User login
Informed consent: The more you know, the more you and your patient are protected
CASE: Surgeon accused of performing tubal ligation without consent
A patient was scheduled for an elective cesarean delivery to be performed by her ObGyn (Dr. Surgeon) at the nearby medical center. The patient was asked to sign an electronic signature pad in her ObGyn’s office, which transposed her signature onto an electronic form that she could not see at the time. She signed it. The consent was not printed out in the office but was added to her electronic medical record, and a copy was sent to her via email. Among other things, the consent included, “[Name] hereby agrees that all appropriate medical and surgical procedures as determined by the physicians and others in this hospital are in my best interest. No further consent is required to any of the treatment in this hospital.”
In the hospital, Dr. Surgeon spoke preoper- atively with the patient about cesarean delivery, the various risks and benefits, and the possibility and risks of an alternative trial of labor. Dr. Surgeon noted the conversation in the patient’s chart.
A nurse brought a standard hard copy “Zee Hospital Surgical Consent Form” to the patient. In a relevant part it provided, “I hereby consent to the surgical procedure Dr. Surgeon has discussed with me: _______” (the blank was filled in with “cesarean delivery”). The form continued: “He/She has explained the risks and benefits. I also authorize Dr. Surgeon, and such assistants as he/she may select, to perform this procedure. In his/her medical judgment, if additional procedures are appropriate, I hereby consent to their performance, in addition to the procedures listed in this form.” The patient signed the form.
While Dr. Surgeon was scrubbing for the delivery, the patient’s husband (also a surgeon at the hospital; Dr. Husband), stopped by, thanked Dr. Surgeon, and said, “Oh, by the way, my wife would like you to do a tubal ligation as well—she really wants it for health reasons. Her chronic hypertension skyrocketed during this pregnancy, and we don’t want any more children.”
“She didn’t mention that a little earlier while I was talking with her,” replied Dr. Surgeon, “but I can see how it would have slipped her mind.”
Dr. Surgeon performed the cesarean delivery and tubal ligation. All went well, with a healthy baby and mother. Several months later, the patient and Dr. Husband separated and sought divorce.
The patient, surprised by the cost of the hospital bill (Dr. Surgeon did not bill for his surgical services as a professional courtesy), was astonished to see a charge related to tubal ligation. Knowing how common billing mistakes were at Zee Hospital, she called to have the bill corrected. The clerk informed her that her medical record showed that a tubal ligation had been performed and that the bill was correct.
The patient sued Dr. Surgeon, Zee Hospital, and her (now former) husband, Dr. Husband, both for the cesarean delivery and the tubal ligation. Her claims are primarily based on the lack of informed consent.
What’s the verdict?
The patient likely has a strong case regarding the tubal ligation claim, but a weak case related to the cesarean delivery claim.
Read the ethical, medical, and legal implications of this case
Ethical and medical considerations
Although this case seems too strange for fiction, the basic facts are taken from events that did occur at a major institution. The puzzling features of this case are meant to be a cautionary tale: it is easy in the rush with the pressure of clinical practice to view informed consent as a bothersome technical detail. Yet as the following discussion suggests, adhering closely to the tenets of informed consent protects not only the fundamental interests of the patient but also the physicians and medical institutions.
Informed consent serves as protective communication
Informed consent at its core is a “process of communication” that involves you as the health care provider and the patient. It provides authority for an activity based upon an understanding of what that activity entails.1,2 Aspects of informed consent, from the physician−patient perspective, include the following:
- disclosure
- comprehension
- voluntary choice
- authorization.
In one other sense, informed consent is based on a fiduciary relationship between the ObGyn and patient.3 Overall, the process consists of an educational communication by the physician to the patient. Ideally, providers perceive the process from an ethical point of view that has been formalized by cases and statutes.4
Informed consent protects one of the most basic values of medicine and society: autonomy. From the perspective of moral philosophers, the principle of autonomy establishes the moral right to choose and follow one’s own plan for life and action.5,6 For ObGyns, the patient’s autonomy and her ability to participate in the medical decision-making process is of paramount importance. Informed consent is also a reflection of trust inherent to the physician−patient relationship.4
Informed consent is too often viewed as a mere legal formality. In truth, it melds legal and ethical values and concerns. The President’s Commission reflected this, noting that informed consent is rooted in “the fundamental recognition that adults are entitled to accept or reject health care intervention(s) on the basis of their own personal values and in furtherance of their own personal goals.”7
The historic perspective of informed consent dates back to Egyptian, Greek, and Roman eras. Dhar and Dhar suggest that the concept of “physicians’ love for humanity—philantropia” dates back to Plato and is complemented by the term “philotechnia” (love of medicine), all of which have evolved into today’s use of the terms “risks, benefits, and alternatives.”8
We emphasize that informed consent is much more than a legal concept. It has strong clinical roots because it provides an opportunity for physicians to improve communication with their patients. Informed consent is not a form; it is a process to be taken seriously.
Legal principles of informed consent
The famous New York case of Mary Schloendorff v. Society of New York Hospital, in 1914, heralded a principle that remains central in American law. Justice Benjamin Cardozo, writing for the majority, held that, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages.”9 The surgeon in the Schloendorff case had undertaken a gynecologic procedure—removal of a fibroid tumor—without patient consent. (In that case the hospital rather than the physician was sued, but the principle clearly applied to the physician.)
Over the last century, the American law of informed consent has developed in a number of ways.10 Lack of informed consent is now almost always considered a form of negligence rather than an intentional tort of battery. The details of the legal requirements vary from state to state as a result of statutory changes and court decisions. But in one way or another, to be “informed,” consent generally must include 4 things:
- a description of the procedure or intervention that is proposed
- the risks and benefits of the proposal—the focus here is generally on the risks of the treatment
- alternatives, if there are any (eg, pharmacologic vs surgical treatment)
- the consequences of not undertaking the proposed treatment (eg, the refusal to have a Papanicolaou smear).
A fifth point might be added—the offer to answer any questions or provide additional information.
These 4 or 5 basic items and the expanded list are efforts to simply describe the information that a reasonable person would need in order to make a decision that represents the patient’s values, personality, and preferences. (Informed consent is in some ways an ongoing process—since a patient may withdraw his/her consent.)
Exceptions to the informed consent requirement
Before turning to the facts in the hypothetical case, it is worth noting that there are 2 common exceptions to the informed consent requirement. The first is an emergency exception. When someone requires immediate attention and the patient is not conscious or capable of consent (nor is a “next of kin” available), treatment may proceed.
The second is therapeutic exception. Its designation is narrow, and it is risky to rely on it except in extreme circumstances. But when the very process of informing the patient of all the risks of a proposed treatment would create significant additional risks for the patient, the consent process may be modified. For example, for an extremely suggestable patient, describing certain risks might, in a psychosomatic way, cause the risk to be realized. In such cases, the record must be clearly documented. It is generally best to discuss the matter with a family member or other surrogate decision maker.
Read what went wrong in this case
What went wrong with consent in this case?
Our case illustrates a number of problems that occur when informed consent is not properly completed.
The electronic signature on the broadly stated consent form the patient initially signed in the office was nearly useless. She did not know what she was signing, did not have any chance to read it before signing, and was provided no help with any of the information factors of informed consent.
The surgical consent form is among the most interesting elements of this case. The form itself was seriously flawed because it contained no real evidence that the patient received information about the risks and alternatives. If the form is all there was, it would be a problem. But the conversation that Dr. Surgeon documented with the patient seemed to provide the basic elements of informed consent, including discussion of risks and benefits.
Oral informed consent is recognized in most states. To his credit, Dr. Surgeon appropriately recorded the conversation in the record. The risk of oral informed consent not backed up by text signature is that, if a dispute arises about the consent, it is difficult to prove details of what was said. (There was, of course, no such dispute about the cesarean delivery as it turned out in this case.)
Technological add-ons to consent: Pros and cons
Video and computer software are increasingly becoming an integral part of the informed consent process, and may improve comprehension by patients.11 Electronic consent may be helpful in proving what the patient was told during the consent process. A difficulty can result from overreliance on the electronic aspect and forgetting the human part of the informed consent equation. The health care team often can be productive parts of the informed consent process, but the surgeon must take ultimate responsibility for the informed consent.12
Was there informed consent for the tubal ligation?
The major problem in this case, of course, was the tubal ligation. It does not take much of an understanding of the legal niceties of informed consent to know that there was no real consent to this procedure. Dr. Husband did not have authority to consent, and his comment to Dr. Surgeon did not qualify as consent.
The hospital consent form may appear to provide some legal protection (“In his medical judgment, if additional procedures are appropriate, I hereby consent to doing those….”). Such language was once common in informed consent forms, but it offered little real consent except for trivial incidental processes (removal of an appendix) or where there was a real medical necessity for doing an expanded procedure (removal of a previously unknown cancerous growth).
Thus, Dr. Surgeon performed the sterilization without consent and may well be liable for that part of the surgery even though it did not turn out badly in a medical sense. If not for the tubal ligation, the damages would probably have been trivial. The real loss here is not a medical injury; it is the loss of reproductive capacity.
Protecting reproductive capacity. Modern law has been especially sensitive to protecting decisions regarding reproductive capacity. Therefore, the absence of clear consent to permanent sterilization is legally problematic. Dr. Surgeon may claim that he reasonably believed that the husband could give surrogate consent and it was too late to check with the patient herself. This situation does not fit well with the emergency exception, and it appears from the facts that Dr. Surgeon acted without informed consent to the sterilization.
Was it negligence or battery?
Dr. Surgeon. The most likely basis for liability for Dr. Surgeon is negligence. There is some argument that the tort of battery is a possibility because there was no consent at all for the sterilization. The claim would be that it was not the “information” that was lacking; it was the consent itself. The fact that Dr. Surgeon did not charge for his services would not absolve him of liability.
Dr. Husband. The potential liability of Dr. Husband is complicated by questions of whether he was acting in the capacity of a physician (which would likely involve the question of whether his malpractice insurance would be available), the degree to which he was acting in good faith, and facts we do not have in this case. If Dr. Husband gave consent (and thereby “caused”) the sterilization knowing that his wife did not want to have it or because of animus toward her (they were about to be separated and divorced, after all), there is the possibility of liability. (In some states a form of interspousal liability might complicate some of these claims—but that is a topic for another day.) He essentially took action for the purpose of wrongly causing the sterilization—which may be a battery (an intentional offensive or harmful touching). The legal rules around battery allow punitive damages as well as compensatory damages. In addition, many malpractice insurance policies provide limited coverage for intentional torts. To complicate matters further, it is not clear that Dr. Husband’s actions were related to his practice of medicine in any event (although Dr. Surgeon might claim that Dr. Husband’s expressed concern about his wife’s hypertension was enough to create a malpractice issue if Dr. Surgeon did not perform the verbally requested tubal ligation).
If, as we have speculated, Dr. Husband’s actions were motivated by improper personal considerations at the expense of a patient, he may also face medical board complaints from the patient. It is plausible that a state law makes it a criminal offense to wrongfully (or fraudulently) consent to medical treatment, particularly if related to reproductive capacity.
The hospital may face liability on several grounds, depending in part on the relationships between the hospital, Dr. Surgeon, and Dr. Husband. If Dr. Surgeon is an employee or agent of the hospital, he would be liable for his negligence. Even if Dr. Surgeon is technically an independent contractor, the failure of the hospital to offer more oversight concerning the surgical procedures in its facilities could give rise to a claim of negligence.
As to Dr. Husband, many of the same considerations are present. In addition, even if he is an agent of the hospital, the hospital may claim that his actions (especially if motivated by personal considerations) were a “lark of his own” and not in the course of his employment by the hospital.
Read about the clinical opportunity of informed consent
The clinical opportunity of informed consent
More than a technical legal doctrine, informed consent provides ObGyns an important opportunity for better communications with patients, and is a chance to create reasonable expectations and a more therapeutic relationship that involves the patient in care and decision making. It is likely that engaging the patient in good informed consent processes can set the stage for improved outcomes.
Interactive dialogue with the patient is one advised approach.10 This undertaking in part reflects that, as patients have more ready access to information in the digital age, they are positioned to play a more active role in health care decision making.
The benefits of informed consent are likely to be greatest if you view the process not as a technical legal requirement but as an excellent opportunity to engage the patient in her own care and treatment. Planning, intervention, and evaluation of care options as well as education regarding the medical problem at hand are integral to the informed consent process. And, of course, the right to consent is a “basic patient right” that in a sense guarantees that he/she has the right to make informed decisions regarding one’s care.6
Special considerations
Informed consent most often is associated with but not limited to surgical procedures (often performed with the use of surgical instruments and/or devices). It applies to diagnostic interventions as well as treatment. The more invasive or risky an intervention, the more important it is that the information is thorough.14,15
Pharmaceuticals have informed consent issues. The theory has been that pharmaceutical companies inform physicians of the risks and instructions for the use of pharmaceuticals and the physicians inform the patients. Indeed, traditionally pharmaceutical companies have gained immunity for “failure to warn” patients because the physicians were the “learned intermediaries” providing information to the public. Patient package inserts and pharmacists have taken over the informational role, but informed consent does apply to pharmaceuticals.
It is also worth noting that informed consent in any formal research study or the trial of new techniques, compounds, or devices requires a special process of approval by an institutional review board.
Set the stage for best outcomes
The main objective of informed consent is promoting the autonomy of your patient. That requires that she understand the risks, benefits, and alternatives associated with the procedure and the risks associated with a refusal of treatment. Done properly, this can result in your patient gaining confidence and trust in you as her provider.
Informed consent is a process that reflects our interactions with our patients. It is part of the broader commitment by the medical profession to “first do no harm.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Grady C. Enduring and emerging challenges of informed consent. N Engl J Med. 2015;372(22):855–862.
- Faden RR, Beauchamp TL. History and theory of informed consent. New York, New York: Oxford University Press; 1986.
- Paterick TJ, Carson G, Allen M, Paterick TE. Medical informed consent: general considerations for physicians. Mayo Clin Proc. 2008;83(3):313–319.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: Informed consent (reaffirmed 2015). Obstet Gynecol. 2009;114(2 pt 1):401–408.
- Jonsen A, Siegler M, Winslade W. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. New York, New York: McGraw Hill; 2010.
- Menendez J. Informed consent: essential legal and ethical principles for nurses. JONAS Healthc Law Ethics Regul. 2013;15(4):140–144.
- Abram MB, Ballantine HT, Dunlop GR, et al; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. Volume One: Report. https://repository.library.georgetown.edu/bitstream/handle/10822/559354/making_health_care_decisions.pdf?sequence=1. Published October 1982. Accessed January 9, 2017.
- Dhar H, Dhar D. Informed consent in clinical practice and literature overview. Arch Gynecol Obstet. 2012;286(3):649–651.
- NE Schloendorff v Society of New York Hospital, 211 NY 125, 106 NE 93 1914.
- Avery D. Summary of informed consent and refusal. Am J Clinical Med. 2009;6(3):28–29.
- Pallett A, Phippen N, Miller C, Barnett J. Informed consent for hysterectomy: Does a video presentation improve patient comprehension? [poster 17F]. Obstet Gynecol. 2016;127(suppl):55S.
- Cainzos M, Gonzalez-Vinagre S. Informed consent in surgery. World J Surg. 2014;38(7):1587–1593.
- Weaver J. A problem with informed consent. J Am Coll Surg. 2009;209(2):286–287.
- Bunch W. Informed consent. Clin Orthop Relat Res. 2000;378:71–77.
- Peltier LF. Orthopedics: a history and iconography (Norman Orthopedic, No. 3). San Francisco, California: Jeremy Norman Co; 1993.
CASE: Surgeon accused of performing tubal ligation without consent
A patient was scheduled for an elective cesarean delivery to be performed by her ObGyn (Dr. Surgeon) at the nearby medical center. The patient was asked to sign an electronic signature pad in her ObGyn’s office, which transposed her signature onto an electronic form that she could not see at the time. She signed it. The consent was not printed out in the office but was added to her electronic medical record, and a copy was sent to her via email. Among other things, the consent included, “[Name] hereby agrees that all appropriate medical and surgical procedures as determined by the physicians and others in this hospital are in my best interest. No further consent is required to any of the treatment in this hospital.”
In the hospital, Dr. Surgeon spoke preoper- atively with the patient about cesarean delivery, the various risks and benefits, and the possibility and risks of an alternative trial of labor. Dr. Surgeon noted the conversation in the patient’s chart.
A nurse brought a standard hard copy “Zee Hospital Surgical Consent Form” to the patient. In a relevant part it provided, “I hereby consent to the surgical procedure Dr. Surgeon has discussed with me: _______” (the blank was filled in with “cesarean delivery”). The form continued: “He/She has explained the risks and benefits. I also authorize Dr. Surgeon, and such assistants as he/she may select, to perform this procedure. In his/her medical judgment, if additional procedures are appropriate, I hereby consent to their performance, in addition to the procedures listed in this form.” The patient signed the form.
While Dr. Surgeon was scrubbing for the delivery, the patient’s husband (also a surgeon at the hospital; Dr. Husband), stopped by, thanked Dr. Surgeon, and said, “Oh, by the way, my wife would like you to do a tubal ligation as well—she really wants it for health reasons. Her chronic hypertension skyrocketed during this pregnancy, and we don’t want any more children.”
“She didn’t mention that a little earlier while I was talking with her,” replied Dr. Surgeon, “but I can see how it would have slipped her mind.”
Dr. Surgeon performed the cesarean delivery and tubal ligation. All went well, with a healthy baby and mother. Several months later, the patient and Dr. Husband separated and sought divorce.
The patient, surprised by the cost of the hospital bill (Dr. Surgeon did not bill for his surgical services as a professional courtesy), was astonished to see a charge related to tubal ligation. Knowing how common billing mistakes were at Zee Hospital, she called to have the bill corrected. The clerk informed her that her medical record showed that a tubal ligation had been performed and that the bill was correct.
The patient sued Dr. Surgeon, Zee Hospital, and her (now former) husband, Dr. Husband, both for the cesarean delivery and the tubal ligation. Her claims are primarily based on the lack of informed consent.
What’s the verdict?
The patient likely has a strong case regarding the tubal ligation claim, but a weak case related to the cesarean delivery claim.
Read the ethical, medical, and legal implications of this case
Ethical and medical considerations
Although this case seems too strange for fiction, the basic facts are taken from events that did occur at a major institution. The puzzling features of this case are meant to be a cautionary tale: it is easy in the rush with the pressure of clinical practice to view informed consent as a bothersome technical detail. Yet as the following discussion suggests, adhering closely to the tenets of informed consent protects not only the fundamental interests of the patient but also the physicians and medical institutions.
Informed consent serves as protective communication
Informed consent at its core is a “process of communication” that involves you as the health care provider and the patient. It provides authority for an activity based upon an understanding of what that activity entails.1,2 Aspects of informed consent, from the physician−patient perspective, include the following:
- disclosure
- comprehension
- voluntary choice
- authorization.
In one other sense, informed consent is based on a fiduciary relationship between the ObGyn and patient.3 Overall, the process consists of an educational communication by the physician to the patient. Ideally, providers perceive the process from an ethical point of view that has been formalized by cases and statutes.4
Informed consent protects one of the most basic values of medicine and society: autonomy. From the perspective of moral philosophers, the principle of autonomy establishes the moral right to choose and follow one’s own plan for life and action.5,6 For ObGyns, the patient’s autonomy and her ability to participate in the medical decision-making process is of paramount importance. Informed consent is also a reflection of trust inherent to the physician−patient relationship.4
Informed consent is too often viewed as a mere legal formality. In truth, it melds legal and ethical values and concerns. The President’s Commission reflected this, noting that informed consent is rooted in “the fundamental recognition that adults are entitled to accept or reject health care intervention(s) on the basis of their own personal values and in furtherance of their own personal goals.”7
The historic perspective of informed consent dates back to Egyptian, Greek, and Roman eras. Dhar and Dhar suggest that the concept of “physicians’ love for humanity—philantropia” dates back to Plato and is complemented by the term “philotechnia” (love of medicine), all of which have evolved into today’s use of the terms “risks, benefits, and alternatives.”8
We emphasize that informed consent is much more than a legal concept. It has strong clinical roots because it provides an opportunity for physicians to improve communication with their patients. Informed consent is not a form; it is a process to be taken seriously.
Legal principles of informed consent
The famous New York case of Mary Schloendorff v. Society of New York Hospital, in 1914, heralded a principle that remains central in American law. Justice Benjamin Cardozo, writing for the majority, held that, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages.”9 The surgeon in the Schloendorff case had undertaken a gynecologic procedure—removal of a fibroid tumor—without patient consent. (In that case the hospital rather than the physician was sued, but the principle clearly applied to the physician.)
Over the last century, the American law of informed consent has developed in a number of ways.10 Lack of informed consent is now almost always considered a form of negligence rather than an intentional tort of battery. The details of the legal requirements vary from state to state as a result of statutory changes and court decisions. But in one way or another, to be “informed,” consent generally must include 4 things:
- a description of the procedure or intervention that is proposed
- the risks and benefits of the proposal—the focus here is generally on the risks of the treatment
- alternatives, if there are any (eg, pharmacologic vs surgical treatment)
- the consequences of not undertaking the proposed treatment (eg, the refusal to have a Papanicolaou smear).
A fifth point might be added—the offer to answer any questions or provide additional information.
These 4 or 5 basic items and the expanded list are efforts to simply describe the information that a reasonable person would need in order to make a decision that represents the patient’s values, personality, and preferences. (Informed consent is in some ways an ongoing process—since a patient may withdraw his/her consent.)
Exceptions to the informed consent requirement
Before turning to the facts in the hypothetical case, it is worth noting that there are 2 common exceptions to the informed consent requirement. The first is an emergency exception. When someone requires immediate attention and the patient is not conscious or capable of consent (nor is a “next of kin” available), treatment may proceed.
The second is therapeutic exception. Its designation is narrow, and it is risky to rely on it except in extreme circumstances. But when the very process of informing the patient of all the risks of a proposed treatment would create significant additional risks for the patient, the consent process may be modified. For example, for an extremely suggestable patient, describing certain risks might, in a psychosomatic way, cause the risk to be realized. In such cases, the record must be clearly documented. It is generally best to discuss the matter with a family member or other surrogate decision maker.
Read what went wrong in this case
What went wrong with consent in this case?
Our case illustrates a number of problems that occur when informed consent is not properly completed.
The electronic signature on the broadly stated consent form the patient initially signed in the office was nearly useless. She did not know what she was signing, did not have any chance to read it before signing, and was provided no help with any of the information factors of informed consent.
The surgical consent form is among the most interesting elements of this case. The form itself was seriously flawed because it contained no real evidence that the patient received information about the risks and alternatives. If the form is all there was, it would be a problem. But the conversation that Dr. Surgeon documented with the patient seemed to provide the basic elements of informed consent, including discussion of risks and benefits.
Oral informed consent is recognized in most states. To his credit, Dr. Surgeon appropriately recorded the conversation in the record. The risk of oral informed consent not backed up by text signature is that, if a dispute arises about the consent, it is difficult to prove details of what was said. (There was, of course, no such dispute about the cesarean delivery as it turned out in this case.)
Technological add-ons to consent: Pros and cons
Video and computer software are increasingly becoming an integral part of the informed consent process, and may improve comprehension by patients.11 Electronic consent may be helpful in proving what the patient was told during the consent process. A difficulty can result from overreliance on the electronic aspect and forgetting the human part of the informed consent equation. The health care team often can be productive parts of the informed consent process, but the surgeon must take ultimate responsibility for the informed consent.12
Was there informed consent for the tubal ligation?
The major problem in this case, of course, was the tubal ligation. It does not take much of an understanding of the legal niceties of informed consent to know that there was no real consent to this procedure. Dr. Husband did not have authority to consent, and his comment to Dr. Surgeon did not qualify as consent.
The hospital consent form may appear to provide some legal protection (“In his medical judgment, if additional procedures are appropriate, I hereby consent to doing those….”). Such language was once common in informed consent forms, but it offered little real consent except for trivial incidental processes (removal of an appendix) or where there was a real medical necessity for doing an expanded procedure (removal of a previously unknown cancerous growth).
Thus, Dr. Surgeon performed the sterilization without consent and may well be liable for that part of the surgery even though it did not turn out badly in a medical sense. If not for the tubal ligation, the damages would probably have been trivial. The real loss here is not a medical injury; it is the loss of reproductive capacity.
Protecting reproductive capacity. Modern law has been especially sensitive to protecting decisions regarding reproductive capacity. Therefore, the absence of clear consent to permanent sterilization is legally problematic. Dr. Surgeon may claim that he reasonably believed that the husband could give surrogate consent and it was too late to check with the patient herself. This situation does not fit well with the emergency exception, and it appears from the facts that Dr. Surgeon acted without informed consent to the sterilization.
Was it negligence or battery?
Dr. Surgeon. The most likely basis for liability for Dr. Surgeon is negligence. There is some argument that the tort of battery is a possibility because there was no consent at all for the sterilization. The claim would be that it was not the “information” that was lacking; it was the consent itself. The fact that Dr. Surgeon did not charge for his services would not absolve him of liability.
Dr. Husband. The potential liability of Dr. Husband is complicated by questions of whether he was acting in the capacity of a physician (which would likely involve the question of whether his malpractice insurance would be available), the degree to which he was acting in good faith, and facts we do not have in this case. If Dr. Husband gave consent (and thereby “caused”) the sterilization knowing that his wife did not want to have it or because of animus toward her (they were about to be separated and divorced, after all), there is the possibility of liability. (In some states a form of interspousal liability might complicate some of these claims—but that is a topic for another day.) He essentially took action for the purpose of wrongly causing the sterilization—which may be a battery (an intentional offensive or harmful touching). The legal rules around battery allow punitive damages as well as compensatory damages. In addition, many malpractice insurance policies provide limited coverage for intentional torts. To complicate matters further, it is not clear that Dr. Husband’s actions were related to his practice of medicine in any event (although Dr. Surgeon might claim that Dr. Husband’s expressed concern about his wife’s hypertension was enough to create a malpractice issue if Dr. Surgeon did not perform the verbally requested tubal ligation).
If, as we have speculated, Dr. Husband’s actions were motivated by improper personal considerations at the expense of a patient, he may also face medical board complaints from the patient. It is plausible that a state law makes it a criminal offense to wrongfully (or fraudulently) consent to medical treatment, particularly if related to reproductive capacity.
The hospital may face liability on several grounds, depending in part on the relationships between the hospital, Dr. Surgeon, and Dr. Husband. If Dr. Surgeon is an employee or agent of the hospital, he would be liable for his negligence. Even if Dr. Surgeon is technically an independent contractor, the failure of the hospital to offer more oversight concerning the surgical procedures in its facilities could give rise to a claim of negligence.
As to Dr. Husband, many of the same considerations are present. In addition, even if he is an agent of the hospital, the hospital may claim that his actions (especially if motivated by personal considerations) were a “lark of his own” and not in the course of his employment by the hospital.
Read about the clinical opportunity of informed consent
The clinical opportunity of informed consent
More than a technical legal doctrine, informed consent provides ObGyns an important opportunity for better communications with patients, and is a chance to create reasonable expectations and a more therapeutic relationship that involves the patient in care and decision making. It is likely that engaging the patient in good informed consent processes can set the stage for improved outcomes.
Interactive dialogue with the patient is one advised approach.10 This undertaking in part reflects that, as patients have more ready access to information in the digital age, they are positioned to play a more active role in health care decision making.
The benefits of informed consent are likely to be greatest if you view the process not as a technical legal requirement but as an excellent opportunity to engage the patient in her own care and treatment. Planning, intervention, and evaluation of care options as well as education regarding the medical problem at hand are integral to the informed consent process. And, of course, the right to consent is a “basic patient right” that in a sense guarantees that he/she has the right to make informed decisions regarding one’s care.6
Special considerations
Informed consent most often is associated with but not limited to surgical procedures (often performed with the use of surgical instruments and/or devices). It applies to diagnostic interventions as well as treatment. The more invasive or risky an intervention, the more important it is that the information is thorough.14,15
Pharmaceuticals have informed consent issues. The theory has been that pharmaceutical companies inform physicians of the risks and instructions for the use of pharmaceuticals and the physicians inform the patients. Indeed, traditionally pharmaceutical companies have gained immunity for “failure to warn” patients because the physicians were the “learned intermediaries” providing information to the public. Patient package inserts and pharmacists have taken over the informational role, but informed consent does apply to pharmaceuticals.
It is also worth noting that informed consent in any formal research study or the trial of new techniques, compounds, or devices requires a special process of approval by an institutional review board.
Set the stage for best outcomes
The main objective of informed consent is promoting the autonomy of your patient. That requires that she understand the risks, benefits, and alternatives associated with the procedure and the risks associated with a refusal of treatment. Done properly, this can result in your patient gaining confidence and trust in you as her provider.
Informed consent is a process that reflects our interactions with our patients. It is part of the broader commitment by the medical profession to “first do no harm.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: Surgeon accused of performing tubal ligation without consent
A patient was scheduled for an elective cesarean delivery to be performed by her ObGyn (Dr. Surgeon) at the nearby medical center. The patient was asked to sign an electronic signature pad in her ObGyn’s office, which transposed her signature onto an electronic form that she could not see at the time. She signed it. The consent was not printed out in the office but was added to her electronic medical record, and a copy was sent to her via email. Among other things, the consent included, “[Name] hereby agrees that all appropriate medical and surgical procedures as determined by the physicians and others in this hospital are in my best interest. No further consent is required to any of the treatment in this hospital.”
In the hospital, Dr. Surgeon spoke preoper- atively with the patient about cesarean delivery, the various risks and benefits, and the possibility and risks of an alternative trial of labor. Dr. Surgeon noted the conversation in the patient’s chart.
A nurse brought a standard hard copy “Zee Hospital Surgical Consent Form” to the patient. In a relevant part it provided, “I hereby consent to the surgical procedure Dr. Surgeon has discussed with me: _______” (the blank was filled in with “cesarean delivery”). The form continued: “He/She has explained the risks and benefits. I also authorize Dr. Surgeon, and such assistants as he/she may select, to perform this procedure. In his/her medical judgment, if additional procedures are appropriate, I hereby consent to their performance, in addition to the procedures listed in this form.” The patient signed the form.
While Dr. Surgeon was scrubbing for the delivery, the patient’s husband (also a surgeon at the hospital; Dr. Husband), stopped by, thanked Dr. Surgeon, and said, “Oh, by the way, my wife would like you to do a tubal ligation as well—she really wants it for health reasons. Her chronic hypertension skyrocketed during this pregnancy, and we don’t want any more children.”
“She didn’t mention that a little earlier while I was talking with her,” replied Dr. Surgeon, “but I can see how it would have slipped her mind.”
Dr. Surgeon performed the cesarean delivery and tubal ligation. All went well, with a healthy baby and mother. Several months later, the patient and Dr. Husband separated and sought divorce.
The patient, surprised by the cost of the hospital bill (Dr. Surgeon did not bill for his surgical services as a professional courtesy), was astonished to see a charge related to tubal ligation. Knowing how common billing mistakes were at Zee Hospital, she called to have the bill corrected. The clerk informed her that her medical record showed that a tubal ligation had been performed and that the bill was correct.
The patient sued Dr. Surgeon, Zee Hospital, and her (now former) husband, Dr. Husband, both for the cesarean delivery and the tubal ligation. Her claims are primarily based on the lack of informed consent.
What’s the verdict?
The patient likely has a strong case regarding the tubal ligation claim, but a weak case related to the cesarean delivery claim.
Read the ethical, medical, and legal implications of this case
Ethical and medical considerations
Although this case seems too strange for fiction, the basic facts are taken from events that did occur at a major institution. The puzzling features of this case are meant to be a cautionary tale: it is easy in the rush with the pressure of clinical practice to view informed consent as a bothersome technical detail. Yet as the following discussion suggests, adhering closely to the tenets of informed consent protects not only the fundamental interests of the patient but also the physicians and medical institutions.
Informed consent serves as protective communication
Informed consent at its core is a “process of communication” that involves you as the health care provider and the patient. It provides authority for an activity based upon an understanding of what that activity entails.1,2 Aspects of informed consent, from the physician−patient perspective, include the following:
- disclosure
- comprehension
- voluntary choice
- authorization.
In one other sense, informed consent is based on a fiduciary relationship between the ObGyn and patient.3 Overall, the process consists of an educational communication by the physician to the patient. Ideally, providers perceive the process from an ethical point of view that has been formalized by cases and statutes.4
Informed consent protects one of the most basic values of medicine and society: autonomy. From the perspective of moral philosophers, the principle of autonomy establishes the moral right to choose and follow one’s own plan for life and action.5,6 For ObGyns, the patient’s autonomy and her ability to participate in the medical decision-making process is of paramount importance. Informed consent is also a reflection of trust inherent to the physician−patient relationship.4
Informed consent is too often viewed as a mere legal formality. In truth, it melds legal and ethical values and concerns. The President’s Commission reflected this, noting that informed consent is rooted in “the fundamental recognition that adults are entitled to accept or reject health care intervention(s) on the basis of their own personal values and in furtherance of their own personal goals.”7
The historic perspective of informed consent dates back to Egyptian, Greek, and Roman eras. Dhar and Dhar suggest that the concept of “physicians’ love for humanity—philantropia” dates back to Plato and is complemented by the term “philotechnia” (love of medicine), all of which have evolved into today’s use of the terms “risks, benefits, and alternatives.”8
We emphasize that informed consent is much more than a legal concept. It has strong clinical roots because it provides an opportunity for physicians to improve communication with their patients. Informed consent is not a form; it is a process to be taken seriously.
Legal principles of informed consent
The famous New York case of Mary Schloendorff v. Society of New York Hospital, in 1914, heralded a principle that remains central in American law. Justice Benjamin Cardozo, writing for the majority, held that, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages.”9 The surgeon in the Schloendorff case had undertaken a gynecologic procedure—removal of a fibroid tumor—without patient consent. (In that case the hospital rather than the physician was sued, but the principle clearly applied to the physician.)
Over the last century, the American law of informed consent has developed in a number of ways.10 Lack of informed consent is now almost always considered a form of negligence rather than an intentional tort of battery. The details of the legal requirements vary from state to state as a result of statutory changes and court decisions. But in one way or another, to be “informed,” consent generally must include 4 things:
- a description of the procedure or intervention that is proposed
- the risks and benefits of the proposal—the focus here is generally on the risks of the treatment
- alternatives, if there are any (eg, pharmacologic vs surgical treatment)
- the consequences of not undertaking the proposed treatment (eg, the refusal to have a Papanicolaou smear).
A fifth point might be added—the offer to answer any questions or provide additional information.
These 4 or 5 basic items and the expanded list are efforts to simply describe the information that a reasonable person would need in order to make a decision that represents the patient’s values, personality, and preferences. (Informed consent is in some ways an ongoing process—since a patient may withdraw his/her consent.)
Exceptions to the informed consent requirement
Before turning to the facts in the hypothetical case, it is worth noting that there are 2 common exceptions to the informed consent requirement. The first is an emergency exception. When someone requires immediate attention and the patient is not conscious or capable of consent (nor is a “next of kin” available), treatment may proceed.
The second is therapeutic exception. Its designation is narrow, and it is risky to rely on it except in extreme circumstances. But when the very process of informing the patient of all the risks of a proposed treatment would create significant additional risks for the patient, the consent process may be modified. For example, for an extremely suggestable patient, describing certain risks might, in a psychosomatic way, cause the risk to be realized. In such cases, the record must be clearly documented. It is generally best to discuss the matter with a family member or other surrogate decision maker.
Read what went wrong in this case
What went wrong with consent in this case?
Our case illustrates a number of problems that occur when informed consent is not properly completed.
The electronic signature on the broadly stated consent form the patient initially signed in the office was nearly useless. She did not know what she was signing, did not have any chance to read it before signing, and was provided no help with any of the information factors of informed consent.
The surgical consent form is among the most interesting elements of this case. The form itself was seriously flawed because it contained no real evidence that the patient received information about the risks and alternatives. If the form is all there was, it would be a problem. But the conversation that Dr. Surgeon documented with the patient seemed to provide the basic elements of informed consent, including discussion of risks and benefits.
Oral informed consent is recognized in most states. To his credit, Dr. Surgeon appropriately recorded the conversation in the record. The risk of oral informed consent not backed up by text signature is that, if a dispute arises about the consent, it is difficult to prove details of what was said. (There was, of course, no such dispute about the cesarean delivery as it turned out in this case.)
Technological add-ons to consent: Pros and cons
Video and computer software are increasingly becoming an integral part of the informed consent process, and may improve comprehension by patients.11 Electronic consent may be helpful in proving what the patient was told during the consent process. A difficulty can result from overreliance on the electronic aspect and forgetting the human part of the informed consent equation. The health care team often can be productive parts of the informed consent process, but the surgeon must take ultimate responsibility for the informed consent.12
Was there informed consent for the tubal ligation?
The major problem in this case, of course, was the tubal ligation. It does not take much of an understanding of the legal niceties of informed consent to know that there was no real consent to this procedure. Dr. Husband did not have authority to consent, and his comment to Dr. Surgeon did not qualify as consent.
The hospital consent form may appear to provide some legal protection (“In his medical judgment, if additional procedures are appropriate, I hereby consent to doing those….”). Such language was once common in informed consent forms, but it offered little real consent except for trivial incidental processes (removal of an appendix) or where there was a real medical necessity for doing an expanded procedure (removal of a previously unknown cancerous growth).
Thus, Dr. Surgeon performed the sterilization without consent and may well be liable for that part of the surgery even though it did not turn out badly in a medical sense. If not for the tubal ligation, the damages would probably have been trivial. The real loss here is not a medical injury; it is the loss of reproductive capacity.
Protecting reproductive capacity. Modern law has been especially sensitive to protecting decisions regarding reproductive capacity. Therefore, the absence of clear consent to permanent sterilization is legally problematic. Dr. Surgeon may claim that he reasonably believed that the husband could give surrogate consent and it was too late to check with the patient herself. This situation does not fit well with the emergency exception, and it appears from the facts that Dr. Surgeon acted without informed consent to the sterilization.
Was it negligence or battery?
Dr. Surgeon. The most likely basis for liability for Dr. Surgeon is negligence. There is some argument that the tort of battery is a possibility because there was no consent at all for the sterilization. The claim would be that it was not the “information” that was lacking; it was the consent itself. The fact that Dr. Surgeon did not charge for his services would not absolve him of liability.
Dr. Husband. The potential liability of Dr. Husband is complicated by questions of whether he was acting in the capacity of a physician (which would likely involve the question of whether his malpractice insurance would be available), the degree to which he was acting in good faith, and facts we do not have in this case. If Dr. Husband gave consent (and thereby “caused”) the sterilization knowing that his wife did not want to have it or because of animus toward her (they were about to be separated and divorced, after all), there is the possibility of liability. (In some states a form of interspousal liability might complicate some of these claims—but that is a topic for another day.) He essentially took action for the purpose of wrongly causing the sterilization—which may be a battery (an intentional offensive or harmful touching). The legal rules around battery allow punitive damages as well as compensatory damages. In addition, many malpractice insurance policies provide limited coverage for intentional torts. To complicate matters further, it is not clear that Dr. Husband’s actions were related to his practice of medicine in any event (although Dr. Surgeon might claim that Dr. Husband’s expressed concern about his wife’s hypertension was enough to create a malpractice issue if Dr. Surgeon did not perform the verbally requested tubal ligation).
If, as we have speculated, Dr. Husband’s actions were motivated by improper personal considerations at the expense of a patient, he may also face medical board complaints from the patient. It is plausible that a state law makes it a criminal offense to wrongfully (or fraudulently) consent to medical treatment, particularly if related to reproductive capacity.
The hospital may face liability on several grounds, depending in part on the relationships between the hospital, Dr. Surgeon, and Dr. Husband. If Dr. Surgeon is an employee or agent of the hospital, he would be liable for his negligence. Even if Dr. Surgeon is technically an independent contractor, the failure of the hospital to offer more oversight concerning the surgical procedures in its facilities could give rise to a claim of negligence.
As to Dr. Husband, many of the same considerations are present. In addition, even if he is an agent of the hospital, the hospital may claim that his actions (especially if motivated by personal considerations) were a “lark of his own” and not in the course of his employment by the hospital.
Read about the clinical opportunity of informed consent
The clinical opportunity of informed consent
More than a technical legal doctrine, informed consent provides ObGyns an important opportunity for better communications with patients, and is a chance to create reasonable expectations and a more therapeutic relationship that involves the patient in care and decision making. It is likely that engaging the patient in good informed consent processes can set the stage for improved outcomes.
Interactive dialogue with the patient is one advised approach.10 This undertaking in part reflects that, as patients have more ready access to information in the digital age, they are positioned to play a more active role in health care decision making.
The benefits of informed consent are likely to be greatest if you view the process not as a technical legal requirement but as an excellent opportunity to engage the patient in her own care and treatment. Planning, intervention, and evaluation of care options as well as education regarding the medical problem at hand are integral to the informed consent process. And, of course, the right to consent is a “basic patient right” that in a sense guarantees that he/she has the right to make informed decisions regarding one’s care.6
Special considerations
Informed consent most often is associated with but not limited to surgical procedures (often performed with the use of surgical instruments and/or devices). It applies to diagnostic interventions as well as treatment. The more invasive or risky an intervention, the more important it is that the information is thorough.14,15
Pharmaceuticals have informed consent issues. The theory has been that pharmaceutical companies inform physicians of the risks and instructions for the use of pharmaceuticals and the physicians inform the patients. Indeed, traditionally pharmaceutical companies have gained immunity for “failure to warn” patients because the physicians were the “learned intermediaries” providing information to the public. Patient package inserts and pharmacists have taken over the informational role, but informed consent does apply to pharmaceuticals.
It is also worth noting that informed consent in any formal research study or the trial of new techniques, compounds, or devices requires a special process of approval by an institutional review board.
Set the stage for best outcomes
The main objective of informed consent is promoting the autonomy of your patient. That requires that she understand the risks, benefits, and alternatives associated with the procedure and the risks associated with a refusal of treatment. Done properly, this can result in your patient gaining confidence and trust in you as her provider.
Informed consent is a process that reflects our interactions with our patients. It is part of the broader commitment by the medical profession to “first do no harm.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Grady C. Enduring and emerging challenges of informed consent. N Engl J Med. 2015;372(22):855–862.
- Faden RR, Beauchamp TL. History and theory of informed consent. New York, New York: Oxford University Press; 1986.
- Paterick TJ, Carson G, Allen M, Paterick TE. Medical informed consent: general considerations for physicians. Mayo Clin Proc. 2008;83(3):313–319.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: Informed consent (reaffirmed 2015). Obstet Gynecol. 2009;114(2 pt 1):401–408.
- Jonsen A, Siegler M, Winslade W. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. New York, New York: McGraw Hill; 2010.
- Menendez J. Informed consent: essential legal and ethical principles for nurses. JONAS Healthc Law Ethics Regul. 2013;15(4):140–144.
- Abram MB, Ballantine HT, Dunlop GR, et al; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. Volume One: Report. https://repository.library.georgetown.edu/bitstream/handle/10822/559354/making_health_care_decisions.pdf?sequence=1. Published October 1982. Accessed January 9, 2017.
- Dhar H, Dhar D. Informed consent in clinical practice and literature overview. Arch Gynecol Obstet. 2012;286(3):649–651.
- NE Schloendorff v Society of New York Hospital, 211 NY 125, 106 NE 93 1914.
- Avery D. Summary of informed consent and refusal. Am J Clinical Med. 2009;6(3):28–29.
- Pallett A, Phippen N, Miller C, Barnett J. Informed consent for hysterectomy: Does a video presentation improve patient comprehension? [poster 17F]. Obstet Gynecol. 2016;127(suppl):55S.
- Cainzos M, Gonzalez-Vinagre S. Informed consent in surgery. World J Surg. 2014;38(7):1587–1593.
- Weaver J. A problem with informed consent. J Am Coll Surg. 2009;209(2):286–287.
- Bunch W. Informed consent. Clin Orthop Relat Res. 2000;378:71–77.
- Peltier LF. Orthopedics: a history and iconography (Norman Orthopedic, No. 3). San Francisco, California: Jeremy Norman Co; 1993.
- Grady C. Enduring and emerging challenges of informed consent. N Engl J Med. 2015;372(22):855–862.
- Faden RR, Beauchamp TL. History and theory of informed consent. New York, New York: Oxford University Press; 1986.
- Paterick TJ, Carson G, Allen M, Paterick TE. Medical informed consent: general considerations for physicians. Mayo Clin Proc. 2008;83(3):313–319.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: Informed consent (reaffirmed 2015). Obstet Gynecol. 2009;114(2 pt 1):401–408.
- Jonsen A, Siegler M, Winslade W. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. New York, New York: McGraw Hill; 2010.
- Menendez J. Informed consent: essential legal and ethical principles for nurses. JONAS Healthc Law Ethics Regul. 2013;15(4):140–144.
- Abram MB, Ballantine HT, Dunlop GR, et al; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. Volume One: Report. https://repository.library.georgetown.edu/bitstream/handle/10822/559354/making_health_care_decisions.pdf?sequence=1. Published October 1982. Accessed January 9, 2017.
- Dhar H, Dhar D. Informed consent in clinical practice and literature overview. Arch Gynecol Obstet. 2012;286(3):649–651.
- NE Schloendorff v Society of New York Hospital, 211 NY 125, 106 NE 93 1914.
- Avery D. Summary of informed consent and refusal. Am J Clinical Med. 2009;6(3):28–29.
- Pallett A, Phippen N, Miller C, Barnett J. Informed consent for hysterectomy: Does a video presentation improve patient comprehension? [poster 17F]. Obstet Gynecol. 2016;127(suppl):55S.
- Cainzos M, Gonzalez-Vinagre S. Informed consent in surgery. World J Surg. 2014;38(7):1587–1593.
- Weaver J. A problem with informed consent. J Am Coll Surg. 2009;209(2):286–287.
- Bunch W. Informed consent. Clin Orthop Relat Res. 2000;378:71–77.
- Peltier LF. Orthopedics: a history and iconography (Norman Orthopedic, No. 3). San Francisco, California: Jeremy Norman Co; 1993.
Disrupted placenta: Infant anemia
Disrupted placenta: Infant anemia
An Obgyn recommended an elective transverse low incision cesarean delivery at a prenatal visit. Due to severe weather, the ObGyn was unable to come to the hospital; an on-call ObGyn consulted with the ObGyn by phone. Cesarean delivery resulted in disruption of the placenta. When the infant’s blood gasses test results were abnormal, he was transferred to the neonatal intensive care unit, where anemia was diagnosed. The infant was hospitalized for 31 days.
PARENTS’ CLAIM:
The on-call ObGyn caused the child’s injury by performing a transverse low incision. A testifying radiology expert said that ultrasonography (US) taken 5 weeks before delivery showed an anterior low-lying placenta but a clear field existed that would have allowed a vertical incision without placental disruption.
PHYSICIAN’S DEFENSE:
The delivery was within the standard of care. The ObGyn did not have access to the US cited by the testifying radiologist; standard of care did not require that she have access to them. A transverse incision minimizes blood loss; a vertical incision would have disrupted a larger area of placenta. The infant had normal blood gasses at delivery; any injury was not related to placental disruption.
VERDICT:
A Virginia defense verdict was returned.
Child has spastic CP after long labor
A 17-year-old woman's baby was delivered using vacuum extraction after a prolonged labor. Two days after birth, US results revealed diffuse brain edema in the baby. Magnetic resonance imaging demonstrated an absence of brain parenchyma in the left and right hemispheres. The baby received a diagnosis of spastic cerebral palsy (CP). She has little voluntary movement and requires a feeding tube, a portable aspiration device, and in-home attendant care.
PARENT’S CLAIM:
The baby underwent a hypoxic ischemic event during labor. Four hospital physicians
DEFENDANTS’ DEFENSE:
The fetus did not have a fetal heart rate pattern that would have required an earlier delivery. The injury sustained by the baby was not compatible with a prolonged hypoxic event and was more likely caused by a genetic defect. The infant suffered a subacute brain injury at least 1 week before delivery.
VERDICT:
The hospital settled for $1.25 million. A California defense verdict was returned for the physicians.
Misdiagnosed ectopic pregnancy
After a home pregnancy test was positive, a 27-year-old woman reported vaginal spotting and cramping to her ObGyn. When no uterine contents showed on US, the ObGyn suspected an ectopic pregnancy and recommended termination of pregnancy. The woman requested another US; an appointment was scheduled for the next day. Instead of waiting, the woman went to an emergency department (ED) that night. Bloodwork confirmed the pregnancy but US results showed no evidence of an intrauterine pregnancy. The ED physician diagnosed an ectopic pregnancy. The on-call ObGyn concurred and recommended termination of pregnancy by surgical intervention or methotrexate. The patient chose methotrexate, which was administered, and she was discharged.
In the on-call ObGyn’s office a week later, the patient’s beta-hGC levels had not decreased. US revealed 2 intrauterine pregnancies, one with a heartbeat. The on-call ObGyn immediately referred the patient to a maternal-fetal medicine specialist. New US results showed evidence of an abnormal intrauterine pregnancy and a second gestational sac with no embryo. Two days later US showed a twin pregnancy: a 6-week fetal pole with no heartbeat and the other with no fetal pole or yolk sac. A dilation and curettage was performed.
PARENTS’ CLAIM:
The on-call ObGyn misdiagnosed an ectopic pregnancy, failed to order additional testing, and failed to observe the patient for 48 to 72 hours before administering methotrexate. This led to the loss of twins.
DEFENDANTS’ DEFENSE:
An ectopic pregnancy is an emergency that requires prompt diagnosis and treatment. There were sufficient signs for the on-call ObGyn to diagnose an ectopic pregnancy. She would have violated the standard of care if she had not administered treatment.
VERDICT:
The hospital settled for $127,000 before trial. An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Disrupted placenta: Infant anemia
An Obgyn recommended an elective transverse low incision cesarean delivery at a prenatal visit. Due to severe weather, the ObGyn was unable to come to the hospital; an on-call ObGyn consulted with the ObGyn by phone. Cesarean delivery resulted in disruption of the placenta. When the infant’s blood gasses test results were abnormal, he was transferred to the neonatal intensive care unit, where anemia was diagnosed. The infant was hospitalized for 31 days.
PARENTS’ CLAIM:
The on-call ObGyn caused the child’s injury by performing a transverse low incision. A testifying radiology expert said that ultrasonography (US) taken 5 weeks before delivery showed an anterior low-lying placenta but a clear field existed that would have allowed a vertical incision without placental disruption.
PHYSICIAN’S DEFENSE:
The delivery was within the standard of care. The ObGyn did not have access to the US cited by the testifying radiologist; standard of care did not require that she have access to them. A transverse incision minimizes blood loss; a vertical incision would have disrupted a larger area of placenta. The infant had normal blood gasses at delivery; any injury was not related to placental disruption.
VERDICT:
A Virginia defense verdict was returned.
Child has spastic CP after long labor
A 17-year-old woman's baby was delivered using vacuum extraction after a prolonged labor. Two days after birth, US results revealed diffuse brain edema in the baby. Magnetic resonance imaging demonstrated an absence of brain parenchyma in the left and right hemispheres. The baby received a diagnosis of spastic cerebral palsy (CP). She has little voluntary movement and requires a feeding tube, a portable aspiration device, and in-home attendant care.
PARENT’S CLAIM:
The baby underwent a hypoxic ischemic event during labor. Four hospital physicians
DEFENDANTS’ DEFENSE:
The fetus did not have a fetal heart rate pattern that would have required an earlier delivery. The injury sustained by the baby was not compatible with a prolonged hypoxic event and was more likely caused by a genetic defect. The infant suffered a subacute brain injury at least 1 week before delivery.
VERDICT:
The hospital settled for $1.25 million. A California defense verdict was returned for the physicians.
Misdiagnosed ectopic pregnancy
After a home pregnancy test was positive, a 27-year-old woman reported vaginal spotting and cramping to her ObGyn. When no uterine contents showed on US, the ObGyn suspected an ectopic pregnancy and recommended termination of pregnancy. The woman requested another US; an appointment was scheduled for the next day. Instead of waiting, the woman went to an emergency department (ED) that night. Bloodwork confirmed the pregnancy but US results showed no evidence of an intrauterine pregnancy. The ED physician diagnosed an ectopic pregnancy. The on-call ObGyn concurred and recommended termination of pregnancy by surgical intervention or methotrexate. The patient chose methotrexate, which was administered, and she was discharged.
In the on-call ObGyn’s office a week later, the patient’s beta-hGC levels had not decreased. US revealed 2 intrauterine pregnancies, one with a heartbeat. The on-call ObGyn immediately referred the patient to a maternal-fetal medicine specialist. New US results showed evidence of an abnormal intrauterine pregnancy and a second gestational sac with no embryo. Two days later US showed a twin pregnancy: a 6-week fetal pole with no heartbeat and the other with no fetal pole or yolk sac. A dilation and curettage was performed.
PARENTS’ CLAIM:
The on-call ObGyn misdiagnosed an ectopic pregnancy, failed to order additional testing, and failed to observe the patient for 48 to 72 hours before administering methotrexate. This led to the loss of twins.
DEFENDANTS’ DEFENSE:
An ectopic pregnancy is an emergency that requires prompt diagnosis and treatment. There were sufficient signs for the on-call ObGyn to diagnose an ectopic pregnancy. She would have violated the standard of care if she had not administered treatment.
VERDICT:
The hospital settled for $127,000 before trial. An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Disrupted placenta: Infant anemia
An Obgyn recommended an elective transverse low incision cesarean delivery at a prenatal visit. Due to severe weather, the ObGyn was unable to come to the hospital; an on-call ObGyn consulted with the ObGyn by phone. Cesarean delivery resulted in disruption of the placenta. When the infant’s blood gasses test results were abnormal, he was transferred to the neonatal intensive care unit, where anemia was diagnosed. The infant was hospitalized for 31 days.
PARENTS’ CLAIM:
The on-call ObGyn caused the child’s injury by performing a transverse low incision. A testifying radiology expert said that ultrasonography (US) taken 5 weeks before delivery showed an anterior low-lying placenta but a clear field existed that would have allowed a vertical incision without placental disruption.
PHYSICIAN’S DEFENSE:
The delivery was within the standard of care. The ObGyn did not have access to the US cited by the testifying radiologist; standard of care did not require that she have access to them. A transverse incision minimizes blood loss; a vertical incision would have disrupted a larger area of placenta. The infant had normal blood gasses at delivery; any injury was not related to placental disruption.
VERDICT:
A Virginia defense verdict was returned.
Child has spastic CP after long labor
A 17-year-old woman's baby was delivered using vacuum extraction after a prolonged labor. Two days after birth, US results revealed diffuse brain edema in the baby. Magnetic resonance imaging demonstrated an absence of brain parenchyma in the left and right hemispheres. The baby received a diagnosis of spastic cerebral palsy (CP). She has little voluntary movement and requires a feeding tube, a portable aspiration device, and in-home attendant care.
PARENT’S CLAIM:
The baby underwent a hypoxic ischemic event during labor. Four hospital physicians
DEFENDANTS’ DEFENSE:
The fetus did not have a fetal heart rate pattern that would have required an earlier delivery. The injury sustained by the baby was not compatible with a prolonged hypoxic event and was more likely caused by a genetic defect. The infant suffered a subacute brain injury at least 1 week before delivery.
VERDICT:
The hospital settled for $1.25 million. A California defense verdict was returned for the physicians.
Misdiagnosed ectopic pregnancy
After a home pregnancy test was positive, a 27-year-old woman reported vaginal spotting and cramping to her ObGyn. When no uterine contents showed on US, the ObGyn suspected an ectopic pregnancy and recommended termination of pregnancy. The woman requested another US; an appointment was scheduled for the next day. Instead of waiting, the woman went to an emergency department (ED) that night. Bloodwork confirmed the pregnancy but US results showed no evidence of an intrauterine pregnancy. The ED physician diagnosed an ectopic pregnancy. The on-call ObGyn concurred and recommended termination of pregnancy by surgical intervention or methotrexate. The patient chose methotrexate, which was administered, and she was discharged.
In the on-call ObGyn’s office a week later, the patient’s beta-hGC levels had not decreased. US revealed 2 intrauterine pregnancies, one with a heartbeat. The on-call ObGyn immediately referred the patient to a maternal-fetal medicine specialist. New US results showed evidence of an abnormal intrauterine pregnancy and a second gestational sac with no embryo. Two days later US showed a twin pregnancy: a 6-week fetal pole with no heartbeat and the other with no fetal pole or yolk sac. A dilation and curettage was performed.
PARENTS’ CLAIM:
The on-call ObGyn misdiagnosed an ectopic pregnancy, failed to order additional testing, and failed to observe the patient for 48 to 72 hours before administering methotrexate. This led to the loss of twins.
DEFENDANTS’ DEFENSE:
An ectopic pregnancy is an emergency that requires prompt diagnosis and treatment. There were sufficient signs for the on-call ObGyn to diagnose an ectopic pregnancy. She would have violated the standard of care if she had not administered treatment.
VERDICT:
The hospital settled for $127,000 before trial. An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Did mother’s allergic reaction cause fetal injury?
Did mother’s allergic reaction cause fetal injury?
When a mother was admitted to the labor and delivery unit, she had strep throat; ampicillin was administered. She experienced anaphylactic symptoms that were attended to. The baby, delivered vaginally 3 hours later, was severely distressed and showed signs of asphyxia. He was found to have a permanent brain injury.
PARENTS’ CLAIM:
The ObGyn and hospital nurses failed to properly manage the mother’s anaphylactic reaction to ampicillin. Fetal heart-rate tracings indicated fetal distress. Standard of care required prompt intervention with epinephrine and/or emergency cesarean delivery. Brain injury occurred because these procedures were not performed.
DEFENDANTS’ DEFENSE:
The nurses denied fault and explained that they appropriately and immediately responded to mild anaphylactic symptoms in the mother. They could not administer epinephrine because the ObGyn did not order it.
The ObGyn denied violating the standard of care that included minimizing the mother’s allergic reaction. Because the mother didn’t have a rash, it was not necessary to order epinephrine. The baby sustained an unknown injury earlier in the pregnancy that was unrelated to labor.
VERDICT:
A Tennessee defense verdict was returned.
Resident blamed for shoulder dystocia
A mother presented to a federally funded health center in labor. A first-year resident managed labor and delivery under the supervision of the attending physician. Shoulder dystocia was encountered and the baby suffered a permanent brachial plexus injury.
PARENTS’ CLAIM:
Negligence occurred when the resident used excessive force by pulling on the infant’s neck during delivery. The resident, who had just received his medical license, was poorly supervised by the attending physician.
DEFENDANTS’ DEFENSE:
Suit was brought against the resident, the attending physician, the federal government, and the hospital’s residency program. The resident denied using excessive force. As soon as delivery became complex, the attending physician completed the delivery. The baby’s injuries were unpredictable and unavoidable.
VERDICT:
A $290,000 settlement with the federal government was reached before trial. A Pennsylvania defense verdict was returned for the other parties.
Related Article:
Tackle the challenging shoulder dystocia emergency by practicing delivery of the posterior arm
What caused brachial plexus injury?
An experienced midwife delivered a baby who sustained a brachial plexus injury resulting in flail arm syndrome.
PARENTS’ CLAIM:
The midwife mismanaged the delivery causing permanent injury. The child has gained little improvement with surgery and physical therapy.
DEFENDANTS’ DEFENSE:
The injury was caused by the natural forces of labor. The midwife used appropriate techniques during the birth.
VERDICT:
A Washington defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Did mother’s allergic reaction cause fetal injury?
When a mother was admitted to the labor and delivery unit, she had strep throat; ampicillin was administered. She experienced anaphylactic symptoms that were attended to. The baby, delivered vaginally 3 hours later, was severely distressed and showed signs of asphyxia. He was found to have a permanent brain injury.
PARENTS’ CLAIM:
The ObGyn and hospital nurses failed to properly manage the mother’s anaphylactic reaction to ampicillin. Fetal heart-rate tracings indicated fetal distress. Standard of care required prompt intervention with epinephrine and/or emergency cesarean delivery. Brain injury occurred because these procedures were not performed.
DEFENDANTS’ DEFENSE:
The nurses denied fault and explained that they appropriately and immediately responded to mild anaphylactic symptoms in the mother. They could not administer epinephrine because the ObGyn did not order it.
The ObGyn denied violating the standard of care that included minimizing the mother’s allergic reaction. Because the mother didn’t have a rash, it was not necessary to order epinephrine. The baby sustained an unknown injury earlier in the pregnancy that was unrelated to labor.
VERDICT:
A Tennessee defense verdict was returned.
Resident blamed for shoulder dystocia
A mother presented to a federally funded health center in labor. A first-year resident managed labor and delivery under the supervision of the attending physician. Shoulder dystocia was encountered and the baby suffered a permanent brachial plexus injury.
PARENTS’ CLAIM:
Negligence occurred when the resident used excessive force by pulling on the infant’s neck during delivery. The resident, who had just received his medical license, was poorly supervised by the attending physician.
DEFENDANTS’ DEFENSE:
Suit was brought against the resident, the attending physician, the federal government, and the hospital’s residency program. The resident denied using excessive force. As soon as delivery became complex, the attending physician completed the delivery. The baby’s injuries were unpredictable and unavoidable.
VERDICT:
A $290,000 settlement with the federal government was reached before trial. A Pennsylvania defense verdict was returned for the other parties.
Related Article:
Tackle the challenging shoulder dystocia emergency by practicing delivery of the posterior arm
What caused brachial plexus injury?
An experienced midwife delivered a baby who sustained a brachial plexus injury resulting in flail arm syndrome.
PARENTS’ CLAIM:
The midwife mismanaged the delivery causing permanent injury. The child has gained little improvement with surgery and physical therapy.
DEFENDANTS’ DEFENSE:
The injury was caused by the natural forces of labor. The midwife used appropriate techniques during the birth.
VERDICT:
A Washington defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Did mother’s allergic reaction cause fetal injury?
When a mother was admitted to the labor and delivery unit, she had strep throat; ampicillin was administered. She experienced anaphylactic symptoms that were attended to. The baby, delivered vaginally 3 hours later, was severely distressed and showed signs of asphyxia. He was found to have a permanent brain injury.
PARENTS’ CLAIM:
The ObGyn and hospital nurses failed to properly manage the mother’s anaphylactic reaction to ampicillin. Fetal heart-rate tracings indicated fetal distress. Standard of care required prompt intervention with epinephrine and/or emergency cesarean delivery. Brain injury occurred because these procedures were not performed.
DEFENDANTS’ DEFENSE:
The nurses denied fault and explained that they appropriately and immediately responded to mild anaphylactic symptoms in the mother. They could not administer epinephrine because the ObGyn did not order it.
The ObGyn denied violating the standard of care that included minimizing the mother’s allergic reaction. Because the mother didn’t have a rash, it was not necessary to order epinephrine. The baby sustained an unknown injury earlier in the pregnancy that was unrelated to labor.
VERDICT:
A Tennessee defense verdict was returned.
Resident blamed for shoulder dystocia
A mother presented to a federally funded health center in labor. A first-year resident managed labor and delivery under the supervision of the attending physician. Shoulder dystocia was encountered and the baby suffered a permanent brachial plexus injury.
PARENTS’ CLAIM:
Negligence occurred when the resident used excessive force by pulling on the infant’s neck during delivery. The resident, who had just received his medical license, was poorly supervised by the attending physician.
DEFENDANTS’ DEFENSE:
Suit was brought against the resident, the attending physician, the federal government, and the hospital’s residency program. The resident denied using excessive force. As soon as delivery became complex, the attending physician completed the delivery. The baby’s injuries were unpredictable and unavoidable.
VERDICT:
A $290,000 settlement with the federal government was reached before trial. A Pennsylvania defense verdict was returned for the other parties.
Related Article:
Tackle the challenging shoulder dystocia emergency by practicing delivery of the posterior arm
What caused brachial plexus injury?
An experienced midwife delivered a baby who sustained a brachial plexus injury resulting in flail arm syndrome.
PARENTS’ CLAIM:
The midwife mismanaged the delivery causing permanent injury. The child has gained little improvement with surgery and physical therapy.
DEFENDANTS’ DEFENSE:
The injury was caused by the natural forces of labor. The midwife used appropriate techniques during the birth.
VERDICT:
A Washington defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Removal of wrong ovary?
Removal of wrong ovary?
Several years earlier, a patient had undergone a hysterectomy but retained her ovaries and fallopian tubes. She reported recurrent pelvic pain, especially on the left side, to a gynecologic surgeon. Ultrasonography (US) results showed a small follicular cyst on the right ovary and a simple cyst on the left ovary. The patient consented to diagnostic laparoscopy with possible left salpingo-oophorectomy. During the procedure, the surgeon removed the right fallopian tube and ovary. After recovery, the patient continued to have left-sided pelvic pain. When she saw another surgeon a year later, US results showed that the left ovary and tube were still intact. The patient underwent left salpingo-oophorectomy.
PATIENT’S CLAIM:
The surgeon removed the wrong ovary and tube, a breach of the standard of care, and didn’t adequately explain his surgical actions.
DEFENDANTS’ DEFENSE:
Standard of care was maintained. During surgery, the surgeon encountered severe adhesions on the patient’s left side and was unable to visualize her left ovary. He decided that what had appeared to be an ovary on US most likely was a fluid collection, and that the patient’s left ovary must have been removed at hysterectomy. The surgeon concluded that the hemorrhagic cyst on the right ovary and adhesions were causing the patient’s pain, and removed them. The patient had given him permission to perform laparoscopic surgery, but he did not have her consent to convert to laparotomy, which would have been necessary to confirm the absence of her left ovary.
VERDICT:
An Alabama defense verdict was returned.
Related Article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Was wrong hysterectomy procedure chosen?
After being treated by her ObGyn for postmenopausal bleeding with medication and dilation and curettage, a 50-year-old woman underwent total abdominal hysterectomy (TAH). At an office visit 3 weeks postsurgery, she reported uncontrollable urination. The patient was admitted to a hospital, where cystogram results showed a vesico-vaginal fistula (VVF). She was treated with catheter drainage and referred to a urologist. The patient underwent 2 unsuccessful repair operations. A third repair, performed 10 months after the TAH, was successful.
PATIENT’S CLAIM:
The ObGyn should have performed laparoscopic supracervical hysterectomy (LSH) instead of TAH because the patient’s cervix would have remained intact and VVF would not have developed. Medical bills totaled $194,000.
PHYSICIAN’S DEFENSE:
The standard of care did not require LSH. Had the ObGyn left the cervix intact, the patient could have continued bleeding with increased risk of cervical cancer. A bladder injury is a known complication of hysterectomy.
VERDICT:
A Mississippi defense verdict was returned.
Woman dies after uterine fibroid removal
A 39-year-old woman with a history of hypertension, diabetes, moderate obesity, and end-stage renal disease underwent myomectomy. A first-year resident assisted the attending anesthesiologist during the procedure. While the patient was under general anesthesia, her blood pressure (BP) dropped rapidly and remained at an abnormally low level for 45 minutes. Then the patient’s heart rate dropped to around 30 bpm and remained at that level for 15 minutes before her BP and heart rate were finally restored. The patient never regained consciousness and remained in an irreversible coma until she died 6 days later.
ESTATE’S CLAIM:
The anesthesiologist and resident negligently allowed the patient’s BP and heart rate to fall to dangerously low levels. Because the patient had hypertension, diabetes, and obesity, she required a higher BP to maintain adequate cerebral perfusion. The physicians precipitated the patient’s hypotension by giving her an excessive dose of morphine and bupivacaine via epidural catheter prior to induction of general anesthesia, and then failed to give her sufficient doses of vasopressors to increase her BP to safe levels. They failed to properly treat the condition in a timely manner, causing brain damage, and ultimately, death.
DEFENDANTS’ DEFENSE:
The case was settled during mediation.
VERDICT:
A $900,000 Massachusetts settlement was reached.
Related Article:
Total abdominal hysterectomy the Mayo Clinic way
Ureter injured during hysterectomy
A 47-year-old woman’s right ureter was damaged during laparoscopic hysterectomy. During surgery, the gynecologist called in a urologist to repair the injury. The patient reported postsurgical complications including renal function impairment. A computed tomography scan showed a right ureter obstruction. When surgery confirmed complete obstruction of the ureter, she had a temporary nephrostomy drain placed. After 4 weeks, the patient returned to the operating room to have the right ureter implanted into the bladder. The patient reported occasional painful urination with increased urinary frequency and decreased right kidney size.
PATIENT’S CLAIM:
The gynecologist lacerated the ureter because he did not adequately identify and protect the ureter; this error represented a departure from the standard of care. The urologist failed to properly repair the injury. The patient sought recovery of $990,000 for past and future pain and suffering.
DEFENDANTS’ CLAIM:
The suit against the urologist and hospital was dropped, but continued against the gynecologist. The gynecologist claimed that the patient’s injury was a thermal burn, and is a known complication of the procedure.
VERDICT:
A $500,000 New York verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Removal of wrong ovary?
Several years earlier, a patient had undergone a hysterectomy but retained her ovaries and fallopian tubes. She reported recurrent pelvic pain, especially on the left side, to a gynecologic surgeon. Ultrasonography (US) results showed a small follicular cyst on the right ovary and a simple cyst on the left ovary. The patient consented to diagnostic laparoscopy with possible left salpingo-oophorectomy. During the procedure, the surgeon removed the right fallopian tube and ovary. After recovery, the patient continued to have left-sided pelvic pain. When she saw another surgeon a year later, US results showed that the left ovary and tube were still intact. The patient underwent left salpingo-oophorectomy.
PATIENT’S CLAIM:
The surgeon removed the wrong ovary and tube, a breach of the standard of care, and didn’t adequately explain his surgical actions.
DEFENDANTS’ DEFENSE:
Standard of care was maintained. During surgery, the surgeon encountered severe adhesions on the patient’s left side and was unable to visualize her left ovary. He decided that what had appeared to be an ovary on US most likely was a fluid collection, and that the patient’s left ovary must have been removed at hysterectomy. The surgeon concluded that the hemorrhagic cyst on the right ovary and adhesions were causing the patient’s pain, and removed them. The patient had given him permission to perform laparoscopic surgery, but he did not have her consent to convert to laparotomy, which would have been necessary to confirm the absence of her left ovary.
VERDICT:
An Alabama defense verdict was returned.
Related Article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Was wrong hysterectomy procedure chosen?
After being treated by her ObGyn for postmenopausal bleeding with medication and dilation and curettage, a 50-year-old woman underwent total abdominal hysterectomy (TAH). At an office visit 3 weeks postsurgery, she reported uncontrollable urination. The patient was admitted to a hospital, where cystogram results showed a vesico-vaginal fistula (VVF). She was treated with catheter drainage and referred to a urologist. The patient underwent 2 unsuccessful repair operations. A third repair, performed 10 months after the TAH, was successful.
PATIENT’S CLAIM:
The ObGyn should have performed laparoscopic supracervical hysterectomy (LSH) instead of TAH because the patient’s cervix would have remained intact and VVF would not have developed. Medical bills totaled $194,000.
PHYSICIAN’S DEFENSE:
The standard of care did not require LSH. Had the ObGyn left the cervix intact, the patient could have continued bleeding with increased risk of cervical cancer. A bladder injury is a known complication of hysterectomy.
VERDICT:
A Mississippi defense verdict was returned.
Woman dies after uterine fibroid removal
A 39-year-old woman with a history of hypertension, diabetes, moderate obesity, and end-stage renal disease underwent myomectomy. A first-year resident assisted the attending anesthesiologist during the procedure. While the patient was under general anesthesia, her blood pressure (BP) dropped rapidly and remained at an abnormally low level for 45 minutes. Then the patient’s heart rate dropped to around 30 bpm and remained at that level for 15 minutes before her BP and heart rate were finally restored. The patient never regained consciousness and remained in an irreversible coma until she died 6 days later.
ESTATE’S CLAIM:
The anesthesiologist and resident negligently allowed the patient’s BP and heart rate to fall to dangerously low levels. Because the patient had hypertension, diabetes, and obesity, she required a higher BP to maintain adequate cerebral perfusion. The physicians precipitated the patient’s hypotension by giving her an excessive dose of morphine and bupivacaine via epidural catheter prior to induction of general anesthesia, and then failed to give her sufficient doses of vasopressors to increase her BP to safe levels. They failed to properly treat the condition in a timely manner, causing brain damage, and ultimately, death.
DEFENDANTS’ DEFENSE:
The case was settled during mediation.
VERDICT:
A $900,000 Massachusetts settlement was reached.
Related Article:
Total abdominal hysterectomy the Mayo Clinic way
Ureter injured during hysterectomy
A 47-year-old woman’s right ureter was damaged during laparoscopic hysterectomy. During surgery, the gynecologist called in a urologist to repair the injury. The patient reported postsurgical complications including renal function impairment. A computed tomography scan showed a right ureter obstruction. When surgery confirmed complete obstruction of the ureter, she had a temporary nephrostomy drain placed. After 4 weeks, the patient returned to the operating room to have the right ureter implanted into the bladder. The patient reported occasional painful urination with increased urinary frequency and decreased right kidney size.
PATIENT’S CLAIM:
The gynecologist lacerated the ureter because he did not adequately identify and protect the ureter; this error represented a departure from the standard of care. The urologist failed to properly repair the injury. The patient sought recovery of $990,000 for past and future pain and suffering.
DEFENDANTS’ CLAIM:
The suit against the urologist and hospital was dropped, but continued against the gynecologist. The gynecologist claimed that the patient’s injury was a thermal burn, and is a known complication of the procedure.
VERDICT:
A $500,000 New York verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Removal of wrong ovary?
Several years earlier, a patient had undergone a hysterectomy but retained her ovaries and fallopian tubes. She reported recurrent pelvic pain, especially on the left side, to a gynecologic surgeon. Ultrasonography (US) results showed a small follicular cyst on the right ovary and a simple cyst on the left ovary. The patient consented to diagnostic laparoscopy with possible left salpingo-oophorectomy. During the procedure, the surgeon removed the right fallopian tube and ovary. After recovery, the patient continued to have left-sided pelvic pain. When she saw another surgeon a year later, US results showed that the left ovary and tube were still intact. The patient underwent left salpingo-oophorectomy.
PATIENT’S CLAIM:
The surgeon removed the wrong ovary and tube, a breach of the standard of care, and didn’t adequately explain his surgical actions.
DEFENDANTS’ DEFENSE:
Standard of care was maintained. During surgery, the surgeon encountered severe adhesions on the patient’s left side and was unable to visualize her left ovary. He decided that what had appeared to be an ovary on US most likely was a fluid collection, and that the patient’s left ovary must have been removed at hysterectomy. The surgeon concluded that the hemorrhagic cyst on the right ovary and adhesions were causing the patient’s pain, and removed them. The patient had given him permission to perform laparoscopic surgery, but he did not have her consent to convert to laparotomy, which would have been necessary to confirm the absence of her left ovary.
VERDICT:
An Alabama defense verdict was returned.
Related Article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Was wrong hysterectomy procedure chosen?
After being treated by her ObGyn for postmenopausal bleeding with medication and dilation and curettage, a 50-year-old woman underwent total abdominal hysterectomy (TAH). At an office visit 3 weeks postsurgery, she reported uncontrollable urination. The patient was admitted to a hospital, where cystogram results showed a vesico-vaginal fistula (VVF). She was treated with catheter drainage and referred to a urologist. The patient underwent 2 unsuccessful repair operations. A third repair, performed 10 months after the TAH, was successful.
PATIENT’S CLAIM:
The ObGyn should have performed laparoscopic supracervical hysterectomy (LSH) instead of TAH because the patient’s cervix would have remained intact and VVF would not have developed. Medical bills totaled $194,000.
PHYSICIAN’S DEFENSE:
The standard of care did not require LSH. Had the ObGyn left the cervix intact, the patient could have continued bleeding with increased risk of cervical cancer. A bladder injury is a known complication of hysterectomy.
VERDICT:
A Mississippi defense verdict was returned.
Woman dies after uterine fibroid removal
A 39-year-old woman with a history of hypertension, diabetes, moderate obesity, and end-stage renal disease underwent myomectomy. A first-year resident assisted the attending anesthesiologist during the procedure. While the patient was under general anesthesia, her blood pressure (BP) dropped rapidly and remained at an abnormally low level for 45 minutes. Then the patient’s heart rate dropped to around 30 bpm and remained at that level for 15 minutes before her BP and heart rate were finally restored. The patient never regained consciousness and remained in an irreversible coma until she died 6 days later.
ESTATE’S CLAIM:
The anesthesiologist and resident negligently allowed the patient’s BP and heart rate to fall to dangerously low levels. Because the patient had hypertension, diabetes, and obesity, she required a higher BP to maintain adequate cerebral perfusion. The physicians precipitated the patient’s hypotension by giving her an excessive dose of morphine and bupivacaine via epidural catheter prior to induction of general anesthesia, and then failed to give her sufficient doses of vasopressors to increase her BP to safe levels. They failed to properly treat the condition in a timely manner, causing brain damage, and ultimately, death.
DEFENDANTS’ DEFENSE:
The case was settled during mediation.
VERDICT:
A $900,000 Massachusetts settlement was reached.
Related Article:
Total abdominal hysterectomy the Mayo Clinic way
Ureter injured during hysterectomy
A 47-year-old woman’s right ureter was damaged during laparoscopic hysterectomy. During surgery, the gynecologist called in a urologist to repair the injury. The patient reported postsurgical complications including renal function impairment. A computed tomography scan showed a right ureter obstruction. When surgery confirmed complete obstruction of the ureter, she had a temporary nephrostomy drain placed. After 4 weeks, the patient returned to the operating room to have the right ureter implanted into the bladder. The patient reported occasional painful urination with increased urinary frequency and decreased right kidney size.
PATIENT’S CLAIM:
The gynecologist lacerated the ureter because he did not adequately identify and protect the ureter; this error represented a departure from the standard of care. The urologist failed to properly repair the injury. The patient sought recovery of $990,000 for past and future pain and suffering.
DEFENDANTS’ CLAIM:
The suit against the urologist and hospital was dropped, but continued against the gynecologist. The gynecologist claimed that the patient’s injury was a thermal burn, and is a known complication of the procedure.
VERDICT:
A $500,000 New York verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Sample Professional Contract
See the PDF below.
See the PDF below.
See the PDF below.
Negotiating The Professional Contract
For the freshly minted NP or PA, finding the right place to practice and negotiating a reasonable professional contract can be a challenge. The keys to successful negotiation are similar to those for attaining proficiency in your clinical practice—providing insight into your personality, an evaluation of your personal and professional goals, and a commitment of time for preparation. For most NPs and PAs, employment opportunities do not just happen. Preparation, persistence, and personal contacts are basic requirements for finding the right position.
Of great interest to NPs and PAs—especially those with looming loan payments—is the compensation package. There are many important questions and topics to discuss regarding compensation (see Table 1). However, salaries are often determined by the “going rate” for particular services in your geographic region, in addition to your specialty, experience, and credentials. Your professional association (AAPA for PAs, AANP for NPs) has robust data on salaries in your particular specialty, practice setting, and geographic region; the average salary for both professions is currently about $97,000.1,2
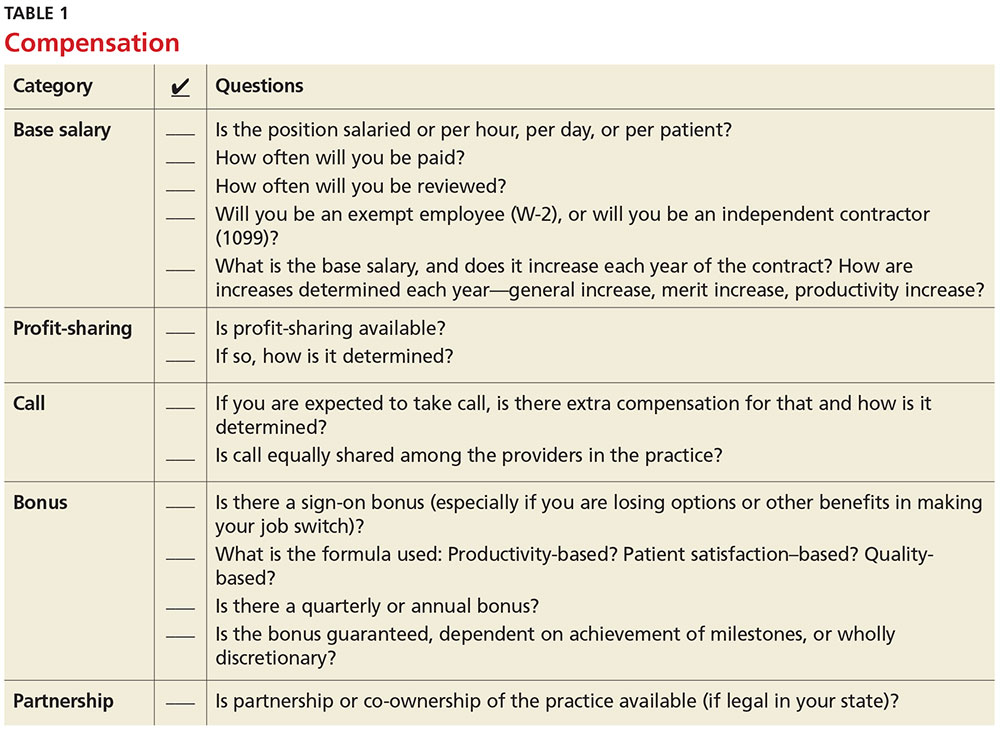
Familiarize yourself with the statutes and regulations that govern the scope of practice in your state—this is especially important if there are specific supervision or collaboration rules. Be prepared to present applicable statutes, rules, and regulations to the physician and/or office manager. Know whether any reimbursement restrictions exist. Be sure to review IRS guidelines for employee status versus independent contractor status.
The diversity of NP and PA practices means one size does not fit all, so it is best to identify the practice that complements your own personality. So, before you open negotiations, it is important that you research the practice. (For suggestions on what to inquire about, see Table 2). It is also a good idea to check the Docinfo website (http://docinfo.org/#/search/query), sponsored by the Federation of State Medical Boards, to research disciplinary records of the physician(s). Additional information can be acquired at each state regulatory board site.
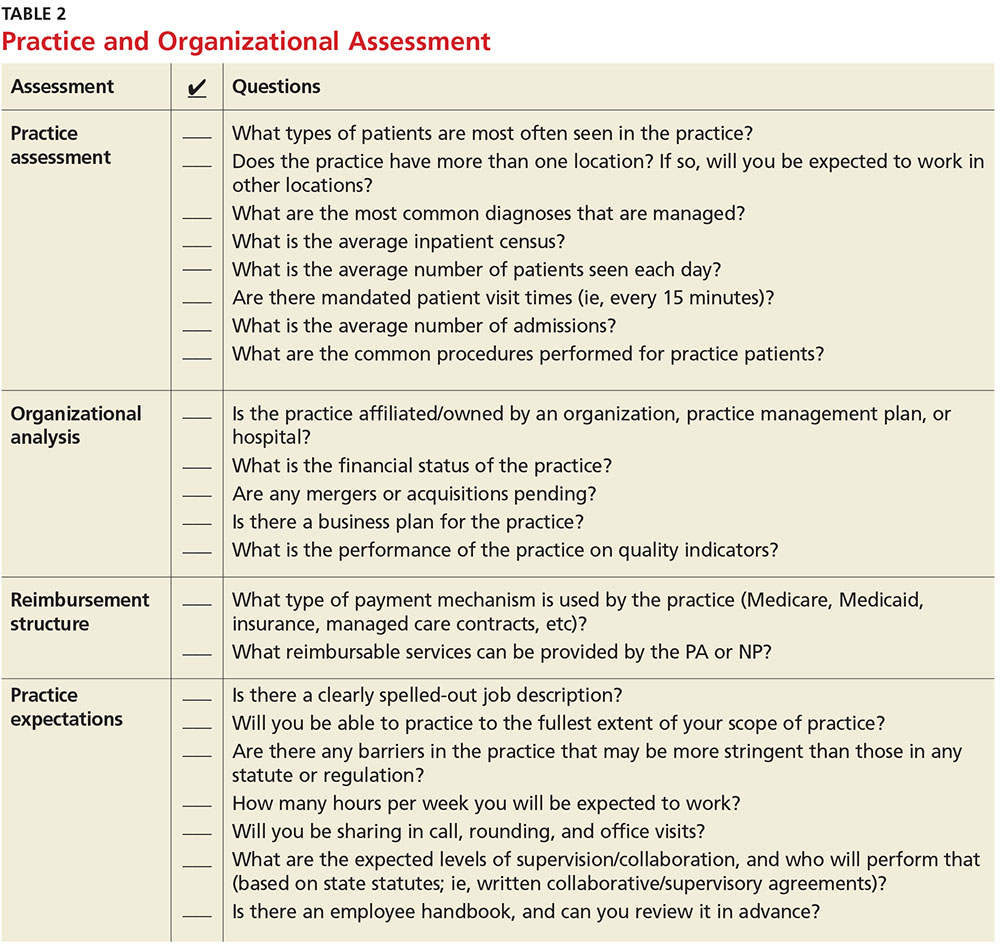
NEGOTIATION
When you’ve decided which employment offer to pursue, it’s time to think about how you want to negotiate your contract. Many people feel that negotiation is equivalent to confrontation, inevitably leading to an awkward disagreement with the practice. This is rarely the case; negotiation is simply a professional conversation, best had one-on-one with the key decision maker, rather than a group.
Never assume that your compensation package is predetermined. Whether you are starting a new job or looking to enhance your current situation, you can make a difference by asking for what you need.3 Knowing the local market and data is essential. Research the average salary in the region (for experienced versus new NP or PA). Be sure to think beyond salary and evaluate which benefits you’d like to have as part of your compensation package (see Table 3, as well as our survey results).
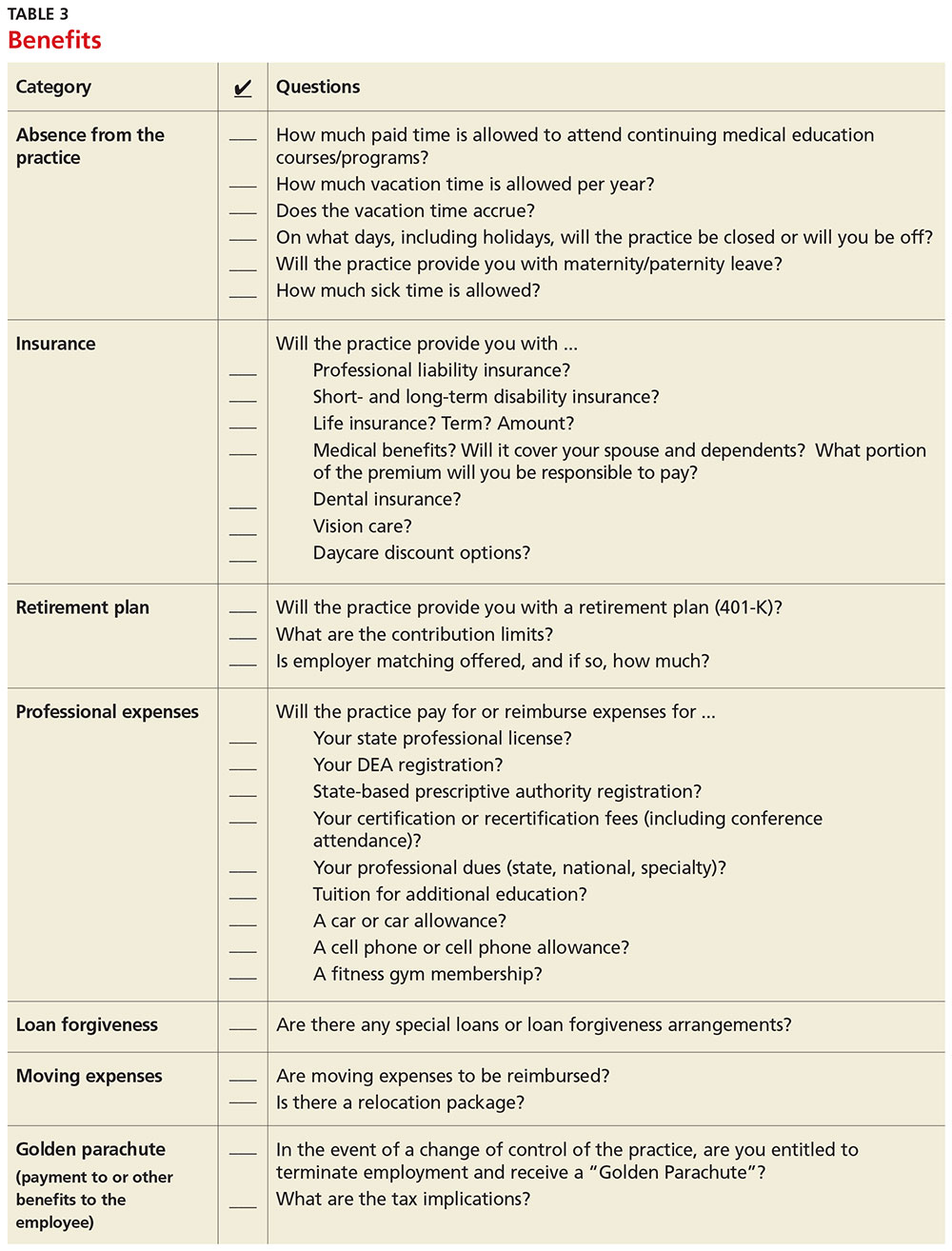
Carolyn Buppert, a specialist in legal and reimbursement issues for NPs and PAs, suggests three “P’s” of negotiation: Prepare, probe, and propose.4
Prepare. Learn how to calculate the projected revenue you would bring into a practice. You can determine the profit you generate by asking the practice administrator for data, noting Current Procedural Terminology codes and dates and becoming familiar with the fee schedule. According to Buppert, your salary and benefits should amount to about one-third of your total billings, and the benefits should equate to about 25% of your base salary.4 It is worthwhile to discuss nonmonetary contributions to the practice, such as improvements in patient satisfaction or reduction in no-shows.
Probe. Ask about the practice’s financial health during your interview and determine employer expectations for profits.
Propose. Once your prospective employer proves their value to you and after you have done due diligence researching the practice, do not hesitate to ask for what you deserve. When doing this, it is important to maintain neutral body language, keep an unemotional tone of voice, and convey an understanding of the employer’s point of view.4
Most successful negotiations occur over a couple of meetings. Careful listening is essential to avoid misunderstandings and false assumptions. By listening intently, you can identify the issues most important to the employer (eg, pay may be negotiable, but moonlighting not; or control over shift schedules is a hot button, but pay is not). Evaluating and weighing those against your own requirements may avoid an unnecessary impasse and result in a better outcome for you.
One question lives at the heart of negotiations: Should agreements be in writing? Written agreements carry more weight and prevent misunderstandings, a benefit to both parties involved. Formal, written negotiation of a contract forces the parties to discuss issues and provides a record for future reference.5
CONTRACTS
Because courses in negotiations, contract law, and business principles are rarely taught in educational programs, you should consider consulting an attorney who is familiar with contract and business issues. Avoid attorneys who have to research the laws regarding NP and PA practice—there are many who are well versed in these contracts. It is also usually more acceptable to conduct initial negotiations yourself, rather than through an attorney.
First, ask the attorney to review the contract and advise you of any troublesome provision or obvious omissions (see Table 4; a sample contract is also available on our website).6-8 Many attorneys with experience reviewing and negotiating such contracts will be willing to do an initial read and consultation for a fixed, predetermined fee. Following that consultation, it is best to discuss your concerns and questions directly with your potential employer. If you can come to a general agreement on revisions, either your lawyer or the employer’s can make the necessary changes.
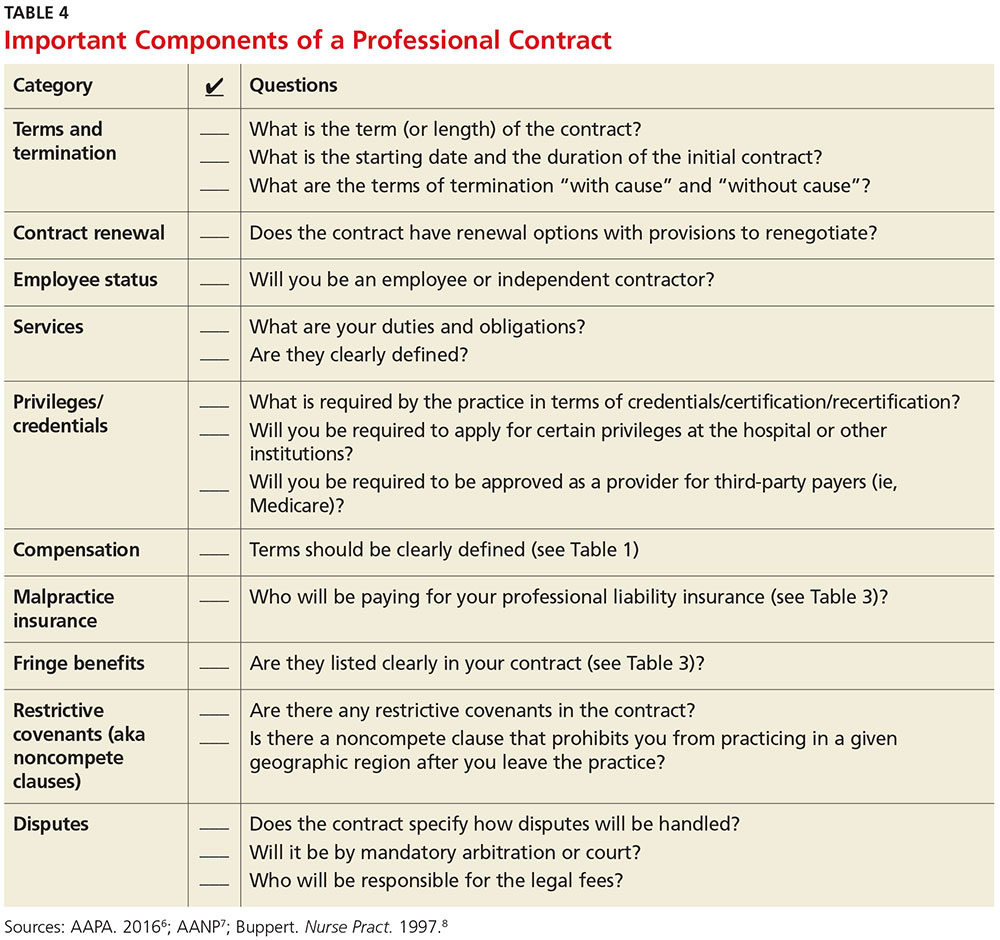
When considering an employment agreement, there are specific issues and potential hurdles to look out for. Following is a brief discussion of some of them.
Liability insurance
Find out which type of liability insurance is offered (occurrence-based or claims-made), as well as the limits of liability. Occurrence-based insurance is usually recommended. However, if the policy is claims-made, it’s important to know if the tail coverage will be paid by the employer, or if there is a rider on the physician’s policy. Determine if your contract will allow for the cost of the tail to be deducted from final amounts that may be owed to you upon termination. Be prepared to acquire the tail, if needed, to ensure coverage.
Restrictive covenants (noncompete clauses)
Unfortunately, not all employment relationships work out in the long term. In recognition of this, many professional contracts contain an agreement known as a restrictive covenant, which impedes the NP’s or PA’s ability to practice in the community following a relationship cessation. Depending on where the practice is located, such restrictions can be devastating and may even require the NP or PA to move in order to pursue a career. The law of restrictive covenants varies greatly from state to state. Your attorney can help you evaluate the enforceability and effect of a restrictive covenant, advise you on what is or isn’t reasonable in the community, and give you suggestions on how to negotiate a more reasonable one.
Moonlighting
Whether or not you can moonlight—and where—is often negotiable. An employer certainly has the right to require that moonlighting not interfere with your regular duties or schedule; endorse competitors of your employer or potentially divert patients; or expose the employer to malpractice liability. If you can assure your employer that these three situations will not transpire, then moonlighting (with advance scheduling notice and permission) should be acceptable.
Training/continuing education
It is typical for the employer to reimburse some or all of the cost of continuing education, up to a maximum annual amount. It is also reasonable for the employer (if paying for the CME) to pre-approve the curriculum, as well as the timing to avoid scheduling problems.
Salary and bonus
Compensation systems can be entirely objective (ie, production based), subjective (entirely up to the discretion of the employer based on internal criteria), or a combination of both. It is important to get a clear understanding of the system so that you know what is expected of you and what the rewards are for meeting performance goals.
Income guarantee/advanced expenses/repayment obligation
It is not uncommon for a local hospital to help a medical practice by guaranteeing the salary for a certain period of time. In this situation, the guarantee can be structured in a number of different ways—but it typically involves an obligation to repay a predetermined amount if you leave the practice area before the expiration of the term. Often, the practice will seek to pass that liability on to you. The same may apply for advanced moving expenses, CME, etc. A practice may require you to be employed for a specified amount of time to “earn” those advanced expenses, or to pay them back if an early termination occurs. In any case, it is important to know what the expectations are, and what circumstances could lead to an early termination and/or repayment obligation.
Terms and termination
Pay particular attention to the terms of your agreement. In one paragraph, it may say that the contract is for one year with annual renewals, but later on it explains that it can be terminated by either party upon 30 days notice. In that case, it is not a one-year contract; it is a 30-day contract. If there is a possibility of early termination and a restrictive covenant, or even a repayment obligation, you could really be at risk. Pay attention to whether early termination is “for cause” or “without cause.” If it is only for cause, inquire what constitutes a cause and whether there are any opportunities to rectify a perceived problem.
CONCLUSION
Constant changes in the health care marketplace will continue to generate opportunities for NPs and PAs. This is especially true for clinicians who demonstrate competence, enthusiasm, and commitment to quality patient care. The same clinical skills you learned in school and practice will help you find a clinical position and negotiate a good professional contract. Attention to detail, evidence-based research, and excellent communication skills will enable you to land a position beneficial to both parties.
1. American Academy of Physician Assistants. 2016 AAPA Salary Report. www.aapa.org/research/salary-report. Accessed November 4, 2016.
2. American Academy of Nurse Practitioners. Annual income for full-time nurse practitioners up 10% since 2011. www.aanp.org/press-room/press-releases/166-press-room/2015-press-releases/1803-annual- income-for-full-time-nurse-practitioners-up-10-since-2011. Accessed November 4, 2016.
3. Bourne H. A Great Deal! Compensation Negotiation for Nurse Practitioners & Physician Assistants. 3rd ed. Arcata, CA: Open Spaces; 1998.
4. Buppert C. Nurse Practitioner’s Business Practice and Legal Guide. 5th ed. Burlington, MA: Jones & Bartlett Learning; 2015.
5. Henley MB. Finding your ideal job and negotiating your contract: where to get the information and numbers you need to know. J Orthop Trauma. 2012;26(1):S9-S13.
6. AAPA. Contacts and contracts: a guide to your PA career. www.aapa.org/WorkArea/DownloadAsset.aspx?id=2147486883. Accessed November 4, 2016.
7. AANP. Employment negotiations. www.aanp.org/practice/reimbursement/68-articles/579-employment-negotiations. Accessed November 4, 2016.
8. Buppert C. Employment agreements: clauses that can change an NP’s life. Nurse Pract. 1997;22(8):108-109.
For the freshly minted NP or PA, finding the right place to practice and negotiating a reasonable professional contract can be a challenge. The keys to successful negotiation are similar to those for attaining proficiency in your clinical practice—providing insight into your personality, an evaluation of your personal and professional goals, and a commitment of time for preparation. For most NPs and PAs, employment opportunities do not just happen. Preparation, persistence, and personal contacts are basic requirements for finding the right position.
Of great interest to NPs and PAs—especially those with looming loan payments—is the compensation package. There are many important questions and topics to discuss regarding compensation (see Table 1). However, salaries are often determined by the “going rate” for particular services in your geographic region, in addition to your specialty, experience, and credentials. Your professional association (AAPA for PAs, AANP for NPs) has robust data on salaries in your particular specialty, practice setting, and geographic region; the average salary for both professions is currently about $97,000.1,2
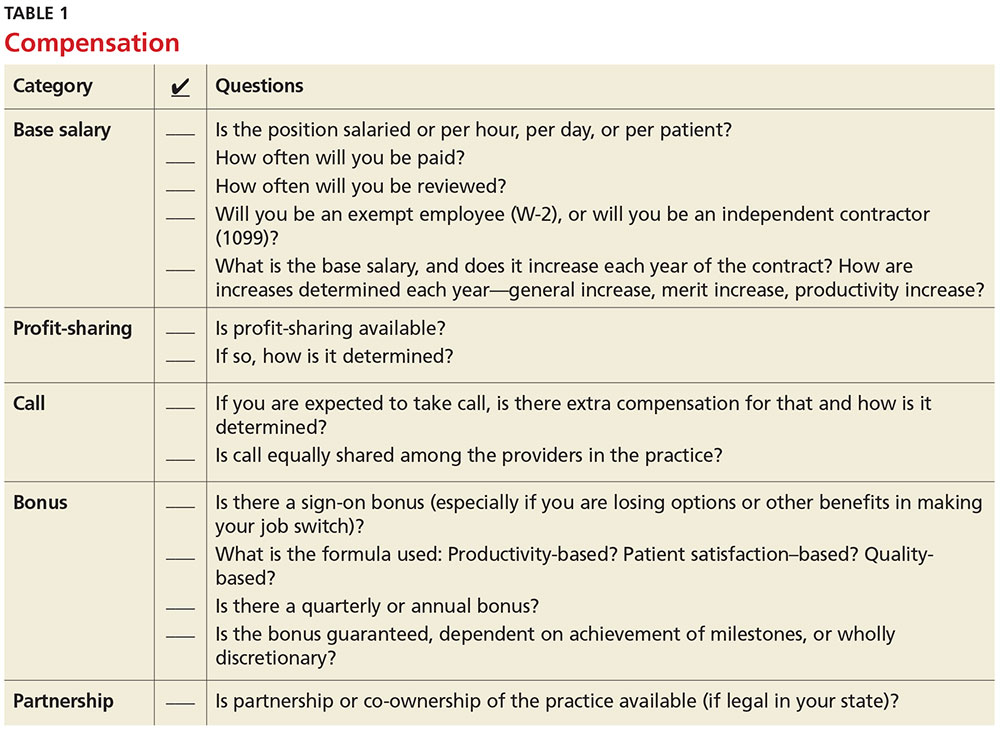
Familiarize yourself with the statutes and regulations that govern the scope of practice in your state—this is especially important if there are specific supervision or collaboration rules. Be prepared to present applicable statutes, rules, and regulations to the physician and/or office manager. Know whether any reimbursement restrictions exist. Be sure to review IRS guidelines for employee status versus independent contractor status.
The diversity of NP and PA practices means one size does not fit all, so it is best to identify the practice that complements your own personality. So, before you open negotiations, it is important that you research the practice. (For suggestions on what to inquire about, see Table 2). It is also a good idea to check the Docinfo website (http://docinfo.org/#/search/query), sponsored by the Federation of State Medical Boards, to research disciplinary records of the physician(s). Additional information can be acquired at each state regulatory board site.
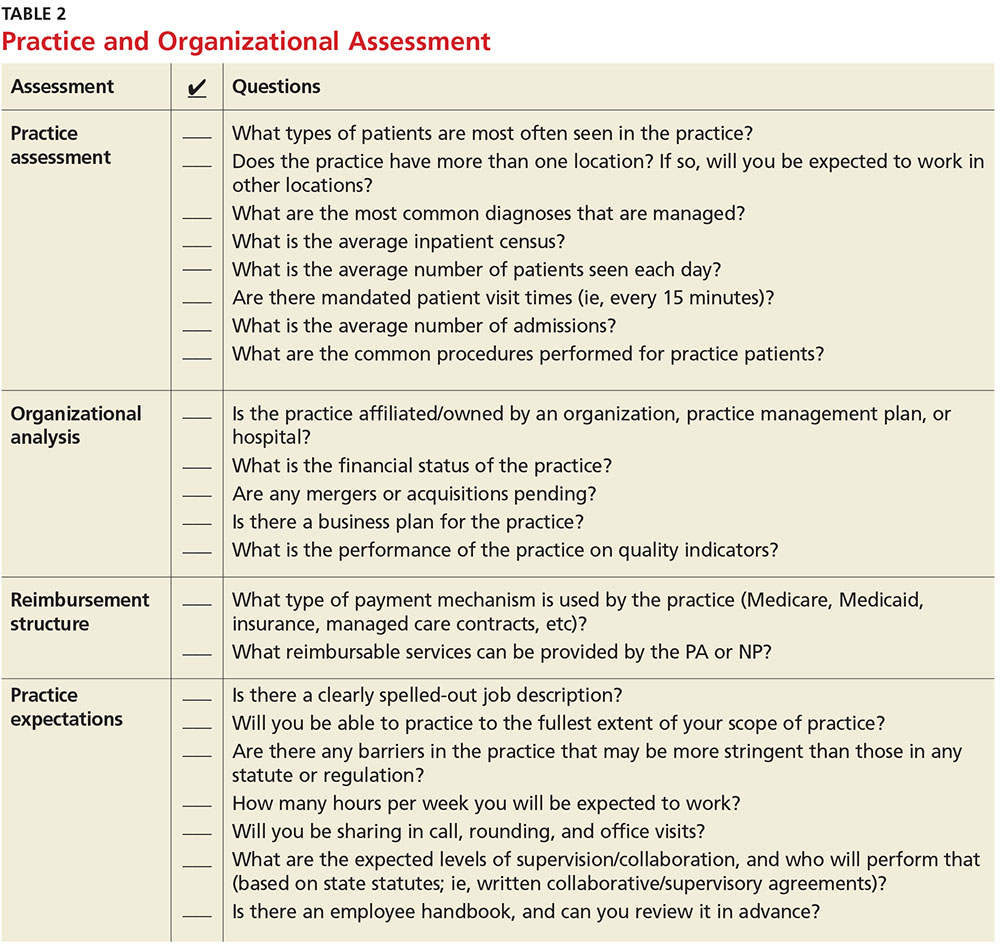
NEGOTIATION
When you’ve decided which employment offer to pursue, it’s time to think about how you want to negotiate your contract. Many people feel that negotiation is equivalent to confrontation, inevitably leading to an awkward disagreement with the practice. This is rarely the case; negotiation is simply a professional conversation, best had one-on-one with the key decision maker, rather than a group.
Never assume that your compensation package is predetermined. Whether you are starting a new job or looking to enhance your current situation, you can make a difference by asking for what you need.3 Knowing the local market and data is essential. Research the average salary in the region (for experienced versus new NP or PA). Be sure to think beyond salary and evaluate which benefits you’d like to have as part of your compensation package (see Table 3, as well as our survey results).
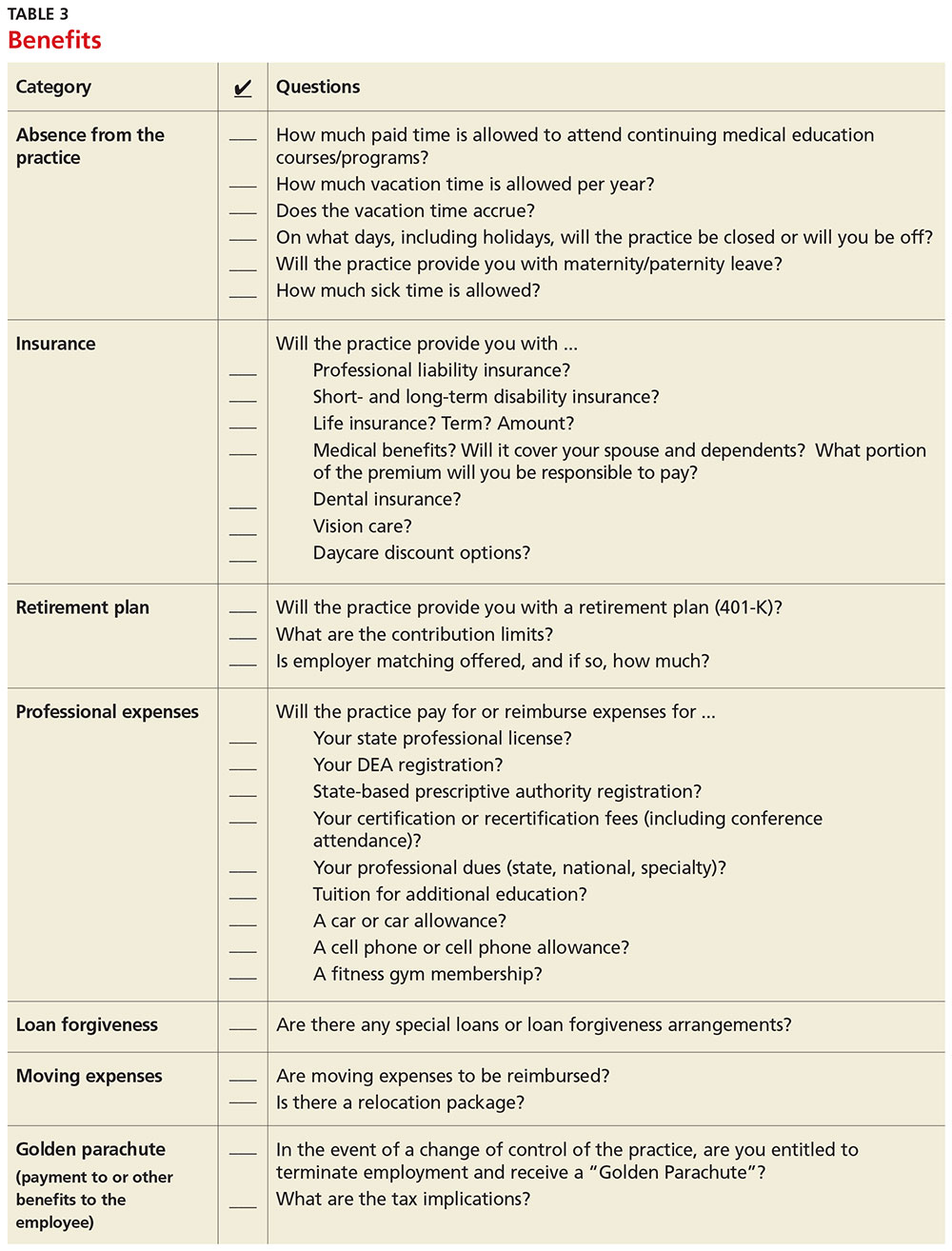
Carolyn Buppert, a specialist in legal and reimbursement issues for NPs and PAs, suggests three “P’s” of negotiation: Prepare, probe, and propose.4
Prepare. Learn how to calculate the projected revenue you would bring into a practice. You can determine the profit you generate by asking the practice administrator for data, noting Current Procedural Terminology codes and dates and becoming familiar with the fee schedule. According to Buppert, your salary and benefits should amount to about one-third of your total billings, and the benefits should equate to about 25% of your base salary.4 It is worthwhile to discuss nonmonetary contributions to the practice, such as improvements in patient satisfaction or reduction in no-shows.
Probe. Ask about the practice’s financial health during your interview and determine employer expectations for profits.
Propose. Once your prospective employer proves their value to you and after you have done due diligence researching the practice, do not hesitate to ask for what you deserve. When doing this, it is important to maintain neutral body language, keep an unemotional tone of voice, and convey an understanding of the employer’s point of view.4
Most successful negotiations occur over a couple of meetings. Careful listening is essential to avoid misunderstandings and false assumptions. By listening intently, you can identify the issues most important to the employer (eg, pay may be negotiable, but moonlighting not; or control over shift schedules is a hot button, but pay is not). Evaluating and weighing those against your own requirements may avoid an unnecessary impasse and result in a better outcome for you.
One question lives at the heart of negotiations: Should agreements be in writing? Written agreements carry more weight and prevent misunderstandings, a benefit to both parties involved. Formal, written negotiation of a contract forces the parties to discuss issues and provides a record for future reference.5
CONTRACTS
Because courses in negotiations, contract law, and business principles are rarely taught in educational programs, you should consider consulting an attorney who is familiar with contract and business issues. Avoid attorneys who have to research the laws regarding NP and PA practice—there are many who are well versed in these contracts. It is also usually more acceptable to conduct initial negotiations yourself, rather than through an attorney.
First, ask the attorney to review the contract and advise you of any troublesome provision or obvious omissions (see Table 4; a sample contract is also available on our website).6-8 Many attorneys with experience reviewing and negotiating such contracts will be willing to do an initial read and consultation for a fixed, predetermined fee. Following that consultation, it is best to discuss your concerns and questions directly with your potential employer. If you can come to a general agreement on revisions, either your lawyer or the employer’s can make the necessary changes.
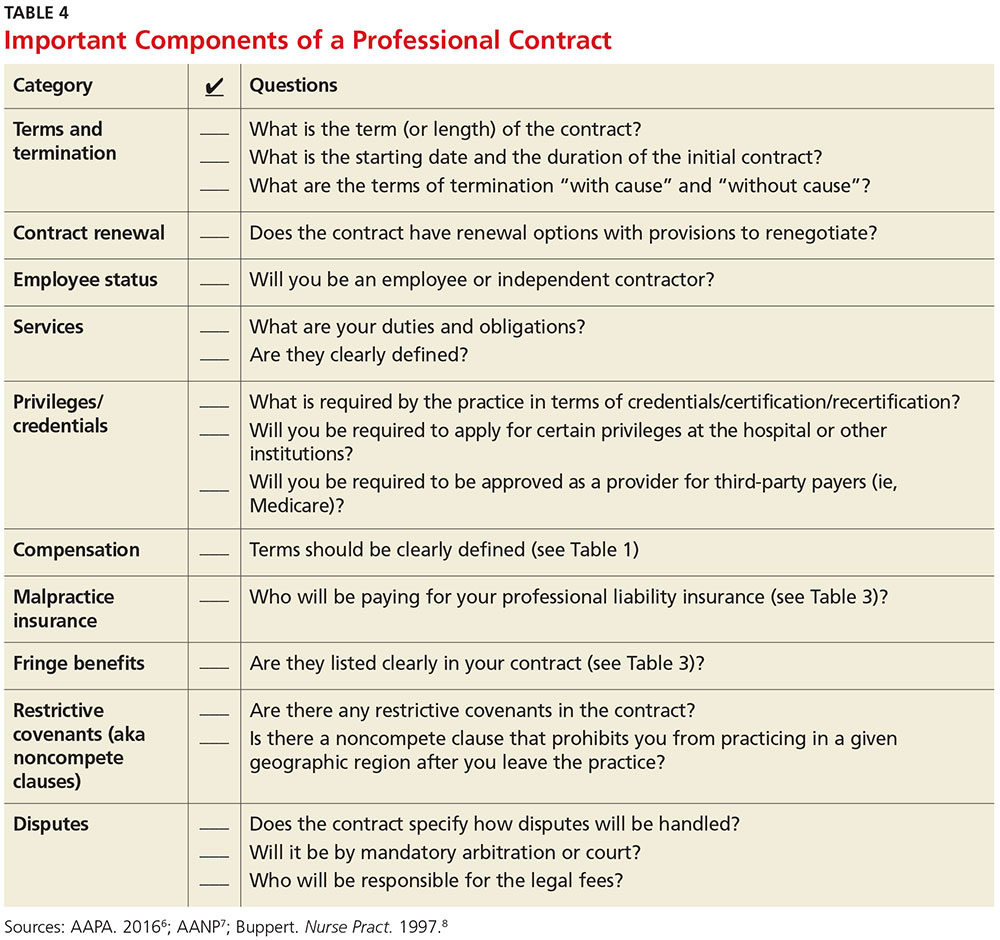
When considering an employment agreement, there are specific issues and potential hurdles to look out for. Following is a brief discussion of some of them.
Liability insurance
Find out which type of liability insurance is offered (occurrence-based or claims-made), as well as the limits of liability. Occurrence-based insurance is usually recommended. However, if the policy is claims-made, it’s important to know if the tail coverage will be paid by the employer, or if there is a rider on the physician’s policy. Determine if your contract will allow for the cost of the tail to be deducted from final amounts that may be owed to you upon termination. Be prepared to acquire the tail, if needed, to ensure coverage.
Restrictive covenants (noncompete clauses)
Unfortunately, not all employment relationships work out in the long term. In recognition of this, many professional contracts contain an agreement known as a restrictive covenant, which impedes the NP’s or PA’s ability to practice in the community following a relationship cessation. Depending on where the practice is located, such restrictions can be devastating and may even require the NP or PA to move in order to pursue a career. The law of restrictive covenants varies greatly from state to state. Your attorney can help you evaluate the enforceability and effect of a restrictive covenant, advise you on what is or isn’t reasonable in the community, and give you suggestions on how to negotiate a more reasonable one.
Moonlighting
Whether or not you can moonlight—and where—is often negotiable. An employer certainly has the right to require that moonlighting not interfere with your regular duties or schedule; endorse competitors of your employer or potentially divert patients; or expose the employer to malpractice liability. If you can assure your employer that these three situations will not transpire, then moonlighting (with advance scheduling notice and permission) should be acceptable.
Training/continuing education
It is typical for the employer to reimburse some or all of the cost of continuing education, up to a maximum annual amount. It is also reasonable for the employer (if paying for the CME) to pre-approve the curriculum, as well as the timing to avoid scheduling problems.
Salary and bonus
Compensation systems can be entirely objective (ie, production based), subjective (entirely up to the discretion of the employer based on internal criteria), or a combination of both. It is important to get a clear understanding of the system so that you know what is expected of you and what the rewards are for meeting performance goals.
Income guarantee/advanced expenses/repayment obligation
It is not uncommon for a local hospital to help a medical practice by guaranteeing the salary for a certain period of time. In this situation, the guarantee can be structured in a number of different ways—but it typically involves an obligation to repay a predetermined amount if you leave the practice area before the expiration of the term. Often, the practice will seek to pass that liability on to you. The same may apply for advanced moving expenses, CME, etc. A practice may require you to be employed for a specified amount of time to “earn” those advanced expenses, or to pay them back if an early termination occurs. In any case, it is important to know what the expectations are, and what circumstances could lead to an early termination and/or repayment obligation.
Terms and termination
Pay particular attention to the terms of your agreement. In one paragraph, it may say that the contract is for one year with annual renewals, but later on it explains that it can be terminated by either party upon 30 days notice. In that case, it is not a one-year contract; it is a 30-day contract. If there is a possibility of early termination and a restrictive covenant, or even a repayment obligation, you could really be at risk. Pay attention to whether early termination is “for cause” or “without cause.” If it is only for cause, inquire what constitutes a cause and whether there are any opportunities to rectify a perceived problem.
CONCLUSION
Constant changes in the health care marketplace will continue to generate opportunities for NPs and PAs. This is especially true for clinicians who demonstrate competence, enthusiasm, and commitment to quality patient care. The same clinical skills you learned in school and practice will help you find a clinical position and negotiate a good professional contract. Attention to detail, evidence-based research, and excellent communication skills will enable you to land a position beneficial to both parties.
For the freshly minted NP or PA, finding the right place to practice and negotiating a reasonable professional contract can be a challenge. The keys to successful negotiation are similar to those for attaining proficiency in your clinical practice—providing insight into your personality, an evaluation of your personal and professional goals, and a commitment of time for preparation. For most NPs and PAs, employment opportunities do not just happen. Preparation, persistence, and personal contacts are basic requirements for finding the right position.
Of great interest to NPs and PAs—especially those with looming loan payments—is the compensation package. There are many important questions and topics to discuss regarding compensation (see Table 1). However, salaries are often determined by the “going rate” for particular services in your geographic region, in addition to your specialty, experience, and credentials. Your professional association (AAPA for PAs, AANP for NPs) has robust data on salaries in your particular specialty, practice setting, and geographic region; the average salary for both professions is currently about $97,000.1,2
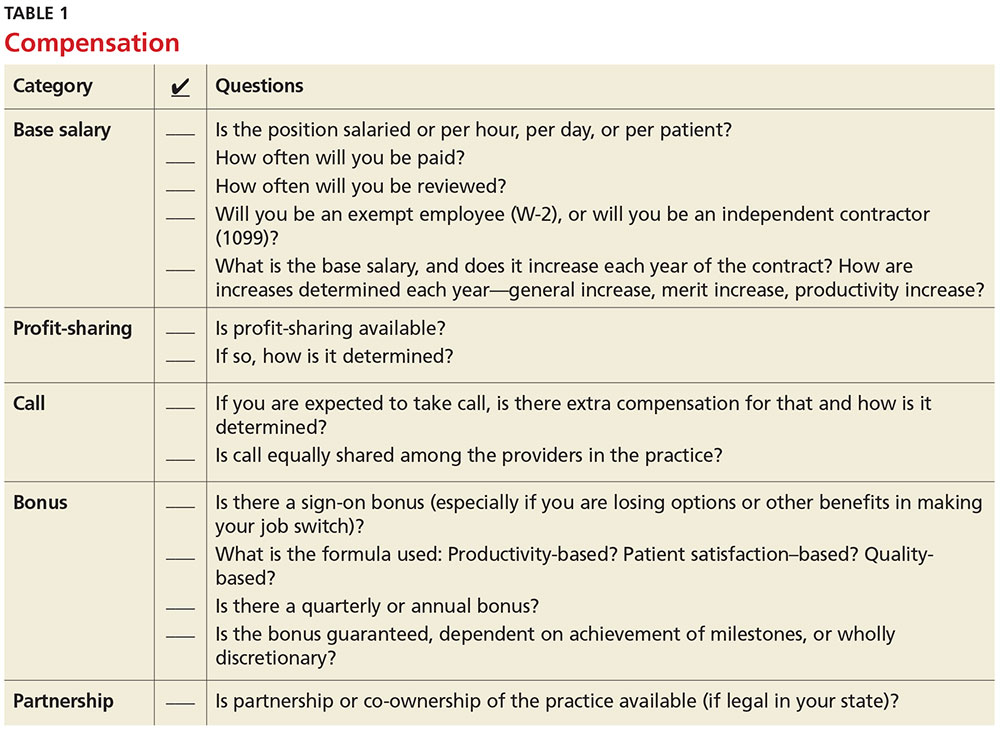
Familiarize yourself with the statutes and regulations that govern the scope of practice in your state—this is especially important if there are specific supervision or collaboration rules. Be prepared to present applicable statutes, rules, and regulations to the physician and/or office manager. Know whether any reimbursement restrictions exist. Be sure to review IRS guidelines for employee status versus independent contractor status.
The diversity of NP and PA practices means one size does not fit all, so it is best to identify the practice that complements your own personality. So, before you open negotiations, it is important that you research the practice. (For suggestions on what to inquire about, see Table 2). It is also a good idea to check the Docinfo website (http://docinfo.org/#/search/query), sponsored by the Federation of State Medical Boards, to research disciplinary records of the physician(s). Additional information can be acquired at each state regulatory board site.
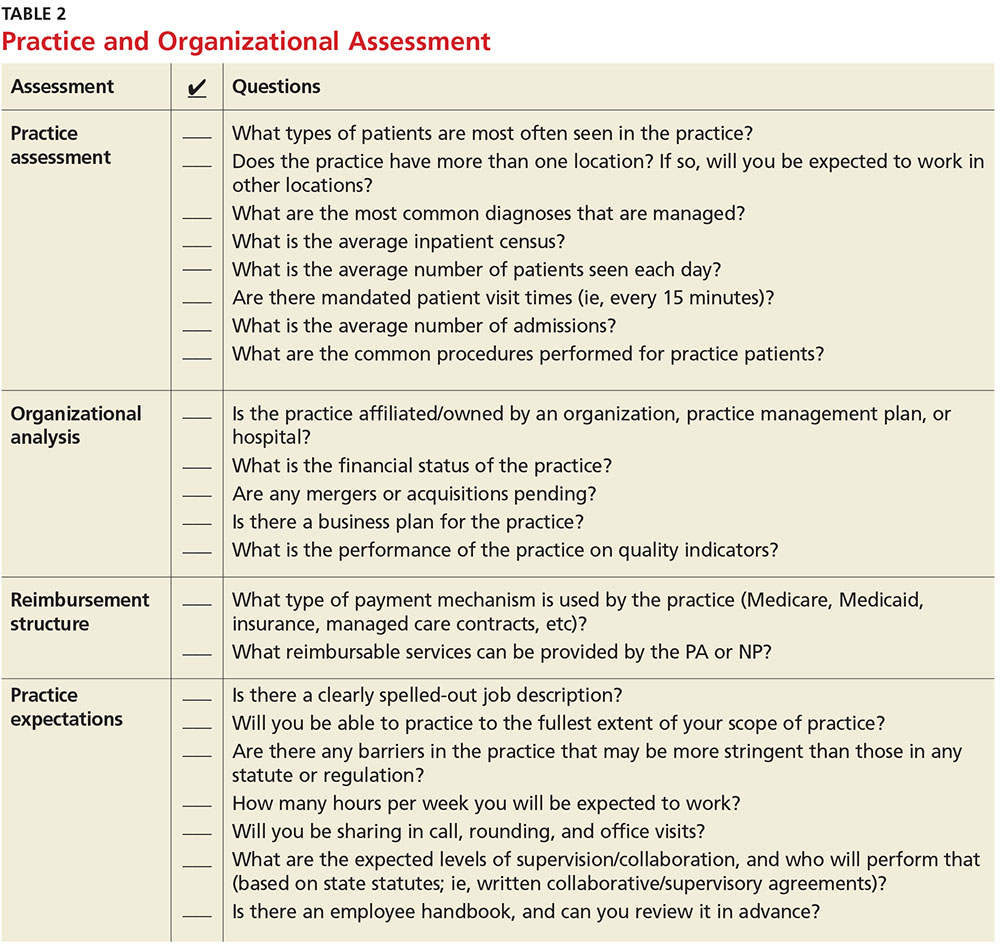
NEGOTIATION
When you’ve decided which employment offer to pursue, it’s time to think about how you want to negotiate your contract. Many people feel that negotiation is equivalent to confrontation, inevitably leading to an awkward disagreement with the practice. This is rarely the case; negotiation is simply a professional conversation, best had one-on-one with the key decision maker, rather than a group.
Never assume that your compensation package is predetermined. Whether you are starting a new job or looking to enhance your current situation, you can make a difference by asking for what you need.3 Knowing the local market and data is essential. Research the average salary in the region (for experienced versus new NP or PA). Be sure to think beyond salary and evaluate which benefits you’d like to have as part of your compensation package (see Table 3, as well as our survey results).
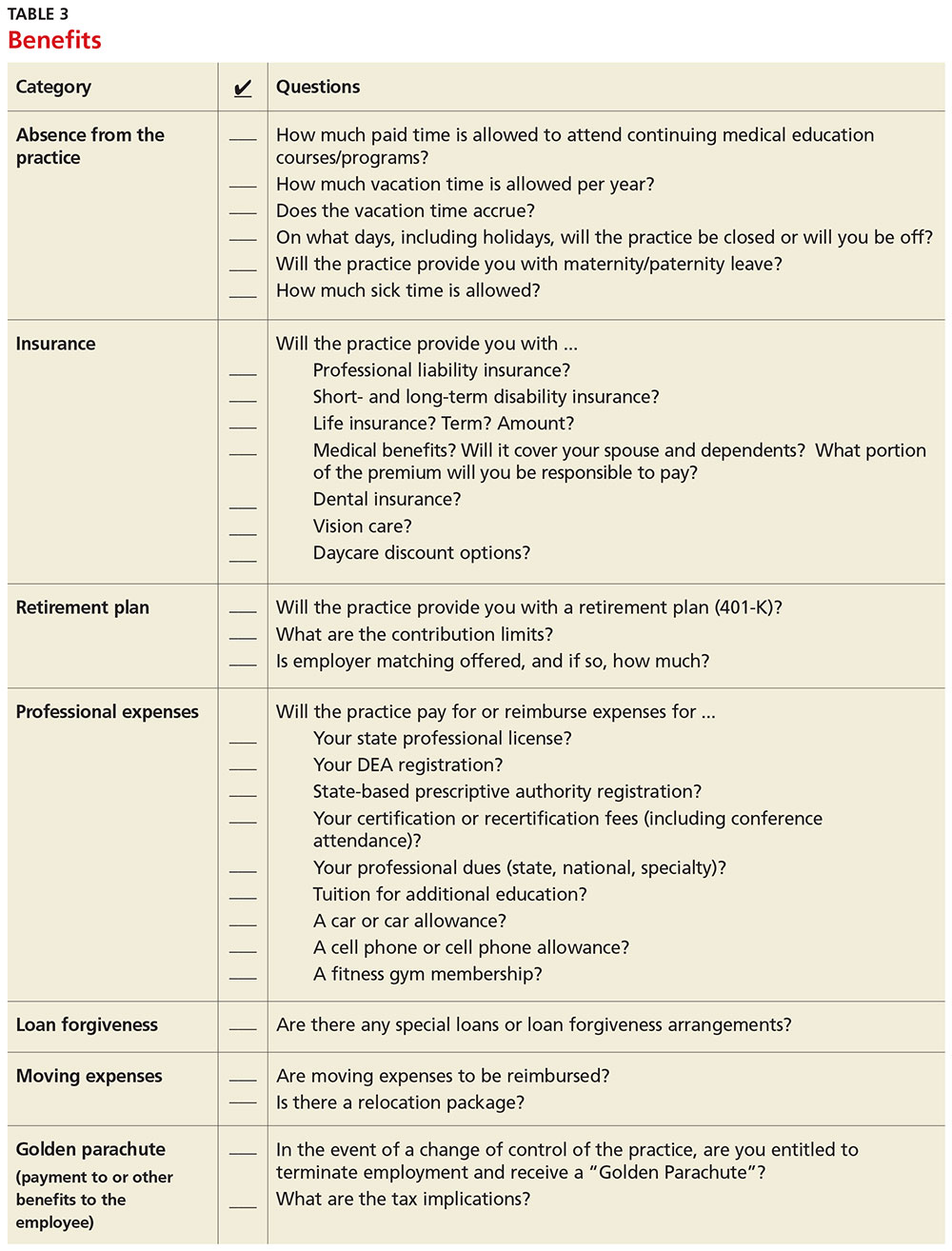
Carolyn Buppert, a specialist in legal and reimbursement issues for NPs and PAs, suggests three “P’s” of negotiation: Prepare, probe, and propose.4
Prepare. Learn how to calculate the projected revenue you would bring into a practice. You can determine the profit you generate by asking the practice administrator for data, noting Current Procedural Terminology codes and dates and becoming familiar with the fee schedule. According to Buppert, your salary and benefits should amount to about one-third of your total billings, and the benefits should equate to about 25% of your base salary.4 It is worthwhile to discuss nonmonetary contributions to the practice, such as improvements in patient satisfaction or reduction in no-shows.
Probe. Ask about the practice’s financial health during your interview and determine employer expectations for profits.
Propose. Once your prospective employer proves their value to you and after you have done due diligence researching the practice, do not hesitate to ask for what you deserve. When doing this, it is important to maintain neutral body language, keep an unemotional tone of voice, and convey an understanding of the employer’s point of view.4
Most successful negotiations occur over a couple of meetings. Careful listening is essential to avoid misunderstandings and false assumptions. By listening intently, you can identify the issues most important to the employer (eg, pay may be negotiable, but moonlighting not; or control over shift schedules is a hot button, but pay is not). Evaluating and weighing those against your own requirements may avoid an unnecessary impasse and result in a better outcome for you.
One question lives at the heart of negotiations: Should agreements be in writing? Written agreements carry more weight and prevent misunderstandings, a benefit to both parties involved. Formal, written negotiation of a contract forces the parties to discuss issues and provides a record for future reference.5
CONTRACTS
Because courses in negotiations, contract law, and business principles are rarely taught in educational programs, you should consider consulting an attorney who is familiar with contract and business issues. Avoid attorneys who have to research the laws regarding NP and PA practice—there are many who are well versed in these contracts. It is also usually more acceptable to conduct initial negotiations yourself, rather than through an attorney.
First, ask the attorney to review the contract and advise you of any troublesome provision or obvious omissions (see Table 4; a sample contract is also available on our website).6-8 Many attorneys with experience reviewing and negotiating such contracts will be willing to do an initial read and consultation for a fixed, predetermined fee. Following that consultation, it is best to discuss your concerns and questions directly with your potential employer. If you can come to a general agreement on revisions, either your lawyer or the employer’s can make the necessary changes.
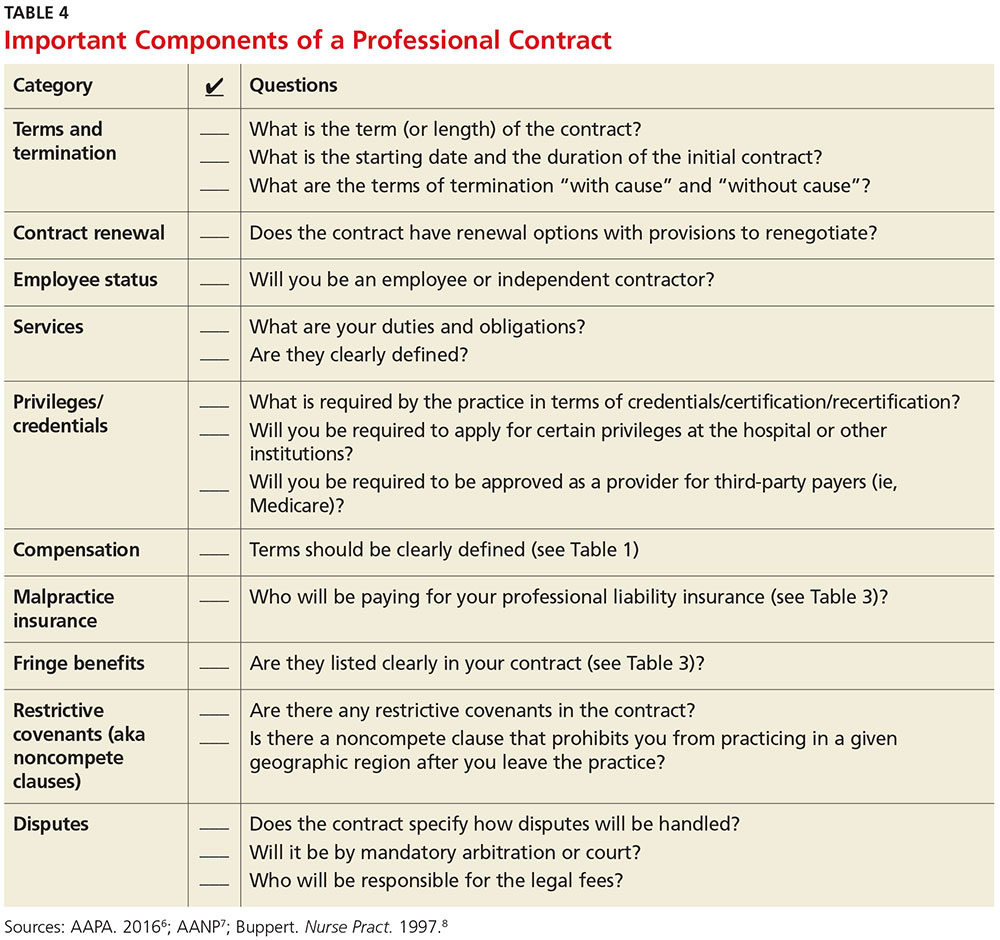
When considering an employment agreement, there are specific issues and potential hurdles to look out for. Following is a brief discussion of some of them.
Liability insurance
Find out which type of liability insurance is offered (occurrence-based or claims-made), as well as the limits of liability. Occurrence-based insurance is usually recommended. However, if the policy is claims-made, it’s important to know if the tail coverage will be paid by the employer, or if there is a rider on the physician’s policy. Determine if your contract will allow for the cost of the tail to be deducted from final amounts that may be owed to you upon termination. Be prepared to acquire the tail, if needed, to ensure coverage.
Restrictive covenants (noncompete clauses)
Unfortunately, not all employment relationships work out in the long term. In recognition of this, many professional contracts contain an agreement known as a restrictive covenant, which impedes the NP’s or PA’s ability to practice in the community following a relationship cessation. Depending on where the practice is located, such restrictions can be devastating and may even require the NP or PA to move in order to pursue a career. The law of restrictive covenants varies greatly from state to state. Your attorney can help you evaluate the enforceability and effect of a restrictive covenant, advise you on what is or isn’t reasonable in the community, and give you suggestions on how to negotiate a more reasonable one.
Moonlighting
Whether or not you can moonlight—and where—is often negotiable. An employer certainly has the right to require that moonlighting not interfere with your regular duties or schedule; endorse competitors of your employer or potentially divert patients; or expose the employer to malpractice liability. If you can assure your employer that these three situations will not transpire, then moonlighting (with advance scheduling notice and permission) should be acceptable.
Training/continuing education
It is typical for the employer to reimburse some or all of the cost of continuing education, up to a maximum annual amount. It is also reasonable for the employer (if paying for the CME) to pre-approve the curriculum, as well as the timing to avoid scheduling problems.
Salary and bonus
Compensation systems can be entirely objective (ie, production based), subjective (entirely up to the discretion of the employer based on internal criteria), or a combination of both. It is important to get a clear understanding of the system so that you know what is expected of you and what the rewards are for meeting performance goals.
Income guarantee/advanced expenses/repayment obligation
It is not uncommon for a local hospital to help a medical practice by guaranteeing the salary for a certain period of time. In this situation, the guarantee can be structured in a number of different ways—but it typically involves an obligation to repay a predetermined amount if you leave the practice area before the expiration of the term. Often, the practice will seek to pass that liability on to you. The same may apply for advanced moving expenses, CME, etc. A practice may require you to be employed for a specified amount of time to “earn” those advanced expenses, or to pay them back if an early termination occurs. In any case, it is important to know what the expectations are, and what circumstances could lead to an early termination and/or repayment obligation.
Terms and termination
Pay particular attention to the terms of your agreement. In one paragraph, it may say that the contract is for one year with annual renewals, but later on it explains that it can be terminated by either party upon 30 days notice. In that case, it is not a one-year contract; it is a 30-day contract. If there is a possibility of early termination and a restrictive covenant, or even a repayment obligation, you could really be at risk. Pay attention to whether early termination is “for cause” or “without cause.” If it is only for cause, inquire what constitutes a cause and whether there are any opportunities to rectify a perceived problem.
CONCLUSION
Constant changes in the health care marketplace will continue to generate opportunities for NPs and PAs. This is especially true for clinicians who demonstrate competence, enthusiasm, and commitment to quality patient care. The same clinical skills you learned in school and practice will help you find a clinical position and negotiate a good professional contract. Attention to detail, evidence-based research, and excellent communication skills will enable you to land a position beneficial to both parties.
1. American Academy of Physician Assistants. 2016 AAPA Salary Report. www.aapa.org/research/salary-report. Accessed November 4, 2016.
2. American Academy of Nurse Practitioners. Annual income for full-time nurse practitioners up 10% since 2011. www.aanp.org/press-room/press-releases/166-press-room/2015-press-releases/1803-annual- income-for-full-time-nurse-practitioners-up-10-since-2011. Accessed November 4, 2016.
3. Bourne H. A Great Deal! Compensation Negotiation for Nurse Practitioners & Physician Assistants. 3rd ed. Arcata, CA: Open Spaces; 1998.
4. Buppert C. Nurse Practitioner’s Business Practice and Legal Guide. 5th ed. Burlington, MA: Jones & Bartlett Learning; 2015.
5. Henley MB. Finding your ideal job and negotiating your contract: where to get the information and numbers you need to know. J Orthop Trauma. 2012;26(1):S9-S13.
6. AAPA. Contacts and contracts: a guide to your PA career. www.aapa.org/WorkArea/DownloadAsset.aspx?id=2147486883. Accessed November 4, 2016.
7. AANP. Employment negotiations. www.aanp.org/practice/reimbursement/68-articles/579-employment-negotiations. Accessed November 4, 2016.
8. Buppert C. Employment agreements: clauses that can change an NP’s life. Nurse Pract. 1997;22(8):108-109.
1. American Academy of Physician Assistants. 2016 AAPA Salary Report. www.aapa.org/research/salary-report. Accessed November 4, 2016.
2. American Academy of Nurse Practitioners. Annual income for full-time nurse practitioners up 10% since 2011. www.aanp.org/press-room/press-releases/166-press-room/2015-press-releases/1803-annual- income-for-full-time-nurse-practitioners-up-10-since-2011. Accessed November 4, 2016.
3. Bourne H. A Great Deal! Compensation Negotiation for Nurse Practitioners & Physician Assistants. 3rd ed. Arcata, CA: Open Spaces; 1998.
4. Buppert C. Nurse Practitioner’s Business Practice and Legal Guide. 5th ed. Burlington, MA: Jones & Bartlett Learning; 2015.
5. Henley MB. Finding your ideal job and negotiating your contract: where to get the information and numbers you need to know. J Orthop Trauma. 2012;26(1):S9-S13.
6. AAPA. Contacts and contracts: a guide to your PA career. www.aapa.org/WorkArea/DownloadAsset.aspx?id=2147486883. Accessed November 4, 2016.
7. AANP. Employment negotiations. www.aanp.org/practice/reimbursement/68-articles/579-employment-negotiations. Accessed November 4, 2016.
8. Buppert C. Employment agreements: clauses that can change an NP’s life. Nurse Pract. 1997;22(8):108-109.
Beyond Salary—Are You Happy With Your Work?
Would you say you're satisfied with your job? If you had to do it all over again, what—if anything—would you change? We asked, you answered! Here are the results of our first annual Job Satisfaction Survey, including a comprehensive list of the nonmonetary benefits you deem most important.
Would you say you're satisfied with your job? If you had to do it all over again, what—if anything—would you change? We asked, you answered! Here are the results of our first annual Job Satisfaction Survey, including a comprehensive list of the nonmonetary benefits you deem most important.
Would you say you're satisfied with your job? If you had to do it all over again, what—if anything—would you change? We asked, you answered! Here are the results of our first annual Job Satisfaction Survey, including a comprehensive list of the nonmonetary benefits you deem most important.
Malpractice Counsel: Abdominal pain in an elderly patient
Case
An 89-year-old woman presented to the ED with the chief complaints of abdominal pain and nausea with vomiting. The patient stated that several hours prior, she had ingested an expired beverage, which she related to the sudden onset of her symptoms. The patient denied fever, chills, dysuria, or frequency. Her medical history was significant for chronic atrial fibrillation (AF) and congestive heart failure. The patient’s medications included metoprolol and furosemide; she was not on any anticoagulation medication.
On physical examination, the patient appeared her stated age, and was in moderate distress secondary to the abdominal pain. Vital signs were: temperature, 98.8oF; heart rate, 98 beats/min; respiratory rate, 20 breaths/min; and blood pressure, 116/72 mm Hg. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was unremarkable. On lung examination, breath sounds were equal bilaterally with bibasilar rales. The heart rhythm was irregularly irregular without murmurs, rubs, or gallops. The abdomen was soft to palpitation, but diffusely tender, without rebound, guarding, or mass. Rectal examination revealed normal tone and brown stool, and was trace positive for heme.
The emergency physician (EP) ordered an electrocardiogram (ECG), complete blood count, basic metabolic profile (BMP), urinalysis, and lipase test. The patient was administered intravenous (IV) normal saline at 75 cc/h, and morphine 4 mg and ondansetron 4 mg IV for the abdominal pain, nausea, and vomiting. She required several more doses of morphine due to the severity of the pain. The laboratory results included an elevated white blood count of 18.4 x 109/L with a left shift, but normal hemoglobin and hematocrit values. The ECG demonstrated AF with a controlled ventricular rate; there was no evidence of ischemia or injury. The BMP was remarkable for a slightly depressed potassium level (3.3 mEq/L), a decreased serum bicarbonate of 20 mEq/L, and evidence of renal insufficiency with a blood urea nitrogen of 28 mg/dL and a serum creatinine of 1.6 mg/dL. Given the ongoing severe pain, leukocytosis, metabolic acidosis, and lack of clear etiology, the EP ordered a computed tomography (CT) scan of the abdomen and pelvis; no IV contrast was ordered because of the abnormal renal function studies.
The radiologist interpreted the CT scan as essentially normal. The EP admitted the patient to the on-call hospitalist, who consulted both cardiology and gastroenterology services. During the night, the patient complained of increasing abdominal pain, and her abdomen became distended with peritoneal signs. She was taken emergently to the operating room in the early morning hours. A large segment of gangrenous small intestine was found upon exploration. The surgery was discontinued and comfort care measures were instituted. The patient died the following day.
The patient’s family sued the EP and the hospital for failure to make a timely diagnosis of mesenteric ischemia. They further stated that the EP should have ordered a CT angiogram (CTA) of the abdomen and pelvis. The defense argued that a contrast CT scan was contraindicated because of the patient’s poor renal function. A defense verdict was returned at trial.
Discussion
Elderly patients (defined as older than age 65 years) presenting to the ED with abdominal pain remain a diagnostic challenge for even the most seasoned clinician. While elderly patients with a chief complaint of abdominal pain represent only a small percentage of ED patients, approximately 50% to 66% of these patients will require hospitalization, while one-third will require a surgical intervention.1 The seriousness of this complaint in elderly patients is further emphasized by the fact that older patients with abdominal pain have a 6- to 8-fold increase in mortality compared to younger patients.2,3 This can be partially explained by the simple fact that the life-threatening causes of abdominal pain—abdominal aortic aneurysm, mesenteric ischemia, bowel perforation, volvulus, and acute bowel obstruction—occur more frequently (but not exclusively) in elderly patients. Historical risk factors for life-threatening causes of abdominal pain include: age older than 65 years, immunocompromised state, alcohol abuse, cardiovascular (CV) disease (eg, coronary artery disease, hypertension, AF), major comorbidities (eg, cancer, renal failure), and prior surgery or recent gastrointestinal instrumentation.1
The patient in this case had two risk factors for life-threatening causes of lower abdominal pain—age and AF. These are also two of the major risk factors for mesenteric ischemia, which was her ultimate diagnosis.
Acute mesenteric ischemia refers to the sudden onset of small intestinal hypoperfusion, frequently due to acute occlusion (embolism or thrombosis) of an intestinal artery, most commonly the superior mesenteric artery (SMA).4 The SMA supplies the entire small intestine except for the proximal duodenum. Other causes of acute mesenteric ischemia include venous occlusion (thrombosis) and nonocclusive mesenteric ischemia secondary to vasoconstriction from low-cardiac output or use of vasopressors.4
Thromboembolic occlusion of the SMA is the most common cause of acute mesenteric ischemia, accounting for 67% to 95% of cases.4 In addition to AF, the risk of arterial embolism is increased in patients with valvular disease, infective endocarditis, recent myocardial infarction, aortic atherosclerosis, or aortic aneurysm.4 Risk factors for thrombotic arterial occlusion include peripheral artery disease, advanced age, and low-cardiac output states.5
A frequent presentation of embolic mesenteric arterial ischemia, occurring in approximately one-third of cases, is an elderly patient with AF (or other source of embolism) and onset of severe, sudden abdominal pain out of proportion to physical examination. While nausea and vomiting are also common, bloody bowel movements are less frequent in the early course of the disease process.4 A history of a prior embolic event is present in approximately one-third of such patients.
On physical examination, the abdomen may be normal initially, or demonstrate only mild distention and tenderness without peritoneal signs. However, as the ischemia progresses, the abdomen becomes more distended, bowel sounds become absent, and peritoneal signs (ie, guarding and rebound) become apparent.6
The results of laboratory studies can suggest the diagnosis, but none are confirmatory. Laboratory findings may include a marked leukocytosis with left shift, an elevated hematocrit secondary to hemoconcentration, and metabolic acidosis. A helpful clinical pearl is to consider intestinal ischemia in the differential diagnosis of any patient with acute abdominal pain and metabolic acidosis.6 Serum lactate is frequently elevated (73%-94%) but a very nonspecific marker. Similarly, an arterial blood gas analysis may demonstrate metabolic acidosis. More recently, a normal D-dimer result has been used to help exclude the diagnosis of acute intestinal ischemia, since it is elevated in 96% of patients with the disease.6 Similar to lactate, an abnormal D-dimer result has a poor specificity (40%).6 Early in the disease course, nearly all laboratory studies may be normal.
Depending on the severity of the presentation, imaging can help make the definitive diagnosis. For patients with peritonitis or obvious bowel perforation, IV fluid resuscitation, IV antibiotics, and immediate surgical exploration are indicated. Plain radiographs of the abdomen offer little help, as many of the findings early in the disease course are nonspecific, and radiographs can be normal in 25% of cases.6 Ultrasound can identify arterial stenosis or occlusion of the SMA, but is frequently technically limited by the presence of air-filled loops of distended bowel.6 Magnetic resonance angiography has similar sensitivity and specificity as CTA for mesenteric arterial ischemia, and is actually more sensitive than CTA for mesenteric venous thrombosis; it also can be performed in patients with contrast allergy.6 However, CTA is performed more commonly because of its lower cost, greater speed, and wide availability.6 A CTA of the abdomen and pelvis (without oral contrast) is probably the best study for patients in whom mesenteric ischemia is high on the differential diagnosis.6 For patients with a less clear picture and a broader differential diagnosis, a CT scan of the abdomen/pelvis with both IV and oral contrast is preferred.7 Common findings on CT scan with IV/oral contrast in acute mesenteric ischemia include the following: bowel wall thickening, dilatation, stranding, bowel wall attenuation, abnormal enhancement, and pneumatosis. Unfortunately, many of these findings are nonspecific.7
Once the diagnosis of acute mesenteric ischemia is made, patients should be designated “nothing by mouth” and a nasogastric tube placed to decompress the bowel. These patients will require IV fluid resuscitation with normal saline. The amount and rate will depend on their clinical presentation and underlying CV status. Any electrolyte abnormalities should be corrected and broad spectrum IV antibiotics initiated. Vascular surgery or general surgery services should be consulted to determine the optimal management. Most patients with acute intestinal ischemia due to mesenteric arterial occlusion (or venous occlusive or nonocclusive mesenteric ischemia) will be started on anticoagulation, typically IV heparin, unless contraindications are present.6 Surgical treatment options include arterial embolectomy, arterial bypass, arterial stenting, arterial thrombolysis, or intra-arterial vasodilator infusion.
1. Kendall JL, Moreira ME. Evaluation of the adult with abdominal pain in the emergency department. UpToDate Web site. http://www.uptodate.com/contents/evaluation-of-the-adult-with-abdominal-pain-in-the-emergency-department. Updated September 29, 2016. Accessed November 30, 2016.
2. Lewis LM, Banet GA, Blanda M, Hustey FM, Meldon SW, Gerson LW. Etiology and clinical course of abdominal pain in senior patients: a prospective, multicenter study. J Gerontol A Biol Sci Med Sci. 2005;60(8):1071-1076.
3. Sanson TG, O’Keefe KP. Evaluation of abdominal pain in the elderly. Emerg Med Clin North Am. 1996;14(3):615.
4. Tendler DA, Lamont JT, Pearl G. Acute mesenteric arterial occlusion. UpToDate Web site. http://www.uptodate.com/contents/acute-mesenteric-arterial-occlusion. Updated May 27, 2015. Accessed November 30, 2016.
5. McKinsey JF, Gewertz BL. Acute mesenteric ischemia. Surg Clin North Am. 1997;77(2):307-318.
6. Tendler DA, Lamont JT. Overview of intestinal ischemia in adults. UpToDate Web site. http://www.uptodate.com/contents/overview-of-intestinal-ischemia-in-adults. Updated February 23, 2016. Accessed November 30, 2016.
7. Wiesner W. Khurana B, Ji H, Ros PR. CT of acute bowel ischemia. Radiology. 2003;226(3):635-650.
Case
An 89-year-old woman presented to the ED with the chief complaints of abdominal pain and nausea with vomiting. The patient stated that several hours prior, she had ingested an expired beverage, which she related to the sudden onset of her symptoms. The patient denied fever, chills, dysuria, or frequency. Her medical history was significant for chronic atrial fibrillation (AF) and congestive heart failure. The patient’s medications included metoprolol and furosemide; she was not on any anticoagulation medication.
On physical examination, the patient appeared her stated age, and was in moderate distress secondary to the abdominal pain. Vital signs were: temperature, 98.8oF; heart rate, 98 beats/min; respiratory rate, 20 breaths/min; and blood pressure, 116/72 mm Hg. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was unremarkable. On lung examination, breath sounds were equal bilaterally with bibasilar rales. The heart rhythm was irregularly irregular without murmurs, rubs, or gallops. The abdomen was soft to palpitation, but diffusely tender, without rebound, guarding, or mass. Rectal examination revealed normal tone and brown stool, and was trace positive for heme.
The emergency physician (EP) ordered an electrocardiogram (ECG), complete blood count, basic metabolic profile (BMP), urinalysis, and lipase test. The patient was administered intravenous (IV) normal saline at 75 cc/h, and morphine 4 mg and ondansetron 4 mg IV for the abdominal pain, nausea, and vomiting. She required several more doses of morphine due to the severity of the pain. The laboratory results included an elevated white blood count of 18.4 x 109/L with a left shift, but normal hemoglobin and hematocrit values. The ECG demonstrated AF with a controlled ventricular rate; there was no evidence of ischemia or injury. The BMP was remarkable for a slightly depressed potassium level (3.3 mEq/L), a decreased serum bicarbonate of 20 mEq/L, and evidence of renal insufficiency with a blood urea nitrogen of 28 mg/dL and a serum creatinine of 1.6 mg/dL. Given the ongoing severe pain, leukocytosis, metabolic acidosis, and lack of clear etiology, the EP ordered a computed tomography (CT) scan of the abdomen and pelvis; no IV contrast was ordered because of the abnormal renal function studies.
The radiologist interpreted the CT scan as essentially normal. The EP admitted the patient to the on-call hospitalist, who consulted both cardiology and gastroenterology services. During the night, the patient complained of increasing abdominal pain, and her abdomen became distended with peritoneal signs. She was taken emergently to the operating room in the early morning hours. A large segment of gangrenous small intestine was found upon exploration. The surgery was discontinued and comfort care measures were instituted. The patient died the following day.
The patient’s family sued the EP and the hospital for failure to make a timely diagnosis of mesenteric ischemia. They further stated that the EP should have ordered a CT angiogram (CTA) of the abdomen and pelvis. The defense argued that a contrast CT scan was contraindicated because of the patient’s poor renal function. A defense verdict was returned at trial.
Discussion
Elderly patients (defined as older than age 65 years) presenting to the ED with abdominal pain remain a diagnostic challenge for even the most seasoned clinician. While elderly patients with a chief complaint of abdominal pain represent only a small percentage of ED patients, approximately 50% to 66% of these patients will require hospitalization, while one-third will require a surgical intervention.1 The seriousness of this complaint in elderly patients is further emphasized by the fact that older patients with abdominal pain have a 6- to 8-fold increase in mortality compared to younger patients.2,3 This can be partially explained by the simple fact that the life-threatening causes of abdominal pain—abdominal aortic aneurysm, mesenteric ischemia, bowel perforation, volvulus, and acute bowel obstruction—occur more frequently (but not exclusively) in elderly patients. Historical risk factors for life-threatening causes of abdominal pain include: age older than 65 years, immunocompromised state, alcohol abuse, cardiovascular (CV) disease (eg, coronary artery disease, hypertension, AF), major comorbidities (eg, cancer, renal failure), and prior surgery or recent gastrointestinal instrumentation.1
The patient in this case had two risk factors for life-threatening causes of lower abdominal pain—age and AF. These are also two of the major risk factors for mesenteric ischemia, which was her ultimate diagnosis.
Acute mesenteric ischemia refers to the sudden onset of small intestinal hypoperfusion, frequently due to acute occlusion (embolism or thrombosis) of an intestinal artery, most commonly the superior mesenteric artery (SMA).4 The SMA supplies the entire small intestine except for the proximal duodenum. Other causes of acute mesenteric ischemia include venous occlusion (thrombosis) and nonocclusive mesenteric ischemia secondary to vasoconstriction from low-cardiac output or use of vasopressors.4
Thromboembolic occlusion of the SMA is the most common cause of acute mesenteric ischemia, accounting for 67% to 95% of cases.4 In addition to AF, the risk of arterial embolism is increased in patients with valvular disease, infective endocarditis, recent myocardial infarction, aortic atherosclerosis, or aortic aneurysm.4 Risk factors for thrombotic arterial occlusion include peripheral artery disease, advanced age, and low-cardiac output states.5
A frequent presentation of embolic mesenteric arterial ischemia, occurring in approximately one-third of cases, is an elderly patient with AF (or other source of embolism) and onset of severe, sudden abdominal pain out of proportion to physical examination. While nausea and vomiting are also common, bloody bowel movements are less frequent in the early course of the disease process.4 A history of a prior embolic event is present in approximately one-third of such patients.
On physical examination, the abdomen may be normal initially, or demonstrate only mild distention and tenderness without peritoneal signs. However, as the ischemia progresses, the abdomen becomes more distended, bowel sounds become absent, and peritoneal signs (ie, guarding and rebound) become apparent.6
The results of laboratory studies can suggest the diagnosis, but none are confirmatory. Laboratory findings may include a marked leukocytosis with left shift, an elevated hematocrit secondary to hemoconcentration, and metabolic acidosis. A helpful clinical pearl is to consider intestinal ischemia in the differential diagnosis of any patient with acute abdominal pain and metabolic acidosis.6 Serum lactate is frequently elevated (73%-94%) but a very nonspecific marker. Similarly, an arterial blood gas analysis may demonstrate metabolic acidosis. More recently, a normal D-dimer result has been used to help exclude the diagnosis of acute intestinal ischemia, since it is elevated in 96% of patients with the disease.6 Similar to lactate, an abnormal D-dimer result has a poor specificity (40%).6 Early in the disease course, nearly all laboratory studies may be normal.
Depending on the severity of the presentation, imaging can help make the definitive diagnosis. For patients with peritonitis or obvious bowel perforation, IV fluid resuscitation, IV antibiotics, and immediate surgical exploration are indicated. Plain radiographs of the abdomen offer little help, as many of the findings early in the disease course are nonspecific, and radiographs can be normal in 25% of cases.6 Ultrasound can identify arterial stenosis or occlusion of the SMA, but is frequently technically limited by the presence of air-filled loops of distended bowel.6 Magnetic resonance angiography has similar sensitivity and specificity as CTA for mesenteric arterial ischemia, and is actually more sensitive than CTA for mesenteric venous thrombosis; it also can be performed in patients with contrast allergy.6 However, CTA is performed more commonly because of its lower cost, greater speed, and wide availability.6 A CTA of the abdomen and pelvis (without oral contrast) is probably the best study for patients in whom mesenteric ischemia is high on the differential diagnosis.6 For patients with a less clear picture and a broader differential diagnosis, a CT scan of the abdomen/pelvis with both IV and oral contrast is preferred.7 Common findings on CT scan with IV/oral contrast in acute mesenteric ischemia include the following: bowel wall thickening, dilatation, stranding, bowel wall attenuation, abnormal enhancement, and pneumatosis. Unfortunately, many of these findings are nonspecific.7
Once the diagnosis of acute mesenteric ischemia is made, patients should be designated “nothing by mouth” and a nasogastric tube placed to decompress the bowel. These patients will require IV fluid resuscitation with normal saline. The amount and rate will depend on their clinical presentation and underlying CV status. Any electrolyte abnormalities should be corrected and broad spectrum IV antibiotics initiated. Vascular surgery or general surgery services should be consulted to determine the optimal management. Most patients with acute intestinal ischemia due to mesenteric arterial occlusion (or venous occlusive or nonocclusive mesenteric ischemia) will be started on anticoagulation, typically IV heparin, unless contraindications are present.6 Surgical treatment options include arterial embolectomy, arterial bypass, arterial stenting, arterial thrombolysis, or intra-arterial vasodilator infusion.
Case
An 89-year-old woman presented to the ED with the chief complaints of abdominal pain and nausea with vomiting. The patient stated that several hours prior, she had ingested an expired beverage, which she related to the sudden onset of her symptoms. The patient denied fever, chills, dysuria, or frequency. Her medical history was significant for chronic atrial fibrillation (AF) and congestive heart failure. The patient’s medications included metoprolol and furosemide; she was not on any anticoagulation medication.
On physical examination, the patient appeared her stated age, and was in moderate distress secondary to the abdominal pain. Vital signs were: temperature, 98.8oF; heart rate, 98 beats/min; respiratory rate, 20 breaths/min; and blood pressure, 116/72 mm Hg. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was unremarkable. On lung examination, breath sounds were equal bilaterally with bibasilar rales. The heart rhythm was irregularly irregular without murmurs, rubs, or gallops. The abdomen was soft to palpitation, but diffusely tender, without rebound, guarding, or mass. Rectal examination revealed normal tone and brown stool, and was trace positive for heme.
The emergency physician (EP) ordered an electrocardiogram (ECG), complete blood count, basic metabolic profile (BMP), urinalysis, and lipase test. The patient was administered intravenous (IV) normal saline at 75 cc/h, and morphine 4 mg and ondansetron 4 mg IV for the abdominal pain, nausea, and vomiting. She required several more doses of morphine due to the severity of the pain. The laboratory results included an elevated white blood count of 18.4 x 109/L with a left shift, but normal hemoglobin and hematocrit values. The ECG demonstrated AF with a controlled ventricular rate; there was no evidence of ischemia or injury. The BMP was remarkable for a slightly depressed potassium level (3.3 mEq/L), a decreased serum bicarbonate of 20 mEq/L, and evidence of renal insufficiency with a blood urea nitrogen of 28 mg/dL and a serum creatinine of 1.6 mg/dL. Given the ongoing severe pain, leukocytosis, metabolic acidosis, and lack of clear etiology, the EP ordered a computed tomography (CT) scan of the abdomen and pelvis; no IV contrast was ordered because of the abnormal renal function studies.
The radiologist interpreted the CT scan as essentially normal. The EP admitted the patient to the on-call hospitalist, who consulted both cardiology and gastroenterology services. During the night, the patient complained of increasing abdominal pain, and her abdomen became distended with peritoneal signs. She was taken emergently to the operating room in the early morning hours. A large segment of gangrenous small intestine was found upon exploration. The surgery was discontinued and comfort care measures were instituted. The patient died the following day.
The patient’s family sued the EP and the hospital for failure to make a timely diagnosis of mesenteric ischemia. They further stated that the EP should have ordered a CT angiogram (CTA) of the abdomen and pelvis. The defense argued that a contrast CT scan was contraindicated because of the patient’s poor renal function. A defense verdict was returned at trial.
Discussion
Elderly patients (defined as older than age 65 years) presenting to the ED with abdominal pain remain a diagnostic challenge for even the most seasoned clinician. While elderly patients with a chief complaint of abdominal pain represent only a small percentage of ED patients, approximately 50% to 66% of these patients will require hospitalization, while one-third will require a surgical intervention.1 The seriousness of this complaint in elderly patients is further emphasized by the fact that older patients with abdominal pain have a 6- to 8-fold increase in mortality compared to younger patients.2,3 This can be partially explained by the simple fact that the life-threatening causes of abdominal pain—abdominal aortic aneurysm, mesenteric ischemia, bowel perforation, volvulus, and acute bowel obstruction—occur more frequently (but not exclusively) in elderly patients. Historical risk factors for life-threatening causes of abdominal pain include: age older than 65 years, immunocompromised state, alcohol abuse, cardiovascular (CV) disease (eg, coronary artery disease, hypertension, AF), major comorbidities (eg, cancer, renal failure), and prior surgery or recent gastrointestinal instrumentation.1
The patient in this case had two risk factors for life-threatening causes of lower abdominal pain—age and AF. These are also two of the major risk factors for mesenteric ischemia, which was her ultimate diagnosis.
Acute mesenteric ischemia refers to the sudden onset of small intestinal hypoperfusion, frequently due to acute occlusion (embolism or thrombosis) of an intestinal artery, most commonly the superior mesenteric artery (SMA).4 The SMA supplies the entire small intestine except for the proximal duodenum. Other causes of acute mesenteric ischemia include venous occlusion (thrombosis) and nonocclusive mesenteric ischemia secondary to vasoconstriction from low-cardiac output or use of vasopressors.4
Thromboembolic occlusion of the SMA is the most common cause of acute mesenteric ischemia, accounting for 67% to 95% of cases.4 In addition to AF, the risk of arterial embolism is increased in patients with valvular disease, infective endocarditis, recent myocardial infarction, aortic atherosclerosis, or aortic aneurysm.4 Risk factors for thrombotic arterial occlusion include peripheral artery disease, advanced age, and low-cardiac output states.5
A frequent presentation of embolic mesenteric arterial ischemia, occurring in approximately one-third of cases, is an elderly patient with AF (or other source of embolism) and onset of severe, sudden abdominal pain out of proportion to physical examination. While nausea and vomiting are also common, bloody bowel movements are less frequent in the early course of the disease process.4 A history of a prior embolic event is present in approximately one-third of such patients.
On physical examination, the abdomen may be normal initially, or demonstrate only mild distention and tenderness without peritoneal signs. However, as the ischemia progresses, the abdomen becomes more distended, bowel sounds become absent, and peritoneal signs (ie, guarding and rebound) become apparent.6
The results of laboratory studies can suggest the diagnosis, but none are confirmatory. Laboratory findings may include a marked leukocytosis with left shift, an elevated hematocrit secondary to hemoconcentration, and metabolic acidosis. A helpful clinical pearl is to consider intestinal ischemia in the differential diagnosis of any patient with acute abdominal pain and metabolic acidosis.6 Serum lactate is frequently elevated (73%-94%) but a very nonspecific marker. Similarly, an arterial blood gas analysis may demonstrate metabolic acidosis. More recently, a normal D-dimer result has been used to help exclude the diagnosis of acute intestinal ischemia, since it is elevated in 96% of patients with the disease.6 Similar to lactate, an abnormal D-dimer result has a poor specificity (40%).6 Early in the disease course, nearly all laboratory studies may be normal.
Depending on the severity of the presentation, imaging can help make the definitive diagnosis. For patients with peritonitis or obvious bowel perforation, IV fluid resuscitation, IV antibiotics, and immediate surgical exploration are indicated. Plain radiographs of the abdomen offer little help, as many of the findings early in the disease course are nonspecific, and radiographs can be normal in 25% of cases.6 Ultrasound can identify arterial stenosis or occlusion of the SMA, but is frequently technically limited by the presence of air-filled loops of distended bowel.6 Magnetic resonance angiography has similar sensitivity and specificity as CTA for mesenteric arterial ischemia, and is actually more sensitive than CTA for mesenteric venous thrombosis; it also can be performed in patients with contrast allergy.6 However, CTA is performed more commonly because of its lower cost, greater speed, and wide availability.6 A CTA of the abdomen and pelvis (without oral contrast) is probably the best study for patients in whom mesenteric ischemia is high on the differential diagnosis.6 For patients with a less clear picture and a broader differential diagnosis, a CT scan of the abdomen/pelvis with both IV and oral contrast is preferred.7 Common findings on CT scan with IV/oral contrast in acute mesenteric ischemia include the following: bowel wall thickening, dilatation, stranding, bowel wall attenuation, abnormal enhancement, and pneumatosis. Unfortunately, many of these findings are nonspecific.7
Once the diagnosis of acute mesenteric ischemia is made, patients should be designated “nothing by mouth” and a nasogastric tube placed to decompress the bowel. These patients will require IV fluid resuscitation with normal saline. The amount and rate will depend on their clinical presentation and underlying CV status. Any electrolyte abnormalities should be corrected and broad spectrum IV antibiotics initiated. Vascular surgery or general surgery services should be consulted to determine the optimal management. Most patients with acute intestinal ischemia due to mesenteric arterial occlusion (or venous occlusive or nonocclusive mesenteric ischemia) will be started on anticoagulation, typically IV heparin, unless contraindications are present.6 Surgical treatment options include arterial embolectomy, arterial bypass, arterial stenting, arterial thrombolysis, or intra-arterial vasodilator infusion.
1. Kendall JL, Moreira ME. Evaluation of the adult with abdominal pain in the emergency department. UpToDate Web site. http://www.uptodate.com/contents/evaluation-of-the-adult-with-abdominal-pain-in-the-emergency-department. Updated September 29, 2016. Accessed November 30, 2016.
2. Lewis LM, Banet GA, Blanda M, Hustey FM, Meldon SW, Gerson LW. Etiology and clinical course of abdominal pain in senior patients: a prospective, multicenter study. J Gerontol A Biol Sci Med Sci. 2005;60(8):1071-1076.
3. Sanson TG, O’Keefe KP. Evaluation of abdominal pain in the elderly. Emerg Med Clin North Am. 1996;14(3):615.
4. Tendler DA, Lamont JT, Pearl G. Acute mesenteric arterial occlusion. UpToDate Web site. http://www.uptodate.com/contents/acute-mesenteric-arterial-occlusion. Updated May 27, 2015. Accessed November 30, 2016.
5. McKinsey JF, Gewertz BL. Acute mesenteric ischemia. Surg Clin North Am. 1997;77(2):307-318.
6. Tendler DA, Lamont JT. Overview of intestinal ischemia in adults. UpToDate Web site. http://www.uptodate.com/contents/overview-of-intestinal-ischemia-in-adults. Updated February 23, 2016. Accessed November 30, 2016.
7. Wiesner W. Khurana B, Ji H, Ros PR. CT of acute bowel ischemia. Radiology. 2003;226(3):635-650.
1. Kendall JL, Moreira ME. Evaluation of the adult with abdominal pain in the emergency department. UpToDate Web site. http://www.uptodate.com/contents/evaluation-of-the-adult-with-abdominal-pain-in-the-emergency-department. Updated September 29, 2016. Accessed November 30, 2016.
2. Lewis LM, Banet GA, Blanda M, Hustey FM, Meldon SW, Gerson LW. Etiology and clinical course of abdominal pain in senior patients: a prospective, multicenter study. J Gerontol A Biol Sci Med Sci. 2005;60(8):1071-1076.
3. Sanson TG, O’Keefe KP. Evaluation of abdominal pain in the elderly. Emerg Med Clin North Am. 1996;14(3):615.
4. Tendler DA, Lamont JT, Pearl G. Acute mesenteric arterial occlusion. UpToDate Web site. http://www.uptodate.com/contents/acute-mesenteric-arterial-occlusion. Updated May 27, 2015. Accessed November 30, 2016.
5. McKinsey JF, Gewertz BL. Acute mesenteric ischemia. Surg Clin North Am. 1997;77(2):307-318.
6. Tendler DA, Lamont JT. Overview of intestinal ischemia in adults. UpToDate Web site. http://www.uptodate.com/contents/overview-of-intestinal-ischemia-in-adults. Updated February 23, 2016. Accessed November 30, 2016.
7. Wiesner W. Khurana B, Ji H, Ros PR. CT of acute bowel ischemia. Radiology. 2003;226(3):635-650.
We can work it out: Should I hire my patient?
Dear Dr. Mossman,
Each month, I see my patient, Mr. R, for a 15-minute medication management appointment. At his latest visit, Mr. R mentioned his financial difficulties. He also observed that our office needed to have some carpentry work done—not a surprise, because he’s known in our area as one of the best carpenters around. He suggested that I hire him as payment for the next 6 appointments. What risks might I encounter if I oblige him?
Submitted by “Dr. Z”
Nearly 29 million Americans are uninsured,1 and even more have trouble accessing mental health care.2 Many psychiatrists struggle to provide affordable services while remaining financially viable.3,4 For outpatients with limited means to pay for care, spacing appointments to fit their budgets might compromise treatment.5 Simply not charging patients poses its own clinical and ethical challenges.6-8
As a result, some mental health professionals make barter arrangements to help their patients enter or continue treatment. To answer Dr. Z’s question on whether exchanging services might be a way to arrange matters with some patients, we explore:
- the idea of bartering for psychiatric treatment
- related ethical and legal considerations
- when and in what situations bartering might be appropriate.
Think of what I’m saying: Bartering for treatment
“Barter” refers to exchanging commodities, products, or services of equivalent value without using money.9 In 2010, Nevada Republican Senate candidate Sue Lowden encouraged barter for health care and harkened back to an earlier time where “they would bring a chicken to the doctor; they would say ‘I’ll paint your house.’”10
Such payment arrangements have been encouraged as health care has become increasingly commoditized.11-13 This happens through both direct barter between physician and patient and barter exchanges. Barter exchange systems have been set up on Web sites (as of 2013, at least 400 such online exchanges were available14), local communities,11,15 and social programs. For example, through the “Swapping Guns for Therapy” program, psychologists in California gave free or reduced-fee care for people who traded in their guns.16
Try to see it my way: A prevailing view of barter
Several psychiatrists recommend against bartering for treatment, for a variety of reasons.7,8,17-19 Simon18 argues that a stable fee policy is part of a proper therapeutic framework, and money is “the only acceptable medium of exchange when receiving payment from patients.” Emotional distress and the power differential inherent in treatment might prevent a patient from making an accurate assessment of the value of the bartered goods or services,7,8,17,18,20 which could lead to future claims of undue influence from trading goods or services below market value.17 To avoid the possibility of exploitating the patient, Simon18 recommends that the psychiatrist’s professional fee be “the only material benefit received from the patient.”
The American Psychiatric Association’s code of ethics states that “it is not ethical to switch a doctor–patient relationship to an employer–employee one … and, in most cases, such an arrangement would be unethical.”21 In some therapeutic settings, employing a patient risks inappropriate self-disclosure and intrusion.16
More than other physicians, psychiatrists pay special attention to professional boundaries, the technical term for the “edge of appropriate behavior,” within which safe, effective care can occur.22,23 Although some boundary crossings can be harmless and even constructive, repeated boundary crossings are the forerunners to improper behavior, including sexual relationships with patients.24-26
Out of concern that bartering could become the first step down a slippery ethical slope toward patient exploitation, mental health clinicians have deemed the practice “ethically troubling,”19 said it did “not usually work out well,”7 and declared it “so fraught with risks for both parties that it seem[ed] illogical to even consider it as an option.”27
While I see it your way: What barter proponents say
Reports of bartering for chickens28 and purchasing fuel from a patient in remote Alaska29 show that not all physicians agree and why they feel that professional codes of ethics reflect an urban bias.28,29 In many rural areas and small towns, access to mental health services is limited, and patients often interact with their doctors outside of clinical encounters.23,29-31
Bartering can benefit a physician’s practice by:
- reducing the need to discount services
- eliminating bureaucratic burdens of traditional insurance arrangements
- facilitating development of a patient base
- allowing patients choice and flexibility in seeking medical care.6,16,32
Bartering could confer certain clinical benefits, such as:
- enhancing trust and empathy32
- encouraging patients to make their needs known constructively6
- modeling financial self-care6
- helping the doctor to feel fairly compensated for providing thoughtful care6
- acknowledging the patient’s cultural values15,33
- affirming that patients and doctors both produce things of value.16
I have always thought: Other ethical models
An ethical approach to bartering that requires careful thought and respect for the patient’s needs appears consistent with a primary goal of treatment: “to increase the capacity of individuals to make more rational choices in their lives and to be relatively freer from disabling conflicts.”20 Some authors criticize slippery-slope arguments and strict-rule ethical approaches as being too rigid, limiting, or risk-averse.22,26,34 In Table 1,6,8,16,18,27,29-31,35-37 we list several factors that might weigh for or against a decision to enter into a barter arrangement as payment for care.
In a similar manner, Martinez33,38 proposed a graded-risk framework that encourages examination of potential harms and benefits of a decision, potential coercive or exploitative elements, the clinician’s intentions and aspiration to professional ideals, and the context of the decision. Within this framework, some bartering arrangements might be encouraged and, perhaps, even obligatory because of the potential benefits to the patient; other arrangements (eg, trading psychotherapy for menial services) might be unjustifiable. Martinez38 argues that this approach fosters mutual decision-making with patients, discourages physician paternalism, and “demands that we struggle with the particulars with each case.”
Gottlieb’s decision-making model35 recognizes that trying to avoid all dual relationships is unrealistic and not all dual relationships are exploitative. Instead, a clinician must assess 3 dimensions of current and proposed relationships:
- the degree of power differential
- the duration of treatment
- the clarity of termination.
The decision-making process also requires involvement of the patient, who if “unable to recognize the dilemma or is unwilling to consider the issues before deciding, should be considered at risk, and the contemplated relationship rejected.”35
So I will ask you once again: Dr. Z’s decision
In the case of Dr. Z and Mr. R, a barter arrangement might work in the sense of permitting and sustaining good care. Mr. R suggested the idea and might not be able to afford care without it. Nothing in Dr. Z’s description suggests that Mr. R has personality characteristics or other conditions that would compromise his ability to give informed consent or to understand the nuances of a barter arrangement. Dr. Z is not providing a treatment (eg, psychodynamic therapy) that a barter arrangement could contaminate. That the arrangement would be circumscribed limits the effect of a power differential, as would its brief duration and defined termination endpoint. Dr. Z’s letter to the authors also shows his willingness to seek consultation.
There’s a chance that we may fall apart: Reasons for caution
Martinez’s graded-risk approach recognizes reasons for caution:
- the risk of harm to the patient or doctor–patient relationship
- the uncertain benefit to the patient
- the blurring of Dr. Z’s self-interest and Mr. R’s needs
- some ambiguity about possible exploitation.
Dr. Z and Mr. R have not discussed the value of Mr. R’s work—which might create a rift between them—and despite Mr. R’s reputation, other carpenters are available. Future med-check appointments will give them little time to explore and discuss the meanings of the barter.
Any proposed barter arrangement creates some clinical perils that can be particularly salient in mental health treatment. Patients could view themselves as “special” or entitled to enhanced access to the doctor because of exchanged services, which could take a toll on the doctor.39 The physician’s objectivity might diminish, and the business aspect of their relationship could make both parties less comfortable when discussing sensitive information relevant to treatment.31,40 Also, the suggested barter is for services to be provided at Dr. Z’s office, where confidentiality may be breeched and transference issues could arise.
A medical malpractice claim states that a doctor has breached a duty of care to a patient such that harm (or “damages”) resulted.41 Should Dr. Z and Mr. R’s barter agreement turn sour and harm follow, Mr. R could sue for recovery of damages based of a claim of duress, undue influence, or other aspects of the doctor–patient power differential.27,42,43 Given the published views we have described, a psychiatrist who barters also may be viewed as violating state regulations that measure the standard of care against generally accepted practice.
Only time will tell if I am right or I am wrong
If you face a situation similar to Dr. Z’s and want to consider a barter arrangement, you can take several steps to mitigate potential risk to your patient and ensure competent care (Table 25,6,15,16,32,35,39,40,44-47). One of the most important steps is to seek ongoing consultation, both before and after a decision to barter. Ideally, the consulting colleague would know you and your circumstances and would have sufficient clinical grasp of the patient to make an informed assessment of risks and benefits.35 This consultation, as well as your own rationale for acting on recommendations, should be thoroughly documented in the patient’s records.26,44,45
Certain types of barter should be off limits, including:
- trading prescription drugs for goods or services
- trading for services that tie into the success of one’s business (eg, business advising or marketing)16
- offering treatment in exchange for illegal or ethically unacceptable services.48
Beyond ethical considerations are some practical issues. The Internal Revenue Service has specific rules regarding taxation of bartered goods and services, which must be included as taxable income.46 If possible, an independent agent should appraise the traded goods or services before the agreement.6 When working in a group practice, the clinician might have to figure out how to allocate the received goods or services such as shared overhead costs.28 Preferably, the patient’s goods or services should be provided before care is delivered.16 If not, the duration of services rendered should be limited, and either party should have the option to disengage from the relationship if one feels dissatisfied.16
A written contract, discussed ahead of time, can be a sound way to summarize the terms of the arrangement. Both sides also should consider what would happen if an injury occurred.16 Finally, you must adhere to any relevant state laws regarding payment for services, particularly if the patient has health insurance.32
If the bartering arrangement does not work, you should take an open and non-defensive approach. If you believe you have made a mistake, consider apologizing.45
1. Kaiser Commission on Medicaid and the Uninsured. Key facts about the uninsured population. http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population. Published September 29, 2016. Accessed October 7, 2016.
2. National Alliance on Mental Illness. A long road ahead: achieving true parity in mental health and substance use care. https://www.nami.org/About-NAMI/Publications-Reports/Public-Policy-Reports/A-Long-Road-Ahead/2015-ALongRoadAhead.pdf. Published April 2015. Accessed October 7, 2016.
3. Insel T. Director’s blog: the paradox of parity. May 30, 2014. https://www.nimh.nih.gov/about/director/2014/the-paradox-of-parity.shtml. Published May 30, 2014. Accessed October 7, 2016.
4. Bishop TF, Press MJ, Keyhani S, et al. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181.
5. What do you do when patients cannot pay? Psychiatry (Edgmont). 2009;6(5):51-52.
6. Hill M. Barter: ethical considerations in psychotherapy. Women Ther. 2000;22(3):81-91.
7. Simon RI. Commentary: treatment boundaries—flexible guidelines, not rigid standards. J Am Acad Psychiatry Law. 2001;29(3):287-289.
8. Simon RI, Williams IC. Maintaining treatment boundaries in small communities and rural areas. Psychiatr Serv. 1999;50(11):1440-1446.
9. Compact edition of the Oxford English dictionary. New York, NY: Oxford University Press; 1971:171.
10. Coolican JP. Sue Lowden stands by health care plan. Las Vegas Sun. http://lasvegassun.com/news/2010/apr/20/sue-lowden-draws-fire-repeating-health-care-barter. Published April 20, 2010. Accessed September 20, 2016.
11. Consumer Reports. Barter sometimes allow patients to pay for health care they otherwise could not afford. Washington Post. https://www.washingtonpost.com/national/health-science/barter-sometimes-allow-patients-to-pay-for-health-care-they-otherwise-could-not-afford/2013/09/30/e7e5a55e-069d-11e3-88d6-d5795fab4637_story.html. Published September 20, 2013. Accessed September 27, 2016.
12. Ellis B. MediBid auction site lets doctors bid for patients. CNN Money. http://money.cnn.com/2014/01/09/pf/insurance/medibid. Published January 9, 2014. Accessed September 23, 2016.
13. Ambrosino B. Surgery for sale: the ethics of health care bartering in a social media marketplace. http://hub.jhu.edu/2014/01/16/hopkins-ethicist-ponders-medibid. Published January 16, 2014. Accessed September 23, 2016.
14. Thomas C. When patients barter for health care. https://ethicalnag.org/2013/07/30/barter. Published July 30, 2016. Accessed October 9, 2016.
15. Syme G. Fetters or freedom: dual relationships in counselling. Int J Adv Counselling. 2006;28(1):57-69.
16. Zur O. Bartering in psychotherapy and counselling: complexities, case studies and guidelines. New Therapist. 2008;58:18-26.
17. Simon RI. The psychiatrist as a fiduciary: avoiding the double agent role. Psychiatric Annals. 1987;17(9):622-626.
18. Simon RI. Treatment boundary violations: clinical, ethical, and legal considerations. Bull Am Acad Psychiatry Law. 1992;20(3):269-288.
19. Walker R, Clark JJ. Heading off boundary problems: clinical supervision as risk management. Psychiatr Serv. 1999;50(11):1435-1439.
20. Malmquist CP, Norman MT. Psychiatrist-patient boundary issues following treatment termination. Am J Psychiatry. 2001;158(7):1010-1018.
21. American Psychiatric Association. The opinions of the ethics committee on the principles of medical ethics, with annotations especially applicable to psychiatry. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2016. Accessed October 4, 2016.
22. Gutheil TG, Gabbard GO. Misuses and misunderstandings of boundary theory in clinical and regulatory settings. Am J Psychiatry. 1998;155(3):409-414.
23. Crowden A. Professional boundaries and the ethics of dual and multiple overlapping relationships in psychotherapy. Monash Bioeth Rev. 2008;27(4):10-27.
24. Gabbard GO. Commentary: boundaries, culture, and psychotherapy. J Am Acad Psychiatry Law. 2001;29(3):284-286.
25. Kroll J. Boundary violations: a culture-bound syndrome. J Am Acad Psychiatry Law. 2001;29(3):274-283.
26. Gottlieb MC, Younggren JN. Is there a slippery slope? Considerations regarding multiple relationships and risk management. Professional Psychology: Research and Practice. 2009;40(6):564-557.
27. Woody RH. Bartering for psychological services. Professional Psychology: Research and Practice. 1998;29(2):174-178.
28. Bartering for medical care. MGMA Connex. 2008;8(6):11.
29. Roberts LW, Battaglia J, Epstein RS. Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatr Serv. 1994;50(4):497-503.
30. Endacott R, Wood A, Judd F, et al. Impact and management of dual relationships in metropolitan, regional and rural mental health practice. Aust N Z J Psychiatry. 2006;40(11-12):987-994.
31. Scopelliti J, Judd F, Grigg M, et al. Dual relationships in mental health practice: issues for clinicians in rural settings. Aust N Z J Psychiatry. 2004;38(11-12):953-959.
32. Ayers AA. Bartering basics for the urgent care operator. http://www.alanayersurgentcare.com/Linked_Files/2013_Articles/Ayers_UCAOA_Bartering_%20Basics_2012_01_09.pdf. Accessed September 23, 2016.
33. Savin D, Martinez R. Cross-cultural boundary dilemmas: a graded-risk assessment approach. Transcult Psychiatry. 2006;42(2):243-258.
34. Glass LL. The gray areas of boundary crossings and violations. Am J Psychother. 2003;57(4):429-444.
35. Gottlieb MC. Avoiding exploitive dual relationships: a decision-making model. Psychotherapy (Chic). 1993;30(1):41-48.
36. Lane JA. The ethical implications of bartering for mental health services: examining interdisciplinary ethical standards. http://pdxscholar.library.pdx.edu/coun_fac/36. Published 2012. Accessed October 17, 2016.
37. Miller RD, Maier GJ. Nonsexual boundary violations: sauce for the gander. J Psychiatry Law. 2002;30(3):309-329.
38. Martinez R. A model for boundary dilemmas: ethical decision-making in the patient-professional relationship. Ethical Hum Sci Serv. 2000;2(1):43-61.
39. Salmon K, Klijnsma M. Boundary issues: employing patients as staff? Br J Gen Pract. 2009;59(558):56-57.
40. College of Physicians and Surgeons Ontario. Hiring patients may compromise physician-patient relationship. Dialogue. 2015;3:47.
41. Bal S. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467(2):339-347.
42. What puts a psychiatrist at risk for a malpractice lawsuit? Psychiatry (Edgmont). 2009;6(8):38-39.
43. Geis v Landau, 117 Misc2d 396 (NY Misc 1983).
44. Nisselle P. Danger zone. When boundaries are crossed in the doctor-patient relationship. Aust Fam Physician. 2000;29(6):541-544.
45. Pope KS, Keith-Spiegel P. A practical approach to boundaries in psychotherapy: making decisions, bypassing blunders, and mending fences. J Clin Psychol. 2008;64(5):638-652.
46. IRS Publication 17. https://www.irs.gov/publications/p17/ch12.html. Published 2015. Accessed October 5, 2016.
47. Epstein RS, Simon RI. The exploitation index: an early warning indicator of boundary violations in psychotherapy. Bull Menninger Clin. 1990;54(4):450-465.
48. Skutch J. Savannah doctor accused of trading drugs for sex with strippers. Augusta Chronicle. http://chronicle.augusta.com/news/crime-courts/2013-01-31/savannah-doctor-accused-trading-drugs-sex-strippers. Published January 31, 2013. Accessed October 16, 2016.
Dear Dr. Mossman,
Each month, I see my patient, Mr. R, for a 15-minute medication management appointment. At his latest visit, Mr. R mentioned his financial difficulties. He also observed that our office needed to have some carpentry work done—not a surprise, because he’s known in our area as one of the best carpenters around. He suggested that I hire him as payment for the next 6 appointments. What risks might I encounter if I oblige him?
Submitted by “Dr. Z”
Nearly 29 million Americans are uninsured,1 and even more have trouble accessing mental health care.2 Many psychiatrists struggle to provide affordable services while remaining financially viable.3,4 For outpatients with limited means to pay for care, spacing appointments to fit their budgets might compromise treatment.5 Simply not charging patients poses its own clinical and ethical challenges.6-8
As a result, some mental health professionals make barter arrangements to help their patients enter or continue treatment. To answer Dr. Z’s question on whether exchanging services might be a way to arrange matters with some patients, we explore:
- the idea of bartering for psychiatric treatment
- related ethical and legal considerations
- when and in what situations bartering might be appropriate.
Think of what I’m saying: Bartering for treatment
“Barter” refers to exchanging commodities, products, or services of equivalent value without using money.9 In 2010, Nevada Republican Senate candidate Sue Lowden encouraged barter for health care and harkened back to an earlier time where “they would bring a chicken to the doctor; they would say ‘I’ll paint your house.’”10
Such payment arrangements have been encouraged as health care has become increasingly commoditized.11-13 This happens through both direct barter between physician and patient and barter exchanges. Barter exchange systems have been set up on Web sites (as of 2013, at least 400 such online exchanges were available14), local communities,11,15 and social programs. For example, through the “Swapping Guns for Therapy” program, psychologists in California gave free or reduced-fee care for people who traded in their guns.16
Try to see it my way: A prevailing view of barter
Several psychiatrists recommend against bartering for treatment, for a variety of reasons.7,8,17-19 Simon18 argues that a stable fee policy is part of a proper therapeutic framework, and money is “the only acceptable medium of exchange when receiving payment from patients.” Emotional distress and the power differential inherent in treatment might prevent a patient from making an accurate assessment of the value of the bartered goods or services,7,8,17,18,20 which could lead to future claims of undue influence from trading goods or services below market value.17 To avoid the possibility of exploitating the patient, Simon18 recommends that the psychiatrist’s professional fee be “the only material benefit received from the patient.”
The American Psychiatric Association’s code of ethics states that “it is not ethical to switch a doctor–patient relationship to an employer–employee one … and, in most cases, such an arrangement would be unethical.”21 In some therapeutic settings, employing a patient risks inappropriate self-disclosure and intrusion.16
More than other physicians, psychiatrists pay special attention to professional boundaries, the technical term for the “edge of appropriate behavior,” within which safe, effective care can occur.22,23 Although some boundary crossings can be harmless and even constructive, repeated boundary crossings are the forerunners to improper behavior, including sexual relationships with patients.24-26
Out of concern that bartering could become the first step down a slippery ethical slope toward patient exploitation, mental health clinicians have deemed the practice “ethically troubling,”19 said it did “not usually work out well,”7 and declared it “so fraught with risks for both parties that it seem[ed] illogical to even consider it as an option.”27
While I see it your way: What barter proponents say
Reports of bartering for chickens28 and purchasing fuel from a patient in remote Alaska29 show that not all physicians agree and why they feel that professional codes of ethics reflect an urban bias.28,29 In many rural areas and small towns, access to mental health services is limited, and patients often interact with their doctors outside of clinical encounters.23,29-31
Bartering can benefit a physician’s practice by:
- reducing the need to discount services
- eliminating bureaucratic burdens of traditional insurance arrangements
- facilitating development of a patient base
- allowing patients choice and flexibility in seeking medical care.6,16,32
Bartering could confer certain clinical benefits, such as:
- enhancing trust and empathy32
- encouraging patients to make their needs known constructively6
- modeling financial self-care6
- helping the doctor to feel fairly compensated for providing thoughtful care6
- acknowledging the patient’s cultural values15,33
- affirming that patients and doctors both produce things of value.16
I have always thought: Other ethical models
An ethical approach to bartering that requires careful thought and respect for the patient’s needs appears consistent with a primary goal of treatment: “to increase the capacity of individuals to make more rational choices in their lives and to be relatively freer from disabling conflicts.”20 Some authors criticize slippery-slope arguments and strict-rule ethical approaches as being too rigid, limiting, or risk-averse.22,26,34 In Table 1,6,8,16,18,27,29-31,35-37 we list several factors that might weigh for or against a decision to enter into a barter arrangement as payment for care.
In a similar manner, Martinez33,38 proposed a graded-risk framework that encourages examination of potential harms and benefits of a decision, potential coercive or exploitative elements, the clinician’s intentions and aspiration to professional ideals, and the context of the decision. Within this framework, some bartering arrangements might be encouraged and, perhaps, even obligatory because of the potential benefits to the patient; other arrangements (eg, trading psychotherapy for menial services) might be unjustifiable. Martinez38 argues that this approach fosters mutual decision-making with patients, discourages physician paternalism, and “demands that we struggle with the particulars with each case.”
Gottlieb’s decision-making model35 recognizes that trying to avoid all dual relationships is unrealistic and not all dual relationships are exploitative. Instead, a clinician must assess 3 dimensions of current and proposed relationships:
- the degree of power differential
- the duration of treatment
- the clarity of termination.
The decision-making process also requires involvement of the patient, who if “unable to recognize the dilemma or is unwilling to consider the issues before deciding, should be considered at risk, and the contemplated relationship rejected.”35
So I will ask you once again: Dr. Z’s decision
In the case of Dr. Z and Mr. R, a barter arrangement might work in the sense of permitting and sustaining good care. Mr. R suggested the idea and might not be able to afford care without it. Nothing in Dr. Z’s description suggests that Mr. R has personality characteristics or other conditions that would compromise his ability to give informed consent or to understand the nuances of a barter arrangement. Dr. Z is not providing a treatment (eg, psychodynamic therapy) that a barter arrangement could contaminate. That the arrangement would be circumscribed limits the effect of a power differential, as would its brief duration and defined termination endpoint. Dr. Z’s letter to the authors also shows his willingness to seek consultation.
There’s a chance that we may fall apart: Reasons for caution
Martinez’s graded-risk approach recognizes reasons for caution:
- the risk of harm to the patient or doctor–patient relationship
- the uncertain benefit to the patient
- the blurring of Dr. Z’s self-interest and Mr. R’s needs
- some ambiguity about possible exploitation.
Dr. Z and Mr. R have not discussed the value of Mr. R’s work—which might create a rift between them—and despite Mr. R’s reputation, other carpenters are available. Future med-check appointments will give them little time to explore and discuss the meanings of the barter.
Any proposed barter arrangement creates some clinical perils that can be particularly salient in mental health treatment. Patients could view themselves as “special” or entitled to enhanced access to the doctor because of exchanged services, which could take a toll on the doctor.39 The physician’s objectivity might diminish, and the business aspect of their relationship could make both parties less comfortable when discussing sensitive information relevant to treatment.31,40 Also, the suggested barter is for services to be provided at Dr. Z’s office, where confidentiality may be breeched and transference issues could arise.
A medical malpractice claim states that a doctor has breached a duty of care to a patient such that harm (or “damages”) resulted.41 Should Dr. Z and Mr. R’s barter agreement turn sour and harm follow, Mr. R could sue for recovery of damages based of a claim of duress, undue influence, or other aspects of the doctor–patient power differential.27,42,43 Given the published views we have described, a psychiatrist who barters also may be viewed as violating state regulations that measure the standard of care against generally accepted practice.
Only time will tell if I am right or I am wrong
If you face a situation similar to Dr. Z’s and want to consider a barter arrangement, you can take several steps to mitigate potential risk to your patient and ensure competent care (Table 25,6,15,16,32,35,39,40,44-47). One of the most important steps is to seek ongoing consultation, both before and after a decision to barter. Ideally, the consulting colleague would know you and your circumstances and would have sufficient clinical grasp of the patient to make an informed assessment of risks and benefits.35 This consultation, as well as your own rationale for acting on recommendations, should be thoroughly documented in the patient’s records.26,44,45
Certain types of barter should be off limits, including:
- trading prescription drugs for goods or services
- trading for services that tie into the success of one’s business (eg, business advising or marketing)16
- offering treatment in exchange for illegal or ethically unacceptable services.48
Beyond ethical considerations are some practical issues. The Internal Revenue Service has specific rules regarding taxation of bartered goods and services, which must be included as taxable income.46 If possible, an independent agent should appraise the traded goods or services before the agreement.6 When working in a group practice, the clinician might have to figure out how to allocate the received goods or services such as shared overhead costs.28 Preferably, the patient’s goods or services should be provided before care is delivered.16 If not, the duration of services rendered should be limited, and either party should have the option to disengage from the relationship if one feels dissatisfied.16
A written contract, discussed ahead of time, can be a sound way to summarize the terms of the arrangement. Both sides also should consider what would happen if an injury occurred.16 Finally, you must adhere to any relevant state laws regarding payment for services, particularly if the patient has health insurance.32
If the bartering arrangement does not work, you should take an open and non-defensive approach. If you believe you have made a mistake, consider apologizing.45
Dear Dr. Mossman,
Each month, I see my patient, Mr. R, for a 15-minute medication management appointment. At his latest visit, Mr. R mentioned his financial difficulties. He also observed that our office needed to have some carpentry work done—not a surprise, because he’s known in our area as one of the best carpenters around. He suggested that I hire him as payment for the next 6 appointments. What risks might I encounter if I oblige him?
Submitted by “Dr. Z”
Nearly 29 million Americans are uninsured,1 and even more have trouble accessing mental health care.2 Many psychiatrists struggle to provide affordable services while remaining financially viable.3,4 For outpatients with limited means to pay for care, spacing appointments to fit their budgets might compromise treatment.5 Simply not charging patients poses its own clinical and ethical challenges.6-8
As a result, some mental health professionals make barter arrangements to help their patients enter or continue treatment. To answer Dr. Z’s question on whether exchanging services might be a way to arrange matters with some patients, we explore:
- the idea of bartering for psychiatric treatment
- related ethical and legal considerations
- when and in what situations bartering might be appropriate.
Think of what I’m saying: Bartering for treatment
“Barter” refers to exchanging commodities, products, or services of equivalent value without using money.9 In 2010, Nevada Republican Senate candidate Sue Lowden encouraged barter for health care and harkened back to an earlier time where “they would bring a chicken to the doctor; they would say ‘I’ll paint your house.’”10
Such payment arrangements have been encouraged as health care has become increasingly commoditized.11-13 This happens through both direct barter between physician and patient and barter exchanges. Barter exchange systems have been set up on Web sites (as of 2013, at least 400 such online exchanges were available14), local communities,11,15 and social programs. For example, through the “Swapping Guns for Therapy” program, psychologists in California gave free or reduced-fee care for people who traded in their guns.16
Try to see it my way: A prevailing view of barter
Several psychiatrists recommend against bartering for treatment, for a variety of reasons.7,8,17-19 Simon18 argues that a stable fee policy is part of a proper therapeutic framework, and money is “the only acceptable medium of exchange when receiving payment from patients.” Emotional distress and the power differential inherent in treatment might prevent a patient from making an accurate assessment of the value of the bartered goods or services,7,8,17,18,20 which could lead to future claims of undue influence from trading goods or services below market value.17 To avoid the possibility of exploitating the patient, Simon18 recommends that the psychiatrist’s professional fee be “the only material benefit received from the patient.”
The American Psychiatric Association’s code of ethics states that “it is not ethical to switch a doctor–patient relationship to an employer–employee one … and, in most cases, such an arrangement would be unethical.”21 In some therapeutic settings, employing a patient risks inappropriate self-disclosure and intrusion.16
More than other physicians, psychiatrists pay special attention to professional boundaries, the technical term for the “edge of appropriate behavior,” within which safe, effective care can occur.22,23 Although some boundary crossings can be harmless and even constructive, repeated boundary crossings are the forerunners to improper behavior, including sexual relationships with patients.24-26
Out of concern that bartering could become the first step down a slippery ethical slope toward patient exploitation, mental health clinicians have deemed the practice “ethically troubling,”19 said it did “not usually work out well,”7 and declared it “so fraught with risks for both parties that it seem[ed] illogical to even consider it as an option.”27
While I see it your way: What barter proponents say
Reports of bartering for chickens28 and purchasing fuel from a patient in remote Alaska29 show that not all physicians agree and why they feel that professional codes of ethics reflect an urban bias.28,29 In many rural areas and small towns, access to mental health services is limited, and patients often interact with their doctors outside of clinical encounters.23,29-31
Bartering can benefit a physician’s practice by:
- reducing the need to discount services
- eliminating bureaucratic burdens of traditional insurance arrangements
- facilitating development of a patient base
- allowing patients choice and flexibility in seeking medical care.6,16,32
Bartering could confer certain clinical benefits, such as:
- enhancing trust and empathy32
- encouraging patients to make their needs known constructively6
- modeling financial self-care6
- helping the doctor to feel fairly compensated for providing thoughtful care6
- acknowledging the patient’s cultural values15,33
- affirming that patients and doctors both produce things of value.16
I have always thought: Other ethical models
An ethical approach to bartering that requires careful thought and respect for the patient’s needs appears consistent with a primary goal of treatment: “to increase the capacity of individuals to make more rational choices in their lives and to be relatively freer from disabling conflicts.”20 Some authors criticize slippery-slope arguments and strict-rule ethical approaches as being too rigid, limiting, or risk-averse.22,26,34 In Table 1,6,8,16,18,27,29-31,35-37 we list several factors that might weigh for or against a decision to enter into a barter arrangement as payment for care.
In a similar manner, Martinez33,38 proposed a graded-risk framework that encourages examination of potential harms and benefits of a decision, potential coercive or exploitative elements, the clinician’s intentions and aspiration to professional ideals, and the context of the decision. Within this framework, some bartering arrangements might be encouraged and, perhaps, even obligatory because of the potential benefits to the patient; other arrangements (eg, trading psychotherapy for menial services) might be unjustifiable. Martinez38 argues that this approach fosters mutual decision-making with patients, discourages physician paternalism, and “demands that we struggle with the particulars with each case.”
Gottlieb’s decision-making model35 recognizes that trying to avoid all dual relationships is unrealistic and not all dual relationships are exploitative. Instead, a clinician must assess 3 dimensions of current and proposed relationships:
- the degree of power differential
- the duration of treatment
- the clarity of termination.
The decision-making process also requires involvement of the patient, who if “unable to recognize the dilemma or is unwilling to consider the issues before deciding, should be considered at risk, and the contemplated relationship rejected.”35
So I will ask you once again: Dr. Z’s decision
In the case of Dr. Z and Mr. R, a barter arrangement might work in the sense of permitting and sustaining good care. Mr. R suggested the idea and might not be able to afford care without it. Nothing in Dr. Z’s description suggests that Mr. R has personality characteristics or other conditions that would compromise his ability to give informed consent or to understand the nuances of a barter arrangement. Dr. Z is not providing a treatment (eg, psychodynamic therapy) that a barter arrangement could contaminate. That the arrangement would be circumscribed limits the effect of a power differential, as would its brief duration and defined termination endpoint. Dr. Z’s letter to the authors also shows his willingness to seek consultation.
There’s a chance that we may fall apart: Reasons for caution
Martinez’s graded-risk approach recognizes reasons for caution:
- the risk of harm to the patient or doctor–patient relationship
- the uncertain benefit to the patient
- the blurring of Dr. Z’s self-interest and Mr. R’s needs
- some ambiguity about possible exploitation.
Dr. Z and Mr. R have not discussed the value of Mr. R’s work—which might create a rift between them—and despite Mr. R’s reputation, other carpenters are available. Future med-check appointments will give them little time to explore and discuss the meanings of the barter.
Any proposed barter arrangement creates some clinical perils that can be particularly salient in mental health treatment. Patients could view themselves as “special” or entitled to enhanced access to the doctor because of exchanged services, which could take a toll on the doctor.39 The physician’s objectivity might diminish, and the business aspect of their relationship could make both parties less comfortable when discussing sensitive information relevant to treatment.31,40 Also, the suggested barter is for services to be provided at Dr. Z’s office, where confidentiality may be breeched and transference issues could arise.
A medical malpractice claim states that a doctor has breached a duty of care to a patient such that harm (or “damages”) resulted.41 Should Dr. Z and Mr. R’s barter agreement turn sour and harm follow, Mr. R could sue for recovery of damages based of a claim of duress, undue influence, or other aspects of the doctor–patient power differential.27,42,43 Given the published views we have described, a psychiatrist who barters also may be viewed as violating state regulations that measure the standard of care against generally accepted practice.
Only time will tell if I am right or I am wrong
If you face a situation similar to Dr. Z’s and want to consider a barter arrangement, you can take several steps to mitigate potential risk to your patient and ensure competent care (Table 25,6,15,16,32,35,39,40,44-47). One of the most important steps is to seek ongoing consultation, both before and after a decision to barter. Ideally, the consulting colleague would know you and your circumstances and would have sufficient clinical grasp of the patient to make an informed assessment of risks and benefits.35 This consultation, as well as your own rationale for acting on recommendations, should be thoroughly documented in the patient’s records.26,44,45
Certain types of barter should be off limits, including:
- trading prescription drugs for goods or services
- trading for services that tie into the success of one’s business (eg, business advising or marketing)16
- offering treatment in exchange for illegal or ethically unacceptable services.48
Beyond ethical considerations are some practical issues. The Internal Revenue Service has specific rules regarding taxation of bartered goods and services, which must be included as taxable income.46 If possible, an independent agent should appraise the traded goods or services before the agreement.6 When working in a group practice, the clinician might have to figure out how to allocate the received goods or services such as shared overhead costs.28 Preferably, the patient’s goods or services should be provided before care is delivered.16 If not, the duration of services rendered should be limited, and either party should have the option to disengage from the relationship if one feels dissatisfied.16
A written contract, discussed ahead of time, can be a sound way to summarize the terms of the arrangement. Both sides also should consider what would happen if an injury occurred.16 Finally, you must adhere to any relevant state laws regarding payment for services, particularly if the patient has health insurance.32
If the bartering arrangement does not work, you should take an open and non-defensive approach. If you believe you have made a mistake, consider apologizing.45
1. Kaiser Commission on Medicaid and the Uninsured. Key facts about the uninsured population. http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population. Published September 29, 2016. Accessed October 7, 2016.
2. National Alliance on Mental Illness. A long road ahead: achieving true parity in mental health and substance use care. https://www.nami.org/About-NAMI/Publications-Reports/Public-Policy-Reports/A-Long-Road-Ahead/2015-ALongRoadAhead.pdf. Published April 2015. Accessed October 7, 2016.
3. Insel T. Director’s blog: the paradox of parity. May 30, 2014. https://www.nimh.nih.gov/about/director/2014/the-paradox-of-parity.shtml. Published May 30, 2014. Accessed October 7, 2016.
4. Bishop TF, Press MJ, Keyhani S, et al. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181.
5. What do you do when patients cannot pay? Psychiatry (Edgmont). 2009;6(5):51-52.
6. Hill M. Barter: ethical considerations in psychotherapy. Women Ther. 2000;22(3):81-91.
7. Simon RI. Commentary: treatment boundaries—flexible guidelines, not rigid standards. J Am Acad Psychiatry Law. 2001;29(3):287-289.
8. Simon RI, Williams IC. Maintaining treatment boundaries in small communities and rural areas. Psychiatr Serv. 1999;50(11):1440-1446.
9. Compact edition of the Oxford English dictionary. New York, NY: Oxford University Press; 1971:171.
10. Coolican JP. Sue Lowden stands by health care plan. Las Vegas Sun. http://lasvegassun.com/news/2010/apr/20/sue-lowden-draws-fire-repeating-health-care-barter. Published April 20, 2010. Accessed September 20, 2016.
11. Consumer Reports. Barter sometimes allow patients to pay for health care they otherwise could not afford. Washington Post. https://www.washingtonpost.com/national/health-science/barter-sometimes-allow-patients-to-pay-for-health-care-they-otherwise-could-not-afford/2013/09/30/e7e5a55e-069d-11e3-88d6-d5795fab4637_story.html. Published September 20, 2013. Accessed September 27, 2016.
12. Ellis B. MediBid auction site lets doctors bid for patients. CNN Money. http://money.cnn.com/2014/01/09/pf/insurance/medibid. Published January 9, 2014. Accessed September 23, 2016.
13. Ambrosino B. Surgery for sale: the ethics of health care bartering in a social media marketplace. http://hub.jhu.edu/2014/01/16/hopkins-ethicist-ponders-medibid. Published January 16, 2014. Accessed September 23, 2016.
14. Thomas C. When patients barter for health care. https://ethicalnag.org/2013/07/30/barter. Published July 30, 2016. Accessed October 9, 2016.
15. Syme G. Fetters or freedom: dual relationships in counselling. Int J Adv Counselling. 2006;28(1):57-69.
16. Zur O. Bartering in psychotherapy and counselling: complexities, case studies and guidelines. New Therapist. 2008;58:18-26.
17. Simon RI. The psychiatrist as a fiduciary: avoiding the double agent role. Psychiatric Annals. 1987;17(9):622-626.
18. Simon RI. Treatment boundary violations: clinical, ethical, and legal considerations. Bull Am Acad Psychiatry Law. 1992;20(3):269-288.
19. Walker R, Clark JJ. Heading off boundary problems: clinical supervision as risk management. Psychiatr Serv. 1999;50(11):1435-1439.
20. Malmquist CP, Norman MT. Psychiatrist-patient boundary issues following treatment termination. Am J Psychiatry. 2001;158(7):1010-1018.
21. American Psychiatric Association. The opinions of the ethics committee on the principles of medical ethics, with annotations especially applicable to psychiatry. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2016. Accessed October 4, 2016.
22. Gutheil TG, Gabbard GO. Misuses and misunderstandings of boundary theory in clinical and regulatory settings. Am J Psychiatry. 1998;155(3):409-414.
23. Crowden A. Professional boundaries and the ethics of dual and multiple overlapping relationships in psychotherapy. Monash Bioeth Rev. 2008;27(4):10-27.
24. Gabbard GO. Commentary: boundaries, culture, and psychotherapy. J Am Acad Psychiatry Law. 2001;29(3):284-286.
25. Kroll J. Boundary violations: a culture-bound syndrome. J Am Acad Psychiatry Law. 2001;29(3):274-283.
26. Gottlieb MC, Younggren JN. Is there a slippery slope? Considerations regarding multiple relationships and risk management. Professional Psychology: Research and Practice. 2009;40(6):564-557.
27. Woody RH. Bartering for psychological services. Professional Psychology: Research and Practice. 1998;29(2):174-178.
28. Bartering for medical care. MGMA Connex. 2008;8(6):11.
29. Roberts LW, Battaglia J, Epstein RS. Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatr Serv. 1994;50(4):497-503.
30. Endacott R, Wood A, Judd F, et al. Impact and management of dual relationships in metropolitan, regional and rural mental health practice. Aust N Z J Psychiatry. 2006;40(11-12):987-994.
31. Scopelliti J, Judd F, Grigg M, et al. Dual relationships in mental health practice: issues for clinicians in rural settings. Aust N Z J Psychiatry. 2004;38(11-12):953-959.
32. Ayers AA. Bartering basics for the urgent care operator. http://www.alanayersurgentcare.com/Linked_Files/2013_Articles/Ayers_UCAOA_Bartering_%20Basics_2012_01_09.pdf. Accessed September 23, 2016.
33. Savin D, Martinez R. Cross-cultural boundary dilemmas: a graded-risk assessment approach. Transcult Psychiatry. 2006;42(2):243-258.
34. Glass LL. The gray areas of boundary crossings and violations. Am J Psychother. 2003;57(4):429-444.
35. Gottlieb MC. Avoiding exploitive dual relationships: a decision-making model. Psychotherapy (Chic). 1993;30(1):41-48.
36. Lane JA. The ethical implications of bartering for mental health services: examining interdisciplinary ethical standards. http://pdxscholar.library.pdx.edu/coun_fac/36. Published 2012. Accessed October 17, 2016.
37. Miller RD, Maier GJ. Nonsexual boundary violations: sauce for the gander. J Psychiatry Law. 2002;30(3):309-329.
38. Martinez R. A model for boundary dilemmas: ethical decision-making in the patient-professional relationship. Ethical Hum Sci Serv. 2000;2(1):43-61.
39. Salmon K, Klijnsma M. Boundary issues: employing patients as staff? Br J Gen Pract. 2009;59(558):56-57.
40. College of Physicians and Surgeons Ontario. Hiring patients may compromise physician-patient relationship. Dialogue. 2015;3:47.
41. Bal S. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467(2):339-347.
42. What puts a psychiatrist at risk for a malpractice lawsuit? Psychiatry (Edgmont). 2009;6(8):38-39.
43. Geis v Landau, 117 Misc2d 396 (NY Misc 1983).
44. Nisselle P. Danger zone. When boundaries are crossed in the doctor-patient relationship. Aust Fam Physician. 2000;29(6):541-544.
45. Pope KS, Keith-Spiegel P. A practical approach to boundaries in psychotherapy: making decisions, bypassing blunders, and mending fences. J Clin Psychol. 2008;64(5):638-652.
46. IRS Publication 17. https://www.irs.gov/publications/p17/ch12.html. Published 2015. Accessed October 5, 2016.
47. Epstein RS, Simon RI. The exploitation index: an early warning indicator of boundary violations in psychotherapy. Bull Menninger Clin. 1990;54(4):450-465.
48. Skutch J. Savannah doctor accused of trading drugs for sex with strippers. Augusta Chronicle. http://chronicle.augusta.com/news/crime-courts/2013-01-31/savannah-doctor-accused-trading-drugs-sex-strippers. Published January 31, 2013. Accessed October 16, 2016.
1. Kaiser Commission on Medicaid and the Uninsured. Key facts about the uninsured population. http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population. Published September 29, 2016. Accessed October 7, 2016.
2. National Alliance on Mental Illness. A long road ahead: achieving true parity in mental health and substance use care. https://www.nami.org/About-NAMI/Publications-Reports/Public-Policy-Reports/A-Long-Road-Ahead/2015-ALongRoadAhead.pdf. Published April 2015. Accessed October 7, 2016.
3. Insel T. Director’s blog: the paradox of parity. May 30, 2014. https://www.nimh.nih.gov/about/director/2014/the-paradox-of-parity.shtml. Published May 30, 2014. Accessed October 7, 2016.
4. Bishop TF, Press MJ, Keyhani S, et al. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181.
5. What do you do when patients cannot pay? Psychiatry (Edgmont). 2009;6(5):51-52.
6. Hill M. Barter: ethical considerations in psychotherapy. Women Ther. 2000;22(3):81-91.
7. Simon RI. Commentary: treatment boundaries—flexible guidelines, not rigid standards. J Am Acad Psychiatry Law. 2001;29(3):287-289.
8. Simon RI, Williams IC. Maintaining treatment boundaries in small communities and rural areas. Psychiatr Serv. 1999;50(11):1440-1446.
9. Compact edition of the Oxford English dictionary. New York, NY: Oxford University Press; 1971:171.
10. Coolican JP. Sue Lowden stands by health care plan. Las Vegas Sun. http://lasvegassun.com/news/2010/apr/20/sue-lowden-draws-fire-repeating-health-care-barter. Published April 20, 2010. Accessed September 20, 2016.
11. Consumer Reports. Barter sometimes allow patients to pay for health care they otherwise could not afford. Washington Post. https://www.washingtonpost.com/national/health-science/barter-sometimes-allow-patients-to-pay-for-health-care-they-otherwise-could-not-afford/2013/09/30/e7e5a55e-069d-11e3-88d6-d5795fab4637_story.html. Published September 20, 2013. Accessed September 27, 2016.
12. Ellis B. MediBid auction site lets doctors bid for patients. CNN Money. http://money.cnn.com/2014/01/09/pf/insurance/medibid. Published January 9, 2014. Accessed September 23, 2016.
13. Ambrosino B. Surgery for sale: the ethics of health care bartering in a social media marketplace. http://hub.jhu.edu/2014/01/16/hopkins-ethicist-ponders-medibid. Published January 16, 2014. Accessed September 23, 2016.
14. Thomas C. When patients barter for health care. https://ethicalnag.org/2013/07/30/barter. Published July 30, 2016. Accessed October 9, 2016.
15. Syme G. Fetters or freedom: dual relationships in counselling. Int J Adv Counselling. 2006;28(1):57-69.
16. Zur O. Bartering in psychotherapy and counselling: complexities, case studies and guidelines. New Therapist. 2008;58:18-26.
17. Simon RI. The psychiatrist as a fiduciary: avoiding the double agent role. Psychiatric Annals. 1987;17(9):622-626.
18. Simon RI. Treatment boundary violations: clinical, ethical, and legal considerations. Bull Am Acad Psychiatry Law. 1992;20(3):269-288.
19. Walker R, Clark JJ. Heading off boundary problems: clinical supervision as risk management. Psychiatr Serv. 1999;50(11):1435-1439.
20. Malmquist CP, Norman MT. Psychiatrist-patient boundary issues following treatment termination. Am J Psychiatry. 2001;158(7):1010-1018.
21. American Psychiatric Association. The opinions of the ethics committee on the principles of medical ethics, with annotations especially applicable to psychiatry. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2016. Accessed October 4, 2016.
22. Gutheil TG, Gabbard GO. Misuses and misunderstandings of boundary theory in clinical and regulatory settings. Am J Psychiatry. 1998;155(3):409-414.
23. Crowden A. Professional boundaries and the ethics of dual and multiple overlapping relationships in psychotherapy. Monash Bioeth Rev. 2008;27(4):10-27.
24. Gabbard GO. Commentary: boundaries, culture, and psychotherapy. J Am Acad Psychiatry Law. 2001;29(3):284-286.
25. Kroll J. Boundary violations: a culture-bound syndrome. J Am Acad Psychiatry Law. 2001;29(3):274-283.
26. Gottlieb MC, Younggren JN. Is there a slippery slope? Considerations regarding multiple relationships and risk management. Professional Psychology: Research and Practice. 2009;40(6):564-557.
27. Woody RH. Bartering for psychological services. Professional Psychology: Research and Practice. 1998;29(2):174-178.
28. Bartering for medical care. MGMA Connex. 2008;8(6):11.
29. Roberts LW, Battaglia J, Epstein RS. Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatr Serv. 1994;50(4):497-503.
30. Endacott R, Wood A, Judd F, et al. Impact and management of dual relationships in metropolitan, regional and rural mental health practice. Aust N Z J Psychiatry. 2006;40(11-12):987-994.
31. Scopelliti J, Judd F, Grigg M, et al. Dual relationships in mental health practice: issues for clinicians in rural settings. Aust N Z J Psychiatry. 2004;38(11-12):953-959.
32. Ayers AA. Bartering basics for the urgent care operator. http://www.alanayersurgentcare.com/Linked_Files/2013_Articles/Ayers_UCAOA_Bartering_%20Basics_2012_01_09.pdf. Accessed September 23, 2016.
33. Savin D, Martinez R. Cross-cultural boundary dilemmas: a graded-risk assessment approach. Transcult Psychiatry. 2006;42(2):243-258.
34. Glass LL. The gray areas of boundary crossings and violations. Am J Psychother. 2003;57(4):429-444.
35. Gottlieb MC. Avoiding exploitive dual relationships: a decision-making model. Psychotherapy (Chic). 1993;30(1):41-48.
36. Lane JA. The ethical implications of bartering for mental health services: examining interdisciplinary ethical standards. http://pdxscholar.library.pdx.edu/coun_fac/36. Published 2012. Accessed October 17, 2016.
37. Miller RD, Maier GJ. Nonsexual boundary violations: sauce for the gander. J Psychiatry Law. 2002;30(3):309-329.
38. Martinez R. A model for boundary dilemmas: ethical decision-making in the patient-professional relationship. Ethical Hum Sci Serv. 2000;2(1):43-61.
39. Salmon K, Klijnsma M. Boundary issues: employing patients as staff? Br J Gen Pract. 2009;59(558):56-57.
40. College of Physicians and Surgeons Ontario. Hiring patients may compromise physician-patient relationship. Dialogue. 2015;3:47.
41. Bal S. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467(2):339-347.
42. What puts a psychiatrist at risk for a malpractice lawsuit? Psychiatry (Edgmont). 2009;6(8):38-39.
43. Geis v Landau, 117 Misc2d 396 (NY Misc 1983).
44. Nisselle P. Danger zone. When boundaries are crossed in the doctor-patient relationship. Aust Fam Physician. 2000;29(6):541-544.
45. Pope KS, Keith-Spiegel P. A practical approach to boundaries in psychotherapy: making decisions, bypassing blunders, and mending fences. J Clin Psychol. 2008;64(5):638-652.
46. IRS Publication 17. https://www.irs.gov/publications/p17/ch12.html. Published 2015. Accessed October 5, 2016.
47. Epstein RS, Simon RI. The exploitation index: an early warning indicator of boundary violations in psychotherapy. Bull Menninger Clin. 1990;54(4):450-465.
48. Skutch J. Savannah doctor accused of trading drugs for sex with strippers. Augusta Chronicle. http://chronicle.augusta.com/news/crime-courts/2013-01-31/savannah-doctor-accused-trading-drugs-sex-strippers. Published January 31, 2013. Accessed October 16, 2016.