User login
Patient with a breast mass: Why did she pursue litigation?
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
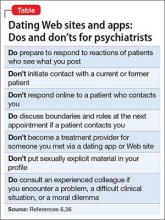
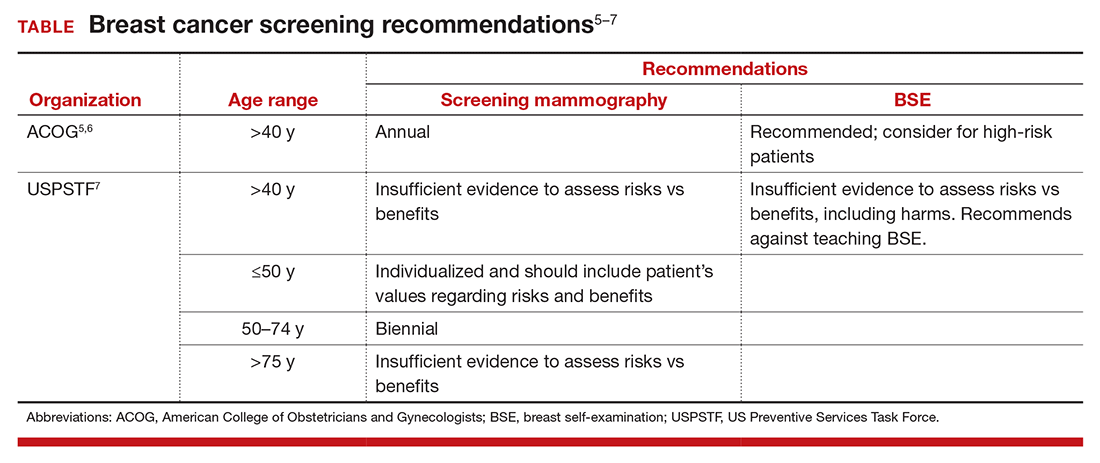
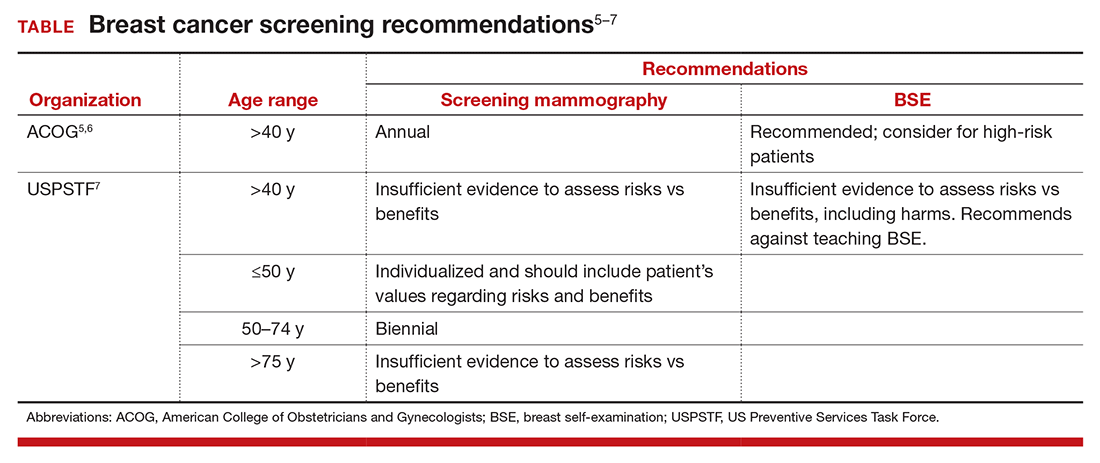
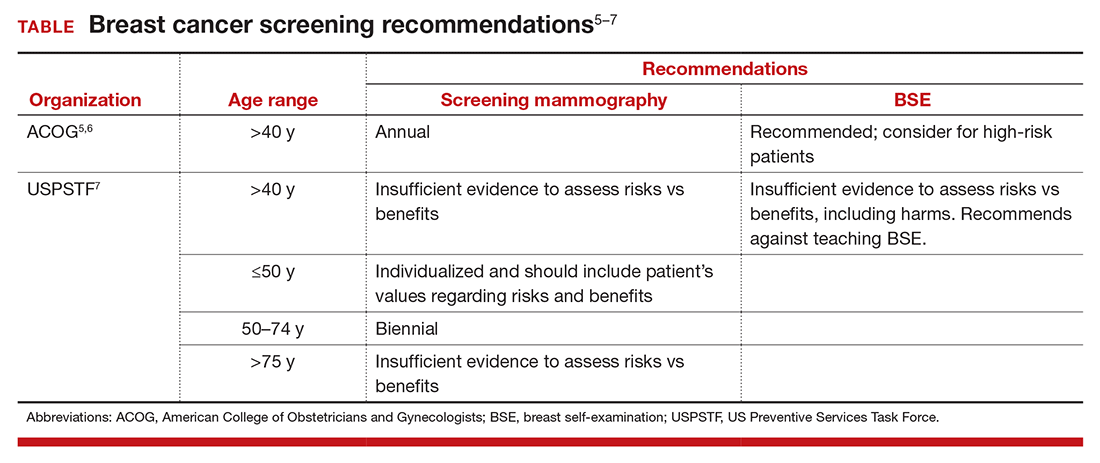
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
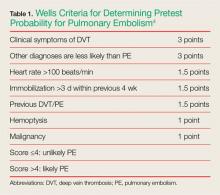
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
Malpractice Counsel: Missed Nodule
Case
A 48-year-old man presented to the ED with a 2-day history of cough and congestion. He described the cough as gradual in onset and, though initially nonproductive, it was now productive of green sputum. He denied fevers or chills, chest pain, nausea, vomiting, or diarrhea, and complained of only mild shortness of breath. His medical history was significant for hypertension, which was well managed with daily lisinopril-hydrochlorothiazide. He admitted to smoking one pack of cigarettes per day for the past 25 years, but denied alcohol or illicit drug use.
On physical examination, the patient’s vital signs were: blood pressure, 112/64 mm Hg; heart rate, 84 beats/min; respiratory rate, 20 breaths/min; and temperature, 98oF. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was normal. Auscultation of the lungs revealed bilateral breath sounds with scattered, faint expiratory wheezing; the heart had a regular rate and rhythm, without murmurs, rubs, or gallops.
The emergency physician (EP) ordered posteroanterior and lateral chest X-rays (CXR), which he interpreted as normal. He also ordered an albuterol handheld nebulizer treatment for the patient. After the albuterol treatment, the patient felt he was breathing more easily. The frequency of his cough had also decreased following treatment and, on re-examination, he exhibited no wheezing and was given azithromycin 500 mg orally in the ED. The EP diagnosed the patient with acute bronchitis and discharged him home with an albuterol metered dose inhaler with a spacer, and a 4-day course of azithromycin. He also encouraged the patient to quit smoking.
The next day the radiologist’s official reading of the patient’s radiographs included the finding of a very small pulmonary nodule, which was seen only on the lateral X-ray. The radiologist recommended a repeat CXR or a computed tomography (CT) scan of the chest in 6 months.
Unfortunately, the EP never saw this information, and the patient was not contacted regarding the abnormal radiology finding and the need for follow-up. Approximately 20 months later, the patient was diagnosed with lung cancer with metastasis to the thoracic spine and liver. Despite chemotherapy and radiation treatment, he died from the cancer.
The patient’s family brought a malpractice suit against the EP, stating that the cancer could have been successfully treated prior to any metastasis if the patient had been informed of the abnormal radiology findings at his ED visit 20 months prior. The EP argued that he never saw the official radiology report, and therefore had no knowledge of the need for follow-up. At trial, a jury verdict was returned in favor of the defendant.
Discussion
Unfortunately, some version of this scenario occurs on a frequent basis. While imaging studies account for the majority of such cases, the same situation can occur with abnormal laboratory results, body-fluid cultures, or pathology reports in which an abnormality is identified (eg, positive blood culture, missed fracture) but, for a myriad of reasons, the critical information does not get related to the patient.
Because of the episodic nature of the practice of emergency medicine (EM), a process must be in place to ensure any “positive” test results or findings discovered after patient discharge are reviewed and compared to the ED diagnosis, and that any “misses” result in notifying the patient and/or his or her primary care physician and arranging follow-up. In cases such as the one presented here, a system issue existed—one that was not due to any fault or oversight of the EP. Ideally, EM leadership should work closely with leadership from radiology and laboratory services and hospital risk management to develop such a process—one that will be effective every day, including weekends and holidays.
Missed fractures on radiographs are a common cause of malpractice litigation against EPs. In one review by Kachalia et al1 examining malpractice claims involving EPs, missed fractures on radiographs accounted for 19% (the most common) of the 79 missed diagnoses identified in their study.In a similar study by Karcz et al,2 missed fractures ranked second in frequency and dollars lost in malpractice cases against EPs in Massachusetts.
While missed lesions on CXR do not occur with the same frequency as missed fractures, the results are much more devastating when the lesion turns out to be malignant. Three common areas where such lesions are missed on CXR include: the apex of the lung, obscured by overlying clavicle and ribs; the retrocardiac region (as in the patient in this case); and the lung bases obscured by the diaphragm.
Emergency physicians are neither trained nor expected to identify every single abnormality—especially subtle radiographic abnormalities. This is why there are radiology overreads, and a system or process must be in place to ensure patients are informed of any positive findings and to arrange proper follow-up.
1. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
2. Karcz A, Korn R, Burke MC, et al. Malpractice claims against emergency physicians in Massachusetts: 1975-1993. Am J Emerg Med. 1996;14(4):341-345.
Case
A 48-year-old man presented to the ED with a 2-day history of cough and congestion. He described the cough as gradual in onset and, though initially nonproductive, it was now productive of green sputum. He denied fevers or chills, chest pain, nausea, vomiting, or diarrhea, and complained of only mild shortness of breath. His medical history was significant for hypertension, which was well managed with daily lisinopril-hydrochlorothiazide. He admitted to smoking one pack of cigarettes per day for the past 25 years, but denied alcohol or illicit drug use.
On physical examination, the patient’s vital signs were: blood pressure, 112/64 mm Hg; heart rate, 84 beats/min; respiratory rate, 20 breaths/min; and temperature, 98oF. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was normal. Auscultation of the lungs revealed bilateral breath sounds with scattered, faint expiratory wheezing; the heart had a regular rate and rhythm, without murmurs, rubs, or gallops.
The emergency physician (EP) ordered posteroanterior and lateral chest X-rays (CXR), which he interpreted as normal. He also ordered an albuterol handheld nebulizer treatment for the patient. After the albuterol treatment, the patient felt he was breathing more easily. The frequency of his cough had also decreased following treatment and, on re-examination, he exhibited no wheezing and was given azithromycin 500 mg orally in the ED. The EP diagnosed the patient with acute bronchitis and discharged him home with an albuterol metered dose inhaler with a spacer, and a 4-day course of azithromycin. He also encouraged the patient to quit smoking.
The next day the radiologist’s official reading of the patient’s radiographs included the finding of a very small pulmonary nodule, which was seen only on the lateral X-ray. The radiologist recommended a repeat CXR or a computed tomography (CT) scan of the chest in 6 months.
Unfortunately, the EP never saw this information, and the patient was not contacted regarding the abnormal radiology finding and the need for follow-up. Approximately 20 months later, the patient was diagnosed with lung cancer with metastasis to the thoracic spine and liver. Despite chemotherapy and radiation treatment, he died from the cancer.
The patient’s family brought a malpractice suit against the EP, stating that the cancer could have been successfully treated prior to any metastasis if the patient had been informed of the abnormal radiology findings at his ED visit 20 months prior. The EP argued that he never saw the official radiology report, and therefore had no knowledge of the need for follow-up. At trial, a jury verdict was returned in favor of the defendant.
Discussion
Unfortunately, some version of this scenario occurs on a frequent basis. While imaging studies account for the majority of such cases, the same situation can occur with abnormal laboratory results, body-fluid cultures, or pathology reports in which an abnormality is identified (eg, positive blood culture, missed fracture) but, for a myriad of reasons, the critical information does not get related to the patient.
Because of the episodic nature of the practice of emergency medicine (EM), a process must be in place to ensure any “positive” test results or findings discovered after patient discharge are reviewed and compared to the ED diagnosis, and that any “misses” result in notifying the patient and/or his or her primary care physician and arranging follow-up. In cases such as the one presented here, a system issue existed—one that was not due to any fault or oversight of the EP. Ideally, EM leadership should work closely with leadership from radiology and laboratory services and hospital risk management to develop such a process—one that will be effective every day, including weekends and holidays.
Missed fractures on radiographs are a common cause of malpractice litigation against EPs. In one review by Kachalia et al1 examining malpractice claims involving EPs, missed fractures on radiographs accounted for 19% (the most common) of the 79 missed diagnoses identified in their study.In a similar study by Karcz et al,2 missed fractures ranked second in frequency and dollars lost in malpractice cases against EPs in Massachusetts.
While missed lesions on CXR do not occur with the same frequency as missed fractures, the results are much more devastating when the lesion turns out to be malignant. Three common areas where such lesions are missed on CXR include: the apex of the lung, obscured by overlying clavicle and ribs; the retrocardiac region (as in the patient in this case); and the lung bases obscured by the diaphragm.
Emergency physicians are neither trained nor expected to identify every single abnormality—especially subtle radiographic abnormalities. This is why there are radiology overreads, and a system or process must be in place to ensure patients are informed of any positive findings and to arrange proper follow-up.
Case
A 48-year-old man presented to the ED with a 2-day history of cough and congestion. He described the cough as gradual in onset and, though initially nonproductive, it was now productive of green sputum. He denied fevers or chills, chest pain, nausea, vomiting, or diarrhea, and complained of only mild shortness of breath. His medical history was significant for hypertension, which was well managed with daily lisinopril-hydrochlorothiazide. He admitted to smoking one pack of cigarettes per day for the past 25 years, but denied alcohol or illicit drug use.
On physical examination, the patient’s vital signs were: blood pressure, 112/64 mm Hg; heart rate, 84 beats/min; respiratory rate, 20 breaths/min; and temperature, 98oF. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was normal. Auscultation of the lungs revealed bilateral breath sounds with scattered, faint expiratory wheezing; the heart had a regular rate and rhythm, without murmurs, rubs, or gallops.
The emergency physician (EP) ordered posteroanterior and lateral chest X-rays (CXR), which he interpreted as normal. He also ordered an albuterol handheld nebulizer treatment for the patient. After the albuterol treatment, the patient felt he was breathing more easily. The frequency of his cough had also decreased following treatment and, on re-examination, he exhibited no wheezing and was given azithromycin 500 mg orally in the ED. The EP diagnosed the patient with acute bronchitis and discharged him home with an albuterol metered dose inhaler with a spacer, and a 4-day course of azithromycin. He also encouraged the patient to quit smoking.
The next day the radiologist’s official reading of the patient’s radiographs included the finding of a very small pulmonary nodule, which was seen only on the lateral X-ray. The radiologist recommended a repeat CXR or a computed tomography (CT) scan of the chest in 6 months.
Unfortunately, the EP never saw this information, and the patient was not contacted regarding the abnormal radiology finding and the need for follow-up. Approximately 20 months later, the patient was diagnosed with lung cancer with metastasis to the thoracic spine and liver. Despite chemotherapy and radiation treatment, he died from the cancer.
The patient’s family brought a malpractice suit against the EP, stating that the cancer could have been successfully treated prior to any metastasis if the patient had been informed of the abnormal radiology findings at his ED visit 20 months prior. The EP argued that he never saw the official radiology report, and therefore had no knowledge of the need for follow-up. At trial, a jury verdict was returned in favor of the defendant.
Discussion
Unfortunately, some version of this scenario occurs on a frequent basis. While imaging studies account for the majority of such cases, the same situation can occur with abnormal laboratory results, body-fluid cultures, or pathology reports in which an abnormality is identified (eg, positive blood culture, missed fracture) but, for a myriad of reasons, the critical information does not get related to the patient.
Because of the episodic nature of the practice of emergency medicine (EM), a process must be in place to ensure any “positive” test results or findings discovered after patient discharge are reviewed and compared to the ED diagnosis, and that any “misses” result in notifying the patient and/or his or her primary care physician and arranging follow-up. In cases such as the one presented here, a system issue existed—one that was not due to any fault or oversight of the EP. Ideally, EM leadership should work closely with leadership from radiology and laboratory services and hospital risk management to develop such a process—one that will be effective every day, including weekends and holidays.
Missed fractures on radiographs are a common cause of malpractice litigation against EPs. In one review by Kachalia et al1 examining malpractice claims involving EPs, missed fractures on radiographs accounted for 19% (the most common) of the 79 missed diagnoses identified in their study.In a similar study by Karcz et al,2 missed fractures ranked second in frequency and dollars lost in malpractice cases against EPs in Massachusetts.
While missed lesions on CXR do not occur with the same frequency as missed fractures, the results are much more devastating when the lesion turns out to be malignant. Three common areas where such lesions are missed on CXR include: the apex of the lung, obscured by overlying clavicle and ribs; the retrocardiac region (as in the patient in this case); and the lung bases obscured by the diaphragm.
Emergency physicians are neither trained nor expected to identify every single abnormality—especially subtle radiographic abnormalities. This is why there are radiology overreads, and a system or process must be in place to ensure patients are informed of any positive findings and to arrange proper follow-up.
1. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
2. Karcz A, Korn R, Burke MC, et al. Malpractice claims against emergency physicians in Massachusetts: 1975-1993. Am J Emerg Med. 1996;14(4):341-345.
1. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
2. Karcz A, Korn R, Burke MC, et al. Malpractice claims against emergency physicians in Massachusetts: 1975-1993. Am J Emerg Med. 1996;14(4):341-345.
Claimed missteps lead to brain damage: $53M award
Claimed missteps lead to brain damage: $53M award
At 2:00 AM, a woman at 40 weeks’ gestation went to a hospital because she felt a decrease in fetal movement. At birth, the baby was not breathing. He was rushed to the neonatal intensive care unit where he was resuscitated and placed on life support. He remained in critical care for 4 weeks. The child has cerebral palsy and cannot walk, talk, or care for himself. He will need 24-hour care for the rest of his life.
PARENT’S CLAIM:
The lawsuit cited 20 alleged missteps by physicians and nurses, including failure to: react to abnormal fetal heart-rate patterns that indicated fetal distress, perform a timely cesarean delivery, and follow a chain of command. During the 12 hours that the mother was in labor at the hospital, nurses and physicians allegedly ignored her. Although the fetal heart-rate monitor showed fetal distress, the mother continued to lie unattended. At 12:40 PM, physicians called for cesarean delivery due to fetal distress, but it took an hour for the child to be born.
The negligence of the hospital staff and delay in delivery caused hypoxia, resulting in cerebral palsy. All medical records from the hospital’s neonatal clinic show that he suffered hypoxia at birth.
HOSPITAL’S DEFENSE:
The mother and child were treated for an infection, which is a recognized cause of cerebral palsy. The child was born with normal blood oxygen levels. His injury occurred before the mother came to the hospital.
VERDICT:
A $53 million Illinois verdict was returned. The hospital applied for a mistrial based on allegedly inflammatory comments by the prosecuting attorney, but that was dismissed.
Birth trauma: $2.75M settlement
A woman had her first prenatal visit at 21 weeks’ gestation. Her advanced maternal age (39 years) and poor health history, including prior delivery of a baby with intrauterine growth restriction (IUGR), put her at risk; her prenatal care was transferred to a high-risk clinic.
At her next prenatal visit, records noted that the mother’s job required excessive standing, that she tested positive for marijuana, and that she was at risk for IUGR. Notes did not say that the mother was informed of her IUGR risk nor was a plan created for additional testing to monitor IUGR.
Ultrasonography (US) performed at 25 weeks’ gestation estimated that the baby’s weight was in the 11th- to 12th-week percentile. Amniotic fluid volume was noted as normal.
The mother missed her next appointment but returned at 28 weeks’ gestation, when she reported a headache and was found to have high blood pressure. US revealed normal fetal heart anatomy but amniotic fluid volume was noted to have decreased since the first US. The mother missed the next several appointments.
When she presented at 33 weeks’ gestation, her blood pressure was 160/97 mm Hg, fetal heart-rate tones were normal, and there was positive fetal movement. Fundal height measurement revealed a 3-cm discrepancy in date and size, suggesting a small baby, decreased amniotic fluid, or both. The ObGyn ordered testing for the next day. When a nonstress test performed from 8:44 AM to 9:10 AM was nonreassuring, the mother was ordered to immediately go to the hospital. She did not arrive at the hospital until 11:13 AM, when she was placed on fetal heart-rate monitor; test results were nonreassuring. At 11:30 AM, US revealed IUGR and oligohydramnios. An urgent cesarean delivery was performed and the baby was born at 11:56 AM.
The child’s Apgar scores were 4 and 9 at 1 and 5 minutes, respectively. The baby developed white matter brain damage and grade III and IV intraventricular hemorrhages due to hypoxia, ischemia, and metabolic acidosis. A maternal drug screen was positive for marijuana. Placental pathology revealed multiple abnormalities including placental infarcts involving approximately 50% of placental tissue, abnormal vascular changes, intervillous fibrin deposition, and chronic villitis.
At trial, the child had developmental delays, cognitive defects, learning disabilities, and breakthrough seizures.
PARENT’S CLAIM:
The mother claimed that the high-risk clinic was negligent. A plan should have been put into place at her first visit to monitor for IUGR based on her history. She was not advised of her risk of having another IUGR baby. Fundal height measurement, US to test for IUGR, or assessments of fetal heart-rate tones and fetal movement were not performed regularly. If a nonstress test had been performed earlier than 33 weeks’ gestation, she might have been admitted to the hospital for monitoring and earlier delivery, resulting in a healthier baby.
DEFENDANTS’ DEFENSE:
The mother was noncompliant and missed most of her prenatal appointments. She also continued to smoke marijuana throughout her pregnancy although she was told to stop. When the mother arrived at the prenatal clinic at 33 weeks’ gestation, tests were ordered and delivery occurred in a timely fashion. Any problems suffered by the child were a result of prematurity and damage that occurred during the 5 weeks of missed prenatal appointments.
VERDICT:
A $2.75M Missouri settlement was reached.
Who should have delivered the baby?
A mother’s prenatal care was managed by her family practitioner (FP). The mother went to the FP for induction of labor, but it was unsuccessful. Three days later, the baby was delivered by the FP and began having seizures a few minutes after birth. The child is quadriplegic and has severe cerebral palsy.
PARENTS’ CLAIM:
The FP was negligent in managing labor and delivery. She should have called an ObGyn to manage the labor. She failed to monitor fetal heart-rate tracings and failed to order an emergency cesarean delivery. The FP mismanaged the baby’s condition upon delivery and seizures started.
PHYSICIAN’S DEFENSE:
The FP properly managed the delivery and postdelivery complications. The brain injury had nothing to do with the birth; it was instead caused by a stroke disorder that occurred 3 to 7 days before delivery.
VERDICT:
A Minnesota defense verdict was returned.
Undiagnosed H1N1 influenza (swine flu) during pregnancy; mother and child die: $16.7M verdict
At 7 months’ gestation, a 27-year-old woman presented to a clinic on June 26 with a runny nose, congestion, cough, wheezing, chills, and sweats. The physician noted concern about proteinuria and that the patient reported chills and sweats, but that he was uncertain as to the symptoms’ cause. He recommended that she see her ObGyn immediately and report to the emergency department (ED) if symptoms worsened. The patient called her ObGyn to report having a temperature between 94˚F and 103˚F and taking acetaminophen. The next day, she saw a nurse practitioner in the ObGyn’s office who documented that the patient was not given antiviral medication.
On June 29, the patient was still feeling ill and went to the ED. Although a physician planned to discharge her, an ObGyn nurse recognized that the patient was too ill to leave and had her admitted.
The patient’s condition worsened overnight and she was transferred to the intensive care unit (ICU), where she was intubated and put on a ventilator. Medical notes read “as whether influenza was present was unclear…Tamiflu will be started, but the efficacy of it this late into a possible influenza episode is extremely questionable.” ICU physicians believed that the best option was to deliver the child. After the patient’s husband gave permission, the child was born by cesarean delivery. The mother never regained full consciousness and remained in a medically induced coma. She died on August 11 after the family decided to remove life support.
After being given the diagnosis of intrauterine hypoxia, the child remained in intensive care for several weeks and then was discharged home. Seven months later, the father found his daughter in bed, not breathing, which physicians believed was an episode of sudden infant death syndrome. The father performed CPR and rushed her to the hospital. Physicians tried twice to take the child off the ventilator, but she could not breathe without assistance. On February 21, life support was removed and the child died.
ESTATES’ CLAIM:
The clinic and its physician were negligent for failing to recognize that the mother had influenza; she presented with classic flu symptoms during a worldwide pandemic. In the several months before the patient’s visit, the clinic had received notices from health authorities alerting medical professionals to the dangers of H1N1 influenza, or Swine Flu. The clinic also had received, before the patient’s visit, information warning of an elevated risk of H1N1 to pregnant women, with instructions to administer oseltamivir phosphate (Tamiflu) to any pregnant woman suspected of having influenza.
DEFENDANTS’ DEFENSE:
The clinic and physician denied negligence, claiming that treatment of the mother was appropriate.
VERDICT:
A $16.7 million Washington verdict was returned.
Mother claims to being uninformed of antiepileptics’ risks
A woman with epilepsy gave birth to a child with physical and cognitive birth defects.
PARENT’S CLAIM:
The mother claimed that, although she was of child-bearing age, she had never been informed of the risk of birth defects associated with taking an antiepileptic medication. Had she known of the risk, she would not have chosen to conceive. The physicians should have prescribed a different antiepileptic drug.
DEFENDANTS’ DEFENSE:
The clinic’s physicians met the standard of care in prescribing the drug. They properly informed the mother of the risks of taking the antiepileptic drug during pregnancy. The patient was allergic to all other antiepileptic drugs available at the time, so an alternative was not available.
VERDICT:
An Illinois defense verdict was returned for the clinic.
Mother has stroke during delivery: $3M settlement
A 42-year-old woman had a hemorrhagic stroke during the delivery of her first child. She remained hospitalized for observation with a medical plan to insert a drain if her condition worsened. Initially she did well, but she then began to have episodes of decreased consciousness and loss of function and later became unresponsive. Her physicians then undertook an emergency procedure to attempt to drain blood from her brain, but the surgical measure did not prevent her from incurring significant cognitive and physical injuries.
PATIENT’S CLAIM:
The agreed-upon medical plan of treatment was not followed, resulting in severe brain damage to the patient.
DEFENDANTS’ DEFENSE:
The case was settled during the trial.
VERDICT:
A $3 million Massachusetts settlement was reached.
Did delayed cesarean cause cognitive defects?
When fetal distress was detected, the nurse called the patient’s ObGyn at 12:30 AM. The ObGyn arrived at the hospital at 12:48 AM, ordered a cesarean delivery at 12:56 AM, and the baby was born at 1:20 AM.
PARENTS’ CLAIM:
The ObGyn was negligent for not calling for the hospital’s on-duty resident physician to become involved in the case when the nurse phoned at 12:30 AM. If the ObGyn had done so, cesarean delivery would have been ordered and completed earlier, which would have averted the child’s injuries, including cognitive and physical impairments.
PHYSICIAN’S DEFENSE:
The ObGyn asserted that, based on the information provided to her, there was no reason to request the resident’s involvement. An earlier cesarean delivery was not necessary based on fetal heart-rate monitoring strip results. The ObGyn acted in a timely manner when calling for cesarean delivery. There was no concrete evidence that any alleged delay caused the child’s injuries.
VERDICT:
An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Claimed missteps lead to brain damage: $53M award
At 2:00 AM, a woman at 40 weeks’ gestation went to a hospital because she felt a decrease in fetal movement. At birth, the baby was not breathing. He was rushed to the neonatal intensive care unit where he was resuscitated and placed on life support. He remained in critical care for 4 weeks. The child has cerebral palsy and cannot walk, talk, or care for himself. He will need 24-hour care for the rest of his life.
PARENT’S CLAIM:
The lawsuit cited 20 alleged missteps by physicians and nurses, including failure to: react to abnormal fetal heart-rate patterns that indicated fetal distress, perform a timely cesarean delivery, and follow a chain of command. During the 12 hours that the mother was in labor at the hospital, nurses and physicians allegedly ignored her. Although the fetal heart-rate monitor showed fetal distress, the mother continued to lie unattended. At 12:40 PM, physicians called for cesarean delivery due to fetal distress, but it took an hour for the child to be born.
The negligence of the hospital staff and delay in delivery caused hypoxia, resulting in cerebral palsy. All medical records from the hospital’s neonatal clinic show that he suffered hypoxia at birth.
HOSPITAL’S DEFENSE:
The mother and child were treated for an infection, which is a recognized cause of cerebral palsy. The child was born with normal blood oxygen levels. His injury occurred before the mother came to the hospital.
VERDICT:
A $53 million Illinois verdict was returned. The hospital applied for a mistrial based on allegedly inflammatory comments by the prosecuting attorney, but that was dismissed.
Birth trauma: $2.75M settlement
A woman had her first prenatal visit at 21 weeks’ gestation. Her advanced maternal age (39 years) and poor health history, including prior delivery of a baby with intrauterine growth restriction (IUGR), put her at risk; her prenatal care was transferred to a high-risk clinic.
At her next prenatal visit, records noted that the mother’s job required excessive standing, that she tested positive for marijuana, and that she was at risk for IUGR. Notes did not say that the mother was informed of her IUGR risk nor was a plan created for additional testing to monitor IUGR.
Ultrasonography (US) performed at 25 weeks’ gestation estimated that the baby’s weight was in the 11th- to 12th-week percentile. Amniotic fluid volume was noted as normal.
The mother missed her next appointment but returned at 28 weeks’ gestation, when she reported a headache and was found to have high blood pressure. US revealed normal fetal heart anatomy but amniotic fluid volume was noted to have decreased since the first US. The mother missed the next several appointments.
When she presented at 33 weeks’ gestation, her blood pressure was 160/97 mm Hg, fetal heart-rate tones were normal, and there was positive fetal movement. Fundal height measurement revealed a 3-cm discrepancy in date and size, suggesting a small baby, decreased amniotic fluid, or both. The ObGyn ordered testing for the next day. When a nonstress test performed from 8:44 AM to 9:10 AM was nonreassuring, the mother was ordered to immediately go to the hospital. She did not arrive at the hospital until 11:13 AM, when she was placed on fetal heart-rate monitor; test results were nonreassuring. At 11:30 AM, US revealed IUGR and oligohydramnios. An urgent cesarean delivery was performed and the baby was born at 11:56 AM.
The child’s Apgar scores were 4 and 9 at 1 and 5 minutes, respectively. The baby developed white matter brain damage and grade III and IV intraventricular hemorrhages due to hypoxia, ischemia, and metabolic acidosis. A maternal drug screen was positive for marijuana. Placental pathology revealed multiple abnormalities including placental infarcts involving approximately 50% of placental tissue, abnormal vascular changes, intervillous fibrin deposition, and chronic villitis.
At trial, the child had developmental delays, cognitive defects, learning disabilities, and breakthrough seizures.
PARENT’S CLAIM:
The mother claimed that the high-risk clinic was negligent. A plan should have been put into place at her first visit to monitor for IUGR based on her history. She was not advised of her risk of having another IUGR baby. Fundal height measurement, US to test for IUGR, or assessments of fetal heart-rate tones and fetal movement were not performed regularly. If a nonstress test had been performed earlier than 33 weeks’ gestation, she might have been admitted to the hospital for monitoring and earlier delivery, resulting in a healthier baby.
DEFENDANTS’ DEFENSE:
The mother was noncompliant and missed most of her prenatal appointments. She also continued to smoke marijuana throughout her pregnancy although she was told to stop. When the mother arrived at the prenatal clinic at 33 weeks’ gestation, tests were ordered and delivery occurred in a timely fashion. Any problems suffered by the child were a result of prematurity and damage that occurred during the 5 weeks of missed prenatal appointments.
VERDICT:
A $2.75M Missouri settlement was reached.
Who should have delivered the baby?
A mother’s prenatal care was managed by her family practitioner (FP). The mother went to the FP for induction of labor, but it was unsuccessful. Three days later, the baby was delivered by the FP and began having seizures a few minutes after birth. The child is quadriplegic and has severe cerebral palsy.
PARENTS’ CLAIM:
The FP was negligent in managing labor and delivery. She should have called an ObGyn to manage the labor. She failed to monitor fetal heart-rate tracings and failed to order an emergency cesarean delivery. The FP mismanaged the baby’s condition upon delivery and seizures started.
PHYSICIAN’S DEFENSE:
The FP properly managed the delivery and postdelivery complications. The brain injury had nothing to do with the birth; it was instead caused by a stroke disorder that occurred 3 to 7 days before delivery.
VERDICT:
A Minnesota defense verdict was returned.
Undiagnosed H1N1 influenza (swine flu) during pregnancy; mother and child die: $16.7M verdict
At 7 months’ gestation, a 27-year-old woman presented to a clinic on June 26 with a runny nose, congestion, cough, wheezing, chills, and sweats. The physician noted concern about proteinuria and that the patient reported chills and sweats, but that he was uncertain as to the symptoms’ cause. He recommended that she see her ObGyn immediately and report to the emergency department (ED) if symptoms worsened. The patient called her ObGyn to report having a temperature between 94˚F and 103˚F and taking acetaminophen. The next day, she saw a nurse practitioner in the ObGyn’s office who documented that the patient was not given antiviral medication.
On June 29, the patient was still feeling ill and went to the ED. Although a physician planned to discharge her, an ObGyn nurse recognized that the patient was too ill to leave and had her admitted.
The patient’s condition worsened overnight and she was transferred to the intensive care unit (ICU), where she was intubated and put on a ventilator. Medical notes read “as whether influenza was present was unclear…Tamiflu will be started, but the efficacy of it this late into a possible influenza episode is extremely questionable.” ICU physicians believed that the best option was to deliver the child. After the patient’s husband gave permission, the child was born by cesarean delivery. The mother never regained full consciousness and remained in a medically induced coma. She died on August 11 after the family decided to remove life support.
After being given the diagnosis of intrauterine hypoxia, the child remained in intensive care for several weeks and then was discharged home. Seven months later, the father found his daughter in bed, not breathing, which physicians believed was an episode of sudden infant death syndrome. The father performed CPR and rushed her to the hospital. Physicians tried twice to take the child off the ventilator, but she could not breathe without assistance. On February 21, life support was removed and the child died.
ESTATES’ CLAIM:
The clinic and its physician were negligent for failing to recognize that the mother had influenza; she presented with classic flu symptoms during a worldwide pandemic. In the several months before the patient’s visit, the clinic had received notices from health authorities alerting medical professionals to the dangers of H1N1 influenza, or Swine Flu. The clinic also had received, before the patient’s visit, information warning of an elevated risk of H1N1 to pregnant women, with instructions to administer oseltamivir phosphate (Tamiflu) to any pregnant woman suspected of having influenza.
DEFENDANTS’ DEFENSE:
The clinic and physician denied negligence, claiming that treatment of the mother was appropriate.
VERDICT:
A $16.7 million Washington verdict was returned.
Mother claims to being uninformed of antiepileptics’ risks
A woman with epilepsy gave birth to a child with physical and cognitive birth defects.
PARENT’S CLAIM:
The mother claimed that, although she was of child-bearing age, she had never been informed of the risk of birth defects associated with taking an antiepileptic medication. Had she known of the risk, she would not have chosen to conceive. The physicians should have prescribed a different antiepileptic drug.
DEFENDANTS’ DEFENSE:
The clinic’s physicians met the standard of care in prescribing the drug. They properly informed the mother of the risks of taking the antiepileptic drug during pregnancy. The patient was allergic to all other antiepileptic drugs available at the time, so an alternative was not available.
VERDICT:
An Illinois defense verdict was returned for the clinic.
Mother has stroke during delivery: $3M settlement
A 42-year-old woman had a hemorrhagic stroke during the delivery of her first child. She remained hospitalized for observation with a medical plan to insert a drain if her condition worsened. Initially she did well, but she then began to have episodes of decreased consciousness and loss of function and later became unresponsive. Her physicians then undertook an emergency procedure to attempt to drain blood from her brain, but the surgical measure did not prevent her from incurring significant cognitive and physical injuries.
PATIENT’S CLAIM:
The agreed-upon medical plan of treatment was not followed, resulting in severe brain damage to the patient.
DEFENDANTS’ DEFENSE:
The case was settled during the trial.
VERDICT:
A $3 million Massachusetts settlement was reached.
Did delayed cesarean cause cognitive defects?
When fetal distress was detected, the nurse called the patient’s ObGyn at 12:30 AM. The ObGyn arrived at the hospital at 12:48 AM, ordered a cesarean delivery at 12:56 AM, and the baby was born at 1:20 AM.
PARENTS’ CLAIM:
The ObGyn was negligent for not calling for the hospital’s on-duty resident physician to become involved in the case when the nurse phoned at 12:30 AM. If the ObGyn had done so, cesarean delivery would have been ordered and completed earlier, which would have averted the child’s injuries, including cognitive and physical impairments.
PHYSICIAN’S DEFENSE:
The ObGyn asserted that, based on the information provided to her, there was no reason to request the resident’s involvement. An earlier cesarean delivery was not necessary based on fetal heart-rate monitoring strip results. The ObGyn acted in a timely manner when calling for cesarean delivery. There was no concrete evidence that any alleged delay caused the child’s injuries.
VERDICT:
An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Claimed missteps lead to brain damage: $53M award
At 2:00 AM, a woman at 40 weeks’ gestation went to a hospital because she felt a decrease in fetal movement. At birth, the baby was not breathing. He was rushed to the neonatal intensive care unit where he was resuscitated and placed on life support. He remained in critical care for 4 weeks. The child has cerebral palsy and cannot walk, talk, or care for himself. He will need 24-hour care for the rest of his life.
PARENT’S CLAIM:
The lawsuit cited 20 alleged missteps by physicians and nurses, including failure to: react to abnormal fetal heart-rate patterns that indicated fetal distress, perform a timely cesarean delivery, and follow a chain of command. During the 12 hours that the mother was in labor at the hospital, nurses and physicians allegedly ignored her. Although the fetal heart-rate monitor showed fetal distress, the mother continued to lie unattended. At 12:40 PM, physicians called for cesarean delivery due to fetal distress, but it took an hour for the child to be born.
The negligence of the hospital staff and delay in delivery caused hypoxia, resulting in cerebral palsy. All medical records from the hospital’s neonatal clinic show that he suffered hypoxia at birth.
HOSPITAL’S DEFENSE:
The mother and child were treated for an infection, which is a recognized cause of cerebral palsy. The child was born with normal blood oxygen levels. His injury occurred before the mother came to the hospital.
VERDICT:
A $53 million Illinois verdict was returned. The hospital applied for a mistrial based on allegedly inflammatory comments by the prosecuting attorney, but that was dismissed.
Birth trauma: $2.75M settlement
A woman had her first prenatal visit at 21 weeks’ gestation. Her advanced maternal age (39 years) and poor health history, including prior delivery of a baby with intrauterine growth restriction (IUGR), put her at risk; her prenatal care was transferred to a high-risk clinic.
At her next prenatal visit, records noted that the mother’s job required excessive standing, that she tested positive for marijuana, and that she was at risk for IUGR. Notes did not say that the mother was informed of her IUGR risk nor was a plan created for additional testing to monitor IUGR.
Ultrasonography (US) performed at 25 weeks’ gestation estimated that the baby’s weight was in the 11th- to 12th-week percentile. Amniotic fluid volume was noted as normal.
The mother missed her next appointment but returned at 28 weeks’ gestation, when she reported a headache and was found to have high blood pressure. US revealed normal fetal heart anatomy but amniotic fluid volume was noted to have decreased since the first US. The mother missed the next several appointments.
When she presented at 33 weeks’ gestation, her blood pressure was 160/97 mm Hg, fetal heart-rate tones were normal, and there was positive fetal movement. Fundal height measurement revealed a 3-cm discrepancy in date and size, suggesting a small baby, decreased amniotic fluid, or both. The ObGyn ordered testing for the next day. When a nonstress test performed from 8:44 AM to 9:10 AM was nonreassuring, the mother was ordered to immediately go to the hospital. She did not arrive at the hospital until 11:13 AM, when she was placed on fetal heart-rate monitor; test results were nonreassuring. At 11:30 AM, US revealed IUGR and oligohydramnios. An urgent cesarean delivery was performed and the baby was born at 11:56 AM.
The child’s Apgar scores were 4 and 9 at 1 and 5 minutes, respectively. The baby developed white matter brain damage and grade III and IV intraventricular hemorrhages due to hypoxia, ischemia, and metabolic acidosis. A maternal drug screen was positive for marijuana. Placental pathology revealed multiple abnormalities including placental infarcts involving approximately 50% of placental tissue, abnormal vascular changes, intervillous fibrin deposition, and chronic villitis.
At trial, the child had developmental delays, cognitive defects, learning disabilities, and breakthrough seizures.
PARENT’S CLAIM:
The mother claimed that the high-risk clinic was negligent. A plan should have been put into place at her first visit to monitor for IUGR based on her history. She was not advised of her risk of having another IUGR baby. Fundal height measurement, US to test for IUGR, or assessments of fetal heart-rate tones and fetal movement were not performed regularly. If a nonstress test had been performed earlier than 33 weeks’ gestation, she might have been admitted to the hospital for monitoring and earlier delivery, resulting in a healthier baby.
DEFENDANTS’ DEFENSE:
The mother was noncompliant and missed most of her prenatal appointments. She also continued to smoke marijuana throughout her pregnancy although she was told to stop. When the mother arrived at the prenatal clinic at 33 weeks’ gestation, tests were ordered and delivery occurred in a timely fashion. Any problems suffered by the child were a result of prematurity and damage that occurred during the 5 weeks of missed prenatal appointments.
VERDICT:
A $2.75M Missouri settlement was reached.
Who should have delivered the baby?
A mother’s prenatal care was managed by her family practitioner (FP). The mother went to the FP for induction of labor, but it was unsuccessful. Three days later, the baby was delivered by the FP and began having seizures a few minutes after birth. The child is quadriplegic and has severe cerebral palsy.
PARENTS’ CLAIM:
The FP was negligent in managing labor and delivery. She should have called an ObGyn to manage the labor. She failed to monitor fetal heart-rate tracings and failed to order an emergency cesarean delivery. The FP mismanaged the baby’s condition upon delivery and seizures started.
PHYSICIAN’S DEFENSE:
The FP properly managed the delivery and postdelivery complications. The brain injury had nothing to do with the birth; it was instead caused by a stroke disorder that occurred 3 to 7 days before delivery.
VERDICT:
A Minnesota defense verdict was returned.
Undiagnosed H1N1 influenza (swine flu) during pregnancy; mother and child die: $16.7M verdict
At 7 months’ gestation, a 27-year-old woman presented to a clinic on June 26 with a runny nose, congestion, cough, wheezing, chills, and sweats. The physician noted concern about proteinuria and that the patient reported chills and sweats, but that he was uncertain as to the symptoms’ cause. He recommended that she see her ObGyn immediately and report to the emergency department (ED) if symptoms worsened. The patient called her ObGyn to report having a temperature between 94˚F and 103˚F and taking acetaminophen. The next day, she saw a nurse practitioner in the ObGyn’s office who documented that the patient was not given antiviral medication.
On June 29, the patient was still feeling ill and went to the ED. Although a physician planned to discharge her, an ObGyn nurse recognized that the patient was too ill to leave and had her admitted.
The patient’s condition worsened overnight and she was transferred to the intensive care unit (ICU), where she was intubated and put on a ventilator. Medical notes read “as whether influenza was present was unclear…Tamiflu will be started, but the efficacy of it this late into a possible influenza episode is extremely questionable.” ICU physicians believed that the best option was to deliver the child. After the patient’s husband gave permission, the child was born by cesarean delivery. The mother never regained full consciousness and remained in a medically induced coma. She died on August 11 after the family decided to remove life support.
After being given the diagnosis of intrauterine hypoxia, the child remained in intensive care for several weeks and then was discharged home. Seven months later, the father found his daughter in bed, not breathing, which physicians believed was an episode of sudden infant death syndrome. The father performed CPR and rushed her to the hospital. Physicians tried twice to take the child off the ventilator, but she could not breathe without assistance. On February 21, life support was removed and the child died.
ESTATES’ CLAIM:
The clinic and its physician were negligent for failing to recognize that the mother had influenza; she presented with classic flu symptoms during a worldwide pandemic. In the several months before the patient’s visit, the clinic had received notices from health authorities alerting medical professionals to the dangers of H1N1 influenza, or Swine Flu. The clinic also had received, before the patient’s visit, information warning of an elevated risk of H1N1 to pregnant women, with instructions to administer oseltamivir phosphate (Tamiflu) to any pregnant woman suspected of having influenza.
DEFENDANTS’ DEFENSE:
The clinic and physician denied negligence, claiming that treatment of the mother was appropriate.
VERDICT:
A $16.7 million Washington verdict was returned.
Mother claims to being uninformed of antiepileptics’ risks
A woman with epilepsy gave birth to a child with physical and cognitive birth defects.
PARENT’S CLAIM:
The mother claimed that, although she was of child-bearing age, she had never been informed of the risk of birth defects associated with taking an antiepileptic medication. Had she known of the risk, she would not have chosen to conceive. The physicians should have prescribed a different antiepileptic drug.
DEFENDANTS’ DEFENSE:
The clinic’s physicians met the standard of care in prescribing the drug. They properly informed the mother of the risks of taking the antiepileptic drug during pregnancy. The patient was allergic to all other antiepileptic drugs available at the time, so an alternative was not available.
VERDICT:
An Illinois defense verdict was returned for the clinic.
Mother has stroke during delivery: $3M settlement
A 42-year-old woman had a hemorrhagic stroke during the delivery of her first child. She remained hospitalized for observation with a medical plan to insert a drain if her condition worsened. Initially she did well, but she then began to have episodes of decreased consciousness and loss of function and later became unresponsive. Her physicians then undertook an emergency procedure to attempt to drain blood from her brain, but the surgical measure did not prevent her from incurring significant cognitive and physical injuries.
PATIENT’S CLAIM:
The agreed-upon medical plan of treatment was not followed, resulting in severe brain damage to the patient.
DEFENDANTS’ DEFENSE:
The case was settled during the trial.
VERDICT:
A $3 million Massachusetts settlement was reached.
Did delayed cesarean cause cognitive defects?
When fetal distress was detected, the nurse called the patient’s ObGyn at 12:30 AM. The ObGyn arrived at the hospital at 12:48 AM, ordered a cesarean delivery at 12:56 AM, and the baby was born at 1:20 AM.
PARENTS’ CLAIM:
The ObGyn was negligent for not calling for the hospital’s on-duty resident physician to become involved in the case when the nurse phoned at 12:30 AM. If the ObGyn had done so, cesarean delivery would have been ordered and completed earlier, which would have averted the child’s injuries, including cognitive and physical impairments.
PHYSICIAN’S DEFENSE:
The ObGyn asserted that, based on the information provided to her, there was no reason to request the resident’s involvement. An earlier cesarean delivery was not necessary based on fetal heart-rate monitoring strip results. The ObGyn acted in a timely manner when calling for cesarean delivery. There was no concrete evidence that any alleged delay caused the child’s injuries.
VERDICT:
An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Malpractice Counsel: Acute Pulmonary Embolism Masquerading as Acute Coronary Syndrome
Case
A 37-year-old woman presented to the ED with a 90-minute history of chest tightness and shortness of breath. She admitted to feeling anxious but denied nausea, vomiting, or diaphoresis. The patient was in good health overall and had no history of similar symptoms. The only medication she took on a regular basis was a combination oral contraceptive (OC). Regarding the patient’s social history, she admitted to smoking one-half of a pack of cigarettes per day and occasional alcohol use.
On physical examination, the patient’s vital signs were: heart rate (HR), 102 beats/min; blood pressure, 118/64 mm Hg; respiratory rate, 20 breaths/min; and temperature, 98.6˚F. Oxygen saturation was 95% on room air. The head, eyes, ears, nose, and throat examination was normal. The cardiopulmonary examination revealed slight tachycardia with a regular rhythm but no murmurs, rubs, or gallops; the lungs were clear to auscultation bilaterally. The abdominal examination revealed a soft, nontender abdomen, without mass, and no guarding or rebound was present. An examination of the lower extremities was not documented.
The emergency physician (EP) ordered laboratory studies, which included a complete blood count (CBC), basic metabolic profile (BMP), and troponin I level. A chest X-ray and electrocardiogram (ECG) were also ordered. The chest X-ray was interpreted as normal, and the ECG revealed mild sinus tachycardia with nonspecific ST-T segment changes in V1 through V3. The CBC and BMP were all within normal limits, but the troponin I level was slightly elevated.
Given the patient’s clinical presentation and slightly elevated troponin I level, the EP was concerned for an acute coronary syndrome (ACS) and admitted the patient to the care of the on-call cardiologist. Prior to transfer, the patient was given 325 mg of aspirin by mouth, but no anticoagulation therapy was ordered. The cardiologist, who evaluated the patient after she was admitted to the inpatient floor, was concerned the patient had a pulmonary embolism (PE), and ordered a stat computed tomography angiography (CTA) scan of the chest. While the patient was undergoing the chest CTA scan, she went into cardiac arrest. Despite aggressive resuscitative measures, the patient could not be revived and was pronounced dead. An autopsy revealed a PE as the cause of death.
Plaintiff’s Claim
The patient’s estate sued the EP for failure to properly diagnose the PE, stating the hospital was vicariously liable for the EP’s actions. The emergency medicine (EM) expert for the plaintiff opined that the decedent’s symptoms should have prompted the EP to suspect she was suffering from a PE, and he should have immediately ordered anticoagulation, a D-dimer test, or a chest CTA scan. The expert cardiologist for the plaintiff stated the EP should have immediately started the patient on anticoagulation prior to the chest CTA scan.
The Defense
The defense EM expert stated the defendant’s diagnosis of ACS was appropriate given the patient’s overall clinical presentation, and the defense expert cardiologist stated the standard of care did not require the EP to administer anticoagulation prior to her diagnosis of PE, since the bleeding risks outweighed the benefits.
Verdict
At trial, the jury returned a defense verdict.
Discussion
This is not the first (nor probably the last) malpractice case in this column to involve a missed PE. While there have been improvements to the tools we currently possess to evaluate patients for suspected PE, it remains a difficult condition to reliably and timely identify in the ED. Although the two predominating symptoms—shortness of breath and chest pain—are common presentations in the ED, each is associated with large differential diagnoses.
Acute Coronary Syndrome Versus Pulmonary Embolism
From what we know of the published details of this case, the patient had only one risk factor for ACS (cigarette smoking) and two risk factors for PE (cigarette smoking and estrogen-containing contraceptive use). The only abnormal physical finding (tachycardia) was slightly more suggestive of PE than ACS. This patient’s primary complaint was chest fullness and shortness of breath. According to the Prospective Investigation of Pulmonary Embolism Diagnosis II study, shortness of breath is the most common complaint in PE (73%), followed by pleuritic chest pain (44%).1
In ACS, which is more common in men versus women and in patients of both sexes over age 55 years, the clinical presentation most commonly involves chest pain that patients describe as a pressure or fullness (as demonstrated in this patient). Unfortunately, in certain patient populations (eg, women, elderly patients, patients with diabetes mellitus) the presenting complaint can be shortness of breath, weakness, or nausea and vomiting. In a study evaluating how frequently an acute PE can mimic ACS, Kukla et al2 found that one-third of patients with an acute PE can present with all of the manifestations suggestive of ACS (ie, chest pain, ECG changes, and elevated troponin).
It is probably safe to assume the elevated troponin I level played a factor in influencing the EP to diagnose ACS, rather than pursuing an alternative diagnosis such as PE. Unfortunately, since both serum troponin T and I can be markers of right ventricle dysfunction, they are elevated in 30% to 50% of patients with moderate-to-large PE.3 However, neither serum troponin T nor troponin I is specific for myocardial infarction or unstable angina.
Pretest Probability: Wells Criteria
Determining pretest probability for any disease process is important when evaluating complaints in the ED; this is especially true for PE. One of the most frequently used tools for determining the likelihood of PE in ED patients is the Wells criteria (Table 1).4
Based on the published information available, the patient in this case would have scored a 1.5, placing her in the unlikely or low-risk category for PE. Patients whose Wells score places them in the low-risk group can benefit from serum D-dimer testing to help diagnose PE. However, serum D-dimer testing should not be ordered for patients in the likely or high-risk categories; these patients should instead be sent directly for imaging studies such as a chest CTA scan.
Pulmonary Embolism Rule-Out Criteria
For patients whose Wells criteria score places them in the “unlikely group,” the PE rule-out criteria (PERC) can be used to determine the need for ordering a D-dimer. If all eight criteria are met, no further testing is necessary to exclude PE from the differential diagnosis (Table 2).5
Summary
Evaluating chest pain and shortness of breath in the ED is a humbling experience for even the most seasoned EP. Thoroughly reviewing the patient’s history and physical examination, and determining the pretest probability of disease entities high on the differential diagnoses list, go a long way in helping make the correct diagnosis—and in turn initiating possible life-saving interventions and treatment.
1. Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879.
2. Kukla P, Dlugopolski R, Krupa E, et al. How often pulmonary embolism mimics acute coronary syndrome? Kardiol Pol. 2011;69(3):235-240.
3. Meyer T, Binder L, Hruska N, Luthe H, Buchwald AB. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632-1636.
4. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
5. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772-780. doi: 10.1111/j.1538-7836.2008.02944.x.
Case
A 37-year-old woman presented to the ED with a 90-minute history of chest tightness and shortness of breath. She admitted to feeling anxious but denied nausea, vomiting, or diaphoresis. The patient was in good health overall and had no history of similar symptoms. The only medication she took on a regular basis was a combination oral contraceptive (OC). Regarding the patient’s social history, she admitted to smoking one-half of a pack of cigarettes per day and occasional alcohol use.
On physical examination, the patient’s vital signs were: heart rate (HR), 102 beats/min; blood pressure, 118/64 mm Hg; respiratory rate, 20 breaths/min; and temperature, 98.6˚F. Oxygen saturation was 95% on room air. The head, eyes, ears, nose, and throat examination was normal. The cardiopulmonary examination revealed slight tachycardia with a regular rhythm but no murmurs, rubs, or gallops; the lungs were clear to auscultation bilaterally. The abdominal examination revealed a soft, nontender abdomen, without mass, and no guarding or rebound was present. An examination of the lower extremities was not documented.
The emergency physician (EP) ordered laboratory studies, which included a complete blood count (CBC), basic metabolic profile (BMP), and troponin I level. A chest X-ray and electrocardiogram (ECG) were also ordered. The chest X-ray was interpreted as normal, and the ECG revealed mild sinus tachycardia with nonspecific ST-T segment changes in V1 through V3. The CBC and BMP were all within normal limits, but the troponin I level was slightly elevated.
Given the patient’s clinical presentation and slightly elevated troponin I level, the EP was concerned for an acute coronary syndrome (ACS) and admitted the patient to the care of the on-call cardiologist. Prior to transfer, the patient was given 325 mg of aspirin by mouth, but no anticoagulation therapy was ordered. The cardiologist, who evaluated the patient after she was admitted to the inpatient floor, was concerned the patient had a pulmonary embolism (PE), and ordered a stat computed tomography angiography (CTA) scan of the chest. While the patient was undergoing the chest CTA scan, she went into cardiac arrest. Despite aggressive resuscitative measures, the patient could not be revived and was pronounced dead. An autopsy revealed a PE as the cause of death.
Plaintiff’s Claim
The patient’s estate sued the EP for failure to properly diagnose the PE, stating the hospital was vicariously liable for the EP’s actions. The emergency medicine (EM) expert for the plaintiff opined that the decedent’s symptoms should have prompted the EP to suspect she was suffering from a PE, and he should have immediately ordered anticoagulation, a D-dimer test, or a chest CTA scan. The expert cardiologist for the plaintiff stated the EP should have immediately started the patient on anticoagulation prior to the chest CTA scan.
The Defense
The defense EM expert stated the defendant’s diagnosis of ACS was appropriate given the patient’s overall clinical presentation, and the defense expert cardiologist stated the standard of care did not require the EP to administer anticoagulation prior to her diagnosis of PE, since the bleeding risks outweighed the benefits.
Verdict
At trial, the jury returned a defense verdict.
Discussion
This is not the first (nor probably the last) malpractice case in this column to involve a missed PE. While there have been improvements to the tools we currently possess to evaluate patients for suspected PE, it remains a difficult condition to reliably and timely identify in the ED. Although the two predominating symptoms—shortness of breath and chest pain—are common presentations in the ED, each is associated with large differential diagnoses.
Acute Coronary Syndrome Versus Pulmonary Embolism
From what we know of the published details of this case, the patient had only one risk factor for ACS (cigarette smoking) and two risk factors for PE (cigarette smoking and estrogen-containing contraceptive use). The only abnormal physical finding (tachycardia) was slightly more suggestive of PE than ACS. This patient’s primary complaint was chest fullness and shortness of breath. According to the Prospective Investigation of Pulmonary Embolism Diagnosis II study, shortness of breath is the most common complaint in PE (73%), followed by pleuritic chest pain (44%).1
In ACS, which is more common in men versus women and in patients of both sexes over age 55 years, the clinical presentation most commonly involves chest pain that patients describe as a pressure or fullness (as demonstrated in this patient). Unfortunately, in certain patient populations (eg, women, elderly patients, patients with diabetes mellitus) the presenting complaint can be shortness of breath, weakness, or nausea and vomiting. In a study evaluating how frequently an acute PE can mimic ACS, Kukla et al2 found that one-third of patients with an acute PE can present with all of the manifestations suggestive of ACS (ie, chest pain, ECG changes, and elevated troponin).
It is probably safe to assume the elevated troponin I level played a factor in influencing the EP to diagnose ACS, rather than pursuing an alternative diagnosis such as PE. Unfortunately, since both serum troponin T and I can be markers of right ventricle dysfunction, they are elevated in 30% to 50% of patients with moderate-to-large PE.3 However, neither serum troponin T nor troponin I is specific for myocardial infarction or unstable angina.
Pretest Probability: Wells Criteria
Determining pretest probability for any disease process is important when evaluating complaints in the ED; this is especially true for PE. One of the most frequently used tools for determining the likelihood of PE in ED patients is the Wells criteria (Table 1).4
Based on the published information available, the patient in this case would have scored a 1.5, placing her in the unlikely or low-risk category for PE. Patients whose Wells score places them in the low-risk group can benefit from serum D-dimer testing to help diagnose PE. However, serum D-dimer testing should not be ordered for patients in the likely or high-risk categories; these patients should instead be sent directly for imaging studies such as a chest CTA scan.
Pulmonary Embolism Rule-Out Criteria
For patients whose Wells criteria score places them in the “unlikely group,” the PE rule-out criteria (PERC) can be used to determine the need for ordering a D-dimer. If all eight criteria are met, no further testing is necessary to exclude PE from the differential diagnosis (Table 2).5
Summary
Evaluating chest pain and shortness of breath in the ED is a humbling experience for even the most seasoned EP. Thoroughly reviewing the patient’s history and physical examination, and determining the pretest probability of disease entities high on the differential diagnoses list, go a long way in helping make the correct diagnosis—and in turn initiating possible life-saving interventions and treatment.
Case
A 37-year-old woman presented to the ED with a 90-minute history of chest tightness and shortness of breath. She admitted to feeling anxious but denied nausea, vomiting, or diaphoresis. The patient was in good health overall and had no history of similar symptoms. The only medication she took on a regular basis was a combination oral contraceptive (OC). Regarding the patient’s social history, she admitted to smoking one-half of a pack of cigarettes per day and occasional alcohol use.
On physical examination, the patient’s vital signs were: heart rate (HR), 102 beats/min; blood pressure, 118/64 mm Hg; respiratory rate, 20 breaths/min; and temperature, 98.6˚F. Oxygen saturation was 95% on room air. The head, eyes, ears, nose, and throat examination was normal. The cardiopulmonary examination revealed slight tachycardia with a regular rhythm but no murmurs, rubs, or gallops; the lungs were clear to auscultation bilaterally. The abdominal examination revealed a soft, nontender abdomen, without mass, and no guarding or rebound was present. An examination of the lower extremities was not documented.
The emergency physician (EP) ordered laboratory studies, which included a complete blood count (CBC), basic metabolic profile (BMP), and troponin I level. A chest X-ray and electrocardiogram (ECG) were also ordered. The chest X-ray was interpreted as normal, and the ECG revealed mild sinus tachycardia with nonspecific ST-T segment changes in V1 through V3. The CBC and BMP were all within normal limits, but the troponin I level was slightly elevated.
Given the patient’s clinical presentation and slightly elevated troponin I level, the EP was concerned for an acute coronary syndrome (ACS) and admitted the patient to the care of the on-call cardiologist. Prior to transfer, the patient was given 325 mg of aspirin by mouth, but no anticoagulation therapy was ordered. The cardiologist, who evaluated the patient after she was admitted to the inpatient floor, was concerned the patient had a pulmonary embolism (PE), and ordered a stat computed tomography angiography (CTA) scan of the chest. While the patient was undergoing the chest CTA scan, she went into cardiac arrest. Despite aggressive resuscitative measures, the patient could not be revived and was pronounced dead. An autopsy revealed a PE as the cause of death.
Plaintiff’s Claim
The patient’s estate sued the EP for failure to properly diagnose the PE, stating the hospital was vicariously liable for the EP’s actions. The emergency medicine (EM) expert for the plaintiff opined that the decedent’s symptoms should have prompted the EP to suspect she was suffering from a PE, and he should have immediately ordered anticoagulation, a D-dimer test, or a chest CTA scan. The expert cardiologist for the plaintiff stated the EP should have immediately started the patient on anticoagulation prior to the chest CTA scan.
The Defense
The defense EM expert stated the defendant’s diagnosis of ACS was appropriate given the patient’s overall clinical presentation, and the defense expert cardiologist stated the standard of care did not require the EP to administer anticoagulation prior to her diagnosis of PE, since the bleeding risks outweighed the benefits.
Verdict
At trial, the jury returned a defense verdict.
Discussion
This is not the first (nor probably the last) malpractice case in this column to involve a missed PE. While there have been improvements to the tools we currently possess to evaluate patients for suspected PE, it remains a difficult condition to reliably and timely identify in the ED. Although the two predominating symptoms—shortness of breath and chest pain—are common presentations in the ED, each is associated with large differential diagnoses.
Acute Coronary Syndrome Versus Pulmonary Embolism
From what we know of the published details of this case, the patient had only one risk factor for ACS (cigarette smoking) and two risk factors for PE (cigarette smoking and estrogen-containing contraceptive use). The only abnormal physical finding (tachycardia) was slightly more suggestive of PE than ACS. This patient’s primary complaint was chest fullness and shortness of breath. According to the Prospective Investigation of Pulmonary Embolism Diagnosis II study, shortness of breath is the most common complaint in PE (73%), followed by pleuritic chest pain (44%).1
In ACS, which is more common in men versus women and in patients of both sexes over age 55 years, the clinical presentation most commonly involves chest pain that patients describe as a pressure or fullness (as demonstrated in this patient). Unfortunately, in certain patient populations (eg, women, elderly patients, patients with diabetes mellitus) the presenting complaint can be shortness of breath, weakness, or nausea and vomiting. In a study evaluating how frequently an acute PE can mimic ACS, Kukla et al2 found that one-third of patients with an acute PE can present with all of the manifestations suggestive of ACS (ie, chest pain, ECG changes, and elevated troponin).
It is probably safe to assume the elevated troponin I level played a factor in influencing the EP to diagnose ACS, rather than pursuing an alternative diagnosis such as PE. Unfortunately, since both serum troponin T and I can be markers of right ventricle dysfunction, they are elevated in 30% to 50% of patients with moderate-to-large PE.3 However, neither serum troponin T nor troponin I is specific for myocardial infarction or unstable angina.
Pretest Probability: Wells Criteria
Determining pretest probability for any disease process is important when evaluating complaints in the ED; this is especially true for PE. One of the most frequently used tools for determining the likelihood of PE in ED patients is the Wells criteria (Table 1).4
Based on the published information available, the patient in this case would have scored a 1.5, placing her in the unlikely or low-risk category for PE. Patients whose Wells score places them in the low-risk group can benefit from serum D-dimer testing to help diagnose PE. However, serum D-dimer testing should not be ordered for patients in the likely or high-risk categories; these patients should instead be sent directly for imaging studies such as a chest CTA scan.
Pulmonary Embolism Rule-Out Criteria
For patients whose Wells criteria score places them in the “unlikely group,” the PE rule-out criteria (PERC) can be used to determine the need for ordering a D-dimer. If all eight criteria are met, no further testing is necessary to exclude PE from the differential diagnosis (Table 2).5
Summary
Evaluating chest pain and shortness of breath in the ED is a humbling experience for even the most seasoned EP. Thoroughly reviewing the patient’s history and physical examination, and determining the pretest probability of disease entities high on the differential diagnoses list, go a long way in helping make the correct diagnosis—and in turn initiating possible life-saving interventions and treatment.
1. Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879.
2. Kukla P, Dlugopolski R, Krupa E, et al. How often pulmonary embolism mimics acute coronary syndrome? Kardiol Pol. 2011;69(3):235-240.
3. Meyer T, Binder L, Hruska N, Luthe H, Buchwald AB. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632-1636.
4. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
5. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772-780. doi: 10.1111/j.1538-7836.2008.02944.x.
1. Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879.
2. Kukla P, Dlugopolski R, Krupa E, et al. How often pulmonary embolism mimics acute coronary syndrome? Kardiol Pol. 2011;69(3):235-240.
3. Meyer T, Binder L, Hruska N, Luthe H, Buchwald AB. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632-1636.
4. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
5. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772-780. doi: 10.1111/j.1538-7836.2008.02944.x.
4 Supreme Court decisions important to ObGyns from the 2015−2016 term
Each year, the decisions of the Supreme Court have a significant impact on ObGyn practice. During the 2015–2016 term, which ended in June, the Court issued important rulings on abortion facilities, Affordable Care Act (ACA) contraception coverage, health care False Claims Act (FCA) liability, and state health care data collection. The American Medical Association (AMA), the Association of American Medical Colleges (AAMC), the American College of Obstetricians and Gynecologists (ACOG), and other organizations that represent health care professionals play an important role in health-related Supreme Court cases. For example, amicus curiae (“friend of the Court”) briefs are filed not by parties to a case but by organizations that have a special insight into or interest in a case. Although the extent to which amicus briefs influence cases is often unclear, organization representatives think their briefs make a difference, and briefs undoubtedly do in some cases.
The 2016 presidential election will determine the Supreme Court make-up for the next term, but in this article we consider recent cases that affect ObGyns’ practice in particular. We start with the cases in which professional organizations filed amicus briefs and then turn to other notable cases.
1. Abortion access in Texas and other states
The most important ObGyn case of the 2015–2016 term was Whole Woman’s Health v Hellerstedt.1
At stake. Texas adopted a statute requiring 1) that physicians who perform abortions have admitting privileges at a hospital within 30 miles of the clinic and 2) that abortion clinics meet the state’s standards for ambulatory surgical centers. The current law, upheld by the Court some years ago, is that state laws affecting abortion are unconstitutional if they “unduly burden” the right to abortion. By undue burden, the Court meant, “Regulations that have the purpose or effect of presenting a substantial obstacle to a woman seeking an abortion impose an undue burden on the right.” The question in the Texas case was whether the statute’s 2 requirements were undue.
ACOG, AMA, and other groups filed a brief stating that the Texas law did not promote the welfare of women but instead was unnecessary and not “supported by accepted medical practice or scientific evidence.”2 In another brief the Society of Hospital Medicine and the Society of ObGyn Hospitalists also indicated that having admitting privileges is appropriate only for physicians who regularly admit patients to a hospital.3
A brief filed by the American Association of Pro-Life Obstetricians and Gynecologists and several other organizations argued the other side: “The surgical center and admitting privileges requirements imposed by the Act reflect the professional standard of practice for outpatient gynecological and similar surgery.”4
Final ruling. In a 5−3 decision, the Court struck down the Texas law for providing little or no health benefits while significantly burdening abortion facility access. Many clinics had closed or were in plans to because of the difficulty and expense of complying with the law. This case has national implications. Similar laws, either in place or being considered in other states, will almost certainly be ruled unconstitutional.
2. Contraceptive coverage
The case of Zubik v Burwell was closely watched this past year.
At stake. Under the ACA, a nonprofit religious organization may certify its objection to its insurance plan’s contraception coverage, at which point other arrangements are made to provide contraceptive coverage through the same plan. Religious organizations objected to the certification requirement.
A brief filed by ACOG, Physicians for Reproductive Health, and other groups emphasized the importance of providing contraceptives and contraceptive counseling as part of regular health care and suggested that the current accommodation for religious organizations is appropriate.5
After hearing the formal oral arguments, the Court asked for additional briefs on “whether contraceptive coverage could be provided to petitioners’ employees, through petitioners’ insurance companies, without any such notice from petitioners.”6
Final ruling. The parties agreed such a system would resolve the issue, so the Court sent the case back to the lower court to work out the details. In effect, the case was mediated—an unusual if not unique action for the Court. The resolution probably will achieve what the briefs sought—access to contraceptives and continuity of care.
3. Fraud and abuse litigation
The FCA, which provides for triple damages (3 times actual damages) and stiff civil penalties for anyone who presents the federal government (Medicare, Medicaid) with false claims for goods or services, is a major means of uncovering and punishing health care fraud and abuse. In health care, this law has been used to prosecute cases involving services paid for but not provided, unnecessary services, and off-label pharmaceutical promotion.
An important part of the FCA is that it allows a private intervenor (whistleblower) to initiate an action against a health care provider. The government may then take up the case. If not, the intervenor may pursue it; the incentive is 15% to 30% of the damages the government is awarded.
At stake. The Court was asked if “implied certification” applies to FCA cases.7 Implied certification means that requesting a payment from Medicare or Medicaid implies that the provider is not knowingly withholding information material to the government’s decision to pay the claim. In separately filed briefs, AMA et al8 and American Hospital Association (AHA) et al9 argued that applying implied certification to FCA cases would expand FCA litigation (particularly by intervenors), which is already expensive for health care institutions.
Final ruling. The Court unanimously adopted implied certification but noted that nondisclosure of information must be shown to be a material misrepresentation rather than a trivial regulatory or contractual violation. Furthermore, the Court emphasized that the basis for a claim must be an allegation of fraud, not of malpractice. These findings, which certainly are not what the health care organizations had hoped for, likely will lead to an increase in FCA cases.
4. Collection of state health care data
In Vermont, and about 20 other states that collect data on health care utilization and costs, health insurers and other entities are required to submit detailed reports about health care claims.10 Some insurers objected to this requirement.
At stake. An AHA–AAMC brief noted the importance of health care data and of Vermont’s collecting these data as contributing to better, more efficient health care delivery.11 Another brief, filed by AMA and the Vermont Medical Society, presented more legal or statutory arguments.12
Final ruling. The Court held that the Vermont plan and similar plans violate the federal Employee Retirement Income Security Act of 1974. As health insurance companies and other entities already provide detailed utilization and cost data to the federal government, producing up to 50 additional reports for state governments would be burdensome. Any state that wants the information, the Court said, should obtain it from the federal government.
More notable 2015-2016 Supreme Court decisions.
The Court:
- permitted limited consideration of race in university admissions. ACOG, AAMC, and AMA with many other groups filed an amicus brief supporting medical school and university affirmative action programs.1
- held that a state must give full faith and credit to the adoption orders of the courts of other states (this case involved an LGBT couple).2
- held that states may require (without a search warrant) a breathalyzer test, but not a blood test, for a driver suspected of drinking.3
- narrowed the ability of the federal government to seize or restrain (before trial) the assets of a person charged with criminal health care offenses.4
- temporarily stayed the August 2016 US Department of Education order to schools to allow transgender students to use the facilities in which they feel "most comfortable." The Court likely will take up this case very soon.5
- Fisher v University of Texas at Austin et al, No. 14-981 (2016). https://www.supremecourt.gov/opinions/15pdf/14-981_4g15.pdf. Accessed August 30, 2016.
- V.L. v E.L. et al, No. 15-648 (2016). https://www.supremecourt.gov/opinions/15pdf/15-648_d18e.pdf. Accessed August 30, 2016.
- Birchfield v North Dakota, No. 14-1468 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1468_8n59.pdf. Accessed August 30, 2016.
- Luis v United States, No. 14-419 (2016). https://www.supremecourt.gov/opinions/15pdf/14-419_nmip.pdf. Accessed August 30, 2016.
- Gloucester County School Board v G.G., by his next friend and mother, Deidre Grimm, No. 16A52 (2016). https://www.supremecourt.gov/opinions/15pdf/16a52_8759.pdf. Accessed August 30, 2016.
What’s to come
The Court’s recent decisions on access to abortion services and contraceptives were good for patients of ObGyns, but its decisions on health care FCA liability and state health care data collection were, arguably, not as good for ObGyn business practices.
The Court itself had an unusual year. Justice Scalia died in February, and Congress’s inaction on seating a replacement meant that most of the term’s cases were decided by an 8-member Court. Nevertheless, the Court was deadlocked 4−4 on only 4 of the 80 cases it heard. In addition, it was relatively agreed on outcomes; in only about one-third of cases were there more than 2 justices disagreeing with the outcome.
It is unlikely that a replacement for Justice Scalia will be confirmed before the Court begins its new term in October. The need to replace Justice Scalia and the potential turnover of other Court members—Justice Ginsburg is 83, Justice Kennedy is 80, and Justice Breyer is 78—are reminders of the importance of this year’s presidential election. In the meantime, the Court is accepting the cases that will make up the coming term’s docket, and ObGyns undoubtedly will play a role in cases that involve health care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). https://www.supremecourt.gov/opinions/15pdf/15-274_new_e18f.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, American Medical Association, American Academy of Family Physicians, American Osteopathic Association, and American Academy of Pediatrics in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/ACOG-WilmerHale.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by Society of Hospital Medicine and Society of Ob/Gyn Hospitalists in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/Society-of-Hospital-Medicine-Crowell.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Association of Pro-Life Obstetricians and Gynecologists, American College of Pediatricians, Christian Medical & Dental Association, Catholic Medical Association, and Physicians for Life in support of respondents. Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al. http://www.scotusblog.com/wp-content/uploads/2016/02/15-274-bsac-American-Association-of-Pro-Life-Obstetricians-and-Gynecolog....pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, Physicians for Reproductive Health, American Academy of Family Physicians, American Nurses Association, et al in support of the government and affirmance. Zubik et al v Burwell, Secretary of Health and Human Services, et al, Nos. 14-1418, 14-1458, 14-1505, 15-35, 15-105, 15-119, and 15-191. http://www.scotusblog.com/wp-content/uploads/2016/02/Docfoc.com-Amicus-Brief-Zubik-v.-Burwell.pdf. Accessed August 30, 2016.
- Zubik et al v Burwell, Secretary of Health and Human Services, et al, No. 14-1418 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1418_8758.pdf. Accessed August 30, 2016.
- Universal Health Services, Inc v United States et al ex rel. Escobar et al, No. 15-7 (2016). https://www.supremecourt.gov/opinions/15pdf/15-7_a074.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association, National Association of Chain Drug Stores, National Association of Manufacturers, American Tort Reform Association and NFIB Small Business Legal Center in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7-tsac-American-Medical-Association.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association, Federation of American Hospitals, and Association of American Medical Colleges in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7tsacAHAFAHAAMC.pdf. Accessed August 30, 2016.
- Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). https://www.supremecourt.gov/opinions/15pdf/14-181_5426.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association and Association of American Medical Colleges in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/150904-amicus-gobeille-liberty.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association and Vermont Medical Society in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/VHCURES-Amicus-Brief-of-American-Medical-Association.pdf. Accessed August 30, 2016.
Each year, the decisions of the Supreme Court have a significant impact on ObGyn practice. During the 2015–2016 term, which ended in June, the Court issued important rulings on abortion facilities, Affordable Care Act (ACA) contraception coverage, health care False Claims Act (FCA) liability, and state health care data collection. The American Medical Association (AMA), the Association of American Medical Colleges (AAMC), the American College of Obstetricians and Gynecologists (ACOG), and other organizations that represent health care professionals play an important role in health-related Supreme Court cases. For example, amicus curiae (“friend of the Court”) briefs are filed not by parties to a case but by organizations that have a special insight into or interest in a case. Although the extent to which amicus briefs influence cases is often unclear, organization representatives think their briefs make a difference, and briefs undoubtedly do in some cases.
The 2016 presidential election will determine the Supreme Court make-up for the next term, but in this article we consider recent cases that affect ObGyns’ practice in particular. We start with the cases in which professional organizations filed amicus briefs and then turn to other notable cases.
1. Abortion access in Texas and other states
The most important ObGyn case of the 2015–2016 term was Whole Woman’s Health v Hellerstedt.1
At stake. Texas adopted a statute requiring 1) that physicians who perform abortions have admitting privileges at a hospital within 30 miles of the clinic and 2) that abortion clinics meet the state’s standards for ambulatory surgical centers. The current law, upheld by the Court some years ago, is that state laws affecting abortion are unconstitutional if they “unduly burden” the right to abortion. By undue burden, the Court meant, “Regulations that have the purpose or effect of presenting a substantial obstacle to a woman seeking an abortion impose an undue burden on the right.” The question in the Texas case was whether the statute’s 2 requirements were undue.
ACOG, AMA, and other groups filed a brief stating that the Texas law did not promote the welfare of women but instead was unnecessary and not “supported by accepted medical practice or scientific evidence.”2 In another brief the Society of Hospital Medicine and the Society of ObGyn Hospitalists also indicated that having admitting privileges is appropriate only for physicians who regularly admit patients to a hospital.3
A brief filed by the American Association of Pro-Life Obstetricians and Gynecologists and several other organizations argued the other side: “The surgical center and admitting privileges requirements imposed by the Act reflect the professional standard of practice for outpatient gynecological and similar surgery.”4
Final ruling. In a 5−3 decision, the Court struck down the Texas law for providing little or no health benefits while significantly burdening abortion facility access. Many clinics had closed or were in plans to because of the difficulty and expense of complying with the law. This case has national implications. Similar laws, either in place or being considered in other states, will almost certainly be ruled unconstitutional.
2. Contraceptive coverage
The case of Zubik v Burwell was closely watched this past year.
At stake. Under the ACA, a nonprofit religious organization may certify its objection to its insurance plan’s contraception coverage, at which point other arrangements are made to provide contraceptive coverage through the same plan. Religious organizations objected to the certification requirement.
A brief filed by ACOG, Physicians for Reproductive Health, and other groups emphasized the importance of providing contraceptives and contraceptive counseling as part of regular health care and suggested that the current accommodation for religious organizations is appropriate.5
After hearing the formal oral arguments, the Court asked for additional briefs on “whether contraceptive coverage could be provided to petitioners’ employees, through petitioners’ insurance companies, without any such notice from petitioners.”6
Final ruling. The parties agreed such a system would resolve the issue, so the Court sent the case back to the lower court to work out the details. In effect, the case was mediated—an unusual if not unique action for the Court. The resolution probably will achieve what the briefs sought—access to contraceptives and continuity of care.
3. Fraud and abuse litigation
The FCA, which provides for triple damages (3 times actual damages) and stiff civil penalties for anyone who presents the federal government (Medicare, Medicaid) with false claims for goods or services, is a major means of uncovering and punishing health care fraud and abuse. In health care, this law has been used to prosecute cases involving services paid for but not provided, unnecessary services, and off-label pharmaceutical promotion.
An important part of the FCA is that it allows a private intervenor (whistleblower) to initiate an action against a health care provider. The government may then take up the case. If not, the intervenor may pursue it; the incentive is 15% to 30% of the damages the government is awarded.
At stake. The Court was asked if “implied certification” applies to FCA cases.7 Implied certification means that requesting a payment from Medicare or Medicaid implies that the provider is not knowingly withholding information material to the government’s decision to pay the claim. In separately filed briefs, AMA et al8 and American Hospital Association (AHA) et al9 argued that applying implied certification to FCA cases would expand FCA litigation (particularly by intervenors), which is already expensive for health care institutions.
Final ruling. The Court unanimously adopted implied certification but noted that nondisclosure of information must be shown to be a material misrepresentation rather than a trivial regulatory or contractual violation. Furthermore, the Court emphasized that the basis for a claim must be an allegation of fraud, not of malpractice. These findings, which certainly are not what the health care organizations had hoped for, likely will lead to an increase in FCA cases.
4. Collection of state health care data
In Vermont, and about 20 other states that collect data on health care utilization and costs, health insurers and other entities are required to submit detailed reports about health care claims.10 Some insurers objected to this requirement.
At stake. An AHA–AAMC brief noted the importance of health care data and of Vermont’s collecting these data as contributing to better, more efficient health care delivery.11 Another brief, filed by AMA and the Vermont Medical Society, presented more legal or statutory arguments.12
Final ruling. The Court held that the Vermont plan and similar plans violate the federal Employee Retirement Income Security Act of 1974. As health insurance companies and other entities already provide detailed utilization and cost data to the federal government, producing up to 50 additional reports for state governments would be burdensome. Any state that wants the information, the Court said, should obtain it from the federal government.
More notable 2015-2016 Supreme Court decisions.
The Court:
- permitted limited consideration of race in university admissions. ACOG, AAMC, and AMA with many other groups filed an amicus brief supporting medical school and university affirmative action programs.1
- held that a state must give full faith and credit to the adoption orders of the courts of other states (this case involved an LGBT couple).2
- held that states may require (without a search warrant) a breathalyzer test, but not a blood test, for a driver suspected of drinking.3
- narrowed the ability of the federal government to seize or restrain (before trial) the assets of a person charged with criminal health care offenses.4
- temporarily stayed the August 2016 US Department of Education order to schools to allow transgender students to use the facilities in which they feel "most comfortable." The Court likely will take up this case very soon.5
- Fisher v University of Texas at Austin et al, No. 14-981 (2016). https://www.supremecourt.gov/opinions/15pdf/14-981_4g15.pdf. Accessed August 30, 2016.
- V.L. v E.L. et al, No. 15-648 (2016). https://www.supremecourt.gov/opinions/15pdf/15-648_d18e.pdf. Accessed August 30, 2016.
- Birchfield v North Dakota, No. 14-1468 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1468_8n59.pdf. Accessed August 30, 2016.
- Luis v United States, No. 14-419 (2016). https://www.supremecourt.gov/opinions/15pdf/14-419_nmip.pdf. Accessed August 30, 2016.
- Gloucester County School Board v G.G., by his next friend and mother, Deidre Grimm, No. 16A52 (2016). https://www.supremecourt.gov/opinions/15pdf/16a52_8759.pdf. Accessed August 30, 2016.
What’s to come
The Court’s recent decisions on access to abortion services and contraceptives were good for patients of ObGyns, but its decisions on health care FCA liability and state health care data collection were, arguably, not as good for ObGyn business practices.
The Court itself had an unusual year. Justice Scalia died in February, and Congress’s inaction on seating a replacement meant that most of the term’s cases were decided by an 8-member Court. Nevertheless, the Court was deadlocked 4−4 on only 4 of the 80 cases it heard. In addition, it was relatively agreed on outcomes; in only about one-third of cases were there more than 2 justices disagreeing with the outcome.
It is unlikely that a replacement for Justice Scalia will be confirmed before the Court begins its new term in October. The need to replace Justice Scalia and the potential turnover of other Court members—Justice Ginsburg is 83, Justice Kennedy is 80, and Justice Breyer is 78—are reminders of the importance of this year’s presidential election. In the meantime, the Court is accepting the cases that will make up the coming term’s docket, and ObGyns undoubtedly will play a role in cases that involve health care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Each year, the decisions of the Supreme Court have a significant impact on ObGyn practice. During the 2015–2016 term, which ended in June, the Court issued important rulings on abortion facilities, Affordable Care Act (ACA) contraception coverage, health care False Claims Act (FCA) liability, and state health care data collection. The American Medical Association (AMA), the Association of American Medical Colleges (AAMC), the American College of Obstetricians and Gynecologists (ACOG), and other organizations that represent health care professionals play an important role in health-related Supreme Court cases. For example, amicus curiae (“friend of the Court”) briefs are filed not by parties to a case but by organizations that have a special insight into or interest in a case. Although the extent to which amicus briefs influence cases is often unclear, organization representatives think their briefs make a difference, and briefs undoubtedly do in some cases.
The 2016 presidential election will determine the Supreme Court make-up for the next term, but in this article we consider recent cases that affect ObGyns’ practice in particular. We start with the cases in which professional organizations filed amicus briefs and then turn to other notable cases.
1. Abortion access in Texas and other states
The most important ObGyn case of the 2015–2016 term was Whole Woman’s Health v Hellerstedt.1
At stake. Texas adopted a statute requiring 1) that physicians who perform abortions have admitting privileges at a hospital within 30 miles of the clinic and 2) that abortion clinics meet the state’s standards for ambulatory surgical centers. The current law, upheld by the Court some years ago, is that state laws affecting abortion are unconstitutional if they “unduly burden” the right to abortion. By undue burden, the Court meant, “Regulations that have the purpose or effect of presenting a substantial obstacle to a woman seeking an abortion impose an undue burden on the right.” The question in the Texas case was whether the statute’s 2 requirements were undue.
ACOG, AMA, and other groups filed a brief stating that the Texas law did not promote the welfare of women but instead was unnecessary and not “supported by accepted medical practice or scientific evidence.”2 In another brief the Society of Hospital Medicine and the Society of ObGyn Hospitalists also indicated that having admitting privileges is appropriate only for physicians who regularly admit patients to a hospital.3
A brief filed by the American Association of Pro-Life Obstetricians and Gynecologists and several other organizations argued the other side: “The surgical center and admitting privileges requirements imposed by the Act reflect the professional standard of practice for outpatient gynecological and similar surgery.”4
Final ruling. In a 5−3 decision, the Court struck down the Texas law for providing little or no health benefits while significantly burdening abortion facility access. Many clinics had closed or were in plans to because of the difficulty and expense of complying with the law. This case has national implications. Similar laws, either in place or being considered in other states, will almost certainly be ruled unconstitutional.
2. Contraceptive coverage
The case of Zubik v Burwell was closely watched this past year.
At stake. Under the ACA, a nonprofit religious organization may certify its objection to its insurance plan’s contraception coverage, at which point other arrangements are made to provide contraceptive coverage through the same plan. Religious organizations objected to the certification requirement.
A brief filed by ACOG, Physicians for Reproductive Health, and other groups emphasized the importance of providing contraceptives and contraceptive counseling as part of regular health care and suggested that the current accommodation for religious organizations is appropriate.5
After hearing the formal oral arguments, the Court asked for additional briefs on “whether contraceptive coverage could be provided to petitioners’ employees, through petitioners’ insurance companies, without any such notice from petitioners.”6
Final ruling. The parties agreed such a system would resolve the issue, so the Court sent the case back to the lower court to work out the details. In effect, the case was mediated—an unusual if not unique action for the Court. The resolution probably will achieve what the briefs sought—access to contraceptives and continuity of care.
3. Fraud and abuse litigation
The FCA, which provides for triple damages (3 times actual damages) and stiff civil penalties for anyone who presents the federal government (Medicare, Medicaid) with false claims for goods or services, is a major means of uncovering and punishing health care fraud and abuse. In health care, this law has been used to prosecute cases involving services paid for but not provided, unnecessary services, and off-label pharmaceutical promotion.
An important part of the FCA is that it allows a private intervenor (whistleblower) to initiate an action against a health care provider. The government may then take up the case. If not, the intervenor may pursue it; the incentive is 15% to 30% of the damages the government is awarded.
At stake. The Court was asked if “implied certification” applies to FCA cases.7 Implied certification means that requesting a payment from Medicare or Medicaid implies that the provider is not knowingly withholding information material to the government’s decision to pay the claim. In separately filed briefs, AMA et al8 and American Hospital Association (AHA) et al9 argued that applying implied certification to FCA cases would expand FCA litigation (particularly by intervenors), which is already expensive for health care institutions.
Final ruling. The Court unanimously adopted implied certification but noted that nondisclosure of information must be shown to be a material misrepresentation rather than a trivial regulatory or contractual violation. Furthermore, the Court emphasized that the basis for a claim must be an allegation of fraud, not of malpractice. These findings, which certainly are not what the health care organizations had hoped for, likely will lead to an increase in FCA cases.
4. Collection of state health care data
In Vermont, and about 20 other states that collect data on health care utilization and costs, health insurers and other entities are required to submit detailed reports about health care claims.10 Some insurers objected to this requirement.
At stake. An AHA–AAMC brief noted the importance of health care data and of Vermont’s collecting these data as contributing to better, more efficient health care delivery.11 Another brief, filed by AMA and the Vermont Medical Society, presented more legal or statutory arguments.12
Final ruling. The Court held that the Vermont plan and similar plans violate the federal Employee Retirement Income Security Act of 1974. As health insurance companies and other entities already provide detailed utilization and cost data to the federal government, producing up to 50 additional reports for state governments would be burdensome. Any state that wants the information, the Court said, should obtain it from the federal government.
More notable 2015-2016 Supreme Court decisions.
The Court:
- permitted limited consideration of race in university admissions. ACOG, AAMC, and AMA with many other groups filed an amicus brief supporting medical school and university affirmative action programs.1
- held that a state must give full faith and credit to the adoption orders of the courts of other states (this case involved an LGBT couple).2
- held that states may require (without a search warrant) a breathalyzer test, but not a blood test, for a driver suspected of drinking.3
- narrowed the ability of the federal government to seize or restrain (before trial) the assets of a person charged with criminal health care offenses.4
- temporarily stayed the August 2016 US Department of Education order to schools to allow transgender students to use the facilities in which they feel "most comfortable." The Court likely will take up this case very soon.5
- Fisher v University of Texas at Austin et al, No. 14-981 (2016). https://www.supremecourt.gov/opinions/15pdf/14-981_4g15.pdf. Accessed August 30, 2016.
- V.L. v E.L. et al, No. 15-648 (2016). https://www.supremecourt.gov/opinions/15pdf/15-648_d18e.pdf. Accessed August 30, 2016.
- Birchfield v North Dakota, No. 14-1468 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1468_8n59.pdf. Accessed August 30, 2016.
- Luis v United States, No. 14-419 (2016). https://www.supremecourt.gov/opinions/15pdf/14-419_nmip.pdf. Accessed August 30, 2016.
- Gloucester County School Board v G.G., by his next friend and mother, Deidre Grimm, No. 16A52 (2016). https://www.supremecourt.gov/opinions/15pdf/16a52_8759.pdf. Accessed August 30, 2016.
What’s to come
The Court’s recent decisions on access to abortion services and contraceptives were good for patients of ObGyns, but its decisions on health care FCA liability and state health care data collection were, arguably, not as good for ObGyn business practices.
The Court itself had an unusual year. Justice Scalia died in February, and Congress’s inaction on seating a replacement meant that most of the term’s cases were decided by an 8-member Court. Nevertheless, the Court was deadlocked 4−4 on only 4 of the 80 cases it heard. In addition, it was relatively agreed on outcomes; in only about one-third of cases were there more than 2 justices disagreeing with the outcome.
It is unlikely that a replacement for Justice Scalia will be confirmed before the Court begins its new term in October. The need to replace Justice Scalia and the potential turnover of other Court members—Justice Ginsburg is 83, Justice Kennedy is 80, and Justice Breyer is 78—are reminders of the importance of this year’s presidential election. In the meantime, the Court is accepting the cases that will make up the coming term’s docket, and ObGyns undoubtedly will play a role in cases that involve health care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). https://www.supremecourt.gov/opinions/15pdf/15-274_new_e18f.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, American Medical Association, American Academy of Family Physicians, American Osteopathic Association, and American Academy of Pediatrics in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/ACOG-WilmerHale.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by Society of Hospital Medicine and Society of Ob/Gyn Hospitalists in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/Society-of-Hospital-Medicine-Crowell.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Association of Pro-Life Obstetricians and Gynecologists, American College of Pediatricians, Christian Medical & Dental Association, Catholic Medical Association, and Physicians for Life in support of respondents. Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al. http://www.scotusblog.com/wp-content/uploads/2016/02/15-274-bsac-American-Association-of-Pro-Life-Obstetricians-and-Gynecolog....pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, Physicians for Reproductive Health, American Academy of Family Physicians, American Nurses Association, et al in support of the government and affirmance. Zubik et al v Burwell, Secretary of Health and Human Services, et al, Nos. 14-1418, 14-1458, 14-1505, 15-35, 15-105, 15-119, and 15-191. http://www.scotusblog.com/wp-content/uploads/2016/02/Docfoc.com-Amicus-Brief-Zubik-v.-Burwell.pdf. Accessed August 30, 2016.
- Zubik et al v Burwell, Secretary of Health and Human Services, et al, No. 14-1418 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1418_8758.pdf. Accessed August 30, 2016.
- Universal Health Services, Inc v United States et al ex rel. Escobar et al, No. 15-7 (2016). https://www.supremecourt.gov/opinions/15pdf/15-7_a074.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association, National Association of Chain Drug Stores, National Association of Manufacturers, American Tort Reform Association and NFIB Small Business Legal Center in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7-tsac-American-Medical-Association.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association, Federation of American Hospitals, and Association of American Medical Colleges in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7tsacAHAFAHAAMC.pdf. Accessed August 30, 2016.
- Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). https://www.supremecourt.gov/opinions/15pdf/14-181_5426.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association and Association of American Medical Colleges in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/150904-amicus-gobeille-liberty.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association and Vermont Medical Society in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/VHCURES-Amicus-Brief-of-American-Medical-Association.pdf. Accessed August 30, 2016.
- Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). https://www.supremecourt.gov/opinions/15pdf/15-274_new_e18f.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, American Medical Association, American Academy of Family Physicians, American Osteopathic Association, and American Academy of Pediatrics in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/ACOG-WilmerHale.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by Society of Hospital Medicine and Society of Ob/Gyn Hospitalists in support of petitioners. Whole Woman's Health et al v Cole, Commissioner, Texas Department of State Health Services, et al, No. 15-274 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/Society-of-Hospital-Medicine-Crowell.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Association of Pro-Life Obstetricians and Gynecologists, American College of Pediatricians, Christian Medical & Dental Association, Catholic Medical Association, and Physicians for Life in support of respondents. Whole Woman's Health et al v Hellerstedt, Commissioner, Texas Department of State Health Services, et al. http://www.scotusblog.com/wp-content/uploads/2016/02/15-274-bsac-American-Association-of-Pro-Life-Obstetricians-and-Gynecolog....pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American College of Obstetricians and Gynecologists, Physicians for Reproductive Health, American Academy of Family Physicians, American Nurses Association, et al in support of the government and affirmance. Zubik et al v Burwell, Secretary of Health and Human Services, et al, Nos. 14-1418, 14-1458, 14-1505, 15-35, 15-105, 15-119, and 15-191. http://www.scotusblog.com/wp-content/uploads/2016/02/Docfoc.com-Amicus-Brief-Zubik-v.-Burwell.pdf. Accessed August 30, 2016.
- Zubik et al v Burwell, Secretary of Health and Human Services, et al, No. 14-1418 (2016). https://www.supremecourt.gov/opinions/15pdf/14-1418_8758.pdf. Accessed August 30, 2016.
- Universal Health Services, Inc v United States et al ex rel. Escobar et al, No. 15-7 (2016). https://www.supremecourt.gov/opinions/15pdf/15-7_a074.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association, National Association of Chain Drug Stores, National Association of Manufacturers, American Tort Reform Association and NFIB Small Business Legal Center in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7-tsac-American-Medical-Association.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association, Federation of American Hospitals, and Association of American Medical Colleges in support of petitioner. Universal Health Services, Inc v United States and Commonwealth of Massachusetts ex rel. Escobar and Correa, No. 15-7 (2016). http://www.scotusblog.com/wp-content/uploads/2016/01/15-7tsacAHAFAHAAMC.pdf. Accessed August 30, 2016.
- Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). https://www.supremecourt.gov/opinions/15pdf/14-181_5426.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Hospital Association and Association of American Medical Colleges in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/150904-amicus-gobeille-liberty.pdf. Accessed August 30, 2016.
- Amici curiae brief filed by American Medical Association and Vermont Medical Society in support of petitioner. Gobeille, Chair, Vermont Green Mountain Care Board, v Liberty Mutual Insurance Co, No. 14-181 (2016). http://www.scotusblog.com/wp-content/uploads/2015/09/VHCURES-Amicus-Brief-of-American-Medical-Association.pdf. Accessed August 30, 2016.
In this Article
- Whole Woman’s Health v Hellerstedt
- Fraud and abuse litigation
- What’s to come
Online dating and personal information: Pause before you post
Most adults want to have happy romantic relationships. But meeting eligible companions and finding the time to date can feel nearly impossible to many physicians, especially residents, whose 80-hour work weeks limit opportunities to meet potential partners.1
So it’s no surprise that Dr. R’s friends have suggested that she try online dating. If she does, she would be far from alone: 15% of U.S. adults have sought relationships online, and one-fourth of people in their 20s have used a mobile dating app.2,3 Online dating might work well for Dr. R, too. Between 2005 and 2012, more than one-third of U.S. marriages started online, and these marriages seemed happier and ended in separation or divorce less often than marriages that started in more traditional ways.4
Online dating is just one example of how “the permeation of online and social media into everyday life is placing doctors in new situations that they find difficult to navigate.”5 Many physicians—psychiatrists among them—date online. Yet, like Dr. R, physicians are cautious about using social media because of worries about public exposure and legal concerns.5 Moreover, medical associations haven’t developed guidelines that would help physicians reconcile their professional and personal lives if they seek companionship online.6
Although we don’t have complete answers to Dr. R’s questions, we have gathered some ideas and information that she might find helpful. Read on as we explore:
- potential benefits for psychiatrists who try online dating
- problems when physicians use social media
- how to minimize mishaps if you seek companionship online.
Advantages and benefits
Online dating is most popular among young adults. But singles and divorcees of all ages, sexual orientations, and backgrounds are increasingly seeking long-term relationships with internet-based dating tools rather than hoping to meet people through family, friends, church, and the workplace. It has become common—and no longer stigmatizing—for couples to say they met online.2,7
A dating Web site or app is a simple, fast, low-investment way to increase your opportunities to meet other singles and to make contact with more potential partners than you would meet otherwise. This is particularly helpful for people in thinner dating markets (eg, gays, lesbians, middle-age heterosexuals, and rural dwellers) or people seeking a companion of a particular type or lifestyle.7,8 Many internet dating tools claim that their matching algorithms can increase your chances of meeting someone you will find compatible (although research questions whether the algorithms really work8). Dating sites and apps also let users engage in brief, computer-mediated communications that can foster greater attraction and comfort before meeting for a first date.8
Appeal to psychiatrists
Online dating may have special appeal to young psychiatrists such as Dr. R. Oddly enough, being a mental health professional can leave you socially isolated. Many people react cautiously when they learn you are a psychiatrist—they think you are evaluating them (and let’s face it: often, this is true).9 Psychiatrists should be cordial but circumspect in conducting work relationships, which limits the type and amount of social life they might generate in the setting where many people meet their future spouses.10
Online dating can help single psychiatrists overcome these barriers. Scientifically minded physicians can find plenty of research-grounded advice for improving online dating chances.11-14 Two medical researchers even published a meta-analysis of evidence-based methods that can improve the chances of converting online contacts to a first date.15
Caution: Hazards ahead
When seeking romance online, psychiatrists shouldn’t forget their professional obligations, including the duty to maintain clear boundaries between their social and work lives.16 If Dr. R decides to try online dating, she will be making it possible for curious patients to gain access to some of her personal information. She will have to figure out how to avoid jeopardizing her professional reputation or inadvertently opening the door to sexual misconduct.17
Boundaries online. Psychiatrists use the term “boundaries” to refer to how they structure appointments and monitor their behavior during therapy to keep the treatment relationship free of personal, sexual, and romantic influences. Keeping one’s emotional life out of treatment helps prevent exploitation of patients and fosters a sense of safety and assurance that the physician is acting solely with the patient’s interest in mind. Breaching boundaries in ways that exploit patients or serve the doctor’s needs can undermine treatment, harm patients, and result in serious professional consequences.18
Maintaining appropriate boundaries can be challenging for psychiatrists who want to date online because the outside-the-office context can muddy the distinction between one’s professional and personal identity. Online dating environments make it easier for physicians to inadvertently initiate social or romantic interactions with people they have treated but don’t recognize (something the authors know has happened to colleagues). Additionally, the internet’s anonymity leaves users vulnerable to being lured into interactions with someone who is using a fictional online persona—an activity colloquially called “catfishing.”19
Although patients may play an active role in boundary breaches, the physician bears sole responsibility for maintaining proper limits within the therapeutic relationship.18 For many psychiatrists, innocuous but non-professional interactions with patients have been the first steps down a “slippery slope” toward serious boundary violations, including sexual contact—an activity that both the American Medical Association (AMA) and the American Psychiatric Association deem categorically unethical and that can lead to malpractice lawsuits, sanctions by medical license boards, and (in some jurisdictions) criminal prosecution.20 When using social media and online dating tools, psychiatrists should avoid even seemingly minor boundary violations as a safeguard against more serious transgressions.20,21
Reports of online misconduct by medical trainees and practitioners are plentiful.22,23 In response, several medical organizations, including the AMA and the American College of Physicians, have developed professional guidelines for appropriate behavior on social media by physicians.24,25 These guidelines stress the importance of maintaining a professional presence when one’s online activity is publicly viewable.
How much self-disclosure is appropriate?
Traditionally, psychiatrists (including psychoanalysts) have felt that occasional, limited, well-considered references to oneself are acceptable and even helpful in treatment.26 The majority of therapists report using therapy-relevant self-disclosure, but they are cautious about what they say. Conscientious therapists avoid self-disclosure to satisfy their own needs, and they avoid self-disclosure with patients for whom it would have detrimental effects.18,27
Dating Web sites contain a lot of personal information that physicians don’t usually share with patients. Although physicians who use social media are advised to be careful about the information they make available to the public,28 this is more difficult to do with dating applications, where revealing some information about yourself is necessary for making meaningful connections. Creating an online dating profile means that you are potentially letting patients or patients’ relatives know about your place of residence, income, sexual orientation, number of children, and interests. You will need to think about how you will respond if a patient unexpectedly comments on your dating profile during a session or asks you out.
Beyond creating awkward situations, self-disclosure can have treatment implications, and it’s impossible to know how a particular comment will affect a particular client in a particular situation.29 Psychiatrists who engage in online dating may want to limit their posted personal information only to what they would feel reasonably comfortable with having patients know about them, and hope this will suffice to capture the attention of potential partners.
Sustaining professionalism while remaining human. The term “medical professionalism” originally referred to ethical conduct during the practice of medicine30 and to sustaining one’s commitment to patients, fellow professionals, and the institutions within which health care is provided.31 More recently, however, discussions of medical professionalism have encompassed how physicians comport themselves away from work. Physicians’ actions outside the office or hospital—and especially what they say, do, or post online—have a powerful effect on perceptions of their institutions and the medical profession as a whole.25,32
Photos and comments posted by physicians can be seen by millions and can have major repercussions for employment prospects and public perceptions.25 Questionable postings by physicians on social media outlets have resulted in disciplinary actions by licensing authorities and have damaged physicians’ careers.23
What seems appropriate for a dating Web site varies from person to person. A suggestive smile or flirtatious joke that most people would find harmless may strike others as provocative. Derogatory language, depictions of intoxication or substance abuse, and inappropriate patient-related comments are clear-cut mistakes.32-34 But also keep in mind that what medical professionals find acceptable to post on social networking sites does not always match what the general public thinks.35
Bottom Line
1. Miller JA. Romance in residency: is dating even possible? Medscape. http://www.medscape.com/viewarticle/844059. Published May 5, 2016. Accessed June 27, 2016.
2. Smith A, Anderson M. 5 facts about online dating. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/02/29/5-facts-about-online-dating. Published February 29, 2016. Accessed June 27, 2016.
3. Smith A. 15% of American adults have used online dating sites or mobile dating apps. http://www.pewinternet.org/2016/02/11/15-percent-of-american-adults-have-used-online-dating-sites-or-mobile-dating-apps/. Published February 11, 2016. Accessed June 27, 2016.
4. Cacioppo JT, Cacioppo S, Gonzaga GC, et al. Marital satisfaction and break-ups differ across on-line and off-line meeting venues. Proc Natl Acad Sci U S A. 2013;110(25):10135-10140.
5. Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16(12):e267.
6. Berlin R. The professional ethics of online dating: need for guidance. J Am Acad Child Adolesc Psychiatry. 2014;53(9):935-937.
7. Rosenfeld MJ, Thomas RJ. Searching for a mate: the rise of the Internet as a social intermediary. Am Sociol Rev. 2012;77(4):523-547.
8. Finkel EJ, Eastwick PW, Karney BR, et al. Online dating: a critical analysis from the perspective of psychological science. Psychol Sci Public Interest. 2012;13(1):3-66.
9. Pierre J. A mad world: a diagnosis of mental illness is more common than ever—did psychiatrists create the problem, or just recognise it? Aeon.co. https://aeon.co/essays/do-psychiatrists-really-think-that-everyone-is-crazy. Published March 19, 2014. Accessed June 28, 2016.
10. Pearce A, Gambrell D. This chart shows who marries CEOs, doctors, chefs and janitors. Bloomberg. http://www.bloomberg.com/graphics/2016-who-marries-whom. February 11, 2016. Accessed June 28, 2016.
11. Lowin R. Proofread that text before sending! Bad grammar is a dating deal breaker, most say. Today. http://www.today.com/health/can-your-awesome-grammar-really-get-you-date-according-new-t77376. Published March 2, 2016. Accessed June 28, 2016.
12. Reilly K. This strategy will make your Tinder game much stronger. Time. http://time.com/4263598/tinder-gif-messages-response-rate. Published March 17, 2016. Accessed June 28, 2016.
13. Wotipka CD, High AC. Providing a foundation for a satisfying relationship: a direct test of warranting versus selective self-presentation as predictors of attraction to online dating profiles. Presentation at the 101st Annual Meeting of the National Communication Association; November 20, 2014; Chicago, IL.
14. Vacharkulksemsuk T, Reit E, Khambatta P, et al. Dominant, open nonverbal displays are attractive at zero-acquaintance. Proc Natl Acad Sci U S A. 2016;113(15):4009-4014.
15. Khan KS, Chaudhry S. An evidence-based approach to an ancient pursuit: systematic review on converting online contact into a first date. Evid Based Med. 2015;20(2):48-56.
16. Chretien KC, Tuck MG. Online professionalism: a synthetic review. Int Rev Psychiatry. 2015;27(2):106-117.
17. Jackson WC. When patients are normal people: strategies for managing dual relationships. Prim Care Companion J Clin Psychiatry. 2002;4(3):100-103.
18. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
19. D’Costa K. Catfishing: the truth about deception online. ScientificAmerican.com. http://blogs.scientificamerican.com/anthropology-in-practice/catfishing-the-truth-about-deception-online. Published April 25, 2014. Accessed June 29, 2016.
20. Sarkar SP. Boundary violation and sexual exploitation in psychiatry and psychotherapy: a review. Adv Psychiatr Treat. 2004;10(4):312-320.
21. Nadelson C, Notman MT. Boundaries in the doctor-patient relationship. Theor Med Bioeth. 2002;23(3):191-201.
22. Walton JM, White J, Ross S. What’s on YOUR Facebook profile? Evaluation of an educational intervention to promote appropriate use of privacy settings by medical students on social networking sites. Med Educ Online. 2015;20:28708. doi: 10.3402/meo.v20.28708.
23. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
24. Decamp M. Physicians, social media, and conflict of interest. J Gen Intern Med. 2013;28(2):299-303.
25. Farnan JM, Snyder Sulmasy L, Worster BK, et al; American College of Physicians Ethics, Professionalism and Human Rights Committee; American College of Physicians Council of Associates; Federation of State Medical Boards Special Committee on Ethics and Professionalism. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620-627.
26. Meissner WW. The problem of self-disclosure in psychoanalysis. J Am Psychoanal Assoc. 2002;50(3):827-867.
27. Henretty JR, Levitt HM. The role of therapist self-disclosure in psychotherapy: a qualitative review. Clin Psychol Rev. 2010;30(1):63-77.
28. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
29. Peterson ZD. More than a mirror: the ethics of therapist self-disclosure. Psychotherapy: Theory Research & Practice. 2002;39(1):21-31.
30. Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226-235.
31. Wass V. Doctors in society: medical professionalism in a changing world. Clin Med (Lond). 2006;6(1):109-113.
32. Langenfeld SJ, Cook G, Sudbeck C, et al. An assessment of unprofessional behavior among surgical residents on Facebook: a warning of the dangers of social media. J Surg Educ. 2014;71(6):e28-e32.
33. Chauhan B, George R, Coffin J. Social media and you: what every physician needs to know. J Med Pract Manage. 2012;28(3):206-209.
34. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
35. Jain A, Petty EM, Jaber RM, et al. What is appropriate to post on social media? Ratings from students, faculty members and the public. Med Educ. 2014;48(2):157-169.
36. Gabbard GO, Roberts LW, Crisp-Han H, et al. Professionalism in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2012.
Most adults want to have happy romantic relationships. But meeting eligible companions and finding the time to date can feel nearly impossible to many physicians, especially residents, whose 80-hour work weeks limit opportunities to meet potential partners.1
So it’s no surprise that Dr. R’s friends have suggested that she try online dating. If she does, she would be far from alone: 15% of U.S. adults have sought relationships online, and one-fourth of people in their 20s have used a mobile dating app.2,3 Online dating might work well for Dr. R, too. Between 2005 and 2012, more than one-third of U.S. marriages started online, and these marriages seemed happier and ended in separation or divorce less often than marriages that started in more traditional ways.4
Online dating is just one example of how “the permeation of online and social media into everyday life is placing doctors in new situations that they find difficult to navigate.”5 Many physicians—psychiatrists among them—date online. Yet, like Dr. R, physicians are cautious about using social media because of worries about public exposure and legal concerns.5 Moreover, medical associations haven’t developed guidelines that would help physicians reconcile their professional and personal lives if they seek companionship online.6
Although we don’t have complete answers to Dr. R’s questions, we have gathered some ideas and information that she might find helpful. Read on as we explore:
- potential benefits for psychiatrists who try online dating
- problems when physicians use social media
- how to minimize mishaps if you seek companionship online.
Advantages and benefits
Online dating is most popular among young adults. But singles and divorcees of all ages, sexual orientations, and backgrounds are increasingly seeking long-term relationships with internet-based dating tools rather than hoping to meet people through family, friends, church, and the workplace. It has become common—and no longer stigmatizing—for couples to say they met online.2,7
A dating Web site or app is a simple, fast, low-investment way to increase your opportunities to meet other singles and to make contact with more potential partners than you would meet otherwise. This is particularly helpful for people in thinner dating markets (eg, gays, lesbians, middle-age heterosexuals, and rural dwellers) or people seeking a companion of a particular type or lifestyle.7,8 Many internet dating tools claim that their matching algorithms can increase your chances of meeting someone you will find compatible (although research questions whether the algorithms really work8). Dating sites and apps also let users engage in brief, computer-mediated communications that can foster greater attraction and comfort before meeting for a first date.8
Appeal to psychiatrists
Online dating may have special appeal to young psychiatrists such as Dr. R. Oddly enough, being a mental health professional can leave you socially isolated. Many people react cautiously when they learn you are a psychiatrist—they think you are evaluating them (and let’s face it: often, this is true).9 Psychiatrists should be cordial but circumspect in conducting work relationships, which limits the type and amount of social life they might generate in the setting where many people meet their future spouses.10
Online dating can help single psychiatrists overcome these barriers. Scientifically minded physicians can find plenty of research-grounded advice for improving online dating chances.11-14 Two medical researchers even published a meta-analysis of evidence-based methods that can improve the chances of converting online contacts to a first date.15
Caution: Hazards ahead
When seeking romance online, psychiatrists shouldn’t forget their professional obligations, including the duty to maintain clear boundaries between their social and work lives.16 If Dr. R decides to try online dating, she will be making it possible for curious patients to gain access to some of her personal information. She will have to figure out how to avoid jeopardizing her professional reputation or inadvertently opening the door to sexual misconduct.17
Boundaries online. Psychiatrists use the term “boundaries” to refer to how they structure appointments and monitor their behavior during therapy to keep the treatment relationship free of personal, sexual, and romantic influences. Keeping one’s emotional life out of treatment helps prevent exploitation of patients and fosters a sense of safety and assurance that the physician is acting solely with the patient’s interest in mind. Breaching boundaries in ways that exploit patients or serve the doctor’s needs can undermine treatment, harm patients, and result in serious professional consequences.18
Maintaining appropriate boundaries can be challenging for psychiatrists who want to date online because the outside-the-office context can muddy the distinction between one’s professional and personal identity. Online dating environments make it easier for physicians to inadvertently initiate social or romantic interactions with people they have treated but don’t recognize (something the authors know has happened to colleagues). Additionally, the internet’s anonymity leaves users vulnerable to being lured into interactions with someone who is using a fictional online persona—an activity colloquially called “catfishing.”19
Although patients may play an active role in boundary breaches, the physician bears sole responsibility for maintaining proper limits within the therapeutic relationship.18 For many psychiatrists, innocuous but non-professional interactions with patients have been the first steps down a “slippery slope” toward serious boundary violations, including sexual contact—an activity that both the American Medical Association (AMA) and the American Psychiatric Association deem categorically unethical and that can lead to malpractice lawsuits, sanctions by medical license boards, and (in some jurisdictions) criminal prosecution.20 When using social media and online dating tools, psychiatrists should avoid even seemingly minor boundary violations as a safeguard against more serious transgressions.20,21
Reports of online misconduct by medical trainees and practitioners are plentiful.22,23 In response, several medical organizations, including the AMA and the American College of Physicians, have developed professional guidelines for appropriate behavior on social media by physicians.24,25 These guidelines stress the importance of maintaining a professional presence when one’s online activity is publicly viewable.
How much self-disclosure is appropriate?
Traditionally, psychiatrists (including psychoanalysts) have felt that occasional, limited, well-considered references to oneself are acceptable and even helpful in treatment.26 The majority of therapists report using therapy-relevant self-disclosure, but they are cautious about what they say. Conscientious therapists avoid self-disclosure to satisfy their own needs, and they avoid self-disclosure with patients for whom it would have detrimental effects.18,27
Dating Web sites contain a lot of personal information that physicians don’t usually share with patients. Although physicians who use social media are advised to be careful about the information they make available to the public,28 this is more difficult to do with dating applications, where revealing some information about yourself is necessary for making meaningful connections. Creating an online dating profile means that you are potentially letting patients or patients’ relatives know about your place of residence, income, sexual orientation, number of children, and interests. You will need to think about how you will respond if a patient unexpectedly comments on your dating profile during a session or asks you out.
Beyond creating awkward situations, self-disclosure can have treatment implications, and it’s impossible to know how a particular comment will affect a particular client in a particular situation.29 Psychiatrists who engage in online dating may want to limit their posted personal information only to what they would feel reasonably comfortable with having patients know about them, and hope this will suffice to capture the attention of potential partners.
Sustaining professionalism while remaining human. The term “medical professionalism” originally referred to ethical conduct during the practice of medicine30 and to sustaining one’s commitment to patients, fellow professionals, and the institutions within which health care is provided.31 More recently, however, discussions of medical professionalism have encompassed how physicians comport themselves away from work. Physicians’ actions outside the office or hospital—and especially what they say, do, or post online—have a powerful effect on perceptions of their institutions and the medical profession as a whole.25,32
Photos and comments posted by physicians can be seen by millions and can have major repercussions for employment prospects and public perceptions.25 Questionable postings by physicians on social media outlets have resulted in disciplinary actions by licensing authorities and have damaged physicians’ careers.23
What seems appropriate for a dating Web site varies from person to person. A suggestive smile or flirtatious joke that most people would find harmless may strike others as provocative. Derogatory language, depictions of intoxication or substance abuse, and inappropriate patient-related comments are clear-cut mistakes.32-34 But also keep in mind that what medical professionals find acceptable to post on social networking sites does not always match what the general public thinks.35
Bottom Line
Most adults want to have happy romantic relationships. But meeting eligible companions and finding the time to date can feel nearly impossible to many physicians, especially residents, whose 80-hour work weeks limit opportunities to meet potential partners.1
So it’s no surprise that Dr. R’s friends have suggested that she try online dating. If she does, she would be far from alone: 15% of U.S. adults have sought relationships online, and one-fourth of people in their 20s have used a mobile dating app.2,3 Online dating might work well for Dr. R, too. Between 2005 and 2012, more than one-third of U.S. marriages started online, and these marriages seemed happier and ended in separation or divorce less often than marriages that started in more traditional ways.4
Online dating is just one example of how “the permeation of online and social media into everyday life is placing doctors in new situations that they find difficult to navigate.”5 Many physicians—psychiatrists among them—date online. Yet, like Dr. R, physicians are cautious about using social media because of worries about public exposure and legal concerns.5 Moreover, medical associations haven’t developed guidelines that would help physicians reconcile their professional and personal lives if they seek companionship online.6
Although we don’t have complete answers to Dr. R’s questions, we have gathered some ideas and information that she might find helpful. Read on as we explore:
- potential benefits for psychiatrists who try online dating
- problems when physicians use social media
- how to minimize mishaps if you seek companionship online.
Advantages and benefits
Online dating is most popular among young adults. But singles and divorcees of all ages, sexual orientations, and backgrounds are increasingly seeking long-term relationships with internet-based dating tools rather than hoping to meet people through family, friends, church, and the workplace. It has become common—and no longer stigmatizing—for couples to say they met online.2,7
A dating Web site or app is a simple, fast, low-investment way to increase your opportunities to meet other singles and to make contact with more potential partners than you would meet otherwise. This is particularly helpful for people in thinner dating markets (eg, gays, lesbians, middle-age heterosexuals, and rural dwellers) or people seeking a companion of a particular type or lifestyle.7,8 Many internet dating tools claim that their matching algorithms can increase your chances of meeting someone you will find compatible (although research questions whether the algorithms really work8). Dating sites and apps also let users engage in brief, computer-mediated communications that can foster greater attraction and comfort before meeting for a first date.8
Appeal to psychiatrists
Online dating may have special appeal to young psychiatrists such as Dr. R. Oddly enough, being a mental health professional can leave you socially isolated. Many people react cautiously when they learn you are a psychiatrist—they think you are evaluating them (and let’s face it: often, this is true).9 Psychiatrists should be cordial but circumspect in conducting work relationships, which limits the type and amount of social life they might generate in the setting where many people meet their future spouses.10
Online dating can help single psychiatrists overcome these barriers. Scientifically minded physicians can find plenty of research-grounded advice for improving online dating chances.11-14 Two medical researchers even published a meta-analysis of evidence-based methods that can improve the chances of converting online contacts to a first date.15
Caution: Hazards ahead
When seeking romance online, psychiatrists shouldn’t forget their professional obligations, including the duty to maintain clear boundaries between their social and work lives.16 If Dr. R decides to try online dating, she will be making it possible for curious patients to gain access to some of her personal information. She will have to figure out how to avoid jeopardizing her professional reputation or inadvertently opening the door to sexual misconduct.17
Boundaries online. Psychiatrists use the term “boundaries” to refer to how they structure appointments and monitor their behavior during therapy to keep the treatment relationship free of personal, sexual, and romantic influences. Keeping one’s emotional life out of treatment helps prevent exploitation of patients and fosters a sense of safety and assurance that the physician is acting solely with the patient’s interest in mind. Breaching boundaries in ways that exploit patients or serve the doctor’s needs can undermine treatment, harm patients, and result in serious professional consequences.18
Maintaining appropriate boundaries can be challenging for psychiatrists who want to date online because the outside-the-office context can muddy the distinction between one’s professional and personal identity. Online dating environments make it easier for physicians to inadvertently initiate social or romantic interactions with people they have treated but don’t recognize (something the authors know has happened to colleagues). Additionally, the internet’s anonymity leaves users vulnerable to being lured into interactions with someone who is using a fictional online persona—an activity colloquially called “catfishing.”19
Although patients may play an active role in boundary breaches, the physician bears sole responsibility for maintaining proper limits within the therapeutic relationship.18 For many psychiatrists, innocuous but non-professional interactions with patients have been the first steps down a “slippery slope” toward serious boundary violations, including sexual contact—an activity that both the American Medical Association (AMA) and the American Psychiatric Association deem categorically unethical and that can lead to malpractice lawsuits, sanctions by medical license boards, and (in some jurisdictions) criminal prosecution.20 When using social media and online dating tools, psychiatrists should avoid even seemingly minor boundary violations as a safeguard against more serious transgressions.20,21
Reports of online misconduct by medical trainees and practitioners are plentiful.22,23 In response, several medical organizations, including the AMA and the American College of Physicians, have developed professional guidelines for appropriate behavior on social media by physicians.24,25 These guidelines stress the importance of maintaining a professional presence when one’s online activity is publicly viewable.
How much self-disclosure is appropriate?
Traditionally, psychiatrists (including psychoanalysts) have felt that occasional, limited, well-considered references to oneself are acceptable and even helpful in treatment.26 The majority of therapists report using therapy-relevant self-disclosure, but they are cautious about what they say. Conscientious therapists avoid self-disclosure to satisfy their own needs, and they avoid self-disclosure with patients for whom it would have detrimental effects.18,27
Dating Web sites contain a lot of personal information that physicians don’t usually share with patients. Although physicians who use social media are advised to be careful about the information they make available to the public,28 this is more difficult to do with dating applications, where revealing some information about yourself is necessary for making meaningful connections. Creating an online dating profile means that you are potentially letting patients or patients’ relatives know about your place of residence, income, sexual orientation, number of children, and interests. You will need to think about how you will respond if a patient unexpectedly comments on your dating profile during a session or asks you out.
Beyond creating awkward situations, self-disclosure can have treatment implications, and it’s impossible to know how a particular comment will affect a particular client in a particular situation.29 Psychiatrists who engage in online dating may want to limit their posted personal information only to what they would feel reasonably comfortable with having patients know about them, and hope this will suffice to capture the attention of potential partners.
Sustaining professionalism while remaining human. The term “medical professionalism” originally referred to ethical conduct during the practice of medicine30 and to sustaining one’s commitment to patients, fellow professionals, and the institutions within which health care is provided.31 More recently, however, discussions of medical professionalism have encompassed how physicians comport themselves away from work. Physicians’ actions outside the office or hospital—and especially what they say, do, or post online—have a powerful effect on perceptions of their institutions and the medical profession as a whole.25,32
Photos and comments posted by physicians can be seen by millions and can have major repercussions for employment prospects and public perceptions.25 Questionable postings by physicians on social media outlets have resulted in disciplinary actions by licensing authorities and have damaged physicians’ careers.23
What seems appropriate for a dating Web site varies from person to person. A suggestive smile or flirtatious joke that most people would find harmless may strike others as provocative. Derogatory language, depictions of intoxication or substance abuse, and inappropriate patient-related comments are clear-cut mistakes.32-34 But also keep in mind that what medical professionals find acceptable to post on social networking sites does not always match what the general public thinks.35
Bottom Line
1. Miller JA. Romance in residency: is dating even possible? Medscape. http://www.medscape.com/viewarticle/844059. Published May 5, 2016. Accessed June 27, 2016.
2. Smith A, Anderson M. 5 facts about online dating. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/02/29/5-facts-about-online-dating. Published February 29, 2016. Accessed June 27, 2016.
3. Smith A. 15% of American adults have used online dating sites or mobile dating apps. http://www.pewinternet.org/2016/02/11/15-percent-of-american-adults-have-used-online-dating-sites-or-mobile-dating-apps/. Published February 11, 2016. Accessed June 27, 2016.
4. Cacioppo JT, Cacioppo S, Gonzaga GC, et al. Marital satisfaction and break-ups differ across on-line and off-line meeting venues. Proc Natl Acad Sci U S A. 2013;110(25):10135-10140.
5. Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16(12):e267.
6. Berlin R. The professional ethics of online dating: need for guidance. J Am Acad Child Adolesc Psychiatry. 2014;53(9):935-937.
7. Rosenfeld MJ, Thomas RJ. Searching for a mate: the rise of the Internet as a social intermediary. Am Sociol Rev. 2012;77(4):523-547.
8. Finkel EJ, Eastwick PW, Karney BR, et al. Online dating: a critical analysis from the perspective of psychological science. Psychol Sci Public Interest. 2012;13(1):3-66.
9. Pierre J. A mad world: a diagnosis of mental illness is more common than ever—did psychiatrists create the problem, or just recognise it? Aeon.co. https://aeon.co/essays/do-psychiatrists-really-think-that-everyone-is-crazy. Published March 19, 2014. Accessed June 28, 2016.
10. Pearce A, Gambrell D. This chart shows who marries CEOs, doctors, chefs and janitors. Bloomberg. http://www.bloomberg.com/graphics/2016-who-marries-whom. February 11, 2016. Accessed June 28, 2016.
11. Lowin R. Proofread that text before sending! Bad grammar is a dating deal breaker, most say. Today. http://www.today.com/health/can-your-awesome-grammar-really-get-you-date-according-new-t77376. Published March 2, 2016. Accessed June 28, 2016.
12. Reilly K. This strategy will make your Tinder game much stronger. Time. http://time.com/4263598/tinder-gif-messages-response-rate. Published March 17, 2016. Accessed June 28, 2016.
13. Wotipka CD, High AC. Providing a foundation for a satisfying relationship: a direct test of warranting versus selective self-presentation as predictors of attraction to online dating profiles. Presentation at the 101st Annual Meeting of the National Communication Association; November 20, 2014; Chicago, IL.
14. Vacharkulksemsuk T, Reit E, Khambatta P, et al. Dominant, open nonverbal displays are attractive at zero-acquaintance. Proc Natl Acad Sci U S A. 2016;113(15):4009-4014.
15. Khan KS, Chaudhry S. An evidence-based approach to an ancient pursuit: systematic review on converting online contact into a first date. Evid Based Med. 2015;20(2):48-56.
16. Chretien KC, Tuck MG. Online professionalism: a synthetic review. Int Rev Psychiatry. 2015;27(2):106-117.
17. Jackson WC. When patients are normal people: strategies for managing dual relationships. Prim Care Companion J Clin Psychiatry. 2002;4(3):100-103.
18. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
19. D’Costa K. Catfishing: the truth about deception online. ScientificAmerican.com. http://blogs.scientificamerican.com/anthropology-in-practice/catfishing-the-truth-about-deception-online. Published April 25, 2014. Accessed June 29, 2016.
20. Sarkar SP. Boundary violation and sexual exploitation in psychiatry and psychotherapy: a review. Adv Psychiatr Treat. 2004;10(4):312-320.
21. Nadelson C, Notman MT. Boundaries in the doctor-patient relationship. Theor Med Bioeth. 2002;23(3):191-201.
22. Walton JM, White J, Ross S. What’s on YOUR Facebook profile? Evaluation of an educational intervention to promote appropriate use of privacy settings by medical students on social networking sites. Med Educ Online. 2015;20:28708. doi: 10.3402/meo.v20.28708.
23. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
24. Decamp M. Physicians, social media, and conflict of interest. J Gen Intern Med. 2013;28(2):299-303.
25. Farnan JM, Snyder Sulmasy L, Worster BK, et al; American College of Physicians Ethics, Professionalism and Human Rights Committee; American College of Physicians Council of Associates; Federation of State Medical Boards Special Committee on Ethics and Professionalism. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620-627.
26. Meissner WW. The problem of self-disclosure in psychoanalysis. J Am Psychoanal Assoc. 2002;50(3):827-867.
27. Henretty JR, Levitt HM. The role of therapist self-disclosure in psychotherapy: a qualitative review. Clin Psychol Rev. 2010;30(1):63-77.
28. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
29. Peterson ZD. More than a mirror: the ethics of therapist self-disclosure. Psychotherapy: Theory Research & Practice. 2002;39(1):21-31.
30. Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226-235.
31. Wass V. Doctors in society: medical professionalism in a changing world. Clin Med (Lond). 2006;6(1):109-113.
32. Langenfeld SJ, Cook G, Sudbeck C, et al. An assessment of unprofessional behavior among surgical residents on Facebook: a warning of the dangers of social media. J Surg Educ. 2014;71(6):e28-e32.
33. Chauhan B, George R, Coffin J. Social media and you: what every physician needs to know. J Med Pract Manage. 2012;28(3):206-209.
34. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
35. Jain A, Petty EM, Jaber RM, et al. What is appropriate to post on social media? Ratings from students, faculty members and the public. Med Educ. 2014;48(2):157-169.
36. Gabbard GO, Roberts LW, Crisp-Han H, et al. Professionalism in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2012.
1. Miller JA. Romance in residency: is dating even possible? Medscape. http://www.medscape.com/viewarticle/844059. Published May 5, 2016. Accessed June 27, 2016.
2. Smith A, Anderson M. 5 facts about online dating. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/02/29/5-facts-about-online-dating. Published February 29, 2016. Accessed June 27, 2016.
3. Smith A. 15% of American adults have used online dating sites or mobile dating apps. http://www.pewinternet.org/2016/02/11/15-percent-of-american-adults-have-used-online-dating-sites-or-mobile-dating-apps/. Published February 11, 2016. Accessed June 27, 2016.
4. Cacioppo JT, Cacioppo S, Gonzaga GC, et al. Marital satisfaction and break-ups differ across on-line and off-line meeting venues. Proc Natl Acad Sci U S A. 2013;110(25):10135-10140.
5. Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16(12):e267.
6. Berlin R. The professional ethics of online dating: need for guidance. J Am Acad Child Adolesc Psychiatry. 2014;53(9):935-937.
7. Rosenfeld MJ, Thomas RJ. Searching for a mate: the rise of the Internet as a social intermediary. Am Sociol Rev. 2012;77(4):523-547.
8. Finkel EJ, Eastwick PW, Karney BR, et al. Online dating: a critical analysis from the perspective of psychological science. Psychol Sci Public Interest. 2012;13(1):3-66.
9. Pierre J. A mad world: a diagnosis of mental illness is more common than ever—did psychiatrists create the problem, or just recognise it? Aeon.co. https://aeon.co/essays/do-psychiatrists-really-think-that-everyone-is-crazy. Published March 19, 2014. Accessed June 28, 2016.
10. Pearce A, Gambrell D. This chart shows who marries CEOs, doctors, chefs and janitors. Bloomberg. http://www.bloomberg.com/graphics/2016-who-marries-whom. February 11, 2016. Accessed June 28, 2016.
11. Lowin R. Proofread that text before sending! Bad grammar is a dating deal breaker, most say. Today. http://www.today.com/health/can-your-awesome-grammar-really-get-you-date-according-new-t77376. Published March 2, 2016. Accessed June 28, 2016.
12. Reilly K. This strategy will make your Tinder game much stronger. Time. http://time.com/4263598/tinder-gif-messages-response-rate. Published March 17, 2016. Accessed June 28, 2016.
13. Wotipka CD, High AC. Providing a foundation for a satisfying relationship: a direct test of warranting versus selective self-presentation as predictors of attraction to online dating profiles. Presentation at the 101st Annual Meeting of the National Communication Association; November 20, 2014; Chicago, IL.
14. Vacharkulksemsuk T, Reit E, Khambatta P, et al. Dominant, open nonverbal displays are attractive at zero-acquaintance. Proc Natl Acad Sci U S A. 2016;113(15):4009-4014.
15. Khan KS, Chaudhry S. An evidence-based approach to an ancient pursuit: systematic review on converting online contact into a first date. Evid Based Med. 2015;20(2):48-56.
16. Chretien KC, Tuck MG. Online professionalism: a synthetic review. Int Rev Psychiatry. 2015;27(2):106-117.
17. Jackson WC. When patients are normal people: strategies for managing dual relationships. Prim Care Companion J Clin Psychiatry. 2002;4(3):100-103.
18. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
19. D’Costa K. Catfishing: the truth about deception online. ScientificAmerican.com. http://blogs.scientificamerican.com/anthropology-in-practice/catfishing-the-truth-about-deception-online. Published April 25, 2014. Accessed June 29, 2016.
20. Sarkar SP. Boundary violation and sexual exploitation in psychiatry and psychotherapy: a review. Adv Psychiatr Treat. 2004;10(4):312-320.
21. Nadelson C, Notman MT. Boundaries in the doctor-patient relationship. Theor Med Bioeth. 2002;23(3):191-201.
22. Walton JM, White J, Ross S. What’s on YOUR Facebook profile? Evaluation of an educational intervention to promote appropriate use of privacy settings by medical students on social networking sites. Med Educ Online. 2015;20:28708. doi: 10.3402/meo.v20.28708.
23. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
24. Decamp M. Physicians, social media, and conflict of interest. J Gen Intern Med. 2013;28(2):299-303.
25. Farnan JM, Snyder Sulmasy L, Worster BK, et al; American College of Physicians Ethics, Professionalism and Human Rights Committee; American College of Physicians Council of Associates; Federation of State Medical Boards Special Committee on Ethics and Professionalism. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620-627.
26. Meissner WW. The problem of self-disclosure in psychoanalysis. J Am Psychoanal Assoc. 2002;50(3):827-867.
27. Henretty JR, Levitt HM. The role of therapist self-disclosure in psychotherapy: a qualitative review. Clin Psychol Rev. 2010;30(1):63-77.
28. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
29. Peterson ZD. More than a mirror: the ethics of therapist self-disclosure. Psychotherapy: Theory Research & Practice. 2002;39(1):21-31.
30. Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226-235.
31. Wass V. Doctors in society: medical professionalism in a changing world. Clin Med (Lond). 2006;6(1):109-113.
32. Langenfeld SJ, Cook G, Sudbeck C, et al. An assessment of unprofessional behavior among surgical residents on Facebook: a warning of the dangers of social media. J Surg Educ. 2014;71(6):e28-e32.
33. Chauhan B, George R, Coffin J. Social media and you: what every physician needs to know. J Med Pract Manage. 2012;28(3):206-209.
34. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
35. Jain A, Petty EM, Jaber RM, et al. What is appropriate to post on social media? Ratings from students, faculty members and the public. Med Educ. 2014;48(2):157-169.
36. Gabbard GO, Roberts LW, Crisp-Han H, et al. Professionalism in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2012.
Medical errors: Meeting ethical obligations and reducing liability with proper communication
In her position as Chief Medical Officer, Dr. Patrice Weiss leads efforts not only to assure clinical excellence from the more than 900 clinicians at the Carilion Clinic in Roanoke, Virginia, but also to improve patient experience. She lectures extensively on one of her passions in medicine: medical errors, and the concept of the second victim. OBG
OBG Management: What is the definition of a medical error?
Patrice M. Weiss, MD: Clinicians may be somewhat surprised to learn that there is no universal definition of a medical error that sets standardized nomenclature. The Institute of Medicine, in its landmark work To Err Is Human, adopted this definition: “failure of a planned action to be completed as intended, or the use of a wrong plan to achieve an aim.”1
In general terms, a medical error is an act of commission or omission, meaning that something was done or not done, that has negative consequences for the patient and is judged as wrong by our peers. An unanticipated outcome can be due to a medical error or can occur without a medical error. An unpredicted side effect, for instance—one that may have a low probability of drug–drug interaction or drug reaction occurrence—is an unexpected outcome. If the incidence of a drug reaction is 1 in 1,000 and your patient is that one, it does not necessarily mean that there was a medical error.
Often, if the outcome is unanticipated, patients and their families will assume, rightly or wrongly, that a medical error did occur.
OBG Management: Are physicians required to disclose medical errors?
Dr. Weiss: Yes. The Joint Commission’s standard principle states that the responsible licensed independent practitioner, or his or her designee, clearly explain the outcome of any treatment or procedure to the patient and, when appropriate, the patient’s family, whenever those outcomes differ significantly from the anticipated outcome.2
This can even include unanticipated outcomes that are not due to an error. Specifically speaking about medical errors, however, we do have the responsibility, both from this standard and from a professional and ethical standard to disclose what, why, and how the error occurred and what we are going to do to ensure it does not happen again.
OBG Management: How does a physician best communicate to a patient an unanticipated outcome that was not due to a medical error?
Dr. Weiss: Usually we as health care providers are more comfortable talking about unanticipated outcomes without medical errors. It is important to, when speaking with patients, be clear and concise, describing what you best know at the time, in language that patients can understand. I often jokingly say that, at a minimum, all of us in health care are bilingual: We speak our native language, and we speak “medicine.”
After describing unanticipated outcomes to patients and their families in terms they understand, affirm their understanding with a follow-up open-ended question. “Do you understand what I just said to you?” is ineffective. A better approach is saying, “Mrs. Jones, in your own words, will you describe back to me what your understanding is as to why this happened?” The answer received will allow you to know the patient’s level of understanding. It also will give you the opportunity to clear up points that are not clear or were misinterpreted. Do not leave patients feeling in a “lurch,” left to wonder or with a lack of understanding, or worse yet, with a sense that you are holding something back.
OBG Management: What is the best approach to disclosing an unanticipated outcome that was due to a medical error?
Dr. Weiss: First and foremost, you must be certain that a medical error did actually occur. There can be speculation at first, and that speculation should occur behind the scenes, with peer review or a root cause analysis on the event. Speculation should not enter into your conversation with the patient. Notional language can add to their anxiety, create mistrust on the patient’s part, and perhaps make a patient feel as if you are not giving the answers that he or she needs.
When it is believed that a medical error did occur, there are several things that need to be done:
- Gather as much information at the event as possible.
- Notify the hospital (ie, risk management or quality or patient safety). This is important because it is an organizational approach to medical errors when they do occur.
- Support the patient and the patient’s family through the entire process. Speaking to the patient and the family may be a part of ascertaining what happened and contributing factors. Clinicians have said to me, “Well, I can’t really go talk to the patient or the patient’s family right now because I don’t really know everything that happened.” Keep in mind, however, that the longer you wait to talk to the patient and family, the more time they have to speculate and to ask other people, perhaps those not involved and with no knowledge of, what happened.
OBG Management: What is the best timing and location for the disclosure conversation?
Dr. Weiss: The person who is responsible for the patient who was involved in the medical error needs to have the disclosure conversation. The conversation with the patient, and the family if the patient so desires, should occur as soon as possible. However, take into consideration the patient being awake, coherent, and not under the influence of medications. With those caveats, the best time to speak is when it is convenient for the patient. Do not plug this conversation into a 10-minute opening in your busy schedule. The conversation could take an hour, or it could take 15 minutes. It should not be conducted as a matter of convenience to the clinician.
In addition, often times the recovery room is not the best location—it is not private and confidential, and the patient is still groggy and will be unable to remember most of what is said or ask questions as needed.
OBG Management: You advocate a “TEAM” approach when speaking with the patient. What is TEAM?
Dr. Weiss: Disclosure conversations are not easy to have. The patient and the patient’s family are often upset. Medical errors challenge a physician’s humility and integrity, and they can lead to questioning of one’s own ability. I adopted the helpful pneumonic TEAM after first learning about it at what is now known as the Institute for Healthcare Communication. It refers to what parties need to be notified and who needs to be present with you when having a disclosure conversation. Of course, you want someone there who not only can serve as a witness but also can help facilitate the gathering of answers for questions that will be asked. The best person for this job could be the lead physician involved in the care of the patient, a hospital risk manager, a colleague, or the patient safety officer.
The “T” stands for truthful. When you begin the conversation, tell the patient at that point what you know to be true and what you know may have happened or definitely did not happen that contributed to the outcome. Again, do not speculate in answering the patient’s questions. A good approach is to say, “This is what I know happened. As of right now, this is what I know may have contributed or did contribute. We are going to be looking into this more thoroughly. As I learn more, you will be the first to know.”
These are not one-time conversations. As you do learn more, circle back and talk to the patient and family. This can be a dialogue that goes on for weeks or even months.
“E” equals empathy. Allow the patient and the patient’s family to ventilate. Try to understand what is it that they are most upset about, and try to soothe these upset feelings. For example, do not make the assumption that they are most upset about paying for a surgery in which there was a medical error. In fact, they really may be most upset about staying in the hospital 2 additional days, and they are going to now miss the visit of a relative, their child’s graduation, or something important to them.
Let patients talk. Do not interrupt them. Do not stand over them while they are in the bed; sit down at eye level with them. Talk in a voice and tone that the patient understands and try to soothe and empathetically relate to what is being said.
The “A” is important: Apology. There are 2 things that patients want when a medical error occurs: 1) to hear the clinician say, “I’m sorry”—and you should be sorry if a medical error occurred, and you should say that you are sorry this happened—and 2) what you or your organization is going to do so that this does not happen to the next person. Incorporate these 2 factors into the apology piece.
OBG Management: Can saying, “I’m sorry” expose a clinician unnecessarily to malpractice risk?
Dr. Weiss: Saying “I’m sorry,” of course, has come under a lot of scrutiny. There are various state laws, and you should be aware of your state’s apology laws. In many states an apology, with “I’m sorry,” cannot be used against a provider. However, there is not 100% absolution of the event if an apology occurs. In other words, “I’m sorry” cannot be held against you, but saying “I’m sorry” does not negate the error that occurred.
Even when practicing in a state in which there is not an apology law, however, and a clinician does apologize and that apology comes up in the legal setting of a true medical error, we would need to ask, is it really that bad that an apology was made on behalf of the medical error that was committed? Isn’t that compassion? Isn’t that empathy? Isn’t that showing that I as the physician care for the patient and the medical team cares for the patient?
Finally, abide by the disclosure policy and standards of your organization.
OBG Management: What does the “M” in TEAM stand for?
Dr. Weiss: Management. There may be times when a medical error occurs that the patient or the patient’s family are angry and upset to the point that they no longer want you to continue to care for them. Be empathetic and helpful by offering to assist them in finding someone else to continue to provide their care. Also let them know that you are more than happy to continue to care for them and assist them in their healing and restoration to health in any way that you can: “Of course the ongoing management of your care is your decision, and we will do whatever your wishes are.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- To err is human: Building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, eds. Washington, DC: National Academy Press; 2000. http://www.nap.edu/books/0309068371/html. Accessed August 22, 2016.
- The Joint Commission on Health Care Accreditation, Patient Safety Standard RI.1.2.2.
In her position as Chief Medical Officer, Dr. Patrice Weiss leads efforts not only to assure clinical excellence from the more than 900 clinicians at the Carilion Clinic in Roanoke, Virginia, but also to improve patient experience. She lectures extensively on one of her passions in medicine: medical errors, and the concept of the second victim. OBG
OBG Management: What is the definition of a medical error?
Patrice M. Weiss, MD: Clinicians may be somewhat surprised to learn that there is no universal definition of a medical error that sets standardized nomenclature. The Institute of Medicine, in its landmark work To Err Is Human, adopted this definition: “failure of a planned action to be completed as intended, or the use of a wrong plan to achieve an aim.”1
In general terms, a medical error is an act of commission or omission, meaning that something was done or not done, that has negative consequences for the patient and is judged as wrong by our peers. An unanticipated outcome can be due to a medical error or can occur without a medical error. An unpredicted side effect, for instance—one that may have a low probability of drug–drug interaction or drug reaction occurrence—is an unexpected outcome. If the incidence of a drug reaction is 1 in 1,000 and your patient is that one, it does not necessarily mean that there was a medical error.
Often, if the outcome is unanticipated, patients and their families will assume, rightly or wrongly, that a medical error did occur.
OBG Management: Are physicians required to disclose medical errors?
Dr. Weiss: Yes. The Joint Commission’s standard principle states that the responsible licensed independent practitioner, or his or her designee, clearly explain the outcome of any treatment or procedure to the patient and, when appropriate, the patient’s family, whenever those outcomes differ significantly from the anticipated outcome.2
This can even include unanticipated outcomes that are not due to an error. Specifically speaking about medical errors, however, we do have the responsibility, both from this standard and from a professional and ethical standard to disclose what, why, and how the error occurred and what we are going to do to ensure it does not happen again.
OBG Management: How does a physician best communicate to a patient an unanticipated outcome that was not due to a medical error?
Dr. Weiss: Usually we as health care providers are more comfortable talking about unanticipated outcomes without medical errors. It is important to, when speaking with patients, be clear and concise, describing what you best know at the time, in language that patients can understand. I often jokingly say that, at a minimum, all of us in health care are bilingual: We speak our native language, and we speak “medicine.”
After describing unanticipated outcomes to patients and their families in terms they understand, affirm their understanding with a follow-up open-ended question. “Do you understand what I just said to you?” is ineffective. A better approach is saying, “Mrs. Jones, in your own words, will you describe back to me what your understanding is as to why this happened?” The answer received will allow you to know the patient’s level of understanding. It also will give you the opportunity to clear up points that are not clear or were misinterpreted. Do not leave patients feeling in a “lurch,” left to wonder or with a lack of understanding, or worse yet, with a sense that you are holding something back.
OBG Management: What is the best approach to disclosing an unanticipated outcome that was due to a medical error?
Dr. Weiss: First and foremost, you must be certain that a medical error did actually occur. There can be speculation at first, and that speculation should occur behind the scenes, with peer review or a root cause analysis on the event. Speculation should not enter into your conversation with the patient. Notional language can add to their anxiety, create mistrust on the patient’s part, and perhaps make a patient feel as if you are not giving the answers that he or she needs.
When it is believed that a medical error did occur, there are several things that need to be done:
- Gather as much information at the event as possible.
- Notify the hospital (ie, risk management or quality or patient safety). This is important because it is an organizational approach to medical errors when they do occur.
- Support the patient and the patient’s family through the entire process. Speaking to the patient and the family may be a part of ascertaining what happened and contributing factors. Clinicians have said to me, “Well, I can’t really go talk to the patient or the patient’s family right now because I don’t really know everything that happened.” Keep in mind, however, that the longer you wait to talk to the patient and family, the more time they have to speculate and to ask other people, perhaps those not involved and with no knowledge of, what happened.
OBG Management: What is the best timing and location for the disclosure conversation?
Dr. Weiss: The person who is responsible for the patient who was involved in the medical error needs to have the disclosure conversation. The conversation with the patient, and the family if the patient so desires, should occur as soon as possible. However, take into consideration the patient being awake, coherent, and not under the influence of medications. With those caveats, the best time to speak is when it is convenient for the patient. Do not plug this conversation into a 10-minute opening in your busy schedule. The conversation could take an hour, or it could take 15 minutes. It should not be conducted as a matter of convenience to the clinician.
In addition, often times the recovery room is not the best location—it is not private and confidential, and the patient is still groggy and will be unable to remember most of what is said or ask questions as needed.
OBG Management: You advocate a “TEAM” approach when speaking with the patient. What is TEAM?
Dr. Weiss: Disclosure conversations are not easy to have. The patient and the patient’s family are often upset. Medical errors challenge a physician’s humility and integrity, and they can lead to questioning of one’s own ability. I adopted the helpful pneumonic TEAM after first learning about it at what is now known as the Institute for Healthcare Communication. It refers to what parties need to be notified and who needs to be present with you when having a disclosure conversation. Of course, you want someone there who not only can serve as a witness but also can help facilitate the gathering of answers for questions that will be asked. The best person for this job could be the lead physician involved in the care of the patient, a hospital risk manager, a colleague, or the patient safety officer.
The “T” stands for truthful. When you begin the conversation, tell the patient at that point what you know to be true and what you know may have happened or definitely did not happen that contributed to the outcome. Again, do not speculate in answering the patient’s questions. A good approach is to say, “This is what I know happened. As of right now, this is what I know may have contributed or did contribute. We are going to be looking into this more thoroughly. As I learn more, you will be the first to know.”
These are not one-time conversations. As you do learn more, circle back and talk to the patient and family. This can be a dialogue that goes on for weeks or even months.
“E” equals empathy. Allow the patient and the patient’s family to ventilate. Try to understand what is it that they are most upset about, and try to soothe these upset feelings. For example, do not make the assumption that they are most upset about paying for a surgery in which there was a medical error. In fact, they really may be most upset about staying in the hospital 2 additional days, and they are going to now miss the visit of a relative, their child’s graduation, or something important to them.
Let patients talk. Do not interrupt them. Do not stand over them while they are in the bed; sit down at eye level with them. Talk in a voice and tone that the patient understands and try to soothe and empathetically relate to what is being said.
The “A” is important: Apology. There are 2 things that patients want when a medical error occurs: 1) to hear the clinician say, “I’m sorry”—and you should be sorry if a medical error occurred, and you should say that you are sorry this happened—and 2) what you or your organization is going to do so that this does not happen to the next person. Incorporate these 2 factors into the apology piece.
OBG Management: Can saying, “I’m sorry” expose a clinician unnecessarily to malpractice risk?
Dr. Weiss: Saying “I’m sorry,” of course, has come under a lot of scrutiny. There are various state laws, and you should be aware of your state’s apology laws. In many states an apology, with “I’m sorry,” cannot be used against a provider. However, there is not 100% absolution of the event if an apology occurs. In other words, “I’m sorry” cannot be held against you, but saying “I’m sorry” does not negate the error that occurred.
Even when practicing in a state in which there is not an apology law, however, and a clinician does apologize and that apology comes up in the legal setting of a true medical error, we would need to ask, is it really that bad that an apology was made on behalf of the medical error that was committed? Isn’t that compassion? Isn’t that empathy? Isn’t that showing that I as the physician care for the patient and the medical team cares for the patient?
Finally, abide by the disclosure policy and standards of your organization.
OBG Management: What does the “M” in TEAM stand for?
Dr. Weiss: Management. There may be times when a medical error occurs that the patient or the patient’s family are angry and upset to the point that they no longer want you to continue to care for them. Be empathetic and helpful by offering to assist them in finding someone else to continue to provide their care. Also let them know that you are more than happy to continue to care for them and assist them in their healing and restoration to health in any way that you can: “Of course the ongoing management of your care is your decision, and we will do whatever your wishes are.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In her position as Chief Medical Officer, Dr. Patrice Weiss leads efforts not only to assure clinical excellence from the more than 900 clinicians at the Carilion Clinic in Roanoke, Virginia, but also to improve patient experience. She lectures extensively on one of her passions in medicine: medical errors, and the concept of the second victim. OBG
OBG Management: What is the definition of a medical error?
Patrice M. Weiss, MD: Clinicians may be somewhat surprised to learn that there is no universal definition of a medical error that sets standardized nomenclature. The Institute of Medicine, in its landmark work To Err Is Human, adopted this definition: “failure of a planned action to be completed as intended, or the use of a wrong plan to achieve an aim.”1
In general terms, a medical error is an act of commission or omission, meaning that something was done or not done, that has negative consequences for the patient and is judged as wrong by our peers. An unanticipated outcome can be due to a medical error or can occur without a medical error. An unpredicted side effect, for instance—one that may have a low probability of drug–drug interaction or drug reaction occurrence—is an unexpected outcome. If the incidence of a drug reaction is 1 in 1,000 and your patient is that one, it does not necessarily mean that there was a medical error.
Often, if the outcome is unanticipated, patients and their families will assume, rightly or wrongly, that a medical error did occur.
OBG Management: Are physicians required to disclose medical errors?
Dr. Weiss: Yes. The Joint Commission’s standard principle states that the responsible licensed independent practitioner, or his or her designee, clearly explain the outcome of any treatment or procedure to the patient and, when appropriate, the patient’s family, whenever those outcomes differ significantly from the anticipated outcome.2
This can even include unanticipated outcomes that are not due to an error. Specifically speaking about medical errors, however, we do have the responsibility, both from this standard and from a professional and ethical standard to disclose what, why, and how the error occurred and what we are going to do to ensure it does not happen again.
OBG Management: How does a physician best communicate to a patient an unanticipated outcome that was not due to a medical error?
Dr. Weiss: Usually we as health care providers are more comfortable talking about unanticipated outcomes without medical errors. It is important to, when speaking with patients, be clear and concise, describing what you best know at the time, in language that patients can understand. I often jokingly say that, at a minimum, all of us in health care are bilingual: We speak our native language, and we speak “medicine.”
After describing unanticipated outcomes to patients and their families in terms they understand, affirm their understanding with a follow-up open-ended question. “Do you understand what I just said to you?” is ineffective. A better approach is saying, “Mrs. Jones, in your own words, will you describe back to me what your understanding is as to why this happened?” The answer received will allow you to know the patient’s level of understanding. It also will give you the opportunity to clear up points that are not clear or were misinterpreted. Do not leave patients feeling in a “lurch,” left to wonder or with a lack of understanding, or worse yet, with a sense that you are holding something back.
OBG Management: What is the best approach to disclosing an unanticipated outcome that was due to a medical error?
Dr. Weiss: First and foremost, you must be certain that a medical error did actually occur. There can be speculation at first, and that speculation should occur behind the scenes, with peer review or a root cause analysis on the event. Speculation should not enter into your conversation with the patient. Notional language can add to their anxiety, create mistrust on the patient’s part, and perhaps make a patient feel as if you are not giving the answers that he or she needs.
When it is believed that a medical error did occur, there are several things that need to be done:
- Gather as much information at the event as possible.
- Notify the hospital (ie, risk management or quality or patient safety). This is important because it is an organizational approach to medical errors when they do occur.
- Support the patient and the patient’s family through the entire process. Speaking to the patient and the family may be a part of ascertaining what happened and contributing factors. Clinicians have said to me, “Well, I can’t really go talk to the patient or the patient’s family right now because I don’t really know everything that happened.” Keep in mind, however, that the longer you wait to talk to the patient and family, the more time they have to speculate and to ask other people, perhaps those not involved and with no knowledge of, what happened.
OBG Management: What is the best timing and location for the disclosure conversation?
Dr. Weiss: The person who is responsible for the patient who was involved in the medical error needs to have the disclosure conversation. The conversation with the patient, and the family if the patient so desires, should occur as soon as possible. However, take into consideration the patient being awake, coherent, and not under the influence of medications. With those caveats, the best time to speak is when it is convenient for the patient. Do not plug this conversation into a 10-minute opening in your busy schedule. The conversation could take an hour, or it could take 15 minutes. It should not be conducted as a matter of convenience to the clinician.
In addition, often times the recovery room is not the best location—it is not private and confidential, and the patient is still groggy and will be unable to remember most of what is said or ask questions as needed.
OBG Management: You advocate a “TEAM” approach when speaking with the patient. What is TEAM?
Dr. Weiss: Disclosure conversations are not easy to have. The patient and the patient’s family are often upset. Medical errors challenge a physician’s humility and integrity, and they can lead to questioning of one’s own ability. I adopted the helpful pneumonic TEAM after first learning about it at what is now known as the Institute for Healthcare Communication. It refers to what parties need to be notified and who needs to be present with you when having a disclosure conversation. Of course, you want someone there who not only can serve as a witness but also can help facilitate the gathering of answers for questions that will be asked. The best person for this job could be the lead physician involved in the care of the patient, a hospital risk manager, a colleague, or the patient safety officer.
The “T” stands for truthful. When you begin the conversation, tell the patient at that point what you know to be true and what you know may have happened or definitely did not happen that contributed to the outcome. Again, do not speculate in answering the patient’s questions. A good approach is to say, “This is what I know happened. As of right now, this is what I know may have contributed or did contribute. We are going to be looking into this more thoroughly. As I learn more, you will be the first to know.”
These are not one-time conversations. As you do learn more, circle back and talk to the patient and family. This can be a dialogue that goes on for weeks or even months.
“E” equals empathy. Allow the patient and the patient’s family to ventilate. Try to understand what is it that they are most upset about, and try to soothe these upset feelings. For example, do not make the assumption that they are most upset about paying for a surgery in which there was a medical error. In fact, they really may be most upset about staying in the hospital 2 additional days, and they are going to now miss the visit of a relative, their child’s graduation, or something important to them.
Let patients talk. Do not interrupt them. Do not stand over them while they are in the bed; sit down at eye level with them. Talk in a voice and tone that the patient understands and try to soothe and empathetically relate to what is being said.
The “A” is important: Apology. There are 2 things that patients want when a medical error occurs: 1) to hear the clinician say, “I’m sorry”—and you should be sorry if a medical error occurred, and you should say that you are sorry this happened—and 2) what you or your organization is going to do so that this does not happen to the next person. Incorporate these 2 factors into the apology piece.
OBG Management: Can saying, “I’m sorry” expose a clinician unnecessarily to malpractice risk?
Dr. Weiss: Saying “I’m sorry,” of course, has come under a lot of scrutiny. There are various state laws, and you should be aware of your state’s apology laws. In many states an apology, with “I’m sorry,” cannot be used against a provider. However, there is not 100% absolution of the event if an apology occurs. In other words, “I’m sorry” cannot be held against you, but saying “I’m sorry” does not negate the error that occurred.
Even when practicing in a state in which there is not an apology law, however, and a clinician does apologize and that apology comes up in the legal setting of a true medical error, we would need to ask, is it really that bad that an apology was made on behalf of the medical error that was committed? Isn’t that compassion? Isn’t that empathy? Isn’t that showing that I as the physician care for the patient and the medical team cares for the patient?
Finally, abide by the disclosure policy and standards of your organization.
OBG Management: What does the “M” in TEAM stand for?
Dr. Weiss: Management. There may be times when a medical error occurs that the patient or the patient’s family are angry and upset to the point that they no longer want you to continue to care for them. Be empathetic and helpful by offering to assist them in finding someone else to continue to provide their care. Also let them know that you are more than happy to continue to care for them and assist them in their healing and restoration to health in any way that you can: “Of course the ongoing management of your care is your decision, and we will do whatever your wishes are.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- To err is human: Building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, eds. Washington, DC: National Academy Press; 2000. http://www.nap.edu/books/0309068371/html. Accessed August 22, 2016.
- The Joint Commission on Health Care Accreditation, Patient Safety Standard RI.1.2.2.
- To err is human: Building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, eds. Washington, DC: National Academy Press; 2000. http://www.nap.edu/books/0309068371/html. Accessed August 22, 2016.
- The Joint Commission on Health Care Accreditation, Patient Safety Standard RI.1.2.2.
In this Article
- Medical error disclosure requirements
- The TEAM approach to disclosure
- Saying “I’m sorry” and malpractice risk
Delayed delivery blamed for brain injury: $9.6M
Delayed delivery blamed for brain injury: $9.6M 
At 5:00 AM, the ObGyn called for emergency cesarean delivery, requesting assistance from a surgeon and surgical scrub technician. The baby was delivered at 5:28 AM with a nuchal cord. She was limp, blue, and not breathing, with Apgar scores of 0, 2, and 3, at 1, 5, and 10 minutes, respectively. After full resuscitation, the baby was transferred to another hospital where she was treated for hypoxic-ischemic encephalopathy with therapeutic hypothermia; a feeding tube was placed.
At trial, the 3.5-year-old child is totally blind, has cerebral palsy, a seizure disorder, speech and language impairments, and continues to require frequent suctioning. She will require 24-hour licensed nursing care for life.
PARENTS’ CLAIM:
Standard of care required delivery before 4:00
DEFENDANTS’ DEFENSE:
The ObGyn observed that labor was progressing, indicating that vaginal delivery was appropriate. A cesarean delivery was not required earlier because FHR variability persisted, showing that the fetus was not acidotic. Delivery occurred less than 30 minutes after cesarean delivery was ordered, consistent with guidelines. The infant’s injury was caused by an unpredictable cord accident and had nothing to do with an alleged delivery delay.
VERDICT:
The case was filed as a Federal Tort Claims Act case because the ObGyn was employed by a federal clinic. A California judge awarded $9,609,305 after concluding that the cesarean delivery should have occurred earlier. The hospital settled for a confidential amount.
Mother dies of PPH: $9.2 million
A woman gave birth by cesarean delivery. Shortly after surgery ended at 10:55
ESTATE’S CLAIM:
The ObGyn’s postoperative care of the patient was negligent. After surgery, he was absent from the OR and did not follow up with the patient after he left the hospital. The ICU nurses’ notes indicated that the patient was still actively bleeding when she entered the ICU. Despite repeated calls to the critical care specialist, the patient was left untreated by any physician until Code Blue was called.
PHYSICIANS’ DEFENSE:
After the hospital reached a pretrial confidential settlement, the suit continued against the ObGyn and critical care specialist.
The ObGyn reported that he remained in the OR and left only after placing an intrauterine balloon and administering medications that successfully controlled the PPH. He disputed the accuracy of the ICU nurses’ notes that related that the patient’s vital signs indicating active bleeding “at all times.”
The critical care specialist contended that he had recommended that the patient be kept in the OR instead of transferring her to ICU. He denied hearing from the ICU staff after 12:35
VERDICT:
A $9,284,464 California verdict was returned against the ObGyn. The jury found the critical care specialist not guilty.
Delayed delivery blamed for brain injury: $9.6M 
At 5:00 AM, the ObGyn called for emergency cesarean delivery, requesting assistance from a surgeon and surgical scrub technician. The baby was delivered at 5:28 AM with a nuchal cord. She was limp, blue, and not breathing, with Apgar scores of 0, 2, and 3, at 1, 5, and 10 minutes, respectively. After full resuscitation, the baby was transferred to another hospital where she was treated for hypoxic-ischemic encephalopathy with therapeutic hypothermia; a feeding tube was placed.
At trial, the 3.5-year-old child is totally blind, has cerebral palsy, a seizure disorder, speech and language impairments, and continues to require frequent suctioning. She will require 24-hour licensed nursing care for life.
PARENTS’ CLAIM:
Standard of care required delivery before 4:00
DEFENDANTS’ DEFENSE:
The ObGyn observed that labor was progressing, indicating that vaginal delivery was appropriate. A cesarean delivery was not required earlier because FHR variability persisted, showing that the fetus was not acidotic. Delivery occurred less than 30 minutes after cesarean delivery was ordered, consistent with guidelines. The infant’s injury was caused by an unpredictable cord accident and had nothing to do with an alleged delivery delay.
VERDICT:
The case was filed as a Federal Tort Claims Act case because the ObGyn was employed by a federal clinic. A California judge awarded $9,609,305 after concluding that the cesarean delivery should have occurred earlier. The hospital settled for a confidential amount.
Mother dies of PPH: $9.2 million
A woman gave birth by cesarean delivery. Shortly after surgery ended at 10:55
ESTATE’S CLAIM:
The ObGyn’s postoperative care of the patient was negligent. After surgery, he was absent from the OR and did not follow up with the patient after he left the hospital. The ICU nurses’ notes indicated that the patient was still actively bleeding when she entered the ICU. Despite repeated calls to the critical care specialist, the patient was left untreated by any physician until Code Blue was called.
PHYSICIANS’ DEFENSE:
After the hospital reached a pretrial confidential settlement, the suit continued against the ObGyn and critical care specialist.
The ObGyn reported that he remained in the OR and left only after placing an intrauterine balloon and administering medications that successfully controlled the PPH. He disputed the accuracy of the ICU nurses’ notes that related that the patient’s vital signs indicating active bleeding “at all times.”
The critical care specialist contended that he had recommended that the patient be kept in the OR instead of transferring her to ICU. He denied hearing from the ICU staff after 12:35
VERDICT:
A $9,284,464 California verdict was returned against the ObGyn. The jury found the critical care specialist not guilty.
Delayed delivery blamed for brain injury: $9.6M 
At 5:00 AM, the ObGyn called for emergency cesarean delivery, requesting assistance from a surgeon and surgical scrub technician. The baby was delivered at 5:28 AM with a nuchal cord. She was limp, blue, and not breathing, with Apgar scores of 0, 2, and 3, at 1, 5, and 10 minutes, respectively. After full resuscitation, the baby was transferred to another hospital where she was treated for hypoxic-ischemic encephalopathy with therapeutic hypothermia; a feeding tube was placed.
At trial, the 3.5-year-old child is totally blind, has cerebral palsy, a seizure disorder, speech and language impairments, and continues to require frequent suctioning. She will require 24-hour licensed nursing care for life.
PARENTS’ CLAIM:
Standard of care required delivery before 4:00
DEFENDANTS’ DEFENSE:
The ObGyn observed that labor was progressing, indicating that vaginal delivery was appropriate. A cesarean delivery was not required earlier because FHR variability persisted, showing that the fetus was not acidotic. Delivery occurred less than 30 minutes after cesarean delivery was ordered, consistent with guidelines. The infant’s injury was caused by an unpredictable cord accident and had nothing to do with an alleged delivery delay.
VERDICT:
The case was filed as a Federal Tort Claims Act case because the ObGyn was employed by a federal clinic. A California judge awarded $9,609,305 after concluding that the cesarean delivery should have occurred earlier. The hospital settled for a confidential amount.
Mother dies of PPH: $9.2 million
A woman gave birth by cesarean delivery. Shortly after surgery ended at 10:55
ESTATE’S CLAIM:
The ObGyn’s postoperative care of the patient was negligent. After surgery, he was absent from the OR and did not follow up with the patient after he left the hospital. The ICU nurses’ notes indicated that the patient was still actively bleeding when she entered the ICU. Despite repeated calls to the critical care specialist, the patient was left untreated by any physician until Code Blue was called.
PHYSICIANS’ DEFENSE:
After the hospital reached a pretrial confidential settlement, the suit continued against the ObGyn and critical care specialist.
The ObGyn reported that he remained in the OR and left only after placing an intrauterine balloon and administering medications that successfully controlled the PPH. He disputed the accuracy of the ICU nurses’ notes that related that the patient’s vital signs indicating active bleeding “at all times.”
The critical care specialist contended that he had recommended that the patient be kept in the OR instead of transferring her to ICU. He denied hearing from the ICU staff after 12:35
VERDICT:
A $9,284,464 California verdict was returned against the ObGyn. The jury found the critical care specialist not guilty.
Was the pregnancy ectopic or intrauterine?
Was the pregnancy ectopic or intrauterine?A 40-year-old woman underwent ultrasonography (US) during an office visit with her ObGyn. Results indicated that there was no gestational sac in the uterus. Following repeat US at a radiology facility, the radiologist reported that he saw no evidence of pregnancy in the uterus but did see a complex structure outside the uterus. He recommended follow-up US to further investigate the possibility of an ectopic pregnancy. After reading the radiologist’s report, the ObGyn concluded that it was highly likely that the woman had an ectopic pregnancy. He sent her to a hospital’s emergency department (ED) for an injection of methotrexate to manage the ectopic pregnancy.
Two days later, the patient returned to the ED with abdominal pain and vaginal spotting. US results showed an intrauterine pregnancy. However, based on the high risk of fetal deformity or death caused by methotrexate, the patient agreed to undergo surgical removal of fetal remains.
PARENT'S CLAIM: The patient and her husband sued the radiologist, alleging that his misreading of the subsequent US fell below the standard of care. If he had not misread the US, the ObGyn would not have ordered termination of an ectopic pregnancy with a teratogenic medication.
PHYSICIAN'S DEFENSE: The case was settled during trial.
VERDICT: An undisclosed Arizona settlement was reached with the radiologist.
Have you read this Editorial by Dr. Barbieri?
Stop using the hCG discriminatory zone of 1,500 to 2,000 mIU/mL to guide intervention during early pregnancy. (Editorial; January 2015)
Increasing pain after ovarian cystectomy: $1.5MA woman in her 40s underwent ovarian cystectomy performed by her gynecologist. After surgery, the patient reported increasingly intense abdominal pain to the gynecologist. After 10 days, laboratory testing showed an increase in the patient’s white blood cell count. During exploratory surgery, a perforation was found in her sigmoid colon, and a colostomy was performed.
PATIENT'S CLAIM: The gynecologist was negligent in injuring the colon and then not intraoperatively identifying and repairing the damage. Postoperatively, the gynecologist failed to address the injury in a timely manner.
PHYSICIAN'S DEFENSE: A colon injury is a known complication of the procedure. Such injuries are often not identified until days after the surgery.
VERDICT: A $1.52 million New York verdict was returned.
Bladder injury causes multiple operations A woman in her 30s underwent a hysterectomy performed by her ObGyn. During the procedure, the ObGyn perforated the patient’s bladder. The ObGyn attempted to repair the injury, but then called in a urologist to complete the procedure. The urologist had to reduce the size of the bladder in order to complete the repair. The patient underwent additional operations to treat a postsurgical infection and adhesions. During an operation to treat infection, a surgeon found that the ureter had been reimplanted.
PATIENT'S CLAIM: During the first repair procedure, the urologist was negligent in not inspecting adjacent organs for damage before closing. Infection developed because the repair was improperly performed.
PHYSICIAN'S DEFENSE: The urologist denied negligence. Infection is a known complication of an intraoperative bladder injury.
VERDICT: A Michigan defense verdict was reached.
These cases were selected by the editors of OBG Management from "Medical Malpractice Verdicts, Settlements, & Experts," with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Was the pregnancy ectopic or intrauterine?A 40-year-old woman underwent ultrasonography (US) during an office visit with her ObGyn. Results indicated that there was no gestational sac in the uterus. Following repeat US at a radiology facility, the radiologist reported that he saw no evidence of pregnancy in the uterus but did see a complex structure outside the uterus. He recommended follow-up US to further investigate the possibility of an ectopic pregnancy. After reading the radiologist’s report, the ObGyn concluded that it was highly likely that the woman had an ectopic pregnancy. He sent her to a hospital’s emergency department (ED) for an injection of methotrexate to manage the ectopic pregnancy.
Two days later, the patient returned to the ED with abdominal pain and vaginal spotting. US results showed an intrauterine pregnancy. However, based on the high risk of fetal deformity or death caused by methotrexate, the patient agreed to undergo surgical removal of fetal remains.
PARENT'S CLAIM: The patient and her husband sued the radiologist, alleging that his misreading of the subsequent US fell below the standard of care. If he had not misread the US, the ObGyn would not have ordered termination of an ectopic pregnancy with a teratogenic medication.
PHYSICIAN'S DEFENSE: The case was settled during trial.
VERDICT: An undisclosed Arizona settlement was reached with the radiologist.
Have you read this Editorial by Dr. Barbieri?
Stop using the hCG discriminatory zone of 1,500 to 2,000 mIU/mL to guide intervention during early pregnancy. (Editorial; January 2015)
Increasing pain after ovarian cystectomy: $1.5MA woman in her 40s underwent ovarian cystectomy performed by her gynecologist. After surgery, the patient reported increasingly intense abdominal pain to the gynecologist. After 10 days, laboratory testing showed an increase in the patient’s white blood cell count. During exploratory surgery, a perforation was found in her sigmoid colon, and a colostomy was performed.
PATIENT'S CLAIM: The gynecologist was negligent in injuring the colon and then not intraoperatively identifying and repairing the damage. Postoperatively, the gynecologist failed to address the injury in a timely manner.
PHYSICIAN'S DEFENSE: A colon injury is a known complication of the procedure. Such injuries are often not identified until days after the surgery.
VERDICT: A $1.52 million New York verdict was returned.
Bladder injury causes multiple operations A woman in her 30s underwent a hysterectomy performed by her ObGyn. During the procedure, the ObGyn perforated the patient’s bladder. The ObGyn attempted to repair the injury, but then called in a urologist to complete the procedure. The urologist had to reduce the size of the bladder in order to complete the repair. The patient underwent additional operations to treat a postsurgical infection and adhesions. During an operation to treat infection, a surgeon found that the ureter had been reimplanted.
PATIENT'S CLAIM: During the first repair procedure, the urologist was negligent in not inspecting adjacent organs for damage before closing. Infection developed because the repair was improperly performed.
PHYSICIAN'S DEFENSE: The urologist denied negligence. Infection is a known complication of an intraoperative bladder injury.
VERDICT: A Michigan defense verdict was reached.
These cases were selected by the editors of OBG Management from "Medical Malpractice Verdicts, Settlements, & Experts," with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Was the pregnancy ectopic or intrauterine?A 40-year-old woman underwent ultrasonography (US) during an office visit with her ObGyn. Results indicated that there was no gestational sac in the uterus. Following repeat US at a radiology facility, the radiologist reported that he saw no evidence of pregnancy in the uterus but did see a complex structure outside the uterus. He recommended follow-up US to further investigate the possibility of an ectopic pregnancy. After reading the radiologist’s report, the ObGyn concluded that it was highly likely that the woman had an ectopic pregnancy. He sent her to a hospital’s emergency department (ED) for an injection of methotrexate to manage the ectopic pregnancy.
Two days later, the patient returned to the ED with abdominal pain and vaginal spotting. US results showed an intrauterine pregnancy. However, based on the high risk of fetal deformity or death caused by methotrexate, the patient agreed to undergo surgical removal of fetal remains.
PARENT'S CLAIM: The patient and her husband sued the radiologist, alleging that his misreading of the subsequent US fell below the standard of care. If he had not misread the US, the ObGyn would not have ordered termination of an ectopic pregnancy with a teratogenic medication.
PHYSICIAN'S DEFENSE: The case was settled during trial.
VERDICT: An undisclosed Arizona settlement was reached with the radiologist.
Have you read this Editorial by Dr. Barbieri?
Stop using the hCG discriminatory zone of 1,500 to 2,000 mIU/mL to guide intervention during early pregnancy. (Editorial; January 2015)
Increasing pain after ovarian cystectomy: $1.5MA woman in her 40s underwent ovarian cystectomy performed by her gynecologist. After surgery, the patient reported increasingly intense abdominal pain to the gynecologist. After 10 days, laboratory testing showed an increase in the patient’s white blood cell count. During exploratory surgery, a perforation was found in her sigmoid colon, and a colostomy was performed.
PATIENT'S CLAIM: The gynecologist was negligent in injuring the colon and then not intraoperatively identifying and repairing the damage. Postoperatively, the gynecologist failed to address the injury in a timely manner.
PHYSICIAN'S DEFENSE: A colon injury is a known complication of the procedure. Such injuries are often not identified until days after the surgery.
VERDICT: A $1.52 million New York verdict was returned.
Bladder injury causes multiple operations A woman in her 30s underwent a hysterectomy performed by her ObGyn. During the procedure, the ObGyn perforated the patient’s bladder. The ObGyn attempted to repair the injury, but then called in a urologist to complete the procedure. The urologist had to reduce the size of the bladder in order to complete the repair. The patient underwent additional operations to treat a postsurgical infection and adhesions. During an operation to treat infection, a surgeon found that the ureter had been reimplanted.
PATIENT'S CLAIM: During the first repair procedure, the urologist was negligent in not inspecting adjacent organs for damage before closing. Infection developed because the repair was improperly performed.
PHYSICIAN'S DEFENSE: The urologist denied negligence. Infection is a known complication of an intraoperative bladder injury.
VERDICT: A Michigan defense verdict was reached.
These cases were selected by the editors of OBG Management from "Medical Malpractice Verdicts, Settlements, & Experts," with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.