User login
Bladder Cancer: Is Active Surveillance the Way Forward?
PARIS — Should clinicians promote active surveillance for non–muscle-invasive bladder tumors (NMIBT) and establish it as a comprehensive management approach, as with prostate and kidney cancers?
During the 117th congress of the French Association of Urology (AFU), Benjamin Pradère, MD, urologic surgeon at Croix du Sud Clinic in Quint-Fonsegrives, France, advocated for this approach, suggesting that the use of biomarkers could enhance its effectiveness.
However, it requires careful patient selection, proper information, and relevant follow-up,” said Dr. Pradère, who is a member of the AFU Cancer Committee (CCAFU).
Low-Grade Tumors
NMIBTs are precancerous lesions and constitute 70%-80% of diagnosed bladder tumors. The remaining tumors are more severe invasive tumors that infiltrate deep tissues. NMIBTs, however, entail a high risk for recurrence (reaching 80% after endoscopic resection), as well as a high risk for progression.
As a result, the diagnosis of NMIBT involves follow-up that significantly impacts patients’ quality of life due to repeated cystoscopies and endovesical treatments. “Tumors with the most impact are low-grade Ta tumors”, with longer-term monitoring required for these low-risk tumors.
Hematuria is the most frequent clinical sign. NMIBT diagnosis occurs after endoscopic tumor resection via transurethral resection, followed by an anatomopathological analysis to determine cell grade and tumor stage. Treatment depends on the risk of recurrence and progression, as well as the risk of therapeutic failure after the initial resection.
Risk stratification distinguishes the following four levels:
- Low-risk tumors: Low-grade pTa urothelial tumors, unifocal, < 3 cm, no history of bladder tumors. Low risk of recurrence and progression.
- Intermediate-risk tumors: Other low-grade pTa urothelial tumors with no high-risk criteria. Low risk of progression but high risk of recurrence.
- High-risk tumors: Tumors with at least one risk factor: Stage pT1, high grade, presence of carcinoma in situ. High risks of progression and recurrence.
- Very high-risk tumors: Tumors combining all risk factors (pT1 grade with carcinoma in situ). Very high and early risk of progression.
“We know that low-grade NMIBTs have no impact on survival,” said Dr. Pradère. For these tumors, which represent 60% of diagnosed NMIBTs, or approximately 250,000 new cases annually in France, specific survival is > 99%, meaning that most diagnosed patients will not die of bladder cancer.
The recurrence rate for low-grade tumors is 50%, but recurrences are “almost always low-grade and rarely invade the basement membrane,” said Pradère. Implementing active surveillance to limit surgical intervention to more advanced forms seems to be relevant for these tumors.
Cystoscopy Every 3 Months
According to CCAFU recommendations, “active surveillance is a therapeutic alternative that can be proposed for patients with recurrent low-risk NMIBT after the initial diagnosis.” Criteria include low-grade pTa, fewer than five tumors, size ≤ 15 mm, negative urinary cytology, asymptomatic nature, and the patient’s acceptance of closer monitoring.
While active surveillance has become the standard treatment for low-risk prostate cancer, this therapeutic option remains marginal in bladder cancer, as in kidney cancer. The goal is to defer or avoid surgical treatment by closely monitoring the natural progression of the disease.
For NMIBTs, follow-up modalities are not yet specifically recommended because of a lack of data, said Dr. Pradère. According to a consensus, cystoscopy should be repeated every 3 months for a year and then every 6 months. Unlike standard follow-up, it includes cytology “to not miss the transition to high grade.”
CCAFU recommends discontinuing active surveillance if any of the following criteria are present:
- More than 10 lesions
- Size > 30 mm
- Positive cytology
- Symptoms (hematuria, micturition disorders, and recurring infections).
Literature on the benefits of active surveillance in bladder tumors is still limited. Only seven studies are available. Overall, for nearly 600 included patients, tumors progressed in about 12% of cases. Progression to invasive tumors occurred in 0.8% of patients (n = 5).
13 Months’ Surveillance
According to a long-term study (median follow-up of 38 months), patients mostly exit active surveillance in the first year. The median duration of active surveillance is 13 months. Active surveillance is discontinued to surgically treat tumors that turn out to be low-grade Ta tumors in 70% of cases.
The following factors predicting recurrence and progression of tumors have been identified: Multiple tumors, early recurrence (within a year of initial diagnosis), frequent recurrence (more than one recurrence per year), tumors > 3 cm, and failure of previous endovesical treatment.
Recent studies have shown that with at least three of these recurrence and progression factors, the median duration under active surveillance is 15 months compared with 28 months in the absence of such factors. “Considering these factors, it is possible to assess the benefit of active surveillance for the patient,” said Dr. Pradère.
If active surveillance for bladder tumors is still not widely practiced, then the contribution of imaging (MRI and ultrasound) and biomarkers could promote its adoption. “The use of biomarkers should change the game and encourage active surveillance in patients with small polyps,” said Dr. Pradère.
ADXBladder Test Utility
A study highlighted the importance of evaluating minichromosome maintenance protein 5 expression during active surveillance using the ADXBladder ELISA test on a urine sample. This test is usually used in bladder cancer diagnosis.
“This study showed that a negative result in two consecutive tests during active surveillance is associated with an almost zero recurrence risk. After two negative tests, most patients do not exit active surveillance,” said Dr. Pradère. But the positive predictive value of biomarkers remains low for low-grade tumors.
The future of active surveillance in bladder cancer should involve better patient selection that relies on risk factors, enhanced modalities through imaging and biomarkers, and the advent of artificial intelligence to analyze cystoscopy results, concluded Dr. Pradère.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
PARIS — Should clinicians promote active surveillance for non–muscle-invasive bladder tumors (NMIBT) and establish it as a comprehensive management approach, as with prostate and kidney cancers?
During the 117th congress of the French Association of Urology (AFU), Benjamin Pradère, MD, urologic surgeon at Croix du Sud Clinic in Quint-Fonsegrives, France, advocated for this approach, suggesting that the use of biomarkers could enhance its effectiveness.
However, it requires careful patient selection, proper information, and relevant follow-up,” said Dr. Pradère, who is a member of the AFU Cancer Committee (CCAFU).
Low-Grade Tumors
NMIBTs are precancerous lesions and constitute 70%-80% of diagnosed bladder tumors. The remaining tumors are more severe invasive tumors that infiltrate deep tissues. NMIBTs, however, entail a high risk for recurrence (reaching 80% after endoscopic resection), as well as a high risk for progression.
As a result, the diagnosis of NMIBT involves follow-up that significantly impacts patients’ quality of life due to repeated cystoscopies and endovesical treatments. “Tumors with the most impact are low-grade Ta tumors”, with longer-term monitoring required for these low-risk tumors.
Hematuria is the most frequent clinical sign. NMIBT diagnosis occurs after endoscopic tumor resection via transurethral resection, followed by an anatomopathological analysis to determine cell grade and tumor stage. Treatment depends on the risk of recurrence and progression, as well as the risk of therapeutic failure after the initial resection.
Risk stratification distinguishes the following four levels:
- Low-risk tumors: Low-grade pTa urothelial tumors, unifocal, < 3 cm, no history of bladder tumors. Low risk of recurrence and progression.
- Intermediate-risk tumors: Other low-grade pTa urothelial tumors with no high-risk criteria. Low risk of progression but high risk of recurrence.
- High-risk tumors: Tumors with at least one risk factor: Stage pT1, high grade, presence of carcinoma in situ. High risks of progression and recurrence.
- Very high-risk tumors: Tumors combining all risk factors (pT1 grade with carcinoma in situ). Very high and early risk of progression.
“We know that low-grade NMIBTs have no impact on survival,” said Dr. Pradère. For these tumors, which represent 60% of diagnosed NMIBTs, or approximately 250,000 new cases annually in France, specific survival is > 99%, meaning that most diagnosed patients will not die of bladder cancer.
The recurrence rate for low-grade tumors is 50%, but recurrences are “almost always low-grade and rarely invade the basement membrane,” said Pradère. Implementing active surveillance to limit surgical intervention to more advanced forms seems to be relevant for these tumors.
Cystoscopy Every 3 Months
According to CCAFU recommendations, “active surveillance is a therapeutic alternative that can be proposed for patients with recurrent low-risk NMIBT after the initial diagnosis.” Criteria include low-grade pTa, fewer than five tumors, size ≤ 15 mm, negative urinary cytology, asymptomatic nature, and the patient’s acceptance of closer monitoring.
While active surveillance has become the standard treatment for low-risk prostate cancer, this therapeutic option remains marginal in bladder cancer, as in kidney cancer. The goal is to defer or avoid surgical treatment by closely monitoring the natural progression of the disease.
For NMIBTs, follow-up modalities are not yet specifically recommended because of a lack of data, said Dr. Pradère. According to a consensus, cystoscopy should be repeated every 3 months for a year and then every 6 months. Unlike standard follow-up, it includes cytology “to not miss the transition to high grade.”
CCAFU recommends discontinuing active surveillance if any of the following criteria are present:
- More than 10 lesions
- Size > 30 mm
- Positive cytology
- Symptoms (hematuria, micturition disorders, and recurring infections).
Literature on the benefits of active surveillance in bladder tumors is still limited. Only seven studies are available. Overall, for nearly 600 included patients, tumors progressed in about 12% of cases. Progression to invasive tumors occurred in 0.8% of patients (n = 5).
13 Months’ Surveillance
According to a long-term study (median follow-up of 38 months), patients mostly exit active surveillance in the first year. The median duration of active surveillance is 13 months. Active surveillance is discontinued to surgically treat tumors that turn out to be low-grade Ta tumors in 70% of cases.
The following factors predicting recurrence and progression of tumors have been identified: Multiple tumors, early recurrence (within a year of initial diagnosis), frequent recurrence (more than one recurrence per year), tumors > 3 cm, and failure of previous endovesical treatment.
Recent studies have shown that with at least three of these recurrence and progression factors, the median duration under active surveillance is 15 months compared with 28 months in the absence of such factors. “Considering these factors, it is possible to assess the benefit of active surveillance for the patient,” said Dr. Pradère.
If active surveillance for bladder tumors is still not widely practiced, then the contribution of imaging (MRI and ultrasound) and biomarkers could promote its adoption. “The use of biomarkers should change the game and encourage active surveillance in patients with small polyps,” said Dr. Pradère.
ADXBladder Test Utility
A study highlighted the importance of evaluating minichromosome maintenance protein 5 expression during active surveillance using the ADXBladder ELISA test on a urine sample. This test is usually used in bladder cancer diagnosis.
“This study showed that a negative result in two consecutive tests during active surveillance is associated with an almost zero recurrence risk. After two negative tests, most patients do not exit active surveillance,” said Dr. Pradère. But the positive predictive value of biomarkers remains low for low-grade tumors.
The future of active surveillance in bladder cancer should involve better patient selection that relies on risk factors, enhanced modalities through imaging and biomarkers, and the advent of artificial intelligence to analyze cystoscopy results, concluded Dr. Pradère.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
PARIS — Should clinicians promote active surveillance for non–muscle-invasive bladder tumors (NMIBT) and establish it as a comprehensive management approach, as with prostate and kidney cancers?
During the 117th congress of the French Association of Urology (AFU), Benjamin Pradère, MD, urologic surgeon at Croix du Sud Clinic in Quint-Fonsegrives, France, advocated for this approach, suggesting that the use of biomarkers could enhance its effectiveness.
However, it requires careful patient selection, proper information, and relevant follow-up,” said Dr. Pradère, who is a member of the AFU Cancer Committee (CCAFU).
Low-Grade Tumors
NMIBTs are precancerous lesions and constitute 70%-80% of diagnosed bladder tumors. The remaining tumors are more severe invasive tumors that infiltrate deep tissues. NMIBTs, however, entail a high risk for recurrence (reaching 80% after endoscopic resection), as well as a high risk for progression.
As a result, the diagnosis of NMIBT involves follow-up that significantly impacts patients’ quality of life due to repeated cystoscopies and endovesical treatments. “Tumors with the most impact are low-grade Ta tumors”, with longer-term monitoring required for these low-risk tumors.
Hematuria is the most frequent clinical sign. NMIBT diagnosis occurs after endoscopic tumor resection via transurethral resection, followed by an anatomopathological analysis to determine cell grade and tumor stage. Treatment depends on the risk of recurrence and progression, as well as the risk of therapeutic failure after the initial resection.
Risk stratification distinguishes the following four levels:
- Low-risk tumors: Low-grade pTa urothelial tumors, unifocal, < 3 cm, no history of bladder tumors. Low risk of recurrence and progression.
- Intermediate-risk tumors: Other low-grade pTa urothelial tumors with no high-risk criteria. Low risk of progression but high risk of recurrence.
- High-risk tumors: Tumors with at least one risk factor: Stage pT1, high grade, presence of carcinoma in situ. High risks of progression and recurrence.
- Very high-risk tumors: Tumors combining all risk factors (pT1 grade with carcinoma in situ). Very high and early risk of progression.
“We know that low-grade NMIBTs have no impact on survival,” said Dr. Pradère. For these tumors, which represent 60% of diagnosed NMIBTs, or approximately 250,000 new cases annually in France, specific survival is > 99%, meaning that most diagnosed patients will not die of bladder cancer.
The recurrence rate for low-grade tumors is 50%, but recurrences are “almost always low-grade and rarely invade the basement membrane,” said Pradère. Implementing active surveillance to limit surgical intervention to more advanced forms seems to be relevant for these tumors.
Cystoscopy Every 3 Months
According to CCAFU recommendations, “active surveillance is a therapeutic alternative that can be proposed for patients with recurrent low-risk NMIBT after the initial diagnosis.” Criteria include low-grade pTa, fewer than five tumors, size ≤ 15 mm, negative urinary cytology, asymptomatic nature, and the patient’s acceptance of closer monitoring.
While active surveillance has become the standard treatment for low-risk prostate cancer, this therapeutic option remains marginal in bladder cancer, as in kidney cancer. The goal is to defer or avoid surgical treatment by closely monitoring the natural progression of the disease.
For NMIBTs, follow-up modalities are not yet specifically recommended because of a lack of data, said Dr. Pradère. According to a consensus, cystoscopy should be repeated every 3 months for a year and then every 6 months. Unlike standard follow-up, it includes cytology “to not miss the transition to high grade.”
CCAFU recommends discontinuing active surveillance if any of the following criteria are present:
- More than 10 lesions
- Size > 30 mm
- Positive cytology
- Symptoms (hematuria, micturition disorders, and recurring infections).
Literature on the benefits of active surveillance in bladder tumors is still limited. Only seven studies are available. Overall, for nearly 600 included patients, tumors progressed in about 12% of cases. Progression to invasive tumors occurred in 0.8% of patients (n = 5).
13 Months’ Surveillance
According to a long-term study (median follow-up of 38 months), patients mostly exit active surveillance in the first year. The median duration of active surveillance is 13 months. Active surveillance is discontinued to surgically treat tumors that turn out to be low-grade Ta tumors in 70% of cases.
The following factors predicting recurrence and progression of tumors have been identified: Multiple tumors, early recurrence (within a year of initial diagnosis), frequent recurrence (more than one recurrence per year), tumors > 3 cm, and failure of previous endovesical treatment.
Recent studies have shown that with at least three of these recurrence and progression factors, the median duration under active surveillance is 15 months compared with 28 months in the absence of such factors. “Considering these factors, it is possible to assess the benefit of active surveillance for the patient,” said Dr. Pradère.
If active surveillance for bladder tumors is still not widely practiced, then the contribution of imaging (MRI and ultrasound) and biomarkers could promote its adoption. “The use of biomarkers should change the game and encourage active surveillance in patients with small polyps,” said Dr. Pradère.
ADXBladder Test Utility
A study highlighted the importance of evaluating minichromosome maintenance protein 5 expression during active surveillance using the ADXBladder ELISA test on a urine sample. This test is usually used in bladder cancer diagnosis.
“This study showed that a negative result in two consecutive tests during active surveillance is associated with an almost zero recurrence risk. After two negative tests, most patients do not exit active surveillance,” said Dr. Pradère. But the positive predictive value of biomarkers remains low for low-grade tumors.
The future of active surveillance in bladder cancer should involve better patient selection that relies on risk factors, enhanced modalities through imaging and biomarkers, and the advent of artificial intelligence to analyze cystoscopy results, concluded Dr. Pradère.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
Shelf Life for Opioid Overdose Drug Naloxone Extended
At the request of the US Food and Drug Administration (FDA), Emergent BioSolutions has extended the shelf life of the rapid opioid overdose reversal agent, naloxone (4 mg) nasal spray (Narcan), from 3 to 4 years.
Naloxone is “an important tool” in addressing opioid overdoses, and this extension supports the FDA’s “efforts to ensure more OTC naloxone products remain available to the public,” Marta Sokolowska, PhD, with the FDA Center for Drug Evaluation and Research, said in a statement.
Naloxone nasal spray was first approved by the FDA in 2015 as a prescription drug. Last spring, the agency approved the drug for over-the-counter use.
“The shelf life of products that were produced and distributed prior to this announcement is not affected and remains unchanged. Prescribers, patients, and caregivers are advised to continue to abide by the expiration date printed on each product’s packaging and within the product’s labeling,” the FDA advised.
“FDA’s request for this shelf-life extension is a testament to the agency’s continuing progress toward implementing the FDA Overdose Prevention Framework, which provides our vision to undertake impactful, creative actions to encourage harm reduction and innovation in reducing controlled substance-related overdoses and deaths,” the agency said.
According to the US Centers for Disease Control and Prevention, from 1999 to 2021, nearly 645,000 people died from an overdose involving any opioid, including prescription and illicit opioids.
A version of this article appeared on Medscape.com.
At the request of the US Food and Drug Administration (FDA), Emergent BioSolutions has extended the shelf life of the rapid opioid overdose reversal agent, naloxone (4 mg) nasal spray (Narcan), from 3 to 4 years.
Naloxone is “an important tool” in addressing opioid overdoses, and this extension supports the FDA’s “efforts to ensure more OTC naloxone products remain available to the public,” Marta Sokolowska, PhD, with the FDA Center for Drug Evaluation and Research, said in a statement.
Naloxone nasal spray was first approved by the FDA in 2015 as a prescription drug. Last spring, the agency approved the drug for over-the-counter use.
“The shelf life of products that were produced and distributed prior to this announcement is not affected and remains unchanged. Prescribers, patients, and caregivers are advised to continue to abide by the expiration date printed on each product’s packaging and within the product’s labeling,” the FDA advised.
“FDA’s request for this shelf-life extension is a testament to the agency’s continuing progress toward implementing the FDA Overdose Prevention Framework, which provides our vision to undertake impactful, creative actions to encourage harm reduction and innovation in reducing controlled substance-related overdoses and deaths,” the agency said.
According to the US Centers for Disease Control and Prevention, from 1999 to 2021, nearly 645,000 people died from an overdose involving any opioid, including prescription and illicit opioids.
A version of this article appeared on Medscape.com.
At the request of the US Food and Drug Administration (FDA), Emergent BioSolutions has extended the shelf life of the rapid opioid overdose reversal agent, naloxone (4 mg) nasal spray (Narcan), from 3 to 4 years.
Naloxone is “an important tool” in addressing opioid overdoses, and this extension supports the FDA’s “efforts to ensure more OTC naloxone products remain available to the public,” Marta Sokolowska, PhD, with the FDA Center for Drug Evaluation and Research, said in a statement.
Naloxone nasal spray was first approved by the FDA in 2015 as a prescription drug. Last spring, the agency approved the drug for over-the-counter use.
“The shelf life of products that were produced and distributed prior to this announcement is not affected and remains unchanged. Prescribers, patients, and caregivers are advised to continue to abide by the expiration date printed on each product’s packaging and within the product’s labeling,” the FDA advised.
“FDA’s request for this shelf-life extension is a testament to the agency’s continuing progress toward implementing the FDA Overdose Prevention Framework, which provides our vision to undertake impactful, creative actions to encourage harm reduction and innovation in reducing controlled substance-related overdoses and deaths,” the agency said.
According to the US Centers for Disease Control and Prevention, from 1999 to 2021, nearly 645,000 people died from an overdose involving any opioid, including prescription and illicit opioids.
A version of this article appeared on Medscape.com.
Even Intentional Weight Loss Linked With Cancer
This transcript has been edited for clarity.
As anyone who has been through medical training will tell you, some little scenes just stick with you. I had been seeing a patient in our resident clinic in West Philly for a couple of years. She was in her mid-60s with diabetes and hypertension and a distant smoking history. She was overweight and had been trying to improve her diet and lose weight since I started seeing her. One day she came in and was delighted to report that she had finally started shedding some pounds — about 15 in the past 2 months.
I enthusiastically told my preceptor that my careful dietary counseling had finally done the job. She looked through the chart for a moment and asked, “Is she up to date on her cancer screening?” A workup revealed adenocarcinoma of the lung. The patient did well, actually, but the story stuck with me.
The textbooks call it “unintentional weight loss,” often in big, scary letters, and every doctor will go just a bit pale if a patient tells them that, despite efforts not to, they are losing weight. But true unintentional weight loss is not that common. After all, most of us are at least half-heartedly trying to lose weight all the time. Should doctors be worried when we are successful?
A new study suggests that perhaps they should. We’re talking about this study, appearing in JAMA, which combined participants from two long-running observational cohorts: 120,000 women from the Nurses’ Health Study, and 50,000 men from the Health Professionals Follow-Up Study. (These cohorts started in the 1970s and 1980s, so we’ll give them a pass on the gender-specific study designs.)
The rationale of enrolling healthcare providers in these cohort studies is that they would be reliable witnesses of their own health status. If a nurse or doctor says they have pancreatic cancer, it’s likely that they truly have pancreatic cancer. Detailed health surveys were distributed to the participants every other year, and the average follow-up was more than a decade.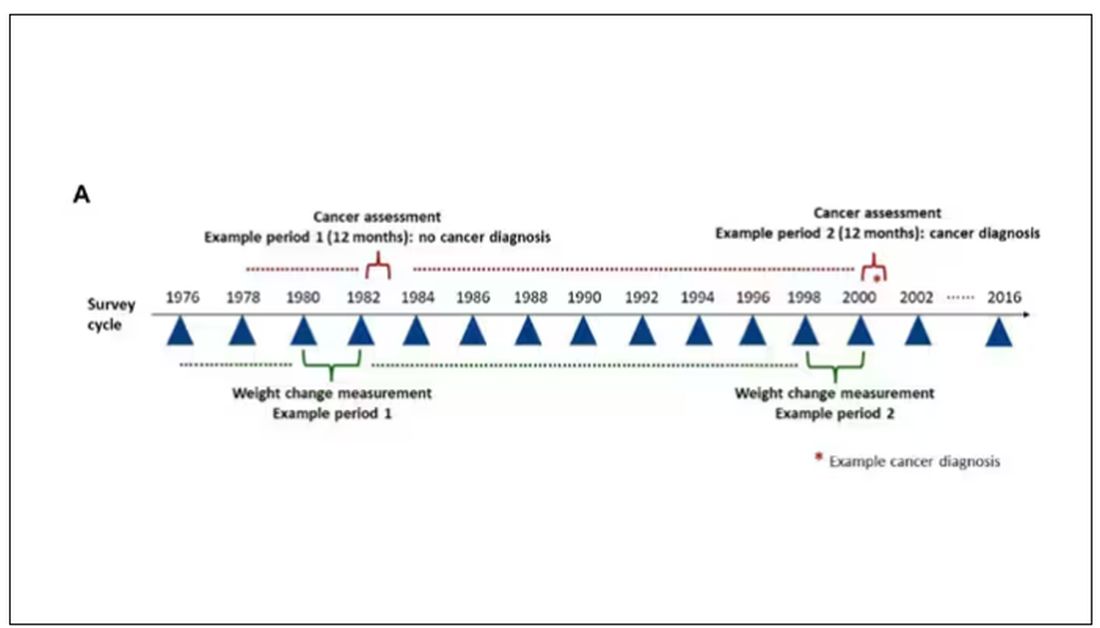
Participants recorded their weight — as an aside, a nested study found that self-reported rate was extremely well correlated with professionally measured weight — and whether they had received a cancer diagnosis since the last survey.
This allowed researchers to look at the phenomenon described above. Would weight loss precede a new diagnosis of cancer? And, more interestingly, would intentional weight loss precede a new diagnosis of cancer.
I don’t think it will surprise you to hear that individuals in the highest category of weight loss, those who lost more than 10% of their body weight over a 2-year period, had a larger risk of being diagnosed with cancer in the next year. That’s the yellow line in this graph. In fact, they had about a 40% higher risk than those who did not lose weight.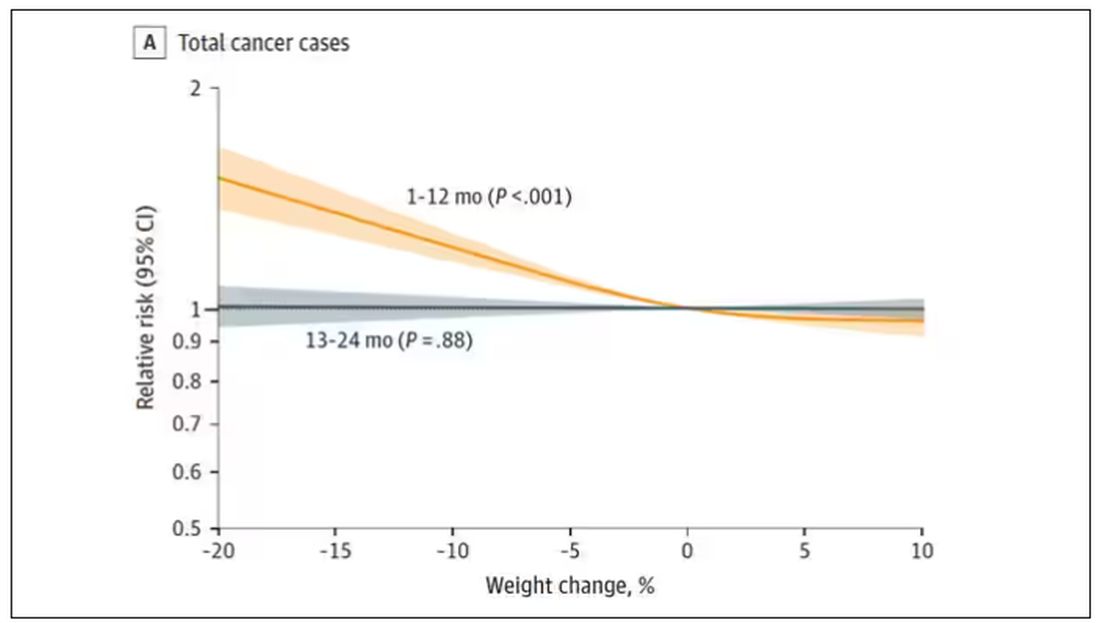
Increased risk was found across multiple cancer types, though cancers of the gastrointestinal tract, not surprisingly, were most strongly associated with antecedent weight loss.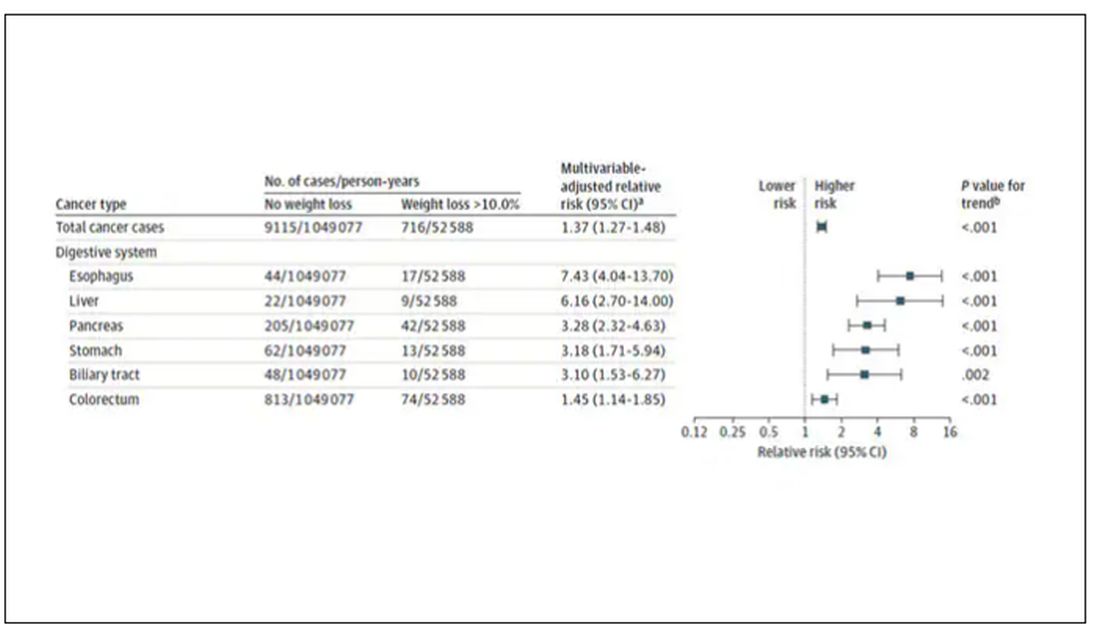
What about intentionality of weight loss? Unfortunately, the surveys did not ask participants whether they were trying to lose weight. Rather, the surveys asked about exercise and dietary habits. The researchers leveraged these responses to create three categories of participants: those who seemed to be trying to lose weight (defined as people who had increased their exercise and dietary quality); those who didn’t seem to be trying to lose weight (they changed neither exercise nor dietary behaviors); and a middle group, which changed one or the other of these behaviors but not both.
Let’s look at those who really seemed to be trying to lose weight. Over 2 years, they got more exercise and improved their diet.
If they succeeded in losing 10% or more of their body weight, they still had a higher risk for cancer than those who had not lost weight — about 30% higher, which is not that different from the 40% increased risk when you include those folks who weren’t changing their lifestyle.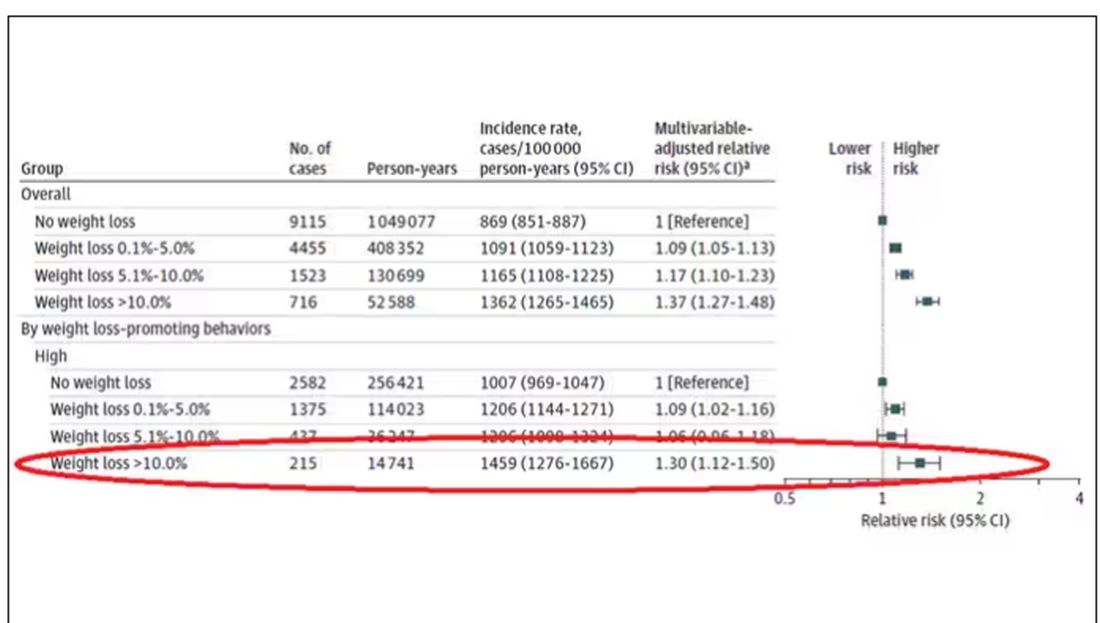
This is why this study is important. The classic teaching is that unintentional weight loss is a bad thing and needs a workup. That’s fine. But we live in a world where perhaps the majority of people are, at any given time, trying to lose weight.
We need to be careful here. I am not by any means trying to say that people who have successfully lost weight have cancer. Both of the following statements can be true:
Significant weight loss, whether intentional or not, is associated with a higher risk for cancer.
Most people with significant weight loss will not have cancer.
Both of these can be true because cancer is, fortunately, rare. Of people who lose weight, the vast majority will lose weight because they are engaging in healthier behaviors. A small number may lose weight because something else is wrong. It’s just hard to tell the two apart.
Out of the nearly 200,000 people in this study, only around 16,000 developed cancer during follow-up. Again, although the chance of having cancer is slightly higher if someone has experienced weight loss, the chance is still very low.
We also need to avoid suggesting that weight loss causes cancer. Some people lose weight because of an existing, as of yet undiagnosed cancer and its metabolic effects. This is borne out if you look at the risk of being diagnosed with cancer as you move further away from the interval of weight loss.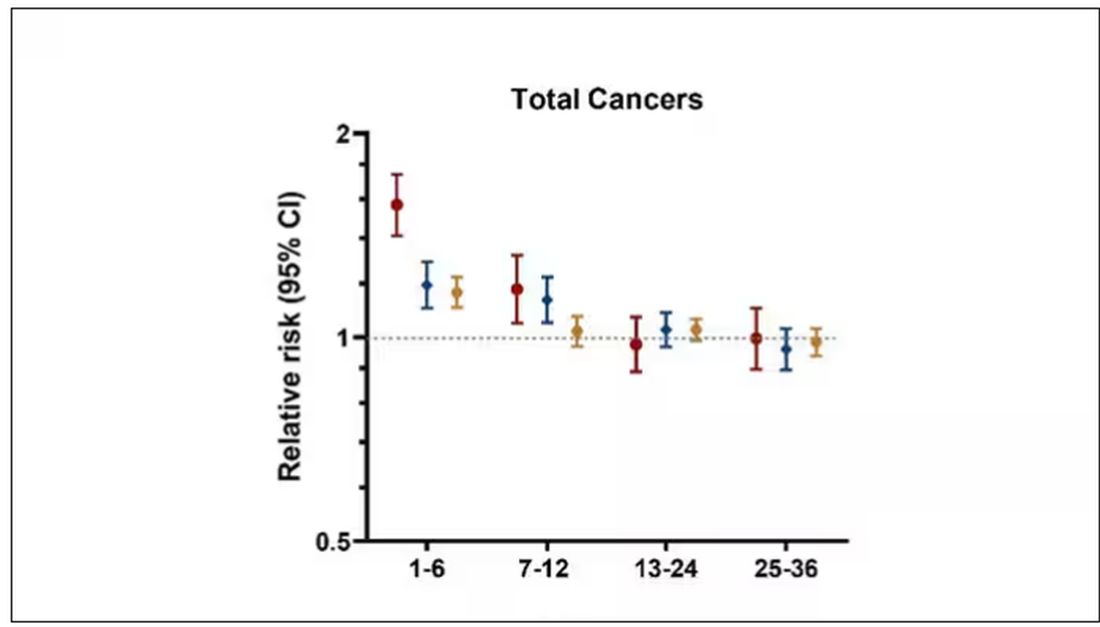
The further you get from the year of that 10% weight loss, the less likely you are to be diagnosed with cancer. Most of these cancers are diagnosed within a year of losing weight. In other words, if you’re reading this and getting worried that you lost weight 10 years ago, you’re probably out of the woods. That was, most likely, just you getting healthier.
Last thing: We have methods for weight loss now that are way more effective than diet or exercise. I’m looking at you, Ozempic. But aside from the weight loss wonder drugs, we have surgery and other interventions. This study did not capture any of that data. Ozempic wasn’t even on the market during this study, so we can’t say anything about the relationship between weight loss and cancer among people using nonlifestyle mechanisms to lose weight.
It’s a complicated system. But the clinically actionable point here is to notice if patients have lost weight. If they’ve lost it without trying, further workup is reasonable. If they’ve lost it but were trying to lose it, tell them “good job.” And consider a workup anyway.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
As anyone who has been through medical training will tell you, some little scenes just stick with you. I had been seeing a patient in our resident clinic in West Philly for a couple of years. She was in her mid-60s with diabetes and hypertension and a distant smoking history. She was overweight and had been trying to improve her diet and lose weight since I started seeing her. One day she came in and was delighted to report that she had finally started shedding some pounds — about 15 in the past 2 months.
I enthusiastically told my preceptor that my careful dietary counseling had finally done the job. She looked through the chart for a moment and asked, “Is she up to date on her cancer screening?” A workup revealed adenocarcinoma of the lung. The patient did well, actually, but the story stuck with me.
The textbooks call it “unintentional weight loss,” often in big, scary letters, and every doctor will go just a bit pale if a patient tells them that, despite efforts not to, they are losing weight. But true unintentional weight loss is not that common. After all, most of us are at least half-heartedly trying to lose weight all the time. Should doctors be worried when we are successful?
A new study suggests that perhaps they should. We’re talking about this study, appearing in JAMA, which combined participants from two long-running observational cohorts: 120,000 women from the Nurses’ Health Study, and 50,000 men from the Health Professionals Follow-Up Study. (These cohorts started in the 1970s and 1980s, so we’ll give them a pass on the gender-specific study designs.)
The rationale of enrolling healthcare providers in these cohort studies is that they would be reliable witnesses of their own health status. If a nurse or doctor says they have pancreatic cancer, it’s likely that they truly have pancreatic cancer. Detailed health surveys were distributed to the participants every other year, and the average follow-up was more than a decade.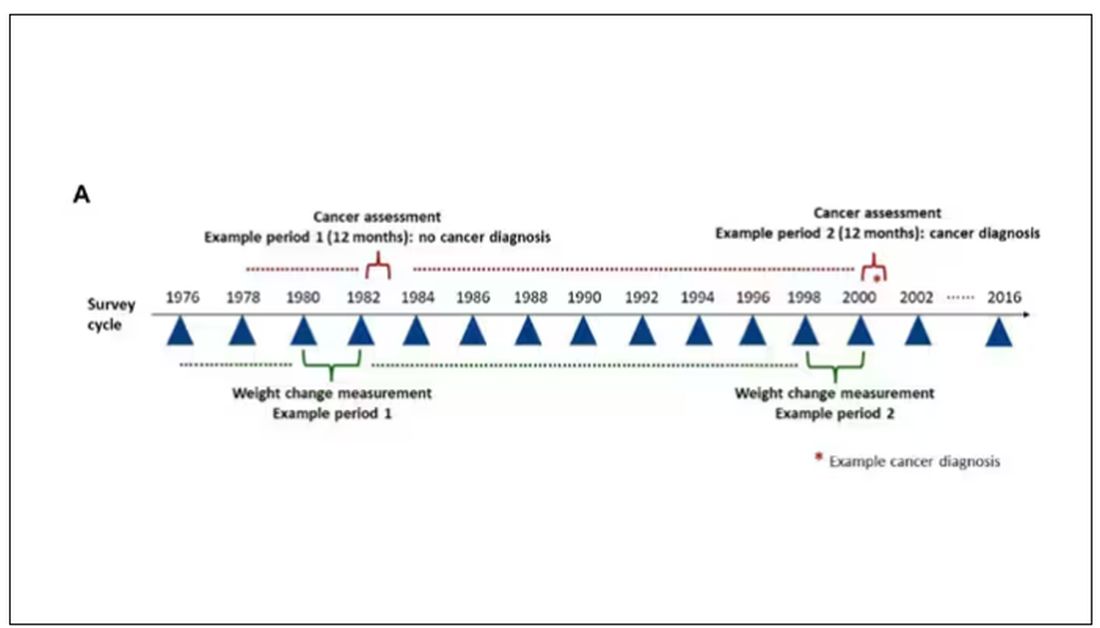
Participants recorded their weight — as an aside, a nested study found that self-reported rate was extremely well correlated with professionally measured weight — and whether they had received a cancer diagnosis since the last survey.
This allowed researchers to look at the phenomenon described above. Would weight loss precede a new diagnosis of cancer? And, more interestingly, would intentional weight loss precede a new diagnosis of cancer.
I don’t think it will surprise you to hear that individuals in the highest category of weight loss, those who lost more than 10% of their body weight over a 2-year period, had a larger risk of being diagnosed with cancer in the next year. That’s the yellow line in this graph. In fact, they had about a 40% higher risk than those who did not lose weight.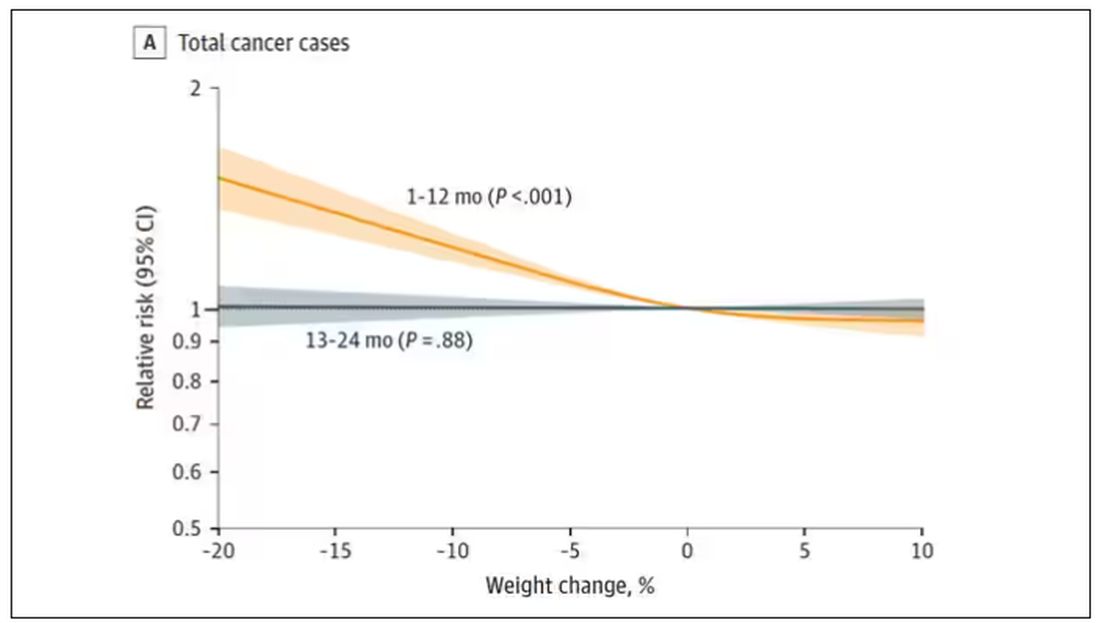
Increased risk was found across multiple cancer types, though cancers of the gastrointestinal tract, not surprisingly, were most strongly associated with antecedent weight loss.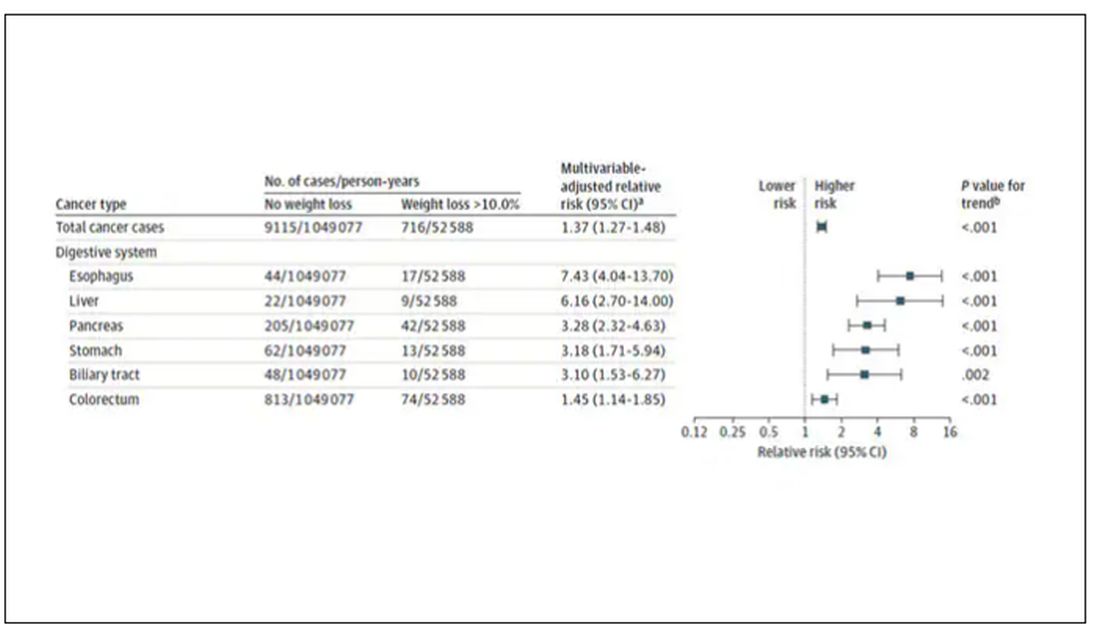
What about intentionality of weight loss? Unfortunately, the surveys did not ask participants whether they were trying to lose weight. Rather, the surveys asked about exercise and dietary habits. The researchers leveraged these responses to create three categories of participants: those who seemed to be trying to lose weight (defined as people who had increased their exercise and dietary quality); those who didn’t seem to be trying to lose weight (they changed neither exercise nor dietary behaviors); and a middle group, which changed one or the other of these behaviors but not both.
Let’s look at those who really seemed to be trying to lose weight. Over 2 years, they got more exercise and improved their diet.
If they succeeded in losing 10% or more of their body weight, they still had a higher risk for cancer than those who had not lost weight — about 30% higher, which is not that different from the 40% increased risk when you include those folks who weren’t changing their lifestyle.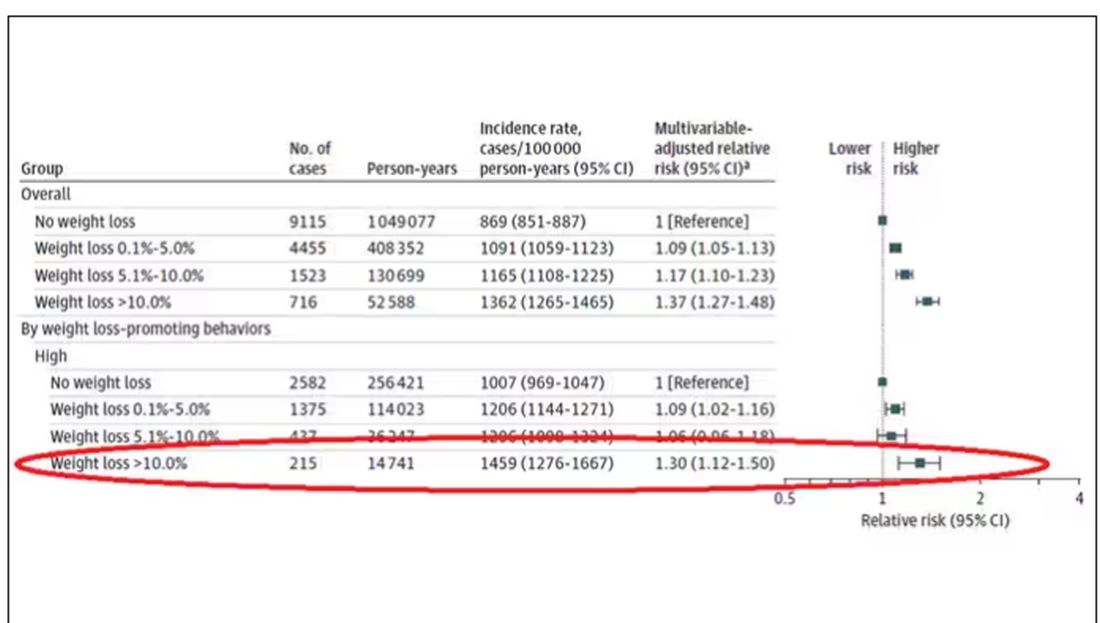
This is why this study is important. The classic teaching is that unintentional weight loss is a bad thing and needs a workup. That’s fine. But we live in a world where perhaps the majority of people are, at any given time, trying to lose weight.
We need to be careful here. I am not by any means trying to say that people who have successfully lost weight have cancer. Both of the following statements can be true:
Significant weight loss, whether intentional or not, is associated with a higher risk for cancer.
Most people with significant weight loss will not have cancer.
Both of these can be true because cancer is, fortunately, rare. Of people who lose weight, the vast majority will lose weight because they are engaging in healthier behaviors. A small number may lose weight because something else is wrong. It’s just hard to tell the two apart.
Out of the nearly 200,000 people in this study, only around 16,000 developed cancer during follow-up. Again, although the chance of having cancer is slightly higher if someone has experienced weight loss, the chance is still very low.
We also need to avoid suggesting that weight loss causes cancer. Some people lose weight because of an existing, as of yet undiagnosed cancer and its metabolic effects. This is borne out if you look at the risk of being diagnosed with cancer as you move further away from the interval of weight loss.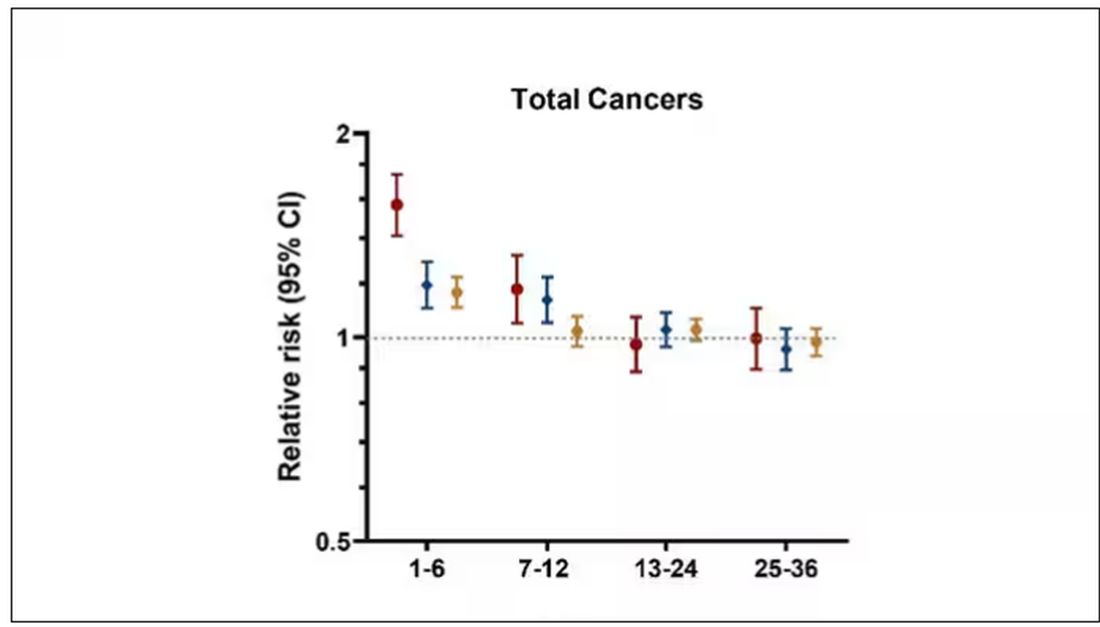
The further you get from the year of that 10% weight loss, the less likely you are to be diagnosed with cancer. Most of these cancers are diagnosed within a year of losing weight. In other words, if you’re reading this and getting worried that you lost weight 10 years ago, you’re probably out of the woods. That was, most likely, just you getting healthier.
Last thing: We have methods for weight loss now that are way more effective than diet or exercise. I’m looking at you, Ozempic. But aside from the weight loss wonder drugs, we have surgery and other interventions. This study did not capture any of that data. Ozempic wasn’t even on the market during this study, so we can’t say anything about the relationship between weight loss and cancer among people using nonlifestyle mechanisms to lose weight.
It’s a complicated system. But the clinically actionable point here is to notice if patients have lost weight. If they’ve lost it without trying, further workup is reasonable. If they’ve lost it but were trying to lose it, tell them “good job.” And consider a workup anyway.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
As anyone who has been through medical training will tell you, some little scenes just stick with you. I had been seeing a patient in our resident clinic in West Philly for a couple of years. She was in her mid-60s with diabetes and hypertension and a distant smoking history. She was overweight and had been trying to improve her diet and lose weight since I started seeing her. One day she came in and was delighted to report that she had finally started shedding some pounds — about 15 in the past 2 months.
I enthusiastically told my preceptor that my careful dietary counseling had finally done the job. She looked through the chart for a moment and asked, “Is she up to date on her cancer screening?” A workup revealed adenocarcinoma of the lung. The patient did well, actually, but the story stuck with me.
The textbooks call it “unintentional weight loss,” often in big, scary letters, and every doctor will go just a bit pale if a patient tells them that, despite efforts not to, they are losing weight. But true unintentional weight loss is not that common. After all, most of us are at least half-heartedly trying to lose weight all the time. Should doctors be worried when we are successful?
A new study suggests that perhaps they should. We’re talking about this study, appearing in JAMA, which combined participants from two long-running observational cohorts: 120,000 women from the Nurses’ Health Study, and 50,000 men from the Health Professionals Follow-Up Study. (These cohorts started in the 1970s and 1980s, so we’ll give them a pass on the gender-specific study designs.)
The rationale of enrolling healthcare providers in these cohort studies is that they would be reliable witnesses of their own health status. If a nurse or doctor says they have pancreatic cancer, it’s likely that they truly have pancreatic cancer. Detailed health surveys were distributed to the participants every other year, and the average follow-up was more than a decade.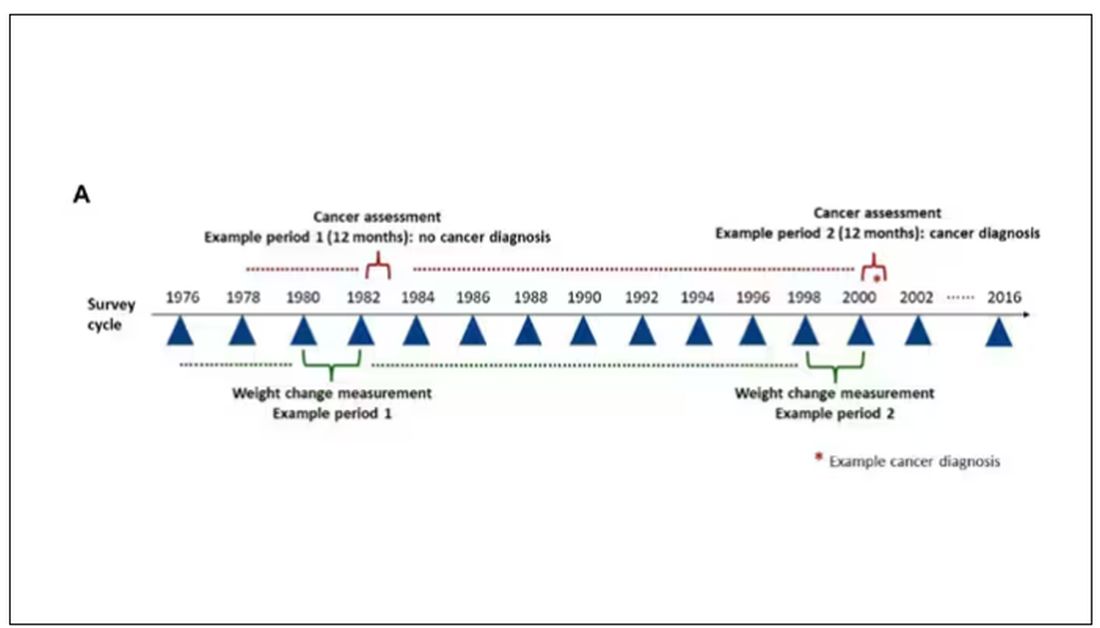
Participants recorded their weight — as an aside, a nested study found that self-reported rate was extremely well correlated with professionally measured weight — and whether they had received a cancer diagnosis since the last survey.
This allowed researchers to look at the phenomenon described above. Would weight loss precede a new diagnosis of cancer? And, more interestingly, would intentional weight loss precede a new diagnosis of cancer.
I don’t think it will surprise you to hear that individuals in the highest category of weight loss, those who lost more than 10% of their body weight over a 2-year period, had a larger risk of being diagnosed with cancer in the next year. That’s the yellow line in this graph. In fact, they had about a 40% higher risk than those who did not lose weight.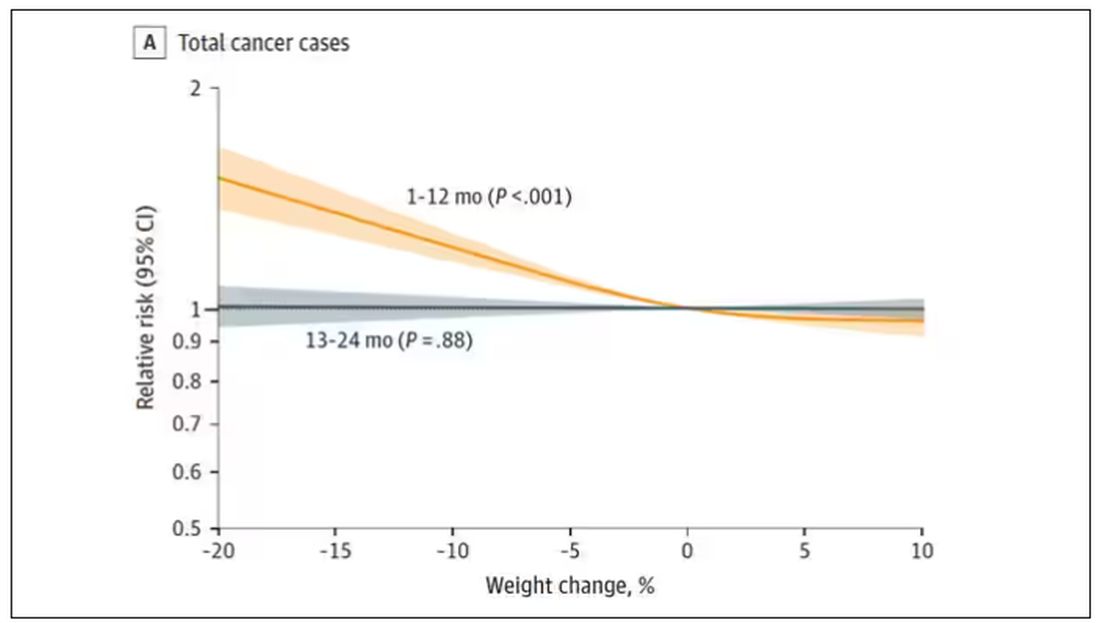
Increased risk was found across multiple cancer types, though cancers of the gastrointestinal tract, not surprisingly, were most strongly associated with antecedent weight loss.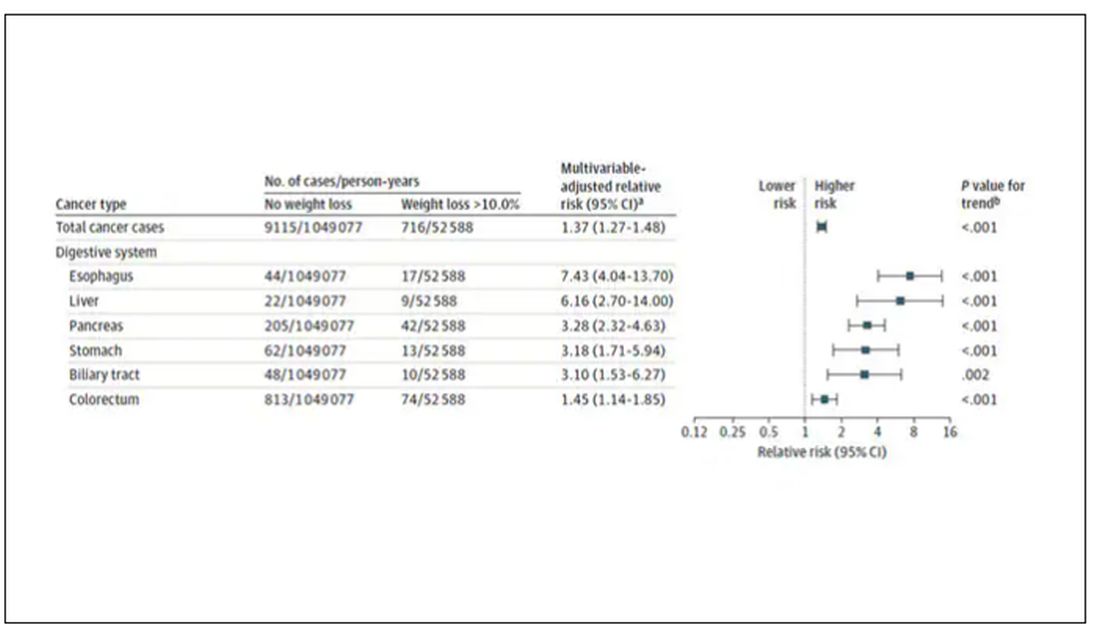
What about intentionality of weight loss? Unfortunately, the surveys did not ask participants whether they were trying to lose weight. Rather, the surveys asked about exercise and dietary habits. The researchers leveraged these responses to create three categories of participants: those who seemed to be trying to lose weight (defined as people who had increased their exercise and dietary quality); those who didn’t seem to be trying to lose weight (they changed neither exercise nor dietary behaviors); and a middle group, which changed one or the other of these behaviors but not both.
Let’s look at those who really seemed to be trying to lose weight. Over 2 years, they got more exercise and improved their diet.
If they succeeded in losing 10% or more of their body weight, they still had a higher risk for cancer than those who had not lost weight — about 30% higher, which is not that different from the 40% increased risk when you include those folks who weren’t changing their lifestyle.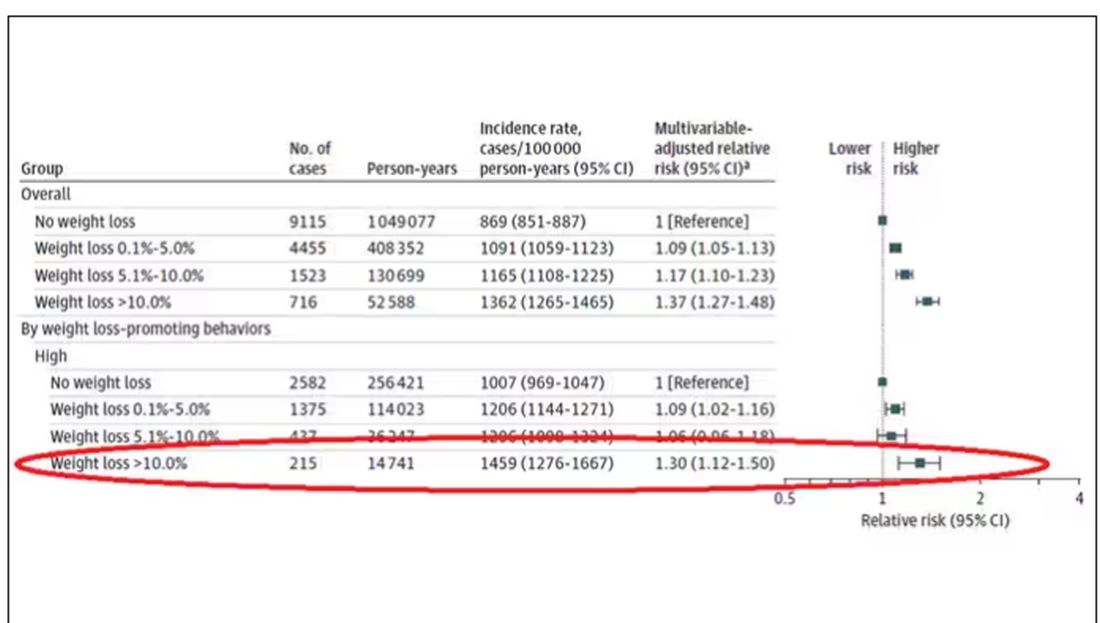
This is why this study is important. The classic teaching is that unintentional weight loss is a bad thing and needs a workup. That’s fine. But we live in a world where perhaps the majority of people are, at any given time, trying to lose weight.
We need to be careful here. I am not by any means trying to say that people who have successfully lost weight have cancer. Both of the following statements can be true:
Significant weight loss, whether intentional or not, is associated with a higher risk for cancer.
Most people with significant weight loss will not have cancer.
Both of these can be true because cancer is, fortunately, rare. Of people who lose weight, the vast majority will lose weight because they are engaging in healthier behaviors. A small number may lose weight because something else is wrong. It’s just hard to tell the two apart.
Out of the nearly 200,000 people in this study, only around 16,000 developed cancer during follow-up. Again, although the chance of having cancer is slightly higher if someone has experienced weight loss, the chance is still very low.
We also need to avoid suggesting that weight loss causes cancer. Some people lose weight because of an existing, as of yet undiagnosed cancer and its metabolic effects. This is borne out if you look at the risk of being diagnosed with cancer as you move further away from the interval of weight loss.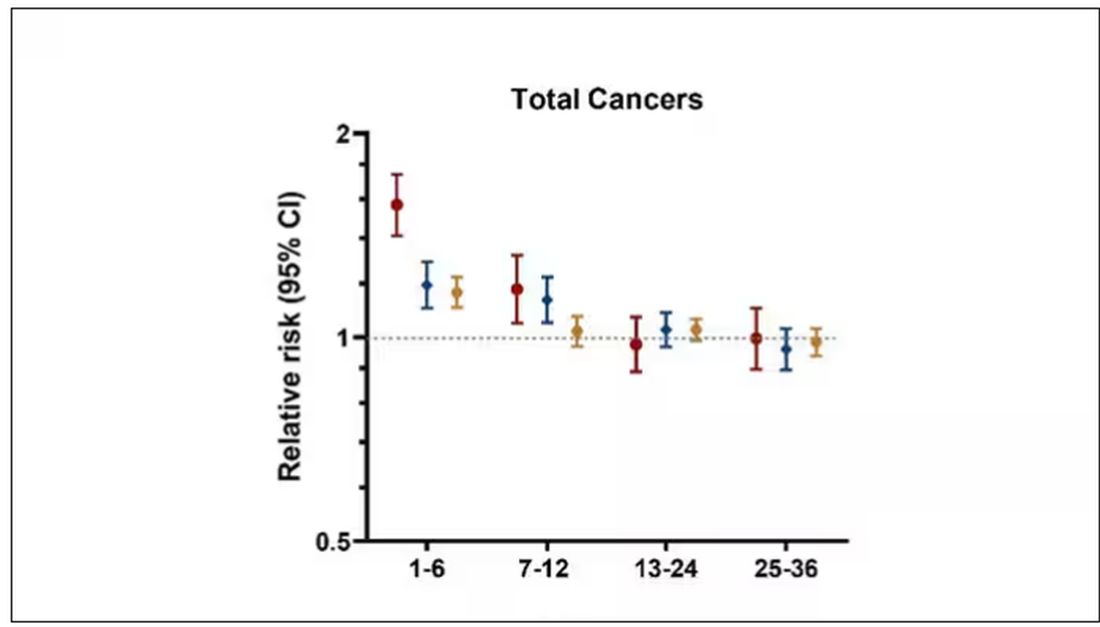
The further you get from the year of that 10% weight loss, the less likely you are to be diagnosed with cancer. Most of these cancers are diagnosed within a year of losing weight. In other words, if you’re reading this and getting worried that you lost weight 10 years ago, you’re probably out of the woods. That was, most likely, just you getting healthier.
Last thing: We have methods for weight loss now that are way more effective than diet or exercise. I’m looking at you, Ozempic. But aside from the weight loss wonder drugs, we have surgery and other interventions. This study did not capture any of that data. Ozempic wasn’t even on the market during this study, so we can’t say anything about the relationship between weight loss and cancer among people using nonlifestyle mechanisms to lose weight.
It’s a complicated system. But the clinically actionable point here is to notice if patients have lost weight. If they’ve lost it without trying, further workup is reasonable. If they’ve lost it but were trying to lose it, tell them “good job.” And consider a workup anyway.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
More Cardiologists Failing the Boards: Why and How to Fix?
Recent evidence suggests that more cardiologists are failing to pass their boards. , experts said.
Among the 1061 candidates who took their first American Board of Internal Medicine (ABIM) cardiovascular (CV) disease exam in 2022, about 80 fellows failed who might have passed had they trained in 2016-2019, according to Anis John Kadado, MD, University of Massachusetts Medical School–Baystate Campus, Springfield, Massachusetts, and colleagues, writing in a viewpoint article published in the Journal of the American College of Cardiology.
“The purpose of board examinations is to test the knowledge, core concepts, and fundamental principles of trainees as they deliver patient care,” said Dr. Kadado. “The decline in CV board pass rates reflects a potential gap in training, which may translate to suboptimal patient care.”
Why the Downturn?
Reasons for the increased failures are likely multifactorial, Dr. Kadado said. While some blame the ABIM, the exam has remained about the same over the past 6 years, so the test itself seems unlikely to explain the decline.
The main culprit, according to the viewpoint authors, is “the educational fallout from the disruptions caused by changes made in response to the COVID pandemic.” Changes that Dr. Kadado and colleagues said put the current class of graduating fellows at “high risk” of failing their boards in the fall.
The typical cardiology fellowship is 3 years or more for subspecialty training. Candidates who took the ABIM exam in 2021 had 18 months of training that overlapped with the pandemic response, and those who took the exam in 2022 had about 30 months of training disrupted by COVID. However, fellows who first took the exam in 2023 had essentially 36 months of training affected by COVID, potentially reducing their odds of passing.
“It is hard, if not impossible, to understand the driving forces for this recent decrease in performance on the initial ABIM certification examination, nor is it possible to forecast if there will be an end to this slide,” Jeffrey T. Kuvin, MD, chair of cardiology at the Zucker School of Medicine at Northwell Health, Manhasset, New York, and colleagues wrote in response to the viewpoint article.
The authors acknowledged that COVID disrupted graduate medical training and that the long-term effects of the disruption are now emerging. However, they also pinpoint other potential issues affecting fellows, including information/technology overload, a focus on patient volume over education, lack of attention to core concepts, and, as Dr. Kadado and colleagues noted, high burnout rates among fellows and knowledge gaps due to easy access to electronic resources rather than reading and studying to retain information.
COVID disruptions included limits on in-person learning, clinic exposure, research opportunities, and conference travel, according to the authors. From a 2020 viewpoint, Dr. Kuvin also noted the loss of bedside teaching and on-site grand rounds.
Furthermore, with deferrals of elective cardiac, endovascular, and structural catheterization procedures during the pandemic, elective cases normally done by fellows were postponed or canceled.
Restoring Education, Board Passing Rates
“Having recently passed the ABIM cardiovascular board exam myself, my take-home message at this point is for current fellows-in-training to remain organized, track training milestones, and foresee any training shortcomings,” Dr. Kadado said. Adding that fellows, graduates and leadership should “identify deficiencies and work on overcoming them.”
The viewpoint authors suggested strategies that fellowship leadership can use. These include:
- Regularly assessing faculty emotional well-being and burnout to ensure that they are engaged in meaningful teaching activities
- Emphasizing in-person learning, meaningful participation in conferences, and faculty oversight
- Encouraging fellows to pursue “self-directed learning” during off-hours
- Developing and implementing checklists, competency-based models, curricula, and rotations to ensure that training milestones are being met
- Returning to in-person imaging interpretation for imaging modalities such as echocardiography, cardiac CT, and cardiac MRI
- Ensuring that fellows take the American College of Cardiology in-training examination
- Providing practice question banks so that fellows can assess their knowledge gaps
“This might also be an opportune time to assess the assessment,” Dr. Kuvin and colleagues noted. “There are likely alternative or additional approaches that could provide a more comprehensive, modern tool to gauge clinical competence in a supportive manner.”
They suggested that these tools could include assessment by simulation for interventional cardiology and electrophysiology, oral case reviews, objective structured clinical exams, and evaluations of nonclinical competencies such as professionalism and health equity.
Implications for the New Cardiology Board
While the ABIM cardiology board exam days may be numbered, board certification via some type of exam process is not going away.
The American College of Cardiology and four other US CV societies — the American Heart Association, the Heart Failure Society of America, the Heart Rhythm Society, and the Society for Cardiovascular Angiography & Interventions — formally announced in September that they have joined forces to propose a new professional certification board called the American Board of Cardiovascular Medicine (ABCVM). The application to the ABMS for a separate cardiology board is still ongoing and will take time.
An initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured.
Preparing for the new board will likely be “largely the same” as for the ABIM board, Dr. Kadado said. “This includes access to practice question banks, faculty oversight, strong clinical exposure and practice, regular didactic sessions, and self-directed learning.”
“Passing the board exam is just one step in our ongoing journey as a cardiologist,” he added. “Our field is rapidly evolving, and continuous learning and adaptation are part of the very essence of being a healthcare professional.”
Dr. Kadado had no relevant relationships to disclose. Dr. Kuvin is an ACC trustee and has been heading up the working group to develop the ABCVM.
A version of this article appeared on Medscape.com.
Recent evidence suggests that more cardiologists are failing to pass their boards. , experts said.
Among the 1061 candidates who took their first American Board of Internal Medicine (ABIM) cardiovascular (CV) disease exam in 2022, about 80 fellows failed who might have passed had they trained in 2016-2019, according to Anis John Kadado, MD, University of Massachusetts Medical School–Baystate Campus, Springfield, Massachusetts, and colleagues, writing in a viewpoint article published in the Journal of the American College of Cardiology.
“The purpose of board examinations is to test the knowledge, core concepts, and fundamental principles of trainees as they deliver patient care,” said Dr. Kadado. “The decline in CV board pass rates reflects a potential gap in training, which may translate to suboptimal patient care.”
Why the Downturn?
Reasons for the increased failures are likely multifactorial, Dr. Kadado said. While some blame the ABIM, the exam has remained about the same over the past 6 years, so the test itself seems unlikely to explain the decline.
The main culprit, according to the viewpoint authors, is “the educational fallout from the disruptions caused by changes made in response to the COVID pandemic.” Changes that Dr. Kadado and colleagues said put the current class of graduating fellows at “high risk” of failing their boards in the fall.
The typical cardiology fellowship is 3 years or more for subspecialty training. Candidates who took the ABIM exam in 2021 had 18 months of training that overlapped with the pandemic response, and those who took the exam in 2022 had about 30 months of training disrupted by COVID. However, fellows who first took the exam in 2023 had essentially 36 months of training affected by COVID, potentially reducing their odds of passing.
“It is hard, if not impossible, to understand the driving forces for this recent decrease in performance on the initial ABIM certification examination, nor is it possible to forecast if there will be an end to this slide,” Jeffrey T. Kuvin, MD, chair of cardiology at the Zucker School of Medicine at Northwell Health, Manhasset, New York, and colleagues wrote in response to the viewpoint article.
The authors acknowledged that COVID disrupted graduate medical training and that the long-term effects of the disruption are now emerging. However, they also pinpoint other potential issues affecting fellows, including information/technology overload, a focus on patient volume over education, lack of attention to core concepts, and, as Dr. Kadado and colleagues noted, high burnout rates among fellows and knowledge gaps due to easy access to electronic resources rather than reading and studying to retain information.
COVID disruptions included limits on in-person learning, clinic exposure, research opportunities, and conference travel, according to the authors. From a 2020 viewpoint, Dr. Kuvin also noted the loss of bedside teaching and on-site grand rounds.
Furthermore, with deferrals of elective cardiac, endovascular, and structural catheterization procedures during the pandemic, elective cases normally done by fellows were postponed or canceled.
Restoring Education, Board Passing Rates
“Having recently passed the ABIM cardiovascular board exam myself, my take-home message at this point is for current fellows-in-training to remain organized, track training milestones, and foresee any training shortcomings,” Dr. Kadado said. Adding that fellows, graduates and leadership should “identify deficiencies and work on overcoming them.”
The viewpoint authors suggested strategies that fellowship leadership can use. These include:
- Regularly assessing faculty emotional well-being and burnout to ensure that they are engaged in meaningful teaching activities
- Emphasizing in-person learning, meaningful participation in conferences, and faculty oversight
- Encouraging fellows to pursue “self-directed learning” during off-hours
- Developing and implementing checklists, competency-based models, curricula, and rotations to ensure that training milestones are being met
- Returning to in-person imaging interpretation for imaging modalities such as echocardiography, cardiac CT, and cardiac MRI
- Ensuring that fellows take the American College of Cardiology in-training examination
- Providing practice question banks so that fellows can assess their knowledge gaps
“This might also be an opportune time to assess the assessment,” Dr. Kuvin and colleagues noted. “There are likely alternative or additional approaches that could provide a more comprehensive, modern tool to gauge clinical competence in a supportive manner.”
They suggested that these tools could include assessment by simulation for interventional cardiology and electrophysiology, oral case reviews, objective structured clinical exams, and evaluations of nonclinical competencies such as professionalism and health equity.
Implications for the New Cardiology Board
While the ABIM cardiology board exam days may be numbered, board certification via some type of exam process is not going away.
The American College of Cardiology and four other US CV societies — the American Heart Association, the Heart Failure Society of America, the Heart Rhythm Society, and the Society for Cardiovascular Angiography & Interventions — formally announced in September that they have joined forces to propose a new professional certification board called the American Board of Cardiovascular Medicine (ABCVM). The application to the ABMS for a separate cardiology board is still ongoing and will take time.
An initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured.
Preparing for the new board will likely be “largely the same” as for the ABIM board, Dr. Kadado said. “This includes access to practice question banks, faculty oversight, strong clinical exposure and practice, regular didactic sessions, and self-directed learning.”
“Passing the board exam is just one step in our ongoing journey as a cardiologist,” he added. “Our field is rapidly evolving, and continuous learning and adaptation are part of the very essence of being a healthcare professional.”
Dr. Kadado had no relevant relationships to disclose. Dr. Kuvin is an ACC trustee and has been heading up the working group to develop the ABCVM.
A version of this article appeared on Medscape.com.
Recent evidence suggests that more cardiologists are failing to pass their boards. , experts said.
Among the 1061 candidates who took their first American Board of Internal Medicine (ABIM) cardiovascular (CV) disease exam in 2022, about 80 fellows failed who might have passed had they trained in 2016-2019, according to Anis John Kadado, MD, University of Massachusetts Medical School–Baystate Campus, Springfield, Massachusetts, and colleagues, writing in a viewpoint article published in the Journal of the American College of Cardiology.
“The purpose of board examinations is to test the knowledge, core concepts, and fundamental principles of trainees as they deliver patient care,” said Dr. Kadado. “The decline in CV board pass rates reflects a potential gap in training, which may translate to suboptimal patient care.”
Why the Downturn?
Reasons for the increased failures are likely multifactorial, Dr. Kadado said. While some blame the ABIM, the exam has remained about the same over the past 6 years, so the test itself seems unlikely to explain the decline.
The main culprit, according to the viewpoint authors, is “the educational fallout from the disruptions caused by changes made in response to the COVID pandemic.” Changes that Dr. Kadado and colleagues said put the current class of graduating fellows at “high risk” of failing their boards in the fall.
The typical cardiology fellowship is 3 years or more for subspecialty training. Candidates who took the ABIM exam in 2021 had 18 months of training that overlapped with the pandemic response, and those who took the exam in 2022 had about 30 months of training disrupted by COVID. However, fellows who first took the exam in 2023 had essentially 36 months of training affected by COVID, potentially reducing their odds of passing.
“It is hard, if not impossible, to understand the driving forces for this recent decrease in performance on the initial ABIM certification examination, nor is it possible to forecast if there will be an end to this slide,” Jeffrey T. Kuvin, MD, chair of cardiology at the Zucker School of Medicine at Northwell Health, Manhasset, New York, and colleagues wrote in response to the viewpoint article.
The authors acknowledged that COVID disrupted graduate medical training and that the long-term effects of the disruption are now emerging. However, they also pinpoint other potential issues affecting fellows, including information/technology overload, a focus on patient volume over education, lack of attention to core concepts, and, as Dr. Kadado and colleagues noted, high burnout rates among fellows and knowledge gaps due to easy access to electronic resources rather than reading and studying to retain information.
COVID disruptions included limits on in-person learning, clinic exposure, research opportunities, and conference travel, according to the authors. From a 2020 viewpoint, Dr. Kuvin also noted the loss of bedside teaching and on-site grand rounds.
Furthermore, with deferrals of elective cardiac, endovascular, and structural catheterization procedures during the pandemic, elective cases normally done by fellows were postponed or canceled.
Restoring Education, Board Passing Rates
“Having recently passed the ABIM cardiovascular board exam myself, my take-home message at this point is for current fellows-in-training to remain organized, track training milestones, and foresee any training shortcomings,” Dr. Kadado said. Adding that fellows, graduates and leadership should “identify deficiencies and work on overcoming them.”
The viewpoint authors suggested strategies that fellowship leadership can use. These include:
- Regularly assessing faculty emotional well-being and burnout to ensure that they are engaged in meaningful teaching activities
- Emphasizing in-person learning, meaningful participation in conferences, and faculty oversight
- Encouraging fellows to pursue “self-directed learning” during off-hours
- Developing and implementing checklists, competency-based models, curricula, and rotations to ensure that training milestones are being met
- Returning to in-person imaging interpretation for imaging modalities such as echocardiography, cardiac CT, and cardiac MRI
- Ensuring that fellows take the American College of Cardiology in-training examination
- Providing practice question banks so that fellows can assess their knowledge gaps
“This might also be an opportune time to assess the assessment,” Dr. Kuvin and colleagues noted. “There are likely alternative or additional approaches that could provide a more comprehensive, modern tool to gauge clinical competence in a supportive manner.”
They suggested that these tools could include assessment by simulation for interventional cardiology and electrophysiology, oral case reviews, objective structured clinical exams, and evaluations of nonclinical competencies such as professionalism and health equity.
Implications for the New Cardiology Board
While the ABIM cardiology board exam days may be numbered, board certification via some type of exam process is not going away.
The American College of Cardiology and four other US CV societies — the American Heart Association, the Heart Failure Society of America, the Heart Rhythm Society, and the Society for Cardiovascular Angiography & Interventions — formally announced in September that they have joined forces to propose a new professional certification board called the American Board of Cardiovascular Medicine (ABCVM). The application to the ABMS for a separate cardiology board is still ongoing and will take time.
An initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured.
Preparing for the new board will likely be “largely the same” as for the ABIM board, Dr. Kadado said. “This includes access to practice question banks, faculty oversight, strong clinical exposure and practice, regular didactic sessions, and self-directed learning.”
“Passing the board exam is just one step in our ongoing journey as a cardiologist,” he added. “Our field is rapidly evolving, and continuous learning and adaptation are part of the very essence of being a healthcare professional.”
Dr. Kadado had no relevant relationships to disclose. Dr. Kuvin is an ACC trustee and has been heading up the working group to develop the ABCVM.
A version of this article appeared on Medscape.com.
Will New Lung Cancer Screening Guidelines Save More Lives?
When the American Cancer Society recently unveiled changes to its lung cancer screening guidance, the aim was to remove barriers to screening and catch more cancers in high-risk people earlier.
Although the lung cancer death rate has declined significantly over the past few decades, lung cancer remains the leading cause of cancer deaths worldwide.
Detecting lung cancer early is key to improving survival. Still, lung cancer screening rates are poor. In 2021, the American Lung Association estimated that 14 million US adults qualified for lung cancer screening, but only 5.8% received it.
Smokers or former smokers without symptoms may forgo regular screening and only receive their screening scan after symptoms emerge, explained Janani S. Reisenauer, MD, Division Chair of Thoracic Surgery at Mayo Clinic, Rochester, Minnesota. But by the time symptoms develop, the cancer is typically more advanced, and treatment options become more limited.
The goal of the new American Cancer Society guidelines, published in early November 2023 in CA: A Cancer Journal for Physicians, is to identify lung cancers at earlier stages when they are easier to treat.
Almost 5 million more high-risk people will now qualify for regular lung cancer screening, the guideline authors estimated.
But will expanding screening help reduce deaths from lung cancer? And perhaps just as important, will the guidelines move the needle on the “disappointingly low” lung cancer screening rates up to this point?
“I definitely think it’s a step in the right direction,” said Lecia V. Sequist, MD, MPH, clinical researcher and lung cancer medical oncologist, Massachusetts General Hospital Cancer Center, Boston, Massachusetts.
The new guidelines lowered the age for annual lung cancer screening among asymptomatic former or current smokers from 55-74 years to 50-80 years. The update also now considers a high-risk person anyone with a 20-pack-year history, down from a 30-pack-year history, and removes the requirement that former smokers must have quit within 15 years to be eligible for screening.
As people age, their risk for lung cancer increases, so it makes sense to screen all former smokers regardless of when they quit, explained Kim Lori Sandler, MD, from Vanderbilt University Medical Center, Nashville, Tennessee, and cochair of the American College of Radiology’s Lung Cancer Screening Steering Committee.
“There’s really nothing magical or drastic that happens at the 15-year mark,” Dr. Sequist agreed. For “someone who quit 14 years ago versus 16 years ago, it is essentially the same risk, and so scientifically it doesn’t really make sense to impose an artificial cut-off where no change in risk exists.”
The latest evidence reviewed in the new guidelines shows that expanding the guidelines would identify more early-stage cancers and potentially save lives. The authors modeled the benefits and harms of lung cancer screening using several scenarios.
Moving the start age from 55 to 50 years would lead to a 15% reduction in lung cancer mortality in men aged 50-54 years, the model suggested.
Removing the 15-year timeline for quitting smoking also would also improve outcomes. Compared with scenarios that included the 15-year quit timeline for former smokers, those that removed the limit would result in a 37.3% increase in screening exams, a 21% increase in would avert lung cancer deaths, and offer a 19% increase in life-years gained per 100,000 population.
Overall, the evidence indicates that, “if fully implemented, these recommendations have a high likelihood of significantly reducing death and suffering from lung cancer in the United States,” the guideline authors wrote.
But screening more people also comes with risks, such as more false-positive findings, which could lead to extra scans, invasive tests for tissue sampling, or even procedures for benign disease, Dr. Sandler explained. The latter “is what we really need to avoid.”
Even so, Dr. Sandler believes the current guidelines show that the benefit of screening “is great enough that it’s worth including these additional individuals.”
Guidelines Are Not Enough
But will expanding the screening criteria prompt more eligible individuals to receive their CT scans?
Simply expanding the eligibility criteria, by itself, likely won’t measurably improve screening uptake, said Paolo Boffetta, MD, MPH, of Stony Brook Cancer Center, Stony Brook, New York.
Healthcare and insurance access along with patient demand may present the most significant barriers to improving screening uptake.
The “issue is not the guideline as much as it’s the healthcare system,” said Otis W. Brawley, MD, professor of oncology at the Johns Hopkins University School of Medicine, Baltimore, Maryland.
Access to screening at hospitals with limited CT scanners and staff could present one major issue.
When Dr. Brawley worked at a large inner-city safety net hospital in Atlanta, patients with lung cancer frequently had to wait over a week to use one of the four CT scanners, he recalled. Adding to these delays, we didn’t have enough people to read the screens or enough people to do the diagnostics for those who had abnormalities, said Dr. Brawley.
To increase lung cancer screening in this context would increase the wait time for patients who do have cancer, he said.
Insurance coverage could present a roadblock for some as well. While the 2021 US Preventive Services Task Force (USPSTF) recommendations largely align with the new ones from the American Cancer Society, there’s one key difference: The USPSTF still requires former smokers to have quit within 15 years to be eligible for annual screening.
Because the USPSTF recommendations dictate insurance coverage, some former smokers — those who quit more than 15 years ago — may not qualify for coverage and would have to pay out-of-pocket for screening.
Dr. Sequist, however, had a more optimistic outlook about screening uptake.
The American Cancer Society guidelines should remove some of the stigma surrounding lung cancer screening. Most people, when asked a lot of questions about their tobacco use and history, tend to downplay it because there’s shame associated with smoking, Dr. Sequist said. The new guidelines limit the information needed to determine eligibility.
Dr. Sequist also noted that the updated American Cancer Society guideline would improve screening rates because it simplifies the eligibility criteria and makes it easier for physicians to determine who qualifies.
The issue, however, is that some of these individuals — those who quit over 15 years ago — may not have their scan covered by insurance, which could preclude lower-income individuals from getting screened.
The American Cancer Society guidelines” do not necessarily translate into a change in policy,” which is “dictated by the USPSTF and payors such as Medicare,” explained Peter Mazzone, MD, MPH, director of the Lung Cancer Program and Lung Cancer Screening Program for the Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
On the patient side, Dr. Brawley noted, “we don’t yet have a large demand” for screening.
Many current and former smokers may put off lung cancer screening or not seek it out. Some may be unaware of their eligibility, while others may fear the outcome of a scan. Even among eligible individuals who do receive an initial scan, most — more than 75% — do not return for their next scan a year later, research showed.
Enhancing patient education and launching strong marketing campaigns would be a key element to encourage more people to get their annual screening and reduce the stigma associated with lung cancer as a smoker’s disease.
“Primary care physicians are integral in ensuring all eligible patients receive appropriate screening for lung cancer,” said Steven P. Furr, MD, president of the American Academy of Family Physicians and a family physician in Jackson, Alabama. “It is imperative that family physicians encourage screening in at-risk patients and counsel them on the importance of continued screening, as well as smoking cessation, if needed.”
Two authors of the new guidelines reported financial relationships with Seno Medical Instruments, the Genentech Foundation, Crispr Therapeutics, BEAM Therapeutics, Intellia Therapeutics, Editas Medicine, Freenome, and Guardant Health.
A version of this article appeared on Medscape.com.
When the American Cancer Society recently unveiled changes to its lung cancer screening guidance, the aim was to remove barriers to screening and catch more cancers in high-risk people earlier.
Although the lung cancer death rate has declined significantly over the past few decades, lung cancer remains the leading cause of cancer deaths worldwide.
Detecting lung cancer early is key to improving survival. Still, lung cancer screening rates are poor. In 2021, the American Lung Association estimated that 14 million US adults qualified for lung cancer screening, but only 5.8% received it.
Smokers or former smokers without symptoms may forgo regular screening and only receive their screening scan after symptoms emerge, explained Janani S. Reisenauer, MD, Division Chair of Thoracic Surgery at Mayo Clinic, Rochester, Minnesota. But by the time symptoms develop, the cancer is typically more advanced, and treatment options become more limited.
The goal of the new American Cancer Society guidelines, published in early November 2023 in CA: A Cancer Journal for Physicians, is to identify lung cancers at earlier stages when they are easier to treat.
Almost 5 million more high-risk people will now qualify for regular lung cancer screening, the guideline authors estimated.
But will expanding screening help reduce deaths from lung cancer? And perhaps just as important, will the guidelines move the needle on the “disappointingly low” lung cancer screening rates up to this point?
“I definitely think it’s a step in the right direction,” said Lecia V. Sequist, MD, MPH, clinical researcher and lung cancer medical oncologist, Massachusetts General Hospital Cancer Center, Boston, Massachusetts.
The new guidelines lowered the age for annual lung cancer screening among asymptomatic former or current smokers from 55-74 years to 50-80 years. The update also now considers a high-risk person anyone with a 20-pack-year history, down from a 30-pack-year history, and removes the requirement that former smokers must have quit within 15 years to be eligible for screening.
As people age, their risk for lung cancer increases, so it makes sense to screen all former smokers regardless of when they quit, explained Kim Lori Sandler, MD, from Vanderbilt University Medical Center, Nashville, Tennessee, and cochair of the American College of Radiology’s Lung Cancer Screening Steering Committee.
“There’s really nothing magical or drastic that happens at the 15-year mark,” Dr. Sequist agreed. For “someone who quit 14 years ago versus 16 years ago, it is essentially the same risk, and so scientifically it doesn’t really make sense to impose an artificial cut-off where no change in risk exists.”
The latest evidence reviewed in the new guidelines shows that expanding the guidelines would identify more early-stage cancers and potentially save lives. The authors modeled the benefits and harms of lung cancer screening using several scenarios.
Moving the start age from 55 to 50 years would lead to a 15% reduction in lung cancer mortality in men aged 50-54 years, the model suggested.
Removing the 15-year timeline for quitting smoking also would also improve outcomes. Compared with scenarios that included the 15-year quit timeline for former smokers, those that removed the limit would result in a 37.3% increase in screening exams, a 21% increase in would avert lung cancer deaths, and offer a 19% increase in life-years gained per 100,000 population.
Overall, the evidence indicates that, “if fully implemented, these recommendations have a high likelihood of significantly reducing death and suffering from lung cancer in the United States,” the guideline authors wrote.
But screening more people also comes with risks, such as more false-positive findings, which could lead to extra scans, invasive tests for tissue sampling, or even procedures for benign disease, Dr. Sandler explained. The latter “is what we really need to avoid.”
Even so, Dr. Sandler believes the current guidelines show that the benefit of screening “is great enough that it’s worth including these additional individuals.”
Guidelines Are Not Enough
But will expanding the screening criteria prompt more eligible individuals to receive their CT scans?
Simply expanding the eligibility criteria, by itself, likely won’t measurably improve screening uptake, said Paolo Boffetta, MD, MPH, of Stony Brook Cancer Center, Stony Brook, New York.
Healthcare and insurance access along with patient demand may present the most significant barriers to improving screening uptake.
The “issue is not the guideline as much as it’s the healthcare system,” said Otis W. Brawley, MD, professor of oncology at the Johns Hopkins University School of Medicine, Baltimore, Maryland.
Access to screening at hospitals with limited CT scanners and staff could present one major issue.
When Dr. Brawley worked at a large inner-city safety net hospital in Atlanta, patients with lung cancer frequently had to wait over a week to use one of the four CT scanners, he recalled. Adding to these delays, we didn’t have enough people to read the screens or enough people to do the diagnostics for those who had abnormalities, said Dr. Brawley.
To increase lung cancer screening in this context would increase the wait time for patients who do have cancer, he said.
Insurance coverage could present a roadblock for some as well. While the 2021 US Preventive Services Task Force (USPSTF) recommendations largely align with the new ones from the American Cancer Society, there’s one key difference: The USPSTF still requires former smokers to have quit within 15 years to be eligible for annual screening.
Because the USPSTF recommendations dictate insurance coverage, some former smokers — those who quit more than 15 years ago — may not qualify for coverage and would have to pay out-of-pocket for screening.
Dr. Sequist, however, had a more optimistic outlook about screening uptake.
The American Cancer Society guidelines should remove some of the stigma surrounding lung cancer screening. Most people, when asked a lot of questions about their tobacco use and history, tend to downplay it because there’s shame associated with smoking, Dr. Sequist said. The new guidelines limit the information needed to determine eligibility.
Dr. Sequist also noted that the updated American Cancer Society guideline would improve screening rates because it simplifies the eligibility criteria and makes it easier for physicians to determine who qualifies.
The issue, however, is that some of these individuals — those who quit over 15 years ago — may not have their scan covered by insurance, which could preclude lower-income individuals from getting screened.
The American Cancer Society guidelines” do not necessarily translate into a change in policy,” which is “dictated by the USPSTF and payors such as Medicare,” explained Peter Mazzone, MD, MPH, director of the Lung Cancer Program and Lung Cancer Screening Program for the Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
On the patient side, Dr. Brawley noted, “we don’t yet have a large demand” for screening.
Many current and former smokers may put off lung cancer screening or not seek it out. Some may be unaware of their eligibility, while others may fear the outcome of a scan. Even among eligible individuals who do receive an initial scan, most — more than 75% — do not return for their next scan a year later, research showed.
Enhancing patient education and launching strong marketing campaigns would be a key element to encourage more people to get their annual screening and reduce the stigma associated with lung cancer as a smoker’s disease.
“Primary care physicians are integral in ensuring all eligible patients receive appropriate screening for lung cancer,” said Steven P. Furr, MD, president of the American Academy of Family Physicians and a family physician in Jackson, Alabama. “It is imperative that family physicians encourage screening in at-risk patients and counsel them on the importance of continued screening, as well as smoking cessation, if needed.”
Two authors of the new guidelines reported financial relationships with Seno Medical Instruments, the Genentech Foundation, Crispr Therapeutics, BEAM Therapeutics, Intellia Therapeutics, Editas Medicine, Freenome, and Guardant Health.
A version of this article appeared on Medscape.com.
When the American Cancer Society recently unveiled changes to its lung cancer screening guidance, the aim was to remove barriers to screening and catch more cancers in high-risk people earlier.
Although the lung cancer death rate has declined significantly over the past few decades, lung cancer remains the leading cause of cancer deaths worldwide.
Detecting lung cancer early is key to improving survival. Still, lung cancer screening rates are poor. In 2021, the American Lung Association estimated that 14 million US adults qualified for lung cancer screening, but only 5.8% received it.
Smokers or former smokers without symptoms may forgo regular screening and only receive their screening scan after symptoms emerge, explained Janani S. Reisenauer, MD, Division Chair of Thoracic Surgery at Mayo Clinic, Rochester, Minnesota. But by the time symptoms develop, the cancer is typically more advanced, and treatment options become more limited.
The goal of the new American Cancer Society guidelines, published in early November 2023 in CA: A Cancer Journal for Physicians, is to identify lung cancers at earlier stages when they are easier to treat.
Almost 5 million more high-risk people will now qualify for regular lung cancer screening, the guideline authors estimated.
But will expanding screening help reduce deaths from lung cancer? And perhaps just as important, will the guidelines move the needle on the “disappointingly low” lung cancer screening rates up to this point?
“I definitely think it’s a step in the right direction,” said Lecia V. Sequist, MD, MPH, clinical researcher and lung cancer medical oncologist, Massachusetts General Hospital Cancer Center, Boston, Massachusetts.
The new guidelines lowered the age for annual lung cancer screening among asymptomatic former or current smokers from 55-74 years to 50-80 years. The update also now considers a high-risk person anyone with a 20-pack-year history, down from a 30-pack-year history, and removes the requirement that former smokers must have quit within 15 years to be eligible for screening.
As people age, their risk for lung cancer increases, so it makes sense to screen all former smokers regardless of when they quit, explained Kim Lori Sandler, MD, from Vanderbilt University Medical Center, Nashville, Tennessee, and cochair of the American College of Radiology’s Lung Cancer Screening Steering Committee.
“There’s really nothing magical or drastic that happens at the 15-year mark,” Dr. Sequist agreed. For “someone who quit 14 years ago versus 16 years ago, it is essentially the same risk, and so scientifically it doesn’t really make sense to impose an artificial cut-off where no change in risk exists.”
The latest evidence reviewed in the new guidelines shows that expanding the guidelines would identify more early-stage cancers and potentially save lives. The authors modeled the benefits and harms of lung cancer screening using several scenarios.
Moving the start age from 55 to 50 years would lead to a 15% reduction in lung cancer mortality in men aged 50-54 years, the model suggested.
Removing the 15-year timeline for quitting smoking also would also improve outcomes. Compared with scenarios that included the 15-year quit timeline for former smokers, those that removed the limit would result in a 37.3% increase in screening exams, a 21% increase in would avert lung cancer deaths, and offer a 19% increase in life-years gained per 100,000 population.
Overall, the evidence indicates that, “if fully implemented, these recommendations have a high likelihood of significantly reducing death and suffering from lung cancer in the United States,” the guideline authors wrote.
But screening more people also comes with risks, such as more false-positive findings, which could lead to extra scans, invasive tests for tissue sampling, or even procedures for benign disease, Dr. Sandler explained. The latter “is what we really need to avoid.”
Even so, Dr. Sandler believes the current guidelines show that the benefit of screening “is great enough that it’s worth including these additional individuals.”
Guidelines Are Not Enough
But will expanding the screening criteria prompt more eligible individuals to receive their CT scans?
Simply expanding the eligibility criteria, by itself, likely won’t measurably improve screening uptake, said Paolo Boffetta, MD, MPH, of Stony Brook Cancer Center, Stony Brook, New York.
Healthcare and insurance access along with patient demand may present the most significant barriers to improving screening uptake.
The “issue is not the guideline as much as it’s the healthcare system,” said Otis W. Brawley, MD, professor of oncology at the Johns Hopkins University School of Medicine, Baltimore, Maryland.
Access to screening at hospitals with limited CT scanners and staff could present one major issue.
When Dr. Brawley worked at a large inner-city safety net hospital in Atlanta, patients with lung cancer frequently had to wait over a week to use one of the four CT scanners, he recalled. Adding to these delays, we didn’t have enough people to read the screens or enough people to do the diagnostics for those who had abnormalities, said Dr. Brawley.
To increase lung cancer screening in this context would increase the wait time for patients who do have cancer, he said.
Insurance coverage could present a roadblock for some as well. While the 2021 US Preventive Services Task Force (USPSTF) recommendations largely align with the new ones from the American Cancer Society, there’s one key difference: The USPSTF still requires former smokers to have quit within 15 years to be eligible for annual screening.
Because the USPSTF recommendations dictate insurance coverage, some former smokers — those who quit more than 15 years ago — may not qualify for coverage and would have to pay out-of-pocket for screening.
Dr. Sequist, however, had a more optimistic outlook about screening uptake.
The American Cancer Society guidelines should remove some of the stigma surrounding lung cancer screening. Most people, when asked a lot of questions about their tobacco use and history, tend to downplay it because there’s shame associated with smoking, Dr. Sequist said. The new guidelines limit the information needed to determine eligibility.
Dr. Sequist also noted that the updated American Cancer Society guideline would improve screening rates because it simplifies the eligibility criteria and makes it easier for physicians to determine who qualifies.
The issue, however, is that some of these individuals — those who quit over 15 years ago — may not have their scan covered by insurance, which could preclude lower-income individuals from getting screened.
The American Cancer Society guidelines” do not necessarily translate into a change in policy,” which is “dictated by the USPSTF and payors such as Medicare,” explained Peter Mazzone, MD, MPH, director of the Lung Cancer Program and Lung Cancer Screening Program for the Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
On the patient side, Dr. Brawley noted, “we don’t yet have a large demand” for screening.
Many current and former smokers may put off lung cancer screening or not seek it out. Some may be unaware of their eligibility, while others may fear the outcome of a scan. Even among eligible individuals who do receive an initial scan, most — more than 75% — do not return for their next scan a year later, research showed.
Enhancing patient education and launching strong marketing campaigns would be a key element to encourage more people to get their annual screening and reduce the stigma associated with lung cancer as a smoker’s disease.
“Primary care physicians are integral in ensuring all eligible patients receive appropriate screening for lung cancer,” said Steven P. Furr, MD, president of the American Academy of Family Physicians and a family physician in Jackson, Alabama. “It is imperative that family physicians encourage screening in at-risk patients and counsel them on the importance of continued screening, as well as smoking cessation, if needed.”
Two authors of the new guidelines reported financial relationships with Seno Medical Instruments, the Genentech Foundation, Crispr Therapeutics, BEAM Therapeutics, Intellia Therapeutics, Editas Medicine, Freenome, and Guardant Health.
A version of this article appeared on Medscape.com.
Functional Outcomes in Localized Prostate Cancer: Treatment Choice, Time, Prognosis All Matter
New research published Jan. 23 in JAMA parses functional outcome results from a population-based study of men diagnosed with localized prostate cancer. For their research, Bashir Al Hussein Al Awamlh, MD, of Vanderbilt University in Nashville, Tennessee, and his colleagues, looked at sexual function, urinary health, bowel function, hormonal function, and other outcomes in this cohort at 10 years’ follow-up.
Among 2455 patients for whom 10-year data were available, 1877 were deemed at baseline to have a favorable prognosis (defined as cT1-cT2bN0M0, prostate-specific antigen level less than 20 ng/mL, and grade group 1-2) and 568 had unfavorable-prognosis prostate cancer (defined as cT2cN0M0, prostate-specific antigen level of 20-50 ng/mL, or grade group 3-5). Follow-up data were collected by questionnaire through February 1, 2022. The men in the study were all younger than 80 years, and three-quarters of them were White.
At 10 years, outcomes differed based on the amount of time that had passed since diagnosis (they found different results at 3 and 5 year follow up, for example) and which treatment a patient received.
Among men with favorable prognoses at diagnosis, 20% underwent active surveillance for at least 1 year, while 56% received radical prostatectomy, 19% had external beam radiotherapy (EBRT) without ADT, and 5% had brachytherapy. Nearly a third of men originally opting for surveillance went on to undergo a therapeutic intervention by 10 years.
Dr. Al Hussein Al Awamlh and his colleagues found that while 3- and 5-year follow-up studies in this cohort had shown declines in sexual function among men who underwent surgery compared with those who had radiation or active surveillance, by 10 years those differences had faded, with no clinically meaningful differences in sexual function scores between the surgery and surveillance groups. In an interview, Dr. Al Hussein Al Awamlh said that this finding likely reflected mainly age-related declines in function across the study population — though it could also reflect declines after converting from surveillance to surgery or gradual decline with radiation treatment, he acknowledged.
Men with favorable prognoses at baseline who underwent surgery saw significantly worse urinary incontinence at 10 years compared with those started on radiotherapy or active surveillance. And EBRT was associated with fewer incontinence issues compared with active surveillance.
Among the group of men with an unfavorable prognosis at baseline, 64% of whom underwent radical prostatectomy and 36% EBRT with ADT, surgery was associated with worse urinary incontinence but not worse sexual function throughout 10 years of follow up, compared to radiotherapy with androgen deprivation therapy.
Radiation-treated patients with unfavorable prognoses, meanwhile, saw significantly worse bowel function and hormone function at 10 years compared with patients who had undergone surgery.
Dr. Al Hussein Al Awamlh said that a strength of this study was that “we had enough patients to stratify functional outcomes based on disease prognosis.” Another key finding was that some of the outcomes changed over time. “For example, among the patients with unfavorable prognoses, at 10-year follow-up there was slightly worse bowel and hormone function seen associated with radiation with ADT compared with surgery,” he said — something not seen at earlier follow-up points.
The findings may help offer a more nuanced way to counsel patients, Dr. Al Hussein Al Awamlh noted. For example, the side effects associated with sexual function “are not as relevant for those with unfavorable disease,” he said.
While current prostate cancer guidelines do address quality of life in shared decision-making, he said, “hopefully this data may provide more insight on that.” For patients with favorable prognosis, the findings reinforce that “active surveillance is a great option because it avoids the effects associated with those other treatments.”
Ultimately, Dr. Al Hussein Al Awamlh said, “this is a patient preference issue. It’s important for patients to understand how different functions are affected and to decide what is better for them — what they can live with and what they cannot, provided all the options are oncologically safe.”
The study authors disclosed as limitations of their study its observational design, the potential for response bias among study participants, and small numbers for some of the measured outcomes.
In an interview, urologist Mark S. Litwin, MD, of the University of California Los Angeles, characterized the study as “a well-conducted very-long-term longitudinal cohort that tracked men long past the initial diagnosis and treatment. That empowered the Vanderbilt team to find differences in quality of life many years later and compare them to other older men who had not received treatment.”
The new findings, Dr. Litwin said, “are critical in showing that most men with prostate cancer do not die from it; hence, the quality-of-life effects end up being the key issues for decision-making.”
Dr. Al Hussein Al Awamlh and colleagues’ study was funded by grants from the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Patient-Centered Outcomes Research Institute. Several coauthors disclosed funding from pharmaceutical and/or device manufacturers. Dr. Litwin disclosed no conflicts of interest related to his comment.
New research published Jan. 23 in JAMA parses functional outcome results from a population-based study of men diagnosed with localized prostate cancer. For their research, Bashir Al Hussein Al Awamlh, MD, of Vanderbilt University in Nashville, Tennessee, and his colleagues, looked at sexual function, urinary health, bowel function, hormonal function, and other outcomes in this cohort at 10 years’ follow-up.
Among 2455 patients for whom 10-year data were available, 1877 were deemed at baseline to have a favorable prognosis (defined as cT1-cT2bN0M0, prostate-specific antigen level less than 20 ng/mL, and grade group 1-2) and 568 had unfavorable-prognosis prostate cancer (defined as cT2cN0M0, prostate-specific antigen level of 20-50 ng/mL, or grade group 3-5). Follow-up data were collected by questionnaire through February 1, 2022. The men in the study were all younger than 80 years, and three-quarters of them were White.
At 10 years, outcomes differed based on the amount of time that had passed since diagnosis (they found different results at 3 and 5 year follow up, for example) and which treatment a patient received.
Among men with favorable prognoses at diagnosis, 20% underwent active surveillance for at least 1 year, while 56% received radical prostatectomy, 19% had external beam radiotherapy (EBRT) without ADT, and 5% had brachytherapy. Nearly a third of men originally opting for surveillance went on to undergo a therapeutic intervention by 10 years.
Dr. Al Hussein Al Awamlh and his colleagues found that while 3- and 5-year follow-up studies in this cohort had shown declines in sexual function among men who underwent surgery compared with those who had radiation or active surveillance, by 10 years those differences had faded, with no clinically meaningful differences in sexual function scores between the surgery and surveillance groups. In an interview, Dr. Al Hussein Al Awamlh said that this finding likely reflected mainly age-related declines in function across the study population — though it could also reflect declines after converting from surveillance to surgery or gradual decline with radiation treatment, he acknowledged.
Men with favorable prognoses at baseline who underwent surgery saw significantly worse urinary incontinence at 10 years compared with those started on radiotherapy or active surveillance. And EBRT was associated with fewer incontinence issues compared with active surveillance.
Among the group of men with an unfavorable prognosis at baseline, 64% of whom underwent radical prostatectomy and 36% EBRT with ADT, surgery was associated with worse urinary incontinence but not worse sexual function throughout 10 years of follow up, compared to radiotherapy with androgen deprivation therapy.
Radiation-treated patients with unfavorable prognoses, meanwhile, saw significantly worse bowel function and hormone function at 10 years compared with patients who had undergone surgery.
Dr. Al Hussein Al Awamlh said that a strength of this study was that “we had enough patients to stratify functional outcomes based on disease prognosis.” Another key finding was that some of the outcomes changed over time. “For example, among the patients with unfavorable prognoses, at 10-year follow-up there was slightly worse bowel and hormone function seen associated with radiation with ADT compared with surgery,” he said — something not seen at earlier follow-up points.
The findings may help offer a more nuanced way to counsel patients, Dr. Al Hussein Al Awamlh noted. For example, the side effects associated with sexual function “are not as relevant for those with unfavorable disease,” he said.
While current prostate cancer guidelines do address quality of life in shared decision-making, he said, “hopefully this data may provide more insight on that.” For patients with favorable prognosis, the findings reinforce that “active surveillance is a great option because it avoids the effects associated with those other treatments.”
Ultimately, Dr. Al Hussein Al Awamlh said, “this is a patient preference issue. It’s important for patients to understand how different functions are affected and to decide what is better for them — what they can live with and what they cannot, provided all the options are oncologically safe.”
The study authors disclosed as limitations of their study its observational design, the potential for response bias among study participants, and small numbers for some of the measured outcomes.
In an interview, urologist Mark S. Litwin, MD, of the University of California Los Angeles, characterized the study as “a well-conducted very-long-term longitudinal cohort that tracked men long past the initial diagnosis and treatment. That empowered the Vanderbilt team to find differences in quality of life many years later and compare them to other older men who had not received treatment.”
The new findings, Dr. Litwin said, “are critical in showing that most men with prostate cancer do not die from it; hence, the quality-of-life effects end up being the key issues for decision-making.”
Dr. Al Hussein Al Awamlh and colleagues’ study was funded by grants from the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Patient-Centered Outcomes Research Institute. Several coauthors disclosed funding from pharmaceutical and/or device manufacturers. Dr. Litwin disclosed no conflicts of interest related to his comment.
New research published Jan. 23 in JAMA parses functional outcome results from a population-based study of men diagnosed with localized prostate cancer. For their research, Bashir Al Hussein Al Awamlh, MD, of Vanderbilt University in Nashville, Tennessee, and his colleagues, looked at sexual function, urinary health, bowel function, hormonal function, and other outcomes in this cohort at 10 years’ follow-up.
Among 2455 patients for whom 10-year data were available, 1877 were deemed at baseline to have a favorable prognosis (defined as cT1-cT2bN0M0, prostate-specific antigen level less than 20 ng/mL, and grade group 1-2) and 568 had unfavorable-prognosis prostate cancer (defined as cT2cN0M0, prostate-specific antigen level of 20-50 ng/mL, or grade group 3-5). Follow-up data were collected by questionnaire through February 1, 2022. The men in the study were all younger than 80 years, and three-quarters of them were White.
At 10 years, outcomes differed based on the amount of time that had passed since diagnosis (they found different results at 3 and 5 year follow up, for example) and which treatment a patient received.
Among men with favorable prognoses at diagnosis, 20% underwent active surveillance for at least 1 year, while 56% received radical prostatectomy, 19% had external beam radiotherapy (EBRT) without ADT, and 5% had brachytherapy. Nearly a third of men originally opting for surveillance went on to undergo a therapeutic intervention by 10 years.
Dr. Al Hussein Al Awamlh and his colleagues found that while 3- and 5-year follow-up studies in this cohort had shown declines in sexual function among men who underwent surgery compared with those who had radiation or active surveillance, by 10 years those differences had faded, with no clinically meaningful differences in sexual function scores between the surgery and surveillance groups. In an interview, Dr. Al Hussein Al Awamlh said that this finding likely reflected mainly age-related declines in function across the study population — though it could also reflect declines after converting from surveillance to surgery or gradual decline with radiation treatment, he acknowledged.
Men with favorable prognoses at baseline who underwent surgery saw significantly worse urinary incontinence at 10 years compared with those started on radiotherapy or active surveillance. And EBRT was associated with fewer incontinence issues compared with active surveillance.
Among the group of men with an unfavorable prognosis at baseline, 64% of whom underwent radical prostatectomy and 36% EBRT with ADT, surgery was associated with worse urinary incontinence but not worse sexual function throughout 10 years of follow up, compared to radiotherapy with androgen deprivation therapy.
Radiation-treated patients with unfavorable prognoses, meanwhile, saw significantly worse bowel function and hormone function at 10 years compared with patients who had undergone surgery.
Dr. Al Hussein Al Awamlh said that a strength of this study was that “we had enough patients to stratify functional outcomes based on disease prognosis.” Another key finding was that some of the outcomes changed over time. “For example, among the patients with unfavorable prognoses, at 10-year follow-up there was slightly worse bowel and hormone function seen associated with radiation with ADT compared with surgery,” he said — something not seen at earlier follow-up points.
The findings may help offer a more nuanced way to counsel patients, Dr. Al Hussein Al Awamlh noted. For example, the side effects associated with sexual function “are not as relevant for those with unfavorable disease,” he said.
While current prostate cancer guidelines do address quality of life in shared decision-making, he said, “hopefully this data may provide more insight on that.” For patients with favorable prognosis, the findings reinforce that “active surveillance is a great option because it avoids the effects associated with those other treatments.”
Ultimately, Dr. Al Hussein Al Awamlh said, “this is a patient preference issue. It’s important for patients to understand how different functions are affected and to decide what is better for them — what they can live with and what they cannot, provided all the options are oncologically safe.”
The study authors disclosed as limitations of their study its observational design, the potential for response bias among study participants, and small numbers for some of the measured outcomes.
In an interview, urologist Mark S. Litwin, MD, of the University of California Los Angeles, characterized the study as “a well-conducted very-long-term longitudinal cohort that tracked men long past the initial diagnosis and treatment. That empowered the Vanderbilt team to find differences in quality of life many years later and compare them to other older men who had not received treatment.”
The new findings, Dr. Litwin said, “are critical in showing that most men with prostate cancer do not die from it; hence, the quality-of-life effects end up being the key issues for decision-making.”
Dr. Al Hussein Al Awamlh and colleagues’ study was funded by grants from the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Patient-Centered Outcomes Research Institute. Several coauthors disclosed funding from pharmaceutical and/or device manufacturers. Dr. Litwin disclosed no conflicts of interest related to his comment.
FROM JAMA
The Case for Biomarker Testing in Gastroesophageal Cancer
For patients to fully benefit from the latest targeted therapies, biomarker testing needs to improve, explained Yelena Janjigian, MD, chief of gastrointestinal oncology at the Memorial Sloan Kettering Cancer Center in New York City.
“The biomarker revolution in this disease has been quite remarkable in the last 10 years, so it’s very important to routinely test for these biomarkers,” Dr. Janjigian said in a presentation at the 2024 ASCO Gastrointestinal Cancers Symposium.
Dr. Janjigian suspected that inertia and logistics are the main reasons biomarker testing rates have lagged. “Even at tertiary cancer centers like ours, we fall short,” she said. For practices that don’t see many patients with gastroesophageal cancer, the rates are probably worse.
Biomarker testing, however, is readily available, Dr. Janjigian said, and overall, it’s about “being obsessive about doing it and following up on it and training your staff.”
As for how to prioritize biomarker testing for treatment selection, Dr. Janjigian provided her top three picks.
Microsatellite instability (MSI) is the most important biomarker, followed by human epidermal growth factor receptor 2 (HER2) as well as tumors expressing programmed death–ligand 1 (PD-L1) with a combined positive score (CPS) of 5 or higher.
Claudin 18.2 testing is “a great newcomer” worth mentioning as well, she noted. Claudin 18.2 is “very druggable,” and several claudin-targeting drugs are currently being assessed, including zolbetuximab.
MSI testing earned the top spot for Dr. Janjigian given the overall survival results from the CHECKMATE 649 trial.
The trial, which Dr. Janjigian led, assessed treatment with first-line nivolumab plus chemotherapy, nivolumab plus ipilimumab, or chemotherapy alone in patients with advanced gastric cancer, gastroesophageal junction cancer, or esophageal adenocarcinoma.
Median overall survival among the small subset of patients with high MSI who received nivolumab plus chemotherapy (n = 23) was more than three times longer than that among those who received chemotherapy alone (n = 21) — 38.7 months vs 12.3 months. Median overall survival was not reached in patients with high MSI who received nivolumab plus ipilimumab at the trial’s 36-month follow-up.
Dr. Janjigian’s case for a PD-L1 CPS of 5 or higher also came, in part, from the CHECKMATE 649 trial. In a subgroup analysis, patients with a CPS of 5 or higher receiving nivolumab plus chemotherapy had a significantly higher median overall survival of 14.4 months vs 11.1 months with chemotherapy alone.
Dr. Janjigian made the case for HER2 testing based on outcomes from the KEYNOTE 811 trial.
This trial, also led by Dr. Janjigian, randomized HER2-positive patients with unresectable advanced gastroesophageal junction adenocarcinoma irrespective of PDL-1 status to pembrolizumab plus trastuzumab and chemotherapy or trastuzumab and chemotherapy alone.
Past studies have reported that targeting HER2 by itself is not a good idea, Dr. Janjigian said, but this trial demonstrated that dual PD-L1/HER2 blockade improves survival outcomes.
Median overall survival in HER2-positive patients with a PD-L1 CPS of 1 or more was 20.0 months vs 15.7 months (hazard ratio [HR], 0.81; 95% CI, 0.67-0.98) compared with 20.0 vs 16.8 months in the overall cohort (HR, 0.84; 95% CI, 0.70-1.01). However, patients with PD-L1 CPS below 1 showed limited benefit from pembrolizumab (HR, 1.41 for overall survival; 95% CI, 0.90-2.20).
To take advantage of the benefit, HER2 testing is “critical,” Dr. Janjigian said.
Overall, when it comes to targeted therapy for advanced disease, the evolution has been rapid. But “we are not done yet,” she said. “We need to be smarter about patient selection” by using biomarker testing.
Dr. Janjigian reported a range of industry ties, including travel expenses, honoraria, and research funding from nivolumab maker Bristol Myers Squibb and Merck, the maker of pembrolizumab. She also advises both companies.
A version of this article first appeared on Medscape.com.
For patients to fully benefit from the latest targeted therapies, biomarker testing needs to improve, explained Yelena Janjigian, MD, chief of gastrointestinal oncology at the Memorial Sloan Kettering Cancer Center in New York City.
“The biomarker revolution in this disease has been quite remarkable in the last 10 years, so it’s very important to routinely test for these biomarkers,” Dr. Janjigian said in a presentation at the 2024 ASCO Gastrointestinal Cancers Symposium.
Dr. Janjigian suspected that inertia and logistics are the main reasons biomarker testing rates have lagged. “Even at tertiary cancer centers like ours, we fall short,” she said. For practices that don’t see many patients with gastroesophageal cancer, the rates are probably worse.
Biomarker testing, however, is readily available, Dr. Janjigian said, and overall, it’s about “being obsessive about doing it and following up on it and training your staff.”
As for how to prioritize biomarker testing for treatment selection, Dr. Janjigian provided her top three picks.
Microsatellite instability (MSI) is the most important biomarker, followed by human epidermal growth factor receptor 2 (HER2) as well as tumors expressing programmed death–ligand 1 (PD-L1) with a combined positive score (CPS) of 5 or higher.
Claudin 18.2 testing is “a great newcomer” worth mentioning as well, she noted. Claudin 18.2 is “very druggable,” and several claudin-targeting drugs are currently being assessed, including zolbetuximab.
MSI testing earned the top spot for Dr. Janjigian given the overall survival results from the CHECKMATE 649 trial.
The trial, which Dr. Janjigian led, assessed treatment with first-line nivolumab plus chemotherapy, nivolumab plus ipilimumab, or chemotherapy alone in patients with advanced gastric cancer, gastroesophageal junction cancer, or esophageal adenocarcinoma.
Median overall survival among the small subset of patients with high MSI who received nivolumab plus chemotherapy (n = 23) was more than three times longer than that among those who received chemotherapy alone (n = 21) — 38.7 months vs 12.3 months. Median overall survival was not reached in patients with high MSI who received nivolumab plus ipilimumab at the trial’s 36-month follow-up.
Dr. Janjigian’s case for a PD-L1 CPS of 5 or higher also came, in part, from the CHECKMATE 649 trial. In a subgroup analysis, patients with a CPS of 5 or higher receiving nivolumab plus chemotherapy had a significantly higher median overall survival of 14.4 months vs 11.1 months with chemotherapy alone.
Dr. Janjigian made the case for HER2 testing based on outcomes from the KEYNOTE 811 trial.
This trial, also led by Dr. Janjigian, randomized HER2-positive patients with unresectable advanced gastroesophageal junction adenocarcinoma irrespective of PDL-1 status to pembrolizumab plus trastuzumab and chemotherapy or trastuzumab and chemotherapy alone.
Past studies have reported that targeting HER2 by itself is not a good idea, Dr. Janjigian said, but this trial demonstrated that dual PD-L1/HER2 blockade improves survival outcomes.
Median overall survival in HER2-positive patients with a PD-L1 CPS of 1 or more was 20.0 months vs 15.7 months (hazard ratio [HR], 0.81; 95% CI, 0.67-0.98) compared with 20.0 vs 16.8 months in the overall cohort (HR, 0.84; 95% CI, 0.70-1.01). However, patients with PD-L1 CPS below 1 showed limited benefit from pembrolizumab (HR, 1.41 for overall survival; 95% CI, 0.90-2.20).
To take advantage of the benefit, HER2 testing is “critical,” Dr. Janjigian said.
Overall, when it comes to targeted therapy for advanced disease, the evolution has been rapid. But “we are not done yet,” she said. “We need to be smarter about patient selection” by using biomarker testing.
Dr. Janjigian reported a range of industry ties, including travel expenses, honoraria, and research funding from nivolumab maker Bristol Myers Squibb and Merck, the maker of pembrolizumab. She also advises both companies.
A version of this article first appeared on Medscape.com.
For patients to fully benefit from the latest targeted therapies, biomarker testing needs to improve, explained Yelena Janjigian, MD, chief of gastrointestinal oncology at the Memorial Sloan Kettering Cancer Center in New York City.
“The biomarker revolution in this disease has been quite remarkable in the last 10 years, so it’s very important to routinely test for these biomarkers,” Dr. Janjigian said in a presentation at the 2024 ASCO Gastrointestinal Cancers Symposium.
Dr. Janjigian suspected that inertia and logistics are the main reasons biomarker testing rates have lagged. “Even at tertiary cancer centers like ours, we fall short,” she said. For practices that don’t see many patients with gastroesophageal cancer, the rates are probably worse.
Biomarker testing, however, is readily available, Dr. Janjigian said, and overall, it’s about “being obsessive about doing it and following up on it and training your staff.”
As for how to prioritize biomarker testing for treatment selection, Dr. Janjigian provided her top three picks.
Microsatellite instability (MSI) is the most important biomarker, followed by human epidermal growth factor receptor 2 (HER2) as well as tumors expressing programmed death–ligand 1 (PD-L1) with a combined positive score (CPS) of 5 or higher.
Claudin 18.2 testing is “a great newcomer” worth mentioning as well, she noted. Claudin 18.2 is “very druggable,” and several claudin-targeting drugs are currently being assessed, including zolbetuximab.
MSI testing earned the top spot for Dr. Janjigian given the overall survival results from the CHECKMATE 649 trial.
The trial, which Dr. Janjigian led, assessed treatment with first-line nivolumab plus chemotherapy, nivolumab plus ipilimumab, or chemotherapy alone in patients with advanced gastric cancer, gastroesophageal junction cancer, or esophageal adenocarcinoma.
Median overall survival among the small subset of patients with high MSI who received nivolumab plus chemotherapy (n = 23) was more than three times longer than that among those who received chemotherapy alone (n = 21) — 38.7 months vs 12.3 months. Median overall survival was not reached in patients with high MSI who received nivolumab plus ipilimumab at the trial’s 36-month follow-up.
Dr. Janjigian’s case for a PD-L1 CPS of 5 or higher also came, in part, from the CHECKMATE 649 trial. In a subgroup analysis, patients with a CPS of 5 or higher receiving nivolumab plus chemotherapy had a significantly higher median overall survival of 14.4 months vs 11.1 months with chemotherapy alone.
Dr. Janjigian made the case for HER2 testing based on outcomes from the KEYNOTE 811 trial.
This trial, also led by Dr. Janjigian, randomized HER2-positive patients with unresectable advanced gastroesophageal junction adenocarcinoma irrespective of PDL-1 status to pembrolizumab plus trastuzumab and chemotherapy or trastuzumab and chemotherapy alone.
Past studies have reported that targeting HER2 by itself is not a good idea, Dr. Janjigian said, but this trial demonstrated that dual PD-L1/HER2 blockade improves survival outcomes.
Median overall survival in HER2-positive patients with a PD-L1 CPS of 1 or more was 20.0 months vs 15.7 months (hazard ratio [HR], 0.81; 95% CI, 0.67-0.98) compared with 20.0 vs 16.8 months in the overall cohort (HR, 0.84; 95% CI, 0.70-1.01). However, patients with PD-L1 CPS below 1 showed limited benefit from pembrolizumab (HR, 1.41 for overall survival; 95% CI, 0.90-2.20).
To take advantage of the benefit, HER2 testing is “critical,” Dr. Janjigian said.
Overall, when it comes to targeted therapy for advanced disease, the evolution has been rapid. But “we are not done yet,” she said. “We need to be smarter about patient selection” by using biomarker testing.
Dr. Janjigian reported a range of industry ties, including travel expenses, honoraria, and research funding from nivolumab maker Bristol Myers Squibb and Merck, the maker of pembrolizumab. She also advises both companies.
A version of this article first appeared on Medscape.com.
FROM ASCO GI 2024
Targeted Colorectal Cancer Combo Improves QoL
Dominik Modest, MD, presented these new results of the phase 3 CodeBreaK 300 trial at the 2024 ASCO Gastrointestinal Cancers Symposium.
The KRAS G12C mutation occurs in 3%-4% of metastatic colorectal cancer cases, according to Dr. Modest and the other authors of a paper published in the New England Journal of Medicine describing the primary outcome of the trial. The study included 160 patients who were randomized to once daily sotorasib (960 mg) plus panitumumab (Soto960), once daily sotorasib (240 mg) plus panitumumab (Soto240), or investigator’s choice of trifluridine–tipiracil or regorafenib.
The December 2023 paper described improvements in median progression-free survival, progression or death, and objective response (OR). The authors described statistically significant improvements in disease progression or death in the Soto960 group (hazard ratio [HR], 0.49; P = .006) and the Soto240 group (HR, 0.58; P = .03). The objective response rate was highest in the Soto960 group (26.4%; 95% CI, 15.3%-40.3%), followed by the Soto240 group (5.7%; 95% CI, 1.2%-15.7%), and the control group (0%; 95% CI, 0.0%-6.6%). Grade 3 or higher treatment-related adverse events were generally similar at 35.8% (Soto960), 30.2% (Soto240), and 43.1% (control) in each group. The most common adverse events associated with sotorasib-panitumumab were skin-related toxicity and hypomagnesemia.
The new analysis showed that both doses of sotorasib also improved patient-reported outcomes from baseline to week 8, Dr. Modest, professor of medicine at Charité University of Medicine in Berlin, said at the meeting.
Compared with the chemotherapy group, there were statistically significant differences in least square mean change from baseline to week 8 for: pain at its worst in the Soto240 group (Brief Pain Inventory [BPI], –1.18; 95% CI, –2.05 to –0.32) and the Soto960 group (BPI, –1.49; 95% CI, –2.36 to –0.61); and physical functioning, as measured by the European Organisation for Research and Treatment of Cancer Core 30-item Quality of Life questionnaire, in the Soto240 (7.95; 95% CI, 2.39-13.51) and Soto960 (6.73; 95% CI, 1.05-12.41) groups. Nearly all other measures trended toward favoring the sotorasib/panitumumab groups, but did not reach statistical significance. A similar pattern was seen in time to deterioration measures. Among adverse events, diarrhea trended toward being more frequent in the intervention arms.
At week 9, 63% of patients in Soto960 and 84% in Soto240 reported improvement in the Patient Global Impression of Change score (PGI-C), versus 37% in the chemotherapy arm. At week 17, the percentages were 77%, 59%, and 21%, respectively.
“The clinical benefits and the better quality of life outcomes associated with sotorasib at the high dose of 960 milligrams plus panitumumab establishes this combination as a potential new standard [therapy] for patients with chemorefractory KRAS G12C mutant colorectal cancer, and I think it’s quite reassuring that even if you compare two active drugs versus one active drug, this does not necessarily translate into impaired quality of life assessments by the patients,” Dr. Modest said during his presentation.
CodeBreaK 300 may point the way to other dual therapies involving kinase inhibitors, according to Rona Yaeger, MD, who wrote an accompanying editorial to the NEJM paper. Dr. Yaeger noted that clinical and preclinical studies had shown that targeted oncogenes like KRAS G12C and BRAF V600E alone would be insufficient in colorectal cancer.
When combined with KRAS G12C inhibitors, EGFR inhibitors prevent EGFR from participating in negative feedback loops that can otherwise lead to drug resistance. “Whether targeting [receptor tyrosine kinases like EGFR] in epithelial tumors other than those associated with colorectal cancers would improve the incidence of response to KRAS G12C inhibitors remains unknown,” wrote Dr. Yaeger, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York. There is an ongoing clinical trial evaluating KRAS G12C inhibitors combined with EGFR antibodies in both lung and pancreatic cancer.
She noted that colorectal tumors have high levels of receptor tyrosine kinases, and argued that this will require higher doses of KRAS G12C inhibitors or novel drugs with higher activity. This is supported by the higher frequency of response and longer PFS at the higher dose in CodeBreaK 300, but could present a challenge: “Lowering the drug dose to manage toxic effects may limit the efficacy of the drug against some cancers,” she wrote.
Dr. Yaeger highlighted the KRYSTAL-10 phase 3 randomized trial, which is assessing the KRAS G12C inhibitor adagrasib in combination with the EGFR antibody cetuximab versus chemotherapy in advanced solid tumors with the KRAS G12C mutation.
“The CodeBreaK 300 trial is an exciting first step for targeting KRAS in colorectal cancer,” Dr. Yaeger wrote.
Dr. Modest has financial relationships with Amgen, AstraZeneca/MedImmune, Bristol-Myers Squibb, Incyte, Lily, Merck Serono, Merck Sharp & Dohme, Onkowissen, Pierre Fabre, Roche, and SERVIER. Dr. Yaeger has financial relationships with Amgen, Boehringer Ingelheim, Daiichi Sankyo, Mirati, Pfizer, and Zai Lab.
Dominik Modest, MD, presented these new results of the phase 3 CodeBreaK 300 trial at the 2024 ASCO Gastrointestinal Cancers Symposium.
The KRAS G12C mutation occurs in 3%-4% of metastatic colorectal cancer cases, according to Dr. Modest and the other authors of a paper published in the New England Journal of Medicine describing the primary outcome of the trial. The study included 160 patients who were randomized to once daily sotorasib (960 mg) plus panitumumab (Soto960), once daily sotorasib (240 mg) plus panitumumab (Soto240), or investigator’s choice of trifluridine–tipiracil or regorafenib.
The December 2023 paper described improvements in median progression-free survival, progression or death, and objective response (OR). The authors described statistically significant improvements in disease progression or death in the Soto960 group (hazard ratio [HR], 0.49; P = .006) and the Soto240 group (HR, 0.58; P = .03). The objective response rate was highest in the Soto960 group (26.4%; 95% CI, 15.3%-40.3%), followed by the Soto240 group (5.7%; 95% CI, 1.2%-15.7%), and the control group (0%; 95% CI, 0.0%-6.6%). Grade 3 or higher treatment-related adverse events were generally similar at 35.8% (Soto960), 30.2% (Soto240), and 43.1% (control) in each group. The most common adverse events associated with sotorasib-panitumumab were skin-related toxicity and hypomagnesemia.
The new analysis showed that both doses of sotorasib also improved patient-reported outcomes from baseline to week 8, Dr. Modest, professor of medicine at Charité University of Medicine in Berlin, said at the meeting.
Compared with the chemotherapy group, there were statistically significant differences in least square mean change from baseline to week 8 for: pain at its worst in the Soto240 group (Brief Pain Inventory [BPI], –1.18; 95% CI, –2.05 to –0.32) and the Soto960 group (BPI, –1.49; 95% CI, –2.36 to –0.61); and physical functioning, as measured by the European Organisation for Research and Treatment of Cancer Core 30-item Quality of Life questionnaire, in the Soto240 (7.95; 95% CI, 2.39-13.51) and Soto960 (6.73; 95% CI, 1.05-12.41) groups. Nearly all other measures trended toward favoring the sotorasib/panitumumab groups, but did not reach statistical significance. A similar pattern was seen in time to deterioration measures. Among adverse events, diarrhea trended toward being more frequent in the intervention arms.
At week 9, 63% of patients in Soto960 and 84% in Soto240 reported improvement in the Patient Global Impression of Change score (PGI-C), versus 37% in the chemotherapy arm. At week 17, the percentages were 77%, 59%, and 21%, respectively.
“The clinical benefits and the better quality of life outcomes associated with sotorasib at the high dose of 960 milligrams plus panitumumab establishes this combination as a potential new standard [therapy] for patients with chemorefractory KRAS G12C mutant colorectal cancer, and I think it’s quite reassuring that even if you compare two active drugs versus one active drug, this does not necessarily translate into impaired quality of life assessments by the patients,” Dr. Modest said during his presentation.
CodeBreaK 300 may point the way to other dual therapies involving kinase inhibitors, according to Rona Yaeger, MD, who wrote an accompanying editorial to the NEJM paper. Dr. Yaeger noted that clinical and preclinical studies had shown that targeted oncogenes like KRAS G12C and BRAF V600E alone would be insufficient in colorectal cancer.
When combined with KRAS G12C inhibitors, EGFR inhibitors prevent EGFR from participating in negative feedback loops that can otherwise lead to drug resistance. “Whether targeting [receptor tyrosine kinases like EGFR] in epithelial tumors other than those associated with colorectal cancers would improve the incidence of response to KRAS G12C inhibitors remains unknown,” wrote Dr. Yaeger, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York. There is an ongoing clinical trial evaluating KRAS G12C inhibitors combined with EGFR antibodies in both lung and pancreatic cancer.
She noted that colorectal tumors have high levels of receptor tyrosine kinases, and argued that this will require higher doses of KRAS G12C inhibitors or novel drugs with higher activity. This is supported by the higher frequency of response and longer PFS at the higher dose in CodeBreaK 300, but could present a challenge: “Lowering the drug dose to manage toxic effects may limit the efficacy of the drug against some cancers,” she wrote.
Dr. Yaeger highlighted the KRYSTAL-10 phase 3 randomized trial, which is assessing the KRAS G12C inhibitor adagrasib in combination with the EGFR antibody cetuximab versus chemotherapy in advanced solid tumors with the KRAS G12C mutation.
“The CodeBreaK 300 trial is an exciting first step for targeting KRAS in colorectal cancer,” Dr. Yaeger wrote.
Dr. Modest has financial relationships with Amgen, AstraZeneca/MedImmune, Bristol-Myers Squibb, Incyte, Lily, Merck Serono, Merck Sharp & Dohme, Onkowissen, Pierre Fabre, Roche, and SERVIER. Dr. Yaeger has financial relationships with Amgen, Boehringer Ingelheim, Daiichi Sankyo, Mirati, Pfizer, and Zai Lab.
Dominik Modest, MD, presented these new results of the phase 3 CodeBreaK 300 trial at the 2024 ASCO Gastrointestinal Cancers Symposium.
The KRAS G12C mutation occurs in 3%-4% of metastatic colorectal cancer cases, according to Dr. Modest and the other authors of a paper published in the New England Journal of Medicine describing the primary outcome of the trial. The study included 160 patients who were randomized to once daily sotorasib (960 mg) plus panitumumab (Soto960), once daily sotorasib (240 mg) plus panitumumab (Soto240), or investigator’s choice of trifluridine–tipiracil or regorafenib.
The December 2023 paper described improvements in median progression-free survival, progression or death, and objective response (OR). The authors described statistically significant improvements in disease progression or death in the Soto960 group (hazard ratio [HR], 0.49; P = .006) and the Soto240 group (HR, 0.58; P = .03). The objective response rate was highest in the Soto960 group (26.4%; 95% CI, 15.3%-40.3%), followed by the Soto240 group (5.7%; 95% CI, 1.2%-15.7%), and the control group (0%; 95% CI, 0.0%-6.6%). Grade 3 or higher treatment-related adverse events were generally similar at 35.8% (Soto960), 30.2% (Soto240), and 43.1% (control) in each group. The most common adverse events associated with sotorasib-panitumumab were skin-related toxicity and hypomagnesemia.
The new analysis showed that both doses of sotorasib also improved patient-reported outcomes from baseline to week 8, Dr. Modest, professor of medicine at Charité University of Medicine in Berlin, said at the meeting.
Compared with the chemotherapy group, there were statistically significant differences in least square mean change from baseline to week 8 for: pain at its worst in the Soto240 group (Brief Pain Inventory [BPI], –1.18; 95% CI, –2.05 to –0.32) and the Soto960 group (BPI, –1.49; 95% CI, –2.36 to –0.61); and physical functioning, as measured by the European Organisation for Research and Treatment of Cancer Core 30-item Quality of Life questionnaire, in the Soto240 (7.95; 95% CI, 2.39-13.51) and Soto960 (6.73; 95% CI, 1.05-12.41) groups. Nearly all other measures trended toward favoring the sotorasib/panitumumab groups, but did not reach statistical significance. A similar pattern was seen in time to deterioration measures. Among adverse events, diarrhea trended toward being more frequent in the intervention arms.
At week 9, 63% of patients in Soto960 and 84% in Soto240 reported improvement in the Patient Global Impression of Change score (PGI-C), versus 37% in the chemotherapy arm. At week 17, the percentages were 77%, 59%, and 21%, respectively.
“The clinical benefits and the better quality of life outcomes associated with sotorasib at the high dose of 960 milligrams plus panitumumab establishes this combination as a potential new standard [therapy] for patients with chemorefractory KRAS G12C mutant colorectal cancer, and I think it’s quite reassuring that even if you compare two active drugs versus one active drug, this does not necessarily translate into impaired quality of life assessments by the patients,” Dr. Modest said during his presentation.
CodeBreaK 300 may point the way to other dual therapies involving kinase inhibitors, according to Rona Yaeger, MD, who wrote an accompanying editorial to the NEJM paper. Dr. Yaeger noted that clinical and preclinical studies had shown that targeted oncogenes like KRAS G12C and BRAF V600E alone would be insufficient in colorectal cancer.
When combined with KRAS G12C inhibitors, EGFR inhibitors prevent EGFR from participating in negative feedback loops that can otherwise lead to drug resistance. “Whether targeting [receptor tyrosine kinases like EGFR] in epithelial tumors other than those associated with colorectal cancers would improve the incidence of response to KRAS G12C inhibitors remains unknown,” wrote Dr. Yaeger, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York. There is an ongoing clinical trial evaluating KRAS G12C inhibitors combined with EGFR antibodies in both lung and pancreatic cancer.
She noted that colorectal tumors have high levels of receptor tyrosine kinases, and argued that this will require higher doses of KRAS G12C inhibitors or novel drugs with higher activity. This is supported by the higher frequency of response and longer PFS at the higher dose in CodeBreaK 300, but could present a challenge: “Lowering the drug dose to manage toxic effects may limit the efficacy of the drug against some cancers,” she wrote.
Dr. Yaeger highlighted the KRYSTAL-10 phase 3 randomized trial, which is assessing the KRAS G12C inhibitor adagrasib in combination with the EGFR antibody cetuximab versus chemotherapy in advanced solid tumors with the KRAS G12C mutation.
“The CodeBreaK 300 trial is an exciting first step for targeting KRAS in colorectal cancer,” Dr. Yaeger wrote.
Dr. Modest has financial relationships with Amgen, AstraZeneca/MedImmune, Bristol-Myers Squibb, Incyte, Lily, Merck Serono, Merck Sharp & Dohme, Onkowissen, Pierre Fabre, Roche, and SERVIER. Dr. Yaeger has financial relationships with Amgen, Boehringer Ingelheim, Daiichi Sankyo, Mirati, Pfizer, and Zai Lab.
FROM ASCO GI
Immunotherapy Combo Wins Big on PFS in First-Line Mets CRC
SAN FRANCISCO —
Findings from the CHECKMATE-8HW trial revealed that first-line nivolumab plus ipilimumab led to a significant improvement in progression-free survival (PFS) compared with chemotherapy among patients with metastatic CRC.
More specifically, at 2 years, PFS was 72% among patients with microsatellite instability–high (MSI-H) or deficient mismatch repair (dMMR) randomized to the immunotherapy combination compared with just 14% among those randomized to chemotherapy with or without targeted therapy.
The magnitude of the benefit was unexpected, especially considering patients received only four cycles of the immunotherapy combination in the trial. “It’s a good surprise,” said lead investigator Thierry Andre, MD, who presented the findings at the 2024 ASCO Gastrointestinal Cancers Symposium.
The findings indicate that nivolumab plus ipilimumab should really be “a new standard,” said Andre, a medical oncologist at Sorbonne University, Paris.
The combination as well as nivolumab alone has received US Food and Drug Administration’s (FDA’s) approval to treat MSI-H or dMMR metastatic CRC in the second line, following chemotherapy failure.
The FDA also approved pembrolizumab as first-line monotherapy for this CRC indication in 2020. The KEYNOTE-177 trial, which led to the pembrolizumab approval, reported a 2-year PFS of 48% among patients receiving the monotherapy. Andre was the lead investigator on KEYNOTE-177.
To compare PFS results for pembrolizumab and nivolumab alone, the CHECKMATE-8HW trial included a nivolumab monotherapy arm, but these results are pending, as are the overall survival findings, Andre said.
Overall, CHECKMATE-8HW must be taken into context with KEYNOTE-177, and “we need a little bit more trial data” for oncologists to decide between the two options, said Neil Newman, MD, a radiation oncologist at the University of Texas Health Science Center, San Antonio, Texas, who co-moderated Dr. Andre’s presentation.
Andre noted, however, that if the nivolumab and pembrolizumab monotherapy results are similar, most patients will likely receive the nivolumab/ipilimumab combination, given the improved PFS outcomes.
In CHECKMATE-8HW, patients were randomized to three regimens. The 202 patients in the combination arm received nivolumab 240 mg plus ipilimumab 1 mg/kg every 3 weeks for four doses, followed by nivolumab 480 mg every 4 weeks. The 101 patients in the chemotherapy group received investigator’s choice of mFOLFOX6 or FOLFIRI with or without bevacizumab or cetuximab. And the nivolumab monotherapy arm received nivolumab 240 mg every 2 weeks for six doses, followed by nivolumab 480 mg every 4 weeks.
Treatment continued until disease progression or unacceptable toxicity over a maximum of 2 years. The median duration of treatment was 13.5 months in the nivolumab/ipilimumab arm vs 4 months in the chemotherapy arm.
PFS curves started to separate between nivolumab/ipilimumab and chemotherapy at about 3 months.
Patients receiving the combination exhibited a 79% reduction in the risk for disease progression or death at 2 years (72% vs 14%; hazard ratio, 0.21; P < .0001). The median PFS was not reached with the combination vs 5.9 months with chemotherapy. The PFS benefit of nivolumab/ipilimumab held across various subgroups, including patients with KRAS or NRAS mutations and baseline lung, liver, or peritoneal metastases.
The incidence of grade 3/4 treatment-related adverse events was 23% with nivolumab/ipilimumab vs 48% in the chemotherapy arm. The most common grade 3/4 events with nivolumab/ipilimumab were diarrhea/colitis (5%), adrenal insufficiency (4%), hepatitis (3%), and inflammation of the pituitary gland (3%).
Two treatment-related deaths occurred in the combination arm — one from pneumonitis and the second from myocarditis — and none occurred in the chemotherapy arm.
Mark A. Lewis, MD, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, was impressed with the CHECKMATE-8HW findings. The data are shaping up to make nivolumab/ipilimumab “the next great step in metastatic CRC management beyond KEYNOTE-177,” Dr. Lewis said.
Dr. Lewis noted that the new trial makes it “imperative” to standardize testing for immunotherapy candidacy upfront. “It is completely unacceptable for any patient with metastatic CRC to not have their MMR/MSI status assessed,” he said. “Much as no oncologist would dare treat breast cancer without testing ER, PR, HER2 status, biomarkers cannot be a later-line afterthought in stage IV CRC.”
Drugmaker Bristol-Myers Squibb told this news organization that the company will be seeking a first-line indication for the combination, and anticipates approval early next year or possibly sooner, if the FDA grants a priority review.
The work was funded by Bristol-Myers Squibb and the ONO Pharmaceutical Company. Dr. Andre had numerous industry ties, including being a consultant for both BMS and Merck. He also reported honoraria from both companies. Dr. Newman and Dr. Lewis didn’t have any disclosures.
A version of this article appeared on Medscape.com.
SAN FRANCISCO —
Findings from the CHECKMATE-8HW trial revealed that first-line nivolumab plus ipilimumab led to a significant improvement in progression-free survival (PFS) compared with chemotherapy among patients with metastatic CRC.
More specifically, at 2 years, PFS was 72% among patients with microsatellite instability–high (MSI-H) or deficient mismatch repair (dMMR) randomized to the immunotherapy combination compared with just 14% among those randomized to chemotherapy with or without targeted therapy.
The magnitude of the benefit was unexpected, especially considering patients received only four cycles of the immunotherapy combination in the trial. “It’s a good surprise,” said lead investigator Thierry Andre, MD, who presented the findings at the 2024 ASCO Gastrointestinal Cancers Symposium.
The findings indicate that nivolumab plus ipilimumab should really be “a new standard,” said Andre, a medical oncologist at Sorbonne University, Paris.
The combination as well as nivolumab alone has received US Food and Drug Administration’s (FDA’s) approval to treat MSI-H or dMMR metastatic CRC in the second line, following chemotherapy failure.
The FDA also approved pembrolizumab as first-line monotherapy for this CRC indication in 2020. The KEYNOTE-177 trial, which led to the pembrolizumab approval, reported a 2-year PFS of 48% among patients receiving the monotherapy. Andre was the lead investigator on KEYNOTE-177.
To compare PFS results for pembrolizumab and nivolumab alone, the CHECKMATE-8HW trial included a nivolumab monotherapy arm, but these results are pending, as are the overall survival findings, Andre said.
Overall, CHECKMATE-8HW must be taken into context with KEYNOTE-177, and “we need a little bit more trial data” for oncologists to decide between the two options, said Neil Newman, MD, a radiation oncologist at the University of Texas Health Science Center, San Antonio, Texas, who co-moderated Dr. Andre’s presentation.
Andre noted, however, that if the nivolumab and pembrolizumab monotherapy results are similar, most patients will likely receive the nivolumab/ipilimumab combination, given the improved PFS outcomes.
In CHECKMATE-8HW, patients were randomized to three regimens. The 202 patients in the combination arm received nivolumab 240 mg plus ipilimumab 1 mg/kg every 3 weeks for four doses, followed by nivolumab 480 mg every 4 weeks. The 101 patients in the chemotherapy group received investigator’s choice of mFOLFOX6 or FOLFIRI with or without bevacizumab or cetuximab. And the nivolumab monotherapy arm received nivolumab 240 mg every 2 weeks for six doses, followed by nivolumab 480 mg every 4 weeks.
Treatment continued until disease progression or unacceptable toxicity over a maximum of 2 years. The median duration of treatment was 13.5 months in the nivolumab/ipilimumab arm vs 4 months in the chemotherapy arm.
PFS curves started to separate between nivolumab/ipilimumab and chemotherapy at about 3 months.
Patients receiving the combination exhibited a 79% reduction in the risk for disease progression or death at 2 years (72% vs 14%; hazard ratio, 0.21; P < .0001). The median PFS was not reached with the combination vs 5.9 months with chemotherapy. The PFS benefit of nivolumab/ipilimumab held across various subgroups, including patients with KRAS or NRAS mutations and baseline lung, liver, or peritoneal metastases.
The incidence of grade 3/4 treatment-related adverse events was 23% with nivolumab/ipilimumab vs 48% in the chemotherapy arm. The most common grade 3/4 events with nivolumab/ipilimumab were diarrhea/colitis (5%), adrenal insufficiency (4%), hepatitis (3%), and inflammation of the pituitary gland (3%).
Two treatment-related deaths occurred in the combination arm — one from pneumonitis and the second from myocarditis — and none occurred in the chemotherapy arm.
Mark A. Lewis, MD, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, was impressed with the CHECKMATE-8HW findings. The data are shaping up to make nivolumab/ipilimumab “the next great step in metastatic CRC management beyond KEYNOTE-177,” Dr. Lewis said.
Dr. Lewis noted that the new trial makes it “imperative” to standardize testing for immunotherapy candidacy upfront. “It is completely unacceptable for any patient with metastatic CRC to not have their MMR/MSI status assessed,” he said. “Much as no oncologist would dare treat breast cancer without testing ER, PR, HER2 status, biomarkers cannot be a later-line afterthought in stage IV CRC.”
Drugmaker Bristol-Myers Squibb told this news organization that the company will be seeking a first-line indication for the combination, and anticipates approval early next year or possibly sooner, if the FDA grants a priority review.
The work was funded by Bristol-Myers Squibb and the ONO Pharmaceutical Company. Dr. Andre had numerous industry ties, including being a consultant for both BMS and Merck. He also reported honoraria from both companies. Dr. Newman and Dr. Lewis didn’t have any disclosures.
A version of this article appeared on Medscape.com.
SAN FRANCISCO —
Findings from the CHECKMATE-8HW trial revealed that first-line nivolumab plus ipilimumab led to a significant improvement in progression-free survival (PFS) compared with chemotherapy among patients with metastatic CRC.
More specifically, at 2 years, PFS was 72% among patients with microsatellite instability–high (MSI-H) or deficient mismatch repair (dMMR) randomized to the immunotherapy combination compared with just 14% among those randomized to chemotherapy with or without targeted therapy.
The magnitude of the benefit was unexpected, especially considering patients received only four cycles of the immunotherapy combination in the trial. “It’s a good surprise,” said lead investigator Thierry Andre, MD, who presented the findings at the 2024 ASCO Gastrointestinal Cancers Symposium.
The findings indicate that nivolumab plus ipilimumab should really be “a new standard,” said Andre, a medical oncologist at Sorbonne University, Paris.
The combination as well as nivolumab alone has received US Food and Drug Administration’s (FDA’s) approval to treat MSI-H or dMMR metastatic CRC in the second line, following chemotherapy failure.
The FDA also approved pembrolizumab as first-line monotherapy for this CRC indication in 2020. The KEYNOTE-177 trial, which led to the pembrolizumab approval, reported a 2-year PFS of 48% among patients receiving the monotherapy. Andre was the lead investigator on KEYNOTE-177.
To compare PFS results for pembrolizumab and nivolumab alone, the CHECKMATE-8HW trial included a nivolumab monotherapy arm, but these results are pending, as are the overall survival findings, Andre said.
Overall, CHECKMATE-8HW must be taken into context with KEYNOTE-177, and “we need a little bit more trial data” for oncologists to decide between the two options, said Neil Newman, MD, a radiation oncologist at the University of Texas Health Science Center, San Antonio, Texas, who co-moderated Dr. Andre’s presentation.
Andre noted, however, that if the nivolumab and pembrolizumab monotherapy results are similar, most patients will likely receive the nivolumab/ipilimumab combination, given the improved PFS outcomes.
In CHECKMATE-8HW, patients were randomized to three regimens. The 202 patients in the combination arm received nivolumab 240 mg plus ipilimumab 1 mg/kg every 3 weeks for four doses, followed by nivolumab 480 mg every 4 weeks. The 101 patients in the chemotherapy group received investigator’s choice of mFOLFOX6 or FOLFIRI with or without bevacizumab or cetuximab. And the nivolumab monotherapy arm received nivolumab 240 mg every 2 weeks for six doses, followed by nivolumab 480 mg every 4 weeks.
Treatment continued until disease progression or unacceptable toxicity over a maximum of 2 years. The median duration of treatment was 13.5 months in the nivolumab/ipilimumab arm vs 4 months in the chemotherapy arm.
PFS curves started to separate between nivolumab/ipilimumab and chemotherapy at about 3 months.
Patients receiving the combination exhibited a 79% reduction in the risk for disease progression or death at 2 years (72% vs 14%; hazard ratio, 0.21; P < .0001). The median PFS was not reached with the combination vs 5.9 months with chemotherapy. The PFS benefit of nivolumab/ipilimumab held across various subgroups, including patients with KRAS or NRAS mutations and baseline lung, liver, or peritoneal metastases.
The incidence of grade 3/4 treatment-related adverse events was 23% with nivolumab/ipilimumab vs 48% in the chemotherapy arm. The most common grade 3/4 events with nivolumab/ipilimumab were diarrhea/colitis (5%), adrenal insufficiency (4%), hepatitis (3%), and inflammation of the pituitary gland (3%).
Two treatment-related deaths occurred in the combination arm — one from pneumonitis and the second from myocarditis — and none occurred in the chemotherapy arm.
Mark A. Lewis, MD, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, was impressed with the CHECKMATE-8HW findings. The data are shaping up to make nivolumab/ipilimumab “the next great step in metastatic CRC management beyond KEYNOTE-177,” Dr. Lewis said.
Dr. Lewis noted that the new trial makes it “imperative” to standardize testing for immunotherapy candidacy upfront. “It is completely unacceptable for any patient with metastatic CRC to not have their MMR/MSI status assessed,” he said. “Much as no oncologist would dare treat breast cancer without testing ER, PR, HER2 status, biomarkers cannot be a later-line afterthought in stage IV CRC.”
Drugmaker Bristol-Myers Squibb told this news organization that the company will be seeking a first-line indication for the combination, and anticipates approval early next year or possibly sooner, if the FDA grants a priority review.
The work was funded by Bristol-Myers Squibb and the ONO Pharmaceutical Company. Dr. Andre had numerous industry ties, including being a consultant for both BMS and Merck. He also reported honoraria from both companies. Dr. Newman and Dr. Lewis didn’t have any disclosures.
A version of this article appeared on Medscape.com.
FROM ASCO-GI 2024
Corticosteroid Injections Don’t Move Blood Sugar for Most
TOPLINE:
Intra-articular corticosteroid (IACS) injections pose a minimal risk of accelerating diabetes for most people, despite temporarily elevating blood glucose levels, according to a study published in Clinical Diabetes.
METHODOLOGY:
- Almost half of Americans with diabetes have arthritis, so glycemic control is a concern for many receiving IACS injections.
- IACS injections are known to cause short-term hyperglycemia, but their long-term effects on glycemic control are not well studied.
- For the retrospective cohort study, researchers at Mayo Clinic in Rochester, Minnesota, used electronic health records from 1169 adults who had received an IACS injection in one large joint between 2012 and 2018.
- They analyzed data on A1C levels for study participants from 18 months before and after the injections.
- Researchers assessed if participants had a greater-than-expected (defined as an increase of more than 0.5% above expected) concentration of A1C after the injection, and examined rates of diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome in the 30 days following an injection.
TAKEAWAY:
- Nearly 16% of people experienced a greater-than-expected A1C level after receiving an injection.
- A1C levels rose by an average of 1.2% in the greater-than-expected group, but decreased by an average of 0.2% in the average group.
- One patient had an episode of severe hyperglycemia that was linked to the injection.
- A baseline level of A1C above 8% was the only factor associated with a greater-than-expected increase in the marker after an IACS injection.
IN PRACTICE:
“Although most patients do not experience an increase in A1C after IACS, clinicians should counsel patients with suboptimally controlled diabetes about risks of further hyperglycemia after IACS administration,” the researchers wrote.
SOURCE:
The study was led by Terin T. Sytsma, MD, of Mayo Clinic in Rochester, Minnesota.
LIMITATIONS:
The study was retrospective and could not establish causation. In addition, the population was of residents from one county in Minnesota, and was not racially or ethnically diverse. Details about the injection, such as location and total dose, were not available. The study also did not include a control group.
DISCLOSURES:
The study was funded by Mayo Clinic and the National Center for Advancing Translational Sciences. The authors reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
Intra-articular corticosteroid (IACS) injections pose a minimal risk of accelerating diabetes for most people, despite temporarily elevating blood glucose levels, according to a study published in Clinical Diabetes.
METHODOLOGY:
- Almost half of Americans with diabetes have arthritis, so glycemic control is a concern for many receiving IACS injections.
- IACS injections are known to cause short-term hyperglycemia, but their long-term effects on glycemic control are not well studied.
- For the retrospective cohort study, researchers at Mayo Clinic in Rochester, Minnesota, used electronic health records from 1169 adults who had received an IACS injection in one large joint between 2012 and 2018.
- They analyzed data on A1C levels for study participants from 18 months before and after the injections.
- Researchers assessed if participants had a greater-than-expected (defined as an increase of more than 0.5% above expected) concentration of A1C after the injection, and examined rates of diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome in the 30 days following an injection.
TAKEAWAY:
- Nearly 16% of people experienced a greater-than-expected A1C level after receiving an injection.
- A1C levels rose by an average of 1.2% in the greater-than-expected group, but decreased by an average of 0.2% in the average group.
- One patient had an episode of severe hyperglycemia that was linked to the injection.
- A baseline level of A1C above 8% was the only factor associated with a greater-than-expected increase in the marker after an IACS injection.
IN PRACTICE:
“Although most patients do not experience an increase in A1C after IACS, clinicians should counsel patients with suboptimally controlled diabetes about risks of further hyperglycemia after IACS administration,” the researchers wrote.
SOURCE:
The study was led by Terin T. Sytsma, MD, of Mayo Clinic in Rochester, Minnesota.
LIMITATIONS:
The study was retrospective and could not establish causation. In addition, the population was of residents from one county in Minnesota, and was not racially or ethnically diverse. Details about the injection, such as location and total dose, were not available. The study also did not include a control group.
DISCLOSURES:
The study was funded by Mayo Clinic and the National Center for Advancing Translational Sciences. The authors reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
Intra-articular corticosteroid (IACS) injections pose a minimal risk of accelerating diabetes for most people, despite temporarily elevating blood glucose levels, according to a study published in Clinical Diabetes.
METHODOLOGY:
- Almost half of Americans with diabetes have arthritis, so glycemic control is a concern for many receiving IACS injections.
- IACS injections are known to cause short-term hyperglycemia, but their long-term effects on glycemic control are not well studied.
- For the retrospective cohort study, researchers at Mayo Clinic in Rochester, Minnesota, used electronic health records from 1169 adults who had received an IACS injection in one large joint between 2012 and 2018.
- They analyzed data on A1C levels for study participants from 18 months before and after the injections.
- Researchers assessed if participants had a greater-than-expected (defined as an increase of more than 0.5% above expected) concentration of A1C after the injection, and examined rates of diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome in the 30 days following an injection.
TAKEAWAY:
- Nearly 16% of people experienced a greater-than-expected A1C level after receiving an injection.
- A1C levels rose by an average of 1.2% in the greater-than-expected group, but decreased by an average of 0.2% in the average group.
- One patient had an episode of severe hyperglycemia that was linked to the injection.
- A baseline level of A1C above 8% was the only factor associated with a greater-than-expected increase in the marker after an IACS injection.
IN PRACTICE:
“Although most patients do not experience an increase in A1C after IACS, clinicians should counsel patients with suboptimally controlled diabetes about risks of further hyperglycemia after IACS administration,” the researchers wrote.
SOURCE:
The study was led by Terin T. Sytsma, MD, of Mayo Clinic in Rochester, Minnesota.
LIMITATIONS:
The study was retrospective and could not establish causation. In addition, the population was of residents from one county in Minnesota, and was not racially or ethnically diverse. Details about the injection, such as location and total dose, were not available. The study also did not include a control group.
DISCLOSURES:
The study was funded by Mayo Clinic and the National Center for Advancing Translational Sciences. The authors reported no relevant disclosures.
A version of this article first appeared on Medscape.com.

