User login
Five Situations Where Hospitalists Need a Healthcare Attorney
It is inevitable that, at some point in your career, you will need to hire a healthcare attorney. Proper representation is the best way to ensure a positive outcome in any situation.
Physicians often consider tackling certain issues on their own to reduce costs and avoid complicating matters. However, there are at least five situations in which you must retain an experienced healthcare attorney, or you could end up underpaid, subject to overreaching restrictive covenants, severely fined, or responsible for a large settlement.
1. Negotiating an Employment Contract
Whether you are considering a position as an employee of a physician group, hospital, or health system, it is critical that you understand the employment agreement presented to you so you can be sure it is fair and represents your best interests. The agreement itself defines the scope and conditions of your employment and consequently impacts your personal and professional satisfaction. It usually contains confusing legal terminology, such as noncompetition and nonsolicitation clauses. If you do not understand these terms, problems may arise in the future regarding your rights and capabilities upon termination of employment.
For these reasons, it is critical to engage a healthcare attorney who is well-versed in physician employment agreements. At a minimum, an attorney can confirm whether the compensation offered is comparable to that of physicians with similar experience and skills in your geographical area. The attorney can decipher confusing bonus compensation and may be able to negotiate more favorable terms. The same is true of understanding the benefits offered and establishing your call coverage.
An attorney will be able to advise you when it is appropriate to push back and request additional benefits or propose more favorable changes to your call coverage. Most important, the attorney will clarify the term of the employment agreement, the corresponding termination provisions, and any restrictions on your ability to practice upon termination of the agreement. Although the ultimate decision to accept the employment offer rests solely with you, an experienced healthcare attorney can help you understand the agreement and give you confidence in that decision.
2. Leaving a Practice for New Opportunities or Retirement
Whether you decide to leave a practice to pursue a new opportunity or because you are retiring, it is critical that you engage a healthcare attorney to help you navigate this road. If you are leaving to pursue new opportunities, an attorney can help you understand any restrictive covenants that may apply upon your departure and who retains ownership of the medical records of patients you treated while employed by the practice. In addition, you’ll be assisted in drafting any required notifications to patients alerting them of your departure.
If you are leaving the practice due to retirement, there are additional concerns. If you own the practice, you will need to decide whether to sell the practice or wind it down. If you decide to sell, an attorney can help you negotiate a favorable merger agreement and file any required change of ownership forms. If you choose to wind down your practice, your employee agreements and service and vendor contracts, including managed care participation agreements, will need to be reviewed for specific termination and notice requirements.
As with departure from a practice, there are certain notifications that must be issued to your patients detailing the closure of your practice and addressing patient options for continuity of care. An attorney can draft such notifications for you and, in addition, will be able to assist with notifying your malpractice carrier of your retirement and ensuring you have proper continuing coverage.
Finally, an attorney can arrange custody of your medical records in accordance with applicable state record retention requirements, help wind down your financial matters, and terminate your practice’s professional entity.
3. Practice Mergers
Engaging a healthcare transaction attorney protects your investment in your practice and in the practice with which you decide to merge. Healthcare mergers, due to the complex rules and regulations governing the industry, are uniquely complicated. A traditional business lawyer with merger experience likely will not understand regulations that solely impact healthcare mergers, which can lead to regulatory fines and penalties.
Therefore, if you are considering merging your practice, it is critical that you engage an attorney who is highly experienced in the legal implications of healthcare transactions and who has a deep understanding of the Anti-Kickback Statute, Stark Law, and other applicable regulations. Doing so is the only way to ensure compliance with healthcare rules and regulations.
4. Payor Audits
The number of payor audits is increasing dramatically. Payor audits can involve Medicare, Medicaid, or third-party payors. When an audit notice is received, there often is a limited time period to respond. Therefore, it is imperative that you engage an experienced healthcare attorney upon receipt of such a notice to draft a professional response to the audit request and help you gather the requested documents in accordance with the time frames specified in the notice.
In addition, an attorney can address procedural, legal, or factual flaws in the auditor’s position, which can prevent repayment of significant monetary penalties and suspension or revocation of billing privileges.
5. Malpractice Allegations
Without question, if you are subject to a medical malpractice lawsuit, you absolutely must retain an experienced healthcare attorney. Your insurance company will usually hire one for you, but that is not always the case.
Medical malpractice cases are extremely complicated. To prevail, you need an attorney who not only understands the law but also the practice of medicine. A healthcare attorney will not only know what litigation filings are required but will be able to arrange expert witnesses to help prove that you acted in accordance with professional standards.
In Sum
It is critical that an experienced healthcare attorney be hired to help manage these situations and many more. There is no better way to protect the professional and personal interests you have worked so hard to build. TH
It is inevitable that, at some point in your career, you will need to hire a healthcare attorney. Proper representation is the best way to ensure a positive outcome in any situation.
Physicians often consider tackling certain issues on their own to reduce costs and avoid complicating matters. However, there are at least five situations in which you must retain an experienced healthcare attorney, or you could end up underpaid, subject to overreaching restrictive covenants, severely fined, or responsible for a large settlement.
1. Negotiating an Employment Contract
Whether you are considering a position as an employee of a physician group, hospital, or health system, it is critical that you understand the employment agreement presented to you so you can be sure it is fair and represents your best interests. The agreement itself defines the scope and conditions of your employment and consequently impacts your personal and professional satisfaction. It usually contains confusing legal terminology, such as noncompetition and nonsolicitation clauses. If you do not understand these terms, problems may arise in the future regarding your rights and capabilities upon termination of employment.
For these reasons, it is critical to engage a healthcare attorney who is well-versed in physician employment agreements. At a minimum, an attorney can confirm whether the compensation offered is comparable to that of physicians with similar experience and skills in your geographical area. The attorney can decipher confusing bonus compensation and may be able to negotiate more favorable terms. The same is true of understanding the benefits offered and establishing your call coverage.
An attorney will be able to advise you when it is appropriate to push back and request additional benefits or propose more favorable changes to your call coverage. Most important, the attorney will clarify the term of the employment agreement, the corresponding termination provisions, and any restrictions on your ability to practice upon termination of the agreement. Although the ultimate decision to accept the employment offer rests solely with you, an experienced healthcare attorney can help you understand the agreement and give you confidence in that decision.
2. Leaving a Practice for New Opportunities or Retirement
Whether you decide to leave a practice to pursue a new opportunity or because you are retiring, it is critical that you engage a healthcare attorney to help you navigate this road. If you are leaving to pursue new opportunities, an attorney can help you understand any restrictive covenants that may apply upon your departure and who retains ownership of the medical records of patients you treated while employed by the practice. In addition, you’ll be assisted in drafting any required notifications to patients alerting them of your departure.
If you are leaving the practice due to retirement, there are additional concerns. If you own the practice, you will need to decide whether to sell the practice or wind it down. If you decide to sell, an attorney can help you negotiate a favorable merger agreement and file any required change of ownership forms. If you choose to wind down your practice, your employee agreements and service and vendor contracts, including managed care participation agreements, will need to be reviewed for specific termination and notice requirements.
As with departure from a practice, there are certain notifications that must be issued to your patients detailing the closure of your practice and addressing patient options for continuity of care. An attorney can draft such notifications for you and, in addition, will be able to assist with notifying your malpractice carrier of your retirement and ensuring you have proper continuing coverage.
Finally, an attorney can arrange custody of your medical records in accordance with applicable state record retention requirements, help wind down your financial matters, and terminate your practice’s professional entity.
3. Practice Mergers
Engaging a healthcare transaction attorney protects your investment in your practice and in the practice with which you decide to merge. Healthcare mergers, due to the complex rules and regulations governing the industry, are uniquely complicated. A traditional business lawyer with merger experience likely will not understand regulations that solely impact healthcare mergers, which can lead to regulatory fines and penalties.
Therefore, if you are considering merging your practice, it is critical that you engage an attorney who is highly experienced in the legal implications of healthcare transactions and who has a deep understanding of the Anti-Kickback Statute, Stark Law, and other applicable regulations. Doing so is the only way to ensure compliance with healthcare rules and regulations.
4. Payor Audits
The number of payor audits is increasing dramatically. Payor audits can involve Medicare, Medicaid, or third-party payors. When an audit notice is received, there often is a limited time period to respond. Therefore, it is imperative that you engage an experienced healthcare attorney upon receipt of such a notice to draft a professional response to the audit request and help you gather the requested documents in accordance with the time frames specified in the notice.
In addition, an attorney can address procedural, legal, or factual flaws in the auditor’s position, which can prevent repayment of significant monetary penalties and suspension or revocation of billing privileges.
5. Malpractice Allegations
Without question, if you are subject to a medical malpractice lawsuit, you absolutely must retain an experienced healthcare attorney. Your insurance company will usually hire one for you, but that is not always the case.
Medical malpractice cases are extremely complicated. To prevail, you need an attorney who not only understands the law but also the practice of medicine. A healthcare attorney will not only know what litigation filings are required but will be able to arrange expert witnesses to help prove that you acted in accordance with professional standards.
In Sum
It is critical that an experienced healthcare attorney be hired to help manage these situations and many more. There is no better way to protect the professional and personal interests you have worked so hard to build. TH
It is inevitable that, at some point in your career, you will need to hire a healthcare attorney. Proper representation is the best way to ensure a positive outcome in any situation.
Physicians often consider tackling certain issues on their own to reduce costs and avoid complicating matters. However, there are at least five situations in which you must retain an experienced healthcare attorney, or you could end up underpaid, subject to overreaching restrictive covenants, severely fined, or responsible for a large settlement.
1. Negotiating an Employment Contract
Whether you are considering a position as an employee of a physician group, hospital, or health system, it is critical that you understand the employment agreement presented to you so you can be sure it is fair and represents your best interests. The agreement itself defines the scope and conditions of your employment and consequently impacts your personal and professional satisfaction. It usually contains confusing legal terminology, such as noncompetition and nonsolicitation clauses. If you do not understand these terms, problems may arise in the future regarding your rights and capabilities upon termination of employment.
For these reasons, it is critical to engage a healthcare attorney who is well-versed in physician employment agreements. At a minimum, an attorney can confirm whether the compensation offered is comparable to that of physicians with similar experience and skills in your geographical area. The attorney can decipher confusing bonus compensation and may be able to negotiate more favorable terms. The same is true of understanding the benefits offered and establishing your call coverage.
An attorney will be able to advise you when it is appropriate to push back and request additional benefits or propose more favorable changes to your call coverage. Most important, the attorney will clarify the term of the employment agreement, the corresponding termination provisions, and any restrictions on your ability to practice upon termination of the agreement. Although the ultimate decision to accept the employment offer rests solely with you, an experienced healthcare attorney can help you understand the agreement and give you confidence in that decision.
2. Leaving a Practice for New Opportunities or Retirement
Whether you decide to leave a practice to pursue a new opportunity or because you are retiring, it is critical that you engage a healthcare attorney to help you navigate this road. If you are leaving to pursue new opportunities, an attorney can help you understand any restrictive covenants that may apply upon your departure and who retains ownership of the medical records of patients you treated while employed by the practice. In addition, you’ll be assisted in drafting any required notifications to patients alerting them of your departure.
If you are leaving the practice due to retirement, there are additional concerns. If you own the practice, you will need to decide whether to sell the practice or wind it down. If you decide to sell, an attorney can help you negotiate a favorable merger agreement and file any required change of ownership forms. If you choose to wind down your practice, your employee agreements and service and vendor contracts, including managed care participation agreements, will need to be reviewed for specific termination and notice requirements.
As with departure from a practice, there are certain notifications that must be issued to your patients detailing the closure of your practice and addressing patient options for continuity of care. An attorney can draft such notifications for you and, in addition, will be able to assist with notifying your malpractice carrier of your retirement and ensuring you have proper continuing coverage.
Finally, an attorney can arrange custody of your medical records in accordance with applicable state record retention requirements, help wind down your financial matters, and terminate your practice’s professional entity.
3. Practice Mergers
Engaging a healthcare transaction attorney protects your investment in your practice and in the practice with which you decide to merge. Healthcare mergers, due to the complex rules and regulations governing the industry, are uniquely complicated. A traditional business lawyer with merger experience likely will not understand regulations that solely impact healthcare mergers, which can lead to regulatory fines and penalties.
Therefore, if you are considering merging your practice, it is critical that you engage an attorney who is highly experienced in the legal implications of healthcare transactions and who has a deep understanding of the Anti-Kickback Statute, Stark Law, and other applicable regulations. Doing so is the only way to ensure compliance with healthcare rules and regulations.
4. Payor Audits
The number of payor audits is increasing dramatically. Payor audits can involve Medicare, Medicaid, or third-party payors. When an audit notice is received, there often is a limited time period to respond. Therefore, it is imperative that you engage an experienced healthcare attorney upon receipt of such a notice to draft a professional response to the audit request and help you gather the requested documents in accordance with the time frames specified in the notice.
In addition, an attorney can address procedural, legal, or factual flaws in the auditor’s position, which can prevent repayment of significant monetary penalties and suspension or revocation of billing privileges.
5. Malpractice Allegations
Without question, if you are subject to a medical malpractice lawsuit, you absolutely must retain an experienced healthcare attorney. Your insurance company will usually hire one for you, but that is not always the case.
Medical malpractice cases are extremely complicated. To prevail, you need an attorney who not only understands the law but also the practice of medicine. A healthcare attorney will not only know what litigation filings are required but will be able to arrange expert witnesses to help prove that you acted in accordance with professional standards.
In Sum
It is critical that an experienced healthcare attorney be hired to help manage these situations and many more. There is no better way to protect the professional and personal interests you have worked so hard to build. TH
Fistula developed after delivery: $50M verdict
Fistula developed after delivery: $50M verdict
During delivery of a 31-year-old woman's baby, a nuchal cord was encountered. In order to safely deliver the child, the ObGyn performed an episiotomy.
After delivery, the patient reported an odorous vaginal discharge. The ObGyn explained that the condition was a natural byproduct of delivery and suggested that it would resolve without treatment.
The patient became pregnant a second time shortly after her first delivery and was evaluated by a midwife. The patient again reported the odorous discharge, but the condition was not addressed. At delivery of her second child, the ObGyn determined that the patient had a rectovaginal fistula. The patient underwent 13 repair operations.
PATIENT’S CLAIM:
The fistula was a byproduct of the episiotomy performed during the first delivery. The episiotomy should not have been performed. The ObGyn should have diagnosed and treated the fistula prior to delivery of the second child and performed a cesarean delivery.
DEFENDANT'S DEFENSE:
The ObGyn reported that the patient's medical records showed that she did not report the odorous discharge until after her second delivery.
VERDICT:
A New York $50 million verdict was returned.
Related article:
Management of wound complications following obstetric anal sphincter injury (OASIS)
Abdominal wall hematoma during pregnancy: $2.5M award
At 35 weeks' gestation, a 38-year-old woman presented to the emergency department (ED) with right upper abdominal pain. Her pregnancy was at high risk because of her age and the fact that she had thrombophilia involving both factor V and protein S deficiency. During pregnancy she was anticoagulated. She had been coughing from bronchitis, which was treated with antibiotics and an inhaler.
In the ED, laboratory testing determined that her blood was not properly clotting. Upper abdominal ultrasonography (US) showed an abdominal wall hematoma and gall stones. The ED physician, after contacting the on-call ObGyn, told the patient that nothing further could be done until after the baby's birth and prescribed medications for nausea and pain. The patient was discharged.
Thirty-three hours later, the patient was rushed to the hospital after she was found barely responsive, pale, and in severe pain. US results showed that the hematoma had grown extensively. The patient was in hypovolemic shock having lost more than 50% of her blood volume. She was admitted to the intensive care unit.
After induced labor, a stillborn son was delivered. The autopsy report revealed that the child died from either asphyxiation or an hypoxic ischemic event that occurred when the mother went into shock.
PATIENT’S CLAIM:
The ED physician and staff were negligent. Once the hematoma was identified, the standard of care is to monitor the hematoma with regular US. Instead, the ED physician discharged the patient. The ED physician contacted the on-call ObGyn but did not ask for a consult. The patient should have been admitted for monitoring.
DEFENDANT'S DEFENSE:
The ED physician met the standard of care. The mother's condition would likely have been detected during a nonstress test scheduled for the following day but the mother missed the prenatal exam because she had just left the hospital.
VERDICT:
A $2.5 million Missouri verdict was returned.
Incorrect due date, child with brain injuries: $1.2M
When a pregnant woman presented for her first prenatal visit, she was unsure of the date of her last menstrual period. During subsequent prenatal visits, she underwent 3 ultrasounds.
Labor was induced on August 1 because she reported gastrointestinal reflux. The infant appeared healthy at birth but soon went into respiratory distress. He was slow to meet developmental goals and was believed to be autistic. At age 5 years, he was given a diagnosis of periventricular leukomalacia.
PARENT’S CLAIM:
The child, 11 years old at the time of trial, has permanent brain injuries due to premature delivery. The mother's due date should have been projected as August 25 according to prenatal US measurements. The ObGyn misinterpreted the US data and estimated a due date of August 15. Therefore induction on August 1st caused him to be premature.
PHYSICIAN’S DEFENSE:
The standard of care was met. Gestational age evaluation using US is an estimate based on the child's size at specific time points, not an exact calculation, especially if the mother is not sure about the date of her last menses.
VERDICT:
A $1.2 million New Jersey verdict was returned.
Related article:
Three good apps for calculating the date of delivery
Bacterial infection blamed for birth injury
A woman was at 28 weeks' gestation when her membranes ruptured on September 28. She began to leak amniotic fluid and was put on bed rest. She saw her ObGyn on October 13 with signs of a bacterial infection of her membranes. The ObGyn decided to induce labor; a baby girl was born 11 hours later. The child had meningitis at birth and other infection-related complications including a brain hemorrhage. She continues to have permanent neurologic deficits.
PARENT’S CLAIM:
The ObGyn was negligent in not immediately delivering the child via cesarean delivery on October 13. The delay exposed the baby to infection for 11 more hours; the extended exposure led to her permanent injury.
PHYSICIAN’S DEFENSE:
The patient's treatment met the standard of care.
VERDICT:
A Virginia defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Fistula developed after delivery: $50M verdict
During delivery of a 31-year-old woman's baby, a nuchal cord was encountered. In order to safely deliver the child, the ObGyn performed an episiotomy.
After delivery, the patient reported an odorous vaginal discharge. The ObGyn explained that the condition was a natural byproduct of delivery and suggested that it would resolve without treatment.
The patient became pregnant a second time shortly after her first delivery and was evaluated by a midwife. The patient again reported the odorous discharge, but the condition was not addressed. At delivery of her second child, the ObGyn determined that the patient had a rectovaginal fistula. The patient underwent 13 repair operations.
PATIENT’S CLAIM:
The fistula was a byproduct of the episiotomy performed during the first delivery. The episiotomy should not have been performed. The ObGyn should have diagnosed and treated the fistula prior to delivery of the second child and performed a cesarean delivery.
DEFENDANT'S DEFENSE:
The ObGyn reported that the patient's medical records showed that she did not report the odorous discharge until after her second delivery.
VERDICT:
A New York $50 million verdict was returned.
Related article:
Management of wound complications following obstetric anal sphincter injury (OASIS)
Abdominal wall hematoma during pregnancy: $2.5M award
At 35 weeks' gestation, a 38-year-old woman presented to the emergency department (ED) with right upper abdominal pain. Her pregnancy was at high risk because of her age and the fact that she had thrombophilia involving both factor V and protein S deficiency. During pregnancy she was anticoagulated. She had been coughing from bronchitis, which was treated with antibiotics and an inhaler.
In the ED, laboratory testing determined that her blood was not properly clotting. Upper abdominal ultrasonography (US) showed an abdominal wall hematoma and gall stones. The ED physician, after contacting the on-call ObGyn, told the patient that nothing further could be done until after the baby's birth and prescribed medications for nausea and pain. The patient was discharged.
Thirty-three hours later, the patient was rushed to the hospital after she was found barely responsive, pale, and in severe pain. US results showed that the hematoma had grown extensively. The patient was in hypovolemic shock having lost more than 50% of her blood volume. She was admitted to the intensive care unit.
After induced labor, a stillborn son was delivered. The autopsy report revealed that the child died from either asphyxiation or an hypoxic ischemic event that occurred when the mother went into shock.
PATIENT’S CLAIM:
The ED physician and staff were negligent. Once the hematoma was identified, the standard of care is to monitor the hematoma with regular US. Instead, the ED physician discharged the patient. The ED physician contacted the on-call ObGyn but did not ask for a consult. The patient should have been admitted for monitoring.
DEFENDANT'S DEFENSE:
The ED physician met the standard of care. The mother's condition would likely have been detected during a nonstress test scheduled for the following day but the mother missed the prenatal exam because she had just left the hospital.
VERDICT:
A $2.5 million Missouri verdict was returned.
Incorrect due date, child with brain injuries: $1.2M
When a pregnant woman presented for her first prenatal visit, she was unsure of the date of her last menstrual period. During subsequent prenatal visits, she underwent 3 ultrasounds.
Labor was induced on August 1 because she reported gastrointestinal reflux. The infant appeared healthy at birth but soon went into respiratory distress. He was slow to meet developmental goals and was believed to be autistic. At age 5 years, he was given a diagnosis of periventricular leukomalacia.
PARENT’S CLAIM:
The child, 11 years old at the time of trial, has permanent brain injuries due to premature delivery. The mother's due date should have been projected as August 25 according to prenatal US measurements. The ObGyn misinterpreted the US data and estimated a due date of August 15. Therefore induction on August 1st caused him to be premature.
PHYSICIAN’S DEFENSE:
The standard of care was met. Gestational age evaluation using US is an estimate based on the child's size at specific time points, not an exact calculation, especially if the mother is not sure about the date of her last menses.
VERDICT:
A $1.2 million New Jersey verdict was returned.
Related article:
Three good apps for calculating the date of delivery
Bacterial infection blamed for birth injury
A woman was at 28 weeks' gestation when her membranes ruptured on September 28. She began to leak amniotic fluid and was put on bed rest. She saw her ObGyn on October 13 with signs of a bacterial infection of her membranes. The ObGyn decided to induce labor; a baby girl was born 11 hours later. The child had meningitis at birth and other infection-related complications including a brain hemorrhage. She continues to have permanent neurologic deficits.
PARENT’S CLAIM:
The ObGyn was negligent in not immediately delivering the child via cesarean delivery on October 13. The delay exposed the baby to infection for 11 more hours; the extended exposure led to her permanent injury.
PHYSICIAN’S DEFENSE:
The patient's treatment met the standard of care.
VERDICT:
A Virginia defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Fistula developed after delivery: $50M verdict
During delivery of a 31-year-old woman's baby, a nuchal cord was encountered. In order to safely deliver the child, the ObGyn performed an episiotomy.
After delivery, the patient reported an odorous vaginal discharge. The ObGyn explained that the condition was a natural byproduct of delivery and suggested that it would resolve without treatment.
The patient became pregnant a second time shortly after her first delivery and was evaluated by a midwife. The patient again reported the odorous discharge, but the condition was not addressed. At delivery of her second child, the ObGyn determined that the patient had a rectovaginal fistula. The patient underwent 13 repair operations.
PATIENT’S CLAIM:
The fistula was a byproduct of the episiotomy performed during the first delivery. The episiotomy should not have been performed. The ObGyn should have diagnosed and treated the fistula prior to delivery of the second child and performed a cesarean delivery.
DEFENDANT'S DEFENSE:
The ObGyn reported that the patient's medical records showed that she did not report the odorous discharge until after her second delivery.
VERDICT:
A New York $50 million verdict was returned.
Related article:
Management of wound complications following obstetric anal sphincter injury (OASIS)
Abdominal wall hematoma during pregnancy: $2.5M award
At 35 weeks' gestation, a 38-year-old woman presented to the emergency department (ED) with right upper abdominal pain. Her pregnancy was at high risk because of her age and the fact that she had thrombophilia involving both factor V and protein S deficiency. During pregnancy she was anticoagulated. She had been coughing from bronchitis, which was treated with antibiotics and an inhaler.
In the ED, laboratory testing determined that her blood was not properly clotting. Upper abdominal ultrasonography (US) showed an abdominal wall hematoma and gall stones. The ED physician, after contacting the on-call ObGyn, told the patient that nothing further could be done until after the baby's birth and prescribed medications for nausea and pain. The patient was discharged.
Thirty-three hours later, the patient was rushed to the hospital after she was found barely responsive, pale, and in severe pain. US results showed that the hematoma had grown extensively. The patient was in hypovolemic shock having lost more than 50% of her blood volume. She was admitted to the intensive care unit.
After induced labor, a stillborn son was delivered. The autopsy report revealed that the child died from either asphyxiation or an hypoxic ischemic event that occurred when the mother went into shock.
PATIENT’S CLAIM:
The ED physician and staff were negligent. Once the hematoma was identified, the standard of care is to monitor the hematoma with regular US. Instead, the ED physician discharged the patient. The ED physician contacted the on-call ObGyn but did not ask for a consult. The patient should have been admitted for monitoring.
DEFENDANT'S DEFENSE:
The ED physician met the standard of care. The mother's condition would likely have been detected during a nonstress test scheduled for the following day but the mother missed the prenatal exam because she had just left the hospital.
VERDICT:
A $2.5 million Missouri verdict was returned.
Incorrect due date, child with brain injuries: $1.2M
When a pregnant woman presented for her first prenatal visit, she was unsure of the date of her last menstrual period. During subsequent prenatal visits, she underwent 3 ultrasounds.
Labor was induced on August 1 because she reported gastrointestinal reflux. The infant appeared healthy at birth but soon went into respiratory distress. He was slow to meet developmental goals and was believed to be autistic. At age 5 years, he was given a diagnosis of periventricular leukomalacia.
PARENT’S CLAIM:
The child, 11 years old at the time of trial, has permanent brain injuries due to premature delivery. The mother's due date should have been projected as August 25 according to prenatal US measurements. The ObGyn misinterpreted the US data and estimated a due date of August 15. Therefore induction on August 1st caused him to be premature.
PHYSICIAN’S DEFENSE:
The standard of care was met. Gestational age evaluation using US is an estimate based on the child's size at specific time points, not an exact calculation, especially if the mother is not sure about the date of her last menses.
VERDICT:
A $1.2 million New Jersey verdict was returned.
Related article:
Three good apps for calculating the date of delivery
Bacterial infection blamed for birth injury
A woman was at 28 weeks' gestation when her membranes ruptured on September 28. She began to leak amniotic fluid and was put on bed rest. She saw her ObGyn on October 13 with signs of a bacterial infection of her membranes. The ObGyn decided to induce labor; a baby girl was born 11 hours later. The child had meningitis at birth and other infection-related complications including a brain hemorrhage. She continues to have permanent neurologic deficits.
PARENT’S CLAIM:
The ObGyn was negligent in not immediately delivering the child via cesarean delivery on October 13. The delay exposed the baby to infection for 11 more hours; the extended exposure led to her permanent injury.
PHYSICIAN’S DEFENSE:
The patient's treatment met the standard of care.
VERDICT:
A Virginia defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Ectopic pregnancy misdiagnosed
Ectopic pregnancy misdiagnosed
When a patient called her ObGyn (Dr. A) to report that she was 6 weeks' pregnant and had lower abdominal pain, she was seen by his partner (Dr. B). Dr. B could not identify an intrauterine pregnancy using ultrasonography (US), but the patient's hCG level was highly suggestive of an ectopic pregnancy. The next day, Dr. B performed exploratory laparoscopy, found no evidence of an ectopic pregnancy, and removed the patient's appendix. He continued to be concerned about the possibility of an ectopic pregnancy and suggested that the patient terminate the pregnancy. The next day he prescribed methotrexate. A week later, US revealed a fetus in utero with a beating heart. Because of the likelihood of birth defects after methotrexate use, Dr. B recommended terminating the pregnancy; an abortion was performed a month later.
PATIENT’S CLAIM:
Dr. B should have waited for the pathology report on the appendix and repeated the US before rushing into advising termination of pregnancy.
PHYSICIAN’S CLAIM :
Dr. B acted reasonably based on the patient's symptoms.
VERDICT:
A Kentucky defense verdict was returned.
Related article:
Stop using the hCG discriminatory zone of 1,500 to 2,000 mIU/mL to guide intervention during early pregnancy
Hemorrhage after trocar insertion
A gynecologist performed laparoscopic hysterectomy on his 46-year-old patient. During trocar insertion, the patient's iliac artery, iliac vein, and small bowel were injured. The patient hemorrhaged and went into cardiac arrest. The patient was given several transfusions and the injuries were repaired.
One day after discharge, she returned to the hospital with symptoms of an embolism; she was treated with anticoagulants for 1 year. A year after surgery, she was informed that she was transfused during surgery with HIV-positive blood. Her initial HIV test came back negative.
PATIENT’S CLAIM:
The gynecologist deviated from the standard of care by performing a "blind" trocar insertion, which caused the major vessels to be more susceptible to injury.
PHYSICIAN’S DEFENSE:
There was no deviation from the standard of care. Blind insertion of a trocar is an acceptable procedure.
VERDICT:
A $383,000 Illinois verdict was returned.
Related article:
How to avoid major vessel injury during gynecologic laparoscopy
Delay in ovarian cancer diagnosis: $1.9M settlement
A 64-year-old woman reported worsening abdominal pain, fatigue, and unexplained weight loss to her primary care physician. The physician did not order tests to assess the patient's status; he diagnosed gastritis. Several months later the patient saw another physician, who ordered imaging and identified stage IV ovarian clear cell carcinoma.
PATIENT’S CLAIM:
Timely imaging would have diagnosed ovarian cancer at stage I or II and given her a 90% survival rate at 10 years. Due to the diagnostic delay, her survival rate was less than 10% at 10 years.
PHYSICIAN’S DEFENSE:
The case settled before trial.
VERDICT:
A $1.9 million Illinois settlement was reached.
Late breast cancer diagnosis: $1.7M settlement
When a 25-year-old woman found a lump in her left breast she saw her gynecologist, who recommended US and fine-needle aspiration biopsy. US results indicated possible cancer; biopsy results were reported as negative for cancer. No further action was taken.
Eight months later, a second physician diagnosed stage IV breast cancer requiring chemotherapy, radiation therapy, and multiple surgeries.
PATIENT’S CLAIM:
The radiologist misread the fine-needle aspiration biopsy results. The gynecologist should have ordered a core needle biopsy because it is more reliable.
PHYSICIAN’S DEFENSE:
The case was settled during the trial.
VERDICT:
A $3.5 million Illinois settlement was reached.
Perforated colon after oophorectomy
A 55-year-old woman underwent laparoscopic oophorectomy to address pelvic pain and a right ovarian mass. Following surgery she developed peritonitis and sepsis. She underwent a colon resection with colostomy and had severe keloid scarring.
PATIENT’S CLAIM:
The surgeon was well aware of her history of extensive pelvic adhesions. Given her medical history, he should have performed an open laparotomy.
PHYSICIAN’S DEFENSE:
The case settled during trial.
VERDICT:
A $700,000 Illinois settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Ectopic pregnancy misdiagnosed
When a patient called her ObGyn (Dr. A) to report that she was 6 weeks' pregnant and had lower abdominal pain, she was seen by his partner (Dr. B). Dr. B could not identify an intrauterine pregnancy using ultrasonography (US), but the patient's hCG level was highly suggestive of an ectopic pregnancy. The next day, Dr. B performed exploratory laparoscopy, found no evidence of an ectopic pregnancy, and removed the patient's appendix. He continued to be concerned about the possibility of an ectopic pregnancy and suggested that the patient terminate the pregnancy. The next day he prescribed methotrexate. A week later, US revealed a fetus in utero with a beating heart. Because of the likelihood of birth defects after methotrexate use, Dr. B recommended terminating the pregnancy; an abortion was performed a month later.
PATIENT’S CLAIM:
Dr. B should have waited for the pathology report on the appendix and repeated the US before rushing into advising termination of pregnancy.
PHYSICIAN’S CLAIM :
Dr. B acted reasonably based on the patient's symptoms.
VERDICT:
A Kentucky defense verdict was returned.
Related article:
Stop using the hCG discriminatory zone of 1,500 to 2,000 mIU/mL to guide intervention during early pregnancy
Hemorrhage after trocar insertion
A gynecologist performed laparoscopic hysterectomy on his 46-year-old patient. During trocar insertion, the patient's iliac artery, iliac vein, and small bowel were injured. The patient hemorrhaged and went into cardiac arrest. The patient was given several transfusions and the injuries were repaired.
One day after discharge, she returned to the hospital with symptoms of an embolism; she was treated with anticoagulants for 1 year. A year after surgery, she was informed that she was transfused during surgery with HIV-positive blood. Her initial HIV test came back negative.
PATIENT’S CLAIM:
The gynecologist deviated from the standard of care by performing a "blind" trocar insertion, which caused the major vessels to be more susceptible to injury.
PHYSICIAN’S DEFENSE:
There was no deviation from the standard of care. Blind insertion of a trocar is an acceptable procedure.
VERDICT:
A $383,000 Illinois verdict was returned.
Related article:
How to avoid major vessel injury during gynecologic laparoscopy
Delay in ovarian cancer diagnosis: $1.9M settlement
A 64-year-old woman reported worsening abdominal pain, fatigue, and unexplained weight loss to her primary care physician. The physician did not order tests to assess the patient's status; he diagnosed gastritis. Several months later the patient saw another physician, who ordered imaging and identified stage IV ovarian clear cell carcinoma.
PATIENT’S CLAIM:
Timely imaging would have diagnosed ovarian cancer at stage I or II and given her a 90% survival rate at 10 years. Due to the diagnostic delay, her survival rate was less than 10% at 10 years.
PHYSICIAN’S DEFENSE:
The case settled before trial.
VERDICT:
A $1.9 million Illinois settlement was reached.
Late breast cancer diagnosis: $1.7M settlement
When a 25-year-old woman found a lump in her left breast she saw her gynecologist, who recommended US and fine-needle aspiration biopsy. US results indicated possible cancer; biopsy results were reported as negative for cancer. No further action was taken.
Eight months later, a second physician diagnosed stage IV breast cancer requiring chemotherapy, radiation therapy, and multiple surgeries.
PATIENT’S CLAIM:
The radiologist misread the fine-needle aspiration biopsy results. The gynecologist should have ordered a core needle biopsy because it is more reliable.
PHYSICIAN’S DEFENSE:
The case was settled during the trial.
VERDICT:
A $3.5 million Illinois settlement was reached.
Perforated colon after oophorectomy
A 55-year-old woman underwent laparoscopic oophorectomy to address pelvic pain and a right ovarian mass. Following surgery she developed peritonitis and sepsis. She underwent a colon resection with colostomy and had severe keloid scarring.
PATIENT’S CLAIM:
The surgeon was well aware of her history of extensive pelvic adhesions. Given her medical history, he should have performed an open laparotomy.
PHYSICIAN’S DEFENSE:
The case settled during trial.
VERDICT:
A $700,000 Illinois settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Ectopic pregnancy misdiagnosed
When a patient called her ObGyn (Dr. A) to report that she was 6 weeks' pregnant and had lower abdominal pain, she was seen by his partner (Dr. B). Dr. B could not identify an intrauterine pregnancy using ultrasonography (US), but the patient's hCG level was highly suggestive of an ectopic pregnancy. The next day, Dr. B performed exploratory laparoscopy, found no evidence of an ectopic pregnancy, and removed the patient's appendix. He continued to be concerned about the possibility of an ectopic pregnancy and suggested that the patient terminate the pregnancy. The next day he prescribed methotrexate. A week later, US revealed a fetus in utero with a beating heart. Because of the likelihood of birth defects after methotrexate use, Dr. B recommended terminating the pregnancy; an abortion was performed a month later.
PATIENT’S CLAIM:
Dr. B should have waited for the pathology report on the appendix and repeated the US before rushing into advising termination of pregnancy.
PHYSICIAN’S CLAIM :
Dr. B acted reasonably based on the patient's symptoms.
VERDICT:
A Kentucky defense verdict was returned.
Related article:
Stop using the hCG discriminatory zone of 1,500 to 2,000 mIU/mL to guide intervention during early pregnancy
Hemorrhage after trocar insertion
A gynecologist performed laparoscopic hysterectomy on his 46-year-old patient. During trocar insertion, the patient's iliac artery, iliac vein, and small bowel were injured. The patient hemorrhaged and went into cardiac arrest. The patient was given several transfusions and the injuries were repaired.
One day after discharge, she returned to the hospital with symptoms of an embolism; she was treated with anticoagulants for 1 year. A year after surgery, she was informed that she was transfused during surgery with HIV-positive blood. Her initial HIV test came back negative.
PATIENT’S CLAIM:
The gynecologist deviated from the standard of care by performing a "blind" trocar insertion, which caused the major vessels to be more susceptible to injury.
PHYSICIAN’S DEFENSE:
There was no deviation from the standard of care. Blind insertion of a trocar is an acceptable procedure.
VERDICT:
A $383,000 Illinois verdict was returned.
Related article:
How to avoid major vessel injury during gynecologic laparoscopy
Delay in ovarian cancer diagnosis: $1.9M settlement
A 64-year-old woman reported worsening abdominal pain, fatigue, and unexplained weight loss to her primary care physician. The physician did not order tests to assess the patient's status; he diagnosed gastritis. Several months later the patient saw another physician, who ordered imaging and identified stage IV ovarian clear cell carcinoma.
PATIENT’S CLAIM:
Timely imaging would have diagnosed ovarian cancer at stage I or II and given her a 90% survival rate at 10 years. Due to the diagnostic delay, her survival rate was less than 10% at 10 years.
PHYSICIAN’S DEFENSE:
The case settled before trial.
VERDICT:
A $1.9 million Illinois settlement was reached.
Late breast cancer diagnosis: $1.7M settlement
When a 25-year-old woman found a lump in her left breast she saw her gynecologist, who recommended US and fine-needle aspiration biopsy. US results indicated possible cancer; biopsy results were reported as negative for cancer. No further action was taken.
Eight months later, a second physician diagnosed stage IV breast cancer requiring chemotherapy, radiation therapy, and multiple surgeries.
PATIENT’S CLAIM:
The radiologist misread the fine-needle aspiration biopsy results. The gynecologist should have ordered a core needle biopsy because it is more reliable.
PHYSICIAN’S DEFENSE:
The case was settled during the trial.
VERDICT:
A $3.5 million Illinois settlement was reached.
Perforated colon after oophorectomy
A 55-year-old woman underwent laparoscopic oophorectomy to address pelvic pain and a right ovarian mass. Following surgery she developed peritonitis and sepsis. She underwent a colon resection with colostomy and had severe keloid scarring.
PATIENT’S CLAIM:
The surgeon was well aware of her history of extensive pelvic adhesions. Given her medical history, he should have performed an open laparotomy.
PHYSICIAN’S DEFENSE:
The case settled during trial.
VERDICT:
A $700,000 Illinois settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Preeclampsia test cancelled: $5M settlement, and more
Preeclampsia test cancelled: $5M settlement
A 35-year-old woman was pregnant with her first child. Prior to and during her pregnancy, she took medication for chronic hypertension. Although another ObGyn had ordered a 24-hour urinalysis to test for preeclampsia, the ObGyn who saw the mother in early May for a third trimester visit cancelled the test.
The mother delivered the child by cesarean delivery when the fetal heart-rate monitor indicated fetal distress. After birth, the child received a diagnosis of cerebral palsy, spastic quadriplegia, and dystonia.
Parents' claim: The decision by the second ObGyn to cancel the 24-hour urinalysis eliminated the opportunity to diagnose preeclampsia superimposed on chronic hypertension. Over time, preeclampsia impaired blood flow to the placenta and fetus. If the mother had been assessed in early May, the injury could have been prevented.
Defendants' defense: The case was settled during trial.
Verdict: A $5,000,000 Illinois settlement was reached through mediation with the hospital physicians’ group and 2 ObGyns.
Umbilical cord damaged at delivery: $1.5M settlement
A mother at full term presented to the hospital in labor. During delivery, the umbilical cord was severed during maneuvers to address shoulder dystocia. The fetus was stillborn.
Parents' claim: The patient told the nurses that shoulder dystocia had been encountered during a previous delivery. Shoulder dystocia maneuvers were not performed correctly. Cesarean delivery was never offered.
Hospital's Defense: The nurses called the certified nurse midwife who was managing labor and delivery to alert her of the patient’s history. The midwife denied receiving such a call. The case was settled during trial.
Verdict: A $1.5 million Illinois settlement was reached.
What caused sepsis after oophorectomy?
A woman had a cyst on her left ovary. The ObGyn began surgery laparoscopically but converted to open salpingo-oophorectomy because of extensive adhesions. Four days after surgery, the patient received a diagnosis of peritonitis and sepsis due to spillage from the sigmoid colon. She required a second surgery to repair the damage, followed by a long recovery.
Patient's claim: The ObGyn should not have attempted laparoscopic surgery; he knew of her extensive surgical history and should have anticipated the presence of adhesions. If the laparoscopic entry site had been examined properly intraoperatively, the injury could have been repaired immediately.
Physician's defense: The ObGyn had no reason to believe the patient would have adhesions in the umbilical area; prior surgeries occurred in the upper abdomen. Laparoscopic surgery with Veress needle access is an accepted method used by obstetric surgeons. The ObGyn carefully irrigated and inspected the abdomen before closing. Injury to the sigmoid colon is a known complication of left oophorectomy.
At the time of surgery, the patient was likely suffering from diverticulosis, a long-term condition that can lead to a leak in the large colon. The weakness in the patient’s colon caused a postsurgical leak; signs and symptoms did not appear until 4 days after surgery.
Verdict: A California defense verdict was returned.
Ectopic pregnancy misdiagnosed
A 39-year-old woman reported abdominal pain to her ObGyn. After ultrasonography (US), she was given a diagnosis of ectopic pregnancy. The ObGyn administered methotrexate to terminate the pregnancy. Five days later, repeat US showed a viable uterine pregnancy. Based on the risks posed by methotrexate, the patient terminated the pregnancy.
Patient's claim: The ObGyn misdiagnosed the pregnancy as ectopic.
Hospital's Defense: The case was settled during trial.
Verdict: A $625,000 Illinois settlement was reached.
Infant dies. was it fetal hydrops?
A woman was admitted to the hospital in full-term labor. She was cared for by a team of residents and nurses supervised by an attending ObGyn. During labor, the staff documented late, variable decelerations with periods of minimal or undetectable variability on the fetal heart-rate monitor. The fetal heart rate, however, was reported as being reassuring overall.
After 90 minutes, fetal heart-rate tracings became non-reassuring. Because the baby's head was crowning, the ObGyn used vacuum extraction for delivery. The infant was born without signs of life. A neonatologist thought the infant appeared hydropic with generalized edema, ascites, and pleural effusion. Efforts at resuscitation were unsuccessful until the neonatologist performed thoracentesis. The infant died several hours later. Cause of death has charted as hypoxic ischemic encephalopathy and multisystem organ failure.
Estate's claim: The hospital staff deviated from the standard of care by failing to appropriately communicate, failing to recognize fetal distress, and failing to perform a cesarean delivery when tracings were nonreassuring. An expert neonatologist claimed that failure to react to fetal distress caused the fetus to develop severe intrauterine hypoxic ischemia causing death.
Defendants' defense: Overall, the fetal heart-rate tracings were reassuring. The team communicated appropriately and kept the attending ObGyn alerted to the status. Delivery was expedited when fetal distress was evident.
Fetal hydrops was the end result of a serious problem in utero that could not have developed during the hours of labor and delivery; it most likely arose days to weeks before delivery. Nothing that occurred during labor and delivery caused hypoxic ischemic encephalopathy.
Verdict: An Illinois defense verdict was returned.
Child has permanent shoulder injury: $1M verdict
A mother was admitted to a hospital in full-term labor. During delivery, anterior shoulder dystocia was encountered.
The child received a diagnosis of a left brachial plexus injury and extracranial and intracranial bleeding. She underwent 3 surgeries to reattach nerve roots and move muscles and tendons in her shoulder and forearm in an effort to improve function in her left arm, wrist, and hand. She has undergone extensive physical and occupational therapy. Her left arm is smaller than her right arm and she has minimal strength, dexterity, and only 20% functionality of her left arm.
Parent's claim: The ObGyn exerted excessive traction when delivering the child. Alternate methods should have been used to manage shoulder dystocia. The hospital nurses should not have used fundal pressure.
Defendants' defense: The suit was brought against the ObGyn, his practice, and the hospital. The ObGyn claimed that he used several maneuvers to manage shoulder dystocia. The child’s injuries were a result of the maternal forces of labor and were not caused by negligence on the part of the ObGyn or nurses. The nurses denied using fundal pressure; they were trained to use suprapubic pressure.
Verdict: A $1,012,00 Illinois verdict was returned, finding the ObGyn’s practice 100% liable.
Parvovirus exposure: Fetal death
When a woman first saw an ObGyn, ultrasonography (US) indicated that her fetus was at 8 to 9 weeks’ gestation. One month later, she told the same ObGyn that she had been exposed to Fifth disease. Because blood work was positive for parvovirus B19, the ObGyn ordered the patient to undergo US every 2 weeks for the next 10 weeks. Two weeks later, the patient saw a second ObGyn at the same clinic. Although the first ObGyn had ordered US, none was performed; the patient’s next appointment was scheduled in 4 weeks. At that time, the patient saw a third ObGyn, who ordered US. He noted in her chart that the fetus had a nuchal fold, indicating Down syndrome. He told the patient to return in 2 weeks for a follow-up US. The results of that US showed that the fetus had died. Fetal cord blood tested positive for parvovirus B19.
Parent's claim: All 3 ObGyns failed to react properly to indications of parvovirus infection. Regular US should have been performed, as suggested by the first ObGyn. The mother should have been referred to a perinatologist or other maternal-fetal specialist when blood work was positive for parvovirus B19. A specialist could have provided treatment for the virus.
Physician's defense: The ObGyns denied any breach in the standard of care. They claimed that results would have been the same if they had referred the patient to a specialist.
Verdict: An Alabama defense verdict was returned.
Preeclampsia test cancelled: $5M settlement
A 35-year-old woman was pregnant with her first child. Prior to and during her pregnancy, she took medication for chronic hypertension. Although another ObGyn had ordered a 24-hour urinalysis to test for preeclampsia, the ObGyn who saw the mother in early May for a third trimester visit cancelled the test.
The mother delivered the child by cesarean delivery when the fetal heart-rate monitor indicated fetal distress. After birth, the child received a diagnosis of cerebral palsy, spastic quadriplegia, and dystonia.
Parents' claim: The decision by the second ObGyn to cancel the 24-hour urinalysis eliminated the opportunity to diagnose preeclampsia superimposed on chronic hypertension. Over time, preeclampsia impaired blood flow to the placenta and fetus. If the mother had been assessed in early May, the injury could have been prevented.
Defendants' defense: The case was settled during trial.
Verdict: A $5,000,000 Illinois settlement was reached through mediation with the hospital physicians’ group and 2 ObGyns.
Umbilical cord damaged at delivery: $1.5M settlement
A mother at full term presented to the hospital in labor. During delivery, the umbilical cord was severed during maneuvers to address shoulder dystocia. The fetus was stillborn.
Parents' claim: The patient told the nurses that shoulder dystocia had been encountered during a previous delivery. Shoulder dystocia maneuvers were not performed correctly. Cesarean delivery was never offered.
Hospital's Defense: The nurses called the certified nurse midwife who was managing labor and delivery to alert her of the patient’s history. The midwife denied receiving such a call. The case was settled during trial.
Verdict: A $1.5 million Illinois settlement was reached.
What caused sepsis after oophorectomy?
A woman had a cyst on her left ovary. The ObGyn began surgery laparoscopically but converted to open salpingo-oophorectomy because of extensive adhesions. Four days after surgery, the patient received a diagnosis of peritonitis and sepsis due to spillage from the sigmoid colon. She required a second surgery to repair the damage, followed by a long recovery.
Patient's claim: The ObGyn should not have attempted laparoscopic surgery; he knew of her extensive surgical history and should have anticipated the presence of adhesions. If the laparoscopic entry site had been examined properly intraoperatively, the injury could have been repaired immediately.
Physician's defense: The ObGyn had no reason to believe the patient would have adhesions in the umbilical area; prior surgeries occurred in the upper abdomen. Laparoscopic surgery with Veress needle access is an accepted method used by obstetric surgeons. The ObGyn carefully irrigated and inspected the abdomen before closing. Injury to the sigmoid colon is a known complication of left oophorectomy.
At the time of surgery, the patient was likely suffering from diverticulosis, a long-term condition that can lead to a leak in the large colon. The weakness in the patient’s colon caused a postsurgical leak; signs and symptoms did not appear until 4 days after surgery.
Verdict: A California defense verdict was returned.
Ectopic pregnancy misdiagnosed
A 39-year-old woman reported abdominal pain to her ObGyn. After ultrasonography (US), she was given a diagnosis of ectopic pregnancy. The ObGyn administered methotrexate to terminate the pregnancy. Five days later, repeat US showed a viable uterine pregnancy. Based on the risks posed by methotrexate, the patient terminated the pregnancy.
Patient's claim: The ObGyn misdiagnosed the pregnancy as ectopic.
Hospital's Defense: The case was settled during trial.
Verdict: A $625,000 Illinois settlement was reached.
Infant dies. was it fetal hydrops?
A woman was admitted to the hospital in full-term labor. She was cared for by a team of residents and nurses supervised by an attending ObGyn. During labor, the staff documented late, variable decelerations with periods of minimal or undetectable variability on the fetal heart-rate monitor. The fetal heart rate, however, was reported as being reassuring overall.
After 90 minutes, fetal heart-rate tracings became non-reassuring. Because the baby's head was crowning, the ObGyn used vacuum extraction for delivery. The infant was born without signs of life. A neonatologist thought the infant appeared hydropic with generalized edema, ascites, and pleural effusion. Efforts at resuscitation were unsuccessful until the neonatologist performed thoracentesis. The infant died several hours later. Cause of death has charted as hypoxic ischemic encephalopathy and multisystem organ failure.
Estate's claim: The hospital staff deviated from the standard of care by failing to appropriately communicate, failing to recognize fetal distress, and failing to perform a cesarean delivery when tracings were nonreassuring. An expert neonatologist claimed that failure to react to fetal distress caused the fetus to develop severe intrauterine hypoxic ischemia causing death.
Defendants' defense: Overall, the fetal heart-rate tracings were reassuring. The team communicated appropriately and kept the attending ObGyn alerted to the status. Delivery was expedited when fetal distress was evident.
Fetal hydrops was the end result of a serious problem in utero that could not have developed during the hours of labor and delivery; it most likely arose days to weeks before delivery. Nothing that occurred during labor and delivery caused hypoxic ischemic encephalopathy.
Verdict: An Illinois defense verdict was returned.
Child has permanent shoulder injury: $1M verdict
A mother was admitted to a hospital in full-term labor. During delivery, anterior shoulder dystocia was encountered.
The child received a diagnosis of a left brachial plexus injury and extracranial and intracranial bleeding. She underwent 3 surgeries to reattach nerve roots and move muscles and tendons in her shoulder and forearm in an effort to improve function in her left arm, wrist, and hand. She has undergone extensive physical and occupational therapy. Her left arm is smaller than her right arm and she has minimal strength, dexterity, and only 20% functionality of her left arm.
Parent's claim: The ObGyn exerted excessive traction when delivering the child. Alternate methods should have been used to manage shoulder dystocia. The hospital nurses should not have used fundal pressure.
Defendants' defense: The suit was brought against the ObGyn, his practice, and the hospital. The ObGyn claimed that he used several maneuvers to manage shoulder dystocia. The child’s injuries were a result of the maternal forces of labor and were not caused by negligence on the part of the ObGyn or nurses. The nurses denied using fundal pressure; they were trained to use suprapubic pressure.
Verdict: A $1,012,00 Illinois verdict was returned, finding the ObGyn’s practice 100% liable.
Parvovirus exposure: Fetal death
When a woman first saw an ObGyn, ultrasonography (US) indicated that her fetus was at 8 to 9 weeks’ gestation. One month later, she told the same ObGyn that she had been exposed to Fifth disease. Because blood work was positive for parvovirus B19, the ObGyn ordered the patient to undergo US every 2 weeks for the next 10 weeks. Two weeks later, the patient saw a second ObGyn at the same clinic. Although the first ObGyn had ordered US, none was performed; the patient’s next appointment was scheduled in 4 weeks. At that time, the patient saw a third ObGyn, who ordered US. He noted in her chart that the fetus had a nuchal fold, indicating Down syndrome. He told the patient to return in 2 weeks for a follow-up US. The results of that US showed that the fetus had died. Fetal cord blood tested positive for parvovirus B19.
Parent's claim: All 3 ObGyns failed to react properly to indications of parvovirus infection. Regular US should have been performed, as suggested by the first ObGyn. The mother should have been referred to a perinatologist or other maternal-fetal specialist when blood work was positive for parvovirus B19. A specialist could have provided treatment for the virus.
Physician's defense: The ObGyns denied any breach in the standard of care. They claimed that results would have been the same if they had referred the patient to a specialist.
Verdict: An Alabama defense verdict was returned.
Preeclampsia test cancelled: $5M settlement
A 35-year-old woman was pregnant with her first child. Prior to and during her pregnancy, she took medication for chronic hypertension. Although another ObGyn had ordered a 24-hour urinalysis to test for preeclampsia, the ObGyn who saw the mother in early May for a third trimester visit cancelled the test.
The mother delivered the child by cesarean delivery when the fetal heart-rate monitor indicated fetal distress. After birth, the child received a diagnosis of cerebral palsy, spastic quadriplegia, and dystonia.
Parents' claim: The decision by the second ObGyn to cancel the 24-hour urinalysis eliminated the opportunity to diagnose preeclampsia superimposed on chronic hypertension. Over time, preeclampsia impaired blood flow to the placenta and fetus. If the mother had been assessed in early May, the injury could have been prevented.
Defendants' defense: The case was settled during trial.
Verdict: A $5,000,000 Illinois settlement was reached through mediation with the hospital physicians’ group and 2 ObGyns.
Umbilical cord damaged at delivery: $1.5M settlement
A mother at full term presented to the hospital in labor. During delivery, the umbilical cord was severed during maneuvers to address shoulder dystocia. The fetus was stillborn.
Parents' claim: The patient told the nurses that shoulder dystocia had been encountered during a previous delivery. Shoulder dystocia maneuvers were not performed correctly. Cesarean delivery was never offered.
Hospital's Defense: The nurses called the certified nurse midwife who was managing labor and delivery to alert her of the patient’s history. The midwife denied receiving such a call. The case was settled during trial.
Verdict: A $1.5 million Illinois settlement was reached.
What caused sepsis after oophorectomy?
A woman had a cyst on her left ovary. The ObGyn began surgery laparoscopically but converted to open salpingo-oophorectomy because of extensive adhesions. Four days after surgery, the patient received a diagnosis of peritonitis and sepsis due to spillage from the sigmoid colon. She required a second surgery to repair the damage, followed by a long recovery.
Patient's claim: The ObGyn should not have attempted laparoscopic surgery; he knew of her extensive surgical history and should have anticipated the presence of adhesions. If the laparoscopic entry site had been examined properly intraoperatively, the injury could have been repaired immediately.
Physician's defense: The ObGyn had no reason to believe the patient would have adhesions in the umbilical area; prior surgeries occurred in the upper abdomen. Laparoscopic surgery with Veress needle access is an accepted method used by obstetric surgeons. The ObGyn carefully irrigated and inspected the abdomen before closing. Injury to the sigmoid colon is a known complication of left oophorectomy.
At the time of surgery, the patient was likely suffering from diverticulosis, a long-term condition that can lead to a leak in the large colon. The weakness in the patient’s colon caused a postsurgical leak; signs and symptoms did not appear until 4 days after surgery.
Verdict: A California defense verdict was returned.
Ectopic pregnancy misdiagnosed
A 39-year-old woman reported abdominal pain to her ObGyn. After ultrasonography (US), she was given a diagnosis of ectopic pregnancy. The ObGyn administered methotrexate to terminate the pregnancy. Five days later, repeat US showed a viable uterine pregnancy. Based on the risks posed by methotrexate, the patient terminated the pregnancy.
Patient's claim: The ObGyn misdiagnosed the pregnancy as ectopic.
Hospital's Defense: The case was settled during trial.
Verdict: A $625,000 Illinois settlement was reached.
Infant dies. was it fetal hydrops?
A woman was admitted to the hospital in full-term labor. She was cared for by a team of residents and nurses supervised by an attending ObGyn. During labor, the staff documented late, variable decelerations with periods of minimal or undetectable variability on the fetal heart-rate monitor. The fetal heart rate, however, was reported as being reassuring overall.
After 90 minutes, fetal heart-rate tracings became non-reassuring. Because the baby's head was crowning, the ObGyn used vacuum extraction for delivery. The infant was born without signs of life. A neonatologist thought the infant appeared hydropic with generalized edema, ascites, and pleural effusion. Efforts at resuscitation were unsuccessful until the neonatologist performed thoracentesis. The infant died several hours later. Cause of death has charted as hypoxic ischemic encephalopathy and multisystem organ failure.
Estate's claim: The hospital staff deviated from the standard of care by failing to appropriately communicate, failing to recognize fetal distress, and failing to perform a cesarean delivery when tracings were nonreassuring. An expert neonatologist claimed that failure to react to fetal distress caused the fetus to develop severe intrauterine hypoxic ischemia causing death.
Defendants' defense: Overall, the fetal heart-rate tracings were reassuring. The team communicated appropriately and kept the attending ObGyn alerted to the status. Delivery was expedited when fetal distress was evident.
Fetal hydrops was the end result of a serious problem in utero that could not have developed during the hours of labor and delivery; it most likely arose days to weeks before delivery. Nothing that occurred during labor and delivery caused hypoxic ischemic encephalopathy.
Verdict: An Illinois defense verdict was returned.
Child has permanent shoulder injury: $1M verdict
A mother was admitted to a hospital in full-term labor. During delivery, anterior shoulder dystocia was encountered.
The child received a diagnosis of a left brachial plexus injury and extracranial and intracranial bleeding. She underwent 3 surgeries to reattach nerve roots and move muscles and tendons in her shoulder and forearm in an effort to improve function in her left arm, wrist, and hand. She has undergone extensive physical and occupational therapy. Her left arm is smaller than her right arm and she has minimal strength, dexterity, and only 20% functionality of her left arm.
Parent's claim: The ObGyn exerted excessive traction when delivering the child. Alternate methods should have been used to manage shoulder dystocia. The hospital nurses should not have used fundal pressure.
Defendants' defense: The suit was brought against the ObGyn, his practice, and the hospital. The ObGyn claimed that he used several maneuvers to manage shoulder dystocia. The child’s injuries were a result of the maternal forces of labor and were not caused by negligence on the part of the ObGyn or nurses. The nurses denied using fundal pressure; they were trained to use suprapubic pressure.
Verdict: A $1,012,00 Illinois verdict was returned, finding the ObGyn’s practice 100% liable.
Parvovirus exposure: Fetal death
When a woman first saw an ObGyn, ultrasonography (US) indicated that her fetus was at 8 to 9 weeks’ gestation. One month later, she told the same ObGyn that she had been exposed to Fifth disease. Because blood work was positive for parvovirus B19, the ObGyn ordered the patient to undergo US every 2 weeks for the next 10 weeks. Two weeks later, the patient saw a second ObGyn at the same clinic. Although the first ObGyn had ordered US, none was performed; the patient’s next appointment was scheduled in 4 weeks. At that time, the patient saw a third ObGyn, who ordered US. He noted in her chart that the fetus had a nuchal fold, indicating Down syndrome. He told the patient to return in 2 weeks for a follow-up US. The results of that US showed that the fetus had died. Fetal cord blood tested positive for parvovirus B19.
Parent's claim: All 3 ObGyns failed to react properly to indications of parvovirus infection. Regular US should have been performed, as suggested by the first ObGyn. The mother should have been referred to a perinatologist or other maternal-fetal specialist when blood work was positive for parvovirus B19. A specialist could have provided treatment for the virus.
Physician's defense: The ObGyns denied any breach in the standard of care. They claimed that results would have been the same if they had referred the patient to a specialist.
Verdict: An Alabama defense verdict was returned.
Additional Medical Verdicts
• Umbilical cord damaged at delivery: $1.5M settlement
• What caused sepsis after oophorectomy?
• Ectopic pregnancy misdiagnosed
• Infant dies. Was it fetal hydrops?
• Child has permanent shoulder injury: $1M verdict
• Parvovirus exposure: fetal death
WATCH: It's All in Your Hospitalist Contract
Steve Harris, Esq., legal columnist for The Hospitalist, explains the ins and outs of a hospitalist contract.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Steve Harris, Esq., legal columnist for The Hospitalist, explains the ins and outs of a hospitalist contract.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Steve Harris, Esq., legal columnist for The Hospitalist, explains the ins and outs of a hospitalist contract.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The medicolegal considerations of interacting with your patients online
CASE: Patient discloses personal information in electronic communication. How to respond and what’s at stake?
Your nurse comes to you with a dilemma. Last Friday she received an email from a patient, sent to the nurse’s personal email account (G-mail) that conveyed information regarding the patient’s recent treatment for a herpetic vulvar lesion. The text details presumed exposure, date and time, number of sexual partners, concernfor “spread of disease,” and the patient’s desire to have a comprehensive sexually transmitted infection screening as soon as possible.
Your nurse has years of professional experience, but she is perhaps not the most savvy with regard to current information technology and social media. Nonetheless, she knows it is best not to immediately respond to the patient’s email without checking with you. She tracks you down on Monday morning to review the email and the dilemma she feels she has been placed in. What’s the best next step?
While discussing the general question with the staff, another nurse notes that there have been some reviews of the office on social media. It seems that this second nurse tweets and texts with patients all the time. The office manager strongly suggests that the office “join the 21st Century” by setting up a Facebook page and using their webpage to attract new patients and communicate with current patients.
How do you prepare for this? Is your staff knowledgeable about the dos and don’ts of social media?
The use of social media by health care providers has been growing for several years. Back in 2011 a large survey by QuantiaMD revealed that 87% of physicians used social media for personal reasons, and 67% of them used it professionally.1 How they used it for professional purposes also was explored in 2011, with almost 3 of 4 physicians using it for social networking and more than half engaging with their own institution’s social media (FIGURE).2 In 2013, 53% of physicians indicated that their practice had a Facebook platform, 28% had a presence on LinkedIn, and 21% were on Twitter.3 Not surprisingly, social media use is higher among younger physicians4; the 2016 equivalents to these percentages most likely are higher.
| Health providers’ use of social media for professional reasons2 |
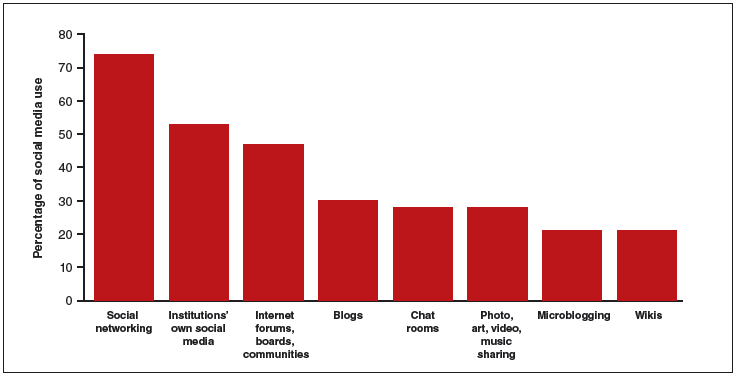
|
In 2011, a survey found that most health providers used social networking, their institutions’ own social media, and Internet forums, boards, and communities for professional reasons. |
Patients’ outreach through social media regarding health care information continues to grow, with 33.8% asking for health advice using social media.5 While email and other social media open the possibility of improved communication with patients, they also present a number of important professional and legal issues that deserve special consideration.6 Each medium presents its own challenges, but there are 4 categories of concern related to basic values and rights that we consider important to review:
- confidentiality
- dual relationships and conflicts of interest
- quality of care and advice
- general professionalism (including advertising).
Confidentiality
Few values of the medical profession are of longer standing than the commitment to maintain patient privacy. Fifth Century BC obligations continue to apply to the technology of the 21st Century AD. And the challenges are significant.
Email is not secure
In the opening case, the choice to email her clinician was apparently the patient’s. She probably does not realize that email is not very confidential, although it is undoubtedly in the Terms of Service Agreement she clicked through. Her email was likely scanned by her email service provider—Google, in this case—as well as the nurse. If, however, the physician’s office responds by email, it may well compound the confidentiality problem by further distributing the information through yet another email provider.
If, as a physician, you encourage email communication by your patients, a smart approach is to emphasize that such communications are not very confidential. At a minimum, until a secure email system can be established, it is best not to transmit medical information via email and to inform patients of the risk of such communication. In the case above, the nurse who received the email should respond to the patient by telephone (much more secure). Or she can respond to the patient by email (not including the patient’s message in the return), writing that, because email communications are inherently not confidential, she suggests a phone call or personal visit.
This case also notes that the patient sent the email to the nurse’s personal account, not to an office email account. Sending medical emails to an employee’s personal account raises additional problems of confidentiality and appropriate controls. It should be made clear that employees should not be discussing private medical matters via their own email accounts.
Other forms of social media are also not secure
Similar concerns arise about texting and using Twitter by the second nurse. These activities apparently had been unknown to the physician, but the practice still may be responsible for her actions. These are insecure forms of communication and raise serious ethical and legal concerns.
Other social media pose confidentiality risks as well. For example, a physician was dismissed from a position and reprimanded by the medical board for posting patient information on Facebook,7 and an ObGyn caused problems by posting a nasty note about a patient who showed up late for an appointment.8 Too many patients may not understand that posting on social media is the equivalent of standing on a street corner yelling private information. Social media sites that invite the discussion of personal matters are an invitation to trouble.
Physicians are ethically obliged to protect confidentiality
Professional standards place significant ethical obligations on physicians to protect patient confidentiality. The American Medical Association (AMA) has an ethics opinion on professionalism with social media,9 as does the American College of Obstetricians and Gynecologists (ACOG).10 Another excellent discussion of ethical and practical issues is a joint position paper by the American College of Physicians and the Federation of State Medical Boards.11 Both documents focus attention on issues of confidentiality.
Physicians are legally obliged to protect confidentiality
There are many legal protections for confidentiality that can be implicated by electronic communications and social media. All states provide protection for unwarranted disclosure of private patient information. Such disclosures made electronically are included.12 Indeed, because electronic disclosures may be broadcast more widely, they may be especially dangerous. The misuse of social media may result in license discipline by the state board, regulatory sanctions, or civil liability (rare, but criminal sanctions are a possibility in extreme circumstances).
In addition to state laws regarding confidentiality, there are a number of federal laws that cover confidential medical information. None is more important than the Health Insurance Portability and Accountability Act (HIPAA) and the more recent HITECH amendments (Health Information Technology for Economic and Clinical Health).13 These laws have both privacy provisions and security (including “encryption”) requirements. These are complicated laws but at their core are the notions that health care providers and some others:
- are responsible for maintaining the security and privacy of health information
- may not transmit (even unintentionally) such information to others without patient permission or legal authority.14
- may not transmit (even unintentionally) such information to others without patient permission or legal authority.
A good source of step-by-step information about these laws is “Health information privacy: Covered entities and business associates,” on the US Health and Human Services website.14
HITECH also provides for notice to patients when health information is inappropriately transmitted. Thus, a missing USB flash drive with patient information may require notification to thousands of patients.15 Any consideration of the use of email or social media in medical practice must take into account the HIPAA/HITECH obligations to protect the security of patient health information. There can be serious professional consequences for failing to follow the HIPAA requirements.16
Dual relationships and conflicts of interest
In our hypothetical case, the office manager’s suggestion that the office use Facebook and their website to attract new patients also may raise confidentiality problems. The Facebook suggestion especially needs to be considered carefully. Facebook use is estimated to be 63% to 96% among students and 13% to 47% among health care professionals.17 Facebook is most often seen as an interactive social site; it risks blurring the lines between personal and professional relationships.9 There is a consensus that a physician should not “friend” patients on Facebook. The AMA ethics opinion notes that “physicians must maintain appropriate boundaries of the patient-physician relationship in accordance with professional ethical guidelines, just as they would in any other context.”9
Separate personal and professional contacts
Difficulties with interactive social media are not limited to the physicians in a practice. The problems increase with the number of staff members who post or respond on social media. Control of social media is essential. The practice must ensure that staff members do not slip into inappropriate personal comments and relationships. Staff should understand (and be reminded of) the necessity of separating personal and professional contacts.
Avoid misunderstandings
In addition, whatever the intent of the physician and staff may be, it is essentially impossible to know how patients will interpret interactions on these social media. The very informal, off-the-cuff, chatty way in which Facebook and similar sites are used invites misunderstandings, and maintaining professional boundaries is necessary.
Ground rules
All of this is not to say that professionals should never use Facebook or similar sites. Rather, if used, ground rules need to be established.
Social media communications must:
- be professional and not related to personal matters
- not be used to give medical advice
- be controlled by high level staff
- be reviewed periodically.
Staff training
Particularly for interactive social media (email, texts, Twitter, Facebook, etc), it is essential that there be both clear policies and good staff training (TABLE).9–11,18 There really should be no “making it up as we go along.” Staff on a social media lark of their own can be disastrous for the practice. Policies need to be updated frequently, and staff training reinforced and repeated periodically.
Quality of care and advice
Start with your website
Institutions’ websites are major sources of health care information: Nearly 32% of US adults would be very likely to prefer a hospital based on its website.5 Your website can be an important face of your practice to the community—for good or for bad. On one hand, the practice can control what is on a website and, unlike some social media, it will not be directed to individual patients. Done well, it “provides golden opportunities for marketing physician services, as well as for contributing to public health by providing high-quality online content that is both accurate and understandable to laypeople.”19 Done badly, it can convey incorrect and harmful information and discredit the medical practice that established it.
Your website introduces the practice and settings, but it will serve another purpose to thousands of people who likely will see it over time as a source of credible health information. The importance of ensuring that your website is carefully constructed to provide, or link to, good medical advice that contributes to quality of care cannot be overstated.
A good website begins with a clear statement of the reasons and goals for having the site. Professional design assistance generally is used to create the site, but that design process needs to be overseen by a medical professional to ensure that it conveys the sense of the practice and provides completely accurate information. A homepage of dancing clowns with stethoscopes may seem good to a 20-something-year-old designer, but it is not appropriate for a physician. It will be the practice, not the designer, who is held accountable for the site content. Links to other sites need to be vetted and used with care. Patients and other members of the public may well take the links as carrying the endorsement of the practice and its physicians.
Perhaps the greatest risk of a website is that it will not be kept current. Unfortunately, they do not update themselves. Some knowledgeable staff member must frequently review it to update everything from office hours and personnel to links to other sites. In addition, the physicians periodically must review it to ensure that all medical information is up to date and accurate. Old, outdated information about the office can put off potential patients. Outdated medical information may be harmful to patients who rely on it.
Any professional website should include disclaimers informing users that the site is not intended to establish a professional relationship or to give professional advice. The nature and extent of the disclaimer will depend on the type of information on the site. An example of a particularly thorough disclaimer is the Mayo Clinic disclaimer and terms of use (http://www.mayoclinic.org/about-this-site/terms-conditions-use-policy).
General professionalism
At the end of the day, social media are an outreach from a medical practice and from the profession to the public.20 Failure to treat these platforms with appropriate professional standards may result in professional discipline, damages, or civil penalties. Almost all of the reviews of social media use in health care practice note that the risks of inappropriate use are not only to the individual physician but also to the general medical profession, which may be undermined. Consider posting policies of the relevent state medical boards, the AMA, and ACOG in your office after you have had a discussion with your staff about them.21
The AMA statement includes a provision that a physician seeing unprofessional social media conduct by a colleague has the responsibility to bring that to the attention of the colleague. If the colleague does not correct a significant problem, “the physician should report the matter to appropriate authorities.”9
Bottom line
Any practitioner considering the use of social media must view it as a major step that requires caution, expert assistance, and constant attention to potential privacy, quality, and professionalism issues. If you are considering it, ensure that all staff associated with the practice understand and agree to the established limits on social media use.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Modahl M, Tompsett L, Moorhead T. Doctors, patients, & social media. Quantia MD website. http://www.quantiamd.com/q-qcp/DoctorsPatientSocialMedia.pdf. Published September 2011. Accessed February 18, 2016.
- Kuberacka A, Wengrojj J, Fabozzi N. Social media use in U.S. healthcare provider institutions: Insights from Frost & Sullivan and iHT2 survey. Frost and Sullivan website. http://ihealthtran.com/pdf/frostiht2survey.pdf. Published August 30, 2011. Accessed February 18, 2016.
- O’Connor ME. How do tech savvy physicians use health technology and social media? Health Care Social Media website. http://hcsmmonitor.com/2014/01/08/how-do-tech-savvy-physicians-use-health-technology-and-social-media/. Published January 8, 2014. Accessed February 18, 2016.
- American Medical Association (AMA) Insurance. 2014 work/life profiles of today’s U.S. physician. AMA Insurance website. https://www.amainsure.com/work-life-profiles-of-todays-us-physician.html. Published April 2014. Accessed February 18, 2016.
- National Research Corporation. 2013 National Market Insights Survey: Health care social media website. https://healthcaresocialmedia.files.wordpress.com/2014/04/nrc-infographiclong.jpg. Accessed February 18, 2016.
- Suby C. Social media in health care: benefits, concerns and guidelines for use. Creat Nurs. 2013;19(3):140–147.
- Conaboy C. For doctors, social media a tricky case. Boston Globe. http://www.boston.com/lifestyle/health/articles/2011/04/20/for_doctors_social_media_a_tricky_case/?page=full. Published April 20, 2011. Accessed February 18, 2016.
- Matyszczyk C. Outcry as ob-gyn uses Facebook to complain about patient. CNET. http://www.cnet.com/news/outcry-as-ob-gyn-uses-facebook-to-complain-about-patient/Minion Pro. Published February 9, 2013. Accessed February 18, 2016.
- American Medical Association (AMA). Opinion 9.124: Professionalism in the use of social media. AMA website. http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion9124.page? Published June 2011. Accessed February 18, 2016.
- American College of Obstetricians and Gynecologists (ACOG) Committee on Professional Liability. ACOG Committee Opinion No. 622: professional use of digital and social media. Obstet Gynecol. 2015;125(2):516-520.
- Farnan JM, Sulmasy LS, Worster BK, et al. Online medical professionalism: patient and public relationships: Policy Statement From the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620–627.
- Hader A, Drown E. Patient privacy and social media. AANA J. 2010;78(4):270–274.
- Kavoussi SC, Huang JJ, Tsai JC, Kempton JE. HIPAA for physicians in the information age. Conn Med. 2014;78(7):425–427.
- U.S. Department of Health & Human Services (HHS). Health information privacy: Covered entities and business associates. HHS website. http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/. Published March 14, 2012. Accessed February 18, 2016.
- Perna G. Breach report: lost flash drive at Kaiser Permanente affects 49,000 patients. Healthcare Informatics website. http://www.healthcare-informatics.com/news-item/breach-report-lost-flash-drive-kaiser-permanente-affects-49000-patients. Published December 11, 2013. Accessed February 18, 2016.
- McBride M. How to ensure your social media efforts are HIPAA-compliant. Med Econ. 2012;89:70–74.
- Von Muhlen M, Ohno-Machado L. Reviewing social media use by clinicians. J Am Med Inform Assoc. 2012;19(5):777–781.
- Omurtag K, Turek P. Incorporating social media into practice: a blueprint for reproductive health providers. Clin Obstet Gynecol. 2013;56(3):463–470.
- Radmanesh A, Duszak R, Fitzgerald R. Social media and public outreach: a physician primer. Am J Neuroradiol. 2015;36(7):1223–1224.
- Grajales FJ 3rd, Sheps S, Ho K, Novak-Lauscher H, Eysenbach G. Social media: a review and tutorial of applications in medicine and health care. J Med Internet Res. 2014;16(2):e13.
- ACOG Today. Social media guide: how to comment with patients and spread women’s health messages. American Congress of Obstetricians and Gynecologists website. http://www.acog.org/-/media/ACOG-Today/acogToday201211.pdf. Published November 2012. Accessed February 18, 2016.
CASE: Patient discloses personal information in electronic communication. How to respond and what’s at stake?
Your nurse comes to you with a dilemma. Last Friday she received an email from a patient, sent to the nurse’s personal email account (G-mail) that conveyed information regarding the patient’s recent treatment for a herpetic vulvar lesion. The text details presumed exposure, date and time, number of sexual partners, concernfor “spread of disease,” and the patient’s desire to have a comprehensive sexually transmitted infection screening as soon as possible.
Your nurse has years of professional experience, but she is perhaps not the most savvy with regard to current information technology and social media. Nonetheless, she knows it is best not to immediately respond to the patient’s email without checking with you. She tracks you down on Monday morning to review the email and the dilemma she feels she has been placed in. What’s the best next step?
While discussing the general question with the staff, another nurse notes that there have been some reviews of the office on social media. It seems that this second nurse tweets and texts with patients all the time. The office manager strongly suggests that the office “join the 21st Century” by setting up a Facebook page and using their webpage to attract new patients and communicate with current patients.
How do you prepare for this? Is your staff knowledgeable about the dos and don’ts of social media?
The use of social media by health care providers has been growing for several years. Back in 2011 a large survey by QuantiaMD revealed that 87% of physicians used social media for personal reasons, and 67% of them used it professionally.1 How they used it for professional purposes also was explored in 2011, with almost 3 of 4 physicians using it for social networking and more than half engaging with their own institution’s social media (FIGURE).2 In 2013, 53% of physicians indicated that their practice had a Facebook platform, 28% had a presence on LinkedIn, and 21% were on Twitter.3 Not surprisingly, social media use is higher among younger physicians4; the 2016 equivalents to these percentages most likely are higher.
| Health providers’ use of social media for professional reasons2 |
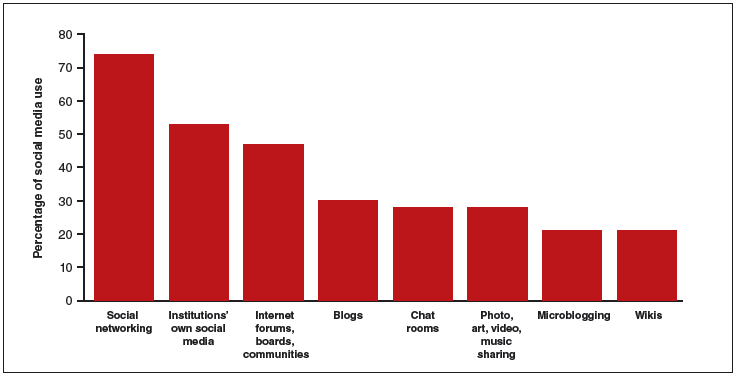
|
In 2011, a survey found that most health providers used social networking, their institutions’ own social media, and Internet forums, boards, and communities for professional reasons. |
Patients’ outreach through social media regarding health care information continues to grow, with 33.8% asking for health advice using social media.5 While email and other social media open the possibility of improved communication with patients, they also present a number of important professional and legal issues that deserve special consideration.6 Each medium presents its own challenges, but there are 4 categories of concern related to basic values and rights that we consider important to review:
- confidentiality
- dual relationships and conflicts of interest
- quality of care and advice
- general professionalism (including advertising).
Confidentiality
Few values of the medical profession are of longer standing than the commitment to maintain patient privacy. Fifth Century BC obligations continue to apply to the technology of the 21st Century AD. And the challenges are significant.
Email is not secure
In the opening case, the choice to email her clinician was apparently the patient’s. She probably does not realize that email is not very confidential, although it is undoubtedly in the Terms of Service Agreement she clicked through. Her email was likely scanned by her email service provider—Google, in this case—as well as the nurse. If, however, the physician’s office responds by email, it may well compound the confidentiality problem by further distributing the information through yet another email provider.
If, as a physician, you encourage email communication by your patients, a smart approach is to emphasize that such communications are not very confidential. At a minimum, until a secure email system can be established, it is best not to transmit medical information via email and to inform patients of the risk of such communication. In the case above, the nurse who received the email should respond to the patient by telephone (much more secure). Or she can respond to the patient by email (not including the patient’s message in the return), writing that, because email communications are inherently not confidential, she suggests a phone call or personal visit.
This case also notes that the patient sent the email to the nurse’s personal account, not to an office email account. Sending medical emails to an employee’s personal account raises additional problems of confidentiality and appropriate controls. It should be made clear that employees should not be discussing private medical matters via their own email accounts.
Other forms of social media are also not secure
Similar concerns arise about texting and using Twitter by the second nurse. These activities apparently had been unknown to the physician, but the practice still may be responsible for her actions. These are insecure forms of communication and raise serious ethical and legal concerns.
Other social media pose confidentiality risks as well. For example, a physician was dismissed from a position and reprimanded by the medical board for posting patient information on Facebook,7 and an ObGyn caused problems by posting a nasty note about a patient who showed up late for an appointment.8 Too many patients may not understand that posting on social media is the equivalent of standing on a street corner yelling private information. Social media sites that invite the discussion of personal matters are an invitation to trouble.
Physicians are ethically obliged to protect confidentiality
Professional standards place significant ethical obligations on physicians to protect patient confidentiality. The American Medical Association (AMA) has an ethics opinion on professionalism with social media,9 as does the American College of Obstetricians and Gynecologists (ACOG).10 Another excellent discussion of ethical and practical issues is a joint position paper by the American College of Physicians and the Federation of State Medical Boards.11 Both documents focus attention on issues of confidentiality.
Physicians are legally obliged to protect confidentiality
There are many legal protections for confidentiality that can be implicated by electronic communications and social media. All states provide protection for unwarranted disclosure of private patient information. Such disclosures made electronically are included.12 Indeed, because electronic disclosures may be broadcast more widely, they may be especially dangerous. The misuse of social media may result in license discipline by the state board, regulatory sanctions, or civil liability (rare, but criminal sanctions are a possibility in extreme circumstances).
In addition to state laws regarding confidentiality, there are a number of federal laws that cover confidential medical information. None is more important than the Health Insurance Portability and Accountability Act (HIPAA) and the more recent HITECH amendments (Health Information Technology for Economic and Clinical Health).13 These laws have both privacy provisions and security (including “encryption”) requirements. These are complicated laws but at their core are the notions that health care providers and some others:
- are responsible for maintaining the security and privacy of health information
- may not transmit (even unintentionally) such information to others without patient permission or legal authority.14
- may not transmit (even unintentionally) such information to others without patient permission or legal authority.
A good source of step-by-step information about these laws is “Health information privacy: Covered entities and business associates,” on the US Health and Human Services website.14
HITECH also provides for notice to patients when health information is inappropriately transmitted. Thus, a missing USB flash drive with patient information may require notification to thousands of patients.15 Any consideration of the use of email or social media in medical practice must take into account the HIPAA/HITECH obligations to protect the security of patient health information. There can be serious professional consequences for failing to follow the HIPAA requirements.16
Dual relationships and conflicts of interest
In our hypothetical case, the office manager’s suggestion that the office use Facebook and their website to attract new patients also may raise confidentiality problems. The Facebook suggestion especially needs to be considered carefully. Facebook use is estimated to be 63% to 96% among students and 13% to 47% among health care professionals.17 Facebook is most often seen as an interactive social site; it risks blurring the lines between personal and professional relationships.9 There is a consensus that a physician should not “friend” patients on Facebook. The AMA ethics opinion notes that “physicians must maintain appropriate boundaries of the patient-physician relationship in accordance with professional ethical guidelines, just as they would in any other context.”9
Separate personal and professional contacts
Difficulties with interactive social media are not limited to the physicians in a practice. The problems increase with the number of staff members who post or respond on social media. Control of social media is essential. The practice must ensure that staff members do not slip into inappropriate personal comments and relationships. Staff should understand (and be reminded of) the necessity of separating personal and professional contacts.
Avoid misunderstandings
In addition, whatever the intent of the physician and staff may be, it is essentially impossible to know how patients will interpret interactions on these social media. The very informal, off-the-cuff, chatty way in which Facebook and similar sites are used invites misunderstandings, and maintaining professional boundaries is necessary.
Ground rules
All of this is not to say that professionals should never use Facebook or similar sites. Rather, if used, ground rules need to be established.
Social media communications must:
- be professional and not related to personal matters
- not be used to give medical advice
- be controlled by high level staff
- be reviewed periodically.
Staff training
Particularly for interactive social media (email, texts, Twitter, Facebook, etc), it is essential that there be both clear policies and good staff training (TABLE).9–11,18 There really should be no “making it up as we go along.” Staff on a social media lark of their own can be disastrous for the practice. Policies need to be updated frequently, and staff training reinforced and repeated periodically.
Quality of care and advice
Start with your website
Institutions’ websites are major sources of health care information: Nearly 32% of US adults would be very likely to prefer a hospital based on its website.5 Your website can be an important face of your practice to the community—for good or for bad. On one hand, the practice can control what is on a website and, unlike some social media, it will not be directed to individual patients. Done well, it “provides golden opportunities for marketing physician services, as well as for contributing to public health by providing high-quality online content that is both accurate and understandable to laypeople.”19 Done badly, it can convey incorrect and harmful information and discredit the medical practice that established it.
Your website introduces the practice and settings, but it will serve another purpose to thousands of people who likely will see it over time as a source of credible health information. The importance of ensuring that your website is carefully constructed to provide, or link to, good medical advice that contributes to quality of care cannot be overstated.
A good website begins with a clear statement of the reasons and goals for having the site. Professional design assistance generally is used to create the site, but that design process needs to be overseen by a medical professional to ensure that it conveys the sense of the practice and provides completely accurate information. A homepage of dancing clowns with stethoscopes may seem good to a 20-something-year-old designer, but it is not appropriate for a physician. It will be the practice, not the designer, who is held accountable for the site content. Links to other sites need to be vetted and used with care. Patients and other members of the public may well take the links as carrying the endorsement of the practice and its physicians.
Perhaps the greatest risk of a website is that it will not be kept current. Unfortunately, they do not update themselves. Some knowledgeable staff member must frequently review it to update everything from office hours and personnel to links to other sites. In addition, the physicians periodically must review it to ensure that all medical information is up to date and accurate. Old, outdated information about the office can put off potential patients. Outdated medical information may be harmful to patients who rely on it.
Any professional website should include disclaimers informing users that the site is not intended to establish a professional relationship or to give professional advice. The nature and extent of the disclaimer will depend on the type of information on the site. An example of a particularly thorough disclaimer is the Mayo Clinic disclaimer and terms of use (http://www.mayoclinic.org/about-this-site/terms-conditions-use-policy).
General professionalism
At the end of the day, social media are an outreach from a medical practice and from the profession to the public.20 Failure to treat these platforms with appropriate professional standards may result in professional discipline, damages, or civil penalties. Almost all of the reviews of social media use in health care practice note that the risks of inappropriate use are not only to the individual physician but also to the general medical profession, which may be undermined. Consider posting policies of the relevent state medical boards, the AMA, and ACOG in your office after you have had a discussion with your staff about them.21
The AMA statement includes a provision that a physician seeing unprofessional social media conduct by a colleague has the responsibility to bring that to the attention of the colleague. If the colleague does not correct a significant problem, “the physician should report the matter to appropriate authorities.”9
Bottom line
Any practitioner considering the use of social media must view it as a major step that requires caution, expert assistance, and constant attention to potential privacy, quality, and professionalism issues. If you are considering it, ensure that all staff associated with the practice understand and agree to the established limits on social media use.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: Patient discloses personal information in electronic communication. How to respond and what’s at stake?
Your nurse comes to you with a dilemma. Last Friday she received an email from a patient, sent to the nurse’s personal email account (G-mail) that conveyed information regarding the patient’s recent treatment for a herpetic vulvar lesion. The text details presumed exposure, date and time, number of sexual partners, concernfor “spread of disease,” and the patient’s desire to have a comprehensive sexually transmitted infection screening as soon as possible.
Your nurse has years of professional experience, but she is perhaps not the most savvy with regard to current information technology and social media. Nonetheless, she knows it is best not to immediately respond to the patient’s email without checking with you. She tracks you down on Monday morning to review the email and the dilemma she feels she has been placed in. What’s the best next step?
While discussing the general question with the staff, another nurse notes that there have been some reviews of the office on social media. It seems that this second nurse tweets and texts with patients all the time. The office manager strongly suggests that the office “join the 21st Century” by setting up a Facebook page and using their webpage to attract new patients and communicate with current patients.
How do you prepare for this? Is your staff knowledgeable about the dos and don’ts of social media?
The use of social media by health care providers has been growing for several years. Back in 2011 a large survey by QuantiaMD revealed that 87% of physicians used social media for personal reasons, and 67% of them used it professionally.1 How they used it for professional purposes also was explored in 2011, with almost 3 of 4 physicians using it for social networking and more than half engaging with their own institution’s social media (FIGURE).2 In 2013, 53% of physicians indicated that their practice had a Facebook platform, 28% had a presence on LinkedIn, and 21% were on Twitter.3 Not surprisingly, social media use is higher among younger physicians4; the 2016 equivalents to these percentages most likely are higher.
| Health providers’ use of social media for professional reasons2 |
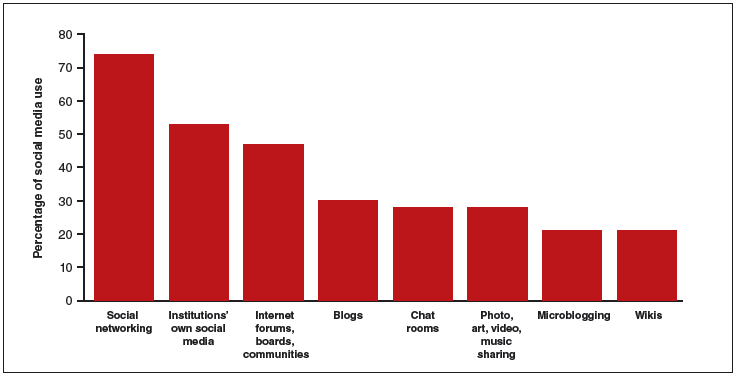
|
In 2011, a survey found that most health providers used social networking, their institutions’ own social media, and Internet forums, boards, and communities for professional reasons. |
Patients’ outreach through social media regarding health care information continues to grow, with 33.8% asking for health advice using social media.5 While email and other social media open the possibility of improved communication with patients, they also present a number of important professional and legal issues that deserve special consideration.6 Each medium presents its own challenges, but there are 4 categories of concern related to basic values and rights that we consider important to review:
- confidentiality
- dual relationships and conflicts of interest
- quality of care and advice
- general professionalism (including advertising).
Confidentiality
Few values of the medical profession are of longer standing than the commitment to maintain patient privacy. Fifth Century BC obligations continue to apply to the technology of the 21st Century AD. And the challenges are significant.
Email is not secure
In the opening case, the choice to email her clinician was apparently the patient’s. She probably does not realize that email is not very confidential, although it is undoubtedly in the Terms of Service Agreement she clicked through. Her email was likely scanned by her email service provider—Google, in this case—as well as the nurse. If, however, the physician’s office responds by email, it may well compound the confidentiality problem by further distributing the information through yet another email provider.
If, as a physician, you encourage email communication by your patients, a smart approach is to emphasize that such communications are not very confidential. At a minimum, until a secure email system can be established, it is best not to transmit medical information via email and to inform patients of the risk of such communication. In the case above, the nurse who received the email should respond to the patient by telephone (much more secure). Or she can respond to the patient by email (not including the patient’s message in the return), writing that, because email communications are inherently not confidential, she suggests a phone call or personal visit.
This case also notes that the patient sent the email to the nurse’s personal account, not to an office email account. Sending medical emails to an employee’s personal account raises additional problems of confidentiality and appropriate controls. It should be made clear that employees should not be discussing private medical matters via their own email accounts.
Other forms of social media are also not secure
Similar concerns arise about texting and using Twitter by the second nurse. These activities apparently had been unknown to the physician, but the practice still may be responsible for her actions. These are insecure forms of communication and raise serious ethical and legal concerns.
Other social media pose confidentiality risks as well. For example, a physician was dismissed from a position and reprimanded by the medical board for posting patient information on Facebook,7 and an ObGyn caused problems by posting a nasty note about a patient who showed up late for an appointment.8 Too many patients may not understand that posting on social media is the equivalent of standing on a street corner yelling private information. Social media sites that invite the discussion of personal matters are an invitation to trouble.
Physicians are ethically obliged to protect confidentiality
Professional standards place significant ethical obligations on physicians to protect patient confidentiality. The American Medical Association (AMA) has an ethics opinion on professionalism with social media,9 as does the American College of Obstetricians and Gynecologists (ACOG).10 Another excellent discussion of ethical and practical issues is a joint position paper by the American College of Physicians and the Federation of State Medical Boards.11 Both documents focus attention on issues of confidentiality.
Physicians are legally obliged to protect confidentiality
There are many legal protections for confidentiality that can be implicated by electronic communications and social media. All states provide protection for unwarranted disclosure of private patient information. Such disclosures made electronically are included.12 Indeed, because electronic disclosures may be broadcast more widely, they may be especially dangerous. The misuse of social media may result in license discipline by the state board, regulatory sanctions, or civil liability (rare, but criminal sanctions are a possibility in extreme circumstances).
In addition to state laws regarding confidentiality, there are a number of federal laws that cover confidential medical information. None is more important than the Health Insurance Portability and Accountability Act (HIPAA) and the more recent HITECH amendments (Health Information Technology for Economic and Clinical Health).13 These laws have both privacy provisions and security (including “encryption”) requirements. These are complicated laws but at their core are the notions that health care providers and some others:
- are responsible for maintaining the security and privacy of health information
- may not transmit (even unintentionally) such information to others without patient permission or legal authority.14
- may not transmit (even unintentionally) such information to others without patient permission or legal authority.
A good source of step-by-step information about these laws is “Health information privacy: Covered entities and business associates,” on the US Health and Human Services website.14
HITECH also provides for notice to patients when health information is inappropriately transmitted. Thus, a missing USB flash drive with patient information may require notification to thousands of patients.15 Any consideration of the use of email or social media in medical practice must take into account the HIPAA/HITECH obligations to protect the security of patient health information. There can be serious professional consequences for failing to follow the HIPAA requirements.16
Dual relationships and conflicts of interest
In our hypothetical case, the office manager’s suggestion that the office use Facebook and their website to attract new patients also may raise confidentiality problems. The Facebook suggestion especially needs to be considered carefully. Facebook use is estimated to be 63% to 96% among students and 13% to 47% among health care professionals.17 Facebook is most often seen as an interactive social site; it risks blurring the lines between personal and professional relationships.9 There is a consensus that a physician should not “friend” patients on Facebook. The AMA ethics opinion notes that “physicians must maintain appropriate boundaries of the patient-physician relationship in accordance with professional ethical guidelines, just as they would in any other context.”9
Separate personal and professional contacts
Difficulties with interactive social media are not limited to the physicians in a practice. The problems increase with the number of staff members who post or respond on social media. Control of social media is essential. The practice must ensure that staff members do not slip into inappropriate personal comments and relationships. Staff should understand (and be reminded of) the necessity of separating personal and professional contacts.
Avoid misunderstandings
In addition, whatever the intent of the physician and staff may be, it is essentially impossible to know how patients will interpret interactions on these social media. The very informal, off-the-cuff, chatty way in which Facebook and similar sites are used invites misunderstandings, and maintaining professional boundaries is necessary.
Ground rules
All of this is not to say that professionals should never use Facebook or similar sites. Rather, if used, ground rules need to be established.
Social media communications must:
- be professional and not related to personal matters
- not be used to give medical advice
- be controlled by high level staff
- be reviewed periodically.
Staff training
Particularly for interactive social media (email, texts, Twitter, Facebook, etc), it is essential that there be both clear policies and good staff training (TABLE).9–11,18 There really should be no “making it up as we go along.” Staff on a social media lark of their own can be disastrous for the practice. Policies need to be updated frequently, and staff training reinforced and repeated periodically.
Quality of care and advice
Start with your website
Institutions’ websites are major sources of health care information: Nearly 32% of US adults would be very likely to prefer a hospital based on its website.5 Your website can be an important face of your practice to the community—for good or for bad. On one hand, the practice can control what is on a website and, unlike some social media, it will not be directed to individual patients. Done well, it “provides golden opportunities for marketing physician services, as well as for contributing to public health by providing high-quality online content that is both accurate and understandable to laypeople.”19 Done badly, it can convey incorrect and harmful information and discredit the medical practice that established it.
Your website introduces the practice and settings, but it will serve another purpose to thousands of people who likely will see it over time as a source of credible health information. The importance of ensuring that your website is carefully constructed to provide, or link to, good medical advice that contributes to quality of care cannot be overstated.
A good website begins with a clear statement of the reasons and goals for having the site. Professional design assistance generally is used to create the site, but that design process needs to be overseen by a medical professional to ensure that it conveys the sense of the practice and provides completely accurate information. A homepage of dancing clowns with stethoscopes may seem good to a 20-something-year-old designer, but it is not appropriate for a physician. It will be the practice, not the designer, who is held accountable for the site content. Links to other sites need to be vetted and used with care. Patients and other members of the public may well take the links as carrying the endorsement of the practice and its physicians.
Perhaps the greatest risk of a website is that it will not be kept current. Unfortunately, they do not update themselves. Some knowledgeable staff member must frequently review it to update everything from office hours and personnel to links to other sites. In addition, the physicians periodically must review it to ensure that all medical information is up to date and accurate. Old, outdated information about the office can put off potential patients. Outdated medical information may be harmful to patients who rely on it.
Any professional website should include disclaimers informing users that the site is not intended to establish a professional relationship or to give professional advice. The nature and extent of the disclaimer will depend on the type of information on the site. An example of a particularly thorough disclaimer is the Mayo Clinic disclaimer and terms of use (http://www.mayoclinic.org/about-this-site/terms-conditions-use-policy).
General professionalism
At the end of the day, social media are an outreach from a medical practice and from the profession to the public.20 Failure to treat these platforms with appropriate professional standards may result in professional discipline, damages, or civil penalties. Almost all of the reviews of social media use in health care practice note that the risks of inappropriate use are not only to the individual physician but also to the general medical profession, which may be undermined. Consider posting policies of the relevent state medical boards, the AMA, and ACOG in your office after you have had a discussion with your staff about them.21
The AMA statement includes a provision that a physician seeing unprofessional social media conduct by a colleague has the responsibility to bring that to the attention of the colleague. If the colleague does not correct a significant problem, “the physician should report the matter to appropriate authorities.”9
Bottom line
Any practitioner considering the use of social media must view it as a major step that requires caution, expert assistance, and constant attention to potential privacy, quality, and professionalism issues. If you are considering it, ensure that all staff associated with the practice understand and agree to the established limits on social media use.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Modahl M, Tompsett L, Moorhead T. Doctors, patients, & social media. Quantia MD website. http://www.quantiamd.com/q-qcp/DoctorsPatientSocialMedia.pdf. Published September 2011. Accessed February 18, 2016.
- Kuberacka A, Wengrojj J, Fabozzi N. Social media use in U.S. healthcare provider institutions: Insights from Frost & Sullivan and iHT2 survey. Frost and Sullivan website. http://ihealthtran.com/pdf/frostiht2survey.pdf. Published August 30, 2011. Accessed February 18, 2016.
- O’Connor ME. How do tech savvy physicians use health technology and social media? Health Care Social Media website. http://hcsmmonitor.com/2014/01/08/how-do-tech-savvy-physicians-use-health-technology-and-social-media/. Published January 8, 2014. Accessed February 18, 2016.
- American Medical Association (AMA) Insurance. 2014 work/life profiles of today’s U.S. physician. AMA Insurance website. https://www.amainsure.com/work-life-profiles-of-todays-us-physician.html. Published April 2014. Accessed February 18, 2016.
- National Research Corporation. 2013 National Market Insights Survey: Health care social media website. https://healthcaresocialmedia.files.wordpress.com/2014/04/nrc-infographiclong.jpg. Accessed February 18, 2016.
- Suby C. Social media in health care: benefits, concerns and guidelines for use. Creat Nurs. 2013;19(3):140–147.
- Conaboy C. For doctors, social media a tricky case. Boston Globe. http://www.boston.com/lifestyle/health/articles/2011/04/20/for_doctors_social_media_a_tricky_case/?page=full. Published April 20, 2011. Accessed February 18, 2016.
- Matyszczyk C. Outcry as ob-gyn uses Facebook to complain about patient. CNET. http://www.cnet.com/news/outcry-as-ob-gyn-uses-facebook-to-complain-about-patient/Minion Pro. Published February 9, 2013. Accessed February 18, 2016.
- American Medical Association (AMA). Opinion 9.124: Professionalism in the use of social media. AMA website. http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion9124.page? Published June 2011. Accessed February 18, 2016.
- American College of Obstetricians and Gynecologists (ACOG) Committee on Professional Liability. ACOG Committee Opinion No. 622: professional use of digital and social media. Obstet Gynecol. 2015;125(2):516-520.
- Farnan JM, Sulmasy LS, Worster BK, et al. Online medical professionalism: patient and public relationships: Policy Statement From the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620–627.
- Hader A, Drown E. Patient privacy and social media. AANA J. 2010;78(4):270–274.
- Kavoussi SC, Huang JJ, Tsai JC, Kempton JE. HIPAA for physicians in the information age. Conn Med. 2014;78(7):425–427.
- U.S. Department of Health & Human Services (HHS). Health information privacy: Covered entities and business associates. HHS website. http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/. Published March 14, 2012. Accessed February 18, 2016.
- Perna G. Breach report: lost flash drive at Kaiser Permanente affects 49,000 patients. Healthcare Informatics website. http://www.healthcare-informatics.com/news-item/breach-report-lost-flash-drive-kaiser-permanente-affects-49000-patients. Published December 11, 2013. Accessed February 18, 2016.
- McBride M. How to ensure your social media efforts are HIPAA-compliant. Med Econ. 2012;89:70–74.
- Von Muhlen M, Ohno-Machado L. Reviewing social media use by clinicians. J Am Med Inform Assoc. 2012;19(5):777–781.
- Omurtag K, Turek P. Incorporating social media into practice: a blueprint for reproductive health providers. Clin Obstet Gynecol. 2013;56(3):463–470.
- Radmanesh A, Duszak R, Fitzgerald R. Social media and public outreach: a physician primer. Am J Neuroradiol. 2015;36(7):1223–1224.
- Grajales FJ 3rd, Sheps S, Ho K, Novak-Lauscher H, Eysenbach G. Social media: a review and tutorial of applications in medicine and health care. J Med Internet Res. 2014;16(2):e13.
- ACOG Today. Social media guide: how to comment with patients and spread women’s health messages. American Congress of Obstetricians and Gynecologists website. http://www.acog.org/-/media/ACOG-Today/acogToday201211.pdf. Published November 2012. Accessed February 18, 2016.
- Modahl M, Tompsett L, Moorhead T. Doctors, patients, & social media. Quantia MD website. http://www.quantiamd.com/q-qcp/DoctorsPatientSocialMedia.pdf. Published September 2011. Accessed February 18, 2016.
- Kuberacka A, Wengrojj J, Fabozzi N. Social media use in U.S. healthcare provider institutions: Insights from Frost & Sullivan and iHT2 survey. Frost and Sullivan website. http://ihealthtran.com/pdf/frostiht2survey.pdf. Published August 30, 2011. Accessed February 18, 2016.
- O’Connor ME. How do tech savvy physicians use health technology and social media? Health Care Social Media website. http://hcsmmonitor.com/2014/01/08/how-do-tech-savvy-physicians-use-health-technology-and-social-media/. Published January 8, 2014. Accessed February 18, 2016.
- American Medical Association (AMA) Insurance. 2014 work/life profiles of today’s U.S. physician. AMA Insurance website. https://www.amainsure.com/work-life-profiles-of-todays-us-physician.html. Published April 2014. Accessed February 18, 2016.
- National Research Corporation. 2013 National Market Insights Survey: Health care social media website. https://healthcaresocialmedia.files.wordpress.com/2014/04/nrc-infographiclong.jpg. Accessed February 18, 2016.
- Suby C. Social media in health care: benefits, concerns and guidelines for use. Creat Nurs. 2013;19(3):140–147.
- Conaboy C. For doctors, social media a tricky case. Boston Globe. http://www.boston.com/lifestyle/health/articles/2011/04/20/for_doctors_social_media_a_tricky_case/?page=full. Published April 20, 2011. Accessed February 18, 2016.
- Matyszczyk C. Outcry as ob-gyn uses Facebook to complain about patient. CNET. http://www.cnet.com/news/outcry-as-ob-gyn-uses-facebook-to-complain-about-patient/Minion Pro. Published February 9, 2013. Accessed February 18, 2016.
- American Medical Association (AMA). Opinion 9.124: Professionalism in the use of social media. AMA website. http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion9124.page? Published June 2011. Accessed February 18, 2016.
- American College of Obstetricians and Gynecologists (ACOG) Committee on Professional Liability. ACOG Committee Opinion No. 622: professional use of digital and social media. Obstet Gynecol. 2015;125(2):516-520.
- Farnan JM, Sulmasy LS, Worster BK, et al. Online medical professionalism: patient and public relationships: Policy Statement From the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620–627.
- Hader A, Drown E. Patient privacy and social media. AANA J. 2010;78(4):270–274.
- Kavoussi SC, Huang JJ, Tsai JC, Kempton JE. HIPAA for physicians in the information age. Conn Med. 2014;78(7):425–427.
- U.S. Department of Health & Human Services (HHS). Health information privacy: Covered entities and business associates. HHS website. http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/. Published March 14, 2012. Accessed February 18, 2016.
- Perna G. Breach report: lost flash drive at Kaiser Permanente affects 49,000 patients. Healthcare Informatics website. http://www.healthcare-informatics.com/news-item/breach-report-lost-flash-drive-kaiser-permanente-affects-49000-patients. Published December 11, 2013. Accessed February 18, 2016.
- McBride M. How to ensure your social media efforts are HIPAA-compliant. Med Econ. 2012;89:70–74.
- Von Muhlen M, Ohno-Machado L. Reviewing social media use by clinicians. J Am Med Inform Assoc. 2012;19(5):777–781.
- Omurtag K, Turek P. Incorporating social media into practice: a blueprint for reproductive health providers. Clin Obstet Gynecol. 2013;56(3):463–470.
- Radmanesh A, Duszak R, Fitzgerald R. Social media and public outreach: a physician primer. Am J Neuroradiol. 2015;36(7):1223–1224.
- Grajales FJ 3rd, Sheps S, Ho K, Novak-Lauscher H, Eysenbach G. Social media: a review and tutorial of applications in medicine and health care. J Med Internet Res. 2014;16(2):e13.
- ACOG Today. Social media guide: how to comment with patients and spread women’s health messages. American Congress of Obstetricians and Gynecologists website. http://www.acog.org/-/media/ACOG-Today/acogToday201211.pdf. Published November 2012. Accessed February 18, 2016.
In this Article
- Health providers’ use of social media
- Protecting confidentiality
- Creating a social media policy
Postpartum life-threatening strep infection
Postpartum life-threatening strep infection
A pregnant woman received prenatal care from a midwifery practice. A week before her scheduled delivery, the patient became ill with fever and vomiting and visited her midwife. While tests were still pending, the midwife decided to admit the mother to the hospital for induction of labor. The baby was born by vaginal delivery under the midwife’s care. The mother remained in the hospital for observation.
Two days after delivery, the mother began to have nausea, vomiting, and a low-grade fever. The nurse called the midwife, who ordered acetaminophen (Tylenol) but did not come to examine the patient. Two hours later, the nurse notified the midwife that the patient’s condition had worsened and that she was experiencing abdominal pain; the midwife ordered oxycodone. Over the next few hours, the midwife was apprised of the patient’s condition several times by telephone, but she never came to examine the patient nor did she ask her supervising ObGyn to examine the patient.
The next morning, a second midwife noted that the patient was experiencing an itchy rash on her extremities and abdomen. A complete blood count (CBC) showed a “critical lab value” of 44% band neutrophils (normal, 0% to 10% for the hospital laboratory). The second midwife and nurse told the supervising ObGyn that the patient otherwise looked well; he discharged the patient.
At home, the patient’s condition worsened. Her husband called the ObGyn several times and took her to the emergency department (ED) that evening. Her condition deteriorated and she was transferred to another facility where she was diagnosed with a life-threatening Group A Streptococcus (GAS) infection. After weeks of treatment for sepsis, the patient’s foot was amputated.
Patient's claim: The first midwife was negligent in her postpartum treatment of the patient; she should have come to the hospital to examine the patient or have requested that the supervising ObGyn examine the patient. The rash and CBC test results should have initiated further treatment and investigation; the patient should not have been discharged. GAS was not found or treated in a timely manner, resulting in sepsis and amputation.
Defendants' defense: The case was settled during the trial.
Verdict: A $2,500,000 Massachusetts settlement was reached with the midwife, her practice, and the ObGyn.
Failure to follow-up on abnormal Pap
A woman in her 50s reported abnormal bleeding to her gynecologist. Results of an endometrial biopsy were negative for cancer; the gynecologist prescribed hormone therapy. The patient continued to bleed until she entered menopause.
Ten years later, the bleeding returned. Results of a Pap test indicated atypical endometrial cells; an ultrasound showed a markedly abnormal endometrium. The gynecologist recommended a hysteroscopic dilation and curettage (D&C). When he attempted the procedure it ended prematurely because he was unable to enter the patient’s endometrium. The patient’s discharge instructions indicated that she should call the physician for follow up. In a letter to the patient written a month later, the physician discussed the abnormal Pap test results and indicated that the patient had 2 options: another D&C under ultrasound guidance or hysterectomy. He also noted that he would contact the patient’s primary care physician (PCP) for input.
Two years later, the patient returned to the gynecologist because the bleeding, which had never stopped, had increased in intensity. Endometrial cancer was diagnosed.
Patient's claim: The gynecologist never followed up with the patient or her PCP after the incomplete D&C. There is no record that communication ever occurred between the gynecologist and PCP. Lack of follow-up and treatment resulted in progression of the cancer from stage 1 to stage 3C, with a 5-year survivability of 47% (stage 1 survivability is 83%).
Physician's defense: The gynecologist was surprised that no one had ever followed up with the patient. The patient was comparatively negligent for failing to seek medical care for the 2-year period.
Verdict: A $430,000 Minnesota settlement was reached at mediation.
LIVER DISEASE LED TO STILLBIRTH
A 37-year-old woman reported nausea, vomiting, headaches, heartburn, and upper abdominal pain to her ObGyn several times during her third trimester. She had been pregnant before and knew that this pregnancy “felt” different. She went to the ED 1 week before the birth of her child, but she was discharged. The child was stillborn.
Parent's claim: Neither the ObGyn who provided prenatal care nor the on-call ED ObGyn ordered laboratory testing, which would have revealed a rare disease: acute fatty liver of pregnancy. Action could have saved the life of her child.
The patient’s ObGyn disregarded the patient’s reported symptoms; no blood work or liver testing was done. The ObGyn should have recognized the symptoms of liver disease that presented during the third trimester. A diagnosis of liver disease would have initiated induction of labor.
The patient’s expert witness noted that the severity of the third trimester symptoms warranted follow-up testing; the patient should not have had all of those symptoms so late in pregnancy. Testing would have revealed that, by not functioning properly, the liver was creating a toxic environment for the fetus. Labor should have been induced at 36 weeks when the fetal heart testing was still normal.
The ED nurses contacted the on-call ObGyn by telephone to discuss the patient’s symptoms; the ObGyn did not come to the ED to examine the patient or order testing.
The patient suffered emotional distress as a result of the loss of her child.
Defendants' defense: The medical center and the on-call ObGyn settled prior to trial.
The ObGyn claimed that the patient’s symptoms were common for pregnancy and that the disease could not be diagnosed based on the presented symptoms. It was not a violation of the standard of care for the extremely rare liver disease to not be diagnosed. The defense’s expert claimed that the symptoms reported by the patient did not warrant follow-up blood work. There was no way to determine whether or not the fetus died as a result of the mother’s liver disease or nuchal cord involvement.
A placental pathologist noted that the placenta was injured by thrombosis; the fetus’ death was most likely idiopathic. He later acknowledged that thrombosis can be related to liver disease.
Verdict: Jurors were instructed to consider this a personal injury case for the mother due to an unborn fetus’ lacks standing for injury or death under California law. A $160,090 California verdict was returned against the ObGyn who provided prenatal care.
Postpartum life-threatening strep infection
A pregnant woman received prenatal care from a midwifery practice. A week before her scheduled delivery, the patient became ill with fever and vomiting and visited her midwife. While tests were still pending, the midwife decided to admit the mother to the hospital for induction of labor. The baby was born by vaginal delivery under the midwife’s care. The mother remained in the hospital for observation.
Two days after delivery, the mother began to have nausea, vomiting, and a low-grade fever. The nurse called the midwife, who ordered acetaminophen (Tylenol) but did not come to examine the patient. Two hours later, the nurse notified the midwife that the patient’s condition had worsened and that she was experiencing abdominal pain; the midwife ordered oxycodone. Over the next few hours, the midwife was apprised of the patient’s condition several times by telephone, but she never came to examine the patient nor did she ask her supervising ObGyn to examine the patient.
The next morning, a second midwife noted that the patient was experiencing an itchy rash on her extremities and abdomen. A complete blood count (CBC) showed a “critical lab value” of 44% band neutrophils (normal, 0% to 10% for the hospital laboratory). The second midwife and nurse told the supervising ObGyn that the patient otherwise looked well; he discharged the patient.
At home, the patient’s condition worsened. Her husband called the ObGyn several times and took her to the emergency department (ED) that evening. Her condition deteriorated and she was transferred to another facility where she was diagnosed with a life-threatening Group A Streptococcus (GAS) infection. After weeks of treatment for sepsis, the patient’s foot was amputated.
Patient's claim: The first midwife was negligent in her postpartum treatment of the patient; she should have come to the hospital to examine the patient or have requested that the supervising ObGyn examine the patient. The rash and CBC test results should have initiated further treatment and investigation; the patient should not have been discharged. GAS was not found or treated in a timely manner, resulting in sepsis and amputation.
Defendants' defense: The case was settled during the trial.
Verdict: A $2,500,000 Massachusetts settlement was reached with the midwife, her practice, and the ObGyn.
Failure to follow-up on abnormal Pap
A woman in her 50s reported abnormal bleeding to her gynecologist. Results of an endometrial biopsy were negative for cancer; the gynecologist prescribed hormone therapy. The patient continued to bleed until she entered menopause.
Ten years later, the bleeding returned. Results of a Pap test indicated atypical endometrial cells; an ultrasound showed a markedly abnormal endometrium. The gynecologist recommended a hysteroscopic dilation and curettage (D&C). When he attempted the procedure it ended prematurely because he was unable to enter the patient’s endometrium. The patient’s discharge instructions indicated that she should call the physician for follow up. In a letter to the patient written a month later, the physician discussed the abnormal Pap test results and indicated that the patient had 2 options: another D&C under ultrasound guidance or hysterectomy. He also noted that he would contact the patient’s primary care physician (PCP) for input.
Two years later, the patient returned to the gynecologist because the bleeding, which had never stopped, had increased in intensity. Endometrial cancer was diagnosed.
Patient's claim: The gynecologist never followed up with the patient or her PCP after the incomplete D&C. There is no record that communication ever occurred between the gynecologist and PCP. Lack of follow-up and treatment resulted in progression of the cancer from stage 1 to stage 3C, with a 5-year survivability of 47% (stage 1 survivability is 83%).
Physician's defense: The gynecologist was surprised that no one had ever followed up with the patient. The patient was comparatively negligent for failing to seek medical care for the 2-year period.
Verdict: A $430,000 Minnesota settlement was reached at mediation.
LIVER DISEASE LED TO STILLBIRTH
A 37-year-old woman reported nausea, vomiting, headaches, heartburn, and upper abdominal pain to her ObGyn several times during her third trimester. She had been pregnant before and knew that this pregnancy “felt” different. She went to the ED 1 week before the birth of her child, but she was discharged. The child was stillborn.
Parent's claim: Neither the ObGyn who provided prenatal care nor the on-call ED ObGyn ordered laboratory testing, which would have revealed a rare disease: acute fatty liver of pregnancy. Action could have saved the life of her child.
The patient’s ObGyn disregarded the patient’s reported symptoms; no blood work or liver testing was done. The ObGyn should have recognized the symptoms of liver disease that presented during the third trimester. A diagnosis of liver disease would have initiated induction of labor.
The patient’s expert witness noted that the severity of the third trimester symptoms warranted follow-up testing; the patient should not have had all of those symptoms so late in pregnancy. Testing would have revealed that, by not functioning properly, the liver was creating a toxic environment for the fetus. Labor should have been induced at 36 weeks when the fetal heart testing was still normal.
The ED nurses contacted the on-call ObGyn by telephone to discuss the patient’s symptoms; the ObGyn did not come to the ED to examine the patient or order testing.
The patient suffered emotional distress as a result of the loss of her child.
Defendants' defense: The medical center and the on-call ObGyn settled prior to trial.
The ObGyn claimed that the patient’s symptoms were common for pregnancy and that the disease could not be diagnosed based on the presented symptoms. It was not a violation of the standard of care for the extremely rare liver disease to not be diagnosed. The defense’s expert claimed that the symptoms reported by the patient did not warrant follow-up blood work. There was no way to determine whether or not the fetus died as a result of the mother’s liver disease or nuchal cord involvement.
A placental pathologist noted that the placenta was injured by thrombosis; the fetus’ death was most likely idiopathic. He later acknowledged that thrombosis can be related to liver disease.
Verdict: Jurors were instructed to consider this a personal injury case for the mother due to an unborn fetus’ lacks standing for injury or death under California law. A $160,090 California verdict was returned against the ObGyn who provided prenatal care.
Postpartum life-threatening strep infection
A pregnant woman received prenatal care from a midwifery practice. A week before her scheduled delivery, the patient became ill with fever and vomiting and visited her midwife. While tests were still pending, the midwife decided to admit the mother to the hospital for induction of labor. The baby was born by vaginal delivery under the midwife’s care. The mother remained in the hospital for observation.
Two days after delivery, the mother began to have nausea, vomiting, and a low-grade fever. The nurse called the midwife, who ordered acetaminophen (Tylenol) but did not come to examine the patient. Two hours later, the nurse notified the midwife that the patient’s condition had worsened and that she was experiencing abdominal pain; the midwife ordered oxycodone. Over the next few hours, the midwife was apprised of the patient’s condition several times by telephone, but she never came to examine the patient nor did she ask her supervising ObGyn to examine the patient.
The next morning, a second midwife noted that the patient was experiencing an itchy rash on her extremities and abdomen. A complete blood count (CBC) showed a “critical lab value” of 44% band neutrophils (normal, 0% to 10% for the hospital laboratory). The second midwife and nurse told the supervising ObGyn that the patient otherwise looked well; he discharged the patient.
At home, the patient’s condition worsened. Her husband called the ObGyn several times and took her to the emergency department (ED) that evening. Her condition deteriorated and she was transferred to another facility where she was diagnosed with a life-threatening Group A Streptococcus (GAS) infection. After weeks of treatment for sepsis, the patient’s foot was amputated.
Patient's claim: The first midwife was negligent in her postpartum treatment of the patient; she should have come to the hospital to examine the patient or have requested that the supervising ObGyn examine the patient. The rash and CBC test results should have initiated further treatment and investigation; the patient should not have been discharged. GAS was not found or treated in a timely manner, resulting in sepsis and amputation.
Defendants' defense: The case was settled during the trial.
Verdict: A $2,500,000 Massachusetts settlement was reached with the midwife, her practice, and the ObGyn.
Failure to follow-up on abnormal Pap
A woman in her 50s reported abnormal bleeding to her gynecologist. Results of an endometrial biopsy were negative for cancer; the gynecologist prescribed hormone therapy. The patient continued to bleed until she entered menopause.
Ten years later, the bleeding returned. Results of a Pap test indicated atypical endometrial cells; an ultrasound showed a markedly abnormal endometrium. The gynecologist recommended a hysteroscopic dilation and curettage (D&C). When he attempted the procedure it ended prematurely because he was unable to enter the patient’s endometrium. The patient’s discharge instructions indicated that she should call the physician for follow up. In a letter to the patient written a month later, the physician discussed the abnormal Pap test results and indicated that the patient had 2 options: another D&C under ultrasound guidance or hysterectomy. He also noted that he would contact the patient’s primary care physician (PCP) for input.
Two years later, the patient returned to the gynecologist because the bleeding, which had never stopped, had increased in intensity. Endometrial cancer was diagnosed.
Patient's claim: The gynecologist never followed up with the patient or her PCP after the incomplete D&C. There is no record that communication ever occurred between the gynecologist and PCP. Lack of follow-up and treatment resulted in progression of the cancer from stage 1 to stage 3C, with a 5-year survivability of 47% (stage 1 survivability is 83%).
Physician's defense: The gynecologist was surprised that no one had ever followed up with the patient. The patient was comparatively negligent for failing to seek medical care for the 2-year period.
Verdict: A $430,000 Minnesota settlement was reached at mediation.
LIVER DISEASE LED TO STILLBIRTH
A 37-year-old woman reported nausea, vomiting, headaches, heartburn, and upper abdominal pain to her ObGyn several times during her third trimester. She had been pregnant before and knew that this pregnancy “felt” different. She went to the ED 1 week before the birth of her child, but she was discharged. The child was stillborn.
Parent's claim: Neither the ObGyn who provided prenatal care nor the on-call ED ObGyn ordered laboratory testing, which would have revealed a rare disease: acute fatty liver of pregnancy. Action could have saved the life of her child.
The patient’s ObGyn disregarded the patient’s reported symptoms; no blood work or liver testing was done. The ObGyn should have recognized the symptoms of liver disease that presented during the third trimester. A diagnosis of liver disease would have initiated induction of labor.
The patient’s expert witness noted that the severity of the third trimester symptoms warranted follow-up testing; the patient should not have had all of those symptoms so late in pregnancy. Testing would have revealed that, by not functioning properly, the liver was creating a toxic environment for the fetus. Labor should have been induced at 36 weeks when the fetal heart testing was still normal.
The ED nurses contacted the on-call ObGyn by telephone to discuss the patient’s symptoms; the ObGyn did not come to the ED to examine the patient or order testing.
The patient suffered emotional distress as a result of the loss of her child.
Defendants' defense: The medical center and the on-call ObGyn settled prior to trial.
The ObGyn claimed that the patient’s symptoms were common for pregnancy and that the disease could not be diagnosed based on the presented symptoms. It was not a violation of the standard of care for the extremely rare liver disease to not be diagnosed. The defense’s expert claimed that the symptoms reported by the patient did not warrant follow-up blood work. There was no way to determine whether or not the fetus died as a result of the mother’s liver disease or nuchal cord involvement.
A placental pathologist noted that the placenta was injured by thrombosis; the fetus’ death was most likely idiopathic. He later acknowledged that thrombosis can be related to liver disease.
Verdict: Jurors were instructed to consider this a personal injury case for the mother due to an unborn fetus’ lacks standing for injury or death under California law. A $160,090 California verdict was returned against the ObGyn who provided prenatal care.
Additional Medical Verdicts
• Failure to follow-up on abnormal Pap
• Liver disease led to stillbirth
Malpractice Counsel: Bicycle fall, hemodialysis complication
Fall
A 52-year-old man presented to the ED with complaints of left shoulder and left chest pain following a bicycle accident. The patient stated he had fallen from his bicycle and landed on his left side after he turned sharply to miss a speeding car. He denied head injury, loss of consciousness, or neck pain. The patient was ambulatory after the fall and had driven himself to the ED, and complained primarily of the left shoulder and left chest pain. He described the chest pain as sharp, worsening with movement and deep inspiration. The pain also was associated with mild shortness of breath. The patient denied headache, nausea, vomiting, abdominal pain, or back pain. He was otherwise in good health and on no medications.
The patient’s vital signs on presentation were normal and his head was atraumatic. He exhibited no midline posterior cervical tenderness to palpation. The head, eyes, ears, nose, and throat (HEENT) and mouth examinations were unremarkable. The patient did have tenderness to palpation over the left clavicle and left anterior chest; there was no crepitus or subcutaneous emphysema appreciated. Breath sounds were normal, and the heart had a regular rate and rhythm without murmurs, rubs, or gallops. The abdomen was soft and nontender, without guarding or rebound. The pelvis was stable, and the patient moved all four extremities with good strength. However, he did exhibit pain with movement of his left shoulder. Peripheral pulses were 2+ and symmetrical.
The emergency physician (EP) ordered an X-ray of the chest and left shoulder, as well as urinalysis. The X-rays revealed a small left pneumothorax, a minimally displaced left clavicular fracture, and fractures of the left fourth and fifth ribs. The urinalysis results were normal. The patient was administered intravenous (IV) morphine for pain and placed on 2 L/minute oxygen via nasal cannula, with 100% oxygen saturation on pulse oximetry.
The EP consulted a pulmonologist regarding management of the pneumothorax, who recommended a 4-hour observation period in the ED, followed by a repeat chest X-ray. During the observation period, the patient remained on oxygen and continued to deny any new complaints, including headache, dizziness, or abdominal pain. His vital signs remained normal throughout the entire observation period.
While in radiology services for a repeat chest X-ray, the patient fainted and struck his head on the floor. The EP immediately ordered a noncontrast computed tomography scan of the head, which demonstrated a large intracranial bleed. The patient was taken immediately to the operating room by neurosurgery. His recovery was uneventful, and he was discharged home without obvious sequelae.
The patient sued the EP and hospital for negligent care, claiming the EP underestimated the patient’s injuries and that additional testing was warranted. The defendants argued the patient was properly evaluated based on the history and physical examination. A defense verdict was returned.
Discussion
One possible criticism of this case is the consulting of a pulmonologist for the traumatic pneumothorax rather than a trauma surgeon or general surgeon. It is unclear if these specialists were not available for consult. Nevertheless, the pulmonologist’s advice to the EP was reasonable. Until just recently, it was dogma that all traumatic pneumothoraces required tube thoracostomy for management. This is still true for tension pneumothorax, hemothorax, moderate-to-large pneumothorax, symptomatic pneumothorax, or if mechanical ventilation is anticipated or needed.1 For small pneumothoraces, several management options exist, including close observation, needle or catheter aspiration, or placement of a pigtail catheter—in addition to the placement of a small (ie, 10-14 French) thoracostomy tube.2
Regardless, it does not appear the pneumothorax played a role in the patient’s hospital fall. More likely, the patient experienced a vasovagal episode. Interestingly, he never required treatment for the pneumothorax, despite requiring mechanical ventilation.
A Tragic Complication of Hemodialysis
A 58-year-old man presented to the ED with the chief complaint of bleeding from his dialysis fistula. The patient had end-stage renal disease and had been on hemodialysis (HD) for the past 3 years. He had an arteriovenous fistula (AVF) in his left arm for dialysis access, and received HD 3 days per week—every Tuesday, Thursday, and Saturday. He had completed a scheduled run of dialysis 5 hours prior to presentation, but had continued to bleed intermittently from the AVF site. The patient stated he had applied pressure multiple times to the site, but was unsuccessful in stopping the bleeding. His medical history was significant for hypertension and coronary artery disease. Regarding his social history, the patient admitted to smoking one pack of cigarettes per day and consuming alcohol on a regular basis.
The patient’s vital signs at presentation were: heart rate, 98 beats/minute; blood pressure, 146/85 mm Hg; respiratory rate, 20 breaths/minute; and temperature, 98.6°F. Oxygen saturation was 96% on room air. The HEENT examination was unremarkable. Examination of the heart revealed a normal rate and regular rhythm with a grade of 1/6 systolic murmur, heard best at the left sternal border. The breath sounds were equal bilaterally and clear to auscultation; the abdominal examination was unremarkable. The patient had an AVF in his left forearm that was not actively bleeding. There was a palpable thrill and a bruit present on auscultation over the site; there was no increased warmth or drainage.
The EP ordered a complete blood count (CBC) on the patient. The hemoglobin and hematocrit levels were essentially unchanged from a previous CBC 1 month prior, and the platelet count was normal. After approximately 1 hour of observation in the ED, there was no rebleeding at the site, and the patient was discharged home.
Unfortunately, the bleeding resumed the following day. The patient went into cardiac arrest and died at home prior to arrival of emergency medical services. The patient’s family sued the EP and hospital for discharging the patient home without first obtaining a surgical consult. The EP and hospital settled the case with the family for $2 million.
Discussion
Many patients who present to the ED with bleeding from the vascular access site can be managed simply with direct pressure, typically for a minimum of 5 to 10 minutes. In more severe cases, the EP can apply direct pressure with an absorbable gelatin sponge (eg, Gelfoam). If the patient presents soon after completion of dialysis, the EP should consider heparin anticoagulation as the etiology. In such cases, the use of IV protamine should be considered. One milligram of protamine can reverse 100 units of heparin. Since typically 1,000 to 2,000 units of heparin are administered at dialysis, a dose of 10 to 20 mg of protamine IV should be sufficient to reverse bleeding.
Other strategies to control hemorrhage from the access site include the use of topical thrombin or an IV drip of desmopressin. Once bleeding has been controlled, the patient should be observed for a minimum of 1 to 2 hours in the ED. If the bleeding still cannot be controlled, emergent consultation with vascular surgery services is required. Placing a suture at the site, or the use of a tourniquet proximal to the access site, can be used as a temporary measure until the surgeon arrives. The disadvantage of applying direct pressure is that it can cause thrombosis within the fistula or graft. However, given the alternative, this is an acceptable risk.
It is unfortunate that this case settled because it does not appear that any malpractice was committed. Vascular surgeons do not come to the ED to see functioning, nonbleeding AVFs. There was no published information explaining why the patient experienced rebleeding 10 to 12 hours after the initial event (perhaps some minor trauma precipitated it). Even if this patient had been observed in the ED for 8 hours, he would not have experienced rebleeding in the ED, but the tragic outcome would remain the same.
- Fall
- Legome E. Initial evaluation and management of blunt thoracic trauma in adults. UpToDate Web site. Available at http://www.uptodate.com/contents/initial-evaluation-and-management-of-blunt-thoracic-trauma-in-adults?source=search_result&search=Initial+evaluation+and+management+of+blunt+thoracic+trauma+in+adults.&selectedTitle=1~150. Updated September 21, 2015. Accessed February 21, 2016.
- Nicks BA, Manthey D. Pneumothorax. In: Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. New York, NY: McGraw Hill Education; 2016:464-468.
- A Tragic Complication of Hemodialysis
- Stolic R. Most important chronic complications of arteriovenous fistulas for hemodialysis. Med Princ Pract. 2013;22(3):220-228.
- Lutz J, Menke J, Sollinger D, Schinzel H, Thurmel K. Haemostasis in chronic kidney disease. Nephrol Dial Transplant. 2014;29(1):29-40.
Fall
A 52-year-old man presented to the ED with complaints of left shoulder and left chest pain following a bicycle accident. The patient stated he had fallen from his bicycle and landed on his left side after he turned sharply to miss a speeding car. He denied head injury, loss of consciousness, or neck pain. The patient was ambulatory after the fall and had driven himself to the ED, and complained primarily of the left shoulder and left chest pain. He described the chest pain as sharp, worsening with movement and deep inspiration. The pain also was associated with mild shortness of breath. The patient denied headache, nausea, vomiting, abdominal pain, or back pain. He was otherwise in good health and on no medications.
The patient’s vital signs on presentation were normal and his head was atraumatic. He exhibited no midline posterior cervical tenderness to palpation. The head, eyes, ears, nose, and throat (HEENT) and mouth examinations were unremarkable. The patient did have tenderness to palpation over the left clavicle and left anterior chest; there was no crepitus or subcutaneous emphysema appreciated. Breath sounds were normal, and the heart had a regular rate and rhythm without murmurs, rubs, or gallops. The abdomen was soft and nontender, without guarding or rebound. The pelvis was stable, and the patient moved all four extremities with good strength. However, he did exhibit pain with movement of his left shoulder. Peripheral pulses were 2+ and symmetrical.
The emergency physician (EP) ordered an X-ray of the chest and left shoulder, as well as urinalysis. The X-rays revealed a small left pneumothorax, a minimally displaced left clavicular fracture, and fractures of the left fourth and fifth ribs. The urinalysis results were normal. The patient was administered intravenous (IV) morphine for pain and placed on 2 L/minute oxygen via nasal cannula, with 100% oxygen saturation on pulse oximetry.
The EP consulted a pulmonologist regarding management of the pneumothorax, who recommended a 4-hour observation period in the ED, followed by a repeat chest X-ray. During the observation period, the patient remained on oxygen and continued to deny any new complaints, including headache, dizziness, or abdominal pain. His vital signs remained normal throughout the entire observation period.
While in radiology services for a repeat chest X-ray, the patient fainted and struck his head on the floor. The EP immediately ordered a noncontrast computed tomography scan of the head, which demonstrated a large intracranial bleed. The patient was taken immediately to the operating room by neurosurgery. His recovery was uneventful, and he was discharged home without obvious sequelae.
The patient sued the EP and hospital for negligent care, claiming the EP underestimated the patient’s injuries and that additional testing was warranted. The defendants argued the patient was properly evaluated based on the history and physical examination. A defense verdict was returned.
Discussion
One possible criticism of this case is the consulting of a pulmonologist for the traumatic pneumothorax rather than a trauma surgeon or general surgeon. It is unclear if these specialists were not available for consult. Nevertheless, the pulmonologist’s advice to the EP was reasonable. Until just recently, it was dogma that all traumatic pneumothoraces required tube thoracostomy for management. This is still true for tension pneumothorax, hemothorax, moderate-to-large pneumothorax, symptomatic pneumothorax, or if mechanical ventilation is anticipated or needed.1 For small pneumothoraces, several management options exist, including close observation, needle or catheter aspiration, or placement of a pigtail catheter—in addition to the placement of a small (ie, 10-14 French) thoracostomy tube.2
Regardless, it does not appear the pneumothorax played a role in the patient’s hospital fall. More likely, the patient experienced a vasovagal episode. Interestingly, he never required treatment for the pneumothorax, despite requiring mechanical ventilation.
A Tragic Complication of Hemodialysis
A 58-year-old man presented to the ED with the chief complaint of bleeding from his dialysis fistula. The patient had end-stage renal disease and had been on hemodialysis (HD) for the past 3 years. He had an arteriovenous fistula (AVF) in his left arm for dialysis access, and received HD 3 days per week—every Tuesday, Thursday, and Saturday. He had completed a scheduled run of dialysis 5 hours prior to presentation, but had continued to bleed intermittently from the AVF site. The patient stated he had applied pressure multiple times to the site, but was unsuccessful in stopping the bleeding. His medical history was significant for hypertension and coronary artery disease. Regarding his social history, the patient admitted to smoking one pack of cigarettes per day and consuming alcohol on a regular basis.
The patient’s vital signs at presentation were: heart rate, 98 beats/minute; blood pressure, 146/85 mm Hg; respiratory rate, 20 breaths/minute; and temperature, 98.6°F. Oxygen saturation was 96% on room air. The HEENT examination was unremarkable. Examination of the heart revealed a normal rate and regular rhythm with a grade of 1/6 systolic murmur, heard best at the left sternal border. The breath sounds were equal bilaterally and clear to auscultation; the abdominal examination was unremarkable. The patient had an AVF in his left forearm that was not actively bleeding. There was a palpable thrill and a bruit present on auscultation over the site; there was no increased warmth or drainage.
The EP ordered a complete blood count (CBC) on the patient. The hemoglobin and hematocrit levels were essentially unchanged from a previous CBC 1 month prior, and the platelet count was normal. After approximately 1 hour of observation in the ED, there was no rebleeding at the site, and the patient was discharged home.
Unfortunately, the bleeding resumed the following day. The patient went into cardiac arrest and died at home prior to arrival of emergency medical services. The patient’s family sued the EP and hospital for discharging the patient home without first obtaining a surgical consult. The EP and hospital settled the case with the family for $2 million.
Discussion
Many patients who present to the ED with bleeding from the vascular access site can be managed simply with direct pressure, typically for a minimum of 5 to 10 minutes. In more severe cases, the EP can apply direct pressure with an absorbable gelatin sponge (eg, Gelfoam). If the patient presents soon after completion of dialysis, the EP should consider heparin anticoagulation as the etiology. In such cases, the use of IV protamine should be considered. One milligram of protamine can reverse 100 units of heparin. Since typically 1,000 to 2,000 units of heparin are administered at dialysis, a dose of 10 to 20 mg of protamine IV should be sufficient to reverse bleeding.
Other strategies to control hemorrhage from the access site include the use of topical thrombin or an IV drip of desmopressin. Once bleeding has been controlled, the patient should be observed for a minimum of 1 to 2 hours in the ED. If the bleeding still cannot be controlled, emergent consultation with vascular surgery services is required. Placing a suture at the site, or the use of a tourniquet proximal to the access site, can be used as a temporary measure until the surgeon arrives. The disadvantage of applying direct pressure is that it can cause thrombosis within the fistula or graft. However, given the alternative, this is an acceptable risk.
It is unfortunate that this case settled because it does not appear that any malpractice was committed. Vascular surgeons do not come to the ED to see functioning, nonbleeding AVFs. There was no published information explaining why the patient experienced rebleeding 10 to 12 hours after the initial event (perhaps some minor trauma precipitated it). Even if this patient had been observed in the ED for 8 hours, he would not have experienced rebleeding in the ED, but the tragic outcome would remain the same.
Fall
A 52-year-old man presented to the ED with complaints of left shoulder and left chest pain following a bicycle accident. The patient stated he had fallen from his bicycle and landed on his left side after he turned sharply to miss a speeding car. He denied head injury, loss of consciousness, or neck pain. The patient was ambulatory after the fall and had driven himself to the ED, and complained primarily of the left shoulder and left chest pain. He described the chest pain as sharp, worsening with movement and deep inspiration. The pain also was associated with mild shortness of breath. The patient denied headache, nausea, vomiting, abdominal pain, or back pain. He was otherwise in good health and on no medications.
The patient’s vital signs on presentation were normal and his head was atraumatic. He exhibited no midline posterior cervical tenderness to palpation. The head, eyes, ears, nose, and throat (HEENT) and mouth examinations were unremarkable. The patient did have tenderness to palpation over the left clavicle and left anterior chest; there was no crepitus or subcutaneous emphysema appreciated. Breath sounds were normal, and the heart had a regular rate and rhythm without murmurs, rubs, or gallops. The abdomen was soft and nontender, without guarding or rebound. The pelvis was stable, and the patient moved all four extremities with good strength. However, he did exhibit pain with movement of his left shoulder. Peripheral pulses were 2+ and symmetrical.
The emergency physician (EP) ordered an X-ray of the chest and left shoulder, as well as urinalysis. The X-rays revealed a small left pneumothorax, a minimally displaced left clavicular fracture, and fractures of the left fourth and fifth ribs. The urinalysis results were normal. The patient was administered intravenous (IV) morphine for pain and placed on 2 L/minute oxygen via nasal cannula, with 100% oxygen saturation on pulse oximetry.
The EP consulted a pulmonologist regarding management of the pneumothorax, who recommended a 4-hour observation period in the ED, followed by a repeat chest X-ray. During the observation period, the patient remained on oxygen and continued to deny any new complaints, including headache, dizziness, or abdominal pain. His vital signs remained normal throughout the entire observation period.
While in radiology services for a repeat chest X-ray, the patient fainted and struck his head on the floor. The EP immediately ordered a noncontrast computed tomography scan of the head, which demonstrated a large intracranial bleed. The patient was taken immediately to the operating room by neurosurgery. His recovery was uneventful, and he was discharged home without obvious sequelae.
The patient sued the EP and hospital for negligent care, claiming the EP underestimated the patient’s injuries and that additional testing was warranted. The defendants argued the patient was properly evaluated based on the history and physical examination. A defense verdict was returned.
Discussion
One possible criticism of this case is the consulting of a pulmonologist for the traumatic pneumothorax rather than a trauma surgeon or general surgeon. It is unclear if these specialists were not available for consult. Nevertheless, the pulmonologist’s advice to the EP was reasonable. Until just recently, it was dogma that all traumatic pneumothoraces required tube thoracostomy for management. This is still true for tension pneumothorax, hemothorax, moderate-to-large pneumothorax, symptomatic pneumothorax, or if mechanical ventilation is anticipated or needed.1 For small pneumothoraces, several management options exist, including close observation, needle or catheter aspiration, or placement of a pigtail catheter—in addition to the placement of a small (ie, 10-14 French) thoracostomy tube.2
Regardless, it does not appear the pneumothorax played a role in the patient’s hospital fall. More likely, the patient experienced a vasovagal episode. Interestingly, he never required treatment for the pneumothorax, despite requiring mechanical ventilation.
A Tragic Complication of Hemodialysis
A 58-year-old man presented to the ED with the chief complaint of bleeding from his dialysis fistula. The patient had end-stage renal disease and had been on hemodialysis (HD) for the past 3 years. He had an arteriovenous fistula (AVF) in his left arm for dialysis access, and received HD 3 days per week—every Tuesday, Thursday, and Saturday. He had completed a scheduled run of dialysis 5 hours prior to presentation, but had continued to bleed intermittently from the AVF site. The patient stated he had applied pressure multiple times to the site, but was unsuccessful in stopping the bleeding. His medical history was significant for hypertension and coronary artery disease. Regarding his social history, the patient admitted to smoking one pack of cigarettes per day and consuming alcohol on a regular basis.
The patient’s vital signs at presentation were: heart rate, 98 beats/minute; blood pressure, 146/85 mm Hg; respiratory rate, 20 breaths/minute; and temperature, 98.6°F. Oxygen saturation was 96% on room air. The HEENT examination was unremarkable. Examination of the heart revealed a normal rate and regular rhythm with a grade of 1/6 systolic murmur, heard best at the left sternal border. The breath sounds were equal bilaterally and clear to auscultation; the abdominal examination was unremarkable. The patient had an AVF in his left forearm that was not actively bleeding. There was a palpable thrill and a bruit present on auscultation over the site; there was no increased warmth or drainage.
The EP ordered a complete blood count (CBC) on the patient. The hemoglobin and hematocrit levels were essentially unchanged from a previous CBC 1 month prior, and the platelet count was normal. After approximately 1 hour of observation in the ED, there was no rebleeding at the site, and the patient was discharged home.
Unfortunately, the bleeding resumed the following day. The patient went into cardiac arrest and died at home prior to arrival of emergency medical services. The patient’s family sued the EP and hospital for discharging the patient home without first obtaining a surgical consult. The EP and hospital settled the case with the family for $2 million.
Discussion
Many patients who present to the ED with bleeding from the vascular access site can be managed simply with direct pressure, typically for a minimum of 5 to 10 minutes. In more severe cases, the EP can apply direct pressure with an absorbable gelatin sponge (eg, Gelfoam). If the patient presents soon after completion of dialysis, the EP should consider heparin anticoagulation as the etiology. In such cases, the use of IV protamine should be considered. One milligram of protamine can reverse 100 units of heparin. Since typically 1,000 to 2,000 units of heparin are administered at dialysis, a dose of 10 to 20 mg of protamine IV should be sufficient to reverse bleeding.
Other strategies to control hemorrhage from the access site include the use of topical thrombin or an IV drip of desmopressin. Once bleeding has been controlled, the patient should be observed for a minimum of 1 to 2 hours in the ED. If the bleeding still cannot be controlled, emergent consultation with vascular surgery services is required. Placing a suture at the site, or the use of a tourniquet proximal to the access site, can be used as a temporary measure until the surgeon arrives. The disadvantage of applying direct pressure is that it can cause thrombosis within the fistula or graft. However, given the alternative, this is an acceptable risk.
It is unfortunate that this case settled because it does not appear that any malpractice was committed. Vascular surgeons do not come to the ED to see functioning, nonbleeding AVFs. There was no published information explaining why the patient experienced rebleeding 10 to 12 hours after the initial event (perhaps some minor trauma precipitated it). Even if this patient had been observed in the ED for 8 hours, he would not have experienced rebleeding in the ED, but the tragic outcome would remain the same.
- Fall
- Legome E. Initial evaluation and management of blunt thoracic trauma in adults. UpToDate Web site. Available at http://www.uptodate.com/contents/initial-evaluation-and-management-of-blunt-thoracic-trauma-in-adults?source=search_result&search=Initial+evaluation+and+management+of+blunt+thoracic+trauma+in+adults.&selectedTitle=1~150. Updated September 21, 2015. Accessed February 21, 2016.
- Nicks BA, Manthey D. Pneumothorax. In: Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. New York, NY: McGraw Hill Education; 2016:464-468.
- A Tragic Complication of Hemodialysis
- Stolic R. Most important chronic complications of arteriovenous fistulas for hemodialysis. Med Princ Pract. 2013;22(3):220-228.
- Lutz J, Menke J, Sollinger D, Schinzel H, Thurmel K. Haemostasis in chronic kidney disease. Nephrol Dial Transplant. 2014;29(1):29-40.
- Fall
- Legome E. Initial evaluation and management of blunt thoracic trauma in adults. UpToDate Web site. Available at http://www.uptodate.com/contents/initial-evaluation-and-management-of-blunt-thoracic-trauma-in-adults?source=search_result&search=Initial+evaluation+and+management+of+blunt+thoracic+trauma+in+adults.&selectedTitle=1~150. Updated September 21, 2015. Accessed February 21, 2016.
- Nicks BA, Manthey D. Pneumothorax. In: Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. New York, NY: McGraw Hill Education; 2016:464-468.
- A Tragic Complication of Hemodialysis
- Stolic R. Most important chronic complications of arteriovenous fistulas for hemodialysis. Med Princ Pract. 2013;22(3):220-228.
- Lutz J, Menke J, Sollinger D, Schinzel H, Thurmel K. Haemostasis in chronic kidney disease. Nephrol Dial Transplant. 2014;29(1):29-40.
Imposing treatment on patients with eating disorders: What are the legal risks?
Dear Dr. Mossman,
At the general hospital where I perform consultations, the medical service asked me to fill out psychiatric “hold” documents to keep a severely malnourished young woman with anorexia nervosa from leaving the hospital. Ms. Q, whose body mass index (BMI) was 12 (yes, 12), came to the hospital to have her “electrolytes fixed.” She was willing to stay the night for electrolyte repletion, but insisted she could gain weight on her own at home.
I’m worried that she might die without prompt inpatient treatment; she needs to stay on the medical service. Should I fill out a psychiatric hold to keep her there? What legal risks could I face if Ms. Q is detained and force-fed against her will? What are the legal risks of letting her leave the hospital before she is medically stable?
Submitted by “Dr. F”
When a severely malnourished patient with an eating disorder arrives on a medical floor, treatment teams often ask psychiatric consultants to help them impose care the patient desperately needs but doesn’t want. This reaction is understandable. After all, an eating disorder is a psychiatric illness, and hospital-based psychiatrists have experience with treating involuntary patients. A psychiatric hold may seem like a sensible way to save the life of a hospitalized patient with a mental illness.
But filling out a psychiatric hold only scratches the surface of what a psychiatric consultant’s contribution should include; in Ms. Q’s case, initiating a psychiatric hold is probably the wrong thing to do.
Why would filling out a psychiatric hold be inappropriate for Ms. Q? What clinical factors and legal issues should a psychiatrist consider when helping medical colleagues provide unwanted treatment to a severely malnourished patient with an eating disorder? We’ll explore these matters as we consider the case of Ms. Q (Figure) and the following questions:
- What type of care is most appropriate for her now?
- Can she refuse medical treatment?
- What are the medicolegal risks of letting her leave the hospital?
- What are the medicolegal risks of detaining and force-feeding her against her will?
- When is a psychiatric “hold” appropriate?
What care is appropriate?
Given her state of self-starvation, Ms. Q’s treatment plan could require close monitoring of her electrolytes and cardiac status, as well as watching her for signs of “refeeding syndrome”—rapid, potentially fatal fluid shifts and metabolic derangements that malnourished patients could experience when they receive artificial refeeding.1
First, the physicians who are caring for Ms. Q should determine whether she needs more intensive medical supervision than is usually available on a psychiatric unit. If she does, but she won’t agree to stay on a medical unit for care, a psychiatric hold is the wrong step, for 2 reasons:
- Once a psychiatric hold has been executed, state statutes require the patient to be placed in a psychiatric facility—a state-approved psychiatric treatment setting, such as a psychiatric unit or free-standing psychiatric hospital—within a specified period.2,3 Most nonpsychiatric medical units would not meet state’s statutory definition for such a facility.
- A psychiatric hold only permits short-term detention. It does not provide legal authority to impose unwanted medical treatment.
Does Ms. Q have capacity?
In the United States, Ms. Q has a legal right to refuse medical care—even if she needs it urgently—provided that her refusal is made competently.4 As Appelbaum and Grisso5 explained in a now-classic 1988 article:
The legal standards for competence include the four related skills of communicating a choice, understanding relevant information, appreciating the current situation and its consequences, and manipulating information rationally.
The Table5 describes these abilities in more detail.
Only courts can make legal determinations of competence, so physicians refer to an evaluation of a patient’s competence-related abilities as a “capacity assessment.” The decision as to whether a patient has capacity ultimately rests with the primary treatment team; however, physicians in other specialties often enlist psychiatrists’ help with this matter because of their interviewing skills and knowledge of how mental illness can impair capacity.
No easy-to-use instrument for evaluating capacity is available. However, Appelbaum6 provides examples of questions that often prove useful in such assessments, and a review by Sessums et al7 on several capacity evaluation tools suggests that the Aid to Capacity Evaluation8 may be the best instrument for performing capacity assessments.
Patients with anorexia nervosa often differ substantially from healthy people in how they assign values to life and death,9 which can make it difficult to evaluate their capacity to refuse life-saving treatment. Malnutrition can alter patients’ ability to think clearly, a phenomenon that some patients with anorexia mention as a reason they are grateful (in retrospect) for the compulsory treatment they received.10 Yet, if an evaluation shows that the patient has the decision-making capacity to refuse care, then her (his) caregivers should carefully document this conclusion and the basis for it. Although caregivers might encourage her to accept the treatment they believe she needs, they should not provide treatment that conflicts with their patient’s wishes.
If evaluation shows that the patient lacks capacity, however, the findings that support this conclusion should be documented clearly. The team then should consult the hospital attorney to determine how to best proceed. The attorney might recommend that a physician on the primary treatment team initiate a “medical hold”—an order that the patient may not leave against medical advice (AMA)—and then seek an emergency guardianship to permit medical treatment, such as refeeding.
To treat or not to treat?
What are the legal risks of allowing Ms. Q to leave AMA before she reaches medical stability?
Powers and Cloak11 describe a case of a 26-year-old woman with anorexia nervosa who came to the hospital with dizziness, weakness, and a very low blood glucose level. She was discharged after 6 days without having received any feeding, only to return to the emergency department 2 days later. This time, she had a letter from her physician stating that she needed medical supervision to start refeeding, yet she was discharged from the emergency department within a few hours. She was re-admitted to the hospital the next day.
Powers and Cloak11 do not report this woman’s medical outcome. But what if she had suffered a fatal cardiac arrhythmia before her third presentation to the emergency department or suffered another injury attributable to her nutritional state: Could her physicians be found at fault?
On Cohen & Associates’ Web site, they essentially answer, “Yes.” They describe a case of “Miss McIntosh,” who had anorexia nervosa and was discharged home from a hospital despite “chronic metabolic problems and not eating properly.” She went into a “hypoglycemic encephalopathic coma” and “suffered irreversible brain damage.” A subsequent lawsuit against the hospital resulted in a 7-figure settlement,12 illustrating the potential for adverse medicolegal consequences if failure to treat a patient with anorexia nervosa could be linked to subsequent physical harm. On the other hand, could a patient with anorexia who is being force-fed take legal action against her providers? At least 3 recent British cases suggest that this is possible.13-15 A British medical student with anorexia, E, made an emergency application to the Court of Protection in London, claiming that being fed against her will was akin to reliving her past experience of sexual abuse. In E’s case, the judge ruled “that the balance tips slowly but unmistakably in the direction of life preserving treatment” and authorized feeding over her objection.6 In 2 other cases, however, British courts have ruled that force-feeding anorexic patients would be futile and disallowed the practice.14,15
Faced with possible legal action, no matter what course you take, how should you respond? Getting legal and ethical consultation is prudent if time allows. In many cases, hospital attorneys might prefer that physicians err on the side of preserving life(D. Vanderpool, MBA, JD, personal communication, February 3, 2016)—even if that means detaining a patient without clear legal authorization to do so—because attorneys would prefer to defend a doctor who acted to save someone’s life than to defend a doctor who knowingly allowed a patient to die.
When might persons with an eating disorder be civilly committed?
Suppose that Ms. Q does not need urgent nonpsychiatric medical care, or that her life-threatening physical problems now have been addressed. Her physicians strongly recommend that she undergo inpatient psychiatric treatment for her eating disorder, but she wants to leave. Would it now be appropriate to fill out paperwork to initiate a psychiatric hold?
All U.S. jurisdictions authorize “civil commitment” proceedings that can lead to involuntary psychiatric hospitalization of people who have a mental disorder and pose a risk to themselves or others because of the disorder.16
In general, to be subject to civil commitment, a person must have a substantial disorder of thought, mood, perception, orientation, or memory. In addition, that disorder must grossly impair her (his) judgment, behavior, reality testing, or ability to meet the demands of everyday life.17
People with psychosis, a severe mood disorder, or dementia often meet these criteria. However, psychiatrists do not usually consider anorexia nervosa to be a thought disorder, mood disorder, or memory disorder. Does this mean that people with anorexia nervosa cannot meet the “substantial” mental disorder criterion?
It does not. Courts interpret the words in statutes based on their “ordinary and natural meaning.”18 If Ms. Q perceived herself as fat, despite having a BMI that was far below the healthy range, most people would regard her thinking to be disordered. If, in addition, her mental disorder impaired her “judgment, behavior, and capacity to meet the ordinary demands of sustaining existence,” then her anorexia nervosa “would qualify as a mental disorder for commitment purposes.”19
To be subject to civil commitment, a person with a substantial mental disorder also must pose a risk of harm to herself or others because of the disorder. That risk can be evidenced via an action, attempt, or threat to do direct physical harm, or it might inhere in the potential for developing grave disability through neglect of one’s basic needs, such as failing to eat adequately. In Ms. Q’s case, if the evidence shows her eating-disordered behavior has placed her at imminent risk of permanent injury or death, she has satisfied the legal criteria that justify court-ordered psychiatric hospitalization.
Bottom Line
When a severely malnourished patient with anorexia nervosa does not agree to allow recommended care, an appropriate clinical response should include judgment about the urgency of the proposed treatment, what treatment setting is best suited to the patient’s condition, and whether the patient has the mental capacity to refuse potentially life-saving care.
1. Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008;336(7659):1495-1498.
2. Ohio Revised Code §5122.01(F).
3. Oregon Revised Statutes §426.005(c).
4. Schloendorff v Society of New York Hospital, 211 N.Y. 125, 105 N.E. 92 (N1914).
5. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
6. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
7. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-427.
8. Community tools: Aid to Capacity Evaluation (ACE). University of Toronto Joint Centre for Bioethics. http://www.jcb.utoronto.ca/tools/ace_download.shtml. Updated May 8, 2008. Accessed December 21, 2015.
9. Tan J, Hope T, Stewart A. Competence to refuse treatment in anorexia nervosa. Int J Law Psychiatry. 2003;26(6):697-707.
10. Elzakkers IF, Danner UN, Hoek HW, et al. Compulsory treatment in anorexia nervosa: a review. Int J Eat Disord. 2014;47(8):845-852.
11. Powers PS, Cloak NL. Failure to feed patients with anorexia nervosa and other perils and perplexities in the medical care of eating disorder patients. Eat Disord. 2013;21(1):81-89.
12. “Failure to properly treat anorexia nervosa.” Harry S. Cohen & Associates. http://medmal1.com/article/failure-to-properly-treat-anorexia-nervosa. Accessed February 1, 2016.
13. A Local Authority v E. and Others [2012] EWHC 1639 (COP).
14. A NHS Foundation Trust v Ms. X [2014] EWCOP 35.
15. NHS Trust v L [2012] EWHC 2741 (COP).
16. Pinals DA, Mossman D. Evaluation for civil commitment. New York, NY: Oxford University Press; 2011.
17. Castellano-Hoyt DW. Enhancing police response to persons in mental health crisis: providing strategies, communication techniques, and crisis intervention preparation in overcoming institutional challenges. Springfield, IL: Charles C. Thomas Publisher, Ltd; 2003.
18. FDIC v Meyer, 510 U.S. 471 (1994).
19. Appelbaum PS, Rumpf T. Civil commitment of the anorexic patient. Gen Hosp Psychiatry. 1998;20(4):225-230.
Dear Dr. Mossman,
At the general hospital where I perform consultations, the medical service asked me to fill out psychiatric “hold” documents to keep a severely malnourished young woman with anorexia nervosa from leaving the hospital. Ms. Q, whose body mass index (BMI) was 12 (yes, 12), came to the hospital to have her “electrolytes fixed.” She was willing to stay the night for electrolyte repletion, but insisted she could gain weight on her own at home.
I’m worried that she might die without prompt inpatient treatment; she needs to stay on the medical service. Should I fill out a psychiatric hold to keep her there? What legal risks could I face if Ms. Q is detained and force-fed against her will? What are the legal risks of letting her leave the hospital before she is medically stable?
Submitted by “Dr. F”
When a severely malnourished patient with an eating disorder arrives on a medical floor, treatment teams often ask psychiatric consultants to help them impose care the patient desperately needs but doesn’t want. This reaction is understandable. After all, an eating disorder is a psychiatric illness, and hospital-based psychiatrists have experience with treating involuntary patients. A psychiatric hold may seem like a sensible way to save the life of a hospitalized patient with a mental illness.
But filling out a psychiatric hold only scratches the surface of what a psychiatric consultant’s contribution should include; in Ms. Q’s case, initiating a psychiatric hold is probably the wrong thing to do.
Why would filling out a psychiatric hold be inappropriate for Ms. Q? What clinical factors and legal issues should a psychiatrist consider when helping medical colleagues provide unwanted treatment to a severely malnourished patient with an eating disorder? We’ll explore these matters as we consider the case of Ms. Q (Figure) and the following questions:
- What type of care is most appropriate for her now?
- Can she refuse medical treatment?
- What are the medicolegal risks of letting her leave the hospital?
- What are the medicolegal risks of detaining and force-feeding her against her will?
- When is a psychiatric “hold” appropriate?
What care is appropriate?
Given her state of self-starvation, Ms. Q’s treatment plan could require close monitoring of her electrolytes and cardiac status, as well as watching her for signs of “refeeding syndrome”—rapid, potentially fatal fluid shifts and metabolic derangements that malnourished patients could experience when they receive artificial refeeding.1
First, the physicians who are caring for Ms. Q should determine whether she needs more intensive medical supervision than is usually available on a psychiatric unit. If she does, but she won’t agree to stay on a medical unit for care, a psychiatric hold is the wrong step, for 2 reasons:
- Once a psychiatric hold has been executed, state statutes require the patient to be placed in a psychiatric facility—a state-approved psychiatric treatment setting, such as a psychiatric unit or free-standing psychiatric hospital—within a specified period.2,3 Most nonpsychiatric medical units would not meet state’s statutory definition for such a facility.
- A psychiatric hold only permits short-term detention. It does not provide legal authority to impose unwanted medical treatment.
Does Ms. Q have capacity?
In the United States, Ms. Q has a legal right to refuse medical care—even if she needs it urgently—provided that her refusal is made competently.4 As Appelbaum and Grisso5 explained in a now-classic 1988 article:
The legal standards for competence include the four related skills of communicating a choice, understanding relevant information, appreciating the current situation and its consequences, and manipulating information rationally.
The Table5 describes these abilities in more detail.
Only courts can make legal determinations of competence, so physicians refer to an evaluation of a patient’s competence-related abilities as a “capacity assessment.” The decision as to whether a patient has capacity ultimately rests with the primary treatment team; however, physicians in other specialties often enlist psychiatrists’ help with this matter because of their interviewing skills and knowledge of how mental illness can impair capacity.
No easy-to-use instrument for evaluating capacity is available. However, Appelbaum6 provides examples of questions that often prove useful in such assessments, and a review by Sessums et al7 on several capacity evaluation tools suggests that the Aid to Capacity Evaluation8 may be the best instrument for performing capacity assessments.
Patients with anorexia nervosa often differ substantially from healthy people in how they assign values to life and death,9 which can make it difficult to evaluate their capacity to refuse life-saving treatment. Malnutrition can alter patients’ ability to think clearly, a phenomenon that some patients with anorexia mention as a reason they are grateful (in retrospect) for the compulsory treatment they received.10 Yet, if an evaluation shows that the patient has the decision-making capacity to refuse care, then her (his) caregivers should carefully document this conclusion and the basis for it. Although caregivers might encourage her to accept the treatment they believe she needs, they should not provide treatment that conflicts with their patient’s wishes.
If evaluation shows that the patient lacks capacity, however, the findings that support this conclusion should be documented clearly. The team then should consult the hospital attorney to determine how to best proceed. The attorney might recommend that a physician on the primary treatment team initiate a “medical hold”—an order that the patient may not leave against medical advice (AMA)—and then seek an emergency guardianship to permit medical treatment, such as refeeding.
To treat or not to treat?
What are the legal risks of allowing Ms. Q to leave AMA before she reaches medical stability?
Powers and Cloak11 describe a case of a 26-year-old woman with anorexia nervosa who came to the hospital with dizziness, weakness, and a very low blood glucose level. She was discharged after 6 days without having received any feeding, only to return to the emergency department 2 days later. This time, she had a letter from her physician stating that she needed medical supervision to start refeeding, yet she was discharged from the emergency department within a few hours. She was re-admitted to the hospital the next day.
Powers and Cloak11 do not report this woman’s medical outcome. But what if she had suffered a fatal cardiac arrhythmia before her third presentation to the emergency department or suffered another injury attributable to her nutritional state: Could her physicians be found at fault?
On Cohen & Associates’ Web site, they essentially answer, “Yes.” They describe a case of “Miss McIntosh,” who had anorexia nervosa and was discharged home from a hospital despite “chronic metabolic problems and not eating properly.” She went into a “hypoglycemic encephalopathic coma” and “suffered irreversible brain damage.” A subsequent lawsuit against the hospital resulted in a 7-figure settlement,12 illustrating the potential for adverse medicolegal consequences if failure to treat a patient with anorexia nervosa could be linked to subsequent physical harm. On the other hand, could a patient with anorexia who is being force-fed take legal action against her providers? At least 3 recent British cases suggest that this is possible.13-15 A British medical student with anorexia, E, made an emergency application to the Court of Protection in London, claiming that being fed against her will was akin to reliving her past experience of sexual abuse. In E’s case, the judge ruled “that the balance tips slowly but unmistakably in the direction of life preserving treatment” and authorized feeding over her objection.6 In 2 other cases, however, British courts have ruled that force-feeding anorexic patients would be futile and disallowed the practice.14,15
Faced with possible legal action, no matter what course you take, how should you respond? Getting legal and ethical consultation is prudent if time allows. In many cases, hospital attorneys might prefer that physicians err on the side of preserving life(D. Vanderpool, MBA, JD, personal communication, February 3, 2016)—even if that means detaining a patient without clear legal authorization to do so—because attorneys would prefer to defend a doctor who acted to save someone’s life than to defend a doctor who knowingly allowed a patient to die.
When might persons with an eating disorder be civilly committed?
Suppose that Ms. Q does not need urgent nonpsychiatric medical care, or that her life-threatening physical problems now have been addressed. Her physicians strongly recommend that she undergo inpatient psychiatric treatment for her eating disorder, but she wants to leave. Would it now be appropriate to fill out paperwork to initiate a psychiatric hold?
All U.S. jurisdictions authorize “civil commitment” proceedings that can lead to involuntary psychiatric hospitalization of people who have a mental disorder and pose a risk to themselves or others because of the disorder.16
In general, to be subject to civil commitment, a person must have a substantial disorder of thought, mood, perception, orientation, or memory. In addition, that disorder must grossly impair her (his) judgment, behavior, reality testing, or ability to meet the demands of everyday life.17
People with psychosis, a severe mood disorder, or dementia often meet these criteria. However, psychiatrists do not usually consider anorexia nervosa to be a thought disorder, mood disorder, or memory disorder. Does this mean that people with anorexia nervosa cannot meet the “substantial” mental disorder criterion?
It does not. Courts interpret the words in statutes based on their “ordinary and natural meaning.”18 If Ms. Q perceived herself as fat, despite having a BMI that was far below the healthy range, most people would regard her thinking to be disordered. If, in addition, her mental disorder impaired her “judgment, behavior, and capacity to meet the ordinary demands of sustaining existence,” then her anorexia nervosa “would qualify as a mental disorder for commitment purposes.”19
To be subject to civil commitment, a person with a substantial mental disorder also must pose a risk of harm to herself or others because of the disorder. That risk can be evidenced via an action, attempt, or threat to do direct physical harm, or it might inhere in the potential for developing grave disability through neglect of one’s basic needs, such as failing to eat adequately. In Ms. Q’s case, if the evidence shows her eating-disordered behavior has placed her at imminent risk of permanent injury or death, she has satisfied the legal criteria that justify court-ordered psychiatric hospitalization.
Bottom Line
When a severely malnourished patient with anorexia nervosa does not agree to allow recommended care, an appropriate clinical response should include judgment about the urgency of the proposed treatment, what treatment setting is best suited to the patient’s condition, and whether the patient has the mental capacity to refuse potentially life-saving care.
Dear Dr. Mossman,
At the general hospital where I perform consultations, the medical service asked me to fill out psychiatric “hold” documents to keep a severely malnourished young woman with anorexia nervosa from leaving the hospital. Ms. Q, whose body mass index (BMI) was 12 (yes, 12), came to the hospital to have her “electrolytes fixed.” She was willing to stay the night for electrolyte repletion, but insisted she could gain weight on her own at home.
I’m worried that she might die without prompt inpatient treatment; she needs to stay on the medical service. Should I fill out a psychiatric hold to keep her there? What legal risks could I face if Ms. Q is detained and force-fed against her will? What are the legal risks of letting her leave the hospital before she is medically stable?
Submitted by “Dr. F”
When a severely malnourished patient with an eating disorder arrives on a medical floor, treatment teams often ask psychiatric consultants to help them impose care the patient desperately needs but doesn’t want. This reaction is understandable. After all, an eating disorder is a psychiatric illness, and hospital-based psychiatrists have experience with treating involuntary patients. A psychiatric hold may seem like a sensible way to save the life of a hospitalized patient with a mental illness.
But filling out a psychiatric hold only scratches the surface of what a psychiatric consultant’s contribution should include; in Ms. Q’s case, initiating a psychiatric hold is probably the wrong thing to do.
Why would filling out a psychiatric hold be inappropriate for Ms. Q? What clinical factors and legal issues should a psychiatrist consider when helping medical colleagues provide unwanted treatment to a severely malnourished patient with an eating disorder? We’ll explore these matters as we consider the case of Ms. Q (Figure) and the following questions:
- What type of care is most appropriate for her now?
- Can she refuse medical treatment?
- What are the medicolegal risks of letting her leave the hospital?
- What are the medicolegal risks of detaining and force-feeding her against her will?
- When is a psychiatric “hold” appropriate?
What care is appropriate?
Given her state of self-starvation, Ms. Q’s treatment plan could require close monitoring of her electrolytes and cardiac status, as well as watching her for signs of “refeeding syndrome”—rapid, potentially fatal fluid shifts and metabolic derangements that malnourished patients could experience when they receive artificial refeeding.1
First, the physicians who are caring for Ms. Q should determine whether she needs more intensive medical supervision than is usually available on a psychiatric unit. If she does, but she won’t agree to stay on a medical unit for care, a psychiatric hold is the wrong step, for 2 reasons:
- Once a psychiatric hold has been executed, state statutes require the patient to be placed in a psychiatric facility—a state-approved psychiatric treatment setting, such as a psychiatric unit or free-standing psychiatric hospital—within a specified period.2,3 Most nonpsychiatric medical units would not meet state’s statutory definition for such a facility.
- A psychiatric hold only permits short-term detention. It does not provide legal authority to impose unwanted medical treatment.
Does Ms. Q have capacity?
In the United States, Ms. Q has a legal right to refuse medical care—even if she needs it urgently—provided that her refusal is made competently.4 As Appelbaum and Grisso5 explained in a now-classic 1988 article:
The legal standards for competence include the four related skills of communicating a choice, understanding relevant information, appreciating the current situation and its consequences, and manipulating information rationally.
The Table5 describes these abilities in more detail.
Only courts can make legal determinations of competence, so physicians refer to an evaluation of a patient’s competence-related abilities as a “capacity assessment.” The decision as to whether a patient has capacity ultimately rests with the primary treatment team; however, physicians in other specialties often enlist psychiatrists’ help with this matter because of their interviewing skills and knowledge of how mental illness can impair capacity.
No easy-to-use instrument for evaluating capacity is available. However, Appelbaum6 provides examples of questions that often prove useful in such assessments, and a review by Sessums et al7 on several capacity evaluation tools suggests that the Aid to Capacity Evaluation8 may be the best instrument for performing capacity assessments.
Patients with anorexia nervosa often differ substantially from healthy people in how they assign values to life and death,9 which can make it difficult to evaluate their capacity to refuse life-saving treatment. Malnutrition can alter patients’ ability to think clearly, a phenomenon that some patients with anorexia mention as a reason they are grateful (in retrospect) for the compulsory treatment they received.10 Yet, if an evaluation shows that the patient has the decision-making capacity to refuse care, then her (his) caregivers should carefully document this conclusion and the basis for it. Although caregivers might encourage her to accept the treatment they believe she needs, they should not provide treatment that conflicts with their patient’s wishes.
If evaluation shows that the patient lacks capacity, however, the findings that support this conclusion should be documented clearly. The team then should consult the hospital attorney to determine how to best proceed. The attorney might recommend that a physician on the primary treatment team initiate a “medical hold”—an order that the patient may not leave against medical advice (AMA)—and then seek an emergency guardianship to permit medical treatment, such as refeeding.
To treat or not to treat?
What are the legal risks of allowing Ms. Q to leave AMA before she reaches medical stability?
Powers and Cloak11 describe a case of a 26-year-old woman with anorexia nervosa who came to the hospital with dizziness, weakness, and a very low blood glucose level. She was discharged after 6 days without having received any feeding, only to return to the emergency department 2 days later. This time, she had a letter from her physician stating that she needed medical supervision to start refeeding, yet she was discharged from the emergency department within a few hours. She was re-admitted to the hospital the next day.
Powers and Cloak11 do not report this woman’s medical outcome. But what if she had suffered a fatal cardiac arrhythmia before her third presentation to the emergency department or suffered another injury attributable to her nutritional state: Could her physicians be found at fault?
On Cohen & Associates’ Web site, they essentially answer, “Yes.” They describe a case of “Miss McIntosh,” who had anorexia nervosa and was discharged home from a hospital despite “chronic metabolic problems and not eating properly.” She went into a “hypoglycemic encephalopathic coma” and “suffered irreversible brain damage.” A subsequent lawsuit against the hospital resulted in a 7-figure settlement,12 illustrating the potential for adverse medicolegal consequences if failure to treat a patient with anorexia nervosa could be linked to subsequent physical harm. On the other hand, could a patient with anorexia who is being force-fed take legal action against her providers? At least 3 recent British cases suggest that this is possible.13-15 A British medical student with anorexia, E, made an emergency application to the Court of Protection in London, claiming that being fed against her will was akin to reliving her past experience of sexual abuse. In E’s case, the judge ruled “that the balance tips slowly but unmistakably in the direction of life preserving treatment” and authorized feeding over her objection.6 In 2 other cases, however, British courts have ruled that force-feeding anorexic patients would be futile and disallowed the practice.14,15
Faced with possible legal action, no matter what course you take, how should you respond? Getting legal and ethical consultation is prudent if time allows. In many cases, hospital attorneys might prefer that physicians err on the side of preserving life(D. Vanderpool, MBA, JD, personal communication, February 3, 2016)—even if that means detaining a patient without clear legal authorization to do so—because attorneys would prefer to defend a doctor who acted to save someone’s life than to defend a doctor who knowingly allowed a patient to die.
When might persons with an eating disorder be civilly committed?
Suppose that Ms. Q does not need urgent nonpsychiatric medical care, or that her life-threatening physical problems now have been addressed. Her physicians strongly recommend that she undergo inpatient psychiatric treatment for her eating disorder, but she wants to leave. Would it now be appropriate to fill out paperwork to initiate a psychiatric hold?
All U.S. jurisdictions authorize “civil commitment” proceedings that can lead to involuntary psychiatric hospitalization of people who have a mental disorder and pose a risk to themselves or others because of the disorder.16
In general, to be subject to civil commitment, a person must have a substantial disorder of thought, mood, perception, orientation, or memory. In addition, that disorder must grossly impair her (his) judgment, behavior, reality testing, or ability to meet the demands of everyday life.17
People with psychosis, a severe mood disorder, or dementia often meet these criteria. However, psychiatrists do not usually consider anorexia nervosa to be a thought disorder, mood disorder, or memory disorder. Does this mean that people with anorexia nervosa cannot meet the “substantial” mental disorder criterion?
It does not. Courts interpret the words in statutes based on their “ordinary and natural meaning.”18 If Ms. Q perceived herself as fat, despite having a BMI that was far below the healthy range, most people would regard her thinking to be disordered. If, in addition, her mental disorder impaired her “judgment, behavior, and capacity to meet the ordinary demands of sustaining existence,” then her anorexia nervosa “would qualify as a mental disorder for commitment purposes.”19
To be subject to civil commitment, a person with a substantial mental disorder also must pose a risk of harm to herself or others because of the disorder. That risk can be evidenced via an action, attempt, or threat to do direct physical harm, or it might inhere in the potential for developing grave disability through neglect of one’s basic needs, such as failing to eat adequately. In Ms. Q’s case, if the evidence shows her eating-disordered behavior has placed her at imminent risk of permanent injury or death, she has satisfied the legal criteria that justify court-ordered psychiatric hospitalization.
Bottom Line
When a severely malnourished patient with anorexia nervosa does not agree to allow recommended care, an appropriate clinical response should include judgment about the urgency of the proposed treatment, what treatment setting is best suited to the patient’s condition, and whether the patient has the mental capacity to refuse potentially life-saving care.
1. Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008;336(7659):1495-1498.
2. Ohio Revised Code §5122.01(F).
3. Oregon Revised Statutes §426.005(c).
4. Schloendorff v Society of New York Hospital, 211 N.Y. 125, 105 N.E. 92 (N1914).
5. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
6. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
7. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-427.
8. Community tools: Aid to Capacity Evaluation (ACE). University of Toronto Joint Centre for Bioethics. http://www.jcb.utoronto.ca/tools/ace_download.shtml. Updated May 8, 2008. Accessed December 21, 2015.
9. Tan J, Hope T, Stewart A. Competence to refuse treatment in anorexia nervosa. Int J Law Psychiatry. 2003;26(6):697-707.
10. Elzakkers IF, Danner UN, Hoek HW, et al. Compulsory treatment in anorexia nervosa: a review. Int J Eat Disord. 2014;47(8):845-852.
11. Powers PS, Cloak NL. Failure to feed patients with anorexia nervosa and other perils and perplexities in the medical care of eating disorder patients. Eat Disord. 2013;21(1):81-89.
12. “Failure to properly treat anorexia nervosa.” Harry S. Cohen & Associates. http://medmal1.com/article/failure-to-properly-treat-anorexia-nervosa. Accessed February 1, 2016.
13. A Local Authority v E. and Others [2012] EWHC 1639 (COP).
14. A NHS Foundation Trust v Ms. X [2014] EWCOP 35.
15. NHS Trust v L [2012] EWHC 2741 (COP).
16. Pinals DA, Mossman D. Evaluation for civil commitment. New York, NY: Oxford University Press; 2011.
17. Castellano-Hoyt DW. Enhancing police response to persons in mental health crisis: providing strategies, communication techniques, and crisis intervention preparation in overcoming institutional challenges. Springfield, IL: Charles C. Thomas Publisher, Ltd; 2003.
18. FDIC v Meyer, 510 U.S. 471 (1994).
19. Appelbaum PS, Rumpf T. Civil commitment of the anorexic patient. Gen Hosp Psychiatry. 1998;20(4):225-230.
1. Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008;336(7659):1495-1498.
2. Ohio Revised Code §5122.01(F).
3. Oregon Revised Statutes §426.005(c).
4. Schloendorff v Society of New York Hospital, 211 N.Y. 125, 105 N.E. 92 (N1914).
5. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
6. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
7. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-427.
8. Community tools: Aid to Capacity Evaluation (ACE). University of Toronto Joint Centre for Bioethics. http://www.jcb.utoronto.ca/tools/ace_download.shtml. Updated May 8, 2008. Accessed December 21, 2015.
9. Tan J, Hope T, Stewart A. Competence to refuse treatment in anorexia nervosa. Int J Law Psychiatry. 2003;26(6):697-707.
10. Elzakkers IF, Danner UN, Hoek HW, et al. Compulsory treatment in anorexia nervosa: a review. Int J Eat Disord. 2014;47(8):845-852.
11. Powers PS, Cloak NL. Failure to feed patients with anorexia nervosa and other perils and perplexities in the medical care of eating disorder patients. Eat Disord. 2013;21(1):81-89.
12. “Failure to properly treat anorexia nervosa.” Harry S. Cohen & Associates. http://medmal1.com/article/failure-to-properly-treat-anorexia-nervosa. Accessed February 1, 2016.
13. A Local Authority v E. and Others [2012] EWHC 1639 (COP).
14. A NHS Foundation Trust v Ms. X [2014] EWCOP 35.
15. NHS Trust v L [2012] EWHC 2741 (COP).
16. Pinals DA, Mossman D. Evaluation for civil commitment. New York, NY: Oxford University Press; 2011.
17. Castellano-Hoyt DW. Enhancing police response to persons in mental health crisis: providing strategies, communication techniques, and crisis intervention preparation in overcoming institutional challenges. Springfield, IL: Charles C. Thomas Publisher, Ltd; 2003.
18. FDIC v Meyer, 510 U.S. 471 (1994).
19. Appelbaum PS, Rumpf T. Civil commitment of the anorexic patient. Gen Hosp Psychiatry. 1998;20(4):225-230.
Law & Medicine: Which doctors get sued?
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]