User login
Creating better performance incentives
P4P programs suffer from several flaws
Many performance improvement programs try to create a higher value health system by incentivizing physicians and health systems to behave in particular ways. These have often been pay-for-performance programs that offer bonuses or impose penalties depending on how providers perform on various metrics.
“In theory, this makes sense,” said Dhruv Khullar, MD, MPP, lead author of a JAMA article about the future of incentives, and assistant professor at Weill Cornell Medicine in New York. “But in practice, these programs have not been successful in consistently improving quality, and sometimes they have been counterproductive. In our article, we argued that focusing too narrowly on financial rewards is not the right strategy to improve health system performance – and is sometimes at odds with the physician professionalism and what really motivates most clinicians.”
Pay-for-performance programs suffer from several fundamental flaws: they focus too narrowly on financial incentives and use centralized accountability instead of local culture, for example, Dr. Khullar said.
“A better future state would involve capitalizing on physician professionalism through nonfinancial rewards, resources for quality improvement, team-based assessments, and emphasizing continuous learning and organizational culture,” he noted. Performance programs would take a more global view of clinical care by emphasizing culture, teams, trust, and learning. Such a system would allow hospitalists and other physicians to worry less about meeting specific metrics and focus more on providing high-quality care to their patients.
“I would hope physicians, payers, and administrators would reconsider some previously held beliefs about quality improvement, especially the idea that better quality requires giving people bonus payments or imposing financial penalties,” Dr. Khullar said. “We believe the next wave of performance improvement programs should entertain other paths to better quality, which are more in line with human motivation and physician professionalism.”
Reference
1. Khullar D, Wolfson D, Casalino LP. Professionalism, Performance, and the Future of Physician Incentives. JAMA. 2018 Nov 26 (Epub ahead of print). doi: 10.1001/jama.2018.17719. Accessed Dec. 11, 2018.
P4P programs suffer from several flaws
P4P programs suffer from several flaws
Many performance improvement programs try to create a higher value health system by incentivizing physicians and health systems to behave in particular ways. These have often been pay-for-performance programs that offer bonuses or impose penalties depending on how providers perform on various metrics.
“In theory, this makes sense,” said Dhruv Khullar, MD, MPP, lead author of a JAMA article about the future of incentives, and assistant professor at Weill Cornell Medicine in New York. “But in practice, these programs have not been successful in consistently improving quality, and sometimes they have been counterproductive. In our article, we argued that focusing too narrowly on financial rewards is not the right strategy to improve health system performance – and is sometimes at odds with the physician professionalism and what really motivates most clinicians.”
Pay-for-performance programs suffer from several fundamental flaws: they focus too narrowly on financial incentives and use centralized accountability instead of local culture, for example, Dr. Khullar said.
“A better future state would involve capitalizing on physician professionalism through nonfinancial rewards, resources for quality improvement, team-based assessments, and emphasizing continuous learning and organizational culture,” he noted. Performance programs would take a more global view of clinical care by emphasizing culture, teams, trust, and learning. Such a system would allow hospitalists and other physicians to worry less about meeting specific metrics and focus more on providing high-quality care to their patients.
“I would hope physicians, payers, and administrators would reconsider some previously held beliefs about quality improvement, especially the idea that better quality requires giving people bonus payments or imposing financial penalties,” Dr. Khullar said. “We believe the next wave of performance improvement programs should entertain other paths to better quality, which are more in line with human motivation and physician professionalism.”
Reference
1. Khullar D, Wolfson D, Casalino LP. Professionalism, Performance, and the Future of Physician Incentives. JAMA. 2018 Nov 26 (Epub ahead of print). doi: 10.1001/jama.2018.17719. Accessed Dec. 11, 2018.
Many performance improvement programs try to create a higher value health system by incentivizing physicians and health systems to behave in particular ways. These have often been pay-for-performance programs that offer bonuses or impose penalties depending on how providers perform on various metrics.
“In theory, this makes sense,” said Dhruv Khullar, MD, MPP, lead author of a JAMA article about the future of incentives, and assistant professor at Weill Cornell Medicine in New York. “But in practice, these programs have not been successful in consistently improving quality, and sometimes they have been counterproductive. In our article, we argued that focusing too narrowly on financial rewards is not the right strategy to improve health system performance – and is sometimes at odds with the physician professionalism and what really motivates most clinicians.”
Pay-for-performance programs suffer from several fundamental flaws: they focus too narrowly on financial incentives and use centralized accountability instead of local culture, for example, Dr. Khullar said.
“A better future state would involve capitalizing on physician professionalism through nonfinancial rewards, resources for quality improvement, team-based assessments, and emphasizing continuous learning and organizational culture,” he noted. Performance programs would take a more global view of clinical care by emphasizing culture, teams, trust, and learning. Such a system would allow hospitalists and other physicians to worry less about meeting specific metrics and focus more on providing high-quality care to their patients.
“I would hope physicians, payers, and administrators would reconsider some previously held beliefs about quality improvement, especially the idea that better quality requires giving people bonus payments or imposing financial penalties,” Dr. Khullar said. “We believe the next wave of performance improvement programs should entertain other paths to better quality, which are more in line with human motivation and physician professionalism.”
Reference
1. Khullar D, Wolfson D, Casalino LP. Professionalism, Performance, and the Future of Physician Incentives. JAMA. 2018 Nov 26 (Epub ahead of print). doi: 10.1001/jama.2018.17719. Accessed Dec. 11, 2018.
A “Ray of light”
Finding inspiration in our patients
I rush into the room at 4:30 p.m., hoping for a quick visit and maybe an early exit from the hospital; I had been asked to see Mr. Bryant in room 6765 with sigmoid volvulus.
“Hey, Dr. Hass, my brother!” he says with a huge smile. Somehow, he must have gotten a glimpse of me before I could see him. I peek over the nurse’s shoulder, and then I see that unforgettable smile with only a few teeth and big bright eyes. Immediately I recognize him and think, “How could I have forgotten his name? Ray – like a beam of light.” He certainly had not forgotten me.
“It’s been more than a year since I was last here,” he says proudly.
When we met during his last hospitalization, I was struck by a thought that implanted itself deep in my brain: This guy is the happiest person I have ever met. And after what must have been 18 hard months for him, he is still smiling – and more than that, he is radiating love.
The fact that he is the “happiest person” is made more remarkable by all the hardship he has endured. Ray was born with cerebral palsy and didn’t walk until he was 10. The continuous spasms in his muscles led to severe cervical disc disease. His worsening pain and weakness were missed by his health care providers until he had lost significant strength in his hands and legs. When he finally got an MRI and then emergency surgery, it was too late. He never regained the dexterity of his hands or the ability to walk. He can climb onto his scooter chair only with the help of a lift.
“Wow! How you been, Ray?”
He replies with a phrase that jumped back out from my memory as he was saying it: “I just wake up every day and think about what I can do to make people happy.”
The goosebumps rise on my arms; I remember feeling this same sense of awe the last time we met – a feeling of real spiritual love for this guy.
“Today I feel so much better, too. I want to thank y’all who helped my stomach go down. Man, it got so huge, I thought I might blow up.” One of the consequences of the nerve damage he sustained is a very slow gut that has led to a stretched-out colon. The other day, his big, floppy colon got twisted, and neither our gastroenterologist nor radiologist was able to untwist it. He still has a tube in his rectum to help decompress his bowel.
Ray fills me in on the details in the slightly strained and slurred speech that sometimes comes with cerebral palsy. As he relays his story, my mind goes to work trying to diagnosis this mysterious case of happiness. How can I not try to get to the origins of this wellspring of love? I can’t help but thinking: Was it Ray’s joy and his speech impediment that made him seem childlike, or was it some brain injury that blessedly knocked out his self-pity? I would be wallowing in self-pity if I were as gravely disabled as him.
After a moment’s reflection, I recall the research on the amazing stability of our happiness set point: Good things and bad only move our happiness for a while before we return to our innate level of happiness. I see I had likely fallen prey to a stereotype of the disabled as heroic for just being themselves. Ray’s happiness is largely because of his lack of self-absorption and his focus on service and love.
Finishing our conversation and leaving the room feeling enlivened, I realize that Ray‘s generous spirit is a gift.
That night, my heart aches. I think about the inadequate care that led to Ray’s profound loss of function, leading to a surge of anger toward our flawed health care system – one that routinely lets down the most vulnerable among us.
The next day, two sisters and an aunt join Ray in his room. They ask for hugs, and I happily supply them. “Ray told us about you,” says Sheila, one of his sisters.
“Well, we have been talking about him here at the hospital, because he brightens everyone’s day. He is truly amazing. Has Ray always been so full of love?” I say, hoping to get some insight into his remarkable spirit.
Tonya, his aunt, responds first. “We were raised that way – to look for the good and keep love in our hearts. But Ray has always been the best. He never, ever complains. He brings joy to so many people. You should see him every day out on his scooter. That’s how he got that big sore on his butt.”
Ray indeed had developed a pressure sore, one that was going to need some thoughtful, ongoing care.
“But I finally got the right kind of cushion, before it was real hard,” he says.
I move from hospitalist mode to primary care mode and ask about his home equipment and his dental care. But they all want to keep talking about love.
“If doctors showed more love and their human side, they could bring more healing,” his sister says.
After 20 minutes of chatting, I pause. It is my last day on service, I had run out of medical reason to stay and I have others to see. So, I reluctantly give my goodbye hugs and leave. At the door, I turn back around. “Hey, Ray, can I get a picture with you?”
“Yeah, I want one with you, too!”
So, not surprisingly, Ray never complains. Maybe his spinal cord injury wasn’t from negligent care. Maybe he was so accustomed to looking past discomfort and too busy with his ministry of love, it didn’t occur to him to seek care.
Still, such a tragedy that he lost so much of the little mobility he did have. But maybe not so bad. His injury brought him back in contact with me and our staff. He is still waking up trying to make people happy and I can see his efforts are working. “He made my day!” I hear from a nurse. There is a healthy buzz at the nurses’ station after visits to his room.
Before walking out the door, he gives me an awkward fist bump from the bed and says, “I want to thank y’all again for everything. And I want you to know I love you.”
I find myself tearing up. “I love you too, my brother. And I am the one who should be grateful, Ray.” Saying it, I feel myself playing a part in the cycle of gratitude. Even small gifts put us under an obligation to give back. With great gifts, the desire to give is inescapable.
There is only one Ray, but he has given me something to aspire toward and what feels like urgency to do it. I want to “wake up each day thinking about ways to make other people happy.”
And understanding the potency of the gift from him has alerted me to the value of looking for other gifts and other inspirations from those I care for – something those of us who tend to be in the “doing” part of the provider-patient relationship can easy miss.
I will never be the beacon of light and love that Ray is, but being compelled to be my most authentic caring self with him, I see that for years I have held back – in the name of professionalism – the positive emotions that naturally arise from the work I do. I will try to shine and try to connect with that “Ray of light” residing in all my patients. I hope, too, that the cycle of giving Ray started will continue spreading to all those I care for.
Dr. Hass is a hospitalist at Sutter Health in Oakland, Calif. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
Finding inspiration in our patients
Finding inspiration in our patients
I rush into the room at 4:30 p.m., hoping for a quick visit and maybe an early exit from the hospital; I had been asked to see Mr. Bryant in room 6765 with sigmoid volvulus.
“Hey, Dr. Hass, my brother!” he says with a huge smile. Somehow, he must have gotten a glimpse of me before I could see him. I peek over the nurse’s shoulder, and then I see that unforgettable smile with only a few teeth and big bright eyes. Immediately I recognize him and think, “How could I have forgotten his name? Ray – like a beam of light.” He certainly had not forgotten me.
“It’s been more than a year since I was last here,” he says proudly.
When we met during his last hospitalization, I was struck by a thought that implanted itself deep in my brain: This guy is the happiest person I have ever met. And after what must have been 18 hard months for him, he is still smiling – and more than that, he is radiating love.
The fact that he is the “happiest person” is made more remarkable by all the hardship he has endured. Ray was born with cerebral palsy and didn’t walk until he was 10. The continuous spasms in his muscles led to severe cervical disc disease. His worsening pain and weakness were missed by his health care providers until he had lost significant strength in his hands and legs. When he finally got an MRI and then emergency surgery, it was too late. He never regained the dexterity of his hands or the ability to walk. He can climb onto his scooter chair only with the help of a lift.
“Wow! How you been, Ray?”
He replies with a phrase that jumped back out from my memory as he was saying it: “I just wake up every day and think about what I can do to make people happy.”
The goosebumps rise on my arms; I remember feeling this same sense of awe the last time we met – a feeling of real spiritual love for this guy.
“Today I feel so much better, too. I want to thank y’all who helped my stomach go down. Man, it got so huge, I thought I might blow up.” One of the consequences of the nerve damage he sustained is a very slow gut that has led to a stretched-out colon. The other day, his big, floppy colon got twisted, and neither our gastroenterologist nor radiologist was able to untwist it. He still has a tube in his rectum to help decompress his bowel.
Ray fills me in on the details in the slightly strained and slurred speech that sometimes comes with cerebral palsy. As he relays his story, my mind goes to work trying to diagnosis this mysterious case of happiness. How can I not try to get to the origins of this wellspring of love? I can’t help but thinking: Was it Ray’s joy and his speech impediment that made him seem childlike, or was it some brain injury that blessedly knocked out his self-pity? I would be wallowing in self-pity if I were as gravely disabled as him.
After a moment’s reflection, I recall the research on the amazing stability of our happiness set point: Good things and bad only move our happiness for a while before we return to our innate level of happiness. I see I had likely fallen prey to a stereotype of the disabled as heroic for just being themselves. Ray’s happiness is largely because of his lack of self-absorption and his focus on service and love.
Finishing our conversation and leaving the room feeling enlivened, I realize that Ray‘s generous spirit is a gift.
That night, my heart aches. I think about the inadequate care that led to Ray’s profound loss of function, leading to a surge of anger toward our flawed health care system – one that routinely lets down the most vulnerable among us.
The next day, two sisters and an aunt join Ray in his room. They ask for hugs, and I happily supply them. “Ray told us about you,” says Sheila, one of his sisters.
“Well, we have been talking about him here at the hospital, because he brightens everyone’s day. He is truly amazing. Has Ray always been so full of love?” I say, hoping to get some insight into his remarkable spirit.
Tonya, his aunt, responds first. “We were raised that way – to look for the good and keep love in our hearts. But Ray has always been the best. He never, ever complains. He brings joy to so many people. You should see him every day out on his scooter. That’s how he got that big sore on his butt.”
Ray indeed had developed a pressure sore, one that was going to need some thoughtful, ongoing care.
“But I finally got the right kind of cushion, before it was real hard,” he says.
I move from hospitalist mode to primary care mode and ask about his home equipment and his dental care. But they all want to keep talking about love.
“If doctors showed more love and their human side, they could bring more healing,” his sister says.
After 20 minutes of chatting, I pause. It is my last day on service, I had run out of medical reason to stay and I have others to see. So, I reluctantly give my goodbye hugs and leave. At the door, I turn back around. “Hey, Ray, can I get a picture with you?”
“Yeah, I want one with you, too!”
So, not surprisingly, Ray never complains. Maybe his spinal cord injury wasn’t from negligent care. Maybe he was so accustomed to looking past discomfort and too busy with his ministry of love, it didn’t occur to him to seek care.
Still, such a tragedy that he lost so much of the little mobility he did have. But maybe not so bad. His injury brought him back in contact with me and our staff. He is still waking up trying to make people happy and I can see his efforts are working. “He made my day!” I hear from a nurse. There is a healthy buzz at the nurses’ station after visits to his room.
Before walking out the door, he gives me an awkward fist bump from the bed and says, “I want to thank y’all again for everything. And I want you to know I love you.”
I find myself tearing up. “I love you too, my brother. And I am the one who should be grateful, Ray.” Saying it, I feel myself playing a part in the cycle of gratitude. Even small gifts put us under an obligation to give back. With great gifts, the desire to give is inescapable.
There is only one Ray, but he has given me something to aspire toward and what feels like urgency to do it. I want to “wake up each day thinking about ways to make other people happy.”
And understanding the potency of the gift from him has alerted me to the value of looking for other gifts and other inspirations from those I care for – something those of us who tend to be in the “doing” part of the provider-patient relationship can easy miss.
I will never be the beacon of light and love that Ray is, but being compelled to be my most authentic caring self with him, I see that for years I have held back – in the name of professionalism – the positive emotions that naturally arise from the work I do. I will try to shine and try to connect with that “Ray of light” residing in all my patients. I hope, too, that the cycle of giving Ray started will continue spreading to all those I care for.
Dr. Hass is a hospitalist at Sutter Health in Oakland, Calif. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
I rush into the room at 4:30 p.m., hoping for a quick visit and maybe an early exit from the hospital; I had been asked to see Mr. Bryant in room 6765 with sigmoid volvulus.
“Hey, Dr. Hass, my brother!” he says with a huge smile. Somehow, he must have gotten a glimpse of me before I could see him. I peek over the nurse’s shoulder, and then I see that unforgettable smile with only a few teeth and big bright eyes. Immediately I recognize him and think, “How could I have forgotten his name? Ray – like a beam of light.” He certainly had not forgotten me.
“It’s been more than a year since I was last here,” he says proudly.
When we met during his last hospitalization, I was struck by a thought that implanted itself deep in my brain: This guy is the happiest person I have ever met. And after what must have been 18 hard months for him, he is still smiling – and more than that, he is radiating love.
The fact that he is the “happiest person” is made more remarkable by all the hardship he has endured. Ray was born with cerebral palsy and didn’t walk until he was 10. The continuous spasms in his muscles led to severe cervical disc disease. His worsening pain and weakness were missed by his health care providers until he had lost significant strength in his hands and legs. When he finally got an MRI and then emergency surgery, it was too late. He never regained the dexterity of his hands or the ability to walk. He can climb onto his scooter chair only with the help of a lift.
“Wow! How you been, Ray?”
He replies with a phrase that jumped back out from my memory as he was saying it: “I just wake up every day and think about what I can do to make people happy.”
The goosebumps rise on my arms; I remember feeling this same sense of awe the last time we met – a feeling of real spiritual love for this guy.
“Today I feel so much better, too. I want to thank y’all who helped my stomach go down. Man, it got so huge, I thought I might blow up.” One of the consequences of the nerve damage he sustained is a very slow gut that has led to a stretched-out colon. The other day, his big, floppy colon got twisted, and neither our gastroenterologist nor radiologist was able to untwist it. He still has a tube in his rectum to help decompress his bowel.
Ray fills me in on the details in the slightly strained and slurred speech that sometimes comes with cerebral palsy. As he relays his story, my mind goes to work trying to diagnosis this mysterious case of happiness. How can I not try to get to the origins of this wellspring of love? I can’t help but thinking: Was it Ray’s joy and his speech impediment that made him seem childlike, or was it some brain injury that blessedly knocked out his self-pity? I would be wallowing in self-pity if I were as gravely disabled as him.
After a moment’s reflection, I recall the research on the amazing stability of our happiness set point: Good things and bad only move our happiness for a while before we return to our innate level of happiness. I see I had likely fallen prey to a stereotype of the disabled as heroic for just being themselves. Ray’s happiness is largely because of his lack of self-absorption and his focus on service and love.
Finishing our conversation and leaving the room feeling enlivened, I realize that Ray‘s generous spirit is a gift.
That night, my heart aches. I think about the inadequate care that led to Ray’s profound loss of function, leading to a surge of anger toward our flawed health care system – one that routinely lets down the most vulnerable among us.
The next day, two sisters and an aunt join Ray in his room. They ask for hugs, and I happily supply them. “Ray told us about you,” says Sheila, one of his sisters.
“Well, we have been talking about him here at the hospital, because he brightens everyone’s day. He is truly amazing. Has Ray always been so full of love?” I say, hoping to get some insight into his remarkable spirit.
Tonya, his aunt, responds first. “We were raised that way – to look for the good and keep love in our hearts. But Ray has always been the best. He never, ever complains. He brings joy to so many people. You should see him every day out on his scooter. That’s how he got that big sore on his butt.”
Ray indeed had developed a pressure sore, one that was going to need some thoughtful, ongoing care.
“But I finally got the right kind of cushion, before it was real hard,” he says.
I move from hospitalist mode to primary care mode and ask about his home equipment and his dental care. But they all want to keep talking about love.
“If doctors showed more love and their human side, they could bring more healing,” his sister says.
After 20 minutes of chatting, I pause. It is my last day on service, I had run out of medical reason to stay and I have others to see. So, I reluctantly give my goodbye hugs and leave. At the door, I turn back around. “Hey, Ray, can I get a picture with you?”
“Yeah, I want one with you, too!”
So, not surprisingly, Ray never complains. Maybe his spinal cord injury wasn’t from negligent care. Maybe he was so accustomed to looking past discomfort and too busy with his ministry of love, it didn’t occur to him to seek care.
Still, such a tragedy that he lost so much of the little mobility he did have. But maybe not so bad. His injury brought him back in contact with me and our staff. He is still waking up trying to make people happy and I can see his efforts are working. “He made my day!” I hear from a nurse. There is a healthy buzz at the nurses’ station after visits to his room.
Before walking out the door, he gives me an awkward fist bump from the bed and says, “I want to thank y’all again for everything. And I want you to know I love you.”
I find myself tearing up. “I love you too, my brother. And I am the one who should be grateful, Ray.” Saying it, I feel myself playing a part in the cycle of gratitude. Even small gifts put us under an obligation to give back. With great gifts, the desire to give is inescapable.
There is only one Ray, but he has given me something to aspire toward and what feels like urgency to do it. I want to “wake up each day thinking about ways to make other people happy.”
And understanding the potency of the gift from him has alerted me to the value of looking for other gifts and other inspirations from those I care for – something those of us who tend to be in the “doing” part of the provider-patient relationship can easy miss.
I will never be the beacon of light and love that Ray is, but being compelled to be my most authentic caring self with him, I see that for years I have held back – in the name of professionalism – the positive emotions that naturally arise from the work I do. I will try to shine and try to connect with that “Ray of light” residing in all my patients. I hope, too, that the cycle of giving Ray started will continue spreading to all those I care for.
Dr. Hass is a hospitalist at Sutter Health in Oakland, Calif. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
Are hospitalists being more highly valued?
An uptrend in financial support
Since the inception of hospital medicine more than 2 decades ago, the total number of hospitalists has rapidly increased to more than 60,000. The Society of Hospital Medicine’s State of Hospital Medicine Report (SoHM), published biennially, captures new changes in our growing field and sheds light on current practice trends.
Among its findings, the 2018 SoHM Report reassuringly reveals that financial support from hospitals to hospital medicine groups (HMGs) continues to climb, even in the setting of rising health care costs and ongoing budget pressure.
The median amount of financial support per full-time equivalent (FTE) physician for HMGs serving adults was $176,658, according to the 2018 SoHM Report, which is up 12% from the 2016 median of $157,535. While there is no correlation between group sizes and the amount of financial support per FTE physician, there are significant differences across regions, with HMGs in the Midwest garnering the highest median support, at $193,121 per FTE physician.
The report also reveals big differences by employment model. For example, private multispecialty and primary care medical groups receive much less financial support ($58,396 per FTE physician) than HMGs employed by hospitals. This likely signifies that their main source of revenue is from professional service fees. Regardless of the types of employment models, past surveys have reported more than 95% of HMGs receive support from their hospitals to help cover expenses.
The median amount of financial support per FTE provider (including nurse practitioners, physician assistants, and locum tenens) was $134,300, which represents a 3.3% decrease, compared with the 2016 SoHM Report. For the first time, the 2018 SoHM also collected data on financial support per “work relative value unit” (wRVU) in addition to support per FTE physician and support per FTE provider. HMGs and their hospitals can use support per wRVU data to evaluate the support per unit of work, regardless of who (whether it is a physician, an advanced practice provider, and/or others) performed that work.
The median amount of financial support per wRVU for HMGs serving adults in 2018 was $41.92, with academic HMGs reporting a higher amount ($45.81) than nonacademic HMGs ($41.28). It will be interesting to track these numbers over time.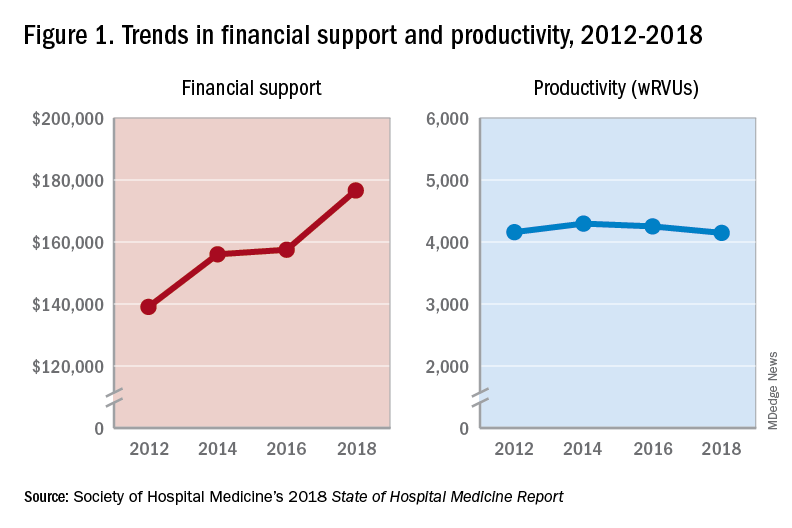
One of the most intriguing findings from the SHM’s 2018 SoHM Report is that financial support has risen despite relatively flat professional fee productivity (see Figure 1). Productivity, calculated as work relative value units (wRVUs) per physician declined slightly from 4,252 in 2016 to 4,147 in 2018.
There may be a few reasons why wRVUs per physician has remained relatively unchanged over the years. Many hospitals emphasize quality of care above provider productivity. The volume-to-value shift in theory serves as a means to reduce hospital-associated complications, length of stay, and readmission rates, thereby avoiding penalties and saving the overall costs for the hospitals in the long run.
Hospitalists involved in quality improvement projects and other essential nonclinical work perform tasks that are rarely captured in the wRVU metric. Improving patient experience, one of the Triple Aim components, necessitates extra time and effort, which also are nonbillable. In addition, increasing productivity can be challenging, a double-edged sword that may further escalate burnout and turnover rates. The static productivity may portend that it has leveled off or hit the ceiling in spite of ongoing efforts to improve efficacy.
In my view, the decision to invest in hospitalists for their contributions and dedications should not be determined based on a single metric such as wRVUs per physician. Hospitalist work on quality improvements; patient safety; efficiency, from direct bedside patient care to nonclinical efforts; teaching; research; involvements in various committees; administrative tasks; and leadership roles in improving health care systems are immeasurable. These are the reasons that most hospitals chose to adopt the hospitalist model and continue to support it. In fact, demand for hospitalists still outstrips supply, as evidenced by more than half of the hospital medicine groups with unfilled positions and an overall high turnover rate per 2018 SoHM data.
Although hospitalists are needed for the value that they provide, they should not take the status quo for granted. Instead, in return for the favorable financial support and in appreciation of being valued, hospitalists have a responsibility to prove that they are the right group chosen to do the work and help achieve their hospital’s mission and goals.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
References
Afsar N. Looking into the Future and Making History. Hospitalist. 2019;23(1):31.
Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
FitzGerald S. Not a Time for Modesty. Oct. 2009. Retrieved from https://acphospitalist.org/archives/2009/10/value.htm.
Watcher RM et al. Zero to 50,000 – The 20th Anniversary of the Hospitalist. N Eng J Med. 2016. 375(11):1009-11.
An uptrend in financial support
An uptrend in financial support
Since the inception of hospital medicine more than 2 decades ago, the total number of hospitalists has rapidly increased to more than 60,000. The Society of Hospital Medicine’s State of Hospital Medicine Report (SoHM), published biennially, captures new changes in our growing field and sheds light on current practice trends.
Among its findings, the 2018 SoHM Report reassuringly reveals that financial support from hospitals to hospital medicine groups (HMGs) continues to climb, even in the setting of rising health care costs and ongoing budget pressure.
The median amount of financial support per full-time equivalent (FTE) physician for HMGs serving adults was $176,658, according to the 2018 SoHM Report, which is up 12% from the 2016 median of $157,535. While there is no correlation between group sizes and the amount of financial support per FTE physician, there are significant differences across regions, with HMGs in the Midwest garnering the highest median support, at $193,121 per FTE physician.
The report also reveals big differences by employment model. For example, private multispecialty and primary care medical groups receive much less financial support ($58,396 per FTE physician) than HMGs employed by hospitals. This likely signifies that their main source of revenue is from professional service fees. Regardless of the types of employment models, past surveys have reported more than 95% of HMGs receive support from their hospitals to help cover expenses.
The median amount of financial support per FTE provider (including nurse practitioners, physician assistants, and locum tenens) was $134,300, which represents a 3.3% decrease, compared with the 2016 SoHM Report. For the first time, the 2018 SoHM also collected data on financial support per “work relative value unit” (wRVU) in addition to support per FTE physician and support per FTE provider. HMGs and their hospitals can use support per wRVU data to evaluate the support per unit of work, regardless of who (whether it is a physician, an advanced practice provider, and/or others) performed that work.
The median amount of financial support per wRVU for HMGs serving adults in 2018 was $41.92, with academic HMGs reporting a higher amount ($45.81) than nonacademic HMGs ($41.28). It will be interesting to track these numbers over time.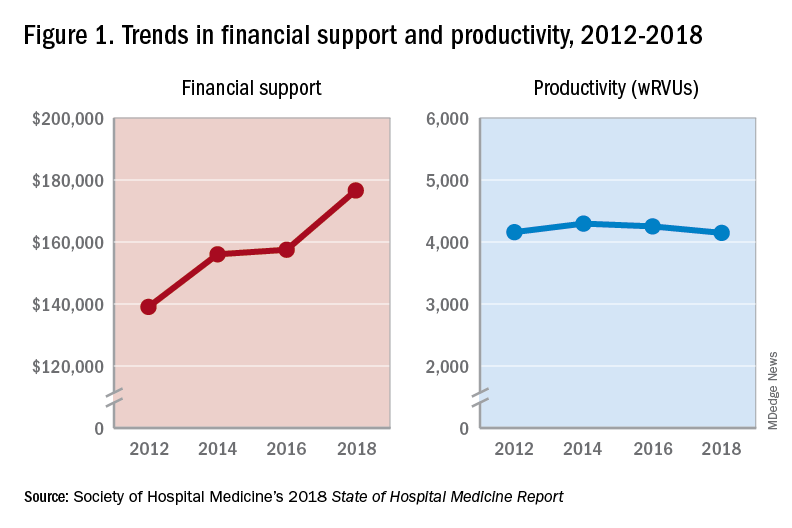
One of the most intriguing findings from the SHM’s 2018 SoHM Report is that financial support has risen despite relatively flat professional fee productivity (see Figure 1). Productivity, calculated as work relative value units (wRVUs) per physician declined slightly from 4,252 in 2016 to 4,147 in 2018.
There may be a few reasons why wRVUs per physician has remained relatively unchanged over the years. Many hospitals emphasize quality of care above provider productivity. The volume-to-value shift in theory serves as a means to reduce hospital-associated complications, length of stay, and readmission rates, thereby avoiding penalties and saving the overall costs for the hospitals in the long run.
Hospitalists involved in quality improvement projects and other essential nonclinical work perform tasks that are rarely captured in the wRVU metric. Improving patient experience, one of the Triple Aim components, necessitates extra time and effort, which also are nonbillable. In addition, increasing productivity can be challenging, a double-edged sword that may further escalate burnout and turnover rates. The static productivity may portend that it has leveled off or hit the ceiling in spite of ongoing efforts to improve efficacy.
In my view, the decision to invest in hospitalists for their contributions and dedications should not be determined based on a single metric such as wRVUs per physician. Hospitalist work on quality improvements; patient safety; efficiency, from direct bedside patient care to nonclinical efforts; teaching; research; involvements in various committees; administrative tasks; and leadership roles in improving health care systems are immeasurable. These are the reasons that most hospitals chose to adopt the hospitalist model and continue to support it. In fact, demand for hospitalists still outstrips supply, as evidenced by more than half of the hospital medicine groups with unfilled positions and an overall high turnover rate per 2018 SoHM data.
Although hospitalists are needed for the value that they provide, they should not take the status quo for granted. Instead, in return for the favorable financial support and in appreciation of being valued, hospitalists have a responsibility to prove that they are the right group chosen to do the work and help achieve their hospital’s mission and goals.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
References
Afsar N. Looking into the Future and Making History. Hospitalist. 2019;23(1):31.
Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
FitzGerald S. Not a Time for Modesty. Oct. 2009. Retrieved from https://acphospitalist.org/archives/2009/10/value.htm.
Watcher RM et al. Zero to 50,000 – The 20th Anniversary of the Hospitalist. N Eng J Med. 2016. 375(11):1009-11.
Since the inception of hospital medicine more than 2 decades ago, the total number of hospitalists has rapidly increased to more than 60,000. The Society of Hospital Medicine’s State of Hospital Medicine Report (SoHM), published biennially, captures new changes in our growing field and sheds light on current practice trends.
Among its findings, the 2018 SoHM Report reassuringly reveals that financial support from hospitals to hospital medicine groups (HMGs) continues to climb, even in the setting of rising health care costs and ongoing budget pressure.
The median amount of financial support per full-time equivalent (FTE) physician for HMGs serving adults was $176,658, according to the 2018 SoHM Report, which is up 12% from the 2016 median of $157,535. While there is no correlation between group sizes and the amount of financial support per FTE physician, there are significant differences across regions, with HMGs in the Midwest garnering the highest median support, at $193,121 per FTE physician.
The report also reveals big differences by employment model. For example, private multispecialty and primary care medical groups receive much less financial support ($58,396 per FTE physician) than HMGs employed by hospitals. This likely signifies that their main source of revenue is from professional service fees. Regardless of the types of employment models, past surveys have reported more than 95% of HMGs receive support from their hospitals to help cover expenses.
The median amount of financial support per FTE provider (including nurse practitioners, physician assistants, and locum tenens) was $134,300, which represents a 3.3% decrease, compared with the 2016 SoHM Report. For the first time, the 2018 SoHM also collected data on financial support per “work relative value unit” (wRVU) in addition to support per FTE physician and support per FTE provider. HMGs and their hospitals can use support per wRVU data to evaluate the support per unit of work, regardless of who (whether it is a physician, an advanced practice provider, and/or others) performed that work.
The median amount of financial support per wRVU for HMGs serving adults in 2018 was $41.92, with academic HMGs reporting a higher amount ($45.81) than nonacademic HMGs ($41.28). It will be interesting to track these numbers over time.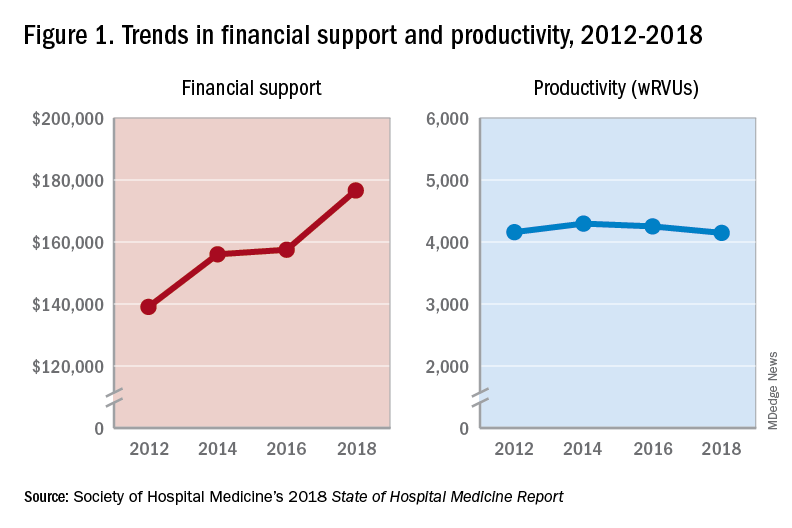
One of the most intriguing findings from the SHM’s 2018 SoHM Report is that financial support has risen despite relatively flat professional fee productivity (see Figure 1). Productivity, calculated as work relative value units (wRVUs) per physician declined slightly from 4,252 in 2016 to 4,147 in 2018.
There may be a few reasons why wRVUs per physician has remained relatively unchanged over the years. Many hospitals emphasize quality of care above provider productivity. The volume-to-value shift in theory serves as a means to reduce hospital-associated complications, length of stay, and readmission rates, thereby avoiding penalties and saving the overall costs for the hospitals in the long run.
Hospitalists involved in quality improvement projects and other essential nonclinical work perform tasks that are rarely captured in the wRVU metric. Improving patient experience, one of the Triple Aim components, necessitates extra time and effort, which also are nonbillable. In addition, increasing productivity can be challenging, a double-edged sword that may further escalate burnout and turnover rates. The static productivity may portend that it has leveled off or hit the ceiling in spite of ongoing efforts to improve efficacy.
In my view, the decision to invest in hospitalists for their contributions and dedications should not be determined based on a single metric such as wRVUs per physician. Hospitalist work on quality improvements; patient safety; efficiency, from direct bedside patient care to nonclinical efforts; teaching; research; involvements in various committees; administrative tasks; and leadership roles in improving health care systems are immeasurable. These are the reasons that most hospitals chose to adopt the hospitalist model and continue to support it. In fact, demand for hospitalists still outstrips supply, as evidenced by more than half of the hospital medicine groups with unfilled positions and an overall high turnover rate per 2018 SoHM data.
Although hospitalists are needed for the value that they provide, they should not take the status quo for granted. Instead, in return for the favorable financial support and in appreciation of being valued, hospitalists have a responsibility to prove that they are the right group chosen to do the work and help achieve their hospital’s mission and goals.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
References
Afsar N. Looking into the Future and Making History. Hospitalist. 2019;23(1):31.
Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
FitzGerald S. Not a Time for Modesty. Oct. 2009. Retrieved from https://acphospitalist.org/archives/2009/10/value.htm.
Watcher RM et al. Zero to 50,000 – The 20th Anniversary of the Hospitalist. N Eng J Med. 2016. 375(11):1009-11.
Reducing adverse drug reactions
Easing the inpatient/outpatient transition
Adverse drug reactions are a problem hospitalists encounter often. An estimated 9% of hospital admissions in older adults are the result of adverse drug reactions, and up to one in five adults experience an adverse drug reaction during hospitalization.
“Many interventions have been tried to solve this problem, and certain of them have worked, but to date we don’t have any great solutions that meaningfully impact the rate of these events in a way that’s feasible in most health care environments, so any efforts to reduce the burden of these problems in older adults could be hugely beneficial,” said Michael Steinman, MD, author of an editorial highlighting a new approach.
His editorial in BMJ Quality & Safety cites research on the Pharm2Pharm program, implemented in six Hawaiian hospitals, in which hospital-based pharmacists identified inpatients at high risk of medication misadventures with criteria such as use of multiple medications, presence of high-risk medications such as warfarin or glucose-lowering drugs, and a history of previous acute care use resulting from medication-related problems. The hospital pharmacist would then meet with the patient to reconcile medications and facilitate a coordinated hand-off to a community pharmacist, who would meet with the patient after discharge.
In addition to a 36% reduction in the rate of medication-related hospitalizations, the intervention generated an estimated savings of $6.6 million per year in avoided hospitalizations.
There are two major takeaways, said Dr. Steinman, who is based in the division of geriatrics at the University of California, San Francisco: It’s critical to focus on transitions and coordination between inpatient and outpatient care to address medication-related problems, and pharmacists can be extremely helpful in that.
“Decisions about drug therapy in the hospital may seem reasonable in the short term but often won’t stick in the long term unless there is a coordinated care that can help ensure appropriate follow-through once patients return home,” Dr. Steinman said. “The study that the editorial references is a systems intervention that hospitalists can advocate for in their own institutions, but in the immediate day-to-day, trying to ensure solid coordination of medication management from the inpatient to outpatient setting is likely to be very helpful for their patients.”
The long-term outcomes of hospitalized patients are largely influenced by getting them set up with appropriate community resources and supports once they leave the hospital, he added, and the hospital can play a critical role in putting these pieces into place.
Reference
1. Steinman MA. Reducing hospital admissions for adverse drug events through coordinated pharmacist care: learning from Hawai’i without a field trip. BMJ Qual Saf. Epub 2018 Nov 24. doi: 10.1136/bmjqs-2018-008815. Accessed Dec. 11, 2018.
Easing the inpatient/outpatient transition
Easing the inpatient/outpatient transition
Adverse drug reactions are a problem hospitalists encounter often. An estimated 9% of hospital admissions in older adults are the result of adverse drug reactions, and up to one in five adults experience an adverse drug reaction during hospitalization.
“Many interventions have been tried to solve this problem, and certain of them have worked, but to date we don’t have any great solutions that meaningfully impact the rate of these events in a way that’s feasible in most health care environments, so any efforts to reduce the burden of these problems in older adults could be hugely beneficial,” said Michael Steinman, MD, author of an editorial highlighting a new approach.
His editorial in BMJ Quality & Safety cites research on the Pharm2Pharm program, implemented in six Hawaiian hospitals, in which hospital-based pharmacists identified inpatients at high risk of medication misadventures with criteria such as use of multiple medications, presence of high-risk medications such as warfarin or glucose-lowering drugs, and a history of previous acute care use resulting from medication-related problems. The hospital pharmacist would then meet with the patient to reconcile medications and facilitate a coordinated hand-off to a community pharmacist, who would meet with the patient after discharge.
In addition to a 36% reduction in the rate of medication-related hospitalizations, the intervention generated an estimated savings of $6.6 million per year in avoided hospitalizations.
There are two major takeaways, said Dr. Steinman, who is based in the division of geriatrics at the University of California, San Francisco: It’s critical to focus on transitions and coordination between inpatient and outpatient care to address medication-related problems, and pharmacists can be extremely helpful in that.
“Decisions about drug therapy in the hospital may seem reasonable in the short term but often won’t stick in the long term unless there is a coordinated care that can help ensure appropriate follow-through once patients return home,” Dr. Steinman said. “The study that the editorial references is a systems intervention that hospitalists can advocate for in their own institutions, but in the immediate day-to-day, trying to ensure solid coordination of medication management from the inpatient to outpatient setting is likely to be very helpful for their patients.”
The long-term outcomes of hospitalized patients are largely influenced by getting them set up with appropriate community resources and supports once they leave the hospital, he added, and the hospital can play a critical role in putting these pieces into place.
Reference
1. Steinman MA. Reducing hospital admissions for adverse drug events through coordinated pharmacist care: learning from Hawai’i without a field trip. BMJ Qual Saf. Epub 2018 Nov 24. doi: 10.1136/bmjqs-2018-008815. Accessed Dec. 11, 2018.
Adverse drug reactions are a problem hospitalists encounter often. An estimated 9% of hospital admissions in older adults are the result of adverse drug reactions, and up to one in five adults experience an adverse drug reaction during hospitalization.
“Many interventions have been tried to solve this problem, and certain of them have worked, but to date we don’t have any great solutions that meaningfully impact the rate of these events in a way that’s feasible in most health care environments, so any efforts to reduce the burden of these problems in older adults could be hugely beneficial,” said Michael Steinman, MD, author of an editorial highlighting a new approach.
His editorial in BMJ Quality & Safety cites research on the Pharm2Pharm program, implemented in six Hawaiian hospitals, in which hospital-based pharmacists identified inpatients at high risk of medication misadventures with criteria such as use of multiple medications, presence of high-risk medications such as warfarin or glucose-lowering drugs, and a history of previous acute care use resulting from medication-related problems. The hospital pharmacist would then meet with the patient to reconcile medications and facilitate a coordinated hand-off to a community pharmacist, who would meet with the patient after discharge.
In addition to a 36% reduction in the rate of medication-related hospitalizations, the intervention generated an estimated savings of $6.6 million per year in avoided hospitalizations.
There are two major takeaways, said Dr. Steinman, who is based in the division of geriatrics at the University of California, San Francisco: It’s critical to focus on transitions and coordination between inpatient and outpatient care to address medication-related problems, and pharmacists can be extremely helpful in that.
“Decisions about drug therapy in the hospital may seem reasonable in the short term but often won’t stick in the long term unless there is a coordinated care that can help ensure appropriate follow-through once patients return home,” Dr. Steinman said. “The study that the editorial references is a systems intervention that hospitalists can advocate for in their own institutions, but in the immediate day-to-day, trying to ensure solid coordination of medication management from the inpatient to outpatient setting is likely to be very helpful for their patients.”
The long-term outcomes of hospitalized patients are largely influenced by getting them set up with appropriate community resources and supports once they leave the hospital, he added, and the hospital can play a critical role in putting these pieces into place.
Reference
1. Steinman MA. Reducing hospital admissions for adverse drug events through coordinated pharmacist care: learning from Hawai’i without a field trip. BMJ Qual Saf. Epub 2018 Nov 24. doi: 10.1136/bmjqs-2018-008815. Accessed Dec. 11, 2018.
Bringing QI training to an IM residency program
Consider a formal step-wise curriculum
For current and future hospitalists, there’s no doubt that knowledge of quality improvement (QI) fundamentals is an important component of a successful practice. One physician team set out to provide their trainees with that QI foundation and described the results.
“We believed that implementing a formal step-wise QI curriculum would not only meet the Accreditation Council of Graduate Medical Education (ACGME) requirements, but also increase residents’ knowledge of QI fundamentals and ultimately establish a culture of continuous improvement aiming to provide high-value care to our health care consumers,” said lead author J. Colt Cowdell, MD, MBA, of Mayo Clinic in Jacksonville, Fla.
Prior to any interventions, the team surveyed internal medicine residents regarding three unique patient scenarios and scored their answers. Residents were then assigned to one of five unique QI projects for the academic year in combination with a structured didactic QI curriculum.
After the structured progressive curriculum, in combination with team-based QI projects, residents were surveyed again. Results showed not only increased QI knowledge, but also improved patient safety and reduced waste.
“Keys to successful implementation included a thorough explanation of the need for this curriculum to the learners and ensuring that QI teams were multidisciplinary – residents, QI experts, nurses, techs, pharmacy, administrators, etc.,” said Dr. Cowdell.
For hospitalists in an academic setting, this work can provide a framework to incorporate QI into their residency programs. “I hope, if they have a passion for QI, they would seek out opportunities to mentor residents and help lead multidisciplinary team-based projects,” Dr. Cowdell said.
Reference
1. Cowdell, JC; Trautman, C; Lewis, M; Dawson, N. Integration of a Novel Quality Improvement Curriculum into an Internal Medicine Residency Program. Abstract published at Hospital Medicine 2018; April 8-11; Orlando, Fla. Abstract 54. https://www.shmabstracts.com/abstract/integration-of-a-novel-quality-improvement-curriculum-into-an-internal-medicine-residency-program/. Accessed Dec. 11, 2018.
Consider a formal step-wise curriculum
Consider a formal step-wise curriculum
For current and future hospitalists, there’s no doubt that knowledge of quality improvement (QI) fundamentals is an important component of a successful practice. One physician team set out to provide their trainees with that QI foundation and described the results.
“We believed that implementing a formal step-wise QI curriculum would not only meet the Accreditation Council of Graduate Medical Education (ACGME) requirements, but also increase residents’ knowledge of QI fundamentals and ultimately establish a culture of continuous improvement aiming to provide high-value care to our health care consumers,” said lead author J. Colt Cowdell, MD, MBA, of Mayo Clinic in Jacksonville, Fla.
Prior to any interventions, the team surveyed internal medicine residents regarding three unique patient scenarios and scored their answers. Residents were then assigned to one of five unique QI projects for the academic year in combination with a structured didactic QI curriculum.
After the structured progressive curriculum, in combination with team-based QI projects, residents were surveyed again. Results showed not only increased QI knowledge, but also improved patient safety and reduced waste.
“Keys to successful implementation included a thorough explanation of the need for this curriculum to the learners and ensuring that QI teams were multidisciplinary – residents, QI experts, nurses, techs, pharmacy, administrators, etc.,” said Dr. Cowdell.
For hospitalists in an academic setting, this work can provide a framework to incorporate QI into their residency programs. “I hope, if they have a passion for QI, they would seek out opportunities to mentor residents and help lead multidisciplinary team-based projects,” Dr. Cowdell said.
Reference
1. Cowdell, JC; Trautman, C; Lewis, M; Dawson, N. Integration of a Novel Quality Improvement Curriculum into an Internal Medicine Residency Program. Abstract published at Hospital Medicine 2018; April 8-11; Orlando, Fla. Abstract 54. https://www.shmabstracts.com/abstract/integration-of-a-novel-quality-improvement-curriculum-into-an-internal-medicine-residency-program/. Accessed Dec. 11, 2018.
For current and future hospitalists, there’s no doubt that knowledge of quality improvement (QI) fundamentals is an important component of a successful practice. One physician team set out to provide their trainees with that QI foundation and described the results.
“We believed that implementing a formal step-wise QI curriculum would not only meet the Accreditation Council of Graduate Medical Education (ACGME) requirements, but also increase residents’ knowledge of QI fundamentals and ultimately establish a culture of continuous improvement aiming to provide high-value care to our health care consumers,” said lead author J. Colt Cowdell, MD, MBA, of Mayo Clinic in Jacksonville, Fla.
Prior to any interventions, the team surveyed internal medicine residents regarding three unique patient scenarios and scored their answers. Residents were then assigned to one of five unique QI projects for the academic year in combination with a structured didactic QI curriculum.
After the structured progressive curriculum, in combination with team-based QI projects, residents were surveyed again. Results showed not only increased QI knowledge, but also improved patient safety and reduced waste.
“Keys to successful implementation included a thorough explanation of the need for this curriculum to the learners and ensuring that QI teams were multidisciplinary – residents, QI experts, nurses, techs, pharmacy, administrators, etc.,” said Dr. Cowdell.
For hospitalists in an academic setting, this work can provide a framework to incorporate QI into their residency programs. “I hope, if they have a passion for QI, they would seek out opportunities to mentor residents and help lead multidisciplinary team-based projects,” Dr. Cowdell said.
Reference
1. Cowdell, JC; Trautman, C; Lewis, M; Dawson, N. Integration of a Novel Quality Improvement Curriculum into an Internal Medicine Residency Program. Abstract published at Hospital Medicine 2018; April 8-11; Orlando, Fla. Abstract 54. https://www.shmabstracts.com/abstract/integration-of-a-novel-quality-improvement-curriculum-into-an-internal-medicine-residency-program/. Accessed Dec. 11, 2018.
Discharge before noon: An appropriate metric for efficiency?
I first heard the term “discharge before noon” (DCBN) as a third-year medical student starting my internal medicine rotation. The basic idea made sense: Get patients out of the hospital early so rooms can be cleaned more quickly and new patients wouldn’t have to wait so long in the ED.
It quickly became apparent, however, that a lot of moving parts had to align perfectly for DCBN. Even if we prioritized rounding on dischargeable patients (starting 8-9 a.m. depending on the service/day), they still needed prescriptions filled, normal clothes to wear, and a way to get home, which wasn’t easy to coordinate while we were still trying to see all the other patients.
Fast forward through 5 years of residency/fellowship experience and DCBN seems even more unrealistic in hospitalized pediatric patients. As a simple example, discharge criteria for dehydration (one of the most common reasons for pediatric hospitalization) include demonstrating the ability to drink enough liquids to stay hydrated. Who’s going to force children to stay up all night sipping fluids (plus changing all those diapers or taking them to the bathroom)? If the child stays on intravenous fluids overnight, we have to monitor at least through breakfast, likely lunch, thus making DCBN nearly impossible.
In a January 2019 article in the Journal of Hospital Medicine, Hailey James, MHA, (@Haileyjms on Twitter) and her colleagues demonstrated an association between DCBN and decreased length of stay (LOS) for medical but not surgical pediatric discharges.1 This made them question if DCBN is an appropriate metric for discharge efficiency, as well as workflow differences between services. Many hospitals, however, still try to push DCBN as a goal (see Destino et al in the same January 2019 issue of JHM2), which could potentially lead to people trying to game the system.
How does your institution try to make discharge processes more efficient? Is it actually possible to do everything more quickly without sacrificing quality or trainee education? Whether your patients are kids, adults, or both, there are likely many issues in common where we could all learn from each other.
We discussed this topic in #JHMChat on April 15 on Twitter. New to Twitter or not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed dozens of articles spanning a wide variety of topics related to caring for hospitalized patients. All are welcome to join, including medical students, residents, nurses, practicing hospitalists, and more. It’s a great opportunity to virtually meet and learn from others while earning free CME.
To participate in future chats, type #JHMChat in the search box on the top right corner of your Twitter homepage, click on the “Latest” tab at the top left to see the most recent tweets, and join the conversation (don’t forget the hashtag)!
Dr. Chen is a pediatric hospital medicine fellow at Rady Children’s Hospital, University of California, San Diego. She is one of the cofounders/moderators of #PHMFellowJC, serves as a fellow district representative for the American Academy of Pediatrics, and is an active #tweetiatrician at @DrJenChen4kids. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
References
1. James HJ et al. The Association of Discharge Before Noon and Length of Stay in Hospitalized Pediatric Patients. J Hosp Med. 2019;14(1):28-32. doi: 10.12788/jhm.3111.
2. Destino L et al. Improving Patient Flow: Analysis of an Initiative to Improve Early Discharge. J Hosp Med. 2019;14(1):22-7. doi: 10.12788/jhm.3133.
I first heard the term “discharge before noon” (DCBN) as a third-year medical student starting my internal medicine rotation. The basic idea made sense: Get patients out of the hospital early so rooms can be cleaned more quickly and new patients wouldn’t have to wait so long in the ED.
It quickly became apparent, however, that a lot of moving parts had to align perfectly for DCBN. Even if we prioritized rounding on dischargeable patients (starting 8-9 a.m. depending on the service/day), they still needed prescriptions filled, normal clothes to wear, and a way to get home, which wasn’t easy to coordinate while we were still trying to see all the other patients.
Fast forward through 5 years of residency/fellowship experience and DCBN seems even more unrealistic in hospitalized pediatric patients. As a simple example, discharge criteria for dehydration (one of the most common reasons for pediatric hospitalization) include demonstrating the ability to drink enough liquids to stay hydrated. Who’s going to force children to stay up all night sipping fluids (plus changing all those diapers or taking them to the bathroom)? If the child stays on intravenous fluids overnight, we have to monitor at least through breakfast, likely lunch, thus making DCBN nearly impossible.
In a January 2019 article in the Journal of Hospital Medicine, Hailey James, MHA, (@Haileyjms on Twitter) and her colleagues demonstrated an association between DCBN and decreased length of stay (LOS) for medical but not surgical pediatric discharges.1 This made them question if DCBN is an appropriate metric for discharge efficiency, as well as workflow differences between services. Many hospitals, however, still try to push DCBN as a goal (see Destino et al in the same January 2019 issue of JHM2), which could potentially lead to people trying to game the system.
How does your institution try to make discharge processes more efficient? Is it actually possible to do everything more quickly without sacrificing quality or trainee education? Whether your patients are kids, adults, or both, there are likely many issues in common where we could all learn from each other.
We discussed this topic in #JHMChat on April 15 on Twitter. New to Twitter or not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed dozens of articles spanning a wide variety of topics related to caring for hospitalized patients. All are welcome to join, including medical students, residents, nurses, practicing hospitalists, and more. It’s a great opportunity to virtually meet and learn from others while earning free CME.
To participate in future chats, type #JHMChat in the search box on the top right corner of your Twitter homepage, click on the “Latest” tab at the top left to see the most recent tweets, and join the conversation (don’t forget the hashtag)!
Dr. Chen is a pediatric hospital medicine fellow at Rady Children’s Hospital, University of California, San Diego. She is one of the cofounders/moderators of #PHMFellowJC, serves as a fellow district representative for the American Academy of Pediatrics, and is an active #tweetiatrician at @DrJenChen4kids. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
References
1. James HJ et al. The Association of Discharge Before Noon and Length of Stay in Hospitalized Pediatric Patients. J Hosp Med. 2019;14(1):28-32. doi: 10.12788/jhm.3111.
2. Destino L et al. Improving Patient Flow: Analysis of an Initiative to Improve Early Discharge. J Hosp Med. 2019;14(1):22-7. doi: 10.12788/jhm.3133.
I first heard the term “discharge before noon” (DCBN) as a third-year medical student starting my internal medicine rotation. The basic idea made sense: Get patients out of the hospital early so rooms can be cleaned more quickly and new patients wouldn’t have to wait so long in the ED.
It quickly became apparent, however, that a lot of moving parts had to align perfectly for DCBN. Even if we prioritized rounding on dischargeable patients (starting 8-9 a.m. depending on the service/day), they still needed prescriptions filled, normal clothes to wear, and a way to get home, which wasn’t easy to coordinate while we were still trying to see all the other patients.
Fast forward through 5 years of residency/fellowship experience and DCBN seems even more unrealistic in hospitalized pediatric patients. As a simple example, discharge criteria for dehydration (one of the most common reasons for pediatric hospitalization) include demonstrating the ability to drink enough liquids to stay hydrated. Who’s going to force children to stay up all night sipping fluids (plus changing all those diapers or taking them to the bathroom)? If the child stays on intravenous fluids overnight, we have to monitor at least through breakfast, likely lunch, thus making DCBN nearly impossible.
In a January 2019 article in the Journal of Hospital Medicine, Hailey James, MHA, (@Haileyjms on Twitter) and her colleagues demonstrated an association between DCBN and decreased length of stay (LOS) for medical but not surgical pediatric discharges.1 This made them question if DCBN is an appropriate metric for discharge efficiency, as well as workflow differences between services. Many hospitals, however, still try to push DCBN as a goal (see Destino et al in the same January 2019 issue of JHM2), which could potentially lead to people trying to game the system.
How does your institution try to make discharge processes more efficient? Is it actually possible to do everything more quickly without sacrificing quality or trainee education? Whether your patients are kids, adults, or both, there are likely many issues in common where we could all learn from each other.
We discussed this topic in #JHMChat on April 15 on Twitter. New to Twitter or not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed dozens of articles spanning a wide variety of topics related to caring for hospitalized patients. All are welcome to join, including medical students, residents, nurses, practicing hospitalists, and more. It’s a great opportunity to virtually meet and learn from others while earning free CME.
To participate in future chats, type #JHMChat in the search box on the top right corner of your Twitter homepage, click on the “Latest” tab at the top left to see the most recent tweets, and join the conversation (don’t forget the hashtag)!
Dr. Chen is a pediatric hospital medicine fellow at Rady Children’s Hospital, University of California, San Diego. She is one of the cofounders/moderators of #PHMFellowJC, serves as a fellow district representative for the American Academy of Pediatrics, and is an active #tweetiatrician at @DrJenChen4kids. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
References
1. James HJ et al. The Association of Discharge Before Noon and Length of Stay in Hospitalized Pediatric Patients. J Hosp Med. 2019;14(1):28-32. doi: 10.12788/jhm.3111.
2. Destino L et al. Improving Patient Flow: Analysis of an Initiative to Improve Early Discharge. J Hosp Med. 2019;14(1):22-7. doi: 10.12788/jhm.3133.
Opioid prescriptions declined 33% over 5 years
Fewer opioid retail prescriptions are being filled, according to a new report issued by the American Medical Association Opioid Task Force.
Opioid prescribing declined by 33% over a 5-year period based on the total number of opioid retail prescriptions filled. Total prescriptions declined from 251.8 million in 2013 to 168.8 million in 2018, according to the report.
The numbers come as the most recent data from the Centers for Disease Control and Prevention show a leveling of deaths involving prescription opioids. The CDC data were most recently updated in January 2019 and cover the period 1999-2017.
A closer look shows that deaths involving prescription opioids, but not other synthetic narcotics, peaked in 2011 and have generally declined since then. Deaths involving other synthetic narcotics, however, have been rising, offsetting the reduction and keeping the total number of deaths involving opioids relatively stable between 2016 and 2017.
Other data released by the AMA Opioid Task Force show that physicians are increasing their use of state-level prescription drug monitoring programs (PDMPs).
In 2017, there were 1.5 million physicians registered to use state PDMPs. That number rose to 1.97 million in 2019. And the physicians are using PDMPs. In 2018, physicians made 460 million PDMP queries, up 56% from 2017 and up 651% from 2014.
More education about opioid prescribing is being sought, with 700,000 physicians completing CME training and accessing other training related to opioid prescribing, pain management, screening for substance use disorders, and other related topics.
While the report does show positive trends, the task force is calling for more action, including more access to naloxone and better access to mental health treatment.
The report notes that more than 66,000 physicians and other health professionals have a federal waiver to prescribe buprenorphine, up more than 28,000 since 2016.
A number of policy recommendations are made in the report, including removing inappropriate administrative burdens or barriers that delay access to medications used in medication-assisted treatment (MAT); removing barriers to comprehensive pain care and rehabilitation programs, and reforming the civil and criminal justice system to help ensure access to high-quality, evidence-based care for opioid use disorder.
“We are at a crossroads in our nation’s efforts to end the opioid epidemic,” AMA Opioid Task Force Chair Patrice A. Harris, MD, stated in the report. “It is time to end delays and barriers to medication-assisted treatment – evidence based care proven to save lives; time for payers, [pharmacy benefit managers] and pharmacy chains to reevaluate and revise policies that restrict opioid therapy to patients based on arbitrary thresholds; and time to commit to helping all patients access evidence-based care for pain and substance use disorders.”
Dr. Harris continued: “Physicians must continue to demonstrate leadership, but unless these actions occur, the progress we are making will not stop patients from dying.”
Fewer opioid retail prescriptions are being filled, according to a new report issued by the American Medical Association Opioid Task Force.
Opioid prescribing declined by 33% over a 5-year period based on the total number of opioid retail prescriptions filled. Total prescriptions declined from 251.8 million in 2013 to 168.8 million in 2018, according to the report.
The numbers come as the most recent data from the Centers for Disease Control and Prevention show a leveling of deaths involving prescription opioids. The CDC data were most recently updated in January 2019 and cover the period 1999-2017.
A closer look shows that deaths involving prescription opioids, but not other synthetic narcotics, peaked in 2011 and have generally declined since then. Deaths involving other synthetic narcotics, however, have been rising, offsetting the reduction and keeping the total number of deaths involving opioids relatively stable between 2016 and 2017.
Other data released by the AMA Opioid Task Force show that physicians are increasing their use of state-level prescription drug monitoring programs (PDMPs).
In 2017, there were 1.5 million physicians registered to use state PDMPs. That number rose to 1.97 million in 2019. And the physicians are using PDMPs. In 2018, physicians made 460 million PDMP queries, up 56% from 2017 and up 651% from 2014.
More education about opioid prescribing is being sought, with 700,000 physicians completing CME training and accessing other training related to opioid prescribing, pain management, screening for substance use disorders, and other related topics.
While the report does show positive trends, the task force is calling for more action, including more access to naloxone and better access to mental health treatment.
The report notes that more than 66,000 physicians and other health professionals have a federal waiver to prescribe buprenorphine, up more than 28,000 since 2016.
A number of policy recommendations are made in the report, including removing inappropriate administrative burdens or barriers that delay access to medications used in medication-assisted treatment (MAT); removing barriers to comprehensive pain care and rehabilitation programs, and reforming the civil and criminal justice system to help ensure access to high-quality, evidence-based care for opioid use disorder.
“We are at a crossroads in our nation’s efforts to end the opioid epidemic,” AMA Opioid Task Force Chair Patrice A. Harris, MD, stated in the report. “It is time to end delays and barriers to medication-assisted treatment – evidence based care proven to save lives; time for payers, [pharmacy benefit managers] and pharmacy chains to reevaluate and revise policies that restrict opioid therapy to patients based on arbitrary thresholds; and time to commit to helping all patients access evidence-based care for pain and substance use disorders.”
Dr. Harris continued: “Physicians must continue to demonstrate leadership, but unless these actions occur, the progress we are making will not stop patients from dying.”
Fewer opioid retail prescriptions are being filled, according to a new report issued by the American Medical Association Opioid Task Force.
Opioid prescribing declined by 33% over a 5-year period based on the total number of opioid retail prescriptions filled. Total prescriptions declined from 251.8 million in 2013 to 168.8 million in 2018, according to the report.
The numbers come as the most recent data from the Centers for Disease Control and Prevention show a leveling of deaths involving prescription opioids. The CDC data were most recently updated in January 2019 and cover the period 1999-2017.
A closer look shows that deaths involving prescription opioids, but not other synthetic narcotics, peaked in 2011 and have generally declined since then. Deaths involving other synthetic narcotics, however, have been rising, offsetting the reduction and keeping the total number of deaths involving opioids relatively stable between 2016 and 2017.
Other data released by the AMA Opioid Task Force show that physicians are increasing their use of state-level prescription drug monitoring programs (PDMPs).
In 2017, there were 1.5 million physicians registered to use state PDMPs. That number rose to 1.97 million in 2019. And the physicians are using PDMPs. In 2018, physicians made 460 million PDMP queries, up 56% from 2017 and up 651% from 2014.
More education about opioid prescribing is being sought, with 700,000 physicians completing CME training and accessing other training related to opioid prescribing, pain management, screening for substance use disorders, and other related topics.
While the report does show positive trends, the task force is calling for more action, including more access to naloxone and better access to mental health treatment.
The report notes that more than 66,000 physicians and other health professionals have a federal waiver to prescribe buprenorphine, up more than 28,000 since 2016.
A number of policy recommendations are made in the report, including removing inappropriate administrative burdens or barriers that delay access to medications used in medication-assisted treatment (MAT); removing barriers to comprehensive pain care and rehabilitation programs, and reforming the civil and criminal justice system to help ensure access to high-quality, evidence-based care for opioid use disorder.
“We are at a crossroads in our nation’s efforts to end the opioid epidemic,” AMA Opioid Task Force Chair Patrice A. Harris, MD, stated in the report. “It is time to end delays and barriers to medication-assisted treatment – evidence based care proven to save lives; time for payers, [pharmacy benefit managers] and pharmacy chains to reevaluate and revise policies that restrict opioid therapy to patients based on arbitrary thresholds; and time to commit to helping all patients access evidence-based care for pain and substance use disorders.”
Dr. Harris continued: “Physicians must continue to demonstrate leadership, but unless these actions occur, the progress we are making will not stop patients from dying.”
New help for peanut allergies
Breakthrough therapy holds potential
When it comes to anaphylaxis episodes leading to pediatric intensive care–unit stays, peanuts are the most common culprit. Now the results of a recent clinical trial may lead to approval of the first oral medication to ameliorate reactions in children with severe peanut allergies.
After 6 months of treatment and 6 months of maintenance therapy, two-thirds of the 372 children who received this treatment could ingest the equivalent of two peanuts without allergic symptoms. Just 4% of the 124 children given a placebo powder were able to consume that amount of peanut without reacting. The treatment was not effective for the small number of adults in the study.
This trial of the drug, called AR101 and developed by Aimmune Therapeutics, was published in Nov. 2018 in the New England Journal of Medicine. The company has submitted a biologics license application to the U.S. Food and Drug Administration, and because the drug has been designated a breakthrough therapy, it will go through an accelerated approval process. It could be on the market by the end of 2019.
Reference
1. Rabin RC. New Peanut Allergy Drug Shows ‘Lifesaving’ Potential. New York Times. Nov. 18, 2018. https://www.nytimes.com/2018/11/18/well/live/new-peanut-allergy-drug-shows-lifesaving-potential.html. Accessed Nov. 26, 2018.
Breakthrough therapy holds potential
Breakthrough therapy holds potential
When it comes to anaphylaxis episodes leading to pediatric intensive care–unit stays, peanuts are the most common culprit. Now the results of a recent clinical trial may lead to approval of the first oral medication to ameliorate reactions in children with severe peanut allergies.
After 6 months of treatment and 6 months of maintenance therapy, two-thirds of the 372 children who received this treatment could ingest the equivalent of two peanuts without allergic symptoms. Just 4% of the 124 children given a placebo powder were able to consume that amount of peanut without reacting. The treatment was not effective for the small number of adults in the study.
This trial of the drug, called AR101 and developed by Aimmune Therapeutics, was published in Nov. 2018 in the New England Journal of Medicine. The company has submitted a biologics license application to the U.S. Food and Drug Administration, and because the drug has been designated a breakthrough therapy, it will go through an accelerated approval process. It could be on the market by the end of 2019.
Reference
1. Rabin RC. New Peanut Allergy Drug Shows ‘Lifesaving’ Potential. New York Times. Nov. 18, 2018. https://www.nytimes.com/2018/11/18/well/live/new-peanut-allergy-drug-shows-lifesaving-potential.html. Accessed Nov. 26, 2018.
When it comes to anaphylaxis episodes leading to pediatric intensive care–unit stays, peanuts are the most common culprit. Now the results of a recent clinical trial may lead to approval of the first oral medication to ameliorate reactions in children with severe peanut allergies.
After 6 months of treatment and 6 months of maintenance therapy, two-thirds of the 372 children who received this treatment could ingest the equivalent of two peanuts without allergic symptoms. Just 4% of the 124 children given a placebo powder were able to consume that amount of peanut without reacting. The treatment was not effective for the small number of adults in the study.
This trial of the drug, called AR101 and developed by Aimmune Therapeutics, was published in Nov. 2018 in the New England Journal of Medicine. The company has submitted a biologics license application to the U.S. Food and Drug Administration, and because the drug has been designated a breakthrough therapy, it will go through an accelerated approval process. It could be on the market by the end of 2019.
Reference
1. Rabin RC. New Peanut Allergy Drug Shows ‘Lifesaving’ Potential. New York Times. Nov. 18, 2018. https://www.nytimes.com/2018/11/18/well/live/new-peanut-allergy-drug-shows-lifesaving-potential.html. Accessed Nov. 26, 2018.
Following the path of leadership
VA Hospitalist Dr. Matthew Tuck
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
VA Hospitalist Dr. Matthew Tuck
VA Hospitalist Dr. Matthew Tuck
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
Focus on science, not format
How JHM is improving the author experience
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
How JHM is improving the author experience
How JHM is improving the author experience
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.