User login
Predictors of Length of Stay Among Older Veterans With Schizophrenia Living in VA Community Living Centers
Peanut Allergy Awareness
Among all persons with food allergies, those who are allergic to peanuts are at greatest risk for anaphylactic symptoms.1 About 30,000 cases of food allergy–related anaphylaxis are seen in the nation’s emergency departments (EDs) each year, and the food most commonly responsible is peanuts.2 What can primary care providers do to reduce the number of peanut allergy–associated anaphylactic reactions and fatalities, both in the ED and in the larger community?
According to a guideline from the National Institute of Allergy and Infectious Diseases (NIAID),3 prevalence of peanut allergy is about 0.6% of the US population, although in an 11-year survey involving more than 13,000 respondents, Sicherer et al4 reported allergy to peanuts, tree nuts, or both in 1.4%, possibly translating to some three million Americans; British researchers have reported peanut allergy in 1.8% of an 1,100-member children’s cohort.5 The risk of exposure to peanuts and the associated risk for severe and possibly fatal anaphylaxis present a lifelong struggle for both patient and family.
ETIOLOGY OF PEANUT ALLERGIES
Food allergy prevalence has reportedly doubled in recent decades, with a significant increase also seen in allergy severity.6 Allergies involving eggs, nuts, fish, milk, and other foods represent the leading cause of hospital-treated anaphylaxis throughout the world.1 Unlike other allergenic foods that affect only one age-group, peanuts are among the foods that trigger the “vast majority” of allergic reactions in young children, teenagers, and adults alike.3
Increases in reported episodes of peanut allergy reactions may be occurring for several reasons:
• Many people have adopted vegetarian diets, and nuts are considered a good protein source6
• Environmental exposures are increasingly common
• More people are genetically vulnerable, as the role of family history becomes clearer
• Food preparation methods (eg, shared processing equipment, contaminated raw materials, formulation errors) and inaccurate labeling lead to accidental exposures7,8
• Exposure to nuts in utero or during breastfeeding is more common.9 Nowak-Wegrzyn and Sampson6 point to the promotion of peanut butter as an economical, nutritious food source for children and for women during pregnancy and lactation; mothers’ consumption of peanuts more than once a week during pregnancy and lactation have been linked to overexposure for their children.9
Other trends that may contribute to peanut allergy prevalence are the early introduction of solid foods in the infant diet and the use of skin products that contain peanut oil.6
Environment and Genetics
The body of knowledge regarding the specific causes of peanut allergy is increasing constantly. Several known peanut proteins (Ara h1, Ara h2, Ara h3, Ara h6, Ara h7, and Ara h9; Ara h8 is a homologous allergen that may account for peanut/birch cross-reactivity) are thought to be responsible for the initial sensitization to peanuts in vulnerable persons, triggering the associated immunoglobulin E (IgE)–mediated response.10-12 Approximately 75% of known peanut-allergic patients will react to these proteins on their first ingestion after being sensitized.9
Since IgE antibodies do not cross the placenta, it is believed that sensitization to peanut proteins must occur in utero or through breast milk. This form of sensitization predisposes these patients to the initial life-threatening anaphylactic reaction.9
There is strong evidence that genetic factors may play a role in peanut allergies.2 In a study of 58 pairs of twins by Sicherer et al,13 heritability of peanut allergy was estimated at 82%, with 64% of monozygotic pairs, versus 7% of dizygotic pairs, showing concordance for peanut allergy. However, the genetic loci that may be responsible for specific food allergies have not yet been identified.2
It is believed that manifestations of food allergy are very similar to those of asthma and atopic dermatitis. According to Green and colleagues,14 82% of peanut-allergic children who visited a referral clinic also had atopic dermatitis. These conditions appear to be triggered by similar mechanisms, mediated by both environmental and genetic factors.2,14-16 Hong et al2 are optimistic about the advances being made in food allergy genetics. Increased understanding, they feel, may lead to new treatment options for potentially fatal food allergies.2
PATIENT PRESENTATION AND HISTORY
As with any IgE-mediated immune response, the patient must have been exposed to the allergen in question. Most patients present with a history of having ingested raw or boiled peanuts and/or foods produced in a facility that also processes nuts.1,18 Clinical symptoms of peanut allergy may develop within seconds of ingestion. For some patients, consumption of as little as 5 to 50 mg of peanut protein can trigger symptoms.19 (A single peanut from a jar of commercially processed peanuts contains approximately 300 mg of potentially allergenic protein.1)
Typically, the most dramatically affected patients have a medical history of asthma or other IgE-mediated immune reactions.1 In one study, young adults with IgE-mediated peanut allergy were found at especially high risk for severe anaphylaxis.6 Seventy-five percent of patients who have a reaction to peanuts do so following their first ingestion (after the initial exposure).
The mean patient age for a diagnosis of peanut allergy is about 14 months; only 20% of the patients diagnosed with a peanut allergy (most likely those with a baseline peanut-specific serum IgE level 18) will outgrow it by the time they reach school age.18,20 Those who do should be encouraged to consume peanuts on a regular basis; according to Byrne et al,21 8% of patients with allergy resolution experience recurrence, a possible result of infrequent peanut consumption.
PHYSICAL EXAMINATION
Patients with peanut allergies can present with a range of symptoms, possibly involving cutaneous, cardiovascular, gastrointestinal, and/or respiratory systems (see Table 115,22). The more notable symptoms, possibly developing within 15 minutes of exposure, are progressive upper and lower respiratory difficulties, vomiting, diarrhea, hypotension, edema of the face and hands, arrhythmia, throat tightness (in serious cases, approaching anaphylaxis), and possibly loss of consciousness. Such severe reactions often occur in the child who has ingested raw peanuts or tree nuts.22
Milder physical exam findings include erythema, pruritus, conjunctivitis, abdominal pain, nasal congestion, itchy throat, and sneezing. These reactions may have been triggered by foods produced in a facility that also processes nuts, household utensils used to prepare foods that contain nuts, or cross-contamination from another child.9,15,24
DIAGNOSTIC WORK-UP
The diagnosis of a patient with a peanut allergy is made through thorough history taking, careful physical examination, allergy testing with either a skin prick test (SPT) or serum-specific IgE, and oral food challenges. The gold standard for diagnosing food allergy is the double-blind, placebo-controlled oral food challenge,2,25-27 as this test alone can determine the amount of peanut protein needed to trigger a reaction in the given patient.9 However, this is a difficult test to administer and must be performed under strict medical supervision.21
It has been determined that a wheal size of 8.0 mm or greater on the SPT has a 95% to 100% positive predictive value for peanut allergy.1,26,27 Although conflicting results have been reported in some patients between SPT and the oral food challenge, a negative SPT result is considered useful for excluding IgE-mediated allergic responses.22
Researchers examining the peanut-specific serum IgE have demonstrated a 95% to 99% positive predictive value when serum levels exceed 15 kU/L.26,27 This cutoff value in peanut allergy patients is considered suggestive of allergic reactivity, although negative results on an oral food challenge have been reported in more than 25% of children with serum levels exceeding the cutoff.25-27 Testing may have been to whole peanut extract rather than the molecular components (eg, Ara h8).11,12
This past summer, the FDA approved a component test that detects allergen components that include Ara h1, h2, h3, h8, and h9.11,12 Another specific version of the serum IgE test has been in development, one that measures the patient’s IgE reactions to the Ara h2 and Ara h8 components in peanut protein. Johnson and colleagues10,28 have found an increasing level of serum IgE anti–Ara h2 in children who were unable to pass the oral peanut challenge, whereas serum IgE anti–Ara h8 was higher in those who did pass the challenge.28
DIAGNOSING ANAPHYLAXIS
The manifestation of anaphylaxis in patients allergic to peanuts or tree nuts can be life-threatening.29 Symptoms include intense pruritus with flushing of the skin, urticaria, and angioedema, upper-respiratory obstruction resulting from laryngeal edema, and hypotension.30 The clinical criteria for diagnosing anaphylaxis can be found in Table 2.30,31
It is important to recognize the signs and symptoms of anaphylaxis in patients with a peanut allergy; many patients who present to the ED represent first-time reactions. Among patients with life-threatening symptoms on initial reaction, 71% will have similarly severe reactions in subsequent episodes (compared with 44% of patients whose first reaction was not life-threatening).3
TREATMENT, INCLUDING PATIENT EDUCATION
Currently there is no cure for peanut allergy, and no appropriate therapies yet exist to reduce allergy severity. Modest gains have been reported in raising tolerance threshold levels through peanut oral immunotherapy—a long, painstaking process.19,21,32 For now, treatment for peanut allergy is directed at controlling symptoms, once a reaction has occurred. Therefore, the clinician’s goal is to educate peanut-allergic patients and their families on avoiding accidental peanut ingestion, recognizing signs and symptoms of an allergic reaction, and preparing an emergency plan.4
Because four in five patients can expect peanut allergy to last for a lifetime,18,20 strict avoidance of peanuts and peanut products is essential—though difficult because of accidental exposure to food allergens (for example, when dining in restaurants or purchasing bakery products22,32), cross-contamination (as can occur when a food preparation area is not properly cleaned), and allergen cross-reactivity (such as consumption of other legumes).1 Patients must be taught to read food labels carefully for possible hidden sources of peanuts (see Table 37,8); in some cases, product labels bear helpful advisory wording, such as “may contain peanuts.”34,35 US legislation mandates that listed ingredients on food packaging include the eight foods that account for 90% of allergic reactions:
• Peanuts
• Tree nuts
• Egg
• Milk
• Wheat
• Soybeans
• Fish
• Crustacean shellfish.34
Treatment for Anaphylaxis
In pediatric patients, administration of epinephrine is the definitive treatment for anaphylaxis; both the child and parents should carry an epinephrine self-injection device at all times in the event of accidental peanut ingestion. These devices are available in two strengths, based on the child’s weight, and expiration dates should be noted with care. Correct use of the epinephrine self-injection device should be reviewed at each office visit.6
Early-stage allergic reactions can be managed by oral antihistamines, such as diphenhydramine (1 mg/kg body weight up to 75 mg) and an intramuscular injection of epinephrine.1 Prompt transport to the ED should follow (see “Management of Anaphylaxis in the ED”1,9).
PREVENTION
A 2010 expert panel on diagnosis and management of food allergy sponsored by the NIAID, NIH,3 does not advise women to restrict their diet during pregnancy and lactation. Similarly, the United Kingdom’s Department of Health and the Food Standards Agency (DHFSA)36,37 does not support the belief that eating peanuts and peanut-containing foods during pregnancy correlates with a child’s potential for developing a peanut allergy.
The DHFSA does recommend breastfeeding infants for the first six months, if possible, and that mothers refrain from introducing peanut-containing foods during that time. They also recommend that foods associated with a high risk for allergy be introduced into a child’s diet one at a time, to make it easier to identify any allergenic substance.36,37
Lastly, the DHFSA advises parents with a family history of peanut allergy to introduce peanuts only after consulting with their health care provider. The same consideration is advised if a child has already been diagnosed with another allergy.34 According to the American Academy of Pediatrics,6,38 children at high risk for food allergy (eg, atopic disease in both parents or one parent and one sibling) should be breastfed or be given hypoallergenic formula until age 1 year, with no solid foods before age 6 months; peanut-containing foods should not be given before age 3 or 4 years.
CONCLUSION
Peanut allergy can present a lifelong battle for affected patients. Eating one peanut or being exposed even to minute amounts of peanut protein could mean life or death without appropriate management. Reading food labels carefully, preparing peanut-free foods, recognizing the signs and symptoms of anaphylaxis, and obtaining the necessary treatment when allergic reactions occur are essential for peanut-allergic patients and their families.
REFERENCES
1. Burks AW. Peanut allergy. Lancet. 2008;371 (9623):1538-1546.
2. Hong X, Tsai HJ, Wang X. Genetics of food allergy. Curr Opin Pediatr. 2009;21(6):770-776.
3. Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 suppl):S1-S58.
4. Sicherer S, Muñoz-Furlong A, Godbold JH, Sampson HA. US prevalence of self-reported peanut, tree nut, and sesame allergy: 11-year follow-up. J Allergy Clin Immunol. 2010;125(6):1322-1326.
5. Hourihane JO, Aiken R, Briggs R, et al. The impact of government advice to pregnant mothers regarding peanut avoidance on the prevalence of peanut allergy in United Kingdom children at school entry. J Allergy Clin Immunol. 2007;312(5):1197-1202.
6. Nowak-Wegrzyn A, Sampson HA. Adverse reactions to foods. Med Clin North Am. 2006;90(1):97-127.
7. Puglisi G, Frieri M. Update on hidden food allergens and food labeling. Allergy Asthma Proc. 2007;28(6):634-639.
8. Hefle SL. Hidden food allergens. Curr Opin Allergy Clin Immunol. 2001;1(3):269-271.
9. Lee CW, Sheffer AL. Peanut allergy. Allergy Asthma Proc. 2003;24(4):259-264.
10. Boughton B. New test for peanut allergy a step forward. www.medscape.com/viewarticle/740133. Accessed November 16, 2011.
11. Asarnoj A, Movérare R, Östblom E, et al. IgE to peanut allergen components: relation to peanut symptoms and pollen sensitization in 8-year-olds. Allergy. 2010;65(9):1189-1195.
12. Codreanu F, Collignon O, Roitel O, et al. A novel immunoassay using recombinant allergens simplifies peanut allergy diagnosis. Int Arch Allergy Immunol. 2011;154(3):216-226.
13. Sicherer SH, Furlong TJ, Maes HH, et al. Genetics of peanut allergy: a twin study. J Allergy Clin Immunol. 2000;106(1 pt 1):53-56.
14. Green TD, LaBelle VS, Steele PH, et al. Clinical characteristics of peanut-allergic children: recent changes. Pediatrics. 2007;120(6):1304-1310.
15. Al-ahmed N, Alsowaidi S, Vadas P. Peanut allergy: an overview. Allergy Asthma Clin Immunol. 2008;4(4):139-143.
16. Björkstén B. Genetic and environmental risk factors for the development of food allergy. Curr Opin Allergy Clin Immunol. 2005;5(3):249-253.
17. Lack G. Epidemiologic risks for food allergy. J Allergy Clin Immunol. 2008;121(6):1331-1336.
18. Skolnick HS, Conover-Walker MK, Koerner CB, et al. The natural history of peanut allergy. J Allergy Clin Immunol. 2001;107(2):367-374.
19. Clark AT, Islam S, King Y, et al. Successful oral tolerance induction in severe peanut allergy. Allergy. 2009;64(8):1218-1220.
20. Busse PJ, Nowak-Wegrzyn AH, Noone SA, et al. Recurrent peanut allergy. N Engl J Med. 2002; 347(19):1535-1536.
21. Byrne AM, Malka-Rais J, Burks AW, Fleischer DM. How do we know when peanut and tree nut allergy have resolved, and how do we keep it resolved? Clin Exp Allergy. 2010;49(9):1303-1311.
22. Sampson HA. Update on food allergy. J Allergy Clin Immunol. 2004;113(5):805-819.
23. Furlong TJ, Desimone J, Sicherer SH. Peanut and tree nut allergic reactions in restaurants and other establishments. J Allergy Clin Immunol. 2001;108(5):866-870.
24. Nelson HS, Lahr J, Rule R, et al. Treatment of anaphylactic sensitivity to peanuts by immunotherapy with injections of aqueous peanut extract. J Allergy Clin Immunol. 1997;99(6 pt 1):744-751.
25. Du Toit G, Santos A, Roberts G, et al. The diagnosis of IgE-mediated food allergy in childhood. Pediatr Allergy Immunol. 2009;20(4):309-319.
26. Roberts G, Lack G. Diagnosing peanut allergy with skin prick and specific IgE testing. J Allergy Clin Immunol. 2005;115(6):1291-1296.
27. Wainstein BK, Yee A, Jelley D, et al. Combining skin prick, immediate skin application and specific-IgE testing in the diagnosis of peanut allergy in children. Pediatr Allergy Immunol. 2007;18(3):231-239.
28. Johnson K, Keet C, Hamilton R, Wood R. Predictive value of peanut component specific IgE in a clinical population. Presented at: 2011 Annual Meeting, American Academy of Allergy, Asthma and Immunology; March 19, 2011; San Francisco, CA. Abstract 267.
29. Sheffer AL. Allergen avoidance to reduce asthma-related morbidity. N Engl J Med. 2004;351(11):1134-1136.
30. Russell S, Monroe K, Losek JD. Anaphylaxis management in the pediatric emergency department: opportunities for improvement. Pediatr Emerg Care. 2010;26(2):71-76.
31. Sampson HA, Munoz-Furlong A, Campbell RL, et al. Second symposium on the definition and management of anaphylaxis: summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117(2):391-397.
32. Blumchen K, Ulbricht H, Staden U, et al. Oral peanut immunotherapy in children with peanut anaphylaxis. J Allergy Clin Immunol. 2010; 126(1):83-91.
33. Yu JW, Kagan R, Verreault N, et al. Accidental ingestions in children with peanut allergy. J Allergy Clin Immunol. 2006;118(2):466-472.
34. Taylor SL, Hefle SL. Food allergen labeling in the USA and Europe. Curr Opin Allergy Clin Immunol. 2006;6(3):186-190.
35. Sampson HA, Srivastava K, Li XM, Burks AW. New perspectives for the treatment of food allergy (peanut). Arb Paul Ehrlich Inst Bundesamt Sera Impfstoffe Frankf A M. 2003;(94):236-244.
36. McLean S, Sheikh A. Does avoidance of peanuts in early life reduce the risk of peanut allergy? BMJ. 2010 Mar 11;340:c424.
37. Department of Health. Revised government advice on consumption of peanut during pregnancy, breastfeeding, and early life and development of peanut allergy (Aug 2009). www.dh.gov.uk/en/Healthcare/Children/Maternity/Maternalandinfantnutrition/DH_104490. Accessed November 16, 2011.
38. American Academy of Pediatrics. Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106(2):346-349.
Among all persons with food allergies, those who are allergic to peanuts are at greatest risk for anaphylactic symptoms.1 About 30,000 cases of food allergy–related anaphylaxis are seen in the nation’s emergency departments (EDs) each year, and the food most commonly responsible is peanuts.2 What can primary care providers do to reduce the number of peanut allergy–associated anaphylactic reactions and fatalities, both in the ED and in the larger community?
According to a guideline from the National Institute of Allergy and Infectious Diseases (NIAID),3 prevalence of peanut allergy is about 0.6% of the US population, although in an 11-year survey involving more than 13,000 respondents, Sicherer et al4 reported allergy to peanuts, tree nuts, or both in 1.4%, possibly translating to some three million Americans; British researchers have reported peanut allergy in 1.8% of an 1,100-member children’s cohort.5 The risk of exposure to peanuts and the associated risk for severe and possibly fatal anaphylaxis present a lifelong struggle for both patient and family.
ETIOLOGY OF PEANUT ALLERGIES
Food allergy prevalence has reportedly doubled in recent decades, with a significant increase also seen in allergy severity.6 Allergies involving eggs, nuts, fish, milk, and other foods represent the leading cause of hospital-treated anaphylaxis throughout the world.1 Unlike other allergenic foods that affect only one age-group, peanuts are among the foods that trigger the “vast majority” of allergic reactions in young children, teenagers, and adults alike.3
Increases in reported episodes of peanut allergy reactions may be occurring for several reasons:
• Many people have adopted vegetarian diets, and nuts are considered a good protein source6
• Environmental exposures are increasingly common
• More people are genetically vulnerable, as the role of family history becomes clearer
• Food preparation methods (eg, shared processing equipment, contaminated raw materials, formulation errors) and inaccurate labeling lead to accidental exposures7,8
• Exposure to nuts in utero or during breastfeeding is more common.9 Nowak-Wegrzyn and Sampson6 point to the promotion of peanut butter as an economical, nutritious food source for children and for women during pregnancy and lactation; mothers’ consumption of peanuts more than once a week during pregnancy and lactation have been linked to overexposure for their children.9
Other trends that may contribute to peanut allergy prevalence are the early introduction of solid foods in the infant diet and the use of skin products that contain peanut oil.6
Environment and Genetics
The body of knowledge regarding the specific causes of peanut allergy is increasing constantly. Several known peanut proteins (Ara h1, Ara h2, Ara h3, Ara h6, Ara h7, and Ara h9; Ara h8 is a homologous allergen that may account for peanut/birch cross-reactivity) are thought to be responsible for the initial sensitization to peanuts in vulnerable persons, triggering the associated immunoglobulin E (IgE)–mediated response.10-12 Approximately 75% of known peanut-allergic patients will react to these proteins on their first ingestion after being sensitized.9
Since IgE antibodies do not cross the placenta, it is believed that sensitization to peanut proteins must occur in utero or through breast milk. This form of sensitization predisposes these patients to the initial life-threatening anaphylactic reaction.9
There is strong evidence that genetic factors may play a role in peanut allergies.2 In a study of 58 pairs of twins by Sicherer et al,13 heritability of peanut allergy was estimated at 82%, with 64% of monozygotic pairs, versus 7% of dizygotic pairs, showing concordance for peanut allergy. However, the genetic loci that may be responsible for specific food allergies have not yet been identified.2
It is believed that manifestations of food allergy are very similar to those of asthma and atopic dermatitis. According to Green and colleagues,14 82% of peanut-allergic children who visited a referral clinic also had atopic dermatitis. These conditions appear to be triggered by similar mechanisms, mediated by both environmental and genetic factors.2,14-16 Hong et al2 are optimistic about the advances being made in food allergy genetics. Increased understanding, they feel, may lead to new treatment options for potentially fatal food allergies.2
PATIENT PRESENTATION AND HISTORY
As with any IgE-mediated immune response, the patient must have been exposed to the allergen in question. Most patients present with a history of having ingested raw or boiled peanuts and/or foods produced in a facility that also processes nuts.1,18 Clinical symptoms of peanut allergy may develop within seconds of ingestion. For some patients, consumption of as little as 5 to 50 mg of peanut protein can trigger symptoms.19 (A single peanut from a jar of commercially processed peanuts contains approximately 300 mg of potentially allergenic protein.1)
Typically, the most dramatically affected patients have a medical history of asthma or other IgE-mediated immune reactions.1 In one study, young adults with IgE-mediated peanut allergy were found at especially high risk for severe anaphylaxis.6 Seventy-five percent of patients who have a reaction to peanuts do so following their first ingestion (after the initial exposure).
The mean patient age for a diagnosis of peanut allergy is about 14 months; only 20% of the patients diagnosed with a peanut allergy (most likely those with a baseline peanut-specific serum IgE level 18) will outgrow it by the time they reach school age.18,20 Those who do should be encouraged to consume peanuts on a regular basis; according to Byrne et al,21 8% of patients with allergy resolution experience recurrence, a possible result of infrequent peanut consumption.
PHYSICAL EXAMINATION
Patients with peanut allergies can present with a range of symptoms, possibly involving cutaneous, cardiovascular, gastrointestinal, and/or respiratory systems (see Table 115,22). The more notable symptoms, possibly developing within 15 minutes of exposure, are progressive upper and lower respiratory difficulties, vomiting, diarrhea, hypotension, edema of the face and hands, arrhythmia, throat tightness (in serious cases, approaching anaphylaxis), and possibly loss of consciousness. Such severe reactions often occur in the child who has ingested raw peanuts or tree nuts.22
Milder physical exam findings include erythema, pruritus, conjunctivitis, abdominal pain, nasal congestion, itchy throat, and sneezing. These reactions may have been triggered by foods produced in a facility that also processes nuts, household utensils used to prepare foods that contain nuts, or cross-contamination from another child.9,15,24
DIAGNOSTIC WORK-UP
The diagnosis of a patient with a peanut allergy is made through thorough history taking, careful physical examination, allergy testing with either a skin prick test (SPT) or serum-specific IgE, and oral food challenges. The gold standard for diagnosing food allergy is the double-blind, placebo-controlled oral food challenge,2,25-27 as this test alone can determine the amount of peanut protein needed to trigger a reaction in the given patient.9 However, this is a difficult test to administer and must be performed under strict medical supervision.21
It has been determined that a wheal size of 8.0 mm or greater on the SPT has a 95% to 100% positive predictive value for peanut allergy.1,26,27 Although conflicting results have been reported in some patients between SPT and the oral food challenge, a negative SPT result is considered useful for excluding IgE-mediated allergic responses.22
Researchers examining the peanut-specific serum IgE have demonstrated a 95% to 99% positive predictive value when serum levels exceed 15 kU/L.26,27 This cutoff value in peanut allergy patients is considered suggestive of allergic reactivity, although negative results on an oral food challenge have been reported in more than 25% of children with serum levels exceeding the cutoff.25-27 Testing may have been to whole peanut extract rather than the molecular components (eg, Ara h8).11,12
This past summer, the FDA approved a component test that detects allergen components that include Ara h1, h2, h3, h8, and h9.11,12 Another specific version of the serum IgE test has been in development, one that measures the patient’s IgE reactions to the Ara h2 and Ara h8 components in peanut protein. Johnson and colleagues10,28 have found an increasing level of serum IgE anti–Ara h2 in children who were unable to pass the oral peanut challenge, whereas serum IgE anti–Ara h8 was higher in those who did pass the challenge.28
DIAGNOSING ANAPHYLAXIS
The manifestation of anaphylaxis in patients allergic to peanuts or tree nuts can be life-threatening.29 Symptoms include intense pruritus with flushing of the skin, urticaria, and angioedema, upper-respiratory obstruction resulting from laryngeal edema, and hypotension.30 The clinical criteria for diagnosing anaphylaxis can be found in Table 2.30,31
It is important to recognize the signs and symptoms of anaphylaxis in patients with a peanut allergy; many patients who present to the ED represent first-time reactions. Among patients with life-threatening symptoms on initial reaction, 71% will have similarly severe reactions in subsequent episodes (compared with 44% of patients whose first reaction was not life-threatening).3
TREATMENT, INCLUDING PATIENT EDUCATION
Currently there is no cure for peanut allergy, and no appropriate therapies yet exist to reduce allergy severity. Modest gains have been reported in raising tolerance threshold levels through peanut oral immunotherapy—a long, painstaking process.19,21,32 For now, treatment for peanut allergy is directed at controlling symptoms, once a reaction has occurred. Therefore, the clinician’s goal is to educate peanut-allergic patients and their families on avoiding accidental peanut ingestion, recognizing signs and symptoms of an allergic reaction, and preparing an emergency plan.4
Because four in five patients can expect peanut allergy to last for a lifetime,18,20 strict avoidance of peanuts and peanut products is essential—though difficult because of accidental exposure to food allergens (for example, when dining in restaurants or purchasing bakery products22,32), cross-contamination (as can occur when a food preparation area is not properly cleaned), and allergen cross-reactivity (such as consumption of other legumes).1 Patients must be taught to read food labels carefully for possible hidden sources of peanuts (see Table 37,8); in some cases, product labels bear helpful advisory wording, such as “may contain peanuts.”34,35 US legislation mandates that listed ingredients on food packaging include the eight foods that account for 90% of allergic reactions:
• Peanuts
• Tree nuts
• Egg
• Milk
• Wheat
• Soybeans
• Fish
• Crustacean shellfish.34
Treatment for Anaphylaxis
In pediatric patients, administration of epinephrine is the definitive treatment for anaphylaxis; both the child and parents should carry an epinephrine self-injection device at all times in the event of accidental peanut ingestion. These devices are available in two strengths, based on the child’s weight, and expiration dates should be noted with care. Correct use of the epinephrine self-injection device should be reviewed at each office visit.6
Early-stage allergic reactions can be managed by oral antihistamines, such as diphenhydramine (1 mg/kg body weight up to 75 mg) and an intramuscular injection of epinephrine.1 Prompt transport to the ED should follow (see “Management of Anaphylaxis in the ED”1,9).
PREVENTION
A 2010 expert panel on diagnosis and management of food allergy sponsored by the NIAID, NIH,3 does not advise women to restrict their diet during pregnancy and lactation. Similarly, the United Kingdom’s Department of Health and the Food Standards Agency (DHFSA)36,37 does not support the belief that eating peanuts and peanut-containing foods during pregnancy correlates with a child’s potential for developing a peanut allergy.
The DHFSA does recommend breastfeeding infants for the first six months, if possible, and that mothers refrain from introducing peanut-containing foods during that time. They also recommend that foods associated with a high risk for allergy be introduced into a child’s diet one at a time, to make it easier to identify any allergenic substance.36,37
Lastly, the DHFSA advises parents with a family history of peanut allergy to introduce peanuts only after consulting with their health care provider. The same consideration is advised if a child has already been diagnosed with another allergy.34 According to the American Academy of Pediatrics,6,38 children at high risk for food allergy (eg, atopic disease in both parents or one parent and one sibling) should be breastfed or be given hypoallergenic formula until age 1 year, with no solid foods before age 6 months; peanut-containing foods should not be given before age 3 or 4 years.
CONCLUSION
Peanut allergy can present a lifelong battle for affected patients. Eating one peanut or being exposed even to minute amounts of peanut protein could mean life or death without appropriate management. Reading food labels carefully, preparing peanut-free foods, recognizing the signs and symptoms of anaphylaxis, and obtaining the necessary treatment when allergic reactions occur are essential for peanut-allergic patients and their families.
REFERENCES
1. Burks AW. Peanut allergy. Lancet. 2008;371 (9623):1538-1546.
2. Hong X, Tsai HJ, Wang X. Genetics of food allergy. Curr Opin Pediatr. 2009;21(6):770-776.
3. Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 suppl):S1-S58.
4. Sicherer S, Muñoz-Furlong A, Godbold JH, Sampson HA. US prevalence of self-reported peanut, tree nut, and sesame allergy: 11-year follow-up. J Allergy Clin Immunol. 2010;125(6):1322-1326.
5. Hourihane JO, Aiken R, Briggs R, et al. The impact of government advice to pregnant mothers regarding peanut avoidance on the prevalence of peanut allergy in United Kingdom children at school entry. J Allergy Clin Immunol. 2007;312(5):1197-1202.
6. Nowak-Wegrzyn A, Sampson HA. Adverse reactions to foods. Med Clin North Am. 2006;90(1):97-127.
7. Puglisi G, Frieri M. Update on hidden food allergens and food labeling. Allergy Asthma Proc. 2007;28(6):634-639.
8. Hefle SL. Hidden food allergens. Curr Opin Allergy Clin Immunol. 2001;1(3):269-271.
9. Lee CW, Sheffer AL. Peanut allergy. Allergy Asthma Proc. 2003;24(4):259-264.
10. Boughton B. New test for peanut allergy a step forward. www.medscape.com/viewarticle/740133. Accessed November 16, 2011.
11. Asarnoj A, Movérare R, Östblom E, et al. IgE to peanut allergen components: relation to peanut symptoms and pollen sensitization in 8-year-olds. Allergy. 2010;65(9):1189-1195.
12. Codreanu F, Collignon O, Roitel O, et al. A novel immunoassay using recombinant allergens simplifies peanut allergy diagnosis. Int Arch Allergy Immunol. 2011;154(3):216-226.
13. Sicherer SH, Furlong TJ, Maes HH, et al. Genetics of peanut allergy: a twin study. J Allergy Clin Immunol. 2000;106(1 pt 1):53-56.
14. Green TD, LaBelle VS, Steele PH, et al. Clinical characteristics of peanut-allergic children: recent changes. Pediatrics. 2007;120(6):1304-1310.
15. Al-ahmed N, Alsowaidi S, Vadas P. Peanut allergy: an overview. Allergy Asthma Clin Immunol. 2008;4(4):139-143.
16. Björkstén B. Genetic and environmental risk factors for the development of food allergy. Curr Opin Allergy Clin Immunol. 2005;5(3):249-253.
17. Lack G. Epidemiologic risks for food allergy. J Allergy Clin Immunol. 2008;121(6):1331-1336.
18. Skolnick HS, Conover-Walker MK, Koerner CB, et al. The natural history of peanut allergy. J Allergy Clin Immunol. 2001;107(2):367-374.
19. Clark AT, Islam S, King Y, et al. Successful oral tolerance induction in severe peanut allergy. Allergy. 2009;64(8):1218-1220.
20. Busse PJ, Nowak-Wegrzyn AH, Noone SA, et al. Recurrent peanut allergy. N Engl J Med. 2002; 347(19):1535-1536.
21. Byrne AM, Malka-Rais J, Burks AW, Fleischer DM. How do we know when peanut and tree nut allergy have resolved, and how do we keep it resolved? Clin Exp Allergy. 2010;49(9):1303-1311.
22. Sampson HA. Update on food allergy. J Allergy Clin Immunol. 2004;113(5):805-819.
23. Furlong TJ, Desimone J, Sicherer SH. Peanut and tree nut allergic reactions in restaurants and other establishments. J Allergy Clin Immunol. 2001;108(5):866-870.
24. Nelson HS, Lahr J, Rule R, et al. Treatment of anaphylactic sensitivity to peanuts by immunotherapy with injections of aqueous peanut extract. J Allergy Clin Immunol. 1997;99(6 pt 1):744-751.
25. Du Toit G, Santos A, Roberts G, et al. The diagnosis of IgE-mediated food allergy in childhood. Pediatr Allergy Immunol. 2009;20(4):309-319.
26. Roberts G, Lack G. Diagnosing peanut allergy with skin prick and specific IgE testing. J Allergy Clin Immunol. 2005;115(6):1291-1296.
27. Wainstein BK, Yee A, Jelley D, et al. Combining skin prick, immediate skin application and specific-IgE testing in the diagnosis of peanut allergy in children. Pediatr Allergy Immunol. 2007;18(3):231-239.
28. Johnson K, Keet C, Hamilton R, Wood R. Predictive value of peanut component specific IgE in a clinical population. Presented at: 2011 Annual Meeting, American Academy of Allergy, Asthma and Immunology; March 19, 2011; San Francisco, CA. Abstract 267.
29. Sheffer AL. Allergen avoidance to reduce asthma-related morbidity. N Engl J Med. 2004;351(11):1134-1136.
30. Russell S, Monroe K, Losek JD. Anaphylaxis management in the pediatric emergency department: opportunities for improvement. Pediatr Emerg Care. 2010;26(2):71-76.
31. Sampson HA, Munoz-Furlong A, Campbell RL, et al. Second symposium on the definition and management of anaphylaxis: summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117(2):391-397.
32. Blumchen K, Ulbricht H, Staden U, et al. Oral peanut immunotherapy in children with peanut anaphylaxis. J Allergy Clin Immunol. 2010; 126(1):83-91.
33. Yu JW, Kagan R, Verreault N, et al. Accidental ingestions in children with peanut allergy. J Allergy Clin Immunol. 2006;118(2):466-472.
34. Taylor SL, Hefle SL. Food allergen labeling in the USA and Europe. Curr Opin Allergy Clin Immunol. 2006;6(3):186-190.
35. Sampson HA, Srivastava K, Li XM, Burks AW. New perspectives for the treatment of food allergy (peanut). Arb Paul Ehrlich Inst Bundesamt Sera Impfstoffe Frankf A M. 2003;(94):236-244.
36. McLean S, Sheikh A. Does avoidance of peanuts in early life reduce the risk of peanut allergy? BMJ. 2010 Mar 11;340:c424.
37. Department of Health. Revised government advice on consumption of peanut during pregnancy, breastfeeding, and early life and development of peanut allergy (Aug 2009). www.dh.gov.uk/en/Healthcare/Children/Maternity/Maternalandinfantnutrition/DH_104490. Accessed November 16, 2011.
38. American Academy of Pediatrics. Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106(2):346-349.
Among all persons with food allergies, those who are allergic to peanuts are at greatest risk for anaphylactic symptoms.1 About 30,000 cases of food allergy–related anaphylaxis are seen in the nation’s emergency departments (EDs) each year, and the food most commonly responsible is peanuts.2 What can primary care providers do to reduce the number of peanut allergy–associated anaphylactic reactions and fatalities, both in the ED and in the larger community?
According to a guideline from the National Institute of Allergy and Infectious Diseases (NIAID),3 prevalence of peanut allergy is about 0.6% of the US population, although in an 11-year survey involving more than 13,000 respondents, Sicherer et al4 reported allergy to peanuts, tree nuts, or both in 1.4%, possibly translating to some three million Americans; British researchers have reported peanut allergy in 1.8% of an 1,100-member children’s cohort.5 The risk of exposure to peanuts and the associated risk for severe and possibly fatal anaphylaxis present a lifelong struggle for both patient and family.
ETIOLOGY OF PEANUT ALLERGIES
Food allergy prevalence has reportedly doubled in recent decades, with a significant increase also seen in allergy severity.6 Allergies involving eggs, nuts, fish, milk, and other foods represent the leading cause of hospital-treated anaphylaxis throughout the world.1 Unlike other allergenic foods that affect only one age-group, peanuts are among the foods that trigger the “vast majority” of allergic reactions in young children, teenagers, and adults alike.3
Increases in reported episodes of peanut allergy reactions may be occurring for several reasons:
• Many people have adopted vegetarian diets, and nuts are considered a good protein source6
• Environmental exposures are increasingly common
• More people are genetically vulnerable, as the role of family history becomes clearer
• Food preparation methods (eg, shared processing equipment, contaminated raw materials, formulation errors) and inaccurate labeling lead to accidental exposures7,8
• Exposure to nuts in utero or during breastfeeding is more common.9 Nowak-Wegrzyn and Sampson6 point to the promotion of peanut butter as an economical, nutritious food source for children and for women during pregnancy and lactation; mothers’ consumption of peanuts more than once a week during pregnancy and lactation have been linked to overexposure for their children.9
Other trends that may contribute to peanut allergy prevalence are the early introduction of solid foods in the infant diet and the use of skin products that contain peanut oil.6
Environment and Genetics
The body of knowledge regarding the specific causes of peanut allergy is increasing constantly. Several known peanut proteins (Ara h1, Ara h2, Ara h3, Ara h6, Ara h7, and Ara h9; Ara h8 is a homologous allergen that may account for peanut/birch cross-reactivity) are thought to be responsible for the initial sensitization to peanuts in vulnerable persons, triggering the associated immunoglobulin E (IgE)–mediated response.10-12 Approximately 75% of known peanut-allergic patients will react to these proteins on their first ingestion after being sensitized.9
Since IgE antibodies do not cross the placenta, it is believed that sensitization to peanut proteins must occur in utero or through breast milk. This form of sensitization predisposes these patients to the initial life-threatening anaphylactic reaction.9
There is strong evidence that genetic factors may play a role in peanut allergies.2 In a study of 58 pairs of twins by Sicherer et al,13 heritability of peanut allergy was estimated at 82%, with 64% of monozygotic pairs, versus 7% of dizygotic pairs, showing concordance for peanut allergy. However, the genetic loci that may be responsible for specific food allergies have not yet been identified.2
It is believed that manifestations of food allergy are very similar to those of asthma and atopic dermatitis. According to Green and colleagues,14 82% of peanut-allergic children who visited a referral clinic also had atopic dermatitis. These conditions appear to be triggered by similar mechanisms, mediated by both environmental and genetic factors.2,14-16 Hong et al2 are optimistic about the advances being made in food allergy genetics. Increased understanding, they feel, may lead to new treatment options for potentially fatal food allergies.2
PATIENT PRESENTATION AND HISTORY
As with any IgE-mediated immune response, the patient must have been exposed to the allergen in question. Most patients present with a history of having ingested raw or boiled peanuts and/or foods produced in a facility that also processes nuts.1,18 Clinical symptoms of peanut allergy may develop within seconds of ingestion. For some patients, consumption of as little as 5 to 50 mg of peanut protein can trigger symptoms.19 (A single peanut from a jar of commercially processed peanuts contains approximately 300 mg of potentially allergenic protein.1)
Typically, the most dramatically affected patients have a medical history of asthma or other IgE-mediated immune reactions.1 In one study, young adults with IgE-mediated peanut allergy were found at especially high risk for severe anaphylaxis.6 Seventy-five percent of patients who have a reaction to peanuts do so following their first ingestion (after the initial exposure).
The mean patient age for a diagnosis of peanut allergy is about 14 months; only 20% of the patients diagnosed with a peanut allergy (most likely those with a baseline peanut-specific serum IgE level 18) will outgrow it by the time they reach school age.18,20 Those who do should be encouraged to consume peanuts on a regular basis; according to Byrne et al,21 8% of patients with allergy resolution experience recurrence, a possible result of infrequent peanut consumption.
PHYSICAL EXAMINATION
Patients with peanut allergies can present with a range of symptoms, possibly involving cutaneous, cardiovascular, gastrointestinal, and/or respiratory systems (see Table 115,22). The more notable symptoms, possibly developing within 15 minutes of exposure, are progressive upper and lower respiratory difficulties, vomiting, diarrhea, hypotension, edema of the face and hands, arrhythmia, throat tightness (in serious cases, approaching anaphylaxis), and possibly loss of consciousness. Such severe reactions often occur in the child who has ingested raw peanuts or tree nuts.22
Milder physical exam findings include erythema, pruritus, conjunctivitis, abdominal pain, nasal congestion, itchy throat, and sneezing. These reactions may have been triggered by foods produced in a facility that also processes nuts, household utensils used to prepare foods that contain nuts, or cross-contamination from another child.9,15,24
DIAGNOSTIC WORK-UP
The diagnosis of a patient with a peanut allergy is made through thorough history taking, careful physical examination, allergy testing with either a skin prick test (SPT) or serum-specific IgE, and oral food challenges. The gold standard for diagnosing food allergy is the double-blind, placebo-controlled oral food challenge,2,25-27 as this test alone can determine the amount of peanut protein needed to trigger a reaction in the given patient.9 However, this is a difficult test to administer and must be performed under strict medical supervision.21
It has been determined that a wheal size of 8.0 mm or greater on the SPT has a 95% to 100% positive predictive value for peanut allergy.1,26,27 Although conflicting results have been reported in some patients between SPT and the oral food challenge, a negative SPT result is considered useful for excluding IgE-mediated allergic responses.22
Researchers examining the peanut-specific serum IgE have demonstrated a 95% to 99% positive predictive value when serum levels exceed 15 kU/L.26,27 This cutoff value in peanut allergy patients is considered suggestive of allergic reactivity, although negative results on an oral food challenge have been reported in more than 25% of children with serum levels exceeding the cutoff.25-27 Testing may have been to whole peanut extract rather than the molecular components (eg, Ara h8).11,12
This past summer, the FDA approved a component test that detects allergen components that include Ara h1, h2, h3, h8, and h9.11,12 Another specific version of the serum IgE test has been in development, one that measures the patient’s IgE reactions to the Ara h2 and Ara h8 components in peanut protein. Johnson and colleagues10,28 have found an increasing level of serum IgE anti–Ara h2 in children who were unable to pass the oral peanut challenge, whereas serum IgE anti–Ara h8 was higher in those who did pass the challenge.28
DIAGNOSING ANAPHYLAXIS
The manifestation of anaphylaxis in patients allergic to peanuts or tree nuts can be life-threatening.29 Symptoms include intense pruritus with flushing of the skin, urticaria, and angioedema, upper-respiratory obstruction resulting from laryngeal edema, and hypotension.30 The clinical criteria for diagnosing anaphylaxis can be found in Table 2.30,31
It is important to recognize the signs and symptoms of anaphylaxis in patients with a peanut allergy; many patients who present to the ED represent first-time reactions. Among patients with life-threatening symptoms on initial reaction, 71% will have similarly severe reactions in subsequent episodes (compared with 44% of patients whose first reaction was not life-threatening).3
TREATMENT, INCLUDING PATIENT EDUCATION
Currently there is no cure for peanut allergy, and no appropriate therapies yet exist to reduce allergy severity. Modest gains have been reported in raising tolerance threshold levels through peanut oral immunotherapy—a long, painstaking process.19,21,32 For now, treatment for peanut allergy is directed at controlling symptoms, once a reaction has occurred. Therefore, the clinician’s goal is to educate peanut-allergic patients and their families on avoiding accidental peanut ingestion, recognizing signs and symptoms of an allergic reaction, and preparing an emergency plan.4
Because four in five patients can expect peanut allergy to last for a lifetime,18,20 strict avoidance of peanuts and peanut products is essential—though difficult because of accidental exposure to food allergens (for example, when dining in restaurants or purchasing bakery products22,32), cross-contamination (as can occur when a food preparation area is not properly cleaned), and allergen cross-reactivity (such as consumption of other legumes).1 Patients must be taught to read food labels carefully for possible hidden sources of peanuts (see Table 37,8); in some cases, product labels bear helpful advisory wording, such as “may contain peanuts.”34,35 US legislation mandates that listed ingredients on food packaging include the eight foods that account for 90% of allergic reactions:
• Peanuts
• Tree nuts
• Egg
• Milk
• Wheat
• Soybeans
• Fish
• Crustacean shellfish.34
Treatment for Anaphylaxis
In pediatric patients, administration of epinephrine is the definitive treatment for anaphylaxis; both the child and parents should carry an epinephrine self-injection device at all times in the event of accidental peanut ingestion. These devices are available in two strengths, based on the child’s weight, and expiration dates should be noted with care. Correct use of the epinephrine self-injection device should be reviewed at each office visit.6
Early-stage allergic reactions can be managed by oral antihistamines, such as diphenhydramine (1 mg/kg body weight up to 75 mg) and an intramuscular injection of epinephrine.1 Prompt transport to the ED should follow (see “Management of Anaphylaxis in the ED”1,9).
PREVENTION
A 2010 expert panel on diagnosis and management of food allergy sponsored by the NIAID, NIH,3 does not advise women to restrict their diet during pregnancy and lactation. Similarly, the United Kingdom’s Department of Health and the Food Standards Agency (DHFSA)36,37 does not support the belief that eating peanuts and peanut-containing foods during pregnancy correlates with a child’s potential for developing a peanut allergy.
The DHFSA does recommend breastfeeding infants for the first six months, if possible, and that mothers refrain from introducing peanut-containing foods during that time. They also recommend that foods associated with a high risk for allergy be introduced into a child’s diet one at a time, to make it easier to identify any allergenic substance.36,37
Lastly, the DHFSA advises parents with a family history of peanut allergy to introduce peanuts only after consulting with their health care provider. The same consideration is advised if a child has already been diagnosed with another allergy.34 According to the American Academy of Pediatrics,6,38 children at high risk for food allergy (eg, atopic disease in both parents or one parent and one sibling) should be breastfed or be given hypoallergenic formula until age 1 year, with no solid foods before age 6 months; peanut-containing foods should not be given before age 3 or 4 years.
CONCLUSION
Peanut allergy can present a lifelong battle for affected patients. Eating one peanut or being exposed even to minute amounts of peanut protein could mean life or death without appropriate management. Reading food labels carefully, preparing peanut-free foods, recognizing the signs and symptoms of anaphylaxis, and obtaining the necessary treatment when allergic reactions occur are essential for peanut-allergic patients and their families.
REFERENCES
1. Burks AW. Peanut allergy. Lancet. 2008;371 (9623):1538-1546.
2. Hong X, Tsai HJ, Wang X. Genetics of food allergy. Curr Opin Pediatr. 2009;21(6):770-776.
3. Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 suppl):S1-S58.
4. Sicherer S, Muñoz-Furlong A, Godbold JH, Sampson HA. US prevalence of self-reported peanut, tree nut, and sesame allergy: 11-year follow-up. J Allergy Clin Immunol. 2010;125(6):1322-1326.
5. Hourihane JO, Aiken R, Briggs R, et al. The impact of government advice to pregnant mothers regarding peanut avoidance on the prevalence of peanut allergy in United Kingdom children at school entry. J Allergy Clin Immunol. 2007;312(5):1197-1202.
6. Nowak-Wegrzyn A, Sampson HA. Adverse reactions to foods. Med Clin North Am. 2006;90(1):97-127.
7. Puglisi G, Frieri M. Update on hidden food allergens and food labeling. Allergy Asthma Proc. 2007;28(6):634-639.
8. Hefle SL. Hidden food allergens. Curr Opin Allergy Clin Immunol. 2001;1(3):269-271.
9. Lee CW, Sheffer AL. Peanut allergy. Allergy Asthma Proc. 2003;24(4):259-264.
10. Boughton B. New test for peanut allergy a step forward. www.medscape.com/viewarticle/740133. Accessed November 16, 2011.
11. Asarnoj A, Movérare R, Östblom E, et al. IgE to peanut allergen components: relation to peanut symptoms and pollen sensitization in 8-year-olds. Allergy. 2010;65(9):1189-1195.
12. Codreanu F, Collignon O, Roitel O, et al. A novel immunoassay using recombinant allergens simplifies peanut allergy diagnosis. Int Arch Allergy Immunol. 2011;154(3):216-226.
13. Sicherer SH, Furlong TJ, Maes HH, et al. Genetics of peanut allergy: a twin study. J Allergy Clin Immunol. 2000;106(1 pt 1):53-56.
14. Green TD, LaBelle VS, Steele PH, et al. Clinical characteristics of peanut-allergic children: recent changes. Pediatrics. 2007;120(6):1304-1310.
15. Al-ahmed N, Alsowaidi S, Vadas P. Peanut allergy: an overview. Allergy Asthma Clin Immunol. 2008;4(4):139-143.
16. Björkstén B. Genetic and environmental risk factors for the development of food allergy. Curr Opin Allergy Clin Immunol. 2005;5(3):249-253.
17. Lack G. Epidemiologic risks for food allergy. J Allergy Clin Immunol. 2008;121(6):1331-1336.
18. Skolnick HS, Conover-Walker MK, Koerner CB, et al. The natural history of peanut allergy. J Allergy Clin Immunol. 2001;107(2):367-374.
19. Clark AT, Islam S, King Y, et al. Successful oral tolerance induction in severe peanut allergy. Allergy. 2009;64(8):1218-1220.
20. Busse PJ, Nowak-Wegrzyn AH, Noone SA, et al. Recurrent peanut allergy. N Engl J Med. 2002; 347(19):1535-1536.
21. Byrne AM, Malka-Rais J, Burks AW, Fleischer DM. How do we know when peanut and tree nut allergy have resolved, and how do we keep it resolved? Clin Exp Allergy. 2010;49(9):1303-1311.
22. Sampson HA. Update on food allergy. J Allergy Clin Immunol. 2004;113(5):805-819.
23. Furlong TJ, Desimone J, Sicherer SH. Peanut and tree nut allergic reactions in restaurants and other establishments. J Allergy Clin Immunol. 2001;108(5):866-870.
24. Nelson HS, Lahr J, Rule R, et al. Treatment of anaphylactic sensitivity to peanuts by immunotherapy with injections of aqueous peanut extract. J Allergy Clin Immunol. 1997;99(6 pt 1):744-751.
25. Du Toit G, Santos A, Roberts G, et al. The diagnosis of IgE-mediated food allergy in childhood. Pediatr Allergy Immunol. 2009;20(4):309-319.
26. Roberts G, Lack G. Diagnosing peanut allergy with skin prick and specific IgE testing. J Allergy Clin Immunol. 2005;115(6):1291-1296.
27. Wainstein BK, Yee A, Jelley D, et al. Combining skin prick, immediate skin application and specific-IgE testing in the diagnosis of peanut allergy in children. Pediatr Allergy Immunol. 2007;18(3):231-239.
28. Johnson K, Keet C, Hamilton R, Wood R. Predictive value of peanut component specific IgE in a clinical population. Presented at: 2011 Annual Meeting, American Academy of Allergy, Asthma and Immunology; March 19, 2011; San Francisco, CA. Abstract 267.
29. Sheffer AL. Allergen avoidance to reduce asthma-related morbidity. N Engl J Med. 2004;351(11):1134-1136.
30. Russell S, Monroe K, Losek JD. Anaphylaxis management in the pediatric emergency department: opportunities for improvement. Pediatr Emerg Care. 2010;26(2):71-76.
31. Sampson HA, Munoz-Furlong A, Campbell RL, et al. Second symposium on the definition and management of anaphylaxis: summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117(2):391-397.
32. Blumchen K, Ulbricht H, Staden U, et al. Oral peanut immunotherapy in children with peanut anaphylaxis. J Allergy Clin Immunol. 2010; 126(1):83-91.
33. Yu JW, Kagan R, Verreault N, et al. Accidental ingestions in children with peanut allergy. J Allergy Clin Immunol. 2006;118(2):466-472.
34. Taylor SL, Hefle SL. Food allergen labeling in the USA and Europe. Curr Opin Allergy Clin Immunol. 2006;6(3):186-190.
35. Sampson HA, Srivastava K, Li XM, Burks AW. New perspectives for the treatment of food allergy (peanut). Arb Paul Ehrlich Inst Bundesamt Sera Impfstoffe Frankf A M. 2003;(94):236-244.
36. McLean S, Sheikh A. Does avoidance of peanuts in early life reduce the risk of peanut allergy? BMJ. 2010 Mar 11;340:c424.
37. Department of Health. Revised government advice on consumption of peanut during pregnancy, breastfeeding, and early life and development of peanut allergy (Aug 2009). www.dh.gov.uk/en/Healthcare/Children/Maternity/Maternalandinfantnutrition/DH_104490. Accessed November 16, 2011.
38. American Academy of Pediatrics. Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106(2):346-349.
Grand Rounds: Pregnant Woman, 33, With Leg Pain and Numbness
A 33-year-old woman in her 32nd week of pregnancy (gravida 3, para 2) presented to the emergency department (ED) with a five-day history of weakness and ascending numbness below the right knee. She related a two-week history of right-sided low back pain that radiated to the right buttock and was associated with severe right lower extremity (RLE) pain, most prominent in the posterolateral aspect of the right calf. She denied perianal numbness, incontinence, or other changes in bowel or bladder function. She also denied left lower extremity involvement or trauma.
The patient had had one uneventful pregnancy to date. Her medical history included hypothyroidism, treated with levothyroxine; and anxiety, for which she was taking sertraline. She denied any history of allergies, alcohol consumption, smoking, or illicit drug use. She had been evaluated twice and received reassurance in the two weeks before her presentation to the ED. She was admitted to the obstetric service secondary to pain, and a stat MRI rather than x-ray was ordered by obstetrics. An orthopedic consult was ordered. A spine surgeon happened to be on call.
Examination revealed that the patient walked plantigrade, with her right foot slightly externally rotated. She was unable to dorsiflex or plantarflex her right foot. She was unable to heel- or toe-walk on the right side, possessed 0 out of 5 strength at the right extensor hallucis longus and 2 to 3 out of 5 at the right tibialis anterior and gastroc soleus complex. She complained of pain with right leg elevation exceeding 30° and had very limited sensation to light touch in the right L5 and S1 dermatomes. Deep tendon reflex was absent at the right ankle. The patient refused a rectal exam or post-void evaluation.
The initial diagnosis considered by the ED clinician was sciatica, with a differential diagnosis that included pelvic pain of pregnancy, lumbar sprain strain, sciatica, lumbar disk, herniated nucleus pulposus with radiculopathy, and cauda equina syndrome. Trauma was considered and ruled out, as were malignancies; inflammatory, infectious, or degenerative conditions; or other compressive processes.1
Lumbar MRI demonstrated a very large, right-sided disk herniation at L5-S1 with an extruded fragment that was severely compressing the thecal sac and the right S1 nerve root, causing severe right foraminal stenosis at the level of L5-S1. Degenerative changes were noted at L4-5 with disk dessication and no lesions seen.
The patient was diagnosed with cauda equina syndrome, which was felt to be causing severe RLE weakness and ascending numbness. The options of observation, analgesia, physical therapy, and epidural injections were discussed with the patient; however, surgery was strongly recommended due to her profound weakness and the severity of pain she was experiencing, in addition to the size of the disk herniation. She opted for surgery.
The patient was given epidural anesthesia at the L3-4 level, with a catheter left in place during the procedure. A test dose of lidocaine (1.5 cc) with epinephrine was injected to ensure proper placement, and bupivacaine 0.5% was given in increments of 5.0 cc three times during the case. Propofol was administered for sedation, and a 2.0-mg dose of a long-acting morphine was given to the patient before removal of the epidural catheter. Fetal monitoring was performed by obstetrics throughout the procedure.
A laminotomy, partial facetectomy, and diskectomy were performed at L5-S1 with excision of a free fragment. Surgical pathology described the disk as fibrocartilaginous tissue measuring 3.5 cm x 1.4 cm x 0.6 cm.
DISCUSSION
Although nearly half of pregnant women experience low back pain, cauda equina syndrome (CES), a complication of lumbar disk herniation, is extremely rare in the gravid patient.2 In a decade-long review of 48,760 consecutive deliveries, LaBan et al3 identified symptomatic lumbar herniated nucleus pulposus in only five patients (approximately one in 10,000 pregnancies). In pregnant women who do experience CES, symptoms most commonly develop between the fifth and seventh month of pregnancy.4 According to Small et al,5 “The major pitfall in diagnosis is not including CES in the back pain differential.”
True CES presents as a triad of symptoms: lower extremity weakness, altered sensation in the skin of the buttocks and upper posterior thighs (saddle anesthesia), and dysfunction or paralysis of the bowel and bladder. However, few patients present with all of the classic symptoms,6 and patients with CES are often dismissed by several clinicians in their search for relief before presenting to a subspecialist. Kostuik et al7 consider “unilateral sciatica with motor and sensory disturbance” a more common presentation of CES; also indicative of this condition, they report, is “urinary dysfunction combined with motor and sensory loss in the presence of a disc lesion.”
The polypeptide relaxin, which is secreted by the corpus luteum to promote joint laxity in late pregnancy, has been associated with low back pain and pelvic pain of pregnancy; it has also been suggested as a possible contributing cause of CES during pregnancy.8,9 Additionally, increased lumbar lordosis with positional and postural stress may cause direct pressure by the gravid uterus on nerve roots. The great vessels may also be compressed by the uterus, resulting in ischemia of the neural element and back pain that radiates to the legs.10 Many cases of lumbar disk prolapse occur during the first and second trimesters. The most clinically incapacitated patients have been found to have the highest levels of relaxin.9
The Diagnosis
Early diagnosis of CES, through proper physical examination and radiologic studies, is paramount. A rectal examination should be performed to assess for sphincter tone (which may be diminished in 80% of patients) and to assess for perineal sensation.5 Catheterization yielding a postvoid residual urine greater than 100/200 cc is reported to have a specificity and sensitivity of 90% or greater for CES. Small et al5 recommend a straight leg raise maneuver to assess for radiculopathy.
Various studies in the literature support the use of MRI in the gravid patient to confirm the diagnosis of CES and to identify the degree and level of disk protrusion.2-4,11
Treatment
CES requires urgent surgical decompression.11 Early recognition of CES attributable to lumbar disk prolapse, report O’Laoire et al,12 is essential to prevent irreversible sphincter paralysis. They liken the condition’s urgency to that of extradural hematoma in a head injury.
Disk surgery during pregnancy—preferably a team effort, with obstetrics performing perioperative fetal monitoring—has been deemed a safe management method.2,4 Spinal or general anesthesia during nonobstetric surgery is generally considered safe for both mother and fetus.13,14 Adequate oxygenation without risk for hyperventilation is considered essential.15
PATIENT OUTCOME
In the immediate postoperative period, the patient continued to complain of RLE pain, which abated significantly by the time she was discharged. When she was seen in follow-up four days later, she was able to heel- and toe-walk on the right side, and her strength had improved to 3 or 4 out of 5 at the RLE. She continued to experience diminished sensation to the plantar aspect of the right foot, which persisted at the one-month follow up. At that visit, the patient also reported occasional pain in the right buttock. Physical therapy was started to strengthen the RLE.
By three months postsurgery, the patient had undergone uneventful vaginal delivery. She had an entirely benign exam with 5 out of 5 strength at the RLE and no neurologic deficits. She was cleared to return to light weightlifting with good technique and lumbar support but was told to refrain from running until the sixth month postsurgery.
CONCLUSION
Although the case patient did not have a “true” (ie, typical) presentation of CES, her symptoms warranted a full workup and treatment to prevent possible long-term sequelae. Medical practitioners should be familiar with the triad presentation of CES. They must differentiate lower back pain of muscular origin from lumbar disk herniation and be able to appreciate the degree of symptom severity reported by the gravid patient. A thorough history and physical assessment must be performed in every such case. When in doubt, the clinician must err on the side of caution, referring the patient for MRI and consulting with a specialist.
REFERENCES
1. Johnston RA. The management of acute spinal cord compression. J Neurol Neurosurg Psychiatr. 1993;56(10):1046-1054.
2. Brown MD, Levi AD. Surgery for lumbar disc herniation during pregnancy. Spine (Phila PA 1976). 2001;26(5):440-443.
3. LaBan MM, Perrin JCS, Latimer FR. Pregnancy and the herniated lumbar disc. Arch Phys Med Rehabil. 1983;64(7):319-321.
4. LaBan MM, Rapp NS, Van Oeyen P, Meerschaert JR. The lumbar herniated disk of pregnancy: a report of six cases identified by magnetic resonance imaging. Arch Phys Med Rehabil. 1995;76(5):476-479.
5. Small SA, Perron AD, Brady WJ. Orthopedic pitfalls: cauda equina syndrome. Am J Emerg Med. 2005;23(2):159-163.
6. Tay EC, Chacha PB. Midline prolapse of a lumbar intervertebral disc with compression of the cauda equina. J Bone Joint Surg. 1979;61(1):43-46.
7. Kostuik JP, Harrington I, Alexander D, et al. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am. 1986;68(3):386-391.
8. Russell R, Reynolds F. Back pain, pregnancy, and childbirth. BMJ. 1997;314(7087):1062-1063.
9. MacLennan AH, Nicholson R, Green RC, Bath M. Serum relaxin and pelvic pain of pregnancy. Lancet. 1986;2(8501):243-245.
10. Ashkan K, Casey AT, Powell M, Crockard HA. Back pain during pregnancy and after childbirth: an unusual cause not to miss. J R Soc Med. 1998;91(2):88-90.
11. Busse JW, Bhandari M, Schnittker JB, et al. Delayed presentation of cauda equina syndrome secondary to lumbar disc herniation: functional outcomes and health-related quality of life. CJEM. 2001;3(4):285-291.
12. O’Laoire SA, Crockard HA, Thomas DG. Prognosis for sphincter recovery after operation for cauda equina compression owing to lumbar disc prolapse. Br Med J (Clin Res Ed). 1981;282(6279):1852-1854.
13. Kuczkowski KM. The safety of anaesthetics in pregnant women. Expert Opin Drug Saf. 2006; 5(2):251-264.
14. Kuczkowski KM. Nonobstetric surgery during pregnancy: what are the risks of anesthesia? Obstet Gynecol Surv. 2004;59(1):52-56.
15. Birnbach DJ, Browne IM. Anesthesia for obstetrics. In: Miller RD, Eriksson LI, Fleisher LA, et al. Miller’s Anesthesia. Philadelphia, PA: Churchill Livingston, Elsevier Health Science; 2010: 2203-2240.
A 33-year-old woman in her 32nd week of pregnancy (gravida 3, para 2) presented to the emergency department (ED) with a five-day history of weakness and ascending numbness below the right knee. She related a two-week history of right-sided low back pain that radiated to the right buttock and was associated with severe right lower extremity (RLE) pain, most prominent in the posterolateral aspect of the right calf. She denied perianal numbness, incontinence, or other changes in bowel or bladder function. She also denied left lower extremity involvement or trauma.
The patient had had one uneventful pregnancy to date. Her medical history included hypothyroidism, treated with levothyroxine; and anxiety, for which she was taking sertraline. She denied any history of allergies, alcohol consumption, smoking, or illicit drug use. She had been evaluated twice and received reassurance in the two weeks before her presentation to the ED. She was admitted to the obstetric service secondary to pain, and a stat MRI rather than x-ray was ordered by obstetrics. An orthopedic consult was ordered. A spine surgeon happened to be on call.
Examination revealed that the patient walked plantigrade, with her right foot slightly externally rotated. She was unable to dorsiflex or plantarflex her right foot. She was unable to heel- or toe-walk on the right side, possessed 0 out of 5 strength at the right extensor hallucis longus and 2 to 3 out of 5 at the right tibialis anterior and gastroc soleus complex. She complained of pain with right leg elevation exceeding 30° and had very limited sensation to light touch in the right L5 and S1 dermatomes. Deep tendon reflex was absent at the right ankle. The patient refused a rectal exam or post-void evaluation.
The initial diagnosis considered by the ED clinician was sciatica, with a differential diagnosis that included pelvic pain of pregnancy, lumbar sprain strain, sciatica, lumbar disk, herniated nucleus pulposus with radiculopathy, and cauda equina syndrome. Trauma was considered and ruled out, as were malignancies; inflammatory, infectious, or degenerative conditions; or other compressive processes.1
Lumbar MRI demonstrated a very large, right-sided disk herniation at L5-S1 with an extruded fragment that was severely compressing the thecal sac and the right S1 nerve root, causing severe right foraminal stenosis at the level of L5-S1. Degenerative changes were noted at L4-5 with disk dessication and no lesions seen.
The patient was diagnosed with cauda equina syndrome, which was felt to be causing severe RLE weakness and ascending numbness. The options of observation, analgesia, physical therapy, and epidural injections were discussed with the patient; however, surgery was strongly recommended due to her profound weakness and the severity of pain she was experiencing, in addition to the size of the disk herniation. She opted for surgery.
The patient was given epidural anesthesia at the L3-4 level, with a catheter left in place during the procedure. A test dose of lidocaine (1.5 cc) with epinephrine was injected to ensure proper placement, and bupivacaine 0.5% was given in increments of 5.0 cc three times during the case. Propofol was administered for sedation, and a 2.0-mg dose of a long-acting morphine was given to the patient before removal of the epidural catheter. Fetal monitoring was performed by obstetrics throughout the procedure.
A laminotomy, partial facetectomy, and diskectomy were performed at L5-S1 with excision of a free fragment. Surgical pathology described the disk as fibrocartilaginous tissue measuring 3.5 cm x 1.4 cm x 0.6 cm.
DISCUSSION
Although nearly half of pregnant women experience low back pain, cauda equina syndrome (CES), a complication of lumbar disk herniation, is extremely rare in the gravid patient.2 In a decade-long review of 48,760 consecutive deliveries, LaBan et al3 identified symptomatic lumbar herniated nucleus pulposus in only five patients (approximately one in 10,000 pregnancies). In pregnant women who do experience CES, symptoms most commonly develop between the fifth and seventh month of pregnancy.4 According to Small et al,5 “The major pitfall in diagnosis is not including CES in the back pain differential.”
True CES presents as a triad of symptoms: lower extremity weakness, altered sensation in the skin of the buttocks and upper posterior thighs (saddle anesthesia), and dysfunction or paralysis of the bowel and bladder. However, few patients present with all of the classic symptoms,6 and patients with CES are often dismissed by several clinicians in their search for relief before presenting to a subspecialist. Kostuik et al7 consider “unilateral sciatica with motor and sensory disturbance” a more common presentation of CES; also indicative of this condition, they report, is “urinary dysfunction combined with motor and sensory loss in the presence of a disc lesion.”
The polypeptide relaxin, which is secreted by the corpus luteum to promote joint laxity in late pregnancy, has been associated with low back pain and pelvic pain of pregnancy; it has also been suggested as a possible contributing cause of CES during pregnancy.8,9 Additionally, increased lumbar lordosis with positional and postural stress may cause direct pressure by the gravid uterus on nerve roots. The great vessels may also be compressed by the uterus, resulting in ischemia of the neural element and back pain that radiates to the legs.10 Many cases of lumbar disk prolapse occur during the first and second trimesters. The most clinically incapacitated patients have been found to have the highest levels of relaxin.9
The Diagnosis
Early diagnosis of CES, through proper physical examination and radiologic studies, is paramount. A rectal examination should be performed to assess for sphincter tone (which may be diminished in 80% of patients) and to assess for perineal sensation.5 Catheterization yielding a postvoid residual urine greater than 100/200 cc is reported to have a specificity and sensitivity of 90% or greater for CES. Small et al5 recommend a straight leg raise maneuver to assess for radiculopathy.
Various studies in the literature support the use of MRI in the gravid patient to confirm the diagnosis of CES and to identify the degree and level of disk protrusion.2-4,11
Treatment
CES requires urgent surgical decompression.11 Early recognition of CES attributable to lumbar disk prolapse, report O’Laoire et al,12 is essential to prevent irreversible sphincter paralysis. They liken the condition’s urgency to that of extradural hematoma in a head injury.
Disk surgery during pregnancy—preferably a team effort, with obstetrics performing perioperative fetal monitoring—has been deemed a safe management method.2,4 Spinal or general anesthesia during nonobstetric surgery is generally considered safe for both mother and fetus.13,14 Adequate oxygenation without risk for hyperventilation is considered essential.15
PATIENT OUTCOME
In the immediate postoperative period, the patient continued to complain of RLE pain, which abated significantly by the time she was discharged. When she was seen in follow-up four days later, she was able to heel- and toe-walk on the right side, and her strength had improved to 3 or 4 out of 5 at the RLE. She continued to experience diminished sensation to the plantar aspect of the right foot, which persisted at the one-month follow up. At that visit, the patient also reported occasional pain in the right buttock. Physical therapy was started to strengthen the RLE.
By three months postsurgery, the patient had undergone uneventful vaginal delivery. She had an entirely benign exam with 5 out of 5 strength at the RLE and no neurologic deficits. She was cleared to return to light weightlifting with good technique and lumbar support but was told to refrain from running until the sixth month postsurgery.
CONCLUSION
Although the case patient did not have a “true” (ie, typical) presentation of CES, her symptoms warranted a full workup and treatment to prevent possible long-term sequelae. Medical practitioners should be familiar with the triad presentation of CES. They must differentiate lower back pain of muscular origin from lumbar disk herniation and be able to appreciate the degree of symptom severity reported by the gravid patient. A thorough history and physical assessment must be performed in every such case. When in doubt, the clinician must err on the side of caution, referring the patient for MRI and consulting with a specialist.
REFERENCES
1. Johnston RA. The management of acute spinal cord compression. J Neurol Neurosurg Psychiatr. 1993;56(10):1046-1054.
2. Brown MD, Levi AD. Surgery for lumbar disc herniation during pregnancy. Spine (Phila PA 1976). 2001;26(5):440-443.
3. LaBan MM, Perrin JCS, Latimer FR. Pregnancy and the herniated lumbar disc. Arch Phys Med Rehabil. 1983;64(7):319-321.
4. LaBan MM, Rapp NS, Van Oeyen P, Meerschaert JR. The lumbar herniated disk of pregnancy: a report of six cases identified by magnetic resonance imaging. Arch Phys Med Rehabil. 1995;76(5):476-479.
5. Small SA, Perron AD, Brady WJ. Orthopedic pitfalls: cauda equina syndrome. Am J Emerg Med. 2005;23(2):159-163.
6. Tay EC, Chacha PB. Midline prolapse of a lumbar intervertebral disc with compression of the cauda equina. J Bone Joint Surg. 1979;61(1):43-46.
7. Kostuik JP, Harrington I, Alexander D, et al. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am. 1986;68(3):386-391.
8. Russell R, Reynolds F. Back pain, pregnancy, and childbirth. BMJ. 1997;314(7087):1062-1063.
9. MacLennan AH, Nicholson R, Green RC, Bath M. Serum relaxin and pelvic pain of pregnancy. Lancet. 1986;2(8501):243-245.
10. Ashkan K, Casey AT, Powell M, Crockard HA. Back pain during pregnancy and after childbirth: an unusual cause not to miss. J R Soc Med. 1998;91(2):88-90.
11. Busse JW, Bhandari M, Schnittker JB, et al. Delayed presentation of cauda equina syndrome secondary to lumbar disc herniation: functional outcomes and health-related quality of life. CJEM. 2001;3(4):285-291.
12. O’Laoire SA, Crockard HA, Thomas DG. Prognosis for sphincter recovery after operation for cauda equina compression owing to lumbar disc prolapse. Br Med J (Clin Res Ed). 1981;282(6279):1852-1854.
13. Kuczkowski KM. The safety of anaesthetics in pregnant women. Expert Opin Drug Saf. 2006; 5(2):251-264.
14. Kuczkowski KM. Nonobstetric surgery during pregnancy: what are the risks of anesthesia? Obstet Gynecol Surv. 2004;59(1):52-56.
15. Birnbach DJ, Browne IM. Anesthesia for obstetrics. In: Miller RD, Eriksson LI, Fleisher LA, et al. Miller’s Anesthesia. Philadelphia, PA: Churchill Livingston, Elsevier Health Science; 2010: 2203-2240.
A 33-year-old woman in her 32nd week of pregnancy (gravida 3, para 2) presented to the emergency department (ED) with a five-day history of weakness and ascending numbness below the right knee. She related a two-week history of right-sided low back pain that radiated to the right buttock and was associated with severe right lower extremity (RLE) pain, most prominent in the posterolateral aspect of the right calf. She denied perianal numbness, incontinence, or other changes in bowel or bladder function. She also denied left lower extremity involvement or trauma.
The patient had had one uneventful pregnancy to date. Her medical history included hypothyroidism, treated with levothyroxine; and anxiety, for which she was taking sertraline. She denied any history of allergies, alcohol consumption, smoking, or illicit drug use. She had been evaluated twice and received reassurance in the two weeks before her presentation to the ED. She was admitted to the obstetric service secondary to pain, and a stat MRI rather than x-ray was ordered by obstetrics. An orthopedic consult was ordered. A spine surgeon happened to be on call.
Examination revealed that the patient walked plantigrade, with her right foot slightly externally rotated. She was unable to dorsiflex or plantarflex her right foot. She was unable to heel- or toe-walk on the right side, possessed 0 out of 5 strength at the right extensor hallucis longus and 2 to 3 out of 5 at the right tibialis anterior and gastroc soleus complex. She complained of pain with right leg elevation exceeding 30° and had very limited sensation to light touch in the right L5 and S1 dermatomes. Deep tendon reflex was absent at the right ankle. The patient refused a rectal exam or post-void evaluation.
The initial diagnosis considered by the ED clinician was sciatica, with a differential diagnosis that included pelvic pain of pregnancy, lumbar sprain strain, sciatica, lumbar disk, herniated nucleus pulposus with radiculopathy, and cauda equina syndrome. Trauma was considered and ruled out, as were malignancies; inflammatory, infectious, or degenerative conditions; or other compressive processes.1
Lumbar MRI demonstrated a very large, right-sided disk herniation at L5-S1 with an extruded fragment that was severely compressing the thecal sac and the right S1 nerve root, causing severe right foraminal stenosis at the level of L5-S1. Degenerative changes were noted at L4-5 with disk dessication and no lesions seen.
The patient was diagnosed with cauda equina syndrome, which was felt to be causing severe RLE weakness and ascending numbness. The options of observation, analgesia, physical therapy, and epidural injections were discussed with the patient; however, surgery was strongly recommended due to her profound weakness and the severity of pain she was experiencing, in addition to the size of the disk herniation. She opted for surgery.
The patient was given epidural anesthesia at the L3-4 level, with a catheter left in place during the procedure. A test dose of lidocaine (1.5 cc) with epinephrine was injected to ensure proper placement, and bupivacaine 0.5% was given in increments of 5.0 cc three times during the case. Propofol was administered for sedation, and a 2.0-mg dose of a long-acting morphine was given to the patient before removal of the epidural catheter. Fetal monitoring was performed by obstetrics throughout the procedure.
A laminotomy, partial facetectomy, and diskectomy were performed at L5-S1 with excision of a free fragment. Surgical pathology described the disk as fibrocartilaginous tissue measuring 3.5 cm x 1.4 cm x 0.6 cm.
DISCUSSION
Although nearly half of pregnant women experience low back pain, cauda equina syndrome (CES), a complication of lumbar disk herniation, is extremely rare in the gravid patient.2 In a decade-long review of 48,760 consecutive deliveries, LaBan et al3 identified symptomatic lumbar herniated nucleus pulposus in only five patients (approximately one in 10,000 pregnancies). In pregnant women who do experience CES, symptoms most commonly develop between the fifth and seventh month of pregnancy.4 According to Small et al,5 “The major pitfall in diagnosis is not including CES in the back pain differential.”
True CES presents as a triad of symptoms: lower extremity weakness, altered sensation in the skin of the buttocks and upper posterior thighs (saddle anesthesia), and dysfunction or paralysis of the bowel and bladder. However, few patients present with all of the classic symptoms,6 and patients with CES are often dismissed by several clinicians in their search for relief before presenting to a subspecialist. Kostuik et al7 consider “unilateral sciatica with motor and sensory disturbance” a more common presentation of CES; also indicative of this condition, they report, is “urinary dysfunction combined with motor and sensory loss in the presence of a disc lesion.”
The polypeptide relaxin, which is secreted by the corpus luteum to promote joint laxity in late pregnancy, has been associated with low back pain and pelvic pain of pregnancy; it has also been suggested as a possible contributing cause of CES during pregnancy.8,9 Additionally, increased lumbar lordosis with positional and postural stress may cause direct pressure by the gravid uterus on nerve roots. The great vessels may also be compressed by the uterus, resulting in ischemia of the neural element and back pain that radiates to the legs.10 Many cases of lumbar disk prolapse occur during the first and second trimesters. The most clinically incapacitated patients have been found to have the highest levels of relaxin.9
The Diagnosis
Early diagnosis of CES, through proper physical examination and radiologic studies, is paramount. A rectal examination should be performed to assess for sphincter tone (which may be diminished in 80% of patients) and to assess for perineal sensation.5 Catheterization yielding a postvoid residual urine greater than 100/200 cc is reported to have a specificity and sensitivity of 90% or greater for CES. Small et al5 recommend a straight leg raise maneuver to assess for radiculopathy.
Various studies in the literature support the use of MRI in the gravid patient to confirm the diagnosis of CES and to identify the degree and level of disk protrusion.2-4,11
Treatment
CES requires urgent surgical decompression.11 Early recognition of CES attributable to lumbar disk prolapse, report O’Laoire et al,12 is essential to prevent irreversible sphincter paralysis. They liken the condition’s urgency to that of extradural hematoma in a head injury.
Disk surgery during pregnancy—preferably a team effort, with obstetrics performing perioperative fetal monitoring—has been deemed a safe management method.2,4 Spinal or general anesthesia during nonobstetric surgery is generally considered safe for both mother and fetus.13,14 Adequate oxygenation without risk for hyperventilation is considered essential.15
PATIENT OUTCOME
In the immediate postoperative period, the patient continued to complain of RLE pain, which abated significantly by the time she was discharged. When she was seen in follow-up four days later, she was able to heel- and toe-walk on the right side, and her strength had improved to 3 or 4 out of 5 at the RLE. She continued to experience diminished sensation to the plantar aspect of the right foot, which persisted at the one-month follow up. At that visit, the patient also reported occasional pain in the right buttock. Physical therapy was started to strengthen the RLE.
By three months postsurgery, the patient had undergone uneventful vaginal delivery. She had an entirely benign exam with 5 out of 5 strength at the RLE and no neurologic deficits. She was cleared to return to light weightlifting with good technique and lumbar support but was told to refrain from running until the sixth month postsurgery.
CONCLUSION
Although the case patient did not have a “true” (ie, typical) presentation of CES, her symptoms warranted a full workup and treatment to prevent possible long-term sequelae. Medical practitioners should be familiar with the triad presentation of CES. They must differentiate lower back pain of muscular origin from lumbar disk herniation and be able to appreciate the degree of symptom severity reported by the gravid patient. A thorough history and physical assessment must be performed in every such case. When in doubt, the clinician must err on the side of caution, referring the patient for MRI and consulting with a specialist.
REFERENCES
1. Johnston RA. The management of acute spinal cord compression. J Neurol Neurosurg Psychiatr. 1993;56(10):1046-1054.
2. Brown MD, Levi AD. Surgery for lumbar disc herniation during pregnancy. Spine (Phila PA 1976). 2001;26(5):440-443.
3. LaBan MM, Perrin JCS, Latimer FR. Pregnancy and the herniated lumbar disc. Arch Phys Med Rehabil. 1983;64(7):319-321.
4. LaBan MM, Rapp NS, Van Oeyen P, Meerschaert JR. The lumbar herniated disk of pregnancy: a report of six cases identified by magnetic resonance imaging. Arch Phys Med Rehabil. 1995;76(5):476-479.
5. Small SA, Perron AD, Brady WJ. Orthopedic pitfalls: cauda equina syndrome. Am J Emerg Med. 2005;23(2):159-163.
6. Tay EC, Chacha PB. Midline prolapse of a lumbar intervertebral disc with compression of the cauda equina. J Bone Joint Surg. 1979;61(1):43-46.
7. Kostuik JP, Harrington I, Alexander D, et al. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am. 1986;68(3):386-391.
8. Russell R, Reynolds F. Back pain, pregnancy, and childbirth. BMJ. 1997;314(7087):1062-1063.
9. MacLennan AH, Nicholson R, Green RC, Bath M. Serum relaxin and pelvic pain of pregnancy. Lancet. 1986;2(8501):243-245.
10. Ashkan K, Casey AT, Powell M, Crockard HA. Back pain during pregnancy and after childbirth: an unusual cause not to miss. J R Soc Med. 1998;91(2):88-90.
11. Busse JW, Bhandari M, Schnittker JB, et al. Delayed presentation of cauda equina syndrome secondary to lumbar disc herniation: functional outcomes and health-related quality of life. CJEM. 2001;3(4):285-291.
12. O’Laoire SA, Crockard HA, Thomas DG. Prognosis for sphincter recovery after operation for cauda equina compression owing to lumbar disc prolapse. Br Med J (Clin Res Ed). 1981;282(6279):1852-1854.
13. Kuczkowski KM. The safety of anaesthetics in pregnant women. Expert Opin Drug Saf. 2006; 5(2):251-264.
14. Kuczkowski KM. Nonobstetric surgery during pregnancy: what are the risks of anesthesia? Obstet Gynecol Surv. 2004;59(1):52-56.
15. Birnbach DJ, Browne IM. Anesthesia for obstetrics. In: Miller RD, Eriksson LI, Fleisher LA, et al. Miller’s Anesthesia. Philadelphia, PA: Churchill Livingston, Elsevier Health Science; 2010: 2203-2240.
Cover
Diffuse Muscle Weakness:
The Toxicologist's Approach
Postoperative Infections of the Spine
UPDATE ON URINARY INCONTINENCE
- Update on urinary incontinence: Occult incontinence in women who have pelvic organ prolapse
Maria Fidela Paraiso, MD; Elena Tunitsky-Bitton, MD (December 2010)
Urinary incontinence affects as many as 50% of adult women1; 16% have bothersome symptoms2 and as many as 10% undergo surgical correction of their condition.3 The prevalence of urinary incontinence increases with age; with the aging US population expected to more than double by 2050,4 more and more women will seek treatment.
This notion of a growing population of women who want treatment is supported by a recent article that evaluated trends in surgery for urinary incontinence between 1998 and 2007: The researchers found that the number of inpatient urinary incontinence surgeries nearly tripled over 1 decade.5
Therapeutic revolution
Introduction of the retropubic mid-urethral sling in 19966 transformed the surgical management of stress incontinence; the procedure has become the gold standard. Subsequent iterations of the sling procedure include a transobturator approach7 (known as the “TOT” sling) and, more recently, single-incision slings—alternatives intended primarily to improve the safety profile and ease of the procedure while maintaining its efficacy.
The newer sling procedures—many including novel mesh materials, some delivered in kit form—came to market under the US Food and Drug Administration’s so-called 510(k) rule, however, allowing manufacturers to launch them with little or no data supporting safety and efficacy. Given those circumstances, the optimal surgical management of stress urinary incontinence (SUI) remains controversial, and surgeons must take into account individual patient characteristics and treatment goals when developing a plan for surgical management. Providers must also remember that not all women will opt for, or are good candidates for, surgical intervention. These women need alternatives to operative management.
In this Update, we review and comment on four published papers that 1) highlight recent developments in the treatment of SUI and 2) provide concrete guidance to clinicians for providing optimal management:
- A randomized trial of nonsurgical management of stress incontinence using a continence pessary, compared with behavioral therapy and with combined (pessary plus behavioral therapy) treatment (the ATLAS trial)
- A randomized clinical trial that compared the efficacy of retropubic slings and TOT slings, with 1-year follow-up (the TOMUS trial)
- A randomized clinical trial that compared the efficacy of retropubic slings and TOT slings in women who have intrinsic sphincter deficiency
- A meta-analysis of the safety and efficacy of single-incision slings.
Conservative therapy is still an important, effective option for SUI
Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115(3):609–617.
Conservative treatment options for SUI are limited. They include:
- a pessary
- behavioral/pelvic floor physical therapy
- duloxetine (Cymbalta), a serotonin and norepinephrine reuptake inhibitor antidepressant (as an off-label use).
Level-I evidence exists to support utilization of behavioral pelvic floor therapy, based on a Cochrane review.8 Yet, little evidence exists by which we can compare the efficacy of various incontinence pessaries and their efficacy when combined with behavioral therapy.
Study design. This multi-center, randomized trial was conducted to fill this gap in the evidence. Four hundred forty-six women who had SUI were randomized to three groups: pessary only (149); behavioral therapy only (146); and pessary plus behavioral therapy (151). Women 18 years and older who had either SUI alone or stress-predominant incontinence were eligible. At baseline, 20.7% of subjects had undergone nonsurgical incontinence treatment; 6.9% had had surgical management. There was no significant difference in regard to prior treatment among the study groups.
Behavioral therapy comprised four visits at 2-week intervals, conducted by a nurse or a physical therapist who had undergone standardized training. Visits focused on engaging pelvic floor muscles; subjects received a “prescription” for home practice.
Women in the pessary groups were fitted at as many as three clinic visits with an incontinence ring or dish.
Measures of primary outcomes included the Patient Global Impression of Improvement (PGI-I) and the stress incontinence subset of the Pelvic Floor Distress Inventory (PFDI) at 3 months (follow-up continued to 12 months).
Findings. At 3 months, 40% of subjects in the pessary-only group, 49% in the behavioral therapy-only group, and 53% in the combined group reported (on the PGI-I) that their symptoms were “much” or “very much” better. Furthermore, 33% in the pessary-only group, 49% in the behavioral therapy-only group, and 44% in the combined group reported (on the PFDI) no bothersome stress incontinence.
Only PFDI measures were significantly different between pessary and behavioral therapy groups. Both PFDI and PGI-I demonstrated a significant difference in combined therapy compared to a pessary, but not in combined therapy compared to behavioral therapy. Because combination therapy was not superior to both single-therapies, the researchers concluded that combination therapy was not superior to single therapy.
By 12 months, efficacy declined in all groups: 32% of all women reported they were “much” or “very much” better, and 36% denied symptoms of stress incontinence. There was no difference in efficacy across the three groups by the end of the follow-up period.
The modest success rate of the conservative measures for treating SUI that were studied here, and the decline in their efficacy over time, might be discouraging at first glance. But more than one third of patients experienced benefit in the end—in the face of low risk. Consider a pessary or behavioral therapy to be a workable, low-risk option for your patients who have SUI, therefore. Combining those two measures does not, however, provide superior results.
TOT, retropubic slings equally effective for SUI—but complications differ
Richter H, Albo M, Zyczynski H, et al; Urinary Incontinence Treatment Network. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362(22):2066–2076.
This large, randomized, prospective multi-center study from the well-respected Pelvic Floor Disorders Network demonstrated that the efficacy of retropubic and TOT slings is equivalent. At the same time, the trial highlighted important differences in the complication profiles of these two surgical approaches. Given the high success rate of retropubic slings, the study was designed as an equivalence trial, with the principal aim of demonstrating whether both approaches share a similar success rate.
Study design. Investigators recruited women who had been given a diagnosis of SUI and were planning to undergo surgical correction, randomizing 597 who had predominant stress loss symptoms and a positive stress test (urodynamics were not required); 565 completed the 12-month follow-up.
Findings. Objective and subjective cure rates were similar in both groups at 12 months. (“Objective cure” was defined as a negative stress test, negative pad test, and no re-treatment within the follow-up period; “subjective cure” was defined as no re-treatment, no episodes of leakage on a voiding diary, and no self-report of stress loss.)
At 12 months, the objective cure rate was 81% for the retropubic sling and 78% for the TOT sling (the difference of three percentage points had a 95% confidence interval [CI] of –3.6–9.6). Despite very close findings, the subjective cure rate was lower in the TOT group (56%) than in the retropubic group (62%) (the difference of just over six percentage points had a 95% CI of –1.6–14.3) and did not meet criteria for equivalence.
There was no difference between the two groups in the incidence of urge incontinence; patient satisfaction; and quality-of-life outcomes.
But divergence was seen in complications. A higher incidence of voiding dysfunction that required re-operation was seen in the retropubic group (2.7%) than in the TOT group (0%) (P = .004). The retropubic sling group also exhibited a higher incidence of mesh exposure and bladder perforation. The TOT group had a higher incidence of neurologic sequelae (numbness, weakness) than the retropubic group (9.4% and 0.04%, respectively) (P = .01).
This well-designed trial confirmed the current standard of practice and supports the findings of a recent Cochrane review that reported a success rate of 88% for the retropubic approach and 84% for the TOT approach.9 The trial also demonstrated that you can anticipate similar success rates with retropubic and TOT approaches to placing a mid-urethral sling.
Note: The design of this study did not call for urodynamic evaluation, but more than 85% of subjects did undergo such testing, including measurement of the Valsalva leak-point pressure (VLPP) and the maximum urethral-closure pressure (MUCP). The investigators’ linear regression analysis revealed no change in outcomes between the two approaches when adjusting for VLPP and MUCP. This supportive finding suggests that a TOT sling would be just as beneficial as a retropubic sling in women who have ISD—although other recent studies that specifically addressed this matter came to a different conclusion.
Intrinsic sphincter deficiency might be a risk factor for failure of a TOT sling
Schierlitz L, Dwyer P, Rosamilla A, et al. Effectiveness of tension-free vaginal tape compared with TOT tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol. 2008;112(6):1253–1261.
In the trial by Richter and colleagues that we reviewed above, the investigators found that ISD—defined as low VLPP or low MUCP—did not have an impact on outcomes after placement of retropubic and TOT slings. Yet, other recent studies have concluded differently: In this trial from Australia, researchers concluded that a retropubic sling was more effective than a TOT sling in women who had ISD.
Study design. This randomized, prospective study of 164 women who had SUI and ISD (defined as MUCP <20 cm H2O or VLPP <60 cm H2O) randomized subjects to placement of a retropubic sling or a TOT sling. The primary outcome was the presence or absence of urodynamically documented stress incontinence at 6 months. Secondary outcomes included complications, self-reported SUI, and findings on a quality-of-life questionnaire.
Findings. At 6 months, 138 patients completed an evaluation, including repeat urodynamic study. The success rate in the retropubic group was 79%, compared with only 55% in the TOT group (P = .004). Nine women in the TOT group underwent repeat surgery; none did in the retropubic group. There was no difference between groups in de novo overactive bladder symptoms; overactive bladder symptoms resolved at a nearly equivalent rate: 40% in the TOT group and 36% in the retropubic group. No difference was seen in the rate of intraoperative or postoperative complications, although the rate of bladder perforation was higher in the retropubic group, leaning toward significance (P = .06).
Women who have ISD are better served by having a retropubic sling, not a TOT sling, placed.
Single-incision slings demonstrate lower efficacy than traditional slings
Adbel-Fattah M, Ford JA, Lim CP, Madhuvrata P. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: a meta-analysis of effectiveness and complications. Eur Urol. 2011;60(3):468–480.
The single-incision sling was introduced in 2006 to, ostensibly, simplify surgery and reduce the risk of complications. Yet, essentially, no data on the efficacy or safety of single-incision kits existed when they entered the market!
Study design. This meta-analysis of single-incision slings analyzed the surgical literature from 1996 through early 2011. Investigators found nine studies that met criteria for objective and subjective outcomes in randomized or quasi-randomized clinical trials. They performed the analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
A total of 758 women who participated in nine randomized clinical trials were included for analysis. Seven studies reported on the subjective cure rate; six reported on the objective cure rate.
Findings. The analysis showed that single-incision slings are associated with lower subjective and objective cure rates than traditional slings (for single-incision slings, the risk ratio [RR] was 0.83 [95% CI, 0.70–0.99]; for traditional slings, RR was 0.85 [95% CI, 0.74–0.97]). In addition, re-operation rates were significantly higher in the single-incision sling group (RR, 6.72 [95% CI, 2.4–18.9]).
The single-incision sling was associated with a shorter operating time and less postoperative pain, but had a higher rate of mesh exposure (RR, 3.86 [95% CI, 1.45–10.3]).
This is important information about the relative effectiveness of the single-incision sling compared to more traditional retropubic and TOT approaches. If you are going to offer a single-incision sling, you must 1) select patients carefully and 2) counsel appropriate candidates on two key points: data on the success of single-incision slings are limited and an inferior (that is, inferior to traditional techniques) result is possible.
From stem-cell research. This expanding component of a number of medical specialties includes urologic applications. Animal-based studies have been supportive here,1-3 and two studies have translated the use of stem cells for correcting SUI to humans.4,5
Taken together, the human studies treated 20 women with autologous muscle-derived stem cells or muscle progenitor cells that were injected periurethrally or intrasphincterically. Seventeen subjects completed follow-up; improvement was demonstrated in all but two of them.4,5
The promise of stem-cell applications for treating SUI is exciting. We need additional investigation into methods and safety, however—making widespread application in humans not yet suitable. Still, the field is rapidly expanding and this remains a hopeful treatment option for the future.
For repairing vaginal prolapse. Unpublished findings from the Outcomes Following Vaginal Prolapse Repair and Mid Urethral Sling (OPUS) trial—the “vaginal counterpart,” one could say, to the notable CARE trial of cholesterol level management—were presented at the annual scientific meeting of the American Urogynecologic Society (AUGS) in September. This landmark study demonstrated that a prophylactic midurethral sling placed at the time of vaginal prolapse repair results in superior continence at 3 and 12 months in women who did not have preoperative symptoms of incontinence. Publication of this study—it has been submitted to a leading medical journal—will have a significant impact on the counseling that providers offer to asymptomatic patients who are undergoing vaginal reconstructive surgery about having a prophylactic sling placed.
REFERENCES
1. Wu G, Song Y, Zheng X, Jiang Z. Adipose-derived stromal cell transplantation for treatment of stress urinary incontinence. Tissue Cell. 2011;43(4):246–253.
2. Kim SO, Na HS, Kwon D, Joo SY, Kim HS, Ahn Y. Bone-marrow-derived mesenchymal stem cell transplantation enhances closing pressure and leak point pressure in a female urinary incontinence rat model. Urol Int. 2011;86(1):110–116.
3. Corcos J, Loutochin O, Campeau L, et al. Bone marrow mesenchymal stromal cell therapy for external urethral sphincter restoration in a rat model of stress urinary incontinence. Neurourol Urodyn. 2011;30(3):447–455.
4. Carr LK, Steele D, Steele S, et al. 1-year follow-up of autologous muscle-derived stem cell injection pilot study to treat stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):881–883.
5. Sebe P, Doucet C, Cornu JN, et al. Intrasphincteric injections of autologous muscular cells in women with refractory stress urinary incontinence: a prospective study. Int Urogynecol J. 2011;22(2):183–189.
We want to hear from you! Tell us what you think.
1. Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165(5):537-542.
2. Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311-1316.
3. Thom DH, Nygaard IE, Calhoun EA. Urologic diseases in America project: urinary incontinence in women-national trends in hospitalizations office visits, treatment and economic impact. J Urol. 2005;173(4):1295-1301.
4. Vincent GK, Velkoff VA. The Next Four Decades. The older population in the United States: 2010 to 2050. Current Populations Reports. Washington DC: US Census Bureau; May 2010. http://www.census.gov/prod/2010pubs/p25-1138.pdf. Accessed October 26, 2011.
5. Wu JM, Gandhi MP, Shah AD, Shah JY, Fulton RG, Weidner AC. Trends in inpatient urinary incontinence surgery in the USA 1998-2007. Int Urogynecol J. 2011;22(11):1437-1443.
6. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7(2):81-86.
7. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women[in French]. Prog Urol. 2001;11(6):1306-1313.
8. Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment for urinary incontinence in women. A Cochrane systematic review. Eur J Phys Rehabil Med. 2008;44(1):47-63.
9. Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2009:CD006375.
- Update on urinary incontinence: Occult incontinence in women who have pelvic organ prolapse
Maria Fidela Paraiso, MD; Elena Tunitsky-Bitton, MD (December 2010)
Urinary incontinence affects as many as 50% of adult women1; 16% have bothersome symptoms2 and as many as 10% undergo surgical correction of their condition.3 The prevalence of urinary incontinence increases with age; with the aging US population expected to more than double by 2050,4 more and more women will seek treatment.
This notion of a growing population of women who want treatment is supported by a recent article that evaluated trends in surgery for urinary incontinence between 1998 and 2007: The researchers found that the number of inpatient urinary incontinence surgeries nearly tripled over 1 decade.5
Therapeutic revolution
Introduction of the retropubic mid-urethral sling in 19966 transformed the surgical management of stress incontinence; the procedure has become the gold standard. Subsequent iterations of the sling procedure include a transobturator approach7 (known as the “TOT” sling) and, more recently, single-incision slings—alternatives intended primarily to improve the safety profile and ease of the procedure while maintaining its efficacy.
The newer sling procedures—many including novel mesh materials, some delivered in kit form—came to market under the US Food and Drug Administration’s so-called 510(k) rule, however, allowing manufacturers to launch them with little or no data supporting safety and efficacy. Given those circumstances, the optimal surgical management of stress urinary incontinence (SUI) remains controversial, and surgeons must take into account individual patient characteristics and treatment goals when developing a plan for surgical management. Providers must also remember that not all women will opt for, or are good candidates for, surgical intervention. These women need alternatives to operative management.
In this Update, we review and comment on four published papers that 1) highlight recent developments in the treatment of SUI and 2) provide concrete guidance to clinicians for providing optimal management:
- A randomized trial of nonsurgical management of stress incontinence using a continence pessary, compared with behavioral therapy and with combined (pessary plus behavioral therapy) treatment (the ATLAS trial)
- A randomized clinical trial that compared the efficacy of retropubic slings and TOT slings, with 1-year follow-up (the TOMUS trial)
- A randomized clinical trial that compared the efficacy of retropubic slings and TOT slings in women who have intrinsic sphincter deficiency
- A meta-analysis of the safety and efficacy of single-incision slings.
Conservative therapy is still an important, effective option for SUI
Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115(3):609–617.
Conservative treatment options for SUI are limited. They include:
- a pessary
- behavioral/pelvic floor physical therapy
- duloxetine (Cymbalta), a serotonin and norepinephrine reuptake inhibitor antidepressant (as an off-label use).
Level-I evidence exists to support utilization of behavioral pelvic floor therapy, based on a Cochrane review.8 Yet, little evidence exists by which we can compare the efficacy of various incontinence pessaries and their efficacy when combined with behavioral therapy.
Study design. This multi-center, randomized trial was conducted to fill this gap in the evidence. Four hundred forty-six women who had SUI were randomized to three groups: pessary only (149); behavioral therapy only (146); and pessary plus behavioral therapy (151). Women 18 years and older who had either SUI alone or stress-predominant incontinence were eligible. At baseline, 20.7% of subjects had undergone nonsurgical incontinence treatment; 6.9% had had surgical management. There was no significant difference in regard to prior treatment among the study groups.
Behavioral therapy comprised four visits at 2-week intervals, conducted by a nurse or a physical therapist who had undergone standardized training. Visits focused on engaging pelvic floor muscles; subjects received a “prescription” for home practice.
Women in the pessary groups were fitted at as many as three clinic visits with an incontinence ring or dish.
Measures of primary outcomes included the Patient Global Impression of Improvement (PGI-I) and the stress incontinence subset of the Pelvic Floor Distress Inventory (PFDI) at 3 months (follow-up continued to 12 months).
Findings. At 3 months, 40% of subjects in the pessary-only group, 49% in the behavioral therapy-only group, and 53% in the combined group reported (on the PGI-I) that their symptoms were “much” or “very much” better. Furthermore, 33% in the pessary-only group, 49% in the behavioral therapy-only group, and 44% in the combined group reported (on the PFDI) no bothersome stress incontinence.
Only PFDI measures were significantly different between pessary and behavioral therapy groups. Both PFDI and PGI-I demonstrated a significant difference in combined therapy compared to a pessary, but not in combined therapy compared to behavioral therapy. Because combination therapy was not superior to both single-therapies, the researchers concluded that combination therapy was not superior to single therapy.
By 12 months, efficacy declined in all groups: 32% of all women reported they were “much” or “very much” better, and 36% denied symptoms of stress incontinence. There was no difference in efficacy across the three groups by the end of the follow-up period.
The modest success rate of the conservative measures for treating SUI that were studied here, and the decline in their efficacy over time, might be discouraging at first glance. But more than one third of patients experienced benefit in the end—in the face of low risk. Consider a pessary or behavioral therapy to be a workable, low-risk option for your patients who have SUI, therefore. Combining those two measures does not, however, provide superior results.
TOT, retropubic slings equally effective for SUI—but complications differ
Richter H, Albo M, Zyczynski H, et al; Urinary Incontinence Treatment Network. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362(22):2066–2076.
This large, randomized, prospective multi-center study from the well-respected Pelvic Floor Disorders Network demonstrated that the efficacy of retropubic and TOT slings is equivalent. At the same time, the trial highlighted important differences in the complication profiles of these two surgical approaches. Given the high success rate of retropubic slings, the study was designed as an equivalence trial, with the principal aim of demonstrating whether both approaches share a similar success rate.
Study design. Investigators recruited women who had been given a diagnosis of SUI and were planning to undergo surgical correction, randomizing 597 who had predominant stress loss symptoms and a positive stress test (urodynamics were not required); 565 completed the 12-month follow-up.
Findings. Objective and subjective cure rates were similar in both groups at 12 months. (“Objective cure” was defined as a negative stress test, negative pad test, and no re-treatment within the follow-up period; “subjective cure” was defined as no re-treatment, no episodes of leakage on a voiding diary, and no self-report of stress loss.)
At 12 months, the objective cure rate was 81% for the retropubic sling and 78% for the TOT sling (the difference of three percentage points had a 95% confidence interval [CI] of –3.6–9.6). Despite very close findings, the subjective cure rate was lower in the TOT group (56%) than in the retropubic group (62%) (the difference of just over six percentage points had a 95% CI of –1.6–14.3) and did not meet criteria for equivalence.
There was no difference between the two groups in the incidence of urge incontinence; patient satisfaction; and quality-of-life outcomes.
But divergence was seen in complications. A higher incidence of voiding dysfunction that required re-operation was seen in the retropubic group (2.7%) than in the TOT group (0%) (P = .004). The retropubic sling group also exhibited a higher incidence of mesh exposure and bladder perforation. The TOT group had a higher incidence of neurologic sequelae (numbness, weakness) than the retropubic group (9.4% and 0.04%, respectively) (P = .01).
This well-designed trial confirmed the current standard of practice and supports the findings of a recent Cochrane review that reported a success rate of 88% for the retropubic approach and 84% for the TOT approach.9 The trial also demonstrated that you can anticipate similar success rates with retropubic and TOT approaches to placing a mid-urethral sling.
Note: The design of this study did not call for urodynamic evaluation, but more than 85% of subjects did undergo such testing, including measurement of the Valsalva leak-point pressure (VLPP) and the maximum urethral-closure pressure (MUCP). The investigators’ linear regression analysis revealed no change in outcomes between the two approaches when adjusting for VLPP and MUCP. This supportive finding suggests that a TOT sling would be just as beneficial as a retropubic sling in women who have ISD—although other recent studies that specifically addressed this matter came to a different conclusion.
Intrinsic sphincter deficiency might be a risk factor for failure of a TOT sling
Schierlitz L, Dwyer P, Rosamilla A, et al. Effectiveness of tension-free vaginal tape compared with TOT tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol. 2008;112(6):1253–1261.
In the trial by Richter and colleagues that we reviewed above, the investigators found that ISD—defined as low VLPP or low MUCP—did not have an impact on outcomes after placement of retropubic and TOT slings. Yet, other recent studies have concluded differently: In this trial from Australia, researchers concluded that a retropubic sling was more effective than a TOT sling in women who had ISD.
Study design. This randomized, prospective study of 164 women who had SUI and ISD (defined as MUCP <20 cm H2O or VLPP <60 cm H2O) randomized subjects to placement of a retropubic sling or a TOT sling. The primary outcome was the presence or absence of urodynamically documented stress incontinence at 6 months. Secondary outcomes included complications, self-reported SUI, and findings on a quality-of-life questionnaire.
Findings. At 6 months, 138 patients completed an evaluation, including repeat urodynamic study. The success rate in the retropubic group was 79%, compared with only 55% in the TOT group (P = .004). Nine women in the TOT group underwent repeat surgery; none did in the retropubic group. There was no difference between groups in de novo overactive bladder symptoms; overactive bladder symptoms resolved at a nearly equivalent rate: 40% in the TOT group and 36% in the retropubic group. No difference was seen in the rate of intraoperative or postoperative complications, although the rate of bladder perforation was higher in the retropubic group, leaning toward significance (P = .06).
Women who have ISD are better served by having a retropubic sling, not a TOT sling, placed.
Single-incision slings demonstrate lower efficacy than traditional slings
Adbel-Fattah M, Ford JA, Lim CP, Madhuvrata P. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: a meta-analysis of effectiveness and complications. Eur Urol. 2011;60(3):468–480.
The single-incision sling was introduced in 2006 to, ostensibly, simplify surgery and reduce the risk of complications. Yet, essentially, no data on the efficacy or safety of single-incision kits existed when they entered the market!
Study design. This meta-analysis of single-incision slings analyzed the surgical literature from 1996 through early 2011. Investigators found nine studies that met criteria for objective and subjective outcomes in randomized or quasi-randomized clinical trials. They performed the analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
A total of 758 women who participated in nine randomized clinical trials were included for analysis. Seven studies reported on the subjective cure rate; six reported on the objective cure rate.
Findings. The analysis showed that single-incision slings are associated with lower subjective and objective cure rates than traditional slings (for single-incision slings, the risk ratio [RR] was 0.83 [95% CI, 0.70–0.99]; for traditional slings, RR was 0.85 [95% CI, 0.74–0.97]). In addition, re-operation rates were significantly higher in the single-incision sling group (RR, 6.72 [95% CI, 2.4–18.9]).
The single-incision sling was associated with a shorter operating time and less postoperative pain, but had a higher rate of mesh exposure (RR, 3.86 [95% CI, 1.45–10.3]).
This is important information about the relative effectiveness of the single-incision sling compared to more traditional retropubic and TOT approaches. If you are going to offer a single-incision sling, you must 1) select patients carefully and 2) counsel appropriate candidates on two key points: data on the success of single-incision slings are limited and an inferior (that is, inferior to traditional techniques) result is possible.
From stem-cell research. This expanding component of a number of medical specialties includes urologic applications. Animal-based studies have been supportive here,1-3 and two studies have translated the use of stem cells for correcting SUI to humans.4,5
Taken together, the human studies treated 20 women with autologous muscle-derived stem cells or muscle progenitor cells that were injected periurethrally or intrasphincterically. Seventeen subjects completed follow-up; improvement was demonstrated in all but two of them.4,5
The promise of stem-cell applications for treating SUI is exciting. We need additional investigation into methods and safety, however—making widespread application in humans not yet suitable. Still, the field is rapidly expanding and this remains a hopeful treatment option for the future.
For repairing vaginal prolapse. Unpublished findings from the Outcomes Following Vaginal Prolapse Repair and Mid Urethral Sling (OPUS) trial—the “vaginal counterpart,” one could say, to the notable CARE trial of cholesterol level management—were presented at the annual scientific meeting of the American Urogynecologic Society (AUGS) in September. This landmark study demonstrated that a prophylactic midurethral sling placed at the time of vaginal prolapse repair results in superior continence at 3 and 12 months in women who did not have preoperative symptoms of incontinence. Publication of this study—it has been submitted to a leading medical journal—will have a significant impact on the counseling that providers offer to asymptomatic patients who are undergoing vaginal reconstructive surgery about having a prophylactic sling placed.
REFERENCES
1. Wu G, Song Y, Zheng X, Jiang Z. Adipose-derived stromal cell transplantation for treatment of stress urinary incontinence. Tissue Cell. 2011;43(4):246–253.
2. Kim SO, Na HS, Kwon D, Joo SY, Kim HS, Ahn Y. Bone-marrow-derived mesenchymal stem cell transplantation enhances closing pressure and leak point pressure in a female urinary incontinence rat model. Urol Int. 2011;86(1):110–116.
3. Corcos J, Loutochin O, Campeau L, et al. Bone marrow mesenchymal stromal cell therapy for external urethral sphincter restoration in a rat model of stress urinary incontinence. Neurourol Urodyn. 2011;30(3):447–455.
4. Carr LK, Steele D, Steele S, et al. 1-year follow-up of autologous muscle-derived stem cell injection pilot study to treat stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):881–883.
5. Sebe P, Doucet C, Cornu JN, et al. Intrasphincteric injections of autologous muscular cells in women with refractory stress urinary incontinence: a prospective study. Int Urogynecol J. 2011;22(2):183–189.
We want to hear from you! Tell us what you think.
- Update on urinary incontinence: Occult incontinence in women who have pelvic organ prolapse
Maria Fidela Paraiso, MD; Elena Tunitsky-Bitton, MD (December 2010)
Urinary incontinence affects as many as 50% of adult women1; 16% have bothersome symptoms2 and as many as 10% undergo surgical correction of their condition.3 The prevalence of urinary incontinence increases with age; with the aging US population expected to more than double by 2050,4 more and more women will seek treatment.
This notion of a growing population of women who want treatment is supported by a recent article that evaluated trends in surgery for urinary incontinence between 1998 and 2007: The researchers found that the number of inpatient urinary incontinence surgeries nearly tripled over 1 decade.5
Therapeutic revolution
Introduction of the retropubic mid-urethral sling in 19966 transformed the surgical management of stress incontinence; the procedure has become the gold standard. Subsequent iterations of the sling procedure include a transobturator approach7 (known as the “TOT” sling) and, more recently, single-incision slings—alternatives intended primarily to improve the safety profile and ease of the procedure while maintaining its efficacy.
The newer sling procedures—many including novel mesh materials, some delivered in kit form—came to market under the US Food and Drug Administration’s so-called 510(k) rule, however, allowing manufacturers to launch them with little or no data supporting safety and efficacy. Given those circumstances, the optimal surgical management of stress urinary incontinence (SUI) remains controversial, and surgeons must take into account individual patient characteristics and treatment goals when developing a plan for surgical management. Providers must also remember that not all women will opt for, or are good candidates for, surgical intervention. These women need alternatives to operative management.
In this Update, we review and comment on four published papers that 1) highlight recent developments in the treatment of SUI and 2) provide concrete guidance to clinicians for providing optimal management:
- A randomized trial of nonsurgical management of stress incontinence using a continence pessary, compared with behavioral therapy and with combined (pessary plus behavioral therapy) treatment (the ATLAS trial)
- A randomized clinical trial that compared the efficacy of retropubic slings and TOT slings, with 1-year follow-up (the TOMUS trial)
- A randomized clinical trial that compared the efficacy of retropubic slings and TOT slings in women who have intrinsic sphincter deficiency
- A meta-analysis of the safety and efficacy of single-incision slings.
Conservative therapy is still an important, effective option for SUI
Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115(3):609–617.
Conservative treatment options for SUI are limited. They include:
- a pessary
- behavioral/pelvic floor physical therapy
- duloxetine (Cymbalta), a serotonin and norepinephrine reuptake inhibitor antidepressant (as an off-label use).
Level-I evidence exists to support utilization of behavioral pelvic floor therapy, based on a Cochrane review.8 Yet, little evidence exists by which we can compare the efficacy of various incontinence pessaries and their efficacy when combined with behavioral therapy.
Study design. This multi-center, randomized trial was conducted to fill this gap in the evidence. Four hundred forty-six women who had SUI were randomized to three groups: pessary only (149); behavioral therapy only (146); and pessary plus behavioral therapy (151). Women 18 years and older who had either SUI alone or stress-predominant incontinence were eligible. At baseline, 20.7% of subjects had undergone nonsurgical incontinence treatment; 6.9% had had surgical management. There was no significant difference in regard to prior treatment among the study groups.
Behavioral therapy comprised four visits at 2-week intervals, conducted by a nurse or a physical therapist who had undergone standardized training. Visits focused on engaging pelvic floor muscles; subjects received a “prescription” for home practice.
Women in the pessary groups were fitted at as many as three clinic visits with an incontinence ring or dish.
Measures of primary outcomes included the Patient Global Impression of Improvement (PGI-I) and the stress incontinence subset of the Pelvic Floor Distress Inventory (PFDI) at 3 months (follow-up continued to 12 months).
Findings. At 3 months, 40% of subjects in the pessary-only group, 49% in the behavioral therapy-only group, and 53% in the combined group reported (on the PGI-I) that their symptoms were “much” or “very much” better. Furthermore, 33% in the pessary-only group, 49% in the behavioral therapy-only group, and 44% in the combined group reported (on the PFDI) no bothersome stress incontinence.
Only PFDI measures were significantly different between pessary and behavioral therapy groups. Both PFDI and PGI-I demonstrated a significant difference in combined therapy compared to a pessary, but not in combined therapy compared to behavioral therapy. Because combination therapy was not superior to both single-therapies, the researchers concluded that combination therapy was not superior to single therapy.
By 12 months, efficacy declined in all groups: 32% of all women reported they were “much” or “very much” better, and 36% denied symptoms of stress incontinence. There was no difference in efficacy across the three groups by the end of the follow-up period.
The modest success rate of the conservative measures for treating SUI that were studied here, and the decline in their efficacy over time, might be discouraging at first glance. But more than one third of patients experienced benefit in the end—in the face of low risk. Consider a pessary or behavioral therapy to be a workable, low-risk option for your patients who have SUI, therefore. Combining those two measures does not, however, provide superior results.
TOT, retropubic slings equally effective for SUI—but complications differ
Richter H, Albo M, Zyczynski H, et al; Urinary Incontinence Treatment Network. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362(22):2066–2076.
This large, randomized, prospective multi-center study from the well-respected Pelvic Floor Disorders Network demonstrated that the efficacy of retropubic and TOT slings is equivalent. At the same time, the trial highlighted important differences in the complication profiles of these two surgical approaches. Given the high success rate of retropubic slings, the study was designed as an equivalence trial, with the principal aim of demonstrating whether both approaches share a similar success rate.
Study design. Investigators recruited women who had been given a diagnosis of SUI and were planning to undergo surgical correction, randomizing 597 who had predominant stress loss symptoms and a positive stress test (urodynamics were not required); 565 completed the 12-month follow-up.
Findings. Objective and subjective cure rates were similar in both groups at 12 months. (“Objective cure” was defined as a negative stress test, negative pad test, and no re-treatment within the follow-up period; “subjective cure” was defined as no re-treatment, no episodes of leakage on a voiding diary, and no self-report of stress loss.)
At 12 months, the objective cure rate was 81% for the retropubic sling and 78% for the TOT sling (the difference of three percentage points had a 95% confidence interval [CI] of –3.6–9.6). Despite very close findings, the subjective cure rate was lower in the TOT group (56%) than in the retropubic group (62%) (the difference of just over six percentage points had a 95% CI of –1.6–14.3) and did not meet criteria for equivalence.
There was no difference between the two groups in the incidence of urge incontinence; patient satisfaction; and quality-of-life outcomes.
But divergence was seen in complications. A higher incidence of voiding dysfunction that required re-operation was seen in the retropubic group (2.7%) than in the TOT group (0%) (P = .004). The retropubic sling group also exhibited a higher incidence of mesh exposure and bladder perforation. The TOT group had a higher incidence of neurologic sequelae (numbness, weakness) than the retropubic group (9.4% and 0.04%, respectively) (P = .01).
This well-designed trial confirmed the current standard of practice and supports the findings of a recent Cochrane review that reported a success rate of 88% for the retropubic approach and 84% for the TOT approach.9 The trial also demonstrated that you can anticipate similar success rates with retropubic and TOT approaches to placing a mid-urethral sling.
Note: The design of this study did not call for urodynamic evaluation, but more than 85% of subjects did undergo such testing, including measurement of the Valsalva leak-point pressure (VLPP) and the maximum urethral-closure pressure (MUCP). The investigators’ linear regression analysis revealed no change in outcomes between the two approaches when adjusting for VLPP and MUCP. This supportive finding suggests that a TOT sling would be just as beneficial as a retropubic sling in women who have ISD—although other recent studies that specifically addressed this matter came to a different conclusion.
Intrinsic sphincter deficiency might be a risk factor for failure of a TOT sling
Schierlitz L, Dwyer P, Rosamilla A, et al. Effectiveness of tension-free vaginal tape compared with TOT tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol. 2008;112(6):1253–1261.
In the trial by Richter and colleagues that we reviewed above, the investigators found that ISD—defined as low VLPP or low MUCP—did not have an impact on outcomes after placement of retropubic and TOT slings. Yet, other recent studies have concluded differently: In this trial from Australia, researchers concluded that a retropubic sling was more effective than a TOT sling in women who had ISD.
Study design. This randomized, prospective study of 164 women who had SUI and ISD (defined as MUCP <20 cm H2O or VLPP <60 cm H2O) randomized subjects to placement of a retropubic sling or a TOT sling. The primary outcome was the presence or absence of urodynamically documented stress incontinence at 6 months. Secondary outcomes included complications, self-reported SUI, and findings on a quality-of-life questionnaire.
Findings. At 6 months, 138 patients completed an evaluation, including repeat urodynamic study. The success rate in the retropubic group was 79%, compared with only 55% in the TOT group (P = .004). Nine women in the TOT group underwent repeat surgery; none did in the retropubic group. There was no difference between groups in de novo overactive bladder symptoms; overactive bladder symptoms resolved at a nearly equivalent rate: 40% in the TOT group and 36% in the retropubic group. No difference was seen in the rate of intraoperative or postoperative complications, although the rate of bladder perforation was higher in the retropubic group, leaning toward significance (P = .06).
Women who have ISD are better served by having a retropubic sling, not a TOT sling, placed.
Single-incision slings demonstrate lower efficacy than traditional slings
Adbel-Fattah M, Ford JA, Lim CP, Madhuvrata P. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: a meta-analysis of effectiveness and complications. Eur Urol. 2011;60(3):468–480.
The single-incision sling was introduced in 2006 to, ostensibly, simplify surgery and reduce the risk of complications. Yet, essentially, no data on the efficacy or safety of single-incision kits existed when they entered the market!
Study design. This meta-analysis of single-incision slings analyzed the surgical literature from 1996 through early 2011. Investigators found nine studies that met criteria for objective and subjective outcomes in randomized or quasi-randomized clinical trials. They performed the analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
A total of 758 women who participated in nine randomized clinical trials were included for analysis. Seven studies reported on the subjective cure rate; six reported on the objective cure rate.
Findings. The analysis showed that single-incision slings are associated with lower subjective and objective cure rates than traditional slings (for single-incision slings, the risk ratio [RR] was 0.83 [95% CI, 0.70–0.99]; for traditional slings, RR was 0.85 [95% CI, 0.74–0.97]). In addition, re-operation rates were significantly higher in the single-incision sling group (RR, 6.72 [95% CI, 2.4–18.9]).
The single-incision sling was associated with a shorter operating time and less postoperative pain, but had a higher rate of mesh exposure (RR, 3.86 [95% CI, 1.45–10.3]).
This is important information about the relative effectiveness of the single-incision sling compared to more traditional retropubic and TOT approaches. If you are going to offer a single-incision sling, you must 1) select patients carefully and 2) counsel appropriate candidates on two key points: data on the success of single-incision slings are limited and an inferior (that is, inferior to traditional techniques) result is possible.
From stem-cell research. This expanding component of a number of medical specialties includes urologic applications. Animal-based studies have been supportive here,1-3 and two studies have translated the use of stem cells for correcting SUI to humans.4,5
Taken together, the human studies treated 20 women with autologous muscle-derived stem cells or muscle progenitor cells that were injected periurethrally or intrasphincterically. Seventeen subjects completed follow-up; improvement was demonstrated in all but two of them.4,5
The promise of stem-cell applications for treating SUI is exciting. We need additional investigation into methods and safety, however—making widespread application in humans not yet suitable. Still, the field is rapidly expanding and this remains a hopeful treatment option for the future.
For repairing vaginal prolapse. Unpublished findings from the Outcomes Following Vaginal Prolapse Repair and Mid Urethral Sling (OPUS) trial—the “vaginal counterpart,” one could say, to the notable CARE trial of cholesterol level management—were presented at the annual scientific meeting of the American Urogynecologic Society (AUGS) in September. This landmark study demonstrated that a prophylactic midurethral sling placed at the time of vaginal prolapse repair results in superior continence at 3 and 12 months in women who did not have preoperative symptoms of incontinence. Publication of this study—it has been submitted to a leading medical journal—will have a significant impact on the counseling that providers offer to asymptomatic patients who are undergoing vaginal reconstructive surgery about having a prophylactic sling placed.
REFERENCES
1. Wu G, Song Y, Zheng X, Jiang Z. Adipose-derived stromal cell transplantation for treatment of stress urinary incontinence. Tissue Cell. 2011;43(4):246–253.
2. Kim SO, Na HS, Kwon D, Joo SY, Kim HS, Ahn Y. Bone-marrow-derived mesenchymal stem cell transplantation enhances closing pressure and leak point pressure in a female urinary incontinence rat model. Urol Int. 2011;86(1):110–116.
3. Corcos J, Loutochin O, Campeau L, et al. Bone marrow mesenchymal stromal cell therapy for external urethral sphincter restoration in a rat model of stress urinary incontinence. Neurourol Urodyn. 2011;30(3):447–455.
4. Carr LK, Steele D, Steele S, et al. 1-year follow-up of autologous muscle-derived stem cell injection pilot study to treat stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):881–883.
5. Sebe P, Doucet C, Cornu JN, et al. Intrasphincteric injections of autologous muscular cells in women with refractory stress urinary incontinence: a prospective study. Int Urogynecol J. 2011;22(2):183–189.
We want to hear from you! Tell us what you think.
1. Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165(5):537-542.
2. Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311-1316.
3. Thom DH, Nygaard IE, Calhoun EA. Urologic diseases in America project: urinary incontinence in women-national trends in hospitalizations office visits, treatment and economic impact. J Urol. 2005;173(4):1295-1301.
4. Vincent GK, Velkoff VA. The Next Four Decades. The older population in the United States: 2010 to 2050. Current Populations Reports. Washington DC: US Census Bureau; May 2010. http://www.census.gov/prod/2010pubs/p25-1138.pdf. Accessed October 26, 2011.
5. Wu JM, Gandhi MP, Shah AD, Shah JY, Fulton RG, Weidner AC. Trends in inpatient urinary incontinence surgery in the USA 1998-2007. Int Urogynecol J. 2011;22(11):1437-1443.
6. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7(2):81-86.
7. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women[in French]. Prog Urol. 2001;11(6):1306-1313.
8. Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment for urinary incontinence in women. A Cochrane systematic review. Eur J Phys Rehabil Med. 2008;44(1):47-63.
9. Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2009:CD006375.
1. Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165(5):537-542.
2. Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311-1316.
3. Thom DH, Nygaard IE, Calhoun EA. Urologic diseases in America project: urinary incontinence in women-national trends in hospitalizations office visits, treatment and economic impact. J Urol. 2005;173(4):1295-1301.
4. Vincent GK, Velkoff VA. The Next Four Decades. The older population in the United States: 2010 to 2050. Current Populations Reports. Washington DC: US Census Bureau; May 2010. http://www.census.gov/prod/2010pubs/p25-1138.pdf. Accessed October 26, 2011.
5. Wu JM, Gandhi MP, Shah AD, Shah JY, Fulton RG, Weidner AC. Trends in inpatient urinary incontinence surgery in the USA 1998-2007. Int Urogynecol J. 2011;22(11):1437-1443.
6. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7(2):81-86.
7. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women[in French]. Prog Urol. 2001;11(6):1306-1313.
8. Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment for urinary incontinence in women. A Cochrane systematic review. Eur J Phys Rehabil Med. 2008;44(1):47-63.
9. Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2009:CD006375.
A reasoned plan to manage a persistent Category-II FHR tracing
- Stop staring at that Category-II fetal heart-rate tracing…
Robert L. Barbieri, MD (Editorial, April 2011) - Guidelines on fetal monitoring aim to codify normal, abnormal FHR
Robert L. Barbieri, MD (Editorial, October 2008)
CASE An uncertain interlude during labor
An obstetrician checks on her laboring patient, only to discover that the fetal heart-rate (FHR) tracing has moved from Category I, a normal classification, into Category II—a gray zone. The OB decides to be proactive, not simply to wait for the tracing to return to normal. She has the patient move from a supine to a lateral position, provides oxygen, and administers a bolus of 500 to 1,000 mL of lactated Ringer’s solution over 20 minutes.
The tracing remains in Category II.
What should the OB do next?
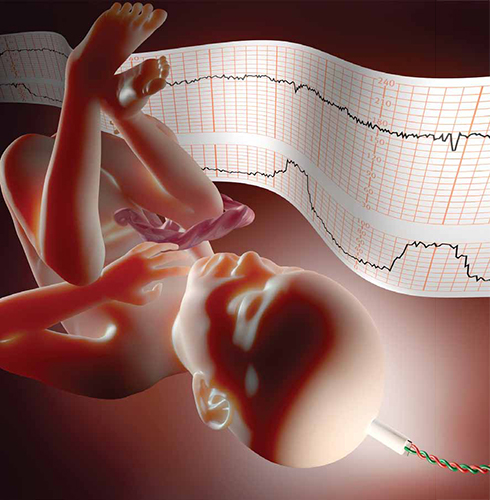
When a fetal heart-rate tracing remains in Category II despite well-considered conservative corrective measures, a reasoned, rather than passive, approach is recommended.In 2008, the National Institute of Child Health and Human Development proposed a three-tier classification system for electronic FHR tracings (TABLE 1).1 Tracings in Category I are considered normal and can be managed routinely.1-3 Category-III tracings are considered abnormal and require additional attention; if corrective measures do not result in improvement, rapid delivery usually is warranted.1-3 Category II includes all FHR tracings that do not fit into either of the other categories. Because Category II encompasses such a wide range of FHR tracings, there are many options for management.
TABLE 1
3-tier fetal heart-rate classification system
| Category | Description |
|---|---|
| I | Fetal heart-rate (FHR) tracings include all of the following:
|
| II | Includes all FHR tracings not included in Category I or Category III |
| III | FHR tracings include:
|
| Source: Adapted from Macones GA, et al.1 | |
If the case described above sounds familiar, it may be that you read Editor in Chief Dr. Robert L. Barbieri’s editorial on Category-II FHR tracings in the April 2011 issue of OBG Management.4 That essay described a number of common conservative corrective measures applicable for Category-II tracings, including the three interventions the OB performed.
Other measures:
- reduce or stop infusion of oxytocin
- discontinue cervical ripening agents
- consider administering a tocolytic, such as terbutaline, if tachysystole is present or if uterine contractions are prolonged or coupled
- consider the option of amnioinfusion if variable decelerations are present.4,5
Systematic review of the oxygen pathway, from the environment to the fetus (maternal lungs, heart, vasculature, uterus, placenta, and umbilical cord), can facilitate recollection of all of these measures. In addition, a simplified “A-B-C-D” approach to the management of a Category-II FHR tracing is helpful (TABLES 2 and 3):
- Assess the oxygen pathway
- Begin conservative corrective measures
- Clear obstacles to rapid delivery
- Determine decision-to-delivery time.6,7
TABLE 2
Conservative corrective measures to improve fetal oxygenation
| “A” Assess oxygen pathway | “B” Begin corrective measures if indicated | |
|---|---|---|
| Lungs | Airway and breathing | Supplemental oxygen (10 L) using a tight-fitting, non-rebreather face mask for at least 15 minutes |
| Heart | Heart rate and rhythm | Position changes IV fluid bolus (500–1,000 cc of isotonic fluid over 20 min) Correct hypotension |
| Vasculature | Blood pressure Volume status | |
| Uterus | Contraction strength Contraction frequency Baseline uterine tone Exclude uterine rupture | Stop or reduce uterine stimulants (oxytocin, prostaglandin) Consider uterine relaxant (terbutaline) |
| Placenta | Placental separation Bleeding vasa previa | |
| Cord | Vaginal exam Exclude cord prolapse | Consider amnioinfusion |
| Courtesy of David A. Miller, MD | ||
As the obstetrician in the opening scenario knows all too well, conservative corrective measures do not always transform FHR tracings from Category II to Category I. In fact, it is extremely common for a Category-II tracing to remain in Category II despite every conservative corrective measure in the book. This article presents a practical, systematic, standardized approach to the management of a persistent Category-II FHR tracing.
TABLE 3
Steps involved in preparing for delivery
| “C” Clear obstacles to rapid delivery | “D” Determine decision-to-delivery time | |
|---|---|---|
| Facility | Operating room availability Equipment | Facility response time |
| Staff | Notify: Obstetrician Surgical assistant Anesthesiologist Neonatologist Pediatrician Nursing staff | Consider staff: Availability Training Experience |
| Mother | Informed consent Anesthesia options Laboratory tests Blood products Intravenous access Urinary catheter Abdominal prep Transfer to OR | Surgical considerations (prior abdominal or uterine surgery) Medical considerations (obesity, hypertension, diabetes, SLE) Obstetric considerations (parity, pelvimetry, placental location) |
| Fetus | Confirm: Estimated fetal weight Gestational age Presentation Position | Consider factors such as: Estimated fetal weight Gestational age Presentation Position |
| Labor | Confirm adequate monitoring of uterine contractions | Consider factors such as: Arrest disorder Protracted labor Remote from delivery Poor expulsive efforts |
| Courtesy of David A. Miller, MD | ||
CASE Continued
When the OB’s preliminary interventions fail to nudge the FHR tracing back to Category I, she stops oxytocin and administers terbutaline. She even tries amnioinfusion. Still, the FHR tracing remains in Category II.
“What now?,” she wonders.
If conservative measures do not correct the FHR tracing to the satisfaction of the clinician, it is prudent to plan ahead for the possible need for rapid delivery. In a standardized “A-B-C-D” approach to FHR management, the next step is “C”: Clear obstacles to rapid delivery. This step does not constitute a commitment to a particular time or method of delivery. It simply serves as a reminder of common sources of unnecessary delay so that they can be addressed in a standardized, timely manner (FIGURE).

Decision model for management of intrapartum fetal heart rate (FHR)Standardization has long been recognized as an essential element of patient safety, and a growing body of contemporary evidence confirms that standardization can reduce adverse outcomes and malpractice claims.8-10 In FHR monitoring, standardization can help ensure that common obstacles to rapid delivery are not overlooked and that decisions are made in a timely fashion. TABLE 3 identifies common obstacles to rapid delivery, groups them in five major categories, and organizes them in non-random order. From largest to smallest, these categories include the facility, staff, mother, fetus, and labor.
Because many of these examples are viewed by clinicians as “common sense,” they do not always receive the serious, systematic attention they deserve. Instead, they are often left to the vagaries of random recall and are frequently overlooked, jeopardizing patient safety and inviting criticism. An easy way to minimize the error inherent in random recall is to use a simple checklist and to post it in a conspicuous location on the labor-and-delivery unit.
Next step: “D” – Determine the decision-to-delivery time
After appropriate conservative measures have been implemented and obstacles to rapid delivery have been cleared away, it is sensible to take a moment to estimate the time needed to accomplish delivery in the event of a sudden emergency. This step should be addressed by the clinician who is ultimately responsible for performing operative delivery, should it become necessary. The time between decision and delivery can be estimated systematically by considering individual characteristics of the facility, staff, mother, fetus, and labor. TABLE 3 summarizes examples of factors that can have an impact on this estimate.
Clinical judgment is required
Management steps A, B, C, and D are relatively uncontroversial, readily amenable to standardization, and represent the overwhelming majority of decisions that must be made during labor. These steps do not replace clinical judgment. On the contrary, they encourage the systematic, timely application of clinical judgment.
However, if the FHR tracing has not returned to Category I by the time A, B, C, and D are completed, the clinician must make a decision about whether to continue to wait for spontaneous vaginal delivery or to expedite delivery by other means. This decision balances the estimated time until vaginal delivery against the estimated time until the onset of metabolic acidemia and potential injury.
The estimate of the time until vaginal delivery is guided by the usual obstetric considerations, including the three “P’s”:
- Power – uterine contractions
- Passenger – the fetus
- Passage – the pelvis.
The estimate of the time until the onset of metabolic acidemia and potential injury is guided by limited data suggesting that metabolic acidemia usually does not appear suddenly, but can evolve gradually over a period of approximately 60 minutes.15 This general statement applies only to FHR tracings that are normal initially and subsequently develop minimal to absent variability with recurrent decelerations and no acute events.15 It does not constitute a “safe harbor.”
The inherent imprecision of these estimates can make the decision difficult. One of the most common preventable errors at this stage of FHR management is to postpone a difficult but clinically necessary decision in the hope that the situation will resolve on its own. Despite the difficulty, the standard of care mandates that a decision must be made using the best information available.
If a decision is made to expedite delivery, the rationale should be documented, and the plan should be implemented as rapidly and safely as feasible. If a decision is made to continue to wait, the rationale and plan should be documented, and the decision should be revisited after a reasonable period of time, usually in the range of 5 to 15 minutes in the second stage of labor.
“Deciding to wait” is distinctly different from “waiting to decide.” The former reflects the timely application of clinical judgment; the latter suggests procrastination.
CASE Resolved
The OB evaluates the patient again. The FHR tracing remains in Category II. The baseline rate is 150 bpm, variability is moderate, accelerations are present, and there are variable decelerations with every other contraction. The cervix remains dilated to 6 cm despite more than 2 hours of adequate contractions. Secondary arrest of dilatation is diagnosed, and cesarean delivery is recommended. Shortly thereafter, a vigorous baby is born. As the presence of moderate variability and accelerations predicted, the 5-minute Apgar score is normal. Assessment of the umbilical artery blood gas confirms the absence of metabolic acidemia, and the newborn course is uneventful.
The paradox of FHR monitoring
The greatest strength of intrapartum FHR monitoring is the ability of moderate variability or accelerations, or both, to predict normal neurologic outcome with an extremely high degree of reliability.1,11,12 One of the greatest weaknesses of FHR monitoring is the inability of an “abnormal” tracing to predict abnormal neurologic outcome with any clinically relevant degree of accuracy. The false-positive rate of FHR monitoring for predicting cerebral palsy has been reported to exceed 99%, yielding a positive predictive value of less than 1%.1,13 This imprecision is explained in part by the relative rarity of intrapartum hypoxic neurologic injury, and in part by the mitigating interventions that are frequently prompted by FHR “abnormalities.”14 However, these explanations do not alter the fact that the positive predictive value of intrapartum FHR monitoring, as it is used in actual clinical practice, is essentially zero.
Reasonable management decisions simply cannot be based on the results of a test that is virtually always wrong. On the other hand, the negative predictive value of intrapartum FHR monitoring is nearly 100%. A test that is virtually always right is the ideal foundation for rational decision-making.
Standardization of intrapartum FHR monitoring promotes safety by reducing unnecessary complexity and minimizing the error inherent in random recall. However, the technology can achieve its potential only if it is used appropriately. Trying to use intrapartum FHR monitoring to diagnose neurologic injury is a recipe for failure. In contrast, relying on the presence of moderate variability or accelerations, or both, to confirm adequate fetal oxygenation allows the clinician to formulate and articulate a rational, evidence-based plan of management that reflects consensus in the literature.
We want to hear from you! Tell us what you think.
1. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions interpretation, and research guidelines. Obstet Gynecol. 2008;112(3):661-666.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin number 106: Intrapartum fetal heart rate monitoring: nomenclature interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192-202.
3. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116(5):1232-1240.
4. Barbieri RL. Stop staring at that Category-II fetal heart-rate tracing…and do something instead to improve fetal status! OBG Manage. 2011;23(4):6-9.
5. Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005;105(6):1362-1368.
6. Miller DA. Intrapartum fetal heart rate definitions and interpretation: evolving consensus. Clin Obstet Gynecol. 2011;54(1):16-21.
7. Miller DA. Intrapartum fetal heart monitoring: a standardized approach to management. Clin Obstet Gynecol. 2011;54(1):22-27.
8. To Err is Human: Building a Safer Health System. Kohn LT Corrigan JM, Donaldson MS, eds. Committee on Quality of Health Care in America. Institute of Medicine. Washington, DC: National Academy of Sciences;1999:14.
9. Pettker CM, Thung SF, Norwitz ER, et al. Impact of a comprehensive patient safety strategy on obstetric adverse events. Am J Obstet Gynecol. 2009;200(5):492.e1-8.
10. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
11. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ. 1999;319(7216):1054-1059.
12. American College of Obstetricians and Gynecologists. Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology. Washington DC: American College of Obstetricians and Gynecologists; 2003.
13. Nelson KB, Dambrosia JM, Ting TY, Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med. 1996;334(10):613-618.
14. Freeman RK, Nageotte MP. Comments on American College of Obstetricians and Gynecologists Practice Bulletin No. 106. Am J Obstet Gynecol. 2010;202(5):411-412.
15. Parer JT, King T, Flanders S, Fox M, Kilpatrick SJ. Fetal acidemia and electronic fetal heart rate patterns: is there evidence of an association? J Matern Fetal Neonatal Med. 2006;19(5):289-294.
- Stop staring at that Category-II fetal heart-rate tracing…
Robert L. Barbieri, MD (Editorial, April 2011) - Guidelines on fetal monitoring aim to codify normal, abnormal FHR
Robert L. Barbieri, MD (Editorial, October 2008)
CASE An uncertain interlude during labor
An obstetrician checks on her laboring patient, only to discover that the fetal heart-rate (FHR) tracing has moved from Category I, a normal classification, into Category II—a gray zone. The OB decides to be proactive, not simply to wait for the tracing to return to normal. She has the patient move from a supine to a lateral position, provides oxygen, and administers a bolus of 500 to 1,000 mL of lactated Ringer’s solution over 20 minutes.
The tracing remains in Category II.
What should the OB do next?
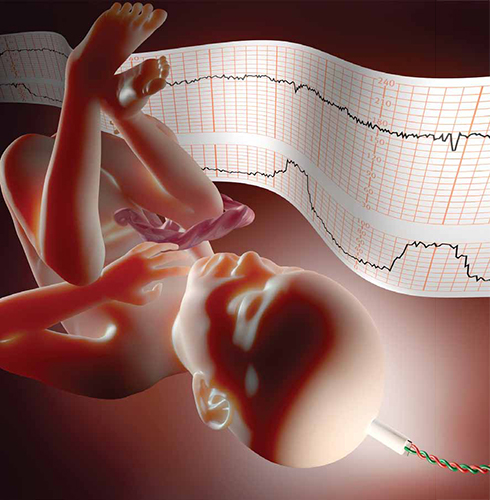
When a fetal heart-rate tracing remains in Category II despite well-considered conservative corrective measures, a reasoned, rather than passive, approach is recommended.In 2008, the National Institute of Child Health and Human Development proposed a three-tier classification system for electronic FHR tracings (TABLE 1).1 Tracings in Category I are considered normal and can be managed routinely.1-3 Category-III tracings are considered abnormal and require additional attention; if corrective measures do not result in improvement, rapid delivery usually is warranted.1-3 Category II includes all FHR tracings that do not fit into either of the other categories. Because Category II encompasses such a wide range of FHR tracings, there are many options for management.
TABLE 1
3-tier fetal heart-rate classification system
| Category | Description |
|---|---|
| I | Fetal heart-rate (FHR) tracings include all of the following:
|
| II | Includes all FHR tracings not included in Category I or Category III |
| III | FHR tracings include:
|
| Source: Adapted from Macones GA, et al.1 | |
If the case described above sounds familiar, it may be that you read Editor in Chief Dr. Robert L. Barbieri’s editorial on Category-II FHR tracings in the April 2011 issue of OBG Management.4 That essay described a number of common conservative corrective measures applicable for Category-II tracings, including the three interventions the OB performed.
Other measures:
- reduce or stop infusion of oxytocin
- discontinue cervical ripening agents
- consider administering a tocolytic, such as terbutaline, if tachysystole is present or if uterine contractions are prolonged or coupled
- consider the option of amnioinfusion if variable decelerations are present.4,5
Systematic review of the oxygen pathway, from the environment to the fetus (maternal lungs, heart, vasculature, uterus, placenta, and umbilical cord), can facilitate recollection of all of these measures. In addition, a simplified “A-B-C-D” approach to the management of a Category-II FHR tracing is helpful (TABLES 2 and 3):
- Assess the oxygen pathway
- Begin conservative corrective measures
- Clear obstacles to rapid delivery
- Determine decision-to-delivery time.6,7
TABLE 2
Conservative corrective measures to improve fetal oxygenation
| “A” Assess oxygen pathway | “B” Begin corrective measures if indicated | |
|---|---|---|
| Lungs | Airway and breathing | Supplemental oxygen (10 L) using a tight-fitting, non-rebreather face mask for at least 15 minutes |
| Heart | Heart rate and rhythm | Position changes IV fluid bolus (500–1,000 cc of isotonic fluid over 20 min) Correct hypotension |
| Vasculature | Blood pressure Volume status | |
| Uterus | Contraction strength Contraction frequency Baseline uterine tone Exclude uterine rupture | Stop or reduce uterine stimulants (oxytocin, prostaglandin) Consider uterine relaxant (terbutaline) |
| Placenta | Placental separation Bleeding vasa previa | |
| Cord | Vaginal exam Exclude cord prolapse | Consider amnioinfusion |
| Courtesy of David A. Miller, MD | ||
As the obstetrician in the opening scenario knows all too well, conservative corrective measures do not always transform FHR tracings from Category II to Category I. In fact, it is extremely common for a Category-II tracing to remain in Category II despite every conservative corrective measure in the book. This article presents a practical, systematic, standardized approach to the management of a persistent Category-II FHR tracing.
TABLE 3
Steps involved in preparing for delivery
| “C” Clear obstacles to rapid delivery | “D” Determine decision-to-delivery time | |
|---|---|---|
| Facility | Operating room availability Equipment | Facility response time |
| Staff | Notify: Obstetrician Surgical assistant Anesthesiologist Neonatologist Pediatrician Nursing staff | Consider staff: Availability Training Experience |
| Mother | Informed consent Anesthesia options Laboratory tests Blood products Intravenous access Urinary catheter Abdominal prep Transfer to OR | Surgical considerations (prior abdominal or uterine surgery) Medical considerations (obesity, hypertension, diabetes, SLE) Obstetric considerations (parity, pelvimetry, placental location) |
| Fetus | Confirm: Estimated fetal weight Gestational age Presentation Position | Consider factors such as: Estimated fetal weight Gestational age Presentation Position |
| Labor | Confirm adequate monitoring of uterine contractions | Consider factors such as: Arrest disorder Protracted labor Remote from delivery Poor expulsive efforts |
| Courtesy of David A. Miller, MD | ||
CASE Continued
When the OB’s preliminary interventions fail to nudge the FHR tracing back to Category I, she stops oxytocin and administers terbutaline. She even tries amnioinfusion. Still, the FHR tracing remains in Category II.
“What now?,” she wonders.
If conservative measures do not correct the FHR tracing to the satisfaction of the clinician, it is prudent to plan ahead for the possible need for rapid delivery. In a standardized “A-B-C-D” approach to FHR management, the next step is “C”: Clear obstacles to rapid delivery. This step does not constitute a commitment to a particular time or method of delivery. It simply serves as a reminder of common sources of unnecessary delay so that they can be addressed in a standardized, timely manner (FIGURE).

Decision model for management of intrapartum fetal heart rate (FHR)Standardization has long been recognized as an essential element of patient safety, and a growing body of contemporary evidence confirms that standardization can reduce adverse outcomes and malpractice claims.8-10 In FHR monitoring, standardization can help ensure that common obstacles to rapid delivery are not overlooked and that decisions are made in a timely fashion. TABLE 3 identifies common obstacles to rapid delivery, groups them in five major categories, and organizes them in non-random order. From largest to smallest, these categories include the facility, staff, mother, fetus, and labor.
Because many of these examples are viewed by clinicians as “common sense,” they do not always receive the serious, systematic attention they deserve. Instead, they are often left to the vagaries of random recall and are frequently overlooked, jeopardizing patient safety and inviting criticism. An easy way to minimize the error inherent in random recall is to use a simple checklist and to post it in a conspicuous location on the labor-and-delivery unit.
Next step: “D” – Determine the decision-to-delivery time
After appropriate conservative measures have been implemented and obstacles to rapid delivery have been cleared away, it is sensible to take a moment to estimate the time needed to accomplish delivery in the event of a sudden emergency. This step should be addressed by the clinician who is ultimately responsible for performing operative delivery, should it become necessary. The time between decision and delivery can be estimated systematically by considering individual characteristics of the facility, staff, mother, fetus, and labor. TABLE 3 summarizes examples of factors that can have an impact on this estimate.
Clinical judgment is required
Management steps A, B, C, and D are relatively uncontroversial, readily amenable to standardization, and represent the overwhelming majority of decisions that must be made during labor. These steps do not replace clinical judgment. On the contrary, they encourage the systematic, timely application of clinical judgment.
However, if the FHR tracing has not returned to Category I by the time A, B, C, and D are completed, the clinician must make a decision about whether to continue to wait for spontaneous vaginal delivery or to expedite delivery by other means. This decision balances the estimated time until vaginal delivery against the estimated time until the onset of metabolic acidemia and potential injury.
The estimate of the time until vaginal delivery is guided by the usual obstetric considerations, including the three “P’s”:
- Power – uterine contractions
- Passenger – the fetus
- Passage – the pelvis.
The estimate of the time until the onset of metabolic acidemia and potential injury is guided by limited data suggesting that metabolic acidemia usually does not appear suddenly, but can evolve gradually over a period of approximately 60 minutes.15 This general statement applies only to FHR tracings that are normal initially and subsequently develop minimal to absent variability with recurrent decelerations and no acute events.15 It does not constitute a “safe harbor.”
The inherent imprecision of these estimates can make the decision difficult. One of the most common preventable errors at this stage of FHR management is to postpone a difficult but clinically necessary decision in the hope that the situation will resolve on its own. Despite the difficulty, the standard of care mandates that a decision must be made using the best information available.
If a decision is made to expedite delivery, the rationale should be documented, and the plan should be implemented as rapidly and safely as feasible. If a decision is made to continue to wait, the rationale and plan should be documented, and the decision should be revisited after a reasonable period of time, usually in the range of 5 to 15 minutes in the second stage of labor.
“Deciding to wait” is distinctly different from “waiting to decide.” The former reflects the timely application of clinical judgment; the latter suggests procrastination.
CASE Resolved
The OB evaluates the patient again. The FHR tracing remains in Category II. The baseline rate is 150 bpm, variability is moderate, accelerations are present, and there are variable decelerations with every other contraction. The cervix remains dilated to 6 cm despite more than 2 hours of adequate contractions. Secondary arrest of dilatation is diagnosed, and cesarean delivery is recommended. Shortly thereafter, a vigorous baby is born. As the presence of moderate variability and accelerations predicted, the 5-minute Apgar score is normal. Assessment of the umbilical artery blood gas confirms the absence of metabolic acidemia, and the newborn course is uneventful.
The paradox of FHR monitoring
The greatest strength of intrapartum FHR monitoring is the ability of moderate variability or accelerations, or both, to predict normal neurologic outcome with an extremely high degree of reliability.1,11,12 One of the greatest weaknesses of FHR monitoring is the inability of an “abnormal” tracing to predict abnormal neurologic outcome with any clinically relevant degree of accuracy. The false-positive rate of FHR monitoring for predicting cerebral palsy has been reported to exceed 99%, yielding a positive predictive value of less than 1%.1,13 This imprecision is explained in part by the relative rarity of intrapartum hypoxic neurologic injury, and in part by the mitigating interventions that are frequently prompted by FHR “abnormalities.”14 However, these explanations do not alter the fact that the positive predictive value of intrapartum FHR monitoring, as it is used in actual clinical practice, is essentially zero.
Reasonable management decisions simply cannot be based on the results of a test that is virtually always wrong. On the other hand, the negative predictive value of intrapartum FHR monitoring is nearly 100%. A test that is virtually always right is the ideal foundation for rational decision-making.
Standardization of intrapartum FHR monitoring promotes safety by reducing unnecessary complexity and minimizing the error inherent in random recall. However, the technology can achieve its potential only if it is used appropriately. Trying to use intrapartum FHR monitoring to diagnose neurologic injury is a recipe for failure. In contrast, relying on the presence of moderate variability or accelerations, or both, to confirm adequate fetal oxygenation allows the clinician to formulate and articulate a rational, evidence-based plan of management that reflects consensus in the literature.
We want to hear from you! Tell us what you think.
- Stop staring at that Category-II fetal heart-rate tracing…
Robert L. Barbieri, MD (Editorial, April 2011) - Guidelines on fetal monitoring aim to codify normal, abnormal FHR
Robert L. Barbieri, MD (Editorial, October 2008)
CASE An uncertain interlude during labor
An obstetrician checks on her laboring patient, only to discover that the fetal heart-rate (FHR) tracing has moved from Category I, a normal classification, into Category II—a gray zone. The OB decides to be proactive, not simply to wait for the tracing to return to normal. She has the patient move from a supine to a lateral position, provides oxygen, and administers a bolus of 500 to 1,000 mL of lactated Ringer’s solution over 20 minutes.
The tracing remains in Category II.
What should the OB do next?
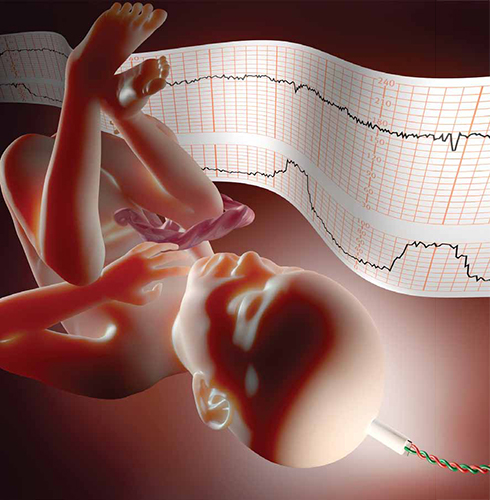
When a fetal heart-rate tracing remains in Category II despite well-considered conservative corrective measures, a reasoned, rather than passive, approach is recommended.In 2008, the National Institute of Child Health and Human Development proposed a three-tier classification system for electronic FHR tracings (TABLE 1).1 Tracings in Category I are considered normal and can be managed routinely.1-3 Category-III tracings are considered abnormal and require additional attention; if corrective measures do not result in improvement, rapid delivery usually is warranted.1-3 Category II includes all FHR tracings that do not fit into either of the other categories. Because Category II encompasses such a wide range of FHR tracings, there are many options for management.
TABLE 1
3-tier fetal heart-rate classification system
| Category | Description |
|---|---|
| I | Fetal heart-rate (FHR) tracings include all of the following:
|
| II | Includes all FHR tracings not included in Category I or Category III |
| III | FHR tracings include:
|
| Source: Adapted from Macones GA, et al.1 | |
If the case described above sounds familiar, it may be that you read Editor in Chief Dr. Robert L. Barbieri’s editorial on Category-II FHR tracings in the April 2011 issue of OBG Management.4 That essay described a number of common conservative corrective measures applicable for Category-II tracings, including the three interventions the OB performed.
Other measures:
- reduce or stop infusion of oxytocin
- discontinue cervical ripening agents
- consider administering a tocolytic, such as terbutaline, if tachysystole is present or if uterine contractions are prolonged or coupled
- consider the option of amnioinfusion if variable decelerations are present.4,5
Systematic review of the oxygen pathway, from the environment to the fetus (maternal lungs, heart, vasculature, uterus, placenta, and umbilical cord), can facilitate recollection of all of these measures. In addition, a simplified “A-B-C-D” approach to the management of a Category-II FHR tracing is helpful (TABLES 2 and 3):
- Assess the oxygen pathway
- Begin conservative corrective measures
- Clear obstacles to rapid delivery
- Determine decision-to-delivery time.6,7
TABLE 2
Conservative corrective measures to improve fetal oxygenation
| “A” Assess oxygen pathway | “B” Begin corrective measures if indicated | |
|---|---|---|
| Lungs | Airway and breathing | Supplemental oxygen (10 L) using a tight-fitting, non-rebreather face mask for at least 15 minutes |
| Heart | Heart rate and rhythm | Position changes IV fluid bolus (500–1,000 cc of isotonic fluid over 20 min) Correct hypotension |
| Vasculature | Blood pressure Volume status | |
| Uterus | Contraction strength Contraction frequency Baseline uterine tone Exclude uterine rupture | Stop or reduce uterine stimulants (oxytocin, prostaglandin) Consider uterine relaxant (terbutaline) |
| Placenta | Placental separation Bleeding vasa previa | |
| Cord | Vaginal exam Exclude cord prolapse | Consider amnioinfusion |
| Courtesy of David A. Miller, MD | ||
As the obstetrician in the opening scenario knows all too well, conservative corrective measures do not always transform FHR tracings from Category II to Category I. In fact, it is extremely common for a Category-II tracing to remain in Category II despite every conservative corrective measure in the book. This article presents a practical, systematic, standardized approach to the management of a persistent Category-II FHR tracing.
TABLE 3
Steps involved in preparing for delivery
| “C” Clear obstacles to rapid delivery | “D” Determine decision-to-delivery time | |
|---|---|---|
| Facility | Operating room availability Equipment | Facility response time |
| Staff | Notify: Obstetrician Surgical assistant Anesthesiologist Neonatologist Pediatrician Nursing staff | Consider staff: Availability Training Experience |
| Mother | Informed consent Anesthesia options Laboratory tests Blood products Intravenous access Urinary catheter Abdominal prep Transfer to OR | Surgical considerations (prior abdominal or uterine surgery) Medical considerations (obesity, hypertension, diabetes, SLE) Obstetric considerations (parity, pelvimetry, placental location) |
| Fetus | Confirm: Estimated fetal weight Gestational age Presentation Position | Consider factors such as: Estimated fetal weight Gestational age Presentation Position |
| Labor | Confirm adequate monitoring of uterine contractions | Consider factors such as: Arrest disorder Protracted labor Remote from delivery Poor expulsive efforts |
| Courtesy of David A. Miller, MD | ||
CASE Continued
When the OB’s preliminary interventions fail to nudge the FHR tracing back to Category I, she stops oxytocin and administers terbutaline. She even tries amnioinfusion. Still, the FHR tracing remains in Category II.
“What now?,” she wonders.
If conservative measures do not correct the FHR tracing to the satisfaction of the clinician, it is prudent to plan ahead for the possible need for rapid delivery. In a standardized “A-B-C-D” approach to FHR management, the next step is “C”: Clear obstacles to rapid delivery. This step does not constitute a commitment to a particular time or method of delivery. It simply serves as a reminder of common sources of unnecessary delay so that they can be addressed in a standardized, timely manner (FIGURE).

Decision model for management of intrapartum fetal heart rate (FHR)Standardization has long been recognized as an essential element of patient safety, and a growing body of contemporary evidence confirms that standardization can reduce adverse outcomes and malpractice claims.8-10 In FHR monitoring, standardization can help ensure that common obstacles to rapid delivery are not overlooked and that decisions are made in a timely fashion. TABLE 3 identifies common obstacles to rapid delivery, groups them in five major categories, and organizes them in non-random order. From largest to smallest, these categories include the facility, staff, mother, fetus, and labor.
Because many of these examples are viewed by clinicians as “common sense,” they do not always receive the serious, systematic attention they deserve. Instead, they are often left to the vagaries of random recall and are frequently overlooked, jeopardizing patient safety and inviting criticism. An easy way to minimize the error inherent in random recall is to use a simple checklist and to post it in a conspicuous location on the labor-and-delivery unit.
Next step: “D” – Determine the decision-to-delivery time
After appropriate conservative measures have been implemented and obstacles to rapid delivery have been cleared away, it is sensible to take a moment to estimate the time needed to accomplish delivery in the event of a sudden emergency. This step should be addressed by the clinician who is ultimately responsible for performing operative delivery, should it become necessary. The time between decision and delivery can be estimated systematically by considering individual characteristics of the facility, staff, mother, fetus, and labor. TABLE 3 summarizes examples of factors that can have an impact on this estimate.
Clinical judgment is required
Management steps A, B, C, and D are relatively uncontroversial, readily amenable to standardization, and represent the overwhelming majority of decisions that must be made during labor. These steps do not replace clinical judgment. On the contrary, they encourage the systematic, timely application of clinical judgment.
However, if the FHR tracing has not returned to Category I by the time A, B, C, and D are completed, the clinician must make a decision about whether to continue to wait for spontaneous vaginal delivery or to expedite delivery by other means. This decision balances the estimated time until vaginal delivery against the estimated time until the onset of metabolic acidemia and potential injury.
The estimate of the time until vaginal delivery is guided by the usual obstetric considerations, including the three “P’s”:
- Power – uterine contractions
- Passenger – the fetus
- Passage – the pelvis.
The estimate of the time until the onset of metabolic acidemia and potential injury is guided by limited data suggesting that metabolic acidemia usually does not appear suddenly, but can evolve gradually over a period of approximately 60 minutes.15 This general statement applies only to FHR tracings that are normal initially and subsequently develop minimal to absent variability with recurrent decelerations and no acute events.15 It does not constitute a “safe harbor.”
The inherent imprecision of these estimates can make the decision difficult. One of the most common preventable errors at this stage of FHR management is to postpone a difficult but clinically necessary decision in the hope that the situation will resolve on its own. Despite the difficulty, the standard of care mandates that a decision must be made using the best information available.
If a decision is made to expedite delivery, the rationale should be documented, and the plan should be implemented as rapidly and safely as feasible. If a decision is made to continue to wait, the rationale and plan should be documented, and the decision should be revisited after a reasonable period of time, usually in the range of 5 to 15 minutes in the second stage of labor.
“Deciding to wait” is distinctly different from “waiting to decide.” The former reflects the timely application of clinical judgment; the latter suggests procrastination.
CASE Resolved
The OB evaluates the patient again. The FHR tracing remains in Category II. The baseline rate is 150 bpm, variability is moderate, accelerations are present, and there are variable decelerations with every other contraction. The cervix remains dilated to 6 cm despite more than 2 hours of adequate contractions. Secondary arrest of dilatation is diagnosed, and cesarean delivery is recommended. Shortly thereafter, a vigorous baby is born. As the presence of moderate variability and accelerations predicted, the 5-minute Apgar score is normal. Assessment of the umbilical artery blood gas confirms the absence of metabolic acidemia, and the newborn course is uneventful.
The paradox of FHR monitoring
The greatest strength of intrapartum FHR monitoring is the ability of moderate variability or accelerations, or both, to predict normal neurologic outcome with an extremely high degree of reliability.1,11,12 One of the greatest weaknesses of FHR monitoring is the inability of an “abnormal” tracing to predict abnormal neurologic outcome with any clinically relevant degree of accuracy. The false-positive rate of FHR monitoring for predicting cerebral palsy has been reported to exceed 99%, yielding a positive predictive value of less than 1%.1,13 This imprecision is explained in part by the relative rarity of intrapartum hypoxic neurologic injury, and in part by the mitigating interventions that are frequently prompted by FHR “abnormalities.”14 However, these explanations do not alter the fact that the positive predictive value of intrapartum FHR monitoring, as it is used in actual clinical practice, is essentially zero.
Reasonable management decisions simply cannot be based on the results of a test that is virtually always wrong. On the other hand, the negative predictive value of intrapartum FHR monitoring is nearly 100%. A test that is virtually always right is the ideal foundation for rational decision-making.
Standardization of intrapartum FHR monitoring promotes safety by reducing unnecessary complexity and minimizing the error inherent in random recall. However, the technology can achieve its potential only if it is used appropriately. Trying to use intrapartum FHR monitoring to diagnose neurologic injury is a recipe for failure. In contrast, relying on the presence of moderate variability or accelerations, or both, to confirm adequate fetal oxygenation allows the clinician to formulate and articulate a rational, evidence-based plan of management that reflects consensus in the literature.
We want to hear from you! Tell us what you think.
1. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions interpretation, and research guidelines. Obstet Gynecol. 2008;112(3):661-666.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin number 106: Intrapartum fetal heart rate monitoring: nomenclature interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192-202.
3. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116(5):1232-1240.
4. Barbieri RL. Stop staring at that Category-II fetal heart-rate tracing…and do something instead to improve fetal status! OBG Manage. 2011;23(4):6-9.
5. Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005;105(6):1362-1368.
6. Miller DA. Intrapartum fetal heart rate definitions and interpretation: evolving consensus. Clin Obstet Gynecol. 2011;54(1):16-21.
7. Miller DA. Intrapartum fetal heart monitoring: a standardized approach to management. Clin Obstet Gynecol. 2011;54(1):22-27.
8. To Err is Human: Building a Safer Health System. Kohn LT Corrigan JM, Donaldson MS, eds. Committee on Quality of Health Care in America. Institute of Medicine. Washington, DC: National Academy of Sciences;1999:14.
9. Pettker CM, Thung SF, Norwitz ER, et al. Impact of a comprehensive patient safety strategy on obstetric adverse events. Am J Obstet Gynecol. 2009;200(5):492.e1-8.
10. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
11. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ. 1999;319(7216):1054-1059.
12. American College of Obstetricians and Gynecologists. Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology. Washington DC: American College of Obstetricians and Gynecologists; 2003.
13. Nelson KB, Dambrosia JM, Ting TY, Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med. 1996;334(10):613-618.
14. Freeman RK, Nageotte MP. Comments on American College of Obstetricians and Gynecologists Practice Bulletin No. 106. Am J Obstet Gynecol. 2010;202(5):411-412.
15. Parer JT, King T, Flanders S, Fox M, Kilpatrick SJ. Fetal acidemia and electronic fetal heart rate patterns: is there evidence of an association? J Matern Fetal Neonatal Med. 2006;19(5):289-294.
1. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions interpretation, and research guidelines. Obstet Gynecol. 2008;112(3):661-666.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin number 106: Intrapartum fetal heart rate monitoring: nomenclature interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192-202.
3. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116(5):1232-1240.
4. Barbieri RL. Stop staring at that Category-II fetal heart-rate tracing…and do something instead to improve fetal status! OBG Manage. 2011;23(4):6-9.
5. Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005;105(6):1362-1368.
6. Miller DA. Intrapartum fetal heart rate definitions and interpretation: evolving consensus. Clin Obstet Gynecol. 2011;54(1):16-21.
7. Miller DA. Intrapartum fetal heart monitoring: a standardized approach to management. Clin Obstet Gynecol. 2011;54(1):22-27.
8. To Err is Human: Building a Safer Health System. Kohn LT Corrigan JM, Donaldson MS, eds. Committee on Quality of Health Care in America. Institute of Medicine. Washington, DC: National Academy of Sciences;1999:14.
9. Pettker CM, Thung SF, Norwitz ER, et al. Impact of a comprehensive patient safety strategy on obstetric adverse events. Am J Obstet Gynecol. 2009;200(5):492.e1-8.
10. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
11. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ. 1999;319(7216):1054-1059.
12. American College of Obstetricians and Gynecologists. Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology. Washington DC: American College of Obstetricians and Gynecologists; 2003.
13. Nelson KB, Dambrosia JM, Ting TY, Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med. 1996;334(10):613-618.
14. Freeman RK, Nageotte MP. Comments on American College of Obstetricians and Gynecologists Practice Bulletin No. 106. Am J Obstet Gynecol. 2010;202(5):411-412.
15. Parer JT, King T, Flanders S, Fox M, Kilpatrick SJ. Fetal acidemia and electronic fetal heart rate patterns: is there evidence of an association? J Matern Fetal Neonatal Med. 2006;19(5):289-294.
Insulin Pump Therapy for the Patient With Diabetes
The FDA has reported that in 2007, 375,000 Americans with diabetes were using an insulin pump.1 Improvements in pump technology (including the addition of continuous glucose monitoring2,3), more data on the use of pumps in type 2 diabetes,4-7 improved insurance coverage,8 and the general population’s comfort with technology-based solutions may lead more patients with diabetes to choose a pump to deliver their insulin.
As a result, primary care practitioners will be increasingly likely to have patients who use continuous subcutaneous insulin infusion (CSII) pumps. While the initiation of pump therapy and follow-up with patients who use pumps have traditionally been the purview of endocrinologists, it is important for primary care providers to understand the basics of insulin pump therapy, enabling them to work collaboratively with the patient and the diabetes care team.
REVIEW OF INSULIN ACTION IN THE BODY
The body’s own (endogenous) insulin is secreted by the beta cells of the pancreas. Basal insulin is the background amount of insulin continuously released by the body in order to regulate hepatic glucose production and lipolysis. In response to food intake, the body releases additional insulin to match the glycemic effect of carbohydrates, fat, and protein.9
Insulin regimens attempt to mimic the body’s physiologic release of insulin by administering long-acting insulin to provide basal coverage, and rapid- or short-acting insulin to metabolize meals. The first long-acting insulin developed was NPH (still in use today), which was created by the addition of neutral protamine Hagedorn to regular insulin to delay insulin absorption.10
There are a few reasons that NPH use has fallen out of favor, especially for patients with type 1 diabetes, who do not produce endogenous insulin. One is a pronounced peak in action that requires patients to time their consumption of meals and snacks around peaks. If food consumption is insufficient, hypoglycemia may occur. Additionally, after the peak follows a valley in which low levels of exogenous insulin can lead to hyperglycemia.11
The second problem with NPH surrounds the inconsistency in both intersubject and intrasubject absorption rates. Absorption variability as great as 50% has been reported.12,13 This, of course, may lead to an increase in glycemic variability, that is, the magnitude of glucose fluctuation14 within a day. (Note: It has been hypothesized that, in conjunction with the A1C measure, glycemic variability may account in part for the long-term complications of diabetes.14)
Insulin Analogs
Radical advances in the potential for improved glucose control emerged with the development of insulin analogs.15,16 On the market now are three rapid-acting insulin analogs: lispro, aspart, and glulisine. Long-acting analogs are glargine and detemir, either of which may be given once or twice a day.17 Clinically, detemir is generally given twice per day in most patients with type 1 diabetes due to its shorter duration of action.
Most patients with type 1 diabetes are now managed with a once- or twice-daily injection of a long-acting insulin analog and one short-acting analog before each meal; thus, patients must take four or more insulin injections each day. While this multiple daily injection (MDI) insulin regimen approximates the body’s endogenous production of insulin more closely than the traditional split/mix regimens of NPH and regular insulin, there are still shortcomings. Once the long-acting insulin has been injected, it provides a steady level of insulin that cannot be adjusted for changes in the patient’s routine, such as exercise, delayed meals, or sleep, or for changes in the metabolic milieu, such as infection or other illness.18
PUMP BASICS
The CSII pump is a programmable insulin delivery system that provides continuous amounts of insulin and allows the user to deliver extra insulin to metabolize meals or to correct high blood glucose levels. Typically, rapid-acting insulin is used in the pump, although for patients with severe insulin resistance who need high doses of insulin, U-500 regular insulin may be used.19 U-500 regular insulin is a concentrated insulin dosed at one-fifth of U-100 regular insulin; that is, 100 units of regular insulin would equate to 20 units of U-500 insulin. (To clarify further, “U-100” refers to 100 U/mL, and “U-500” means 500 U/mL.) Understanding the indications for U-500 insulin and its adjustment is a specialized skill of the diabetologist experienced in its use.
A traditional pump consists of a beeper-sized device. It contains a reservoir that the user fills with insulin, then connects to an infusion set. The infusion set consists of tubing connected to a flexible catheter or needle that is inserted into the subcutaneous tissue. A mechanism to attach and detach the tubing from the infusion site is included so that users can disconnect it for bathing, sexual activity, contact sports, or other circumstances. Infusion sets are available in different sizes and styles to accommodate patients with different body weights, body fat levels, and lifestyle needs.
The “patch” or “wireless” pump, as it is sometimes called, is a self-contained unit or “pod” that resides directly on the skin, delivers insulin through a flexible catheter, and is disposed of or recycled every two to three days; it does not require tubing.
Potential pump users have a variety of manufacturers and models from which to choose, all providing similar features. Considerations for selecting a pump should include its particular features, cost of supplies, insurance coverage, customer service and support, and personal preference.
Basal and Bolus Insulin
The continuous background delivery in the pump is known as the basal; the rate at which the pump delivers the basal can be changed at different times of day to allow for changes in the patient’s routine and metabolic milieu (see Figure 1). Basal rates can be set anywhere between 0.025 and 35 units per hour. Most pumps allow for basal rates to last for as little as 30 minutes, but pump users commonly set one to four basal rates over 24 hours.
Some diabetic patients experience the dawn phenomenon, that is, fasting hyperglycemia resulting from the body’s release of growth hormone, cortisol, and adrenaline. These hormones, which produce a state of insulin resistance, are released beginning at about 2:00 to 3:00 am. A patient who is taking 24 units per day of total basal insulin might set a basal rate of one unit per hour; adjustments can be made if the patient needs less insulin at night and is prone to the dawn phenomenon.
All pumps begin basal rate programming at midnight. A basal rate profile for a patient who is prone to the dawn phenomenon and who needs 24 units/d of basal, goes to bed at 10:00 pm, and wakes up at 6:00 am, might look like this:
12:00 am: 0.8 units/h
3:00 am: 1.2 units/h
9:00 am: 1.0 units/h
10:00 pm: 0.8 units/h
Temporary basal rates may be set lower to account for exercise, or higher during times of illness. The pumper selects the amount released, the rate, and the length of time the temporary rate should last. After that selected time period is over, the pump automatically reverts to the regular basal rate. Setting lower basal rates before, during, or after exercise may benefit a patient who experiences exercise-related hypoglycemia. A patient who needs to adjust for exercise might select a temporary basal rate set to begin one hour before exercise and continue during exercise and for one hour after exercise.20
Even with these adjustments, however, low blood sugars may still occur, and delayed hypoglycemia may develop hours after exercise is completed.21 Muscle and liver tissue store excess sugar in the form of glycogen; glycogen stores are depleted during exercise, and blood sugar may decline when the muscle and liver take up blood sugar to replace the stores. In such instances, an extra carbohydrate snack and/or use of the temporary basal may prevent hypoglycemia.20
Setting temporary basal rates may also prevent hyperglycemia. In the absence of sufficient insulin, patients with type 1 diabetes produce ketones. Setting higher basal rates during illness, combined with frequent monitoring of blood sugars and ketones in the blood or urine, can prevent diabetic ketoacidosis (DKA). It is important for patients to understand that illness may increase their metabolic need for insulin.9 Even if the appetite decreases during illness, extra insulin may be needed. Frequent blood glucose monitoring and testing for ketones, when necessary, are essential for the patient with type 1 diabetes.
The supplemental insulin that patients take to compensate for carbohydrate intake and to correct high blood glucose is called the bolus. More recent pump technology, sometimes called the “smart” pump, includes features that will calculate for the patient how much of a bolus should be taken, based on three factors: carbohydrates ingested, current blood glucose level, and active insulin, that is, the amount of insulin that is still considered active after the patient takes a bolus based on the pharmacodynamic profile of the insulin.15,22
Carbohydrate-Counting
By the time a patient is started on an insulin pump, he or she should be proficient in carbohydrate-counting.8 There are several books on the market that list carbohydrate content of foods, including popular restaurant menu items and products sold in supermarkets. There are also apps available for PDAs and smart phones. The American Diabetes Association Web site (www.diabetes.org) offers carbohydrate-counting and menu-planning tools. For patients who eat out, it may be helpful to look up the restaurant’s menu online in advance and if possible, research the nutrition facts associated with each course selection. Even for patients with good carbohydrate-counting skills, it is often a challenge to get blood sugars into a desirable postprandial range.
The glycemic index is an important consideration. This 0-to-100–point scale is used to indicate how quickly specific foods raise blood sugar. Foods higher on the index (such as white potatoes and fruit juice) raise blood sugar more quickly than do foods that are lower on the index (whole grains, milk, nuts, and seeds).23 The caveat to using the glycemic index is that foods are often consumed as part of a mixed meal of proteins, fats, and carbohydrates—each of which will have a different effect on how rapidly blood sugars rise. Since fat slows digestion, meals that are high in both fats and carbohydrates can cause extended elevations in blood glucose.
To address this concern, smart pumps are equipped with an extended bolus feature that allows delivery of the bolus over a preset period of time.24 A percentage of the bolus may be delivered immediately and the remainder over time (dual-wave bolus). A typical split may be 50% now and 50% over the next two hours. This takes into account not only carbohydrate intake, but the components of a meal high in carbs and fat, such as pizza.
Several factors can impact the accuracy with which the patient calculates boluses to lower blood sugars for meals and other times of elevated blood glucose. Optimally, the total amount of correction insulin should represent only a small portion of the total daily bolus amount if the patient is being proactive. Ask patients about their carbohydrate-counting. Are they counting at a high skill level? Is their insulin-to-carbohydrate ratio correct? What about their inputs into their bolus calculator? Are their targets set too high or too low? Is their sensitivity correct? Is their active insulin time correct?
To assess postprandial control, patients should be instructed to check their blood glucose two hours after they started to ingest each meal.15 Consistent elevations mean that an adjustment to the insulin-to-carbohydrate ratio is indicated; alternatively, the patient may choose to consume fewer carbohydrates if weight is a concern.
If patients are not consistently measuring their foods (a discipline that is important but challenging to maintain), portion creep may be occurring. Encourage the patient to start measuring food again, at least for a while. A refresher visit to the nutritionist or diabetes educator may also be helpful. If patients are eating out often, they should be encouraged to limit themselves to meals with a known carbohydrate content.
Response to various foods is often idiosyncratic. Having patients keep a detailed log of foods eaten, exercise performed, and corresponding blood glucose levels will often clear up mysterious blood sugar elevations.
Correction Insulin
Depending on their personal approach and regimen, patients are taught to monitor their glucose either prior to eating, after eating, or both; and to take insulin to achieve a correction if the glucose is outside their target zone. A typical preprandial target range is 80 to 120 mg/dL, with 140 to 180 mg/dL two hours postprandial. (The American Association of Clinical Endocrinologists, while emphasizing the importance of individualizing glucose targets, suggests a fasting plasma glucose level below 110 mg/dL and a two-hour postprandial concentration below 140 mg/dL to achieve a target A1C level ≤ 6.5% in the nonpregnant adult.16 The American Diabetes Association’s comparable recommendations are 70 to 130 mg/dL preprandial and 180 mg/dL peak postprandial.15)
In today’s pumps, as part of the bolus calculation, a number can be programmed that represents the number of points in mg/dL by which one unit of insulin will reduce blood sugars. This may be known as a sensitivity or correction factor.
For example, a pumper who is making a postprandial correction and is not eating has a target blood sugar between 140 and 180 mg/dL and a sensitivity of 40; at present, his blood sugar is 230 mg/dL. Assuming no active insulin, the pump would calculate a dose of about 1.25 units of rapid-acting insulin.
How active insulin, or insulin on board, is calculated differs among pump manufacturers but is loosely based on original insulin pharmacodynamic studies.15,22 In smart pumps, the bolus calculator takes into consideration how much insulin is still active when it recommends a correction dose for hyperglycemia. This allows the user to address hyperglycemia quickly and effectively but prevents “stacking” of insulin doses and subsequent hypoglycemia.18
The active insulin time is preset in some pumps, but many diabetes clinicians use three or four hours (anecdotal evidence). The pumper can test the validity of active insulin by administering a correction bolus when blood glucose exceeds 250 mg/dL, then checking blood glucose levels every 30 to 60 minutes for six hours with no further food intake.9 The length of time it takes for blood sugars to return to target and remain steady is determined to be the correct duration of insulin action. In the example above, if the pump determined that there was active insulin remaining from the prior meal, it would subtract that amount from the calculation to prevent insulin stacking—which would most likely lead to overcorrection and hypoglycemia.
PUMP OPTIONS AND GLUCOSE MONITORING
In addition to using wireless communication, current “disposable” (“patch”) pumps operate without the conventional infusion set and tubing. Some smart pumps are now equipped with a combination device: a diabetes-specific, PDA-like apparatus with an integrated glucose monitor that links to the pump through infrared technology (see Figure 2). Another pump has a “linked” glucose monitor (see Figure 3) that allows the user to test blood sugar, with the reading downloaded to the pump. The pump (or PDA) calculates the needed dose, based on programmed insulin-to-carbohydrate ratios and correction factors.22
A bolus calculator on the PDA helps the user calculate the bolus dose to be delivered to the pump without the user’s having to remove the pump to administer a dose. The pumper can discreetly administer insulin, even when the patient is eating out.
The one patch pump that is currently on the market requires the user to set the PDA to bolus, since the pod has no buttons with which to input instructions for a bolus. Use of the PDA or linked meter requires the pumper to use a particular brand of test strips. If insurance does not cover that brand, the patient can use another manufacturer’s monitor and enter blood sugar readings manually.
Potential Pump Problems
Patients who are considering any CSII pump must be willing to check blood glucose levels frequently. Malfunction of insulin pumps (including a blockage or pump failure) is associated with an increased risk for DKA,8 because the pump delivers only short-acting insulin. Without the presence of long-acting insulin as a backup, DKA can develop rapidly. All pumps have pressure-sensing alarms to detect blockages; in patients who receive small doses of insulin, however, it may take time for the alarm to be triggered. Thus, the importance of frequent blood glucose monitoring is evident. (Additionally, in case of pump failure, patients should know their basal rates and insulin-to-carbohydrate ratios or keep them written down.)
Pumpers are taught that if they experience two or more unexplained high glucose readings in a row to troubleshoot the infusion set for air bubbles or a clog. They should also take an injection of insulin to correct the high glucose and change the reservoir and infusion set.
Continuous Glucose Monitor
Some patients use continuous glucose monitoring (CGM) with a sensor that measures glucose levels in the interstitial fluid. At the time of this writing, one currently available pump is equipped with an integrated glucose sensor (see Figure 3). This device monitors interstitial fluid glucose levels continuously and can provide trend data, letting the user know whether blood sugars are rising or falling and how rapidly.25
Recently, researchers for the Sensor-Augmented Pump Therapy for A1C Reduction (STAR 3) study26,27 reported that use of sensor-augmented insulin pumps (SAP) reduces A1C without increasing hypoglycemia, compared with MDI insulin regimens. Additional markers of success in SAP use, compared with an MDI regimen, are sensor glucose values that are closer to target, bolus-calculator interactions, amount of sensor use, and lower glycemic variability—especially in patients who achieve lower A1C.28,29
Even when the patient is using a glucose sensor, however, blood sugars must still be tested at least twice a day to calibrate the sensor. There is a common misperception that CGM serves as a substitute for blood glucose (finger-stick) monitoring, but there is a lag time between interstitial fluid glucose levels and blood glucose levels.30 Blood glucose monitoring by finger-stick is still considered the gold standard for measuring glucose; sensor manufacturers recommend that patients not take a treatment action based on sensor data without confirming first with a finger-stick.
Barriers to effective glucose sensor use include the high cost of sensors and variability in insurance coverage, user factors (patients’ not using sensors daily, calibrating them inaccurately), insertion-site infections, and technology issues, like sensor failure.27,31
Memory Features
Pump technology makes it possible to review bolus history (ie, the amount of bolus and the time at which it was given) as well as the dosage of insulin taken throughout the day. Based on these data, several assessments can be made:
• Is the basal-to-bolus ratio appropriate? (It should be about 40% to 50% basal / 50% to 60% bolus.)8
• Is the amount of insulin adequate? Adults and prepubertal children with type 1 diabetes usually require 0.6 to 0.9 units/kg/d.15 During puberty, insulin requirements can rise to 1.5 units/kg/d32 due to increased insulin resistance, surges in pubertal hormones, and greater caloric intake during growth spurts. Pump manufacturers offer data management software that allows the user to produce graphs, track trends, and monitor basal-to-bolus ratios.
• Is the patient actually bolusing for meals? Does the patient check blood glucose postprandially and bolus when the reading is high?
PATIENT TRAINING BEFORE PUMP INITIATION
Insurance coverage is generally favorable for pumps and associated supplies, since their cost benefit (ie, decreases in use of antidiabetic drugs and of health care resources6) is well proven for patients with type 1 diabetes. For those with type 2 diabetes, obtaining coverage is more challenging5 but can be supported if the patient has a history of severe hypoglycemia, insulin resistance, or uncontrolled blood sugar levels.6,7
Pump manufacturers employ insurance specialists to work with patients and providers in order to facilitate the insurance reimbursement process. Payment plans are available for what insurance does not cover, and pump warranties last for several years. Many insurance plans do not cover an automatic upgrade to a newer pump when the warranty expires, but the patient may be eligible for a discount on a newer pump.
Before initiating pump use, patients receive instruction from certified pump trainers—generally health professionals, such as nurses and registered dietitians, who may be employees of the endocrine practice or of the pump manufacturing company, or independent contractors; many are certified diabetes educators (CDEs). Training may be conducted in the patient’s home or in the medical office. Typically, patients are given some sort of DVD or CD-ROM and workbook to complete before pump training takes place.
Pump trainers make sure patients understand the basics of carbohydrate-counting, sick day management, and treatment of hypoglycemia and hyperglycemia. Training may comprise two sessions, one during which the patient can wear the pump with a saline administration and practice with it for a few days before starting on insulin at the second session. Training should be individualized to allow for different speeds and styles of learning.
Careful patient selection is the key to successful pump use. Optimally, patients should be motivated to improve their blood glucose control, compliant with their current regimen, and proficient in their diabetes self-management skills, including carbohydrate-counting, troubleshooting, and making adjustments for day-to-day variability in their circumstances.8
Pump trainers can make suggestions to the patient’s diabetologist regarding basal rates, correction factors, and insulin-to-carbohydrate ratios, but a health care provider’s order is necessary to initiate use of a pump.
RESOURCES FOR PATIENTS
Referral to a CDE and/or an endocrinology specialist may be helpful for any patient who was started on a pump in the past but is now struggling with management or would like to fine-tune his or her control. Patients who are unable to reduce an A1C of 8% may also benefit from referral. Not all of these practitioners operate at an expert level in pump therapy, however.
Given the shortage of endocrinologists and CDEs, especially in rural areas, finding a qualified practitioner is sometimes challenging. The American Association of Diabetes Educators maintains a referral service at www.diabeteseduca tor.org/find or (800) TeamUp4.
Patients can also contact the pump manufacturer to ask about local resources. Classes in advanced pumping skills and local pump support groups are often sponsored by pump manufacturers. Additionally, excellent books have been published on pump therapy and carbohydrate-counting, including those listed below.
RISKS AND BENEFITS OF INSULIN PUMP THERAPY
Risks of insulin pump therapy include DKA, infusion-site problems, and infection leading to abscess.27,33,34
In the absence of insulin, patients with type 1 diabetes produce ketones; because a pump uses only rapid- or short-acting insulin, a failure to deliver that insulin can lead to acute insulin deficiency, resulting in DKA. All pumps are equipped with pressure-sensitive alarms that will alert the user to a blockage that may result in failure to deliver insulin. Pump users who receive low doses of insulin (the absence of which may not cause sufficient pressure to trigger the alarm) or who experience pump blockages that cause only partial delivery may experience alarm failure. It is crucial for patients to monitor their blood sugar frequently; those who are unwilling to do so are not good candidates for insulin pump therapy.8
Infusion-site problems can include skin reactions to tape or infections resulting from inadequate cleansing or from failure to cleanse the site and change the infusion set, as recommended by the manufacturer, every two to three days. Pump trainers or the pump manufacturer’s customer service team can offer solutions to infusion-site skin care problems. Scrupulous handwashing, timely site changes, and cleansing of the skin are essential to preventing site problems.
Benefits of insulin pump therapy include the opportunity to individualize therapy for specific medical needs and lifestyle differences. Basal profiles can be individually adjusted for metabolic concerns, such as the dawn phenomenon or temporary illness—as well as day-to-day changes, such as increased physical activity. Bolus calculators allow for more accurate matching of the insulin-to-carbohydrate ratio and the amount of correction insulin necessary before meals.
CONCLUSION
CSII pumps may offer significant benefits to diabetic patients, compared with their current MDI regimen. These include reduction in A1C without increases in hypoglycemia, greater flexibility, improved quality of life—and, especially when used in conjunction with continuous glucose monitoring, reduction in glycemic variability. Patients and providers must bear in mind, however, that the pump is a tool, not a substitute for what guarantees success in diabetes management—namely, attention to meal planning, carbohydrate-counting, frequent blood sugar monitoring, competent sick day management, regular exercise, and target blood sugar and A1C goals. The patient most likely to benefit from insulin pump use is one with the motivation to make the lifestyle changes that effective therapy requires.
REFERENCES
1. General Hospital and Personal Use Medical Devices Panel Meeting—March 5, 2010. www .fda.gov/downloads/AdvisoryCommittees/Com mitteesMeetingMaterials/MedicalDevices/
MedicalDevicesAdvisoryCommittee/General HospitalandPersonalUseDevicesPanel/
UCM203749.pdf. Accessed October 21, 2011.
2. Fabiato K, Buse J, Duclos M, et al. Clinical experience with continuous glucose monitoring in adults. Diabetes Technol Ther. 2009;11 suppl 1:S93-S103.
3. Battelino T, Phillip M, Bratina N, et al. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care. 2011; 34(4):795-800
4. Edelman SV, Bode BW, Bailey TS, et al. Insulin pump therapy in patients with type 2 diabetes safely improved glycemic control using a simple insulin dosing regimen. Diabetes Technol Ther. 2010;12(8):627-633.
5. Skladany MJ, Miller M, Guthermann JS, Ludwig CR. Patch-pump technology to manage type 2 diabetes mellitus: hurdles to market acceptance. J Diabetes Sci Technol. 2008;2(6): 1147-1150.
6. Lynch PM, Riedel AA, Samant N, et al. Resource utilization with insulin pump therapy for type 2 diabetes mellitus. Am J Manag Care. 2010;16(12):892-896.
7. Nielsen S, Kain D, Szudzik E, et al. Use of continuous subcutaneous insulin infusion pump in patients with type 2 diabetes mellitus. Diabetes Educ. 2005;31(6):843-848.
8. Scheiner G, Sobel RJ, Smith DE, et al. Insulin pump therapy: guidelines for successful outcomes. Diabetes Educ. 2009;35 suppl 2:29S-41S.
9. Unger J. Insulin pump therapy. In: Unger J. Diabetes Management in Primary Care. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:265-320.
10. Hagedorn HC. Modifications of insulin. Physician’s Bull. 1947;12(5):26-33.
11. Salemyr J, Bang P, Örtqvist E. Lower HbA1c after 1 year, in children with type 1 diabetes treated with insulin glargine vs. NPH insulin from diagnosis: a retrospective study. Pediatr Diabetes. 2011;12(5):501-505.
12. Lauritzen T, Pramming S, Deckert T, Binder C. Pharmacokinetics of continuous subcutaneous insulin infusion. Diabetologia. 1983;24(5): 326-329.
13. Binder C, Lauritzen T, Faber O, Pramming S. Insulin pharmacokinetics. Diabetes Care. 1984; 7(2):188-199.
14. Brownlee M, Hirsch IB. Glycemic variability: a hemoglobin A1c–independent risk factor for diabetic complications. JAMA. 2006;295(14): 1707-1708.
15. American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care. 2008;31 suppl 1:S12-S54.
16. Handelsman Y, Mechanick JI, Blonde L, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for developing a diabetes mellitus comprehensive care plan. Endocrine Pract. 2011;17(suppl 2):1-53.
17. Kaufman F. Insulin treatment. In: Kaufman F, ed. Medical Management of Type 1 Diabetes. 5th ed. Alexandria, VA: American Diabetes Association; 2008:57-82.
18. Hirsch IB. Insulin analogues. N Engl J Med. 2005;352(2):174-183.
19. Cochran E, Musso C, Gorden P. The use of U-500 in patients with extreme insulin resistance. Diabetes Care. 2005;28(5):1240-1244.
20. Diabetes Research in Children Network (DirecNet) Study Group. Prevention of hypoglycemia during exercise in children with type 1 diabetes by suspending basal insulin. Diabetes Care. 2006;29(10):2200-2204.
21. Maran A, Pavan P, Bonsembiante B, et al. Continuous glucose monitoring reveals delayed nocturnal hypoglycemia after intermittent high-intensity exercise in nontrained patients with type 1 diabetes. Diabetes Technol Ther. 2010; 12(10):763-768.
22. Davidson PC, Hebblewhite HR, Steed RD, Bode BW. Analysis of guidelines for basal-bolus insulin dosing: basal insulin, correction factor, and carbohydrate-to-insulin ratio. Endocr Pract. 2008;14(9):1095-1101.
23. Glycemic Index Foundation, Sydney University Glycemic Index Research Service (SUGiRS). GI testing and research. www.glycemicindex
.com. Accessed October 21, 2011.
24. Pankowska E, Błazik M. Bolus calculator with nutrition database software, a new concept of prandial insulin programming for pump users.
J Diabetes Sci Technol. 2010;4(3):571-576.
25. Davis SN, Horton ES, Battelino T, et al. STAR 3 randomized controlled trial to compare sensor-augmented insulin pump therapy with multiple daily injections in the treatment of type 1 diabetes: research design, methods, and baseline characteristics of enrolled subjects. Diabetes Technol Ther. 2010;12(4):249-255.
26. Buse JB, Dailey G, Ahmann AA, et al. Baseline predictors of A1C reduction in adults using sensor-augmented pump therapy or multiple daily injection therapy: the STAR 3 experience. Diabetes Technol Ther. 2011;13(6):601-606.
27. Bergenstal RM, Tamborlane WV, Ahmann A, et al. Sensor-Augmented Pump Therapy for A1C Reduction (STAR 3) Study: results from the 6-month continuation phase. Diabetes Care. 2011 Sep 20. Epub ahead of print.
28. Green JB, Lane WS, Bergenstal RM, et al. Insulin Pump Settings Associated with Degree of Glycemic Improvement in Adults with Type 1 Diabetes Using Sensor-Augmented Pump Therapy. Presented at: Diabetes Technology Meeting; November 11-13, 2010; Bethesda, MD. Abstract A51.
29. Buse JB, Kidva YC, Guthrie RA, et al. Assessment of glycemic variability and CD40 ligand in the STAR 3 Study. Presented at: American Diabetes Association Scientific Sessions; June 2, 2011; San Diego, CA. Abstract 0923-P.
30. Hirsch IB. Algorithms for care in adults using continuous glucose monitoring. J Diabetes Sci Technol. 2007;1(1):126-129.
31. Wolpert HA. Continuous glucose monitoring: coming of age (editorial). N Engl J Med. 2010;363(4):383-384.
32. Wiegand S, Raile K, Reinehr T, et al; DPV-Wiss Study Group. Daily insulin requirement of children and adolescents with type 1 diabetes: effect of age, body mass index and mode of therapy. Eur J Endocrinol. 2008;158(4):543-549.
33. Hanas R, Ludvigsson J. Hypoglycemia and ketoacidosis with insulin pump therapy in children and adolescents. Pediatr Diabetes. 2006;7 suppl 4:32-38.
34. Unger J. A primary care approach to continuous subcutaneous insulin infusion. Clin Diabetes. 1999;17(3). http://journal.diabetes.org/clinicaldiabetes/V17N31999/Pg113.htm. Accessed October 21, 2011.
The FDA has reported that in 2007, 375,000 Americans with diabetes were using an insulin pump.1 Improvements in pump technology (including the addition of continuous glucose monitoring2,3), more data on the use of pumps in type 2 diabetes,4-7 improved insurance coverage,8 and the general population’s comfort with technology-based solutions may lead more patients with diabetes to choose a pump to deliver their insulin.
As a result, primary care practitioners will be increasingly likely to have patients who use continuous subcutaneous insulin infusion (CSII) pumps. While the initiation of pump therapy and follow-up with patients who use pumps have traditionally been the purview of endocrinologists, it is important for primary care providers to understand the basics of insulin pump therapy, enabling them to work collaboratively with the patient and the diabetes care team.
REVIEW OF INSULIN ACTION IN THE BODY
The body’s own (endogenous) insulin is secreted by the beta cells of the pancreas. Basal insulin is the background amount of insulin continuously released by the body in order to regulate hepatic glucose production and lipolysis. In response to food intake, the body releases additional insulin to match the glycemic effect of carbohydrates, fat, and protein.9
Insulin regimens attempt to mimic the body’s physiologic release of insulin by administering long-acting insulin to provide basal coverage, and rapid- or short-acting insulin to metabolize meals. The first long-acting insulin developed was NPH (still in use today), which was created by the addition of neutral protamine Hagedorn to regular insulin to delay insulin absorption.10
There are a few reasons that NPH use has fallen out of favor, especially for patients with type 1 diabetes, who do not produce endogenous insulin. One is a pronounced peak in action that requires patients to time their consumption of meals and snacks around peaks. If food consumption is insufficient, hypoglycemia may occur. Additionally, after the peak follows a valley in which low levels of exogenous insulin can lead to hyperglycemia.11
The second problem with NPH surrounds the inconsistency in both intersubject and intrasubject absorption rates. Absorption variability as great as 50% has been reported.12,13 This, of course, may lead to an increase in glycemic variability, that is, the magnitude of glucose fluctuation14 within a day. (Note: It has been hypothesized that, in conjunction with the A1C measure, glycemic variability may account in part for the long-term complications of diabetes.14)
Insulin Analogs
Radical advances in the potential for improved glucose control emerged with the development of insulin analogs.15,16 On the market now are three rapid-acting insulin analogs: lispro, aspart, and glulisine. Long-acting analogs are glargine and detemir, either of which may be given once or twice a day.17 Clinically, detemir is generally given twice per day in most patients with type 1 diabetes due to its shorter duration of action.
Most patients with type 1 diabetes are now managed with a once- or twice-daily injection of a long-acting insulin analog and one short-acting analog before each meal; thus, patients must take four or more insulin injections each day. While this multiple daily injection (MDI) insulin regimen approximates the body’s endogenous production of insulin more closely than the traditional split/mix regimens of NPH and regular insulin, there are still shortcomings. Once the long-acting insulin has been injected, it provides a steady level of insulin that cannot be adjusted for changes in the patient’s routine, such as exercise, delayed meals, or sleep, or for changes in the metabolic milieu, such as infection or other illness.18
PUMP BASICS
The CSII pump is a programmable insulin delivery system that provides continuous amounts of insulin and allows the user to deliver extra insulin to metabolize meals or to correct high blood glucose levels. Typically, rapid-acting insulin is used in the pump, although for patients with severe insulin resistance who need high doses of insulin, U-500 regular insulin may be used.19 U-500 regular insulin is a concentrated insulin dosed at one-fifth of U-100 regular insulin; that is, 100 units of regular insulin would equate to 20 units of U-500 insulin. (To clarify further, “U-100” refers to 100 U/mL, and “U-500” means 500 U/mL.) Understanding the indications for U-500 insulin and its adjustment is a specialized skill of the diabetologist experienced in its use.
A traditional pump consists of a beeper-sized device. It contains a reservoir that the user fills with insulin, then connects to an infusion set. The infusion set consists of tubing connected to a flexible catheter or needle that is inserted into the subcutaneous tissue. A mechanism to attach and detach the tubing from the infusion site is included so that users can disconnect it for bathing, sexual activity, contact sports, or other circumstances. Infusion sets are available in different sizes and styles to accommodate patients with different body weights, body fat levels, and lifestyle needs.
The “patch” or “wireless” pump, as it is sometimes called, is a self-contained unit or “pod” that resides directly on the skin, delivers insulin through a flexible catheter, and is disposed of or recycled every two to three days; it does not require tubing.
Potential pump users have a variety of manufacturers and models from which to choose, all providing similar features. Considerations for selecting a pump should include its particular features, cost of supplies, insurance coverage, customer service and support, and personal preference.
Basal and Bolus Insulin
The continuous background delivery in the pump is known as the basal; the rate at which the pump delivers the basal can be changed at different times of day to allow for changes in the patient’s routine and metabolic milieu (see Figure 1). Basal rates can be set anywhere between 0.025 and 35 units per hour. Most pumps allow for basal rates to last for as little as 30 minutes, but pump users commonly set one to four basal rates over 24 hours.
Some diabetic patients experience the dawn phenomenon, that is, fasting hyperglycemia resulting from the body’s release of growth hormone, cortisol, and adrenaline. These hormones, which produce a state of insulin resistance, are released beginning at about 2:00 to 3:00 am. A patient who is taking 24 units per day of total basal insulin might set a basal rate of one unit per hour; adjustments can be made if the patient needs less insulin at night and is prone to the dawn phenomenon.
All pumps begin basal rate programming at midnight. A basal rate profile for a patient who is prone to the dawn phenomenon and who needs 24 units/d of basal, goes to bed at 10:00 pm, and wakes up at 6:00 am, might look like this:
12:00 am: 0.8 units/h
3:00 am: 1.2 units/h
9:00 am: 1.0 units/h
10:00 pm: 0.8 units/h
Temporary basal rates may be set lower to account for exercise, or higher during times of illness. The pumper selects the amount released, the rate, and the length of time the temporary rate should last. After that selected time period is over, the pump automatically reverts to the regular basal rate. Setting lower basal rates before, during, or after exercise may benefit a patient who experiences exercise-related hypoglycemia. A patient who needs to adjust for exercise might select a temporary basal rate set to begin one hour before exercise and continue during exercise and for one hour after exercise.20
Even with these adjustments, however, low blood sugars may still occur, and delayed hypoglycemia may develop hours after exercise is completed.21 Muscle and liver tissue store excess sugar in the form of glycogen; glycogen stores are depleted during exercise, and blood sugar may decline when the muscle and liver take up blood sugar to replace the stores. In such instances, an extra carbohydrate snack and/or use of the temporary basal may prevent hypoglycemia.20
Setting temporary basal rates may also prevent hyperglycemia. In the absence of sufficient insulin, patients with type 1 diabetes produce ketones. Setting higher basal rates during illness, combined with frequent monitoring of blood sugars and ketones in the blood or urine, can prevent diabetic ketoacidosis (DKA). It is important for patients to understand that illness may increase their metabolic need for insulin.9 Even if the appetite decreases during illness, extra insulin may be needed. Frequent blood glucose monitoring and testing for ketones, when necessary, are essential for the patient with type 1 diabetes.
The supplemental insulin that patients take to compensate for carbohydrate intake and to correct high blood glucose is called the bolus. More recent pump technology, sometimes called the “smart” pump, includes features that will calculate for the patient how much of a bolus should be taken, based on three factors: carbohydrates ingested, current blood glucose level, and active insulin, that is, the amount of insulin that is still considered active after the patient takes a bolus based on the pharmacodynamic profile of the insulin.15,22
Carbohydrate-Counting
By the time a patient is started on an insulin pump, he or she should be proficient in carbohydrate-counting.8 There are several books on the market that list carbohydrate content of foods, including popular restaurant menu items and products sold in supermarkets. There are also apps available for PDAs and smart phones. The American Diabetes Association Web site (www.diabetes.org) offers carbohydrate-counting and menu-planning tools. For patients who eat out, it may be helpful to look up the restaurant’s menu online in advance and if possible, research the nutrition facts associated with each course selection. Even for patients with good carbohydrate-counting skills, it is often a challenge to get blood sugars into a desirable postprandial range.
The glycemic index is an important consideration. This 0-to-100–point scale is used to indicate how quickly specific foods raise blood sugar. Foods higher on the index (such as white potatoes and fruit juice) raise blood sugar more quickly than do foods that are lower on the index (whole grains, milk, nuts, and seeds).23 The caveat to using the glycemic index is that foods are often consumed as part of a mixed meal of proteins, fats, and carbohydrates—each of which will have a different effect on how rapidly blood sugars rise. Since fat slows digestion, meals that are high in both fats and carbohydrates can cause extended elevations in blood glucose.
To address this concern, smart pumps are equipped with an extended bolus feature that allows delivery of the bolus over a preset period of time.24 A percentage of the bolus may be delivered immediately and the remainder over time (dual-wave bolus). A typical split may be 50% now and 50% over the next two hours. This takes into account not only carbohydrate intake, but the components of a meal high in carbs and fat, such as pizza.
Several factors can impact the accuracy with which the patient calculates boluses to lower blood sugars for meals and other times of elevated blood glucose. Optimally, the total amount of correction insulin should represent only a small portion of the total daily bolus amount if the patient is being proactive. Ask patients about their carbohydrate-counting. Are they counting at a high skill level? Is their insulin-to-carbohydrate ratio correct? What about their inputs into their bolus calculator? Are their targets set too high or too low? Is their sensitivity correct? Is their active insulin time correct?
To assess postprandial control, patients should be instructed to check their blood glucose two hours after they started to ingest each meal.15 Consistent elevations mean that an adjustment to the insulin-to-carbohydrate ratio is indicated; alternatively, the patient may choose to consume fewer carbohydrates if weight is a concern.
If patients are not consistently measuring their foods (a discipline that is important but challenging to maintain), portion creep may be occurring. Encourage the patient to start measuring food again, at least for a while. A refresher visit to the nutritionist or diabetes educator may also be helpful. If patients are eating out often, they should be encouraged to limit themselves to meals with a known carbohydrate content.
Response to various foods is often idiosyncratic. Having patients keep a detailed log of foods eaten, exercise performed, and corresponding blood glucose levels will often clear up mysterious blood sugar elevations.
Correction Insulin
Depending on their personal approach and regimen, patients are taught to monitor their glucose either prior to eating, after eating, or both; and to take insulin to achieve a correction if the glucose is outside their target zone. A typical preprandial target range is 80 to 120 mg/dL, with 140 to 180 mg/dL two hours postprandial. (The American Association of Clinical Endocrinologists, while emphasizing the importance of individualizing glucose targets, suggests a fasting plasma glucose level below 110 mg/dL and a two-hour postprandial concentration below 140 mg/dL to achieve a target A1C level ≤ 6.5% in the nonpregnant adult.16 The American Diabetes Association’s comparable recommendations are 70 to 130 mg/dL preprandial and 180 mg/dL peak postprandial.15)
In today’s pumps, as part of the bolus calculation, a number can be programmed that represents the number of points in mg/dL by which one unit of insulin will reduce blood sugars. This may be known as a sensitivity or correction factor.
For example, a pumper who is making a postprandial correction and is not eating has a target blood sugar between 140 and 180 mg/dL and a sensitivity of 40; at present, his blood sugar is 230 mg/dL. Assuming no active insulin, the pump would calculate a dose of about 1.25 units of rapid-acting insulin.
How active insulin, or insulin on board, is calculated differs among pump manufacturers but is loosely based on original insulin pharmacodynamic studies.15,22 In smart pumps, the bolus calculator takes into consideration how much insulin is still active when it recommends a correction dose for hyperglycemia. This allows the user to address hyperglycemia quickly and effectively but prevents “stacking” of insulin doses and subsequent hypoglycemia.18
The active insulin time is preset in some pumps, but many diabetes clinicians use three or four hours (anecdotal evidence). The pumper can test the validity of active insulin by administering a correction bolus when blood glucose exceeds 250 mg/dL, then checking blood glucose levels every 30 to 60 minutes for six hours with no further food intake.9 The length of time it takes for blood sugars to return to target and remain steady is determined to be the correct duration of insulin action. In the example above, if the pump determined that there was active insulin remaining from the prior meal, it would subtract that amount from the calculation to prevent insulin stacking—which would most likely lead to overcorrection and hypoglycemia.
PUMP OPTIONS AND GLUCOSE MONITORING
In addition to using wireless communication, current “disposable” (“patch”) pumps operate without the conventional infusion set and tubing. Some smart pumps are now equipped with a combination device: a diabetes-specific, PDA-like apparatus with an integrated glucose monitor that links to the pump through infrared technology (see Figure 2). Another pump has a “linked” glucose monitor (see Figure 3) that allows the user to test blood sugar, with the reading downloaded to the pump. The pump (or PDA) calculates the needed dose, based on programmed insulin-to-carbohydrate ratios and correction factors.22
A bolus calculator on the PDA helps the user calculate the bolus dose to be delivered to the pump without the user’s having to remove the pump to administer a dose. The pumper can discreetly administer insulin, even when the patient is eating out.
The one patch pump that is currently on the market requires the user to set the PDA to bolus, since the pod has no buttons with which to input instructions for a bolus. Use of the PDA or linked meter requires the pumper to use a particular brand of test strips. If insurance does not cover that brand, the patient can use another manufacturer’s monitor and enter blood sugar readings manually.
Potential Pump Problems
Patients who are considering any CSII pump must be willing to check blood glucose levels frequently. Malfunction of insulin pumps (including a blockage or pump failure) is associated with an increased risk for DKA,8 because the pump delivers only short-acting insulin. Without the presence of long-acting insulin as a backup, DKA can develop rapidly. All pumps have pressure-sensing alarms to detect blockages; in patients who receive small doses of insulin, however, it may take time for the alarm to be triggered. Thus, the importance of frequent blood glucose monitoring is evident. (Additionally, in case of pump failure, patients should know their basal rates and insulin-to-carbohydrate ratios or keep them written down.)
Pumpers are taught that if they experience two or more unexplained high glucose readings in a row to troubleshoot the infusion set for air bubbles or a clog. They should also take an injection of insulin to correct the high glucose and change the reservoir and infusion set.
Continuous Glucose Monitor
Some patients use continuous glucose monitoring (CGM) with a sensor that measures glucose levels in the interstitial fluid. At the time of this writing, one currently available pump is equipped with an integrated glucose sensor (see Figure 3). This device monitors interstitial fluid glucose levels continuously and can provide trend data, letting the user know whether blood sugars are rising or falling and how rapidly.25
Recently, researchers for the Sensor-Augmented Pump Therapy for A1C Reduction (STAR 3) study26,27 reported that use of sensor-augmented insulin pumps (SAP) reduces A1C without increasing hypoglycemia, compared with MDI insulin regimens. Additional markers of success in SAP use, compared with an MDI regimen, are sensor glucose values that are closer to target, bolus-calculator interactions, amount of sensor use, and lower glycemic variability—especially in patients who achieve lower A1C.28,29
Even when the patient is using a glucose sensor, however, blood sugars must still be tested at least twice a day to calibrate the sensor. There is a common misperception that CGM serves as a substitute for blood glucose (finger-stick) monitoring, but there is a lag time between interstitial fluid glucose levels and blood glucose levels.30 Blood glucose monitoring by finger-stick is still considered the gold standard for measuring glucose; sensor manufacturers recommend that patients not take a treatment action based on sensor data without confirming first with a finger-stick.
Barriers to effective glucose sensor use include the high cost of sensors and variability in insurance coverage, user factors (patients’ not using sensors daily, calibrating them inaccurately), insertion-site infections, and technology issues, like sensor failure.27,31
Memory Features
Pump technology makes it possible to review bolus history (ie, the amount of bolus and the time at which it was given) as well as the dosage of insulin taken throughout the day. Based on these data, several assessments can be made:
• Is the basal-to-bolus ratio appropriate? (It should be about 40% to 50% basal / 50% to 60% bolus.)8
• Is the amount of insulin adequate? Adults and prepubertal children with type 1 diabetes usually require 0.6 to 0.9 units/kg/d.15 During puberty, insulin requirements can rise to 1.5 units/kg/d32 due to increased insulin resistance, surges in pubertal hormones, and greater caloric intake during growth spurts. Pump manufacturers offer data management software that allows the user to produce graphs, track trends, and monitor basal-to-bolus ratios.
• Is the patient actually bolusing for meals? Does the patient check blood glucose postprandially and bolus when the reading is high?
PATIENT TRAINING BEFORE PUMP INITIATION
Insurance coverage is generally favorable for pumps and associated supplies, since their cost benefit (ie, decreases in use of antidiabetic drugs and of health care resources6) is well proven for patients with type 1 diabetes. For those with type 2 diabetes, obtaining coverage is more challenging5 but can be supported if the patient has a history of severe hypoglycemia, insulin resistance, or uncontrolled blood sugar levels.6,7
Pump manufacturers employ insurance specialists to work with patients and providers in order to facilitate the insurance reimbursement process. Payment plans are available for what insurance does not cover, and pump warranties last for several years. Many insurance plans do not cover an automatic upgrade to a newer pump when the warranty expires, but the patient may be eligible for a discount on a newer pump.
Before initiating pump use, patients receive instruction from certified pump trainers—generally health professionals, such as nurses and registered dietitians, who may be employees of the endocrine practice or of the pump manufacturing company, or independent contractors; many are certified diabetes educators (CDEs). Training may be conducted in the patient’s home or in the medical office. Typically, patients are given some sort of DVD or CD-ROM and workbook to complete before pump training takes place.
Pump trainers make sure patients understand the basics of carbohydrate-counting, sick day management, and treatment of hypoglycemia and hyperglycemia. Training may comprise two sessions, one during which the patient can wear the pump with a saline administration and practice with it for a few days before starting on insulin at the second session. Training should be individualized to allow for different speeds and styles of learning.
Careful patient selection is the key to successful pump use. Optimally, patients should be motivated to improve their blood glucose control, compliant with their current regimen, and proficient in their diabetes self-management skills, including carbohydrate-counting, troubleshooting, and making adjustments for day-to-day variability in their circumstances.8
Pump trainers can make suggestions to the patient’s diabetologist regarding basal rates, correction factors, and insulin-to-carbohydrate ratios, but a health care provider’s order is necessary to initiate use of a pump.
RESOURCES FOR PATIENTS
Referral to a CDE and/or an endocrinology specialist may be helpful for any patient who was started on a pump in the past but is now struggling with management or would like to fine-tune his or her control. Patients who are unable to reduce an A1C of 8% may also benefit from referral. Not all of these practitioners operate at an expert level in pump therapy, however.
Given the shortage of endocrinologists and CDEs, especially in rural areas, finding a qualified practitioner is sometimes challenging. The American Association of Diabetes Educators maintains a referral service at www.diabeteseduca tor.org/find or (800) TeamUp4.
Patients can also contact the pump manufacturer to ask about local resources. Classes in advanced pumping skills and local pump support groups are often sponsored by pump manufacturers. Additionally, excellent books have been published on pump therapy and carbohydrate-counting, including those listed below.
RISKS AND BENEFITS OF INSULIN PUMP THERAPY
Risks of insulin pump therapy include DKA, infusion-site problems, and infection leading to abscess.27,33,34
In the absence of insulin, patients with type 1 diabetes produce ketones; because a pump uses only rapid- or short-acting insulin, a failure to deliver that insulin can lead to acute insulin deficiency, resulting in DKA. All pumps are equipped with pressure-sensitive alarms that will alert the user to a blockage that may result in failure to deliver insulin. Pump users who receive low doses of insulin (the absence of which may not cause sufficient pressure to trigger the alarm) or who experience pump blockages that cause only partial delivery may experience alarm failure. It is crucial for patients to monitor their blood sugar frequently; those who are unwilling to do so are not good candidates for insulin pump therapy.8
Infusion-site problems can include skin reactions to tape or infections resulting from inadequate cleansing or from failure to cleanse the site and change the infusion set, as recommended by the manufacturer, every two to three days. Pump trainers or the pump manufacturer’s customer service team can offer solutions to infusion-site skin care problems. Scrupulous handwashing, timely site changes, and cleansing of the skin are essential to preventing site problems.
Benefits of insulin pump therapy include the opportunity to individualize therapy for specific medical needs and lifestyle differences. Basal profiles can be individually adjusted for metabolic concerns, such as the dawn phenomenon or temporary illness—as well as day-to-day changes, such as increased physical activity. Bolus calculators allow for more accurate matching of the insulin-to-carbohydrate ratio and the amount of correction insulin necessary before meals.
CONCLUSION
CSII pumps may offer significant benefits to diabetic patients, compared with their current MDI regimen. These include reduction in A1C without increases in hypoglycemia, greater flexibility, improved quality of life—and, especially when used in conjunction with continuous glucose monitoring, reduction in glycemic variability. Patients and providers must bear in mind, however, that the pump is a tool, not a substitute for what guarantees success in diabetes management—namely, attention to meal planning, carbohydrate-counting, frequent blood sugar monitoring, competent sick day management, regular exercise, and target blood sugar and A1C goals. The patient most likely to benefit from insulin pump use is one with the motivation to make the lifestyle changes that effective therapy requires.
REFERENCES
1. General Hospital and Personal Use Medical Devices Panel Meeting—March 5, 2010. www .fda.gov/downloads/AdvisoryCommittees/Com mitteesMeetingMaterials/MedicalDevices/
MedicalDevicesAdvisoryCommittee/General HospitalandPersonalUseDevicesPanel/
UCM203749.pdf. Accessed October 21, 2011.
2. Fabiato K, Buse J, Duclos M, et al. Clinical experience with continuous glucose monitoring in adults. Diabetes Technol Ther. 2009;11 suppl 1:S93-S103.
3. Battelino T, Phillip M, Bratina N, et al. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care. 2011; 34(4):795-800
4. Edelman SV, Bode BW, Bailey TS, et al. Insulin pump therapy in patients with type 2 diabetes safely improved glycemic control using a simple insulin dosing regimen. Diabetes Technol Ther. 2010;12(8):627-633.
5. Skladany MJ, Miller M, Guthermann JS, Ludwig CR. Patch-pump technology to manage type 2 diabetes mellitus: hurdles to market acceptance. J Diabetes Sci Technol. 2008;2(6): 1147-1150.
6. Lynch PM, Riedel AA, Samant N, et al. Resource utilization with insulin pump therapy for type 2 diabetes mellitus. Am J Manag Care. 2010;16(12):892-896.
7. Nielsen S, Kain D, Szudzik E, et al. Use of continuous subcutaneous insulin infusion pump in patients with type 2 diabetes mellitus. Diabetes Educ. 2005;31(6):843-848.
8. Scheiner G, Sobel RJ, Smith DE, et al. Insulin pump therapy: guidelines for successful outcomes. Diabetes Educ. 2009;35 suppl 2:29S-41S.
9. Unger J. Insulin pump therapy. In: Unger J. Diabetes Management in Primary Care. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:265-320.
10. Hagedorn HC. Modifications of insulin. Physician’s Bull. 1947;12(5):26-33.
11. Salemyr J, Bang P, Örtqvist E. Lower HbA1c after 1 year, in children with type 1 diabetes treated with insulin glargine vs. NPH insulin from diagnosis: a retrospective study. Pediatr Diabetes. 2011;12(5):501-505.
12. Lauritzen T, Pramming S, Deckert T, Binder C. Pharmacokinetics of continuous subcutaneous insulin infusion. Diabetologia. 1983;24(5): 326-329.
13. Binder C, Lauritzen T, Faber O, Pramming S. Insulin pharmacokinetics. Diabetes Care. 1984; 7(2):188-199.
14. Brownlee M, Hirsch IB. Glycemic variability: a hemoglobin A1c–independent risk factor for diabetic complications. JAMA. 2006;295(14): 1707-1708.
15. American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care. 2008;31 suppl 1:S12-S54.
16. Handelsman Y, Mechanick JI, Blonde L, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for developing a diabetes mellitus comprehensive care plan. Endocrine Pract. 2011;17(suppl 2):1-53.
17. Kaufman F. Insulin treatment. In: Kaufman F, ed. Medical Management of Type 1 Diabetes. 5th ed. Alexandria, VA: American Diabetes Association; 2008:57-82.
18. Hirsch IB. Insulin analogues. N Engl J Med. 2005;352(2):174-183.
19. Cochran E, Musso C, Gorden P. The use of U-500 in patients with extreme insulin resistance. Diabetes Care. 2005;28(5):1240-1244.
20. Diabetes Research in Children Network (DirecNet) Study Group. Prevention of hypoglycemia during exercise in children with type 1 diabetes by suspending basal insulin. Diabetes Care. 2006;29(10):2200-2204.
21. Maran A, Pavan P, Bonsembiante B, et al. Continuous glucose monitoring reveals delayed nocturnal hypoglycemia after intermittent high-intensity exercise in nontrained patients with type 1 diabetes. Diabetes Technol Ther. 2010; 12(10):763-768.
22. Davidson PC, Hebblewhite HR, Steed RD, Bode BW. Analysis of guidelines for basal-bolus insulin dosing: basal insulin, correction factor, and carbohydrate-to-insulin ratio. Endocr Pract. 2008;14(9):1095-1101.
23. Glycemic Index Foundation, Sydney University Glycemic Index Research Service (SUGiRS). GI testing and research. www.glycemicindex
.com. Accessed October 21, 2011.
24. Pankowska E, Błazik M. Bolus calculator with nutrition database software, a new concept of prandial insulin programming for pump users.
J Diabetes Sci Technol. 2010;4(3):571-576.
25. Davis SN, Horton ES, Battelino T, et al. STAR 3 randomized controlled trial to compare sensor-augmented insulin pump therapy with multiple daily injections in the treatment of type 1 diabetes: research design, methods, and baseline characteristics of enrolled subjects. Diabetes Technol Ther. 2010;12(4):249-255.
26. Buse JB, Dailey G, Ahmann AA, et al. Baseline predictors of A1C reduction in adults using sensor-augmented pump therapy or multiple daily injection therapy: the STAR 3 experience. Diabetes Technol Ther. 2011;13(6):601-606.
27. Bergenstal RM, Tamborlane WV, Ahmann A, et al. Sensor-Augmented Pump Therapy for A1C Reduction (STAR 3) Study: results from the 6-month continuation phase. Diabetes Care. 2011 Sep 20. Epub ahead of print.
28. Green JB, Lane WS, Bergenstal RM, et al. Insulin Pump Settings Associated with Degree of Glycemic Improvement in Adults with Type 1 Diabetes Using Sensor-Augmented Pump Therapy. Presented at: Diabetes Technology Meeting; November 11-13, 2010; Bethesda, MD. Abstract A51.
29. Buse JB, Kidva YC, Guthrie RA, et al. Assessment of glycemic variability and CD40 ligand in the STAR 3 Study. Presented at: American Diabetes Association Scientific Sessions; June 2, 2011; San Diego, CA. Abstract 0923-P.
30. Hirsch IB. Algorithms for care in adults using continuous glucose monitoring. J Diabetes Sci Technol. 2007;1(1):126-129.
31. Wolpert HA. Continuous glucose monitoring: coming of age (editorial). N Engl J Med. 2010;363(4):383-384.
32. Wiegand S, Raile K, Reinehr T, et al; DPV-Wiss Study Group. Daily insulin requirement of children and adolescents with type 1 diabetes: effect of age, body mass index and mode of therapy. Eur J Endocrinol. 2008;158(4):543-549.
33. Hanas R, Ludvigsson J. Hypoglycemia and ketoacidosis with insulin pump therapy in children and adolescents. Pediatr Diabetes. 2006;7 suppl 4:32-38.
34. Unger J. A primary care approach to continuous subcutaneous insulin infusion. Clin Diabetes. 1999;17(3). http://journal.diabetes.org/clinicaldiabetes/V17N31999/Pg113.htm. Accessed October 21, 2011.
The FDA has reported that in 2007, 375,000 Americans with diabetes were using an insulin pump.1 Improvements in pump technology (including the addition of continuous glucose monitoring2,3), more data on the use of pumps in type 2 diabetes,4-7 improved insurance coverage,8 and the general population’s comfort with technology-based solutions may lead more patients with diabetes to choose a pump to deliver their insulin.
As a result, primary care practitioners will be increasingly likely to have patients who use continuous subcutaneous insulin infusion (CSII) pumps. While the initiation of pump therapy and follow-up with patients who use pumps have traditionally been the purview of endocrinologists, it is important for primary care providers to understand the basics of insulin pump therapy, enabling them to work collaboratively with the patient and the diabetes care team.
REVIEW OF INSULIN ACTION IN THE BODY
The body’s own (endogenous) insulin is secreted by the beta cells of the pancreas. Basal insulin is the background amount of insulin continuously released by the body in order to regulate hepatic glucose production and lipolysis. In response to food intake, the body releases additional insulin to match the glycemic effect of carbohydrates, fat, and protein.9
Insulin regimens attempt to mimic the body’s physiologic release of insulin by administering long-acting insulin to provide basal coverage, and rapid- or short-acting insulin to metabolize meals. The first long-acting insulin developed was NPH (still in use today), which was created by the addition of neutral protamine Hagedorn to regular insulin to delay insulin absorption.10
There are a few reasons that NPH use has fallen out of favor, especially for patients with type 1 diabetes, who do not produce endogenous insulin. One is a pronounced peak in action that requires patients to time their consumption of meals and snacks around peaks. If food consumption is insufficient, hypoglycemia may occur. Additionally, after the peak follows a valley in which low levels of exogenous insulin can lead to hyperglycemia.11
The second problem with NPH surrounds the inconsistency in both intersubject and intrasubject absorption rates. Absorption variability as great as 50% has been reported.12,13 This, of course, may lead to an increase in glycemic variability, that is, the magnitude of glucose fluctuation14 within a day. (Note: It has been hypothesized that, in conjunction with the A1C measure, glycemic variability may account in part for the long-term complications of diabetes.14)
Insulin Analogs
Radical advances in the potential for improved glucose control emerged with the development of insulin analogs.15,16 On the market now are three rapid-acting insulin analogs: lispro, aspart, and glulisine. Long-acting analogs are glargine and detemir, either of which may be given once or twice a day.17 Clinically, detemir is generally given twice per day in most patients with type 1 diabetes due to its shorter duration of action.
Most patients with type 1 diabetes are now managed with a once- or twice-daily injection of a long-acting insulin analog and one short-acting analog before each meal; thus, patients must take four or more insulin injections each day. While this multiple daily injection (MDI) insulin regimen approximates the body’s endogenous production of insulin more closely than the traditional split/mix regimens of NPH and regular insulin, there are still shortcomings. Once the long-acting insulin has been injected, it provides a steady level of insulin that cannot be adjusted for changes in the patient’s routine, such as exercise, delayed meals, or sleep, or for changes in the metabolic milieu, such as infection or other illness.18
PUMP BASICS
The CSII pump is a programmable insulin delivery system that provides continuous amounts of insulin and allows the user to deliver extra insulin to metabolize meals or to correct high blood glucose levels. Typically, rapid-acting insulin is used in the pump, although for patients with severe insulin resistance who need high doses of insulin, U-500 regular insulin may be used.19 U-500 regular insulin is a concentrated insulin dosed at one-fifth of U-100 regular insulin; that is, 100 units of regular insulin would equate to 20 units of U-500 insulin. (To clarify further, “U-100” refers to 100 U/mL, and “U-500” means 500 U/mL.) Understanding the indications for U-500 insulin and its adjustment is a specialized skill of the diabetologist experienced in its use.
A traditional pump consists of a beeper-sized device. It contains a reservoir that the user fills with insulin, then connects to an infusion set. The infusion set consists of tubing connected to a flexible catheter or needle that is inserted into the subcutaneous tissue. A mechanism to attach and detach the tubing from the infusion site is included so that users can disconnect it for bathing, sexual activity, contact sports, or other circumstances. Infusion sets are available in different sizes and styles to accommodate patients with different body weights, body fat levels, and lifestyle needs.
The “patch” or “wireless” pump, as it is sometimes called, is a self-contained unit or “pod” that resides directly on the skin, delivers insulin through a flexible catheter, and is disposed of or recycled every two to three days; it does not require tubing.
Potential pump users have a variety of manufacturers and models from which to choose, all providing similar features. Considerations for selecting a pump should include its particular features, cost of supplies, insurance coverage, customer service and support, and personal preference.
Basal and Bolus Insulin
The continuous background delivery in the pump is known as the basal; the rate at which the pump delivers the basal can be changed at different times of day to allow for changes in the patient’s routine and metabolic milieu (see Figure 1). Basal rates can be set anywhere between 0.025 and 35 units per hour. Most pumps allow for basal rates to last for as little as 30 minutes, but pump users commonly set one to four basal rates over 24 hours.
Some diabetic patients experience the dawn phenomenon, that is, fasting hyperglycemia resulting from the body’s release of growth hormone, cortisol, and adrenaline. These hormones, which produce a state of insulin resistance, are released beginning at about 2:00 to 3:00 am. A patient who is taking 24 units per day of total basal insulin might set a basal rate of one unit per hour; adjustments can be made if the patient needs less insulin at night and is prone to the dawn phenomenon.
All pumps begin basal rate programming at midnight. A basal rate profile for a patient who is prone to the dawn phenomenon and who needs 24 units/d of basal, goes to bed at 10:00 pm, and wakes up at 6:00 am, might look like this:
12:00 am: 0.8 units/h
3:00 am: 1.2 units/h
9:00 am: 1.0 units/h
10:00 pm: 0.8 units/h
Temporary basal rates may be set lower to account for exercise, or higher during times of illness. The pumper selects the amount released, the rate, and the length of time the temporary rate should last. After that selected time period is over, the pump automatically reverts to the regular basal rate. Setting lower basal rates before, during, or after exercise may benefit a patient who experiences exercise-related hypoglycemia. A patient who needs to adjust for exercise might select a temporary basal rate set to begin one hour before exercise and continue during exercise and for one hour after exercise.20
Even with these adjustments, however, low blood sugars may still occur, and delayed hypoglycemia may develop hours after exercise is completed.21 Muscle and liver tissue store excess sugar in the form of glycogen; glycogen stores are depleted during exercise, and blood sugar may decline when the muscle and liver take up blood sugar to replace the stores. In such instances, an extra carbohydrate snack and/or use of the temporary basal may prevent hypoglycemia.20
Setting temporary basal rates may also prevent hyperglycemia. In the absence of sufficient insulin, patients with type 1 diabetes produce ketones. Setting higher basal rates during illness, combined with frequent monitoring of blood sugars and ketones in the blood or urine, can prevent diabetic ketoacidosis (DKA). It is important for patients to understand that illness may increase their metabolic need for insulin.9 Even if the appetite decreases during illness, extra insulin may be needed. Frequent blood glucose monitoring and testing for ketones, when necessary, are essential for the patient with type 1 diabetes.
The supplemental insulin that patients take to compensate for carbohydrate intake and to correct high blood glucose is called the bolus. More recent pump technology, sometimes called the “smart” pump, includes features that will calculate for the patient how much of a bolus should be taken, based on three factors: carbohydrates ingested, current blood glucose level, and active insulin, that is, the amount of insulin that is still considered active after the patient takes a bolus based on the pharmacodynamic profile of the insulin.15,22
Carbohydrate-Counting
By the time a patient is started on an insulin pump, he or she should be proficient in carbohydrate-counting.8 There are several books on the market that list carbohydrate content of foods, including popular restaurant menu items and products sold in supermarkets. There are also apps available for PDAs and smart phones. The American Diabetes Association Web site (www.diabetes.org) offers carbohydrate-counting and menu-planning tools. For patients who eat out, it may be helpful to look up the restaurant’s menu online in advance and if possible, research the nutrition facts associated with each course selection. Even for patients with good carbohydrate-counting skills, it is often a challenge to get blood sugars into a desirable postprandial range.
The glycemic index is an important consideration. This 0-to-100–point scale is used to indicate how quickly specific foods raise blood sugar. Foods higher on the index (such as white potatoes and fruit juice) raise blood sugar more quickly than do foods that are lower on the index (whole grains, milk, nuts, and seeds).23 The caveat to using the glycemic index is that foods are often consumed as part of a mixed meal of proteins, fats, and carbohydrates—each of which will have a different effect on how rapidly blood sugars rise. Since fat slows digestion, meals that are high in both fats and carbohydrates can cause extended elevations in blood glucose.
To address this concern, smart pumps are equipped with an extended bolus feature that allows delivery of the bolus over a preset period of time.24 A percentage of the bolus may be delivered immediately and the remainder over time (dual-wave bolus). A typical split may be 50% now and 50% over the next two hours. This takes into account not only carbohydrate intake, but the components of a meal high in carbs and fat, such as pizza.
Several factors can impact the accuracy with which the patient calculates boluses to lower blood sugars for meals and other times of elevated blood glucose. Optimally, the total amount of correction insulin should represent only a small portion of the total daily bolus amount if the patient is being proactive. Ask patients about their carbohydrate-counting. Are they counting at a high skill level? Is their insulin-to-carbohydrate ratio correct? What about their inputs into their bolus calculator? Are their targets set too high or too low? Is their sensitivity correct? Is their active insulin time correct?
To assess postprandial control, patients should be instructed to check their blood glucose two hours after they started to ingest each meal.15 Consistent elevations mean that an adjustment to the insulin-to-carbohydrate ratio is indicated; alternatively, the patient may choose to consume fewer carbohydrates if weight is a concern.
If patients are not consistently measuring their foods (a discipline that is important but challenging to maintain), portion creep may be occurring. Encourage the patient to start measuring food again, at least for a while. A refresher visit to the nutritionist or diabetes educator may also be helpful. If patients are eating out often, they should be encouraged to limit themselves to meals with a known carbohydrate content.
Response to various foods is often idiosyncratic. Having patients keep a detailed log of foods eaten, exercise performed, and corresponding blood glucose levels will often clear up mysterious blood sugar elevations.
Correction Insulin
Depending on their personal approach and regimen, patients are taught to monitor their glucose either prior to eating, after eating, or both; and to take insulin to achieve a correction if the glucose is outside their target zone. A typical preprandial target range is 80 to 120 mg/dL, with 140 to 180 mg/dL two hours postprandial. (The American Association of Clinical Endocrinologists, while emphasizing the importance of individualizing glucose targets, suggests a fasting plasma glucose level below 110 mg/dL and a two-hour postprandial concentration below 140 mg/dL to achieve a target A1C level ≤ 6.5% in the nonpregnant adult.16 The American Diabetes Association’s comparable recommendations are 70 to 130 mg/dL preprandial and 180 mg/dL peak postprandial.15)
In today’s pumps, as part of the bolus calculation, a number can be programmed that represents the number of points in mg/dL by which one unit of insulin will reduce blood sugars. This may be known as a sensitivity or correction factor.
For example, a pumper who is making a postprandial correction and is not eating has a target blood sugar between 140 and 180 mg/dL and a sensitivity of 40; at present, his blood sugar is 230 mg/dL. Assuming no active insulin, the pump would calculate a dose of about 1.25 units of rapid-acting insulin.
How active insulin, or insulin on board, is calculated differs among pump manufacturers but is loosely based on original insulin pharmacodynamic studies.15,22 In smart pumps, the bolus calculator takes into consideration how much insulin is still active when it recommends a correction dose for hyperglycemia. This allows the user to address hyperglycemia quickly and effectively but prevents “stacking” of insulin doses and subsequent hypoglycemia.18
The active insulin time is preset in some pumps, but many diabetes clinicians use three or four hours (anecdotal evidence). The pumper can test the validity of active insulin by administering a correction bolus when blood glucose exceeds 250 mg/dL, then checking blood glucose levels every 30 to 60 minutes for six hours with no further food intake.9 The length of time it takes for blood sugars to return to target and remain steady is determined to be the correct duration of insulin action. In the example above, if the pump determined that there was active insulin remaining from the prior meal, it would subtract that amount from the calculation to prevent insulin stacking—which would most likely lead to overcorrection and hypoglycemia.
PUMP OPTIONS AND GLUCOSE MONITORING
In addition to using wireless communication, current “disposable” (“patch”) pumps operate without the conventional infusion set and tubing. Some smart pumps are now equipped with a combination device: a diabetes-specific, PDA-like apparatus with an integrated glucose monitor that links to the pump through infrared technology (see Figure 2). Another pump has a “linked” glucose monitor (see Figure 3) that allows the user to test blood sugar, with the reading downloaded to the pump. The pump (or PDA) calculates the needed dose, based on programmed insulin-to-carbohydrate ratios and correction factors.22
A bolus calculator on the PDA helps the user calculate the bolus dose to be delivered to the pump without the user’s having to remove the pump to administer a dose. The pumper can discreetly administer insulin, even when the patient is eating out.
The one patch pump that is currently on the market requires the user to set the PDA to bolus, since the pod has no buttons with which to input instructions for a bolus. Use of the PDA or linked meter requires the pumper to use a particular brand of test strips. If insurance does not cover that brand, the patient can use another manufacturer’s monitor and enter blood sugar readings manually.
Potential Pump Problems
Patients who are considering any CSII pump must be willing to check blood glucose levels frequently. Malfunction of insulin pumps (including a blockage or pump failure) is associated with an increased risk for DKA,8 because the pump delivers only short-acting insulin. Without the presence of long-acting insulin as a backup, DKA can develop rapidly. All pumps have pressure-sensing alarms to detect blockages; in patients who receive small doses of insulin, however, it may take time for the alarm to be triggered. Thus, the importance of frequent blood glucose monitoring is evident. (Additionally, in case of pump failure, patients should know their basal rates and insulin-to-carbohydrate ratios or keep them written down.)
Pumpers are taught that if they experience two or more unexplained high glucose readings in a row to troubleshoot the infusion set for air bubbles or a clog. They should also take an injection of insulin to correct the high glucose and change the reservoir and infusion set.
Continuous Glucose Monitor
Some patients use continuous glucose monitoring (CGM) with a sensor that measures glucose levels in the interstitial fluid. At the time of this writing, one currently available pump is equipped with an integrated glucose sensor (see Figure 3). This device monitors interstitial fluid glucose levels continuously and can provide trend data, letting the user know whether blood sugars are rising or falling and how rapidly.25
Recently, researchers for the Sensor-Augmented Pump Therapy for A1C Reduction (STAR 3) study26,27 reported that use of sensor-augmented insulin pumps (SAP) reduces A1C without increasing hypoglycemia, compared with MDI insulin regimens. Additional markers of success in SAP use, compared with an MDI regimen, are sensor glucose values that are closer to target, bolus-calculator interactions, amount of sensor use, and lower glycemic variability—especially in patients who achieve lower A1C.28,29
Even when the patient is using a glucose sensor, however, blood sugars must still be tested at least twice a day to calibrate the sensor. There is a common misperception that CGM serves as a substitute for blood glucose (finger-stick) monitoring, but there is a lag time between interstitial fluid glucose levels and blood glucose levels.30 Blood glucose monitoring by finger-stick is still considered the gold standard for measuring glucose; sensor manufacturers recommend that patients not take a treatment action based on sensor data without confirming first with a finger-stick.
Barriers to effective glucose sensor use include the high cost of sensors and variability in insurance coverage, user factors (patients’ not using sensors daily, calibrating them inaccurately), insertion-site infections, and technology issues, like sensor failure.27,31
Memory Features
Pump technology makes it possible to review bolus history (ie, the amount of bolus and the time at which it was given) as well as the dosage of insulin taken throughout the day. Based on these data, several assessments can be made:
• Is the basal-to-bolus ratio appropriate? (It should be about 40% to 50% basal / 50% to 60% bolus.)8
• Is the amount of insulin adequate? Adults and prepubertal children with type 1 diabetes usually require 0.6 to 0.9 units/kg/d.15 During puberty, insulin requirements can rise to 1.5 units/kg/d32 due to increased insulin resistance, surges in pubertal hormones, and greater caloric intake during growth spurts. Pump manufacturers offer data management software that allows the user to produce graphs, track trends, and monitor basal-to-bolus ratios.
• Is the patient actually bolusing for meals? Does the patient check blood glucose postprandially and bolus when the reading is high?
PATIENT TRAINING BEFORE PUMP INITIATION
Insurance coverage is generally favorable for pumps and associated supplies, since their cost benefit (ie, decreases in use of antidiabetic drugs and of health care resources6) is well proven for patients with type 1 diabetes. For those with type 2 diabetes, obtaining coverage is more challenging5 but can be supported if the patient has a history of severe hypoglycemia, insulin resistance, or uncontrolled blood sugar levels.6,7
Pump manufacturers employ insurance specialists to work with patients and providers in order to facilitate the insurance reimbursement process. Payment plans are available for what insurance does not cover, and pump warranties last for several years. Many insurance plans do not cover an automatic upgrade to a newer pump when the warranty expires, but the patient may be eligible for a discount on a newer pump.
Before initiating pump use, patients receive instruction from certified pump trainers—generally health professionals, such as nurses and registered dietitians, who may be employees of the endocrine practice or of the pump manufacturing company, or independent contractors; many are certified diabetes educators (CDEs). Training may be conducted in the patient’s home or in the medical office. Typically, patients are given some sort of DVD or CD-ROM and workbook to complete before pump training takes place.
Pump trainers make sure patients understand the basics of carbohydrate-counting, sick day management, and treatment of hypoglycemia and hyperglycemia. Training may comprise two sessions, one during which the patient can wear the pump with a saline administration and practice with it for a few days before starting on insulin at the second session. Training should be individualized to allow for different speeds and styles of learning.
Careful patient selection is the key to successful pump use. Optimally, patients should be motivated to improve their blood glucose control, compliant with their current regimen, and proficient in their diabetes self-management skills, including carbohydrate-counting, troubleshooting, and making adjustments for day-to-day variability in their circumstances.8
Pump trainers can make suggestions to the patient’s diabetologist regarding basal rates, correction factors, and insulin-to-carbohydrate ratios, but a health care provider’s order is necessary to initiate use of a pump.
RESOURCES FOR PATIENTS
Referral to a CDE and/or an endocrinology specialist may be helpful for any patient who was started on a pump in the past but is now struggling with management or would like to fine-tune his or her control. Patients who are unable to reduce an A1C of 8% may also benefit from referral. Not all of these practitioners operate at an expert level in pump therapy, however.
Given the shortage of endocrinologists and CDEs, especially in rural areas, finding a qualified practitioner is sometimes challenging. The American Association of Diabetes Educators maintains a referral service at www.diabeteseduca tor.org/find or (800) TeamUp4.
Patients can also contact the pump manufacturer to ask about local resources. Classes in advanced pumping skills and local pump support groups are often sponsored by pump manufacturers. Additionally, excellent books have been published on pump therapy and carbohydrate-counting, including those listed below.
RISKS AND BENEFITS OF INSULIN PUMP THERAPY
Risks of insulin pump therapy include DKA, infusion-site problems, and infection leading to abscess.27,33,34
In the absence of insulin, patients with type 1 diabetes produce ketones; because a pump uses only rapid- or short-acting insulin, a failure to deliver that insulin can lead to acute insulin deficiency, resulting in DKA. All pumps are equipped with pressure-sensitive alarms that will alert the user to a blockage that may result in failure to deliver insulin. Pump users who receive low doses of insulin (the absence of which may not cause sufficient pressure to trigger the alarm) or who experience pump blockages that cause only partial delivery may experience alarm failure. It is crucial for patients to monitor their blood sugar frequently; those who are unwilling to do so are not good candidates for insulin pump therapy.8
Infusion-site problems can include skin reactions to tape or infections resulting from inadequate cleansing or from failure to cleanse the site and change the infusion set, as recommended by the manufacturer, every two to three days. Pump trainers or the pump manufacturer’s customer service team can offer solutions to infusion-site skin care problems. Scrupulous handwashing, timely site changes, and cleansing of the skin are essential to preventing site problems.
Benefits of insulin pump therapy include the opportunity to individualize therapy for specific medical needs and lifestyle differences. Basal profiles can be individually adjusted for metabolic concerns, such as the dawn phenomenon or temporary illness—as well as day-to-day changes, such as increased physical activity. Bolus calculators allow for more accurate matching of the insulin-to-carbohydrate ratio and the amount of correction insulin necessary before meals.
CONCLUSION
CSII pumps may offer significant benefits to diabetic patients, compared with their current MDI regimen. These include reduction in A1C without increases in hypoglycemia, greater flexibility, improved quality of life—and, especially when used in conjunction with continuous glucose monitoring, reduction in glycemic variability. Patients and providers must bear in mind, however, that the pump is a tool, not a substitute for what guarantees success in diabetes management—namely, attention to meal planning, carbohydrate-counting, frequent blood sugar monitoring, competent sick day management, regular exercise, and target blood sugar and A1C goals. The patient most likely to benefit from insulin pump use is one with the motivation to make the lifestyle changes that effective therapy requires.
REFERENCES
1. General Hospital and Personal Use Medical Devices Panel Meeting—March 5, 2010. www .fda.gov/downloads/AdvisoryCommittees/Com mitteesMeetingMaterials/MedicalDevices/
MedicalDevicesAdvisoryCommittee/General HospitalandPersonalUseDevicesPanel/
UCM203749.pdf. Accessed October 21, 2011.
2. Fabiato K, Buse J, Duclos M, et al. Clinical experience with continuous glucose monitoring in adults. Diabetes Technol Ther. 2009;11 suppl 1:S93-S103.
3. Battelino T, Phillip M, Bratina N, et al. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care. 2011; 34(4):795-800
4. Edelman SV, Bode BW, Bailey TS, et al. Insulin pump therapy in patients with type 2 diabetes safely improved glycemic control using a simple insulin dosing regimen. Diabetes Technol Ther. 2010;12(8):627-633.
5. Skladany MJ, Miller M, Guthermann JS, Ludwig CR. Patch-pump technology to manage type 2 diabetes mellitus: hurdles to market acceptance. J Diabetes Sci Technol. 2008;2(6): 1147-1150.
6. Lynch PM, Riedel AA, Samant N, et al. Resource utilization with insulin pump therapy for type 2 diabetes mellitus. Am J Manag Care. 2010;16(12):892-896.
7. Nielsen S, Kain D, Szudzik E, et al. Use of continuous subcutaneous insulin infusion pump in patients with type 2 diabetes mellitus. Diabetes Educ. 2005;31(6):843-848.
8. Scheiner G, Sobel RJ, Smith DE, et al. Insulin pump therapy: guidelines for successful outcomes. Diabetes Educ. 2009;35 suppl 2:29S-41S.
9. Unger J. Insulin pump therapy. In: Unger J. Diabetes Management in Primary Care. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:265-320.
10. Hagedorn HC. Modifications of insulin. Physician’s Bull. 1947;12(5):26-33.
11. Salemyr J, Bang P, Örtqvist E. Lower HbA1c after 1 year, in children with type 1 diabetes treated with insulin glargine vs. NPH insulin from diagnosis: a retrospective study. Pediatr Diabetes. 2011;12(5):501-505.
12. Lauritzen T, Pramming S, Deckert T, Binder C. Pharmacokinetics of continuous subcutaneous insulin infusion. Diabetologia. 1983;24(5): 326-329.
13. Binder C, Lauritzen T, Faber O, Pramming S. Insulin pharmacokinetics. Diabetes Care. 1984; 7(2):188-199.
14. Brownlee M, Hirsch IB. Glycemic variability: a hemoglobin A1c–independent risk factor for diabetic complications. JAMA. 2006;295(14): 1707-1708.
15. American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care. 2008;31 suppl 1:S12-S54.
16. Handelsman Y, Mechanick JI, Blonde L, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for developing a diabetes mellitus comprehensive care plan. Endocrine Pract. 2011;17(suppl 2):1-53.
17. Kaufman F. Insulin treatment. In: Kaufman F, ed. Medical Management of Type 1 Diabetes. 5th ed. Alexandria, VA: American Diabetes Association; 2008:57-82.
18. Hirsch IB. Insulin analogues. N Engl J Med. 2005;352(2):174-183.
19. Cochran E, Musso C, Gorden P. The use of U-500 in patients with extreme insulin resistance. Diabetes Care. 2005;28(5):1240-1244.
20. Diabetes Research in Children Network (DirecNet) Study Group. Prevention of hypoglycemia during exercise in children with type 1 diabetes by suspending basal insulin. Diabetes Care. 2006;29(10):2200-2204.
21. Maran A, Pavan P, Bonsembiante B, et al. Continuous glucose monitoring reveals delayed nocturnal hypoglycemia after intermittent high-intensity exercise in nontrained patients with type 1 diabetes. Diabetes Technol Ther. 2010; 12(10):763-768.
22. Davidson PC, Hebblewhite HR, Steed RD, Bode BW. Analysis of guidelines for basal-bolus insulin dosing: basal insulin, correction factor, and carbohydrate-to-insulin ratio. Endocr Pract. 2008;14(9):1095-1101.
23. Glycemic Index Foundation, Sydney University Glycemic Index Research Service (SUGiRS). GI testing and research. www.glycemicindex
.com. Accessed October 21, 2011.
24. Pankowska E, Błazik M. Bolus calculator with nutrition database software, a new concept of prandial insulin programming for pump users.
J Diabetes Sci Technol. 2010;4(3):571-576.
25. Davis SN, Horton ES, Battelino T, et al. STAR 3 randomized controlled trial to compare sensor-augmented insulin pump therapy with multiple daily injections in the treatment of type 1 diabetes: research design, methods, and baseline characteristics of enrolled subjects. Diabetes Technol Ther. 2010;12(4):249-255.
26. Buse JB, Dailey G, Ahmann AA, et al. Baseline predictors of A1C reduction in adults using sensor-augmented pump therapy or multiple daily injection therapy: the STAR 3 experience. Diabetes Technol Ther. 2011;13(6):601-606.
27. Bergenstal RM, Tamborlane WV, Ahmann A, et al. Sensor-Augmented Pump Therapy for A1C Reduction (STAR 3) Study: results from the 6-month continuation phase. Diabetes Care. 2011 Sep 20. Epub ahead of print.
28. Green JB, Lane WS, Bergenstal RM, et al. Insulin Pump Settings Associated with Degree of Glycemic Improvement in Adults with Type 1 Diabetes Using Sensor-Augmented Pump Therapy. Presented at: Diabetes Technology Meeting; November 11-13, 2010; Bethesda, MD. Abstract A51.
29. Buse JB, Kidva YC, Guthrie RA, et al. Assessment of glycemic variability and CD40 ligand in the STAR 3 Study. Presented at: American Diabetes Association Scientific Sessions; June 2, 2011; San Diego, CA. Abstract 0923-P.
30. Hirsch IB. Algorithms for care in adults using continuous glucose monitoring. J Diabetes Sci Technol. 2007;1(1):126-129.
31. Wolpert HA. Continuous glucose monitoring: coming of age (editorial). N Engl J Med. 2010;363(4):383-384.
32. Wiegand S, Raile K, Reinehr T, et al; DPV-Wiss Study Group. Daily insulin requirement of children and adolescents with type 1 diabetes: effect of age, body mass index and mode of therapy. Eur J Endocrinol. 2008;158(4):543-549.
33. Hanas R, Ludvigsson J. Hypoglycemia and ketoacidosis with insulin pump therapy in children and adolescents. Pediatr Diabetes. 2006;7 suppl 4:32-38.
34. Unger J. A primary care approach to continuous subcutaneous insulin infusion. Clin Diabetes. 1999;17(3). http://journal.diabetes.org/clinicaldiabetes/V17N31999/Pg113.htm. Accessed October 21, 2011.