User login
How Hospitalist Groups Make Time for Leadership
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
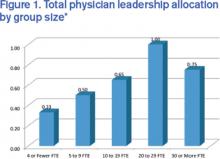
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Time-Based Physician Services Require Proper Documentation
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
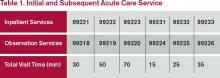
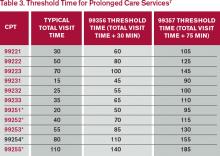
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Joining forces, Part 2
The ongoing sea change in medicine has led to a substantial erosion of physician autonomy, and to ever-increasing administrative burdens that hit small practices the hardest. Does this mean that the independent private physician practice model is doomed, as some predict? Absolutely not; but it will force many solo practitioners and small groups to join forces to protect themselves.
Those practices that offer unique services, or fill an unmet niche, may be able to remain small; but most smaller practices will need to consider a larger alternative. In a previous column, I outlined the basics of one such protective strategy – merging two or more small practices into a larger entity – but there are other options to consider.
One attractive and relatively straightforward strategy is the formation of a cooperative group. In most areas, there are very likely several small practices in similar predicaments that might be receptive to discussing a collaboration on billing and purchasing. This allows each participant to maintain independence as a private practice, while pooling resources to ease the administrative burdens of all. Once that arrangement is in place, the group can consider more ambitious projects, such as the joint purchase of an EHR system, sharing of personnel to lower staffing costs, and an integrated scheduling system. The latter will be particularly attractive to participants in later stages of their careers who are considering an intermediate option, somewhere between full-time work and complete retirement.
After a time, when the structure is stabilized and everyone agrees that his or her individual and shared interests and goals are being met, an outright merger can be contemplated. Projects of this scope require careful planning and implementation, and should not be undertaken without the help of competent legal counsel and an experienced business consultant.
A more complex but increasingly popular option is to join other small practices and providers in an independent practice association (IPA). An IPA is a legal entity organized and directed by physicians for the purpose of negotiating contracts with insurance companies on their behalf. Because of its structure, an IPA is better positioned to enter into such financial arrangements, and to counterbalance the leverage of insurers, but there are legal issues to consider. Many IPAs are vulnerable to antitrust charges because they include competing health care providers. You should check with legal counsel before signing on to an IPA, to make sure that it abides by antitrust and price fixing laws. IPAs have also been known to fail, particularly in states where they are not adequately regulated.
A possible successor to IPAs is the accountable care organization (ACO), an entity born as a component of the Affordable Care Act. While the official definition remains nebulous, an ACO is basically a network of doctors and hospitals that shares financial and medical responsibility for providing coordinated and efficient care to patients. The goal of ACO participants is to limit unnecessary spending, both individually and collectively, according to criteria established by the Centers for Medicare & Medicaid Services, without compromising quality of care in the process. More than 600 ACOs had been approved by the CMS as of the beginning of 2014.
It is important to remember that the ACO model remains very much a work in progress. ACOs make providers jointly accountable for the health of their patients. They offer financial incentives to cooperate, and to save money by avoiding unnecessary tests and procedures. A key component is the sharing of information. Providers who save money while also meeting quality targets are theoretically entitled to a portion of the savings.
As with IPAs, ACO ventures involve a measure of risk. ACOs that fail to meet the CMS performance and savings benchmarks can be stuck with the bill for investments made to improve care, such as equipment and computer purchases and the hiring of mid-level providers and managers, and they may be assessed monetary penalties as well. ACOs sponsored by physicians or rural providers, however, can apply to receive payments in advance to help finance infrastructure investments – a concession the Obama administration made after receiving complaints from rural hospitals.
Clearly, the price of remaining autonomous will be significant, and many private practitioners will be unwilling to pay it: Only 36% of physicians remained in independent practice at the end of the 2013, according to data from the American Medical Association – down from 57% in 2000 – but those of us who remain committed to independence will find ways to preserve it. In medicine, as in life, those most responsive to change will survive and flourish.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
The ongoing sea change in medicine has led to a substantial erosion of physician autonomy, and to ever-increasing administrative burdens that hit small practices the hardest. Does this mean that the independent private physician practice model is doomed, as some predict? Absolutely not; but it will force many solo practitioners and small groups to join forces to protect themselves.
Those practices that offer unique services, or fill an unmet niche, may be able to remain small; but most smaller practices will need to consider a larger alternative. In a previous column, I outlined the basics of one such protective strategy – merging two or more small practices into a larger entity – but there are other options to consider.
One attractive and relatively straightforward strategy is the formation of a cooperative group. In most areas, there are very likely several small practices in similar predicaments that might be receptive to discussing a collaboration on billing and purchasing. This allows each participant to maintain independence as a private practice, while pooling resources to ease the administrative burdens of all. Once that arrangement is in place, the group can consider more ambitious projects, such as the joint purchase of an EHR system, sharing of personnel to lower staffing costs, and an integrated scheduling system. The latter will be particularly attractive to participants in later stages of their careers who are considering an intermediate option, somewhere between full-time work and complete retirement.
After a time, when the structure is stabilized and everyone agrees that his or her individual and shared interests and goals are being met, an outright merger can be contemplated. Projects of this scope require careful planning and implementation, and should not be undertaken without the help of competent legal counsel and an experienced business consultant.
A more complex but increasingly popular option is to join other small practices and providers in an independent practice association (IPA). An IPA is a legal entity organized and directed by physicians for the purpose of negotiating contracts with insurance companies on their behalf. Because of its structure, an IPA is better positioned to enter into such financial arrangements, and to counterbalance the leverage of insurers, but there are legal issues to consider. Many IPAs are vulnerable to antitrust charges because they include competing health care providers. You should check with legal counsel before signing on to an IPA, to make sure that it abides by antitrust and price fixing laws. IPAs have also been known to fail, particularly in states where they are not adequately regulated.
A possible successor to IPAs is the accountable care organization (ACO), an entity born as a component of the Affordable Care Act. While the official definition remains nebulous, an ACO is basically a network of doctors and hospitals that shares financial and medical responsibility for providing coordinated and efficient care to patients. The goal of ACO participants is to limit unnecessary spending, both individually and collectively, according to criteria established by the Centers for Medicare & Medicaid Services, without compromising quality of care in the process. More than 600 ACOs had been approved by the CMS as of the beginning of 2014.
It is important to remember that the ACO model remains very much a work in progress. ACOs make providers jointly accountable for the health of their patients. They offer financial incentives to cooperate, and to save money by avoiding unnecessary tests and procedures. A key component is the sharing of information. Providers who save money while also meeting quality targets are theoretically entitled to a portion of the savings.
As with IPAs, ACO ventures involve a measure of risk. ACOs that fail to meet the CMS performance and savings benchmarks can be stuck with the bill for investments made to improve care, such as equipment and computer purchases and the hiring of mid-level providers and managers, and they may be assessed monetary penalties as well. ACOs sponsored by physicians or rural providers, however, can apply to receive payments in advance to help finance infrastructure investments – a concession the Obama administration made after receiving complaints from rural hospitals.
Clearly, the price of remaining autonomous will be significant, and many private practitioners will be unwilling to pay it: Only 36% of physicians remained in independent practice at the end of the 2013, according to data from the American Medical Association – down from 57% in 2000 – but those of us who remain committed to independence will find ways to preserve it. In medicine, as in life, those most responsive to change will survive and flourish.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
The ongoing sea change in medicine has led to a substantial erosion of physician autonomy, and to ever-increasing administrative burdens that hit small practices the hardest. Does this mean that the independent private physician practice model is doomed, as some predict? Absolutely not; but it will force many solo practitioners and small groups to join forces to protect themselves.
Those practices that offer unique services, or fill an unmet niche, may be able to remain small; but most smaller practices will need to consider a larger alternative. In a previous column, I outlined the basics of one such protective strategy – merging two or more small practices into a larger entity – but there are other options to consider.
One attractive and relatively straightforward strategy is the formation of a cooperative group. In most areas, there are very likely several small practices in similar predicaments that might be receptive to discussing a collaboration on billing and purchasing. This allows each participant to maintain independence as a private practice, while pooling resources to ease the administrative burdens of all. Once that arrangement is in place, the group can consider more ambitious projects, such as the joint purchase of an EHR system, sharing of personnel to lower staffing costs, and an integrated scheduling system. The latter will be particularly attractive to participants in later stages of their careers who are considering an intermediate option, somewhere between full-time work and complete retirement.
After a time, when the structure is stabilized and everyone agrees that his or her individual and shared interests and goals are being met, an outright merger can be contemplated. Projects of this scope require careful planning and implementation, and should not be undertaken without the help of competent legal counsel and an experienced business consultant.
A more complex but increasingly popular option is to join other small practices and providers in an independent practice association (IPA). An IPA is a legal entity organized and directed by physicians for the purpose of negotiating contracts with insurance companies on their behalf. Because of its structure, an IPA is better positioned to enter into such financial arrangements, and to counterbalance the leverage of insurers, but there are legal issues to consider. Many IPAs are vulnerable to antitrust charges because they include competing health care providers. You should check with legal counsel before signing on to an IPA, to make sure that it abides by antitrust and price fixing laws. IPAs have also been known to fail, particularly in states where they are not adequately regulated.
A possible successor to IPAs is the accountable care organization (ACO), an entity born as a component of the Affordable Care Act. While the official definition remains nebulous, an ACO is basically a network of doctors and hospitals that shares financial and medical responsibility for providing coordinated and efficient care to patients. The goal of ACO participants is to limit unnecessary spending, both individually and collectively, according to criteria established by the Centers for Medicare & Medicaid Services, without compromising quality of care in the process. More than 600 ACOs had been approved by the CMS as of the beginning of 2014.
It is important to remember that the ACO model remains very much a work in progress. ACOs make providers jointly accountable for the health of their patients. They offer financial incentives to cooperate, and to save money by avoiding unnecessary tests and procedures. A key component is the sharing of information. Providers who save money while also meeting quality targets are theoretically entitled to a portion of the savings.
As with IPAs, ACO ventures involve a measure of risk. ACOs that fail to meet the CMS performance and savings benchmarks can be stuck with the bill for investments made to improve care, such as equipment and computer purchases and the hiring of mid-level providers and managers, and they may be assessed monetary penalties as well. ACOs sponsored by physicians or rural providers, however, can apply to receive payments in advance to help finance infrastructure investments – a concession the Obama administration made after receiving complaints from rural hospitals.
Clearly, the price of remaining autonomous will be significant, and many private practitioners will be unwilling to pay it: Only 36% of physicians remained in independent practice at the end of the 2013, according to data from the American Medical Association – down from 57% in 2000 – but those of us who remain committed to independence will find ways to preserve it. In medicine, as in life, those most responsive to change will survive and flourish.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Fit Direct Observation of Medical Trainees Into Your Day
All of us who work with housestaff understand that a crucial component of teaching clinical medicine is to take the time to both supervise resident work and deliver constructive feedback on its quality. In the assessment of competence, trainees have “direct supervision” when an attending, senior resident, or other individual is physically present and guiding the care in real time or “indirect supervision” when work is being checked after the care has been administered.
Regardless of the level of supervision, checking in with direct observations (watching trainees do the actual work in real time) provides invaluable information for both patient care and resident assessment. Given that assessment and supervision are key components of the Accreditation Council for Graduate Medical Education’s (ACGME) Next Accreditation System, many programs are now placing particular emphasis on the time we spend observing our trainees.
How can faculty fit direct observation into an already busy day? Here are some ideas for how to adapt and leverage your workflow to create new opportunities for resident skills assessment.
Micro-Observations Matter
Gone are the days of sitting in a patient room for an hour observing a long history and physical performed by the resident or student that you are supervising. In spite of time constraints, you should aim to be at the bedside at the same time as the trainee as much as possible. Once there, take note of all that you see. For example, we often observe residents and students during bedside rounds or critical family discussions. Here are additional opportunities for trainee observation that might fit into your workflow:
- First thing in the morning, when the team is pre-rounding (this is perfect for when you are worried about a patient or are scheduled for a busy afternoon). Do NOT interrupt the resident workflow. Instruct them at the beginning of the rotation that you plan to observe unannounced. If they see you, they should continue with their normal activities. Pop in and out to catch key points, and gather the information necessary to guide patient care. Don’t take over to do teaching or feedback; that will come later in the day.
- During a procedure performed by a supervising resident who already has demonstrated technical competence. Bring a computer on wheels into the patient’s room, sit down, and catch up on charting while listening to and observing the explanations, teaching, and interaction between the patient and the resident. You can still intervene if necessary, but take appropriate steps to allow resident autonomy and the observation of high-level communication skills.
- At the bedside of a clinically unstable patient. If you are together with the team when a nurse calls with a concern, you can instruct the resident to go ahead and intervene with close follow-up in a few minutes. This allows residents to get a head start, gather information, and establish themselves as the decision-makers, while still providing an opportunity for close observation by the faculty.
- Finalizing a discharge first thing in the morning. With most hospitals focusing on discharge timeliness, faculty often discuss patients scheduled for discharge prior to or outside of formal rounds. Get to the patient! Observe the resident interacting with the patient and multidisciplinary team, confirming medication reconciliation, finalizing the discharge diagnosis and instructions, and inquiring further about barriers to adherence with the discharge regimen.
Vary Your Approach
Use a variety of formats to tell your learners what was observed. Specific, quick comments made in real time can be encouraging, and brief suggestions are usually welcome in the context of a particular patient. Other observations and feedback that need to be more sensitive or require more time are perfect to wrap up at the end of the day. Finally, the message function in the electronic medical record is another great and timely format for providing feedback on observations related to clinical documentation, differential diagnosis, and management plan.
Real-Time Recordkeeping
Record your observations as you go. Even though you are providing formative feedback throughout the month, you likely also will be expected to translate those observations into a summative end-of-rotation assessment. Whether it is on a notecard with the name of each trainee being supervised or on a printed blank copy of the end of the month assessment or other program-specific assessments, jotting down specific observations will help you recall key information.
When feedback is provided, note the date in order to guide your summative feedback discussion and the final assessment.
Keep in mind that program assessment tools often serve to remind faculty of specific behaviors that have not historically been evaluated. For example, faculty might be in the habit of providing feedback on communication skills after a family meeting but may not specifically listen for trainees to use “teach-back” concepts when explaining the plan for discharge or noting whether they actively seek input from the multidisciplinary team. A tool that lists “teach-back” or “seeks out interprofessional collaboration” as line items on the form can help to remind you of the qualities you are being asked to assess.
Although direct observation is essential in providing useful assessments during the course of supervision of trainees, there are additional ways that faculty can “see” how a trainee is doing. For example, faculty or supervising residents can “observe” an intern’s completed discharge summary in real time for important and key components. Checking this work enables you to provide an assessment of additional skills (i.e., medication reconciliation, medical knowledge, management of clinical conditions, and appropriate handoff to future care providers). As trainees progressively demonstrate competence, the degree of supervision evolves to the point of a quick verification rather than the initial detailed review.
In summary, supervising trainees well means both thinking critically about their care of patients and providing feedback. As much as we have adapted our clinical workflow to meet increasing regulatory, quality, or patient throughput requirements, we must also change our educational workflow to meet the needs of our learners.
This adaptation should not be onerous. A few simple adjustments, as outlined above, can lead to higher-quality assessments and increased satisfaction in your role as teacher. So, get back out on the wards and observe!
Dr. O’Malley is the internal medicine residency program director at Banner Good Samaritan in Phoenix, Ariz., and an assistant professor of medicine at the University of Arizona College of Medicine. She currently serves as SHM’s representative on the Alliance for Academic Internal Medicine’s Internal Medicine Education Redesign Advisory Board, along with Dr. Caverzagie, who is associate dean for educational strategy at the University of Nebraska College of Medicine in Omaha and vice president for education, clinical enterprise of the Nebraska Medical Center. Dr. Caverzagie also was a member of the ABIM and ACGME milestone writing groups.
All of us who work with housestaff understand that a crucial component of teaching clinical medicine is to take the time to both supervise resident work and deliver constructive feedback on its quality. In the assessment of competence, trainees have “direct supervision” when an attending, senior resident, or other individual is physically present and guiding the care in real time or “indirect supervision” when work is being checked after the care has been administered.
Regardless of the level of supervision, checking in with direct observations (watching trainees do the actual work in real time) provides invaluable information for both patient care and resident assessment. Given that assessment and supervision are key components of the Accreditation Council for Graduate Medical Education’s (ACGME) Next Accreditation System, many programs are now placing particular emphasis on the time we spend observing our trainees.
How can faculty fit direct observation into an already busy day? Here are some ideas for how to adapt and leverage your workflow to create new opportunities for resident skills assessment.
Micro-Observations Matter
Gone are the days of sitting in a patient room for an hour observing a long history and physical performed by the resident or student that you are supervising. In spite of time constraints, you should aim to be at the bedside at the same time as the trainee as much as possible. Once there, take note of all that you see. For example, we often observe residents and students during bedside rounds or critical family discussions. Here are additional opportunities for trainee observation that might fit into your workflow:
- First thing in the morning, when the team is pre-rounding (this is perfect for when you are worried about a patient or are scheduled for a busy afternoon). Do NOT interrupt the resident workflow. Instruct them at the beginning of the rotation that you plan to observe unannounced. If they see you, they should continue with their normal activities. Pop in and out to catch key points, and gather the information necessary to guide patient care. Don’t take over to do teaching or feedback; that will come later in the day.
- During a procedure performed by a supervising resident who already has demonstrated technical competence. Bring a computer on wheels into the patient’s room, sit down, and catch up on charting while listening to and observing the explanations, teaching, and interaction between the patient and the resident. You can still intervene if necessary, but take appropriate steps to allow resident autonomy and the observation of high-level communication skills.
- At the bedside of a clinically unstable patient. If you are together with the team when a nurse calls with a concern, you can instruct the resident to go ahead and intervene with close follow-up in a few minutes. This allows residents to get a head start, gather information, and establish themselves as the decision-makers, while still providing an opportunity for close observation by the faculty.
- Finalizing a discharge first thing in the morning. With most hospitals focusing on discharge timeliness, faculty often discuss patients scheduled for discharge prior to or outside of formal rounds. Get to the patient! Observe the resident interacting with the patient and multidisciplinary team, confirming medication reconciliation, finalizing the discharge diagnosis and instructions, and inquiring further about barriers to adherence with the discharge regimen.
Vary Your Approach
Use a variety of formats to tell your learners what was observed. Specific, quick comments made in real time can be encouraging, and brief suggestions are usually welcome in the context of a particular patient. Other observations and feedback that need to be more sensitive or require more time are perfect to wrap up at the end of the day. Finally, the message function in the electronic medical record is another great and timely format for providing feedback on observations related to clinical documentation, differential diagnosis, and management plan.
Real-Time Recordkeeping
Record your observations as you go. Even though you are providing formative feedback throughout the month, you likely also will be expected to translate those observations into a summative end-of-rotation assessment. Whether it is on a notecard with the name of each trainee being supervised or on a printed blank copy of the end of the month assessment or other program-specific assessments, jotting down specific observations will help you recall key information.
When feedback is provided, note the date in order to guide your summative feedback discussion and the final assessment.
Keep in mind that program assessment tools often serve to remind faculty of specific behaviors that have not historically been evaluated. For example, faculty might be in the habit of providing feedback on communication skills after a family meeting but may not specifically listen for trainees to use “teach-back” concepts when explaining the plan for discharge or noting whether they actively seek input from the multidisciplinary team. A tool that lists “teach-back” or “seeks out interprofessional collaboration” as line items on the form can help to remind you of the qualities you are being asked to assess.
Although direct observation is essential in providing useful assessments during the course of supervision of trainees, there are additional ways that faculty can “see” how a trainee is doing. For example, faculty or supervising residents can “observe” an intern’s completed discharge summary in real time for important and key components. Checking this work enables you to provide an assessment of additional skills (i.e., medication reconciliation, medical knowledge, management of clinical conditions, and appropriate handoff to future care providers). As trainees progressively demonstrate competence, the degree of supervision evolves to the point of a quick verification rather than the initial detailed review.
In summary, supervising trainees well means both thinking critically about their care of patients and providing feedback. As much as we have adapted our clinical workflow to meet increasing regulatory, quality, or patient throughput requirements, we must also change our educational workflow to meet the needs of our learners.
This adaptation should not be onerous. A few simple adjustments, as outlined above, can lead to higher-quality assessments and increased satisfaction in your role as teacher. So, get back out on the wards and observe!
Dr. O’Malley is the internal medicine residency program director at Banner Good Samaritan in Phoenix, Ariz., and an assistant professor of medicine at the University of Arizona College of Medicine. She currently serves as SHM’s representative on the Alliance for Academic Internal Medicine’s Internal Medicine Education Redesign Advisory Board, along with Dr. Caverzagie, who is associate dean for educational strategy at the University of Nebraska College of Medicine in Omaha and vice president for education, clinical enterprise of the Nebraska Medical Center. Dr. Caverzagie also was a member of the ABIM and ACGME milestone writing groups.
All of us who work with housestaff understand that a crucial component of teaching clinical medicine is to take the time to both supervise resident work and deliver constructive feedback on its quality. In the assessment of competence, trainees have “direct supervision” when an attending, senior resident, or other individual is physically present and guiding the care in real time or “indirect supervision” when work is being checked after the care has been administered.
Regardless of the level of supervision, checking in with direct observations (watching trainees do the actual work in real time) provides invaluable information for both patient care and resident assessment. Given that assessment and supervision are key components of the Accreditation Council for Graduate Medical Education’s (ACGME) Next Accreditation System, many programs are now placing particular emphasis on the time we spend observing our trainees.
How can faculty fit direct observation into an already busy day? Here are some ideas for how to adapt and leverage your workflow to create new opportunities for resident skills assessment.
Micro-Observations Matter
Gone are the days of sitting in a patient room for an hour observing a long history and physical performed by the resident or student that you are supervising. In spite of time constraints, you should aim to be at the bedside at the same time as the trainee as much as possible. Once there, take note of all that you see. For example, we often observe residents and students during bedside rounds or critical family discussions. Here are additional opportunities for trainee observation that might fit into your workflow:
- First thing in the morning, when the team is pre-rounding (this is perfect for when you are worried about a patient or are scheduled for a busy afternoon). Do NOT interrupt the resident workflow. Instruct them at the beginning of the rotation that you plan to observe unannounced. If they see you, they should continue with their normal activities. Pop in and out to catch key points, and gather the information necessary to guide patient care. Don’t take over to do teaching or feedback; that will come later in the day.
- During a procedure performed by a supervising resident who already has demonstrated technical competence. Bring a computer on wheels into the patient’s room, sit down, and catch up on charting while listening to and observing the explanations, teaching, and interaction between the patient and the resident. You can still intervene if necessary, but take appropriate steps to allow resident autonomy and the observation of high-level communication skills.
- At the bedside of a clinically unstable patient. If you are together with the team when a nurse calls with a concern, you can instruct the resident to go ahead and intervene with close follow-up in a few minutes. This allows residents to get a head start, gather information, and establish themselves as the decision-makers, while still providing an opportunity for close observation by the faculty.
- Finalizing a discharge first thing in the morning. With most hospitals focusing on discharge timeliness, faculty often discuss patients scheduled for discharge prior to or outside of formal rounds. Get to the patient! Observe the resident interacting with the patient and multidisciplinary team, confirming medication reconciliation, finalizing the discharge diagnosis and instructions, and inquiring further about barriers to adherence with the discharge regimen.
Vary Your Approach
Use a variety of formats to tell your learners what was observed. Specific, quick comments made in real time can be encouraging, and brief suggestions are usually welcome in the context of a particular patient. Other observations and feedback that need to be more sensitive or require more time are perfect to wrap up at the end of the day. Finally, the message function in the electronic medical record is another great and timely format for providing feedback on observations related to clinical documentation, differential diagnosis, and management plan.
Real-Time Recordkeeping
Record your observations as you go. Even though you are providing formative feedback throughout the month, you likely also will be expected to translate those observations into a summative end-of-rotation assessment. Whether it is on a notecard with the name of each trainee being supervised or on a printed blank copy of the end of the month assessment or other program-specific assessments, jotting down specific observations will help you recall key information.
When feedback is provided, note the date in order to guide your summative feedback discussion and the final assessment.
Keep in mind that program assessment tools often serve to remind faculty of specific behaviors that have not historically been evaluated. For example, faculty might be in the habit of providing feedback on communication skills after a family meeting but may not specifically listen for trainees to use “teach-back” concepts when explaining the plan for discharge or noting whether they actively seek input from the multidisciplinary team. A tool that lists “teach-back” or “seeks out interprofessional collaboration” as line items on the form can help to remind you of the qualities you are being asked to assess.
Although direct observation is essential in providing useful assessments during the course of supervision of trainees, there are additional ways that faculty can “see” how a trainee is doing. For example, faculty or supervising residents can “observe” an intern’s completed discharge summary in real time for important and key components. Checking this work enables you to provide an assessment of additional skills (i.e., medication reconciliation, medical knowledge, management of clinical conditions, and appropriate handoff to future care providers). As trainees progressively demonstrate competence, the degree of supervision evolves to the point of a quick verification rather than the initial detailed review.
In summary, supervising trainees well means both thinking critically about their care of patients and providing feedback. As much as we have adapted our clinical workflow to meet increasing regulatory, quality, or patient throughput requirements, we must also change our educational workflow to meet the needs of our learners.
This adaptation should not be onerous. A few simple adjustments, as outlined above, can lead to higher-quality assessments and increased satisfaction in your role as teacher. So, get back out on the wards and observe!
Dr. O’Malley is the internal medicine residency program director at Banner Good Samaritan in Phoenix, Ariz., and an assistant professor of medicine at the University of Arizona College of Medicine. She currently serves as SHM’s representative on the Alliance for Academic Internal Medicine’s Internal Medicine Education Redesign Advisory Board, along with Dr. Caverzagie, who is associate dean for educational strategy at the University of Nebraska College of Medicine in Omaha and vice president for education, clinical enterprise of the Nebraska Medical Center. Dr. Caverzagie also was a member of the ABIM and ACGME milestone writing groups.
Academic Hospitalist Groups Use Observation Status More Frequently
Insurers’ use of certain criteria to separate hospital stays into inpatient or observation status remains widespread. Observation status ensures provider reimbursement for hospitalizations deemed necessary by clinical judgment but not qualifying as inpatient care. Admission under observation status impacts the patient’s financial burden, as well, with observation admissions typically associated with increased out-of-pocket costs.
Although hospitals have always faced decreased reimbursement for observation admissions (compared to inpatient admissions), new penalties attached to readmission for patients discharged from an inpatient stay raise the potential to impact hospitalist practice by incentivizing increased use of observation status for hospitalizations in order to avoid readmission penalties.
Have readmission penalties associated with inpatient admissions actually led to increased use of observation status by hospitalist groups?
SHM’s 2014 State of Hospital Medicine report provides insight into this question. In groups serving adults only, observation discharges accounted for 16.1% of all discharges (see Figure 1). If the survey’s reported same-day admission and discharge rate of 3.5%, collected separately this year, can be assumed to be largely reflective of observation status discharges, then the true percentage of discharges under observation status is likely closer to 19.6%.

–Dr. Smith
The question of determining whether to bill episodes as inpatient or observation status was asked in the 2012 survey, as well, though by a different methodology: 20% of admissions were billed as observation status by hospitalist practices seeing adults only. Even with some observation admissions in 2012 being converted to inpatient status later in the hospital stay (a factor accounted for in the 2014 survey by changing the wording of the survey so that it asks about status at discharge), not much overall change in hospitalist group practice can be appreciated.
Does the overall observation status use rate tell the whole story?
When 2012 and 2014 survey data are separated by academic status, a clear change in practice over time can be seen. Academic HMGs experienced an increase in use of observation status, from 15.3% of admissions in 2012 to 19.4% of discharges in 2014 (or 22.8% in 2014, if same-day hospital stay responses are added to the observation data). In comparison, nonacademic hospitalist practices reported a decrease in observation status utilization, from 20.4% of admissions in 2012 to 15.6% of discharges in 2014 (or 19.2%, accounting for same-day discharges as observation status).
Academic HMGs, which frequently rely on housestaff for the finer points of patient care documentation, must consequently rely on documentation largely written by providers with less experience and incentive to optimize documentation for billing, compared to experienced hospitalists. It’s plausible to speculate that the benefits associated with compensation for inpatient status for hospitals, compared to the risks of financial penalty associated with billing under inpatient status, could be different for academic than for nonacademic hospitalist groups, due to the differences in the quality of documentation between the two practice types, and that academic HMGs, or the hospitals they work with, see the risks associated with inpatient status billing as high enough to change billing practices. Nonacademic hospitalist groups, on the other hand, may rely on the experience of their retained hospitalists to document justification for inpatient status more effectively, and may thus maximize the financial benefit of inpatient status utilization sufficiently to overcome associated financial risks.
In an ever-changing reimbursement and political advocacy landscape, future SHM surveys will be pivotal in assessing what happens with trends surrounding use of observation status for episodes of hospital care.
Dr. Smith is a hospitalist and assistant professor at Northwestern University in Chicago, Ill., and a member of SHM’s Practice Analysis Committee.
Insurers’ use of certain criteria to separate hospital stays into inpatient or observation status remains widespread. Observation status ensures provider reimbursement for hospitalizations deemed necessary by clinical judgment but not qualifying as inpatient care. Admission under observation status impacts the patient’s financial burden, as well, with observation admissions typically associated with increased out-of-pocket costs.
Although hospitals have always faced decreased reimbursement for observation admissions (compared to inpatient admissions), new penalties attached to readmission for patients discharged from an inpatient stay raise the potential to impact hospitalist practice by incentivizing increased use of observation status for hospitalizations in order to avoid readmission penalties.
Have readmission penalties associated with inpatient admissions actually led to increased use of observation status by hospitalist groups?
SHM’s 2014 State of Hospital Medicine report provides insight into this question. In groups serving adults only, observation discharges accounted for 16.1% of all discharges (see Figure 1). If the survey’s reported same-day admission and discharge rate of 3.5%, collected separately this year, can be assumed to be largely reflective of observation status discharges, then the true percentage of discharges under observation status is likely closer to 19.6%.

–Dr. Smith
The question of determining whether to bill episodes as inpatient or observation status was asked in the 2012 survey, as well, though by a different methodology: 20% of admissions were billed as observation status by hospitalist practices seeing adults only. Even with some observation admissions in 2012 being converted to inpatient status later in the hospital stay (a factor accounted for in the 2014 survey by changing the wording of the survey so that it asks about status at discharge), not much overall change in hospitalist group practice can be appreciated.
Does the overall observation status use rate tell the whole story?
When 2012 and 2014 survey data are separated by academic status, a clear change in practice over time can be seen. Academic HMGs experienced an increase in use of observation status, from 15.3% of admissions in 2012 to 19.4% of discharges in 2014 (or 22.8% in 2014, if same-day hospital stay responses are added to the observation data). In comparison, nonacademic hospitalist practices reported a decrease in observation status utilization, from 20.4% of admissions in 2012 to 15.6% of discharges in 2014 (or 19.2%, accounting for same-day discharges as observation status).
Academic HMGs, which frequently rely on housestaff for the finer points of patient care documentation, must consequently rely on documentation largely written by providers with less experience and incentive to optimize documentation for billing, compared to experienced hospitalists. It’s plausible to speculate that the benefits associated with compensation for inpatient status for hospitals, compared to the risks of financial penalty associated with billing under inpatient status, could be different for academic than for nonacademic hospitalist groups, due to the differences in the quality of documentation between the two practice types, and that academic HMGs, or the hospitals they work with, see the risks associated with inpatient status billing as high enough to change billing practices. Nonacademic hospitalist groups, on the other hand, may rely on the experience of their retained hospitalists to document justification for inpatient status more effectively, and may thus maximize the financial benefit of inpatient status utilization sufficiently to overcome associated financial risks.
In an ever-changing reimbursement and political advocacy landscape, future SHM surveys will be pivotal in assessing what happens with trends surrounding use of observation status for episodes of hospital care.
Dr. Smith is a hospitalist and assistant professor at Northwestern University in Chicago, Ill., and a member of SHM’s Practice Analysis Committee.
Insurers’ use of certain criteria to separate hospital stays into inpatient or observation status remains widespread. Observation status ensures provider reimbursement for hospitalizations deemed necessary by clinical judgment but not qualifying as inpatient care. Admission under observation status impacts the patient’s financial burden, as well, with observation admissions typically associated with increased out-of-pocket costs.
Although hospitals have always faced decreased reimbursement for observation admissions (compared to inpatient admissions), new penalties attached to readmission for patients discharged from an inpatient stay raise the potential to impact hospitalist practice by incentivizing increased use of observation status for hospitalizations in order to avoid readmission penalties.
Have readmission penalties associated with inpatient admissions actually led to increased use of observation status by hospitalist groups?
SHM’s 2014 State of Hospital Medicine report provides insight into this question. In groups serving adults only, observation discharges accounted for 16.1% of all discharges (see Figure 1). If the survey’s reported same-day admission and discharge rate of 3.5%, collected separately this year, can be assumed to be largely reflective of observation status discharges, then the true percentage of discharges under observation status is likely closer to 19.6%.

–Dr. Smith
The question of determining whether to bill episodes as inpatient or observation status was asked in the 2012 survey, as well, though by a different methodology: 20% of admissions were billed as observation status by hospitalist practices seeing adults only. Even with some observation admissions in 2012 being converted to inpatient status later in the hospital stay (a factor accounted for in the 2014 survey by changing the wording of the survey so that it asks about status at discharge), not much overall change in hospitalist group practice can be appreciated.
Does the overall observation status use rate tell the whole story?
When 2012 and 2014 survey data are separated by academic status, a clear change in practice over time can be seen. Academic HMGs experienced an increase in use of observation status, from 15.3% of admissions in 2012 to 19.4% of discharges in 2014 (or 22.8% in 2014, if same-day hospital stay responses are added to the observation data). In comparison, nonacademic hospitalist practices reported a decrease in observation status utilization, from 20.4% of admissions in 2012 to 15.6% of discharges in 2014 (or 19.2%, accounting for same-day discharges as observation status).
Academic HMGs, which frequently rely on housestaff for the finer points of patient care documentation, must consequently rely on documentation largely written by providers with less experience and incentive to optimize documentation for billing, compared to experienced hospitalists. It’s plausible to speculate that the benefits associated with compensation for inpatient status for hospitals, compared to the risks of financial penalty associated with billing under inpatient status, could be different for academic than for nonacademic hospitalist groups, due to the differences in the quality of documentation between the two practice types, and that academic HMGs, or the hospitals they work with, see the risks associated with inpatient status billing as high enough to change billing practices. Nonacademic hospitalist groups, on the other hand, may rely on the experience of their retained hospitalists to document justification for inpatient status more effectively, and may thus maximize the financial benefit of inpatient status utilization sufficiently to overcome associated financial risks.
In an ever-changing reimbursement and political advocacy landscape, future SHM surveys will be pivotal in assessing what happens with trends surrounding use of observation status for episodes of hospital care.
Dr. Smith is a hospitalist and assistant professor at Northwestern University in Chicago, Ill., and a member of SHM’s Practice Analysis Committee.
Are ObGyns getting “bumped” out of deserved Medicaid reimbursement?
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
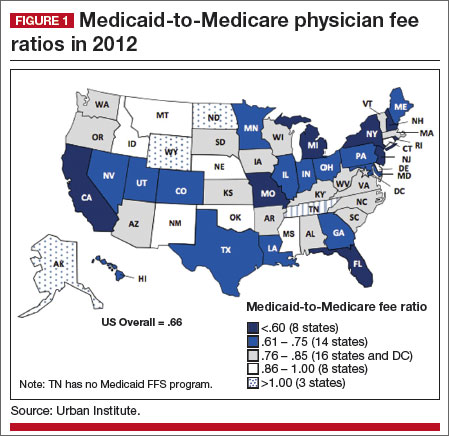
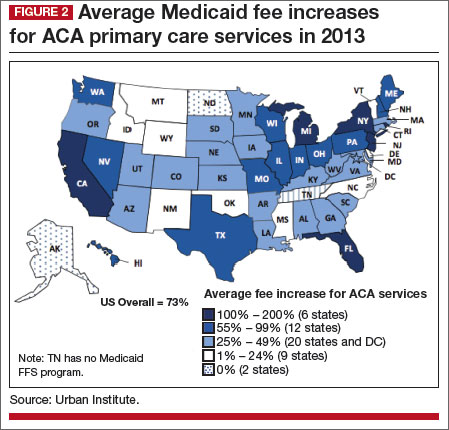
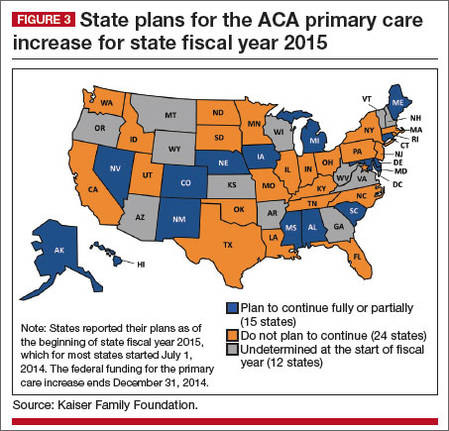
|
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
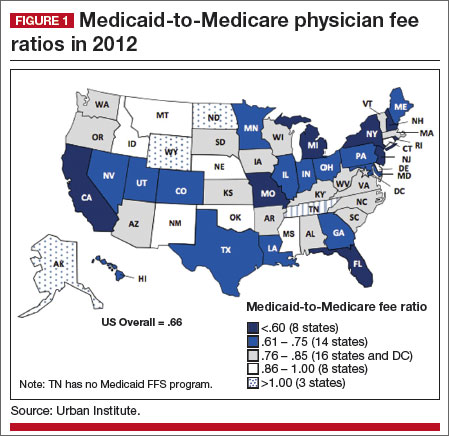
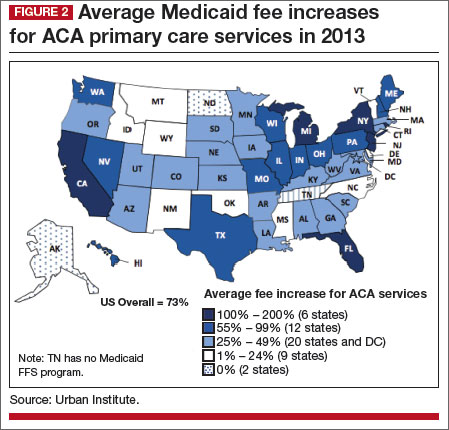
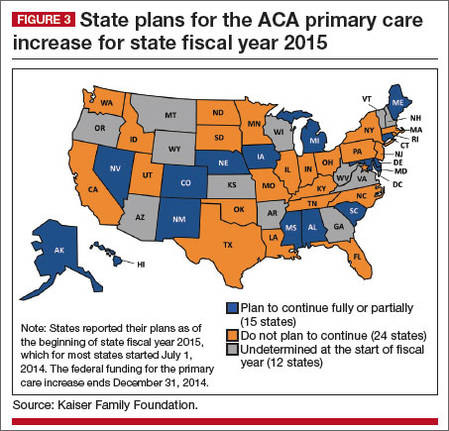
|
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
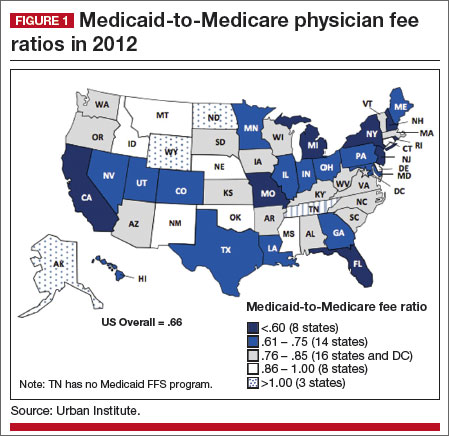
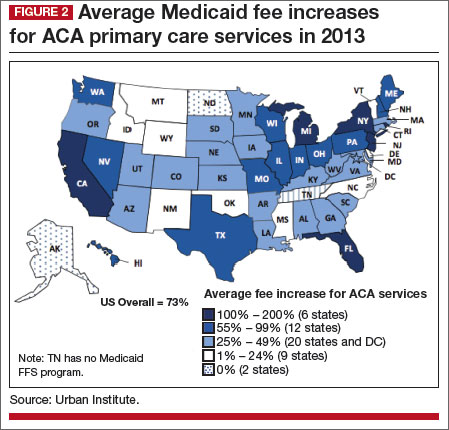
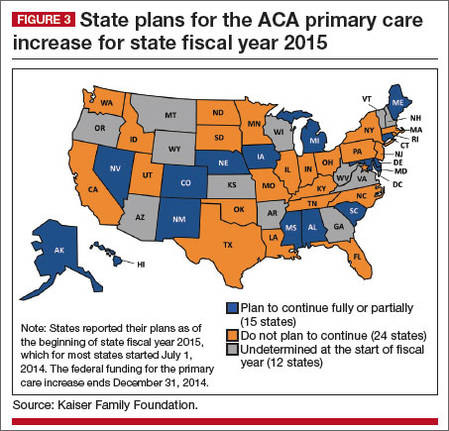
|
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
The Patient Relations and Service Recovery Guide: A Colorful Approach to Handling Upset and Angry Patients
Tearful breakdowns and loud outbursts—they happen with orthopedic patients even in the best of practices. And if you are an orthopedic surgeon who has rarely or never experienced a patient in emotional distress, just talk with your staff—they have no doubt experienced this many times.
There is something about orthopedic conditions—they carry with them an increased likelihood of emotional adverse effects for patients and their loved ones. Inhibited movement can lead to palpable frustration and depression. Time off from work may cause financial hardship and an identity crisis for a family breadwinner. Physical pain can cause the patient to become depressed, angry, or dependent on prescription medication. Medications can cause a change in disposition or outlook. These realities make orthopedic surgery practices particularly predisposed to patient relations risks and service recovery opportunities.
As a practice management consultant and former executive director of an orthopedic practice, I have observed and participated in patient relations and service recovery efforts at many levels. Particularly proud of the way our staff and physicians prevented and handled these and having spent many years traveling by air under the color-coded TSA (Transportation Security Administration) security level indicator system, I created the Patient Relations and Service Recovery Guide (Figure) to help practices gain perspective, have a vocabulary, and develop practical methods for mitigating patient relations risks and responding to incidents and complaints.
The Patient Relations and Service Recovery Guide
The Patient Relations and Service Recovery Guide shows the relationship between the practice as a whole and the patient as an individual.
Green and Red
Green describes the elements of service orientation that the practice must consistently demonstrate and convey to each individual from the point of access, through treatment, and, finally, during account settlement. If you think you have a systemic problem with anything under the Green heading, you probably need a practice management or service orientation consultant, not this article. Red shows the other end of the spectrum—a complete degeneration, worst-case scenario. As with problems in the Green category, this article will not help you in these Red situations, for which you need experienced legal counsel immediately.
We’ll now explore the stories, challenges, opportunities, and practical suggestions for the Blue, Yellow, and Orange categories. The Blue and Yellow categories in the Figure are shaded in grey as a depiction of the interactive, fluid nature of these situations. In addition, they are situations that have developed and can be resolved within and by the practice.
Blue
Patients are very comfortable complaining to the receptionist, x-ray technician, and medical assistant about any number of perceived shortcomings, but when you walk in the examination room, not a word. This is a reality I am sure you have heard about from your staff, and it puts them in a position to observe and determine if a patient’s frustration is escalating. Telephone and front desk receptions are first in line. Patients will say to a telephone receptionist, “I have called 3 times yesterday and twice today and the doctor/nurse still hasn’t called back.” Front desk receptionists will also observe dynamics in the seating area. Staff are your partners in patient relations and service recovery. Working together effectively will help you address issues in the Blue and Yellow areas.
Create an environment that prevents patient discontent and supports service orientation goals. A hospital-based practice that I once managed was a flagship for service excellence goals of a Fortune 150 corporation, had a large seating area, and was close to the airport in a city with multiple company properties; we frequently had executives showing up unannounced, and, because of company politics, it seemed like they were actively looking for instances of substandard service. More importantly, though, we had patients. We established “Waiting Stories” as a performance standard for the receptionists. That is, at any moment, the receptionist was able to recap the “story” of each person in the seating area. The “story” is the reason the person was there, the appointment time, and the cause of the delay, if the wait time was excessive. We all knew this was a performance standard for our practice, so if a receptionist called back to the clinic to find out the reason for a backup in throughput, everyone was respectful and responsive to the inquiry.
The receptionists quickly became effective in judging situations and mitigating or avoiding breakdowns in service and communication. We also implemented an easy and quick notification code for when they needed help handling a service recovery situation. The responses and support in those situations were unwavering, consistent, and blame-free. We would debrief after a significant situation was resolved to determine if there were systemic or response improvement opportunities.
Communication among staff is essential for preventing or mitigating patient discontent. All practices experience service and throughput errors occasionally: a quiet, uncomplaining patient inadvertently doesn’t get called back and remains in the seating area unnoticed; a call doesn’t get returned; x-ray breaks down and a spine patient has to make a painful walk; the physician has to interrupt the encounter to take an important call; etc. Stuff happens. Individually, these breaches are tolerable to most patients. Unfortunately, there can be a cumulative element—when various service mishaps happen to the same patient. This is when communication and support among the staff and with the manager become especially important. If a patient has weathered a rough or long wait or has expressed some dissatisfaction while in the reception area, it’s probably a good idea to let the back-office staff know, so they can show a little extra compassion and be cognizant of additional situations.
Clinical staff and the physicians must convey support and appreciation to front-line staff who observe and share that a patient may be prone to distress, so that they will continue to participate in active incident prevention and service recovery.
Heightening awareness on the part of your staff—especially, receptionists, technicians, medical assistants, and collectors—goes a long way toward getting patient discontent issues settled before they get out of hand. As executive director of a large orthopedic surgery practice, I was particularly proud of our staff’s sensitivity to patient discontent, their sense of when it might be helpful to bring in a manager, and the managers’ ability both to recover many situations and to know when it was most effective to get help and support from either one of the executive team or physicians.
I can remember one patient that both front-line staff and the manager determined needed some service recovery intervention. She had been visibly upset at the end of her final postoperative visit with the physician. The staff noticed and called the manager in. The patient mentioned to the manager that she had been to another orthopedic surgeon who had told her that the surgery our physician had performed was not the right one and that he would have done things differently. The patient said she just didn’t know what to do. Our manager had the keen sense to know that she should get help to recover the situation within our practice. She and all of the staff were always supported when they asked for help, and the physicians were good about expressing their gratitude to the staff for their efforts. The manager escorted the upset patient to my office where we talked—well, she mostly talked and I listened. It turned out that her injuries had prevented her from attending games during her only child’s senior soccer season. I know, it sounds more like therapy—it was a lot of listening and compassion on my part. Eventually, she got around to thanking me for listening. And while that was not the end of it (there was another conversation), she did not take any action against our physician. See the “Talking It Through” Box.
Another group of staff who can identify issues is billing and collections. Often a patient will experience a minor cumulative series of service breaches (eg, long wait, perceived physician distraction, long hold times on the phone) and then lose it when they receive a bill that is incorrect, late, or confusing. The staff members answering those calls also need to feel supported in asking for help from a manager or another associate, either during the call or by suggesting that someone call the patient back.
Empowering staff or managers with tangible service recovery courtesies is also a good idea. We gave our staff coupons from the sundries shop in the building, so that when experiencing a particularly long wait, the patient could go down and get a complimentary snack. We also had 1 or 2 occasions when a patient drove a great distance to see the physician and experienced a significant service breach. As part of our response, we gave the patient a gas card.
Blue is the category in which the staff’s keen observation and true teamwork and support come into play when a situation or developing situation is identified.
Yellow
Yellow, while still contained within the practice, is overt. There has been an incident and/or a communication (letter or call) to the manager or physician. In Yellow, we are beyond the cooperative staff observation and sensory skills—we know something has happened. A situation might be physical- and/or facility-based, eg, a patient or family member had a minor stumble on a doormat, and though luckily they had not appeared injured and the physician checked them out, it was an incident. The other sign of a Yellow situation is that a patient or family member has written a letter to the practice to express their dissatisfaction. In either case, as dreadful as it may seem or as busy as you may be, follow up promptly.
In the case of an incident in the practice, the doctor or manager can call the patient that evening to check in and make sure all is well. Upon receiving a letter, the treating physician and manager should take a minute to discuss and agree on a response plan. Sometimes the situation may call for patient discharge from the practice—only the physician can determine that. Other times, the content of the letter may cause you to consult an attorney or your malpractice insurance carrier. The letters sometimes voice service-oriented complaints and can be addressed by the manager with a phone call and conversation as described in the Blue section above.
Orange
As a consultant, I have assisted many physicians in responding to individual patient complaints to their state medical board (SMB). I have seen a 15-page, single-spaced, typewritten letter with photographs (of the patient’s 70-lb pannus, no less), a 4-sentence letter in childlike grammar and handwriting, and many in between. The spelling, grammar, punctuation, coherence, and brevity of the letter do not matter. Your feelings on the validity of the complaint (ie, “That’s total BS!”) don’t matter. The perceived mental health of the patient (ie,“Well, he’s crazy! Ask my nurse.”) does not matter. Your SMB takes each and every complaint letter very seriously and so must you. One complaint spiraling out of control can be all it takes for you to lose your license. Having said that, individual patient SMB complaints are not uncommon; even the best physicians receive them.
Here are some thoughts to keep in mind regarding individual patient SMB complaints. An individual patient SMB complaint:
◾ Typically comes to you via US mail with no receipt signature required. Lots of us do so much online these days we can go weeks, perhaps months, without looking at our mail—even if staff members have opened it.
Suggestion: Make sure the staff looks at mail and is able to judge what requires action and what should be brought to your attention. Provide appreciation and detailed feedback when staff members bring something to you and do not misdirect negative reactions regardless of the content. You would rather staff members feel comfortable bringing something to your attention that is immaterial than keep something important from you out of fear of displeasing you.
◾ Includes a SMB response deadline that may give you as little as 1 or 2 weeks.
Suggestion: Meet the deadline. If you have or are going to miss the deadline or know that you cannot meet it, have your staff call the SMB office and abjectly request an extension.
◾ Is coming from physicians as members of the SMB, even though it may have the names of physicians you know, perhaps friends, on the letterhead.
Suggestions:
1. The physicians are not your colleagues in this situation. In this capacity, each physician is a member of an oversight board that serves and protects the people of your state. Don’t try to address the situation with a phone call or comment on the golf course.
2. Reply in the format the board has requested—a letter. Open your response letter with a statement that acknowledges the work and responsibility of the SMB and your appreciation, for example:
Esteemed Board,
While I regret that a patient complaint associated with me has come to your attention, I am grateful that the physicians and the people of [your state] have an oversight body to ensure the integrity of medical care delivered and received. Thank you for your service.
◾ Is likely to make you feel angry, indignant, unappreciated, hurt, bewildered, etc.
Suggestion: Breathe, vent to someone you can trust, exercise, get a good night’s sleep, and/or other calming, self-preservation tactics. Repeat as necessary so as not to allow these emotions a place in your response.
◾ May or may not include a request for a copy of the complete medical record.
Suggestion: If the medical record is not requested, do not send it. If the medical record is requested, send it in its entirety, as is. Do not make changes, edits, or amendments to the medical record as a response to the complaint.
◾ May be brief, vague, long, articulate, well thought-out and well structured, and/or ridiculous. Regardless of education level, profession, age, and socioeconomic status, any of your patients may write a complaint letter to the SMB, who then must address it.
Suggestions:
1. Demonstrate respect for the board’s time and service by writing a response letter of respectable length and substance regardless of the brevity of the complaint. Brief responses to the SMB may be perceived as arrogant and irreverent, and this is the exact situation and group of people in the entire state in which and before whom you do not want to be thought of that way.
2. Summarize the case with detail and substance in the letter, even if the medical record will be included in the response. Identify the actual complaints and address them in an organized way, an objective voice, and a logical order. Describe the time, thought, and follow-up you have put into addressing the situation. For instance, if the complaint includes a legitimate reference to a delay in test results or an unreturned phone call, provide a broad description of having reviewed and modified the process with your staff to understand where the gap occurred and having taken measures to help keep it from happening again.
◾ Will likely require that a copy of your response be made available or sent to the complainant.
Suggestions:
1. You are writing to 2, maybe 3, recipients: the SMB, the complainant, and the complainant’s attorney. Even if it is clear the patient did not consult a lawyer to write the complaint, it is best to write the response as though it will be read by an attorney.
2. Take the time and deliberation necessary for a multiple-draft writing process. Get help from someone to assure you have addressed all the issues in an organized, objective way.
◾ May lead to a request from the SMB that you appear before them in response to the original complaint letter and/or to clarify your response to a complaint letter. This is an indication of an investigation that has escalated beyond the patient SMB complaint letters addressed in this article; consult an experienced attorney who represents you.
Sometimes other state oversight bodies will receive complaints directly from patients and follow up with you. Consult your attorney, risk management consultant, or malpractice coverage representative for guidance if you are unsure as to the jurisdiction or how to respond.
Conclusion
Most of your practice operates in the Green, no doubt. It is simply not noticeable or memorable when everything goes smoothly. When incidents occur that require service recovery, I hope this guide and commentary will offer perspective on the full range of patient relations and service recovery, provide stories and experiences that might help, and offer general tips and suggestions.
Tearful breakdowns and loud outbursts—they happen with orthopedic patients even in the best of practices. And if you are an orthopedic surgeon who has rarely or never experienced a patient in emotional distress, just talk with your staff—they have no doubt experienced this many times.
There is something about orthopedic conditions—they carry with them an increased likelihood of emotional adverse effects for patients and their loved ones. Inhibited movement can lead to palpable frustration and depression. Time off from work may cause financial hardship and an identity crisis for a family breadwinner. Physical pain can cause the patient to become depressed, angry, or dependent on prescription medication. Medications can cause a change in disposition or outlook. These realities make orthopedic surgery practices particularly predisposed to patient relations risks and service recovery opportunities.
As a practice management consultant and former executive director of an orthopedic practice, I have observed and participated in patient relations and service recovery efforts at many levels. Particularly proud of the way our staff and physicians prevented and handled these and having spent many years traveling by air under the color-coded TSA (Transportation Security Administration) security level indicator system, I created the Patient Relations and Service Recovery Guide (Figure) to help practices gain perspective, have a vocabulary, and develop practical methods for mitigating patient relations risks and responding to incidents and complaints.
The Patient Relations and Service Recovery Guide
The Patient Relations and Service Recovery Guide shows the relationship between the practice as a whole and the patient as an individual.
Green and Red
Green describes the elements of service orientation that the practice must consistently demonstrate and convey to each individual from the point of access, through treatment, and, finally, during account settlement. If you think you have a systemic problem with anything under the Green heading, you probably need a practice management or service orientation consultant, not this article. Red shows the other end of the spectrum—a complete degeneration, worst-case scenario. As with problems in the Green category, this article will not help you in these Red situations, for which you need experienced legal counsel immediately.
We’ll now explore the stories, challenges, opportunities, and practical suggestions for the Blue, Yellow, and Orange categories. The Blue and Yellow categories in the Figure are shaded in grey as a depiction of the interactive, fluid nature of these situations. In addition, they are situations that have developed and can be resolved within and by the practice.
Blue
Patients are very comfortable complaining to the receptionist, x-ray technician, and medical assistant about any number of perceived shortcomings, but when you walk in the examination room, not a word. This is a reality I am sure you have heard about from your staff, and it puts them in a position to observe and determine if a patient’s frustration is escalating. Telephone and front desk receptions are first in line. Patients will say to a telephone receptionist, “I have called 3 times yesterday and twice today and the doctor/nurse still hasn’t called back.” Front desk receptionists will also observe dynamics in the seating area. Staff are your partners in patient relations and service recovery. Working together effectively will help you address issues in the Blue and Yellow areas.
Create an environment that prevents patient discontent and supports service orientation goals. A hospital-based practice that I once managed was a flagship for service excellence goals of a Fortune 150 corporation, had a large seating area, and was close to the airport in a city with multiple company properties; we frequently had executives showing up unannounced, and, because of company politics, it seemed like they were actively looking for instances of substandard service. More importantly, though, we had patients. We established “Waiting Stories” as a performance standard for the receptionists. That is, at any moment, the receptionist was able to recap the “story” of each person in the seating area. The “story” is the reason the person was there, the appointment time, and the cause of the delay, if the wait time was excessive. We all knew this was a performance standard for our practice, so if a receptionist called back to the clinic to find out the reason for a backup in throughput, everyone was respectful and responsive to the inquiry.
The receptionists quickly became effective in judging situations and mitigating or avoiding breakdowns in service and communication. We also implemented an easy and quick notification code for when they needed help handling a service recovery situation. The responses and support in those situations were unwavering, consistent, and blame-free. We would debrief after a significant situation was resolved to determine if there were systemic or response improvement opportunities.
Communication among staff is essential for preventing or mitigating patient discontent. All practices experience service and throughput errors occasionally: a quiet, uncomplaining patient inadvertently doesn’t get called back and remains in the seating area unnoticed; a call doesn’t get returned; x-ray breaks down and a spine patient has to make a painful walk; the physician has to interrupt the encounter to take an important call; etc. Stuff happens. Individually, these breaches are tolerable to most patients. Unfortunately, there can be a cumulative element—when various service mishaps happen to the same patient. This is when communication and support among the staff and with the manager become especially important. If a patient has weathered a rough or long wait or has expressed some dissatisfaction while in the reception area, it’s probably a good idea to let the back-office staff know, so they can show a little extra compassion and be cognizant of additional situations.
Clinical staff and the physicians must convey support and appreciation to front-line staff who observe and share that a patient may be prone to distress, so that they will continue to participate in active incident prevention and service recovery.
Heightening awareness on the part of your staff—especially, receptionists, technicians, medical assistants, and collectors—goes a long way toward getting patient discontent issues settled before they get out of hand. As executive director of a large orthopedic surgery practice, I was particularly proud of our staff’s sensitivity to patient discontent, their sense of when it might be helpful to bring in a manager, and the managers’ ability both to recover many situations and to know when it was most effective to get help and support from either one of the executive team or physicians.
I can remember one patient that both front-line staff and the manager determined needed some service recovery intervention. She had been visibly upset at the end of her final postoperative visit with the physician. The staff noticed and called the manager in. The patient mentioned to the manager that she had been to another orthopedic surgeon who had told her that the surgery our physician had performed was not the right one and that he would have done things differently. The patient said she just didn’t know what to do. Our manager had the keen sense to know that she should get help to recover the situation within our practice. She and all of the staff were always supported when they asked for help, and the physicians were good about expressing their gratitude to the staff for their efforts. The manager escorted the upset patient to my office where we talked—well, she mostly talked and I listened. It turned out that her injuries had prevented her from attending games during her only child’s senior soccer season. I know, it sounds more like therapy—it was a lot of listening and compassion on my part. Eventually, she got around to thanking me for listening. And while that was not the end of it (there was another conversation), she did not take any action against our physician. See the “Talking It Through” Box.
Another group of staff who can identify issues is billing and collections. Often a patient will experience a minor cumulative series of service breaches (eg, long wait, perceived physician distraction, long hold times on the phone) and then lose it when they receive a bill that is incorrect, late, or confusing. The staff members answering those calls also need to feel supported in asking for help from a manager or another associate, either during the call or by suggesting that someone call the patient back.
Empowering staff or managers with tangible service recovery courtesies is also a good idea. We gave our staff coupons from the sundries shop in the building, so that when experiencing a particularly long wait, the patient could go down and get a complimentary snack. We also had 1 or 2 occasions when a patient drove a great distance to see the physician and experienced a significant service breach. As part of our response, we gave the patient a gas card.
Blue is the category in which the staff’s keen observation and true teamwork and support come into play when a situation or developing situation is identified.
Yellow
Yellow, while still contained within the practice, is overt. There has been an incident and/or a communication (letter or call) to the manager or physician. In Yellow, we are beyond the cooperative staff observation and sensory skills—we know something has happened. A situation might be physical- and/or facility-based, eg, a patient or family member had a minor stumble on a doormat, and though luckily they had not appeared injured and the physician checked them out, it was an incident. The other sign of a Yellow situation is that a patient or family member has written a letter to the practice to express their dissatisfaction. In either case, as dreadful as it may seem or as busy as you may be, follow up promptly.
In the case of an incident in the practice, the doctor or manager can call the patient that evening to check in and make sure all is well. Upon receiving a letter, the treating physician and manager should take a minute to discuss and agree on a response plan. Sometimes the situation may call for patient discharge from the practice—only the physician can determine that. Other times, the content of the letter may cause you to consult an attorney or your malpractice insurance carrier. The letters sometimes voice service-oriented complaints and can be addressed by the manager with a phone call and conversation as described in the Blue section above.
Orange
As a consultant, I have assisted many physicians in responding to individual patient complaints to their state medical board (SMB). I have seen a 15-page, single-spaced, typewritten letter with photographs (of the patient’s 70-lb pannus, no less), a 4-sentence letter in childlike grammar and handwriting, and many in between. The spelling, grammar, punctuation, coherence, and brevity of the letter do not matter. Your feelings on the validity of the complaint (ie, “That’s total BS!”) don’t matter. The perceived mental health of the patient (ie,“Well, he’s crazy! Ask my nurse.”) does not matter. Your SMB takes each and every complaint letter very seriously and so must you. One complaint spiraling out of control can be all it takes for you to lose your license. Having said that, individual patient SMB complaints are not uncommon; even the best physicians receive them.
Here are some thoughts to keep in mind regarding individual patient SMB complaints. An individual patient SMB complaint:
◾ Typically comes to you via US mail with no receipt signature required. Lots of us do so much online these days we can go weeks, perhaps months, without looking at our mail—even if staff members have opened it.
Suggestion: Make sure the staff looks at mail and is able to judge what requires action and what should be brought to your attention. Provide appreciation and detailed feedback when staff members bring something to you and do not misdirect negative reactions regardless of the content. You would rather staff members feel comfortable bringing something to your attention that is immaterial than keep something important from you out of fear of displeasing you.
◾ Includes a SMB response deadline that may give you as little as 1 or 2 weeks.
Suggestion: Meet the deadline. If you have or are going to miss the deadline or know that you cannot meet it, have your staff call the SMB office and abjectly request an extension.
◾ Is coming from physicians as members of the SMB, even though it may have the names of physicians you know, perhaps friends, on the letterhead.
Suggestions:
1. The physicians are not your colleagues in this situation. In this capacity, each physician is a member of an oversight board that serves and protects the people of your state. Don’t try to address the situation with a phone call or comment on the golf course.
2. Reply in the format the board has requested—a letter. Open your response letter with a statement that acknowledges the work and responsibility of the SMB and your appreciation, for example:
Esteemed Board,
While I regret that a patient complaint associated with me has come to your attention, I am grateful that the physicians and the people of [your state] have an oversight body to ensure the integrity of medical care delivered and received. Thank you for your service.
◾ Is likely to make you feel angry, indignant, unappreciated, hurt, bewildered, etc.
Suggestion: Breathe, vent to someone you can trust, exercise, get a good night’s sleep, and/or other calming, self-preservation tactics. Repeat as necessary so as not to allow these emotions a place in your response.
◾ May or may not include a request for a copy of the complete medical record.
Suggestion: If the medical record is not requested, do not send it. If the medical record is requested, send it in its entirety, as is. Do not make changes, edits, or amendments to the medical record as a response to the complaint.
◾ May be brief, vague, long, articulate, well thought-out and well structured, and/or ridiculous. Regardless of education level, profession, age, and socioeconomic status, any of your patients may write a complaint letter to the SMB, who then must address it.
Suggestions:
1. Demonstrate respect for the board’s time and service by writing a response letter of respectable length and substance regardless of the brevity of the complaint. Brief responses to the SMB may be perceived as arrogant and irreverent, and this is the exact situation and group of people in the entire state in which and before whom you do not want to be thought of that way.
2. Summarize the case with detail and substance in the letter, even if the medical record will be included in the response. Identify the actual complaints and address them in an organized way, an objective voice, and a logical order. Describe the time, thought, and follow-up you have put into addressing the situation. For instance, if the complaint includes a legitimate reference to a delay in test results or an unreturned phone call, provide a broad description of having reviewed and modified the process with your staff to understand where the gap occurred and having taken measures to help keep it from happening again.
◾ Will likely require that a copy of your response be made available or sent to the complainant.
Suggestions:
1. You are writing to 2, maybe 3, recipients: the SMB, the complainant, and the complainant’s attorney. Even if it is clear the patient did not consult a lawyer to write the complaint, it is best to write the response as though it will be read by an attorney.
2. Take the time and deliberation necessary for a multiple-draft writing process. Get help from someone to assure you have addressed all the issues in an organized, objective way.
◾ May lead to a request from the SMB that you appear before them in response to the original complaint letter and/or to clarify your response to a complaint letter. This is an indication of an investigation that has escalated beyond the patient SMB complaint letters addressed in this article; consult an experienced attorney who represents you.
Sometimes other state oversight bodies will receive complaints directly from patients and follow up with you. Consult your attorney, risk management consultant, or malpractice coverage representative for guidance if you are unsure as to the jurisdiction or how to respond.
Conclusion
Most of your practice operates in the Green, no doubt. It is simply not noticeable or memorable when everything goes smoothly. When incidents occur that require service recovery, I hope this guide and commentary will offer perspective on the full range of patient relations and service recovery, provide stories and experiences that might help, and offer general tips and suggestions.
Tearful breakdowns and loud outbursts—they happen with orthopedic patients even in the best of practices. And if you are an orthopedic surgeon who has rarely or never experienced a patient in emotional distress, just talk with your staff—they have no doubt experienced this many times.
There is something about orthopedic conditions—they carry with them an increased likelihood of emotional adverse effects for patients and their loved ones. Inhibited movement can lead to palpable frustration and depression. Time off from work may cause financial hardship and an identity crisis for a family breadwinner. Physical pain can cause the patient to become depressed, angry, or dependent on prescription medication. Medications can cause a change in disposition or outlook. These realities make orthopedic surgery practices particularly predisposed to patient relations risks and service recovery opportunities.
As a practice management consultant and former executive director of an orthopedic practice, I have observed and participated in patient relations and service recovery efforts at many levels. Particularly proud of the way our staff and physicians prevented and handled these and having spent many years traveling by air under the color-coded TSA (Transportation Security Administration) security level indicator system, I created the Patient Relations and Service Recovery Guide (Figure) to help practices gain perspective, have a vocabulary, and develop practical methods for mitigating patient relations risks and responding to incidents and complaints.
The Patient Relations and Service Recovery Guide
The Patient Relations and Service Recovery Guide shows the relationship between the practice as a whole and the patient as an individual.
Green and Red
Green describes the elements of service orientation that the practice must consistently demonstrate and convey to each individual from the point of access, through treatment, and, finally, during account settlement. If you think you have a systemic problem with anything under the Green heading, you probably need a practice management or service orientation consultant, not this article. Red shows the other end of the spectrum—a complete degeneration, worst-case scenario. As with problems in the Green category, this article will not help you in these Red situations, for which you need experienced legal counsel immediately.
We’ll now explore the stories, challenges, opportunities, and practical suggestions for the Blue, Yellow, and Orange categories. The Blue and Yellow categories in the Figure are shaded in grey as a depiction of the interactive, fluid nature of these situations. In addition, they are situations that have developed and can be resolved within and by the practice.
Blue
Patients are very comfortable complaining to the receptionist, x-ray technician, and medical assistant about any number of perceived shortcomings, but when you walk in the examination room, not a word. This is a reality I am sure you have heard about from your staff, and it puts them in a position to observe and determine if a patient’s frustration is escalating. Telephone and front desk receptions are first in line. Patients will say to a telephone receptionist, “I have called 3 times yesterday and twice today and the doctor/nurse still hasn’t called back.” Front desk receptionists will also observe dynamics in the seating area. Staff are your partners in patient relations and service recovery. Working together effectively will help you address issues in the Blue and Yellow areas.
Create an environment that prevents patient discontent and supports service orientation goals. A hospital-based practice that I once managed was a flagship for service excellence goals of a Fortune 150 corporation, had a large seating area, and was close to the airport in a city with multiple company properties; we frequently had executives showing up unannounced, and, because of company politics, it seemed like they were actively looking for instances of substandard service. More importantly, though, we had patients. We established “Waiting Stories” as a performance standard for the receptionists. That is, at any moment, the receptionist was able to recap the “story” of each person in the seating area. The “story” is the reason the person was there, the appointment time, and the cause of the delay, if the wait time was excessive. We all knew this was a performance standard for our practice, so if a receptionist called back to the clinic to find out the reason for a backup in throughput, everyone was respectful and responsive to the inquiry.
The receptionists quickly became effective in judging situations and mitigating or avoiding breakdowns in service and communication. We also implemented an easy and quick notification code for when they needed help handling a service recovery situation. The responses and support in those situations were unwavering, consistent, and blame-free. We would debrief after a significant situation was resolved to determine if there were systemic or response improvement opportunities.
Communication among staff is essential for preventing or mitigating patient discontent. All practices experience service and throughput errors occasionally: a quiet, uncomplaining patient inadvertently doesn’t get called back and remains in the seating area unnoticed; a call doesn’t get returned; x-ray breaks down and a spine patient has to make a painful walk; the physician has to interrupt the encounter to take an important call; etc. Stuff happens. Individually, these breaches are tolerable to most patients. Unfortunately, there can be a cumulative element—when various service mishaps happen to the same patient. This is when communication and support among the staff and with the manager become especially important. If a patient has weathered a rough or long wait or has expressed some dissatisfaction while in the reception area, it’s probably a good idea to let the back-office staff know, so they can show a little extra compassion and be cognizant of additional situations.
Clinical staff and the physicians must convey support and appreciation to front-line staff who observe and share that a patient may be prone to distress, so that they will continue to participate in active incident prevention and service recovery.
Heightening awareness on the part of your staff—especially, receptionists, technicians, medical assistants, and collectors—goes a long way toward getting patient discontent issues settled before they get out of hand. As executive director of a large orthopedic surgery practice, I was particularly proud of our staff’s sensitivity to patient discontent, their sense of when it might be helpful to bring in a manager, and the managers’ ability both to recover many situations and to know when it was most effective to get help and support from either one of the executive team or physicians.
I can remember one patient that both front-line staff and the manager determined needed some service recovery intervention. She had been visibly upset at the end of her final postoperative visit with the physician. The staff noticed and called the manager in. The patient mentioned to the manager that she had been to another orthopedic surgeon who had told her that the surgery our physician had performed was not the right one and that he would have done things differently. The patient said she just didn’t know what to do. Our manager had the keen sense to know that she should get help to recover the situation within our practice. She and all of the staff were always supported when they asked for help, and the physicians were good about expressing their gratitude to the staff for their efforts. The manager escorted the upset patient to my office where we talked—well, she mostly talked and I listened. It turned out that her injuries had prevented her from attending games during her only child’s senior soccer season. I know, it sounds more like therapy—it was a lot of listening and compassion on my part. Eventually, she got around to thanking me for listening. And while that was not the end of it (there was another conversation), she did not take any action against our physician. See the “Talking It Through” Box.
Another group of staff who can identify issues is billing and collections. Often a patient will experience a minor cumulative series of service breaches (eg, long wait, perceived physician distraction, long hold times on the phone) and then lose it when they receive a bill that is incorrect, late, or confusing. The staff members answering those calls also need to feel supported in asking for help from a manager or another associate, either during the call or by suggesting that someone call the patient back.
Empowering staff or managers with tangible service recovery courtesies is also a good idea. We gave our staff coupons from the sundries shop in the building, so that when experiencing a particularly long wait, the patient could go down and get a complimentary snack. We also had 1 or 2 occasions when a patient drove a great distance to see the physician and experienced a significant service breach. As part of our response, we gave the patient a gas card.
Blue is the category in which the staff’s keen observation and true teamwork and support come into play when a situation or developing situation is identified.
Yellow
Yellow, while still contained within the practice, is overt. There has been an incident and/or a communication (letter or call) to the manager or physician. In Yellow, we are beyond the cooperative staff observation and sensory skills—we know something has happened. A situation might be physical- and/or facility-based, eg, a patient or family member had a minor stumble on a doormat, and though luckily they had not appeared injured and the physician checked them out, it was an incident. The other sign of a Yellow situation is that a patient or family member has written a letter to the practice to express their dissatisfaction. In either case, as dreadful as it may seem or as busy as you may be, follow up promptly.
In the case of an incident in the practice, the doctor or manager can call the patient that evening to check in and make sure all is well. Upon receiving a letter, the treating physician and manager should take a minute to discuss and agree on a response plan. Sometimes the situation may call for patient discharge from the practice—only the physician can determine that. Other times, the content of the letter may cause you to consult an attorney or your malpractice insurance carrier. The letters sometimes voice service-oriented complaints and can be addressed by the manager with a phone call and conversation as described in the Blue section above.
Orange
As a consultant, I have assisted many physicians in responding to individual patient complaints to their state medical board (SMB). I have seen a 15-page, single-spaced, typewritten letter with photographs (of the patient’s 70-lb pannus, no less), a 4-sentence letter in childlike grammar and handwriting, and many in between. The spelling, grammar, punctuation, coherence, and brevity of the letter do not matter. Your feelings on the validity of the complaint (ie, “That’s total BS!”) don’t matter. The perceived mental health of the patient (ie,“Well, he’s crazy! Ask my nurse.”) does not matter. Your SMB takes each and every complaint letter very seriously and so must you. One complaint spiraling out of control can be all it takes for you to lose your license. Having said that, individual patient SMB complaints are not uncommon; even the best physicians receive them.
Here are some thoughts to keep in mind regarding individual patient SMB complaints. An individual patient SMB complaint:
◾ Typically comes to you via US mail with no receipt signature required. Lots of us do so much online these days we can go weeks, perhaps months, without looking at our mail—even if staff members have opened it.
Suggestion: Make sure the staff looks at mail and is able to judge what requires action and what should be brought to your attention. Provide appreciation and detailed feedback when staff members bring something to you and do not misdirect negative reactions regardless of the content. You would rather staff members feel comfortable bringing something to your attention that is immaterial than keep something important from you out of fear of displeasing you.
◾ Includes a SMB response deadline that may give you as little as 1 or 2 weeks.
Suggestion: Meet the deadline. If you have or are going to miss the deadline or know that you cannot meet it, have your staff call the SMB office and abjectly request an extension.
◾ Is coming from physicians as members of the SMB, even though it may have the names of physicians you know, perhaps friends, on the letterhead.
Suggestions:
1. The physicians are not your colleagues in this situation. In this capacity, each physician is a member of an oversight board that serves and protects the people of your state. Don’t try to address the situation with a phone call or comment on the golf course.
2. Reply in the format the board has requested—a letter. Open your response letter with a statement that acknowledges the work and responsibility of the SMB and your appreciation, for example:
Esteemed Board,
While I regret that a patient complaint associated with me has come to your attention, I am grateful that the physicians and the people of [your state] have an oversight body to ensure the integrity of medical care delivered and received. Thank you for your service.
◾ Is likely to make you feel angry, indignant, unappreciated, hurt, bewildered, etc.
Suggestion: Breathe, vent to someone you can trust, exercise, get a good night’s sleep, and/or other calming, self-preservation tactics. Repeat as necessary so as not to allow these emotions a place in your response.
◾ May or may not include a request for a copy of the complete medical record.
Suggestion: If the medical record is not requested, do not send it. If the medical record is requested, send it in its entirety, as is. Do not make changes, edits, or amendments to the medical record as a response to the complaint.
◾ May be brief, vague, long, articulate, well thought-out and well structured, and/or ridiculous. Regardless of education level, profession, age, and socioeconomic status, any of your patients may write a complaint letter to the SMB, who then must address it.
Suggestions:
1. Demonstrate respect for the board’s time and service by writing a response letter of respectable length and substance regardless of the brevity of the complaint. Brief responses to the SMB may be perceived as arrogant and irreverent, and this is the exact situation and group of people in the entire state in which and before whom you do not want to be thought of that way.
2. Summarize the case with detail and substance in the letter, even if the medical record will be included in the response. Identify the actual complaints and address them in an organized way, an objective voice, and a logical order. Describe the time, thought, and follow-up you have put into addressing the situation. For instance, if the complaint includes a legitimate reference to a delay in test results or an unreturned phone call, provide a broad description of having reviewed and modified the process with your staff to understand where the gap occurred and having taken measures to help keep it from happening again.
◾ Will likely require that a copy of your response be made available or sent to the complainant.
Suggestions:
1. You are writing to 2, maybe 3, recipients: the SMB, the complainant, and the complainant’s attorney. Even if it is clear the patient did not consult a lawyer to write the complaint, it is best to write the response as though it will be read by an attorney.
2. Take the time and deliberation necessary for a multiple-draft writing process. Get help from someone to assure you have addressed all the issues in an organized, objective way.
◾ May lead to a request from the SMB that you appear before them in response to the original complaint letter and/or to clarify your response to a complaint letter. This is an indication of an investigation that has escalated beyond the patient SMB complaint letters addressed in this article; consult an experienced attorney who represents you.
Sometimes other state oversight bodies will receive complaints directly from patients and follow up with you. Consult your attorney, risk management consultant, or malpractice coverage representative for guidance if you are unsure as to the jurisdiction or how to respond.
Conclusion
Most of your practice operates in the Green, no doubt. It is simply not noticeable or memorable when everything goes smoothly. When incidents occur that require service recovery, I hope this guide and commentary will offer perspective on the full range of patient relations and service recovery, provide stories and experiences that might help, and offer general tips and suggestions.
Using the Internet in your practice. Part 4: Reputation management—how to gather kudos and combat negative online reviews
“It takes 20 years to build a reputation and 5 minutes to ruin it. If you think about that, you’ll do things differently.”
—Warren Buffet
CASE: Decline in new patients
A well-respected physician—one of the best in his field—notices that the number of new patients in his practice has fallen off drastically over the past year. Baffled, he hires a consultant, who discovers that the doctor’s online reputation has plummeted, thanks to four negative reviews and no positive ones.
What can the physician do to remedy the situation and restore his reputation?
The problem can be fixed, but it takes time—like major surgery. Rather than wait until negative reviews are posted, we recommend that you become proactive and take steps as soon as possible to secure your online reputation. That way, you won’t get caught by surprise when one or two unhappy patients try to smear your good name. In this article, we step you through a number of remedies and proactive strategies for boosting positive online reviews and combating negative ones.
The Internet: A one-stop source of information
The Internet has become everyone’s go-to source for pretty much any kind of data, including details on products, services, and people. Anyone can access all kinds of information simply by asking.
Today, people research medical conditions on the Web, often using Google. If you have done your search engine optimization, your Web site will come up in the first page of search results, making it possible for prospective patients to click through to your homepage. (For the scoop on search engine optimization, see Part 3 of this series, “Maximizing your online reach through SEO and pay-per-click,” which appeared in the September 2014 issue of OBG Management.)
If visitors like what they see at your site, they may make an appointment. But they are more likely to visit three or four other sites before making a decision. And in all likelihood, they will research each physician to find out what patients have to say about her or him. It’s no different than looking at the reviews of hotels or products you are considering.
You are an open book on the Internet. Only a few short years ago, your peers and patients knew your reputation primarily through word of mouth, which traveled at the speed of molasses. For the most part, that information was favorable. Today your exposure is much greater, and negative comments about you can be viewed by thousands of potential patients. The speed of information has increased, as well. What is posted on the Internet can become readily available to hundreds, thousands, and even millions of Web users in a nanosecond.
The Internet provides a forum for people to say whatever they want about their experiences, both positive and negative. Regrettably, the positive experiences do not find their way online nearly as often as the negative ones!
The bottom line? In today’s Internet-savvy world, you need to pay regular attention to your online reputation. You need to take steps to ensure that your name and practice look their best and to negate any complaints that may appear.
What patients share about their experience with you
Many online review sites provide an opportunity for your patients to describe their experience with you and your practice. To name a few: RateMDs.com, Vitals.com, ZocDoc.com, healthgrades.com, UcompareHealth.com, Citysearch.com, yelp.com, and, of course, Google Plus reviews.
And when patients post comments on the Internet, you likely will be rated on:
- the patient’s wait time
- how your staff treated the patient
- the diagnosis
- your attitude
- the level of trust in your decisions
- treatment and outcome.
The online surfer searching for a reputable physician is likely to believe whatever he or she finds on the leading review sites.
The good news: Most physicians have a very favorable rating, averaging 9.3 out of 10 on a scale of 1 to 10. In fact, 70% of doctors have perfect scores!1
The bad news: Someone who is unhappy with her treatment or outcome will go out of her way to find every online review site possible and proclaim your faults to the cyber-world, using the Internet as a forum, whether her facts are straight or not. Patients who are pleased and satisfied rarely bother to place a positive review.
How you can control your online reputation
It is incumbent upon you to keep an eye on your online reputation at all times. Here are some tips for taking charge:
- If someone posts a negative review, respond to them directly in the review site. Doing so does not violate privacy laws as long as you do not mention the patient’s name or give other identifying details. Explain your side of the story without confirming or denying that the reviewer is or was a patient. Do not mention the specifics of any patient’s condition.
- If you feel that a negative review is completely unjustified, file a dispute with the review site. Many review sites will remove the unfavorable content if you can convince them that the patient is merely ranting.
- To protect your reputation over the long term, use your name or practice name to set up an alert with Google Alerts by visiting the site Google.com/alerts.
- Do a Google search of your name and the name of your practice at least once a month and check out all the review sites that come up. Read the comments!
Develop a proactive system
You have a lot of control when it comes to protecting your online reputation, provided you are willing to take the time to set up a system to regularly request feedback or testimonials from your patients.
Regrettably, this is where most medical practices fall short, by failing to establish a system to solicit positive reviews.
The process need not be complicated. Such a system can be set in motion by scheduling a quick meeting with your staff to announce your plans to solicit testimonials from patients. Often there will be a flurry of activity for a couple of weeks before the task is forgotten. To keep your system from falling through the cracks, make a checklist and decide who on your staff is responsible for each step in the process. Go over the results in your staff meetings on a regular basis—ie, at least monthly.
You want to solicit positive reviews for use in two places:
- your Web site
- the review sites we mentioned earlier.
Posting testimonials on your Web site
Your site is the place prospective patients visit when they are looking for information about you and your services. Here are a few tips on gathering and posting testimonials:
- The best time to solicit feedback from the patient is after the follow-up appointment, when her needs have been met and she has had at least two experiences with your practice. If she is happy with her outcome, she is likely to be receptive to the idea of providing a testimonial while the details are fresh in her mind.
- Post testimonials on your homepage and every other page at your site. They should be visible when each page loads without the need to scroll down. A testimonial is worthless if it can’t be easily seen.
- Post testimonials in italics, with quotation marks around the comments to distinguish them from other elements on the page.
- Give each testimonial a headline in bold italics. Use key words likely to resonate with the reader. For example, if the patient reports: “I had a surgical procedure and it was a game changer. You turned my life around! Thank you!” the headline might be: “You turned my life around.”
- Create a Web page just for testimonials and order the comments and headlines so that they will appeal to a diversity of prospective patients. The visitor may not read every testimonial, but she will at least read and scroll through the headlines.
Gathering feedback: Your options
- One option for automating the gathering of feedback is to include a patient feedback survey on your Web site. It’s a convenient way to ask for comments. When the patient is in the office, you or your staff can simply ask her to visit the survey page on your site and answer the questions. The problem with this approach is that many patients will agree to complete the survey but few will actually follow through.
- A far more effective way to get patients to complete a survey while they are still in your office is to have the receptionist hand the patient an iPad after her appointment and ask her to take a couple of minutes to complete the survey. You can then transcribe her comments and post them on your site.
- Asking patients to post positive comments on review sites such as healthgrades.com is another option—but, again, patients are unlikely to follow through unless you make it as easy and fast as possible. The best way to do this is to provide your patient with a blueprint for how to proceed. We offer a “patient feedback” form that contains four or five questions (FIGURE). The answers to these questions will provide a great testimonial for the doctor and the practice. Providing your patients with the right questions to elicit an emotional response will help them describe their experiences more fully. If you let the patient create a testimonial on her own, you’ll probably just receive comments such as, “I’m very happy with my results” or “She is a great doctor.”
- Also provide patients with a step-by-step process for entering their feedback on the desired review sites. This can be a daunting task for your patient, so your instructions should be clear and simple. Better yet, have someone on your staff sit with the patient at a computer or iPad to help her through the process.
- Another way to control your online reputation is to capture positive comments at the point of service. In our practice, we have a testimonial poster in every exam room as well as the reception area. It contains a quick response (QR) code that can be scanned to allow the patient to submit a testimonial about her experience with the practice. With this system, we are able to collect three to five positive reviews every day.
FIGURE: Patient follow-up satisfaction survey
| It is our intention to provide our patients with the absolute best medical care available to produce optimal results. Your feedback about your procedure and patient care is an important measure of our performance. Please take the time to let us know how you feel about your results:
Your name: _______________________________ Date: ________ Thank you for telling us about the results of your procedure. How you feel about your experience helps us better understand the physical and emotional needs of our patients. We would like to share your experience with others who might be struggling with the same issues. By signing this form, you agree to let us share this information on our Web site and informational material to help other patients understand the benefits of having these types of procedures performed. |
CASE: Resolved
The physician institutes a process in his practice to gather testimonials and positive feedback, and his staff takes time to help willing patients post their reviews online. He also disputes the negative comments that have already been posted online, offering an objective response to the complaints and asking the Web sites to take down the reviews that are merely ranting. In addition, he posts selected testimonials on the homepage of his Web site and adds a page that is just for testimonials.
Within a few weeks, the number of new patients scheduling appointments with him begins to increase until he once again enjoys a bustling practice.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Schwartz SK. Online patient feedback: what to do. Physicianspractice.com. http://www.physicianspractice.com/health-it/online-patient-feedback-what-do. Published December 27, 2012. Accessed November 15, 2014.
“It takes 20 years to build a reputation and 5 minutes to ruin it. If you think about that, you’ll do things differently.”
—Warren Buffet
CASE: Decline in new patients
A well-respected physician—one of the best in his field—notices that the number of new patients in his practice has fallen off drastically over the past year. Baffled, he hires a consultant, who discovers that the doctor’s online reputation has plummeted, thanks to four negative reviews and no positive ones.
What can the physician do to remedy the situation and restore his reputation?
The problem can be fixed, but it takes time—like major surgery. Rather than wait until negative reviews are posted, we recommend that you become proactive and take steps as soon as possible to secure your online reputation. That way, you won’t get caught by surprise when one or two unhappy patients try to smear your good name. In this article, we step you through a number of remedies and proactive strategies for boosting positive online reviews and combating negative ones.
The Internet: A one-stop source of information
The Internet has become everyone’s go-to source for pretty much any kind of data, including details on products, services, and people. Anyone can access all kinds of information simply by asking.
Today, people research medical conditions on the Web, often using Google. If you have done your search engine optimization, your Web site will come up in the first page of search results, making it possible for prospective patients to click through to your homepage. (For the scoop on search engine optimization, see Part 3 of this series, “Maximizing your online reach through SEO and pay-per-click,” which appeared in the September 2014 issue of OBG Management.)
If visitors like what they see at your site, they may make an appointment. But they are more likely to visit three or four other sites before making a decision. And in all likelihood, they will research each physician to find out what patients have to say about her or him. It’s no different than looking at the reviews of hotels or products you are considering.
You are an open book on the Internet. Only a few short years ago, your peers and patients knew your reputation primarily through word of mouth, which traveled at the speed of molasses. For the most part, that information was favorable. Today your exposure is much greater, and negative comments about you can be viewed by thousands of potential patients. The speed of information has increased, as well. What is posted on the Internet can become readily available to hundreds, thousands, and even millions of Web users in a nanosecond.
The Internet provides a forum for people to say whatever they want about their experiences, both positive and negative. Regrettably, the positive experiences do not find their way online nearly as often as the negative ones!
The bottom line? In today’s Internet-savvy world, you need to pay regular attention to your online reputation. You need to take steps to ensure that your name and practice look their best and to negate any complaints that may appear.
What patients share about their experience with you
Many online review sites provide an opportunity for your patients to describe their experience with you and your practice. To name a few: RateMDs.com, Vitals.com, ZocDoc.com, healthgrades.com, UcompareHealth.com, Citysearch.com, yelp.com, and, of course, Google Plus reviews.
And when patients post comments on the Internet, you likely will be rated on:
- the patient’s wait time
- how your staff treated the patient
- the diagnosis
- your attitude
- the level of trust in your decisions
- treatment and outcome.
The online surfer searching for a reputable physician is likely to believe whatever he or she finds on the leading review sites.
The good news: Most physicians have a very favorable rating, averaging 9.3 out of 10 on a scale of 1 to 10. In fact, 70% of doctors have perfect scores!1
The bad news: Someone who is unhappy with her treatment or outcome will go out of her way to find every online review site possible and proclaim your faults to the cyber-world, using the Internet as a forum, whether her facts are straight or not. Patients who are pleased and satisfied rarely bother to place a positive review.
How you can control your online reputation
It is incumbent upon you to keep an eye on your online reputation at all times. Here are some tips for taking charge:
- If someone posts a negative review, respond to them directly in the review site. Doing so does not violate privacy laws as long as you do not mention the patient’s name or give other identifying details. Explain your side of the story without confirming or denying that the reviewer is or was a patient. Do not mention the specifics of any patient’s condition.
- If you feel that a negative review is completely unjustified, file a dispute with the review site. Many review sites will remove the unfavorable content if you can convince them that the patient is merely ranting.
- To protect your reputation over the long term, use your name or practice name to set up an alert with Google Alerts by visiting the site Google.com/alerts.
- Do a Google search of your name and the name of your practice at least once a month and check out all the review sites that come up. Read the comments!
Develop a proactive system
You have a lot of control when it comes to protecting your online reputation, provided you are willing to take the time to set up a system to regularly request feedback or testimonials from your patients.
Regrettably, this is where most medical practices fall short, by failing to establish a system to solicit positive reviews.
The process need not be complicated. Such a system can be set in motion by scheduling a quick meeting with your staff to announce your plans to solicit testimonials from patients. Often there will be a flurry of activity for a couple of weeks before the task is forgotten. To keep your system from falling through the cracks, make a checklist and decide who on your staff is responsible for each step in the process. Go over the results in your staff meetings on a regular basis—ie, at least monthly.
You want to solicit positive reviews for use in two places:
- your Web site
- the review sites we mentioned earlier.
Posting testimonials on your Web site
Your site is the place prospective patients visit when they are looking for information about you and your services. Here are a few tips on gathering and posting testimonials:
- The best time to solicit feedback from the patient is after the follow-up appointment, when her needs have been met and she has had at least two experiences with your practice. If she is happy with her outcome, she is likely to be receptive to the idea of providing a testimonial while the details are fresh in her mind.
- Post testimonials on your homepage and every other page at your site. They should be visible when each page loads without the need to scroll down. A testimonial is worthless if it can’t be easily seen.
- Post testimonials in italics, with quotation marks around the comments to distinguish them from other elements on the page.
- Give each testimonial a headline in bold italics. Use key words likely to resonate with the reader. For example, if the patient reports: “I had a surgical procedure and it was a game changer. You turned my life around! Thank you!” the headline might be: “You turned my life around.”
- Create a Web page just for testimonials and order the comments and headlines so that they will appeal to a diversity of prospective patients. The visitor may not read every testimonial, but she will at least read and scroll through the headlines.
Gathering feedback: Your options
- One option for automating the gathering of feedback is to include a patient feedback survey on your Web site. It’s a convenient way to ask for comments. When the patient is in the office, you or your staff can simply ask her to visit the survey page on your site and answer the questions. The problem with this approach is that many patients will agree to complete the survey but few will actually follow through.
- A far more effective way to get patients to complete a survey while they are still in your office is to have the receptionist hand the patient an iPad after her appointment and ask her to take a couple of minutes to complete the survey. You can then transcribe her comments and post them on your site.
- Asking patients to post positive comments on review sites such as healthgrades.com is another option—but, again, patients are unlikely to follow through unless you make it as easy and fast as possible. The best way to do this is to provide your patient with a blueprint for how to proceed. We offer a “patient feedback” form that contains four or five questions (FIGURE). The answers to these questions will provide a great testimonial for the doctor and the practice. Providing your patients with the right questions to elicit an emotional response will help them describe their experiences more fully. If you let the patient create a testimonial on her own, you’ll probably just receive comments such as, “I’m very happy with my results” or “She is a great doctor.”
- Also provide patients with a step-by-step process for entering their feedback on the desired review sites. This can be a daunting task for your patient, so your instructions should be clear and simple. Better yet, have someone on your staff sit with the patient at a computer or iPad to help her through the process.
- Another way to control your online reputation is to capture positive comments at the point of service. In our practice, we have a testimonial poster in every exam room as well as the reception area. It contains a quick response (QR) code that can be scanned to allow the patient to submit a testimonial about her experience with the practice. With this system, we are able to collect three to five positive reviews every day.
FIGURE: Patient follow-up satisfaction survey
| It is our intention to provide our patients with the absolute best medical care available to produce optimal results. Your feedback about your procedure and patient care is an important measure of our performance. Please take the time to let us know how you feel about your results:
Your name: _______________________________ Date: ________ Thank you for telling us about the results of your procedure. How you feel about your experience helps us better understand the physical and emotional needs of our patients. We would like to share your experience with others who might be struggling with the same issues. By signing this form, you agree to let us share this information on our Web site and informational material to help other patients understand the benefits of having these types of procedures performed. |
CASE: Resolved
The physician institutes a process in his practice to gather testimonials and positive feedback, and his staff takes time to help willing patients post their reviews online. He also disputes the negative comments that have already been posted online, offering an objective response to the complaints and asking the Web sites to take down the reviews that are merely ranting. In addition, he posts selected testimonials on the homepage of his Web site and adds a page that is just for testimonials.
Within a few weeks, the number of new patients scheduling appointments with him begins to increase until he once again enjoys a bustling practice.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“It takes 20 years to build a reputation and 5 minutes to ruin it. If you think about that, you’ll do things differently.”
—Warren Buffet
CASE: Decline in new patients
A well-respected physician—one of the best in his field—notices that the number of new patients in his practice has fallen off drastically over the past year. Baffled, he hires a consultant, who discovers that the doctor’s online reputation has plummeted, thanks to four negative reviews and no positive ones.
What can the physician do to remedy the situation and restore his reputation?
The problem can be fixed, but it takes time—like major surgery. Rather than wait until negative reviews are posted, we recommend that you become proactive and take steps as soon as possible to secure your online reputation. That way, you won’t get caught by surprise when one or two unhappy patients try to smear your good name. In this article, we step you through a number of remedies and proactive strategies for boosting positive online reviews and combating negative ones.
The Internet: A one-stop source of information
The Internet has become everyone’s go-to source for pretty much any kind of data, including details on products, services, and people. Anyone can access all kinds of information simply by asking.
Today, people research medical conditions on the Web, often using Google. If you have done your search engine optimization, your Web site will come up in the first page of search results, making it possible for prospective patients to click through to your homepage. (For the scoop on search engine optimization, see Part 3 of this series, “Maximizing your online reach through SEO and pay-per-click,” which appeared in the September 2014 issue of OBG Management.)
If visitors like what they see at your site, they may make an appointment. But they are more likely to visit three or four other sites before making a decision. And in all likelihood, they will research each physician to find out what patients have to say about her or him. It’s no different than looking at the reviews of hotels or products you are considering.
You are an open book on the Internet. Only a few short years ago, your peers and patients knew your reputation primarily through word of mouth, which traveled at the speed of molasses. For the most part, that information was favorable. Today your exposure is much greater, and negative comments about you can be viewed by thousands of potential patients. The speed of information has increased, as well. What is posted on the Internet can become readily available to hundreds, thousands, and even millions of Web users in a nanosecond.
The Internet provides a forum for people to say whatever they want about their experiences, both positive and negative. Regrettably, the positive experiences do not find their way online nearly as often as the negative ones!
The bottom line? In today’s Internet-savvy world, you need to pay regular attention to your online reputation. You need to take steps to ensure that your name and practice look their best and to negate any complaints that may appear.
What patients share about their experience with you
Many online review sites provide an opportunity for your patients to describe their experience with you and your practice. To name a few: RateMDs.com, Vitals.com, ZocDoc.com, healthgrades.com, UcompareHealth.com, Citysearch.com, yelp.com, and, of course, Google Plus reviews.
And when patients post comments on the Internet, you likely will be rated on:
- the patient’s wait time
- how your staff treated the patient
- the diagnosis
- your attitude
- the level of trust in your decisions
- treatment and outcome.
The online surfer searching for a reputable physician is likely to believe whatever he or she finds on the leading review sites.
The good news: Most physicians have a very favorable rating, averaging 9.3 out of 10 on a scale of 1 to 10. In fact, 70% of doctors have perfect scores!1
The bad news: Someone who is unhappy with her treatment or outcome will go out of her way to find every online review site possible and proclaim your faults to the cyber-world, using the Internet as a forum, whether her facts are straight or not. Patients who are pleased and satisfied rarely bother to place a positive review.
How you can control your online reputation
It is incumbent upon you to keep an eye on your online reputation at all times. Here are some tips for taking charge:
- If someone posts a negative review, respond to them directly in the review site. Doing so does not violate privacy laws as long as you do not mention the patient’s name or give other identifying details. Explain your side of the story without confirming or denying that the reviewer is or was a patient. Do not mention the specifics of any patient’s condition.
- If you feel that a negative review is completely unjustified, file a dispute with the review site. Many review sites will remove the unfavorable content if you can convince them that the patient is merely ranting.
- To protect your reputation over the long term, use your name or practice name to set up an alert with Google Alerts by visiting the site Google.com/alerts.
- Do a Google search of your name and the name of your practice at least once a month and check out all the review sites that come up. Read the comments!
Develop a proactive system
You have a lot of control when it comes to protecting your online reputation, provided you are willing to take the time to set up a system to regularly request feedback or testimonials from your patients.
Regrettably, this is where most medical practices fall short, by failing to establish a system to solicit positive reviews.
The process need not be complicated. Such a system can be set in motion by scheduling a quick meeting with your staff to announce your plans to solicit testimonials from patients. Often there will be a flurry of activity for a couple of weeks before the task is forgotten. To keep your system from falling through the cracks, make a checklist and decide who on your staff is responsible for each step in the process. Go over the results in your staff meetings on a regular basis—ie, at least monthly.
You want to solicit positive reviews for use in two places:
- your Web site
- the review sites we mentioned earlier.
Posting testimonials on your Web site
Your site is the place prospective patients visit when they are looking for information about you and your services. Here are a few tips on gathering and posting testimonials:
- The best time to solicit feedback from the patient is after the follow-up appointment, when her needs have been met and she has had at least two experiences with your practice. If she is happy with her outcome, she is likely to be receptive to the idea of providing a testimonial while the details are fresh in her mind.
- Post testimonials on your homepage and every other page at your site. They should be visible when each page loads without the need to scroll down. A testimonial is worthless if it can’t be easily seen.
- Post testimonials in italics, with quotation marks around the comments to distinguish them from other elements on the page.
- Give each testimonial a headline in bold italics. Use key words likely to resonate with the reader. For example, if the patient reports: “I had a surgical procedure and it was a game changer. You turned my life around! Thank you!” the headline might be: “You turned my life around.”
- Create a Web page just for testimonials and order the comments and headlines so that they will appeal to a diversity of prospective patients. The visitor may not read every testimonial, but she will at least read and scroll through the headlines.
Gathering feedback: Your options
- One option for automating the gathering of feedback is to include a patient feedback survey on your Web site. It’s a convenient way to ask for comments. When the patient is in the office, you or your staff can simply ask her to visit the survey page on your site and answer the questions. The problem with this approach is that many patients will agree to complete the survey but few will actually follow through.
- A far more effective way to get patients to complete a survey while they are still in your office is to have the receptionist hand the patient an iPad after her appointment and ask her to take a couple of minutes to complete the survey. You can then transcribe her comments and post them on your site.
- Asking patients to post positive comments on review sites such as healthgrades.com is another option—but, again, patients are unlikely to follow through unless you make it as easy and fast as possible. The best way to do this is to provide your patient with a blueprint for how to proceed. We offer a “patient feedback” form that contains four or five questions (FIGURE). The answers to these questions will provide a great testimonial for the doctor and the practice. Providing your patients with the right questions to elicit an emotional response will help them describe their experiences more fully. If you let the patient create a testimonial on her own, you’ll probably just receive comments such as, “I’m very happy with my results” or “She is a great doctor.”
- Also provide patients with a step-by-step process for entering their feedback on the desired review sites. This can be a daunting task for your patient, so your instructions should be clear and simple. Better yet, have someone on your staff sit with the patient at a computer or iPad to help her through the process.
- Another way to control your online reputation is to capture positive comments at the point of service. In our practice, we have a testimonial poster in every exam room as well as the reception area. It contains a quick response (QR) code that can be scanned to allow the patient to submit a testimonial about her experience with the practice. With this system, we are able to collect three to five positive reviews every day.
FIGURE: Patient follow-up satisfaction survey
| It is our intention to provide our patients with the absolute best medical care available to produce optimal results. Your feedback about your procedure and patient care is an important measure of our performance. Please take the time to let us know how you feel about your results:
Your name: _______________________________ Date: ________ Thank you for telling us about the results of your procedure. How you feel about your experience helps us better understand the physical and emotional needs of our patients. We would like to share your experience with others who might be struggling with the same issues. By signing this form, you agree to let us share this information on our Web site and informational material to help other patients understand the benefits of having these types of procedures performed. |
CASE: Resolved
The physician institutes a process in his practice to gather testimonials and positive feedback, and his staff takes time to help willing patients post their reviews online. He also disputes the negative comments that have already been posted online, offering an objective response to the complaints and asking the Web sites to take down the reviews that are merely ranting. In addition, he posts selected testimonials on the homepage of his Web site and adds a page that is just for testimonials.
Within a few weeks, the number of new patients scheduling appointments with him begins to increase until he once again enjoys a bustling practice.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Schwartz SK. Online patient feedback: what to do. Physicianspractice.com. http://www.physicianspractice.com/health-it/online-patient-feedback-what-do. Published December 27, 2012. Accessed November 15, 2014.
Reference
- Schwartz SK. Online patient feedback: what to do. Physicianspractice.com. http://www.physicianspractice.com/health-it/online-patient-feedback-what-do. Published December 27, 2012. Accessed November 15, 2014.
Joining forces
Tough economic times and the unpredictable consequences of health care reform are making a growing number of solo practitioners and small private groups very nervous. I’ve received many inquiries about protective options, such as joining a multispecialty group, or merging two or more small practices into larger entities.
If becoming an employee of a large corporation does not appeal to you, a merger can offer significant advantages in stabilization of income and expenses; but careful planning, and a written agreement, are essential.
If you are considering this option, here are some things to think about:
What is the compensation formula? Will everyone be paid only for what they do individually, or will revenue be shared equally? I favor a combination; productivity is rewarded, but your income doesn’t drop to zero when you take time off.
Who will be in charge, and what percentage vote will be needed to approve important decisions? Typically, the majority rules, but you may wish to create a list of pivotal moves that will require unanimous approval, such as purchasing expensive equipment, borrowing money, or adding new partners.
Will you keep your retirement plans separate, or combine them? If the latter, you will have to agree on the terms of the new plan, which can be the same or different from any of the existing plans. You’ll probably need some legal guidance to ensure that assets from existing plans can be transferred into a new plan without tax issues.
Since most private practices are incorporated, there are two basic options for combining them: Corporation A can simply absorb corporation B; the latter ceases to exist, and corporation A, the so-called “surviving entity,” assumes all assets and liabilities of both old corporations. Corporation B shareholders exchange shares of its stock for shares of corporation A, with adjustments for any inequalities in stock value.
The second option is to start a completely new corporation. Both separate entities dissolve and distribute their equipment and charts to their shareholders, who then transfer the assets to the new corporation.
Option 2 is popular, but I am not a fan. It is billed as an opportunity to start fresh, shielding everyone from exposure to malpractice suits and other liabilities. However, the reality is that anyone looking to sue either old corporation will simply sue the new entity as the so-called “successor” corporation, on the grounds that it has assumed responsibility for its predecessors’ liabilities. You also will need new provider numbers, which may impede cash flow for months. Plus, the IRS treats corporate liquidations, even for merger purposes, as sales of assets, and taxes them.
In general, most experts that I’ve talked with favor outright merger of the corporations. This option is tax neutral, and while it may theoretically be less satisfactory liability-wise, you can minimize risk by examining financial and legal records, and by identifying any glaring flaws in charting or coding. Your lawyers can add “hold harmless” clauses to the merger agreement, indemnifying each party against the others’ liabilities. This area in particular is where you need experienced, competent legal advice.
Another common sticking point is known as “equalization.” Ideally, each party brings an equal amount of assets to the table, but in the real world that is rarely the case. One party may contribute more equipment, for example, and the others are often asked to make up the difference (“equalize”) with something else, usually cash.
An alternative is to agree that any inequalities will be compensated at the other end, in the form of buyout value; that is, physicians contributing more assets will receive larger buyouts when they leave or retire than those contributing less.
Non-compete provisions are always a difficult issue, mostly because they are so hard (and expensive) to enforce. An increasingly popular alternative is, once again, to deal with it at the other end, with a buyout penalty. An unhappy partner can leave, and compete, but at the cost of a substantially reduced buyout. This permits competition, but discourages it; and it compensates the remaining partners.
These are only some of the pivotal business and legal issues that must be settled in advance. A little planning and negotiation can prevent a lot of grief, regret, and legal expenses in the future. I’ll mention some other, more complicated merger options in a future column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News. Additional columns are available online at edermatologynews.com.
Tough economic times and the unpredictable consequences of health care reform are making a growing number of solo practitioners and small private groups very nervous. I’ve received many inquiries about protective options, such as joining a multispecialty group, or merging two or more small practices into larger entities.
If becoming an employee of a large corporation does not appeal to you, a merger can offer significant advantages in stabilization of income and expenses; but careful planning, and a written agreement, are essential.
If you are considering this option, here are some things to think about:
What is the compensation formula? Will everyone be paid only for what they do individually, or will revenue be shared equally? I favor a combination; productivity is rewarded, but your income doesn’t drop to zero when you take time off.
Who will be in charge, and what percentage vote will be needed to approve important decisions? Typically, the majority rules, but you may wish to create a list of pivotal moves that will require unanimous approval, such as purchasing expensive equipment, borrowing money, or adding new partners.
Will you keep your retirement plans separate, or combine them? If the latter, you will have to agree on the terms of the new plan, which can be the same or different from any of the existing plans. You’ll probably need some legal guidance to ensure that assets from existing plans can be transferred into a new plan without tax issues.
Since most private practices are incorporated, there are two basic options for combining them: Corporation A can simply absorb corporation B; the latter ceases to exist, and corporation A, the so-called “surviving entity,” assumes all assets and liabilities of both old corporations. Corporation B shareholders exchange shares of its stock for shares of corporation A, with adjustments for any inequalities in stock value.
The second option is to start a completely new corporation. Both separate entities dissolve and distribute their equipment and charts to their shareholders, who then transfer the assets to the new corporation.
Option 2 is popular, but I am not a fan. It is billed as an opportunity to start fresh, shielding everyone from exposure to malpractice suits and other liabilities. However, the reality is that anyone looking to sue either old corporation will simply sue the new entity as the so-called “successor” corporation, on the grounds that it has assumed responsibility for its predecessors’ liabilities. You also will need new provider numbers, which may impede cash flow for months. Plus, the IRS treats corporate liquidations, even for merger purposes, as sales of assets, and taxes them.
In general, most experts that I’ve talked with favor outright merger of the corporations. This option is tax neutral, and while it may theoretically be less satisfactory liability-wise, you can minimize risk by examining financial and legal records, and by identifying any glaring flaws in charting or coding. Your lawyers can add “hold harmless” clauses to the merger agreement, indemnifying each party against the others’ liabilities. This area in particular is where you need experienced, competent legal advice.
Another common sticking point is known as “equalization.” Ideally, each party brings an equal amount of assets to the table, but in the real world that is rarely the case. One party may contribute more equipment, for example, and the others are often asked to make up the difference (“equalize”) with something else, usually cash.
An alternative is to agree that any inequalities will be compensated at the other end, in the form of buyout value; that is, physicians contributing more assets will receive larger buyouts when they leave or retire than those contributing less.
Non-compete provisions are always a difficult issue, mostly because they are so hard (and expensive) to enforce. An increasingly popular alternative is, once again, to deal with it at the other end, with a buyout penalty. An unhappy partner can leave, and compete, but at the cost of a substantially reduced buyout. This permits competition, but discourages it; and it compensates the remaining partners.
These are only some of the pivotal business and legal issues that must be settled in advance. A little planning and negotiation can prevent a lot of grief, regret, and legal expenses in the future. I’ll mention some other, more complicated merger options in a future column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News. Additional columns are available online at edermatologynews.com.
Tough economic times and the unpredictable consequences of health care reform are making a growing number of solo practitioners and small private groups very nervous. I’ve received many inquiries about protective options, such as joining a multispecialty group, or merging two or more small practices into larger entities.
If becoming an employee of a large corporation does not appeal to you, a merger can offer significant advantages in stabilization of income and expenses; but careful planning, and a written agreement, are essential.
If you are considering this option, here are some things to think about:
What is the compensation formula? Will everyone be paid only for what they do individually, or will revenue be shared equally? I favor a combination; productivity is rewarded, but your income doesn’t drop to zero when you take time off.
Who will be in charge, and what percentage vote will be needed to approve important decisions? Typically, the majority rules, but you may wish to create a list of pivotal moves that will require unanimous approval, such as purchasing expensive equipment, borrowing money, or adding new partners.
Will you keep your retirement plans separate, or combine them? If the latter, you will have to agree on the terms of the new plan, which can be the same or different from any of the existing plans. You’ll probably need some legal guidance to ensure that assets from existing plans can be transferred into a new plan without tax issues.
Since most private practices are incorporated, there are two basic options for combining them: Corporation A can simply absorb corporation B; the latter ceases to exist, and corporation A, the so-called “surviving entity,” assumes all assets and liabilities of both old corporations. Corporation B shareholders exchange shares of its stock for shares of corporation A, with adjustments for any inequalities in stock value.
The second option is to start a completely new corporation. Both separate entities dissolve and distribute their equipment and charts to their shareholders, who then transfer the assets to the new corporation.
Option 2 is popular, but I am not a fan. It is billed as an opportunity to start fresh, shielding everyone from exposure to malpractice suits and other liabilities. However, the reality is that anyone looking to sue either old corporation will simply sue the new entity as the so-called “successor” corporation, on the grounds that it has assumed responsibility for its predecessors’ liabilities. You also will need new provider numbers, which may impede cash flow for months. Plus, the IRS treats corporate liquidations, even for merger purposes, as sales of assets, and taxes them.
In general, most experts that I’ve talked with favor outright merger of the corporations. This option is tax neutral, and while it may theoretically be less satisfactory liability-wise, you can minimize risk by examining financial and legal records, and by identifying any glaring flaws in charting or coding. Your lawyers can add “hold harmless” clauses to the merger agreement, indemnifying each party against the others’ liabilities. This area in particular is where you need experienced, competent legal advice.
Another common sticking point is known as “equalization.” Ideally, each party brings an equal amount of assets to the table, but in the real world that is rarely the case. One party may contribute more equipment, for example, and the others are often asked to make up the difference (“equalize”) with something else, usually cash.
An alternative is to agree that any inequalities will be compensated at the other end, in the form of buyout value; that is, physicians contributing more assets will receive larger buyouts when they leave or retire than those contributing less.
Non-compete provisions are always a difficult issue, mostly because they are so hard (and expensive) to enforce. An increasingly popular alternative is, once again, to deal with it at the other end, with a buyout penalty. An unhappy partner can leave, and compete, but at the cost of a substantially reduced buyout. This permits competition, but discourages it; and it compensates the remaining partners.
These are only some of the pivotal business and legal issues that must be settled in advance. A little planning and negotiation can prevent a lot of grief, regret, and legal expenses in the future. I’ll mention some other, more complicated merger options in a future column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Skin & Allergy News. Additional columns are available online at edermatologynews.com.
Best practices for the surgical management of adnexal masses in pregnancy
During the 43rd AAGL Global Congress, held November 17–21 in Vancouver, British Columbia, Sarah L. Cohen, MD, MPH, of Brigham and Women’s Hospital in Boston, Massachusetts, stepped attendees through diagnosis and surgical management of adnexal masses in pregnancy, noting the approaches backed by the highest-quality data.
The incidence of adnexal masses in pregnancy is 1 in every 600 live births. A mass can be benign or malignant. Among benign masses found in pregnancy are functional cysts, teratomas, and the corpus luteum.
Work-up
Ultrasound imaging is a valuable component of the work-up, owing to its risk-free nature. Magnetic resonance imaging may be appropriate in selected cases, but gadolinium contrast should be avoided.
In pregnancy, the aim is to limit ionizing radiation to less than 5 to 10 rads to minimize the risk of childhood malignancy/leukemia, with no single imaging study exceeding 5 rads.
Tumor markers may be helpful, but careful interpretation is critical, taking into account the effects of pregnancy itself on CA-125 (which peaks in the first trimester), human chorionic gonadotropin, alpha fetoprotein, inhibin A, and lactate dehydrogenase.
When expectant management may be appropriate
Watchful waiting may be considered for simple cysts less than 6 cm in size, provided the patient is asymptomatic with no signs of malignancy.
Surgery is indicated when the patient is symptomatic, when there is a concern for malignancy, and when a persistent mass exceeds 10 cm in size.
As always, elective surgery is preferable, as emergent surgery in pregnancy is associated with a risk of preterm labor of 22% to 35%.
Optimal timing of surgery
Surgery can be performed safely in any trimester, provided the gynecologist is aware of special concerns. For example, in the first trimester, organogenesis is under way and the corpus luteum is still present. If the corpus luteum is removed, progesterone supplementation is necessary.
When surgery can be postponed to the second trimester, it allows time for possible resolution of the mass.
Mode of surgery
Laparoscopy allows for faster recovery, less pain (and, therefore, lower narcotic exposure to the fetus), and improved maternal ventilation.
Prophylaxis for venous thromboembolism is indicated through the use of pneumatic compression devices and, when appropriate, heparin.
Initial port placement can be performed using a Hassan technique, Veress needle, or optical trocar.
Insufflation pressures of 10 to 15 mm Hg are safe, with intraoperative monitoring of carbon dioxide.
Availability of guidelines
Surgeons should make use of guidelines, when feasible, to guide surgery. For example, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) publishes guidelines on surgery during pregnancy. The American College of Obstetricians and Gynecologists also offers guidelines.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
During the 43rd AAGL Global Congress, held November 17–21 in Vancouver, British Columbia, Sarah L. Cohen, MD, MPH, of Brigham and Women’s Hospital in Boston, Massachusetts, stepped attendees through diagnosis and surgical management of adnexal masses in pregnancy, noting the approaches backed by the highest-quality data.
The incidence of adnexal masses in pregnancy is 1 in every 600 live births. A mass can be benign or malignant. Among benign masses found in pregnancy are functional cysts, teratomas, and the corpus luteum.
Work-up
Ultrasound imaging is a valuable component of the work-up, owing to its risk-free nature. Magnetic resonance imaging may be appropriate in selected cases, but gadolinium contrast should be avoided.
In pregnancy, the aim is to limit ionizing radiation to less than 5 to 10 rads to minimize the risk of childhood malignancy/leukemia, with no single imaging study exceeding 5 rads.
Tumor markers may be helpful, but careful interpretation is critical, taking into account the effects of pregnancy itself on CA-125 (which peaks in the first trimester), human chorionic gonadotropin, alpha fetoprotein, inhibin A, and lactate dehydrogenase.
When expectant management may be appropriate
Watchful waiting may be considered for simple cysts less than 6 cm in size, provided the patient is asymptomatic with no signs of malignancy.
Surgery is indicated when the patient is symptomatic, when there is a concern for malignancy, and when a persistent mass exceeds 10 cm in size.
As always, elective surgery is preferable, as emergent surgery in pregnancy is associated with a risk of preterm labor of 22% to 35%.
Optimal timing of surgery
Surgery can be performed safely in any trimester, provided the gynecologist is aware of special concerns. For example, in the first trimester, organogenesis is under way and the corpus luteum is still present. If the corpus luteum is removed, progesterone supplementation is necessary.
When surgery can be postponed to the second trimester, it allows time for possible resolution of the mass.
Mode of surgery
Laparoscopy allows for faster recovery, less pain (and, therefore, lower narcotic exposure to the fetus), and improved maternal ventilation.
Prophylaxis for venous thromboembolism is indicated through the use of pneumatic compression devices and, when appropriate, heparin.
Initial port placement can be performed using a Hassan technique, Veress needle, or optical trocar.
Insufflation pressures of 10 to 15 mm Hg are safe, with intraoperative monitoring of carbon dioxide.
Availability of guidelines
Surgeons should make use of guidelines, when feasible, to guide surgery. For example, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) publishes guidelines on surgery during pregnancy. The American College of Obstetricians and Gynecologists also offers guidelines.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
During the 43rd AAGL Global Congress, held November 17–21 in Vancouver, British Columbia, Sarah L. Cohen, MD, MPH, of Brigham and Women’s Hospital in Boston, Massachusetts, stepped attendees through diagnosis and surgical management of adnexal masses in pregnancy, noting the approaches backed by the highest-quality data.
The incidence of adnexal masses in pregnancy is 1 in every 600 live births. A mass can be benign or malignant. Among benign masses found in pregnancy are functional cysts, teratomas, and the corpus luteum.
Work-up
Ultrasound imaging is a valuable component of the work-up, owing to its risk-free nature. Magnetic resonance imaging may be appropriate in selected cases, but gadolinium contrast should be avoided.
In pregnancy, the aim is to limit ionizing radiation to less than 5 to 10 rads to minimize the risk of childhood malignancy/leukemia, with no single imaging study exceeding 5 rads.
Tumor markers may be helpful, but careful interpretation is critical, taking into account the effects of pregnancy itself on CA-125 (which peaks in the first trimester), human chorionic gonadotropin, alpha fetoprotein, inhibin A, and lactate dehydrogenase.
When expectant management may be appropriate
Watchful waiting may be considered for simple cysts less than 6 cm in size, provided the patient is asymptomatic with no signs of malignancy.
Surgery is indicated when the patient is symptomatic, when there is a concern for malignancy, and when a persistent mass exceeds 10 cm in size.
As always, elective surgery is preferable, as emergent surgery in pregnancy is associated with a risk of preterm labor of 22% to 35%.
Optimal timing of surgery
Surgery can be performed safely in any trimester, provided the gynecologist is aware of special concerns. For example, in the first trimester, organogenesis is under way and the corpus luteum is still present. If the corpus luteum is removed, progesterone supplementation is necessary.
When surgery can be postponed to the second trimester, it allows time for possible resolution of the mass.
Mode of surgery
Laparoscopy allows for faster recovery, less pain (and, therefore, lower narcotic exposure to the fetus), and improved maternal ventilation.
Prophylaxis for venous thromboembolism is indicated through the use of pneumatic compression devices and, when appropriate, heparin.
Initial port placement can be performed using a Hassan technique, Veress needle, or optical trocar.
Insufflation pressures of 10 to 15 mm Hg are safe, with intraoperative monitoring of carbon dioxide.
Availability of guidelines
Surgeons should make use of guidelines, when feasible, to guide surgery. For example, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) publishes guidelines on surgery during pregnancy. The American College of Obstetricians and Gynecologists also offers guidelines.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.