User login
A dermatologist’s bad dream?
My plane doesn’t leave till 2:30. Glad I cut off seeing patients at 11, which should give me plenty of time. I’m getting smarter in my old age.
Smooth morning, paperwork pretty much done. Just one patient left. Look, a nice little old man. He has such a sweet smile.
“How can I help you, Mr. Goldfarb?”
“It’s complicated. This letter explains everything that’s happened the past 3 years,”
Oh-oh, that doesn’t sound good. “OK, let’s have a look.”
“My, you read fast, Doctor.”
When the first line says, ‘The lice all over my body don’t go away even after I apply bug shampoo every day,’ I’m pretty much done.
“Doctor, this bag has everything I’ve used: lice shampoo, insect spray, itch lotion. I forgot to bring in all the little bugs I collected from my combs and sheets.”
No! This can’t be happening! How do I negotiate with a delusion and still make my plane?
“Sometimes it feels like bugs are crawling on my skin.”
“Itching often feels that way ... ”
“I brought pictures. Want to see?”
No! Not an album! Snap after snap: scabs on the scalp, scaling at the corners of the mouth, linear scratches on the extremities.
“You know, Mr. Goldfarb – maybe firm confidence will let me regain control of this interview – what you’re describing does not sound like lice or bugs of any kind ... ”
“But Doctor, how do you explain this?” Another photo, this of a comb filled with brownish epidermal fragments. “I meant to bring some in, but I forgot.”
Enough. Time to look grim and speak briskly. “Mr. Goldfarb, this cannot be lice because ... ”
“I see them coming out of all my pores ... ”
“Mr. Goldfarb!” Now it’s my turn to interrupt. “I would appreciate it if you would let me finish my sentence.”
“Yes, Doctor. If it’s not lice, what do you think it is?”
Must think fast. “Sensitivity. Sensitive skin, especially if you’ve scratched it, can certainly feel as though there are things crawling on you. Patients often say that the skin feels this way. I will therefore treat this sensitivity with anti-inflammatory creams and lotion you will apply to the scalp, face, and the rest of your body respectively.”
Goldfarb is still listening. I’m almost there.
“I want you to use this medication for 2 weeks without stopping, and not use any more of the bug shampoos and creams because they can be irritating and increase itch and sensitivity. Please call me on my private extension at that point with your progress.” Easier to deny a delusion when not standing face to face.
“That’s good news, Doctor. I’ll pick up the medication and let you know.”
At most, he’ll stop scratching for a while. By the time he starts again, I’ll have made my plane and come back to the office. Meantime: Depart exam room briskly!
I can still make it if I leave right away. One last check of my office e-mail. There’s one from Zelda. She has a small scaly patch on one forearm. Claims it’s responded neither to topical antifungals nor steroids.
Here’s the text of her e-mail: “Doctor, I showed my rash to my neighbor Mary. She did some Internet research, and she’s convinced it’s chromoblastomycosis. I’m pretty sure she’s right. What do you think?”
I think I better leave right now.
My reply: “Dear Zelda, pretty unlikely. Try the new cream I’m going to prescribe for 2 weeks, and let me check on how you’re doing.”
How does evil dermatologic karma know that I’m trying to leave town? Parasitosis and chromoblastomycosis! Can this be a bad dream? If so, why don’t I wake up?
Mr. Goldfarb, still looking sweet and mild, sits in the waiting room, awaiting the elder shuttle to take him home.
Walk fast. Do not smile and meet his gaze. This is no time for politeness.
No, sir. I am outta here.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Write to him at [email protected].
My plane doesn’t leave till 2:30. Glad I cut off seeing patients at 11, which should give me plenty of time. I’m getting smarter in my old age.
Smooth morning, paperwork pretty much done. Just one patient left. Look, a nice little old man. He has such a sweet smile.
“How can I help you, Mr. Goldfarb?”
“It’s complicated. This letter explains everything that’s happened the past 3 years,”
Oh-oh, that doesn’t sound good. “OK, let’s have a look.”
“My, you read fast, Doctor.”
When the first line says, ‘The lice all over my body don’t go away even after I apply bug shampoo every day,’ I’m pretty much done.
“Doctor, this bag has everything I’ve used: lice shampoo, insect spray, itch lotion. I forgot to bring in all the little bugs I collected from my combs and sheets.”
No! This can’t be happening! How do I negotiate with a delusion and still make my plane?
“Sometimes it feels like bugs are crawling on my skin.”
“Itching often feels that way ... ”
“I brought pictures. Want to see?”
No! Not an album! Snap after snap: scabs on the scalp, scaling at the corners of the mouth, linear scratches on the extremities.
“You know, Mr. Goldfarb – maybe firm confidence will let me regain control of this interview – what you’re describing does not sound like lice or bugs of any kind ... ”
“But Doctor, how do you explain this?” Another photo, this of a comb filled with brownish epidermal fragments. “I meant to bring some in, but I forgot.”
Enough. Time to look grim and speak briskly. “Mr. Goldfarb, this cannot be lice because ... ”
“I see them coming out of all my pores ... ”
“Mr. Goldfarb!” Now it’s my turn to interrupt. “I would appreciate it if you would let me finish my sentence.”
“Yes, Doctor. If it’s not lice, what do you think it is?”
Must think fast. “Sensitivity. Sensitive skin, especially if you’ve scratched it, can certainly feel as though there are things crawling on you. Patients often say that the skin feels this way. I will therefore treat this sensitivity with anti-inflammatory creams and lotion you will apply to the scalp, face, and the rest of your body respectively.”
Goldfarb is still listening. I’m almost there.
“I want you to use this medication for 2 weeks without stopping, and not use any more of the bug shampoos and creams because they can be irritating and increase itch and sensitivity. Please call me on my private extension at that point with your progress.” Easier to deny a delusion when not standing face to face.
“That’s good news, Doctor. I’ll pick up the medication and let you know.”
At most, he’ll stop scratching for a while. By the time he starts again, I’ll have made my plane and come back to the office. Meantime: Depart exam room briskly!
I can still make it if I leave right away. One last check of my office e-mail. There’s one from Zelda. She has a small scaly patch on one forearm. Claims it’s responded neither to topical antifungals nor steroids.
Here’s the text of her e-mail: “Doctor, I showed my rash to my neighbor Mary. She did some Internet research, and she’s convinced it’s chromoblastomycosis. I’m pretty sure she’s right. What do you think?”
I think I better leave right now.
My reply: “Dear Zelda, pretty unlikely. Try the new cream I’m going to prescribe for 2 weeks, and let me check on how you’re doing.”
How does evil dermatologic karma know that I’m trying to leave town? Parasitosis and chromoblastomycosis! Can this be a bad dream? If so, why don’t I wake up?
Mr. Goldfarb, still looking sweet and mild, sits in the waiting room, awaiting the elder shuttle to take him home.
Walk fast. Do not smile and meet his gaze. This is no time for politeness.
No, sir. I am outta here.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Write to him at [email protected].
My plane doesn’t leave till 2:30. Glad I cut off seeing patients at 11, which should give me plenty of time. I’m getting smarter in my old age.
Smooth morning, paperwork pretty much done. Just one patient left. Look, a nice little old man. He has such a sweet smile.
“How can I help you, Mr. Goldfarb?”
“It’s complicated. This letter explains everything that’s happened the past 3 years,”
Oh-oh, that doesn’t sound good. “OK, let’s have a look.”
“My, you read fast, Doctor.”
When the first line says, ‘The lice all over my body don’t go away even after I apply bug shampoo every day,’ I’m pretty much done.
“Doctor, this bag has everything I’ve used: lice shampoo, insect spray, itch lotion. I forgot to bring in all the little bugs I collected from my combs and sheets.”
No! This can’t be happening! How do I negotiate with a delusion and still make my plane?
“Sometimes it feels like bugs are crawling on my skin.”
“Itching often feels that way ... ”
“I brought pictures. Want to see?”
No! Not an album! Snap after snap: scabs on the scalp, scaling at the corners of the mouth, linear scratches on the extremities.
“You know, Mr. Goldfarb – maybe firm confidence will let me regain control of this interview – what you’re describing does not sound like lice or bugs of any kind ... ”
“But Doctor, how do you explain this?” Another photo, this of a comb filled with brownish epidermal fragments. “I meant to bring some in, but I forgot.”
Enough. Time to look grim and speak briskly. “Mr. Goldfarb, this cannot be lice because ... ”
“I see them coming out of all my pores ... ”
“Mr. Goldfarb!” Now it’s my turn to interrupt. “I would appreciate it if you would let me finish my sentence.”
“Yes, Doctor. If it’s not lice, what do you think it is?”
Must think fast. “Sensitivity. Sensitive skin, especially if you’ve scratched it, can certainly feel as though there are things crawling on you. Patients often say that the skin feels this way. I will therefore treat this sensitivity with anti-inflammatory creams and lotion you will apply to the scalp, face, and the rest of your body respectively.”
Goldfarb is still listening. I’m almost there.
“I want you to use this medication for 2 weeks without stopping, and not use any more of the bug shampoos and creams because they can be irritating and increase itch and sensitivity. Please call me on my private extension at that point with your progress.” Easier to deny a delusion when not standing face to face.
“That’s good news, Doctor. I’ll pick up the medication and let you know.”
At most, he’ll stop scratching for a while. By the time he starts again, I’ll have made my plane and come back to the office. Meantime: Depart exam room briskly!
I can still make it if I leave right away. One last check of my office e-mail. There’s one from Zelda. She has a small scaly patch on one forearm. Claims it’s responded neither to topical antifungals nor steroids.
Here’s the text of her e-mail: “Doctor, I showed my rash to my neighbor Mary. She did some Internet research, and she’s convinced it’s chromoblastomycosis. I’m pretty sure she’s right. What do you think?”
I think I better leave right now.
My reply: “Dear Zelda, pretty unlikely. Try the new cream I’m going to prescribe for 2 weeks, and let me check on how you’re doing.”
How does evil dermatologic karma know that I’m trying to leave town? Parasitosis and chromoblastomycosis! Can this be a bad dream? If so, why don’t I wake up?
Mr. Goldfarb, still looking sweet and mild, sits in the waiting room, awaiting the elder shuttle to take him home.
Walk fast. Do not smile and meet his gaze. This is no time for politeness.
No, sir. I am outta here.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Write to him at [email protected].
Caring for gender-nonconforming youth in a primary care setting – Part 2
Gender identity typically develops in early childhood, and by age 4 years, most children consistently refer to themselves as a girl or a boy.1 For the majority of children, natal sex or sex assigned at birth, aligns with gender identity (a person’s innate sense of feeling male, female, or somewhere in between). However, this is not always the case. Gender identity can be understood as a spectrum with youth identifying as a gender that aligns with their natal sex (cisgender), is opposite of their natal sex (transgender), no gender (agender), or somewhere in between (genderqueer). The distress that can result from an incongruence between natal sex and gender identity is called gender dysphoria. Youth with gender dysphoria are at increased risk for a number of conditions, including suicide and self-harm. Early identification and appropriate care of these youth can reduce these risks. This month’s column will briefly review assessment of these youth in the pediatric setting.
Many youth who have a gender-nonconforming identity in childhood will not go on to have one in adulthood.2,3 Those who have a consistent, insistent, and persistent nonconforming identity are more likely to have this identity persist into adulthood. Youth who experience increased gender dysphoria with the onset of puberty rarely have this subside.
As it can be difficult to predict the trajectory of gender identity from childhood to adolescence, the approach to the prepubertal and pubertal gender nonconforming patient is different. It is important to note that research suggests that gender identity is innate and cannot be changed with interventions. The goals of care for gender-nonconforming (GN) youth include providing a safe environment where youth can explore their identities, and individualizing treatment to meet the needs of each patient and family.
Care for prepubertal GN youth
For parents:
Have you noticed, or are you concerned about your child’s:
• Preference or rejection of particular toys/games?
• Hair and clothing preferences or rejections?
• Preferred (if any) gender of playmates?
Has your child ever expressed:
• A desire to be or insistence that they are the other gender?
• A dislike of their sexual anatomy?
• A desire for primary (penis, vagina) or secondary (periods, facial hair) sex characteristics of the other gender?
Are you concerned about bullying ?
Do you have any concerns about your child’s mood or concerns for self-harm?
For children:
• Do you feel more like a girl, boy, neither, both?
• How would you like to play, cut your hair, dress?
• What name or pronoun (she for girl, he for boy) fits you?4
The goal for prepubertal youth with nonconforming identities is to ensure that they are safe at home, school, and at play. Some youth may express a desire to “transition” or live as their identified gender by changing their name and dressing as their identified gender. Some youth and families may choose to transition only in certain settings (at home, but not at school). Some youth and families may want a safe space where the child can grow, develop, and continue to explore their identity without transitioning. Mental health providers trained in the care of GN youth can help patients and families decide if transition is appropriate for them and support them with the process and timing of transitioning. For youth who experience depression, anxiety, bullying, or thoughts of self-harm related to their gender identity, care by an experienced mental health provider is essential. It is important to recognize that each patient and family will need an individualized approach based on their needs.
Care for pubertal GN youth
The development of secondary sex characteristics can be particularly distressing for GN youth. Some youth may first experience gender dysphoria at this time. This distress combined with the psychosocial stressors of adolescent development can lead to depression, anxiety, suicidal ideation, self-harm, and other risk taking behaviors. Visits with pubertal GN youth, as with any adolescent, should include confidential time alone with the medical provider to discuss any concerns. Youth should be informed that information will be kept confidential, but parents will need to be notified of any safety concerns (such as suicidality or self-harm). As with prepubertal youth, a history related to hair and clothing preferences; distress related to genital anatomy; and the desire to be the other gender should be obtained. A pubertal history and any related symptoms of distress also should be obtained.
DO
• Ask preferred name and pronoun.
• Perform confidential strength and risk assessment.
• Assess for family and social support.
• Refer to appropriate mental health and transgender providers.
DON’T
• Assume names and pronouns.
• Interview patient only with parent in the room.
• Disclose identity without patient consent.
• Dismiss parents as sources of support.
• Refer for reparative therapy.4
Youth who are suspected to have a diagnosis of gender dysphoria should be referred to mental health and medical providers with experience caring for transgender youth. These specialists can work with patients and families, and determine when and if youth are eligible for puberty blocking therapy with GnRH analogues and/or hormone therapy. GnRH analogues, if appropriate, can be prescribed after patients have reached sexual maturity rating stage 2. The rationale for this treatment is to prevent the development of unwanted secondary sex characteristics while giving the youth a chance to continue with psychotherapy and explore their gender identity.5 Hormone therapy, if appropriate, can be prescribed a few years later under the care of a transgender specialist and mental health provider.
Summary
It is normal to experiment with gender roles and expression in childhood. Providing a safe space to do this is important.
Individuals who have a persistent, consistent, and insistent gender-nonconforming identification and who have increased distress with puberty are unlikely to have this subside.
Pediatricians can assess for gender dysphoria and screen for related mood disorders and behaviors in the primary care setting. Appropriate referral to trained professionals is important.
Care should be individualized and focused on the health and safety of the patient.
Resources
For health care professionals
• World Professional Association for Transgender Health: Standards of care on care of transgender patients and provider directory. www.wpath.org• Physicians for Reproductive Health’s adolescent reproductive and sexual health education program (ARSHEP): Best practices for adolescent and reproductive health: Module on caring for transgender adolescent patients. prh.org/teen-reproductive-health/arshep-downloads/
For patients and families
• Family Acceptance Project: familyproject.sfsu.edu/
• Healthychildren.org: Parenting website supported by the American Academy of Pediatrics. Links to articles on gender nonconforming and transgender children; gender identity development in children. www.healthychildren.org
References
1. Caring for Your School Age Child: Ages 5-12 by the American Academy of Pediatrics (New York: Bantam Books, 1995).
2. Dev Psychol. 2008 Jan;44(1):34-45.
3. J Am Acad Child and Adolesc Psychiatry. 2008;47(12):1413-23
4. Caring for Transgender Adolescent Patients. Physicians for Reproductive Health’s Adolescent Reproductive and Sexual Health Education Program (ARSHEP): Best practices for adolescent and reproductive health: prh.org/teen-reproductive-health/arshep-downloads/
5. World Professional Association of Transgender Health, Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, 7th Edition (International Journal of Transgenderism. 2011;13:165-232)
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus.
Gender identity typically develops in early childhood, and by age 4 years, most children consistently refer to themselves as a girl or a boy.1 For the majority of children, natal sex or sex assigned at birth, aligns with gender identity (a person’s innate sense of feeling male, female, or somewhere in between). However, this is not always the case. Gender identity can be understood as a spectrum with youth identifying as a gender that aligns with their natal sex (cisgender), is opposite of their natal sex (transgender), no gender (agender), or somewhere in between (genderqueer). The distress that can result from an incongruence between natal sex and gender identity is called gender dysphoria. Youth with gender dysphoria are at increased risk for a number of conditions, including suicide and self-harm. Early identification and appropriate care of these youth can reduce these risks. This month’s column will briefly review assessment of these youth in the pediatric setting.
Many youth who have a gender-nonconforming identity in childhood will not go on to have one in adulthood.2,3 Those who have a consistent, insistent, and persistent nonconforming identity are more likely to have this identity persist into adulthood. Youth who experience increased gender dysphoria with the onset of puberty rarely have this subside.
As it can be difficult to predict the trajectory of gender identity from childhood to adolescence, the approach to the prepubertal and pubertal gender nonconforming patient is different. It is important to note that research suggests that gender identity is innate and cannot be changed with interventions. The goals of care for gender-nonconforming (GN) youth include providing a safe environment where youth can explore their identities, and individualizing treatment to meet the needs of each patient and family.
Care for prepubertal GN youth
For parents:
Have you noticed, or are you concerned about your child’s:
• Preference or rejection of particular toys/games?
• Hair and clothing preferences or rejections?
• Preferred (if any) gender of playmates?
Has your child ever expressed:
• A desire to be or insistence that they are the other gender?
• A dislike of their sexual anatomy?
• A desire for primary (penis, vagina) or secondary (periods, facial hair) sex characteristics of the other gender?
Are you concerned about bullying ?
Do you have any concerns about your child’s mood or concerns for self-harm?
For children:
• Do you feel more like a girl, boy, neither, both?
• How would you like to play, cut your hair, dress?
• What name or pronoun (she for girl, he for boy) fits you?4
The goal for prepubertal youth with nonconforming identities is to ensure that they are safe at home, school, and at play. Some youth may express a desire to “transition” or live as their identified gender by changing their name and dressing as their identified gender. Some youth and families may choose to transition only in certain settings (at home, but not at school). Some youth and families may want a safe space where the child can grow, develop, and continue to explore their identity without transitioning. Mental health providers trained in the care of GN youth can help patients and families decide if transition is appropriate for them and support them with the process and timing of transitioning. For youth who experience depression, anxiety, bullying, or thoughts of self-harm related to their gender identity, care by an experienced mental health provider is essential. It is important to recognize that each patient and family will need an individualized approach based on their needs.
Care for pubertal GN youth
The development of secondary sex characteristics can be particularly distressing for GN youth. Some youth may first experience gender dysphoria at this time. This distress combined with the psychosocial stressors of adolescent development can lead to depression, anxiety, suicidal ideation, self-harm, and other risk taking behaviors. Visits with pubertal GN youth, as with any adolescent, should include confidential time alone with the medical provider to discuss any concerns. Youth should be informed that information will be kept confidential, but parents will need to be notified of any safety concerns (such as suicidality or self-harm). As with prepubertal youth, a history related to hair and clothing preferences; distress related to genital anatomy; and the desire to be the other gender should be obtained. A pubertal history and any related symptoms of distress also should be obtained.
DO
• Ask preferred name and pronoun.
• Perform confidential strength and risk assessment.
• Assess for family and social support.
• Refer to appropriate mental health and transgender providers.
DON’T
• Assume names and pronouns.
• Interview patient only with parent in the room.
• Disclose identity without patient consent.
• Dismiss parents as sources of support.
• Refer for reparative therapy.4
Youth who are suspected to have a diagnosis of gender dysphoria should be referred to mental health and medical providers with experience caring for transgender youth. These specialists can work with patients and families, and determine when and if youth are eligible for puberty blocking therapy with GnRH analogues and/or hormone therapy. GnRH analogues, if appropriate, can be prescribed after patients have reached sexual maturity rating stage 2. The rationale for this treatment is to prevent the development of unwanted secondary sex characteristics while giving the youth a chance to continue with psychotherapy and explore their gender identity.5 Hormone therapy, if appropriate, can be prescribed a few years later under the care of a transgender specialist and mental health provider.
Summary
It is normal to experiment with gender roles and expression in childhood. Providing a safe space to do this is important.
Individuals who have a persistent, consistent, and insistent gender-nonconforming identification and who have increased distress with puberty are unlikely to have this subside.
Pediatricians can assess for gender dysphoria and screen for related mood disorders and behaviors in the primary care setting. Appropriate referral to trained professionals is important.
Care should be individualized and focused on the health and safety of the patient.
Resources
For health care professionals
• World Professional Association for Transgender Health: Standards of care on care of transgender patients and provider directory. www.wpath.org• Physicians for Reproductive Health’s adolescent reproductive and sexual health education program (ARSHEP): Best practices for adolescent and reproductive health: Module on caring for transgender adolescent patients. prh.org/teen-reproductive-health/arshep-downloads/
For patients and families
• Family Acceptance Project: familyproject.sfsu.edu/
• Healthychildren.org: Parenting website supported by the American Academy of Pediatrics. Links to articles on gender nonconforming and transgender children; gender identity development in children. www.healthychildren.org
References
1. Caring for Your School Age Child: Ages 5-12 by the American Academy of Pediatrics (New York: Bantam Books, 1995).
2. Dev Psychol. 2008 Jan;44(1):34-45.
3. J Am Acad Child and Adolesc Psychiatry. 2008;47(12):1413-23
4. Caring for Transgender Adolescent Patients. Physicians for Reproductive Health’s Adolescent Reproductive and Sexual Health Education Program (ARSHEP): Best practices for adolescent and reproductive health: prh.org/teen-reproductive-health/arshep-downloads/
5. World Professional Association of Transgender Health, Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, 7th Edition (International Journal of Transgenderism. 2011;13:165-232)
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus.
Gender identity typically develops in early childhood, and by age 4 years, most children consistently refer to themselves as a girl or a boy.1 For the majority of children, natal sex or sex assigned at birth, aligns with gender identity (a person’s innate sense of feeling male, female, or somewhere in between). However, this is not always the case. Gender identity can be understood as a spectrum with youth identifying as a gender that aligns with their natal sex (cisgender), is opposite of their natal sex (transgender), no gender (agender), or somewhere in between (genderqueer). The distress that can result from an incongruence between natal sex and gender identity is called gender dysphoria. Youth with gender dysphoria are at increased risk for a number of conditions, including suicide and self-harm. Early identification and appropriate care of these youth can reduce these risks. This month’s column will briefly review assessment of these youth in the pediatric setting.
Many youth who have a gender-nonconforming identity in childhood will not go on to have one in adulthood.2,3 Those who have a consistent, insistent, and persistent nonconforming identity are more likely to have this identity persist into adulthood. Youth who experience increased gender dysphoria with the onset of puberty rarely have this subside.
As it can be difficult to predict the trajectory of gender identity from childhood to adolescence, the approach to the prepubertal and pubertal gender nonconforming patient is different. It is important to note that research suggests that gender identity is innate and cannot be changed with interventions. The goals of care for gender-nonconforming (GN) youth include providing a safe environment where youth can explore their identities, and individualizing treatment to meet the needs of each patient and family.
Care for prepubertal GN youth
For parents:
Have you noticed, or are you concerned about your child’s:
• Preference or rejection of particular toys/games?
• Hair and clothing preferences or rejections?
• Preferred (if any) gender of playmates?
Has your child ever expressed:
• A desire to be or insistence that they are the other gender?
• A dislike of their sexual anatomy?
• A desire for primary (penis, vagina) or secondary (periods, facial hair) sex characteristics of the other gender?
Are you concerned about bullying ?
Do you have any concerns about your child’s mood or concerns for self-harm?
For children:
• Do you feel more like a girl, boy, neither, both?
• How would you like to play, cut your hair, dress?
• What name or pronoun (she for girl, he for boy) fits you?4
The goal for prepubertal youth with nonconforming identities is to ensure that they are safe at home, school, and at play. Some youth may express a desire to “transition” or live as their identified gender by changing their name and dressing as their identified gender. Some youth and families may choose to transition only in certain settings (at home, but not at school). Some youth and families may want a safe space where the child can grow, develop, and continue to explore their identity without transitioning. Mental health providers trained in the care of GN youth can help patients and families decide if transition is appropriate for them and support them with the process and timing of transitioning. For youth who experience depression, anxiety, bullying, or thoughts of self-harm related to their gender identity, care by an experienced mental health provider is essential. It is important to recognize that each patient and family will need an individualized approach based on their needs.
Care for pubertal GN youth
The development of secondary sex characteristics can be particularly distressing for GN youth. Some youth may first experience gender dysphoria at this time. This distress combined with the psychosocial stressors of adolescent development can lead to depression, anxiety, suicidal ideation, self-harm, and other risk taking behaviors. Visits with pubertal GN youth, as with any adolescent, should include confidential time alone with the medical provider to discuss any concerns. Youth should be informed that information will be kept confidential, but parents will need to be notified of any safety concerns (such as suicidality or self-harm). As with prepubertal youth, a history related to hair and clothing preferences; distress related to genital anatomy; and the desire to be the other gender should be obtained. A pubertal history and any related symptoms of distress also should be obtained.
DO
• Ask preferred name and pronoun.
• Perform confidential strength and risk assessment.
• Assess for family and social support.
• Refer to appropriate mental health and transgender providers.
DON’T
• Assume names and pronouns.
• Interview patient only with parent in the room.
• Disclose identity without patient consent.
• Dismiss parents as sources of support.
• Refer for reparative therapy.4
Youth who are suspected to have a diagnosis of gender dysphoria should be referred to mental health and medical providers with experience caring for transgender youth. These specialists can work with patients and families, and determine when and if youth are eligible for puberty blocking therapy with GnRH analogues and/or hormone therapy. GnRH analogues, if appropriate, can be prescribed after patients have reached sexual maturity rating stage 2. The rationale for this treatment is to prevent the development of unwanted secondary sex characteristics while giving the youth a chance to continue with psychotherapy and explore their gender identity.5 Hormone therapy, if appropriate, can be prescribed a few years later under the care of a transgender specialist and mental health provider.
Summary
It is normal to experiment with gender roles and expression in childhood. Providing a safe space to do this is important.
Individuals who have a persistent, consistent, and insistent gender-nonconforming identification and who have increased distress with puberty are unlikely to have this subside.
Pediatricians can assess for gender dysphoria and screen for related mood disorders and behaviors in the primary care setting. Appropriate referral to trained professionals is important.
Care should be individualized and focused on the health and safety of the patient.
Resources
For health care professionals
• World Professional Association for Transgender Health: Standards of care on care of transgender patients and provider directory. www.wpath.org• Physicians for Reproductive Health’s adolescent reproductive and sexual health education program (ARSHEP): Best practices for adolescent and reproductive health: Module on caring for transgender adolescent patients. prh.org/teen-reproductive-health/arshep-downloads/
For patients and families
• Family Acceptance Project: familyproject.sfsu.edu/
• Healthychildren.org: Parenting website supported by the American Academy of Pediatrics. Links to articles on gender nonconforming and transgender children; gender identity development in children. www.healthychildren.org
References
1. Caring for Your School Age Child: Ages 5-12 by the American Academy of Pediatrics (New York: Bantam Books, 1995).
2. Dev Psychol. 2008 Jan;44(1):34-45.
3. J Am Acad Child and Adolesc Psychiatry. 2008;47(12):1413-23
4. Caring for Transgender Adolescent Patients. Physicians for Reproductive Health’s Adolescent Reproductive and Sexual Health Education Program (ARSHEP): Best practices for adolescent and reproductive health: prh.org/teen-reproductive-health/arshep-downloads/
5. World Professional Association of Transgender Health, Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, 7th Edition (International Journal of Transgenderism. 2011;13:165-232)
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus.
Examining the medical needs of military women
A supplement recently published in Military Medicine seeks to examine how the Defense Department meets the medical needs of its women warriors. Called “Combat: Framing the Issues of Health and Health Research for America’s Servicewomen,” the articles go a long way toward shining a light on an important issue.
Several of the articles in the supplement highlight mental health issues for women in the military. They include the pieces about sexual harassment, the many faces of military families, alcohol use, and the corrosive effects of ostracism.
One of the articles by Kate McGraw, Ph.D., of the Deployment Health Clinical Center, Silver Spring, Md., focuses on the mental well-being of servicewomen and sexual trauma. Underlying the supplement is the recognition that the most robust mental health research repeatedly conducted in Afghanistan, for example, did not include a single woman because of the sampling methodology. A dedicated group addressing service women’s health and inclusion in health research would have prevented this oversight.
The health of female service members has long been an interest of mine, partly because I was in the Army for 28 years and deployed to a lot of austere environments. They included the rice fields of Camp Edwards, near the DMZ in Korea; Mogadishu and other “cities” in Somalia; and various Forward Operating Bases in Iraq.
Many years ago, I published an article on health concerns of deployed women. That focused on concerns about how to avoid urinary tract infections (UTIs) while in the field – where bathrooms are often scarce and dirty – and other seemingly mundane issues.
Mundane unless you have a UTI, or are trying to figure out how to manage your menses with no tampons or places to wash your hands.
Since then the literature has grown. For example, I published a volume called “Women at War” (Oxford University Press, 2015) last spring. This recent supplement advances those discussions, including articles on avoiding anemia and stress fractures.
But the way forward has been spotty. Many political issues delay an open discussion, especially on reproductive concerns. Further, there is no driving function within the Department of Defense that focuses on funding research in support of service women and reporting back to the department and civilian leadership.
For example: Female service members have a rate of unintended pregnancy twice that of the civilian world. This leads to early attrition from the military, and in turn, to young female veterans with children who are homeless.
Some have said, highlighting these concerns, that females should not be in the military because our presence is a risk to operational readiness. However, this is not an issue without tested solutions.
Taking this one issue further, consider that all service women are included in the Military Health System and have access to a variety of forms of birth control. If female service members can be put on oral contraceptives, that would both suppress their menses and avoid unwanted pregnancies. However, longer lasting methods of birth control would enable service women to enjoy decreased menses, avoid unwanted pregnancies, and avoid access issues during deployment.
The supplement contains numerous health policy and research recommendations as well as a detailed look at the unique health and lifestyle challenges of service women. Other issues include: the reproductive health of women in austere environments, nutritional factors, avoiding musculoskeletal injuries, combat-related injuries, designing military equipment (including uniforms) for optimal performance, and the role of leadership. It concludes with 20 research gaps and accompanying recommendations.
The number of women serving in the military is increasing, while all jobs, particularly those in the ground combat element, are now open to women. The time is now to focus on establishing and tracking health and well-being issues to ensure the success of this population – and the Military Medicine special issue is just a first step.
Dr. Ritchie serves as professor of psychiatry at the Uniformed Services University of the Health Services in Bethesda, Md., and at Georgetown University in Washington. She helped write one of the articles in the supplement with Dr. McGraw and Tracey Perez Koehlmoos, Ph.D., an associate professor with the Uniformed Services University.
A supplement recently published in Military Medicine seeks to examine how the Defense Department meets the medical needs of its women warriors. Called “Combat: Framing the Issues of Health and Health Research for America’s Servicewomen,” the articles go a long way toward shining a light on an important issue.
Several of the articles in the supplement highlight mental health issues for women in the military. They include the pieces about sexual harassment, the many faces of military families, alcohol use, and the corrosive effects of ostracism.
One of the articles by Kate McGraw, Ph.D., of the Deployment Health Clinical Center, Silver Spring, Md., focuses on the mental well-being of servicewomen and sexual trauma. Underlying the supplement is the recognition that the most robust mental health research repeatedly conducted in Afghanistan, for example, did not include a single woman because of the sampling methodology. A dedicated group addressing service women’s health and inclusion in health research would have prevented this oversight.
The health of female service members has long been an interest of mine, partly because I was in the Army for 28 years and deployed to a lot of austere environments. They included the rice fields of Camp Edwards, near the DMZ in Korea; Mogadishu and other “cities” in Somalia; and various Forward Operating Bases in Iraq.
Many years ago, I published an article on health concerns of deployed women. That focused on concerns about how to avoid urinary tract infections (UTIs) while in the field – where bathrooms are often scarce and dirty – and other seemingly mundane issues.
Mundane unless you have a UTI, or are trying to figure out how to manage your menses with no tampons or places to wash your hands.
Since then the literature has grown. For example, I published a volume called “Women at War” (Oxford University Press, 2015) last spring. This recent supplement advances those discussions, including articles on avoiding anemia and stress fractures.
But the way forward has been spotty. Many political issues delay an open discussion, especially on reproductive concerns. Further, there is no driving function within the Department of Defense that focuses on funding research in support of service women and reporting back to the department and civilian leadership.
For example: Female service members have a rate of unintended pregnancy twice that of the civilian world. This leads to early attrition from the military, and in turn, to young female veterans with children who are homeless.
Some have said, highlighting these concerns, that females should not be in the military because our presence is a risk to operational readiness. However, this is not an issue without tested solutions.
Taking this one issue further, consider that all service women are included in the Military Health System and have access to a variety of forms of birth control. If female service members can be put on oral contraceptives, that would both suppress their menses and avoid unwanted pregnancies. However, longer lasting methods of birth control would enable service women to enjoy decreased menses, avoid unwanted pregnancies, and avoid access issues during deployment.
The supplement contains numerous health policy and research recommendations as well as a detailed look at the unique health and lifestyle challenges of service women. Other issues include: the reproductive health of women in austere environments, nutritional factors, avoiding musculoskeletal injuries, combat-related injuries, designing military equipment (including uniforms) for optimal performance, and the role of leadership. It concludes with 20 research gaps and accompanying recommendations.
The number of women serving in the military is increasing, while all jobs, particularly those in the ground combat element, are now open to women. The time is now to focus on establishing and tracking health and well-being issues to ensure the success of this population – and the Military Medicine special issue is just a first step.
Dr. Ritchie serves as professor of psychiatry at the Uniformed Services University of the Health Services in Bethesda, Md., and at Georgetown University in Washington. She helped write one of the articles in the supplement with Dr. McGraw and Tracey Perez Koehlmoos, Ph.D., an associate professor with the Uniformed Services University.
A supplement recently published in Military Medicine seeks to examine how the Defense Department meets the medical needs of its women warriors. Called “Combat: Framing the Issues of Health and Health Research for America’s Servicewomen,” the articles go a long way toward shining a light on an important issue.
Several of the articles in the supplement highlight mental health issues for women in the military. They include the pieces about sexual harassment, the many faces of military families, alcohol use, and the corrosive effects of ostracism.
One of the articles by Kate McGraw, Ph.D., of the Deployment Health Clinical Center, Silver Spring, Md., focuses on the mental well-being of servicewomen and sexual trauma. Underlying the supplement is the recognition that the most robust mental health research repeatedly conducted in Afghanistan, for example, did not include a single woman because of the sampling methodology. A dedicated group addressing service women’s health and inclusion in health research would have prevented this oversight.
The health of female service members has long been an interest of mine, partly because I was in the Army for 28 years and deployed to a lot of austere environments. They included the rice fields of Camp Edwards, near the DMZ in Korea; Mogadishu and other “cities” in Somalia; and various Forward Operating Bases in Iraq.
Many years ago, I published an article on health concerns of deployed women. That focused on concerns about how to avoid urinary tract infections (UTIs) while in the field – where bathrooms are often scarce and dirty – and other seemingly mundane issues.
Mundane unless you have a UTI, or are trying to figure out how to manage your menses with no tampons or places to wash your hands.
Since then the literature has grown. For example, I published a volume called “Women at War” (Oxford University Press, 2015) last spring. This recent supplement advances those discussions, including articles on avoiding anemia and stress fractures.
But the way forward has been spotty. Many political issues delay an open discussion, especially on reproductive concerns. Further, there is no driving function within the Department of Defense that focuses on funding research in support of service women and reporting back to the department and civilian leadership.
For example: Female service members have a rate of unintended pregnancy twice that of the civilian world. This leads to early attrition from the military, and in turn, to young female veterans with children who are homeless.
Some have said, highlighting these concerns, that females should not be in the military because our presence is a risk to operational readiness. However, this is not an issue without tested solutions.
Taking this one issue further, consider that all service women are included in the Military Health System and have access to a variety of forms of birth control. If female service members can be put on oral contraceptives, that would both suppress their menses and avoid unwanted pregnancies. However, longer lasting methods of birth control would enable service women to enjoy decreased menses, avoid unwanted pregnancies, and avoid access issues during deployment.
The supplement contains numerous health policy and research recommendations as well as a detailed look at the unique health and lifestyle challenges of service women. Other issues include: the reproductive health of women in austere environments, nutritional factors, avoiding musculoskeletal injuries, combat-related injuries, designing military equipment (including uniforms) for optimal performance, and the role of leadership. It concludes with 20 research gaps and accompanying recommendations.
The number of women serving in the military is increasing, while all jobs, particularly those in the ground combat element, are now open to women. The time is now to focus on establishing and tracking health and well-being issues to ensure the success of this population – and the Military Medicine special issue is just a first step.
Dr. Ritchie serves as professor of psychiatry at the Uniformed Services University of the Health Services in Bethesda, Md., and at Georgetown University in Washington. She helped write one of the articles in the supplement with Dr. McGraw and Tracey Perez Koehlmoos, Ph.D., an associate professor with the Uniformed Services University.
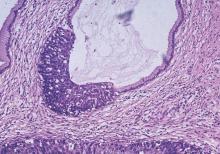
Fertility preservation in early cervical cancer
Historically, the standard of care for women diagnosed with early cervical cancer has been radical hysterectomy. Thus, young women are not only being confronted with a cancer diagnosis, but may also be forced to cope with the loss of their fertility.
As many young women with cervical cancer were not accepting of this treatment, Dr. Daniel Dargent pioneered the vaginal radical trachelectomy as a fertility-preserving treatment option for early cervical cancer in 1994. There have now been more than 900 vaginal radical trachelectomies performed and they have been shown to have oncologic outcomes similar to those of traditional radical hysterectomy, while sparing a woman’s fertility (Int J Gynecol Cancer. 2013 Jul;23[6]:982-9).
Obstetric outcomes following vaginal radical trachelectomy are acceptable with 17% miscarriage rate in the first trimester (compared to 10%-20% in the general population) and 8% in the second trimester (compared to 1%-5% in the general population) (Am Fam Physician. 2007 Nov 1;76[9]:1341-6). Following vaginal radical trachelectomy, 64% of pregnancies deliver at term.
The usual criteria required to undergo radical trachelectomy include:
1) Reproductive age with desire for fertility.
2) Stage IA1 with LVSI (lymphovascular space invasion), IA2, or IB1 with tumor less than 2 cm.
3) Limited endocervical involvement via preoperative MRI.
4) Negative pelvic lymph nodes.
Preoperative PET scan can be used to evaluate nodal status, but suspicious lymph nodes should be evaluated on frozen section at the time of surgery. The presence of LVSI alone is not a contraindication to trachelectomy.
A key limitation of vaginal radical trachelectomy is the specialized training required to perform this technically challenging procedure. Few surgeons in the United States are trained to perform vaginal radical trachelectomy. In response to this limitation, surgeons began to attempt radical trachelectomy via laparotomy (Gynecol Oncol. 2006 Dec;103[3]:807-13). Oncologic outcomes following fertility-sparing abdominal radical trachelectomy have been reported to be equivalent to radical hysterectomy. Concerns regarding the abdominal approach to radical trachelectomy include higher rates of second trimester loss (19%) when compared to the vaginal approach (8%), higher rate of loss of fertility (30%), and risk of postoperative adhesions.
The advent of minimally invasive surgery, particularly robotic surgery, now offers surgeons the ability to perform a procedure technically similar to radical hysterectomy using a minimally invasive approach. Given the similarity of procedural steps of radical trachelectomy to radical hysterectomy using the robotic platform, this procedure is gaining acceptance in the United States with an associated improved surgeon learning curve (Gynecol Oncol. 2008 Nov;111[2]:255-60). In addition, the use of minimally invasive surgery should result in less adhesion formation facilitating natural fertility options postoperatively.
Obstetric and fertility outcomes are limited following minimally invasive radical trachelectomy via laparoscopy or robotic surgery given the novelty of this procedure. Emerging obstetric outcomes appear reassuring, but further data are needed to fully understand the effects of this procedure on pregnancy outcomes and the need for assisted reproductive techniques to achieve pregnancy.
The management of pregnancies following radical trachelectomy is also an area with limited data, which presents a clinical challenge to obstetricians. Many gynecologic oncologists perform a permanent cerclage at the time of trachelectomy and recommend delivery via scheduled cesarean at term for all subsequent pregnancies prior to labor (usually 37-38 weeks).
At our institution, we recommend the use of progesterone from 16 to 36 weeks despite no clear evidence on the role of progesterone in this setting. Maternal-fetal medicine consultation should be considered to either follow these patients during their pregnancies or to perform a single consultative visit to guide antepartum care.
Some have advocated for less radical surgery, such as simple trachelectomy or large cold knife conization, as the risk of parametrial extension in these patients is low (Gynecol Oncol. 2011 Dec;123[3]:557-60). More data are needed to determine if this is a safe approach. Further, the use of neoadjuvant chemotherapy followed by cold knife conization for fertility preservation in women with larger tumors has been proposed. This may be a feasible option in women with chemo-sensitive tumors, but progression on chemotherapy and increased recurrences have been reported with this approach (Gynecol Oncol. 2008 Dec;111[3]:438-43).
Women of reproductive age diagnosed with early cervical cancer now have multiple options for fertility preservation. Ongoing research regarding obstetric and fertility outcomes is needed; however, oncologic outcomes appear to be equivalent.
Dr. Clark is a fellow in the division of gynecologic oncology, department of obstetrics and gynecology, at the University of North Carolina, Chapel Hill. Dr. Boggess is an expert in robotic surgery in gynecologic oncology and is a professor in the division of gynecologic oncology at UNC–Chapel Hill. They reported having no financial disclosures relevant to this column. Email them at [email protected].
Historically, the standard of care for women diagnosed with early cervical cancer has been radical hysterectomy. Thus, young women are not only being confronted with a cancer diagnosis, but may also be forced to cope with the loss of their fertility.
As many young women with cervical cancer were not accepting of this treatment, Dr. Daniel Dargent pioneered the vaginal radical trachelectomy as a fertility-preserving treatment option for early cervical cancer in 1994. There have now been more than 900 vaginal radical trachelectomies performed and they have been shown to have oncologic outcomes similar to those of traditional radical hysterectomy, while sparing a woman’s fertility (Int J Gynecol Cancer. 2013 Jul;23[6]:982-9).
Obstetric outcomes following vaginal radical trachelectomy are acceptable with 17% miscarriage rate in the first trimester (compared to 10%-20% in the general population) and 8% in the second trimester (compared to 1%-5% in the general population) (Am Fam Physician. 2007 Nov 1;76[9]:1341-6). Following vaginal radical trachelectomy, 64% of pregnancies deliver at term.
The usual criteria required to undergo radical trachelectomy include:
1) Reproductive age with desire for fertility.
2) Stage IA1 with LVSI (lymphovascular space invasion), IA2, or IB1 with tumor less than 2 cm.
3) Limited endocervical involvement via preoperative MRI.
4) Negative pelvic lymph nodes.
Preoperative PET scan can be used to evaluate nodal status, but suspicious lymph nodes should be evaluated on frozen section at the time of surgery. The presence of LVSI alone is not a contraindication to trachelectomy.
A key limitation of vaginal radical trachelectomy is the specialized training required to perform this technically challenging procedure. Few surgeons in the United States are trained to perform vaginal radical trachelectomy. In response to this limitation, surgeons began to attempt radical trachelectomy via laparotomy (Gynecol Oncol. 2006 Dec;103[3]:807-13). Oncologic outcomes following fertility-sparing abdominal radical trachelectomy have been reported to be equivalent to radical hysterectomy. Concerns regarding the abdominal approach to radical trachelectomy include higher rates of second trimester loss (19%) when compared to the vaginal approach (8%), higher rate of loss of fertility (30%), and risk of postoperative adhesions.
The advent of minimally invasive surgery, particularly robotic surgery, now offers surgeons the ability to perform a procedure technically similar to radical hysterectomy using a minimally invasive approach. Given the similarity of procedural steps of radical trachelectomy to radical hysterectomy using the robotic platform, this procedure is gaining acceptance in the United States with an associated improved surgeon learning curve (Gynecol Oncol. 2008 Nov;111[2]:255-60). In addition, the use of minimally invasive surgery should result in less adhesion formation facilitating natural fertility options postoperatively.
Obstetric and fertility outcomes are limited following minimally invasive radical trachelectomy via laparoscopy or robotic surgery given the novelty of this procedure. Emerging obstetric outcomes appear reassuring, but further data are needed to fully understand the effects of this procedure on pregnancy outcomes and the need for assisted reproductive techniques to achieve pregnancy.
The management of pregnancies following radical trachelectomy is also an area with limited data, which presents a clinical challenge to obstetricians. Many gynecologic oncologists perform a permanent cerclage at the time of trachelectomy and recommend delivery via scheduled cesarean at term for all subsequent pregnancies prior to labor (usually 37-38 weeks).
At our institution, we recommend the use of progesterone from 16 to 36 weeks despite no clear evidence on the role of progesterone in this setting. Maternal-fetal medicine consultation should be considered to either follow these patients during their pregnancies or to perform a single consultative visit to guide antepartum care.
Some have advocated for less radical surgery, such as simple trachelectomy or large cold knife conization, as the risk of parametrial extension in these patients is low (Gynecol Oncol. 2011 Dec;123[3]:557-60). More data are needed to determine if this is a safe approach. Further, the use of neoadjuvant chemotherapy followed by cold knife conization for fertility preservation in women with larger tumors has been proposed. This may be a feasible option in women with chemo-sensitive tumors, but progression on chemotherapy and increased recurrences have been reported with this approach (Gynecol Oncol. 2008 Dec;111[3]:438-43).
Women of reproductive age diagnosed with early cervical cancer now have multiple options for fertility preservation. Ongoing research regarding obstetric and fertility outcomes is needed; however, oncologic outcomes appear to be equivalent.
Dr. Clark is a fellow in the division of gynecologic oncology, department of obstetrics and gynecology, at the University of North Carolina, Chapel Hill. Dr. Boggess is an expert in robotic surgery in gynecologic oncology and is a professor in the division of gynecologic oncology at UNC–Chapel Hill. They reported having no financial disclosures relevant to this column. Email them at [email protected].
Historically, the standard of care for women diagnosed with early cervical cancer has been radical hysterectomy. Thus, young women are not only being confronted with a cancer diagnosis, but may also be forced to cope with the loss of their fertility.
As many young women with cervical cancer were not accepting of this treatment, Dr. Daniel Dargent pioneered the vaginal radical trachelectomy as a fertility-preserving treatment option for early cervical cancer in 1994. There have now been more than 900 vaginal radical trachelectomies performed and they have been shown to have oncologic outcomes similar to those of traditional radical hysterectomy, while sparing a woman’s fertility (Int J Gynecol Cancer. 2013 Jul;23[6]:982-9).
Obstetric outcomes following vaginal radical trachelectomy are acceptable with 17% miscarriage rate in the first trimester (compared to 10%-20% in the general population) and 8% in the second trimester (compared to 1%-5% in the general population) (Am Fam Physician. 2007 Nov 1;76[9]:1341-6). Following vaginal radical trachelectomy, 64% of pregnancies deliver at term.
The usual criteria required to undergo radical trachelectomy include:
1) Reproductive age with desire for fertility.
2) Stage IA1 with LVSI (lymphovascular space invasion), IA2, or IB1 with tumor less than 2 cm.
3) Limited endocervical involvement via preoperative MRI.
4) Negative pelvic lymph nodes.
Preoperative PET scan can be used to evaluate nodal status, but suspicious lymph nodes should be evaluated on frozen section at the time of surgery. The presence of LVSI alone is not a contraindication to trachelectomy.
A key limitation of vaginal radical trachelectomy is the specialized training required to perform this technically challenging procedure. Few surgeons in the United States are trained to perform vaginal radical trachelectomy. In response to this limitation, surgeons began to attempt radical trachelectomy via laparotomy (Gynecol Oncol. 2006 Dec;103[3]:807-13). Oncologic outcomes following fertility-sparing abdominal radical trachelectomy have been reported to be equivalent to radical hysterectomy. Concerns regarding the abdominal approach to radical trachelectomy include higher rates of second trimester loss (19%) when compared to the vaginal approach (8%), higher rate of loss of fertility (30%), and risk of postoperative adhesions.
The advent of minimally invasive surgery, particularly robotic surgery, now offers surgeons the ability to perform a procedure technically similar to radical hysterectomy using a minimally invasive approach. Given the similarity of procedural steps of radical trachelectomy to radical hysterectomy using the robotic platform, this procedure is gaining acceptance in the United States with an associated improved surgeon learning curve (Gynecol Oncol. 2008 Nov;111[2]:255-60). In addition, the use of minimally invasive surgery should result in less adhesion formation facilitating natural fertility options postoperatively.
Obstetric and fertility outcomes are limited following minimally invasive radical trachelectomy via laparoscopy or robotic surgery given the novelty of this procedure. Emerging obstetric outcomes appear reassuring, but further data are needed to fully understand the effects of this procedure on pregnancy outcomes and the need for assisted reproductive techniques to achieve pregnancy.
The management of pregnancies following radical trachelectomy is also an area with limited data, which presents a clinical challenge to obstetricians. Many gynecologic oncologists perform a permanent cerclage at the time of trachelectomy and recommend delivery via scheduled cesarean at term for all subsequent pregnancies prior to labor (usually 37-38 weeks).
At our institution, we recommend the use of progesterone from 16 to 36 weeks despite no clear evidence on the role of progesterone in this setting. Maternal-fetal medicine consultation should be considered to either follow these patients during their pregnancies or to perform a single consultative visit to guide antepartum care.
Some have advocated for less radical surgery, such as simple trachelectomy or large cold knife conization, as the risk of parametrial extension in these patients is low (Gynecol Oncol. 2011 Dec;123[3]:557-60). More data are needed to determine if this is a safe approach. Further, the use of neoadjuvant chemotherapy followed by cold knife conization for fertility preservation in women with larger tumors has been proposed. This may be a feasible option in women with chemo-sensitive tumors, but progression on chemotherapy and increased recurrences have been reported with this approach (Gynecol Oncol. 2008 Dec;111[3]:438-43).
Women of reproductive age diagnosed with early cervical cancer now have multiple options for fertility preservation. Ongoing research regarding obstetric and fertility outcomes is needed; however, oncologic outcomes appear to be equivalent.
Dr. Clark is a fellow in the division of gynecologic oncology, department of obstetrics and gynecology, at the University of North Carolina, Chapel Hill. Dr. Boggess is an expert in robotic surgery in gynecologic oncology and is a professor in the division of gynecologic oncology at UNC–Chapel Hill. They reported having no financial disclosures relevant to this column. Email them at [email protected].
Understanding stillbirth
When a couple learns that “they are pregnant,” it is often one of the most joyous moments in their lives. However, despite the modern prenatal care available to women in the United States, pregnancy loss remains a real concern. Miscarriage is estimated to occur in 15%-20% of pregnancies; recurrent pregnancy loss in about 1%-2% of pregnancies; and stillbirth in as many as 1% of pregnancies. The causes of pregnancy loss can range from those we can diagnose, such as genetic factors, anatomic complications, and thrombophilia, to those that elude us completely.
In December 2015, investigators from Karolinska Institutet in Stockholm published a study indicating that women who gained weight between their first and second pregnancies, but who were a healthy weight prior to their first pregnancy, had an increased risk of experiencing a stillbirth (30%-50%), or having an infant who died within the first year (27%-60%) (Lancet 2015. doi: 10.1016/S0140-6736(15)00990-3). We have devoted a number of Master Class columns to the link between obesity and pregnancy complications, and this study further reinforces the influence of a healthy weight on pregnancy outcomes.
In addition to lifestyle modifications, evidence has suggested that low-molecular-weight heparin, aspirin, or vitamin supplements, in combination with appropriate surveillance and management, may reduce risk of pregnancy loss. However, more work is needed to fully understand why fetal death occurs if we are to better equip ourselves, and our patients, with all the information necessary to prevent loss from happening.
For this reason, we have invited Dr. Uma M. Reddy of the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health, to address one of the most devastating types of pregnancy losses: stillbirth. As a program scientist for large research studies, such as the Stillbirth Collaborative Research Network, Dr. Reddy’s unique perspective will add greatly to our understanding of pregnancy loss.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece reported having no relevant financial disclosures. He is the medical editor of this column.
When a couple learns that “they are pregnant,” it is often one of the most joyous moments in their lives. However, despite the modern prenatal care available to women in the United States, pregnancy loss remains a real concern. Miscarriage is estimated to occur in 15%-20% of pregnancies; recurrent pregnancy loss in about 1%-2% of pregnancies; and stillbirth in as many as 1% of pregnancies. The causes of pregnancy loss can range from those we can diagnose, such as genetic factors, anatomic complications, and thrombophilia, to those that elude us completely.
In December 2015, investigators from Karolinska Institutet in Stockholm published a study indicating that women who gained weight between their first and second pregnancies, but who were a healthy weight prior to their first pregnancy, had an increased risk of experiencing a stillbirth (30%-50%), or having an infant who died within the first year (27%-60%) (Lancet 2015. doi: 10.1016/S0140-6736(15)00990-3). We have devoted a number of Master Class columns to the link between obesity and pregnancy complications, and this study further reinforces the influence of a healthy weight on pregnancy outcomes.
In addition to lifestyle modifications, evidence has suggested that low-molecular-weight heparin, aspirin, or vitamin supplements, in combination with appropriate surveillance and management, may reduce risk of pregnancy loss. However, more work is needed to fully understand why fetal death occurs if we are to better equip ourselves, and our patients, with all the information necessary to prevent loss from happening.
For this reason, we have invited Dr. Uma M. Reddy of the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health, to address one of the most devastating types of pregnancy losses: stillbirth. As a program scientist for large research studies, such as the Stillbirth Collaborative Research Network, Dr. Reddy’s unique perspective will add greatly to our understanding of pregnancy loss.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece reported having no relevant financial disclosures. He is the medical editor of this column.
When a couple learns that “they are pregnant,” it is often one of the most joyous moments in their lives. However, despite the modern prenatal care available to women in the United States, pregnancy loss remains a real concern. Miscarriage is estimated to occur in 15%-20% of pregnancies; recurrent pregnancy loss in about 1%-2% of pregnancies; and stillbirth in as many as 1% of pregnancies. The causes of pregnancy loss can range from those we can diagnose, such as genetic factors, anatomic complications, and thrombophilia, to those that elude us completely.
In December 2015, investigators from Karolinska Institutet in Stockholm published a study indicating that women who gained weight between their first and second pregnancies, but who were a healthy weight prior to their first pregnancy, had an increased risk of experiencing a stillbirth (30%-50%), or having an infant who died within the first year (27%-60%) (Lancet 2015. doi: 10.1016/S0140-6736(15)00990-3). We have devoted a number of Master Class columns to the link between obesity and pregnancy complications, and this study further reinforces the influence of a healthy weight on pregnancy outcomes.
In addition to lifestyle modifications, evidence has suggested that low-molecular-weight heparin, aspirin, or vitamin supplements, in combination with appropriate surveillance and management, may reduce risk of pregnancy loss. However, more work is needed to fully understand why fetal death occurs if we are to better equip ourselves, and our patients, with all the information necessary to prevent loss from happening.
For this reason, we have invited Dr. Uma M. Reddy of the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health, to address one of the most devastating types of pregnancy losses: stillbirth. As a program scientist for large research studies, such as the Stillbirth Collaborative Research Network, Dr. Reddy’s unique perspective will add greatly to our understanding of pregnancy loss.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece reported having no relevant financial disclosures. He is the medical editor of this column.
Research adds insight on stillbirth risk factors
Stillbirth is a major public health problem, occurring in approximately 1 of every 160 pregnancies in the United States. The rate has remained stagnant since 2006. Prior to that time, from 1990 to 2006, the rate declined somewhat, but only half as much as the decline in infant mortality during this time period. Racial disparities also have persisted, with non-Hispanic black women having more than a twofold increase in risk (Natl Vital Stat Rep. 2012;60:1-22).
Research conducted by the Stillbirth Collaborative Research Network (SCRN) and others has provided us with insight on risk factors and on probable and possible causes of death among stillbirths, which are defined as fetal deaths at 20 or more weeks’ gestation. We know from SCRN data, for instance, that black women are more likely to have stillbirths associated with obstetric complications and infections than white and Hispanic women. However, we still cannot explain a substantial proportion of stillbirths, despite a complete evaluation, or predict who will have a stillbirth.
What we can do as obstetricians is be aware that stillbirth is one of the most common adverse pregnancy outcomes in the United States and counsel women regarding risk factors that are modifiable. Moreover, when stillbirth happens, a complete postmortem evaluation that includes autopsy, placental pathology, karyotype or microarray analysis, and fetal-maternal hemorrhage testing is recommended (Obstet Gynecol. 2009;113[3]:748-61). Recent data show that each of these four components is valuable and should be considered the basic work-up for stillbirth.
Risks and causes
Pregnancy history was the strongest baseline risk factor for stillbirth in an analysis of 614 stillbirths and 1,816 live births in the SCRN’s population-based, case-control study conducted between 2006 and 2008. The SCRN was initiated by the Eunice Kennedy Shriver National Institute of Child Health and Human Development in 2003. This critical population-based study was conducted at 59 U.S. tertiary care and community hospitals in five catchment areas and has been analyzed in more than 15 published reports.
Women with a previous stillbirth have been known to be at 5- to 10-fold increased risk of a recurrence of stillbirth, and the SCRN findings confirmed this. The study added to our knowledge, however, with the finding that even a prior pregnancy loss at less than 20 weeks’ gestation increased the risk for stillbirth.
Other risk factors identified in the study, in addition to race, included having a multifetal pregnancy (adjusted odds ratio of 4.59), diabetes (AOR of 2.50), maternal age of 40 years or older (AOR of 2.41), maternal AB blood type (AOR of 1.96, compared with type O), a history of drug addiction (AOR of 2.08), smoking during the 3 months prior to pregnancy (AOR of 1.55-1.57, depending on amount), and being unmarried and not cohabitating (AOR of 1.69). Regarding racial disparity, the study showed that elevated risk of stillbirth for non-Hispanic blacks occurred predominantly prior to 24 weeks of gestation.
As in prior research, overweight and obesity also conferred elevated risks in the SCRN study (AORs of 1.43 and 1.72, respectively), and these risks were not explained by either diabetes or hypertension (JAMA. 2011;306:2469-79).
The use of assisted reproductive technology was not included in the study’s multivariate model, but previous research has shown a fourfold increased risk of stillbirth for singleton IVF/ICSI pregnancies. The reason is unclear, but the risk appears to be more related to IVF/ICSI rather than the underlying infertility (Hum Reprod. 2010 May;25[5]:1312-6).
A previous preterm or small-for-gestational-age birth has also been shown in prior research to be a significant risk factor for stillbirth. Less clear is the role of previous cesarean delivery in stillbirth risk. An association has been demonstrated in several studies, however, including one involving about 180,000 singleton pregnancies of 23 or more weeks’ gestation. Women in this cohort who had a previous cesarean delivery had a 1.3-fold increased risk of antepartum stillbirth, after controlling for important factors such as race, body mass index (BMI), and maternal disease (Obstet Gynecol. 2010 Nov;116[5]:1119-26).
In another analysis of the SCRN study looking specifically at causes of stillbirth, a “probable” cause of death was found in 61% of cases and a “possible or probable” cause of death in more than 76% of cases. The most common causes were obstetric complications (29.3%), placental abnormalities (23.6%), fetal genetic/structural abnormalities (13.7%), infection (12.9%), umbilical cord abnormalities (10.4%), hypertensive disorders (9.2%), and other maternal medical conditions (7.8%).
A higher proportion of stillbirths in non-Hispanic black women, compared with non-Hispanic white women and Hispanic women was associated with obstetric complications (43.5%) and infections (25.2%). This finding combined with the finding that stillbirth in black women often occurs at less than 24 weeks’ gestation suggests that measures aimed at reducing the rate of spontaneous preterm birth in black women could potentially reduce the rate of stillbirth as well (JAMA. 2011 Dec 14;306[22]:2459-68).
Work-up and prevention
Prevention of stillbirth requires that we identify the women at highest risk, and thus far this ability still eludes us. Apart from occurrence of previous stillbirth or pregnancy loss, other risk factors have had limited predictive value in the SCRN analyses and other research.
Biomarkers such as a low PAPP-A during the first trimester and a high AFP in the second trimester – as well as Doppler imaging of the uterine artery – have also been associated with stillbirth, but again, the positive predictive value has been shown to be low (Clin Obstet Gynecol. 2010 Sep;53[3]:597-606). More research is needed to determine if some combination of biochemical markers, imaging, and other risk factors can predict which women are at highest risk.
In the meantime, attention can be paid – in the preconception period if possible – to modifiable risk factors such as maternal obesity, diabetes, and smoking. About 10% of stillbirths are associated with maternal conditions such as hypertension and diabetes, and late stillbirths in particular (28 weeks or later) are associated with maternal medical conditions that are potentially preventable.
Normalization of prepregnancy weight should be a goal, since the overall risk of stillbirth appears to increase independently with increasing BMI. Glycemic control should also be achieved: A recent meta-analysis of preconception and prenatal care of diabetic women estimated “conservatively” that 10% of diabetes-associated stillbirths could be prevented with early detection and glycemic control (BMC Public Health. 2011;11 Suppl 3:S2). Research has also shown that women who quit smoking between their first and second pregnancy reduce their stillbirth risk to that of nonsmokers in the second pregnancy (BJOG. 2007 Jun;114[6]:699-704).
When stillbirth happens, a thorough work-up is recommended in order to counsel for future pregnancies and decrease the risk of recurrence. Evaluations for causes of stillbirth are too often incomplete in the United States for various reasons, including emotional, cultural, and resource factors. Even if a cause is not found, many families appreciate knowing that every effort has been made to determine a cause of death.
Four components of evaluation – autopsy, placental examination, karyotype or microarray analysis, and fetal-maternal hemorrhage testing – have proven to be high-yield tests when performed in all cases of stillbirth.
In the SCRN study, of 512 stillbirths undergoing a complete evaluation, 66.4% had a positive result – defined as abnormalities contributing to a probable or possible cause – for at least one of the first three tests (JAMA. 2011 Dec 14;306[22]:2459-68).
A Dutch study of 1,025 stillbirths similarly demonstrated that all four tests are justified. A test was defined as valuable in this study if it established or excluded a cause of stillbirth. Placental examination was determined to be the most valuable test, helping to determine a cause of death in 95.7% of cases. Autopsy was valuable 72.6% of the time, and cytogenetic analysis was valuable in 29% of cases.
Kleihauer-Betke testing for fetal-maternal hemorrhage was positive in 11.9% of women. However, fetal maternal hemorrhage was considered the cause of death in only 1.3%.of cases because, beyond a positive Kleihauer-Betke test, evidence of fetal anemia confirmed by placental examination and/or autopsy was required for hemorrhage to be considered the cause of death (Am. J. Obstet. Gynecol. 2012;206:53.e1-12). Because Kleihauer-Betke testing is ideally performed before induction, authors of both the SCRN study and the Dutch study believe it is a valuable test to be offered in all cases.
In both studies, the yield of other stillbirth diagnostic tests (for example, maternal serology, hormone assessment, and toxicology screen) was low, indicating that these tests are considered sequential and can be performed only when the clinical history or findings of the four core tests raise suspicion of particular potential causes. Antinuclear antibody testing and TORCH (toxoplasmosis, rubella, cytomegalovirus, herpes simplex) titers have an extremely low yield and are generally not useful.
For detecting genetic abnormalities after stillbirth, it appears that microarray analysis is superior to karyotype analysis. In a SCRN analysis of samples from 532 stillbirths, microarray yielded results more often and identified more genetic abnormalities. Unlike karyotype, it does not require live cells, which makes it preferable for stillbirth evaluation (N Engl J Med. 2012 Dec 6;367[23]:2185-93).
Current research
One of the more significant studies underway on prevention is looking at labor induction as an intervention for reducing stillbirths and improving other perinatal outcomes. The ARRIVE trial (“A Randomized Trial of Induction Versus Expectant Management”), currently in the recruitment stage, will examine outcomes after induction at 39 weeks’ gestation, compared with expectant management in 6,000 patients (clinicaltrials.gov/ct2/show/NCT01990612).
Common wisdom informed by retrospective cohort studies has long told us that inducing labor prior to 41 weeks’ gestation is associated with a higher risk of cesarean delivery in nulliparous women. However, recent observational data have suggested that women whose labor is induced actually have fewer cesarean deliveries and better perinatal outcomes, including a lower risk of stillbirth (AJOG 2012;207:502.e1-8).
In addition, a meta-analysis published in 2014, as the ARRIVE trial was taking shape, reported a 12% reduction in cesarean delivery, and a reduced risk of stillbirth, among women whose labor was induced. The initial cervical score did not impact the main findings (CMAJ. 2014 Jun 10;186[9]:665-73). If these findings are confirmed in the ARRIVE trial, we could see a new opportunity for stillbirth prevention.
Another ongoing study of 10,000 singleton pregnancies – the Nulliparous Pregnancy Outcomes: Monitoring Mothers-to-Be (nuMoM2b) study – may also lead to prevention strategies in women for whom the current pregnancy will lead to their first delivery. Among the questions being examined in this eight-site study are whether sleep-disordered breathing, or apnea, and a supine sleep position are risk factors for adverse pregnancy outcomes including stillbirth.
Supine sleeping in the last month of pregnancy was strongly associated with stillbirth in a recent analysis from the Sydney Stillbirth Study (Obstet Gynecol. 2015 Feb;125[2]:347-55), and an early analysis of a nuMoM2b subset has shown associations between sleep-disordered breathing in midpregnancy and the development of hypertensive disorders of pregnancy, and between sleep-disordered breathing in early- and mid-pregnancy and gestational diabetes (Am J Obstet Gynecol. 2015;212:S424-425).
The possible role of low-dose aspirin in preventing stillbirth also needs more exploration. A recent randomized trial of women attempting to become pregnant after having had one or two prior pregnancy losses found no difference overall in live birth rates between those who took low-dose aspirin and those assigned to placebo. However, there was one subgroup – women with a single loss at less than 20 weeks’ gestation during the previous year – in which live birth rates were higher in the aspirin group (Lancet. 2014 Jul 5;384[9937]:29-36). More research is necessary to determine if low-dose aspirin administration in women with a previous stillbirth improves pregnancy outcome.
Dr. Reddy is a member at the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. She is a board-certified ob.gyn. and maternal-fetal medicine specialist. She is the program scientist for the Maternal-Fetal Medicine Units Network and for the Stillbirth Collaborative Research Network. The comments and views of the author do not necessarily represent the views of the NICHD.
Stillbirth is a major public health problem, occurring in approximately 1 of every 160 pregnancies in the United States. The rate has remained stagnant since 2006. Prior to that time, from 1990 to 2006, the rate declined somewhat, but only half as much as the decline in infant mortality during this time period. Racial disparities also have persisted, with non-Hispanic black women having more than a twofold increase in risk (Natl Vital Stat Rep. 2012;60:1-22).
Research conducted by the Stillbirth Collaborative Research Network (SCRN) and others has provided us with insight on risk factors and on probable and possible causes of death among stillbirths, which are defined as fetal deaths at 20 or more weeks’ gestation. We know from SCRN data, for instance, that black women are more likely to have stillbirths associated with obstetric complications and infections than white and Hispanic women. However, we still cannot explain a substantial proportion of stillbirths, despite a complete evaluation, or predict who will have a stillbirth.
What we can do as obstetricians is be aware that stillbirth is one of the most common adverse pregnancy outcomes in the United States and counsel women regarding risk factors that are modifiable. Moreover, when stillbirth happens, a complete postmortem evaluation that includes autopsy, placental pathology, karyotype or microarray analysis, and fetal-maternal hemorrhage testing is recommended (Obstet Gynecol. 2009;113[3]:748-61). Recent data show that each of these four components is valuable and should be considered the basic work-up for stillbirth.
Risks and causes
Pregnancy history was the strongest baseline risk factor for stillbirth in an analysis of 614 stillbirths and 1,816 live births in the SCRN’s population-based, case-control study conducted between 2006 and 2008. The SCRN was initiated by the Eunice Kennedy Shriver National Institute of Child Health and Human Development in 2003. This critical population-based study was conducted at 59 U.S. tertiary care and community hospitals in five catchment areas and has been analyzed in more than 15 published reports.
Women with a previous stillbirth have been known to be at 5- to 10-fold increased risk of a recurrence of stillbirth, and the SCRN findings confirmed this. The study added to our knowledge, however, with the finding that even a prior pregnancy loss at less than 20 weeks’ gestation increased the risk for stillbirth.
Other risk factors identified in the study, in addition to race, included having a multifetal pregnancy (adjusted odds ratio of 4.59), diabetes (AOR of 2.50), maternal age of 40 years or older (AOR of 2.41), maternal AB blood type (AOR of 1.96, compared with type O), a history of drug addiction (AOR of 2.08), smoking during the 3 months prior to pregnancy (AOR of 1.55-1.57, depending on amount), and being unmarried and not cohabitating (AOR of 1.69). Regarding racial disparity, the study showed that elevated risk of stillbirth for non-Hispanic blacks occurred predominantly prior to 24 weeks of gestation.
As in prior research, overweight and obesity also conferred elevated risks in the SCRN study (AORs of 1.43 and 1.72, respectively), and these risks were not explained by either diabetes or hypertension (JAMA. 2011;306:2469-79).
The use of assisted reproductive technology was not included in the study’s multivariate model, but previous research has shown a fourfold increased risk of stillbirth for singleton IVF/ICSI pregnancies. The reason is unclear, but the risk appears to be more related to IVF/ICSI rather than the underlying infertility (Hum Reprod. 2010 May;25[5]:1312-6).
A previous preterm or small-for-gestational-age birth has also been shown in prior research to be a significant risk factor for stillbirth. Less clear is the role of previous cesarean delivery in stillbirth risk. An association has been demonstrated in several studies, however, including one involving about 180,000 singleton pregnancies of 23 or more weeks’ gestation. Women in this cohort who had a previous cesarean delivery had a 1.3-fold increased risk of antepartum stillbirth, after controlling for important factors such as race, body mass index (BMI), and maternal disease (Obstet Gynecol. 2010 Nov;116[5]:1119-26).
In another analysis of the SCRN study looking specifically at causes of stillbirth, a “probable” cause of death was found in 61% of cases and a “possible or probable” cause of death in more than 76% of cases. The most common causes were obstetric complications (29.3%), placental abnormalities (23.6%), fetal genetic/structural abnormalities (13.7%), infection (12.9%), umbilical cord abnormalities (10.4%), hypertensive disorders (9.2%), and other maternal medical conditions (7.8%).
A higher proportion of stillbirths in non-Hispanic black women, compared with non-Hispanic white women and Hispanic women was associated with obstetric complications (43.5%) and infections (25.2%). This finding combined with the finding that stillbirth in black women often occurs at less than 24 weeks’ gestation suggests that measures aimed at reducing the rate of spontaneous preterm birth in black women could potentially reduce the rate of stillbirth as well (JAMA. 2011 Dec 14;306[22]:2459-68).
Work-up and prevention
Prevention of stillbirth requires that we identify the women at highest risk, and thus far this ability still eludes us. Apart from occurrence of previous stillbirth or pregnancy loss, other risk factors have had limited predictive value in the SCRN analyses and other research.
Biomarkers such as a low PAPP-A during the first trimester and a high AFP in the second trimester – as well as Doppler imaging of the uterine artery – have also been associated with stillbirth, but again, the positive predictive value has been shown to be low (Clin Obstet Gynecol. 2010 Sep;53[3]:597-606). More research is needed to determine if some combination of biochemical markers, imaging, and other risk factors can predict which women are at highest risk.
In the meantime, attention can be paid – in the preconception period if possible – to modifiable risk factors such as maternal obesity, diabetes, and smoking. About 10% of stillbirths are associated with maternal conditions such as hypertension and diabetes, and late stillbirths in particular (28 weeks or later) are associated with maternal medical conditions that are potentially preventable.
Normalization of prepregnancy weight should be a goal, since the overall risk of stillbirth appears to increase independently with increasing BMI. Glycemic control should also be achieved: A recent meta-analysis of preconception and prenatal care of diabetic women estimated “conservatively” that 10% of diabetes-associated stillbirths could be prevented with early detection and glycemic control (BMC Public Health. 2011;11 Suppl 3:S2). Research has also shown that women who quit smoking between their first and second pregnancy reduce their stillbirth risk to that of nonsmokers in the second pregnancy (BJOG. 2007 Jun;114[6]:699-704).
When stillbirth happens, a thorough work-up is recommended in order to counsel for future pregnancies and decrease the risk of recurrence. Evaluations for causes of stillbirth are too often incomplete in the United States for various reasons, including emotional, cultural, and resource factors. Even if a cause is not found, many families appreciate knowing that every effort has been made to determine a cause of death.
Four components of evaluation – autopsy, placental examination, karyotype or microarray analysis, and fetal-maternal hemorrhage testing – have proven to be high-yield tests when performed in all cases of stillbirth.
In the SCRN study, of 512 stillbirths undergoing a complete evaluation, 66.4% had a positive result – defined as abnormalities contributing to a probable or possible cause – for at least one of the first three tests (JAMA. 2011 Dec 14;306[22]:2459-68).
A Dutch study of 1,025 stillbirths similarly demonstrated that all four tests are justified. A test was defined as valuable in this study if it established or excluded a cause of stillbirth. Placental examination was determined to be the most valuable test, helping to determine a cause of death in 95.7% of cases. Autopsy was valuable 72.6% of the time, and cytogenetic analysis was valuable in 29% of cases.
Kleihauer-Betke testing for fetal-maternal hemorrhage was positive in 11.9% of women. However, fetal maternal hemorrhage was considered the cause of death in only 1.3%.of cases because, beyond a positive Kleihauer-Betke test, evidence of fetal anemia confirmed by placental examination and/or autopsy was required for hemorrhage to be considered the cause of death (Am. J. Obstet. Gynecol. 2012;206:53.e1-12). Because Kleihauer-Betke testing is ideally performed before induction, authors of both the SCRN study and the Dutch study believe it is a valuable test to be offered in all cases.
In both studies, the yield of other stillbirth diagnostic tests (for example, maternal serology, hormone assessment, and toxicology screen) was low, indicating that these tests are considered sequential and can be performed only when the clinical history or findings of the four core tests raise suspicion of particular potential causes. Antinuclear antibody testing and TORCH (toxoplasmosis, rubella, cytomegalovirus, herpes simplex) titers have an extremely low yield and are generally not useful.
For detecting genetic abnormalities after stillbirth, it appears that microarray analysis is superior to karyotype analysis. In a SCRN analysis of samples from 532 stillbirths, microarray yielded results more often and identified more genetic abnormalities. Unlike karyotype, it does not require live cells, which makes it preferable for stillbirth evaluation (N Engl J Med. 2012 Dec 6;367[23]:2185-93).
Current research
One of the more significant studies underway on prevention is looking at labor induction as an intervention for reducing stillbirths and improving other perinatal outcomes. The ARRIVE trial (“A Randomized Trial of Induction Versus Expectant Management”), currently in the recruitment stage, will examine outcomes after induction at 39 weeks’ gestation, compared with expectant management in 6,000 patients (clinicaltrials.gov/ct2/show/NCT01990612).
Common wisdom informed by retrospective cohort studies has long told us that inducing labor prior to 41 weeks’ gestation is associated with a higher risk of cesarean delivery in nulliparous women. However, recent observational data have suggested that women whose labor is induced actually have fewer cesarean deliveries and better perinatal outcomes, including a lower risk of stillbirth (AJOG 2012;207:502.e1-8).
In addition, a meta-analysis published in 2014, as the ARRIVE trial was taking shape, reported a 12% reduction in cesarean delivery, and a reduced risk of stillbirth, among women whose labor was induced. The initial cervical score did not impact the main findings (CMAJ. 2014 Jun 10;186[9]:665-73). If these findings are confirmed in the ARRIVE trial, we could see a new opportunity for stillbirth prevention.
Another ongoing study of 10,000 singleton pregnancies – the Nulliparous Pregnancy Outcomes: Monitoring Mothers-to-Be (nuMoM2b) study – may also lead to prevention strategies in women for whom the current pregnancy will lead to their first delivery. Among the questions being examined in this eight-site study are whether sleep-disordered breathing, or apnea, and a supine sleep position are risk factors for adverse pregnancy outcomes including stillbirth.
Supine sleeping in the last month of pregnancy was strongly associated with stillbirth in a recent analysis from the Sydney Stillbirth Study (Obstet Gynecol. 2015 Feb;125[2]:347-55), and an early analysis of a nuMoM2b subset has shown associations between sleep-disordered breathing in midpregnancy and the development of hypertensive disorders of pregnancy, and between sleep-disordered breathing in early- and mid-pregnancy and gestational diabetes (Am J Obstet Gynecol. 2015;212:S424-425).
The possible role of low-dose aspirin in preventing stillbirth also needs more exploration. A recent randomized trial of women attempting to become pregnant after having had one or two prior pregnancy losses found no difference overall in live birth rates between those who took low-dose aspirin and those assigned to placebo. However, there was one subgroup – women with a single loss at less than 20 weeks’ gestation during the previous year – in which live birth rates were higher in the aspirin group (Lancet. 2014 Jul 5;384[9937]:29-36). More research is necessary to determine if low-dose aspirin administration in women with a previous stillbirth improves pregnancy outcome.
Dr. Reddy is a member at the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. She is a board-certified ob.gyn. and maternal-fetal medicine specialist. She is the program scientist for the Maternal-Fetal Medicine Units Network and for the Stillbirth Collaborative Research Network. The comments and views of the author do not necessarily represent the views of the NICHD.
Stillbirth is a major public health problem, occurring in approximately 1 of every 160 pregnancies in the United States. The rate has remained stagnant since 2006. Prior to that time, from 1990 to 2006, the rate declined somewhat, but only half as much as the decline in infant mortality during this time period. Racial disparities also have persisted, with non-Hispanic black women having more than a twofold increase in risk (Natl Vital Stat Rep. 2012;60:1-22).
Research conducted by the Stillbirth Collaborative Research Network (SCRN) and others has provided us with insight on risk factors and on probable and possible causes of death among stillbirths, which are defined as fetal deaths at 20 or more weeks’ gestation. We know from SCRN data, for instance, that black women are more likely to have stillbirths associated with obstetric complications and infections than white and Hispanic women. However, we still cannot explain a substantial proportion of stillbirths, despite a complete evaluation, or predict who will have a stillbirth.
What we can do as obstetricians is be aware that stillbirth is one of the most common adverse pregnancy outcomes in the United States and counsel women regarding risk factors that are modifiable. Moreover, when stillbirth happens, a complete postmortem evaluation that includes autopsy, placental pathology, karyotype or microarray analysis, and fetal-maternal hemorrhage testing is recommended (Obstet Gynecol. 2009;113[3]:748-61). Recent data show that each of these four components is valuable and should be considered the basic work-up for stillbirth.
Risks and causes
Pregnancy history was the strongest baseline risk factor for stillbirth in an analysis of 614 stillbirths and 1,816 live births in the SCRN’s population-based, case-control study conducted between 2006 and 2008. The SCRN was initiated by the Eunice Kennedy Shriver National Institute of Child Health and Human Development in 2003. This critical population-based study was conducted at 59 U.S. tertiary care and community hospitals in five catchment areas and has been analyzed in more than 15 published reports.
Women with a previous stillbirth have been known to be at 5- to 10-fold increased risk of a recurrence of stillbirth, and the SCRN findings confirmed this. The study added to our knowledge, however, with the finding that even a prior pregnancy loss at less than 20 weeks’ gestation increased the risk for stillbirth.
Other risk factors identified in the study, in addition to race, included having a multifetal pregnancy (adjusted odds ratio of 4.59), diabetes (AOR of 2.50), maternal age of 40 years or older (AOR of 2.41), maternal AB blood type (AOR of 1.96, compared with type O), a history of drug addiction (AOR of 2.08), smoking during the 3 months prior to pregnancy (AOR of 1.55-1.57, depending on amount), and being unmarried and not cohabitating (AOR of 1.69). Regarding racial disparity, the study showed that elevated risk of stillbirth for non-Hispanic blacks occurred predominantly prior to 24 weeks of gestation.
As in prior research, overweight and obesity also conferred elevated risks in the SCRN study (AORs of 1.43 and 1.72, respectively), and these risks were not explained by either diabetes or hypertension (JAMA. 2011;306:2469-79).
The use of assisted reproductive technology was not included in the study’s multivariate model, but previous research has shown a fourfold increased risk of stillbirth for singleton IVF/ICSI pregnancies. The reason is unclear, but the risk appears to be more related to IVF/ICSI rather than the underlying infertility (Hum Reprod. 2010 May;25[5]:1312-6).
A previous preterm or small-for-gestational-age birth has also been shown in prior research to be a significant risk factor for stillbirth. Less clear is the role of previous cesarean delivery in stillbirth risk. An association has been demonstrated in several studies, however, including one involving about 180,000 singleton pregnancies of 23 or more weeks’ gestation. Women in this cohort who had a previous cesarean delivery had a 1.3-fold increased risk of antepartum stillbirth, after controlling for important factors such as race, body mass index (BMI), and maternal disease (Obstet Gynecol. 2010 Nov;116[5]:1119-26).
In another analysis of the SCRN study looking specifically at causes of stillbirth, a “probable” cause of death was found in 61% of cases and a “possible or probable” cause of death in more than 76% of cases. The most common causes were obstetric complications (29.3%), placental abnormalities (23.6%), fetal genetic/structural abnormalities (13.7%), infection (12.9%), umbilical cord abnormalities (10.4%), hypertensive disorders (9.2%), and other maternal medical conditions (7.8%).
A higher proportion of stillbirths in non-Hispanic black women, compared with non-Hispanic white women and Hispanic women was associated with obstetric complications (43.5%) and infections (25.2%). This finding combined with the finding that stillbirth in black women often occurs at less than 24 weeks’ gestation suggests that measures aimed at reducing the rate of spontaneous preterm birth in black women could potentially reduce the rate of stillbirth as well (JAMA. 2011 Dec 14;306[22]:2459-68).
Work-up and prevention
Prevention of stillbirth requires that we identify the women at highest risk, and thus far this ability still eludes us. Apart from occurrence of previous stillbirth or pregnancy loss, other risk factors have had limited predictive value in the SCRN analyses and other research.
Biomarkers such as a low PAPP-A during the first trimester and a high AFP in the second trimester – as well as Doppler imaging of the uterine artery – have also been associated with stillbirth, but again, the positive predictive value has been shown to be low (Clin Obstet Gynecol. 2010 Sep;53[3]:597-606). More research is needed to determine if some combination of biochemical markers, imaging, and other risk factors can predict which women are at highest risk.
In the meantime, attention can be paid – in the preconception period if possible – to modifiable risk factors such as maternal obesity, diabetes, and smoking. About 10% of stillbirths are associated with maternal conditions such as hypertension and diabetes, and late stillbirths in particular (28 weeks or later) are associated with maternal medical conditions that are potentially preventable.
Normalization of prepregnancy weight should be a goal, since the overall risk of stillbirth appears to increase independently with increasing BMI. Glycemic control should also be achieved: A recent meta-analysis of preconception and prenatal care of diabetic women estimated “conservatively” that 10% of diabetes-associated stillbirths could be prevented with early detection and glycemic control (BMC Public Health. 2011;11 Suppl 3:S2). Research has also shown that women who quit smoking between their first and second pregnancy reduce their stillbirth risk to that of nonsmokers in the second pregnancy (BJOG. 2007 Jun;114[6]:699-704).
When stillbirth happens, a thorough work-up is recommended in order to counsel for future pregnancies and decrease the risk of recurrence. Evaluations for causes of stillbirth are too often incomplete in the United States for various reasons, including emotional, cultural, and resource factors. Even if a cause is not found, many families appreciate knowing that every effort has been made to determine a cause of death.
Four components of evaluation – autopsy, placental examination, karyotype or microarray analysis, and fetal-maternal hemorrhage testing – have proven to be high-yield tests when performed in all cases of stillbirth.
In the SCRN study, of 512 stillbirths undergoing a complete evaluation, 66.4% had a positive result – defined as abnormalities contributing to a probable or possible cause – for at least one of the first three tests (JAMA. 2011 Dec 14;306[22]:2459-68).
A Dutch study of 1,025 stillbirths similarly demonstrated that all four tests are justified. A test was defined as valuable in this study if it established or excluded a cause of stillbirth. Placental examination was determined to be the most valuable test, helping to determine a cause of death in 95.7% of cases. Autopsy was valuable 72.6% of the time, and cytogenetic analysis was valuable in 29% of cases.
Kleihauer-Betke testing for fetal-maternal hemorrhage was positive in 11.9% of women. However, fetal maternal hemorrhage was considered the cause of death in only 1.3%.of cases because, beyond a positive Kleihauer-Betke test, evidence of fetal anemia confirmed by placental examination and/or autopsy was required for hemorrhage to be considered the cause of death (Am. J. Obstet. Gynecol. 2012;206:53.e1-12). Because Kleihauer-Betke testing is ideally performed before induction, authors of both the SCRN study and the Dutch study believe it is a valuable test to be offered in all cases.
In both studies, the yield of other stillbirth diagnostic tests (for example, maternal serology, hormone assessment, and toxicology screen) was low, indicating that these tests are considered sequential and can be performed only when the clinical history or findings of the four core tests raise suspicion of particular potential causes. Antinuclear antibody testing and TORCH (toxoplasmosis, rubella, cytomegalovirus, herpes simplex) titers have an extremely low yield and are generally not useful.
For detecting genetic abnormalities after stillbirth, it appears that microarray analysis is superior to karyotype analysis. In a SCRN analysis of samples from 532 stillbirths, microarray yielded results more often and identified more genetic abnormalities. Unlike karyotype, it does not require live cells, which makes it preferable for stillbirth evaluation (N Engl J Med. 2012 Dec 6;367[23]:2185-93).
Current research
One of the more significant studies underway on prevention is looking at labor induction as an intervention for reducing stillbirths and improving other perinatal outcomes. The ARRIVE trial (“A Randomized Trial of Induction Versus Expectant Management”), currently in the recruitment stage, will examine outcomes after induction at 39 weeks’ gestation, compared with expectant management in 6,000 patients (clinicaltrials.gov/ct2/show/NCT01990612).
Common wisdom informed by retrospective cohort studies has long told us that inducing labor prior to 41 weeks’ gestation is associated with a higher risk of cesarean delivery in nulliparous women. However, recent observational data have suggested that women whose labor is induced actually have fewer cesarean deliveries and better perinatal outcomes, including a lower risk of stillbirth (AJOG 2012;207:502.e1-8).
In addition, a meta-analysis published in 2014, as the ARRIVE trial was taking shape, reported a 12% reduction in cesarean delivery, and a reduced risk of stillbirth, among women whose labor was induced. The initial cervical score did not impact the main findings (CMAJ. 2014 Jun 10;186[9]:665-73). If these findings are confirmed in the ARRIVE trial, we could see a new opportunity for stillbirth prevention.
Another ongoing study of 10,000 singleton pregnancies – the Nulliparous Pregnancy Outcomes: Monitoring Mothers-to-Be (nuMoM2b) study – may also lead to prevention strategies in women for whom the current pregnancy will lead to their first delivery. Among the questions being examined in this eight-site study are whether sleep-disordered breathing, or apnea, and a supine sleep position are risk factors for adverse pregnancy outcomes including stillbirth.
Supine sleeping in the last month of pregnancy was strongly associated with stillbirth in a recent analysis from the Sydney Stillbirth Study (Obstet Gynecol. 2015 Feb;125[2]:347-55), and an early analysis of a nuMoM2b subset has shown associations between sleep-disordered breathing in midpregnancy and the development of hypertensive disorders of pregnancy, and between sleep-disordered breathing in early- and mid-pregnancy and gestational diabetes (Am J Obstet Gynecol. 2015;212:S424-425).
The possible role of low-dose aspirin in preventing stillbirth also needs more exploration. A recent randomized trial of women attempting to become pregnant after having had one or two prior pregnancy losses found no difference overall in live birth rates between those who took low-dose aspirin and those assigned to placebo. However, there was one subgroup – women with a single loss at less than 20 weeks’ gestation during the previous year – in which live birth rates were higher in the aspirin group (Lancet. 2014 Jul 5;384[9937]:29-36). More research is necessary to determine if low-dose aspirin administration in women with a previous stillbirth improves pregnancy outcome.
Dr. Reddy is a member at the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. She is a board-certified ob.gyn. and maternal-fetal medicine specialist. She is the program scientist for the Maternal-Fetal Medicine Units Network and for the Stillbirth Collaborative Research Network. The comments and views of the author do not necessarily represent the views of the NICHD.
Biologic treatment in pregnancy requires balancing risks
The effectiveness of immunoglobulin biologic treatments in controlling chronic and potentially debilitating autoimmune diseases such as rheumatoid arthritis and ulcerative colitis means that more physicians are faced with the question of how to handle the use of these drugs in pregnancy.
While immunoglobulin G (IgG) biologicals are large molecules, there is no doubt that they cross the placenta through specific transport systems with a long half life in infants, creating potential risks for immunocompromise in early life. At the same time, these biologicals are essential, in many cases, for controlling the pregnant woman’s disease and allowing her to carry a pregnancy successfully by avoiding disease flare.
For ob.gyns., successful management of a pregnancy in which the woman is taking an immunoglobulin biological, such as an anti–tumor necrosis factor (TNF)-alpha agent, requires an understanding of not only which drugs cross the placenta, but when they do so and at what levels.
Crossing the placenta
Along with my student Juejing Ling, I recently reviewed the question of how the use of immunoglobulin biologicals in pregnancy affects the vaccination of infants in an article published in Expert Review of Vaccines (2015 Dec 7:1-18 doi: 10.1586/14760584.2016.1115351). Our analysis relates only to biologicals with partial or full IgG structure, as they are capable of crossing the placenta.
Data are still limited about the use of immunoglobulin biologicals in pregnancy, but measurement of umbilical cord blood has shown high levels of anti-TNF IgG in newborn serum, raising concerns about how these neonates will respond to vaccinations.
Neonates rely on maternal IgG transport to prevent infection in the first few months of life and that transport process begins around 12 weeks gestation. Fetal IgG levels begin to rise at 13-18 weeks and reach 120%-130% of maternal levels when the fetus reaches full term. In contrast, fusion proteins that contain the Fc portion and Fab fragment appear to have limited ability to cross the placenta. As a result, chimeric and full human IgG antibodies such as infliximab, adalimumab, and rituximab have demonstrated high levels of placental transport, while other agents, such as etanercept, appear to cross the placenta at lower levels.
Hence, due to the ineffective clearance, certain immunoglobulin biologicals actually have a higher concentration and a longer half life in neonates than in mothers. For instance, with infliximab, studies show that levels in the umbilical cord were up to fourfold higher than maternal levels, even when the drug was discontinued at 30 weeks of pregnancy or earlier. Due to long neonatal half life, infliximab levels became undetectable in infant serum only between 2-7 months, compared with 1-2 weeks in adults. Adalimumab is similar, where concentrations of the drug in neonates can be 150% of the maternal serum level and detectable for about 3 months after birth.
Transport of anti-TNFs is also possible through breastfeeding, although studies indicate that the levels are very low.
Infection risk
Due to the immunosuppressive effect of anti-TNF immunoglobulin biologicals, newborn infection is a real concern. Review of the literature showed that severe and moderate neutropenia and skin infection were reported in four neonates born to two women with ulcerative colitis who had taken infliximab throughout pregnancy.
Some other studies have followed infants who had detectable biological levels at birth after in utero exposure. In general, there is normal development in the first year without overt infection. However, there have been case reports of infections with varicella or upper respiratory infections in infants exposed to infliximab before 30 weeks’ gestation.
There is very little data on the long-term immune system impacts for infants exposed to immunoglobulin biologicals in utero. However, these agents are generally not at detectable levels after 1 year.
Impact on vaccination
Although these IgG biologicals will clear the infants’ systems after several months of life (generally by 8 months), another concern is for how their presence in the early months impacts neonatal vaccination, specifically live attenuated vaccines such as MMR (measles, mumps and rubella), BCG for tuberculosis, oral polio, rotavirus vaccine, and the intranasal influenza vaccine.
Generally, outcomes among infants exposed to anti-TNFs have been good. For instance, reports looking at 24 children with exposure to anti-TNFs found no complications with the MMR vaccine. But a famous case report identified one infant who died at 4.5 months after receiving the BCG vaccine at 3 months. The mother, who had Crohn’s disease, had been taking infliximab 10 mg/kg every 8 weeks throughout her pregnancy.
Another study of 15 infants in the Czech Republic who were exposed to infliximab in utero and received BCG vaccination within 1 week of birth found that three of the infants developed large local skin reactions. One of the three children also developed axillary lymphadenopathy. All of the children recovered without the need for anti-tuberculosis therapy.
So what do these complications mean for vaccination strategies? Both the European Crohn’s and Colitis Organisation and the World Congress of Gastroenterology recommend that in terms of non-live vaccines, it’s safe to follow the same vaccine schedule as infants not exposed to biologicals in utero. When it comes to live attenuated vaccines such as rotavirus, oral polio, and BCG, these infants should be treated as immunocompromised and not receive these vaccines until after 6 months of age, when the biologicals should be at undetectable levels.
Future directions
Given that most infections and other adverse events happen after late exposure in pregnancy, some have recommended discontinuing anti-TNF treatment before the third trimester. In fact, this has become a common management practice. However, this should be an individualized decision made after discussion between a woman and her physician or physicians. Any benefits from early discontinuation of an immunoglobulin biological therapy should be weighed against the risk of disease flare, which also has real potential to complicate pregnancy.
The evidence presented here not only shines a light on the possible risk to infants, but also on the need for more high-quality evidence on which physicians can base decisions. Most of the available evidence is drawn from case reports and registry databases. Both of these suffer from a lack of control groups. To answer these questions definitively, we need more well-controlled studies of large populations. I strongly urge readers to follow the amazing work led by Dr. Uma Mahadevan and her colleagues at the University of California, San Francisco on biological use in pregnancy and long-term outcomes. As we wait for more evidence, we all look forward to the development of newer biologic agents that can help women control autoimmune disease without crossing the placenta.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He reported having no financial disclosures related to this article. Email him at [email protected].
The effectiveness of immunoglobulin biologic treatments in controlling chronic and potentially debilitating autoimmune diseases such as rheumatoid arthritis and ulcerative colitis means that more physicians are faced with the question of how to handle the use of these drugs in pregnancy.
While immunoglobulin G (IgG) biologicals are large molecules, there is no doubt that they cross the placenta through specific transport systems with a long half life in infants, creating potential risks for immunocompromise in early life. At the same time, these biologicals are essential, in many cases, for controlling the pregnant woman’s disease and allowing her to carry a pregnancy successfully by avoiding disease flare.
For ob.gyns., successful management of a pregnancy in which the woman is taking an immunoglobulin biological, such as an anti–tumor necrosis factor (TNF)-alpha agent, requires an understanding of not only which drugs cross the placenta, but when they do so and at what levels.
Crossing the placenta
Along with my student Juejing Ling, I recently reviewed the question of how the use of immunoglobulin biologicals in pregnancy affects the vaccination of infants in an article published in Expert Review of Vaccines (2015 Dec 7:1-18 doi: 10.1586/14760584.2016.1115351). Our analysis relates only to biologicals with partial or full IgG structure, as they are capable of crossing the placenta.
Data are still limited about the use of immunoglobulin biologicals in pregnancy, but measurement of umbilical cord blood has shown high levels of anti-TNF IgG in newborn serum, raising concerns about how these neonates will respond to vaccinations.
Neonates rely on maternal IgG transport to prevent infection in the first few months of life and that transport process begins around 12 weeks gestation. Fetal IgG levels begin to rise at 13-18 weeks and reach 120%-130% of maternal levels when the fetus reaches full term. In contrast, fusion proteins that contain the Fc portion and Fab fragment appear to have limited ability to cross the placenta. As a result, chimeric and full human IgG antibodies such as infliximab, adalimumab, and rituximab have demonstrated high levels of placental transport, while other agents, such as etanercept, appear to cross the placenta at lower levels.
Hence, due to the ineffective clearance, certain immunoglobulin biologicals actually have a higher concentration and a longer half life in neonates than in mothers. For instance, with infliximab, studies show that levels in the umbilical cord were up to fourfold higher than maternal levels, even when the drug was discontinued at 30 weeks of pregnancy or earlier. Due to long neonatal half life, infliximab levels became undetectable in infant serum only between 2-7 months, compared with 1-2 weeks in adults. Adalimumab is similar, where concentrations of the drug in neonates can be 150% of the maternal serum level and detectable for about 3 months after birth.
Transport of anti-TNFs is also possible through breastfeeding, although studies indicate that the levels are very low.
Infection risk
Due to the immunosuppressive effect of anti-TNF immunoglobulin biologicals, newborn infection is a real concern. Review of the literature showed that severe and moderate neutropenia and skin infection were reported in four neonates born to two women with ulcerative colitis who had taken infliximab throughout pregnancy.
Some other studies have followed infants who had detectable biological levels at birth after in utero exposure. In general, there is normal development in the first year without overt infection. However, there have been case reports of infections with varicella or upper respiratory infections in infants exposed to infliximab before 30 weeks’ gestation.
There is very little data on the long-term immune system impacts for infants exposed to immunoglobulin biologicals in utero. However, these agents are generally not at detectable levels after 1 year.
Impact on vaccination
Although these IgG biologicals will clear the infants’ systems after several months of life (generally by 8 months), another concern is for how their presence in the early months impacts neonatal vaccination, specifically live attenuated vaccines such as MMR (measles, mumps and rubella), BCG for tuberculosis, oral polio, rotavirus vaccine, and the intranasal influenza vaccine.
Generally, outcomes among infants exposed to anti-TNFs have been good. For instance, reports looking at 24 children with exposure to anti-TNFs found no complications with the MMR vaccine. But a famous case report identified one infant who died at 4.5 months after receiving the BCG vaccine at 3 months. The mother, who had Crohn’s disease, had been taking infliximab 10 mg/kg every 8 weeks throughout her pregnancy.
Another study of 15 infants in the Czech Republic who were exposed to infliximab in utero and received BCG vaccination within 1 week of birth found that three of the infants developed large local skin reactions. One of the three children also developed axillary lymphadenopathy. All of the children recovered without the need for anti-tuberculosis therapy.
So what do these complications mean for vaccination strategies? Both the European Crohn’s and Colitis Organisation and the World Congress of Gastroenterology recommend that in terms of non-live vaccines, it’s safe to follow the same vaccine schedule as infants not exposed to biologicals in utero. When it comes to live attenuated vaccines such as rotavirus, oral polio, and BCG, these infants should be treated as immunocompromised and not receive these vaccines until after 6 months of age, when the biologicals should be at undetectable levels.
Future directions
Given that most infections and other adverse events happen after late exposure in pregnancy, some have recommended discontinuing anti-TNF treatment before the third trimester. In fact, this has become a common management practice. However, this should be an individualized decision made after discussion between a woman and her physician or physicians. Any benefits from early discontinuation of an immunoglobulin biological therapy should be weighed against the risk of disease flare, which also has real potential to complicate pregnancy.
The evidence presented here not only shines a light on the possible risk to infants, but also on the need for more high-quality evidence on which physicians can base decisions. Most of the available evidence is drawn from case reports and registry databases. Both of these suffer from a lack of control groups. To answer these questions definitively, we need more well-controlled studies of large populations. I strongly urge readers to follow the amazing work led by Dr. Uma Mahadevan and her colleagues at the University of California, San Francisco on biological use in pregnancy and long-term outcomes. As we wait for more evidence, we all look forward to the development of newer biologic agents that can help women control autoimmune disease without crossing the placenta.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He reported having no financial disclosures related to this article. Email him at [email protected].
The effectiveness of immunoglobulin biologic treatments in controlling chronic and potentially debilitating autoimmune diseases such as rheumatoid arthritis and ulcerative colitis means that more physicians are faced with the question of how to handle the use of these drugs in pregnancy.
While immunoglobulin G (IgG) biologicals are large molecules, there is no doubt that they cross the placenta through specific transport systems with a long half life in infants, creating potential risks for immunocompromise in early life. At the same time, these biologicals are essential, in many cases, for controlling the pregnant woman’s disease and allowing her to carry a pregnancy successfully by avoiding disease flare.
For ob.gyns., successful management of a pregnancy in which the woman is taking an immunoglobulin biological, such as an anti–tumor necrosis factor (TNF)-alpha agent, requires an understanding of not only which drugs cross the placenta, but when they do so and at what levels.
Crossing the placenta
Along with my student Juejing Ling, I recently reviewed the question of how the use of immunoglobulin biologicals in pregnancy affects the vaccination of infants in an article published in Expert Review of Vaccines (2015 Dec 7:1-18 doi: 10.1586/14760584.2016.1115351). Our analysis relates only to biologicals with partial or full IgG structure, as they are capable of crossing the placenta.
Data are still limited about the use of immunoglobulin biologicals in pregnancy, but measurement of umbilical cord blood has shown high levels of anti-TNF IgG in newborn serum, raising concerns about how these neonates will respond to vaccinations.
Neonates rely on maternal IgG transport to prevent infection in the first few months of life and that transport process begins around 12 weeks gestation. Fetal IgG levels begin to rise at 13-18 weeks and reach 120%-130% of maternal levels when the fetus reaches full term. In contrast, fusion proteins that contain the Fc portion and Fab fragment appear to have limited ability to cross the placenta. As a result, chimeric and full human IgG antibodies such as infliximab, adalimumab, and rituximab have demonstrated high levels of placental transport, while other agents, such as etanercept, appear to cross the placenta at lower levels.
Hence, due to the ineffective clearance, certain immunoglobulin biologicals actually have a higher concentration and a longer half life in neonates than in mothers. For instance, with infliximab, studies show that levels in the umbilical cord were up to fourfold higher than maternal levels, even when the drug was discontinued at 30 weeks of pregnancy or earlier. Due to long neonatal half life, infliximab levels became undetectable in infant serum only between 2-7 months, compared with 1-2 weeks in adults. Adalimumab is similar, where concentrations of the drug in neonates can be 150% of the maternal serum level and detectable for about 3 months after birth.
Transport of anti-TNFs is also possible through breastfeeding, although studies indicate that the levels are very low.
Infection risk
Due to the immunosuppressive effect of anti-TNF immunoglobulin biologicals, newborn infection is a real concern. Review of the literature showed that severe and moderate neutropenia and skin infection were reported in four neonates born to two women with ulcerative colitis who had taken infliximab throughout pregnancy.
Some other studies have followed infants who had detectable biological levels at birth after in utero exposure. In general, there is normal development in the first year without overt infection. However, there have been case reports of infections with varicella or upper respiratory infections in infants exposed to infliximab before 30 weeks’ gestation.
There is very little data on the long-term immune system impacts for infants exposed to immunoglobulin biologicals in utero. However, these agents are generally not at detectable levels after 1 year.
Impact on vaccination
Although these IgG biologicals will clear the infants’ systems after several months of life (generally by 8 months), another concern is for how their presence in the early months impacts neonatal vaccination, specifically live attenuated vaccines such as MMR (measles, mumps and rubella), BCG for tuberculosis, oral polio, rotavirus vaccine, and the intranasal influenza vaccine.
Generally, outcomes among infants exposed to anti-TNFs have been good. For instance, reports looking at 24 children with exposure to anti-TNFs found no complications with the MMR vaccine. But a famous case report identified one infant who died at 4.5 months after receiving the BCG vaccine at 3 months. The mother, who had Crohn’s disease, had been taking infliximab 10 mg/kg every 8 weeks throughout her pregnancy.
Another study of 15 infants in the Czech Republic who were exposed to infliximab in utero and received BCG vaccination within 1 week of birth found that three of the infants developed large local skin reactions. One of the three children also developed axillary lymphadenopathy. All of the children recovered without the need for anti-tuberculosis therapy.
So what do these complications mean for vaccination strategies? Both the European Crohn’s and Colitis Organisation and the World Congress of Gastroenterology recommend that in terms of non-live vaccines, it’s safe to follow the same vaccine schedule as infants not exposed to biologicals in utero. When it comes to live attenuated vaccines such as rotavirus, oral polio, and BCG, these infants should be treated as immunocompromised and not receive these vaccines until after 6 months of age, when the biologicals should be at undetectable levels.
Future directions
Given that most infections and other adverse events happen after late exposure in pregnancy, some have recommended discontinuing anti-TNF treatment before the third trimester. In fact, this has become a common management practice. However, this should be an individualized decision made after discussion between a woman and her physician or physicians. Any benefits from early discontinuation of an immunoglobulin biological therapy should be weighed against the risk of disease flare, which also has real potential to complicate pregnancy.
The evidence presented here not only shines a light on the possible risk to infants, but also on the need for more high-quality evidence on which physicians can base decisions. Most of the available evidence is drawn from case reports and registry databases. Both of these suffer from a lack of control groups. To answer these questions definitively, we need more well-controlled studies of large populations. I strongly urge readers to follow the amazing work led by Dr. Uma Mahadevan and her colleagues at the University of California, San Francisco on biological use in pregnancy and long-term outcomes. As we wait for more evidence, we all look forward to the development of newer biologic agents that can help women control autoimmune disease without crossing the placenta.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He reported having no financial disclosures related to this article. Email him at [email protected].
Pretreatment hydroquinone for nonablative laser resurfacing of acne scars?
Pretreatment of skin prior to nonablative or ablative laser resurfacing is common practice, particularly in darker skin types. Treatment regimens include using hydroquinone 4% (and other hydroquinone-containing combinations) once to twice daily for 1-2 weeks prior to the laser procedure. The rationale makes sense. Quieting melanin production by inhibiting tyrosinase would seem to decrease the incidence of postinflammatory hyperpigmentation after laser resurfacing procedures. But is this common practice effective?
For ablative CO2 resurfacing in 100 patients Fitzpatrick Skin Types (FST) I-III, there was no significant difference in the incidence of hyperpigmentation in those randomized to be pretreated with either hydroquinone, glycolic acid, tretinoin, or to no treatment.1 The thought was that the follicular melanocytes involved in re-epithelialization were not affected by the pretreatment. This is the only published laser resurfacing today to date examining various pretreatment protocols with hyperpigmentation as a primary study outcome. From this study, it seems as though pretreatment before laser resurfacing is not helpful, but what about for nonablative resurfacing in darker skin types (FST IV-VI)?
In darker skin types (FST IV-VI), the risk of postinflammatory hyperpigmentation (PIH) is inherently higher and the incidence after laser resurfacing is greater. While the incidence of PIH is lower with nonablative fractional resurfacing, compared with ablative resurfacing, PIH can still occur whether pretreatment hydroquinone is used or not.2,3,4 To date, there are no published studies looking at the incidence of PIH when comparing pretreatment antipigment agents versus no pretreatment for laser resurfacing for acne scars in darker skin types. A split-face study comparing pretreatment on one side and no pretreatment on the other could help delineate whether this practice is evidence based.
For nonablative fractional laser resurfacing of acne scars, lower densities in darker skin types are recommended and may help reduce PIH risk. There is no statistically significant difference in improvement of acne scars in using low versus high densities using the same fluences. However, some studies note that higher densities clinically resulted in a mild improvement of acne scars over lower densities (not statistically significant); thus, if lower densities are used, it is possible that more treatments may be needed.4,5
Vigorous sun protection before and after treatment is prudent, with sun avoidance and physical sunscreens reducing the risk of PIH in darker skin from irritant or allergic contact dermatitis, compared with chemical sunscreens. If PIH occurs, it is often self limited (up to 1-2 months). Sun protection and posttreatment regimens of hydroquinone (or other lightening agent) aid in hastening improvement.
If the patient is undergoing nonablative laser resurfacing to treat pigmentation, such as melasma, then hydroquinone pre- and postlaser is appropriate. In my opinion, laser treatment of melasma should not be first line because of safety and efficacy concerns. However, in these cases, hydroquinone prior to laser has shown benefit.6 In addition, hydroquinone after nonablative fractional resurfacing may enhance penetration of the topical and improve efficacy.
In summary, the evidence shows that pretreatment with antipigment agents is not warranted in skin types I-III for ablative laser resurfacing. Pretreatment with antipigment agents for nonablative laser resurfacing for melasma (which should not be considered a first line treatment for melasma) is warranted. However, at this time, it is not clear whether pretreatment with antipigments for nonablative laser resurfacing for acne scars in darker skin types is useful. Lower densities should be used and if PIH does occur, it is usually self limited, and posttreatment hydroquinone or other antipigment agents may be useful.
References
1. Dermatol Surg. 1999 Jan;25(1):15-7.
2. Dermatol Surg. 2010 May;36(5):602-9.
3. Br J Dermatol. 2012 Jun;166(6):1160-9.
4.Lasers Surg Med. 2007 Jun;39(5):381-5.
5. Lasers Surg Med. 2007 Apr;39(4):311-4.
6. Dermatol Surg. 2010 Jun;36(6):909-18.
Dr. Wesley and Dr. Talakoub are co-contributors to the monthly Aesthetic Dermatology column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
Pretreatment of skin prior to nonablative or ablative laser resurfacing is common practice, particularly in darker skin types. Treatment regimens include using hydroquinone 4% (and other hydroquinone-containing combinations) once to twice daily for 1-2 weeks prior to the laser procedure. The rationale makes sense. Quieting melanin production by inhibiting tyrosinase would seem to decrease the incidence of postinflammatory hyperpigmentation after laser resurfacing procedures. But is this common practice effective?
For ablative CO2 resurfacing in 100 patients Fitzpatrick Skin Types (FST) I-III, there was no significant difference in the incidence of hyperpigmentation in those randomized to be pretreated with either hydroquinone, glycolic acid, tretinoin, or to no treatment.1 The thought was that the follicular melanocytes involved in re-epithelialization were not affected by the pretreatment. This is the only published laser resurfacing today to date examining various pretreatment protocols with hyperpigmentation as a primary study outcome. From this study, it seems as though pretreatment before laser resurfacing is not helpful, but what about for nonablative resurfacing in darker skin types (FST IV-VI)?
In darker skin types (FST IV-VI), the risk of postinflammatory hyperpigmentation (PIH) is inherently higher and the incidence after laser resurfacing is greater. While the incidence of PIH is lower with nonablative fractional resurfacing, compared with ablative resurfacing, PIH can still occur whether pretreatment hydroquinone is used or not.2,3,4 To date, there are no published studies looking at the incidence of PIH when comparing pretreatment antipigment agents versus no pretreatment for laser resurfacing for acne scars in darker skin types. A split-face study comparing pretreatment on one side and no pretreatment on the other could help delineate whether this practice is evidence based.
For nonablative fractional laser resurfacing of acne scars, lower densities in darker skin types are recommended and may help reduce PIH risk. There is no statistically significant difference in improvement of acne scars in using low versus high densities using the same fluences. However, some studies note that higher densities clinically resulted in a mild improvement of acne scars over lower densities (not statistically significant); thus, if lower densities are used, it is possible that more treatments may be needed.4,5
Vigorous sun protection before and after treatment is prudent, with sun avoidance and physical sunscreens reducing the risk of PIH in darker skin from irritant or allergic contact dermatitis, compared with chemical sunscreens. If PIH occurs, it is often self limited (up to 1-2 months). Sun protection and posttreatment regimens of hydroquinone (or other lightening agent) aid in hastening improvement.
If the patient is undergoing nonablative laser resurfacing to treat pigmentation, such as melasma, then hydroquinone pre- and postlaser is appropriate. In my opinion, laser treatment of melasma should not be first line because of safety and efficacy concerns. However, in these cases, hydroquinone prior to laser has shown benefit.6 In addition, hydroquinone after nonablative fractional resurfacing may enhance penetration of the topical and improve efficacy.
In summary, the evidence shows that pretreatment with antipigment agents is not warranted in skin types I-III for ablative laser resurfacing. Pretreatment with antipigment agents for nonablative laser resurfacing for melasma (which should not be considered a first line treatment for melasma) is warranted. However, at this time, it is not clear whether pretreatment with antipigments for nonablative laser resurfacing for acne scars in darker skin types is useful. Lower densities should be used and if PIH does occur, it is usually self limited, and posttreatment hydroquinone or other antipigment agents may be useful.
References
1. Dermatol Surg. 1999 Jan;25(1):15-7.
2. Dermatol Surg. 2010 May;36(5):602-9.
3. Br J Dermatol. 2012 Jun;166(6):1160-9.
4.Lasers Surg Med. 2007 Jun;39(5):381-5.
5. Lasers Surg Med. 2007 Apr;39(4):311-4.
6. Dermatol Surg. 2010 Jun;36(6):909-18.
Dr. Wesley and Dr. Talakoub are co-contributors to the monthly Aesthetic Dermatology column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
Pretreatment of skin prior to nonablative or ablative laser resurfacing is common practice, particularly in darker skin types. Treatment regimens include using hydroquinone 4% (and other hydroquinone-containing combinations) once to twice daily for 1-2 weeks prior to the laser procedure. The rationale makes sense. Quieting melanin production by inhibiting tyrosinase would seem to decrease the incidence of postinflammatory hyperpigmentation after laser resurfacing procedures. But is this common practice effective?
For ablative CO2 resurfacing in 100 patients Fitzpatrick Skin Types (FST) I-III, there was no significant difference in the incidence of hyperpigmentation in those randomized to be pretreated with either hydroquinone, glycolic acid, tretinoin, or to no treatment.1 The thought was that the follicular melanocytes involved in re-epithelialization were not affected by the pretreatment. This is the only published laser resurfacing today to date examining various pretreatment protocols with hyperpigmentation as a primary study outcome. From this study, it seems as though pretreatment before laser resurfacing is not helpful, but what about for nonablative resurfacing in darker skin types (FST IV-VI)?
In darker skin types (FST IV-VI), the risk of postinflammatory hyperpigmentation (PIH) is inherently higher and the incidence after laser resurfacing is greater. While the incidence of PIH is lower with nonablative fractional resurfacing, compared with ablative resurfacing, PIH can still occur whether pretreatment hydroquinone is used or not.2,3,4 To date, there are no published studies looking at the incidence of PIH when comparing pretreatment antipigment agents versus no pretreatment for laser resurfacing for acne scars in darker skin types. A split-face study comparing pretreatment on one side and no pretreatment on the other could help delineate whether this practice is evidence based.
For nonablative fractional laser resurfacing of acne scars, lower densities in darker skin types are recommended and may help reduce PIH risk. There is no statistically significant difference in improvement of acne scars in using low versus high densities using the same fluences. However, some studies note that higher densities clinically resulted in a mild improvement of acne scars over lower densities (not statistically significant); thus, if lower densities are used, it is possible that more treatments may be needed.4,5
Vigorous sun protection before and after treatment is prudent, with sun avoidance and physical sunscreens reducing the risk of PIH in darker skin from irritant or allergic contact dermatitis, compared with chemical sunscreens. If PIH occurs, it is often self limited (up to 1-2 months). Sun protection and posttreatment regimens of hydroquinone (or other lightening agent) aid in hastening improvement.
If the patient is undergoing nonablative laser resurfacing to treat pigmentation, such as melasma, then hydroquinone pre- and postlaser is appropriate. In my opinion, laser treatment of melasma should not be first line because of safety and efficacy concerns. However, in these cases, hydroquinone prior to laser has shown benefit.6 In addition, hydroquinone after nonablative fractional resurfacing may enhance penetration of the topical and improve efficacy.
In summary, the evidence shows that pretreatment with antipigment agents is not warranted in skin types I-III for ablative laser resurfacing. Pretreatment with antipigment agents for nonablative laser resurfacing for melasma (which should not be considered a first line treatment for melasma) is warranted. However, at this time, it is not clear whether pretreatment with antipigments for nonablative laser resurfacing for acne scars in darker skin types is useful. Lower densities should be used and if PIH does occur, it is usually self limited, and posttreatment hydroquinone or other antipigment agents may be useful.
References
1. Dermatol Surg. 1999 Jan;25(1):15-7.
2. Dermatol Surg. 2010 May;36(5):602-9.
3. Br J Dermatol. 2012 Jun;166(6):1160-9.
4.Lasers Surg Med. 2007 Jun;39(5):381-5.
5. Lasers Surg Med. 2007 Apr;39(4):311-4.
6. Dermatol Surg. 2010 Jun;36(6):909-18.
Dr. Wesley and Dr. Talakoub are co-contributors to the monthly Aesthetic Dermatology column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
Transitions
This month will mark the end of my 10-year tenure as Editor-in-Chief of The American Journal of Orthopedics (AJO). Every successful organization goes through periodic transitions, where past successes are reviewed and future challenges addressed. AJO is no different. I would like to reflect on these past 10 years, share some highlights, and acknowledge those who have contributed to the success of AJO.
The Editorial Staff of the Journal has consistently performed beyond the call of duty, producing outstanding issues month after month. Of this excellent team, several members deserve special mention: Group Editor Glenn Williams, Managing Editor Joseph Kinsley, and Assistant Editor Kellie DeSantis. I offer my gratitude to all for a job well done.
I am particularly proud that under my leadership, the Editorial Board nearly doubled and clinical submissions increased almost 4-fold. I want to thank all members of the Editorial Board. Your expertise and dedication has enabled AJO to accommodate the vast increase in submissions and greatly improved the quality of papers published in recent years. I have so appreciated your efforts and hard work.
The addition of the Residency Advisory Board several years ago provided an excellent forum for orthopedic surgeons in training to share their thoughts on subjects of particular interest and address issues not typically covered during the course of their clinical training; such as the importance of mentorship, how to organize a practice, and how to decipher an employment contract for one’s first “real” job. I have been immensely impressed with residents’ insights and their willingness to share them with their colleagues. I hope that this experience at AJO will encourage them to join other Editorial Boards during their professional careers.
Over these past 10 years, I have tried to satisfy the mission of The American Journal of Orthopedics: “… to provide timely, practical, and readable technical information of the highest caliber to the orthopedic surgeon involved in the everyday practice of orthopedics.” To this end, I expanded the “expert opinion” 5 Points series originally introduced by John Gould, MD, my predecessor as Editor-in-Chief. In addition, I added the Practice Management articles, prepared by Karen Zupko and her associates, which have been especially informative and popular.
I have thoroughly enjoyed sharing with you my nonclinical editorials touching on the “topics of the day.” Among my favorites were “Customer Satisfaction: Are Hospitals ‘Hospitable’?”1 which anticipated the growing influence of patient satisfaction scores in our professional lives; and “Are Surgeons Accepting Bribes?”,2 addressing a subject that predated the 2007 Deferred Prosecution Agreement3 which has transformed the relationships between orthopedic surgeons and the orthopedic device industry. I hope you have enjoyed reading my musings as much as I enjoyed writing them.
Our incoming Editor-in-Chief is Bryan T. Hanypsiak, MD, Director of Sports Medicine, Peconic Bay Medical Center in Riverhead, New York, and Chairman of the September 2015 Innovative Techniques: The Knee Course, sponsored by AJO in Las Vegas. Bryan will remain committed to the original mission of AJO and its high editorial and peer reviewed standards. However, the format will change with the March 2016 issue and have the feel of a clinical magazine. I have every confidence that, with Dr. Hanypsiak’s leadership and the support of the publisher, the AJO brand will continue to thrive in an ever-changing and challenging marketplace.
Finally, I wish to thank all the readers of AJO who have supported the Journal, one of only a handful of orthopedic publications that still caters to the professional interests of the general orthopedic surgeon with a comprehensive scope of clinical and non-clinical topics. Leading the Board as Editor-in-Chief has been one of the most fulfilling and rewarding activities of my professional career, and it has truly been my honor to serve you. I wish all of you the best.
1. McCann PD. Customer satisfaction: are hospitals “hospitable”? Am J Orthop. 2006;35(2):59.
2. McCann PD. Are surgeons accepting bribes? Am J Orthop. 2006;35(3):114.
3. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed January 11, 2016.
This month will mark the end of my 10-year tenure as Editor-in-Chief of The American Journal of Orthopedics (AJO). Every successful organization goes through periodic transitions, where past successes are reviewed and future challenges addressed. AJO is no different. I would like to reflect on these past 10 years, share some highlights, and acknowledge those who have contributed to the success of AJO.
The Editorial Staff of the Journal has consistently performed beyond the call of duty, producing outstanding issues month after month. Of this excellent team, several members deserve special mention: Group Editor Glenn Williams, Managing Editor Joseph Kinsley, and Assistant Editor Kellie DeSantis. I offer my gratitude to all for a job well done.
I am particularly proud that under my leadership, the Editorial Board nearly doubled and clinical submissions increased almost 4-fold. I want to thank all members of the Editorial Board. Your expertise and dedication has enabled AJO to accommodate the vast increase in submissions and greatly improved the quality of papers published in recent years. I have so appreciated your efforts and hard work.
The addition of the Residency Advisory Board several years ago provided an excellent forum for orthopedic surgeons in training to share their thoughts on subjects of particular interest and address issues not typically covered during the course of their clinical training; such as the importance of mentorship, how to organize a practice, and how to decipher an employment contract for one’s first “real” job. I have been immensely impressed with residents’ insights and their willingness to share them with their colleagues. I hope that this experience at AJO will encourage them to join other Editorial Boards during their professional careers.
Over these past 10 years, I have tried to satisfy the mission of The American Journal of Orthopedics: “… to provide timely, practical, and readable technical information of the highest caliber to the orthopedic surgeon involved in the everyday practice of orthopedics.” To this end, I expanded the “expert opinion” 5 Points series originally introduced by John Gould, MD, my predecessor as Editor-in-Chief. In addition, I added the Practice Management articles, prepared by Karen Zupko and her associates, which have been especially informative and popular.
I have thoroughly enjoyed sharing with you my nonclinical editorials touching on the “topics of the day.” Among my favorites were “Customer Satisfaction: Are Hospitals ‘Hospitable’?”1 which anticipated the growing influence of patient satisfaction scores in our professional lives; and “Are Surgeons Accepting Bribes?”,2 addressing a subject that predated the 2007 Deferred Prosecution Agreement3 which has transformed the relationships between orthopedic surgeons and the orthopedic device industry. I hope you have enjoyed reading my musings as much as I enjoyed writing them.
Our incoming Editor-in-Chief is Bryan T. Hanypsiak, MD, Director of Sports Medicine, Peconic Bay Medical Center in Riverhead, New York, and Chairman of the September 2015 Innovative Techniques: The Knee Course, sponsored by AJO in Las Vegas. Bryan will remain committed to the original mission of AJO and its high editorial and peer reviewed standards. However, the format will change with the March 2016 issue and have the feel of a clinical magazine. I have every confidence that, with Dr. Hanypsiak’s leadership and the support of the publisher, the AJO brand will continue to thrive in an ever-changing and challenging marketplace.
Finally, I wish to thank all the readers of AJO who have supported the Journal, one of only a handful of orthopedic publications that still caters to the professional interests of the general orthopedic surgeon with a comprehensive scope of clinical and non-clinical topics. Leading the Board as Editor-in-Chief has been one of the most fulfilling and rewarding activities of my professional career, and it has truly been my honor to serve you. I wish all of you the best.
This month will mark the end of my 10-year tenure as Editor-in-Chief of The American Journal of Orthopedics (AJO). Every successful organization goes through periodic transitions, where past successes are reviewed and future challenges addressed. AJO is no different. I would like to reflect on these past 10 years, share some highlights, and acknowledge those who have contributed to the success of AJO.
The Editorial Staff of the Journal has consistently performed beyond the call of duty, producing outstanding issues month after month. Of this excellent team, several members deserve special mention: Group Editor Glenn Williams, Managing Editor Joseph Kinsley, and Assistant Editor Kellie DeSantis. I offer my gratitude to all for a job well done.
I am particularly proud that under my leadership, the Editorial Board nearly doubled and clinical submissions increased almost 4-fold. I want to thank all members of the Editorial Board. Your expertise and dedication has enabled AJO to accommodate the vast increase in submissions and greatly improved the quality of papers published in recent years. I have so appreciated your efforts and hard work.
The addition of the Residency Advisory Board several years ago provided an excellent forum for orthopedic surgeons in training to share their thoughts on subjects of particular interest and address issues not typically covered during the course of their clinical training; such as the importance of mentorship, how to organize a practice, and how to decipher an employment contract for one’s first “real” job. I have been immensely impressed with residents’ insights and their willingness to share them with their colleagues. I hope that this experience at AJO will encourage them to join other Editorial Boards during their professional careers.
Over these past 10 years, I have tried to satisfy the mission of The American Journal of Orthopedics: “… to provide timely, practical, and readable technical information of the highest caliber to the orthopedic surgeon involved in the everyday practice of orthopedics.” To this end, I expanded the “expert opinion” 5 Points series originally introduced by John Gould, MD, my predecessor as Editor-in-Chief. In addition, I added the Practice Management articles, prepared by Karen Zupko and her associates, which have been especially informative and popular.
I have thoroughly enjoyed sharing with you my nonclinical editorials touching on the “topics of the day.” Among my favorites were “Customer Satisfaction: Are Hospitals ‘Hospitable’?”1 which anticipated the growing influence of patient satisfaction scores in our professional lives; and “Are Surgeons Accepting Bribes?”,2 addressing a subject that predated the 2007 Deferred Prosecution Agreement3 which has transformed the relationships between orthopedic surgeons and the orthopedic device industry. I hope you have enjoyed reading my musings as much as I enjoyed writing them.
Our incoming Editor-in-Chief is Bryan T. Hanypsiak, MD, Director of Sports Medicine, Peconic Bay Medical Center in Riverhead, New York, and Chairman of the September 2015 Innovative Techniques: The Knee Course, sponsored by AJO in Las Vegas. Bryan will remain committed to the original mission of AJO and its high editorial and peer reviewed standards. However, the format will change with the March 2016 issue and have the feel of a clinical magazine. I have every confidence that, with Dr. Hanypsiak’s leadership and the support of the publisher, the AJO brand will continue to thrive in an ever-changing and challenging marketplace.
Finally, I wish to thank all the readers of AJO who have supported the Journal, one of only a handful of orthopedic publications that still caters to the professional interests of the general orthopedic surgeon with a comprehensive scope of clinical and non-clinical topics. Leading the Board as Editor-in-Chief has been one of the most fulfilling and rewarding activities of my professional career, and it has truly been my honor to serve you. I wish all of you the best.
1. McCann PD. Customer satisfaction: are hospitals “hospitable”? Am J Orthop. 2006;35(2):59.
2. McCann PD. Are surgeons accepting bribes? Am J Orthop. 2006;35(3):114.
3. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed January 11, 2016.
1. McCann PD. Customer satisfaction: are hospitals “hospitable”? Am J Orthop. 2006;35(2):59.
2. McCann PD. Are surgeons accepting bribes? Am J Orthop. 2006;35(3):114.
3. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed January 11, 2016.
Precision medicine in cardiology
The possibility that we can define the specific and unique treatment for an individual’s specific disease is the holy grail of therapeutics. Our current therapy is largely defined by randomized clinical trials (RCTs), which provide an average response of therapy in a given disease tested in hundreds or thousands of patients.
RCTs identify the statistical benefit of a particular treatment when compared with a placebo in heterogeneous patients who, at best, are demographically similar but do not truly represent the general population.
Dr. Sidney Goldstein
Although an RCT shows an average statistical benefit, some individuals may have a profound benefit; others in the trial may not benefit at all, and some may do worse than placebo. The reason for the differential response is poorly understood. Therefore, treatment programs based on RCT data by definition are crude and imprecise by design for a variety of conditions, including cancer and cardiovascular diseases.
There has been a call for more personalization and precision in defining and developing predictably successful therapy. It is proposed that precision medicine will lead to optimal targeted individualized treatment based on patients’ genetic profile. This has led oncologists to use genetic profiling of therapy based on cells derived from patient’s tumor. Cancer therapy is in the forefront of genomic analysis of tumor tissue in order to guide specific tumor therapy. Unique DNA gene mutations are now being identified that may explain the genesis, spread, and growth of a tumor. It also provides a potential link between the genetic characteristics of the tumor to specific therapy. As a result, a number of laboratories have developed genetic probes that can mitigate gene expression or overexpression and thereby modify progression of disease.
To some degree, the field of cardiology has found some precision in defining individual therapy for the treatment of a variety of expressions of cardiovascular disease. We have drugs that are aimed at the treatment of hypertension, hypercholesterolemia, heart failure, and vascular thrombogenesis, to name some of the major targets. Just as the oncologists are searching for specific treatments of individual tumors, cardiology is searching for specific targets based on our understanding of the pathophysiologic mechanism leading to the expression and progression of disease. We have been fortunate in a large part to be able to measure pathophysiology and therapy at the bedside.
For some time, investigators have been examining the genetic variants in human tissue in order to understand drug responsiveness in several cardiovascular environments. Single nucleotide polymorphisms (SNP) have been discovered in beta-receptors that may define risk factors for disease and function as modifiers of disease once it has occurred. These factors also have the potential to modify beta-receptor response to adrenergic agonists and antagonists. The understanding of the SNP expression is anticipated to lead to the individualization of drug therapy and define or predict an individual’s response to particular drug therapy. As a result, they may explain the spectrum of clinical response observed in RCTs. Similar observations have been observed with the genetic polymorphism, of renin-angiotensin-aldosterone system and sympathetic systems. The understanding of genetic polymorphism may also provide insight into the expression of disease in particular demographic groups.
So far, the cost of these drugs is huge when applied to just a few individuals who are potential beneficiaries of the therapy. Consequently, patient and society and your insurance company are asked to pay the cost of the drugs to treat just a few patients. Over time, it is possible that these unique genomic characteristics can be applied to larger populations and may spread the costs over a larger number of patients. So far, the potential for this to happen is limited.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The possibility that we can define the specific and unique treatment for an individual’s specific disease is the holy grail of therapeutics. Our current therapy is largely defined by randomized clinical trials (RCTs), which provide an average response of therapy in a given disease tested in hundreds or thousands of patients.
RCTs identify the statistical benefit of a particular treatment when compared with a placebo in heterogeneous patients who, at best, are demographically similar but do not truly represent the general population.
Dr. Sidney Goldstein
Although an RCT shows an average statistical benefit, some individuals may have a profound benefit; others in the trial may not benefit at all, and some may do worse than placebo. The reason for the differential response is poorly understood. Therefore, treatment programs based on RCT data by definition are crude and imprecise by design for a variety of conditions, including cancer and cardiovascular diseases.
There has been a call for more personalization and precision in defining and developing predictably successful therapy. It is proposed that precision medicine will lead to optimal targeted individualized treatment based on patients’ genetic profile. This has led oncologists to use genetic profiling of therapy based on cells derived from patient’s tumor. Cancer therapy is in the forefront of genomic analysis of tumor tissue in order to guide specific tumor therapy. Unique DNA gene mutations are now being identified that may explain the genesis, spread, and growth of a tumor. It also provides a potential link between the genetic characteristics of the tumor to specific therapy. As a result, a number of laboratories have developed genetic probes that can mitigate gene expression or overexpression and thereby modify progression of disease.
To some degree, the field of cardiology has found some precision in defining individual therapy for the treatment of a variety of expressions of cardiovascular disease. We have drugs that are aimed at the treatment of hypertension, hypercholesterolemia, heart failure, and vascular thrombogenesis, to name some of the major targets. Just as the oncologists are searching for specific treatments of individual tumors, cardiology is searching for specific targets based on our understanding of the pathophysiologic mechanism leading to the expression and progression of disease. We have been fortunate in a large part to be able to measure pathophysiology and therapy at the bedside.
For some time, investigators have been examining the genetic variants in human tissue in order to understand drug responsiveness in several cardiovascular environments. Single nucleotide polymorphisms (SNP) have been discovered in beta-receptors that may define risk factors for disease and function as modifiers of disease once it has occurred. These factors also have the potential to modify beta-receptor response to adrenergic agonists and antagonists. The understanding of the SNP expression is anticipated to lead to the individualization of drug therapy and define or predict an individual’s response to particular drug therapy. As a result, they may explain the spectrum of clinical response observed in RCTs. Similar observations have been observed with the genetic polymorphism, of renin-angiotensin-aldosterone system and sympathetic systems. The understanding of genetic polymorphism may also provide insight into the expression of disease in particular demographic groups.
So far, the cost of these drugs is huge when applied to just a few individuals who are potential beneficiaries of the therapy. Consequently, patient and society and your insurance company are asked to pay the cost of the drugs to treat just a few patients. Over time, it is possible that these unique genomic characteristics can be applied to larger populations and may spread the costs over a larger number of patients. So far, the potential for this to happen is limited.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The possibility that we can define the specific and unique treatment for an individual’s specific disease is the holy grail of therapeutics. Our current therapy is largely defined by randomized clinical trials (RCTs), which provide an average response of therapy in a given disease tested in hundreds or thousands of patients.
RCTs identify the statistical benefit of a particular treatment when compared with a placebo in heterogeneous patients who, at best, are demographically similar but do not truly represent the general population.
Dr. Sidney Goldstein
Although an RCT shows an average statistical benefit, some individuals may have a profound benefit; others in the trial may not benefit at all, and some may do worse than placebo. The reason for the differential response is poorly understood. Therefore, treatment programs based on RCT data by definition are crude and imprecise by design for a variety of conditions, including cancer and cardiovascular diseases.
There has been a call for more personalization and precision in defining and developing predictably successful therapy. It is proposed that precision medicine will lead to optimal targeted individualized treatment based on patients’ genetic profile. This has led oncologists to use genetic profiling of therapy based on cells derived from patient’s tumor. Cancer therapy is in the forefront of genomic analysis of tumor tissue in order to guide specific tumor therapy. Unique DNA gene mutations are now being identified that may explain the genesis, spread, and growth of a tumor. It also provides a potential link between the genetic characteristics of the tumor to specific therapy. As a result, a number of laboratories have developed genetic probes that can mitigate gene expression or overexpression and thereby modify progression of disease.
To some degree, the field of cardiology has found some precision in defining individual therapy for the treatment of a variety of expressions of cardiovascular disease. We have drugs that are aimed at the treatment of hypertension, hypercholesterolemia, heart failure, and vascular thrombogenesis, to name some of the major targets. Just as the oncologists are searching for specific treatments of individual tumors, cardiology is searching for specific targets based on our understanding of the pathophysiologic mechanism leading to the expression and progression of disease. We have been fortunate in a large part to be able to measure pathophysiology and therapy at the bedside.
For some time, investigators have been examining the genetic variants in human tissue in order to understand drug responsiveness in several cardiovascular environments. Single nucleotide polymorphisms (SNP) have been discovered in beta-receptors that may define risk factors for disease and function as modifiers of disease once it has occurred. These factors also have the potential to modify beta-receptor response to adrenergic agonists and antagonists. The understanding of the SNP expression is anticipated to lead to the individualization of drug therapy and define or predict an individual’s response to particular drug therapy. As a result, they may explain the spectrum of clinical response observed in RCTs. Similar observations have been observed with the genetic polymorphism, of renin-angiotensin-aldosterone system and sympathetic systems. The understanding of genetic polymorphism may also provide insight into the expression of disease in particular demographic groups.
So far, the cost of these drugs is huge when applied to just a few individuals who are potential beneficiaries of the therapy. Consequently, patient and society and your insurance company are asked to pay the cost of the drugs to treat just a few patients. Over time, it is possible that these unique genomic characteristics can be applied to larger populations and may spread the costs over a larger number of patients. So far, the potential for this to happen is limited.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.