment.20
Applying the evidence: Medical treatment
Choose any of the therapies least likely to do harm and supported by evidence of efficacy: topical 50% DMSO cream (SOR: B), intravenous bisphosphonates (SOR: A), or limited courses of oral corticosteroids (SOR: B). Despite some contradictory findings in the literature,6,17,18 other studies demonstrate that physical therapy18,19 and calcitonin7 reduce pain, and neither is likely to cause harm (SOR: B).
Epidural clonidine injection,6 IRSB with bretylium,6-8 and spinal cord stimulation9,16 have demonstrated some efficacy, but due to the invasiveness of the treatments and the modest benefits, patients should be counseled carefully before initiating these therapies (SOR: B) (TABLE 1).
Therapies to avoid. Therapies to avoid due to lack of evidence, lack of efficacy, or likelihood of adverse outcomes include IV regional blocks with everything but bretylium,6-8 sympathetic ganglion blocks with local anesthetics (very short duration of analgesia),13 systemic intravenous sympathetic inhibition,6 acupuncture,20 and sympathectomy (SOR: B).12
TABLE 1
Effectiveness of treatments for CRPS type 1
| TREATMENT | STUDY TYPE | STUDY QUALITY | EFFECT* |
|---|---|---|---|
| DMSO | SR6 | 2 – small RCT (n=32)21 | (+): Analgesia during therapy |
| Bisphosphonates | RCTs14,15 | 1 – multiple RCTs (n=32)15 and (n=20)14 | (+): Long-term (4 weeks14 to 180 days15) overall clinical improvement with significant analgesia |
| Corticosteroids | 2 SRs6,11 | 2 – 2 small RCTs, 1 in post-traumatic CRPS type 1 (n=23)22 and 1 (poor-quality) in shoulder-hand syndrome (n=36)3 | (+): 75% clinical improvement to 12 wk in CRPS type 1;22 and resolution of symptoms in shoulder-hand syndrome3 |
| Clonidine | SR6 | 2 – small RCT (n=26)23 | (+): Temporary analgesia |
| Spinal cord stimulation | SR9-11 | 2 – multiple SRs based on 1 RCT (n=36)16 | (+): Modest long-term (2-y)16 analgesic effect, improved health-related quality of life, no improvement in patient functioning and 34% rate of adverse occurrences9 |
| Physical therapy and occupational therapy | RCT17-19 | 1 – RCT (n=135) | (+/–): Contradictory analyses using different methods of measuring impairment, 1 showing no advantage of PT or OT over control,17 the other showing improvement with both.18 Significant improvement in pain at 1 y with PT over OT and control, no significant improvement in active ROM.19 |
| Calcitonin | SR6,7 | 1 – multiple RCTs24-26 | (+/–): Contradictory results – 1 SR indicating a significant analgesic effect7 the other suggesting no analgesic effect6 |
| IRSBs (bretylium, ketanserin, guanethidine, reserpine, droperidol, or atropine) | SR6-8 | 1 and 2 – Good-quality RCTs | (+/–): When collectively analyzed, no overall positive of guanethidine, otherwise effect.7,8 When evaluated by particular medication, small or poor quality RCTs limited evidence for analgesia with bretylium and ketanserin (not available in the US),6,8 and no analgesia with guanethidine, reserpine, droperidol and atropine6 |
| Sympathetic ganglion blocks (lidocaine/bupivacaine) | RCT13 | 2 – small RCT (n=7) | (+/–): Short-term analgesia with longer duration of pain control in treatment group (3.5 days) vs placebo (1 day) |
| Sympathectomy (chemical or surgical) | SR12 | 2 – SR based on poor-quality evidence, no placebo controlled RCTs | (+/–): No evidence of effectiveness, high rates (>10%) of adverse effects including worse pain, new neuropathic pain and pathological body sweating |
| Acupuncture (30 min 5x/wk for 3 wk | RCT20 | 2 – small RCT (n=14) | (–): Immediate and long-term (6-mo) clinical improvement and analgesia in sham/acupuncture treatment groups |
| Sympathetic inhibition | SR6 | 1 & 2 – variable-quality RCTs27-29 | (+/–): Contradictory results, with the best-designed study showing only a 9% short-term relief of pain28 |
| DOSAGES: DMSO: 50% cream applied 5x/d for at least 2 mo.21 | |||
| Bisphosphonates: IV alendronate 7.5 mg once daily for 3 days14 or intravenous clodronate 300 mg once daily for 10 days.15 | |||
| Calcitonin: intranasal 400 IU once daily26 or 100 IU 3 times daily27 or intramuscular 100 IU once daily for 3 weeks.28 | |||
| Corticosteroids: prednisone 10 mg 3 times daily until remission, max. up to 12 weeks,22 or prednisolone 32 mg daily for 2 wk with a 2-wk taper.4 | |||
| Clonidine: 300 μg epidural injection.23 | |||
| Sympathetic inhibition: IV phentolamine.27-29 | |||
| *Effect: (+) = positive, (+/–) = contradictory results or poor quality evidence, (–) = no effect. | |||
| SR, systematic review; MA, meta-analysis; RCT, randomized controlled trial; DMSO, dimethylsulfoxide; PT, physical therapy; OT, occupational therapy; ROM, range of motion. | |||
Acknowledgments
The authors would like to express their appreciation to Cheryl Mongillo, Peggy Lardear, and Brian Pellini for their assistance in preparing the manuscript, Dolores Moran and Diane Wolfe for their assistance in finding articles, and to Roger Rodrigue, MD for reviewing the manuscript. Funding for this project was provided by a grant from the Delaware Department of Health and Social Services, Division of Public Health.
CORRESPONDING AUTHOR
Anna Quisel, MD, c/o Cheryl Mongillo, Family Medicine Center, 1401 Foulk Road, Wilmington, DE 19803. E-mail: [email protected]
1. Stanton-Hicks MD, Burton AW, Bruehl SP, et al. An updated interdisciplinary clinical pathway for CRPS: Report of an expert panel. Pain Practice 2002;2:1-16.
2. Commentary on RSD focus article Bandolier 2002. Available at:www.jr2.ox.ac.uk/bandolier/booth/painpag/wisdom/RSD.html.
3. Petchkrua W, Weiss DJ, Patel RR. Reassessment of the incidence of complex regional pain syndrome type 1 following stroke. Neurorehabil Neural Repair 2000;14:59-63.
4. Braus DF, Krauss JK, Strobel J. The shoulder-hand syndrome after stroke: a prospective clinical trial. Ann Neurol 1994;36:728-733.
5. Zollinger PE, Tuienebreijer WE, Kreis RW, Breederveld RS. Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: a randomised trial. Lancet 1999;354:2025-2028.
6. Kingery WS. A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes. Pain 1997;73:123-139.
7. Perez RS, Kwakkel G, Zuurmond WW, de Lange JJ. Treatment of reflex sympathetic dystrophy (CRPS type 1). a research synthesis of 21 randomized clinical trials. J Pain Symptom Manage 2001;21:511-526.
8. Jadad AR, Carroll D, Glynn CJ, McQuay HJ. Intravenous regional sympathetic blockade for pain relief in reflex sympathetic dystrophy: a systematic review and a randomized, double-blind crossover study. J Pain Symptom Manage 1995;10:13-20.
9. Turner JA, Loeser JD, Deyo RA, Sanders SB. Spinal cord stimulation for patients with failed back surgery syndrome or complex regional pain syndrome: a systematic review of effectiveness and complications. Pain 2004;108:137-147.
10. Grabow TS, Tella PK, Raja SN. Spinal cord stimulation for complex regional pain syndrome: an evidencebased medicine review of the literature. Clin J Pain 2003;19:371-383.
11. Geurts AC, Visschers BA, van Limbeek J, et al. Systematic review of aetiology and treatment of post-stroke hand oedma and shoulder-hand syndrome. Scan J Rehabil Med 2000;32:4-10.
12. Mailis A, Furlan A. Sympathectomy for neuropathic pain. Cochrane Database Syst Rev 2003;2.-
13. Price DD, Long S, Wilsey B, Rafii A. Analysis of peak magnitude and duration of analgesia produced by local anesthetics injected into sympathetic ganglia of complex regional pain syndrome patients. Clin J Pain 1998;14:216-226.
14. Adami S, Fossaluzza V, Gatti D, et al. Bisphosphonate therapy of reflex sympathetic dystrophy syndrome. Ann Rheum Dis 1997;56:201-204.
15. Varenna M, Zucchi F, Ghiringhelli D, et al. Intravenous clodronate in the treatment of reflex sympathetic dystrophy syndrome. A randomized double blind, placebo controlled study. J Rheumatol 2000;27:1477-1483.
16. Kemler MA, De Vet HC, Barendse GA, Van Den Wildenberg FA, Van Kleef M. The effect of spinal cord stimulation in patients with chronic reflex sympathetic dystrophy: two years’ follow-up of the randomized controlled trial. Ann Neurol 2004;55:13-18.
17. Oerlemans HM, Goris JA, de Boo T, Oostendorp RA. Do physical therapy and occupational therapy reduce the impairment percentage in reflex sympathetic dystrophy? Am J Phys Med Rehabil 1999;78:533-539.
18. Oerlemans HM, Oostendorp RA, de Boo T, van der Laan L, Severens JL, Goris JA. Adjuvant physical therapy versus occupational therapy in patients with reflex sympathetic dystrophy/complex regional pain syndrome type I. Arch Phys Med Rehabil 2000;81:49-56.
19. Oerlemans HM, Oostendorp RA, de Boo T, Goris RJ. Pain and reduced mobility in complex regional pain syndrome I: outcome of a prospective randomised controlled clinical trial of adjuvant physical therapy versus occupational therapy. Pain 1999;83:77-83.
20. Korpan MI, Dezu Y, Schneider B, Leitha T, Fialka-Moser V. Acupuncture in the treatment of posttraumatic pain syndrome. Acta Orthop Belg 1999;65:197-201.
21. Zuurmond WW, Langendijk PN, Bezemer PD, Brink HE, de Lange JJ, van loenen AC. Treatment of acute reflex sympathetic dystrophy with DMSO 50% in a fatty cream. Acta Anaesthesiol Scand 1996;40:364-367.
22. Christensen K, Jensen EM, Noer I. The reflex dystrophy syndrome response to treatment with systemic corticosteroids. Acta Chirurgica Scandinavica 1982;148:653-655.
23. Rauck RL, Eisenach JC, Jackson K, Young LD, Southern J. Epidural clonidine treatment for refractory reflex sympathetic dystrophy. Anesthesiology 1993;79:1163-1169.
24. Bickerstaff DR, Kanis JA. The use of nasal calcitonin in the treatment of post-traumatic algodystrophy. Br J Rheumatol 1991;30:291-294.
25. Gobelet C, Waldburger M, Meier JL. The effect of adding calcitonin to physical treatment on reflex sympathetic dystrophy. Pain 1992;48:171-175.
26. Gobelet C, Meier J, Schaffner W, et al. Calcitonin and reflex sympathetic dystrophy syndrome. Clin Rheumatol 1986;5:382-388.
27. Raja AN, Treed RD, Davis KD, Campbell JN. Systematic alpha-adrenergic blockade with phentolamine: a diagnostic test for sympathetically maintained pain. Anesthesiol 1991;74:691-698.
28. Verdugo RJ, Ochoa JL. Sympathetically maintained pain. I. Phentolamine block questions the concept. Neurology 1994;44:1003-1010.
29. Verdugo RJ, Campero M, Ochoa JL. Phentolamine sympathetic block in painful polyneuropathies. II. Further questioning of the concept of “sympathetically maintained pain.” Neurology 1994;44:1010-1014.
- Treatments for CRPS type 1 supported by evidence of efficacy and little likelihood for harm are: topical DMSO cream (B), IV bisphosphonates (A) and limited courses of oral corticosteroids (B). Despite some contradictory evidence, physical therapy and calcitonin (intranasal or intramuscular) are likely to benefit patients with CRPS type 1 (B).
- Due to modest benefits and the invasiveness of the therapies, epidural clonidine injection, intravenous regional sympathetic block with bretylium and spinal cord stimulation should be offered only after careful counseling (B).
- Therapies to avoid due to lack of efficacy, lack of evidence, or a high likelihood of adverse outcomes are IV regional sympathetic blocks with anything but bretylium, sympathetic ganglion blocks with local anesthetics, systemic IV sympathetic inhibition, acupuncture, and sympathectomy (B).
In last issue of the Journal of Family Practice, we discussed diagnosis of CRPS type 1 (“Complex regional pain syndrome underdiagnosed,” 2005; 54: 524–532). Once other conditions have been ruled out, a primary care practitioner can diagnose CRPS type 1 right in the office using clinical findings and the patient’s report of symptoms. Similarly, primary care practitioners can provide most of the best treatments for CRPS type 1. In fact, evidence indicates that no benefit has been proven from more invasive treatments such as sympathectomy which continue to be included in recommendations by experts.1
Evidence for intervention less than compelling
A review of the literature on treating CRPS type 1 raises a question: is there any evidence that treatment makes a difference in outcomes that matter to patients, such as returning to work, regaining functionality of the affected limb, or resolution of pain? The large discrepancy between the high rates of CRPS type 1 documented in prospective studies of post-traumatic patients and the low rates of diagnosis of CRPS type 1 in actual practice suggests that most cases of CRPS type 1 resolve without being diagnosed and treated. This is not proven because, unfortunately, the natural history of persons diagnosed in the first 9 weeks after injury is not known.2
Are there benefits to early treatment?
From the clinician’s perspective, persons diagnosed with CRPS type 1 early appear more likely to respond to treatment. There is an “oft-quoted contention that results of early treatment will be better than those when the pain is treated late.”2 Yet, the great majority of these patients may have improved just as readily without treatment. For the few cases of undiagnosed CRPS type 1 that will persist to become chronic and treatment resistant, it is unknown whether early treatment would have been preventive2 or how clinicians could distinguish these cases early enough to target them for treatment.
Intriguing but limited data exist for using preventive therapies in all at-risk patients. One prospective cohort study documented a lower rate of CRPS type 1 in stroke patients who underwent early inpatient rehabilitation, compared with patients in earlier studies who rarely received early rehabilitation. This finding indirectly suggests a possible preventive effect of physical/occupational therapy (LOE: 3, cross-study comparison).3 Luckily, early inpatient rehabilitation in stroke patients has become the standard of care, which may prevent many cases of CRPS type 1 as a side effect.
It also appears that injury to a newly hemiplegic arm may contribute to the shoulder-hand syndrome; a study that alerted patients and care-takers to the risk of injury reduced the rate of shoulder hand syndrome from 27 to 8% (LOE: 2, lowerquality RCT).4 Among post-traumatic patients with wrist fracture, a double-blind randomized placebo controlled trial (n=115) of vitamin C 500 mg tabs initiated upon diagnosis of fracture and continued for 50 days resulted in a marked decrease of CRPS type 1 from 22% in the placebo group to 7% in the vitamin C group (relative risk=0.17) (LOE: 1, high-quality RCT).5 These results have not been tested in subsequent trials, however.
Guideline recommendations: Physical and psychological therapy, pain management
Many treatments for CRPS have been tried and are summarized without a systematic or evidence-based approach to the literature in a consensus statement released in 2002 by an interdisciplinary expert panel (LOE: 3, consensus guideline).1 These guidelines suggest rapid initiation of multidisciplinary treatment with advancement to higher levels of intervention if no benefit from initial therapy occurs in 2 weeks. Simultaneous physical rehabilitation, psychological therapy, and pain management are recommended.
Rehabilitation through physical therapy and occupational therapy starts with desensitization and stress loading, progresses to increasing flexibility with gentle active range of motion and stretching, and eventually to normalization of use.
Psychological therapy starts with teaching patients that 1) pain sensations in CRPS type 1 do not indicate tissue damage, and 2) reactivation of the affected limb is important. With persistent symptoms, clinical psychological assessment is recommended, eventually followed by cognitive behavioral therapy.
Pain management starts with oral or topical medications typically used for other neuropathic pain conditions (eg, amitriptyline (Elavil), gabapentin (Neurontin), opioids, and nonsteroidal antidepressants). The guideline also recommends steroids, calcitonin, and alpha-1 adrenoceptor antagonists (terazosin [Hytrin] or phenoxybenzamine [Dibenzylene]). With persistent symptoms, intravenous regional sympathetic blocks (IRSBs) and somatic nerve blocks are recommended. According to the guideline, treatment for resistant cases may progress to epidural catheters for sympathetic blockade, spinal cord stimulation, intrathecal baclofen (Lioresal), or sympathectomy.1
Reviews of medication trials show minimal effectiveness
Meta-analyses and systematic reviews of the literature reveal that many of the treatments recommended in the guidelines are minimally if at all effective, or have been inadequately researched.6-12 This is particularly so concerning invasive therapies such as sympathetic ganglion block,13 sympathectomy,12 and spinal cord stimulation9,10 that introduce the possibility of adverse effects. Yet, evidence is equally sparse for common pain therapies in CRPS type 1, such as nonsteroidal anti-inflammatory drugs, antidepressants, opiates, or antiseizure medications.
Systematic review and meta-analysis of medication trials for CRPS only partially agree.6-8,11 A 1999 systematic review concluded that oral corticosteroids demonstrated a consistent and long-term analgesic effect in CRPS.6 This review identified only limited data to suggest an analgesic effect from topical dimethylsulfoxide (DMSO), epidural clonidine and IRSB with ketanserin (not available in the US), and bretylium. The review concluded there was contradictory evidence of an analgesic effect from calcitonin or intravenous phentolamine and most likely no effect, and evidence against the effectiveness of guanethidine and reserpine IRSBs, and droperidol and atropine IRSBs.6
A 1995 systematic review of IRSBs concluded as well that overall there was no effect on pain, but a single RCT of each bretylium and ketanserin showed an analgesic effect.8 In a systematic review focused on upper extremity post-stroke CRPS (also known as shoulder-hand syndrome), 1 RCT was identified, and indicated that corticosteroids had an analgesic effect.11 High-quality evidence for the use of intramuscular calcitonin was lacking.11
Calcitonin may be one exception. A systematic review of medical treatment for CRPS type 1 identified 21 randomized trials, enough to undertake a statistical analysis of the analgesic effect of 4 types of treatment: sympathetic suppressors, guanethidine, intravenous regional blocks, and calcitonin.7 Of the 4, only calcitonin appeared to have a significant beneficial effect on pain.7
IV bisphosphonates show promise. More recently, intravenous bisphosphonates have demonstrated clinical and analgesic benefits in 2 small but high-quality RCTs.14,15 Strikingly, short-term therapy of 3 to 10 days of IV alendronate (Fosamax) or clodronate (Bonefos) without adverse effects resulted in significant overall improvements for the duration of the 2 trials, 4 weeks14 and 180 days.15
Nonpharmacologic treatments
Nonmedical treatments that have been studied include spinal cord stimulation, physical therapy, occupational therapy, and acupuncture. Spinal cord stimulation demonstrated a modest long-term (2-year) reduction in pain and improvement in health related quality of life in 1 RCT,16 but with no improvement in patient functioning and a 34% rate of adverse occurrences.9 Similarly, physical therapy and occupational therapy have been studied only in 1 large RCT (n=135).
Treatment with physical therapy did decrease pain compared with occupational therapy and control therapy,17 but revealed no improvement in active range of motion with physical or occupational therapy compared with control therapy.17 Furthermore, physical therapy led only to uncertain diminishment of impairment when data were analyzed in 2 different ways, 1 of which showed a benefit of physical and occupational therapy over control treatment,18 1 of which did not.19
Acupuncture demonstrated no improvement over sham treatment.20
Applying the evidence: Medical treatment
Choose any of the therapies least likely to do harm and supported by evidence of efficacy: topical 50% DMSO cream (SOR: B), intravenous bisphosphonates (SOR: A), or limited courses of oral corticosteroids (SOR: B). Despite some contradictory findings in the literature,6,17,18 other studies demonstrate that physical therapy18,19 and calcitonin7 reduce pain, and neither is likely to cause harm (SOR: B).
Epidural clonidine injection,6 IRSB with bretylium,6-8 and spinal cord stimulation9,16 have demonstrated some efficacy, but due to the invasiveness of the treatments and the modest benefits, patients should be counseled carefully before initiating these therapies (SOR: B) (TABLE 1).
Therapies to avoid. Therapies to avoid due to lack of evidence, lack of efficacy, or likelihood of adverse outcomes include IV regional blocks with everything but bretylium,6-8 sympathetic ganglion blocks with local anesthetics (very short duration of analgesia),13 systemic intravenous sympathetic inhibition,6 acupuncture,20 and sympathectomy (SOR: B).12
TABLE 1
Effectiveness of treatments for CRPS type 1
| TREATMENT | STUDY TYPE | STUDY QUALITY | EFFECT* |
|---|---|---|---|
| DMSO | SR6 | 2 – small RCT (n=32)21 | (+): Analgesia during therapy |
| Bisphosphonates | RCTs14,15 | 1 – multiple RCTs (n=32)15 and (n=20)14 | (+): Long-term (4 weeks14 to 180 days15) overall clinical improvement with significant analgesia |
| Corticosteroids | 2 SRs6,11 | 2 – 2 small RCTs, 1 in post-traumatic CRPS type 1 (n=23)22 and 1 (poor-quality) in shoulder-hand syndrome (n=36)3 | (+): 75% clinical improvement to 12 wk in CRPS type 1;22 and resolution of symptoms in shoulder-hand syndrome3 |
| Clonidine | SR6 | 2 – small RCT (n=26)23 | (+): Temporary analgesia |
| Spinal cord stimulation | SR9-11 | 2 – multiple SRs based on 1 RCT (n=36)16 | (+): Modest long-term (2-y)16 analgesic effect, improved health-related quality of life, no improvement in patient functioning and 34% rate of adverse occurrences9 |
| Physical therapy and occupational therapy | RCT17-19 | 1 – RCT (n=135) | (+/–): Contradictory analyses using different methods of measuring impairment, 1 showing no advantage of PT or OT over control,17 the other showing improvement with both.18 Significant improvement in pain at 1 y with PT over OT and control, no significant improvement in active ROM.19 |
| Calcitonin | SR6,7 | 1 – multiple RCTs24-26 | (+/–): Contradictory results – 1 SR indicating a significant analgesic effect7 the other suggesting no analgesic effect6 |
| IRSBs (bretylium, ketanserin, guanethidine, reserpine, droperidol, or atropine) | SR6-8 | 1 and 2 – Good-quality RCTs | (+/–): When collectively analyzed, no overall positive of guanethidine, otherwise effect.7,8 When evaluated by particular medication, small or poor quality RCTs limited evidence for analgesia with bretylium and ketanserin (not available in the US),6,8 and no analgesia with guanethidine, reserpine, droperidol and atropine6 |
| Sympathetic ganglion blocks (lidocaine/bupivacaine) | RCT13 | 2 – small RCT (n=7) | (+/–): Short-term analgesia with longer duration of pain control in treatment group (3.5 days) vs placebo (1 day) |
| Sympathectomy (chemical or surgical) | SR12 | 2 – SR based on poor-quality evidence, no placebo controlled RCTs | (+/–): No evidence of effectiveness, high rates (>10%) of adverse effects including worse pain, new neuropathic pain and pathological body sweating |
| Acupuncture (30 min 5x/wk for 3 wk | RCT20 | 2 – small RCT (n=14) | (–): Immediate and long-term (6-mo) clinical improvement and analgesia in sham/acupuncture treatment groups |
| Sympathetic inhibition | SR6 | 1 & 2 – variable-quality RCTs27-29 | (+/–): Contradictory results, with the best-designed study showing only a 9% short-term relief of pain28 |
| DOSAGES: DMSO: 50% cream applied 5x/d for at least 2 mo.21 | |||
| Bisphosphonates: IV alendronate 7.5 mg once daily for 3 days14 or intravenous clodronate 300 mg once daily for 10 days.15 | |||
| Calcitonin: intranasal 400 IU once daily26 or 100 IU 3 times daily27 or intramuscular 100 IU once daily for 3 weeks.28 | |||
| Corticosteroids: prednisone 10 mg 3 times daily until remission, max. up to 12 weeks,22 or prednisolone 32 mg daily for 2 wk with a 2-wk taper.4 | |||
| Clonidine: 300 μg epidural injection.23 | |||
| Sympathetic inhibition: IV phentolamine.27-29 | |||
| *Effect: (+) = positive, (+/–) = contradictory results or poor quality evidence, (–) = no effect. | |||
| SR, systematic review; MA, meta-analysis; RCT, randomized controlled trial; DMSO, dimethylsulfoxide; PT, physical therapy; OT, occupational therapy; ROM, range of motion. | |||
Acknowledgments
The authors would like to express their appreciation to Cheryl Mongillo, Peggy Lardear, and Brian Pellini for their assistance in preparing the manuscript, Dolores Moran and Diane Wolfe for their assistance in finding articles, and to Roger Rodrigue, MD for reviewing the manuscript. Funding for this project was provided by a grant from the Delaware Department of Health and Social Services, Division of Public Health.
CORRESPONDING AUTHOR
Anna Quisel, MD, c/o Cheryl Mongillo, Family Medicine Center, 1401 Foulk Road, Wilmington, DE 19803. E-mail: [email protected]
- Treatments for CRPS type 1 supported by evidence of efficacy and little likelihood for harm are: topical DMSO cream (B), IV bisphosphonates (A) and limited courses of oral corticosteroids (B). Despite some contradictory evidence, physical therapy and calcitonin (intranasal or intramuscular) are likely to benefit patients with CRPS type 1 (B).
- Due to modest benefits and the invasiveness of the therapies, epidural clonidine injection, intravenous regional sympathetic block with bretylium and spinal cord stimulation should be offered only after careful counseling (B).
- Therapies to avoid due to lack of efficacy, lack of evidence, or a high likelihood of adverse outcomes are IV regional sympathetic blocks with anything but bretylium, sympathetic ganglion blocks with local anesthetics, systemic IV sympathetic inhibition, acupuncture, and sympathectomy (B).
In last issue of the Journal of Family Practice, we discussed diagnosis of CRPS type 1 (“Complex regional pain syndrome underdiagnosed,” 2005; 54: 524–532). Once other conditions have been ruled out, a primary care practitioner can diagnose CRPS type 1 right in the office using clinical findings and the patient’s report of symptoms. Similarly, primary care practitioners can provide most of the best treatments for CRPS type 1. In fact, evidence indicates that no benefit has been proven from more invasive treatments such as sympathectomy which continue to be included in recommendations by experts.1
Evidence for intervention less than compelling
A review of the literature on treating CRPS type 1 raises a question: is there any evidence that treatment makes a difference in outcomes that matter to patients, such as returning to work, regaining functionality of the affected limb, or resolution of pain? The large discrepancy between the high rates of CRPS type 1 documented in prospective studies of post-traumatic patients and the low rates of diagnosis of CRPS type 1 in actual practice suggests that most cases of CRPS type 1 resolve without being diagnosed and treated. This is not proven because, unfortunately, the natural history of persons diagnosed in the first 9 weeks after injury is not known.2
Are there benefits to early treatment?
From the clinician’s perspective, persons diagnosed with CRPS type 1 early appear more likely to respond to treatment. There is an “oft-quoted contention that results of early treatment will be better than those when the pain is treated late.”2 Yet, the great majority of these patients may have improved just as readily without treatment. For the few cases of undiagnosed CRPS type 1 that will persist to become chronic and treatment resistant, it is unknown whether early treatment would have been preventive2 or how clinicians could distinguish these cases early enough to target them for treatment.
Intriguing but limited data exist for using preventive therapies in all at-risk patients. One prospective cohort study documented a lower rate of CRPS type 1 in stroke patients who underwent early inpatient rehabilitation, compared with patients in earlier studies who rarely received early rehabilitation. This finding indirectly suggests a possible preventive effect of physical/occupational therapy (LOE: 3, cross-study comparison).3 Luckily, early inpatient rehabilitation in stroke patients has become the standard of care, which may prevent many cases of CRPS type 1 as a side effect.
It also appears that injury to a newly hemiplegic arm may contribute to the shoulder-hand syndrome; a study that alerted patients and care-takers to the risk of injury reduced the rate of shoulder hand syndrome from 27 to 8% (LOE: 2, lowerquality RCT).4 Among post-traumatic patients with wrist fracture, a double-blind randomized placebo controlled trial (n=115) of vitamin C 500 mg tabs initiated upon diagnosis of fracture and continued for 50 days resulted in a marked decrease of CRPS type 1 from 22% in the placebo group to 7% in the vitamin C group (relative risk=0.17) (LOE: 1, high-quality RCT).5 These results have not been tested in subsequent trials, however.
Guideline recommendations: Physical and psychological therapy, pain management
Many treatments for CRPS have been tried and are summarized without a systematic or evidence-based approach to the literature in a consensus statement released in 2002 by an interdisciplinary expert panel (LOE: 3, consensus guideline).1 These guidelines suggest rapid initiation of multidisciplinary treatment with advancement to higher levels of intervention if no benefit from initial therapy occurs in 2 weeks. Simultaneous physical rehabilitation, psychological therapy, and pain management are recommended.
Rehabilitation through physical therapy and occupational therapy starts with desensitization and stress loading, progresses to increasing flexibility with gentle active range of motion and stretching, and eventually to normalization of use.
Psychological therapy starts with teaching patients that 1) pain sensations in CRPS type 1 do not indicate tissue damage, and 2) reactivation of the affected limb is important. With persistent symptoms, clinical psychological assessment is recommended, eventually followed by cognitive behavioral therapy.
Pain management starts with oral or topical medications typically used for other neuropathic pain conditions (eg, amitriptyline (Elavil), gabapentin (Neurontin), opioids, and nonsteroidal antidepressants). The guideline also recommends steroids, calcitonin, and alpha-1 adrenoceptor antagonists (terazosin [Hytrin] or phenoxybenzamine [Dibenzylene]). With persistent symptoms, intravenous regional sympathetic blocks (IRSBs) and somatic nerve blocks are recommended. According to the guideline, treatment for resistant cases may progress to epidural catheters for sympathetic blockade, spinal cord stimulation, intrathecal baclofen (Lioresal), or sympathectomy.1
Reviews of medication trials show minimal effectiveness
Meta-analyses and systematic reviews of the literature reveal that many of the treatments recommended in the guidelines are minimally if at all effective, or have been inadequately researched.6-12 This is particularly so concerning invasive therapies such as sympathetic ganglion block,13 sympathectomy,12 and spinal cord stimulation9,10 that introduce the possibility of adverse effects. Yet, evidence is equally sparse for common pain therapies in CRPS type 1, such as nonsteroidal anti-inflammatory drugs, antidepressants, opiates, or antiseizure medications.
Systematic review and meta-analysis of medication trials for CRPS only partially agree.6-8,11 A 1999 systematic review concluded that oral corticosteroids demonstrated a consistent and long-term analgesic effect in CRPS.6 This review identified only limited data to suggest an analgesic effect from topical dimethylsulfoxide (DMSO), epidural clonidine and IRSB with ketanserin (not available in the US), and bretylium. The review concluded there was contradictory evidence of an analgesic effect from calcitonin or intravenous phentolamine and most likely no effect, and evidence against the effectiveness of guanethidine and reserpine IRSBs, and droperidol and atropine IRSBs.6
A 1995 systematic review of IRSBs concluded as well that overall there was no effect on pain, but a single RCT of each bretylium and ketanserin showed an analgesic effect.8 In a systematic review focused on upper extremity post-stroke CRPS (also known as shoulder-hand syndrome), 1 RCT was identified, and indicated that corticosteroids had an analgesic effect.11 High-quality evidence for the use of intramuscular calcitonin was lacking.11
Calcitonin may be one exception. A systematic review of medical treatment for CRPS type 1 identified 21 randomized trials, enough to undertake a statistical analysis of the analgesic effect of 4 types of treatment: sympathetic suppressors, guanethidine, intravenous regional blocks, and calcitonin.7 Of the 4, only calcitonin appeared to have a significant beneficial effect on pain.7
IV bisphosphonates show promise. More recently, intravenous bisphosphonates have demonstrated clinical and analgesic benefits in 2 small but high-quality RCTs.14,15 Strikingly, short-term therapy of 3 to 10 days of IV alendronate (Fosamax) or clodronate (Bonefos) without adverse effects resulted in significant overall improvements for the duration of the 2 trials, 4 weeks14 and 180 days.15
Nonpharmacologic treatments
Nonmedical treatments that have been studied include spinal cord stimulation, physical therapy, occupational therapy, and acupuncture. Spinal cord stimulation demonstrated a modest long-term (2-year) reduction in pain and improvement in health related quality of life in 1 RCT,16 but with no improvement in patient functioning and a 34% rate of adverse occurrences.9 Similarly, physical therapy and occupational therapy have been studied only in 1 large RCT (n=135).
Treatment with physical therapy did decrease pain compared with occupational therapy and control therapy,17 but revealed no improvement in active range of motion with physical or occupational therapy compared with control therapy.17 Furthermore, physical therapy led only to uncertain diminishment of impairment when data were analyzed in 2 different ways, 1 of which showed a benefit of physical and occupational therapy over control treatment,18 1 of which did not.19
Acupuncture demonstrated no improvement over sham treatment.20
Applying the evidence: Medical treatment
Choose any of the therapies least likely to do harm and supported by evidence of efficacy: topical 50% DMSO cream (SOR: B), intravenous bisphosphonates (SOR: A), or limited courses of oral corticosteroids (SOR: B). Despite some contradictory findings in the literature,6,17,18 other studies demonstrate that physical therapy18,19 and calcitonin7 reduce pain, and neither is likely to cause harm (SOR: B).
Epidural clonidine injection,6 IRSB with bretylium,6-8 and spinal cord stimulation9,16 have demonstrated some efficacy, but due to the invasiveness of the treatments and the modest benefits, patients should be counseled carefully before initiating these therapies (SOR: B) (TABLE 1).
Therapies to avoid. Therapies to avoid due to lack of evidence, lack of efficacy, or likelihood of adverse outcomes include IV regional blocks with everything but bretylium,6-8 sympathetic ganglion blocks with local anesthetics (very short duration of analgesia),13 systemic intravenous sympathetic inhibition,6 acupuncture,20 and sympathectomy (SOR: B).12
TABLE 1
Effectiveness of treatments for CRPS type 1
| TREATMENT | STUDY TYPE | STUDY QUALITY | EFFECT* |
|---|---|---|---|
| DMSO | SR6 | 2 – small RCT (n=32)21 | (+): Analgesia during therapy |
| Bisphosphonates | RCTs14,15 | 1 – multiple RCTs (n=32)15 and (n=20)14 | (+): Long-term (4 weeks14 to 180 days15) overall clinical improvement with significant analgesia |
| Corticosteroids | 2 SRs6,11 | 2 – 2 small RCTs, 1 in post-traumatic CRPS type 1 (n=23)22 and 1 (poor-quality) in shoulder-hand syndrome (n=36)3 | (+): 75% clinical improvement to 12 wk in CRPS type 1;22 and resolution of symptoms in shoulder-hand syndrome3 |
| Clonidine | SR6 | 2 – small RCT (n=26)23 | (+): Temporary analgesia |
| Spinal cord stimulation | SR9-11 | 2 – multiple SRs based on 1 RCT (n=36)16 | (+): Modest long-term (2-y)16 analgesic effect, improved health-related quality of life, no improvement in patient functioning and 34% rate of adverse occurrences9 |
| Physical therapy and occupational therapy | RCT17-19 | 1 – RCT (n=135) | (+/–): Contradictory analyses using different methods of measuring impairment, 1 showing no advantage of PT or OT over control,17 the other showing improvement with both.18 Significant improvement in pain at 1 y with PT over OT and control, no significant improvement in active ROM.19 |
| Calcitonin | SR6,7 | 1 – multiple RCTs24-26 | (+/–): Contradictory results – 1 SR indicating a significant analgesic effect7 the other suggesting no analgesic effect6 |
| IRSBs (bretylium, ketanserin, guanethidine, reserpine, droperidol, or atropine) | SR6-8 | 1 and 2 – Good-quality RCTs | (+/–): When collectively analyzed, no overall positive of guanethidine, otherwise effect.7,8 When evaluated by particular medication, small or poor quality RCTs limited evidence for analgesia with bretylium and ketanserin (not available in the US),6,8 and no analgesia with guanethidine, reserpine, droperidol and atropine6 |
| Sympathetic ganglion blocks (lidocaine/bupivacaine) | RCT13 | 2 – small RCT (n=7) | (+/–): Short-term analgesia with longer duration of pain control in treatment group (3.5 days) vs placebo (1 day) |
| Sympathectomy (chemical or surgical) | SR12 | 2 – SR based on poor-quality evidence, no placebo controlled RCTs | (+/–): No evidence of effectiveness, high rates (>10%) of adverse effects including worse pain, new neuropathic pain and pathological body sweating |
| Acupuncture (30 min 5x/wk for 3 wk | RCT20 | 2 – small RCT (n=14) | (–): Immediate and long-term (6-mo) clinical improvement and analgesia in sham/acupuncture treatment groups |
| Sympathetic inhibition | SR6 | 1 & 2 – variable-quality RCTs27-29 | (+/–): Contradictory results, with the best-designed study showing only a 9% short-term relief of pain28 |
| DOSAGES: DMSO: 50% cream applied 5x/d for at least 2 mo.21 | |||
| Bisphosphonates: IV alendronate 7.5 mg once daily for 3 days14 or intravenous clodronate 300 mg once daily for 10 days.15 | |||
| Calcitonin: intranasal 400 IU once daily26 or 100 IU 3 times daily27 or intramuscular 100 IU once daily for 3 weeks.28 | |||
| Corticosteroids: prednisone 10 mg 3 times daily until remission, max. up to 12 weeks,22 or prednisolone 32 mg daily for 2 wk with a 2-wk taper.4 | |||
| Clonidine: 300 μg epidural injection.23 | |||
| Sympathetic inhibition: IV phentolamine.27-29 | |||
| *Effect: (+) = positive, (+/–) = contradictory results or poor quality evidence, (–) = no effect. | |||
| SR, systematic review; MA, meta-analysis; RCT, randomized controlled trial; DMSO, dimethylsulfoxide; PT, physical therapy; OT, occupational therapy; ROM, range of motion. | |||
Acknowledgments
The authors would like to express their appreciation to Cheryl Mongillo, Peggy Lardear, and Brian Pellini for their assistance in preparing the manuscript, Dolores Moran and Diane Wolfe for their assistance in finding articles, and to Roger Rodrigue, MD for reviewing the manuscript. Funding for this project was provided by a grant from the Delaware Department of Health and Social Services, Division of Public Health.
CORRESPONDING AUTHOR
Anna Quisel, MD, c/o Cheryl Mongillo, Family Medicine Center, 1401 Foulk Road, Wilmington, DE 19803. E-mail: [email protected]
1. Stanton-Hicks MD, Burton AW, Bruehl SP, et al. An updated interdisciplinary clinical pathway for CRPS: Report of an expert panel. Pain Practice 2002;2:1-16.
2. Commentary on RSD focus article Bandolier 2002. Available at:www.jr2.ox.ac.uk/bandolier/booth/painpag/wisdom/RSD.html.
3. Petchkrua W, Weiss DJ, Patel RR. Reassessment of the incidence of complex regional pain syndrome type 1 following stroke. Neurorehabil Neural Repair 2000;14:59-63.
4. Braus DF, Krauss JK, Strobel J. The shoulder-hand syndrome after stroke: a prospective clinical trial. Ann Neurol 1994;36:728-733.
5. Zollinger PE, Tuienebreijer WE, Kreis RW, Breederveld RS. Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: a randomised trial. Lancet 1999;354:2025-2028.
6. Kingery WS. A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes. Pain 1997;73:123-139.
7. Perez RS, Kwakkel G, Zuurmond WW, de Lange JJ. Treatment of reflex sympathetic dystrophy (CRPS type 1). a research synthesis of 21 randomized clinical trials. J Pain Symptom Manage 2001;21:511-526.
8. Jadad AR, Carroll D, Glynn CJ, McQuay HJ. Intravenous regional sympathetic blockade for pain relief in reflex sympathetic dystrophy: a systematic review and a randomized, double-blind crossover study. J Pain Symptom Manage 1995;10:13-20.
9. Turner JA, Loeser JD, Deyo RA, Sanders SB. Spinal cord stimulation for patients with failed back surgery syndrome or complex regional pain syndrome: a systematic review of effectiveness and complications. Pain 2004;108:137-147.
10. Grabow TS, Tella PK, Raja SN. Spinal cord stimulation for complex regional pain syndrome: an evidencebased medicine review of the literature. Clin J Pain 2003;19:371-383.
11. Geurts AC, Visschers BA, van Limbeek J, et al. Systematic review of aetiology and treatment of post-stroke hand oedma and shoulder-hand syndrome. Scan J Rehabil Med 2000;32:4-10.
12. Mailis A, Furlan A. Sympathectomy for neuropathic pain. Cochrane Database Syst Rev 2003;2.-
13. Price DD, Long S, Wilsey B, Rafii A. Analysis of peak magnitude and duration of analgesia produced by local anesthetics injected into sympathetic ganglia of complex regional pain syndrome patients. Clin J Pain 1998;14:216-226.
14. Adami S, Fossaluzza V, Gatti D, et al. Bisphosphonate therapy of reflex sympathetic dystrophy syndrome. Ann Rheum Dis 1997;56:201-204.
15. Varenna M, Zucchi F, Ghiringhelli D, et al. Intravenous clodronate in the treatment of reflex sympathetic dystrophy syndrome. A randomized double blind, placebo controlled study. J Rheumatol 2000;27:1477-1483.
16. Kemler MA, De Vet HC, Barendse GA, Van Den Wildenberg FA, Van Kleef M. The effect of spinal cord stimulation in patients with chronic reflex sympathetic dystrophy: two years’ follow-up of the randomized controlled trial. Ann Neurol 2004;55:13-18.
17. Oerlemans HM, Goris JA, de Boo T, Oostendorp RA. Do physical therapy and occupational therapy reduce the impairment percentage in reflex sympathetic dystrophy? Am J Phys Med Rehabil 1999;78:533-539.
18. Oerlemans HM, Oostendorp RA, de Boo T, van der Laan L, Severens JL, Goris JA. Adjuvant physical therapy versus occupational therapy in patients with reflex sympathetic dystrophy/complex regional pain syndrome type I. Arch Phys Med Rehabil 2000;81:49-56.
19. Oerlemans HM, Oostendorp RA, de Boo T, Goris RJ. Pain and reduced mobility in complex regional pain syndrome I: outcome of a prospective randomised controlled clinical trial of adjuvant physical therapy versus occupational therapy. Pain 1999;83:77-83.
20. Korpan MI, Dezu Y, Schneider B, Leitha T, Fialka-Moser V. Acupuncture in the treatment of posttraumatic pain syndrome. Acta Orthop Belg 1999;65:197-201.
21. Zuurmond WW, Langendijk PN, Bezemer PD, Brink HE, de Lange JJ, van loenen AC. Treatment of acute reflex sympathetic dystrophy with DMSO 50% in a fatty cream. Acta Anaesthesiol Scand 1996;40:364-367.
22. Christensen K, Jensen EM, Noer I. The reflex dystrophy syndrome response to treatment with systemic corticosteroids. Acta Chirurgica Scandinavica 1982;148:653-655.
23. Rauck RL, Eisenach JC, Jackson K, Young LD, Southern J. Epidural clonidine treatment for refractory reflex sympathetic dystrophy. Anesthesiology 1993;79:1163-1169.
24. Bickerstaff DR, Kanis JA. The use of nasal calcitonin in the treatment of post-traumatic algodystrophy. Br J Rheumatol 1991;30:291-294.
25. Gobelet C, Waldburger M, Meier JL. The effect of adding calcitonin to physical treatment on reflex sympathetic dystrophy. Pain 1992;48:171-175.
26. Gobelet C, Meier J, Schaffner W, et al. Calcitonin and reflex sympathetic dystrophy syndrome. Clin Rheumatol 1986;5:382-388.
27. Raja AN, Treed RD, Davis KD, Campbell JN. Systematic alpha-adrenergic blockade with phentolamine: a diagnostic test for sympathetically maintained pain. Anesthesiol 1991;74:691-698.
28. Verdugo RJ, Ochoa JL. Sympathetically maintained pain. I. Phentolamine block questions the concept. Neurology 1994;44:1003-1010.
29. Verdugo RJ, Campero M, Ochoa JL. Phentolamine sympathetic block in painful polyneuropathies. II. Further questioning of the concept of “sympathetically maintained pain.” Neurology 1994;44:1010-1014.
1. Stanton-Hicks MD, Burton AW, Bruehl SP, et al. An updated interdisciplinary clinical pathway for CRPS: Report of an expert panel. Pain Practice 2002;2:1-16.
2. Commentary on RSD focus article Bandolier 2002. Available at:www.jr2.ox.ac.uk/bandolier/booth/painpag/wisdom/RSD.html.
3. Petchkrua W, Weiss DJ, Patel RR. Reassessment of the incidence of complex regional pain syndrome type 1 following stroke. Neurorehabil Neural Repair 2000;14:59-63.
4. Braus DF, Krauss JK, Strobel J. The shoulder-hand syndrome after stroke: a prospective clinical trial. Ann Neurol 1994;36:728-733.
5. Zollinger PE, Tuienebreijer WE, Kreis RW, Breederveld RS. Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: a randomised trial. Lancet 1999;354:2025-2028.
6. Kingery WS. A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes. Pain 1997;73:123-139.
7. Perez RS, Kwakkel G, Zuurmond WW, de Lange JJ. Treatment of reflex sympathetic dystrophy (CRPS type 1). a research synthesis of 21 randomized clinical trials. J Pain Symptom Manage 2001;21:511-526.
8. Jadad AR, Carroll D, Glynn CJ, McQuay HJ. Intravenous regional sympathetic blockade for pain relief in reflex sympathetic dystrophy: a systematic review and a randomized, double-blind crossover study. J Pain Symptom Manage 1995;10:13-20.
9. Turner JA, Loeser JD, Deyo RA, Sanders SB. Spinal cord stimulation for patients with failed back surgery syndrome or complex regional pain syndrome: a systematic review of effectiveness and complications. Pain 2004;108:137-147.
10. Grabow TS, Tella PK, Raja SN. Spinal cord stimulation for complex regional pain syndrome: an evidencebased medicine review of the literature. Clin J Pain 2003;19:371-383.
11. Geurts AC, Visschers BA, van Limbeek J, et al. Systematic review of aetiology and treatment of post-stroke hand oedma and shoulder-hand syndrome. Scan J Rehabil Med 2000;32:4-10.
12. Mailis A, Furlan A. Sympathectomy for neuropathic pain. Cochrane Database Syst Rev 2003;2.-
13. Price DD, Long S, Wilsey B, Rafii A. Analysis of peak magnitude and duration of analgesia produced by local anesthetics injected into sympathetic ganglia of complex regional pain syndrome patients. Clin J Pain 1998;14:216-226.
14. Adami S, Fossaluzza V, Gatti D, et al. Bisphosphonate therapy of reflex sympathetic dystrophy syndrome. Ann Rheum Dis 1997;56:201-204.
15. Varenna M, Zucchi F, Ghiringhelli D, et al. Intravenous clodronate in the treatment of reflex sympathetic dystrophy syndrome. A randomized double blind, placebo controlled study. J Rheumatol 2000;27:1477-1483.
16. Kemler MA, De Vet HC, Barendse GA, Van Den Wildenberg FA, Van Kleef M. The effect of spinal cord stimulation in patients with chronic reflex sympathetic dystrophy: two years’ follow-up of the randomized controlled trial. Ann Neurol 2004;55:13-18.
17. Oerlemans HM, Goris JA, de Boo T, Oostendorp RA. Do physical therapy and occupational therapy reduce the impairment percentage in reflex sympathetic dystrophy? Am J Phys Med Rehabil 1999;78:533-539.
18. Oerlemans HM, Oostendorp RA, de Boo T, van der Laan L, Severens JL, Goris JA. Adjuvant physical therapy versus occupational therapy in patients with reflex sympathetic dystrophy/complex regional pain syndrome type I. Arch Phys Med Rehabil 2000;81:49-56.
19. Oerlemans HM, Oostendorp RA, de Boo T, Goris RJ. Pain and reduced mobility in complex regional pain syndrome I: outcome of a prospective randomised controlled clinical trial of adjuvant physical therapy versus occupational therapy. Pain 1999;83:77-83.
20. Korpan MI, Dezu Y, Schneider B, Leitha T, Fialka-Moser V. Acupuncture in the treatment of posttraumatic pain syndrome. Acta Orthop Belg 1999;65:197-201.
21. Zuurmond WW, Langendijk PN, Bezemer PD, Brink HE, de Lange JJ, van loenen AC. Treatment of acute reflex sympathetic dystrophy with DMSO 50% in a fatty cream. Acta Anaesthesiol Scand 1996;40:364-367.
22. Christensen K, Jensen EM, Noer I. The reflex dystrophy syndrome response to treatment with systemic corticosteroids. Acta Chirurgica Scandinavica 1982;148:653-655.
23. Rauck RL, Eisenach JC, Jackson K, Young LD, Southern J. Epidural clonidine treatment for refractory reflex sympathetic dystrophy. Anesthesiology 1993;79:1163-1169.
24. Bickerstaff DR, Kanis JA. The use of nasal calcitonin in the treatment of post-traumatic algodystrophy. Br J Rheumatol 1991;30:291-294.
25. Gobelet C, Waldburger M, Meier JL. The effect of adding calcitonin to physical treatment on reflex sympathetic dystrophy. Pain 1992;48:171-175.
26. Gobelet C, Meier J, Schaffner W, et al. Calcitonin and reflex sympathetic dystrophy syndrome. Clin Rheumatol 1986;5:382-388.
27. Raja AN, Treed RD, Davis KD, Campbell JN. Systematic alpha-adrenergic blockade with phentolamine: a diagnostic test for sympathetically maintained pain. Anesthesiol 1991;74:691-698.
28. Verdugo RJ, Ochoa JL. Sympathetically maintained pain. I. Phentolamine block questions the concept. Neurology 1994;44:1003-1010.
29. Verdugo RJ, Campero M, Ochoa JL. Phentolamine sympathetic block in painful polyneuropathies. II. Further questioning of the concept of “sympathetically maintained pain.” Neurology 1994;44:1010-1014.