User login
Migraine after concussion linked to worse outcomes
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Focused ultrasound ablation reduces dyskinesia in Parkinson’s disease
, new research shows.
The technique requires no sedation or brain implants. Surgeons use MRI to identify the globus pallidus internus, a part of the basal ganglia involved in movement disorders, and a focused ultrasound beam to heat and destroy the tissue.
Investigators performed the procedure with a device called Exablate Neuro, which was first approved by the Food and Drug Administration in 2016 to treat essential tremor.
On the basis of the results of a multicenter, randomized, sham-controlled trial, the agency expanded the indication in 2021 to include unilateral pallidotomy to treat advanced Parkinson’s disease for patients with mobility, rigidity, or dyskinesia symptoms.
“In some patients with Parkinson’s disease, you get dyskinesias, and ablation of the globus pallidus significantly reduces those dyskinesias and motor impairment,” said lead investigator Vibhor Krishna, MD, associate professor of neurosurgery at the University of North Carolina at Chapel Hill. “It could be used to treat patients when other surgical procedures can’t be applied.”
The study was published online in the New England Journal of Medicine.
Strong response
For the study, 94 patients with advanced Parkinson’s disease who had dyskinesias or motor fluctuations and motor impairment in the off-medication state wore transducer helmets while lying in an MRI scanner. Patients were awake during the entire procedure.
The treatment group received unilateral FUSA on the side of the brain with the greatest motor impairment. The device initially delivered target temperatures of 40°-45° C. Ablative temperatures were gradually increased following evaluations to test for improvement of motor symptoms. The maximum temperature used was 54.3° C.
Patients in the control group underwent an identical procedure with the sonication energy disabled.
The primary outcome was a response to therapy at 3 months, defined as a decrease of at least three points from baseline either in the score on the Movement Disorders Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), part III, while off medication or in the score on the Unified Dyskinesia Rating Scale (UDRS) while on medication.
At 3 months, 69% of the treatment group reported a response, compared with 32% of the control group (P = .003).
When researchers analyzed MDS-UPDRS scores, they found that 29% of the treatment group and 27% of the control group showed improvement. For UDRS scores, 12% of the treatment group demonstrated improvement. In the control group, there was no improvement on this score. Improvements in both scores were reported in 28% of the treatment group and 5% of the control group.
Among those who reported a response at 3 months, 77% continued to show a response at 12 months.
‘Unforgiving’ area of the brain
While the response rate was a promising sign of this finding, it was not what interested Dr. Krishna the most. “The most surprising finding of this trial is how safe focused ultrasound pallidotomy is in treating patients with Parkinson’s disease,” he said.
The globus pallidus internus is an area of the brain that Dr. Krishna calls “unforgiving.”
“One side is motor fibers, and any problem with that can paralyze the patient, and just below that is the optic tract, and any problem there, you would lose vision,” Dr. Krishna said. “It is a very tough neighborhood to be in.”
By using MRI-guided ultrasound, surgeons can change the target and temperature of the ultrasound beam during the procedure to allow more precise treatment.
Pallidotomy-related adverse events in the treatment group included dysarthria, gait disturbance, loss of taste, visual disturbance, and facial weakness. All were mild to moderate, Dr. Krishna said.
More study is needed
Dyskinesia is a challenge in the management of Parkinson’s disease. Patients need antiparkinsonian medications to slow deterioration of motor function, but those medications can cause the involuntary movements that are a hallmark of dyskinesia.
The most common treatment for this complication, deep-brain stimulation (DBS), has its own drawbacks. It’s an open procedure, and there is a low-level risk for intracranial bleeding and infection. In addition, the electrode implants require ongoing maintenance and adjustment.
But the findings of this study show that, for patients who aren’t candidates for other therapies, such as DBS and ablative radiofrequency, FUSA may be an alternative, wrote Anette Schrag, PhD, professor of clinical neurosciences at University College London, in an accompanying commentary.
“The results confirm that it is effective in reducing motor complications of Parkinson’s disease, at least in the short term,” Dr. Schrag wrote. However, more long-term studies are needed, she added.
One-third of patients in the treatment group had no response to the treatment, and investigators aren’t sure why. Dr. Krishna noted that the benefits of the procedure waned in about a quarter of patients within a year of treatment.
Investigators plan to probe these questions in future trials.
“The results of this trial are promising,” Dr. Schrag wrote, “but given the nonreversible nature of the intervention and the progressive nature of the disease, it will be important to establish whether improvements in motor complications are maintained over longer periods and whether treatment results in improved overall functioning and quality of life for patients.”
The study was funded by Insightec. Disclosure forms for Dr. Krishna and Dr. Schrag are provided on the journal’s website.
A version of this article originally appeared on Medscape.com.
, new research shows.
The technique requires no sedation or brain implants. Surgeons use MRI to identify the globus pallidus internus, a part of the basal ganglia involved in movement disorders, and a focused ultrasound beam to heat and destroy the tissue.
Investigators performed the procedure with a device called Exablate Neuro, which was first approved by the Food and Drug Administration in 2016 to treat essential tremor.
On the basis of the results of a multicenter, randomized, sham-controlled trial, the agency expanded the indication in 2021 to include unilateral pallidotomy to treat advanced Parkinson’s disease for patients with mobility, rigidity, or dyskinesia symptoms.
“In some patients with Parkinson’s disease, you get dyskinesias, and ablation of the globus pallidus significantly reduces those dyskinesias and motor impairment,” said lead investigator Vibhor Krishna, MD, associate professor of neurosurgery at the University of North Carolina at Chapel Hill. “It could be used to treat patients when other surgical procedures can’t be applied.”
The study was published online in the New England Journal of Medicine.
Strong response
For the study, 94 patients with advanced Parkinson’s disease who had dyskinesias or motor fluctuations and motor impairment in the off-medication state wore transducer helmets while lying in an MRI scanner. Patients were awake during the entire procedure.
The treatment group received unilateral FUSA on the side of the brain with the greatest motor impairment. The device initially delivered target temperatures of 40°-45° C. Ablative temperatures were gradually increased following evaluations to test for improvement of motor symptoms. The maximum temperature used was 54.3° C.
Patients in the control group underwent an identical procedure with the sonication energy disabled.
The primary outcome was a response to therapy at 3 months, defined as a decrease of at least three points from baseline either in the score on the Movement Disorders Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), part III, while off medication or in the score on the Unified Dyskinesia Rating Scale (UDRS) while on medication.
At 3 months, 69% of the treatment group reported a response, compared with 32% of the control group (P = .003).
When researchers analyzed MDS-UPDRS scores, they found that 29% of the treatment group and 27% of the control group showed improvement. For UDRS scores, 12% of the treatment group demonstrated improvement. In the control group, there was no improvement on this score. Improvements in both scores were reported in 28% of the treatment group and 5% of the control group.
Among those who reported a response at 3 months, 77% continued to show a response at 12 months.
‘Unforgiving’ area of the brain
While the response rate was a promising sign of this finding, it was not what interested Dr. Krishna the most. “The most surprising finding of this trial is how safe focused ultrasound pallidotomy is in treating patients with Parkinson’s disease,” he said.
The globus pallidus internus is an area of the brain that Dr. Krishna calls “unforgiving.”
“One side is motor fibers, and any problem with that can paralyze the patient, and just below that is the optic tract, and any problem there, you would lose vision,” Dr. Krishna said. “It is a very tough neighborhood to be in.”
By using MRI-guided ultrasound, surgeons can change the target and temperature of the ultrasound beam during the procedure to allow more precise treatment.
Pallidotomy-related adverse events in the treatment group included dysarthria, gait disturbance, loss of taste, visual disturbance, and facial weakness. All were mild to moderate, Dr. Krishna said.
More study is needed
Dyskinesia is a challenge in the management of Parkinson’s disease. Patients need antiparkinsonian medications to slow deterioration of motor function, but those medications can cause the involuntary movements that are a hallmark of dyskinesia.
The most common treatment for this complication, deep-brain stimulation (DBS), has its own drawbacks. It’s an open procedure, and there is a low-level risk for intracranial bleeding and infection. In addition, the electrode implants require ongoing maintenance and adjustment.
But the findings of this study show that, for patients who aren’t candidates for other therapies, such as DBS and ablative radiofrequency, FUSA may be an alternative, wrote Anette Schrag, PhD, professor of clinical neurosciences at University College London, in an accompanying commentary.
“The results confirm that it is effective in reducing motor complications of Parkinson’s disease, at least in the short term,” Dr. Schrag wrote. However, more long-term studies are needed, she added.
One-third of patients in the treatment group had no response to the treatment, and investigators aren’t sure why. Dr. Krishna noted that the benefits of the procedure waned in about a quarter of patients within a year of treatment.
Investigators plan to probe these questions in future trials.
“The results of this trial are promising,” Dr. Schrag wrote, “but given the nonreversible nature of the intervention and the progressive nature of the disease, it will be important to establish whether improvements in motor complications are maintained over longer periods and whether treatment results in improved overall functioning and quality of life for patients.”
The study was funded by Insightec. Disclosure forms for Dr. Krishna and Dr. Schrag are provided on the journal’s website.
A version of this article originally appeared on Medscape.com.
, new research shows.
The technique requires no sedation or brain implants. Surgeons use MRI to identify the globus pallidus internus, a part of the basal ganglia involved in movement disorders, and a focused ultrasound beam to heat and destroy the tissue.
Investigators performed the procedure with a device called Exablate Neuro, which was first approved by the Food and Drug Administration in 2016 to treat essential tremor.
On the basis of the results of a multicenter, randomized, sham-controlled trial, the agency expanded the indication in 2021 to include unilateral pallidotomy to treat advanced Parkinson’s disease for patients with mobility, rigidity, or dyskinesia symptoms.
“In some patients with Parkinson’s disease, you get dyskinesias, and ablation of the globus pallidus significantly reduces those dyskinesias and motor impairment,” said lead investigator Vibhor Krishna, MD, associate professor of neurosurgery at the University of North Carolina at Chapel Hill. “It could be used to treat patients when other surgical procedures can’t be applied.”
The study was published online in the New England Journal of Medicine.
Strong response
For the study, 94 patients with advanced Parkinson’s disease who had dyskinesias or motor fluctuations and motor impairment in the off-medication state wore transducer helmets while lying in an MRI scanner. Patients were awake during the entire procedure.
The treatment group received unilateral FUSA on the side of the brain with the greatest motor impairment. The device initially delivered target temperatures of 40°-45° C. Ablative temperatures were gradually increased following evaluations to test for improvement of motor symptoms. The maximum temperature used was 54.3° C.
Patients in the control group underwent an identical procedure with the sonication energy disabled.
The primary outcome was a response to therapy at 3 months, defined as a decrease of at least three points from baseline either in the score on the Movement Disorders Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), part III, while off medication or in the score on the Unified Dyskinesia Rating Scale (UDRS) while on medication.
At 3 months, 69% of the treatment group reported a response, compared with 32% of the control group (P = .003).
When researchers analyzed MDS-UPDRS scores, they found that 29% of the treatment group and 27% of the control group showed improvement. For UDRS scores, 12% of the treatment group demonstrated improvement. In the control group, there was no improvement on this score. Improvements in both scores were reported in 28% of the treatment group and 5% of the control group.
Among those who reported a response at 3 months, 77% continued to show a response at 12 months.
‘Unforgiving’ area of the brain
While the response rate was a promising sign of this finding, it was not what interested Dr. Krishna the most. “The most surprising finding of this trial is how safe focused ultrasound pallidotomy is in treating patients with Parkinson’s disease,” he said.
The globus pallidus internus is an area of the brain that Dr. Krishna calls “unforgiving.”
“One side is motor fibers, and any problem with that can paralyze the patient, and just below that is the optic tract, and any problem there, you would lose vision,” Dr. Krishna said. “It is a very tough neighborhood to be in.”
By using MRI-guided ultrasound, surgeons can change the target and temperature of the ultrasound beam during the procedure to allow more precise treatment.
Pallidotomy-related adverse events in the treatment group included dysarthria, gait disturbance, loss of taste, visual disturbance, and facial weakness. All were mild to moderate, Dr. Krishna said.
More study is needed
Dyskinesia is a challenge in the management of Parkinson’s disease. Patients need antiparkinsonian medications to slow deterioration of motor function, but those medications can cause the involuntary movements that are a hallmark of dyskinesia.
The most common treatment for this complication, deep-brain stimulation (DBS), has its own drawbacks. It’s an open procedure, and there is a low-level risk for intracranial bleeding and infection. In addition, the electrode implants require ongoing maintenance and adjustment.
But the findings of this study show that, for patients who aren’t candidates for other therapies, such as DBS and ablative radiofrequency, FUSA may be an alternative, wrote Anette Schrag, PhD, professor of clinical neurosciences at University College London, in an accompanying commentary.
“The results confirm that it is effective in reducing motor complications of Parkinson’s disease, at least in the short term,” Dr. Schrag wrote. However, more long-term studies are needed, she added.
One-third of patients in the treatment group had no response to the treatment, and investigators aren’t sure why. Dr. Krishna noted that the benefits of the procedure waned in about a quarter of patients within a year of treatment.
Investigators plan to probe these questions in future trials.
“The results of this trial are promising,” Dr. Schrag wrote, “but given the nonreversible nature of the intervention and the progressive nature of the disease, it will be important to establish whether improvements in motor complications are maintained over longer periods and whether treatment results in improved overall functioning and quality of life for patients.”
The study was funded by Insightec. Disclosure forms for Dr. Krishna and Dr. Schrag are provided on the journal’s website.
A version of this article originally appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Which nonopioid meds are best for easing acute low back pain?
based on data from more than 3,000 individuals.
Acute low back pain (LBP) remains a common cause of disability worldwide, with a high socioeconomic burden, write Alice Baroncini, MD, of RWTH University Hospital, Aachen, Germany, and colleagues.
In an analysis published in the Journal of Orthopaedic Research, a team of investigators from Germany examined which nonopioid drugs are best for treating LBP.
The researchers identified 18 studies totaling 3,478 patients with acute low back pain of less than 12 weeks’ duration. They selected studies that only investigated the lumbar spine, and studies involving opioids were excluded. The mean age of the patients across all the studies was 42.5 years, and 54% were women. The mean duration of symptoms before treatment was 15.1 days.
Overall, muscle relaxants and NSAIDs demonstrated effectiveness in reducing pain and disability for acute LBP patients after about 1 week of use.
In addition, studies of a combination of NSAIDs and paracetamol (also known as acetaminophen) showed a greater improvement than NSAIDs alone, but paracetamol/acetaminophen alone had no significant impact on LBP.
Most patients with acute LBP experience spontaneous recovery and reduction of symptoms, thus the real impact of most medications is uncertain, the researchers write in their discussion. The lack of a placebo effect in the selected studies reinforces the hypothesis that nonopioid medications improve LBP symptoms, they say.
However, “while this work only focuses on the pharmacological management of acute LBP, it is fundamental to highlight that the use of drugs should always be a second-line strategy once other nonpharmacological, noninvasive therapies have proved to be insufficient,” the researchers write.
The study findings were limited by several factors, including the inability to distinguish among different NSAID classes, the inability to conduct a subanalysis of the best drug or treatment protocol for a given drug class, and the short follow-up period for the included studies, the researchers note.
More research is needed to address the effects of different drugs on LBP recurrence, they add.
However, the results support the current opinion that NSAIDs can be effectively used for LBP, strengthened by the large number of studies and relatively low risk of bias, the researchers conclude.
The current study addresses a common cause of morbidity among patients and highlights alternatives to opioid analgesics for its management, Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview.
Dr. Pal said he was not surprised by the results. “The findings of the study mirror prior studies,” he said. “However, the lack of benefit of paracetamol alone needs to be highlighted as important to clinical practice.”
A key message for clinicians is the role of NSAIDs in LBP, Dr. Pal said. “NSAIDs, either alone or in combination with paracetamol or myorelaxants, can be effective therapy for select patients with acute LBP.” However, “further research is needed to better identify which patients would derive most benefit from this approach,” he said.
Other research needs include more evidence to better understand the appropriate duration of therapy, given the potential for adverse effects with chronic NSAID use, Dr. Pal said.
The study received no outside funding. The researchers and Dr. Pal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
based on data from more than 3,000 individuals.
Acute low back pain (LBP) remains a common cause of disability worldwide, with a high socioeconomic burden, write Alice Baroncini, MD, of RWTH University Hospital, Aachen, Germany, and colleagues.
In an analysis published in the Journal of Orthopaedic Research, a team of investigators from Germany examined which nonopioid drugs are best for treating LBP.
The researchers identified 18 studies totaling 3,478 patients with acute low back pain of less than 12 weeks’ duration. They selected studies that only investigated the lumbar spine, and studies involving opioids were excluded. The mean age of the patients across all the studies was 42.5 years, and 54% were women. The mean duration of symptoms before treatment was 15.1 days.
Overall, muscle relaxants and NSAIDs demonstrated effectiveness in reducing pain and disability for acute LBP patients after about 1 week of use.
In addition, studies of a combination of NSAIDs and paracetamol (also known as acetaminophen) showed a greater improvement than NSAIDs alone, but paracetamol/acetaminophen alone had no significant impact on LBP.
Most patients with acute LBP experience spontaneous recovery and reduction of symptoms, thus the real impact of most medications is uncertain, the researchers write in their discussion. The lack of a placebo effect in the selected studies reinforces the hypothesis that nonopioid medications improve LBP symptoms, they say.
However, “while this work only focuses on the pharmacological management of acute LBP, it is fundamental to highlight that the use of drugs should always be a second-line strategy once other nonpharmacological, noninvasive therapies have proved to be insufficient,” the researchers write.
The study findings were limited by several factors, including the inability to distinguish among different NSAID classes, the inability to conduct a subanalysis of the best drug or treatment protocol for a given drug class, and the short follow-up period for the included studies, the researchers note.
More research is needed to address the effects of different drugs on LBP recurrence, they add.
However, the results support the current opinion that NSAIDs can be effectively used for LBP, strengthened by the large number of studies and relatively low risk of bias, the researchers conclude.
The current study addresses a common cause of morbidity among patients and highlights alternatives to opioid analgesics for its management, Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview.
Dr. Pal said he was not surprised by the results. “The findings of the study mirror prior studies,” he said. “However, the lack of benefit of paracetamol alone needs to be highlighted as important to clinical practice.”
A key message for clinicians is the role of NSAIDs in LBP, Dr. Pal said. “NSAIDs, either alone or in combination with paracetamol or myorelaxants, can be effective therapy for select patients with acute LBP.” However, “further research is needed to better identify which patients would derive most benefit from this approach,” he said.
Other research needs include more evidence to better understand the appropriate duration of therapy, given the potential for adverse effects with chronic NSAID use, Dr. Pal said.
The study received no outside funding. The researchers and Dr. Pal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
based on data from more than 3,000 individuals.
Acute low back pain (LBP) remains a common cause of disability worldwide, with a high socioeconomic burden, write Alice Baroncini, MD, of RWTH University Hospital, Aachen, Germany, and colleagues.
In an analysis published in the Journal of Orthopaedic Research, a team of investigators from Germany examined which nonopioid drugs are best for treating LBP.
The researchers identified 18 studies totaling 3,478 patients with acute low back pain of less than 12 weeks’ duration. They selected studies that only investigated the lumbar spine, and studies involving opioids were excluded. The mean age of the patients across all the studies was 42.5 years, and 54% were women. The mean duration of symptoms before treatment was 15.1 days.
Overall, muscle relaxants and NSAIDs demonstrated effectiveness in reducing pain and disability for acute LBP patients after about 1 week of use.
In addition, studies of a combination of NSAIDs and paracetamol (also known as acetaminophen) showed a greater improvement than NSAIDs alone, but paracetamol/acetaminophen alone had no significant impact on LBP.
Most patients with acute LBP experience spontaneous recovery and reduction of symptoms, thus the real impact of most medications is uncertain, the researchers write in their discussion. The lack of a placebo effect in the selected studies reinforces the hypothesis that nonopioid medications improve LBP symptoms, they say.
However, “while this work only focuses on the pharmacological management of acute LBP, it is fundamental to highlight that the use of drugs should always be a second-line strategy once other nonpharmacological, noninvasive therapies have proved to be insufficient,” the researchers write.
The study findings were limited by several factors, including the inability to distinguish among different NSAID classes, the inability to conduct a subanalysis of the best drug or treatment protocol for a given drug class, and the short follow-up period for the included studies, the researchers note.
More research is needed to address the effects of different drugs on LBP recurrence, they add.
However, the results support the current opinion that NSAIDs can be effectively used for LBP, strengthened by the large number of studies and relatively low risk of bias, the researchers conclude.
The current study addresses a common cause of morbidity among patients and highlights alternatives to opioid analgesics for its management, Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview.
Dr. Pal said he was not surprised by the results. “The findings of the study mirror prior studies,” he said. “However, the lack of benefit of paracetamol alone needs to be highlighted as important to clinical practice.”
A key message for clinicians is the role of NSAIDs in LBP, Dr. Pal said. “NSAIDs, either alone or in combination with paracetamol or myorelaxants, can be effective therapy for select patients with acute LBP.” However, “further research is needed to better identify which patients would derive most benefit from this approach,” he said.
Other research needs include more evidence to better understand the appropriate duration of therapy, given the potential for adverse effects with chronic NSAID use, Dr. Pal said.
The study received no outside funding. The researchers and Dr. Pal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF ORTHOPAEDIC RESEARCH
Spinal cord stimulation restores poststroke arm, hand function in two patients
The results provide “promising, albeit preliminary, evidence that spinal cord stimulation could be an assistive as well as a restorative approach for upper-limb recovery after stroke,” wrote first author Marc P. Powell, PhD, of Reach Neuro Inc., Pittsburgh, and colleagues.
The findings were published online in Nature Medicine.
Top cause of paralysis
“Stroke is the largest cause of paralysis in the world,” with nearly three-quarters of patients with stroke experiencing lasting deficits in motor control of their arm and hand, co–senior study author Marco Capogrosso, PhD, assistant professor of neurological surgery at the University of Pittsburgh, said during a press briefing.
Stroke can disrupt communication between the brain and the spinal cord, leading to motor deficits in the arm and hand. However, below the lesion, the spinal circuits that control movement remain intact and could be targeted to restore function, Dr. Capogrosso noted.
Spinal cord stimulation has shown promise in promoting long-lasting recovery of leg motor function in patients with spinal cord injury; but until now, it’s been largely unexplored for upper-limb recovery.
In this “first-in-human” study, the investigators percutaneously implanted two linear leads in the dorsolateral epidural space targeting neural circuits that control arm and hand muscles in two patients.
One of the patients was a woman (age, 31 years) who had experienced a right thalamic hemorrhagic stroke secondary to a cavernous malformation 9 years before enrolling in the pilot study.
The other patient was a woman (age, 47 years) who experienced a right ischemic middle cerebral artery (MCA) stroke secondary to a right carotid dissection, resulting in a large MCA territory infarct 3 years before entering the study.
In both patients, continuous stimulation of the targeted neural circuits led to significant and immediate improvement in arm and hand strength and dexterity. This enabled the patients to perform movements that they couldn’t perform without spinal cord stimulation.
The process also enabled fine motor skills, such as opening a lock and using utensils to eat independently – tasks that the younger woman had not been able to do for 9 years.
“Perhaps even more interesting, we found that after a few weeks of use, some of these improvements endure when the stimulation is switched off, indicating exciting avenues for the future of stroke therapies,” Dr. Capogrosso said in a news release.
No serious adverse events were reported.
‘Easily translated’
Dr. Capogrosso said that, thanks to years of preclinical research, the investigators have developed a practical, easy-to-use stimulation protocol adapting existing clinical technologies that “could be easily translated to the hospital and quickly moved from the lab to the clinic.”
The researchers noted, however, that further studies in larger cohorts will be required to validate the safety and efficacy of this approach.
They are currently working with more patients with stroke to fine-tune placement of the leads and stimulation protocol, as well as determine which patients are best suited for the approach.
“Creating effective neurorehabilitation solutions for people affected by movement impairment after stroke is becoming ever more urgent,” co–senior author Elvira Pirondini, PhD, assistant professor of physical medicine and rehabilitation at the University of Pittsburgh, said in the release.
“Even mild deficits resulting from a stroke can isolate people from social and professional lives and become very debilitating, with motor impairments in the arm and hand being especially taxing and impeding simple daily activities, such as writing, eating, and getting dressed,” she added.
This research was funded by the National Institutes of Health BRAIN Initiative, with additional research support provided by the Department of Neurological Surgery and the Department of Physical Medicine and Rehabilitation at Pitt, and the Department of Mechanical Engineering and the Neuroscience Institute at Carnegie Mellon University. Three investigators have financial interests in Reach Neuro, which has an interest in the technology being evaluated in this study.
A version of this article first appeared on Medscape.com.
The results provide “promising, albeit preliminary, evidence that spinal cord stimulation could be an assistive as well as a restorative approach for upper-limb recovery after stroke,” wrote first author Marc P. Powell, PhD, of Reach Neuro Inc., Pittsburgh, and colleagues.
The findings were published online in Nature Medicine.
Top cause of paralysis
“Stroke is the largest cause of paralysis in the world,” with nearly three-quarters of patients with stroke experiencing lasting deficits in motor control of their arm and hand, co–senior study author Marco Capogrosso, PhD, assistant professor of neurological surgery at the University of Pittsburgh, said during a press briefing.
Stroke can disrupt communication between the brain and the spinal cord, leading to motor deficits in the arm and hand. However, below the lesion, the spinal circuits that control movement remain intact and could be targeted to restore function, Dr. Capogrosso noted.
Spinal cord stimulation has shown promise in promoting long-lasting recovery of leg motor function in patients with spinal cord injury; but until now, it’s been largely unexplored for upper-limb recovery.
In this “first-in-human” study, the investigators percutaneously implanted two linear leads in the dorsolateral epidural space targeting neural circuits that control arm and hand muscles in two patients.
One of the patients was a woman (age, 31 years) who had experienced a right thalamic hemorrhagic stroke secondary to a cavernous malformation 9 years before enrolling in the pilot study.
The other patient was a woman (age, 47 years) who experienced a right ischemic middle cerebral artery (MCA) stroke secondary to a right carotid dissection, resulting in a large MCA territory infarct 3 years before entering the study.
In both patients, continuous stimulation of the targeted neural circuits led to significant and immediate improvement in arm and hand strength and dexterity. This enabled the patients to perform movements that they couldn’t perform without spinal cord stimulation.
The process also enabled fine motor skills, such as opening a lock and using utensils to eat independently – tasks that the younger woman had not been able to do for 9 years.
“Perhaps even more interesting, we found that after a few weeks of use, some of these improvements endure when the stimulation is switched off, indicating exciting avenues for the future of stroke therapies,” Dr. Capogrosso said in a news release.
No serious adverse events were reported.
‘Easily translated’
Dr. Capogrosso said that, thanks to years of preclinical research, the investigators have developed a practical, easy-to-use stimulation protocol adapting existing clinical technologies that “could be easily translated to the hospital and quickly moved from the lab to the clinic.”
The researchers noted, however, that further studies in larger cohorts will be required to validate the safety and efficacy of this approach.
They are currently working with more patients with stroke to fine-tune placement of the leads and stimulation protocol, as well as determine which patients are best suited for the approach.
“Creating effective neurorehabilitation solutions for people affected by movement impairment after stroke is becoming ever more urgent,” co–senior author Elvira Pirondini, PhD, assistant professor of physical medicine and rehabilitation at the University of Pittsburgh, said in the release.
“Even mild deficits resulting from a stroke can isolate people from social and professional lives and become very debilitating, with motor impairments in the arm and hand being especially taxing and impeding simple daily activities, such as writing, eating, and getting dressed,” she added.
This research was funded by the National Institutes of Health BRAIN Initiative, with additional research support provided by the Department of Neurological Surgery and the Department of Physical Medicine and Rehabilitation at Pitt, and the Department of Mechanical Engineering and the Neuroscience Institute at Carnegie Mellon University. Three investigators have financial interests in Reach Neuro, which has an interest in the technology being evaluated in this study.
A version of this article first appeared on Medscape.com.
The results provide “promising, albeit preliminary, evidence that spinal cord stimulation could be an assistive as well as a restorative approach for upper-limb recovery after stroke,” wrote first author Marc P. Powell, PhD, of Reach Neuro Inc., Pittsburgh, and colleagues.
The findings were published online in Nature Medicine.
Top cause of paralysis
“Stroke is the largest cause of paralysis in the world,” with nearly three-quarters of patients with stroke experiencing lasting deficits in motor control of their arm and hand, co–senior study author Marco Capogrosso, PhD, assistant professor of neurological surgery at the University of Pittsburgh, said during a press briefing.
Stroke can disrupt communication between the brain and the spinal cord, leading to motor deficits in the arm and hand. However, below the lesion, the spinal circuits that control movement remain intact and could be targeted to restore function, Dr. Capogrosso noted.
Spinal cord stimulation has shown promise in promoting long-lasting recovery of leg motor function in patients with spinal cord injury; but until now, it’s been largely unexplored for upper-limb recovery.
In this “first-in-human” study, the investigators percutaneously implanted two linear leads in the dorsolateral epidural space targeting neural circuits that control arm and hand muscles in two patients.
One of the patients was a woman (age, 31 years) who had experienced a right thalamic hemorrhagic stroke secondary to a cavernous malformation 9 years before enrolling in the pilot study.
The other patient was a woman (age, 47 years) who experienced a right ischemic middle cerebral artery (MCA) stroke secondary to a right carotid dissection, resulting in a large MCA territory infarct 3 years before entering the study.
In both patients, continuous stimulation of the targeted neural circuits led to significant and immediate improvement in arm and hand strength and dexterity. This enabled the patients to perform movements that they couldn’t perform without spinal cord stimulation.
The process also enabled fine motor skills, such as opening a lock and using utensils to eat independently – tasks that the younger woman had not been able to do for 9 years.
“Perhaps even more interesting, we found that after a few weeks of use, some of these improvements endure when the stimulation is switched off, indicating exciting avenues for the future of stroke therapies,” Dr. Capogrosso said in a news release.
No serious adverse events were reported.
‘Easily translated’
Dr. Capogrosso said that, thanks to years of preclinical research, the investigators have developed a practical, easy-to-use stimulation protocol adapting existing clinical technologies that “could be easily translated to the hospital and quickly moved from the lab to the clinic.”
The researchers noted, however, that further studies in larger cohorts will be required to validate the safety and efficacy of this approach.
They are currently working with more patients with stroke to fine-tune placement of the leads and stimulation protocol, as well as determine which patients are best suited for the approach.
“Creating effective neurorehabilitation solutions for people affected by movement impairment after stroke is becoming ever more urgent,” co–senior author Elvira Pirondini, PhD, assistant professor of physical medicine and rehabilitation at the University of Pittsburgh, said in the release.
“Even mild deficits resulting from a stroke can isolate people from social and professional lives and become very debilitating, with motor impairments in the arm and hand being especially taxing and impeding simple daily activities, such as writing, eating, and getting dressed,” she added.
This research was funded by the National Institutes of Health BRAIN Initiative, with additional research support provided by the Department of Neurological Surgery and the Department of Physical Medicine and Rehabilitation at Pitt, and the Department of Mechanical Engineering and the Neuroscience Institute at Carnegie Mellon University. Three investigators have financial interests in Reach Neuro, which has an interest in the technology being evaluated in this study.
A version of this article first appeared on Medscape.com.
FROM NATURE MEDICINE
‘Quick, affordable’ test helps predict CGRP response for migraine
new research suggests.
The ictal phase refers to “sensitization occurring during a time when central trigeminovascular neurons receive massive nociceptive input from active meningeal nociceptors,” whereas the nonictal phase refers to “sensitization occurring during a time when central trigeminovascular neurons receive no or subliminal nociceptive input from meningeal nociceptors,” investigators noted.
In an observational, open-label cohort study, pretreatment nonictal cephalic allodynia identified galcanezumab responders with nearly 80% accuracy, and it identified nonresponders with nearly 85% accuracy.
“Detection of nonictal allodynia with a simplified paradigm of Quantitative Sensory Testing (QST) may provide a quick, affordable, noninvasive, and patient-friendly way to prospectively distinguish between responders and nonresponders to the prophylactic treatment of chronic and high-frequency episodic migraine with drugs that reduce CGRP signaling,” Sait Ashina, MD, of Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, and colleagues wrote.
The findings were published online in Cephalalgia.
Immediate clinical relevance
Investigator Rami Burstein, PhD, also with Beth Israel Deaconess Medical Center and Harvard Medical School, developed the concept of predicting response to anti-CGRP treatment by testing for the presence or absence of nonictal cephalic allodynia in collaboration with the company CGRP Diagnostics.
In 43 anti–CGRP-naive patients with migraine, the researchers used a simplified QST algorithm to determine the presence/absence of cephalic or extracephalic allodynia during the nonictal phase of migraine – defined as the period from less than 12 hours after a migraine attack to less than 12 hours before the next attack.
Patients were considered to have allodynia if heat pain thresholds were between 32° C and 40° C, if cold pain thresholds were between 32° C and 20° C, or if the mechanical pain was threshold was less than 60 g.
Using these strict criteria, pretreatment nonictal cephalic allodynia was a statistically significant predictor of response to anti-CGRP therapy. It was present in 84% of the 19 nonresponders and was absent in 79% of the 24 responders, for an overall accuracy rate of 86% (P < .0001).
Nonictal cephalic allodynia was “consistently” predictive of response for patients with chronic migraine as well as for those with high-frequency episodic migraine, the researchers reported.
In contrast, they noted that assessing nonictal extracephalic allodynia with QST missed nearly 50% of the patients with allodynia among the nonresponders (accuracy rate of 42%) and added little to the assessment of allodynia among the responders.
Mark Hasleton, PhD, CEO of CGRP Diagnostics, said in an interview that the study shows it’s possible to determine response to anti-CGRP therapy and to prescribe these medications to patients who are most likely to respond.
Dr. Hasleton, who was not personally involved with the current study, noted that pretreatment testing for nonictal cephalic allodynia may also allow for earlier prescription of anti-CGRP therapy and potentially dispense without the need for the current trial-and-error approach to prescribing. He noted that if one anti-CGRP fails the patient, it is highly likely that others will also fail.
Given the “very high correlation of the presence of nonictal cephalic allodynia in responders to galcanezumab, our recommendation would be to routinely pretest all potential anti-CGRP candidates prior to prescription,” he said.
End of trial-and-error prescribing
In a comment, Shaheen Lakhan, MD, a neurologist and researcher in Boston, said this research is “very noteworthy, moving us one step closer to predictive, precision medicine and away from the practice of trial-and-error prescribing.
“The trial-and-error approach to migraine management is daunting. These are very costly therapies, and when they don’t work, there is continued tremendous suffering and loss of quality of life for patients,” said Dr. Lakhan, who was not involved in the study.
He added that the failure of drugs to benefit individual patients “may lead to distrust of the health care provider” and to the system as a whole, which in turn could lead to less access to care for other conditions or for preventive measures.
“I envision a time when these predictive measures collectively (interictal allodynia, as in this study, plus biobehavioral data) will assist us neurologists in appropriately selecting migraine therapies,” Dr. Lakhan said.
“Beyond that, we will eventually test new therapies not in cells, animals, and even humans but in silico. In the very near future, we will have solutions tailored to not people suffering a disease but to you – an individual with a unique genetic, protein, physical, developmental, psychological, and behavioral makeup,” he added.
The study was funded in part by Eli Lilly, the National Institutes of Health, and the anesthesia department at Beth Israel Deaconess Medical Center. Galcanezumab was provided by Eli Lilly. Dr. Lakhan reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
The ictal phase refers to “sensitization occurring during a time when central trigeminovascular neurons receive massive nociceptive input from active meningeal nociceptors,” whereas the nonictal phase refers to “sensitization occurring during a time when central trigeminovascular neurons receive no or subliminal nociceptive input from meningeal nociceptors,” investigators noted.
In an observational, open-label cohort study, pretreatment nonictal cephalic allodynia identified galcanezumab responders with nearly 80% accuracy, and it identified nonresponders with nearly 85% accuracy.
“Detection of nonictal allodynia with a simplified paradigm of Quantitative Sensory Testing (QST) may provide a quick, affordable, noninvasive, and patient-friendly way to prospectively distinguish between responders and nonresponders to the prophylactic treatment of chronic and high-frequency episodic migraine with drugs that reduce CGRP signaling,” Sait Ashina, MD, of Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, and colleagues wrote.
The findings were published online in Cephalalgia.
Immediate clinical relevance
Investigator Rami Burstein, PhD, also with Beth Israel Deaconess Medical Center and Harvard Medical School, developed the concept of predicting response to anti-CGRP treatment by testing for the presence or absence of nonictal cephalic allodynia in collaboration with the company CGRP Diagnostics.
In 43 anti–CGRP-naive patients with migraine, the researchers used a simplified QST algorithm to determine the presence/absence of cephalic or extracephalic allodynia during the nonictal phase of migraine – defined as the period from less than 12 hours after a migraine attack to less than 12 hours before the next attack.
Patients were considered to have allodynia if heat pain thresholds were between 32° C and 40° C, if cold pain thresholds were between 32° C and 20° C, or if the mechanical pain was threshold was less than 60 g.
Using these strict criteria, pretreatment nonictal cephalic allodynia was a statistically significant predictor of response to anti-CGRP therapy. It was present in 84% of the 19 nonresponders and was absent in 79% of the 24 responders, for an overall accuracy rate of 86% (P < .0001).
Nonictal cephalic allodynia was “consistently” predictive of response for patients with chronic migraine as well as for those with high-frequency episodic migraine, the researchers reported.
In contrast, they noted that assessing nonictal extracephalic allodynia with QST missed nearly 50% of the patients with allodynia among the nonresponders (accuracy rate of 42%) and added little to the assessment of allodynia among the responders.
Mark Hasleton, PhD, CEO of CGRP Diagnostics, said in an interview that the study shows it’s possible to determine response to anti-CGRP therapy and to prescribe these medications to patients who are most likely to respond.
Dr. Hasleton, who was not personally involved with the current study, noted that pretreatment testing for nonictal cephalic allodynia may also allow for earlier prescription of anti-CGRP therapy and potentially dispense without the need for the current trial-and-error approach to prescribing. He noted that if one anti-CGRP fails the patient, it is highly likely that others will also fail.
Given the “very high correlation of the presence of nonictal cephalic allodynia in responders to galcanezumab, our recommendation would be to routinely pretest all potential anti-CGRP candidates prior to prescription,” he said.
End of trial-and-error prescribing
In a comment, Shaheen Lakhan, MD, a neurologist and researcher in Boston, said this research is “very noteworthy, moving us one step closer to predictive, precision medicine and away from the practice of trial-and-error prescribing.
“The trial-and-error approach to migraine management is daunting. These are very costly therapies, and when they don’t work, there is continued tremendous suffering and loss of quality of life for patients,” said Dr. Lakhan, who was not involved in the study.
He added that the failure of drugs to benefit individual patients “may lead to distrust of the health care provider” and to the system as a whole, which in turn could lead to less access to care for other conditions or for preventive measures.
“I envision a time when these predictive measures collectively (interictal allodynia, as in this study, plus biobehavioral data) will assist us neurologists in appropriately selecting migraine therapies,” Dr. Lakhan said.
“Beyond that, we will eventually test new therapies not in cells, animals, and even humans but in silico. In the very near future, we will have solutions tailored to not people suffering a disease but to you – an individual with a unique genetic, protein, physical, developmental, psychological, and behavioral makeup,” he added.
The study was funded in part by Eli Lilly, the National Institutes of Health, and the anesthesia department at Beth Israel Deaconess Medical Center. Galcanezumab was provided by Eli Lilly. Dr. Lakhan reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
The ictal phase refers to “sensitization occurring during a time when central trigeminovascular neurons receive massive nociceptive input from active meningeal nociceptors,” whereas the nonictal phase refers to “sensitization occurring during a time when central trigeminovascular neurons receive no or subliminal nociceptive input from meningeal nociceptors,” investigators noted.
In an observational, open-label cohort study, pretreatment nonictal cephalic allodynia identified galcanezumab responders with nearly 80% accuracy, and it identified nonresponders with nearly 85% accuracy.
“Detection of nonictal allodynia with a simplified paradigm of Quantitative Sensory Testing (QST) may provide a quick, affordable, noninvasive, and patient-friendly way to prospectively distinguish between responders and nonresponders to the prophylactic treatment of chronic and high-frequency episodic migraine with drugs that reduce CGRP signaling,” Sait Ashina, MD, of Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, and colleagues wrote.
The findings were published online in Cephalalgia.
Immediate clinical relevance
Investigator Rami Burstein, PhD, also with Beth Israel Deaconess Medical Center and Harvard Medical School, developed the concept of predicting response to anti-CGRP treatment by testing for the presence or absence of nonictal cephalic allodynia in collaboration with the company CGRP Diagnostics.
In 43 anti–CGRP-naive patients with migraine, the researchers used a simplified QST algorithm to determine the presence/absence of cephalic or extracephalic allodynia during the nonictal phase of migraine – defined as the period from less than 12 hours after a migraine attack to less than 12 hours before the next attack.
Patients were considered to have allodynia if heat pain thresholds were between 32° C and 40° C, if cold pain thresholds were between 32° C and 20° C, or if the mechanical pain was threshold was less than 60 g.
Using these strict criteria, pretreatment nonictal cephalic allodynia was a statistically significant predictor of response to anti-CGRP therapy. It was present in 84% of the 19 nonresponders and was absent in 79% of the 24 responders, for an overall accuracy rate of 86% (P < .0001).
Nonictal cephalic allodynia was “consistently” predictive of response for patients with chronic migraine as well as for those with high-frequency episodic migraine, the researchers reported.
In contrast, they noted that assessing nonictal extracephalic allodynia with QST missed nearly 50% of the patients with allodynia among the nonresponders (accuracy rate of 42%) and added little to the assessment of allodynia among the responders.
Mark Hasleton, PhD, CEO of CGRP Diagnostics, said in an interview that the study shows it’s possible to determine response to anti-CGRP therapy and to prescribe these medications to patients who are most likely to respond.
Dr. Hasleton, who was not personally involved with the current study, noted that pretreatment testing for nonictal cephalic allodynia may also allow for earlier prescription of anti-CGRP therapy and potentially dispense without the need for the current trial-and-error approach to prescribing. He noted that if one anti-CGRP fails the patient, it is highly likely that others will also fail.
Given the “very high correlation of the presence of nonictal cephalic allodynia in responders to galcanezumab, our recommendation would be to routinely pretest all potential anti-CGRP candidates prior to prescription,” he said.
End of trial-and-error prescribing
In a comment, Shaheen Lakhan, MD, a neurologist and researcher in Boston, said this research is “very noteworthy, moving us one step closer to predictive, precision medicine and away from the practice of trial-and-error prescribing.
“The trial-and-error approach to migraine management is daunting. These are very costly therapies, and when they don’t work, there is continued tremendous suffering and loss of quality of life for patients,” said Dr. Lakhan, who was not involved in the study.
He added that the failure of drugs to benefit individual patients “may lead to distrust of the health care provider” and to the system as a whole, which in turn could lead to less access to care for other conditions or for preventive measures.
“I envision a time when these predictive measures collectively (interictal allodynia, as in this study, plus biobehavioral data) will assist us neurologists in appropriately selecting migraine therapies,” Dr. Lakhan said.
“Beyond that, we will eventually test new therapies not in cells, animals, and even humans but in silico. In the very near future, we will have solutions tailored to not people suffering a disease but to you – an individual with a unique genetic, protein, physical, developmental, psychological, and behavioral makeup,” he added.
The study was funded in part by Eli Lilly, the National Institutes of Health, and the anesthesia department at Beth Israel Deaconess Medical Center. Galcanezumab was provided by Eli Lilly. Dr. Lakhan reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CEPHALALGIA
Adult brains contain millions of ‘silent synapses’
according to neuroscientists from the Massachusetts Institute of Technology.
What to know:
- An estimated 30% of all synapses in the brain’s cortex are silent and become active to allow the adult brain to continually form new memories and leave existing conventional synapses unmodified.
- Silent synapses are looking for new connections, and when important new information is presented, connections between the relevant neurons are strengthened to allow the brain to remember new things.
- Using the silent synapses for the new memories does not overwrite the important memories stored in more mature synapses, which are harder to change.
- The brain’s neurons display a wide range of plasticity mechanisms that account for how brains can efficiently learn new things and retain them in long-term memory.
- Flexibility of synapses is critical for acquiring new information, and stability is required to retain important information, enabling one to more easily adjust and change behaviors and habits or incorporate new information.
This is a summary of the article, “Filopodia Are a Structural Substrate for Silent Synapses in Adult Neocortex,” published in Nature Nov. 30, 2022. The full article can be found at nature.com .
A version of this article first appeared on Medscape.com.
according to neuroscientists from the Massachusetts Institute of Technology.
What to know:
- An estimated 30% of all synapses in the brain’s cortex are silent and become active to allow the adult brain to continually form new memories and leave existing conventional synapses unmodified.
- Silent synapses are looking for new connections, and when important new information is presented, connections between the relevant neurons are strengthened to allow the brain to remember new things.
- Using the silent synapses for the new memories does not overwrite the important memories stored in more mature synapses, which are harder to change.
- The brain’s neurons display a wide range of plasticity mechanisms that account for how brains can efficiently learn new things and retain them in long-term memory.
- Flexibility of synapses is critical for acquiring new information, and stability is required to retain important information, enabling one to more easily adjust and change behaviors and habits or incorporate new information.
This is a summary of the article, “Filopodia Are a Structural Substrate for Silent Synapses in Adult Neocortex,” published in Nature Nov. 30, 2022. The full article can be found at nature.com .
A version of this article first appeared on Medscape.com.
according to neuroscientists from the Massachusetts Institute of Technology.
What to know:
- An estimated 30% of all synapses in the brain’s cortex are silent and become active to allow the adult brain to continually form new memories and leave existing conventional synapses unmodified.
- Silent synapses are looking for new connections, and when important new information is presented, connections between the relevant neurons are strengthened to allow the brain to remember new things.
- Using the silent synapses for the new memories does not overwrite the important memories stored in more mature synapses, which are harder to change.
- The brain’s neurons display a wide range of plasticity mechanisms that account for how brains can efficiently learn new things and retain them in long-term memory.
- Flexibility of synapses is critical for acquiring new information, and stability is required to retain important information, enabling one to more easily adjust and change behaviors and habits or incorporate new information.
This is a summary of the article, “Filopodia Are a Structural Substrate for Silent Synapses in Adult Neocortex,” published in Nature Nov. 30, 2022. The full article can be found at nature.com .
A version of this article first appeared on Medscape.com.
Diabetes drug tied to lower dementia risk
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY
Immunodeficiencies tied to psychiatric disorders in offspring
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.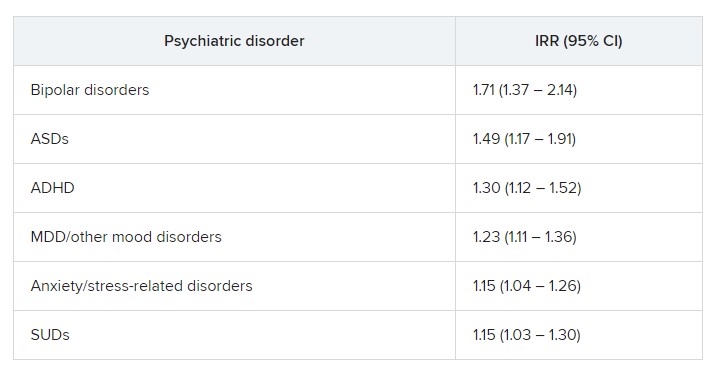
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.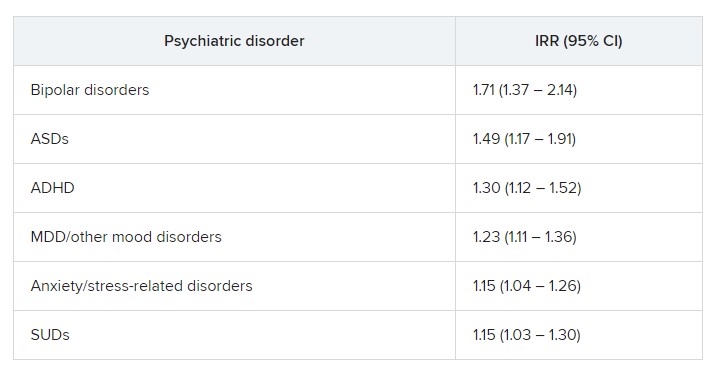
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.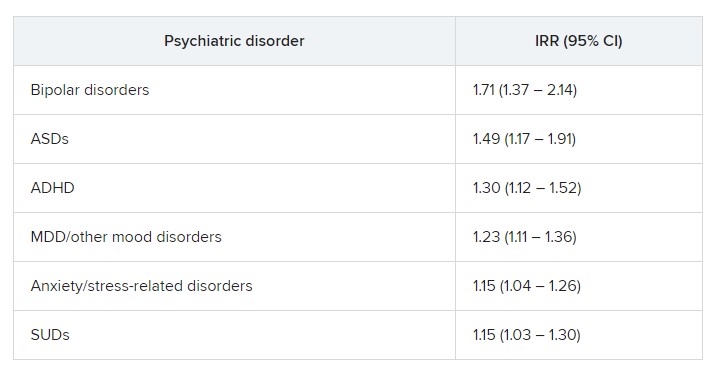
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Be aware of hepatic encephalopathy, dementia overlap in older patients with cirrhosis
, according to a new study involving U.S. veterans.
The overlap between dementia and HE was also independent of alcohol use, brain injury, age, and other metabolic risk factors.
“The aging of patients with cirrhosis leads us to encounter several individuals who may be prone to both of these diseases,” senior author Jasmohan Bajaj, MD, a professor of gastroenterology, hepatology, and nutrition at Virginia Commonwealth University Medical Center and GI section of the Central Virginia Veterans Healthcare System in Richmond, said in an interview.
“Given the epidemic of metabolic syndrome and alcohol, consider excluding cirrhosis in your patient [for] whom the presumptive diagnosis is dementia, since they could have concomitant HE,” he said.
“On the flip side, in those with HE who have predominant long-term memory issues and persistent cognitive changes, consider consulting a neuropsychiatrist or neurologist to ensure there is a resolution of the underlying disease process,” Dr. Bajaj added.
The study was published online in The American Journal of Gastroenterology.
Analyzing associations
HE is a common decompensating event in patients with cirrhosis. Because of the aging population of patients with cirrhosis, however, it’s important to differentiate HE from nonhepatic etiologies of cognitive impairment, such as dementia, the authors note.
Using data from the VA Corporate Data Warehouse, Dr. Bajaj and colleagues identified veterans with cirrhosis who received VA care between October 2019 and September 2021 and compared baseline characteristics between the cohorts based on the presence or absence of dementia. The research team then evaluated factors associated with having a diagnosis of dementia, adjusting for demographics, comorbid illnesses, cirrhosis etiology, and cirrhosis complications.
Investigators identified 71,522 veterans with diagnostic codes for cirrhosis who were engaged in VA care in 2019. They were mostly men (96.2%) and had a median age of 66. The most common etiologies of cirrhosis were alcohol and hepatitis C, followed by nonalcoholic steatohepatitis (NASH). The group also included veterans with predominantly compensated cirrhosis and a median MELD-Na score of 9. The MELD-Na score gauges the severity of chronic liver disease using values such as serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time and sodium to predict survival.
Among those with cirrhosis, 5,647 (7.9%) also had dementia diagnosis codes. This rate is higher than the prevalence of dementia in the general population and equivalent to the rate of dementia in veterans without cirrhosis who are older than 65, the authors note.
In general, veterans with dementia tended to be older, to be White, to live in an urban area, and to have higher MELD-Na scores, and they were more frequently diagnosed with alcohol-related cirrhosis, alcohol and tobacco use disorder, diabetes, chronic kidney disease, chronic heart failure, brain trauma, and cerebrovascular disease.
In a multivariable analysis, the presence of any decompensating event was significantly associated with dementia. In subsequent analyses of individual decompensating events, however, the strongest association was with HE, while ascites or variceal bleeding did not add to the risk.
When HE was defined as patients who filled prescriptions for lactulose or rifaximin, the frequency of patients with HE decreased from 13.7% to 10.9%. In an analysis with HE as the decompensating event, the association between HE and dementia remained significant compared to when HE was defined by diagnostic codes alone.
“We were surprised by the high proportion of patients with dementia who also had cirrhosis, and given the genuine difficulty that clinicians have with defining HE vs. dementia, we were not very surprised at that overlap,” Dr. Bajaj said.
“We were also surprised at the specificity of this overlap only with HE and not with other decompensating events, which was also independent of head injury, alcohol use, and PTSD,” he added.
Additional research needed
Future research should look at the characteristics of HE, including the number of episodes or breakthrough episodes, and should focus on objective biomarkers to differentiate dementia and HE, the study authors write.
“The distinction and study of potential overlapping features among HE and dementia is important because HE is often treatable with medications and reverses after liver transplant, while this does not occur with dementia,” they add.
Dr. Bajaj and colleagues call for a greater awareness of disease processes and complications in older patients with cirrhosis, particularly since diagnostic imprecision can lead to patient and family confusion, distrust, and ineffective treatment.
The study will help physicians better understand the important overlap between dementia and HE, said Eric Orman, MD, an associate professor of medicine at Indiana University, Indianapolis.
Dr. Orman, who wasn’t involved with this study, has researched recent trends in the characteristics and outcomes of patients with newly diagnosed cirrhosis and has found that the proportion of older adults has increased, as well as those with alcoholic cirrhosis and NASH, which has implications for future patient care.
“It is important to recognize that both dementia and HE can occur either separately or concurrently in individuals with cirrhosis,” Dr. Orman told this news organization. “When seeing patients with cognitive impairment, having a high index of suspicion for both conditions is critical to ensure appropriate diagnosis and treatment.”
The study’s findings “represent the tip of the iceberg,” Neal Parikh, MD, an assistant professor of neurology and neuroscience at Weill Cornell Medicine in New York, said in an interview. “There is a tremendous amount left to be discovered regarding the role of the liver in brain health.”
Dr. Parikh, who wasn’t associated with this study, has researched the impact of chronic liver conditions on cognitive impairment and dementia. He is working on a project that addresses HE in detail.
“There is growing recognition of a so-called ‘liver-brain axis,’ with several researchers, including my group, showing that a range of chronic liver conditions may detrimentally impact cognitive function and increase the risk of dementia,” he said. “Studying the specific contributions of cirrhosis is critical for understanding the role of hepatic encephalopathy in age-related cognitive decline.”
The study received no financial support. The authors reported no potential competing interests.
A version of this article first appeared on Medscape.com.
, according to a new study involving U.S. veterans.
The overlap between dementia and HE was also independent of alcohol use, brain injury, age, and other metabolic risk factors.
“The aging of patients with cirrhosis leads us to encounter several individuals who may be prone to both of these diseases,” senior author Jasmohan Bajaj, MD, a professor of gastroenterology, hepatology, and nutrition at Virginia Commonwealth University Medical Center and GI section of the Central Virginia Veterans Healthcare System in Richmond, said in an interview.
“Given the epidemic of metabolic syndrome and alcohol, consider excluding cirrhosis in your patient [for] whom the presumptive diagnosis is dementia, since they could have concomitant HE,” he said.
“On the flip side, in those with HE who have predominant long-term memory issues and persistent cognitive changes, consider consulting a neuropsychiatrist or neurologist to ensure there is a resolution of the underlying disease process,” Dr. Bajaj added.
The study was published online in The American Journal of Gastroenterology.
Analyzing associations
HE is a common decompensating event in patients with cirrhosis. Because of the aging population of patients with cirrhosis, however, it’s important to differentiate HE from nonhepatic etiologies of cognitive impairment, such as dementia, the authors note.
Using data from the VA Corporate Data Warehouse, Dr. Bajaj and colleagues identified veterans with cirrhosis who received VA care between October 2019 and September 2021 and compared baseline characteristics between the cohorts based on the presence or absence of dementia. The research team then evaluated factors associated with having a diagnosis of dementia, adjusting for demographics, comorbid illnesses, cirrhosis etiology, and cirrhosis complications.
Investigators identified 71,522 veterans with diagnostic codes for cirrhosis who were engaged in VA care in 2019. They were mostly men (96.2%) and had a median age of 66. The most common etiologies of cirrhosis were alcohol and hepatitis C, followed by nonalcoholic steatohepatitis (NASH). The group also included veterans with predominantly compensated cirrhosis and a median MELD-Na score of 9. The MELD-Na score gauges the severity of chronic liver disease using values such as serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time and sodium to predict survival.
Among those with cirrhosis, 5,647 (7.9%) also had dementia diagnosis codes. This rate is higher than the prevalence of dementia in the general population and equivalent to the rate of dementia in veterans without cirrhosis who are older than 65, the authors note.
In general, veterans with dementia tended to be older, to be White, to live in an urban area, and to have higher MELD-Na scores, and they were more frequently diagnosed with alcohol-related cirrhosis, alcohol and tobacco use disorder, diabetes, chronic kidney disease, chronic heart failure, brain trauma, and cerebrovascular disease.
In a multivariable analysis, the presence of any decompensating event was significantly associated with dementia. In subsequent analyses of individual decompensating events, however, the strongest association was with HE, while ascites or variceal bleeding did not add to the risk.
When HE was defined as patients who filled prescriptions for lactulose or rifaximin, the frequency of patients with HE decreased from 13.7% to 10.9%. In an analysis with HE as the decompensating event, the association between HE and dementia remained significant compared to when HE was defined by diagnostic codes alone.
“We were surprised by the high proportion of patients with dementia who also had cirrhosis, and given the genuine difficulty that clinicians have with defining HE vs. dementia, we were not very surprised at that overlap,” Dr. Bajaj said.
“We were also surprised at the specificity of this overlap only with HE and not with other decompensating events, which was also independent of head injury, alcohol use, and PTSD,” he added.
Additional research needed
Future research should look at the characteristics of HE, including the number of episodes or breakthrough episodes, and should focus on objective biomarkers to differentiate dementia and HE, the study authors write.
“The distinction and study of potential overlapping features among HE and dementia is important because HE is often treatable with medications and reverses after liver transplant, while this does not occur with dementia,” they add.
Dr. Bajaj and colleagues call for a greater awareness of disease processes and complications in older patients with cirrhosis, particularly since diagnostic imprecision can lead to patient and family confusion, distrust, and ineffective treatment.
The study will help physicians better understand the important overlap between dementia and HE, said Eric Orman, MD, an associate professor of medicine at Indiana University, Indianapolis.
Dr. Orman, who wasn’t involved with this study, has researched recent trends in the characteristics and outcomes of patients with newly diagnosed cirrhosis and has found that the proportion of older adults has increased, as well as those with alcoholic cirrhosis and NASH, which has implications for future patient care.
“It is important to recognize that both dementia and HE can occur either separately or concurrently in individuals with cirrhosis,” Dr. Orman told this news organization. “When seeing patients with cognitive impairment, having a high index of suspicion for both conditions is critical to ensure appropriate diagnosis and treatment.”
The study’s findings “represent the tip of the iceberg,” Neal Parikh, MD, an assistant professor of neurology and neuroscience at Weill Cornell Medicine in New York, said in an interview. “There is a tremendous amount left to be discovered regarding the role of the liver in brain health.”
Dr. Parikh, who wasn’t associated with this study, has researched the impact of chronic liver conditions on cognitive impairment and dementia. He is working on a project that addresses HE in detail.
“There is growing recognition of a so-called ‘liver-brain axis,’ with several researchers, including my group, showing that a range of chronic liver conditions may detrimentally impact cognitive function and increase the risk of dementia,” he said. “Studying the specific contributions of cirrhosis is critical for understanding the role of hepatic encephalopathy in age-related cognitive decline.”
The study received no financial support. The authors reported no potential competing interests.
A version of this article first appeared on Medscape.com.
, according to a new study involving U.S. veterans.
The overlap between dementia and HE was also independent of alcohol use, brain injury, age, and other metabolic risk factors.
“The aging of patients with cirrhosis leads us to encounter several individuals who may be prone to both of these diseases,” senior author Jasmohan Bajaj, MD, a professor of gastroenterology, hepatology, and nutrition at Virginia Commonwealth University Medical Center and GI section of the Central Virginia Veterans Healthcare System in Richmond, said in an interview.
“Given the epidemic of metabolic syndrome and alcohol, consider excluding cirrhosis in your patient [for] whom the presumptive diagnosis is dementia, since they could have concomitant HE,” he said.
“On the flip side, in those with HE who have predominant long-term memory issues and persistent cognitive changes, consider consulting a neuropsychiatrist or neurologist to ensure there is a resolution of the underlying disease process,” Dr. Bajaj added.
The study was published online in The American Journal of Gastroenterology.
Analyzing associations
HE is a common decompensating event in patients with cirrhosis. Because of the aging population of patients with cirrhosis, however, it’s important to differentiate HE from nonhepatic etiologies of cognitive impairment, such as dementia, the authors note.
Using data from the VA Corporate Data Warehouse, Dr. Bajaj and colleagues identified veterans with cirrhosis who received VA care between October 2019 and September 2021 and compared baseline characteristics between the cohorts based on the presence or absence of dementia. The research team then evaluated factors associated with having a diagnosis of dementia, adjusting for demographics, comorbid illnesses, cirrhosis etiology, and cirrhosis complications.
Investigators identified 71,522 veterans with diagnostic codes for cirrhosis who were engaged in VA care in 2019. They were mostly men (96.2%) and had a median age of 66. The most common etiologies of cirrhosis were alcohol and hepatitis C, followed by nonalcoholic steatohepatitis (NASH). The group also included veterans with predominantly compensated cirrhosis and a median MELD-Na score of 9. The MELD-Na score gauges the severity of chronic liver disease using values such as serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time and sodium to predict survival.
Among those with cirrhosis, 5,647 (7.9%) also had dementia diagnosis codes. This rate is higher than the prevalence of dementia in the general population and equivalent to the rate of dementia in veterans without cirrhosis who are older than 65, the authors note.
In general, veterans with dementia tended to be older, to be White, to live in an urban area, and to have higher MELD-Na scores, and they were more frequently diagnosed with alcohol-related cirrhosis, alcohol and tobacco use disorder, diabetes, chronic kidney disease, chronic heart failure, brain trauma, and cerebrovascular disease.
In a multivariable analysis, the presence of any decompensating event was significantly associated with dementia. In subsequent analyses of individual decompensating events, however, the strongest association was with HE, while ascites or variceal bleeding did not add to the risk.
When HE was defined as patients who filled prescriptions for lactulose or rifaximin, the frequency of patients with HE decreased from 13.7% to 10.9%. In an analysis with HE as the decompensating event, the association between HE and dementia remained significant compared to when HE was defined by diagnostic codes alone.
“We were surprised by the high proportion of patients with dementia who also had cirrhosis, and given the genuine difficulty that clinicians have with defining HE vs. dementia, we were not very surprised at that overlap,” Dr. Bajaj said.
“We were also surprised at the specificity of this overlap only with HE and not with other decompensating events, which was also independent of head injury, alcohol use, and PTSD,” he added.
Additional research needed
Future research should look at the characteristics of HE, including the number of episodes or breakthrough episodes, and should focus on objective biomarkers to differentiate dementia and HE, the study authors write.
“The distinction and study of potential overlapping features among HE and dementia is important because HE is often treatable with medications and reverses after liver transplant, while this does not occur with dementia,” they add.
Dr. Bajaj and colleagues call for a greater awareness of disease processes and complications in older patients with cirrhosis, particularly since diagnostic imprecision can lead to patient and family confusion, distrust, and ineffective treatment.
The study will help physicians better understand the important overlap between dementia and HE, said Eric Orman, MD, an associate professor of medicine at Indiana University, Indianapolis.
Dr. Orman, who wasn’t involved with this study, has researched recent trends in the characteristics and outcomes of patients with newly diagnosed cirrhosis and has found that the proportion of older adults has increased, as well as those with alcoholic cirrhosis and NASH, which has implications for future patient care.
“It is important to recognize that both dementia and HE can occur either separately or concurrently in individuals with cirrhosis,” Dr. Orman told this news organization. “When seeing patients with cognitive impairment, having a high index of suspicion for both conditions is critical to ensure appropriate diagnosis and treatment.”
The study’s findings “represent the tip of the iceberg,” Neal Parikh, MD, an assistant professor of neurology and neuroscience at Weill Cornell Medicine in New York, said in an interview. “There is a tremendous amount left to be discovered regarding the role of the liver in brain health.”
Dr. Parikh, who wasn’t associated with this study, has researched the impact of chronic liver conditions on cognitive impairment and dementia. He is working on a project that addresses HE in detail.
“There is growing recognition of a so-called ‘liver-brain axis,’ with several researchers, including my group, showing that a range of chronic liver conditions may detrimentally impact cognitive function and increase the risk of dementia,” he said. “Studying the specific contributions of cirrhosis is critical for understanding the role of hepatic encephalopathy in age-related cognitive decline.”
The study received no financial support. The authors reported no potential competing interests.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
We don’t lose our keys (or other things) as much as we think
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
FROM CURRENT BIOLOGY