User login
In search of high-value care
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
Six steps that can help your team
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
IVC filter placement increases mortality in some VTE patients
Clinical question: How does inferior vena cava (IVC) filter placement affect 30-day mortality in patients with venous thromboembolism (VTE) with increased risk of bleeding when anticoagulation is not feasible?
Background: Standard treatment for VTE, including deep venous thrombosis (DVT) and pulmonary embolism (PE), is anticoagulation. However, for patients with active bleeding or increased risk of bleeding, anticoagulation may be contraindicated. In these circumstances, placing an IVC filter is recommended by major professional societies; however, the mortality benefit of IVC filter placement is uncertain.
Study design: A retrospective cohort study.
Setting: State Inpatient and Emergency Department Databases from California, Florida, and New York hospitals from 2005 to 2012.
Synopsis: The authors compared the 30-day mortality rates in 45,771 hospitalized adult patients with inpatient diagnosis codes of PE and/or DVT, as well as a contraindication to anticoagulation, who underwent IVC filter placement with 80,259 similar patients who did not undergo IVC filter placement. Baseline characteristics and coexisting conditions were similar in the two populations. The authors found that patients with IVC filter placement had an increased risk of 30-day mortality, compared with patients without an IVC filter placed (HR, 1.18; 95% CI, 1.13-1.22; P less than .001).
This study used observational data derived from reimbursement codes, which lacked unmeasured confounders (for example, severity of VTE and fragility score), so randomized, controlled trials are required to confirm the results. Nevertheless, this study should prompt physicians to carefully consider decisions to place an IVC filter in the setting of a contraindication to anticoagulation.
Bottom line: IVC filter placement in patients with VTE and contraindication for anticoagulation was associated with an increased 30-day mortality. Randomized, controlled trials are required to confirm the observed results.
Citation: Turner TE et al. Association of inferior vena cava filter placement for venous thromboembolic disease and a contraindication to anticoagulation with 30-day mortality. JAMA Network Open. 2018;1(3):e180452.
Dr. Kobaidze is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Clinical question: How does inferior vena cava (IVC) filter placement affect 30-day mortality in patients with venous thromboembolism (VTE) with increased risk of bleeding when anticoagulation is not feasible?
Background: Standard treatment for VTE, including deep venous thrombosis (DVT) and pulmonary embolism (PE), is anticoagulation. However, for patients with active bleeding or increased risk of bleeding, anticoagulation may be contraindicated. In these circumstances, placing an IVC filter is recommended by major professional societies; however, the mortality benefit of IVC filter placement is uncertain.
Study design: A retrospective cohort study.
Setting: State Inpatient and Emergency Department Databases from California, Florida, and New York hospitals from 2005 to 2012.
Synopsis: The authors compared the 30-day mortality rates in 45,771 hospitalized adult patients with inpatient diagnosis codes of PE and/or DVT, as well as a contraindication to anticoagulation, who underwent IVC filter placement with 80,259 similar patients who did not undergo IVC filter placement. Baseline characteristics and coexisting conditions were similar in the two populations. The authors found that patients with IVC filter placement had an increased risk of 30-day mortality, compared with patients without an IVC filter placed (HR, 1.18; 95% CI, 1.13-1.22; P less than .001).
This study used observational data derived from reimbursement codes, which lacked unmeasured confounders (for example, severity of VTE and fragility score), so randomized, controlled trials are required to confirm the results. Nevertheless, this study should prompt physicians to carefully consider decisions to place an IVC filter in the setting of a contraindication to anticoagulation.
Bottom line: IVC filter placement in patients with VTE and contraindication for anticoagulation was associated with an increased 30-day mortality. Randomized, controlled trials are required to confirm the observed results.
Citation: Turner TE et al. Association of inferior vena cava filter placement for venous thromboembolic disease and a contraindication to anticoagulation with 30-day mortality. JAMA Network Open. 2018;1(3):e180452.
Dr. Kobaidze is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Clinical question: How does inferior vena cava (IVC) filter placement affect 30-day mortality in patients with venous thromboembolism (VTE) with increased risk of bleeding when anticoagulation is not feasible?
Background: Standard treatment for VTE, including deep venous thrombosis (DVT) and pulmonary embolism (PE), is anticoagulation. However, for patients with active bleeding or increased risk of bleeding, anticoagulation may be contraindicated. In these circumstances, placing an IVC filter is recommended by major professional societies; however, the mortality benefit of IVC filter placement is uncertain.
Study design: A retrospective cohort study.
Setting: State Inpatient and Emergency Department Databases from California, Florida, and New York hospitals from 2005 to 2012.
Synopsis: The authors compared the 30-day mortality rates in 45,771 hospitalized adult patients with inpatient diagnosis codes of PE and/or DVT, as well as a contraindication to anticoagulation, who underwent IVC filter placement with 80,259 similar patients who did not undergo IVC filter placement. Baseline characteristics and coexisting conditions were similar in the two populations. The authors found that patients with IVC filter placement had an increased risk of 30-day mortality, compared with patients without an IVC filter placed (HR, 1.18; 95% CI, 1.13-1.22; P less than .001).
This study used observational data derived from reimbursement codes, which lacked unmeasured confounders (for example, severity of VTE and fragility score), so randomized, controlled trials are required to confirm the results. Nevertheless, this study should prompt physicians to carefully consider decisions to place an IVC filter in the setting of a contraindication to anticoagulation.
Bottom line: IVC filter placement in patients with VTE and contraindication for anticoagulation was associated with an increased 30-day mortality. Randomized, controlled trials are required to confirm the observed results.
Citation: Turner TE et al. Association of inferior vena cava filter placement for venous thromboembolic disease and a contraindication to anticoagulation with 30-day mortality. JAMA Network Open. 2018;1(3):e180452.
Dr. Kobaidze is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
How common are noninfectious complications of Foley catheters?
CLINICAL QUESTION: How common are noninfectious complications of Foley catheters?
BACKGROUND: Approximately 20% of hospitalized patients have a Foley catheter inserted at some time during their admission. Infectious complications associated with the use of Foley catheters are widely recognized; however, much less is known about noninfectious complications.
STUDY DESIGN: Prospective cohort study.
SETTING: Four U.S. hospitals in two states.SYNOPSIS: The study included 2,076 hospitalized patients with a Foley catheter. They were followed for 30 days after its insertion, even if catheter removal occurred during this time period. Data about infectious and noninfectious complications were collected through patient interviews.
At least one complication was noted in 1,184 of 2,076 patients (57%) during the 30-day period following Foley catheter insertion. While infectious complications occurred in 219 of 2,076 patients (10.5%), noninfectious complications (such as pain, urinary urgency, hematuria) were reported by 1,150 patients (55.4%; P less than .001). For those with catheters still in place, the most common complication was pain or discomfort (54.5%). Postremoval leaking urine (20.3%) and/or urgency and bladder spasms (24.0%) were the most common complications.
The study only included patients who had a Foley catheter placed during a hospitalization; the results may not apply to patients who receive catheters in other settings.
BOTTOM LINE: Noninfectious complications affect over half of patients with a Foley catheters. These types of complications should be targeted in future harm prevention efforts and should be considered when deciding to place a Foley catheter.
CITATION: Saint S et al. A multicenter study of patient-reported infectious and noninfectious complications associated with indwelling urethral catheters. JAMA Intern Med. 2018;178(8):1078-85.
Dr. Clarke is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
CLINICAL QUESTION: How common are noninfectious complications of Foley catheters?
BACKGROUND: Approximately 20% of hospitalized patients have a Foley catheter inserted at some time during their admission. Infectious complications associated with the use of Foley catheters are widely recognized; however, much less is known about noninfectious complications.
STUDY DESIGN: Prospective cohort study.
SETTING: Four U.S. hospitals in two states.SYNOPSIS: The study included 2,076 hospitalized patients with a Foley catheter. They were followed for 30 days after its insertion, even if catheter removal occurred during this time period. Data about infectious and noninfectious complications were collected through patient interviews.
At least one complication was noted in 1,184 of 2,076 patients (57%) during the 30-day period following Foley catheter insertion. While infectious complications occurred in 219 of 2,076 patients (10.5%), noninfectious complications (such as pain, urinary urgency, hematuria) were reported by 1,150 patients (55.4%; P less than .001). For those with catheters still in place, the most common complication was pain or discomfort (54.5%). Postremoval leaking urine (20.3%) and/or urgency and bladder spasms (24.0%) were the most common complications.
The study only included patients who had a Foley catheter placed during a hospitalization; the results may not apply to patients who receive catheters in other settings.
BOTTOM LINE: Noninfectious complications affect over half of patients with a Foley catheters. These types of complications should be targeted in future harm prevention efforts and should be considered when deciding to place a Foley catheter.
CITATION: Saint S et al. A multicenter study of patient-reported infectious and noninfectious complications associated with indwelling urethral catheters. JAMA Intern Med. 2018;178(8):1078-85.
Dr. Clarke is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
CLINICAL QUESTION: How common are noninfectious complications of Foley catheters?
BACKGROUND: Approximately 20% of hospitalized patients have a Foley catheter inserted at some time during their admission. Infectious complications associated with the use of Foley catheters are widely recognized; however, much less is known about noninfectious complications.
STUDY DESIGN: Prospective cohort study.
SETTING: Four U.S. hospitals in two states.SYNOPSIS: The study included 2,076 hospitalized patients with a Foley catheter. They were followed for 30 days after its insertion, even if catheter removal occurred during this time period. Data about infectious and noninfectious complications were collected through patient interviews.
At least one complication was noted in 1,184 of 2,076 patients (57%) during the 30-day period following Foley catheter insertion. While infectious complications occurred in 219 of 2,076 patients (10.5%), noninfectious complications (such as pain, urinary urgency, hematuria) were reported by 1,150 patients (55.4%; P less than .001). For those with catheters still in place, the most common complication was pain or discomfort (54.5%). Postremoval leaking urine (20.3%) and/or urgency and bladder spasms (24.0%) were the most common complications.
The study only included patients who had a Foley catheter placed during a hospitalization; the results may not apply to patients who receive catheters in other settings.
BOTTOM LINE: Noninfectious complications affect over half of patients with a Foley catheters. These types of complications should be targeted in future harm prevention efforts and should be considered when deciding to place a Foley catheter.
CITATION: Saint S et al. A multicenter study of patient-reported infectious and noninfectious complications associated with indwelling urethral catheters. JAMA Intern Med. 2018;178(8):1078-85.
Dr. Clarke is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
One-dose-fits-all aspirin administration strategy may not be advisable
Clinical question: Are the same doses of aspirin equally effective in preventing cardiovascular (CV) events and long-term colorectal risk reduction in patients of various body sizes?
Background: Strong evidence for the one-dose-fits-all approach to use of aspirin in long-term prevention of CV events is lacking. Aspirin effect may be dependent on patient’s body size. Excess dosing of aspirin in patients of small body size might negatively affect their outcomes.
Study design: Meta-analysis.
Setting: Trials from the Antithrombotic Trialists’ Collaboration, other systematic reviews of trials of aspirin, and from the Cochrane Database of Systematic Reviews.
Synopsis: The authors included 10 trials (117,279 participants altogether) and analyzed the association of body weight with the effectiveness of aspirin doses on CV event and colon cancer prevention. The greatest benefit of low-dose aspirin (75-100 mg) in reducing CV events was seen in patients weighing 50-69 kg (hazard ratio, 0.75; 95% confidence interval, 0.65-0.85; P less than .0001), with CV events increasing with increasing weights (P interaction = .0072). There was an increased rate of fatality with low-dose aspirin among patients at body weights greater than 70 kg (HR, 1.33; 95% CI, 1.08-1.64; P = .0082) or less than 50 kg (HR, 1.52; 95% CI, 1.04-2.21; P = .031). Higher doses of aspirin were more effective at higher body weights (P interaction = .017). Similar weight-dependent effects were seen in the 20-year risk of colorectal cancer.
While findings are consistent across trials looking at dose-dependent aspirin effects in patients of various body sizes, limitations included lack of generalizability of the results in secondary prevention trials, inclusion of older trials, variability of participants’ characteristics, and aspirin compliance across trials.
Bottom line: Weight-based aspirin dosing may be required for prevention of CV events, sudden cardiac death, and cancer. Based on the results of this meta-analysis, one-dose-fits-all aspirin administration strategy may not be advisable.
Citation: Rothwell PM et al. Effects of aspirin on risks of vascular events and cancer according to body weight and dose: Analysis of individual patient data from randomized trials. Lancet. 2018;392:387-99.
Dr. Burklin is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Clinical question: Are the same doses of aspirin equally effective in preventing cardiovascular (CV) events and long-term colorectal risk reduction in patients of various body sizes?
Background: Strong evidence for the one-dose-fits-all approach to use of aspirin in long-term prevention of CV events is lacking. Aspirin effect may be dependent on patient’s body size. Excess dosing of aspirin in patients of small body size might negatively affect their outcomes.
Study design: Meta-analysis.
Setting: Trials from the Antithrombotic Trialists’ Collaboration, other systematic reviews of trials of aspirin, and from the Cochrane Database of Systematic Reviews.
Synopsis: The authors included 10 trials (117,279 participants altogether) and analyzed the association of body weight with the effectiveness of aspirin doses on CV event and colon cancer prevention. The greatest benefit of low-dose aspirin (75-100 mg) in reducing CV events was seen in patients weighing 50-69 kg (hazard ratio, 0.75; 95% confidence interval, 0.65-0.85; P less than .0001), with CV events increasing with increasing weights (P interaction = .0072). There was an increased rate of fatality with low-dose aspirin among patients at body weights greater than 70 kg (HR, 1.33; 95% CI, 1.08-1.64; P = .0082) or less than 50 kg (HR, 1.52; 95% CI, 1.04-2.21; P = .031). Higher doses of aspirin were more effective at higher body weights (P interaction = .017). Similar weight-dependent effects were seen in the 20-year risk of colorectal cancer.
While findings are consistent across trials looking at dose-dependent aspirin effects in patients of various body sizes, limitations included lack of generalizability of the results in secondary prevention trials, inclusion of older trials, variability of participants’ characteristics, and aspirin compliance across trials.
Bottom line: Weight-based aspirin dosing may be required for prevention of CV events, sudden cardiac death, and cancer. Based on the results of this meta-analysis, one-dose-fits-all aspirin administration strategy may not be advisable.
Citation: Rothwell PM et al. Effects of aspirin on risks of vascular events and cancer according to body weight and dose: Analysis of individual patient data from randomized trials. Lancet. 2018;392:387-99.
Dr. Burklin is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Clinical question: Are the same doses of aspirin equally effective in preventing cardiovascular (CV) events and long-term colorectal risk reduction in patients of various body sizes?
Background: Strong evidence for the one-dose-fits-all approach to use of aspirin in long-term prevention of CV events is lacking. Aspirin effect may be dependent on patient’s body size. Excess dosing of aspirin in patients of small body size might negatively affect their outcomes.
Study design: Meta-analysis.
Setting: Trials from the Antithrombotic Trialists’ Collaboration, other systematic reviews of trials of aspirin, and from the Cochrane Database of Systematic Reviews.
Synopsis: The authors included 10 trials (117,279 participants altogether) and analyzed the association of body weight with the effectiveness of aspirin doses on CV event and colon cancer prevention. The greatest benefit of low-dose aspirin (75-100 mg) in reducing CV events was seen in patients weighing 50-69 kg (hazard ratio, 0.75; 95% confidence interval, 0.65-0.85; P less than .0001), with CV events increasing with increasing weights (P interaction = .0072). There was an increased rate of fatality with low-dose aspirin among patients at body weights greater than 70 kg (HR, 1.33; 95% CI, 1.08-1.64; P = .0082) or less than 50 kg (HR, 1.52; 95% CI, 1.04-2.21; P = .031). Higher doses of aspirin were more effective at higher body weights (P interaction = .017). Similar weight-dependent effects were seen in the 20-year risk of colorectal cancer.
While findings are consistent across trials looking at dose-dependent aspirin effects in patients of various body sizes, limitations included lack of generalizability of the results in secondary prevention trials, inclusion of older trials, variability of participants’ characteristics, and aspirin compliance across trials.
Bottom line: Weight-based aspirin dosing may be required for prevention of CV events, sudden cardiac death, and cancer. Based on the results of this meta-analysis, one-dose-fits-all aspirin administration strategy may not be advisable.
Citation: Rothwell PM et al. Effects of aspirin on risks of vascular events and cancer according to body weight and dose: Analysis of individual patient data from randomized trials. Lancet. 2018;392:387-99.
Dr. Burklin is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Creating innovative discharge plans
‘Long Stay Committee’ may help
Hospitalists pay attention to length of stay as a measure of hospital efficiency and resource utilization; outliers on that measure – “long stay patients” – who present complex discharges are a barrier to length of stay reduction. To address this challenge, one institution formed a multidisciplinary Long Stay Committee and described the results in an abstract.
The Long Stay Committee is composed of medical directors, the chief quality officer, directors in nursing, directors of case management/social work, hospitalists, risk management, finance, ethics, psychiatry, and directors of rehabilitation. The most complex patient discharges, identified by case management and social work, are brought to the Long Stay Committee.
“Lack of guardianship is one of the most encountered barriers,” according to the authors. “The Long Stay Committee played an integral part in our institution partnering with the local county to form a guardian service board which facilitates guardianship appointments. Other solutions have included working with the patient and support persons to find appropriate discharge levels of care throughout the United States and other countries as well as guiding them through the process to gain the necessary financial resources.”
The authors conclude that the foundation of the committee’s success in coming up with innovative discharge solutions is the broad range of disciplines that attend this committee and the atmosphere of teamwork it creates.
Reference
Heacock A et al. Long Stay Committee finds innovative discharge plans for difficult discharges. Hospital Medicine 2018, Abstract 312. .
‘Long Stay Committee’ may help
‘Long Stay Committee’ may help
Hospitalists pay attention to length of stay as a measure of hospital efficiency and resource utilization; outliers on that measure – “long stay patients” – who present complex discharges are a barrier to length of stay reduction. To address this challenge, one institution formed a multidisciplinary Long Stay Committee and described the results in an abstract.
The Long Stay Committee is composed of medical directors, the chief quality officer, directors in nursing, directors of case management/social work, hospitalists, risk management, finance, ethics, psychiatry, and directors of rehabilitation. The most complex patient discharges, identified by case management and social work, are brought to the Long Stay Committee.
“Lack of guardianship is one of the most encountered barriers,” according to the authors. “The Long Stay Committee played an integral part in our institution partnering with the local county to form a guardian service board which facilitates guardianship appointments. Other solutions have included working with the patient and support persons to find appropriate discharge levels of care throughout the United States and other countries as well as guiding them through the process to gain the necessary financial resources.”
The authors conclude that the foundation of the committee’s success in coming up with innovative discharge solutions is the broad range of disciplines that attend this committee and the atmosphere of teamwork it creates.
Reference
Heacock A et al. Long Stay Committee finds innovative discharge plans for difficult discharges. Hospital Medicine 2018, Abstract 312. .
Hospitalists pay attention to length of stay as a measure of hospital efficiency and resource utilization; outliers on that measure – “long stay patients” – who present complex discharges are a barrier to length of stay reduction. To address this challenge, one institution formed a multidisciplinary Long Stay Committee and described the results in an abstract.
The Long Stay Committee is composed of medical directors, the chief quality officer, directors in nursing, directors of case management/social work, hospitalists, risk management, finance, ethics, psychiatry, and directors of rehabilitation. The most complex patient discharges, identified by case management and social work, are brought to the Long Stay Committee.
“Lack of guardianship is one of the most encountered barriers,” according to the authors. “The Long Stay Committee played an integral part in our institution partnering with the local county to form a guardian service board which facilitates guardianship appointments. Other solutions have included working with the patient and support persons to find appropriate discharge levels of care throughout the United States and other countries as well as guiding them through the process to gain the necessary financial resources.”
The authors conclude that the foundation of the committee’s success in coming up with innovative discharge solutions is the broad range of disciplines that attend this committee and the atmosphere of teamwork it creates.
Reference
Heacock A et al. Long Stay Committee finds innovative discharge plans for difficult discharges. Hospital Medicine 2018, Abstract 312. .
Malpractice: More lawsuits does not equal more relocations
David M. Studdert of Stanford (Calif.) University and his colleagues analyzed data from Medicare and the National Practitioner Data Bank (NPDB) to assess associations between the number of paid malpractice claims that doctors accrued and exits from medical practice, changes in clinical volume, geographic relocation, and change in practice-group size. The study population included 480,894 physicians who had 68,956 paid claims from 2003 to 2015. Of the study group, 89% had no claims, 9% had one claim, and the remaining 2% had two or more claims that accounted for 40% of all claims. Nearly three-quarters of the doctors studied were men, and the majority of specialties were internal medicine (17%), general practice/family medicine (15%), emergency medicine (7%), radiology (6%), and anesthesiology (6%).
Physicians with a higher number of claims against them did not relocate at a greater rate than physicians who had fewer or no claims, the investigators wrote in the New England Journal of Medicine.
More claims against a doctor were associated with a higher likelihood of leaving medicine and more shifts into smaller practice settings. For instance, physicians with one claim had 9% higher odds of leaving the practice than doctors with no claims, and physicians with five or more claims had a 45% higher chance of leaving medicine than doctors with no claims, the researchers found.
In addition, investigators found that doctors with two to four claims had 50%-60% higher odds of entering solo practice than physicians with no claims, and physicians with five or more claims had nearly 150% higher odds of moving to solo practice than doctors who had never been sued. Physicians with three or more claims were more likely to be male, work in surgical specialties, and be at least age 50 years.
The study addresses concerns that physicians with troubling legal records were moving across state lines for a fresh start, Mr. Studdert said in an interview. “We were surprised to find that physicians who accumulated multiple malpractice claims were no more likely to relocate their practices than physicians without claims. The National Practitioner Data Bank probably has something to do with that.”
Established by Congress in 1986, the NPDB was started, in part, to restrict the ability of incompetent physicians to move across states to hide their track records. By requiring hospitals to query doctors records before granting them clinical privileges and encouraging physician groups, health plans, and professional societies to do the same, the NPDB has “almost certainly increased the difficulty of relocation for physicians with legal problems,” the authors noted in the study.
A primary takeaway from the analysis is that, while a single malpractice claim is a relatively weak signal that a quality problem exists, multiple paid claims over a relatively short period of time are a strong signal that a physician may have a quality deficiency, Mr. Studdert said in the interview.
“Regulators and malpractice insurers should be paying closer attention to this signal,” he added. “To the extent that physicians are aware of a colleague’s checkered malpractice history, they may have a role to play too. Vigilance about signs of further problems, for one, but also careful thought about the wisdom of referring patients to such physicians.”
Michelle M. Mello, JD, PhD, and Mr. Studdert both reported receiving grants from SUMIT Insurance during the conduct of the study.
Source: Studdert DM et al. N Engl J Med. 2019 Mar 28. doi: 10.1056/NEJMsa1809981.
David M. Studdert of Stanford (Calif.) University and his colleagues analyzed data from Medicare and the National Practitioner Data Bank (NPDB) to assess associations between the number of paid malpractice claims that doctors accrued and exits from medical practice, changes in clinical volume, geographic relocation, and change in practice-group size. The study population included 480,894 physicians who had 68,956 paid claims from 2003 to 2015. Of the study group, 89% had no claims, 9% had one claim, and the remaining 2% had two or more claims that accounted for 40% of all claims. Nearly three-quarters of the doctors studied were men, and the majority of specialties were internal medicine (17%), general practice/family medicine (15%), emergency medicine (7%), radiology (6%), and anesthesiology (6%).
Physicians with a higher number of claims against them did not relocate at a greater rate than physicians who had fewer or no claims, the investigators wrote in the New England Journal of Medicine.
More claims against a doctor were associated with a higher likelihood of leaving medicine and more shifts into smaller practice settings. For instance, physicians with one claim had 9% higher odds of leaving the practice than doctors with no claims, and physicians with five or more claims had a 45% higher chance of leaving medicine than doctors with no claims, the researchers found.
In addition, investigators found that doctors with two to four claims had 50%-60% higher odds of entering solo practice than physicians with no claims, and physicians with five or more claims had nearly 150% higher odds of moving to solo practice than doctors who had never been sued. Physicians with three or more claims were more likely to be male, work in surgical specialties, and be at least age 50 years.
The study addresses concerns that physicians with troubling legal records were moving across state lines for a fresh start, Mr. Studdert said in an interview. “We were surprised to find that physicians who accumulated multiple malpractice claims were no more likely to relocate their practices than physicians without claims. The National Practitioner Data Bank probably has something to do with that.”
Established by Congress in 1986, the NPDB was started, in part, to restrict the ability of incompetent physicians to move across states to hide their track records. By requiring hospitals to query doctors records before granting them clinical privileges and encouraging physician groups, health plans, and professional societies to do the same, the NPDB has “almost certainly increased the difficulty of relocation for physicians with legal problems,” the authors noted in the study.
A primary takeaway from the analysis is that, while a single malpractice claim is a relatively weak signal that a quality problem exists, multiple paid claims over a relatively short period of time are a strong signal that a physician may have a quality deficiency, Mr. Studdert said in the interview.
“Regulators and malpractice insurers should be paying closer attention to this signal,” he added. “To the extent that physicians are aware of a colleague’s checkered malpractice history, they may have a role to play too. Vigilance about signs of further problems, for one, but also careful thought about the wisdom of referring patients to such physicians.”
Michelle M. Mello, JD, PhD, and Mr. Studdert both reported receiving grants from SUMIT Insurance during the conduct of the study.
Source: Studdert DM et al. N Engl J Med. 2019 Mar 28. doi: 10.1056/NEJMsa1809981.
David M. Studdert of Stanford (Calif.) University and his colleagues analyzed data from Medicare and the National Practitioner Data Bank (NPDB) to assess associations between the number of paid malpractice claims that doctors accrued and exits from medical practice, changes in clinical volume, geographic relocation, and change in practice-group size. The study population included 480,894 physicians who had 68,956 paid claims from 2003 to 2015. Of the study group, 89% had no claims, 9% had one claim, and the remaining 2% had two or more claims that accounted for 40% of all claims. Nearly three-quarters of the doctors studied were men, and the majority of specialties were internal medicine (17%), general practice/family medicine (15%), emergency medicine (7%), radiology (6%), and anesthesiology (6%).
Physicians with a higher number of claims against them did not relocate at a greater rate than physicians who had fewer or no claims, the investigators wrote in the New England Journal of Medicine.
More claims against a doctor were associated with a higher likelihood of leaving medicine and more shifts into smaller practice settings. For instance, physicians with one claim had 9% higher odds of leaving the practice than doctors with no claims, and physicians with five or more claims had a 45% higher chance of leaving medicine than doctors with no claims, the researchers found.
In addition, investigators found that doctors with two to four claims had 50%-60% higher odds of entering solo practice than physicians with no claims, and physicians with five or more claims had nearly 150% higher odds of moving to solo practice than doctors who had never been sued. Physicians with three or more claims were more likely to be male, work in surgical specialties, and be at least age 50 years.
The study addresses concerns that physicians with troubling legal records were moving across state lines for a fresh start, Mr. Studdert said in an interview. “We were surprised to find that physicians who accumulated multiple malpractice claims were no more likely to relocate their practices than physicians without claims. The National Practitioner Data Bank probably has something to do with that.”
Established by Congress in 1986, the NPDB was started, in part, to restrict the ability of incompetent physicians to move across states to hide their track records. By requiring hospitals to query doctors records before granting them clinical privileges and encouraging physician groups, health plans, and professional societies to do the same, the NPDB has “almost certainly increased the difficulty of relocation for physicians with legal problems,” the authors noted in the study.
A primary takeaway from the analysis is that, while a single malpractice claim is a relatively weak signal that a quality problem exists, multiple paid claims over a relatively short period of time are a strong signal that a physician may have a quality deficiency, Mr. Studdert said in the interview.
“Regulators and malpractice insurers should be paying closer attention to this signal,” he added. “To the extent that physicians are aware of a colleague’s checkered malpractice history, they may have a role to play too. Vigilance about signs of further problems, for one, but also careful thought about the wisdom of referring patients to such physicians.”
Michelle M. Mello, JD, PhD, and Mr. Studdert both reported receiving grants from SUMIT Insurance during the conduct of the study.
Source: Studdert DM et al. N Engl J Med. 2019 Mar 28. doi: 10.1056/NEJMsa1809981.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Highlighting the value in high-value care
Helping consumers learn
Hospitalists can have a role in helping patients choose and receive high-value care from the vast array of health care choices they face. Helping them use quality and cost reports is one way to do that, according to a recent editorial by Jeffrey T. Kullgren, MD, MS, MPH.
We know that if consumers used public reporting of quality and costs to choose facilities that generate the best health outcomes for the resources utilized, it might improve the overall value of health care spending. But most people choose health care services based on personal recommendations or the requirements of their insurance network. Even if they wanted to use reports of quality or cost, the information in these reports is meant for providers and would likely be unhelpful for consumers.
Research suggests that different presentation of the information could make a difference. “Simpler presentations of information in public reports may be more likely to help consumers choose higher-value providers and facilities,” Dr. Kullgren said.
He concluded that consumers may also need additional incentives, “such as financial incentives to encourage high-value choices or programs that educate consumers about how to use cost and quality information when seeking care,” he said.
There’s an opportunity for hospitalists to help consumers learn to use that information. “This strategy would approach consumerism as a teachable health behavior and could be particularly helpful for consumers with ongoing medical needs who face high cost sharing,” he wrote.
“Some hospitalists may be involved in the implementation of programs to publicly report quality and costs for their institutions,” he said. “Others may treat patients who have chosen hospitals based on publicly reported information, or patients who might be interested in using such information to choose sites of postdischarge outpatient care. In each of these cases, it is important for hospitalists to understand the opportunities and limits of such public reports so as to best help patients receive high-value care.”
Reference
Kullgren JT. Helping consumers make high value health care choices: The devil is in the details. Health Serv Res. 2018;53(4). http://www.hsr.org/hsr/abstract.jsp?aid=53301961729.
Helping consumers learn
Helping consumers learn
Hospitalists can have a role in helping patients choose and receive high-value care from the vast array of health care choices they face. Helping them use quality and cost reports is one way to do that, according to a recent editorial by Jeffrey T. Kullgren, MD, MS, MPH.
We know that if consumers used public reporting of quality and costs to choose facilities that generate the best health outcomes for the resources utilized, it might improve the overall value of health care spending. But most people choose health care services based on personal recommendations or the requirements of their insurance network. Even if they wanted to use reports of quality or cost, the information in these reports is meant for providers and would likely be unhelpful for consumers.
Research suggests that different presentation of the information could make a difference. “Simpler presentations of information in public reports may be more likely to help consumers choose higher-value providers and facilities,” Dr. Kullgren said.
He concluded that consumers may also need additional incentives, “such as financial incentives to encourage high-value choices or programs that educate consumers about how to use cost and quality information when seeking care,” he said.
There’s an opportunity for hospitalists to help consumers learn to use that information. “This strategy would approach consumerism as a teachable health behavior and could be particularly helpful for consumers with ongoing medical needs who face high cost sharing,” he wrote.
“Some hospitalists may be involved in the implementation of programs to publicly report quality and costs for their institutions,” he said. “Others may treat patients who have chosen hospitals based on publicly reported information, or patients who might be interested in using such information to choose sites of postdischarge outpatient care. In each of these cases, it is important for hospitalists to understand the opportunities and limits of such public reports so as to best help patients receive high-value care.”
Reference
Kullgren JT. Helping consumers make high value health care choices: The devil is in the details. Health Serv Res. 2018;53(4). http://www.hsr.org/hsr/abstract.jsp?aid=53301961729.
Hospitalists can have a role in helping patients choose and receive high-value care from the vast array of health care choices they face. Helping them use quality and cost reports is one way to do that, according to a recent editorial by Jeffrey T. Kullgren, MD, MS, MPH.
We know that if consumers used public reporting of quality and costs to choose facilities that generate the best health outcomes for the resources utilized, it might improve the overall value of health care spending. But most people choose health care services based on personal recommendations or the requirements of their insurance network. Even if they wanted to use reports of quality or cost, the information in these reports is meant for providers and would likely be unhelpful for consumers.
Research suggests that different presentation of the information could make a difference. “Simpler presentations of information in public reports may be more likely to help consumers choose higher-value providers and facilities,” Dr. Kullgren said.
He concluded that consumers may also need additional incentives, “such as financial incentives to encourage high-value choices or programs that educate consumers about how to use cost and quality information when seeking care,” he said.
There’s an opportunity for hospitalists to help consumers learn to use that information. “This strategy would approach consumerism as a teachable health behavior and could be particularly helpful for consumers with ongoing medical needs who face high cost sharing,” he wrote.
“Some hospitalists may be involved in the implementation of programs to publicly report quality and costs for their institutions,” he said. “Others may treat patients who have chosen hospitals based on publicly reported information, or patients who might be interested in using such information to choose sites of postdischarge outpatient care. In each of these cases, it is important for hospitalists to understand the opportunities and limits of such public reports so as to best help patients receive high-value care.”
Reference
Kullgren JT. Helping consumers make high value health care choices: The devil is in the details. Health Serv Res. 2018;53(4). http://www.hsr.org/hsr/abstract.jsp?aid=53301961729.
AI will change the practice of medicine
Remembering the importance of caring
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
Remembering the importance of caring
Remembering the importance of caring
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
Report calls for focus on ‘subpopulations’ to fight opioid epidemic
Most people who could benefit from FDA-approved medications for opioid use disorder do not receive them, and access to those treatments is not equitable, according to a new consensus study report from the National Academies of Sciences, Engineering, and Medicine.
“Methadone, buprenorphine, and extended-release naltrexone are safe and highly effective medications that are already approved by the U.S. Food and Drug Administration to treat OUD,” the report said. “These medications save lives, but the majority of people with OUD in the United States receive no treatment at all.”
It also said additional research will be needed to address opioid use disorder among subpopulations in the United States, such as adolescents, older adults, people with comorbidities, racial and ethnic groups, and people with low socioeconomic status. The National Academies’ report was sponsored by NIDA and SAMHSA.
A few weeks before the release of National Academies report, the National Academy of Medicine (NAM) held a webinar providing details on its Action Collaborative on Countering the U.S. Opioid Epidemic. The collaborative, a partnership of public and private stakeholders, aims to address the opioid crisis through a multidisciplinary, cross-sector effort.
The collaborative is represented by federal agencies, state and local governments, health care systems, provider groups, nonprofits, payers, industry, academia, patient organizations, and communities across about 55 organizations, according to Victor J. Dzau, MD, chair of the Action Collaborative and current NAM president. Over a 2-year period, the collaborative’s goal is to accelerate progress in overcoming the opioid crisis by recognizing the challenges, research gaps, and needs of organizations involved in the crisis and “elevate and accelerate evidence-based, multisectoral, and interprofessional solutions,” he said.
“This is not a problem that can be solved by a single sector. It is truly a whole of society problem,” said Adm. Brett P. Giroir, MD, assistant secretary for health at the U.S. Department of Health and Human Services, said during the webinar. “And the only way that we are going to be able to begin making inroads to reverse the trends of this crisis is if we work together.” Dr. Giroir also serves as cochair of the steering committee for the collaborative.
In its overview of the collaborative, the NAM outlined four working groups developed through a series of surveys and planning meetings that would identify the resources that currently exist to combat the opioid epidemic and determine which resources still need to be developed. In the Health Professional Education and Training Working Group, for example, the objective is to examine what is being taught to health professionals about acute and chronic pain management at an accreditation, certification, and regulatory level to develop educational tools based around knowledge gaps in those areas and analyze how the new resources are affecting health professions after they have been adopted, said Steve Singer, PhD, vice president of education and outreach at the Accreditation Council for Graduate Medical Education and colead of the working group.“Our goal is really to provide guidance and resources across the continuum of health professions and education with an interprofessional – and patient-informed view,” he said.
The Opioid Prescribing Guidelines and Evidence Standards Working Group plans to address the disparities in prescribing and tapering guidelines for acute and chronic pain as well as identify where pain management guidelines in different specialties “cannot be justified,” based on available evidence.
“Further, we think it’s really important to not just have guidelines that will sit on a shelf, but we also want to think about how we can support implementation of these guidelines into practice ... ” said Helen Burstin, MD, MPH, executive vice president and CEO for the Council of Medical Specialty Societies and colead of the working group.
Alonzo L. Plough, PhD, MPH, vice president of research-evaluation-learning at the Robert Wood Johnson Foundation and colead of the Prevention, Treatment, and Recovery Services Working Group, explained that the goal of his group is to identify the “essential elements and components” and best practices of prevention, treatment, and recovery for OUD. He noted that, although the working group will not be able to reach all patient populations affected by OUD, it has discussed targeting vulnerable high-risk populations, such as those involved in the criminal justice system, homeless veterans, mothers, and children.
“This is an ecosystem that requires great concentration and effort to make sure that there are integrated approaches throughout the continuum that work for patients and clients from different walks of life, and I think that our overall guidance is how we can recognize and use evidence to find those approaches and build on them for guidance,” he said.
The Research, Data, and Metrics Needs Working Group is tasked with collaborating with the other groups to obtain currently available information and identify what barriers exist to greater transparency, sharing and interoperability of data as well as what gaps in research currently exist that would further the collaborative’s mission, said Kelly J. Clark, MD, MBA, of the ASAM. “It is simply critical for us to utilize the data that’s out there, to pool it into more actionable information – and then to act on it,” Dr. Clark said.
The NAM is seeking new organizations interested in joining the collaborative as a network organization, which would receive updates and provide input on the collaborative but would not be a part of the working groups.
The first public meeting of the Action Collaborative on Countering the U.S. Opioid Epidemic will take place on April 30, 2019, in Washington.
Most people who could benefit from FDA-approved medications for opioid use disorder do not receive them, and access to those treatments is not equitable, according to a new consensus study report from the National Academies of Sciences, Engineering, and Medicine.
“Methadone, buprenorphine, and extended-release naltrexone are safe and highly effective medications that are already approved by the U.S. Food and Drug Administration to treat OUD,” the report said. “These medications save lives, but the majority of people with OUD in the United States receive no treatment at all.”
It also said additional research will be needed to address opioid use disorder among subpopulations in the United States, such as adolescents, older adults, people with comorbidities, racial and ethnic groups, and people with low socioeconomic status. The National Academies’ report was sponsored by NIDA and SAMHSA.
A few weeks before the release of National Academies report, the National Academy of Medicine (NAM) held a webinar providing details on its Action Collaborative on Countering the U.S. Opioid Epidemic. The collaborative, a partnership of public and private stakeholders, aims to address the opioid crisis through a multidisciplinary, cross-sector effort.
The collaborative is represented by federal agencies, state and local governments, health care systems, provider groups, nonprofits, payers, industry, academia, patient organizations, and communities across about 55 organizations, according to Victor J. Dzau, MD, chair of the Action Collaborative and current NAM president. Over a 2-year period, the collaborative’s goal is to accelerate progress in overcoming the opioid crisis by recognizing the challenges, research gaps, and needs of organizations involved in the crisis and “elevate and accelerate evidence-based, multisectoral, and interprofessional solutions,” he said.
“This is not a problem that can be solved by a single sector. It is truly a whole of society problem,” said Adm. Brett P. Giroir, MD, assistant secretary for health at the U.S. Department of Health and Human Services, said during the webinar. “And the only way that we are going to be able to begin making inroads to reverse the trends of this crisis is if we work together.” Dr. Giroir also serves as cochair of the steering committee for the collaborative.
In its overview of the collaborative, the NAM outlined four working groups developed through a series of surveys and planning meetings that would identify the resources that currently exist to combat the opioid epidemic and determine which resources still need to be developed. In the Health Professional Education and Training Working Group, for example, the objective is to examine what is being taught to health professionals about acute and chronic pain management at an accreditation, certification, and regulatory level to develop educational tools based around knowledge gaps in those areas and analyze how the new resources are affecting health professions after they have been adopted, said Steve Singer, PhD, vice president of education and outreach at the Accreditation Council for Graduate Medical Education and colead of the working group.“Our goal is really to provide guidance and resources across the continuum of health professions and education with an interprofessional – and patient-informed view,” he said.
The Opioid Prescribing Guidelines and Evidence Standards Working Group plans to address the disparities in prescribing and tapering guidelines for acute and chronic pain as well as identify where pain management guidelines in different specialties “cannot be justified,” based on available evidence.
“Further, we think it’s really important to not just have guidelines that will sit on a shelf, but we also want to think about how we can support implementation of these guidelines into practice ... ” said Helen Burstin, MD, MPH, executive vice president and CEO for the Council of Medical Specialty Societies and colead of the working group.
Alonzo L. Plough, PhD, MPH, vice president of research-evaluation-learning at the Robert Wood Johnson Foundation and colead of the Prevention, Treatment, and Recovery Services Working Group, explained that the goal of his group is to identify the “essential elements and components” and best practices of prevention, treatment, and recovery for OUD. He noted that, although the working group will not be able to reach all patient populations affected by OUD, it has discussed targeting vulnerable high-risk populations, such as those involved in the criminal justice system, homeless veterans, mothers, and children.
“This is an ecosystem that requires great concentration and effort to make sure that there are integrated approaches throughout the continuum that work for patients and clients from different walks of life, and I think that our overall guidance is how we can recognize and use evidence to find those approaches and build on them for guidance,” he said.
The Research, Data, and Metrics Needs Working Group is tasked with collaborating with the other groups to obtain currently available information and identify what barriers exist to greater transparency, sharing and interoperability of data as well as what gaps in research currently exist that would further the collaborative’s mission, said Kelly J. Clark, MD, MBA, of the ASAM. “It is simply critical for us to utilize the data that’s out there, to pool it into more actionable information – and then to act on it,” Dr. Clark said.
The NAM is seeking new organizations interested in joining the collaborative as a network organization, which would receive updates and provide input on the collaborative but would not be a part of the working groups.
The first public meeting of the Action Collaborative on Countering the U.S. Opioid Epidemic will take place on April 30, 2019, in Washington.
Most people who could benefit from FDA-approved medications for opioid use disorder do not receive them, and access to those treatments is not equitable, according to a new consensus study report from the National Academies of Sciences, Engineering, and Medicine.
“Methadone, buprenorphine, and extended-release naltrexone are safe and highly effective medications that are already approved by the U.S. Food and Drug Administration to treat OUD,” the report said. “These medications save lives, but the majority of people with OUD in the United States receive no treatment at all.”
It also said additional research will be needed to address opioid use disorder among subpopulations in the United States, such as adolescents, older adults, people with comorbidities, racial and ethnic groups, and people with low socioeconomic status. The National Academies’ report was sponsored by NIDA and SAMHSA.
A few weeks before the release of National Academies report, the National Academy of Medicine (NAM) held a webinar providing details on its Action Collaborative on Countering the U.S. Opioid Epidemic. The collaborative, a partnership of public and private stakeholders, aims to address the opioid crisis through a multidisciplinary, cross-sector effort.
The collaborative is represented by federal agencies, state and local governments, health care systems, provider groups, nonprofits, payers, industry, academia, patient organizations, and communities across about 55 organizations, according to Victor J. Dzau, MD, chair of the Action Collaborative and current NAM president. Over a 2-year period, the collaborative’s goal is to accelerate progress in overcoming the opioid crisis by recognizing the challenges, research gaps, and needs of organizations involved in the crisis and “elevate and accelerate evidence-based, multisectoral, and interprofessional solutions,” he said.
“This is not a problem that can be solved by a single sector. It is truly a whole of society problem,” said Adm. Brett P. Giroir, MD, assistant secretary for health at the U.S. Department of Health and Human Services, said during the webinar. “And the only way that we are going to be able to begin making inroads to reverse the trends of this crisis is if we work together.” Dr. Giroir also serves as cochair of the steering committee for the collaborative.
In its overview of the collaborative, the NAM outlined four working groups developed through a series of surveys and planning meetings that would identify the resources that currently exist to combat the opioid epidemic and determine which resources still need to be developed. In the Health Professional Education and Training Working Group, for example, the objective is to examine what is being taught to health professionals about acute and chronic pain management at an accreditation, certification, and regulatory level to develop educational tools based around knowledge gaps in those areas and analyze how the new resources are affecting health professions after they have been adopted, said Steve Singer, PhD, vice president of education and outreach at the Accreditation Council for Graduate Medical Education and colead of the working group.“Our goal is really to provide guidance and resources across the continuum of health professions and education with an interprofessional – and patient-informed view,” he said.
The Opioid Prescribing Guidelines and Evidence Standards Working Group plans to address the disparities in prescribing and tapering guidelines for acute and chronic pain as well as identify where pain management guidelines in different specialties “cannot be justified,” based on available evidence.
“Further, we think it’s really important to not just have guidelines that will sit on a shelf, but we also want to think about how we can support implementation of these guidelines into practice ... ” said Helen Burstin, MD, MPH, executive vice president and CEO for the Council of Medical Specialty Societies and colead of the working group.
Alonzo L. Plough, PhD, MPH, vice president of research-evaluation-learning at the Robert Wood Johnson Foundation and colead of the Prevention, Treatment, and Recovery Services Working Group, explained that the goal of his group is to identify the “essential elements and components” and best practices of prevention, treatment, and recovery for OUD. He noted that, although the working group will not be able to reach all patient populations affected by OUD, it has discussed targeting vulnerable high-risk populations, such as those involved in the criminal justice system, homeless veterans, mothers, and children.
“This is an ecosystem that requires great concentration and effort to make sure that there are integrated approaches throughout the continuum that work for patients and clients from different walks of life, and I think that our overall guidance is how we can recognize and use evidence to find those approaches and build on them for guidance,” he said.
The Research, Data, and Metrics Needs Working Group is tasked with collaborating with the other groups to obtain currently available information and identify what barriers exist to greater transparency, sharing and interoperability of data as well as what gaps in research currently exist that would further the collaborative’s mission, said Kelly J. Clark, MD, MBA, of the ASAM. “It is simply critical for us to utilize the data that’s out there, to pool it into more actionable information – and then to act on it,” Dr. Clark said.
The NAM is seeking new organizations interested in joining the collaborative as a network organization, which would receive updates and provide input on the collaborative but would not be a part of the working groups.
The first public meeting of the Action Collaborative on Countering the U.S. Opioid Epidemic will take place on April 30, 2019, in Washington.
Gender wage gap varies by specialty
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
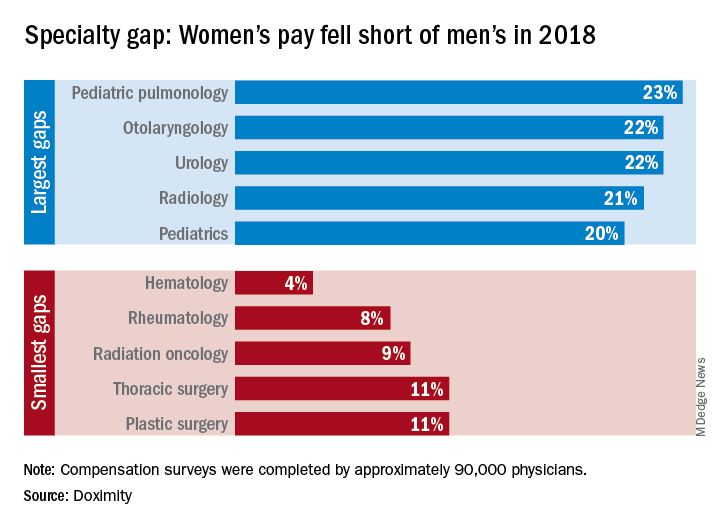
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
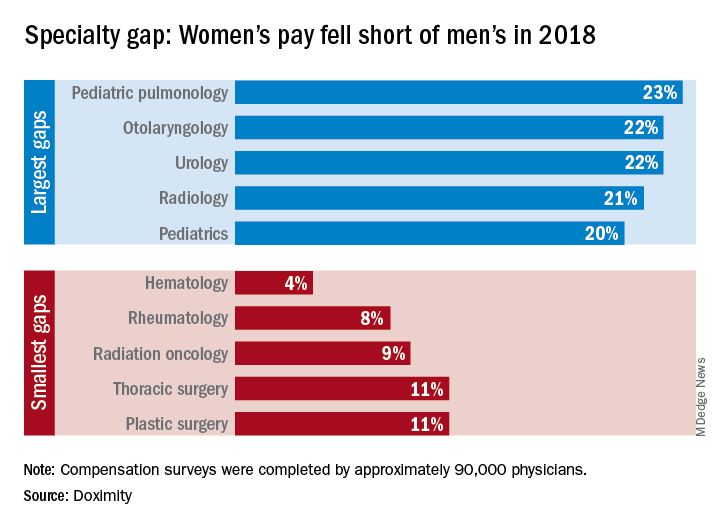
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
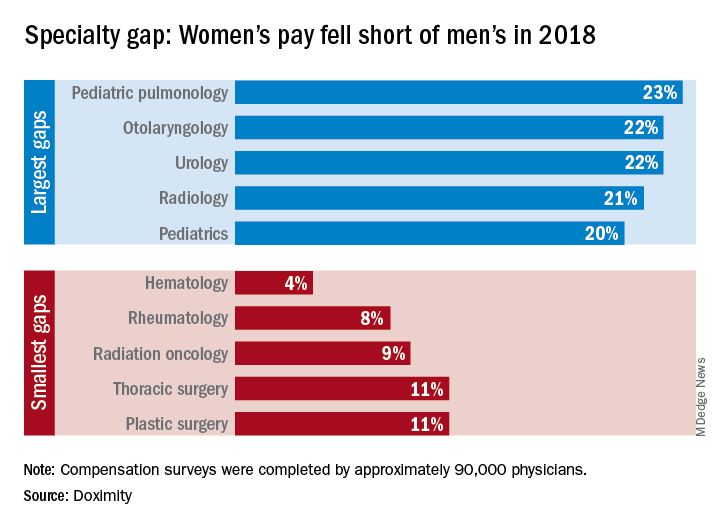
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.