User login
What Matters: Probiotics for colds
In the midst of the cold and flu season, we should reflect on the fact that our patients are laying down billions of dollars annually on preventions and cures for respiratory tract infections.
An aside: I am frequently turned down on my offer of the influenza vaccine, for which we probably have the best evidence. But $60 per month for a completely unproven preventive/curative agent made in some random factory in some random foreign land with no guarantee of good manufacturing practices (never mind the lack of active ingredients)? Stores can’t keep it in stock.
But I digress.
Our patients may lack the awareness of where to access evidence-based information when seeking answers about efficacy for cold remedies. So, it’s up to us to have at least some sense of where to get reliable information.
Truth be told, I am an enormous fan of safe and effective nonmedication therapies for the treatment and prevention of disease. So, when time permits, I will do a quick PubMed.gov search limiting my articles to randomized trials or systematic reviews on the latest and greatest home remedy.
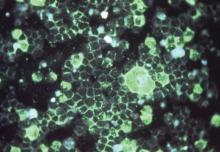
Probiotics have been around for a while, and I think of them as a cure in search of a disease. The Cochrane Collaboration conducted a systematic review evaluating probiotics for the prevention of upper respiratory tract infection. In this review, 13 randomized, controlled trials were included (Explore [NY]. 2015 Sep-Oct;11[5]:418-20).
Probiotics were observed to be significantly better than placebo for reducing episodes of upper respiratory tract infection, the mean duration of episodes, antibiotic prescription rates, and cold-related absences. The evidence was of moderate to low quality.
Some may wonder how an ingested probiotic helps the respiratory tract stave off or fight infection. The prevailing theory appears to be that probiotics may function by mobilizing cells from the intestine to immunomodulate respiratory mucosa.
As for what probiotic/organism to prescribe? On this issue, there is a lot of smoke and not a lot of heat.
In general, the product should be encapsulated, and the label should include the genus and species of the strains (e.g., Lactobacillus acidophilus), the number of organisms (e.g., 5 billion), storage conditions (e.g., refrigerated or room temperature), and the shelf life. Pharmacy chain house brands may be cheaper. Gummy and chewable products tend to have 92% fewer beneficial bacteria than standard formulations.
How can we ensure purity?
That is tough, because supplements like probiotics are not regulated by the Food and Drug Administration above and beyond the agency’s trying to ensure good manufacturing practices. However, companies such as LabDoor (which generates revenue through affiliate links) test and grade supplements for label accuracy and purity. Websites like this might be the best place to start.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
In the midst of the cold and flu season, we should reflect on the fact that our patients are laying down billions of dollars annually on preventions and cures for respiratory tract infections.
An aside: I am frequently turned down on my offer of the influenza vaccine, for which we probably have the best evidence. But $60 per month for a completely unproven preventive/curative agent made in some random factory in some random foreign land with no guarantee of good manufacturing practices (never mind the lack of active ingredients)? Stores can’t keep it in stock.
But I digress.
Our patients may lack the awareness of where to access evidence-based information when seeking answers about efficacy for cold remedies. So, it’s up to us to have at least some sense of where to get reliable information.
Truth be told, I am an enormous fan of safe and effective nonmedication therapies for the treatment and prevention of disease. So, when time permits, I will do a quick PubMed.gov search limiting my articles to randomized trials or systematic reviews on the latest and greatest home remedy.
Probiotics have been around for a while, and I think of them as a cure in search of a disease. The Cochrane Collaboration conducted a systematic review evaluating probiotics for the prevention of upper respiratory tract infection. In this review, 13 randomized, controlled trials were included (Explore [NY]. 2015 Sep-Oct;11[5]:418-20).
Probiotics were observed to be significantly better than placebo for reducing episodes of upper respiratory tract infection, the mean duration of episodes, antibiotic prescription rates, and cold-related absences. The evidence was of moderate to low quality.
Some may wonder how an ingested probiotic helps the respiratory tract stave off or fight infection. The prevailing theory appears to be that probiotics may function by mobilizing cells from the intestine to immunomodulate respiratory mucosa.
As for what probiotic/organism to prescribe? On this issue, there is a lot of smoke and not a lot of heat.
In general, the product should be encapsulated, and the label should include the genus and species of the strains (e.g., Lactobacillus acidophilus), the number of organisms (e.g., 5 billion), storage conditions (e.g., refrigerated or room temperature), and the shelf life. Pharmacy chain house brands may be cheaper. Gummy and chewable products tend to have 92% fewer beneficial bacteria than standard formulations.
How can we ensure purity?
That is tough, because supplements like probiotics are not regulated by the Food and Drug Administration above and beyond the agency’s trying to ensure good manufacturing practices. However, companies such as LabDoor (which generates revenue through affiliate links) test and grade supplements for label accuracy and purity. Websites like this might be the best place to start.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
In the midst of the cold and flu season, we should reflect on the fact that our patients are laying down billions of dollars annually on preventions and cures for respiratory tract infections.
An aside: I am frequently turned down on my offer of the influenza vaccine, for which we probably have the best evidence. But $60 per month for a completely unproven preventive/curative agent made in some random factory in some random foreign land with no guarantee of good manufacturing practices (never mind the lack of active ingredients)? Stores can’t keep it in stock.
But I digress.
Our patients may lack the awareness of where to access evidence-based information when seeking answers about efficacy for cold remedies. So, it’s up to us to have at least some sense of where to get reliable information.
Truth be told, I am an enormous fan of safe and effective nonmedication therapies for the treatment and prevention of disease. So, when time permits, I will do a quick PubMed.gov search limiting my articles to randomized trials or systematic reviews on the latest and greatest home remedy.
Probiotics have been around for a while, and I think of them as a cure in search of a disease. The Cochrane Collaboration conducted a systematic review evaluating probiotics for the prevention of upper respiratory tract infection. In this review, 13 randomized, controlled trials were included (Explore [NY]. 2015 Sep-Oct;11[5]:418-20).
Probiotics were observed to be significantly better than placebo for reducing episodes of upper respiratory tract infection, the mean duration of episodes, antibiotic prescription rates, and cold-related absences. The evidence was of moderate to low quality.
Some may wonder how an ingested probiotic helps the respiratory tract stave off or fight infection. The prevailing theory appears to be that probiotics may function by mobilizing cells from the intestine to immunomodulate respiratory mucosa.
As for what probiotic/organism to prescribe? On this issue, there is a lot of smoke and not a lot of heat.
In general, the product should be encapsulated, and the label should include the genus and species of the strains (e.g., Lactobacillus acidophilus), the number of organisms (e.g., 5 billion), storage conditions (e.g., refrigerated or room temperature), and the shelf life. Pharmacy chain house brands may be cheaper. Gummy and chewable products tend to have 92% fewer beneficial bacteria than standard formulations.
How can we ensure purity?
That is tough, because supplements like probiotics are not regulated by the Food and Drug Administration above and beyond the agency’s trying to ensure good manufacturing practices. However, companies such as LabDoor (which generates revenue through affiliate links) test and grade supplements for label accuracy and purity. Websites like this might be the best place to start.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
Vascular surgery – it’s personal
Let’s get personal for a moment. The next time you walk past your local cancer center, pay attention to the signs, the branding, and the message. I’ll bet you won’t have to look too hard to see reference to personalized or precision medicine. Our oncology colleagues have completely invested in these principles and it’s easy to see why.
The concept of personalized medicine involves therapeutic strategies that take individual variability into account. Along with advances in patient care this strategy has resonated with patients, funding agencies, philanthropists, and governments. Most recently, President Obama announced a new precision medicine initiative in his State of the Union Address, and this month we’ve seen these ideas reflected in Vice President Biden’s “moonshot” to cure cancer.
All well and good, but what about vascular surgery? Let’s see – making therapeutic decisions at the individual patient level, taking patient variability into account, whether its anatomy, comorbidities, genetic profile – isn’t this what we do every day? Of course, it is! We just haven’t been as forthright in owning it or broadcasting it.
If we think about it, we are further along the path to personalized vascular therapy than we think (Vascular. 2016 Jan 13. pii:1708538115624810). In a practical sense, we do it every day, whether its custom devices for aortic therapy, applying data from registries and randomized, controlled trials to individual patients, or using genetic information to make recommendations regarding medical, surgical, or endovascular therapy, we regularly make recommendations “taking individual patient variability into account.”
There are ongoing advances in all of these areas by our innovative vascular surgery colleagues. Dr. Benjamin W. Starnes is using 3-D printing to develop custom templates for personalized “point of care” aortic endograft fenestration (J Vasc Surg. 2015;61:1637-41). Genetic variability is being considered when applying medical therapy, known as pharmacogenetics, but also when applying surgical therapy, as “surgicogenetics.”
A prime example is the pioneering work led by Dr. Michael S. Conte and the late Dr. Alexander Clowes, who are attempting to explain some of the variability in outcomes following infrainguinal bypass surgery by differences in a single nucleotide polymorphism (J Vasc Surg. 2013 May;57:1179-85). Genetics drives surgical outcomes, surgicogenetics indeed!
These are just some of the examples of “Personalized Vascular Therapy” that all vascular surgeons practice to a certain extent and where there are lively areas of investigation.
So the time has come for us to not only practice personalized medicine, but to own it, to broadcast it, to leverage it, as well. Personalized Vascular Therapy has a nice ring to it, don’t you think? We do it, let’s not by shy about it.
Dr. Forbes is professor and chair of the division of vascular surgery at the University of Toronto.
Let’s get personal for a moment. The next time you walk past your local cancer center, pay attention to the signs, the branding, and the message. I’ll bet you won’t have to look too hard to see reference to personalized or precision medicine. Our oncology colleagues have completely invested in these principles and it’s easy to see why.
The concept of personalized medicine involves therapeutic strategies that take individual variability into account. Along with advances in patient care this strategy has resonated with patients, funding agencies, philanthropists, and governments. Most recently, President Obama announced a new precision medicine initiative in his State of the Union Address, and this month we’ve seen these ideas reflected in Vice President Biden’s “moonshot” to cure cancer.
All well and good, but what about vascular surgery? Let’s see – making therapeutic decisions at the individual patient level, taking patient variability into account, whether its anatomy, comorbidities, genetic profile – isn’t this what we do every day? Of course, it is! We just haven’t been as forthright in owning it or broadcasting it.
If we think about it, we are further along the path to personalized vascular therapy than we think (Vascular. 2016 Jan 13. pii:1708538115624810). In a practical sense, we do it every day, whether its custom devices for aortic therapy, applying data from registries and randomized, controlled trials to individual patients, or using genetic information to make recommendations regarding medical, surgical, or endovascular therapy, we regularly make recommendations “taking individual patient variability into account.”
There are ongoing advances in all of these areas by our innovative vascular surgery colleagues. Dr. Benjamin W. Starnes is using 3-D printing to develop custom templates for personalized “point of care” aortic endograft fenestration (J Vasc Surg. 2015;61:1637-41). Genetic variability is being considered when applying medical therapy, known as pharmacogenetics, but also when applying surgical therapy, as “surgicogenetics.”
A prime example is the pioneering work led by Dr. Michael S. Conte and the late Dr. Alexander Clowes, who are attempting to explain some of the variability in outcomes following infrainguinal bypass surgery by differences in a single nucleotide polymorphism (J Vasc Surg. 2013 May;57:1179-85). Genetics drives surgical outcomes, surgicogenetics indeed!
These are just some of the examples of “Personalized Vascular Therapy” that all vascular surgeons practice to a certain extent and where there are lively areas of investigation.
So the time has come for us to not only practice personalized medicine, but to own it, to broadcast it, to leverage it, as well. Personalized Vascular Therapy has a nice ring to it, don’t you think? We do it, let’s not by shy about it.
Dr. Forbes is professor and chair of the division of vascular surgery at the University of Toronto.
Let’s get personal for a moment. The next time you walk past your local cancer center, pay attention to the signs, the branding, and the message. I’ll bet you won’t have to look too hard to see reference to personalized or precision medicine. Our oncology colleagues have completely invested in these principles and it’s easy to see why.
The concept of personalized medicine involves therapeutic strategies that take individual variability into account. Along with advances in patient care this strategy has resonated with patients, funding agencies, philanthropists, and governments. Most recently, President Obama announced a new precision medicine initiative in his State of the Union Address, and this month we’ve seen these ideas reflected in Vice President Biden’s “moonshot” to cure cancer.
All well and good, but what about vascular surgery? Let’s see – making therapeutic decisions at the individual patient level, taking patient variability into account, whether its anatomy, comorbidities, genetic profile – isn’t this what we do every day? Of course, it is! We just haven’t been as forthright in owning it or broadcasting it.
If we think about it, we are further along the path to personalized vascular therapy than we think (Vascular. 2016 Jan 13. pii:1708538115624810). In a practical sense, we do it every day, whether its custom devices for aortic therapy, applying data from registries and randomized, controlled trials to individual patients, or using genetic information to make recommendations regarding medical, surgical, or endovascular therapy, we regularly make recommendations “taking individual patient variability into account.”
There are ongoing advances in all of these areas by our innovative vascular surgery colleagues. Dr. Benjamin W. Starnes is using 3-D printing to develop custom templates for personalized “point of care” aortic endograft fenestration (J Vasc Surg. 2015;61:1637-41). Genetic variability is being considered when applying medical therapy, known as pharmacogenetics, but also when applying surgical therapy, as “surgicogenetics.”
A prime example is the pioneering work led by Dr. Michael S. Conte and the late Dr. Alexander Clowes, who are attempting to explain some of the variability in outcomes following infrainguinal bypass surgery by differences in a single nucleotide polymorphism (J Vasc Surg. 2013 May;57:1179-85). Genetics drives surgical outcomes, surgicogenetics indeed!
These are just some of the examples of “Personalized Vascular Therapy” that all vascular surgeons practice to a certain extent and where there are lively areas of investigation.
So the time has come for us to not only practice personalized medicine, but to own it, to broadcast it, to leverage it, as well. Personalized Vascular Therapy has a nice ring to it, don’t you think? We do it, let’s not by shy about it.
Dr. Forbes is professor and chair of the division of vascular surgery at the University of Toronto.
On my own during an employee’s maternity leave
Recently, my secretary was out on maternity leave for 6 weeks.
I run a small practice, and my medical assistant works from home on the far side of town. So I was on my own at the office. My MA and I split things up, and since I was the only one physically in the building, I took over all the front office stuff and she took the back office.
I ran the front desk for the whole time – checking people in and out, taking copays, copying insurance cards, giving referrals to therapy places, sending logs to the billing company, and doing other everyday stuff.
Plenty of people asked why I didn’t hire a temp, obviously not knowing how close to the edge a modern solo practice runs. If I hire a temp, that’s another salary to pay, meaning one of the other three of us here would have to skip a few paychecks. I’m not going to put my secretary on unpaid leave for that time. She’s awesome, has been with me since 2004, and has stuck with me through good and bad years. If I don’t pay her that time, she can’t pay her rent, and I don’t have the heart to do that to her. Maybe a big corporate person wouldn’t lose any sleep about it, but I would. Great people are hard to find, and I want to keep the ones I have.
Besides, if I hired a temp, I’d have to train them from the beginning. I don’t use off-the-shelf medical software, just a system I designed myself. It would take time out of my day to teach them how to use it, where I send patients for tests and referrals, and how to sort documents accurately into the correct e-charts. So, for 6 weeks it just seemed easier to do it myself. I know how I like it done.
It wasn’t easy for my MA as well. She had to take over scheduling appointments, handling billing questions, making reminder calls, and doing other miscellaneous stuff. Even after work was over, I’d be at home catching up on all the dictations I hadn’t had time to do, and we’d be going back and forth by phone and email to settle different issues until 8:00 at night or so. By the end of the 6 weeks, we were both pretty burned out and exhausted.
I’m sure the patients weren’t thrilled, either. During that time, they could only reach a voice mail box telling them to leave a message and we’d get back to them as quickly as possible.
I assumed my practice was the only one dinky (or poor, by medical standards) enough to have to resort to this – until I had a chance conversation with a local family practice doctor, when he mentioned he’d had to do something similar when his secretary retired and he didn’t find a replacement for several weeks. A cardiologist mentioned doing the same thing while we were chatting at the hospital. Like me, they were both in solo practice.
This is, apparently, the nature of a modern small practice. The revenue and expense streams are too tight to allow for an extra salary, so even the doctor pitches in to cover. I’m sure my colleagues in large groups will laugh at the thought, but I don’t care. I have to do what’s right for my practice and to survive in the modern medical climate. And if working the front desk for a few weeks is what’s needed to stay independent, so be it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, my secretary was out on maternity leave for 6 weeks.
I run a small practice, and my medical assistant works from home on the far side of town. So I was on my own at the office. My MA and I split things up, and since I was the only one physically in the building, I took over all the front office stuff and she took the back office.
I ran the front desk for the whole time – checking people in and out, taking copays, copying insurance cards, giving referrals to therapy places, sending logs to the billing company, and doing other everyday stuff.
Plenty of people asked why I didn’t hire a temp, obviously not knowing how close to the edge a modern solo practice runs. If I hire a temp, that’s another salary to pay, meaning one of the other three of us here would have to skip a few paychecks. I’m not going to put my secretary on unpaid leave for that time. She’s awesome, has been with me since 2004, and has stuck with me through good and bad years. If I don’t pay her that time, she can’t pay her rent, and I don’t have the heart to do that to her. Maybe a big corporate person wouldn’t lose any sleep about it, but I would. Great people are hard to find, and I want to keep the ones I have.
Besides, if I hired a temp, I’d have to train them from the beginning. I don’t use off-the-shelf medical software, just a system I designed myself. It would take time out of my day to teach them how to use it, where I send patients for tests and referrals, and how to sort documents accurately into the correct e-charts. So, for 6 weeks it just seemed easier to do it myself. I know how I like it done.
It wasn’t easy for my MA as well. She had to take over scheduling appointments, handling billing questions, making reminder calls, and doing other miscellaneous stuff. Even after work was over, I’d be at home catching up on all the dictations I hadn’t had time to do, and we’d be going back and forth by phone and email to settle different issues until 8:00 at night or so. By the end of the 6 weeks, we were both pretty burned out and exhausted.
I’m sure the patients weren’t thrilled, either. During that time, they could only reach a voice mail box telling them to leave a message and we’d get back to them as quickly as possible.
I assumed my practice was the only one dinky (or poor, by medical standards) enough to have to resort to this – until I had a chance conversation with a local family practice doctor, when he mentioned he’d had to do something similar when his secretary retired and he didn’t find a replacement for several weeks. A cardiologist mentioned doing the same thing while we were chatting at the hospital. Like me, they were both in solo practice.
This is, apparently, the nature of a modern small practice. The revenue and expense streams are too tight to allow for an extra salary, so even the doctor pitches in to cover. I’m sure my colleagues in large groups will laugh at the thought, but I don’t care. I have to do what’s right for my practice and to survive in the modern medical climate. And if working the front desk for a few weeks is what’s needed to stay independent, so be it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, my secretary was out on maternity leave for 6 weeks.
I run a small practice, and my medical assistant works from home on the far side of town. So I was on my own at the office. My MA and I split things up, and since I was the only one physically in the building, I took over all the front office stuff and she took the back office.
I ran the front desk for the whole time – checking people in and out, taking copays, copying insurance cards, giving referrals to therapy places, sending logs to the billing company, and doing other everyday stuff.
Plenty of people asked why I didn’t hire a temp, obviously not knowing how close to the edge a modern solo practice runs. If I hire a temp, that’s another salary to pay, meaning one of the other three of us here would have to skip a few paychecks. I’m not going to put my secretary on unpaid leave for that time. She’s awesome, has been with me since 2004, and has stuck with me through good and bad years. If I don’t pay her that time, she can’t pay her rent, and I don’t have the heart to do that to her. Maybe a big corporate person wouldn’t lose any sleep about it, but I would. Great people are hard to find, and I want to keep the ones I have.
Besides, if I hired a temp, I’d have to train them from the beginning. I don’t use off-the-shelf medical software, just a system I designed myself. It would take time out of my day to teach them how to use it, where I send patients for tests and referrals, and how to sort documents accurately into the correct e-charts. So, for 6 weeks it just seemed easier to do it myself. I know how I like it done.
It wasn’t easy for my MA as well. She had to take over scheduling appointments, handling billing questions, making reminder calls, and doing other miscellaneous stuff. Even after work was over, I’d be at home catching up on all the dictations I hadn’t had time to do, and we’d be going back and forth by phone and email to settle different issues until 8:00 at night or so. By the end of the 6 weeks, we were both pretty burned out and exhausted.
I’m sure the patients weren’t thrilled, either. During that time, they could only reach a voice mail box telling them to leave a message and we’d get back to them as quickly as possible.
I assumed my practice was the only one dinky (or poor, by medical standards) enough to have to resort to this – until I had a chance conversation with a local family practice doctor, when he mentioned he’d had to do something similar when his secretary retired and he didn’t find a replacement for several weeks. A cardiologist mentioned doing the same thing while we were chatting at the hospital. Like me, they were both in solo practice.
This is, apparently, the nature of a modern small practice. The revenue and expense streams are too tight to allow for an extra salary, so even the doctor pitches in to cover. I’m sure my colleagues in large groups will laugh at the thought, but I don’t care. I have to do what’s right for my practice and to survive in the modern medical climate. And if working the front desk for a few weeks is what’s needed to stay independent, so be it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Quo vadis, Psychiatry?
Psychiatrists frequently complain about their lack of recognition by other specialties, stigmatization of mental illness and the practice of psychiatry, and diminishing sense of identity as a specialty. Although I share these concerns, there is another trend that worries me perhaps more: the deliberate abandonment of more and more areas of what has traditionally been and should be psychiatry’s area of expertise and skills. Not all of this is our own doing; the fact is that other clinicians would like to get “a piece of our pie”—a trend seen in other specialties as well (eg, parts of radiology taken over by cardiologists). However, I view our role in this process as larger than other specialties’ or disciplines’ efforts.
Many of us choose not to treat substance abuse patients and instead refer them to “specialists”; yet, don’t we have enough of our own trained specialists and don’t we fill our addiction psychiatry fellowship training positions? Similarly, many do not like to treat patients with comorbid psychiatric illness and substance abuse, although this occurs frequently in our practice. Cognitive disorders often are left to neurologists and our role in managing these patients is diminishing. Pulmonologists gradually are taking over sleep disorders; one wonders why. We do not like to ask our patients about their sexual history, not even talking about treating their sexual problems! Most psychiatrists are afraid of prescribing phosphodiesterase-5 inhibitors. We are leaving the entire field of human sexuality to gynecologists, urologists, and other specialists. Paraphilic disorders are something we do not want to manage and we would rather get the whole area out of our classification systems, with the implication that these are not really mental health problems.
Many of us prefer not to treat personality disorder patients—especially those with borderline personality disorder—because they are “difficult.” Some do not even feel comfortable managing adverse effects of psychotropics such as the metabolic syndrome, or use “unusual” augmentations such as thyroid hormone. We prescribe fewer and fewer older, yet efficacious, psychotropic medications; only a small fraction of psychiatrists still prescribes monoamine oxidase inhibitors. Other disciplines, eg, primary care and pain medicine, prescribe some tricyclic antidepressants more than we do. We irrationally avoid benzodiazepines and do not like prescribing lithium, because it requires ordering blood levels and lab tests. We seem comfortable only with newer antidepressants and antipsychotics. How is this way of prescribing different from what is done in primary care? Some of our leaders sneer at the idea of psychiatrists practicing psychotherapy, perhaps feeling that such a “lowly art” should be provided by psychologists and social workers. We do not address relational issues. Last but not least, I hear colleagues saying that they do not like to treat “difficult” patients.
What are we aspiring to be and to do? To treat schizophrenia, bipolar disorder, and maybe depression, with a limited medication armamentarium we feel comfortable with and no psychotherapy? I am sure that many will say I am exaggerating, but I think not. We have, as Pogo said, met the enemy and he is us. We should get off the slippery slope of selling out psychiatry piece-by-piece, and fully embrace—clinically and research-wise (funding!)—all of what has been part of psychiatry.
Psychiatrists frequently complain about their lack of recognition by other specialties, stigmatization of mental illness and the practice of psychiatry, and diminishing sense of identity as a specialty. Although I share these concerns, there is another trend that worries me perhaps more: the deliberate abandonment of more and more areas of what has traditionally been and should be psychiatry’s area of expertise and skills. Not all of this is our own doing; the fact is that other clinicians would like to get “a piece of our pie”—a trend seen in other specialties as well (eg, parts of radiology taken over by cardiologists). However, I view our role in this process as larger than other specialties’ or disciplines’ efforts.
Many of us choose not to treat substance abuse patients and instead refer them to “specialists”; yet, don’t we have enough of our own trained specialists and don’t we fill our addiction psychiatry fellowship training positions? Similarly, many do not like to treat patients with comorbid psychiatric illness and substance abuse, although this occurs frequently in our practice. Cognitive disorders often are left to neurologists and our role in managing these patients is diminishing. Pulmonologists gradually are taking over sleep disorders; one wonders why. We do not like to ask our patients about their sexual history, not even talking about treating their sexual problems! Most psychiatrists are afraid of prescribing phosphodiesterase-5 inhibitors. We are leaving the entire field of human sexuality to gynecologists, urologists, and other specialists. Paraphilic disorders are something we do not want to manage and we would rather get the whole area out of our classification systems, with the implication that these are not really mental health problems.
Many of us prefer not to treat personality disorder patients—especially those with borderline personality disorder—because they are “difficult.” Some do not even feel comfortable managing adverse effects of psychotropics such as the metabolic syndrome, or use “unusual” augmentations such as thyroid hormone. We prescribe fewer and fewer older, yet efficacious, psychotropic medications; only a small fraction of psychiatrists still prescribes monoamine oxidase inhibitors. Other disciplines, eg, primary care and pain medicine, prescribe some tricyclic antidepressants more than we do. We irrationally avoid benzodiazepines and do not like prescribing lithium, because it requires ordering blood levels and lab tests. We seem comfortable only with newer antidepressants and antipsychotics. How is this way of prescribing different from what is done in primary care? Some of our leaders sneer at the idea of psychiatrists practicing psychotherapy, perhaps feeling that such a “lowly art” should be provided by psychologists and social workers. We do not address relational issues. Last but not least, I hear colleagues saying that they do not like to treat “difficult” patients.
What are we aspiring to be and to do? To treat schizophrenia, bipolar disorder, and maybe depression, with a limited medication armamentarium we feel comfortable with and no psychotherapy? I am sure that many will say I am exaggerating, but I think not. We have, as Pogo said, met the enemy and he is us. We should get off the slippery slope of selling out psychiatry piece-by-piece, and fully embrace—clinically and research-wise (funding!)—all of what has been part of psychiatry.
Psychiatrists frequently complain about their lack of recognition by other specialties, stigmatization of mental illness and the practice of psychiatry, and diminishing sense of identity as a specialty. Although I share these concerns, there is another trend that worries me perhaps more: the deliberate abandonment of more and more areas of what has traditionally been and should be psychiatry’s area of expertise and skills. Not all of this is our own doing; the fact is that other clinicians would like to get “a piece of our pie”—a trend seen in other specialties as well (eg, parts of radiology taken over by cardiologists). However, I view our role in this process as larger than other specialties’ or disciplines’ efforts.
Many of us choose not to treat substance abuse patients and instead refer them to “specialists”; yet, don’t we have enough of our own trained specialists and don’t we fill our addiction psychiatry fellowship training positions? Similarly, many do not like to treat patients with comorbid psychiatric illness and substance abuse, although this occurs frequently in our practice. Cognitive disorders often are left to neurologists and our role in managing these patients is diminishing. Pulmonologists gradually are taking over sleep disorders; one wonders why. We do not like to ask our patients about their sexual history, not even talking about treating their sexual problems! Most psychiatrists are afraid of prescribing phosphodiesterase-5 inhibitors. We are leaving the entire field of human sexuality to gynecologists, urologists, and other specialists. Paraphilic disorders are something we do not want to manage and we would rather get the whole area out of our classification systems, with the implication that these are not really mental health problems.
Many of us prefer not to treat personality disorder patients—especially those with borderline personality disorder—because they are “difficult.” Some do not even feel comfortable managing adverse effects of psychotropics such as the metabolic syndrome, or use “unusual” augmentations such as thyroid hormone. We prescribe fewer and fewer older, yet efficacious, psychotropic medications; only a small fraction of psychiatrists still prescribes monoamine oxidase inhibitors. Other disciplines, eg, primary care and pain medicine, prescribe some tricyclic antidepressants more than we do. We irrationally avoid benzodiazepines and do not like prescribing lithium, because it requires ordering blood levels and lab tests. We seem comfortable only with newer antidepressants and antipsychotics. How is this way of prescribing different from what is done in primary care? Some of our leaders sneer at the idea of psychiatrists practicing psychotherapy, perhaps feeling that such a “lowly art” should be provided by psychologists and social workers. We do not address relational issues. Last but not least, I hear colleagues saying that they do not like to treat “difficult” patients.
What are we aspiring to be and to do? To treat schizophrenia, bipolar disorder, and maybe depression, with a limited medication armamentarium we feel comfortable with and no psychotherapy? I am sure that many will say I am exaggerating, but I think not. We have, as Pogo said, met the enemy and he is us. We should get off the slippery slope of selling out psychiatry piece-by-piece, and fully embrace—clinically and research-wise (funding!)—all of what has been part of psychiatry.
The newest ‘rage’: disruptive mood dysregulation disorder
Outbursts by children when frustrated or when asked to “do something they don’t want to do” are among the most common behavioral complaints voiced by parents. But behavioral outbursts, beyond the typical tantrums of children up to age 4 years, can be signs of very severe mental health disorders and are the most common reason for psychiatric admission (50%-60%).
While behavioral dysregulation is undeniably a huge problem for families, there has been an unreasonable 40-fold rise in diagnosis of bipolar disorder from 1994 to 2003, and 48% were prescribed atypical neuroleptics – medications with serious side effects. In response to this overdiagnosis as bipolar disorder, in 2013 the DSM-5 created a new diagnosis called disruptive mood dysregulation disorder (DMDD) to differentiate children who experience explosive outbursts who have a different outcome. This new classification includes children aged 6-12 years with persistent irritability most of the time, nearly every day, lasting at least 12 months and starting before age 10 years. DMDD diagnosis is not used after age 18 years.
To be diagnosed, the child has to have frequent, severe temper outbursts “grossly out of proportion” to the situation, averaging at least three times per week. The outbursts can be verbal or physical aggression to people, things, or themselves. While tantrums can be severe in children with delayed development, for the DMDD diagnosis these behaviors must be inconsistent with developmental level and must occur in at least two settings, and in one setting it must be severe. While outbursts are common, only half of children in one study of severe tantrum behavior in 5- to 9-year-olds also had the required persistent irritability.
If this does sound a lot like bipolar disorder so far, you are right. So what is different? DMDD has a prevalence of 2%-5% and occurs mostly in boys, whereas bipolar disorder affects boys and girls equally and affects less than 1% prior to adolescence.
The key features distinguishing DMDD from bipolar disorder are lack of an episodic nature to the irritability and lack of mania. Irritability in DMDD has to be persistently present with breaks of no more than 3 consecutive months in the defining 12-month period. There also cannot be any more than 1 day of the elevated mood features of mania or hypomania. Identifying mania is the hardest part, even in diagnosing adult bipolar, where it occurs only 1% of the year, much less in children who are generally lively! Hypomania, while less intense than mania, is when the person is energetic, talkative, and confident to an extreme extent, often with a flight of creative ideas. Excitement over birthdays or Christmas specifically does not count! So getting this history has to be done carefully, generally by a mental health professional, to make the distinction.
Interestingly, DMDD is not diagnosed when outbursts and irritability are better explained by autism spectrum disorder, separation anxiety disorder, or PTSD. To me, these exclusions point out the importance of sorting out the “set conditions” for all problematic behaviors, not always an easy task. Symptoms of autism in high functioning individuals can be quite subtle. Was the upset from change in a rigid routine known only to the child? Were sensory stimuli such as loud noises intolerable to this child? Was a nonverbal signal of a peer mistaken as a threat? While violent outbursts precipitated by these factors would still be considered “grossly out of proportion to the situation” for a typical child, they are not uncommon in atypical children. Similarly, children with separation anxiety disorder experience a high level of threat from even thinking about being apart from their caregivers, setting them up for alarm by situations other children would not find difficult.
The American Academy of Pediatrics emphasizes the need to assess all children for a history of psychological trauma. Traumas are quite common, and their sequelae affect many aspects of the child’s life; in the case of outbursts, it is emotional resilience that is impaired. As for all DSM-5 diagnoses, DMDD is not diagnosed when the irritability is due to physiological effects of a substance (e.g. steroids) or another medical or neurological disorder. Children with chronic pain conditions such as rheumatoid arthritis or sickle cell usually cope remarkably well, but when they don’t, their irritability should not be considered a mental health disorder. More commonly, sleep debt can produce chronic irritability and always should be assessed.
When coaching families about outbursts, I work to help them recognize that the child is not just angry, but very distressed. While “typical” tantrums last 1-5 minutes and show a rise then decline in intensity of the anger and distress, anger outbursts are longer and have an initial short and rapid burst of anger that then declines over the duration of the outburst, and with a steady but lower level of distress throughout.
The option to hug and verbally console the child’s distress is sometimes effective and does not reinforce the behavior unless the parent also yields to demands. But once outbursts begin, I liken them to a bomb going off – there is no intervention possible then. Instead, the task of the family, and over time that of the child, is to recognize and better manage the triggers.
Dr. Ross Greene, in his book, “The Explosive Child: A New Approach for Understanding and Parenting Easily Frustrated, Chronically Inflexible Children,” asserts that the child’s anger and distress can be interpreted as frustration from a gap in skills. This has treatment implications for identifying, educating about, and ameliorating the child’s weaknesses (deficits in understanding, communication, emotion regulation, flexibility or performance; or excess jealousy or hypersensitivity), and coaching parents to recognize, acknowledge, and avoid stressing these areas, if possible. I coach families to give points to the child for progressive little steps toward being able to recognize, verbalize, and inhibit outbursts with a reward system for the points. This helps put the parents and child “on the same team” in working on improving these skills.
Research on children with DMDD indicates that they show less positive affect when winning a “fixed” video game and are less able to suppress negative affect when losing. (Don’t forget to examine the role of real video games as precipitants of tantrums and contingently remove them!) Threshold for upset is lower and the degree of the upsets less well handled by children with DMDD.
In another study, when presented with a series of ambiguous facial expressions, children with DMDD were more likely to see anger in the faces than were controls. One hopeful result was that they could be taught to shift their perceptions significantly away from seeing anger, also reducing irritability and resulting in functional MRI changes. Such hostile bias attribution (tending to see threat) is well known to predispose to aggression. Cognitive behavioral therapy, the most effective counseling intervention, similarly teaches children to rethink their own negative thoughts before acting.
If irritability and rages were not enough, most children with DMDD have other psychiatric disorders; 39% having two, and 51% three or more (J Child Adolesc Psychopharmacol. 2013 Nov;23[9]:588-96). If not for the DMDD diagnosis, 82% would meet criteria for oppositional defiant disorder (ODD). The other common comorbidities are attention-deficit/hyperactivity disorder (ADHD) (74.5%), anxiety disorders (49.0%), and depression that is not major depressive disorder (MDD)(33.3%). When MDD is present, that diagnosis takes precedence. One cannot diagnose ODD, intermittent explosive disorder, or bipolar disorder along with DMDD, conditions from which it is intended to differentiate. Each of these comorbid disorders can be difficult to manage alone much less in combination, making DMDD a disorder deserving diagnosis and treatment by a mental health professional.
One of the main reasons DMDD was created is that children with these features go on to depressive or anxiety disorder in adolescence, not bipolar disorder.
While there is no treatment specific to DMDD, the depression component and prognosis suggest use of SSRIs, in addition to psychosocial therapies, and stimulants for the comorbid ADHD. Unfortunately, these two classes of medication are relatively contraindicated in bipolar disorder because they can lead to treatment-induced episodic mania (TEM). TEM occurs twice as often with antidepressants compared with stimulants (44% vs. 18%) in children with bipolar disorder (J Affect Disord. 2004 Oct 1;82[1]:149-58). Getting the diagnosis correct is, therefore, of great importance when medication is considered.
Approaches such as behavior modification, family therapy, and inpatient treatment can be effective for chronic irritability and aggression. Stimulant treatment of comorbid ADHD can decrease aggression and irritability. Alpha agonists such as guanfacine or clonidine also can help. In cases of partial improvement, adding either risperidone or divalproex may further decrease aggression in ADHD. In refractory aggression, risperidone has the best evidence. The Affective Reactivity Index or Outburst Monitoring Scale can be helpful in assessing severity and monitoring outcomes.
While a prognosis for depression rather than bipolar disorder sounds like a plus, in a longitudinal study, adults who had DMDD as children had worse outcomes, including being more likely to have adverse health outcomes (smoking, sexually transmitted infection), police contact, and low educational attainment, and being more likely to live in poverty, compared with controls who had other psychiatric disorders. While DMDD is a new and different diagnosis, it is similar to bipolar in having a potential course of life disruption, dangerous behaviors, suicide risk, and hospitalization.
Dr. Howard is assistant professor of pediatrics at the Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline. E-mail her at [email protected].
Outbursts by children when frustrated or when asked to “do something they don’t want to do” are among the most common behavioral complaints voiced by parents. But behavioral outbursts, beyond the typical tantrums of children up to age 4 years, can be signs of very severe mental health disorders and are the most common reason for psychiatric admission (50%-60%).
While behavioral dysregulation is undeniably a huge problem for families, there has been an unreasonable 40-fold rise in diagnosis of bipolar disorder from 1994 to 2003, and 48% were prescribed atypical neuroleptics – medications with serious side effects. In response to this overdiagnosis as bipolar disorder, in 2013 the DSM-5 created a new diagnosis called disruptive mood dysregulation disorder (DMDD) to differentiate children who experience explosive outbursts who have a different outcome. This new classification includes children aged 6-12 years with persistent irritability most of the time, nearly every day, lasting at least 12 months and starting before age 10 years. DMDD diagnosis is not used after age 18 years.
To be diagnosed, the child has to have frequent, severe temper outbursts “grossly out of proportion” to the situation, averaging at least three times per week. The outbursts can be verbal or physical aggression to people, things, or themselves. While tantrums can be severe in children with delayed development, for the DMDD diagnosis these behaviors must be inconsistent with developmental level and must occur in at least two settings, and in one setting it must be severe. While outbursts are common, only half of children in one study of severe tantrum behavior in 5- to 9-year-olds also had the required persistent irritability.
If this does sound a lot like bipolar disorder so far, you are right. So what is different? DMDD has a prevalence of 2%-5% and occurs mostly in boys, whereas bipolar disorder affects boys and girls equally and affects less than 1% prior to adolescence.
The key features distinguishing DMDD from bipolar disorder are lack of an episodic nature to the irritability and lack of mania. Irritability in DMDD has to be persistently present with breaks of no more than 3 consecutive months in the defining 12-month period. There also cannot be any more than 1 day of the elevated mood features of mania or hypomania. Identifying mania is the hardest part, even in diagnosing adult bipolar, where it occurs only 1% of the year, much less in children who are generally lively! Hypomania, while less intense than mania, is when the person is energetic, talkative, and confident to an extreme extent, often with a flight of creative ideas. Excitement over birthdays or Christmas specifically does not count! So getting this history has to be done carefully, generally by a mental health professional, to make the distinction.
Interestingly, DMDD is not diagnosed when outbursts and irritability are better explained by autism spectrum disorder, separation anxiety disorder, or PTSD. To me, these exclusions point out the importance of sorting out the “set conditions” for all problematic behaviors, not always an easy task. Symptoms of autism in high functioning individuals can be quite subtle. Was the upset from change in a rigid routine known only to the child? Were sensory stimuli such as loud noises intolerable to this child? Was a nonverbal signal of a peer mistaken as a threat? While violent outbursts precipitated by these factors would still be considered “grossly out of proportion to the situation” for a typical child, they are not uncommon in atypical children. Similarly, children with separation anxiety disorder experience a high level of threat from even thinking about being apart from their caregivers, setting them up for alarm by situations other children would not find difficult.
The American Academy of Pediatrics emphasizes the need to assess all children for a history of psychological trauma. Traumas are quite common, and their sequelae affect many aspects of the child’s life; in the case of outbursts, it is emotional resilience that is impaired. As for all DSM-5 diagnoses, DMDD is not diagnosed when the irritability is due to physiological effects of a substance (e.g. steroids) or another medical or neurological disorder. Children with chronic pain conditions such as rheumatoid arthritis or sickle cell usually cope remarkably well, but when they don’t, their irritability should not be considered a mental health disorder. More commonly, sleep debt can produce chronic irritability and always should be assessed.
When coaching families about outbursts, I work to help them recognize that the child is not just angry, but very distressed. While “typical” tantrums last 1-5 minutes and show a rise then decline in intensity of the anger and distress, anger outbursts are longer and have an initial short and rapid burst of anger that then declines over the duration of the outburst, and with a steady but lower level of distress throughout.
The option to hug and verbally console the child’s distress is sometimes effective and does not reinforce the behavior unless the parent also yields to demands. But once outbursts begin, I liken them to a bomb going off – there is no intervention possible then. Instead, the task of the family, and over time that of the child, is to recognize and better manage the triggers.
Dr. Ross Greene, in his book, “The Explosive Child: A New Approach for Understanding and Parenting Easily Frustrated, Chronically Inflexible Children,” asserts that the child’s anger and distress can be interpreted as frustration from a gap in skills. This has treatment implications for identifying, educating about, and ameliorating the child’s weaknesses (deficits in understanding, communication, emotion regulation, flexibility or performance; or excess jealousy or hypersensitivity), and coaching parents to recognize, acknowledge, and avoid stressing these areas, if possible. I coach families to give points to the child for progressive little steps toward being able to recognize, verbalize, and inhibit outbursts with a reward system for the points. This helps put the parents and child “on the same team” in working on improving these skills.
Research on children with DMDD indicates that they show less positive affect when winning a “fixed” video game and are less able to suppress negative affect when losing. (Don’t forget to examine the role of real video games as precipitants of tantrums and contingently remove them!) Threshold for upset is lower and the degree of the upsets less well handled by children with DMDD.
In another study, when presented with a series of ambiguous facial expressions, children with DMDD were more likely to see anger in the faces than were controls. One hopeful result was that they could be taught to shift their perceptions significantly away from seeing anger, also reducing irritability and resulting in functional MRI changes. Such hostile bias attribution (tending to see threat) is well known to predispose to aggression. Cognitive behavioral therapy, the most effective counseling intervention, similarly teaches children to rethink their own negative thoughts before acting.
If irritability and rages were not enough, most children with DMDD have other psychiatric disorders; 39% having two, and 51% three or more (J Child Adolesc Psychopharmacol. 2013 Nov;23[9]:588-96). If not for the DMDD diagnosis, 82% would meet criteria for oppositional defiant disorder (ODD). The other common comorbidities are attention-deficit/hyperactivity disorder (ADHD) (74.5%), anxiety disorders (49.0%), and depression that is not major depressive disorder (MDD)(33.3%). When MDD is present, that diagnosis takes precedence. One cannot diagnose ODD, intermittent explosive disorder, or bipolar disorder along with DMDD, conditions from which it is intended to differentiate. Each of these comorbid disorders can be difficult to manage alone much less in combination, making DMDD a disorder deserving diagnosis and treatment by a mental health professional.
One of the main reasons DMDD was created is that children with these features go on to depressive or anxiety disorder in adolescence, not bipolar disorder.
While there is no treatment specific to DMDD, the depression component and prognosis suggest use of SSRIs, in addition to psychosocial therapies, and stimulants for the comorbid ADHD. Unfortunately, these two classes of medication are relatively contraindicated in bipolar disorder because they can lead to treatment-induced episodic mania (TEM). TEM occurs twice as often with antidepressants compared with stimulants (44% vs. 18%) in children with bipolar disorder (J Affect Disord. 2004 Oct 1;82[1]:149-58). Getting the diagnosis correct is, therefore, of great importance when medication is considered.
Approaches such as behavior modification, family therapy, and inpatient treatment can be effective for chronic irritability and aggression. Stimulant treatment of comorbid ADHD can decrease aggression and irritability. Alpha agonists such as guanfacine or clonidine also can help. In cases of partial improvement, adding either risperidone or divalproex may further decrease aggression in ADHD. In refractory aggression, risperidone has the best evidence. The Affective Reactivity Index or Outburst Monitoring Scale can be helpful in assessing severity and monitoring outcomes.
While a prognosis for depression rather than bipolar disorder sounds like a plus, in a longitudinal study, adults who had DMDD as children had worse outcomes, including being more likely to have adverse health outcomes (smoking, sexually transmitted infection), police contact, and low educational attainment, and being more likely to live in poverty, compared with controls who had other psychiatric disorders. While DMDD is a new and different diagnosis, it is similar to bipolar in having a potential course of life disruption, dangerous behaviors, suicide risk, and hospitalization.
Dr. Howard is assistant professor of pediatrics at the Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline. E-mail her at [email protected].
Outbursts by children when frustrated or when asked to “do something they don’t want to do” are among the most common behavioral complaints voiced by parents. But behavioral outbursts, beyond the typical tantrums of children up to age 4 years, can be signs of very severe mental health disorders and are the most common reason for psychiatric admission (50%-60%).
While behavioral dysregulation is undeniably a huge problem for families, there has been an unreasonable 40-fold rise in diagnosis of bipolar disorder from 1994 to 2003, and 48% were prescribed atypical neuroleptics – medications with serious side effects. In response to this overdiagnosis as bipolar disorder, in 2013 the DSM-5 created a new diagnosis called disruptive mood dysregulation disorder (DMDD) to differentiate children who experience explosive outbursts who have a different outcome. This new classification includes children aged 6-12 years with persistent irritability most of the time, nearly every day, lasting at least 12 months and starting before age 10 years. DMDD diagnosis is not used after age 18 years.
To be diagnosed, the child has to have frequent, severe temper outbursts “grossly out of proportion” to the situation, averaging at least three times per week. The outbursts can be verbal or physical aggression to people, things, or themselves. While tantrums can be severe in children with delayed development, for the DMDD diagnosis these behaviors must be inconsistent with developmental level and must occur in at least two settings, and in one setting it must be severe. While outbursts are common, only half of children in one study of severe tantrum behavior in 5- to 9-year-olds also had the required persistent irritability.
If this does sound a lot like bipolar disorder so far, you are right. So what is different? DMDD has a prevalence of 2%-5% and occurs mostly in boys, whereas bipolar disorder affects boys and girls equally and affects less than 1% prior to adolescence.
The key features distinguishing DMDD from bipolar disorder are lack of an episodic nature to the irritability and lack of mania. Irritability in DMDD has to be persistently present with breaks of no more than 3 consecutive months in the defining 12-month period. There also cannot be any more than 1 day of the elevated mood features of mania or hypomania. Identifying mania is the hardest part, even in diagnosing adult bipolar, where it occurs only 1% of the year, much less in children who are generally lively! Hypomania, while less intense than mania, is when the person is energetic, talkative, and confident to an extreme extent, often with a flight of creative ideas. Excitement over birthdays or Christmas specifically does not count! So getting this history has to be done carefully, generally by a mental health professional, to make the distinction.
Interestingly, DMDD is not diagnosed when outbursts and irritability are better explained by autism spectrum disorder, separation anxiety disorder, or PTSD. To me, these exclusions point out the importance of sorting out the “set conditions” for all problematic behaviors, not always an easy task. Symptoms of autism in high functioning individuals can be quite subtle. Was the upset from change in a rigid routine known only to the child? Were sensory stimuli such as loud noises intolerable to this child? Was a nonverbal signal of a peer mistaken as a threat? While violent outbursts precipitated by these factors would still be considered “grossly out of proportion to the situation” for a typical child, they are not uncommon in atypical children. Similarly, children with separation anxiety disorder experience a high level of threat from even thinking about being apart from their caregivers, setting them up for alarm by situations other children would not find difficult.
The American Academy of Pediatrics emphasizes the need to assess all children for a history of psychological trauma. Traumas are quite common, and their sequelae affect many aspects of the child’s life; in the case of outbursts, it is emotional resilience that is impaired. As for all DSM-5 diagnoses, DMDD is not diagnosed when the irritability is due to physiological effects of a substance (e.g. steroids) or another medical or neurological disorder. Children with chronic pain conditions such as rheumatoid arthritis or sickle cell usually cope remarkably well, but when they don’t, their irritability should not be considered a mental health disorder. More commonly, sleep debt can produce chronic irritability and always should be assessed.
When coaching families about outbursts, I work to help them recognize that the child is not just angry, but very distressed. While “typical” tantrums last 1-5 minutes and show a rise then decline in intensity of the anger and distress, anger outbursts are longer and have an initial short and rapid burst of anger that then declines over the duration of the outburst, and with a steady but lower level of distress throughout.
The option to hug and verbally console the child’s distress is sometimes effective and does not reinforce the behavior unless the parent also yields to demands. But once outbursts begin, I liken them to a bomb going off – there is no intervention possible then. Instead, the task of the family, and over time that of the child, is to recognize and better manage the triggers.
Dr. Ross Greene, in his book, “The Explosive Child: A New Approach for Understanding and Parenting Easily Frustrated, Chronically Inflexible Children,” asserts that the child’s anger and distress can be interpreted as frustration from a gap in skills. This has treatment implications for identifying, educating about, and ameliorating the child’s weaknesses (deficits in understanding, communication, emotion regulation, flexibility or performance; or excess jealousy or hypersensitivity), and coaching parents to recognize, acknowledge, and avoid stressing these areas, if possible. I coach families to give points to the child for progressive little steps toward being able to recognize, verbalize, and inhibit outbursts with a reward system for the points. This helps put the parents and child “on the same team” in working on improving these skills.
Research on children with DMDD indicates that they show less positive affect when winning a “fixed” video game and are less able to suppress negative affect when losing. (Don’t forget to examine the role of real video games as precipitants of tantrums and contingently remove them!) Threshold for upset is lower and the degree of the upsets less well handled by children with DMDD.
In another study, when presented with a series of ambiguous facial expressions, children with DMDD were more likely to see anger in the faces than were controls. One hopeful result was that they could be taught to shift their perceptions significantly away from seeing anger, also reducing irritability and resulting in functional MRI changes. Such hostile bias attribution (tending to see threat) is well known to predispose to aggression. Cognitive behavioral therapy, the most effective counseling intervention, similarly teaches children to rethink their own negative thoughts before acting.
If irritability and rages were not enough, most children with DMDD have other psychiatric disorders; 39% having two, and 51% three or more (J Child Adolesc Psychopharmacol. 2013 Nov;23[9]:588-96). If not for the DMDD diagnosis, 82% would meet criteria for oppositional defiant disorder (ODD). The other common comorbidities are attention-deficit/hyperactivity disorder (ADHD) (74.5%), anxiety disorders (49.0%), and depression that is not major depressive disorder (MDD)(33.3%). When MDD is present, that diagnosis takes precedence. One cannot diagnose ODD, intermittent explosive disorder, or bipolar disorder along with DMDD, conditions from which it is intended to differentiate. Each of these comorbid disorders can be difficult to manage alone much less in combination, making DMDD a disorder deserving diagnosis and treatment by a mental health professional.
One of the main reasons DMDD was created is that children with these features go on to depressive or anxiety disorder in adolescence, not bipolar disorder.
While there is no treatment specific to DMDD, the depression component and prognosis suggest use of SSRIs, in addition to psychosocial therapies, and stimulants for the comorbid ADHD. Unfortunately, these two classes of medication are relatively contraindicated in bipolar disorder because they can lead to treatment-induced episodic mania (TEM). TEM occurs twice as often with antidepressants compared with stimulants (44% vs. 18%) in children with bipolar disorder (J Affect Disord. 2004 Oct 1;82[1]:149-58). Getting the diagnosis correct is, therefore, of great importance when medication is considered.
Approaches such as behavior modification, family therapy, and inpatient treatment can be effective for chronic irritability and aggression. Stimulant treatment of comorbid ADHD can decrease aggression and irritability. Alpha agonists such as guanfacine or clonidine also can help. In cases of partial improvement, adding either risperidone or divalproex may further decrease aggression in ADHD. In refractory aggression, risperidone has the best evidence. The Affective Reactivity Index or Outburst Monitoring Scale can be helpful in assessing severity and monitoring outcomes.
While a prognosis for depression rather than bipolar disorder sounds like a plus, in a longitudinal study, adults who had DMDD as children had worse outcomes, including being more likely to have adverse health outcomes (smoking, sexually transmitted infection), police contact, and low educational attainment, and being more likely to live in poverty, compared with controls who had other psychiatric disorders. While DMDD is a new and different diagnosis, it is similar to bipolar in having a potential course of life disruption, dangerous behaviors, suicide risk, and hospitalization.
Dr. Howard is assistant professor of pediatrics at the Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline. E-mail her at [email protected].
The Starbucks generation
Iced, Half-Caff, Ristretto, Venti, 4-Pump, Sugar Free, Cinnamon, Dolce Soy Skinny Latte. Or Non-Fat Frappuccino with Extra Whipped Cream and Chocolate Sauce. Sorry, let me simplify: Triple, Venti, Soy, No Foam Latte. If you’re thinking I am speaking a foreign language, just ask a teen and they likely will be able to translate for you. This is normal Starbucks lingo. If you’re not a coffee drinker, you’re likely completely lost, but for those of us who live by the bean, it’s the language of love, caffeine love.
Twenty years ago, the thought of a teen drinking coffee was unheard of. Sure, soda has been there for decades, and in many cultures tea is a common drink, but today many kids are lining up at Starbucks for the caffeine jolt, and the new drinks such as 5-Hour Energy, Jolt, and Red Bull are making this generation the most sleep-deprived ever.
But how bad is caffeine for teens? The average adult consumes approximately 300 mg of caffeine per day,1 which is equivalent to 2-4 cups of coffee; this is considered to be a moderate intake. But the average teen intake of caffeine is not limited to just coffee. Many are consuming their favorite drink from Starbucks, then a few cans of soda, chocolate candy, and maybe even an energy drink – all before the school day is over. When we consider the content of caffeine in these products, the intake of caffeine is staggering.
For example, the average soda contains 35-55 mg of caffeine. Energy drinks such as Red Bull, Amp, and Monster contain approximately 150 mg of caffeine. A tall (small) Starbucks coffee also contains about 150 mg of caffeine, and when we increase the size to a grande, then we are looking at 320 mg.2,4 Simple math will show that the average teen likely has excessive intake of caffeine, resulting in adverse health effects.
The most concerning adverse effect is sleep deprivation.5 Physiologically, the circadian rhythm of adolescents changes and decreases the secretion of melatonin naturally, making it more difficult for them to fall asleep. With the addition of caffeine in high amounts, this is making falling asleep a greater challenge. Sleep deprivation leads to daytime sleepiness and inattention, resulting in learning issues.
Other ill effects found in some studies is that consumption of more than 220 mg of caffeine per day is associated with increased impulsivity, sensation seeking, and risk-taking behaviors.2 In people who are predisposed to arrhythmias, excessive intake can result in the onset of arrhythmias. Nervousness and jitteriness are other common effects.
Another consideration beyond the direct effects of caffeine is that it is usually coupled with sugary substances like those found in syrups used in Starbucks drinks, chocolate candy, and energy drinks. This has led to concerns of obesity as well as dental decay.
Now, when caffeine is taken in small to moderate amounts, less than 300 mg, there are health benefits. It certainly does improve concentration by attaching to the adenosine receptors that block the adenosine effect of sedation on the brain. This leads to improved concentration, memory retention, auditory vigilance, and reaction time.
Recent studies have shown that caffeine in moderate amounts can protect against Alzheimer’s, and is linked to a small decreased risk of cancer and liver disease. Coffee drinkers have also shown a moderate decrease in Parkinson’s disease and stroke.3,6
Regardless of the benefits of caffeine, the American Academy of Pediatrics has been very clear that it does not recommend caffeine in children. In its 2011 guideline,7 the extra calories, the risk of impulsive behavior, and sleep deprivation far outweighed any benefit that caffeine would have. It is critical that physicians educate their patients about foods that contain caffeine and the cumulative effect these foods have on their well-being, now and in the future.
References
1. “Trends in Caffeine Intake Among US Children and Adolescents” (Pediatrics 2014;133:386-93).
2. Caffeine Consumption Among Children and Adolescents. National Council on Strength and Fitness.
3. What is it about coffee? Harvard Health Letter (www.health.harvard.edu/staying-healthy/what-is-it-about-coffee).
4. Caffeine counts. American Physiological Association (Monitor on Psychology. 2001 June;32[6]).
5. J Pediatrics. 2011 March;158(3):508-9.
6. J Alzheimers Dis. 2010;20(suppl 1):s167-74.
7. Pediatrics 2011 June;127(6):1182-9
Dr. Pearce is a pediatrician in Frankfort, Ill.
Iced, Half-Caff, Ristretto, Venti, 4-Pump, Sugar Free, Cinnamon, Dolce Soy Skinny Latte. Or Non-Fat Frappuccino with Extra Whipped Cream and Chocolate Sauce. Sorry, let me simplify: Triple, Venti, Soy, No Foam Latte. If you’re thinking I am speaking a foreign language, just ask a teen and they likely will be able to translate for you. This is normal Starbucks lingo. If you’re not a coffee drinker, you’re likely completely lost, but for those of us who live by the bean, it’s the language of love, caffeine love.
Twenty years ago, the thought of a teen drinking coffee was unheard of. Sure, soda has been there for decades, and in many cultures tea is a common drink, but today many kids are lining up at Starbucks for the caffeine jolt, and the new drinks such as 5-Hour Energy, Jolt, and Red Bull are making this generation the most sleep-deprived ever.
But how bad is caffeine for teens? The average adult consumes approximately 300 mg of caffeine per day,1 which is equivalent to 2-4 cups of coffee; this is considered to be a moderate intake. But the average teen intake of caffeine is not limited to just coffee. Many are consuming their favorite drink from Starbucks, then a few cans of soda, chocolate candy, and maybe even an energy drink – all before the school day is over. When we consider the content of caffeine in these products, the intake of caffeine is staggering.
For example, the average soda contains 35-55 mg of caffeine. Energy drinks such as Red Bull, Amp, and Monster contain approximately 150 mg of caffeine. A tall (small) Starbucks coffee also contains about 150 mg of caffeine, and when we increase the size to a grande, then we are looking at 320 mg.2,4 Simple math will show that the average teen likely has excessive intake of caffeine, resulting in adverse health effects.
The most concerning adverse effect is sleep deprivation.5 Physiologically, the circadian rhythm of adolescents changes and decreases the secretion of melatonin naturally, making it more difficult for them to fall asleep. With the addition of caffeine in high amounts, this is making falling asleep a greater challenge. Sleep deprivation leads to daytime sleepiness and inattention, resulting in learning issues.
Other ill effects found in some studies is that consumption of more than 220 mg of caffeine per day is associated with increased impulsivity, sensation seeking, and risk-taking behaviors.2 In people who are predisposed to arrhythmias, excessive intake can result in the onset of arrhythmias. Nervousness and jitteriness are other common effects.
Another consideration beyond the direct effects of caffeine is that it is usually coupled with sugary substances like those found in syrups used in Starbucks drinks, chocolate candy, and energy drinks. This has led to concerns of obesity as well as dental decay.
Now, when caffeine is taken in small to moderate amounts, less than 300 mg, there are health benefits. It certainly does improve concentration by attaching to the adenosine receptors that block the adenosine effect of sedation on the brain. This leads to improved concentration, memory retention, auditory vigilance, and reaction time.
Recent studies have shown that caffeine in moderate amounts can protect against Alzheimer’s, and is linked to a small decreased risk of cancer and liver disease. Coffee drinkers have also shown a moderate decrease in Parkinson’s disease and stroke.3,6
Regardless of the benefits of caffeine, the American Academy of Pediatrics has been very clear that it does not recommend caffeine in children. In its 2011 guideline,7 the extra calories, the risk of impulsive behavior, and sleep deprivation far outweighed any benefit that caffeine would have. It is critical that physicians educate their patients about foods that contain caffeine and the cumulative effect these foods have on their well-being, now and in the future.
References
1. “Trends in Caffeine Intake Among US Children and Adolescents” (Pediatrics 2014;133:386-93).
2. Caffeine Consumption Among Children and Adolescents. National Council on Strength and Fitness.
3. What is it about coffee? Harvard Health Letter (www.health.harvard.edu/staying-healthy/what-is-it-about-coffee).
4. Caffeine counts. American Physiological Association (Monitor on Psychology. 2001 June;32[6]).
5. J Pediatrics. 2011 March;158(3):508-9.
6. J Alzheimers Dis. 2010;20(suppl 1):s167-74.
7. Pediatrics 2011 June;127(6):1182-9
Dr. Pearce is a pediatrician in Frankfort, Ill.
Iced, Half-Caff, Ristretto, Venti, 4-Pump, Sugar Free, Cinnamon, Dolce Soy Skinny Latte. Or Non-Fat Frappuccino with Extra Whipped Cream and Chocolate Sauce. Sorry, let me simplify: Triple, Venti, Soy, No Foam Latte. If you’re thinking I am speaking a foreign language, just ask a teen and they likely will be able to translate for you. This is normal Starbucks lingo. If you’re not a coffee drinker, you’re likely completely lost, but for those of us who live by the bean, it’s the language of love, caffeine love.
Twenty years ago, the thought of a teen drinking coffee was unheard of. Sure, soda has been there for decades, and in many cultures tea is a common drink, but today many kids are lining up at Starbucks for the caffeine jolt, and the new drinks such as 5-Hour Energy, Jolt, and Red Bull are making this generation the most sleep-deprived ever.
But how bad is caffeine for teens? The average adult consumes approximately 300 mg of caffeine per day,1 which is equivalent to 2-4 cups of coffee; this is considered to be a moderate intake. But the average teen intake of caffeine is not limited to just coffee. Many are consuming their favorite drink from Starbucks, then a few cans of soda, chocolate candy, and maybe even an energy drink – all before the school day is over. When we consider the content of caffeine in these products, the intake of caffeine is staggering.
For example, the average soda contains 35-55 mg of caffeine. Energy drinks such as Red Bull, Amp, and Monster contain approximately 150 mg of caffeine. A tall (small) Starbucks coffee also contains about 150 mg of caffeine, and when we increase the size to a grande, then we are looking at 320 mg.2,4 Simple math will show that the average teen likely has excessive intake of caffeine, resulting in adverse health effects.
The most concerning adverse effect is sleep deprivation.5 Physiologically, the circadian rhythm of adolescents changes and decreases the secretion of melatonin naturally, making it more difficult for them to fall asleep. With the addition of caffeine in high amounts, this is making falling asleep a greater challenge. Sleep deprivation leads to daytime sleepiness and inattention, resulting in learning issues.
Other ill effects found in some studies is that consumption of more than 220 mg of caffeine per day is associated with increased impulsivity, sensation seeking, and risk-taking behaviors.2 In people who are predisposed to arrhythmias, excessive intake can result in the onset of arrhythmias. Nervousness and jitteriness are other common effects.
Another consideration beyond the direct effects of caffeine is that it is usually coupled with sugary substances like those found in syrups used in Starbucks drinks, chocolate candy, and energy drinks. This has led to concerns of obesity as well as dental decay.
Now, when caffeine is taken in small to moderate amounts, less than 300 mg, there are health benefits. It certainly does improve concentration by attaching to the adenosine receptors that block the adenosine effect of sedation on the brain. This leads to improved concentration, memory retention, auditory vigilance, and reaction time.
Recent studies have shown that caffeine in moderate amounts can protect against Alzheimer’s, and is linked to a small decreased risk of cancer and liver disease. Coffee drinkers have also shown a moderate decrease in Parkinson’s disease and stroke.3,6
Regardless of the benefits of caffeine, the American Academy of Pediatrics has been very clear that it does not recommend caffeine in children. In its 2011 guideline,7 the extra calories, the risk of impulsive behavior, and sleep deprivation far outweighed any benefit that caffeine would have. It is critical that physicians educate their patients about foods that contain caffeine and the cumulative effect these foods have on their well-being, now and in the future.
References
1. “Trends in Caffeine Intake Among US Children and Adolescents” (Pediatrics 2014;133:386-93).
2. Caffeine Consumption Among Children and Adolescents. National Council on Strength and Fitness.
3. What is it about coffee? Harvard Health Letter (www.health.harvard.edu/staying-healthy/what-is-it-about-coffee).
4. Caffeine counts. American Physiological Association (Monitor on Psychology. 2001 June;32[6]).
5. J Pediatrics. 2011 March;158(3):508-9.
6. J Alzheimers Dis. 2010;20(suppl 1):s167-74.
7. Pediatrics 2011 June;127(6):1182-9
Dr. Pearce is a pediatrician in Frankfort, Ill.
Behavior problems in youth: Are things worse today than in the past?
Every generation of adults seems to worry that the next generation of youth is in trouble. The perception of kids today is no different, with theories abounding as to why the mental health of the newest generation is slipping, compared with previous standards. From mobile phones to helicopter parents, it might seem like a foregone conclusion that our current crop of young people is destined to be insecure, inattentive, and unable to cope with challenges and stress. Many news headlines on the latest mass shooting or standardized test results often seem to confirm these widespread concerns.
Pediatricians often hear parents lamenting the “good old days” when such things as corporal punishment were more easily accepted to help keep kids in line. But taking a step back, it may be worth a more objective look to examine the assumption that child behavioral problems are worse than ever. Measuring overall mental health is not an easy task, but looking at several important metrics indicate that things may not be nearly as bad as many people think.
Substance use
From the latest data from the Monitoring the Future Study, one of the nation’s most reliable sources on teen substance use, the use of both alcohol and tobacco among youth is at the lowest level since the study began in 1975. Use of drugs like heroin and ecstasy also are declining. The only major exception to this trend seems to be cannabis use, which has generally shown stable rates during this climate of marijuana decriminalization and, for some states, legalization.
Teen pregnancy rates
One area where there continues to be sustained progress is in teen pregnancy. According to the government’s Centers for Disease Control and Prevention, the overall pregnancy rate among adolescent females has been cut in half from 1991 to 2011, across many different ethnic groups. The rate fell from 61.8/1,000 teenagers aged 15-19 years to 31.3/1,000 teenagers.
Delinquency
Far fewer adolescents are being held against their will in juvenile detention centers. The number of youth who are incarcerated have dropped from a high of 381/100,000 in 1995 to 225/100,000 in 2010, according to a report by the Annie E. Casey Foundation.
Bullying
Bullying has been increasingly recognized as the public health problem that it is. The use of online technology also has created many new settings in which bullying can take place. Nevertheless, there is reason to be optimistic. From the National Center for Education Statistics and the National Crime Victimization Survey, the number of students who report being bullied at school has dropped from 32% in 2007 to an all-time low of 22% in 2013. Another recent study reached similar conclusions for bullying and many other forms of child victimization between 2003 and 2011 (JAMA Pediatr. 2014 Jun;168[6]:540-6).
Suicide
According to the CDC, the rate of completed suicide in youth peaked in the early1990s and then dropped and stabilized before starting to creep up again over the past 5 or so years. The trends are somewhat different, based on gender and the specific age group that is examined. The majority of completed youth suicides occur in males, with current rates still well below those historical highs.
Psychiatric disorders
This one is particularly tricky. While the rates of many specific psychiatric disorders such as ADHD and bipolar disorder have been rising in youth, as well as the use of psychiatric medications, it is much less clear whether this represents a true rise in these disorders versus other factors such as improved detection and a lower diagnostic threshold. One study by Achenbach et al. that measured quantitative levels of child behavior problems from the same rating scale over a 23-year time span found some increases in overall levels from the 1970s to the early 1990s, but then levels began to fall by the end of the millennium (J Abnorm Child Psychol. 2003 Feb;31[1]:1-11).
Of course, these hopeful trends in many significant areas do not mean that these problems have been overcome. While much work remains to be done on many fronts, it is still worth keeping in mind that the overall condition of youth mental health may not be as dire as we might be led to believe and that there is evidence that our efforts, perhaps, are leading to some progress.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. He said he has no relevant financial disclosures. Follow him on Twitter @pedipsych. E-mail him at [email protected].
Every generation of adults seems to worry that the next generation of youth is in trouble. The perception of kids today is no different, with theories abounding as to why the mental health of the newest generation is slipping, compared with previous standards. From mobile phones to helicopter parents, it might seem like a foregone conclusion that our current crop of young people is destined to be insecure, inattentive, and unable to cope with challenges and stress. Many news headlines on the latest mass shooting or standardized test results often seem to confirm these widespread concerns.
Pediatricians often hear parents lamenting the “good old days” when such things as corporal punishment were more easily accepted to help keep kids in line. But taking a step back, it may be worth a more objective look to examine the assumption that child behavioral problems are worse than ever. Measuring overall mental health is not an easy task, but looking at several important metrics indicate that things may not be nearly as bad as many people think.
Substance use
From the latest data from the Monitoring the Future Study, one of the nation’s most reliable sources on teen substance use, the use of both alcohol and tobacco among youth is at the lowest level since the study began in 1975. Use of drugs like heroin and ecstasy also are declining. The only major exception to this trend seems to be cannabis use, which has generally shown stable rates during this climate of marijuana decriminalization and, for some states, legalization.
Teen pregnancy rates
One area where there continues to be sustained progress is in teen pregnancy. According to the government’s Centers for Disease Control and Prevention, the overall pregnancy rate among adolescent females has been cut in half from 1991 to 2011, across many different ethnic groups. The rate fell from 61.8/1,000 teenagers aged 15-19 years to 31.3/1,000 teenagers.
Delinquency
Far fewer adolescents are being held against their will in juvenile detention centers. The number of youth who are incarcerated have dropped from a high of 381/100,000 in 1995 to 225/100,000 in 2010, according to a report by the Annie E. Casey Foundation.
Bullying
Bullying has been increasingly recognized as the public health problem that it is. The use of online technology also has created many new settings in which bullying can take place. Nevertheless, there is reason to be optimistic. From the National Center for Education Statistics and the National Crime Victimization Survey, the number of students who report being bullied at school has dropped from 32% in 2007 to an all-time low of 22% in 2013. Another recent study reached similar conclusions for bullying and many other forms of child victimization between 2003 and 2011 (JAMA Pediatr. 2014 Jun;168[6]:540-6).
Suicide
According to the CDC, the rate of completed suicide in youth peaked in the early1990s and then dropped and stabilized before starting to creep up again over the past 5 or so years. The trends are somewhat different, based on gender and the specific age group that is examined. The majority of completed youth suicides occur in males, with current rates still well below those historical highs.
Psychiatric disorders
This one is particularly tricky. While the rates of many specific psychiatric disorders such as ADHD and bipolar disorder have been rising in youth, as well as the use of psychiatric medications, it is much less clear whether this represents a true rise in these disorders versus other factors such as improved detection and a lower diagnostic threshold. One study by Achenbach et al. that measured quantitative levels of child behavior problems from the same rating scale over a 23-year time span found some increases in overall levels from the 1970s to the early 1990s, but then levels began to fall by the end of the millennium (J Abnorm Child Psychol. 2003 Feb;31[1]:1-11).
Of course, these hopeful trends in many significant areas do not mean that these problems have been overcome. While much work remains to be done on many fronts, it is still worth keeping in mind that the overall condition of youth mental health may not be as dire as we might be led to believe and that there is evidence that our efforts, perhaps, are leading to some progress.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. He said he has no relevant financial disclosures. Follow him on Twitter @pedipsych. E-mail him at [email protected].
Every generation of adults seems to worry that the next generation of youth is in trouble. The perception of kids today is no different, with theories abounding as to why the mental health of the newest generation is slipping, compared with previous standards. From mobile phones to helicopter parents, it might seem like a foregone conclusion that our current crop of young people is destined to be insecure, inattentive, and unable to cope with challenges and stress. Many news headlines on the latest mass shooting or standardized test results often seem to confirm these widespread concerns.
Pediatricians often hear parents lamenting the “good old days” when such things as corporal punishment were more easily accepted to help keep kids in line. But taking a step back, it may be worth a more objective look to examine the assumption that child behavioral problems are worse than ever. Measuring overall mental health is not an easy task, but looking at several important metrics indicate that things may not be nearly as bad as many people think.
Substance use
From the latest data from the Monitoring the Future Study, one of the nation’s most reliable sources on teen substance use, the use of both alcohol and tobacco among youth is at the lowest level since the study began in 1975. Use of drugs like heroin and ecstasy also are declining. The only major exception to this trend seems to be cannabis use, which has generally shown stable rates during this climate of marijuana decriminalization and, for some states, legalization.
Teen pregnancy rates
One area where there continues to be sustained progress is in teen pregnancy. According to the government’s Centers for Disease Control and Prevention, the overall pregnancy rate among adolescent females has been cut in half from 1991 to 2011, across many different ethnic groups. The rate fell from 61.8/1,000 teenagers aged 15-19 years to 31.3/1,000 teenagers.
Delinquency
Far fewer adolescents are being held against their will in juvenile detention centers. The number of youth who are incarcerated have dropped from a high of 381/100,000 in 1995 to 225/100,000 in 2010, according to a report by the Annie E. Casey Foundation.
Bullying
Bullying has been increasingly recognized as the public health problem that it is. The use of online technology also has created many new settings in which bullying can take place. Nevertheless, there is reason to be optimistic. From the National Center for Education Statistics and the National Crime Victimization Survey, the number of students who report being bullied at school has dropped from 32% in 2007 to an all-time low of 22% in 2013. Another recent study reached similar conclusions for bullying and many other forms of child victimization between 2003 and 2011 (JAMA Pediatr. 2014 Jun;168[6]:540-6).
Suicide
According to the CDC, the rate of completed suicide in youth peaked in the early1990s and then dropped and stabilized before starting to creep up again over the past 5 or so years. The trends are somewhat different, based on gender and the specific age group that is examined. The majority of completed youth suicides occur in males, with current rates still well below those historical highs.
Psychiatric disorders
This one is particularly tricky. While the rates of many specific psychiatric disorders such as ADHD and bipolar disorder have been rising in youth, as well as the use of psychiatric medications, it is much less clear whether this represents a true rise in these disorders versus other factors such as improved detection and a lower diagnostic threshold. One study by Achenbach et al. that measured quantitative levels of child behavior problems from the same rating scale over a 23-year time span found some increases in overall levels from the 1970s to the early 1990s, but then levels began to fall by the end of the millennium (J Abnorm Child Psychol. 2003 Feb;31[1]:1-11).
Of course, these hopeful trends in many significant areas do not mean that these problems have been overcome. While much work remains to be done on many fronts, it is still worth keeping in mind that the overall condition of youth mental health may not be as dire as we might be led to believe and that there is evidence that our efforts, perhaps, are leading to some progress.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. He said he has no relevant financial disclosures. Follow him on Twitter @pedipsych. E-mail him at [email protected].
Epic fail
A couple of years ago, “epic fail” was the phrase my teenage son used as I unsuccessfully attempted to beat him in a game we were playing. At the time, I thought to myself it was a harsh, but accurate assessment of my performance. And I was certainly motivated to practice on my own so that the next time, things would be different.
That same phrase came to mind as I read an October 2015 online article published in Cancer Epidemiology, Biomarkers & Prevention titled “Quality of Physician Communication about Human Papillomavirus Vaccine: Findings from a National Survey” (Nov:24[11];1673). The article describes well the poor performance of the medical community – primarily pediatricians and family physicians – in providing this vaccine. Another source, the most recent National Immunization Survey–Teen 2014, reports another alarming trend: HPV vaccine series initiation and completion continues to lag far behind what it should be.
It came as no surprise to me that the journal article clearly showed what I have suspected for some time and what has been hinted at by previous studies. The epic failure in providing what is essentially a cancer-prevention vaccine to the recommended population of 11- to 12-year-old boys and girls lies not at the feet of the antivaccine movement or hesitant parents. Rather, the failure belongs to us.
The article describes findings from an online survey sent to 2,368 pediatricians and family physicians in 2014. Respondents (776) self-reported their own performance on strength of endorsement (saying the vaccine is important), timeliness (recommending it at ages 11 and 12 years), consistency (recommending it routinely versus using a risk-based approach), and urgency (recommending same-day vaccination).
More than one-quarter stated they did not strongly endorse the HPV vaccine, and a similar number reported they did not recommend it be given at 11-12 years of age. Amazingly, 59% stated they used a risk-based approach versus a routine approach to recommending the HPV vaccine, and only half of the respondents recommended giving the vaccine at the current encounter when discussing the HPV vaccine. Because this is self-reported data, these results represent a best-case scenario because respondents would be unlikely to paint an unflattering picture of their own performance.
Clearly, we have a major problem with physicians struggling with their own discomfort in talking about the HPV vaccine and who erroneously believe parents do not value it. The physician’s lack of competency in communicating effectively – overtly and covertly – leads to a lack of an affirmative recommendation that is so important in any preventive intervention. We are at risk of being the generation of pediatricians and family physicians who collectively failed to protect our patients from a preventable cause of cancer. Only we can fix what is wrong with us. Only we can turn around this epic failure.
Physicians and other providers of medical care to adolescents can access resources to help themselves improve their provision of the HPV vaccine to their patients. One of the best collections of resources can be found online at the American Academy of Pediatrics' Champion Toolkit. This includes material from the Centers for Disease Control and Prevention and AAP as well as some illuminating video vignettes that illustrate the do's and don'ts of communicating with families about HPV vaccination. This must become part of our mission!
Dr. Terk is a pediatrician in Keller, Tx., and is the immediate past president of the Texas Pediatric Society.
*Updated 1/26/2016
A couple of years ago, “epic fail” was the phrase my teenage son used as I unsuccessfully attempted to beat him in a game we were playing. At the time, I thought to myself it was a harsh, but accurate assessment of my performance. And I was certainly motivated to practice on my own so that the next time, things would be different.
That same phrase came to mind as I read an October 2015 online article published in Cancer Epidemiology, Biomarkers & Prevention titled “Quality of Physician Communication about Human Papillomavirus Vaccine: Findings from a National Survey” (Nov:24[11];1673). The article describes well the poor performance of the medical community – primarily pediatricians and family physicians – in providing this vaccine. Another source, the most recent National Immunization Survey–Teen 2014, reports another alarming trend: HPV vaccine series initiation and completion continues to lag far behind what it should be.
It came as no surprise to me that the journal article clearly showed what I have suspected for some time and what has been hinted at by previous studies. The epic failure in providing what is essentially a cancer-prevention vaccine to the recommended population of 11- to 12-year-old boys and girls lies not at the feet of the antivaccine movement or hesitant parents. Rather, the failure belongs to us.
The article describes findings from an online survey sent to 2,368 pediatricians and family physicians in 2014. Respondents (776) self-reported their own performance on strength of endorsement (saying the vaccine is important), timeliness (recommending it at ages 11 and 12 years), consistency (recommending it routinely versus using a risk-based approach), and urgency (recommending same-day vaccination).
More than one-quarter stated they did not strongly endorse the HPV vaccine, and a similar number reported they did not recommend it be given at 11-12 years of age. Amazingly, 59% stated they used a risk-based approach versus a routine approach to recommending the HPV vaccine, and only half of the respondents recommended giving the vaccine at the current encounter when discussing the HPV vaccine. Because this is self-reported data, these results represent a best-case scenario because respondents would be unlikely to paint an unflattering picture of their own performance.
Clearly, we have a major problem with physicians struggling with their own discomfort in talking about the HPV vaccine and who erroneously believe parents do not value it. The physician’s lack of competency in communicating effectively – overtly and covertly – leads to a lack of an affirmative recommendation that is so important in any preventive intervention. We are at risk of being the generation of pediatricians and family physicians who collectively failed to protect our patients from a preventable cause of cancer. Only we can fix what is wrong with us. Only we can turn around this epic failure.
Physicians and other providers of medical care to adolescents can access resources to help themselves improve their provision of the HPV vaccine to their patients. One of the best collections of resources can be found online at the American Academy of Pediatrics' Champion Toolkit. This includes material from the Centers for Disease Control and Prevention and AAP as well as some illuminating video vignettes that illustrate the do's and don'ts of communicating with families about HPV vaccination. This must become part of our mission!
Dr. Terk is a pediatrician in Keller, Tx., and is the immediate past president of the Texas Pediatric Society.
*Updated 1/26/2016
A couple of years ago, “epic fail” was the phrase my teenage son used as I unsuccessfully attempted to beat him in a game we were playing. At the time, I thought to myself it was a harsh, but accurate assessment of my performance. And I was certainly motivated to practice on my own so that the next time, things would be different.
That same phrase came to mind as I read an October 2015 online article published in Cancer Epidemiology, Biomarkers & Prevention titled “Quality of Physician Communication about Human Papillomavirus Vaccine: Findings from a National Survey” (Nov:24[11];1673). The article describes well the poor performance of the medical community – primarily pediatricians and family physicians – in providing this vaccine. Another source, the most recent National Immunization Survey–Teen 2014, reports another alarming trend: HPV vaccine series initiation and completion continues to lag far behind what it should be.
It came as no surprise to me that the journal article clearly showed what I have suspected for some time and what has been hinted at by previous studies. The epic failure in providing what is essentially a cancer-prevention vaccine to the recommended population of 11- to 12-year-old boys and girls lies not at the feet of the antivaccine movement or hesitant parents. Rather, the failure belongs to us.
The article describes findings from an online survey sent to 2,368 pediatricians and family physicians in 2014. Respondents (776) self-reported their own performance on strength of endorsement (saying the vaccine is important), timeliness (recommending it at ages 11 and 12 years), consistency (recommending it routinely versus using a risk-based approach), and urgency (recommending same-day vaccination).
More than one-quarter stated they did not strongly endorse the HPV vaccine, and a similar number reported they did not recommend it be given at 11-12 years of age. Amazingly, 59% stated they used a risk-based approach versus a routine approach to recommending the HPV vaccine, and only half of the respondents recommended giving the vaccine at the current encounter when discussing the HPV vaccine. Because this is self-reported data, these results represent a best-case scenario because respondents would be unlikely to paint an unflattering picture of their own performance.
Clearly, we have a major problem with physicians struggling with their own discomfort in talking about the HPV vaccine and who erroneously believe parents do not value it. The physician’s lack of competency in communicating effectively – overtly and covertly – leads to a lack of an affirmative recommendation that is so important in any preventive intervention. We are at risk of being the generation of pediatricians and family physicians who collectively failed to protect our patients from a preventable cause of cancer. Only we can fix what is wrong with us. Only we can turn around this epic failure.
Physicians and other providers of medical care to adolescents can access resources to help themselves improve their provision of the HPV vaccine to their patients. One of the best collections of resources can be found online at the American Academy of Pediatrics' Champion Toolkit. This includes material from the Centers for Disease Control and Prevention and AAP as well as some illuminating video vignettes that illustrate the do's and don'ts of communicating with families about HPV vaccination. This must become part of our mission!
Dr. Terk is a pediatrician in Keller, Tx., and is the immediate past president of the Texas Pediatric Society.
*Updated 1/26/2016
Maternal immunization during pregnancy: lessons learned, and emerging opportunities
Pediatricians and our teams are the immunization experts. We educate, advocate, and incorporate vaccines into much of our daily routine. As such, we recognize the importance of working with our colleagues in family medicine, internal medicine, and obstetrics to optimize immunization programs for high-risk individuals, including pregnant women. Recent advances in vaccine recommendations during pregnancy are a result of the collaborative efforts of the health care providers for these women, and from systematic evaluation of immunization programs, vaccine pregnancy registries, and disease epidemiology.
Vaccinating women during pregnancy should be considered when a vaccine is known to be safe and when the following apply:
• The risk of severe infection is high during or augmented by pregnancy.
• The specific infection during pregnancy threatens the fetus.
• Maternal protection against infection benefits the newborn.
• Passive transfer of antibody from mother to fetus benefits the newborn.
Examples of safe vaccines immediately come to mind that fulfill one of more of these criteria, yet substantial obstacles exist even where safety and effectiveness data are robust. Because clinical vaccine trials traditionally exclude pregnant women, safety and effectiveness data for this group and their newborns are limited and often must come through experience. In a climate of increased vaccine hesitancy in general, both among providers and patients, vaccine delivery can be fragmented and particularly difficult to streamline. Additional obstacles that exist for any immunization program, including one that targets pregnant women specifically, are immunization delivery logistics and cost.
One of the major success stories of maternal immunization that is easily forgotten or overlooked in developed parts of the world is in the prevention of maternal and neonatal tetanus (MNT). A review of recent history reminds us that between the years 2000 and 2014, 35 countries were finally successful in eliminating MNT, including China, Turkey, Egypt, and South Africa. In addition, 24 of 36 states in the country of India, 30 of 34 provinces of Indonesia, and most of Ethiopia have met with success. This has been accomplished through aggressive tetanus vaccination programs, and through education programs targeted at optimal umbilical cord stump care after delivery.
In the United States, the Advisory Committee on Immunization Practices recommends that all pregnant women should receive inactivated influenza vaccine and Tdap vaccine. In addition, several other vaccines are recommended under certain circumstances. Live attenuated vaccines are considered contraindicated, although yellow fever vaccine is an exception during epidemics, or when travel to a highly endemic area during pregnancy cannot be avoided.
Influenza vaccine administered during pregnancy reduces maternal morbidity and mortality. Moreover, safety and benefits for the fetus are clearly documented. Both retrospective cohort analysis studies and randomized controlled trials have consistently demonstrated lower risk of preterm birth and lower risk for delivering newborns small for gestational age among women who received inactivated influenza vaccine during pregnancy. The benefit extends to term healthy infants who are less likely to be hospitalized during the first months of life if their mother was vaccinated against influenza during pregnancy. Because the mother was immunized during pregnancy, it reduces her risk of infection, thereby reducing the potential that the newborn will be exposed to a mother who is contagious. Perhaps more importantly, infants born at or near term have the benefit of transplacental antibody endowment from their mother, including vaccine induced anti-influenza antibodies. This passive protection is expected to last for several months. Active immunization against influenza during infancy begins at 6 months of age.
Tdap vaccine is also recommended during each pregnancy. In the United States, MNT is eliminated. Here, as in other developed countries, Tdap is administered to reduce infant pertussis morbidity. Pertussis remains endemic to the United States, and infants who develop whooping cough during the first 2-3 months of life are at the highest risk for morbidity and mortality.
Historically, one-third of infants infected with pertussis were infected by their mother, although more recent evidence suggests that older siblings are at least as likely a source. Looking back to the paradigm for protection against influenza infection in the first few months of life, it becomes clear why the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention has recommended Tdap vaccine for all mothers during each pregnancy.
The first goal is to prevent pertussis in the mother so that she will not transmit the infection to her newborn. The additional goal, and the rationale for vaccinating pregnant women during every pregnancy, is to optimize levels of anti-pertussis antibody in the mother, so that the transplacental endowment to the infant is as robust as possible.
Serologic studies have demonstrated that Tdap vaccine induces high anti-pertussis antibodies when administered during pregnancy, but that the half-life of those antibodies is brief. When Tdap is given during pregnancy, and the infant is born at or near term, the antibody transfer to the infant is expected to provide passive protection for several months. Maternal immunization during pregnancy thereby reduces the risk that the mother will develop pertussis and transmit it to her newborn, while at the same time allows a degree of passive immunoprotection to the infant during the most vulnerable period of life. Active immunization against pertussis in the infant begins between 6-8 weeks of age.
Another infection that is exceedingly common during the first several months of life is respiratory syncytial virus (RSV). RSV remains the most common reason for infant hospitalization in the United States and other developed countries. The source of the virus can be any other person with a mild or moderate respiratory tract infection as the virus is ubiquitous, and can re-infect individuals throughout their lifetime. The first infection, however, is the worst. It is estimated that between 3% and 4% of the U.S. birth cohort is hospitalized with RSV. With a U.S. birth cohort of about 4 million, the result is 120,000-160,000 infant admissions annually.
The RSV epidemic is seasonal, fairly predictable, and dreaded by primary care pediatricians and hospitalists alike. Lower respiratory tract infection with RSV, in the form of RSV bronchiolitis, presents all too commonly in the young infant with cough, coryza, tachypnea, and wheezing. When the work of breathing increases, and the cough symptoms predominate, the infant is unable to feed efficiently. Hospitalizations may be for dehydration, concerns for impending respiratory failure, or for the administration of supplemental oxygen or other respiratory support. No specific therapeutic interventions reliably reduce the symptoms or the length of hospital stay, nor do they reduce the possibility that intensive care with mechanical ventilation may be required. Treatments are only supportive. An effective vaccine remains elusive.
All other common infections that once resulted in high rates of hospitalization in the first year of life are now substantially reduced through vaccination. Why not this one? The development of a safe and effective vaccine to prevent infant RSV infection or to reduce RSV-associated hospitalizations is especially challenging for multiple reasons.
Some of these reasons have met with substantial advances quite recently, including the discovery of antigen structures needed to induce neutralizing antibody responses. There also are challenges specific to the infant group we need most to protect. Infant RSV infection itself confers only modest protection against subsequent infection. Repeated infections over time are necessary for protection against illness when re-exposed. A vaccine that is able to induce a response similar to natural infection would therefore require multiple doses, presumably over time (the so called ‘primary series’) before a substantial clinical benefit would be expected. This is particularly important because most RSV-associated hospitalizations occur during the first several months of life, reducing the timeline for which a protective vaccine series could be administered.
The challenges are parallel to the issues described earlier for protection against both influenza and pertussis. Infant protection against both of these infections are now addressed, at least to start with, by vaccinating the mother during her pregnancy. In the infant, the pertussis vaccine primary series is then initiated between 6 and 8 weeks of age, and the influenza series initiated at 6 months of age. It is the passive protection, in the form of transplacental maternal antibody, that offers the interim protection during the highest-risk first months of life.
For infants at very high risk of serious RSV infection, passive antibody protection is already administered in the form of the pharmacobiologic medication palivizumab. Its half-life dictates monthly injections for those eligible, and its cost precludes its use for any but the highest risk infants (those born prematurely, and those with chronic lung disease and/or congenital heart disease). This strategy, however, has proven effective in preventing RSV-associated hospitalization in every group in which it has been studied. This “proof of concept” strongly suggests that if the right RSV vaccine is given to women during pregnancy to induce a robust neutralizing anti-RSV antibody response, and that antibody is transferred to the fetus prior to birth, the newborn will benefit from protection against RSV for a period of time.
Several questions emerge. If RSV is ubiquitous, and can re-infect individuals throughout their lifetime, then some women will be infected during their pregnancy. Do their infants benefit? As a re-infection, the maternal symptoms would be expected to be mild, but the infection could boost the women’s natural immunity with a robust anamnestic antibody response. This possibility has not been studied systematically, but might help to explain why some healthy term infants exposed to RSV develop little or no symptoms, while others (mothers who have not recently had a natural RSV infection) develop severe illness requiring hospitalization.
There are data to support the contention that term infants born to mothers with higher naturally occurring anti-RSV neutralizing antibodies benefit from those antibodies. In a large prospective cohort study performed in Kenya, cord blood anti-RSV antibody concentrations correlated directly with the length of time before the infant’s first RSV infection. It’s therefore logical to conclude that administering an effective RSV vaccine during pregnancy could augment that natural antibody response, be transferred to the infant at birth, and offer protection against RSV when exposed.
Several candidate vaccines for study already exist and have undergone phase I testing in nonpregnant adults. Once safety is demonstrated, the next step is to identify the vaccine formulation resulting in the most robust anti-RSV neutralizing antibody concentrations. Such a candidate vaccine will be chosen for future phase III trials during pregnancy. Safety, and maternal/cord blood RSV antibody titers will be of interest during that clinical trial, but the rates and timing of RSV infection and RSV-associated hospitalizations among the infants born to those mothers will be the most instructive.
Ideally, a candidate RSV vaccine shown to be as safe and as effective during pregnancy as inactivated influenza vaccines and/or Tdap vaccines would be implemented immediately and universally. Unfortunately, substantial vaccine hesitancy for the use of influenza and Tdap vaccines continues among pregnant patients and their providers. Acceptance of an RSV vaccine for use during pregnancy will not come easily, or immediately. As with all of our successful vaccine programs, launching such an effort will require education, patience, and careful post-licensure documentation of the impact that the intervention has in the real world.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University, Syracuse, N.Y. Dr. Domachowske is performing clinical trials and has grants in the area of RSV prevention with Astra Zeneca, Regeneron, and Glaxo Smith Kline.
Pediatricians and our teams are the immunization experts. We educate, advocate, and incorporate vaccines into much of our daily routine. As such, we recognize the importance of working with our colleagues in family medicine, internal medicine, and obstetrics to optimize immunization programs for high-risk individuals, including pregnant women. Recent advances in vaccine recommendations during pregnancy are a result of the collaborative efforts of the health care providers for these women, and from systematic evaluation of immunization programs, vaccine pregnancy registries, and disease epidemiology.
Vaccinating women during pregnancy should be considered when a vaccine is known to be safe and when the following apply:
• The risk of severe infection is high during or augmented by pregnancy.
• The specific infection during pregnancy threatens the fetus.
• Maternal protection against infection benefits the newborn.
• Passive transfer of antibody from mother to fetus benefits the newborn.
Examples of safe vaccines immediately come to mind that fulfill one of more of these criteria, yet substantial obstacles exist even where safety and effectiveness data are robust. Because clinical vaccine trials traditionally exclude pregnant women, safety and effectiveness data for this group and their newborns are limited and often must come through experience. In a climate of increased vaccine hesitancy in general, both among providers and patients, vaccine delivery can be fragmented and particularly difficult to streamline. Additional obstacles that exist for any immunization program, including one that targets pregnant women specifically, are immunization delivery logistics and cost.
One of the major success stories of maternal immunization that is easily forgotten or overlooked in developed parts of the world is in the prevention of maternal and neonatal tetanus (MNT). A review of recent history reminds us that between the years 2000 and 2014, 35 countries were finally successful in eliminating MNT, including China, Turkey, Egypt, and South Africa. In addition, 24 of 36 states in the country of India, 30 of 34 provinces of Indonesia, and most of Ethiopia have met with success. This has been accomplished through aggressive tetanus vaccination programs, and through education programs targeted at optimal umbilical cord stump care after delivery.
In the United States, the Advisory Committee on Immunization Practices recommends that all pregnant women should receive inactivated influenza vaccine and Tdap vaccine. In addition, several other vaccines are recommended under certain circumstances. Live attenuated vaccines are considered contraindicated, although yellow fever vaccine is an exception during epidemics, or when travel to a highly endemic area during pregnancy cannot be avoided.
Influenza vaccine administered during pregnancy reduces maternal morbidity and mortality. Moreover, safety and benefits for the fetus are clearly documented. Both retrospective cohort analysis studies and randomized controlled trials have consistently demonstrated lower risk of preterm birth and lower risk for delivering newborns small for gestational age among women who received inactivated influenza vaccine during pregnancy. The benefit extends to term healthy infants who are less likely to be hospitalized during the first months of life if their mother was vaccinated against influenza during pregnancy. Because the mother was immunized during pregnancy, it reduces her risk of infection, thereby reducing the potential that the newborn will be exposed to a mother who is contagious. Perhaps more importantly, infants born at or near term have the benefit of transplacental antibody endowment from their mother, including vaccine induced anti-influenza antibodies. This passive protection is expected to last for several months. Active immunization against influenza during infancy begins at 6 months of age.
Tdap vaccine is also recommended during each pregnancy. In the United States, MNT is eliminated. Here, as in other developed countries, Tdap is administered to reduce infant pertussis morbidity. Pertussis remains endemic to the United States, and infants who develop whooping cough during the first 2-3 months of life are at the highest risk for morbidity and mortality.
Historically, one-third of infants infected with pertussis were infected by their mother, although more recent evidence suggests that older siblings are at least as likely a source. Looking back to the paradigm for protection against influenza infection in the first few months of life, it becomes clear why the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention has recommended Tdap vaccine for all mothers during each pregnancy.
The first goal is to prevent pertussis in the mother so that she will not transmit the infection to her newborn. The additional goal, and the rationale for vaccinating pregnant women during every pregnancy, is to optimize levels of anti-pertussis antibody in the mother, so that the transplacental endowment to the infant is as robust as possible.
Serologic studies have demonstrated that Tdap vaccine induces high anti-pertussis antibodies when administered during pregnancy, but that the half-life of those antibodies is brief. When Tdap is given during pregnancy, and the infant is born at or near term, the antibody transfer to the infant is expected to provide passive protection for several months. Maternal immunization during pregnancy thereby reduces the risk that the mother will develop pertussis and transmit it to her newborn, while at the same time allows a degree of passive immunoprotection to the infant during the most vulnerable period of life. Active immunization against pertussis in the infant begins between 6-8 weeks of age.
Another infection that is exceedingly common during the first several months of life is respiratory syncytial virus (RSV). RSV remains the most common reason for infant hospitalization in the United States and other developed countries. The source of the virus can be any other person with a mild or moderate respiratory tract infection as the virus is ubiquitous, and can re-infect individuals throughout their lifetime. The first infection, however, is the worst. It is estimated that between 3% and 4% of the U.S. birth cohort is hospitalized with RSV. With a U.S. birth cohort of about 4 million, the result is 120,000-160,000 infant admissions annually.
The RSV epidemic is seasonal, fairly predictable, and dreaded by primary care pediatricians and hospitalists alike. Lower respiratory tract infection with RSV, in the form of RSV bronchiolitis, presents all too commonly in the young infant with cough, coryza, tachypnea, and wheezing. When the work of breathing increases, and the cough symptoms predominate, the infant is unable to feed efficiently. Hospitalizations may be for dehydration, concerns for impending respiratory failure, or for the administration of supplemental oxygen or other respiratory support. No specific therapeutic interventions reliably reduce the symptoms or the length of hospital stay, nor do they reduce the possibility that intensive care with mechanical ventilation may be required. Treatments are only supportive. An effective vaccine remains elusive.
All other common infections that once resulted in high rates of hospitalization in the first year of life are now substantially reduced through vaccination. Why not this one? The development of a safe and effective vaccine to prevent infant RSV infection or to reduce RSV-associated hospitalizations is especially challenging for multiple reasons.
Some of these reasons have met with substantial advances quite recently, including the discovery of antigen structures needed to induce neutralizing antibody responses. There also are challenges specific to the infant group we need most to protect. Infant RSV infection itself confers only modest protection against subsequent infection. Repeated infections over time are necessary for protection against illness when re-exposed. A vaccine that is able to induce a response similar to natural infection would therefore require multiple doses, presumably over time (the so called ‘primary series’) before a substantial clinical benefit would be expected. This is particularly important because most RSV-associated hospitalizations occur during the first several months of life, reducing the timeline for which a protective vaccine series could be administered.
The challenges are parallel to the issues described earlier for protection against both influenza and pertussis. Infant protection against both of these infections are now addressed, at least to start with, by vaccinating the mother during her pregnancy. In the infant, the pertussis vaccine primary series is then initiated between 6 and 8 weeks of age, and the influenza series initiated at 6 months of age. It is the passive protection, in the form of transplacental maternal antibody, that offers the interim protection during the highest-risk first months of life.
For infants at very high risk of serious RSV infection, passive antibody protection is already administered in the form of the pharmacobiologic medication palivizumab. Its half-life dictates monthly injections for those eligible, and its cost precludes its use for any but the highest risk infants (those born prematurely, and those with chronic lung disease and/or congenital heart disease). This strategy, however, has proven effective in preventing RSV-associated hospitalization in every group in which it has been studied. This “proof of concept” strongly suggests that if the right RSV vaccine is given to women during pregnancy to induce a robust neutralizing anti-RSV antibody response, and that antibody is transferred to the fetus prior to birth, the newborn will benefit from protection against RSV for a period of time.
Several questions emerge. If RSV is ubiquitous, and can re-infect individuals throughout their lifetime, then some women will be infected during their pregnancy. Do their infants benefit? As a re-infection, the maternal symptoms would be expected to be mild, but the infection could boost the women’s natural immunity with a robust anamnestic antibody response. This possibility has not been studied systematically, but might help to explain why some healthy term infants exposed to RSV develop little or no symptoms, while others (mothers who have not recently had a natural RSV infection) develop severe illness requiring hospitalization.
There are data to support the contention that term infants born to mothers with higher naturally occurring anti-RSV neutralizing antibodies benefit from those antibodies. In a large prospective cohort study performed in Kenya, cord blood anti-RSV antibody concentrations correlated directly with the length of time before the infant’s first RSV infection. It’s therefore logical to conclude that administering an effective RSV vaccine during pregnancy could augment that natural antibody response, be transferred to the infant at birth, and offer protection against RSV when exposed.
Several candidate vaccines for study already exist and have undergone phase I testing in nonpregnant adults. Once safety is demonstrated, the next step is to identify the vaccine formulation resulting in the most robust anti-RSV neutralizing antibody concentrations. Such a candidate vaccine will be chosen for future phase III trials during pregnancy. Safety, and maternal/cord blood RSV antibody titers will be of interest during that clinical trial, but the rates and timing of RSV infection and RSV-associated hospitalizations among the infants born to those mothers will be the most instructive.
Ideally, a candidate RSV vaccine shown to be as safe and as effective during pregnancy as inactivated influenza vaccines and/or Tdap vaccines would be implemented immediately and universally. Unfortunately, substantial vaccine hesitancy for the use of influenza and Tdap vaccines continues among pregnant patients and their providers. Acceptance of an RSV vaccine for use during pregnancy will not come easily, or immediately. As with all of our successful vaccine programs, launching such an effort will require education, patience, and careful post-licensure documentation of the impact that the intervention has in the real world.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University, Syracuse, N.Y. Dr. Domachowske is performing clinical trials and has grants in the area of RSV prevention with Astra Zeneca, Regeneron, and Glaxo Smith Kline.
Pediatricians and our teams are the immunization experts. We educate, advocate, and incorporate vaccines into much of our daily routine. As such, we recognize the importance of working with our colleagues in family medicine, internal medicine, and obstetrics to optimize immunization programs for high-risk individuals, including pregnant women. Recent advances in vaccine recommendations during pregnancy are a result of the collaborative efforts of the health care providers for these women, and from systematic evaluation of immunization programs, vaccine pregnancy registries, and disease epidemiology.
Vaccinating women during pregnancy should be considered when a vaccine is known to be safe and when the following apply:
• The risk of severe infection is high during or augmented by pregnancy.
• The specific infection during pregnancy threatens the fetus.
• Maternal protection against infection benefits the newborn.
• Passive transfer of antibody from mother to fetus benefits the newborn.
Examples of safe vaccines immediately come to mind that fulfill one of more of these criteria, yet substantial obstacles exist even where safety and effectiveness data are robust. Because clinical vaccine trials traditionally exclude pregnant women, safety and effectiveness data for this group and their newborns are limited and often must come through experience. In a climate of increased vaccine hesitancy in general, both among providers and patients, vaccine delivery can be fragmented and particularly difficult to streamline. Additional obstacles that exist for any immunization program, including one that targets pregnant women specifically, are immunization delivery logistics and cost.
One of the major success stories of maternal immunization that is easily forgotten or overlooked in developed parts of the world is in the prevention of maternal and neonatal tetanus (MNT). A review of recent history reminds us that between the years 2000 and 2014, 35 countries were finally successful in eliminating MNT, including China, Turkey, Egypt, and South Africa. In addition, 24 of 36 states in the country of India, 30 of 34 provinces of Indonesia, and most of Ethiopia have met with success. This has been accomplished through aggressive tetanus vaccination programs, and through education programs targeted at optimal umbilical cord stump care after delivery.
In the United States, the Advisory Committee on Immunization Practices recommends that all pregnant women should receive inactivated influenza vaccine and Tdap vaccine. In addition, several other vaccines are recommended under certain circumstances. Live attenuated vaccines are considered contraindicated, although yellow fever vaccine is an exception during epidemics, or when travel to a highly endemic area during pregnancy cannot be avoided.
Influenza vaccine administered during pregnancy reduces maternal morbidity and mortality. Moreover, safety and benefits for the fetus are clearly documented. Both retrospective cohort analysis studies and randomized controlled trials have consistently demonstrated lower risk of preterm birth and lower risk for delivering newborns small for gestational age among women who received inactivated influenza vaccine during pregnancy. The benefit extends to term healthy infants who are less likely to be hospitalized during the first months of life if their mother was vaccinated against influenza during pregnancy. Because the mother was immunized during pregnancy, it reduces her risk of infection, thereby reducing the potential that the newborn will be exposed to a mother who is contagious. Perhaps more importantly, infants born at or near term have the benefit of transplacental antibody endowment from their mother, including vaccine induced anti-influenza antibodies. This passive protection is expected to last for several months. Active immunization against influenza during infancy begins at 6 months of age.
Tdap vaccine is also recommended during each pregnancy. In the United States, MNT is eliminated. Here, as in other developed countries, Tdap is administered to reduce infant pertussis morbidity. Pertussis remains endemic to the United States, and infants who develop whooping cough during the first 2-3 months of life are at the highest risk for morbidity and mortality.
Historically, one-third of infants infected with pertussis were infected by their mother, although more recent evidence suggests that older siblings are at least as likely a source. Looking back to the paradigm for protection against influenza infection in the first few months of life, it becomes clear why the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention has recommended Tdap vaccine for all mothers during each pregnancy.
The first goal is to prevent pertussis in the mother so that she will not transmit the infection to her newborn. The additional goal, and the rationale for vaccinating pregnant women during every pregnancy, is to optimize levels of anti-pertussis antibody in the mother, so that the transplacental endowment to the infant is as robust as possible.
Serologic studies have demonstrated that Tdap vaccine induces high anti-pertussis antibodies when administered during pregnancy, but that the half-life of those antibodies is brief. When Tdap is given during pregnancy, and the infant is born at or near term, the antibody transfer to the infant is expected to provide passive protection for several months. Maternal immunization during pregnancy thereby reduces the risk that the mother will develop pertussis and transmit it to her newborn, while at the same time allows a degree of passive immunoprotection to the infant during the most vulnerable period of life. Active immunization against pertussis in the infant begins between 6-8 weeks of age.
Another infection that is exceedingly common during the first several months of life is respiratory syncytial virus (RSV). RSV remains the most common reason for infant hospitalization in the United States and other developed countries. The source of the virus can be any other person with a mild or moderate respiratory tract infection as the virus is ubiquitous, and can re-infect individuals throughout their lifetime. The first infection, however, is the worst. It is estimated that between 3% and 4% of the U.S. birth cohort is hospitalized with RSV. With a U.S. birth cohort of about 4 million, the result is 120,000-160,000 infant admissions annually.
The RSV epidemic is seasonal, fairly predictable, and dreaded by primary care pediatricians and hospitalists alike. Lower respiratory tract infection with RSV, in the form of RSV bronchiolitis, presents all too commonly in the young infant with cough, coryza, tachypnea, and wheezing. When the work of breathing increases, and the cough symptoms predominate, the infant is unable to feed efficiently. Hospitalizations may be for dehydration, concerns for impending respiratory failure, or for the administration of supplemental oxygen or other respiratory support. No specific therapeutic interventions reliably reduce the symptoms or the length of hospital stay, nor do they reduce the possibility that intensive care with mechanical ventilation may be required. Treatments are only supportive. An effective vaccine remains elusive.
All other common infections that once resulted in high rates of hospitalization in the first year of life are now substantially reduced through vaccination. Why not this one? The development of a safe and effective vaccine to prevent infant RSV infection or to reduce RSV-associated hospitalizations is especially challenging for multiple reasons.
Some of these reasons have met with substantial advances quite recently, including the discovery of antigen structures needed to induce neutralizing antibody responses. There also are challenges specific to the infant group we need most to protect. Infant RSV infection itself confers only modest protection against subsequent infection. Repeated infections over time are necessary for protection against illness when re-exposed. A vaccine that is able to induce a response similar to natural infection would therefore require multiple doses, presumably over time (the so called ‘primary series’) before a substantial clinical benefit would be expected. This is particularly important because most RSV-associated hospitalizations occur during the first several months of life, reducing the timeline for which a protective vaccine series could be administered.
The challenges are parallel to the issues described earlier for protection against both influenza and pertussis. Infant protection against both of these infections are now addressed, at least to start with, by vaccinating the mother during her pregnancy. In the infant, the pertussis vaccine primary series is then initiated between 6 and 8 weeks of age, and the influenza series initiated at 6 months of age. It is the passive protection, in the form of transplacental maternal antibody, that offers the interim protection during the highest-risk first months of life.
For infants at very high risk of serious RSV infection, passive antibody protection is already administered in the form of the pharmacobiologic medication palivizumab. Its half-life dictates monthly injections for those eligible, and its cost precludes its use for any but the highest risk infants (those born prematurely, and those with chronic lung disease and/or congenital heart disease). This strategy, however, has proven effective in preventing RSV-associated hospitalization in every group in which it has been studied. This “proof of concept” strongly suggests that if the right RSV vaccine is given to women during pregnancy to induce a robust neutralizing anti-RSV antibody response, and that antibody is transferred to the fetus prior to birth, the newborn will benefit from protection against RSV for a period of time.
Several questions emerge. If RSV is ubiquitous, and can re-infect individuals throughout their lifetime, then some women will be infected during their pregnancy. Do their infants benefit? As a re-infection, the maternal symptoms would be expected to be mild, but the infection could boost the women’s natural immunity with a robust anamnestic antibody response. This possibility has not been studied systematically, but might help to explain why some healthy term infants exposed to RSV develop little or no symptoms, while others (mothers who have not recently had a natural RSV infection) develop severe illness requiring hospitalization.
There are data to support the contention that term infants born to mothers with higher naturally occurring anti-RSV neutralizing antibodies benefit from those antibodies. In a large prospective cohort study performed in Kenya, cord blood anti-RSV antibody concentrations correlated directly with the length of time before the infant’s first RSV infection. It’s therefore logical to conclude that administering an effective RSV vaccine during pregnancy could augment that natural antibody response, be transferred to the infant at birth, and offer protection against RSV when exposed.
Several candidate vaccines for study already exist and have undergone phase I testing in nonpregnant adults. Once safety is demonstrated, the next step is to identify the vaccine formulation resulting in the most robust anti-RSV neutralizing antibody concentrations. Such a candidate vaccine will be chosen for future phase III trials during pregnancy. Safety, and maternal/cord blood RSV antibody titers will be of interest during that clinical trial, but the rates and timing of RSV infection and RSV-associated hospitalizations among the infants born to those mothers will be the most instructive.
Ideally, a candidate RSV vaccine shown to be as safe and as effective during pregnancy as inactivated influenza vaccines and/or Tdap vaccines would be implemented immediately and universally. Unfortunately, substantial vaccine hesitancy for the use of influenza and Tdap vaccines continues among pregnant patients and their providers. Acceptance of an RSV vaccine for use during pregnancy will not come easily, or immediately. As with all of our successful vaccine programs, launching such an effort will require education, patience, and careful post-licensure documentation of the impact that the intervention has in the real world.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University, Syracuse, N.Y. Dr. Domachowske is performing clinical trials and has grants in the area of RSV prevention with Astra Zeneca, Regeneron, and Glaxo Smith Kline.
Why you need a new SVS tie or scarf
Congratulations! You noticed that Vascular Specialist has a new look. And with your well-honed powers of observation you also noticed the inauguration of the new logo for the Society for Vascular Surgery. However, you may be somewhat nonplussed. Because of the new logo you may have to buy a whole new wardrobe of SVS garments. I must admit I was confused as to the rationale behind changing the logo.
Surely it wasn’t because patients went elsewhere for treatment because they didn’t approve of the old one. I had never heard “Sorry Dr. Samson, I’m going to a cardiologist, I prefer the American College of Cardiology logo,” However, I now understand the reason behind this change is not so trivial. Rather, the new logo and Vascular Specialist’s appearance portends momentous changes in the aspirations and objectives of SVS and its publications.
Let me start with SVS. Long considered a staid, conservative organization geared mainly to promote academic and research achievements, it now fully embraces a commitment to the entire field of vascular surgery, its practitioners and patients. Under the leadership of current President Bruce Perler, the Executive Committee realized it is an imperative that government, health industries, and other medical specialists recognize the uniqueness of the spectrum of vascular surgeons’ services. Further, that this message is conveyed by SVS as our official mouthpiece.
You may ask how changing the logo conveys such a message. Simply put, the old logo does not work well with different color backgrounds and modern electronic media. It does not scale in updated websites, web browsers, or mobile apps. The new logo overcomes all these problems and by so doing confirms a change in direction for SVS. It acknowledges that our Society is part of the “Now” generation that understands the importance of all these new forms of communication. It affirms that branding and marketing the Society and its member vascular surgeons has become a priority.
Also, SVS recognized that this could only be achieved through an aggressive marketing campaign utilizing all that modern media has to offer. The first item on the Executive’s agenda was updating the SVS web site and for this a more workable logo was essential. The new website is in development and will debut soon. Concurrently, all aspects of branding will be revamped and the new logo will become omnipresent. It will now appear proudly on position papers, the JVS, SVS guidelines and all documents authored by the Society. I admit that to bolster this effort I have championed a complete name change to the American College of Vascular Surgery – but I have come to believe that this would be time consuming and entail so much cajoling that it would delay the SVS’s program. The website is a priority and our Society needs to move forward with its marketing campaign. The new logo is symbolic of the new SVS and it looks great!
The new design for Vascular Specialist begins as it enters its second decade as the official newspaper of SVS. Like SVS, our newspaper has also changed with the times. Although print has become very expensive, through the generosity of our many industry supporters, we have been able to expand the print editions to at least 20 pages every month and it is now mailed to over 5,000 members and affiliates worldwide.
A recent survey of SVS members confirmed that Vascular Specialist is the most widely read of all the vascular related periodicals. Importantly, Vascular Specialist also takes advantage of all the new methods of communication. It is now not only presented in print, but has an electronic presence with a website (www.vascularspecialistonline.com) and a mobile app containing many articles beyond those you will read in the print edition. We hope that vascular specialistonline.com will become your go to site for news and conversation related to all things vascular. One of my goals as Medical editor is to encourage you to not only be an avid reader, but also a contributor.
There are many ways you can help grow Vascular Specialist. Write a letter to the editor, contribute a Tips and Tricks, volunteer to write a Point/Counter Point column, submit an Opinion piece or simply respond to one of our online polls. Perhaps you wrote an article or made a presentation that you would like to reach a wider audience. You could send it to us and our reporters will convert it into newsworthy reports that can be printed or added to our online edition. Don’t fret over the chore of grammar and style; our writing staff will help make you seem like Shakespeare!
Of course patients did not avoid us because of our old logo and members read Vascular Specialist even though the font was old fashioned. However, these are important and exciting times and we want you to take part. We hope you will continue to read about your accomplishments and SVS achievements in print and electronic versions of Vascular Specialist. And yes, you may have to spring for a new SVS tie or scarf because the old ones are no longer current.
But, hopefully, the powers that be will recognize that a document or electronic media emblazoned with speaks authoritatively on behalf of vascular surgeons and our patients.
Dr. Samson is clinical professor of surgery (vascular) at Florida State University Medical School, is president of Mote Vascular Foundation, and an attending vascular surgeon, Sarasota (Fla.) Vascular Specialists.
Congratulations! You noticed that Vascular Specialist has a new look. And with your well-honed powers of observation you also noticed the inauguration of the new logo for the Society for Vascular Surgery. However, you may be somewhat nonplussed. Because of the new logo you may have to buy a whole new wardrobe of SVS garments. I must admit I was confused as to the rationale behind changing the logo.
Surely it wasn’t because patients went elsewhere for treatment because they didn’t approve of the old one. I had never heard “Sorry Dr. Samson, I’m going to a cardiologist, I prefer the American College of Cardiology logo,” However, I now understand the reason behind this change is not so trivial. Rather, the new logo and Vascular Specialist’s appearance portends momentous changes in the aspirations and objectives of SVS and its publications.
Let me start with SVS. Long considered a staid, conservative organization geared mainly to promote academic and research achievements, it now fully embraces a commitment to the entire field of vascular surgery, its practitioners and patients. Under the leadership of current President Bruce Perler, the Executive Committee realized it is an imperative that government, health industries, and other medical specialists recognize the uniqueness of the spectrum of vascular surgeons’ services. Further, that this message is conveyed by SVS as our official mouthpiece.
You may ask how changing the logo conveys such a message. Simply put, the old logo does not work well with different color backgrounds and modern electronic media. It does not scale in updated websites, web browsers, or mobile apps. The new logo overcomes all these problems and by so doing confirms a change in direction for SVS. It acknowledges that our Society is part of the “Now” generation that understands the importance of all these new forms of communication. It affirms that branding and marketing the Society and its member vascular surgeons has become a priority.
Also, SVS recognized that this could only be achieved through an aggressive marketing campaign utilizing all that modern media has to offer. The first item on the Executive’s agenda was updating the SVS web site and for this a more workable logo was essential. The new website is in development and will debut soon. Concurrently, all aspects of branding will be revamped and the new logo will become omnipresent. It will now appear proudly on position papers, the JVS, SVS guidelines and all documents authored by the Society. I admit that to bolster this effort I have championed a complete name change to the American College of Vascular Surgery – but I have come to believe that this would be time consuming and entail so much cajoling that it would delay the SVS’s program. The website is a priority and our Society needs to move forward with its marketing campaign. The new logo is symbolic of the new SVS and it looks great!
The new design for Vascular Specialist begins as it enters its second decade as the official newspaper of SVS. Like SVS, our newspaper has also changed with the times. Although print has become very expensive, through the generosity of our many industry supporters, we have been able to expand the print editions to at least 20 pages every month and it is now mailed to over 5,000 members and affiliates worldwide.
A recent survey of SVS members confirmed that Vascular Specialist is the most widely read of all the vascular related periodicals. Importantly, Vascular Specialist also takes advantage of all the new methods of communication. It is now not only presented in print, but has an electronic presence with a website (www.vascularspecialistonline.com) and a mobile app containing many articles beyond those you will read in the print edition. We hope that vascular specialistonline.com will become your go to site for news and conversation related to all things vascular. One of my goals as Medical editor is to encourage you to not only be an avid reader, but also a contributor.
There are many ways you can help grow Vascular Specialist. Write a letter to the editor, contribute a Tips and Tricks, volunteer to write a Point/Counter Point column, submit an Opinion piece or simply respond to one of our online polls. Perhaps you wrote an article or made a presentation that you would like to reach a wider audience. You could send it to us and our reporters will convert it into newsworthy reports that can be printed or added to our online edition. Don’t fret over the chore of grammar and style; our writing staff will help make you seem like Shakespeare!
Of course patients did not avoid us because of our old logo and members read Vascular Specialist even though the font was old fashioned. However, these are important and exciting times and we want you to take part. We hope you will continue to read about your accomplishments and SVS achievements in print and electronic versions of Vascular Specialist. And yes, you may have to spring for a new SVS tie or scarf because the old ones are no longer current.
But, hopefully, the powers that be will recognize that a document or electronic media emblazoned with speaks authoritatively on behalf of vascular surgeons and our patients.
Dr. Samson is clinical professor of surgery (vascular) at Florida State University Medical School, is president of Mote Vascular Foundation, and an attending vascular surgeon, Sarasota (Fla.) Vascular Specialists.
Congratulations! You noticed that Vascular Specialist has a new look. And with your well-honed powers of observation you also noticed the inauguration of the new logo for the Society for Vascular Surgery. However, you may be somewhat nonplussed. Because of the new logo you may have to buy a whole new wardrobe of SVS garments. I must admit I was confused as to the rationale behind changing the logo.
Surely it wasn’t because patients went elsewhere for treatment because they didn’t approve of the old one. I had never heard “Sorry Dr. Samson, I’m going to a cardiologist, I prefer the American College of Cardiology logo,” However, I now understand the reason behind this change is not so trivial. Rather, the new logo and Vascular Specialist’s appearance portends momentous changes in the aspirations and objectives of SVS and its publications.
Let me start with SVS. Long considered a staid, conservative organization geared mainly to promote academic and research achievements, it now fully embraces a commitment to the entire field of vascular surgery, its practitioners and patients. Under the leadership of current President Bruce Perler, the Executive Committee realized it is an imperative that government, health industries, and other medical specialists recognize the uniqueness of the spectrum of vascular surgeons’ services. Further, that this message is conveyed by SVS as our official mouthpiece.
You may ask how changing the logo conveys such a message. Simply put, the old logo does not work well with different color backgrounds and modern electronic media. It does not scale in updated websites, web browsers, or mobile apps. The new logo overcomes all these problems and by so doing confirms a change in direction for SVS. It acknowledges that our Society is part of the “Now” generation that understands the importance of all these new forms of communication. It affirms that branding and marketing the Society and its member vascular surgeons has become a priority.
Also, SVS recognized that this could only be achieved through an aggressive marketing campaign utilizing all that modern media has to offer. The first item on the Executive’s agenda was updating the SVS web site and for this a more workable logo was essential. The new website is in development and will debut soon. Concurrently, all aspects of branding will be revamped and the new logo will become omnipresent. It will now appear proudly on position papers, the JVS, SVS guidelines and all documents authored by the Society. I admit that to bolster this effort I have championed a complete name change to the American College of Vascular Surgery – but I have come to believe that this would be time consuming and entail so much cajoling that it would delay the SVS’s program. The website is a priority and our Society needs to move forward with its marketing campaign. The new logo is symbolic of the new SVS and it looks great!
The new design for Vascular Specialist begins as it enters its second decade as the official newspaper of SVS. Like SVS, our newspaper has also changed with the times. Although print has become very expensive, through the generosity of our many industry supporters, we have been able to expand the print editions to at least 20 pages every month and it is now mailed to over 5,000 members and affiliates worldwide.
A recent survey of SVS members confirmed that Vascular Specialist is the most widely read of all the vascular related periodicals. Importantly, Vascular Specialist also takes advantage of all the new methods of communication. It is now not only presented in print, but has an electronic presence with a website (www.vascularspecialistonline.com) and a mobile app containing many articles beyond those you will read in the print edition. We hope that vascular specialistonline.com will become your go to site for news and conversation related to all things vascular. One of my goals as Medical editor is to encourage you to not only be an avid reader, but also a contributor.
There are many ways you can help grow Vascular Specialist. Write a letter to the editor, contribute a Tips and Tricks, volunteer to write a Point/Counter Point column, submit an Opinion piece or simply respond to one of our online polls. Perhaps you wrote an article or made a presentation that you would like to reach a wider audience. You could send it to us and our reporters will convert it into newsworthy reports that can be printed or added to our online edition. Don’t fret over the chore of grammar and style; our writing staff will help make you seem like Shakespeare!
Of course patients did not avoid us because of our old logo and members read Vascular Specialist even though the font was old fashioned. However, these are important and exciting times and we want you to take part. We hope you will continue to read about your accomplishments and SVS achievements in print and electronic versions of Vascular Specialist. And yes, you may have to spring for a new SVS tie or scarf because the old ones are no longer current.
But, hopefully, the powers that be will recognize that a document or electronic media emblazoned with speaks authoritatively on behalf of vascular surgeons and our patients.
Dr. Samson is clinical professor of surgery (vascular) at Florida State University Medical School, is president of Mote Vascular Foundation, and an attending vascular surgeon, Sarasota (Fla.) Vascular Specialists.