User login
HM15 Session Analysis: Innovative Hospitalist Staffing Models
HM15 Presenters: John Nelson, MD, MHM; Daniel Hanson, MD, FHM; Darren Thomas, MD
Summation: The presenters, from three entirely different geographic regions across the U.S., walked the audience through several different innovative hospitalist staffing models, from staffing in a multi-hospital system to integrating of advanced practice clinicians to deploying staggered staffing techniques to match the patient demand and enhance continuity of care.
Many multi-hospital systems are challenged to consider creative solutions on how to meet individual hospital staffing needs, while also creating staffing efficiencies across the system, such as cross coverage at night and back-up staffing solutions for increased patient volumes and unexpected staffing vacancies.
Examples to enhance patient continuity were presented throughout, such as pairing together a hospitalist from one week to a hospitalist from an alternate week to care for the same patients.
Similarly, the experts provided a compelling case to consider pairing hospitalist providers with patients, and referring physicians longitudinally across multiple admissions.
Key Takeaways:
1. Patients Come First - consider patient alignment, or continuity, in determing provider scheduling options.
2. Multi-hospital Systems - establish the onboarding parameters needed for providers to be successful in covering more than one hospital and how to build into your scheduling model.
3. Integrate the Care Team - ensure the roles of the integrated provider team (e.g., physicians and advanced practice clinicians) are clearly understood when developing the schedule.
4. Know Your Numbers - clearly understand the workload demands to properly balance the scheduling needs before establishing the schedule.
5. Regular Review - regularly review all of these areas and revise your schedule based on the changing landscape of demands on your hospital medicine group.
HM15 Presenters: John Nelson, MD, MHM; Daniel Hanson, MD, FHM; Darren Thomas, MD
Summation: The presenters, from three entirely different geographic regions across the U.S., walked the audience through several different innovative hospitalist staffing models, from staffing in a multi-hospital system to integrating of advanced practice clinicians to deploying staggered staffing techniques to match the patient demand and enhance continuity of care.
Many multi-hospital systems are challenged to consider creative solutions on how to meet individual hospital staffing needs, while also creating staffing efficiencies across the system, such as cross coverage at night and back-up staffing solutions for increased patient volumes and unexpected staffing vacancies.
Examples to enhance patient continuity were presented throughout, such as pairing together a hospitalist from one week to a hospitalist from an alternate week to care for the same patients.
Similarly, the experts provided a compelling case to consider pairing hospitalist providers with patients, and referring physicians longitudinally across multiple admissions.
Key Takeaways:
1. Patients Come First - consider patient alignment, or continuity, in determing provider scheduling options.
2. Multi-hospital Systems - establish the onboarding parameters needed for providers to be successful in covering more than one hospital and how to build into your scheduling model.
3. Integrate the Care Team - ensure the roles of the integrated provider team (e.g., physicians and advanced practice clinicians) are clearly understood when developing the schedule.
4. Know Your Numbers - clearly understand the workload demands to properly balance the scheduling needs before establishing the schedule.
5. Regular Review - regularly review all of these areas and revise your schedule based on the changing landscape of demands on your hospital medicine group.
HM15 Presenters: John Nelson, MD, MHM; Daniel Hanson, MD, FHM; Darren Thomas, MD
Summation: The presenters, from three entirely different geographic regions across the U.S., walked the audience through several different innovative hospitalist staffing models, from staffing in a multi-hospital system to integrating of advanced practice clinicians to deploying staggered staffing techniques to match the patient demand and enhance continuity of care.
Many multi-hospital systems are challenged to consider creative solutions on how to meet individual hospital staffing needs, while also creating staffing efficiencies across the system, such as cross coverage at night and back-up staffing solutions for increased patient volumes and unexpected staffing vacancies.
Examples to enhance patient continuity were presented throughout, such as pairing together a hospitalist from one week to a hospitalist from an alternate week to care for the same patients.
Similarly, the experts provided a compelling case to consider pairing hospitalist providers with patients, and referring physicians longitudinally across multiple admissions.
Key Takeaways:
1. Patients Come First - consider patient alignment, or continuity, in determing provider scheduling options.
2. Multi-hospital Systems - establish the onboarding parameters needed for providers to be successful in covering more than one hospital and how to build into your scheduling model.
3. Integrate the Care Team - ensure the roles of the integrated provider team (e.g., physicians and advanced practice clinicians) are clearly understood when developing the schedule.
4. Know Your Numbers - clearly understand the workload demands to properly balance the scheduling needs before establishing the schedule.
5. Regular Review - regularly review all of these areas and revise your schedule based on the changing landscape of demands on your hospital medicine group.
Implementing Physician Value-Based Purchasing in Your Practice: HM15 Session Analysis
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
Hot Topics in Practice Management; HM15 Session Analysis
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
Medicare Standard Practical Solution to Medical Coding Complexity
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
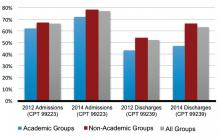
Academic Hospitalist Groups Lag Behind in Admissions, Discharges
In 2012, SHM reported increasing numbers of hospital encounters coded for high-level evaluation and management services, as reported by the 2012 State of Hospital Medicine (SOHM) survey respondents. The 2014 SOHM report shows a solid continuation of this trend, with high-level CPT codes predominating in admission and discharge services by wider margins than ever before.
The 2014 report provides CPT code data from 173 hospitalist groups, who reported the number of inpatient admissions with CPT codes corresponding to Level 1, Level 2, or Level 3. Inpatient discharges have codes corresponding to either Level 1 or Level 2.
Compared to 2012, Level 3 admissions (CPT 99223) increased by 14% in 2014 and now account for 77% of all admissions (see Figure 1). Level 2 discharges (CPT 99239) have increased by 17% since 2012 and now account for 63% of discharges.
In 2014, SOHM added CPT code distribution data for observation care. Observation admissions and inpatient and observation subsequent care are also reported as Level 1, 2, or 3 by the corresponding CPT codes. Observation discharges, which have only one code level, are also reported, in addition to the three levels of same-day admit/discharge encounters.
The rate of Level 3 CPT codes reported for observation admissions, which was 72%, roughly approximated that of inpatient admissions. For subsequent care, Level 2 accounts for the majority of both observation and inpatient codes.
Despite the general predominance of Level 3 admissions and now Level 2 inpatient discharges, not all hospitalist groups deal equally in these higher billing evaluation and management services. Groups in the West region previously dominated the high-level encounters in both admissions and discharges; in 2014, the South took the lead in high-level admissions.

One factor that has consistently signaled lower rates of high-level coding, however, is academic status. A likely reason, as alluded to in a previous “Survey Insights” column, relates to the fact that residents’ time is not billable. This is particularly important in the discharge coding, in which the higher Level 2 code is strictly based on the statement by an attending that discharge services were personally provided for more than 30 minutes. Understandably, this happens less often when a resident’s education includes providing discharge services.
If attending face-to-face time is a major factor in the discharge coding differential, it does not explain where academic groups are missing the boat on the admission side, where residents’ documentation is incorporated by attendings—and can have a substantial effect on accurate billing. This assumes that academic groups are not treating far fewer sick patients, less comprehensively, across the board.
In my own public academic hospital, I see reviewing the required elements of the history and physical examination (H&P) as survival for our hospital and our mission, as well as an opportunity to educate residents simultaneously in patient interviewing skills and system-based practice.
But before I get too far into waxing altruistic, let me recognize another factor suggested by the SOHM report: I am not 100% salaried. That means thorough documentation and accurate coding directly impact my personal compensation.
The 2014 SOHM report shows, as it did in 2012, an inverse correlation between high-level admissions and percent salaried compensation. Although this relationship remains less clear in follow-ups and discharges, perhaps hospitalists pay more attention to coding criteria when it’s bread on the table…and if time permits.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
In 2012, SHM reported increasing numbers of hospital encounters coded for high-level evaluation and management services, as reported by the 2012 State of Hospital Medicine (SOHM) survey respondents. The 2014 SOHM report shows a solid continuation of this trend, with high-level CPT codes predominating in admission and discharge services by wider margins than ever before.
The 2014 report provides CPT code data from 173 hospitalist groups, who reported the number of inpatient admissions with CPT codes corresponding to Level 1, Level 2, or Level 3. Inpatient discharges have codes corresponding to either Level 1 or Level 2.
Compared to 2012, Level 3 admissions (CPT 99223) increased by 14% in 2014 and now account for 77% of all admissions (see Figure 1). Level 2 discharges (CPT 99239) have increased by 17% since 2012 and now account for 63% of discharges.
In 2014, SOHM added CPT code distribution data for observation care. Observation admissions and inpatient and observation subsequent care are also reported as Level 1, 2, or 3 by the corresponding CPT codes. Observation discharges, which have only one code level, are also reported, in addition to the three levels of same-day admit/discharge encounters.
The rate of Level 3 CPT codes reported for observation admissions, which was 72%, roughly approximated that of inpatient admissions. For subsequent care, Level 2 accounts for the majority of both observation and inpatient codes.
Despite the general predominance of Level 3 admissions and now Level 2 inpatient discharges, not all hospitalist groups deal equally in these higher billing evaluation and management services. Groups in the West region previously dominated the high-level encounters in both admissions and discharges; in 2014, the South took the lead in high-level admissions.

One factor that has consistently signaled lower rates of high-level coding, however, is academic status. A likely reason, as alluded to in a previous “Survey Insights” column, relates to the fact that residents’ time is not billable. This is particularly important in the discharge coding, in which the higher Level 2 code is strictly based on the statement by an attending that discharge services were personally provided for more than 30 minutes. Understandably, this happens less often when a resident’s education includes providing discharge services.
If attending face-to-face time is a major factor in the discharge coding differential, it does not explain where academic groups are missing the boat on the admission side, where residents’ documentation is incorporated by attendings—and can have a substantial effect on accurate billing. This assumes that academic groups are not treating far fewer sick patients, less comprehensively, across the board.
In my own public academic hospital, I see reviewing the required elements of the history and physical examination (H&P) as survival for our hospital and our mission, as well as an opportunity to educate residents simultaneously in patient interviewing skills and system-based practice.
But before I get too far into waxing altruistic, let me recognize another factor suggested by the SOHM report: I am not 100% salaried. That means thorough documentation and accurate coding directly impact my personal compensation.
The 2014 SOHM report shows, as it did in 2012, an inverse correlation between high-level admissions and percent salaried compensation. Although this relationship remains less clear in follow-ups and discharges, perhaps hospitalists pay more attention to coding criteria when it’s bread on the table…and if time permits.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
In 2012, SHM reported increasing numbers of hospital encounters coded for high-level evaluation and management services, as reported by the 2012 State of Hospital Medicine (SOHM) survey respondents. The 2014 SOHM report shows a solid continuation of this trend, with high-level CPT codes predominating in admission and discharge services by wider margins than ever before.
The 2014 report provides CPT code data from 173 hospitalist groups, who reported the number of inpatient admissions with CPT codes corresponding to Level 1, Level 2, or Level 3. Inpatient discharges have codes corresponding to either Level 1 or Level 2.
Compared to 2012, Level 3 admissions (CPT 99223) increased by 14% in 2014 and now account for 77% of all admissions (see Figure 1). Level 2 discharges (CPT 99239) have increased by 17% since 2012 and now account for 63% of discharges.
In 2014, SOHM added CPT code distribution data for observation care. Observation admissions and inpatient and observation subsequent care are also reported as Level 1, 2, or 3 by the corresponding CPT codes. Observation discharges, which have only one code level, are also reported, in addition to the three levels of same-day admit/discharge encounters.
The rate of Level 3 CPT codes reported for observation admissions, which was 72%, roughly approximated that of inpatient admissions. For subsequent care, Level 2 accounts for the majority of both observation and inpatient codes.
Despite the general predominance of Level 3 admissions and now Level 2 inpatient discharges, not all hospitalist groups deal equally in these higher billing evaluation and management services. Groups in the West region previously dominated the high-level encounters in both admissions and discharges; in 2014, the South took the lead in high-level admissions.

One factor that has consistently signaled lower rates of high-level coding, however, is academic status. A likely reason, as alluded to in a previous “Survey Insights” column, relates to the fact that residents’ time is not billable. This is particularly important in the discharge coding, in which the higher Level 2 code is strictly based on the statement by an attending that discharge services were personally provided for more than 30 minutes. Understandably, this happens less often when a resident’s education includes providing discharge services.
If attending face-to-face time is a major factor in the discharge coding differential, it does not explain where academic groups are missing the boat on the admission side, where residents’ documentation is incorporated by attendings—and can have a substantial effect on accurate billing. This assumes that academic groups are not treating far fewer sick patients, less comprehensively, across the board.
In my own public academic hospital, I see reviewing the required elements of the history and physical examination (H&P) as survival for our hospital and our mission, as well as an opportunity to educate residents simultaneously in patient interviewing skills and system-based practice.
But before I get too far into waxing altruistic, let me recognize another factor suggested by the SOHM report: I am not 100% salaried. That means thorough documentation and accurate coding directly impact my personal compensation.
The 2014 SOHM report shows, as it did in 2012, an inverse correlation between high-level admissions and percent salaried compensation. Although this relationship remains less clear in follow-ups and discharges, perhaps hospitalists pay more attention to coding criteria when it’s bread on the table…and if time permits.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
5 ways to wake up your Web site
Web sites are not like wine and cheese—they don’t necessarily get better with age. You may have started your Web page 20 years ago by moving your 3-color trifold brochure onto the Internet. It may have worked then, but to compete today you must have a robust, interactive, attractive Web site that is continuously being updated with new content. What prospective patients are looking for in a Web site has evolved rapidly. How to get these patients to take action and call for an appointment requires a process or a system.
Trying to keep your Web site current can be daunting for most medical practices. If you find that your Web site is not generating new patients and that your existing patients are not using the site in an interactive fashion, then it is time to upgrade. In this article we suggest 5 practical ways to make your Web site a useful adjunct to your medical practice—an automatic patient conversion system.
1. Go mobile
Make your Web site “thumb friendly.” Mobile technology has taken over the desktop and laptop worlds. Now nearly everyone is using a hand-held smartphone or tablet for their Internet needs.
To attract patients your Web page must be responsive to the screen size of a smartphone or tablet—very different from your Web site, which is accessed from a desktop or a laptop computer. The majority of users navigate not with a mouse but with their fingers and thumbs. To ensure they can find their way on your Web page on a mobile device, the screen view should adjust automatically to the mobile device being used. Whether that is accomplished through a mobile responsive design or an entirely different mobile Web site, you do not want the user to have to resize, zoom, or pinch their way through the page in order to read the content. All the buttons must be large enough to be easily pressed without having to zoom in, and the font should be easy-to-read in style and size.
Having your current Web site programmed to be responsive to these devices will increase the time a mobile user spends on your site and make it easier for her to make an appointment.
2. Add patient reviews
What others say about you is far more important than anything you can say about yourself. Almost half of prospective patients will check out your online reviews before calling you to schedule an appointment.1 Therefore, it is very important that you ask for positive feedback from your patients and post it to your Web site. We recommend that you capture compliments from your existing patients when they are in the office. Have a computer or iPad handy for them to create a positive review; patients who “promise” to do it when they get back to the office or home rarely follow through. Testimonials should be visible on your homepage and can link to another testimonial page or review site.
“as many as 8 out of 10 people will look online for information about individual doctors. And all of that happens long before they make an appointment … and what they find—positive, negative, neutral or nothing at all—influences their decision to call or not to call.”2
Always invite your patients to evaluate you, your practice partners, and the practice online. There are numerous patient review Web sites, including: Google Plus, http://www.RateMDs.com, http://www.Vitals.com, and http://www.HealthGrades.com. And check out what your patients are saying about you on a regular basis. Just type “Reviews for Dr. <your name>” into your search bar to find the results.
Although we hope they will, happy patients rarely fill out these online reviews. However, it takes just 2 or 3 unhappy patients to ruin your online reputation. That could be costing you tens of thousands of dollars in lost billing.
3. Share your videos
What’s hot and what’s not? To answer that, just take a look at how many people watch videos on YouTube every day! People don’t want to read anymore; they want to be entertained and spoon-fed information.
Take advantage of this trend by placing videos on your homepage. Post a video that introduces your practice, provides testimonials of satisfied patients, explains some of the procedures you perform, or shows you describing the latest breakthrough in medical technology.
Your videos don’t have to be long. One to 2 minutes is plenty. They don’t have to feature you talking about medical symptoms or procedures (what’s called a talking head video). Use a PowerPoint presentation with voice overlay—and you don’t have to be the one talking.
Your Web site isn’t the only place you’ll want to post your videos. YouTube is second only to Google as the most popular search engine.3 Just about everyone goes to YouTube to view videos on whatever interests them. See our April 2014 article, titled “Using the Internet in your practice. Part 2: Generating new patients using social media,” to learn more on getting started with YouTube.
Videos will improve your Web site rankings and will increase the time visitors spend on the site. When done properly—labeling the videos with relevant keywords, making the videos short, and presenting information in layman’s language with reasons why it is important to seek a professional if the viewer is experiencing these types of symptoms—they are a great way to convert visitors to patients.
4. Hook‘em on the homepage
If you want your Web site to create a favorable first impression, your homepage should reflect that positive impression. Remember, the homepage, as the face of your practice, is the first thing that a patient will see long before she picks up the phone or comes to the office.
A potential patient visiting your site will make a snap judgment within a few seconds. Think of your homepage as a highway billboard. There are about 3 seconds to make an impression and for a driver to decide whether or not she will exit the highway to buy gas or eat at a restaurant or even contact a business in the future by telephone or, most likely, online. A visit to your Web site has the same attraction timing.
Your homepage must be attractive; provide useful, current information; and have pleasing graphics—all without requiring the visitor to scroll down too far. Your Web site is your opportunity to create a good first impression—an opportunity that won’t happen again.
Use compelling headlines with keyword-related content. You want to make sure you use keywords that a prospective patient might search for in a main headline and in the main body of your homepage. But patients are not the only ones who spot those key terms. Search engines also crawl your Web site for keywords that prospective patients may type into the Google search bar—words like gynecologist, ObGyn, urinary leakage, breast lump, pelvic pain, menopause, etc. Using those keywords helps your site to be found more often by patients and helps those prospective patients find information relevant to their medical needs.
5. Place calls to action on every page
Contact us! This is so rudimentary, yet many Web sites do not have easy-to-find contact information on their homepages. Be sure to include your phone number (which could be different than your regular phone office number so you can track how many calls you get from your Web site).
Add a “schedule an appointment” icon in a prominent position on the homepage so the visitor does not have to scroll down to search for it. But don’t just stop at the homepage. Your contact information should be on every page so that, when the visitor is on a page reading about a condition or procedure, the “schedule an appointment” button is right there for her to click.
Be sure to evaluate your contact page. Make sure it’s easy for patients to find multiple ways to connect with you and your office: phone, fax, email, and snail mail.
Interactivity is important. Why not have an “Ask the doctor your question” field? It makes the site interactive and gives you the opportunity to communicate and develop a relationship with your patients.
Additional interactivity
Social media is the new buzz word-of-mouth. Your patients use Facebook, YouTube, blogging, and Twitter every day. It is the easiest way to stay connected and make your practice and your brand part of their daily lives. Social media builds loyalty. Integrating social media into your Web site provides new opportunities to engage your existing patients and to attract new ones to your practice.
Connect to medical records. Your Web site should have an easy portal for patients to connect to their medical records and laboratory results in a secure, encrypted fashion to comply with HIPAA regulations.
You can do this yourself!
You and your staff should be able to make changes on your Web site without having to contact your Web developer, even if you do not have full-time IT assistance. For example, in Dr. Baum’s practice, his support staff can add testimonials, content, and pictures without contacting the Web developer or knowing code.
Make sure that function is designed into your site and that your Web developer teaches you and your staff how to keep your site updated.
The bottom line
Web sites are like a farmer’s fence, they are always under construction. Merely having a Web site, regardless of the size, specialty, or location of your practice, is not enough. Be sure your site attracts, holds, and converts viewers into paying patients. We hope you will consider these 5 suggestions as a roadmap to develop a robust site, so that when you ask a patient who referred her to your practice, her answer will be “your Web site” or “the Internet.” This will bring cockles to your heart and bucks in your bank account.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Online reputation management for doctors. Vanguard Communications Web site. http://vanguardcommuni cations.net/medical-marketing-portfolio/reputation-management. Accessed March 17, 2015.
2. Gandolf S. Ten commandments of online reputation management for physicians [Part one]. Healthcare Success Web site. http://www.healthcaresuccess.com/blog/internet-marketing-advertising/10-commandments-online-reputation-management-physicians-2.html. Published May 12, 2014. Accessed March 9, 2015.
3. YouTube—The 2nd Largest Search Engine. Mushroom Networks Web site. http://www.mushroomnetworks.com/infographics/youtube---the-2nd-largest-search-engine-infographic. Accessed March 17, 2015.
Web sites are not like wine and cheese—they don’t necessarily get better with age. You may have started your Web page 20 years ago by moving your 3-color trifold brochure onto the Internet. It may have worked then, but to compete today you must have a robust, interactive, attractive Web site that is continuously being updated with new content. What prospective patients are looking for in a Web site has evolved rapidly. How to get these patients to take action and call for an appointment requires a process or a system.
Trying to keep your Web site current can be daunting for most medical practices. If you find that your Web site is not generating new patients and that your existing patients are not using the site in an interactive fashion, then it is time to upgrade. In this article we suggest 5 practical ways to make your Web site a useful adjunct to your medical practice—an automatic patient conversion system.
1. Go mobile
Make your Web site “thumb friendly.” Mobile technology has taken over the desktop and laptop worlds. Now nearly everyone is using a hand-held smartphone or tablet for their Internet needs.
To attract patients your Web page must be responsive to the screen size of a smartphone or tablet—very different from your Web site, which is accessed from a desktop or a laptop computer. The majority of users navigate not with a mouse but with their fingers and thumbs. To ensure they can find their way on your Web page on a mobile device, the screen view should adjust automatically to the mobile device being used. Whether that is accomplished through a mobile responsive design or an entirely different mobile Web site, you do not want the user to have to resize, zoom, or pinch their way through the page in order to read the content. All the buttons must be large enough to be easily pressed without having to zoom in, and the font should be easy-to-read in style and size.
Having your current Web site programmed to be responsive to these devices will increase the time a mobile user spends on your site and make it easier for her to make an appointment.
2. Add patient reviews
What others say about you is far more important than anything you can say about yourself. Almost half of prospective patients will check out your online reviews before calling you to schedule an appointment.1 Therefore, it is very important that you ask for positive feedback from your patients and post it to your Web site. We recommend that you capture compliments from your existing patients when they are in the office. Have a computer or iPad handy for them to create a positive review; patients who “promise” to do it when they get back to the office or home rarely follow through. Testimonials should be visible on your homepage and can link to another testimonial page or review site.
“as many as 8 out of 10 people will look online for information about individual doctors. And all of that happens long before they make an appointment … and what they find—positive, negative, neutral or nothing at all—influences their decision to call or not to call.”2
Always invite your patients to evaluate you, your practice partners, and the practice online. There are numerous patient review Web sites, including: Google Plus, http://www.RateMDs.com, http://www.Vitals.com, and http://www.HealthGrades.com. And check out what your patients are saying about you on a regular basis. Just type “Reviews for Dr. <your name>” into your search bar to find the results.
Although we hope they will, happy patients rarely fill out these online reviews. However, it takes just 2 or 3 unhappy patients to ruin your online reputation. That could be costing you tens of thousands of dollars in lost billing.
3. Share your videos
What’s hot and what’s not? To answer that, just take a look at how many people watch videos on YouTube every day! People don’t want to read anymore; they want to be entertained and spoon-fed information.
Take advantage of this trend by placing videos on your homepage. Post a video that introduces your practice, provides testimonials of satisfied patients, explains some of the procedures you perform, or shows you describing the latest breakthrough in medical technology.
Your videos don’t have to be long. One to 2 minutes is plenty. They don’t have to feature you talking about medical symptoms or procedures (what’s called a talking head video). Use a PowerPoint presentation with voice overlay—and you don’t have to be the one talking.
Your Web site isn’t the only place you’ll want to post your videos. YouTube is second only to Google as the most popular search engine.3 Just about everyone goes to YouTube to view videos on whatever interests them. See our April 2014 article, titled “Using the Internet in your practice. Part 2: Generating new patients using social media,” to learn more on getting started with YouTube.
Videos will improve your Web site rankings and will increase the time visitors spend on the site. When done properly—labeling the videos with relevant keywords, making the videos short, and presenting information in layman’s language with reasons why it is important to seek a professional if the viewer is experiencing these types of symptoms—they are a great way to convert visitors to patients.
4. Hook‘em on the homepage
If you want your Web site to create a favorable first impression, your homepage should reflect that positive impression. Remember, the homepage, as the face of your practice, is the first thing that a patient will see long before she picks up the phone or comes to the office.
A potential patient visiting your site will make a snap judgment within a few seconds. Think of your homepage as a highway billboard. There are about 3 seconds to make an impression and for a driver to decide whether or not she will exit the highway to buy gas or eat at a restaurant or even contact a business in the future by telephone or, most likely, online. A visit to your Web site has the same attraction timing.
Your homepage must be attractive; provide useful, current information; and have pleasing graphics—all without requiring the visitor to scroll down too far. Your Web site is your opportunity to create a good first impression—an opportunity that won’t happen again.
Use compelling headlines with keyword-related content. You want to make sure you use keywords that a prospective patient might search for in a main headline and in the main body of your homepage. But patients are not the only ones who spot those key terms. Search engines also crawl your Web site for keywords that prospective patients may type into the Google search bar—words like gynecologist, ObGyn, urinary leakage, breast lump, pelvic pain, menopause, etc. Using those keywords helps your site to be found more often by patients and helps those prospective patients find information relevant to their medical needs.
5. Place calls to action on every page
Contact us! This is so rudimentary, yet many Web sites do not have easy-to-find contact information on their homepages. Be sure to include your phone number (which could be different than your regular phone office number so you can track how many calls you get from your Web site).
Add a “schedule an appointment” icon in a prominent position on the homepage so the visitor does not have to scroll down to search for it. But don’t just stop at the homepage. Your contact information should be on every page so that, when the visitor is on a page reading about a condition or procedure, the “schedule an appointment” button is right there for her to click.
Be sure to evaluate your contact page. Make sure it’s easy for patients to find multiple ways to connect with you and your office: phone, fax, email, and snail mail.
Interactivity is important. Why not have an “Ask the doctor your question” field? It makes the site interactive and gives you the opportunity to communicate and develop a relationship with your patients.
Additional interactivity
Social media is the new buzz word-of-mouth. Your patients use Facebook, YouTube, blogging, and Twitter every day. It is the easiest way to stay connected and make your practice and your brand part of their daily lives. Social media builds loyalty. Integrating social media into your Web site provides new opportunities to engage your existing patients and to attract new ones to your practice.
Connect to medical records. Your Web site should have an easy portal for patients to connect to their medical records and laboratory results in a secure, encrypted fashion to comply with HIPAA regulations.
You can do this yourself!
You and your staff should be able to make changes on your Web site without having to contact your Web developer, even if you do not have full-time IT assistance. For example, in Dr. Baum’s practice, his support staff can add testimonials, content, and pictures without contacting the Web developer or knowing code.
Make sure that function is designed into your site and that your Web developer teaches you and your staff how to keep your site updated.
The bottom line
Web sites are like a farmer’s fence, they are always under construction. Merely having a Web site, regardless of the size, specialty, or location of your practice, is not enough. Be sure your site attracts, holds, and converts viewers into paying patients. We hope you will consider these 5 suggestions as a roadmap to develop a robust site, so that when you ask a patient who referred her to your practice, her answer will be “your Web site” or “the Internet.” This will bring cockles to your heart and bucks in your bank account.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Web sites are not like wine and cheese—they don’t necessarily get better with age. You may have started your Web page 20 years ago by moving your 3-color trifold brochure onto the Internet. It may have worked then, but to compete today you must have a robust, interactive, attractive Web site that is continuously being updated with new content. What prospective patients are looking for in a Web site has evolved rapidly. How to get these patients to take action and call for an appointment requires a process or a system.
Trying to keep your Web site current can be daunting for most medical practices. If you find that your Web site is not generating new patients and that your existing patients are not using the site in an interactive fashion, then it is time to upgrade. In this article we suggest 5 practical ways to make your Web site a useful adjunct to your medical practice—an automatic patient conversion system.
1. Go mobile
Make your Web site “thumb friendly.” Mobile technology has taken over the desktop and laptop worlds. Now nearly everyone is using a hand-held smartphone or tablet for their Internet needs.
To attract patients your Web page must be responsive to the screen size of a smartphone or tablet—very different from your Web site, which is accessed from a desktop or a laptop computer. The majority of users navigate not with a mouse but with their fingers and thumbs. To ensure they can find their way on your Web page on a mobile device, the screen view should adjust automatically to the mobile device being used. Whether that is accomplished through a mobile responsive design or an entirely different mobile Web site, you do not want the user to have to resize, zoom, or pinch their way through the page in order to read the content. All the buttons must be large enough to be easily pressed without having to zoom in, and the font should be easy-to-read in style and size.
Having your current Web site programmed to be responsive to these devices will increase the time a mobile user spends on your site and make it easier for her to make an appointment.
2. Add patient reviews
What others say about you is far more important than anything you can say about yourself. Almost half of prospective patients will check out your online reviews before calling you to schedule an appointment.1 Therefore, it is very important that you ask for positive feedback from your patients and post it to your Web site. We recommend that you capture compliments from your existing patients when they are in the office. Have a computer or iPad handy for them to create a positive review; patients who “promise” to do it when they get back to the office or home rarely follow through. Testimonials should be visible on your homepage and can link to another testimonial page or review site.
“as many as 8 out of 10 people will look online for information about individual doctors. And all of that happens long before they make an appointment … and what they find—positive, negative, neutral or nothing at all—influences their decision to call or not to call.”2
Always invite your patients to evaluate you, your practice partners, and the practice online. There are numerous patient review Web sites, including: Google Plus, http://www.RateMDs.com, http://www.Vitals.com, and http://www.HealthGrades.com. And check out what your patients are saying about you on a regular basis. Just type “Reviews for Dr. <your name>” into your search bar to find the results.
Although we hope they will, happy patients rarely fill out these online reviews. However, it takes just 2 or 3 unhappy patients to ruin your online reputation. That could be costing you tens of thousands of dollars in lost billing.
3. Share your videos
What’s hot and what’s not? To answer that, just take a look at how many people watch videos on YouTube every day! People don’t want to read anymore; they want to be entertained and spoon-fed information.
Take advantage of this trend by placing videos on your homepage. Post a video that introduces your practice, provides testimonials of satisfied patients, explains some of the procedures you perform, or shows you describing the latest breakthrough in medical technology.
Your videos don’t have to be long. One to 2 minutes is plenty. They don’t have to feature you talking about medical symptoms or procedures (what’s called a talking head video). Use a PowerPoint presentation with voice overlay—and you don’t have to be the one talking.
Your Web site isn’t the only place you’ll want to post your videos. YouTube is second only to Google as the most popular search engine.3 Just about everyone goes to YouTube to view videos on whatever interests them. See our April 2014 article, titled “Using the Internet in your practice. Part 2: Generating new patients using social media,” to learn more on getting started with YouTube.
Videos will improve your Web site rankings and will increase the time visitors spend on the site. When done properly—labeling the videos with relevant keywords, making the videos short, and presenting information in layman’s language with reasons why it is important to seek a professional if the viewer is experiencing these types of symptoms—they are a great way to convert visitors to patients.
4. Hook‘em on the homepage
If you want your Web site to create a favorable first impression, your homepage should reflect that positive impression. Remember, the homepage, as the face of your practice, is the first thing that a patient will see long before she picks up the phone or comes to the office.
A potential patient visiting your site will make a snap judgment within a few seconds. Think of your homepage as a highway billboard. There are about 3 seconds to make an impression and for a driver to decide whether or not she will exit the highway to buy gas or eat at a restaurant or even contact a business in the future by telephone or, most likely, online. A visit to your Web site has the same attraction timing.
Your homepage must be attractive; provide useful, current information; and have pleasing graphics—all without requiring the visitor to scroll down too far. Your Web site is your opportunity to create a good first impression—an opportunity that won’t happen again.
Use compelling headlines with keyword-related content. You want to make sure you use keywords that a prospective patient might search for in a main headline and in the main body of your homepage. But patients are not the only ones who spot those key terms. Search engines also crawl your Web site for keywords that prospective patients may type into the Google search bar—words like gynecologist, ObGyn, urinary leakage, breast lump, pelvic pain, menopause, etc. Using those keywords helps your site to be found more often by patients and helps those prospective patients find information relevant to their medical needs.
5. Place calls to action on every page
Contact us! This is so rudimentary, yet many Web sites do not have easy-to-find contact information on their homepages. Be sure to include your phone number (which could be different than your regular phone office number so you can track how many calls you get from your Web site).
Add a “schedule an appointment” icon in a prominent position on the homepage so the visitor does not have to scroll down to search for it. But don’t just stop at the homepage. Your contact information should be on every page so that, when the visitor is on a page reading about a condition or procedure, the “schedule an appointment” button is right there for her to click.
Be sure to evaluate your contact page. Make sure it’s easy for patients to find multiple ways to connect with you and your office: phone, fax, email, and snail mail.
Interactivity is important. Why not have an “Ask the doctor your question” field? It makes the site interactive and gives you the opportunity to communicate and develop a relationship with your patients.
Additional interactivity
Social media is the new buzz word-of-mouth. Your patients use Facebook, YouTube, blogging, and Twitter every day. It is the easiest way to stay connected and make your practice and your brand part of their daily lives. Social media builds loyalty. Integrating social media into your Web site provides new opportunities to engage your existing patients and to attract new ones to your practice.
Connect to medical records. Your Web site should have an easy portal for patients to connect to their medical records and laboratory results in a secure, encrypted fashion to comply with HIPAA regulations.
You can do this yourself!
You and your staff should be able to make changes on your Web site without having to contact your Web developer, even if you do not have full-time IT assistance. For example, in Dr. Baum’s practice, his support staff can add testimonials, content, and pictures without contacting the Web developer or knowing code.
Make sure that function is designed into your site and that your Web developer teaches you and your staff how to keep your site updated.
The bottom line
Web sites are like a farmer’s fence, they are always under construction. Merely having a Web site, regardless of the size, specialty, or location of your practice, is not enough. Be sure your site attracts, holds, and converts viewers into paying patients. We hope you will consider these 5 suggestions as a roadmap to develop a robust site, so that when you ask a patient who referred her to your practice, her answer will be “your Web site” or “the Internet.” This will bring cockles to your heart and bucks in your bank account.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Online reputation management for doctors. Vanguard Communications Web site. http://vanguardcommuni cations.net/medical-marketing-portfolio/reputation-management. Accessed March 17, 2015.
2. Gandolf S. Ten commandments of online reputation management for physicians [Part one]. Healthcare Success Web site. http://www.healthcaresuccess.com/blog/internet-marketing-advertising/10-commandments-online-reputation-management-physicians-2.html. Published May 12, 2014. Accessed March 9, 2015.
3. YouTube—The 2nd Largest Search Engine. Mushroom Networks Web site. http://www.mushroomnetworks.com/infographics/youtube---the-2nd-largest-search-engine-infographic. Accessed March 17, 2015.
1. Online reputation management for doctors. Vanguard Communications Web site. http://vanguardcommuni cations.net/medical-marketing-portfolio/reputation-management. Accessed March 17, 2015.
2. Gandolf S. Ten commandments of online reputation management for physicians [Part one]. Healthcare Success Web site. http://www.healthcaresuccess.com/blog/internet-marketing-advertising/10-commandments-online-reputation-management-physicians-2.html. Published May 12, 2014. Accessed March 9, 2015.
3. YouTube—The 2nd Largest Search Engine. Mushroom Networks Web site. http://www.mushroomnetworks.com/infographics/youtube---the-2nd-largest-search-engine-infographic. Accessed March 17, 2015.
Sharpening the saw
Recently, I wrote that springtime is an excellent time to spruce up your office, to check your equipment for malfunctions, to resharpen your curettes and scissors, and to back up your computer files and upgrade software. More important than any of that, though, is reevaluating your most important asset: yourself.
I write this reminder every couple of years because it’s so easy to lose sight of the big picture among the pressures of our daily routines. Sooner or later, no matter how dedicated we are, the grind gets to all of us, leading to fatigue, irritability, and a progressive decline in motivation. And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well-being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of 1 a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a piano or sailing lesson; or a long weekend away with my wife. And I take no less than 4 weeks vacation per year.
I know how some of you feel about “wasting” a workday. Vacations are even worse, because patients might go elsewhere while we’re gone, and every day the office is idle we “lose money.”
That whole paradigm is wrong. Stop thinking day to day; think year to year instead. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacation days; it all averages out in the end.
Besides, this is much more important than money. This is breaking the routine, clearing the cobwebs, living your life. Trust me – your practice will still be there when you return.
Last month, my wife and I hiked up a mountain in the Himalayas to the fabled Tiger’s Nest Monastery in Bhutan. As I huffed and puffed up the trail, I didn’t have the time – or the slightest inclination – to worry about the office. When the trek was over, I returned ready to take on the world, and my practice, anew.
And I jotted down some great ideas – practical, medical, and literary. Original thoughts are hard to come by during the daily grind, but they often appear, unannounced, in a new and refreshing environment.
Creative people have long recognized the value of “sharpening the saw.” A classic example is the oft-told story of Swiss physicist K. Alex Müller and German physicist J. Georg Bednorz. In 1986, they reached a major impasse in their superconductivity research; it appeared 2 decades of work might be for naught. The harder they pressed, the more elusive the answer became. So Müller decided to take some time off, put aside his troubles, and research a subject that had always interested him: ceramics.
Nothing could have been further from his research field, of course, since ceramics are among the poorest conductors known. Yet, as he relaxed, it occurred to Müller that a unique property of ceramics might apply to their project. Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor.
The rest, as they say, is history; Müller and Bednorz won a Nobel Prize and triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically levitated trains, and many other applications that are still being realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at the same old problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember Eastern’s First Law: Your last words will NOT be, “I wish I had spent more time in the office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Recently, I wrote that springtime is an excellent time to spruce up your office, to check your equipment for malfunctions, to resharpen your curettes and scissors, and to back up your computer files and upgrade software. More important than any of that, though, is reevaluating your most important asset: yourself.
I write this reminder every couple of years because it’s so easy to lose sight of the big picture among the pressures of our daily routines. Sooner or later, no matter how dedicated we are, the grind gets to all of us, leading to fatigue, irritability, and a progressive decline in motivation. And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well-being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of 1 a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a piano or sailing lesson; or a long weekend away with my wife. And I take no less than 4 weeks vacation per year.
I know how some of you feel about “wasting” a workday. Vacations are even worse, because patients might go elsewhere while we’re gone, and every day the office is idle we “lose money.”
That whole paradigm is wrong. Stop thinking day to day; think year to year instead. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacation days; it all averages out in the end.
Besides, this is much more important than money. This is breaking the routine, clearing the cobwebs, living your life. Trust me – your practice will still be there when you return.
Last month, my wife and I hiked up a mountain in the Himalayas to the fabled Tiger’s Nest Monastery in Bhutan. As I huffed and puffed up the trail, I didn’t have the time – or the slightest inclination – to worry about the office. When the trek was over, I returned ready to take on the world, and my practice, anew.
And I jotted down some great ideas – practical, medical, and literary. Original thoughts are hard to come by during the daily grind, but they often appear, unannounced, in a new and refreshing environment.
Creative people have long recognized the value of “sharpening the saw.” A classic example is the oft-told story of Swiss physicist K. Alex Müller and German physicist J. Georg Bednorz. In 1986, they reached a major impasse in their superconductivity research; it appeared 2 decades of work might be for naught. The harder they pressed, the more elusive the answer became. So Müller decided to take some time off, put aside his troubles, and research a subject that had always interested him: ceramics.
Nothing could have been further from his research field, of course, since ceramics are among the poorest conductors known. Yet, as he relaxed, it occurred to Müller that a unique property of ceramics might apply to their project. Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor.
The rest, as they say, is history; Müller and Bednorz won a Nobel Prize and triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically levitated trains, and many other applications that are still being realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at the same old problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember Eastern’s First Law: Your last words will NOT be, “I wish I had spent more time in the office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Recently, I wrote that springtime is an excellent time to spruce up your office, to check your equipment for malfunctions, to resharpen your curettes and scissors, and to back up your computer files and upgrade software. More important than any of that, though, is reevaluating your most important asset: yourself.
I write this reminder every couple of years because it’s so easy to lose sight of the big picture among the pressures of our daily routines. Sooner or later, no matter how dedicated we are, the grind gets to all of us, leading to fatigue, irritability, and a progressive decline in motivation. And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well-being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of 1 a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a piano or sailing lesson; or a long weekend away with my wife. And I take no less than 4 weeks vacation per year.
I know how some of you feel about “wasting” a workday. Vacations are even worse, because patients might go elsewhere while we’re gone, and every day the office is idle we “lose money.”
That whole paradigm is wrong. Stop thinking day to day; think year to year instead. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacation days; it all averages out in the end.
Besides, this is much more important than money. This is breaking the routine, clearing the cobwebs, living your life. Trust me – your practice will still be there when you return.
Last month, my wife and I hiked up a mountain in the Himalayas to the fabled Tiger’s Nest Monastery in Bhutan. As I huffed and puffed up the trail, I didn’t have the time – or the slightest inclination – to worry about the office. When the trek was over, I returned ready to take on the world, and my practice, anew.
And I jotted down some great ideas – practical, medical, and literary. Original thoughts are hard to come by during the daily grind, but they often appear, unannounced, in a new and refreshing environment.
Creative people have long recognized the value of “sharpening the saw.” A classic example is the oft-told story of Swiss physicist K. Alex Müller and German physicist J. Georg Bednorz. In 1986, they reached a major impasse in their superconductivity research; it appeared 2 decades of work might be for naught. The harder they pressed, the more elusive the answer became. So Müller decided to take some time off, put aside his troubles, and research a subject that had always interested him: ceramics.
Nothing could have been further from his research field, of course, since ceramics are among the poorest conductors known. Yet, as he relaxed, it occurred to Müller that a unique property of ceramics might apply to their project. Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor.
The rest, as they say, is history; Müller and Bednorz won a Nobel Prize and triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically levitated trains, and many other applications that are still being realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at the same old problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember Eastern’s First Law: Your last words will NOT be, “I wish I had spent more time in the office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
How Academic Hospitalists Can Balance Teaching, Nonteaching Roles
As a group director at a growing, university-based hospitalist program, I often interview aspiring academic hospitalists. Inevitably, the conversation turns to a coveted aspect of the job. I’m not talking about the salary. Applicants want to know, “How much time will I spend on teaching services?”
Because hospitalists at academic institutions typically are passionate about their work as instructors and mentors, they highly value time with trainees. Unfortunately, the 2011 Accreditation Council for Graduate Medical Education (ACGME) work hour rules triggered an expansion in non-teaching services at many teaching hospitals, forcing groups either to divide teaching service among an increasing number of attending physicians or to allocate this commodity unevenly on grounds such as seniority. For many group leaders, striking the right balance between teaching and non-teaching service can be an important contributor to recruitment and retention. During these interviews, I’ve often wondered how our group compares to others around the country.
The 2014 State of Hospital Medicine report (SOHM) shines light on this topic.
Among the 422 groups that only care for adults, 52 self-reported as academic groups. The groups were then asked to describe how they distribute work duties. In these academic practices, about half (52.5%) of the group’s full-time equivalents (FTEs) were devoted to clinical work in which the attending supervises learners delivering care. The remaining FTEs were devoted to a mix of clinical work on non-teaching services, administration, and protected time for research.
Interestingly, the portion devoted to clinical teaching differs substantially between university-based and affiliated community teaching hospitals (36.2% vs. 79.1%), suggesting that hospitalists face tough competition for teaching time at the main campuses of academic systems but might have more opportunities to teach at the bedside in faculty jobs at affiliated hospitals.
The above FTE figures represent averages, which don’t tell the whole story. Groups might not distribute teaching time evenly; the approach to allocation ranges from a completely egalitarian approach to a system with two tiers that separate teaching and non-teaching hospitalists.
To address the ranges, the State of Hospital Medicine survey asked respondents to divide their faculty into five categories of individual job types, ranging from “No clinical activity with trainees” to “>75% of clinical activity with trainees” (see Figure 1). The results show a broad array of teaching responsibilities, with 20% of academic hospitalists spending no time teaching and another 21% spending almost all of their time teaching.
I suspect this distribution partially reflects the underlying interests of the individual hospitalists, but it is also a product of the available opportunities. A few factors might influence those opportunities, such as decisions by the hospital to hire hospitalists rather than nurse practitioners and physicians assistants to cover new services, or the presence of specialists and general internists who share teaching service slots with hospitalists.
One of the great things about SHM’s State of Hospital Medicine report is how it depicts the wide variety of careers available to hospitalists; the teaching environment is no exception. Although I strive to help my colleagues tailor positions to suit their interests, we never have quite enough resident service time to meet the demands of our enthusiastic teachers. Fortunately, this report allows me to discuss our job openings with candidates knowing how we stack up against academic programs around the country.
Dr. White is assistant professor of medicine at the University of Washington and hospitalist group director at the University of Washington Medical Center in Seattle.
As a group director at a growing, university-based hospitalist program, I often interview aspiring academic hospitalists. Inevitably, the conversation turns to a coveted aspect of the job. I’m not talking about the salary. Applicants want to know, “How much time will I spend on teaching services?”
Because hospitalists at academic institutions typically are passionate about their work as instructors and mentors, they highly value time with trainees. Unfortunately, the 2011 Accreditation Council for Graduate Medical Education (ACGME) work hour rules triggered an expansion in non-teaching services at many teaching hospitals, forcing groups either to divide teaching service among an increasing number of attending physicians or to allocate this commodity unevenly on grounds such as seniority. For many group leaders, striking the right balance between teaching and non-teaching service can be an important contributor to recruitment and retention. During these interviews, I’ve often wondered how our group compares to others around the country.
The 2014 State of Hospital Medicine report (SOHM) shines light on this topic.
Among the 422 groups that only care for adults, 52 self-reported as academic groups. The groups were then asked to describe how they distribute work duties. In these academic practices, about half (52.5%) of the group’s full-time equivalents (FTEs) were devoted to clinical work in which the attending supervises learners delivering care. The remaining FTEs were devoted to a mix of clinical work on non-teaching services, administration, and protected time for research.
Interestingly, the portion devoted to clinical teaching differs substantially between university-based and affiliated community teaching hospitals (36.2% vs. 79.1%), suggesting that hospitalists face tough competition for teaching time at the main campuses of academic systems but might have more opportunities to teach at the bedside in faculty jobs at affiliated hospitals.
The above FTE figures represent averages, which don’t tell the whole story. Groups might not distribute teaching time evenly; the approach to allocation ranges from a completely egalitarian approach to a system with two tiers that separate teaching and non-teaching hospitalists.
To address the ranges, the State of Hospital Medicine survey asked respondents to divide their faculty into five categories of individual job types, ranging from “No clinical activity with trainees” to “>75% of clinical activity with trainees” (see Figure 1). The results show a broad array of teaching responsibilities, with 20% of academic hospitalists spending no time teaching and another 21% spending almost all of their time teaching.
I suspect this distribution partially reflects the underlying interests of the individual hospitalists, but it is also a product of the available opportunities. A few factors might influence those opportunities, such as decisions by the hospital to hire hospitalists rather than nurse practitioners and physicians assistants to cover new services, or the presence of specialists and general internists who share teaching service slots with hospitalists.
One of the great things about SHM’s State of Hospital Medicine report is how it depicts the wide variety of careers available to hospitalists; the teaching environment is no exception. Although I strive to help my colleagues tailor positions to suit their interests, we never have quite enough resident service time to meet the demands of our enthusiastic teachers. Fortunately, this report allows me to discuss our job openings with candidates knowing how we stack up against academic programs around the country.
Dr. White is assistant professor of medicine at the University of Washington and hospitalist group director at the University of Washington Medical Center in Seattle.
As a group director at a growing, university-based hospitalist program, I often interview aspiring academic hospitalists. Inevitably, the conversation turns to a coveted aspect of the job. I’m not talking about the salary. Applicants want to know, “How much time will I spend on teaching services?”
Because hospitalists at academic institutions typically are passionate about their work as instructors and mentors, they highly value time with trainees. Unfortunately, the 2011 Accreditation Council for Graduate Medical Education (ACGME) work hour rules triggered an expansion in non-teaching services at many teaching hospitals, forcing groups either to divide teaching service among an increasing number of attending physicians or to allocate this commodity unevenly on grounds such as seniority. For many group leaders, striking the right balance between teaching and non-teaching service can be an important contributor to recruitment and retention. During these interviews, I’ve often wondered how our group compares to others around the country.
The 2014 State of Hospital Medicine report (SOHM) shines light on this topic.
Among the 422 groups that only care for adults, 52 self-reported as academic groups. The groups were then asked to describe how they distribute work duties. In these academic practices, about half (52.5%) of the group’s full-time equivalents (FTEs) were devoted to clinical work in which the attending supervises learners delivering care. The remaining FTEs were devoted to a mix of clinical work on non-teaching services, administration, and protected time for research.
Interestingly, the portion devoted to clinical teaching differs substantially between university-based and affiliated community teaching hospitals (36.2% vs. 79.1%), suggesting that hospitalists face tough competition for teaching time at the main campuses of academic systems but might have more opportunities to teach at the bedside in faculty jobs at affiliated hospitals.
The above FTE figures represent averages, which don’t tell the whole story. Groups might not distribute teaching time evenly; the approach to allocation ranges from a completely egalitarian approach to a system with two tiers that separate teaching and non-teaching hospitalists.
To address the ranges, the State of Hospital Medicine survey asked respondents to divide their faculty into five categories of individual job types, ranging from “No clinical activity with trainees” to “>75% of clinical activity with trainees” (see Figure 1). The results show a broad array of teaching responsibilities, with 20% of academic hospitalists spending no time teaching and another 21% spending almost all of their time teaching.
I suspect this distribution partially reflects the underlying interests of the individual hospitalists, but it is also a product of the available opportunities. A few factors might influence those opportunities, such as decisions by the hospital to hire hospitalists rather than nurse practitioners and physicians assistants to cover new services, or the presence of specialists and general internists who share teaching service slots with hospitalists.
One of the great things about SHM’s State of Hospital Medicine report is how it depicts the wide variety of careers available to hospitalists; the teaching environment is no exception. Although I strive to help my colleagues tailor positions to suit their interests, we never have quite enough resident service time to meet the demands of our enthusiastic teachers. Fortunately, this report allows me to discuss our job openings with candidates knowing how we stack up against academic programs around the country.
Dr. White is assistant professor of medicine at the University of Washington and hospitalist group director at the University of Washington Medical Center in Seattle.
Meaningful Use for Surgeons—It’s Not as Complicated as You Think
It’s spring. Have you started your Meaningful Use reporting yet? More important, have you begun reporting at all?
“Say the words Meaningful Use to most orthopedists, and they usually roll their eyes or shake their heads,” says Cheyenne Brinson, MBA, CPA, a KarenZupko & Associates consultant who has been advising surgical practices on Meaningful Use since the program’s inception. Although many orthopedists are successfully using certified electronic health records (EHRs) to e-prescribe and enter radiology and laboratory orders, Brinson says many other requirements are misunderstood and perceived as overly complex. In many cases, practices are doing more work than they need to in order to attest.
“It’s actually not that complicated to meet Meaningful Use requirements,” she says. “The trick is to zero in on what’s relevant only for surgeons. This isn’t crystal clear in the CMS [Centers for Medicare & Medicaid Services] documents, and it’s not the forte of most EHR vendors or trainers either.” In fact, in Brinson’s experience, most EHR trainers present Meaningful Use to every practice as if it were primary care. Yet, the requirements for surgeons are different for primary care and are, frankly, less involved.
That’s good news. Because if you didn’t attest for Meaningful Use in 2014, the first year that reporting was required, you’re automatically getting dinged 2% on your Medicare payments in 2015. So, it’s time to get organized and get moving to avoid further penalties.
Avoid These Four Common Faux Pas
Brinson says the Clinical Quality Measures (CQMs) are hands down the most misunderstood component of Meaningful Use. “When I explain Meaningful Use to surgeons, I can’t jump up and down and wave my hands in the air enough to call attention to this,” she quips.
At issue: There are 64 CQMs, but very few are applicable to surgeons. Yet, many surgeons think they have to perform them for Meaningful Use. Not so, says Brinson. “Surgeons have to report a CQM only if it’s clinically relevant. If none of the CQMs are clinically relevant in your practice, it’s okay to report a zero value if you have not actually performed it.”
Here’s how this plays out. In Stage 2, physicians must report 9 CQMs across 3 domains; Population/Public Health, Patient Safety, and Efficient Use of Healthcare Resources are examples of domains that are most applicable to orthopedists. “If you choose Low Back Pain: Use of Imaging Studies as one of these, it’s possible an orthopedist would have a numeric value to report,” Brinson says. “But if you also choose Use of High-Risk Medications in the Elderly, an orthopedist will probably report a zero value. And that’s totally acceptable. You will not be penalized for reporting zero.”
Another common misconception is around the Vital Signs and Smoking Status measures. “We have worked with surgical practices that think Meaningful Use is requiring them to collect vital signs and smoking status at every visit, even though they may not be clinically relevant,” says Brinson. Again, not true.
“Height and/or weight and blood pressure, as well as smoking status measures, need to be reported only once per patient during the reporting period,” Brinson clarifies. “So from a practical standpoint, most orthopedic practices can collect this data from new patients and then again as clinically necessary,” adding there are even exclusions for physicians who attest that either height and weight and/or blood pressure has no relevance to their scope of practice at all.
Brinson also sees practices do more work than they need to when it comes to Patient Care Reminders. She recently worked with a surgery practice that sent reminders for colonoscopies. “Not exactly clinically relevant,” she says, “and an unnecessary step for staff.” That’s because physicians aren’t required to send reminders that aren’t relevant to their specialty.
The Federal Register states, “An eligible provider (EP) should use clinically relevant information stored within the [EHR] to identify patients who should receive reminders…. The EP is best positioned to decide which information is clinically relevant for this purpose.”
“In orthopedics, clinically relevant reminders could be for an outside referral, a follow-up on an MRI or other test, or a reminder to schedule a postoperative appointment,” Brinson explains. “Work with your EHR vendor to create the reminders that are most appropriate for your patient base.”
The final faux pas that Brinson finds: “Meaningful Use requires you to report data for all patients, not just Medicare patients. That seems to be a point of confusion for many.”
Three Cheers for the Patient Portal Requirement
Stage 2 saw the addition of the Patient Portal Requirement, and Brinson suggests that the benefits of this tool go far beyond Meaningful Use. “Patient portals are essential to a modern practice,” she says. “Patients use them to complete a health history prior to their appointment, pay their bill, schedule follow-up appointments, and more.” Further, the patient portal facilitates another Meaningful Use Stage 2 requirement: secure electronic messaging with patients. For both Meaningful Use and risk management, moving away from e-mail and texting and toward secure/encrypted messaging is a must. The patient portal has this feature already built in, and all messages are stored securely and archived—which meets the HIPAA (Health Insurance Portability and Accountability Act) Omnibus requirements, too.
So if you’ve implemented a patient portal, that’s good for your practice and your patients on many levels. But there is a caveat about meeting the Meaningful Use requirement. “For this requirement, 5% of the unique patients seen during the reporting period must ‘view, download, or transmit to a third party their health information,’” Brinson explains. “So the onus is on your practice to ‘sell’ the benefits of the patient portal and get patients to use it so you can achieve the 5% threshold.”
Clinical Decision Support and Summaries
The requirements of Clinical Decision Support Interventions and Clinical Summaries may seem daunting, but, if you think beyond Meaningful Use for a moment, both facilitate better care.
Take Clinical Decision Support Interventions. What would be helpful for you to know about a patient before surgery? What information would enable you to deliver better care?
“One surgeon told me that a family history of malignant hyperthermia would mean the difference between performing the case in the operating room versus the ambulatory surgery center,” Brinson says. “This is a good example of an intervention that a surgeon would work with their EHR vendor to set up.”
The objective states that each intervention is to be an evidence-based decision-support intervention based on each one and at least one combination of the following data: problem list, medication list, medication allergy list, demographics, laboratory tests and values/results, and vital signs. “Stage 1 requires physicians to implement 1 Clinical Decision Support Intervention, and Stage 2 requires 5,” reminds Brinson.
And here’s all you need to know about Clinical Summaries. Although there are 20 specific required elements of a clinical summary, physicians themselves need to provide details only for clinical instructions and the care plan, including goals and instructions. Ancillary staff can populate the other elements.
Brinson points out that surgeons are not expected to provide a copy of the patient’s note, or to complete the note, before the patient checks out. The requirement under Stage 2 is that the clinical summary is provided to the patient within 1 business day. “From a practical standpoint, practices can print the clinical summary for patients at checkout. A well-done clinical summary is a practice efficiency tool as much as a clinical document. It can reduce phone calls from patients asking, ‘Now what did the doctor tell me to do?’”
Often Overlooked
There are requirements that, Brinson says, surgeons often gloss over: Protect Electronic Health Information and Text-Searchable Progress Notes.
“Stage 2 requires physicians to conduct a privacy risk analysis to protect electronic health information,” she explains. “Most EHR vendors don’t offer this as part of their product, so it’s frequently overlooked.” Such an analysis typically requires an outside vendor, but there are free, do-it-yourself tools available, such as the Privacy and Security Toolkit for Small Provider Organizations,* from the Healthcare Information and Management Systems Society (HIMSS).
The analysis should follow HIPAA guidelines, and the most intensive part of this requirement is to conduct or review a privacy risk analysis of the clinical technology. “You’ve also got to address data encryption and security in the EHR, and ensure HIPAA policies and procedures are in place,” Brinson states.
Text-Searchable Progress Notes are also a new requirement in Stage 2. All progress notes must be text searchable—practices can no longer include progress notes as scanned attachments. “That means no more PDFs,” Brinson says. “Surgeons can still dictate, but the dictation must be entered into the EHR in such a way that it’s searchable. In Stage 2, 30% of unique patients must have a minimum of 1 text-searchable electronic progress note created, edited, and signed in the EHR.”
Conclusion
Meaningful Use does not have to be cumbersome. Focus on what surgical practices need to know, and attestation won’t be as complicated as you think.
*http://www.himss.org/library/healthcare-privacy-security/small-provider-toolkit?navItemNumber=16493.
It’s spring. Have you started your Meaningful Use reporting yet? More important, have you begun reporting at all?
“Say the words Meaningful Use to most orthopedists, and they usually roll their eyes or shake their heads,” says Cheyenne Brinson, MBA, CPA, a KarenZupko & Associates consultant who has been advising surgical practices on Meaningful Use since the program’s inception. Although many orthopedists are successfully using certified electronic health records (EHRs) to e-prescribe and enter radiology and laboratory orders, Brinson says many other requirements are misunderstood and perceived as overly complex. In many cases, practices are doing more work than they need to in order to attest.
“It’s actually not that complicated to meet Meaningful Use requirements,” she says. “The trick is to zero in on what’s relevant only for surgeons. This isn’t crystal clear in the CMS [Centers for Medicare & Medicaid Services] documents, and it’s not the forte of most EHR vendors or trainers either.” In fact, in Brinson’s experience, most EHR trainers present Meaningful Use to every practice as if it were primary care. Yet, the requirements for surgeons are different for primary care and are, frankly, less involved.
That’s good news. Because if you didn’t attest for Meaningful Use in 2014, the first year that reporting was required, you’re automatically getting dinged 2% on your Medicare payments in 2015. So, it’s time to get organized and get moving to avoid further penalties.
Avoid These Four Common Faux Pas
Brinson says the Clinical Quality Measures (CQMs) are hands down the most misunderstood component of Meaningful Use. “When I explain Meaningful Use to surgeons, I can’t jump up and down and wave my hands in the air enough to call attention to this,” she quips.
At issue: There are 64 CQMs, but very few are applicable to surgeons. Yet, many surgeons think they have to perform them for Meaningful Use. Not so, says Brinson. “Surgeons have to report a CQM only if it’s clinically relevant. If none of the CQMs are clinically relevant in your practice, it’s okay to report a zero value if you have not actually performed it.”
Here’s how this plays out. In Stage 2, physicians must report 9 CQMs across 3 domains; Population/Public Health, Patient Safety, and Efficient Use of Healthcare Resources are examples of domains that are most applicable to orthopedists. “If you choose Low Back Pain: Use of Imaging Studies as one of these, it’s possible an orthopedist would have a numeric value to report,” Brinson says. “But if you also choose Use of High-Risk Medications in the Elderly, an orthopedist will probably report a zero value. And that’s totally acceptable. You will not be penalized for reporting zero.”
Another common misconception is around the Vital Signs and Smoking Status measures. “We have worked with surgical practices that think Meaningful Use is requiring them to collect vital signs and smoking status at every visit, even though they may not be clinically relevant,” says Brinson. Again, not true.
“Height and/or weight and blood pressure, as well as smoking status measures, need to be reported only once per patient during the reporting period,” Brinson clarifies. “So from a practical standpoint, most orthopedic practices can collect this data from new patients and then again as clinically necessary,” adding there are even exclusions for physicians who attest that either height and weight and/or blood pressure has no relevance to their scope of practice at all.
Brinson also sees practices do more work than they need to when it comes to Patient Care Reminders. She recently worked with a surgery practice that sent reminders for colonoscopies. “Not exactly clinically relevant,” she says, “and an unnecessary step for staff.” That’s because physicians aren’t required to send reminders that aren’t relevant to their specialty.
The Federal Register states, “An eligible provider (EP) should use clinically relevant information stored within the [EHR] to identify patients who should receive reminders…. The EP is best positioned to decide which information is clinically relevant for this purpose.”
“In orthopedics, clinically relevant reminders could be for an outside referral, a follow-up on an MRI or other test, or a reminder to schedule a postoperative appointment,” Brinson explains. “Work with your EHR vendor to create the reminders that are most appropriate for your patient base.”
The final faux pas that Brinson finds: “Meaningful Use requires you to report data for all patients, not just Medicare patients. That seems to be a point of confusion for many.”
Three Cheers for the Patient Portal Requirement
Stage 2 saw the addition of the Patient Portal Requirement, and Brinson suggests that the benefits of this tool go far beyond Meaningful Use. “Patient portals are essential to a modern practice,” she says. “Patients use them to complete a health history prior to their appointment, pay their bill, schedule follow-up appointments, and more.” Further, the patient portal facilitates another Meaningful Use Stage 2 requirement: secure electronic messaging with patients. For both Meaningful Use and risk management, moving away from e-mail and texting and toward secure/encrypted messaging is a must. The patient portal has this feature already built in, and all messages are stored securely and archived—which meets the HIPAA (Health Insurance Portability and Accountability Act) Omnibus requirements, too.
So if you’ve implemented a patient portal, that’s good for your practice and your patients on many levels. But there is a caveat about meeting the Meaningful Use requirement. “For this requirement, 5% of the unique patients seen during the reporting period must ‘view, download, or transmit to a third party their health information,’” Brinson explains. “So the onus is on your practice to ‘sell’ the benefits of the patient portal and get patients to use it so you can achieve the 5% threshold.”
Clinical Decision Support and Summaries
The requirements of Clinical Decision Support Interventions and Clinical Summaries may seem daunting, but, if you think beyond Meaningful Use for a moment, both facilitate better care.
Take Clinical Decision Support Interventions. What would be helpful for you to know about a patient before surgery? What information would enable you to deliver better care?
“One surgeon told me that a family history of malignant hyperthermia would mean the difference between performing the case in the operating room versus the ambulatory surgery center,” Brinson says. “This is a good example of an intervention that a surgeon would work with their EHR vendor to set up.”
The objective states that each intervention is to be an evidence-based decision-support intervention based on each one and at least one combination of the following data: problem list, medication list, medication allergy list, demographics, laboratory tests and values/results, and vital signs. “Stage 1 requires physicians to implement 1 Clinical Decision Support Intervention, and Stage 2 requires 5,” reminds Brinson.
And here’s all you need to know about Clinical Summaries. Although there are 20 specific required elements of a clinical summary, physicians themselves need to provide details only for clinical instructions and the care plan, including goals and instructions. Ancillary staff can populate the other elements.
Brinson points out that surgeons are not expected to provide a copy of the patient’s note, or to complete the note, before the patient checks out. The requirement under Stage 2 is that the clinical summary is provided to the patient within 1 business day. “From a practical standpoint, practices can print the clinical summary for patients at checkout. A well-done clinical summary is a practice efficiency tool as much as a clinical document. It can reduce phone calls from patients asking, ‘Now what did the doctor tell me to do?’”
Often Overlooked
There are requirements that, Brinson says, surgeons often gloss over: Protect Electronic Health Information and Text-Searchable Progress Notes.
“Stage 2 requires physicians to conduct a privacy risk analysis to protect electronic health information,” she explains. “Most EHR vendors don’t offer this as part of their product, so it’s frequently overlooked.” Such an analysis typically requires an outside vendor, but there are free, do-it-yourself tools available, such as the Privacy and Security Toolkit for Small Provider Organizations,* from the Healthcare Information and Management Systems Society (HIMSS).
The analysis should follow HIPAA guidelines, and the most intensive part of this requirement is to conduct or review a privacy risk analysis of the clinical technology. “You’ve also got to address data encryption and security in the EHR, and ensure HIPAA policies and procedures are in place,” Brinson states.
Text-Searchable Progress Notes are also a new requirement in Stage 2. All progress notes must be text searchable—practices can no longer include progress notes as scanned attachments. “That means no more PDFs,” Brinson says. “Surgeons can still dictate, but the dictation must be entered into the EHR in such a way that it’s searchable. In Stage 2, 30% of unique patients must have a minimum of 1 text-searchable electronic progress note created, edited, and signed in the EHR.”
Conclusion
Meaningful Use does not have to be cumbersome. Focus on what surgical practices need to know, and attestation won’t be as complicated as you think.
It’s spring. Have you started your Meaningful Use reporting yet? More important, have you begun reporting at all?
“Say the words Meaningful Use to most orthopedists, and they usually roll their eyes or shake their heads,” says Cheyenne Brinson, MBA, CPA, a KarenZupko & Associates consultant who has been advising surgical practices on Meaningful Use since the program’s inception. Although many orthopedists are successfully using certified electronic health records (EHRs) to e-prescribe and enter radiology and laboratory orders, Brinson says many other requirements are misunderstood and perceived as overly complex. In many cases, practices are doing more work than they need to in order to attest.
“It’s actually not that complicated to meet Meaningful Use requirements,” she says. “The trick is to zero in on what’s relevant only for surgeons. This isn’t crystal clear in the CMS [Centers for Medicare & Medicaid Services] documents, and it’s not the forte of most EHR vendors or trainers either.” In fact, in Brinson’s experience, most EHR trainers present Meaningful Use to every practice as if it were primary care. Yet, the requirements for surgeons are different for primary care and are, frankly, less involved.
That’s good news. Because if you didn’t attest for Meaningful Use in 2014, the first year that reporting was required, you’re automatically getting dinged 2% on your Medicare payments in 2015. So, it’s time to get organized and get moving to avoid further penalties.
Avoid These Four Common Faux Pas
Brinson says the Clinical Quality Measures (CQMs) are hands down the most misunderstood component of Meaningful Use. “When I explain Meaningful Use to surgeons, I can’t jump up and down and wave my hands in the air enough to call attention to this,” she quips.
At issue: There are 64 CQMs, but very few are applicable to surgeons. Yet, many surgeons think they have to perform them for Meaningful Use. Not so, says Brinson. “Surgeons have to report a CQM only if it’s clinically relevant. If none of the CQMs are clinically relevant in your practice, it’s okay to report a zero value if you have not actually performed it.”
Here’s how this plays out. In Stage 2, physicians must report 9 CQMs across 3 domains; Population/Public Health, Patient Safety, and Efficient Use of Healthcare Resources are examples of domains that are most applicable to orthopedists. “If you choose Low Back Pain: Use of Imaging Studies as one of these, it’s possible an orthopedist would have a numeric value to report,” Brinson says. “But if you also choose Use of High-Risk Medications in the Elderly, an orthopedist will probably report a zero value. And that’s totally acceptable. You will not be penalized for reporting zero.”
Another common misconception is around the Vital Signs and Smoking Status measures. “We have worked with surgical practices that think Meaningful Use is requiring them to collect vital signs and smoking status at every visit, even though they may not be clinically relevant,” says Brinson. Again, not true.
“Height and/or weight and blood pressure, as well as smoking status measures, need to be reported only once per patient during the reporting period,” Brinson clarifies. “So from a practical standpoint, most orthopedic practices can collect this data from new patients and then again as clinically necessary,” adding there are even exclusions for physicians who attest that either height and weight and/or blood pressure has no relevance to their scope of practice at all.
Brinson also sees practices do more work than they need to when it comes to Patient Care Reminders. She recently worked with a surgery practice that sent reminders for colonoscopies. “Not exactly clinically relevant,” she says, “and an unnecessary step for staff.” That’s because physicians aren’t required to send reminders that aren’t relevant to their specialty.
The Federal Register states, “An eligible provider (EP) should use clinically relevant information stored within the [EHR] to identify patients who should receive reminders…. The EP is best positioned to decide which information is clinically relevant for this purpose.”
“In orthopedics, clinically relevant reminders could be for an outside referral, a follow-up on an MRI or other test, or a reminder to schedule a postoperative appointment,” Brinson explains. “Work with your EHR vendor to create the reminders that are most appropriate for your patient base.”
The final faux pas that Brinson finds: “Meaningful Use requires you to report data for all patients, not just Medicare patients. That seems to be a point of confusion for many.”
Three Cheers for the Patient Portal Requirement
Stage 2 saw the addition of the Patient Portal Requirement, and Brinson suggests that the benefits of this tool go far beyond Meaningful Use. “Patient portals are essential to a modern practice,” she says. “Patients use them to complete a health history prior to their appointment, pay their bill, schedule follow-up appointments, and more.” Further, the patient portal facilitates another Meaningful Use Stage 2 requirement: secure electronic messaging with patients. For both Meaningful Use and risk management, moving away from e-mail and texting and toward secure/encrypted messaging is a must. The patient portal has this feature already built in, and all messages are stored securely and archived—which meets the HIPAA (Health Insurance Portability and Accountability Act) Omnibus requirements, too.
So if you’ve implemented a patient portal, that’s good for your practice and your patients on many levels. But there is a caveat about meeting the Meaningful Use requirement. “For this requirement, 5% of the unique patients seen during the reporting period must ‘view, download, or transmit to a third party their health information,’” Brinson explains. “So the onus is on your practice to ‘sell’ the benefits of the patient portal and get patients to use it so you can achieve the 5% threshold.”
Clinical Decision Support and Summaries
The requirements of Clinical Decision Support Interventions and Clinical Summaries may seem daunting, but, if you think beyond Meaningful Use for a moment, both facilitate better care.
Take Clinical Decision Support Interventions. What would be helpful for you to know about a patient before surgery? What information would enable you to deliver better care?
“One surgeon told me that a family history of malignant hyperthermia would mean the difference between performing the case in the operating room versus the ambulatory surgery center,” Brinson says. “This is a good example of an intervention that a surgeon would work with their EHR vendor to set up.”
The objective states that each intervention is to be an evidence-based decision-support intervention based on each one and at least one combination of the following data: problem list, medication list, medication allergy list, demographics, laboratory tests and values/results, and vital signs. “Stage 1 requires physicians to implement 1 Clinical Decision Support Intervention, and Stage 2 requires 5,” reminds Brinson.
And here’s all you need to know about Clinical Summaries. Although there are 20 specific required elements of a clinical summary, physicians themselves need to provide details only for clinical instructions and the care plan, including goals and instructions. Ancillary staff can populate the other elements.
Brinson points out that surgeons are not expected to provide a copy of the patient’s note, or to complete the note, before the patient checks out. The requirement under Stage 2 is that the clinical summary is provided to the patient within 1 business day. “From a practical standpoint, practices can print the clinical summary for patients at checkout. A well-done clinical summary is a practice efficiency tool as much as a clinical document. It can reduce phone calls from patients asking, ‘Now what did the doctor tell me to do?’”
Often Overlooked
There are requirements that, Brinson says, surgeons often gloss over: Protect Electronic Health Information and Text-Searchable Progress Notes.
“Stage 2 requires physicians to conduct a privacy risk analysis to protect electronic health information,” she explains. “Most EHR vendors don’t offer this as part of their product, so it’s frequently overlooked.” Such an analysis typically requires an outside vendor, but there are free, do-it-yourself tools available, such as the Privacy and Security Toolkit for Small Provider Organizations,* from the Healthcare Information and Management Systems Society (HIMSS).
The analysis should follow HIPAA guidelines, and the most intensive part of this requirement is to conduct or review a privacy risk analysis of the clinical technology. “You’ve also got to address data encryption and security in the EHR, and ensure HIPAA policies and procedures are in place,” Brinson states.
Text-Searchable Progress Notes are also a new requirement in Stage 2. All progress notes must be text searchable—practices can no longer include progress notes as scanned attachments. “That means no more PDFs,” Brinson says. “Surgeons can still dictate, but the dictation must be entered into the EHR in such a way that it’s searchable. In Stage 2, 30% of unique patients must have a minimum of 1 text-searchable electronic progress note created, edited, and signed in the EHR.”
Conclusion
Meaningful Use does not have to be cumbersome. Focus on what surgical practices need to know, and attestation won’t be as complicated as you think.
*http://www.himss.org/library/healthcare-privacy-security/small-provider-toolkit?navItemNumber=16493.
*http://www.himss.org/library/healthcare-privacy-security/small-provider-toolkit?navItemNumber=16493.
Visit your office
Every year around now, as spring begins to revive the landscape, I like to take a tour of my office from the perspective of a patient visiting our facility for the first time, because more often than not, the internal environment could use a bit of a revival as well.
We tend not to notice gradual deterioration in the workplace we inhabit every day: Carpets fade and dull with constant traffic and cleaning; wallpaper and paint accumulate dirt, stains, and damage; furniture gets dirty and dented, fabric rips, hardware goes missing.
When did you last take a good look at your waiting room? Have your patients been snacking and spilling drinks in there, despite the signs begging them not to? Is the wallpaper smudged on the walls behind chairs, where they rest their heads? How are the carpeting and upholstery holding up?
Even if you don’t find anything obvious, it’s wise to check periodically for subtle evidence of age: Find some patches of protected carpeting and flooring – under desks, for example – and compare them with exposed floors.
And look at the decor itself; is it dated or just plain old looking? Any interior designer will tell you he or she can determine quite accurately when a space was last decorated, simply by the color and style of the materials used. If your office is stuck in the ’90s, it’s probably time for a change.
If you’re planning a vacation this summer (and I hope you are), that would be the perfect time for a redo. Your patients will be spared the dust and turmoil, tradespeople won’t have to work around your office hours, and you won’t have to cancel any hours that weren’t already canceled. Best of all, you’ll come back to a clean, fresh environment.
Start by reviewing your color scheme. If it’s hopelessly out of date and style, or if you are just tired of it, change it. Wallpaper and carpeting should be long-wearing industrial quality, paint should be high-quality eggshell finish to facilitate cleaning, and everything should be professionally applied. (This is neither the time nor place for do-it-yourself experiments.) And get your building’s maintenance crew to fix any nagging plumbing, electrical, or heating/air conditioning problems while pipes, ducts, and wires are more readily accessible.
If your wall decorations are dated and unattractive, now would be a good time to replace at least some of them. This need not be an expensive proposition. I recently redecorated my exam room walls with framed photos from my travel adventures, to very positive responses from patients and staff alike. If you’re not an artist or photographer, invite family members, local artists, or talented patients to display some of their creations on your walls.
Plants are great accents and excellent stress reducers for apprehensive patients, yet many offices have little or no plant life. If you are hesitant to take on the extra work of plant upkeep, consider using one of the many corporate plant services that rent you the plants, keep them healthy, and replace them as necessary.
Furniture is another important element in keeping your office environment fresh and inviting. You may be able to resurface and reupholster what you have now, but if not, shop carefully. Beware of nonmedical products promoted specifically to physicians, as they tend to be overpriced. If you shop online, remember to factor in shipping costs, which can be considerable for furniture. Don’t be afraid to ask for discounts; you won’t get them if you don’t ask.
This is also a good time to clear out old textbooks, magazines, and files that you will never open again – not in this digital age.
Finally, spruce-up time is an excellent opportunity to inventory your medical equipment. We’ve all seen vintage offices full of gadgets that were state-of-the-art decades ago. Nostalgia is nice, but would you want to be treated by a physician whose office could be a Smithsonian exhibit titled, “Doctor’s Office Circa 1975?” Neither would your patients, for the most part. In fact, many of them – particularly younger ones – assume that doctors who don’t keep up with technologic innovations don’t keep up with anything else, either.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Every year around now, as spring begins to revive the landscape, I like to take a tour of my office from the perspective of a patient visiting our facility for the first time, because more often than not, the internal environment could use a bit of a revival as well.
We tend not to notice gradual deterioration in the workplace we inhabit every day: Carpets fade and dull with constant traffic and cleaning; wallpaper and paint accumulate dirt, stains, and damage; furniture gets dirty and dented, fabric rips, hardware goes missing.
When did you last take a good look at your waiting room? Have your patients been snacking and spilling drinks in there, despite the signs begging them not to? Is the wallpaper smudged on the walls behind chairs, where they rest their heads? How are the carpeting and upholstery holding up?
Even if you don’t find anything obvious, it’s wise to check periodically for subtle evidence of age: Find some patches of protected carpeting and flooring – under desks, for example – and compare them with exposed floors.
And look at the decor itself; is it dated or just plain old looking? Any interior designer will tell you he or she can determine quite accurately when a space was last decorated, simply by the color and style of the materials used. If your office is stuck in the ’90s, it’s probably time for a change.
If you’re planning a vacation this summer (and I hope you are), that would be the perfect time for a redo. Your patients will be spared the dust and turmoil, tradespeople won’t have to work around your office hours, and you won’t have to cancel any hours that weren’t already canceled. Best of all, you’ll come back to a clean, fresh environment.
Start by reviewing your color scheme. If it’s hopelessly out of date and style, or if you are just tired of it, change it. Wallpaper and carpeting should be long-wearing industrial quality, paint should be high-quality eggshell finish to facilitate cleaning, and everything should be professionally applied. (This is neither the time nor place for do-it-yourself experiments.) And get your building’s maintenance crew to fix any nagging plumbing, electrical, or heating/air conditioning problems while pipes, ducts, and wires are more readily accessible.
If your wall decorations are dated and unattractive, now would be a good time to replace at least some of them. This need not be an expensive proposition. I recently redecorated my exam room walls with framed photos from my travel adventures, to very positive responses from patients and staff alike. If you’re not an artist or photographer, invite family members, local artists, or talented patients to display some of their creations on your walls.
Plants are great accents and excellent stress reducers for apprehensive patients, yet many offices have little or no plant life. If you are hesitant to take on the extra work of plant upkeep, consider using one of the many corporate plant services that rent you the plants, keep them healthy, and replace them as necessary.
Furniture is another important element in keeping your office environment fresh and inviting. You may be able to resurface and reupholster what you have now, but if not, shop carefully. Beware of nonmedical products promoted specifically to physicians, as they tend to be overpriced. If you shop online, remember to factor in shipping costs, which can be considerable for furniture. Don’t be afraid to ask for discounts; you won’t get them if you don’t ask.
This is also a good time to clear out old textbooks, magazines, and files that you will never open again – not in this digital age.
Finally, spruce-up time is an excellent opportunity to inventory your medical equipment. We’ve all seen vintage offices full of gadgets that were state-of-the-art decades ago. Nostalgia is nice, but would you want to be treated by a physician whose office could be a Smithsonian exhibit titled, “Doctor’s Office Circa 1975?” Neither would your patients, for the most part. In fact, many of them – particularly younger ones – assume that doctors who don’t keep up with technologic innovations don’t keep up with anything else, either.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Every year around now, as spring begins to revive the landscape, I like to take a tour of my office from the perspective of a patient visiting our facility for the first time, because more often than not, the internal environment could use a bit of a revival as well.
We tend not to notice gradual deterioration in the workplace we inhabit every day: Carpets fade and dull with constant traffic and cleaning; wallpaper and paint accumulate dirt, stains, and damage; furniture gets dirty and dented, fabric rips, hardware goes missing.
When did you last take a good look at your waiting room? Have your patients been snacking and spilling drinks in there, despite the signs begging them not to? Is the wallpaper smudged on the walls behind chairs, where they rest their heads? How are the carpeting and upholstery holding up?
Even if you don’t find anything obvious, it’s wise to check periodically for subtle evidence of age: Find some patches of protected carpeting and flooring – under desks, for example – and compare them with exposed floors.
And look at the decor itself; is it dated or just plain old looking? Any interior designer will tell you he or she can determine quite accurately when a space was last decorated, simply by the color and style of the materials used. If your office is stuck in the ’90s, it’s probably time for a change.
If you’re planning a vacation this summer (and I hope you are), that would be the perfect time for a redo. Your patients will be spared the dust and turmoil, tradespeople won’t have to work around your office hours, and you won’t have to cancel any hours that weren’t already canceled. Best of all, you’ll come back to a clean, fresh environment.
Start by reviewing your color scheme. If it’s hopelessly out of date and style, or if you are just tired of it, change it. Wallpaper and carpeting should be long-wearing industrial quality, paint should be high-quality eggshell finish to facilitate cleaning, and everything should be professionally applied. (This is neither the time nor place for do-it-yourself experiments.) And get your building’s maintenance crew to fix any nagging plumbing, electrical, or heating/air conditioning problems while pipes, ducts, and wires are more readily accessible.
If your wall decorations are dated and unattractive, now would be a good time to replace at least some of them. This need not be an expensive proposition. I recently redecorated my exam room walls with framed photos from my travel adventures, to very positive responses from patients and staff alike. If you’re not an artist or photographer, invite family members, local artists, or talented patients to display some of their creations on your walls.
Plants are great accents and excellent stress reducers for apprehensive patients, yet many offices have little or no plant life. If you are hesitant to take on the extra work of plant upkeep, consider using one of the many corporate plant services that rent you the plants, keep them healthy, and replace them as necessary.
Furniture is another important element in keeping your office environment fresh and inviting. You may be able to resurface and reupholster what you have now, but if not, shop carefully. Beware of nonmedical products promoted specifically to physicians, as they tend to be overpriced. If you shop online, remember to factor in shipping costs, which can be considerable for furniture. Don’t be afraid to ask for discounts; you won’t get them if you don’t ask.
This is also a good time to clear out old textbooks, magazines, and files that you will never open again – not in this digital age.
Finally, spruce-up time is an excellent opportunity to inventory your medical equipment. We’ve all seen vintage offices full of gadgets that were state-of-the-art decades ago. Nostalgia is nice, but would you want to be treated by a physician whose office could be a Smithsonian exhibit titled, “Doctor’s Office Circa 1975?” Neither would your patients, for the most part. In fact, many of them – particularly younger ones – assume that doctors who don’t keep up with technologic innovations don’t keep up with anything else, either.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.