User login
COVID-19 in pediatric patients: What the hospitalist needs to know
Coronavirus disease (COVID-19) was declared a pandemic by the World Health Organization on March 11. This rapidly spreading disease is caused by the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection has spread to more than 140 countries, including the United States. As of March 16, more than 170,400 people had tested positive for SARS-CoV-2 and more than 6,619 people have died across the globe.
The number of new COVID-19 cases appears to be decreasing in China, but the number of cases are rapidly increasing worldwide. Based on available data, primarily from China, children (aged 0-19 years) account for only about 2% of all cases. Despite the probable low virulence and incidence of infection in children, they could act as potential vectors and transmit infection to more vulnerable populations. As of March 16, approximately 3,823 cases and more than 67 deaths had been reported in the United States with few pediatric patients testing positive for the disease.
SARS-CoV2 transmission mainly occurs via respiratory route through close contact with infected individuals and through fomites. The incubation period ranges from 2-14 days with an average of about 5 days. Adult patients present with cough and fever, which may progress to lower respiratory tract symptoms, including shortness of breath. Approximately 10% of all patients develop severe disease and acute respiratory distress syndrome (ARDS), requiring mechanical ventilation.
COVID-19 carries a mortality rate of up to 3%, but has been significantly higher in the elderly population, and those with chronic health conditions. Available data so far shows that children are at lower risk and the severity of the disease has been milder compared to adults. The reasons for this are not clear at this time. As of March 16, there were no reported COVID-19 related deaths in children under age 9 years.
The pediatric population: Disease patterns and transmission
The epidemiology and spectrum of disease for COVID-19 is poorly understood in pediatrics because of the low number of reported pediatric cases and limited data available from these patients. Small numbers of reported cases in children has led some to believe that children are relatively immune to the infection by SARS-CoV-2. However, Oifang et al. found that children are equally as likely as adults to be infected.1
Liu et al. found that of 366 children admitted to a hospital in Wuhan with respiratory infections in January 2020, 1.6% (six patients) cases were positive for SARS-CoV-2.2 These six children were aged 1-7 years and had all been previously healthy; all six presented with cough and fever of 102.2° F or greater. Four of the children also had vomiting. Laboratory findings were notable for lymphopenia (six of six), leukopenia (four of six), and neutropenia (3/6) with mild to moderate elevation in C-reactive protein (6.8-58.8 mg/L). Five of six children had chest CT scans. One child’s CT scan showed “bilateral ground-glass opacities” (similar to what is reported in adults), three showed “bilateral patchy shadows,” and one was normal. One child (aged 3 years) was admitted to the ICU. All of the children were treated with supportive measures, empiric antibiotics, and antivirals (six of six received oseltamivir and four of six received ribavirin). All six children recovered completely and their median hospital stay was 7.5 days with a range of 5-13 days.
Xia et al. reviewed 20 children (aged 1 day to 14 years) admitted to a hospital in Wuhan during Jan. 23–Feb. 8.3 The study reported that fever and cough were the most common presenting symptoms (approximately 65%). Less common symptoms included rhinorrhea (15%), diarrhea (15%), vomiting (10%), and sore throat (5%). WBC count was normal in majority of children (70%) with leukopenia in 20% and leukocytosis in 10%. Lymphopenia was noted to be 35%. Elevated procalcitonin was noted in 80% of children, although the degree of elevation is unclear. In this study, 8 of 20 children were coinfected with other respiratory pathogens such as influenza, respiratory syncytial virus, mycoplasma, and cytomegalovirus. All children had chest CT scans. Ten of 20 children had bilateral pulmonary lesions, 6 of 20 had unilateral pulmonary lesions, 12 of 20 had ground-glass opacities and 10 of 20 had lung consolidations with halo signs.
Wei et al., retrospective chart review of nine infants admitted for COVID-19 found that all nine had at least one infected family member.4 This study reported that seven of nine were female infants, four of nine had fever, two had mild upper respiratory infection symptoms, and one had no symptoms. The study did report that two infants did not have any information available related to symptoms. None of the infants developed severe symptoms or required ICU admission.
The youngest patient to be diagnosed with COVID-19 was a newborn of less than 24 hours old from England, whose mother also tested positive for SARS-CoV-2. However, Chen et al. found no evidence of vertical transmission of the virus from infected pregnant women to their newborns.5
Although the risk of infection in children has been reported to be low, the infection has been shown to be particularly severe in adults with compromised immune systems and chronic health conditions. Thus immunocompromised children and those with chronic health conditions are thought to be at a higher risk for contracting the infection, with the probability for increased morbidity and mortality. Some of these risk groups include premature infants, young infants, immunocompromised children, and children with chronic health conditions like asthma, diabetes, and others. It is essential that caregivers, healthy siblings, and other family members are protected from contracting the infection in order to protect these vulnerable children. Given the high infectivity of SARS-CoV-2, the implications of infected children attending schools and daycares may be far reaching if there is delayed identification of the infection. For these reasons, it is important to closely monitor and promptly test children living with infected adults to prevent the spread. It may become necessary to close schools to mitigate transmission.
Schools and daycares should work with their local health departments and physicians in case of infected individuals in their community. In China, authorities closed schools and allowed students to receive virtual education from home, which may be a reasonable choice depending on resources.
Current challenges
Given the aggressive transmission of COVID-19, these numbers seem to be increasing exponentially with a significant impact on the life of the entire country. Therefore, we must focus on containing the spread and mitigating the transmission with a multimodality approach.
Some of the initial challenges faced by physicians in the United States were related to difficulty in access to testing in persons under investigation (PUI), which in turn resulted in a delay in diagnosis and infection control. At this time, the need is to increase surge testing capabilities across the country through a variety of innovative approaches including public-private partnerships with commercial labs through Emergency Use Authorization (EUA) issued by the Centers for Disease Control and Prevention and the Department of Health and Human Services. To minimize exposure to health care professionals, telemedicine and telehealth capabilities should be exploited. This will minimize the exposure to infected patients and reduce the need for already limited personal protective equipment (PPE). As the number of cases rise, hospitals should expect and prepare for a surge in COVID-19–related hospitalizations and health care utilization.
Conclusion
Various theories are being proposed as to why children are not experiencing severe disease with COVID-19. Children may have cross-protective immunity from infection with other coronaviruses. Children may not have the same exposures from work, travel, and caregiving that adults experience as they are typically exposed by someone in their home. At this time, not enough is known about clinical presentations in children as the situation continues to evolve across the globe.
Respiratory infections in children pose unique infection control challenges with respect to compliant hand hygiene, cough etiquette, and the use of PPE when indicated. There is also concern for persistent fecal shedding of virus in infected pediatric patients, which could be another mode of transmission.6 Children could, however, be very efficient vectors of COVID-19, similar to flu, and potentially spread the pathogen to very vulnerable populations leading to high morbidity and mortality. School closures are an effective social distancing measure needed to flatten the curve and avoid overwhelming the health care structure of the United States.
Dr. Konanki is a board-certified pediatrician doing inpatient work at Wellspan Chambersburg Hospital and outpatient work at Keystone Pediatrics in Chambersburg, Pa. He also serves as the physician member of the hospital’s Code Blue Jr. committee and as a member of Quality Metrics committee at Keystone Health. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson.
References
1. Bi Q et al. Epidemiology and transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. medRxiv 2020.03.03.20028423.
2. Liu W et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
3. Xia W et al. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718.
4. Wei M et al. Novel Coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 Feb. 14. doi: 10.1001/jama.2020.2131.
5. Huijun C et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020 Mar 7 395;10226:809-15.
6. Xu Y et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020 Mar 13. doi. org/10.1038/s41591-020-0817-4.
Coronavirus disease (COVID-19) was declared a pandemic by the World Health Organization on March 11. This rapidly spreading disease is caused by the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection has spread to more than 140 countries, including the United States. As of March 16, more than 170,400 people had tested positive for SARS-CoV-2 and more than 6,619 people have died across the globe.
The number of new COVID-19 cases appears to be decreasing in China, but the number of cases are rapidly increasing worldwide. Based on available data, primarily from China, children (aged 0-19 years) account for only about 2% of all cases. Despite the probable low virulence and incidence of infection in children, they could act as potential vectors and transmit infection to more vulnerable populations. As of March 16, approximately 3,823 cases and more than 67 deaths had been reported in the United States with few pediatric patients testing positive for the disease.
SARS-CoV2 transmission mainly occurs via respiratory route through close contact with infected individuals and through fomites. The incubation period ranges from 2-14 days with an average of about 5 days. Adult patients present with cough and fever, which may progress to lower respiratory tract symptoms, including shortness of breath. Approximately 10% of all patients develop severe disease and acute respiratory distress syndrome (ARDS), requiring mechanical ventilation.
COVID-19 carries a mortality rate of up to 3%, but has been significantly higher in the elderly population, and those with chronic health conditions. Available data so far shows that children are at lower risk and the severity of the disease has been milder compared to adults. The reasons for this are not clear at this time. As of March 16, there were no reported COVID-19 related deaths in children under age 9 years.
The pediatric population: Disease patterns and transmission
The epidemiology and spectrum of disease for COVID-19 is poorly understood in pediatrics because of the low number of reported pediatric cases and limited data available from these patients. Small numbers of reported cases in children has led some to believe that children are relatively immune to the infection by SARS-CoV-2. However, Oifang et al. found that children are equally as likely as adults to be infected.1
Liu et al. found that of 366 children admitted to a hospital in Wuhan with respiratory infections in January 2020, 1.6% (six patients) cases were positive for SARS-CoV-2.2 These six children were aged 1-7 years and had all been previously healthy; all six presented with cough and fever of 102.2° F or greater. Four of the children also had vomiting. Laboratory findings were notable for lymphopenia (six of six), leukopenia (four of six), and neutropenia (3/6) with mild to moderate elevation in C-reactive protein (6.8-58.8 mg/L). Five of six children had chest CT scans. One child’s CT scan showed “bilateral ground-glass opacities” (similar to what is reported in adults), three showed “bilateral patchy shadows,” and one was normal. One child (aged 3 years) was admitted to the ICU. All of the children were treated with supportive measures, empiric antibiotics, and antivirals (six of six received oseltamivir and four of six received ribavirin). All six children recovered completely and their median hospital stay was 7.5 days with a range of 5-13 days.
Xia et al. reviewed 20 children (aged 1 day to 14 years) admitted to a hospital in Wuhan during Jan. 23–Feb. 8.3 The study reported that fever and cough were the most common presenting symptoms (approximately 65%). Less common symptoms included rhinorrhea (15%), diarrhea (15%), vomiting (10%), and sore throat (5%). WBC count was normal in majority of children (70%) with leukopenia in 20% and leukocytosis in 10%. Lymphopenia was noted to be 35%. Elevated procalcitonin was noted in 80% of children, although the degree of elevation is unclear. In this study, 8 of 20 children were coinfected with other respiratory pathogens such as influenza, respiratory syncytial virus, mycoplasma, and cytomegalovirus. All children had chest CT scans. Ten of 20 children had bilateral pulmonary lesions, 6 of 20 had unilateral pulmonary lesions, 12 of 20 had ground-glass opacities and 10 of 20 had lung consolidations with halo signs.
Wei et al., retrospective chart review of nine infants admitted for COVID-19 found that all nine had at least one infected family member.4 This study reported that seven of nine were female infants, four of nine had fever, two had mild upper respiratory infection symptoms, and one had no symptoms. The study did report that two infants did not have any information available related to symptoms. None of the infants developed severe symptoms or required ICU admission.
The youngest patient to be diagnosed with COVID-19 was a newborn of less than 24 hours old from England, whose mother also tested positive for SARS-CoV-2. However, Chen et al. found no evidence of vertical transmission of the virus from infected pregnant women to their newborns.5
Although the risk of infection in children has been reported to be low, the infection has been shown to be particularly severe in adults with compromised immune systems and chronic health conditions. Thus immunocompromised children and those with chronic health conditions are thought to be at a higher risk for contracting the infection, with the probability for increased morbidity and mortality. Some of these risk groups include premature infants, young infants, immunocompromised children, and children with chronic health conditions like asthma, diabetes, and others. It is essential that caregivers, healthy siblings, and other family members are protected from contracting the infection in order to protect these vulnerable children. Given the high infectivity of SARS-CoV-2, the implications of infected children attending schools and daycares may be far reaching if there is delayed identification of the infection. For these reasons, it is important to closely monitor and promptly test children living with infected adults to prevent the spread. It may become necessary to close schools to mitigate transmission.
Schools and daycares should work with their local health departments and physicians in case of infected individuals in their community. In China, authorities closed schools and allowed students to receive virtual education from home, which may be a reasonable choice depending on resources.
Current challenges
Given the aggressive transmission of COVID-19, these numbers seem to be increasing exponentially with a significant impact on the life of the entire country. Therefore, we must focus on containing the spread and mitigating the transmission with a multimodality approach.
Some of the initial challenges faced by physicians in the United States were related to difficulty in access to testing in persons under investigation (PUI), which in turn resulted in a delay in diagnosis and infection control. At this time, the need is to increase surge testing capabilities across the country through a variety of innovative approaches including public-private partnerships with commercial labs through Emergency Use Authorization (EUA) issued by the Centers for Disease Control and Prevention and the Department of Health and Human Services. To minimize exposure to health care professionals, telemedicine and telehealth capabilities should be exploited. This will minimize the exposure to infected patients and reduce the need for already limited personal protective equipment (PPE). As the number of cases rise, hospitals should expect and prepare for a surge in COVID-19–related hospitalizations and health care utilization.
Conclusion
Various theories are being proposed as to why children are not experiencing severe disease with COVID-19. Children may have cross-protective immunity from infection with other coronaviruses. Children may not have the same exposures from work, travel, and caregiving that adults experience as they are typically exposed by someone in their home. At this time, not enough is known about clinical presentations in children as the situation continues to evolve across the globe.
Respiratory infections in children pose unique infection control challenges with respect to compliant hand hygiene, cough etiquette, and the use of PPE when indicated. There is also concern for persistent fecal shedding of virus in infected pediatric patients, which could be another mode of transmission.6 Children could, however, be very efficient vectors of COVID-19, similar to flu, and potentially spread the pathogen to very vulnerable populations leading to high morbidity and mortality. School closures are an effective social distancing measure needed to flatten the curve and avoid overwhelming the health care structure of the United States.
Dr. Konanki is a board-certified pediatrician doing inpatient work at Wellspan Chambersburg Hospital and outpatient work at Keystone Pediatrics in Chambersburg, Pa. He also serves as the physician member of the hospital’s Code Blue Jr. committee and as a member of Quality Metrics committee at Keystone Health. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson.
References
1. Bi Q et al. Epidemiology and transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. medRxiv 2020.03.03.20028423.
2. Liu W et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
3. Xia W et al. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718.
4. Wei M et al. Novel Coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 Feb. 14. doi: 10.1001/jama.2020.2131.
5. Huijun C et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020 Mar 7 395;10226:809-15.
6. Xu Y et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020 Mar 13. doi. org/10.1038/s41591-020-0817-4.
Coronavirus disease (COVID-19) was declared a pandemic by the World Health Organization on March 11. This rapidly spreading disease is caused by the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection has spread to more than 140 countries, including the United States. As of March 16, more than 170,400 people had tested positive for SARS-CoV-2 and more than 6,619 people have died across the globe.
The number of new COVID-19 cases appears to be decreasing in China, but the number of cases are rapidly increasing worldwide. Based on available data, primarily from China, children (aged 0-19 years) account for only about 2% of all cases. Despite the probable low virulence and incidence of infection in children, they could act as potential vectors and transmit infection to more vulnerable populations. As of March 16, approximately 3,823 cases and more than 67 deaths had been reported in the United States with few pediatric patients testing positive for the disease.
SARS-CoV2 transmission mainly occurs via respiratory route through close contact with infected individuals and through fomites. The incubation period ranges from 2-14 days with an average of about 5 days. Adult patients present with cough and fever, which may progress to lower respiratory tract symptoms, including shortness of breath. Approximately 10% of all patients develop severe disease and acute respiratory distress syndrome (ARDS), requiring mechanical ventilation.
COVID-19 carries a mortality rate of up to 3%, but has been significantly higher in the elderly population, and those with chronic health conditions. Available data so far shows that children are at lower risk and the severity of the disease has been milder compared to adults. The reasons for this are not clear at this time. As of March 16, there were no reported COVID-19 related deaths in children under age 9 years.
The pediatric population: Disease patterns and transmission
The epidemiology and spectrum of disease for COVID-19 is poorly understood in pediatrics because of the low number of reported pediatric cases and limited data available from these patients. Small numbers of reported cases in children has led some to believe that children are relatively immune to the infection by SARS-CoV-2. However, Oifang et al. found that children are equally as likely as adults to be infected.1
Liu et al. found that of 366 children admitted to a hospital in Wuhan with respiratory infections in January 2020, 1.6% (six patients) cases were positive for SARS-CoV-2.2 These six children were aged 1-7 years and had all been previously healthy; all six presented with cough and fever of 102.2° F or greater. Four of the children also had vomiting. Laboratory findings were notable for lymphopenia (six of six), leukopenia (four of six), and neutropenia (3/6) with mild to moderate elevation in C-reactive protein (6.8-58.8 mg/L). Five of six children had chest CT scans. One child’s CT scan showed “bilateral ground-glass opacities” (similar to what is reported in adults), three showed “bilateral patchy shadows,” and one was normal. One child (aged 3 years) was admitted to the ICU. All of the children were treated with supportive measures, empiric antibiotics, and antivirals (six of six received oseltamivir and four of six received ribavirin). All six children recovered completely and their median hospital stay was 7.5 days with a range of 5-13 days.
Xia et al. reviewed 20 children (aged 1 day to 14 years) admitted to a hospital in Wuhan during Jan. 23–Feb. 8.3 The study reported that fever and cough were the most common presenting symptoms (approximately 65%). Less common symptoms included rhinorrhea (15%), diarrhea (15%), vomiting (10%), and sore throat (5%). WBC count was normal in majority of children (70%) with leukopenia in 20% and leukocytosis in 10%. Lymphopenia was noted to be 35%. Elevated procalcitonin was noted in 80% of children, although the degree of elevation is unclear. In this study, 8 of 20 children were coinfected with other respiratory pathogens such as influenza, respiratory syncytial virus, mycoplasma, and cytomegalovirus. All children had chest CT scans. Ten of 20 children had bilateral pulmonary lesions, 6 of 20 had unilateral pulmonary lesions, 12 of 20 had ground-glass opacities and 10 of 20 had lung consolidations with halo signs.
Wei et al., retrospective chart review of nine infants admitted for COVID-19 found that all nine had at least one infected family member.4 This study reported that seven of nine were female infants, four of nine had fever, two had mild upper respiratory infection symptoms, and one had no symptoms. The study did report that two infants did not have any information available related to symptoms. None of the infants developed severe symptoms or required ICU admission.
The youngest patient to be diagnosed with COVID-19 was a newborn of less than 24 hours old from England, whose mother also tested positive for SARS-CoV-2. However, Chen et al. found no evidence of vertical transmission of the virus from infected pregnant women to their newborns.5
Although the risk of infection in children has been reported to be low, the infection has been shown to be particularly severe in adults with compromised immune systems and chronic health conditions. Thus immunocompromised children and those with chronic health conditions are thought to be at a higher risk for contracting the infection, with the probability for increased morbidity and mortality. Some of these risk groups include premature infants, young infants, immunocompromised children, and children with chronic health conditions like asthma, diabetes, and others. It is essential that caregivers, healthy siblings, and other family members are protected from contracting the infection in order to protect these vulnerable children. Given the high infectivity of SARS-CoV-2, the implications of infected children attending schools and daycares may be far reaching if there is delayed identification of the infection. For these reasons, it is important to closely monitor and promptly test children living with infected adults to prevent the spread. It may become necessary to close schools to mitigate transmission.
Schools and daycares should work with their local health departments and physicians in case of infected individuals in their community. In China, authorities closed schools and allowed students to receive virtual education from home, which may be a reasonable choice depending on resources.
Current challenges
Given the aggressive transmission of COVID-19, these numbers seem to be increasing exponentially with a significant impact on the life of the entire country. Therefore, we must focus on containing the spread and mitigating the transmission with a multimodality approach.
Some of the initial challenges faced by physicians in the United States were related to difficulty in access to testing in persons under investigation (PUI), which in turn resulted in a delay in diagnosis and infection control. At this time, the need is to increase surge testing capabilities across the country through a variety of innovative approaches including public-private partnerships with commercial labs through Emergency Use Authorization (EUA) issued by the Centers for Disease Control and Prevention and the Department of Health and Human Services. To minimize exposure to health care professionals, telemedicine and telehealth capabilities should be exploited. This will minimize the exposure to infected patients and reduce the need for already limited personal protective equipment (PPE). As the number of cases rise, hospitals should expect and prepare for a surge in COVID-19–related hospitalizations and health care utilization.
Conclusion
Various theories are being proposed as to why children are not experiencing severe disease with COVID-19. Children may have cross-protective immunity from infection with other coronaviruses. Children may not have the same exposures from work, travel, and caregiving that adults experience as they are typically exposed by someone in their home. At this time, not enough is known about clinical presentations in children as the situation continues to evolve across the globe.
Respiratory infections in children pose unique infection control challenges with respect to compliant hand hygiene, cough etiquette, and the use of PPE when indicated. There is also concern for persistent fecal shedding of virus in infected pediatric patients, which could be another mode of transmission.6 Children could, however, be very efficient vectors of COVID-19, similar to flu, and potentially spread the pathogen to very vulnerable populations leading to high morbidity and mortality. School closures are an effective social distancing measure needed to flatten the curve and avoid overwhelming the health care structure of the United States.
Dr. Konanki is a board-certified pediatrician doing inpatient work at Wellspan Chambersburg Hospital and outpatient work at Keystone Pediatrics in Chambersburg, Pa. He also serves as the physician member of the hospital’s Code Blue Jr. committee and as a member of Quality Metrics committee at Keystone Health. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson.
References
1. Bi Q et al. Epidemiology and transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. medRxiv 2020.03.03.20028423.
2. Liu W et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
3. Xia W et al. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718.
4. Wei M et al. Novel Coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 Feb. 14. doi: 10.1001/jama.2020.2131.
5. Huijun C et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020 Mar 7 395;10226:809-15.
6. Xu Y et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020 Mar 13. doi. org/10.1038/s41591-020-0817-4.
Coronavirus stays in aerosols for hours, on surfaces for days
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
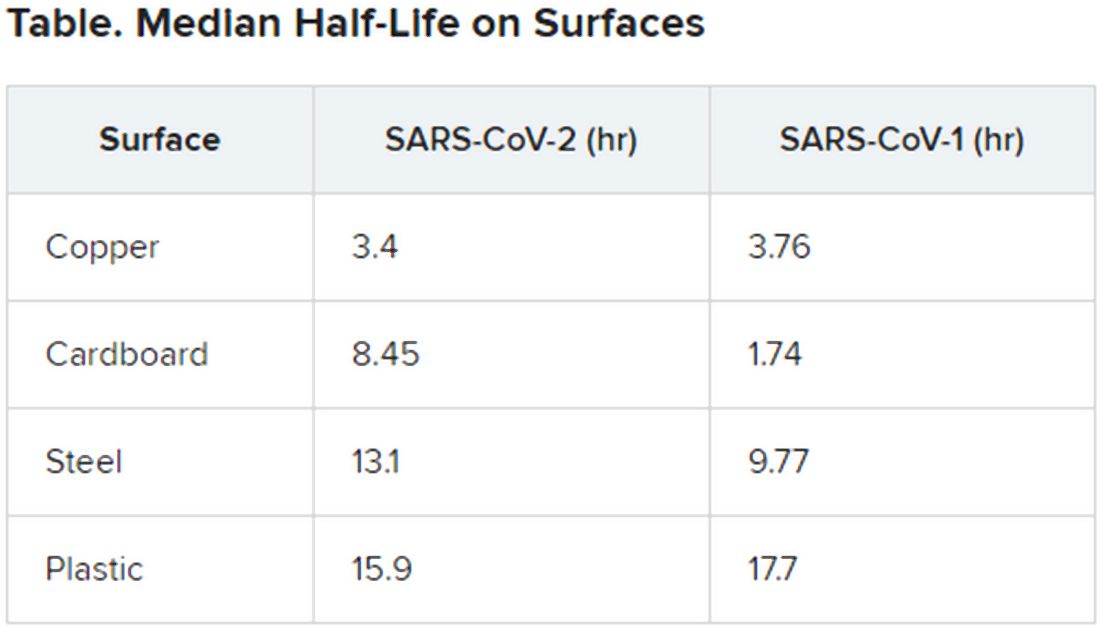
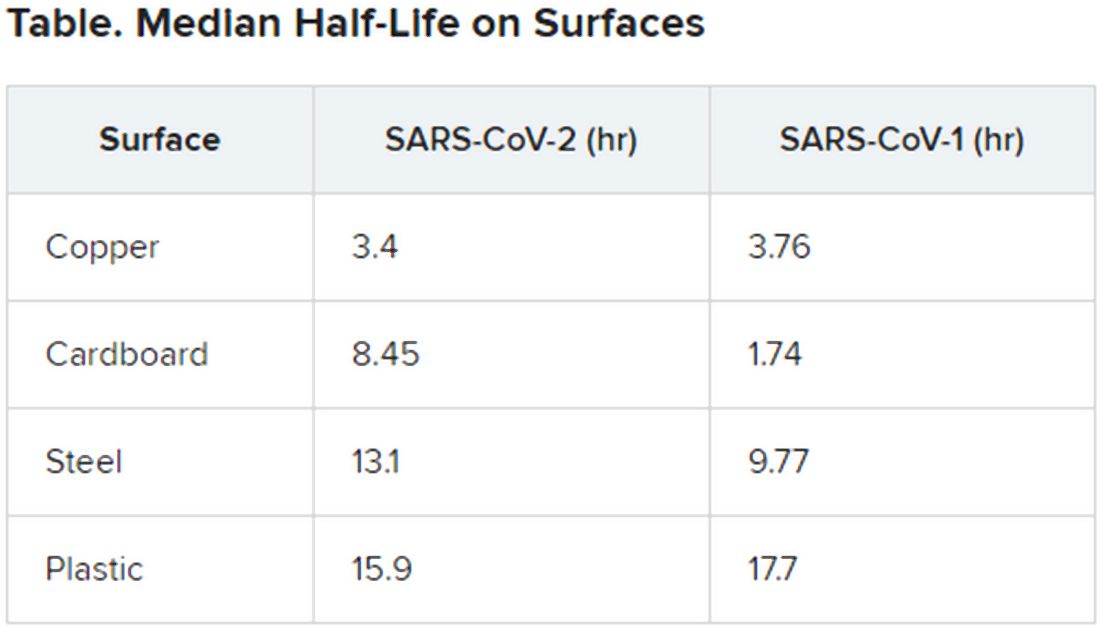
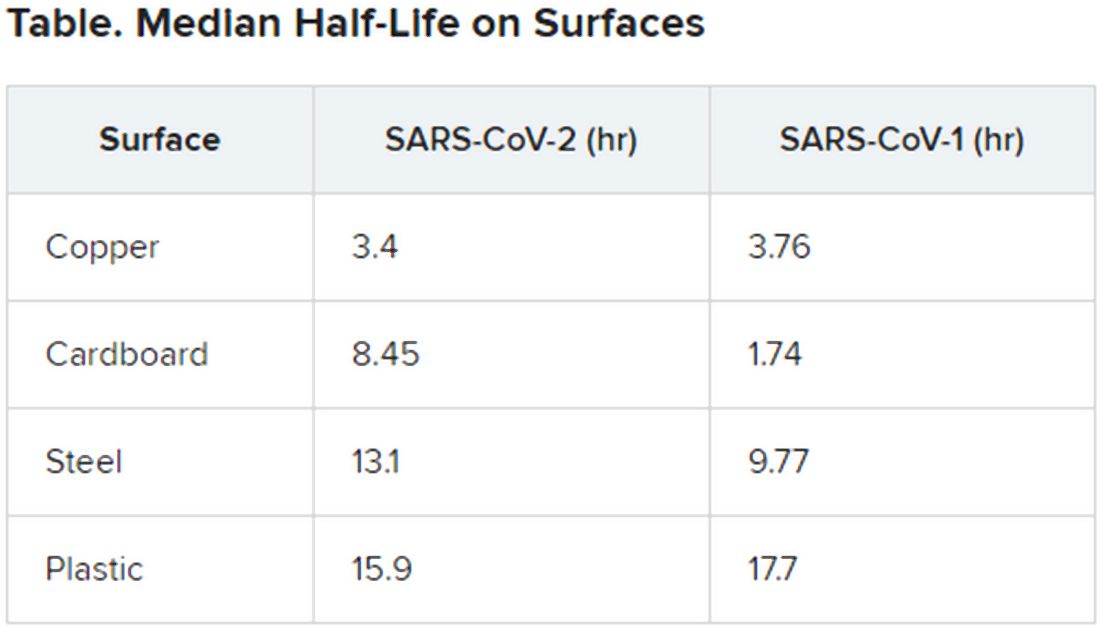
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Treating COVID-19 in patients with diabetes
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
CDC expert answers top COVID-19 questions
With new developments daily and lingering uncertainty about COVID-19, questions about testing and treatment for the coronavirus are at the forefront.
To address these top questions, Jay C. Butler, MD, deputy director for infectious diseases at the Centers for Disease Control and Prevention, sat down with JAMA editor Howard Bauchner, MD, to discuss the latest data on COVID-19 and to outline updated guidance from the agency. The following question-and-answer session was part of a live stream interview hosted by JAMA on March 16, 2020. The questions have been edited for length and clarity.
What test is being used to identify COVID-19?
In the United States, the most common and widely available test is the RT-polymerase chain reaction (rRT-PCR), which over the past few weeks has become available at public health labs across the country, Dr. Butler said during the JAMA interview. Capacity for the test is now possible in all 50 states and in Washington, D.C.
“More recently, there’s been a number of commercial labs that have come online to be able to do the testing,” Dr. Butler said. “Additionally, a number of academic centers are now able to run [Food and Drug Administration]–approved testing using slightly different PCR platforms.”
How accurate is the test?
Dr. Butler called PCR the “gold standard,” for testing COVID-19, and said it’s safe to say the test’s likelihood of identifying infection or past infection is extremely high. However, data on test sensitivity is limited.
“This may be frustrating to those of us who really like to know specifics of how to interpret the test results, but it’s important to keep in mind, we’re talking about a virus that we didn’t know existed 3 months ago,” he said.
At what point does a person with coronavirus test positive?
When exactly a test becomes positive is an unknown, Dr. Butler said. The assumption is that a patient who tests positive is more likely to be infectious, and data suggest the level of infectiousness is greatest after the onset of symptoms.
“There is at least some anecdotal reports that suggest that transmission could occur before onset of symptoms, but the data is still very limited,” he said. “Of course that has big implications in terms of how well we can really slow the spread of the virus.”
Who should get tested?
Dr. Butler said the focus should be individuals who are symptomatic with evidence of respiratory tract infection. People who are concerned about the virus and want a test are not the target.
“It’s important when talking to patients to help them to understand, this is different than a test for HIV or hepatitis C, where much of the message is: ‘Please get tested.’ ” he said. “This a situation where we’re trying to diagnose an acute infection. We do have a resource that may become limited again as some of the equipment required for running the test or collecting the specimen may come into short supply, so we want to focus on those people who are symptomatic and particularly on people who may be at higher risk of more severe illness.”
If a previously infected patient tests negative, can they still shed virus?
The CDC is currently analyzing how a negative PCR test relates to viral load, according to Dr. Butler. He added there have been situations in which a patient has twice tested negative for the virus, but a third swab resulted in a weakly positive result.
“It’s not clear if those are people who are actually infectious,” he said. “The PCR is detecting viral RNA, it doesn’t necessarily indicate there is viable virus present in the respiratory tract. So in general, I think it is safe to go back to work, but a positive test in a situation like that can be very difficult to interpret because we think it probably doesn’t reflect infectivity, but we don’t know for sure.”
Do we have an adequate supply of tests in the United States?
The CDC has addressed supply concerns by broadening the number of PCR platforms that can be used to run COVID-19 analyses, Dr. Butler said. Expansion of these platforms has been one way the government is furthering testing options and enabling consumer labs and academic centers to contribute to testing.
When can people who test positive go back to work?
The CDC is still researching that question and reviewing the data, Dr. Butler said. The current recommendation is that a patient who tests positive is considered clear to return to work after two negative tests at least 24 hours apart, following the resolution of symptoms. The CDC has not yet made an official recommendation on an exact time frame, but the CDC is considering a 14-day minimum of quarantine.
“The one caveat I’ll add is that someone who is a health care worker, even if they have resolved symptoms, it’s still a good idea to wear a surgical mask [when they return to work], just as an extra precaution.”
What do we know about immunity? Can patients get reinfected?
Long-term immunity after exposure and infection is virtually unknown, Dr. Butler said. Investigators know those with COVID-19 have an antibody response, but whether that is protective or not, is unclear. In regard to older coronaviruses, such as those that cause colds, patients generally develop an antibody response and may have a period of immunity, but that immunity eventually wanes and reinfection can occur.
What is the latest on therapies?
A number of trials are underway in China and in the United States to test possible therapies for COVID-19, Dr. Butler said. One of the candidate drugs is the broad spectrum antiviral drug remdesivir, which was developed for the treatment of the Ebola virus. Additionally, the National Institutes of Health is studying the potential for monoclonal antibodies to treat COVID-19.
“Of course these are drugs not yet FDA approved,” he said. “We all want to have them in our toolbox as soon as possible, but we want to make sure these drugs are going to benefit and not harm, and that they really do have the utility that we hope for.”
Is there specific guidance for healthcare workers about COVID-19?
Health care workers have a much higher likelihood of being exposed or exposing others who are at high risk of severe infection, Dr. Butler said. That’s why, if a health care worker becomes infected and recovers, it’s still important to take extra precautions when going back to work, such as wearing a mask.
“These are recommendations that are in-draft,” he said. “I want to be clear, I’m floating concepts out there that people can consider. ... I recognize as a former infection control medical director at a hospital that sometimes you have to adapt those guidelines based on your local conditions.”
With new developments daily and lingering uncertainty about COVID-19, questions about testing and treatment for the coronavirus are at the forefront.
To address these top questions, Jay C. Butler, MD, deputy director for infectious diseases at the Centers for Disease Control and Prevention, sat down with JAMA editor Howard Bauchner, MD, to discuss the latest data on COVID-19 and to outline updated guidance from the agency. The following question-and-answer session was part of a live stream interview hosted by JAMA on March 16, 2020. The questions have been edited for length and clarity.
What test is being used to identify COVID-19?
In the United States, the most common and widely available test is the RT-polymerase chain reaction (rRT-PCR), which over the past few weeks has become available at public health labs across the country, Dr. Butler said during the JAMA interview. Capacity for the test is now possible in all 50 states and in Washington, D.C.
“More recently, there’s been a number of commercial labs that have come online to be able to do the testing,” Dr. Butler said. “Additionally, a number of academic centers are now able to run [Food and Drug Administration]–approved testing using slightly different PCR platforms.”
How accurate is the test?
Dr. Butler called PCR the “gold standard,” for testing COVID-19, and said it’s safe to say the test’s likelihood of identifying infection or past infection is extremely high. However, data on test sensitivity is limited.
“This may be frustrating to those of us who really like to know specifics of how to interpret the test results, but it’s important to keep in mind, we’re talking about a virus that we didn’t know existed 3 months ago,” he said.
At what point does a person with coronavirus test positive?
When exactly a test becomes positive is an unknown, Dr. Butler said. The assumption is that a patient who tests positive is more likely to be infectious, and data suggest the level of infectiousness is greatest after the onset of symptoms.
“There is at least some anecdotal reports that suggest that transmission could occur before onset of symptoms, but the data is still very limited,” he said. “Of course that has big implications in terms of how well we can really slow the spread of the virus.”
Who should get tested?
Dr. Butler said the focus should be individuals who are symptomatic with evidence of respiratory tract infection. People who are concerned about the virus and want a test are not the target.
“It’s important when talking to patients to help them to understand, this is different than a test for HIV or hepatitis C, where much of the message is: ‘Please get tested.’ ” he said. “This a situation where we’re trying to diagnose an acute infection. We do have a resource that may become limited again as some of the equipment required for running the test or collecting the specimen may come into short supply, so we want to focus on those people who are symptomatic and particularly on people who may be at higher risk of more severe illness.”
If a previously infected patient tests negative, can they still shed virus?
The CDC is currently analyzing how a negative PCR test relates to viral load, according to Dr. Butler. He added there have been situations in which a patient has twice tested negative for the virus, but a third swab resulted in a weakly positive result.
“It’s not clear if those are people who are actually infectious,” he said. “The PCR is detecting viral RNA, it doesn’t necessarily indicate there is viable virus present in the respiratory tract. So in general, I think it is safe to go back to work, but a positive test in a situation like that can be very difficult to interpret because we think it probably doesn’t reflect infectivity, but we don’t know for sure.”
Do we have an adequate supply of tests in the United States?
The CDC has addressed supply concerns by broadening the number of PCR platforms that can be used to run COVID-19 analyses, Dr. Butler said. Expansion of these platforms has been one way the government is furthering testing options and enabling consumer labs and academic centers to contribute to testing.
When can people who test positive go back to work?
The CDC is still researching that question and reviewing the data, Dr. Butler said. The current recommendation is that a patient who tests positive is considered clear to return to work after two negative tests at least 24 hours apart, following the resolution of symptoms. The CDC has not yet made an official recommendation on an exact time frame, but the CDC is considering a 14-day minimum of quarantine.
“The one caveat I’ll add is that someone who is a health care worker, even if they have resolved symptoms, it’s still a good idea to wear a surgical mask [when they return to work], just as an extra precaution.”
What do we know about immunity? Can patients get reinfected?
Long-term immunity after exposure and infection is virtually unknown, Dr. Butler said. Investigators know those with COVID-19 have an antibody response, but whether that is protective or not, is unclear. In regard to older coronaviruses, such as those that cause colds, patients generally develop an antibody response and may have a period of immunity, but that immunity eventually wanes and reinfection can occur.
What is the latest on therapies?
A number of trials are underway in China and in the United States to test possible therapies for COVID-19, Dr. Butler said. One of the candidate drugs is the broad spectrum antiviral drug remdesivir, which was developed for the treatment of the Ebola virus. Additionally, the National Institutes of Health is studying the potential for monoclonal antibodies to treat COVID-19.
“Of course these are drugs not yet FDA approved,” he said. “We all want to have them in our toolbox as soon as possible, but we want to make sure these drugs are going to benefit and not harm, and that they really do have the utility that we hope for.”
Is there specific guidance for healthcare workers about COVID-19?
Health care workers have a much higher likelihood of being exposed or exposing others who are at high risk of severe infection, Dr. Butler said. That’s why, if a health care worker becomes infected and recovers, it’s still important to take extra precautions when going back to work, such as wearing a mask.
“These are recommendations that are in-draft,” he said. “I want to be clear, I’m floating concepts out there that people can consider. ... I recognize as a former infection control medical director at a hospital that sometimes you have to adapt those guidelines based on your local conditions.”
With new developments daily and lingering uncertainty about COVID-19, questions about testing and treatment for the coronavirus are at the forefront.
To address these top questions, Jay C. Butler, MD, deputy director for infectious diseases at the Centers for Disease Control and Prevention, sat down with JAMA editor Howard Bauchner, MD, to discuss the latest data on COVID-19 and to outline updated guidance from the agency. The following question-and-answer session was part of a live stream interview hosted by JAMA on March 16, 2020. The questions have been edited for length and clarity.
What test is being used to identify COVID-19?
In the United States, the most common and widely available test is the RT-polymerase chain reaction (rRT-PCR), which over the past few weeks has become available at public health labs across the country, Dr. Butler said during the JAMA interview. Capacity for the test is now possible in all 50 states and in Washington, D.C.
“More recently, there’s been a number of commercial labs that have come online to be able to do the testing,” Dr. Butler said. “Additionally, a number of academic centers are now able to run [Food and Drug Administration]–approved testing using slightly different PCR platforms.”
How accurate is the test?
Dr. Butler called PCR the “gold standard,” for testing COVID-19, and said it’s safe to say the test’s likelihood of identifying infection or past infection is extremely high. However, data on test sensitivity is limited.
“This may be frustrating to those of us who really like to know specifics of how to interpret the test results, but it’s important to keep in mind, we’re talking about a virus that we didn’t know existed 3 months ago,” he said.
At what point does a person with coronavirus test positive?
When exactly a test becomes positive is an unknown, Dr. Butler said. The assumption is that a patient who tests positive is more likely to be infectious, and data suggest the level of infectiousness is greatest after the onset of symptoms.
“There is at least some anecdotal reports that suggest that transmission could occur before onset of symptoms, but the data is still very limited,” he said. “Of course that has big implications in terms of how well we can really slow the spread of the virus.”
Who should get tested?
Dr. Butler said the focus should be individuals who are symptomatic with evidence of respiratory tract infection. People who are concerned about the virus and want a test are not the target.
“It’s important when talking to patients to help them to understand, this is different than a test for HIV or hepatitis C, where much of the message is: ‘Please get tested.’ ” he said. “This a situation where we’re trying to diagnose an acute infection. We do have a resource that may become limited again as some of the equipment required for running the test or collecting the specimen may come into short supply, so we want to focus on those people who are symptomatic and particularly on people who may be at higher risk of more severe illness.”
If a previously infected patient tests negative, can they still shed virus?
The CDC is currently analyzing how a negative PCR test relates to viral load, according to Dr. Butler. He added there have been situations in which a patient has twice tested negative for the virus, but a third swab resulted in a weakly positive result.
“It’s not clear if those are people who are actually infectious,” he said. “The PCR is detecting viral RNA, it doesn’t necessarily indicate there is viable virus present in the respiratory tract. So in general, I think it is safe to go back to work, but a positive test in a situation like that can be very difficult to interpret because we think it probably doesn’t reflect infectivity, but we don’t know for sure.”
Do we have an adequate supply of tests in the United States?
The CDC has addressed supply concerns by broadening the number of PCR platforms that can be used to run COVID-19 analyses, Dr. Butler said. Expansion of these platforms has been one way the government is furthering testing options and enabling consumer labs and academic centers to contribute to testing.
When can people who test positive go back to work?
The CDC is still researching that question and reviewing the data, Dr. Butler said. The current recommendation is that a patient who tests positive is considered clear to return to work after two negative tests at least 24 hours apart, following the resolution of symptoms. The CDC has not yet made an official recommendation on an exact time frame, but the CDC is considering a 14-day minimum of quarantine.
“The one caveat I’ll add is that someone who is a health care worker, even if they have resolved symptoms, it’s still a good idea to wear a surgical mask [when they return to work], just as an extra precaution.”
What do we know about immunity? Can patients get reinfected?
Long-term immunity after exposure and infection is virtually unknown, Dr. Butler said. Investigators know those with COVID-19 have an antibody response, but whether that is protective or not, is unclear. In regard to older coronaviruses, such as those that cause colds, patients generally develop an antibody response and may have a period of immunity, but that immunity eventually wanes and reinfection can occur.
What is the latest on therapies?
A number of trials are underway in China and in the United States to test possible therapies for COVID-19, Dr. Butler said. One of the candidate drugs is the broad spectrum antiviral drug remdesivir, which was developed for the treatment of the Ebola virus. Additionally, the National Institutes of Health is studying the potential for monoclonal antibodies to treat COVID-19.
“Of course these are drugs not yet FDA approved,” he said. “We all want to have them in our toolbox as soon as possible, but we want to make sure these drugs are going to benefit and not harm, and that they really do have the utility that we hope for.”
Is there specific guidance for healthcare workers about COVID-19?
Health care workers have a much higher likelihood of being exposed or exposing others who are at high risk of severe infection, Dr. Butler said. That’s why, if a health care worker becomes infected and recovers, it’s still important to take extra precautions when going back to work, such as wearing a mask.
“These are recommendations that are in-draft,” he said. “I want to be clear, I’m floating concepts out there that people can consider. ... I recognize as a former infection control medical director at a hospital that sometimes you have to adapt those guidelines based on your local conditions.”
Here’s what ICUs are putting up against COVID-19
As COVID-19 spreads across the United States, it is important to understand the extent of the nation’s ICU resources, according to the Society of Critical Care Medicine. The SCCM has updated its statistics on the resources available to care for what could become “an overwhelming number of critically ill patients, many of whom may require mechanical ventilation,” the society said in a blog post on March 13.
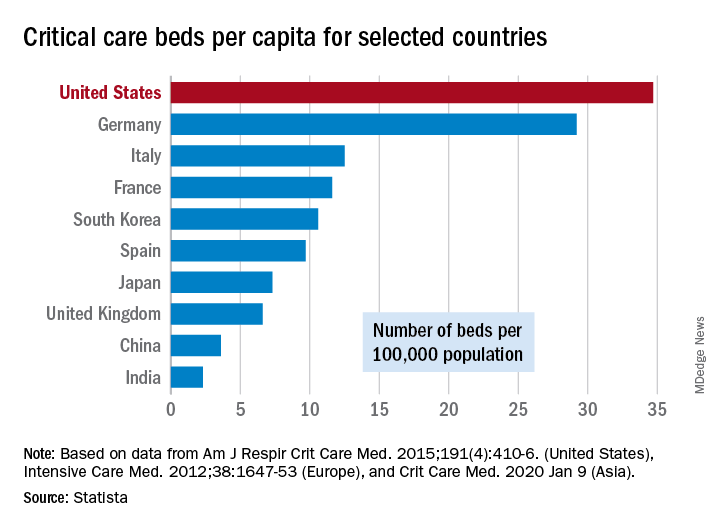
That overwhelming number was considered at an American Hospital Association webinar in February: Investigators projected that 4.8 million patients could be hospitalized with COVID-19, of whom 1.9 million would be admitted to ICUs and 960,000 would require ventilator support, Neil A. Halpern, MD, director of the critical care center at Memorial Sloan Kettering Cancer Center, New York, and Kay See Tan, PhD, of the hospital’s department of epidemiology and biostatistics, reported in that post.
As far as critical care beds are concerned, the United States is in better shape than are other countries dealing with the coronavirus. The United States’ 34.7 critical care beds per 100,000 population put it a good bit ahead of Germany, which has 29.2 beds per 100,000, while other countries in both Europe and Asia are well behind, Dr. Halpern and Dr. Tan noted.
More recent data from the AHA show that just over half of its registered community hospitals deliver ICU services and have at least 10 acute care beds and one ICU bed, they reported.
Those 2,704 hospitals have nearly 535,000 acute care beds, of which almost 97,000 are ICU beds. Almost 71% of those ICU beds are for adults, with the rest located in neonatal and pediatric units, data from an AHA 2018 survey show.
Since patients with COVID-19 are most often admitted to ICUs with severe hypoxic respiratory failure, the nation’s supply of ventilators also may be tested. U.S. acute care hospitals own about 62,000 full-featured mechanical ventilators and almost 99,000 older ventilators that “may not be capable of adequately supporting patients with severe acute respiratory failure,” Dr. Halpern and Dr. Tan said.
As U.S. hospitals reach the crisis levels anticipated in the COVID-19 pandemic, staffing shortages can be expected as well. Almost half (48%) of acute care hospitals have no intensivists, so “other physicians (e.g., pulmonologists, surgeons, anesthesiologists, etc) may be pressed into service as outpatient clinics and elective surgery are suspended,” they wrote.
The blog post includes a tiered staffing strategy that the SCCM “encourages hospitals to adopt in pandemic situations such as COVID-19.”
As COVID-19 spreads across the United States, it is important to understand the extent of the nation’s ICU resources, according to the Society of Critical Care Medicine. The SCCM has updated its statistics on the resources available to care for what could become “an overwhelming number of critically ill patients, many of whom may require mechanical ventilation,” the society said in a blog post on March 13.
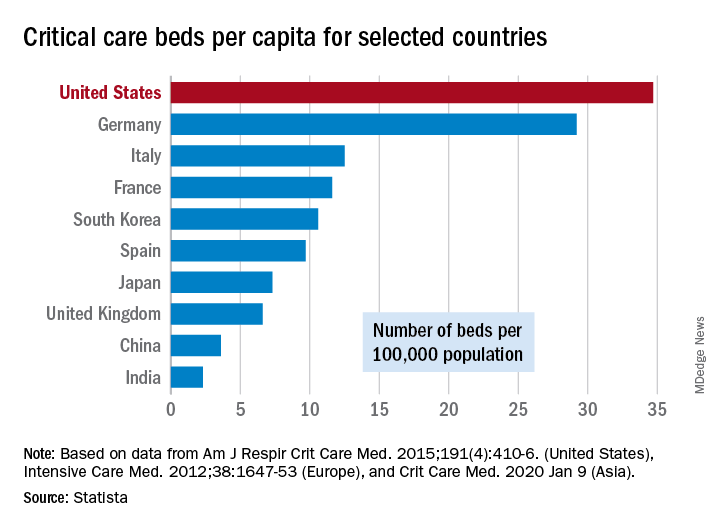
That overwhelming number was considered at an American Hospital Association webinar in February: Investigators projected that 4.8 million patients could be hospitalized with COVID-19, of whom 1.9 million would be admitted to ICUs and 960,000 would require ventilator support, Neil A. Halpern, MD, director of the critical care center at Memorial Sloan Kettering Cancer Center, New York, and Kay See Tan, PhD, of the hospital’s department of epidemiology and biostatistics, reported in that post.
As far as critical care beds are concerned, the United States is in better shape than are other countries dealing with the coronavirus. The United States’ 34.7 critical care beds per 100,000 population put it a good bit ahead of Germany, which has 29.2 beds per 100,000, while other countries in both Europe and Asia are well behind, Dr. Halpern and Dr. Tan noted.
More recent data from the AHA show that just over half of its registered community hospitals deliver ICU services and have at least 10 acute care beds and one ICU bed, they reported.
Those 2,704 hospitals have nearly 535,000 acute care beds, of which almost 97,000 are ICU beds. Almost 71% of those ICU beds are for adults, with the rest located in neonatal and pediatric units, data from an AHA 2018 survey show.
Since patients with COVID-19 are most often admitted to ICUs with severe hypoxic respiratory failure, the nation’s supply of ventilators also may be tested. U.S. acute care hospitals own about 62,000 full-featured mechanical ventilators and almost 99,000 older ventilators that “may not be capable of adequately supporting patients with severe acute respiratory failure,” Dr. Halpern and Dr. Tan said.
As U.S. hospitals reach the crisis levels anticipated in the COVID-19 pandemic, staffing shortages can be expected as well. Almost half (48%) of acute care hospitals have no intensivists, so “other physicians (e.g., pulmonologists, surgeons, anesthesiologists, etc) may be pressed into service as outpatient clinics and elective surgery are suspended,” they wrote.
The blog post includes a tiered staffing strategy that the SCCM “encourages hospitals to adopt in pandemic situations such as COVID-19.”
As COVID-19 spreads across the United States, it is important to understand the extent of the nation’s ICU resources, according to the Society of Critical Care Medicine. The SCCM has updated its statistics on the resources available to care for what could become “an overwhelming number of critically ill patients, many of whom may require mechanical ventilation,” the society said in a blog post on March 13.
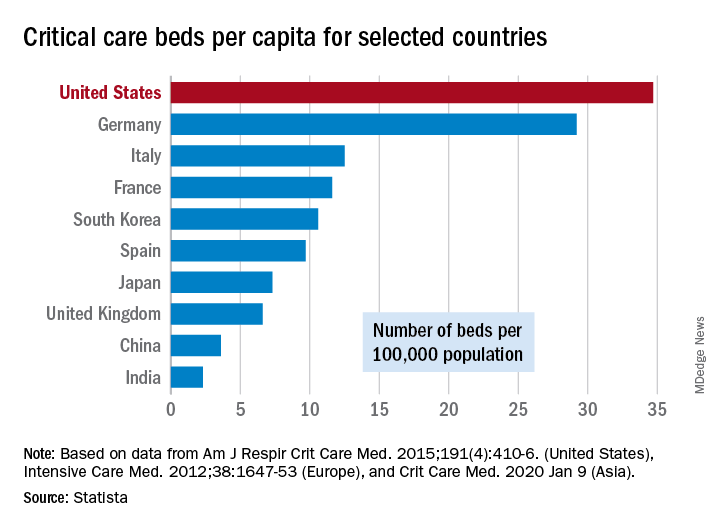
That overwhelming number was considered at an American Hospital Association webinar in February: Investigators projected that 4.8 million patients could be hospitalized with COVID-19, of whom 1.9 million would be admitted to ICUs and 960,000 would require ventilator support, Neil A. Halpern, MD, director of the critical care center at Memorial Sloan Kettering Cancer Center, New York, and Kay See Tan, PhD, of the hospital’s department of epidemiology and biostatistics, reported in that post.
As far as critical care beds are concerned, the United States is in better shape than are other countries dealing with the coronavirus. The United States’ 34.7 critical care beds per 100,000 population put it a good bit ahead of Germany, which has 29.2 beds per 100,000, while other countries in both Europe and Asia are well behind, Dr. Halpern and Dr. Tan noted.
More recent data from the AHA show that just over half of its registered community hospitals deliver ICU services and have at least 10 acute care beds and one ICU bed, they reported.
Those 2,704 hospitals have nearly 535,000 acute care beds, of which almost 97,000 are ICU beds. Almost 71% of those ICU beds are for adults, with the rest located in neonatal and pediatric units, data from an AHA 2018 survey show.
Since patients with COVID-19 are most often admitted to ICUs with severe hypoxic respiratory failure, the nation’s supply of ventilators also may be tested. U.S. acute care hospitals own about 62,000 full-featured mechanical ventilators and almost 99,000 older ventilators that “may not be capable of adequately supporting patients with severe acute respiratory failure,” Dr. Halpern and Dr. Tan said.
As U.S. hospitals reach the crisis levels anticipated in the COVID-19 pandemic, staffing shortages can be expected as well. Almost half (48%) of acute care hospitals have no intensivists, so “other physicians (e.g., pulmonologists, surgeons, anesthesiologists, etc) may be pressed into service as outpatient clinics and elective surgery are suspended,” they wrote.
The blog post includes a tiered staffing strategy that the SCCM “encourages hospitals to adopt in pandemic situations such as COVID-19.”
Detection of COVID-19 in children in early January 2020 in Wuhan, China
Clinical question: What were the clinical characteristics of children in Wuhan, China hospitalized with SARS-CoV-2?
Background: The coronavirus disease 2019 (COVID-19) was recently described by researchers in Wuhan, China.1 However, there has been limited discussion on how the disease has affected children. Based on the Chinese Center for Disease Control and Prevention report, Wu et al. found that 1% of the affected population was less than 10 years, and another 1% of the affected population was 10-19 years.2 However, little information regarding hospitalizations of children with viral infections was previously reported.
Study design: A retrospective analysis of hospitalized children.
Setting: Three sites of a multisite urban teaching hospital in central Wuhan, China.
Synopsis: Over an 8-day period, hospitalized pediatric patients were retrospectively enrolled into this study. The authors defined pediatric patients as those aged 16 years or younger. The patients had one throat swab specimen collected on admission. Throat swab specimens were tested for viral etiologies. In response to the COVID-19 outbreak, the throat samples were retrospectively tested for SARS-CoV-2. If two independent experiments and a clinically verified diagnostic test confirmed the SARS-CoV-2, the cases were confirmed as COVID-19 cases. During the 8-day period, 366 hospitalized pediatric patients were included in the study. Of the 366 patients, 6 tested positive for SARS-CoV-2, while 23 tested positive for influenza A and 20 tested positive for influenza B. The median age of the six patients was 3 years (range, 1-7 years), and all were previously healthy. All six pediatric patients with COVID-19 had high fevers (greater than 39°C), cough, and lymphopenia. Four of the six affected patients had vomiting and leukopenia, while three of the six patients had neutropenia. Four of the six affected patients had pneumonia, as diagnosed on CT scans. Of the six patients, one patient was admitted to the ICU and received intravenous immunoglobulin. The patient admitted to ICU underwent a CT scan which showed “patchy ground-glass opacities in both lungs,” while three of the five children requiring non-ICU hospitalization had chest radiographs showing “patchy shadows in both lungs.” The median length of stay in the hospital was 7.5 days (range, 5-13 days).
Bottom line: COVID-19 causes moderate to severe respiratory illness in pediatric patients with SARS-CoV-2, possibly leading to critical illness. During this time period of the Wuhan COVID-19 outbreak, pediatric patients were more likely to be hospitalized with influenza A or B, than they were with SARS-CoV-2.
Citation: Liu W et al. Detection of Covid-19 in Children in Early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
Dr. Kumar is clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of the Hospitalist.
References
1. Zhu N et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727-33.
2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 Feb 24 (Epub ahead of print).
From the Hospitalist editors: The pediatrics “In the Literature” series generally focuses on original articles. However, given the urgency to learn more about SARS-CoV-2/COVID-19 pandemic and the limited literature about hospitalized pediatric patients with the disease, the editors of the Hospitalist thought it was appropriate to share an article reviewing this letter that was recently published in the New England Journal of Medicine.
Clinical question: What were the clinical characteristics of children in Wuhan, China hospitalized with SARS-CoV-2?
Background: The coronavirus disease 2019 (COVID-19) was recently described by researchers in Wuhan, China.1 However, there has been limited discussion on how the disease has affected children. Based on the Chinese Center for Disease Control and Prevention report, Wu et al. found that 1% of the affected population was less than 10 years, and another 1% of the affected population was 10-19 years.2 However, little information regarding hospitalizations of children with viral infections was previously reported.
Study design: A retrospective analysis of hospitalized children.
Setting: Three sites of a multisite urban teaching hospital in central Wuhan, China.
Synopsis: Over an 8-day period, hospitalized pediatric patients were retrospectively enrolled into this study. The authors defined pediatric patients as those aged 16 years or younger. The patients had one throat swab specimen collected on admission. Throat swab specimens were tested for viral etiologies. In response to the COVID-19 outbreak, the throat samples were retrospectively tested for SARS-CoV-2. If two independent experiments and a clinically verified diagnostic test confirmed the SARS-CoV-2, the cases were confirmed as COVID-19 cases. During the 8-day period, 366 hospitalized pediatric patients were included in the study. Of the 366 patients, 6 tested positive for SARS-CoV-2, while 23 tested positive for influenza A and 20 tested positive for influenza B. The median age of the six patients was 3 years (range, 1-7 years), and all were previously healthy. All six pediatric patients with COVID-19 had high fevers (greater than 39°C), cough, and lymphopenia. Four of the six affected patients had vomiting and leukopenia, while three of the six patients had neutropenia. Four of the six affected patients had pneumonia, as diagnosed on CT scans. Of the six patients, one patient was admitted to the ICU and received intravenous immunoglobulin. The patient admitted to ICU underwent a CT scan which showed “patchy ground-glass opacities in both lungs,” while three of the five children requiring non-ICU hospitalization had chest radiographs showing “patchy shadows in both lungs.” The median length of stay in the hospital was 7.5 days (range, 5-13 days).
Bottom line: COVID-19 causes moderate to severe respiratory illness in pediatric patients with SARS-CoV-2, possibly leading to critical illness. During this time period of the Wuhan COVID-19 outbreak, pediatric patients were more likely to be hospitalized with influenza A or B, than they were with SARS-CoV-2.
Citation: Liu W et al. Detection of Covid-19 in Children in Early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
Dr. Kumar is clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of the Hospitalist.
References
1. Zhu N et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727-33.
2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 Feb 24 (Epub ahead of print).
From the Hospitalist editors: The pediatrics “In the Literature” series generally focuses on original articles. However, given the urgency to learn more about SARS-CoV-2/COVID-19 pandemic and the limited literature about hospitalized pediatric patients with the disease, the editors of the Hospitalist thought it was appropriate to share an article reviewing this letter that was recently published in the New England Journal of Medicine.
Clinical question: What were the clinical characteristics of children in Wuhan, China hospitalized with SARS-CoV-2?
Background: The coronavirus disease 2019 (COVID-19) was recently described by researchers in Wuhan, China.1 However, there has been limited discussion on how the disease has affected children. Based on the Chinese Center for Disease Control and Prevention report, Wu et al. found that 1% of the affected population was less than 10 years, and another 1% of the affected population was 10-19 years.2 However, little information regarding hospitalizations of children with viral infections was previously reported.
Study design: A retrospective analysis of hospitalized children.
Setting: Three sites of a multisite urban teaching hospital in central Wuhan, China.
Synopsis: Over an 8-day period, hospitalized pediatric patients were retrospectively enrolled into this study. The authors defined pediatric patients as those aged 16 years or younger. The patients had one throat swab specimen collected on admission. Throat swab specimens were tested for viral etiologies. In response to the COVID-19 outbreak, the throat samples were retrospectively tested for SARS-CoV-2. If two independent experiments and a clinically verified diagnostic test confirmed the SARS-CoV-2, the cases were confirmed as COVID-19 cases. During the 8-day period, 366 hospitalized pediatric patients were included in the study. Of the 366 patients, 6 tested positive for SARS-CoV-2, while 23 tested positive for influenza A and 20 tested positive for influenza B. The median age of the six patients was 3 years (range, 1-7 years), and all were previously healthy. All six pediatric patients with COVID-19 had high fevers (greater than 39°C), cough, and lymphopenia. Four of the six affected patients had vomiting and leukopenia, while three of the six patients had neutropenia. Four of the six affected patients had pneumonia, as diagnosed on CT scans. Of the six patients, one patient was admitted to the ICU and received intravenous immunoglobulin. The patient admitted to ICU underwent a CT scan which showed “patchy ground-glass opacities in both lungs,” while three of the five children requiring non-ICU hospitalization had chest radiographs showing “patchy shadows in both lungs.” The median length of stay in the hospital was 7.5 days (range, 5-13 days).
Bottom line: COVID-19 causes moderate to severe respiratory illness in pediatric patients with SARS-CoV-2, possibly leading to critical illness. During this time period of the Wuhan COVID-19 outbreak, pediatric patients were more likely to be hospitalized with influenza A or B, than they were with SARS-CoV-2.
Citation: Liu W et al. Detection of Covid-19 in Children in Early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
Dr. Kumar is clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of the Hospitalist.
References
1. Zhu N et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727-33.
2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 Feb 24 (Epub ahead of print).
From the Hospitalist editors: The pediatrics “In the Literature” series generally focuses on original articles. However, given the urgency to learn more about SARS-CoV-2/COVID-19 pandemic and the limited literature about hospitalized pediatric patients with the disease, the editors of the Hospitalist thought it was appropriate to share an article reviewing this letter that was recently published in the New England Journal of Medicine.
Society of Hospital Medicine cancels 2020 Annual Conference
The Society of Hospital Medicine (SHM) has canceled its annual conference, scheduled for mid-April, joining a growing list of events shuttered by coronavirus (COVID-19) concerns.
In a March 13 announcement, SHM said it would be impossible for the society to host the Hospital Medicine 2020 conference amid the escalating health concerns regarding the global COVID-19 outbreak. For more information about the cancellation and the society’s refund policies, see the SHM website for a list of frequently answered questions.
The Society of Hospital Medicine (SHM) has canceled its annual conference, scheduled for mid-April, joining a growing list of events shuttered by coronavirus (COVID-19) concerns.
In a March 13 announcement, SHM said it would be impossible for the society to host the Hospital Medicine 2020 conference amid the escalating health concerns regarding the global COVID-19 outbreak. For more information about the cancellation and the society’s refund policies, see the SHM website for a list of frequently answered questions.
The Society of Hospital Medicine (SHM) has canceled its annual conference, scheduled for mid-April, joining a growing list of events shuttered by coronavirus (COVID-19) concerns.
In a March 13 announcement, SHM said it would be impossible for the society to host the Hospital Medicine 2020 conference amid the escalating health concerns regarding the global COVID-19 outbreak. For more information about the cancellation and the society’s refund policies, see the SHM website for a list of frequently answered questions.
Hospital medicine physician leaders
The right skills and time to develop them
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
The right skills and time to develop them
The right skills and time to develop them
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
A match made in medicine: Match Day 2020
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Health professionals fight against COVID-19 myths and misinformation
Misinformation about the COVID-19 travels faster than the virus and complicates the job of doctors who are treating those infected and responding to concerns of their other patients.
An array of myths springing up around this disease can be found on the Internet. The main themes appear to be false narratives about the origin of the virus, the size of the outbreak in the United States and in other countries, the availability of cures and treatments, and ways to prevent infection. Widespread misinformation hampers public health efforts to control the disease outbreak, confuses the public, and requires medical professionals to spend time refuting myths and re-educating patients.
A group of infectious disease experts became so alarmed by the misinformation trend they published a statement in The Lancet decrying the spread of false statements being circulated by some media outlets. “The rapid, open, and transparent sharing of data on this outbreak is now being threatened by rumours and misinformation ... Conspiracy theories do nothing but create fear, rumours, and prejudice that jeopardise our global collaboration in the fight against this virus,” wrote Charles H. Calisher, PhD, of Colorado State University, Fort Collins, and colleagues.
What can physicians do to counter misinformation?
Pulmonologist and critical care physician Cedric “Jamie” Rutland, MD, who practices in Riverside, Calif., sees misinformation about the novel coronavirus every day at home and on the job. His patients worry that everyone who gets infected will die or end up in the ICU. His neighbors ask him to pilfer surgical masks to protect them from the false notion that Chinese people in their community posed some kind of COVID-19 risk.
As he pondered how to counter myths with facts, Dr. Rutland turned to an unusual resource: His 7-year-old daughter Amelia. He explained to her how COVID-19 works and found that she could easily understand the basics. Now, Dr. Rutland draws upon the lessons from chats with his daughter as he explains COVID-19 to his patient audience on his YouTube channel “Medicine Deconstructed.” Simplicity, but not too much simplicity, is key, he said. Dr. Rutland uses a visual aid – a rough drawing of a virus – and shows how inflammation and antibodies enter the picture after infection. “I just teach them that if you’re a healthy person, this is how the body works, and this is what the immune system will do,” he said. “For the most part, you can calm people down when you make time for education.”
What are best practices? In a series of interviews, specialists emphasized the importance of fact-finding, wide-ranging communication, and – perhaps most difficult of all – humility.
Dr. Rutland emphasizes thoughtful communication based on facts and humility when communicating to patients about this potential health risk. “A lot of people finish medical school and think, ‘Everyone should trust me because I’m the pulmonologist or the GI doc.’ That’s not how it works. You still have to earn people’s trust,” he said.
Make sure all staff get reliable information
Hospitals are scrambling to keep staff safe with up-to-date directives and debunk false narratives about the virus. Keeping all hospital staff informed with verified and authoritative facts about the coronavirus is a key objective of the Massachusetts General Hospital’s Center for Disaster Medicine. The Center’s coronavirus educational materials are distributed to all staffers from physicians to janitors. “These provide information that they need to understand the risks and keep themselves safe,” said Eileen Searle, PhD, the Biothreats Clinical Operations program manager in the CDM.
According to Dr. Searle, the hospital keeps a continually updated COVID-19 Frequently Asked Questions document in its internal computer system. All employees can access it, she said, and it’s updated to include questions as they come up.
Even valets and front-desk volunteers are encouraged to read the FAQ, she said, since “they’re the first people that family and patients are interacting with.” The document “gives them reassurance about delivering messages,” she said.
Use patience with your patients
Dr. Rutland urges colleagues to take the time to listen to patients and educate them. “Reduce the gap between you and them,” said Dr. Rutland, who treats patients in Orange and Riverside counties. “Take off your white coat, sit down, and talk to the person about their concerns.”
Boston cardiologist Haider Warraich, MD, of Brigham and Women’s Hospital, Boston, said it’s important to “put medical information into a greater human context.” For example, he has told patients that he’s still taking his daughter to school despite COVID-19 risks. “I take the information I provide and apply it to my own life,” he said.
The Washington State Department of Health offers this advice to physicians to counter false information and stigma: “Stay updated and informed on COVID-19 to avoid miscommunication or inaccurate information. Talk openly about the harm of stigma. View people directly impacted by stigma as people first. Be conscious of your language. Acknowledge access and language barriers.”
Speak out on social media – but don’t fight
Should medical professionals speak out about COVID-19 misinformation via social media? It’s an individual decision, Dr. Warraich said, “but my sense is that it’s never been more important for physicians to be part of the fray and help quell the epidemic of misinformation that almost always follows any type of medial calamity.”
Dr. Rutland, vice president and founding member of the Association for Healthcare Social Media, cautioned that effective communication via social media requires care. Avoid confrontation, he advised. “Don’t call people stupid or say things like, ‘I went to medical school and I’m smarter than you.’ ”
Instead, he said, “it’s important to just state the facts: These are the people who are dying, these are the people who are getting infected.”
And, he added, remember to push the most important message of all: Wash your hands!
Public health organizations fight the ‘infodemic’
In a trend that hearkens back to the days of snake oil cures for all maladies, advertisements for fake treatments are popping up on the Internet and on other media.
Facebook and Amazon have acted to remove these ads but these messages continue to flood social media such as Twitter, WhatsApp, and other sites. Discussion groups on platforms such as Reddit continue to pump out misinformation about COVID-19. Conspiracy theories that link the virus to espionage and bioweapons are making the rounds on the Internet and talk radio. Wrong information about the effectiveness of non-N95 face masks to protect wearers against infection is widespread, leading to shortages for medical personnel and price gouging. Pernicious rumors about the effectiveness of substances such a vinegar, silver, garlic, lemon juice, and even vodka to disinfect hands and surfaces abound on the Internet. An especially dangerous stream of misinformation stigmatizes ethnic groups and individuals as sources of the infection.
The World Health Organization identified early in the COVID-19 outbreak the global wave of misinformation about the virus and dubbed the problem the “infodemic.” The WHO “Q & A” page on COVID-19 is updated frequently and addresses myths and rumors currently circulating.
According to the WHO website, the agency has reached out to social media players such as Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, and Weibo, the microblogging site in China. WHO has worked with these sites to curb the “infodemic” of misinformation and has used these sites for public education outreach on COVID-19. “Myth busting” infographics posted on a WHO web page are also reposted on major social media sites.
The CDC has followed with its own “frequently asked questions” page to address questions and rumors. State health agencies have put up COVID-19 pages to address public concerns and offer advice on prevention. The Maryland Department of Health web page directly addresses dangerous misinformation: “Do not stigmatize people of any specific ethnicities or racial background. Viruses do not target people from specific populations, ethnicities or racial backgrounds. Stay informed and seek information from reliable, official sources. Be wary of myths, rumors and misinformation circulating online and elsewhere. Health information shared through social media is frequently inaccurate, unless coming from an official, reliable source such as the CDC, MDH or local health departments.”
The Washington State Department of Health has taken a more assertive stance on stigma. The COVID-19 web page recommends to the public: “Show compassion and support for individuals and communities more closely impacted. Avoid stigmatizing people who are in quarantine. They are making the right choice for their communities. Do not make assumptions about someone’s health status based on their ethnicity, race or national origin.”
Misinformation about the COVID-19 travels faster than the virus and complicates the job of doctors who are treating those infected and responding to concerns of their other patients.
An array of myths springing up around this disease can be found on the Internet. The main themes appear to be false narratives about the origin of the virus, the size of the outbreak in the United States and in other countries, the availability of cures and treatments, and ways to prevent infection. Widespread misinformation hampers public health efforts to control the disease outbreak, confuses the public, and requires medical professionals to spend time refuting myths and re-educating patients.
A group of infectious disease experts became so alarmed by the misinformation trend they published a statement in The Lancet decrying the spread of false statements being circulated by some media outlets. “The rapid, open, and transparent sharing of data on this outbreak is now being threatened by rumours and misinformation ... Conspiracy theories do nothing but create fear, rumours, and prejudice that jeopardise our global collaboration in the fight against this virus,” wrote Charles H. Calisher, PhD, of Colorado State University, Fort Collins, and colleagues.
What can physicians do to counter misinformation?
Pulmonologist and critical care physician Cedric “Jamie” Rutland, MD, who practices in Riverside, Calif., sees misinformation about the novel coronavirus every day at home and on the job. His patients worry that everyone who gets infected will die or end up in the ICU. His neighbors ask him to pilfer surgical masks to protect them from the false notion that Chinese people in their community posed some kind of COVID-19 risk.
As he pondered how to counter myths with facts, Dr. Rutland turned to an unusual resource: His 7-year-old daughter Amelia. He explained to her how COVID-19 works and found that she could easily understand the basics. Now, Dr. Rutland draws upon the lessons from chats with his daughter as he explains COVID-19 to his patient audience on his YouTube channel “Medicine Deconstructed.” Simplicity, but not too much simplicity, is key, he said. Dr. Rutland uses a visual aid – a rough drawing of a virus – and shows how inflammation and antibodies enter the picture after infection. “I just teach them that if you’re a healthy person, this is how the body works, and this is what the immune system will do,” he said. “For the most part, you can calm people down when you make time for education.”
What are best practices? In a series of interviews, specialists emphasized the importance of fact-finding, wide-ranging communication, and – perhaps most difficult of all – humility.
Dr. Rutland emphasizes thoughtful communication based on facts and humility when communicating to patients about this potential health risk. “A lot of people finish medical school and think, ‘Everyone should trust me because I’m the pulmonologist or the GI doc.’ That’s not how it works. You still have to earn people’s trust,” he said.
Make sure all staff get reliable information
Hospitals are scrambling to keep staff safe with up-to-date directives and debunk false narratives about the virus. Keeping all hospital staff informed with verified and authoritative facts about the coronavirus is a key objective of the Massachusetts General Hospital’s Center for Disaster Medicine. The Center’s coronavirus educational materials are distributed to all staffers from physicians to janitors. “These provide information that they need to understand the risks and keep themselves safe,” said Eileen Searle, PhD, the Biothreats Clinical Operations program manager in the CDM.
According to Dr. Searle, the hospital keeps a continually updated COVID-19 Frequently Asked Questions document in its internal computer system. All employees can access it, she said, and it’s updated to include questions as they come up.
Even valets and front-desk volunteers are encouraged to read the FAQ, she said, since “they’re the first people that family and patients are interacting with.” The document “gives them reassurance about delivering messages,” she said.
Use patience with your patients
Dr. Rutland urges colleagues to take the time to listen to patients and educate them. “Reduce the gap between you and them,” said Dr. Rutland, who treats patients in Orange and Riverside counties. “Take off your white coat, sit down, and talk to the person about their concerns.”
Boston cardiologist Haider Warraich, MD, of Brigham and Women’s Hospital, Boston, said it’s important to “put medical information into a greater human context.” For example, he has told patients that he’s still taking his daughter to school despite COVID-19 risks. “I take the information I provide and apply it to my own life,” he said.
The Washington State Department of Health offers this advice to physicians to counter false information and stigma: “Stay updated and informed on COVID-19 to avoid miscommunication or inaccurate information. Talk openly about the harm of stigma. View people directly impacted by stigma as people first. Be conscious of your language. Acknowledge access and language barriers.”
Speak out on social media – but don’t fight
Should medical professionals speak out about COVID-19 misinformation via social media? It’s an individual decision, Dr. Warraich said, “but my sense is that it’s never been more important for physicians to be part of the fray and help quell the epidemic of misinformation that almost always follows any type of medial calamity.”
Dr. Rutland, vice president and founding member of the Association for Healthcare Social Media, cautioned that effective communication via social media requires care. Avoid confrontation, he advised. “Don’t call people stupid or say things like, ‘I went to medical school and I’m smarter than you.’ ”
Instead, he said, “it’s important to just state the facts: These are the people who are dying, these are the people who are getting infected.”
And, he added, remember to push the most important message of all: Wash your hands!
Public health organizations fight the ‘infodemic’
In a trend that hearkens back to the days of snake oil cures for all maladies, advertisements for fake treatments are popping up on the Internet and on other media.
Facebook and Amazon have acted to remove these ads but these messages continue to flood social media such as Twitter, WhatsApp, and other sites. Discussion groups on platforms such as Reddit continue to pump out misinformation about COVID-19. Conspiracy theories that link the virus to espionage and bioweapons are making the rounds on the Internet and talk radio. Wrong information about the effectiveness of non-N95 face masks to protect wearers against infection is widespread, leading to shortages for medical personnel and price gouging. Pernicious rumors about the effectiveness of substances such a vinegar, silver, garlic, lemon juice, and even vodka to disinfect hands and surfaces abound on the Internet. An especially dangerous stream of misinformation stigmatizes ethnic groups and individuals as sources of the infection.
The World Health Organization identified early in the COVID-19 outbreak the global wave of misinformation about the virus and dubbed the problem the “infodemic.” The WHO “Q & A” page on COVID-19 is updated frequently and addresses myths and rumors currently circulating.
According to the WHO website, the agency has reached out to social media players such as Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, and Weibo, the microblogging site in China. WHO has worked with these sites to curb the “infodemic” of misinformation and has used these sites for public education outreach on COVID-19. “Myth busting” infographics posted on a WHO web page are also reposted on major social media sites.
The CDC has followed with its own “frequently asked questions” page to address questions and rumors. State health agencies have put up COVID-19 pages to address public concerns and offer advice on prevention. The Maryland Department of Health web page directly addresses dangerous misinformation: “Do not stigmatize people of any specific ethnicities or racial background. Viruses do not target people from specific populations, ethnicities or racial backgrounds. Stay informed and seek information from reliable, official sources. Be wary of myths, rumors and misinformation circulating online and elsewhere. Health information shared through social media is frequently inaccurate, unless coming from an official, reliable source such as the CDC, MDH or local health departments.”
The Washington State Department of Health has taken a more assertive stance on stigma. The COVID-19 web page recommends to the public: “Show compassion and support for individuals and communities more closely impacted. Avoid stigmatizing people who are in quarantine. They are making the right choice for their communities. Do not make assumptions about someone’s health status based on their ethnicity, race or national origin.”
Misinformation about the COVID-19 travels faster than the virus and complicates the job of doctors who are treating those infected and responding to concerns of their other patients.
An array of myths springing up around this disease can be found on the Internet. The main themes appear to be false narratives about the origin of the virus, the size of the outbreak in the United States and in other countries, the availability of cures and treatments, and ways to prevent infection. Widespread misinformation hampers public health efforts to control the disease outbreak, confuses the public, and requires medical professionals to spend time refuting myths and re-educating patients.
A group of infectious disease experts became so alarmed by the misinformation trend they published a statement in The Lancet decrying the spread of false statements being circulated by some media outlets. “The rapid, open, and transparent sharing of data on this outbreak is now being threatened by rumours and misinformation ... Conspiracy theories do nothing but create fear, rumours, and prejudice that jeopardise our global collaboration in the fight against this virus,” wrote Charles H. Calisher, PhD, of Colorado State University, Fort Collins, and colleagues.
What can physicians do to counter misinformation?
Pulmonologist and critical care physician Cedric “Jamie” Rutland, MD, who practices in Riverside, Calif., sees misinformation about the novel coronavirus every day at home and on the job. His patients worry that everyone who gets infected will die or end up in the ICU. His neighbors ask him to pilfer surgical masks to protect them from the false notion that Chinese people in their community posed some kind of COVID-19 risk.
As he pondered how to counter myths with facts, Dr. Rutland turned to an unusual resource: His 7-year-old daughter Amelia. He explained to her how COVID-19 works and found that she could easily understand the basics. Now, Dr. Rutland draws upon the lessons from chats with his daughter as he explains COVID-19 to his patient audience on his YouTube channel “Medicine Deconstructed.” Simplicity, but not too much simplicity, is key, he said. Dr. Rutland uses a visual aid – a rough drawing of a virus – and shows how inflammation and antibodies enter the picture after infection. “I just teach them that if you’re a healthy person, this is how the body works, and this is what the immune system will do,” he said. “For the most part, you can calm people down when you make time for education.”
What are best practices? In a series of interviews, specialists emphasized the importance of fact-finding, wide-ranging communication, and – perhaps most difficult of all – humility.
Dr. Rutland emphasizes thoughtful communication based on facts and humility when communicating to patients about this potential health risk. “A lot of people finish medical school and think, ‘Everyone should trust me because I’m the pulmonologist or the GI doc.’ That’s not how it works. You still have to earn people’s trust,” he said.
Make sure all staff get reliable information
Hospitals are scrambling to keep staff safe with up-to-date directives and debunk false narratives about the virus. Keeping all hospital staff informed with verified and authoritative facts about the coronavirus is a key objective of the Massachusetts General Hospital’s Center for Disaster Medicine. The Center’s coronavirus educational materials are distributed to all staffers from physicians to janitors. “These provide information that they need to understand the risks and keep themselves safe,” said Eileen Searle, PhD, the Biothreats Clinical Operations program manager in the CDM.
According to Dr. Searle, the hospital keeps a continually updated COVID-19 Frequently Asked Questions document in its internal computer system. All employees can access it, she said, and it’s updated to include questions as they come up.
Even valets and front-desk volunteers are encouraged to read the FAQ, she said, since “they’re the first people that family and patients are interacting with.” The document “gives them reassurance about delivering messages,” she said.
Use patience with your patients
Dr. Rutland urges colleagues to take the time to listen to patients and educate them. “Reduce the gap between you and them,” said Dr. Rutland, who treats patients in Orange and Riverside counties. “Take off your white coat, sit down, and talk to the person about their concerns.”
Boston cardiologist Haider Warraich, MD, of Brigham and Women’s Hospital, Boston, said it’s important to “put medical information into a greater human context.” For example, he has told patients that he’s still taking his daughter to school despite COVID-19 risks. “I take the information I provide and apply it to my own life,” he said.
The Washington State Department of Health offers this advice to physicians to counter false information and stigma: “Stay updated and informed on COVID-19 to avoid miscommunication or inaccurate information. Talk openly about the harm of stigma. View people directly impacted by stigma as people first. Be conscious of your language. Acknowledge access and language barriers.”
Speak out on social media – but don’t fight
Should medical professionals speak out about COVID-19 misinformation via social media? It’s an individual decision, Dr. Warraich said, “but my sense is that it’s never been more important for physicians to be part of the fray and help quell the epidemic of misinformation that almost always follows any type of medial calamity.”
Dr. Rutland, vice president and founding member of the Association for Healthcare Social Media, cautioned that effective communication via social media requires care. Avoid confrontation, he advised. “Don’t call people stupid or say things like, ‘I went to medical school and I’m smarter than you.’ ”
Instead, he said, “it’s important to just state the facts: These are the people who are dying, these are the people who are getting infected.”
And, he added, remember to push the most important message of all: Wash your hands!
Public health organizations fight the ‘infodemic’
In a trend that hearkens back to the days of snake oil cures for all maladies, advertisements for fake treatments are popping up on the Internet and on other media.
Facebook and Amazon have acted to remove these ads but these messages continue to flood social media such as Twitter, WhatsApp, and other sites. Discussion groups on platforms such as Reddit continue to pump out misinformation about COVID-19. Conspiracy theories that link the virus to espionage and bioweapons are making the rounds on the Internet and talk radio. Wrong information about the effectiveness of non-N95 face masks to protect wearers against infection is widespread, leading to shortages for medical personnel and price gouging. Pernicious rumors about the effectiveness of substances such a vinegar, silver, garlic, lemon juice, and even vodka to disinfect hands and surfaces abound on the Internet. An especially dangerous stream of misinformation stigmatizes ethnic groups and individuals as sources of the infection.
The World Health Organization identified early in the COVID-19 outbreak the global wave of misinformation about the virus and dubbed the problem the “infodemic.” The WHO “Q & A” page on COVID-19 is updated frequently and addresses myths and rumors currently circulating.
According to the WHO website, the agency has reached out to social media players such as Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, and Weibo, the microblogging site in China. WHO has worked with these sites to curb the “infodemic” of misinformation and has used these sites for public education outreach on COVID-19. “Myth busting” infographics posted on a WHO web page are also reposted on major social media sites.
The CDC has followed with its own “frequently asked questions” page to address questions and rumors. State health agencies have put up COVID-19 pages to address public concerns and offer advice on prevention. The Maryland Department of Health web page directly addresses dangerous misinformation: “Do not stigmatize people of any specific ethnicities or racial background. Viruses do not target people from specific populations, ethnicities or racial backgrounds. Stay informed and seek information from reliable, official sources. Be wary of myths, rumors and misinformation circulating online and elsewhere. Health information shared through social media is frequently inaccurate, unless coming from an official, reliable source such as the CDC, MDH or local health departments.”
The Washington State Department of Health has taken a more assertive stance on stigma. The COVID-19 web page recommends to the public: “Show compassion and support for individuals and communities more closely impacted. Avoid stigmatizing people who are in quarantine. They are making the right choice for their communities. Do not make assumptions about someone’s health status based on their ethnicity, race or national origin.”