User login
At U.S. Ground Zero for coronavirus, a hospital is transformed
David Baker, MD, a hospitalist at EvergreenHealth in Kirkland, Wash., had just come off a 7-day stretch of work and was early into his usual 7 days off. He’d helped care for some patients from a nearby assisted living facility who had been admitted with puzzlingly severe viral pneumonia that wasn’t influenza.
Though COVID-19, the novel coronavirus that was sickening tens of thousands in the Chinese province of Hubei, was in the back of everyone’s mind in late February, he said he wasn’t really expecting the call notifying him that two of the patients with pneumonia had tested positive for COVID-19.
Michael Chu, MD, was coming onto EvergreenHealth’s hospitalist service at about the time Dr. Baker was rotating off. He recalled learning of the first two positive COVID-19 tests on the evening of Feb. 28 – a Friday. He and his colleagues took in this information, coming to the realization that they were seeing other patients from the same facility who had viral pneumonia and negative influenza tests. “The first cohort of coronavirus patients all came from Life Care,” the Kirkland assisted living facility that was the epicenter of the first identified U.S. outbreak of community-transmitted coronavirus, said Dr. Chu. “They all fit a clinical syndrome” and many of them were critically ill or failing fast, since they were aged and with multiple risk factors, he said during the interviews he and his colleagues participated in.
As he processed the news of the positive tests and his inadvertent exposure to COVID-19, Dr. Baker realized that his duty schedule worked in his favor, since he wasn’t expected back for several more days. When he did come back to work after remaining asymptomatic, he found a much-changed environment as the coronavirus cases poured in and continual adaptations were made to accommodate these patients – and to keep staff and other patients safe.
The hospital adapts to a new normal
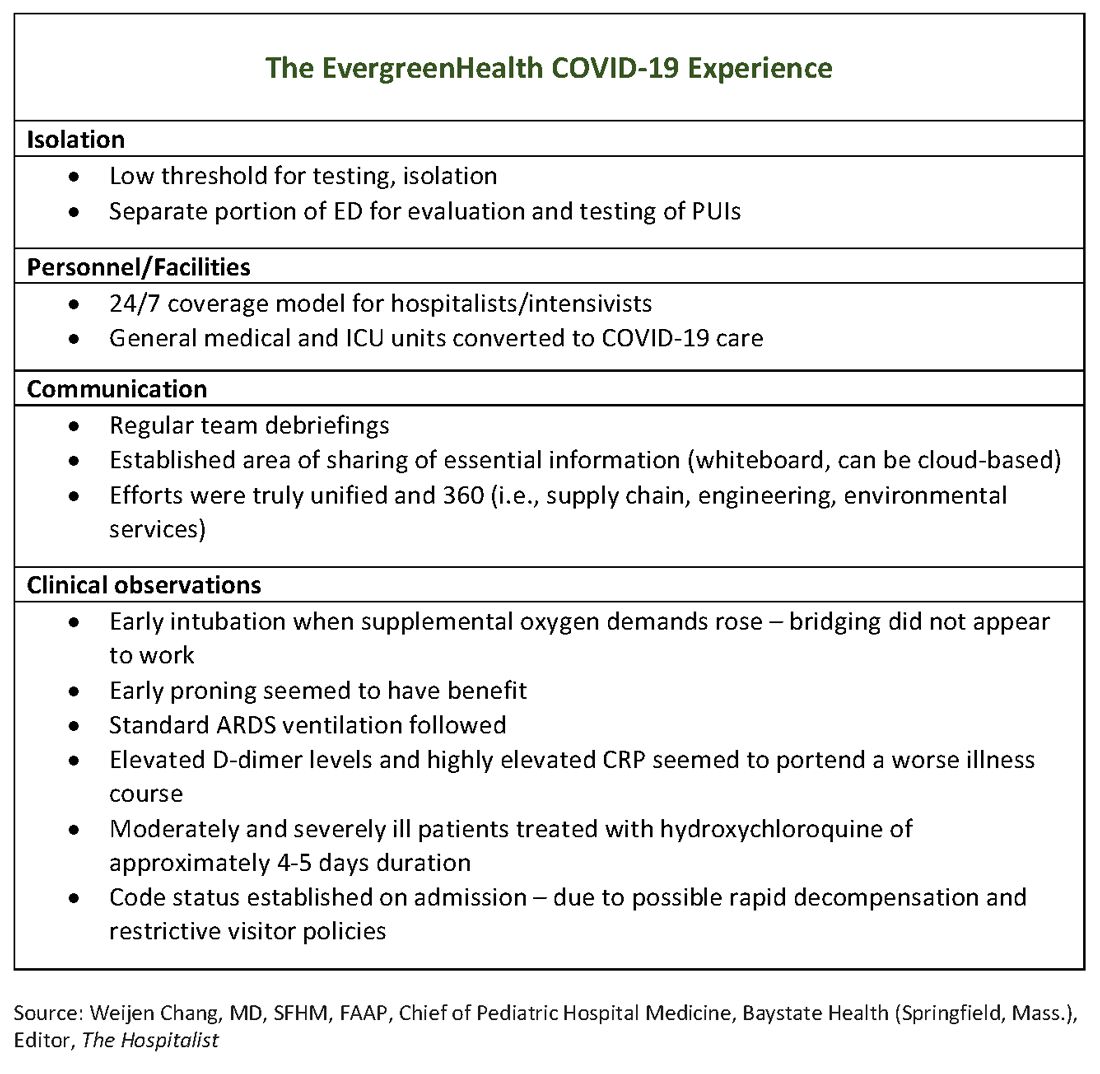
The usual protocol in EvergreenHealth’s ICU is for the nocturnist hospitalists, such as Dr. Baker, to staff that unit, with intensivists readily available for phone consultation. However, as the numbers of critically ill, ventilated COVID-19 patients climbed, the facility switched to 24/7 staffing with intensivists to augment the hospitalist team, said Nancy Marshall, MD, the director of EvergreenHealth’s hospitalist service.
Dr. Marshall related how the entire hospital rallied to create appropriate – but flexible – staffing and environmental adaptations to the influx of coronavirus patients. “Early on, we established a separate portion of the emergency department to evaluate and test persons under investigation,” for COVID-19, she said. When they realized that they were seeing the nation’s first cluster of community coronavirus transmission, they used “appropriate isolation precautions” when indicated. Triggers for clinical suspicion included not just fever or cough, but also a new requirement for supplemental oxygen and new abnormal findings on chest radiographs.
Patients with confirmed or suspected coronavirus, once admitted, were placed in negative-pressure rooms, and droplet precautions were used with these patients. In the absence of aerosol-generating procedures, those caring for these patients used a standard surgical mask, goggles or face shield, an isolation gown, and gloves. For intubations, bronchoscopies, and other aerosol-generating procedures, N95 masks were used; the facility also has some powered and controlled air-purifying respirators.
In short order, once the size of the outbreak was appreciated, said Dr. Marshall, the entire ICU and half of another general medical floor in the hospital were converted to negative-pressure rooms.
Dr. Marshall said that having daily team debriefings has been essential. The hospitalist team room has a big whiteboard where essential information can be put up and shared. Frequent video conferencing has allowed physicians and advanced practice clinicians on the hospitalist team to ask questions, share concerns, and develop a shared knowledge base and vocabulary as they confronted this novel illness.
The rapid adaptations that EvergreenHealth successfully made depended on a responsive administration, good communication among physician services and with nursing staff, and the active participation of engineering and environmental services teams in adjusting to shifting patient needs, said Dr. Marshall.
“Preparedness is key,” Dr. Chu noted. “Managing this has required a unified effort” that addresses everything from the supply chain for personal protective equipment, to cleaning procedures, to engineering fixes that quickly added negative-pressure rooms.
“I can’t emphasize enough that this is a team sport,” said Dr. Marshall.
The unpredictable clinical course of COVID-19
The chimeric clinical course of COVID-19 means clinicians need to keep an open mind and be ready to act nimbly, said the EvergreenHealth hospitalists. Pattern recognition is a key to competent clinical management of hospitalized patients, but the course of coronavirus thus far defies any convenient application of heuristics.
Those first two patients had some characteristics in common, aside from their arrival from the same long-term care facility They each had unexplained acute respiratory distress syndrome and ground-glass opacities seen on chest CT, said Dr. Marshall. But all agreed it is still not clear who will fare well, and who will do poorly once they are admitted with coronavirus.
“We have noticed that these patients tend to have a rough course,” said Dr. Marshall. The “brisk inflammatory response” seen in some patients manifests in persistent fevers, big C-reactive protein (CRP) elevations, and likely is part of the picture of yet-unknown host factors that contribute to a worse disease course for some, she said. “These patients look toxic for a long time.”
Dr. Chu said that he’s seen even younger, healthier-looking patients admitted from the emergency department who are already quite dyspneic and may be headed for ventilation. These patients may have a low procalcitonin, and will often turn out to have an “impressive-looking” chest x-ray or CT that will show prominent bilateral infiltrates.
On the other hand, said Dr. Marshall, she and her colleagues have admitted frail-appearing nonagenarians who “just kind of sleep it off,” with little more than a cough and intermittent fevers.
Dr. Chu concurred: “So many of these patients had risk factors for severe disease and only had mild illness. Many were really quite stable.”
In terms of managing respiratory status, Dr. Baker said that the time to start planning for intubation is when the supplemental oxygen demands of COVID-19 patients start to go up. Unlike with patients who may be in some respiratory distress from other causes, once these patients have increased Fi02 needs, bridging “doesn’t work. ... They need to be intubated. Early intubation is important.” Clinicians’ level of concern should spike when they see increased work of breathing in a coronavirus patient, regardless of what the numbers are saying, he added.
For coronavirus patients with acute respiratory distress syndrome (ARDS), early proning also seems to provide some benefit, he said. At EvergreenHealth, standard ARDS ventilation protocols are being followed, including low tidal volume ventilation and positive end-expiratory pressure (PEEP) ladders. Coronavirus ventilation management has thus far been “pretty similar to standard practice with ARDS patients,” he said.
The hospitalist team was able to tap into the building knowledge base in China: Two of the EvergreenHealth hospitalists spoke fluent Mandarin, and one had contacts in China that allowed her to connect with Chinese physicians who had been treating COVID-19 patients since that outbreak had started. They established regular communication on WeChat, checking in frequently for updates on therapies and diagnostics being used in China as well.
One benefit of being in communication with colleagues in China, said Dr. Baker, was that they were able to get anecdotal evidence that elevated D-dimer levels and highly elevated CRP levels can portend a worse illness course. These findings seem to have held generally true for EvergreenHealth patients, he said. Dr. Marshall also spoke to the value of early communication with Chinese teams, who confirmed that the picture of a febrile illness with elevated CRP and leukopenia should raise the index of suspicion for coronavirus.
“Patients might improve over a few days, and then in the final 24 hours of their lives, we see changes in hemodynamics,” including reduced ejection fraction consistent with cardiogenic shock, as well as arrhythmias, said Dr. Baker. Some of the early patient deaths at EvergreenHealth followed this pattern, he said, noting that others have called for investigation into whether viral myocarditis is at play in some coronavirus deaths.
Moderately and severely ill coronavirus patients at EvergreenHealth currently receive a course of hydroxychloroquine of approximately 4-5 days’ duration. The hospital obtained remdesivir from Gilead through its compassionate-use program early on, and now is participating in a clinical trial for COVID-19 patients in the ICU.
By March 23, the facility had seen 162 confirmed COVID-19 cases, and 30 patients had died. Twenty-two inpatients had been discharged, and an additional 58 who were seen in the emergency department had been discharged home without admission.
Be suspicious – and prepared
When asked what he’d like his colleagues around the country to know as they diagnose and admit their first patients who are ill with coronavirus, Dr. Baker advised maintaining a high index of suspicion and a low threshold for testing. “I’ve given some thought to this,” he said. “From our reading and what information is out there, we are geared to pick up on the classic symptoms of coronavirus – cough, fever, some gastrointestinal symptoms.” However, many elderly patients “are not good historians. Some may have advanced dementia. ... When patients arrive with no history, we do our best to gather information,” but sometimes a case can still take clinicians by surprise, he said.
Dr. Baker told a cautionary tale of one of his patients, a woman who was admitted for a hip fracture after a fall at an assisted living facility. The patient was mildly hypoxic, but had an unremarkable physical exam, no fever, and a clear chest x-ray. She went to surgery and then to a postoperative floor with no isolation measures. When her respiratory status unexpectedly deteriorated, she was tested for COVID-19 – and was positive.
“When in doubt, isolate,” said Dr. Baker.
Dr. Chu concurred: “As soon as you suspect, move them, rather than testing first.”
Dr. Baker acknowledged, though, that when testing criteria and availability of personal protective equipment and test materials may vary by region, “it’s a challenge, especially with limited resources.”
Dr. Chu said that stringent isolation, though necessary, creates great hardship for patients and families. “It’s really important for us to check in with family members,” he said; patients are alone and afraid, and family members feel cut off – and also afraid on behalf of their ill loved ones. Workflow planning should acknowledge this and allocate extra time for patient connection and a little more time on the phone with families.
Dr. Chu offered a sobering final word. Make sure family members know their ill loved one’s wishes for care, he said: “There’s never been a better time to clarify code status on admission.”
Physicians at EvergreenHealth have created a document that contains consolidated information on what to anticipate and how to prepare for the arrival of COVID-19+ patients, recommendations on maximizing safety in the hospital environment, and key clinical management considerations. The document will be updated as new information arises.
Correction, 3/27/20: An earlier version of this article referenced white blood counts, presence of lymphopenia, and elevated hepatic enzymes for patients at EvergreenHealth when in fact that information pertained to patients in China. That paragraph has been deleted.
David Baker, MD, a hospitalist at EvergreenHealth in Kirkland, Wash., had just come off a 7-day stretch of work and was early into his usual 7 days off. He’d helped care for some patients from a nearby assisted living facility who had been admitted with puzzlingly severe viral pneumonia that wasn’t influenza.
Though COVID-19, the novel coronavirus that was sickening tens of thousands in the Chinese province of Hubei, was in the back of everyone’s mind in late February, he said he wasn’t really expecting the call notifying him that two of the patients with pneumonia had tested positive for COVID-19.
Michael Chu, MD, was coming onto EvergreenHealth’s hospitalist service at about the time Dr. Baker was rotating off. He recalled learning of the first two positive COVID-19 tests on the evening of Feb. 28 – a Friday. He and his colleagues took in this information, coming to the realization that they were seeing other patients from the same facility who had viral pneumonia and negative influenza tests. “The first cohort of coronavirus patients all came from Life Care,” the Kirkland assisted living facility that was the epicenter of the first identified U.S. outbreak of community-transmitted coronavirus, said Dr. Chu. “They all fit a clinical syndrome” and many of them were critically ill or failing fast, since they were aged and with multiple risk factors, he said during the interviews he and his colleagues participated in.
As he processed the news of the positive tests and his inadvertent exposure to COVID-19, Dr. Baker realized that his duty schedule worked in his favor, since he wasn’t expected back for several more days. When he did come back to work after remaining asymptomatic, he found a much-changed environment as the coronavirus cases poured in and continual adaptations were made to accommodate these patients – and to keep staff and other patients safe.
The hospital adapts to a new normal
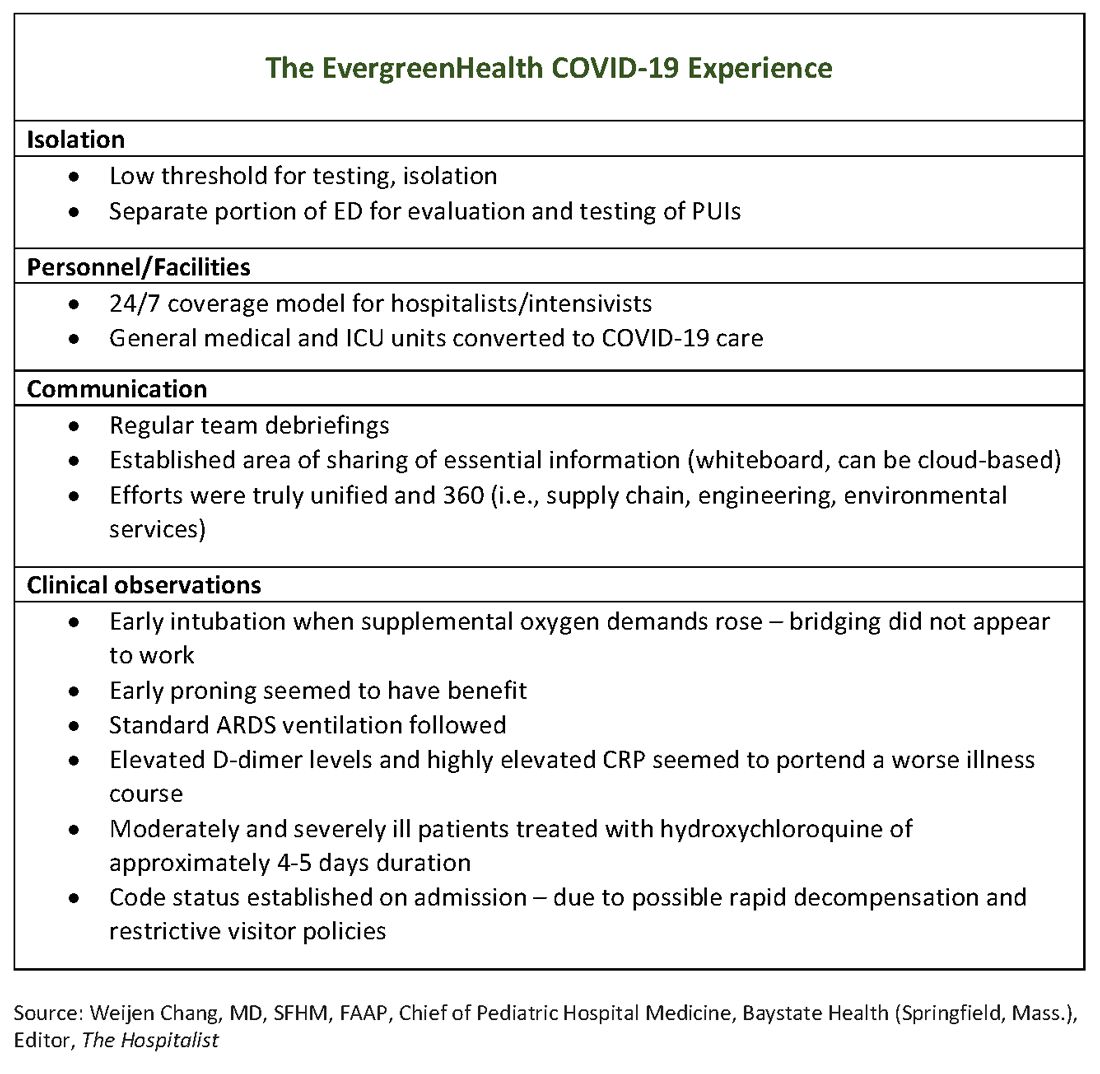
The usual protocol in EvergreenHealth’s ICU is for the nocturnist hospitalists, such as Dr. Baker, to staff that unit, with intensivists readily available for phone consultation. However, as the numbers of critically ill, ventilated COVID-19 patients climbed, the facility switched to 24/7 staffing with intensivists to augment the hospitalist team, said Nancy Marshall, MD, the director of EvergreenHealth’s hospitalist service.
Dr. Marshall related how the entire hospital rallied to create appropriate – but flexible – staffing and environmental adaptations to the influx of coronavirus patients. “Early on, we established a separate portion of the emergency department to evaluate and test persons under investigation,” for COVID-19, she said. When they realized that they were seeing the nation’s first cluster of community coronavirus transmission, they used “appropriate isolation precautions” when indicated. Triggers for clinical suspicion included not just fever or cough, but also a new requirement for supplemental oxygen and new abnormal findings on chest radiographs.
Patients with confirmed or suspected coronavirus, once admitted, were placed in negative-pressure rooms, and droplet precautions were used with these patients. In the absence of aerosol-generating procedures, those caring for these patients used a standard surgical mask, goggles or face shield, an isolation gown, and gloves. For intubations, bronchoscopies, and other aerosol-generating procedures, N95 masks were used; the facility also has some powered and controlled air-purifying respirators.
In short order, once the size of the outbreak was appreciated, said Dr. Marshall, the entire ICU and half of another general medical floor in the hospital were converted to negative-pressure rooms.
Dr. Marshall said that having daily team debriefings has been essential. The hospitalist team room has a big whiteboard where essential information can be put up and shared. Frequent video conferencing has allowed physicians and advanced practice clinicians on the hospitalist team to ask questions, share concerns, and develop a shared knowledge base and vocabulary as they confronted this novel illness.
The rapid adaptations that EvergreenHealth successfully made depended on a responsive administration, good communication among physician services and with nursing staff, and the active participation of engineering and environmental services teams in adjusting to shifting patient needs, said Dr. Marshall.
“Preparedness is key,” Dr. Chu noted. “Managing this has required a unified effort” that addresses everything from the supply chain for personal protective equipment, to cleaning procedures, to engineering fixes that quickly added negative-pressure rooms.
“I can’t emphasize enough that this is a team sport,” said Dr. Marshall.
The unpredictable clinical course of COVID-19
The chimeric clinical course of COVID-19 means clinicians need to keep an open mind and be ready to act nimbly, said the EvergreenHealth hospitalists. Pattern recognition is a key to competent clinical management of hospitalized patients, but the course of coronavirus thus far defies any convenient application of heuristics.
Those first two patients had some characteristics in common, aside from their arrival from the same long-term care facility They each had unexplained acute respiratory distress syndrome and ground-glass opacities seen on chest CT, said Dr. Marshall. But all agreed it is still not clear who will fare well, and who will do poorly once they are admitted with coronavirus.
“We have noticed that these patients tend to have a rough course,” said Dr. Marshall. The “brisk inflammatory response” seen in some patients manifests in persistent fevers, big C-reactive protein (CRP) elevations, and likely is part of the picture of yet-unknown host factors that contribute to a worse disease course for some, she said. “These patients look toxic for a long time.”
Dr. Chu said that he’s seen even younger, healthier-looking patients admitted from the emergency department who are already quite dyspneic and may be headed for ventilation. These patients may have a low procalcitonin, and will often turn out to have an “impressive-looking” chest x-ray or CT that will show prominent bilateral infiltrates.
On the other hand, said Dr. Marshall, she and her colleagues have admitted frail-appearing nonagenarians who “just kind of sleep it off,” with little more than a cough and intermittent fevers.
Dr. Chu concurred: “So many of these patients had risk factors for severe disease and only had mild illness. Many were really quite stable.”
In terms of managing respiratory status, Dr. Baker said that the time to start planning for intubation is when the supplemental oxygen demands of COVID-19 patients start to go up. Unlike with patients who may be in some respiratory distress from other causes, once these patients have increased Fi02 needs, bridging “doesn’t work. ... They need to be intubated. Early intubation is important.” Clinicians’ level of concern should spike when they see increased work of breathing in a coronavirus patient, regardless of what the numbers are saying, he added.
For coronavirus patients with acute respiratory distress syndrome (ARDS), early proning also seems to provide some benefit, he said. At EvergreenHealth, standard ARDS ventilation protocols are being followed, including low tidal volume ventilation and positive end-expiratory pressure (PEEP) ladders. Coronavirus ventilation management has thus far been “pretty similar to standard practice with ARDS patients,” he said.
The hospitalist team was able to tap into the building knowledge base in China: Two of the EvergreenHealth hospitalists spoke fluent Mandarin, and one had contacts in China that allowed her to connect with Chinese physicians who had been treating COVID-19 patients since that outbreak had started. They established regular communication on WeChat, checking in frequently for updates on therapies and diagnostics being used in China as well.
One benefit of being in communication with colleagues in China, said Dr. Baker, was that they were able to get anecdotal evidence that elevated D-dimer levels and highly elevated CRP levels can portend a worse illness course. These findings seem to have held generally true for EvergreenHealth patients, he said. Dr. Marshall also spoke to the value of early communication with Chinese teams, who confirmed that the picture of a febrile illness with elevated CRP and leukopenia should raise the index of suspicion for coronavirus.
“Patients might improve over a few days, and then in the final 24 hours of their lives, we see changes in hemodynamics,” including reduced ejection fraction consistent with cardiogenic shock, as well as arrhythmias, said Dr. Baker. Some of the early patient deaths at EvergreenHealth followed this pattern, he said, noting that others have called for investigation into whether viral myocarditis is at play in some coronavirus deaths.
Moderately and severely ill coronavirus patients at EvergreenHealth currently receive a course of hydroxychloroquine of approximately 4-5 days’ duration. The hospital obtained remdesivir from Gilead through its compassionate-use program early on, and now is participating in a clinical trial for COVID-19 patients in the ICU.
By March 23, the facility had seen 162 confirmed COVID-19 cases, and 30 patients had died. Twenty-two inpatients had been discharged, and an additional 58 who were seen in the emergency department had been discharged home without admission.
Be suspicious – and prepared
When asked what he’d like his colleagues around the country to know as they diagnose and admit their first patients who are ill with coronavirus, Dr. Baker advised maintaining a high index of suspicion and a low threshold for testing. “I’ve given some thought to this,” he said. “From our reading and what information is out there, we are geared to pick up on the classic symptoms of coronavirus – cough, fever, some gastrointestinal symptoms.” However, many elderly patients “are not good historians. Some may have advanced dementia. ... When patients arrive with no history, we do our best to gather information,” but sometimes a case can still take clinicians by surprise, he said.
Dr. Baker told a cautionary tale of one of his patients, a woman who was admitted for a hip fracture after a fall at an assisted living facility. The patient was mildly hypoxic, but had an unremarkable physical exam, no fever, and a clear chest x-ray. She went to surgery and then to a postoperative floor with no isolation measures. When her respiratory status unexpectedly deteriorated, she was tested for COVID-19 – and was positive.
“When in doubt, isolate,” said Dr. Baker.
Dr. Chu concurred: “As soon as you suspect, move them, rather than testing first.”
Dr. Baker acknowledged, though, that when testing criteria and availability of personal protective equipment and test materials may vary by region, “it’s a challenge, especially with limited resources.”
Dr. Chu said that stringent isolation, though necessary, creates great hardship for patients and families. “It’s really important for us to check in with family members,” he said; patients are alone and afraid, and family members feel cut off – and also afraid on behalf of their ill loved ones. Workflow planning should acknowledge this and allocate extra time for patient connection and a little more time on the phone with families.
Dr. Chu offered a sobering final word. Make sure family members know their ill loved one’s wishes for care, he said: “There’s never been a better time to clarify code status on admission.”
Physicians at EvergreenHealth have created a document that contains consolidated information on what to anticipate and how to prepare for the arrival of COVID-19+ patients, recommendations on maximizing safety in the hospital environment, and key clinical management considerations. The document will be updated as new information arises.
Correction, 3/27/20: An earlier version of this article referenced white blood counts, presence of lymphopenia, and elevated hepatic enzymes for patients at EvergreenHealth when in fact that information pertained to patients in China. That paragraph has been deleted.
David Baker, MD, a hospitalist at EvergreenHealth in Kirkland, Wash., had just come off a 7-day stretch of work and was early into his usual 7 days off. He’d helped care for some patients from a nearby assisted living facility who had been admitted with puzzlingly severe viral pneumonia that wasn’t influenza.
Though COVID-19, the novel coronavirus that was sickening tens of thousands in the Chinese province of Hubei, was in the back of everyone’s mind in late February, he said he wasn’t really expecting the call notifying him that two of the patients with pneumonia had tested positive for COVID-19.
Michael Chu, MD, was coming onto EvergreenHealth’s hospitalist service at about the time Dr. Baker was rotating off. He recalled learning of the first two positive COVID-19 tests on the evening of Feb. 28 – a Friday. He and his colleagues took in this information, coming to the realization that they were seeing other patients from the same facility who had viral pneumonia and negative influenza tests. “The first cohort of coronavirus patients all came from Life Care,” the Kirkland assisted living facility that was the epicenter of the first identified U.S. outbreak of community-transmitted coronavirus, said Dr. Chu. “They all fit a clinical syndrome” and many of them were critically ill or failing fast, since they were aged and with multiple risk factors, he said during the interviews he and his colleagues participated in.
As he processed the news of the positive tests and his inadvertent exposure to COVID-19, Dr. Baker realized that his duty schedule worked in his favor, since he wasn’t expected back for several more days. When he did come back to work after remaining asymptomatic, he found a much-changed environment as the coronavirus cases poured in and continual adaptations were made to accommodate these patients – and to keep staff and other patients safe.
The hospital adapts to a new normal
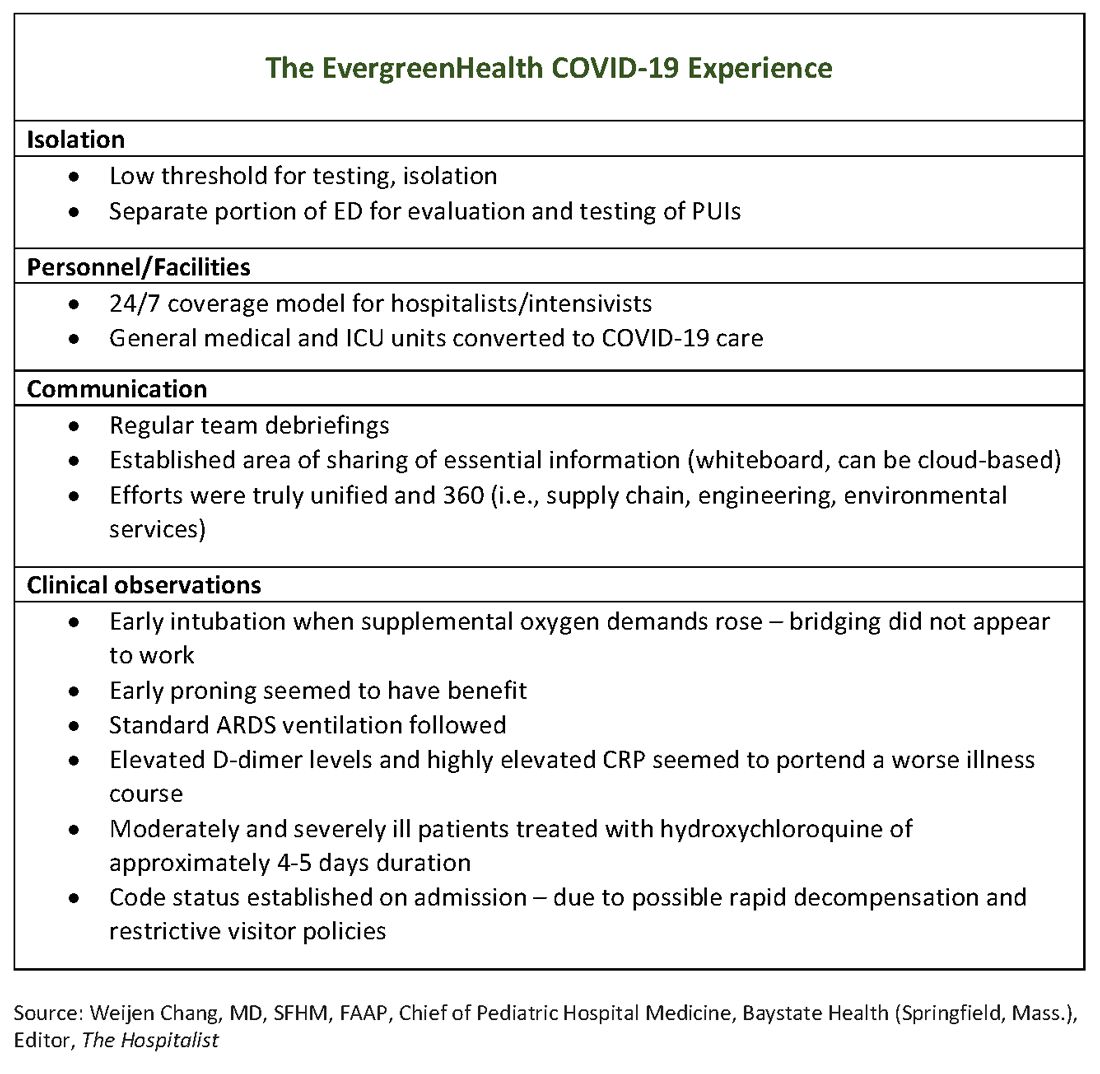
The usual protocol in EvergreenHealth’s ICU is for the nocturnist hospitalists, such as Dr. Baker, to staff that unit, with intensivists readily available for phone consultation. However, as the numbers of critically ill, ventilated COVID-19 patients climbed, the facility switched to 24/7 staffing with intensivists to augment the hospitalist team, said Nancy Marshall, MD, the director of EvergreenHealth’s hospitalist service.
Dr. Marshall related how the entire hospital rallied to create appropriate – but flexible – staffing and environmental adaptations to the influx of coronavirus patients. “Early on, we established a separate portion of the emergency department to evaluate and test persons under investigation,” for COVID-19, she said. When they realized that they were seeing the nation’s first cluster of community coronavirus transmission, they used “appropriate isolation precautions” when indicated. Triggers for clinical suspicion included not just fever or cough, but also a new requirement for supplemental oxygen and new abnormal findings on chest radiographs.
Patients with confirmed or suspected coronavirus, once admitted, were placed in negative-pressure rooms, and droplet precautions were used with these patients. In the absence of aerosol-generating procedures, those caring for these patients used a standard surgical mask, goggles or face shield, an isolation gown, and gloves. For intubations, bronchoscopies, and other aerosol-generating procedures, N95 masks were used; the facility also has some powered and controlled air-purifying respirators.
In short order, once the size of the outbreak was appreciated, said Dr. Marshall, the entire ICU and half of another general medical floor in the hospital were converted to negative-pressure rooms.
Dr. Marshall said that having daily team debriefings has been essential. The hospitalist team room has a big whiteboard where essential information can be put up and shared. Frequent video conferencing has allowed physicians and advanced practice clinicians on the hospitalist team to ask questions, share concerns, and develop a shared knowledge base and vocabulary as they confronted this novel illness.
The rapid adaptations that EvergreenHealth successfully made depended on a responsive administration, good communication among physician services and with nursing staff, and the active participation of engineering and environmental services teams in adjusting to shifting patient needs, said Dr. Marshall.
“Preparedness is key,” Dr. Chu noted. “Managing this has required a unified effort” that addresses everything from the supply chain for personal protective equipment, to cleaning procedures, to engineering fixes that quickly added negative-pressure rooms.
“I can’t emphasize enough that this is a team sport,” said Dr. Marshall.
The unpredictable clinical course of COVID-19
The chimeric clinical course of COVID-19 means clinicians need to keep an open mind and be ready to act nimbly, said the EvergreenHealth hospitalists. Pattern recognition is a key to competent clinical management of hospitalized patients, but the course of coronavirus thus far defies any convenient application of heuristics.
Those first two patients had some characteristics in common, aside from their arrival from the same long-term care facility They each had unexplained acute respiratory distress syndrome and ground-glass opacities seen on chest CT, said Dr. Marshall. But all agreed it is still not clear who will fare well, and who will do poorly once they are admitted with coronavirus.
“We have noticed that these patients tend to have a rough course,” said Dr. Marshall. The “brisk inflammatory response” seen in some patients manifests in persistent fevers, big C-reactive protein (CRP) elevations, and likely is part of the picture of yet-unknown host factors that contribute to a worse disease course for some, she said. “These patients look toxic for a long time.”
Dr. Chu said that he’s seen even younger, healthier-looking patients admitted from the emergency department who are already quite dyspneic and may be headed for ventilation. These patients may have a low procalcitonin, and will often turn out to have an “impressive-looking” chest x-ray or CT that will show prominent bilateral infiltrates.
On the other hand, said Dr. Marshall, she and her colleagues have admitted frail-appearing nonagenarians who “just kind of sleep it off,” with little more than a cough and intermittent fevers.
Dr. Chu concurred: “So many of these patients had risk factors for severe disease and only had mild illness. Many were really quite stable.”
In terms of managing respiratory status, Dr. Baker said that the time to start planning for intubation is when the supplemental oxygen demands of COVID-19 patients start to go up. Unlike with patients who may be in some respiratory distress from other causes, once these patients have increased Fi02 needs, bridging “doesn’t work. ... They need to be intubated. Early intubation is important.” Clinicians’ level of concern should spike when they see increased work of breathing in a coronavirus patient, regardless of what the numbers are saying, he added.
For coronavirus patients with acute respiratory distress syndrome (ARDS), early proning also seems to provide some benefit, he said. At EvergreenHealth, standard ARDS ventilation protocols are being followed, including low tidal volume ventilation and positive end-expiratory pressure (PEEP) ladders. Coronavirus ventilation management has thus far been “pretty similar to standard practice with ARDS patients,” he said.
The hospitalist team was able to tap into the building knowledge base in China: Two of the EvergreenHealth hospitalists spoke fluent Mandarin, and one had contacts in China that allowed her to connect with Chinese physicians who had been treating COVID-19 patients since that outbreak had started. They established regular communication on WeChat, checking in frequently for updates on therapies and diagnostics being used in China as well.
One benefit of being in communication with colleagues in China, said Dr. Baker, was that they were able to get anecdotal evidence that elevated D-dimer levels and highly elevated CRP levels can portend a worse illness course. These findings seem to have held generally true for EvergreenHealth patients, he said. Dr. Marshall also spoke to the value of early communication with Chinese teams, who confirmed that the picture of a febrile illness with elevated CRP and leukopenia should raise the index of suspicion for coronavirus.
“Patients might improve over a few days, and then in the final 24 hours of their lives, we see changes in hemodynamics,” including reduced ejection fraction consistent with cardiogenic shock, as well as arrhythmias, said Dr. Baker. Some of the early patient deaths at EvergreenHealth followed this pattern, he said, noting that others have called for investigation into whether viral myocarditis is at play in some coronavirus deaths.
Moderately and severely ill coronavirus patients at EvergreenHealth currently receive a course of hydroxychloroquine of approximately 4-5 days’ duration. The hospital obtained remdesivir from Gilead through its compassionate-use program early on, and now is participating in a clinical trial for COVID-19 patients in the ICU.
By March 23, the facility had seen 162 confirmed COVID-19 cases, and 30 patients had died. Twenty-two inpatients had been discharged, and an additional 58 who were seen in the emergency department had been discharged home without admission.
Be suspicious – and prepared
When asked what he’d like his colleagues around the country to know as they diagnose and admit their first patients who are ill with coronavirus, Dr. Baker advised maintaining a high index of suspicion and a low threshold for testing. “I’ve given some thought to this,” he said. “From our reading and what information is out there, we are geared to pick up on the classic symptoms of coronavirus – cough, fever, some gastrointestinal symptoms.” However, many elderly patients “are not good historians. Some may have advanced dementia. ... When patients arrive with no history, we do our best to gather information,” but sometimes a case can still take clinicians by surprise, he said.
Dr. Baker told a cautionary tale of one of his patients, a woman who was admitted for a hip fracture after a fall at an assisted living facility. The patient was mildly hypoxic, but had an unremarkable physical exam, no fever, and a clear chest x-ray. She went to surgery and then to a postoperative floor with no isolation measures. When her respiratory status unexpectedly deteriorated, she was tested for COVID-19 – and was positive.
“When in doubt, isolate,” said Dr. Baker.
Dr. Chu concurred: “As soon as you suspect, move them, rather than testing first.”
Dr. Baker acknowledged, though, that when testing criteria and availability of personal protective equipment and test materials may vary by region, “it’s a challenge, especially with limited resources.”
Dr. Chu said that stringent isolation, though necessary, creates great hardship for patients and families. “It’s really important for us to check in with family members,” he said; patients are alone and afraid, and family members feel cut off – and also afraid on behalf of their ill loved ones. Workflow planning should acknowledge this and allocate extra time for patient connection and a little more time on the phone with families.
Dr. Chu offered a sobering final word. Make sure family members know their ill loved one’s wishes for care, he said: “There’s never been a better time to clarify code status on admission.”
Physicians at EvergreenHealth have created a document that contains consolidated information on what to anticipate and how to prepare for the arrival of COVID-19+ patients, recommendations on maximizing safety in the hospital environment, and key clinical management considerations. The document will be updated as new information arises.
Correction, 3/27/20: An earlier version of this article referenced white blood counts, presence of lymphopenia, and elevated hepatic enzymes for patients at EvergreenHealth when in fact that information pertained to patients in China. That paragraph has been deleted.
Step 1 scoring moves to pass/fail: Hospitalists’ role and unintended consequences
The National Board of Medical Examiners recently announced a change in the United States Medical Licensing Examination (USMLE) Step 1 score reporting from a 3-digit score to a pass/fail score beginning in 2022.1 Endorsed by a broad coalition of organizations involved in undergraduate (UME) and graduate medical education (GME), this change is intended as a first step toward systemic improvements in the UME-GME transition to residency by promoting holistic reviews of applicants. Additionally, it is meant to tackle widespread concerns about medical student distress brought about by the residency selection process. For example, switching to pass/fail preclinical curricula has resulted in an improvement in medical student well-being at many medical schools.2 It is the hope that a mirrored change in Step 1 may similarly improve mental health and encourage a growth mindset towards learning.
On the other hand, many residency programs rely on USMLE scores for screening potential candidates, especially as application inflation has burdened programs with thousands of applications.3 The change to a pass/fail Step 1 score will likely shift emphasis and stress to the Step 2 CK Exam, essentially negating the intended effect. Furthermore, for schools still reporting NBME Subject (shelf) Exam scores and Clerkship grades, there will likely be a greater emphasis placed on these metrics as well. The need for objective assessment methods are seen by many as so critical that some GME leaders have advocated for instituting entrance exams or requiring a Standardized Letter of Evaluation as a prerequisite to residency application. Finally, medical students jockeying for competitive residency positions may also feel pressured to distinguish themselves by boosting other aspects of their portfolio by taking a research year or applying for away electives, which risks marginalizing students of lesser means or with family responsibilities.
Ultimately, the change to a pass/fail Step 1 exam will likely do little to address the expanding gulf between the UME and GME communities. Residency program directors are searching for students with qualities of a good physician, such as interpersonal skills, “teamsmanship,” compassion, and professionalism, but reliable, objective, and standardized assessment tools are not available. Currently our best tools are clinical evaluations which are subject to grade inflation and implicit racial and gender biases. Furthermore, other components of a residency application, such as letters of recommendation, Chair’s letters, and the Medical Student Performance Evaluation (Dean’s letter), are regarded to be less informative as schools move toward no student rankings, pass/fail grading schemes, and nonstandardized summative adjectives to describe medical students overall medical school performance.
Finally, medical student distress in the residency application process may stem from the perpetuation of elitism that extends from medical school to fellowship training and academic hospital medicine. Rankings of medical schools, residencies, fellowships, and hospitals serve to create a hierarchical system. Competitive residency applicants see admittance into the best training programs as opening doors to opportunities, while not getting into these programs is seen as closing doors to career paths and opportunities.
With this change in Step 1 score reporting, where do we as hospitalists fit in? Hospitalists are at the forefront of educating and evaluating medical students in academic medical centers, and we are often asked to write letters of recommendation and serve as mentors. If done well, these activities can have a positive impact on medical student applications to residency by alleviating some of the stresses and mitigating the downsides to the new Step 1 scoring system. Writing impactful letters and thoughtful evaluations are all skills that should be incorporated in hospitalist faculty development programs. Moreover, in order to serve as better advocates for our students, it is important that academic hospitalists understand the evolving landscape of the residency application process and are mindful of the stresses that medical students face. Changing Step 1 scoring to pass/fail will likely have unintended consequences for our medical students, and we as hospitalists must be ready to improve our knowledge and skills in order to continue to support and advocate for our medical students.
Dr. Esquivel is a hospitalist and assistant professor at Weill Cornell Medical College in New York; Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis; Dr. Ricotta is a hospitalist at Beth Israel Deaconess Medical Center, Boston, and instructor in medicine at Harvard Medical School; Dr. Rendon is a hospitalist at the University of New Mexico in Albuquerque; Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee.
References
1. United States Medical Licensing Examination (2020 Feb). Change to pass/fail score reporting for Step 1.
2. Slavin SJ and Chibnall JT. Finding the why, changing the how: Improving the mental health of medical students, residents, and physicians. Academic Medicine. 2016;91(9):1194‐6.
3. Pereira AG, Chelminski PR, et al. Application inflation for internal medicine applicants in the Match: Drivers, consequences, and potential solutions. Am J Med. 2016 Aug;129(8): 885-91.
The National Board of Medical Examiners recently announced a change in the United States Medical Licensing Examination (USMLE) Step 1 score reporting from a 3-digit score to a pass/fail score beginning in 2022.1 Endorsed by a broad coalition of organizations involved in undergraduate (UME) and graduate medical education (GME), this change is intended as a first step toward systemic improvements in the UME-GME transition to residency by promoting holistic reviews of applicants. Additionally, it is meant to tackle widespread concerns about medical student distress brought about by the residency selection process. For example, switching to pass/fail preclinical curricula has resulted in an improvement in medical student well-being at many medical schools.2 It is the hope that a mirrored change in Step 1 may similarly improve mental health and encourage a growth mindset towards learning.
On the other hand, many residency programs rely on USMLE scores for screening potential candidates, especially as application inflation has burdened programs with thousands of applications.3 The change to a pass/fail Step 1 score will likely shift emphasis and stress to the Step 2 CK Exam, essentially negating the intended effect. Furthermore, for schools still reporting NBME Subject (shelf) Exam scores and Clerkship grades, there will likely be a greater emphasis placed on these metrics as well. The need for objective assessment methods are seen by many as so critical that some GME leaders have advocated for instituting entrance exams or requiring a Standardized Letter of Evaluation as a prerequisite to residency application. Finally, medical students jockeying for competitive residency positions may also feel pressured to distinguish themselves by boosting other aspects of their portfolio by taking a research year or applying for away electives, which risks marginalizing students of lesser means or with family responsibilities.
Ultimately, the change to a pass/fail Step 1 exam will likely do little to address the expanding gulf between the UME and GME communities. Residency program directors are searching for students with qualities of a good physician, such as interpersonal skills, “teamsmanship,” compassion, and professionalism, but reliable, objective, and standardized assessment tools are not available. Currently our best tools are clinical evaluations which are subject to grade inflation and implicit racial and gender biases. Furthermore, other components of a residency application, such as letters of recommendation, Chair’s letters, and the Medical Student Performance Evaluation (Dean’s letter), are regarded to be less informative as schools move toward no student rankings, pass/fail grading schemes, and nonstandardized summative adjectives to describe medical students overall medical school performance.
Finally, medical student distress in the residency application process may stem from the perpetuation of elitism that extends from medical school to fellowship training and academic hospital medicine. Rankings of medical schools, residencies, fellowships, and hospitals serve to create a hierarchical system. Competitive residency applicants see admittance into the best training programs as opening doors to opportunities, while not getting into these programs is seen as closing doors to career paths and opportunities.
With this change in Step 1 score reporting, where do we as hospitalists fit in? Hospitalists are at the forefront of educating and evaluating medical students in academic medical centers, and we are often asked to write letters of recommendation and serve as mentors. If done well, these activities can have a positive impact on medical student applications to residency by alleviating some of the stresses and mitigating the downsides to the new Step 1 scoring system. Writing impactful letters and thoughtful evaluations are all skills that should be incorporated in hospitalist faculty development programs. Moreover, in order to serve as better advocates for our students, it is important that academic hospitalists understand the evolving landscape of the residency application process and are mindful of the stresses that medical students face. Changing Step 1 scoring to pass/fail will likely have unintended consequences for our medical students, and we as hospitalists must be ready to improve our knowledge and skills in order to continue to support and advocate for our medical students.
Dr. Esquivel is a hospitalist and assistant professor at Weill Cornell Medical College in New York; Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis; Dr. Ricotta is a hospitalist at Beth Israel Deaconess Medical Center, Boston, and instructor in medicine at Harvard Medical School; Dr. Rendon is a hospitalist at the University of New Mexico in Albuquerque; Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee.
References
1. United States Medical Licensing Examination (2020 Feb). Change to pass/fail score reporting for Step 1.
2. Slavin SJ and Chibnall JT. Finding the why, changing the how: Improving the mental health of medical students, residents, and physicians. Academic Medicine. 2016;91(9):1194‐6.
3. Pereira AG, Chelminski PR, et al. Application inflation for internal medicine applicants in the Match: Drivers, consequences, and potential solutions. Am J Med. 2016 Aug;129(8): 885-91.
The National Board of Medical Examiners recently announced a change in the United States Medical Licensing Examination (USMLE) Step 1 score reporting from a 3-digit score to a pass/fail score beginning in 2022.1 Endorsed by a broad coalition of organizations involved in undergraduate (UME) and graduate medical education (GME), this change is intended as a first step toward systemic improvements in the UME-GME transition to residency by promoting holistic reviews of applicants. Additionally, it is meant to tackle widespread concerns about medical student distress brought about by the residency selection process. For example, switching to pass/fail preclinical curricula has resulted in an improvement in medical student well-being at many medical schools.2 It is the hope that a mirrored change in Step 1 may similarly improve mental health and encourage a growth mindset towards learning.
On the other hand, many residency programs rely on USMLE scores for screening potential candidates, especially as application inflation has burdened programs with thousands of applications.3 The change to a pass/fail Step 1 score will likely shift emphasis and stress to the Step 2 CK Exam, essentially negating the intended effect. Furthermore, for schools still reporting NBME Subject (shelf) Exam scores and Clerkship grades, there will likely be a greater emphasis placed on these metrics as well. The need for objective assessment methods are seen by many as so critical that some GME leaders have advocated for instituting entrance exams or requiring a Standardized Letter of Evaluation as a prerequisite to residency application. Finally, medical students jockeying for competitive residency positions may also feel pressured to distinguish themselves by boosting other aspects of their portfolio by taking a research year or applying for away electives, which risks marginalizing students of lesser means or with family responsibilities.
Ultimately, the change to a pass/fail Step 1 exam will likely do little to address the expanding gulf between the UME and GME communities. Residency program directors are searching for students with qualities of a good physician, such as interpersonal skills, “teamsmanship,” compassion, and professionalism, but reliable, objective, and standardized assessment tools are not available. Currently our best tools are clinical evaluations which are subject to grade inflation and implicit racial and gender biases. Furthermore, other components of a residency application, such as letters of recommendation, Chair’s letters, and the Medical Student Performance Evaluation (Dean’s letter), are regarded to be less informative as schools move toward no student rankings, pass/fail grading schemes, and nonstandardized summative adjectives to describe medical students overall medical school performance.
Finally, medical student distress in the residency application process may stem from the perpetuation of elitism that extends from medical school to fellowship training and academic hospital medicine. Rankings of medical schools, residencies, fellowships, and hospitals serve to create a hierarchical system. Competitive residency applicants see admittance into the best training programs as opening doors to opportunities, while not getting into these programs is seen as closing doors to career paths and opportunities.
With this change in Step 1 score reporting, where do we as hospitalists fit in? Hospitalists are at the forefront of educating and evaluating medical students in academic medical centers, and we are often asked to write letters of recommendation and serve as mentors. If done well, these activities can have a positive impact on medical student applications to residency by alleviating some of the stresses and mitigating the downsides to the new Step 1 scoring system. Writing impactful letters and thoughtful evaluations are all skills that should be incorporated in hospitalist faculty development programs. Moreover, in order to serve as better advocates for our students, it is important that academic hospitalists understand the evolving landscape of the residency application process and are mindful of the stresses that medical students face. Changing Step 1 scoring to pass/fail will likely have unintended consequences for our medical students, and we as hospitalists must be ready to improve our knowledge and skills in order to continue to support and advocate for our medical students.
Dr. Esquivel is a hospitalist and assistant professor at Weill Cornell Medical College in New York; Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis; Dr. Ricotta is a hospitalist at Beth Israel Deaconess Medical Center, Boston, and instructor in medicine at Harvard Medical School; Dr. Rendon is a hospitalist at the University of New Mexico in Albuquerque; Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee.
References
1. United States Medical Licensing Examination (2020 Feb). Change to pass/fail score reporting for Step 1.
2. Slavin SJ and Chibnall JT. Finding the why, changing the how: Improving the mental health of medical students, residents, and physicians. Academic Medicine. 2016;91(9):1194‐6.
3. Pereira AG, Chelminski PR, et al. Application inflation for internal medicine applicants in the Match: Drivers, consequences, and potential solutions. Am J Med. 2016 Aug;129(8): 885-91.
Treatment options for COVID-19: Dr. Annie Luetkemeyer
Annie Luetkemeyer, MD, professor of infectious diseases at UCSF, is an expert on the treatment of viral infections. Robert Wachter, MD, MHM, chair of the UCSF Department of Medicine, interviewed her about the evidence behind potential treatments for COVID-19 (including chloroquine/hydroxychloroquine, remdesivir, and others), as well as how to assess new and existing drugs in a pandemic.
Annie Luetkemeyer, MD, professor of infectious diseases at UCSF, is an expert on the treatment of viral infections. Robert Wachter, MD, MHM, chair of the UCSF Department of Medicine, interviewed her about the evidence behind potential treatments for COVID-19 (including chloroquine/hydroxychloroquine, remdesivir, and others), as well as how to assess new and existing drugs in a pandemic.
Annie Luetkemeyer, MD, professor of infectious diseases at UCSF, is an expert on the treatment of viral infections. Robert Wachter, MD, MHM, chair of the UCSF Department of Medicine, interviewed her about the evidence behind potential treatments for COVID-19 (including chloroquine/hydroxychloroquine, remdesivir, and others), as well as how to assess new and existing drugs in a pandemic.
Get out the inpatient vote
Disenfranchisement undeniably remains a major problem across the United States. While it is challenging for health care providers to find time to vote, hospitalized patients are an underrecognized vulnerable group, often unable to exercise this constitutional right. With the 2020 election approaching, voting is as important as ever.
On morning rounds after the 2018 election, we discussed the impact of a changing majority in the House of Representatives and its potential impact on health care in America. We discussed where, when, and how we voted, and then suddenly considered a question that we were unable to answer: How do our hospitalized patients vote and did any of them vote in this important election?
Inpatients rarely know when or how long they will be hospitalized. They often have no chance to prepare by paying bills, arranging care for loved ones, or finding coverage for employment responsibilities. The sickest patients can do little more than wonder about anything other than their short-term health. As a result of restricted voting laws, they, like too many others, are effectively disenfranchised.
We asked administrators in multiple hospitals across New York City how to help our patients vote. Unfortunately, the process is overwhelmingly complex and varies by state. Absentee ballots, which are easily accessible in New York if it they are requested no later than 7 days before the election, are harder to come by on the same day. Most people struggle to vote in general – with only 61% voting in the 2016 election.1 To combat this, individual hospitals have created initiatives such as Penn Votes, which has helped 65 hospitalized Pennsylvania residents vote in the last three elections2 – a success, but still leaving so many without a voice.
With health care being a major policy issue for the 2020 election, voting has never been more important for patients. With nearly 1 million hospital beds in America,3 hospitalized patients represent a significant number of potential voters who are functionally disenfranchised. Most importantly, these patients are directly under our care, and we are their strongest advocates. Therefore, we ask our fellow health care providers to start planning today how we will help our patients exercise their voices, participate in our health care policy debate, and choose the future leaders of our country.
Dr. Rosenblatt is assistant professor of medicine, Division of Gastroenterology and Hepatology, at Weill Cornell Medicine, New York. Dr. Verna is assistant professor of medicine, Department of Surgery, at Columbia University Irving Medical School, New York. Dr. Rosenblatt and Dr. Verna reported having no relevant conflicts of interest.
References
1. File T. Voting in America: A Look at the 2016 Presidential Election [Internet]. 2017 [cited 2020 Jan 7];Available from: https://www.census.gov/newsroom/blogs/random-samplings/2017/05/voting_in_america.html.
2. Vigodner S. Penn students are helping hospitalized patients cast emergency ballots for Tuesday’s election [Internet]. Dly. Pennsylvanian. 2018;Available from: https://www.thedp.com/article/2018/11/penn-med-votes-emergency-hospital-patients-upenn-philadelphia-elections.
3. Association AH. Fast facts on US hospitals [Internet]. 2019 [cited 2020 Jan 7];Available from: https://www.aha.org/statistics/fast-facts-us-hospitals.
Disenfranchisement undeniably remains a major problem across the United States. While it is challenging for health care providers to find time to vote, hospitalized patients are an underrecognized vulnerable group, often unable to exercise this constitutional right. With the 2020 election approaching, voting is as important as ever.
On morning rounds after the 2018 election, we discussed the impact of a changing majority in the House of Representatives and its potential impact on health care in America. We discussed where, when, and how we voted, and then suddenly considered a question that we were unable to answer: How do our hospitalized patients vote and did any of them vote in this important election?
Inpatients rarely know when or how long they will be hospitalized. They often have no chance to prepare by paying bills, arranging care for loved ones, or finding coverage for employment responsibilities. The sickest patients can do little more than wonder about anything other than their short-term health. As a result of restricted voting laws, they, like too many others, are effectively disenfranchised.
We asked administrators in multiple hospitals across New York City how to help our patients vote. Unfortunately, the process is overwhelmingly complex and varies by state. Absentee ballots, which are easily accessible in New York if it they are requested no later than 7 days before the election, are harder to come by on the same day. Most people struggle to vote in general – with only 61% voting in the 2016 election.1 To combat this, individual hospitals have created initiatives such as Penn Votes, which has helped 65 hospitalized Pennsylvania residents vote in the last three elections2 – a success, but still leaving so many without a voice.
With health care being a major policy issue for the 2020 election, voting has never been more important for patients. With nearly 1 million hospital beds in America,3 hospitalized patients represent a significant number of potential voters who are functionally disenfranchised. Most importantly, these patients are directly under our care, and we are their strongest advocates. Therefore, we ask our fellow health care providers to start planning today how we will help our patients exercise their voices, participate in our health care policy debate, and choose the future leaders of our country.
Dr. Rosenblatt is assistant professor of medicine, Division of Gastroenterology and Hepatology, at Weill Cornell Medicine, New York. Dr. Verna is assistant professor of medicine, Department of Surgery, at Columbia University Irving Medical School, New York. Dr. Rosenblatt and Dr. Verna reported having no relevant conflicts of interest.
References
1. File T. Voting in America: A Look at the 2016 Presidential Election [Internet]. 2017 [cited 2020 Jan 7];Available from: https://www.census.gov/newsroom/blogs/random-samplings/2017/05/voting_in_america.html.
2. Vigodner S. Penn students are helping hospitalized patients cast emergency ballots for Tuesday’s election [Internet]. Dly. Pennsylvanian. 2018;Available from: https://www.thedp.com/article/2018/11/penn-med-votes-emergency-hospital-patients-upenn-philadelphia-elections.
3. Association AH. Fast facts on US hospitals [Internet]. 2019 [cited 2020 Jan 7];Available from: https://www.aha.org/statistics/fast-facts-us-hospitals.
Disenfranchisement undeniably remains a major problem across the United States. While it is challenging for health care providers to find time to vote, hospitalized patients are an underrecognized vulnerable group, often unable to exercise this constitutional right. With the 2020 election approaching, voting is as important as ever.
On morning rounds after the 2018 election, we discussed the impact of a changing majority in the House of Representatives and its potential impact on health care in America. We discussed where, when, and how we voted, and then suddenly considered a question that we were unable to answer: How do our hospitalized patients vote and did any of them vote in this important election?
Inpatients rarely know when or how long they will be hospitalized. They often have no chance to prepare by paying bills, arranging care for loved ones, or finding coverage for employment responsibilities. The sickest patients can do little more than wonder about anything other than their short-term health. As a result of restricted voting laws, they, like too many others, are effectively disenfranchised.
We asked administrators in multiple hospitals across New York City how to help our patients vote. Unfortunately, the process is overwhelmingly complex and varies by state. Absentee ballots, which are easily accessible in New York if it they are requested no later than 7 days before the election, are harder to come by on the same day. Most people struggle to vote in general – with only 61% voting in the 2016 election.1 To combat this, individual hospitals have created initiatives such as Penn Votes, which has helped 65 hospitalized Pennsylvania residents vote in the last three elections2 – a success, but still leaving so many without a voice.
With health care being a major policy issue for the 2020 election, voting has never been more important for patients. With nearly 1 million hospital beds in America,3 hospitalized patients represent a significant number of potential voters who are functionally disenfranchised. Most importantly, these patients are directly under our care, and we are their strongest advocates. Therefore, we ask our fellow health care providers to start planning today how we will help our patients exercise their voices, participate in our health care policy debate, and choose the future leaders of our country.
Dr. Rosenblatt is assistant professor of medicine, Division of Gastroenterology and Hepatology, at Weill Cornell Medicine, New York. Dr. Verna is assistant professor of medicine, Department of Surgery, at Columbia University Irving Medical School, New York. Dr. Rosenblatt and Dr. Verna reported having no relevant conflicts of interest.
References
1. File T. Voting in America: A Look at the 2016 Presidential Election [Internet]. 2017 [cited 2020 Jan 7];Available from: https://www.census.gov/newsroom/blogs/random-samplings/2017/05/voting_in_america.html.
2. Vigodner S. Penn students are helping hospitalized patients cast emergency ballots for Tuesday’s election [Internet]. Dly. Pennsylvanian. 2018;Available from: https://www.thedp.com/article/2018/11/penn-med-votes-emergency-hospital-patients-upenn-philadelphia-elections.
3. Association AH. Fast facts on US hospitals [Internet]. 2019 [cited 2020 Jan 7];Available from: https://www.aha.org/statistics/fast-facts-us-hospitals.
Managing the COVID-19 isolation floor at UCSF Medical Center
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Dramatic rise in hypertension-related deaths in the United States
There has been a dramatic rise in hypertension-related deaths in the United States between 2007 and 2017, a new study shows. The authors, led by Lakshmi Nambiar, MD, Larner College of Medicine, University of Vermont, Burlington, analyzed data from the Centers for Disease Control and Prevention, which collates information from every death certificate in the country, amounting to more than 10 million deaths.
They found that age-adjusted hypertension-related deaths had increased from 18.3 per 100,000 in 2007 to 23.0 per 100,000 in 2017 (P < .001 for decade-long temporal trend).
Nambiar reported results of the study at an American College of Cardiology 2020/World Congress of Cardiology press conference on March 19. It was also published online on the same day in the Journal of the American College of Cardiology.
She noted that death rates due to cardiovascular disease have been falling over the past 20 years largely attributable to statins to treat high cholesterol and stents to treat coronary artery disease. But since 2011, the rate of decline in cardiovascular deaths has slowed. One contributing factor is an increase in heart failure-related deaths but there hasn’t been any data in recent years on hypertension-related deaths.
“Our data show an increase in hypertension-related deaths in all age groups, in all regions of the United States, and in both sexes. These findings are alarming and warrant further investigation, as well as preventative efforts,” Nambiar said. “This is a public health emergency that has not been fully recognized,” she added.
“We were surprised to see how dramatically these deaths were increasing, and we think this is related to the rise in diabetes, obesity, and the aging of the population. We need targeted public health measures to address some of those factors,” Nambiar told Medscape Medical News.
“We are winning the battle against coronary artery disease with statins and stents but we are not winning the battle against hypertension,” she added.
Worst Figures in Rural South
Results showed that hypertension-related deaths increased in both rural and urban regions, but the increase was much steeper in rural areas — a 72% increase over the decade compared with a 20% increase in urban areas.
The highest death risk was identified in the rural South, which demonstrated an age-adjusted 2.5-fold higher death rate compared with other regions (P < .001).
The urban South also demonstrated increasing hypertension-related cardiovascular death rates over time: age-adjusted death rates in the urban South increased by 27% compared with all other urban regions (P < .001).
But the absolute mortality rates and slope of the curves demonstrate the highest risk in patients in the rural South, the researchers report. Age-adjusted hypertension-related death rates increased in the rural South from 23.9 deaths per 100,000 in 2007 to 39.5 deaths per 100,000 in 2017.
Nambiar said the trends in the rural South could be related to social factors and lack of access to healthcare in the area, which has been exacerbated by failure to adopt Medicaid expansion in many of the states in this region.
“When it comes to the management of hypertension you need to be seen regularly by a primary care doctor to get the best treatment and regular assessments,” she stressed.
Chair of the ACC press conference at which the data were presented, Martha Gulati, MD, University of Arizona School of Medicine, Phoenix, said: “In this day and time, there is less smoking, which should translate into lower rates of hypertension, but these trends reported here are very different from what we would expect and are probably associated with the rise in other risk factors such as diabetes and obesity, especially in the rural South.”
Nambiar praised the new ACC/AHA hypertension guidelines that recommend a lower diagnostic threshold, “so more people now fit the criteria for raised blood pressure and need treatment.”
“It is important for all primary care physicians and cardiologists to recognize the new threshold and treat people accordingly,” she said. “High blood pressure is the leading cause of cardiovascular disease. If we can control it better, we may be able to control some of this increased mortality we are seeing.”
This article first appeared on Medscape.com.
There has been a dramatic rise in hypertension-related deaths in the United States between 2007 and 2017, a new study shows. The authors, led by Lakshmi Nambiar, MD, Larner College of Medicine, University of Vermont, Burlington, analyzed data from the Centers for Disease Control and Prevention, which collates information from every death certificate in the country, amounting to more than 10 million deaths.
They found that age-adjusted hypertension-related deaths had increased from 18.3 per 100,000 in 2007 to 23.0 per 100,000 in 2017 (P < .001 for decade-long temporal trend).
Nambiar reported results of the study at an American College of Cardiology 2020/World Congress of Cardiology press conference on March 19. It was also published online on the same day in the Journal of the American College of Cardiology.
She noted that death rates due to cardiovascular disease have been falling over the past 20 years largely attributable to statins to treat high cholesterol and stents to treat coronary artery disease. But since 2011, the rate of decline in cardiovascular deaths has slowed. One contributing factor is an increase in heart failure-related deaths but there hasn’t been any data in recent years on hypertension-related deaths.
“Our data show an increase in hypertension-related deaths in all age groups, in all regions of the United States, and in both sexes. These findings are alarming and warrant further investigation, as well as preventative efforts,” Nambiar said. “This is a public health emergency that has not been fully recognized,” she added.
“We were surprised to see how dramatically these deaths were increasing, and we think this is related to the rise in diabetes, obesity, and the aging of the population. We need targeted public health measures to address some of those factors,” Nambiar told Medscape Medical News.
“We are winning the battle against coronary artery disease with statins and stents but we are not winning the battle against hypertension,” she added.
Worst Figures in Rural South
Results showed that hypertension-related deaths increased in both rural and urban regions, but the increase was much steeper in rural areas — a 72% increase over the decade compared with a 20% increase in urban areas.
The highest death risk was identified in the rural South, which demonstrated an age-adjusted 2.5-fold higher death rate compared with other regions (P < .001).
The urban South also demonstrated increasing hypertension-related cardiovascular death rates over time: age-adjusted death rates in the urban South increased by 27% compared with all other urban regions (P < .001).
But the absolute mortality rates and slope of the curves demonstrate the highest risk in patients in the rural South, the researchers report. Age-adjusted hypertension-related death rates increased in the rural South from 23.9 deaths per 100,000 in 2007 to 39.5 deaths per 100,000 in 2017.
Nambiar said the trends in the rural South could be related to social factors and lack of access to healthcare in the area, which has been exacerbated by failure to adopt Medicaid expansion in many of the states in this region.
“When it comes to the management of hypertension you need to be seen regularly by a primary care doctor to get the best treatment and regular assessments,” she stressed.
Chair of the ACC press conference at which the data were presented, Martha Gulati, MD, University of Arizona School of Medicine, Phoenix, said: “In this day and time, there is less smoking, which should translate into lower rates of hypertension, but these trends reported here are very different from what we would expect and are probably associated with the rise in other risk factors such as diabetes and obesity, especially in the rural South.”
Nambiar praised the new ACC/AHA hypertension guidelines that recommend a lower diagnostic threshold, “so more people now fit the criteria for raised blood pressure and need treatment.”
“It is important for all primary care physicians and cardiologists to recognize the new threshold and treat people accordingly,” she said. “High blood pressure is the leading cause of cardiovascular disease. If we can control it better, we may be able to control some of this increased mortality we are seeing.”
This article first appeared on Medscape.com.
There has been a dramatic rise in hypertension-related deaths in the United States between 2007 and 2017, a new study shows. The authors, led by Lakshmi Nambiar, MD, Larner College of Medicine, University of Vermont, Burlington, analyzed data from the Centers for Disease Control and Prevention, which collates information from every death certificate in the country, amounting to more than 10 million deaths.
They found that age-adjusted hypertension-related deaths had increased from 18.3 per 100,000 in 2007 to 23.0 per 100,000 in 2017 (P < .001 for decade-long temporal trend).
Nambiar reported results of the study at an American College of Cardiology 2020/World Congress of Cardiology press conference on March 19. It was also published online on the same day in the Journal of the American College of Cardiology.
She noted that death rates due to cardiovascular disease have been falling over the past 20 years largely attributable to statins to treat high cholesterol and stents to treat coronary artery disease. But since 2011, the rate of decline in cardiovascular deaths has slowed. One contributing factor is an increase in heart failure-related deaths but there hasn’t been any data in recent years on hypertension-related deaths.
“Our data show an increase in hypertension-related deaths in all age groups, in all regions of the United States, and in both sexes. These findings are alarming and warrant further investigation, as well as preventative efforts,” Nambiar said. “This is a public health emergency that has not been fully recognized,” she added.
“We were surprised to see how dramatically these deaths were increasing, and we think this is related to the rise in diabetes, obesity, and the aging of the population. We need targeted public health measures to address some of those factors,” Nambiar told Medscape Medical News.
“We are winning the battle against coronary artery disease with statins and stents but we are not winning the battle against hypertension,” she added.
Worst Figures in Rural South
Results showed that hypertension-related deaths increased in both rural and urban regions, but the increase was much steeper in rural areas — a 72% increase over the decade compared with a 20% increase in urban areas.
The highest death risk was identified in the rural South, which demonstrated an age-adjusted 2.5-fold higher death rate compared with other regions (P < .001).
The urban South also demonstrated increasing hypertension-related cardiovascular death rates over time: age-adjusted death rates in the urban South increased by 27% compared with all other urban regions (P < .001).
But the absolute mortality rates and slope of the curves demonstrate the highest risk in patients in the rural South, the researchers report. Age-adjusted hypertension-related death rates increased in the rural South from 23.9 deaths per 100,000 in 2007 to 39.5 deaths per 100,000 in 2017.
Nambiar said the trends in the rural South could be related to social factors and lack of access to healthcare in the area, which has been exacerbated by failure to adopt Medicaid expansion in many of the states in this region.
“When it comes to the management of hypertension you need to be seen regularly by a primary care doctor to get the best treatment and regular assessments,” she stressed.
Chair of the ACC press conference at which the data were presented, Martha Gulati, MD, University of Arizona School of Medicine, Phoenix, said: “In this day and time, there is less smoking, which should translate into lower rates of hypertension, but these trends reported here are very different from what we would expect and are probably associated with the rise in other risk factors such as diabetes and obesity, especially in the rural South.”
Nambiar praised the new ACC/AHA hypertension guidelines that recommend a lower diagnostic threshold, “so more people now fit the criteria for raised blood pressure and need treatment.”
“It is important for all primary care physicians and cardiologists to recognize the new threshold and treat people accordingly,” she said. “High blood pressure is the leading cause of cardiovascular disease. If we can control it better, we may be able to control some of this increased mortality we are seeing.”
This article first appeared on Medscape.com.
The hospitalized postbariatric surgery patient
What every hospitalist should know
With the prevalence of obesity worldwide topping 650 million people1 and nearly 40% of U.S. adults having obesity,2 bariatric surgery is increasingly used to treat this disease and its associated comorbidities.
The American Society for Metabolic & Bariatric Surgery estimates that 228,000 bariatric procedures were performed on Americans in 2017, up from 158,000 in 2011.3 Despite lowering the risks of diabetes, stroke, myocardial infarction, cancer, and all-cause mortality,4 bariatric surgery is associated with increased health care use. Neovius et al. found that people who underwent bariatric surgery used 54 mean cumulative hospital days in the 20 years following their procedures, compared with just 40 inpatient days used by controls.5
Although hospitalists are caring for increasing numbers of patients who have undergone bariatric surgery, many of us may not be aware of some of the things that can lead to hospitalization or otherwise affect inpatient medical care. Here are a few points to keep in mind the next time you care for an inpatient with prior bariatric surgery.
Pharmacokinetics change after surgery
Gastrointestinal anatomy necessarily changes after bariatric surgery and can affect the oral absorption of drugs. Because gastric motility may be impaired and the pH in the stomach is increased after bariatric surgery, the disintegration and dissolution of immediate-release solid pills or caps may be compromised.
It is therefore prudent to crush solid forms or switch to liquid or chewable formulations of immediate-release drugs for the first few weeks to months after surgery. Enteric-coated or long-acting drug formulations should not be crushed and should generally be avoided in patients who have undergone bypass procedures such as Roux-en-Y gastric bypass (RYGB) or biliopancreatic diversion with duodenal switch (BPD/DS), as they can demonstrate either enhanced or diminished absorption (depending on the drug).
Reduced intestinal transit times and changes in intestinal pH can alter the absorption of certain drugs as well, and the expression of some drug transporter proteins and enzymes such as the CYP3A4 variant of cytochrome P450 – which is estimated to metabolize up to half of currently available drugs – varies between the upper and the lower small intestine, potentially leading to increased bioavailability of medications metabolized by this enzyme in patients who have undergone bypass surgeries.
Interestingly, longer-term studies have reexamined drug absorption in patients 2-4 years after RYGB and found that initially-increased drug plasma levels often return to preoperative levels or even lower over time,6 likely because of adaptive changes in the GI tract. Because research on the pharmacokinetics of individual drugs after bariatric surgery is lacking, the hospitalist should be aware that the bioavailability of oral drugs is often altered and should monitor patients for the desired therapeutic effect as well as potential toxicities for any drug administered to postbariatric surgery patients.
Finally, note that nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and corticosteroids should be avoided after bariatric surgery unless the benefit clearly outweighs the risk, as they increase the risk of ulcers even in patients without underlying surgical disruptions to the gastric mucosa.
Micronutrient deficiencies are common and can occur at any time
While many clinicians recognize that vitamin deficiencies can occur after weight loss surgeries which bypass the duodenum, such as the RYGB or the BPD/DS, it is important to note that vitamin and mineral deficiencies occur commonly even in patients with intact intestinal absorption such as those who underwent sleeve gastrectomy (SG) and even despite regained weight due to greater volumes of food (and micronutrient) intake over time.
The most common vitamin deficiencies include iron, vitamin B12, thiamine (vitamin B1), and vitamin D, but deficiencies in other vitamins and minerals may found as well. Anemia, bone fractures, heart failure, and encephalopathy can all be related to postoperative vitamin deficiencies. Most bariatric surgery patients should have micronutrient levels monitored on a yearly basis and should be taking at least a multivitamin with minerals (including zinc, copper, selenium and iron), a form of vitamin B12, and vitamin D with calcium supplementation. Additional supplements may be appropriate depending on the type of surgery the patient had or whether a deficiency is found.
The differential diagnosis for abdominal pain after bariatric surgery is unique
While the usual suspects such as diverticulitis or gastritis should be considered in postbariatric surgery patients just as in others, a few specific complications can arise after weight loss surgery.
Marginal ulcerations (ulcers at the surgical anastomotic sites) have been reported in up to a third of patients complaining of abdominal pain or dysphagia after RYGB, with tobacco, alcohol, or NSAID use conferring even greater risk.7 Early upper endoscopy may be warranted in symptomatic patients.
Small bowel obstruction (SBO) may occur due to surgical adhesions as in other patients, but catastrophic internal hernias with associated volvulus can occur due to specific anatomical defects that are created by the RYGB and BPD/DS procedures. CT imaging is insensitive and can miss up to 30% of these cases,8 and nasogastric tubes placed blindly for decompression of an SBO can lead to perforation of the end of the alimentary limb at the gastric pouch outlet, so post-RYGB or BPD/DS patients presenting with signs of small bowel obstruction should have an early surgical consult for expeditious surgical management rather than a trial of conservative medical management.9
Cholelithiasis is a very common postoperative complication, occurring in about 25% of SG patients and 32% of RYGB patients in the first year following surgery. The risk of gallstone formation can be significantly reduced with the postoperative use of ursodeoxycholic acid.10
Onset of abdominal cramping, nausea and diarrhea (sometimes accompanied by vasomotor symptoms) within 15-60 minutes of eating may be due to early dumping syndrome. Rapid delivery of food from the gastric pouch into the small intestine causes the release of gut peptides and an osmotic fluid shift into the intestinal lumen that can trigger these symptoms even in patients with a preserved pyloric sphincter, such as those who underwent SG. Simply eliminating sugars and simple carbohydrates from the diet usually resolves the problem, and eliminating lactose can often be helpful as well.
Postprandial hyperinsulinemic hypoglycemia (“late dumping syndrome”) can develop years after surgery
Vasomotor symptoms such as flushing/sweating, shaking, tachycardia/palpitations, lightheadedness, or difficulty concentrating occurring 1-3 hours after a meal should prompt blood glucose testing, as delayed hypoglycemia can occur after a large insulin surge.
Most commonly seen after RYGB, late dumping syndrome, like early dumping syndrome, can often be managed by eliminating sugars and simple carbohydrates from the diet. The onset of late dumping syndrome has been reported as late as 8 years after surgery,11 so the etiology of symptoms can be elusive. If the diagnosis is unclear, an oral glucose tolerance test may be helpful.
Alcohol use disorder is more prevalent after weight loss surgery
Changes to the gastrointestinal anatomy allow for more rapid absorption of ethanol into the bloodstream, making the drug more potent in postop patients. Simultaneously, many patients who undergo bariatric surgery have a history of using food to buffer negative emotions. Abruptly depriving them of that comfort in the context of the increased potency of alcohol could potentially leave bariatric surgery patients vulnerable to the development of alcohol use disorder, even when they did not misuse alcohol preoperatively.
Of note, alcohol misuse becomes more prevalent after the first postoperative year.12 Screening for alcohol misuse on admission to the hospital is wise in all cases, but perhaps even more so in the postbariatric surgery patient. If a patient does report excessive alcohol use, keep possible thiamine deficiency in mind.
The risk of suicide and self-harm increases after bariatric surgery
While all-cause mortality rates decrease after bariatric surgery compared with matched controls, the risk of suicide and nonfatal self-harm increases.
About half of bariatric surgery patients with nonfatal events have substance misuse.13 Notably, several studies have found reduced plasma levels of SSRIs in patients after RYGB,6 so pharmacotherapy for mood disorders could be less effective after bariatric surgery as well. The hospitalist could positively impact patients by screening for both substance misuse and depression and by having a low threshold for referral to a mental health professional.
As we see ever-increasing numbers of inpatients who have a history of bariatric surgery, being aware of these common and important complications can help today’s hospitalist provide the best care possible.
Dr. Kerns is a hospitalist and codirector of bariatric surgery at the Washington DC VA Medical Center.
References
1. Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published Feb 16, 2018.
2. Hales CM et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. 2017.
3. Estimate of Bariatric Surgery Numbers, 2011-2018. ASMBS.org. Published June 2018.
4. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013 Mar;273(3):219-34. doi: 10.1111/joim.12012.
5. Neovius M et al. Health care use during 20 years following bariatric surgery. JAMA. 2012 Sep 19; 308(11):1132-41. doi: 10.1001/2012.jama.11792.
6. Azran C. et al. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes Rev. 2016 Nov;17(11):1050-66. doi: 10.1111/obr.12434.
7. El-hayek KM et al. Marginal ulcer after Roux-en-Y gastric bypass: What have we really learned? Surg Endosc. 2012 Oct;26(10):2789-96. Epub 2012 Apr 28. (Abstract presented at Society of American Gastrointestinal and Endoscopic Surgeons 2012 annual meeting, San Diego.) 8. Iannelli A et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16:1265-71. doi: 10.1381/096089206778663689.
9. Lim R et al. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018 Oct 9;3(1): e000219. doi: 10.1136/tsaco-2018-000219.
10. Coupaye M et al. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg Obes Relat Dis. 2017;13(4):681-5. doi: 10.1016/j.soard.2016.11.022.
11. Eisenberg D et al. ASMBS position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery. Surg Obes Relat Dis. 2017 Mar;13(3):371-8. doi: 10.1016/j.soard.2016.12.005.
12. King WC et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147.
13. Neovius M et al. Risk of suicide and non-fatal self-harm after bariatric surgery: Results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018 Mar;6(3):197-207. doi: 10.1016/S2213-8587(17)30437-0.
What every hospitalist should know
What every hospitalist should know
With the prevalence of obesity worldwide topping 650 million people1 and nearly 40% of U.S. adults having obesity,2 bariatric surgery is increasingly used to treat this disease and its associated comorbidities.
The American Society for Metabolic & Bariatric Surgery estimates that 228,000 bariatric procedures were performed on Americans in 2017, up from 158,000 in 2011.3 Despite lowering the risks of diabetes, stroke, myocardial infarction, cancer, and all-cause mortality,4 bariatric surgery is associated with increased health care use. Neovius et al. found that people who underwent bariatric surgery used 54 mean cumulative hospital days in the 20 years following their procedures, compared with just 40 inpatient days used by controls.5
Although hospitalists are caring for increasing numbers of patients who have undergone bariatric surgery, many of us may not be aware of some of the things that can lead to hospitalization or otherwise affect inpatient medical care. Here are a few points to keep in mind the next time you care for an inpatient with prior bariatric surgery.
Pharmacokinetics change after surgery
Gastrointestinal anatomy necessarily changes after bariatric surgery and can affect the oral absorption of drugs. Because gastric motility may be impaired and the pH in the stomach is increased after bariatric surgery, the disintegration and dissolution of immediate-release solid pills or caps may be compromised.
It is therefore prudent to crush solid forms or switch to liquid or chewable formulations of immediate-release drugs for the first few weeks to months after surgery. Enteric-coated or long-acting drug formulations should not be crushed and should generally be avoided in patients who have undergone bypass procedures such as Roux-en-Y gastric bypass (RYGB) or biliopancreatic diversion with duodenal switch (BPD/DS), as they can demonstrate either enhanced or diminished absorption (depending on the drug).
Reduced intestinal transit times and changes in intestinal pH can alter the absorption of certain drugs as well, and the expression of some drug transporter proteins and enzymes such as the CYP3A4 variant of cytochrome P450 – which is estimated to metabolize up to half of currently available drugs – varies between the upper and the lower small intestine, potentially leading to increased bioavailability of medications metabolized by this enzyme in patients who have undergone bypass surgeries.
Interestingly, longer-term studies have reexamined drug absorption in patients 2-4 years after RYGB and found that initially-increased drug plasma levels often return to preoperative levels or even lower over time,6 likely because of adaptive changes in the GI tract. Because research on the pharmacokinetics of individual drugs after bariatric surgery is lacking, the hospitalist should be aware that the bioavailability of oral drugs is often altered and should monitor patients for the desired therapeutic effect as well as potential toxicities for any drug administered to postbariatric surgery patients.
Finally, note that nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and corticosteroids should be avoided after bariatric surgery unless the benefit clearly outweighs the risk, as they increase the risk of ulcers even in patients without underlying surgical disruptions to the gastric mucosa.
Micronutrient deficiencies are common and can occur at any time
While many clinicians recognize that vitamin deficiencies can occur after weight loss surgeries which bypass the duodenum, such as the RYGB or the BPD/DS, it is important to note that vitamin and mineral deficiencies occur commonly even in patients with intact intestinal absorption such as those who underwent sleeve gastrectomy (SG) and even despite regained weight due to greater volumes of food (and micronutrient) intake over time.
The most common vitamin deficiencies include iron, vitamin B12, thiamine (vitamin B1), and vitamin D, but deficiencies in other vitamins and minerals may found as well. Anemia, bone fractures, heart failure, and encephalopathy can all be related to postoperative vitamin deficiencies. Most bariatric surgery patients should have micronutrient levels monitored on a yearly basis and should be taking at least a multivitamin with minerals (including zinc, copper, selenium and iron), a form of vitamin B12, and vitamin D with calcium supplementation. Additional supplements may be appropriate depending on the type of surgery the patient had or whether a deficiency is found.
The differential diagnosis for abdominal pain after bariatric surgery is unique
While the usual suspects such as diverticulitis or gastritis should be considered in postbariatric surgery patients just as in others, a few specific complications can arise after weight loss surgery.
Marginal ulcerations (ulcers at the surgical anastomotic sites) have been reported in up to a third of patients complaining of abdominal pain or dysphagia after RYGB, with tobacco, alcohol, or NSAID use conferring even greater risk.7 Early upper endoscopy may be warranted in symptomatic patients.
Small bowel obstruction (SBO) may occur due to surgical adhesions as in other patients, but catastrophic internal hernias with associated volvulus can occur due to specific anatomical defects that are created by the RYGB and BPD/DS procedures. CT imaging is insensitive and can miss up to 30% of these cases,8 and nasogastric tubes placed blindly for decompression of an SBO can lead to perforation of the end of the alimentary limb at the gastric pouch outlet, so post-RYGB or BPD/DS patients presenting with signs of small bowel obstruction should have an early surgical consult for expeditious surgical management rather than a trial of conservative medical management.9
Cholelithiasis is a very common postoperative complication, occurring in about 25% of SG patients and 32% of RYGB patients in the first year following surgery. The risk of gallstone formation can be significantly reduced with the postoperative use of ursodeoxycholic acid.10
Onset of abdominal cramping, nausea and diarrhea (sometimes accompanied by vasomotor symptoms) within 15-60 minutes of eating may be due to early dumping syndrome. Rapid delivery of food from the gastric pouch into the small intestine causes the release of gut peptides and an osmotic fluid shift into the intestinal lumen that can trigger these symptoms even in patients with a preserved pyloric sphincter, such as those who underwent SG. Simply eliminating sugars and simple carbohydrates from the diet usually resolves the problem, and eliminating lactose can often be helpful as well.
Postprandial hyperinsulinemic hypoglycemia (“late dumping syndrome”) can develop years after surgery
Vasomotor symptoms such as flushing/sweating, shaking, tachycardia/palpitations, lightheadedness, or difficulty concentrating occurring 1-3 hours after a meal should prompt blood glucose testing, as delayed hypoglycemia can occur after a large insulin surge.
Most commonly seen after RYGB, late dumping syndrome, like early dumping syndrome, can often be managed by eliminating sugars and simple carbohydrates from the diet. The onset of late dumping syndrome has been reported as late as 8 years after surgery,11 so the etiology of symptoms can be elusive. If the diagnosis is unclear, an oral glucose tolerance test may be helpful.
Alcohol use disorder is more prevalent after weight loss surgery
Changes to the gastrointestinal anatomy allow for more rapid absorption of ethanol into the bloodstream, making the drug more potent in postop patients. Simultaneously, many patients who undergo bariatric surgery have a history of using food to buffer negative emotions. Abruptly depriving them of that comfort in the context of the increased potency of alcohol could potentially leave bariatric surgery patients vulnerable to the development of alcohol use disorder, even when they did not misuse alcohol preoperatively.
Of note, alcohol misuse becomes more prevalent after the first postoperative year.12 Screening for alcohol misuse on admission to the hospital is wise in all cases, but perhaps even more so in the postbariatric surgery patient. If a patient does report excessive alcohol use, keep possible thiamine deficiency in mind.
The risk of suicide and self-harm increases after bariatric surgery
While all-cause mortality rates decrease after bariatric surgery compared with matched controls, the risk of suicide and nonfatal self-harm increases.
About half of bariatric surgery patients with nonfatal events have substance misuse.13 Notably, several studies have found reduced plasma levels of SSRIs in patients after RYGB,6 so pharmacotherapy for mood disorders could be less effective after bariatric surgery as well. The hospitalist could positively impact patients by screening for both substance misuse and depression and by having a low threshold for referral to a mental health professional.
As we see ever-increasing numbers of inpatients who have a history of bariatric surgery, being aware of these common and important complications can help today’s hospitalist provide the best care possible.
Dr. Kerns is a hospitalist and codirector of bariatric surgery at the Washington DC VA Medical Center.
References
1. Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published Feb 16, 2018.
2. Hales CM et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. 2017.
3. Estimate of Bariatric Surgery Numbers, 2011-2018. ASMBS.org. Published June 2018.
4. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013 Mar;273(3):219-34. doi: 10.1111/joim.12012.
5. Neovius M et al. Health care use during 20 years following bariatric surgery. JAMA. 2012 Sep 19; 308(11):1132-41. doi: 10.1001/2012.jama.11792.
6. Azran C. et al. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes Rev. 2016 Nov;17(11):1050-66. doi: 10.1111/obr.12434.
7. El-hayek KM et al. Marginal ulcer after Roux-en-Y gastric bypass: What have we really learned? Surg Endosc. 2012 Oct;26(10):2789-96. Epub 2012 Apr 28. (Abstract presented at Society of American Gastrointestinal and Endoscopic Surgeons 2012 annual meeting, San Diego.) 8. Iannelli A et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16:1265-71. doi: 10.1381/096089206778663689.
9. Lim R et al. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018 Oct 9;3(1): e000219. doi: 10.1136/tsaco-2018-000219.
10. Coupaye M et al. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg Obes Relat Dis. 2017;13(4):681-5. doi: 10.1016/j.soard.2016.11.022.
11. Eisenberg D et al. ASMBS position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery. Surg Obes Relat Dis. 2017 Mar;13(3):371-8. doi: 10.1016/j.soard.2016.12.005.
12. King WC et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147.
13. Neovius M et al. Risk of suicide and non-fatal self-harm after bariatric surgery: Results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018 Mar;6(3):197-207. doi: 10.1016/S2213-8587(17)30437-0.
With the prevalence of obesity worldwide topping 650 million people1 and nearly 40% of U.S. adults having obesity,2 bariatric surgery is increasingly used to treat this disease and its associated comorbidities.
The American Society for Metabolic & Bariatric Surgery estimates that 228,000 bariatric procedures were performed on Americans in 2017, up from 158,000 in 2011.3 Despite lowering the risks of diabetes, stroke, myocardial infarction, cancer, and all-cause mortality,4 bariatric surgery is associated with increased health care use. Neovius et al. found that people who underwent bariatric surgery used 54 mean cumulative hospital days in the 20 years following their procedures, compared with just 40 inpatient days used by controls.5
Although hospitalists are caring for increasing numbers of patients who have undergone bariatric surgery, many of us may not be aware of some of the things that can lead to hospitalization or otherwise affect inpatient medical care. Here are a few points to keep in mind the next time you care for an inpatient with prior bariatric surgery.
Pharmacokinetics change after surgery
Gastrointestinal anatomy necessarily changes after bariatric surgery and can affect the oral absorption of drugs. Because gastric motility may be impaired and the pH in the stomach is increased after bariatric surgery, the disintegration and dissolution of immediate-release solid pills or caps may be compromised.
It is therefore prudent to crush solid forms or switch to liquid or chewable formulations of immediate-release drugs for the first few weeks to months after surgery. Enteric-coated or long-acting drug formulations should not be crushed and should generally be avoided in patients who have undergone bypass procedures such as Roux-en-Y gastric bypass (RYGB) or biliopancreatic diversion with duodenal switch (BPD/DS), as they can demonstrate either enhanced or diminished absorption (depending on the drug).
Reduced intestinal transit times and changes in intestinal pH can alter the absorption of certain drugs as well, and the expression of some drug transporter proteins and enzymes such as the CYP3A4 variant of cytochrome P450 – which is estimated to metabolize up to half of currently available drugs – varies between the upper and the lower small intestine, potentially leading to increased bioavailability of medications metabolized by this enzyme in patients who have undergone bypass surgeries.
Interestingly, longer-term studies have reexamined drug absorption in patients 2-4 years after RYGB and found that initially-increased drug plasma levels often return to preoperative levels or even lower over time,6 likely because of adaptive changes in the GI tract. Because research on the pharmacokinetics of individual drugs after bariatric surgery is lacking, the hospitalist should be aware that the bioavailability of oral drugs is often altered and should monitor patients for the desired therapeutic effect as well as potential toxicities for any drug administered to postbariatric surgery patients.
Finally, note that nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and corticosteroids should be avoided after bariatric surgery unless the benefit clearly outweighs the risk, as they increase the risk of ulcers even in patients without underlying surgical disruptions to the gastric mucosa.
Micronutrient deficiencies are common and can occur at any time
While many clinicians recognize that vitamin deficiencies can occur after weight loss surgeries which bypass the duodenum, such as the RYGB or the BPD/DS, it is important to note that vitamin and mineral deficiencies occur commonly even in patients with intact intestinal absorption such as those who underwent sleeve gastrectomy (SG) and even despite regained weight due to greater volumes of food (and micronutrient) intake over time.
The most common vitamin deficiencies include iron, vitamin B12, thiamine (vitamin B1), and vitamin D, but deficiencies in other vitamins and minerals may found as well. Anemia, bone fractures, heart failure, and encephalopathy can all be related to postoperative vitamin deficiencies. Most bariatric surgery patients should have micronutrient levels monitored on a yearly basis and should be taking at least a multivitamin with minerals (including zinc, copper, selenium and iron), a form of vitamin B12, and vitamin D with calcium supplementation. Additional supplements may be appropriate depending on the type of surgery the patient had or whether a deficiency is found.
The differential diagnosis for abdominal pain after bariatric surgery is unique
While the usual suspects such as diverticulitis or gastritis should be considered in postbariatric surgery patients just as in others, a few specific complications can arise after weight loss surgery.
Marginal ulcerations (ulcers at the surgical anastomotic sites) have been reported in up to a third of patients complaining of abdominal pain or dysphagia after RYGB, with tobacco, alcohol, or NSAID use conferring even greater risk.7 Early upper endoscopy may be warranted in symptomatic patients.
Small bowel obstruction (SBO) may occur due to surgical adhesions as in other patients, but catastrophic internal hernias with associated volvulus can occur due to specific anatomical defects that are created by the RYGB and BPD/DS procedures. CT imaging is insensitive and can miss up to 30% of these cases,8 and nasogastric tubes placed blindly for decompression of an SBO can lead to perforation of the end of the alimentary limb at the gastric pouch outlet, so post-RYGB or BPD/DS patients presenting with signs of small bowel obstruction should have an early surgical consult for expeditious surgical management rather than a trial of conservative medical management.9
Cholelithiasis is a very common postoperative complication, occurring in about 25% of SG patients and 32% of RYGB patients in the first year following surgery. The risk of gallstone formation can be significantly reduced with the postoperative use of ursodeoxycholic acid.10
Onset of abdominal cramping, nausea and diarrhea (sometimes accompanied by vasomotor symptoms) within 15-60 minutes of eating may be due to early dumping syndrome. Rapid delivery of food from the gastric pouch into the small intestine causes the release of gut peptides and an osmotic fluid shift into the intestinal lumen that can trigger these symptoms even in patients with a preserved pyloric sphincter, such as those who underwent SG. Simply eliminating sugars and simple carbohydrates from the diet usually resolves the problem, and eliminating lactose can often be helpful as well.
Postprandial hyperinsulinemic hypoglycemia (“late dumping syndrome”) can develop years after surgery
Vasomotor symptoms such as flushing/sweating, shaking, tachycardia/palpitations, lightheadedness, or difficulty concentrating occurring 1-3 hours after a meal should prompt blood glucose testing, as delayed hypoglycemia can occur after a large insulin surge.
Most commonly seen after RYGB, late dumping syndrome, like early dumping syndrome, can often be managed by eliminating sugars and simple carbohydrates from the diet. The onset of late dumping syndrome has been reported as late as 8 years after surgery,11 so the etiology of symptoms can be elusive. If the diagnosis is unclear, an oral glucose tolerance test may be helpful.
Alcohol use disorder is more prevalent after weight loss surgery
Changes to the gastrointestinal anatomy allow for more rapid absorption of ethanol into the bloodstream, making the drug more potent in postop patients. Simultaneously, many patients who undergo bariatric surgery have a history of using food to buffer negative emotions. Abruptly depriving them of that comfort in the context of the increased potency of alcohol could potentially leave bariatric surgery patients vulnerable to the development of alcohol use disorder, even when they did not misuse alcohol preoperatively.
Of note, alcohol misuse becomes more prevalent after the first postoperative year.12 Screening for alcohol misuse on admission to the hospital is wise in all cases, but perhaps even more so in the postbariatric surgery patient. If a patient does report excessive alcohol use, keep possible thiamine deficiency in mind.
The risk of suicide and self-harm increases after bariatric surgery
While all-cause mortality rates decrease after bariatric surgery compared with matched controls, the risk of suicide and nonfatal self-harm increases.
About half of bariatric surgery patients with nonfatal events have substance misuse.13 Notably, several studies have found reduced plasma levels of SSRIs in patients after RYGB,6 so pharmacotherapy for mood disorders could be less effective after bariatric surgery as well. The hospitalist could positively impact patients by screening for both substance misuse and depression and by having a low threshold for referral to a mental health professional.
As we see ever-increasing numbers of inpatients who have a history of bariatric surgery, being aware of these common and important complications can help today’s hospitalist provide the best care possible.
Dr. Kerns is a hospitalist and codirector of bariatric surgery at the Washington DC VA Medical Center.
References
1. Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published Feb 16, 2018.
2. Hales CM et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. 2017.
3. Estimate of Bariatric Surgery Numbers, 2011-2018. ASMBS.org. Published June 2018.
4. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013 Mar;273(3):219-34. doi: 10.1111/joim.12012.
5. Neovius M et al. Health care use during 20 years following bariatric surgery. JAMA. 2012 Sep 19; 308(11):1132-41. doi: 10.1001/2012.jama.11792.
6. Azran C. et al. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes Rev. 2016 Nov;17(11):1050-66. doi: 10.1111/obr.12434.
7. El-hayek KM et al. Marginal ulcer after Roux-en-Y gastric bypass: What have we really learned? Surg Endosc. 2012 Oct;26(10):2789-96. Epub 2012 Apr 28. (Abstract presented at Society of American Gastrointestinal and Endoscopic Surgeons 2012 annual meeting, San Diego.) 8. Iannelli A et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16:1265-71. doi: 10.1381/096089206778663689.
9. Lim R et al. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018 Oct 9;3(1): e000219. doi: 10.1136/tsaco-2018-000219.
10. Coupaye M et al. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg Obes Relat Dis. 2017;13(4):681-5. doi: 10.1016/j.soard.2016.11.022.
11. Eisenberg D et al. ASMBS position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery. Surg Obes Relat Dis. 2017 Mar;13(3):371-8. doi: 10.1016/j.soard.2016.12.005.
12. King WC et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147.
13. Neovius M et al. Risk of suicide and non-fatal self-harm after bariatric surgery: Results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018 Mar;6(3):197-207. doi: 10.1016/S2213-8587(17)30437-0.
Designing an effective onboarding program
It goes beyond welcoming and orientation
As I gear up to welcome and onboard new hires to our hospitalist group, I could not help but reflect on my first day as a hospitalist. Fresh out of residency, my orientation was a day and a half long.
The medical director gave me a brief overview of the program. The program administrator handed me a thick folder of policies followed by a quick tour of the hospital and an afternoon training for the computerized order entry system (that was a time before EHRs). The next morning, I was given my full panel of patients, my new lab coat, and sent off into the battlefield.
I can vividly remember feeling anxious, a bit confused, and quite overwhelmed as I went through my day. The days turned into a week and the next. I kept wondering if I was doing everything right. It took me a month to feel a little more comfortable. It all turned out fine. Since nobody told me otherwise, I assumed it did.
Quite a bit has changed since then in hospital medicine. Hospital medicine groups, nowadays, have to tackle the changing landscape of payment reform, take on responsibility for an increasing range of hospital quality metrics and juggle a swath of subspecialty comanagement agreements. Hospital medicine providers function from the inpatient to the post-acute care arena, all while continuing to demonstrate their value to the hospital administration. Simultaneously, they have to ensure their providers are engaged and functioning at their optimal level while battling the ever-increasing threat of burnout.
Thus, for new hires, all the above aspects of my orientation have become critical but alas terribly insufficient. Well into its third decade, the hospital medicine job market continues to boom but remains a revolving door. Hospital medicine groups continue to grow in size and integrate across hospitals in a given health system. The vast majority of the new hires tend to be fresh out of residency. The first year remains the most vulnerable period for a new hospitalist. Hospital medicine groups must design and implement a robust onboarding program for their new hires. It goes beyond welcoming and orientation of new hires to full integration and assimilation in order to transform them into highly efficient and productive team members. Effective onboarding is table stakes for a successful and thriving hospital medicine group.
The content
An effective onboarding program should focus on three key dimensions: the organizational, the technical, and the social.1
1. The organizational or administrative aspect: The most common aspect of onboarding is providing new hires with information on the group’s policies and procedures: what to do and how to do it. Equally essential is giving them the tools and contacts that will help them understand and navigate their first few months. Information on how to contact consultants, signing on and off shifts, and so on can be easily conveyed through documents. However, having peers and the critical administrative staff communicate other aspects such as a detailed tour of the hospital, scheduling, and vacation policies is far more effective. It provides an excellent opportunity to introduce new hires to the key personnel in the group and vice versa as new hires get familiar with the unofficial workplace language. Breaking down all this information into meaningful, absorbable boluses, spread over time, is key to avoiding information overload. Allowing new hires to assimilate and adapt to the group norms requires follow-up and reinforcement. Group leaders should plan to meet with them at predetermined intervals, such as at 30, 60, 90 days, to engage them in conversations about the group’s values, performance measurements, rewards, and the opportunities for growth that exist within the group and institution.
2. The technical or the clinical aspect: The majority of physicians and advanced providers hired to a hospital medicine group have come immediately from training. Transition into the autonomous role of an attending, or a semi-autonomous role for advanced providers, with a larger patient panel can be quite unnerving and stressful. It can be disorientating even for experienced providers transitioning into a new health system. A well-structured onboarding can allow providers to deploy their training and experience at your organization effectively. Many onboarding programs have a clinical ramp-up period. The providers begin with a limited patient panel and gradually acclimatize into a full patient load. Many programs pair a senior hospitalist with the new hire during this period – a ‘buddy.’ Buddies are available to help new hires navigate the health system and familiarize them with the stakeholders. They help new hires by providing context to understand their new role and how they can contribute to the group’s success. In many instances, buddies help outline the unspoken rules of the group.
3. The social aspect – enculturation and networking: This is probably the most important of the three elements. It is quite common for new hires to feel like a stranger in a new land. A well-designed onboarding program provides new hires the space to forge relationships with each other and existing members of the hospital medicine team. Groups can do this in myriad ways – an informal welcome social, a meet and greet breakfast or lunch, in-person orientation when designing the administrative onboarding, and assignment of buddies or mentors during their clinical ramp-up period. It is all about providing a space to establish and nurture lasting relationships between the new hires and the group. When done well, this helps transform a group into a community. It also lays the groundwork to avoid stress and loneliness, some of the culprits that lead to physician burnout. It is through these interpersonal connections that new hires adapt to a hospital medicine group’s prevailing culture.
The personnel
Effective onboarding should be more than mere orientation. Group leaders should make an active attempt at understanding the core values and needs of the group. A good onboarding process assists new hires to internalize and accept the norms of the group. This process is not just a result of what comes from top management but also what they see and hear from the rank and file providers in the group. Hence it is critical to have the right people who understand and embody these values at the planning table. It is equally essential that necessary time and resources are devoted to building a program that meets the needs of the group. The practice management committee at SHM interviewed five different programs across a spectrum of settings. All of them had a designated onboarding program leader with a planning committee that included the administrative staff and senior frontline hospitalists.
The costs
According to one estimate, the cost of physician turnover is $400,000-$600,000 per provider.2 Given such staggering costs, it is not difficult to justify the financial resources required to structure an effective onboarding program. Activities such as a detailed facility tour, a welcome breakfast, and a peer buddy system cost virtually nothing. They go a long way in building comradery, make new hires feel like they are part of a team, and reduce burnout and turnover. Costs of an onboarding program are typically related to wages during shadowing and clinical ramp-up. However, all the programs we interviewed acknowledged that the costs associated with onboarding, in the broader context, were small and necessary.
The bottom line
An effective onboarding program that is well planned, well structured, and well executed is inherently valuable. It sends a positive signal to new hires, reassuring them that they made a great decision by joining the group. It also reminds the existing providers why they want to be a part of the group and its culture.
It is not about what is said or done during the onboarding process or how long it lasts. It need not be overly complicated. It is how the process makes everyone feel about the group. At the end of the day, like in all aspects of life, that is what ultimately matters.
The SHM Practice Management Committee has created a document that outlines the guiding principles for effective onboarding with attached case studies. Visit the SHM website for more information: https://www.hospitalmedicine.org.
Dr. Irani is a hospitalist affiliated with Baystate Health in Springfield, Mass. He would like to thank Joshua Lapps, Luke Heisenger, and all the members of the SHM Practice Management Committee for their assistance and input in drafting the guiding principles of onboarding and the case studies that have heavily inspired the above article.
References
1. Carucci R. To Retain New Hires, Spend More Time Onboarding Them. Harvard Busines Review. Dec 3, 2018. https://hbr.org/2018/12/to-retain-new-hires-spend-more-time-onboarding-them
2. Franz D. The staggering costs of physician turnover. Today’s Hospitalist. August 2016. https://www.todayshospitalist.com/staggering-costs-physician-turnover/
It goes beyond welcoming and orientation
It goes beyond welcoming and orientation
As I gear up to welcome and onboard new hires to our hospitalist group, I could not help but reflect on my first day as a hospitalist. Fresh out of residency, my orientation was a day and a half long.
The medical director gave me a brief overview of the program. The program administrator handed me a thick folder of policies followed by a quick tour of the hospital and an afternoon training for the computerized order entry system (that was a time before EHRs). The next morning, I was given my full panel of patients, my new lab coat, and sent off into the battlefield.
I can vividly remember feeling anxious, a bit confused, and quite overwhelmed as I went through my day. The days turned into a week and the next. I kept wondering if I was doing everything right. It took me a month to feel a little more comfortable. It all turned out fine. Since nobody told me otherwise, I assumed it did.
Quite a bit has changed since then in hospital medicine. Hospital medicine groups, nowadays, have to tackle the changing landscape of payment reform, take on responsibility for an increasing range of hospital quality metrics and juggle a swath of subspecialty comanagement agreements. Hospital medicine providers function from the inpatient to the post-acute care arena, all while continuing to demonstrate their value to the hospital administration. Simultaneously, they have to ensure their providers are engaged and functioning at their optimal level while battling the ever-increasing threat of burnout.
Thus, for new hires, all the above aspects of my orientation have become critical but alas terribly insufficient. Well into its third decade, the hospital medicine job market continues to boom but remains a revolving door. Hospital medicine groups continue to grow in size and integrate across hospitals in a given health system. The vast majority of the new hires tend to be fresh out of residency. The first year remains the most vulnerable period for a new hospitalist. Hospital medicine groups must design and implement a robust onboarding program for their new hires. It goes beyond welcoming and orientation of new hires to full integration and assimilation in order to transform them into highly efficient and productive team members. Effective onboarding is table stakes for a successful and thriving hospital medicine group.
The content
An effective onboarding program should focus on three key dimensions: the organizational, the technical, and the social.1
1. The organizational or administrative aspect: The most common aspect of onboarding is providing new hires with information on the group’s policies and procedures: what to do and how to do it. Equally essential is giving them the tools and contacts that will help them understand and navigate their first few months. Information on how to contact consultants, signing on and off shifts, and so on can be easily conveyed through documents. However, having peers and the critical administrative staff communicate other aspects such as a detailed tour of the hospital, scheduling, and vacation policies is far more effective. It provides an excellent opportunity to introduce new hires to the key personnel in the group and vice versa as new hires get familiar with the unofficial workplace language. Breaking down all this information into meaningful, absorbable boluses, spread over time, is key to avoiding information overload. Allowing new hires to assimilate and adapt to the group norms requires follow-up and reinforcement. Group leaders should plan to meet with them at predetermined intervals, such as at 30, 60, 90 days, to engage them in conversations about the group’s values, performance measurements, rewards, and the opportunities for growth that exist within the group and institution.
2. The technical or the clinical aspect: The majority of physicians and advanced providers hired to a hospital medicine group have come immediately from training. Transition into the autonomous role of an attending, or a semi-autonomous role for advanced providers, with a larger patient panel can be quite unnerving and stressful. It can be disorientating even for experienced providers transitioning into a new health system. A well-structured onboarding can allow providers to deploy their training and experience at your organization effectively. Many onboarding programs have a clinical ramp-up period. The providers begin with a limited patient panel and gradually acclimatize into a full patient load. Many programs pair a senior hospitalist with the new hire during this period – a ‘buddy.’ Buddies are available to help new hires navigate the health system and familiarize them with the stakeholders. They help new hires by providing context to understand their new role and how they can contribute to the group’s success. In many instances, buddies help outline the unspoken rules of the group.
3. The social aspect – enculturation and networking: This is probably the most important of the three elements. It is quite common for new hires to feel like a stranger in a new land. A well-designed onboarding program provides new hires the space to forge relationships with each other and existing members of the hospital medicine team. Groups can do this in myriad ways – an informal welcome social, a meet and greet breakfast or lunch, in-person orientation when designing the administrative onboarding, and assignment of buddies or mentors during their clinical ramp-up period. It is all about providing a space to establish and nurture lasting relationships between the new hires and the group. When done well, this helps transform a group into a community. It also lays the groundwork to avoid stress and loneliness, some of the culprits that lead to physician burnout. It is through these interpersonal connections that new hires adapt to a hospital medicine group’s prevailing culture.
The personnel
Effective onboarding should be more than mere orientation. Group leaders should make an active attempt at understanding the core values and needs of the group. A good onboarding process assists new hires to internalize and accept the norms of the group. This process is not just a result of what comes from top management but also what they see and hear from the rank and file providers in the group. Hence it is critical to have the right people who understand and embody these values at the planning table. It is equally essential that necessary time and resources are devoted to building a program that meets the needs of the group. The practice management committee at SHM interviewed five different programs across a spectrum of settings. All of them had a designated onboarding program leader with a planning committee that included the administrative staff and senior frontline hospitalists.
The costs
According to one estimate, the cost of physician turnover is $400,000-$600,000 per provider.2 Given such staggering costs, it is not difficult to justify the financial resources required to structure an effective onboarding program. Activities such as a detailed facility tour, a welcome breakfast, and a peer buddy system cost virtually nothing. They go a long way in building comradery, make new hires feel like they are part of a team, and reduce burnout and turnover. Costs of an onboarding program are typically related to wages during shadowing and clinical ramp-up. However, all the programs we interviewed acknowledged that the costs associated with onboarding, in the broader context, were small and necessary.
The bottom line
An effective onboarding program that is well planned, well structured, and well executed is inherently valuable. It sends a positive signal to new hires, reassuring them that they made a great decision by joining the group. It also reminds the existing providers why they want to be a part of the group and its culture.
It is not about what is said or done during the onboarding process or how long it lasts. It need not be overly complicated. It is how the process makes everyone feel about the group. At the end of the day, like in all aspects of life, that is what ultimately matters.
The SHM Practice Management Committee has created a document that outlines the guiding principles for effective onboarding with attached case studies. Visit the SHM website for more information: https://www.hospitalmedicine.org.
Dr. Irani is a hospitalist affiliated with Baystate Health in Springfield, Mass. He would like to thank Joshua Lapps, Luke Heisenger, and all the members of the SHM Practice Management Committee for their assistance and input in drafting the guiding principles of onboarding and the case studies that have heavily inspired the above article.
References
1. Carucci R. To Retain New Hires, Spend More Time Onboarding Them. Harvard Busines Review. Dec 3, 2018. https://hbr.org/2018/12/to-retain-new-hires-spend-more-time-onboarding-them
2. Franz D. The staggering costs of physician turnover. Today’s Hospitalist. August 2016. https://www.todayshospitalist.com/staggering-costs-physician-turnover/
As I gear up to welcome and onboard new hires to our hospitalist group, I could not help but reflect on my first day as a hospitalist. Fresh out of residency, my orientation was a day and a half long.
The medical director gave me a brief overview of the program. The program administrator handed me a thick folder of policies followed by a quick tour of the hospital and an afternoon training for the computerized order entry system (that was a time before EHRs). The next morning, I was given my full panel of patients, my new lab coat, and sent off into the battlefield.
I can vividly remember feeling anxious, a bit confused, and quite overwhelmed as I went through my day. The days turned into a week and the next. I kept wondering if I was doing everything right. It took me a month to feel a little more comfortable. It all turned out fine. Since nobody told me otherwise, I assumed it did.
Quite a bit has changed since then in hospital medicine. Hospital medicine groups, nowadays, have to tackle the changing landscape of payment reform, take on responsibility for an increasing range of hospital quality metrics and juggle a swath of subspecialty comanagement agreements. Hospital medicine providers function from the inpatient to the post-acute care arena, all while continuing to demonstrate their value to the hospital administration. Simultaneously, they have to ensure their providers are engaged and functioning at their optimal level while battling the ever-increasing threat of burnout.
Thus, for new hires, all the above aspects of my orientation have become critical but alas terribly insufficient. Well into its third decade, the hospital medicine job market continues to boom but remains a revolving door. Hospital medicine groups continue to grow in size and integrate across hospitals in a given health system. The vast majority of the new hires tend to be fresh out of residency. The first year remains the most vulnerable period for a new hospitalist. Hospital medicine groups must design and implement a robust onboarding program for their new hires. It goes beyond welcoming and orientation of new hires to full integration and assimilation in order to transform them into highly efficient and productive team members. Effective onboarding is table stakes for a successful and thriving hospital medicine group.
The content
An effective onboarding program should focus on three key dimensions: the organizational, the technical, and the social.1
1. The organizational or administrative aspect: The most common aspect of onboarding is providing new hires with information on the group’s policies and procedures: what to do and how to do it. Equally essential is giving them the tools and contacts that will help them understand and navigate their first few months. Information on how to contact consultants, signing on and off shifts, and so on can be easily conveyed through documents. However, having peers and the critical administrative staff communicate other aspects such as a detailed tour of the hospital, scheduling, and vacation policies is far more effective. It provides an excellent opportunity to introduce new hires to the key personnel in the group and vice versa as new hires get familiar with the unofficial workplace language. Breaking down all this information into meaningful, absorbable boluses, spread over time, is key to avoiding information overload. Allowing new hires to assimilate and adapt to the group norms requires follow-up and reinforcement. Group leaders should plan to meet with them at predetermined intervals, such as at 30, 60, 90 days, to engage them in conversations about the group’s values, performance measurements, rewards, and the opportunities for growth that exist within the group and institution.
2. The technical or the clinical aspect: The majority of physicians and advanced providers hired to a hospital medicine group have come immediately from training. Transition into the autonomous role of an attending, or a semi-autonomous role for advanced providers, with a larger patient panel can be quite unnerving and stressful. It can be disorientating even for experienced providers transitioning into a new health system. A well-structured onboarding can allow providers to deploy their training and experience at your organization effectively. Many onboarding programs have a clinical ramp-up period. The providers begin with a limited patient panel and gradually acclimatize into a full patient load. Many programs pair a senior hospitalist with the new hire during this period – a ‘buddy.’ Buddies are available to help new hires navigate the health system and familiarize them with the stakeholders. They help new hires by providing context to understand their new role and how they can contribute to the group’s success. In many instances, buddies help outline the unspoken rules of the group.
3. The social aspect – enculturation and networking: This is probably the most important of the three elements. It is quite common for new hires to feel like a stranger in a new land. A well-designed onboarding program provides new hires the space to forge relationships with each other and existing members of the hospital medicine team. Groups can do this in myriad ways – an informal welcome social, a meet and greet breakfast or lunch, in-person orientation when designing the administrative onboarding, and assignment of buddies or mentors during their clinical ramp-up period. It is all about providing a space to establish and nurture lasting relationships between the new hires and the group. When done well, this helps transform a group into a community. It also lays the groundwork to avoid stress and loneliness, some of the culprits that lead to physician burnout. It is through these interpersonal connections that new hires adapt to a hospital medicine group’s prevailing culture.
The personnel
Effective onboarding should be more than mere orientation. Group leaders should make an active attempt at understanding the core values and needs of the group. A good onboarding process assists new hires to internalize and accept the norms of the group. This process is not just a result of what comes from top management but also what they see and hear from the rank and file providers in the group. Hence it is critical to have the right people who understand and embody these values at the planning table. It is equally essential that necessary time and resources are devoted to building a program that meets the needs of the group. The practice management committee at SHM interviewed five different programs across a spectrum of settings. All of them had a designated onboarding program leader with a planning committee that included the administrative staff and senior frontline hospitalists.
The costs
According to one estimate, the cost of physician turnover is $400,000-$600,000 per provider.2 Given such staggering costs, it is not difficult to justify the financial resources required to structure an effective onboarding program. Activities such as a detailed facility tour, a welcome breakfast, and a peer buddy system cost virtually nothing. They go a long way in building comradery, make new hires feel like they are part of a team, and reduce burnout and turnover. Costs of an onboarding program are typically related to wages during shadowing and clinical ramp-up. However, all the programs we interviewed acknowledged that the costs associated with onboarding, in the broader context, were small and necessary.
The bottom line
An effective onboarding program that is well planned, well structured, and well executed is inherently valuable. It sends a positive signal to new hires, reassuring them that they made a great decision by joining the group. It also reminds the existing providers why they want to be a part of the group and its culture.
It is not about what is said or done during the onboarding process or how long it lasts. It need not be overly complicated. It is how the process makes everyone feel about the group. At the end of the day, like in all aspects of life, that is what ultimately matters.
The SHM Practice Management Committee has created a document that outlines the guiding principles for effective onboarding with attached case studies. Visit the SHM website for more information: https://www.hospitalmedicine.org.
Dr. Irani is a hospitalist affiliated with Baystate Health in Springfield, Mass. He would like to thank Joshua Lapps, Luke Heisenger, and all the members of the SHM Practice Management Committee for their assistance and input in drafting the guiding principles of onboarding and the case studies that have heavily inspired the above article.
References
1. Carucci R. To Retain New Hires, Spend More Time Onboarding Them. Harvard Busines Review. Dec 3, 2018. https://hbr.org/2018/12/to-retain-new-hires-spend-more-time-onboarding-them
2. Franz D. The staggering costs of physician turnover. Today’s Hospitalist. August 2016. https://www.todayshospitalist.com/staggering-costs-physician-turnover/
COVID-19 in pregnant women and the impact on newborns
Clinical question: How does infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in pregnant mothers affect their newborns?
Background: A novel coronavirus, now named SARS-CoV-2 by the World Health Organization (previously referred to as 2019-nCoV), is currently causing a worldwide pandemic. It is believed to have originated in Hubei province, China, but is now rapidly spreading in other countries. Although its effects are most severe in the elderly, SARS-CoV-2 has been infecting younger patients, including pregnant women. The effect of COVID-19, the disease caused by SARS-CoV-2, in pregnant women on their newborn children, is unknown, as is the nature of perinatal transmission of SARS-CoV-2.
Study design: Retrospective analysis.
Setting: Five hospitals in Hubei province, China.
Synopsis: Researchers retrospectively analyzed the clinical features and outcomes of 10 neonates (including two twins) born to nine mothers with confirmed SARS-CoV-2 infection in five hospitals in Hubei province, China, during Jan. 20–Feb. 5, 2020. The mothers were, on average, 30 years of age, but their prior state of health was not described. SARS-CoV-2 infection was confirmed in eight mothers by SARS-CoV-2 nucleic acid testing (NAT). The twins’ mother was diagnosed with COVID-19 based on chest CT scan showing viral interstitial pneumonia with other causes of fever and lung infection being “excluded,” despite a negative SARS-CoV-2 NAT test.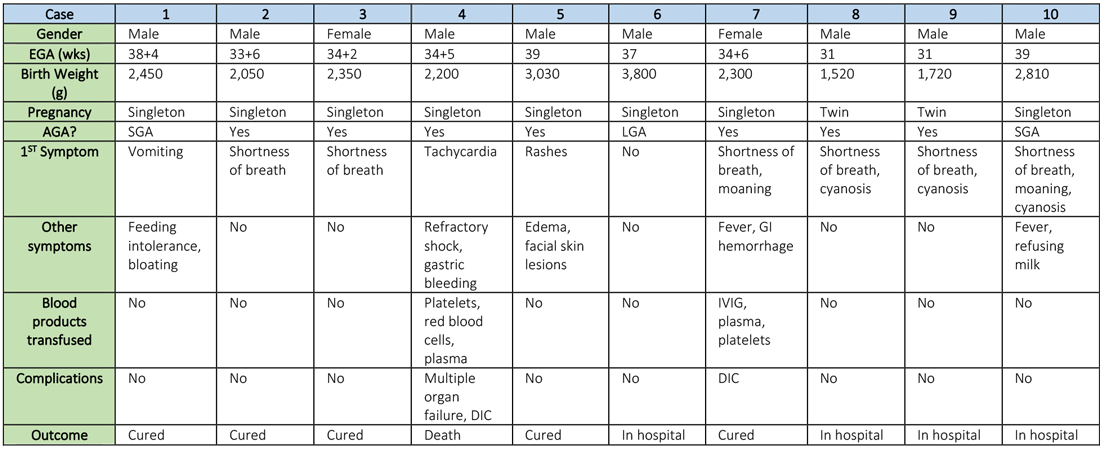
Symptoms occurred in the following:
- Before delivery in four mothers, three of whom were treated with oseltamivir (Tamiflu) after delivery.
- On the day of delivery in two mothers, one of whom was treated with oseltamivir and nebulized inhaled interferon after delivery.
- After delivery in three mothers.
Seven mothers delivered by cesarean section and two by vaginal delivery. Prenatal complications included intrauterine distress in six mothers, premature rupture of membranes in three (5-7 hours before onset of true labor), abnormal amniotic fluid in two, “abnormal” umbilical cord in two, and placenta previa in one.
The neonates born to these mothers included two females and eight males; four were full-term and six were premature (degree of prematurity not described). Symptoms first observed in these newborns included shortness of breath (six), fevers (two), tachycardia (one), and vomiting, feeding intolerance, “bloating,” refusing milk, and “gastric bleeding.” Chest radiographs were abnormal in seven newborns, including evidence of “infection” (four), neonatal respiratory distress syndrome (two), and pneumothorax (one). Two cases were described in detail:
- A neonate delivered at 34+5/7 weeks gestational age, was admitted due to shortness of breath and “moaning.” Eight days later, the neonate developed refractory shock, multiple organ failure, disseminated intravascular coagulation requiring transfusions of platelets, red blood cells, and plasma. He died on the ninth day.
- A neonate delivered at 34+6 weeks gestational age and was admitted 25 minutes after delivery due to shortness of breath and “moaning.” He required 2 days of noninvasive support/oxygen therapy and was observed to later develop “oxygen fluctuations” and thrombocytopenia at 3 days of life. The neonate was treated with “respiratory support,” intravenous immunoglobulin, transfusions of platelets and plasma, hydrocortisone (5 mg/kg per day for 6 days), low-dose heparin (2 units/kg per hr for 6 days), and low molecular weight heparin (2 units/kg per hr for 6 days). He was described to be “cured” 15 days later.
All nine neonates underwent pharyngeal swabs for SARS-CoV-2 NAT, and all were negative.
Bottom line: Although data are currently very limited, neonates born to mothers with COVID-19 appear to be at risk for adverse outcomes, including fetal distress, respiratory distress, thrombocytopenia associated with abnormal liver function, and death. There was no evidence of vertical transmission in this study.
Citation: Zhu H et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020 Feb;9(1):51-60.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
Clinical question: How does infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in pregnant mothers affect their newborns?
Background: A novel coronavirus, now named SARS-CoV-2 by the World Health Organization (previously referred to as 2019-nCoV), is currently causing a worldwide pandemic. It is believed to have originated in Hubei province, China, but is now rapidly spreading in other countries. Although its effects are most severe in the elderly, SARS-CoV-2 has been infecting younger patients, including pregnant women. The effect of COVID-19, the disease caused by SARS-CoV-2, in pregnant women on their newborn children, is unknown, as is the nature of perinatal transmission of SARS-CoV-2.
Study design: Retrospective analysis.
Setting: Five hospitals in Hubei province, China.
Synopsis: Researchers retrospectively analyzed the clinical features and outcomes of 10 neonates (including two twins) born to nine mothers with confirmed SARS-CoV-2 infection in five hospitals in Hubei province, China, during Jan. 20–Feb. 5, 2020. The mothers were, on average, 30 years of age, but their prior state of health was not described. SARS-CoV-2 infection was confirmed in eight mothers by SARS-CoV-2 nucleic acid testing (NAT). The twins’ mother was diagnosed with COVID-19 based on chest CT scan showing viral interstitial pneumonia with other causes of fever and lung infection being “excluded,” despite a negative SARS-CoV-2 NAT test.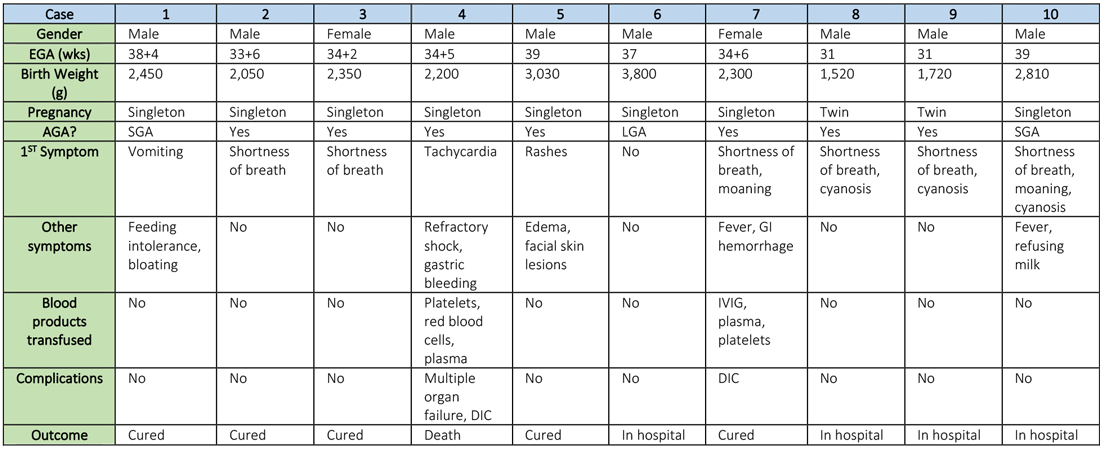
Symptoms occurred in the following:
- Before delivery in four mothers, three of whom were treated with oseltamivir (Tamiflu) after delivery.
- On the day of delivery in two mothers, one of whom was treated with oseltamivir and nebulized inhaled interferon after delivery.
- After delivery in three mothers.
Seven mothers delivered by cesarean section and two by vaginal delivery. Prenatal complications included intrauterine distress in six mothers, premature rupture of membranes in three (5-7 hours before onset of true labor), abnormal amniotic fluid in two, “abnormal” umbilical cord in two, and placenta previa in one.
The neonates born to these mothers included two females and eight males; four were full-term and six were premature (degree of prematurity not described). Symptoms first observed in these newborns included shortness of breath (six), fevers (two), tachycardia (one), and vomiting, feeding intolerance, “bloating,” refusing milk, and “gastric bleeding.” Chest radiographs were abnormal in seven newborns, including evidence of “infection” (four), neonatal respiratory distress syndrome (two), and pneumothorax (one). Two cases were described in detail:
- A neonate delivered at 34+5/7 weeks gestational age, was admitted due to shortness of breath and “moaning.” Eight days later, the neonate developed refractory shock, multiple organ failure, disseminated intravascular coagulation requiring transfusions of platelets, red blood cells, and plasma. He died on the ninth day.
- A neonate delivered at 34+6 weeks gestational age and was admitted 25 minutes after delivery due to shortness of breath and “moaning.” He required 2 days of noninvasive support/oxygen therapy and was observed to later develop “oxygen fluctuations” and thrombocytopenia at 3 days of life. The neonate was treated with “respiratory support,” intravenous immunoglobulin, transfusions of platelets and plasma, hydrocortisone (5 mg/kg per day for 6 days), low-dose heparin (2 units/kg per hr for 6 days), and low molecular weight heparin (2 units/kg per hr for 6 days). He was described to be “cured” 15 days later.
All nine neonates underwent pharyngeal swabs for SARS-CoV-2 NAT, and all were negative.
Bottom line: Although data are currently very limited, neonates born to mothers with COVID-19 appear to be at risk for adverse outcomes, including fetal distress, respiratory distress, thrombocytopenia associated with abnormal liver function, and death. There was no evidence of vertical transmission in this study.
Citation: Zhu H et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020 Feb;9(1):51-60.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
Clinical question: How does infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in pregnant mothers affect their newborns?
Background: A novel coronavirus, now named SARS-CoV-2 by the World Health Organization (previously referred to as 2019-nCoV), is currently causing a worldwide pandemic. It is believed to have originated in Hubei province, China, but is now rapidly spreading in other countries. Although its effects are most severe in the elderly, SARS-CoV-2 has been infecting younger patients, including pregnant women. The effect of COVID-19, the disease caused by SARS-CoV-2, in pregnant women on their newborn children, is unknown, as is the nature of perinatal transmission of SARS-CoV-2.
Study design: Retrospective analysis.
Setting: Five hospitals in Hubei province, China.
Synopsis: Researchers retrospectively analyzed the clinical features and outcomes of 10 neonates (including two twins) born to nine mothers with confirmed SARS-CoV-2 infection in five hospitals in Hubei province, China, during Jan. 20–Feb. 5, 2020. The mothers were, on average, 30 years of age, but their prior state of health was not described. SARS-CoV-2 infection was confirmed in eight mothers by SARS-CoV-2 nucleic acid testing (NAT). The twins’ mother was diagnosed with COVID-19 based on chest CT scan showing viral interstitial pneumonia with other causes of fever and lung infection being “excluded,” despite a negative SARS-CoV-2 NAT test.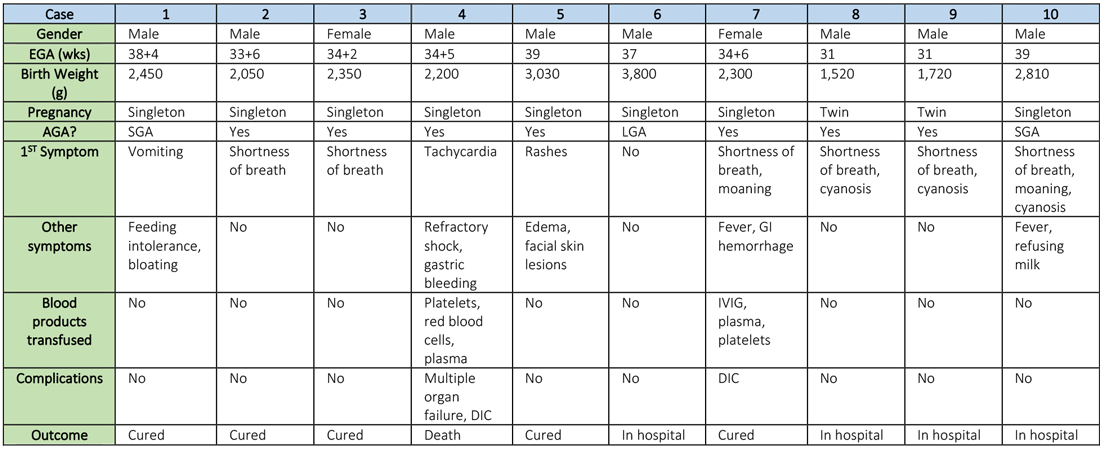
Symptoms occurred in the following:
- Before delivery in four mothers, three of whom were treated with oseltamivir (Tamiflu) after delivery.
- On the day of delivery in two mothers, one of whom was treated with oseltamivir and nebulized inhaled interferon after delivery.
- After delivery in three mothers.
Seven mothers delivered by cesarean section and two by vaginal delivery. Prenatal complications included intrauterine distress in six mothers, premature rupture of membranes in three (5-7 hours before onset of true labor), abnormal amniotic fluid in two, “abnormal” umbilical cord in two, and placenta previa in one.
The neonates born to these mothers included two females and eight males; four were full-term and six were premature (degree of prematurity not described). Symptoms first observed in these newborns included shortness of breath (six), fevers (two), tachycardia (one), and vomiting, feeding intolerance, “bloating,” refusing milk, and “gastric bleeding.” Chest radiographs were abnormal in seven newborns, including evidence of “infection” (four), neonatal respiratory distress syndrome (two), and pneumothorax (one). Two cases were described in detail:
- A neonate delivered at 34+5/7 weeks gestational age, was admitted due to shortness of breath and “moaning.” Eight days later, the neonate developed refractory shock, multiple organ failure, disseminated intravascular coagulation requiring transfusions of platelets, red blood cells, and plasma. He died on the ninth day.
- A neonate delivered at 34+6 weeks gestational age and was admitted 25 minutes after delivery due to shortness of breath and “moaning.” He required 2 days of noninvasive support/oxygen therapy and was observed to later develop “oxygen fluctuations” and thrombocytopenia at 3 days of life. The neonate was treated with “respiratory support,” intravenous immunoglobulin, transfusions of platelets and plasma, hydrocortisone (5 mg/kg per day for 6 days), low-dose heparin (2 units/kg per hr for 6 days), and low molecular weight heparin (2 units/kg per hr for 6 days). He was described to be “cured” 15 days later.
All nine neonates underwent pharyngeal swabs for SARS-CoV-2 NAT, and all were negative.
Bottom line: Although data are currently very limited, neonates born to mothers with COVID-19 appear to be at risk for adverse outcomes, including fetal distress, respiratory distress, thrombocytopenia associated with abnormal liver function, and death. There was no evidence of vertical transmission in this study.
Citation: Zhu H et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020 Feb;9(1):51-60.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
Hospitalist movers and shakers – March 2020
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.