User login
Maintaining Board Certification Has High Hidden Cost
NEW YORK (Reuters Health) - The American Board of Internal Medicine (ABIM) maintenance-of-certification (MOC) program could cost $5.7 billion in physicians' time and fees over the next decade, according to a new model study.
"We estimate that physicians will spend 33 million hours over 10 years to fulfill MOC requirements," Dr. Dhruv S. Kazi from the University of California, San Francisco, told Reuters Health by email.
"This is approximately equivalent to the total clinical work load of 1785 physicians over 10 years," Dr. Kazi said. "This demand on physician time comes during a period of expanding insurance coverage and anticipated physician workforce shortfalls; it may therefore adversely affect access to care, particularly elective care."
The ABIM's substantial expansion in 2014 of its MOC requirements for the more than 250,000 board-certified internists, hospitalists and internal medicine subspecialists ignited an intense debate about the societal value of the program, resulting in temporary suspension of some of the new requirements.
Dr. Kazi's team sought to quantify the costs of the 2015 version of the MOC program and compare them with the costs that would have been incurred had the 2013 version remained unchanged.
The new MOC requirements would cost board-certified internal medicine physicians an average of $23,607 over 10 years, including $2,349 in fees to the ABIM and $21,259 in time costs, the researchers report in Annals of Internal Medicine, online July 28.
Average costs would range from $16,725 for general internists to $40,495 for hematologists-oncologists.
The overall program would cost $5.7 billion ($561 million in fees to ABIM and $5.1 billion in time costs) over the next 10 years, an increase of $1.2 billion over the previous MOC program.
"The ABIM has previously suggested that participation in MOC will cost $200 to $400 per year," the researchers note. "This is a substantial underestimate precisely because it overlooks time costs."
"While we had anticipated that physician time would be an important driver of costs of the program, we were surprised to see that 9 out of every 10 dollars in MOC costs were related to the program's demands on physician time," Dr. Kazi said. "In fact, every additional hour spent by physicians on MOC increased the costs of the program by approximately 13 million dollars."
"The internal medicine community has embraced the principle of evidence-based medicine in clinical practice; expensive policy interventions such as MOC should be held to the same evidentiary standards," Dr. Kazi concluded.
"Instead of piecemeal evaluations, the entire MOC program should be compared head-to-head with other policy interventions or health systems interventions that improve healthcare quality, thus providing an empirical basis for choosing MOC over alternative strategies for quality improvement," Dr. Kazi said.
"We hope that the high costs of MOC catalyze future studies examining the impact of MOC on the quality and economics of care delivered by board-certified physicians in the United States," Dr. Kazi added.
Dr. Robert B. Baron from the American Board of Internal Medicine told Reuters Health by email, "Their analysis is less about time and cost of doing MOC than it is about the time physicians take staying up-to-date. They estimate that it is about an hour a month, and about 40 hours to prepare for the exam every decade. While the researchers attribute that time to MOC, I suspect most physicians would be spending this time staying abreast of the latest developments in their field, with or without MOC. What MOC offers them is a structured framework to keep up and a marker for the public that they are."
"Our MOC program already recognizes so much of what physicians are doing in practice to stay up to date," said Dr. Baron, also of the University of California, San Francisco. "We can and should do more in that area. We are getting a lot of feedback from physicians about how we can improve MOC, and this feedback will help us shape what we know will be an evolving program."
"In conversations we have already had with the community, one thing physicians have shared loud and clear is that they deeply value staying current in their field," he added. "They believe they should spend time staying abreast of the latest updates in their discipline. We are talking with the community to assure that MOC gives them a structured way to stay current, and we all agree it is an important marker for patients that they have done so."
"The researchers make some claims about overall costs to the health care system," Dr. Baron said. "If you accept their methodology, which is a stretch, other research that appeared in JAMA in December showed greater overall savings - 30 times as much as the costs reported here - just in Medicare costs for physicians who participated in MOC. So maybe all those hours spent keeping up are worth it, not just for the physicians and the patients we take care of but for our entire health care system."
NEW YORK (Reuters Health) - The American Board of Internal Medicine (ABIM) maintenance-of-certification (MOC) program could cost $5.7 billion in physicians' time and fees over the next decade, according to a new model study.
"We estimate that physicians will spend 33 million hours over 10 years to fulfill MOC requirements," Dr. Dhruv S. Kazi from the University of California, San Francisco, told Reuters Health by email.
"This is approximately equivalent to the total clinical work load of 1785 physicians over 10 years," Dr. Kazi said. "This demand on physician time comes during a period of expanding insurance coverage and anticipated physician workforce shortfalls; it may therefore adversely affect access to care, particularly elective care."
The ABIM's substantial expansion in 2014 of its MOC requirements for the more than 250,000 board-certified internists, hospitalists and internal medicine subspecialists ignited an intense debate about the societal value of the program, resulting in temporary suspension of some of the new requirements.
Dr. Kazi's team sought to quantify the costs of the 2015 version of the MOC program and compare them with the costs that would have been incurred had the 2013 version remained unchanged.
The new MOC requirements would cost board-certified internal medicine physicians an average of $23,607 over 10 years, including $2,349 in fees to the ABIM and $21,259 in time costs, the researchers report in Annals of Internal Medicine, online July 28.
Average costs would range from $16,725 for general internists to $40,495 for hematologists-oncologists.
The overall program would cost $5.7 billion ($561 million in fees to ABIM and $5.1 billion in time costs) over the next 10 years, an increase of $1.2 billion over the previous MOC program.
"The ABIM has previously suggested that participation in MOC will cost $200 to $400 per year," the researchers note. "This is a substantial underestimate precisely because it overlooks time costs."
"While we had anticipated that physician time would be an important driver of costs of the program, we were surprised to see that 9 out of every 10 dollars in MOC costs were related to the program's demands on physician time," Dr. Kazi said. "In fact, every additional hour spent by physicians on MOC increased the costs of the program by approximately 13 million dollars."
"The internal medicine community has embraced the principle of evidence-based medicine in clinical practice; expensive policy interventions such as MOC should be held to the same evidentiary standards," Dr. Kazi concluded.
"Instead of piecemeal evaluations, the entire MOC program should be compared head-to-head with other policy interventions or health systems interventions that improve healthcare quality, thus providing an empirical basis for choosing MOC over alternative strategies for quality improvement," Dr. Kazi said.
"We hope that the high costs of MOC catalyze future studies examining the impact of MOC on the quality and economics of care delivered by board-certified physicians in the United States," Dr. Kazi added.
Dr. Robert B. Baron from the American Board of Internal Medicine told Reuters Health by email, "Their analysis is less about time and cost of doing MOC than it is about the time physicians take staying up-to-date. They estimate that it is about an hour a month, and about 40 hours to prepare for the exam every decade. While the researchers attribute that time to MOC, I suspect most physicians would be spending this time staying abreast of the latest developments in their field, with or without MOC. What MOC offers them is a structured framework to keep up and a marker for the public that they are."
"Our MOC program already recognizes so much of what physicians are doing in practice to stay up to date," said Dr. Baron, also of the University of California, San Francisco. "We can and should do more in that area. We are getting a lot of feedback from physicians about how we can improve MOC, and this feedback will help us shape what we know will be an evolving program."
"In conversations we have already had with the community, one thing physicians have shared loud and clear is that they deeply value staying current in their field," he added. "They believe they should spend time staying abreast of the latest updates in their discipline. We are talking with the community to assure that MOC gives them a structured way to stay current, and we all agree it is an important marker for patients that they have done so."
"The researchers make some claims about overall costs to the health care system," Dr. Baron said. "If you accept their methodology, which is a stretch, other research that appeared in JAMA in December showed greater overall savings - 30 times as much as the costs reported here - just in Medicare costs for physicians who participated in MOC. So maybe all those hours spent keeping up are worth it, not just for the physicians and the patients we take care of but for our entire health care system."
NEW YORK (Reuters Health) - The American Board of Internal Medicine (ABIM) maintenance-of-certification (MOC) program could cost $5.7 billion in physicians' time and fees over the next decade, according to a new model study.
"We estimate that physicians will spend 33 million hours over 10 years to fulfill MOC requirements," Dr. Dhruv S. Kazi from the University of California, San Francisco, told Reuters Health by email.
"This is approximately equivalent to the total clinical work load of 1785 physicians over 10 years," Dr. Kazi said. "This demand on physician time comes during a period of expanding insurance coverage and anticipated physician workforce shortfalls; it may therefore adversely affect access to care, particularly elective care."
The ABIM's substantial expansion in 2014 of its MOC requirements for the more than 250,000 board-certified internists, hospitalists and internal medicine subspecialists ignited an intense debate about the societal value of the program, resulting in temporary suspension of some of the new requirements.
Dr. Kazi's team sought to quantify the costs of the 2015 version of the MOC program and compare them with the costs that would have been incurred had the 2013 version remained unchanged.
The new MOC requirements would cost board-certified internal medicine physicians an average of $23,607 over 10 years, including $2,349 in fees to the ABIM and $21,259 in time costs, the researchers report in Annals of Internal Medicine, online July 28.
Average costs would range from $16,725 for general internists to $40,495 for hematologists-oncologists.
The overall program would cost $5.7 billion ($561 million in fees to ABIM and $5.1 billion in time costs) over the next 10 years, an increase of $1.2 billion over the previous MOC program.
"The ABIM has previously suggested that participation in MOC will cost $200 to $400 per year," the researchers note. "This is a substantial underestimate precisely because it overlooks time costs."
"While we had anticipated that physician time would be an important driver of costs of the program, we were surprised to see that 9 out of every 10 dollars in MOC costs were related to the program's demands on physician time," Dr. Kazi said. "In fact, every additional hour spent by physicians on MOC increased the costs of the program by approximately 13 million dollars."
"The internal medicine community has embraced the principle of evidence-based medicine in clinical practice; expensive policy interventions such as MOC should be held to the same evidentiary standards," Dr. Kazi concluded.
"Instead of piecemeal evaluations, the entire MOC program should be compared head-to-head with other policy interventions or health systems interventions that improve healthcare quality, thus providing an empirical basis for choosing MOC over alternative strategies for quality improvement," Dr. Kazi said.
"We hope that the high costs of MOC catalyze future studies examining the impact of MOC on the quality and economics of care delivered by board-certified physicians in the United States," Dr. Kazi added.
Dr. Robert B. Baron from the American Board of Internal Medicine told Reuters Health by email, "Their analysis is less about time and cost of doing MOC than it is about the time physicians take staying up-to-date. They estimate that it is about an hour a month, and about 40 hours to prepare for the exam every decade. While the researchers attribute that time to MOC, I suspect most physicians would be spending this time staying abreast of the latest developments in their field, with or without MOC. What MOC offers them is a structured framework to keep up and a marker for the public that they are."
"Our MOC program already recognizes so much of what physicians are doing in practice to stay up to date," said Dr. Baron, also of the University of California, San Francisco. "We can and should do more in that area. We are getting a lot of feedback from physicians about how we can improve MOC, and this feedback will help us shape what we know will be an evolving program."
"In conversations we have already had with the community, one thing physicians have shared loud and clear is that they deeply value staying current in their field," he added. "They believe they should spend time staying abreast of the latest updates in their discipline. We are talking with the community to assure that MOC gives them a structured way to stay current, and we all agree it is an important marker for patients that they have done so."
"The researchers make some claims about overall costs to the health care system," Dr. Baron said. "If you accept their methodology, which is a stretch, other research that appeared in JAMA in December showed greater overall savings - 30 times as much as the costs reported here - just in Medicare costs for physicians who participated in MOC. So maybe all those hours spent keeping up are worth it, not just for the physicians and the patients we take care of but for our entire health care system."
TeamHealth Announces $1.6 Billion Acquisition of IPC Healthcare
What the Supreme Court ruling in King v. Burwell means for women’s health
In a widely anticipated judgment on the Affordable Care Act (ACA), the US Supreme Court ruled 6-3 in favor of the law on June 26, 2015. The case at hand, King v. Burwell, challenged whether individuals purchasing health insurance through federal exchanges were eligible for federal premium subsidies. This ruling cemented the ACA into law and avoided a potential calamity in the private health insurance market. Let’s take a closer look.
What the case was about
The ACA allows states to set up their own health insurance exchanges or participate in a federally run exchange. Although the drafters of the ACA had expected each state to set up its own exchange, two-thirds of the states declined to do so, many in opposition to the ACA. As a result, 7 million citizens in 34 states now purchase their health insurance through federally created exchanges.
The plaintiffs in King v. Burwell argued that, because the legislation refers to those enrolled “through an Exchange established by the State,” individuals in states with federally run exchanges are not eligible for subsidies.
The law states:
(A) the monthly premiums for such month for 1 or more qualified health plans offered in the individual market within a State which cover the taxpayer, the taxpayer’s spouse, or any dependent (as defined in section 152) of the taxpayer and which were enrolled in through an Exchange established by the State under 1311 of the Patient Protection and Affordable Care Act…[emphasis added].
The Supreme Court was asked to decide whether to adhere to those exact words or to honor Congress’ intent to allow individuals to purchase subsidized insurance on any type of exchange.
What might have happened
We’ve explored in previous articles the interconnectedness of many sections of the ACA. Nowhere is that interconnectedness more clearly demonstrated than here. In order to ensure that private health insurers provide better coverage, the law requires them to abide by important consumer protections, including the elimination of “preexisting condition” exclusions. In order to prevent adverse selection and keep insurers solvent under these new rules, all individuals are required to have health care coverage—the individual mandate. If everyone is required to purchase health insurance, it has to be affordable, so lower-income individuals were promised subsidies, paid for 100% by the federal government, to help them cover their premiums when insurance is purchased through an exchange. Take away the subsidies and the whole thing starts to unravel.
The Urban Institute estimated that a Supreme Court ruling in favor of King, which would have eliminated the subsidies in states using a federal exchange, would have reduced federal tax subsidies by $29 billion in 2016, making coverage unaffordable for many and increasing the ranks of the uninsured by 8.2 million people.1
Louise Sheiner and Brendan Mochoruk of the Brookings Institute speculated that healthy individuals would disproportionately leave the marketplace, triggering 35% increases in insurance premiums for those remaining, as well as significant increases in premiums for those who just lost their subsidies.2 Many observers, including these experts, forecast that insurance companies would exit the federal exchanges altogether, triggering a health insurance “death spiral”: As premiums rise, the healthiest customers leave the marketplace, causing premiums to rise more, causing more healthy people to leave, and so on.
Clearly, this Supreme Court decision has had dramatic, long-term, real-world effects on millions of Americans. On the national level, 6,387,789 individuals were at risk of losing their tax credits if the Supreme Court had ruled in favor of King. That number represents more than $1.7 billion in total monthly tax credits. For a look at how a judgment in favor of King would have affected subsidies on a state-by-state basis, see TABLE 1.
What other commentators are saying about the King v. Burwell decision
In his majority opinion, Chief Justice John Roberts noted that the “meaning of the phrase ‘established by the State’ is not so clear.” And as Amy Howe articulated on SCOTUSblog: “if the phrase…is in fact not clear…then the next step is to look at the Affordable Care Act more broadly to determine what Congress meant by the phrase. And when you do that, the Court reasoned, it becomes apparent that Congress actually intended for the subsidies to be available to everyone who buys health insurance on an exchange, no matter who created it. If the subsidies weren’t available in the states with federal exchanges, the Court explained, the insurance markets in those states simply wouldn’t work properly: without the subsidies, almost all of the people who purchased insurance on the exchanges would no longer be required to purchase insurance because it would be too expensive. This would create a ‘death spiral’….”
—Amy Howe, SCOTUSblog3
“Additional court challenges to other ACA provisions are still possible, but King’s six-member majority shows little appetite for challenges threatening the Act’s core structure. Even Scalia’s dissent recognizes that the ACA may one day ‘attain the enduring status of the Social Security Act.’ Thus, the decision may usher in a new era of policy maturity, in which efforts to undermine the ACA diminish, as focus shifts to efforts to implement and improve it.”
—Mark A. Hall, JD, New England Journal of Medicine4
“With the Court upholding the administration’s interpretation of the law, the Obama administration has little reason to accede to
Republican proposals. The Court’s decision effectively puts the future of the ACA on hold until the 2016 elections, when the people will decide whether to stay the course or to chart a very different path.”
—Timothy Jost, Health Affairs5
“A case that 6 months ago seemed to offer the Court’s conservatives a low-risk opportunity to accomplish what they almost did in 2012—kill the Affordable Care Act—became suffused with danger, for the millions of newly insured Americans, of course, but also for the Supreme Court itself. Ideology came face to face with reality, and reality prevailed.”
—Linda Greenhouse, New York Times6
How premium subsidies work
Premium subsidies are actually tax credits. Individuals and families can qualify for them to purchase any type of health insurance offered on an exchange, except catastrophic coverage. To receive the premium tax credit for coverage starting in 2015, a marketplace enrollee must:
- have a household income that is 1 to4 times the federal poverty level. In 2015, the range of incomes that qualify for subsidies is $11,670 for an individual and $23,850 for a family of 4 at 100% of the federal poverty level. At 400% of the federal poverty level, it is $46,680 for an individual and $95,400 for a family of 4.
- lack access to affordable coverage through an employer (including a family member’s employer)
- be ineligible for coverage through Medicare, Medicaid, the Children’s Health Insurance Program, or other forms of public assistance
- have US citizenship or proof of legal residency
- file taxes jointly if married.
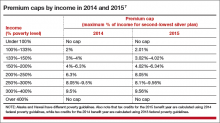
The premium tax credit caps the amount that an individual or family must spend on their monthly payments for health insurance. The cap depends on the family’s income; lower-income families have a lower cap. The amount of the tax credit remains the same, so a person who purchases a more expensive plan pays the cost difference (TABLE 2).
The ruling’s effect on women’s health
On June 26, American College of Obstetricians and Gynecologists President Mark S. DeFrancesco, MD, MBA, hailed the Supreme Court decision, saying, “Importantly, recent data have shown that newly insured adults under the ACA were more likely to be women. Those who did gain coverage through the ACA reported better access to health care and better financial security from medical costs.”
“Without question, many women enrollees were able to purchase health insurance coverage due, in part, to the ACA subsidies that helped make this purchase affordable. In fact, government data have suggested that roughly 85% of health exchange enrollees received subsidies,” Dr. DeFrancesco said.
“If the Supreme Court had overturned this important assistance, approximately 4.8 million women would have been unable to afford the coverage that they need. The impact also would have been widespread; as these women were forced to leave the insurance marketplace, it is likely that premiums throughout the marketplace would have risen dramatically,” he continued.
“Instead, patients—especially the low- and moderate-income American women who have particularly benefited from ACA subsidies—will continue to have the peace of mind that comes with insurance coverage.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Blumberg LJ, Buettgens M, Holahan J. The implications of a Supreme Court finding for the plaintiff in King v. Burwell: 8.2 million more uninsured and 35% higher premiums. Urban Institute. http://www.urban.org/research/publication/implications-supreme-court-finding-plaintiff-king-vs-burwell-82-million-more-uninsured-and-35-higher-premiums. Published January 8, 2015. Accessed July 2, 2015.
2. Sheiner L, Mochoruk B. King v. Burwell explained. Brookings Institute. http://www.brookings.edu/blogs/health360/posts/2015/03/03-king-v-burwell-explainer-sheiner. Published March 3, 2015. Accessed July 2, 2015.
3. Howe A. Court backs Obama administration on health care subsidies: In plain English. SCOTUSblog. http://www.scotusblog.com/2015/06/court-backs-obama-administration-on-health-care-subsidies-in-plain-english/. Published June 25, 2015. Accessed July 1, 2015.
4. Hall MA. King v. Burwell—ACA Armageddon averted. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMp1504077. Published July 1, 2015. Accessed July 2, 2015.
5. Jost T. Implementing health reform: The Supreme Court upholds tax credits in the federal exchange. Health Affairs blog. http://healthaffairs.org/blog/2015/06/25/implementing-health-reform-the-supreme-court-upholds-tax-credits-in-the-federal-exchange/. Published June 25, 2015. Accessed July 1, 2015.
6. Greenhouse L. The Roberts Court’s reality check. New York Times. http://www.nytimes.com/2015/06/26/opinion/the-roberts-courts-reality-check.html. Published June 25, 2015. Accessed July 1, 2015.
7. Henry J. Kaiser Family Foundation. Explaining health care reform: questions about health insurance subsidies. Table 2. http://kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/. Published October 27, 2014. Accessed July 2, 2015.
In a widely anticipated judgment on the Affordable Care Act (ACA), the US Supreme Court ruled 6-3 in favor of the law on June 26, 2015. The case at hand, King v. Burwell, challenged whether individuals purchasing health insurance through federal exchanges were eligible for federal premium subsidies. This ruling cemented the ACA into law and avoided a potential calamity in the private health insurance market. Let’s take a closer look.
What the case was about
The ACA allows states to set up their own health insurance exchanges or participate in a federally run exchange. Although the drafters of the ACA had expected each state to set up its own exchange, two-thirds of the states declined to do so, many in opposition to the ACA. As a result, 7 million citizens in 34 states now purchase their health insurance through federally created exchanges.
The plaintiffs in King v. Burwell argued that, because the legislation refers to those enrolled “through an Exchange established by the State,” individuals in states with federally run exchanges are not eligible for subsidies.
The law states:
(A) the monthly premiums for such month for 1 or more qualified health plans offered in the individual market within a State which cover the taxpayer, the taxpayer’s spouse, or any dependent (as defined in section 152) of the taxpayer and which were enrolled in through an Exchange established by the State under 1311 of the Patient Protection and Affordable Care Act…[emphasis added].
The Supreme Court was asked to decide whether to adhere to those exact words or to honor Congress’ intent to allow individuals to purchase subsidized insurance on any type of exchange.
What might have happened
We’ve explored in previous articles the interconnectedness of many sections of the ACA. Nowhere is that interconnectedness more clearly demonstrated than here. In order to ensure that private health insurers provide better coverage, the law requires them to abide by important consumer protections, including the elimination of “preexisting condition” exclusions. In order to prevent adverse selection and keep insurers solvent under these new rules, all individuals are required to have health care coverage—the individual mandate. If everyone is required to purchase health insurance, it has to be affordable, so lower-income individuals were promised subsidies, paid for 100% by the federal government, to help them cover their premiums when insurance is purchased through an exchange. Take away the subsidies and the whole thing starts to unravel.
The Urban Institute estimated that a Supreme Court ruling in favor of King, which would have eliminated the subsidies in states using a federal exchange, would have reduced federal tax subsidies by $29 billion in 2016, making coverage unaffordable for many and increasing the ranks of the uninsured by 8.2 million people.1
Louise Sheiner and Brendan Mochoruk of the Brookings Institute speculated that healthy individuals would disproportionately leave the marketplace, triggering 35% increases in insurance premiums for those remaining, as well as significant increases in premiums for those who just lost their subsidies.2 Many observers, including these experts, forecast that insurance companies would exit the federal exchanges altogether, triggering a health insurance “death spiral”: As premiums rise, the healthiest customers leave the marketplace, causing premiums to rise more, causing more healthy people to leave, and so on.
Clearly, this Supreme Court decision has had dramatic, long-term, real-world effects on millions of Americans. On the national level, 6,387,789 individuals were at risk of losing their tax credits if the Supreme Court had ruled in favor of King. That number represents more than $1.7 billion in total monthly tax credits. For a look at how a judgment in favor of King would have affected subsidies on a state-by-state basis, see TABLE 1.
What other commentators are saying about the King v. Burwell decision
In his majority opinion, Chief Justice John Roberts noted that the “meaning of the phrase ‘established by the State’ is not so clear.” And as Amy Howe articulated on SCOTUSblog: “if the phrase…is in fact not clear…then the next step is to look at the Affordable Care Act more broadly to determine what Congress meant by the phrase. And when you do that, the Court reasoned, it becomes apparent that Congress actually intended for the subsidies to be available to everyone who buys health insurance on an exchange, no matter who created it. If the subsidies weren’t available in the states with federal exchanges, the Court explained, the insurance markets in those states simply wouldn’t work properly: without the subsidies, almost all of the people who purchased insurance on the exchanges would no longer be required to purchase insurance because it would be too expensive. This would create a ‘death spiral’….”
—Amy Howe, SCOTUSblog3
“Additional court challenges to other ACA provisions are still possible, but King’s six-member majority shows little appetite for challenges threatening the Act’s core structure. Even Scalia’s dissent recognizes that the ACA may one day ‘attain the enduring status of the Social Security Act.’ Thus, the decision may usher in a new era of policy maturity, in which efforts to undermine the ACA diminish, as focus shifts to efforts to implement and improve it.”
—Mark A. Hall, JD, New England Journal of Medicine4
“With the Court upholding the administration’s interpretation of the law, the Obama administration has little reason to accede to
Republican proposals. The Court’s decision effectively puts the future of the ACA on hold until the 2016 elections, when the people will decide whether to stay the course or to chart a very different path.”
—Timothy Jost, Health Affairs5
“A case that 6 months ago seemed to offer the Court’s conservatives a low-risk opportunity to accomplish what they almost did in 2012—kill the Affordable Care Act—became suffused with danger, for the millions of newly insured Americans, of course, but also for the Supreme Court itself. Ideology came face to face with reality, and reality prevailed.”
—Linda Greenhouse, New York Times6
How premium subsidies work
Premium subsidies are actually tax credits. Individuals and families can qualify for them to purchase any type of health insurance offered on an exchange, except catastrophic coverage. To receive the premium tax credit for coverage starting in 2015, a marketplace enrollee must:
- have a household income that is 1 to4 times the federal poverty level. In 2015, the range of incomes that qualify for subsidies is $11,670 for an individual and $23,850 for a family of 4 at 100% of the federal poverty level. At 400% of the federal poverty level, it is $46,680 for an individual and $95,400 for a family of 4.
- lack access to affordable coverage through an employer (including a family member’s employer)
- be ineligible for coverage through Medicare, Medicaid, the Children’s Health Insurance Program, or other forms of public assistance
- have US citizenship or proof of legal residency
- file taxes jointly if married.
The premium tax credit caps the amount that an individual or family must spend on their monthly payments for health insurance. The cap depends on the family’s income; lower-income families have a lower cap. The amount of the tax credit remains the same, so a person who purchases a more expensive plan pays the cost difference (TABLE 2).
The ruling’s effect on women’s health
On June 26, American College of Obstetricians and Gynecologists President Mark S. DeFrancesco, MD, MBA, hailed the Supreme Court decision, saying, “Importantly, recent data have shown that newly insured adults under the ACA were more likely to be women. Those who did gain coverage through the ACA reported better access to health care and better financial security from medical costs.”
“Without question, many women enrollees were able to purchase health insurance coverage due, in part, to the ACA subsidies that helped make this purchase affordable. In fact, government data have suggested that roughly 85% of health exchange enrollees received subsidies,” Dr. DeFrancesco said.
“If the Supreme Court had overturned this important assistance, approximately 4.8 million women would have been unable to afford the coverage that they need. The impact also would have been widespread; as these women were forced to leave the insurance marketplace, it is likely that premiums throughout the marketplace would have risen dramatically,” he continued.
“Instead, patients—especially the low- and moderate-income American women who have particularly benefited from ACA subsidies—will continue to have the peace of mind that comes with insurance coverage.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In a widely anticipated judgment on the Affordable Care Act (ACA), the US Supreme Court ruled 6-3 in favor of the law on June 26, 2015. The case at hand, King v. Burwell, challenged whether individuals purchasing health insurance through federal exchanges were eligible for federal premium subsidies. This ruling cemented the ACA into law and avoided a potential calamity in the private health insurance market. Let’s take a closer look.
What the case was about
The ACA allows states to set up their own health insurance exchanges or participate in a federally run exchange. Although the drafters of the ACA had expected each state to set up its own exchange, two-thirds of the states declined to do so, many in opposition to the ACA. As a result, 7 million citizens in 34 states now purchase their health insurance through federally created exchanges.
The plaintiffs in King v. Burwell argued that, because the legislation refers to those enrolled “through an Exchange established by the State,” individuals in states with federally run exchanges are not eligible for subsidies.
The law states:
(A) the monthly premiums for such month for 1 or more qualified health plans offered in the individual market within a State which cover the taxpayer, the taxpayer’s spouse, or any dependent (as defined in section 152) of the taxpayer and which were enrolled in through an Exchange established by the State under 1311 of the Patient Protection and Affordable Care Act…[emphasis added].
The Supreme Court was asked to decide whether to adhere to those exact words or to honor Congress’ intent to allow individuals to purchase subsidized insurance on any type of exchange.
What might have happened
We’ve explored in previous articles the interconnectedness of many sections of the ACA. Nowhere is that interconnectedness more clearly demonstrated than here. In order to ensure that private health insurers provide better coverage, the law requires them to abide by important consumer protections, including the elimination of “preexisting condition” exclusions. In order to prevent adverse selection and keep insurers solvent under these new rules, all individuals are required to have health care coverage—the individual mandate. If everyone is required to purchase health insurance, it has to be affordable, so lower-income individuals were promised subsidies, paid for 100% by the federal government, to help them cover their premiums when insurance is purchased through an exchange. Take away the subsidies and the whole thing starts to unravel.
The Urban Institute estimated that a Supreme Court ruling in favor of King, which would have eliminated the subsidies in states using a federal exchange, would have reduced federal tax subsidies by $29 billion in 2016, making coverage unaffordable for many and increasing the ranks of the uninsured by 8.2 million people.1
Louise Sheiner and Brendan Mochoruk of the Brookings Institute speculated that healthy individuals would disproportionately leave the marketplace, triggering 35% increases in insurance premiums for those remaining, as well as significant increases in premiums for those who just lost their subsidies.2 Many observers, including these experts, forecast that insurance companies would exit the federal exchanges altogether, triggering a health insurance “death spiral”: As premiums rise, the healthiest customers leave the marketplace, causing premiums to rise more, causing more healthy people to leave, and so on.
Clearly, this Supreme Court decision has had dramatic, long-term, real-world effects on millions of Americans. On the national level, 6,387,789 individuals were at risk of losing their tax credits if the Supreme Court had ruled in favor of King. That number represents more than $1.7 billion in total monthly tax credits. For a look at how a judgment in favor of King would have affected subsidies on a state-by-state basis, see TABLE 1.
What other commentators are saying about the King v. Burwell decision
In his majority opinion, Chief Justice John Roberts noted that the “meaning of the phrase ‘established by the State’ is not so clear.” And as Amy Howe articulated on SCOTUSblog: “if the phrase…is in fact not clear…then the next step is to look at the Affordable Care Act more broadly to determine what Congress meant by the phrase. And when you do that, the Court reasoned, it becomes apparent that Congress actually intended for the subsidies to be available to everyone who buys health insurance on an exchange, no matter who created it. If the subsidies weren’t available in the states with federal exchanges, the Court explained, the insurance markets in those states simply wouldn’t work properly: without the subsidies, almost all of the people who purchased insurance on the exchanges would no longer be required to purchase insurance because it would be too expensive. This would create a ‘death spiral’….”
—Amy Howe, SCOTUSblog3
“Additional court challenges to other ACA provisions are still possible, but King’s six-member majority shows little appetite for challenges threatening the Act’s core structure. Even Scalia’s dissent recognizes that the ACA may one day ‘attain the enduring status of the Social Security Act.’ Thus, the decision may usher in a new era of policy maturity, in which efforts to undermine the ACA diminish, as focus shifts to efforts to implement and improve it.”
—Mark A. Hall, JD, New England Journal of Medicine4
“With the Court upholding the administration’s interpretation of the law, the Obama administration has little reason to accede to
Republican proposals. The Court’s decision effectively puts the future of the ACA on hold until the 2016 elections, when the people will decide whether to stay the course or to chart a very different path.”
—Timothy Jost, Health Affairs5
“A case that 6 months ago seemed to offer the Court’s conservatives a low-risk opportunity to accomplish what they almost did in 2012—kill the Affordable Care Act—became suffused with danger, for the millions of newly insured Americans, of course, but also for the Supreme Court itself. Ideology came face to face with reality, and reality prevailed.”
—Linda Greenhouse, New York Times6
How premium subsidies work
Premium subsidies are actually tax credits. Individuals and families can qualify for them to purchase any type of health insurance offered on an exchange, except catastrophic coverage. To receive the premium tax credit for coverage starting in 2015, a marketplace enrollee must:
- have a household income that is 1 to4 times the federal poverty level. In 2015, the range of incomes that qualify for subsidies is $11,670 for an individual and $23,850 for a family of 4 at 100% of the federal poverty level. At 400% of the federal poverty level, it is $46,680 for an individual and $95,400 for a family of 4.
- lack access to affordable coverage through an employer (including a family member’s employer)
- be ineligible for coverage through Medicare, Medicaid, the Children’s Health Insurance Program, or other forms of public assistance
- have US citizenship or proof of legal residency
- file taxes jointly if married.
The premium tax credit caps the amount that an individual or family must spend on their monthly payments for health insurance. The cap depends on the family’s income; lower-income families have a lower cap. The amount of the tax credit remains the same, so a person who purchases a more expensive plan pays the cost difference (TABLE 2).
The ruling’s effect on women’s health
On June 26, American College of Obstetricians and Gynecologists President Mark S. DeFrancesco, MD, MBA, hailed the Supreme Court decision, saying, “Importantly, recent data have shown that newly insured adults under the ACA were more likely to be women. Those who did gain coverage through the ACA reported better access to health care and better financial security from medical costs.”
“Without question, many women enrollees were able to purchase health insurance coverage due, in part, to the ACA subsidies that helped make this purchase affordable. In fact, government data have suggested that roughly 85% of health exchange enrollees received subsidies,” Dr. DeFrancesco said.
“If the Supreme Court had overturned this important assistance, approximately 4.8 million women would have been unable to afford the coverage that they need. The impact also would have been widespread; as these women were forced to leave the insurance marketplace, it is likely that premiums throughout the marketplace would have risen dramatically,” he continued.
“Instead, patients—especially the low- and moderate-income American women who have particularly benefited from ACA subsidies—will continue to have the peace of mind that comes with insurance coverage.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Blumberg LJ, Buettgens M, Holahan J. The implications of a Supreme Court finding for the plaintiff in King v. Burwell: 8.2 million more uninsured and 35% higher premiums. Urban Institute. http://www.urban.org/research/publication/implications-supreme-court-finding-plaintiff-king-vs-burwell-82-million-more-uninsured-and-35-higher-premiums. Published January 8, 2015. Accessed July 2, 2015.
2. Sheiner L, Mochoruk B. King v. Burwell explained. Brookings Institute. http://www.brookings.edu/blogs/health360/posts/2015/03/03-king-v-burwell-explainer-sheiner. Published March 3, 2015. Accessed July 2, 2015.
3. Howe A. Court backs Obama administration on health care subsidies: In plain English. SCOTUSblog. http://www.scotusblog.com/2015/06/court-backs-obama-administration-on-health-care-subsidies-in-plain-english/. Published June 25, 2015. Accessed July 1, 2015.
4. Hall MA. King v. Burwell—ACA Armageddon averted. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMp1504077. Published July 1, 2015. Accessed July 2, 2015.
5. Jost T. Implementing health reform: The Supreme Court upholds tax credits in the federal exchange. Health Affairs blog. http://healthaffairs.org/blog/2015/06/25/implementing-health-reform-the-supreme-court-upholds-tax-credits-in-the-federal-exchange/. Published June 25, 2015. Accessed July 1, 2015.
6. Greenhouse L. The Roberts Court’s reality check. New York Times. http://www.nytimes.com/2015/06/26/opinion/the-roberts-courts-reality-check.html. Published June 25, 2015. Accessed July 1, 2015.
7. Henry J. Kaiser Family Foundation. Explaining health care reform: questions about health insurance subsidies. Table 2. http://kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/. Published October 27, 2014. Accessed July 2, 2015.
1. Blumberg LJ, Buettgens M, Holahan J. The implications of a Supreme Court finding for the plaintiff in King v. Burwell: 8.2 million more uninsured and 35% higher premiums. Urban Institute. http://www.urban.org/research/publication/implications-supreme-court-finding-plaintiff-king-vs-burwell-82-million-more-uninsured-and-35-higher-premiums. Published January 8, 2015. Accessed July 2, 2015.
2. Sheiner L, Mochoruk B. King v. Burwell explained. Brookings Institute. http://www.brookings.edu/blogs/health360/posts/2015/03/03-king-v-burwell-explainer-sheiner. Published March 3, 2015. Accessed July 2, 2015.
3. Howe A. Court backs Obama administration on health care subsidies: In plain English. SCOTUSblog. http://www.scotusblog.com/2015/06/court-backs-obama-administration-on-health-care-subsidies-in-plain-english/. Published June 25, 2015. Accessed July 1, 2015.
4. Hall MA. King v. Burwell—ACA Armageddon averted. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMp1504077. Published July 1, 2015. Accessed July 2, 2015.
5. Jost T. Implementing health reform: The Supreme Court upholds tax credits in the federal exchange. Health Affairs blog. http://healthaffairs.org/blog/2015/06/25/implementing-health-reform-the-supreme-court-upholds-tax-credits-in-the-federal-exchange/. Published June 25, 2015. Accessed July 1, 2015.
6. Greenhouse L. The Roberts Court’s reality check. New York Times. http://www.nytimes.com/2015/06/26/opinion/the-roberts-courts-reality-check.html. Published June 25, 2015. Accessed July 1, 2015.
7. Henry J. Kaiser Family Foundation. Explaining health care reform: questions about health insurance subsidies. Table 2. http://kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/. Published October 27, 2014. Accessed July 2, 2015.
Tips for Hospitalists on Spending More of Their Time at the Top of Their License
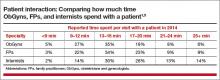
Hospitalists spend too little time working at the top of their license. Put differently, I think a hospitalist often spends only about 1.5 to two hours in a 10- or 12-hour workday making use of the knowledge base and skills developed in training. (I wrote about this and referenced some hospitalist time-motion studies in my December 2010 column.)
The remaining hours are typically spent in activities such as figuring out which surgeon is on call and tracking her down, managing patient lists, filling out paper or electronic forms, explaining observation status to patients, and so on.
When I first became a hospitalist in the 1980s, there was already a lot of talk about the paperwork burden faced by doctors across all specialties. I recall the gnashing of teeth that ensued—lots of articles and seminars, and it seems to me even a few legislative proposals, focused on the topic. It appears that nearly every recruitment ad at the time mentioned something like “Let us take care of running the business, so you can focus solely on patient care.” Clearly, doctors were seeking relief from the burden of nonclinical work even back then.
I can’t recall reading or hearing anyone talk about the “paperwork” burden of physician practice in the past few years. This isn’t because things have gotten better; in fact, I think the burden of “non-doctoring activities” has steadily increased. We hear less about the problem of excessive paperwork simply because, more recently, it has been framed differently—it is now typically referred to as the problem of too little time spent practicing at the top of license.
Search the Internet for “top of license” and a number of interesting things turn up. Most are healthcare related—maybe other professions don’t use the term—and there are just as many links referring to nurses as physicians. Much is written about the need for primary care physicians to spend more time working at the top of their license, but I couldn’t find anything addressing this issue specifically for hospitalists.
What Can Be Done?
Moving your work as a hospitalist more to the top of your license isn’t a simple thing, and our whole field will need to work on this over time. The most effective interventions will vary some from place to place, but here are some ideas that may be relevant for many hospitalist groups.
Medication reconciliation. I fully support the idea of careful medication reconciliation, but, given that such a large portion of hospitalist patients are on so many medications, this is a time-consuming task. And, in many or most hospitals, the task suffers from diffusion of responsibility; for example, the ED nurse makes only a half-hearted attempt to get an accurate list, and the hospitalist believes that whatever the ED nurse entered into the record regarding patient medications is probably the best obtainable list.
A pharmacy technician stationed in the ED and charged with recording the best obtainable list of medicines on patient arrival can address both of these problems (for more information, the American Society of Health-System Pharmacists offers webinars and other resources on this topic). This would include calling family members, pharmacies, and physician offices for clarification in some cases. Hospitalists working in such an environment nearly always say it is extremely valuable in reducing inaccuracies in the pre-hospital medication list, as well as saving hospitalists time when they are admitting patients.
Unfortunately, hospitals may resist adding pharmacy technicians because of the expense or, in some cases, because of concerns that such work may exceed the legal scope of work for technicians.
Post-hospital appointments. I think arranging post-hospital appointments should be no more difficult for the hospitalist than ordering a complete blood count (CBC). It shouldn’t matter whether I want the patient to follow up with the PCP he has been seeing for years, or see a neurologist or diabetes educator as a new patient consult. Any treating doctor in the hospital should be able to arrange such post-hospital visits with just a click or two in the EHR, or a stroke of the pen. And the patient should leave the hospital with a written date and time of the appointment that has been made for them.
Few hospitals can reliably provide this, however, so, all too often, hospitalists spend their time calling clerical staff at outpatient clinics to arrange appointments, writing them down, and delivering them to patients. This is far from what anyone would consider top of license work. (I wrote a little more about this in last month’s column.)
Medicare benefits specialist. Many hospitalists end up spending significant time explaining to patients and families the reason a patient is on observation status and trying to defuse the resulting frustration and anger. As I stated in my November 2014 column, I think observation status is so frustrating to patients that it is often the root cause of complaints about care and, potentially, the source of malpractice suits.
Physicians have an unavoidable role in determining observation versus inpatient status, but I think hospitals should work hard to ensure that someone other than the doctor is available to explain to patients and families the reason for observation status, along with its implications, and to provide sympathy for their frustrations. This allows the doctor to stay focused on clinical care.
Limit reliance on a “triage hospitalist.” Hospitalist groups larger than about 20 providers often have one provider devoted through much of a daytime shift to triaging and assigning new referrals across all providers working that day. For larger practices, this triage work may consume all of the provider’s shift, so that person has no time left for clinical care. It is hard for me to see this as top of license work that only a physician or advanced practice clinician can do. In my December 2010 column, I provided some potential alternatives to dedicating a physician or other provider to a triage role.
Your list of important changes that are needed to move hospitalists toward more time spent working at the top of their license will likely differ a lot from the issues above. But every group could benefit from deliberately thinking about what would be most valuable for them and trying to make that a reality.

Hospitalists spend too little time working at the top of their license. Put differently, I think a hospitalist often spends only about 1.5 to two hours in a 10- or 12-hour workday making use of the knowledge base and skills developed in training. (I wrote about this and referenced some hospitalist time-motion studies in my December 2010 column.)
The remaining hours are typically spent in activities such as figuring out which surgeon is on call and tracking her down, managing patient lists, filling out paper or electronic forms, explaining observation status to patients, and so on.
When I first became a hospitalist in the 1980s, there was already a lot of talk about the paperwork burden faced by doctors across all specialties. I recall the gnashing of teeth that ensued—lots of articles and seminars, and it seems to me even a few legislative proposals, focused on the topic. It appears that nearly every recruitment ad at the time mentioned something like “Let us take care of running the business, so you can focus solely on patient care.” Clearly, doctors were seeking relief from the burden of nonclinical work even back then.
I can’t recall reading or hearing anyone talk about the “paperwork” burden of physician practice in the past few years. This isn’t because things have gotten better; in fact, I think the burden of “non-doctoring activities” has steadily increased. We hear less about the problem of excessive paperwork simply because, more recently, it has been framed differently—it is now typically referred to as the problem of too little time spent practicing at the top of license.
Search the Internet for “top of license” and a number of interesting things turn up. Most are healthcare related—maybe other professions don’t use the term—and there are just as many links referring to nurses as physicians. Much is written about the need for primary care physicians to spend more time working at the top of their license, but I couldn’t find anything addressing this issue specifically for hospitalists.
What Can Be Done?
Moving your work as a hospitalist more to the top of your license isn’t a simple thing, and our whole field will need to work on this over time. The most effective interventions will vary some from place to place, but here are some ideas that may be relevant for many hospitalist groups.
Medication reconciliation. I fully support the idea of careful medication reconciliation, but, given that such a large portion of hospitalist patients are on so many medications, this is a time-consuming task. And, in many or most hospitals, the task suffers from diffusion of responsibility; for example, the ED nurse makes only a half-hearted attempt to get an accurate list, and the hospitalist believes that whatever the ED nurse entered into the record regarding patient medications is probably the best obtainable list.
A pharmacy technician stationed in the ED and charged with recording the best obtainable list of medicines on patient arrival can address both of these problems (for more information, the American Society of Health-System Pharmacists offers webinars and other resources on this topic). This would include calling family members, pharmacies, and physician offices for clarification in some cases. Hospitalists working in such an environment nearly always say it is extremely valuable in reducing inaccuracies in the pre-hospital medication list, as well as saving hospitalists time when they are admitting patients.
Unfortunately, hospitals may resist adding pharmacy technicians because of the expense or, in some cases, because of concerns that such work may exceed the legal scope of work for technicians.
Post-hospital appointments. I think arranging post-hospital appointments should be no more difficult for the hospitalist than ordering a complete blood count (CBC). It shouldn’t matter whether I want the patient to follow up with the PCP he has been seeing for years, or see a neurologist or diabetes educator as a new patient consult. Any treating doctor in the hospital should be able to arrange such post-hospital visits with just a click or two in the EHR, or a stroke of the pen. And the patient should leave the hospital with a written date and time of the appointment that has been made for them.
Few hospitals can reliably provide this, however, so, all too often, hospitalists spend their time calling clerical staff at outpatient clinics to arrange appointments, writing them down, and delivering them to patients. This is far from what anyone would consider top of license work. (I wrote a little more about this in last month’s column.)
Medicare benefits specialist. Many hospitalists end up spending significant time explaining to patients and families the reason a patient is on observation status and trying to defuse the resulting frustration and anger. As I stated in my November 2014 column, I think observation status is so frustrating to patients that it is often the root cause of complaints about care and, potentially, the source of malpractice suits.
Physicians have an unavoidable role in determining observation versus inpatient status, but I think hospitals should work hard to ensure that someone other than the doctor is available to explain to patients and families the reason for observation status, along with its implications, and to provide sympathy for their frustrations. This allows the doctor to stay focused on clinical care.
Limit reliance on a “triage hospitalist.” Hospitalist groups larger than about 20 providers often have one provider devoted through much of a daytime shift to triaging and assigning new referrals across all providers working that day. For larger practices, this triage work may consume all of the provider’s shift, so that person has no time left for clinical care. It is hard for me to see this as top of license work that only a physician or advanced practice clinician can do. In my December 2010 column, I provided some potential alternatives to dedicating a physician or other provider to a triage role.
Your list of important changes that are needed to move hospitalists toward more time spent working at the top of their license will likely differ a lot from the issues above. But every group could benefit from deliberately thinking about what would be most valuable for them and trying to make that a reality.

Hospitalists spend too little time working at the top of their license. Put differently, I think a hospitalist often spends only about 1.5 to two hours in a 10- or 12-hour workday making use of the knowledge base and skills developed in training. (I wrote about this and referenced some hospitalist time-motion studies in my December 2010 column.)
The remaining hours are typically spent in activities such as figuring out which surgeon is on call and tracking her down, managing patient lists, filling out paper or electronic forms, explaining observation status to patients, and so on.
When I first became a hospitalist in the 1980s, there was already a lot of talk about the paperwork burden faced by doctors across all specialties. I recall the gnashing of teeth that ensued—lots of articles and seminars, and it seems to me even a few legislative proposals, focused on the topic. It appears that nearly every recruitment ad at the time mentioned something like “Let us take care of running the business, so you can focus solely on patient care.” Clearly, doctors were seeking relief from the burden of nonclinical work even back then.
I can’t recall reading or hearing anyone talk about the “paperwork” burden of physician practice in the past few years. This isn’t because things have gotten better; in fact, I think the burden of “non-doctoring activities” has steadily increased. We hear less about the problem of excessive paperwork simply because, more recently, it has been framed differently—it is now typically referred to as the problem of too little time spent practicing at the top of license.
Search the Internet for “top of license” and a number of interesting things turn up. Most are healthcare related—maybe other professions don’t use the term—and there are just as many links referring to nurses as physicians. Much is written about the need for primary care physicians to spend more time working at the top of their license, but I couldn’t find anything addressing this issue specifically for hospitalists.
What Can Be Done?
Moving your work as a hospitalist more to the top of your license isn’t a simple thing, and our whole field will need to work on this over time. The most effective interventions will vary some from place to place, but here are some ideas that may be relevant for many hospitalist groups.
Medication reconciliation. I fully support the idea of careful medication reconciliation, but, given that such a large portion of hospitalist patients are on so many medications, this is a time-consuming task. And, in many or most hospitals, the task suffers from diffusion of responsibility; for example, the ED nurse makes only a half-hearted attempt to get an accurate list, and the hospitalist believes that whatever the ED nurse entered into the record regarding patient medications is probably the best obtainable list.
A pharmacy technician stationed in the ED and charged with recording the best obtainable list of medicines on patient arrival can address both of these problems (for more information, the American Society of Health-System Pharmacists offers webinars and other resources on this topic). This would include calling family members, pharmacies, and physician offices for clarification in some cases. Hospitalists working in such an environment nearly always say it is extremely valuable in reducing inaccuracies in the pre-hospital medication list, as well as saving hospitalists time when they are admitting patients.
Unfortunately, hospitals may resist adding pharmacy technicians because of the expense or, in some cases, because of concerns that such work may exceed the legal scope of work for technicians.
Post-hospital appointments. I think arranging post-hospital appointments should be no more difficult for the hospitalist than ordering a complete blood count (CBC). It shouldn’t matter whether I want the patient to follow up with the PCP he has been seeing for years, or see a neurologist or diabetes educator as a new patient consult. Any treating doctor in the hospital should be able to arrange such post-hospital visits with just a click or two in the EHR, or a stroke of the pen. And the patient should leave the hospital with a written date and time of the appointment that has been made for them.
Few hospitals can reliably provide this, however, so, all too often, hospitalists spend their time calling clerical staff at outpatient clinics to arrange appointments, writing them down, and delivering them to patients. This is far from what anyone would consider top of license work. (I wrote a little more about this in last month’s column.)
Medicare benefits specialist. Many hospitalists end up spending significant time explaining to patients and families the reason a patient is on observation status and trying to defuse the resulting frustration and anger. As I stated in my November 2014 column, I think observation status is so frustrating to patients that it is often the root cause of complaints about care and, potentially, the source of malpractice suits.
Physicians have an unavoidable role in determining observation versus inpatient status, but I think hospitals should work hard to ensure that someone other than the doctor is available to explain to patients and families the reason for observation status, along with its implications, and to provide sympathy for their frustrations. This allows the doctor to stay focused on clinical care.
Limit reliance on a “triage hospitalist.” Hospitalist groups larger than about 20 providers often have one provider devoted through much of a daytime shift to triaging and assigning new referrals across all providers working that day. For larger practices, this triage work may consume all of the provider’s shift, so that person has no time left for clinical care. It is hard for me to see this as top of license work that only a physician or advanced practice clinician can do. In my December 2010 column, I provided some potential alternatives to dedicating a physician or other provider to a triage role.
Your list of important changes that are needed to move hospitalists toward more time spent working at the top of their license will likely differ a lot from the issues above. But every group could benefit from deliberately thinking about what would be most valuable for them and trying to make that a reality.

Specialty Hospitalists May Be Coming to Your Hospital Soon
Nearly 20 years ago, Bob Wachter, MD, coined the term “hospitalist,” defining a new specialty caring for the hospitalized medical patient. Since that time, we’ve seen rapid growth in the numbers of physicians who identify themselves as hospitalists, dominated by training in internal medicine and, to a lesser extent, family practice and pediatrics.
But, what about other specialty hospitalists, trained in the medicine or surgical specialties? How much of a presence do they have in our institutions today and in which specialties? To help us better understand this, a new question in 2014 State of Hospital Medicine survey asked whether specialty hospitalists practice in your hospital or health system.

—Carolyn Sites, DO, FHM
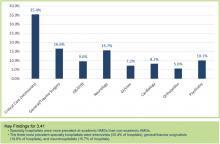
Results show the top three specialty hospitalists to be critical care, at (35.4%), followed by general surgery/trauma (16.6%) and neurology (15.7%), based on the responses of survey participants representing hospital medicine groups (HMGs) that care for adults only. Other specialties included obstetrics (OB), psychiatry, GI, cardiology, and orthopedics (see Figure 1).
Perhaps not too surprising, the greatest number of specialty hospitalists are found in university and academic settings. These are our primary training centers, offering fellowship programs and further subspecialization programs. Much like in our own field of hospital medicine, some academic centers have created one-year fellowships for those interested in specific hospital specialty fields, such as OB hospitalist.
For reasons that are less clear, the survey also shows percentages are highest in the western U.S. and lowest in the East.
Critical care hospitalists, also known as intensivists, dominate the spectrum, being present in academic and nonacademic centers, regardless of the employment model of the medical hospitalists at those facilities. This is not unexpected, given the Leapfrog Group’s endorsement of ICU physician staffing with intensivists.
What’s driving the other specialty hospitalist fields? I suspect the reasons are similar to those of our own specialty. OB and neuro hospitalists at my health system cite the challenges of managing outpatient and inpatient practices, the higher inpatient acuity and focused skill set that are required, immediate availability demands, and work-life balance as key factors. Further drivers include external quality/safety governing agencies or groups, such as the Leapfrog example above, or The Joint Commission’s requirements for certification as a Comprehensive Stroke Center with neurointensive care units.
Much like our own field’s exponential growth, we are likely to see further expansion of specialty hospitalists over the next several years. It will be interesting to watch how much and how fast this occurs, and what impact and influence these groups will bring to the care of the hospitalized patient. I’m already looking forward to next year’s SOHM report to see those results.
Dr. Sites is regional medical director of hospital medicine at Providence Health Systems in Oregon and a member of the SHM Practice Analysis Committee.
Nearly 20 years ago, Bob Wachter, MD, coined the term “hospitalist,” defining a new specialty caring for the hospitalized medical patient. Since that time, we’ve seen rapid growth in the numbers of physicians who identify themselves as hospitalists, dominated by training in internal medicine and, to a lesser extent, family practice and pediatrics.
But, what about other specialty hospitalists, trained in the medicine or surgical specialties? How much of a presence do they have in our institutions today and in which specialties? To help us better understand this, a new question in 2014 State of Hospital Medicine survey asked whether specialty hospitalists practice in your hospital or health system.

—Carolyn Sites, DO, FHM
Results show the top three specialty hospitalists to be critical care, at (35.4%), followed by general surgery/trauma (16.6%) and neurology (15.7%), based on the responses of survey participants representing hospital medicine groups (HMGs) that care for adults only. Other specialties included obstetrics (OB), psychiatry, GI, cardiology, and orthopedics (see Figure 1).
Perhaps not too surprising, the greatest number of specialty hospitalists are found in university and academic settings. These are our primary training centers, offering fellowship programs and further subspecialization programs. Much like in our own field of hospital medicine, some academic centers have created one-year fellowships for those interested in specific hospital specialty fields, such as OB hospitalist.
For reasons that are less clear, the survey also shows percentages are highest in the western U.S. and lowest in the East.
Critical care hospitalists, also known as intensivists, dominate the spectrum, being present in academic and nonacademic centers, regardless of the employment model of the medical hospitalists at those facilities. This is not unexpected, given the Leapfrog Group’s endorsement of ICU physician staffing with intensivists.
What’s driving the other specialty hospitalist fields? I suspect the reasons are similar to those of our own specialty. OB and neuro hospitalists at my health system cite the challenges of managing outpatient and inpatient practices, the higher inpatient acuity and focused skill set that are required, immediate availability demands, and work-life balance as key factors. Further drivers include external quality/safety governing agencies or groups, such as the Leapfrog example above, or The Joint Commission’s requirements for certification as a Comprehensive Stroke Center with neurointensive care units.
Much like our own field’s exponential growth, we are likely to see further expansion of specialty hospitalists over the next several years. It will be interesting to watch how much and how fast this occurs, and what impact and influence these groups will bring to the care of the hospitalized patient. I’m already looking forward to next year’s SOHM report to see those results.
Dr. Sites is regional medical director of hospital medicine at Providence Health Systems in Oregon and a member of the SHM Practice Analysis Committee.
Nearly 20 years ago, Bob Wachter, MD, coined the term “hospitalist,” defining a new specialty caring for the hospitalized medical patient. Since that time, we’ve seen rapid growth in the numbers of physicians who identify themselves as hospitalists, dominated by training in internal medicine and, to a lesser extent, family practice and pediatrics.
But, what about other specialty hospitalists, trained in the medicine or surgical specialties? How much of a presence do they have in our institutions today and in which specialties? To help us better understand this, a new question in 2014 State of Hospital Medicine survey asked whether specialty hospitalists practice in your hospital or health system.

—Carolyn Sites, DO, FHM
Results show the top three specialty hospitalists to be critical care, at (35.4%), followed by general surgery/trauma (16.6%) and neurology (15.7%), based on the responses of survey participants representing hospital medicine groups (HMGs) that care for adults only. Other specialties included obstetrics (OB), psychiatry, GI, cardiology, and orthopedics (see Figure 1).
Perhaps not too surprising, the greatest number of specialty hospitalists are found in university and academic settings. These are our primary training centers, offering fellowship programs and further subspecialization programs. Much like in our own field of hospital medicine, some academic centers have created one-year fellowships for those interested in specific hospital specialty fields, such as OB hospitalist.
For reasons that are less clear, the survey also shows percentages are highest in the western U.S. and lowest in the East.
Critical care hospitalists, also known as intensivists, dominate the spectrum, being present in academic and nonacademic centers, regardless of the employment model of the medical hospitalists at those facilities. This is not unexpected, given the Leapfrog Group’s endorsement of ICU physician staffing with intensivists.
What’s driving the other specialty hospitalist fields? I suspect the reasons are similar to those of our own specialty. OB and neuro hospitalists at my health system cite the challenges of managing outpatient and inpatient practices, the higher inpatient acuity and focused skill set that are required, immediate availability demands, and work-life balance as key factors. Further drivers include external quality/safety governing agencies or groups, such as the Leapfrog example above, or The Joint Commission’s requirements for certification as a Comprehensive Stroke Center with neurointensive care units.
Much like our own field’s exponential growth, we are likely to see further expansion of specialty hospitalists over the next several years. It will be interesting to watch how much and how fast this occurs, and what impact and influence these groups will bring to the care of the hospitalized patient. I’m already looking forward to next year’s SOHM report to see those results.
Dr. Sites is regional medical director of hospital medicine at Providence Health Systems in Oregon and a member of the SHM Practice Analysis Committee.
Business associate agreements
Revision of the Health Insurance Portability and Accountability Act (HIPAA) rules has prompted numerous questions about business associates (BAs) and business associate agreements (BAAs). Apparently there is confusion about exactly which businesses qualify as BAs and how your BAAs should be modified to reflect the new provisions.
The criteria for identifying BAs are admittedly vague: The act defines them as nonemployees, performing “functions or activities” on behalf of the “covered entity” (your practice) that involve “creating, receiving, maintaining, or transmitting” personal health information (PHI).
Clearly, answering and billing services, independent transcriptionists, hardware and software companies, and any other vendors involved in creating or maintaining your medical records always qualify as BAs. Other businesses may or may not qualify, depending on whether they need direct access to PHI in order to provide their service. These include practice management consultants, attorneys, companies that store or microfilm medical records, and record-shredding services.
Specialty pharmacies are seldom mentioned in the BA discussion, but they probably should be. Pharmaceutical manufacturers are increasingly using them as intermediaries for their products – particularly the more expensive ones, such as biologics. Many of them ship products directly to patients, for which they require home addresses and other personal information, and in order to file payment paperwork and claim forms, they usually request diagnoses and associated medical information. By any reasonable interpretation of the new rules, this makes them BAs, and you should have BAAs in place before allowing them to fill your prescriptions.
To further complicate the situation, manufacturers and insurers routinely compile information about the real world uses of their products. To that end, they often ask specialty pharmacies to provide them with any patient data that they collect. Under the new rules, patients may restrict any PHI shared with third parties when patients pay for the drugs or services themselves. Your specialty pharmacy BAA should include a provision noting that the pharmacy is forbidden from disclosing any data to pharmaceutical companies or insurers from patients who self-pay and request confidentiality.
Mail carriers, package delivery people, cleaning services, copier repairmen, bank employees, and the like are not considered BAs. While they might conceivably come in contact with PHI on occasion, they don’t need it to do their job. You are required to use “reasonable diligence” in limiting the PHI that these folks may encounter, but you do not need to enter into written BA agreements with them.
Independent contractors who work within your practice – aestheticians and physical therapists, for example – are not considered BAs either, and do not need to sign a BA agreement. Just train them, as you do your employees.
Another source of confusion is the provision in the new rules that makes BAs directly responsible for their own HIPAA violations. While this might seem to eliminate the need for BAAs entirely, unfortunately that is not the case. In fact, even more responsibility has been placed on physicians for confidentiality breaches committed by their BAs. It is not enough to simply have a BAA in place; you are expected to use “reasonable diligence” in monitoring the work of your BAs. While BAs and their subcontractors are responsible for their own actions, the primary responsibility remains with you. Furthermore, you now must assume the worst-case scenario. Previously, when PHI was compromised, you would have to notify affected patients (and the government) only if there was a “significant risk of financial or reputational harm”; but now, any incident involving patient records is assumed to be a breach, and must be reported. Failure to do so could subject your practice, as well as the contractor, to significant fines.
If you haven’t yet revised your Notice of Privacy Practices (NPP) to explain your relationships with BAs, and their status under the new rules, do it now. (You should have done it last September.) You need to explain the breach notification process too, as well as the new patient rights mentioned above. You must post your revised NPP in your office, and make copies available there, but you need not mail a copy to every patient.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Revision of the Health Insurance Portability and Accountability Act (HIPAA) rules has prompted numerous questions about business associates (BAs) and business associate agreements (BAAs). Apparently there is confusion about exactly which businesses qualify as BAs and how your BAAs should be modified to reflect the new provisions.
The criteria for identifying BAs are admittedly vague: The act defines them as nonemployees, performing “functions or activities” on behalf of the “covered entity” (your practice) that involve “creating, receiving, maintaining, or transmitting” personal health information (PHI).
Clearly, answering and billing services, independent transcriptionists, hardware and software companies, and any other vendors involved in creating or maintaining your medical records always qualify as BAs. Other businesses may or may not qualify, depending on whether they need direct access to PHI in order to provide their service. These include practice management consultants, attorneys, companies that store or microfilm medical records, and record-shredding services.
Specialty pharmacies are seldom mentioned in the BA discussion, but they probably should be. Pharmaceutical manufacturers are increasingly using them as intermediaries for their products – particularly the more expensive ones, such as biologics. Many of them ship products directly to patients, for which they require home addresses and other personal information, and in order to file payment paperwork and claim forms, they usually request diagnoses and associated medical information. By any reasonable interpretation of the new rules, this makes them BAs, and you should have BAAs in place before allowing them to fill your prescriptions.
To further complicate the situation, manufacturers and insurers routinely compile information about the real world uses of their products. To that end, they often ask specialty pharmacies to provide them with any patient data that they collect. Under the new rules, patients may restrict any PHI shared with third parties when patients pay for the drugs or services themselves. Your specialty pharmacy BAA should include a provision noting that the pharmacy is forbidden from disclosing any data to pharmaceutical companies or insurers from patients who self-pay and request confidentiality.
Mail carriers, package delivery people, cleaning services, copier repairmen, bank employees, and the like are not considered BAs. While they might conceivably come in contact with PHI on occasion, they don’t need it to do their job. You are required to use “reasonable diligence” in limiting the PHI that these folks may encounter, but you do not need to enter into written BA agreements with them.
Independent contractors who work within your practice – aestheticians and physical therapists, for example – are not considered BAs either, and do not need to sign a BA agreement. Just train them, as you do your employees.
Another source of confusion is the provision in the new rules that makes BAs directly responsible for their own HIPAA violations. While this might seem to eliminate the need for BAAs entirely, unfortunately that is not the case. In fact, even more responsibility has been placed on physicians for confidentiality breaches committed by their BAs. It is not enough to simply have a BAA in place; you are expected to use “reasonable diligence” in monitoring the work of your BAs. While BAs and their subcontractors are responsible for their own actions, the primary responsibility remains with you. Furthermore, you now must assume the worst-case scenario. Previously, when PHI was compromised, you would have to notify affected patients (and the government) only if there was a “significant risk of financial or reputational harm”; but now, any incident involving patient records is assumed to be a breach, and must be reported. Failure to do so could subject your practice, as well as the contractor, to significant fines.
If you haven’t yet revised your Notice of Privacy Practices (NPP) to explain your relationships with BAs, and their status under the new rules, do it now. (You should have done it last September.) You need to explain the breach notification process too, as well as the new patient rights mentioned above. You must post your revised NPP in your office, and make copies available there, but you need not mail a copy to every patient.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Revision of the Health Insurance Portability and Accountability Act (HIPAA) rules has prompted numerous questions about business associates (BAs) and business associate agreements (BAAs). Apparently there is confusion about exactly which businesses qualify as BAs and how your BAAs should be modified to reflect the new provisions.
The criteria for identifying BAs are admittedly vague: The act defines them as nonemployees, performing “functions or activities” on behalf of the “covered entity” (your practice) that involve “creating, receiving, maintaining, or transmitting” personal health information (PHI).
Clearly, answering and billing services, independent transcriptionists, hardware and software companies, and any other vendors involved in creating or maintaining your medical records always qualify as BAs. Other businesses may or may not qualify, depending on whether they need direct access to PHI in order to provide their service. These include practice management consultants, attorneys, companies that store or microfilm medical records, and record-shredding services.
Specialty pharmacies are seldom mentioned in the BA discussion, but they probably should be. Pharmaceutical manufacturers are increasingly using them as intermediaries for their products – particularly the more expensive ones, such as biologics. Many of them ship products directly to patients, for which they require home addresses and other personal information, and in order to file payment paperwork and claim forms, they usually request diagnoses and associated medical information. By any reasonable interpretation of the new rules, this makes them BAs, and you should have BAAs in place before allowing them to fill your prescriptions.
To further complicate the situation, manufacturers and insurers routinely compile information about the real world uses of their products. To that end, they often ask specialty pharmacies to provide them with any patient data that they collect. Under the new rules, patients may restrict any PHI shared with third parties when patients pay for the drugs or services themselves. Your specialty pharmacy BAA should include a provision noting that the pharmacy is forbidden from disclosing any data to pharmaceutical companies or insurers from patients who self-pay and request confidentiality.
Mail carriers, package delivery people, cleaning services, copier repairmen, bank employees, and the like are not considered BAs. While they might conceivably come in contact with PHI on occasion, they don’t need it to do their job. You are required to use “reasonable diligence” in limiting the PHI that these folks may encounter, but you do not need to enter into written BA agreements with them.
Independent contractors who work within your practice – aestheticians and physical therapists, for example – are not considered BAs either, and do not need to sign a BA agreement. Just train them, as you do your employees.
Another source of confusion is the provision in the new rules that makes BAs directly responsible for their own HIPAA violations. While this might seem to eliminate the need for BAAs entirely, unfortunately that is not the case. In fact, even more responsibility has been placed on physicians for confidentiality breaches committed by their BAs. It is not enough to simply have a BAA in place; you are expected to use “reasonable diligence” in monitoring the work of your BAs. While BAs and their subcontractors are responsible for their own actions, the primary responsibility remains with you. Furthermore, you now must assume the worst-case scenario. Previously, when PHI was compromised, you would have to notify affected patients (and the government) only if there was a “significant risk of financial or reputational harm”; but now, any incident involving patient records is assumed to be a breach, and must be reported. Failure to do so could subject your practice, as well as the contractor, to significant fines.
If you haven’t yet revised your Notice of Privacy Practices (NPP) to explain your relationships with BAs, and their status under the new rules, do it now. (You should have done it last September.) You need to explain the breach notification process too, as well as the new patient rights mentioned above. You must post your revised NPP in your office, and make copies available there, but you need not mail a copy to every patient.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Get more patients with backlinks
The medical profession has its jargon. So does the Internet world. Some of that jargon can be important to your success. “Backlinks” or “inbound links” are terms that should get your attention.
Why?
By developing them, you can attract more patients to your practice.
Backlinks are one piece of the Internet marketing puzzle that can help get your Web site on the first page of Google search results.
And just how important is it to be on page 1?
Well, consider that 91.5% of Web surfers do not go beyond the first page of results. That’s what an online advertising network called Chitika found when it examined tens of millions of online ad impressions in which the user was referred to the page via a Google search.1
Just what are backlinks? They are links to your Web page from another site. In basic link terminology, a backlink is any link received by a Web page, directory, Web site, or top-level domain from another, similar site. In this article we discuss the importance of these links and ways to use them in your social media to attract new patients to your site and your practice.
Start with good site design
If you can get listed on the first page of Google search results for the keywords your patients are using, more traffic will come to your Web site. That won’t help if you have a poorly designed site that has no patient conversion strategies, techniques, and systems to transform Web site visitors to patients.
You see, everything has to work together in a coordinated, integrated manner if you want to increase the number of patients who are looking for your services online. We’ve covered many of the basics in earlier articles on Web site design and improvement (see the box below). If you have a nonoptimal site, consider starting with these articles.
Articles on Web design and Internet usage by Ron Romano and Neil H. Baum, MD
5 ways to wake up your Web site
April 2015
Using the Internet in your practice
Part 1: Why social media are important and how to get started
February 2014
Part 2: Generating new patients using social media
April 2014
Part 3: Maximizing your online reach through SEO and pay-per-click
September 2014
Part 4: Reputation management: How to gather kudos and combat negative online reviews
December 2014
These articles are available in the archive at obgmanagement.com
Why backlinks are important
Google uses more than 200 algorithms to rank your Web site. Some are more important than others and have a greater influence on search engine positioning. Backlinks are one of those important influencers.
The number of backlinks you have is an indication of the popularity or importance of your Web site. Google considers a site more significant or relevant than others if it has a large number of quality backlinks from other directories, ezines, blogs, and social media Web sites. These backlinks must be relevant to your keywords. For example, because you are a medical professional, a link to your site from the American Cancer Society or the Mayo Clinic is considered more credible than a link from a local spa or health club.
A search engine such as Google considers the content of the sites it places at the top of the search results page. When links to your site come from other credible and popular sites, and those sites have content related to your site, these backlinks are considered more relevant to your site.
If backlinks come from sites with unrelated content, they are considered less relevant. You may even be penalized by Google for adding backlinks that have no content value.
For example, if a Web master has a site that focuses on urinary incontinence and receives a backlink from another site with information or articles about urinary incontinence, that backlink will be considered more relevant than a link from a site about mortgages that somehow also includes urinary incontinence on its page. Therefore, the higher the relevance of the site linking back to yours, the better the quality of that link.
Top 7 inbound links—and how to obtain them
1. Directories
Directories are indexes of online sites, typically organized by category. You want to ensure that each of your keywords is manually submitted to each directory so it is listed separately. This way you get maximum link value for each keyword.
Links back to your site from directories such as Yahoo Directory and DMOZ.org are valuable. DMOZ.org is edited by humans. Although it is free, it may take some time for your site to be added. A listing in Yahoo’s Directory costs $299 per year.
2. Press releases
If you are writing press releases, make sure they contain keywords that someone would use to find a business like yours. Also ensure that they include links back to your site.
Once the press release is written, submit it to all the news agencies. Then you must wait and see if any of them pick it up and publish it.
You may want to consider having a press release professionally written and distributed by a public relations firm to boost your chances of having the release picked up. PRWeb.com has an excellent reputation. Its distribution network includes the search engines Google, Yahoo, and Bing; media outlets such as USA Today, CNN, and the Wall Street Journal; Associated Press distribution through major newspapers; and health and medical digests such as the Mayo Clinic, WebMD, Women’s Health, and many more.
3. Article directories
By writing and distributing articles through high-traffic article directories, such as EzineArticles.com, Articles.org, and Hubpages.com, you can attract valuable inbound links from a high-traffic site. Craft an effective link at the close of your article to drive traffic back to your site. An example of what your link might say is, “To view a short video on Kegel exercises for pelvic organ prolapse, visit our Web site at www.neilbaum.com/videos.”
4. Social bookmarking
Like Web browser bookmarks, social bookmarking sites such as Digg.com, Reddit.com, and Del.icio.us.com store individual pages (bookmarks) online and allow users to tag (with keywords), organize, search, and manage these bookmarks as well as share them with others. If you bookmark your content on these sites, you get a link from the service. By producing content that your readers enjoy and bookmark to their friends, you gain a link that increases in search engine optimization (SEO) value.
5. Blog comments
To find blog posts on which to comment, you can use blog-specific search engines such as Google Blog Search. Make sure these are blogs read by your target market, not your colleagues. Brand yourself by always using the same name and remember to link back to your site. Always leave a comment that adds to the conversation.
6. Social media
Google also indexes your Twitter updates and social networking profiles. Add that to Web 2.0 hubsites like Scribd or HubPage and you’ve got a way to create many inbound links in a very short time. Scribd is a digital library featuring an ebook and audiobook subscription service that includes New York Times best sellers and classics. HubPages is a user-generated content, revenue-sharing Web site.
7. Video syndication
YouTube is one of the most visited sites online, and the number of sites that syndicate videos is growing every day. These sites often allow you to link to your site in your video’s description, on your profile page, or both.
The importance of being consistent—and honest
For best results, you need to build these links monthly with regularity, and over time, you will reap the benefits of improved rankings. While it is fairly easy to modify your Web pages to make them more SEO-friendly, it is harder to influence other Web sites and get them to link to yours. This is the reason search engines consider backlinks such an important factor.
Moreover, search engines’ criteria for quality backlinks have gotten tougher, thanks to unscrupulous Web masters trying to achieve these backlinks by deceptive techniques, such as hidden links or automatically generated pages whose sole purpose is to provide backlinks to Web sites. These pages are called link farms. Not only are they disregarded by search engines, but linking to one could get your site banned entirely. This strategy is often referred to as “black hat” linking and is to be avoided.
“White hat” methods to increase backlinks
Blog posting is one of the easiest, least expensive, and most effective ways to garner links from other sites. However, to reap this benefit, you must post blog entries consistently. We suggest posting at least once weekly. Your blog will gain more attention if you have something newsworthy to report. For example, if you attend a meeting where a revolutionary new development is reported, and you write about it before the media, you can be sure others will want to connect and link to your site.
Conduct a survey and share your results on your site. Others will want to link to your report.
Share any templates your office uses to be more efficient and productive. For example, Dr. Baum has a template, or checklist, for starting and ending every day in the office. It is shared on his Web site so that other sites can link to it and make use of it.
Show your funny bone. Humor often travels in a viral direction. If something funny happens in your practice, share it with others and they will frequently link to the source.
Join a forum. Forums are a great source of high-quality traffic and links. You can use a forum to reach out to a specific community.By placing valid, useful contributions, you gain legitimate authority for your site.
The bottom line
You want to attract as many visitors to your Web site as possible. Your own content and the frequency of your postings are mainstays of making your Web site relevant to existing and potential patients. Also useful are backlinks. The number and quality of your inbound links are major factors in SEO. Search engines place high value on trust and authority, and an inbound link from a very high-ranking and trusted Web site tells the search engine that someone trusted also trusts you. So start linking.
Reference
1. The value of Google result positioning. Chitika.com. http://chitika.com/google-positioning-value. Updated June 12, 2013. Accessed June 9, 2015.
The medical profession has its jargon. So does the Internet world. Some of that jargon can be important to your success. “Backlinks” or “inbound links” are terms that should get your attention.
Why?
By developing them, you can attract more patients to your practice.
Backlinks are one piece of the Internet marketing puzzle that can help get your Web site on the first page of Google search results.
And just how important is it to be on page 1?
Well, consider that 91.5% of Web surfers do not go beyond the first page of results. That’s what an online advertising network called Chitika found when it examined tens of millions of online ad impressions in which the user was referred to the page via a Google search.1
Just what are backlinks? They are links to your Web page from another site. In basic link terminology, a backlink is any link received by a Web page, directory, Web site, or top-level domain from another, similar site. In this article we discuss the importance of these links and ways to use them in your social media to attract new patients to your site and your practice.
Start with good site design
If you can get listed on the first page of Google search results for the keywords your patients are using, more traffic will come to your Web site. That won’t help if you have a poorly designed site that has no patient conversion strategies, techniques, and systems to transform Web site visitors to patients.
You see, everything has to work together in a coordinated, integrated manner if you want to increase the number of patients who are looking for your services online. We’ve covered many of the basics in earlier articles on Web site design and improvement (see the box below). If you have a nonoptimal site, consider starting with these articles.
Articles on Web design and Internet usage by Ron Romano and Neil H. Baum, MD
5 ways to wake up your Web site
April 2015
Using the Internet in your practice
Part 1: Why social media are important and how to get started
February 2014
Part 2: Generating new patients using social media
April 2014
Part 3: Maximizing your online reach through SEO and pay-per-click
September 2014
Part 4: Reputation management: How to gather kudos and combat negative online reviews
December 2014
These articles are available in the archive at obgmanagement.com
Why backlinks are important
Google uses more than 200 algorithms to rank your Web site. Some are more important than others and have a greater influence on search engine positioning. Backlinks are one of those important influencers.
The number of backlinks you have is an indication of the popularity or importance of your Web site. Google considers a site more significant or relevant than others if it has a large number of quality backlinks from other directories, ezines, blogs, and social media Web sites. These backlinks must be relevant to your keywords. For example, because you are a medical professional, a link to your site from the American Cancer Society or the Mayo Clinic is considered more credible than a link from a local spa or health club.
A search engine such as Google considers the content of the sites it places at the top of the search results page. When links to your site come from other credible and popular sites, and those sites have content related to your site, these backlinks are considered more relevant to your site.
If backlinks come from sites with unrelated content, they are considered less relevant. You may even be penalized by Google for adding backlinks that have no content value.
For example, if a Web master has a site that focuses on urinary incontinence and receives a backlink from another site with information or articles about urinary incontinence, that backlink will be considered more relevant than a link from a site about mortgages that somehow also includes urinary incontinence on its page. Therefore, the higher the relevance of the site linking back to yours, the better the quality of that link.
Top 7 inbound links—and how to obtain them
1. Directories
Directories are indexes of online sites, typically organized by category. You want to ensure that each of your keywords is manually submitted to each directory so it is listed separately. This way you get maximum link value for each keyword.
Links back to your site from directories such as Yahoo Directory and DMOZ.org are valuable. DMOZ.org is edited by humans. Although it is free, it may take some time for your site to be added. A listing in Yahoo’s Directory costs $299 per year.
2. Press releases
If you are writing press releases, make sure they contain keywords that someone would use to find a business like yours. Also ensure that they include links back to your site.
Once the press release is written, submit it to all the news agencies. Then you must wait and see if any of them pick it up and publish it.
You may want to consider having a press release professionally written and distributed by a public relations firm to boost your chances of having the release picked up. PRWeb.com has an excellent reputation. Its distribution network includes the search engines Google, Yahoo, and Bing; media outlets such as USA Today, CNN, and the Wall Street Journal; Associated Press distribution through major newspapers; and health and medical digests such as the Mayo Clinic, WebMD, Women’s Health, and many more.
3. Article directories
By writing and distributing articles through high-traffic article directories, such as EzineArticles.com, Articles.org, and Hubpages.com, you can attract valuable inbound links from a high-traffic site. Craft an effective link at the close of your article to drive traffic back to your site. An example of what your link might say is, “To view a short video on Kegel exercises for pelvic organ prolapse, visit our Web site at www.neilbaum.com/videos.”
4. Social bookmarking
Like Web browser bookmarks, social bookmarking sites such as Digg.com, Reddit.com, and Del.icio.us.com store individual pages (bookmarks) online and allow users to tag (with keywords), organize, search, and manage these bookmarks as well as share them with others. If you bookmark your content on these sites, you get a link from the service. By producing content that your readers enjoy and bookmark to their friends, you gain a link that increases in search engine optimization (SEO) value.
5. Blog comments
To find blog posts on which to comment, you can use blog-specific search engines such as Google Blog Search. Make sure these are blogs read by your target market, not your colleagues. Brand yourself by always using the same name and remember to link back to your site. Always leave a comment that adds to the conversation.
6. Social media
Google also indexes your Twitter updates and social networking profiles. Add that to Web 2.0 hubsites like Scribd or HubPage and you’ve got a way to create many inbound links in a very short time. Scribd is a digital library featuring an ebook and audiobook subscription service that includes New York Times best sellers and classics. HubPages is a user-generated content, revenue-sharing Web site.
7. Video syndication
YouTube is one of the most visited sites online, and the number of sites that syndicate videos is growing every day. These sites often allow you to link to your site in your video’s description, on your profile page, or both.
The importance of being consistent—and honest
For best results, you need to build these links monthly with regularity, and over time, you will reap the benefits of improved rankings. While it is fairly easy to modify your Web pages to make them more SEO-friendly, it is harder to influence other Web sites and get them to link to yours. This is the reason search engines consider backlinks such an important factor.
Moreover, search engines’ criteria for quality backlinks have gotten tougher, thanks to unscrupulous Web masters trying to achieve these backlinks by deceptive techniques, such as hidden links or automatically generated pages whose sole purpose is to provide backlinks to Web sites. These pages are called link farms. Not only are they disregarded by search engines, but linking to one could get your site banned entirely. This strategy is often referred to as “black hat” linking and is to be avoided.
“White hat” methods to increase backlinks
Blog posting is one of the easiest, least expensive, and most effective ways to garner links from other sites. However, to reap this benefit, you must post blog entries consistently. We suggest posting at least once weekly. Your blog will gain more attention if you have something newsworthy to report. For example, if you attend a meeting where a revolutionary new development is reported, and you write about it before the media, you can be sure others will want to connect and link to your site.
Conduct a survey and share your results on your site. Others will want to link to your report.
Share any templates your office uses to be more efficient and productive. For example, Dr. Baum has a template, or checklist, for starting and ending every day in the office. It is shared on his Web site so that other sites can link to it and make use of it.
Show your funny bone. Humor often travels in a viral direction. If something funny happens in your practice, share it with others and they will frequently link to the source.
Join a forum. Forums are a great source of high-quality traffic and links. You can use a forum to reach out to a specific community.By placing valid, useful contributions, you gain legitimate authority for your site.
The bottom line
You want to attract as many visitors to your Web site as possible. Your own content and the frequency of your postings are mainstays of making your Web site relevant to existing and potential patients. Also useful are backlinks. The number and quality of your inbound links are major factors in SEO. Search engines place high value on trust and authority, and an inbound link from a very high-ranking and trusted Web site tells the search engine that someone trusted also trusts you. So start linking.
The medical profession has its jargon. So does the Internet world. Some of that jargon can be important to your success. “Backlinks” or “inbound links” are terms that should get your attention.
Why?
By developing them, you can attract more patients to your practice.
Backlinks are one piece of the Internet marketing puzzle that can help get your Web site on the first page of Google search results.
And just how important is it to be on page 1?
Well, consider that 91.5% of Web surfers do not go beyond the first page of results. That’s what an online advertising network called Chitika found when it examined tens of millions of online ad impressions in which the user was referred to the page via a Google search.1
Just what are backlinks? They are links to your Web page from another site. In basic link terminology, a backlink is any link received by a Web page, directory, Web site, or top-level domain from another, similar site. In this article we discuss the importance of these links and ways to use them in your social media to attract new patients to your site and your practice.
Start with good site design
If you can get listed on the first page of Google search results for the keywords your patients are using, more traffic will come to your Web site. That won’t help if you have a poorly designed site that has no patient conversion strategies, techniques, and systems to transform Web site visitors to patients.
You see, everything has to work together in a coordinated, integrated manner if you want to increase the number of patients who are looking for your services online. We’ve covered many of the basics in earlier articles on Web site design and improvement (see the box below). If you have a nonoptimal site, consider starting with these articles.
Articles on Web design and Internet usage by Ron Romano and Neil H. Baum, MD
5 ways to wake up your Web site
April 2015
Using the Internet in your practice
Part 1: Why social media are important and how to get started
February 2014
Part 2: Generating new patients using social media
April 2014
Part 3: Maximizing your online reach through SEO and pay-per-click
September 2014
Part 4: Reputation management: How to gather kudos and combat negative online reviews
December 2014
These articles are available in the archive at obgmanagement.com
Why backlinks are important
Google uses more than 200 algorithms to rank your Web site. Some are more important than others and have a greater influence on search engine positioning. Backlinks are one of those important influencers.
The number of backlinks you have is an indication of the popularity or importance of your Web site. Google considers a site more significant or relevant than others if it has a large number of quality backlinks from other directories, ezines, blogs, and social media Web sites. These backlinks must be relevant to your keywords. For example, because you are a medical professional, a link to your site from the American Cancer Society or the Mayo Clinic is considered more credible than a link from a local spa or health club.
A search engine such as Google considers the content of the sites it places at the top of the search results page. When links to your site come from other credible and popular sites, and those sites have content related to your site, these backlinks are considered more relevant to your site.
If backlinks come from sites with unrelated content, they are considered less relevant. You may even be penalized by Google for adding backlinks that have no content value.
For example, if a Web master has a site that focuses on urinary incontinence and receives a backlink from another site with information or articles about urinary incontinence, that backlink will be considered more relevant than a link from a site about mortgages that somehow also includes urinary incontinence on its page. Therefore, the higher the relevance of the site linking back to yours, the better the quality of that link.
Top 7 inbound links—and how to obtain them
1. Directories
Directories are indexes of online sites, typically organized by category. You want to ensure that each of your keywords is manually submitted to each directory so it is listed separately. This way you get maximum link value for each keyword.
Links back to your site from directories such as Yahoo Directory and DMOZ.org are valuable. DMOZ.org is edited by humans. Although it is free, it may take some time for your site to be added. A listing in Yahoo’s Directory costs $299 per year.
2. Press releases
If you are writing press releases, make sure they contain keywords that someone would use to find a business like yours. Also ensure that they include links back to your site.
Once the press release is written, submit it to all the news agencies. Then you must wait and see if any of them pick it up and publish it.
You may want to consider having a press release professionally written and distributed by a public relations firm to boost your chances of having the release picked up. PRWeb.com has an excellent reputation. Its distribution network includes the search engines Google, Yahoo, and Bing; media outlets such as USA Today, CNN, and the Wall Street Journal; Associated Press distribution through major newspapers; and health and medical digests such as the Mayo Clinic, WebMD, Women’s Health, and many more.
3. Article directories
By writing and distributing articles through high-traffic article directories, such as EzineArticles.com, Articles.org, and Hubpages.com, you can attract valuable inbound links from a high-traffic site. Craft an effective link at the close of your article to drive traffic back to your site. An example of what your link might say is, “To view a short video on Kegel exercises for pelvic organ prolapse, visit our Web site at www.neilbaum.com/videos.”
4. Social bookmarking
Like Web browser bookmarks, social bookmarking sites such as Digg.com, Reddit.com, and Del.icio.us.com store individual pages (bookmarks) online and allow users to tag (with keywords), organize, search, and manage these bookmarks as well as share them with others. If you bookmark your content on these sites, you get a link from the service. By producing content that your readers enjoy and bookmark to their friends, you gain a link that increases in search engine optimization (SEO) value.
5. Blog comments
To find blog posts on which to comment, you can use blog-specific search engines such as Google Blog Search. Make sure these are blogs read by your target market, not your colleagues. Brand yourself by always using the same name and remember to link back to your site. Always leave a comment that adds to the conversation.
6. Social media
Google also indexes your Twitter updates and social networking profiles. Add that to Web 2.0 hubsites like Scribd or HubPage and you’ve got a way to create many inbound links in a very short time. Scribd is a digital library featuring an ebook and audiobook subscription service that includes New York Times best sellers and classics. HubPages is a user-generated content, revenue-sharing Web site.
7. Video syndication
YouTube is one of the most visited sites online, and the number of sites that syndicate videos is growing every day. These sites often allow you to link to your site in your video’s description, on your profile page, or both.
The importance of being consistent—and honest
For best results, you need to build these links monthly with regularity, and over time, you will reap the benefits of improved rankings. While it is fairly easy to modify your Web pages to make them more SEO-friendly, it is harder to influence other Web sites and get them to link to yours. This is the reason search engines consider backlinks such an important factor.
Moreover, search engines’ criteria for quality backlinks have gotten tougher, thanks to unscrupulous Web masters trying to achieve these backlinks by deceptive techniques, such as hidden links or automatically generated pages whose sole purpose is to provide backlinks to Web sites. These pages are called link farms. Not only are they disregarded by search engines, but linking to one could get your site banned entirely. This strategy is often referred to as “black hat” linking and is to be avoided.
“White hat” methods to increase backlinks
Blog posting is one of the easiest, least expensive, and most effective ways to garner links from other sites. However, to reap this benefit, you must post blog entries consistently. We suggest posting at least once weekly. Your blog will gain more attention if you have something newsworthy to report. For example, if you attend a meeting where a revolutionary new development is reported, and you write about it before the media, you can be sure others will want to connect and link to your site.
Conduct a survey and share your results on your site. Others will want to link to your report.
Share any templates your office uses to be more efficient and productive. For example, Dr. Baum has a template, or checklist, for starting and ending every day in the office. It is shared on his Web site so that other sites can link to it and make use of it.
Show your funny bone. Humor often travels in a viral direction. If something funny happens in your practice, share it with others and they will frequently link to the source.
Join a forum. Forums are a great source of high-quality traffic and links. You can use a forum to reach out to a specific community.By placing valid, useful contributions, you gain legitimate authority for your site.
The bottom line
You want to attract as many visitors to your Web site as possible. Your own content and the frequency of your postings are mainstays of making your Web site relevant to existing and potential patients. Also useful are backlinks. The number and quality of your inbound links are major factors in SEO. Search engines place high value on trust and authority, and an inbound link from a very high-ranking and trusted Web site tells the search engine that someone trusted also trusts you. So start linking.
Reference
1. The value of Google result positioning. Chitika.com. http://chitika.com/google-positioning-value. Updated June 12, 2013. Accessed June 9, 2015.
Reference
1. The value of Google result positioning. Chitika.com. http://chitika.com/google-positioning-value. Updated June 12, 2013. Accessed June 9, 2015.
ObGyn salaries continue gradual improvement
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
In this article
- Which practice settings pay better?
- Would you select a career in ObGyn again?
- Comparing time spent with patients
ICD-10 Race to the Finish: 8 High Priorities in the 11th Hour
As late as mid-April 2015, a survey of 121 orthopedic practices indicated that 30% had done nothing to start preparing for ICD-10 (International Classification of Diseases, Tenth Revision).1 That’s scary. And even the practices that had begun to prepare had not completed a number of key tasks (Figure 1).
Certainly, the will-they-or-won’t-they possibility of another congressional delay had many practices sitting on their hands this year. But now that the October 1, 2015, implementation is set in stone, this lack of inertia has many practices woefully behind. If your practice is one of many that hasn’t mapped your common ICD-9 (International Classification of Diseases, Ninth Revision) codes to ICD-10 codes, completed payer testing, or attended training, it’s time for a “full-court press.”
Being unprepared for ICD-10 will cause more than just an increase in claim denials. If your surgery schedule is booked a few months out, your staff will need to pre-authorize cases using ICD-10 as early as August 1—and they won’t be able to do that if you haven’t dictated the clinical terms required to choose an ICD-10 code. Without an understanding of ICD-10, severity of illness coding will suffer, and that will affect your bundled and value-based payments. And, if you don’t provide an adequate diagnosis when sending patients off-site for physical therapy, you’ll soon be getting phone calls from their billing staff demanding more specifics.
The clock is ticking and time is short. Here’s a prioritized list of what needs to get done.
1. Generate an ICD-9 frequency report
Identifying which diagnosis codes are the most frequently used, and therefore drive a significant portion of practice revenue, is an absolute must. The data will help prioritize training and code-mapping activities.
Most practices generate Current Procedural Terminology (CPT) code-frequency reports regularly, but few have ever run an ICD-9 code-frequency report. Call your vendor and ask for assistance, as there are multiple ways to run this report and they vary by practice management system. Sort the data elements and generate the ICD-9 frequency report by:
- Primary diagnosis.
- Unique patient.
- Revenue. (If your practice management system can’t give you diagnosis data by revenue, which enables you to focus on the codes that generate the most revenue, generate it by charges.)
The result should be a report that identifies the 20 to 25 diagnosis codes (or charges, depending on the reports generated) that drive the most revenue for the practice. Use the data to focus and prioritize your training and code-mapping activities.
2. Schedule training
Forget about “general” ICD-10 training courses. You need orthopedic-specific guidance. That’s because ICD-10 for orthopedics is more complex than for other specialties. Dictating fractures under ICD-10 is not so simple. Selecting an injury code requires confidence in correctly using the seventh character.
“Everyone who uses diagnosis codes must have baseline knowledge: surgeons, billing staff, surgical coordinators, and clinical team,” according to Sarah Wiskerchen, MBA, CPC, consultant and ICD-10 educator with KarenZupko & Associates (KZA). Training must include the practical details of ICD-10, such as assigning laterality, understanding the system architecture, and limiting the use of unspecified codes.
The American Academy of Orthopaedic Surgeons (AAOS) offers a self-paced, online training series that provides details for the top 3 diagnosis codes for each subspecialty. The 10-program course, ICD-10-CM: By the Numbers, is available at www.aaos.org ($299 for members, $399 for nonmembers). If you prefer live instruction, there is one more AAOS-sponsored, regional ICD-10 workshop left before the October 1 deadline, and more may be added. (Details at www.karenzupko.com)
These courses provide highly specific and granular ICD-10 knowledge and incorporate the use of Code-X, an AAOS-developed software tool. They also feature tools for handling the complexities of fractures and injury codes, such as Leo C. Far, an acronym developed by KZA consultant and coding educator Margie Maley, BSN, MS, to make ICD-10 diagnosis coding for fractures easier (Figure 2).
Some subspecialty societies also offer ICD-10 training. The American Society for Surgery of the Hand (www.assh.org), for example, offers a series of webinars and member-developed ICD-9-to-ICD-10 code maps.
3. Crosswalk your common codes from ICD-9 to ICD-10
Crosswalking is the process of mapping your most commonly used ICD-9 codes to their equivalent ICD-10 codes. This exercise familiarizes your team with ICD-10 language and terms, and gives a sense of which ICD-9 codes expand to just 1 or 2 ICD-10 codes and which codes expand into 10 or more codes—as some injury codes do (Table).
“Attempting to map the codes before completing ICD-10 training is like trying to write a letter in Greek when you only speak English,” Wiskerchen warns. “So start this process after at least some of your team have grasped the fundamentals of ICD-10.” This is where the data from your ICD-9 frequency report comes in. Use it to prioritize which codes to map first with a goal of mapping your top 25 ICD-9 codes to their ICD-10 equivalents by August 31.
Invest in good tools to support your mapping efforts. Avoid general mapping equivalent (GEM) coding tools, which are free for a good reason—they are incomplete and don’t always lead you to the correct ICD-10 code. Instead, purchase resources from credible sources, such as the American Medical Association (AMA; www.ama-assn.org). The AMA publishes ICD-10-CM 2016: The Complete Official Codebook as well as ICD-10-CM Mappings 2016, which links ICD-9 codes to all valid ICD-10 alternatives. The AMA also offers electronic ICD-10-CM Express Reference Mapping Cards for multiple specialties.
Practice makes perfect and crosswalking from ICD-9 to ICD-10 is one of the best ways for your team to become aware of the nuances in the new coding system. Like learning a new language, “speaking” ICD-10 does not become automatic just because you’ve attended training or completed the coding maps. Training teaches the architecture of the new coding system. Mapping provides a structured way to become familiar with the codes the practice will use most often. Once these 2 primary pieces are understood and assimilated, most physicians find that dictating the necessary new terms becomes quite easy.
4. Conduct a gap analysis to identify the ICD-10 terms missing from each provider’s current documentation
Conduct the gap analysis after your team has completed training, and once you’ve at least begun the process of mapping codes from ICD-9 to ICD-10. Here’s how:
- Generate a CPT frequency report.
- Select the top 5 procedures for each physician.
- Pull 2 patients’ notes for each of the top procedures.
- Review the notes and try to select ICD-10 code(s).
If key ICD-10 terms are not included in current documentation, physicians should modify the templates or macros they rely on for dictation.
“This simple exercise makes it obvious which clinical information physicians must add for ICD-10,” Wiskerchen says. For example, if the patient had an arthroscopy, but the note doesn’t specify on which leg, that’s a clear indication that the physician must dictate laterality. “The gap analysis is a great way to coach physicians about the clinical details to document, so staff can bill under ICD-10,” Wiskerchen says.
5. Contact technology vendors
Given the number of new ICD-10 codes in orthopedics, paper cheat sheets will be obsolete. Instead, you’ll need to rely on pull-down menus and/or search fields in the electronic health record (EHR) and practice management systems.
“Get clarity about how the new features and workflow processes will work in your systems,” suggests Wiskerchen. “Ask questions such as: Which features will be added or changed to accommodate the new codes? Will there be new screens or pick lists for ICD-10, or search fields? How will new screens and features change our current workflow? And schedule any necessary training as soon as possible.”
In addition to software upgrades and training, vendors and clearinghouses offer an array of services to help practices make the transition. Some vendors even provide help coordinating your internal plan with their new product features and training. Contact vendors to find out what they offer.
6. Use completed code maps to build diagnosis code databases, EHR templates, charge tickets, pick lists, prompters, and other coding tools
“Provide the code crosswalks and results of your documentation gap analysis to the IT [information technology] team so they can get started,” Wiskerchen advises. “And assign a physician or midlevel provider to work with IT so that the tools are clinically accurate.”
7. Schedule testing with clearinghouses and payers
“Successful testing indicates that your hard work has paid off, and that claims will be processed with few, if any, ICD-10–related hiccups,” Wiskerchen says. Essentially, the testing confirms that your ICD-10 code database, pick lists, vendor features, and other coding fields are working properly. “Testing with a clearinghouse is good. Testing directly with the payer is even better, if you are a direct submitter and it is allowed,” Wiskerchen suggests. Contact your clearinghouse and/or payers for testing opportunities prior to October 1.
8. Develop a plan for a potential cash flow crunch
So what happens if your best efforts in the 11th hour still aren’t enough to get your practice to the ICD-10 finish line? Prepare for the possibility of increased claim denials and temporary cash flow stalls, and put a plan in place to deal with them.
Start now by cleaning up as much of the accounts receivable as possible, and moving patient collections up front. Ask the billing team for a weekly status update of the largest unpaid balances in the 60-day aging column, and what has been done to appeal or otherwise address them. Analyze denial patterns and trends and fix their causes at the source—some may be ICD-10–related, others may simply be a gap in the reimbursement process that needs improvement.
Use payer cost estimators to calculate patient out-of-pocket cost and to collect unmet deductibles, coinsurance, and noncovered services prior to surgery. The surgeon-developed iPhone app Health Insurance Arithmetic2 ($1.99 in the iTunes Store) can help staff do this math on one, simple screen.
Finally, secure a line of credit to guard against a claim denial pile up this fall. A line of credit mitigates financial risk by making cash available quickly, should you need it to cover temporary revenue shortfalls, meet payroll, or pay operational expenses. It’s not too late to meet with your banker and apply for this protection, and the peace of mind may even help you sleep better.
1. KarenZupko & Associates, Inc. Pre-course survey of Q1 2015 coding and reimbursement workshop attendees. [Workshops are cosponsored by the American Academy of Orthopaedic Surgeons.] Unpublished data, April 2015.
2. Health Insurance Arithmetic. iTunes Store website. https://itunes.apple.com/us/app/healthinsurancearithmetic/id953262818. Accessed May 12, 2015.
As late as mid-April 2015, a survey of 121 orthopedic practices indicated that 30% had done nothing to start preparing for ICD-10 (International Classification of Diseases, Tenth Revision).1 That’s scary. And even the practices that had begun to prepare had not completed a number of key tasks (Figure 1).
Certainly, the will-they-or-won’t-they possibility of another congressional delay had many practices sitting on their hands this year. But now that the October 1, 2015, implementation is set in stone, this lack of inertia has many practices woefully behind. If your practice is one of many that hasn’t mapped your common ICD-9 (International Classification of Diseases, Ninth Revision) codes to ICD-10 codes, completed payer testing, or attended training, it’s time for a “full-court press.”
Being unprepared for ICD-10 will cause more than just an increase in claim denials. If your surgery schedule is booked a few months out, your staff will need to pre-authorize cases using ICD-10 as early as August 1—and they won’t be able to do that if you haven’t dictated the clinical terms required to choose an ICD-10 code. Without an understanding of ICD-10, severity of illness coding will suffer, and that will affect your bundled and value-based payments. And, if you don’t provide an adequate diagnosis when sending patients off-site for physical therapy, you’ll soon be getting phone calls from their billing staff demanding more specifics.
The clock is ticking and time is short. Here’s a prioritized list of what needs to get done.
1. Generate an ICD-9 frequency report
Identifying which diagnosis codes are the most frequently used, and therefore drive a significant portion of practice revenue, is an absolute must. The data will help prioritize training and code-mapping activities.
Most practices generate Current Procedural Terminology (CPT) code-frequency reports regularly, but few have ever run an ICD-9 code-frequency report. Call your vendor and ask for assistance, as there are multiple ways to run this report and they vary by practice management system. Sort the data elements and generate the ICD-9 frequency report by:
- Primary diagnosis.
- Unique patient.
- Revenue. (If your practice management system can’t give you diagnosis data by revenue, which enables you to focus on the codes that generate the most revenue, generate it by charges.)
The result should be a report that identifies the 20 to 25 diagnosis codes (or charges, depending on the reports generated) that drive the most revenue for the practice. Use the data to focus and prioritize your training and code-mapping activities.
2. Schedule training
Forget about “general” ICD-10 training courses. You need orthopedic-specific guidance. That’s because ICD-10 for orthopedics is more complex than for other specialties. Dictating fractures under ICD-10 is not so simple. Selecting an injury code requires confidence in correctly using the seventh character.
“Everyone who uses diagnosis codes must have baseline knowledge: surgeons, billing staff, surgical coordinators, and clinical team,” according to Sarah Wiskerchen, MBA, CPC, consultant and ICD-10 educator with KarenZupko & Associates (KZA). Training must include the practical details of ICD-10, such as assigning laterality, understanding the system architecture, and limiting the use of unspecified codes.
The American Academy of Orthopaedic Surgeons (AAOS) offers a self-paced, online training series that provides details for the top 3 diagnosis codes for each subspecialty. The 10-program course, ICD-10-CM: By the Numbers, is available at www.aaos.org ($299 for members, $399 for nonmembers). If you prefer live instruction, there is one more AAOS-sponsored, regional ICD-10 workshop left before the October 1 deadline, and more may be added. (Details at www.karenzupko.com)
These courses provide highly specific and granular ICD-10 knowledge and incorporate the use of Code-X, an AAOS-developed software tool. They also feature tools for handling the complexities of fractures and injury codes, such as Leo C. Far, an acronym developed by KZA consultant and coding educator Margie Maley, BSN, MS, to make ICD-10 diagnosis coding for fractures easier (Figure 2).
Some subspecialty societies also offer ICD-10 training. The American Society for Surgery of the Hand (www.assh.org), for example, offers a series of webinars and member-developed ICD-9-to-ICD-10 code maps.
3. Crosswalk your common codes from ICD-9 to ICD-10
Crosswalking is the process of mapping your most commonly used ICD-9 codes to their equivalent ICD-10 codes. This exercise familiarizes your team with ICD-10 language and terms, and gives a sense of which ICD-9 codes expand to just 1 or 2 ICD-10 codes and which codes expand into 10 or more codes—as some injury codes do (Table).
“Attempting to map the codes before completing ICD-10 training is like trying to write a letter in Greek when you only speak English,” Wiskerchen warns. “So start this process after at least some of your team have grasped the fundamentals of ICD-10.” This is where the data from your ICD-9 frequency report comes in. Use it to prioritize which codes to map first with a goal of mapping your top 25 ICD-9 codes to their ICD-10 equivalents by August 31.
Invest in good tools to support your mapping efforts. Avoid general mapping equivalent (GEM) coding tools, which are free for a good reason—they are incomplete and don’t always lead you to the correct ICD-10 code. Instead, purchase resources from credible sources, such as the American Medical Association (AMA; www.ama-assn.org). The AMA publishes ICD-10-CM 2016: The Complete Official Codebook as well as ICD-10-CM Mappings 2016, which links ICD-9 codes to all valid ICD-10 alternatives. The AMA also offers electronic ICD-10-CM Express Reference Mapping Cards for multiple specialties.
Practice makes perfect and crosswalking from ICD-9 to ICD-10 is one of the best ways for your team to become aware of the nuances in the new coding system. Like learning a new language, “speaking” ICD-10 does not become automatic just because you’ve attended training or completed the coding maps. Training teaches the architecture of the new coding system. Mapping provides a structured way to become familiar with the codes the practice will use most often. Once these 2 primary pieces are understood and assimilated, most physicians find that dictating the necessary new terms becomes quite easy.
4. Conduct a gap analysis to identify the ICD-10 terms missing from each provider’s current documentation
Conduct the gap analysis after your team has completed training, and once you’ve at least begun the process of mapping codes from ICD-9 to ICD-10. Here’s how:
- Generate a CPT frequency report.
- Select the top 5 procedures for each physician.
- Pull 2 patients’ notes for each of the top procedures.
- Review the notes and try to select ICD-10 code(s).
If key ICD-10 terms are not included in current documentation, physicians should modify the templates or macros they rely on for dictation.
“This simple exercise makes it obvious which clinical information physicians must add for ICD-10,” Wiskerchen says. For example, if the patient had an arthroscopy, but the note doesn’t specify on which leg, that’s a clear indication that the physician must dictate laterality. “The gap analysis is a great way to coach physicians about the clinical details to document, so staff can bill under ICD-10,” Wiskerchen says.
5. Contact technology vendors
Given the number of new ICD-10 codes in orthopedics, paper cheat sheets will be obsolete. Instead, you’ll need to rely on pull-down menus and/or search fields in the electronic health record (EHR) and practice management systems.
“Get clarity about how the new features and workflow processes will work in your systems,” suggests Wiskerchen. “Ask questions such as: Which features will be added or changed to accommodate the new codes? Will there be new screens or pick lists for ICD-10, or search fields? How will new screens and features change our current workflow? And schedule any necessary training as soon as possible.”
In addition to software upgrades and training, vendors and clearinghouses offer an array of services to help practices make the transition. Some vendors even provide help coordinating your internal plan with their new product features and training. Contact vendors to find out what they offer.
6. Use completed code maps to build diagnosis code databases, EHR templates, charge tickets, pick lists, prompters, and other coding tools
“Provide the code crosswalks and results of your documentation gap analysis to the IT [information technology] team so they can get started,” Wiskerchen advises. “And assign a physician or midlevel provider to work with IT so that the tools are clinically accurate.”
7. Schedule testing with clearinghouses and payers
“Successful testing indicates that your hard work has paid off, and that claims will be processed with few, if any, ICD-10–related hiccups,” Wiskerchen says. Essentially, the testing confirms that your ICD-10 code database, pick lists, vendor features, and other coding fields are working properly. “Testing with a clearinghouse is good. Testing directly with the payer is even better, if you are a direct submitter and it is allowed,” Wiskerchen suggests. Contact your clearinghouse and/or payers for testing opportunities prior to October 1.
8. Develop a plan for a potential cash flow crunch
So what happens if your best efforts in the 11th hour still aren’t enough to get your practice to the ICD-10 finish line? Prepare for the possibility of increased claim denials and temporary cash flow stalls, and put a plan in place to deal with them.
Start now by cleaning up as much of the accounts receivable as possible, and moving patient collections up front. Ask the billing team for a weekly status update of the largest unpaid balances in the 60-day aging column, and what has been done to appeal or otherwise address them. Analyze denial patterns and trends and fix their causes at the source—some may be ICD-10–related, others may simply be a gap in the reimbursement process that needs improvement.
Use payer cost estimators to calculate patient out-of-pocket cost and to collect unmet deductibles, coinsurance, and noncovered services prior to surgery. The surgeon-developed iPhone app Health Insurance Arithmetic2 ($1.99 in the iTunes Store) can help staff do this math on one, simple screen.
Finally, secure a line of credit to guard against a claim denial pile up this fall. A line of credit mitigates financial risk by making cash available quickly, should you need it to cover temporary revenue shortfalls, meet payroll, or pay operational expenses. It’s not too late to meet with your banker and apply for this protection, and the peace of mind may even help you sleep better.
As late as mid-April 2015, a survey of 121 orthopedic practices indicated that 30% had done nothing to start preparing for ICD-10 (International Classification of Diseases, Tenth Revision).1 That’s scary. And even the practices that had begun to prepare had not completed a number of key tasks (Figure 1).
Certainly, the will-they-or-won’t-they possibility of another congressional delay had many practices sitting on their hands this year. But now that the October 1, 2015, implementation is set in stone, this lack of inertia has many practices woefully behind. If your practice is one of many that hasn’t mapped your common ICD-9 (International Classification of Diseases, Ninth Revision) codes to ICD-10 codes, completed payer testing, or attended training, it’s time for a “full-court press.”
Being unprepared for ICD-10 will cause more than just an increase in claim denials. If your surgery schedule is booked a few months out, your staff will need to pre-authorize cases using ICD-10 as early as August 1—and they won’t be able to do that if you haven’t dictated the clinical terms required to choose an ICD-10 code. Without an understanding of ICD-10, severity of illness coding will suffer, and that will affect your bundled and value-based payments. And, if you don’t provide an adequate diagnosis when sending patients off-site for physical therapy, you’ll soon be getting phone calls from their billing staff demanding more specifics.
The clock is ticking and time is short. Here’s a prioritized list of what needs to get done.
1. Generate an ICD-9 frequency report
Identifying which diagnosis codes are the most frequently used, and therefore drive a significant portion of practice revenue, is an absolute must. The data will help prioritize training and code-mapping activities.
Most practices generate Current Procedural Terminology (CPT) code-frequency reports regularly, but few have ever run an ICD-9 code-frequency report. Call your vendor and ask for assistance, as there are multiple ways to run this report and they vary by practice management system. Sort the data elements and generate the ICD-9 frequency report by:
- Primary diagnosis.
- Unique patient.
- Revenue. (If your practice management system can’t give you diagnosis data by revenue, which enables you to focus on the codes that generate the most revenue, generate it by charges.)
The result should be a report that identifies the 20 to 25 diagnosis codes (or charges, depending on the reports generated) that drive the most revenue for the practice. Use the data to focus and prioritize your training and code-mapping activities.
2. Schedule training
Forget about “general” ICD-10 training courses. You need orthopedic-specific guidance. That’s because ICD-10 for orthopedics is more complex than for other specialties. Dictating fractures under ICD-10 is not so simple. Selecting an injury code requires confidence in correctly using the seventh character.
“Everyone who uses diagnosis codes must have baseline knowledge: surgeons, billing staff, surgical coordinators, and clinical team,” according to Sarah Wiskerchen, MBA, CPC, consultant and ICD-10 educator with KarenZupko & Associates (KZA). Training must include the practical details of ICD-10, such as assigning laterality, understanding the system architecture, and limiting the use of unspecified codes.
The American Academy of Orthopaedic Surgeons (AAOS) offers a self-paced, online training series that provides details for the top 3 diagnosis codes for each subspecialty. The 10-program course, ICD-10-CM: By the Numbers, is available at www.aaos.org ($299 for members, $399 for nonmembers). If you prefer live instruction, there is one more AAOS-sponsored, regional ICD-10 workshop left before the October 1 deadline, and more may be added. (Details at www.karenzupko.com)
These courses provide highly specific and granular ICD-10 knowledge and incorporate the use of Code-X, an AAOS-developed software tool. They also feature tools for handling the complexities of fractures and injury codes, such as Leo C. Far, an acronym developed by KZA consultant and coding educator Margie Maley, BSN, MS, to make ICD-10 diagnosis coding for fractures easier (Figure 2).
Some subspecialty societies also offer ICD-10 training. The American Society for Surgery of the Hand (www.assh.org), for example, offers a series of webinars and member-developed ICD-9-to-ICD-10 code maps.
3. Crosswalk your common codes from ICD-9 to ICD-10
Crosswalking is the process of mapping your most commonly used ICD-9 codes to their equivalent ICD-10 codes. This exercise familiarizes your team with ICD-10 language and terms, and gives a sense of which ICD-9 codes expand to just 1 or 2 ICD-10 codes and which codes expand into 10 or more codes—as some injury codes do (Table).
“Attempting to map the codes before completing ICD-10 training is like trying to write a letter in Greek when you only speak English,” Wiskerchen warns. “So start this process after at least some of your team have grasped the fundamentals of ICD-10.” This is where the data from your ICD-9 frequency report comes in. Use it to prioritize which codes to map first with a goal of mapping your top 25 ICD-9 codes to their ICD-10 equivalents by August 31.
Invest in good tools to support your mapping efforts. Avoid general mapping equivalent (GEM) coding tools, which are free for a good reason—they are incomplete and don’t always lead you to the correct ICD-10 code. Instead, purchase resources from credible sources, such as the American Medical Association (AMA; www.ama-assn.org). The AMA publishes ICD-10-CM 2016: The Complete Official Codebook as well as ICD-10-CM Mappings 2016, which links ICD-9 codes to all valid ICD-10 alternatives. The AMA also offers electronic ICD-10-CM Express Reference Mapping Cards for multiple specialties.
Practice makes perfect and crosswalking from ICD-9 to ICD-10 is one of the best ways for your team to become aware of the nuances in the new coding system. Like learning a new language, “speaking” ICD-10 does not become automatic just because you’ve attended training or completed the coding maps. Training teaches the architecture of the new coding system. Mapping provides a structured way to become familiar with the codes the practice will use most often. Once these 2 primary pieces are understood and assimilated, most physicians find that dictating the necessary new terms becomes quite easy.
4. Conduct a gap analysis to identify the ICD-10 terms missing from each provider’s current documentation
Conduct the gap analysis after your team has completed training, and once you’ve at least begun the process of mapping codes from ICD-9 to ICD-10. Here’s how:
- Generate a CPT frequency report.
- Select the top 5 procedures for each physician.
- Pull 2 patients’ notes for each of the top procedures.
- Review the notes and try to select ICD-10 code(s).
If key ICD-10 terms are not included in current documentation, physicians should modify the templates or macros they rely on for dictation.
“This simple exercise makes it obvious which clinical information physicians must add for ICD-10,” Wiskerchen says. For example, if the patient had an arthroscopy, but the note doesn’t specify on which leg, that’s a clear indication that the physician must dictate laterality. “The gap analysis is a great way to coach physicians about the clinical details to document, so staff can bill under ICD-10,” Wiskerchen says.
5. Contact technology vendors
Given the number of new ICD-10 codes in orthopedics, paper cheat sheets will be obsolete. Instead, you’ll need to rely on pull-down menus and/or search fields in the electronic health record (EHR) and practice management systems.
“Get clarity about how the new features and workflow processes will work in your systems,” suggests Wiskerchen. “Ask questions such as: Which features will be added or changed to accommodate the new codes? Will there be new screens or pick lists for ICD-10, or search fields? How will new screens and features change our current workflow? And schedule any necessary training as soon as possible.”
In addition to software upgrades and training, vendors and clearinghouses offer an array of services to help practices make the transition. Some vendors even provide help coordinating your internal plan with their new product features and training. Contact vendors to find out what they offer.
6. Use completed code maps to build diagnosis code databases, EHR templates, charge tickets, pick lists, prompters, and other coding tools
“Provide the code crosswalks and results of your documentation gap analysis to the IT [information technology] team so they can get started,” Wiskerchen advises. “And assign a physician or midlevel provider to work with IT so that the tools are clinically accurate.”
7. Schedule testing with clearinghouses and payers
“Successful testing indicates that your hard work has paid off, and that claims will be processed with few, if any, ICD-10–related hiccups,” Wiskerchen says. Essentially, the testing confirms that your ICD-10 code database, pick lists, vendor features, and other coding fields are working properly. “Testing with a clearinghouse is good. Testing directly with the payer is even better, if you are a direct submitter and it is allowed,” Wiskerchen suggests. Contact your clearinghouse and/or payers for testing opportunities prior to October 1.
8. Develop a plan for a potential cash flow crunch
So what happens if your best efforts in the 11th hour still aren’t enough to get your practice to the ICD-10 finish line? Prepare for the possibility of increased claim denials and temporary cash flow stalls, and put a plan in place to deal with them.
Start now by cleaning up as much of the accounts receivable as possible, and moving patient collections up front. Ask the billing team for a weekly status update of the largest unpaid balances in the 60-day aging column, and what has been done to appeal or otherwise address them. Analyze denial patterns and trends and fix their causes at the source—some may be ICD-10–related, others may simply be a gap in the reimbursement process that needs improvement.
Use payer cost estimators to calculate patient out-of-pocket cost and to collect unmet deductibles, coinsurance, and noncovered services prior to surgery. The surgeon-developed iPhone app Health Insurance Arithmetic2 ($1.99 in the iTunes Store) can help staff do this math on one, simple screen.
Finally, secure a line of credit to guard against a claim denial pile up this fall. A line of credit mitigates financial risk by making cash available quickly, should you need it to cover temporary revenue shortfalls, meet payroll, or pay operational expenses. It’s not too late to meet with your banker and apply for this protection, and the peace of mind may even help you sleep better.
1. KarenZupko & Associates, Inc. Pre-course survey of Q1 2015 coding and reimbursement workshop attendees. [Workshops are cosponsored by the American Academy of Orthopaedic Surgeons.] Unpublished data, April 2015.
2. Health Insurance Arithmetic. iTunes Store website. https://itunes.apple.com/us/app/healthinsurancearithmetic/id953262818. Accessed May 12, 2015.
1. KarenZupko & Associates, Inc. Pre-course survey of Q1 2015 coding and reimbursement workshop attendees. [Workshops are cosponsored by the American Academy of Orthopaedic Surgeons.] Unpublished data, April 2015.
2. Health Insurance Arithmetic. iTunes Store website. https://itunes.apple.com/us/app/healthinsurancearithmetic/id953262818. Accessed May 12, 2015.
Small practices, say hello to the VBM
While much has been written about the Center for Medicare & Medicaid Services (CMS) plan to shift its payment system away from fee for service and toward a “value-based” structure, most physicians in small and solo private settings have given little, if any, thought to its potential impact on their practices. That is about to change.
The principal vehicle for the CMS plan is something called the Value-Based Payment Modifier (VBM), a component of the Affordable Care Act (ACA). The VBM has been off the radar of smaller private practices, because up until now it has applied only to groups with more than 10 providers. Starting this year, it applies to everyone. If you accept Medicare patients, regardless of the size of your practice, VBM will become part of your life – because your 2017 Medicare payments will be adjusted based on your 2015 VBM “score.”
That score will be based on your “quality of care” (as defined by the CMS) and how much your care costs the system, compared with care provided by other physicians. The quality component will be calculated from measures reported through the Physician Quality Reporting System (PQRS). Your practice will then be “tiered” to determine whether your performance is statistically better, the same, or worse than the national mean. The CMS has not shared all the details of its “quality tiering” formula, but you can get an idea of their general criteria by reviewing the recently released “Quality Benchmarks for the 2015 Value Modifier” at CMS.org.
To calculate the cost component, the CMS will evaluate measures that include total overall costs per beneficiary, and total costs for a composite of chronic conditions, such as (for internists) chronic obstructive pulmonary disease, heart failure, coronary artery disease, and diabetes; no one has speculated on which diseases might be used for dermatology. Practitioners are eligible for a 1% bonus if their average score is in the top 25% of all scores nationwide. You can get some sense of where you stand in the national hierarchy by studying your Quality Resource and Use Report (QRUR), which gathers information about each practice’s quality and performance rates for the VBM. Reports for the first half of 2014 were released by the CMS in April, and can be downloaded from the QRUR section of CMS.gov.
The ACA requires that the program be budget neutral – which means that all bonuses to physicians in the highest 25% must be offset by penalties – “negative adjustments” – to those in the lowest 25%. The good news is that groups with two to nine providers, and solo practitioners who report successfully for PQRS, receive only the upward or neutral adjustment for 2017, with no downward adjustments. That means you will have at least one penalty-free year to determine where you stand in the VBM pecking order – and perhaps earn a bonus.
So in summary, here is what you have to do now, in 2015, to maximize your chances of earning that upward adjustment in 2017:
• If you haven’t already, make sure your practice data are correct in the Medicare Provider Enrollment, Chain, and Ownership System (PECOS). This is where CMS will gather data for the VBM and the Physician Feedback Reports.
• Study the Quality Benchmarks and download your practice’s QRUR, as mentioned.
• Report successfully for PQRS in 2015, which will also avoid an automatic penalty of 4% in 2017.
Are there serious potential consequences inherent in this unprecedented new system? I think so. For all the talk that the transition from fee-for-service to “value-based” reimbursement would result in better care at a lower cost, there is little evidence that care is improving, and even less that costs are decreasing.
In essence, the VBM establishes arbitrary practice standards and spending ceilings. It creates new incentives to practice “cookbook” medicine, and new disincentives to order tests, consults, or medications, even when doing so would clearly be in a patient’s best interest. Physicians who have the temerity to practice medicine as they see fit, irrespective of the costs involved, will be punished.
Patients will certainly not welcome their physicians’ new reluctance to recommend appropriate interventions for fear of generating excessive costs, and should a less-than-thorough work-up lead to a missed diagnosis, the ACA offers no protection at all from any resulting malpractice litigation.
All of that said, the VBM is a reality, and can no longer be ignored if you treat Medicare patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters.
While much has been written about the Center for Medicare & Medicaid Services (CMS) plan to shift its payment system away from fee for service and toward a “value-based” structure, most physicians in small and solo private settings have given little, if any, thought to its potential impact on their practices. That is about to change.
The principal vehicle for the CMS plan is something called the Value-Based Payment Modifier (VBM), a component of the Affordable Care Act (ACA). The VBM has been off the radar of smaller private practices, because up until now it has applied only to groups with more than 10 providers. Starting this year, it applies to everyone. If you accept Medicare patients, regardless of the size of your practice, VBM will become part of your life – because your 2017 Medicare payments will be adjusted based on your 2015 VBM “score.”
That score will be based on your “quality of care” (as defined by the CMS) and how much your care costs the system, compared with care provided by other physicians. The quality component will be calculated from measures reported through the Physician Quality Reporting System (PQRS). Your practice will then be “tiered” to determine whether your performance is statistically better, the same, or worse than the national mean. The CMS has not shared all the details of its “quality tiering” formula, but you can get an idea of their general criteria by reviewing the recently released “Quality Benchmarks for the 2015 Value Modifier” at CMS.org.
To calculate the cost component, the CMS will evaluate measures that include total overall costs per beneficiary, and total costs for a composite of chronic conditions, such as (for internists) chronic obstructive pulmonary disease, heart failure, coronary artery disease, and diabetes; no one has speculated on which diseases might be used for dermatology. Practitioners are eligible for a 1% bonus if their average score is in the top 25% of all scores nationwide. You can get some sense of where you stand in the national hierarchy by studying your Quality Resource and Use Report (QRUR), which gathers information about each practice’s quality and performance rates for the VBM. Reports for the first half of 2014 were released by the CMS in April, and can be downloaded from the QRUR section of CMS.gov.
The ACA requires that the program be budget neutral – which means that all bonuses to physicians in the highest 25% must be offset by penalties – “negative adjustments” – to those in the lowest 25%. The good news is that groups with two to nine providers, and solo practitioners who report successfully for PQRS, receive only the upward or neutral adjustment for 2017, with no downward adjustments. That means you will have at least one penalty-free year to determine where you stand in the VBM pecking order – and perhaps earn a bonus.
So in summary, here is what you have to do now, in 2015, to maximize your chances of earning that upward adjustment in 2017:
• If you haven’t already, make sure your practice data are correct in the Medicare Provider Enrollment, Chain, and Ownership System (PECOS). This is where CMS will gather data for the VBM and the Physician Feedback Reports.
• Study the Quality Benchmarks and download your practice’s QRUR, as mentioned.
• Report successfully for PQRS in 2015, which will also avoid an automatic penalty of 4% in 2017.
Are there serious potential consequences inherent in this unprecedented new system? I think so. For all the talk that the transition from fee-for-service to “value-based” reimbursement would result in better care at a lower cost, there is little evidence that care is improving, and even less that costs are decreasing.
In essence, the VBM establishes arbitrary practice standards and spending ceilings. It creates new incentives to practice “cookbook” medicine, and new disincentives to order tests, consults, or medications, even when doing so would clearly be in a patient’s best interest. Physicians who have the temerity to practice medicine as they see fit, irrespective of the costs involved, will be punished.
Patients will certainly not welcome their physicians’ new reluctance to recommend appropriate interventions for fear of generating excessive costs, and should a less-than-thorough work-up lead to a missed diagnosis, the ACA offers no protection at all from any resulting malpractice litigation.
All of that said, the VBM is a reality, and can no longer be ignored if you treat Medicare patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters.
While much has been written about the Center for Medicare & Medicaid Services (CMS) plan to shift its payment system away from fee for service and toward a “value-based” structure, most physicians in small and solo private settings have given little, if any, thought to its potential impact on their practices. That is about to change.
The principal vehicle for the CMS plan is something called the Value-Based Payment Modifier (VBM), a component of the Affordable Care Act (ACA). The VBM has been off the radar of smaller private practices, because up until now it has applied only to groups with more than 10 providers. Starting this year, it applies to everyone. If you accept Medicare patients, regardless of the size of your practice, VBM will become part of your life – because your 2017 Medicare payments will be adjusted based on your 2015 VBM “score.”
That score will be based on your “quality of care” (as defined by the CMS) and how much your care costs the system, compared with care provided by other physicians. The quality component will be calculated from measures reported through the Physician Quality Reporting System (PQRS). Your practice will then be “tiered” to determine whether your performance is statistically better, the same, or worse than the national mean. The CMS has not shared all the details of its “quality tiering” formula, but you can get an idea of their general criteria by reviewing the recently released “Quality Benchmarks for the 2015 Value Modifier” at CMS.org.
To calculate the cost component, the CMS will evaluate measures that include total overall costs per beneficiary, and total costs for a composite of chronic conditions, such as (for internists) chronic obstructive pulmonary disease, heart failure, coronary artery disease, and diabetes; no one has speculated on which diseases might be used for dermatology. Practitioners are eligible for a 1% bonus if their average score is in the top 25% of all scores nationwide. You can get some sense of where you stand in the national hierarchy by studying your Quality Resource and Use Report (QRUR), which gathers information about each practice’s quality and performance rates for the VBM. Reports for the first half of 2014 were released by the CMS in April, and can be downloaded from the QRUR section of CMS.gov.
The ACA requires that the program be budget neutral – which means that all bonuses to physicians in the highest 25% must be offset by penalties – “negative adjustments” – to those in the lowest 25%. The good news is that groups with two to nine providers, and solo practitioners who report successfully for PQRS, receive only the upward or neutral adjustment for 2017, with no downward adjustments. That means you will have at least one penalty-free year to determine where you stand in the VBM pecking order – and perhaps earn a bonus.
So in summary, here is what you have to do now, in 2015, to maximize your chances of earning that upward adjustment in 2017:
• If you haven’t already, make sure your practice data are correct in the Medicare Provider Enrollment, Chain, and Ownership System (PECOS). This is where CMS will gather data for the VBM and the Physician Feedback Reports.
• Study the Quality Benchmarks and download your practice’s QRUR, as mentioned.
• Report successfully for PQRS in 2015, which will also avoid an automatic penalty of 4% in 2017.
Are there serious potential consequences inherent in this unprecedented new system? I think so. For all the talk that the transition from fee-for-service to “value-based” reimbursement would result in better care at a lower cost, there is little evidence that care is improving, and even less that costs are decreasing.
In essence, the VBM establishes arbitrary practice standards and spending ceilings. It creates new incentives to practice “cookbook” medicine, and new disincentives to order tests, consults, or medications, even when doing so would clearly be in a patient’s best interest. Physicians who have the temerity to practice medicine as they see fit, irrespective of the costs involved, will be punished.
Patients will certainly not welcome their physicians’ new reluctance to recommend appropriate interventions for fear of generating excessive costs, and should a less-than-thorough work-up lead to a missed diagnosis, the ACA offers no protection at all from any resulting malpractice litigation.
All of that said, the VBM is a reality, and can no longer be ignored if you treat Medicare patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters.