User login
VIDEO: How should you respond to a possible privacy breach?
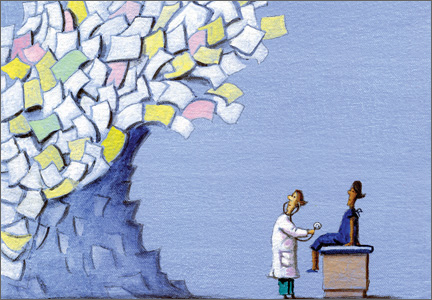
CHICAGO – Overreact, don’t underreact, when it comes to possible health care privacy breaches, attorney Clinton Mikel advised at a conference held by the American Bar Association.
The actions that physicians take immediately following a potential data exposure will significantly impact how the Health and Human Services Department’s Office for Civil Rights (OCR) responds to the incident and whether physicians face penalties, said Mr. Mikel, who specializes in the Health Insurance Portability and Accountability Act (HIPAA) and state privacy laws.
In an interview at the conference, Mr. Mikel, who practices law in Southfield, Mich., discussed common misconceptions that physicians have about privacy breaches and the best ways in which to respond internally to possible exposures. He also offered guidance on the top mistakes to avoid when confronted with possible security breaches and shared perspective on how the OCR might address such issues in the future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
CHICAGO – Overreact, don’t underreact, when it comes to possible health care privacy breaches, attorney Clinton Mikel advised at a conference held by the American Bar Association.
The actions that physicians take immediately following a potential data exposure will significantly impact how the Health and Human Services Department’s Office for Civil Rights (OCR) responds to the incident and whether physicians face penalties, said Mr. Mikel, who specializes in the Health Insurance Portability and Accountability Act (HIPAA) and state privacy laws.
In an interview at the conference, Mr. Mikel, who practices law in Southfield, Mich., discussed common misconceptions that physicians have about privacy breaches and the best ways in which to respond internally to possible exposures. He also offered guidance on the top mistakes to avoid when confronted with possible security breaches and shared perspective on how the OCR might address such issues in the future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
CHICAGO – Overreact, don’t underreact, when it comes to possible health care privacy breaches, attorney Clinton Mikel advised at a conference held by the American Bar Association.
The actions that physicians take immediately following a potential data exposure will significantly impact how the Health and Human Services Department’s Office for Civil Rights (OCR) responds to the incident and whether physicians face penalties, said Mr. Mikel, who specializes in the Health Insurance Portability and Accountability Act (HIPAA) and state privacy laws.
In an interview at the conference, Mr. Mikel, who practices law in Southfield, Mich., discussed common misconceptions that physicians have about privacy breaches and the best ways in which to respond internally to possible exposures. He also offered guidance on the top mistakes to avoid when confronted with possible security breaches and shared perspective on how the OCR might address such issues in the future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS LEGAL ISSUES CONFERENCE
The SGR is abolished! What comes next?
Congratulations, OBG Management readers! After years of hard work and collective advocacy on your part, the US Congress finally passed, and President Barack Obama quickly signed into law, a permanent repeal of the Medicare Sustainable Growth Rate (SGR) physician payment system. Yes, celebrations are in order.
The US House of Representatives passed the bill, HR 2, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), sponsored by American College of Obstetricians and Gynecologists (ACOG) Fellow and US Rep. Michael Burgess (R-TX), on March 26, with 382 Republicans and Democrats voting “Yes.” The Senate followed, on April 14, and agreed with the House to repeal, forever, the Medicare SGR, passing the Burgess bill without amendment, on a bipartisan vote of 92–8. With only hours to go before the scheduled 21.2% cut took effect, the President signed the bill, now Public Law (PL) 114-10, on April 16. The President noted that he was “proud to sign the bill into law.” ACOG is proud to have been such an important part of this landmark moment.
SGR: the perennial nemesis of physicians
The SGR has wreaked havoc on medicine and patient care for 15 years or more. Approximately 30,000 ObGyns participate in Medicare, and many private health insurers use Medicare payment policies, as does TriCare, the nation’s health care coverage for military members and their families. The SGR’s effect was felt widely across medicine, making it nearly impossible for physician practices to invest in health information technology and other patient safety advances, or even to plan for the next year or continue accepting Medicare patients.
When it was introduced last year, HR 2 was supported by more than 600 national and state medical societies and specialty organizations, plus patient and provider organizations, policy think tanks, and advocacy groups across the political spectrum.
ACOG Fellows petitioned their members of Congress with incredible passion, perseverance, and commitment to put an end to the SGR wrecking ball. Hundreds flew into Washington, DC, sent thousands of emails, made phone calls, wrote letters, and personally lobbied at home and in the halls of Congress.
Special kudos, too, to our champions in Congress, and there are many, led by ACOG Fellows and US Reps. Dr. Burgess and Phil Roe, MD (R-TN). Burgess wrote the House bill and, together with Roe, pushed nonstop to get this bill over the finish line. It wouldn’t have happened without them.
ACOG worked tirelessly on its own and in coalition with the American Medical Association, surgical groups, and many other partners. We were able to win important provisions in the statute that we anticipate will greatly help ObGyns successfully transition to this new payment system.
PL114-10 replaces the SGR with a new payment system intended to promote care coordination and quality improvement and lead to better health for our nation’s seniors. Congress developed this new payment plan with the physician community, rather than imposing it on us. That’s why throughout the statute, we see repeated requirements that the Secretary of Health and Human Services must develop quality measures, alternative payment models, and a host of key aspects with input from and in consultation with physicians and the relevant medical specialties, ensuring that physicians retain their preeminent roles in these areas. Funding is provided for quality measure development at $15 million per year from 2015 to 2019.
This law will likely change physician practices more than the ACA ever will, and Congress agreed that physicians should be integral to its development to ensure that they can continue to thrive and provide high-quality care and access for their patients.
Let’s take a closer look at the new Medicare payment system—especially what it will mean for your practice.
What the new law does
Important provisions
- MACRA retains the fee-for-service payment model, now called the Merit-based Incentive Payment System, or MIPS. Physician participation in the Advanced Payment Models (APMs) is entirely voluntary. But physicians who participate in APMs and who score better each year will earn more.
- All physician types are treated equally. Congress didn’t pick specialty winners and losers.
- The new payment system rewards physicians for continuous improvement. You can determine how financially well you do.
- Beginning in 2019, Medicare physician payments will reflect each individual physician’s performance, based on a range of measures developed by the relevant medical specialty that will give individuals options that best reflect their practices.
- Individual physicians will receive confidential quarterly feedback on their performance.
- Technical support is provided for smaller practices, funded at $20 million per year from 2016 to 2020, to help them transition to MIPS and APMs. And physicians in small practices can opt to join a “virtual MIPS group,” associating with other practices or hospitals in the same geographic region or by specialty types.
- The law protects physicians from liability from federal or state standards of care. No health care guideline or other standard developed under federal or state requirements associated with this law may be used as a standard of care or duty of care owed by a health care professional to a patient in a medical liability lawsuit.
MACRA stabilizes the Medicare payment system by permanently repealing the SGR and scheduling payments into the future:
- through June 2015: Stable payments with no cuts
- July 2015–2019: 0.5% annual payment increases to all Medicare physicians
- 2020–2025: No automatic annual payment changes but opportunities for payment increases based on individual performance
- 2026 and beyond: 0.75% annual payment increases for qualifying APMs, 0.25% for MIPS providers, with opportunities in both systems for higher payments based on individual performance.
Top ACOG wins
Among the most meaningful accomplishments achieved by ACOG in its work to repeal the sustainable growth rate are:
- Reliable payment increases for the first 5 years. The law ensures a period of stability with modest Medicare payment in-
creases for 5 years and no cuts, with opportunity for payment increases for the next 5 years. This 5-year period gives physicians time to get ready for the new payment systems. - Protection for low-Medicare–volume physician practices. ObGyns and other physicians with a small Medicare patient population are exempt from many program requirements and penalties.
- Stops the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes, reinstating 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, including urogynecologists and gynecologic oncologists.
- Physician liability protections. The law ensures that federal quality measurements cannot be used to imply medical negligence and generate lawsuits.
- Protection for ultrasound. There are no cuts to ultrasound reimbursement.
- An end, in 2018, to penalties related to electronic health record (EHR) meaningful use, Physician Quality Reporting Systems, and the use of the value-based modifier.
- APM bonus payments. Bonus eligibility for Alternative Payment Model (APM) participation is based on patient volume, not just revenue, to make it easier for ObGyns to qualify.
- 2-year extension of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country.
- Quality-measure development. The law helps professional organizations, such as ACOG, develop quality measures for the Merit-Based Incentive Payment System (MIPS) rather than allow these measures to be developed by a federal agency, ensuring that this new program works for physicians and our patients.
Two payment system options reward continuous quality improvement
Option 1: MIPS. MACRA consolidates and expands pay-for-performance incentives within the old SGR fee-for-service system, creating the new MIPS. Under MIPS, the Physician Quality Reporting System (PQRS), electronic health record (EHR) meaningful use incentive program, and physician value-based modifiers (VBMs) become a single program. In 2019, a physician’s individual score on these measures will be used to adjust his or her Medicare payments, and the penalties previously associated with these programs come to an end.
MACRA creates 4 categories of measures that are weighted to calculate an individual physician’s MIPS score:
- Quality (50% of total adjustment in 2019, shrinking to 30% of total adjustment in 2021). Quality measures currently in use in the PQRS, VBM, and EHR meaningful use programs will continue to be used. The Secretary of Health and Human Services must fund and work with specialty societies to develop any additional measures, and measures utilized in clinical data registries can be used for this category as well. Measures will be updated annually, and ACOG and other specialties can submit measures directly for approval, rather than rely on an outside entity.
- Resource use (10% of total adjustment in 2019, growing to 30% of total adjustment by 2021). Resource use measures are risk-adjusted and include those already used in the VBM program; others must be developed with physicians, reflecting both the physician’s role in treating the patient (eg, primary or specialty care) and the type of treatment (eg, chronic or acute).
- EHR use (25% of total adjustment). Current meaningful use systems will qualify for this category. The law also requires EHR interoperability by 2018 and prohibits the blocking of information sharing between EHR vendors.
- Clinical improvement (15% of total adjustment). This is a new component of physician measurement, intended to give physicians credit for working to improve their practices and help them participate in APMs, which have higher reimbursement potential. This menu of qualifying activities—including 24-hour availability, safety, and patient satisfaction—must be developed with physicians and must be attainable by all specialties and practice types, including small practices and those in rural and underserved areas. Maintenance of certification can be used to qual-ify for a high score.
Physicians will only be assessed on the categories, measures, and activities that apply to them. A physician’s composite score (0–100) will be compared with a performance threshold that reflects all physicians. Those who score above the threshold will receive increased payments; those who score below the threshold will receive reduced payments. Physicians will know these thresholds in advance and will know the score they must reach to avoid penalties and win higher reimbursements in each performance period.
As physicians as a whole improve their performance, the threshold will move with them. So each year, physicians will have the incentive to keep improving their quality, resource use, clinical improvement, and EHR use. A physician’s payment adjustment in one year will not affect his or her payment adjustment in the next year.
The range of potential payment adjustments based on MIPS performance measures increases each year through 2022. Providers who have high scores are rewarded with a 4% increase in 2019. By 2022, the reward is 9%. The program is budget-neutral, so total positive adjustments across all providers will equal total negative adjustments across all providers to poor performers. Separate funds are set aside to reward the highest performers, who will earn bonuses of up to 10% of their fee-for-service payment rate from 2019 through 2024, as well as to help low performers improve and qualify for increased payments from 2016 through 2020.
Help for physicians includes:
- flexibility to participate in a way that best reflects their practice, using risk-adjusted clinical outcome measures
- option to participate in a virtual MIPS group rather than go it alone
- technical assistance to practices with 15 or fewer professionals, $20 million annually from 2016 through 2020, with preference to practices with low MIPS scores and those in rural and underserved areas
- quarterly confidential feedback on performance in the quality and resource use categories
- advance notification to each physician of the score needed to reach higher payment levels
- exclusion from MIPS of physicians who treat few Medicare patients, as well as those who receive a significant portion of their revenues from APMs.
Option 2: APMs. Physicians can earn higher fees by opting out of MIPS fee for service and participating in APMs. The law defines qualifying APMs as those that require participating providers to take on “more than nominal” financial risk, report quality measures, and use certified EHR technology.
APMs will cover multiple services, show that they can limit the growth of spending, and use performance-based methods of compensation. These and other provisions will likely continue the trend away from physicians practicing in solo or small-group fee-for-service practices into risk-based multispecialty settings that are subject to increased management and oversight.
From 2019 to 2024, qualified APM physicians will receive a 5% annual lump sum bonus based on their prior year’s physician fee-schedule payments plus shared savings from participation. This bonus is based on patient volume, not just revenue, to make it easier for ObGyns to qualify. To make the bonus widely available, the Secretary of Health and Human Services must test APMs designed for specific specialties and physicians in small practices. As in MIPS, top APM performers will also receive an additional bonus.
To qualify, physicians must meet increasing thresholds for the percentage of their revenue that they receive through APMs. Those who are below but near the required level of APM revenue can be exempted from MIPS adjustments.
- 2019–2020: 25% of Medicare revenue must be received through APMs.
- 2021–2022: 50% of Medicare revenue or 50% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
- 2023 and beyond: 75% of Medicare revenue or 75% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
Who pays the bill?
Medicare beneficiaries pay more
The new law increases the percentage of Medicare Parts B and D premiums that high-income beneficiaries must pay beginning in 2018:
- Single seniors reporting income of more than $133,500 and married couples with income of more than $267,000 will see their share of premiums rise from 50% to 65%.
- Single seniors reporting income above $160,000 and married couples with income above $320,000 will see their premium share rise from 65% to 80%.
This change will affect about 2% of Medicare beneficiaries; half of all Medicare beneficiaries currently have annual incomes below $26,000.1
Medigap “first-dollar coverage” will end
Many Medigap plans on the market today provide “first-dollar coverage” for beneficiaries, which means that the plans pay the deductibles and copayments so that the beneficiaries have no out-of-pocket costs. Beginning in 2020, Medigap plans will only be available to cover costs above the Medicare Part B deductible, currently $147 per year, for new Medigap enrollees. Many lawmakers thought it was important for Medicare beneficiaries to have “skin in the game.”
The law cuts payments for some providers
To partially offset the cost of repealing the SGR, MACRA cuts Medicare payments to hospitals and postacute providers. It:
- delays Disproportionate Share Hospital (DSH) cuts scheduled to begin in 2017 by a year and extends them through 2025
- requires an increase in payments to hospitals scheduled for 2018 to instead be phased in over 6 years
- limits the 2018 payment update for post-acute providers to 1%.
The law extends many programs
These programs are vital to support the future ObGyn workforce and access to health care. Among these programs are:
- a halt to the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes. The law reinstates 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
- renewal of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country
- establishment of a Medicaid/CHIP Pediatric Quality Measures Program, supporting the development and physician adoption of quality measures, including for prenatal and preconception care
- funding for the Maternal, Infant, and Early Childhood Home Visiting Program, helping at-risk pregnant women and their families to promote healthy births and early childhood development
- funding for community health centers, an important source of care for 13 million women and girls in all 50 states and the District of Columbia
- funding for the National Health Service Corps, bringing ObGyns and other primary care providers to underserved rural and urban areas through scholarships and loan repayment programs
- funding for the Teaching Health Center Graduate Medical Education Payment Program, enhancing training for ObGyns and other primary care providers in community-based settings
- extending the Medicare Geographic Practice Cost Index floor, helping ensure access to care for women in rural areas
- extending the Personal Responsibility Education Program to help prevent teen pregnancies and sexually transmitted infections.
Next steps
It’s very important that ObGyns and other physicians use these early years to understand and get ready for the new payment systems. ACOG is developing educational material for our members, and will work closely with our colleague medical organizations and the Department of Health and Human Services to develop key aspects of the law and ensure that it is properly implemented to work for physicians and patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
1. Aaron HJ. Three cheers for log-rolling: The demise of the SGR. Brookings Health360. http://www.brookings.edu/blogs/health360/posts/2015/04/22-medicare-sgr-repeal-doc-fix-aaron. Published April 22, 2015. Accessed May 12, 2015.
Congratulations, OBG Management readers! After years of hard work and collective advocacy on your part, the US Congress finally passed, and President Barack Obama quickly signed into law, a permanent repeal of the Medicare Sustainable Growth Rate (SGR) physician payment system. Yes, celebrations are in order.
The US House of Representatives passed the bill, HR 2, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), sponsored by American College of Obstetricians and Gynecologists (ACOG) Fellow and US Rep. Michael Burgess (R-TX), on March 26, with 382 Republicans and Democrats voting “Yes.” The Senate followed, on April 14, and agreed with the House to repeal, forever, the Medicare SGR, passing the Burgess bill without amendment, on a bipartisan vote of 92–8. With only hours to go before the scheduled 21.2% cut took effect, the President signed the bill, now Public Law (PL) 114-10, on April 16. The President noted that he was “proud to sign the bill into law.” ACOG is proud to have been such an important part of this landmark moment.
SGR: the perennial nemesis of physicians
The SGR has wreaked havoc on medicine and patient care for 15 years or more. Approximately 30,000 ObGyns participate in Medicare, and many private health insurers use Medicare payment policies, as does TriCare, the nation’s health care coverage for military members and their families. The SGR’s effect was felt widely across medicine, making it nearly impossible for physician practices to invest in health information technology and other patient safety advances, or even to plan for the next year or continue accepting Medicare patients.
When it was introduced last year, HR 2 was supported by more than 600 national and state medical societies and specialty organizations, plus patient and provider organizations, policy think tanks, and advocacy groups across the political spectrum.
ACOG Fellows petitioned their members of Congress with incredible passion, perseverance, and commitment to put an end to the SGR wrecking ball. Hundreds flew into Washington, DC, sent thousands of emails, made phone calls, wrote letters, and personally lobbied at home and in the halls of Congress.
Special kudos, too, to our champions in Congress, and there are many, led by ACOG Fellows and US Reps. Dr. Burgess and Phil Roe, MD (R-TN). Burgess wrote the House bill and, together with Roe, pushed nonstop to get this bill over the finish line. It wouldn’t have happened without them.
ACOG worked tirelessly on its own and in coalition with the American Medical Association, surgical groups, and many other partners. We were able to win important provisions in the statute that we anticipate will greatly help ObGyns successfully transition to this new payment system.
PL114-10 replaces the SGR with a new payment system intended to promote care coordination and quality improvement and lead to better health for our nation’s seniors. Congress developed this new payment plan with the physician community, rather than imposing it on us. That’s why throughout the statute, we see repeated requirements that the Secretary of Health and Human Services must develop quality measures, alternative payment models, and a host of key aspects with input from and in consultation with physicians and the relevant medical specialties, ensuring that physicians retain their preeminent roles in these areas. Funding is provided for quality measure development at $15 million per year from 2015 to 2019.
This law will likely change physician practices more than the ACA ever will, and Congress agreed that physicians should be integral to its development to ensure that they can continue to thrive and provide high-quality care and access for their patients.
Let’s take a closer look at the new Medicare payment system—especially what it will mean for your practice.
What the new law does
Important provisions
- MACRA retains the fee-for-service payment model, now called the Merit-based Incentive Payment System, or MIPS. Physician participation in the Advanced Payment Models (APMs) is entirely voluntary. But physicians who participate in APMs and who score better each year will earn more.
- All physician types are treated equally. Congress didn’t pick specialty winners and losers.
- The new payment system rewards physicians for continuous improvement. You can determine how financially well you do.
- Beginning in 2019, Medicare physician payments will reflect each individual physician’s performance, based on a range of measures developed by the relevant medical specialty that will give individuals options that best reflect their practices.
- Individual physicians will receive confidential quarterly feedback on their performance.
- Technical support is provided for smaller practices, funded at $20 million per year from 2016 to 2020, to help them transition to MIPS and APMs. And physicians in small practices can opt to join a “virtual MIPS group,” associating with other practices or hospitals in the same geographic region or by specialty types.
- The law protects physicians from liability from federal or state standards of care. No health care guideline or other standard developed under federal or state requirements associated with this law may be used as a standard of care or duty of care owed by a health care professional to a patient in a medical liability lawsuit.
MACRA stabilizes the Medicare payment system by permanently repealing the SGR and scheduling payments into the future:
- through June 2015: Stable payments with no cuts
- July 2015–2019: 0.5% annual payment increases to all Medicare physicians
- 2020–2025: No automatic annual payment changes but opportunities for payment increases based on individual performance
- 2026 and beyond: 0.75% annual payment increases for qualifying APMs, 0.25% for MIPS providers, with opportunities in both systems for higher payments based on individual performance.
Top ACOG wins
Among the most meaningful accomplishments achieved by ACOG in its work to repeal the sustainable growth rate are:
- Reliable payment increases for the first 5 years. The law ensures a period of stability with modest Medicare payment in-
creases for 5 years and no cuts, with opportunity for payment increases for the next 5 years. This 5-year period gives physicians time to get ready for the new payment systems. - Protection for low-Medicare–volume physician practices. ObGyns and other physicians with a small Medicare patient population are exempt from many program requirements and penalties.
- Stops the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes, reinstating 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, including urogynecologists and gynecologic oncologists.
- Physician liability protections. The law ensures that federal quality measurements cannot be used to imply medical negligence and generate lawsuits.
- Protection for ultrasound. There are no cuts to ultrasound reimbursement.
- An end, in 2018, to penalties related to electronic health record (EHR) meaningful use, Physician Quality Reporting Systems, and the use of the value-based modifier.
- APM bonus payments. Bonus eligibility for Alternative Payment Model (APM) participation is based on patient volume, not just revenue, to make it easier for ObGyns to qualify.
- 2-year extension of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country.
- Quality-measure development. The law helps professional organizations, such as ACOG, develop quality measures for the Merit-Based Incentive Payment System (MIPS) rather than allow these measures to be developed by a federal agency, ensuring that this new program works for physicians and our patients.
Two payment system options reward continuous quality improvement
Option 1: MIPS. MACRA consolidates and expands pay-for-performance incentives within the old SGR fee-for-service system, creating the new MIPS. Under MIPS, the Physician Quality Reporting System (PQRS), electronic health record (EHR) meaningful use incentive program, and physician value-based modifiers (VBMs) become a single program. In 2019, a physician’s individual score on these measures will be used to adjust his or her Medicare payments, and the penalties previously associated with these programs come to an end.
MACRA creates 4 categories of measures that are weighted to calculate an individual physician’s MIPS score:
- Quality (50% of total adjustment in 2019, shrinking to 30% of total adjustment in 2021). Quality measures currently in use in the PQRS, VBM, and EHR meaningful use programs will continue to be used. The Secretary of Health and Human Services must fund and work with specialty societies to develop any additional measures, and measures utilized in clinical data registries can be used for this category as well. Measures will be updated annually, and ACOG and other specialties can submit measures directly for approval, rather than rely on an outside entity.
- Resource use (10% of total adjustment in 2019, growing to 30% of total adjustment by 2021). Resource use measures are risk-adjusted and include those already used in the VBM program; others must be developed with physicians, reflecting both the physician’s role in treating the patient (eg, primary or specialty care) and the type of treatment (eg, chronic or acute).
- EHR use (25% of total adjustment). Current meaningful use systems will qualify for this category. The law also requires EHR interoperability by 2018 and prohibits the blocking of information sharing between EHR vendors.
- Clinical improvement (15% of total adjustment). This is a new component of physician measurement, intended to give physicians credit for working to improve their practices and help them participate in APMs, which have higher reimbursement potential. This menu of qualifying activities—including 24-hour availability, safety, and patient satisfaction—must be developed with physicians and must be attainable by all specialties and practice types, including small practices and those in rural and underserved areas. Maintenance of certification can be used to qual-ify for a high score.
Physicians will only be assessed on the categories, measures, and activities that apply to them. A physician’s composite score (0–100) will be compared with a performance threshold that reflects all physicians. Those who score above the threshold will receive increased payments; those who score below the threshold will receive reduced payments. Physicians will know these thresholds in advance and will know the score they must reach to avoid penalties and win higher reimbursements in each performance period.
As physicians as a whole improve their performance, the threshold will move with them. So each year, physicians will have the incentive to keep improving their quality, resource use, clinical improvement, and EHR use. A physician’s payment adjustment in one year will not affect his or her payment adjustment in the next year.
The range of potential payment adjustments based on MIPS performance measures increases each year through 2022. Providers who have high scores are rewarded with a 4% increase in 2019. By 2022, the reward is 9%. The program is budget-neutral, so total positive adjustments across all providers will equal total negative adjustments across all providers to poor performers. Separate funds are set aside to reward the highest performers, who will earn bonuses of up to 10% of their fee-for-service payment rate from 2019 through 2024, as well as to help low performers improve and qualify for increased payments from 2016 through 2020.
Help for physicians includes:
- flexibility to participate in a way that best reflects their practice, using risk-adjusted clinical outcome measures
- option to participate in a virtual MIPS group rather than go it alone
- technical assistance to practices with 15 or fewer professionals, $20 million annually from 2016 through 2020, with preference to practices with low MIPS scores and those in rural and underserved areas
- quarterly confidential feedback on performance in the quality and resource use categories
- advance notification to each physician of the score needed to reach higher payment levels
- exclusion from MIPS of physicians who treat few Medicare patients, as well as those who receive a significant portion of their revenues from APMs.
Option 2: APMs. Physicians can earn higher fees by opting out of MIPS fee for service and participating in APMs. The law defines qualifying APMs as those that require participating providers to take on “more than nominal” financial risk, report quality measures, and use certified EHR technology.
APMs will cover multiple services, show that they can limit the growth of spending, and use performance-based methods of compensation. These and other provisions will likely continue the trend away from physicians practicing in solo or small-group fee-for-service practices into risk-based multispecialty settings that are subject to increased management and oversight.
From 2019 to 2024, qualified APM physicians will receive a 5% annual lump sum bonus based on their prior year’s physician fee-schedule payments plus shared savings from participation. This bonus is based on patient volume, not just revenue, to make it easier for ObGyns to qualify. To make the bonus widely available, the Secretary of Health and Human Services must test APMs designed for specific specialties and physicians in small practices. As in MIPS, top APM performers will also receive an additional bonus.
To qualify, physicians must meet increasing thresholds for the percentage of their revenue that they receive through APMs. Those who are below but near the required level of APM revenue can be exempted from MIPS adjustments.
- 2019–2020: 25% of Medicare revenue must be received through APMs.
- 2021–2022: 50% of Medicare revenue or 50% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
- 2023 and beyond: 75% of Medicare revenue or 75% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
Who pays the bill?
Medicare beneficiaries pay more
The new law increases the percentage of Medicare Parts B and D premiums that high-income beneficiaries must pay beginning in 2018:
- Single seniors reporting income of more than $133,500 and married couples with income of more than $267,000 will see their share of premiums rise from 50% to 65%.
- Single seniors reporting income above $160,000 and married couples with income above $320,000 will see their premium share rise from 65% to 80%.
This change will affect about 2% of Medicare beneficiaries; half of all Medicare beneficiaries currently have annual incomes below $26,000.1
Medigap “first-dollar coverage” will end
Many Medigap plans on the market today provide “first-dollar coverage” for beneficiaries, which means that the plans pay the deductibles and copayments so that the beneficiaries have no out-of-pocket costs. Beginning in 2020, Medigap plans will only be available to cover costs above the Medicare Part B deductible, currently $147 per year, for new Medigap enrollees. Many lawmakers thought it was important for Medicare beneficiaries to have “skin in the game.”
The law cuts payments for some providers
To partially offset the cost of repealing the SGR, MACRA cuts Medicare payments to hospitals and postacute providers. It:
- delays Disproportionate Share Hospital (DSH) cuts scheduled to begin in 2017 by a year and extends them through 2025
- requires an increase in payments to hospitals scheduled for 2018 to instead be phased in over 6 years
- limits the 2018 payment update for post-acute providers to 1%.
The law extends many programs
These programs are vital to support the future ObGyn workforce and access to health care. Among these programs are:
- a halt to the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes. The law reinstates 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
- renewal of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country
- establishment of a Medicaid/CHIP Pediatric Quality Measures Program, supporting the development and physician adoption of quality measures, including for prenatal and preconception care
- funding for the Maternal, Infant, and Early Childhood Home Visiting Program, helping at-risk pregnant women and their families to promote healthy births and early childhood development
- funding for community health centers, an important source of care for 13 million women and girls in all 50 states and the District of Columbia
- funding for the National Health Service Corps, bringing ObGyns and other primary care providers to underserved rural and urban areas through scholarships and loan repayment programs
- funding for the Teaching Health Center Graduate Medical Education Payment Program, enhancing training for ObGyns and other primary care providers in community-based settings
- extending the Medicare Geographic Practice Cost Index floor, helping ensure access to care for women in rural areas
- extending the Personal Responsibility Education Program to help prevent teen pregnancies and sexually transmitted infections.
Next steps
It’s very important that ObGyns and other physicians use these early years to understand and get ready for the new payment systems. ACOG is developing educational material for our members, and will work closely with our colleague medical organizations and the Department of Health and Human Services to develop key aspects of the law and ensure that it is properly implemented to work for physicians and patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Congratulations, OBG Management readers! After years of hard work and collective advocacy on your part, the US Congress finally passed, and President Barack Obama quickly signed into law, a permanent repeal of the Medicare Sustainable Growth Rate (SGR) physician payment system. Yes, celebrations are in order.
The US House of Representatives passed the bill, HR 2, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), sponsored by American College of Obstetricians and Gynecologists (ACOG) Fellow and US Rep. Michael Burgess (R-TX), on March 26, with 382 Republicans and Democrats voting “Yes.” The Senate followed, on April 14, and agreed with the House to repeal, forever, the Medicare SGR, passing the Burgess bill without amendment, on a bipartisan vote of 92–8. With only hours to go before the scheduled 21.2% cut took effect, the President signed the bill, now Public Law (PL) 114-10, on April 16. The President noted that he was “proud to sign the bill into law.” ACOG is proud to have been such an important part of this landmark moment.
SGR: the perennial nemesis of physicians
The SGR has wreaked havoc on medicine and patient care for 15 years or more. Approximately 30,000 ObGyns participate in Medicare, and many private health insurers use Medicare payment policies, as does TriCare, the nation’s health care coverage for military members and their families. The SGR’s effect was felt widely across medicine, making it nearly impossible for physician practices to invest in health information technology and other patient safety advances, or even to plan for the next year or continue accepting Medicare patients.
When it was introduced last year, HR 2 was supported by more than 600 national and state medical societies and specialty organizations, plus patient and provider organizations, policy think tanks, and advocacy groups across the political spectrum.
ACOG Fellows petitioned their members of Congress with incredible passion, perseverance, and commitment to put an end to the SGR wrecking ball. Hundreds flew into Washington, DC, sent thousands of emails, made phone calls, wrote letters, and personally lobbied at home and in the halls of Congress.
Special kudos, too, to our champions in Congress, and there are many, led by ACOG Fellows and US Reps. Dr. Burgess and Phil Roe, MD (R-TN). Burgess wrote the House bill and, together with Roe, pushed nonstop to get this bill over the finish line. It wouldn’t have happened without them.
ACOG worked tirelessly on its own and in coalition with the American Medical Association, surgical groups, and many other partners. We were able to win important provisions in the statute that we anticipate will greatly help ObGyns successfully transition to this new payment system.
PL114-10 replaces the SGR with a new payment system intended to promote care coordination and quality improvement and lead to better health for our nation’s seniors. Congress developed this new payment plan with the physician community, rather than imposing it on us. That’s why throughout the statute, we see repeated requirements that the Secretary of Health and Human Services must develop quality measures, alternative payment models, and a host of key aspects with input from and in consultation with physicians and the relevant medical specialties, ensuring that physicians retain their preeminent roles in these areas. Funding is provided for quality measure development at $15 million per year from 2015 to 2019.
This law will likely change physician practices more than the ACA ever will, and Congress agreed that physicians should be integral to its development to ensure that they can continue to thrive and provide high-quality care and access for their patients.
Let’s take a closer look at the new Medicare payment system—especially what it will mean for your practice.
What the new law does
Important provisions
- MACRA retains the fee-for-service payment model, now called the Merit-based Incentive Payment System, or MIPS. Physician participation in the Advanced Payment Models (APMs) is entirely voluntary. But physicians who participate in APMs and who score better each year will earn more.
- All physician types are treated equally. Congress didn’t pick specialty winners and losers.
- The new payment system rewards physicians for continuous improvement. You can determine how financially well you do.
- Beginning in 2019, Medicare physician payments will reflect each individual physician’s performance, based on a range of measures developed by the relevant medical specialty that will give individuals options that best reflect their practices.
- Individual physicians will receive confidential quarterly feedback on their performance.
- Technical support is provided for smaller practices, funded at $20 million per year from 2016 to 2020, to help them transition to MIPS and APMs. And physicians in small practices can opt to join a “virtual MIPS group,” associating with other practices or hospitals in the same geographic region or by specialty types.
- The law protects physicians from liability from federal or state standards of care. No health care guideline or other standard developed under federal or state requirements associated with this law may be used as a standard of care or duty of care owed by a health care professional to a patient in a medical liability lawsuit.
MACRA stabilizes the Medicare payment system by permanently repealing the SGR and scheduling payments into the future:
- through June 2015: Stable payments with no cuts
- July 2015–2019: 0.5% annual payment increases to all Medicare physicians
- 2020–2025: No automatic annual payment changes but opportunities for payment increases based on individual performance
- 2026 and beyond: 0.75% annual payment increases for qualifying APMs, 0.25% for MIPS providers, with opportunities in both systems for higher payments based on individual performance.
Top ACOG wins
Among the most meaningful accomplishments achieved by ACOG in its work to repeal the sustainable growth rate are:
- Reliable payment increases for the first 5 years. The law ensures a period of stability with modest Medicare payment in-
creases for 5 years and no cuts, with opportunity for payment increases for the next 5 years. This 5-year period gives physicians time to get ready for the new payment systems. - Protection for low-Medicare–volume physician practices. ObGyns and other physicians with a small Medicare patient population are exempt from many program requirements and penalties.
- Stops the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes, reinstating 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, including urogynecologists and gynecologic oncologists.
- Physician liability protections. The law ensures that federal quality measurements cannot be used to imply medical negligence and generate lawsuits.
- Protection for ultrasound. There are no cuts to ultrasound reimbursement.
- An end, in 2018, to penalties related to electronic health record (EHR) meaningful use, Physician Quality Reporting Systems, and the use of the value-based modifier.
- APM bonus payments. Bonus eligibility for Alternative Payment Model (APM) participation is based on patient volume, not just revenue, to make it easier for ObGyns to qualify.
- 2-year extension of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country.
- Quality-measure development. The law helps professional organizations, such as ACOG, develop quality measures for the Merit-Based Incentive Payment System (MIPS) rather than allow these measures to be developed by a federal agency, ensuring that this new program works for physicians and our patients.
Two payment system options reward continuous quality improvement
Option 1: MIPS. MACRA consolidates and expands pay-for-performance incentives within the old SGR fee-for-service system, creating the new MIPS. Under MIPS, the Physician Quality Reporting System (PQRS), electronic health record (EHR) meaningful use incentive program, and physician value-based modifiers (VBMs) become a single program. In 2019, a physician’s individual score on these measures will be used to adjust his or her Medicare payments, and the penalties previously associated with these programs come to an end.
MACRA creates 4 categories of measures that are weighted to calculate an individual physician’s MIPS score:
- Quality (50% of total adjustment in 2019, shrinking to 30% of total adjustment in 2021). Quality measures currently in use in the PQRS, VBM, and EHR meaningful use programs will continue to be used. The Secretary of Health and Human Services must fund and work with specialty societies to develop any additional measures, and measures utilized in clinical data registries can be used for this category as well. Measures will be updated annually, and ACOG and other specialties can submit measures directly for approval, rather than rely on an outside entity.
- Resource use (10% of total adjustment in 2019, growing to 30% of total adjustment by 2021). Resource use measures are risk-adjusted and include those already used in the VBM program; others must be developed with physicians, reflecting both the physician’s role in treating the patient (eg, primary or specialty care) and the type of treatment (eg, chronic or acute).
- EHR use (25% of total adjustment). Current meaningful use systems will qualify for this category. The law also requires EHR interoperability by 2018 and prohibits the blocking of information sharing between EHR vendors.
- Clinical improvement (15% of total adjustment). This is a new component of physician measurement, intended to give physicians credit for working to improve their practices and help them participate in APMs, which have higher reimbursement potential. This menu of qualifying activities—including 24-hour availability, safety, and patient satisfaction—must be developed with physicians and must be attainable by all specialties and practice types, including small practices and those in rural and underserved areas. Maintenance of certification can be used to qual-ify for a high score.
Physicians will only be assessed on the categories, measures, and activities that apply to them. A physician’s composite score (0–100) will be compared with a performance threshold that reflects all physicians. Those who score above the threshold will receive increased payments; those who score below the threshold will receive reduced payments. Physicians will know these thresholds in advance and will know the score they must reach to avoid penalties and win higher reimbursements in each performance period.
As physicians as a whole improve their performance, the threshold will move with them. So each year, physicians will have the incentive to keep improving their quality, resource use, clinical improvement, and EHR use. A physician’s payment adjustment in one year will not affect his or her payment adjustment in the next year.
The range of potential payment adjustments based on MIPS performance measures increases each year through 2022. Providers who have high scores are rewarded with a 4% increase in 2019. By 2022, the reward is 9%. The program is budget-neutral, so total positive adjustments across all providers will equal total negative adjustments across all providers to poor performers. Separate funds are set aside to reward the highest performers, who will earn bonuses of up to 10% of their fee-for-service payment rate from 2019 through 2024, as well as to help low performers improve and qualify for increased payments from 2016 through 2020.
Help for physicians includes:
- flexibility to participate in a way that best reflects their practice, using risk-adjusted clinical outcome measures
- option to participate in a virtual MIPS group rather than go it alone
- technical assistance to practices with 15 or fewer professionals, $20 million annually from 2016 through 2020, with preference to practices with low MIPS scores and those in rural and underserved areas
- quarterly confidential feedback on performance in the quality and resource use categories
- advance notification to each physician of the score needed to reach higher payment levels
- exclusion from MIPS of physicians who treat few Medicare patients, as well as those who receive a significant portion of their revenues from APMs.
Option 2: APMs. Physicians can earn higher fees by opting out of MIPS fee for service and participating in APMs. The law defines qualifying APMs as those that require participating providers to take on “more than nominal” financial risk, report quality measures, and use certified EHR technology.
APMs will cover multiple services, show that they can limit the growth of spending, and use performance-based methods of compensation. These and other provisions will likely continue the trend away from physicians practicing in solo or small-group fee-for-service practices into risk-based multispecialty settings that are subject to increased management and oversight.
From 2019 to 2024, qualified APM physicians will receive a 5% annual lump sum bonus based on their prior year’s physician fee-schedule payments plus shared savings from participation. This bonus is based on patient volume, not just revenue, to make it easier for ObGyns to qualify. To make the bonus widely available, the Secretary of Health and Human Services must test APMs designed for specific specialties and physicians in small practices. As in MIPS, top APM performers will also receive an additional bonus.
To qualify, physicians must meet increasing thresholds for the percentage of their revenue that they receive through APMs. Those who are below but near the required level of APM revenue can be exempted from MIPS adjustments.
- 2019–2020: 25% of Medicare revenue must be received through APMs.
- 2021–2022: 50% of Medicare revenue or 50% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
- 2023 and beyond: 75% of Medicare revenue or 75% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
Who pays the bill?
Medicare beneficiaries pay more
The new law increases the percentage of Medicare Parts B and D premiums that high-income beneficiaries must pay beginning in 2018:
- Single seniors reporting income of more than $133,500 and married couples with income of more than $267,000 will see their share of premiums rise from 50% to 65%.
- Single seniors reporting income above $160,000 and married couples with income above $320,000 will see their premium share rise from 65% to 80%.
This change will affect about 2% of Medicare beneficiaries; half of all Medicare beneficiaries currently have annual incomes below $26,000.1
Medigap “first-dollar coverage” will end
Many Medigap plans on the market today provide “first-dollar coverage” for beneficiaries, which means that the plans pay the deductibles and copayments so that the beneficiaries have no out-of-pocket costs. Beginning in 2020, Medigap plans will only be available to cover costs above the Medicare Part B deductible, currently $147 per year, for new Medigap enrollees. Many lawmakers thought it was important for Medicare beneficiaries to have “skin in the game.”
The law cuts payments for some providers
To partially offset the cost of repealing the SGR, MACRA cuts Medicare payments to hospitals and postacute providers. It:
- delays Disproportionate Share Hospital (DSH) cuts scheduled to begin in 2017 by a year and extends them through 2025
- requires an increase in payments to hospitals scheduled for 2018 to instead be phased in over 6 years
- limits the 2018 payment update for post-acute providers to 1%.
The law extends many programs
These programs are vital to support the future ObGyn workforce and access to health care. Among these programs are:
- a halt to the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes. The law reinstates 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
- renewal of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country
- establishment of a Medicaid/CHIP Pediatric Quality Measures Program, supporting the development and physician adoption of quality measures, including for prenatal and preconception care
- funding for the Maternal, Infant, and Early Childhood Home Visiting Program, helping at-risk pregnant women and their families to promote healthy births and early childhood development
- funding for community health centers, an important source of care for 13 million women and girls in all 50 states and the District of Columbia
- funding for the National Health Service Corps, bringing ObGyns and other primary care providers to underserved rural and urban areas through scholarships and loan repayment programs
- funding for the Teaching Health Center Graduate Medical Education Payment Program, enhancing training for ObGyns and other primary care providers in community-based settings
- extending the Medicare Geographic Practice Cost Index floor, helping ensure access to care for women in rural areas
- extending the Personal Responsibility Education Program to help prevent teen pregnancies and sexually transmitted infections.
Next steps
It’s very important that ObGyns and other physicians use these early years to understand and get ready for the new payment systems. ACOG is developing educational material for our members, and will work closely with our colleague medical organizations and the Department of Health and Human Services to develop key aspects of the law and ensure that it is properly implemented to work for physicians and patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
1. Aaron HJ. Three cheers for log-rolling: The demise of the SGR. Brookings Health360. http://www.brookings.edu/blogs/health360/posts/2015/04/22-medicare-sgr-repeal-doc-fix-aaron. Published April 22, 2015. Accessed May 12, 2015.
Reference
1. Aaron HJ. Three cheers for log-rolling: The demise of the SGR. Brookings Health360. http://www.brookings.edu/blogs/health360/posts/2015/04/22-medicare-sgr-repeal-doc-fix-aaron. Published April 22, 2015. Accessed May 12, 2015.
Sunshine Act – another reminder
I’ve written about the Physician Payment Sunshine Act several times since it became law in 2013. My basic opinion – that it is a tempest in a teapot – has not changed. Nonetheless, now is the time to review the 2014 data reported under your name – and if necessary, initiate a dispute – before the information is posted publicly on June 30.
A quick review: The Sunshine Act, known officially as the “Open Payments Program,” requires all manufacturers of drugs, devices, and medical supplies covered by federal health care programs to report to the Centers for Medicare & Medicaid Services any financial interactions with physicians and teaching hospitals.
Reportable interactions include consulting, food, ownership or investment interest, direct compensation for speakers at education programs, and research. Compensation for clinical trials must be reported but is not made public until the product receives FDA approval, or until 4 years after the payment, whichever is earlier. Payments for trials involving a new indication for an approved drug are posted the following year.
Exemptions include CME activities funded by manufacturers and product samples for patient use. Medical students and residents are exempted entirely.
You are allowed to review your data and request corrections before information is posted publicly. You will have an additional 2 years to pursue corrections after the content goes live at the end of June, but any erroneous information will remain online until the next scheduled update, so you should find and fix errors as promptly as possible.
If you don’t see drug reps, accept sponsored lunches, or give sponsored talks, don’t assume that you won’t be on the website. Check anyway: You might be indirectly involved in a compensation that you were not aware of, or you might have been reported in error.
To review your data, register at the CMS Enterprise Portal (https://portal.cms.gov/wps/portal/unauthportal/home/) and request access to the Open Payments system.
The question remains as to what effect the law might be having on research, continuing education, or physicians’ relationships with the pharmaceutical industry. The short answer is that no one knows. The first data posting this past September came and went with little fanfare, and no repercussions directly attributable to the program have been reported as of this writing.
Sunshine laws have been in effect for several years in six states: California, Colorado, Massachusetts, Minnesota, Vermont, and West Virginia, plus the District of Columbia. (Maine repealed its law in 2011.) Observers disagree on their impact. Studies in Maine and West Virginia showed no significant public reaction or changes in prescribing patterns, according to a 2012 article in the Archives of Internal Medicine (now JAMA Internal Medicine).
Reactions from the public are equally inscrutable. Do citizens think less of doctors who accept the occasional industry-sponsored lunch for their employees? Do they think more of doctors who speak at meetings, or conduct industry-sponsored clinical research? There are no objective data. Anecdotally, I haven’t heard a peep – positive, negative, or indifferent – from any of my patients, nor have any other physicians that I’ve asked.
As of now, I stand by my initial prediction that attorneys, activists, and the occasional reporter will data-mine the information for various purposes, but few patients will bother to visit. Of course, that doesn’t mean you should ignore it as well. As always, I suggest you review the accuracy of anything posted about you, in any form or context, on any venue. This year’s data (reflecting all 2014 reports) have been available for review since April 6. You can initiate a dispute at any time over the next 2 years, before or after public release on June 30, but the sooner the better. Corrections are made each time CMS updates the system.
Maintaining accurate financial records has always been important, but it will be even more important now to support your disputes. CMS won’t simply take your word for it. A free app is available to help you track payments and other reportable industry interactions; search for “Open Payments” at your favorite app store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
I’ve written about the Physician Payment Sunshine Act several times since it became law in 2013. My basic opinion – that it is a tempest in a teapot – has not changed. Nonetheless, now is the time to review the 2014 data reported under your name – and if necessary, initiate a dispute – before the information is posted publicly on June 30.
A quick review: The Sunshine Act, known officially as the “Open Payments Program,” requires all manufacturers of drugs, devices, and medical supplies covered by federal health care programs to report to the Centers for Medicare & Medicaid Services any financial interactions with physicians and teaching hospitals.
Reportable interactions include consulting, food, ownership or investment interest, direct compensation for speakers at education programs, and research. Compensation for clinical trials must be reported but is not made public until the product receives FDA approval, or until 4 years after the payment, whichever is earlier. Payments for trials involving a new indication for an approved drug are posted the following year.
Exemptions include CME activities funded by manufacturers and product samples for patient use. Medical students and residents are exempted entirely.
You are allowed to review your data and request corrections before information is posted publicly. You will have an additional 2 years to pursue corrections after the content goes live at the end of June, but any erroneous information will remain online until the next scheduled update, so you should find and fix errors as promptly as possible.
If you don’t see drug reps, accept sponsored lunches, or give sponsored talks, don’t assume that you won’t be on the website. Check anyway: You might be indirectly involved in a compensation that you were not aware of, or you might have been reported in error.
To review your data, register at the CMS Enterprise Portal (https://portal.cms.gov/wps/portal/unauthportal/home/) and request access to the Open Payments system.
The question remains as to what effect the law might be having on research, continuing education, or physicians’ relationships with the pharmaceutical industry. The short answer is that no one knows. The first data posting this past September came and went with little fanfare, and no repercussions directly attributable to the program have been reported as of this writing.
Sunshine laws have been in effect for several years in six states: California, Colorado, Massachusetts, Minnesota, Vermont, and West Virginia, plus the District of Columbia. (Maine repealed its law in 2011.) Observers disagree on their impact. Studies in Maine and West Virginia showed no significant public reaction or changes in prescribing patterns, according to a 2012 article in the Archives of Internal Medicine (now JAMA Internal Medicine).
Reactions from the public are equally inscrutable. Do citizens think less of doctors who accept the occasional industry-sponsored lunch for their employees? Do they think more of doctors who speak at meetings, or conduct industry-sponsored clinical research? There are no objective data. Anecdotally, I haven’t heard a peep – positive, negative, or indifferent – from any of my patients, nor have any other physicians that I’ve asked.
As of now, I stand by my initial prediction that attorneys, activists, and the occasional reporter will data-mine the information for various purposes, but few patients will bother to visit. Of course, that doesn’t mean you should ignore it as well. As always, I suggest you review the accuracy of anything posted about you, in any form or context, on any venue. This year’s data (reflecting all 2014 reports) have been available for review since April 6. You can initiate a dispute at any time over the next 2 years, before or after public release on June 30, but the sooner the better. Corrections are made each time CMS updates the system.
Maintaining accurate financial records has always been important, but it will be even more important now to support your disputes. CMS won’t simply take your word for it. A free app is available to help you track payments and other reportable industry interactions; search for “Open Payments” at your favorite app store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
I’ve written about the Physician Payment Sunshine Act several times since it became law in 2013. My basic opinion – that it is a tempest in a teapot – has not changed. Nonetheless, now is the time to review the 2014 data reported under your name – and if necessary, initiate a dispute – before the information is posted publicly on June 30.
A quick review: The Sunshine Act, known officially as the “Open Payments Program,” requires all manufacturers of drugs, devices, and medical supplies covered by federal health care programs to report to the Centers for Medicare & Medicaid Services any financial interactions with physicians and teaching hospitals.
Reportable interactions include consulting, food, ownership or investment interest, direct compensation for speakers at education programs, and research. Compensation for clinical trials must be reported but is not made public until the product receives FDA approval, or until 4 years after the payment, whichever is earlier. Payments for trials involving a new indication for an approved drug are posted the following year.
Exemptions include CME activities funded by manufacturers and product samples for patient use. Medical students and residents are exempted entirely.
You are allowed to review your data and request corrections before information is posted publicly. You will have an additional 2 years to pursue corrections after the content goes live at the end of June, but any erroneous information will remain online until the next scheduled update, so you should find and fix errors as promptly as possible.
If you don’t see drug reps, accept sponsored lunches, or give sponsored talks, don’t assume that you won’t be on the website. Check anyway: You might be indirectly involved in a compensation that you were not aware of, or you might have been reported in error.
To review your data, register at the CMS Enterprise Portal (https://portal.cms.gov/wps/portal/unauthportal/home/) and request access to the Open Payments system.
The question remains as to what effect the law might be having on research, continuing education, or physicians’ relationships with the pharmaceutical industry. The short answer is that no one knows. The first data posting this past September came and went with little fanfare, and no repercussions directly attributable to the program have been reported as of this writing.
Sunshine laws have been in effect for several years in six states: California, Colorado, Massachusetts, Minnesota, Vermont, and West Virginia, plus the District of Columbia. (Maine repealed its law in 2011.) Observers disagree on their impact. Studies in Maine and West Virginia showed no significant public reaction or changes in prescribing patterns, according to a 2012 article in the Archives of Internal Medicine (now JAMA Internal Medicine).
Reactions from the public are equally inscrutable. Do citizens think less of doctors who accept the occasional industry-sponsored lunch for their employees? Do they think more of doctors who speak at meetings, or conduct industry-sponsored clinical research? There are no objective data. Anecdotally, I haven’t heard a peep – positive, negative, or indifferent – from any of my patients, nor have any other physicians that I’ve asked.
As of now, I stand by my initial prediction that attorneys, activists, and the occasional reporter will data-mine the information for various purposes, but few patients will bother to visit. Of course, that doesn’t mean you should ignore it as well. As always, I suggest you review the accuracy of anything posted about you, in any form or context, on any venue. This year’s data (reflecting all 2014 reports) have been available for review since April 6. You can initiate a dispute at any time over the next 2 years, before or after public release on June 30, but the sooner the better. Corrections are made each time CMS updates the system.
Maintaining accurate financial records has always been important, but it will be even more important now to support your disputes. CMS won’t simply take your word for it. A free app is available to help you track payments and other reportable industry interactions; search for “Open Payments” at your favorite app store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Family Medicine’s Increasing Presence in Hospital Medicine
Years ago, I struggled with a difficult decision. Given the fact that the military disallowed dual training tracks, such as internal medicine/pediatrics (med/peds), I had to choose from internal medicine (IM), pediatrics (Peds), or family practice (FP) residencies. My personal history and experiential data remained incomplete and the view ahead blurry; still, the choice remained.
Over time, I’ve embraced the uncertainty inherent in most analyses. Such is the case with the current composition of specialties that make up hospital medicine nationwide. Available data remains in flux, yet I see apparent trends.
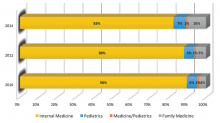
A new question in the 2014 State of Hospital Medicine (SOHM) report asked, “Did your hospital medicine group employ hospitalist physicians trained and certified in the following specialties…?” Strikingly, a full 59% of groups serving adult patients only reported having at least one family medicine-trained provider in their midst! And in these adult-only practices, 98% of groups utilized at least one internal medicine physician, 24% reported a med/peds doc, and none reported pediatricians.
Meanwhile, of 40 groups caring for children only, 95% reported using pediatrics, 2.5% internal medicine (huh?), 22.5% med/peds, and zero FPs. The 19 groups serving both adults and children revealed participation from all four nonsurgical hospitalist specialties (IM, peds, FP, med/peds).
So what is the specialty distribution of medical hospitalists overall? There’s no good data about this.
The 2014 Medical Group Management Association (MGMA) sample, licensed for use in SOHM, reported data for roughly 4,200 community hospital medicine providers: 82% were internal medicine, 10% family medicine, 7% pediatrics, and <1% med/peds. MGMA, however, cautions against assuming that this represents the entire population of hospitalists and their training. Although representative of the groups who participated in the survey, it may not be representative of groups that didn’t participate, and thus it would be misleading to suggest that this distribution holds true nationally.
In an effort to corroborate the MGMA distribution, I reviewed other compensation and productivity surveys; one such survey, conducted by the American Medical Group Association, reported hospitalists by training program. It contained over 3,700 community hospital providers—89% internal medicine, 6% family medicine, 5% pediatrics—but did not inquire about medicine/pediatrics.
Finally, if one combines the academic and community provider samples from MGMA (n=4,867), the distribution is 80% IM, 8.5% FP, 10% peds, and <1% med/peds.
Which of these, if any, is the actual distribution of nonprocedural hospitalists? Although we cannot know exactly, I believe something close to the following to be current state: internal medicine 80%, family medicine 10%, pediatrics 10%, and medicine/pediatrics <1%.
It is clear from survey trends that the proportion of family medicine providers is growing, while the internal medicine super-majority is shrinking somewhat. Pediatrics appears to remain stable as a proportion of the total, as does med/peds, with the latter unable to grow in numbers proportionally given the small number of providers nationally compared to the other three fields.
The growth of family medicine-trained hospitalists relates to the continued high demand for the profession, with such residents comprising the largest pool of available providers, second only to internal medicine.
Based on the SHM survey, family medicine hospitalists seem to practice similarly to IM; they generally see adults only. It appears that they are accepted into traditional adult hospitalist practices, readily contrasting with groups serving children, which report no FP participation. Meanwhile, med/peds hospitalists provide care across the spectrum of hospitalist groups, though they often report splitting their duties between adults-only services and pediatric services.
As for me, a generation removed from my election of a family practice internship and subsequent transition to internal medicine residency, I should not have worried so. Both paths can lead to hospital medicine.
Dr. Ahlstrom is a hospitalist at Indigo Health Partners in Traverse City, Mich., and a member of SHM’s Practice Analysis Committee.
Years ago, I struggled with a difficult decision. Given the fact that the military disallowed dual training tracks, such as internal medicine/pediatrics (med/peds), I had to choose from internal medicine (IM), pediatrics (Peds), or family practice (FP) residencies. My personal history and experiential data remained incomplete and the view ahead blurry; still, the choice remained.
Over time, I’ve embraced the uncertainty inherent in most analyses. Such is the case with the current composition of specialties that make up hospital medicine nationwide. Available data remains in flux, yet I see apparent trends.
A new question in the 2014 State of Hospital Medicine (SOHM) report asked, “Did your hospital medicine group employ hospitalist physicians trained and certified in the following specialties…?” Strikingly, a full 59% of groups serving adult patients only reported having at least one family medicine-trained provider in their midst! And in these adult-only practices, 98% of groups utilized at least one internal medicine physician, 24% reported a med/peds doc, and none reported pediatricians.
Meanwhile, of 40 groups caring for children only, 95% reported using pediatrics, 2.5% internal medicine (huh?), 22.5% med/peds, and zero FPs. The 19 groups serving both adults and children revealed participation from all four nonsurgical hospitalist specialties (IM, peds, FP, med/peds).
So what is the specialty distribution of medical hospitalists overall? There’s no good data about this.
The 2014 Medical Group Management Association (MGMA) sample, licensed for use in SOHM, reported data for roughly 4,200 community hospital medicine providers: 82% were internal medicine, 10% family medicine, 7% pediatrics, and <1% med/peds. MGMA, however, cautions against assuming that this represents the entire population of hospitalists and their training. Although representative of the groups who participated in the survey, it may not be representative of groups that didn’t participate, and thus it would be misleading to suggest that this distribution holds true nationally.
In an effort to corroborate the MGMA distribution, I reviewed other compensation and productivity surveys; one such survey, conducted by the American Medical Group Association, reported hospitalists by training program. It contained over 3,700 community hospital providers—89% internal medicine, 6% family medicine, 5% pediatrics—but did not inquire about medicine/pediatrics.
Finally, if one combines the academic and community provider samples from MGMA (n=4,867), the distribution is 80% IM, 8.5% FP, 10% peds, and <1% med/peds.
Which of these, if any, is the actual distribution of nonprocedural hospitalists? Although we cannot know exactly, I believe something close to the following to be current state: internal medicine 80%, family medicine 10%, pediatrics 10%, and medicine/pediatrics <1%.
It is clear from survey trends that the proportion of family medicine providers is growing, while the internal medicine super-majority is shrinking somewhat. Pediatrics appears to remain stable as a proportion of the total, as does med/peds, with the latter unable to grow in numbers proportionally given the small number of providers nationally compared to the other three fields.
The growth of family medicine-trained hospitalists relates to the continued high demand for the profession, with such residents comprising the largest pool of available providers, second only to internal medicine.
Based on the SHM survey, family medicine hospitalists seem to practice similarly to IM; they generally see adults only. It appears that they are accepted into traditional adult hospitalist practices, readily contrasting with groups serving children, which report no FP participation. Meanwhile, med/peds hospitalists provide care across the spectrum of hospitalist groups, though they often report splitting their duties between adults-only services and pediatric services.
As for me, a generation removed from my election of a family practice internship and subsequent transition to internal medicine residency, I should not have worried so. Both paths can lead to hospital medicine.
Dr. Ahlstrom is a hospitalist at Indigo Health Partners in Traverse City, Mich., and a member of SHM’s Practice Analysis Committee.
Years ago, I struggled with a difficult decision. Given the fact that the military disallowed dual training tracks, such as internal medicine/pediatrics (med/peds), I had to choose from internal medicine (IM), pediatrics (Peds), or family practice (FP) residencies. My personal history and experiential data remained incomplete and the view ahead blurry; still, the choice remained.
Over time, I’ve embraced the uncertainty inherent in most analyses. Such is the case with the current composition of specialties that make up hospital medicine nationwide. Available data remains in flux, yet I see apparent trends.
A new question in the 2014 State of Hospital Medicine (SOHM) report asked, “Did your hospital medicine group employ hospitalist physicians trained and certified in the following specialties…?” Strikingly, a full 59% of groups serving adult patients only reported having at least one family medicine-trained provider in their midst! And in these adult-only practices, 98% of groups utilized at least one internal medicine physician, 24% reported a med/peds doc, and none reported pediatricians.
Meanwhile, of 40 groups caring for children only, 95% reported using pediatrics, 2.5% internal medicine (huh?), 22.5% med/peds, and zero FPs. The 19 groups serving both adults and children revealed participation from all four nonsurgical hospitalist specialties (IM, peds, FP, med/peds).
So what is the specialty distribution of medical hospitalists overall? There’s no good data about this.
The 2014 Medical Group Management Association (MGMA) sample, licensed for use in SOHM, reported data for roughly 4,200 community hospital medicine providers: 82% were internal medicine, 10% family medicine, 7% pediatrics, and <1% med/peds. MGMA, however, cautions against assuming that this represents the entire population of hospitalists and their training. Although representative of the groups who participated in the survey, it may not be representative of groups that didn’t participate, and thus it would be misleading to suggest that this distribution holds true nationally.
In an effort to corroborate the MGMA distribution, I reviewed other compensation and productivity surveys; one such survey, conducted by the American Medical Group Association, reported hospitalists by training program. It contained over 3,700 community hospital providers—89% internal medicine, 6% family medicine, 5% pediatrics—but did not inquire about medicine/pediatrics.
Finally, if one combines the academic and community provider samples from MGMA (n=4,867), the distribution is 80% IM, 8.5% FP, 10% peds, and <1% med/peds.
Which of these, if any, is the actual distribution of nonprocedural hospitalists? Although we cannot know exactly, I believe something close to the following to be current state: internal medicine 80%, family medicine 10%, pediatrics 10%, and medicine/pediatrics <1%.
It is clear from survey trends that the proportion of family medicine providers is growing, while the internal medicine super-majority is shrinking somewhat. Pediatrics appears to remain stable as a proportion of the total, as does med/peds, with the latter unable to grow in numbers proportionally given the small number of providers nationally compared to the other three fields.
The growth of family medicine-trained hospitalists relates to the continued high demand for the profession, with such residents comprising the largest pool of available providers, second only to internal medicine.
Based on the SHM survey, family medicine hospitalists seem to practice similarly to IM; they generally see adults only. It appears that they are accepted into traditional adult hospitalist practices, readily contrasting with groups serving children, which report no FP participation. Meanwhile, med/peds hospitalists provide care across the spectrum of hospitalist groups, though they often report splitting their duties between adults-only services and pediatric services.
As for me, a generation removed from my election of a family practice internship and subsequent transition to internal medicine residency, I should not have worried so. Both paths can lead to hospital medicine.
Dr. Ahlstrom is a hospitalist at Indigo Health Partners in Traverse City, Mich., and a member of SHM’s Practice Analysis Committee.
LISTEN NOW: David Weidig, MD, talks about best practices for multi-site hospital medicine
Excerpts from our interview with Team Hospitalist member David Weidig, MD, director of hospital medicine for Aurora Medical Group in West Allis, Wis., about best practices for multi-site hospital medicine.
[audio mp3="http://www.the-hospitalist.org/wp-content/uploads/2015/05/David-Weidig_HM15_FINAL_050215.mp3"][/audio]
Excerpts from our interview with Team Hospitalist member David Weidig, MD, director of hospital medicine for Aurora Medical Group in West Allis, Wis., about best practices for multi-site hospital medicine.
[audio mp3="http://www.the-hospitalist.org/wp-content/uploads/2015/05/David-Weidig_HM15_FINAL_050215.mp3"][/audio]
Excerpts from our interview with Team Hospitalist member David Weidig, MD, director of hospital medicine for Aurora Medical Group in West Allis, Wis., about best practices for multi-site hospital medicine.
[audio mp3="http://www.the-hospitalist.org/wp-content/uploads/2015/05/David-Weidig_HM15_FINAL_050215.mp3"][/audio]
Why CMS’ plan to unbundle global surgery periods should be scrapped
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
21st-Century Patient Collections: Implement a Point-of-Service Collections Program Now
An 8-surgeon group in the Southeast had a history of high patient receivables, the result of a long-held culture of “We’ll submit to your insurance and bill you after insurance pays.”
The billing and collections staff worked in the basement—far away and out of sight of the patients who showed up for their postoperative visits owing big bucks.
In a flash of wisdom, the administrator agreed to move the patient-balance collector into a converted closet near the check-out area, and provided the information, tools, and training that enabled her to speak with patients about their balances when they came in for an appointment. In her first month in this role and location, this employee collected more than her annual salary from patients.
It Takes a Program
This is one of our favorite client success stories, and it illustrates a key point: point-of-service (POS) collections do not have to be complicated. But the process does have to be deliberate and coordinated. Practices cannot simply update the financial policy and hope the staff members magically begin collecting. If this is your strategy, we promise that it will fail.
Successful POS collecting requires a program approach. And this approach starts at the front-end of the billing cycle, not “after insurance pays.”
POS collections have never been more important. Health insurance exchanges and payers are increasing deductibles and coinsurances. Physicians are opting out of network. Given these realities, POS collections are vital to your cash flow and effective receivables management.
If you are starting practice, you have a perfect opportunity to open with POS collecting in place. A solo surgeon whom we set up in practice did so, and has collected up-front for office services, scans, and surgeries from his first day in practice. Today, the practice’s only outstanding patient receivables are those of patients on payment plans—and these are less than 1% of total accounts receivable.
We also converted the “after insurance pays” philosophy of a surgeon in the South, implementing both POS collections and surgical deposits. In the first month, his patient payments increased by 40%. Another solo orthopedist reported an increased take-home salary of $90,000 in the first year after we helped his staff collect surgery deposits.
Six POS Program Elements
In 30 years of implementing or training staff to implement POS collections, we have come to recognize the following 6 key elements to include in your program approach: Policies + Procedures + Technology + Training + Monitoring + Coaching.
At a high level, here are the actions your practice will need to take:
1. Update the financial policy with 1 written standard for all physicians.
2. Develop granular procedures driven by the policy; these are the “how-tos” that enable the staff to collect successfully.
3. Implement new technologies, such as cost estimators, recurring payments, and online bill pay.
4. Schedule formal training to ensure that staff members know how to ask for money. (Do not assume they are, can, or will without training.)
5. Measure and monitor the outcome of patient collections and staff performance.
6. Provide ongoing coaching and oversight to maintain motivation and skills.
A blueprint for addressing each one of these actions follows.
1. Update the financial policy
The policy is the set of expectations on which to build all procedures and training. Dust off this document, and review it as a group with the practice administrator. First, strike old language that says the patient will be balance-billed, or will only be asked in the office for his visit copay. Next, strive for clarity. “You will be asked to pay your financial responsibility at the time of service,” really says nothing. Instead, the policy should be direct:
If you are recommended for surgery, our staff will calculate your coinsurance and unmet deductible amounts: 50% of this amount will be collected as a surgery deposit, and the remaining 50% is due on or before the day of surgery. Payment plans are available.
For office visits and services, break down the policy by coverage type. We find that a table such as the one shown makes expectations clear.
Finally, strive for 1 standard policy for all providers. If every provider is allowed to create his or her own set of collection policies, the practice is setting staff up for complexity overload, and collections will suffer.
2. Develop granular procedures
Few practices take the time to translate the financial policy into written procedures that can be followed by staff. The policy establishes the rules, but the procedures tell staff what to do to implement those rules. For instance:
Create a “POS Playbook” that contains information such as procedures, cost-quotation worksheets, US Poverty guidelines1, and financing brochures. As old-school as it sounds, a 3-ring binder is great for this information, and makes information access and updates easy.
3. Implement collection technologies
Modern practices use inexpensive (and often free) tools that increase patient convenience and staff efficiency. Implement at least 2 of these useful technologies and watch your POS collections increase:
Reports from your practice management system (PMS). Use the technology you already have. There are 2 standard reports in your PMS or clearinghouse that give front-desk staff the data to ask patients for money. Eligibility status and past-due balance reports indicate amounts owed, unmet deductibles, and the ineligible patients they can collect from when they come in for their appointment.
Online cost estimators. These free, online tools are offered by payers and provide staff with real-time data about a patient’s unmet deductible and coinsurance. When staff members enter Current Procedural Terminology (CPT) codes and the patient’s benefit information into the online cost estimator, they can access valuable information. Many insurance plans offer cost estimators on their web sites. Others deliver the data through statewide or regional portals, such as Availity (www.availity.com). The accuracy of cost-estimator data can vary by region and depends on the data links with payers. Ask your team to evaluate which estimators are best for you based on your payer mix.
Online bill pay. Everyone appreciates the convenience of paying bills online. Most patient portals offer this feature. If yours does not or you do not have a portal, you can offer PayPal (www.paypal.com) on your practice website, or use a system such as Intuit Health (www.intuithealth.com).
Recurring billing. Recurring billing is how you pay for services, such as Netflix, Pandora, or your gym membership: it is automatically billed to a credit card each month. Offer this option to patients as a payment plan method, and staff will no longer need to send costly statements, post monthly check payments, or follow up when a patient is delinquent. Plus, it guarantees payment every month; patients can no longer say, “I forgot.”
TransFirst (www.transfirstassociation.com) and a-claim (www.a-claim.com) offer recurring billing through a “virtual terminal” that staff logs in to at checkout, or during the preprocedure patient counseling process. Both vendors also offer the option of automatically charging a patient’s credit card after their insurance pays, speeding patient account pay-off and negating the need for statements.
Real-time collections scripts based on payer rules. Patient Access, offered by Availity, combines real-time payer data with financial policies that are entered during set-up to create instant, patient-specific scripts that staff members read to the patient in front of them.
4. Schedule formal training
Just because someone can collect a copay does not mean he or she is comfortable with or capable of asking patients for past-due balances, surgical deposits, or large coinsurances. It is the rare staff person who is a “natural” at asking patients for money in a polished and professional manner.
That’s why training staff how to ask patients for money is vital. A front-office supervisor or manager should conduct several training sessions to cover policies and procedures. Training materials should include talking points and scenarios for collecting for office services and past-due balances, and calculating what patients owe, using technology tools. Use role-playing to ensure staff can explain payment plan options and how to apply for patient financing or financial assistance.
Few practices can skip this part of the POS program and still be successful. If your manager or supervisor is not capable of training, it is worth the investment to hire an outside expert. Without thorough training, staff efforts will be suboptimal or, at worst, fail because the staff members will not know how or what to collect.
5. Measure and monitor the outcome
The Hawthorne effect is a psychological phenomenon that says people perform better and make more positive changes as a result of increased attention.2 In other words, staff members will perform better, and collect more, if they know someone is paying attention. Trust us on this one.
Employees respect what management inspects. So even if the implementation of POS collections has been a big success, do not take your eyes off the ball.
Stop by the front desk or surgery coordinator’s office a few times a month and ask how much has been collected. Randomly review daily over-the-counter collections logs. And always put POS collections performance on the monthly partner meeting agenda; review a graph that shows monthly collections at checkout and surgery deposits. Keeping tabs on performance enables the practice to take action quickly when collections drop, and before that decline becomes acute.
6. Provide ongoing coaching and oversight
Most practices train once, then wonder why staff motivation (and collections too) fall off after a while. Like that new couch you bought: it was all you could talk about the week after it was delivered. Now, it is only a comfy place to sit. It is the same with collections efforts. When the newness wears off, staff motivation does too, and training principles can be forgotten. That’s human nature. Conduct role-playing in staff meetings each quarter and discuss best practices for handling patient objections. Encourage peer-to-peer observation and coaching to address knowledge gaps and missed collection opportunities. Ongoing training and coaching will tease out training needs and boost your team’s collection confidence and success.
1. 2015 Poverty Guidelines. US Department of Health and Human Services website. http://aspe.hhs.gov/poverty/15poverty.cfm. Accessed March 25, 2015.
2. The Hawthorne effect. The Economist website. http://www.economist.com/node/12510632. Published November 3, 2008. Accessed March 25, 2015.
An 8-surgeon group in the Southeast had a history of high patient receivables, the result of a long-held culture of “We’ll submit to your insurance and bill you after insurance pays.”
The billing and collections staff worked in the basement—far away and out of sight of the patients who showed up for their postoperative visits owing big bucks.
In a flash of wisdom, the administrator agreed to move the patient-balance collector into a converted closet near the check-out area, and provided the information, tools, and training that enabled her to speak with patients about their balances when they came in for an appointment. In her first month in this role and location, this employee collected more than her annual salary from patients.
It Takes a Program
This is one of our favorite client success stories, and it illustrates a key point: point-of-service (POS) collections do not have to be complicated. But the process does have to be deliberate and coordinated. Practices cannot simply update the financial policy and hope the staff members magically begin collecting. If this is your strategy, we promise that it will fail.
Successful POS collecting requires a program approach. And this approach starts at the front-end of the billing cycle, not “after insurance pays.”
POS collections have never been more important. Health insurance exchanges and payers are increasing deductibles and coinsurances. Physicians are opting out of network. Given these realities, POS collections are vital to your cash flow and effective receivables management.
If you are starting practice, you have a perfect opportunity to open with POS collecting in place. A solo surgeon whom we set up in practice did so, and has collected up-front for office services, scans, and surgeries from his first day in practice. Today, the practice’s only outstanding patient receivables are those of patients on payment plans—and these are less than 1% of total accounts receivable.
We also converted the “after insurance pays” philosophy of a surgeon in the South, implementing both POS collections and surgical deposits. In the first month, his patient payments increased by 40%. Another solo orthopedist reported an increased take-home salary of $90,000 in the first year after we helped his staff collect surgery deposits.
Six POS Program Elements
In 30 years of implementing or training staff to implement POS collections, we have come to recognize the following 6 key elements to include in your program approach: Policies + Procedures + Technology + Training + Monitoring + Coaching.
At a high level, here are the actions your practice will need to take:
1. Update the financial policy with 1 written standard for all physicians.
2. Develop granular procedures driven by the policy; these are the “how-tos” that enable the staff to collect successfully.
3. Implement new technologies, such as cost estimators, recurring payments, and online bill pay.
4. Schedule formal training to ensure that staff members know how to ask for money. (Do not assume they are, can, or will without training.)
5. Measure and monitor the outcome of patient collections and staff performance.
6. Provide ongoing coaching and oversight to maintain motivation and skills.
A blueprint for addressing each one of these actions follows.
1. Update the financial policy
The policy is the set of expectations on which to build all procedures and training. Dust off this document, and review it as a group with the practice administrator. First, strike old language that says the patient will be balance-billed, or will only be asked in the office for his visit copay. Next, strive for clarity. “You will be asked to pay your financial responsibility at the time of service,” really says nothing. Instead, the policy should be direct:
If you are recommended for surgery, our staff will calculate your coinsurance and unmet deductible amounts: 50% of this amount will be collected as a surgery deposit, and the remaining 50% is due on or before the day of surgery. Payment plans are available.
For office visits and services, break down the policy by coverage type. We find that a table such as the one shown makes expectations clear.
Finally, strive for 1 standard policy for all providers. If every provider is allowed to create his or her own set of collection policies, the practice is setting staff up for complexity overload, and collections will suffer.
2. Develop granular procedures
Few practices take the time to translate the financial policy into written procedures that can be followed by staff. The policy establishes the rules, but the procedures tell staff what to do to implement those rules. For instance:
Create a “POS Playbook” that contains information such as procedures, cost-quotation worksheets, US Poverty guidelines1, and financing brochures. As old-school as it sounds, a 3-ring binder is great for this information, and makes information access and updates easy.
3. Implement collection technologies
Modern practices use inexpensive (and often free) tools that increase patient convenience and staff efficiency. Implement at least 2 of these useful technologies and watch your POS collections increase:
Reports from your practice management system (PMS). Use the technology you already have. There are 2 standard reports in your PMS or clearinghouse that give front-desk staff the data to ask patients for money. Eligibility status and past-due balance reports indicate amounts owed, unmet deductibles, and the ineligible patients they can collect from when they come in for their appointment.
Online cost estimators. These free, online tools are offered by payers and provide staff with real-time data about a patient’s unmet deductible and coinsurance. When staff members enter Current Procedural Terminology (CPT) codes and the patient’s benefit information into the online cost estimator, they can access valuable information. Many insurance plans offer cost estimators on their web sites. Others deliver the data through statewide or regional portals, such as Availity (www.availity.com). The accuracy of cost-estimator data can vary by region and depends on the data links with payers. Ask your team to evaluate which estimators are best for you based on your payer mix.
Online bill pay. Everyone appreciates the convenience of paying bills online. Most patient portals offer this feature. If yours does not or you do not have a portal, you can offer PayPal (www.paypal.com) on your practice website, or use a system such as Intuit Health (www.intuithealth.com).
Recurring billing. Recurring billing is how you pay for services, such as Netflix, Pandora, or your gym membership: it is automatically billed to a credit card each month. Offer this option to patients as a payment plan method, and staff will no longer need to send costly statements, post monthly check payments, or follow up when a patient is delinquent. Plus, it guarantees payment every month; patients can no longer say, “I forgot.”
TransFirst (www.transfirstassociation.com) and a-claim (www.a-claim.com) offer recurring billing through a “virtual terminal” that staff logs in to at checkout, or during the preprocedure patient counseling process. Both vendors also offer the option of automatically charging a patient’s credit card after their insurance pays, speeding patient account pay-off and negating the need for statements.
Real-time collections scripts based on payer rules. Patient Access, offered by Availity, combines real-time payer data with financial policies that are entered during set-up to create instant, patient-specific scripts that staff members read to the patient in front of them.
4. Schedule formal training
Just because someone can collect a copay does not mean he or she is comfortable with or capable of asking patients for past-due balances, surgical deposits, or large coinsurances. It is the rare staff person who is a “natural” at asking patients for money in a polished and professional manner.
That’s why training staff how to ask patients for money is vital. A front-office supervisor or manager should conduct several training sessions to cover policies and procedures. Training materials should include talking points and scenarios for collecting for office services and past-due balances, and calculating what patients owe, using technology tools. Use role-playing to ensure staff can explain payment plan options and how to apply for patient financing or financial assistance.
Few practices can skip this part of the POS program and still be successful. If your manager or supervisor is not capable of training, it is worth the investment to hire an outside expert. Without thorough training, staff efforts will be suboptimal or, at worst, fail because the staff members will not know how or what to collect.
5. Measure and monitor the outcome
The Hawthorne effect is a psychological phenomenon that says people perform better and make more positive changes as a result of increased attention.2 In other words, staff members will perform better, and collect more, if they know someone is paying attention. Trust us on this one.
Employees respect what management inspects. So even if the implementation of POS collections has been a big success, do not take your eyes off the ball.
Stop by the front desk or surgery coordinator’s office a few times a month and ask how much has been collected. Randomly review daily over-the-counter collections logs. And always put POS collections performance on the monthly partner meeting agenda; review a graph that shows monthly collections at checkout and surgery deposits. Keeping tabs on performance enables the practice to take action quickly when collections drop, and before that decline becomes acute.
6. Provide ongoing coaching and oversight
Most practices train once, then wonder why staff motivation (and collections too) fall off after a while. Like that new couch you bought: it was all you could talk about the week after it was delivered. Now, it is only a comfy place to sit. It is the same with collections efforts. When the newness wears off, staff motivation does too, and training principles can be forgotten. That’s human nature. Conduct role-playing in staff meetings each quarter and discuss best practices for handling patient objections. Encourage peer-to-peer observation and coaching to address knowledge gaps and missed collection opportunities. Ongoing training and coaching will tease out training needs and boost your team’s collection confidence and success.
An 8-surgeon group in the Southeast had a history of high patient receivables, the result of a long-held culture of “We’ll submit to your insurance and bill you after insurance pays.”
The billing and collections staff worked in the basement—far away and out of sight of the patients who showed up for their postoperative visits owing big bucks.
In a flash of wisdom, the administrator agreed to move the patient-balance collector into a converted closet near the check-out area, and provided the information, tools, and training that enabled her to speak with patients about their balances when they came in for an appointment. In her first month in this role and location, this employee collected more than her annual salary from patients.
It Takes a Program
This is one of our favorite client success stories, and it illustrates a key point: point-of-service (POS) collections do not have to be complicated. But the process does have to be deliberate and coordinated. Practices cannot simply update the financial policy and hope the staff members magically begin collecting. If this is your strategy, we promise that it will fail.
Successful POS collecting requires a program approach. And this approach starts at the front-end of the billing cycle, not “after insurance pays.”
POS collections have never been more important. Health insurance exchanges and payers are increasing deductibles and coinsurances. Physicians are opting out of network. Given these realities, POS collections are vital to your cash flow and effective receivables management.
If you are starting practice, you have a perfect opportunity to open with POS collecting in place. A solo surgeon whom we set up in practice did so, and has collected up-front for office services, scans, and surgeries from his first day in practice. Today, the practice’s only outstanding patient receivables are those of patients on payment plans—and these are less than 1% of total accounts receivable.
We also converted the “after insurance pays” philosophy of a surgeon in the South, implementing both POS collections and surgical deposits. In the first month, his patient payments increased by 40%. Another solo orthopedist reported an increased take-home salary of $90,000 in the first year after we helped his staff collect surgery deposits.
Six POS Program Elements
In 30 years of implementing or training staff to implement POS collections, we have come to recognize the following 6 key elements to include in your program approach: Policies + Procedures + Technology + Training + Monitoring + Coaching.
At a high level, here are the actions your practice will need to take:
1. Update the financial policy with 1 written standard for all physicians.
2. Develop granular procedures driven by the policy; these are the “how-tos” that enable the staff to collect successfully.
3. Implement new technologies, such as cost estimators, recurring payments, and online bill pay.
4. Schedule formal training to ensure that staff members know how to ask for money. (Do not assume they are, can, or will without training.)
5. Measure and monitor the outcome of patient collections and staff performance.
6. Provide ongoing coaching and oversight to maintain motivation and skills.
A blueprint for addressing each one of these actions follows.
1. Update the financial policy
The policy is the set of expectations on which to build all procedures and training. Dust off this document, and review it as a group with the practice administrator. First, strike old language that says the patient will be balance-billed, or will only be asked in the office for his visit copay. Next, strive for clarity. “You will be asked to pay your financial responsibility at the time of service,” really says nothing. Instead, the policy should be direct:
If you are recommended for surgery, our staff will calculate your coinsurance and unmet deductible amounts: 50% of this amount will be collected as a surgery deposit, and the remaining 50% is due on or before the day of surgery. Payment plans are available.
For office visits and services, break down the policy by coverage type. We find that a table such as the one shown makes expectations clear.
Finally, strive for 1 standard policy for all providers. If every provider is allowed to create his or her own set of collection policies, the practice is setting staff up for complexity overload, and collections will suffer.
2. Develop granular procedures
Few practices take the time to translate the financial policy into written procedures that can be followed by staff. The policy establishes the rules, but the procedures tell staff what to do to implement those rules. For instance:
Create a “POS Playbook” that contains information such as procedures, cost-quotation worksheets, US Poverty guidelines1, and financing brochures. As old-school as it sounds, a 3-ring binder is great for this information, and makes information access and updates easy.
3. Implement collection technologies
Modern practices use inexpensive (and often free) tools that increase patient convenience and staff efficiency. Implement at least 2 of these useful technologies and watch your POS collections increase:
Reports from your practice management system (PMS). Use the technology you already have. There are 2 standard reports in your PMS or clearinghouse that give front-desk staff the data to ask patients for money. Eligibility status and past-due balance reports indicate amounts owed, unmet deductibles, and the ineligible patients they can collect from when they come in for their appointment.
Online cost estimators. These free, online tools are offered by payers and provide staff with real-time data about a patient’s unmet deductible and coinsurance. When staff members enter Current Procedural Terminology (CPT) codes and the patient’s benefit information into the online cost estimator, they can access valuable information. Many insurance plans offer cost estimators on their web sites. Others deliver the data through statewide or regional portals, such as Availity (www.availity.com). The accuracy of cost-estimator data can vary by region and depends on the data links with payers. Ask your team to evaluate which estimators are best for you based on your payer mix.
Online bill pay. Everyone appreciates the convenience of paying bills online. Most patient portals offer this feature. If yours does not or you do not have a portal, you can offer PayPal (www.paypal.com) on your practice website, or use a system such as Intuit Health (www.intuithealth.com).
Recurring billing. Recurring billing is how you pay for services, such as Netflix, Pandora, or your gym membership: it is automatically billed to a credit card each month. Offer this option to patients as a payment plan method, and staff will no longer need to send costly statements, post monthly check payments, or follow up when a patient is delinquent. Plus, it guarantees payment every month; patients can no longer say, “I forgot.”
TransFirst (www.transfirstassociation.com) and a-claim (www.a-claim.com) offer recurring billing through a “virtual terminal” that staff logs in to at checkout, or during the preprocedure patient counseling process. Both vendors also offer the option of automatically charging a patient’s credit card after their insurance pays, speeding patient account pay-off and negating the need for statements.
Real-time collections scripts based on payer rules. Patient Access, offered by Availity, combines real-time payer data with financial policies that are entered during set-up to create instant, patient-specific scripts that staff members read to the patient in front of them.
4. Schedule formal training
Just because someone can collect a copay does not mean he or she is comfortable with or capable of asking patients for past-due balances, surgical deposits, or large coinsurances. It is the rare staff person who is a “natural” at asking patients for money in a polished and professional manner.
That’s why training staff how to ask patients for money is vital. A front-office supervisor or manager should conduct several training sessions to cover policies and procedures. Training materials should include talking points and scenarios for collecting for office services and past-due balances, and calculating what patients owe, using technology tools. Use role-playing to ensure staff can explain payment plan options and how to apply for patient financing or financial assistance.
Few practices can skip this part of the POS program and still be successful. If your manager or supervisor is not capable of training, it is worth the investment to hire an outside expert. Without thorough training, staff efforts will be suboptimal or, at worst, fail because the staff members will not know how or what to collect.
5. Measure and monitor the outcome
The Hawthorne effect is a psychological phenomenon that says people perform better and make more positive changes as a result of increased attention.2 In other words, staff members will perform better, and collect more, if they know someone is paying attention. Trust us on this one.
Employees respect what management inspects. So even if the implementation of POS collections has been a big success, do not take your eyes off the ball.
Stop by the front desk or surgery coordinator’s office a few times a month and ask how much has been collected. Randomly review daily over-the-counter collections logs. And always put POS collections performance on the monthly partner meeting agenda; review a graph that shows monthly collections at checkout and surgery deposits. Keeping tabs on performance enables the practice to take action quickly when collections drop, and before that decline becomes acute.
6. Provide ongoing coaching and oversight
Most practices train once, then wonder why staff motivation (and collections too) fall off after a while. Like that new couch you bought: it was all you could talk about the week after it was delivered. Now, it is only a comfy place to sit. It is the same with collections efforts. When the newness wears off, staff motivation does too, and training principles can be forgotten. That’s human nature. Conduct role-playing in staff meetings each quarter and discuss best practices for handling patient objections. Encourage peer-to-peer observation and coaching to address knowledge gaps and missed collection opportunities. Ongoing training and coaching will tease out training needs and boost your team’s collection confidence and success.
1. 2015 Poverty Guidelines. US Department of Health and Human Services website. http://aspe.hhs.gov/poverty/15poverty.cfm. Accessed March 25, 2015.
2. The Hawthorne effect. The Economist website. http://www.economist.com/node/12510632. Published November 3, 2008. Accessed March 25, 2015.
1. 2015 Poverty Guidelines. US Department of Health and Human Services website. http://aspe.hhs.gov/poverty/15poverty.cfm. Accessed March 25, 2015.
2. The Hawthorne effect. The Economist website. http://www.economist.com/node/12510632. Published November 3, 2008. Accessed March 25, 2015.
ICD-10 update
When I last wrote about the International Classification of Diseases, 10th Revision (ICD-10) – last year, at about this time – the switchover was scheduled to take place on Oct. 1. Shortly thereafter, of course, Congress decided to delay the inevitable for 1 year. While the House Energy and Commerce Committee has hinted at the possibility of further postponements, we must all assume, until we hear otherwise, that the day of reckoning will arrive as scheduled. You will need to be ready if you expect to be paid come October.
Remember, on Sept. 30 you will be using ICD-9 codes, and the next day you will have to begin using ICD-10. There is no transition period; all ICD-9–coded claims will be rejected from Oct. 1 forward, and no ICD-10 codes can be used before that date. Failure to prepare will be an unmitigated disaster for your practice’s cash flow.
First, decide which parts of your coding and billing systems – and EHR, if you have one – need to be upgraded, how you will do it, and what it will cost. Then, you must get familiar with the new system.
Coders and billers will need the most training on the new methodology, but physicians and other providers must also learn how the new codes are different from the old ones. In general, most differences are in specificity and level of documentation (left/right, acute/chronic, etc.), but there are new codes as well.
I suggest you start by identifying your most-used 20 or 30 diagnosis codes, and then study in detail the differences between the ICD-9 and ICD-10 versions of them. Once you have mastered those, you can go on to other, less-used codes. Take as much time as you need to do this: Remember, everything changes abruptly on Oct. 1, and you will have to get it right the first time.
Be sure to cross-train your coders and other staff members. If a crucial employee quits in the middle of September, you don’t want to have to start from square one. Also, ask your employees to plan their vacations well in advance – and not during the last 3 months of the year. That goes for you, too. This will not be a good time for you to be away, or for the office to run short-staffed.
Next, I suggest you contact all of your third-party payers, billing services, and clearinghouses. Be aggressive; ask them how, exactly, they are preparing for the changeover, and stay in continuous contact with them. Unfortunately, many of these organizations are as behind as most medical practices in their preparations.
Many payers and clearinghouses (including the Centers for Medicare & Medicaid Services) are staging test runs during which you can submit practice claims using the new system. Payers will determine whether your ICD-10 code is in the right place and in the right format; whether the code you used is appropriate; and whether the claim would have been accepted, rejected, or held pending additional information. You will need to do this for each payer, because each will have different coding policies. Many of those policies have not yet been released, and, in some cases, have not even been developed.
You can register for CMS testing sessions through your local Medicare Administrative Contractor (MAC) website. Use the sessions to test your internal system as well, to ensure that everything works smoothly from the time you code a claim until payment is received. Select commonly used ICD-9 claims and practice coding them in ICD-10. The American Academy of Dermatology offers an assortment of training aids at its website, aad.org.
Even the best-laid plans can go awry, however, so it would be prudent to put aside a cash reserve or secure a line of credit to cover expenses during the first few months of the transition, in case the payment machinery falters and large numbers of claims go unpaid. For the same reason, consider postponing major capital investments until early 2016.
You may have heard that ICD-10 is only a transition system; that ICD-11 will be following closely on its heels. I doubt it. In all probability, we will be using ICD-10 a lot longer than CMS originally planned. Besides, ICD-11 is essentially a refinement of ICD-10, not the significant departure that the 10th revision is over the 9th.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
When I last wrote about the International Classification of Diseases, 10th Revision (ICD-10) – last year, at about this time – the switchover was scheduled to take place on Oct. 1. Shortly thereafter, of course, Congress decided to delay the inevitable for 1 year. While the House Energy and Commerce Committee has hinted at the possibility of further postponements, we must all assume, until we hear otherwise, that the day of reckoning will arrive as scheduled. You will need to be ready if you expect to be paid come October.
Remember, on Sept. 30 you will be using ICD-9 codes, and the next day you will have to begin using ICD-10. There is no transition period; all ICD-9–coded claims will be rejected from Oct. 1 forward, and no ICD-10 codes can be used before that date. Failure to prepare will be an unmitigated disaster for your practice’s cash flow.
First, decide which parts of your coding and billing systems – and EHR, if you have one – need to be upgraded, how you will do it, and what it will cost. Then, you must get familiar with the new system.
Coders and billers will need the most training on the new methodology, but physicians and other providers must also learn how the new codes are different from the old ones. In general, most differences are in specificity and level of documentation (left/right, acute/chronic, etc.), but there are new codes as well.
I suggest you start by identifying your most-used 20 or 30 diagnosis codes, and then study in detail the differences between the ICD-9 and ICD-10 versions of them. Once you have mastered those, you can go on to other, less-used codes. Take as much time as you need to do this: Remember, everything changes abruptly on Oct. 1, and you will have to get it right the first time.
Be sure to cross-train your coders and other staff members. If a crucial employee quits in the middle of September, you don’t want to have to start from square one. Also, ask your employees to plan their vacations well in advance – and not during the last 3 months of the year. That goes for you, too. This will not be a good time for you to be away, or for the office to run short-staffed.
Next, I suggest you contact all of your third-party payers, billing services, and clearinghouses. Be aggressive; ask them how, exactly, they are preparing for the changeover, and stay in continuous contact with them. Unfortunately, many of these organizations are as behind as most medical practices in their preparations.
Many payers and clearinghouses (including the Centers for Medicare & Medicaid Services) are staging test runs during which you can submit practice claims using the new system. Payers will determine whether your ICD-10 code is in the right place and in the right format; whether the code you used is appropriate; and whether the claim would have been accepted, rejected, or held pending additional information. You will need to do this for each payer, because each will have different coding policies. Many of those policies have not yet been released, and, in some cases, have not even been developed.
You can register for CMS testing sessions through your local Medicare Administrative Contractor (MAC) website. Use the sessions to test your internal system as well, to ensure that everything works smoothly from the time you code a claim until payment is received. Select commonly used ICD-9 claims and practice coding them in ICD-10. The American Academy of Dermatology offers an assortment of training aids at its website, aad.org.
Even the best-laid plans can go awry, however, so it would be prudent to put aside a cash reserve or secure a line of credit to cover expenses during the first few months of the transition, in case the payment machinery falters and large numbers of claims go unpaid. For the same reason, consider postponing major capital investments until early 2016.
You may have heard that ICD-10 is only a transition system; that ICD-11 will be following closely on its heels. I doubt it. In all probability, we will be using ICD-10 a lot longer than CMS originally planned. Besides, ICD-11 is essentially a refinement of ICD-10, not the significant departure that the 10th revision is over the 9th.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
When I last wrote about the International Classification of Diseases, 10th Revision (ICD-10) – last year, at about this time – the switchover was scheduled to take place on Oct. 1. Shortly thereafter, of course, Congress decided to delay the inevitable for 1 year. While the House Energy and Commerce Committee has hinted at the possibility of further postponements, we must all assume, until we hear otherwise, that the day of reckoning will arrive as scheduled. You will need to be ready if you expect to be paid come October.
Remember, on Sept. 30 you will be using ICD-9 codes, and the next day you will have to begin using ICD-10. There is no transition period; all ICD-9–coded claims will be rejected from Oct. 1 forward, and no ICD-10 codes can be used before that date. Failure to prepare will be an unmitigated disaster for your practice’s cash flow.
First, decide which parts of your coding and billing systems – and EHR, if you have one – need to be upgraded, how you will do it, and what it will cost. Then, you must get familiar with the new system.
Coders and billers will need the most training on the new methodology, but physicians and other providers must also learn how the new codes are different from the old ones. In general, most differences are in specificity and level of documentation (left/right, acute/chronic, etc.), but there are new codes as well.
I suggest you start by identifying your most-used 20 or 30 diagnosis codes, and then study in detail the differences between the ICD-9 and ICD-10 versions of them. Once you have mastered those, you can go on to other, less-used codes. Take as much time as you need to do this: Remember, everything changes abruptly on Oct. 1, and you will have to get it right the first time.
Be sure to cross-train your coders and other staff members. If a crucial employee quits in the middle of September, you don’t want to have to start from square one. Also, ask your employees to plan their vacations well in advance – and not during the last 3 months of the year. That goes for you, too. This will not be a good time for you to be away, or for the office to run short-staffed.
Next, I suggest you contact all of your third-party payers, billing services, and clearinghouses. Be aggressive; ask them how, exactly, they are preparing for the changeover, and stay in continuous contact with them. Unfortunately, many of these organizations are as behind as most medical practices in their preparations.
Many payers and clearinghouses (including the Centers for Medicare & Medicaid Services) are staging test runs during which you can submit practice claims using the new system. Payers will determine whether your ICD-10 code is in the right place and in the right format; whether the code you used is appropriate; and whether the claim would have been accepted, rejected, or held pending additional information. You will need to do this for each payer, because each will have different coding policies. Many of those policies have not yet been released, and, in some cases, have not even been developed.
You can register for CMS testing sessions through your local Medicare Administrative Contractor (MAC) website. Use the sessions to test your internal system as well, to ensure that everything works smoothly from the time you code a claim until payment is received. Select commonly used ICD-9 claims and practice coding them in ICD-10. The American Academy of Dermatology offers an assortment of training aids at its website, aad.org.
Even the best-laid plans can go awry, however, so it would be prudent to put aside a cash reserve or secure a line of credit to cover expenses during the first few months of the transition, in case the payment machinery falters and large numbers of claims go unpaid. For the same reason, consider postponing major capital investments until early 2016.
You may have heard that ICD-10 is only a transition system; that ICD-11 will be following closely on its heels. I doubt it. In all probability, we will be using ICD-10 a lot longer than CMS originally planned. Besides, ICD-11 is essentially a refinement of ICD-10, not the significant departure that the 10th revision is over the 9th.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Multi-Site Hospitalist Leaders: HM15 Session Summary
Session: Multi-site Hospitalist Leaders: Unique Challenges/What You Should Know
HM15 Presenter/Moderator: Scott Rissmiller, MD
Summation: This standing-room-only session was the result of a popular HMX e-community, which has become an active discussion board. As hospitals and health systems continue to consolidate across the country, there has been a rapid growth of multi-hospital systems. The role of the “Chief Hospitalist,” whose job is to lead multiple hospitalist groups within these systems, is evolving. These “Chief Hospitalists” are growing in number and they, as well as their followers, face unique challenges.
These points regarding organization structure were discussed, and as you look at your own organizational structure, these questions deserve your attention:
- Purpose of your structure?
- Is your structure centralized or decentralized?
- How does your organizational structure support decision-making?
- How does the structure ensure proper communication?
- How are resources shared across geography?
- What is your administrative support structure?
- How is administrative time allocated for physician leaders?
- How do you ensure engagement from all providers?
- How does your organization structure create alignment with the healthcare system?
The following compensation issues were discussed, and can be used as a discussion outline for most groups:
- How does your compensation (comp) plan align with the goals and values of the system?
- How does your comp plan account for regional variances?
- How does the comp plan encourage teamwork and sharing of resources?
- How does comp plan account for differences in acuity, hospital size, night frequency, etc.?
- Are goals and incentives group based, site based, or individual based?
- How does the comp plan fairly reward “non-RVU” work? (teaching, committee service, etc.)
- Should all site leaders receive the same comp regardless of group size?
- Does the comp plan incorporate “minimum work standards”/social compact?
Key Points/HM Takeaways:
- Panel discussion was valuable and reassured attendees that there are multiple ways to make groups successful. One common variable of successful groups is open lines of communication at all levels.
- Physician on-boarding is critical and should be utilized to set clear expectations.
- HM Goals/expectations must be aligned with those of the hospital and health system.
- When multiple hospitals are part of a larger system, it is desirable for goals to be aligned across the health system.
- Two-way open communication is necessary for success.
- Try to take a walk in your colleague’s/stakeholder’s shoes:
- How does my hospital administrative partner see this issue?
- How does my regional director/system lead see this issue?
- How does my bedside hospitalist physician/provider see this issue?
- How would my patients view this issue?
- Issues facing different types of groups, academic vs. community and for profit vs. not for profit, are somewhat variable.
- The leadership Dyad consisting of a physician and practice management professional in partnership is an effective and well-proven management model.
Many thanks to Drs. T.J. Richardson and Dan Duzan for their input and assistance with this session summary. Dr. Richardson is a Regional Medical Director and Dr. Duzan is a Facility Medical Director, both work for TeamHealth.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
Session: Multi-site Hospitalist Leaders: Unique Challenges/What You Should Know
HM15 Presenter/Moderator: Scott Rissmiller, MD
Summation: This standing-room-only session was the result of a popular HMX e-community, which has become an active discussion board. As hospitals and health systems continue to consolidate across the country, there has been a rapid growth of multi-hospital systems. The role of the “Chief Hospitalist,” whose job is to lead multiple hospitalist groups within these systems, is evolving. These “Chief Hospitalists” are growing in number and they, as well as their followers, face unique challenges.
These points regarding organization structure were discussed, and as you look at your own organizational structure, these questions deserve your attention:
- Purpose of your structure?
- Is your structure centralized or decentralized?
- How does your organizational structure support decision-making?
- How does the structure ensure proper communication?
- How are resources shared across geography?
- What is your administrative support structure?
- How is administrative time allocated for physician leaders?
- How do you ensure engagement from all providers?
- How does your organization structure create alignment with the healthcare system?
The following compensation issues were discussed, and can be used as a discussion outline for most groups:
- How does your compensation (comp) plan align with the goals and values of the system?
- How does your comp plan account for regional variances?
- How does the comp plan encourage teamwork and sharing of resources?
- How does comp plan account for differences in acuity, hospital size, night frequency, etc.?
- Are goals and incentives group based, site based, or individual based?
- How does the comp plan fairly reward “non-RVU” work? (teaching, committee service, etc.)
- Should all site leaders receive the same comp regardless of group size?
- Does the comp plan incorporate “minimum work standards”/social compact?
Key Points/HM Takeaways:
- Panel discussion was valuable and reassured attendees that there are multiple ways to make groups successful. One common variable of successful groups is open lines of communication at all levels.
- Physician on-boarding is critical and should be utilized to set clear expectations.
- HM Goals/expectations must be aligned with those of the hospital and health system.
- When multiple hospitals are part of a larger system, it is desirable for goals to be aligned across the health system.
- Two-way open communication is necessary for success.
- Try to take a walk in your colleague’s/stakeholder’s shoes:
- How does my hospital administrative partner see this issue?
- How does my regional director/system lead see this issue?
- How does my bedside hospitalist physician/provider see this issue?
- How would my patients view this issue?
- Issues facing different types of groups, academic vs. community and for profit vs. not for profit, are somewhat variable.
- The leadership Dyad consisting of a physician and practice management professional in partnership is an effective and well-proven management model.
Many thanks to Drs. T.J. Richardson and Dan Duzan for their input and assistance with this session summary. Dr. Richardson is a Regional Medical Director and Dr. Duzan is a Facility Medical Director, both work for TeamHealth.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
Session: Multi-site Hospitalist Leaders: Unique Challenges/What You Should Know
HM15 Presenter/Moderator: Scott Rissmiller, MD
Summation: This standing-room-only session was the result of a popular HMX e-community, which has become an active discussion board. As hospitals and health systems continue to consolidate across the country, there has been a rapid growth of multi-hospital systems. The role of the “Chief Hospitalist,” whose job is to lead multiple hospitalist groups within these systems, is evolving. These “Chief Hospitalists” are growing in number and they, as well as their followers, face unique challenges.
These points regarding organization structure were discussed, and as you look at your own organizational structure, these questions deserve your attention:
- Purpose of your structure?
- Is your structure centralized or decentralized?
- How does your organizational structure support decision-making?
- How does the structure ensure proper communication?
- How are resources shared across geography?
- What is your administrative support structure?
- How is administrative time allocated for physician leaders?
- How do you ensure engagement from all providers?
- How does your organization structure create alignment with the healthcare system?
The following compensation issues were discussed, and can be used as a discussion outline for most groups:
- How does your compensation (comp) plan align with the goals and values of the system?
- How does your comp plan account for regional variances?
- How does the comp plan encourage teamwork and sharing of resources?
- How does comp plan account for differences in acuity, hospital size, night frequency, etc.?
- Are goals and incentives group based, site based, or individual based?
- How does the comp plan fairly reward “non-RVU” work? (teaching, committee service, etc.)
- Should all site leaders receive the same comp regardless of group size?
- Does the comp plan incorporate “minimum work standards”/social compact?
Key Points/HM Takeaways:
- Panel discussion was valuable and reassured attendees that there are multiple ways to make groups successful. One common variable of successful groups is open lines of communication at all levels.
- Physician on-boarding is critical and should be utilized to set clear expectations.
- HM Goals/expectations must be aligned with those of the hospital and health system.
- When multiple hospitals are part of a larger system, it is desirable for goals to be aligned across the health system.
- Two-way open communication is necessary for success.
- Try to take a walk in your colleague’s/stakeholder’s shoes:
- How does my hospital administrative partner see this issue?
- How does my regional director/system lead see this issue?
- How does my bedside hospitalist physician/provider see this issue?
- How would my patients view this issue?
- Issues facing different types of groups, academic vs. community and for profit vs. not for profit, are somewhat variable.
- The leadership Dyad consisting of a physician and practice management professional in partnership is an effective and well-proven management model.
Many thanks to Drs. T.J. Richardson and Dan Duzan for their input and assistance with this session summary. Dr. Richardson is a Regional Medical Director and Dr. Duzan is a Facility Medical Director, both work for TeamHealth.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
HM15 Session Analysis: The Physician-Administrator Management Dyad
Hm15 Presenters: Chuck Ainsworth, MD, MCC,; Dan Virnich, MD, MBA; Roberta Himebaugh, MBA, SFHM; Robert Hickling, MHA; Sendil Krishnan, MD
Summation: The presenters, a group of physicians and administrators for hospital medicine groups, explored three dyad models. These three models were:
- Office of the Executive, where there is one senior executive and a junior executive;
- Coordinated Co-Leadership, where each of the two co-leaders has separate direct reports; and
- Integrated Co-Leadership, where there are two co-leaders and the staff report to the co-leader team.
The discussion ensued to outline the benefit of a dyad leadership model, which can lead to growth and success in advancing the commitment to patient care. The group also emphasized the importance of providing leadership training and education to optimize the dyad leadership model. Bringing together physician and administrator dyads enables an organization to have complimentary expertise to advance hospital medicine programs into the next era.
Hm15 Presenters: Chuck Ainsworth, MD, MCC,; Dan Virnich, MD, MBA; Roberta Himebaugh, MBA, SFHM; Robert Hickling, MHA; Sendil Krishnan, MD
Summation: The presenters, a group of physicians and administrators for hospital medicine groups, explored three dyad models. These three models were:
- Office of the Executive, where there is one senior executive and a junior executive;
- Coordinated Co-Leadership, where each of the two co-leaders has separate direct reports; and
- Integrated Co-Leadership, where there are two co-leaders and the staff report to the co-leader team.
The discussion ensued to outline the benefit of a dyad leadership model, which can lead to growth and success in advancing the commitment to patient care. The group also emphasized the importance of providing leadership training and education to optimize the dyad leadership model. Bringing together physician and administrator dyads enables an organization to have complimentary expertise to advance hospital medicine programs into the next era.
Hm15 Presenters: Chuck Ainsworth, MD, MCC,; Dan Virnich, MD, MBA; Roberta Himebaugh, MBA, SFHM; Robert Hickling, MHA; Sendil Krishnan, MD
Summation: The presenters, a group of physicians and administrators for hospital medicine groups, explored three dyad models. These three models were:
- Office of the Executive, where there is one senior executive and a junior executive;
- Coordinated Co-Leadership, where each of the two co-leaders has separate direct reports; and
- Integrated Co-Leadership, where there are two co-leaders and the staff report to the co-leader team.
The discussion ensued to outline the benefit of a dyad leadership model, which can lead to growth and success in advancing the commitment to patient care. The group also emphasized the importance of providing leadership training and education to optimize the dyad leadership model. Bringing together physician and administrator dyads enables an organization to have complimentary expertise to advance hospital medicine programs into the next era.