User login
Key ways to differentiate a benign from a malignant adnexal mass
Click here to register for PAGS 2014 December 4 to 6 at the Bellagio in Las Vegas
More from PAGS 2013:
Lichen sclerosis: My approach to treatment
Michael Baggish, MD
Click here to register for PAGS 2014 December 4 to 6 at the Bellagio in Las Vegas
More from PAGS 2013:
Lichen sclerosis: My approach to treatment
Michael Baggish, MD
Click here to register for PAGS 2014 December 4 to 6 at the Bellagio in Las Vegas
More from PAGS 2013:
Lichen sclerosis: My approach to treatment
Michael Baggish, MD
Why FDA hearing on morcellation safety could drive innovation
As a member of the Obstetrics & Gynecology Devices Panel FDA Advisory Committee, Dr. Iglesia digested the information presented at the hearing on July 10 and 11 and made her recommendations, along with her fellow panel members, for the fate of laparoscopic power morcellators to the FDA. Tune in to this special audiocast to hear Dr. Iglesia discuss the specific issues the panel weighed when making their final recommendations.
Dr. Iglesia is Director, Section of Female Pelvic Medicine and Reconstructive Surgery, MedStar Washington Hospital Center, and Associate Professor, Departments of ObGyn and Urology, Georgetown University School of Medicine, Washington, DC. She also serves on the OBG Management Board of Editors.
TRANSCRIPT
Janelle Yates: OBG Management Editorial Board Member Dr. Cheryl Iglesia attended the July 10th and 11th FDA hearing on microscopic power morcellation as a member of the Obstetrics and Gynecology Devices Panel Advisory Committee. In this audiocast, she describes the hearing and the panel’s recommendations as well as many of the fine points considered in weighing the risks and benefits of power morcellation. Dr. Iglesia is Director of the Section of Female Pelvic Medicine and Reconstructive Surgery at MedStar Washington Hospital Center, and Associate Professor in the Departments of Ob/Gyn and Neurology at Georgetown University’s School of Medicine in Washington, DC.
Dr. Iglesia, could you describe your role on the FDA’s Obstetrics and Gynecology Device Panel Advisory Committee?
Cheryl B. Iglesia, MD: I’m considered a special government employee and I have a 5-year term on the ObGyn Devices Panel. I was a member of the panel that reviewed vaginal mesh, and this is my second ObGyn devices panel as a consultant on power morcellation for laparoscopy. After the hearing, which was July 10th and 11th, we make recommendations as a panel but no final decisions are made until everything has been reviewed by officials at the FDA, and the FDA will come up with final decisions based in part on some of the recommendations that the panel has made. Therefore I can’t give you an official view, and what I’ll be talking about right now mostly represents my own opinion.
Ms. Yates: Just to review: What was the goal of the 2-day hearing, and whose points of view were represented to the panel?
Dr. Iglesia: The goal was to discuss the risk of disseminating unsuspected uterine malignancy with power morcellation. We talked on the panel about what the risk is of occult leiomyosarcoma in women with uterine fibroids. We talked about the preoperative screening evaluation process, talked about options for interoperative strategies to minimize or mitigate intraperitoneal fragmentation or dissemination of the tissue. They talked about various types of morcellators and, moving forward, if leiomyosarcoma was diagnosed, whether or not power morcellation upgraded an occult malignancy. And what the benchmarks should be for future devices, and whether or not future devices— not just for the power morcellators with containment, like containment bags—how they should be evaluated and tested moving forward. There was also some discussion about the role of registries.
Ms. Yates: What final recommendations did the panel make to the FDA?
Dr. Iglesia: Overall, there was a very long discussion about the risk of having an unsuspected sarcoma and the rates ranged from one in 350 to one in 7,450. What we as a panel realized is that while there are some indicators that could be suspicious for leiomyosarcoma, particularly on an MRI, that one cannot be 100% certain, particularly when you have a fibroid that’s degenerating, that it’s not just leiomyosarcoma but other occult malignancies.
The bottom line is the patients must be adequately worked up, particularly if there is abnormal bleeding. An evaluation would include normal cervical cytology, normal endometrial sampling, either sonograms or MRIs if indicated, and we talked about patient selection. In particular of being very worried about using morcellation in the postmenopausal woman who’s bleeding. We talked a lot about other options for morcellation. In general, if you can remove a uterus through the vagina or intact, that’s ideal because there’s a lot of data about the pros and cons from the vaginal approach to hysterectomy. But we’re not 100% certain that containment bags are going to be the “be-all and end-all.” In that, particularly if you’re doing subtotal hysterectomies, you still might be cutting through cancers and occult malignancies and the containment bags are very thin so that there’s a possibility that there could be leakage and/or breakage or unintended injury to other interperitoneal organs like bowels and vessels, etc. So we can’t be complacent about being 100% certain that things will go right even with the use of a bag.
Ms. Yates: Were there any final recommendations about informed consent?
Dr. Iglesia: A lot of discussion, particularly on the second day, was in the area of labeling special controls and it would be labeling for a patient and practitioners or physician surgeons who are using the morcellator. To the extent that—and there have been some precedents I think in silicon breast and other devices—where both the patient and the physician have to sign off that they’re aware that morcellators may be used, that there’s a potential for dissemination of an occult malignancy or even dissemination of benign disease like leiomyomatosis and incomplete removal. There are risks of using the morcellator in terms of injury, just a whole checklist. But it’s interesting for the labeling, both the patient and the physician in this: One of the recommendations for special controls would be included.
Ms. Yates: And would that involve a black box warning?
Dr. Iglesia: I think there were several discussions about the black box warning; I’m not sure what the final discussion is. Some people believe that with the black box on an administrative level, it sends a signal and a reminder to everyone about the labeling. But labeling can be done without a black box and it can be done with a black box. I’m not 100% certain how that will ultimately be decided upon by the FDA.
Ms. Yates: What were your reactions to the hearing, apart from your role on the panel? Did you feel that adequate testimony was heard from all the parties that have a stake in the immediate and long-term fate of laparoscopic power morcellation?
Dr. Iglesia: I think that the FDA did an excellent job in convening all the players, anybody who has interests in the stake I feel was represented--from industry and companies that make morcellators, companies that make containment bags, medical societies, ACOG, and AAGL gave testimony. AAGL’s testimony was very powerful, particularly by Dr. Jubilee Brown in mentioning that without the morcellator more women may be subjected to abdominal procedure, which in and of itself has some morbidity and mortality associated with that type of operation, and it was a nice study analysis. In terms of a decision tree what the potential harms would be without available morcellators to use, and I thought the MRI imaging that was done by the radiologist was also very interesting and discussed the limits of our ability to detect.
I also found some of the testimony to be extremely powerful from the patients, including that of Dr. Amy Reed and her family and the other women who presented. In some of the cases, we and several people on the panel, including myself, did wonder about the selection or the choice to use the morcellator in the first place in some cases, particularly in women who had uterine fibroids and they were postmenopausal. I think that that would be a particular case where you know go ahead and make an incision because there’s a potential higher index of suspicion for cancer in those kinds of cases.
Ms. Yates: Do you care to predict whether gynecologic surgeons will continue to use power morcellators after this controversy?
Dr. Iglesia: You know, and this was also discussed by Dr. Fisher and some of the officials from the FDA, that if anything this would be a call for innovation and improving products that could morcellate and contain at the same time. I know that we have some hysteroscopic morcellators that you can insert and there’s a vacuum and so things get kind of vacuumed up and whether or not we can develop something that has very little spill—obviously none at all would be key—and I do believe that at some point there will be some ingenuity and some improvements made to the current devices that will allow us to continue this is in our armamentarium.
What was interesting was that one of the questions that was addressed to the panel was, “When do you see that the benefits may outweigh the risks, in what population?” And leiomyosarcoma, which is just one of the occult malignancies—and there’s different types of sarcomas including endometrial stromal sarcomas and other endometrial cancer and malignancies. What’s interesting is that when you look at fibroids and even when you do a myomectomy it’s not necessarily just the power of morcellation, it’s just cutting through cancer or morcellating either vaginally or open. You’re doing an open myomectomy, just removal of the fibroid, and it turns out that that’s cancer. You know that is not a good prognosis to start with, but to spread it clearly is not good for the patient and makes a bad condition even worse.
But it really means that we need to do a better job in pretty accurately identifying patients. And while we’re there, we did mention on the panel that maybe we can develop risk calculators or ways to stratify based on the MRI imaging, patient age, patient race, and whether or not something has a higher index of suspicion for being cancerous. What I meant to say is the two benefits outweigh the risk.
One other case was the young 20-something-year-old fertility patient with the fibroids that clearly have an impact. I mean you don’t want to do a hysterectomy and you still want to remove the fibroid in as noninvasive a way as possible and morcellation may be the best in terms of creating less adhesions. The other case was something that I had mentioned in patients who have prolapse who you’re thinking about placing mesh. Some people do subtotal hysterectomies and then attach the mesh to the cervix as opposed to the vaginal cuff to decrease the risk of cuff erosion and that’s another technique where benefits might outweigh the risk, particularly in older postmenopausal women with not particularly enlarged uteri. So, more to come.
As a member of the Obstetrics & Gynecology Devices Panel FDA Advisory Committee, Dr. Iglesia digested the information presented at the hearing on July 10 and 11 and made her recommendations, along with her fellow panel members, for the fate of laparoscopic power morcellators to the FDA. Tune in to this special audiocast to hear Dr. Iglesia discuss the specific issues the panel weighed when making their final recommendations.
Dr. Iglesia is Director, Section of Female Pelvic Medicine and Reconstructive Surgery, MedStar Washington Hospital Center, and Associate Professor, Departments of ObGyn and Urology, Georgetown University School of Medicine, Washington, DC. She also serves on the OBG Management Board of Editors.
TRANSCRIPT
Janelle Yates: OBG Management Editorial Board Member Dr. Cheryl Iglesia attended the July 10th and 11th FDA hearing on microscopic power morcellation as a member of the Obstetrics and Gynecology Devices Panel Advisory Committee. In this audiocast, she describes the hearing and the panel’s recommendations as well as many of the fine points considered in weighing the risks and benefits of power morcellation. Dr. Iglesia is Director of the Section of Female Pelvic Medicine and Reconstructive Surgery at MedStar Washington Hospital Center, and Associate Professor in the Departments of Ob/Gyn and Neurology at Georgetown University’s School of Medicine in Washington, DC.
Dr. Iglesia, could you describe your role on the FDA’s Obstetrics and Gynecology Device Panel Advisory Committee?
Cheryl B. Iglesia, MD: I’m considered a special government employee and I have a 5-year term on the ObGyn Devices Panel. I was a member of the panel that reviewed vaginal mesh, and this is my second ObGyn devices panel as a consultant on power morcellation for laparoscopy. After the hearing, which was July 10th and 11th, we make recommendations as a panel but no final decisions are made until everything has been reviewed by officials at the FDA, and the FDA will come up with final decisions based in part on some of the recommendations that the panel has made. Therefore I can’t give you an official view, and what I’ll be talking about right now mostly represents my own opinion.
Ms. Yates: Just to review: What was the goal of the 2-day hearing, and whose points of view were represented to the panel?
Dr. Iglesia: The goal was to discuss the risk of disseminating unsuspected uterine malignancy with power morcellation. We talked on the panel about what the risk is of occult leiomyosarcoma in women with uterine fibroids. We talked about the preoperative screening evaluation process, talked about options for interoperative strategies to minimize or mitigate intraperitoneal fragmentation or dissemination of the tissue. They talked about various types of morcellators and, moving forward, if leiomyosarcoma was diagnosed, whether or not power morcellation upgraded an occult malignancy. And what the benchmarks should be for future devices, and whether or not future devices— not just for the power morcellators with containment, like containment bags—how they should be evaluated and tested moving forward. There was also some discussion about the role of registries.
Ms. Yates: What final recommendations did the panel make to the FDA?
Dr. Iglesia: Overall, there was a very long discussion about the risk of having an unsuspected sarcoma and the rates ranged from one in 350 to one in 7,450. What we as a panel realized is that while there are some indicators that could be suspicious for leiomyosarcoma, particularly on an MRI, that one cannot be 100% certain, particularly when you have a fibroid that’s degenerating, that it’s not just leiomyosarcoma but other occult malignancies.
The bottom line is the patients must be adequately worked up, particularly if there is abnormal bleeding. An evaluation would include normal cervical cytology, normal endometrial sampling, either sonograms or MRIs if indicated, and we talked about patient selection. In particular of being very worried about using morcellation in the postmenopausal woman who’s bleeding. We talked a lot about other options for morcellation. In general, if you can remove a uterus through the vagina or intact, that’s ideal because there’s a lot of data about the pros and cons from the vaginal approach to hysterectomy. But we’re not 100% certain that containment bags are going to be the “be-all and end-all.” In that, particularly if you’re doing subtotal hysterectomies, you still might be cutting through cancers and occult malignancies and the containment bags are very thin so that there’s a possibility that there could be leakage and/or breakage or unintended injury to other interperitoneal organs like bowels and vessels, etc. So we can’t be complacent about being 100% certain that things will go right even with the use of a bag.
Ms. Yates: Were there any final recommendations about informed consent?
Dr. Iglesia: A lot of discussion, particularly on the second day, was in the area of labeling special controls and it would be labeling for a patient and practitioners or physician surgeons who are using the morcellator. To the extent that—and there have been some precedents I think in silicon breast and other devices—where both the patient and the physician have to sign off that they’re aware that morcellators may be used, that there’s a potential for dissemination of an occult malignancy or even dissemination of benign disease like leiomyomatosis and incomplete removal. There are risks of using the morcellator in terms of injury, just a whole checklist. But it’s interesting for the labeling, both the patient and the physician in this: One of the recommendations for special controls would be included.
Ms. Yates: And would that involve a black box warning?
Dr. Iglesia: I think there were several discussions about the black box warning; I’m not sure what the final discussion is. Some people believe that with the black box on an administrative level, it sends a signal and a reminder to everyone about the labeling. But labeling can be done without a black box and it can be done with a black box. I’m not 100% certain how that will ultimately be decided upon by the FDA.
Ms. Yates: What were your reactions to the hearing, apart from your role on the panel? Did you feel that adequate testimony was heard from all the parties that have a stake in the immediate and long-term fate of laparoscopic power morcellation?
Dr. Iglesia: I think that the FDA did an excellent job in convening all the players, anybody who has interests in the stake I feel was represented--from industry and companies that make morcellators, companies that make containment bags, medical societies, ACOG, and AAGL gave testimony. AAGL’s testimony was very powerful, particularly by Dr. Jubilee Brown in mentioning that without the morcellator more women may be subjected to abdominal procedure, which in and of itself has some morbidity and mortality associated with that type of operation, and it was a nice study analysis. In terms of a decision tree what the potential harms would be without available morcellators to use, and I thought the MRI imaging that was done by the radiologist was also very interesting and discussed the limits of our ability to detect.
I also found some of the testimony to be extremely powerful from the patients, including that of Dr. Amy Reed and her family and the other women who presented. In some of the cases, we and several people on the panel, including myself, did wonder about the selection or the choice to use the morcellator in the first place in some cases, particularly in women who had uterine fibroids and they were postmenopausal. I think that that would be a particular case where you know go ahead and make an incision because there’s a potential higher index of suspicion for cancer in those kinds of cases.
Ms. Yates: Do you care to predict whether gynecologic surgeons will continue to use power morcellators after this controversy?
Dr. Iglesia: You know, and this was also discussed by Dr. Fisher and some of the officials from the FDA, that if anything this would be a call for innovation and improving products that could morcellate and contain at the same time. I know that we have some hysteroscopic morcellators that you can insert and there’s a vacuum and so things get kind of vacuumed up and whether or not we can develop something that has very little spill—obviously none at all would be key—and I do believe that at some point there will be some ingenuity and some improvements made to the current devices that will allow us to continue this is in our armamentarium.
What was interesting was that one of the questions that was addressed to the panel was, “When do you see that the benefits may outweigh the risks, in what population?” And leiomyosarcoma, which is just one of the occult malignancies—and there’s different types of sarcomas including endometrial stromal sarcomas and other endometrial cancer and malignancies. What’s interesting is that when you look at fibroids and even when you do a myomectomy it’s not necessarily just the power of morcellation, it’s just cutting through cancer or morcellating either vaginally or open. You’re doing an open myomectomy, just removal of the fibroid, and it turns out that that’s cancer. You know that is not a good prognosis to start with, but to spread it clearly is not good for the patient and makes a bad condition even worse.
But it really means that we need to do a better job in pretty accurately identifying patients. And while we’re there, we did mention on the panel that maybe we can develop risk calculators or ways to stratify based on the MRI imaging, patient age, patient race, and whether or not something has a higher index of suspicion for being cancerous. What I meant to say is the two benefits outweigh the risk.
One other case was the young 20-something-year-old fertility patient with the fibroids that clearly have an impact. I mean you don’t want to do a hysterectomy and you still want to remove the fibroid in as noninvasive a way as possible and morcellation may be the best in terms of creating less adhesions. The other case was something that I had mentioned in patients who have prolapse who you’re thinking about placing mesh. Some people do subtotal hysterectomies and then attach the mesh to the cervix as opposed to the vaginal cuff to decrease the risk of cuff erosion and that’s another technique where benefits might outweigh the risk, particularly in older postmenopausal women with not particularly enlarged uteri. So, more to come.
As a member of the Obstetrics & Gynecology Devices Panel FDA Advisory Committee, Dr. Iglesia digested the information presented at the hearing on July 10 and 11 and made her recommendations, along with her fellow panel members, for the fate of laparoscopic power morcellators to the FDA. Tune in to this special audiocast to hear Dr. Iglesia discuss the specific issues the panel weighed when making their final recommendations.
Dr. Iglesia is Director, Section of Female Pelvic Medicine and Reconstructive Surgery, MedStar Washington Hospital Center, and Associate Professor, Departments of ObGyn and Urology, Georgetown University School of Medicine, Washington, DC. She also serves on the OBG Management Board of Editors.
TRANSCRIPT
Janelle Yates: OBG Management Editorial Board Member Dr. Cheryl Iglesia attended the July 10th and 11th FDA hearing on microscopic power morcellation as a member of the Obstetrics and Gynecology Devices Panel Advisory Committee. In this audiocast, she describes the hearing and the panel’s recommendations as well as many of the fine points considered in weighing the risks and benefits of power morcellation. Dr. Iglesia is Director of the Section of Female Pelvic Medicine and Reconstructive Surgery at MedStar Washington Hospital Center, and Associate Professor in the Departments of Ob/Gyn and Neurology at Georgetown University’s School of Medicine in Washington, DC.
Dr. Iglesia, could you describe your role on the FDA’s Obstetrics and Gynecology Device Panel Advisory Committee?
Cheryl B. Iglesia, MD: I’m considered a special government employee and I have a 5-year term on the ObGyn Devices Panel. I was a member of the panel that reviewed vaginal mesh, and this is my second ObGyn devices panel as a consultant on power morcellation for laparoscopy. After the hearing, which was July 10th and 11th, we make recommendations as a panel but no final decisions are made until everything has been reviewed by officials at the FDA, and the FDA will come up with final decisions based in part on some of the recommendations that the panel has made. Therefore I can’t give you an official view, and what I’ll be talking about right now mostly represents my own opinion.
Ms. Yates: Just to review: What was the goal of the 2-day hearing, and whose points of view were represented to the panel?
Dr. Iglesia: The goal was to discuss the risk of disseminating unsuspected uterine malignancy with power morcellation. We talked on the panel about what the risk is of occult leiomyosarcoma in women with uterine fibroids. We talked about the preoperative screening evaluation process, talked about options for interoperative strategies to minimize or mitigate intraperitoneal fragmentation or dissemination of the tissue. They talked about various types of morcellators and, moving forward, if leiomyosarcoma was diagnosed, whether or not power morcellation upgraded an occult malignancy. And what the benchmarks should be for future devices, and whether or not future devices— not just for the power morcellators with containment, like containment bags—how they should be evaluated and tested moving forward. There was also some discussion about the role of registries.
Ms. Yates: What final recommendations did the panel make to the FDA?
Dr. Iglesia: Overall, there was a very long discussion about the risk of having an unsuspected sarcoma and the rates ranged from one in 350 to one in 7,450. What we as a panel realized is that while there are some indicators that could be suspicious for leiomyosarcoma, particularly on an MRI, that one cannot be 100% certain, particularly when you have a fibroid that’s degenerating, that it’s not just leiomyosarcoma but other occult malignancies.
The bottom line is the patients must be adequately worked up, particularly if there is abnormal bleeding. An evaluation would include normal cervical cytology, normal endometrial sampling, either sonograms or MRIs if indicated, and we talked about patient selection. In particular of being very worried about using morcellation in the postmenopausal woman who’s bleeding. We talked a lot about other options for morcellation. In general, if you can remove a uterus through the vagina or intact, that’s ideal because there’s a lot of data about the pros and cons from the vaginal approach to hysterectomy. But we’re not 100% certain that containment bags are going to be the “be-all and end-all.” In that, particularly if you’re doing subtotal hysterectomies, you still might be cutting through cancers and occult malignancies and the containment bags are very thin so that there’s a possibility that there could be leakage and/or breakage or unintended injury to other interperitoneal organs like bowels and vessels, etc. So we can’t be complacent about being 100% certain that things will go right even with the use of a bag.
Ms. Yates: Were there any final recommendations about informed consent?
Dr. Iglesia: A lot of discussion, particularly on the second day, was in the area of labeling special controls and it would be labeling for a patient and practitioners or physician surgeons who are using the morcellator. To the extent that—and there have been some precedents I think in silicon breast and other devices—where both the patient and the physician have to sign off that they’re aware that morcellators may be used, that there’s a potential for dissemination of an occult malignancy or even dissemination of benign disease like leiomyomatosis and incomplete removal. There are risks of using the morcellator in terms of injury, just a whole checklist. But it’s interesting for the labeling, both the patient and the physician in this: One of the recommendations for special controls would be included.
Ms. Yates: And would that involve a black box warning?
Dr. Iglesia: I think there were several discussions about the black box warning; I’m not sure what the final discussion is. Some people believe that with the black box on an administrative level, it sends a signal and a reminder to everyone about the labeling. But labeling can be done without a black box and it can be done with a black box. I’m not 100% certain how that will ultimately be decided upon by the FDA.
Ms. Yates: What were your reactions to the hearing, apart from your role on the panel? Did you feel that adequate testimony was heard from all the parties that have a stake in the immediate and long-term fate of laparoscopic power morcellation?
Dr. Iglesia: I think that the FDA did an excellent job in convening all the players, anybody who has interests in the stake I feel was represented--from industry and companies that make morcellators, companies that make containment bags, medical societies, ACOG, and AAGL gave testimony. AAGL’s testimony was very powerful, particularly by Dr. Jubilee Brown in mentioning that without the morcellator more women may be subjected to abdominal procedure, which in and of itself has some morbidity and mortality associated with that type of operation, and it was a nice study analysis. In terms of a decision tree what the potential harms would be without available morcellators to use, and I thought the MRI imaging that was done by the radiologist was also very interesting and discussed the limits of our ability to detect.
I also found some of the testimony to be extremely powerful from the patients, including that of Dr. Amy Reed and her family and the other women who presented. In some of the cases, we and several people on the panel, including myself, did wonder about the selection or the choice to use the morcellator in the first place in some cases, particularly in women who had uterine fibroids and they were postmenopausal. I think that that would be a particular case where you know go ahead and make an incision because there’s a potential higher index of suspicion for cancer in those kinds of cases.
Ms. Yates: Do you care to predict whether gynecologic surgeons will continue to use power morcellators after this controversy?
Dr. Iglesia: You know, and this was also discussed by Dr. Fisher and some of the officials from the FDA, that if anything this would be a call for innovation and improving products that could morcellate and contain at the same time. I know that we have some hysteroscopic morcellators that you can insert and there’s a vacuum and so things get kind of vacuumed up and whether or not we can develop something that has very little spill—obviously none at all would be key—and I do believe that at some point there will be some ingenuity and some improvements made to the current devices that will allow us to continue this is in our armamentarium.
What was interesting was that one of the questions that was addressed to the panel was, “When do you see that the benefits may outweigh the risks, in what population?” And leiomyosarcoma, which is just one of the occult malignancies—and there’s different types of sarcomas including endometrial stromal sarcomas and other endometrial cancer and malignancies. What’s interesting is that when you look at fibroids and even when you do a myomectomy it’s not necessarily just the power of morcellation, it’s just cutting through cancer or morcellating either vaginally or open. You’re doing an open myomectomy, just removal of the fibroid, and it turns out that that’s cancer. You know that is not a good prognosis to start with, but to spread it clearly is not good for the patient and makes a bad condition even worse.
But it really means that we need to do a better job in pretty accurately identifying patients. And while we’re there, we did mention on the panel that maybe we can develop risk calculators or ways to stratify based on the MRI imaging, patient age, patient race, and whether or not something has a higher index of suspicion for being cancerous. What I meant to say is the two benefits outweigh the risk.
One other case was the young 20-something-year-old fertility patient with the fibroids that clearly have an impact. I mean you don’t want to do a hysterectomy and you still want to remove the fibroid in as noninvasive a way as possible and morcellation may be the best in terms of creating less adhesions. The other case was something that I had mentioned in patients who have prolapse who you’re thinking about placing mesh. Some people do subtotal hysterectomies and then attach the mesh to the cervix as opposed to the vaginal cuff to decrease the risk of cuff erosion and that’s another technique where benefits might outweigh the risk, particularly in older postmenopausal women with not particularly enlarged uteri. So, more to come.
Does prenatal acetaminophen exposure increase the risk of behavioral problems in the child?
In the continuing drive to determine the cause of neurobehavioral complications, particularly ADHD and HKD, a number of studies have reported associations with various substances. These include pesticides,1 hormones,2 hormone disrupters,1 and, possibly, genetics. Nevertheless, the etiology of these disorders remains a mystery. ADHD is a complex and heterogeneous disorder. Although we do not yet understand the cause, genetics (or, more accurately, pharmacogenetics) seems likely to play a role.
This study from a large Danish population appears to suggest that the prenatal use of acetaminophen may increase the risk of ADHD and HKD. It is yet another study in which the data indicate and the authors claim that use of a particular drug during pregnancy is responsible for this condition. However, despite the extremely large sample size (which increases the likelihood of positive findings), the hazard ratios were only marginally significant, suggesting that the relevance of the conclusions is questionable.
Details of the study
The 64,322 live-born children and mothers in the Danish National Birth Cohort from 1996 to 2002 were evaluated three ways:
- through parental reports of behavioral problems in children at age 7 using the Strengths and Difficulties Questionnaire
- through retrieval of HKD diagnoses from the Danish National Hospital Registry or the Danish Psychiatric Central Registry prior to 2011
- through prescriptions for ADHD (primarily methylphenidate [Ritalin]) for children from the Danish Prescription Registry.
Liew and colleagues then estimated hazard ratios for receiving a diagnosis of HKD or using a medication for ADHD, as well as risk ratios for behavioral problems in children after prenatal exposure to acetaminophen.
Stronger associations between prenatal acetaminophen use and HKD or ADHD were found when the mother used the medication in more than one trimester. Exposure-response trends increased with the frequency of acetaminophen use during pregnancy for all three outcomes (HKD diagnosis, ADHD-like behaviors, and ADHD medication use; P trend <.001). Results did not appear to be confounded by maternal inflammation, infection during pregnancy, or the mother’s mental health status.
Related articles:
• How can pregnant women safely relieve low-back pain? Roselyn Jan W. Clemente-Fuentes, MD; Heather Pickett, DO; Misty Carney, MLIS; and Paul Crawford, MD (January 2014)
• Perinatal depression: What you can do to reduce its long-term effects. Janelle Yates (February 2014)
• Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a “re-run” or as a “new series”? John T. Repke, MD (Guest Editorial; June 2014)
Why these findings are less than compelling
Acetaminophen is the most commonly used medication during pregnancy, although few investigators have analyzed neurobehavioral complications in children exposed to this drug in utero. Another recent epidemiologic study from Norway also suggests that long-term exposure (>28 days) to acetaminophen increases the risk of poor gross motor functioning, poor communication skills, and externalizing and internalizing behavior problems.3
The rationale behind an association between acetaminophen and ADHD and HKD is that the medication is an endocrine-disrupting agent. The evidence of this status comes primarily from in vitro experiments from one group of researchers, which may not represent in vivo conditions.4,5
Epidemiologic studies frequently are confounded by poor design and methodology. It also should be noted that correlation is not necessarily the same as causation. In this study, the design and methodology were appropriate considering the data available. Researchers often use large databases like this to research “hot topics” such as the association between ADHD and prenatal acetaminophen use. In this study, acetaminophen cannot be associated definitively with an increased risk of ADHD or HKD. Further research is needed, with greater attention to possible confounding factors, such as why these women consumed chronic doses and for what conditions.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
For the time being, you should probably counsel your patients to use acetaminophen sparingly during pregnancy, and certainly not on a daily basis. We also should encourage nonpharmacologic pain management, such as cognitive behavioral therapy, when appropriate, and caution patients against long-term use of analgesics, when possible, during gestation and lactation.
Thomas W. Hale, RPH, PhD; Aarienne Einarson, RN; and Teresa Baker, MD
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
1. Kajta M, Wojtowicz AK. Impact of endocrine-disrupting chemicals on neural development and the onset of neurological disorders. Pharmacol Rep. 2013;65(6):1632–1639.
2. de Bruin EI, Verheij F, Wiegman T, Ferdinand RF. Differences in finger length ratio between males with autism, pervasive developmental disorder–not otherwise specified, ADHD, and anxiety disorders. Dev Med Child Neurol. 2006;48(12):962–965.
3. Brandlistuen RE, Ystrom E, Nulman I, Koren G, Nordeng H. Prenatal paracetamol exposure and child neurodevelopment: A sibling-controlled cohort study. Int J Epidemiol. 2013;42(6):1702–1713.
4. Kristensen DM, Lesne L, Le Fol V, et al. Paracetamol (acetaminophen), aspirin (acetylsalicylic acid), and indomethacin are anti-androgenic in the rat foetal testis. Int J Androl. 2012;35(3):377–384.
5. Albert O, Desdoits-Lethimonier C, Lesne L, et al. Paracetamol, aspirin, and indomethacin display endocrine disrupting properties in the adult human testis in vitro. Hum Reprod. 2013;28(7):1890–1898.
In the continuing drive to determine the cause of neurobehavioral complications, particularly ADHD and HKD, a number of studies have reported associations with various substances. These include pesticides,1 hormones,2 hormone disrupters,1 and, possibly, genetics. Nevertheless, the etiology of these disorders remains a mystery. ADHD is a complex and heterogeneous disorder. Although we do not yet understand the cause, genetics (or, more accurately, pharmacogenetics) seems likely to play a role.
This study from a large Danish population appears to suggest that the prenatal use of acetaminophen may increase the risk of ADHD and HKD. It is yet another study in which the data indicate and the authors claim that use of a particular drug during pregnancy is responsible for this condition. However, despite the extremely large sample size (which increases the likelihood of positive findings), the hazard ratios were only marginally significant, suggesting that the relevance of the conclusions is questionable.
Details of the study
The 64,322 live-born children and mothers in the Danish National Birth Cohort from 1996 to 2002 were evaluated three ways:
- through parental reports of behavioral problems in children at age 7 using the Strengths and Difficulties Questionnaire
- through retrieval of HKD diagnoses from the Danish National Hospital Registry or the Danish Psychiatric Central Registry prior to 2011
- through prescriptions for ADHD (primarily methylphenidate [Ritalin]) for children from the Danish Prescription Registry.
Liew and colleagues then estimated hazard ratios for receiving a diagnosis of HKD or using a medication for ADHD, as well as risk ratios for behavioral problems in children after prenatal exposure to acetaminophen.
Stronger associations between prenatal acetaminophen use and HKD or ADHD were found when the mother used the medication in more than one trimester. Exposure-response trends increased with the frequency of acetaminophen use during pregnancy for all three outcomes (HKD diagnosis, ADHD-like behaviors, and ADHD medication use; P trend <.001). Results did not appear to be confounded by maternal inflammation, infection during pregnancy, or the mother’s mental health status.
Related articles:
• How can pregnant women safely relieve low-back pain? Roselyn Jan W. Clemente-Fuentes, MD; Heather Pickett, DO; Misty Carney, MLIS; and Paul Crawford, MD (January 2014)
• Perinatal depression: What you can do to reduce its long-term effects. Janelle Yates (February 2014)
• Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a “re-run” or as a “new series”? John T. Repke, MD (Guest Editorial; June 2014)
Why these findings are less than compelling
Acetaminophen is the most commonly used medication during pregnancy, although few investigators have analyzed neurobehavioral complications in children exposed to this drug in utero. Another recent epidemiologic study from Norway also suggests that long-term exposure (>28 days) to acetaminophen increases the risk of poor gross motor functioning, poor communication skills, and externalizing and internalizing behavior problems.3
The rationale behind an association between acetaminophen and ADHD and HKD is that the medication is an endocrine-disrupting agent. The evidence of this status comes primarily from in vitro experiments from one group of researchers, which may not represent in vivo conditions.4,5
Epidemiologic studies frequently are confounded by poor design and methodology. It also should be noted that correlation is not necessarily the same as causation. In this study, the design and methodology were appropriate considering the data available. Researchers often use large databases like this to research “hot topics” such as the association between ADHD and prenatal acetaminophen use. In this study, acetaminophen cannot be associated definitively with an increased risk of ADHD or HKD. Further research is needed, with greater attention to possible confounding factors, such as why these women consumed chronic doses and for what conditions.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
For the time being, you should probably counsel your patients to use acetaminophen sparingly during pregnancy, and certainly not on a daily basis. We also should encourage nonpharmacologic pain management, such as cognitive behavioral therapy, when appropriate, and caution patients against long-term use of analgesics, when possible, during gestation and lactation.
Thomas W. Hale, RPH, PhD; Aarienne Einarson, RN; and Teresa Baker, MD
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
In the continuing drive to determine the cause of neurobehavioral complications, particularly ADHD and HKD, a number of studies have reported associations with various substances. These include pesticides,1 hormones,2 hormone disrupters,1 and, possibly, genetics. Nevertheless, the etiology of these disorders remains a mystery. ADHD is a complex and heterogeneous disorder. Although we do not yet understand the cause, genetics (or, more accurately, pharmacogenetics) seems likely to play a role.
This study from a large Danish population appears to suggest that the prenatal use of acetaminophen may increase the risk of ADHD and HKD. It is yet another study in which the data indicate and the authors claim that use of a particular drug during pregnancy is responsible for this condition. However, despite the extremely large sample size (which increases the likelihood of positive findings), the hazard ratios were only marginally significant, suggesting that the relevance of the conclusions is questionable.
Details of the study
The 64,322 live-born children and mothers in the Danish National Birth Cohort from 1996 to 2002 were evaluated three ways:
- through parental reports of behavioral problems in children at age 7 using the Strengths and Difficulties Questionnaire
- through retrieval of HKD diagnoses from the Danish National Hospital Registry or the Danish Psychiatric Central Registry prior to 2011
- through prescriptions for ADHD (primarily methylphenidate [Ritalin]) for children from the Danish Prescription Registry.
Liew and colleagues then estimated hazard ratios for receiving a diagnosis of HKD or using a medication for ADHD, as well as risk ratios for behavioral problems in children after prenatal exposure to acetaminophen.
Stronger associations between prenatal acetaminophen use and HKD or ADHD were found when the mother used the medication in more than one trimester. Exposure-response trends increased with the frequency of acetaminophen use during pregnancy for all three outcomes (HKD diagnosis, ADHD-like behaviors, and ADHD medication use; P trend <.001). Results did not appear to be confounded by maternal inflammation, infection during pregnancy, or the mother’s mental health status.
Related articles:
• How can pregnant women safely relieve low-back pain? Roselyn Jan W. Clemente-Fuentes, MD; Heather Pickett, DO; Misty Carney, MLIS; and Paul Crawford, MD (January 2014)
• Perinatal depression: What you can do to reduce its long-term effects. Janelle Yates (February 2014)
• Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a “re-run” or as a “new series”? John T. Repke, MD (Guest Editorial; June 2014)
Why these findings are less than compelling
Acetaminophen is the most commonly used medication during pregnancy, although few investigators have analyzed neurobehavioral complications in children exposed to this drug in utero. Another recent epidemiologic study from Norway also suggests that long-term exposure (>28 days) to acetaminophen increases the risk of poor gross motor functioning, poor communication skills, and externalizing and internalizing behavior problems.3
The rationale behind an association between acetaminophen and ADHD and HKD is that the medication is an endocrine-disrupting agent. The evidence of this status comes primarily from in vitro experiments from one group of researchers, which may not represent in vivo conditions.4,5
Epidemiologic studies frequently are confounded by poor design and methodology. It also should be noted that correlation is not necessarily the same as causation. In this study, the design and methodology were appropriate considering the data available. Researchers often use large databases like this to research “hot topics” such as the association between ADHD and prenatal acetaminophen use. In this study, acetaminophen cannot be associated definitively with an increased risk of ADHD or HKD. Further research is needed, with greater attention to possible confounding factors, such as why these women consumed chronic doses and for what conditions.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
For the time being, you should probably counsel your patients to use acetaminophen sparingly during pregnancy, and certainly not on a daily basis. We also should encourage nonpharmacologic pain management, such as cognitive behavioral therapy, when appropriate, and caution patients against long-term use of analgesics, when possible, during gestation and lactation.
Thomas W. Hale, RPH, PhD; Aarienne Einarson, RN; and Teresa Baker, MD
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
1. Kajta M, Wojtowicz AK. Impact of endocrine-disrupting chemicals on neural development and the onset of neurological disorders. Pharmacol Rep. 2013;65(6):1632–1639.
2. de Bruin EI, Verheij F, Wiegman T, Ferdinand RF. Differences in finger length ratio between males with autism, pervasive developmental disorder–not otherwise specified, ADHD, and anxiety disorders. Dev Med Child Neurol. 2006;48(12):962–965.
3. Brandlistuen RE, Ystrom E, Nulman I, Koren G, Nordeng H. Prenatal paracetamol exposure and child neurodevelopment: A sibling-controlled cohort study. Int J Epidemiol. 2013;42(6):1702–1713.
4. Kristensen DM, Lesne L, Le Fol V, et al. Paracetamol (acetaminophen), aspirin (acetylsalicylic acid), and indomethacin are anti-androgenic in the rat foetal testis. Int J Androl. 2012;35(3):377–384.
5. Albert O, Desdoits-Lethimonier C, Lesne L, et al. Paracetamol, aspirin, and indomethacin display endocrine disrupting properties in the adult human testis in vitro. Hum Reprod. 2013;28(7):1890–1898.
1. Kajta M, Wojtowicz AK. Impact of endocrine-disrupting chemicals on neural development and the onset of neurological disorders. Pharmacol Rep. 2013;65(6):1632–1639.
2. de Bruin EI, Verheij F, Wiegman T, Ferdinand RF. Differences in finger length ratio between males with autism, pervasive developmental disorder–not otherwise specified, ADHD, and anxiety disorders. Dev Med Child Neurol. 2006;48(12):962–965.
3. Brandlistuen RE, Ystrom E, Nulman I, Koren G, Nordeng H. Prenatal paracetamol exposure and child neurodevelopment: A sibling-controlled cohort study. Int J Epidemiol. 2013;42(6):1702–1713.
4. Kristensen DM, Lesne L, Le Fol V, et al. Paracetamol (acetaminophen), aspirin (acetylsalicylic acid), and indomethacin are anti-androgenic in the rat foetal testis. Int J Androl. 2012;35(3):377–384.
5. Albert O, Desdoits-Lethimonier C, Lesne L, et al. Paracetamol, aspirin, and indomethacin display endocrine disrupting properties in the adult human testis in vitro. Hum Reprod. 2013;28(7):1890–1898.
Proper Inpatient Documentation, Coding Essential to Avoid a Medicare Audit
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
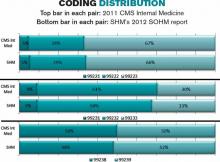
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Hypertension and pregnancy and preventing the first cesarean delivery
This peer to peer discussion focuses on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines1 and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.2
In this 20-minute audiocast, listen to these experts discuss:
Changing diagnostic tools for preeclampsia
- The 24-hour urinary protein estimation: When is it necessary?
- Use of magnesium sulfate for seizure prophylaxis
Preventing the first cesarean delivery
- Redefining the stages of labor: When is the second-stage too long?
- The lost skill of forceps delivery
- Is cesarean delivery rate the optimal metric for measuring neonatal outcome?
John T. Repke, MD, is University Professor and Chairman of the Department of Obstetrics and Gynecology at Penn State University College of Medicine, and Obstetrician-Gynecologist-in-Chief at the Milton S. Hershey Medical Center in Hershey, Pennsylvania. Dr. Repke is a member of the Board of Editors of OBG Management and is author of the June 2014 Guest Editorial on hypertension and pregnancy.
Errol R. Norwitz, MD, PhD, is the Louis E. Phaneuf Professor and Chairman of the Department of Obstetrics and Gynecology at Tufts Medical Center and Tufts University School of Medicine in Boston, Massachusetts. Dr. Norwitz is a member of the Board of Editors of OBG Management and is author of the June 2014 Update on operative vaginal delivery.
The speakers report no financial relationships relevant to this audiocast.
Click here for a downloadable transcript
TRANSCRIPT
ACOG guidelines on hypertension and pregnancy raise some questions
John T. Repke, MD: So, Errol, I was impressed over the first couple of days of being at the meeting. As you know, we had a postgraduate course, and one of the items that we talked about was the new hypertension and pregnancy document that was released by the Task Force on Hypertension and Pregnancy1 charged by the American College of Obstetricians and Gynecologists. I’ve got to say that while the goal of the document was to provide some standardization and clarification, there still seems to be a lot of confusion in my audience about how to interpret some of the guidelines. Have you found that?
Errol R. Norwitz, MD, PhD: Yes, I have. I found it interesting that it was put out as an executive summary, and not as a practice bulletin, which will probably follow in months. That document, which came out in November 2013, helped to address many of the issues we’ve had over the years of preeclampsia, in terms of its definition and some of the management issues. But, it also raised a number of questions that still need to be resolved.
Dr. Repke: Yes. I think one of the things to keep in mind, and I’ve tabulated all of the recommendations, is that about 60 recommendations came out of that document and only six of the 60 were accompanied by a strong quality of evidence, or rather, a high quality of evidence, and a strong recommendation. And a lot of those things were addressing issues that I think most practitioners already did, in so far as using antenatal steroids for maturation; using magnesium sulfate for patients with preeclampsia with severe features; and using magnesium sulfate as a treatment of eclampsia. But a lot of the other recommendations really were based on either moderate- or low-quality evidence, and had qualified recommendations. And, I think that’s what has led to some of the confusion.
Changing diagnostic tools for preeclampsia
Dr. Repke: What sort of specific things are your practitioners asking you about as far as, “Is this gestational hypertension or is this preeclampsia?” The guidelines say proteinuria is not required anymore. How are you dealing with that?
Should we still do the 24-hour urinary protein estimation?
Dr. Norwitz: The biggest change, in my mind, is the statement that you no longer require significant proteinuria to make the diagnosis of preeclampsia, and, indeed, of severe preeclampsia. So, if you do have significant proteinuria, then that would confirm the diagnosis. But, you can also have preeclampsia in the presence of other endorgan injuries, such as kidney injury and liver injury in the absence of significant proteinuria.
So, one of the questions that comes up is, “Should we actually do the 24-hour urinary protein estimation?”
And, my answer is, “yes.” If you have significant proteinuria, then that would confirm the diagnosis. If you don’t, you can still make the diagnosis in the setting of low platelets, elevated liver enzymes, or abnormal renal function. So, the issue is, and I’d be curious to hear your answer, if you have someone with platelets of, let’s say, 78, a new onset of sustained elevation of blood pressure, would you do the 24-hour urine estimation or just defer it?
Dr. Repke: We wouldn’t perform the 24-hour urine test under those circumstances. And, we would consider that nuance of hypertension with a severe feature that is now preeclampsia with severe feature, and the management would be based on gestational age. With a platelet count that low, the management would be stabilization and delivery. Although, if stabilized, I think that’s the type of patient that potentially could have delivery delayed until you could get an effective antenatal steroid if she was less that 34 weeks’ gestation.
Dr. Norwitz: So, that’s one issue I think needs to be clarified. If there’s other evidence of endorgan damage, then you can defer the 24-hour urinary protein. That’s another question that comes up. I’m pleased they could resolve the issue of repeated 24-hour urinary estimations. Once you have your 300 mg suggestive of the diagnosis of preeclampsia, there’s no reason to then repeat it looking for elevation and increased leakage of protein into the urine, because it doesn’t correlate with adverse outcome for the mother or fetus. So, that issue was clarified.
Dr. Repke: I think that two questions that came up in our course, and I think they were very legitimate, are, “Do we even need to do urine protein at all?” Because if you look at the guidelines for management, the only difference between preeclampsia management without severe features and gestational hypertension is frequency of antenatal testing until you decide to begin delivery. Now, in the old days, one would say, “Well, another difference would be that the preeclamptic would get magnesium sulfate.” But the current Hypertension in Pregnancy Guidelines1 suggest that preeclampsia without severe features doesn’t necessarily have to be managed with magnesium sulfate. So, I’m still wrestling with whether, other than the fact that it might be for study purposes or for categorization or research, whether proteinuria adds anything to the equation.
And, then the second question is, “How do you resolve the issue of disagreement?” So, the example is protein:creatinine ratio allows for a more rapid diagnosis of significant proteinuria. If that patient doesn’t have to deliver immediately and a 24-hour urine sample is obtained, which do you believe if you have a protein:creatinine ratio greater than 0.3, but now your 24-hour urine is 212 mg/dL? And, I don’t have the answer to that, but that’s another area of confusion.
Dr. Norwitz: And, I think that confusion will persist. I don’t think this document is going to resolve it.
New terminology: Preeclampsia with or without severe features
Dr. Norwitz: I do like the difference in terminology between preeclampsia with severe features and preeclampsia without severe features. I think the old terminology of severe and mild preeclampsia was somewhat confusing. I certainly appreciate that alteration in terminology, although it may take a while for it to catch on. I’m still seeing the term “mild preeclampsia” used quite widely.
Use of magnesium sulfate for seizure prophylaxis
Dr. Norwitz: You did raise the issue of magnesium sulfate for seizure prophylaxis in the setting of severe preeclampsia without severe features. And I was struck by the statement. Not only is it not necessary to give it, but in the Executive Summary, as you suggest, it is not indicated and you recommended against starting it. Is that how you interpret it as the well?
Dr. Repke: Well, I might have interpreted the statement the way I wanted to interpret it. And, as you know, in our institution, because we feel we are a teaching program, people can progress very quickly intrapartum from not having severe features to having severe features, and we don’t want to miss that window of opportunity. Our practice in that regard does not follow the guidelines. We use intrapartum magnesium prophylaxis for all patients with the diagnosis of preeclampsia, and continue it for 24 hours postpartum.
Dr. Norwitz: And I would have to say we decided do the same. So, once a diagnosis of preeclampsia is made, we would give intrapartum, and then postpartum magnesium seizure prophylaxis for 24 hours, regardless of whether there’s evidence of severe features or no severe features.
Dr. Repke: And there again, I think it’s why, for you and I, it will still be important to assess the proteinuria because that diagnostic difference between preeclampsia and gestational hypertension is going to alter management. But if you follow the document word for word, if you’re not going to use magnesium without severe features, I’m not really sure what proteinuria adds. I guess, at the end of the day, you’ve got to be a good doctor. And, you’ve got to be physically assessing your patient on a very regular basis.
Preventing the first cesarean delivery. Will cesarean rates decline?
Dr. Repke: So, speaking of guidelines, the Society for Maternal Fetal Medicine (SMFM) just came out with a document trying to address this issue of the cesarean-section rate in the United States and are there things that we can be doing to lower the primary C-section rate.2 My feeling is probably disseminated from the recognition that vaginal birth after C-section never got to the levels of acceptance that anybody hoped back when Healthy People 2010 was first written. And, we could eliminate that issue or, at least significantly reduce that issue, if the first C-section never took place.
And, I guess I’d like some of your thoughts about some of the things in that document, some of the things we need to be reconsidering in terms of how we define labor and so on.
Dr. Norwitz: It is true, I think, that there’s been an epidemic of cesarean deliveries in the last decade in the US, but also throughout the world, I think, even in countries that have traditionally had very low cesarean delivery rates, the classic one being Ireland and the UK countries. Their rates are now increasing significantly.
And there are a number of different reasons as to why this may be. I think, certainly the obesity epidemic has contributed to this. You want to deliver patients who have an elevated BMI prior to the postterm period. But, it’s often difficult to monitor these patients, and the cesarean-delivery rate overall is much higher in that population. So, that might be one reason why cesarean-delivery rates overall are going up. But, certainly there are many others.
Dr. Repke: Yes, I think you’re absolutely right: the demographics of change. Childbearing is being delayed. We know that uterine contractility dynamics alter with advanced maternal age. We’ve got a higher incidence of multiple gestations with advanced maternal age. We have more patients that require induction because of supervening medical complications of pregnancy, whether that be Class A2 gestational diabetes, or whether that be pregnancy-induced hypertension.
Redefining the stages of labor
Dr. Repke: I think some of the intriguing data, to me, is a willingness to re-look at how we define the stages of labor. And what are acceptable norms? And, while I have some concerns about how that may be interpreted in the rank and file, I think it’s at least heightened the awareness of my faculty that we just can’t tolerate the C-section at 4 cm, or whether the latent phase of labor should be allowed to go to 6 cm. I don’t think we really have the data for that. But I’d be happy if I could just start to see a reduction in “failure to progress at 4 cm.”
And then the issue of second stage, I think, is also important. What do you think about the guidelines’ recommendation that there may not really be an upper limit of allowability for second-stage labors?
Dr. Norwitz: Well, certainly I think it’s important to think back to the historical context of where the labor curves developed. The original labor curves were actually developed in Zimbabwe (at that time it was Rhodesia) by an obstetrician working in the community called Philpott. And he was trying to determine when it was appropriate to send patients into the tertiary care center. So he designed the labor curve and said if patients failed to progress over a certain number of hours, those are patients that are likely to need an operative delivery, and he would then send them into the tertiary care center.
And, then Dr. Freidman picked up on that idea and developed the Freidman Curve in Boston. But that was an era, again, many years ago when the population demographics were very different, when not many patients received regional anesthesia. I think if you look at the current guidelines, there is a huge discrepancy between women who get epidural anesthesia and those that don’t in terms of the progress of labor, both the first stage and the second stage.
Is it anesthesia?
Dr. Repke: One of the things that, you know, I haven’t looked at this paper in a long time, but you remember at Brigham and Women’s Hospital, probably 20 years ago, we were winding down the Active Management of Labor Study3 that was designed to try to replicate what had gone on at the Dublin Maternity Hospital,4 and if I’m remembering correctly, one of the remarkable things about that is that in Dublin, there were virtually no C-sections in the second stage. And so people assumed that while they were more aggressive with forceps, the operative vaginal delivery rate was no different between Brigham and Women’s Hospital and the Dublin Maternity Hospital. And so there needed to be another explanation.
And, I know I’m going to incur some of the ire of our anesthesia colleagues, but I really wonder whether there is a contribution of regional anesthesia to some of the labor dystocias that we see, and whether that’s a new demographic that we haven’t really adequately assessed. Even though I recognize some of the anesthesia literature5 seems to suggest very strongly that it has no effect. You know, if you were to plot a graph of regional anesthesia rates and cesarean section rates, they would probably parallel each other.
Dr. Norwitz: I think they do. I think we’ve long known that epidural anesthesia slows down the second stage of labor. These analyses suggest that it also has a significant effect on the first stage. And, I think that needs to be taken into account.
The lost skill of forceps delivery
Dr. Norwitz: I personally think that the skill set, in terms of operative vaginal delivery with forceps and vacuum, has really been lost. And I do feel that’s one of the factors contributing to the increase in cesarean delivery rates. I certainly see that in my practice: that I’m comfortable doing rotational forceps and mid-cavity forceps deliveries, where many of my colleagues have lost that skill, and rely now on the vacuum, which in certain circumstances is a less-than-ideal instrument. So, I believe that’s part of the reason why the cesarean delivery rates have gone up.
Lengthy second stage
Dr. Norwitz: But, certainly, I think, epidural anesthesia has made a difference, and I think we need to be cognizant of the fact that there is no “hard stop” now, in terms of the length of the second stage. If you get to 3 hours, even 4 hours, I would say, and there’s continued descent with pushing and fetal heart-rate tracing is reassuring, it’s reasonable to continue beyond those cutoffs.
Dr. Repke: I agree. I also have a concern about that, and I’m going to use a little bit of a parallel example of, you know, 7 or 8 years ago, there was a big push, and I think it was an appropriate push, to try to avoid elective deliveries prior to 39 weeks.6,7 What ended up happening was that people forgot about the term “elective,” and all they heard was 39 weeks. And what we would see on Board Examinations was, “Why do you have this placenta previa delivering at 39 weeks?”
“Well, that’s our hospital policy. We can’t deliver before 39 weeks.”
And, I think, the complications started to arise, and that’s what led to SMFM and ACOG coming out with guidelines for when it is acceptable to deliver prior to 39 weeks.2,6–8
So, the analogy is: I’m afraid that people are only going to see there is no upper limit for latent phase, there is no upper limit for second stage; that clinical judgment may not get its due in making these decisions. And we’ve all been in situations where, when you are trying to extract the head out of the pelvis, a cesarean section after a 5- or 6-hour second stage has its own set of complications. So my concern is that I hope we will recognize that we have to still use some clinical judgment, what I term the so-called “art of obstetrics,” into managing these patients.
Are you optimistic that we’re going to the lower C-section rate?
Dr. Norwitz: No, I think, it’s going to continue to go up. I think, with the increasing number of multiple pregnancies, obesity, maternal age getting further and further along, I think this is only going to continue to rise. And to be honest, I don’t know the correct cesarean delivery rate, or even if that is the metric that we should be measuring.
What is the right metric to measure neonatal outcome?
Dr. Norwitz: Maybe we should be looking at perinatal outcome. If perinatal outcome is improved, then maybe the cesarean rate is less important. Obviously, the first cesarean does have implications for subsequent pregnancy outcomes, and if we do continue to see this rise in cesarean deliveries, we are going to end up with many more placental accretas and hemorrhages in women in years to come.
So, careful counseling is important. If patients plan to have one or two kids only, maybe a cesarean delivery is very reasonable. If they are planning on having six or seven kids, then maybe you have to have a more careful discussion.
Dr. Repke: Yes, I think, that’s a very good point: the number of cesareans and the potential risks for abnormal placentation. I think societal expectations have changed in terms of what they want. Most mothers are willing to sacrifice maternal risk for presumed benefits to the fetus.
I think, where we’ve gotten into trouble as a specialty, though, is that we’ve had a hard time proving that neonatal outcome, in fact, has improved—despite an almost tripling of the cesarean section rate since, probably, the early 1970s. Although, anecdotally, what my pediatric and neonatal colleagues will tell me is they don’t get the kind of damaged babies they used to get. So the neonatologists that are closer to my age that have been doing this for a long time, they’re not seeing the really severe meconium aspiration syndromes; they’re not seeing really severe forceps-related injuries, or vacuum-related injuries that they used to see. So, those may be data that we’re going to need to accumulate with a little bit more rigor, and see if that’s true.
But I tend to agree with you. I don’t know what the right cesarean section rate is. I often tell people, I have yet to meet a patient who doesn’t think her cesarean section was indicated. And that’s where I think we hit the crossroads of individual patient-care management. So, we know across all other disciplines in medicine we’re entering the era of personalized medicine, yet we want to make broad public health policy that may not apply to individuals, and run with that. So, that’s also a concern. But, as they say, a story we will follow with interest.
Dr. Norwitz: I think so. I think the other part of that equation is the stillbirth rate, and the fact that there’s a push now to avoid elective inductions before 39 weeks, which I think is very reasonable, with a focus there again on elective inductions.
There’s also a push to induce patients before 42 weeks. And that bar has been pushed back, and in most practices around the country now, deliveries are being affected and recommended at 41 weeks. And clearly, if you take a nulliparous patient with an unfavorable cervix and induce at 41 weeks, you are going to increase the cesarean rate. I would argue that you are also decreasing the chance that there will be a stillbirth. But that data has not been forthcoming.
So this issue is by no means resolved. I think there are going to be many more years of data and studies and consensus opinions before we have a much better sense of what the right cesarean
rate is.
Dr. Repke: Yes, I think that’s a great point. And, one thing that I think people aren’t maybe that familiar with is when this push came, and again, it is an appropriate push to minimize elective deliveries before 39 weeks. When they looked at neonatal outcomes, all they looked at were the group that delivered at 37 weeks, and the group that delivered at 39 weeks. And they didn’t look at what happened with the other ones.9
So, they did look at the stillbirths of fetal distress or the other complications that happened between 37 and 1, and 38 and 6. They just looked at neonates that were born at 37 weeks and compared them to neonates that were born at 39 weeks, and found reduced instances of things like transient tachypnea of the newborn, hyperbilirubinemia, and thermoregulation issues, and those sorts of things. But, never looked at the neonates in that window, so no question 39 is better than 37, but, 37 is better than not making it to 39. So that, as you said, we’ve got a lot more information we’ve got to gather.
Errol, good talking with you.
Dr. Norwitz: Thank you.
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus: Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Frigoletto FD, Lieberman E, Lang J, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333(12):745–750.
- O’Driscoll K, Meagher D, Boylan P. Active Management of Labor. 3rd ed. London: Mosby- Yearbook; 1993.
- Chestnut DH, McGrath JM, Vincent RD, et al. Does early administration of epidural analgesia effect obstetric outcome in nulliparous women who are in spontaneous labor? Anesthesiology. 1994;80(6):1201–1208.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 560: Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915.
- Spong CY, Mercer BM, D’Alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):323–333.
- Tita ATN, Landon MB, Spong CY, et al; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat Cesarean Delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
This peer to peer discussion focuses on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines1 and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.2
In this 20-minute audiocast, listen to these experts discuss:
Changing diagnostic tools for preeclampsia
- The 24-hour urinary protein estimation: When is it necessary?
- Use of magnesium sulfate for seizure prophylaxis
Preventing the first cesarean delivery
- Redefining the stages of labor: When is the second-stage too long?
- The lost skill of forceps delivery
- Is cesarean delivery rate the optimal metric for measuring neonatal outcome?
John T. Repke, MD, is University Professor and Chairman of the Department of Obstetrics and Gynecology at Penn State University College of Medicine, and Obstetrician-Gynecologist-in-Chief at the Milton S. Hershey Medical Center in Hershey, Pennsylvania. Dr. Repke is a member of the Board of Editors of OBG Management and is author of the June 2014 Guest Editorial on hypertension and pregnancy.
Errol R. Norwitz, MD, PhD, is the Louis E. Phaneuf Professor and Chairman of the Department of Obstetrics and Gynecology at Tufts Medical Center and Tufts University School of Medicine in Boston, Massachusetts. Dr. Norwitz is a member of the Board of Editors of OBG Management and is author of the June 2014 Update on operative vaginal delivery.
The speakers report no financial relationships relevant to this audiocast.
Click here for a downloadable transcript
TRANSCRIPT
ACOG guidelines on hypertension and pregnancy raise some questions
John T. Repke, MD: So, Errol, I was impressed over the first couple of days of being at the meeting. As you know, we had a postgraduate course, and one of the items that we talked about was the new hypertension and pregnancy document that was released by the Task Force on Hypertension and Pregnancy1 charged by the American College of Obstetricians and Gynecologists. I’ve got to say that while the goal of the document was to provide some standardization and clarification, there still seems to be a lot of confusion in my audience about how to interpret some of the guidelines. Have you found that?
Errol R. Norwitz, MD, PhD: Yes, I have. I found it interesting that it was put out as an executive summary, and not as a practice bulletin, which will probably follow in months. That document, which came out in November 2013, helped to address many of the issues we’ve had over the years of preeclampsia, in terms of its definition and some of the management issues. But, it also raised a number of questions that still need to be resolved.
Dr. Repke: Yes. I think one of the things to keep in mind, and I’ve tabulated all of the recommendations, is that about 60 recommendations came out of that document and only six of the 60 were accompanied by a strong quality of evidence, or rather, a high quality of evidence, and a strong recommendation. And a lot of those things were addressing issues that I think most practitioners already did, in so far as using antenatal steroids for maturation; using magnesium sulfate for patients with preeclampsia with severe features; and using magnesium sulfate as a treatment of eclampsia. But a lot of the other recommendations really were based on either moderate- or low-quality evidence, and had qualified recommendations. And, I think that’s what has led to some of the confusion.
Changing diagnostic tools for preeclampsia
Dr. Repke: What sort of specific things are your practitioners asking you about as far as, “Is this gestational hypertension or is this preeclampsia?” The guidelines say proteinuria is not required anymore. How are you dealing with that?
Should we still do the 24-hour urinary protein estimation?
Dr. Norwitz: The biggest change, in my mind, is the statement that you no longer require significant proteinuria to make the diagnosis of preeclampsia, and, indeed, of severe preeclampsia. So, if you do have significant proteinuria, then that would confirm the diagnosis. But, you can also have preeclampsia in the presence of other endorgan injuries, such as kidney injury and liver injury in the absence of significant proteinuria.
So, one of the questions that comes up is, “Should we actually do the 24-hour urinary protein estimation?”
And, my answer is, “yes.” If you have significant proteinuria, then that would confirm the diagnosis. If you don’t, you can still make the diagnosis in the setting of low platelets, elevated liver enzymes, or abnormal renal function. So, the issue is, and I’d be curious to hear your answer, if you have someone with platelets of, let’s say, 78, a new onset of sustained elevation of blood pressure, would you do the 24-hour urine estimation or just defer it?
Dr. Repke: We wouldn’t perform the 24-hour urine test under those circumstances. And, we would consider that nuance of hypertension with a severe feature that is now preeclampsia with severe feature, and the management would be based on gestational age. With a platelet count that low, the management would be stabilization and delivery. Although, if stabilized, I think that’s the type of patient that potentially could have delivery delayed until you could get an effective antenatal steroid if she was less that 34 weeks’ gestation.
Dr. Norwitz: So, that’s one issue I think needs to be clarified. If there’s other evidence of endorgan damage, then you can defer the 24-hour urinary protein. That’s another question that comes up. I’m pleased they could resolve the issue of repeated 24-hour urinary estimations. Once you have your 300 mg suggestive of the diagnosis of preeclampsia, there’s no reason to then repeat it looking for elevation and increased leakage of protein into the urine, because it doesn’t correlate with adverse outcome for the mother or fetus. So, that issue was clarified.
Dr. Repke: I think that two questions that came up in our course, and I think they were very legitimate, are, “Do we even need to do urine protein at all?” Because if you look at the guidelines for management, the only difference between preeclampsia management without severe features and gestational hypertension is frequency of antenatal testing until you decide to begin delivery. Now, in the old days, one would say, “Well, another difference would be that the preeclamptic would get magnesium sulfate.” But the current Hypertension in Pregnancy Guidelines1 suggest that preeclampsia without severe features doesn’t necessarily have to be managed with magnesium sulfate. So, I’m still wrestling with whether, other than the fact that it might be for study purposes or for categorization or research, whether proteinuria adds anything to the equation.
And, then the second question is, “How do you resolve the issue of disagreement?” So, the example is protein:creatinine ratio allows for a more rapid diagnosis of significant proteinuria. If that patient doesn’t have to deliver immediately and a 24-hour urine sample is obtained, which do you believe if you have a protein:creatinine ratio greater than 0.3, but now your 24-hour urine is 212 mg/dL? And, I don’t have the answer to that, but that’s another area of confusion.
Dr. Norwitz: And, I think that confusion will persist. I don’t think this document is going to resolve it.
New terminology: Preeclampsia with or without severe features
Dr. Norwitz: I do like the difference in terminology between preeclampsia with severe features and preeclampsia without severe features. I think the old terminology of severe and mild preeclampsia was somewhat confusing. I certainly appreciate that alteration in terminology, although it may take a while for it to catch on. I’m still seeing the term “mild preeclampsia” used quite widely.
Use of magnesium sulfate for seizure prophylaxis
Dr. Norwitz: You did raise the issue of magnesium sulfate for seizure prophylaxis in the setting of severe preeclampsia without severe features. And I was struck by the statement. Not only is it not necessary to give it, but in the Executive Summary, as you suggest, it is not indicated and you recommended against starting it. Is that how you interpret it as the well?
Dr. Repke: Well, I might have interpreted the statement the way I wanted to interpret it. And, as you know, in our institution, because we feel we are a teaching program, people can progress very quickly intrapartum from not having severe features to having severe features, and we don’t want to miss that window of opportunity. Our practice in that regard does not follow the guidelines. We use intrapartum magnesium prophylaxis for all patients with the diagnosis of preeclampsia, and continue it for 24 hours postpartum.
Dr. Norwitz: And I would have to say we decided do the same. So, once a diagnosis of preeclampsia is made, we would give intrapartum, and then postpartum magnesium seizure prophylaxis for 24 hours, regardless of whether there’s evidence of severe features or no severe features.
Dr. Repke: And there again, I think it’s why, for you and I, it will still be important to assess the proteinuria because that diagnostic difference between preeclampsia and gestational hypertension is going to alter management. But if you follow the document word for word, if you’re not going to use magnesium without severe features, I’m not really sure what proteinuria adds. I guess, at the end of the day, you’ve got to be a good doctor. And, you’ve got to be physically assessing your patient on a very regular basis.
Preventing the first cesarean delivery. Will cesarean rates decline?
Dr. Repke: So, speaking of guidelines, the Society for Maternal Fetal Medicine (SMFM) just came out with a document trying to address this issue of the cesarean-section rate in the United States and are there things that we can be doing to lower the primary C-section rate.2 My feeling is probably disseminated from the recognition that vaginal birth after C-section never got to the levels of acceptance that anybody hoped back when Healthy People 2010 was first written. And, we could eliminate that issue or, at least significantly reduce that issue, if the first C-section never took place.
And, I guess I’d like some of your thoughts about some of the things in that document, some of the things we need to be reconsidering in terms of how we define labor and so on.
Dr. Norwitz: It is true, I think, that there’s been an epidemic of cesarean deliveries in the last decade in the US, but also throughout the world, I think, even in countries that have traditionally had very low cesarean delivery rates, the classic one being Ireland and the UK countries. Their rates are now increasing significantly.
And there are a number of different reasons as to why this may be. I think, certainly the obesity epidemic has contributed to this. You want to deliver patients who have an elevated BMI prior to the postterm period. But, it’s often difficult to monitor these patients, and the cesarean-delivery rate overall is much higher in that population. So, that might be one reason why cesarean-delivery rates overall are going up. But, certainly there are many others.
Dr. Repke: Yes, I think you’re absolutely right: the demographics of change. Childbearing is being delayed. We know that uterine contractility dynamics alter with advanced maternal age. We’ve got a higher incidence of multiple gestations with advanced maternal age. We have more patients that require induction because of supervening medical complications of pregnancy, whether that be Class A2 gestational diabetes, or whether that be pregnancy-induced hypertension.
Redefining the stages of labor
Dr. Repke: I think some of the intriguing data, to me, is a willingness to re-look at how we define the stages of labor. And what are acceptable norms? And, while I have some concerns about how that may be interpreted in the rank and file, I think it’s at least heightened the awareness of my faculty that we just can’t tolerate the C-section at 4 cm, or whether the latent phase of labor should be allowed to go to 6 cm. I don’t think we really have the data for that. But I’d be happy if I could just start to see a reduction in “failure to progress at 4 cm.”
And then the issue of second stage, I think, is also important. What do you think about the guidelines’ recommendation that there may not really be an upper limit of allowability for second-stage labors?
Dr. Norwitz: Well, certainly I think it’s important to think back to the historical context of where the labor curves developed. The original labor curves were actually developed in Zimbabwe (at that time it was Rhodesia) by an obstetrician working in the community called Philpott. And he was trying to determine when it was appropriate to send patients into the tertiary care center. So he designed the labor curve and said if patients failed to progress over a certain number of hours, those are patients that are likely to need an operative delivery, and he would then send them into the tertiary care center.
And, then Dr. Freidman picked up on that idea and developed the Freidman Curve in Boston. But that was an era, again, many years ago when the population demographics were very different, when not many patients received regional anesthesia. I think if you look at the current guidelines, there is a huge discrepancy between women who get epidural anesthesia and those that don’t in terms of the progress of labor, both the first stage and the second stage.
Is it anesthesia?
Dr. Repke: One of the things that, you know, I haven’t looked at this paper in a long time, but you remember at Brigham and Women’s Hospital, probably 20 years ago, we were winding down the Active Management of Labor Study3 that was designed to try to replicate what had gone on at the Dublin Maternity Hospital,4 and if I’m remembering correctly, one of the remarkable things about that is that in Dublin, there were virtually no C-sections in the second stage. And so people assumed that while they were more aggressive with forceps, the operative vaginal delivery rate was no different between Brigham and Women’s Hospital and the Dublin Maternity Hospital. And so there needed to be another explanation.
And, I know I’m going to incur some of the ire of our anesthesia colleagues, but I really wonder whether there is a contribution of regional anesthesia to some of the labor dystocias that we see, and whether that’s a new demographic that we haven’t really adequately assessed. Even though I recognize some of the anesthesia literature5 seems to suggest very strongly that it has no effect. You know, if you were to plot a graph of regional anesthesia rates and cesarean section rates, they would probably parallel each other.
Dr. Norwitz: I think they do. I think we’ve long known that epidural anesthesia slows down the second stage of labor. These analyses suggest that it also has a significant effect on the first stage. And, I think that needs to be taken into account.
The lost skill of forceps delivery
Dr. Norwitz: I personally think that the skill set, in terms of operative vaginal delivery with forceps and vacuum, has really been lost. And I do feel that’s one of the factors contributing to the increase in cesarean delivery rates. I certainly see that in my practice: that I’m comfortable doing rotational forceps and mid-cavity forceps deliveries, where many of my colleagues have lost that skill, and rely now on the vacuum, which in certain circumstances is a less-than-ideal instrument. So, I believe that’s part of the reason why the cesarean delivery rates have gone up.
Lengthy second stage
Dr. Norwitz: But, certainly, I think, epidural anesthesia has made a difference, and I think we need to be cognizant of the fact that there is no “hard stop” now, in terms of the length of the second stage. If you get to 3 hours, even 4 hours, I would say, and there’s continued descent with pushing and fetal heart-rate tracing is reassuring, it’s reasonable to continue beyond those cutoffs.
Dr. Repke: I agree. I also have a concern about that, and I’m going to use a little bit of a parallel example of, you know, 7 or 8 years ago, there was a big push, and I think it was an appropriate push, to try to avoid elective deliveries prior to 39 weeks.6,7 What ended up happening was that people forgot about the term “elective,” and all they heard was 39 weeks. And what we would see on Board Examinations was, “Why do you have this placenta previa delivering at 39 weeks?”
“Well, that’s our hospital policy. We can’t deliver before 39 weeks.”
And, I think, the complications started to arise, and that’s what led to SMFM and ACOG coming out with guidelines for when it is acceptable to deliver prior to 39 weeks.2,6–8
So, the analogy is: I’m afraid that people are only going to see there is no upper limit for latent phase, there is no upper limit for second stage; that clinical judgment may not get its due in making these decisions. And we’ve all been in situations where, when you are trying to extract the head out of the pelvis, a cesarean section after a 5- or 6-hour second stage has its own set of complications. So my concern is that I hope we will recognize that we have to still use some clinical judgment, what I term the so-called “art of obstetrics,” into managing these patients.
Are you optimistic that we’re going to the lower C-section rate?
Dr. Norwitz: No, I think, it’s going to continue to go up. I think, with the increasing number of multiple pregnancies, obesity, maternal age getting further and further along, I think this is only going to continue to rise. And to be honest, I don’t know the correct cesarean delivery rate, or even if that is the metric that we should be measuring.
What is the right metric to measure neonatal outcome?
Dr. Norwitz: Maybe we should be looking at perinatal outcome. If perinatal outcome is improved, then maybe the cesarean rate is less important. Obviously, the first cesarean does have implications for subsequent pregnancy outcomes, and if we do continue to see this rise in cesarean deliveries, we are going to end up with many more placental accretas and hemorrhages in women in years to come.
So, careful counseling is important. If patients plan to have one or two kids only, maybe a cesarean delivery is very reasonable. If they are planning on having six or seven kids, then maybe you have to have a more careful discussion.
Dr. Repke: Yes, I think, that’s a very good point: the number of cesareans and the potential risks for abnormal placentation. I think societal expectations have changed in terms of what they want. Most mothers are willing to sacrifice maternal risk for presumed benefits to the fetus.
I think, where we’ve gotten into trouble as a specialty, though, is that we’ve had a hard time proving that neonatal outcome, in fact, has improved—despite an almost tripling of the cesarean section rate since, probably, the early 1970s. Although, anecdotally, what my pediatric and neonatal colleagues will tell me is they don’t get the kind of damaged babies they used to get. So the neonatologists that are closer to my age that have been doing this for a long time, they’re not seeing the really severe meconium aspiration syndromes; they’re not seeing really severe forceps-related injuries, or vacuum-related injuries that they used to see. So, those may be data that we’re going to need to accumulate with a little bit more rigor, and see if that’s true.
But I tend to agree with you. I don’t know what the right cesarean section rate is. I often tell people, I have yet to meet a patient who doesn’t think her cesarean section was indicated. And that’s where I think we hit the crossroads of individual patient-care management. So, we know across all other disciplines in medicine we’re entering the era of personalized medicine, yet we want to make broad public health policy that may not apply to individuals, and run with that. So, that’s also a concern. But, as they say, a story we will follow with interest.
Dr. Norwitz: I think so. I think the other part of that equation is the stillbirth rate, and the fact that there’s a push now to avoid elective inductions before 39 weeks, which I think is very reasonable, with a focus there again on elective inductions.
There’s also a push to induce patients before 42 weeks. And that bar has been pushed back, and in most practices around the country now, deliveries are being affected and recommended at 41 weeks. And clearly, if you take a nulliparous patient with an unfavorable cervix and induce at 41 weeks, you are going to increase the cesarean rate. I would argue that you are also decreasing the chance that there will be a stillbirth. But that data has not been forthcoming.
So this issue is by no means resolved. I think there are going to be many more years of data and studies and consensus opinions before we have a much better sense of what the right cesarean
rate is.
Dr. Repke: Yes, I think that’s a great point. And, one thing that I think people aren’t maybe that familiar with is when this push came, and again, it is an appropriate push to minimize elective deliveries before 39 weeks. When they looked at neonatal outcomes, all they looked at were the group that delivered at 37 weeks, and the group that delivered at 39 weeks. And they didn’t look at what happened with the other ones.9
So, they did look at the stillbirths of fetal distress or the other complications that happened between 37 and 1, and 38 and 6. They just looked at neonates that were born at 37 weeks and compared them to neonates that were born at 39 weeks, and found reduced instances of things like transient tachypnea of the newborn, hyperbilirubinemia, and thermoregulation issues, and those sorts of things. But, never looked at the neonates in that window, so no question 39 is better than 37, but, 37 is better than not making it to 39. So that, as you said, we’ve got a lot more information we’ve got to gather.
Errol, good talking with you.
Dr. Norwitz: Thank you.
This peer to peer discussion focuses on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines1 and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.2
In this 20-minute audiocast, listen to these experts discuss:
Changing diagnostic tools for preeclampsia
- The 24-hour urinary protein estimation: When is it necessary?
- Use of magnesium sulfate for seizure prophylaxis
Preventing the first cesarean delivery
- Redefining the stages of labor: When is the second-stage too long?
- The lost skill of forceps delivery
- Is cesarean delivery rate the optimal metric for measuring neonatal outcome?
John T. Repke, MD, is University Professor and Chairman of the Department of Obstetrics and Gynecology at Penn State University College of Medicine, and Obstetrician-Gynecologist-in-Chief at the Milton S. Hershey Medical Center in Hershey, Pennsylvania. Dr. Repke is a member of the Board of Editors of OBG Management and is author of the June 2014 Guest Editorial on hypertension and pregnancy.
Errol R. Norwitz, MD, PhD, is the Louis E. Phaneuf Professor and Chairman of the Department of Obstetrics and Gynecology at Tufts Medical Center and Tufts University School of Medicine in Boston, Massachusetts. Dr. Norwitz is a member of the Board of Editors of OBG Management and is author of the June 2014 Update on operative vaginal delivery.
The speakers report no financial relationships relevant to this audiocast.
Click here for a downloadable transcript
TRANSCRIPT
ACOG guidelines on hypertension and pregnancy raise some questions
John T. Repke, MD: So, Errol, I was impressed over the first couple of days of being at the meeting. As you know, we had a postgraduate course, and one of the items that we talked about was the new hypertension and pregnancy document that was released by the Task Force on Hypertension and Pregnancy1 charged by the American College of Obstetricians and Gynecologists. I’ve got to say that while the goal of the document was to provide some standardization and clarification, there still seems to be a lot of confusion in my audience about how to interpret some of the guidelines. Have you found that?
Errol R. Norwitz, MD, PhD: Yes, I have. I found it interesting that it was put out as an executive summary, and not as a practice bulletin, which will probably follow in months. That document, which came out in November 2013, helped to address many of the issues we’ve had over the years of preeclampsia, in terms of its definition and some of the management issues. But, it also raised a number of questions that still need to be resolved.
Dr. Repke: Yes. I think one of the things to keep in mind, and I’ve tabulated all of the recommendations, is that about 60 recommendations came out of that document and only six of the 60 were accompanied by a strong quality of evidence, or rather, a high quality of evidence, and a strong recommendation. And a lot of those things were addressing issues that I think most practitioners already did, in so far as using antenatal steroids for maturation; using magnesium sulfate for patients with preeclampsia with severe features; and using magnesium sulfate as a treatment of eclampsia. But a lot of the other recommendations really were based on either moderate- or low-quality evidence, and had qualified recommendations. And, I think that’s what has led to some of the confusion.
Changing diagnostic tools for preeclampsia
Dr. Repke: What sort of specific things are your practitioners asking you about as far as, “Is this gestational hypertension or is this preeclampsia?” The guidelines say proteinuria is not required anymore. How are you dealing with that?
Should we still do the 24-hour urinary protein estimation?
Dr. Norwitz: The biggest change, in my mind, is the statement that you no longer require significant proteinuria to make the diagnosis of preeclampsia, and, indeed, of severe preeclampsia. So, if you do have significant proteinuria, then that would confirm the diagnosis. But, you can also have preeclampsia in the presence of other endorgan injuries, such as kidney injury and liver injury in the absence of significant proteinuria.
So, one of the questions that comes up is, “Should we actually do the 24-hour urinary protein estimation?”
And, my answer is, “yes.” If you have significant proteinuria, then that would confirm the diagnosis. If you don’t, you can still make the diagnosis in the setting of low platelets, elevated liver enzymes, or abnormal renal function. So, the issue is, and I’d be curious to hear your answer, if you have someone with platelets of, let’s say, 78, a new onset of sustained elevation of blood pressure, would you do the 24-hour urine estimation or just defer it?
Dr. Repke: We wouldn’t perform the 24-hour urine test under those circumstances. And, we would consider that nuance of hypertension with a severe feature that is now preeclampsia with severe feature, and the management would be based on gestational age. With a platelet count that low, the management would be stabilization and delivery. Although, if stabilized, I think that’s the type of patient that potentially could have delivery delayed until you could get an effective antenatal steroid if she was less that 34 weeks’ gestation.
Dr. Norwitz: So, that’s one issue I think needs to be clarified. If there’s other evidence of endorgan damage, then you can defer the 24-hour urinary protein. That’s another question that comes up. I’m pleased they could resolve the issue of repeated 24-hour urinary estimations. Once you have your 300 mg suggestive of the diagnosis of preeclampsia, there’s no reason to then repeat it looking for elevation and increased leakage of protein into the urine, because it doesn’t correlate with adverse outcome for the mother or fetus. So, that issue was clarified.
Dr. Repke: I think that two questions that came up in our course, and I think they were very legitimate, are, “Do we even need to do urine protein at all?” Because if you look at the guidelines for management, the only difference between preeclampsia management without severe features and gestational hypertension is frequency of antenatal testing until you decide to begin delivery. Now, in the old days, one would say, “Well, another difference would be that the preeclamptic would get magnesium sulfate.” But the current Hypertension in Pregnancy Guidelines1 suggest that preeclampsia without severe features doesn’t necessarily have to be managed with magnesium sulfate. So, I’m still wrestling with whether, other than the fact that it might be for study purposes or for categorization or research, whether proteinuria adds anything to the equation.
And, then the second question is, “How do you resolve the issue of disagreement?” So, the example is protein:creatinine ratio allows for a more rapid diagnosis of significant proteinuria. If that patient doesn’t have to deliver immediately and a 24-hour urine sample is obtained, which do you believe if you have a protein:creatinine ratio greater than 0.3, but now your 24-hour urine is 212 mg/dL? And, I don’t have the answer to that, but that’s another area of confusion.
Dr. Norwitz: And, I think that confusion will persist. I don’t think this document is going to resolve it.
New terminology: Preeclampsia with or without severe features
Dr. Norwitz: I do like the difference in terminology between preeclampsia with severe features and preeclampsia without severe features. I think the old terminology of severe and mild preeclampsia was somewhat confusing. I certainly appreciate that alteration in terminology, although it may take a while for it to catch on. I’m still seeing the term “mild preeclampsia” used quite widely.
Use of magnesium sulfate for seizure prophylaxis
Dr. Norwitz: You did raise the issue of magnesium sulfate for seizure prophylaxis in the setting of severe preeclampsia without severe features. And I was struck by the statement. Not only is it not necessary to give it, but in the Executive Summary, as you suggest, it is not indicated and you recommended against starting it. Is that how you interpret it as the well?
Dr. Repke: Well, I might have interpreted the statement the way I wanted to interpret it. And, as you know, in our institution, because we feel we are a teaching program, people can progress very quickly intrapartum from not having severe features to having severe features, and we don’t want to miss that window of opportunity. Our practice in that regard does not follow the guidelines. We use intrapartum magnesium prophylaxis for all patients with the diagnosis of preeclampsia, and continue it for 24 hours postpartum.
Dr. Norwitz: And I would have to say we decided do the same. So, once a diagnosis of preeclampsia is made, we would give intrapartum, and then postpartum magnesium seizure prophylaxis for 24 hours, regardless of whether there’s evidence of severe features or no severe features.
Dr. Repke: And there again, I think it’s why, for you and I, it will still be important to assess the proteinuria because that diagnostic difference between preeclampsia and gestational hypertension is going to alter management. But if you follow the document word for word, if you’re not going to use magnesium without severe features, I’m not really sure what proteinuria adds. I guess, at the end of the day, you’ve got to be a good doctor. And, you’ve got to be physically assessing your patient on a very regular basis.
Preventing the first cesarean delivery. Will cesarean rates decline?
Dr. Repke: So, speaking of guidelines, the Society for Maternal Fetal Medicine (SMFM) just came out with a document trying to address this issue of the cesarean-section rate in the United States and are there things that we can be doing to lower the primary C-section rate.2 My feeling is probably disseminated from the recognition that vaginal birth after C-section never got to the levels of acceptance that anybody hoped back when Healthy People 2010 was first written. And, we could eliminate that issue or, at least significantly reduce that issue, if the first C-section never took place.
And, I guess I’d like some of your thoughts about some of the things in that document, some of the things we need to be reconsidering in terms of how we define labor and so on.
Dr. Norwitz: It is true, I think, that there’s been an epidemic of cesarean deliveries in the last decade in the US, but also throughout the world, I think, even in countries that have traditionally had very low cesarean delivery rates, the classic one being Ireland and the UK countries. Their rates are now increasing significantly.
And there are a number of different reasons as to why this may be. I think, certainly the obesity epidemic has contributed to this. You want to deliver patients who have an elevated BMI prior to the postterm period. But, it’s often difficult to monitor these patients, and the cesarean-delivery rate overall is much higher in that population. So, that might be one reason why cesarean-delivery rates overall are going up. But, certainly there are many others.
Dr. Repke: Yes, I think you’re absolutely right: the demographics of change. Childbearing is being delayed. We know that uterine contractility dynamics alter with advanced maternal age. We’ve got a higher incidence of multiple gestations with advanced maternal age. We have more patients that require induction because of supervening medical complications of pregnancy, whether that be Class A2 gestational diabetes, or whether that be pregnancy-induced hypertension.
Redefining the stages of labor
Dr. Repke: I think some of the intriguing data, to me, is a willingness to re-look at how we define the stages of labor. And what are acceptable norms? And, while I have some concerns about how that may be interpreted in the rank and file, I think it’s at least heightened the awareness of my faculty that we just can’t tolerate the C-section at 4 cm, or whether the latent phase of labor should be allowed to go to 6 cm. I don’t think we really have the data for that. But I’d be happy if I could just start to see a reduction in “failure to progress at 4 cm.”
And then the issue of second stage, I think, is also important. What do you think about the guidelines’ recommendation that there may not really be an upper limit of allowability for second-stage labors?
Dr. Norwitz: Well, certainly I think it’s important to think back to the historical context of where the labor curves developed. The original labor curves were actually developed in Zimbabwe (at that time it was Rhodesia) by an obstetrician working in the community called Philpott. And he was trying to determine when it was appropriate to send patients into the tertiary care center. So he designed the labor curve and said if patients failed to progress over a certain number of hours, those are patients that are likely to need an operative delivery, and he would then send them into the tertiary care center.
And, then Dr. Freidman picked up on that idea and developed the Freidman Curve in Boston. But that was an era, again, many years ago when the population demographics were very different, when not many patients received regional anesthesia. I think if you look at the current guidelines, there is a huge discrepancy between women who get epidural anesthesia and those that don’t in terms of the progress of labor, both the first stage and the second stage.
Is it anesthesia?
Dr. Repke: One of the things that, you know, I haven’t looked at this paper in a long time, but you remember at Brigham and Women’s Hospital, probably 20 years ago, we were winding down the Active Management of Labor Study3 that was designed to try to replicate what had gone on at the Dublin Maternity Hospital,4 and if I’m remembering correctly, one of the remarkable things about that is that in Dublin, there were virtually no C-sections in the second stage. And so people assumed that while they were more aggressive with forceps, the operative vaginal delivery rate was no different between Brigham and Women’s Hospital and the Dublin Maternity Hospital. And so there needed to be another explanation.
And, I know I’m going to incur some of the ire of our anesthesia colleagues, but I really wonder whether there is a contribution of regional anesthesia to some of the labor dystocias that we see, and whether that’s a new demographic that we haven’t really adequately assessed. Even though I recognize some of the anesthesia literature5 seems to suggest very strongly that it has no effect. You know, if you were to plot a graph of regional anesthesia rates and cesarean section rates, they would probably parallel each other.
Dr. Norwitz: I think they do. I think we’ve long known that epidural anesthesia slows down the second stage of labor. These analyses suggest that it also has a significant effect on the first stage. And, I think that needs to be taken into account.
The lost skill of forceps delivery
Dr. Norwitz: I personally think that the skill set, in terms of operative vaginal delivery with forceps and vacuum, has really been lost. And I do feel that’s one of the factors contributing to the increase in cesarean delivery rates. I certainly see that in my practice: that I’m comfortable doing rotational forceps and mid-cavity forceps deliveries, where many of my colleagues have lost that skill, and rely now on the vacuum, which in certain circumstances is a less-than-ideal instrument. So, I believe that’s part of the reason why the cesarean delivery rates have gone up.
Lengthy second stage
Dr. Norwitz: But, certainly, I think, epidural anesthesia has made a difference, and I think we need to be cognizant of the fact that there is no “hard stop” now, in terms of the length of the second stage. If you get to 3 hours, even 4 hours, I would say, and there’s continued descent with pushing and fetal heart-rate tracing is reassuring, it’s reasonable to continue beyond those cutoffs.
Dr. Repke: I agree. I also have a concern about that, and I’m going to use a little bit of a parallel example of, you know, 7 or 8 years ago, there was a big push, and I think it was an appropriate push, to try to avoid elective deliveries prior to 39 weeks.6,7 What ended up happening was that people forgot about the term “elective,” and all they heard was 39 weeks. And what we would see on Board Examinations was, “Why do you have this placenta previa delivering at 39 weeks?”
“Well, that’s our hospital policy. We can’t deliver before 39 weeks.”
And, I think, the complications started to arise, and that’s what led to SMFM and ACOG coming out with guidelines for when it is acceptable to deliver prior to 39 weeks.2,6–8
So, the analogy is: I’m afraid that people are only going to see there is no upper limit for latent phase, there is no upper limit for second stage; that clinical judgment may not get its due in making these decisions. And we’ve all been in situations where, when you are trying to extract the head out of the pelvis, a cesarean section after a 5- or 6-hour second stage has its own set of complications. So my concern is that I hope we will recognize that we have to still use some clinical judgment, what I term the so-called “art of obstetrics,” into managing these patients.
Are you optimistic that we’re going to the lower C-section rate?
Dr. Norwitz: No, I think, it’s going to continue to go up. I think, with the increasing number of multiple pregnancies, obesity, maternal age getting further and further along, I think this is only going to continue to rise. And to be honest, I don’t know the correct cesarean delivery rate, or even if that is the metric that we should be measuring.
What is the right metric to measure neonatal outcome?
Dr. Norwitz: Maybe we should be looking at perinatal outcome. If perinatal outcome is improved, then maybe the cesarean rate is less important. Obviously, the first cesarean does have implications for subsequent pregnancy outcomes, and if we do continue to see this rise in cesarean deliveries, we are going to end up with many more placental accretas and hemorrhages in women in years to come.
So, careful counseling is important. If patients plan to have one or two kids only, maybe a cesarean delivery is very reasonable. If they are planning on having six or seven kids, then maybe you have to have a more careful discussion.
Dr. Repke: Yes, I think, that’s a very good point: the number of cesareans and the potential risks for abnormal placentation. I think societal expectations have changed in terms of what they want. Most mothers are willing to sacrifice maternal risk for presumed benefits to the fetus.
I think, where we’ve gotten into trouble as a specialty, though, is that we’ve had a hard time proving that neonatal outcome, in fact, has improved—despite an almost tripling of the cesarean section rate since, probably, the early 1970s. Although, anecdotally, what my pediatric and neonatal colleagues will tell me is they don’t get the kind of damaged babies they used to get. So the neonatologists that are closer to my age that have been doing this for a long time, they’re not seeing the really severe meconium aspiration syndromes; they’re not seeing really severe forceps-related injuries, or vacuum-related injuries that they used to see. So, those may be data that we’re going to need to accumulate with a little bit more rigor, and see if that’s true.
But I tend to agree with you. I don’t know what the right cesarean section rate is. I often tell people, I have yet to meet a patient who doesn’t think her cesarean section was indicated. And that’s where I think we hit the crossroads of individual patient-care management. So, we know across all other disciplines in medicine we’re entering the era of personalized medicine, yet we want to make broad public health policy that may not apply to individuals, and run with that. So, that’s also a concern. But, as they say, a story we will follow with interest.
Dr. Norwitz: I think so. I think the other part of that equation is the stillbirth rate, and the fact that there’s a push now to avoid elective inductions before 39 weeks, which I think is very reasonable, with a focus there again on elective inductions.
There’s also a push to induce patients before 42 weeks. And that bar has been pushed back, and in most practices around the country now, deliveries are being affected and recommended at 41 weeks. And clearly, if you take a nulliparous patient with an unfavorable cervix and induce at 41 weeks, you are going to increase the cesarean rate. I would argue that you are also decreasing the chance that there will be a stillbirth. But that data has not been forthcoming.
So this issue is by no means resolved. I think there are going to be many more years of data and studies and consensus opinions before we have a much better sense of what the right cesarean
rate is.
Dr. Repke: Yes, I think that’s a great point. And, one thing that I think people aren’t maybe that familiar with is when this push came, and again, it is an appropriate push to minimize elective deliveries before 39 weeks. When they looked at neonatal outcomes, all they looked at were the group that delivered at 37 weeks, and the group that delivered at 39 weeks. And they didn’t look at what happened with the other ones.9
So, they did look at the stillbirths of fetal distress or the other complications that happened between 37 and 1, and 38 and 6. They just looked at neonates that were born at 37 weeks and compared them to neonates that were born at 39 weeks, and found reduced instances of things like transient tachypnea of the newborn, hyperbilirubinemia, and thermoregulation issues, and those sorts of things. But, never looked at the neonates in that window, so no question 39 is better than 37, but, 37 is better than not making it to 39. So that, as you said, we’ve got a lot more information we’ve got to gather.
Errol, good talking with you.
Dr. Norwitz: Thank you.
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus: Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Frigoletto FD, Lieberman E, Lang J, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333(12):745–750.
- O’Driscoll K, Meagher D, Boylan P. Active Management of Labor. 3rd ed. London: Mosby- Yearbook; 1993.
- Chestnut DH, McGrath JM, Vincent RD, et al. Does early administration of epidural analgesia effect obstetric outcome in nulliparous women who are in spontaneous labor? Anesthesiology. 1994;80(6):1201–1208.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 560: Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915.
- Spong CY, Mercer BM, D’Alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):323–333.
- Tita ATN, Landon MB, Spong CY, et al; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat Cesarean Delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus: Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Frigoletto FD, Lieberman E, Lang J, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333(12):745–750.
- O’Driscoll K, Meagher D, Boylan P. Active Management of Labor. 3rd ed. London: Mosby- Yearbook; 1993.
- Chestnut DH, McGrath JM, Vincent RD, et al. Does early administration of epidural analgesia effect obstetric outcome in nulliparous women who are in spontaneous labor? Anesthesiology. 1994;80(6):1201–1208.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 560: Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915.
- Spong CY, Mercer BM, D’Alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):323–333.
- Tita ATN, Landon MB, Spong CY, et al; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat Cesarean Delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
Is neonatal injury more likely outside of a 30-minute decision-to-incision time interval for cesarean delivery?
Cesarean section is one of the most common surgical procedures worldwide. In a review of more than 13 million deliveries, cesarean delivery for nonreassuring fetal heart rate tracing occurred in about 3% of cases.1 Most of these urgent deliveries occur without known predisposing factors.1 A source of consternation for clinicians related to labor and delivery is the decision-to-incision time (DIT) interval for cesarean delivery for nonreassuring fetal heart rate tracing.
Previously, The American College of Obstetricians and Gynecologists (ACOG) suggested the DIT interval should be 30 minutes or less, for prolonged DIT increased the likelihood of neonatal injury.2 A DIT interval of more than 30 minutes became the sine qua non for poor neonatal outcomes and the linchpin for obstetric litigation.3 Starting in the 1990s, publications indicated that neonatal morbidity is not related to DIT and adverse neonatal outcomes may occur with a DIT interval of only a few minutes.4 Most studies, however, were hampered by small sample size.
Related article: 10 practical, evidence-based recommendations for improving maternal outcomes of cesarean delivery. Baha M. Sibai, MD (March 2012)
In an attempt to clarify whether neonatal outcomes differed among cesarean deliveries performed before or after 30 minutes lapsed, Tolcher and colleagues recently published a systematic review and meta-analysis evaluating all published reports that assessed adherence to a DIT policy for cesarean deliveries to be performed within 30 minutes of a nonreassuring fetal heart rate tracing. They reported on the number of emergent (Category 1) and urgent (Category 2) cesarean deliveries accomplished within 30 minutes and compared neonatal outcomes for cesarean deliveries before and after the 30-minute DIT.
Some important observations:
- First, all the studies were observational; only one paper focused exclusively on preterm infants, and only five of the identified 34 publications, involving 22,936 women, were determined to be “high quality.”
- Second, one of five neonates (21%) requiring emergent cesarean delivery were not delivered within 30 minutes. And 64% of urgent deliveries were not performed within 30 minutes.
- Third, and most surprisingly, in the 13 studies that included neonatal outcomes, 5-minute Apgar scores less than 7 and cord pH values less than 7.10 were significantly more common among neonates delivered within 30 minutes than among neonates delivered outside of 30 minutes. When the authors limited analysis to infants requiring emergent versus urgent delivery, however, the difference in Apgar scores and pH values was nonsignificant.
Several strengths of this analysis should be mentioned. The careful study design—meticulous and systematic evaluation of all publications and adherence to established publication evaluation and meta-analysis reporting protocols—strengthen the validity of these results. This report is clinically useful because the authors not only evaluated time frames from decision-to-incision but also reported and correlated neonatal outcomes.
Despite the multiple strengths, some weaknesses are worth mentioning. No maternal outcomes were reported. Mothers who require emergent cesarean delivery are at increased risk for adverse outcomes due to the requirement for general anesthesia and urgency with which the surgery is performed. The report only focused on 5-minute Apgar scores less than 7, neonatal intensive care admissions, and cord pH values less than 7.10 as adverse neonatal outcomes. The absence of additional adverse outcomes, as well as long-term neonatal and infant outcomes, hampers our ability to present the patient with all the facts. Lastly, the authors promulgated the classification of degree of urgency for cesarean delivery proposed by Lucas and colleagues5 without providing evidence that this classification is linked with clinically meaningful outcomes.
While a randomized trial would be unethical, a fact acknowledged by the authors, prospective cohort studies with long-term neonatal and infant follow-up could provide us with much needed information that would help us counsel our patients. The frequency with which cesarean deliveries are performed requires us to offer our patients the best and most comprehensive information available.
Related article:
• Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence; December 2013)
• Mother-, baby-, and family- centered cesarean delivery: It is possible. William Camann, MD, and Robert L. Barbieri, MD (Editorial; March 2013)
What this evidence means for practice
The ideal decision-to-incision time is probably best determined individually and may not encompass a “one-size-fits-all” approach. More studies are needed to elucidate this critical clinical question. In the meantime, we suggest: 1) consulting colleagues if interpretation of the tracing is uncertain, especially with preterm parturients, 2) intrauterine resuscitation, including tocolytics and amnioinfusion when appropriate, 3) scalp or vibroacoustic stimulation to elicit acceleration, 4) administering ephedrine if hypotensive, 5) expeditious delivery considering the clinical situation and logistics, 6) documenting decision-to-incision time in operative notes, and 7) sending umbilical arterial and venous blood for acid-base analysis and the placenta to pathology for evaluation.
Suneet P. Chauhan, MD, and Hector Mendez-Figueroa, MD
TELL US WHAT YOU THINK!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- Chauhan SP, Magann EF, Scott JR, Scardo JA, Hendrix NW, Martin JN Jr. Cesarean delivery for fetal distress: Rate and risk factors. Obstet Gynecol Surv. 2003;58(5):337−350.
- American Academy of Pediatrics; American College of Obstetrics and Gynecology. Guidelines for perinatal care. 2nd ed. Washington, DC: American College of Obstetrics and Gynecology; 1988:71.
- Chauhan SP, Chauhan VB, Cowan BD, Hendrix NW, Magann EF, Morrison JC. Professional liability claims and Central Association of Obstetricians and Gynecologists members: Myth versus reality. Am J Obstet Gynecol. 2005;192(6):1820−1826.
- American College of Obstetricians and Gynecologists and American Academy of Pediatrics Task Force. Neonatal encephalopathy and neurologic outcomes. 2nd ed. Washington, DC: American College of Obstetricians and Gynecologists; 2014.
- Lucas DN, Yentis SM, Kinsella SM, et al. Urgency of caesarean section: A new classification. J R Soc Med. 2000;93(7):346–350.
Cesarean section is one of the most common surgical procedures worldwide. In a review of more than 13 million deliveries, cesarean delivery for nonreassuring fetal heart rate tracing occurred in about 3% of cases.1 Most of these urgent deliveries occur without known predisposing factors.1 A source of consternation for clinicians related to labor and delivery is the decision-to-incision time (DIT) interval for cesarean delivery for nonreassuring fetal heart rate tracing.
Previously, The American College of Obstetricians and Gynecologists (ACOG) suggested the DIT interval should be 30 minutes or less, for prolonged DIT increased the likelihood of neonatal injury.2 A DIT interval of more than 30 minutes became the sine qua non for poor neonatal outcomes and the linchpin for obstetric litigation.3 Starting in the 1990s, publications indicated that neonatal morbidity is not related to DIT and adverse neonatal outcomes may occur with a DIT interval of only a few minutes.4 Most studies, however, were hampered by small sample size.
Related article: 10 practical, evidence-based recommendations for improving maternal outcomes of cesarean delivery. Baha M. Sibai, MD (March 2012)
In an attempt to clarify whether neonatal outcomes differed among cesarean deliveries performed before or after 30 minutes lapsed, Tolcher and colleagues recently published a systematic review and meta-analysis evaluating all published reports that assessed adherence to a DIT policy for cesarean deliveries to be performed within 30 minutes of a nonreassuring fetal heart rate tracing. They reported on the number of emergent (Category 1) and urgent (Category 2) cesarean deliveries accomplished within 30 minutes and compared neonatal outcomes for cesarean deliveries before and after the 30-minute DIT.
Some important observations:
- First, all the studies were observational; only one paper focused exclusively on preterm infants, and only five of the identified 34 publications, involving 22,936 women, were determined to be “high quality.”
- Second, one of five neonates (21%) requiring emergent cesarean delivery were not delivered within 30 minutes. And 64% of urgent deliveries were not performed within 30 minutes.
- Third, and most surprisingly, in the 13 studies that included neonatal outcomes, 5-minute Apgar scores less than 7 and cord pH values less than 7.10 were significantly more common among neonates delivered within 30 minutes than among neonates delivered outside of 30 minutes. When the authors limited analysis to infants requiring emergent versus urgent delivery, however, the difference in Apgar scores and pH values was nonsignificant.
Several strengths of this analysis should be mentioned. The careful study design—meticulous and systematic evaluation of all publications and adherence to established publication evaluation and meta-analysis reporting protocols—strengthen the validity of these results. This report is clinically useful because the authors not only evaluated time frames from decision-to-incision but also reported and correlated neonatal outcomes.
Despite the multiple strengths, some weaknesses are worth mentioning. No maternal outcomes were reported. Mothers who require emergent cesarean delivery are at increased risk for adverse outcomes due to the requirement for general anesthesia and urgency with which the surgery is performed. The report only focused on 5-minute Apgar scores less than 7, neonatal intensive care admissions, and cord pH values less than 7.10 as adverse neonatal outcomes. The absence of additional adverse outcomes, as well as long-term neonatal and infant outcomes, hampers our ability to present the patient with all the facts. Lastly, the authors promulgated the classification of degree of urgency for cesarean delivery proposed by Lucas and colleagues5 without providing evidence that this classification is linked with clinically meaningful outcomes.
While a randomized trial would be unethical, a fact acknowledged by the authors, prospective cohort studies with long-term neonatal and infant follow-up could provide us with much needed information that would help us counsel our patients. The frequency with which cesarean deliveries are performed requires us to offer our patients the best and most comprehensive information available.
Related article:
• Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence; December 2013)
• Mother-, baby-, and family- centered cesarean delivery: It is possible. William Camann, MD, and Robert L. Barbieri, MD (Editorial; March 2013)
What this evidence means for practice
The ideal decision-to-incision time is probably best determined individually and may not encompass a “one-size-fits-all” approach. More studies are needed to elucidate this critical clinical question. In the meantime, we suggest: 1) consulting colleagues if interpretation of the tracing is uncertain, especially with preterm parturients, 2) intrauterine resuscitation, including tocolytics and amnioinfusion when appropriate, 3) scalp or vibroacoustic stimulation to elicit acceleration, 4) administering ephedrine if hypotensive, 5) expeditious delivery considering the clinical situation and logistics, 6) documenting decision-to-incision time in operative notes, and 7) sending umbilical arterial and venous blood for acid-base analysis and the placenta to pathology for evaluation.
Suneet P. Chauhan, MD, and Hector Mendez-Figueroa, MD
TELL US WHAT YOU THINK!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Cesarean section is one of the most common surgical procedures worldwide. In a review of more than 13 million deliveries, cesarean delivery for nonreassuring fetal heart rate tracing occurred in about 3% of cases.1 Most of these urgent deliveries occur without known predisposing factors.1 A source of consternation for clinicians related to labor and delivery is the decision-to-incision time (DIT) interval for cesarean delivery for nonreassuring fetal heart rate tracing.
Previously, The American College of Obstetricians and Gynecologists (ACOG) suggested the DIT interval should be 30 minutes or less, for prolonged DIT increased the likelihood of neonatal injury.2 A DIT interval of more than 30 minutes became the sine qua non for poor neonatal outcomes and the linchpin for obstetric litigation.3 Starting in the 1990s, publications indicated that neonatal morbidity is not related to DIT and adverse neonatal outcomes may occur with a DIT interval of only a few minutes.4 Most studies, however, were hampered by small sample size.
Related article: 10 practical, evidence-based recommendations for improving maternal outcomes of cesarean delivery. Baha M. Sibai, MD (March 2012)
In an attempt to clarify whether neonatal outcomes differed among cesarean deliveries performed before or after 30 minutes lapsed, Tolcher and colleagues recently published a systematic review and meta-analysis evaluating all published reports that assessed adherence to a DIT policy for cesarean deliveries to be performed within 30 minutes of a nonreassuring fetal heart rate tracing. They reported on the number of emergent (Category 1) and urgent (Category 2) cesarean deliveries accomplished within 30 minutes and compared neonatal outcomes for cesarean deliveries before and after the 30-minute DIT.
Some important observations:
- First, all the studies were observational; only one paper focused exclusively on preterm infants, and only five of the identified 34 publications, involving 22,936 women, were determined to be “high quality.”
- Second, one of five neonates (21%) requiring emergent cesarean delivery were not delivered within 30 minutes. And 64% of urgent deliveries were not performed within 30 minutes.
- Third, and most surprisingly, in the 13 studies that included neonatal outcomes, 5-minute Apgar scores less than 7 and cord pH values less than 7.10 were significantly more common among neonates delivered within 30 minutes than among neonates delivered outside of 30 minutes. When the authors limited analysis to infants requiring emergent versus urgent delivery, however, the difference in Apgar scores and pH values was nonsignificant.
Several strengths of this analysis should be mentioned. The careful study design—meticulous and systematic evaluation of all publications and adherence to established publication evaluation and meta-analysis reporting protocols—strengthen the validity of these results. This report is clinically useful because the authors not only evaluated time frames from decision-to-incision but also reported and correlated neonatal outcomes.
Despite the multiple strengths, some weaknesses are worth mentioning. No maternal outcomes were reported. Mothers who require emergent cesarean delivery are at increased risk for adverse outcomes due to the requirement for general anesthesia and urgency with which the surgery is performed. The report only focused on 5-minute Apgar scores less than 7, neonatal intensive care admissions, and cord pH values less than 7.10 as adverse neonatal outcomes. The absence of additional adverse outcomes, as well as long-term neonatal and infant outcomes, hampers our ability to present the patient with all the facts. Lastly, the authors promulgated the classification of degree of urgency for cesarean delivery proposed by Lucas and colleagues5 without providing evidence that this classification is linked with clinically meaningful outcomes.
While a randomized trial would be unethical, a fact acknowledged by the authors, prospective cohort studies with long-term neonatal and infant follow-up could provide us with much needed information that would help us counsel our patients. The frequency with which cesarean deliveries are performed requires us to offer our patients the best and most comprehensive information available.
Related article:
• Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence; December 2013)
• Mother-, baby-, and family- centered cesarean delivery: It is possible. William Camann, MD, and Robert L. Barbieri, MD (Editorial; March 2013)
What this evidence means for practice
The ideal decision-to-incision time is probably best determined individually and may not encompass a “one-size-fits-all” approach. More studies are needed to elucidate this critical clinical question. In the meantime, we suggest: 1) consulting colleagues if interpretation of the tracing is uncertain, especially with preterm parturients, 2) intrauterine resuscitation, including tocolytics and amnioinfusion when appropriate, 3) scalp or vibroacoustic stimulation to elicit acceleration, 4) administering ephedrine if hypotensive, 5) expeditious delivery considering the clinical situation and logistics, 6) documenting decision-to-incision time in operative notes, and 7) sending umbilical arterial and venous blood for acid-base analysis and the placenta to pathology for evaluation.
Suneet P. Chauhan, MD, and Hector Mendez-Figueroa, MD
TELL US WHAT YOU THINK!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- Chauhan SP, Magann EF, Scott JR, Scardo JA, Hendrix NW, Martin JN Jr. Cesarean delivery for fetal distress: Rate and risk factors. Obstet Gynecol Surv. 2003;58(5):337−350.
- American Academy of Pediatrics; American College of Obstetrics and Gynecology. Guidelines for perinatal care. 2nd ed. Washington, DC: American College of Obstetrics and Gynecology; 1988:71.
- Chauhan SP, Chauhan VB, Cowan BD, Hendrix NW, Magann EF, Morrison JC. Professional liability claims and Central Association of Obstetricians and Gynecologists members: Myth versus reality. Am J Obstet Gynecol. 2005;192(6):1820−1826.
- American College of Obstetricians and Gynecologists and American Academy of Pediatrics Task Force. Neonatal encephalopathy and neurologic outcomes. 2nd ed. Washington, DC: American College of Obstetricians and Gynecologists; 2014.
- Lucas DN, Yentis SM, Kinsella SM, et al. Urgency of caesarean section: A new classification. J R Soc Med. 2000;93(7):346–350.
- Chauhan SP, Magann EF, Scott JR, Scardo JA, Hendrix NW, Martin JN Jr. Cesarean delivery for fetal distress: Rate and risk factors. Obstet Gynecol Surv. 2003;58(5):337−350.
- American Academy of Pediatrics; American College of Obstetrics and Gynecology. Guidelines for perinatal care. 2nd ed. Washington, DC: American College of Obstetrics and Gynecology; 1988:71.
- Chauhan SP, Chauhan VB, Cowan BD, Hendrix NW, Magann EF, Morrison JC. Professional liability claims and Central Association of Obstetricians and Gynecologists members: Myth versus reality. Am J Obstet Gynecol. 2005;192(6):1820−1826.
- American College of Obstetricians and Gynecologists and American Academy of Pediatrics Task Force. Neonatal encephalopathy and neurologic outcomes. 2nd ed. Washington, DC: American College of Obstetricians and Gynecologists; 2014.
- Lucas DN, Yentis SM, Kinsella SM, et al. Urgency of caesarean section: A new classification. J R Soc Med. 2000;93(7):346–350.
What is the clinical and economic return on taxpayers’ $260M investment in the WHI?
The WHI estrogen plus progestin (EPT) clinical trial, a $260 million venture, is among the most expensive projects ever undertaken by the National Institutes of Health. Following 2002 publication of its initial findings, use of EPT and estrogen alone (ET) hormone therapy (HT) among US women plummeted. Investigators, including WHI leadership, estimated the clinical and economic impact of this trial from a payer perspective.
Details of the study
For the years 2003 to 2012, the authors used a disease-simulation model to evaluate the effect of the WHI EPT trial on women aged 50 to 79 with an intact uterus (women who were combined-HT [cHT], or EPT, eligible). They compared outcomes between a “WHI scenario,” in which the prevalence of cHT use was based on actual WHI findings, with a “no-WHI” scenario, in which pre-WHI trends in cHT use (from 1998 to 2002) were linearly extrapolated.
The simulation model predicted that 9.5 million women used cHT in the no-WHI scenario, 4.3 million more than actually used cHT in the WHI scenario. The authors estimated that, compared with the no-WHI scenario, 126,000, 76,000, and 80,000 fewer respective cases of breast cancer, cardiovascular disease (CVD), and venous thromboembolism occurred and that 263,000 and 15,000 more respective cases of fractures and colorectal cancer occurred among women as a result of the WHI.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; February 2014)
Regarding economic outcomes, the authors estimated that the WHI resulted in $35.2 billion in direct medical expenditure savings—principally from fewer prescriptions for EPT and associated office visits ($26.2 billion), but also from decreased breast cancer incidence ($4.5 billion) and decreased CVD incidence ($2.2 billion), among other savings, which offset increases in expenditures for greater fracture incidence ($4.8 billion) and colorectal cancer ($1.0 billion).
Related article: In the latest report from the WHI, the data contradict the conclusions. Holly Thacker, MD (Commentary; March 2014)
In addition, the investigators reported a tremendous gain in quality of life years (145,000) in the WHI versus the no-WHI scenario, attributing the difference to the greater health-related quality-of-life effect associated with decreased breast cancer and CVD incidence in the WHI scenario.
What this evidence means for practice
At first glance, the clinical and economic benefits of the WHI EPT trial appear enormous. However, the authors surprisingly failed to take into consideration relevant issues well known to women’s health clinicians: lower use of systemic HT (both in women with an intact uterus and those posthysterectomy) has resulted in many more women suffering from bothersome vasomotor and sleep-related menopausal symptoms, with resultant impairment of quality of life.
In addition, the authors did not account for the major reduction in use of ET after the 2002 WHI findings in women who have had a hysterectomy; given that ET reduces the incidence of breast cancer and cardiovascular disease, declines in ET use have resulted in increased morbidity and mortality from these conditions.1
Finally, as the profound declines in use of systemic HT have not been accompanied by a substantive increase in the use of vaginal estrogen, we have an epidemic of symptomatic vulvovaginal atrophy, with attendant sexual dysfunction and impaired quality of life.
Andrew M. Kaunitz, MD
TELL US WHAT YOU THINK!
Share your thoughts on this article. Send your Letter to the Editor: [email protected]
Reference
- Sarrel PM, Njike VY, Vinante V, Katz DL. The mortality toll of estrogen avoidance: an analysis of excess deaths among hysterectomized women aged 50 to 59 years. Am J Public Health. 2013;103(9):1583–1588.
The WHI estrogen plus progestin (EPT) clinical trial, a $260 million venture, is among the most expensive projects ever undertaken by the National Institutes of Health. Following 2002 publication of its initial findings, use of EPT and estrogen alone (ET) hormone therapy (HT) among US women plummeted. Investigators, including WHI leadership, estimated the clinical and economic impact of this trial from a payer perspective.
Details of the study
For the years 2003 to 2012, the authors used a disease-simulation model to evaluate the effect of the WHI EPT trial on women aged 50 to 79 with an intact uterus (women who were combined-HT [cHT], or EPT, eligible). They compared outcomes between a “WHI scenario,” in which the prevalence of cHT use was based on actual WHI findings, with a “no-WHI” scenario, in which pre-WHI trends in cHT use (from 1998 to 2002) were linearly extrapolated.
The simulation model predicted that 9.5 million women used cHT in the no-WHI scenario, 4.3 million more than actually used cHT in the WHI scenario. The authors estimated that, compared with the no-WHI scenario, 126,000, 76,000, and 80,000 fewer respective cases of breast cancer, cardiovascular disease (CVD), and venous thromboembolism occurred and that 263,000 and 15,000 more respective cases of fractures and colorectal cancer occurred among women as a result of the WHI.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; February 2014)
Regarding economic outcomes, the authors estimated that the WHI resulted in $35.2 billion in direct medical expenditure savings—principally from fewer prescriptions for EPT and associated office visits ($26.2 billion), but also from decreased breast cancer incidence ($4.5 billion) and decreased CVD incidence ($2.2 billion), among other savings, which offset increases in expenditures for greater fracture incidence ($4.8 billion) and colorectal cancer ($1.0 billion).
Related article: In the latest report from the WHI, the data contradict the conclusions. Holly Thacker, MD (Commentary; March 2014)
In addition, the investigators reported a tremendous gain in quality of life years (145,000) in the WHI versus the no-WHI scenario, attributing the difference to the greater health-related quality-of-life effect associated with decreased breast cancer and CVD incidence in the WHI scenario.
What this evidence means for practice
At first glance, the clinical and economic benefits of the WHI EPT trial appear enormous. However, the authors surprisingly failed to take into consideration relevant issues well known to women’s health clinicians: lower use of systemic HT (both in women with an intact uterus and those posthysterectomy) has resulted in many more women suffering from bothersome vasomotor and sleep-related menopausal symptoms, with resultant impairment of quality of life.
In addition, the authors did not account for the major reduction in use of ET after the 2002 WHI findings in women who have had a hysterectomy; given that ET reduces the incidence of breast cancer and cardiovascular disease, declines in ET use have resulted in increased morbidity and mortality from these conditions.1
Finally, as the profound declines in use of systemic HT have not been accompanied by a substantive increase in the use of vaginal estrogen, we have an epidemic of symptomatic vulvovaginal atrophy, with attendant sexual dysfunction and impaired quality of life.
Andrew M. Kaunitz, MD
TELL US WHAT YOU THINK!
Share your thoughts on this article. Send your Letter to the Editor: [email protected]
The WHI estrogen plus progestin (EPT) clinical trial, a $260 million venture, is among the most expensive projects ever undertaken by the National Institutes of Health. Following 2002 publication of its initial findings, use of EPT and estrogen alone (ET) hormone therapy (HT) among US women plummeted. Investigators, including WHI leadership, estimated the clinical and economic impact of this trial from a payer perspective.
Details of the study
For the years 2003 to 2012, the authors used a disease-simulation model to evaluate the effect of the WHI EPT trial on women aged 50 to 79 with an intact uterus (women who were combined-HT [cHT], or EPT, eligible). They compared outcomes between a “WHI scenario,” in which the prevalence of cHT use was based on actual WHI findings, with a “no-WHI” scenario, in which pre-WHI trends in cHT use (from 1998 to 2002) were linearly extrapolated.
The simulation model predicted that 9.5 million women used cHT in the no-WHI scenario, 4.3 million more than actually used cHT in the WHI scenario. The authors estimated that, compared with the no-WHI scenario, 126,000, 76,000, and 80,000 fewer respective cases of breast cancer, cardiovascular disease (CVD), and venous thromboembolism occurred and that 263,000 and 15,000 more respective cases of fractures and colorectal cancer occurred among women as a result of the WHI.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; February 2014)
Regarding economic outcomes, the authors estimated that the WHI resulted in $35.2 billion in direct medical expenditure savings—principally from fewer prescriptions for EPT and associated office visits ($26.2 billion), but also from decreased breast cancer incidence ($4.5 billion) and decreased CVD incidence ($2.2 billion), among other savings, which offset increases in expenditures for greater fracture incidence ($4.8 billion) and colorectal cancer ($1.0 billion).
Related article: In the latest report from the WHI, the data contradict the conclusions. Holly Thacker, MD (Commentary; March 2014)
In addition, the investigators reported a tremendous gain in quality of life years (145,000) in the WHI versus the no-WHI scenario, attributing the difference to the greater health-related quality-of-life effect associated with decreased breast cancer and CVD incidence in the WHI scenario.
What this evidence means for practice
At first glance, the clinical and economic benefits of the WHI EPT trial appear enormous. However, the authors surprisingly failed to take into consideration relevant issues well known to women’s health clinicians: lower use of systemic HT (both in women with an intact uterus and those posthysterectomy) has resulted in many more women suffering from bothersome vasomotor and sleep-related menopausal symptoms, with resultant impairment of quality of life.
In addition, the authors did not account for the major reduction in use of ET after the 2002 WHI findings in women who have had a hysterectomy; given that ET reduces the incidence of breast cancer and cardiovascular disease, declines in ET use have resulted in increased morbidity and mortality from these conditions.1
Finally, as the profound declines in use of systemic HT have not been accompanied by a substantive increase in the use of vaginal estrogen, we have an epidemic of symptomatic vulvovaginal atrophy, with attendant sexual dysfunction and impaired quality of life.
Andrew M. Kaunitz, MD
TELL US WHAT YOU THINK!
Share your thoughts on this article. Send your Letter to the Editor: [email protected]
Reference
- Sarrel PM, Njike VY, Vinante V, Katz DL. The mortality toll of estrogen avoidance: an analysis of excess deaths among hysterectomized women aged 50 to 59 years. Am J Public Health. 2013;103(9):1583–1588.
Reference
- Sarrel PM, Njike VY, Vinante V, Katz DL. The mortality toll of estrogen avoidance: an analysis of excess deaths among hysterectomized women aged 50 to 59 years. Am J Public Health. 2013;103(9):1583–1588.
Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a “re-run” or as a “new series”?
In November 2013, The American College of Obstetricians and Gynecologists (ACOG) published the results of its Task Force on Hypertension in Pregnancy.1 The Task Force aimed to help clinicians become familiar with the state of research in hypertension during pregnancy as well as to assist us in standardizing management approaches to such patients.
The Task Force reported that, worldwide, hypertensive disorders complicate approximately 10% of pregnancies. In addition, in the United States, the past 20 years have brought a 25% increase in the incidence of preeclampsia. According to past ACOG President James N. Martin, Jr, MD, in the last 10 years, the pathophysiology of preeclampsia has become better understood, but the etiology remains unclear and evidence that has emerged to guide therapy has not translated into clinical practice.1
Related articles:
The latest guidance from ACOG on hypertension in pregnancy. Jaimey E. Pauli, MD (Audiocast, January 2014)
Update on Obstetrics. Jaimey E. Pauli, MD, and John T. Repke, MD (January 2014)
The Task Force document contained 60 recommendations for the prevention, prediction, and management of hypertensive disorders of pregnancy, including preeclampsia, gestational hypertension, chronic hypertension, HELLP syndrome, and preeclampsia superimposed on an underlying hypertensive disorder (see box below). One recommendation was that women at high risk for preeclampsia, particularly those with a history of preeclampsia that required delivery before 34 weeks, could possibly benefit from taking aspirin (60–81 mg) daily starting at the end of the first trimester. They further noted that this benefit could include prevention of recurrent severe preeclampsia, or at least a reduction in recurrence risk.
The ACOG Task Force made its recommendation based on results of a meta-analysis of low-dose aspirin trials, involving more than 30,000 patients,2 suggesting a small decrease in the risk of preeclampsia and associated morbidity. More precise risk reduction estimates were difficult to make due to the heterogeneity of the studies reviewed. And the Task Force further stated that this (low-dose aspirin) approach had no demonstrable acute adverse fetal effects, although long-term adverse effects could not be entirely excluded based on the current data.
Unfortunately, according to the ACOG document, the strength of the evidence supporting their recommendation was “moderate” and the strength of the recommendation was “qualified” so, not exactly a resounding endorsement of this approach, but a recommendation nonetheless.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery

John T. Repke, MD, author of this Guest Editorial, recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
Data suggest aspirin for high-risk women could be reasonable
A recent study by Henderson and colleagues presented a systematic review for the US Preventive Services Task Force (USPSTF) on the potential for low-dose aspirin to prevent morbidity and mortality from preeclampsia.3 The design was a meta-analysis of 28 studies: two large, multisite, randomized clinical trials (RCTs); 13 smaller RCTs of high-risk women, of which eight were deemed “good quality”; and six RCTs and two observational studies of average-risk women, of which seven were deemed to be good quality.
The results essentially supported the notion that low-dose aspirin had a beneficial effect with respect to prevention of preeclampsia and perinatal morbidity in women at high risk for preeclampsia. Additionally, no harmful effects were identified, although the authors acknowledged potential rare or long-term harm could not be excluded.
Questions remain
While somewhat gratifying, the results of the USPSTF systematic review still leave many questions. First, the dose of aspirin used in the studies analyzed ranged from 50 mg/d to 150 mg/d. In the United States, “low-dose” aspirin is usually prescribed at 81 mg/d, so the applicability of this review’s findings to US clinical practice is not exact. Second, the authors acknowledged that the putative positive effects observed could be secondary to so-called “small study effects,” and that when only the larger studies were analyzed the effects were less impressive.
Related article: A stepwise approach to managing eclampsia and other hypertensive emergencies. Baha M. Sibai (October 2013)
In my opinion, both the USPSTF study and the recommendations from the ACOG Task Force provide some reassurance for clinicians that the use of daily, low-dose aspirin by women at high risk for preeclampsia probably does afford some benefit, and seems to be a safe approach—as we have known from the initial Maternal-Fetal Medicine Units (MFMU) trial published in 1993 on low-risk women4 and the follow-up MFMU study on high-risk women.5
The need for additional studies is clear, however. The idea that preeclampsia is the same in every patient would seem to make no more sense than thinking all cancer is the same, with the same risk factors, the same epidemiology and pathophysiology, and the same response to similar treatments. Fundamentally, we need to further explore the different pathways through which preeclampsia develops in women and then apply the strategy best suited to treating (or preventing) their form of the disease—a personalized medicine approach.
In the meantime, most patients who have delivered at 34 weeks or less because of preeclampsia and who are contemplating another pregnancy are really not interested in hearing us tell them that we cannot do anything to prevent recurrent preeclampsia because we are awaiting further studies. At least the ACOG recommendations and the results of the USPSTF’s systematic review provide us with a reasonable, although perhaps not yet optimal, therapeutic option.
Related article: 10 practical, evidence-based recommendations to improve outcomes in women who have eclampsia. Baha M. Sibai (November 2011)
The bottom line
In my own practice, I discuss the option of initiating low-dose aspirin (81 mg/d) as early as 12 weeks’ gestation for patients who had either prior early-onset preeclampsia requiring delivery before 34 weeks’ gestation or preeclampsia during more than one pregnancy.
QUICK POLL
Do you offer low-dose aspirin for preeclampsia prevention?
When faced with a patient with prior preeclampsia in more than one pregnancy or with preeclampsia that resulted in delivery prior to 34 weeks, do you offer low-dose aspirin as an option for preventing preeclampsia?
Visit the Quick Poll on the right column of the OBGManagement.com home page to register your answer and see how your colleagues voted.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- ACOG Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Duley L, Henderson-Smart DJ, Heher S, King JF. Antiplatelet agents for preventing preeclampsia and its complications. Cochrane Database Syst Rev. 2007;(2):CD004659.
- Henderson JT, Whitlock EP, O’Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: A systematic evidence review for the U.S. Preventive Services Task Force [published online ahead of print April 8, 2014]. Ann Intern Med. doi:10.7326/M13-2844.
- Sibai BM, Caritis SN, Thom E, et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1993;329(17):1213–1218.
- Caritis S, Sibai B, Hauth J, et al. Low-dose aspirin to prevent preeclampsia in women at high risk. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;338(11):701–705.
In November 2013, The American College of Obstetricians and Gynecologists (ACOG) published the results of its Task Force on Hypertension in Pregnancy.1 The Task Force aimed to help clinicians become familiar with the state of research in hypertension during pregnancy as well as to assist us in standardizing management approaches to such patients.
The Task Force reported that, worldwide, hypertensive disorders complicate approximately 10% of pregnancies. In addition, in the United States, the past 20 years have brought a 25% increase in the incidence of preeclampsia. According to past ACOG President James N. Martin, Jr, MD, in the last 10 years, the pathophysiology of preeclampsia has become better understood, but the etiology remains unclear and evidence that has emerged to guide therapy has not translated into clinical practice.1
Related articles:
The latest guidance from ACOG on hypertension in pregnancy. Jaimey E. Pauli, MD (Audiocast, January 2014)
Update on Obstetrics. Jaimey E. Pauli, MD, and John T. Repke, MD (January 2014)
The Task Force document contained 60 recommendations for the prevention, prediction, and management of hypertensive disorders of pregnancy, including preeclampsia, gestational hypertension, chronic hypertension, HELLP syndrome, and preeclampsia superimposed on an underlying hypertensive disorder (see box below). One recommendation was that women at high risk for preeclampsia, particularly those with a history of preeclampsia that required delivery before 34 weeks, could possibly benefit from taking aspirin (60–81 mg) daily starting at the end of the first trimester. They further noted that this benefit could include prevention of recurrent severe preeclampsia, or at least a reduction in recurrence risk.
The ACOG Task Force made its recommendation based on results of a meta-analysis of low-dose aspirin trials, involving more than 30,000 patients,2 suggesting a small decrease in the risk of preeclampsia and associated morbidity. More precise risk reduction estimates were difficult to make due to the heterogeneity of the studies reviewed. And the Task Force further stated that this (low-dose aspirin) approach had no demonstrable acute adverse fetal effects, although long-term adverse effects could not be entirely excluded based on the current data.
Unfortunately, according to the ACOG document, the strength of the evidence supporting their recommendation was “moderate” and the strength of the recommendation was “qualified” so, not exactly a resounding endorsement of this approach, but a recommendation nonetheless.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery

John T. Repke, MD, author of this Guest Editorial, recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
Data suggest aspirin for high-risk women could be reasonable
A recent study by Henderson and colleagues presented a systematic review for the US Preventive Services Task Force (USPSTF) on the potential for low-dose aspirin to prevent morbidity and mortality from preeclampsia.3 The design was a meta-analysis of 28 studies: two large, multisite, randomized clinical trials (RCTs); 13 smaller RCTs of high-risk women, of which eight were deemed “good quality”; and six RCTs and two observational studies of average-risk women, of which seven were deemed to be good quality.
The results essentially supported the notion that low-dose aspirin had a beneficial effect with respect to prevention of preeclampsia and perinatal morbidity in women at high risk for preeclampsia. Additionally, no harmful effects were identified, although the authors acknowledged potential rare or long-term harm could not be excluded.
Questions remain
While somewhat gratifying, the results of the USPSTF systematic review still leave many questions. First, the dose of aspirin used in the studies analyzed ranged from 50 mg/d to 150 mg/d. In the United States, “low-dose” aspirin is usually prescribed at 81 mg/d, so the applicability of this review’s findings to US clinical practice is not exact. Second, the authors acknowledged that the putative positive effects observed could be secondary to so-called “small study effects,” and that when only the larger studies were analyzed the effects were less impressive.
Related article: A stepwise approach to managing eclampsia and other hypertensive emergencies. Baha M. Sibai (October 2013)
In my opinion, both the USPSTF study and the recommendations from the ACOG Task Force provide some reassurance for clinicians that the use of daily, low-dose aspirin by women at high risk for preeclampsia probably does afford some benefit, and seems to be a safe approach—as we have known from the initial Maternal-Fetal Medicine Units (MFMU) trial published in 1993 on low-risk women4 and the follow-up MFMU study on high-risk women.5
The need for additional studies is clear, however. The idea that preeclampsia is the same in every patient would seem to make no more sense than thinking all cancer is the same, with the same risk factors, the same epidemiology and pathophysiology, and the same response to similar treatments. Fundamentally, we need to further explore the different pathways through which preeclampsia develops in women and then apply the strategy best suited to treating (or preventing) their form of the disease—a personalized medicine approach.
In the meantime, most patients who have delivered at 34 weeks or less because of preeclampsia and who are contemplating another pregnancy are really not interested in hearing us tell them that we cannot do anything to prevent recurrent preeclampsia because we are awaiting further studies. At least the ACOG recommendations and the results of the USPSTF’s systematic review provide us with a reasonable, although perhaps not yet optimal, therapeutic option.
Related article: 10 practical, evidence-based recommendations to improve outcomes in women who have eclampsia. Baha M. Sibai (November 2011)
The bottom line
In my own practice, I discuss the option of initiating low-dose aspirin (81 mg/d) as early as 12 weeks’ gestation for patients who had either prior early-onset preeclampsia requiring delivery before 34 weeks’ gestation or preeclampsia during more than one pregnancy.
QUICK POLL
Do you offer low-dose aspirin for preeclampsia prevention?
When faced with a patient with prior preeclampsia in more than one pregnancy or with preeclampsia that resulted in delivery prior to 34 weeks, do you offer low-dose aspirin as an option for preventing preeclampsia?
Visit the Quick Poll on the right column of the OBGManagement.com home page to register your answer and see how your colleagues voted.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
In November 2013, The American College of Obstetricians and Gynecologists (ACOG) published the results of its Task Force on Hypertension in Pregnancy.1 The Task Force aimed to help clinicians become familiar with the state of research in hypertension during pregnancy as well as to assist us in standardizing management approaches to such patients.
The Task Force reported that, worldwide, hypertensive disorders complicate approximately 10% of pregnancies. In addition, in the United States, the past 20 years have brought a 25% increase in the incidence of preeclampsia. According to past ACOG President James N. Martin, Jr, MD, in the last 10 years, the pathophysiology of preeclampsia has become better understood, but the etiology remains unclear and evidence that has emerged to guide therapy has not translated into clinical practice.1
Related articles:
The latest guidance from ACOG on hypertension in pregnancy. Jaimey E. Pauli, MD (Audiocast, January 2014)
Update on Obstetrics. Jaimey E. Pauli, MD, and John T. Repke, MD (January 2014)
The Task Force document contained 60 recommendations for the prevention, prediction, and management of hypertensive disorders of pregnancy, including preeclampsia, gestational hypertension, chronic hypertension, HELLP syndrome, and preeclampsia superimposed on an underlying hypertensive disorder (see box below). One recommendation was that women at high risk for preeclampsia, particularly those with a history of preeclampsia that required delivery before 34 weeks, could possibly benefit from taking aspirin (60–81 mg) daily starting at the end of the first trimester. They further noted that this benefit could include prevention of recurrent severe preeclampsia, or at least a reduction in recurrence risk.
The ACOG Task Force made its recommendation based on results of a meta-analysis of low-dose aspirin trials, involving more than 30,000 patients,2 suggesting a small decrease in the risk of preeclampsia and associated morbidity. More precise risk reduction estimates were difficult to make due to the heterogeneity of the studies reviewed. And the Task Force further stated that this (low-dose aspirin) approach had no demonstrable acute adverse fetal effects, although long-term adverse effects could not be entirely excluded based on the current data.
Unfortunately, according to the ACOG document, the strength of the evidence supporting their recommendation was “moderate” and the strength of the recommendation was “qualified” so, not exactly a resounding endorsement of this approach, but a recommendation nonetheless.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery

John T. Repke, MD, author of this Guest Editorial, recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
Data suggest aspirin for high-risk women could be reasonable
A recent study by Henderson and colleagues presented a systematic review for the US Preventive Services Task Force (USPSTF) on the potential for low-dose aspirin to prevent morbidity and mortality from preeclampsia.3 The design was a meta-analysis of 28 studies: two large, multisite, randomized clinical trials (RCTs); 13 smaller RCTs of high-risk women, of which eight were deemed “good quality”; and six RCTs and two observational studies of average-risk women, of which seven were deemed to be good quality.
The results essentially supported the notion that low-dose aspirin had a beneficial effect with respect to prevention of preeclampsia and perinatal morbidity in women at high risk for preeclampsia. Additionally, no harmful effects were identified, although the authors acknowledged potential rare or long-term harm could not be excluded.
Questions remain
While somewhat gratifying, the results of the USPSTF systematic review still leave many questions. First, the dose of aspirin used in the studies analyzed ranged from 50 mg/d to 150 mg/d. In the United States, “low-dose” aspirin is usually prescribed at 81 mg/d, so the applicability of this review’s findings to US clinical practice is not exact. Second, the authors acknowledged that the putative positive effects observed could be secondary to so-called “small study effects,” and that when only the larger studies were analyzed the effects were less impressive.
Related article: A stepwise approach to managing eclampsia and other hypertensive emergencies. Baha M. Sibai (October 2013)
In my opinion, both the USPSTF study and the recommendations from the ACOG Task Force provide some reassurance for clinicians that the use of daily, low-dose aspirin by women at high risk for preeclampsia probably does afford some benefit, and seems to be a safe approach—as we have known from the initial Maternal-Fetal Medicine Units (MFMU) trial published in 1993 on low-risk women4 and the follow-up MFMU study on high-risk women.5
The need for additional studies is clear, however. The idea that preeclampsia is the same in every patient would seem to make no more sense than thinking all cancer is the same, with the same risk factors, the same epidemiology and pathophysiology, and the same response to similar treatments. Fundamentally, we need to further explore the different pathways through which preeclampsia develops in women and then apply the strategy best suited to treating (or preventing) their form of the disease—a personalized medicine approach.
In the meantime, most patients who have delivered at 34 weeks or less because of preeclampsia and who are contemplating another pregnancy are really not interested in hearing us tell them that we cannot do anything to prevent recurrent preeclampsia because we are awaiting further studies. At least the ACOG recommendations and the results of the USPSTF’s systematic review provide us with a reasonable, although perhaps not yet optimal, therapeutic option.
Related article: 10 practical, evidence-based recommendations to improve outcomes in women who have eclampsia. Baha M. Sibai (November 2011)
The bottom line
In my own practice, I discuss the option of initiating low-dose aspirin (81 mg/d) as early as 12 weeks’ gestation for patients who had either prior early-onset preeclampsia requiring delivery before 34 weeks’ gestation or preeclampsia during more than one pregnancy.
QUICK POLL
Do you offer low-dose aspirin for preeclampsia prevention?
When faced with a patient with prior preeclampsia in more than one pregnancy or with preeclampsia that resulted in delivery prior to 34 weeks, do you offer low-dose aspirin as an option for preventing preeclampsia?
Visit the Quick Poll on the right column of the OBGManagement.com home page to register your answer and see how your colleagues voted.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- ACOG Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Duley L, Henderson-Smart DJ, Heher S, King JF. Antiplatelet agents for preventing preeclampsia and its complications. Cochrane Database Syst Rev. 2007;(2):CD004659.
- Henderson JT, Whitlock EP, O’Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: A systematic evidence review for the U.S. Preventive Services Task Force [published online ahead of print April 8, 2014]. Ann Intern Med. doi:10.7326/M13-2844.
- Sibai BM, Caritis SN, Thom E, et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1993;329(17):1213–1218.
- Caritis S, Sibai B, Hauth J, et al. Low-dose aspirin to prevent preeclampsia in women at high risk. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;338(11):701–705.
- ACOG Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Duley L, Henderson-Smart DJ, Heher S, King JF. Antiplatelet agents for preventing preeclampsia and its complications. Cochrane Database Syst Rev. 2007;(2):CD004659.
- Henderson JT, Whitlock EP, O’Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: A systematic evidence review for the U.S. Preventive Services Task Force [published online ahead of print April 8, 2014]. Ann Intern Med. doi:10.7326/M13-2844.
- Sibai BM, Caritis SN, Thom E, et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1993;329(17):1213–1218.
- Caritis S, Sibai B, Hauth J, et al. Low-dose aspirin to prevent preeclampsia in women at high risk. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;338(11):701–705.
Have you read Dr. Errol R. Norwitz's Update on Operative Vaginal Delivery? Click here to access.
How I am adapting my morcellation practice: Voices from across the country
Hear from:
Michael Baggish, MD (St. Helena, California)
Rupen Baxi, MD (Royal Oak, Michigan)
Jennifer Hollings, MD (Richmond, Virginia)
Gwinnett Ladson, MD (Nashville, Tennessee)
Rich Persino, MD (McHenry, Illinois)
Teresa Tam, MD (Chicago, Illinois)
Yvonne Wolny, MD (Chicago, Illinois)
Hear from:
Michael Baggish, MD (St. Helena, California)
Rupen Baxi, MD (Royal Oak, Michigan)
Jennifer Hollings, MD (Richmond, Virginia)
Gwinnett Ladson, MD (Nashville, Tennessee)
Rich Persino, MD (McHenry, Illinois)
Teresa Tam, MD (Chicago, Illinois)
Yvonne Wolny, MD (Chicago, Illinois)
Hear from:
Michael Baggish, MD (St. Helena, California)
Rupen Baxi, MD (Royal Oak, Michigan)
Jennifer Hollings, MD (Richmond, Virginia)
Gwinnett Ladson, MD (Nashville, Tennessee)
Rich Persino, MD (McHenry, Illinois)
Teresa Tam, MD (Chicago, Illinois)
Yvonne Wolny, MD (Chicago, Illinois)
Does the LNG-IUS treat endometrial hyperplasia as effectively as MPA?
Endometrial cancer is the most common gynecologic cancer in the developed world, and its incidence is rising—increasing 50% in the past 10 years in Norway alone. Because endometrial hyperplasia is a precursor to cancer, it is vital that we ensure effective treatment for this prevalent problem. Hysterectomy is one option—used most commonly for complex atypical hyperplasia—but oral progestins have become the norm in women who desire to preserve their uterus when surgery is not the best option.
In this randomized trial from Norway, Orbo and colleagues randomly assigned 170 women aged 30 to 70 years to one of three treatment groups:
- placement of an LNG-IUS (Mirena)
- medroxyprogesterone acetate (MPA) 10 mg for 10 days per cycle
- continuous MPA 10 mg.
All women in the trial had low- or medium-risk endometrial hyperplasia.
After 6 months, women in the LNG-IUS arm had a 100% response rate, compared with 96% for the continuous MPA group and 69% for cyclic MPA.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; March 2014)
Histologic interpretation of hyperplasia is highly subjective
There are several problems inherent in a study like this. Although Orbo and colleagues address these problems tangentially, the problems affect the interpretation of results.
For example, the histologic interpretation of endometrial hyperplasia is known to be associated with low interobserver agreement.1 Clinical trials that use endometrial safety as an outcome require two primary pathologists to review the histology, with a third pathologist standing by in case of disagreement.
In the current study, two pathologists in the same department independently reviewed the histology. Orbo and colleagues used World Health Organization criteria for hyperplasia. However, as an adjunct, they also used a D-evaluation morphometric assessment.2 When I put in a casual call to local gynecologic pathologists, they told me that neither the D-classification nor the immunochemical-detected PTEN protein is used in routine clinical practice to determine the risk of progression.3
Intermittent use of oral MPA is known to be ineffective
The cyclic use of MPA for only 10 days overlooks epidemiology from estrogen-progestin replacement regimens in postmenopausal women. Use of a progestin for fewer than 12 days during estrogen replacement increases the risk of endometrial cancer.4 Exogenous progestin must be given for more than 12 days to inhibit hyperplasia and neoplasia. The dose itself is not critical; the duration of administration is.
In the current study, both the LNG-IUS and continuous MPA met this criterion. Local delivery of the progestin with the LNG-IUS allows for a reduction of the delivered dose and mitigates side effects even as it uses a more potent progestin than MPA.5–8
Assessment of outcomes was questionable
Although Orbo and colleagues suggest that there is no evidence of progression with the LNG-IUS and continuous MPA, they relied on a Pipelle biopsy of the endometrium performed after 6 months of treatment. The clinical settings that led to the hyperplasia in the first place are poorly characterized as either pre- or postmenopausal, and the cause of the hyperplasia is not identified. This approach overlooks such realities as the increased incidence of simple hyperplasia in many perimenopausal women, which appears to regress with further reduction in ovarian estrogen.9
The final outcomes for women in the cyclic MPA arm are not provided. Hyperplasia without atypia progresses to carcinoma in 1.6% of cases, but when atypia is present, the progression rate is 23%.1
What this evidence means for practice
In low-risk women with simple hyperplasia, the use of targeted low-dose progestins—oral or intrauterine—is appealing. While Orbo and colleagues present an interesting study, they do not definitively establish the optimal intervention.
As we enter a cost-conscious phase of medicine in the United States, we may discover that oral generic MPA (given continuously) may be the most cost-effective treatment despite the option of delivering a low-dose progestin via intrauterine device.
David F. Archer, MD
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter in a future issue. Send your letter to: [email protected] Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
- Pickar JH, Yeh IT, Wheeler JE, Cunnane MF, Speroff L. Endometrial effects of lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001;76(1):25–31.
- Orbo A, Ames M, Hancke C, Vereide AB, Pettersen I, Larsen K. Treatment results of endometrial hyperplasia after prospective D-score classification: A follow-up study comparing effect of LNG-IUD and oral progestins versus observation only. Gynecol Oncol. 2008;111(1):68–73.
- Lacey JV Jr, Mutter GL, Ronnett BM, et al. PTEN expression in endometrial biopsies as a marker of progression to endometrial carcinoma. Cancer Res. 2008;68(14):6014–6020.
- Archer DF. Neoplasia of the female reproductive tract: Effects of hormone therapy. Endocrine. 2004;24(3):259–263.
- Moe BT, Vereide AB, Orbo A, Jaeger R, Sager G. Levonorgestrel, medroxyprogesterone, and progesterone cause a concentration-dependent reduction in endometrial cancer (Ishikawa) cell density, and high concentrations of progesterone and mifepristone act in synergy. Anticancer Res. 2009;29(4):1047–1052.
- Phillips A, Hahn DW, Kimek S, McGuire JL. A comparison of the potencies and activities of progestogens used in contraceptives. Contraception. 1987;36(2):181–192.
- Archer DF. Delivery of therapeutic agents to the target tissue. Menopause. 2011;18(10):1040–1041.
- Somboonporn W, Panna S, Temtanakitpaisan T, Kaewrudee S, Soontrapa S. Effects of the levonorgestrel-releasing intrauterine system plus estrogen therapy in perimenopausal and postmenopausal women: systematic review and meta-analysis. Menopause. 2011;18(10):1060–1066.
- Archer DF, McIntyre-Seltman K, Wilborn WW Jr, et al. Endometrial morphology in asymptomatic postmenopausal women. Am J Obstet Gynecol. 1991;165(2):317–322.
Endometrial cancer is the most common gynecologic cancer in the developed world, and its incidence is rising—increasing 50% in the past 10 years in Norway alone. Because endometrial hyperplasia is a precursor to cancer, it is vital that we ensure effective treatment for this prevalent problem. Hysterectomy is one option—used most commonly for complex atypical hyperplasia—but oral progestins have become the norm in women who desire to preserve their uterus when surgery is not the best option.
In this randomized trial from Norway, Orbo and colleagues randomly assigned 170 women aged 30 to 70 years to one of three treatment groups:
- placement of an LNG-IUS (Mirena)
- medroxyprogesterone acetate (MPA) 10 mg for 10 days per cycle
- continuous MPA 10 mg.
All women in the trial had low- or medium-risk endometrial hyperplasia.
After 6 months, women in the LNG-IUS arm had a 100% response rate, compared with 96% for the continuous MPA group and 69% for cyclic MPA.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; March 2014)
Histologic interpretation of hyperplasia is highly subjective
There are several problems inherent in a study like this. Although Orbo and colleagues address these problems tangentially, the problems affect the interpretation of results.
For example, the histologic interpretation of endometrial hyperplasia is known to be associated with low interobserver agreement.1 Clinical trials that use endometrial safety as an outcome require two primary pathologists to review the histology, with a third pathologist standing by in case of disagreement.
In the current study, two pathologists in the same department independently reviewed the histology. Orbo and colleagues used World Health Organization criteria for hyperplasia. However, as an adjunct, they also used a D-evaluation morphometric assessment.2 When I put in a casual call to local gynecologic pathologists, they told me that neither the D-classification nor the immunochemical-detected PTEN protein is used in routine clinical practice to determine the risk of progression.3
Intermittent use of oral MPA is known to be ineffective
The cyclic use of MPA for only 10 days overlooks epidemiology from estrogen-progestin replacement regimens in postmenopausal women. Use of a progestin for fewer than 12 days during estrogen replacement increases the risk of endometrial cancer.4 Exogenous progestin must be given for more than 12 days to inhibit hyperplasia and neoplasia. The dose itself is not critical; the duration of administration is.
In the current study, both the LNG-IUS and continuous MPA met this criterion. Local delivery of the progestin with the LNG-IUS allows for a reduction of the delivered dose and mitigates side effects even as it uses a more potent progestin than MPA.5–8
Assessment of outcomes was questionable
Although Orbo and colleagues suggest that there is no evidence of progression with the LNG-IUS and continuous MPA, they relied on a Pipelle biopsy of the endometrium performed after 6 months of treatment. The clinical settings that led to the hyperplasia in the first place are poorly characterized as either pre- or postmenopausal, and the cause of the hyperplasia is not identified. This approach overlooks such realities as the increased incidence of simple hyperplasia in many perimenopausal women, which appears to regress with further reduction in ovarian estrogen.9
The final outcomes for women in the cyclic MPA arm are not provided. Hyperplasia without atypia progresses to carcinoma in 1.6% of cases, but when atypia is present, the progression rate is 23%.1
What this evidence means for practice
In low-risk women with simple hyperplasia, the use of targeted low-dose progestins—oral or intrauterine—is appealing. While Orbo and colleagues present an interesting study, they do not definitively establish the optimal intervention.
As we enter a cost-conscious phase of medicine in the United States, we may discover that oral generic MPA (given continuously) may be the most cost-effective treatment despite the option of delivering a low-dose progestin via intrauterine device.
David F. Archer, MD
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter in a future issue. Send your letter to: [email protected] Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Endometrial cancer is the most common gynecologic cancer in the developed world, and its incidence is rising—increasing 50% in the past 10 years in Norway alone. Because endometrial hyperplasia is a precursor to cancer, it is vital that we ensure effective treatment for this prevalent problem. Hysterectomy is one option—used most commonly for complex atypical hyperplasia—but oral progestins have become the norm in women who desire to preserve their uterus when surgery is not the best option.
In this randomized trial from Norway, Orbo and colleagues randomly assigned 170 women aged 30 to 70 years to one of three treatment groups:
- placement of an LNG-IUS (Mirena)
- medroxyprogesterone acetate (MPA) 10 mg for 10 days per cycle
- continuous MPA 10 mg.
All women in the trial had low- or medium-risk endometrial hyperplasia.
After 6 months, women in the LNG-IUS arm had a 100% response rate, compared with 96% for the continuous MPA group and 69% for cyclic MPA.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; March 2014)
Histologic interpretation of hyperplasia is highly subjective
There are several problems inherent in a study like this. Although Orbo and colleagues address these problems tangentially, the problems affect the interpretation of results.
For example, the histologic interpretation of endometrial hyperplasia is known to be associated with low interobserver agreement.1 Clinical trials that use endometrial safety as an outcome require two primary pathologists to review the histology, with a third pathologist standing by in case of disagreement.
In the current study, two pathologists in the same department independently reviewed the histology. Orbo and colleagues used World Health Organization criteria for hyperplasia. However, as an adjunct, they also used a D-evaluation morphometric assessment.2 When I put in a casual call to local gynecologic pathologists, they told me that neither the D-classification nor the immunochemical-detected PTEN protein is used in routine clinical practice to determine the risk of progression.3
Intermittent use of oral MPA is known to be ineffective
The cyclic use of MPA for only 10 days overlooks epidemiology from estrogen-progestin replacement regimens in postmenopausal women. Use of a progestin for fewer than 12 days during estrogen replacement increases the risk of endometrial cancer.4 Exogenous progestin must be given for more than 12 days to inhibit hyperplasia and neoplasia. The dose itself is not critical; the duration of administration is.
In the current study, both the LNG-IUS and continuous MPA met this criterion. Local delivery of the progestin with the LNG-IUS allows for a reduction of the delivered dose and mitigates side effects even as it uses a more potent progestin than MPA.5–8
Assessment of outcomes was questionable
Although Orbo and colleagues suggest that there is no evidence of progression with the LNG-IUS and continuous MPA, they relied on a Pipelle biopsy of the endometrium performed after 6 months of treatment. The clinical settings that led to the hyperplasia in the first place are poorly characterized as either pre- or postmenopausal, and the cause of the hyperplasia is not identified. This approach overlooks such realities as the increased incidence of simple hyperplasia in many perimenopausal women, which appears to regress with further reduction in ovarian estrogen.9
The final outcomes for women in the cyclic MPA arm are not provided. Hyperplasia without atypia progresses to carcinoma in 1.6% of cases, but when atypia is present, the progression rate is 23%.1
What this evidence means for practice
In low-risk women with simple hyperplasia, the use of targeted low-dose progestins—oral or intrauterine—is appealing. While Orbo and colleagues present an interesting study, they do not definitively establish the optimal intervention.
As we enter a cost-conscious phase of medicine in the United States, we may discover that oral generic MPA (given continuously) may be the most cost-effective treatment despite the option of delivering a low-dose progestin via intrauterine device.
David F. Archer, MD
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter in a future issue. Send your letter to: [email protected] Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
- Pickar JH, Yeh IT, Wheeler JE, Cunnane MF, Speroff L. Endometrial effects of lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001;76(1):25–31.
- Orbo A, Ames M, Hancke C, Vereide AB, Pettersen I, Larsen K. Treatment results of endometrial hyperplasia after prospective D-score classification: A follow-up study comparing effect of LNG-IUD and oral progestins versus observation only. Gynecol Oncol. 2008;111(1):68–73.
- Lacey JV Jr, Mutter GL, Ronnett BM, et al. PTEN expression in endometrial biopsies as a marker of progression to endometrial carcinoma. Cancer Res. 2008;68(14):6014–6020.
- Archer DF. Neoplasia of the female reproductive tract: Effects of hormone therapy. Endocrine. 2004;24(3):259–263.
- Moe BT, Vereide AB, Orbo A, Jaeger R, Sager G. Levonorgestrel, medroxyprogesterone, and progesterone cause a concentration-dependent reduction in endometrial cancer (Ishikawa) cell density, and high concentrations of progesterone and mifepristone act in synergy. Anticancer Res. 2009;29(4):1047–1052.
- Phillips A, Hahn DW, Kimek S, McGuire JL. A comparison of the potencies and activities of progestogens used in contraceptives. Contraception. 1987;36(2):181–192.
- Archer DF. Delivery of therapeutic agents to the target tissue. Menopause. 2011;18(10):1040–1041.
- Somboonporn W, Panna S, Temtanakitpaisan T, Kaewrudee S, Soontrapa S. Effects of the levonorgestrel-releasing intrauterine system plus estrogen therapy in perimenopausal and postmenopausal women: systematic review and meta-analysis. Menopause. 2011;18(10):1060–1066.
- Archer DF, McIntyre-Seltman K, Wilborn WW Jr, et al. Endometrial morphology in asymptomatic postmenopausal women. Am J Obstet Gynecol. 1991;165(2):317–322.
- Pickar JH, Yeh IT, Wheeler JE, Cunnane MF, Speroff L. Endometrial effects of lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001;76(1):25–31.
- Orbo A, Ames M, Hancke C, Vereide AB, Pettersen I, Larsen K. Treatment results of endometrial hyperplasia after prospective D-score classification: A follow-up study comparing effect of LNG-IUD and oral progestins versus observation only. Gynecol Oncol. 2008;111(1):68–73.
- Lacey JV Jr, Mutter GL, Ronnett BM, et al. PTEN expression in endometrial biopsies as a marker of progression to endometrial carcinoma. Cancer Res. 2008;68(14):6014–6020.
- Archer DF. Neoplasia of the female reproductive tract: Effects of hormone therapy. Endocrine. 2004;24(3):259–263.
- Moe BT, Vereide AB, Orbo A, Jaeger R, Sager G. Levonorgestrel, medroxyprogesterone, and progesterone cause a concentration-dependent reduction in endometrial cancer (Ishikawa) cell density, and high concentrations of progesterone and mifepristone act in synergy. Anticancer Res. 2009;29(4):1047–1052.
- Phillips A, Hahn DW, Kimek S, McGuire JL. A comparison of the potencies and activities of progestogens used in contraceptives. Contraception. 1987;36(2):181–192.
- Archer DF. Delivery of therapeutic agents to the target tissue. Menopause. 2011;18(10):1040–1041.
- Somboonporn W, Panna S, Temtanakitpaisan T, Kaewrudee S, Soontrapa S. Effects of the levonorgestrel-releasing intrauterine system plus estrogen therapy in perimenopausal and postmenopausal women: systematic review and meta-analysis. Menopause. 2011;18(10):1060–1066.
- Archer DF, McIntyre-Seltman K, Wilborn WW Jr, et al. Endometrial morphology in asymptomatic postmenopausal women. Am J Obstet Gynecol. 1991;165(2):317–322.