User login
Pride profile: Keshav Khanijow, MD
Keshav Khanijow, MD, is a hospitalist at Northwestern Memorial Hospital and assistant professor at Northwestern University, Chicago. Originally from the San Francisco Bay area, he studied anthropology as an undergrad at Johns Hopkins University, Baltimore, then went to medical school at the University of California, San Francisco, followed by internal medicine residency and a hospital medicine fellowship at Johns Hopkins Bayview Medical Center. He came out as gay in 2006 as an undergrad. He is a founding member of the Society of Hospital Medicine’s LGBTQ+ Task Force and is involved with SHM’s Diversity and Inclusion Special Interest Group.
What challenges have you faced because of your sexual orientation in the different stages of your career, from training to now as a practicing physician?
In my early training, there weren’t a lot of accessible LGBTQ role models to talk about balancing my personal identities with my professional aspirations. Being a double minority as both South Asian and a gay male, made it that much more difficult. “What is it like to work in health care as a gay cismale? Will being out on my personal statement affect my entry into medical school? Should I list my LGBTQ activism activities or not?” Those were important to me.
And did you make your activism known?
Thankfully, I did. I joke that my application might as well have been printed on rainbow paper, if you will. I decided to be out because I wanted to be part of an environment that would accept me for who I was. But it was a difficult decision.
In medical school at UCSF, it’s San Francisco, so they were a little ahead of the game. They had a lot of social networking opportunities with LGBTQ and ally faculty. Those connections were important in helping me explore different fields, and I even got to write my first publication. That said, networking could sometimes be challenging, especially when it came to residency interviews. While many people would talk about family activities and engagements, I’d only been out to my family for a few years. As such, there would be somewhat of a disconnect. On the flip side, there were LGBTQ celebrations and cultural concepts important to me, but I couldn’t always connect on those fronts either.
When it comes to patients, I do have a bit of a higher-pitched voice, and my mannerisms can be gender nonconforming. While it did make me the target of some cruel middle school humor, I’ve come to be proud of myself, mannerisms and all. That said, I have had patients make remarks to me about being gay, whether it be positive or negative. For LGBTQ patients, they’re like, “this is great, I have a gay doctor. They’ll know a bit more about what I’m talking about or be able to relate to the community pressures I face.”
But sometimes homophobic patients can be a bit more cold. I’ve never had anyone say that they don’t want to have me as their physician, but I definitely have patients who disagree with me and say, essentially, “oh well, you don’t know what you’re talking about because you’re gay.” Of course, there have also been comments based on my ethnicity as well.
What specific progress could you point to that you’ve seen over the course of your training and your career so far with regard to LGBTQ health care workers’ experience and LGBTQ patients?
When I was in college, there was a case in 2007 where a woman wasn’t able to see her partner or children before dying in a Florida hospital. Since then, there’s been great strides with a 2011 executive order extending hospital visitation rights to LGBTQ families. In 2013, there was the legalization of same-sex marriage. More recently, in June 2020, the Supreme Court extended protections against workplace discrimination to LGBTQ employees.
But there are certain things that continue to be problems, such as the recent Final Rule from the Department of Health & Human Services that fails to protect our LGBTQ patients and friends against discrimination in health care.
Can you remember a specific episode with a patient who was in the LGBTQ community that was particularly satisfying or moving?
There are two that I think about. In medical school, I was working in a more conservative area of California, and there was a patient who identified as lesbian. She felt more able to talk about her fears of raising a family in a conservative area. She even said, “I feel you can understand the stuff, I can talk to you a bit more about it freely, which is really nice.” Later on, I was able to see them on another rotation I was on, after she’d had a baby with her partner. I was honored that they considered me a part of their family’s journey.
A couple years ago as an attending hospitalist, I had a gay male patient that came in for hepatitis A treatment. Although we typically think of hepatitis A as a foodborne illness, oral-anal sex (rimming) is also a risk factor. After having an open discussion with him about his sexual practices, I said, “it was probably an STI in your case,” and was able to give him guidelines on how to prevent giving it to anyone else during the recovery period. He was very appreciative, and I was glad to have been there for that patient.
What is SHM’s role in regard to improving the care of LGBTQ patients, improving inclusiveness for LGBTQ health professionals?
Continuing to have educational activities, whether it be lectures at the annual conference or online learning modules, will be critical to care for our LGBTQ patients. With regard to membership, we need to make sure that hospitalists feel included and protected. To this end, our Diversity and Inclusion Special Interest Group was working toward having gender-neutral bathrooms and personal pronoun tags for the in-person 2020 annual conference before it was converted to an online format.
Does it ever get tiring for you to work on “social issues” in addition to strictly medical issues?
I will say I definitely experienced a moment in time during residency where I had to take a step back and recenter myself. Sometimes, realizing how much work needs to get done, coupled with the challenges of one’s personal life, can be daunting. That said, I can only stare at a problem so long before needing to work on creating a solution. At the end of the day I didn’t want to run away from these newfound problems of exclusion – I wanted to be a part of the solution.
In my hospital medicine fellowship, I was lucky to have Flora Kisuule, MD, as a mentor who encouraged me to take my prior work with LGBTQ health and leverage it into hospital medicine projects. As such, I was able to combine a topic I was passionate about with my interests in research and teaching so that they work synergistically. After all, the social issues affect our medical histories, just as our medical issues affect our social being. They go hand in hand.
Keshav Khanijow, MD, is a hospitalist at Northwestern Memorial Hospital and assistant professor at Northwestern University, Chicago. Originally from the San Francisco Bay area, he studied anthropology as an undergrad at Johns Hopkins University, Baltimore, then went to medical school at the University of California, San Francisco, followed by internal medicine residency and a hospital medicine fellowship at Johns Hopkins Bayview Medical Center. He came out as gay in 2006 as an undergrad. He is a founding member of the Society of Hospital Medicine’s LGBTQ+ Task Force and is involved with SHM’s Diversity and Inclusion Special Interest Group.
What challenges have you faced because of your sexual orientation in the different stages of your career, from training to now as a practicing physician?
In my early training, there weren’t a lot of accessible LGBTQ role models to talk about balancing my personal identities with my professional aspirations. Being a double minority as both South Asian and a gay male, made it that much more difficult. “What is it like to work in health care as a gay cismale? Will being out on my personal statement affect my entry into medical school? Should I list my LGBTQ activism activities or not?” Those were important to me.
And did you make your activism known?
Thankfully, I did. I joke that my application might as well have been printed on rainbow paper, if you will. I decided to be out because I wanted to be part of an environment that would accept me for who I was. But it was a difficult decision.
In medical school at UCSF, it’s San Francisco, so they were a little ahead of the game. They had a lot of social networking opportunities with LGBTQ and ally faculty. Those connections were important in helping me explore different fields, and I even got to write my first publication. That said, networking could sometimes be challenging, especially when it came to residency interviews. While many people would talk about family activities and engagements, I’d only been out to my family for a few years. As such, there would be somewhat of a disconnect. On the flip side, there were LGBTQ celebrations and cultural concepts important to me, but I couldn’t always connect on those fronts either.
When it comes to patients, I do have a bit of a higher-pitched voice, and my mannerisms can be gender nonconforming. While it did make me the target of some cruel middle school humor, I’ve come to be proud of myself, mannerisms and all. That said, I have had patients make remarks to me about being gay, whether it be positive or negative. For LGBTQ patients, they’re like, “this is great, I have a gay doctor. They’ll know a bit more about what I’m talking about or be able to relate to the community pressures I face.”
But sometimes homophobic patients can be a bit more cold. I’ve never had anyone say that they don’t want to have me as their physician, but I definitely have patients who disagree with me and say, essentially, “oh well, you don’t know what you’re talking about because you’re gay.” Of course, there have also been comments based on my ethnicity as well.
What specific progress could you point to that you’ve seen over the course of your training and your career so far with regard to LGBTQ health care workers’ experience and LGBTQ patients?
When I was in college, there was a case in 2007 where a woman wasn’t able to see her partner or children before dying in a Florida hospital. Since then, there’s been great strides with a 2011 executive order extending hospital visitation rights to LGBTQ families. In 2013, there was the legalization of same-sex marriage. More recently, in June 2020, the Supreme Court extended protections against workplace discrimination to LGBTQ employees.
But there are certain things that continue to be problems, such as the recent Final Rule from the Department of Health & Human Services that fails to protect our LGBTQ patients and friends against discrimination in health care.
Can you remember a specific episode with a patient who was in the LGBTQ community that was particularly satisfying or moving?
There are two that I think about. In medical school, I was working in a more conservative area of California, and there was a patient who identified as lesbian. She felt more able to talk about her fears of raising a family in a conservative area. She even said, “I feel you can understand the stuff, I can talk to you a bit more about it freely, which is really nice.” Later on, I was able to see them on another rotation I was on, after she’d had a baby with her partner. I was honored that they considered me a part of their family’s journey.
A couple years ago as an attending hospitalist, I had a gay male patient that came in for hepatitis A treatment. Although we typically think of hepatitis A as a foodborne illness, oral-anal sex (rimming) is also a risk factor. After having an open discussion with him about his sexual practices, I said, “it was probably an STI in your case,” and was able to give him guidelines on how to prevent giving it to anyone else during the recovery period. He was very appreciative, and I was glad to have been there for that patient.
What is SHM’s role in regard to improving the care of LGBTQ patients, improving inclusiveness for LGBTQ health professionals?
Continuing to have educational activities, whether it be lectures at the annual conference or online learning modules, will be critical to care for our LGBTQ patients. With regard to membership, we need to make sure that hospitalists feel included and protected. To this end, our Diversity and Inclusion Special Interest Group was working toward having gender-neutral bathrooms and personal pronoun tags for the in-person 2020 annual conference before it was converted to an online format.
Does it ever get tiring for you to work on “social issues” in addition to strictly medical issues?
I will say I definitely experienced a moment in time during residency where I had to take a step back and recenter myself. Sometimes, realizing how much work needs to get done, coupled with the challenges of one’s personal life, can be daunting. That said, I can only stare at a problem so long before needing to work on creating a solution. At the end of the day I didn’t want to run away from these newfound problems of exclusion – I wanted to be a part of the solution.
In my hospital medicine fellowship, I was lucky to have Flora Kisuule, MD, as a mentor who encouraged me to take my prior work with LGBTQ health and leverage it into hospital medicine projects. As such, I was able to combine a topic I was passionate about with my interests in research and teaching so that they work synergistically. After all, the social issues affect our medical histories, just as our medical issues affect our social being. They go hand in hand.
Keshav Khanijow, MD, is a hospitalist at Northwestern Memorial Hospital and assistant professor at Northwestern University, Chicago. Originally from the San Francisco Bay area, he studied anthropology as an undergrad at Johns Hopkins University, Baltimore, then went to medical school at the University of California, San Francisco, followed by internal medicine residency and a hospital medicine fellowship at Johns Hopkins Bayview Medical Center. He came out as gay in 2006 as an undergrad. He is a founding member of the Society of Hospital Medicine’s LGBTQ+ Task Force and is involved with SHM’s Diversity and Inclusion Special Interest Group.
What challenges have you faced because of your sexual orientation in the different stages of your career, from training to now as a practicing physician?
In my early training, there weren’t a lot of accessible LGBTQ role models to talk about balancing my personal identities with my professional aspirations. Being a double minority as both South Asian and a gay male, made it that much more difficult. “What is it like to work in health care as a gay cismale? Will being out on my personal statement affect my entry into medical school? Should I list my LGBTQ activism activities or not?” Those were important to me.
And did you make your activism known?
Thankfully, I did. I joke that my application might as well have been printed on rainbow paper, if you will. I decided to be out because I wanted to be part of an environment that would accept me for who I was. But it was a difficult decision.
In medical school at UCSF, it’s San Francisco, so they were a little ahead of the game. They had a lot of social networking opportunities with LGBTQ and ally faculty. Those connections were important in helping me explore different fields, and I even got to write my first publication. That said, networking could sometimes be challenging, especially when it came to residency interviews. While many people would talk about family activities and engagements, I’d only been out to my family for a few years. As such, there would be somewhat of a disconnect. On the flip side, there were LGBTQ celebrations and cultural concepts important to me, but I couldn’t always connect on those fronts either.
When it comes to patients, I do have a bit of a higher-pitched voice, and my mannerisms can be gender nonconforming. While it did make me the target of some cruel middle school humor, I’ve come to be proud of myself, mannerisms and all. That said, I have had patients make remarks to me about being gay, whether it be positive or negative. For LGBTQ patients, they’re like, “this is great, I have a gay doctor. They’ll know a bit more about what I’m talking about or be able to relate to the community pressures I face.”
But sometimes homophobic patients can be a bit more cold. I’ve never had anyone say that they don’t want to have me as their physician, but I definitely have patients who disagree with me and say, essentially, “oh well, you don’t know what you’re talking about because you’re gay.” Of course, there have also been comments based on my ethnicity as well.
What specific progress could you point to that you’ve seen over the course of your training and your career so far with regard to LGBTQ health care workers’ experience and LGBTQ patients?
When I was in college, there was a case in 2007 where a woman wasn’t able to see her partner or children before dying in a Florida hospital. Since then, there’s been great strides with a 2011 executive order extending hospital visitation rights to LGBTQ families. In 2013, there was the legalization of same-sex marriage. More recently, in June 2020, the Supreme Court extended protections against workplace discrimination to LGBTQ employees.
But there are certain things that continue to be problems, such as the recent Final Rule from the Department of Health & Human Services that fails to protect our LGBTQ patients and friends against discrimination in health care.
Can you remember a specific episode with a patient who was in the LGBTQ community that was particularly satisfying or moving?
There are two that I think about. In medical school, I was working in a more conservative area of California, and there was a patient who identified as lesbian. She felt more able to talk about her fears of raising a family in a conservative area. She even said, “I feel you can understand the stuff, I can talk to you a bit more about it freely, which is really nice.” Later on, I was able to see them on another rotation I was on, after she’d had a baby with her partner. I was honored that they considered me a part of their family’s journey.
A couple years ago as an attending hospitalist, I had a gay male patient that came in for hepatitis A treatment. Although we typically think of hepatitis A as a foodborne illness, oral-anal sex (rimming) is also a risk factor. After having an open discussion with him about his sexual practices, I said, “it was probably an STI in your case,” and was able to give him guidelines on how to prevent giving it to anyone else during the recovery period. He was very appreciative, and I was glad to have been there for that patient.
What is SHM’s role in regard to improving the care of LGBTQ patients, improving inclusiveness for LGBTQ health professionals?
Continuing to have educational activities, whether it be lectures at the annual conference or online learning modules, will be critical to care for our LGBTQ patients. With regard to membership, we need to make sure that hospitalists feel included and protected. To this end, our Diversity and Inclusion Special Interest Group was working toward having gender-neutral bathrooms and personal pronoun tags for the in-person 2020 annual conference before it was converted to an online format.
Does it ever get tiring for you to work on “social issues” in addition to strictly medical issues?
I will say I definitely experienced a moment in time during residency where I had to take a step back and recenter myself. Sometimes, realizing how much work needs to get done, coupled with the challenges of one’s personal life, can be daunting. That said, I can only stare at a problem so long before needing to work on creating a solution. At the end of the day I didn’t want to run away from these newfound problems of exclusion – I wanted to be a part of the solution.
In my hospital medicine fellowship, I was lucky to have Flora Kisuule, MD, as a mentor who encouraged me to take my prior work with LGBTQ health and leverage it into hospital medicine projects. As such, I was able to combine a topic I was passionate about with my interests in research and teaching so that they work synergistically. After all, the social issues affect our medical histories, just as our medical issues affect our social being. They go hand in hand.
Treatment developments in obstructive hypertrophic cardiomyopathy (oHCM)
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Manage the pandemic with a multidisciplinary coalition
Implement a 6-P framework
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.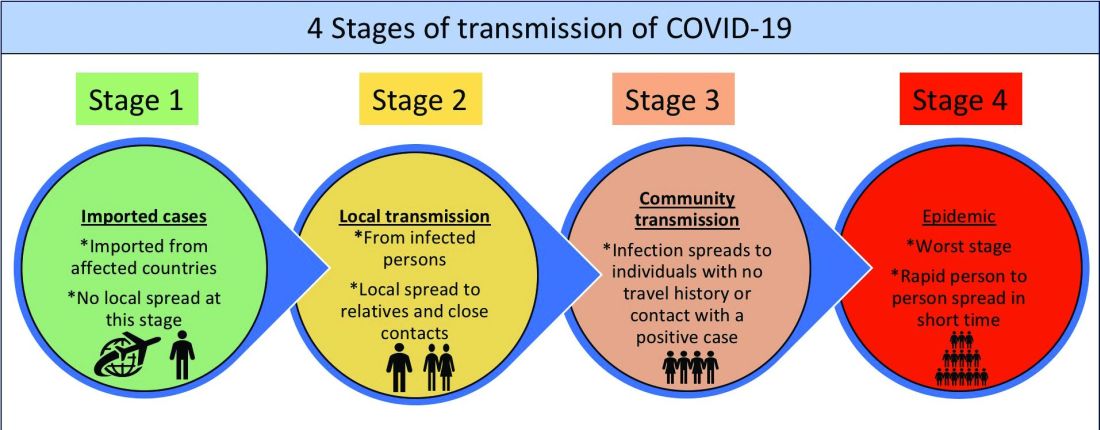
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
Implement a 6-P framework
Implement a 6-P framework
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.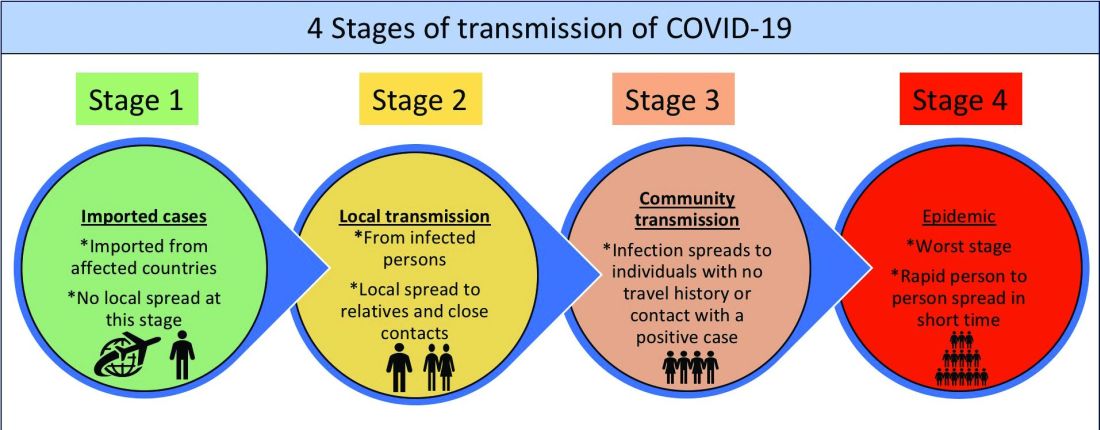
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.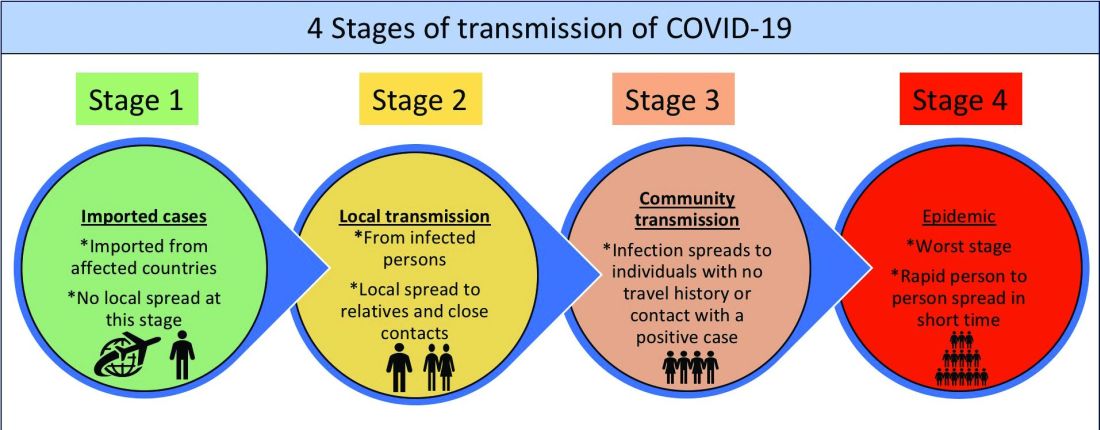
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
Suboptimal statin response predicts future risk
Background: Rates of LDL-C reduction with statin therapy vary based on biological and genetic factors, as well as adherence. In a general primary prevention population at cardiovascular risk, little is known about the extent of this variability or its impact on outcomes.
Study design: Prospective cohort study.
Setting: Primary care practices in England and Wales.
Synopsis: Across a cohort of 183,213 patients, 51.2% had a suboptimal response, defined as a less than 40% proportional reduction in LDL-C. During more than 1 million person-years of follow-up, suboptimal statin response at 2 years was associated with a 20% higher hazard ratio for incident cardiovascular disease.Bottom line: Half of patients do not have a sufficient response to statins, with higher attendant future risk.
Citation: Akyea RK et al. Suboptimal cholesterol response to initiation of statins and future risk of cardiovascular disease. Heart. 2019 Apr 15;0:1-7. doi: 10.1136/heartjnl-2018-314253.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
Background: Rates of LDL-C reduction with statin therapy vary based on biological and genetic factors, as well as adherence. In a general primary prevention population at cardiovascular risk, little is known about the extent of this variability or its impact on outcomes.
Study design: Prospective cohort study.
Setting: Primary care practices in England and Wales.
Synopsis: Across a cohort of 183,213 patients, 51.2% had a suboptimal response, defined as a less than 40% proportional reduction in LDL-C. During more than 1 million person-years of follow-up, suboptimal statin response at 2 years was associated with a 20% higher hazard ratio for incident cardiovascular disease.Bottom line: Half of patients do not have a sufficient response to statins, with higher attendant future risk.
Citation: Akyea RK et al. Suboptimal cholesterol response to initiation of statins and future risk of cardiovascular disease. Heart. 2019 Apr 15;0:1-7. doi: 10.1136/heartjnl-2018-314253.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
Background: Rates of LDL-C reduction with statin therapy vary based on biological and genetic factors, as well as adherence. In a general primary prevention population at cardiovascular risk, little is known about the extent of this variability or its impact on outcomes.
Study design: Prospective cohort study.
Setting: Primary care practices in England and Wales.
Synopsis: Across a cohort of 183,213 patients, 51.2% had a suboptimal response, defined as a less than 40% proportional reduction in LDL-C. During more than 1 million person-years of follow-up, suboptimal statin response at 2 years was associated with a 20% higher hazard ratio for incident cardiovascular disease.Bottom line: Half of patients do not have a sufficient response to statins, with higher attendant future risk.
Citation: Akyea RK et al. Suboptimal cholesterol response to initiation of statins and future risk of cardiovascular disease. Heart. 2019 Apr 15;0:1-7. doi: 10.1136/heartjnl-2018-314253.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
PAP use associated with lower mortality
Background: OSA is a key modifiable risk factor for adverse cardiovascular outcomes and is increasingly prevalent in older populations. PAP improves OSA severity, increases oxygenation, and reduces daytime sleepiness. Its effect on major adverse cardiovascular outcomes remains uncertain.
Study design: Retrospective cohort study of the Sleep Heart Health Study.
Setting: Nine existing U.S. epidemiologic studies.
Synopsis: Of the 392 patients analyzed, 81 were prescribed PAP and 311 were not. Investigators controlled for OSA severity, history of stroke or MI, hypertension, diabetes, weight, smoking, and alcohol intake. The adjusted hazard ratio for death at mean 11 years was 42% lower for those prescribed PAP.
Bottom line: PAP markedly lowers mortality in OSA, with survival curves separating at 6-7 years.
Citation: Lisan Q et al. Association of positive airway pressure prescription with mortality in patients with obesity and severe obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2019 Apr 11. doi: 10.1001/jamaoto.2019.0281.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
Background: OSA is a key modifiable risk factor for adverse cardiovascular outcomes and is increasingly prevalent in older populations. PAP improves OSA severity, increases oxygenation, and reduces daytime sleepiness. Its effect on major adverse cardiovascular outcomes remains uncertain.
Study design: Retrospective cohort study of the Sleep Heart Health Study.
Setting: Nine existing U.S. epidemiologic studies.
Synopsis: Of the 392 patients analyzed, 81 were prescribed PAP and 311 were not. Investigators controlled for OSA severity, history of stroke or MI, hypertension, diabetes, weight, smoking, and alcohol intake. The adjusted hazard ratio for death at mean 11 years was 42% lower for those prescribed PAP.
Bottom line: PAP markedly lowers mortality in OSA, with survival curves separating at 6-7 years.
Citation: Lisan Q et al. Association of positive airway pressure prescription with mortality in patients with obesity and severe obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2019 Apr 11. doi: 10.1001/jamaoto.2019.0281.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
Background: OSA is a key modifiable risk factor for adverse cardiovascular outcomes and is increasingly prevalent in older populations. PAP improves OSA severity, increases oxygenation, and reduces daytime sleepiness. Its effect on major adverse cardiovascular outcomes remains uncertain.
Study design: Retrospective cohort study of the Sleep Heart Health Study.
Setting: Nine existing U.S. epidemiologic studies.
Synopsis: Of the 392 patients analyzed, 81 were prescribed PAP and 311 were not. Investigators controlled for OSA severity, history of stroke or MI, hypertension, diabetes, weight, smoking, and alcohol intake. The adjusted hazard ratio for death at mean 11 years was 42% lower for those prescribed PAP.
Bottom line: PAP markedly lowers mortality in OSA, with survival curves separating at 6-7 years.
Citation: Lisan Q et al. Association of positive airway pressure prescription with mortality in patients with obesity and severe obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2019 Apr 11. doi: 10.1001/jamaoto.2019.0281.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
SHM responds to racism in the United States
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
What COVID-19 has taught us about senior care
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at [email protected]. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at [email protected].
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at [email protected]. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at [email protected].
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at [email protected]. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at [email protected].
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
Farewell to Larry Wellikson, MD, MHM
SHM cofounders praise the Society’s outgoing CEO
Setting the table for over 2 decades
I first met Larry in the spring of 1998 after I had made a presentation to the American College of Physicians’ Board of Regents on the Society for Hospital Medicine’s (then the National Association of Inpatient Physicians) new position statement that referral to hospitalists by primary care physicians should be voluntary. At the time, a number of managed care companies around the United States were compelling primary care physicians to use hospitalists to care for their hospitalized patients apparently because they felt hospitalists could do it more efficiently. SHM became the first professional society to voice the position which in turn was broadly endorsed by physician organizations, including the American Medical Association and the ACP.
Larry sought me out, engaged with me, and handed me his business card. He seemed keen on becoming a part of the rapidly accelerating hospitalist movement and, in retrospect, putting his signature on it. He had recently built and exited from a very large and successful independent physician association during the heyday of California managed care and was eager for a new challenge.
Unlike me, who was just a few years out of residency, Larry was at the height of his professional powers, with the right blend of experience on the one hand and energy on the other to take on a project like SHM.
Larry’s first contribution came in the form of facilitating a 2-day strategic planning meeting with the SHM board in the fall of 1998. John Nelson, MD, had moved to Philadelphia for 3 months to establish the operational foundation of SHM and guide SHM’s first staff member, Angela Musial. One of the most notable achievements during that time was a strategic planning board meeting, which largely set the course for SHM’s early years. Larry was a taskmaster, forcing us to make tough choices about what we wanted to accomplish and to establish concrete goals with timelines and milestones. The adult supervision Larry brought was a new and vital thing for us.
There was a lot at stake in ’97, ‘98, and ‘99. The demand for hospitalists across the nation was skyrocketing and there was a strong need for leadership and bold direction. Academics, community-based hospitalists, pediatricians, entrepreneurs, nonphysician hospital team members, heads of organized medicine, and government and industry leaders were just some of the key stakeholders looking for a seat at the HM table. That table would go on to be set for some 2 decades by Larry Wellikson.
From the beginning, many observers remarked that SHM had established an aggressive agenda. There was an unrelenting need to erect a big tent as a home for diverse stakeholders. John and I and the SHM board were doing all we could to continue to build momentum while also leading our local hospitalist groups and trying to maintain a semblance of balance with our young families back home.
It was against this backdrop, in late 1999, while on yet another flight crisscrossing the country to promote HM and SHM, that John; Bob Wachter, MD (who had by that time replaced John and I as SHM president); and I decided we needed a full-time CEO. By that time, each of us had participated in conversations with Larry. We rapidly decided, with buy-in from the board, that we would offer Larry the position. He accepted and became CEO in January 2000.
To list here all of Larry’s accomplishments since taking the helm at SHM would be impossible. Indeed, all that SHM has achieved is closely tied to Larry. Instead, I would like to call out character traits Larry brought to SHM that are now part of SHM’s DNA and a large part of the reason SHM has been so successful over the past 20 years.
Solution oriented. SHM’s culture has always been to take conditions as they are and work to make things better. There is no place for excessively airing grievances and complaining about “what is being done to us.”
Eschewing the status quo. We can do better. There is too much that needs to be done to wait.
Appropriately irreverent of the norms of the medical establishment. Physicians are by nature careful, plodding, considered, cautious, and methodical. The velocity of change in HM called for a different approach in order to be relevant, one better characterized as the move-fast-and-break-things ethos of a Silicon Valley startup.
Bringing diverse stakeholders to the table. A signature move has been to assemble influential people to lay out the issues before setting a course of action.
Strong bias to action. There is a time to analyze and discuss, but all of this ultimately is in service of taking action to achieve a tangible result.
Working to achieve consensus to a point, then moving forward. Considerable resources have been put into bringing stakeholders together, studying problems, and gaining a common understanding of issues. But this has never been at the expense of taking bold action, even if controversial at times.
Involving industry in creative ways to the benefit of patients. SHM pioneered an approach to use resources gained through industry partnerships to perform national scale improvement activities with groups of hospitalist mentor-experts working with local teams to make care more reliable for patients.
Tirelessly connecting to frontline hospitalists. The lifeblood of SHM is frontline hospitalists. Larry has taken the time to develop relationships with as many as possible, often through personally visiting their communities.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of SHM.
Dynamism
By John Nelson, MD, MHM
You probably know a few people with a magnetic personality. Larry Wellikson is the neodymium variety. Boundless energy, confidence that he has the answer or knows exactly where to find it, and ability to instantly recall every conversation he’s had with you, are traits that have energized his years leading SHM and have led countless people to regard him as friend and mentor.
Watch him at the SHM annual conference. There he goes, fast walking to his next commitment while facing backward to complete from a growing distance the conversation with a person he just bumped into along the way. It is like this for Larry from 6 a.m. until midnight. Like Alexander Hamilton, “the man is nonstop.”
Bill Campbell was the “Trillion Dollar Coach” who had his own success as a business leader, but is best known for mentoring Steve Jobs, the Google founders, and many others who went on to become titans of tech. Larry is hospital medicine’s “Coach,” and has inspired and guided the careers of so many clinicians, administrators, and entrepreneurs in hospital medicine and health care more broadly.
The biggest difference between these two highly effective leaders and mentors might be money; SHM has paid him pretty well, but alas, no stock options.
Larry is a great storyteller, and it doesn’t take long for a conversation with him to arrive at the point where he cites the example of how issues faced by someone else have parallels to your situation, the advice he gave that person, and how things turned out. Mostly this advice is about navigating professional life, but he is also happy to share wisdom about parenting, marriage, money, and sports. And most any other topic.
Larry was very accomplished even prior to connecting with SHM. He had a thriving clinical career, and though he left practice long ago he has maintained a close connection with many people he first met when they were his patients. I was surprised years ago when he drove up a new top-of-the-line Lexus – the two-seater with the solid convertible roof that folded into the trunk with the push of a button. I expressed surprise that he’d buy such a swanky car and he explained that a former patient, now long-time friend, was a Lexus distributor and arranged for Larry to drive it away for something like the cost of a Camry.
He also had terrific success forming and leading a large California independent physician association prior to connecting with SHM. Just ask him to show you the magazine with him on the cover and a glowing article detailing his accomplishments. Seriously, ask him, there’s a good chance he’ll have a copy with him.
When Dr. Win Whitcomb and I were trying to figure out how to start a new medical society and position our field to mature into a real specialty we were lucky enough to connect with many health care leaders who we thought could help. Most tended to pat us on the shoulder and say something along the lines of “good luck with your little hobby, now I have to get back to my important work.” But here was Larry with his impressive resume, having served as one of the leaders who crafted the merger of two giant medical societies (ACP and the American Society of Internal Medicine), keenly interested in our tiny new organization, and excited to serve as facilitator for our first strategic planning session.
SHM got a turbocharger when Larry signed on. For me it has felt like speeding down a highway, top down, radio blasting great music, and happy anticipation of what is around the next corner. I have never been disappointed, and certainly don’t plan to get out of Larry’s car just because he’s retiring as CEO.
Dr. Nelson is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants in La Quinta, Calif.
SHM cofounders praise the Society’s outgoing CEO
SHM cofounders praise the Society’s outgoing CEO
Setting the table for over 2 decades
I first met Larry in the spring of 1998 after I had made a presentation to the American College of Physicians’ Board of Regents on the Society for Hospital Medicine’s (then the National Association of Inpatient Physicians) new position statement that referral to hospitalists by primary care physicians should be voluntary. At the time, a number of managed care companies around the United States were compelling primary care physicians to use hospitalists to care for their hospitalized patients apparently because they felt hospitalists could do it more efficiently. SHM became the first professional society to voice the position which in turn was broadly endorsed by physician organizations, including the American Medical Association and the ACP.
Larry sought me out, engaged with me, and handed me his business card. He seemed keen on becoming a part of the rapidly accelerating hospitalist movement and, in retrospect, putting his signature on it. He had recently built and exited from a very large and successful independent physician association during the heyday of California managed care and was eager for a new challenge.
Unlike me, who was just a few years out of residency, Larry was at the height of his professional powers, with the right blend of experience on the one hand and energy on the other to take on a project like SHM.
Larry’s first contribution came in the form of facilitating a 2-day strategic planning meeting with the SHM board in the fall of 1998. John Nelson, MD, had moved to Philadelphia for 3 months to establish the operational foundation of SHM and guide SHM’s first staff member, Angela Musial. One of the most notable achievements during that time was a strategic planning board meeting, which largely set the course for SHM’s early years. Larry was a taskmaster, forcing us to make tough choices about what we wanted to accomplish and to establish concrete goals with timelines and milestones. The adult supervision Larry brought was a new and vital thing for us.
There was a lot at stake in ’97, ‘98, and ‘99. The demand for hospitalists across the nation was skyrocketing and there was a strong need for leadership and bold direction. Academics, community-based hospitalists, pediatricians, entrepreneurs, nonphysician hospital team members, heads of organized medicine, and government and industry leaders were just some of the key stakeholders looking for a seat at the HM table. That table would go on to be set for some 2 decades by Larry Wellikson.
From the beginning, many observers remarked that SHM had established an aggressive agenda. There was an unrelenting need to erect a big tent as a home for diverse stakeholders. John and I and the SHM board were doing all we could to continue to build momentum while also leading our local hospitalist groups and trying to maintain a semblance of balance with our young families back home.
It was against this backdrop, in late 1999, while on yet another flight crisscrossing the country to promote HM and SHM, that John; Bob Wachter, MD (who had by that time replaced John and I as SHM president); and I decided we needed a full-time CEO. By that time, each of us had participated in conversations with Larry. We rapidly decided, with buy-in from the board, that we would offer Larry the position. He accepted and became CEO in January 2000.
To list here all of Larry’s accomplishments since taking the helm at SHM would be impossible. Indeed, all that SHM has achieved is closely tied to Larry. Instead, I would like to call out character traits Larry brought to SHM that are now part of SHM’s DNA and a large part of the reason SHM has been so successful over the past 20 years.
Solution oriented. SHM’s culture has always been to take conditions as they are and work to make things better. There is no place for excessively airing grievances and complaining about “what is being done to us.”
Eschewing the status quo. We can do better. There is too much that needs to be done to wait.
Appropriately irreverent of the norms of the medical establishment. Physicians are by nature careful, plodding, considered, cautious, and methodical. The velocity of change in HM called for a different approach in order to be relevant, one better characterized as the move-fast-and-break-things ethos of a Silicon Valley startup.
Bringing diverse stakeholders to the table. A signature move has been to assemble influential people to lay out the issues before setting a course of action.
Strong bias to action. There is a time to analyze and discuss, but all of this ultimately is in service of taking action to achieve a tangible result.
Working to achieve consensus to a point, then moving forward. Considerable resources have been put into bringing stakeholders together, studying problems, and gaining a common understanding of issues. But this has never been at the expense of taking bold action, even if controversial at times.
Involving industry in creative ways to the benefit of patients. SHM pioneered an approach to use resources gained through industry partnerships to perform national scale improvement activities with groups of hospitalist mentor-experts working with local teams to make care more reliable for patients.
Tirelessly connecting to frontline hospitalists. The lifeblood of SHM is frontline hospitalists. Larry has taken the time to develop relationships with as many as possible, often through personally visiting their communities.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of SHM.
Dynamism
By John Nelson, MD, MHM
You probably know a few people with a magnetic personality. Larry Wellikson is the neodymium variety. Boundless energy, confidence that he has the answer or knows exactly where to find it, and ability to instantly recall every conversation he’s had with you, are traits that have energized his years leading SHM and have led countless people to regard him as friend and mentor.
Watch him at the SHM annual conference. There he goes, fast walking to his next commitment while facing backward to complete from a growing distance the conversation with a person he just bumped into along the way. It is like this for Larry from 6 a.m. until midnight. Like Alexander Hamilton, “the man is nonstop.”
Bill Campbell was the “Trillion Dollar Coach” who had his own success as a business leader, but is best known for mentoring Steve Jobs, the Google founders, and many others who went on to become titans of tech. Larry is hospital medicine’s “Coach,” and has inspired and guided the careers of so many clinicians, administrators, and entrepreneurs in hospital medicine and health care more broadly.
The biggest difference between these two highly effective leaders and mentors might be money; SHM has paid him pretty well, but alas, no stock options.
Larry is a great storyteller, and it doesn’t take long for a conversation with him to arrive at the point where he cites the example of how issues faced by someone else have parallels to your situation, the advice he gave that person, and how things turned out. Mostly this advice is about navigating professional life, but he is also happy to share wisdom about parenting, marriage, money, and sports. And most any other topic.
Larry was very accomplished even prior to connecting with SHM. He had a thriving clinical career, and though he left practice long ago he has maintained a close connection with many people he first met when they were his patients. I was surprised years ago when he drove up a new top-of-the-line Lexus – the two-seater with the solid convertible roof that folded into the trunk with the push of a button. I expressed surprise that he’d buy such a swanky car and he explained that a former patient, now long-time friend, was a Lexus distributor and arranged for Larry to drive it away for something like the cost of a Camry.
He also had terrific success forming and leading a large California independent physician association prior to connecting with SHM. Just ask him to show you the magazine with him on the cover and a glowing article detailing his accomplishments. Seriously, ask him, there’s a good chance he’ll have a copy with him.
When Dr. Win Whitcomb and I were trying to figure out how to start a new medical society and position our field to mature into a real specialty we were lucky enough to connect with many health care leaders who we thought could help. Most tended to pat us on the shoulder and say something along the lines of “good luck with your little hobby, now I have to get back to my important work.” But here was Larry with his impressive resume, having served as one of the leaders who crafted the merger of two giant medical societies (ACP and the American Society of Internal Medicine), keenly interested in our tiny new organization, and excited to serve as facilitator for our first strategic planning session.
SHM got a turbocharger when Larry signed on. For me it has felt like speeding down a highway, top down, radio blasting great music, and happy anticipation of what is around the next corner. I have never been disappointed, and certainly don’t plan to get out of Larry’s car just because he’s retiring as CEO.
Dr. Nelson is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants in La Quinta, Calif.
Setting the table for over 2 decades
I first met Larry in the spring of 1998 after I had made a presentation to the American College of Physicians’ Board of Regents on the Society for Hospital Medicine’s (then the National Association of Inpatient Physicians) new position statement that referral to hospitalists by primary care physicians should be voluntary. At the time, a number of managed care companies around the United States were compelling primary care physicians to use hospitalists to care for their hospitalized patients apparently because they felt hospitalists could do it more efficiently. SHM became the first professional society to voice the position which in turn was broadly endorsed by physician organizations, including the American Medical Association and the ACP.
Larry sought me out, engaged with me, and handed me his business card. He seemed keen on becoming a part of the rapidly accelerating hospitalist movement and, in retrospect, putting his signature on it. He had recently built and exited from a very large and successful independent physician association during the heyday of California managed care and was eager for a new challenge.
Unlike me, who was just a few years out of residency, Larry was at the height of his professional powers, with the right blend of experience on the one hand and energy on the other to take on a project like SHM.
Larry’s first contribution came in the form of facilitating a 2-day strategic planning meeting with the SHM board in the fall of 1998. John Nelson, MD, had moved to Philadelphia for 3 months to establish the operational foundation of SHM and guide SHM’s first staff member, Angela Musial. One of the most notable achievements during that time was a strategic planning board meeting, which largely set the course for SHM’s early years. Larry was a taskmaster, forcing us to make tough choices about what we wanted to accomplish and to establish concrete goals with timelines and milestones. The adult supervision Larry brought was a new and vital thing for us.
There was a lot at stake in ’97, ‘98, and ‘99. The demand for hospitalists across the nation was skyrocketing and there was a strong need for leadership and bold direction. Academics, community-based hospitalists, pediatricians, entrepreneurs, nonphysician hospital team members, heads of organized medicine, and government and industry leaders were just some of the key stakeholders looking for a seat at the HM table. That table would go on to be set for some 2 decades by Larry Wellikson.
From the beginning, many observers remarked that SHM had established an aggressive agenda. There was an unrelenting need to erect a big tent as a home for diverse stakeholders. John and I and the SHM board were doing all we could to continue to build momentum while also leading our local hospitalist groups and trying to maintain a semblance of balance with our young families back home.
It was against this backdrop, in late 1999, while on yet another flight crisscrossing the country to promote HM and SHM, that John; Bob Wachter, MD (who had by that time replaced John and I as SHM president); and I decided we needed a full-time CEO. By that time, each of us had participated in conversations with Larry. We rapidly decided, with buy-in from the board, that we would offer Larry the position. He accepted and became CEO in January 2000.
To list here all of Larry’s accomplishments since taking the helm at SHM would be impossible. Indeed, all that SHM has achieved is closely tied to Larry. Instead, I would like to call out character traits Larry brought to SHM that are now part of SHM’s DNA and a large part of the reason SHM has been so successful over the past 20 years.
Solution oriented. SHM’s culture has always been to take conditions as they are and work to make things better. There is no place for excessively airing grievances and complaining about “what is being done to us.”
Eschewing the status quo. We can do better. There is too much that needs to be done to wait.
Appropriately irreverent of the norms of the medical establishment. Physicians are by nature careful, plodding, considered, cautious, and methodical. The velocity of change in HM called for a different approach in order to be relevant, one better characterized as the move-fast-and-break-things ethos of a Silicon Valley startup.
Bringing diverse stakeholders to the table. A signature move has been to assemble influential people to lay out the issues before setting a course of action.
Strong bias to action. There is a time to analyze and discuss, but all of this ultimately is in service of taking action to achieve a tangible result.
Working to achieve consensus to a point, then moving forward. Considerable resources have been put into bringing stakeholders together, studying problems, and gaining a common understanding of issues. But this has never been at the expense of taking bold action, even if controversial at times.
Involving industry in creative ways to the benefit of patients. SHM pioneered an approach to use resources gained through industry partnerships to perform national scale improvement activities with groups of hospitalist mentor-experts working with local teams to make care more reliable for patients.
Tirelessly connecting to frontline hospitalists. The lifeblood of SHM is frontline hospitalists. Larry has taken the time to develop relationships with as many as possible, often through personally visiting their communities.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of SHM.
Dynamism
By John Nelson, MD, MHM
You probably know a few people with a magnetic personality. Larry Wellikson is the neodymium variety. Boundless energy, confidence that he has the answer or knows exactly where to find it, and ability to instantly recall every conversation he’s had with you, are traits that have energized his years leading SHM and have led countless people to regard him as friend and mentor.
Watch him at the SHM annual conference. There he goes, fast walking to his next commitment while facing backward to complete from a growing distance the conversation with a person he just bumped into along the way. It is like this for Larry from 6 a.m. until midnight. Like Alexander Hamilton, “the man is nonstop.”
Bill Campbell was the “Trillion Dollar Coach” who had his own success as a business leader, but is best known for mentoring Steve Jobs, the Google founders, and many others who went on to become titans of tech. Larry is hospital medicine’s “Coach,” and has inspired and guided the careers of so many clinicians, administrators, and entrepreneurs in hospital medicine and health care more broadly.
The biggest difference between these two highly effective leaders and mentors might be money; SHM has paid him pretty well, but alas, no stock options.
Larry is a great storyteller, and it doesn’t take long for a conversation with him to arrive at the point where he cites the example of how issues faced by someone else have parallels to your situation, the advice he gave that person, and how things turned out. Mostly this advice is about navigating professional life, but he is also happy to share wisdom about parenting, marriage, money, and sports. And most any other topic.
Larry was very accomplished even prior to connecting with SHM. He had a thriving clinical career, and though he left practice long ago he has maintained a close connection with many people he first met when they were his patients. I was surprised years ago when he drove up a new top-of-the-line Lexus – the two-seater with the solid convertible roof that folded into the trunk with the push of a button. I expressed surprise that he’d buy such a swanky car and he explained that a former patient, now long-time friend, was a Lexus distributor and arranged for Larry to drive it away for something like the cost of a Camry.
He also had terrific success forming and leading a large California independent physician association prior to connecting with SHM. Just ask him to show you the magazine with him on the cover and a glowing article detailing his accomplishments. Seriously, ask him, there’s a good chance he’ll have a copy with him.
When Dr. Win Whitcomb and I were trying to figure out how to start a new medical society and position our field to mature into a real specialty we were lucky enough to connect with many health care leaders who we thought could help. Most tended to pat us on the shoulder and say something along the lines of “good luck with your little hobby, now I have to get back to my important work.” But here was Larry with his impressive resume, having served as one of the leaders who crafted the merger of two giant medical societies (ACP and the American Society of Internal Medicine), keenly interested in our tiny new organization, and excited to serve as facilitator for our first strategic planning session.
SHM got a turbocharger when Larry signed on. For me it has felt like speeding down a highway, top down, radio blasting great music, and happy anticipation of what is around the next corner. I have never been disappointed, and certainly don’t plan to get out of Larry’s car just because he’s retiring as CEO.
Dr. Nelson is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants in La Quinta, Calif.
The plague of racism in our society
Here we are, faced with history in real time. A plague upon a plague. A new one and a longstanding one. COVID-19 and racial injustice. Both are plagues upon our medical house, and it’s time for some spring cleaning.
Initially, COVID-19 concerns brought news of an infection coming for anyone and everyone. Like the Black Death, it was supposedly “the great equalizer,” the “Triumph of Death,” regardless of station in life.
Yet, as the COVID-19 story unfurls, it is clear that minorities are disproportionately affected, just as they always seem to be. In Chicago, for example, African Americans make up 70% of the COVID-19 deaths, yet only 29% of the population. Similar results have been found in Milwaukee and Louisiana, and other parts of the country. As an article in the Journal of Law and the Biosciences indicated, “These racial and ethnic disparities in COVID-19 infections and deaths are a result of historical and current practices of racism that cause disparities in exposure, susceptibility and treatment.”
People of color are disproportionately affected, an outcome of racial health disparities. And these disparities are a public health crisis, sitting in the living room of our house. Disparities continue to exist in national infant mortality, maternal health, and deaths from premature heart disease and stroke. They exist in access to care and are playing out in real time during this pandemic.
COVID-19 and racial injustice, in addition to being sociological and economic crises, are both public health crises that are plaguing African American communities. Consider the case of police violence as a public health issue. Black males are three times more likely to be killed by police than are non-Hispanic white males.
This is a dying room in our medical house, with our patient lying alongside a history of medicine littered with racial injustice, telling us, “I can’t breathe.”
As professionals, we must run to that patient. Professionalism bears the pillars of our ethical principles of primacy of patient welfare, patient autonomy, and social justice. We work hard on the first two. Medical errors, quality improvement, communication, patient safety. All important. But we too often dance, or sit silently, about the third.
Here is an excerpt from “Moral choices for today’s physician”, by Donald M. Berwick, MD:
“The work of a physician as healer cannot stop at the door of an office, the threshold of an operating room, or the front gate of a hospital. The rescue of a society and the restoration of a political ethos that remembers to heal have become the physician’s jobs, too. Professional silence in the face of social injustice is wrong.”
It is chilling to see the great institutions of health care, hospitals, physician groups, and scientific bodies assume that the seat of bystander is available. That seat is gone. To try to avoid the political fray through silence is impossible because silence is now political. Either engage or assist the harm. There is no third choice.
Dr. Berwick echoed the words of Rev. Dr. Martin Luther King Jr., from 1959, in Birmingham, Ala.:
“If you fail to act now, history will have to record that the greatest tragedy of this period of social transition was not the strident clamor of the bad people, but the appalling silence of the good people.”
I have this space to write and speak up, and I urge many of you to do the same. Write to your local newspaper. Share your stories. Listen to others. Engage with your society. Create the space in your practice, your group, your hospital, your department for listening, learning, relearning, educating, and acting.
It’s not easy speaking up and speaking out. Yet, this is our foundation, our call, our professional obligation. We must remember George Floyd, Breonna Taylor, Sandra Bland, Eric Garner, Tamir Rice, Trayvon Martin, and too many others. To recognize the humanity behind the injustices, and to call out their names.
This is lesson 101 on the wards. It’s not the heart failure in bed 1 or the sepsis in bed 2, but the mother, brother, father, and sister who seek out just care. Humanity reaching out their hand, and we must grab it.
I came to medicine for the compassion, for the love, for the comforting hand offered to our patients. That compassion, by definition, requires action.
In his book “Altruism: The Power of Compassion to Change Yourself and the World,” Matthieu Ricard wrote “If compassion without wisdom is blind, compassion without action is hypocritical.”
Silence is inaction. Let’s act.
Dr. Messler is the executive director, quality initiatives, at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared first at SHM’s official blog The Hospital Leader.
Here we are, faced with history in real time. A plague upon a plague. A new one and a longstanding one. COVID-19 and racial injustice. Both are plagues upon our medical house, and it’s time for some spring cleaning.
Initially, COVID-19 concerns brought news of an infection coming for anyone and everyone. Like the Black Death, it was supposedly “the great equalizer,” the “Triumph of Death,” regardless of station in life.
Yet, as the COVID-19 story unfurls, it is clear that minorities are disproportionately affected, just as they always seem to be. In Chicago, for example, African Americans make up 70% of the COVID-19 deaths, yet only 29% of the population. Similar results have been found in Milwaukee and Louisiana, and other parts of the country. As an article in the Journal of Law and the Biosciences indicated, “These racial and ethnic disparities in COVID-19 infections and deaths are a result of historical and current practices of racism that cause disparities in exposure, susceptibility and treatment.”
People of color are disproportionately affected, an outcome of racial health disparities. And these disparities are a public health crisis, sitting in the living room of our house. Disparities continue to exist in national infant mortality, maternal health, and deaths from premature heart disease and stroke. They exist in access to care and are playing out in real time during this pandemic.
COVID-19 and racial injustice, in addition to being sociological and economic crises, are both public health crises that are plaguing African American communities. Consider the case of police violence as a public health issue. Black males are three times more likely to be killed by police than are non-Hispanic white males.
This is a dying room in our medical house, with our patient lying alongside a history of medicine littered with racial injustice, telling us, “I can’t breathe.”
As professionals, we must run to that patient. Professionalism bears the pillars of our ethical principles of primacy of patient welfare, patient autonomy, and social justice. We work hard on the first two. Medical errors, quality improvement, communication, patient safety. All important. But we too often dance, or sit silently, about the third.
Here is an excerpt from “Moral choices for today’s physician”, by Donald M. Berwick, MD:
“The work of a physician as healer cannot stop at the door of an office, the threshold of an operating room, or the front gate of a hospital. The rescue of a society and the restoration of a political ethos that remembers to heal have become the physician’s jobs, too. Professional silence in the face of social injustice is wrong.”
It is chilling to see the great institutions of health care, hospitals, physician groups, and scientific bodies assume that the seat of bystander is available. That seat is gone. To try to avoid the political fray through silence is impossible because silence is now political. Either engage or assist the harm. There is no third choice.
Dr. Berwick echoed the words of Rev. Dr. Martin Luther King Jr., from 1959, in Birmingham, Ala.:
“If you fail to act now, history will have to record that the greatest tragedy of this period of social transition was not the strident clamor of the bad people, but the appalling silence of the good people.”
I have this space to write and speak up, and I urge many of you to do the same. Write to your local newspaper. Share your stories. Listen to others. Engage with your society. Create the space in your practice, your group, your hospital, your department for listening, learning, relearning, educating, and acting.
It’s not easy speaking up and speaking out. Yet, this is our foundation, our call, our professional obligation. We must remember George Floyd, Breonna Taylor, Sandra Bland, Eric Garner, Tamir Rice, Trayvon Martin, and too many others. To recognize the humanity behind the injustices, and to call out their names.
This is lesson 101 on the wards. It’s not the heart failure in bed 1 or the sepsis in bed 2, but the mother, brother, father, and sister who seek out just care. Humanity reaching out their hand, and we must grab it.
I came to medicine for the compassion, for the love, for the comforting hand offered to our patients. That compassion, by definition, requires action.
In his book “Altruism: The Power of Compassion to Change Yourself and the World,” Matthieu Ricard wrote “If compassion without wisdom is blind, compassion without action is hypocritical.”
Silence is inaction. Let’s act.
Dr. Messler is the executive director, quality initiatives, at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared first at SHM’s official blog The Hospital Leader.
Here we are, faced with history in real time. A plague upon a plague. A new one and a longstanding one. COVID-19 and racial injustice. Both are plagues upon our medical house, and it’s time for some spring cleaning.
Initially, COVID-19 concerns brought news of an infection coming for anyone and everyone. Like the Black Death, it was supposedly “the great equalizer,” the “Triumph of Death,” regardless of station in life.
Yet, as the COVID-19 story unfurls, it is clear that minorities are disproportionately affected, just as they always seem to be. In Chicago, for example, African Americans make up 70% of the COVID-19 deaths, yet only 29% of the population. Similar results have been found in Milwaukee and Louisiana, and other parts of the country. As an article in the Journal of Law and the Biosciences indicated, “These racial and ethnic disparities in COVID-19 infections and deaths are a result of historical and current practices of racism that cause disparities in exposure, susceptibility and treatment.”
People of color are disproportionately affected, an outcome of racial health disparities. And these disparities are a public health crisis, sitting in the living room of our house. Disparities continue to exist in national infant mortality, maternal health, and deaths from premature heart disease and stroke. They exist in access to care and are playing out in real time during this pandemic.
COVID-19 and racial injustice, in addition to being sociological and economic crises, are both public health crises that are plaguing African American communities. Consider the case of police violence as a public health issue. Black males are three times more likely to be killed by police than are non-Hispanic white males.
This is a dying room in our medical house, with our patient lying alongside a history of medicine littered with racial injustice, telling us, “I can’t breathe.”
As professionals, we must run to that patient. Professionalism bears the pillars of our ethical principles of primacy of patient welfare, patient autonomy, and social justice. We work hard on the first two. Medical errors, quality improvement, communication, patient safety. All important. But we too often dance, or sit silently, about the third.
Here is an excerpt from “Moral choices for today’s physician”, by Donald M. Berwick, MD:
“The work of a physician as healer cannot stop at the door of an office, the threshold of an operating room, or the front gate of a hospital. The rescue of a society and the restoration of a political ethos that remembers to heal have become the physician’s jobs, too. Professional silence in the face of social injustice is wrong.”
It is chilling to see the great institutions of health care, hospitals, physician groups, and scientific bodies assume that the seat of bystander is available. That seat is gone. To try to avoid the political fray through silence is impossible because silence is now political. Either engage or assist the harm. There is no third choice.
Dr. Berwick echoed the words of Rev. Dr. Martin Luther King Jr., from 1959, in Birmingham, Ala.:
“If you fail to act now, history will have to record that the greatest tragedy of this period of social transition was not the strident clamor of the bad people, but the appalling silence of the good people.”
I have this space to write and speak up, and I urge many of you to do the same. Write to your local newspaper. Share your stories. Listen to others. Engage with your society. Create the space in your practice, your group, your hospital, your department for listening, learning, relearning, educating, and acting.
It’s not easy speaking up and speaking out. Yet, this is our foundation, our call, our professional obligation. We must remember George Floyd, Breonna Taylor, Sandra Bland, Eric Garner, Tamir Rice, Trayvon Martin, and too many others. To recognize the humanity behind the injustices, and to call out their names.
This is lesson 101 on the wards. It’s not the heart failure in bed 1 or the sepsis in bed 2, but the mother, brother, father, and sister who seek out just care. Humanity reaching out their hand, and we must grab it.
I came to medicine for the compassion, for the love, for the comforting hand offered to our patients. That compassion, by definition, requires action.
In his book “Altruism: The Power of Compassion to Change Yourself and the World,” Matthieu Ricard wrote “If compassion without wisdom is blind, compassion without action is hypocritical.”
Silence is inaction. Let’s act.
Dr. Messler is the executive director, quality initiatives, at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared first at SHM’s official blog The Hospital Leader.
The evolution of “COVIDists”
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).

The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).

This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
Adapting to the demands placed on hospital resources by COVID-19
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).

The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).

This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).

The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).

This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi