User login
‘I can’t breathe’: Health inequity and state-sanctioned violence
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
Hospitalist well-being during the pandemic
Navigating COVID-19 requires self-care
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
Navigating COVID-19 requires self-care
Navigating COVID-19 requires self-care
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
Learning the ICU
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Perspectives of a black physician in the time of two pandemics
“Hey there – just checking on you and letting you know I’m thinking of you."
"I know words don't suffice right now. You are in my thoughts."
"If there's any way that I can be of support or if there's something you need, just let me know."
The texts and emails have come in waves. Pinging into my already distracted headspace when, like them, I’m supposed to be focused on a Zoom or WebEx department meeting. These somber reminders underscore what I have known for years but struggled to describe with each new “justice for” hashtag accompanying the name of the latest unarmed black person to die. This is grief.
With every headline in prior years, as black Americans we have usually found solace in our collective fellowship of suffering. Social media timelines become flooded with our own amen choirs and outrage along with words of comfort and inspiration. We remind ourselves of the prior atrocities survived by our people. And like them, we vow to rally; clinging to one other and praying to make it to shore. Though intermittently joined by a smattering of allies, our suffering has mostly been a private, repetitive mourning.
The two pandemics
The year 2020 ushered in a new decade along with the novel SARS-CoV2 (COVID-19) global pandemic. In addition to the thousands of lives that have been lost in the United States alone, COVID-19 brought with it a disruption of life in ways never seen by most generations. Schools and businesses were closed to mitigate spread. Mandatory shelter-in-place orders coupled with physical distancing recommendations limited human interactions and canceled everything from hospital visitations to graduations, intergenerational family gatherings, conferences, and weddings. As the data expanded, it quickly became apparent that minorities, particularly black Americans, shouldered a disproportionate burden of COVID-19. Known health disparities were amplified.
While caring for our patients as black physicians in the time of coronavirus, silently we mourned again. The connection and trust once found through racial concordance was now masked figuratively and literally by personal protective equipment (PPE). We ignored the sting of intimations that the staggering numbers of African Americans hospitalized and dying from COVID-19 could be explained by lack of discipline or, worse, genetic differences by race. Years of disenfranchisement and missed economic opportunities forced large numbers of our patients and loved ones out on the front lines to do essential jobs – but without the celebratory cheers or fanfare enjoyed by others. Frantic phone calls from family and acquaintances interrupted our quiet drives home from emotionally grueling shifts in the hospital – each conversation serving as our personal evidence of COVID-19 and her ruthless ravage of the black community. Add to this trying to serve as cultural bridges between the complexities of medical distrust and patient advocacy along with wrestling with our own vulnerability as potential COVID-19 patients, these have been overwhelming times to say the least.
Then came the acute decompensation of the chronic racism we’d always known in the form of three recent killings of more unarmed African Americans. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home after midnight on a “no knock” warrant. The story was buried in the news of COVID-19 – but we knew. Later we’d learn that 26-year-old Ahmaud Arbery was shot and killed by armed neighbors while running through a Brunswick, Georgia, neighborhood. His death on Feb. 23, 2020, initially yielded no criminal charges. Then, on May 25, 2020, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after a law enforcement official kneeled with his full body weight upon Floyd’s neck for more than 8 minutes. The deaths of Arbery and Floyd were captured by cell phone cameras which, aided by social media, quickly reached the eyes of the entire world.
At first, it seemed plausible that this would be like it always has been. A black mother would stand before a podium filled with multiple microphones crying out in anguish. She would be flanked by community leaders and attorneys demanding justice. Hashtags would be formed. Our people would stand up or kneel down in solidarity – holding fast to our historic resilience. Evanescent allies would appear with signs on lawns and held high over heads. A few weeks would pass by and things would go back to normal. Black people would be left with what always remains: heads bowed and praying at dinner tables petitioning a higher power for protection followed by reaffirmations of what, if anything, could be done to keep our own mamas away from that podium. We’ve learned to treat the grief of racism as endemic to us alone, knowing that it has been a pandemic all along.
Dr. Manning is a professor of medicine and the associate vice chair of diversity, equity, and inclusion at Emory University in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. To read the full version of this article, visit the Journal of Hospital Medicine, where it first appeared (doi: 10.12788/jhm.3481).
“Hey there – just checking on you and letting you know I’m thinking of you."
"I know words don't suffice right now. You are in my thoughts."
"If there's any way that I can be of support or if there's something you need, just let me know."
The texts and emails have come in waves. Pinging into my already distracted headspace when, like them, I’m supposed to be focused on a Zoom or WebEx department meeting. These somber reminders underscore what I have known for years but struggled to describe with each new “justice for” hashtag accompanying the name of the latest unarmed black person to die. This is grief.
With every headline in prior years, as black Americans we have usually found solace in our collective fellowship of suffering. Social media timelines become flooded with our own amen choirs and outrage along with words of comfort and inspiration. We remind ourselves of the prior atrocities survived by our people. And like them, we vow to rally; clinging to one other and praying to make it to shore. Though intermittently joined by a smattering of allies, our suffering has mostly been a private, repetitive mourning.
The two pandemics
The year 2020 ushered in a new decade along with the novel SARS-CoV2 (COVID-19) global pandemic. In addition to the thousands of lives that have been lost in the United States alone, COVID-19 brought with it a disruption of life in ways never seen by most generations. Schools and businesses were closed to mitigate spread. Mandatory shelter-in-place orders coupled with physical distancing recommendations limited human interactions and canceled everything from hospital visitations to graduations, intergenerational family gatherings, conferences, and weddings. As the data expanded, it quickly became apparent that minorities, particularly black Americans, shouldered a disproportionate burden of COVID-19. Known health disparities were amplified.
While caring for our patients as black physicians in the time of coronavirus, silently we mourned again. The connection and trust once found through racial concordance was now masked figuratively and literally by personal protective equipment (PPE). We ignored the sting of intimations that the staggering numbers of African Americans hospitalized and dying from COVID-19 could be explained by lack of discipline or, worse, genetic differences by race. Years of disenfranchisement and missed economic opportunities forced large numbers of our patients and loved ones out on the front lines to do essential jobs – but without the celebratory cheers or fanfare enjoyed by others. Frantic phone calls from family and acquaintances interrupted our quiet drives home from emotionally grueling shifts in the hospital – each conversation serving as our personal evidence of COVID-19 and her ruthless ravage of the black community. Add to this trying to serve as cultural bridges between the complexities of medical distrust and patient advocacy along with wrestling with our own vulnerability as potential COVID-19 patients, these have been overwhelming times to say the least.
Then came the acute decompensation of the chronic racism we’d always known in the form of three recent killings of more unarmed African Americans. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home after midnight on a “no knock” warrant. The story was buried in the news of COVID-19 – but we knew. Later we’d learn that 26-year-old Ahmaud Arbery was shot and killed by armed neighbors while running through a Brunswick, Georgia, neighborhood. His death on Feb. 23, 2020, initially yielded no criminal charges. Then, on May 25, 2020, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after a law enforcement official kneeled with his full body weight upon Floyd’s neck for more than 8 minutes. The deaths of Arbery and Floyd were captured by cell phone cameras which, aided by social media, quickly reached the eyes of the entire world.
At first, it seemed plausible that this would be like it always has been. A black mother would stand before a podium filled with multiple microphones crying out in anguish. She would be flanked by community leaders and attorneys demanding justice. Hashtags would be formed. Our people would stand up or kneel down in solidarity – holding fast to our historic resilience. Evanescent allies would appear with signs on lawns and held high over heads. A few weeks would pass by and things would go back to normal. Black people would be left with what always remains: heads bowed and praying at dinner tables petitioning a higher power for protection followed by reaffirmations of what, if anything, could be done to keep our own mamas away from that podium. We’ve learned to treat the grief of racism as endemic to us alone, knowing that it has been a pandemic all along.
Dr. Manning is a professor of medicine and the associate vice chair of diversity, equity, and inclusion at Emory University in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. To read the full version of this article, visit the Journal of Hospital Medicine, where it first appeared (doi: 10.12788/jhm.3481).
“Hey there – just checking on you and letting you know I’m thinking of you."
"I know words don't suffice right now. You are in my thoughts."
"If there's any way that I can be of support or if there's something you need, just let me know."
The texts and emails have come in waves. Pinging into my already distracted headspace when, like them, I’m supposed to be focused on a Zoom or WebEx department meeting. These somber reminders underscore what I have known for years but struggled to describe with each new “justice for” hashtag accompanying the name of the latest unarmed black person to die. This is grief.
With every headline in prior years, as black Americans we have usually found solace in our collective fellowship of suffering. Social media timelines become flooded with our own amen choirs and outrage along with words of comfort and inspiration. We remind ourselves of the prior atrocities survived by our people. And like them, we vow to rally; clinging to one other and praying to make it to shore. Though intermittently joined by a smattering of allies, our suffering has mostly been a private, repetitive mourning.
The two pandemics
The year 2020 ushered in a new decade along with the novel SARS-CoV2 (COVID-19) global pandemic. In addition to the thousands of lives that have been lost in the United States alone, COVID-19 brought with it a disruption of life in ways never seen by most generations. Schools and businesses were closed to mitigate spread. Mandatory shelter-in-place orders coupled with physical distancing recommendations limited human interactions and canceled everything from hospital visitations to graduations, intergenerational family gatherings, conferences, and weddings. As the data expanded, it quickly became apparent that minorities, particularly black Americans, shouldered a disproportionate burden of COVID-19. Known health disparities were amplified.
While caring for our patients as black physicians in the time of coronavirus, silently we mourned again. The connection and trust once found through racial concordance was now masked figuratively and literally by personal protective equipment (PPE). We ignored the sting of intimations that the staggering numbers of African Americans hospitalized and dying from COVID-19 could be explained by lack of discipline or, worse, genetic differences by race. Years of disenfranchisement and missed economic opportunities forced large numbers of our patients and loved ones out on the front lines to do essential jobs – but without the celebratory cheers or fanfare enjoyed by others. Frantic phone calls from family and acquaintances interrupted our quiet drives home from emotionally grueling shifts in the hospital – each conversation serving as our personal evidence of COVID-19 and her ruthless ravage of the black community. Add to this trying to serve as cultural bridges between the complexities of medical distrust and patient advocacy along with wrestling with our own vulnerability as potential COVID-19 patients, these have been overwhelming times to say the least.
Then came the acute decompensation of the chronic racism we’d always known in the form of three recent killings of more unarmed African Americans. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home after midnight on a “no knock” warrant. The story was buried in the news of COVID-19 – but we knew. Later we’d learn that 26-year-old Ahmaud Arbery was shot and killed by armed neighbors while running through a Brunswick, Georgia, neighborhood. His death on Feb. 23, 2020, initially yielded no criminal charges. Then, on May 25, 2020, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after a law enforcement official kneeled with his full body weight upon Floyd’s neck for more than 8 minutes. The deaths of Arbery and Floyd were captured by cell phone cameras which, aided by social media, quickly reached the eyes of the entire world.
At first, it seemed plausible that this would be like it always has been. A black mother would stand before a podium filled with multiple microphones crying out in anguish. She would be flanked by community leaders and attorneys demanding justice. Hashtags would be formed. Our people would stand up or kneel down in solidarity – holding fast to our historic resilience. Evanescent allies would appear with signs on lawns and held high over heads. A few weeks would pass by and things would go back to normal. Black people would be left with what always remains: heads bowed and praying at dinner tables petitioning a higher power for protection followed by reaffirmations of what, if anything, could be done to keep our own mamas away from that podium. We’ve learned to treat the grief of racism as endemic to us alone, knowing that it has been a pandemic all along.
Dr. Manning is a professor of medicine and the associate vice chair of diversity, equity, and inclusion at Emory University in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. To read the full version of this article, visit the Journal of Hospital Medicine, where it first appeared (doi: 10.12788/jhm.3481).
Hospitalists stretch into new roles on COVID-19 front lines
‘Every single day is different’
In the midst of the COVID-19 pandemic, health systems, hospitals, and hospitalists – especially in hot spots like New York, Detroit, or Boston – have been challenged to stretch limits, redefine roles, and redeploy critical staff in response to rapidly changing needs on the ground.
Many hospitalists are working above and beyond their normal duties, sometimes beyond their training, specialty, or comfort zone and are rising to the occasion in ways they never imagined. These include doing shifts in ICUs, working with ventilator patients, and reporting to other atypical sites of care like postanesthesia care units and post-acute or step-down units.
Valerie Vaughn, MD, MSc, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.”
Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care providers, who volunteered to manage COVID-19 patients in the ICU and other hospital units. She was asked to help develop an all-COVID unit called the Regional Infectious Containment Unit or RICU, which opened March 16. Then, when the RICU became full, it was supplemented by two COVID-19 Moderate Care Units staffed by hospitalists who had “learned the ropes” in the RICU.
Both of these new models were defined in relation to the ICUs at Michigan Medicine – which were doubling in capacity, up to 200 beds at last count – and to the provision of intensive-level and long-term ventilator care for the sickest patients. The moderate care units are for patients who are not on ventilators but still very sick, for example, those receiving massive high-flow oxygen, often with a medical do-not-resuscitate/do-not-intubate order. “We established these units to do everything (medically) short of vents,” Dr. Vaughn said.
“We are having in-depth conversations about goals of care with patients soon after they arrive at the hospital. We know outcomes from ventilators are worse for COVID-positive patients who have comorbidities, and we’re using that information to inform these conversations. We’ve given scripts to clinicians to help guide them in leading these conversations. We can do other things than `use ventilators to manage their symptoms. But these are still difficult conversations,” Dr. Vaughn said.

“We also engaged palliative care early on and asked them to round with us on every [COVID] patient – until demand got too high.” The bottleneck has been the number of ICU beds available, she explained. “If you want your patient to come in and take that bed, make sure you’ve talked to the family about it.”
The COVID-19 team developed guidelines printed on pocket cards addressing critical care issues such as a refresher on how to treat acute respiratory distress syndrome and how to use vasopressors. (See the COVID-19 Continuing Medical Education Portal for web-accessible educational resources developed by Michigan Health).
It’s amazing how quickly patients can become very sick with COVID-19, Dr. Vaughn said. “One of the good things to happen from the beginning with our RICU is that a group of doctors became COVID care experts very quickly. We joined four to five hospitalists and their teams with each intensivist, so one critical care expert is there to do teaching and answer clinicians’ questions. The hospitalists coordinate the COVID care and talk to the families.”
Working on the front lines of this crisis, Dr. Vaughn said, has generated a powerful sense of purpose and camaraderie, creating bonds like in war time. “All of us on our days off feel a twinge of guilt for not being there in the hospital. The sense of gratitude we get from patients and families has been enormous, even when we were telling them bad news. That just brings us to tears.”
One of the hardest things for the doctors practicing above their typical scope of practice is that, when something bad happens, they can’t know whether it was a mistake on their part or not, she noted. “But I’ve never been so proud of our group or to be a hospitalist. No one has complained or pushed back. Everyone has responded by saying: ‘What can I do to help?’ ”
Enough work in hospital medicine
Hospitalists had not been deployed to care for ICU patients at Beth Israel Deaconess Medical Center (BIDMC) in Boston, a major hot spot for COVID-19, said Joseph Ming Wah Li, MD, SFHM, director of the hospital medicine program at BIDMC, when he spoke to The Hospitalist in mid-May. That’s because there were plenty of hospital medicine assignments to keep them busy. Dr. Li leads a service of 120 hospitalists practicing at four hospitals.
“As we speak today, we have 300 patients with COVID, with 70 or 80 of them in our ICU. I’m taking care of 17 patients today, 15 of them COVID-positive, and the other two placed in a former radiology holding suite adapted for COVID-negative patients. Our postanesthesia care unit is now an ICU filled with COVID patients,” he said.
“Half of my day is seeing patients and the other half I’m on Zoom calls. I’m also one of the resource allocation officers for BIDMC,” Dr. Li said. He helped to create a standard of care for the hospital, addressing what to do if there weren’t enough ICU beds or ventilators. “We’ve never actualized it and probably won’t, but it was important to go through this exercise, with a lot of discussion up front.”
Haki Laho, MD, an orthopedic hospitalist at New England Baptist Hospital (NEBH), also in Boston, has been redeployed to care for a different population of patients as his system tries to bunch patients. “All of a sudden – within hours and days – at the beginning of the pandemic and based on the recommendations, our whole system decided to stop all elective procedures and devote the resources to COVID,” he said.
NEBH is Beth Israel Lahey Health’s 141-bed orthopedic and surgical hospital, and the system has tried to keep the specialty facility COVID-19–free as much as possible, with the COVID-19 patients grouped together at BIDMC. Dr. Laho’s orthopedic hospitalist group, just five doctors, has been managing the influx of medical patients with multiple comorbidities – not COVID-19–infected but still a different kind of patient than they are used to.
“So far, so good. We’re dealing with it,” he said. “But if one of us got sick, the others would have to step up and do more shifts. We are physicians, internal medicine trained, but since my residency I hadn’t had to deal with these kinds of issues on a daily basis, such as setting up IV lines. I feel like I am back in residency mode.”
Convention Center medicine
Another Boston hospitalist, Amy Baughman, MD, who practices at Massachusetts General Hospital, is using her skills in a new setting, serving as a co-medical director at Boston Hope Medical Center, a 1,000-bed field hospital for patients with COVID-19. Open since April 10 and housed in the Boston Convention and Exhibition Center, it is a four-way collaboration between the Commonwealth of Massachusetts, the City of Boston, Partners HealthCare, and the Boston Health Care for the Homeless Program.
Boston Hope is divided into a post-acute care section for recovering COVID-19 patients and a respite section for undomiciled patients with COVID-19 who need a place to safely quarantine. Built for a maximum of 1,000 beds, it is currently using fewer, with 83 patients on the post-acute side and 73 on the respite side as of May 12. A total of 370 and 315, respectively, had been admitted through May 12.
The team had 5 days to put the field hospital together with the help of the Army National Guard. “During that first week I was installing hand sanitizer dispensers and making [personal protective equipment] signs. Everyone here has had to do things like that,” Dr. Baughman said. “We’ve had to be incredibly creative in our staffing, using doctors from primary care and subspecialties including dermatology, radiology, and orthopedics. We had to fast-track trainings on how to use EPIC and to provide post-acute COVID care. How do you simultaneously build a medical facility and lead teams to provide high quality care?”
Dr. Baughman still works hospitalist shifts half-time at Massachusetts General. Her prior experience providing post-acute care in the VA system was helpful in creating the post-acute level of care at Boston Hope.
“My medical director role involves supervising, staffing, and scheduling. My co-medical director, Dr. Kerri Palamara, and I also supervise the clinical care,” she said. “There are a lot of systems issues, like ordering labs or prescriptions, with couriers going back and forth. And we developed clinical pathways, such as for [deep vein thrombosis] prophylaxis or for COVID retesting to determine when it is safe to end a quarantine. We’re just now rolling out virtual specialist consultations,” she noted.
“It has gone incredibly well. So much of it has been about our ability and willingness to work hard, and take feedback and go forward. We don’t have time to harp on things. We have to be very solution oriented. At the same time, honestly, it’s been fun. Every single day is different,” Dr. Baughman said.
“It’s been an opportunity to use my skills in a totally new setting, and at a level of responsibility I haven’t had before, although that’s probably a common theme with COVID-19. I was put on this team because I am a hospitalist,” she said. “I think hospitalists have been the backbone of the response to COVID in this country. It’s been an opportunity for our specialty to shine. We need to embrace the opportunity.”
Balancing expertise and supervision
Mount Sinai Hospital (MSH) in Manhattan is in the New York epicenter of the COVID-19 crisis and has mobilized large numbers of pulmonary critical care and anesthesia physicians to staff up multiple ICUs for COVID-19 patients, said Andrew Dunn, MD, chief of the division of hospital medicine at Mount Sinai School of Medicine.
“My hospitalist group is covering many step-down units, medical wards, and atypical locations, providing advanced oxygen therapies, [bilevel positive airway pressure], high-flow nasal cannulas, and managing some patients on ventilators,” he said.
MSH has teaching services with house staff and nonteaching services. “We combined them into a unified service with house staff dispersed across all of the teams. We drafted a lot of nonhospitalists from different specialties to be attendings, and that has given us a tiered model, with a hospitalist supervising three or four nonhospitalist-led teams. Although the supervising hospitalists carry no patient caseloads of their own, this is primarily a clinical rather than an administrative role.”
At the peak, there were 40 rounding teams at MSH, each with a typical census of 15 patients or more, which meant that 10 supervisory hospitalists were responsible for 300 to 400 patients. “What we learned first was the need to balance the level of expertise. For example, a team may include a postgraduate year 3 resident and a radiology intern,” Dr. Dunn said. As COVID-19 census has started coming down, supervisory hospitalists are returning to direct care attending roles, and some hospitalists have been shared across the Mount Sinai system’s hospitals.
Dr. Dunn’s advice for hospitalists filling a supervisory role like this in a tiered model: Make sure you talk to your team the night before the first day of a scheduling block and try to address as many of their questions as possible. “If you wait until the morning of the shift to connect with them, anxiety will be high. But after going through a couple of scheduling cycles, we find that things are getting better. I think we’ve paid a lot of attention to the risks of burnout by our physicians. We’re using a model of 4 days on/4 off.”
Another variation on these themes is Joshua Shatzkes, MD, assistant professor of medicine and cardiology at Mount Sinai, who practices outpatient cardiology at MSH and in several off-site offices in Brooklyn. He saw early on that COVID-19 would have a huge effect on his practice, so he volunteered to help out with inpatient care. “I made it known to my chief that I was available, and I was deployed in the first week, after a weekend of cramming webinars and lectures on critical care and pulling out critical concepts that I already knew.”
Dr. Shatzkes said his career path led him into outpatient cardiology 11 years ago, where he was quickly too busy to see his patients when they went into the hospital, even though he missed hospital medicine. Working as a temporary hospitalist with the arrival of COVID-19, he has been invigorated and mobilized by the experience and reminded of why he went to medical school in the first place. “Each day’s shift went quickly but felt long. At the end of the day, I was tired but not exhausted. When I walked out of a patient’s room, they could tell, ‘This is a doctor who cared for me,’ ” he said.
After Dr. Shatzkes volunteered, he got the call from his division chief. “I was officially deployed for a 4-day shift at Mount Sinai and then as a backup.” On his first morning as an inpatient doctor, he was still getting oriented when calls started coming from the nurses. “I had five patients struggling to breathe. Their degree of hypoxia was remarkable. I kept them out of the ICU, at least for that day.”
Since then, he has continued to follow some of those patients in the hospital, along with some from his outpatient practice who were hospitalized, and others referred by colleagues, while remaining available to his outpatients through telemedicine. When this is all over, Dr. Shatzkes said, he would love to find a way to incorporate a hospital practice in his job – depending on the realities of New York traffic.
“Joshua is not a hospitalist, but he went on service and felt so fulfilled and rewarded, he asked me if he could stay on service,” Dr. Dunn said. “I also got an email from the nurse manager on the unit. They want him back.”
‘Every single day is different’
‘Every single day is different’
In the midst of the COVID-19 pandemic, health systems, hospitals, and hospitalists – especially in hot spots like New York, Detroit, or Boston – have been challenged to stretch limits, redefine roles, and redeploy critical staff in response to rapidly changing needs on the ground.
Many hospitalists are working above and beyond their normal duties, sometimes beyond their training, specialty, or comfort zone and are rising to the occasion in ways they never imagined. These include doing shifts in ICUs, working with ventilator patients, and reporting to other atypical sites of care like postanesthesia care units and post-acute or step-down units.
Valerie Vaughn, MD, MSc, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.”
Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care providers, who volunteered to manage COVID-19 patients in the ICU and other hospital units. She was asked to help develop an all-COVID unit called the Regional Infectious Containment Unit or RICU, which opened March 16. Then, when the RICU became full, it was supplemented by two COVID-19 Moderate Care Units staffed by hospitalists who had “learned the ropes” in the RICU.
Both of these new models were defined in relation to the ICUs at Michigan Medicine – which were doubling in capacity, up to 200 beds at last count – and to the provision of intensive-level and long-term ventilator care for the sickest patients. The moderate care units are for patients who are not on ventilators but still very sick, for example, those receiving massive high-flow oxygen, often with a medical do-not-resuscitate/do-not-intubate order. “We established these units to do everything (medically) short of vents,” Dr. Vaughn said.
“We are having in-depth conversations about goals of care with patients soon after they arrive at the hospital. We know outcomes from ventilators are worse for COVID-positive patients who have comorbidities, and we’re using that information to inform these conversations. We’ve given scripts to clinicians to help guide them in leading these conversations. We can do other things than `use ventilators to manage their symptoms. But these are still difficult conversations,” Dr. Vaughn said.

“We also engaged palliative care early on and asked them to round with us on every [COVID] patient – until demand got too high.” The bottleneck has been the number of ICU beds available, she explained. “If you want your patient to come in and take that bed, make sure you’ve talked to the family about it.”
The COVID-19 team developed guidelines printed on pocket cards addressing critical care issues such as a refresher on how to treat acute respiratory distress syndrome and how to use vasopressors. (See the COVID-19 Continuing Medical Education Portal for web-accessible educational resources developed by Michigan Health).
It’s amazing how quickly patients can become very sick with COVID-19, Dr. Vaughn said. “One of the good things to happen from the beginning with our RICU is that a group of doctors became COVID care experts very quickly. We joined four to five hospitalists and their teams with each intensivist, so one critical care expert is there to do teaching and answer clinicians’ questions. The hospitalists coordinate the COVID care and talk to the families.”
Working on the front lines of this crisis, Dr. Vaughn said, has generated a powerful sense of purpose and camaraderie, creating bonds like in war time. “All of us on our days off feel a twinge of guilt for not being there in the hospital. The sense of gratitude we get from patients and families has been enormous, even when we were telling them bad news. That just brings us to tears.”
One of the hardest things for the doctors practicing above their typical scope of practice is that, when something bad happens, they can’t know whether it was a mistake on their part or not, she noted. “But I’ve never been so proud of our group or to be a hospitalist. No one has complained or pushed back. Everyone has responded by saying: ‘What can I do to help?’ ”
Enough work in hospital medicine
Hospitalists had not been deployed to care for ICU patients at Beth Israel Deaconess Medical Center (BIDMC) in Boston, a major hot spot for COVID-19, said Joseph Ming Wah Li, MD, SFHM, director of the hospital medicine program at BIDMC, when he spoke to The Hospitalist in mid-May. That’s because there were plenty of hospital medicine assignments to keep them busy. Dr. Li leads a service of 120 hospitalists practicing at four hospitals.
“As we speak today, we have 300 patients with COVID, with 70 or 80 of them in our ICU. I’m taking care of 17 patients today, 15 of them COVID-positive, and the other two placed in a former radiology holding suite adapted for COVID-negative patients. Our postanesthesia care unit is now an ICU filled with COVID patients,” he said.
“Half of my day is seeing patients and the other half I’m on Zoom calls. I’m also one of the resource allocation officers for BIDMC,” Dr. Li said. He helped to create a standard of care for the hospital, addressing what to do if there weren’t enough ICU beds or ventilators. “We’ve never actualized it and probably won’t, but it was important to go through this exercise, with a lot of discussion up front.”
Haki Laho, MD, an orthopedic hospitalist at New England Baptist Hospital (NEBH), also in Boston, has been redeployed to care for a different population of patients as his system tries to bunch patients. “All of a sudden – within hours and days – at the beginning of the pandemic and based on the recommendations, our whole system decided to stop all elective procedures and devote the resources to COVID,” he said.
NEBH is Beth Israel Lahey Health’s 141-bed orthopedic and surgical hospital, and the system has tried to keep the specialty facility COVID-19–free as much as possible, with the COVID-19 patients grouped together at BIDMC. Dr. Laho’s orthopedic hospitalist group, just five doctors, has been managing the influx of medical patients with multiple comorbidities – not COVID-19–infected but still a different kind of patient than they are used to.
“So far, so good. We’re dealing with it,” he said. “But if one of us got sick, the others would have to step up and do more shifts. We are physicians, internal medicine trained, but since my residency I hadn’t had to deal with these kinds of issues on a daily basis, such as setting up IV lines. I feel like I am back in residency mode.”
Convention Center medicine
Another Boston hospitalist, Amy Baughman, MD, who practices at Massachusetts General Hospital, is using her skills in a new setting, serving as a co-medical director at Boston Hope Medical Center, a 1,000-bed field hospital for patients with COVID-19. Open since April 10 and housed in the Boston Convention and Exhibition Center, it is a four-way collaboration between the Commonwealth of Massachusetts, the City of Boston, Partners HealthCare, and the Boston Health Care for the Homeless Program.
Boston Hope is divided into a post-acute care section for recovering COVID-19 patients and a respite section for undomiciled patients with COVID-19 who need a place to safely quarantine. Built for a maximum of 1,000 beds, it is currently using fewer, with 83 patients on the post-acute side and 73 on the respite side as of May 12. A total of 370 and 315, respectively, had been admitted through May 12.
The team had 5 days to put the field hospital together with the help of the Army National Guard. “During that first week I was installing hand sanitizer dispensers and making [personal protective equipment] signs. Everyone here has had to do things like that,” Dr. Baughman said. “We’ve had to be incredibly creative in our staffing, using doctors from primary care and subspecialties including dermatology, radiology, and orthopedics. We had to fast-track trainings on how to use EPIC and to provide post-acute COVID care. How do you simultaneously build a medical facility and lead teams to provide high quality care?”
Dr. Baughman still works hospitalist shifts half-time at Massachusetts General. Her prior experience providing post-acute care in the VA system was helpful in creating the post-acute level of care at Boston Hope.
“My medical director role involves supervising, staffing, and scheduling. My co-medical director, Dr. Kerri Palamara, and I also supervise the clinical care,” she said. “There are a lot of systems issues, like ordering labs or prescriptions, with couriers going back and forth. And we developed clinical pathways, such as for [deep vein thrombosis] prophylaxis or for COVID retesting to determine when it is safe to end a quarantine. We’re just now rolling out virtual specialist consultations,” she noted.
“It has gone incredibly well. So much of it has been about our ability and willingness to work hard, and take feedback and go forward. We don’t have time to harp on things. We have to be very solution oriented. At the same time, honestly, it’s been fun. Every single day is different,” Dr. Baughman said.
“It’s been an opportunity to use my skills in a totally new setting, and at a level of responsibility I haven’t had before, although that’s probably a common theme with COVID-19. I was put on this team because I am a hospitalist,” she said. “I think hospitalists have been the backbone of the response to COVID in this country. It’s been an opportunity for our specialty to shine. We need to embrace the opportunity.”
Balancing expertise and supervision
Mount Sinai Hospital (MSH) in Manhattan is in the New York epicenter of the COVID-19 crisis and has mobilized large numbers of pulmonary critical care and anesthesia physicians to staff up multiple ICUs for COVID-19 patients, said Andrew Dunn, MD, chief of the division of hospital medicine at Mount Sinai School of Medicine.
“My hospitalist group is covering many step-down units, medical wards, and atypical locations, providing advanced oxygen therapies, [bilevel positive airway pressure], high-flow nasal cannulas, and managing some patients on ventilators,” he said.
MSH has teaching services with house staff and nonteaching services. “We combined them into a unified service with house staff dispersed across all of the teams. We drafted a lot of nonhospitalists from different specialties to be attendings, and that has given us a tiered model, with a hospitalist supervising three or four nonhospitalist-led teams. Although the supervising hospitalists carry no patient caseloads of their own, this is primarily a clinical rather than an administrative role.”
At the peak, there were 40 rounding teams at MSH, each with a typical census of 15 patients or more, which meant that 10 supervisory hospitalists were responsible for 300 to 400 patients. “What we learned first was the need to balance the level of expertise. For example, a team may include a postgraduate year 3 resident and a radiology intern,” Dr. Dunn said. As COVID-19 census has started coming down, supervisory hospitalists are returning to direct care attending roles, and some hospitalists have been shared across the Mount Sinai system’s hospitals.
Dr. Dunn’s advice for hospitalists filling a supervisory role like this in a tiered model: Make sure you talk to your team the night before the first day of a scheduling block and try to address as many of their questions as possible. “If you wait until the morning of the shift to connect with them, anxiety will be high. But after going through a couple of scheduling cycles, we find that things are getting better. I think we’ve paid a lot of attention to the risks of burnout by our physicians. We’re using a model of 4 days on/4 off.”
Another variation on these themes is Joshua Shatzkes, MD, assistant professor of medicine and cardiology at Mount Sinai, who practices outpatient cardiology at MSH and in several off-site offices in Brooklyn. He saw early on that COVID-19 would have a huge effect on his practice, so he volunteered to help out with inpatient care. “I made it known to my chief that I was available, and I was deployed in the first week, after a weekend of cramming webinars and lectures on critical care and pulling out critical concepts that I already knew.”
Dr. Shatzkes said his career path led him into outpatient cardiology 11 years ago, where he was quickly too busy to see his patients when they went into the hospital, even though he missed hospital medicine. Working as a temporary hospitalist with the arrival of COVID-19, he has been invigorated and mobilized by the experience and reminded of why he went to medical school in the first place. “Each day’s shift went quickly but felt long. At the end of the day, I was tired but not exhausted. When I walked out of a patient’s room, they could tell, ‘This is a doctor who cared for me,’ ” he said.
After Dr. Shatzkes volunteered, he got the call from his division chief. “I was officially deployed for a 4-day shift at Mount Sinai and then as a backup.” On his first morning as an inpatient doctor, he was still getting oriented when calls started coming from the nurses. “I had five patients struggling to breathe. Their degree of hypoxia was remarkable. I kept them out of the ICU, at least for that day.”
Since then, he has continued to follow some of those patients in the hospital, along with some from his outpatient practice who were hospitalized, and others referred by colleagues, while remaining available to his outpatients through telemedicine. When this is all over, Dr. Shatzkes said, he would love to find a way to incorporate a hospital practice in his job – depending on the realities of New York traffic.
“Joshua is not a hospitalist, but he went on service and felt so fulfilled and rewarded, he asked me if he could stay on service,” Dr. Dunn said. “I also got an email from the nurse manager on the unit. They want him back.”
In the midst of the COVID-19 pandemic, health systems, hospitals, and hospitalists – especially in hot spots like New York, Detroit, or Boston – have been challenged to stretch limits, redefine roles, and redeploy critical staff in response to rapidly changing needs on the ground.
Many hospitalists are working above and beyond their normal duties, sometimes beyond their training, specialty, or comfort zone and are rising to the occasion in ways they never imagined. These include doing shifts in ICUs, working with ventilator patients, and reporting to other atypical sites of care like postanesthesia care units and post-acute or step-down units.
Valerie Vaughn, MD, MSc, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.”
Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care providers, who volunteered to manage COVID-19 patients in the ICU and other hospital units. She was asked to help develop an all-COVID unit called the Regional Infectious Containment Unit or RICU, which opened March 16. Then, when the RICU became full, it was supplemented by two COVID-19 Moderate Care Units staffed by hospitalists who had “learned the ropes” in the RICU.
Both of these new models were defined in relation to the ICUs at Michigan Medicine – which were doubling in capacity, up to 200 beds at last count – and to the provision of intensive-level and long-term ventilator care for the sickest patients. The moderate care units are for patients who are not on ventilators but still very sick, for example, those receiving massive high-flow oxygen, often with a medical do-not-resuscitate/do-not-intubate order. “We established these units to do everything (medically) short of vents,” Dr. Vaughn said.
“We are having in-depth conversations about goals of care with patients soon after they arrive at the hospital. We know outcomes from ventilators are worse for COVID-positive patients who have comorbidities, and we’re using that information to inform these conversations. We’ve given scripts to clinicians to help guide them in leading these conversations. We can do other things than `use ventilators to manage their symptoms. But these are still difficult conversations,” Dr. Vaughn said.

“We also engaged palliative care early on and asked them to round with us on every [COVID] patient – until demand got too high.” The bottleneck has been the number of ICU beds available, she explained. “If you want your patient to come in and take that bed, make sure you’ve talked to the family about it.”
The COVID-19 team developed guidelines printed on pocket cards addressing critical care issues such as a refresher on how to treat acute respiratory distress syndrome and how to use vasopressors. (See the COVID-19 Continuing Medical Education Portal for web-accessible educational resources developed by Michigan Health).
It’s amazing how quickly patients can become very sick with COVID-19, Dr. Vaughn said. “One of the good things to happen from the beginning with our RICU is that a group of doctors became COVID care experts very quickly. We joined four to five hospitalists and their teams with each intensivist, so one critical care expert is there to do teaching and answer clinicians’ questions. The hospitalists coordinate the COVID care and talk to the families.”
Working on the front lines of this crisis, Dr. Vaughn said, has generated a powerful sense of purpose and camaraderie, creating bonds like in war time. “All of us on our days off feel a twinge of guilt for not being there in the hospital. The sense of gratitude we get from patients and families has been enormous, even when we were telling them bad news. That just brings us to tears.”
One of the hardest things for the doctors practicing above their typical scope of practice is that, when something bad happens, they can’t know whether it was a mistake on their part or not, she noted. “But I’ve never been so proud of our group or to be a hospitalist. No one has complained or pushed back. Everyone has responded by saying: ‘What can I do to help?’ ”
Enough work in hospital medicine
Hospitalists had not been deployed to care for ICU patients at Beth Israel Deaconess Medical Center (BIDMC) in Boston, a major hot spot for COVID-19, said Joseph Ming Wah Li, MD, SFHM, director of the hospital medicine program at BIDMC, when he spoke to The Hospitalist in mid-May. That’s because there were plenty of hospital medicine assignments to keep them busy. Dr. Li leads a service of 120 hospitalists practicing at four hospitals.
“As we speak today, we have 300 patients with COVID, with 70 or 80 of them in our ICU. I’m taking care of 17 patients today, 15 of them COVID-positive, and the other two placed in a former radiology holding suite adapted for COVID-negative patients. Our postanesthesia care unit is now an ICU filled with COVID patients,” he said.
“Half of my day is seeing patients and the other half I’m on Zoom calls. I’m also one of the resource allocation officers for BIDMC,” Dr. Li said. He helped to create a standard of care for the hospital, addressing what to do if there weren’t enough ICU beds or ventilators. “We’ve never actualized it and probably won’t, but it was important to go through this exercise, with a lot of discussion up front.”
Haki Laho, MD, an orthopedic hospitalist at New England Baptist Hospital (NEBH), also in Boston, has been redeployed to care for a different population of patients as his system tries to bunch patients. “All of a sudden – within hours and days – at the beginning of the pandemic and based on the recommendations, our whole system decided to stop all elective procedures and devote the resources to COVID,” he said.
NEBH is Beth Israel Lahey Health’s 141-bed orthopedic and surgical hospital, and the system has tried to keep the specialty facility COVID-19–free as much as possible, with the COVID-19 patients grouped together at BIDMC. Dr. Laho’s orthopedic hospitalist group, just five doctors, has been managing the influx of medical patients with multiple comorbidities – not COVID-19–infected but still a different kind of patient than they are used to.
“So far, so good. We’re dealing with it,” he said. “But if one of us got sick, the others would have to step up and do more shifts. We are physicians, internal medicine trained, but since my residency I hadn’t had to deal with these kinds of issues on a daily basis, such as setting up IV lines. I feel like I am back in residency mode.”
Convention Center medicine
Another Boston hospitalist, Amy Baughman, MD, who practices at Massachusetts General Hospital, is using her skills in a new setting, serving as a co-medical director at Boston Hope Medical Center, a 1,000-bed field hospital for patients with COVID-19. Open since April 10 and housed in the Boston Convention and Exhibition Center, it is a four-way collaboration between the Commonwealth of Massachusetts, the City of Boston, Partners HealthCare, and the Boston Health Care for the Homeless Program.
Boston Hope is divided into a post-acute care section for recovering COVID-19 patients and a respite section for undomiciled patients with COVID-19 who need a place to safely quarantine. Built for a maximum of 1,000 beds, it is currently using fewer, with 83 patients on the post-acute side and 73 on the respite side as of May 12. A total of 370 and 315, respectively, had been admitted through May 12.
The team had 5 days to put the field hospital together with the help of the Army National Guard. “During that first week I was installing hand sanitizer dispensers and making [personal protective equipment] signs. Everyone here has had to do things like that,” Dr. Baughman said. “We’ve had to be incredibly creative in our staffing, using doctors from primary care and subspecialties including dermatology, radiology, and orthopedics. We had to fast-track trainings on how to use EPIC and to provide post-acute COVID care. How do you simultaneously build a medical facility and lead teams to provide high quality care?”
Dr. Baughman still works hospitalist shifts half-time at Massachusetts General. Her prior experience providing post-acute care in the VA system was helpful in creating the post-acute level of care at Boston Hope.
“My medical director role involves supervising, staffing, and scheduling. My co-medical director, Dr. Kerri Palamara, and I also supervise the clinical care,” she said. “There are a lot of systems issues, like ordering labs or prescriptions, with couriers going back and forth. And we developed clinical pathways, such as for [deep vein thrombosis] prophylaxis or for COVID retesting to determine when it is safe to end a quarantine. We’re just now rolling out virtual specialist consultations,” she noted.
“It has gone incredibly well. So much of it has been about our ability and willingness to work hard, and take feedback and go forward. We don’t have time to harp on things. We have to be very solution oriented. At the same time, honestly, it’s been fun. Every single day is different,” Dr. Baughman said.
“It’s been an opportunity to use my skills in a totally new setting, and at a level of responsibility I haven’t had before, although that’s probably a common theme with COVID-19. I was put on this team because I am a hospitalist,” she said. “I think hospitalists have been the backbone of the response to COVID in this country. It’s been an opportunity for our specialty to shine. We need to embrace the opportunity.”
Balancing expertise and supervision
Mount Sinai Hospital (MSH) in Manhattan is in the New York epicenter of the COVID-19 crisis and has mobilized large numbers of pulmonary critical care and anesthesia physicians to staff up multiple ICUs for COVID-19 patients, said Andrew Dunn, MD, chief of the division of hospital medicine at Mount Sinai School of Medicine.
“My hospitalist group is covering many step-down units, medical wards, and atypical locations, providing advanced oxygen therapies, [bilevel positive airway pressure], high-flow nasal cannulas, and managing some patients on ventilators,” he said.
MSH has teaching services with house staff and nonteaching services. “We combined them into a unified service with house staff dispersed across all of the teams. We drafted a lot of nonhospitalists from different specialties to be attendings, and that has given us a tiered model, with a hospitalist supervising three or four nonhospitalist-led teams. Although the supervising hospitalists carry no patient caseloads of their own, this is primarily a clinical rather than an administrative role.”
At the peak, there were 40 rounding teams at MSH, each with a typical census of 15 patients or more, which meant that 10 supervisory hospitalists were responsible for 300 to 400 patients. “What we learned first was the need to balance the level of expertise. For example, a team may include a postgraduate year 3 resident and a radiology intern,” Dr. Dunn said. As COVID-19 census has started coming down, supervisory hospitalists are returning to direct care attending roles, and some hospitalists have been shared across the Mount Sinai system’s hospitals.
Dr. Dunn’s advice for hospitalists filling a supervisory role like this in a tiered model: Make sure you talk to your team the night before the first day of a scheduling block and try to address as many of their questions as possible. “If you wait until the morning of the shift to connect with them, anxiety will be high. But after going through a couple of scheduling cycles, we find that things are getting better. I think we’ve paid a lot of attention to the risks of burnout by our physicians. We’re using a model of 4 days on/4 off.”
Another variation on these themes is Joshua Shatzkes, MD, assistant professor of medicine and cardiology at Mount Sinai, who practices outpatient cardiology at MSH and in several off-site offices in Brooklyn. He saw early on that COVID-19 would have a huge effect on his practice, so he volunteered to help out with inpatient care. “I made it known to my chief that I was available, and I was deployed in the first week, after a weekend of cramming webinars and lectures on critical care and pulling out critical concepts that I already knew.”
Dr. Shatzkes said his career path led him into outpatient cardiology 11 years ago, where he was quickly too busy to see his patients when they went into the hospital, even though he missed hospital medicine. Working as a temporary hospitalist with the arrival of COVID-19, he has been invigorated and mobilized by the experience and reminded of why he went to medical school in the first place. “Each day’s shift went quickly but felt long. At the end of the day, I was tired but not exhausted. When I walked out of a patient’s room, they could tell, ‘This is a doctor who cared for me,’ ” he said.
After Dr. Shatzkes volunteered, he got the call from his division chief. “I was officially deployed for a 4-day shift at Mount Sinai and then as a backup.” On his first morning as an inpatient doctor, he was still getting oriented when calls started coming from the nurses. “I had five patients struggling to breathe. Their degree of hypoxia was remarkable. I kept them out of the ICU, at least for that day.”
Since then, he has continued to follow some of those patients in the hospital, along with some from his outpatient practice who were hospitalized, and others referred by colleagues, while remaining available to his outpatients through telemedicine. When this is all over, Dr. Shatzkes said, he would love to find a way to incorporate a hospital practice in his job – depending on the realities of New York traffic.
“Joshua is not a hospitalist, but he went on service and felt so fulfilled and rewarded, he asked me if he could stay on service,” Dr. Dunn said. “I also got an email from the nurse manager on the unit. They want him back.”
The CDI APP adviser
A novel approach to APP documentation engagement
As hospitals and clinicians, we are facing increased scrutiny of the care we provide to our patients. There is increased demand for more transparency of our outcomes and a need for increased efficiency of the care we provide in the setting of already significant documentation burden and its known impact on provider burnout.
Clinical documentation integrity (CDI) is an instrumental department which supports complete and accurate documentation, serves as a bridge between physicians and hospital coders such that hospital reimbursement is appropriate and quality metrics are attributed appropriately to the hospital, service lines, and individual providers. Complete and accurate documentation also leads to the submission of coded/claims-based data reflecting provider true intent and to clinically valid data for research and patient centric purposes. For this reason, the physician adviser role as a liaison between physicians and CDI and coding, in addition to utilization management and case management, has become more commonplace. The physician adviser role has been a mainstay of CDI programs across the United States since as early as 2012.
At the University of Colorado Health (UCHealth), the physician adviser role first began in 2015 at our major academic medical center, the University of Colorado Hospital (UCH). That physician adviser, after the additional physician adviser FTE at UCH, having established relationships with physicians across service lines, began to focus on CDI-related education and communication as it pertained to inpatient documentation.
At our institution we have approximately 500 advance practice providers (APPs). Approximately two-thirds of the APPs care for inpatients on a myriad of different service lines and, along with physician learners from interns to fellows, complete the bulk of the documentation in the electronic health record.
In early 2018, the UCHealth office of advanced practice collaborated with CDI in its mission to optimize documentation with the aim to have a positive impact on reimbursement and quality metrics while highlighting APP value. In the relatively early stages of the collaboration it became evident that an APP adviser could be an innovative and effective approach in engaging our many APPs with CDI as faculty members who are generally service line based and, as such, invested in hospital and service line outcomes.
A business case for a new position of APP adviser for CDI was formulated based on not only the number of APP faculty and learners at our institution, but also on the premise that the level of consistency APPs provide would increase reliability in the adoption and adaptation of documentation practices as medicine and coding rules evolve. In addition, APP documentation can stand alone without physician attestation or signature, unlike physicians in training, further making them ideally suited collaborators. The position was approved by hospital leadership and the first APP adviser for CDI in the country (of whom we are aware) was hired at UCH in July 2019.
A dedicated APP CDI adviser facilitates the success of a CDI/APP collaboration through a better understanding of APP engagement needs largely by creating new and/or fostering existing relationships between the APP adviser and the APPs for each service line. The APP CDI adviser identifies the needs of the team in order to maximally enhance their documentation while illustrating how the work/collaboration can positively contribute to APP clinical and/or academic goals. The APP CDI adviser possesses a deeper knowledge of APP clinical work flow and how that work flow might be impacting the documentation. He or she utilizes information gathered from the APP team to create more efficient note templates, provide lunch and learns with different service line APPs, and offering 1:1 drop-in documentation support, allowing for more feedback flexibility in context of their clinical work flow.
This real time input may be received more positively and be perceived as less intimidating in the peer-to-peer context. The APP adviser also attends various educational forums to which the physician advisers may not have access. For example, the APP adviser attends monthly APP orientation to meet new APPs for the institution, attends APP council, is a member of the APP steering committee, and provides documentation tips for the APP monthly newsletter.
At this point we are in the process of collecting pre- and post data to illustrate the benefit of a CDI APP adviser (and the CDI APP collaboration as a whole) through metrics such as CC/MCC capture rate, case mix index, and mortality and length of stay as influenced by the level of complexity in documentation. We hope to add APPs as advisers across the UCHealth system over time and to continue to highlight and publish the experience and outcomes related to this innovative role as it evolves such that other institutions across the country will consider this type of collaboration.
Dr. Anoff is associate professor of clinical practice in the division of hospital medicine and medical director of clinical documentation integrity at University of Colorado Health, Denver. Ms. Brill is senior instructor in the department of neurosurgery and APP adviser of clinical documentation integrity at UCHealth Denver Metro.
A novel approach to APP documentation engagement
A novel approach to APP documentation engagement
As hospitals and clinicians, we are facing increased scrutiny of the care we provide to our patients. There is increased demand for more transparency of our outcomes and a need for increased efficiency of the care we provide in the setting of already significant documentation burden and its known impact on provider burnout.
Clinical documentation integrity (CDI) is an instrumental department which supports complete and accurate documentation, serves as a bridge between physicians and hospital coders such that hospital reimbursement is appropriate and quality metrics are attributed appropriately to the hospital, service lines, and individual providers. Complete and accurate documentation also leads to the submission of coded/claims-based data reflecting provider true intent and to clinically valid data for research and patient centric purposes. For this reason, the physician adviser role as a liaison between physicians and CDI and coding, in addition to utilization management and case management, has become more commonplace. The physician adviser role has been a mainstay of CDI programs across the United States since as early as 2012.
At the University of Colorado Health (UCHealth), the physician adviser role first began in 2015 at our major academic medical center, the University of Colorado Hospital (UCH). That physician adviser, after the additional physician adviser FTE at UCH, having established relationships with physicians across service lines, began to focus on CDI-related education and communication as it pertained to inpatient documentation.
At our institution we have approximately 500 advance practice providers (APPs). Approximately two-thirds of the APPs care for inpatients on a myriad of different service lines and, along with physician learners from interns to fellows, complete the bulk of the documentation in the electronic health record.
In early 2018, the UCHealth office of advanced practice collaborated with CDI in its mission to optimize documentation with the aim to have a positive impact on reimbursement and quality metrics while highlighting APP value. In the relatively early stages of the collaboration it became evident that an APP adviser could be an innovative and effective approach in engaging our many APPs with CDI as faculty members who are generally service line based and, as such, invested in hospital and service line outcomes.
A business case for a new position of APP adviser for CDI was formulated based on not only the number of APP faculty and learners at our institution, but also on the premise that the level of consistency APPs provide would increase reliability in the adoption and adaptation of documentation practices as medicine and coding rules evolve. In addition, APP documentation can stand alone without physician attestation or signature, unlike physicians in training, further making them ideally suited collaborators. The position was approved by hospital leadership and the first APP adviser for CDI in the country (of whom we are aware) was hired at UCH in July 2019.
A dedicated APP CDI adviser facilitates the success of a CDI/APP collaboration through a better understanding of APP engagement needs largely by creating new and/or fostering existing relationships between the APP adviser and the APPs for each service line. The APP CDI adviser identifies the needs of the team in order to maximally enhance their documentation while illustrating how the work/collaboration can positively contribute to APP clinical and/or academic goals. The APP CDI adviser possesses a deeper knowledge of APP clinical work flow and how that work flow might be impacting the documentation. He or she utilizes information gathered from the APP team to create more efficient note templates, provide lunch and learns with different service line APPs, and offering 1:1 drop-in documentation support, allowing for more feedback flexibility in context of their clinical work flow.
This real time input may be received more positively and be perceived as less intimidating in the peer-to-peer context. The APP adviser also attends various educational forums to which the physician advisers may not have access. For example, the APP adviser attends monthly APP orientation to meet new APPs for the institution, attends APP council, is a member of the APP steering committee, and provides documentation tips for the APP monthly newsletter.
At this point we are in the process of collecting pre- and post data to illustrate the benefit of a CDI APP adviser (and the CDI APP collaboration as a whole) through metrics such as CC/MCC capture rate, case mix index, and mortality and length of stay as influenced by the level of complexity in documentation. We hope to add APPs as advisers across the UCHealth system over time and to continue to highlight and publish the experience and outcomes related to this innovative role as it evolves such that other institutions across the country will consider this type of collaboration.
Dr. Anoff is associate professor of clinical practice in the division of hospital medicine and medical director of clinical documentation integrity at University of Colorado Health, Denver. Ms. Brill is senior instructor in the department of neurosurgery and APP adviser of clinical documentation integrity at UCHealth Denver Metro.
As hospitals and clinicians, we are facing increased scrutiny of the care we provide to our patients. There is increased demand for more transparency of our outcomes and a need for increased efficiency of the care we provide in the setting of already significant documentation burden and its known impact on provider burnout.
Clinical documentation integrity (CDI) is an instrumental department which supports complete and accurate documentation, serves as a bridge between physicians and hospital coders such that hospital reimbursement is appropriate and quality metrics are attributed appropriately to the hospital, service lines, and individual providers. Complete and accurate documentation also leads to the submission of coded/claims-based data reflecting provider true intent and to clinically valid data for research and patient centric purposes. For this reason, the physician adviser role as a liaison between physicians and CDI and coding, in addition to utilization management and case management, has become more commonplace. The physician adviser role has been a mainstay of CDI programs across the United States since as early as 2012.
At the University of Colorado Health (UCHealth), the physician adviser role first began in 2015 at our major academic medical center, the University of Colorado Hospital (UCH). That physician adviser, after the additional physician adviser FTE at UCH, having established relationships with physicians across service lines, began to focus on CDI-related education and communication as it pertained to inpatient documentation.
At our institution we have approximately 500 advance practice providers (APPs). Approximately two-thirds of the APPs care for inpatients on a myriad of different service lines and, along with physician learners from interns to fellows, complete the bulk of the documentation in the electronic health record.
In early 2018, the UCHealth office of advanced practice collaborated with CDI in its mission to optimize documentation with the aim to have a positive impact on reimbursement and quality metrics while highlighting APP value. In the relatively early stages of the collaboration it became evident that an APP adviser could be an innovative and effective approach in engaging our many APPs with CDI as faculty members who are generally service line based and, as such, invested in hospital and service line outcomes.
A business case for a new position of APP adviser for CDI was formulated based on not only the number of APP faculty and learners at our institution, but also on the premise that the level of consistency APPs provide would increase reliability in the adoption and adaptation of documentation practices as medicine and coding rules evolve. In addition, APP documentation can stand alone without physician attestation or signature, unlike physicians in training, further making them ideally suited collaborators. The position was approved by hospital leadership and the first APP adviser for CDI in the country (of whom we are aware) was hired at UCH in July 2019.
A dedicated APP CDI adviser facilitates the success of a CDI/APP collaboration through a better understanding of APP engagement needs largely by creating new and/or fostering existing relationships between the APP adviser and the APPs for each service line. The APP CDI adviser identifies the needs of the team in order to maximally enhance their documentation while illustrating how the work/collaboration can positively contribute to APP clinical and/or academic goals. The APP CDI adviser possesses a deeper knowledge of APP clinical work flow and how that work flow might be impacting the documentation. He or she utilizes information gathered from the APP team to create more efficient note templates, provide lunch and learns with different service line APPs, and offering 1:1 drop-in documentation support, allowing for more feedback flexibility in context of their clinical work flow.
This real time input may be received more positively and be perceived as less intimidating in the peer-to-peer context. The APP adviser also attends various educational forums to which the physician advisers may not have access. For example, the APP adviser attends monthly APP orientation to meet new APPs for the institution, attends APP council, is a member of the APP steering committee, and provides documentation tips for the APP monthly newsletter.
At this point we are in the process of collecting pre- and post data to illustrate the benefit of a CDI APP adviser (and the CDI APP collaboration as a whole) through metrics such as CC/MCC capture rate, case mix index, and mortality and length of stay as influenced by the level of complexity in documentation. We hope to add APPs as advisers across the UCHealth system over time and to continue to highlight and publish the experience and outcomes related to this innovative role as it evolves such that other institutions across the country will consider this type of collaboration.
Dr. Anoff is associate professor of clinical practice in the division of hospital medicine and medical director of clinical documentation integrity at University of Colorado Health, Denver. Ms. Brill is senior instructor in the department of neurosurgery and APP adviser of clinical documentation integrity at UCHealth Denver Metro.
Aspirin and warfarin together leads to increased bleeding without reducing thrombotic events
Background: Current guidelines recommend against using aspirin in combination with warfarin for patients with AFib, unless the patient has another indication for aspirin such as recent percutaneous coronary intervention (PCI) or a mechanical heart valve. These recommendations are based on limited clinical trial data that showed an increased risk of adverse events with combination therapy without clinical benefit. Despite these recommendations, recent studies have shown that aspirin use without a clinical indication remains common in patients taking warfarin for AFib. The prevalence of aspirin use without a clinical indication in patients taking warfarin for VTE is less well studied.
Study design: Registry-based cohort study.
Setting: Six anticoagulation clinics in Michigan.
Synopsis: Of the 6,539 patients included in the study, 2,453 patients (37.5%) were taking both warfarin and aspirin without an indication for aspirin therapy; 3,688 propensity score–matched patients (1,844 in each group) were compared to assess rates of bleeding and rates of observed thrombosis at 1 year in patients taking warfarin alone versus warfarin plus aspirin. Patients treated with warfarin plus aspirin experienced more bleeding events than did patients on warfarin monotherapy (95% confidence interval, 23.8%-28.3% vs. 95% CI, 18.3%-22.3%; P less than .001). Rates of observed thrombosis were similar between the two groups (95% CI, 1.6%-3.1% vs. 95% CI, 2.0%-3.6%; P = .40). This study demonstrates that aspirin use without a clinical indication remains common in patients taking warfarin for AFib or VTE, and that reducing inappropriate aspirin use in this patient population may help prevent adverse outcomes.
Bottom line: Use of aspirin without a clinical indication in patients taking warfarin is common and is associated with an increased risk of bleeding without significant clinical benefit.
Citation: Schaefer JK et al. Association of adding aspirin to warfarin therapy without an apparent indication with bleeding and other adverse events. JAMA Intern Med. 2019 Mar 4;179(4):533-41.
Dr. Wachter is an associate medical director at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Current guidelines recommend against using aspirin in combination with warfarin for patients with AFib, unless the patient has another indication for aspirin such as recent percutaneous coronary intervention (PCI) or a mechanical heart valve. These recommendations are based on limited clinical trial data that showed an increased risk of adverse events with combination therapy without clinical benefit. Despite these recommendations, recent studies have shown that aspirin use without a clinical indication remains common in patients taking warfarin for AFib. The prevalence of aspirin use without a clinical indication in patients taking warfarin for VTE is less well studied.
Study design: Registry-based cohort study.
Setting: Six anticoagulation clinics in Michigan.
Synopsis: Of the 6,539 patients included in the study, 2,453 patients (37.5%) were taking both warfarin and aspirin without an indication for aspirin therapy; 3,688 propensity score–matched patients (1,844 in each group) were compared to assess rates of bleeding and rates of observed thrombosis at 1 year in patients taking warfarin alone versus warfarin plus aspirin. Patients treated with warfarin plus aspirin experienced more bleeding events than did patients on warfarin monotherapy (95% confidence interval, 23.8%-28.3% vs. 95% CI, 18.3%-22.3%; P less than .001). Rates of observed thrombosis were similar between the two groups (95% CI, 1.6%-3.1% vs. 95% CI, 2.0%-3.6%; P = .40). This study demonstrates that aspirin use without a clinical indication remains common in patients taking warfarin for AFib or VTE, and that reducing inappropriate aspirin use in this patient population may help prevent adverse outcomes.
Bottom line: Use of aspirin without a clinical indication in patients taking warfarin is common and is associated with an increased risk of bleeding without significant clinical benefit.
Citation: Schaefer JK et al. Association of adding aspirin to warfarin therapy without an apparent indication with bleeding and other adverse events. JAMA Intern Med. 2019 Mar 4;179(4):533-41.
Dr. Wachter is an associate medical director at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Current guidelines recommend against using aspirin in combination with warfarin for patients with AFib, unless the patient has another indication for aspirin such as recent percutaneous coronary intervention (PCI) or a mechanical heart valve. These recommendations are based on limited clinical trial data that showed an increased risk of adverse events with combination therapy without clinical benefit. Despite these recommendations, recent studies have shown that aspirin use without a clinical indication remains common in patients taking warfarin for AFib. The prevalence of aspirin use without a clinical indication in patients taking warfarin for VTE is less well studied.
Study design: Registry-based cohort study.
Setting: Six anticoagulation clinics in Michigan.
Synopsis: Of the 6,539 patients included in the study, 2,453 patients (37.5%) were taking both warfarin and aspirin without an indication for aspirin therapy; 3,688 propensity score–matched patients (1,844 in each group) were compared to assess rates of bleeding and rates of observed thrombosis at 1 year in patients taking warfarin alone versus warfarin plus aspirin. Patients treated with warfarin plus aspirin experienced more bleeding events than did patients on warfarin monotherapy (95% confidence interval, 23.8%-28.3% vs. 95% CI, 18.3%-22.3%; P less than .001). Rates of observed thrombosis were similar between the two groups (95% CI, 1.6%-3.1% vs. 95% CI, 2.0%-3.6%; P = .40). This study demonstrates that aspirin use without a clinical indication remains common in patients taking warfarin for AFib or VTE, and that reducing inappropriate aspirin use in this patient population may help prevent adverse outcomes.
Bottom line: Use of aspirin without a clinical indication in patients taking warfarin is common and is associated with an increased risk of bleeding without significant clinical benefit.
Citation: Schaefer JK et al. Association of adding aspirin to warfarin therapy without an apparent indication with bleeding and other adverse events. JAMA Intern Med. 2019 Mar 4;179(4):533-41.
Dr. Wachter is an associate medical director at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Catheter ablation of AFib improves quality of life more than medications do
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
#WhiteCoats4BlackLives: A ‘platform for good’
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
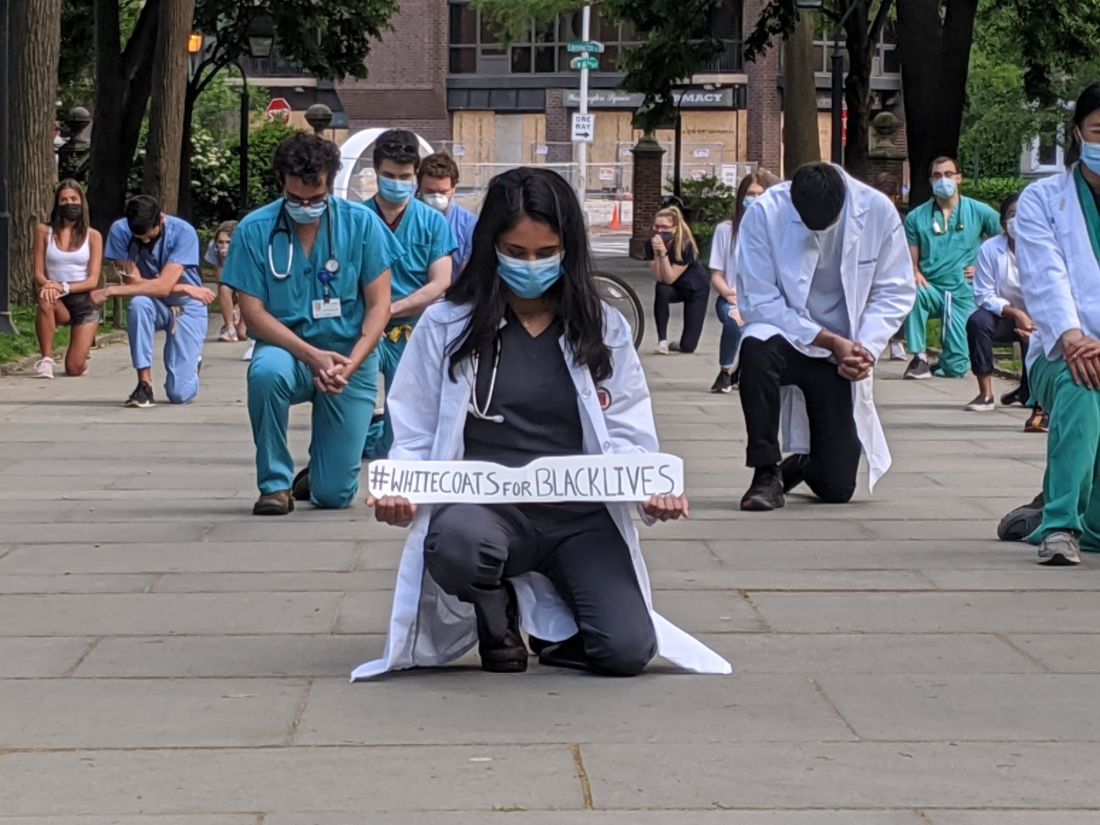
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
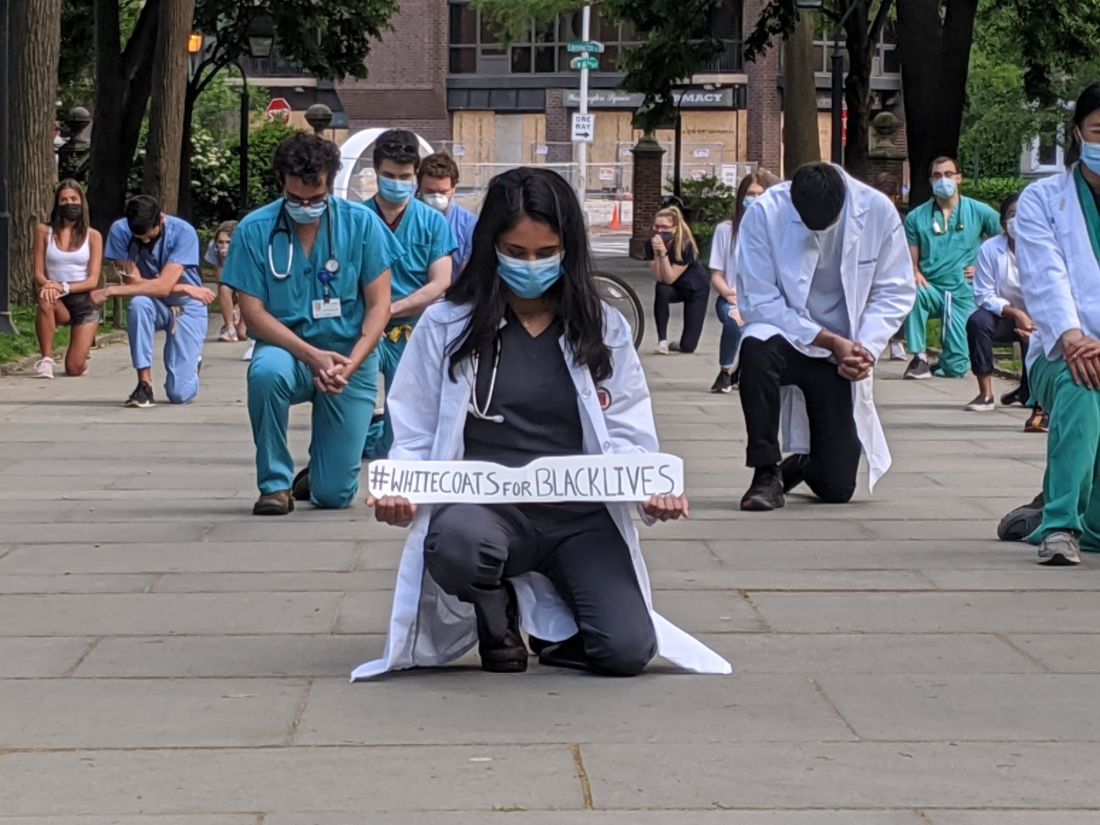
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
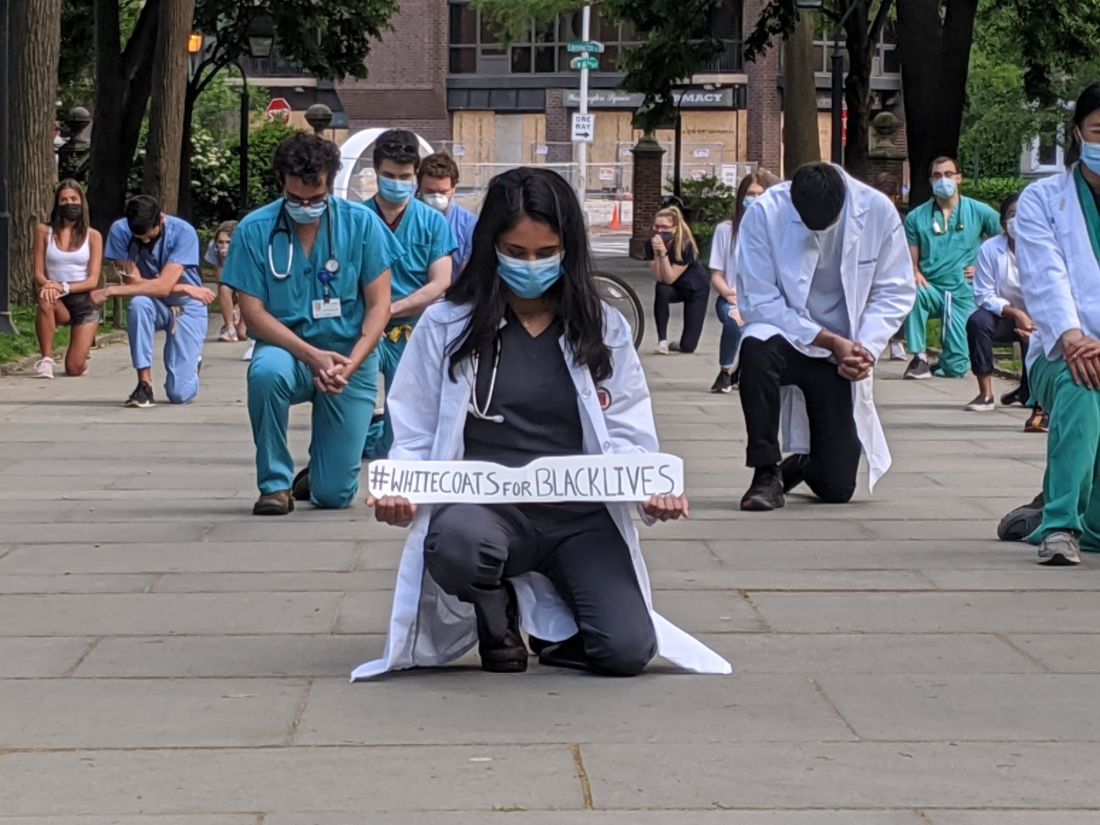
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
QI initiative can decrease unnecessary IV treatment of asymptomatic hypertension
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.