User login
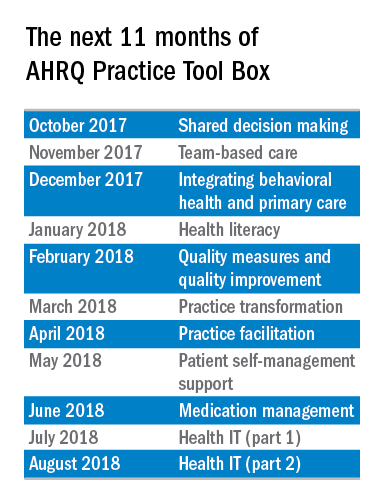
The AHRQ Practice Tool Box
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
The Inflection Point
In the early 1600s, the French playwright Molière wrote one of the great satires of all time, “The Doctor in Spite of Himself.” In that play the main character, Sganarelle, is a woodcutter who wastes all his money on alcohol, so his wife Martine decides she will teach him a lesson. As she is plotting her revenge, Martine overhears two peasants discussing how they have been trying to find a doctor for their rich employer’s daughter, who has become suddenly mute. Martine seizes the opportunity to tell the peasants that her husband is a brilliant – though eccentric – doctor who usually hides his identity. Learning this, the peasants find Sganarelle and beg him to see their master’s daughter. Though he initially refuses, they berate him until he can take it no more, and he finally says that he is a doctor and agrees to assess the ill young woman.
Sganarelle does his best to impersonate a doctor while examining the young woman, and as he is doing so it becomes apparent even to him that she is not truly ill. She is pretending to be mute because she’s being forced to marry a wealthy man she does not love. Sganarelle discusses the diagnosis with her father, stating, “this impediment to the action of the tongue is caused by certain humors.” He goes on to say that her muteness was triggered by, “the vapors that pass from the left side, where the liver resides, to the right side, where the heart dwells.” The rich aristocrat listens intently and accepts the diagnosis, though he seems puzzled about one thing. “Isn’t the heart on the left side of the chest?” he asks. To this insightful and obvious question Sganarelle replies, “Yes, that used to be true; but we’ve changed all that, and we practice medicine now according to a whole new method.”
It is astonishing that Molière, in a farcical comedy written in the 1600s, could have anticipated the dizzying rate of change in modern medicine. While the heart and liver have not changed sides, the ways we are practicing medicine have undergone landmark shifts over the past 10 years. Just look at the new ways in which we record documentation, learn new information, send in prescriptions, manage populations in addition to individual patients, and so many other aspects of care. At times this evolution has its own satirical feel to it. For example, the notion that refusing to refill an opioid prescription for a patient that broke their opioid contract could lead to a bad review on Yelp or points off on a Press Ganey satisfaction survey does not seem reasonable, but it is real.
When we started this column about 10 years ago, we regularly received emails (and even letters written in fine penmanship and mailed in envelopes) from physicians who felt that the EHR was ruining their practice and their lives. Many of the letters talked about early retirement. Some physicians ended up retiring early. Many of these physicians were smart, able people who we believe took great care of patients. But as Leon C. Megginson, interpreting the work of Darwin, observed, “It is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change.” Adaptability favors the young; the young have fewer habits to break, few preconceived ideas of how things should be, and perhaps more energy to give to new tasks.
We believe we have now reached the inflection point – a time in the history of an industry where an event (in this case the advent of the EHR) so fundamentally impacts the industry that the industry is changed from that point forward. The industry, and more importantly those who work in the industry, must adopt new approaches and attitudes in order to survive in the changed environment. Andrew Grove, the former CEO of Intel, talked about Strategic Inflection Points in a keynote address to the Academy of Management: “…what is common to [inflection points] and what is key is that they require a fundamental change in business strategy.” Grove also said, “That change can mean an opportunity to rise to new heights. But it may just as likely signal the beginning of the end.”
Up until recently, the introduction of the EHR lead to discussions about what was good and what was bad about the advent of EHRs. That time is past. We no longer receive letters from physicians expressing their concerns about the EHR, as many of those physicians have taken the change as a signal of the end of their careers, and chosen to retire. The rest have adapted to a new world. And in this new world we are certainly rising to new heights. We are forward-focused and looking at the multi-fold ways that our new technologies can accomplish their many missions – to improve the health of the population, to serve as a source of data to assess the real-world effectiveness of novel therapies, to evaluate and affect the quality of care given by practices and individual physicians, and to take excellent personalized care of individual patients. While we are physicians, not wood cutters as in Molière’s play, it remains incumbent upon us never to stop listening to our patients’ hearts, and to interpret their symptoms and signs with common sense, empathy and even humor when appropriate, all the while embracing approaches that move the health care of our patients forward to new heights.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
In the early 1600s, the French playwright Molière wrote one of the great satires of all time, “The Doctor in Spite of Himself.” In that play the main character, Sganarelle, is a woodcutter who wastes all his money on alcohol, so his wife Martine decides she will teach him a lesson. As she is plotting her revenge, Martine overhears two peasants discussing how they have been trying to find a doctor for their rich employer’s daughter, who has become suddenly mute. Martine seizes the opportunity to tell the peasants that her husband is a brilliant – though eccentric – doctor who usually hides his identity. Learning this, the peasants find Sganarelle and beg him to see their master’s daughter. Though he initially refuses, they berate him until he can take it no more, and he finally says that he is a doctor and agrees to assess the ill young woman.
Sganarelle does his best to impersonate a doctor while examining the young woman, and as he is doing so it becomes apparent even to him that she is not truly ill. She is pretending to be mute because she’s being forced to marry a wealthy man she does not love. Sganarelle discusses the diagnosis with her father, stating, “this impediment to the action of the tongue is caused by certain humors.” He goes on to say that her muteness was triggered by, “the vapors that pass from the left side, where the liver resides, to the right side, where the heart dwells.” The rich aristocrat listens intently and accepts the diagnosis, though he seems puzzled about one thing. “Isn’t the heart on the left side of the chest?” he asks. To this insightful and obvious question Sganarelle replies, “Yes, that used to be true; but we’ve changed all that, and we practice medicine now according to a whole new method.”
It is astonishing that Molière, in a farcical comedy written in the 1600s, could have anticipated the dizzying rate of change in modern medicine. While the heart and liver have not changed sides, the ways we are practicing medicine have undergone landmark shifts over the past 10 years. Just look at the new ways in which we record documentation, learn new information, send in prescriptions, manage populations in addition to individual patients, and so many other aspects of care. At times this evolution has its own satirical feel to it. For example, the notion that refusing to refill an opioid prescription for a patient that broke their opioid contract could lead to a bad review on Yelp or points off on a Press Ganey satisfaction survey does not seem reasonable, but it is real.
When we started this column about 10 years ago, we regularly received emails (and even letters written in fine penmanship and mailed in envelopes) from physicians who felt that the EHR was ruining their practice and their lives. Many of the letters talked about early retirement. Some physicians ended up retiring early. Many of these physicians were smart, able people who we believe took great care of patients. But as Leon C. Megginson, interpreting the work of Darwin, observed, “It is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change.” Adaptability favors the young; the young have fewer habits to break, few preconceived ideas of how things should be, and perhaps more energy to give to new tasks.
We believe we have now reached the inflection point – a time in the history of an industry where an event (in this case the advent of the EHR) so fundamentally impacts the industry that the industry is changed from that point forward. The industry, and more importantly those who work in the industry, must adopt new approaches and attitudes in order to survive in the changed environment. Andrew Grove, the former CEO of Intel, talked about Strategic Inflection Points in a keynote address to the Academy of Management: “…what is common to [inflection points] and what is key is that they require a fundamental change in business strategy.” Grove also said, “That change can mean an opportunity to rise to new heights. But it may just as likely signal the beginning of the end.”
Up until recently, the introduction of the EHR lead to discussions about what was good and what was bad about the advent of EHRs. That time is past. We no longer receive letters from physicians expressing their concerns about the EHR, as many of those physicians have taken the change as a signal of the end of their careers, and chosen to retire. The rest have adapted to a new world. And in this new world we are certainly rising to new heights. We are forward-focused and looking at the multi-fold ways that our new technologies can accomplish their many missions – to improve the health of the population, to serve as a source of data to assess the real-world effectiveness of novel therapies, to evaluate and affect the quality of care given by practices and individual physicians, and to take excellent personalized care of individual patients. While we are physicians, not wood cutters as in Molière’s play, it remains incumbent upon us never to stop listening to our patients’ hearts, and to interpret their symptoms and signs with common sense, empathy and even humor when appropriate, all the while embracing approaches that move the health care of our patients forward to new heights.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
In the early 1600s, the French playwright Molière wrote one of the great satires of all time, “The Doctor in Spite of Himself.” In that play the main character, Sganarelle, is a woodcutter who wastes all his money on alcohol, so his wife Martine decides she will teach him a lesson. As she is plotting her revenge, Martine overhears two peasants discussing how they have been trying to find a doctor for their rich employer’s daughter, who has become suddenly mute. Martine seizes the opportunity to tell the peasants that her husband is a brilliant – though eccentric – doctor who usually hides his identity. Learning this, the peasants find Sganarelle and beg him to see their master’s daughter. Though he initially refuses, they berate him until he can take it no more, and he finally says that he is a doctor and agrees to assess the ill young woman.
Sganarelle does his best to impersonate a doctor while examining the young woman, and as he is doing so it becomes apparent even to him that she is not truly ill. She is pretending to be mute because she’s being forced to marry a wealthy man she does not love. Sganarelle discusses the diagnosis with her father, stating, “this impediment to the action of the tongue is caused by certain humors.” He goes on to say that her muteness was triggered by, “the vapors that pass from the left side, where the liver resides, to the right side, where the heart dwells.” The rich aristocrat listens intently and accepts the diagnosis, though he seems puzzled about one thing. “Isn’t the heart on the left side of the chest?” he asks. To this insightful and obvious question Sganarelle replies, “Yes, that used to be true; but we’ve changed all that, and we practice medicine now according to a whole new method.”
It is astonishing that Molière, in a farcical comedy written in the 1600s, could have anticipated the dizzying rate of change in modern medicine. While the heart and liver have not changed sides, the ways we are practicing medicine have undergone landmark shifts over the past 10 years. Just look at the new ways in which we record documentation, learn new information, send in prescriptions, manage populations in addition to individual patients, and so many other aspects of care. At times this evolution has its own satirical feel to it. For example, the notion that refusing to refill an opioid prescription for a patient that broke their opioid contract could lead to a bad review on Yelp or points off on a Press Ganey satisfaction survey does not seem reasonable, but it is real.
When we started this column about 10 years ago, we regularly received emails (and even letters written in fine penmanship and mailed in envelopes) from physicians who felt that the EHR was ruining their practice and their lives. Many of the letters talked about early retirement. Some physicians ended up retiring early. Many of these physicians were smart, able people who we believe took great care of patients. But as Leon C. Megginson, interpreting the work of Darwin, observed, “It is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change.” Adaptability favors the young; the young have fewer habits to break, few preconceived ideas of how things should be, and perhaps more energy to give to new tasks.
We believe we have now reached the inflection point – a time in the history of an industry where an event (in this case the advent of the EHR) so fundamentally impacts the industry that the industry is changed from that point forward. The industry, and more importantly those who work in the industry, must adopt new approaches and attitudes in order to survive in the changed environment. Andrew Grove, the former CEO of Intel, talked about Strategic Inflection Points in a keynote address to the Academy of Management: “…what is common to [inflection points] and what is key is that they require a fundamental change in business strategy.” Grove also said, “That change can mean an opportunity to rise to new heights. But it may just as likely signal the beginning of the end.”
Up until recently, the introduction of the EHR lead to discussions about what was good and what was bad about the advent of EHRs. That time is past. We no longer receive letters from physicians expressing their concerns about the EHR, as many of those physicians have taken the change as a signal of the end of their careers, and chosen to retire. The rest have adapted to a new world. And in this new world we are certainly rising to new heights. We are forward-focused and looking at the multi-fold ways that our new technologies can accomplish their many missions – to improve the health of the population, to serve as a source of data to assess the real-world effectiveness of novel therapies, to evaluate and affect the quality of care given by practices and individual physicians, and to take excellent personalized care of individual patients. While we are physicians, not wood cutters as in Molière’s play, it remains incumbent upon us never to stop listening to our patients’ hearts, and to interpret their symptoms and signs with common sense, empathy and even humor when appropriate, all the while embracing approaches that move the health care of our patients forward to new heights.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
Climate change may lead to more cellulitis
As a follow-up to our previous column on the effects of climate change on the skin (Dermatology News, June 2016, p. 28), this month’s column will focus on a study recently published in Clinical Infectious Diseases that explores warmer weather as a possible risk factor for cellulitis.1 As the summer continues with sweltering weather, humidity, and the recent spate of hurricanes in North America, it’s interesting to think about how the climate affects our patients and puts them at risk.

Much attention has been given to global warming and climate change over the past several years. The results of this study demonstrate that, if temperatures consistently increase, the odds of cellulitis also may increase in regions exposed to warmer temperatures.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Reference
1. Clin Infect Dis. 2017 Jul 31. doi: 10.1093/cid/cix487.
As a follow-up to our previous column on the effects of climate change on the skin (Dermatology News, June 2016, p. 28), this month’s column will focus on a study recently published in Clinical Infectious Diseases that explores warmer weather as a possible risk factor for cellulitis.1 As the summer continues with sweltering weather, humidity, and the recent spate of hurricanes in North America, it’s interesting to think about how the climate affects our patients and puts them at risk.

Much attention has been given to global warming and climate change over the past several years. The results of this study demonstrate that, if temperatures consistently increase, the odds of cellulitis also may increase in regions exposed to warmer temperatures.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Reference
1. Clin Infect Dis. 2017 Jul 31. doi: 10.1093/cid/cix487.
As a follow-up to our previous column on the effects of climate change on the skin (Dermatology News, June 2016, p. 28), this month’s column will focus on a study recently published in Clinical Infectious Diseases that explores warmer weather as a possible risk factor for cellulitis.1 As the summer continues with sweltering weather, humidity, and the recent spate of hurricanes in North America, it’s interesting to think about how the climate affects our patients and puts them at risk.

Much attention has been given to global warming and climate change over the past several years. The results of this study demonstrate that, if temperatures consistently increase, the odds of cellulitis also may increase in regions exposed to warmer temperatures.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Reference
1. Clin Infect Dis. 2017 Jul 31. doi: 10.1093/cid/cix487.
Ethics in compulsory treatment of patients with severe mental illness
“Ethics is knowing the difference between what you have a right to do and what is right to do.”
– Potter Stewart, U.S. Supreme Court Justice
An understanding of the difference between what is allowed or even recommended and what is ethical often is contemplated in the treatment of mental illness. Mental illnesses can impair judgment in patients confronted with complex decisions about their treatment. A provider, therefore, has to make a decision between respecting autonomy and/or engaging in what may be considered beneficent. While the line separating beneficent care and the respect for the autonomy of a patient may not be present, the question often arises – especially in inpatient care of patients with severe mental illness.
In the inpatient units, I was taught to justify and be mindful of any removal of someone’s right. I learned the responsibility of stripping someone’s freedom. Not only would I find myself preventing someone from going where they wanted or from talking to whomever they wanted, but frequently, we involuntary injected patients with neuroactive chemicals. Those measures are used only in extreme circumstances: In most states, one has to be unable to provide themselves with food, clothing, or shelter secondary to mental illness to be subjected to such aggressive treatment.
Currently, the United States is seeing an increase in the focus on providing more treatment: an emphasis on beneficence over autonomy. This change can be witnessed in the passage of compulsory outpatient treatment laws. Those rulings, such as Laura’s Law in California and Kendra’s Law in New York, have been promoted in response to an increased concern over the consequences of untreated mental illness in crime. In this commentary, I present a case where I felt that despite being given the right and expectation to involuntary treat someone, I did not feel that it was ethical to involuntarily medicate him. (I have made appropriate changes to the patient’s case to maintain confidentiality.)
Our facility
The Psychiatric Stabilization Unit (PSU) of the San Diego Jails is a 30-bed acute psychiatric unit. We serve the 4,500 male inmates and one of the largest mental health systems in the county. The vast majority (from 70% to 90% at any one time) of patients suffer from a psychotic illness, and more than 50% have a comorbid substance use disorder. Contrary to most inpatient units, we do not have pressure from insurance or utilization review to regularly change dosages or medications, and we do not have significant pressure to discharge patients within a certain time frame. The unit serves very disenfranchised patients with most being homeless prior to their arrest and many having no emergency contact or social support of any sort. The unit is staffed by one attending psychiatrist and two therapists. We are subjected to the same involuntary commitment and involuntary medication laws as are community psychiatric hospitals, but we get a significant number of patients under court orders.
The patient presented in this case came under such court order for restoration of his competency to stand trial. In the United States, one cannot stand trial unless competent. Competency is defined as one’s ability to take a meaningful or active part in a trial, the capacity to understand laws, the capacity to understand personal responsibility, the ability to express a plea, and the capability to instruct legal counsel. When patients are found incompetent, they commonly get court ordered to an unit like the PSU with a court order that they cannot understand the risk, benefits, and alternatives of psychotropic treatment and thus can be involuntarily medicated. Often, including in this case, the court order will mention that the patient will not become competent without treatment, including involuntary antipsychotics.
Overview of the case
George is a 50-year-old white male without psychiatric history. He had never been hospitalized psychiatrically voluntarily or involuntarily. He has never engaged in outpatient psychiatric care, has never taken psychotropic medication, and has never been diagnosed with mental illness. He mentions no prior episode of self-harm, suicidality, or suicide attempt. He occasionally drinks alcohol and has smoked marijuana on a few occasions. He despises other drugs, saying that they are “dangerous.” He mentions that his parents had “difficult personalities” but denies any knowledge of them having formal mental illness.
He was born in rural Louisiana to a British mother and an American father. His parents divorced while he was in preschool. His mother remarried, to a salesman, which required them to move frequently to different states for his work. He mentions having performed moderately in school, but poor grades were secondary to his “boredom.” He graduated high school and went to vocational school in technological manufacturing but was unable to graduate. He has since held a series of low-level jobs in retail and janitorial services. He mentions having been in romantic relationships, but when asked to elaborate, he is unable to name any past girlfriends or describe any past relationships. Nonetheless, he describes a wide array of social supports with many friends, though it must be noted that all of his friends have some form of mental illness or intellectual disability.
At this time, he lives with his friend Harry. Harry has a moderate form of autism. George helps him with everything from grocery shopping to financial matters to assistance in personal hygiene. In exchange, Harry provides him with housing that he inherited and financial assistance from his disability benefits. They have lived in the same home for 2 years, since Harry asked George to move in because of concern that he would lose his home over the unsanitary conditions that were present at that time.
George had never been arrested prior to this incarceration. The circumstances of his arrest are unusual. After a neighbor had made complaints that Harry and George were illegally lodging in Harry’s home, the city investigated the matter. George’s report was that Harry was unable to fill out the forms appropriately and was asked to present himself in court. George came along for moral support but became extremely upset when lawyers and judges asked his friend to answer questions he did not have the cognitive ability to answer. Without second thought, George voiced his anger but was asked to remain quiet while not on the stand. He was asked to remain seated and was demanded to follow orders. A few moments later, George was arrested for contempt of court and obstruction to an officer.
Once incarcerated, he declined having any mental illness or needing any treatment during the customary triage visit. He had no problem as an inmate and was never referred to psychiatric services. However, when meeting with his public defender, George derailed into delusions. He talked about how the cops had been conspiring against him all of his life, with his current incarceration as a culmination. He mentioned how the judge was purposely trying to get them evicted so that he could own the house himself. He asked his lawyer to countersue the judge for a violation of his rights. The public defender filed for a competency evaluation of his client.
The forensic psychiatrist evaluated the patient and had a similar interpretation. This was a patient who had delusions and was perseverating on them to the point of being unable to engage in meaningful work with his attorney. The psychiatrist recommended involuntary treatment with an antipsychotic after diagnosing the patient with a psychotic illness.
My interactions with George
George is a loud and bucolic man with an usual mix of Southern idioms, a slightly British accent, and East Coast humor. He insisted on telling me why he wanted the staff to refer to him by his Native American nickname prior to the start our interview. He then asked me to listen to his life story to understand why Harry meant so much to him. Despite recounting their truly meaningful relationship, his affect was odd with poor reactivity; he had an incongruent and somewhat ungenuine joyfulness.
Once I heard his account of their friendship, I asked him about his charges and the incident in the courtroom. His answer was a long diatribe about the wrongs that had been done to him, but most of his speech was a series of illogical delusions. I informed him of my thoughts about his fixed and false beliefs, but he was not able to understand my comments. Nonetheless, I felt that he related to me well and that we had established good rapport.
As I was informing him about the antipsychotic I had chosen for his involuntary treatment, he asked me to hold off. He asked me to consider working with him for some time without medications. After all, he did not believe that he had a mental illness and wanted to attempt to engage in the competency training with our therapist without being medicated.
My conceptualization of him
George is a peculiar case. Practically all patients who are committed to my unit for competency restoration are psychotic, and their psychosis prevents their engagement with their attorneys. They have poor insight into their illness, which leads to their commitment. On admission, I confirm the assessment of the forensic psychiatrist and start the ordered involuntary treatment on patients. Many of them are gravely disabled – making the ethical dilemma easier to navigate. For other patients, the idea that they will be kept incarcerated until found competent also makes the forced treatment a simpler decision.
George was different – his impeccable grooming, his dislike of jail food, and his request for appropriately fitting jail clothes were far from disorganized. More importantly, however, he had adequate shelter outside of jail, income for assisting Harry, and a rich network of friends. Despite being riddled with delusions, his thought process was linear, and he was redirectable – even when discussing his delusions. I conceptualized the ethical conflict as such: Not treating him might lead to a longer period of incompetence and a longer incarceration; treating him would go against his desire to remain untreated.
After contacting Harry, I was fairly certain that George had suffered from his delusions for at least a significant part of his adult life, if not in its entirety. However, Harry was infinitely thankful for George’s assistance and felt that George had a good life. This added another fundamental question: Would forcing George to engage in formal mental health treatment lead him to have a better life? He was happy, had meaningful relationships, and contributed to his life as well as his friends’ lives in a deep way.
I diagnosed him as having an unspecified psychotic disorder, likely schizophrenia; he had delusions and negative symptoms, like his impaired affect. Despite this diagnosis, I decided to hold off from using involuntary treatment. I met with him daily for more than 2 weeks, and we discussed his story, his feelings, and his beliefs. On occasion, it was hard to separate the delusions from justifiable anger at the system. He had felt that he and Harry had been wronged, when society should have protected their vulnerability. He learned to trust me, and his therapist taught him competency training. Despite a possible 1-year commitment, we declared him competent to stand trial in 2 weeks. He had learned and excelled in all facets of the training.
George still had delusions, but he understood his charges, that he had acted inappropriately in the courtroom, and how to discuss his case with his legal counsel. Harry found George to be at his baseline during visits. George acted appropriately; he followed the complex rules set on inmates and engaged in all groups that are held on the unit.
Discussion
I certainly do not question the value of involuntary psychiatric treatment for many patients with grave disabilities, violent tendencies, or incompetence. However, George’s case makes me wonder if many people living with schizophrenia can have rich and meaningful lives without ever being in contact with a mental health provider. I wonder if our almost-obsessive attention to antipsychotics makes us lose sight. Our biological reductionism may lead us to see patients such as George as someone with overactive dopaminergic pathways in need of antidopaminergic antipsychotic. Unfortunately for many, biological reductionism often is based on unsubstantiated evidence.
George reminds me that life, including schizophrenia, is more interesting and complicated than a set of genes, pathways, neurons, or neurotransmitters. Our patients’ lives may be convoluted with delusions, often stemming from truth or impaired affects, which are nonetheless genuine. I don’t know what will happen to George, but his past 50 years suggest that he will continue to have friends, and he will continue to live without being impaired by his delusions. Strangely, I worry less about him than many of my other patients.
Many mental health providers have advocated for a wider and easier access to involuntarily medicate our patients. I think that there is a misguided belief that involuntary antipsychotic treatment will lead to a rise in their use. However, if Carl Rogers, PhD, and others were right in stating that our relationship with our patients was the ultimate factor in their recovery, at what cost are we willing to jeopardize this? My fear is that this cost will be the loss of trust, which is so necessary in treatment. I hope that my short relationship with George did not scare him from ever seeing a psychiatrist again. In some ways, I suspect that by simply listening to George and withholding forced treatment, he will be more inclined to seek treatment in the future.
Take-home points
- Certain patients with psychosis have fairly high functioning.
- Milieu therapy is, in certain cases, able to assuage some symptoms of psychosis.
- Compulsory antipsychotic administration may not be ethical in certain cases of acute psychosis.
- Biological reductionism may undermine a complete ethical understanding of psychosis.
- Psychiatric disorders are etiologically complex and multifactorial.
- Involuntary treatment may provide short-term gains, but prevent long-term trust between patient and provider.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre also mentors several residents on projects, including reduction in the use of solitary confinement of patients with mental illness, reduction in the use of involuntary treatment of the mentally ill, and examination of the mentally ill offender.
“Ethics is knowing the difference between what you have a right to do and what is right to do.”
– Potter Stewart, U.S. Supreme Court Justice
An understanding of the difference between what is allowed or even recommended and what is ethical often is contemplated in the treatment of mental illness. Mental illnesses can impair judgment in patients confronted with complex decisions about their treatment. A provider, therefore, has to make a decision between respecting autonomy and/or engaging in what may be considered beneficent. While the line separating beneficent care and the respect for the autonomy of a patient may not be present, the question often arises – especially in inpatient care of patients with severe mental illness.
In the inpatient units, I was taught to justify and be mindful of any removal of someone’s right. I learned the responsibility of stripping someone’s freedom. Not only would I find myself preventing someone from going where they wanted or from talking to whomever they wanted, but frequently, we involuntary injected patients with neuroactive chemicals. Those measures are used only in extreme circumstances: In most states, one has to be unable to provide themselves with food, clothing, or shelter secondary to mental illness to be subjected to such aggressive treatment.
Currently, the United States is seeing an increase in the focus on providing more treatment: an emphasis on beneficence over autonomy. This change can be witnessed in the passage of compulsory outpatient treatment laws. Those rulings, such as Laura’s Law in California and Kendra’s Law in New York, have been promoted in response to an increased concern over the consequences of untreated mental illness in crime. In this commentary, I present a case where I felt that despite being given the right and expectation to involuntary treat someone, I did not feel that it was ethical to involuntarily medicate him. (I have made appropriate changes to the patient’s case to maintain confidentiality.)
Our facility
The Psychiatric Stabilization Unit (PSU) of the San Diego Jails is a 30-bed acute psychiatric unit. We serve the 4,500 male inmates and one of the largest mental health systems in the county. The vast majority (from 70% to 90% at any one time) of patients suffer from a psychotic illness, and more than 50% have a comorbid substance use disorder. Contrary to most inpatient units, we do not have pressure from insurance or utilization review to regularly change dosages or medications, and we do not have significant pressure to discharge patients within a certain time frame. The unit serves very disenfranchised patients with most being homeless prior to their arrest and many having no emergency contact or social support of any sort. The unit is staffed by one attending psychiatrist and two therapists. We are subjected to the same involuntary commitment and involuntary medication laws as are community psychiatric hospitals, but we get a significant number of patients under court orders.
The patient presented in this case came under such court order for restoration of his competency to stand trial. In the United States, one cannot stand trial unless competent. Competency is defined as one’s ability to take a meaningful or active part in a trial, the capacity to understand laws, the capacity to understand personal responsibility, the ability to express a plea, and the capability to instruct legal counsel. When patients are found incompetent, they commonly get court ordered to an unit like the PSU with a court order that they cannot understand the risk, benefits, and alternatives of psychotropic treatment and thus can be involuntarily medicated. Often, including in this case, the court order will mention that the patient will not become competent without treatment, including involuntary antipsychotics.
Overview of the case
George is a 50-year-old white male without psychiatric history. He had never been hospitalized psychiatrically voluntarily or involuntarily. He has never engaged in outpatient psychiatric care, has never taken psychotropic medication, and has never been diagnosed with mental illness. He mentions no prior episode of self-harm, suicidality, or suicide attempt. He occasionally drinks alcohol and has smoked marijuana on a few occasions. He despises other drugs, saying that they are “dangerous.” He mentions that his parents had “difficult personalities” but denies any knowledge of them having formal mental illness.
He was born in rural Louisiana to a British mother and an American father. His parents divorced while he was in preschool. His mother remarried, to a salesman, which required them to move frequently to different states for his work. He mentions having performed moderately in school, but poor grades were secondary to his “boredom.” He graduated high school and went to vocational school in technological manufacturing but was unable to graduate. He has since held a series of low-level jobs in retail and janitorial services. He mentions having been in romantic relationships, but when asked to elaborate, he is unable to name any past girlfriends or describe any past relationships. Nonetheless, he describes a wide array of social supports with many friends, though it must be noted that all of his friends have some form of mental illness or intellectual disability.
At this time, he lives with his friend Harry. Harry has a moderate form of autism. George helps him with everything from grocery shopping to financial matters to assistance in personal hygiene. In exchange, Harry provides him with housing that he inherited and financial assistance from his disability benefits. They have lived in the same home for 2 years, since Harry asked George to move in because of concern that he would lose his home over the unsanitary conditions that were present at that time.
George had never been arrested prior to this incarceration. The circumstances of his arrest are unusual. After a neighbor had made complaints that Harry and George were illegally lodging in Harry’s home, the city investigated the matter. George’s report was that Harry was unable to fill out the forms appropriately and was asked to present himself in court. George came along for moral support but became extremely upset when lawyers and judges asked his friend to answer questions he did not have the cognitive ability to answer. Without second thought, George voiced his anger but was asked to remain quiet while not on the stand. He was asked to remain seated and was demanded to follow orders. A few moments later, George was arrested for contempt of court and obstruction to an officer.
Once incarcerated, he declined having any mental illness or needing any treatment during the customary triage visit. He had no problem as an inmate and was never referred to psychiatric services. However, when meeting with his public defender, George derailed into delusions. He talked about how the cops had been conspiring against him all of his life, with his current incarceration as a culmination. He mentioned how the judge was purposely trying to get them evicted so that he could own the house himself. He asked his lawyer to countersue the judge for a violation of his rights. The public defender filed for a competency evaluation of his client.
The forensic psychiatrist evaluated the patient and had a similar interpretation. This was a patient who had delusions and was perseverating on them to the point of being unable to engage in meaningful work with his attorney. The psychiatrist recommended involuntary treatment with an antipsychotic after diagnosing the patient with a psychotic illness.
My interactions with George
George is a loud and bucolic man with an usual mix of Southern idioms, a slightly British accent, and East Coast humor. He insisted on telling me why he wanted the staff to refer to him by his Native American nickname prior to the start our interview. He then asked me to listen to his life story to understand why Harry meant so much to him. Despite recounting their truly meaningful relationship, his affect was odd with poor reactivity; he had an incongruent and somewhat ungenuine joyfulness.
Once I heard his account of their friendship, I asked him about his charges and the incident in the courtroom. His answer was a long diatribe about the wrongs that had been done to him, but most of his speech was a series of illogical delusions. I informed him of my thoughts about his fixed and false beliefs, but he was not able to understand my comments. Nonetheless, I felt that he related to me well and that we had established good rapport.
As I was informing him about the antipsychotic I had chosen for his involuntary treatment, he asked me to hold off. He asked me to consider working with him for some time without medications. After all, he did not believe that he had a mental illness and wanted to attempt to engage in the competency training with our therapist without being medicated.
My conceptualization of him
George is a peculiar case. Practically all patients who are committed to my unit for competency restoration are psychotic, and their psychosis prevents their engagement with their attorneys. They have poor insight into their illness, which leads to their commitment. On admission, I confirm the assessment of the forensic psychiatrist and start the ordered involuntary treatment on patients. Many of them are gravely disabled – making the ethical dilemma easier to navigate. For other patients, the idea that they will be kept incarcerated until found competent also makes the forced treatment a simpler decision.
George was different – his impeccable grooming, his dislike of jail food, and his request for appropriately fitting jail clothes were far from disorganized. More importantly, however, he had adequate shelter outside of jail, income for assisting Harry, and a rich network of friends. Despite being riddled with delusions, his thought process was linear, and he was redirectable – even when discussing his delusions. I conceptualized the ethical conflict as such: Not treating him might lead to a longer period of incompetence and a longer incarceration; treating him would go against his desire to remain untreated.
After contacting Harry, I was fairly certain that George had suffered from his delusions for at least a significant part of his adult life, if not in its entirety. However, Harry was infinitely thankful for George’s assistance and felt that George had a good life. This added another fundamental question: Would forcing George to engage in formal mental health treatment lead him to have a better life? He was happy, had meaningful relationships, and contributed to his life as well as his friends’ lives in a deep way.
I diagnosed him as having an unspecified psychotic disorder, likely schizophrenia; he had delusions and negative symptoms, like his impaired affect. Despite this diagnosis, I decided to hold off from using involuntary treatment. I met with him daily for more than 2 weeks, and we discussed his story, his feelings, and his beliefs. On occasion, it was hard to separate the delusions from justifiable anger at the system. He had felt that he and Harry had been wronged, when society should have protected their vulnerability. He learned to trust me, and his therapist taught him competency training. Despite a possible 1-year commitment, we declared him competent to stand trial in 2 weeks. He had learned and excelled in all facets of the training.
George still had delusions, but he understood his charges, that he had acted inappropriately in the courtroom, and how to discuss his case with his legal counsel. Harry found George to be at his baseline during visits. George acted appropriately; he followed the complex rules set on inmates and engaged in all groups that are held on the unit.
Discussion
I certainly do not question the value of involuntary psychiatric treatment for many patients with grave disabilities, violent tendencies, or incompetence. However, George’s case makes me wonder if many people living with schizophrenia can have rich and meaningful lives without ever being in contact with a mental health provider. I wonder if our almost-obsessive attention to antipsychotics makes us lose sight. Our biological reductionism may lead us to see patients such as George as someone with overactive dopaminergic pathways in need of antidopaminergic antipsychotic. Unfortunately for many, biological reductionism often is based on unsubstantiated evidence.
George reminds me that life, including schizophrenia, is more interesting and complicated than a set of genes, pathways, neurons, or neurotransmitters. Our patients’ lives may be convoluted with delusions, often stemming from truth or impaired affects, which are nonetheless genuine. I don’t know what will happen to George, but his past 50 years suggest that he will continue to have friends, and he will continue to live without being impaired by his delusions. Strangely, I worry less about him than many of my other patients.
Many mental health providers have advocated for a wider and easier access to involuntarily medicate our patients. I think that there is a misguided belief that involuntary antipsychotic treatment will lead to a rise in their use. However, if Carl Rogers, PhD, and others were right in stating that our relationship with our patients was the ultimate factor in their recovery, at what cost are we willing to jeopardize this? My fear is that this cost will be the loss of trust, which is so necessary in treatment. I hope that my short relationship with George did not scare him from ever seeing a psychiatrist again. In some ways, I suspect that by simply listening to George and withholding forced treatment, he will be more inclined to seek treatment in the future.
Take-home points
- Certain patients with psychosis have fairly high functioning.
- Milieu therapy is, in certain cases, able to assuage some symptoms of psychosis.
- Compulsory antipsychotic administration may not be ethical in certain cases of acute psychosis.
- Biological reductionism may undermine a complete ethical understanding of psychosis.
- Psychiatric disorders are etiologically complex and multifactorial.
- Involuntary treatment may provide short-term gains, but prevent long-term trust between patient and provider.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre also mentors several residents on projects, including reduction in the use of solitary confinement of patients with mental illness, reduction in the use of involuntary treatment of the mentally ill, and examination of the mentally ill offender.
“Ethics is knowing the difference between what you have a right to do and what is right to do.”
– Potter Stewart, U.S. Supreme Court Justice
An understanding of the difference between what is allowed or even recommended and what is ethical often is contemplated in the treatment of mental illness. Mental illnesses can impair judgment in patients confronted with complex decisions about their treatment. A provider, therefore, has to make a decision between respecting autonomy and/or engaging in what may be considered beneficent. While the line separating beneficent care and the respect for the autonomy of a patient may not be present, the question often arises – especially in inpatient care of patients with severe mental illness.
In the inpatient units, I was taught to justify and be mindful of any removal of someone’s right. I learned the responsibility of stripping someone’s freedom. Not only would I find myself preventing someone from going where they wanted or from talking to whomever they wanted, but frequently, we involuntary injected patients with neuroactive chemicals. Those measures are used only in extreme circumstances: In most states, one has to be unable to provide themselves with food, clothing, or shelter secondary to mental illness to be subjected to such aggressive treatment.
Currently, the United States is seeing an increase in the focus on providing more treatment: an emphasis on beneficence over autonomy. This change can be witnessed in the passage of compulsory outpatient treatment laws. Those rulings, such as Laura’s Law in California and Kendra’s Law in New York, have been promoted in response to an increased concern over the consequences of untreated mental illness in crime. In this commentary, I present a case where I felt that despite being given the right and expectation to involuntary treat someone, I did not feel that it was ethical to involuntarily medicate him. (I have made appropriate changes to the patient’s case to maintain confidentiality.)
Our facility
The Psychiatric Stabilization Unit (PSU) of the San Diego Jails is a 30-bed acute psychiatric unit. We serve the 4,500 male inmates and one of the largest mental health systems in the county. The vast majority (from 70% to 90% at any one time) of patients suffer from a psychotic illness, and more than 50% have a comorbid substance use disorder. Contrary to most inpatient units, we do not have pressure from insurance or utilization review to regularly change dosages or medications, and we do not have significant pressure to discharge patients within a certain time frame. The unit serves very disenfranchised patients with most being homeless prior to their arrest and many having no emergency contact or social support of any sort. The unit is staffed by one attending psychiatrist and two therapists. We are subjected to the same involuntary commitment and involuntary medication laws as are community psychiatric hospitals, but we get a significant number of patients under court orders.
The patient presented in this case came under such court order for restoration of his competency to stand trial. In the United States, one cannot stand trial unless competent. Competency is defined as one’s ability to take a meaningful or active part in a trial, the capacity to understand laws, the capacity to understand personal responsibility, the ability to express a plea, and the capability to instruct legal counsel. When patients are found incompetent, they commonly get court ordered to an unit like the PSU with a court order that they cannot understand the risk, benefits, and alternatives of psychotropic treatment and thus can be involuntarily medicated. Often, including in this case, the court order will mention that the patient will not become competent without treatment, including involuntary antipsychotics.
Overview of the case
George is a 50-year-old white male without psychiatric history. He had never been hospitalized psychiatrically voluntarily or involuntarily. He has never engaged in outpatient psychiatric care, has never taken psychotropic medication, and has never been diagnosed with mental illness. He mentions no prior episode of self-harm, suicidality, or suicide attempt. He occasionally drinks alcohol and has smoked marijuana on a few occasions. He despises other drugs, saying that they are “dangerous.” He mentions that his parents had “difficult personalities” but denies any knowledge of them having formal mental illness.
He was born in rural Louisiana to a British mother and an American father. His parents divorced while he was in preschool. His mother remarried, to a salesman, which required them to move frequently to different states for his work. He mentions having performed moderately in school, but poor grades were secondary to his “boredom.” He graduated high school and went to vocational school in technological manufacturing but was unable to graduate. He has since held a series of low-level jobs in retail and janitorial services. He mentions having been in romantic relationships, but when asked to elaborate, he is unable to name any past girlfriends or describe any past relationships. Nonetheless, he describes a wide array of social supports with many friends, though it must be noted that all of his friends have some form of mental illness or intellectual disability.
At this time, he lives with his friend Harry. Harry has a moderate form of autism. George helps him with everything from grocery shopping to financial matters to assistance in personal hygiene. In exchange, Harry provides him with housing that he inherited and financial assistance from his disability benefits. They have lived in the same home for 2 years, since Harry asked George to move in because of concern that he would lose his home over the unsanitary conditions that were present at that time.
George had never been arrested prior to this incarceration. The circumstances of his arrest are unusual. After a neighbor had made complaints that Harry and George were illegally lodging in Harry’s home, the city investigated the matter. George’s report was that Harry was unable to fill out the forms appropriately and was asked to present himself in court. George came along for moral support but became extremely upset when lawyers and judges asked his friend to answer questions he did not have the cognitive ability to answer. Without second thought, George voiced his anger but was asked to remain quiet while not on the stand. He was asked to remain seated and was demanded to follow orders. A few moments later, George was arrested for contempt of court and obstruction to an officer.
Once incarcerated, he declined having any mental illness or needing any treatment during the customary triage visit. He had no problem as an inmate and was never referred to psychiatric services. However, when meeting with his public defender, George derailed into delusions. He talked about how the cops had been conspiring against him all of his life, with his current incarceration as a culmination. He mentioned how the judge was purposely trying to get them evicted so that he could own the house himself. He asked his lawyer to countersue the judge for a violation of his rights. The public defender filed for a competency evaluation of his client.
The forensic psychiatrist evaluated the patient and had a similar interpretation. This was a patient who had delusions and was perseverating on them to the point of being unable to engage in meaningful work with his attorney. The psychiatrist recommended involuntary treatment with an antipsychotic after diagnosing the patient with a psychotic illness.
My interactions with George
George is a loud and bucolic man with an usual mix of Southern idioms, a slightly British accent, and East Coast humor. He insisted on telling me why he wanted the staff to refer to him by his Native American nickname prior to the start our interview. He then asked me to listen to his life story to understand why Harry meant so much to him. Despite recounting their truly meaningful relationship, his affect was odd with poor reactivity; he had an incongruent and somewhat ungenuine joyfulness.
Once I heard his account of their friendship, I asked him about his charges and the incident in the courtroom. His answer was a long diatribe about the wrongs that had been done to him, but most of his speech was a series of illogical delusions. I informed him of my thoughts about his fixed and false beliefs, but he was not able to understand my comments. Nonetheless, I felt that he related to me well and that we had established good rapport.
As I was informing him about the antipsychotic I had chosen for his involuntary treatment, he asked me to hold off. He asked me to consider working with him for some time without medications. After all, he did not believe that he had a mental illness and wanted to attempt to engage in the competency training with our therapist without being medicated.
My conceptualization of him
George is a peculiar case. Practically all patients who are committed to my unit for competency restoration are psychotic, and their psychosis prevents their engagement with their attorneys. They have poor insight into their illness, which leads to their commitment. On admission, I confirm the assessment of the forensic psychiatrist and start the ordered involuntary treatment on patients. Many of them are gravely disabled – making the ethical dilemma easier to navigate. For other patients, the idea that they will be kept incarcerated until found competent also makes the forced treatment a simpler decision.
George was different – his impeccable grooming, his dislike of jail food, and his request for appropriately fitting jail clothes were far from disorganized. More importantly, however, he had adequate shelter outside of jail, income for assisting Harry, and a rich network of friends. Despite being riddled with delusions, his thought process was linear, and he was redirectable – even when discussing his delusions. I conceptualized the ethical conflict as such: Not treating him might lead to a longer period of incompetence and a longer incarceration; treating him would go against his desire to remain untreated.
After contacting Harry, I was fairly certain that George had suffered from his delusions for at least a significant part of his adult life, if not in its entirety. However, Harry was infinitely thankful for George’s assistance and felt that George had a good life. This added another fundamental question: Would forcing George to engage in formal mental health treatment lead him to have a better life? He was happy, had meaningful relationships, and contributed to his life as well as his friends’ lives in a deep way.
I diagnosed him as having an unspecified psychotic disorder, likely schizophrenia; he had delusions and negative symptoms, like his impaired affect. Despite this diagnosis, I decided to hold off from using involuntary treatment. I met with him daily for more than 2 weeks, and we discussed his story, his feelings, and his beliefs. On occasion, it was hard to separate the delusions from justifiable anger at the system. He had felt that he and Harry had been wronged, when society should have protected their vulnerability. He learned to trust me, and his therapist taught him competency training. Despite a possible 1-year commitment, we declared him competent to stand trial in 2 weeks. He had learned and excelled in all facets of the training.
George still had delusions, but he understood his charges, that he had acted inappropriately in the courtroom, and how to discuss his case with his legal counsel. Harry found George to be at his baseline during visits. George acted appropriately; he followed the complex rules set on inmates and engaged in all groups that are held on the unit.
Discussion
I certainly do not question the value of involuntary psychiatric treatment for many patients with grave disabilities, violent tendencies, or incompetence. However, George’s case makes me wonder if many people living with schizophrenia can have rich and meaningful lives without ever being in contact with a mental health provider. I wonder if our almost-obsessive attention to antipsychotics makes us lose sight. Our biological reductionism may lead us to see patients such as George as someone with overactive dopaminergic pathways in need of antidopaminergic antipsychotic. Unfortunately for many, biological reductionism often is based on unsubstantiated evidence.
George reminds me that life, including schizophrenia, is more interesting and complicated than a set of genes, pathways, neurons, or neurotransmitters. Our patients’ lives may be convoluted with delusions, often stemming from truth or impaired affects, which are nonetheless genuine. I don’t know what will happen to George, but his past 50 years suggest that he will continue to have friends, and he will continue to live without being impaired by his delusions. Strangely, I worry less about him than many of my other patients.
Many mental health providers have advocated for a wider and easier access to involuntarily medicate our patients. I think that there is a misguided belief that involuntary antipsychotic treatment will lead to a rise in their use. However, if Carl Rogers, PhD, and others were right in stating that our relationship with our patients was the ultimate factor in their recovery, at what cost are we willing to jeopardize this? My fear is that this cost will be the loss of trust, which is so necessary in treatment. I hope that my short relationship with George did not scare him from ever seeing a psychiatrist again. In some ways, I suspect that by simply listening to George and withholding forced treatment, he will be more inclined to seek treatment in the future.
Take-home points
- Certain patients with psychosis have fairly high functioning.
- Milieu therapy is, in certain cases, able to assuage some symptoms of psychosis.
- Compulsory antipsychotic administration may not be ethical in certain cases of acute psychosis.
- Biological reductionism may undermine a complete ethical understanding of psychosis.
- Psychiatric disorders are etiologically complex and multifactorial.
- Involuntary treatment may provide short-term gains, but prevent long-term trust between patient and provider.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre also mentors several residents on projects, including reduction in the use of solitary confinement of patients with mental illness, reduction in the use of involuntary treatment of the mentally ill, and examination of the mentally ill offender.
Shinal v. Toms: It’s Now Harder to Get Informed Consent
Question: Which of the following statements regarding Shinal v. Toms, a recent landmark decision on informed consent, is correct?:
A. The case was heard in the Pennsylvania Supreme Court and its decision is binding only in that state.
B. It held that obtaining informed consent is a doctor’s duty that is non-delegable.
C. The decision reversed the lower courts, which had held that the defendant’s qualified assistant could obtain consent.
D. An earlier case heard by the same court had ruled that doctors, not hospitals, owe the legal duty to obtain informed consent.
E. All are correct.
Answer: E.
On Nov. 26, 2007, Megan Shinal and Dr. Steven Toms met for a 20-minute initial consultation to discuss removing a recurrent craniopharyngioma.1 Years earlier, a surgeon had performed a transsphenoidal resection, but was unable to remove all of it. The residual portion of the tumor had increased in size and extended into vital structures of the brain, jeopardizing Mrs. Shinal’s eyesight and her carotid artery, causing headaches, and threatening to impact her pituitary function.
Dr. Toms testified that he reviewed with Mrs. Shinal the alternatives, risks, and benefits of total versus subtotal resection, and shared his opinion that, although a less aggressive approach to removing the tumor was safer in the short term, such an approach would increase the likelihood that the tumor would regrow. Dr. Toms was unable to recall many of the specifics, but he testified that he advised Mrs. Shinal that total surgical resection offered the highest chance for long-term survival. By the end of the visit, Mrs. Shinal had decided to undergo surgery. However, the type of surgery had not yet been determined.
Shortly thereafter, on Dec. 19, 2007, Mrs. Shinal had a telephone conversation with Dr. Toms’ physician assistant. Mrs. Shinal later testified that she asked the physician assistant about scarring that would likely result from surgery, whether radiation would be necessary, and about the date of surgery. The medical record of this telephone call indicated that Dr. Toms’ physician assistant also answered questions about the craniotomy incision. On Jan. 17, 2008, Mrs. Shinal met with the physician assistant at the Geisinger Medical Center’s neurosurgery clinic. The assistant obtained Mrs. Shinal’s medical history, conducted a physical, and provided Mrs. Shinal with information relating to the surgery. Mrs. Shinal signed an informed consent form.
On Jan. 31, 2008, Mrs. Shinal underwent an open craniotomy for a total resection of the pituitary tumor at Geisinger Medical Center. During the operation, Dr. Toms perforated Mrs. Shinal’s carotid artery, which resulted in hemorrhage, stroke, brain injury, and partial blindness.
According to the Shinals’ complaint, Dr. Toms failed to explain the risks of surgery to Mrs. Shinal or to offer her the lower-risk surgical alternative of subtotal resection of the benign tumor, followed by radiation. At trial, Mrs. Shinal was unable to recall being informed of the relative risks of the surgery, other than coma and death. She testified that, had she known the alternative approaches to surgery, i.e., total versus subtotal resection, she would have chosen subtotal resection as the safer, less aggressive alternative.
The trial court instructed the jury with regard to Dr. Toms’ duty to obtain informed consent from Mrs. Shinal as follows: “[I]n considering whether [Dr. Toms] provided consent to [Mrs. Shinal], you may consider any relevant information you find was communicated to [Mrs. Shinal] by any qualified person acting as an assistant to [Dr. Toms].”
On April 21, 2014, the jury returned a verdict in favor of Dr. Toms.
The plaintiffs appealed to the Pennsylvania Superior Court, which affirmed the trial court’s judgment. It rejected the Shinals’ argument that the trial court’s informed consent charge, which permitted the jury to consider information provided by Dr. Toms’ physician assistant to Mrs. Shinal, was erroneous and prejudicial. The Superior Court relied upon two of its prior cases to opine that a qualified professional acting under the attending doctor’s supervision may convey information communicated to a patient for purposes of obtaining informed consent.
The trial court initially instructed the jury that, in assessing whether Dr. Toms obtained Mrs. Shinal’s informed consent, it could consider relevant information communicated by “any qualified person acting as an assistant” to Dr. Toms. The defendant doctor argued that while it is the physician’s duty to obtain the patient’s informed consent, the physician is not required to supply all of the information personally. It is the information conveyed, rather than the person conveying it that determines informed consent. Dr. Toms cited several older Pennsylvania Superior Court cases, which permitted a physician to fulfill through an intermediary the duty to provide sufficient information to obtain a patient’s informed consent.
The plaintiffs then appealed to the Pennsylvania Supreme Court, which led to a reversal. In a 4-3 decision, the court disagreed, citing their ruling in the 2002 case of Valles v. Albert Einstein Medical Center,2 where they held that the duty to obtain informed consent could not be imputed to a hospital. In Valles, the court held that the duty to obtain a patient’s informed consent is a nondelegable duty owed by the physician conducting the surgery or treatment, because obtaining informed consent results directly from the duty of disclosure, which lies solely with the physician, and a hospital therefore cannot be liable for a physician’s failure to obtain informed consent.
Reasoning by extension, the court accordingly ruled that a physician may not delegate to others his or her obligation to provide sufficient information in order to obtain a patient’s informed consent. It declared: “Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.”
The court also held that “a physician cannot rely upon a subordinate to disclose the information required to obtain informed consent. Without direct dialogue and a two-way exchange between the physician and patient, the physician cannot be confident that the patient comprehends the risks, benefits, likelihood of success, and alternatives. ... Informed consent is a product of the physician-patient relationship.
"The patient is in the vulnerable position of entrusting his or her care and well being to the physician based upon the physician’s education, training, and expertise," the court added. "It is incumbent upon the physician to cultivate a relationship with the patient and to familiarize himself or herself with the patient’s understanding and expectations. Were the law to permit physicians to delegate the provision of critical information to staff, it would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider. A regime that would countenance delegation of the informed consent process would undermine the primacy of the physician-patient relationship. Only by personally satisfying the duty of disclosure may the physician ensure that consent truly is informed.”
The facts of the case appear straightforward, and its legal conclusion clear. Whether one agrees with the court’s decision is, however, another matter. The American Medical Association and the Pennsylvania Medical Society (PAMED) had submitted an amicus brief supporting Dr. Toms’ position, arguing that he had fulfilled his obligations under Pennsylvania’s Medical Care Availability and Reduction of Error Act, as well as common law established in previous Pennsylvania court rulings. The final appellate decision therefore came as a big disappointment. The PAMED website notes that the decision “could have significant ramifications for Pennsylvania physicians” in that they can “seemingly no longer rely on the aid of their qualified staff in the informed consent process.”3
The urgent question now is whether other jurisdictions will adopt this Pennsylvania rule that drastically changes the way doctors obtain informed consent from their patients.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Shinal v. Toms, J-106-2016, Supreme Court of Pennsylvania, Decided: June 20, 2017.
2. Valles v. Albert Einstein Medical Center, 805 A.2d (PA, 2002).
3. Informed-consent ruling may have “far-reaching, negative impact.” AMA Wire, Aug 8, 2017.
Question: Which of the following statements regarding Shinal v. Toms, a recent landmark decision on informed consent, is correct?:
A. The case was heard in the Pennsylvania Supreme Court and its decision is binding only in that state.
B. It held that obtaining informed consent is a doctor’s duty that is non-delegable.
C. The decision reversed the lower courts, which had held that the defendant’s qualified assistant could obtain consent.
D. An earlier case heard by the same court had ruled that doctors, not hospitals, owe the legal duty to obtain informed consent.
E. All are correct.
Answer: E.
On Nov. 26, 2007, Megan Shinal and Dr. Steven Toms met for a 20-minute initial consultation to discuss removing a recurrent craniopharyngioma.1 Years earlier, a surgeon had performed a transsphenoidal resection, but was unable to remove all of it. The residual portion of the tumor had increased in size and extended into vital structures of the brain, jeopardizing Mrs. Shinal’s eyesight and her carotid artery, causing headaches, and threatening to impact her pituitary function.
Dr. Toms testified that he reviewed with Mrs. Shinal the alternatives, risks, and benefits of total versus subtotal resection, and shared his opinion that, although a less aggressive approach to removing the tumor was safer in the short term, such an approach would increase the likelihood that the tumor would regrow. Dr. Toms was unable to recall many of the specifics, but he testified that he advised Mrs. Shinal that total surgical resection offered the highest chance for long-term survival. By the end of the visit, Mrs. Shinal had decided to undergo surgery. However, the type of surgery had not yet been determined.
Shortly thereafter, on Dec. 19, 2007, Mrs. Shinal had a telephone conversation with Dr. Toms’ physician assistant. Mrs. Shinal later testified that she asked the physician assistant about scarring that would likely result from surgery, whether radiation would be necessary, and about the date of surgery. The medical record of this telephone call indicated that Dr. Toms’ physician assistant also answered questions about the craniotomy incision. On Jan. 17, 2008, Mrs. Shinal met with the physician assistant at the Geisinger Medical Center’s neurosurgery clinic. The assistant obtained Mrs. Shinal’s medical history, conducted a physical, and provided Mrs. Shinal with information relating to the surgery. Mrs. Shinal signed an informed consent form.
On Jan. 31, 2008, Mrs. Shinal underwent an open craniotomy for a total resection of the pituitary tumor at Geisinger Medical Center. During the operation, Dr. Toms perforated Mrs. Shinal’s carotid artery, which resulted in hemorrhage, stroke, brain injury, and partial blindness.
According to the Shinals’ complaint, Dr. Toms failed to explain the risks of surgery to Mrs. Shinal or to offer her the lower-risk surgical alternative of subtotal resection of the benign tumor, followed by radiation. At trial, Mrs. Shinal was unable to recall being informed of the relative risks of the surgery, other than coma and death. She testified that, had she known the alternative approaches to surgery, i.e., total versus subtotal resection, she would have chosen subtotal resection as the safer, less aggressive alternative.
The trial court instructed the jury with regard to Dr. Toms’ duty to obtain informed consent from Mrs. Shinal as follows: “[I]n considering whether [Dr. Toms] provided consent to [Mrs. Shinal], you may consider any relevant information you find was communicated to [Mrs. Shinal] by any qualified person acting as an assistant to [Dr. Toms].”
On April 21, 2014, the jury returned a verdict in favor of Dr. Toms.
The plaintiffs appealed to the Pennsylvania Superior Court, which affirmed the trial court’s judgment. It rejected the Shinals’ argument that the trial court’s informed consent charge, which permitted the jury to consider information provided by Dr. Toms’ physician assistant to Mrs. Shinal, was erroneous and prejudicial. The Superior Court relied upon two of its prior cases to opine that a qualified professional acting under the attending doctor’s supervision may convey information communicated to a patient for purposes of obtaining informed consent.
The trial court initially instructed the jury that, in assessing whether Dr. Toms obtained Mrs. Shinal’s informed consent, it could consider relevant information communicated by “any qualified person acting as an assistant” to Dr. Toms. The defendant doctor argued that while it is the physician’s duty to obtain the patient’s informed consent, the physician is not required to supply all of the information personally. It is the information conveyed, rather than the person conveying it that determines informed consent. Dr. Toms cited several older Pennsylvania Superior Court cases, which permitted a physician to fulfill through an intermediary the duty to provide sufficient information to obtain a patient’s informed consent.
The plaintiffs then appealed to the Pennsylvania Supreme Court, which led to a reversal. In a 4-3 decision, the court disagreed, citing their ruling in the 2002 case of Valles v. Albert Einstein Medical Center,2 where they held that the duty to obtain informed consent could not be imputed to a hospital. In Valles, the court held that the duty to obtain a patient’s informed consent is a nondelegable duty owed by the physician conducting the surgery or treatment, because obtaining informed consent results directly from the duty of disclosure, which lies solely with the physician, and a hospital therefore cannot be liable for a physician’s failure to obtain informed consent.
Reasoning by extension, the court accordingly ruled that a physician may not delegate to others his or her obligation to provide sufficient information in order to obtain a patient’s informed consent. It declared: “Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.”
The court also held that “a physician cannot rely upon a subordinate to disclose the information required to obtain informed consent. Without direct dialogue and a two-way exchange between the physician and patient, the physician cannot be confident that the patient comprehends the risks, benefits, likelihood of success, and alternatives. ... Informed consent is a product of the physician-patient relationship.
"The patient is in the vulnerable position of entrusting his or her care and well being to the physician based upon the physician’s education, training, and expertise," the court added. "It is incumbent upon the physician to cultivate a relationship with the patient and to familiarize himself or herself with the patient’s understanding and expectations. Were the law to permit physicians to delegate the provision of critical information to staff, it would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider. A regime that would countenance delegation of the informed consent process would undermine the primacy of the physician-patient relationship. Only by personally satisfying the duty of disclosure may the physician ensure that consent truly is informed.”
The facts of the case appear straightforward, and its legal conclusion clear. Whether one agrees with the court’s decision is, however, another matter. The American Medical Association and the Pennsylvania Medical Society (PAMED) had submitted an amicus brief supporting Dr. Toms’ position, arguing that he had fulfilled his obligations under Pennsylvania’s Medical Care Availability and Reduction of Error Act, as well as common law established in previous Pennsylvania court rulings. The final appellate decision therefore came as a big disappointment. The PAMED website notes that the decision “could have significant ramifications for Pennsylvania physicians” in that they can “seemingly no longer rely on the aid of their qualified staff in the informed consent process.”3
The urgent question now is whether other jurisdictions will adopt this Pennsylvania rule that drastically changes the way doctors obtain informed consent from their patients.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Shinal v. Toms, J-106-2016, Supreme Court of Pennsylvania, Decided: June 20, 2017.
2. Valles v. Albert Einstein Medical Center, 805 A.2d (PA, 2002).
3. Informed-consent ruling may have “far-reaching, negative impact.” AMA Wire, Aug 8, 2017.
Question: Which of the following statements regarding Shinal v. Toms, a recent landmark decision on informed consent, is correct?:
A. The case was heard in the Pennsylvania Supreme Court and its decision is binding only in that state.
B. It held that obtaining informed consent is a doctor’s duty that is non-delegable.
C. The decision reversed the lower courts, which had held that the defendant’s qualified assistant could obtain consent.
D. An earlier case heard by the same court had ruled that doctors, not hospitals, owe the legal duty to obtain informed consent.
E. All are correct.
Answer: E.
On Nov. 26, 2007, Megan Shinal and Dr. Steven Toms met for a 20-minute initial consultation to discuss removing a recurrent craniopharyngioma.1 Years earlier, a surgeon had performed a transsphenoidal resection, but was unable to remove all of it. The residual portion of the tumor had increased in size and extended into vital structures of the brain, jeopardizing Mrs. Shinal’s eyesight and her carotid artery, causing headaches, and threatening to impact her pituitary function.
Dr. Toms testified that he reviewed with Mrs. Shinal the alternatives, risks, and benefits of total versus subtotal resection, and shared his opinion that, although a less aggressive approach to removing the tumor was safer in the short term, such an approach would increase the likelihood that the tumor would regrow. Dr. Toms was unable to recall many of the specifics, but he testified that he advised Mrs. Shinal that total surgical resection offered the highest chance for long-term survival. By the end of the visit, Mrs. Shinal had decided to undergo surgery. However, the type of surgery had not yet been determined.
Shortly thereafter, on Dec. 19, 2007, Mrs. Shinal had a telephone conversation with Dr. Toms’ physician assistant. Mrs. Shinal later testified that she asked the physician assistant about scarring that would likely result from surgery, whether radiation would be necessary, and about the date of surgery. The medical record of this telephone call indicated that Dr. Toms’ physician assistant also answered questions about the craniotomy incision. On Jan. 17, 2008, Mrs. Shinal met with the physician assistant at the Geisinger Medical Center’s neurosurgery clinic. The assistant obtained Mrs. Shinal’s medical history, conducted a physical, and provided Mrs. Shinal with information relating to the surgery. Mrs. Shinal signed an informed consent form.
On Jan. 31, 2008, Mrs. Shinal underwent an open craniotomy for a total resection of the pituitary tumor at Geisinger Medical Center. During the operation, Dr. Toms perforated Mrs. Shinal’s carotid artery, which resulted in hemorrhage, stroke, brain injury, and partial blindness.
According to the Shinals’ complaint, Dr. Toms failed to explain the risks of surgery to Mrs. Shinal or to offer her the lower-risk surgical alternative of subtotal resection of the benign tumor, followed by radiation. At trial, Mrs. Shinal was unable to recall being informed of the relative risks of the surgery, other than coma and death. She testified that, had she known the alternative approaches to surgery, i.e., total versus subtotal resection, she would have chosen subtotal resection as the safer, less aggressive alternative.
The trial court instructed the jury with regard to Dr. Toms’ duty to obtain informed consent from Mrs. Shinal as follows: “[I]n considering whether [Dr. Toms] provided consent to [Mrs. Shinal], you may consider any relevant information you find was communicated to [Mrs. Shinal] by any qualified person acting as an assistant to [Dr. Toms].”
On April 21, 2014, the jury returned a verdict in favor of Dr. Toms.
The plaintiffs appealed to the Pennsylvania Superior Court, which affirmed the trial court’s judgment. It rejected the Shinals’ argument that the trial court’s informed consent charge, which permitted the jury to consider information provided by Dr. Toms’ physician assistant to Mrs. Shinal, was erroneous and prejudicial. The Superior Court relied upon two of its prior cases to opine that a qualified professional acting under the attending doctor’s supervision may convey information communicated to a patient for purposes of obtaining informed consent.
The trial court initially instructed the jury that, in assessing whether Dr. Toms obtained Mrs. Shinal’s informed consent, it could consider relevant information communicated by “any qualified person acting as an assistant” to Dr. Toms. The defendant doctor argued that while it is the physician’s duty to obtain the patient’s informed consent, the physician is not required to supply all of the information personally. It is the information conveyed, rather than the person conveying it that determines informed consent. Dr. Toms cited several older Pennsylvania Superior Court cases, which permitted a physician to fulfill through an intermediary the duty to provide sufficient information to obtain a patient’s informed consent.
The plaintiffs then appealed to the Pennsylvania Supreme Court, which led to a reversal. In a 4-3 decision, the court disagreed, citing their ruling in the 2002 case of Valles v. Albert Einstein Medical Center,2 where they held that the duty to obtain informed consent could not be imputed to a hospital. In Valles, the court held that the duty to obtain a patient’s informed consent is a nondelegable duty owed by the physician conducting the surgery or treatment, because obtaining informed consent results directly from the duty of disclosure, which lies solely with the physician, and a hospital therefore cannot be liable for a physician’s failure to obtain informed consent.
Reasoning by extension, the court accordingly ruled that a physician may not delegate to others his or her obligation to provide sufficient information in order to obtain a patient’s informed consent. It declared: “Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.”
The court also held that “a physician cannot rely upon a subordinate to disclose the information required to obtain informed consent. Without direct dialogue and a two-way exchange between the physician and patient, the physician cannot be confident that the patient comprehends the risks, benefits, likelihood of success, and alternatives. ... Informed consent is a product of the physician-patient relationship.
"The patient is in the vulnerable position of entrusting his or her care and well being to the physician based upon the physician’s education, training, and expertise," the court added. "It is incumbent upon the physician to cultivate a relationship with the patient and to familiarize himself or herself with the patient’s understanding and expectations. Were the law to permit physicians to delegate the provision of critical information to staff, it would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider. A regime that would countenance delegation of the informed consent process would undermine the primacy of the physician-patient relationship. Only by personally satisfying the duty of disclosure may the physician ensure that consent truly is informed.”
The facts of the case appear straightforward, and its legal conclusion clear. Whether one agrees with the court’s decision is, however, another matter. The American Medical Association and the Pennsylvania Medical Society (PAMED) had submitted an amicus brief supporting Dr. Toms’ position, arguing that he had fulfilled his obligations under Pennsylvania’s Medical Care Availability and Reduction of Error Act, as well as common law established in previous Pennsylvania court rulings. The final appellate decision therefore came as a big disappointment. The PAMED website notes that the decision “could have significant ramifications for Pennsylvania physicians” in that they can “seemingly no longer rely on the aid of their qualified staff in the informed consent process.”3
The urgent question now is whether other jurisdictions will adopt this Pennsylvania rule that drastically changes the way doctors obtain informed consent from their patients.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Shinal v. Toms, J-106-2016, Supreme Court of Pennsylvania, Decided: June 20, 2017.
2. Valles v. Albert Einstein Medical Center, 805 A.2d (PA, 2002).
3. Informed-consent ruling may have “far-reaching, negative impact.” AMA Wire, Aug 8, 2017.
Back to the Future, Part 2: Community Paramedicine
Following the successful use of ambulances during the Civil War to transport wounded soldiers from the battlefield to safer and better equipped field hospital facilities, many communities adopted the practice for their civilian populations. Between the Civil War and World War II (WWII) "teaching hospitals" sent interns on their ambulances both to improve patient care at the scene, and to further their interns’ postgraduate education. However, as described by Ryan Corbett Bell in his book The Ambulance (Jefferson, NC: McFarland; 2009), by the 1930s, relatively poor reimbursement for ambulance calls followed by the severe doctor shortage due to WWII, effectively ended this practice. Though the interns were initially replaced by "ambulance attendants" or "orderlies," since the 1960s, ambulances have been staffed by trained EMTs and (later) paramedics to provide basic and advanced prehospital care both at the scene and during transport. For almost half a century, paramedics operating with standing protocols and physician medical control have conclusively demonstrated their ability to improve care and save lives.
At present, the increased demand for access to medical care brought about by the Affordable Care Act, an aging homebound population, overcrowded EDs, and inpatient services filled to capacity, along with, in some areas, insufficient numbers of visiting nurses, NPs, and PAs to provide needed home care services, prompted many to consider expanding the role of paramedics and EMTs to provide "community paramedicine," without afterward requiring them to transport patients to hospitals.
Community paramedicine was defined in 2012 by the US Department of Health and Human Services Administration as "an emerging field in health care where EMTs and Paramedics operate in expanded roles in an effort to connect underutilized resources to underserved populations" (https://www.hrsa.gov). A standard curriculum consisting of 114 hours of education in social determinants of health, public health, and tailored learning about chronic diseases, together with 200 hours of laboratory and clinical experiences has been developed and made available free of charge to colleges and universities (https://www.ruralhealthinfo.org).
Among the many individuals and organizations weighing in on the subject of community paramedicine, the American College of Emergency Physicians 2015 policy statement supports the development of properly designed expanded scope of practice programs for EMS personnel with medical oversight, that do not compromise existing emergency response systems (https://www.acep.org/). Dr Bryan Bledsoe, an editorial board member of JEMS (Journal of Emergency Medical Services), provides a thoughtful analysis of the pros and cons of community paramedicine (http://www.jems.com), hile Iyah K. Romm and colleagues, writing in the NEJM Catalyst, offer concrete evidence of the effectiveness of one such mobile integrated healthcare and community paramedicine program (http://catalyst.nejm.org).
Properly trained, experienced paramedics with careful supervision by emergency medical control physicians and consultation with the patients’ primary care physicians, supported by telemedicine and bedside diagnostic tests, can provide essential care in a patient’s home environment. Depending on local circumstances, EMTs and paramedics can provide that care 24/7, supplementing other available home health care to support posthospital-discharge care for congestive heart failure, wound healing, etc, obviating the need for repeated ED and clinic visits or hospitalizations.
In addition to patient benefits, community paramedicine offers an opportunity for experienced paramedics to extend their years of practice similar to the way urgent care clinics have enabled experienced EPs to extend theirs. For all of these reasons, we support an expanded role for EMTs and paramedics in safe, carefully planned community paramedicine programs.
Following the successful use of ambulances during the Civil War to transport wounded soldiers from the battlefield to safer and better equipped field hospital facilities, many communities adopted the practice for their civilian populations. Between the Civil War and World War II (WWII) "teaching hospitals" sent interns on their ambulances both to improve patient care at the scene, and to further their interns’ postgraduate education. However, as described by Ryan Corbett Bell in his book The Ambulance (Jefferson, NC: McFarland; 2009), by the 1930s, relatively poor reimbursement for ambulance calls followed by the severe doctor shortage due to WWII, effectively ended this practice. Though the interns were initially replaced by "ambulance attendants" or "orderlies," since the 1960s, ambulances have been staffed by trained EMTs and (later) paramedics to provide basic and advanced prehospital care both at the scene and during transport. For almost half a century, paramedics operating with standing protocols and physician medical control have conclusively demonstrated their ability to improve care and save lives.
At present, the increased demand for access to medical care brought about by the Affordable Care Act, an aging homebound population, overcrowded EDs, and inpatient services filled to capacity, along with, in some areas, insufficient numbers of visiting nurses, NPs, and PAs to provide needed home care services, prompted many to consider expanding the role of paramedics and EMTs to provide "community paramedicine," without afterward requiring them to transport patients to hospitals.
Community paramedicine was defined in 2012 by the US Department of Health and Human Services Administration as "an emerging field in health care where EMTs and Paramedics operate in expanded roles in an effort to connect underutilized resources to underserved populations" (https://www.hrsa.gov). A standard curriculum consisting of 114 hours of education in social determinants of health, public health, and tailored learning about chronic diseases, together with 200 hours of laboratory and clinical experiences has been developed and made available free of charge to colleges and universities (https://www.ruralhealthinfo.org).
Among the many individuals and organizations weighing in on the subject of community paramedicine, the American College of Emergency Physicians 2015 policy statement supports the development of properly designed expanded scope of practice programs for EMS personnel with medical oversight, that do not compromise existing emergency response systems (https://www.acep.org/). Dr Bryan Bledsoe, an editorial board member of JEMS (Journal of Emergency Medical Services), provides a thoughtful analysis of the pros and cons of community paramedicine (http://www.jems.com), hile Iyah K. Romm and colleagues, writing in the NEJM Catalyst, offer concrete evidence of the effectiveness of one such mobile integrated healthcare and community paramedicine program (http://catalyst.nejm.org).
Properly trained, experienced paramedics with careful supervision by emergency medical control physicians and consultation with the patients’ primary care physicians, supported by telemedicine and bedside diagnostic tests, can provide essential care in a patient’s home environment. Depending on local circumstances, EMTs and paramedics can provide that care 24/7, supplementing other available home health care to support posthospital-discharge care for congestive heart failure, wound healing, etc, obviating the need for repeated ED and clinic visits or hospitalizations.
In addition to patient benefits, community paramedicine offers an opportunity for experienced paramedics to extend their years of practice similar to the way urgent care clinics have enabled experienced EPs to extend theirs. For all of these reasons, we support an expanded role for EMTs and paramedics in safe, carefully planned community paramedicine programs.
Following the successful use of ambulances during the Civil War to transport wounded soldiers from the battlefield to safer and better equipped field hospital facilities, many communities adopted the practice for their civilian populations. Between the Civil War and World War II (WWII) "teaching hospitals" sent interns on their ambulances both to improve patient care at the scene, and to further their interns’ postgraduate education. However, as described by Ryan Corbett Bell in his book The Ambulance (Jefferson, NC: McFarland; 2009), by the 1930s, relatively poor reimbursement for ambulance calls followed by the severe doctor shortage due to WWII, effectively ended this practice. Though the interns were initially replaced by "ambulance attendants" or "orderlies," since the 1960s, ambulances have been staffed by trained EMTs and (later) paramedics to provide basic and advanced prehospital care both at the scene and during transport. For almost half a century, paramedics operating with standing protocols and physician medical control have conclusively demonstrated their ability to improve care and save lives.
At present, the increased demand for access to medical care brought about by the Affordable Care Act, an aging homebound population, overcrowded EDs, and inpatient services filled to capacity, along with, in some areas, insufficient numbers of visiting nurses, NPs, and PAs to provide needed home care services, prompted many to consider expanding the role of paramedics and EMTs to provide "community paramedicine," without afterward requiring them to transport patients to hospitals.
Community paramedicine was defined in 2012 by the US Department of Health and Human Services Administration as "an emerging field in health care where EMTs and Paramedics operate in expanded roles in an effort to connect underutilized resources to underserved populations" (https://www.hrsa.gov). A standard curriculum consisting of 114 hours of education in social determinants of health, public health, and tailored learning about chronic diseases, together with 200 hours of laboratory and clinical experiences has been developed and made available free of charge to colleges and universities (https://www.ruralhealthinfo.org).
Among the many individuals and organizations weighing in on the subject of community paramedicine, the American College of Emergency Physicians 2015 policy statement supports the development of properly designed expanded scope of practice programs for EMS personnel with medical oversight, that do not compromise existing emergency response systems (https://www.acep.org/). Dr Bryan Bledsoe, an editorial board member of JEMS (Journal of Emergency Medical Services), provides a thoughtful analysis of the pros and cons of community paramedicine (http://www.jems.com), hile Iyah K. Romm and colleagues, writing in the NEJM Catalyst, offer concrete evidence of the effectiveness of one such mobile integrated healthcare and community paramedicine program (http://catalyst.nejm.org).
Properly trained, experienced paramedics with careful supervision by emergency medical control physicians and consultation with the patients’ primary care physicians, supported by telemedicine and bedside diagnostic tests, can provide essential care in a patient’s home environment. Depending on local circumstances, EMTs and paramedics can provide that care 24/7, supplementing other available home health care to support posthospital-discharge care for congestive heart failure, wound healing, etc, obviating the need for repeated ED and clinic visits or hospitalizations.
In addition to patient benefits, community paramedicine offers an opportunity for experienced paramedics to extend their years of practice similar to the way urgent care clinics have enabled experienced EPs to extend theirs. For all of these reasons, we support an expanded role for EMTs and paramedics in safe, carefully planned community paramedicine programs.
The Atopic Dermatitis Biologic Era Has Begun
Atopic dermatitis (AD) is a vexing multisystem disorder characterized by frequently recurrent, intrusive, and sometimes disabling itch and dermatitis. The itch may be present throughout the day but crescendos at bedtime or 1 to 2 hours after sleep initiation, resulting in disrupted sleep cycles, lack of rest, more hours scratching, daytime somnolence, poor work attendance and performance, and poor school attendance and performance.1
Atopic dermatitis is a lifelong disease that only remits in approximately half of patients.2 There is a need for a disease-specific systemic drug in AD. Phototherapy, cyclosporine, methotrexate, and azathioprine are nonspecific immunosuppressive agents that can be used off label for AD but may or may not be effective.3 Oral or intramuscular corticosteroids are associated with problematic side effects such as weight gain, osteoporosis, fractures, psychological problems, striae, buffalo hump, and steroid withdrawal symptoms and disease aggravation upon withdrawal (ie, flaring to a state worse than prior to steroid initiation).3,4
A biologic medication for AD has been long overdue. Psoriatic biologic medications have been tried in AD with occasional benefit in case reports but no major response in larger trials. Belloni et al5 reviewed early data on off-label usage of biologics approved by the US Food and Drug Administration for psoriasis or other indications applied to AD patients. In their review of cases, they make the point that results are variable and anti-B-cell activity may hold the greatest promise.5 On the other hand, a recent series of 3 patients showed limited response to rituximab in chronic AD,6 while a combination of omalizumab, an anti-IgE medication, and rituximab was helpful in some patients.7 Ultimately, the issue is that nonspecific biologics may or may not address the underlying disease factors in AD. Therefore, there has been a true need for biologic intervention targeted directly at the pathogenic mechanism of AD. Furthermore, the desire for a biologic targeted at AD is paired with the true need to have a medication so targeted that the drug would have little effect on the rest of the immune system, resulting in targeted immunomodulation without secondary risk of infections.
Wait no longer, that era arrived a few months ago with the rapid US Food and Drug Administration approval of dupilumab, an injectable medication used every 2 weeks for the therapy of moderate to severe AD. This fully human monoclonal antibody against the IL-4Rα subunit blocks IL-4 and IL-13, key inflammatory agents in the triggering of production of IgE and eosinophil activation. Even better than the fact that it is targeted are the excellent outcomes in the therapy of moderate to severe AD in adults and the minimal side-effect profile resulting in no requirements for laboratory screening or ongoing monitoring.8
Dupilumab seems to perform well, both clinically and in improving the lives of AD patients. Meta-analysis of trials involving dupilumab has shown improved health-related quality of life outcomes.9,10 Usage of dupilumab alone in clinical trials for 16 weeks (SOLO 1 and SOLO 2) has resulted in stunning reduction in disease severity with a limited side-effect profile, with patients most commonly reporting conjunctivitis.11 In real-world models where dupilumab is added into a regimen of topical corticosteroid usage (LIBERTY AD CHRONOS trial), patients fared even better with the combination, highlighting that this medication may best be used adjunctively to our skin care guidance as dermatologists.12
A new era for AD patients has arrived and we as practitioners are now fortunate to be able to therapeutically reach the worst cases of AD. The new era has only begun with dozens of new agents addressing a variety of interleukin pathways including IL-17 and IL-22 still under development. Ultimately, we hope that ongoing pediatric trials will allow us to glean the role of early disease intervention at the root cause of AD and address our abilities to prevent comorbidities and disease persistence. Will we be able to avert years of disabling disease? The future holds immense hope.
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351.
- Somanunt S, Chinratanapisit S, Pacharn P, et al. The natural history of atopic dermatitis and its association with Atopic March [published online Dec 12, 2016]. Asian Pac J Allergy Immunol. doi:10.12932/AP0825.
- Sidbury R, Davis DM, Cohen DE, et al; American Academy of Dermatology. Guidelines of care for the management of atopic dermatitis: section 3. management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71:327-349.
- Hajar T, Leshem YA, Hanifin JM, et al; the National Eczema Association Task Force. A systematic review of topical corticosteroid withdrawal ("steroid addiction") in patients with atopic dermatitis and other dermatoses [published online January 13, 2015]. J Am Acad Dermatol. 2015;72:541.e2-549.e2.
- Belloni B, Andres C, Ollert M, et al. Novel immunological approaches in the treatment of atopic eczema. Curr Opin Allergy Clin Immunol. 2008;8:423-427.
- McDonald BS, Jones J, Rustin M. Rituximab as a treatment for severe atopic eczema: failure to improve in three consecutive patients. Clin Exp Dermatol. 2016;41:45-47.
- Sánchez-Ramón S, Eguíluz-Gracia I, Rodríguez-Mazariego ME, et al. Sequential combined therapy with omalizumab and rituximab: a new approach to severe atopic dermatitis. J Investig Allergol Clin Immunol. 2013;23:190-196.
- D'Erme AM, Romanelli M, Chiricozzi A. Spotlight on dupilumab in the treatment of atopic dermatitis: design, development, and potential place in therapy. Drug Des Devel Ther. 2017;11:1473-1480.
- Han Y, Chen Y, Liu X, et al. Efficacy and safety of dupilumab for the treatment of adult atopic dermatitis: a meta-analysis of randomized clinical trials [published online May 4, 2017]. J Allergy Clin Immunol. doi:10.1016/j.jaci.2017.04.015.
- Simpson EL. Dupilumab improves general health-related quality-of-life in patients with moderate-to-severe atopic dermatitis: pooled results from two randomized, controlled phase 3 clinical trials. Dermatol Ther (Heidelb). 2017;7:243-248.
- Simpson EL, Bieber T, Guttman-Yassky E, et al; SOLO 1 and SOLO 2 Investigators. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis [published online Sep 30, 2016]. N Engl J Med. 2016;375:2335-2348.
- Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial [published online May 4, 2017]. Lancet. 2017;389:2287-2303.
Atopic dermatitis (AD) is a vexing multisystem disorder characterized by frequently recurrent, intrusive, and sometimes disabling itch and dermatitis. The itch may be present throughout the day but crescendos at bedtime or 1 to 2 hours after sleep initiation, resulting in disrupted sleep cycles, lack of rest, more hours scratching, daytime somnolence, poor work attendance and performance, and poor school attendance and performance.1
Atopic dermatitis is a lifelong disease that only remits in approximately half of patients.2 There is a need for a disease-specific systemic drug in AD. Phototherapy, cyclosporine, methotrexate, and azathioprine are nonspecific immunosuppressive agents that can be used off label for AD but may or may not be effective.3 Oral or intramuscular corticosteroids are associated with problematic side effects such as weight gain, osteoporosis, fractures, psychological problems, striae, buffalo hump, and steroid withdrawal symptoms and disease aggravation upon withdrawal (ie, flaring to a state worse than prior to steroid initiation).3,4
A biologic medication for AD has been long overdue. Psoriatic biologic medications have been tried in AD with occasional benefit in case reports but no major response in larger trials. Belloni et al5 reviewed early data on off-label usage of biologics approved by the US Food and Drug Administration for psoriasis or other indications applied to AD patients. In their review of cases, they make the point that results are variable and anti-B-cell activity may hold the greatest promise.5 On the other hand, a recent series of 3 patients showed limited response to rituximab in chronic AD,6 while a combination of omalizumab, an anti-IgE medication, and rituximab was helpful in some patients.7 Ultimately, the issue is that nonspecific biologics may or may not address the underlying disease factors in AD. Therefore, there has been a true need for biologic intervention targeted directly at the pathogenic mechanism of AD. Furthermore, the desire for a biologic targeted at AD is paired with the true need to have a medication so targeted that the drug would have little effect on the rest of the immune system, resulting in targeted immunomodulation without secondary risk of infections.
Wait no longer, that era arrived a few months ago with the rapid US Food and Drug Administration approval of dupilumab, an injectable medication used every 2 weeks for the therapy of moderate to severe AD. This fully human monoclonal antibody against the IL-4Rα subunit blocks IL-4 and IL-13, key inflammatory agents in the triggering of production of IgE and eosinophil activation. Even better than the fact that it is targeted are the excellent outcomes in the therapy of moderate to severe AD in adults and the minimal side-effect profile resulting in no requirements for laboratory screening or ongoing monitoring.8
Dupilumab seems to perform well, both clinically and in improving the lives of AD patients. Meta-analysis of trials involving dupilumab has shown improved health-related quality of life outcomes.9,10 Usage of dupilumab alone in clinical trials for 16 weeks (SOLO 1 and SOLO 2) has resulted in stunning reduction in disease severity with a limited side-effect profile, with patients most commonly reporting conjunctivitis.11 In real-world models where dupilumab is added into a regimen of topical corticosteroid usage (LIBERTY AD CHRONOS trial), patients fared even better with the combination, highlighting that this medication may best be used adjunctively to our skin care guidance as dermatologists.12
A new era for AD patients has arrived and we as practitioners are now fortunate to be able to therapeutically reach the worst cases of AD. The new era has only begun with dozens of new agents addressing a variety of interleukin pathways including IL-17 and IL-22 still under development. Ultimately, we hope that ongoing pediatric trials will allow us to glean the role of early disease intervention at the root cause of AD and address our abilities to prevent comorbidities and disease persistence. Will we be able to avert years of disabling disease? The future holds immense hope.
Atopic dermatitis (AD) is a vexing multisystem disorder characterized by frequently recurrent, intrusive, and sometimes disabling itch and dermatitis. The itch may be present throughout the day but crescendos at bedtime or 1 to 2 hours after sleep initiation, resulting in disrupted sleep cycles, lack of rest, more hours scratching, daytime somnolence, poor work attendance and performance, and poor school attendance and performance.1
Atopic dermatitis is a lifelong disease that only remits in approximately half of patients.2 There is a need for a disease-specific systemic drug in AD. Phototherapy, cyclosporine, methotrexate, and azathioprine are nonspecific immunosuppressive agents that can be used off label for AD but may or may not be effective.3 Oral or intramuscular corticosteroids are associated with problematic side effects such as weight gain, osteoporosis, fractures, psychological problems, striae, buffalo hump, and steroid withdrawal symptoms and disease aggravation upon withdrawal (ie, flaring to a state worse than prior to steroid initiation).3,4
A biologic medication for AD has been long overdue. Psoriatic biologic medications have been tried in AD with occasional benefit in case reports but no major response in larger trials. Belloni et al5 reviewed early data on off-label usage of biologics approved by the US Food and Drug Administration for psoriasis or other indications applied to AD patients. In their review of cases, they make the point that results are variable and anti-B-cell activity may hold the greatest promise.5 On the other hand, a recent series of 3 patients showed limited response to rituximab in chronic AD,6 while a combination of omalizumab, an anti-IgE medication, and rituximab was helpful in some patients.7 Ultimately, the issue is that nonspecific biologics may or may not address the underlying disease factors in AD. Therefore, there has been a true need for biologic intervention targeted directly at the pathogenic mechanism of AD. Furthermore, the desire for a biologic targeted at AD is paired with the true need to have a medication so targeted that the drug would have little effect on the rest of the immune system, resulting in targeted immunomodulation without secondary risk of infections.
Wait no longer, that era arrived a few months ago with the rapid US Food and Drug Administration approval of dupilumab, an injectable medication used every 2 weeks for the therapy of moderate to severe AD. This fully human monoclonal antibody against the IL-4Rα subunit blocks IL-4 and IL-13, key inflammatory agents in the triggering of production of IgE and eosinophil activation. Even better than the fact that it is targeted are the excellent outcomes in the therapy of moderate to severe AD in adults and the minimal side-effect profile resulting in no requirements for laboratory screening or ongoing monitoring.8
Dupilumab seems to perform well, both clinically and in improving the lives of AD patients. Meta-analysis of trials involving dupilumab has shown improved health-related quality of life outcomes.9,10 Usage of dupilumab alone in clinical trials for 16 weeks (SOLO 1 and SOLO 2) has resulted in stunning reduction in disease severity with a limited side-effect profile, with patients most commonly reporting conjunctivitis.11 In real-world models where dupilumab is added into a regimen of topical corticosteroid usage (LIBERTY AD CHRONOS trial), patients fared even better with the combination, highlighting that this medication may best be used adjunctively to our skin care guidance as dermatologists.12
A new era for AD patients has arrived and we as practitioners are now fortunate to be able to therapeutically reach the worst cases of AD. The new era has only begun with dozens of new agents addressing a variety of interleukin pathways including IL-17 and IL-22 still under development. Ultimately, we hope that ongoing pediatric trials will allow us to glean the role of early disease intervention at the root cause of AD and address our abilities to prevent comorbidities and disease persistence. Will we be able to avert years of disabling disease? The future holds immense hope.
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351.
- Somanunt S, Chinratanapisit S, Pacharn P, et al. The natural history of atopic dermatitis and its association with Atopic March [published online Dec 12, 2016]. Asian Pac J Allergy Immunol. doi:10.12932/AP0825.
- Sidbury R, Davis DM, Cohen DE, et al; American Academy of Dermatology. Guidelines of care for the management of atopic dermatitis: section 3. management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71:327-349.
- Hajar T, Leshem YA, Hanifin JM, et al; the National Eczema Association Task Force. A systematic review of topical corticosteroid withdrawal ("steroid addiction") in patients with atopic dermatitis and other dermatoses [published online January 13, 2015]. J Am Acad Dermatol. 2015;72:541.e2-549.e2.
- Belloni B, Andres C, Ollert M, et al. Novel immunological approaches in the treatment of atopic eczema. Curr Opin Allergy Clin Immunol. 2008;8:423-427.
- McDonald BS, Jones J, Rustin M. Rituximab as a treatment for severe atopic eczema: failure to improve in three consecutive patients. Clin Exp Dermatol. 2016;41:45-47.
- Sánchez-Ramón S, Eguíluz-Gracia I, Rodríguez-Mazariego ME, et al. Sequential combined therapy with omalizumab and rituximab: a new approach to severe atopic dermatitis. J Investig Allergol Clin Immunol. 2013;23:190-196.
- D'Erme AM, Romanelli M, Chiricozzi A. Spotlight on dupilumab in the treatment of atopic dermatitis: design, development, and potential place in therapy. Drug Des Devel Ther. 2017;11:1473-1480.
- Han Y, Chen Y, Liu X, et al. Efficacy and safety of dupilumab for the treatment of adult atopic dermatitis: a meta-analysis of randomized clinical trials [published online May 4, 2017]. J Allergy Clin Immunol. doi:10.1016/j.jaci.2017.04.015.
- Simpson EL. Dupilumab improves general health-related quality-of-life in patients with moderate-to-severe atopic dermatitis: pooled results from two randomized, controlled phase 3 clinical trials. Dermatol Ther (Heidelb). 2017;7:243-248.
- Simpson EL, Bieber T, Guttman-Yassky E, et al; SOLO 1 and SOLO 2 Investigators. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis [published online Sep 30, 2016]. N Engl J Med. 2016;375:2335-2348.
- Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial [published online May 4, 2017]. Lancet. 2017;389:2287-2303.
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351.
- Somanunt S, Chinratanapisit S, Pacharn P, et al. The natural history of atopic dermatitis and its association with Atopic March [published online Dec 12, 2016]. Asian Pac J Allergy Immunol. doi:10.12932/AP0825.
- Sidbury R, Davis DM, Cohen DE, et al; American Academy of Dermatology. Guidelines of care for the management of atopic dermatitis: section 3. management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71:327-349.
- Hajar T, Leshem YA, Hanifin JM, et al; the National Eczema Association Task Force. A systematic review of topical corticosteroid withdrawal ("steroid addiction") in patients with atopic dermatitis and other dermatoses [published online January 13, 2015]. J Am Acad Dermatol. 2015;72:541.e2-549.e2.
- Belloni B, Andres C, Ollert M, et al. Novel immunological approaches in the treatment of atopic eczema. Curr Opin Allergy Clin Immunol. 2008;8:423-427.
- McDonald BS, Jones J, Rustin M. Rituximab as a treatment for severe atopic eczema: failure to improve in three consecutive patients. Clin Exp Dermatol. 2016;41:45-47.
- Sánchez-Ramón S, Eguíluz-Gracia I, Rodríguez-Mazariego ME, et al. Sequential combined therapy with omalizumab and rituximab: a new approach to severe atopic dermatitis. J Investig Allergol Clin Immunol. 2013;23:190-196.
- D'Erme AM, Romanelli M, Chiricozzi A. Spotlight on dupilumab in the treatment of atopic dermatitis: design, development, and potential place in therapy. Drug Des Devel Ther. 2017;11:1473-1480.
- Han Y, Chen Y, Liu X, et al. Efficacy and safety of dupilumab for the treatment of adult atopic dermatitis: a meta-analysis of randomized clinical trials [published online May 4, 2017]. J Allergy Clin Immunol. doi:10.1016/j.jaci.2017.04.015.
- Simpson EL. Dupilumab improves general health-related quality-of-life in patients with moderate-to-severe atopic dermatitis: pooled results from two randomized, controlled phase 3 clinical trials. Dermatol Ther (Heidelb). 2017;7:243-248.
- Simpson EL, Bieber T, Guttman-Yassky E, et al; SOLO 1 and SOLO 2 Investigators. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis [published online Sep 30, 2016]. N Engl J Med. 2016;375:2335-2348.
- Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial [published online May 4, 2017]. Lancet. 2017;389:2287-2303.
When the waters recede: Hurricane Harvey and PTSD through indirect trauma
It’s been 5 days since Texas came under siege from Hurricane Harvey and it left up to 51 inches of rain in its wake. Several Southern cities suffered almost complete loss of homes and businesses. The Houston metropolitan area reported 14 deaths, including one of a police officer who was trying to report for duty. Hundreds of thousands of homes have been damaged or lost, and thousands of people are now in makeshift shelters across the city. We have slowly begun the process of repair and rebuilding, and many Houstonians are returning to work. Many others, including well-known local celebrities like J.J. Watt and MattressMack, are volunteering their time and giving money to help those who were not so fortunate. The rescue and recovery efforts have been lauded for the absence of issues tied to politics, religion, or race.
Despite this, we must not forget that this was a natural disaster unlike anything that’s been seen in recent decades. Much like Katrina and Sandy, Hurricane Harvey brought to the people who have lived through the initial trauma the fear, nightmares, emotional distress, and sleep disturbances associated with posttraumatic stress disorder (PTSD). They will require significant support and monitoring to determine whether there is a need for medical intervention, such as cognitive-behavioral therapy, behavioral modification, or pharmacotherapy. However, we are also witnessing something psychiatrists are just becoming more knowledgeable about – PTSD due to indirect trauma.

Taking early warnings in stride
When the anchors and journalists began reporting about a tropical cyclone heading toward the Gulf of Mexico on Aug. 17, most Houstonians – myself included – flipped the channel. Living off the Southern Coast of the United States meant seeing more than our fair share of storm systems, including hurricanes. Each time, no matter the damage or the loss, Texans would pull themselves up by their bootstraps and band together to rebuild their beloved city.
So, it’s no surprise that even as Harvey was upgraded to a hurricane and prepared to breach land, we went about business as usual. However, less than a week later, countless residents of the Lone Star State prepared for what promised to be one of the worst storms in recent history.
Moving to Houston from Dallas for college back in 1998, I fell in love with the city and made it my home. I was here when Tropical Storm Allison made landfall in 2001, leaving up to 37 inches of rain and massive flooding in its wake. The Texas Medical Center, where I was working at the Baylor Human Genome Lab for the summer, suffered about $2 billion worth of damage.
I watched as the images and videos of the city under water splashed across my television screen. I witnessed the floodwaters firsthand as my friends and I carefully drove to an overpass and found a vast body of water where a convergence of three highways used to be visible. I was fortunate not to have been affected by the flood, but the fear of West Nile virus worried me for days because of the mosquito infestation that followed. Eventually, the city recovered, the water receded, and we persevered.
In 2005, in the wake of Katrina, Southern Texans were warned of an impending Category 3 hurricane named Rita. Having been inundated with local and national news coverage of the devastation, and hearing the personal stories of evacuees from New Orleans, Houstonians definitely took more notice this time. More than 3 million people from Houston and the surrounding areas evacuated inland before it arrived, but the chaos resulted in indirect deaths from panicked people trying to leave.
I, along with my two best friends and my boyfriend, were among the many who made the lengthy drive to Dallas, where my parents were anxiously waiting. What should have been a 4-hour drive turned into 10, and that was the result of all the back roads we took to get around the majority of the traffic. There were mass outages around the city, but within a few days, we were all back home. Rita left behind much less damage than predicted, and after the water receded, we persevered.
My third encounter with a hurricane was the Category 2 Ike 3 years later. There were mixed emotions going into this one, with many citizens split between evacuating and staying behind. I was in residency by then, and with only a voluntary evacuation for Houston (compared with a mandatory one in Galveston and the coastal cities), I opted to remain. I had already prepared for the worst by barricading all the glass and stocking up on supplies. In addition, I was living in a two-story townhome in an area considered part of a 200-year flood plain, so I figured I was safe. When Ike struck the city, I was up for several hours listening to the howl of the wind and the insistent smacks of rain against my windows. I left town once the coast was clear, not because of flooding, but because Ike knocked out power and water for much of Houston in the middle of a horridly hot September. I stayed with my parents for about a week until my complex had fixed everything, and seeing that the water had receded, I persevered.
Harvey’s vast destruction
This past week, when Category 4 Hurricane Harvey struck my beloved city, I could not have imagined the losses that were waiting for us. After finishing up a short workday on Friday, Aug. 25, I made my last run for supplies before the weekend. Like many others, I had been keeping an eye on the news as we heard about the destruction Harvey had wreaked on Rockport, South Padre, and Corpus Christi. We all knew that this one was the real deal, that Harvey was going to challenge us in every way possible. For the next 4 days I hunkered down in my house, waiting out the periods of torrential rain while keeping a close eye on the news. At worst, my neighborhood flooded up to the front sidewalk, but water never entered my home, as it did for so many unfortunate individuals. I never lost power, air conditioning, or Internet access. The most distressing thing to happen to me was the inability to leave my home for fear of being caught in the floodwater.
We are #The CityWithNoLimits.
We are #HoustonStrong.
We are #TexasStrong.
When the waters recede, we will persevere.
Jennifer Yen, MD, is a board-certified child, adolescent, and adult private practice psychiatrist in Houston. She also is a clinical assistant professor of psychiatry at Baylor College of Medicine and serves on the Consumers Issues Committee of the American Academy of Child and Adolescent Psychiatry.
It’s been 5 days since Texas came under siege from Hurricane Harvey and it left up to 51 inches of rain in its wake. Several Southern cities suffered almost complete loss of homes and businesses. The Houston metropolitan area reported 14 deaths, including one of a police officer who was trying to report for duty. Hundreds of thousands of homes have been damaged or lost, and thousands of people are now in makeshift shelters across the city. We have slowly begun the process of repair and rebuilding, and many Houstonians are returning to work. Many others, including well-known local celebrities like J.J. Watt and MattressMack, are volunteering their time and giving money to help those who were not so fortunate. The rescue and recovery efforts have been lauded for the absence of issues tied to politics, religion, or race.
Despite this, we must not forget that this was a natural disaster unlike anything that’s been seen in recent decades. Much like Katrina and Sandy, Hurricane Harvey brought to the people who have lived through the initial trauma the fear, nightmares, emotional distress, and sleep disturbances associated with posttraumatic stress disorder (PTSD). They will require significant support and monitoring to determine whether there is a need for medical intervention, such as cognitive-behavioral therapy, behavioral modification, or pharmacotherapy. However, we are also witnessing something psychiatrists are just becoming more knowledgeable about – PTSD due to indirect trauma.

Taking early warnings in stride
When the anchors and journalists began reporting about a tropical cyclone heading toward the Gulf of Mexico on Aug. 17, most Houstonians – myself included – flipped the channel. Living off the Southern Coast of the United States meant seeing more than our fair share of storm systems, including hurricanes. Each time, no matter the damage or the loss, Texans would pull themselves up by their bootstraps and band together to rebuild their beloved city.
So, it’s no surprise that even as Harvey was upgraded to a hurricane and prepared to breach land, we went about business as usual. However, less than a week later, countless residents of the Lone Star State prepared for what promised to be one of the worst storms in recent history.
Moving to Houston from Dallas for college back in 1998, I fell in love with the city and made it my home. I was here when Tropical Storm Allison made landfall in 2001, leaving up to 37 inches of rain and massive flooding in its wake. The Texas Medical Center, where I was working at the Baylor Human Genome Lab for the summer, suffered about $2 billion worth of damage.
I watched as the images and videos of the city under water splashed across my television screen. I witnessed the floodwaters firsthand as my friends and I carefully drove to an overpass and found a vast body of water where a convergence of three highways used to be visible. I was fortunate not to have been affected by the flood, but the fear of West Nile virus worried me for days because of the mosquito infestation that followed. Eventually, the city recovered, the water receded, and we persevered.
In 2005, in the wake of Katrina, Southern Texans were warned of an impending Category 3 hurricane named Rita. Having been inundated with local and national news coverage of the devastation, and hearing the personal stories of evacuees from New Orleans, Houstonians definitely took more notice this time. More than 3 million people from Houston and the surrounding areas evacuated inland before it arrived, but the chaos resulted in indirect deaths from panicked people trying to leave.
I, along with my two best friends and my boyfriend, were among the many who made the lengthy drive to Dallas, where my parents were anxiously waiting. What should have been a 4-hour drive turned into 10, and that was the result of all the back roads we took to get around the majority of the traffic. There were mass outages around the city, but within a few days, we were all back home. Rita left behind much less damage than predicted, and after the water receded, we persevered.
My third encounter with a hurricane was the Category 2 Ike 3 years later. There were mixed emotions going into this one, with many citizens split between evacuating and staying behind. I was in residency by then, and with only a voluntary evacuation for Houston (compared with a mandatory one in Galveston and the coastal cities), I opted to remain. I had already prepared for the worst by barricading all the glass and stocking up on supplies. In addition, I was living in a two-story townhome in an area considered part of a 200-year flood plain, so I figured I was safe. When Ike struck the city, I was up for several hours listening to the howl of the wind and the insistent smacks of rain against my windows. I left town once the coast was clear, not because of flooding, but because Ike knocked out power and water for much of Houston in the middle of a horridly hot September. I stayed with my parents for about a week until my complex had fixed everything, and seeing that the water had receded, I persevered.
Harvey’s vast destruction
This past week, when Category 4 Hurricane Harvey struck my beloved city, I could not have imagined the losses that were waiting for us. After finishing up a short workday on Friday, Aug. 25, I made my last run for supplies before the weekend. Like many others, I had been keeping an eye on the news as we heard about the destruction Harvey had wreaked on Rockport, South Padre, and Corpus Christi. We all knew that this one was the real deal, that Harvey was going to challenge us in every way possible. For the next 4 days I hunkered down in my house, waiting out the periods of torrential rain while keeping a close eye on the news. At worst, my neighborhood flooded up to the front sidewalk, but water never entered my home, as it did for so many unfortunate individuals. I never lost power, air conditioning, or Internet access. The most distressing thing to happen to me was the inability to leave my home for fear of being caught in the floodwater.
We are #The CityWithNoLimits.
We are #HoustonStrong.
We are #TexasStrong.
When the waters recede, we will persevere.
Jennifer Yen, MD, is a board-certified child, adolescent, and adult private practice psychiatrist in Houston. She also is a clinical assistant professor of psychiatry at Baylor College of Medicine and serves on the Consumers Issues Committee of the American Academy of Child and Adolescent Psychiatry.
It’s been 5 days since Texas came under siege from Hurricane Harvey and it left up to 51 inches of rain in its wake. Several Southern cities suffered almost complete loss of homes and businesses. The Houston metropolitan area reported 14 deaths, including one of a police officer who was trying to report for duty. Hundreds of thousands of homes have been damaged or lost, and thousands of people are now in makeshift shelters across the city. We have slowly begun the process of repair and rebuilding, and many Houstonians are returning to work. Many others, including well-known local celebrities like J.J. Watt and MattressMack, are volunteering their time and giving money to help those who were not so fortunate. The rescue and recovery efforts have been lauded for the absence of issues tied to politics, religion, or race.
Despite this, we must not forget that this was a natural disaster unlike anything that’s been seen in recent decades. Much like Katrina and Sandy, Hurricane Harvey brought to the people who have lived through the initial trauma the fear, nightmares, emotional distress, and sleep disturbances associated with posttraumatic stress disorder (PTSD). They will require significant support and monitoring to determine whether there is a need for medical intervention, such as cognitive-behavioral therapy, behavioral modification, or pharmacotherapy. However, we are also witnessing something psychiatrists are just becoming more knowledgeable about – PTSD due to indirect trauma.

Taking early warnings in stride
When the anchors and journalists began reporting about a tropical cyclone heading toward the Gulf of Mexico on Aug. 17, most Houstonians – myself included – flipped the channel. Living off the Southern Coast of the United States meant seeing more than our fair share of storm systems, including hurricanes. Each time, no matter the damage or the loss, Texans would pull themselves up by their bootstraps and band together to rebuild their beloved city.
So, it’s no surprise that even as Harvey was upgraded to a hurricane and prepared to breach land, we went about business as usual. However, less than a week later, countless residents of the Lone Star State prepared for what promised to be one of the worst storms in recent history.
Moving to Houston from Dallas for college back in 1998, I fell in love with the city and made it my home. I was here when Tropical Storm Allison made landfall in 2001, leaving up to 37 inches of rain and massive flooding in its wake. The Texas Medical Center, where I was working at the Baylor Human Genome Lab for the summer, suffered about $2 billion worth of damage.
I watched as the images and videos of the city under water splashed across my television screen. I witnessed the floodwaters firsthand as my friends and I carefully drove to an overpass and found a vast body of water where a convergence of three highways used to be visible. I was fortunate not to have been affected by the flood, but the fear of West Nile virus worried me for days because of the mosquito infestation that followed. Eventually, the city recovered, the water receded, and we persevered.
In 2005, in the wake of Katrina, Southern Texans were warned of an impending Category 3 hurricane named Rita. Having been inundated with local and national news coverage of the devastation, and hearing the personal stories of evacuees from New Orleans, Houstonians definitely took more notice this time. More than 3 million people from Houston and the surrounding areas evacuated inland before it arrived, but the chaos resulted in indirect deaths from panicked people trying to leave.
I, along with my two best friends and my boyfriend, were among the many who made the lengthy drive to Dallas, where my parents were anxiously waiting. What should have been a 4-hour drive turned into 10, and that was the result of all the back roads we took to get around the majority of the traffic. There were mass outages around the city, but within a few days, we were all back home. Rita left behind much less damage than predicted, and after the water receded, we persevered.
My third encounter with a hurricane was the Category 2 Ike 3 years later. There were mixed emotions going into this one, with many citizens split between evacuating and staying behind. I was in residency by then, and with only a voluntary evacuation for Houston (compared with a mandatory one in Galveston and the coastal cities), I opted to remain. I had already prepared for the worst by barricading all the glass and stocking up on supplies. In addition, I was living in a two-story townhome in an area considered part of a 200-year flood plain, so I figured I was safe. When Ike struck the city, I was up for several hours listening to the howl of the wind and the insistent smacks of rain against my windows. I left town once the coast was clear, not because of flooding, but because Ike knocked out power and water for much of Houston in the middle of a horridly hot September. I stayed with my parents for about a week until my complex had fixed everything, and seeing that the water had receded, I persevered.
Harvey’s vast destruction
This past week, when Category 4 Hurricane Harvey struck my beloved city, I could not have imagined the losses that were waiting for us. After finishing up a short workday on Friday, Aug. 25, I made my last run for supplies before the weekend. Like many others, I had been keeping an eye on the news as we heard about the destruction Harvey had wreaked on Rockport, South Padre, and Corpus Christi. We all knew that this one was the real deal, that Harvey was going to challenge us in every way possible. For the next 4 days I hunkered down in my house, waiting out the periods of torrential rain while keeping a close eye on the news. At worst, my neighborhood flooded up to the front sidewalk, but water never entered my home, as it did for so many unfortunate individuals. I never lost power, air conditioning, or Internet access. The most distressing thing to happen to me was the inability to leave my home for fear of being caught in the floodwater.
We are #The CityWithNoLimits.
We are #HoustonStrong.
We are #TexasStrong.
When the waters recede, we will persevere.
Jennifer Yen, MD, is a board-certified child, adolescent, and adult private practice psychiatrist in Houston. She also is a clinical assistant professor of psychiatry at Baylor College of Medicine and serves on the Consumers Issues Committee of the American Academy of Child and Adolescent Psychiatry.
The Disease for Which There Is No Cure and Not Enough Conversation
If I simply let the title of this column stand alone, I suspect most readers of Federal Practitioner would fill in the blank with diseases, such as cancer, HIV, or even devastating genetic conditions, just as I would if presented with the statement without explication.
I read the sentence several weeks ago on a website for caregivers of patients with dementia while browsing for quite a different purpose, and it has haunted me ever since. As a consultation psychiatrist who has spent my career as a VA hospitalist, I am well aware of the sad reality of dementia, but against the backdrop of the aging veteran population, the poignancy of the human tragedy overwhelmed me.
Almost every day on the medical and surgical wards of the VA hospital where I have worked for nearly 2 decades, I see an aging veteran population. There are days when the average age of inpatients is pushing 70 years, and there are many patients in their 80s and 90s. The statistics show that my facility is by no means unique in the VA. Data from the American Community Survey Profile of veterans in 2015 indicate that the median age of veterans is 64 years whereas that of nonveterans is 41.1 The survey emphasized that this age factor has a rippling effect on many other demographic parameters, such as disability, income, and employment, all, in turn, impact the epidemiology of health and illness.1
It is not just age that increases the likelihood that a veteran will develop dementia: Research has identified several aspects of military service that raise the risk of being diagnosed with major neurocognitive disorder, the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition designation for dementia. Many families, patients, and even a few health care professionals may not realize that major neurocognitive disorder is the new neuropsychiatric term for dementia.
Also, many health care professionals do not realize that dementia is the sixth leading cause of death in the U.S.2 Traumatic brain injury, posttraumatic stress disorder, and depression are identified as potential contributors to a higher incidence of dementia in service men and women often with onset at an earlier age.3 Given the prevalence of these comorbidities in persons who were in the military, the VA and DoD will face the medical and psychosocial challenges of providing not only clinical treatment, but also a range of social services for military personnel and veterans. Indeed, federal institutions like the GRECC (Geriatric Research Education and Clinical Center) already are engaged in cutting edge research, delivering high-quality medical treatment, and specialized geriatric and dementia care education and support.
Despite these impressive efforts, too often families ask me 2 crucial questions when a patient is already at a moderate or severe stage of the disease: Is there a cure, and will they get better with or without treatment? This lack of knowledge and understanding is by no means confined to federal health care.
A 2015 report from the Alzheimer’s Association found that 45% of patients with Alzheimer disease or their caregivers were not told about the diagnosis by the doctor.2 Doctors reported that they were more likely to have informed the family of a cancer diagnosis at least in part because they felt there were treatments available and in some cases a cure.
Families ask these questions of me and other health care professionals in the hope of finding guidance. Often the veteran has been hospitalized after behavioral disturbances or wandering have made it impossible to care for the loved elder at home. The family is faced with a double blow: learning the patient has an incurable terminal disease and having to make the decision to place a grandmother or father in a nursing facility. Granted this woeful decision may have to be made even when the family has been fully informed at the time of diagnosis, but it is more distressing when the decision is needed immediately based on safety.
Husbands and wives of 50 years or more and adult children, graying themselves, often ask the second question about improvement. Although treatments exist that can help relieve symptoms and slow progression temporarily, the inexorable and tragic course of the wiping away of memory cannot be reversed or halted.
Not surprisingly, practitioners avoid telling patients and families about a dementia diagnosis because those conversations are painful and difficult. However, the news is much less agonizing to hear when there is time to enjoy the good days that remain and to make arrangements for finances and families. For these important reasons, VA emphasizes shared decision making as the cornerstone of geriatric care. Yet there can be no shared decisions without the compassionate and truthful telling about the diagnosis and the prognosis.
1. U.S. Department of Veterans Affairs National Ce- nter for Veterans Analytics and Statistics. Profile of veterans: 2015 data from the American Community Survey. https://www.va.gov/vetdata/docs/Specia lReports/Profile_of_Veterans_2015.pdf. Published March 2017. Accessed August 22, 2017.
2. Alzheimer’s Association. 2015 Alzheimer’s disease facts and figures. Alzheimers Dement. 2015;11(3):332-384.
3. Weiner MW, Friedl KE, Pacifico A, et al. Military risk factors for Alzheimer’s disease. Alzheimers Dement. 2013;9(4):445-451.
If I simply let the title of this column stand alone, I suspect most readers of Federal Practitioner would fill in the blank with diseases, such as cancer, HIV, or even devastating genetic conditions, just as I would if presented with the statement without explication.
I read the sentence several weeks ago on a website for caregivers of patients with dementia while browsing for quite a different purpose, and it has haunted me ever since. As a consultation psychiatrist who has spent my career as a VA hospitalist, I am well aware of the sad reality of dementia, but against the backdrop of the aging veteran population, the poignancy of the human tragedy overwhelmed me.
Almost every day on the medical and surgical wards of the VA hospital where I have worked for nearly 2 decades, I see an aging veteran population. There are days when the average age of inpatients is pushing 70 years, and there are many patients in their 80s and 90s. The statistics show that my facility is by no means unique in the VA. Data from the American Community Survey Profile of veterans in 2015 indicate that the median age of veterans is 64 years whereas that of nonveterans is 41.1 The survey emphasized that this age factor has a rippling effect on many other demographic parameters, such as disability, income, and employment, all, in turn, impact the epidemiology of health and illness.1
It is not just age that increases the likelihood that a veteran will develop dementia: Research has identified several aspects of military service that raise the risk of being diagnosed with major neurocognitive disorder, the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition designation for dementia. Many families, patients, and even a few health care professionals may not realize that major neurocognitive disorder is the new neuropsychiatric term for dementia.
Also, many health care professionals do not realize that dementia is the sixth leading cause of death in the U.S.2 Traumatic brain injury, posttraumatic stress disorder, and depression are identified as potential contributors to a higher incidence of dementia in service men and women often with onset at an earlier age.3 Given the prevalence of these comorbidities in persons who were in the military, the VA and DoD will face the medical and psychosocial challenges of providing not only clinical treatment, but also a range of social services for military personnel and veterans. Indeed, federal institutions like the GRECC (Geriatric Research Education and Clinical Center) already are engaged in cutting edge research, delivering high-quality medical treatment, and specialized geriatric and dementia care education and support.
Despite these impressive efforts, too often families ask me 2 crucial questions when a patient is already at a moderate or severe stage of the disease: Is there a cure, and will they get better with or without treatment? This lack of knowledge and understanding is by no means confined to federal health care.
A 2015 report from the Alzheimer’s Association found that 45% of patients with Alzheimer disease or their caregivers were not told about the diagnosis by the doctor.2 Doctors reported that they were more likely to have informed the family of a cancer diagnosis at least in part because they felt there were treatments available and in some cases a cure.
Families ask these questions of me and other health care professionals in the hope of finding guidance. Often the veteran has been hospitalized after behavioral disturbances or wandering have made it impossible to care for the loved elder at home. The family is faced with a double blow: learning the patient has an incurable terminal disease and having to make the decision to place a grandmother or father in a nursing facility. Granted this woeful decision may have to be made even when the family has been fully informed at the time of diagnosis, but it is more distressing when the decision is needed immediately based on safety.
Husbands and wives of 50 years or more and adult children, graying themselves, often ask the second question about improvement. Although treatments exist that can help relieve symptoms and slow progression temporarily, the inexorable and tragic course of the wiping away of memory cannot be reversed or halted.
Not surprisingly, practitioners avoid telling patients and families about a dementia diagnosis because those conversations are painful and difficult. However, the news is much less agonizing to hear when there is time to enjoy the good days that remain and to make arrangements for finances and families. For these important reasons, VA emphasizes shared decision making as the cornerstone of geriatric care. Yet there can be no shared decisions without the compassionate and truthful telling about the diagnosis and the prognosis.
If I simply let the title of this column stand alone, I suspect most readers of Federal Practitioner would fill in the blank with diseases, such as cancer, HIV, or even devastating genetic conditions, just as I would if presented with the statement without explication.
I read the sentence several weeks ago on a website for caregivers of patients with dementia while browsing for quite a different purpose, and it has haunted me ever since. As a consultation psychiatrist who has spent my career as a VA hospitalist, I am well aware of the sad reality of dementia, but against the backdrop of the aging veteran population, the poignancy of the human tragedy overwhelmed me.
Almost every day on the medical and surgical wards of the VA hospital where I have worked for nearly 2 decades, I see an aging veteran population. There are days when the average age of inpatients is pushing 70 years, and there are many patients in their 80s and 90s. The statistics show that my facility is by no means unique in the VA. Data from the American Community Survey Profile of veterans in 2015 indicate that the median age of veterans is 64 years whereas that of nonveterans is 41.1 The survey emphasized that this age factor has a rippling effect on many other demographic parameters, such as disability, income, and employment, all, in turn, impact the epidemiology of health and illness.1
It is not just age that increases the likelihood that a veteran will develop dementia: Research has identified several aspects of military service that raise the risk of being diagnosed with major neurocognitive disorder, the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition designation for dementia. Many families, patients, and even a few health care professionals may not realize that major neurocognitive disorder is the new neuropsychiatric term for dementia.
Also, many health care professionals do not realize that dementia is the sixth leading cause of death in the U.S.2 Traumatic brain injury, posttraumatic stress disorder, and depression are identified as potential contributors to a higher incidence of dementia in service men and women often with onset at an earlier age.3 Given the prevalence of these comorbidities in persons who were in the military, the VA and DoD will face the medical and psychosocial challenges of providing not only clinical treatment, but also a range of social services for military personnel and veterans. Indeed, federal institutions like the GRECC (Geriatric Research Education and Clinical Center) already are engaged in cutting edge research, delivering high-quality medical treatment, and specialized geriatric and dementia care education and support.
Despite these impressive efforts, too often families ask me 2 crucial questions when a patient is already at a moderate or severe stage of the disease: Is there a cure, and will they get better with or without treatment? This lack of knowledge and understanding is by no means confined to federal health care.
A 2015 report from the Alzheimer’s Association found that 45% of patients with Alzheimer disease or their caregivers were not told about the diagnosis by the doctor.2 Doctors reported that they were more likely to have informed the family of a cancer diagnosis at least in part because they felt there were treatments available and in some cases a cure.
Families ask these questions of me and other health care professionals in the hope of finding guidance. Often the veteran has been hospitalized after behavioral disturbances or wandering have made it impossible to care for the loved elder at home. The family is faced with a double blow: learning the patient has an incurable terminal disease and having to make the decision to place a grandmother or father in a nursing facility. Granted this woeful decision may have to be made even when the family has been fully informed at the time of diagnosis, but it is more distressing when the decision is needed immediately based on safety.
Husbands and wives of 50 years or more and adult children, graying themselves, often ask the second question about improvement. Although treatments exist that can help relieve symptoms and slow progression temporarily, the inexorable and tragic course of the wiping away of memory cannot be reversed or halted.
Not surprisingly, practitioners avoid telling patients and families about a dementia diagnosis because those conversations are painful and difficult. However, the news is much less agonizing to hear when there is time to enjoy the good days that remain and to make arrangements for finances and families. For these important reasons, VA emphasizes shared decision making as the cornerstone of geriatric care. Yet there can be no shared decisions without the compassionate and truthful telling about the diagnosis and the prognosis.
1. U.S. Department of Veterans Affairs National Ce- nter for Veterans Analytics and Statistics. Profile of veterans: 2015 data from the American Community Survey. https://www.va.gov/vetdata/docs/Specia lReports/Profile_of_Veterans_2015.pdf. Published March 2017. Accessed August 22, 2017.
2. Alzheimer’s Association. 2015 Alzheimer’s disease facts and figures. Alzheimers Dement. 2015;11(3):332-384.
3. Weiner MW, Friedl KE, Pacifico A, et al. Military risk factors for Alzheimer’s disease. Alzheimers Dement. 2013;9(4):445-451.
1. U.S. Department of Veterans Affairs National Ce- nter for Veterans Analytics and Statistics. Profile of veterans: 2015 data from the American Community Survey. https://www.va.gov/vetdata/docs/Specia lReports/Profile_of_Veterans_2015.pdf. Published March 2017. Accessed August 22, 2017.
2. Alzheimer’s Association. 2015 Alzheimer’s disease facts and figures. Alzheimers Dement. 2015;11(3):332-384.
3. Weiner MW, Friedl KE, Pacifico A, et al. Military risk factors for Alzheimer’s disease. Alzheimers Dement. 2013;9(4):445-451.
Noxious Nocebos in Dermatology
The medical dictum primum non nocere (first, do no harm) is a fundamental rule by which physicians have lived for centuries.1 Physicians are familiar with the term placebo (I shall please) and the placebo effect of improvement based on expectation of positive results; however, many are not familiar with the term nocebo (I shall harm) and the nocebo effect of lack of improvement or deterioration based on the expectation of negative results. The patient’s expectation of being pleased and/or being harmed may be on the conscious level and/or on one or more subconscious and unconscious levels.
Words can have as much of an impact on some patients as medications or procedures. Rudyard Kipling said, “Words are, of course, the most powerful drug used by mankind.” The words that a dermatologist chooses to use can have either a placebo or a nocebo effect on the patient. The purpose of this commentary is to elevate awareness that there are positive alternatives to unintended negative suggestions that are commonly used in dermatologic practice.
A search of PubMed articles indexed for MEDLINE and Scopus published from January 1966 through July 28, 2016, was conducted using the terms placebo or nocebo and cutaneous or skin. Prior publications in this area related specifically to dermatology include those of Poletti2 and Sonthalia et al.3
Patient expectations play an important role in both positive and negative treatment outcomes. Patient-physician communication can moderate these effects both positively and negatively.4 Nocebo effects can substantially reduce treatment efficacy and patient compliance. Patient expectations of negative results or side effects of a treatment or medication can be self-induced or can be induced by inappropriate physician-patient communication, drug information leaflets, influence of family or peers, or discovery of reported adverse effects through reading materials on the Internet.4 Expectation of negative effects can reduce patient adherence and compliance with treatment, reducing treatment efficacy. The psychosocial context around the patient and the treatment may change the neuronal biochemistry and circuitry in the patient’s brain, and the central and peripheral mechanisms activated by placebos and nocebos have been found to be the same as those activated by the medications, suggesting cognitive/affective enhancing or impeding of drug action.5
The subconscious and unconscious habitual automated parts of the brain hear words on the level of a 5- or 6-year-old child with literal unconscious cognitive interpretation of the words. These parts also do not connect words in a sentence with each other.5 For example, if the dermatologist or nurse says “This will not hurt,” the unconscious brain hears not and hurt but does not connect the two. On the other hand, if the dermatologist or nurse says “ You may experience some discomfort,” the unconscious brain hears comfort. Telling the patient “Don’t scratch” may be heard unconsciously as scratch. See the Table for suggested rephrasing of common nocebos used in dermatology. The conscious parts of the brain help determine cognitions influenced by associated unconscious memories, positive or negative. Both the conscious and unconscious parts of the brain influence affect or emotion.
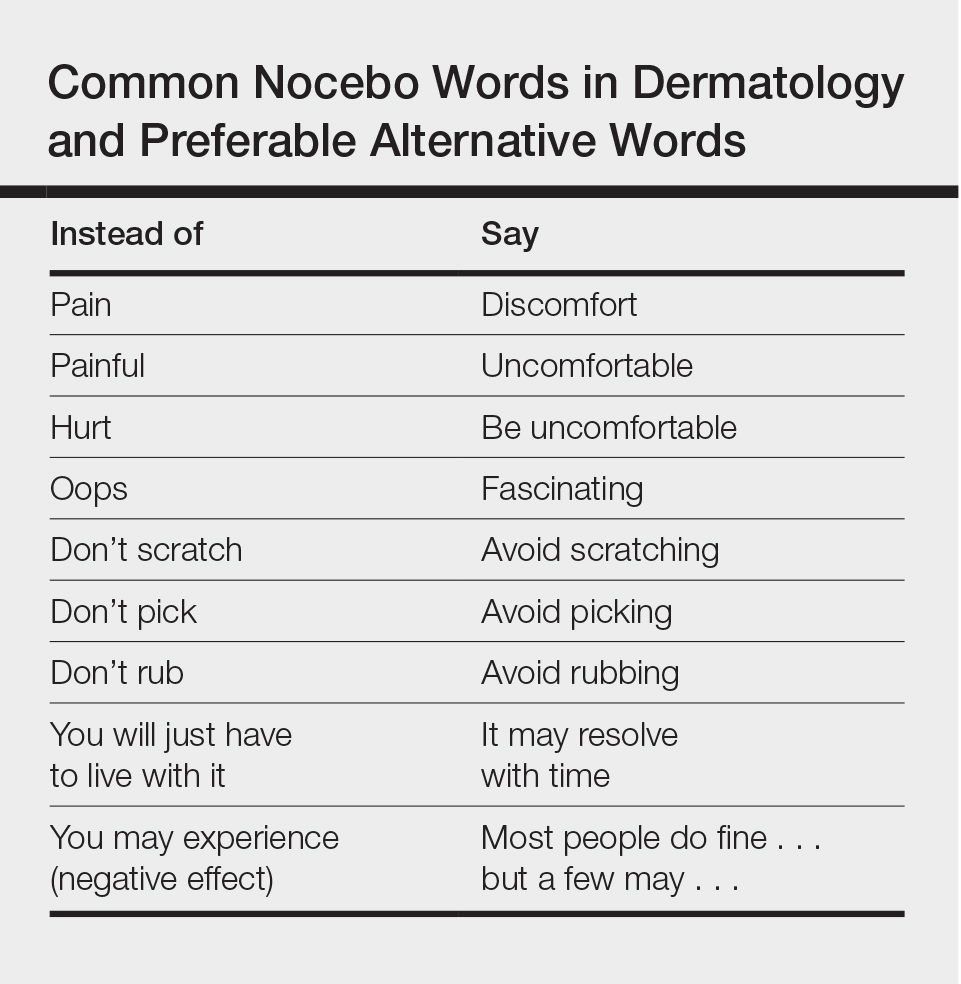
When excess stress occurs, there is a natural shift downward from social communicative newer parasympathetic nervous system to fight or flight sympathetic nervous system, and possibly further shift to the freeze response of older parasympathetic nervous system dominance. Memories that are associated with a strong surge of norepinephrine tend to be much more strongly fixed in the memory than ordinary memories and frequently are associated with overwhelming traumatic experiences. When a threat is perceived, negative interpretations and perceptions generally win out over positive interpretations and perceptions. Unconscious fears generally prevail over conscious thoughts, and stronger emotions generally prevail over weaker emotions. Anxiety often is associated with rapid breathing and activation of the sympathetic nervous system. It can be countered by slow breathing to a rate of approximately 6 breaths per minute, helping to bring back more parasympathetic balance. Pacing a patient’s breathing to slow it and using a soothing tone of voice can help reduce patient anxiety. Reducing anxiety can decrease the patient’s tendency to jump to negative conclusions or have negative perceptions or emotions that can invoke the nocebo effect.
For the dermatologist, as for the patient, changing an old habit and creating a new habit requires repeating something differently and consistently 20 to 40 times. Becoming more conscious of the effects of language on the patient is an important part of the art of medicine. By carefully choosing words, intonation, and body language, it is possible to enhance the placebo effect and decrease the nocebo effect for the benefit of the patient. When describing possible adverse effects of treatments or medications, if the dermatologist says that most people do fine with the treatment but a few can experience the described adverse effect, it usually takes the edge off the potential suggested nocebo effect.
In conclusion, primum non nocere includes careful consideration and use of language, tone, and body language to maximize the placebo effect and minimize the nocebo effect.
- Hippocrates. Epidemics. Jones WHS, trans. Loeb Classical Library: Hippocrates. Vol 1. Cambridge, MA: Harvard University Press; 1923:164-165.
- Poletti ED. El efecto nocebo in dermatología. Dermatol Cosmet Quirg. 2007;5:74.
- Sonthalia S, Sahaya K, Arora R, et al. Nocebo effect in dermatology. Indian J Dermatol Venereol Leprol. 2015;81:242-250.
- Bingel U. Avoiding nocebo effects to optimize treatment outcomes. JAMA. 2014;312:693-694.
- Greenwald AG. New look 3: unconscious cognition reclaimed. Am Psychol. 1992;47:766-779.
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York, NY: W.W. Norton & Co; 2011.
The medical dictum primum non nocere (first, do no harm) is a fundamental rule by which physicians have lived for centuries.1 Physicians are familiar with the term placebo (I shall please) and the placebo effect of improvement based on expectation of positive results; however, many are not familiar with the term nocebo (I shall harm) and the nocebo effect of lack of improvement or deterioration based on the expectation of negative results. The patient’s expectation of being pleased and/or being harmed may be on the conscious level and/or on one or more subconscious and unconscious levels.
Words can have as much of an impact on some patients as medications or procedures. Rudyard Kipling said, “Words are, of course, the most powerful drug used by mankind.” The words that a dermatologist chooses to use can have either a placebo or a nocebo effect on the patient. The purpose of this commentary is to elevate awareness that there are positive alternatives to unintended negative suggestions that are commonly used in dermatologic practice.
A search of PubMed articles indexed for MEDLINE and Scopus published from January 1966 through July 28, 2016, was conducted using the terms placebo or nocebo and cutaneous or skin. Prior publications in this area related specifically to dermatology include those of Poletti2 and Sonthalia et al.3
Patient expectations play an important role in both positive and negative treatment outcomes. Patient-physician communication can moderate these effects both positively and negatively.4 Nocebo effects can substantially reduce treatment efficacy and patient compliance. Patient expectations of negative results or side effects of a treatment or medication can be self-induced or can be induced by inappropriate physician-patient communication, drug information leaflets, influence of family or peers, or discovery of reported adverse effects through reading materials on the Internet.4 Expectation of negative effects can reduce patient adherence and compliance with treatment, reducing treatment efficacy. The psychosocial context around the patient and the treatment may change the neuronal biochemistry and circuitry in the patient’s brain, and the central and peripheral mechanisms activated by placebos and nocebos have been found to be the same as those activated by the medications, suggesting cognitive/affective enhancing or impeding of drug action.5
The subconscious and unconscious habitual automated parts of the brain hear words on the level of a 5- or 6-year-old child with literal unconscious cognitive interpretation of the words. These parts also do not connect words in a sentence with each other.5 For example, if the dermatologist or nurse says “This will not hurt,” the unconscious brain hears not and hurt but does not connect the two. On the other hand, if the dermatologist or nurse says “ You may experience some discomfort,” the unconscious brain hears comfort. Telling the patient “Don’t scratch” may be heard unconsciously as scratch. See the Table for suggested rephrasing of common nocebos used in dermatology. The conscious parts of the brain help determine cognitions influenced by associated unconscious memories, positive or negative. Both the conscious and unconscious parts of the brain influence affect or emotion.
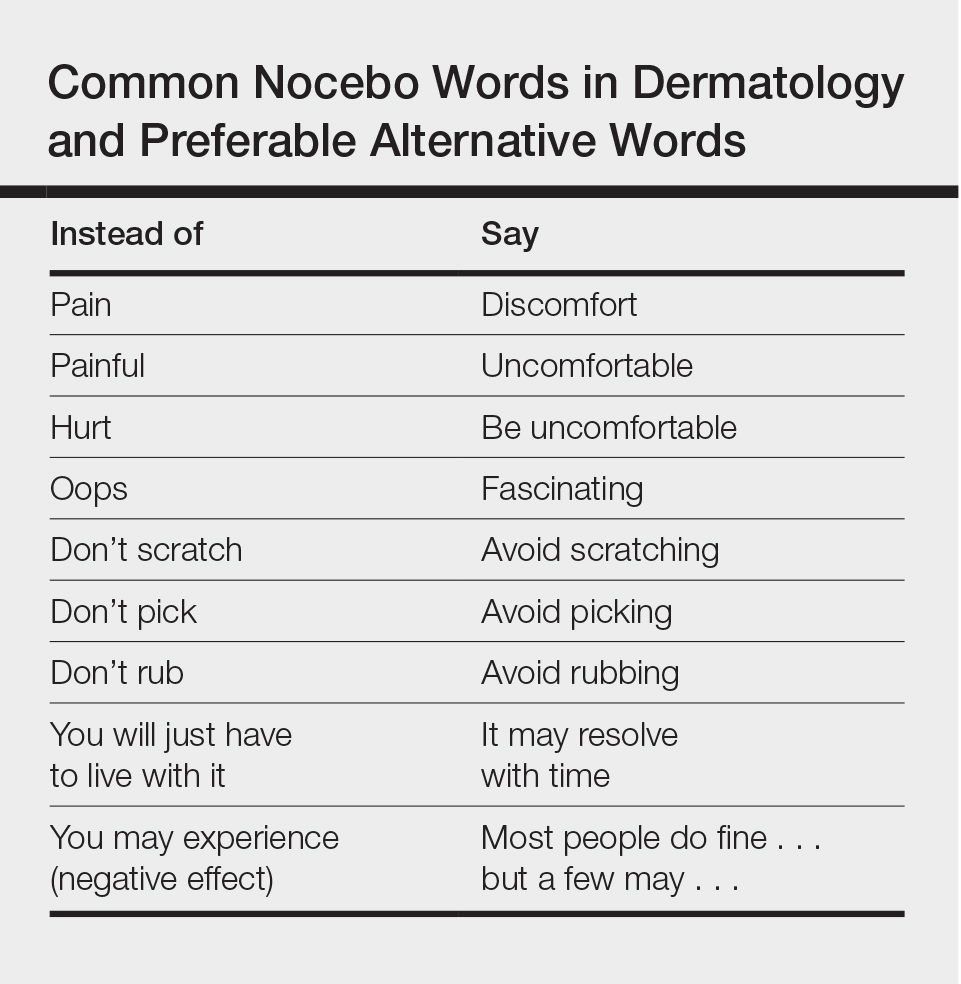
When excess stress occurs, there is a natural shift downward from social communicative newer parasympathetic nervous system to fight or flight sympathetic nervous system, and possibly further shift to the freeze response of older parasympathetic nervous system dominance. Memories that are associated with a strong surge of norepinephrine tend to be much more strongly fixed in the memory than ordinary memories and frequently are associated with overwhelming traumatic experiences. When a threat is perceived, negative interpretations and perceptions generally win out over positive interpretations and perceptions. Unconscious fears generally prevail over conscious thoughts, and stronger emotions generally prevail over weaker emotions. Anxiety often is associated with rapid breathing and activation of the sympathetic nervous system. It can be countered by slow breathing to a rate of approximately 6 breaths per minute, helping to bring back more parasympathetic balance. Pacing a patient’s breathing to slow it and using a soothing tone of voice can help reduce patient anxiety. Reducing anxiety can decrease the patient’s tendency to jump to negative conclusions or have negative perceptions or emotions that can invoke the nocebo effect.
For the dermatologist, as for the patient, changing an old habit and creating a new habit requires repeating something differently and consistently 20 to 40 times. Becoming more conscious of the effects of language on the patient is an important part of the art of medicine. By carefully choosing words, intonation, and body language, it is possible to enhance the placebo effect and decrease the nocebo effect for the benefit of the patient. When describing possible adverse effects of treatments or medications, if the dermatologist says that most people do fine with the treatment but a few can experience the described adverse effect, it usually takes the edge off the potential suggested nocebo effect.
In conclusion, primum non nocere includes careful consideration and use of language, tone, and body language to maximize the placebo effect and minimize the nocebo effect.
The medical dictum primum non nocere (first, do no harm) is a fundamental rule by which physicians have lived for centuries.1 Physicians are familiar with the term placebo (I shall please) and the placebo effect of improvement based on expectation of positive results; however, many are not familiar with the term nocebo (I shall harm) and the nocebo effect of lack of improvement or deterioration based on the expectation of negative results. The patient’s expectation of being pleased and/or being harmed may be on the conscious level and/or on one or more subconscious and unconscious levels.
Words can have as much of an impact on some patients as medications or procedures. Rudyard Kipling said, “Words are, of course, the most powerful drug used by mankind.” The words that a dermatologist chooses to use can have either a placebo or a nocebo effect on the patient. The purpose of this commentary is to elevate awareness that there are positive alternatives to unintended negative suggestions that are commonly used in dermatologic practice.
A search of PubMed articles indexed for MEDLINE and Scopus published from January 1966 through July 28, 2016, was conducted using the terms placebo or nocebo and cutaneous or skin. Prior publications in this area related specifically to dermatology include those of Poletti2 and Sonthalia et al.3
Patient expectations play an important role in both positive and negative treatment outcomes. Patient-physician communication can moderate these effects both positively and negatively.4 Nocebo effects can substantially reduce treatment efficacy and patient compliance. Patient expectations of negative results or side effects of a treatment or medication can be self-induced or can be induced by inappropriate physician-patient communication, drug information leaflets, influence of family or peers, or discovery of reported adverse effects through reading materials on the Internet.4 Expectation of negative effects can reduce patient adherence and compliance with treatment, reducing treatment efficacy. The psychosocial context around the patient and the treatment may change the neuronal biochemistry and circuitry in the patient’s brain, and the central and peripheral mechanisms activated by placebos and nocebos have been found to be the same as those activated by the medications, suggesting cognitive/affective enhancing or impeding of drug action.5
The subconscious and unconscious habitual automated parts of the brain hear words on the level of a 5- or 6-year-old child with literal unconscious cognitive interpretation of the words. These parts also do not connect words in a sentence with each other.5 For example, if the dermatologist or nurse says “This will not hurt,” the unconscious brain hears not and hurt but does not connect the two. On the other hand, if the dermatologist or nurse says “ You may experience some discomfort,” the unconscious brain hears comfort. Telling the patient “Don’t scratch” may be heard unconsciously as scratch. See the Table for suggested rephrasing of common nocebos used in dermatology. The conscious parts of the brain help determine cognitions influenced by associated unconscious memories, positive or negative. Both the conscious and unconscious parts of the brain influence affect or emotion.
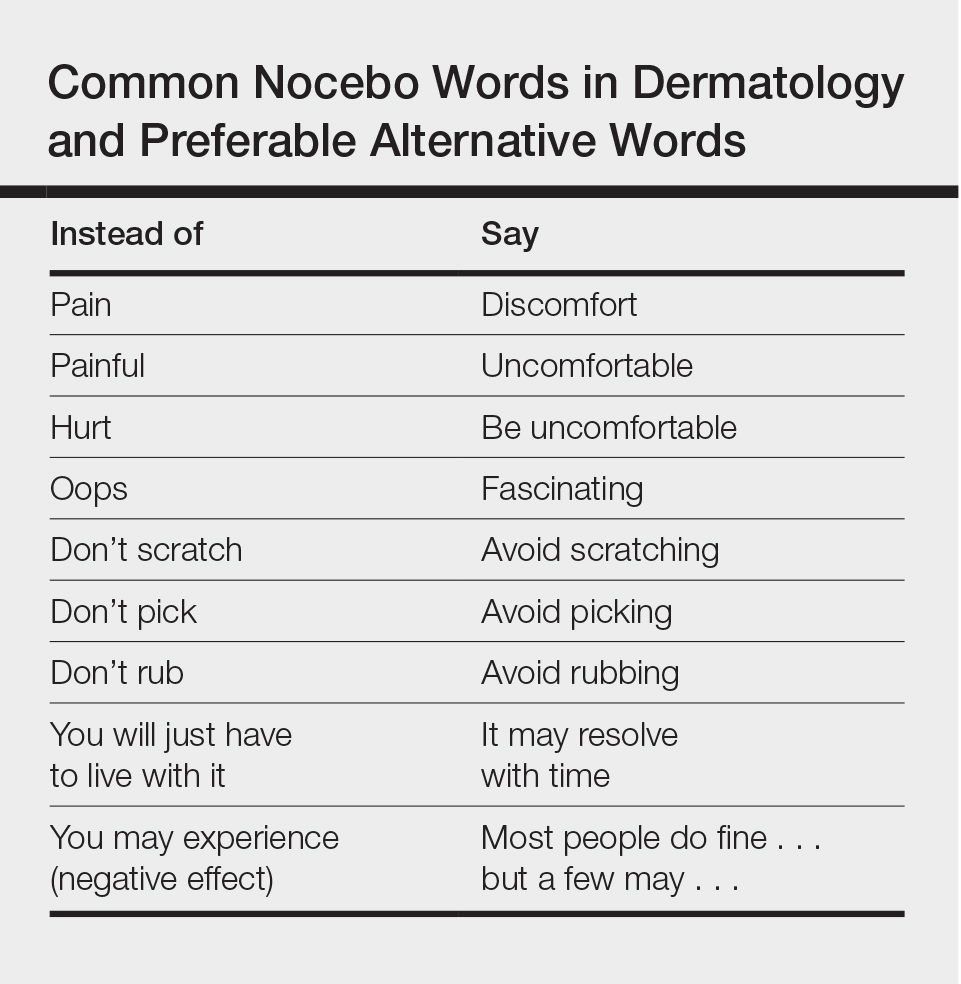
When excess stress occurs, there is a natural shift downward from social communicative newer parasympathetic nervous system to fight or flight sympathetic nervous system, and possibly further shift to the freeze response of older parasympathetic nervous system dominance. Memories that are associated with a strong surge of norepinephrine tend to be much more strongly fixed in the memory than ordinary memories and frequently are associated with overwhelming traumatic experiences. When a threat is perceived, negative interpretations and perceptions generally win out over positive interpretations and perceptions. Unconscious fears generally prevail over conscious thoughts, and stronger emotions generally prevail over weaker emotions. Anxiety often is associated with rapid breathing and activation of the sympathetic nervous system. It can be countered by slow breathing to a rate of approximately 6 breaths per minute, helping to bring back more parasympathetic balance. Pacing a patient’s breathing to slow it and using a soothing tone of voice can help reduce patient anxiety. Reducing anxiety can decrease the patient’s tendency to jump to negative conclusions or have negative perceptions or emotions that can invoke the nocebo effect.
For the dermatologist, as for the patient, changing an old habit and creating a new habit requires repeating something differently and consistently 20 to 40 times. Becoming more conscious of the effects of language on the patient is an important part of the art of medicine. By carefully choosing words, intonation, and body language, it is possible to enhance the placebo effect and decrease the nocebo effect for the benefit of the patient. When describing possible adverse effects of treatments or medications, if the dermatologist says that most people do fine with the treatment but a few can experience the described adverse effect, it usually takes the edge off the potential suggested nocebo effect.
In conclusion, primum non nocere includes careful consideration and use of language, tone, and body language to maximize the placebo effect and minimize the nocebo effect.
- Hippocrates. Epidemics. Jones WHS, trans. Loeb Classical Library: Hippocrates. Vol 1. Cambridge, MA: Harvard University Press; 1923:164-165.
- Poletti ED. El efecto nocebo in dermatología. Dermatol Cosmet Quirg. 2007;5:74.
- Sonthalia S, Sahaya K, Arora R, et al. Nocebo effect in dermatology. Indian J Dermatol Venereol Leprol. 2015;81:242-250.
- Bingel U. Avoiding nocebo effects to optimize treatment outcomes. JAMA. 2014;312:693-694.
- Greenwald AG. New look 3: unconscious cognition reclaimed. Am Psychol. 1992;47:766-779.
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York, NY: W.W. Norton & Co; 2011.
- Hippocrates. Epidemics. Jones WHS, trans. Loeb Classical Library: Hippocrates. Vol 1. Cambridge, MA: Harvard University Press; 1923:164-165.
- Poletti ED. El efecto nocebo in dermatología. Dermatol Cosmet Quirg. 2007;5:74.
- Sonthalia S, Sahaya K, Arora R, et al. Nocebo effect in dermatology. Indian J Dermatol Venereol Leprol. 2015;81:242-250.
- Bingel U. Avoiding nocebo effects to optimize treatment outcomes. JAMA. 2014;312:693-694.
- Greenwald AG. New look 3: unconscious cognition reclaimed. Am Psychol. 1992;47:766-779.
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York, NY: W.W. Norton & Co; 2011.